User login
The Hospitalist only
Visa worries intensify pandemic stress for immigrant hospitalist moms
The COVID-19 pandemic has been difficult for all hospitalists, especially those who are parents of young children. For hospitalist moms who are also immigrants working on temporary H1-B visas, this stress is exacerbated. Though each story is unique, the underlying themes are the same: Worries over visa renewals, the immigration process, family members back home, and the risk of illness, job loss, and deportation.
Supporting the family
Like all health care workers, Prasanna Palabindela, MD, a hospitalist at Jennie Stuart Health in Hopkinsville, Ky., has been worried about bringing COVID-19 home to her family, especially in the beginning. Her in-laws had just arrived from India for a visit in March 2020 when the pandemic began, everything was shut down, and her in-laws were forced to settle in for an unexpected months-long stay.
Along with her elderly in-laws, who also have chronic conditions, Dr. Palabindela had two small children to worry about – a then-5-month-old daughter and a 5-year-old son. “I was more worried about them than me,” she said. “I used to take showers before coming home and just do all precautions as much as I can. I’m glad that I did not bring COVID, so far, to the family.”
Once she could safely send her in-laws back to India, Dr. Palabindela began searching for a nanny. Daycare was out of the question because she didn’t want her children to be exposed to illness. After a long search, she found a nanny who could also help her son with virtual school. “It’s expensive, but still, my family and my family’s health is my priority,” she said.
Working on visas has caused multiple issues for Dr. Palabindela and her husband. After living in different states because of their jobs, her husband joined her in West Virginia for her residency and found a job there. When Dr. Palabindela took her current position, her husband had to quit his job in West Virginia and move with her to Kentucky for them to stay together. Unfortunately, he couldn’t find a good fit for work in Kentucky, so the couple decided to put him on her visa so they wouldn’t have to live apart.
Now Dr. Palabindela is the family’s sole breadwinner. “That means if something happens to me, I always worry what’s going to happen with my family because legally, my husband cannot work. Technically, everyone is deported back to home,” she said. Not being able to work is hard for her husband too. “It’s just so much stress in the family because he worked for 11 years,” said Dr. Palabindela.
Through all the upheavals, Dr. Palabindela has had support from all sides. Her husband has been the biggest source. “He’s my backbone. Every time, he supported me in each and every aspect,” she said. Her parents and her brothers check in on her constantly to make sure she’s staying safe. Even the chief at her hospital has played a significant role, going to bat for his physicians to ensure their safety.
Dr. Palabindela credits everyone who works with COVID-19 patients as heroes. “The nurses, the physicians, the housekeeping, respiratory therapist, speech therapist, physical therapy ... everybody has a role. Everybody is a hero,” she said. “Whoever is wearing a mask is a hero, too, because they are contributing to this community.”
Advocating for immigration reform
A lack of transparency and information in the beginning of the pandemic significantly contributed to anxiety, said Anuradha Amara, MD, MBBS, a hospitalist in Wilmington, Del. She felt that what was on the news and what was actually going on in the hospitals were quite different. Colleagues were getting sick, there wasn’t enough personal protective equipment, and planning went out the window. “It’s like a meteor hitting a place and then we start dealing with the aftermath, but we weren’t ready before,” Dr. Amara said. “We didn’t have a plan for a pandemic.”
Then there was the concern of either her or her husband, a cardiologist, getting sick and potentially losing their jobs and immigration status. “How am I going to go back to my country if I had to? What will happen to my family if I die? If I go on the ventilator? Those are the insecurities we found additional to the pandemic challenges we had,” Dr. Amara said.
Not being able to go see their family in India or have them come visit was difficult – “it was pretty bad up there,” said Dr. Amara. Fortunately, her family members in India remained safe, but there’s a very real uneasiness about returning should an emergency arise. “Should I go back and then take the risk of losing my job and losing my position and my kids are here, they’re going to school here. How do you decide that?” she asked.
One of the worst effects of her visa restrictions was not being able to help in New York when hospitals were so short-staffed, and the morgues were overflowing. “New York is 3 hours away from where I live, but I was in chains. I couldn’t help them because of these visa restrictions,” Dr. Amara said. During the emergency, the state allowed physicians from other states to practice without being licensed in New York, but immigrant physicians were not included. “Even if we wanted to, we couldn’t volunteer,” said Dr. Amara. “I have family in New York, and I was really worried. Out of compassion I wanted to help, but I couldn’t do anything.”
Before the pandemic, Dr. Amara joined in advocacy efforts for immigrant physicians through Physicians for American Healthcare Access (PAHA). “In uncertain times, like COVID, it gets worse that you’re challenged with everything on top of your health, your family, and you have to be worried about deportation,” she said. “We need to strengthen legislation. Nobody should suffer with immigration processes during an active pandemic or otherwise.”
In the United States, 28% of physicians are immigrants. Dr. Amara pointed out that these physicians go through years of expensive training with extensive background checks at every level, yet they’re classified as second preference (EB-2) workers. She believes that physicians as a group should be excluded from this category and allowed to automatically become citizens after 5 years of living in the United States and working in an underserved area.
There have been an estimated 15,000 unused green cards since 2005. And if Congress went back to 1992, there could be more than 220,000 previously unused green cards recaptured. These unused green cards are the basis behind bills H.R.2255 and S.1024, the Healthcare Workforce Resiliency Act, which has been championed by SHM and PAHA. “It will allow the frontline physicians, 15,000 of them, and 25,000 nurses, to obtain their permanent residency,” said Dr. Amara. “These are people who already applied for their permanent residencies and they’re still waiting.”
SHM has consistently advocated for the Act since it was first introduced, written multiple letters on the issue, and supported it both on and off Capitol Hill. The society says the legislation would be an “important first step toward addressing a critical shortage” in the U.S. health care system by “recognizing the vital role immigrant physicians and nurses are playing in the fight against COVID-19.”
Currently, SHM has a live action alert open for the reintroduced bill, and encourages members to contact their legislators and urge them to support the reintroduction of the Act by cosponsoring and working to pass the legislation
Dr. Amara encourages physicians to start engaging in advocacy efforts early. Though she didn’t begin participating until late in her career, she said being aware of and part of policies that affect medicine is important. If more physicians get involved, “there are so many things we can take care of,” said Dr. Amara. “The medical profession doesn’t have to be so difficult and so busy. There are ways we can make it better and I believe that. And obviously I’ll continue to work and advocate for the entire medical profession, their problems, their health and well-being, to prevent burnout.”
Making time for positivity and self-care
Sandhya Tagaram, MD, a hospitalist at UMass Memorial Medical Center in Worcester, Mass., and her husband, also a hospitalist physician, had only ever read about pandemics in books. They certainly never expected to be in the middle of one. “That was a totally different level of anxiety to work as frontline physicians with two kids under 5 years and families away back home in India,” she said.
Dr. Tagaram and her husband work opposite shifts so that one of them is always home with their two young children. “Our schedules became more challenging when the pandemic started. Between both of our schedules and with minimal childcare facilities, we managed to strike a decent work-family balance, although we experience less vacation time together. We are fortunate to have an understanding work group,” said Dr. Tagaram.
Even before COVID-19, Dr. Tagaram found working on the temporary work visa challenging. “I think the pandemic has exposed the layer of uncertainty associated with it,” she said. “It’s incredibly stressful to imagine any minor turbulence that could alter our family and work lives. As a frontline physician mom, I take pride in raising my kids and taking care of my patients. We want to serve our communities and at the same time secure our families.”
Not being able to visit family back home and travel is exceedingly difficult. Dr. Tagaram said it would be helpful if there was a separate permanent residence pathway for physicians because they play a critical role in public health and they have been an integral part of the COVID-19 pandemic response team. A separate pathway could help keep their families secure and enable them to give their best to their communities.
Amid all the anxiety, Dr. Tagaram said she and her husband realized they could not keep living with so much pressure. As parents and as physicians, they did not want their stress to leak out and affect their ability and commitment to care for their children or their patients. They decided they needed to figure out how to be positive and constructive.
“We try some daily fun activities with the kids after returning home from work,” said Dr. Tagaram. They also formed a bubble group with two other physician families so the children could interact safely. She said that it’s critical that physicians take time for themselves. “We have to cultivate a serious hobby that helps to rejuvenate and calm our busy minds,” said Dr. Tagaram.
She makes time every day to exercise and to read at least a few pages from a good book. She is also learning Carnatic music along with one of her daughters. And every month since March 2020, she has journaled about her work and what she learned so her daughters can read it someday. “These things keep me jazzed up,” she said.
The pandemic has highlighted the fact that we are all part of one global community. “Although we hail from different backgrounds, we learned that we do have some common goals of being kind and supportive to each other and to give back to our communities. Hopefully we will continue this spirit,” said Dr. Tagaram. As a physician mother, “I feel it’s a privilege and honor to take care of my family and my community.”
Soldiering on in the COVID-19 war
The uncertainty everyone felt at the beginning of the pandemic was “very, very scary,” said Mamtha Balla, MD, MPH, a hospitalist and clinical assistant professor in northwest Ohio. “Initially, I was so involved in it and I felt like it was like a war, a COVID-19 war, and we are soldiers in that and trying to protect and do whatever we can.”
She and her husband, a geriatrician also working on an H-1B visa, have worked hard not to bring the virus home to their 2-year-old daughter. Going into 2021, the past 2 years have been “the most hectic and emotionally draining – and physically exhausting – years of my life,” said Dr. Balla.
The COVID-19 vaccine has helped reduce some pressure, but Dr. Balla is still concerned about the high risk to health care workers and the new COVID-19 strains coming out. “We are really not sure what we are dealing with and how the COVID will calm,” she said. “It is pretty challenging being a health care worker because not only are you responsible for your patients at the end of the day, but you are also responsible for your families.”
Initially in the United States from India on a student visa in 2008, Dr. Balla was placed on an H-1B visa when she started her residency. It was during this time that her mother was diagnosed with cancer and went through surgeries and chemotherapy. “She was pretty ill,” recalled Dr. Balla.
Despite the situation, Dr. Balla was afraid to go stay with her mother in case her visa application was rejected, and she couldn’t complete her third year of education. “I opted not to go to India at that time because I did not want to take a chance,” Dr. Balla said. “I have tears in my eyes because those are not easy moments, to withhold from seeing your parents, or to be in any other emergency where you cannot travel. That especially puts us at a higher risk emotionally and physically.”
She has not seen her parents in 2½ years. Between the very real possibility of not being able to get her visa stamp and the unpredictability of how other countries are dealing with COVID-19, Dr. Balla feels it is impossible to even think of going to visit. “Even if I go, what if something happens where my visa gets stuck, or the visa office is not open?” she said. If she could not get back to the United States as planned, she would have patients left behind here.
Recently, Dr. Balla did travel to India and her passport stamp did not come on time, so her husband had to come back to the United States by himself. She had to wait for her stamp for a couple more weeks before she could leave and, in the meantime, had to make arrangements at her hospital. “It is so much trauma,” she said.
There’s also the worry she has about getting sick or disabled and not being able to work anymore, resulting in deportation. “Is that what we are doing for people who are working like soldiers? Are we really treating them the correct way?” Dr. Balla asked.
Dr. Balla considers all health care workers to be soldiers in the COVID-19 war. As such, she believes the government should step up to make sure they are supporting and helping these immigrant physician-soldiers who are so necessary. She applauds France’s recent decision to grant citizenship to its frontline immigrant health care workers and feels that the same should be done in the United States. She filed her green card application in 2012, but she is nowhere close to getting it. (The backlog for employment-based green cards is more than 900,000 now.)
As people putting their own and their family’s lives at risk to care for patients with COVID-19, Dr. Balla and her husband have talked about moving to another country or even back to India. “I am a taxpayer; I am a good human being working for the community and for the job. This is my 13th year here. If I am not eligible [for citizenship] still, then I am not sure what else I have to do to prove myself,” she said. “I am owning United States citizens as my people, so please own us and help us out in this difficult scenario.”
The COVID-19 pandemic has been difficult for all hospitalists, especially those who are parents of young children. For hospitalist moms who are also immigrants working on temporary H1-B visas, this stress is exacerbated. Though each story is unique, the underlying themes are the same: Worries over visa renewals, the immigration process, family members back home, and the risk of illness, job loss, and deportation.
Supporting the family
Like all health care workers, Prasanna Palabindela, MD, a hospitalist at Jennie Stuart Health in Hopkinsville, Ky., has been worried about bringing COVID-19 home to her family, especially in the beginning. Her in-laws had just arrived from India for a visit in March 2020 when the pandemic began, everything was shut down, and her in-laws were forced to settle in for an unexpected months-long stay.
Along with her elderly in-laws, who also have chronic conditions, Dr. Palabindela had two small children to worry about – a then-5-month-old daughter and a 5-year-old son. “I was more worried about them than me,” she said. “I used to take showers before coming home and just do all precautions as much as I can. I’m glad that I did not bring COVID, so far, to the family.”
Once she could safely send her in-laws back to India, Dr. Palabindela began searching for a nanny. Daycare was out of the question because she didn’t want her children to be exposed to illness. After a long search, she found a nanny who could also help her son with virtual school. “It’s expensive, but still, my family and my family’s health is my priority,” she said.
Working on visas has caused multiple issues for Dr. Palabindela and her husband. After living in different states because of their jobs, her husband joined her in West Virginia for her residency and found a job there. When Dr. Palabindela took her current position, her husband had to quit his job in West Virginia and move with her to Kentucky for them to stay together. Unfortunately, he couldn’t find a good fit for work in Kentucky, so the couple decided to put him on her visa so they wouldn’t have to live apart.
Now Dr. Palabindela is the family’s sole breadwinner. “That means if something happens to me, I always worry what’s going to happen with my family because legally, my husband cannot work. Technically, everyone is deported back to home,” she said. Not being able to work is hard for her husband too. “It’s just so much stress in the family because he worked for 11 years,” said Dr. Palabindela.
Through all the upheavals, Dr. Palabindela has had support from all sides. Her husband has been the biggest source. “He’s my backbone. Every time, he supported me in each and every aspect,” she said. Her parents and her brothers check in on her constantly to make sure she’s staying safe. Even the chief at her hospital has played a significant role, going to bat for his physicians to ensure their safety.
Dr. Palabindela credits everyone who works with COVID-19 patients as heroes. “The nurses, the physicians, the housekeeping, respiratory therapist, speech therapist, physical therapy ... everybody has a role. Everybody is a hero,” she said. “Whoever is wearing a mask is a hero, too, because they are contributing to this community.”
Advocating for immigration reform
A lack of transparency and information in the beginning of the pandemic significantly contributed to anxiety, said Anuradha Amara, MD, MBBS, a hospitalist in Wilmington, Del. She felt that what was on the news and what was actually going on in the hospitals were quite different. Colleagues were getting sick, there wasn’t enough personal protective equipment, and planning went out the window. “It’s like a meteor hitting a place and then we start dealing with the aftermath, but we weren’t ready before,” Dr. Amara said. “We didn’t have a plan for a pandemic.”
Then there was the concern of either her or her husband, a cardiologist, getting sick and potentially losing their jobs and immigration status. “How am I going to go back to my country if I had to? What will happen to my family if I die? If I go on the ventilator? Those are the insecurities we found additional to the pandemic challenges we had,” Dr. Amara said.
Not being able to go see their family in India or have them come visit was difficult – “it was pretty bad up there,” said Dr. Amara. Fortunately, her family members in India remained safe, but there’s a very real uneasiness about returning should an emergency arise. “Should I go back and then take the risk of losing my job and losing my position and my kids are here, they’re going to school here. How do you decide that?” she asked.
One of the worst effects of her visa restrictions was not being able to help in New York when hospitals were so short-staffed, and the morgues were overflowing. “New York is 3 hours away from where I live, but I was in chains. I couldn’t help them because of these visa restrictions,” Dr. Amara said. During the emergency, the state allowed physicians from other states to practice without being licensed in New York, but immigrant physicians were not included. “Even if we wanted to, we couldn’t volunteer,” said Dr. Amara. “I have family in New York, and I was really worried. Out of compassion I wanted to help, but I couldn’t do anything.”
Before the pandemic, Dr. Amara joined in advocacy efforts for immigrant physicians through Physicians for American Healthcare Access (PAHA). “In uncertain times, like COVID, it gets worse that you’re challenged with everything on top of your health, your family, and you have to be worried about deportation,” she said. “We need to strengthen legislation. Nobody should suffer with immigration processes during an active pandemic or otherwise.”
In the United States, 28% of physicians are immigrants. Dr. Amara pointed out that these physicians go through years of expensive training with extensive background checks at every level, yet they’re classified as second preference (EB-2) workers. She believes that physicians as a group should be excluded from this category and allowed to automatically become citizens after 5 years of living in the United States and working in an underserved area.
There have been an estimated 15,000 unused green cards since 2005. And if Congress went back to 1992, there could be more than 220,000 previously unused green cards recaptured. These unused green cards are the basis behind bills H.R.2255 and S.1024, the Healthcare Workforce Resiliency Act, which has been championed by SHM and PAHA. “It will allow the frontline physicians, 15,000 of them, and 25,000 nurses, to obtain their permanent residency,” said Dr. Amara. “These are people who already applied for their permanent residencies and they’re still waiting.”
SHM has consistently advocated for the Act since it was first introduced, written multiple letters on the issue, and supported it both on and off Capitol Hill. The society says the legislation would be an “important first step toward addressing a critical shortage” in the U.S. health care system by “recognizing the vital role immigrant physicians and nurses are playing in the fight against COVID-19.”
Currently, SHM has a live action alert open for the reintroduced bill, and encourages members to contact their legislators and urge them to support the reintroduction of the Act by cosponsoring and working to pass the legislation
Dr. Amara encourages physicians to start engaging in advocacy efforts early. Though she didn’t begin participating until late in her career, she said being aware of and part of policies that affect medicine is important. If more physicians get involved, “there are so many things we can take care of,” said Dr. Amara. “The medical profession doesn’t have to be so difficult and so busy. There are ways we can make it better and I believe that. And obviously I’ll continue to work and advocate for the entire medical profession, their problems, their health and well-being, to prevent burnout.”
Making time for positivity and self-care
Sandhya Tagaram, MD, a hospitalist at UMass Memorial Medical Center in Worcester, Mass., and her husband, also a hospitalist physician, had only ever read about pandemics in books. They certainly never expected to be in the middle of one. “That was a totally different level of anxiety to work as frontline physicians with two kids under 5 years and families away back home in India,” she said.
Dr. Tagaram and her husband work opposite shifts so that one of them is always home with their two young children. “Our schedules became more challenging when the pandemic started. Between both of our schedules and with minimal childcare facilities, we managed to strike a decent work-family balance, although we experience less vacation time together. We are fortunate to have an understanding work group,” said Dr. Tagaram.
Even before COVID-19, Dr. Tagaram found working on the temporary work visa challenging. “I think the pandemic has exposed the layer of uncertainty associated with it,” she said. “It’s incredibly stressful to imagine any minor turbulence that could alter our family and work lives. As a frontline physician mom, I take pride in raising my kids and taking care of my patients. We want to serve our communities and at the same time secure our families.”
Not being able to visit family back home and travel is exceedingly difficult. Dr. Tagaram said it would be helpful if there was a separate permanent residence pathway for physicians because they play a critical role in public health and they have been an integral part of the COVID-19 pandemic response team. A separate pathway could help keep their families secure and enable them to give their best to their communities.
Amid all the anxiety, Dr. Tagaram said she and her husband realized they could not keep living with so much pressure. As parents and as physicians, they did not want their stress to leak out and affect their ability and commitment to care for their children or their patients. They decided they needed to figure out how to be positive and constructive.
“We try some daily fun activities with the kids after returning home from work,” said Dr. Tagaram. They also formed a bubble group with two other physician families so the children could interact safely. She said that it’s critical that physicians take time for themselves. “We have to cultivate a serious hobby that helps to rejuvenate and calm our busy minds,” said Dr. Tagaram.
She makes time every day to exercise and to read at least a few pages from a good book. She is also learning Carnatic music along with one of her daughters. And every month since March 2020, she has journaled about her work and what she learned so her daughters can read it someday. “These things keep me jazzed up,” she said.
The pandemic has highlighted the fact that we are all part of one global community. “Although we hail from different backgrounds, we learned that we do have some common goals of being kind and supportive to each other and to give back to our communities. Hopefully we will continue this spirit,” said Dr. Tagaram. As a physician mother, “I feel it’s a privilege and honor to take care of my family and my community.”
Soldiering on in the COVID-19 war
The uncertainty everyone felt at the beginning of the pandemic was “very, very scary,” said Mamtha Balla, MD, MPH, a hospitalist and clinical assistant professor in northwest Ohio. “Initially, I was so involved in it and I felt like it was like a war, a COVID-19 war, and we are soldiers in that and trying to protect and do whatever we can.”
She and her husband, a geriatrician also working on an H-1B visa, have worked hard not to bring the virus home to their 2-year-old daughter. Going into 2021, the past 2 years have been “the most hectic and emotionally draining – and physically exhausting – years of my life,” said Dr. Balla.
The COVID-19 vaccine has helped reduce some pressure, but Dr. Balla is still concerned about the high risk to health care workers and the new COVID-19 strains coming out. “We are really not sure what we are dealing with and how the COVID will calm,” she said. “It is pretty challenging being a health care worker because not only are you responsible for your patients at the end of the day, but you are also responsible for your families.”
Initially in the United States from India on a student visa in 2008, Dr. Balla was placed on an H-1B visa when she started her residency. It was during this time that her mother was diagnosed with cancer and went through surgeries and chemotherapy. “She was pretty ill,” recalled Dr. Balla.
Despite the situation, Dr. Balla was afraid to go stay with her mother in case her visa application was rejected, and she couldn’t complete her third year of education. “I opted not to go to India at that time because I did not want to take a chance,” Dr. Balla said. “I have tears in my eyes because those are not easy moments, to withhold from seeing your parents, or to be in any other emergency where you cannot travel. That especially puts us at a higher risk emotionally and physically.”
She has not seen her parents in 2½ years. Between the very real possibility of not being able to get her visa stamp and the unpredictability of how other countries are dealing with COVID-19, Dr. Balla feels it is impossible to even think of going to visit. “Even if I go, what if something happens where my visa gets stuck, or the visa office is not open?” she said. If she could not get back to the United States as planned, she would have patients left behind here.
Recently, Dr. Balla did travel to India and her passport stamp did not come on time, so her husband had to come back to the United States by himself. She had to wait for her stamp for a couple more weeks before she could leave and, in the meantime, had to make arrangements at her hospital. “It is so much trauma,” she said.
There’s also the worry she has about getting sick or disabled and not being able to work anymore, resulting in deportation. “Is that what we are doing for people who are working like soldiers? Are we really treating them the correct way?” Dr. Balla asked.
Dr. Balla considers all health care workers to be soldiers in the COVID-19 war. As such, she believes the government should step up to make sure they are supporting and helping these immigrant physician-soldiers who are so necessary. She applauds France’s recent decision to grant citizenship to its frontline immigrant health care workers and feels that the same should be done in the United States. She filed her green card application in 2012, but she is nowhere close to getting it. (The backlog for employment-based green cards is more than 900,000 now.)
As people putting their own and their family’s lives at risk to care for patients with COVID-19, Dr. Balla and her husband have talked about moving to another country or even back to India. “I am a taxpayer; I am a good human being working for the community and for the job. This is my 13th year here. If I am not eligible [for citizenship] still, then I am not sure what else I have to do to prove myself,” she said. “I am owning United States citizens as my people, so please own us and help us out in this difficult scenario.”
The COVID-19 pandemic has been difficult for all hospitalists, especially those who are parents of young children. For hospitalist moms who are also immigrants working on temporary H1-B visas, this stress is exacerbated. Though each story is unique, the underlying themes are the same: Worries over visa renewals, the immigration process, family members back home, and the risk of illness, job loss, and deportation.
Supporting the family
Like all health care workers, Prasanna Palabindela, MD, a hospitalist at Jennie Stuart Health in Hopkinsville, Ky., has been worried about bringing COVID-19 home to her family, especially in the beginning. Her in-laws had just arrived from India for a visit in March 2020 when the pandemic began, everything was shut down, and her in-laws were forced to settle in for an unexpected months-long stay.
Along with her elderly in-laws, who also have chronic conditions, Dr. Palabindela had two small children to worry about – a then-5-month-old daughter and a 5-year-old son. “I was more worried about them than me,” she said. “I used to take showers before coming home and just do all precautions as much as I can. I’m glad that I did not bring COVID, so far, to the family.”
Once she could safely send her in-laws back to India, Dr. Palabindela began searching for a nanny. Daycare was out of the question because she didn’t want her children to be exposed to illness. After a long search, she found a nanny who could also help her son with virtual school. “It’s expensive, but still, my family and my family’s health is my priority,” she said.
Working on visas has caused multiple issues for Dr. Palabindela and her husband. After living in different states because of their jobs, her husband joined her in West Virginia for her residency and found a job there. When Dr. Palabindela took her current position, her husband had to quit his job in West Virginia and move with her to Kentucky for them to stay together. Unfortunately, he couldn’t find a good fit for work in Kentucky, so the couple decided to put him on her visa so they wouldn’t have to live apart.
Now Dr. Palabindela is the family’s sole breadwinner. “That means if something happens to me, I always worry what’s going to happen with my family because legally, my husband cannot work. Technically, everyone is deported back to home,” she said. Not being able to work is hard for her husband too. “It’s just so much stress in the family because he worked for 11 years,” said Dr. Palabindela.
Through all the upheavals, Dr. Palabindela has had support from all sides. Her husband has been the biggest source. “He’s my backbone. Every time, he supported me in each and every aspect,” she said. Her parents and her brothers check in on her constantly to make sure she’s staying safe. Even the chief at her hospital has played a significant role, going to bat for his physicians to ensure their safety.
Dr. Palabindela credits everyone who works with COVID-19 patients as heroes. “The nurses, the physicians, the housekeeping, respiratory therapist, speech therapist, physical therapy ... everybody has a role. Everybody is a hero,” she said. “Whoever is wearing a mask is a hero, too, because they are contributing to this community.”
Advocating for immigration reform
A lack of transparency and information in the beginning of the pandemic significantly contributed to anxiety, said Anuradha Amara, MD, MBBS, a hospitalist in Wilmington, Del. She felt that what was on the news and what was actually going on in the hospitals were quite different. Colleagues were getting sick, there wasn’t enough personal protective equipment, and planning went out the window. “It’s like a meteor hitting a place and then we start dealing with the aftermath, but we weren’t ready before,” Dr. Amara said. “We didn’t have a plan for a pandemic.”
Then there was the concern of either her or her husband, a cardiologist, getting sick and potentially losing their jobs and immigration status. “How am I going to go back to my country if I had to? What will happen to my family if I die? If I go on the ventilator? Those are the insecurities we found additional to the pandemic challenges we had,” Dr. Amara said.
Not being able to go see their family in India or have them come visit was difficult – “it was pretty bad up there,” said Dr. Amara. Fortunately, her family members in India remained safe, but there’s a very real uneasiness about returning should an emergency arise. “Should I go back and then take the risk of losing my job and losing my position and my kids are here, they’re going to school here. How do you decide that?” she asked.
One of the worst effects of her visa restrictions was not being able to help in New York when hospitals were so short-staffed, and the morgues were overflowing. “New York is 3 hours away from where I live, but I was in chains. I couldn’t help them because of these visa restrictions,” Dr. Amara said. During the emergency, the state allowed physicians from other states to practice without being licensed in New York, but immigrant physicians were not included. “Even if we wanted to, we couldn’t volunteer,” said Dr. Amara. “I have family in New York, and I was really worried. Out of compassion I wanted to help, but I couldn’t do anything.”
Before the pandemic, Dr. Amara joined in advocacy efforts for immigrant physicians through Physicians for American Healthcare Access (PAHA). “In uncertain times, like COVID, it gets worse that you’re challenged with everything on top of your health, your family, and you have to be worried about deportation,” she said. “We need to strengthen legislation. Nobody should suffer with immigration processes during an active pandemic or otherwise.”
In the United States, 28% of physicians are immigrants. Dr. Amara pointed out that these physicians go through years of expensive training with extensive background checks at every level, yet they’re classified as second preference (EB-2) workers. She believes that physicians as a group should be excluded from this category and allowed to automatically become citizens after 5 years of living in the United States and working in an underserved area.
There have been an estimated 15,000 unused green cards since 2005. And if Congress went back to 1992, there could be more than 220,000 previously unused green cards recaptured. These unused green cards are the basis behind bills H.R.2255 and S.1024, the Healthcare Workforce Resiliency Act, which has been championed by SHM and PAHA. “It will allow the frontline physicians, 15,000 of them, and 25,000 nurses, to obtain their permanent residency,” said Dr. Amara. “These are people who already applied for their permanent residencies and they’re still waiting.”
SHM has consistently advocated for the Act since it was first introduced, written multiple letters on the issue, and supported it both on and off Capitol Hill. The society says the legislation would be an “important first step toward addressing a critical shortage” in the U.S. health care system by “recognizing the vital role immigrant physicians and nurses are playing in the fight against COVID-19.”
Currently, SHM has a live action alert open for the reintroduced bill, and encourages members to contact their legislators and urge them to support the reintroduction of the Act by cosponsoring and working to pass the legislation
Dr. Amara encourages physicians to start engaging in advocacy efforts early. Though she didn’t begin participating until late in her career, she said being aware of and part of policies that affect medicine is important. If more physicians get involved, “there are so many things we can take care of,” said Dr. Amara. “The medical profession doesn’t have to be so difficult and so busy. There are ways we can make it better and I believe that. And obviously I’ll continue to work and advocate for the entire medical profession, their problems, their health and well-being, to prevent burnout.”
Making time for positivity and self-care
Sandhya Tagaram, MD, a hospitalist at UMass Memorial Medical Center in Worcester, Mass., and her husband, also a hospitalist physician, had only ever read about pandemics in books. They certainly never expected to be in the middle of one. “That was a totally different level of anxiety to work as frontline physicians with two kids under 5 years and families away back home in India,” she said.
Dr. Tagaram and her husband work opposite shifts so that one of them is always home with their two young children. “Our schedules became more challenging when the pandemic started. Between both of our schedules and with minimal childcare facilities, we managed to strike a decent work-family balance, although we experience less vacation time together. We are fortunate to have an understanding work group,” said Dr. Tagaram.
Even before COVID-19, Dr. Tagaram found working on the temporary work visa challenging. “I think the pandemic has exposed the layer of uncertainty associated with it,” she said. “It’s incredibly stressful to imagine any minor turbulence that could alter our family and work lives. As a frontline physician mom, I take pride in raising my kids and taking care of my patients. We want to serve our communities and at the same time secure our families.”
Not being able to visit family back home and travel is exceedingly difficult. Dr. Tagaram said it would be helpful if there was a separate permanent residence pathway for physicians because they play a critical role in public health and they have been an integral part of the COVID-19 pandemic response team. A separate pathway could help keep their families secure and enable them to give their best to their communities.
Amid all the anxiety, Dr. Tagaram said she and her husband realized they could not keep living with so much pressure. As parents and as physicians, they did not want their stress to leak out and affect their ability and commitment to care for their children or their patients. They decided they needed to figure out how to be positive and constructive.
“We try some daily fun activities with the kids after returning home from work,” said Dr. Tagaram. They also formed a bubble group with two other physician families so the children could interact safely. She said that it’s critical that physicians take time for themselves. “We have to cultivate a serious hobby that helps to rejuvenate and calm our busy minds,” said Dr. Tagaram.
She makes time every day to exercise and to read at least a few pages from a good book. She is also learning Carnatic music along with one of her daughters. And every month since March 2020, she has journaled about her work and what she learned so her daughters can read it someday. “These things keep me jazzed up,” she said.
The pandemic has highlighted the fact that we are all part of one global community. “Although we hail from different backgrounds, we learned that we do have some common goals of being kind and supportive to each other and to give back to our communities. Hopefully we will continue this spirit,” said Dr. Tagaram. As a physician mother, “I feel it’s a privilege and honor to take care of my family and my community.”
Soldiering on in the COVID-19 war
The uncertainty everyone felt at the beginning of the pandemic was “very, very scary,” said Mamtha Balla, MD, MPH, a hospitalist and clinical assistant professor in northwest Ohio. “Initially, I was so involved in it and I felt like it was like a war, a COVID-19 war, and we are soldiers in that and trying to protect and do whatever we can.”
She and her husband, a geriatrician also working on an H-1B visa, have worked hard not to bring the virus home to their 2-year-old daughter. Going into 2021, the past 2 years have been “the most hectic and emotionally draining – and physically exhausting – years of my life,” said Dr. Balla.
The COVID-19 vaccine has helped reduce some pressure, but Dr. Balla is still concerned about the high risk to health care workers and the new COVID-19 strains coming out. “We are really not sure what we are dealing with and how the COVID will calm,” she said. “It is pretty challenging being a health care worker because not only are you responsible for your patients at the end of the day, but you are also responsible for your families.”
Initially in the United States from India on a student visa in 2008, Dr. Balla was placed on an H-1B visa when she started her residency. It was during this time that her mother was diagnosed with cancer and went through surgeries and chemotherapy. “She was pretty ill,” recalled Dr. Balla.
Despite the situation, Dr. Balla was afraid to go stay with her mother in case her visa application was rejected, and she couldn’t complete her third year of education. “I opted not to go to India at that time because I did not want to take a chance,” Dr. Balla said. “I have tears in my eyes because those are not easy moments, to withhold from seeing your parents, or to be in any other emergency where you cannot travel. That especially puts us at a higher risk emotionally and physically.”
She has not seen her parents in 2½ years. Between the very real possibility of not being able to get her visa stamp and the unpredictability of how other countries are dealing with COVID-19, Dr. Balla feels it is impossible to even think of going to visit. “Even if I go, what if something happens where my visa gets stuck, or the visa office is not open?” she said. If she could not get back to the United States as planned, she would have patients left behind here.
Recently, Dr. Balla did travel to India and her passport stamp did not come on time, so her husband had to come back to the United States by himself. She had to wait for her stamp for a couple more weeks before she could leave and, in the meantime, had to make arrangements at her hospital. “It is so much trauma,” she said.
There’s also the worry she has about getting sick or disabled and not being able to work anymore, resulting in deportation. “Is that what we are doing for people who are working like soldiers? Are we really treating them the correct way?” Dr. Balla asked.
Dr. Balla considers all health care workers to be soldiers in the COVID-19 war. As such, she believes the government should step up to make sure they are supporting and helping these immigrant physician-soldiers who are so necessary. She applauds France’s recent decision to grant citizenship to its frontline immigrant health care workers and feels that the same should be done in the United States. She filed her green card application in 2012, but she is nowhere close to getting it. (The backlog for employment-based green cards is more than 900,000 now.)
As people putting their own and their family’s lives at risk to care for patients with COVID-19, Dr. Balla and her husband have talked about moving to another country or even back to India. “I am a taxpayer; I am a good human being working for the community and for the job. This is my 13th year here. If I am not eligible [for citizenship] still, then I am not sure what else I have to do to prove myself,” she said. “I am owning United States citizens as my people, so please own us and help us out in this difficult scenario.”
Hospitalists innovate in ICU management
With intensive care units stretched to their limits – and beyond – during the COVID-19 pandemic, hospitalists became more central than ever in orchestrating the response.
At SHM Converge, the annual conference of the Society of Hospital Medicine, two hospitalists shared how their teams helped to develop new critical care units and strategies for best managing and allocating care to COVID patients in the ICU.
“The pandemic has been a selective pressure on us as a specialty,” said Jason Stein, MD, SFHM, a full-time clinical hospitalist at Roper Hospital, a 332-bed facility in Charleston, S.C.
Dr. Stein explained how hospitalists at Roper helped create the Progressive Care Unit – a negative-pressure unit with 12 high-flow oxygen beds overseen by a hospital medicine team, with the help of a respiratory therapist, pharmacist, and nurses. Patients in this unit had escalating acuity – quickly increasing oxygen needs – or deescalating acuity, such as ICU transfers, Dr. Stein said. Cardiac catheterization space was converted for the unit, which was intended to preserve beds in the hospital ICU for patients needing mechanical ventilation or vasoactive medication.
Interdisciplinary rounds – to assess oxygen and inflammatory marker trends, and run through a COVID care checklist – took place every day at 10 a.m.
“Consistency was the key,” Dr. Stein said.
At Weill Cornell Medical Center in New York, hospitalists helped build the COVID Recovery Unit, which was dedicated to the care of patients coming out of the ICU, said Vishwas Anand Singh, MD, MS, FHM, cochief of hospital medicine at New York Presbyterian–Lower Manhattan Hospital.
“The pandemic created an unprecedented need for critical care, and post-ICU care,” Dr. Singh said. “After extubation, patients remain very complicated and they have unique needs.”
The 30-bed COVID Recovery Unit – converted from a behavioral health unit – was designed to meet those needs. It was staffed by one lead hospitalist, 3 hospitalist physicians, 3 advanced practitioners, about 12 nurses and a neurologist, psychiatrist, and neuropsychologist.
The idea was to integrate medical care with careful attention to rehab and neuropsychological needs, Dr. Singh said. To be in the unit, patients had to be medically stable but with ongoing medical and rehabilitation needs and able to tolerate about half an hour of physical or occupational therapy each day.
The space was set up so that patients could interact with each other as well as staff, and this ability to share their experiences of trauma and recovery “led to an improved sense of psychological well-being and to healing,” according to Dr. Singh. Group therapy and meditation were also held several times a week.
“All this together, we thought we were really meeting the need for a lot of these patients from medical to psychosocial,” he said.
New York Presbyterian––Lower Manhattan Hospital also established a program called ICU Outreach to give hospitalists a “bird’s eye view” of the ICU in order to help move patients from unit to unit for optimized care. One hospitalist acted as a bridge between the ICU, the floors, and the emergency room.
The hospitalist on duty touched based with the ICU each day at 10 a.m., assessed the available beds, compiled a list of patients being discharged, met with all of the hospitalists and individual teams in inpatient and emergency services, and compiled a list of “watchers” – the sickest patients who needed help being managed.
The broad perspective was important, Dr. Singh said.
“We quickly found that each individual team or provider only knew the patients they were caring for, and the ICU Outreach person knew the whole big picture and could put the pieces together,” he said. “They could answer who was next in line for a bed, who benefited from a goals of care discussion, who could be managed on the floor with assistance. And this bridge, having this person fill this role, allowed the intensivists to focus on the patients they had in the unit.”
Palliative care and patient flow
Dr. Singh also described how hospitalists played an important role in palliative care for COVID patients. The hospital medicine team offered hospitalist palliative care services, which included COVIDtalk, a course on communicating about end of life, which helped to expand the pool of palliative care providers. Those trained were taught that these difficult conversations had to be honest and clear, with the goals of care addressed very early in the admission, should a patient decompensate soon after arrival.
A palliative “rapid response team” included a virtual hospitalist, a palliative care nurse practitioner, and a virtual psychiatrist – a team available 24 hours a day to have longer conversations so that clinicians could better tend to their patients when the in-person palliative care service was stretched thin, or at off hours like the middle of the night.
These innovations not only helped serve patients and families better, but also gave hospitalists training and experience in palliative care.
At Roper Hospital, Dr. Stein explained how hospitalists helped improve management of COVID patient flow. Depending on the time of day and the staffing on duty, there could be considerable confusion about where patients should go after the ED, or the COVID progressive unit, or the floor.
Hospitalists helped develop hospitalwide algorithms for escalating and deescalating acuity, Dr. Stein said, providing a “shared mental model for where a patient should go.”
“There are many ways hospitalists can and did rise to meet the unique demands of COVID,” Dr. Singh said, “whether it was innovating a new unit or service or work flow or leading a multidisciplinary team to extend or support other services that may have been strained.”
With intensive care units stretched to their limits – and beyond – during the COVID-19 pandemic, hospitalists became more central than ever in orchestrating the response.
At SHM Converge, the annual conference of the Society of Hospital Medicine, two hospitalists shared how their teams helped to develop new critical care units and strategies for best managing and allocating care to COVID patients in the ICU.
“The pandemic has been a selective pressure on us as a specialty,” said Jason Stein, MD, SFHM, a full-time clinical hospitalist at Roper Hospital, a 332-bed facility in Charleston, S.C.
Dr. Stein explained how hospitalists at Roper helped create the Progressive Care Unit – a negative-pressure unit with 12 high-flow oxygen beds overseen by a hospital medicine team, with the help of a respiratory therapist, pharmacist, and nurses. Patients in this unit had escalating acuity – quickly increasing oxygen needs – or deescalating acuity, such as ICU transfers, Dr. Stein said. Cardiac catheterization space was converted for the unit, which was intended to preserve beds in the hospital ICU for patients needing mechanical ventilation or vasoactive medication.
Interdisciplinary rounds – to assess oxygen and inflammatory marker trends, and run through a COVID care checklist – took place every day at 10 a.m.
“Consistency was the key,” Dr. Stein said.
At Weill Cornell Medical Center in New York, hospitalists helped build the COVID Recovery Unit, which was dedicated to the care of patients coming out of the ICU, said Vishwas Anand Singh, MD, MS, FHM, cochief of hospital medicine at New York Presbyterian–Lower Manhattan Hospital.
“The pandemic created an unprecedented need for critical care, and post-ICU care,” Dr. Singh said. “After extubation, patients remain very complicated and they have unique needs.”
The 30-bed COVID Recovery Unit – converted from a behavioral health unit – was designed to meet those needs. It was staffed by one lead hospitalist, 3 hospitalist physicians, 3 advanced practitioners, about 12 nurses and a neurologist, psychiatrist, and neuropsychologist.
The idea was to integrate medical care with careful attention to rehab and neuropsychological needs, Dr. Singh said. To be in the unit, patients had to be medically stable but with ongoing medical and rehabilitation needs and able to tolerate about half an hour of physical or occupational therapy each day.
The space was set up so that patients could interact with each other as well as staff, and this ability to share their experiences of trauma and recovery “led to an improved sense of psychological well-being and to healing,” according to Dr. Singh. Group therapy and meditation were also held several times a week.
“All this together, we thought we were really meeting the need for a lot of these patients from medical to psychosocial,” he said.
New York Presbyterian––Lower Manhattan Hospital also established a program called ICU Outreach to give hospitalists a “bird’s eye view” of the ICU in order to help move patients from unit to unit for optimized care. One hospitalist acted as a bridge between the ICU, the floors, and the emergency room.
The hospitalist on duty touched based with the ICU each day at 10 a.m., assessed the available beds, compiled a list of patients being discharged, met with all of the hospitalists and individual teams in inpatient and emergency services, and compiled a list of “watchers” – the sickest patients who needed help being managed.
The broad perspective was important, Dr. Singh said.
“We quickly found that each individual team or provider only knew the patients they were caring for, and the ICU Outreach person knew the whole big picture and could put the pieces together,” he said. “They could answer who was next in line for a bed, who benefited from a goals of care discussion, who could be managed on the floor with assistance. And this bridge, having this person fill this role, allowed the intensivists to focus on the patients they had in the unit.”
Palliative care and patient flow
Dr. Singh also described how hospitalists played an important role in palliative care for COVID patients. The hospital medicine team offered hospitalist palliative care services, which included COVIDtalk, a course on communicating about end of life, which helped to expand the pool of palliative care providers. Those trained were taught that these difficult conversations had to be honest and clear, with the goals of care addressed very early in the admission, should a patient decompensate soon after arrival.
A palliative “rapid response team” included a virtual hospitalist, a palliative care nurse practitioner, and a virtual psychiatrist – a team available 24 hours a day to have longer conversations so that clinicians could better tend to their patients when the in-person palliative care service was stretched thin, or at off hours like the middle of the night.
These innovations not only helped serve patients and families better, but also gave hospitalists training and experience in palliative care.
At Roper Hospital, Dr. Stein explained how hospitalists helped improve management of COVID patient flow. Depending on the time of day and the staffing on duty, there could be considerable confusion about where patients should go after the ED, or the COVID progressive unit, or the floor.
Hospitalists helped develop hospitalwide algorithms for escalating and deescalating acuity, Dr. Stein said, providing a “shared mental model for where a patient should go.”
“There are many ways hospitalists can and did rise to meet the unique demands of COVID,” Dr. Singh said, “whether it was innovating a new unit or service or work flow or leading a multidisciplinary team to extend or support other services that may have been strained.”
With intensive care units stretched to their limits – and beyond – during the COVID-19 pandemic, hospitalists became more central than ever in orchestrating the response.
At SHM Converge, the annual conference of the Society of Hospital Medicine, two hospitalists shared how their teams helped to develop new critical care units and strategies for best managing and allocating care to COVID patients in the ICU.
“The pandemic has been a selective pressure on us as a specialty,” said Jason Stein, MD, SFHM, a full-time clinical hospitalist at Roper Hospital, a 332-bed facility in Charleston, S.C.
Dr. Stein explained how hospitalists at Roper helped create the Progressive Care Unit – a negative-pressure unit with 12 high-flow oxygen beds overseen by a hospital medicine team, with the help of a respiratory therapist, pharmacist, and nurses. Patients in this unit had escalating acuity – quickly increasing oxygen needs – or deescalating acuity, such as ICU transfers, Dr. Stein said. Cardiac catheterization space was converted for the unit, which was intended to preserve beds in the hospital ICU for patients needing mechanical ventilation or vasoactive medication.
Interdisciplinary rounds – to assess oxygen and inflammatory marker trends, and run through a COVID care checklist – took place every day at 10 a.m.
“Consistency was the key,” Dr. Stein said.
At Weill Cornell Medical Center in New York, hospitalists helped build the COVID Recovery Unit, which was dedicated to the care of patients coming out of the ICU, said Vishwas Anand Singh, MD, MS, FHM, cochief of hospital medicine at New York Presbyterian–Lower Manhattan Hospital.
“The pandemic created an unprecedented need for critical care, and post-ICU care,” Dr. Singh said. “After extubation, patients remain very complicated and they have unique needs.”
The 30-bed COVID Recovery Unit – converted from a behavioral health unit – was designed to meet those needs. It was staffed by one lead hospitalist, 3 hospitalist physicians, 3 advanced practitioners, about 12 nurses and a neurologist, psychiatrist, and neuropsychologist.
The idea was to integrate medical care with careful attention to rehab and neuropsychological needs, Dr. Singh said. To be in the unit, patients had to be medically stable but with ongoing medical and rehabilitation needs and able to tolerate about half an hour of physical or occupational therapy each day.
The space was set up so that patients could interact with each other as well as staff, and this ability to share their experiences of trauma and recovery “led to an improved sense of psychological well-being and to healing,” according to Dr. Singh. Group therapy and meditation were also held several times a week.
“All this together, we thought we were really meeting the need for a lot of these patients from medical to psychosocial,” he said.
New York Presbyterian––Lower Manhattan Hospital also established a program called ICU Outreach to give hospitalists a “bird’s eye view” of the ICU in order to help move patients from unit to unit for optimized care. One hospitalist acted as a bridge between the ICU, the floors, and the emergency room.
The hospitalist on duty touched based with the ICU each day at 10 a.m., assessed the available beds, compiled a list of patients being discharged, met with all of the hospitalists and individual teams in inpatient and emergency services, and compiled a list of “watchers” – the sickest patients who needed help being managed.
The broad perspective was important, Dr. Singh said.
“We quickly found that each individual team or provider only knew the patients they were caring for, and the ICU Outreach person knew the whole big picture and could put the pieces together,” he said. “They could answer who was next in line for a bed, who benefited from a goals of care discussion, who could be managed on the floor with assistance. And this bridge, having this person fill this role, allowed the intensivists to focus on the patients they had in the unit.”
Palliative care and patient flow
Dr. Singh also described how hospitalists played an important role in palliative care for COVID patients. The hospital medicine team offered hospitalist palliative care services, which included COVIDtalk, a course on communicating about end of life, which helped to expand the pool of palliative care providers. Those trained were taught that these difficult conversations had to be honest and clear, with the goals of care addressed very early in the admission, should a patient decompensate soon after arrival.
A palliative “rapid response team” included a virtual hospitalist, a palliative care nurse practitioner, and a virtual psychiatrist – a team available 24 hours a day to have longer conversations so that clinicians could better tend to their patients when the in-person palliative care service was stretched thin, or at off hours like the middle of the night.
These innovations not only helped serve patients and families better, but also gave hospitalists training and experience in palliative care.
At Roper Hospital, Dr. Stein explained how hospitalists helped improve management of COVID patient flow. Depending on the time of day and the staffing on duty, there could be considerable confusion about where patients should go after the ED, or the COVID progressive unit, or the floor.
Hospitalists helped develop hospitalwide algorithms for escalating and deescalating acuity, Dr. Stein said, providing a “shared mental model for where a patient should go.”
“There are many ways hospitalists can and did rise to meet the unique demands of COVID,” Dr. Singh said, “whether it was innovating a new unit or service or work flow or leading a multidisciplinary team to extend or support other services that may have been strained.”
FROM SHM CONVERGE 2021
Pandemic experience taught lessons about clinician wellness
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
FROM SHM CONVERGE 2021
Making sense of LAMA discharges
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
FROM SHM CONVERGE 2021
Hospital at Home: Delivering hospital-level care without the hospital
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
How to implement a new model of care
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
Physicians’ trust in health care leadership drops in pandemic
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a survey conducted by NORC at the University of Chicago on behalf of the American Board of Internal Medicine Foundation.
Survey results, released May 21, indicate that 30% of physicians say their trust in the U.S. health care system and health care leadership has decreased during the pandemic. Only 18% reported an increase in trust.
Physicians, however, have great trust in their fellow clinicians.
In the survey of 600 physicians, 94% said they trust doctors within their practice; 85% trusted doctors outside of their practice; and 89% trusted nurses. That trust increased during the pandemic, with 41% saying their trust in fellow physicians rose and 37% saying their trust in nurses did.
In a separate survey, NORC asked patients about their trust in various aspects of health care. Among 2,069 respondents, a wide majority reported that they trust doctors (84%) and nurses (85%), but only 64% trusted the health care system as a whole. One in three consumers (32%) said their trust in the health care system decreased during the pandemic, compared with 11% who said their trust increased.
The ABIM Foundation released the research findings on May 21 as part of Building Trust, a national campaign that aims to boost trust among patients, clinicians, system leaders, researchers, and others.
Richard J. Baron, MD, president and chief executive officer of the ABIM Foundation, said in an interview, “Clearly there’s lower trust in health care organization leaders and executives, and that’s troubling.
“Science by itself is not enough,” he said. “Becoming trustworthy has to be a core project of everybody in health care.”
Deterioration in physicians’ trust during the pandemic comes in part from failed promises of adequate personal protective equipment and some physicians’ loss of income as a result of the crisis, Dr. Baron said.
He added that the vaccine rollout was very uneven and that policies as to which elective procedures could be performed were handled differently in different parts of the country.
He also noted that, early on, transparency was lacking as to how many COVID patients hospitals were treating, which may have contributed to the decrease in trust in the system.
Fear of being known as ‘the COVID hospital’
Hospitals were afraid of being known as “the COVID hospital” and losing patients who were afraid to come there, Dr. Baron said.
He said the COVID-19 epidemic exacerbated problems regarding trust, but that trust has been declining for some time. The Building Trust campaign will focus on solutions in breaches of trust as physicians move increasingly toward being employees of huge systems, according to Dr. Baron.
However, trust works both ways, Dr. Baron notes. Physicians can be champions for their health care system or “throw the system under the bus,” he said.
For example, if a patient complains about the appointment system, clinicians who trust their institutions may say the system usually works and that they will try to make sure the patient has a better experience next time. Clinicians without trust may say they agree that the health care system doesn’t know what it is doing, and patients may further lose confidence when physicians validate their complaint, and patients may then go elsewhere.
78% of patients trust primary care doctor
When asked whether they trust their primary care physician, 78% of patients said yes. However, trust in doctors was higher among people who were older (90%), White (82%), or had high income (89%). Among people reporting lower trust, 25% said their physician spends too little time with them, and 14% said their doctor does not know or listen to them.
The survey shows that government agencies have work to do to earn trust. Responses indicate that 43% of physicians said they have “complete trust” in government health care agencies, such as the U.S. Food and Drug Administration and the Centers for Disease Control and Prevention, which is substantially higher than other parts of the health care system. However, trust in agencies declined for 43% of physician respondents and increased for 21%.
Dhruv Khullar, MD, MPP, of the department of health policy and economics at Weill Cornell Medical College in New York, told this news organization the survey results match what he sees anecdotally in medicine – that physicians have been losing trust in the system but not in their colleagues.
He said the sample size of 600 is enough to be influential, though he said he would like to know the response rate, which was not calculated for this survey.
He added that, in large part, physicians’ lack of trust in their systems may come from generally being asked to see more patients and to meet more metrics during the same or shorter periods.
Physicians’ lack of trust in the system can have significant consequences, he said. It can lead to burnout, which has been linked with poorer quality of care and physician turnover, he noted.
COVID-19 led some physicians to wonder whether their system had their best interests at heart, insofar as access to adequate medicines and supplies as well as emotional support were inconsistent, Dr. Khullar said.
He said that to regain trust health care systems need to ask themselves questions in three areas. The first is whether their goals are focused on the best interest of the organization or the best interest of the patient.
“Next is competency,” Dr. Khullar said. “Maybe your motives are right, but are you able to deliver? Are you delivering a good product, whether clinical services or something else?”
The third area is transparency, he said. “Are you going to be honest and forthright in what we’re doing and where we’re going?”
Caroline Pearson, senior vice president of health care strategy for NORC, said the emailed survey was conducted between Dec. 29, 2020, and Feb. 5, 2021, with a health care survey partner that maintains a nationwide panel of physicians across specialties.
She said this report is fairly novel insofar as surveys are more typically conducted regarding patients’ trust of their doctors or of the health care system.
Ms. Pearson said because health care is delivered in teams, understanding the level of trust among the entities helps ensure that care will be delivered effectively and seamlessly with high quality.
“We want our patients to trust our doctors, but we really want doctors to trust each other and trust the hospitals and systems in which they’re working,” she said.
Dr. Baron, Ms. Pearson, and Dr. Khullar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Trends in hospital medicine program operations during COVID-19
Staffing was a challenge for most groups
What a year it has been in the world of hospital medicine with all the changes, challenges, and uncertainties surrounding the COVID-19 pandemic. Some hospitalist programs were hit hard early on with an early surge, when little was known about COVID-19, and other programs have had more time to plan and adapt to later surges.
As many readers of The Hospitalist know, the Society of Hospital Medicine publishes a biennial State of Hospital Medicine (SoHM) Report – last published in September 2020 using data from 2019. The SoHM Report contains a wealth of information that many groups find useful in evaluating their programs, with topics ranging from compensation to staffing to scheduling. As some prior months’ Survey Insights columns have alluded to, with the rapid pace of change in 2020 because of the COVID-19 pandemic, the Society of Hospital Medicine made the decision to publish an addendum highlighting the myriad of adjustments and adaptations that have occurred in such a short period of time. The COVID-19 Addendum is available to all purchasers of the SoHM Report and contains data from survey responses submitted in September 2020.
Let’s take a look at what transpired in 2020, starting with staffing – no doubt a challenge for many groups. During some periods of time, patient volumes may have fallen below historical averages with stay-at-home orders, canceled procedures, and a reluctance by patients to seek medical care. In contrast, for many groups, other parts of the year were all-hands-on-deck scenarios to care for extraordinary surges in patient volume. To compound this, many hospitalist groups had physicians and staff facing quarantine or isolation requirements because of exposures or contracting COVID-19, and locums positions may have been difficult to fill because of travel restrictions and extreme demand.
What operational changes were made in response to these staffing challenges? Perhaps one notable finding from the COVID-19 Addendum was the need for contingency planning and backup systems. From the 2020 SoHM, prior to the pandemic, 47.4% of adult hospital medicine groups had backup systems in place. In our recently published addendum, we found that 61.9% of groups instituted a backup system where none previously existed. In addition, 54.2% of groups modified their existing backup system. Some 39.6% of hospital medicine groups also utilized clinicians from other service lines to help cover service needs.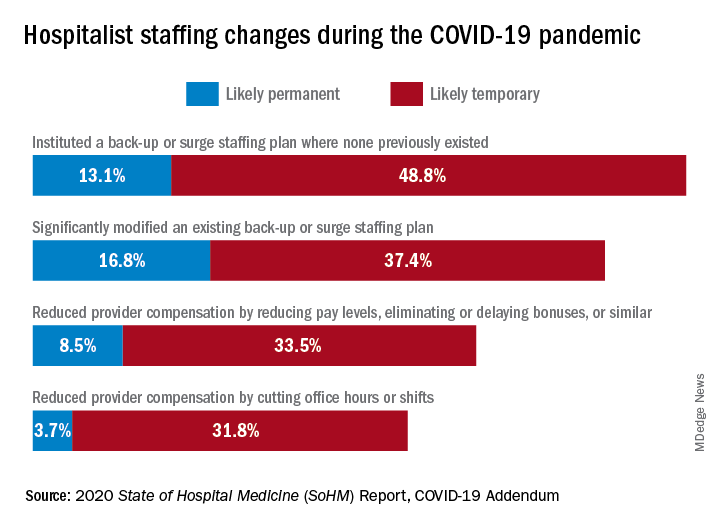
Aside from staffing, hospitals faced unprecedented financial challenges, and these effects rippled through to hospitalists. Our addendum found that 42.0% of hospitalist groups faced reductions in salary or bonuses, and 35.5% of hospital medicine groups reduced provider compensation by a reduction of work hours or shifts. I’ve personally been struck by these findings – that many hospitalists at the front-lines of COVID-19 received salary reductions, albeit temporary for many groups, during one of the most challenging years of their professional careers. Our addendum, interestingly, also found that a smaller 10.7% of groups instituted hazard pay for clinicians caring for COVID-19 patients.
So, are the changes and challenges your group faced similar to what was experienced by other hospital medicine programs? These findings and many more interesting and useful pieces of data are available in the full COVID-19 Addendum. Perhaps my biggest takeaway is that hospitalists have been perhaps the most uniquely positioned specialty to tackle the challenges of the COVID-19 pandemic. We have always been a dynamic, changing field, ready to lead and tackle change – and while change may have happened more quickly and in ways that were unforeseen just a year ago, hospitalists have undoubtedly demonstrated their strengths as leaders ready to adapt and rise to the occasion.
I am optimistic that, as we move beyond the pandemic in the coming months and years, the value that hospitalists have proven yet again will yield long-term recognition and benefits to our programs and our specialty.
Dr. Huang is a physician adviser and clinical professor of medicine in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s Practice Analysis Committee.
Staffing was a challenge for most groups
Staffing was a challenge for most groups
What a year it has been in the world of hospital medicine with all the changes, challenges, and uncertainties surrounding the COVID-19 pandemic. Some hospitalist programs were hit hard early on with an early surge, when little was known about COVID-19, and other programs have had more time to plan and adapt to later surges.
As many readers of The Hospitalist know, the Society of Hospital Medicine publishes a biennial State of Hospital Medicine (SoHM) Report – last published in September 2020 using data from 2019. The SoHM Report contains a wealth of information that many groups find useful in evaluating their programs, with topics ranging from compensation to staffing to scheduling. As some prior months’ Survey Insights columns have alluded to, with the rapid pace of change in 2020 because of the COVID-19 pandemic, the Society of Hospital Medicine made the decision to publish an addendum highlighting the myriad of adjustments and adaptations that have occurred in such a short period of time. The COVID-19 Addendum is available to all purchasers of the SoHM Report and contains data from survey responses submitted in September 2020.
Let’s take a look at what transpired in 2020, starting with staffing – no doubt a challenge for many groups. During some periods of time, patient volumes may have fallen below historical averages with stay-at-home orders, canceled procedures, and a reluctance by patients to seek medical care. In contrast, for many groups, other parts of the year were all-hands-on-deck scenarios to care for extraordinary surges in patient volume. To compound this, many hospitalist groups had physicians and staff facing quarantine or isolation requirements because of exposures or contracting COVID-19, and locums positions may have been difficult to fill because of travel restrictions and extreme demand.
What operational changes were made in response to these staffing challenges? Perhaps one notable finding from the COVID-19 Addendum was the need for contingency planning and backup systems. From the 2020 SoHM, prior to the pandemic, 47.4% of adult hospital medicine groups had backup systems in place. In our recently published addendum, we found that 61.9% of groups instituted a backup system where none previously existed. In addition, 54.2% of groups modified their existing backup system. Some 39.6% of hospital medicine groups also utilized clinicians from other service lines to help cover service needs.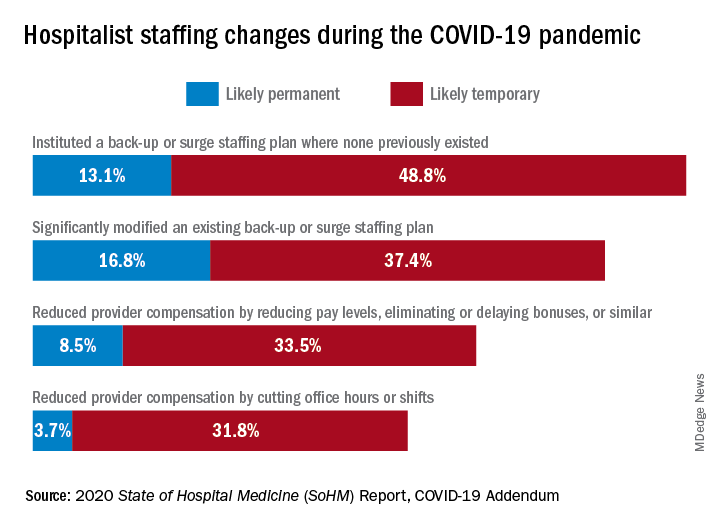
Aside from staffing, hospitals faced unprecedented financial challenges, and these effects rippled through to hospitalists. Our addendum found that 42.0% of hospitalist groups faced reductions in salary or bonuses, and 35.5% of hospital medicine groups reduced provider compensation by a reduction of work hours or shifts. I’ve personally been struck by these findings – that many hospitalists at the front-lines of COVID-19 received salary reductions, albeit temporary for many groups, during one of the most challenging years of their professional careers. Our addendum, interestingly, also found that a smaller 10.7% of groups instituted hazard pay for clinicians caring for COVID-19 patients.
So, are the changes and challenges your group faced similar to what was experienced by other hospital medicine programs? These findings and many more interesting and useful pieces of data are available in the full COVID-19 Addendum. Perhaps my biggest takeaway is that hospitalists have been perhaps the most uniquely positioned specialty to tackle the challenges of the COVID-19 pandemic. We have always been a dynamic, changing field, ready to lead and tackle change – and while change may have happened more quickly and in ways that were unforeseen just a year ago, hospitalists have undoubtedly demonstrated their strengths as leaders ready to adapt and rise to the occasion.
I am optimistic that, as we move beyond the pandemic in the coming months and years, the value that hospitalists have proven yet again will yield long-term recognition and benefits to our programs and our specialty.
Dr. Huang is a physician adviser and clinical professor of medicine in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s Practice Analysis Committee.
What a year it has been in the world of hospital medicine with all the changes, challenges, and uncertainties surrounding the COVID-19 pandemic. Some hospitalist programs were hit hard early on with an early surge, when little was known about COVID-19, and other programs have had more time to plan and adapt to later surges.
As many readers of The Hospitalist know, the Society of Hospital Medicine publishes a biennial State of Hospital Medicine (SoHM) Report – last published in September 2020 using data from 2019. The SoHM Report contains a wealth of information that many groups find useful in evaluating their programs, with topics ranging from compensation to staffing to scheduling. As some prior months’ Survey Insights columns have alluded to, with the rapid pace of change in 2020 because of the COVID-19 pandemic, the Society of Hospital Medicine made the decision to publish an addendum highlighting the myriad of adjustments and adaptations that have occurred in such a short period of time. The COVID-19 Addendum is available to all purchasers of the SoHM Report and contains data from survey responses submitted in September 2020.
Let’s take a look at what transpired in 2020, starting with staffing – no doubt a challenge for many groups. During some periods of time, patient volumes may have fallen below historical averages with stay-at-home orders, canceled procedures, and a reluctance by patients to seek medical care. In contrast, for many groups, other parts of the year were all-hands-on-deck scenarios to care for extraordinary surges in patient volume. To compound this, many hospitalist groups had physicians and staff facing quarantine or isolation requirements because of exposures or contracting COVID-19, and locums positions may have been difficult to fill because of travel restrictions and extreme demand.
What operational changes were made in response to these staffing challenges? Perhaps one notable finding from the COVID-19 Addendum was the need for contingency planning and backup systems. From the 2020 SoHM, prior to the pandemic, 47.4% of adult hospital medicine groups had backup systems in place. In our recently published addendum, we found that 61.9% of groups instituted a backup system where none previously existed. In addition, 54.2% of groups modified their existing backup system. Some 39.6% of hospital medicine groups also utilized clinicians from other service lines to help cover service needs.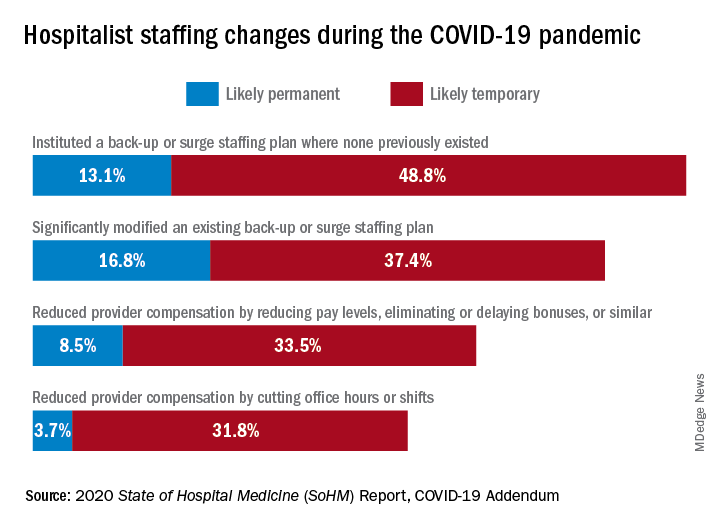
Aside from staffing, hospitals faced unprecedented financial challenges, and these effects rippled through to hospitalists. Our addendum found that 42.0% of hospitalist groups faced reductions in salary or bonuses, and 35.5% of hospital medicine groups reduced provider compensation by a reduction of work hours or shifts. I’ve personally been struck by these findings – that many hospitalists at the front-lines of COVID-19 received salary reductions, albeit temporary for many groups, during one of the most challenging years of their professional careers. Our addendum, interestingly, also found that a smaller 10.7% of groups instituted hazard pay for clinicians caring for COVID-19 patients.
So, are the changes and challenges your group faced similar to what was experienced by other hospital medicine programs? These findings and many more interesting and useful pieces of data are available in the full COVID-19 Addendum. Perhaps my biggest takeaway is that hospitalists have been perhaps the most uniquely positioned specialty to tackle the challenges of the COVID-19 pandemic. We have always been a dynamic, changing field, ready to lead and tackle change – and while change may have happened more quickly and in ways that were unforeseen just a year ago, hospitalists have undoubtedly demonstrated their strengths as leaders ready to adapt and rise to the occasion.
I am optimistic that, as we move beyond the pandemic in the coming months and years, the value that hospitalists have proven yet again will yield long-term recognition and benefits to our programs and our specialty.
Dr. Huang is a physician adviser and clinical professor of medicine in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s Practice Analysis Committee.
Telehealth takeaways for hospitalists outlined
Although the COVID-19 pandemic put telehealth on fast forward, more than one third of patients in the United States engaged with telehealth services before February 2020, according to Ameet Doshi, MD, and Chrisanne Timpe, MD, of HealthPartners in Bloomington, Minn.
Broadly speaking, telehealth is “using virtual tools to evaluate, manage, and care for our patients, regardless of where they are located,” Dr. Doshi said during a May 6 session at SHM Converge, the annual conference of the Society of Hospital Medicine.
The entirety of telehealth includes remote ways to meet almost any patient demand, he said. Some common health terms are used interchangeably, but some use telehealth as a broad term for electronic health care services, while telemedicine may refer specifically to remote patient care, he said.
Telemedicine allows flexibility of delivering patient care in inpatient, outpatient, or at-home settings, said Dr. Doshi. To illustrate the current application of telemedicine, he used an example of a 25-bed critical access hospital serving a growing regional population in which outpatient volume is expanding and ambulatory care services are being added. In this example, inpatient volume is growing, but not enough to support an inpatient consult service, but telehealth access to specialists such as cardiology would be useful in this case, he said.
Hospitalist telehealth means “being able to provide services to changing patient populations regardless of location; we can bring services to where patients are,” said Dr. Doshi.
Benefits of telehealth to patients include less travel and easier access to care, benefits to clinicians include expanding services at lower financial costs, he said.
COVID-19 challenges and opportunities
The COVID-19 pandemic presented both challenges and opportunities for telehealth, Dr. Doshi said. One opportunity was the sudden broad acceptance of virtual care out of necessity and concern for patient and staff safety, and to preserve the use of personal protective equipment, he said. In addition, a loosening of regulatory and financial pressures allowed more institutions to expand and initiate telehealth services.
Challenges included technological limitations and, in some cases, the need to develop a telehealth infrastructure from scratch, Dr. Doshi explained. Concerns also remain regarding how telehealth will evolve in the post-pandemic future, he said.
In the meantime, Medicare data show the impact of the pandemic on telehealth services, said Dr. Doshi. A telehealth waiver issued in March 2020 led to an increase in virtual encounters, and Medicare data show approximately 25 million virtual Medicare encounters between March 2020 and October 2020, representing a 3,000% increase from the same period in 2019, he said.
“Telehealth is here to stay, so the questions are how to craft a hospitalist telehealth program and provide essential patient care,” he said.
Dr. Timpe shared some examples of the evolution of telehealth care during the pandemic, including a case of an asymptomatic but frail patient with diabetes, dementia, and coronary artery disease undergoing outpatient care for a foot infection. The patient presented to an emergency department but refused to be hospitalized because of family concerns about patient isolation (no visitors were allowed at the time) and the concerns about COVID-19 infection.
The need to help treat acutely ill patients such as this patient while avoiding hospital admission during and after the pandemic continues to lead to the development of telehealth programs, Dr. Timpe said. She shared details of the Hospital@Home program developed by her organization, Health Partners. The program is designed to treat acutely ill people in the home, if possible, and avoid the need for hospital admission. Patients receive daily medical management from a hospitalist and care from staff, including registered nurses and community paramedics. Services include provision of IV medications and fluids, but the staff also conduct labs and imaging services, Dr. Timpe said.
Conditions that the program has managed at patients’ homes include pneumonia, COPD, asthma, bronchitis, flu, COVID-19, congestive heart failure, cellulitis, and urinary tract infections, said Dr. Timpe.
“We do not accept people into the program who have treatment needs that can only be met in a hospital,” such as the need for blood products, vasopressor support, telemetry, or positive pressure support, she noted.
Between November 2019 and February 15, 2021, the Hospital@Home program has provided services to 132 patients for a total of 287 visits. The program has averted 50 emergency department visits and 40 hospitalizations, and shorted hospital stays in 57 cases, she noted.
Hospitalists are suited for telehealth for several reasons, including the ability to triage acutely ill patients, familiarity with resource utilization, and expertise in management of complex medical care, said Dr. Timpe.
Looking ahead
Dr. Doshi emphasized several ongoing issues regarding the future of telemedicine, primarily the need for standardized regulation and reimbursement; reduction of health equity disparity and attention to technological barriers (including access and technology literacy); and identification of the next frontiers in telehealth.
Research on the impact and effectiveness of telehealth is limited, but growing, and next frontiers might include making patients more active participants in telehealth via patient-operated kits, or the option of an open telemedicine marketplace, in which patients can select providers from across the country, he said. No matter where telehealth leads in the future, “we need to make sure we have a positive patient outcome,” he concluded.
Dr. Doshi and Dr. Timpe had no financial conflicts to disclose.
Although the COVID-19 pandemic put telehealth on fast forward, more than one third of patients in the United States engaged with telehealth services before February 2020, according to Ameet Doshi, MD, and Chrisanne Timpe, MD, of HealthPartners in Bloomington, Minn.
Broadly speaking, telehealth is “using virtual tools to evaluate, manage, and care for our patients, regardless of where they are located,” Dr. Doshi said during a May 6 session at SHM Converge, the annual conference of the Society of Hospital Medicine.
The entirety of telehealth includes remote ways to meet almost any patient demand, he said. Some common health terms are used interchangeably, but some use telehealth as a broad term for electronic health care services, while telemedicine may refer specifically to remote patient care, he said.
Telemedicine allows flexibility of delivering patient care in inpatient, outpatient, or at-home settings, said Dr. Doshi. To illustrate the current application of telemedicine, he used an example of a 25-bed critical access hospital serving a growing regional population in which outpatient volume is expanding and ambulatory care services are being added. In this example, inpatient volume is growing, but not enough to support an inpatient consult service, but telehealth access to specialists such as cardiology would be useful in this case, he said.
Hospitalist telehealth means “being able to provide services to changing patient populations regardless of location; we can bring services to where patients are,” said Dr. Doshi.
Benefits of telehealth to patients include less travel and easier access to care, benefits to clinicians include expanding services at lower financial costs, he said.
COVID-19 challenges and opportunities
The COVID-19 pandemic presented both challenges and opportunities for telehealth, Dr. Doshi said. One opportunity was the sudden broad acceptance of virtual care out of necessity and concern for patient and staff safety, and to preserve the use of personal protective equipment, he said. In addition, a loosening of regulatory and financial pressures allowed more institutions to expand and initiate telehealth services.
Challenges included technological limitations and, in some cases, the need to develop a telehealth infrastructure from scratch, Dr. Doshi explained. Concerns also remain regarding how telehealth will evolve in the post-pandemic future, he said.
In the meantime, Medicare data show the impact of the pandemic on telehealth services, said Dr. Doshi. A telehealth waiver issued in March 2020 led to an increase in virtual encounters, and Medicare data show approximately 25 million virtual Medicare encounters between March 2020 and October 2020, representing a 3,000% increase from the same period in 2019, he said.
“Telehealth is here to stay, so the questions are how to craft a hospitalist telehealth program and provide essential patient care,” he said.
Dr. Timpe shared some examples of the evolution of telehealth care during the pandemic, including a case of an asymptomatic but frail patient with diabetes, dementia, and coronary artery disease undergoing outpatient care for a foot infection. The patient presented to an emergency department but refused to be hospitalized because of family concerns about patient isolation (no visitors were allowed at the time) and the concerns about COVID-19 infection.
The need to help treat acutely ill patients such as this patient while avoiding hospital admission during and after the pandemic continues to lead to the development of telehealth programs, Dr. Timpe said. She shared details of the Hospital@Home program developed by her organization, Health Partners. The program is designed to treat acutely ill people in the home, if possible, and avoid the need for hospital admission. Patients receive daily medical management from a hospitalist and care from staff, including registered nurses and community paramedics. Services include provision of IV medications and fluids, but the staff also conduct labs and imaging services, Dr. Timpe said.
Conditions that the program has managed at patients’ homes include pneumonia, COPD, asthma, bronchitis, flu, COVID-19, congestive heart failure, cellulitis, and urinary tract infections, said Dr. Timpe.
“We do not accept people into the program who have treatment needs that can only be met in a hospital,” such as the need for blood products, vasopressor support, telemetry, or positive pressure support, she noted.
Between November 2019 and February 15, 2021, the Hospital@Home program has provided services to 132 patients for a total of 287 visits. The program has averted 50 emergency department visits and 40 hospitalizations, and shorted hospital stays in 57 cases, she noted.
Hospitalists are suited for telehealth for several reasons, including the ability to triage acutely ill patients, familiarity with resource utilization, and expertise in management of complex medical care, said Dr. Timpe.
Looking ahead
Dr. Doshi emphasized several ongoing issues regarding the future of telemedicine, primarily the need for standardized regulation and reimbursement; reduction of health equity disparity and attention to technological barriers (including access and technology literacy); and identification of the next frontiers in telehealth.
Research on the impact and effectiveness of telehealth is limited, but growing, and next frontiers might include making patients more active participants in telehealth via patient-operated kits, or the option of an open telemedicine marketplace, in which patients can select providers from across the country, he said. No matter where telehealth leads in the future, “we need to make sure we have a positive patient outcome,” he concluded.
Dr. Doshi and Dr. Timpe had no financial conflicts to disclose.
Although the COVID-19 pandemic put telehealth on fast forward, more than one third of patients in the United States engaged with telehealth services before February 2020, according to Ameet Doshi, MD, and Chrisanne Timpe, MD, of HealthPartners in Bloomington, Minn.
Broadly speaking, telehealth is “using virtual tools to evaluate, manage, and care for our patients, regardless of where they are located,” Dr. Doshi said during a May 6 session at SHM Converge, the annual conference of the Society of Hospital Medicine.
The entirety of telehealth includes remote ways to meet almost any patient demand, he said. Some common health terms are used interchangeably, but some use telehealth as a broad term for electronic health care services, while telemedicine may refer specifically to remote patient care, he said.
Telemedicine allows flexibility of delivering patient care in inpatient, outpatient, or at-home settings, said Dr. Doshi. To illustrate the current application of telemedicine, he used an example of a 25-bed critical access hospital serving a growing regional population in which outpatient volume is expanding and ambulatory care services are being added. In this example, inpatient volume is growing, but not enough to support an inpatient consult service, but telehealth access to specialists such as cardiology would be useful in this case, he said.
Hospitalist telehealth means “being able to provide services to changing patient populations regardless of location; we can bring services to where patients are,” said Dr. Doshi.
Benefits of telehealth to patients include less travel and easier access to care, benefits to clinicians include expanding services at lower financial costs, he said.
COVID-19 challenges and opportunities
The COVID-19 pandemic presented both challenges and opportunities for telehealth, Dr. Doshi said. One opportunity was the sudden broad acceptance of virtual care out of necessity and concern for patient and staff safety, and to preserve the use of personal protective equipment, he said. In addition, a loosening of regulatory and financial pressures allowed more institutions to expand and initiate telehealth services.
Challenges included technological limitations and, in some cases, the need to develop a telehealth infrastructure from scratch, Dr. Doshi explained. Concerns also remain regarding how telehealth will evolve in the post-pandemic future, he said.
In the meantime, Medicare data show the impact of the pandemic on telehealth services, said Dr. Doshi. A telehealth waiver issued in March 2020 led to an increase in virtual encounters, and Medicare data show approximately 25 million virtual Medicare encounters between March 2020 and October 2020, representing a 3,000% increase from the same period in 2019, he said.
“Telehealth is here to stay, so the questions are how to craft a hospitalist telehealth program and provide essential patient care,” he said.
Dr. Timpe shared some examples of the evolution of telehealth care during the pandemic, including a case of an asymptomatic but frail patient with diabetes, dementia, and coronary artery disease undergoing outpatient care for a foot infection. The patient presented to an emergency department but refused to be hospitalized because of family concerns about patient isolation (no visitors were allowed at the time) and the concerns about COVID-19 infection.
The need to help treat acutely ill patients such as this patient while avoiding hospital admission during and after the pandemic continues to lead to the development of telehealth programs, Dr. Timpe said. She shared details of the Hospital@Home program developed by her organization, Health Partners. The program is designed to treat acutely ill people in the home, if possible, and avoid the need for hospital admission. Patients receive daily medical management from a hospitalist and care from staff, including registered nurses and community paramedics. Services include provision of IV medications and fluids, but the staff also conduct labs and imaging services, Dr. Timpe said.
Conditions that the program has managed at patients’ homes include pneumonia, COPD, asthma, bronchitis, flu, COVID-19, congestive heart failure, cellulitis, and urinary tract infections, said Dr. Timpe.
“We do not accept people into the program who have treatment needs that can only be met in a hospital,” such as the need for blood products, vasopressor support, telemetry, or positive pressure support, she noted.
Between November 2019 and February 15, 2021, the Hospital@Home program has provided services to 132 patients for a total of 287 visits. The program has averted 50 emergency department visits and 40 hospitalizations, and shorted hospital stays in 57 cases, she noted.
Hospitalists are suited for telehealth for several reasons, including the ability to triage acutely ill patients, familiarity with resource utilization, and expertise in management of complex medical care, said Dr. Timpe.
Looking ahead
Dr. Doshi emphasized several ongoing issues regarding the future of telemedicine, primarily the need for standardized regulation and reimbursement; reduction of health equity disparity and attention to technological barriers (including access and technology literacy); and identification of the next frontiers in telehealth.
Research on the impact and effectiveness of telehealth is limited, but growing, and next frontiers might include making patients more active participants in telehealth via patient-operated kits, or the option of an open telemedicine marketplace, in which patients can select providers from across the country, he said. No matter where telehealth leads in the future, “we need to make sure we have a positive patient outcome,” he concluded.
Dr. Doshi and Dr. Timpe had no financial conflicts to disclose.
FROM SHM CONVERGE 2021
Survey offers a snapshot of nationwide COVID-19 discharge practices
Discharge practices for COVID-19 patients vary widely at the nation’s academic medical centers, but there are some areas of strong concordance, especially related to procedures for isolation and mitigating transmission of COVID-19.
In addition, most sites use some form of clinical criteria to determine discharge readiness, S. Ryan Greysen, MD, MHS, SFHM, said on May 5 at SHM Converge, the annual conference of the Society of Hospital Medicine.
Those rank among the key findings from of a survey of 22 academic medical centers conducted by the Hospital Medicine Re-engineering Network (HOMERuN), which was launched in 2011 as a way to advance hospital medicine through rigorous research to improve the care of hospitalized patients.
“When COVID came and changed all of our lives, HOMERuN was well positioned to examine the state of practices in member hospitals, and we set out some key principles,” Dr. Greysen said. “First, we wanted to respect the challenges and needs of sites during this extraordinary time. We wanted to support speed and flexibility from our study design to get results to the front lines as quickly as possible. Therefore, we used lightweight research methods such as cross-sectional surveys, periodic evaluations, and we use the data to support operational needs. We have developed linkages to more granular datasets such as electronic health records, but our focus to date has been mostly on the frontline experience of hospitalists and gathering consensus around clinical practice, especially in the early stages of the pandemic.”
In March and April of 2020, Dr. Greysen and colleagues collected and analyzed any discharge protocols, policies, or other documents from 22 academic medical centers. From this they created a follow-up survey containing 21 different domains that was administered to the same institutions in May and June of 2020. “It’s not meant to be a completely comprehensive list, but these 21 domains were the themes we saw coming out of these discharge practice documents,” explained Dr. Greysen, chief of hospital medicine at the University of Pennsylvania, Philadelphia, which is one of the participating sites.
Next, the researchers used a concordance table to help them keep track of which institution responded in which way for which domain, and they bundled the discharge criteria into five higher order domains: procedures for isolation and mitigating transmission; clinical criteria for discharge; nonclinical/nonisolation issues; discharge to settings other than home, and postdischarge instructions, monitoring, and follow-up.
In the procedures for isolation and mitigating transmission domain, Dr. Greysen reported that the use of isolation guidelines was the area of greatest consensus in the study, with 19 of 22 sites (86%) citing the Centers for Disease Control and Prevention and 7 (32%) also citing state department of health guidance. “Specifically, most sites included the ability to socially isolate at home (until no longer necessary per CDC guidance) as part of the criteria,” he said. Most sites (73%) required use of personal protective equipment (PPE) in transportation from the hospital and 73% gave masks and other PPE for use at home.
Session copresenter Maralyssa A. Bann, MD, a hospitalist at the University of Washington/Harborview Medical Center, Seattle, another participating site, pointed out that the institutions surveyed look to the CDC as being “the single source of truth on discharge practices,” specifically material for health care workers related to discharging COVID-19 patients. “Notable specific recent updates include the recommendation that meeting criteria for discontinuation of Transmission-Based Precautions is not a prerequisite for discharge from a health care facility,” Dr. Bann said. “Also, as of August 2020, use of symptom-based strategy for discontinuation of isolation precautions instead of repeat testing is recommended for most patients. This is a rapidly evolving area.”
Practices in the clinical criteria for discharge domain varied by site. Slightly more than one-quarter of sites (27%) gave little or no guidance by using terms like “use clinical judgment,” while 14% gave very specific detailed algorithms. “Most sites fell in between and gave some parameters, usually along the lines of symptom improvement, temperature, and oxygen requirement, but the criteria were variable,” Dr. Greysen said. “For example, in terms of temperature, many sites said that patients should be afebrile for a specific length of time, 24-72 hours, while other sites simply said afebrile at discharge.” Meanwhile, the following criteria for discharge were addressed by relatively few sites: lab criteria (36%), age (36%), high-risk comorbidities (32%), or ID consultation (18%).
In the nonclinical/nonisolation domain, 73% of sites assessed for level of support available, though this was variably defined. Slightly more than half (55%) specifically assessed activities of daily living or the presence of a caregiver to assist, while 18% reported addressing durable medical equipment such as beds and toilets and access to food or medication supplies in ways that were specific for COVID-19 patients.
In the discharge to settings other than home domain, 77% of sites addressed discharge to skilled nursing facilities, inpatient rehabilitation, or long-term care, although specific requirements were often set by the accepting facilities. In addition, 65% of sites gave specific guidance for patients experiencing unstable housing/homelessness, usually recommending a respite facility or similar, and 59% addressed congregate/shared living spaces such as assisted living facilities. “Often the strictest criteria [two negative COVID tests] were applied to discharge to these types of settings,” he said.
In the postdischarge instructions, monitoring, and follow-up domain, 73% of sites reported providing home monitoring and/or virtual follow-up care. Programs ranged from daily texting via SMS or patient portals, RN phone calls, home pulse oximeters, and/or thermometers. In addition, 55% of sites had created COVID-specific brochures, discharge instructions, and other materials to standardize content such as use of PPE, travel restrictions, social distancing, signs and symptoms to watch out for, and what to do if worsening clinically.
Dr. Bann predicted future trends on the heels of the HOMERuN survey, including the development of more evidence and consensus related to discharge criteria. “Clarity is needed specifically around hypoxemia at rest/on ambulation, as well as more flexible criteria for oxygen supplementation,” she said. “We also think there will be a considerable amount of growth in posthospitalization monitoring and support, in particular home-based and virtual/remote monitoring.”
HOMERuN is supported by the Gordon and Betty Moore Foundation, the AAMC, the Patient-Centered Outcomes Research Institute, the Clinical Data Research Networks, the Patient-Powered Research Networks, and Agency for Healthcare Research and Quality. Dr. Greysen and Dr. Bann reported having no financial disclosures.
Discharge practices for COVID-19 patients vary widely at the nation’s academic medical centers, but there are some areas of strong concordance, especially related to procedures for isolation and mitigating transmission of COVID-19.
In addition, most sites use some form of clinical criteria to determine discharge readiness, S. Ryan Greysen, MD, MHS, SFHM, said on May 5 at SHM Converge, the annual conference of the Society of Hospital Medicine.
Those rank among the key findings from of a survey of 22 academic medical centers conducted by the Hospital Medicine Re-engineering Network (HOMERuN), which was launched in 2011 as a way to advance hospital medicine through rigorous research to improve the care of hospitalized patients.
“When COVID came and changed all of our lives, HOMERuN was well positioned to examine the state of practices in member hospitals, and we set out some key principles,” Dr. Greysen said. “First, we wanted to respect the challenges and needs of sites during this extraordinary time. We wanted to support speed and flexibility from our study design to get results to the front lines as quickly as possible. Therefore, we used lightweight research methods such as cross-sectional surveys, periodic evaluations, and we use the data to support operational needs. We have developed linkages to more granular datasets such as electronic health records, but our focus to date has been mostly on the frontline experience of hospitalists and gathering consensus around clinical practice, especially in the early stages of the pandemic.”
In March and April of 2020, Dr. Greysen and colleagues collected and analyzed any discharge protocols, policies, or other documents from 22 academic medical centers. From this they created a follow-up survey containing 21 different domains that was administered to the same institutions in May and June of 2020. “It’s not meant to be a completely comprehensive list, but these 21 domains were the themes we saw coming out of these discharge practice documents,” explained Dr. Greysen, chief of hospital medicine at the University of Pennsylvania, Philadelphia, which is one of the participating sites.
Next, the researchers used a concordance table to help them keep track of which institution responded in which way for which domain, and they bundled the discharge criteria into five higher order domains: procedures for isolation and mitigating transmission; clinical criteria for discharge; nonclinical/nonisolation issues; discharge to settings other than home, and postdischarge instructions, monitoring, and follow-up.
In the procedures for isolation and mitigating transmission domain, Dr. Greysen reported that the use of isolation guidelines was the area of greatest consensus in the study, with 19 of 22 sites (86%) citing the Centers for Disease Control and Prevention and 7 (32%) also citing state department of health guidance. “Specifically, most sites included the ability to socially isolate at home (until no longer necessary per CDC guidance) as part of the criteria,” he said. Most sites (73%) required use of personal protective equipment (PPE) in transportation from the hospital and 73% gave masks and other PPE for use at home.
Session copresenter Maralyssa A. Bann, MD, a hospitalist at the University of Washington/Harborview Medical Center, Seattle, another participating site, pointed out that the institutions surveyed look to the CDC as being “the single source of truth on discharge practices,” specifically material for health care workers related to discharging COVID-19 patients. “Notable specific recent updates include the recommendation that meeting criteria for discontinuation of Transmission-Based Precautions is not a prerequisite for discharge from a health care facility,” Dr. Bann said. “Also, as of August 2020, use of symptom-based strategy for discontinuation of isolation precautions instead of repeat testing is recommended for most patients. This is a rapidly evolving area.”
Practices in the clinical criteria for discharge domain varied by site. Slightly more than one-quarter of sites (27%) gave little or no guidance by using terms like “use clinical judgment,” while 14% gave very specific detailed algorithms. “Most sites fell in between and gave some parameters, usually along the lines of symptom improvement, temperature, and oxygen requirement, but the criteria were variable,” Dr. Greysen said. “For example, in terms of temperature, many sites said that patients should be afebrile for a specific length of time, 24-72 hours, while other sites simply said afebrile at discharge.” Meanwhile, the following criteria for discharge were addressed by relatively few sites: lab criteria (36%), age (36%), high-risk comorbidities (32%), or ID consultation (18%).
In the nonclinical/nonisolation domain, 73% of sites assessed for level of support available, though this was variably defined. Slightly more than half (55%) specifically assessed activities of daily living or the presence of a caregiver to assist, while 18% reported addressing durable medical equipment such as beds and toilets and access to food or medication supplies in ways that were specific for COVID-19 patients.
In the discharge to settings other than home domain, 77% of sites addressed discharge to skilled nursing facilities, inpatient rehabilitation, or long-term care, although specific requirements were often set by the accepting facilities. In addition, 65% of sites gave specific guidance for patients experiencing unstable housing/homelessness, usually recommending a respite facility or similar, and 59% addressed congregate/shared living spaces such as assisted living facilities. “Often the strictest criteria [two negative COVID tests] were applied to discharge to these types of settings,” he said.
In the postdischarge instructions, monitoring, and follow-up domain, 73% of sites reported providing home monitoring and/or virtual follow-up care. Programs ranged from daily texting via SMS or patient portals, RN phone calls, home pulse oximeters, and/or thermometers. In addition, 55% of sites had created COVID-specific brochures, discharge instructions, and other materials to standardize content such as use of PPE, travel restrictions, social distancing, signs and symptoms to watch out for, and what to do if worsening clinically.
Dr. Bann predicted future trends on the heels of the HOMERuN survey, including the development of more evidence and consensus related to discharge criteria. “Clarity is needed specifically around hypoxemia at rest/on ambulation, as well as more flexible criteria for oxygen supplementation,” she said. “We also think there will be a considerable amount of growth in posthospitalization monitoring and support, in particular home-based and virtual/remote monitoring.”
HOMERuN is supported by the Gordon and Betty Moore Foundation, the AAMC, the Patient-Centered Outcomes Research Institute, the Clinical Data Research Networks, the Patient-Powered Research Networks, and Agency for Healthcare Research and Quality. Dr. Greysen and Dr. Bann reported having no financial disclosures.
Discharge practices for COVID-19 patients vary widely at the nation’s academic medical centers, but there are some areas of strong concordance, especially related to procedures for isolation and mitigating transmission of COVID-19.
In addition, most sites use some form of clinical criteria to determine discharge readiness, S. Ryan Greysen, MD, MHS, SFHM, said on May 5 at SHM Converge, the annual conference of the Society of Hospital Medicine.
Those rank among the key findings from of a survey of 22 academic medical centers conducted by the Hospital Medicine Re-engineering Network (HOMERuN), which was launched in 2011 as a way to advance hospital medicine through rigorous research to improve the care of hospitalized patients.
“When COVID came and changed all of our lives, HOMERuN was well positioned to examine the state of practices in member hospitals, and we set out some key principles,” Dr. Greysen said. “First, we wanted to respect the challenges and needs of sites during this extraordinary time. We wanted to support speed and flexibility from our study design to get results to the front lines as quickly as possible. Therefore, we used lightweight research methods such as cross-sectional surveys, periodic evaluations, and we use the data to support operational needs. We have developed linkages to more granular datasets such as electronic health records, but our focus to date has been mostly on the frontline experience of hospitalists and gathering consensus around clinical practice, especially in the early stages of the pandemic.”
In March and April of 2020, Dr. Greysen and colleagues collected and analyzed any discharge protocols, policies, or other documents from 22 academic medical centers. From this they created a follow-up survey containing 21 different domains that was administered to the same institutions in May and June of 2020. “It’s not meant to be a completely comprehensive list, but these 21 domains were the themes we saw coming out of these discharge practice documents,” explained Dr. Greysen, chief of hospital medicine at the University of Pennsylvania, Philadelphia, which is one of the participating sites.
Next, the researchers used a concordance table to help them keep track of which institution responded in which way for which domain, and they bundled the discharge criteria into five higher order domains: procedures for isolation and mitigating transmission; clinical criteria for discharge; nonclinical/nonisolation issues; discharge to settings other than home, and postdischarge instructions, monitoring, and follow-up.
In the procedures for isolation and mitigating transmission domain, Dr. Greysen reported that the use of isolation guidelines was the area of greatest consensus in the study, with 19 of 22 sites (86%) citing the Centers for Disease Control and Prevention and 7 (32%) also citing state department of health guidance. “Specifically, most sites included the ability to socially isolate at home (until no longer necessary per CDC guidance) as part of the criteria,” he said. Most sites (73%) required use of personal protective equipment (PPE) in transportation from the hospital and 73% gave masks and other PPE for use at home.
Session copresenter Maralyssa A. Bann, MD, a hospitalist at the University of Washington/Harborview Medical Center, Seattle, another participating site, pointed out that the institutions surveyed look to the CDC as being “the single source of truth on discharge practices,” specifically material for health care workers related to discharging COVID-19 patients. “Notable specific recent updates include the recommendation that meeting criteria for discontinuation of Transmission-Based Precautions is not a prerequisite for discharge from a health care facility,” Dr. Bann said. “Also, as of August 2020, use of symptom-based strategy for discontinuation of isolation precautions instead of repeat testing is recommended for most patients. This is a rapidly evolving area.”
Practices in the clinical criteria for discharge domain varied by site. Slightly more than one-quarter of sites (27%) gave little or no guidance by using terms like “use clinical judgment,” while 14% gave very specific detailed algorithms. “Most sites fell in between and gave some parameters, usually along the lines of symptom improvement, temperature, and oxygen requirement, but the criteria were variable,” Dr. Greysen said. “For example, in terms of temperature, many sites said that patients should be afebrile for a specific length of time, 24-72 hours, while other sites simply said afebrile at discharge.” Meanwhile, the following criteria for discharge were addressed by relatively few sites: lab criteria (36%), age (36%), high-risk comorbidities (32%), or ID consultation (18%).
In the nonclinical/nonisolation domain, 73% of sites assessed for level of support available, though this was variably defined. Slightly more than half (55%) specifically assessed activities of daily living or the presence of a caregiver to assist, while 18% reported addressing durable medical equipment such as beds and toilets and access to food or medication supplies in ways that were specific for COVID-19 patients.
In the discharge to settings other than home domain, 77% of sites addressed discharge to skilled nursing facilities, inpatient rehabilitation, or long-term care, although specific requirements were often set by the accepting facilities. In addition, 65% of sites gave specific guidance for patients experiencing unstable housing/homelessness, usually recommending a respite facility or similar, and 59% addressed congregate/shared living spaces such as assisted living facilities. “Often the strictest criteria [two negative COVID tests] were applied to discharge to these types of settings,” he said.
In the postdischarge instructions, monitoring, and follow-up domain, 73% of sites reported providing home monitoring and/or virtual follow-up care. Programs ranged from daily texting via SMS or patient portals, RN phone calls, home pulse oximeters, and/or thermometers. In addition, 55% of sites had created COVID-specific brochures, discharge instructions, and other materials to standardize content such as use of PPE, travel restrictions, social distancing, signs and symptoms to watch out for, and what to do if worsening clinically.
Dr. Bann predicted future trends on the heels of the HOMERuN survey, including the development of more evidence and consensus related to discharge criteria. “Clarity is needed specifically around hypoxemia at rest/on ambulation, as well as more flexible criteria for oxygen supplementation,” she said. “We also think there will be a considerable amount of growth in posthospitalization monitoring and support, in particular home-based and virtual/remote monitoring.”
HOMERuN is supported by the Gordon and Betty Moore Foundation, the AAMC, the Patient-Centered Outcomes Research Institute, the Clinical Data Research Networks, the Patient-Powered Research Networks, and Agency for Healthcare Research and Quality. Dr. Greysen and Dr. Bann reported having no financial disclosures.
FROM SHM CONVERGE 2021