User login
Official Newspaper of the American College of Surgeons
Bariatric surgery ups risk of suicide, self-harm
NASHVILLE – , according to findings from a meta-analysis presented at the meeting.
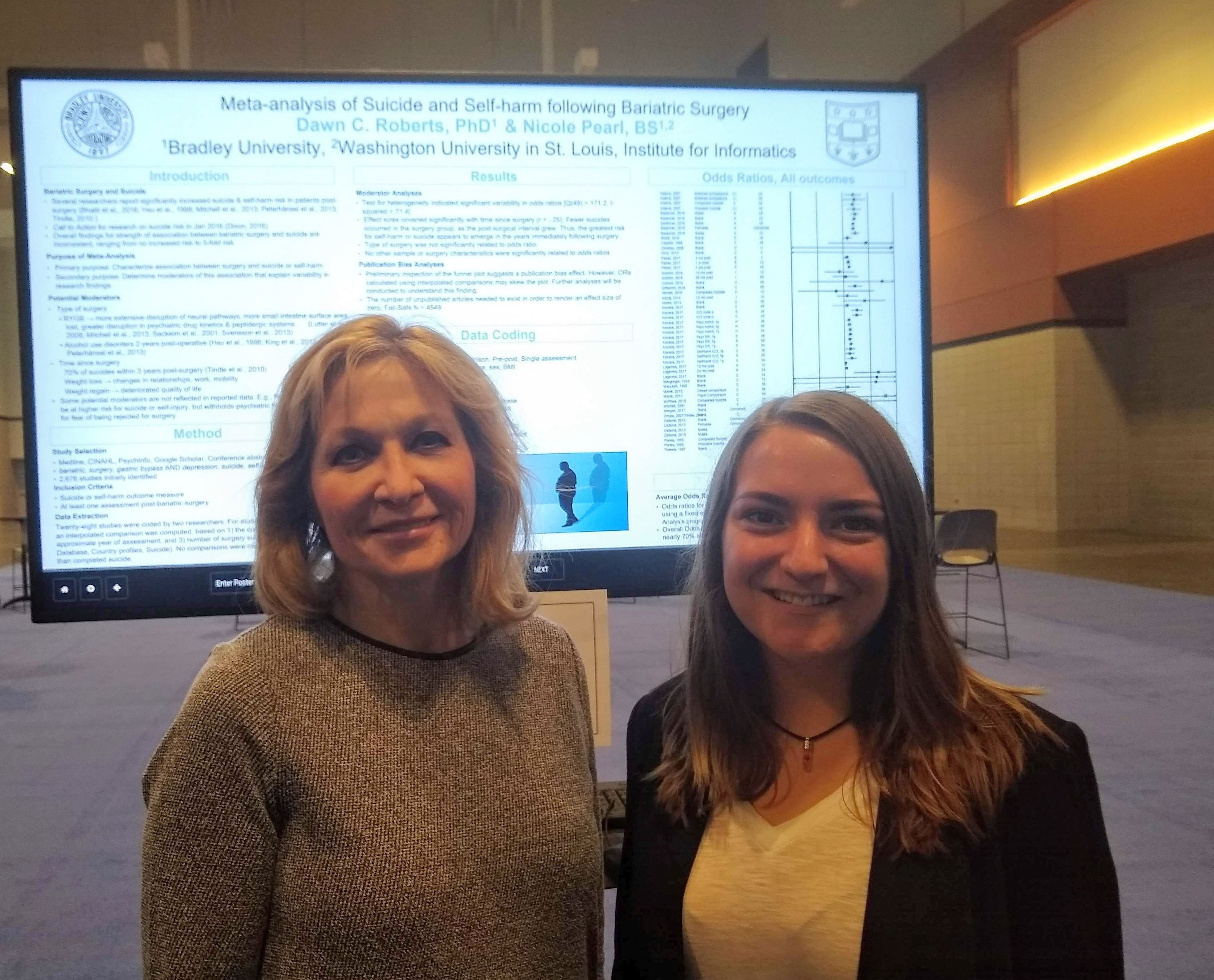
Overall, the odds ratio was 1.69 for self-harm or suicide after bariatric surgery (95% confidence interval, 1.62-1.76; P less than .001), “indicating a nearly 70% increase in risk for self-harm or suicide following bariatric surgery,” wrote Dawn Roberts, PhD, of Bradley University, Peoria, Ill., and her coauthor, Nicole Pearl of Washington University, St. Louis, in the poster accompanying the presentation.
Further, as elapsed time from surgery grew, the suicide rate dropped (effect size covariance, r = –0.25). “Thus, the greatest risk for self-harm or suicide appears to emerge in the years immediately following surgery,” Dr. Roberts said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators had a primary objective of characterizing the association between bariatric surgery and suicide or self-harm. The secondary purpose of the meta-analysis was to find moderators of the association that could explain some of the variability that had previously been seen in studies looking at mental health outcomes after bariatric surgery.
Some of the potential moderators, explained the investigators, included the surgery type. With Roux-en-Y gastric bypass (RYGB), more tissue is removed, potentially causing “more extensive disruption of neural pathways,” the investigators wrote. With greater loss of small-intestine surface area might come more disruption of the gut-brain axis, along with unknown effects on metabolism and pharmacokinetics of psychiatric medication. Additionally, alcohol use disorder might have a more profound effect after gastric bypass surgery.
It had previously been shown that more than two-thirds of suicides happen within the first 3 years after bariatric surgery. With the initial weight loss comes renegotiation of personal relationships, and the potential for more mobility and perhaps expanded career choices; stress accompanies even positive changes in these major life domains. Some patients will also experience weight regain within the first 3 years, after an initial nadir. This also can cause deterioration in quality of life, the investigators explained.
Dr. Roberts and her coinvestigator acknowledge that some of the potential moderators may have been missed in the initial data reporting. For example, the “presurgical sample may be at higher risk for suicide or self-injury but withhold psychiatric history during evaluation for fear of being rejected for surgery.”
From an initial 2,676 studies identified for consideration, investigators in the end extracted data from 28 studies from the United States, Canada, Sweden, and Brazil. The studies had considerable heterogeneity in methods; some included presurgery/postsurgery analyses of the same patients, some had a comparator nonsurgical group, and some used a single postsurgical assessment.
In studies where no nonbariatric comparison sample was available, the investigators assigned interpolated comparison. To arrive at this measure, they drew on the World Health Organization–reported base rate of suicides in the study country at the approximate year of assessment. Suicide was the only interpolated outcome.
Various measures of suicide and self-harm were captured, including completed and probable suicides, suicide attempts, and self-harm events. In some studies, information was drawn from a suicide-specific questionnaire, or from a suicide item on another type of questionnaire.
There was significant variability in the odds ratios for suicide or self-harm across studies, Dr. Roberts said.
The researchers plan to continue analyzing additional measures captured in the meta-analysis, such as gender, age, initial body mass index, surgery type, and the percent of excess weight lost at the time of assessment for suicide or self-harm risk. They reported no outside sources of funding, and no conflicts of interest.
SOURCE: Roberts, D et al. Obesity Week 2018, Poster A433.
NASHVILLE – , according to findings from a meta-analysis presented at the meeting.
Overall, the odds ratio was 1.69 for self-harm or suicide after bariatric surgery (95% confidence interval, 1.62-1.76; P less than .001), “indicating a nearly 70% increase in risk for self-harm or suicide following bariatric surgery,” wrote Dawn Roberts, PhD, of Bradley University, Peoria, Ill., and her coauthor, Nicole Pearl of Washington University, St. Louis, in the poster accompanying the presentation.
Further, as elapsed time from surgery grew, the suicide rate dropped (effect size covariance, r = –0.25). “Thus, the greatest risk for self-harm or suicide appears to emerge in the years immediately following surgery,” Dr. Roberts said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators had a primary objective of characterizing the association between bariatric surgery and suicide or self-harm. The secondary purpose of the meta-analysis was to find moderators of the association that could explain some of the variability that had previously been seen in studies looking at mental health outcomes after bariatric surgery.
Some of the potential moderators, explained the investigators, included the surgery type. With Roux-en-Y gastric bypass (RYGB), more tissue is removed, potentially causing “more extensive disruption of neural pathways,” the investigators wrote. With greater loss of small-intestine surface area might come more disruption of the gut-brain axis, along with unknown effects on metabolism and pharmacokinetics of psychiatric medication. Additionally, alcohol use disorder might have a more profound effect after gastric bypass surgery.
It had previously been shown that more than two-thirds of suicides happen within the first 3 years after bariatric surgery. With the initial weight loss comes renegotiation of personal relationships, and the potential for more mobility and perhaps expanded career choices; stress accompanies even positive changes in these major life domains. Some patients will also experience weight regain within the first 3 years, after an initial nadir. This also can cause deterioration in quality of life, the investigators explained.
Dr. Roberts and her coinvestigator acknowledge that some of the potential moderators may have been missed in the initial data reporting. For example, the “presurgical sample may be at higher risk for suicide or self-injury but withhold psychiatric history during evaluation for fear of being rejected for surgery.”
From an initial 2,676 studies identified for consideration, investigators in the end extracted data from 28 studies from the United States, Canada, Sweden, and Brazil. The studies had considerable heterogeneity in methods; some included presurgery/postsurgery analyses of the same patients, some had a comparator nonsurgical group, and some used a single postsurgical assessment.
In studies where no nonbariatric comparison sample was available, the investigators assigned interpolated comparison. To arrive at this measure, they drew on the World Health Organization–reported base rate of suicides in the study country at the approximate year of assessment. Suicide was the only interpolated outcome.
Various measures of suicide and self-harm were captured, including completed and probable suicides, suicide attempts, and self-harm events. In some studies, information was drawn from a suicide-specific questionnaire, or from a suicide item on another type of questionnaire.
There was significant variability in the odds ratios for suicide or self-harm across studies, Dr. Roberts said.
The researchers plan to continue analyzing additional measures captured in the meta-analysis, such as gender, age, initial body mass index, surgery type, and the percent of excess weight lost at the time of assessment for suicide or self-harm risk. They reported no outside sources of funding, and no conflicts of interest.
SOURCE: Roberts, D et al. Obesity Week 2018, Poster A433.
NASHVILLE – , according to findings from a meta-analysis presented at the meeting.
Overall, the odds ratio was 1.69 for self-harm or suicide after bariatric surgery (95% confidence interval, 1.62-1.76; P less than .001), “indicating a nearly 70% increase in risk for self-harm or suicide following bariatric surgery,” wrote Dawn Roberts, PhD, of Bradley University, Peoria, Ill., and her coauthor, Nicole Pearl of Washington University, St. Louis, in the poster accompanying the presentation.
Further, as elapsed time from surgery grew, the suicide rate dropped (effect size covariance, r = –0.25). “Thus, the greatest risk for self-harm or suicide appears to emerge in the years immediately following surgery,” Dr. Roberts said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators had a primary objective of characterizing the association between bariatric surgery and suicide or self-harm. The secondary purpose of the meta-analysis was to find moderators of the association that could explain some of the variability that had previously been seen in studies looking at mental health outcomes after bariatric surgery.
Some of the potential moderators, explained the investigators, included the surgery type. With Roux-en-Y gastric bypass (RYGB), more tissue is removed, potentially causing “more extensive disruption of neural pathways,” the investigators wrote. With greater loss of small-intestine surface area might come more disruption of the gut-brain axis, along with unknown effects on metabolism and pharmacokinetics of psychiatric medication. Additionally, alcohol use disorder might have a more profound effect after gastric bypass surgery.
It had previously been shown that more than two-thirds of suicides happen within the first 3 years after bariatric surgery. With the initial weight loss comes renegotiation of personal relationships, and the potential for more mobility and perhaps expanded career choices; stress accompanies even positive changes in these major life domains. Some patients will also experience weight regain within the first 3 years, after an initial nadir. This also can cause deterioration in quality of life, the investigators explained.
Dr. Roberts and her coinvestigator acknowledge that some of the potential moderators may have been missed in the initial data reporting. For example, the “presurgical sample may be at higher risk for suicide or self-injury but withhold psychiatric history during evaluation for fear of being rejected for surgery.”
From an initial 2,676 studies identified for consideration, investigators in the end extracted data from 28 studies from the United States, Canada, Sweden, and Brazil. The studies had considerable heterogeneity in methods; some included presurgery/postsurgery analyses of the same patients, some had a comparator nonsurgical group, and some used a single postsurgical assessment.
In studies where no nonbariatric comparison sample was available, the investigators assigned interpolated comparison. To arrive at this measure, they drew on the World Health Organization–reported base rate of suicides in the study country at the approximate year of assessment. Suicide was the only interpolated outcome.
Various measures of suicide and self-harm were captured, including completed and probable suicides, suicide attempts, and self-harm events. In some studies, information was drawn from a suicide-specific questionnaire, or from a suicide item on another type of questionnaire.
There was significant variability in the odds ratios for suicide or self-harm across studies, Dr. Roberts said.
The researchers plan to continue analyzing additional measures captured in the meta-analysis, such as gender, age, initial body mass index, surgery type, and the percent of excess weight lost at the time of assessment for suicide or self-harm risk. They reported no outside sources of funding, and no conflicts of interest.
SOURCE: Roberts, D et al. Obesity Week 2018, Poster A433.
REPORTING FROM OBESITY WEEK 2018
Key clinical point: Bariatric surgery patients have an elevated risk for suicide or self-harm.
Major finding: The odds ratio for suicide or self-harm was 1.69 after bariatric surgery.
Study details: Meta-analysis of 28 studies of bariatric surgery patients.
Disclosures: The authors reported no conflicts of interest and no outside sources of funding.
Source: Roberts D et al. Obesity Week 2018, Poster A433.
All patients with VTE have a high risk of recurrence
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
Recurrence risk is significant among all patients with venous thromboembolism (VTE), though recurrence is most frequent in patients with cancer-related VTE, according to a nationwide Danish study.
Ida Ehlers Albertsen, MD, of Aalborg (Denmark) University Hospital and her coauthors followed 73,993 patients who were diagnosed with incident VTE during January 2000–December 2015. The patients’ VTEs were classified as either cancer-related, unprovoked (occurring in patients without any provoking factors), or provoked (occurring in patients with one or more provoking factors, such as recent major surgery, recent fracture/trauma, obesity, or hormone replacement therapy).
The researchers found similar risks of recurrence among patients with unprovoked and provoked VTE at 6-month follow-up, with rates per 100 person-years of 6.80 and 6.92, respectively. By comparison, the recurrence rate for cancer-related VTE at 6 months was 9.06. The findings were reported in the American Journal of Medicine.
However, at 10-year follow-up the rates were 3.70 for cancer-related VTE, 2.84 for unprovoked VTE, and 2.22 for provoked VTE, which reinforces the belief that “unprovoked venous thromboembolism is associated with long-term higher risk of recurrence than provoked venous thromboembolism.”
Additionally, at 10-year follow-up, the absolute recurrence risk of cancer-related VTE and unprovoked VTE were both at approximately 20%, with recurrence risk of provoked VTE at just above 15%. Compared with the recurrence risk of provoked VTE at 10-year follow-up, the hazard ratios of cancer-related VTE and unprovoked VTE recurrence risk were 1.23 (95% confidence interval, 1.13-1.33) and 1.18 (95% CI, 1.13-1.24), respectively.
The coauthors observed several challenges in comparing their study to previous analyses on recurrent risk, noting that the definition of provoked VTE “varies throughout the literature” and that the majority of VTE studies “provide cumulative incidence proportions and not the actual rates.” They also stated that indefinite or extended therapy for all VTE patients comes with its own potential complications, even with the improved safety of non–vitamin K antagonist oral anticoagulants, writing that “treatment should be given to patients where the benefits outweigh the risks.”
Despite the differences in recurrence rates at 6-month and 10-year follow-up, the coauthors suggested that enough risk was present in all types to warrant additional studies and reconsider how VTE patients are categorized.
“A high recurrence risk in all types of venous thromboembolism indicates that further research is needed to optimize risk stratification for venous thromboembolism patients,” they wrote.
The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
SOURCE: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
FROM THE AMERICAN JOURNAL OF MEDICINE
Key clinical point:
Major finding: At 10-year follow-up, recurrence rates per 100 person-years were 3.70 for patients with cancer-related VTE, 2.84 for patients with unprovoked VTE, and 2.22 for patients with provoked VTE.
Study details: An observational cohort study of 73,993 Danish patients with incident venous thromboembolism during January 2000–December 2015.
Disclosures: The study was partially funded by a grant from the Obel Family Foundation. Some authors reported financial disclosures related to Janssen, Bayer, Roche, and others.
Source: Albertsen IE et al. Am J Med. 2018 Sep;131(9):1067-74.e4.
Hep C–infected livers are safe for transplant
SAN FRANCISCO – A new analysis shows that hepatitis C–infected livers can be safely transplanted into recipients with no effect on graft survival, retransplantation, or mortality. The work confirms that readily available direct-acting antiviral therapy can protect organ recipients and open a source of organs that is typically overlooked.
The work should encourage both physicians and patients to take a closer look at hepatitis C–infected organs, especially for sicker patients, according to Sonali Paul, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Disease 2018.
“A lot of people have an ethical issue with it because we’re actively transplanting a virus into someone. We’re giving someone a disease. My take on it is that we give people Epstein Barr virus or cytomegalovirus all the time – we just [provide] prophylaxis against it, and we don’t even bat an eye. Hepatitis C can be devastating, but we have totally effective treatments for it,” said Dr. Paul, who is an assistant professor of medicine at the University of Chicago.
She cited one colleague at the University of Chicago who several years ago transplanted an organ that had been passed over 700 times, though times have changed since then. “I think people more and more are doing this practice because we know it’s so successful,” said Dr. Paul.
It’s also cost effective. Another study, presented during the same session by Jag Chhatwal, PhD, assistant professor at Harvard Medical School, Boston, showed that accepting a hepatitis C–positive liver is cost effective in patients with Model for End-Stage Liver Disease (MELD) scores ranging from 22 to 40.
“I think we’re going to find across all organ systems, if we can transplant patients rather than keep them on dialysis or keep them on wait lists, it’s got to be cost effective, especially if you think of the health care–associated costs – like a heart transplant patient waiting on the list in the ICU. That’s a huge health care cost,” said Dr. Paul.
Dr. Paul’s team performed an analysis of the Scientific Registry of Transplant Recipients, including single organ transplants from deceased donors, during 2014-2018. Over that period, the number of transplants from hepatitis C–positive donors to hepatitis C–positive recipients rose from 8 in 2014 to 269, and the number of transplants from hepatitis C–positive donors to hepatitis C–negative recipients rose from 0 to 46.
The researchers compared trends from hepatitis C–negative donors with hepatitis C–negative recipients (n = 11,270), negative donors with positive recipients (n = 4,748), positive donors with negative recipients (n = 87), and positive donors with positive recipients (n = 753). Donor status had no effect on graft survival times at 1 or 2 years, with values ranging from 92.6% (negative to negative) to 94.3% (positive to positive) at 1 year and between 85.7% (positive to negative) and 89.7% (positive to positive) at 2 years.
“For someone who has a MELD score of over 20, who has a declining quality of life and really can’t do anything, I think this is a great opportunity. And most patients are absolutely willing to take these organs. We haven’t had many people say no, especially if they feel poorly,” said Dr. Paul.
She also underscored the importance of ensuring that the patient is informed of the status of the donor liver and the need to complete treatment: “The patient has to know what’s happening, and the hospital has to have a safety net if the insurance doesn’t pay for hepatitis C treatment.”
SOURCE: AASLD 2018, Abstract 0249.
SAN FRANCISCO – A new analysis shows that hepatitis C–infected livers can be safely transplanted into recipients with no effect on graft survival, retransplantation, or mortality. The work confirms that readily available direct-acting antiviral therapy can protect organ recipients and open a source of organs that is typically overlooked.
The work should encourage both physicians and patients to take a closer look at hepatitis C–infected organs, especially for sicker patients, according to Sonali Paul, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Disease 2018.
“A lot of people have an ethical issue with it because we’re actively transplanting a virus into someone. We’re giving someone a disease. My take on it is that we give people Epstein Barr virus or cytomegalovirus all the time – we just [provide] prophylaxis against it, and we don’t even bat an eye. Hepatitis C can be devastating, but we have totally effective treatments for it,” said Dr. Paul, who is an assistant professor of medicine at the University of Chicago.
She cited one colleague at the University of Chicago who several years ago transplanted an organ that had been passed over 700 times, though times have changed since then. “I think people more and more are doing this practice because we know it’s so successful,” said Dr. Paul.
It’s also cost effective. Another study, presented during the same session by Jag Chhatwal, PhD, assistant professor at Harvard Medical School, Boston, showed that accepting a hepatitis C–positive liver is cost effective in patients with Model for End-Stage Liver Disease (MELD) scores ranging from 22 to 40.
“I think we’re going to find across all organ systems, if we can transplant patients rather than keep them on dialysis or keep them on wait lists, it’s got to be cost effective, especially if you think of the health care–associated costs – like a heart transplant patient waiting on the list in the ICU. That’s a huge health care cost,” said Dr. Paul.
Dr. Paul’s team performed an analysis of the Scientific Registry of Transplant Recipients, including single organ transplants from deceased donors, during 2014-2018. Over that period, the number of transplants from hepatitis C–positive donors to hepatitis C–positive recipients rose from 8 in 2014 to 269, and the number of transplants from hepatitis C–positive donors to hepatitis C–negative recipients rose from 0 to 46.
The researchers compared trends from hepatitis C–negative donors with hepatitis C–negative recipients (n = 11,270), negative donors with positive recipients (n = 4,748), positive donors with negative recipients (n = 87), and positive donors with positive recipients (n = 753). Donor status had no effect on graft survival times at 1 or 2 years, with values ranging from 92.6% (negative to negative) to 94.3% (positive to positive) at 1 year and between 85.7% (positive to negative) and 89.7% (positive to positive) at 2 years.
“For someone who has a MELD score of over 20, who has a declining quality of life and really can’t do anything, I think this is a great opportunity. And most patients are absolutely willing to take these organs. We haven’t had many people say no, especially if they feel poorly,” said Dr. Paul.
She also underscored the importance of ensuring that the patient is informed of the status of the donor liver and the need to complete treatment: “The patient has to know what’s happening, and the hospital has to have a safety net if the insurance doesn’t pay for hepatitis C treatment.”
SOURCE: AASLD 2018, Abstract 0249.
SAN FRANCISCO – A new analysis shows that hepatitis C–infected livers can be safely transplanted into recipients with no effect on graft survival, retransplantation, or mortality. The work confirms that readily available direct-acting antiviral therapy can protect organ recipients and open a source of organs that is typically overlooked.
The work should encourage both physicians and patients to take a closer look at hepatitis C–infected organs, especially for sicker patients, according to Sonali Paul, MD, who presented the study at the annual meeting of the American Association for the Study of Liver Disease 2018.
“A lot of people have an ethical issue with it because we’re actively transplanting a virus into someone. We’re giving someone a disease. My take on it is that we give people Epstein Barr virus or cytomegalovirus all the time – we just [provide] prophylaxis against it, and we don’t even bat an eye. Hepatitis C can be devastating, but we have totally effective treatments for it,” said Dr. Paul, who is an assistant professor of medicine at the University of Chicago.
She cited one colleague at the University of Chicago who several years ago transplanted an organ that had been passed over 700 times, though times have changed since then. “I think people more and more are doing this practice because we know it’s so successful,” said Dr. Paul.
It’s also cost effective. Another study, presented during the same session by Jag Chhatwal, PhD, assistant professor at Harvard Medical School, Boston, showed that accepting a hepatitis C–positive liver is cost effective in patients with Model for End-Stage Liver Disease (MELD) scores ranging from 22 to 40.
“I think we’re going to find across all organ systems, if we can transplant patients rather than keep them on dialysis or keep them on wait lists, it’s got to be cost effective, especially if you think of the health care–associated costs – like a heart transplant patient waiting on the list in the ICU. That’s a huge health care cost,” said Dr. Paul.
Dr. Paul’s team performed an analysis of the Scientific Registry of Transplant Recipients, including single organ transplants from deceased donors, during 2014-2018. Over that period, the number of transplants from hepatitis C–positive donors to hepatitis C–positive recipients rose from 8 in 2014 to 269, and the number of transplants from hepatitis C–positive donors to hepatitis C–negative recipients rose from 0 to 46.
The researchers compared trends from hepatitis C–negative donors with hepatitis C–negative recipients (n = 11,270), negative donors with positive recipients (n = 4,748), positive donors with negative recipients (n = 87), and positive donors with positive recipients (n = 753). Donor status had no effect on graft survival times at 1 or 2 years, with values ranging from 92.6% (negative to negative) to 94.3% (positive to positive) at 1 year and between 85.7% (positive to negative) and 89.7% (positive to positive) at 2 years.
“For someone who has a MELD score of over 20, who has a declining quality of life and really can’t do anything, I think this is a great opportunity. And most patients are absolutely willing to take these organs. We haven’t had many people say no, especially if they feel poorly,” said Dr. Paul.
She also underscored the importance of ensuring that the patient is informed of the status of the donor liver and the need to complete treatment: “The patient has to know what’s happening, and the hospital has to have a safety net if the insurance doesn’t pay for hepatitis C treatment.”
SOURCE: AASLD 2018, Abstract 0249.
REPORTING FROM THE LIVER MEETING 2018
Key clinical point: Use of hepatitis C–positive livers can significantly increase the donor organ pool.
Major finding: Hepatitis C–infected livers can be safely transplanted into recipients with no effect on graft survival, retransplantation, or mortality.
Study details: Retrospective analysis of 16,858 liver transplants.
Disclosures: The study was funded internally. Dr. Paul has no financial disclosures.
Source: AASLD 2018, Abstract 0249.
Total knee replacement risk soars after arthroscopic surgery for meniscal tear
CHICAGO – A 5-year follow-up of a major randomized trial comparing methods of meniscal tear management in patients with osteoarthritis showed the risk of total knee replacement was 400% greater in patients who underwent arthroscopic partial meniscectomy than in those who received physical therapy alone, Jeffrey N. Katz, MD, reported at the annual meeting of the American College of Rheumatology.
At 5 years, however, the two divergent initial treatment strategies – arthroscopic surgical repair versus physical therapy – resulted in similar degrees of long-term pain improvement, noted Dr. Katz, a rheumatologist who is professor of medicine and orthopedic surgery at Harvard Medical School, Boston.
“Because that’s the case, a reasonable recommendation – and one that most folks around the world who are thinking about this problem would make – is to have the first choice initially be nonoperative; that is, physical therapy, with surgery reserved for those who don’t improve and who have an interest in undertaking the risks of surgery,” he said.
Dr. Katz presented 5-year follow-up data on 341 participants in the MeTeOR trial, a seven-center study in which middle-age or older subjects with knee pain, a meniscal tear, and osteoarthritic changes on x-ray were randomized to arthroscopic repair or physical therapy. A lot rides on the outcomes of this study, as there is a longstanding debate over the balance of risks and benefits of arthroscopic surgery in this common clinical scenario.
Of the 351 participants, 164 were randomized to and received arthroscopic partial meniscectomy, 109 were randomized to and received a standardized program of physical therapy, and 68 were initially randomized to physical therapy but crossed over to arthroscopic surgery within the first few months because of lack of improvement.
At 5 years of follow-up, all three groups showed similar degrees of improvement in Knee Osteoarthritis and Injury Outcome Score Pain Scale scores, from 40-50 out of a possible 100 at baseline to 20-25 at 6 months, with little change thereafter through 5 years.
The eye-catching finding was the difference in the incidence of total knee replacement (TKR) through 5 years: 10% in those who underwent arthroscopic partial meniscectomy, either as initial therapy or after crossing over from the physical therapy group, compared with 2% in patients who underwent physical therapy alone. Given that more than 400,000 arthroscopic partial meniscectomies are done annually in the United States in patients with knee osteoarthritis, extrapolation from the MeTeOR results suggests an excess of 40,000 total knee replacements in surgically treated patients.
“The higher TKR rates that we observed in surgically treated patients are unexplained, concerning, and require further study. The finding is consistent with the observation in the Osteoarthritis Initiative that TKR rates were higher in patients with arthroscopy as opposed to those treated nonsurgically,” the rheumatologist said.
He proposed two possible explanations for the finding. “It does appear that people who have arthroscopic surgery are then, over the next 5 years, more likely to have total knee replacement. We don’t know whether that is because performing arthroscopic surgery is actually damaging the knee further, leading it to deteriorate more quickly and therefore go on to total knee replacement, or whether when patients develop a relationship with a surgeon and have arthroscopic surgery, they get over some of their apprehension about surgery and may become more likely to accept subsequent surgery for total knee replacement. We hope to find the answer. I think this story is still unfolding because 5 years is a relatively brief period of time in the course of osteoarthritis.
“Arthroscopic surgery certainly offers greater shorter-term improvement, and for some patients that’s worth trading off some downstream risk of joint damage, and for others, they would not want to make that trade-off. So I see it ultimately as a matter of patient choice,” Dr. Katz said.
Knee osteoarthritis affects an estimated 15 million Americans. More than one-half of them have a meniscal tear, the majority of which don’t cause symptoms.
Dr. Katz reported having no financial conflicts regarding MeTeOR, which was funded by the National Institutes of Health.
SOURCE: Katz JN et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 1816.
CHICAGO – A 5-year follow-up of a major randomized trial comparing methods of meniscal tear management in patients with osteoarthritis showed the risk of total knee replacement was 400% greater in patients who underwent arthroscopic partial meniscectomy than in those who received physical therapy alone, Jeffrey N. Katz, MD, reported at the annual meeting of the American College of Rheumatology.
At 5 years, however, the two divergent initial treatment strategies – arthroscopic surgical repair versus physical therapy – resulted in similar degrees of long-term pain improvement, noted Dr. Katz, a rheumatologist who is professor of medicine and orthopedic surgery at Harvard Medical School, Boston.
“Because that’s the case, a reasonable recommendation – and one that most folks around the world who are thinking about this problem would make – is to have the first choice initially be nonoperative; that is, physical therapy, with surgery reserved for those who don’t improve and who have an interest in undertaking the risks of surgery,” he said.
Dr. Katz presented 5-year follow-up data on 341 participants in the MeTeOR trial, a seven-center study in which middle-age or older subjects with knee pain, a meniscal tear, and osteoarthritic changes on x-ray were randomized to arthroscopic repair or physical therapy. A lot rides on the outcomes of this study, as there is a longstanding debate over the balance of risks and benefits of arthroscopic surgery in this common clinical scenario.
Of the 351 participants, 164 were randomized to and received arthroscopic partial meniscectomy, 109 were randomized to and received a standardized program of physical therapy, and 68 were initially randomized to physical therapy but crossed over to arthroscopic surgery within the first few months because of lack of improvement.
At 5 years of follow-up, all three groups showed similar degrees of improvement in Knee Osteoarthritis and Injury Outcome Score Pain Scale scores, from 40-50 out of a possible 100 at baseline to 20-25 at 6 months, with little change thereafter through 5 years.
The eye-catching finding was the difference in the incidence of total knee replacement (TKR) through 5 years: 10% in those who underwent arthroscopic partial meniscectomy, either as initial therapy or after crossing over from the physical therapy group, compared with 2% in patients who underwent physical therapy alone. Given that more than 400,000 arthroscopic partial meniscectomies are done annually in the United States in patients with knee osteoarthritis, extrapolation from the MeTeOR results suggests an excess of 40,000 total knee replacements in surgically treated patients.
“The higher TKR rates that we observed in surgically treated patients are unexplained, concerning, and require further study. The finding is consistent with the observation in the Osteoarthritis Initiative that TKR rates were higher in patients with arthroscopy as opposed to those treated nonsurgically,” the rheumatologist said.
He proposed two possible explanations for the finding. “It does appear that people who have arthroscopic surgery are then, over the next 5 years, more likely to have total knee replacement. We don’t know whether that is because performing arthroscopic surgery is actually damaging the knee further, leading it to deteriorate more quickly and therefore go on to total knee replacement, or whether when patients develop a relationship with a surgeon and have arthroscopic surgery, they get over some of their apprehension about surgery and may become more likely to accept subsequent surgery for total knee replacement. We hope to find the answer. I think this story is still unfolding because 5 years is a relatively brief period of time in the course of osteoarthritis.
“Arthroscopic surgery certainly offers greater shorter-term improvement, and for some patients that’s worth trading off some downstream risk of joint damage, and for others, they would not want to make that trade-off. So I see it ultimately as a matter of patient choice,” Dr. Katz said.
Knee osteoarthritis affects an estimated 15 million Americans. More than one-half of them have a meniscal tear, the majority of which don’t cause symptoms.
Dr. Katz reported having no financial conflicts regarding MeTeOR, which was funded by the National Institutes of Health.
SOURCE: Katz JN et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 1816.
CHICAGO – A 5-year follow-up of a major randomized trial comparing methods of meniscal tear management in patients with osteoarthritis showed the risk of total knee replacement was 400% greater in patients who underwent arthroscopic partial meniscectomy than in those who received physical therapy alone, Jeffrey N. Katz, MD, reported at the annual meeting of the American College of Rheumatology.
At 5 years, however, the two divergent initial treatment strategies – arthroscopic surgical repair versus physical therapy – resulted in similar degrees of long-term pain improvement, noted Dr. Katz, a rheumatologist who is professor of medicine and orthopedic surgery at Harvard Medical School, Boston.
“Because that’s the case, a reasonable recommendation – and one that most folks around the world who are thinking about this problem would make – is to have the first choice initially be nonoperative; that is, physical therapy, with surgery reserved for those who don’t improve and who have an interest in undertaking the risks of surgery,” he said.
Dr. Katz presented 5-year follow-up data on 341 participants in the MeTeOR trial, a seven-center study in which middle-age or older subjects with knee pain, a meniscal tear, and osteoarthritic changes on x-ray were randomized to arthroscopic repair or physical therapy. A lot rides on the outcomes of this study, as there is a longstanding debate over the balance of risks and benefits of arthroscopic surgery in this common clinical scenario.
Of the 351 participants, 164 were randomized to and received arthroscopic partial meniscectomy, 109 were randomized to and received a standardized program of physical therapy, and 68 were initially randomized to physical therapy but crossed over to arthroscopic surgery within the first few months because of lack of improvement.
At 5 years of follow-up, all three groups showed similar degrees of improvement in Knee Osteoarthritis and Injury Outcome Score Pain Scale scores, from 40-50 out of a possible 100 at baseline to 20-25 at 6 months, with little change thereafter through 5 years.
The eye-catching finding was the difference in the incidence of total knee replacement (TKR) through 5 years: 10% in those who underwent arthroscopic partial meniscectomy, either as initial therapy or after crossing over from the physical therapy group, compared with 2% in patients who underwent physical therapy alone. Given that more than 400,000 arthroscopic partial meniscectomies are done annually in the United States in patients with knee osteoarthritis, extrapolation from the MeTeOR results suggests an excess of 40,000 total knee replacements in surgically treated patients.
“The higher TKR rates that we observed in surgically treated patients are unexplained, concerning, and require further study. The finding is consistent with the observation in the Osteoarthritis Initiative that TKR rates were higher in patients with arthroscopy as opposed to those treated nonsurgically,” the rheumatologist said.
He proposed two possible explanations for the finding. “It does appear that people who have arthroscopic surgery are then, over the next 5 years, more likely to have total knee replacement. We don’t know whether that is because performing arthroscopic surgery is actually damaging the knee further, leading it to deteriorate more quickly and therefore go on to total knee replacement, or whether when patients develop a relationship with a surgeon and have arthroscopic surgery, they get over some of their apprehension about surgery and may become more likely to accept subsequent surgery for total knee replacement. We hope to find the answer. I think this story is still unfolding because 5 years is a relatively brief period of time in the course of osteoarthritis.
“Arthroscopic surgery certainly offers greater shorter-term improvement, and for some patients that’s worth trading off some downstream risk of joint damage, and for others, they would not want to make that trade-off. So I see it ultimately as a matter of patient choice,” Dr. Katz said.
Knee osteoarthritis affects an estimated 15 million Americans. More than one-half of them have a meniscal tear, the majority of which don’t cause symptoms.
Dr. Katz reported having no financial conflicts regarding MeTeOR, which was funded by the National Institutes of Health.
SOURCE: Katz JN et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 1816.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: Risk of total knee replacement is five times higher after arthroscopic partial meniscectomy.
Major finding: Patients randomized to arthroscopic partial meniscectomy were 400% more likely to subsequently undergo total knee replacement than were those randomized to physical therapy alone.
Study details: This was a presentation of the 5-year follow-up results in 341 participants in the MeTeOR trial, a seven-center study in which middle-age or older subjects with knee pain, a meniscal tear, and osteoarthritic changes on x-ray were randomized to arthroscopic repair or physical therapy.
Disclosures: The presenter reported having no financial conflicts regarding MeTeOR, which was funded by the National Institutes of Health.
Source: Katz JN et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 1816.
Leg ulceration guidelines expected to soon include endovascular ablation
NEW YORK – Guidelines for the management of leg ulcerations will be changed to accommodate the results of the Early Venous Reflux Ablation trial, according to this video interview with the senior author, Alun H Davies, DSc, professor of vascular surgery, Imperial College, London.
In this video interview, conducted at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation, Dr. Davies recaps the major results of the study, which associated immediate endovascular ablation (early intervention) with significantly faster healing than did compression therapy with ablation, considered only after 6 months (delayed intervention).
These data have been published (N Engl J Med 2018 May 31;378:2105-14), but Dr. Davies focused in this interview on the cost efficacy of early intervention with endovascular ablation. In the United Kingdom, where the study was conducted, the data support the cost efficacy, but Dr. Davies predicted even greater savings in the United States because of the expense of frequent wound care visits.
Based on data from a randomized trial, he expects guidelines, including those in the United States, to be revised to list early endovascular ablation as a 1b or 1A recommendation, thereby establishing this intervention as a standard.
If follow-up after 3 years confirms a lower rate of recurrence, an advantage previously shown for open surgery relative to compression healing, the case for early endovascular intervention will be even stronger, according to Dr. Davies.
NEW YORK – Guidelines for the management of leg ulcerations will be changed to accommodate the results of the Early Venous Reflux Ablation trial, according to this video interview with the senior author, Alun H Davies, DSc, professor of vascular surgery, Imperial College, London.
In this video interview, conducted at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation, Dr. Davies recaps the major results of the study, which associated immediate endovascular ablation (early intervention) with significantly faster healing than did compression therapy with ablation, considered only after 6 months (delayed intervention).
These data have been published (N Engl J Med 2018 May 31;378:2105-14), but Dr. Davies focused in this interview on the cost efficacy of early intervention with endovascular ablation. In the United Kingdom, where the study was conducted, the data support the cost efficacy, but Dr. Davies predicted even greater savings in the United States because of the expense of frequent wound care visits.
Based on data from a randomized trial, he expects guidelines, including those in the United States, to be revised to list early endovascular ablation as a 1b or 1A recommendation, thereby establishing this intervention as a standard.
If follow-up after 3 years confirms a lower rate of recurrence, an advantage previously shown for open surgery relative to compression healing, the case for early endovascular intervention will be even stronger, according to Dr. Davies.
NEW YORK – Guidelines for the management of leg ulcerations will be changed to accommodate the results of the Early Venous Reflux Ablation trial, according to this video interview with the senior author, Alun H Davies, DSc, professor of vascular surgery, Imperial College, London.
In this video interview, conducted at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation, Dr. Davies recaps the major results of the study, which associated immediate endovascular ablation (early intervention) with significantly faster healing than did compression therapy with ablation, considered only after 6 months (delayed intervention).
These data have been published (N Engl J Med 2018 May 31;378:2105-14), but Dr. Davies focused in this interview on the cost efficacy of early intervention with endovascular ablation. In the United Kingdom, where the study was conducted, the data support the cost efficacy, but Dr. Davies predicted even greater savings in the United States because of the expense of frequent wound care visits.
Based on data from a randomized trial, he expects guidelines, including those in the United States, to be revised to list early endovascular ablation as a 1b or 1A recommendation, thereby establishing this intervention as a standard.
If follow-up after 3 years confirms a lower rate of recurrence, an advantage previously shown for open surgery relative to compression healing, the case for early endovascular intervention will be even stronger, according to Dr. Davies.
REPORTING FROM VEITHSYMPOSIUM
Tegaderm eliminates corneal abrasions in robotic gynecologic surgery
LAS VEGAS – There hasn’t been a single corneal abrasion in 860 cases of gynecologic robotic surgery at the University of Texas, Austin, since surgeons and anesthesiologists there started sealing women’s eyes shut with a thick layer of ointment and Tegaderm, instead of the usual small squeeze of ointment and tape, according to Michael T. Breen, MD, a gynecologic surgeon at the university.
“Go back to your hospital, meet with your anesthesiologists, and see what you’re doing to protect your patients’ eyes,” Dr. Breen said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
Slathered eyes and Tegaderm are now standard practice at the university. Before the switch was made, there were six corneal abrasions in 231 cases over 6 months. Two of those patients stayed longer in the hospital than they would have otherwise. The changes have eliminated the problem.
The impetus for the switch was a 42-year-old woman who had a robotic hysterectomy. The surgery went fine, but then Dr. Breen had to rush back to the recovery room. The woman was screaming in pain, not from her surgery, but from her left eye.
Corneal abrasions are a well-known risk of surgery because anesthesia decreases tear production and dries the eyes. Robotic gynecologic surgery increases the risk even more, because patients are under longer than with other approaches, and the steep Trendelenburg increases intraocular pressure and eye edema, especially with excess IV fluid.
And “believe it or not, having a pulse oximeter on the dominant hand [also] increases your risk of ocular injury,” Dr. Breen said. Sometimes, patients wake up, go to rub their eyes, and drag the device across their cornea, he said.
The screaming patient – who recovered without permanent damage – prompted Dr. Breen and his colleagues to turn to the literature for solutions. “One was a fully occlusive eye dressing, more than the tape we’ve all been accustomed to, with thick eye ointment application and Tegaderm applying positive pressure to the eye,” he said.
Dr. Breen showed his audience a slide of the setup. “It looks a little unorthodox, but this is how every one of our robotic patients now have their eyes protected. Thick gel which is then covered with a positive pressure Tegaderm,” he said.
, and placing the pulse ox on the nondominant hand. The team already had been decreasing IV fluids as part of their enhanced recovery after surgery protocol, and bringing patients out of steep Trendelenburg as soon as possible.
With the changes, “the rate of corneal abrasions decreased from 2.6% to 0% – and has stayed there,” Dr. Breen said.
There’ve been no allergic reactions to Tegaderm and no eyelid problems. “What we have seen with the simple taping is that, when it comes off, so does some of the eyelid, particularly with geriatric patients. We have not seen that with Tegaderm,” he said.
“Some people use goggles to protect the eyes, and we thought initially that the camera was hitting the face, so we used the Mayo stand to protect it from the camera,” but that didn’t turn out to be the problem, he said. “Goggles actually may make things worse.”
The project had no industry funding, and Dr. Breen had no relevant disclosures.
aotto@mdedge.com
SOURCE: Breen MT et al. 2018 AAGL Global Congress, Abstract 16.
LAS VEGAS – There hasn’t been a single corneal abrasion in 860 cases of gynecologic robotic surgery at the University of Texas, Austin, since surgeons and anesthesiologists there started sealing women’s eyes shut with a thick layer of ointment and Tegaderm, instead of the usual small squeeze of ointment and tape, according to Michael T. Breen, MD, a gynecologic surgeon at the university.
“Go back to your hospital, meet with your anesthesiologists, and see what you’re doing to protect your patients’ eyes,” Dr. Breen said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
Slathered eyes and Tegaderm are now standard practice at the university. Before the switch was made, there were six corneal abrasions in 231 cases over 6 months. Two of those patients stayed longer in the hospital than they would have otherwise. The changes have eliminated the problem.
The impetus for the switch was a 42-year-old woman who had a robotic hysterectomy. The surgery went fine, but then Dr. Breen had to rush back to the recovery room. The woman was screaming in pain, not from her surgery, but from her left eye.
Corneal abrasions are a well-known risk of surgery because anesthesia decreases tear production and dries the eyes. Robotic gynecologic surgery increases the risk even more, because patients are under longer than with other approaches, and the steep Trendelenburg increases intraocular pressure and eye edema, especially with excess IV fluid.
And “believe it or not, having a pulse oximeter on the dominant hand [also] increases your risk of ocular injury,” Dr. Breen said. Sometimes, patients wake up, go to rub their eyes, and drag the device across their cornea, he said.
The screaming patient – who recovered without permanent damage – prompted Dr. Breen and his colleagues to turn to the literature for solutions. “One was a fully occlusive eye dressing, more than the tape we’ve all been accustomed to, with thick eye ointment application and Tegaderm applying positive pressure to the eye,” he said.
Dr. Breen showed his audience a slide of the setup. “It looks a little unorthodox, but this is how every one of our robotic patients now have their eyes protected. Thick gel which is then covered with a positive pressure Tegaderm,” he said.
, and placing the pulse ox on the nondominant hand. The team already had been decreasing IV fluids as part of their enhanced recovery after surgery protocol, and bringing patients out of steep Trendelenburg as soon as possible.
With the changes, “the rate of corneal abrasions decreased from 2.6% to 0% – and has stayed there,” Dr. Breen said.
There’ve been no allergic reactions to Tegaderm and no eyelid problems. “What we have seen with the simple taping is that, when it comes off, so does some of the eyelid, particularly with geriatric patients. We have not seen that with Tegaderm,” he said.
“Some people use goggles to protect the eyes, and we thought initially that the camera was hitting the face, so we used the Mayo stand to protect it from the camera,” but that didn’t turn out to be the problem, he said. “Goggles actually may make things worse.”
The project had no industry funding, and Dr. Breen had no relevant disclosures.
aotto@mdedge.com
SOURCE: Breen MT et al. 2018 AAGL Global Congress, Abstract 16.
LAS VEGAS – There hasn’t been a single corneal abrasion in 860 cases of gynecologic robotic surgery at the University of Texas, Austin, since surgeons and anesthesiologists there started sealing women’s eyes shut with a thick layer of ointment and Tegaderm, instead of the usual small squeeze of ointment and tape, according to Michael T. Breen, MD, a gynecologic surgeon at the university.
“Go back to your hospital, meet with your anesthesiologists, and see what you’re doing to protect your patients’ eyes,” Dr. Breen said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
Slathered eyes and Tegaderm are now standard practice at the university. Before the switch was made, there were six corneal abrasions in 231 cases over 6 months. Two of those patients stayed longer in the hospital than they would have otherwise. The changes have eliminated the problem.
The impetus for the switch was a 42-year-old woman who had a robotic hysterectomy. The surgery went fine, but then Dr. Breen had to rush back to the recovery room. The woman was screaming in pain, not from her surgery, but from her left eye.
Corneal abrasions are a well-known risk of surgery because anesthesia decreases tear production and dries the eyes. Robotic gynecologic surgery increases the risk even more, because patients are under longer than with other approaches, and the steep Trendelenburg increases intraocular pressure and eye edema, especially with excess IV fluid.
And “believe it or not, having a pulse oximeter on the dominant hand [also] increases your risk of ocular injury,” Dr. Breen said. Sometimes, patients wake up, go to rub their eyes, and drag the device across their cornea, he said.
The screaming patient – who recovered without permanent damage – prompted Dr. Breen and his colleagues to turn to the literature for solutions. “One was a fully occlusive eye dressing, more than the tape we’ve all been accustomed to, with thick eye ointment application and Tegaderm applying positive pressure to the eye,” he said.
Dr. Breen showed his audience a slide of the setup. “It looks a little unorthodox, but this is how every one of our robotic patients now have their eyes protected. Thick gel which is then covered with a positive pressure Tegaderm,” he said.
, and placing the pulse ox on the nondominant hand. The team already had been decreasing IV fluids as part of their enhanced recovery after surgery protocol, and bringing patients out of steep Trendelenburg as soon as possible.
With the changes, “the rate of corneal abrasions decreased from 2.6% to 0% – and has stayed there,” Dr. Breen said.
There’ve been no allergic reactions to Tegaderm and no eyelid problems. “What we have seen with the simple taping is that, when it comes off, so does some of the eyelid, particularly with geriatric patients. We have not seen that with Tegaderm,” he said.
“Some people use goggles to protect the eyes, and we thought initially that the camera was hitting the face, so we used the Mayo stand to protect it from the camera,” but that didn’t turn out to be the problem, he said. “Goggles actually may make things worse.”
The project had no industry funding, and Dr. Breen had no relevant disclosures.
aotto@mdedge.com
SOURCE: Breen MT et al. 2018 AAGL Global Congress, Abstract 16.
REPORTING FROM THE AAGL GLOBAL CONGRESS
Key clinical point: “The rate of corneal abrasions decreased from 2.6% to 0% – and has stayed there.”
Major finding: Of the 860 cases of gynecologic robotic surgery at the University of Texas, Austin, there has not been a single case of corneal abrasion since the switch.
Study details: Quality improvement project at the university.
Disclosures: The project had no industry funding, and Dr. Breen had no relevant disclosures.
Source: Breen MT et al. 2018 AAGL Global Congress, Abstract 16.
Smaller assistant ports mean less prolapse repair pain
LAS VEGAS – Patients experience less right-sided pain after laparoscopic sacrocolpopexy when surgeons use an 8-mm assistant port instead of a 12-mm port, results from a small trial show.
In the trial, conducted at Loyola University Medical Center in Maywood, Ill.,17 women were randomized to undergo the procedure with an 8-mm assistant port, and 18 with a 12-mm port, both on the right side of the abdomen.
Overall, pain severity was low at 2 weeks postop in both groups at just over 1 point on a 10-point visual analogue scale and not statistically different. However, patients who had a 12-mm assistant port were more likely to report right-sided pain, compared with those who had an 8-mm assistant port (60% vs.18%, P = 0.027).
“I saw a lot of these patients in the clinic at 2 weeks, and even though the overall pain score was low, they kept complaining about a dull, achy pain on the right side. They were using ibuprofen, and some of them had even restricted [their activities] because they were afraid they were going to pop a stitch,” said study lead Yufan B. Chen, MD, a urogynecology fellow at Loyola.
He said the research team thinks the difference in port-site pain “is clinically significant. . Since our study ended, we have stopped using the 12-mm port in most of our cases; we use the 8-mm port for the assistant,” he said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
The tradeoff was that there were more needle struggles with the 8-mm port, 3.1/case vs. 0.6/case (P = .004). Surgeons found inserting and withdrawing the Gore-Tex needle through the smaller port more difficult. But there were no needle losses in either group and no differences in operative time – an average of about 95 minutes.
“The larger port size essentially benefits the surgeon more than the patient. This is kind of a common theme in minimally invasive surgery where less is actually more,” he said. Since the study, “we have identified why we have challenges with the needle transport; it’s usually because the needle gets bent, so we just unbend it a little bit with our needle drivers before we remove it,” Dr. Chen said.
Even so, “there may be a role in using the 12-mm port when you have assistants who are not [that] experienced,” he said.
Laparoscopic sacrocolpopexy is done through four ports at Loyola: a 12-mm umbilical port for the scope; two 5-mm ports on the left for the primary surgeon; and the right side port for the assistant, through which the Gore-Tex needle is passed.
In the study, there were no demographic or preop differences between the two groups of women. About 60% were white, with a mean age of 61 years. About 10% of the women had had prior abdominal surgery.
The study received no industry funding, and the investigators had no disclosures.
aotto@mdedge.com
SOURCE: Chen YB et al. 2018 AAGL Global Congress, Abstract 197.
LAS VEGAS – Patients experience less right-sided pain after laparoscopic sacrocolpopexy when surgeons use an 8-mm assistant port instead of a 12-mm port, results from a small trial show.
In the trial, conducted at Loyola University Medical Center in Maywood, Ill.,17 women were randomized to undergo the procedure with an 8-mm assistant port, and 18 with a 12-mm port, both on the right side of the abdomen.
Overall, pain severity was low at 2 weeks postop in both groups at just over 1 point on a 10-point visual analogue scale and not statistically different. However, patients who had a 12-mm assistant port were more likely to report right-sided pain, compared with those who had an 8-mm assistant port (60% vs.18%, P = 0.027).
“I saw a lot of these patients in the clinic at 2 weeks, and even though the overall pain score was low, they kept complaining about a dull, achy pain on the right side. They were using ibuprofen, and some of them had even restricted [their activities] because they were afraid they were going to pop a stitch,” said study lead Yufan B. Chen, MD, a urogynecology fellow at Loyola.
He said the research team thinks the difference in port-site pain “is clinically significant. . Since our study ended, we have stopped using the 12-mm port in most of our cases; we use the 8-mm port for the assistant,” he said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
The tradeoff was that there were more needle struggles with the 8-mm port, 3.1/case vs. 0.6/case (P = .004). Surgeons found inserting and withdrawing the Gore-Tex needle through the smaller port more difficult. But there were no needle losses in either group and no differences in operative time – an average of about 95 minutes.
“The larger port size essentially benefits the surgeon more than the patient. This is kind of a common theme in minimally invasive surgery where less is actually more,” he said. Since the study, “we have identified why we have challenges with the needle transport; it’s usually because the needle gets bent, so we just unbend it a little bit with our needle drivers before we remove it,” Dr. Chen said.
Even so, “there may be a role in using the 12-mm port when you have assistants who are not [that] experienced,” he said.
Laparoscopic sacrocolpopexy is done through four ports at Loyola: a 12-mm umbilical port for the scope; two 5-mm ports on the left for the primary surgeon; and the right side port for the assistant, through which the Gore-Tex needle is passed.
In the study, there were no demographic or preop differences between the two groups of women. About 60% were white, with a mean age of 61 years. About 10% of the women had had prior abdominal surgery.
The study received no industry funding, and the investigators had no disclosures.
aotto@mdedge.com
SOURCE: Chen YB et al. 2018 AAGL Global Congress, Abstract 197.
LAS VEGAS – Patients experience less right-sided pain after laparoscopic sacrocolpopexy when surgeons use an 8-mm assistant port instead of a 12-mm port, results from a small trial show.
In the trial, conducted at Loyola University Medical Center in Maywood, Ill.,17 women were randomized to undergo the procedure with an 8-mm assistant port, and 18 with a 12-mm port, both on the right side of the abdomen.
Overall, pain severity was low at 2 weeks postop in both groups at just over 1 point on a 10-point visual analogue scale and not statistically different. However, patients who had a 12-mm assistant port were more likely to report right-sided pain, compared with those who had an 8-mm assistant port (60% vs.18%, P = 0.027).
“I saw a lot of these patients in the clinic at 2 weeks, and even though the overall pain score was low, they kept complaining about a dull, achy pain on the right side. They were using ibuprofen, and some of them had even restricted [their activities] because they were afraid they were going to pop a stitch,” said study lead Yufan B. Chen, MD, a urogynecology fellow at Loyola.
He said the research team thinks the difference in port-site pain “is clinically significant. . Since our study ended, we have stopped using the 12-mm port in most of our cases; we use the 8-mm port for the assistant,” he said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
The tradeoff was that there were more needle struggles with the 8-mm port, 3.1/case vs. 0.6/case (P = .004). Surgeons found inserting and withdrawing the Gore-Tex needle through the smaller port more difficult. But there were no needle losses in either group and no differences in operative time – an average of about 95 minutes.
“The larger port size essentially benefits the surgeon more than the patient. This is kind of a common theme in minimally invasive surgery where less is actually more,” he said. Since the study, “we have identified why we have challenges with the needle transport; it’s usually because the needle gets bent, so we just unbend it a little bit with our needle drivers before we remove it,” Dr. Chen said.
Even so, “there may be a role in using the 12-mm port when you have assistants who are not [that] experienced,” he said.
Laparoscopic sacrocolpopexy is done through four ports at Loyola: a 12-mm umbilical port for the scope; two 5-mm ports on the left for the primary surgeon; and the right side port for the assistant, through which the Gore-Tex needle is passed.
In the study, there were no demographic or preop differences between the two groups of women. About 60% were white, with a mean age of 61 years. About 10% of the women had had prior abdominal surgery.
The study received no industry funding, and the investigators had no disclosures.
aotto@mdedge.com
SOURCE: Chen YB et al. 2018 AAGL Global Congress, Abstract 197.
REPORTING FROM AAGL GLOBAL CONGRESS
Key clinical point: Patients experienced less pain at 2 weeks with a smaller port; there are also more needle struggles, but that can be easily fixed.
Major finding: Patients who had a 12-mm assistant port were more likely to report right-sided pain, compared with those who received an 8- mm assistant port (60% vs. 18%, P = 0.027).
Study details: Randomized trial with 35 women.
Disclosures: The study received no industry funding, and the investigators had no disclosures.
Source: Chen YB et al. 2018 AAGL Global Congress, Abstract 197.
Try to normalize albumin before laparoscopic hysterectomy
LAS VEGAS – Serum albumin is an everyday health marker commonly used for risk assessment in open abdominal procedures, but it’s often not checked before laparoscopic hysterectomies.
Low levels mean something is off, be it malnutrition, inflammation, chronic disease, or other problems. If it can be normalized before surgery, it should be; women probably will do better, according to investigators from the University of Kentucky, Lexington.
“In minimally invasive gynecologic procedures, we haven’t come to adopt this marker just quite yet. It could be included in the routine battery of tests” at minimal cost. “I think it’s something we should consider,” said ob.gyn. resident Suzanne Lababidi, MD.
The team was curious why serum albumin generally is not a part of routine testing for laparoscopic hysterectomy. The first step was to see if it made a difference, so they reviewed 43,289 cases in the National Surgical Quality Improvement Program database. The women were “par for the course;” 51 years old, on average; and had a mean body mass index of 31.9 kg/m2. More than one-third were hypertensive. Mean albumin was in the normal range at 4.1 g/dL, Dr. Lababidi said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
Her team did not come up with a cut-point to delay surgery – that’s the goal of further research – but they noticed on linear regression that women with lower preop albumin had higher rates of surgical site infections and intraoperative transfusions, plus higher rates of postop pneumonia; renal failure; urinary tract infection; sepsis; and deep vein thrombosis, among other issues – and even after controlling for hypertension, diabetes, and other comorbidities. The findings met statistical significance.
It’s true that patients with low albumin might have gone into the operating room sicker, but no matter; Dr. Lababidi’s point was that preop serum albumin is something to pay attention to and correct whenever possible before laparoscopic hysterectomies.
Preop levels are something to consider for “counseling and optimizing patients to improve surgical outcomes,” she said.
The next step toward an albumin cut-point is to weed out confounders by further stratifying patients based on albumin levels, she said.
The work received no industry funding. Dr. Lababidi had no disclosures.
aotto@mdedge.com
SOURCE: Lababidi S et al. 2018 AAGL Global Congress, Abstract 199.
LAS VEGAS – Serum albumin is an everyday health marker commonly used for risk assessment in open abdominal procedures, but it’s often not checked before laparoscopic hysterectomies.
Low levels mean something is off, be it malnutrition, inflammation, chronic disease, or other problems. If it can be normalized before surgery, it should be; women probably will do better, according to investigators from the University of Kentucky, Lexington.
“In minimally invasive gynecologic procedures, we haven’t come to adopt this marker just quite yet. It could be included in the routine battery of tests” at minimal cost. “I think it’s something we should consider,” said ob.gyn. resident Suzanne Lababidi, MD.
The team was curious why serum albumin generally is not a part of routine testing for laparoscopic hysterectomy. The first step was to see if it made a difference, so they reviewed 43,289 cases in the National Surgical Quality Improvement Program database. The women were “par for the course;” 51 years old, on average; and had a mean body mass index of 31.9 kg/m2. More than one-third were hypertensive. Mean albumin was in the normal range at 4.1 g/dL, Dr. Lababidi said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
Her team did not come up with a cut-point to delay surgery – that’s the goal of further research – but they noticed on linear regression that women with lower preop albumin had higher rates of surgical site infections and intraoperative transfusions, plus higher rates of postop pneumonia; renal failure; urinary tract infection; sepsis; and deep vein thrombosis, among other issues – and even after controlling for hypertension, diabetes, and other comorbidities. The findings met statistical significance.
It’s true that patients with low albumin might have gone into the operating room sicker, but no matter; Dr. Lababidi’s point was that preop serum albumin is something to pay attention to and correct whenever possible before laparoscopic hysterectomies.
Preop levels are something to consider for “counseling and optimizing patients to improve surgical outcomes,” she said.
The next step toward an albumin cut-point is to weed out confounders by further stratifying patients based on albumin levels, she said.
The work received no industry funding. Dr. Lababidi had no disclosures.
aotto@mdedge.com
SOURCE: Lababidi S et al. 2018 AAGL Global Congress, Abstract 199.
LAS VEGAS – Serum albumin is an everyday health marker commonly used for risk assessment in open abdominal procedures, but it’s often not checked before laparoscopic hysterectomies.
Low levels mean something is off, be it malnutrition, inflammation, chronic disease, or other problems. If it can be normalized before surgery, it should be; women probably will do better, according to investigators from the University of Kentucky, Lexington.
“In minimally invasive gynecologic procedures, we haven’t come to adopt this marker just quite yet. It could be included in the routine battery of tests” at minimal cost. “I think it’s something we should consider,” said ob.gyn. resident Suzanne Lababidi, MD.
The team was curious why serum albumin generally is not a part of routine testing for laparoscopic hysterectomy. The first step was to see if it made a difference, so they reviewed 43,289 cases in the National Surgical Quality Improvement Program database. The women were “par for the course;” 51 years old, on average; and had a mean body mass index of 31.9 kg/m2. More than one-third were hypertensive. Mean albumin was in the normal range at 4.1 g/dL, Dr. Lababidi said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
Her team did not come up with a cut-point to delay surgery – that’s the goal of further research – but they noticed on linear regression that women with lower preop albumin had higher rates of surgical site infections and intraoperative transfusions, plus higher rates of postop pneumonia; renal failure; urinary tract infection; sepsis; and deep vein thrombosis, among other issues – and even after controlling for hypertension, diabetes, and other comorbidities. The findings met statistical significance.
It’s true that patients with low albumin might have gone into the operating room sicker, but no matter; Dr. Lababidi’s point was that preop serum albumin is something to pay attention to and correct whenever possible before laparoscopic hysterectomies.
Preop levels are something to consider for “counseling and optimizing patients to improve surgical outcomes,” she said.
The next step toward an albumin cut-point is to weed out confounders by further stratifying patients based on albumin levels, she said.
The work received no industry funding. Dr. Lababidi had no disclosures.
aotto@mdedge.com
SOURCE: Lababidi S et al. 2018 AAGL Global Congress, Abstract 199.
REPORTING FROM THE AAGL GLOBAL CONGRESS
Antibiotics backed as standard of care for myomectomies
LAS VEGAS – The surgical site infection rate was 2.9% among women who received perioperative antibiotics for fibroid surgery, but 7.8% among those who did not, in a review of 1,433 cases at Massachusetts General Hospital and Brigham and Women’s Hospital, Boston.
That is despite the fact that antibiotic cases were longer – 155 minutes vs. 89 minutes – and had more blood loss, 200 ml vs. 117 ml. Antibiotic cases also had larger specimen weights – 346 g vs. 176 g – and were more likely to have the uterine cavity entered, 30.2% vs. 14.4%.
“Surgical site infections were more common in the no-antibiotics group despite these being less complex cases.” There was “nearly a fivefold increased odds of surgical site infection or any infectious complication when no antibiotics were given,” after controlling for infection risk factors, including smoking and diabetes, said investigator Nisse V. Clark, MD, a minimally invasive gynecologic surgeon affiliated with Massachusetts General Hospital.
There are no perioperative antibiotic guidelines for myomectomies; maybe there should be. Almost 94% of the women in the review did receive antibiotics at the Harvard-affiliated hospitals, but the nationwide average has been pegged at about two-thirds, she said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
The antibiotic cases usually received a cephalosporin before surgery, and were about evenly about evenly split between abdominal, robotic, and laparoscopic approaches.
About one-third of the 90 women (6.3%) who did not get antibiotics had hysteroscopic procedures in which antibiotics usually are not given because the peritoneal cavity is not breeched. Most of the rest, however, were laparoscopic cases. It’s unknown why they weren’t given antibiotics. In her own practice, Dr. Clark said preop antibiotics are the rule for laparoscopic myomectomies.
The surgical site infection difference was driven largely by higher incidences of pelvic abscesses and other organ space infections in the no-antibiotic group.
The only significant demographic difference between the two groups was that women who received antibiotics were slightly younger (mean 38 versus 39.7 years).
In addition to diabetes and smoking, the team adjusted for age, surgery route, body mass index, uterine entry, intraoperative complications, and myoma weight in their multivariate analysis. Still, women in the no-antibiotic group were 4.59 times more likely to have a surgical site infection, 4.76 more likely to have any infectious complication, and almost 8 times more likely to have a major infectious complication. All of the findings were statistically significant.
The study had no industry funding, and Dr. Clark had no disclosures.
aotto@mdedge.com
LAS VEGAS – The surgical site infection rate was 2.9% among women who received perioperative antibiotics for fibroid surgery, but 7.8% among those who did not, in a review of 1,433 cases at Massachusetts General Hospital and Brigham and Women’s Hospital, Boston.
That is despite the fact that antibiotic cases were longer – 155 minutes vs. 89 minutes – and had more blood loss, 200 ml vs. 117 ml. Antibiotic cases also had larger specimen weights – 346 g vs. 176 g – and were more likely to have the uterine cavity entered, 30.2% vs. 14.4%.
“Surgical site infections were more common in the no-antibiotics group despite these being less complex cases.” There was “nearly a fivefold increased odds of surgical site infection or any infectious complication when no antibiotics were given,” after controlling for infection risk factors, including smoking and diabetes, said investigator Nisse V. Clark, MD, a minimally invasive gynecologic surgeon affiliated with Massachusetts General Hospital.
There are no perioperative antibiotic guidelines for myomectomies; maybe there should be. Almost 94% of the women in the review did receive antibiotics at the Harvard-affiliated hospitals, but the nationwide average has been pegged at about two-thirds, she said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
The antibiotic cases usually received a cephalosporin before surgery, and were about evenly about evenly split between abdominal, robotic, and laparoscopic approaches.
About one-third of the 90 women (6.3%) who did not get antibiotics had hysteroscopic procedures in which antibiotics usually are not given because the peritoneal cavity is not breeched. Most of the rest, however, were laparoscopic cases. It’s unknown why they weren’t given antibiotics. In her own practice, Dr. Clark said preop antibiotics are the rule for laparoscopic myomectomies.
The surgical site infection difference was driven largely by higher incidences of pelvic abscesses and other organ space infections in the no-antibiotic group.
The only significant demographic difference between the two groups was that women who received antibiotics were slightly younger (mean 38 versus 39.7 years).
In addition to diabetes and smoking, the team adjusted for age, surgery route, body mass index, uterine entry, intraoperative complications, and myoma weight in their multivariate analysis. Still, women in the no-antibiotic group were 4.59 times more likely to have a surgical site infection, 4.76 more likely to have any infectious complication, and almost 8 times more likely to have a major infectious complication. All of the findings were statistically significant.
The study had no industry funding, and Dr. Clark had no disclosures.
aotto@mdedge.com
LAS VEGAS – The surgical site infection rate was 2.9% among women who received perioperative antibiotics for fibroid surgery, but 7.8% among those who did not, in a review of 1,433 cases at Massachusetts General Hospital and Brigham and Women’s Hospital, Boston.
That is despite the fact that antibiotic cases were longer – 155 minutes vs. 89 minutes – and had more blood loss, 200 ml vs. 117 ml. Antibiotic cases also had larger specimen weights – 346 g vs. 176 g – and were more likely to have the uterine cavity entered, 30.2% vs. 14.4%.
“Surgical site infections were more common in the no-antibiotics group despite these being less complex cases.” There was “nearly a fivefold increased odds of surgical site infection or any infectious complication when no antibiotics were given,” after controlling for infection risk factors, including smoking and diabetes, said investigator Nisse V. Clark, MD, a minimally invasive gynecologic surgeon affiliated with Massachusetts General Hospital.
There are no perioperative antibiotic guidelines for myomectomies; maybe there should be. Almost 94% of the women in the review did receive antibiotics at the Harvard-affiliated hospitals, but the nationwide average has been pegged at about two-thirds, she said at the meeting, sponsored by the American Association of Gynecologic Laparoscopists.
The antibiotic cases usually received a cephalosporin before surgery, and were about evenly about evenly split between abdominal, robotic, and laparoscopic approaches.
About one-third of the 90 women (6.3%) who did not get antibiotics had hysteroscopic procedures in which antibiotics usually are not given because the peritoneal cavity is not breeched. Most of the rest, however, were laparoscopic cases. It’s unknown why they weren’t given antibiotics. In her own practice, Dr. Clark said preop antibiotics are the rule for laparoscopic myomectomies.
The surgical site infection difference was driven largely by higher incidences of pelvic abscesses and other organ space infections in the no-antibiotic group.
The only significant demographic difference between the two groups was that women who received antibiotics were slightly younger (mean 38 versus 39.7 years).
In addition to diabetes and smoking, the team adjusted for age, surgery route, body mass index, uterine entry, intraoperative complications, and myoma weight in their multivariate analysis. Still, women in the no-antibiotic group were 4.59 times more likely to have a surgical site infection, 4.76 more likely to have any infectious complication, and almost 8 times more likely to have a major infectious complication. All of the findings were statistically significant.
The study had no industry funding, and Dr. Clark had no disclosures.
aotto@mdedge.com
REPORTING FROM THE AAGL GLOBAL CONGRESS
Key clinical point: A Boston study suggests that even low-risk cases benefit from antibiotics.
Major finding: The surgical site infection rate was 2.9% among women who received perioperative antibiotics for fibroid surgery, but 7.8% among those who did not.
Study details: Review of 1,433 myomectomies at two academic medical centers.
Disclosures: The study had no industry funding, and Dr. Clark had no disclosures.
SVS guidelines address scope of practice concerns
NEW YORK – Vascular surgeons are the only specialty qualified to treat all vascular disorders with open surgery and/or endovascular treatment, including the thoracic aorta, according to the updated “Guidelines for hospital privileges in vascular surgery and endovascular interventions: Recommendations of the Society for Vascular Surgery.”
The guidelines, published in May’s Journal of Vascular Surgery, were last updated in 2008, said Keith D. Calligaro, MD, who spoke on their importance and potential benefits to vascular surgeons during his presentation at the VEITHsymposium.
The thoracic aorta component of the guidelines addresses scope of practice concerns between vascular and thoracic surgeons, said Dr. Calligaro, who is a clinical professor of surgery, University of Pennsylvania, and chief of vascular surgery and endovascular therapy at Pennsylvania Hospital, both in Philadelphia.
The guidelines relied on training requirements to provide some of the data to define vascular surgeons and privileges. The open vascular surgery training requirements still are defined by the Residency Review Committee for surgery, and those requirements include 250 major open vascular cases during training, including 30 open abdominal operations, 25 carotid, 45 peripheral open surgery cases, and 10 complex vascular surgeries, said Dr. Calligaro. “In terms of endovascular treatment, the training requirements are over 100 diagnostic caths and over 80 therapeutic interventions, and during training you would have had to have done more than 20 EVARs [endovascular aneurysm repairs].” That number jumped up from five EVARs in the previous guidelines.
Ultimately, “the SVS is basically saying ‘you need to be a vascular surgeon to perform vascular surgery,’ and you need have to have completed an Accreditation Council for Graduate Medical Education–accredited vascular residency.
“So if you are a general surgeon or a heart surgeon and you go to a new hospital and say ‘I want to do vascular,’ the vascular surgeon at that institution can refer to this document and say ‘no, the SVS is saying [the surgeon doesn’t] have the training.’ And I think that’s a pretty gutsy and important call,” said Dr. Calligaro.
It is a different case for endovascular surgery, he said. In this case, the requirement is to have completed an ACGME-accredited program in either vascular surgery, interventional radiology, or interventional cardiology to indicate the appropriate level of training. But SVS agreed with the recommendation by the American College of Cardiology that cardiologists not only had to complete 1 year of coronary interventions but also 1 year of peripheral intervention training, as well.
“So if you are at your hospital and have a cardiologist who is starting to do peripheral vascular stuff, now at least you can wave part of this document and say ‘Hey, look, the most important vascular society in the country is saying that, unless this individual had a year of peripheral training, this cardiologist should not be allowed to do endovascular peripheral interventions,’ ” Dr. Calligaro said.
SOURCE: Calligaro KD et al. J Vasc Surg. 2018 May;67(5):1337-44.
NEW YORK – Vascular surgeons are the only specialty qualified to treat all vascular disorders with open surgery and/or endovascular treatment, including the thoracic aorta, according to the updated “Guidelines for hospital privileges in vascular surgery and endovascular interventions: Recommendations of the Society for Vascular Surgery.”
The guidelines, published in May’s Journal of Vascular Surgery, were last updated in 2008, said Keith D. Calligaro, MD, who spoke on their importance and potential benefits to vascular surgeons during his presentation at the VEITHsymposium.
The thoracic aorta component of the guidelines addresses scope of practice concerns between vascular and thoracic surgeons, said Dr. Calligaro, who is a clinical professor of surgery, University of Pennsylvania, and chief of vascular surgery and endovascular therapy at Pennsylvania Hospital, both in Philadelphia.
The guidelines relied on training requirements to provide some of the data to define vascular surgeons and privileges. The open vascular surgery training requirements still are defined by the Residency Review Committee for surgery, and those requirements include 250 major open vascular cases during training, including 30 open abdominal operations, 25 carotid, 45 peripheral open surgery cases, and 10 complex vascular surgeries, said Dr. Calligaro. “In terms of endovascular treatment, the training requirements are over 100 diagnostic caths and over 80 therapeutic interventions, and during training you would have had to have done more than 20 EVARs [endovascular aneurysm repairs].” That number jumped up from five EVARs in the previous guidelines.
Ultimately, “the SVS is basically saying ‘you need to be a vascular surgeon to perform vascular surgery,’ and you need have to have completed an Accreditation Council for Graduate Medical Education–accredited vascular residency.
“So if you are a general surgeon or a heart surgeon and you go to a new hospital and say ‘I want to do vascular,’ the vascular surgeon at that institution can refer to this document and say ‘no, the SVS is saying [the surgeon doesn’t] have the training.’ And I think that’s a pretty gutsy and important call,” said Dr. Calligaro.
It is a different case for endovascular surgery, he said. In this case, the requirement is to have completed an ACGME-accredited program in either vascular surgery, interventional radiology, or interventional cardiology to indicate the appropriate level of training. But SVS agreed with the recommendation by the American College of Cardiology that cardiologists not only had to complete 1 year of coronary interventions but also 1 year of peripheral intervention training, as well.
“So if you are at your hospital and have a cardiologist who is starting to do peripheral vascular stuff, now at least you can wave part of this document and say ‘Hey, look, the most important vascular society in the country is saying that, unless this individual had a year of peripheral training, this cardiologist should not be allowed to do endovascular peripheral interventions,’ ” Dr. Calligaro said.
SOURCE: Calligaro KD et al. J Vasc Surg. 2018 May;67(5):1337-44.
NEW YORK – Vascular surgeons are the only specialty qualified to treat all vascular disorders with open surgery and/or endovascular treatment, including the thoracic aorta, according to the updated “Guidelines for hospital privileges in vascular surgery and endovascular interventions: Recommendations of the Society for Vascular Surgery.”
The guidelines, published in May’s Journal of Vascular Surgery, were last updated in 2008, said Keith D. Calligaro, MD, who spoke on their importance and potential benefits to vascular surgeons during his presentation at the VEITHsymposium.
The thoracic aorta component of the guidelines addresses scope of practice concerns between vascular and thoracic surgeons, said Dr. Calligaro, who is a clinical professor of surgery, University of Pennsylvania, and chief of vascular surgery and endovascular therapy at Pennsylvania Hospital, both in Philadelphia.
The guidelines relied on training requirements to provide some of the data to define vascular surgeons and privileges. The open vascular surgery training requirements still are defined by the Residency Review Committee for surgery, and those requirements include 250 major open vascular cases during training, including 30 open abdominal operations, 25 carotid, 45 peripheral open surgery cases, and 10 complex vascular surgeries, said Dr. Calligaro. “In terms of endovascular treatment, the training requirements are over 100 diagnostic caths and over 80 therapeutic interventions, and during training you would have had to have done more than 20 EVARs [endovascular aneurysm repairs].” That number jumped up from five EVARs in the previous guidelines.
Ultimately, “the SVS is basically saying ‘you need to be a vascular surgeon to perform vascular surgery,’ and you need have to have completed an Accreditation Council for Graduate Medical Education–accredited vascular residency.
“So if you are a general surgeon or a heart surgeon and you go to a new hospital and say ‘I want to do vascular,’ the vascular surgeon at that institution can refer to this document and say ‘no, the SVS is saying [the surgeon doesn’t] have the training.’ And I think that’s a pretty gutsy and important call,” said Dr. Calligaro.
It is a different case for endovascular surgery, he said. In this case, the requirement is to have completed an ACGME-accredited program in either vascular surgery, interventional radiology, or interventional cardiology to indicate the appropriate level of training. But SVS agreed with the recommendation by the American College of Cardiology that cardiologists not only had to complete 1 year of coronary interventions but also 1 year of peripheral intervention training, as well.
“So if you are at your hospital and have a cardiologist who is starting to do peripheral vascular stuff, now at least you can wave part of this document and say ‘Hey, look, the most important vascular society in the country is saying that, unless this individual had a year of peripheral training, this cardiologist should not be allowed to do endovascular peripheral interventions,’ ” Dr. Calligaro said.
SOURCE: Calligaro KD et al. J Vasc Surg. 2018 May;67(5):1337-44.
REPORTING FROM THE VEITHSYMPOSIUM