User login
The Hospitalist only
Medicare fines half of hospitals for readmitting too many patients
Nearly half the nation’s hospitals, many of which are still wrestling with the financial fallout of the unexpected coronavirus, will get lower payments for all Medicare patients because of their history of readmitting patients, federal records show.
The penalties are the ninth annual round of the Hospital Readmissions Reduction Program created as part of the Affordable Care Act’s broader effort to improve quality and lower costs. The latest penalties are calculated using each hospital case history between July 2016 and June 2019, so the flood of coronavirus patients that have swamped hospitals this year were not included.
The Centers for Medicare & Medicaid Services announced in September it may suspend the penalty program in the future if the chaos surrounding the pandemic, including the spring’s moratorium on elective surgeries, makes it too difficult to assess hospital performance.
For this year, the penalties remain in effect. Retroactive to the federal fiscal year that began Oct. 1, Medicare will lower a year’s worth of payments to 2,545 hospitals, the data show. The average reduction is 0.69%, with 613 hospitals receiving a penalty of 1% or more.
Out of 5,267 hospitals in the country, Congress has exempted 2,176 from the threat of penalties, either because they are critical access hospitals – defined as the only inpatient facility in an area – or hospitals that specialize in psychiatric patients, children, veterans, rehabilitation or long-term care. Of the 3,080 hospitals CMS evaluated, 83% received a penalty.
The number and severity of penalties were comparable to those of recent years, although the number of hospitals receiving the maximum penalty of 3% dropped from 56 to 39. Because the penalties are applied to new admission payments, the total dollar amount each hospital will lose will not be known until after the fiscal year ends on July 30.
“It’s unfortunate that hospitals will face readmission penalties in fiscal year 2021,” said Akin Demehin, director of policy at the American Hospital Association. “Given the financial strain that hospitals are under, every dollar counts, and the impact of any penalty is significant.”
The penalties are based on readmissions of Medicare patients who initially came to the hospital with diagnoses of congestive heart failure, heart attack, pneumonia, chronic obstructive pulmonary disease, hip or knee replacement, or coronary artery bypass graft surgery. Medicare counts as a readmission any of those patients who ended up back in any hospital within 30 days of discharge, except for planned returns like a second phase of surgery.
A hospital will be penalized if its readmission rate is higher than expected given the national trends in any one of those categories.
The industry has disapproved of the program since its inception, complaining the measures aren’t precise and it unfairly punishes hospitals that treat low-income patients, who often don’t have the resources to ensure their recoveries are successful.
Michael Millenson, a health quality consultant who focuses on patient safety, said the penalties are a useful but imperfect mechanism to push hospitals to improve their care. The designers of the penalty system envisioned it as a way to neutralize the economic benefit hospitals get from readmitted patients under Medicare’s fee-for-service payment model, as they are otherwise paid for two stays instead of just one.
“Every industry complains the penalties are too harsh,” he said. “if you’re going to tell me we don’t need any economic incentives to do the right thing because we’re always doing the right thing – that’s not true.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Nearly half the nation’s hospitals, many of which are still wrestling with the financial fallout of the unexpected coronavirus, will get lower payments for all Medicare patients because of their history of readmitting patients, federal records show.
The penalties are the ninth annual round of the Hospital Readmissions Reduction Program created as part of the Affordable Care Act’s broader effort to improve quality and lower costs. The latest penalties are calculated using each hospital case history between July 2016 and June 2019, so the flood of coronavirus patients that have swamped hospitals this year were not included.
The Centers for Medicare & Medicaid Services announced in September it may suspend the penalty program in the future if the chaos surrounding the pandemic, including the spring’s moratorium on elective surgeries, makes it too difficult to assess hospital performance.
For this year, the penalties remain in effect. Retroactive to the federal fiscal year that began Oct. 1, Medicare will lower a year’s worth of payments to 2,545 hospitals, the data show. The average reduction is 0.69%, with 613 hospitals receiving a penalty of 1% or more.
Out of 5,267 hospitals in the country, Congress has exempted 2,176 from the threat of penalties, either because they are critical access hospitals – defined as the only inpatient facility in an area – or hospitals that specialize in psychiatric patients, children, veterans, rehabilitation or long-term care. Of the 3,080 hospitals CMS evaluated, 83% received a penalty.
The number and severity of penalties were comparable to those of recent years, although the number of hospitals receiving the maximum penalty of 3% dropped from 56 to 39. Because the penalties are applied to new admission payments, the total dollar amount each hospital will lose will not be known until after the fiscal year ends on July 30.
“It’s unfortunate that hospitals will face readmission penalties in fiscal year 2021,” said Akin Demehin, director of policy at the American Hospital Association. “Given the financial strain that hospitals are under, every dollar counts, and the impact of any penalty is significant.”
The penalties are based on readmissions of Medicare patients who initially came to the hospital with diagnoses of congestive heart failure, heart attack, pneumonia, chronic obstructive pulmonary disease, hip or knee replacement, or coronary artery bypass graft surgery. Medicare counts as a readmission any of those patients who ended up back in any hospital within 30 days of discharge, except for planned returns like a second phase of surgery.
A hospital will be penalized if its readmission rate is higher than expected given the national trends in any one of those categories.
The industry has disapproved of the program since its inception, complaining the measures aren’t precise and it unfairly punishes hospitals that treat low-income patients, who often don’t have the resources to ensure their recoveries are successful.
Michael Millenson, a health quality consultant who focuses on patient safety, said the penalties are a useful but imperfect mechanism to push hospitals to improve their care. The designers of the penalty system envisioned it as a way to neutralize the economic benefit hospitals get from readmitted patients under Medicare’s fee-for-service payment model, as they are otherwise paid for two stays instead of just one.
“Every industry complains the penalties are too harsh,” he said. “if you’re going to tell me we don’t need any economic incentives to do the right thing because we’re always doing the right thing – that’s not true.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Nearly half the nation’s hospitals, many of which are still wrestling with the financial fallout of the unexpected coronavirus, will get lower payments for all Medicare patients because of their history of readmitting patients, federal records show.
The penalties are the ninth annual round of the Hospital Readmissions Reduction Program created as part of the Affordable Care Act’s broader effort to improve quality and lower costs. The latest penalties are calculated using each hospital case history between July 2016 and June 2019, so the flood of coronavirus patients that have swamped hospitals this year were not included.
The Centers for Medicare & Medicaid Services announced in September it may suspend the penalty program in the future if the chaos surrounding the pandemic, including the spring’s moratorium on elective surgeries, makes it too difficult to assess hospital performance.
For this year, the penalties remain in effect. Retroactive to the federal fiscal year that began Oct. 1, Medicare will lower a year’s worth of payments to 2,545 hospitals, the data show. The average reduction is 0.69%, with 613 hospitals receiving a penalty of 1% or more.
Out of 5,267 hospitals in the country, Congress has exempted 2,176 from the threat of penalties, either because they are critical access hospitals – defined as the only inpatient facility in an area – or hospitals that specialize in psychiatric patients, children, veterans, rehabilitation or long-term care. Of the 3,080 hospitals CMS evaluated, 83% received a penalty.
The number and severity of penalties were comparable to those of recent years, although the number of hospitals receiving the maximum penalty of 3% dropped from 56 to 39. Because the penalties are applied to new admission payments, the total dollar amount each hospital will lose will not be known until after the fiscal year ends on July 30.
“It’s unfortunate that hospitals will face readmission penalties in fiscal year 2021,” said Akin Demehin, director of policy at the American Hospital Association. “Given the financial strain that hospitals are under, every dollar counts, and the impact of any penalty is significant.”
The penalties are based on readmissions of Medicare patients who initially came to the hospital with diagnoses of congestive heart failure, heart attack, pneumonia, chronic obstructive pulmonary disease, hip or knee replacement, or coronary artery bypass graft surgery. Medicare counts as a readmission any of those patients who ended up back in any hospital within 30 days of discharge, except for planned returns like a second phase of surgery.
A hospital will be penalized if its readmission rate is higher than expected given the national trends in any one of those categories.
The industry has disapproved of the program since its inception, complaining the measures aren’t precise and it unfairly punishes hospitals that treat low-income patients, who often don’t have the resources to ensure their recoveries are successful.
Michael Millenson, a health quality consultant who focuses on patient safety, said the penalties are a useful but imperfect mechanism to push hospitals to improve their care. The designers of the penalty system envisioned it as a way to neutralize the economic benefit hospitals get from readmitted patients under Medicare’s fee-for-service payment model, as they are otherwise paid for two stays instead of just one.
“Every industry complains the penalties are too harsh,” he said. “if you’re going to tell me we don’t need any economic incentives to do the right thing because we’re always doing the right thing – that’s not true.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Health sector has spent $464 million on lobbying in 2020
, according to the Center for Responsive Politics.

PhRMA spent $20.7 million on lobbying through the end of September, good enough for third on the overall list of U.S. companies and organizations. Three other members of the health sector made the top 10: the American Hospital Association ($18.3 million), BlueCross/BlueShield ($16.3 million), and the American Medical Association ($15.2 million), the center reported.
Total spending by the health sector was $464 million from Jan. 1 to Sept. 30, topping the finance/insurance/real estate sector at $403 million, and miscellaneous business at $371 million. Miscellaneous business is the home of the U.S. Chamber of Commerce, the annual leader in such spending for the last 20 years, based on data from the Senate Office of Public Records.
The largest share of health sector spending came from pharmaceuticals/health products, with a total of almost $233 million, just slightly more than the sector’s four other constituents combined: hospitals/nursing homes ($80 million), health services/HMOs ($75 million), health professionals ($67 million), and miscellaneous health ($9.5 million), the center said on OpenSecrets.org.
Taking one step down from the sector level, that $233 million made pharmaceuticals/health products the highest spending of about 100 industries in 2020, nearly doubling the efforts of electronics manufacturing and equipment ($118 million), which came a distant second. Hospitals/nursing homes was eighth on the industry list, the center noted.
, according to the Center for Responsive Politics.

PhRMA spent $20.7 million on lobbying through the end of September, good enough for third on the overall list of U.S. companies and organizations. Three other members of the health sector made the top 10: the American Hospital Association ($18.3 million), BlueCross/BlueShield ($16.3 million), and the American Medical Association ($15.2 million), the center reported.
Total spending by the health sector was $464 million from Jan. 1 to Sept. 30, topping the finance/insurance/real estate sector at $403 million, and miscellaneous business at $371 million. Miscellaneous business is the home of the U.S. Chamber of Commerce, the annual leader in such spending for the last 20 years, based on data from the Senate Office of Public Records.
The largest share of health sector spending came from pharmaceuticals/health products, with a total of almost $233 million, just slightly more than the sector’s four other constituents combined: hospitals/nursing homes ($80 million), health services/HMOs ($75 million), health professionals ($67 million), and miscellaneous health ($9.5 million), the center said on OpenSecrets.org.
Taking one step down from the sector level, that $233 million made pharmaceuticals/health products the highest spending of about 100 industries in 2020, nearly doubling the efforts of electronics manufacturing and equipment ($118 million), which came a distant second. Hospitals/nursing homes was eighth on the industry list, the center noted.
, according to the Center for Responsive Politics.

PhRMA spent $20.7 million on lobbying through the end of September, good enough for third on the overall list of U.S. companies and organizations. Three other members of the health sector made the top 10: the American Hospital Association ($18.3 million), BlueCross/BlueShield ($16.3 million), and the American Medical Association ($15.2 million), the center reported.
Total spending by the health sector was $464 million from Jan. 1 to Sept. 30, topping the finance/insurance/real estate sector at $403 million, and miscellaneous business at $371 million. Miscellaneous business is the home of the U.S. Chamber of Commerce, the annual leader in such spending for the last 20 years, based on data from the Senate Office of Public Records.
The largest share of health sector spending came from pharmaceuticals/health products, with a total of almost $233 million, just slightly more than the sector’s four other constituents combined: hospitals/nursing homes ($80 million), health services/HMOs ($75 million), health professionals ($67 million), and miscellaneous health ($9.5 million), the center said on OpenSecrets.org.
Taking one step down from the sector level, that $233 million made pharmaceuticals/health products the highest spending of about 100 industries in 2020, nearly doubling the efforts of electronics manufacturing and equipment ($118 million), which came a distant second. Hospitals/nursing homes was eighth on the industry list, the center noted.
Physician burnout costly to organizations and U.S. health system
Background: Occupational burnout is more prevalent among physicians than among the general population, and physician burnout is associated with several negative clinical outcomes. However, little is known about the economic cost of this widespread issue.
Study design: Cost-consequence analysis using a novel mathematical model.
Setting: Simulated population of U.S. physicians.
Synopsis: Researchers conducted a cost-consequence analysis using a mathematical model designed to determine the financial impact of burnout – or the difference in observed cost and the theoretical cost if physicians did not experience burnout. The model used a hypothetical physician population based on a 2013 profile of U.S. physicians, a 2014 survey of physicians that assessed burnout, and preexisting literature on burnout to generate the input data for their model. The investigators focused on two outcomes: turnover and reduction in clinical hours. They found that approximately $4.6 billion per year is lost in direct cost secondary to physician burnout, with the greatest proportion coming from physician turnover. The figure ranged from $2.6 billion to $6.3 billion in multivariate sensitivity analysis. For an organization, the cost of burnout is about $7,600 per physician per year, with a range of $4,100 to $10,200. Though statistical modeling can be imprecise, and the input data were imperfect, the study was the first to examine the systemwide cost of physician burnout in the United States.
Bottom line: Along with the negative effects on physician and patient well-being, physician burnout is financially costly to the U.S. health care system and to individual organizations. Programs to reduce burnout could be both ethically and economically advantageous.
Citation: Han S et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784-90.
Dr. Suojanen is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Occupational burnout is more prevalent among physicians than among the general population, and physician burnout is associated with several negative clinical outcomes. However, little is known about the economic cost of this widespread issue.
Study design: Cost-consequence analysis using a novel mathematical model.
Setting: Simulated population of U.S. physicians.
Synopsis: Researchers conducted a cost-consequence analysis using a mathematical model designed to determine the financial impact of burnout – or the difference in observed cost and the theoretical cost if physicians did not experience burnout. The model used a hypothetical physician population based on a 2013 profile of U.S. physicians, a 2014 survey of physicians that assessed burnout, and preexisting literature on burnout to generate the input data for their model. The investigators focused on two outcomes: turnover and reduction in clinical hours. They found that approximately $4.6 billion per year is lost in direct cost secondary to physician burnout, with the greatest proportion coming from physician turnover. The figure ranged from $2.6 billion to $6.3 billion in multivariate sensitivity analysis. For an organization, the cost of burnout is about $7,600 per physician per year, with a range of $4,100 to $10,200. Though statistical modeling can be imprecise, and the input data were imperfect, the study was the first to examine the systemwide cost of physician burnout in the United States.
Bottom line: Along with the negative effects on physician and patient well-being, physician burnout is financially costly to the U.S. health care system and to individual organizations. Programs to reduce burnout could be both ethically and economically advantageous.
Citation: Han S et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784-90.
Dr. Suojanen is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Occupational burnout is more prevalent among physicians than among the general population, and physician burnout is associated with several negative clinical outcomes. However, little is known about the economic cost of this widespread issue.
Study design: Cost-consequence analysis using a novel mathematical model.
Setting: Simulated population of U.S. physicians.
Synopsis: Researchers conducted a cost-consequence analysis using a mathematical model designed to determine the financial impact of burnout – or the difference in observed cost and the theoretical cost if physicians did not experience burnout. The model used a hypothetical physician population based on a 2013 profile of U.S. physicians, a 2014 survey of physicians that assessed burnout, and preexisting literature on burnout to generate the input data for their model. The investigators focused on two outcomes: turnover and reduction in clinical hours. They found that approximately $4.6 billion per year is lost in direct cost secondary to physician burnout, with the greatest proportion coming from physician turnover. The figure ranged from $2.6 billion to $6.3 billion in multivariate sensitivity analysis. For an organization, the cost of burnout is about $7,600 per physician per year, with a range of $4,100 to $10,200. Though statistical modeling can be imprecise, and the input data were imperfect, the study was the first to examine the systemwide cost of physician burnout in the United States.
Bottom line: Along with the negative effects on physician and patient well-being, physician burnout is financially costly to the U.S. health care system and to individual organizations. Programs to reduce burnout could be both ethically and economically advantageous.
Citation: Han S et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784-90.
Dr. Suojanen is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Health care workers implore OSHA for more oversight on COVID-19 safety
Last spring, when Cliff Willmeng, RN, was working at United Hospital in St. Paul, Minnesota, he’d take off his personal protective equipment (PPE) in the same hallway where children were transported from ambulances to the neighboring Children’s Hospital emergency department. Stretchers would roll across red tape on the floor that designated the area as a “hot zone.” The door from a break room was about 10 feet away.
Willmeng has been a union activist all his life, but he’d never filed a complaint with the Occupational Safety and Health Administration (OSHA) until the COVID-19 pandemic hit.
Concerned about the inadequate space for doffing PPE and other situations in which the spread of SARS-CoV-2 seemed possible, Willmeng and other colleagues filed multiple OSHA complaints with the Minnesota Department of Labor in March and April. Willmeng was also worried about bringing SARS-CoV-2 on his scrubs home to his wife and kids, and he started wearing hospital-supplied scrubs that were meant for doctors and that were washed on site, which was against hospital policy. The hospital fired Willmeng on May 8, citing code of conduct and respectful workplace violations arising from the uniform dispute.
In August, the state agency issued Willmeng’s hospital a $2,100 fine for failure to comply with guidance regarding “respiratory protection” in response to worker complaints over the fact that they were instructed to restaple elastic bands on N95 masks early in the pandemic. In a statement, United Hospital said it contested the citation, and it is in discussions with Minnesota OSHA. “We have and continue to instruct employees not to alter N95 respirators or reuse damaged or soiled N95 respirators,” such as when the straps are broken, the statement says.
Minnesota OSHA has received three times as many emails and phone calls from workers and employers requesting information and assistance during the pandemic, compared with last year, said spokesperson James Honerman. “If Minnesota OSHA is made aware of a workplace safety or health issue, it assesses the situation and determines how best to respond, including conducting a workplace investigation.”
But Willmeng, who has been out of work since he was fired, says that without a receipt or confirmation from OSHA, he has no way of knowing whether there has been any follow-up regarding his complaints. Minnesota OSHA said workers should receive a letter once a case is resolved.
Like Willmeng’s case, none of the more than 10,000 COVID-related complaints the federal OSHA office has received from across the country have resulted in meaningful sanctions. Unions have picketed local OSHA offices and publicized complaints on behalf of their members to protest what they see as a lack of oversight. Legislators have called on US Department of Labor Secretary Eugene Scalia to step up enforcement.
For many health care workers, complaining to OSHA is a last resort after failing to get satisfactory responses from supervisors and appealing to unions for help. But with such minimal oversight from OSHA, some union leaders and legislators say it’s actually more dangerous than not having workplace safety enforcement at all. Lack of directives from the Trump administration has left the agency without the teeth it has cut under previous administrations, and recent changes to the agency’s rules raise questions about whether companies are ever required to report workers’ hospitalizations due to COVID-19.
“It’s so ineffective that it’s more dangerous to workers,” said Kim Cordova, president of United Food and Commercial Workers (UFCW) Local 7, which represents 22,000 health care and other workers in Colorado and Wyoming. “Employers only do what they’re forced to do.” Instead of deterring a multi-billion-dollar company, she said, such low fines signal that a company doesn’t need to worry about COVID-related safety.
“OSHA is doing a lamentably poor job protecting workers during the pandemic,” said James Brudney, JD, a professor at Fordham Law School, in New York, and former chief counsel of the U.S. Senate Subcommittee on Labor. “I’m not alone in saying that the agency has performed so badly.”
Former government officials writing in JAMA were similarly critical: “In the face of the greatest worker health crisis in recent history, OSHA, the lead government agency responsible for worker health and safety, has not fulfilled its responsibilities.”
What could have been
There were early signs that the agency wouldn’t be heavy-handed about COVID-19 safety concerns, Brudney said.
The agency could have issued Emergency Temporary Standards, rules it can put in place during pandemics that address specific short-term concerns. These rules could have required employers to take infection-control measures to protect workers, including mask wearing, providing proper PPE, and screening for COVID-19 symptoms. “That’s what the agency is supposed to do. They’re supposed to respond to an emergency with emergency measures,” Brudney said.
But despite legislative pressure and a court case, Secretary of Labor Eugene Scalia has declined to do so, saying that the agency would instead rely on its regular general duty clause, which is always in place to keep workplaces free from hazards that “cause death or serious physical harm.” The agency invoked the general duty clause for COVID-19–related violations for the first time in September to levy modest fines.
In response to a request for an interview, a Department of Labor spokesperson said that preexisting OSHA requirements apply to workers during the pandemic, including providing PPE for workers and assessing sanitation and cleanliness standards. The agency has issued specific guidance to companies on pandemic preparedness, she said, and that it responds to all complaints. Additionally, she cited whistleblower laws that make it illegal for employers to retaliate against employees for making safety and health complaints.
The federal OSHA office received 10,868 COVID-related complaints from Feb. 1 through Oct. 20, citing issues ranging from failure to provide proper PPE to not informing workers about exposures. As of Oct. 22, a total of 2,349 of the complaints involved healthcare workers. This count doesn’t include the untold number of “informal” complaints handled by state OSHA offices.
In a recent JAMA opinion piece, two former government officials agreed that “the federal government has not fully utilized OSHA’s public safety authority” and called the issuing of an Emergency Temporary Standard that would require employers to develop and implement infection control plans “the most important action the federal government could take” to protect workers.
“Employers are more likely to implement these controls if they are mandated by a government agency that has adequate enforcement tools to ensure compliance,” wrote former Assistant Secretary of Labor David Michaels, PhD, MPH, now at the Milken Institute School of Public Health of the George Washington University, Washington, and Gregory Wagner, MD, a former senior adviser at the National Institute for Occupational Safety and Health at the Centers for Disease Control and Prevention, now at the Harvard T.H. Chan School of Public Health, Boston.
They cited the success of a standard that OSHA issued in 1991 in response to the HIV/AIDS crisis. “The bloodborne pathogens standard has contributed to a substantial decline in health care worker risk for bloodborne diseases like HIV and hepatitis B and C,” they wrote. In a new report for the Century Foundation, the pair offered recommendations to the federal government for controlling the spread of the disease by ramping up OSHA’s role.
OSHA did issue a response plan that requires employers to report in regard to employees who experienced workplace exposures to SARS-CoV-2 and who were hospitalized with COVID-19 or died of the disease within certain time frames, but recent changes to these rules make experts question whether companies are in fact required to report hospitalizations.
In its second revision of guidelines, added to its FAQ page on Sept. 30, the agency said that, in order to be reportable, “an in-patient hospitalization due to COVID-19 must occur within 24 hours of an exposure to SARS-CoV-2 at work” and that the employer must report the hospitalization within 24 hours of learning both that the employee has been hospitalized and that the reason for the hospitalization was a work-related case of COVID-19. Previously, the 24-hour hospitalization window started at the time of diagnosis of the disease, rather than the work-related exposure.
The agency subsequently dropped the first citation it had issued for a COVID-related violation, even though the company, a nursing home, had already agreed to pay $3,904 for reporting employee hospitalizations late.
“It’s a step backwards from an important workplace and public health function that OSHA should be doing,” said Wagner, coauthor of the JAMA opinion piece.
Even without issuing Emergency Temporary Standards, critics say OSHA could have acted much earlier. OSHA issued its first COVID-related federal citation, the one against the nursing home that was dropped, in May for events that occurred in mid-April. The second COVID-related federal citation came in July.
The agency could also charge much more substantial fines for the citations it has issued. If a medical facility was cited for a PPE violation, such as the Minnesota hospital where workers were told to restaple the elastic bands on N95s, the agency could have cited the hospital for one violation per employee. Such fines based on multiple violations could add up to the hundreds of thousands to millions of dollars.
“It would send a signal to the highest-risk employers that these are violations that need to be addressed immediately,” Brudney said.
Many of the 22 state OSHA offices appear to be more responsive to COVID-related complaints than the federal agency, creating a system in which health care workers have substantially different rights from one state to the next. The governor of California, for example, recently authorized California’s OSHA division to consider COVID-19 an imminent hazard, to prohibit workers from entering areas where the hazard exists, and to require employers to disclose exposures. The state also recently issued large fines for COVID safety issues: $222,075 to frozen food manufacturer Overhill Farms and $214,080 to employment agency Jobsource North America.
Elsewhere, state laws such as New Jersey’s Conscientious Employee Protection Act give workers the right to refuse to work in unsafe situations, Brudney said. “A lot more action is going on at the state level because so little is being done at the federal level,” he said. “Some of it is governors committed to protecting essential workers and their families.”
Unions call for sanctions
Unions are both decrying the lack of enforcement thus far and seeking more oversight going forward.
In August, the National Nurses’ United (NNU) union filed a complaint to implore OSHA to investigate the country’s biggest hospital systems, HCA Healthcare, which operates 184 hospitals and about 2,000 other care sites in 21 states and the United Kingdom. The union describes how, throughout HCA hospitals, there is an environment conducive to the spread of coronavirus. Nurses share space and equipment, such as computers, desks, phones, bathrooms, and break rooms, where staff take off masks to eat and drink. The complaint also describes how there is resistance to testing nurses and a lack of communication about infections among colleagues.
“When they have total disregard for safety, they should be punished to the utmost,” said Markowitz, noting that HCA Healthcare is worth $40 billion. “They can penalize them, but if it’s unsafe conditions for RNs and healthcare workers, we know it’s unsafe for the patients. There needs to be drastic measures to prevent hospital corporations from behaving that way.”
In a statement, HCA spokesman Harlow Sumerford said the company has followed CDC guidance for protecting frontline caregivers. “We’re proud of our response and the significant resources we’ve deployed to help protect our colleagues. Meanwhile, the NNU has chosen to use this pandemic as an opportunity to gain publicity by attacking hospitals across the country,” Sumerford said.
Members of the union recently protested in front of the federal OSHA offices in Denver.
After several months, OSHA finally penalized a meat packing plant where eight workers (six union members) had died of COVID-19 last spring. But the amount – $15,615 – was so low that Cordova worries it will actually have a worse impact than no fine.
“It’s more dangerous to workers because now employers know [they won’t be punished meaningfully],” she said. “During the pandemic, OSHA has been absolutely absent.”
Thus, the recent picketing outside the offices in Denver. But, Cordova noted, it’s unlikely OSHA employees saw them. Their own offices were deemed too risky to stay open during the pandemic. They were vacant.
A version of this article originally appeared on Medscape.com.
Last spring, when Cliff Willmeng, RN, was working at United Hospital in St. Paul, Minnesota, he’d take off his personal protective equipment (PPE) in the same hallway where children were transported from ambulances to the neighboring Children’s Hospital emergency department. Stretchers would roll across red tape on the floor that designated the area as a “hot zone.” The door from a break room was about 10 feet away.
Willmeng has been a union activist all his life, but he’d never filed a complaint with the Occupational Safety and Health Administration (OSHA) until the COVID-19 pandemic hit.
Concerned about the inadequate space for doffing PPE and other situations in which the spread of SARS-CoV-2 seemed possible, Willmeng and other colleagues filed multiple OSHA complaints with the Minnesota Department of Labor in March and April. Willmeng was also worried about bringing SARS-CoV-2 on his scrubs home to his wife and kids, and he started wearing hospital-supplied scrubs that were meant for doctors and that were washed on site, which was against hospital policy. The hospital fired Willmeng on May 8, citing code of conduct and respectful workplace violations arising from the uniform dispute.
In August, the state agency issued Willmeng’s hospital a $2,100 fine for failure to comply with guidance regarding “respiratory protection” in response to worker complaints over the fact that they were instructed to restaple elastic bands on N95 masks early in the pandemic. In a statement, United Hospital said it contested the citation, and it is in discussions with Minnesota OSHA. “We have and continue to instruct employees not to alter N95 respirators or reuse damaged or soiled N95 respirators,” such as when the straps are broken, the statement says.
Minnesota OSHA has received three times as many emails and phone calls from workers and employers requesting information and assistance during the pandemic, compared with last year, said spokesperson James Honerman. “If Minnesota OSHA is made aware of a workplace safety or health issue, it assesses the situation and determines how best to respond, including conducting a workplace investigation.”
But Willmeng, who has been out of work since he was fired, says that without a receipt or confirmation from OSHA, he has no way of knowing whether there has been any follow-up regarding his complaints. Minnesota OSHA said workers should receive a letter once a case is resolved.
Like Willmeng’s case, none of the more than 10,000 COVID-related complaints the federal OSHA office has received from across the country have resulted in meaningful sanctions. Unions have picketed local OSHA offices and publicized complaints on behalf of their members to protest what they see as a lack of oversight. Legislators have called on US Department of Labor Secretary Eugene Scalia to step up enforcement.
For many health care workers, complaining to OSHA is a last resort after failing to get satisfactory responses from supervisors and appealing to unions for help. But with such minimal oversight from OSHA, some union leaders and legislators say it’s actually more dangerous than not having workplace safety enforcement at all. Lack of directives from the Trump administration has left the agency without the teeth it has cut under previous administrations, and recent changes to the agency’s rules raise questions about whether companies are ever required to report workers’ hospitalizations due to COVID-19.
“It’s so ineffective that it’s more dangerous to workers,” said Kim Cordova, president of United Food and Commercial Workers (UFCW) Local 7, which represents 22,000 health care and other workers in Colorado and Wyoming. “Employers only do what they’re forced to do.” Instead of deterring a multi-billion-dollar company, she said, such low fines signal that a company doesn’t need to worry about COVID-related safety.
“OSHA is doing a lamentably poor job protecting workers during the pandemic,” said James Brudney, JD, a professor at Fordham Law School, in New York, and former chief counsel of the U.S. Senate Subcommittee on Labor. “I’m not alone in saying that the agency has performed so badly.”
Former government officials writing in JAMA were similarly critical: “In the face of the greatest worker health crisis in recent history, OSHA, the lead government agency responsible for worker health and safety, has not fulfilled its responsibilities.”
What could have been
There were early signs that the agency wouldn’t be heavy-handed about COVID-19 safety concerns, Brudney said.
The agency could have issued Emergency Temporary Standards, rules it can put in place during pandemics that address specific short-term concerns. These rules could have required employers to take infection-control measures to protect workers, including mask wearing, providing proper PPE, and screening for COVID-19 symptoms. “That’s what the agency is supposed to do. They’re supposed to respond to an emergency with emergency measures,” Brudney said.
But despite legislative pressure and a court case, Secretary of Labor Eugene Scalia has declined to do so, saying that the agency would instead rely on its regular general duty clause, which is always in place to keep workplaces free from hazards that “cause death or serious physical harm.” The agency invoked the general duty clause for COVID-19–related violations for the first time in September to levy modest fines.
In response to a request for an interview, a Department of Labor spokesperson said that preexisting OSHA requirements apply to workers during the pandemic, including providing PPE for workers and assessing sanitation and cleanliness standards. The agency has issued specific guidance to companies on pandemic preparedness, she said, and that it responds to all complaints. Additionally, she cited whistleblower laws that make it illegal for employers to retaliate against employees for making safety and health complaints.
The federal OSHA office received 10,868 COVID-related complaints from Feb. 1 through Oct. 20, citing issues ranging from failure to provide proper PPE to not informing workers about exposures. As of Oct. 22, a total of 2,349 of the complaints involved healthcare workers. This count doesn’t include the untold number of “informal” complaints handled by state OSHA offices.
In a recent JAMA opinion piece, two former government officials agreed that “the federal government has not fully utilized OSHA’s public safety authority” and called the issuing of an Emergency Temporary Standard that would require employers to develop and implement infection control plans “the most important action the federal government could take” to protect workers.
“Employers are more likely to implement these controls if they are mandated by a government agency that has adequate enforcement tools to ensure compliance,” wrote former Assistant Secretary of Labor David Michaels, PhD, MPH, now at the Milken Institute School of Public Health of the George Washington University, Washington, and Gregory Wagner, MD, a former senior adviser at the National Institute for Occupational Safety and Health at the Centers for Disease Control and Prevention, now at the Harvard T.H. Chan School of Public Health, Boston.
They cited the success of a standard that OSHA issued in 1991 in response to the HIV/AIDS crisis. “The bloodborne pathogens standard has contributed to a substantial decline in health care worker risk for bloodborne diseases like HIV and hepatitis B and C,” they wrote. In a new report for the Century Foundation, the pair offered recommendations to the federal government for controlling the spread of the disease by ramping up OSHA’s role.
OSHA did issue a response plan that requires employers to report in regard to employees who experienced workplace exposures to SARS-CoV-2 and who were hospitalized with COVID-19 or died of the disease within certain time frames, but recent changes to these rules make experts question whether companies are in fact required to report hospitalizations.
In its second revision of guidelines, added to its FAQ page on Sept. 30, the agency said that, in order to be reportable, “an in-patient hospitalization due to COVID-19 must occur within 24 hours of an exposure to SARS-CoV-2 at work” and that the employer must report the hospitalization within 24 hours of learning both that the employee has been hospitalized and that the reason for the hospitalization was a work-related case of COVID-19. Previously, the 24-hour hospitalization window started at the time of diagnosis of the disease, rather than the work-related exposure.
The agency subsequently dropped the first citation it had issued for a COVID-related violation, even though the company, a nursing home, had already agreed to pay $3,904 for reporting employee hospitalizations late.
“It’s a step backwards from an important workplace and public health function that OSHA should be doing,” said Wagner, coauthor of the JAMA opinion piece.
Even without issuing Emergency Temporary Standards, critics say OSHA could have acted much earlier. OSHA issued its first COVID-related federal citation, the one against the nursing home that was dropped, in May for events that occurred in mid-April. The second COVID-related federal citation came in July.
The agency could also charge much more substantial fines for the citations it has issued. If a medical facility was cited for a PPE violation, such as the Minnesota hospital where workers were told to restaple the elastic bands on N95s, the agency could have cited the hospital for one violation per employee. Such fines based on multiple violations could add up to the hundreds of thousands to millions of dollars.
“It would send a signal to the highest-risk employers that these are violations that need to be addressed immediately,” Brudney said.
Many of the 22 state OSHA offices appear to be more responsive to COVID-related complaints than the federal agency, creating a system in which health care workers have substantially different rights from one state to the next. The governor of California, for example, recently authorized California’s OSHA division to consider COVID-19 an imminent hazard, to prohibit workers from entering areas where the hazard exists, and to require employers to disclose exposures. The state also recently issued large fines for COVID safety issues: $222,075 to frozen food manufacturer Overhill Farms and $214,080 to employment agency Jobsource North America.
Elsewhere, state laws such as New Jersey’s Conscientious Employee Protection Act give workers the right to refuse to work in unsafe situations, Brudney said. “A lot more action is going on at the state level because so little is being done at the federal level,” he said. “Some of it is governors committed to protecting essential workers and their families.”
Unions call for sanctions
Unions are both decrying the lack of enforcement thus far and seeking more oversight going forward.
In August, the National Nurses’ United (NNU) union filed a complaint to implore OSHA to investigate the country’s biggest hospital systems, HCA Healthcare, which operates 184 hospitals and about 2,000 other care sites in 21 states and the United Kingdom. The union describes how, throughout HCA hospitals, there is an environment conducive to the spread of coronavirus. Nurses share space and equipment, such as computers, desks, phones, bathrooms, and break rooms, where staff take off masks to eat and drink. The complaint also describes how there is resistance to testing nurses and a lack of communication about infections among colleagues.
“When they have total disregard for safety, they should be punished to the utmost,” said Markowitz, noting that HCA Healthcare is worth $40 billion. “They can penalize them, but if it’s unsafe conditions for RNs and healthcare workers, we know it’s unsafe for the patients. There needs to be drastic measures to prevent hospital corporations from behaving that way.”
In a statement, HCA spokesman Harlow Sumerford said the company has followed CDC guidance for protecting frontline caregivers. “We’re proud of our response and the significant resources we’ve deployed to help protect our colleagues. Meanwhile, the NNU has chosen to use this pandemic as an opportunity to gain publicity by attacking hospitals across the country,” Sumerford said.
Members of the union recently protested in front of the federal OSHA offices in Denver.
After several months, OSHA finally penalized a meat packing plant where eight workers (six union members) had died of COVID-19 last spring. But the amount – $15,615 – was so low that Cordova worries it will actually have a worse impact than no fine.
“It’s more dangerous to workers because now employers know [they won’t be punished meaningfully],” she said. “During the pandemic, OSHA has been absolutely absent.”
Thus, the recent picketing outside the offices in Denver. But, Cordova noted, it’s unlikely OSHA employees saw them. Their own offices were deemed too risky to stay open during the pandemic. They were vacant.
A version of this article originally appeared on Medscape.com.
Last spring, when Cliff Willmeng, RN, was working at United Hospital in St. Paul, Minnesota, he’d take off his personal protective equipment (PPE) in the same hallway where children were transported from ambulances to the neighboring Children’s Hospital emergency department. Stretchers would roll across red tape on the floor that designated the area as a “hot zone.” The door from a break room was about 10 feet away.
Willmeng has been a union activist all his life, but he’d never filed a complaint with the Occupational Safety and Health Administration (OSHA) until the COVID-19 pandemic hit.
Concerned about the inadequate space for doffing PPE and other situations in which the spread of SARS-CoV-2 seemed possible, Willmeng and other colleagues filed multiple OSHA complaints with the Minnesota Department of Labor in March and April. Willmeng was also worried about bringing SARS-CoV-2 on his scrubs home to his wife and kids, and he started wearing hospital-supplied scrubs that were meant for doctors and that were washed on site, which was against hospital policy. The hospital fired Willmeng on May 8, citing code of conduct and respectful workplace violations arising from the uniform dispute.
In August, the state agency issued Willmeng’s hospital a $2,100 fine for failure to comply with guidance regarding “respiratory protection” in response to worker complaints over the fact that they were instructed to restaple elastic bands on N95 masks early in the pandemic. In a statement, United Hospital said it contested the citation, and it is in discussions with Minnesota OSHA. “We have and continue to instruct employees not to alter N95 respirators or reuse damaged or soiled N95 respirators,” such as when the straps are broken, the statement says.
Minnesota OSHA has received three times as many emails and phone calls from workers and employers requesting information and assistance during the pandemic, compared with last year, said spokesperson James Honerman. “If Minnesota OSHA is made aware of a workplace safety or health issue, it assesses the situation and determines how best to respond, including conducting a workplace investigation.”
But Willmeng, who has been out of work since he was fired, says that without a receipt or confirmation from OSHA, he has no way of knowing whether there has been any follow-up regarding his complaints. Minnesota OSHA said workers should receive a letter once a case is resolved.
Like Willmeng’s case, none of the more than 10,000 COVID-related complaints the federal OSHA office has received from across the country have resulted in meaningful sanctions. Unions have picketed local OSHA offices and publicized complaints on behalf of their members to protest what they see as a lack of oversight. Legislators have called on US Department of Labor Secretary Eugene Scalia to step up enforcement.
For many health care workers, complaining to OSHA is a last resort after failing to get satisfactory responses from supervisors and appealing to unions for help. But with such minimal oversight from OSHA, some union leaders and legislators say it’s actually more dangerous than not having workplace safety enforcement at all. Lack of directives from the Trump administration has left the agency without the teeth it has cut under previous administrations, and recent changes to the agency’s rules raise questions about whether companies are ever required to report workers’ hospitalizations due to COVID-19.
“It’s so ineffective that it’s more dangerous to workers,” said Kim Cordova, president of United Food and Commercial Workers (UFCW) Local 7, which represents 22,000 health care and other workers in Colorado and Wyoming. “Employers only do what they’re forced to do.” Instead of deterring a multi-billion-dollar company, she said, such low fines signal that a company doesn’t need to worry about COVID-related safety.
“OSHA is doing a lamentably poor job protecting workers during the pandemic,” said James Brudney, JD, a professor at Fordham Law School, in New York, and former chief counsel of the U.S. Senate Subcommittee on Labor. “I’m not alone in saying that the agency has performed so badly.”
Former government officials writing in JAMA were similarly critical: “In the face of the greatest worker health crisis in recent history, OSHA, the lead government agency responsible for worker health and safety, has not fulfilled its responsibilities.”
What could have been
There were early signs that the agency wouldn’t be heavy-handed about COVID-19 safety concerns, Brudney said.
The agency could have issued Emergency Temporary Standards, rules it can put in place during pandemics that address specific short-term concerns. These rules could have required employers to take infection-control measures to protect workers, including mask wearing, providing proper PPE, and screening for COVID-19 symptoms. “That’s what the agency is supposed to do. They’re supposed to respond to an emergency with emergency measures,” Brudney said.
But despite legislative pressure and a court case, Secretary of Labor Eugene Scalia has declined to do so, saying that the agency would instead rely on its regular general duty clause, which is always in place to keep workplaces free from hazards that “cause death or serious physical harm.” The agency invoked the general duty clause for COVID-19–related violations for the first time in September to levy modest fines.
In response to a request for an interview, a Department of Labor spokesperson said that preexisting OSHA requirements apply to workers during the pandemic, including providing PPE for workers and assessing sanitation and cleanliness standards. The agency has issued specific guidance to companies on pandemic preparedness, she said, and that it responds to all complaints. Additionally, she cited whistleblower laws that make it illegal for employers to retaliate against employees for making safety and health complaints.
The federal OSHA office received 10,868 COVID-related complaints from Feb. 1 through Oct. 20, citing issues ranging from failure to provide proper PPE to not informing workers about exposures. As of Oct. 22, a total of 2,349 of the complaints involved healthcare workers. This count doesn’t include the untold number of “informal” complaints handled by state OSHA offices.
In a recent JAMA opinion piece, two former government officials agreed that “the federal government has not fully utilized OSHA’s public safety authority” and called the issuing of an Emergency Temporary Standard that would require employers to develop and implement infection control plans “the most important action the federal government could take” to protect workers.
“Employers are more likely to implement these controls if they are mandated by a government agency that has adequate enforcement tools to ensure compliance,” wrote former Assistant Secretary of Labor David Michaels, PhD, MPH, now at the Milken Institute School of Public Health of the George Washington University, Washington, and Gregory Wagner, MD, a former senior adviser at the National Institute for Occupational Safety and Health at the Centers for Disease Control and Prevention, now at the Harvard T.H. Chan School of Public Health, Boston.
They cited the success of a standard that OSHA issued in 1991 in response to the HIV/AIDS crisis. “The bloodborne pathogens standard has contributed to a substantial decline in health care worker risk for bloodborne diseases like HIV and hepatitis B and C,” they wrote. In a new report for the Century Foundation, the pair offered recommendations to the federal government for controlling the spread of the disease by ramping up OSHA’s role.
OSHA did issue a response plan that requires employers to report in regard to employees who experienced workplace exposures to SARS-CoV-2 and who were hospitalized with COVID-19 or died of the disease within certain time frames, but recent changes to these rules make experts question whether companies are in fact required to report hospitalizations.
In its second revision of guidelines, added to its FAQ page on Sept. 30, the agency said that, in order to be reportable, “an in-patient hospitalization due to COVID-19 must occur within 24 hours of an exposure to SARS-CoV-2 at work” and that the employer must report the hospitalization within 24 hours of learning both that the employee has been hospitalized and that the reason for the hospitalization was a work-related case of COVID-19. Previously, the 24-hour hospitalization window started at the time of diagnosis of the disease, rather than the work-related exposure.
The agency subsequently dropped the first citation it had issued for a COVID-related violation, even though the company, a nursing home, had already agreed to pay $3,904 for reporting employee hospitalizations late.
“It’s a step backwards from an important workplace and public health function that OSHA should be doing,” said Wagner, coauthor of the JAMA opinion piece.
Even without issuing Emergency Temporary Standards, critics say OSHA could have acted much earlier. OSHA issued its first COVID-related federal citation, the one against the nursing home that was dropped, in May for events that occurred in mid-April. The second COVID-related federal citation came in July.
The agency could also charge much more substantial fines for the citations it has issued. If a medical facility was cited for a PPE violation, such as the Minnesota hospital where workers were told to restaple the elastic bands on N95s, the agency could have cited the hospital for one violation per employee. Such fines based on multiple violations could add up to the hundreds of thousands to millions of dollars.
“It would send a signal to the highest-risk employers that these are violations that need to be addressed immediately,” Brudney said.
Many of the 22 state OSHA offices appear to be more responsive to COVID-related complaints than the federal agency, creating a system in which health care workers have substantially different rights from one state to the next. The governor of California, for example, recently authorized California’s OSHA division to consider COVID-19 an imminent hazard, to prohibit workers from entering areas where the hazard exists, and to require employers to disclose exposures. The state also recently issued large fines for COVID safety issues: $222,075 to frozen food manufacturer Overhill Farms and $214,080 to employment agency Jobsource North America.
Elsewhere, state laws such as New Jersey’s Conscientious Employee Protection Act give workers the right to refuse to work in unsafe situations, Brudney said. “A lot more action is going on at the state level because so little is being done at the federal level,” he said. “Some of it is governors committed to protecting essential workers and their families.”
Unions call for sanctions
Unions are both decrying the lack of enforcement thus far and seeking more oversight going forward.
In August, the National Nurses’ United (NNU) union filed a complaint to implore OSHA to investigate the country’s biggest hospital systems, HCA Healthcare, which operates 184 hospitals and about 2,000 other care sites in 21 states and the United Kingdom. The union describes how, throughout HCA hospitals, there is an environment conducive to the spread of coronavirus. Nurses share space and equipment, such as computers, desks, phones, bathrooms, and break rooms, where staff take off masks to eat and drink. The complaint also describes how there is resistance to testing nurses and a lack of communication about infections among colleagues.
“When they have total disregard for safety, they should be punished to the utmost,” said Markowitz, noting that HCA Healthcare is worth $40 billion. “They can penalize them, but if it’s unsafe conditions for RNs and healthcare workers, we know it’s unsafe for the patients. There needs to be drastic measures to prevent hospital corporations from behaving that way.”
In a statement, HCA spokesman Harlow Sumerford said the company has followed CDC guidance for protecting frontline caregivers. “We’re proud of our response and the significant resources we’ve deployed to help protect our colleagues. Meanwhile, the NNU has chosen to use this pandemic as an opportunity to gain publicity by attacking hospitals across the country,” Sumerford said.
Members of the union recently protested in front of the federal OSHA offices in Denver.
After several months, OSHA finally penalized a meat packing plant where eight workers (six union members) had died of COVID-19 last spring. But the amount – $15,615 – was so low that Cordova worries it will actually have a worse impact than no fine.
“It’s more dangerous to workers because now employers know [they won’t be punished meaningfully],” she said. “During the pandemic, OSHA has been absolutely absent.”
Thus, the recent picketing outside the offices in Denver. But, Cordova noted, it’s unlikely OSHA employees saw them. Their own offices were deemed too risky to stay open during the pandemic. They were vacant.
A version of this article originally appeared on Medscape.com.
COVID spikes exacerbate health worker shortages in Rocky Mountains, Great Plains
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Patients can read your clinical notes starting Nov. 2
Starting Nov. 2, all patients in the United States will have immediate access to clinical notes and thus will be able to read their doctors’ writings, as well as test results and reports from pathology and imaging.
The 21st Century Cures Act mandates that patients have fast, electronic access to the following types of notes: consultations, discharge summaries, history, physical examination findings, imaging narratives, laboratory and pathology report narratives, and procedure and progress notes.
But this federal mandate, called “open notes” by many, is potentially confusing and frightening for patients, say some physicians. Others worry that the change will increase workload as clinicians tailor notes for patients and answer related questions.
The law means that inpatient and outpatient notes will be released immediately and that patients will have immediate access to testing and imaging results, including results from sexually transmitted disease tests, Pap tests, cancer biopsies, CT and PET scans, fetal ultrasounds, pneumonia cultures, and mammograms.
Such notes could contain sensitive information, and there is concern that patients could be shocked, confused, or annoyed by what they read, even with more run-of-the-mill notes.
Champions of open notes say that the benefits, including better provider-patient communication, greatly outweigh such risks.
“This is about convenience – a bit like online banking,” commented Charlotte Blease, PhD, resident scholar at OpenNotes, an advocacy nonprofit organization headquartered at the Beth Israel–Deaconess Medical Center in Boston. “But it’s a culture shift for doctors,” she said in an interview.
“It turns physician paternalism on its head,” said C. T. Lin, MD, chief medical information officer, UCHealth, Denver. The change requires “some letting go of old traditions” in medicine, he wrote in an August blog post, referring to the fact that a computer screen – and not a physician – may tell patients about a new health problem.
Dr. Lin summarized the experience at the University of Colorado Cancer Center, which has allowed patients to have access to oncology notes for the past 5 years: “No issues and highly appreciated by patients. We have nothing to fear but fear itself.”
A new audience
Other institutions have also been voluntarily implementing open notes.
UC Davis Health in Sacramento, Calif., has run an optional program for the past year. However, only about two dozen of approximately 1,000 staff physicians opted in to the program.
“This illustrates the point that it’s a new thing that physicians aren’t used to doing. They’ve traditionally written notes for the benefit of their colleagues, for billing, for their own reference,” Scott MacDonald, MD, an internist and electronic health record medical director at UC Davis Health, told this news organization.
“They’ve never –until recently – had the patient as one of the audiences for a note,” he said.
Liam Keating, MD, an otolaryngologist in Martinez, Calif., recalls that he once wrote “globus hystericus,” and the patient wanted to sue him for saying that the patient was hysterical. “I now just code ‘Globus’ (if I don’t jump straight to LPD [lateral pharyngeal diverticulum]),” he commented in response to a commentary on open notes.
Sensitive information occurs more often in certain specialties, for example, psychiatry, genetics, adolescent medicine, and oncology, experts say.
“Cancer is an area that is highly charged for patients and doctors alike,” Dr. MacDonald pointed out. When reading pathology or imaging notes, patients may learn that they have been diagnosed with cancer or that they have a recurrence “without the physician being able to contextualize it and explain things – that’s just new and scary,” he said.
California law dictates that providers cannot post cancer test results without talking with the patient first, said Dr. MacDonald, but not all states have such laws.
Adjustments needed – or not – with open notes
At UCHealth in Aurora, Colo., Robert Breeze, MD, vice-chair of neurosurgery, said he has adjusted his practice to accommodate open notes and to anticipate trouble spots.*
“When I order imaging or send pathology specimens, I have already discussed with the patient the possibilities, including cancer, and what we will do next. Patients deeply appreciate these discussions, before they see the results,” he commented in an institutional white paper issued in anticipation of the changes on Nov. 2.
This is called precounseling, said Trent Rosenbloom, MD, MPH, director of patient portals at Vanderbilt University Medical Center, Nashville, Tenn., which has been a pioneer in information sharing with patients. Their system does delay the release of information in the case of “complicated” results, such as from cancer biopsies, he said in an interview.
However, Christiaan Hoff, MD, PhD, a surgeon at the Medical Center Leeuwarden (the Netherlands), wonders how important it is for the physician to be present when the patient receives bad news, including news about cancer. “We may overestimate our added value in these situations,” he suggested.
“Our empathy may not outweigh” the disadvantages of the situation, and the “finer points of our explanation will often go unnoticed” by the stressed patient, he commented. Dr. Hoff was also responding to the commentary about open notes.
In that commentary, Jack West, MD, a medical oncologist at City of Hope Cancer Center, Duarte, Calif., was concerned about misunderstandings. Oncology is complex, and patients can struggle to understand their prognosis and planned treatment efficacy, especially in cases of metastatic disease, he wrote.
This concern is somewhat refuted by a study published Oct. 5 in Cancer Cell. Responses to two surveys involving 96 oncology clinicians at three U.S. centers found that almost half (44%) believed that their patients “would be confused” by open notes.
However, only 4% of the 3,418 cancer patients from the same surveys reported being confused by open notes. (A majority of participants had more than a high school education, and English was their primary language.)
“Patient and clinician views about open notes in oncology are not aligned, with patients expressing considerably more enthusiasm,” wrote the authors, led by Liz Salmi, senior strategist at OpenNotes, who has been treated for brain cancer.
“All clinicians are anxious at first,” Ms. Salmi told this news organization. “Those patients who have more serious or chronic conditions … are more likely to read their notes.”
The survey results echo the early experience reported from Sweden, where open notes was launched in 2012. “Patients have loved it from the beginning,” said Maria Haggland, PhD, of Uppsala MedTech Science Innovation Center.
However, when the scheme first launched, it was considered to be “very controversial,” and “there were a lot of complaints, from health care professionals, especially,” she added.
Over time, clinicians have embraced open notes, and the program has 7.2 million patient accounts in a country of 10 million people, she observed during an Oct. 5 webinar on open notes.
More work for already overworked clinicians?
An outstanding concern about open notes is that it will cause more work for health care professionals.
Traditionally, doctors have written notes using medical lexicon, including a lot of abbreviations and jargon for efficiency’s sake. Now that patients will read the notes, will clinicians have to spell out things in lay terms, alter their writing so as not to offend, and generally do more work?
William Harvey, MD, chief medical information officer, Tufts Medical Center, Boston, acknowledged that that may be the case.
In a forthcoming note to staff about the Nov. 2 start of open notes, Dr. Harvey will include a reminder to accommodate the patient as a reader. But that may or may not mean an increase in work volume, depending on the provider. “Clinical note writing is highly personal. There’s an art to it,” he said in an interview. “So it’s hard to give standard advice.”
Steven Reidbord, MD, a psychiatrist in private practice in San Francisco and a lecturer at California Pacific Medical Center, is particularly concerned about the impact of open notes on progress notes, which he calls a tool to develop strategies and make observations while working with a patient.
By watering down the language for patients, “you are trading away the technical precision and other advantages of having a professional language,” he told this news organization.
“These notes serve many masters already,” he said, referring to purposes such as utilization review and billing. “The more masters they serve, the less useful they are to get medical work done.”
Dr. MacDonald, the medical information officer, said the new law doesn’t mandate a change in writing style.
In a study published last year, researchers analyzed notes written by oncologists before and after adoption of open notes. They found that, on average, clinicians did not change their note writing. The investigators analyzed more than 100,000 clinical notes written by 35 oncologists at a single center.
Advocates for open notes emphasize that there are benefits for clinicians.
“Doctors are overworked. They’re overburdened. But empowered patients can help the doctor,” said OpenNotes’ Dr. Blease. She cited survey data that show that patients better understand their treatment plan and medication, which can cut down on physician workload.
Open notes are “what you make of it,” said Marlene Millen, MD, an internist at UC San Diego Health, which has had a pilot program for 3 years. Each day, Dr. Millen discusses a shared note with two or three patients. “I actually end all of my appointments with, ‘Don’t forget to read your note later,’ ” she told this news organization.
“I was a little afraid of this initially,” she said, but within the first 3 months of the pilot, about 15 patients gave her direct feedback on how much they appreciated her notes. “It seemed to really reassure them that they were getting good care.”
The persons quoted in this article have disclosed no relevant financial relationships.
Correction, 10/23/20: An earlier version of this article misstated the campus' location.
A version of this article originally appeared on Medscape.com.
Starting Nov. 2, all patients in the United States will have immediate access to clinical notes and thus will be able to read their doctors’ writings, as well as test results and reports from pathology and imaging.
The 21st Century Cures Act mandates that patients have fast, electronic access to the following types of notes: consultations, discharge summaries, history, physical examination findings, imaging narratives, laboratory and pathology report narratives, and procedure and progress notes.
But this federal mandate, called “open notes” by many, is potentially confusing and frightening for patients, say some physicians. Others worry that the change will increase workload as clinicians tailor notes for patients and answer related questions.
The law means that inpatient and outpatient notes will be released immediately and that patients will have immediate access to testing and imaging results, including results from sexually transmitted disease tests, Pap tests, cancer biopsies, CT and PET scans, fetal ultrasounds, pneumonia cultures, and mammograms.
Such notes could contain sensitive information, and there is concern that patients could be shocked, confused, or annoyed by what they read, even with more run-of-the-mill notes.
Champions of open notes say that the benefits, including better provider-patient communication, greatly outweigh such risks.
“This is about convenience – a bit like online banking,” commented Charlotte Blease, PhD, resident scholar at OpenNotes, an advocacy nonprofit organization headquartered at the Beth Israel–Deaconess Medical Center in Boston. “But it’s a culture shift for doctors,” she said in an interview.
“It turns physician paternalism on its head,” said C. T. Lin, MD, chief medical information officer, UCHealth, Denver. The change requires “some letting go of old traditions” in medicine, he wrote in an August blog post, referring to the fact that a computer screen – and not a physician – may tell patients about a new health problem.
Dr. Lin summarized the experience at the University of Colorado Cancer Center, which has allowed patients to have access to oncology notes for the past 5 years: “No issues and highly appreciated by patients. We have nothing to fear but fear itself.”
A new audience
Other institutions have also been voluntarily implementing open notes.
UC Davis Health in Sacramento, Calif., has run an optional program for the past year. However, only about two dozen of approximately 1,000 staff physicians opted in to the program.
“This illustrates the point that it’s a new thing that physicians aren’t used to doing. They’ve traditionally written notes for the benefit of their colleagues, for billing, for their own reference,” Scott MacDonald, MD, an internist and electronic health record medical director at UC Davis Health, told this news organization.
“They’ve never –until recently – had the patient as one of the audiences for a note,” he said.
Liam Keating, MD, an otolaryngologist in Martinez, Calif., recalls that he once wrote “globus hystericus,” and the patient wanted to sue him for saying that the patient was hysterical. “I now just code ‘Globus’ (if I don’t jump straight to LPD [lateral pharyngeal diverticulum]),” he commented in response to a commentary on open notes.
Sensitive information occurs more often in certain specialties, for example, psychiatry, genetics, adolescent medicine, and oncology, experts say.
“Cancer is an area that is highly charged for patients and doctors alike,” Dr. MacDonald pointed out. When reading pathology or imaging notes, patients may learn that they have been diagnosed with cancer or that they have a recurrence “without the physician being able to contextualize it and explain things – that’s just new and scary,” he said.
California law dictates that providers cannot post cancer test results without talking with the patient first, said Dr. MacDonald, but not all states have such laws.
Adjustments needed – or not – with open notes
At UCHealth in Aurora, Colo., Robert Breeze, MD, vice-chair of neurosurgery, said he has adjusted his practice to accommodate open notes and to anticipate trouble spots.*
“When I order imaging or send pathology specimens, I have already discussed with the patient the possibilities, including cancer, and what we will do next. Patients deeply appreciate these discussions, before they see the results,” he commented in an institutional white paper issued in anticipation of the changes on Nov. 2.
This is called precounseling, said Trent Rosenbloom, MD, MPH, director of patient portals at Vanderbilt University Medical Center, Nashville, Tenn., which has been a pioneer in information sharing with patients. Their system does delay the release of information in the case of “complicated” results, such as from cancer biopsies, he said in an interview.
However, Christiaan Hoff, MD, PhD, a surgeon at the Medical Center Leeuwarden (the Netherlands), wonders how important it is for the physician to be present when the patient receives bad news, including news about cancer. “We may overestimate our added value in these situations,” he suggested.
“Our empathy may not outweigh” the disadvantages of the situation, and the “finer points of our explanation will often go unnoticed” by the stressed patient, he commented. Dr. Hoff was also responding to the commentary about open notes.
In that commentary, Jack West, MD, a medical oncologist at City of Hope Cancer Center, Duarte, Calif., was concerned about misunderstandings. Oncology is complex, and patients can struggle to understand their prognosis and planned treatment efficacy, especially in cases of metastatic disease, he wrote.
This concern is somewhat refuted by a study published Oct. 5 in Cancer Cell. Responses to two surveys involving 96 oncology clinicians at three U.S. centers found that almost half (44%) believed that their patients “would be confused” by open notes.
However, only 4% of the 3,418 cancer patients from the same surveys reported being confused by open notes. (A majority of participants had more than a high school education, and English was their primary language.)
“Patient and clinician views about open notes in oncology are not aligned, with patients expressing considerably more enthusiasm,” wrote the authors, led by Liz Salmi, senior strategist at OpenNotes, who has been treated for brain cancer.
“All clinicians are anxious at first,” Ms. Salmi told this news organization. “Those patients who have more serious or chronic conditions … are more likely to read their notes.”
The survey results echo the early experience reported from Sweden, where open notes was launched in 2012. “Patients have loved it from the beginning,” said Maria Haggland, PhD, of Uppsala MedTech Science Innovation Center.
However, when the scheme first launched, it was considered to be “very controversial,” and “there were a lot of complaints, from health care professionals, especially,” she added.
Over time, clinicians have embraced open notes, and the program has 7.2 million patient accounts in a country of 10 million people, she observed during an Oct. 5 webinar on open notes.
More work for already overworked clinicians?
An outstanding concern about open notes is that it will cause more work for health care professionals.
Traditionally, doctors have written notes using medical lexicon, including a lot of abbreviations and jargon for efficiency’s sake. Now that patients will read the notes, will clinicians have to spell out things in lay terms, alter their writing so as not to offend, and generally do more work?
William Harvey, MD, chief medical information officer, Tufts Medical Center, Boston, acknowledged that that may be the case.
In a forthcoming note to staff about the Nov. 2 start of open notes, Dr. Harvey will include a reminder to accommodate the patient as a reader. But that may or may not mean an increase in work volume, depending on the provider. “Clinical note writing is highly personal. There’s an art to it,” he said in an interview. “So it’s hard to give standard advice.”
Steven Reidbord, MD, a psychiatrist in private practice in San Francisco and a lecturer at California Pacific Medical Center, is particularly concerned about the impact of open notes on progress notes, which he calls a tool to develop strategies and make observations while working with a patient.
By watering down the language for patients, “you are trading away the technical precision and other advantages of having a professional language,” he told this news organization.
“These notes serve many masters already,” he said, referring to purposes such as utilization review and billing. “The more masters they serve, the less useful they are to get medical work done.”
Dr. MacDonald, the medical information officer, said the new law doesn’t mandate a change in writing style.
In a study published last year, researchers analyzed notes written by oncologists before and after adoption of open notes. They found that, on average, clinicians did not change their note writing. The investigators analyzed more than 100,000 clinical notes written by 35 oncologists at a single center.
Advocates for open notes emphasize that there are benefits for clinicians.
“Doctors are overworked. They’re overburdened. But empowered patients can help the doctor,” said OpenNotes’ Dr. Blease. She cited survey data that show that patients better understand their treatment plan and medication, which can cut down on physician workload.
Open notes are “what you make of it,” said Marlene Millen, MD, an internist at UC San Diego Health, which has had a pilot program for 3 years. Each day, Dr. Millen discusses a shared note with two or three patients. “I actually end all of my appointments with, ‘Don’t forget to read your note later,’ ” she told this news organization.
“I was a little afraid of this initially,” she said, but within the first 3 months of the pilot, about 15 patients gave her direct feedback on how much they appreciated her notes. “It seemed to really reassure them that they were getting good care.”
The persons quoted in this article have disclosed no relevant financial relationships.
Correction, 10/23/20: An earlier version of this article misstated the campus' location.
A version of this article originally appeared on Medscape.com.
Starting Nov. 2, all patients in the United States will have immediate access to clinical notes and thus will be able to read their doctors’ writings, as well as test results and reports from pathology and imaging.
The 21st Century Cures Act mandates that patients have fast, electronic access to the following types of notes: consultations, discharge summaries, history, physical examination findings, imaging narratives, laboratory and pathology report narratives, and procedure and progress notes.
But this federal mandate, called “open notes” by many, is potentially confusing and frightening for patients, say some physicians. Others worry that the change will increase workload as clinicians tailor notes for patients and answer related questions.
The law means that inpatient and outpatient notes will be released immediately and that patients will have immediate access to testing and imaging results, including results from sexually transmitted disease tests, Pap tests, cancer biopsies, CT and PET scans, fetal ultrasounds, pneumonia cultures, and mammograms.
Such notes could contain sensitive information, and there is concern that patients could be shocked, confused, or annoyed by what they read, even with more run-of-the-mill notes.
Champions of open notes say that the benefits, including better provider-patient communication, greatly outweigh such risks.
“This is about convenience – a bit like online banking,” commented Charlotte Blease, PhD, resident scholar at OpenNotes, an advocacy nonprofit organization headquartered at the Beth Israel–Deaconess Medical Center in Boston. “But it’s a culture shift for doctors,” she said in an interview.
“It turns physician paternalism on its head,” said C. T. Lin, MD, chief medical information officer, UCHealth, Denver. The change requires “some letting go of old traditions” in medicine, he wrote in an August blog post, referring to the fact that a computer screen – and not a physician – may tell patients about a new health problem.
Dr. Lin summarized the experience at the University of Colorado Cancer Center, which has allowed patients to have access to oncology notes for the past 5 years: “No issues and highly appreciated by patients. We have nothing to fear but fear itself.”
A new audience
Other institutions have also been voluntarily implementing open notes.
UC Davis Health in Sacramento, Calif., has run an optional program for the past year. However, only about two dozen of approximately 1,000 staff physicians opted in to the program.
“This illustrates the point that it’s a new thing that physicians aren’t used to doing. They’ve traditionally written notes for the benefit of their colleagues, for billing, for their own reference,” Scott MacDonald, MD, an internist and electronic health record medical director at UC Davis Health, told this news organization.
“They’ve never –until recently – had the patient as one of the audiences for a note,” he said.
Liam Keating, MD, an otolaryngologist in Martinez, Calif., recalls that he once wrote “globus hystericus,” and the patient wanted to sue him for saying that the patient was hysterical. “I now just code ‘Globus’ (if I don’t jump straight to LPD [lateral pharyngeal diverticulum]),” he commented in response to a commentary on open notes.
Sensitive information occurs more often in certain specialties, for example, psychiatry, genetics, adolescent medicine, and oncology, experts say.
“Cancer is an area that is highly charged for patients and doctors alike,” Dr. MacDonald pointed out. When reading pathology or imaging notes, patients may learn that they have been diagnosed with cancer or that they have a recurrence “without the physician being able to contextualize it and explain things – that’s just new and scary,” he said.
California law dictates that providers cannot post cancer test results without talking with the patient first, said Dr. MacDonald, but not all states have such laws.
Adjustments needed – or not – with open notes
At UCHealth in Aurora, Colo., Robert Breeze, MD, vice-chair of neurosurgery, said he has adjusted his practice to accommodate open notes and to anticipate trouble spots.*
“When I order imaging or send pathology specimens, I have already discussed with the patient the possibilities, including cancer, and what we will do next. Patients deeply appreciate these discussions, before they see the results,” he commented in an institutional white paper issued in anticipation of the changes on Nov. 2.
This is called precounseling, said Trent Rosenbloom, MD, MPH, director of patient portals at Vanderbilt University Medical Center, Nashville, Tenn., which has been a pioneer in information sharing with patients. Their system does delay the release of information in the case of “complicated” results, such as from cancer biopsies, he said in an interview.
However, Christiaan Hoff, MD, PhD, a surgeon at the Medical Center Leeuwarden (the Netherlands), wonders how important it is for the physician to be present when the patient receives bad news, including news about cancer. “We may overestimate our added value in these situations,” he suggested.
“Our empathy may not outweigh” the disadvantages of the situation, and the “finer points of our explanation will often go unnoticed” by the stressed patient, he commented. Dr. Hoff was also responding to the commentary about open notes.
In that commentary, Jack West, MD, a medical oncologist at City of Hope Cancer Center, Duarte, Calif., was concerned about misunderstandings. Oncology is complex, and patients can struggle to understand their prognosis and planned treatment efficacy, especially in cases of metastatic disease, he wrote.
This concern is somewhat refuted by a study published Oct. 5 in Cancer Cell. Responses to two surveys involving 96 oncology clinicians at three U.S. centers found that almost half (44%) believed that their patients “would be confused” by open notes.
However, only 4% of the 3,418 cancer patients from the same surveys reported being confused by open notes. (A majority of participants had more than a high school education, and English was their primary language.)
“Patient and clinician views about open notes in oncology are not aligned, with patients expressing considerably more enthusiasm,” wrote the authors, led by Liz Salmi, senior strategist at OpenNotes, who has been treated for brain cancer.
“All clinicians are anxious at first,” Ms. Salmi told this news organization. “Those patients who have more serious or chronic conditions … are more likely to read their notes.”
The survey results echo the early experience reported from Sweden, where open notes was launched in 2012. “Patients have loved it from the beginning,” said Maria Haggland, PhD, of Uppsala MedTech Science Innovation Center.
However, when the scheme first launched, it was considered to be “very controversial,” and “there were a lot of complaints, from health care professionals, especially,” she added.
Over time, clinicians have embraced open notes, and the program has 7.2 million patient accounts in a country of 10 million people, she observed during an Oct. 5 webinar on open notes.
More work for already overworked clinicians?
An outstanding concern about open notes is that it will cause more work for health care professionals.
Traditionally, doctors have written notes using medical lexicon, including a lot of abbreviations and jargon for efficiency’s sake. Now that patients will read the notes, will clinicians have to spell out things in lay terms, alter their writing so as not to offend, and generally do more work?
William Harvey, MD, chief medical information officer, Tufts Medical Center, Boston, acknowledged that that may be the case.
In a forthcoming note to staff about the Nov. 2 start of open notes, Dr. Harvey will include a reminder to accommodate the patient as a reader. But that may or may not mean an increase in work volume, depending on the provider. “Clinical note writing is highly personal. There’s an art to it,” he said in an interview. “So it’s hard to give standard advice.”
Steven Reidbord, MD, a psychiatrist in private practice in San Francisco and a lecturer at California Pacific Medical Center, is particularly concerned about the impact of open notes on progress notes, which he calls a tool to develop strategies and make observations while working with a patient.
By watering down the language for patients, “you are trading away the technical precision and other advantages of having a professional language,” he told this news organization.
“These notes serve many masters already,” he said, referring to purposes such as utilization review and billing. “The more masters they serve, the less useful they are to get medical work done.”
Dr. MacDonald, the medical information officer, said the new law doesn’t mandate a change in writing style.
In a study published last year, researchers analyzed notes written by oncologists before and after adoption of open notes. They found that, on average, clinicians did not change their note writing. The investigators analyzed more than 100,000 clinical notes written by 35 oncologists at a single center.
Advocates for open notes emphasize that there are benefits for clinicians.
“Doctors are overworked. They’re overburdened. But empowered patients can help the doctor,” said OpenNotes’ Dr. Blease. She cited survey data that show that patients better understand their treatment plan and medication, which can cut down on physician workload.
Open notes are “what you make of it,” said Marlene Millen, MD, an internist at UC San Diego Health, which has had a pilot program for 3 years. Each day, Dr. Millen discusses a shared note with two or three patients. “I actually end all of my appointments with, ‘Don’t forget to read your note later,’ ” she told this news organization.
“I was a little afraid of this initially,” she said, but within the first 3 months of the pilot, about 15 patients gave her direct feedback on how much they appreciated her notes. “It seemed to really reassure them that they were getting good care.”
The persons quoted in this article have disclosed no relevant financial relationships.
Correction, 10/23/20: An earlier version of this article misstated the campus' location.
A version of this article originally appeared on Medscape.com.
Increasing racial diversity in hospital medicine’s leadership ranks
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
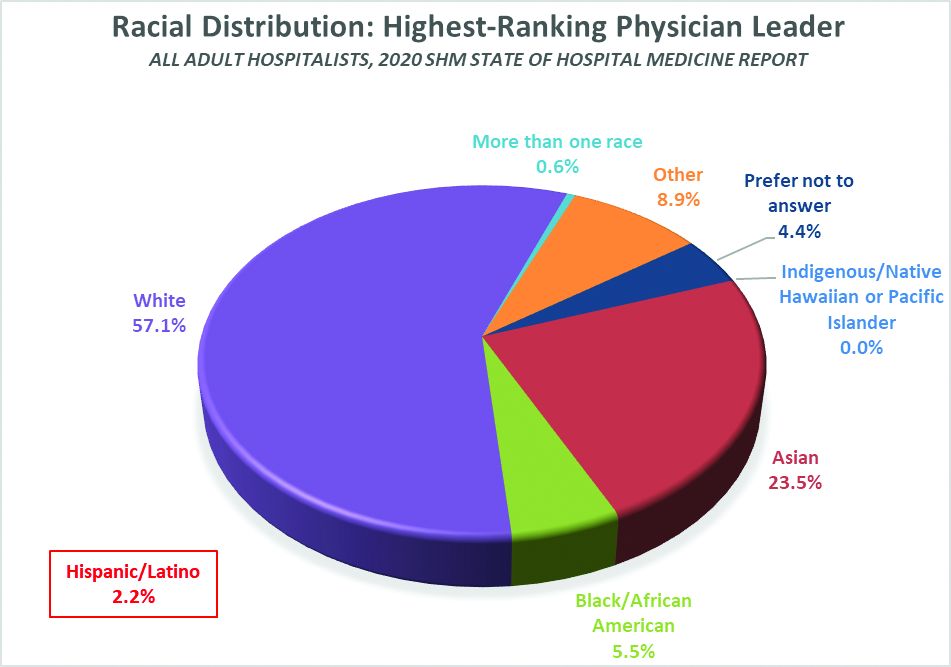
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
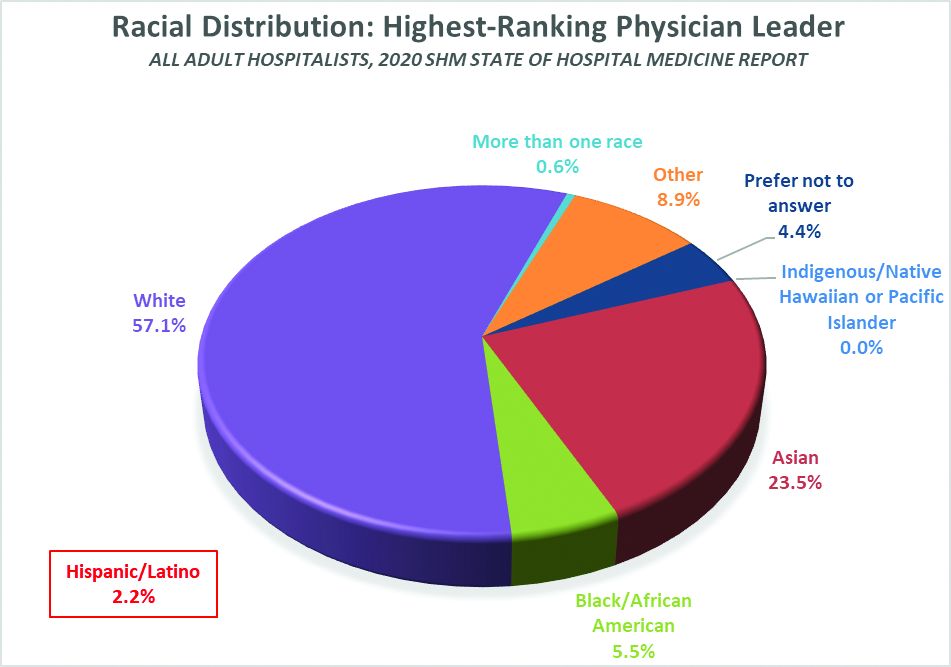
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
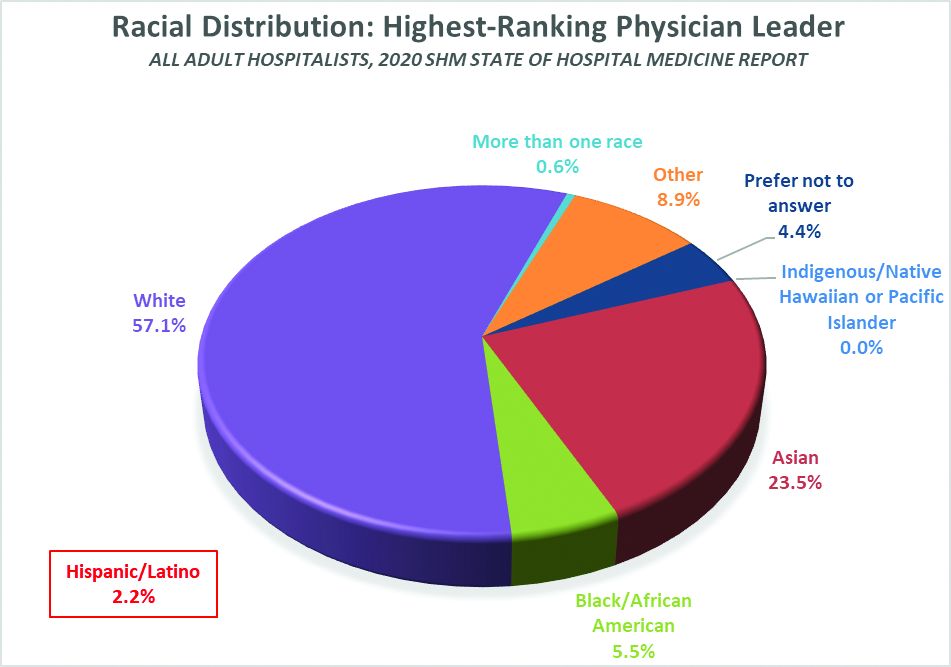
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Hospitalists and unit-based assignments
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
COVID-19 pandemic amplifies uncertainty for immigrant hospitalists
H1-B visa program needs improvement
Statistics tell the tale of immigrants in the American health care workforce in broad strokes. In an interview, though, one hospitalist shared the particulars of his professional and personal journey since arriving in the United States from India 15 years ago.
Mihir Patel, MD, MPH, FHM, came to the United States in 2005 to complete a Master’s in Public Health. Fifteen years later, he is still waiting for the green card that signifies U.S. permanent residency status. The paperwork for the application, he said, was completed in 2012. Since then, he’s been renewing his H-1B visa every three years, and he has no expectation that anything will change soon.
“If you are from India, which has a significant backlog of green cards – up to 50 years…you just wait forever,” he said. “Many people even die waiting for their green card to arrive.”
Arriving on a student visa, Dr. Patel completed his MPH in 2008 and began an internal medicine residency that same year, holding a J-1 visa for the 3 years of his US residency program.
“Post-residency, I started working in a rural hospital in an underserved area of northeast Tennessee as a hospitalist,” thus completing the 3 years of service in a rural underserved area that’s a requirement for J-1 visa holders, said Dr. Patel. “I loved this rural community hospital so much that I ended up staying there for 6 years. During my work at this rural hospital, I was able to enjoy the autonomy of managing a small ICU, doing both critical care procedures and management of intubated critical patients while working as a hospitalist,” he said. Dr. Patel served as chief of staff at the hospital for two years, and also served on the board of directors for his 400-physician medical group.
“I was a proud member of this rural community – Rogersville,” said Dr. Patel. Although he and his wife, who was completing her hospitalist residency, lived in Johnson City, Tenn., “I did not mind driving 120 miles round trip every day to go to my small-town hospital for 6 years,” he said.
Spending this time in rural Tennessee allowed Dr. Patel to finish the requirements necessary for the Physician National Interest Waiver and submit his application for permanent residency. The waiver, though, doesn’t give him priority status in the waiting list for permanent residency status.
After a stint in northern California to be closer to extended family, the pull of “beautiful northeast Tennesse and the rural community” was too strong, so Dr. Patel and his family moved back to Johnson City in 2018.
Now, Dr. Patel is a hospitalist at Ballad Health System in Johnson City. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the COVID-19 Strike Team. He co-founded and is president of the Blue Ridge Chapter of the Society of Hospital Medicine. Under another H-1B visa, Dr. Patel works part-time from home as a telehospitalist, covering six hospitals in 4 different states.
Even in ordinary circumstances, the H-1B visa comes with constraints. Although Dr. Patel’s 6-year old daughter was born in the U.S. and is a citizen, Dr. Patel and his wife have to reapply for their visas every 3 years. “If we travel outside the U.S., we have to get our visas stamped. We cannot change jobs easily due to fear of visa denial, especially with the recent political environment,” said Dr. Patel. “It feels like we are essential health care workers but non-essential immigrants.”
Having recently completed a physician executive MBA program, Dr. Patel said he’d like to start a business of his own using Lean health care principles and telemedicine to improve rural health care. “But while on an H-1B I cannot do anything outside my sponsored employment,” he said.
Ideally, health care organizations would have high flexibility in how and where staff are deployed when a surge of COVID-19 patients hits. Dr. Patel made the point that visa restrictions can make this much harder: “During this COVID crisis, this restriction can cause significant negative impact for small rural hospitals, where local physicians are quarantined and available physicians are on a visa who cannot legally work outside their primary facilities – even though they are willing to work,” he said. “One cannot even work using telemedicine in the same health system, if that is not specifically mentioned during H-1B petition filling. More than 15,000 physicians who are struck by the green card backlog are in the same situation all over U.S.,” he added.
These constraints, though, pale before the consequences of a worst-case pandemic scenario for an immigrant family, where the physician – the primary visa-holder – becomes disabled or dies. In this case, dependent family members must self-deport. “In addition, there would not be any disability or Social Security benefits for the physician or dependents, as they are not citizens or green card holders and they cannot legally stay in the US,” noted Dr. Patel. “Any hospitalist working during the COVID-19 pandemic can have this fate due to our high exposure risk.”
Reauthorizing the H1-B visa program
SHM has been advocating to improve the H1-B visa system for years, Dr. Patel said, The Fairness for High Skilled Immigrants Act passed the U.S. House of Representatives with bipartisan support, and the Society is advocating for its passage in the Senate.
The Fairness for High-Skilled Immigrants Act (S. 386) simplifies the employment-based immigration system by removing per-country caps, converting the employment-based immigration system into a “first-come, first serve” system that does not discriminate on country of origin. The act will also help alleviate the decades-long green card and permanent residency application backlogs.
Dr. Patel emphasized the importance of action by Congress to reauthorize the physician visa waiver program and expediting physician permanent residency. “This is a crisis and we are all physicians who are ready to serve, regardless of our country of origin. Please let us help this great nation by giving us freedom from visa restrictions and providing security for our families.
“During wartime, all frontline soldiers are naturalized and given citizenship by presidential mandate; this is more than war and we are not asking for citizenship – but at least give us a green card which we have already satisfied all requirements for. If not now, then when?” he asked.
H1-B visa program needs improvement
H1-B visa program needs improvement
Statistics tell the tale of immigrants in the American health care workforce in broad strokes. In an interview, though, one hospitalist shared the particulars of his professional and personal journey since arriving in the United States from India 15 years ago.
Mihir Patel, MD, MPH, FHM, came to the United States in 2005 to complete a Master’s in Public Health. Fifteen years later, he is still waiting for the green card that signifies U.S. permanent residency status. The paperwork for the application, he said, was completed in 2012. Since then, he’s been renewing his H-1B visa every three years, and he has no expectation that anything will change soon.
“If you are from India, which has a significant backlog of green cards – up to 50 years…you just wait forever,” he said. “Many people even die waiting for their green card to arrive.”
Arriving on a student visa, Dr. Patel completed his MPH in 2008 and began an internal medicine residency that same year, holding a J-1 visa for the 3 years of his US residency program.
“Post-residency, I started working in a rural hospital in an underserved area of northeast Tennessee as a hospitalist,” thus completing the 3 years of service in a rural underserved area that’s a requirement for J-1 visa holders, said Dr. Patel. “I loved this rural community hospital so much that I ended up staying there for 6 years. During my work at this rural hospital, I was able to enjoy the autonomy of managing a small ICU, doing both critical care procedures and management of intubated critical patients while working as a hospitalist,” he said. Dr. Patel served as chief of staff at the hospital for two years, and also served on the board of directors for his 400-physician medical group.
“I was a proud member of this rural community – Rogersville,” said Dr. Patel. Although he and his wife, who was completing her hospitalist residency, lived in Johnson City, Tenn., “I did not mind driving 120 miles round trip every day to go to my small-town hospital for 6 years,” he said.
Spending this time in rural Tennessee allowed Dr. Patel to finish the requirements necessary for the Physician National Interest Waiver and submit his application for permanent residency. The waiver, though, doesn’t give him priority status in the waiting list for permanent residency status.
After a stint in northern California to be closer to extended family, the pull of “beautiful northeast Tennesse and the rural community” was too strong, so Dr. Patel and his family moved back to Johnson City in 2018.
Now, Dr. Patel is a hospitalist at Ballad Health System in Johnson City. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the COVID-19 Strike Team. He co-founded and is president of the Blue Ridge Chapter of the Society of Hospital Medicine. Under another H-1B visa, Dr. Patel works part-time from home as a telehospitalist, covering six hospitals in 4 different states.
Even in ordinary circumstances, the H-1B visa comes with constraints. Although Dr. Patel’s 6-year old daughter was born in the U.S. and is a citizen, Dr. Patel and his wife have to reapply for their visas every 3 years. “If we travel outside the U.S., we have to get our visas stamped. We cannot change jobs easily due to fear of visa denial, especially with the recent political environment,” said Dr. Patel. “It feels like we are essential health care workers but non-essential immigrants.”
Having recently completed a physician executive MBA program, Dr. Patel said he’d like to start a business of his own using Lean health care principles and telemedicine to improve rural health care. “But while on an H-1B I cannot do anything outside my sponsored employment,” he said.
Ideally, health care organizations would have high flexibility in how and where staff are deployed when a surge of COVID-19 patients hits. Dr. Patel made the point that visa restrictions can make this much harder: “During this COVID crisis, this restriction can cause significant negative impact for small rural hospitals, where local physicians are quarantined and available physicians are on a visa who cannot legally work outside their primary facilities – even though they are willing to work,” he said. “One cannot even work using telemedicine in the same health system, if that is not specifically mentioned during H-1B petition filling. More than 15,000 physicians who are struck by the green card backlog are in the same situation all over U.S.,” he added.
These constraints, though, pale before the consequences of a worst-case pandemic scenario for an immigrant family, where the physician – the primary visa-holder – becomes disabled or dies. In this case, dependent family members must self-deport. “In addition, there would not be any disability or Social Security benefits for the physician or dependents, as they are not citizens or green card holders and they cannot legally stay in the US,” noted Dr. Patel. “Any hospitalist working during the COVID-19 pandemic can have this fate due to our high exposure risk.”
Reauthorizing the H1-B visa program
SHM has been advocating to improve the H1-B visa system for years, Dr. Patel said, The Fairness for High Skilled Immigrants Act passed the U.S. House of Representatives with bipartisan support, and the Society is advocating for its passage in the Senate.
The Fairness for High-Skilled Immigrants Act (S. 386) simplifies the employment-based immigration system by removing per-country caps, converting the employment-based immigration system into a “first-come, first serve” system that does not discriminate on country of origin. The act will also help alleviate the decades-long green card and permanent residency application backlogs.
Dr. Patel emphasized the importance of action by Congress to reauthorize the physician visa waiver program and expediting physician permanent residency. “This is a crisis and we are all physicians who are ready to serve, regardless of our country of origin. Please let us help this great nation by giving us freedom from visa restrictions and providing security for our families.
“During wartime, all frontline soldiers are naturalized and given citizenship by presidential mandate; this is more than war and we are not asking for citizenship – but at least give us a green card which we have already satisfied all requirements for. If not now, then when?” he asked.
Statistics tell the tale of immigrants in the American health care workforce in broad strokes. In an interview, though, one hospitalist shared the particulars of his professional and personal journey since arriving in the United States from India 15 years ago.
Mihir Patel, MD, MPH, FHM, came to the United States in 2005 to complete a Master’s in Public Health. Fifteen years later, he is still waiting for the green card that signifies U.S. permanent residency status. The paperwork for the application, he said, was completed in 2012. Since then, he’s been renewing his H-1B visa every three years, and he has no expectation that anything will change soon.
“If you are from India, which has a significant backlog of green cards – up to 50 years…you just wait forever,” he said. “Many people even die waiting for their green card to arrive.”
Arriving on a student visa, Dr. Patel completed his MPH in 2008 and began an internal medicine residency that same year, holding a J-1 visa for the 3 years of his US residency program.
“Post-residency, I started working in a rural hospital in an underserved area of northeast Tennessee as a hospitalist,” thus completing the 3 years of service in a rural underserved area that’s a requirement for J-1 visa holders, said Dr. Patel. “I loved this rural community hospital so much that I ended up staying there for 6 years. During my work at this rural hospital, I was able to enjoy the autonomy of managing a small ICU, doing both critical care procedures and management of intubated critical patients while working as a hospitalist,” he said. Dr. Patel served as chief of staff at the hospital for two years, and also served on the board of directors for his 400-physician medical group.
“I was a proud member of this rural community – Rogersville,” said Dr. Patel. Although he and his wife, who was completing her hospitalist residency, lived in Johnson City, Tenn., “I did not mind driving 120 miles round trip every day to go to my small-town hospital for 6 years,” he said.
Spending this time in rural Tennessee allowed Dr. Patel to finish the requirements necessary for the Physician National Interest Waiver and submit his application for permanent residency. The waiver, though, doesn’t give him priority status in the waiting list for permanent residency status.
After a stint in northern California to be closer to extended family, the pull of “beautiful northeast Tennesse and the rural community” was too strong, so Dr. Patel and his family moved back to Johnson City in 2018.
Now, Dr. Patel is a hospitalist at Ballad Health System in Johnson City. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the COVID-19 Strike Team. He co-founded and is president of the Blue Ridge Chapter of the Society of Hospital Medicine. Under another H-1B visa, Dr. Patel works part-time from home as a telehospitalist, covering six hospitals in 4 different states.
Even in ordinary circumstances, the H-1B visa comes with constraints. Although Dr. Patel’s 6-year old daughter was born in the U.S. and is a citizen, Dr. Patel and his wife have to reapply for their visas every 3 years. “If we travel outside the U.S., we have to get our visas stamped. We cannot change jobs easily due to fear of visa denial, especially with the recent political environment,” said Dr. Patel. “It feels like we are essential health care workers but non-essential immigrants.”
Having recently completed a physician executive MBA program, Dr. Patel said he’d like to start a business of his own using Lean health care principles and telemedicine to improve rural health care. “But while on an H-1B I cannot do anything outside my sponsored employment,” he said.
Ideally, health care organizations would have high flexibility in how and where staff are deployed when a surge of COVID-19 patients hits. Dr. Patel made the point that visa restrictions can make this much harder: “During this COVID crisis, this restriction can cause significant negative impact for small rural hospitals, where local physicians are quarantined and available physicians are on a visa who cannot legally work outside their primary facilities – even though they are willing to work,” he said. “One cannot even work using telemedicine in the same health system, if that is not specifically mentioned during H-1B petition filling. More than 15,000 physicians who are struck by the green card backlog are in the same situation all over U.S.,” he added.
These constraints, though, pale before the consequences of a worst-case pandemic scenario for an immigrant family, where the physician – the primary visa-holder – becomes disabled or dies. In this case, dependent family members must self-deport. “In addition, there would not be any disability or Social Security benefits for the physician or dependents, as they are not citizens or green card holders and they cannot legally stay in the US,” noted Dr. Patel. “Any hospitalist working during the COVID-19 pandemic can have this fate due to our high exposure risk.”
Reauthorizing the H1-B visa program
SHM has been advocating to improve the H1-B visa system for years, Dr. Patel said, The Fairness for High Skilled Immigrants Act passed the U.S. House of Representatives with bipartisan support, and the Society is advocating for its passage in the Senate.
The Fairness for High-Skilled Immigrants Act (S. 386) simplifies the employment-based immigration system by removing per-country caps, converting the employment-based immigration system into a “first-come, first serve” system that does not discriminate on country of origin. The act will also help alleviate the decades-long green card and permanent residency application backlogs.
Dr. Patel emphasized the importance of action by Congress to reauthorize the physician visa waiver program and expediting physician permanent residency. “This is a crisis and we are all physicians who are ready to serve, regardless of our country of origin. Please let us help this great nation by giving us freedom from visa restrictions and providing security for our families.
“During wartime, all frontline soldiers are naturalized and given citizenship by presidential mandate; this is more than war and we are not asking for citizenship – but at least give us a green card which we have already satisfied all requirements for. If not now, then when?” he asked.