User login
Chronic opioid use may be common in patients with ankylosing spondylitis
About a quarter of all patients with ankylosing spondylitis, and more than half of those patients who were on Medicaid, received at least a 90-day supply of opioids in a year, based on an analysis of U.S. commercial claims data.
The findings were noted in 2012-2017 data from a cohort of 11,945 patients in the Truven Health MarketScan Research database. Of those patients given the International Classification of Diseases (ICD) code 720.0, which is specific for ankylosing spondylitis, 23.5% of patients chronically used opioids. In the broader 720.x commercial claims cohort of 79,190 patients, the proportion who chronically used opioids was 27.3%.
More than 60% of the patients who chronically used opioids had a cumulative drug supply of 270 days or more.
“Patients with ankylosing spondylitis receive opioids with disturbing frequency,” said study author Victor S. Sloan, MD, and research colleagues in the June issue of the Journal of Rheumatology. Ankylosing spondylitis treatment guidelines “specify use of an NSAID as initial pharmacotherapy, with anti-TNF [tumor necrosis factor] therapy in cases of NSAID inefficacy or intolerance. However, for many patients, prescription opioids – while not addressing the underlying inflammation – may offer an inexpensive and rapid means of achieving symptomatic relief.”
Patients who chronically used opioids were more likely to have depression (25.4% vs. 12.5%) and anxiety (20.9% vs. 11.7%) during the baseline period of the study. Patients with chronic opioid use also were more likely to receive muscle relaxants (54.4% vs. 20.2%) and oral corticosteroids (18.4% vs. 9.6%), compared with patients without chronic opioid use, reported Dr. Sloan, vice president and immunology development strategy lead for UCB Pharma and of the Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J., and colleagues.
Claims for anti-TNF therapies, disease-modifying antirheumatic drugs (DMARDs), and NSAIDs were similar for patients with and without chronic opioid use.
The patients in the study had claims with the specified diagnosis codes during Jan. 1, 2013–March 31, 2016 and were enrolled in medical and pharmacy benefits for 12 months before and after the first qualifying ICD code. The study excluded patients with a history of cancer other than nonmelanoma skin cancer. Opioid claims within 7 days of a hospitalization or 2 days of an emergency department or urgent care visit were not included.
The investigators assessed patients’ demographics, clinical characteristics, comorbidities, and prior treatments during a 12-month baseline period prior to the index date. They examined opioid use and exposure to other treatments during a 12-month follow-up period after the index date. They defined chronic opioid use as at least 90 cumulative days of opioid use based on the supply value on opioid pharmacy claims. They summed the days’ supply for all opioid claims during the follow-up period.
Chronic use of opioids was most pronounced in the 917 patients with Medicaid claims with 720.0 diagnosis codes; 57.1% chronically used opioids during follow-up. Among 14,041 patients with Medicaid claims with 720.x codes, 76.7% chronically used opioids.
The data suggest that some patients may receive opioids before they receive recommended therapies. “If this is the case, there may be an opportunity to prevent chronic opioid use by intervening with recommended therapies earlier in the patient’s treatment course,” the authors wrote.
Dr. Sloan and colleagues noted that they had limited information about the timing of opioid use relative to ankylosing spondylitis diagnosis, opioid potency and dose, and the indication for which opioids were prescribed.
UCB Pharma funded the study. The authors are employees of UCB Pharma.
SOURCE: Sloan VS et al. J Rheumatol. 2019 Jan 15. doi: 10.3899/jrheum.180972.
About a quarter of all patients with ankylosing spondylitis, and more than half of those patients who were on Medicaid, received at least a 90-day supply of opioids in a year, based on an analysis of U.S. commercial claims data.
The findings were noted in 2012-2017 data from a cohort of 11,945 patients in the Truven Health MarketScan Research database. Of those patients given the International Classification of Diseases (ICD) code 720.0, which is specific for ankylosing spondylitis, 23.5% of patients chronically used opioids. In the broader 720.x commercial claims cohort of 79,190 patients, the proportion who chronically used opioids was 27.3%.
More than 60% of the patients who chronically used opioids had a cumulative drug supply of 270 days or more.
“Patients with ankylosing spondylitis receive opioids with disturbing frequency,” said study author Victor S. Sloan, MD, and research colleagues in the June issue of the Journal of Rheumatology. Ankylosing spondylitis treatment guidelines “specify use of an NSAID as initial pharmacotherapy, with anti-TNF [tumor necrosis factor] therapy in cases of NSAID inefficacy or intolerance. However, for many patients, prescription opioids – while not addressing the underlying inflammation – may offer an inexpensive and rapid means of achieving symptomatic relief.”
Patients who chronically used opioids were more likely to have depression (25.4% vs. 12.5%) and anxiety (20.9% vs. 11.7%) during the baseline period of the study. Patients with chronic opioid use also were more likely to receive muscle relaxants (54.4% vs. 20.2%) and oral corticosteroids (18.4% vs. 9.6%), compared with patients without chronic opioid use, reported Dr. Sloan, vice president and immunology development strategy lead for UCB Pharma and of the Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J., and colleagues.
Claims for anti-TNF therapies, disease-modifying antirheumatic drugs (DMARDs), and NSAIDs were similar for patients with and without chronic opioid use.
The patients in the study had claims with the specified diagnosis codes during Jan. 1, 2013–March 31, 2016 and were enrolled in medical and pharmacy benefits for 12 months before and after the first qualifying ICD code. The study excluded patients with a history of cancer other than nonmelanoma skin cancer. Opioid claims within 7 days of a hospitalization or 2 days of an emergency department or urgent care visit were not included.
The investigators assessed patients’ demographics, clinical characteristics, comorbidities, and prior treatments during a 12-month baseline period prior to the index date. They examined opioid use and exposure to other treatments during a 12-month follow-up period after the index date. They defined chronic opioid use as at least 90 cumulative days of opioid use based on the supply value on opioid pharmacy claims. They summed the days’ supply for all opioid claims during the follow-up period.
Chronic use of opioids was most pronounced in the 917 patients with Medicaid claims with 720.0 diagnosis codes; 57.1% chronically used opioids during follow-up. Among 14,041 patients with Medicaid claims with 720.x codes, 76.7% chronically used opioids.
The data suggest that some patients may receive opioids before they receive recommended therapies. “If this is the case, there may be an opportunity to prevent chronic opioid use by intervening with recommended therapies earlier in the patient’s treatment course,” the authors wrote.
Dr. Sloan and colleagues noted that they had limited information about the timing of opioid use relative to ankylosing spondylitis diagnosis, opioid potency and dose, and the indication for which opioids were prescribed.
UCB Pharma funded the study. The authors are employees of UCB Pharma.
SOURCE: Sloan VS et al. J Rheumatol. 2019 Jan 15. doi: 10.3899/jrheum.180972.
About a quarter of all patients with ankylosing spondylitis, and more than half of those patients who were on Medicaid, received at least a 90-day supply of opioids in a year, based on an analysis of U.S. commercial claims data.
The findings were noted in 2012-2017 data from a cohort of 11,945 patients in the Truven Health MarketScan Research database. Of those patients given the International Classification of Diseases (ICD) code 720.0, which is specific for ankylosing spondylitis, 23.5% of patients chronically used opioids. In the broader 720.x commercial claims cohort of 79,190 patients, the proportion who chronically used opioids was 27.3%.
More than 60% of the patients who chronically used opioids had a cumulative drug supply of 270 days or more.
“Patients with ankylosing spondylitis receive opioids with disturbing frequency,” said study author Victor S. Sloan, MD, and research colleagues in the June issue of the Journal of Rheumatology. Ankylosing spondylitis treatment guidelines “specify use of an NSAID as initial pharmacotherapy, with anti-TNF [tumor necrosis factor] therapy in cases of NSAID inefficacy or intolerance. However, for many patients, prescription opioids – while not addressing the underlying inflammation – may offer an inexpensive and rapid means of achieving symptomatic relief.”
Patients who chronically used opioids were more likely to have depression (25.4% vs. 12.5%) and anxiety (20.9% vs. 11.7%) during the baseline period of the study. Patients with chronic opioid use also were more likely to receive muscle relaxants (54.4% vs. 20.2%) and oral corticosteroids (18.4% vs. 9.6%), compared with patients without chronic opioid use, reported Dr. Sloan, vice president and immunology development strategy lead for UCB Pharma and of the Rutgers Robert Wood Johnson Medical School in New Brunswick, N.J., and colleagues.
Claims for anti-TNF therapies, disease-modifying antirheumatic drugs (DMARDs), and NSAIDs were similar for patients with and without chronic opioid use.
The patients in the study had claims with the specified diagnosis codes during Jan. 1, 2013–March 31, 2016 and were enrolled in medical and pharmacy benefits for 12 months before and after the first qualifying ICD code. The study excluded patients with a history of cancer other than nonmelanoma skin cancer. Opioid claims within 7 days of a hospitalization or 2 days of an emergency department or urgent care visit were not included.
The investigators assessed patients’ demographics, clinical characteristics, comorbidities, and prior treatments during a 12-month baseline period prior to the index date. They examined opioid use and exposure to other treatments during a 12-month follow-up period after the index date. They defined chronic opioid use as at least 90 cumulative days of opioid use based on the supply value on opioid pharmacy claims. They summed the days’ supply for all opioid claims during the follow-up period.
Chronic use of opioids was most pronounced in the 917 patients with Medicaid claims with 720.0 diagnosis codes; 57.1% chronically used opioids during follow-up. Among 14,041 patients with Medicaid claims with 720.x codes, 76.7% chronically used opioids.
The data suggest that some patients may receive opioids before they receive recommended therapies. “If this is the case, there may be an opportunity to prevent chronic opioid use by intervening with recommended therapies earlier in the patient’s treatment course,” the authors wrote.
Dr. Sloan and colleagues noted that they had limited information about the timing of opioid use relative to ankylosing spondylitis diagnosis, opioid potency and dose, and the indication for which opioids were prescribed.
UCB Pharma funded the study. The authors are employees of UCB Pharma.
SOURCE: Sloan VS et al. J Rheumatol. 2019 Jan 15. doi: 10.3899/jrheum.180972.
FROM THE JOURNAL OF RHEUMATOLOGY
The Opioid Crisis: An MDedge Psychcast Presentation
Opioid prescriptions declined 33% over 5 years
Fewer opioid retail prescriptions are being filled, according to a new report issued by the American Medical Association Opioid Task Force.
Opioid prescribing declined by 33% over a 5-year period based on the total number of opioid retail prescriptions filled. Total prescriptions declined from 251.8 million in 2013 to 168.8 million in 2018, according to the report.
The numbers come as the most recent data from the Centers for Disease Control and Prevention show a leveling of deaths involving prescription opioids. The CDC data were most recently updated in January 2019 and cover the period 1999-2017.
A closer look shows that deaths involving prescription opioids, but not other synthetic narcotics, peaked in 2011 and have generally declined since then. Deaths involving other synthetic narcotics, however, have been rising, offsetting the reduction and keeping the total number of deaths involving opioids relatively stable between 2016 and 2017.
Other data released by the AMA Opioid Task Force show that physicians are increasing their use of state-level prescription drug monitoring programs (PDMPs).
In 2017, there were 1.5 million physicians registered to use state PDMPs. That number rose to 1.97 million in 2019. And the physicians are using PDMPs. In 2018, physicians made 460 million PDMP queries, up 56% from 2017 and up 651% from 2014.
More education about opioid prescribing is being sought, with 700,000 physicians completing CME training and accessing other training related to opioid prescribing, pain management, screening for substance use disorders, and other related topics.
While the report does show positive trends, the task force is calling for more action, including more access to naloxone and better access to mental health treatment.
The report notes that more than 66,000 physicians and other health professionals have a federal waiver to prescribe buprenorphine, up more than 28,000 since 2016.
A number of policy recommendations are made in the report, including removing inappropriate administrative burdens or barriers that delay access to medications used in medication-assisted treatment (MAT); removing barriers to comprehensive pain care and rehabilitation programs, and reforming the civil and criminal justice system to help ensure access to high-quality, evidence-based care for opioid use disorder.
“We are at a crossroads in our nation’s efforts to end the opioid epidemic,” AMA Opioid Task Force Chair Patrice A. Harris, MD, stated in the report. “It is time to end delays and barriers to medication-assisted treatment – evidence based care proven to save lives; time for payers, [pharmacy benefit managers] and pharmacy chains to reevaluate and revise policies that restrict opioid therapy to patients based on arbitrary thresholds; and time to commit to helping all patients access evidence-based care for pain and substance use disorders.”
Dr. Harris continued: “Physicians must continue to demonstrate leadership, but unless these actions occur, the progress we are making will not stop patients from dying.”
Fewer opioid retail prescriptions are being filled, according to a new report issued by the American Medical Association Opioid Task Force.
Opioid prescribing declined by 33% over a 5-year period based on the total number of opioid retail prescriptions filled. Total prescriptions declined from 251.8 million in 2013 to 168.8 million in 2018, according to the report.
The numbers come as the most recent data from the Centers for Disease Control and Prevention show a leveling of deaths involving prescription opioids. The CDC data were most recently updated in January 2019 and cover the period 1999-2017.
A closer look shows that deaths involving prescription opioids, but not other synthetic narcotics, peaked in 2011 and have generally declined since then. Deaths involving other synthetic narcotics, however, have been rising, offsetting the reduction and keeping the total number of deaths involving opioids relatively stable between 2016 and 2017.
Other data released by the AMA Opioid Task Force show that physicians are increasing their use of state-level prescription drug monitoring programs (PDMPs).
In 2017, there were 1.5 million physicians registered to use state PDMPs. That number rose to 1.97 million in 2019. And the physicians are using PDMPs. In 2018, physicians made 460 million PDMP queries, up 56% from 2017 and up 651% from 2014.
More education about opioid prescribing is being sought, with 700,000 physicians completing CME training and accessing other training related to opioid prescribing, pain management, screening for substance use disorders, and other related topics.
While the report does show positive trends, the task force is calling for more action, including more access to naloxone and better access to mental health treatment.
The report notes that more than 66,000 physicians and other health professionals have a federal waiver to prescribe buprenorphine, up more than 28,000 since 2016.
A number of policy recommendations are made in the report, including removing inappropriate administrative burdens or barriers that delay access to medications used in medication-assisted treatment (MAT); removing barriers to comprehensive pain care and rehabilitation programs, and reforming the civil and criminal justice system to help ensure access to high-quality, evidence-based care for opioid use disorder.
“We are at a crossroads in our nation’s efforts to end the opioid epidemic,” AMA Opioid Task Force Chair Patrice A. Harris, MD, stated in the report. “It is time to end delays and barriers to medication-assisted treatment – evidence based care proven to save lives; time for payers, [pharmacy benefit managers] and pharmacy chains to reevaluate and revise policies that restrict opioid therapy to patients based on arbitrary thresholds; and time to commit to helping all patients access evidence-based care for pain and substance use disorders.”
Dr. Harris continued: “Physicians must continue to demonstrate leadership, but unless these actions occur, the progress we are making will not stop patients from dying.”
Fewer opioid retail prescriptions are being filled, according to a new report issued by the American Medical Association Opioid Task Force.
Opioid prescribing declined by 33% over a 5-year period based on the total number of opioid retail prescriptions filled. Total prescriptions declined from 251.8 million in 2013 to 168.8 million in 2018, according to the report.
The numbers come as the most recent data from the Centers for Disease Control and Prevention show a leveling of deaths involving prescription opioids. The CDC data were most recently updated in January 2019 and cover the period 1999-2017.
A closer look shows that deaths involving prescription opioids, but not other synthetic narcotics, peaked in 2011 and have generally declined since then. Deaths involving other synthetic narcotics, however, have been rising, offsetting the reduction and keeping the total number of deaths involving opioids relatively stable between 2016 and 2017.
Other data released by the AMA Opioid Task Force show that physicians are increasing their use of state-level prescription drug monitoring programs (PDMPs).
In 2017, there were 1.5 million physicians registered to use state PDMPs. That number rose to 1.97 million in 2019. And the physicians are using PDMPs. In 2018, physicians made 460 million PDMP queries, up 56% from 2017 and up 651% from 2014.
More education about opioid prescribing is being sought, with 700,000 physicians completing CME training and accessing other training related to opioid prescribing, pain management, screening for substance use disorders, and other related topics.
While the report does show positive trends, the task force is calling for more action, including more access to naloxone and better access to mental health treatment.
The report notes that more than 66,000 physicians and other health professionals have a federal waiver to prescribe buprenorphine, up more than 28,000 since 2016.
A number of policy recommendations are made in the report, including removing inappropriate administrative burdens or barriers that delay access to medications used in medication-assisted treatment (MAT); removing barriers to comprehensive pain care and rehabilitation programs, and reforming the civil and criminal justice system to help ensure access to high-quality, evidence-based care for opioid use disorder.
“We are at a crossroads in our nation’s efforts to end the opioid epidemic,” AMA Opioid Task Force Chair Patrice A. Harris, MD, stated in the report. “It is time to end delays and barriers to medication-assisted treatment – evidence based care proven to save lives; time for payers, [pharmacy benefit managers] and pharmacy chains to reevaluate and revise policies that restrict opioid therapy to patients based on arbitrary thresholds; and time to commit to helping all patients access evidence-based care for pain and substance use disorders.”
Dr. Harris continued: “Physicians must continue to demonstrate leadership, but unless these actions occur, the progress we are making will not stop patients from dying.”
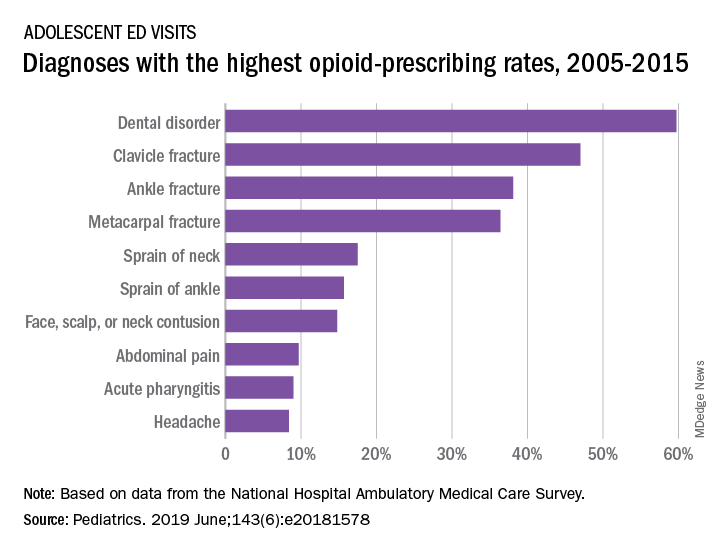
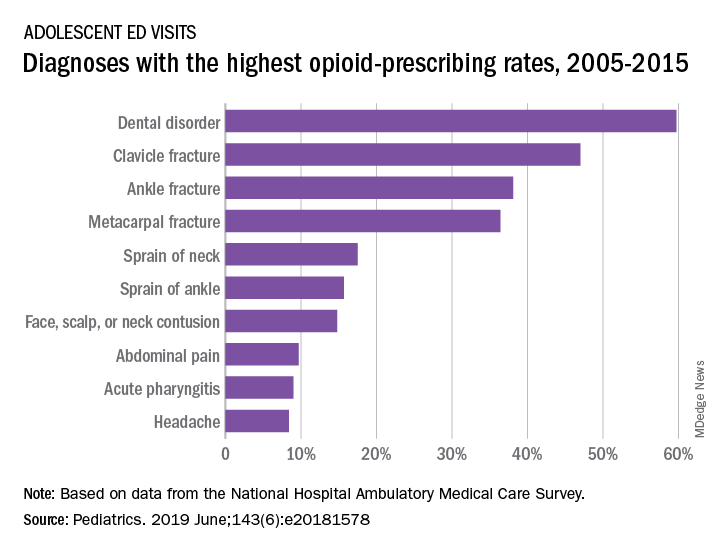
When adolescents visit the ED, 10% leave with an opioid
although there was a small but significant decrease in prescriptions over that time, according to an analysis of two nationwide ambulatory care surveys.
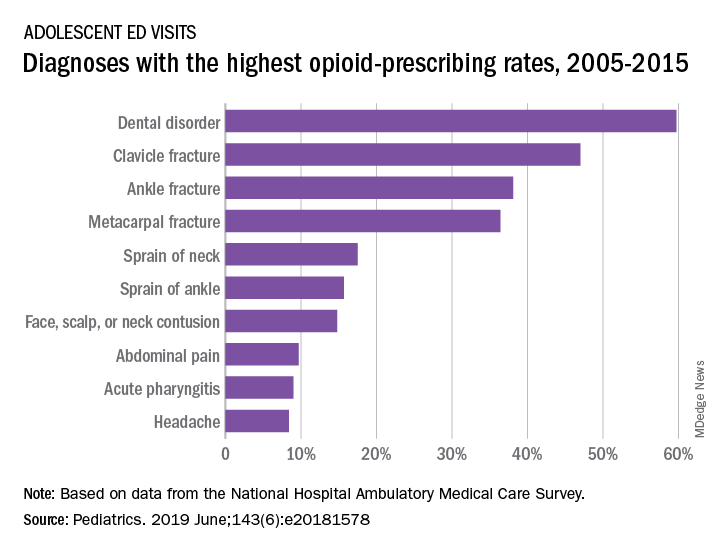
For adolescents aged 13-17 years, 10.4% of ED visits were associated with a prescription for an opioid versus 1.6% among outpatient visits. There was a slight but significant decrease in the rate of opioid prescriptions in the ED setting over the study period, with an odds ratio of 0.95 (95% confidence interval, 0.92-0.97), but there was no significant change in the trend over time in the outpatient setting (OR, 1.02; 95% CI, 0.99-1.09), Joel D. Hudgins, MD, and associates reported in Pediatrics.
“Opioid prescribing in ambulatory care visits is particularly high in the ED setting and … certain diagnoses appear to be routinely treated with an opioid,” said Dr. Hudgins and associates from Boston Children’s Hospital.
The highest rates of opioid prescribing among adolescents visiting the ED involved dental disorders (60%) and acute injuries such as fractures of the clavicle (47%), ankle (38%), and metacarpals (36%). “However, when considering the total volume of opioid prescriptions dispensed [over 7.8 million during 2005-2015], certain common conditions, including abdominal pain, acute pharyngitis, urinary tract infection, and headache, contributed large numbers of prescriptions as well,” they added.
The study involved data from the National Hospital Ambulatory Medical Care Survey (hospital-based EDs) and the National Ambulatory Medical Care Survey (office-based practices), which both are conducted annually by the National Center for Health Statistics.
The senior investigator is supported by an award from the Burroughs Wellcome Fund by the Harvard-MIT Center for Regulatory Science. The authors said that they have no relevant financial relationships.
SOURCE: Hudgins JD et al. Pediatrics. 2019 June. doi: 10.1542/peds.2018-1578.
although there was a small but significant decrease in prescriptions over that time, according to an analysis of two nationwide ambulatory care surveys.
For adolescents aged 13-17 years, 10.4% of ED visits were associated with a prescription for an opioid versus 1.6% among outpatient visits. There was a slight but significant decrease in the rate of opioid prescriptions in the ED setting over the study period, with an odds ratio of 0.95 (95% confidence interval, 0.92-0.97), but there was no significant change in the trend over time in the outpatient setting (OR, 1.02; 95% CI, 0.99-1.09), Joel D. Hudgins, MD, and associates reported in Pediatrics.
“Opioid prescribing in ambulatory care visits is particularly high in the ED setting and … certain diagnoses appear to be routinely treated with an opioid,” said Dr. Hudgins and associates from Boston Children’s Hospital.
The highest rates of opioid prescribing among adolescents visiting the ED involved dental disorders (60%) and acute injuries such as fractures of the clavicle (47%), ankle (38%), and metacarpals (36%). “However, when considering the total volume of opioid prescriptions dispensed [over 7.8 million during 2005-2015], certain common conditions, including abdominal pain, acute pharyngitis, urinary tract infection, and headache, contributed large numbers of prescriptions as well,” they added.
The study involved data from the National Hospital Ambulatory Medical Care Survey (hospital-based EDs) and the National Ambulatory Medical Care Survey (office-based practices), which both are conducted annually by the National Center for Health Statistics.
The senior investigator is supported by an award from the Burroughs Wellcome Fund by the Harvard-MIT Center for Regulatory Science. The authors said that they have no relevant financial relationships.
SOURCE: Hudgins JD et al. Pediatrics. 2019 June. doi: 10.1542/peds.2018-1578.
although there was a small but significant decrease in prescriptions over that time, according to an analysis of two nationwide ambulatory care surveys.
For adolescents aged 13-17 years, 10.4% of ED visits were associated with a prescription for an opioid versus 1.6% among outpatient visits. There was a slight but significant decrease in the rate of opioid prescriptions in the ED setting over the study period, with an odds ratio of 0.95 (95% confidence interval, 0.92-0.97), but there was no significant change in the trend over time in the outpatient setting (OR, 1.02; 95% CI, 0.99-1.09), Joel D. Hudgins, MD, and associates reported in Pediatrics.
“Opioid prescribing in ambulatory care visits is particularly high in the ED setting and … certain diagnoses appear to be routinely treated with an opioid,” said Dr. Hudgins and associates from Boston Children’s Hospital.
The highest rates of opioid prescribing among adolescents visiting the ED involved dental disorders (60%) and acute injuries such as fractures of the clavicle (47%), ankle (38%), and metacarpals (36%). “However, when considering the total volume of opioid prescriptions dispensed [over 7.8 million during 2005-2015], certain common conditions, including abdominal pain, acute pharyngitis, urinary tract infection, and headache, contributed large numbers of prescriptions as well,” they added.
The study involved data from the National Hospital Ambulatory Medical Care Survey (hospital-based EDs) and the National Ambulatory Medical Care Survey (office-based practices), which both are conducted annually by the National Center for Health Statistics.
The senior investigator is supported by an award from the Burroughs Wellcome Fund by the Harvard-MIT Center for Regulatory Science. The authors said that they have no relevant financial relationships.
SOURCE: Hudgins JD et al. Pediatrics. 2019 June. doi: 10.1542/peds.2018-1578.
FROM PEDIATRICS
N.J. law, EMR alerts appear effective at reducing opioid prescriptions
WASHINGTON –
Researchers looked at prescribing patterns of doctors in the Penn Medicine health system, which straddles both the Philadelphia area and southern New Jersey, following the implementation of prescribing limits in New Jersey.
The law in question is a 5-day limit on new opioid prescriptions, which was passed in February 2017 and implemented in May 2017. Penn Medicine implemented an EMR alert in their New Jersey locations to alert physicians within the Penn Medicine system of the change in their state law 2 months after the law went into effect. Researchers looked at prescribing patterns before passage, during the transition between passage and the implementation of the EMR alert and following implementation of the EMR alert, as well as secondary outcomes such as rate of refills, telephone calls, and utilization.
“The implementation of the prescribing limit and EMR alert was associated with a decrease in the volume of opioids prescribed in acute prescriptions without changes in the rates of refills, telephone calls or utilization,” Margaret Lowenstein, MD, of the University of Pennsylvania, Philadelphia, said at the annual meeting of the Society of General Internal Medicine.
“This combination of the policy and the EMR alert may be an effective strategy to influence prescriber behavior,” she added.
Researchers compared outcomes before and after the implementation of the law in New Jersey, using prescribing patterns in Pennsylvania as the control. The cohort of patients was those with a new opioid prescription within Penn Medicine ambulatory nonteaching practices. It excluded specialties not represented in both states as well as patients with cancer, those in hospice and palliative care and those in treatment for opioid use disorder, since the law does not apply to those groups.
In New Jersey, there were 434 patients receiving new prescriptions in the 12 months prior to the implementation of the law, with 234 patients receiving new prescriptions in the 9 months after the EMR alert was implemented in New Jersey. In Pennsylvania, the cohort included 2,961 patients prior to the law going into effect and 1,677 after the EMR intervention went live in New Jersey.
For New Jersey, the morphine milligram equivalent (MME) per prescription was steady at about 350 during the period prior to the law’s implementation, but dropped to nearly 250 by the end of the postintervention period examined. In Pennsylvania, the prelaw implementation period had an MME per prescription a little higher than 200, which leveled off at around 200 during the postintervention period.
“In New Jersey, there is a significantly higher MME than in Pennsylvania and this difference persists in the transition period but what you see in the post period is a significantly greater decline in the MME per prescription in New Jersey as compared to the rate of change in Pa.,” Dr. Lowenstein said. “That difference was statistically significant.”
She said similar results were seen regarding the quantity of tablets prescribed. In New Jersey before the law’s passage, the number of tablets per prescription was close to 50, dropping down to about 35 post period. Pennsylvania saw a slight decrease from about 35 pills per prescription to about 33 during the same period.
No significant changes occurred in the other outcomes measured following implementation of the EMR alert.
Dr. Lowenstein noted that, because the transition period between the law going into effect and the implementation of the EMR alert was so short, whether the greater decreases in opioid prescriptions in New Jersey relative to Pennsylvania was because of the law alone, the EMR alert alone, or both changes is unclear.
Based on the limited amount of change in prescribing patterns during the transition period, it appears that the EMR intervention may be driving the change, “but we weren’t powered to make that determination,” she added.
Dr. Lowenstein and her colleagues reported no disclosures.
WASHINGTON –
Researchers looked at prescribing patterns of doctors in the Penn Medicine health system, which straddles both the Philadelphia area and southern New Jersey, following the implementation of prescribing limits in New Jersey.
The law in question is a 5-day limit on new opioid prescriptions, which was passed in February 2017 and implemented in May 2017. Penn Medicine implemented an EMR alert in their New Jersey locations to alert physicians within the Penn Medicine system of the change in their state law 2 months after the law went into effect. Researchers looked at prescribing patterns before passage, during the transition between passage and the implementation of the EMR alert and following implementation of the EMR alert, as well as secondary outcomes such as rate of refills, telephone calls, and utilization.
“The implementation of the prescribing limit and EMR alert was associated with a decrease in the volume of opioids prescribed in acute prescriptions without changes in the rates of refills, telephone calls or utilization,” Margaret Lowenstein, MD, of the University of Pennsylvania, Philadelphia, said at the annual meeting of the Society of General Internal Medicine.
“This combination of the policy and the EMR alert may be an effective strategy to influence prescriber behavior,” she added.
Researchers compared outcomes before and after the implementation of the law in New Jersey, using prescribing patterns in Pennsylvania as the control. The cohort of patients was those with a new opioid prescription within Penn Medicine ambulatory nonteaching practices. It excluded specialties not represented in both states as well as patients with cancer, those in hospice and palliative care and those in treatment for opioid use disorder, since the law does not apply to those groups.
In New Jersey, there were 434 patients receiving new prescriptions in the 12 months prior to the implementation of the law, with 234 patients receiving new prescriptions in the 9 months after the EMR alert was implemented in New Jersey. In Pennsylvania, the cohort included 2,961 patients prior to the law going into effect and 1,677 after the EMR intervention went live in New Jersey.
For New Jersey, the morphine milligram equivalent (MME) per prescription was steady at about 350 during the period prior to the law’s implementation, but dropped to nearly 250 by the end of the postintervention period examined. In Pennsylvania, the prelaw implementation period had an MME per prescription a little higher than 200, which leveled off at around 200 during the postintervention period.
“In New Jersey, there is a significantly higher MME than in Pennsylvania and this difference persists in the transition period but what you see in the post period is a significantly greater decline in the MME per prescription in New Jersey as compared to the rate of change in Pa.,” Dr. Lowenstein said. “That difference was statistically significant.”
She said similar results were seen regarding the quantity of tablets prescribed. In New Jersey before the law’s passage, the number of tablets per prescription was close to 50, dropping down to about 35 post period. Pennsylvania saw a slight decrease from about 35 pills per prescription to about 33 during the same period.
No significant changes occurred in the other outcomes measured following implementation of the EMR alert.
Dr. Lowenstein noted that, because the transition period between the law going into effect and the implementation of the EMR alert was so short, whether the greater decreases in opioid prescriptions in New Jersey relative to Pennsylvania was because of the law alone, the EMR alert alone, or both changes is unclear.
Based on the limited amount of change in prescribing patterns during the transition period, it appears that the EMR intervention may be driving the change, “but we weren’t powered to make that determination,” she added.
Dr. Lowenstein and her colleagues reported no disclosures.
WASHINGTON –
Researchers looked at prescribing patterns of doctors in the Penn Medicine health system, which straddles both the Philadelphia area and southern New Jersey, following the implementation of prescribing limits in New Jersey.
The law in question is a 5-day limit on new opioid prescriptions, which was passed in February 2017 and implemented in May 2017. Penn Medicine implemented an EMR alert in their New Jersey locations to alert physicians within the Penn Medicine system of the change in their state law 2 months after the law went into effect. Researchers looked at prescribing patterns before passage, during the transition between passage and the implementation of the EMR alert and following implementation of the EMR alert, as well as secondary outcomes such as rate of refills, telephone calls, and utilization.
“The implementation of the prescribing limit and EMR alert was associated with a decrease in the volume of opioids prescribed in acute prescriptions without changes in the rates of refills, telephone calls or utilization,” Margaret Lowenstein, MD, of the University of Pennsylvania, Philadelphia, said at the annual meeting of the Society of General Internal Medicine.
“This combination of the policy and the EMR alert may be an effective strategy to influence prescriber behavior,” she added.
Researchers compared outcomes before and after the implementation of the law in New Jersey, using prescribing patterns in Pennsylvania as the control. The cohort of patients was those with a new opioid prescription within Penn Medicine ambulatory nonteaching practices. It excluded specialties not represented in both states as well as patients with cancer, those in hospice and palliative care and those in treatment for opioid use disorder, since the law does not apply to those groups.
In New Jersey, there were 434 patients receiving new prescriptions in the 12 months prior to the implementation of the law, with 234 patients receiving new prescriptions in the 9 months after the EMR alert was implemented in New Jersey. In Pennsylvania, the cohort included 2,961 patients prior to the law going into effect and 1,677 after the EMR intervention went live in New Jersey.
For New Jersey, the morphine milligram equivalent (MME) per prescription was steady at about 350 during the period prior to the law’s implementation, but dropped to nearly 250 by the end of the postintervention period examined. In Pennsylvania, the prelaw implementation period had an MME per prescription a little higher than 200, which leveled off at around 200 during the postintervention period.
“In New Jersey, there is a significantly higher MME than in Pennsylvania and this difference persists in the transition period but what you see in the post period is a significantly greater decline in the MME per prescription in New Jersey as compared to the rate of change in Pa.,” Dr. Lowenstein said. “That difference was statistically significant.”
She said similar results were seen regarding the quantity of tablets prescribed. In New Jersey before the law’s passage, the number of tablets per prescription was close to 50, dropping down to about 35 post period. Pennsylvania saw a slight decrease from about 35 pills per prescription to about 33 during the same period.
No significant changes occurred in the other outcomes measured following implementation of the EMR alert.
Dr. Lowenstein noted that, because the transition period between the law going into effect and the implementation of the EMR alert was so short, whether the greater decreases in opioid prescriptions in New Jersey relative to Pennsylvania was because of the law alone, the EMR alert alone, or both changes is unclear.
Based on the limited amount of change in prescribing patterns during the transition period, it appears that the EMR intervention may be driving the change, “but we weren’t powered to make that determination,” she added.
Dr. Lowenstein and her colleagues reported no disclosures.
REPORTING FROM SGIM 2019
Risk of suicide attempt is higher in children of opioid users
according to an evaluation of a medical claims database from which a sample of more than 200,00 privately insured parents was evaluated.
Based on data collected between the years 2010 and 2016, the study raises the possibility that rising rates of opioid prescriptions and rising rates of suicide in adolescents and children are linked, said David A. Brent, of the University of Pittsburgh, and associates.
The relationship was considered sufficiently strong that the authors recommended clinicians consider mental health screening of children whose parents are known to have had extensive opioid exposure.
Addressing both opioid use in parents and the mental health in their children “may help, at least in part, to reverse the current upward trend in mortality due to the twin epidemics of suicide and opioid overdose,” said Dr. Brent and associates, whose findings were published in JAMA Psychiatry.
From a pool of more than 1 million parents aged 30-50 years in the claims database, 121,306 parents with extensive opioid use – defined as receiving opioid prescriptions for more than 365 days between 2010 and 2016 – were matched with 121,306 controls in the same age range. Children aged 10-19 years in both groups were compared for suicide attempts.
Overall, the rate of prescription opioid use as defined for inclusion in this study was 5% in the target parent population evaluated in this claims database.
Of the 184,142 children with parents exposed to opioids, 678 (0.37%) attempted suicide versus 212 (0.14%) of the 148,395 children from the nonopioid group. Expressed as a rate per 10,000 person years, the figures were 11.7 and 5.9 for the opioid and nonopioid groups, respectively.
When translated into an odds ratio (OR), the increased risk of suicide was found to be almost twice as high (OR 1.99) among children with parents meeting the study criteria for prescription opioid use. The OR was only slightly reduced (OR 1.85) after adjustment for sex and age.
Suicide attempts overall were higher in daughters than sons and in older children (15 years of age or older) than younger (ages 10 to less than 15 years) whether or not parents were taking opioids, but the relative risk remained consistently higher across all these subgroups when comparing those whose parents were taking prescription opioids with those whose parents were not.
As in past studies, children were more likely to make a suicide attempt if they had a parent who had a history of attempting suicide. However, the authors reported a significantly elevated risk of a suicide attempt for children of prescription opioid users after adjustment for this factor as well as for child depression, parental depression, and parental substance use disorder (OR, 1.45).
The OR of a suicide attempt was not significantly higher for a suicide attempt among those children with both parents taking prescription opioids relative to opioid use in only one parent (OR 1.05).
Dr. Brent and associates acknowledged that these data do not confirm that the rising rate of prescription opioid use is linked to the recent parallel rise in suicide attempts among children. However, they did conclude that children of parents using opioid prescriptions are at risk and might be an appropriate target for suicide prevention.
“Recognition and treatment of patients with opioid use disorder, attendance to comorbid conditions in affected parents, and screening and appropriate referral of their children may help” address both major public health issues, they maintained.
The study was supported by a National Institutes of Health grant. Dr Brent reported receiving royalties from Guilford Press, eRT, and UpToDate. Dr. Gibbons has served as an expert witness in cases related to suicide involving pharmaceutical companies, such as Pfizer and GlaxoSmithKline.
SOURCE: Brent DA et al. JAMA Psychiatry. 2019 May 22 doi: 10.1001/jamapsychiatry.2019.0940.
according to an evaluation of a medical claims database from which a sample of more than 200,00 privately insured parents was evaluated.
Based on data collected between the years 2010 and 2016, the study raises the possibility that rising rates of opioid prescriptions and rising rates of suicide in adolescents and children are linked, said David A. Brent, of the University of Pittsburgh, and associates.
The relationship was considered sufficiently strong that the authors recommended clinicians consider mental health screening of children whose parents are known to have had extensive opioid exposure.
Addressing both opioid use in parents and the mental health in their children “may help, at least in part, to reverse the current upward trend in mortality due to the twin epidemics of suicide and opioid overdose,” said Dr. Brent and associates, whose findings were published in JAMA Psychiatry.
From a pool of more than 1 million parents aged 30-50 years in the claims database, 121,306 parents with extensive opioid use – defined as receiving opioid prescriptions for more than 365 days between 2010 and 2016 – were matched with 121,306 controls in the same age range. Children aged 10-19 years in both groups were compared for suicide attempts.
Overall, the rate of prescription opioid use as defined for inclusion in this study was 5% in the target parent population evaluated in this claims database.
Of the 184,142 children with parents exposed to opioids, 678 (0.37%) attempted suicide versus 212 (0.14%) of the 148,395 children from the nonopioid group. Expressed as a rate per 10,000 person years, the figures were 11.7 and 5.9 for the opioid and nonopioid groups, respectively.
When translated into an odds ratio (OR), the increased risk of suicide was found to be almost twice as high (OR 1.99) among children with parents meeting the study criteria for prescription opioid use. The OR was only slightly reduced (OR 1.85) after adjustment for sex and age.
Suicide attempts overall were higher in daughters than sons and in older children (15 years of age or older) than younger (ages 10 to less than 15 years) whether or not parents were taking opioids, but the relative risk remained consistently higher across all these subgroups when comparing those whose parents were taking prescription opioids with those whose parents were not.
As in past studies, children were more likely to make a suicide attempt if they had a parent who had a history of attempting suicide. However, the authors reported a significantly elevated risk of a suicide attempt for children of prescription opioid users after adjustment for this factor as well as for child depression, parental depression, and parental substance use disorder (OR, 1.45).
The OR of a suicide attempt was not significantly higher for a suicide attempt among those children with both parents taking prescription opioids relative to opioid use in only one parent (OR 1.05).
Dr. Brent and associates acknowledged that these data do not confirm that the rising rate of prescription opioid use is linked to the recent parallel rise in suicide attempts among children. However, they did conclude that children of parents using opioid prescriptions are at risk and might be an appropriate target for suicide prevention.
“Recognition and treatment of patients with opioid use disorder, attendance to comorbid conditions in affected parents, and screening and appropriate referral of their children may help” address both major public health issues, they maintained.
The study was supported by a National Institutes of Health grant. Dr Brent reported receiving royalties from Guilford Press, eRT, and UpToDate. Dr. Gibbons has served as an expert witness in cases related to suicide involving pharmaceutical companies, such as Pfizer and GlaxoSmithKline.
SOURCE: Brent DA et al. JAMA Psychiatry. 2019 May 22 doi: 10.1001/jamapsychiatry.2019.0940.
according to an evaluation of a medical claims database from which a sample of more than 200,00 privately insured parents was evaluated.
Based on data collected between the years 2010 and 2016, the study raises the possibility that rising rates of opioid prescriptions and rising rates of suicide in adolescents and children are linked, said David A. Brent, of the University of Pittsburgh, and associates.
The relationship was considered sufficiently strong that the authors recommended clinicians consider mental health screening of children whose parents are known to have had extensive opioid exposure.
Addressing both opioid use in parents and the mental health in their children “may help, at least in part, to reverse the current upward trend in mortality due to the twin epidemics of suicide and opioid overdose,” said Dr. Brent and associates, whose findings were published in JAMA Psychiatry.
From a pool of more than 1 million parents aged 30-50 years in the claims database, 121,306 parents with extensive opioid use – defined as receiving opioid prescriptions for more than 365 days between 2010 and 2016 – were matched with 121,306 controls in the same age range. Children aged 10-19 years in both groups were compared for suicide attempts.
Overall, the rate of prescription opioid use as defined for inclusion in this study was 5% in the target parent population evaluated in this claims database.
Of the 184,142 children with parents exposed to opioids, 678 (0.37%) attempted suicide versus 212 (0.14%) of the 148,395 children from the nonopioid group. Expressed as a rate per 10,000 person years, the figures were 11.7 and 5.9 for the opioid and nonopioid groups, respectively.
When translated into an odds ratio (OR), the increased risk of suicide was found to be almost twice as high (OR 1.99) among children with parents meeting the study criteria for prescription opioid use. The OR was only slightly reduced (OR 1.85) after adjustment for sex and age.
Suicide attempts overall were higher in daughters than sons and in older children (15 years of age or older) than younger (ages 10 to less than 15 years) whether or not parents were taking opioids, but the relative risk remained consistently higher across all these subgroups when comparing those whose parents were taking prescription opioids with those whose parents were not.
As in past studies, children were more likely to make a suicide attempt if they had a parent who had a history of attempting suicide. However, the authors reported a significantly elevated risk of a suicide attempt for children of prescription opioid users after adjustment for this factor as well as for child depression, parental depression, and parental substance use disorder (OR, 1.45).
The OR of a suicide attempt was not significantly higher for a suicide attempt among those children with both parents taking prescription opioids relative to opioid use in only one parent (OR 1.05).
Dr. Brent and associates acknowledged that these data do not confirm that the rising rate of prescription opioid use is linked to the recent parallel rise in suicide attempts among children. However, they did conclude that children of parents using opioid prescriptions are at risk and might be an appropriate target for suicide prevention.
“Recognition and treatment of patients with opioid use disorder, attendance to comorbid conditions in affected parents, and screening and appropriate referral of their children may help” address both major public health issues, they maintained.
The study was supported by a National Institutes of Health grant. Dr Brent reported receiving royalties from Guilford Press, eRT, and UpToDate. Dr. Gibbons has served as an expert witness in cases related to suicide involving pharmaceutical companies, such as Pfizer and GlaxoSmithKline.
SOURCE: Brent DA et al. JAMA Psychiatry. 2019 May 22 doi: 10.1001/jamapsychiatry.2019.0940.
FROM JAMA PSYCHIATRY
Chronic opioid use linked to low testosterone levels
NEW ORLEANS – About two thirds of men who chronically use opioids have low testosterone levels, based on a literature search of more than 50 randomized and observational studies that examined endocrine function in patients on chronic opioid therapy.
Hypocortisolism, seen in about 20% of the men in these studies, was among the other potentially significant deficiencies in endocrine function, Amir H. Zamanipoor Najafabadi, PhD, reported at the annual meeting of the Endocrine Society.
Dr. Najafabadi of Leiden University in the Netherlands, and Friso de Vries, PhD, analyzed the link between opioid use and changes in the gonadal axis. Most of the subjects in their study were men (J Endocr Soc. 2019. doi. 10.1210/js.2019-SUN-489).
While the data do not support firm conclusions on the health consequences of these endocrine observations, Dr. Najafabadi said that a prospective trial is needed to determine whether there is a potential benefit from screening patients on chronic opioids for potentially treatable endocrine deficiencies.
NEW ORLEANS – About two thirds of men who chronically use opioids have low testosterone levels, based on a literature search of more than 50 randomized and observational studies that examined endocrine function in patients on chronic opioid therapy.
Hypocortisolism, seen in about 20% of the men in these studies, was among the other potentially significant deficiencies in endocrine function, Amir H. Zamanipoor Najafabadi, PhD, reported at the annual meeting of the Endocrine Society.
Dr. Najafabadi of Leiden University in the Netherlands, and Friso de Vries, PhD, analyzed the link between opioid use and changes in the gonadal axis. Most of the subjects in their study were men (J Endocr Soc. 2019. doi. 10.1210/js.2019-SUN-489).
While the data do not support firm conclusions on the health consequences of these endocrine observations, Dr. Najafabadi said that a prospective trial is needed to determine whether there is a potential benefit from screening patients on chronic opioids for potentially treatable endocrine deficiencies.
NEW ORLEANS – About two thirds of men who chronically use opioids have low testosterone levels, based on a literature search of more than 50 randomized and observational studies that examined endocrine function in patients on chronic opioid therapy.
Hypocortisolism, seen in about 20% of the men in these studies, was among the other potentially significant deficiencies in endocrine function, Amir H. Zamanipoor Najafabadi, PhD, reported at the annual meeting of the Endocrine Society.
Dr. Najafabadi of Leiden University in the Netherlands, and Friso de Vries, PhD, analyzed the link between opioid use and changes in the gonadal axis. Most of the subjects in their study were men (J Endocr Soc. 2019. doi. 10.1210/js.2019-SUN-489).
While the data do not support firm conclusions on the health consequences of these endocrine observations, Dr. Najafabadi said that a prospective trial is needed to determine whether there is a potential benefit from screening patients on chronic opioids for potentially treatable endocrine deficiencies.
REPORTING FROM ENDO 2019
Direct pharmacy dispensing of naloxone linked to drop in fatal overdoses
investigators reported.
By contrast, state laws that stopped short of allowing pharmacists to directly dispense the opioid antagonist did not appear to impact mortality, according to the report, which appears in JAMA Internal Medicine (2019 May 6. doi: 10.1001/jamainternmed.2019.0272).
The report, based on state-level trends tracked from 2005 to 2016, indicates that fatal opioid overdoses fell by nearly one-third in states that adopted direct dispensing laws as compared with states that adopted other naloxone laws.
That finding suggests that the policy type determines whether a naloxone law is useful in combating fatal opioid overdoses, said Rahi Abouk, PhD, of William Paterson University, Wayne, N.J. and co-authors of the paper.
“Enabling distribution through various sources, or requiring gatekeepers, will not be as beneficial,” Dr. Abouk and co-authors said in their report.
The current rate of deaths from fentanyl, heroin, and prescription analgesic overdose has outpaced all previous drug epidemics on record, and even surpasses the number of deaths in the peak year of the HIV epidemic of the 1980s, Dr. Abouk and colleagues wrote in their paper.
The number of states with naloxone access laws grew from just 2 in 2005 to 47 by 2016, including 9 states that granted direct authority to pharmacists and 38 that granted indirect authority, according to the researchers.
The analysis of overdose trends from 2005 to 2016 was based on naloxone distribution data from state Medicaid agencies and opioid-related mortality data from a national statistics system. Forty percent of nonelderly adults with an opioid addiction are covered by Medicaid, the researchers said.
They found that naloxone laws granting pharmacists direct dispensing authority were linked to a drop in opioid deaths that increased in magnitude over time, according to researchers. The mean number of opioid deaths dropped by 27% in the second year after adoption of direct authority laws, relative to opioid deaths in states with indirect access laws, while in subsequent years, deaths dropped by 34%.
Emergency department visits related to opioids increased by 15% in direct authority states 3 or more years after adoption, as compared to states that did not adopt direct authority laws. According to investigators, that translated into 15 additional opioid-related emergency department visits each month.
That increase suggests that, alongside direct dispensing laws, “useful interventions” and connections to treatment are needed for the emergency department, according to Dr. Abouk and colleagues.
“This is the location where such programs may be the most effective,” they said in their report.
Future research should be done to determine whether removing gatekeepers increases the value of naloxone distribution policies, they concluded in the report.
Dr. Abouk had no disclosures. Co-authors on the study reported funding and conflict of interest disclosures related to the National Institute on Drug Abuse and the Centers for Disease Control and Prevention.
SOURCE: Abouk R, et al. JAMA Intern Med. 2019 May 6. doi:10.1001/jamainternmed.2019.0272.
investigators reported.
By contrast, state laws that stopped short of allowing pharmacists to directly dispense the opioid antagonist did not appear to impact mortality, according to the report, which appears in JAMA Internal Medicine (2019 May 6. doi: 10.1001/jamainternmed.2019.0272).
The report, based on state-level trends tracked from 2005 to 2016, indicates that fatal opioid overdoses fell by nearly one-third in states that adopted direct dispensing laws as compared with states that adopted other naloxone laws.
That finding suggests that the policy type determines whether a naloxone law is useful in combating fatal opioid overdoses, said Rahi Abouk, PhD, of William Paterson University, Wayne, N.J. and co-authors of the paper.
“Enabling distribution through various sources, or requiring gatekeepers, will not be as beneficial,” Dr. Abouk and co-authors said in their report.
The current rate of deaths from fentanyl, heroin, and prescription analgesic overdose has outpaced all previous drug epidemics on record, and even surpasses the number of deaths in the peak year of the HIV epidemic of the 1980s, Dr. Abouk and colleagues wrote in their paper.
The number of states with naloxone access laws grew from just 2 in 2005 to 47 by 2016, including 9 states that granted direct authority to pharmacists and 38 that granted indirect authority, according to the researchers.
The analysis of overdose trends from 2005 to 2016 was based on naloxone distribution data from state Medicaid agencies and opioid-related mortality data from a national statistics system. Forty percent of nonelderly adults with an opioid addiction are covered by Medicaid, the researchers said.
They found that naloxone laws granting pharmacists direct dispensing authority were linked to a drop in opioid deaths that increased in magnitude over time, according to researchers. The mean number of opioid deaths dropped by 27% in the second year after adoption of direct authority laws, relative to opioid deaths in states with indirect access laws, while in subsequent years, deaths dropped by 34%.
Emergency department visits related to opioids increased by 15% in direct authority states 3 or more years after adoption, as compared to states that did not adopt direct authority laws. According to investigators, that translated into 15 additional opioid-related emergency department visits each month.
That increase suggests that, alongside direct dispensing laws, “useful interventions” and connections to treatment are needed for the emergency department, according to Dr. Abouk and colleagues.
“This is the location where such programs may be the most effective,” they said in their report.
Future research should be done to determine whether removing gatekeepers increases the value of naloxone distribution policies, they concluded in the report.
Dr. Abouk had no disclosures. Co-authors on the study reported funding and conflict of interest disclosures related to the National Institute on Drug Abuse and the Centers for Disease Control and Prevention.
SOURCE: Abouk R, et al. JAMA Intern Med. 2019 May 6. doi:10.1001/jamainternmed.2019.0272.
investigators reported.
By contrast, state laws that stopped short of allowing pharmacists to directly dispense the opioid antagonist did not appear to impact mortality, according to the report, which appears in JAMA Internal Medicine (2019 May 6. doi: 10.1001/jamainternmed.2019.0272).
The report, based on state-level trends tracked from 2005 to 2016, indicates that fatal opioid overdoses fell by nearly one-third in states that adopted direct dispensing laws as compared with states that adopted other naloxone laws.
That finding suggests that the policy type determines whether a naloxone law is useful in combating fatal opioid overdoses, said Rahi Abouk, PhD, of William Paterson University, Wayne, N.J. and co-authors of the paper.
“Enabling distribution through various sources, or requiring gatekeepers, will not be as beneficial,” Dr. Abouk and co-authors said in their report.
The current rate of deaths from fentanyl, heroin, and prescription analgesic overdose has outpaced all previous drug epidemics on record, and even surpasses the number of deaths in the peak year of the HIV epidemic of the 1980s, Dr. Abouk and colleagues wrote in their paper.
The number of states with naloxone access laws grew from just 2 in 2005 to 47 by 2016, including 9 states that granted direct authority to pharmacists and 38 that granted indirect authority, according to the researchers.
The analysis of overdose trends from 2005 to 2016 was based on naloxone distribution data from state Medicaid agencies and opioid-related mortality data from a national statistics system. Forty percent of nonelderly adults with an opioid addiction are covered by Medicaid, the researchers said.
They found that naloxone laws granting pharmacists direct dispensing authority were linked to a drop in opioid deaths that increased in magnitude over time, according to researchers. The mean number of opioid deaths dropped by 27% in the second year after adoption of direct authority laws, relative to opioid deaths in states with indirect access laws, while in subsequent years, deaths dropped by 34%.
Emergency department visits related to opioids increased by 15% in direct authority states 3 or more years after adoption, as compared to states that did not adopt direct authority laws. According to investigators, that translated into 15 additional opioid-related emergency department visits each month.
That increase suggests that, alongside direct dispensing laws, “useful interventions” and connections to treatment are needed for the emergency department, according to Dr. Abouk and colleagues.
“This is the location where such programs may be the most effective,” they said in their report.
Future research should be done to determine whether removing gatekeepers increases the value of naloxone distribution policies, they concluded in the report.
Dr. Abouk had no disclosures. Co-authors on the study reported funding and conflict of interest disclosures related to the National Institute on Drug Abuse and the Centers for Disease Control and Prevention.
SOURCE: Abouk R, et al. JAMA Intern Med. 2019 May 6. doi:10.1001/jamainternmed.2019.0272.
FROM JAMA Internal Medicine
Key clinical point: State laws granting pharmacists direct authority to dispense naloxone were linked to significant drops in opioid-related fatal overdoses.
Major finding: The mean number of opioid deaths dropped by 27% in the second year after adoption of direct authority laws relative to opioid deaths in states with indirect access laws, while in subsequent years, deaths dropped by 34%.
Study details: Analysis of naloxone distribution data and opioid-related mortality data from 2005 to 2016 for all 50 states and the District of Columbia.
Disclosures: Study authors reported funding and conflict of interest disclosures related to the National Institute on Drug Abuse and the Centers for Disease Control and Prevention.
Source: Abouk R, et al. JAMA Intern Med. 2019 May 6.
Only 1.5% of individuals at high risk of opioid overdose receive naloxone
The vast majority of individuals at high risk for opioid overdose do not receive naloxone, despite numerous opportunities, according to Sarah Follman and associates from the University of Chicago.
In a retrospective study published in JAMA Network Open, the study authors analyzed data from individuals in the Truven Health MarketScan Research Database who had ICD-10 codes related to opioid use, misuse, dependence, and overdose. Data from Oct. 1, 2015, through Dec. 31, 2016, were included; a total of 138,108 high-risk individuals were identified as interacting with the health care system nearly 1.2 million times (88,618 hospitalizations, 229,680 ED visits, 298,058 internal medicine visits, and 568,448 family practice visits).
Of the 138,108 individuals in the study, only 2,135 (1.5%) were prescribed naloxone during the study period. Patients who had prior diagnoses of both opioid misuse/dependence and overdose were significantly more likely to receive naloxone than were those who only had a history of opioid dependence (odds ratio, 2.32; 95% confidence interval, 1.98-2.72; P less than .001). In addition, having a history of overdose alone was associated with a decreased chance of receiving naloxone, compared with those with a history of opioid misuse alone (OR, 0.73; 95% CI, 0.57-0.94; P = .01).
Other factors that significantly reduced the odds of receiving naloxone included being aged 30-44 years and being from the Midwest or West. Factors that reduced the odds include having received treatment for opioid use disorder, visiting a detoxification facility, receiving other substance use disorder treatment; and having received outpatient care from a pain specialist, psychologist, or surgeon.
“Most individuals at high risk of opioid overdose do not receive naloxone through direct prescribing,” Ms. Follman and associates wrote. “Clinicians can address this gap by regularly prescribing naloxone to eligible patients. To address barriers to prescribing, hospital systems and medical schools can support clinicians by improving education on screening and treating substance use disorders, clarifying legal concerns, and developing policies and protocols to guide implementation of increased prescribing.
No conflicts of interest were reported; one coauthor reported receiving a grant from the National Institutes of Health.
SOURCE: Follman S et al. JAMA Netw Open. 2019 May 3. doi: 10.1001/jamanetworkopen.2019.3209.
The vast majority of individuals at high risk for opioid overdose do not receive naloxone, despite numerous opportunities, according to Sarah Follman and associates from the University of Chicago.
In a retrospective study published in JAMA Network Open, the study authors analyzed data from individuals in the Truven Health MarketScan Research Database who had ICD-10 codes related to opioid use, misuse, dependence, and overdose. Data from Oct. 1, 2015, through Dec. 31, 2016, were included; a total of 138,108 high-risk individuals were identified as interacting with the health care system nearly 1.2 million times (88,618 hospitalizations, 229,680 ED visits, 298,058 internal medicine visits, and 568,448 family practice visits).
Of the 138,108 individuals in the study, only 2,135 (1.5%) were prescribed naloxone during the study period. Patients who had prior diagnoses of both opioid misuse/dependence and overdose were significantly more likely to receive naloxone than were those who only had a history of opioid dependence (odds ratio, 2.32; 95% confidence interval, 1.98-2.72; P less than .001). In addition, having a history of overdose alone was associated with a decreased chance of receiving naloxone, compared with those with a history of opioid misuse alone (OR, 0.73; 95% CI, 0.57-0.94; P = .01).
Other factors that significantly reduced the odds of receiving naloxone included being aged 30-44 years and being from the Midwest or West. Factors that reduced the odds include having received treatment for opioid use disorder, visiting a detoxification facility, receiving other substance use disorder treatment; and having received outpatient care from a pain specialist, psychologist, or surgeon.
“Most individuals at high risk of opioid overdose do not receive naloxone through direct prescribing,” Ms. Follman and associates wrote. “Clinicians can address this gap by regularly prescribing naloxone to eligible patients. To address barriers to prescribing, hospital systems and medical schools can support clinicians by improving education on screening and treating substance use disorders, clarifying legal concerns, and developing policies and protocols to guide implementation of increased prescribing.
No conflicts of interest were reported; one coauthor reported receiving a grant from the National Institutes of Health.
SOURCE: Follman S et al. JAMA Netw Open. 2019 May 3. doi: 10.1001/jamanetworkopen.2019.3209.
The vast majority of individuals at high risk for opioid overdose do not receive naloxone, despite numerous opportunities, according to Sarah Follman and associates from the University of Chicago.
In a retrospective study published in JAMA Network Open, the study authors analyzed data from individuals in the Truven Health MarketScan Research Database who had ICD-10 codes related to opioid use, misuse, dependence, and overdose. Data from Oct. 1, 2015, through Dec. 31, 2016, were included; a total of 138,108 high-risk individuals were identified as interacting with the health care system nearly 1.2 million times (88,618 hospitalizations, 229,680 ED visits, 298,058 internal medicine visits, and 568,448 family practice visits).
Of the 138,108 individuals in the study, only 2,135 (1.5%) were prescribed naloxone during the study period. Patients who had prior diagnoses of both opioid misuse/dependence and overdose were significantly more likely to receive naloxone than were those who only had a history of opioid dependence (odds ratio, 2.32; 95% confidence interval, 1.98-2.72; P less than .001). In addition, having a history of overdose alone was associated with a decreased chance of receiving naloxone, compared with those with a history of opioid misuse alone (OR, 0.73; 95% CI, 0.57-0.94; P = .01).
Other factors that significantly reduced the odds of receiving naloxone included being aged 30-44 years and being from the Midwest or West. Factors that reduced the odds include having received treatment for opioid use disorder, visiting a detoxification facility, receiving other substance use disorder treatment; and having received outpatient care from a pain specialist, psychologist, or surgeon.
“Most individuals at high risk of opioid overdose do not receive naloxone through direct prescribing,” Ms. Follman and associates wrote. “Clinicians can address this gap by regularly prescribing naloxone to eligible patients. To address barriers to prescribing, hospital systems and medical schools can support clinicians by improving education on screening and treating substance use disorders, clarifying legal concerns, and developing policies and protocols to guide implementation of increased prescribing.
No conflicts of interest were reported; one coauthor reported receiving a grant from the National Institutes of Health.
SOURCE: Follman S et al. JAMA Netw Open. 2019 May 3. doi: 10.1001/jamanetworkopen.2019.3209.
FROM JAMA NETWORK OPEN
Outpatient program successfully tackles substance use and chronic pain
MILWAUKEE – An interdisciplinary intensive outpatient treatment program addressing chronic pain and substance use disorder effectively addressed both diagnoses in a military population.
Intensive outpatient programs (IOPs) frequently address these conditions within a biopsychosocial format, but it’s not common for IOPs to have this dual focus on chronic pain and substance use disorder (SUD), said Michael Stockin, MD, speaking in an interview at the scientific meeting of the American Pain Society.
Dr. Stockin said he and his collaborators recognized that, especially among a military population, the two conditions have considerable overlap, so it made sense to integrate behavioral treatment for both conditions in an intensive outpatient program. “Our hypothesis was that if you can use an intensive outpatient program to address substance use disorder, maybe you can actually add a chronic pain curriculum – like a functional restoration program to it.
“As a result of our study, we did find that there were significant differences in worst pain scores as a result of the program. In the people who took both the substance use disorder and chronic pain curriculum, we found significant reductions in total impairment, worst pain, and they also had less … substance use as well,” said Dr. Stockin.
In a quality improvement project, Dr. Stockin and collaborators compared short-term outcomes for patients who received IOP treatment addressing both chronic pain and SUD with those receiving SUD-only IOP.
For those participating in the joint IOP, scores indicating worst pain on the 0-10 numeric rating scale were reduced significantly, from 7.55 to 6.23 (P = .013). Scores on a functional measure of impairment, the Pain Outcomes Questionnaire Short Form (POQ-SF) also dropped significantly, from 84.92 to 63.50 (P = .034). The vitality domain of the POQ-SF also showed that patients had less impairment after participation in the joint IOP, with scores in that domain dropping from 20.17 to 17.25 (P = .024).
Looking at the total cohort, patient scores on the Brief Addiction Monitor (BAM) dropped significantly from baseline to the end of the intervention, indicating reduced substance use (P = .041). Mean scores for participants in the joint IOP were higher at baseline than for those in the SUD-only IOP (1.000 vs. 0.565). However, those participating in the joint IOP had lower mean postintervention BAM scores than the SUD-only cohort (0.071 vs. 0.174).
American veterans experience more severe pain and have a higher prevalence of chronic pain than nonveterans. Similarly, wrote Dr. Stockin, a chronic pain fellow in pain management at Walter Reed National Military Medical Center, Bethesda, Md., and colleagues in the poster presentation.
The project enrolled a total of 66 patients (10 female and 56 male). Of these, 18 participated in the joint SUD–chronic pain program, and 48 received usual treatment of the SUD-only IOP treatment. The mean overall age was 33.2 years, and 71.2% of participants were white.
Overall, 51 patients (77.3%) of participants had alcohol use disorder. Participants included active duty service members, veterans, and their dependents. Opioid and cannabis use disorders were experienced by a total of eight patients, and seven more patients had diagnoses of alcohol use disorder along with other substance use disorders.
All patients completed the BAM and received urine toxicology and alcohol breath testing at enrollment; drug and alcohol screening was completed at other points during the IOP treatment for both groups as well.
The joint IOP ran 3 full days a week, with a substance use curriculum in the morning and a pain management program in the afternoon; the SUD-only participants had three morning sessions weekly. Both interventions lasted 6 weeks, and Dr. Stockin said he and his colleagues would like to acquire longitudinal data to assess the durability of gains seen from the joint IOP.
The multidisciplinary team running the joint IOP was made up of an addiction/pain medicine physician, a clinical health psychologist, a physical therapist, social workers, and a nurse.
“This project is the first of its kind to find a significant reduction in pain burden while concurrently treating addiction and pain in an outpatient military health care setting,” Dr. Stockin and colleagues wrote in the poster accompanying the presentation.
“We had outcomes in both substance use and chronic pain that were positive, so it suggests that in the military health system, people may actually benefit from treating both chronic pain and substance use disorder concurrently. If you could harmonize those programs, you might be able to get good outcomes for soldiers and their families,” Dr. Stockin said.
Dr. Stockin reported no conflicts of interest. The project was funded by the Defense Health Agency.
MILWAUKEE – An interdisciplinary intensive outpatient treatment program addressing chronic pain and substance use disorder effectively addressed both diagnoses in a military population.
Intensive outpatient programs (IOPs) frequently address these conditions within a biopsychosocial format, but it’s not common for IOPs to have this dual focus on chronic pain and substance use disorder (SUD), said Michael Stockin, MD, speaking in an interview at the scientific meeting of the American Pain Society.
Dr. Stockin said he and his collaborators recognized that, especially among a military population, the two conditions have considerable overlap, so it made sense to integrate behavioral treatment for both conditions in an intensive outpatient program. “Our hypothesis was that if you can use an intensive outpatient program to address substance use disorder, maybe you can actually add a chronic pain curriculum – like a functional restoration program to it.
“As a result of our study, we did find that there were significant differences in worst pain scores as a result of the program. In the people who took both the substance use disorder and chronic pain curriculum, we found significant reductions in total impairment, worst pain, and they also had less … substance use as well,” said Dr. Stockin.
In a quality improvement project, Dr. Stockin and collaborators compared short-term outcomes for patients who received IOP treatment addressing both chronic pain and SUD with those receiving SUD-only IOP.
For those participating in the joint IOP, scores indicating worst pain on the 0-10 numeric rating scale were reduced significantly, from 7.55 to 6.23 (P = .013). Scores on a functional measure of impairment, the Pain Outcomes Questionnaire Short Form (POQ-SF) also dropped significantly, from 84.92 to 63.50 (P = .034). The vitality domain of the POQ-SF also showed that patients had less impairment after participation in the joint IOP, with scores in that domain dropping from 20.17 to 17.25 (P = .024).
Looking at the total cohort, patient scores on the Brief Addiction Monitor (BAM) dropped significantly from baseline to the end of the intervention, indicating reduced substance use (P = .041). Mean scores for participants in the joint IOP were higher at baseline than for those in the SUD-only IOP (1.000 vs. 0.565). However, those participating in the joint IOP had lower mean postintervention BAM scores than the SUD-only cohort (0.071 vs. 0.174).
American veterans experience more severe pain and have a higher prevalence of chronic pain than nonveterans. Similarly, wrote Dr. Stockin, a chronic pain fellow in pain management at Walter Reed National Military Medical Center, Bethesda, Md., and colleagues in the poster presentation.
The project enrolled a total of 66 patients (10 female and 56 male). Of these, 18 participated in the joint SUD–chronic pain program, and 48 received usual treatment of the SUD-only IOP treatment. The mean overall age was 33.2 years, and 71.2% of participants were white.
Overall, 51 patients (77.3%) of participants had alcohol use disorder. Participants included active duty service members, veterans, and their dependents. Opioid and cannabis use disorders were experienced by a total of eight patients, and seven more patients had diagnoses of alcohol use disorder along with other substance use disorders.
All patients completed the BAM and received urine toxicology and alcohol breath testing at enrollment; drug and alcohol screening was completed at other points during the IOP treatment for both groups as well.
The joint IOP ran 3 full days a week, with a substance use curriculum in the morning and a pain management program in the afternoon; the SUD-only participants had three morning sessions weekly. Both interventions lasted 6 weeks, and Dr. Stockin said he and his colleagues would like to acquire longitudinal data to assess the durability of gains seen from the joint IOP.
The multidisciplinary team running the joint IOP was made up of an addiction/pain medicine physician, a clinical health psychologist, a physical therapist, social workers, and a nurse.
“This project is the first of its kind to find a significant reduction in pain burden while concurrently treating addiction and pain in an outpatient military health care setting,” Dr. Stockin and colleagues wrote in the poster accompanying the presentation.
“We had outcomes in both substance use and chronic pain that were positive, so it suggests that in the military health system, people may actually benefit from treating both chronic pain and substance use disorder concurrently. If you could harmonize those programs, you might be able to get good outcomes for soldiers and their families,” Dr. Stockin said.
Dr. Stockin reported no conflicts of interest. The project was funded by the Defense Health Agency.
MILWAUKEE – An interdisciplinary intensive outpatient treatment program addressing chronic pain and substance use disorder effectively addressed both diagnoses in a military population.
Intensive outpatient programs (IOPs) frequently address these conditions within a biopsychosocial format, but it’s not common for IOPs to have this dual focus on chronic pain and substance use disorder (SUD), said Michael Stockin, MD, speaking in an interview at the scientific meeting of the American Pain Society.
Dr. Stockin said he and his collaborators recognized that, especially among a military population, the two conditions have considerable overlap, so it made sense to integrate behavioral treatment for both conditions in an intensive outpatient program. “Our hypothesis was that if you can use an intensive outpatient program to address substance use disorder, maybe you can actually add a chronic pain curriculum – like a functional restoration program to it.
“As a result of our study, we did find that there were significant differences in worst pain scores as a result of the program. In the people who took both the substance use disorder and chronic pain curriculum, we found significant reductions in total impairment, worst pain, and they also had less … substance use as well,” said Dr. Stockin.
In a quality improvement project, Dr. Stockin and collaborators compared short-term outcomes for patients who received IOP treatment addressing both chronic pain and SUD with those receiving SUD-only IOP.
For those participating in the joint IOP, scores indicating worst pain on the 0-10 numeric rating scale were reduced significantly, from 7.55 to 6.23 (P = .013). Scores on a functional measure of impairment, the Pain Outcomes Questionnaire Short Form (POQ-SF) also dropped significantly, from 84.92 to 63.50 (P = .034). The vitality domain of the POQ-SF also showed that patients had less impairment after participation in the joint IOP, with scores in that domain dropping from 20.17 to 17.25 (P = .024).
Looking at the total cohort, patient scores on the Brief Addiction Monitor (BAM) dropped significantly from baseline to the end of the intervention, indicating reduced substance use (P = .041). Mean scores for participants in the joint IOP were higher at baseline than for those in the SUD-only IOP (1.000 vs. 0.565). However, those participating in the joint IOP had lower mean postintervention BAM scores than the SUD-only cohort (0.071 vs. 0.174).
American veterans experience more severe pain and have a higher prevalence of chronic pain than nonveterans. Similarly, wrote Dr. Stockin, a chronic pain fellow in pain management at Walter Reed National Military Medical Center, Bethesda, Md., and colleagues in the poster presentation.
The project enrolled a total of 66 patients (10 female and 56 male). Of these, 18 participated in the joint SUD–chronic pain program, and 48 received usual treatment of the SUD-only IOP treatment. The mean overall age was 33.2 years, and 71.2% of participants were white.
Overall, 51 patients (77.3%) of participants had alcohol use disorder. Participants included active duty service members, veterans, and their dependents. Opioid and cannabis use disorders were experienced by a total of eight patients, and seven more patients had diagnoses of alcohol use disorder along with other substance use disorders.
All patients completed the BAM and received urine toxicology and alcohol breath testing at enrollment; drug and alcohol screening was completed at other points during the IOP treatment for both groups as well.
The joint IOP ran 3 full days a week, with a substance use curriculum in the morning and a pain management program in the afternoon; the SUD-only participants had three morning sessions weekly. Both interventions lasted 6 weeks, and Dr. Stockin said he and his colleagues would like to acquire longitudinal data to assess the durability of gains seen from the joint IOP.
The multidisciplinary team running the joint IOP was made up of an addiction/pain medicine physician, a clinical health psychologist, a physical therapist, social workers, and a nurse.
“This project is the first of its kind to find a significant reduction in pain burden while concurrently treating addiction and pain in an outpatient military health care setting,” Dr. Stockin and colleagues wrote in the poster accompanying the presentation.
“We had outcomes in both substance use and chronic pain that were positive, so it suggests that in the military health system, people may actually benefit from treating both chronic pain and substance use disorder concurrently. If you could harmonize those programs, you might be able to get good outcomes for soldiers and their families,” Dr. Stockin said.
Dr. Stockin reported no conflicts of interest. The project was funded by the Defense Health Agency.
REPORTING FROM APS 2019
Key clinical point: An intensive, 6-week joint substance use disorder and chronic pain intensive outpatient program significantly reduced both substance use and pain.
Major finding: Patients had less pain and reduced substance use after completing the program, compared with baseline (P = .013 and .041, respectively).
Study details: A quality improvement project including 66 patients at a military health facility.
Disclosures: The study was sponsored by the Defense Health Agency. Dr. Stockin reported no conflicts of interest.