User login
Could Resistin Predict Death and Disease Severity in PAH?
Resistin, a cytokine expressed in adipocytes, has been associated with poor clinical outcomes in heart failure and cardiovascular disease, Li Gao, MD, of Johns Hopkins University, Baltimore, Maryland, and colleagues wrote. While mouse studies have shown that human resistin drives pulmonary vascular remodeling and the development of PAH, the role of resistin as a biomarker for PAH remains unclear.
In a study published in Respiratory Research, the researchers reviewed biospecimens and clinical and genetic data from 1121 adults with PAH, 808 with idiopathic PAH (IPAH), and 313 with scleroderma-associated PAH (SSc-PAH). They examined the associations between serum resistin levels and PAH outcomes in multivariate regression models, using machine-learning algorithms to develop models to predict mortality.
Resistin levels were significantly higher in all patients with PAH and patients with the two subtypes than in control participants (all P < .0001). Resistin was also associated with significant discriminative properties, with area under the curve (AUC) measures of 0.84, 0.82, and 0.91 for PAH overall, IPAH, and SSc-PAH, respectively.
Elevated resistin levels (defined as > 4.54 ng/mL) were significantly associated with an increased risk for death (hazard ratio, 2.6; P < .0087) as well as with older age and shorter distance on the 6-minute walk test (P = .001 for both) and reduced cardiac capacity based on the New York Heart Association functional class (P < .014).
Survival models derived from machine learning confirmed the prognostic value of resistin for mortality in PAH as seen in the random forest model, with an AUC of 0.70. “When we used the AUC values of the ROC curve as criteria to evaluate how well resistin levels discerned the presence of PAH, all three tests had excellent discriminative ability (AUCs were 0.84, 0.82, and 0.91 for all PAH, IPAH, and SSc-PAH, respectively),” the researchers wrote.
The researchers also evaluated three RETN genetic variants (rs7408174, rs3219175, and rs3745367) for a specific association with serum resistin levels and measures of PAH severity. Resistin levels were highest among individuals who were carriers of either the rs3219175 or rs3745367 mutation, the researchers noted.
The findings were limited by several factors, including missing data on the 6-minute walk test from several centers, which led to the elimination of that item from the survival analysis. Other limitations included the inability to control for PAH therapy at the time of assessment and the collection of serum at a different time from other clinical variables.
However, “our study provides evidence to support the use of circulating biomarkers as objective and accessible tools for noninvasive PAH risk stratification,” the researchers said. Additional research is needed to strengthen the association, but the findings suggest that resistin represents a novel biomarker for PAH prognostication and risk stratification and may have implications for the development of new treatments.
Biomarker Research Expands Diagnosis and Treatment Horizons
“It is a dynamic time in PAH research and clinical management, given the recent approval and use of the BMP/TGF beta balancing agent sotatercept (Winrevair) as an effective agent to target the molecular origins of this disease,” Stephen Chan, MD, professor of medicine and director of the Vascular Medicine Institute at the University of Pittsburgh, Pittsburgh, Pennsylvania, said in an interview.
The growing number of medications that can be used to treat patients with PAH will likely be more effective if patients are identified and treated early, said Dr. Chan, who was not involved in the study.
However, the time to diagnosis for patients with PAH is still more than 3 years from the start of symptoms, he said. Factors contributing to the delay include the requirement of an invasive cardiac catheterization procedure to make the final diagnosis, the status of PAH as a borderline orphan disease, and the often nonspecific nature of the initial symptoms of PAH.
Consequently, “there is an unmet need to develop effective and preferably noninvasive tools to aid in early diagnosis of PAH,” Dr. Chan added.
The power of the study is in the number of patients included, as much of previous PAH research has involved small studies of patients that could not be replicated or did not generalize to the larger patient population, Dr. Chan said.
The use of the PAH Biobank allows researchers to access a larger population of patients with PAH. “With that in mind, it is not surprising that some markers would emerge as potentially powerful and clinically meaningful,” he said.
“Currently, we do not have a reliable blood-based biomarker that we use in clinical PAH practice, although there are emerging studies that suggest other markers such as metabolites, RNA molecules, and proteins that may serve in the same capacity. If these studies turn out to be reproducible, generalizable, and specific to PAH in larger populations, measuring resistin could be helpful in making early diagnosis, particularly in areas that do not have invasive catheterization facilities (and globally) and for nonspecialists who are puzzled about the nonspecificity of initial symptoms of PAH,” Dr. Chan said.
Resistin could also be incorporated into existing risk stratification scores, such as the REVEAL risk score, that are already used in PAH clinical practice as guidance for when and how to use currently approved medications, he added.
Limitations of the study included the focus only on resistin alone, not in combination with other molecules that might perform better. Also, no independent validation cohort was used, he noted. “While PAH Biobank certainly offered larger numbers than we typically see, we would have to see validation in large independent cohorts for us to be convinced that measurements of resistin should be used in clinical practice.”
Resistin is not specific to PAH, which makes interpretation of the results more complicated, said Dr. Chan. “In this study, the authors used a smaller healthy control cohort of 50 patients as a comparison to their PAH cohort. However, they did not compare their PAH cohort with other cohorts that represent these other ‘resistin-relevant diseases’ and thus do not know whether they can distinguish PAH from any of these other diseases based on simply the resistin levels.” The frequency of comorbidities in patients with PAH, such as obesity, other inflammatory diseases, and cardiovascular disease, could confound the resistin levels.
The study was supported by the National Institutes of Health. Neither the researchers nor Dr. Chan had financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Resistin, a cytokine expressed in adipocytes, has been associated with poor clinical outcomes in heart failure and cardiovascular disease, Li Gao, MD, of Johns Hopkins University, Baltimore, Maryland, and colleagues wrote. While mouse studies have shown that human resistin drives pulmonary vascular remodeling and the development of PAH, the role of resistin as a biomarker for PAH remains unclear.
In a study published in Respiratory Research, the researchers reviewed biospecimens and clinical and genetic data from 1121 adults with PAH, 808 with idiopathic PAH (IPAH), and 313 with scleroderma-associated PAH (SSc-PAH). They examined the associations between serum resistin levels and PAH outcomes in multivariate regression models, using machine-learning algorithms to develop models to predict mortality.
Resistin levels were significantly higher in all patients with PAH and patients with the two subtypes than in control participants (all P < .0001). Resistin was also associated with significant discriminative properties, with area under the curve (AUC) measures of 0.84, 0.82, and 0.91 for PAH overall, IPAH, and SSc-PAH, respectively.
Elevated resistin levels (defined as > 4.54 ng/mL) were significantly associated with an increased risk for death (hazard ratio, 2.6; P < .0087) as well as with older age and shorter distance on the 6-minute walk test (P = .001 for both) and reduced cardiac capacity based on the New York Heart Association functional class (P < .014).
Survival models derived from machine learning confirmed the prognostic value of resistin for mortality in PAH as seen in the random forest model, with an AUC of 0.70. “When we used the AUC values of the ROC curve as criteria to evaluate how well resistin levels discerned the presence of PAH, all three tests had excellent discriminative ability (AUCs were 0.84, 0.82, and 0.91 for all PAH, IPAH, and SSc-PAH, respectively),” the researchers wrote.
The researchers also evaluated three RETN genetic variants (rs7408174, rs3219175, and rs3745367) for a specific association with serum resistin levels and measures of PAH severity. Resistin levels were highest among individuals who were carriers of either the rs3219175 or rs3745367 mutation, the researchers noted.
The findings were limited by several factors, including missing data on the 6-minute walk test from several centers, which led to the elimination of that item from the survival analysis. Other limitations included the inability to control for PAH therapy at the time of assessment and the collection of serum at a different time from other clinical variables.
However, “our study provides evidence to support the use of circulating biomarkers as objective and accessible tools for noninvasive PAH risk stratification,” the researchers said. Additional research is needed to strengthen the association, but the findings suggest that resistin represents a novel biomarker for PAH prognostication and risk stratification and may have implications for the development of new treatments.
Biomarker Research Expands Diagnosis and Treatment Horizons
“It is a dynamic time in PAH research and clinical management, given the recent approval and use of the BMP/TGF beta balancing agent sotatercept (Winrevair) as an effective agent to target the molecular origins of this disease,” Stephen Chan, MD, professor of medicine and director of the Vascular Medicine Institute at the University of Pittsburgh, Pittsburgh, Pennsylvania, said in an interview.
The growing number of medications that can be used to treat patients with PAH will likely be more effective if patients are identified and treated early, said Dr. Chan, who was not involved in the study.
However, the time to diagnosis for patients with PAH is still more than 3 years from the start of symptoms, he said. Factors contributing to the delay include the requirement of an invasive cardiac catheterization procedure to make the final diagnosis, the status of PAH as a borderline orphan disease, and the often nonspecific nature of the initial symptoms of PAH.
Consequently, “there is an unmet need to develop effective and preferably noninvasive tools to aid in early diagnosis of PAH,” Dr. Chan added.
The power of the study is in the number of patients included, as much of previous PAH research has involved small studies of patients that could not be replicated or did not generalize to the larger patient population, Dr. Chan said.
The use of the PAH Biobank allows researchers to access a larger population of patients with PAH. “With that in mind, it is not surprising that some markers would emerge as potentially powerful and clinically meaningful,” he said.
“Currently, we do not have a reliable blood-based biomarker that we use in clinical PAH practice, although there are emerging studies that suggest other markers such as metabolites, RNA molecules, and proteins that may serve in the same capacity. If these studies turn out to be reproducible, generalizable, and specific to PAH in larger populations, measuring resistin could be helpful in making early diagnosis, particularly in areas that do not have invasive catheterization facilities (and globally) and for nonspecialists who are puzzled about the nonspecificity of initial symptoms of PAH,” Dr. Chan said.
Resistin could also be incorporated into existing risk stratification scores, such as the REVEAL risk score, that are already used in PAH clinical practice as guidance for when and how to use currently approved medications, he added.
Limitations of the study included the focus only on resistin alone, not in combination with other molecules that might perform better. Also, no independent validation cohort was used, he noted. “While PAH Biobank certainly offered larger numbers than we typically see, we would have to see validation in large independent cohorts for us to be convinced that measurements of resistin should be used in clinical practice.”
Resistin is not specific to PAH, which makes interpretation of the results more complicated, said Dr. Chan. “In this study, the authors used a smaller healthy control cohort of 50 patients as a comparison to their PAH cohort. However, they did not compare their PAH cohort with other cohorts that represent these other ‘resistin-relevant diseases’ and thus do not know whether they can distinguish PAH from any of these other diseases based on simply the resistin levels.” The frequency of comorbidities in patients with PAH, such as obesity, other inflammatory diseases, and cardiovascular disease, could confound the resistin levels.
The study was supported by the National Institutes of Health. Neither the researchers nor Dr. Chan had financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Resistin, a cytokine expressed in adipocytes, has been associated with poor clinical outcomes in heart failure and cardiovascular disease, Li Gao, MD, of Johns Hopkins University, Baltimore, Maryland, and colleagues wrote. While mouse studies have shown that human resistin drives pulmonary vascular remodeling and the development of PAH, the role of resistin as a biomarker for PAH remains unclear.
In a study published in Respiratory Research, the researchers reviewed biospecimens and clinical and genetic data from 1121 adults with PAH, 808 with idiopathic PAH (IPAH), and 313 with scleroderma-associated PAH (SSc-PAH). They examined the associations between serum resistin levels and PAH outcomes in multivariate regression models, using machine-learning algorithms to develop models to predict mortality.
Resistin levels were significantly higher in all patients with PAH and patients with the two subtypes than in control participants (all P < .0001). Resistin was also associated with significant discriminative properties, with area under the curve (AUC) measures of 0.84, 0.82, and 0.91 for PAH overall, IPAH, and SSc-PAH, respectively.
Elevated resistin levels (defined as > 4.54 ng/mL) were significantly associated with an increased risk for death (hazard ratio, 2.6; P < .0087) as well as with older age and shorter distance on the 6-minute walk test (P = .001 for both) and reduced cardiac capacity based on the New York Heart Association functional class (P < .014).
Survival models derived from machine learning confirmed the prognostic value of resistin for mortality in PAH as seen in the random forest model, with an AUC of 0.70. “When we used the AUC values of the ROC curve as criteria to evaluate how well resistin levels discerned the presence of PAH, all three tests had excellent discriminative ability (AUCs were 0.84, 0.82, and 0.91 for all PAH, IPAH, and SSc-PAH, respectively),” the researchers wrote.
The researchers also evaluated three RETN genetic variants (rs7408174, rs3219175, and rs3745367) for a specific association with serum resistin levels and measures of PAH severity. Resistin levels were highest among individuals who were carriers of either the rs3219175 or rs3745367 mutation, the researchers noted.
The findings were limited by several factors, including missing data on the 6-minute walk test from several centers, which led to the elimination of that item from the survival analysis. Other limitations included the inability to control for PAH therapy at the time of assessment and the collection of serum at a different time from other clinical variables.
However, “our study provides evidence to support the use of circulating biomarkers as objective and accessible tools for noninvasive PAH risk stratification,” the researchers said. Additional research is needed to strengthen the association, but the findings suggest that resistin represents a novel biomarker for PAH prognostication and risk stratification and may have implications for the development of new treatments.
Biomarker Research Expands Diagnosis and Treatment Horizons
“It is a dynamic time in PAH research and clinical management, given the recent approval and use of the BMP/TGF beta balancing agent sotatercept (Winrevair) as an effective agent to target the molecular origins of this disease,” Stephen Chan, MD, professor of medicine and director of the Vascular Medicine Institute at the University of Pittsburgh, Pittsburgh, Pennsylvania, said in an interview.
The growing number of medications that can be used to treat patients with PAH will likely be more effective if patients are identified and treated early, said Dr. Chan, who was not involved in the study.
However, the time to diagnosis for patients with PAH is still more than 3 years from the start of symptoms, he said. Factors contributing to the delay include the requirement of an invasive cardiac catheterization procedure to make the final diagnosis, the status of PAH as a borderline orphan disease, and the often nonspecific nature of the initial symptoms of PAH.
Consequently, “there is an unmet need to develop effective and preferably noninvasive tools to aid in early diagnosis of PAH,” Dr. Chan added.
The power of the study is in the number of patients included, as much of previous PAH research has involved small studies of patients that could not be replicated or did not generalize to the larger patient population, Dr. Chan said.
The use of the PAH Biobank allows researchers to access a larger population of patients with PAH. “With that in mind, it is not surprising that some markers would emerge as potentially powerful and clinically meaningful,” he said.
“Currently, we do not have a reliable blood-based biomarker that we use in clinical PAH practice, although there are emerging studies that suggest other markers such as metabolites, RNA molecules, and proteins that may serve in the same capacity. If these studies turn out to be reproducible, generalizable, and specific to PAH in larger populations, measuring resistin could be helpful in making early diagnosis, particularly in areas that do not have invasive catheterization facilities (and globally) and for nonspecialists who are puzzled about the nonspecificity of initial symptoms of PAH,” Dr. Chan said.
Resistin could also be incorporated into existing risk stratification scores, such as the REVEAL risk score, that are already used in PAH clinical practice as guidance for when and how to use currently approved medications, he added.
Limitations of the study included the focus only on resistin alone, not in combination with other molecules that might perform better. Also, no independent validation cohort was used, he noted. “While PAH Biobank certainly offered larger numbers than we typically see, we would have to see validation in large independent cohorts for us to be convinced that measurements of resistin should be used in clinical practice.”
Resistin is not specific to PAH, which makes interpretation of the results more complicated, said Dr. Chan. “In this study, the authors used a smaller healthy control cohort of 50 patients as a comparison to their PAH cohort. However, they did not compare their PAH cohort with other cohorts that represent these other ‘resistin-relevant diseases’ and thus do not know whether they can distinguish PAH from any of these other diseases based on simply the resistin levels.” The frequency of comorbidities in patients with PAH, such as obesity, other inflammatory diseases, and cardiovascular disease, could confound the resistin levels.
The study was supported by the National Institutes of Health. Neither the researchers nor Dr. Chan had financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Using Telehealth to Increase Lung Cancer Screening Referrals for At-Risk Veterans in Rural Communities
Annual lung cancer screening (LCS) with low-dose computed tomography (LDCT) of the chest has been shown to reduce mortality rates for individuals at risk for lung cancer.1 Despite the benefits, < 5% of those who were eligible for LCS in the United States were screened in 2022.2 Implementation of a LCS program in rural communities is especially challenging because they are sparsely populated, medically underserved, and located far from urban centers.2-7 It is estimated that 1 in 5 people live in rural areas. Rates of tobacco smoking and cancer are higher in rural communities when compared with urban communities.8,9 The scarcity of physicians in rural areas who are familiar with LCS may further impede individuals who are at risk from accessing this life saving service.5,6 As a result, these individuals may not regularly undergo LCS as recommended.9
Telehealth, or the remote delivery of health care services via telecommunications, is an emerging approach for addressing unmet medical needs in rural communities and is being utilized widely by the US Department of Veterans Affairs (VA).4,10-15 The Veterans Integrated Service Network 12 (Great Lakes Network) has established the Clinical Resource Hub (CRH), a telehealth network comprising of licensed independent physicians, nurse practitioners, registered nurses, and ancillary staff. The CRH offers regular, remote health care services to several community-based outpatient clinics (CBOC) primary care clinics located in rural northern Wisconsin and the Upper Peninsula of Michigan.10,14
The utility of telehealth in promoting LCS among at-risk veterans living in rural communities has not been firmly established.4-6 To address this issue, we conducted a proof-of-principle quality improvement project to determine whether a telehealth intervention would increase referrals among at-risk veterans who reside in rural northern Wisconsin and the Upper Peninsula of Michigan who are self-enrolled in a CBOC smoking cessation program in Green Bay, Wisconsin. The CBOC provides primary health care to veterans residing in rural northern Wisconsin and the Upper Peninsula of Michigan as defined by US Department of Agriculture rural-urban commuting area codes.16 The intervention aimed to refer these individuals to the closest available and centralized LCS program, which is located at the Clement J. Zablocki VA Medical Center (CJZVAMC) in Milwaukee, Wisconsin.
METHODS
We reviewed electronic health records (EHR) of LCS-eligible veterans treated by 2 authors (SH and TB) who were self-enrolled in the smoking cessation program at the Green Bay CBOC between October 1, 2020, and September 30, 2021. The program provides comprehensive evidence-based tobacco use treatment, online self-help resources, behavioral counseling, and medicines for smoking cessation.17 Veterans aged 50 to 80 years with a smoking history of ≥ 20 pack-years, who currently smoke cigarettes or quit within the past 15 years, were considered at risk for lung cancer and eligible for LCS. After confirming eligibility, pertinent demographic data were abstracted from each EHR.
Telehealth Intervention
The CJZVAMC centralized LCS program manages all delivery processes and has been previously shown to increase uptake of LCS and improve patient outcomes among veterans as compared to a decentralized approach.18,19 In the centralized approach, eligible veterans were referred by a CBOC primary care practitioner (PCP) to a designated centralized LCS program. The centralized LCS program provides further evaluation and disposition, which includes structured and shared decision making, ordering LDCT of the chest, reporting LDCT results to the patient and PCP, devising a goal-directed care plan, and managing follow-up LDCTs as indicated (Figure 1).18,19
This intervention was initiated before other measures aimed to increase the LCS enrollment for at-risk rural veterans at the CBOC, (eg, mailing LCS education fact sheet to veterans).20 After reviewing prospective veterans’ EHRs, 1 author (TB) contacted LCS-eligible veterans by telephone and left a voicemail if contact could not be established. A second telephone call was placed within 2 months of the initial call if no call back was documented in the EHR. When verbal contact was established, the goals of the centralized LCS program were described and the veteran was invited to participate.21
Veterans were seen at CBOCs affiliated with CJZVAMC. The CJZVAMC LCS coordinator was notified whenever a veteran agreed to enroll into LCS and then ordered LDCT, which was performed and read at CJZVAMC. Once LDCT has been ordered, 1 author (TB) reviewed the veteran’s EHR for LDCT completion over the next 4 months.Upon conclusion of the intervention period, the number of veterans referred for LDCT and the number of LDCTs performed were recorded. Each LDCT was reviewed and coded by medical imaging clinicians according to Lung CT Screening Reporting and Data System (Lung-RADS) version 1.1 and coded as 0, 1, 2, 3, or 4 based on the nodule with the highest degree of suspicion.22 The LDCT and reports were also reviewed by pulmonary physicians at the CJZVAMC Lung Nodule Clinic with recommendations issued and reported to the PCP treating the veteran, such as annual follow-up with LDCT or referral to specialty care for further evaluation as indicated.
RESULTS
Of 117 veterans enrolled in the smoking cessation program at the CBOC during the intervention period, 74 (63%) were eligible to undergo LCS, and 68 (58%) were contacted by telephone (Figure 2). Eligible patients were primarily White male veterans; their mean (SD) age was 65.0 years (7.6). Participation in LCS was discussed with 41 (60%) veterans either during the initial or second telephone call of which 29 (71%) agreed to enroll and 12 (29%) declined. Veterans did not provide reasons for declining participation at the time of the telephone call.
Among the 74 eligible veterans who attended the smoking cessation program, only 3 had LDCT performed before initiation of this project (4%). At the conclusion of the telehealth intervention period, 19 veterans had LDCT performed (26%). Ten LDCTs were coded Lung-RADS 1, 7 Lung-RADS 2, 1 Lung-RADS 3, and 1 Lung-RADS 4B. In each case, annual follow-up LDCT or referral to a LCS clinician was pursued as indicated.22
DISCUSSION
This proof-of-principle quality improvement project found that a high percentage (66%) of individuals in rural communities who were contacted via telehealth agreed to participate in a regional LCS program. The program reviewed LDCT results, ordered follow-up LDCTs, and recommended further evaluations.18,19 Whether this centralized LCS process could also promote adherence with subsequent annual LDCT and/or scheduled clinic appointments with designated clinicians, if abnormal imaging findings are detected, remains unclear.
It has been well established LDCT LCS reduces lung cancer-specific and overall mortality rates among eligible current and former smokers.1,9,23 The 5-year relative survival rate of veterans diagnosed with localized non-small cell lung cancer is 63%; that number drops to 7% in those with advanced disease attesting to the utility of LCS in detecting early stage lung cancer.2 Despite these favorable observations, however, screening rates with free LDCT remains low in rural communities.3-7
This proof-of-principle quality improvement project found that telehealth intervention may increase referrals of at-risk veterans who reside in rural communities to the closest centralized LCS program located at aregional VAMC. This program is responsible for reviewing the results of the initial LDCT, ordering follow-up LDCT, and recommending further evaluation as indicated.18,19 Whether this centralized LCS process would promote adherence with subsequent annual LDCT and/or scheduled clinic appointments with designated clinicians if abnormal imaging findings are detected is yet to be determined.
We found that among 74 LCS-eligible rural veterans attending a CBOC-based smoking cessation program, only 3 (4%) underwent LDCT screening before this telehealth intervention was launched. This low LCS rate among veterans attempting to quit smoking may have been related, in part, to a lack of awareness of this intervention and/or barriers to LCS access.7,10,21,24 Deploying a telehealth intervention targeting LCS could address this life threatening and unmet medical need in rural communities.25 The results of this proof-of-principle quality improvement project support this contention with the reported increased referrals to and completion of initial LDCT within 4 months of the telehealth encounter.
Limitations
This was a small, single site project composed of predominantly White male rural veterans participating in a smoking cessation program associated with a VA facility.26,27 It is not clear whether similar outcomes would be observed in at-risk veterans who do not participate in a smoking cessation program or in more diverse communities. We were unable to contact 40% of LCS-eligible rural veterans by telephone. Twelve veterans reached by telephone declined to participate in LCS without providing a reason, and only 19 of 68 eligible veterans (28%) underwent LDCT screening during the 4-month telehealth intervention. The reasons underlying this overall low accrual rate and whether rural veterans prefer other means of personal communication regarding LCS were not determined. Lastly, generalizability of our initial observations to other veterans living in rural communities is limited because the project was conducted only in rural northern Wisconsin and the Upper Peninsula of Michigan.
Conclusions
At-risk rural veterans may be willing to participate in a centralized LCS program at a regional VA medical facility when contacted and coordinated using telehealth modalities. These findings offer support for future prospective, multisite, VA telehealth-based studies to be conducted in rural areas. The results of this project also suggest that telehealth intervention could increase referrals of at-risk rural veterans to the closest centralized LCS program located at a regional VA medical facility.
1. National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409. doi:10.1056/NEJMoa1102873
2. State of Lung Cancer: 2023 Report. American Lung Association. November 14, 2023. Accessed June 4, 2024. https://www.lung.org/getmedia/186786b6-18c3-46a9-a7e7-810f3ce4deda/SOLC-2023-Print-Report.pdf
3. Okereke IC, Nishi S, Zhou J, Goodwin JS. Trends in lung cancer screening in the United States, 2016-2017. J Thorac Dis. 2019;11(3):873-881. doi:10.21037/jtd.2019.01.105
4. Petraglia AF, Olazagasti JM, Strong A, Dunn B, Anderson RT, Hanley M. Establishing satellite lung cancer screening sites with telehealth to address disparities between high-risk smokers and American College of Radiology-approved Centers of Designation. J Thorac Imaging. 2021;36(1):2-5. doi:10.1097/RTI.0000000000000520
5. Odahowski CL, Zahnd WE, Eberth JM. Challenges and opportunities for lung cancer screening in rural America. J Am Coll Radiol. 2019;16(4 Pt B):590-595. doi:10.1016/j.jacr.2019.01.001
6. Rohatgi KW, Marx CM, Lewis-Thames MW, Liu J, Colditz GA, James AS. Urban-rural disparities in access to low-dose computed tomography lung cancer screening in Missouri and Illinois. Prev Chronic Dis. 2020;17:E140. doi:10.5888/pcd17.200202
7. Boudreau JH, Miller DR, Qian S, Nunez ER, Caverly TJ, Wiener RS. Access to lung cancer screening in the Veterans Health Administration: does geographic distribution match need in the population? Chest. 2021;160(1):358-367. doi:10.1016/j.chest.2021.02.016
8. Howlader N, Noone AM, Krapcho M, et al, eds. SEER Cancer Statistics Review, 1975-2017. National Cancer Institute, US Dept of Health and Human Services; April 15, 2020. Accessed June 4, 2024. https://seer.cancer.gov/archive/csr/1975_2017/index.html
9. US Preventive Services Task Force, Krist AH, Davidson KW, et al. Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(10):962-970. doi:10.1001/jama.2021.1117
10. Gopal RK, Solanki P, Bokhour BG, et al. Provider, staff, and patient perspectives on medical visits using clinical video telehealth: a foundation for educational initiatives to improve medical care in telehealth. J Nurse Pract. 2021;17(5):582-587. doi:10.1016/j.nurpra.2021.02.020
11. Yacoub JH, Swanson CE, Jay AK, Cooper C, Spies J, Krishnan P. The radiology virtual reading room: during and beyond the COVID-19 pandemic. J Digit Imaging. 2021;34(2):308-319. doi:10.1007/s10278-021-00427-4
12. Beswick DM, Vashi A, Song Y, et al. Consultation via telemedicine and access to operative care for patients with head and neck cancer in a Veterans Health Administration population. Head Neck. 2016;38(6):925-929. doi:10.1002/hed.24386
13. Ruco A, Dossa F, Tinmouth J, et al. Social media and mHealth technology for cancer screening: systematic review and meta-analysis. J Med Internet Res. 2021;23(7):e26759. doi:10.2196/26759
14. Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine - a model to access the subspecialist services in underserved rural areas. Int J Med Inform. 2009;78(1):53-59. doi:10.1016/j.ijmedinf.2008.07.010
15. Chen A, Ayub MH, Mishuris RG, et al. Telehealth policy, practice, and education: a position statement of the Society of General Internal Medicine. J Gen Intern Med. 2023;38(11):2613-2620. doi:10.1007/s11606-023-08190-8
16. Rural-Urban Commuting Area Codes. Economic Research Service, US Dept of Agriculture. Updated September 25, 2023. Accessed June 4, 2024. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
17. VHA Directive 1056: National Smoking and Tobacco Use Cessation Program. Veterans Health Administration, US Dept of Veterans Affairs; September 5, 2019. Accessed June 4, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8488
18. Smith HB, Ward R, Frazier C, Angotti J, Tanner NT. Guideline-recommended lung cancer screening adherence is superior with a centralized approach. Chest. 2022;161(3):818-825. doi:10.1016/j.chest.2021.09.002
19. Lewis JA, Samuels LR, Denton J, et al. The association of health care system resources with lung cancer screening implementation: a cohort study. Chest. 2022;162(3):701-711. doi:10.1016/j.chest.2022.03.050
20. US Dept of Veterans Affairs. Lung cancer screening: patient education fact sheet. Accessed July 8, 2024. https://www.cancer.va.gov/assets/pdf/survey/LCSflyer.pdf
21. Melzer AC, Golden SE, Ono SS, Datta S, Crothers K, Slatore CG. What exactly is shared decision-making? A qualitative study of shared decision-making in lung cancer screening. J Gen Intern Med. 2020;35(2):546-553. doi:10.1007/s11606-019-05516-3
22. Chelala L, Hossain R, Kazerooni EA, Christensen JD, Dyer DS, White CS. Lung-RADS Version 1.1: challenges and a look ahead, from the AJR special series on radiology reporting and data systems. AJR Am J Roentgenol. 2021;216(6):1411-1422. doi:10.2214/AJR.20.24807
23. Ritzwoller DP, Meza R, Carroll NM, et al. Evaluation of population-level changes associated with the 2021 US Preventive Services Task Force lung cancer screening recommendations in community-based health care systems. JAMA Netw Open. 2021;4(10):e2128176. doi:10.1001/jamanetworkopen.2021.28176
24. Golden SE, Ono SS, Thakurta SG, et al. “I’m putting my trust in their hands”: a qualitative study of patients’ views on clinician initial communication about lung cancer screening. Chest. 2020;158(3):1260-1267. doi:10.1016/j.chest.2020.02.072
25. Park ER, Chiles C, Cinciripini PM, et al. Impact of the COVID-19 pandemic on telehealth research in cancer prevention and care: a call to sustain telehealth advances. Cancer. 2021;127(3):334-338. doi:10.1002/cncr.33227
26. Tremblay A, Taghizadeh N, Huang J, et al. A randomized controlled study of integrated smoking cessation in a lung cancer screening program. J Thorac Oncol. 2019;14(9):1528-1537. doi:10.1016/j.jtho.2019.04.024
27. Neil JM, Marotta C, Gonzalez I, et al. Integrating tobacco treatment into lung cancer screening practices: study protocol for the Screen ASSIST randomized clinical trial. Contemp Clin Trials. 2021;111:106586. doi:10.1016/j.cct.2021.106586
Annual lung cancer screening (LCS) with low-dose computed tomography (LDCT) of the chest has been shown to reduce mortality rates for individuals at risk for lung cancer.1 Despite the benefits, < 5% of those who were eligible for LCS in the United States were screened in 2022.2 Implementation of a LCS program in rural communities is especially challenging because they are sparsely populated, medically underserved, and located far from urban centers.2-7 It is estimated that 1 in 5 people live in rural areas. Rates of tobacco smoking and cancer are higher in rural communities when compared with urban communities.8,9 The scarcity of physicians in rural areas who are familiar with LCS may further impede individuals who are at risk from accessing this life saving service.5,6 As a result, these individuals may not regularly undergo LCS as recommended.9
Telehealth, or the remote delivery of health care services via telecommunications, is an emerging approach for addressing unmet medical needs in rural communities and is being utilized widely by the US Department of Veterans Affairs (VA).4,10-15 The Veterans Integrated Service Network 12 (Great Lakes Network) has established the Clinical Resource Hub (CRH), a telehealth network comprising of licensed independent physicians, nurse practitioners, registered nurses, and ancillary staff. The CRH offers regular, remote health care services to several community-based outpatient clinics (CBOC) primary care clinics located in rural northern Wisconsin and the Upper Peninsula of Michigan.10,14
The utility of telehealth in promoting LCS among at-risk veterans living in rural communities has not been firmly established.4-6 To address this issue, we conducted a proof-of-principle quality improvement project to determine whether a telehealth intervention would increase referrals among at-risk veterans who reside in rural northern Wisconsin and the Upper Peninsula of Michigan who are self-enrolled in a CBOC smoking cessation program in Green Bay, Wisconsin. The CBOC provides primary health care to veterans residing in rural northern Wisconsin and the Upper Peninsula of Michigan as defined by US Department of Agriculture rural-urban commuting area codes.16 The intervention aimed to refer these individuals to the closest available and centralized LCS program, which is located at the Clement J. Zablocki VA Medical Center (CJZVAMC) in Milwaukee, Wisconsin.
METHODS
We reviewed electronic health records (EHR) of LCS-eligible veterans treated by 2 authors (SH and TB) who were self-enrolled in the smoking cessation program at the Green Bay CBOC between October 1, 2020, and September 30, 2021. The program provides comprehensive evidence-based tobacco use treatment, online self-help resources, behavioral counseling, and medicines for smoking cessation.17 Veterans aged 50 to 80 years with a smoking history of ≥ 20 pack-years, who currently smoke cigarettes or quit within the past 15 years, were considered at risk for lung cancer and eligible for LCS. After confirming eligibility, pertinent demographic data were abstracted from each EHR.
Telehealth Intervention
The CJZVAMC centralized LCS program manages all delivery processes and has been previously shown to increase uptake of LCS and improve patient outcomes among veterans as compared to a decentralized approach.18,19 In the centralized approach, eligible veterans were referred by a CBOC primary care practitioner (PCP) to a designated centralized LCS program. The centralized LCS program provides further evaluation and disposition, which includes structured and shared decision making, ordering LDCT of the chest, reporting LDCT results to the patient and PCP, devising a goal-directed care plan, and managing follow-up LDCTs as indicated (Figure 1).18,19
This intervention was initiated before other measures aimed to increase the LCS enrollment for at-risk rural veterans at the CBOC, (eg, mailing LCS education fact sheet to veterans).20 After reviewing prospective veterans’ EHRs, 1 author (TB) contacted LCS-eligible veterans by telephone and left a voicemail if contact could not be established. A second telephone call was placed within 2 months of the initial call if no call back was documented in the EHR. When verbal contact was established, the goals of the centralized LCS program were described and the veteran was invited to participate.21
Veterans were seen at CBOCs affiliated with CJZVAMC. The CJZVAMC LCS coordinator was notified whenever a veteran agreed to enroll into LCS and then ordered LDCT, which was performed and read at CJZVAMC. Once LDCT has been ordered, 1 author (TB) reviewed the veteran’s EHR for LDCT completion over the next 4 months.Upon conclusion of the intervention period, the number of veterans referred for LDCT and the number of LDCTs performed were recorded. Each LDCT was reviewed and coded by medical imaging clinicians according to Lung CT Screening Reporting and Data System (Lung-RADS) version 1.1 and coded as 0, 1, 2, 3, or 4 based on the nodule with the highest degree of suspicion.22 The LDCT and reports were also reviewed by pulmonary physicians at the CJZVAMC Lung Nodule Clinic with recommendations issued and reported to the PCP treating the veteran, such as annual follow-up with LDCT or referral to specialty care for further evaluation as indicated.
RESULTS
Of 117 veterans enrolled in the smoking cessation program at the CBOC during the intervention period, 74 (63%) were eligible to undergo LCS, and 68 (58%) were contacted by telephone (Figure 2). Eligible patients were primarily White male veterans; their mean (SD) age was 65.0 years (7.6). Participation in LCS was discussed with 41 (60%) veterans either during the initial or second telephone call of which 29 (71%) agreed to enroll and 12 (29%) declined. Veterans did not provide reasons for declining participation at the time of the telephone call.
Among the 74 eligible veterans who attended the smoking cessation program, only 3 had LDCT performed before initiation of this project (4%). At the conclusion of the telehealth intervention period, 19 veterans had LDCT performed (26%). Ten LDCTs were coded Lung-RADS 1, 7 Lung-RADS 2, 1 Lung-RADS 3, and 1 Lung-RADS 4B. In each case, annual follow-up LDCT or referral to a LCS clinician was pursued as indicated.22
DISCUSSION
This proof-of-principle quality improvement project found that a high percentage (66%) of individuals in rural communities who were contacted via telehealth agreed to participate in a regional LCS program. The program reviewed LDCT results, ordered follow-up LDCTs, and recommended further evaluations.18,19 Whether this centralized LCS process could also promote adherence with subsequent annual LDCT and/or scheduled clinic appointments with designated clinicians, if abnormal imaging findings are detected, remains unclear.
It has been well established LDCT LCS reduces lung cancer-specific and overall mortality rates among eligible current and former smokers.1,9,23 The 5-year relative survival rate of veterans diagnosed with localized non-small cell lung cancer is 63%; that number drops to 7% in those with advanced disease attesting to the utility of LCS in detecting early stage lung cancer.2 Despite these favorable observations, however, screening rates with free LDCT remains low in rural communities.3-7
This proof-of-principle quality improvement project found that telehealth intervention may increase referrals of at-risk veterans who reside in rural communities to the closest centralized LCS program located at aregional VAMC. This program is responsible for reviewing the results of the initial LDCT, ordering follow-up LDCT, and recommending further evaluation as indicated.18,19 Whether this centralized LCS process would promote adherence with subsequent annual LDCT and/or scheduled clinic appointments with designated clinicians if abnormal imaging findings are detected is yet to be determined.
We found that among 74 LCS-eligible rural veterans attending a CBOC-based smoking cessation program, only 3 (4%) underwent LDCT screening before this telehealth intervention was launched. This low LCS rate among veterans attempting to quit smoking may have been related, in part, to a lack of awareness of this intervention and/or barriers to LCS access.7,10,21,24 Deploying a telehealth intervention targeting LCS could address this life threatening and unmet medical need in rural communities.25 The results of this proof-of-principle quality improvement project support this contention with the reported increased referrals to and completion of initial LDCT within 4 months of the telehealth encounter.
Limitations
This was a small, single site project composed of predominantly White male rural veterans participating in a smoking cessation program associated with a VA facility.26,27 It is not clear whether similar outcomes would be observed in at-risk veterans who do not participate in a smoking cessation program or in more diverse communities. We were unable to contact 40% of LCS-eligible rural veterans by telephone. Twelve veterans reached by telephone declined to participate in LCS without providing a reason, and only 19 of 68 eligible veterans (28%) underwent LDCT screening during the 4-month telehealth intervention. The reasons underlying this overall low accrual rate and whether rural veterans prefer other means of personal communication regarding LCS were not determined. Lastly, generalizability of our initial observations to other veterans living in rural communities is limited because the project was conducted only in rural northern Wisconsin and the Upper Peninsula of Michigan.
Conclusions
At-risk rural veterans may be willing to participate in a centralized LCS program at a regional VA medical facility when contacted and coordinated using telehealth modalities. These findings offer support for future prospective, multisite, VA telehealth-based studies to be conducted in rural areas. The results of this project also suggest that telehealth intervention could increase referrals of at-risk rural veterans to the closest centralized LCS program located at a regional VA medical facility.
Annual lung cancer screening (LCS) with low-dose computed tomography (LDCT) of the chest has been shown to reduce mortality rates for individuals at risk for lung cancer.1 Despite the benefits, < 5% of those who were eligible for LCS in the United States were screened in 2022.2 Implementation of a LCS program in rural communities is especially challenging because they are sparsely populated, medically underserved, and located far from urban centers.2-7 It is estimated that 1 in 5 people live in rural areas. Rates of tobacco smoking and cancer are higher in rural communities when compared with urban communities.8,9 The scarcity of physicians in rural areas who are familiar with LCS may further impede individuals who are at risk from accessing this life saving service.5,6 As a result, these individuals may not regularly undergo LCS as recommended.9
Telehealth, or the remote delivery of health care services via telecommunications, is an emerging approach for addressing unmet medical needs in rural communities and is being utilized widely by the US Department of Veterans Affairs (VA).4,10-15 The Veterans Integrated Service Network 12 (Great Lakes Network) has established the Clinical Resource Hub (CRH), a telehealth network comprising of licensed independent physicians, nurse practitioners, registered nurses, and ancillary staff. The CRH offers regular, remote health care services to several community-based outpatient clinics (CBOC) primary care clinics located in rural northern Wisconsin and the Upper Peninsula of Michigan.10,14
The utility of telehealth in promoting LCS among at-risk veterans living in rural communities has not been firmly established.4-6 To address this issue, we conducted a proof-of-principle quality improvement project to determine whether a telehealth intervention would increase referrals among at-risk veterans who reside in rural northern Wisconsin and the Upper Peninsula of Michigan who are self-enrolled in a CBOC smoking cessation program in Green Bay, Wisconsin. The CBOC provides primary health care to veterans residing in rural northern Wisconsin and the Upper Peninsula of Michigan as defined by US Department of Agriculture rural-urban commuting area codes.16 The intervention aimed to refer these individuals to the closest available and centralized LCS program, which is located at the Clement J. Zablocki VA Medical Center (CJZVAMC) in Milwaukee, Wisconsin.
METHODS
We reviewed electronic health records (EHR) of LCS-eligible veterans treated by 2 authors (SH and TB) who were self-enrolled in the smoking cessation program at the Green Bay CBOC between October 1, 2020, and September 30, 2021. The program provides comprehensive evidence-based tobacco use treatment, online self-help resources, behavioral counseling, and medicines for smoking cessation.17 Veterans aged 50 to 80 years with a smoking history of ≥ 20 pack-years, who currently smoke cigarettes or quit within the past 15 years, were considered at risk for lung cancer and eligible for LCS. After confirming eligibility, pertinent demographic data were abstracted from each EHR.
Telehealth Intervention
The CJZVAMC centralized LCS program manages all delivery processes and has been previously shown to increase uptake of LCS and improve patient outcomes among veterans as compared to a decentralized approach.18,19 In the centralized approach, eligible veterans were referred by a CBOC primary care practitioner (PCP) to a designated centralized LCS program. The centralized LCS program provides further evaluation and disposition, which includes structured and shared decision making, ordering LDCT of the chest, reporting LDCT results to the patient and PCP, devising a goal-directed care plan, and managing follow-up LDCTs as indicated (Figure 1).18,19
This intervention was initiated before other measures aimed to increase the LCS enrollment for at-risk rural veterans at the CBOC, (eg, mailing LCS education fact sheet to veterans).20 After reviewing prospective veterans’ EHRs, 1 author (TB) contacted LCS-eligible veterans by telephone and left a voicemail if contact could not be established. A second telephone call was placed within 2 months of the initial call if no call back was documented in the EHR. When verbal contact was established, the goals of the centralized LCS program were described and the veteran was invited to participate.21
Veterans were seen at CBOCs affiliated with CJZVAMC. The CJZVAMC LCS coordinator was notified whenever a veteran agreed to enroll into LCS and then ordered LDCT, which was performed and read at CJZVAMC. Once LDCT has been ordered, 1 author (TB) reviewed the veteran’s EHR for LDCT completion over the next 4 months.Upon conclusion of the intervention period, the number of veterans referred for LDCT and the number of LDCTs performed were recorded. Each LDCT was reviewed and coded by medical imaging clinicians according to Lung CT Screening Reporting and Data System (Lung-RADS) version 1.1 and coded as 0, 1, 2, 3, or 4 based on the nodule with the highest degree of suspicion.22 The LDCT and reports were also reviewed by pulmonary physicians at the CJZVAMC Lung Nodule Clinic with recommendations issued and reported to the PCP treating the veteran, such as annual follow-up with LDCT or referral to specialty care for further evaluation as indicated.
RESULTS
Of 117 veterans enrolled in the smoking cessation program at the CBOC during the intervention period, 74 (63%) were eligible to undergo LCS, and 68 (58%) were contacted by telephone (Figure 2). Eligible patients were primarily White male veterans; their mean (SD) age was 65.0 years (7.6). Participation in LCS was discussed with 41 (60%) veterans either during the initial or second telephone call of which 29 (71%) agreed to enroll and 12 (29%) declined. Veterans did not provide reasons for declining participation at the time of the telephone call.
Among the 74 eligible veterans who attended the smoking cessation program, only 3 had LDCT performed before initiation of this project (4%). At the conclusion of the telehealth intervention period, 19 veterans had LDCT performed (26%). Ten LDCTs were coded Lung-RADS 1, 7 Lung-RADS 2, 1 Lung-RADS 3, and 1 Lung-RADS 4B. In each case, annual follow-up LDCT or referral to a LCS clinician was pursued as indicated.22
DISCUSSION
This proof-of-principle quality improvement project found that a high percentage (66%) of individuals in rural communities who were contacted via telehealth agreed to participate in a regional LCS program. The program reviewed LDCT results, ordered follow-up LDCTs, and recommended further evaluations.18,19 Whether this centralized LCS process could also promote adherence with subsequent annual LDCT and/or scheduled clinic appointments with designated clinicians, if abnormal imaging findings are detected, remains unclear.
It has been well established LDCT LCS reduces lung cancer-specific and overall mortality rates among eligible current and former smokers.1,9,23 The 5-year relative survival rate of veterans diagnosed with localized non-small cell lung cancer is 63%; that number drops to 7% in those with advanced disease attesting to the utility of LCS in detecting early stage lung cancer.2 Despite these favorable observations, however, screening rates with free LDCT remains low in rural communities.3-7
This proof-of-principle quality improvement project found that telehealth intervention may increase referrals of at-risk veterans who reside in rural communities to the closest centralized LCS program located at aregional VAMC. This program is responsible for reviewing the results of the initial LDCT, ordering follow-up LDCT, and recommending further evaluation as indicated.18,19 Whether this centralized LCS process would promote adherence with subsequent annual LDCT and/or scheduled clinic appointments with designated clinicians if abnormal imaging findings are detected is yet to be determined.
We found that among 74 LCS-eligible rural veterans attending a CBOC-based smoking cessation program, only 3 (4%) underwent LDCT screening before this telehealth intervention was launched. This low LCS rate among veterans attempting to quit smoking may have been related, in part, to a lack of awareness of this intervention and/or barriers to LCS access.7,10,21,24 Deploying a telehealth intervention targeting LCS could address this life threatening and unmet medical need in rural communities.25 The results of this proof-of-principle quality improvement project support this contention with the reported increased referrals to and completion of initial LDCT within 4 months of the telehealth encounter.
Limitations
This was a small, single site project composed of predominantly White male rural veterans participating in a smoking cessation program associated with a VA facility.26,27 It is not clear whether similar outcomes would be observed in at-risk veterans who do not participate in a smoking cessation program or in more diverse communities. We were unable to contact 40% of LCS-eligible rural veterans by telephone. Twelve veterans reached by telephone declined to participate in LCS without providing a reason, and only 19 of 68 eligible veterans (28%) underwent LDCT screening during the 4-month telehealth intervention. The reasons underlying this overall low accrual rate and whether rural veterans prefer other means of personal communication regarding LCS were not determined. Lastly, generalizability of our initial observations to other veterans living in rural communities is limited because the project was conducted only in rural northern Wisconsin and the Upper Peninsula of Michigan.
Conclusions
At-risk rural veterans may be willing to participate in a centralized LCS program at a regional VA medical facility when contacted and coordinated using telehealth modalities. These findings offer support for future prospective, multisite, VA telehealth-based studies to be conducted in rural areas. The results of this project also suggest that telehealth intervention could increase referrals of at-risk rural veterans to the closest centralized LCS program located at a regional VA medical facility.
1. National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409. doi:10.1056/NEJMoa1102873
2. State of Lung Cancer: 2023 Report. American Lung Association. November 14, 2023. Accessed June 4, 2024. https://www.lung.org/getmedia/186786b6-18c3-46a9-a7e7-810f3ce4deda/SOLC-2023-Print-Report.pdf
3. Okereke IC, Nishi S, Zhou J, Goodwin JS. Trends in lung cancer screening in the United States, 2016-2017. J Thorac Dis. 2019;11(3):873-881. doi:10.21037/jtd.2019.01.105
4. Petraglia AF, Olazagasti JM, Strong A, Dunn B, Anderson RT, Hanley M. Establishing satellite lung cancer screening sites with telehealth to address disparities between high-risk smokers and American College of Radiology-approved Centers of Designation. J Thorac Imaging. 2021;36(1):2-5. doi:10.1097/RTI.0000000000000520
5. Odahowski CL, Zahnd WE, Eberth JM. Challenges and opportunities for lung cancer screening in rural America. J Am Coll Radiol. 2019;16(4 Pt B):590-595. doi:10.1016/j.jacr.2019.01.001
6. Rohatgi KW, Marx CM, Lewis-Thames MW, Liu J, Colditz GA, James AS. Urban-rural disparities in access to low-dose computed tomography lung cancer screening in Missouri and Illinois. Prev Chronic Dis. 2020;17:E140. doi:10.5888/pcd17.200202
7. Boudreau JH, Miller DR, Qian S, Nunez ER, Caverly TJ, Wiener RS. Access to lung cancer screening in the Veterans Health Administration: does geographic distribution match need in the population? Chest. 2021;160(1):358-367. doi:10.1016/j.chest.2021.02.016
8. Howlader N, Noone AM, Krapcho M, et al, eds. SEER Cancer Statistics Review, 1975-2017. National Cancer Institute, US Dept of Health and Human Services; April 15, 2020. Accessed June 4, 2024. https://seer.cancer.gov/archive/csr/1975_2017/index.html
9. US Preventive Services Task Force, Krist AH, Davidson KW, et al. Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(10):962-970. doi:10.1001/jama.2021.1117
10. Gopal RK, Solanki P, Bokhour BG, et al. Provider, staff, and patient perspectives on medical visits using clinical video telehealth: a foundation for educational initiatives to improve medical care in telehealth. J Nurse Pract. 2021;17(5):582-587. doi:10.1016/j.nurpra.2021.02.020
11. Yacoub JH, Swanson CE, Jay AK, Cooper C, Spies J, Krishnan P. The radiology virtual reading room: during and beyond the COVID-19 pandemic. J Digit Imaging. 2021;34(2):308-319. doi:10.1007/s10278-021-00427-4
12. Beswick DM, Vashi A, Song Y, et al. Consultation via telemedicine and access to operative care for patients with head and neck cancer in a Veterans Health Administration population. Head Neck. 2016;38(6):925-929. doi:10.1002/hed.24386
13. Ruco A, Dossa F, Tinmouth J, et al. Social media and mHealth technology for cancer screening: systematic review and meta-analysis. J Med Internet Res. 2021;23(7):e26759. doi:10.2196/26759
14. Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine - a model to access the subspecialist services in underserved rural areas. Int J Med Inform. 2009;78(1):53-59. doi:10.1016/j.ijmedinf.2008.07.010
15. Chen A, Ayub MH, Mishuris RG, et al. Telehealth policy, practice, and education: a position statement of the Society of General Internal Medicine. J Gen Intern Med. 2023;38(11):2613-2620. doi:10.1007/s11606-023-08190-8
16. Rural-Urban Commuting Area Codes. Economic Research Service, US Dept of Agriculture. Updated September 25, 2023. Accessed June 4, 2024. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
17. VHA Directive 1056: National Smoking and Tobacco Use Cessation Program. Veterans Health Administration, US Dept of Veterans Affairs; September 5, 2019. Accessed June 4, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8488
18. Smith HB, Ward R, Frazier C, Angotti J, Tanner NT. Guideline-recommended lung cancer screening adherence is superior with a centralized approach. Chest. 2022;161(3):818-825. doi:10.1016/j.chest.2021.09.002
19. Lewis JA, Samuels LR, Denton J, et al. The association of health care system resources with lung cancer screening implementation: a cohort study. Chest. 2022;162(3):701-711. doi:10.1016/j.chest.2022.03.050
20. US Dept of Veterans Affairs. Lung cancer screening: patient education fact sheet. Accessed July 8, 2024. https://www.cancer.va.gov/assets/pdf/survey/LCSflyer.pdf
21. Melzer AC, Golden SE, Ono SS, Datta S, Crothers K, Slatore CG. What exactly is shared decision-making? A qualitative study of shared decision-making in lung cancer screening. J Gen Intern Med. 2020;35(2):546-553. doi:10.1007/s11606-019-05516-3
22. Chelala L, Hossain R, Kazerooni EA, Christensen JD, Dyer DS, White CS. Lung-RADS Version 1.1: challenges and a look ahead, from the AJR special series on radiology reporting and data systems. AJR Am J Roentgenol. 2021;216(6):1411-1422. doi:10.2214/AJR.20.24807
23. Ritzwoller DP, Meza R, Carroll NM, et al. Evaluation of population-level changes associated with the 2021 US Preventive Services Task Force lung cancer screening recommendations in community-based health care systems. JAMA Netw Open. 2021;4(10):e2128176. doi:10.1001/jamanetworkopen.2021.28176
24. Golden SE, Ono SS, Thakurta SG, et al. “I’m putting my trust in their hands”: a qualitative study of patients’ views on clinician initial communication about lung cancer screening. Chest. 2020;158(3):1260-1267. doi:10.1016/j.chest.2020.02.072
25. Park ER, Chiles C, Cinciripini PM, et al. Impact of the COVID-19 pandemic on telehealth research in cancer prevention and care: a call to sustain telehealth advances. Cancer. 2021;127(3):334-338. doi:10.1002/cncr.33227
26. Tremblay A, Taghizadeh N, Huang J, et al. A randomized controlled study of integrated smoking cessation in a lung cancer screening program. J Thorac Oncol. 2019;14(9):1528-1537. doi:10.1016/j.jtho.2019.04.024
27. Neil JM, Marotta C, Gonzalez I, et al. Integrating tobacco treatment into lung cancer screening practices: study protocol for the Screen ASSIST randomized clinical trial. Contemp Clin Trials. 2021;111:106586. doi:10.1016/j.cct.2021.106586
1. National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409. doi:10.1056/NEJMoa1102873
2. State of Lung Cancer: 2023 Report. American Lung Association. November 14, 2023. Accessed June 4, 2024. https://www.lung.org/getmedia/186786b6-18c3-46a9-a7e7-810f3ce4deda/SOLC-2023-Print-Report.pdf
3. Okereke IC, Nishi S, Zhou J, Goodwin JS. Trends in lung cancer screening in the United States, 2016-2017. J Thorac Dis. 2019;11(3):873-881. doi:10.21037/jtd.2019.01.105
4. Petraglia AF, Olazagasti JM, Strong A, Dunn B, Anderson RT, Hanley M. Establishing satellite lung cancer screening sites with telehealth to address disparities between high-risk smokers and American College of Radiology-approved Centers of Designation. J Thorac Imaging. 2021;36(1):2-5. doi:10.1097/RTI.0000000000000520
5. Odahowski CL, Zahnd WE, Eberth JM. Challenges and opportunities for lung cancer screening in rural America. J Am Coll Radiol. 2019;16(4 Pt B):590-595. doi:10.1016/j.jacr.2019.01.001
6. Rohatgi KW, Marx CM, Lewis-Thames MW, Liu J, Colditz GA, James AS. Urban-rural disparities in access to low-dose computed tomography lung cancer screening in Missouri and Illinois. Prev Chronic Dis. 2020;17:E140. doi:10.5888/pcd17.200202
7. Boudreau JH, Miller DR, Qian S, Nunez ER, Caverly TJ, Wiener RS. Access to lung cancer screening in the Veterans Health Administration: does geographic distribution match need in the population? Chest. 2021;160(1):358-367. doi:10.1016/j.chest.2021.02.016
8. Howlader N, Noone AM, Krapcho M, et al, eds. SEER Cancer Statistics Review, 1975-2017. National Cancer Institute, US Dept of Health and Human Services; April 15, 2020. Accessed June 4, 2024. https://seer.cancer.gov/archive/csr/1975_2017/index.html
9. US Preventive Services Task Force, Krist AH, Davidson KW, et al. Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(10):962-970. doi:10.1001/jama.2021.1117
10. Gopal RK, Solanki P, Bokhour BG, et al. Provider, staff, and patient perspectives on medical visits using clinical video telehealth: a foundation for educational initiatives to improve medical care in telehealth. J Nurse Pract. 2021;17(5):582-587. doi:10.1016/j.nurpra.2021.02.020
11. Yacoub JH, Swanson CE, Jay AK, Cooper C, Spies J, Krishnan P. The radiology virtual reading room: during and beyond the COVID-19 pandemic. J Digit Imaging. 2021;34(2):308-319. doi:10.1007/s10278-021-00427-4
12. Beswick DM, Vashi A, Song Y, et al. Consultation via telemedicine and access to operative care for patients with head and neck cancer in a Veterans Health Administration population. Head Neck. 2016;38(6):925-929. doi:10.1002/hed.24386
13. Ruco A, Dossa F, Tinmouth J, et al. Social media and mHealth technology for cancer screening: systematic review and meta-analysis. J Med Internet Res. 2021;23(7):e26759. doi:10.2196/26759
14. Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine - a model to access the subspecialist services in underserved rural areas. Int J Med Inform. 2009;78(1):53-59. doi:10.1016/j.ijmedinf.2008.07.010
15. Chen A, Ayub MH, Mishuris RG, et al. Telehealth policy, practice, and education: a position statement of the Society of General Internal Medicine. J Gen Intern Med. 2023;38(11):2613-2620. doi:10.1007/s11606-023-08190-8
16. Rural-Urban Commuting Area Codes. Economic Research Service, US Dept of Agriculture. Updated September 25, 2023. Accessed June 4, 2024. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
17. VHA Directive 1056: National Smoking and Tobacco Use Cessation Program. Veterans Health Administration, US Dept of Veterans Affairs; September 5, 2019. Accessed June 4, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8488
18. Smith HB, Ward R, Frazier C, Angotti J, Tanner NT. Guideline-recommended lung cancer screening adherence is superior with a centralized approach. Chest. 2022;161(3):818-825. doi:10.1016/j.chest.2021.09.002
19. Lewis JA, Samuels LR, Denton J, et al. The association of health care system resources with lung cancer screening implementation: a cohort study. Chest. 2022;162(3):701-711. doi:10.1016/j.chest.2022.03.050
20. US Dept of Veterans Affairs. Lung cancer screening: patient education fact sheet. Accessed July 8, 2024. https://www.cancer.va.gov/assets/pdf/survey/LCSflyer.pdf
21. Melzer AC, Golden SE, Ono SS, Datta S, Crothers K, Slatore CG. What exactly is shared decision-making? A qualitative study of shared decision-making in lung cancer screening. J Gen Intern Med. 2020;35(2):546-553. doi:10.1007/s11606-019-05516-3
22. Chelala L, Hossain R, Kazerooni EA, Christensen JD, Dyer DS, White CS. Lung-RADS Version 1.1: challenges and a look ahead, from the AJR special series on radiology reporting and data systems. AJR Am J Roentgenol. 2021;216(6):1411-1422. doi:10.2214/AJR.20.24807
23. Ritzwoller DP, Meza R, Carroll NM, et al. Evaluation of population-level changes associated with the 2021 US Preventive Services Task Force lung cancer screening recommendations in community-based health care systems. JAMA Netw Open. 2021;4(10):e2128176. doi:10.1001/jamanetworkopen.2021.28176
24. Golden SE, Ono SS, Thakurta SG, et al. “I’m putting my trust in their hands”: a qualitative study of patients’ views on clinician initial communication about lung cancer screening. Chest. 2020;158(3):1260-1267. doi:10.1016/j.chest.2020.02.072
25. Park ER, Chiles C, Cinciripini PM, et al. Impact of the COVID-19 pandemic on telehealth research in cancer prevention and care: a call to sustain telehealth advances. Cancer. 2021;127(3):334-338. doi:10.1002/cncr.33227
26. Tremblay A, Taghizadeh N, Huang J, et al. A randomized controlled study of integrated smoking cessation in a lung cancer screening program. J Thorac Oncol. 2019;14(9):1528-1537. doi:10.1016/j.jtho.2019.04.024
27. Neil JM, Marotta C, Gonzalez I, et al. Integrating tobacco treatment into lung cancer screening practices: study protocol for the Screen ASSIST randomized clinical trial. Contemp Clin Trials. 2021;111:106586. doi:10.1016/j.cct.2021.106586
Are Beta-Blockers Safe for COPD?
Everyone takes a pharmacology class in medical school that includes a lecture on beta receptors. They’re in the heart (beta-1) and lungs (beta-2), and drug compounds agonize or antagonize one or both. The professor will caution against using antagonists (beta blockade) for patients with chronic obstructive pulmonary disease (COPD) lest they further impair the patient’s irreversibly narrowed airways. Obsequious students mature into obsequious doctors, intent on “doing no harm.” For better or worse, you withhold beta-blockers from your patient with COPD and comorbid cardiac disease.
Perhaps because the pulmonologist isn’t usually the one who decides whether a beta-blocker is prescribed, I’ve been napping on this topic since training. Early in fellowship, I read an ACP Journal Club article about a Cochrane systematic review (yes, I read a review of a review) that concluded that beta-blockers are fine in patients with COPD. The summary appealed to my bias towards evidence-based medicine (EBM) supplanting physiology, medical school, and everything else. I was more apt to believe my stodgy residency attendings than the stodgy pharmacology professor. Even though COPD and cardiovascular disease share multiple risk factors, I had never reinvestigated the relationship between beta-blockers and COPD.
Turns out that while I was sleeping, the debate continued. Go figure. Just last month a prospective, observational study published in JAMA Network Open found that beta-blockers did not increase the risk for cardiovascular or respiratory events among patients with COPD being discharged after hospitalization for acute myocardial infarction. Although this could be viewed as a triumph for EBM over physiology and a validation of my decade-plus of intellectual laziness, the results are actually pretty thin. These studies, in which patients with an indication for a therapy (a beta-blocker in this case) are analyzed by whether or not they received it, are problematic. The fanciest statistics — in this case, they used propensity scores — can’t control for residual confounding. What drove the physicians to prescribe in some cases but not others? We can only guess.
This might be okay if there hadn’t been a randomized controlled trial (RCT) published in 2019 in The New England Journal of Medicine that found that beta-blockers increase the risk for severe COPD exacerbations. In EBM, the RCT trumps all. Ironically, this trial was designed to test whether beta-blockers reduce severe COPD exacerbations. Yes, we’d come full circle. There was enough biologic plausibility to support a positive effect, or so thought the study authors and the Department of Defense (DOD) — for reasons I can’t possibly guess, the DOD funded this RCT. My pharmacology professor must be rolling over in his tenure.
The RCT did leave beta-blockers some wiggle room. The authors purposely excluded anyone with a cardiovascular indication for a beta-blocker. The intent was to ensure beneficial effects were isolated to respiratory and not cardiovascular outcomes. Of course, the reason I’m writing and you’re reading this is that COPD and cardiovascular disease co-occur at a high rate. The RCT notwithstanding, we prescribe beta-blockers to patients with COPD because they have a cardiac indication, not to reduce acute COPD exacerbations. So, it’s possible there’d be a net beta-blocker benefit in patients with COPD and comorbid heart disease.
That’s where the JAMA Network Open study comes in, but as discussed, methodologic weaknesses preclude its being the final word. That said, I think it’s unlikely we’ll see a COPD with comorbid cardiac disease RCT performed to assess whether beta-blockers provide a net benefit, unless maybe the DOD wants to fund another one of these. In the meantime, I’m calling clinical equipoise and punting. Fortunately for me, I don’t have to prescribe beta-blockers.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
Everyone takes a pharmacology class in medical school that includes a lecture on beta receptors. They’re in the heart (beta-1) and lungs (beta-2), and drug compounds agonize or antagonize one or both. The professor will caution against using antagonists (beta blockade) for patients with chronic obstructive pulmonary disease (COPD) lest they further impair the patient’s irreversibly narrowed airways. Obsequious students mature into obsequious doctors, intent on “doing no harm.” For better or worse, you withhold beta-blockers from your patient with COPD and comorbid cardiac disease.
Perhaps because the pulmonologist isn’t usually the one who decides whether a beta-blocker is prescribed, I’ve been napping on this topic since training. Early in fellowship, I read an ACP Journal Club article about a Cochrane systematic review (yes, I read a review of a review) that concluded that beta-blockers are fine in patients with COPD. The summary appealed to my bias towards evidence-based medicine (EBM) supplanting physiology, medical school, and everything else. I was more apt to believe my stodgy residency attendings than the stodgy pharmacology professor. Even though COPD and cardiovascular disease share multiple risk factors, I had never reinvestigated the relationship between beta-blockers and COPD.
Turns out that while I was sleeping, the debate continued. Go figure. Just last month a prospective, observational study published in JAMA Network Open found that beta-blockers did not increase the risk for cardiovascular or respiratory events among patients with COPD being discharged after hospitalization for acute myocardial infarction. Although this could be viewed as a triumph for EBM over physiology and a validation of my decade-plus of intellectual laziness, the results are actually pretty thin. These studies, in which patients with an indication for a therapy (a beta-blocker in this case) are analyzed by whether or not they received it, are problematic. The fanciest statistics — in this case, they used propensity scores — can’t control for residual confounding. What drove the physicians to prescribe in some cases but not others? We can only guess.
This might be okay if there hadn’t been a randomized controlled trial (RCT) published in 2019 in The New England Journal of Medicine that found that beta-blockers increase the risk for severe COPD exacerbations. In EBM, the RCT trumps all. Ironically, this trial was designed to test whether beta-blockers reduce severe COPD exacerbations. Yes, we’d come full circle. There was enough biologic plausibility to support a positive effect, or so thought the study authors and the Department of Defense (DOD) — for reasons I can’t possibly guess, the DOD funded this RCT. My pharmacology professor must be rolling over in his tenure.
The RCT did leave beta-blockers some wiggle room. The authors purposely excluded anyone with a cardiovascular indication for a beta-blocker. The intent was to ensure beneficial effects were isolated to respiratory and not cardiovascular outcomes. Of course, the reason I’m writing and you’re reading this is that COPD and cardiovascular disease co-occur at a high rate. The RCT notwithstanding, we prescribe beta-blockers to patients with COPD because they have a cardiac indication, not to reduce acute COPD exacerbations. So, it’s possible there’d be a net beta-blocker benefit in patients with COPD and comorbid heart disease.
That’s where the JAMA Network Open study comes in, but as discussed, methodologic weaknesses preclude its being the final word. That said, I think it’s unlikely we’ll see a COPD with comorbid cardiac disease RCT performed to assess whether beta-blockers provide a net benefit, unless maybe the DOD wants to fund another one of these. In the meantime, I’m calling clinical equipoise and punting. Fortunately for me, I don’t have to prescribe beta-blockers.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
Everyone takes a pharmacology class in medical school that includes a lecture on beta receptors. They’re in the heart (beta-1) and lungs (beta-2), and drug compounds agonize or antagonize one or both. The professor will caution against using antagonists (beta blockade) for patients with chronic obstructive pulmonary disease (COPD) lest they further impair the patient’s irreversibly narrowed airways. Obsequious students mature into obsequious doctors, intent on “doing no harm.” For better or worse, you withhold beta-blockers from your patient with COPD and comorbid cardiac disease.
Perhaps because the pulmonologist isn’t usually the one who decides whether a beta-blocker is prescribed, I’ve been napping on this topic since training. Early in fellowship, I read an ACP Journal Club article about a Cochrane systematic review (yes, I read a review of a review) that concluded that beta-blockers are fine in patients with COPD. The summary appealed to my bias towards evidence-based medicine (EBM) supplanting physiology, medical school, and everything else. I was more apt to believe my stodgy residency attendings than the stodgy pharmacology professor. Even though COPD and cardiovascular disease share multiple risk factors, I had never reinvestigated the relationship between beta-blockers and COPD.
Turns out that while I was sleeping, the debate continued. Go figure. Just last month a prospective, observational study published in JAMA Network Open found that beta-blockers did not increase the risk for cardiovascular or respiratory events among patients with COPD being discharged after hospitalization for acute myocardial infarction. Although this could be viewed as a triumph for EBM over physiology and a validation of my decade-plus of intellectual laziness, the results are actually pretty thin. These studies, in which patients with an indication for a therapy (a beta-blocker in this case) are analyzed by whether or not they received it, are problematic. The fanciest statistics — in this case, they used propensity scores — can’t control for residual confounding. What drove the physicians to prescribe in some cases but not others? We can only guess.
This might be okay if there hadn’t been a randomized controlled trial (RCT) published in 2019 in The New England Journal of Medicine that found that beta-blockers increase the risk for severe COPD exacerbations. In EBM, the RCT trumps all. Ironically, this trial was designed to test whether beta-blockers reduce severe COPD exacerbations. Yes, we’d come full circle. There was enough biologic plausibility to support a positive effect, or so thought the study authors and the Department of Defense (DOD) — for reasons I can’t possibly guess, the DOD funded this RCT. My pharmacology professor must be rolling over in his tenure.
The RCT did leave beta-blockers some wiggle room. The authors purposely excluded anyone with a cardiovascular indication for a beta-blocker. The intent was to ensure beneficial effects were isolated to respiratory and not cardiovascular outcomes. Of course, the reason I’m writing and you’re reading this is that COPD and cardiovascular disease co-occur at a high rate. The RCT notwithstanding, we prescribe beta-blockers to patients with COPD because they have a cardiac indication, not to reduce acute COPD exacerbations. So, it’s possible there’d be a net beta-blocker benefit in patients with COPD and comorbid heart disease.
That’s where the JAMA Network Open study comes in, but as discussed, methodologic weaknesses preclude its being the final word. That said, I think it’s unlikely we’ll see a COPD with comorbid cardiac disease RCT performed to assess whether beta-blockers provide a net benefit, unless maybe the DOD wants to fund another one of these. In the meantime, I’m calling clinical equipoise and punting. Fortunately for me, I don’t have to prescribe beta-blockers.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
More Illnesses Possible Related Linked to Counterfeit Botulinum Toxin Reported
— two in the intensive care unit. None of the cases required intubation, according to an announcement of an investigation into these reports in by the Centers for Disease Control and Prevention (CDC).
The report, published online in the Morbidity and Mortality Weekly Report, notes that the four patients in Tennessee received counterfeit BoNT, while product information was not available for the three cases in New York City. “However, one person reported paying less than US wholesale acquisition cost for the administered product, and another reported that the product had been purchased overseas,” the authors of the report wrote. The development underscores that BoNT injections “should be administered only by licensed and trained providers using recommended doses of FDA [Food and Drug Admininstration]-approved products.”
This report follows a CDC advisory published in April 2024 of at least 22 people from 11 states who reported serious reactions after receiving botulinum toxin injections from unlicensed or untrained individuals or in nonhealthcare settings, such as homes and spas.
The median age of the women in the July report was 48 years, and signs and symptoms included ptosis, dry mouth, dysphagia, shortness of breath, and weakness. Onset occurred between February 23 and March 7, 2024.
“This investigation did not determine why these illnesses occurred after cosmetic BoNT injections; potential reasons might include use of counterfeit BoNT, which might be more potent or contain harmful additional ingredients or higher susceptibility to BoNT effects among some persons,” the investigators wrote. They recommended further studies to describe the clinical spectrum of cosmetic BoNT injection effects such as severity of signs and symptoms.
For cases of suspected systemic botulism, the CDC recommends calling the local or state health department for consultation and antitoxin release (as well as information on reporting adverse events). Alternatively, the 24/7 phone number for the CDC clinical botulism service is 770-488-7100.
A version of this article first appeared on Medscape.com.
— two in the intensive care unit. None of the cases required intubation, according to an announcement of an investigation into these reports in by the Centers for Disease Control and Prevention (CDC).
The report, published online in the Morbidity and Mortality Weekly Report, notes that the four patients in Tennessee received counterfeit BoNT, while product information was not available for the three cases in New York City. “However, one person reported paying less than US wholesale acquisition cost for the administered product, and another reported that the product had been purchased overseas,” the authors of the report wrote. The development underscores that BoNT injections “should be administered only by licensed and trained providers using recommended doses of FDA [Food and Drug Admininstration]-approved products.”
This report follows a CDC advisory published in April 2024 of at least 22 people from 11 states who reported serious reactions after receiving botulinum toxin injections from unlicensed or untrained individuals or in nonhealthcare settings, such as homes and spas.
The median age of the women in the July report was 48 years, and signs and symptoms included ptosis, dry mouth, dysphagia, shortness of breath, and weakness. Onset occurred between February 23 and March 7, 2024.
“This investigation did not determine why these illnesses occurred after cosmetic BoNT injections; potential reasons might include use of counterfeit BoNT, which might be more potent or contain harmful additional ingredients or higher susceptibility to BoNT effects among some persons,” the investigators wrote. They recommended further studies to describe the clinical spectrum of cosmetic BoNT injection effects such as severity of signs and symptoms.
For cases of suspected systemic botulism, the CDC recommends calling the local or state health department for consultation and antitoxin release (as well as information on reporting adverse events). Alternatively, the 24/7 phone number for the CDC clinical botulism service is 770-488-7100.
A version of this article first appeared on Medscape.com.
— two in the intensive care unit. None of the cases required intubation, according to an announcement of an investigation into these reports in by the Centers for Disease Control and Prevention (CDC).
The report, published online in the Morbidity and Mortality Weekly Report, notes that the four patients in Tennessee received counterfeit BoNT, while product information was not available for the three cases in New York City. “However, one person reported paying less than US wholesale acquisition cost for the administered product, and another reported that the product had been purchased overseas,” the authors of the report wrote. The development underscores that BoNT injections “should be administered only by licensed and trained providers using recommended doses of FDA [Food and Drug Admininstration]-approved products.”
This report follows a CDC advisory published in April 2024 of at least 22 people from 11 states who reported serious reactions after receiving botulinum toxin injections from unlicensed or untrained individuals or in nonhealthcare settings, such as homes and spas.
The median age of the women in the July report was 48 years, and signs and symptoms included ptosis, dry mouth, dysphagia, shortness of breath, and weakness. Onset occurred between February 23 and March 7, 2024.
“This investigation did not determine why these illnesses occurred after cosmetic BoNT injections; potential reasons might include use of counterfeit BoNT, which might be more potent or contain harmful additional ingredients or higher susceptibility to BoNT effects among some persons,” the investigators wrote. They recommended further studies to describe the clinical spectrum of cosmetic BoNT injection effects such as severity of signs and symptoms.
For cases of suspected systemic botulism, the CDC recommends calling the local or state health department for consultation and antitoxin release (as well as information on reporting adverse events). Alternatively, the 24/7 phone number for the CDC clinical botulism service is 770-488-7100.
A version of this article first appeared on Medscape.com.
FROM THE MMWR
Cost of Drugs Can Be Breathtaking for COPD Patients
For patients with chronic obstructive pulmonary disease (COPD), the Global Initiative on Obstructive Lung Disease recommends long-term term pharmacologic and nonpharmacologic therapies based on each patient’s symptoms and disease severity.
Yet even the most effective drugs work only when patients take them as directed, and according to the World Health Organization, fewer than half of all patients worldwide are fully compliant with long-term COPD drug regimens.
And as a recent cross-sectional study showed, nearly one in six patients in the United States reported missing a COPD drug dose, lowering the dose, or delaying filling a prescription for financial reasons.
“I care for patients with COPD as their pulmonologist, and this is a very common problem that we see in clinical practice,” said Meredith McCormack, MD, a pulmonary and critical care medicine physician and associate director of the Pulmonary & Critical Care Medicine Division at Johns Hopkins University in Baltimore.
Dr. McCormack, a national spokesperson for The American Lung Association, said that she shows new patients the photos of all available inhalers and asks which ones they have and how they take them.
“I would say that a majority of the time people are taking their medicines slightly differently than prescribed, and often, this is due to cost,” she said.
Serious Consequences
Cost-related medication nonadherence (CRN), as investigators term it, can have major health effects and can be significantly more costly in the long run due to increased hospitalization rates, higher morbidity, and greater risk for COPD-related death associated with suboptimal care.
“For some patients even a month or two of being off medications increases the risk of having exacerbations, having more symptoms, [and] having a decline in their lung function,” said Douglas M. Beach, MD, a pulmonologist at Beth Israel Deaconess Medical Center in Boston.
In the aforementioned cross-sectional study, published in the open access journal BMC Public Health, Xin Wen, MD, from the Jiamusi (China) University School of Public Health, and colleagues looked at data on a representative sample of US adults who participated in the US National Health Interview Survey from 2013 through 2020.
The sample included 15,928 persons aged 18 years or older with a self-reported history of COPD who completed a CRN survey including the following questions:
During the past 12 months, have you
- Skipped medication doses to save money?
- Taken less medicine than prescribed to save money?
- Delayed filling a prescription to save money?
The investigators found that a weighted 18.56% of participants representing 2.39 million persons with COPD answered “yes” to one of the questions.
Translated into representative population numbers, that works out to an estimated 1.61 million persons with COPD missing doses, 1.72 million taking lower doses than those prescribed, and 2.03 million delaying filling prescriptions to save money.
A multivariable logistic regression analysis showed that those who were most likely to be nonadherent for financial reasons were patients younger than 65 years, women, persons with low family income, those who lacked health insurance, and patients with multiple comorbidities, the authors found.
Financial Barriers
One of the biggest barriers to COPD medication adherence is, somewhat paradoxically, insurance status, particularly Medicare, said Corinne Young, MSN, FNP-C, FCCP, from Colorado Springs Pulmonary Consultants.
“What’s so unfair about Medicare is that patients have to buy a drug plan, so they have to already pay for an extra plan to have access to drugs, and the plans vary because there are so many choices,” she said in an interview.
Elderly patients may be confused about the available options and may choose the Medicare Advantage plan with the lowest monthly premiums, which have the highest annual deductibles, usually in the $5000-and-up range, she said.
In addition, the Medicare Part D prescription coverage gap, commonly known as the “donut hole,” requires patients to pay a percentage of drug costs above a certain limit ($5030 in 2024) until a yearly out-of-pocket limit (currently $8000) is reached, after which the plan will again pick up most of the costs.
Although makers of inhalers have voluntarily agreed to limit monthly co-pays to $35 for uninsured patients, Medicare plans require insured patients to shell out considerably more, with 30 days of Trelegy Ellipta (fluticasone furoate, umeclidinium, and vilanterol) setting patients back nearly $350 per month, according to a recent search of costs for a United Healthcare Medicare Advantage plan.
Chasing Lower-Cost Options
“I have a lot of patients who use Canadian pharmacies to try to get around it, and I have a lot of patients who make a trip to Mexico every year and load up. I have patients who don’t take their inhalers as they are supposed to in order to make them last longer, and I have patients who take the inhalers of other family members,” Ms. Young said.
Humayun Anjum, MD, FCCP, from Dallas Pulmonary and Critical Care in Dallas, Texas, said in an interview that when patients claim that a prescribed drug isn’t working as expected for them, financial pressures may be partly to blame.
“When you investigate a little bit more, that’s where things become a bit more clear, and the patient may say ‘yeah, I stopped using this inhaler because it was costing me 200 bucks a month and I’m already on other medications,’ ” he said.
He noted that, when possible, he will steer patients toward discount prescription services such as GoodRx, which offers discounts at local pharmacies, or Mark Cuban Cost Plus Drugs, an online pharmacy that offers generic versions of Advair Diskus (fluticasone propionate/salmeterol) at a 100-50 mcg dose for $94.70, a savings of $307.30 over retail pharmacies, according to the company’s website.
Dr. Beach noted that Beth Israel Deaconess has a pharmacist embedded in the pulmonary clinic who can help eligible patients get financial assistance to pay for their medications.
“The influencing factors of CRN are multifaceted and necessitating more rigorous research. Health policy interventions focusing on reducing drug costs, delaying disease progression, preventing exacerbations, and reducing the risk of comorbidities may improve the economic burden of COPD and its outcomes,” Dr. Wen and colleagues wrote.
The study by Dr. Wen and colleagues was funded by grants from Chinese national and academic sources. Dr. McCormack has served as a consultant to Aridis, Boehringer Ingelheim, GlaxoSmithKline, MCG Diagnostics, ndd Medical Technologies, and UpToDate. Ms. Young, Dr. Anjum, and Dr. Beach reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
For patients with chronic obstructive pulmonary disease (COPD), the Global Initiative on Obstructive Lung Disease recommends long-term term pharmacologic and nonpharmacologic therapies based on each patient’s symptoms and disease severity.
Yet even the most effective drugs work only when patients take them as directed, and according to the World Health Organization, fewer than half of all patients worldwide are fully compliant with long-term COPD drug regimens.
And as a recent cross-sectional study showed, nearly one in six patients in the United States reported missing a COPD drug dose, lowering the dose, or delaying filling a prescription for financial reasons.
“I care for patients with COPD as their pulmonologist, and this is a very common problem that we see in clinical practice,” said Meredith McCormack, MD, a pulmonary and critical care medicine physician and associate director of the Pulmonary & Critical Care Medicine Division at Johns Hopkins University in Baltimore.
Dr. McCormack, a national spokesperson for The American Lung Association, said that she shows new patients the photos of all available inhalers and asks which ones they have and how they take them.
“I would say that a majority of the time people are taking their medicines slightly differently than prescribed, and often, this is due to cost,” she said.
Serious Consequences
Cost-related medication nonadherence (CRN), as investigators term it, can have major health effects and can be significantly more costly in the long run due to increased hospitalization rates, higher morbidity, and greater risk for COPD-related death associated with suboptimal care.
“For some patients even a month or two of being off medications increases the risk of having exacerbations, having more symptoms, [and] having a decline in their lung function,” said Douglas M. Beach, MD, a pulmonologist at Beth Israel Deaconess Medical Center in Boston.
In the aforementioned cross-sectional study, published in the open access journal BMC Public Health, Xin Wen, MD, from the Jiamusi (China) University School of Public Health, and colleagues looked at data on a representative sample of US adults who participated in the US National Health Interview Survey from 2013 through 2020.
The sample included 15,928 persons aged 18 years or older with a self-reported history of COPD who completed a CRN survey including the following questions:
During the past 12 months, have you
- Skipped medication doses to save money?
- Taken less medicine than prescribed to save money?
- Delayed filling a prescription to save money?
The investigators found that a weighted 18.56% of participants representing 2.39 million persons with COPD answered “yes” to one of the questions.
Translated into representative population numbers, that works out to an estimated 1.61 million persons with COPD missing doses, 1.72 million taking lower doses than those prescribed, and 2.03 million delaying filling prescriptions to save money.
A multivariable logistic regression analysis showed that those who were most likely to be nonadherent for financial reasons were patients younger than 65 years, women, persons with low family income, those who lacked health insurance, and patients with multiple comorbidities, the authors found.
Financial Barriers
One of the biggest barriers to COPD medication adherence is, somewhat paradoxically, insurance status, particularly Medicare, said Corinne Young, MSN, FNP-C, FCCP, from Colorado Springs Pulmonary Consultants.
“What’s so unfair about Medicare is that patients have to buy a drug plan, so they have to already pay for an extra plan to have access to drugs, and the plans vary because there are so many choices,” she said in an interview.
Elderly patients may be confused about the available options and may choose the Medicare Advantage plan with the lowest monthly premiums, which have the highest annual deductibles, usually in the $5000-and-up range, she said.
In addition, the Medicare Part D prescription coverage gap, commonly known as the “donut hole,” requires patients to pay a percentage of drug costs above a certain limit ($5030 in 2024) until a yearly out-of-pocket limit (currently $8000) is reached, after which the plan will again pick up most of the costs.
Although makers of inhalers have voluntarily agreed to limit monthly co-pays to $35 for uninsured patients, Medicare plans require insured patients to shell out considerably more, with 30 days of Trelegy Ellipta (fluticasone furoate, umeclidinium, and vilanterol) setting patients back nearly $350 per month, according to a recent search of costs for a United Healthcare Medicare Advantage plan.
Chasing Lower-Cost Options
“I have a lot of patients who use Canadian pharmacies to try to get around it, and I have a lot of patients who make a trip to Mexico every year and load up. I have patients who don’t take their inhalers as they are supposed to in order to make them last longer, and I have patients who take the inhalers of other family members,” Ms. Young said.
Humayun Anjum, MD, FCCP, from Dallas Pulmonary and Critical Care in Dallas, Texas, said in an interview that when patients claim that a prescribed drug isn’t working as expected for them, financial pressures may be partly to blame.
“When you investigate a little bit more, that’s where things become a bit more clear, and the patient may say ‘yeah, I stopped using this inhaler because it was costing me 200 bucks a month and I’m already on other medications,’ ” he said.
He noted that, when possible, he will steer patients toward discount prescription services such as GoodRx, which offers discounts at local pharmacies, or Mark Cuban Cost Plus Drugs, an online pharmacy that offers generic versions of Advair Diskus (fluticasone propionate/salmeterol) at a 100-50 mcg dose for $94.70, a savings of $307.30 over retail pharmacies, according to the company’s website.
Dr. Beach noted that Beth Israel Deaconess has a pharmacist embedded in the pulmonary clinic who can help eligible patients get financial assistance to pay for their medications.
“The influencing factors of CRN are multifaceted and necessitating more rigorous research. Health policy interventions focusing on reducing drug costs, delaying disease progression, preventing exacerbations, and reducing the risk of comorbidities may improve the economic burden of COPD and its outcomes,” Dr. Wen and colleagues wrote.
The study by Dr. Wen and colleagues was funded by grants from Chinese national and academic sources. Dr. McCormack has served as a consultant to Aridis, Boehringer Ingelheim, GlaxoSmithKline, MCG Diagnostics, ndd Medical Technologies, and UpToDate. Ms. Young, Dr. Anjum, and Dr. Beach reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
For patients with chronic obstructive pulmonary disease (COPD), the Global Initiative on Obstructive Lung Disease recommends long-term term pharmacologic and nonpharmacologic therapies based on each patient’s symptoms and disease severity.
Yet even the most effective drugs work only when patients take them as directed, and according to the World Health Organization, fewer than half of all patients worldwide are fully compliant with long-term COPD drug regimens.
And as a recent cross-sectional study showed, nearly one in six patients in the United States reported missing a COPD drug dose, lowering the dose, or delaying filling a prescription for financial reasons.
“I care for patients with COPD as their pulmonologist, and this is a very common problem that we see in clinical practice,” said Meredith McCormack, MD, a pulmonary and critical care medicine physician and associate director of the Pulmonary & Critical Care Medicine Division at Johns Hopkins University in Baltimore.
Dr. McCormack, a national spokesperson for The American Lung Association, said that she shows new patients the photos of all available inhalers and asks which ones they have and how they take them.
“I would say that a majority of the time people are taking their medicines slightly differently than prescribed, and often, this is due to cost,” she said.
Serious Consequences
Cost-related medication nonadherence (CRN), as investigators term it, can have major health effects and can be significantly more costly in the long run due to increased hospitalization rates, higher morbidity, and greater risk for COPD-related death associated with suboptimal care.
“For some patients even a month or two of being off medications increases the risk of having exacerbations, having more symptoms, [and] having a decline in their lung function,” said Douglas M. Beach, MD, a pulmonologist at Beth Israel Deaconess Medical Center in Boston.
In the aforementioned cross-sectional study, published in the open access journal BMC Public Health, Xin Wen, MD, from the Jiamusi (China) University School of Public Health, and colleagues looked at data on a representative sample of US adults who participated in the US National Health Interview Survey from 2013 through 2020.
The sample included 15,928 persons aged 18 years or older with a self-reported history of COPD who completed a CRN survey including the following questions:
During the past 12 months, have you
- Skipped medication doses to save money?
- Taken less medicine than prescribed to save money?
- Delayed filling a prescription to save money?
The investigators found that a weighted 18.56% of participants representing 2.39 million persons with COPD answered “yes” to one of the questions.
Translated into representative population numbers, that works out to an estimated 1.61 million persons with COPD missing doses, 1.72 million taking lower doses than those prescribed, and 2.03 million delaying filling prescriptions to save money.
A multivariable logistic regression analysis showed that those who were most likely to be nonadherent for financial reasons were patients younger than 65 years, women, persons with low family income, those who lacked health insurance, and patients with multiple comorbidities, the authors found.
Financial Barriers
One of the biggest barriers to COPD medication adherence is, somewhat paradoxically, insurance status, particularly Medicare, said Corinne Young, MSN, FNP-C, FCCP, from Colorado Springs Pulmonary Consultants.
“What’s so unfair about Medicare is that patients have to buy a drug plan, so they have to already pay for an extra plan to have access to drugs, and the plans vary because there are so many choices,” she said in an interview.
Elderly patients may be confused about the available options and may choose the Medicare Advantage plan with the lowest monthly premiums, which have the highest annual deductibles, usually in the $5000-and-up range, she said.
In addition, the Medicare Part D prescription coverage gap, commonly known as the “donut hole,” requires patients to pay a percentage of drug costs above a certain limit ($5030 in 2024) until a yearly out-of-pocket limit (currently $8000) is reached, after which the plan will again pick up most of the costs.
Although makers of inhalers have voluntarily agreed to limit monthly co-pays to $35 for uninsured patients, Medicare plans require insured patients to shell out considerably more, with 30 days of Trelegy Ellipta (fluticasone furoate, umeclidinium, and vilanterol) setting patients back nearly $350 per month, according to a recent search of costs for a United Healthcare Medicare Advantage plan.
Chasing Lower-Cost Options
“I have a lot of patients who use Canadian pharmacies to try to get around it, and I have a lot of patients who make a trip to Mexico every year and load up. I have patients who don’t take their inhalers as they are supposed to in order to make them last longer, and I have patients who take the inhalers of other family members,” Ms. Young said.
Humayun Anjum, MD, FCCP, from Dallas Pulmonary and Critical Care in Dallas, Texas, said in an interview that when patients claim that a prescribed drug isn’t working as expected for them, financial pressures may be partly to blame.
“When you investigate a little bit more, that’s where things become a bit more clear, and the patient may say ‘yeah, I stopped using this inhaler because it was costing me 200 bucks a month and I’m already on other medications,’ ” he said.
He noted that, when possible, he will steer patients toward discount prescription services such as GoodRx, which offers discounts at local pharmacies, or Mark Cuban Cost Plus Drugs, an online pharmacy that offers generic versions of Advair Diskus (fluticasone propionate/salmeterol) at a 100-50 mcg dose for $94.70, a savings of $307.30 over retail pharmacies, according to the company’s website.
Dr. Beach noted that Beth Israel Deaconess has a pharmacist embedded in the pulmonary clinic who can help eligible patients get financial assistance to pay for their medications.
“The influencing factors of CRN are multifaceted and necessitating more rigorous research. Health policy interventions focusing on reducing drug costs, delaying disease progression, preventing exacerbations, and reducing the risk of comorbidities may improve the economic burden of COPD and its outcomes,” Dr. Wen and colleagues wrote.
The study by Dr. Wen and colleagues was funded by grants from Chinese national and academic sources. Dr. McCormack has served as a consultant to Aridis, Boehringer Ingelheim, GlaxoSmithKline, MCG Diagnostics, ndd Medical Technologies, and UpToDate. Ms. Young, Dr. Anjum, and Dr. Beach reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Measuring Restrictive Lung Disease Severity Using FEV1 vs TLC
Respiratory diseases have varied clinical presentations and are classified as restrictive, obstructive, mixed, or normal. Restrictive lung diseases have reduced lung volumes, either due to an alteration in lung parenchyma or a disease of the pleura, chest wall, or neuromuscular apparatus. If caused by parenchymal lung disease, restrictive lung disorders are accompanied by reduced gas transfer, which may be portrayed clinically by desaturation after exercise. Based on anatomical structures, the causes of lung volume reduction may be intrinsic or extrinsic. Intrinsic causes correspond to diseases of the lung parenchyma, such as idiopathic fibrotic diseases, connective-tissue diseases, drug-induced lung diseases, and other primary diseases of the lungs. Extrinsic causes refer to disorders outside the lungs or extra-pulmonary diseases such as neuromuscular and nonmuscular diseases of the chest wall.1 For example, obesity and myasthenia gravis can cause restrictive lung diseases, one through mechanical interference of lung expansion and the other through neuromuscular impedance of thoracic cage expansion. All these diseases eventually result in lung restriction, impaired lung function, and respiratory failure. This heterogenicity of disease makes establishing a single severity criterion difficult.
Laboratory testing, imaging studies, and examinations are important for determining the pulmonary disease and its course and progression. The pulmonary function test (PFT), which consists of multiple procedures that are performed depending on the information needed, has been an essential tool in practice for the pulmonologist. The PFT includes spirometry, lung volume measurement, respiratory muscle strength, diffusion capacity, and a broncho-provocation test. Each test has a particular role in assisting the diagnosis and/or follow-up of the patient. Spirometry is frequently used due to its range of dynamic physiological parameters, ease of use, and accessibility. It is used for the diagnosis of pulmonary symptoms, in the assessment of disability, and preoperatory evaluation, including lung resection surgery, assisting in the diagnosis, monitoring, and therapy response of pulmonary diseases.
A systematic approach to PFT interpretation is recommended by several societies, such as the American Thoracic Society (ATS) and the European Respiratory Society (ERS).2 The pulmonary function test results must be reproducible and meet established standards to ensure reliable and consistent clinical outcomes. A restrictive respiratory disease is defined by a decrease in total lung capacity (TLC) (< 5% of predicted value) and a normal forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio.2 Although other findings—such as a decrease in vital capacity—should prompt an investigation into whether the patient has a possible restrictive respiratory disease, the sole presence of this parameter is not definitive or diagnostic of a restrictive impairment.2-4 The assessment of severity is typically determined by TLC. Unfortunately, the severity of a restrictive respiratory disease and the degree of patient discomfort do not always correlate when utilizing just TLC. Pulmonary sarcoidosis, for example, is a granulomatous lung disease with a restrictive PFT pattern and a disease burden that may vary over time. Having a more consistent method of grading the severity of the restrictive lung disease may help guide treatment. The modified Medical Research Council (mMRC) scale, a 5-point dyspnea scale, is widely used in assessing the severity of dyspnea in various respiratory conditions, including chronic obstructive pulmonary disease (COPD), where its scores have been associated with patient mortality.1,5 The goal of this study was to document the associations between objective parameters obtained through PFT and other variables, with an established measurement of dyspnea to assess the severity grade of restrictive lung diseases.
Methods
This retrospective record review at the Veterans Affairs Caribbean Healthcare System (VACHS) in San Juan, Puerto Rico, wasconducted using the Veterans Health Information Systems and Technology Architecture to identify patients with a PFT, including spirometry, that indicated a restrictive ventilator pattern based on the current ATS/ERS Task Force on Lung Function Testing.2 Patients were included if they were aged ≥ 21 years, PFT with TLC ≤ 80% predicted, mMRC score documented on PFT, and documented diffusing capacity of the lung for carbon monoxide (DLCO). Patients were excluded if their FEV1/vital capacity (VC) was < 70% predicted using the largest VC, or no mMRC score was available. All patients meeting the inclusion criteria were considered regardless of comorbidities.
The PFT results of all adult patients, including those performed between June 1, 2013, and January 6, 2016, were submitted to spirometry, and lung volume measurements were analyzed. Sociodemographic information was collected, including sex, ethnicity, age, height, weight, and basal metabolic index. Other data found in PFTs, such as smoking status, smoking in packs/year, mMRC score, predicted TLC value, imaging present (chest X-ray, computed tomography), and hospitalizations and exacerbations within 1 year were collected. In addition, we examined the predicted values for FEV1, DLCO, and DLCO/VA (calculated using the Ayer equation), FVC (calculated using the Knudson equation), expiratory reserve volume, inspiratory VC, and slow VC. PaO2, PaCO2, and Alveolar-arterial gradients also were collected.6-9 Information about heart failure status was gathered through medical evaluation of notes and cardiac studies. All categorical variables were correlated with Spearman analysis and quantitative variables with average percentages. P values were calculated with analysis of variance.
Results
Of 6461 VACHS patient records reviewed, 415 met the inclusion criteria. Patients were divided according to their mMRC score: 65 had mMRC score of 0, 87 had an mMRC score of 1, 2 had an mMRC score of 2, 146 had an mMRC of 3, and 115 had an mMRC score of 4. The population was primarily male (98.6%) and of Hispanic ethnicity (96.4%), with a mean age of 72 years (Table 1). Most patients (n = 269, 64.0%) were prior smokers, while 135 patients (32.5%) had never smoked, and 11 (2.7%) were current smokers. At baseline, 169 patients (41.4%) had interstitial lung disease, 39 (9.6%) had chest wall disorders, 29 (7.1%) had occupational exposure, 25 (6.1%) had pneumonitis, and 14 (3.4%) had neuromuscular disorders.
There was a statistically significant relationship between mMRC score and hospitalization and FEV1 but not TLC (Table 2). As mMRC increased, so did hospitalizations: a total of 168 patients (40.5%) were hospitalized; 24 patients (36.9%) had an mMRC score of 0, 30 patients (34.0%) had an mMRC score of 1, 2 patients (100%) had an mMRC score of 2, 54 patients (37.0%) had an mMRC score of 3, and 58 patients (50.0%) had an mMRC score of 4 (P = .04). Mean (SD) TLC values increased as mMRC scores increased. Mean (SD) TLC was 70.5% (33.0) for the entire population; 68.8% (7.2) for patients with an mMRC score of 0, 70.8% (5.8) for patients with an mMRC score of 1, 75.0% (1.4) for patients with an mMRC score of 2, 70.1% (7.2) for patients with an mMRC score of 3, and 71.5% (62.1) for patients with an mMRC score of 4 (P = .10) (Figure 1). There was an associated decrease in mean (SD) FEV1 with mMRC. Mean (SD) FEV1 was 76.2% (18.9) for the entire population; 81.7% (19.3) for patients with an mMRC score of 0, 80.9% (18) for patients with an mMRC score of 1, 93.5% (34.6) for patients with an mMRC score of 2, 76.2% (17.1) for patients with an mMRC score of 3, and 69.2% (19.4) for patients with an mMRC score of 4; (P < .001) (Figure 2).
The correlation between mMRC and FEV1 (r = 0.25, P < .001) was stronger than the correlation between mMRC and TLC (r = 0.15, P < .001). The correlations for DLCO (P < .001), DLCO/VA (P < .001), hemoglobin (P < .02), and PaO2 (P < .001) were all statistically significant (P < .005), but with no strong identifiable trend.
Discussion
The patient population of this study was primarily older males of Hispanic ethnicity with a history of smoking. There was no association between body mass index or smoking status with worsening dyspnea as measured with mMRC scores. We observed no significant correlation between mMRC scores and various factors such as comorbidities including heart conditions, and epidemiological factors like the etiology of lung disease, including both intrinsic and extrinsic causes. This lack of association was anticipated, as restrictive lung diseases in our study predominantly arose from intrinsic pulmonary etiologies, such as interstitial lung disease. A difference between more hospitalizations and worsening dyspnea was identified. There was a slightly higher correlation between FEV1 and mMRC scores when compared with TLC and mMRC scores concerning worsening dyspnea, which could indicate that the use of FEV1 should be preferred over previous recommendations to use TLC.10 Other guidelines have utilized exercise capacity via the 6-minute walk test as a marker of severity with spirometry values and found that DLCO was correlated with severity.11
The latest ERS/ATS guidelines recommend z scores for grading the severity of obstructive lung diseases but do not recommend them for the diagnosis of restrictive lung diseases.12 A z score encompasses diverse variables (eg, age, sex, and ethnicity) to provide more uniform and consistent results. Other studies have been done to relate z scores to other spirometry variables with restrictive lung disease. One such study indicates the potential benefit of using FVC alone to grade restrictive lung diseases.13 There continues to be great diversity in the interpretation of pulmonary function tests, and we believe the information gathered can provide valuable insight for managing patients with restrictive lung diseases.
Limitations
Only 2 patients reported an mMRC score of 2 in our study. This may have affected statistical outcomes. It also may reveal possible deficits in the efficacy of patient education on the mMRC scale. This study was also limited by its small sample size, single center location, and the distribution of patients that reported an mMRC favored either low or high values. The patients in this study, who were all veterans, may not be representative of other patient populations.
Conclusions
There continue to be few factors associated with the physiological severity of the defective oxygen delivery and reported dyspnea of a patient with restrictive lung disease that allows for an accurate, repeatable grading of severity. Using FEV1 instead of TLC to determine the severity of a restrictive lung disease should be reconsidered. We could not find any other strong correlation among other factors studied. Further research should be conducted to continue looking for variables that more accurately depict patient dyspnea in restrictive lung disease.
Acknowledgments
This study is based upon work supported by the Veterans Affairs Caribbean Healthcare System in San Juan, Puerto Rico, and is the result of work supported by Pulmonary & Critical Care Medicine service, with resources and the use of its facilities.
1. Hegewald MJ, Crapo RO. Pulmonary function testing. In: Broaddus VC, Ernst JD, King Jr TE, eds. Murray and Nadel’s Textbook of Respiratory Medicine. 5th ed. Saunders; 2010:522-553.
2. Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948-968. doi:10.1183/09031936.05.00035205
3. Rabe KF, Beghé B, Luppi F, Fabbri LM. Update in chronic obstructive pulmonary disease 2006. Am J Respir Crit Care Med. 2007;175(12):1222-1232. doi:10.1164/rccm.200704-586UP
4. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Spirometry for health care providers Accessed April 30, 2024. https://goldcopd.org/wp-content/uploads/2016/04/GOLD_Spirometry_2010.pdf
5. Mannino DM, Holguin F, Pavlin BI, Ferdinands JM. Risk factors for prevalence of and mortality related to restriction on spirometry: findings from the First National Health and Nutrition Examination Survey and follow-up. Int J Tuberc Lung Dis. 2005;9(6):613-621.
6. Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis. 1983;127(6):725-734. doi:10.1164/arrd.1983.127.6.725
7. Knudson RJ, Burrows B, Lebowitz MD. The maximal expiratory flow-volume curve: its use in the detection of ventilatory abnormalities in a population study. Am Rev Respir Dis. 1976;114(5):871-879. doi:10.1164/arrd.1976.114.5.871
8. Knudson RJ, Lebowitz MD, Burton AP, Knudson DE. The closing volume test: evaluation of nitrogen and bolus methods in a random population. Am Rev Respir Dis. 1977;115(3):423-434. doi:10.1164/arrd.1977.115.3.423
9. Ayers LN, Ginsberg ML, Fein J, Wasserman K. Diffusing capacity, specific diffusing capacity and interpretation of diffusion defects. West J Med. 1975;123(4):255-264.
10. Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Am Rev Respir Dis. 1991;144(5):1202-1218. doi:10.1164/ajrccm/144.5.1202
11. Larson J, Wrzos K, Corazalla E, Wang Q, Kim HJ, Cho RJ. Should FEV1 be used to grade restrictive impairment? A single-center comparison of lung function parameters to 6-minute walk test in patients with restrictive lung disease. HSOA J Pulm Med Respir Res. 2023;9:082. doi:10.24966/PMRR-0177/100082
12. Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2022;60(1):2101499. Published 2022 Jul 13. doi:10.1183/13993003.01499-2021
13. Myrberg T, Lindberg A, Eriksson B, et al. Restrictive spirometry versus restrictive lung function using the GLI reference values. Clin Physiol Funct Imaging. 2022;42(3):181-189. doi:10.1111/cpf.12745
Respiratory diseases have varied clinical presentations and are classified as restrictive, obstructive, mixed, or normal. Restrictive lung diseases have reduced lung volumes, either due to an alteration in lung parenchyma or a disease of the pleura, chest wall, or neuromuscular apparatus. If caused by parenchymal lung disease, restrictive lung disorders are accompanied by reduced gas transfer, which may be portrayed clinically by desaturation after exercise. Based on anatomical structures, the causes of lung volume reduction may be intrinsic or extrinsic. Intrinsic causes correspond to diseases of the lung parenchyma, such as idiopathic fibrotic diseases, connective-tissue diseases, drug-induced lung diseases, and other primary diseases of the lungs. Extrinsic causes refer to disorders outside the lungs or extra-pulmonary diseases such as neuromuscular and nonmuscular diseases of the chest wall.1 For example, obesity and myasthenia gravis can cause restrictive lung diseases, one through mechanical interference of lung expansion and the other through neuromuscular impedance of thoracic cage expansion. All these diseases eventually result in lung restriction, impaired lung function, and respiratory failure. This heterogenicity of disease makes establishing a single severity criterion difficult.
Laboratory testing, imaging studies, and examinations are important for determining the pulmonary disease and its course and progression. The pulmonary function test (PFT), which consists of multiple procedures that are performed depending on the information needed, has been an essential tool in practice for the pulmonologist. The PFT includes spirometry, lung volume measurement, respiratory muscle strength, diffusion capacity, and a broncho-provocation test. Each test has a particular role in assisting the diagnosis and/or follow-up of the patient. Spirometry is frequently used due to its range of dynamic physiological parameters, ease of use, and accessibility. It is used for the diagnosis of pulmonary symptoms, in the assessment of disability, and preoperatory evaluation, including lung resection surgery, assisting in the diagnosis, monitoring, and therapy response of pulmonary diseases.
A systematic approach to PFT interpretation is recommended by several societies, such as the American Thoracic Society (ATS) and the European Respiratory Society (ERS).2 The pulmonary function test results must be reproducible and meet established standards to ensure reliable and consistent clinical outcomes. A restrictive respiratory disease is defined by a decrease in total lung capacity (TLC) (< 5% of predicted value) and a normal forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio.2 Although other findings—such as a decrease in vital capacity—should prompt an investigation into whether the patient has a possible restrictive respiratory disease, the sole presence of this parameter is not definitive or diagnostic of a restrictive impairment.2-4 The assessment of severity is typically determined by TLC. Unfortunately, the severity of a restrictive respiratory disease and the degree of patient discomfort do not always correlate when utilizing just TLC. Pulmonary sarcoidosis, for example, is a granulomatous lung disease with a restrictive PFT pattern and a disease burden that may vary over time. Having a more consistent method of grading the severity of the restrictive lung disease may help guide treatment. The modified Medical Research Council (mMRC) scale, a 5-point dyspnea scale, is widely used in assessing the severity of dyspnea in various respiratory conditions, including chronic obstructive pulmonary disease (COPD), where its scores have been associated with patient mortality.1,5 The goal of this study was to document the associations between objective parameters obtained through PFT and other variables, with an established measurement of dyspnea to assess the severity grade of restrictive lung diseases.
Methods
This retrospective record review at the Veterans Affairs Caribbean Healthcare System (VACHS) in San Juan, Puerto Rico, wasconducted using the Veterans Health Information Systems and Technology Architecture to identify patients with a PFT, including spirometry, that indicated a restrictive ventilator pattern based on the current ATS/ERS Task Force on Lung Function Testing.2 Patients were included if they were aged ≥ 21 years, PFT with TLC ≤ 80% predicted, mMRC score documented on PFT, and documented diffusing capacity of the lung for carbon monoxide (DLCO). Patients were excluded if their FEV1/vital capacity (VC) was < 70% predicted using the largest VC, or no mMRC score was available. All patients meeting the inclusion criteria were considered regardless of comorbidities.
The PFT results of all adult patients, including those performed between June 1, 2013, and January 6, 2016, were submitted to spirometry, and lung volume measurements were analyzed. Sociodemographic information was collected, including sex, ethnicity, age, height, weight, and basal metabolic index. Other data found in PFTs, such as smoking status, smoking in packs/year, mMRC score, predicted TLC value, imaging present (chest X-ray, computed tomography), and hospitalizations and exacerbations within 1 year were collected. In addition, we examined the predicted values for FEV1, DLCO, and DLCO/VA (calculated using the Ayer equation), FVC (calculated using the Knudson equation), expiratory reserve volume, inspiratory VC, and slow VC. PaO2, PaCO2, and Alveolar-arterial gradients also were collected.6-9 Information about heart failure status was gathered through medical evaluation of notes and cardiac studies. All categorical variables were correlated with Spearman analysis and quantitative variables with average percentages. P values were calculated with analysis of variance.
Results
Of 6461 VACHS patient records reviewed, 415 met the inclusion criteria. Patients were divided according to their mMRC score: 65 had mMRC score of 0, 87 had an mMRC score of 1, 2 had an mMRC score of 2, 146 had an mMRC of 3, and 115 had an mMRC score of 4. The population was primarily male (98.6%) and of Hispanic ethnicity (96.4%), with a mean age of 72 years (Table 1). Most patients (n = 269, 64.0%) were prior smokers, while 135 patients (32.5%) had never smoked, and 11 (2.7%) were current smokers. At baseline, 169 patients (41.4%) had interstitial lung disease, 39 (9.6%) had chest wall disorders, 29 (7.1%) had occupational exposure, 25 (6.1%) had pneumonitis, and 14 (3.4%) had neuromuscular disorders.
There was a statistically significant relationship between mMRC score and hospitalization and FEV1 but not TLC (Table 2). As mMRC increased, so did hospitalizations: a total of 168 patients (40.5%) were hospitalized; 24 patients (36.9%) had an mMRC score of 0, 30 patients (34.0%) had an mMRC score of 1, 2 patients (100%) had an mMRC score of 2, 54 patients (37.0%) had an mMRC score of 3, and 58 patients (50.0%) had an mMRC score of 4 (P = .04). Mean (SD) TLC values increased as mMRC scores increased. Mean (SD) TLC was 70.5% (33.0) for the entire population; 68.8% (7.2) for patients with an mMRC score of 0, 70.8% (5.8) for patients with an mMRC score of 1, 75.0% (1.4) for patients with an mMRC score of 2, 70.1% (7.2) for patients with an mMRC score of 3, and 71.5% (62.1) for patients with an mMRC score of 4 (P = .10) (Figure 1). There was an associated decrease in mean (SD) FEV1 with mMRC. Mean (SD) FEV1 was 76.2% (18.9) for the entire population; 81.7% (19.3) for patients with an mMRC score of 0, 80.9% (18) for patients with an mMRC score of 1, 93.5% (34.6) for patients with an mMRC score of 2, 76.2% (17.1) for patients with an mMRC score of 3, and 69.2% (19.4) for patients with an mMRC score of 4; (P < .001) (Figure 2).
The correlation between mMRC and FEV1 (r = 0.25, P < .001) was stronger than the correlation between mMRC and TLC (r = 0.15, P < .001). The correlations for DLCO (P < .001), DLCO/VA (P < .001), hemoglobin (P < .02), and PaO2 (P < .001) were all statistically significant (P < .005), but with no strong identifiable trend.
Discussion
The patient population of this study was primarily older males of Hispanic ethnicity with a history of smoking. There was no association between body mass index or smoking status with worsening dyspnea as measured with mMRC scores. We observed no significant correlation between mMRC scores and various factors such as comorbidities including heart conditions, and epidemiological factors like the etiology of lung disease, including both intrinsic and extrinsic causes. This lack of association was anticipated, as restrictive lung diseases in our study predominantly arose from intrinsic pulmonary etiologies, such as interstitial lung disease. A difference between more hospitalizations and worsening dyspnea was identified. There was a slightly higher correlation between FEV1 and mMRC scores when compared with TLC and mMRC scores concerning worsening dyspnea, which could indicate that the use of FEV1 should be preferred over previous recommendations to use TLC.10 Other guidelines have utilized exercise capacity via the 6-minute walk test as a marker of severity with spirometry values and found that DLCO was correlated with severity.11
The latest ERS/ATS guidelines recommend z scores for grading the severity of obstructive lung diseases but do not recommend them for the diagnosis of restrictive lung diseases.12 A z score encompasses diverse variables (eg, age, sex, and ethnicity) to provide more uniform and consistent results. Other studies have been done to relate z scores to other spirometry variables with restrictive lung disease. One such study indicates the potential benefit of using FVC alone to grade restrictive lung diseases.13 There continues to be great diversity in the interpretation of pulmonary function tests, and we believe the information gathered can provide valuable insight for managing patients with restrictive lung diseases.
Limitations
Only 2 patients reported an mMRC score of 2 in our study. This may have affected statistical outcomes. It also may reveal possible deficits in the efficacy of patient education on the mMRC scale. This study was also limited by its small sample size, single center location, and the distribution of patients that reported an mMRC favored either low or high values. The patients in this study, who were all veterans, may not be representative of other patient populations.
Conclusions
There continue to be few factors associated with the physiological severity of the defective oxygen delivery and reported dyspnea of a patient with restrictive lung disease that allows for an accurate, repeatable grading of severity. Using FEV1 instead of TLC to determine the severity of a restrictive lung disease should be reconsidered. We could not find any other strong correlation among other factors studied. Further research should be conducted to continue looking for variables that more accurately depict patient dyspnea in restrictive lung disease.
Acknowledgments
This study is based upon work supported by the Veterans Affairs Caribbean Healthcare System in San Juan, Puerto Rico, and is the result of work supported by Pulmonary & Critical Care Medicine service, with resources and the use of its facilities.
Respiratory diseases have varied clinical presentations and are classified as restrictive, obstructive, mixed, or normal. Restrictive lung diseases have reduced lung volumes, either due to an alteration in lung parenchyma or a disease of the pleura, chest wall, or neuromuscular apparatus. If caused by parenchymal lung disease, restrictive lung disorders are accompanied by reduced gas transfer, which may be portrayed clinically by desaturation after exercise. Based on anatomical structures, the causes of lung volume reduction may be intrinsic or extrinsic. Intrinsic causes correspond to diseases of the lung parenchyma, such as idiopathic fibrotic diseases, connective-tissue diseases, drug-induced lung diseases, and other primary diseases of the lungs. Extrinsic causes refer to disorders outside the lungs or extra-pulmonary diseases such as neuromuscular and nonmuscular diseases of the chest wall.1 For example, obesity and myasthenia gravis can cause restrictive lung diseases, one through mechanical interference of lung expansion and the other through neuromuscular impedance of thoracic cage expansion. All these diseases eventually result in lung restriction, impaired lung function, and respiratory failure. This heterogenicity of disease makes establishing a single severity criterion difficult.
Laboratory testing, imaging studies, and examinations are important for determining the pulmonary disease and its course and progression. The pulmonary function test (PFT), which consists of multiple procedures that are performed depending on the information needed, has been an essential tool in practice for the pulmonologist. The PFT includes spirometry, lung volume measurement, respiratory muscle strength, diffusion capacity, and a broncho-provocation test. Each test has a particular role in assisting the diagnosis and/or follow-up of the patient. Spirometry is frequently used due to its range of dynamic physiological parameters, ease of use, and accessibility. It is used for the diagnosis of pulmonary symptoms, in the assessment of disability, and preoperatory evaluation, including lung resection surgery, assisting in the diagnosis, monitoring, and therapy response of pulmonary diseases.
A systematic approach to PFT interpretation is recommended by several societies, such as the American Thoracic Society (ATS) and the European Respiratory Society (ERS).2 The pulmonary function test results must be reproducible and meet established standards to ensure reliable and consistent clinical outcomes. A restrictive respiratory disease is defined by a decrease in total lung capacity (TLC) (< 5% of predicted value) and a normal forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio.2 Although other findings—such as a decrease in vital capacity—should prompt an investigation into whether the patient has a possible restrictive respiratory disease, the sole presence of this parameter is not definitive or diagnostic of a restrictive impairment.2-4 The assessment of severity is typically determined by TLC. Unfortunately, the severity of a restrictive respiratory disease and the degree of patient discomfort do not always correlate when utilizing just TLC. Pulmonary sarcoidosis, for example, is a granulomatous lung disease with a restrictive PFT pattern and a disease burden that may vary over time. Having a more consistent method of grading the severity of the restrictive lung disease may help guide treatment. The modified Medical Research Council (mMRC) scale, a 5-point dyspnea scale, is widely used in assessing the severity of dyspnea in various respiratory conditions, including chronic obstructive pulmonary disease (COPD), where its scores have been associated with patient mortality.1,5 The goal of this study was to document the associations between objective parameters obtained through PFT and other variables, with an established measurement of dyspnea to assess the severity grade of restrictive lung diseases.
Methods
This retrospective record review at the Veterans Affairs Caribbean Healthcare System (VACHS) in San Juan, Puerto Rico, wasconducted using the Veterans Health Information Systems and Technology Architecture to identify patients with a PFT, including spirometry, that indicated a restrictive ventilator pattern based on the current ATS/ERS Task Force on Lung Function Testing.2 Patients were included if they were aged ≥ 21 years, PFT with TLC ≤ 80% predicted, mMRC score documented on PFT, and documented diffusing capacity of the lung for carbon monoxide (DLCO). Patients were excluded if their FEV1/vital capacity (VC) was < 70% predicted using the largest VC, or no mMRC score was available. All patients meeting the inclusion criteria were considered regardless of comorbidities.
The PFT results of all adult patients, including those performed between June 1, 2013, and January 6, 2016, were submitted to spirometry, and lung volume measurements were analyzed. Sociodemographic information was collected, including sex, ethnicity, age, height, weight, and basal metabolic index. Other data found in PFTs, such as smoking status, smoking in packs/year, mMRC score, predicted TLC value, imaging present (chest X-ray, computed tomography), and hospitalizations and exacerbations within 1 year were collected. In addition, we examined the predicted values for FEV1, DLCO, and DLCO/VA (calculated using the Ayer equation), FVC (calculated using the Knudson equation), expiratory reserve volume, inspiratory VC, and slow VC. PaO2, PaCO2, and Alveolar-arterial gradients also were collected.6-9 Information about heart failure status was gathered through medical evaluation of notes and cardiac studies. All categorical variables were correlated with Spearman analysis and quantitative variables with average percentages. P values were calculated with analysis of variance.
Results
Of 6461 VACHS patient records reviewed, 415 met the inclusion criteria. Patients were divided according to their mMRC score: 65 had mMRC score of 0, 87 had an mMRC score of 1, 2 had an mMRC score of 2, 146 had an mMRC of 3, and 115 had an mMRC score of 4. The population was primarily male (98.6%) and of Hispanic ethnicity (96.4%), with a mean age of 72 years (Table 1). Most patients (n = 269, 64.0%) were prior smokers, while 135 patients (32.5%) had never smoked, and 11 (2.7%) were current smokers. At baseline, 169 patients (41.4%) had interstitial lung disease, 39 (9.6%) had chest wall disorders, 29 (7.1%) had occupational exposure, 25 (6.1%) had pneumonitis, and 14 (3.4%) had neuromuscular disorders.
There was a statistically significant relationship between mMRC score and hospitalization and FEV1 but not TLC (Table 2). As mMRC increased, so did hospitalizations: a total of 168 patients (40.5%) were hospitalized; 24 patients (36.9%) had an mMRC score of 0, 30 patients (34.0%) had an mMRC score of 1, 2 patients (100%) had an mMRC score of 2, 54 patients (37.0%) had an mMRC score of 3, and 58 patients (50.0%) had an mMRC score of 4 (P = .04). Mean (SD) TLC values increased as mMRC scores increased. Mean (SD) TLC was 70.5% (33.0) for the entire population; 68.8% (7.2) for patients with an mMRC score of 0, 70.8% (5.8) for patients with an mMRC score of 1, 75.0% (1.4) for patients with an mMRC score of 2, 70.1% (7.2) for patients with an mMRC score of 3, and 71.5% (62.1) for patients with an mMRC score of 4 (P = .10) (Figure 1). There was an associated decrease in mean (SD) FEV1 with mMRC. Mean (SD) FEV1 was 76.2% (18.9) for the entire population; 81.7% (19.3) for patients with an mMRC score of 0, 80.9% (18) for patients with an mMRC score of 1, 93.5% (34.6) for patients with an mMRC score of 2, 76.2% (17.1) for patients with an mMRC score of 3, and 69.2% (19.4) for patients with an mMRC score of 4; (P < .001) (Figure 2).
The correlation between mMRC and FEV1 (r = 0.25, P < .001) was stronger than the correlation between mMRC and TLC (r = 0.15, P < .001). The correlations for DLCO (P < .001), DLCO/VA (P < .001), hemoglobin (P < .02), and PaO2 (P < .001) were all statistically significant (P < .005), but with no strong identifiable trend.
Discussion
The patient population of this study was primarily older males of Hispanic ethnicity with a history of smoking. There was no association between body mass index or smoking status with worsening dyspnea as measured with mMRC scores. We observed no significant correlation between mMRC scores and various factors such as comorbidities including heart conditions, and epidemiological factors like the etiology of lung disease, including both intrinsic and extrinsic causes. This lack of association was anticipated, as restrictive lung diseases in our study predominantly arose from intrinsic pulmonary etiologies, such as interstitial lung disease. A difference between more hospitalizations and worsening dyspnea was identified. There was a slightly higher correlation between FEV1 and mMRC scores when compared with TLC and mMRC scores concerning worsening dyspnea, which could indicate that the use of FEV1 should be preferred over previous recommendations to use TLC.10 Other guidelines have utilized exercise capacity via the 6-minute walk test as a marker of severity with spirometry values and found that DLCO was correlated with severity.11
The latest ERS/ATS guidelines recommend z scores for grading the severity of obstructive lung diseases but do not recommend them for the diagnosis of restrictive lung diseases.12 A z score encompasses diverse variables (eg, age, sex, and ethnicity) to provide more uniform and consistent results. Other studies have been done to relate z scores to other spirometry variables with restrictive lung disease. One such study indicates the potential benefit of using FVC alone to grade restrictive lung diseases.13 There continues to be great diversity in the interpretation of pulmonary function tests, and we believe the information gathered can provide valuable insight for managing patients with restrictive lung diseases.
Limitations
Only 2 patients reported an mMRC score of 2 in our study. This may have affected statistical outcomes. It also may reveal possible deficits in the efficacy of patient education on the mMRC scale. This study was also limited by its small sample size, single center location, and the distribution of patients that reported an mMRC favored either low or high values. The patients in this study, who were all veterans, may not be representative of other patient populations.
Conclusions
There continue to be few factors associated with the physiological severity of the defective oxygen delivery and reported dyspnea of a patient with restrictive lung disease that allows for an accurate, repeatable grading of severity. Using FEV1 instead of TLC to determine the severity of a restrictive lung disease should be reconsidered. We could not find any other strong correlation among other factors studied. Further research should be conducted to continue looking for variables that more accurately depict patient dyspnea in restrictive lung disease.
Acknowledgments
This study is based upon work supported by the Veterans Affairs Caribbean Healthcare System in San Juan, Puerto Rico, and is the result of work supported by Pulmonary & Critical Care Medicine service, with resources and the use of its facilities.
1. Hegewald MJ, Crapo RO. Pulmonary function testing. In: Broaddus VC, Ernst JD, King Jr TE, eds. Murray and Nadel’s Textbook of Respiratory Medicine. 5th ed. Saunders; 2010:522-553.
2. Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948-968. doi:10.1183/09031936.05.00035205
3. Rabe KF, Beghé B, Luppi F, Fabbri LM. Update in chronic obstructive pulmonary disease 2006. Am J Respir Crit Care Med. 2007;175(12):1222-1232. doi:10.1164/rccm.200704-586UP
4. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Spirometry for health care providers Accessed April 30, 2024. https://goldcopd.org/wp-content/uploads/2016/04/GOLD_Spirometry_2010.pdf
5. Mannino DM, Holguin F, Pavlin BI, Ferdinands JM. Risk factors for prevalence of and mortality related to restriction on spirometry: findings from the First National Health and Nutrition Examination Survey and follow-up. Int J Tuberc Lung Dis. 2005;9(6):613-621.
6. Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis. 1983;127(6):725-734. doi:10.1164/arrd.1983.127.6.725
7. Knudson RJ, Burrows B, Lebowitz MD. The maximal expiratory flow-volume curve: its use in the detection of ventilatory abnormalities in a population study. Am Rev Respir Dis. 1976;114(5):871-879. doi:10.1164/arrd.1976.114.5.871
8. Knudson RJ, Lebowitz MD, Burton AP, Knudson DE. The closing volume test: evaluation of nitrogen and bolus methods in a random population. Am Rev Respir Dis. 1977;115(3):423-434. doi:10.1164/arrd.1977.115.3.423
9. Ayers LN, Ginsberg ML, Fein J, Wasserman K. Diffusing capacity, specific diffusing capacity and interpretation of diffusion defects. West J Med. 1975;123(4):255-264.
10. Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Am Rev Respir Dis. 1991;144(5):1202-1218. doi:10.1164/ajrccm/144.5.1202
11. Larson J, Wrzos K, Corazalla E, Wang Q, Kim HJ, Cho RJ. Should FEV1 be used to grade restrictive impairment? A single-center comparison of lung function parameters to 6-minute walk test in patients with restrictive lung disease. HSOA J Pulm Med Respir Res. 2023;9:082. doi:10.24966/PMRR-0177/100082
12. Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2022;60(1):2101499. Published 2022 Jul 13. doi:10.1183/13993003.01499-2021
13. Myrberg T, Lindberg A, Eriksson B, et al. Restrictive spirometry versus restrictive lung function using the GLI reference values. Clin Physiol Funct Imaging. 2022;42(3):181-189. doi:10.1111/cpf.12745
1. Hegewald MJ, Crapo RO. Pulmonary function testing. In: Broaddus VC, Ernst JD, King Jr TE, eds. Murray and Nadel’s Textbook of Respiratory Medicine. 5th ed. Saunders; 2010:522-553.
2. Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948-968. doi:10.1183/09031936.05.00035205
3. Rabe KF, Beghé B, Luppi F, Fabbri LM. Update in chronic obstructive pulmonary disease 2006. Am J Respir Crit Care Med. 2007;175(12):1222-1232. doi:10.1164/rccm.200704-586UP
4. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Spirometry for health care providers Accessed April 30, 2024. https://goldcopd.org/wp-content/uploads/2016/04/GOLD_Spirometry_2010.pdf
5. Mannino DM, Holguin F, Pavlin BI, Ferdinands JM. Risk factors for prevalence of and mortality related to restriction on spirometry: findings from the First National Health and Nutrition Examination Survey and follow-up. Int J Tuberc Lung Dis. 2005;9(6):613-621.
6. Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis. 1983;127(6):725-734. doi:10.1164/arrd.1983.127.6.725
7. Knudson RJ, Burrows B, Lebowitz MD. The maximal expiratory flow-volume curve: its use in the detection of ventilatory abnormalities in a population study. Am Rev Respir Dis. 1976;114(5):871-879. doi:10.1164/arrd.1976.114.5.871
8. Knudson RJ, Lebowitz MD, Burton AP, Knudson DE. The closing volume test: evaluation of nitrogen and bolus methods in a random population. Am Rev Respir Dis. 1977;115(3):423-434. doi:10.1164/arrd.1977.115.3.423
9. Ayers LN, Ginsberg ML, Fein J, Wasserman K. Diffusing capacity, specific diffusing capacity and interpretation of diffusion defects. West J Med. 1975;123(4):255-264.
10. Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Am Rev Respir Dis. 1991;144(5):1202-1218. doi:10.1164/ajrccm/144.5.1202
11. Larson J, Wrzos K, Corazalla E, Wang Q, Kim HJ, Cho RJ. Should FEV1 be used to grade restrictive impairment? A single-center comparison of lung function parameters to 6-minute walk test in patients with restrictive lung disease. HSOA J Pulm Med Respir Res. 2023;9:082. doi:10.24966/PMRR-0177/100082
12. Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2022;60(1):2101499. Published 2022 Jul 13. doi:10.1183/13993003.01499-2021
13. Myrberg T, Lindberg A, Eriksson B, et al. Restrictive spirometry versus restrictive lung function using the GLI reference values. Clin Physiol Funct Imaging. 2022;42(3):181-189. doi:10.1111/cpf.12745
Quitting Smoking Boosts Life Expectancy at Any Age
TOPLINE:
Quitting smoking at any age increases life expectancy, with the most significant increases observed in younger individuals. But people who quit over age 65 can extend life expectancy.
METHODOLOGY:
- Researchers analyzed the detrimental effects of smoking and the positive impacts of cessation on life expectancy in individuals aged 35-75 years.
- Age-specific death rates by smoking status were calculated using the relative risks for all-cause mortality derived from the Cancer Prevention Study II data, 2018 National Health Interview Survey smoking prevalence data, and 2018 all-cause mortality rates.
- Life tables were constructed to obtain information on the life expectancies of people who never smoked, those who currently smoked, and those who previously smoked but quit at various ages.
- Estimates of years lost due to smoking and years gained by quitting smoking were calculated for people starting at age 35 and over 10-year increments.
TAKEAWAY:
- Compared with people who never smoked, those who smoked at ages 35, 45, 55, 65, and 75 years and continued smoking throughout their lives would lose 9.1, 8.3, 7.3, 5.9, and 4.4 years, respectively.
- People who quit smoking at ages 35, 45, 55, 65, and 75 years would have life expectancies that are shorter by 1.2, 2.7, 3.9, 4.2, and 3.7 years, respectively, than those of same-age individuals who never smoked.
- Individuals who quit smoking at ages 35, 45, 55, 65, and 75 years would experience an additional 8.0, 5.6, 3.4, 1.7, and 0.7 years of life expectancy compared with those who continued smoking.
- People who quit at ages 65 and 75 years would have a 23.4% and 14.2% chance of gaining at least 1 additional year of life.
IN PRACTICE:
“This cessation benefit is not limited to young- and middle-aged adults who smoke; this study demonstrates its applicability to seniors as well. These findings may be valuable for clinicians seeking scientific evidence to motivate their patients who smoke to quit,” the authors wrote.
SOURCE:
The study was led by Thuy T.T. Le, PhD, from the Department of Health Management and Policy at the University of Michigan School of Public Health in Ann Arbor and published online in the American Journal of Preventive Medicine.
LIMITATIONS:
The study’s estimates were according to data from 2018 and may not reflect current trends. The estimates also did not account for variability in smoking intensity among individuals.
DISCLOSURES:
The study was supported by grants from the National Cancer Institute of the US National Institutes of Health and the US Food and Drug Administration Center for Tobacco Products. The authors declared that they had no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
Quitting smoking at any age increases life expectancy, with the most significant increases observed in younger individuals. But people who quit over age 65 can extend life expectancy.
METHODOLOGY:
- Researchers analyzed the detrimental effects of smoking and the positive impacts of cessation on life expectancy in individuals aged 35-75 years.
- Age-specific death rates by smoking status were calculated using the relative risks for all-cause mortality derived from the Cancer Prevention Study II data, 2018 National Health Interview Survey smoking prevalence data, and 2018 all-cause mortality rates.
- Life tables were constructed to obtain information on the life expectancies of people who never smoked, those who currently smoked, and those who previously smoked but quit at various ages.
- Estimates of years lost due to smoking and years gained by quitting smoking were calculated for people starting at age 35 and over 10-year increments.
TAKEAWAY:
- Compared with people who never smoked, those who smoked at ages 35, 45, 55, 65, and 75 years and continued smoking throughout their lives would lose 9.1, 8.3, 7.3, 5.9, and 4.4 years, respectively.
- People who quit smoking at ages 35, 45, 55, 65, and 75 years would have life expectancies that are shorter by 1.2, 2.7, 3.9, 4.2, and 3.7 years, respectively, than those of same-age individuals who never smoked.
- Individuals who quit smoking at ages 35, 45, 55, 65, and 75 years would experience an additional 8.0, 5.6, 3.4, 1.7, and 0.7 years of life expectancy compared with those who continued smoking.
- People who quit at ages 65 and 75 years would have a 23.4% and 14.2% chance of gaining at least 1 additional year of life.
IN PRACTICE:
“This cessation benefit is not limited to young- and middle-aged adults who smoke; this study demonstrates its applicability to seniors as well. These findings may be valuable for clinicians seeking scientific evidence to motivate their patients who smoke to quit,” the authors wrote.
SOURCE:
The study was led by Thuy T.T. Le, PhD, from the Department of Health Management and Policy at the University of Michigan School of Public Health in Ann Arbor and published online in the American Journal of Preventive Medicine.
LIMITATIONS:
The study’s estimates were according to data from 2018 and may not reflect current trends. The estimates also did not account for variability in smoking intensity among individuals.
DISCLOSURES:
The study was supported by grants from the National Cancer Institute of the US National Institutes of Health and the US Food and Drug Administration Center for Tobacco Products. The authors declared that they had no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
Quitting smoking at any age increases life expectancy, with the most significant increases observed in younger individuals. But people who quit over age 65 can extend life expectancy.
METHODOLOGY:
- Researchers analyzed the detrimental effects of smoking and the positive impacts of cessation on life expectancy in individuals aged 35-75 years.
- Age-specific death rates by smoking status were calculated using the relative risks for all-cause mortality derived from the Cancer Prevention Study II data, 2018 National Health Interview Survey smoking prevalence data, and 2018 all-cause mortality rates.
- Life tables were constructed to obtain information on the life expectancies of people who never smoked, those who currently smoked, and those who previously smoked but quit at various ages.
- Estimates of years lost due to smoking and years gained by quitting smoking were calculated for people starting at age 35 and over 10-year increments.
TAKEAWAY:
- Compared with people who never smoked, those who smoked at ages 35, 45, 55, 65, and 75 years and continued smoking throughout their lives would lose 9.1, 8.3, 7.3, 5.9, and 4.4 years, respectively.
- People who quit smoking at ages 35, 45, 55, 65, and 75 years would have life expectancies that are shorter by 1.2, 2.7, 3.9, 4.2, and 3.7 years, respectively, than those of same-age individuals who never smoked.
- Individuals who quit smoking at ages 35, 45, 55, 65, and 75 years would experience an additional 8.0, 5.6, 3.4, 1.7, and 0.7 years of life expectancy compared with those who continued smoking.
- People who quit at ages 65 and 75 years would have a 23.4% and 14.2% chance of gaining at least 1 additional year of life.
IN PRACTICE:
“This cessation benefit is not limited to young- and middle-aged adults who smoke; this study demonstrates its applicability to seniors as well. These findings may be valuable for clinicians seeking scientific evidence to motivate their patients who smoke to quit,” the authors wrote.
SOURCE:
The study was led by Thuy T.T. Le, PhD, from the Department of Health Management and Policy at the University of Michigan School of Public Health in Ann Arbor and published online in the American Journal of Preventive Medicine.
LIMITATIONS:
The study’s estimates were according to data from 2018 and may not reflect current trends. The estimates also did not account for variability in smoking intensity among individuals.
DISCLOSURES:
The study was supported by grants from the National Cancer Institute of the US National Institutes of Health and the US Food and Drug Administration Center for Tobacco Products. The authors declared that they had no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
Specific Antipsychotics Linked to Increased Pneumonia Risk
TOPLINE:
High-dose antipsychotics, particularly quetiapine, clozapine, and olanzapine, are linked to increased pneumonia risk in patients with schizophrenia, new data show. Monotherapy with high anticholinergic burden also raises pneumonia risk.
METHODOLOGY:
- Using several nationwide data registers, investigators pulled data on individuals who received inpatient care for schizophrenia or schizoaffective disorder (n = 61,889) between 1972 and 2014.
- Data on drug use were gathered from a prescription register and included dispensing dates, cost, dose, package size, and drug formulation. Data on dates and causes of death were obtained from the Causes of Death register.
- After entering the cohort, follow-up started in January 1996 or after the first diagnosis of schizophrenia for those diagnosed between 1996 and 2014.
- The primary outcome was hospitalization caused by pneumonia as the main diagnosis for hospital admission.
TAKEAWAY:
- During 22 years of follow-up, 8917 patients (14.4%) had one or more hospitalizations for pneumonia, and 1137 (12.8%) died within 30 days of admission.
- Pneumonia risk was the highest with the use of high-dose (> 440 mg/d) quetiapine (P = .003), followed by high- (≥ 330 mg/d) and medium-dose (180 to < 330 mg/d) clozapine (both P < .001) and high-dose (≥ 11 mg/d) olanzapine (P = .02).
- Compared with no antipsychotic use, antipsychotic monotherapy was associated with an increased pneumonia risk (P = .03), whereas antipsychotic polytherapy was not.
- Only the use of antipsychotics with high anticholinergic potency was associated with pneumonia risk (P < .001).
IN PRACTICE:
“Identification of antipsychotic drugs that are associated with pneumonia risk may better inform prevention programs (eg, vaccinations),” the researchers noted. “Second, the availability of pneumonia risk estimates for individual antipsychotics and for groups of antipsychotics may foster personalized prescribing guidelines.”
SOURCE:
The study was led by Jurjen Luykx, MD, Amsterdam University Medical Center, Amsterdam, the Netherlands. It was published online in JAMA Psychiatry.
LIMITATIONS:
The investigators could not correct for all possible risk factors that may increase pneumonia risk in individuals with schizophrenia, such as smoking and lifestyle habits. Also, cases of pneumonia that didn’t require hospital admission couldn’t be included in the analysis, so the findings may generalize only to cases of severe pneumonia.
DISCLOSURES:
The study was funded by the Finnish Ministry of Social Affairs and Health.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
High-dose antipsychotics, particularly quetiapine, clozapine, and olanzapine, are linked to increased pneumonia risk in patients with schizophrenia, new data show. Monotherapy with high anticholinergic burden also raises pneumonia risk.
METHODOLOGY:
- Using several nationwide data registers, investigators pulled data on individuals who received inpatient care for schizophrenia or schizoaffective disorder (n = 61,889) between 1972 and 2014.
- Data on drug use were gathered from a prescription register and included dispensing dates, cost, dose, package size, and drug formulation. Data on dates and causes of death were obtained from the Causes of Death register.
- After entering the cohort, follow-up started in January 1996 or after the first diagnosis of schizophrenia for those diagnosed between 1996 and 2014.
- The primary outcome was hospitalization caused by pneumonia as the main diagnosis for hospital admission.
TAKEAWAY:
- During 22 years of follow-up, 8917 patients (14.4%) had one or more hospitalizations for pneumonia, and 1137 (12.8%) died within 30 days of admission.
- Pneumonia risk was the highest with the use of high-dose (> 440 mg/d) quetiapine (P = .003), followed by high- (≥ 330 mg/d) and medium-dose (180 to < 330 mg/d) clozapine (both P < .001) and high-dose (≥ 11 mg/d) olanzapine (P = .02).
- Compared with no antipsychotic use, antipsychotic monotherapy was associated with an increased pneumonia risk (P = .03), whereas antipsychotic polytherapy was not.
- Only the use of antipsychotics with high anticholinergic potency was associated with pneumonia risk (P < .001).
IN PRACTICE:
“Identification of antipsychotic drugs that are associated with pneumonia risk may better inform prevention programs (eg, vaccinations),” the researchers noted. “Second, the availability of pneumonia risk estimates for individual antipsychotics and for groups of antipsychotics may foster personalized prescribing guidelines.”
SOURCE:
The study was led by Jurjen Luykx, MD, Amsterdam University Medical Center, Amsterdam, the Netherlands. It was published online in JAMA Psychiatry.
LIMITATIONS:
The investigators could not correct for all possible risk factors that may increase pneumonia risk in individuals with schizophrenia, such as smoking and lifestyle habits. Also, cases of pneumonia that didn’t require hospital admission couldn’t be included in the analysis, so the findings may generalize only to cases of severe pneumonia.
DISCLOSURES:
The study was funded by the Finnish Ministry of Social Affairs and Health.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
High-dose antipsychotics, particularly quetiapine, clozapine, and olanzapine, are linked to increased pneumonia risk in patients with schizophrenia, new data show. Monotherapy with high anticholinergic burden also raises pneumonia risk.
METHODOLOGY:
- Using several nationwide data registers, investigators pulled data on individuals who received inpatient care for schizophrenia or schizoaffective disorder (n = 61,889) between 1972 and 2014.
- Data on drug use were gathered from a prescription register and included dispensing dates, cost, dose, package size, and drug formulation. Data on dates and causes of death were obtained from the Causes of Death register.
- After entering the cohort, follow-up started in January 1996 or after the first diagnosis of schizophrenia for those diagnosed between 1996 and 2014.
- The primary outcome was hospitalization caused by pneumonia as the main diagnosis for hospital admission.
TAKEAWAY:
- During 22 years of follow-up, 8917 patients (14.4%) had one or more hospitalizations for pneumonia, and 1137 (12.8%) died within 30 days of admission.
- Pneumonia risk was the highest with the use of high-dose (> 440 mg/d) quetiapine (P = .003), followed by high- (≥ 330 mg/d) and medium-dose (180 to < 330 mg/d) clozapine (both P < .001) and high-dose (≥ 11 mg/d) olanzapine (P = .02).
- Compared with no antipsychotic use, antipsychotic monotherapy was associated with an increased pneumonia risk (P = .03), whereas antipsychotic polytherapy was not.
- Only the use of antipsychotics with high anticholinergic potency was associated with pneumonia risk (P < .001).
IN PRACTICE:
“Identification of antipsychotic drugs that are associated with pneumonia risk may better inform prevention programs (eg, vaccinations),” the researchers noted. “Second, the availability of pneumonia risk estimates for individual antipsychotics and for groups of antipsychotics may foster personalized prescribing guidelines.”
SOURCE:
The study was led by Jurjen Luykx, MD, Amsterdam University Medical Center, Amsterdam, the Netherlands. It was published online in JAMA Psychiatry.
LIMITATIONS:
The investigators could not correct for all possible risk factors that may increase pneumonia risk in individuals with schizophrenia, such as smoking and lifestyle habits. Also, cases of pneumonia that didn’t require hospital admission couldn’t be included in the analysis, so the findings may generalize only to cases of severe pneumonia.
DISCLOSURES:
The study was funded by the Finnish Ministry of Social Affairs and Health.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
Top reads from the CHEST journal portfolio
Understanding RA with COPD, lung cancer prediction models, and chronic cardiac dysfunction
Journal CHEST®
Does Rheumatoid Arthritis Increase the Risk of COPD?
By: Chiwook Chung, MD, and colleagues
Notably, individuals with seropositive RA exhibit a greater risk of COPD onset than those with seronegative RA. Although smoking history didn’t affect the relationship between RA and COPD, monitoring respiratory symptoms and pulmonary function in patients with RA, especially patients who are seropositive, is crucial. These findings underscore the importance of interdisciplinary collaboration between rheumatologists and pulmonologists to enhance early detection and management strategies for pulmonary complications in patients with RA.
– Commentary by Corinne Young, MSN, FNP-C, FCCP, Member of the CHEST Physician® Editorial Board
CHEST Pulmonary®
The Lung Cancer Prediction Model “Stress Test”
By: Brent E. Heideman, MD, and colleagues
Current lung cancer prediction models have limited utility in high-risk patients referred for diagnostic biopsy. In a study of 322 indeterminate pulmonary nodules, the Brock, Mayo Clinic, Herder, and Veterans Affairs models showed modest discrimination between benign and malignant nodules (AUCs 0.67-0.77). The models performed poorly for low-risk patients (negative predictive values 63%-71%) and suboptimally for high-risk patients (positive predictive values 73%-87%), suggesting referring physicians use additional clinical information not captured in these models to identify high-risk patients needing biopsy. New prediction models and biomarkers specifically developed and calibrated for high-risk populations are needed to better inform clinical decision-making. Incorporating interval imaging to assess changes in nodule characteristics could potentially improve model performance. Tailored risk assessment tools are crucial for optimizing management and reducing unnecessary invasive procedures in this challenging patient population.
– Commentary by Russell Miller, MD, Member of the CHEST Physician Editorial Board
CHEST Critical Care ®
Characterizing Cardiac Function in ICU Survivors of Sepsis
By: Kevin Garrity, MBChB, and colleagues
While chronic cardiac dysfunction is one of the proposed mechanisms of long-term impairment post critical illness, its prevalence, mechanisms, and associations with disability following admission for sepsis are not well understood. Garrity and colleagues describe the Characterization of Cardiovascular Function in ICU Survivors of Sepsis (CONDUCT-ICU) protocol, a prospective study including two ICUs in Scotland aimed to better define cardiovascular dysfunction in survivors of sepsis. Designed to enroll 69 patients, demographics, cardiac and inflammatory biomarkers, and echocardiograms will be obtained on ICU discharge with additional laboratory data, cardiac magnetic resonance imaging, and patient-reported outcome measures to be obtained at 6 to 10 weeks. This novel multimodal approach will provide understanding into the role of cardiovascular dysfunction following critical illness as well as offer mechanistic insights. The investigators hope to obtain operational and pilot data for larger future studies.
– Commentary by Eugene Yuriditsky, MD, FCCP, Member of the CHEST Physician Editorial Board
Understanding RA with COPD, lung cancer prediction models, and chronic cardiac dysfunction
Understanding RA with COPD, lung cancer prediction models, and chronic cardiac dysfunction
Journal CHEST®
Does Rheumatoid Arthritis Increase the Risk of COPD?
By: Chiwook Chung, MD, and colleagues
Notably, individuals with seropositive RA exhibit a greater risk of COPD onset than those with seronegative RA. Although smoking history didn’t affect the relationship between RA and COPD, monitoring respiratory symptoms and pulmonary function in patients with RA, especially patients who are seropositive, is crucial. These findings underscore the importance of interdisciplinary collaboration between rheumatologists and pulmonologists to enhance early detection and management strategies for pulmonary complications in patients with RA.
– Commentary by Corinne Young, MSN, FNP-C, FCCP, Member of the CHEST Physician® Editorial Board
CHEST Pulmonary®
The Lung Cancer Prediction Model “Stress Test”
By: Brent E. Heideman, MD, and colleagues
Current lung cancer prediction models have limited utility in high-risk patients referred for diagnostic biopsy. In a study of 322 indeterminate pulmonary nodules, the Brock, Mayo Clinic, Herder, and Veterans Affairs models showed modest discrimination between benign and malignant nodules (AUCs 0.67-0.77). The models performed poorly for low-risk patients (negative predictive values 63%-71%) and suboptimally for high-risk patients (positive predictive values 73%-87%), suggesting referring physicians use additional clinical information not captured in these models to identify high-risk patients needing biopsy. New prediction models and biomarkers specifically developed and calibrated for high-risk populations are needed to better inform clinical decision-making. Incorporating interval imaging to assess changes in nodule characteristics could potentially improve model performance. Tailored risk assessment tools are crucial for optimizing management and reducing unnecessary invasive procedures in this challenging patient population.
– Commentary by Russell Miller, MD, Member of the CHEST Physician Editorial Board
CHEST Critical Care ®
Characterizing Cardiac Function in ICU Survivors of Sepsis
By: Kevin Garrity, MBChB, and colleagues
While chronic cardiac dysfunction is one of the proposed mechanisms of long-term impairment post critical illness, its prevalence, mechanisms, and associations with disability following admission for sepsis are not well understood. Garrity and colleagues describe the Characterization of Cardiovascular Function in ICU Survivors of Sepsis (CONDUCT-ICU) protocol, a prospective study including two ICUs in Scotland aimed to better define cardiovascular dysfunction in survivors of sepsis. Designed to enroll 69 patients, demographics, cardiac and inflammatory biomarkers, and echocardiograms will be obtained on ICU discharge with additional laboratory data, cardiac magnetic resonance imaging, and patient-reported outcome measures to be obtained at 6 to 10 weeks. This novel multimodal approach will provide understanding into the role of cardiovascular dysfunction following critical illness as well as offer mechanistic insights. The investigators hope to obtain operational and pilot data for larger future studies.
– Commentary by Eugene Yuriditsky, MD, FCCP, Member of the CHEST Physician Editorial Board
Journal CHEST®
Does Rheumatoid Arthritis Increase the Risk of COPD?
By: Chiwook Chung, MD, and colleagues
Notably, individuals with seropositive RA exhibit a greater risk of COPD onset than those with seronegative RA. Although smoking history didn’t affect the relationship between RA and COPD, monitoring respiratory symptoms and pulmonary function in patients with RA, especially patients who are seropositive, is crucial. These findings underscore the importance of interdisciplinary collaboration between rheumatologists and pulmonologists to enhance early detection and management strategies for pulmonary complications in patients with RA.
– Commentary by Corinne Young, MSN, FNP-C, FCCP, Member of the CHEST Physician® Editorial Board
CHEST Pulmonary®
The Lung Cancer Prediction Model “Stress Test”
By: Brent E. Heideman, MD, and colleagues
Current lung cancer prediction models have limited utility in high-risk patients referred for diagnostic biopsy. In a study of 322 indeterminate pulmonary nodules, the Brock, Mayo Clinic, Herder, and Veterans Affairs models showed modest discrimination between benign and malignant nodules (AUCs 0.67-0.77). The models performed poorly for low-risk patients (negative predictive values 63%-71%) and suboptimally for high-risk patients (positive predictive values 73%-87%), suggesting referring physicians use additional clinical information not captured in these models to identify high-risk patients needing biopsy. New prediction models and biomarkers specifically developed and calibrated for high-risk populations are needed to better inform clinical decision-making. Incorporating interval imaging to assess changes in nodule characteristics could potentially improve model performance. Tailored risk assessment tools are crucial for optimizing management and reducing unnecessary invasive procedures in this challenging patient population.
– Commentary by Russell Miller, MD, Member of the CHEST Physician Editorial Board
CHEST Critical Care ®
Characterizing Cardiac Function in ICU Survivors of Sepsis
By: Kevin Garrity, MBChB, and colleagues
While chronic cardiac dysfunction is one of the proposed mechanisms of long-term impairment post critical illness, its prevalence, mechanisms, and associations with disability following admission for sepsis are not well understood. Garrity and colleagues describe the Characterization of Cardiovascular Function in ICU Survivors of Sepsis (CONDUCT-ICU) protocol, a prospective study including two ICUs in Scotland aimed to better define cardiovascular dysfunction in survivors of sepsis. Designed to enroll 69 patients, demographics, cardiac and inflammatory biomarkers, and echocardiograms will be obtained on ICU discharge with additional laboratory data, cardiac magnetic resonance imaging, and patient-reported outcome measures to be obtained at 6 to 10 weeks. This novel multimodal approach will provide understanding into the role of cardiovascular dysfunction following critical illness as well as offer mechanistic insights. The investigators hope to obtain operational and pilot data for larger future studies.
– Commentary by Eugene Yuriditsky, MD, FCCP, Member of the CHEST Physician Editorial Board
Sex-Related Differences Found in IgG4-Related Disease Epidemiology
TOPLINE:
Men with immunoglobulin G4 (IgG4)-related disease exhibit significantly lower serum lipase levels and a greater likelihood of organ involvement than women, highlighting significant sex-dependent differences in disease manifestations.
METHODOLOGY:
- Researchers conducted a retrospective study of 328 patients (69% men) diagnosed with IgG4-related disease at the Massachusetts General Hospital – Rheumatology Clinic, Boston, who met the American College of Rheumatology–European Alliance of Associations for Rheumatology (ACR-EULAR) classification criteria between January 2008 and May 2023.
- Among the 328 patients, 69% were men and 31% were women, with a significant male-to-female ratio of 2.2:1.0. Men were typically older at diagnosis (median age, 63.7 vs 58.2 years).
- Data on serum lipase levels, renal involvement, and other clinical and laboratory parameters were collected.
TAKEAWAY:
- Men had higher baseline ACR-EULAR scores, indicating more severe disease (median score of 35.0 vs 29.5; P = .0010).
- Male patients demonstrated a median baseline serum lipase concentration of 24.5 U/L, significantly lower than the 33.5 U/L observed in women.
- Pancreatic (50% vs 26%) or renal (36% vs 18%) involvement was more common in men.
- Men exhibited higher IgG4 levels (P = .0050) and active B-cell responses in the blood (P = .0095).
IN PRACTICE:
According to the authors, this work confirms “the impression of an important sex disparity among patients with IgG4-related disease, with most patients being male, and male patients demonstrating strong tendencies toward more severe disease than female patients.”
SOURCE:
The study was led by Isha Jha, MD, Massachusetts General Hospital, Boston. It was published online on May 30, 2024, in The Lancet Rheumatology.
LIMITATIONS:
The study’s retrospective design may limit the ability to establish causality between sex differences and IgG4-related disease manifestations. A relatively small percentage of patients were assessed before receiving any immunosuppressive treatment, potentially influencing the observed clinical parameters.
DISCLOSURES:
This work was supported by the National Institutes of Health/National Institute of Allergy and Infectious Diseases, the Rheumatology Research Foundation, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Some authors declared financial ties outside this work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
Men with immunoglobulin G4 (IgG4)-related disease exhibit significantly lower serum lipase levels and a greater likelihood of organ involvement than women, highlighting significant sex-dependent differences in disease manifestations.
METHODOLOGY:
- Researchers conducted a retrospective study of 328 patients (69% men) diagnosed with IgG4-related disease at the Massachusetts General Hospital – Rheumatology Clinic, Boston, who met the American College of Rheumatology–European Alliance of Associations for Rheumatology (ACR-EULAR) classification criteria between January 2008 and May 2023.
- Among the 328 patients, 69% were men and 31% were women, with a significant male-to-female ratio of 2.2:1.0. Men were typically older at diagnosis (median age, 63.7 vs 58.2 years).
- Data on serum lipase levels, renal involvement, and other clinical and laboratory parameters were collected.
TAKEAWAY:
- Men had higher baseline ACR-EULAR scores, indicating more severe disease (median score of 35.0 vs 29.5; P = .0010).
- Male patients demonstrated a median baseline serum lipase concentration of 24.5 U/L, significantly lower than the 33.5 U/L observed in women.
- Pancreatic (50% vs 26%) or renal (36% vs 18%) involvement was more common in men.
- Men exhibited higher IgG4 levels (P = .0050) and active B-cell responses in the blood (P = .0095).
IN PRACTICE:
According to the authors, this work confirms “the impression of an important sex disparity among patients with IgG4-related disease, with most patients being male, and male patients demonstrating strong tendencies toward more severe disease than female patients.”
SOURCE:
The study was led by Isha Jha, MD, Massachusetts General Hospital, Boston. It was published online on May 30, 2024, in The Lancet Rheumatology.
LIMITATIONS:
The study’s retrospective design may limit the ability to establish causality between sex differences and IgG4-related disease manifestations. A relatively small percentage of patients were assessed before receiving any immunosuppressive treatment, potentially influencing the observed clinical parameters.
DISCLOSURES:
This work was supported by the National Institutes of Health/National Institute of Allergy and Infectious Diseases, the Rheumatology Research Foundation, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Some authors declared financial ties outside this work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
Men with immunoglobulin G4 (IgG4)-related disease exhibit significantly lower serum lipase levels and a greater likelihood of organ involvement than women, highlighting significant sex-dependent differences in disease manifestations.
METHODOLOGY:
- Researchers conducted a retrospective study of 328 patients (69% men) diagnosed with IgG4-related disease at the Massachusetts General Hospital – Rheumatology Clinic, Boston, who met the American College of Rheumatology–European Alliance of Associations for Rheumatology (ACR-EULAR) classification criteria between January 2008 and May 2023.
- Among the 328 patients, 69% were men and 31% were women, with a significant male-to-female ratio of 2.2:1.0. Men were typically older at diagnosis (median age, 63.7 vs 58.2 years).
- Data on serum lipase levels, renal involvement, and other clinical and laboratory parameters were collected.
TAKEAWAY:
- Men had higher baseline ACR-EULAR scores, indicating more severe disease (median score of 35.0 vs 29.5; P = .0010).
- Male patients demonstrated a median baseline serum lipase concentration of 24.5 U/L, significantly lower than the 33.5 U/L observed in women.
- Pancreatic (50% vs 26%) or renal (36% vs 18%) involvement was more common in men.
- Men exhibited higher IgG4 levels (P = .0050) and active B-cell responses in the blood (P = .0095).
IN PRACTICE:
According to the authors, this work confirms “the impression of an important sex disparity among patients with IgG4-related disease, with most patients being male, and male patients demonstrating strong tendencies toward more severe disease than female patients.”
SOURCE:
The study was led by Isha Jha, MD, Massachusetts General Hospital, Boston. It was published online on May 30, 2024, in The Lancet Rheumatology.
LIMITATIONS:
The study’s retrospective design may limit the ability to establish causality between sex differences and IgG4-related disease manifestations. A relatively small percentage of patients were assessed before receiving any immunosuppressive treatment, potentially influencing the observed clinical parameters.
DISCLOSURES:
This work was supported by the National Institutes of Health/National Institute of Allergy and Infectious Diseases, the Rheumatology Research Foundation, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Some authors declared financial ties outside this work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.


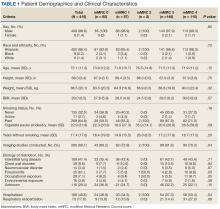

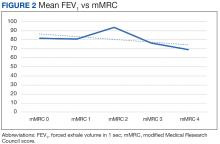
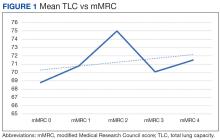
 Author disclosures
Author disclosures


