User login
Antenatal steroids for preterm birth is cost effective
Administering antenatal corticosteroids to pregnant women at high risk for preterm birth was a cost-effective intervention that improved infant respiratory outcomes, according to a new study.
“This intervention has a potential cost saving in the United States of approximately $100 million dollars annually from the benefit in the immediate neonatal outcome alone,” Cynthia Gyamfi-Bannerman, MD, of Columbia University, New York, and her associates reported in JAMA Pediatrics. “Because late preterm birth comprises a large proportion of all preterm births, our findings have the potential for a large influence on public health.”
The researchers conducted a retrospective secondary analysis of the randomized Antenatal Late Preterm Steroids (ALPS) clinical trial October 2010 to February 2015. The trial enrolled randomly assigned antenatal administration of betamethasone or placebo to women pregnant with a singleton and at high risk for preterm birth while between 34 weeks, 6 days, and 36 weeks, 0 days, of gestation.
Antenatal corticosteroid administration was regarded as effective if a newborn did not require treatment in the first 72 hours for respiratory distress or illness. Treatment could include “continuous positive airway pressure or high-flow nasal cannula for 2 hours or more, supplemental oxygen with a fraction of inspired oxygen of 30% or more for 4 hours or more, and extracorporeal membrane oxygenation or mechanical ventilation,” Dr. Gyamfi-Bannerman and her associates wrote.
To tally the costs, the researchers used Medicaid rates to estimate the total in 2015 U.S. dollars for betamethasone, outpatient visits or inpatient stays to administer it, and all direct newborn care costs, including neonatal ICU daily costs stratified by respiratory illness severity. Betamethasone administration included an initial 12-mg intramuscular dose followed by another after 24 hours if the infant had not been delivered.
“Because therapy often persists for longer than this 72-hour duration, we measured costs through hospital discharge,” the authors wrote. “The analysis took the perspective of a third-party payer in which we included direct medical costs and associated overhead accruing to hospitals and medical payers for the care of enrolled patients and their infants.”
Among 2,821 mothers not lost to follow-up during the secondary analysis, 1,426 received betamethasone and 1,395 received placebo. For mothers who received betamethasone antenatally, the total mean cost was $4,681 per mother-infant pair. Total mean cost for those in the placebo group was $5,379 per pair, resulting in a significant mean $698 savings (P = .02). Respiratory morbidity was 2.9% lower in infants whose mothers received antenatal corticosteroid treatment.
“Thus, because the treated group had lower costs and this strategy was more effective, administration of betamethasone to women at risk for late preterm birth was judged to be a dominant strategy, which is defined as one in which costs are lower and effectiveness is higher than a comparator (incremental cost-effectiveness ratio [ICER], −23 986),” Dr. Gyamfi-Bannerman and her associates reported. ICER is defined as the difference in mean total cost per patient in the betamethasone and placebo arms divided by the difference in the effectiveness.
Study limitations were an inability to estimate costs according to quality-adjusted life years or to include families’/caregivers’ costs.
SOURCE: Gyamfi-Bannerman C. JAMA Pediatr. 2019 Mar 11. doi: 10.1001/jamapediatrics.2019.0032.
Administering antenatal corticosteroids to pregnant women at high risk for preterm birth was a cost-effective intervention that improved infant respiratory outcomes, according to a new study.
“This intervention has a potential cost saving in the United States of approximately $100 million dollars annually from the benefit in the immediate neonatal outcome alone,” Cynthia Gyamfi-Bannerman, MD, of Columbia University, New York, and her associates reported in JAMA Pediatrics. “Because late preterm birth comprises a large proportion of all preterm births, our findings have the potential for a large influence on public health.”
The researchers conducted a retrospective secondary analysis of the randomized Antenatal Late Preterm Steroids (ALPS) clinical trial October 2010 to February 2015. The trial enrolled randomly assigned antenatal administration of betamethasone or placebo to women pregnant with a singleton and at high risk for preterm birth while between 34 weeks, 6 days, and 36 weeks, 0 days, of gestation.
Antenatal corticosteroid administration was regarded as effective if a newborn did not require treatment in the first 72 hours for respiratory distress or illness. Treatment could include “continuous positive airway pressure or high-flow nasal cannula for 2 hours or more, supplemental oxygen with a fraction of inspired oxygen of 30% or more for 4 hours or more, and extracorporeal membrane oxygenation or mechanical ventilation,” Dr. Gyamfi-Bannerman and her associates wrote.
To tally the costs, the researchers used Medicaid rates to estimate the total in 2015 U.S. dollars for betamethasone, outpatient visits or inpatient stays to administer it, and all direct newborn care costs, including neonatal ICU daily costs stratified by respiratory illness severity. Betamethasone administration included an initial 12-mg intramuscular dose followed by another after 24 hours if the infant had not been delivered.
“Because therapy often persists for longer than this 72-hour duration, we measured costs through hospital discharge,” the authors wrote. “The analysis took the perspective of a third-party payer in which we included direct medical costs and associated overhead accruing to hospitals and medical payers for the care of enrolled patients and their infants.”
Among 2,821 mothers not lost to follow-up during the secondary analysis, 1,426 received betamethasone and 1,395 received placebo. For mothers who received betamethasone antenatally, the total mean cost was $4,681 per mother-infant pair. Total mean cost for those in the placebo group was $5,379 per pair, resulting in a significant mean $698 savings (P = .02). Respiratory morbidity was 2.9% lower in infants whose mothers received antenatal corticosteroid treatment.
“Thus, because the treated group had lower costs and this strategy was more effective, administration of betamethasone to women at risk for late preterm birth was judged to be a dominant strategy, which is defined as one in which costs are lower and effectiveness is higher than a comparator (incremental cost-effectiveness ratio [ICER], −23 986),” Dr. Gyamfi-Bannerman and her associates reported. ICER is defined as the difference in mean total cost per patient in the betamethasone and placebo arms divided by the difference in the effectiveness.
Study limitations were an inability to estimate costs according to quality-adjusted life years or to include families’/caregivers’ costs.
SOURCE: Gyamfi-Bannerman C. JAMA Pediatr. 2019 Mar 11. doi: 10.1001/jamapediatrics.2019.0032.
Administering antenatal corticosteroids to pregnant women at high risk for preterm birth was a cost-effective intervention that improved infant respiratory outcomes, according to a new study.
“This intervention has a potential cost saving in the United States of approximately $100 million dollars annually from the benefit in the immediate neonatal outcome alone,” Cynthia Gyamfi-Bannerman, MD, of Columbia University, New York, and her associates reported in JAMA Pediatrics. “Because late preterm birth comprises a large proportion of all preterm births, our findings have the potential for a large influence on public health.”
The researchers conducted a retrospective secondary analysis of the randomized Antenatal Late Preterm Steroids (ALPS) clinical trial October 2010 to February 2015. The trial enrolled randomly assigned antenatal administration of betamethasone or placebo to women pregnant with a singleton and at high risk for preterm birth while between 34 weeks, 6 days, and 36 weeks, 0 days, of gestation.
Antenatal corticosteroid administration was regarded as effective if a newborn did not require treatment in the first 72 hours for respiratory distress or illness. Treatment could include “continuous positive airway pressure or high-flow nasal cannula for 2 hours or more, supplemental oxygen with a fraction of inspired oxygen of 30% or more for 4 hours or more, and extracorporeal membrane oxygenation or mechanical ventilation,” Dr. Gyamfi-Bannerman and her associates wrote.
To tally the costs, the researchers used Medicaid rates to estimate the total in 2015 U.S. dollars for betamethasone, outpatient visits or inpatient stays to administer it, and all direct newborn care costs, including neonatal ICU daily costs stratified by respiratory illness severity. Betamethasone administration included an initial 12-mg intramuscular dose followed by another after 24 hours if the infant had not been delivered.
“Because therapy often persists for longer than this 72-hour duration, we measured costs through hospital discharge,” the authors wrote. “The analysis took the perspective of a third-party payer in which we included direct medical costs and associated overhead accruing to hospitals and medical payers for the care of enrolled patients and their infants.”
Among 2,821 mothers not lost to follow-up during the secondary analysis, 1,426 received betamethasone and 1,395 received placebo. For mothers who received betamethasone antenatally, the total mean cost was $4,681 per mother-infant pair. Total mean cost for those in the placebo group was $5,379 per pair, resulting in a significant mean $698 savings (P = .02). Respiratory morbidity was 2.9% lower in infants whose mothers received antenatal corticosteroid treatment.
“Thus, because the treated group had lower costs and this strategy was more effective, administration of betamethasone to women at risk for late preterm birth was judged to be a dominant strategy, which is defined as one in which costs are lower and effectiveness is higher than a comparator (incremental cost-effectiveness ratio [ICER], −23 986),” Dr. Gyamfi-Bannerman and her associates reported. ICER is defined as the difference in mean total cost per patient in the betamethasone and placebo arms divided by the difference in the effectiveness.
Study limitations were an inability to estimate costs according to quality-adjusted life years or to include families’/caregivers’ costs.
SOURCE: Gyamfi-Bannerman C. JAMA Pediatr. 2019 Mar 11. doi: 10.1001/jamapediatrics.2019.0032.
FROM JAMA PEDIATRICS
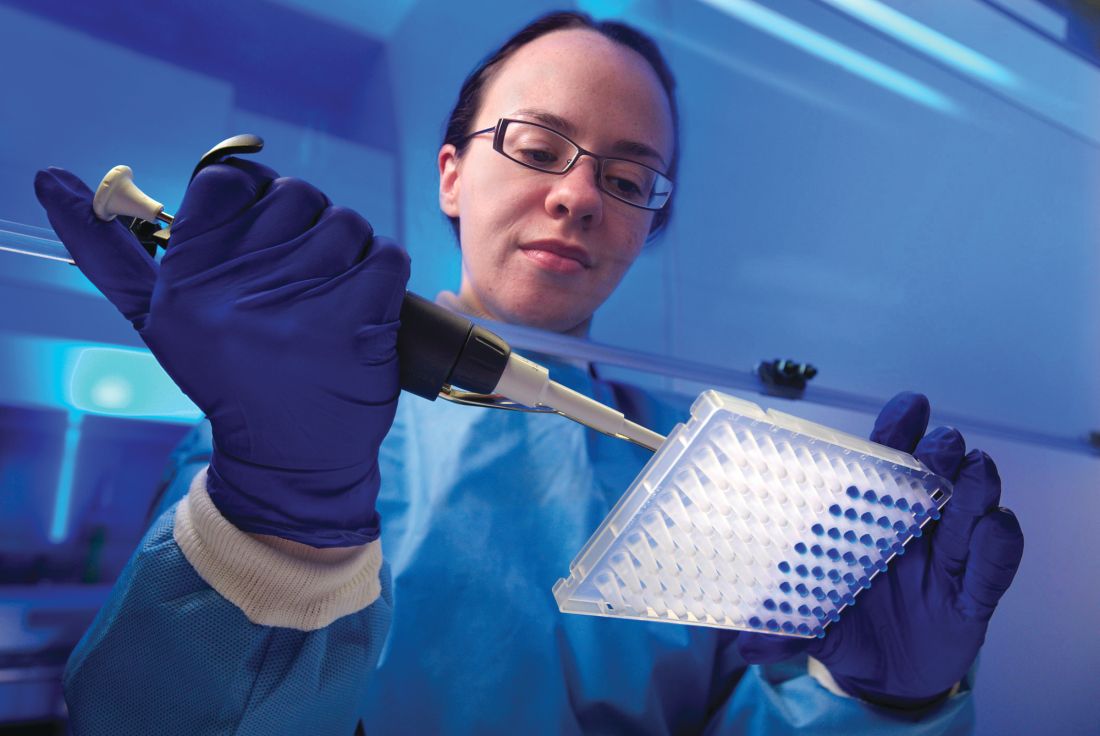
New noninvasive wireless devices aim to more gently monitor neonatal vital signs
and lowering the risk of iatrogenic injuries, according to a series of tests on neonates in two level III NICUs.
“By eliminating wired connections, these platforms also facilitate therapeutic skin-to-skin contact between neonates and parents, which is known to stabilize vital signs, reduce morbidity, and promote parental bonding,” lead author Ha Uk Chung of the University of Illinois at Urbana-Champaign and coauthors wrote in Science.
In an effort to replace current wired systems that rigidly attach to fragile neonate skin, the investigators created a pair of ultrathin, noninvasive devices that can capture and transmit full vital signs with clinical-grade precision. One of the devices is mounted on the chest and captures ECGs; the other records photoplethysmograms from the base of the foot. That data plus skin temperature is wirelessly transmitted and used to measure heart rate, respiration rate, blood oxygenation, and systolic blood pressure via pulse arrival time.
The devices were tested on neonates in two level III NICUs; the infants had gestational ages ranging from 28 weeks to full term, and the results “demonstrate[d] the full range of functions,” the investigators noted. Because the devices are smaller and lighter, they interface with infant skin with forces that are “nearly an order of magnitude smaller” than adhesives used with conventional NICU measuring systems. The coauthors also noted that these cost-effective systems have potential uses beyond typical hospital settings, including “potential relevance to global health.”
No conflicts of interest were reported.
SOURCE: Chung HU et al. Science. 2019 Mar 1. doi: 10.1126/science.aau0780.
and lowering the risk of iatrogenic injuries, according to a series of tests on neonates in two level III NICUs.
“By eliminating wired connections, these platforms also facilitate therapeutic skin-to-skin contact between neonates and parents, which is known to stabilize vital signs, reduce morbidity, and promote parental bonding,” lead author Ha Uk Chung of the University of Illinois at Urbana-Champaign and coauthors wrote in Science.
In an effort to replace current wired systems that rigidly attach to fragile neonate skin, the investigators created a pair of ultrathin, noninvasive devices that can capture and transmit full vital signs with clinical-grade precision. One of the devices is mounted on the chest and captures ECGs; the other records photoplethysmograms from the base of the foot. That data plus skin temperature is wirelessly transmitted and used to measure heart rate, respiration rate, blood oxygenation, and systolic blood pressure via pulse arrival time.
The devices were tested on neonates in two level III NICUs; the infants had gestational ages ranging from 28 weeks to full term, and the results “demonstrate[d] the full range of functions,” the investigators noted. Because the devices are smaller and lighter, they interface with infant skin with forces that are “nearly an order of magnitude smaller” than adhesives used with conventional NICU measuring systems. The coauthors also noted that these cost-effective systems have potential uses beyond typical hospital settings, including “potential relevance to global health.”
No conflicts of interest were reported.
SOURCE: Chung HU et al. Science. 2019 Mar 1. doi: 10.1126/science.aau0780.
and lowering the risk of iatrogenic injuries, according to a series of tests on neonates in two level III NICUs.
“By eliminating wired connections, these platforms also facilitate therapeutic skin-to-skin contact between neonates and parents, which is known to stabilize vital signs, reduce morbidity, and promote parental bonding,” lead author Ha Uk Chung of the University of Illinois at Urbana-Champaign and coauthors wrote in Science.
In an effort to replace current wired systems that rigidly attach to fragile neonate skin, the investigators created a pair of ultrathin, noninvasive devices that can capture and transmit full vital signs with clinical-grade precision. One of the devices is mounted on the chest and captures ECGs; the other records photoplethysmograms from the base of the foot. That data plus skin temperature is wirelessly transmitted and used to measure heart rate, respiration rate, blood oxygenation, and systolic blood pressure via pulse arrival time.
The devices were tested on neonates in two level III NICUs; the infants had gestational ages ranging from 28 weeks to full term, and the results “demonstrate[d] the full range of functions,” the investigators noted. Because the devices are smaller and lighter, they interface with infant skin with forces that are “nearly an order of magnitude smaller” than adhesives used with conventional NICU measuring systems. The coauthors also noted that these cost-effective systems have potential uses beyond typical hospital settings, including “potential relevance to global health.”
No conflicts of interest were reported.
SOURCE: Chung HU et al. Science. 2019 Mar 1. doi: 10.1126/science.aau0780.
FROM SCIENCE
Insulin-treated diabetes in pregnancy carries preterm risk
Women with insulin-treated diabetes are at significantly greater risk of preterm birth and of delivering babies who are large for gestational age (LGA), regardless of prepregnancy body weight, new findings suggest.
Researchers examined the role of maternal diabetes and weight on pregnancy outcomes in the population-based cohort study. The study comprised 649,043 live births in Finland between Jan. 1, 2004, and Dec. 31, 2014, including 4,000 in women with insulin-treated diabetes, 3,740 in women with type 2 diabetes, and 98,568 women with gestational diabetes.
Prepregnancy body mass index was normal for nearly 60% of mothers, while 4% were underweight, 21% were overweight, 8% were moderately obese, and 4% were severely obese.
Overall, the researchers found that women with insulin-treated diabetes had a 43-fold higher odds of having an LGA infant, compared with the reference group of women of normal BMI without diabetes (adjusted odds ratio [aOR], 43.80; 95% confidence interval, 40.88-46.93). And there was an 11-fold greater odds of having a preterm birth in this group (aOR, 11.17; 95% CI, 10.46-11.93).
The findings were published in JAMA Pediatrics.
“Smaller, but clearly statistically significant, increased LGA risks were found also for mothers with type 2 diabetes and gestational diabetes not treated with insulin, especially in combination with prepregnancy overweight or obesity that were stronger for type 2 diabetes than gestational diabetes,” wrote Linghua Kong, MSc, of the department of molecular medicine and surgery at Karolinska Institutet, and coauthors.
The aOR for LGA among women with type 2 diabetes was 9.57 (95% CI, 8.65-10.58), compared with the reference group. And for women with maternal gestational diabetes, the aOR for LGA was 3.80 (95% CI, 3.66-3.96).
Looking at the risk for preterm birth, the researchers found that the aOR among women with type 2 diabetes was 2.12 (95% CI, 1.90-2.36), while there was no association between gestational diabetes and preterm birth.
The researchers also reported that for women with gestational diabetes or no diabetes, the odds of preterm birth increased slightly as maternal prepregnancy BMI increased.
“Maternal glucose metabolism during pregnancy differs from that in the non-pregnant state; insulin resistance is increased, directing fat as the mother’s energy source to ensure adequate carbohydrate supply for the growing fetus,” the researchers wrote. “This increase in insulin resistance is mediated by a number of factors, such as increased levels of progesterone, estrogen, and human placental lactogen.”
The authors noted that their data did not include information on congenital anomalies, maternal complications such as preeclampsia, and grade of diabetes control during pregnancy. In addition, the data on maternal BMI was derived from a single time point.
“These findings may have implications for counseling and managing pregnancies to prevent adverse birth outcomes,” they wrote.
The study and some authors were supported by the THL National Institute for Health and Welfare, the Swedish Research Council, Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. JAMA Pediatr. 2019 Feb 25. doi: 10.1001/jamapediatrics.2018.5541.
Women with insulin-treated diabetes are at significantly greater risk of preterm birth and of delivering babies who are large for gestational age (LGA), regardless of prepregnancy body weight, new findings suggest.
Researchers examined the role of maternal diabetes and weight on pregnancy outcomes in the population-based cohort study. The study comprised 649,043 live births in Finland between Jan. 1, 2004, and Dec. 31, 2014, including 4,000 in women with insulin-treated diabetes, 3,740 in women with type 2 diabetes, and 98,568 women with gestational diabetes.
Prepregnancy body mass index was normal for nearly 60% of mothers, while 4% were underweight, 21% were overweight, 8% were moderately obese, and 4% were severely obese.
Overall, the researchers found that women with insulin-treated diabetes had a 43-fold higher odds of having an LGA infant, compared with the reference group of women of normal BMI without diabetes (adjusted odds ratio [aOR], 43.80; 95% confidence interval, 40.88-46.93). And there was an 11-fold greater odds of having a preterm birth in this group (aOR, 11.17; 95% CI, 10.46-11.93).
The findings were published in JAMA Pediatrics.
“Smaller, but clearly statistically significant, increased LGA risks were found also for mothers with type 2 diabetes and gestational diabetes not treated with insulin, especially in combination with prepregnancy overweight or obesity that were stronger for type 2 diabetes than gestational diabetes,” wrote Linghua Kong, MSc, of the department of molecular medicine and surgery at Karolinska Institutet, and coauthors.
The aOR for LGA among women with type 2 diabetes was 9.57 (95% CI, 8.65-10.58), compared with the reference group. And for women with maternal gestational diabetes, the aOR for LGA was 3.80 (95% CI, 3.66-3.96).
Looking at the risk for preterm birth, the researchers found that the aOR among women with type 2 diabetes was 2.12 (95% CI, 1.90-2.36), while there was no association between gestational diabetes and preterm birth.
The researchers also reported that for women with gestational diabetes or no diabetes, the odds of preterm birth increased slightly as maternal prepregnancy BMI increased.
“Maternal glucose metabolism during pregnancy differs from that in the non-pregnant state; insulin resistance is increased, directing fat as the mother’s energy source to ensure adequate carbohydrate supply for the growing fetus,” the researchers wrote. “This increase in insulin resistance is mediated by a number of factors, such as increased levels of progesterone, estrogen, and human placental lactogen.”
The authors noted that their data did not include information on congenital anomalies, maternal complications such as preeclampsia, and grade of diabetes control during pregnancy. In addition, the data on maternal BMI was derived from a single time point.
“These findings may have implications for counseling and managing pregnancies to prevent adverse birth outcomes,” they wrote.
The study and some authors were supported by the THL National Institute for Health and Welfare, the Swedish Research Council, Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. JAMA Pediatr. 2019 Feb 25. doi: 10.1001/jamapediatrics.2018.5541.
Women with insulin-treated diabetes are at significantly greater risk of preterm birth and of delivering babies who are large for gestational age (LGA), regardless of prepregnancy body weight, new findings suggest.
Researchers examined the role of maternal diabetes and weight on pregnancy outcomes in the population-based cohort study. The study comprised 649,043 live births in Finland between Jan. 1, 2004, and Dec. 31, 2014, including 4,000 in women with insulin-treated diabetes, 3,740 in women with type 2 diabetes, and 98,568 women with gestational diabetes.
Prepregnancy body mass index was normal for nearly 60% of mothers, while 4% were underweight, 21% were overweight, 8% were moderately obese, and 4% were severely obese.
Overall, the researchers found that women with insulin-treated diabetes had a 43-fold higher odds of having an LGA infant, compared with the reference group of women of normal BMI without diabetes (adjusted odds ratio [aOR], 43.80; 95% confidence interval, 40.88-46.93). And there was an 11-fold greater odds of having a preterm birth in this group (aOR, 11.17; 95% CI, 10.46-11.93).
The findings were published in JAMA Pediatrics.
“Smaller, but clearly statistically significant, increased LGA risks were found also for mothers with type 2 diabetes and gestational diabetes not treated with insulin, especially in combination with prepregnancy overweight or obesity that were stronger for type 2 diabetes than gestational diabetes,” wrote Linghua Kong, MSc, of the department of molecular medicine and surgery at Karolinska Institutet, and coauthors.
The aOR for LGA among women with type 2 diabetes was 9.57 (95% CI, 8.65-10.58), compared with the reference group. And for women with maternal gestational diabetes, the aOR for LGA was 3.80 (95% CI, 3.66-3.96).
Looking at the risk for preterm birth, the researchers found that the aOR among women with type 2 diabetes was 2.12 (95% CI, 1.90-2.36), while there was no association between gestational diabetes and preterm birth.
The researchers also reported that for women with gestational diabetes or no diabetes, the odds of preterm birth increased slightly as maternal prepregnancy BMI increased.
“Maternal glucose metabolism during pregnancy differs from that in the non-pregnant state; insulin resistance is increased, directing fat as the mother’s energy source to ensure adequate carbohydrate supply for the growing fetus,” the researchers wrote. “This increase in insulin resistance is mediated by a number of factors, such as increased levels of progesterone, estrogen, and human placental lactogen.”
The authors noted that their data did not include information on congenital anomalies, maternal complications such as preeclampsia, and grade of diabetes control during pregnancy. In addition, the data on maternal BMI was derived from a single time point.
“These findings may have implications for counseling and managing pregnancies to prevent adverse birth outcomes,” they wrote.
The study and some authors were supported by the THL National Institute for Health and Welfare, the Swedish Research Council, Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
SOURCE: Kong L et al. JAMA Pediatr. 2019 Feb 25. doi: 10.1001/jamapediatrics.2018.5541.
FROM JAMA PEDIATRICS
Key clinical point:
Major finding: Pregnant women with insulin-treated diabetes have a 43-fold higher odds of having a child who is large for gestational age and 11-fold high risk for preterm birth.
Study details: A population-based cohort study of 649,043 live births in Finland between 2004 and 2014.
Disclosures: The study and some authors were supported by the THL National Institute for Health and Welfare, the Swedish Research Council, Stockholm County Council, the China Scholarship Council, and the Swedish Brain Foundation.
Source: Kong L et al. JAMA Pediatr. 2019 Feb 25. doi: 10.1001/jamapediatrics.2018.5541.
Umbilical cord milking tied to severe IVH in very premature neonates
Delayed cord clamping and cutting is safer
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
Delayed cord clamping and cutting is safer
Delayed cord clamping and cutting is safer
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
REPORTING FROM THE PREGNANCY MEETING
Buprenorphine for NAS shows promise in reducing length of stay
In what is believed to be the first study of its kind to compare all available pharmacologic treatment options for relief of symptoms associated with neonatal abstinence syndrome (NAS), buprenorphine has the greatest probability of reducing duration of treatment and length of stay among newborns, reported Timothy Disher, PhD, of Dalhousie University School of Nursing, Halifax, N.S., and his associates.

It was noteworthy that the study also found morphine and phenobarbital monotherapies to be worst in overall effectiveness and ranking because these pharmacotherapies are the most frequently used treatments in the United States, according to the authors. Dr. Disher and his associates underscored the need for concern over the common rationale of treatment centers, especially in using phenobarbital, since the American Academy of Pediatrics “highlights that phenobarbital is most commonly used only as adjuvant therapy” and was not intended as a first-line treatment.
In their efforts to identify treatments that are most effective at easing the symptoms of NAS, Dr. Disher and his colleagues conducted a systematic review and network meta-analysis in June 2018, which included a search of the Cochrane Central Register of Controlled Trials, Ovid MEDLINE, Embase, and the Web of Science Core Collection. In addition, they referenced ClinicalTrials.gov to identify relevant ongoing trials. Studies ultimately included in the review were randomized clinical trials comparing at least two pharmacotherapies prescribed for NAS that had been published in peer-reviewed journals.
Eighteen studies examining treatment for NAS among 1,072 newborns, including 10 studies published since 2000, were identified; the remaining studies were published between 1977 and 1986. Altogether, eight treatment interventions were examined across 10 studies
Dr. Disher and his associates reported that, during 2004-2014, there was a fivefold increase in the number of babies presenting with NAS, from 1.5/1,000 live births to 8.0/1,000, which represented a sevenfold increase in treatment cost in the Medicaid population during the same period, from $65.4 million to $462 million.
Although Dr. Disher and his colleagues acknowledged that buprenorphine was identified as best treatment by median ranks, “the ranks for most treatments are imprecise,” they said. According to results of their analysis, buprenorphine was associated with a reduction in 2.19 days of treatment, compared with clonidine, and 12.75 days, compared with morphine. In terms of secondary outcomes, buprenorphine was associated with a reduction in length of stay of 5.35 days, compared with clonidine, and 11.43 days, compared with morphine.
Seven of the studies evaluated (n = 394) included infants requiring adjuvant treatment. Agthe et al. reported that no infants in the concomitant diluted tincture of opium (DTO) and clonidine arm needed adjuvant treatment compared with five infants in the DTO-only arm who did. Surran et al. reported 2 of 32 infants who failed attempts to wean in the concomitant morphine and clonidine group compared with none of the 34 who were in the morphine and phenobarbital group.
In terms of adverse events, one study reported a seizure that was unrelated to treatment (Kraft et al). Agthe et al. reported three infants experiencing seizure in the DTO-only group compared with no infants who received concomitant clonidine. In Surran et al., three infants receiving concomitant phenobarbital and morphine were reported to be oversedated.
In general, the rationale explaining differences in why pharmacologic therapies affect treatment length is underdeveloped, the authors said. Buprenorphine, in particular, is favored because of its ease of dosing schedule and the possible improved safety profile given its longer half-life and greater micro-opioid receptor activity. It has been further suggested that the prolonged half-life of buprenorphine may be responsible for preventing sudden withdrawal symptoms. The researchers found no significant adverse events associated with buprenorphine treatment.
Although there were differences across buprenorphine treatment protocols, Dr. Disher and his colleagues noted that they were “broadly similar.” The authors conceded, however, that there is reason to question “how much of the observed improvement in buprenorphine may be attributable to the differences in optimization of the treatment and weaning protocols.”
Based on findings in this review, the authors caution that it is unlikely “that the current evidence base is sufficient to recommend specific large-scale changes in treatment away from the current standard of care.”
Despite recent research, which proposes trying nonpharmacologic treatments first and incorporating shared rooms for families and infants to reduce length of stay when treatment is required, up to 70% of infants ultimately require pharmacologic treatment. When drug therapy is needed, the average length of stay and overall treatment costs double, 10.9 vs. 22 days and $20,708 vs. $44,720, respectively.
Since results of the analysis show benefit, however variable, in reducing the length of treatment, “continued efforts to identify the optimal pharmacological agents are justified,” urged Dr. Disher and his associates.
Ultimately, before buprenorphine can be considered as a universally accepted standard of care in the treatment of NAS, “a large multisite pragmatic trial that compares buprenorphine with other treatments” will be needed.
One of the researchers – Chris Cameron, PhD – is an employee and holds shares of the Cornerstone Research Group, which provides consultant services to various pharmaceutical and device companies. Dr. Disher is a subcontractor for the Cornerstone Research Group. There were no other disclosures to report.
SOURCE: Disher T et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.5044.
Most of the 50%-80% of newborns treated for NAS are treated pharmacologically in newborn ICUs at significant cost ($93,400 for mean stay of 23 days). To date, the wide variations in care, including pharmacologic options for treating NAS, leave clinicians with no consensus regarding which medication is best. The further absence of high-quality studies that depict effective management strategies for NAS offers “little guidance to inform best practice recommendations,” Elisha M. Wachman, MD, and Martha M. Werler, DSc, wrote in an editorial published with the study.
The network analysis approach followed by Disher et al. requires some assumptions, namely “minimal bias and homogeneity of methods,” the authors observed. Yet, some of the randomized, clinical trials included in their evaluation were “not blinded and thus carry high risk of bias.” In addition, given the varied methods employed across the studies cited, “the primary findings of this meta-analysis warrant further discussion.”
Disher et al. concede that the benefits afforded with buprenorphine treatment could be more pronounced because of the dosing and weaning methods rather than from the effect of the medicine alone. Given that some studies cited did experience a shorter absolute median length of treatment with morphine, it is possible that the shortened lengths of treatment and stay concerning buprenorphine treatment “may be overestimates,” suggested Dr. Wachman and Dr. Werler.
Because of the extent of variability across studies cited, “results of the network meta-analysis by Disher et al. should be interpreted with caution.” It is worth noting that most of the studies evaluated did not “examine long-term outcomes beyond the initial birth hospitalization.” The question is: Does shorter length of treatment lead to improved long-term outcomes, or “does it put the infant at risk for readmission and altered neurobehavior and development?”
Although the researchers provide evidence of buprenorphine’s effectiveness in significantly shortening length of treatment, compared with morphine, “results should be interpreted with caution given the small number of RCTs, small sample sizes, heterogeneous methods and study populations, and lack of long-term outcome data.”
Dr. Wachman is affiliated with the department of pediatrics, Boston Medical Center. Dr. Werler is chair of the department of epidemiology, Boston University School of Public Health. The authors were supported by a grant from the National Institute of Child Health and Human Development. Dr. Werler also is supported by a grant from the Centers for Disease Control and Prevention/Massachusetts Department of Public Health. This editorial accompanied the article by Disher et al. (JAMA Pediatrics. 2019. doi: 10. 1001/jamapediatric.2018.5029).
Most of the 50%-80% of newborns treated for NAS are treated pharmacologically in newborn ICUs at significant cost ($93,400 for mean stay of 23 days). To date, the wide variations in care, including pharmacologic options for treating NAS, leave clinicians with no consensus regarding which medication is best. The further absence of high-quality studies that depict effective management strategies for NAS offers “little guidance to inform best practice recommendations,” Elisha M. Wachman, MD, and Martha M. Werler, DSc, wrote in an editorial published with the study.
The network analysis approach followed by Disher et al. requires some assumptions, namely “minimal bias and homogeneity of methods,” the authors observed. Yet, some of the randomized, clinical trials included in their evaluation were “not blinded and thus carry high risk of bias.” In addition, given the varied methods employed across the studies cited, “the primary findings of this meta-analysis warrant further discussion.”
Disher et al. concede that the benefits afforded with buprenorphine treatment could be more pronounced because of the dosing and weaning methods rather than from the effect of the medicine alone. Given that some studies cited did experience a shorter absolute median length of treatment with morphine, it is possible that the shortened lengths of treatment and stay concerning buprenorphine treatment “may be overestimates,” suggested Dr. Wachman and Dr. Werler.
Because of the extent of variability across studies cited, “results of the network meta-analysis by Disher et al. should be interpreted with caution.” It is worth noting that most of the studies evaluated did not “examine long-term outcomes beyond the initial birth hospitalization.” The question is: Does shorter length of treatment lead to improved long-term outcomes, or “does it put the infant at risk for readmission and altered neurobehavior and development?”
Although the researchers provide evidence of buprenorphine’s effectiveness in significantly shortening length of treatment, compared with morphine, “results should be interpreted with caution given the small number of RCTs, small sample sizes, heterogeneous methods and study populations, and lack of long-term outcome data.”
Dr. Wachman is affiliated with the department of pediatrics, Boston Medical Center. Dr. Werler is chair of the department of epidemiology, Boston University School of Public Health. The authors were supported by a grant from the National Institute of Child Health and Human Development. Dr. Werler also is supported by a grant from the Centers for Disease Control and Prevention/Massachusetts Department of Public Health. This editorial accompanied the article by Disher et al. (JAMA Pediatrics. 2019. doi: 10. 1001/jamapediatric.2018.5029).
Most of the 50%-80% of newborns treated for NAS are treated pharmacologically in newborn ICUs at significant cost ($93,400 for mean stay of 23 days). To date, the wide variations in care, including pharmacologic options for treating NAS, leave clinicians with no consensus regarding which medication is best. The further absence of high-quality studies that depict effective management strategies for NAS offers “little guidance to inform best practice recommendations,” Elisha M. Wachman, MD, and Martha M. Werler, DSc, wrote in an editorial published with the study.
The network analysis approach followed by Disher et al. requires some assumptions, namely “minimal bias and homogeneity of methods,” the authors observed. Yet, some of the randomized, clinical trials included in their evaluation were “not blinded and thus carry high risk of bias.” In addition, given the varied methods employed across the studies cited, “the primary findings of this meta-analysis warrant further discussion.”
Disher et al. concede that the benefits afforded with buprenorphine treatment could be more pronounced because of the dosing and weaning methods rather than from the effect of the medicine alone. Given that some studies cited did experience a shorter absolute median length of treatment with morphine, it is possible that the shortened lengths of treatment and stay concerning buprenorphine treatment “may be overestimates,” suggested Dr. Wachman and Dr. Werler.
Because of the extent of variability across studies cited, “results of the network meta-analysis by Disher et al. should be interpreted with caution.” It is worth noting that most of the studies evaluated did not “examine long-term outcomes beyond the initial birth hospitalization.” The question is: Does shorter length of treatment lead to improved long-term outcomes, or “does it put the infant at risk for readmission and altered neurobehavior and development?”
Although the researchers provide evidence of buprenorphine’s effectiveness in significantly shortening length of treatment, compared with morphine, “results should be interpreted with caution given the small number of RCTs, small sample sizes, heterogeneous methods and study populations, and lack of long-term outcome data.”
Dr. Wachman is affiliated with the department of pediatrics, Boston Medical Center. Dr. Werler is chair of the department of epidemiology, Boston University School of Public Health. The authors were supported by a grant from the National Institute of Child Health and Human Development. Dr. Werler also is supported by a grant from the Centers for Disease Control and Prevention/Massachusetts Department of Public Health. This editorial accompanied the article by Disher et al. (JAMA Pediatrics. 2019. doi: 10. 1001/jamapediatric.2018.5029).
In what is believed to be the first study of its kind to compare all available pharmacologic treatment options for relief of symptoms associated with neonatal abstinence syndrome (NAS), buprenorphine has the greatest probability of reducing duration of treatment and length of stay among newborns, reported Timothy Disher, PhD, of Dalhousie University School of Nursing, Halifax, N.S., and his associates.

It was noteworthy that the study also found morphine and phenobarbital monotherapies to be worst in overall effectiveness and ranking because these pharmacotherapies are the most frequently used treatments in the United States, according to the authors. Dr. Disher and his associates underscored the need for concern over the common rationale of treatment centers, especially in using phenobarbital, since the American Academy of Pediatrics “highlights that phenobarbital is most commonly used only as adjuvant therapy” and was not intended as a first-line treatment.
In their efforts to identify treatments that are most effective at easing the symptoms of NAS, Dr. Disher and his colleagues conducted a systematic review and network meta-analysis in June 2018, which included a search of the Cochrane Central Register of Controlled Trials, Ovid MEDLINE, Embase, and the Web of Science Core Collection. In addition, they referenced ClinicalTrials.gov to identify relevant ongoing trials. Studies ultimately included in the review were randomized clinical trials comparing at least two pharmacotherapies prescribed for NAS that had been published in peer-reviewed journals.
Eighteen studies examining treatment for NAS among 1,072 newborns, including 10 studies published since 2000, were identified; the remaining studies were published between 1977 and 1986. Altogether, eight treatment interventions were examined across 10 studies
Dr. Disher and his associates reported that, during 2004-2014, there was a fivefold increase in the number of babies presenting with NAS, from 1.5/1,000 live births to 8.0/1,000, which represented a sevenfold increase in treatment cost in the Medicaid population during the same period, from $65.4 million to $462 million.
Although Dr. Disher and his colleagues acknowledged that buprenorphine was identified as best treatment by median ranks, “the ranks for most treatments are imprecise,” they said. According to results of their analysis, buprenorphine was associated with a reduction in 2.19 days of treatment, compared with clonidine, and 12.75 days, compared with morphine. In terms of secondary outcomes, buprenorphine was associated with a reduction in length of stay of 5.35 days, compared with clonidine, and 11.43 days, compared with morphine.
Seven of the studies evaluated (n = 394) included infants requiring adjuvant treatment. Agthe et al. reported that no infants in the concomitant diluted tincture of opium (DTO) and clonidine arm needed adjuvant treatment compared with five infants in the DTO-only arm who did. Surran et al. reported 2 of 32 infants who failed attempts to wean in the concomitant morphine and clonidine group compared with none of the 34 who were in the morphine and phenobarbital group.
In terms of adverse events, one study reported a seizure that was unrelated to treatment (Kraft et al). Agthe et al. reported three infants experiencing seizure in the DTO-only group compared with no infants who received concomitant clonidine. In Surran et al., three infants receiving concomitant phenobarbital and morphine were reported to be oversedated.
In general, the rationale explaining differences in why pharmacologic therapies affect treatment length is underdeveloped, the authors said. Buprenorphine, in particular, is favored because of its ease of dosing schedule and the possible improved safety profile given its longer half-life and greater micro-opioid receptor activity. It has been further suggested that the prolonged half-life of buprenorphine may be responsible for preventing sudden withdrawal symptoms. The researchers found no significant adverse events associated with buprenorphine treatment.
Although there were differences across buprenorphine treatment protocols, Dr. Disher and his colleagues noted that they were “broadly similar.” The authors conceded, however, that there is reason to question “how much of the observed improvement in buprenorphine may be attributable to the differences in optimization of the treatment and weaning protocols.”
Based on findings in this review, the authors caution that it is unlikely “that the current evidence base is sufficient to recommend specific large-scale changes in treatment away from the current standard of care.”
Despite recent research, which proposes trying nonpharmacologic treatments first and incorporating shared rooms for families and infants to reduce length of stay when treatment is required, up to 70% of infants ultimately require pharmacologic treatment. When drug therapy is needed, the average length of stay and overall treatment costs double, 10.9 vs. 22 days and $20,708 vs. $44,720, respectively.
Since results of the analysis show benefit, however variable, in reducing the length of treatment, “continued efforts to identify the optimal pharmacological agents are justified,” urged Dr. Disher and his associates.
Ultimately, before buprenorphine can be considered as a universally accepted standard of care in the treatment of NAS, “a large multisite pragmatic trial that compares buprenorphine with other treatments” will be needed.
One of the researchers – Chris Cameron, PhD – is an employee and holds shares of the Cornerstone Research Group, which provides consultant services to various pharmaceutical and device companies. Dr. Disher is a subcontractor for the Cornerstone Research Group. There were no other disclosures to report.
SOURCE: Disher T et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.5044.
In what is believed to be the first study of its kind to compare all available pharmacologic treatment options for relief of symptoms associated with neonatal abstinence syndrome (NAS), buprenorphine has the greatest probability of reducing duration of treatment and length of stay among newborns, reported Timothy Disher, PhD, of Dalhousie University School of Nursing, Halifax, N.S., and his associates.

It was noteworthy that the study also found morphine and phenobarbital monotherapies to be worst in overall effectiveness and ranking because these pharmacotherapies are the most frequently used treatments in the United States, according to the authors. Dr. Disher and his associates underscored the need for concern over the common rationale of treatment centers, especially in using phenobarbital, since the American Academy of Pediatrics “highlights that phenobarbital is most commonly used only as adjuvant therapy” and was not intended as a first-line treatment.
In their efforts to identify treatments that are most effective at easing the symptoms of NAS, Dr. Disher and his colleagues conducted a systematic review and network meta-analysis in June 2018, which included a search of the Cochrane Central Register of Controlled Trials, Ovid MEDLINE, Embase, and the Web of Science Core Collection. In addition, they referenced ClinicalTrials.gov to identify relevant ongoing trials. Studies ultimately included in the review were randomized clinical trials comparing at least two pharmacotherapies prescribed for NAS that had been published in peer-reviewed journals.
Eighteen studies examining treatment for NAS among 1,072 newborns, including 10 studies published since 2000, were identified; the remaining studies were published between 1977 and 1986. Altogether, eight treatment interventions were examined across 10 studies
Dr. Disher and his associates reported that, during 2004-2014, there was a fivefold increase in the number of babies presenting with NAS, from 1.5/1,000 live births to 8.0/1,000, which represented a sevenfold increase in treatment cost in the Medicaid population during the same period, from $65.4 million to $462 million.
Although Dr. Disher and his colleagues acknowledged that buprenorphine was identified as best treatment by median ranks, “the ranks for most treatments are imprecise,” they said. According to results of their analysis, buprenorphine was associated with a reduction in 2.19 days of treatment, compared with clonidine, and 12.75 days, compared with morphine. In terms of secondary outcomes, buprenorphine was associated with a reduction in length of stay of 5.35 days, compared with clonidine, and 11.43 days, compared with morphine.
Seven of the studies evaluated (n = 394) included infants requiring adjuvant treatment. Agthe et al. reported that no infants in the concomitant diluted tincture of opium (DTO) and clonidine arm needed adjuvant treatment compared with five infants in the DTO-only arm who did. Surran et al. reported 2 of 32 infants who failed attempts to wean in the concomitant morphine and clonidine group compared with none of the 34 who were in the morphine and phenobarbital group.
In terms of adverse events, one study reported a seizure that was unrelated to treatment (Kraft et al). Agthe et al. reported three infants experiencing seizure in the DTO-only group compared with no infants who received concomitant clonidine. In Surran et al., three infants receiving concomitant phenobarbital and morphine were reported to be oversedated.
In general, the rationale explaining differences in why pharmacologic therapies affect treatment length is underdeveloped, the authors said. Buprenorphine, in particular, is favored because of its ease of dosing schedule and the possible improved safety profile given its longer half-life and greater micro-opioid receptor activity. It has been further suggested that the prolonged half-life of buprenorphine may be responsible for preventing sudden withdrawal symptoms. The researchers found no significant adverse events associated with buprenorphine treatment.
Although there were differences across buprenorphine treatment protocols, Dr. Disher and his colleagues noted that they were “broadly similar.” The authors conceded, however, that there is reason to question “how much of the observed improvement in buprenorphine may be attributable to the differences in optimization of the treatment and weaning protocols.”
Based on findings in this review, the authors caution that it is unlikely “that the current evidence base is sufficient to recommend specific large-scale changes in treatment away from the current standard of care.”
Despite recent research, which proposes trying nonpharmacologic treatments first and incorporating shared rooms for families and infants to reduce length of stay when treatment is required, up to 70% of infants ultimately require pharmacologic treatment. When drug therapy is needed, the average length of stay and overall treatment costs double, 10.9 vs. 22 days and $20,708 vs. $44,720, respectively.
Since results of the analysis show benefit, however variable, in reducing the length of treatment, “continued efforts to identify the optimal pharmacological agents are justified,” urged Dr. Disher and his associates.
Ultimately, before buprenorphine can be considered as a universally accepted standard of care in the treatment of NAS, “a large multisite pragmatic trial that compares buprenorphine with other treatments” will be needed.
One of the researchers – Chris Cameron, PhD – is an employee and holds shares of the Cornerstone Research Group, which provides consultant services to various pharmaceutical and device companies. Dr. Disher is a subcontractor for the Cornerstone Research Group. There were no other disclosures to report.
SOURCE: Disher T et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.5044.
FROM JAMA PEDIATRICS
Key clinical point: A larger study comparing buprenorphine and morphine is needed to confirm study findings.
Major finding: Although morphine and phenobarbital are prescribed most frequently in the United States, they were found to be the least effective treatments available.
Study details: Systematic review and network meta-analysis.
Disclosures: The authors had no financial relationships relevant to this article to disclose.
Source: Disher T et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.5044.
Device approved to treat PDA in premature infants
weighing as little as 2 pounds.
PDA is a life-threatening opening between two blood vessels leading from the heart and commonly occurs in premature infants, with about one in five infants born prematurely having a hemodynamically significant PDA. The Amplatzer Piccolo Occluder is a self-expanding, wire mesh device that is minimally invasive and is the first device approved for use in very-low-birth-weight infants.
FDA approval was based on results of the ADO II AS trial, which evaluated the device in 50 patients with PDA who were older than 3 days. In addition, the safety and efficacy of the Amplatzer Piccolo Occluder was supported by a continued access protocol involving 150 more patients.
“This approval is a potentially life-saving advance for the very smallest premature infants that will help us treat these delicate babies who might otherwise not be able to survive,” said Evan Zahn, MD, principal investigator of ADO II AS and director of the congenital heart program at Cedars-Sinai’s Smidt Heart Institute in Los Angeles.
Find the full press release on the Abbott website.
weighing as little as 2 pounds.
PDA is a life-threatening opening between two blood vessels leading from the heart and commonly occurs in premature infants, with about one in five infants born prematurely having a hemodynamically significant PDA. The Amplatzer Piccolo Occluder is a self-expanding, wire mesh device that is minimally invasive and is the first device approved for use in very-low-birth-weight infants.
FDA approval was based on results of the ADO II AS trial, which evaluated the device in 50 patients with PDA who were older than 3 days. In addition, the safety and efficacy of the Amplatzer Piccolo Occluder was supported by a continued access protocol involving 150 more patients.
“This approval is a potentially life-saving advance for the very smallest premature infants that will help us treat these delicate babies who might otherwise not be able to survive,” said Evan Zahn, MD, principal investigator of ADO II AS and director of the congenital heart program at Cedars-Sinai’s Smidt Heart Institute in Los Angeles.
Find the full press release on the Abbott website.
weighing as little as 2 pounds.
PDA is a life-threatening opening between two blood vessels leading from the heart and commonly occurs in premature infants, with about one in five infants born prematurely having a hemodynamically significant PDA. The Amplatzer Piccolo Occluder is a self-expanding, wire mesh device that is minimally invasive and is the first device approved for use in very-low-birth-weight infants.
FDA approval was based on results of the ADO II AS trial, which evaluated the device in 50 patients with PDA who were older than 3 days. In addition, the safety and efficacy of the Amplatzer Piccolo Occluder was supported by a continued access protocol involving 150 more patients.
“This approval is a potentially life-saving advance for the very smallest premature infants that will help us treat these delicate babies who might otherwise not be able to survive,” said Evan Zahn, MD, principal investigator of ADO II AS and director of the congenital heart program at Cedars-Sinai’s Smidt Heart Institute in Los Angeles.
Find the full press release on the Abbott website.
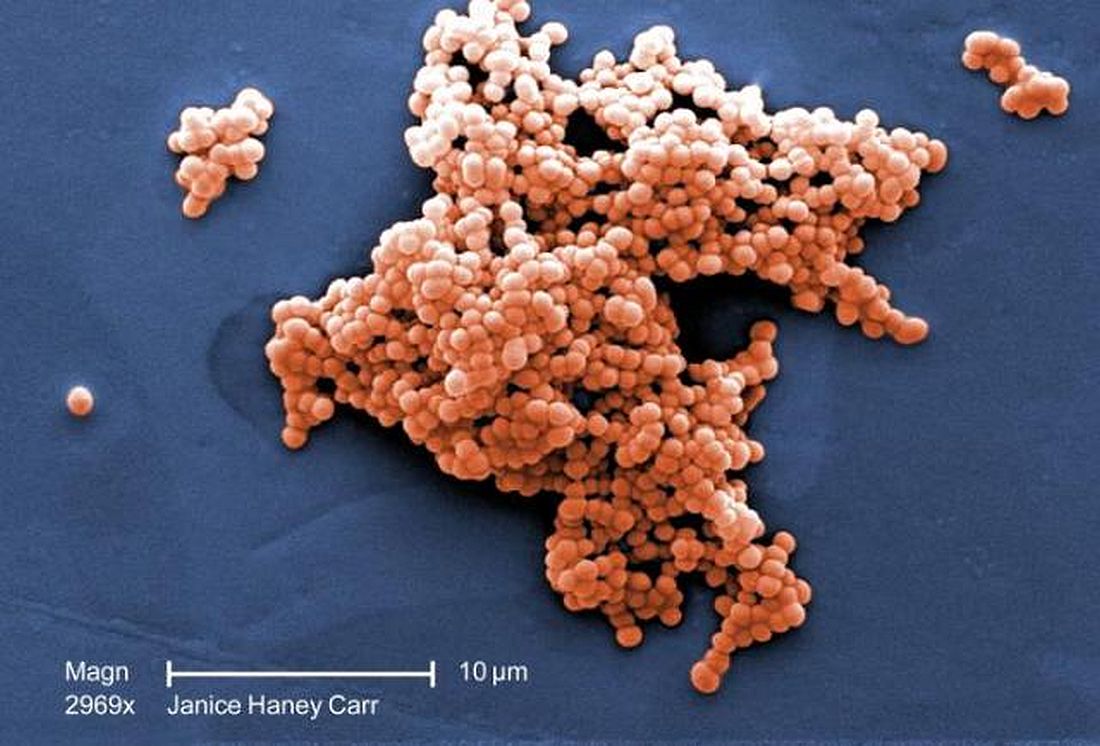
Intrapartum molecular GBS screening reduced newborn early-onset disease, antibiotic use
Point-of-care intrapartum molecular screening of group B Streptococcus reduced the incidence of early-onset disease cases and antibiotic use, according to research published in Obstetrics & Gynecology.
Najoua El Helali, PharmD, from the Service de Microbiologie Clinique at Groupe Hospitalier Paris Saint-Joseph, and her colleagues measured the rate of early-onset disease group B Streptococcus (GBS) in a single-center study analyzing antenatal culture screening for 4 years prior to implementation (2006-2009) of polymerase chain reaction (PCR) screening (2010-2015). There were 11,226 deliveries (11,818 live births) during the antenatal screening period and 18,835 deliveries (18,980 live births) during the PCR screening period. Overall, 4% of deliveries during the antenatal period and 0.1% of deliveries during the intrapartum period were not screened for GBS (P less than .001).
During 2006-2015, the rate of early-onset disease of GBS decreased to 0.21/1,000 cases from 1.01/1,000 cases (risk ratio, 0.25; 95% confidence interval, 0.14-0.43; P = .026), while the rate of probable early-onset disease GBS decreased to 0.73/1,000 cases from 2.8/1,000 cases (RR, 0.25; (95% CI, 0.14-0.43; P less than .001).
For patients with early-onset GBS, length of stay in hospital decreased by 64%, and antibiotic therapy decreased by 60%, but there was no significant difference in average length of stay or duration of antibiotic therapy during the study period. There was a reduction in annual delivery- and treatment-associated costs of early-onset disease GBS from $41,875 to $11,945, while the estimated extra cost of PCR screening to avoid one additional case of early-onset disease GBS was $5,819 and a cost increase of $49 per newborn.
“The additional PCR costs were offset in part by the reduction in early-onset GBS disease treatment costs,” the investigators said.
“A randomized, controlled multicenter study is probably needed to evaluate the cost-effectiveness of this prevention strategy and demonstrate a better efficacy in populations where poorly followed women are of unknown GBS status at presentation for delivery,” the researchers said. “In term newborns, however, using infection rate as an endpoint is problematic given the sample size needed.”
The researchers said their study was potentially limited by lack of a control group and population selection, and described mothers in their center as “mostly well-informed and well-monitored during their pregnancy.”
The authors reported no relevant conflicts of interest.
SOURCE: El Helali N et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003057.
Point-of-care intrapartum molecular screening of group B Streptococcus reduced the incidence of early-onset disease cases and antibiotic use, according to research published in Obstetrics & Gynecology.
Najoua El Helali, PharmD, from the Service de Microbiologie Clinique at Groupe Hospitalier Paris Saint-Joseph, and her colleagues measured the rate of early-onset disease group B Streptococcus (GBS) in a single-center study analyzing antenatal culture screening for 4 years prior to implementation (2006-2009) of polymerase chain reaction (PCR) screening (2010-2015). There were 11,226 deliveries (11,818 live births) during the antenatal screening period and 18,835 deliveries (18,980 live births) during the PCR screening period. Overall, 4% of deliveries during the antenatal period and 0.1% of deliveries during the intrapartum period were not screened for GBS (P less than .001).
During 2006-2015, the rate of early-onset disease of GBS decreased to 0.21/1,000 cases from 1.01/1,000 cases (risk ratio, 0.25; 95% confidence interval, 0.14-0.43; P = .026), while the rate of probable early-onset disease GBS decreased to 0.73/1,000 cases from 2.8/1,000 cases (RR, 0.25; (95% CI, 0.14-0.43; P less than .001).
For patients with early-onset GBS, length of stay in hospital decreased by 64%, and antibiotic therapy decreased by 60%, but there was no significant difference in average length of stay or duration of antibiotic therapy during the study period. There was a reduction in annual delivery- and treatment-associated costs of early-onset disease GBS from $41,875 to $11,945, while the estimated extra cost of PCR screening to avoid one additional case of early-onset disease GBS was $5,819 and a cost increase of $49 per newborn.
“The additional PCR costs were offset in part by the reduction in early-onset GBS disease treatment costs,” the investigators said.
“A randomized, controlled multicenter study is probably needed to evaluate the cost-effectiveness of this prevention strategy and demonstrate a better efficacy in populations where poorly followed women are of unknown GBS status at presentation for delivery,” the researchers said. “In term newborns, however, using infection rate as an endpoint is problematic given the sample size needed.”
The researchers said their study was potentially limited by lack of a control group and population selection, and described mothers in their center as “mostly well-informed and well-monitored during their pregnancy.”
The authors reported no relevant conflicts of interest.
SOURCE: El Helali N et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003057.
Point-of-care intrapartum molecular screening of group B Streptococcus reduced the incidence of early-onset disease cases and antibiotic use, according to research published in Obstetrics & Gynecology.
Najoua El Helali, PharmD, from the Service de Microbiologie Clinique at Groupe Hospitalier Paris Saint-Joseph, and her colleagues measured the rate of early-onset disease group B Streptococcus (GBS) in a single-center study analyzing antenatal culture screening for 4 years prior to implementation (2006-2009) of polymerase chain reaction (PCR) screening (2010-2015). There were 11,226 deliveries (11,818 live births) during the antenatal screening period and 18,835 deliveries (18,980 live births) during the PCR screening period. Overall, 4% of deliveries during the antenatal period and 0.1% of deliveries during the intrapartum period were not screened for GBS (P less than .001).
During 2006-2015, the rate of early-onset disease of GBS decreased to 0.21/1,000 cases from 1.01/1,000 cases (risk ratio, 0.25; 95% confidence interval, 0.14-0.43; P = .026), while the rate of probable early-onset disease GBS decreased to 0.73/1,000 cases from 2.8/1,000 cases (RR, 0.25; (95% CI, 0.14-0.43; P less than .001).
For patients with early-onset GBS, length of stay in hospital decreased by 64%, and antibiotic therapy decreased by 60%, but there was no significant difference in average length of stay or duration of antibiotic therapy during the study period. There was a reduction in annual delivery- and treatment-associated costs of early-onset disease GBS from $41,875 to $11,945, while the estimated extra cost of PCR screening to avoid one additional case of early-onset disease GBS was $5,819 and a cost increase of $49 per newborn.
“The additional PCR costs were offset in part by the reduction in early-onset GBS disease treatment costs,” the investigators said.
“A randomized, controlled multicenter study is probably needed to evaluate the cost-effectiveness of this prevention strategy and demonstrate a better efficacy in populations where poorly followed women are of unknown GBS status at presentation for delivery,” the researchers said. “In term newborns, however, using infection rate as an endpoint is problematic given the sample size needed.”
The researchers said their study was potentially limited by lack of a control group and population selection, and described mothers in their center as “mostly well-informed and well-monitored during their pregnancy.”
The authors reported no relevant conflicts of interest.
SOURCE: El Helali N et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003057.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: The rate of early-onset disease group B Streptococcus decreased from 1.01/1,000 cases to 0.21/1,000 cases across the antenatal and intrapartum periods.
Study details: A single-center study of antenatal culture screening for 11,226 deliveries during 2006-2009 and intrapartum PCR screening for 18,835 deliveries during 2010-2015.
Disclosures: The authors reported no relevant conflicts of interest.
Source: El Helali N et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003057.
Incidence of late-onset GBS cases are higher than early-onset disease
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
FROM JAMA PEDIATRICS
Key clinical point: Between 2006 and 2015, early-onset disease cases of group B Streptococcus (GBS) declined, while the incidence of late-onset cases did not change.
Major finding: The rate of early-onset GBS declined from 0.37 to 0.23 per 1,000 live births and the rate of late-onset GBS cases remained at a mean 0.31 per 1,000 live births.
Study details: A population-based study of infants with early-onset disease and late-onset disease GBS from 10 different states in the Active Bacterial Core surveillance program between 2006 and 2015.
Disclosures: This study was funded in part by the Centers for Disease Control and Prevention. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
Source: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
Tests can identify leukemia risk in newborns with Down syndrome
SAN DIEGO – Research into hundreds of babies with Down syndrome is providing valuable insight into the genetic roots of leukemia and offering a route to identify newborns at high risk.
“We can now identify children at high risk of developing myeloid leukemia within 4 years” through blood or genetic tests, Irene Roberts, MD, a pediatric hematologist at the University of Oxford’s (England) MRC Weatherall Institute of Molecular Medicine, said at the annual meeting of the American Society of Hematology.
About 2%-3% of children with Down syndrome will develop acute lymphocytic leukemia (ALL) or acute myeloid leukemia (AML), according to the National Cancer Institute, rates that are much higher than in the general population.
Research suggests that among children aged 0-4 years with Down syndrome, the standardized incidence ratio (SIR) of AML is 114, compared with other children, Dr. Roberts said. The SIR of ALL is 27 in children aged 1-4 years, she said.
For people with Down syndrome aged 0-60 years, the SIRs are 12 and 13 in AML and ALL, respectively, she said.
In her presentation, Dr. Roberts focused on AML that appears before age 4 years and is preceded by a neonatal preleukemia – transient abnormal myelopoiesis (TAM) – that only occurs in Down syndrome. In most cases, TAM, which occurs with GATA1 mutations, resolves on its own after birth, she said. But in others, the GATA1 mutations continue and cause AML to develop.
Dr. Roberts highlighted her institution’s Oxford Down Syndrome Cohort Study and offered an update to a 2013 report (Blood. 2013 Dec 5;122[24]:3908–17). The study recruited 471 neonates with Down syndrome and followed them for up to 4 years: 341 with no GATA1 mutation and 130 (28%) with the mutation. Dr. Roberts called the latter number a “very high frequency.”
Of those with the mutation, 7 patients (5%) developed AML at a median age of 16 months. None of those without the mutation developed AML.
Also, among the 130 neonates with the mutation, 42% were considered to have “clinical” TAM (more than 10% blasts) and 58% were considered to have “silent” TAM (fewer than 10% blasts).
“We predicted that these babies with clinical TAM would have more severe clinical disease ... and that in fact turned out to be the case,” Dr. Roberts said.
Why is the GATA1 mutation so significant? Research suggests that platelet production is abnormal in neonates with Down syndrome, compared with neonates without it, regardless of whether they have the mutation, Dr. Roberts said.
The mutation doesn’t reduce further platelet count, but does disrupt megakaryopoiesis – the process of the production of platelets. As a result, giant platelets and megakaryocyte fragments are more common, she explained.
Moving forward, research data can be used to identify which children are most at risk, Dr. Roberts said. Newborns with Down syndrome are more likely to survive without leukemia if they have silent TAM, compared with those who have clinical TAM, and if they have an estimated variant allele frequency above 15%, according to findings from the Oxford study.
Children at high risk of AML before age 4 years can be identified by analyzing the percentage of blasts on a smear and/or by analyzing mutation of GATA1, according to Dr. Roberts. However, this cannot be accomplished by the use of a complete blood count (CBC) test, she said, which is used to check for leukemia.
Dr. Roberts called for the development of more guidelines for screening newborns with Down syndrome for leukemia risk. The British Society for Haematology issued testing guidelines, coauthored by Dr. Roberts, in 2018 (Br J Haematol. 2018 Jul;182[2]:200-11).
Dr. Roberts reported having no financial disclosures.
SAN DIEGO – Research into hundreds of babies with Down syndrome is providing valuable insight into the genetic roots of leukemia and offering a route to identify newborns at high risk.
“We can now identify children at high risk of developing myeloid leukemia within 4 years” through blood or genetic tests, Irene Roberts, MD, a pediatric hematologist at the University of Oxford’s (England) MRC Weatherall Institute of Molecular Medicine, said at the annual meeting of the American Society of Hematology.
About 2%-3% of children with Down syndrome will develop acute lymphocytic leukemia (ALL) or acute myeloid leukemia (AML), according to the National Cancer Institute, rates that are much higher than in the general population.
Research suggests that among children aged 0-4 years with Down syndrome, the standardized incidence ratio (SIR) of AML is 114, compared with other children, Dr. Roberts said. The SIR of ALL is 27 in children aged 1-4 years, she said.
For people with Down syndrome aged 0-60 years, the SIRs are 12 and 13 in AML and ALL, respectively, she said.
In her presentation, Dr. Roberts focused on AML that appears before age 4 years and is preceded by a neonatal preleukemia – transient abnormal myelopoiesis (TAM) – that only occurs in Down syndrome. In most cases, TAM, which occurs with GATA1 mutations, resolves on its own after birth, she said. But in others, the GATA1 mutations continue and cause AML to develop.
Dr. Roberts highlighted her institution’s Oxford Down Syndrome Cohort Study and offered an update to a 2013 report (Blood. 2013 Dec 5;122[24]:3908–17). The study recruited 471 neonates with Down syndrome and followed them for up to 4 years: 341 with no GATA1 mutation and 130 (28%) with the mutation. Dr. Roberts called the latter number a “very high frequency.”
Of those with the mutation, 7 patients (5%) developed AML at a median age of 16 months. None of those without the mutation developed AML.
Also, among the 130 neonates with the mutation, 42% were considered to have “clinical” TAM (more than 10% blasts) and 58% were considered to have “silent” TAM (fewer than 10% blasts).
“We predicted that these babies with clinical TAM would have more severe clinical disease ... and that in fact turned out to be the case,” Dr. Roberts said.
Why is the GATA1 mutation so significant? Research suggests that platelet production is abnormal in neonates with Down syndrome, compared with neonates without it, regardless of whether they have the mutation, Dr. Roberts said.
The mutation doesn’t reduce further platelet count, but does disrupt megakaryopoiesis – the process of the production of platelets. As a result, giant platelets and megakaryocyte fragments are more common, she explained.
Moving forward, research data can be used to identify which children are most at risk, Dr. Roberts said. Newborns with Down syndrome are more likely to survive without leukemia if they have silent TAM, compared with those who have clinical TAM, and if they have an estimated variant allele frequency above 15%, according to findings from the Oxford study.
Children at high risk of AML before age 4 years can be identified by analyzing the percentage of blasts on a smear and/or by analyzing mutation of GATA1, according to Dr. Roberts. However, this cannot be accomplished by the use of a complete blood count (CBC) test, she said, which is used to check for leukemia.
Dr. Roberts called for the development of more guidelines for screening newborns with Down syndrome for leukemia risk. The British Society for Haematology issued testing guidelines, coauthored by Dr. Roberts, in 2018 (Br J Haematol. 2018 Jul;182[2]:200-11).
Dr. Roberts reported having no financial disclosures.
SAN DIEGO – Research into hundreds of babies with Down syndrome is providing valuable insight into the genetic roots of leukemia and offering a route to identify newborns at high risk.
“We can now identify children at high risk of developing myeloid leukemia within 4 years” through blood or genetic tests, Irene Roberts, MD, a pediatric hematologist at the University of Oxford’s (England) MRC Weatherall Institute of Molecular Medicine, said at the annual meeting of the American Society of Hematology.
About 2%-3% of children with Down syndrome will develop acute lymphocytic leukemia (ALL) or acute myeloid leukemia (AML), according to the National Cancer Institute, rates that are much higher than in the general population.
Research suggests that among children aged 0-4 years with Down syndrome, the standardized incidence ratio (SIR) of AML is 114, compared with other children, Dr. Roberts said. The SIR of ALL is 27 in children aged 1-4 years, she said.
For people with Down syndrome aged 0-60 years, the SIRs are 12 and 13 in AML and ALL, respectively, she said.
In her presentation, Dr. Roberts focused on AML that appears before age 4 years and is preceded by a neonatal preleukemia – transient abnormal myelopoiesis (TAM) – that only occurs in Down syndrome. In most cases, TAM, which occurs with GATA1 mutations, resolves on its own after birth, she said. But in others, the GATA1 mutations continue and cause AML to develop.
Dr. Roberts highlighted her institution’s Oxford Down Syndrome Cohort Study and offered an update to a 2013 report (Blood. 2013 Dec 5;122[24]:3908–17). The study recruited 471 neonates with Down syndrome and followed them for up to 4 years: 341 with no GATA1 mutation and 130 (28%) with the mutation. Dr. Roberts called the latter number a “very high frequency.”
Of those with the mutation, 7 patients (5%) developed AML at a median age of 16 months. None of those without the mutation developed AML.
Also, among the 130 neonates with the mutation, 42% were considered to have “clinical” TAM (more than 10% blasts) and 58% were considered to have “silent” TAM (fewer than 10% blasts).
“We predicted that these babies with clinical TAM would have more severe clinical disease ... and that in fact turned out to be the case,” Dr. Roberts said.
Why is the GATA1 mutation so significant? Research suggests that platelet production is abnormal in neonates with Down syndrome, compared with neonates without it, regardless of whether they have the mutation, Dr. Roberts said.
The mutation doesn’t reduce further platelet count, but does disrupt megakaryopoiesis – the process of the production of platelets. As a result, giant platelets and megakaryocyte fragments are more common, she explained.
Moving forward, research data can be used to identify which children are most at risk, Dr. Roberts said. Newborns with Down syndrome are more likely to survive without leukemia if they have silent TAM, compared with those who have clinical TAM, and if they have an estimated variant allele frequency above 15%, according to findings from the Oxford study.
Children at high risk of AML before age 4 years can be identified by analyzing the percentage of blasts on a smear and/or by analyzing mutation of GATA1, according to Dr. Roberts. However, this cannot be accomplished by the use of a complete blood count (CBC) test, she said, which is used to check for leukemia.
Dr. Roberts called for the development of more guidelines for screening newborns with Down syndrome for leukemia risk. The British Society for Haematology issued testing guidelines, coauthored by Dr. Roberts, in 2018 (Br J Haematol. 2018 Jul;182[2]:200-11).
Dr. Roberts reported having no financial disclosures.
EXPERT ANALYSIS FROM ASH 2018
Chronic opioid use during pregnancy linked with reduced head circumference in NAS newborns
(HC), reported Craig V. Towers, MD, and his associates at the University of Tennessee Medical Center in Knoxville in Pediatrics.
In the first large prospective cohort study to compare HC in newborns being treated for NAS, a total of 858 neonates, including 429 with NAS and 429 controls, were enrolled and assessed at the University of Tennessee Medical Center, Knoxville, from April 1, 2014, to Dec. 31, 2016.
Dr. Towers and his associates found that mean HC in those neonates with NAS was significantly smaller, by 9.5 mm, than it was in controls. Of the 429 newborns with NAS, 62% had a normal HC, 30% had an HC less than the 10th percentile, and 8% had an HC less than or equal to the third percentile. Of the controls, 12% had an HC less than the 10th percentile.
The authors identified a significant 3% reduction in mean HC as well as a 2% reduction in mean birth weight. “Because newborn HC is an indirect measure of brain volume, further research is necessary to determine if this finding increases the risk for long-term neurodevelopmental delay,” they said.
Even though the newborns with NAS were found to experience greater coexposure to benzodiazepines, stimulants, marijuana, gabapentin, tobacco, and SSRIs, compared with controls, none of these coexposures was determined to be a significant risk factor for smaller head circumference at birth when individual drug exposure relationships within the newborn population alone were assessed, the researchers observed.
Dr. Towers and his associates did consider it noteworthy, however, that the majority of NAS cases included in the study were born to mothers receiving opioid agonist medication–assisted treatment (MAT), which is the recommended treatment in cases where opioid use disorder is addressed during pregnancy. Among the 429 NAS cases, the mothers of 372 (87%) were on opioid agonist MAT (320 buprenorphine and 52 methadone); the remaining 13% were born to mothers who were prescribed other opioid drugs.
There is limited data available to determine whether detoxification during pregnancy for patients with opioid use disorder (OUD) has any effect on lessening the risk of lower HC. In fact, the authors caution that detoxification during pregnancy is not recommended for managing OUD. To date, there are only a few locations in the United States and other countries offering such treatment. If the practice becomes more widespread, they cautioned, further research examining new born HC and long-term outcomes “is of paramount importance.”
Further prospective studies evaluating the effects of opioid exposure in newborns who do not develop NAS also are needed. Such data could provide clues concerning whether there is a crucial period of exposure that leads to reduced HC or whether the effects of opioid exposure are in fact cumulative. In cases where newborns are exposed as a result of maintenance MAT, through illicit use, or as a result of maternal detoxification, such studies also could assist with determining whether it is necessary to reconsider current practices for managing OUD in pregnancy.
The study was partially funded through the Blue Cross Blue Shield Research Foundation. The authors reported no relevant financial disclosures.
SOURCE: Towers CV et al. Pediatrics. 2019;143(1):e20180541.
At a time when more people in the United States are dying from opioid overdose than from automobile trauma, the number of newborns with NAS has virtually exploded, rising fivefold since 2000. In some states, more than 30 infants per 1,000 live births develop NAS “effectively transforming some NICUs into NAS wards,” Mark L. Hudak, MD, and Kartikeya Makker, MD, wrote in an accompanying editorial.
Among the strengths of the current study, they cited “universal dating of pregnancies by early ultrasound, multiple antenatal maternal urine drug tests for exposures in both cases and controls, and the use of a fairly robust statistical methodology to account for confounding exposures.”
Among the findings of the study were that, “compared with well-matched controls, newborns with NAS demonstrated a highly significant (nearly 1 cm) decrease in the mean head circumference. Another finding was that newborns with NAS showed proportionately greater decreases in head circumference than in birth weight,” the editorialists said.
Dr. Hadak and Dr. Makker noted that, while NAS can be challenging to manage, the acute effects of withdrawal are transient. The more important questions, they propose are: “What are the best methods to prevent NAS?” and “What, if any, are the long-term effects of fetal and neonatal opioid exposure on the developing child?”
Dr. Hudak and Dr. Makker question the practicality of closely following maternal opioid usage during pregnancy, but they do foresee value in the anticipated findings of a current study in which Dr. Towers and his associates are observing newborns with reduced fetal exposure to opioids who have not developed NAS.
“Additional evidence revealing that the reduction of maternal opioid use can protect normal fetal head and brain growth should energize discussion about refining the management of the opioid-maintained maternal-fetal dyad, with the goal not solely to prevent NAS but more importantly to optimize the outcome of the child,” they said.
Dr. Hudak and Dr. Makker are affiliated with the department of pediatrics at the University of Florida, Jacksonville. These comments are summarized from an editorial commenting on the study by Towers et al. (Pediatrics. 2019;143[1]:e20183376). Dr. Hudak and Dr. Makker said they had no relevant financial disclosures.
At a time when more people in the United States are dying from opioid overdose than from automobile trauma, the number of newborns with NAS has virtually exploded, rising fivefold since 2000. In some states, more than 30 infants per 1,000 live births develop NAS “effectively transforming some NICUs into NAS wards,” Mark L. Hudak, MD, and Kartikeya Makker, MD, wrote in an accompanying editorial.
Among the strengths of the current study, they cited “universal dating of pregnancies by early ultrasound, multiple antenatal maternal urine drug tests for exposures in both cases and controls, and the use of a fairly robust statistical methodology to account for confounding exposures.”
Among the findings of the study were that, “compared with well-matched controls, newborns with NAS demonstrated a highly significant (nearly 1 cm) decrease in the mean head circumference. Another finding was that newborns with NAS showed proportionately greater decreases in head circumference than in birth weight,” the editorialists said.
Dr. Hadak and Dr. Makker noted that, while NAS can be challenging to manage, the acute effects of withdrawal are transient. The more important questions, they propose are: “What are the best methods to prevent NAS?” and “What, if any, are the long-term effects of fetal and neonatal opioid exposure on the developing child?”
Dr. Hudak and Dr. Makker question the practicality of closely following maternal opioid usage during pregnancy, but they do foresee value in the anticipated findings of a current study in which Dr. Towers and his associates are observing newborns with reduced fetal exposure to opioids who have not developed NAS.
“Additional evidence revealing that the reduction of maternal opioid use can protect normal fetal head and brain growth should energize discussion about refining the management of the opioid-maintained maternal-fetal dyad, with the goal not solely to prevent NAS but more importantly to optimize the outcome of the child,” they said.
Dr. Hudak and Dr. Makker are affiliated with the department of pediatrics at the University of Florida, Jacksonville. These comments are summarized from an editorial commenting on the study by Towers et al. (Pediatrics. 2019;143[1]:e20183376). Dr. Hudak and Dr. Makker said they had no relevant financial disclosures.
At a time when more people in the United States are dying from opioid overdose than from automobile trauma, the number of newborns with NAS has virtually exploded, rising fivefold since 2000. In some states, more than 30 infants per 1,000 live births develop NAS “effectively transforming some NICUs into NAS wards,” Mark L. Hudak, MD, and Kartikeya Makker, MD, wrote in an accompanying editorial.
Among the strengths of the current study, they cited “universal dating of pregnancies by early ultrasound, multiple antenatal maternal urine drug tests for exposures in both cases and controls, and the use of a fairly robust statistical methodology to account for confounding exposures.”
Among the findings of the study were that, “compared with well-matched controls, newborns with NAS demonstrated a highly significant (nearly 1 cm) decrease in the mean head circumference. Another finding was that newborns with NAS showed proportionately greater decreases in head circumference than in birth weight,” the editorialists said.
Dr. Hadak and Dr. Makker noted that, while NAS can be challenging to manage, the acute effects of withdrawal are transient. The more important questions, they propose are: “What are the best methods to prevent NAS?” and “What, if any, are the long-term effects of fetal and neonatal opioid exposure on the developing child?”
Dr. Hudak and Dr. Makker question the practicality of closely following maternal opioid usage during pregnancy, but they do foresee value in the anticipated findings of a current study in which Dr. Towers and his associates are observing newborns with reduced fetal exposure to opioids who have not developed NAS.
“Additional evidence revealing that the reduction of maternal opioid use can protect normal fetal head and brain growth should energize discussion about refining the management of the opioid-maintained maternal-fetal dyad, with the goal not solely to prevent NAS but more importantly to optimize the outcome of the child,” they said.
Dr. Hudak and Dr. Makker are affiliated with the department of pediatrics at the University of Florida, Jacksonville. These comments are summarized from an editorial commenting on the study by Towers et al. (Pediatrics. 2019;143[1]:e20183376). Dr. Hudak and Dr. Makker said they had no relevant financial disclosures.
(HC), reported Craig V. Towers, MD, and his associates at the University of Tennessee Medical Center in Knoxville in Pediatrics.
In the first large prospective cohort study to compare HC in newborns being treated for NAS, a total of 858 neonates, including 429 with NAS and 429 controls, were enrolled and assessed at the University of Tennessee Medical Center, Knoxville, from April 1, 2014, to Dec. 31, 2016.
Dr. Towers and his associates found that mean HC in those neonates with NAS was significantly smaller, by 9.5 mm, than it was in controls. Of the 429 newborns with NAS, 62% had a normal HC, 30% had an HC less than the 10th percentile, and 8% had an HC less than or equal to the third percentile. Of the controls, 12% had an HC less than the 10th percentile.
The authors identified a significant 3% reduction in mean HC as well as a 2% reduction in mean birth weight. “Because newborn HC is an indirect measure of brain volume, further research is necessary to determine if this finding increases the risk for long-term neurodevelopmental delay,” they said.
Even though the newborns with NAS were found to experience greater coexposure to benzodiazepines, stimulants, marijuana, gabapentin, tobacco, and SSRIs, compared with controls, none of these coexposures was determined to be a significant risk factor for smaller head circumference at birth when individual drug exposure relationships within the newborn population alone were assessed, the researchers observed.
Dr. Towers and his associates did consider it noteworthy, however, that the majority of NAS cases included in the study were born to mothers receiving opioid agonist medication–assisted treatment (MAT), which is the recommended treatment in cases where opioid use disorder is addressed during pregnancy. Among the 429 NAS cases, the mothers of 372 (87%) were on opioid agonist MAT (320 buprenorphine and 52 methadone); the remaining 13% were born to mothers who were prescribed other opioid drugs.
There is limited data available to determine whether detoxification during pregnancy for patients with opioid use disorder (OUD) has any effect on lessening the risk of lower HC. In fact, the authors caution that detoxification during pregnancy is not recommended for managing OUD. To date, there are only a few locations in the United States and other countries offering such treatment. If the practice becomes more widespread, they cautioned, further research examining new born HC and long-term outcomes “is of paramount importance.”
Further prospective studies evaluating the effects of opioid exposure in newborns who do not develop NAS also are needed. Such data could provide clues concerning whether there is a crucial period of exposure that leads to reduced HC or whether the effects of opioid exposure are in fact cumulative. In cases where newborns are exposed as a result of maintenance MAT, through illicit use, or as a result of maternal detoxification, such studies also could assist with determining whether it is necessary to reconsider current practices for managing OUD in pregnancy.
The study was partially funded through the Blue Cross Blue Shield Research Foundation. The authors reported no relevant financial disclosures.
SOURCE: Towers CV et al. Pediatrics. 2019;143(1):e20180541.
(HC), reported Craig V. Towers, MD, and his associates at the University of Tennessee Medical Center in Knoxville in Pediatrics.
In the first large prospective cohort study to compare HC in newborns being treated for NAS, a total of 858 neonates, including 429 with NAS and 429 controls, were enrolled and assessed at the University of Tennessee Medical Center, Knoxville, from April 1, 2014, to Dec. 31, 2016.
Dr. Towers and his associates found that mean HC in those neonates with NAS was significantly smaller, by 9.5 mm, than it was in controls. Of the 429 newborns with NAS, 62% had a normal HC, 30% had an HC less than the 10th percentile, and 8% had an HC less than or equal to the third percentile. Of the controls, 12% had an HC less than the 10th percentile.
The authors identified a significant 3% reduction in mean HC as well as a 2% reduction in mean birth weight. “Because newborn HC is an indirect measure of brain volume, further research is necessary to determine if this finding increases the risk for long-term neurodevelopmental delay,” they said.
Even though the newborns with NAS were found to experience greater coexposure to benzodiazepines, stimulants, marijuana, gabapentin, tobacco, and SSRIs, compared with controls, none of these coexposures was determined to be a significant risk factor for smaller head circumference at birth when individual drug exposure relationships within the newborn population alone were assessed, the researchers observed.
Dr. Towers and his associates did consider it noteworthy, however, that the majority of NAS cases included in the study were born to mothers receiving opioid agonist medication–assisted treatment (MAT), which is the recommended treatment in cases where opioid use disorder is addressed during pregnancy. Among the 429 NAS cases, the mothers of 372 (87%) were on opioid agonist MAT (320 buprenorphine and 52 methadone); the remaining 13% were born to mothers who were prescribed other opioid drugs.
There is limited data available to determine whether detoxification during pregnancy for patients with opioid use disorder (OUD) has any effect on lessening the risk of lower HC. In fact, the authors caution that detoxification during pregnancy is not recommended for managing OUD. To date, there are only a few locations in the United States and other countries offering such treatment. If the practice becomes more widespread, they cautioned, further research examining new born HC and long-term outcomes “is of paramount importance.”
Further prospective studies evaluating the effects of opioid exposure in newborns who do not develop NAS also are needed. Such data could provide clues concerning whether there is a crucial period of exposure that leads to reduced HC or whether the effects of opioid exposure are in fact cumulative. In cases where newborns are exposed as a result of maintenance MAT, through illicit use, or as a result of maternal detoxification, such studies also could assist with determining whether it is necessary to reconsider current practices for managing OUD in pregnancy.
The study was partially funded through the Blue Cross Blue Shield Research Foundation. The authors reported no relevant financial disclosures.
SOURCE: Towers CV et al. Pediatrics. 2019;143(1):e20180541.
FROM PEDIATRICS
Key clinical point: Detoxification during pregnancy may be ill advised for patients with opioid use disorder.
Major finding: Head circumference was smaller by a mean 9.5 mm.
Study details: Prospective cohort study of 429 NAS neonates and 429 controls.
Disclosures: The study was partially funded through the Blue Cross Blue Shield Research Foundation. The authors reported no relevant financial disclosures.
Source: Towers CV et al. Pediatrics. 2019;143(1):e20180541.