User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Treating fractures in elderly patients: Beyond the broken bone
While half the fracture-prevention battle is getting people diagnosed with low bone density, nearly 80% of older Americans who suffer bone breaks are not tested or treated for osteoporosis. Fractures associated with aging and diminished bone mineral density exact an enormous toll on patients’ lives and cost the health care system billions of dollars annually according to Bone Health and Osteoporosis: A Report of the Surgeon General. But current gaps in patient education and bone density screening are huge.
“It’s concerning that older patients at risk for fracture are often not screened to determine their risk factors contributing to osteoporosis and patients are not educated about fracture prevention,” said Meryl S. LeBoff, MD, an endocrinologist at Brigham and Women’s Hospital, and chief of calcium and bone section, and professor of medicine, at Harvard Medical School, Boston. “Furthermore, the majority of highest-risk women and men who do have fractures are not screened and they do not receive effective, [Food and Drug Administration]–approved therapies.”
Recent guidelines
Screening with dual-energy x-ray absorptiometry (DEXA) is recommended for all women at age 65 and all men at age 70. But the occasion of a fracture in an older person who has not yet met these age thresholds should prompt a bone density assessment.
“Doctors need to stress that one in two women and one in four men over age 50 will have a fracture in their remaining lifetimes,” Dr. LeBoff said. ”Primary care doctors play a critical role in ordering timely bone densitometry for both sexes.
If an older patient has been treated for a fracture, the main goal going forward is to prevent another one, for which the risk is highest in the 2 years after the incident fracture.”
According to Kendall F. Moseley, MD, clinical director of the division of endocrinology, diabetes & metabolism at Johns Hopkins Medicine in Baltimore, “Elderly patients need to understand that a fracture at their age is like a heart attack of the bone,” she said, adding that just as cardiovascular risk factors such as high blood pressure and blood lipids are silent before a stroke or infarction, the bone thinning of old age is also silent.
Endocrinologist Jennifer J. Kelly, DO, director of the metabolic bone program and an associate professor at the University of Vermont Medical Center in Burlington, said a fracture in anyone over age 50 that appears not to have resulted from a traumatic blow, is a compelling reason to order a DEXA exam.
Nahid J. Rianon, MBBS/MD, DrPH, assistant professor of the division of geriatric medicine at the UTHealth McGovern Medical School, Houston, goes further: “Any fracture in someone age 50 and older warrants screening for osteoporosis. And if the fracture is nontraumatic, that is by definition a clinical diagnosis of osteoporosis regardless of normal results on bone density tests and they should be treated medically. There are aspects of bone that we still can’t measure in the clinical setting.”
If DEXA is not accessible, fracture risk over the next 10 years can be evaluated based on multiple patient characteristics and medical history using the online FRAX calculator.
Just a 3% risk of hip fracture on FRAX is considered an indication to begin medical osteoporosis treatment in the United States regardless of bone density test results, Dr. Rianon said.
Fracture management
Whether a senior suffers a traumatic fracture or an osteoporosis-related fragility fracture, older age can impede the healing process in some. Senescence may also increase systemic proinflammatory status, according to Clark and colleagues, writing in Current Osteoporosis Reports.
They called for research to develop more directed treatment options for the elderly population.
Dr. Rianon noted that healing may also be affected by a decrease in muscle mass, which plays a role in holding the bone in place. “But it is still controversial how changing metabolic factors affect bone healing in the elderly.”
However, countered Dr. Kelly, fractures in elderly patients are not necessarily less likely to mend – if osteoporosis is not present. “Many heal very well – it really depends more upon their overall health and medical history. Whether or not a person requires surgery depends more upon the extent of the fracture and if the bone is able to align and heal appropriately without surgery.”
Fracture sites
Spine. According to the American Academy of Orthopedic Surgeons the earliest and most frequent site of fragility fractures in the elderly is the spine. Most vertebral fracture pain improves within 3 months without specific treatment. A short period of rest, limited analgesic use, and possible back bracing may help as the fractures heal on their own. But if pain is severe and persistent, vertebral augmentation with percutaneous kyphoplasty or vertebroplasty may be an option. These procedures, however, can destabilize surrounding discs because of the greater thickness of the injected cement.
Hip. The most dangerous fractures occur in the hip. These carry at least a 20% risk of death in the first postoperative year and must be treated surgically. Those in the proximal femur, the head, or the femoral neck will usually need hip replacement, but if the break is farther down, it may be repaired with cement, screws, plates, and rods.
Distal radius. Outcomes of wrist fractures may be positive without surgical intervention, according to a recent retrospective analysis from Turkey by Yalin and colleagues. In a comparison of clinical outcomes in seniors aged 70-89 and assigned to cast immobilization or various surgical treatments for distal radius fractures, no statistically significant difference was found in patient-reported disability scores and range of motion values between casting and surgery in the first postoperative year.
Other sites. Fractures in the elderly are not uncommon in the shoulder, distal radius, cubitus, proximal humerus, and humerus. These fractures are often treated without surgery, but nevertheless signal a high risk for additional fractures.
Bone-enhancing medications
Even in the absence of diagnosed low bone density or osteoporosis, anabolic agents such as the synthetic human parathyroid hormones abaloparatide (Tymlos) and teriparatide (Forteo) may be used to help in some cases with a bad healing prognosis and may also be used for people undergoing surgeries such as a spinal fusion, but there are not clinical guidelines. “We receive referrals regularly for this treatment from our orthopedics colleagues, but it is considered an off-label use,” Dr. Kelly said.
The anabolics teriparatide and romosozumab (Evenity) have proved effective in lowering fractures in high-risk older women.
Post fracture
After recovering from a fracture, elderly people are strongly advised to make lifestyle changes to boost bone health and reduce risk of further fractures, said Willy M. Valencia, MD, a geriatrician-endocrinologist at the Cleveland Clinic. Apart from active daily living, he recommends several types of formal exercise to promote bone formation; increase muscle mass, strength, and flexibility; and improve endurance, balance, and gait. The National Institute on Aging outlines suitable exercise programs for seniors.
“These exercises will help reduce the risk of falling and to avoid more fractures,” he said. “Whether a patient has been exercising before the fracture or not, they may feel some reticence or reluctance to take up exercise afterwards because they’re afraid of having another fracture, but they should understand that their fracture risk increases if they remain sedentary. They should start slowly but they can’t be sitting all day.”
Even before it’s possible to exercise at the healing fracture site, added Dr. Rianon, its advisable to work other areas of the body. “Overall mobility is important, and exercising other parts of the body can stimulate strength and help prevent falling.”
In other postsurgical measures, a bone-friendly diet rich in calcium and vitamin D, as well as supplementation with these vital nutrients, is essential to lower the risk of falling.
Fall prevention is paramount, said Dr. Valencia. While exercise can improve, gait, balance, and endurance, logistical measures may also be necessary. Seniors may have to move to a one-floor domicile with no stairs to negotiate. At the very least, they need to fall-proof their daily lives by upgrading their eyeglasses and home lighting, eliminating obstacles and loose carpets, fixing bannisters, and installing bathroom handrails. Some may need assistive devices for walking, especially outdoors in slippery conditions.
At the end of the day, the role of the primary physician in screening for bone problems before fracture and postsurgical care is key. “Risk factors for osteoporosis and fracture risk must be added to the patient’s chart,” said Dr. Rianon. Added Dr. Moseley. “No matter how busy they are, my hope is that primary care physicians will not put patients’ bone health at the bottom of the clinical agenda.”
While half the fracture-prevention battle is getting people diagnosed with low bone density, nearly 80% of older Americans who suffer bone breaks are not tested or treated for osteoporosis. Fractures associated with aging and diminished bone mineral density exact an enormous toll on patients’ lives and cost the health care system billions of dollars annually according to Bone Health and Osteoporosis: A Report of the Surgeon General. But current gaps in patient education and bone density screening are huge.
“It’s concerning that older patients at risk for fracture are often not screened to determine their risk factors contributing to osteoporosis and patients are not educated about fracture prevention,” said Meryl S. LeBoff, MD, an endocrinologist at Brigham and Women’s Hospital, and chief of calcium and bone section, and professor of medicine, at Harvard Medical School, Boston. “Furthermore, the majority of highest-risk women and men who do have fractures are not screened and they do not receive effective, [Food and Drug Administration]–approved therapies.”
Recent guidelines
Screening with dual-energy x-ray absorptiometry (DEXA) is recommended for all women at age 65 and all men at age 70. But the occasion of a fracture in an older person who has not yet met these age thresholds should prompt a bone density assessment.
“Doctors need to stress that one in two women and one in four men over age 50 will have a fracture in their remaining lifetimes,” Dr. LeBoff said. ”Primary care doctors play a critical role in ordering timely bone densitometry for both sexes.
If an older patient has been treated for a fracture, the main goal going forward is to prevent another one, for which the risk is highest in the 2 years after the incident fracture.”
According to Kendall F. Moseley, MD, clinical director of the division of endocrinology, diabetes & metabolism at Johns Hopkins Medicine in Baltimore, “Elderly patients need to understand that a fracture at their age is like a heart attack of the bone,” she said, adding that just as cardiovascular risk factors such as high blood pressure and blood lipids are silent before a stroke or infarction, the bone thinning of old age is also silent.
Endocrinologist Jennifer J. Kelly, DO, director of the metabolic bone program and an associate professor at the University of Vermont Medical Center in Burlington, said a fracture in anyone over age 50 that appears not to have resulted from a traumatic blow, is a compelling reason to order a DEXA exam.
Nahid J. Rianon, MBBS/MD, DrPH, assistant professor of the division of geriatric medicine at the UTHealth McGovern Medical School, Houston, goes further: “Any fracture in someone age 50 and older warrants screening for osteoporosis. And if the fracture is nontraumatic, that is by definition a clinical diagnosis of osteoporosis regardless of normal results on bone density tests and they should be treated medically. There are aspects of bone that we still can’t measure in the clinical setting.”
If DEXA is not accessible, fracture risk over the next 10 years can be evaluated based on multiple patient characteristics and medical history using the online FRAX calculator.
Just a 3% risk of hip fracture on FRAX is considered an indication to begin medical osteoporosis treatment in the United States regardless of bone density test results, Dr. Rianon said.
Fracture management
Whether a senior suffers a traumatic fracture or an osteoporosis-related fragility fracture, older age can impede the healing process in some. Senescence may also increase systemic proinflammatory status, according to Clark and colleagues, writing in Current Osteoporosis Reports.
They called for research to develop more directed treatment options for the elderly population.
Dr. Rianon noted that healing may also be affected by a decrease in muscle mass, which plays a role in holding the bone in place. “But it is still controversial how changing metabolic factors affect bone healing in the elderly.”
However, countered Dr. Kelly, fractures in elderly patients are not necessarily less likely to mend – if osteoporosis is not present. “Many heal very well – it really depends more upon their overall health and medical history. Whether or not a person requires surgery depends more upon the extent of the fracture and if the bone is able to align and heal appropriately without surgery.”
Fracture sites
Spine. According to the American Academy of Orthopedic Surgeons the earliest and most frequent site of fragility fractures in the elderly is the spine. Most vertebral fracture pain improves within 3 months without specific treatment. A short period of rest, limited analgesic use, and possible back bracing may help as the fractures heal on their own. But if pain is severe and persistent, vertebral augmentation with percutaneous kyphoplasty or vertebroplasty may be an option. These procedures, however, can destabilize surrounding discs because of the greater thickness of the injected cement.
Hip. The most dangerous fractures occur in the hip. These carry at least a 20% risk of death in the first postoperative year and must be treated surgically. Those in the proximal femur, the head, or the femoral neck will usually need hip replacement, but if the break is farther down, it may be repaired with cement, screws, plates, and rods.
Distal radius. Outcomes of wrist fractures may be positive without surgical intervention, according to a recent retrospective analysis from Turkey by Yalin and colleagues. In a comparison of clinical outcomes in seniors aged 70-89 and assigned to cast immobilization or various surgical treatments for distal radius fractures, no statistically significant difference was found in patient-reported disability scores and range of motion values between casting and surgery in the first postoperative year.
Other sites. Fractures in the elderly are not uncommon in the shoulder, distal radius, cubitus, proximal humerus, and humerus. These fractures are often treated without surgery, but nevertheless signal a high risk for additional fractures.
Bone-enhancing medications
Even in the absence of diagnosed low bone density or osteoporosis, anabolic agents such as the synthetic human parathyroid hormones abaloparatide (Tymlos) and teriparatide (Forteo) may be used to help in some cases with a bad healing prognosis and may also be used for people undergoing surgeries such as a spinal fusion, but there are not clinical guidelines. “We receive referrals regularly for this treatment from our orthopedics colleagues, but it is considered an off-label use,” Dr. Kelly said.
The anabolics teriparatide and romosozumab (Evenity) have proved effective in lowering fractures in high-risk older women.
Post fracture
After recovering from a fracture, elderly people are strongly advised to make lifestyle changes to boost bone health and reduce risk of further fractures, said Willy M. Valencia, MD, a geriatrician-endocrinologist at the Cleveland Clinic. Apart from active daily living, he recommends several types of formal exercise to promote bone formation; increase muscle mass, strength, and flexibility; and improve endurance, balance, and gait. The National Institute on Aging outlines suitable exercise programs for seniors.
“These exercises will help reduce the risk of falling and to avoid more fractures,” he said. “Whether a patient has been exercising before the fracture or not, they may feel some reticence or reluctance to take up exercise afterwards because they’re afraid of having another fracture, but they should understand that their fracture risk increases if they remain sedentary. They should start slowly but they can’t be sitting all day.”
Even before it’s possible to exercise at the healing fracture site, added Dr. Rianon, its advisable to work other areas of the body. “Overall mobility is important, and exercising other parts of the body can stimulate strength and help prevent falling.”
In other postsurgical measures, a bone-friendly diet rich in calcium and vitamin D, as well as supplementation with these vital nutrients, is essential to lower the risk of falling.
Fall prevention is paramount, said Dr. Valencia. While exercise can improve, gait, balance, and endurance, logistical measures may also be necessary. Seniors may have to move to a one-floor domicile with no stairs to negotiate. At the very least, they need to fall-proof their daily lives by upgrading their eyeglasses and home lighting, eliminating obstacles and loose carpets, fixing bannisters, and installing bathroom handrails. Some may need assistive devices for walking, especially outdoors in slippery conditions.
At the end of the day, the role of the primary physician in screening for bone problems before fracture and postsurgical care is key. “Risk factors for osteoporosis and fracture risk must be added to the patient’s chart,” said Dr. Rianon. Added Dr. Moseley. “No matter how busy they are, my hope is that primary care physicians will not put patients’ bone health at the bottom of the clinical agenda.”
While half the fracture-prevention battle is getting people diagnosed with low bone density, nearly 80% of older Americans who suffer bone breaks are not tested or treated for osteoporosis. Fractures associated with aging and diminished bone mineral density exact an enormous toll on patients’ lives and cost the health care system billions of dollars annually according to Bone Health and Osteoporosis: A Report of the Surgeon General. But current gaps in patient education and bone density screening are huge.
“It’s concerning that older patients at risk for fracture are often not screened to determine their risk factors contributing to osteoporosis and patients are not educated about fracture prevention,” said Meryl S. LeBoff, MD, an endocrinologist at Brigham and Women’s Hospital, and chief of calcium and bone section, and professor of medicine, at Harvard Medical School, Boston. “Furthermore, the majority of highest-risk women and men who do have fractures are not screened and they do not receive effective, [Food and Drug Administration]–approved therapies.”
Recent guidelines
Screening with dual-energy x-ray absorptiometry (DEXA) is recommended for all women at age 65 and all men at age 70. But the occasion of a fracture in an older person who has not yet met these age thresholds should prompt a bone density assessment.
“Doctors need to stress that one in two women and one in four men over age 50 will have a fracture in their remaining lifetimes,” Dr. LeBoff said. ”Primary care doctors play a critical role in ordering timely bone densitometry for both sexes.
If an older patient has been treated for a fracture, the main goal going forward is to prevent another one, for which the risk is highest in the 2 years after the incident fracture.”
According to Kendall F. Moseley, MD, clinical director of the division of endocrinology, diabetes & metabolism at Johns Hopkins Medicine in Baltimore, “Elderly patients need to understand that a fracture at their age is like a heart attack of the bone,” she said, adding that just as cardiovascular risk factors such as high blood pressure and blood lipids are silent before a stroke or infarction, the bone thinning of old age is also silent.
Endocrinologist Jennifer J. Kelly, DO, director of the metabolic bone program and an associate professor at the University of Vermont Medical Center in Burlington, said a fracture in anyone over age 50 that appears not to have resulted from a traumatic blow, is a compelling reason to order a DEXA exam.
Nahid J. Rianon, MBBS/MD, DrPH, assistant professor of the division of geriatric medicine at the UTHealth McGovern Medical School, Houston, goes further: “Any fracture in someone age 50 and older warrants screening for osteoporosis. And if the fracture is nontraumatic, that is by definition a clinical diagnosis of osteoporosis regardless of normal results on bone density tests and they should be treated medically. There are aspects of bone that we still can’t measure in the clinical setting.”
If DEXA is not accessible, fracture risk over the next 10 years can be evaluated based on multiple patient characteristics and medical history using the online FRAX calculator.
Just a 3% risk of hip fracture on FRAX is considered an indication to begin medical osteoporosis treatment in the United States regardless of bone density test results, Dr. Rianon said.
Fracture management
Whether a senior suffers a traumatic fracture or an osteoporosis-related fragility fracture, older age can impede the healing process in some. Senescence may also increase systemic proinflammatory status, according to Clark and colleagues, writing in Current Osteoporosis Reports.
They called for research to develop more directed treatment options for the elderly population.
Dr. Rianon noted that healing may also be affected by a decrease in muscle mass, which plays a role in holding the bone in place. “But it is still controversial how changing metabolic factors affect bone healing in the elderly.”
However, countered Dr. Kelly, fractures in elderly patients are not necessarily less likely to mend – if osteoporosis is not present. “Many heal very well – it really depends more upon their overall health and medical history. Whether or not a person requires surgery depends more upon the extent of the fracture and if the bone is able to align and heal appropriately without surgery.”
Fracture sites
Spine. According to the American Academy of Orthopedic Surgeons the earliest and most frequent site of fragility fractures in the elderly is the spine. Most vertebral fracture pain improves within 3 months without specific treatment. A short period of rest, limited analgesic use, and possible back bracing may help as the fractures heal on their own. But if pain is severe and persistent, vertebral augmentation with percutaneous kyphoplasty or vertebroplasty may be an option. These procedures, however, can destabilize surrounding discs because of the greater thickness of the injected cement.
Hip. The most dangerous fractures occur in the hip. These carry at least a 20% risk of death in the first postoperative year and must be treated surgically. Those in the proximal femur, the head, or the femoral neck will usually need hip replacement, but if the break is farther down, it may be repaired with cement, screws, plates, and rods.
Distal radius. Outcomes of wrist fractures may be positive without surgical intervention, according to a recent retrospective analysis from Turkey by Yalin and colleagues. In a comparison of clinical outcomes in seniors aged 70-89 and assigned to cast immobilization or various surgical treatments for distal radius fractures, no statistically significant difference was found in patient-reported disability scores and range of motion values between casting and surgery in the first postoperative year.
Other sites. Fractures in the elderly are not uncommon in the shoulder, distal radius, cubitus, proximal humerus, and humerus. These fractures are often treated without surgery, but nevertheless signal a high risk for additional fractures.
Bone-enhancing medications
Even in the absence of diagnosed low bone density or osteoporosis, anabolic agents such as the synthetic human parathyroid hormones abaloparatide (Tymlos) and teriparatide (Forteo) may be used to help in some cases with a bad healing prognosis and may also be used for people undergoing surgeries such as a spinal fusion, but there are not clinical guidelines. “We receive referrals regularly for this treatment from our orthopedics colleagues, but it is considered an off-label use,” Dr. Kelly said.
The anabolics teriparatide and romosozumab (Evenity) have proved effective in lowering fractures in high-risk older women.
Post fracture
After recovering from a fracture, elderly people are strongly advised to make lifestyle changes to boost bone health and reduce risk of further fractures, said Willy M. Valencia, MD, a geriatrician-endocrinologist at the Cleveland Clinic. Apart from active daily living, he recommends several types of formal exercise to promote bone formation; increase muscle mass, strength, and flexibility; and improve endurance, balance, and gait. The National Institute on Aging outlines suitable exercise programs for seniors.
“These exercises will help reduce the risk of falling and to avoid more fractures,” he said. “Whether a patient has been exercising before the fracture or not, they may feel some reticence or reluctance to take up exercise afterwards because they’re afraid of having another fracture, but they should understand that their fracture risk increases if they remain sedentary. They should start slowly but they can’t be sitting all day.”
Even before it’s possible to exercise at the healing fracture site, added Dr. Rianon, its advisable to work other areas of the body. “Overall mobility is important, and exercising other parts of the body can stimulate strength and help prevent falling.”
In other postsurgical measures, a bone-friendly diet rich in calcium and vitamin D, as well as supplementation with these vital nutrients, is essential to lower the risk of falling.
Fall prevention is paramount, said Dr. Valencia. While exercise can improve, gait, balance, and endurance, logistical measures may also be necessary. Seniors may have to move to a one-floor domicile with no stairs to negotiate. At the very least, they need to fall-proof their daily lives by upgrading their eyeglasses and home lighting, eliminating obstacles and loose carpets, fixing bannisters, and installing bathroom handrails. Some may need assistive devices for walking, especially outdoors in slippery conditions.
At the end of the day, the role of the primary physician in screening for bone problems before fracture and postsurgical care is key. “Risk factors for osteoporosis and fracture risk must be added to the patient’s chart,” said Dr. Rianon. Added Dr. Moseley. “No matter how busy they are, my hope is that primary care physicians will not put patients’ bone health at the bottom of the clinical agenda.”
Abdominal fat linked to lower brain volume in midlife
In a large study of healthy middle-aged adults, greater visceral and subcutaneous abdominal fat on abdominal MRI predicted brain atrophy on imaging, especially in women.
“The study shows that excess fat is bad for the brain and worse in women, including in Alzheimer’s disease risk regions,” lead author Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, Mo., said in an interview.
The study was published online in the journal Aging and Disease
Modifiable risk factor
Multiple studies have suggested a connection between body fat accumulation and increased dementia risk. But few have examined the relationship between types of fat (visceral and subcutaneous) and brain volume.
For the new study, 10,000 healthy adults aged 20-80 years (mean age, 52.9 years; 53% men) underwent a short whole-body MRI protocol. Regression analyses of abdominal fat types and normalized brain volumes were evaluated, controlling for age and sex.
The research team found that higher amounts of both visceral and subcutaneous abdominal fat predicted lower total gray and white matter volume, as well as lower volume in the hippocampus, frontal cortex, and temporal, parietal, and occipital lobes.
“The findings are quite dramatic,” Dr. Raji told this news organization. “Overall, we found that both subcutaneous and visceral fat has similar levels of negative relationships with brain volumes.”
Women had a higher burden of brain atrophy with increased visceral fat than men. However, it’s difficult to place the sex differences in context because of the lack of prior work specifically investigating visceral fat, brain volume loss, and sex differences, the researchers caution.
They also note that while statistically significant relationships were observed between visceral fat levels and gray matter volume changes, their effect sizes were generally small.
“Thus, the statistical significance of this work is influenced by the large sample size and less so by large effect size in any given set of regions,” the investigators write.
Other limitations include the cross-sectional nature of the study, which precludes conclusions about causality. The analysis also did not account for other lifestyle factors such as physical activity, diet, and genetic variables.
The researchers call for further investigation “to better elucidate underlying mechanisms and discover possible interventions targeting abdominal fat reduction as a strategy to maintain brain health.”
‘Helpful addition to the literature’
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, noted that “previous studies have linked obesity with cognitive decline and increased risk of dementia. Rather than using BMI as a proxy for body fat, the current study examined visceral and subcutaneous fat directly using imaging techniques.”
Dr. Sexton, who was not associated with this study, said the finding that increased body fat was associated with reduced brain volumes suggests “a possible mechanism to explain the previously reported associations between obesity and cognition.”
“Though some degree of atrophy and brain shrinkage is common with old age, awareness of this association is important because reduced brain volume may be associated with problems with thinking, memory, and performing everyday tasks, and because rates of obesity continue to rise in the United States, along with obesity-related conditions including heart disease, stroke, type 2 diabetes and certain types of cancer,” she added.
“While a helpful addition to the literature, the study does have important limitations. As an observational study, it cannot establish whether higher levels of body fat directly causes reduced brain volumes,” Dr. Sexton cautioned.
In addition, the study did not take into account important related factors like physical activity and diet, which may influence any relationship between body fat and brain volumes, she noted. “Overall, it is not just one factor that is important to consider when considering risk for cognitive decline and dementia, but multiple factors.
“Obesity and the location of body fat must be considered in combination with one’s total lived experience and habits, including physical activity, education, head injury, sleep, mental health, and the health of your heart/cardiovascular system and other key bodily systems,” Dr. Sexton said.
The Alzheimer’s Association is leading a 2-year clinical trial known as U.S. POINTER to see whether combining physical activity, healthy nutrition, social and intellectual challenges, and improved self-management of medical conditions can protect cognitive function in older adults who are at increased risk for cognitive decline.
This work was supported in part by Providence St. Joseph Health in Seattle; Saint John’s Health Center Foundation; Pacific Neuroscience Institute and Foundation; Will and Cary Singleton; and the McLoughlin family. Dr. Raji is a consultant for Brainreader, Apollo Health, Voxelwise, Neurevolution, Pacific Neuroscience Institute Foundation, and Icometrix. Dr. Sexton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large study of healthy middle-aged adults, greater visceral and subcutaneous abdominal fat on abdominal MRI predicted brain atrophy on imaging, especially in women.
“The study shows that excess fat is bad for the brain and worse in women, including in Alzheimer’s disease risk regions,” lead author Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, Mo., said in an interview.
The study was published online in the journal Aging and Disease
Modifiable risk factor
Multiple studies have suggested a connection between body fat accumulation and increased dementia risk. But few have examined the relationship between types of fat (visceral and subcutaneous) and brain volume.
For the new study, 10,000 healthy adults aged 20-80 years (mean age, 52.9 years; 53% men) underwent a short whole-body MRI protocol. Regression analyses of abdominal fat types and normalized brain volumes were evaluated, controlling for age and sex.
The research team found that higher amounts of both visceral and subcutaneous abdominal fat predicted lower total gray and white matter volume, as well as lower volume in the hippocampus, frontal cortex, and temporal, parietal, and occipital lobes.
“The findings are quite dramatic,” Dr. Raji told this news organization. “Overall, we found that both subcutaneous and visceral fat has similar levels of negative relationships with brain volumes.”
Women had a higher burden of brain atrophy with increased visceral fat than men. However, it’s difficult to place the sex differences in context because of the lack of prior work specifically investigating visceral fat, brain volume loss, and sex differences, the researchers caution.
They also note that while statistically significant relationships were observed between visceral fat levels and gray matter volume changes, their effect sizes were generally small.
“Thus, the statistical significance of this work is influenced by the large sample size and less so by large effect size in any given set of regions,” the investigators write.
Other limitations include the cross-sectional nature of the study, which precludes conclusions about causality. The analysis also did not account for other lifestyle factors such as physical activity, diet, and genetic variables.
The researchers call for further investigation “to better elucidate underlying mechanisms and discover possible interventions targeting abdominal fat reduction as a strategy to maintain brain health.”
‘Helpful addition to the literature’
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, noted that “previous studies have linked obesity with cognitive decline and increased risk of dementia. Rather than using BMI as a proxy for body fat, the current study examined visceral and subcutaneous fat directly using imaging techniques.”
Dr. Sexton, who was not associated with this study, said the finding that increased body fat was associated with reduced brain volumes suggests “a possible mechanism to explain the previously reported associations between obesity and cognition.”
“Though some degree of atrophy and brain shrinkage is common with old age, awareness of this association is important because reduced brain volume may be associated with problems with thinking, memory, and performing everyday tasks, and because rates of obesity continue to rise in the United States, along with obesity-related conditions including heart disease, stroke, type 2 diabetes and certain types of cancer,” she added.
“While a helpful addition to the literature, the study does have important limitations. As an observational study, it cannot establish whether higher levels of body fat directly causes reduced brain volumes,” Dr. Sexton cautioned.
In addition, the study did not take into account important related factors like physical activity and diet, which may influence any relationship between body fat and brain volumes, she noted. “Overall, it is not just one factor that is important to consider when considering risk for cognitive decline and dementia, but multiple factors.
“Obesity and the location of body fat must be considered in combination with one’s total lived experience and habits, including physical activity, education, head injury, sleep, mental health, and the health of your heart/cardiovascular system and other key bodily systems,” Dr. Sexton said.
The Alzheimer’s Association is leading a 2-year clinical trial known as U.S. POINTER to see whether combining physical activity, healthy nutrition, social and intellectual challenges, and improved self-management of medical conditions can protect cognitive function in older adults who are at increased risk for cognitive decline.
This work was supported in part by Providence St. Joseph Health in Seattle; Saint John’s Health Center Foundation; Pacific Neuroscience Institute and Foundation; Will and Cary Singleton; and the McLoughlin family. Dr. Raji is a consultant for Brainreader, Apollo Health, Voxelwise, Neurevolution, Pacific Neuroscience Institute Foundation, and Icometrix. Dr. Sexton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large study of healthy middle-aged adults, greater visceral and subcutaneous abdominal fat on abdominal MRI predicted brain atrophy on imaging, especially in women.
“The study shows that excess fat is bad for the brain and worse in women, including in Alzheimer’s disease risk regions,” lead author Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, Mo., said in an interview.
The study was published online in the journal Aging and Disease
Modifiable risk factor
Multiple studies have suggested a connection between body fat accumulation and increased dementia risk. But few have examined the relationship between types of fat (visceral and subcutaneous) and brain volume.
For the new study, 10,000 healthy adults aged 20-80 years (mean age, 52.9 years; 53% men) underwent a short whole-body MRI protocol. Regression analyses of abdominal fat types and normalized brain volumes were evaluated, controlling for age and sex.
The research team found that higher amounts of both visceral and subcutaneous abdominal fat predicted lower total gray and white matter volume, as well as lower volume in the hippocampus, frontal cortex, and temporal, parietal, and occipital lobes.
“The findings are quite dramatic,” Dr. Raji told this news organization. “Overall, we found that both subcutaneous and visceral fat has similar levels of negative relationships with brain volumes.”
Women had a higher burden of brain atrophy with increased visceral fat than men. However, it’s difficult to place the sex differences in context because of the lack of prior work specifically investigating visceral fat, brain volume loss, and sex differences, the researchers caution.
They also note that while statistically significant relationships were observed between visceral fat levels and gray matter volume changes, their effect sizes were generally small.
“Thus, the statistical significance of this work is influenced by the large sample size and less so by large effect size in any given set of regions,” the investigators write.
Other limitations include the cross-sectional nature of the study, which precludes conclusions about causality. The analysis also did not account for other lifestyle factors such as physical activity, diet, and genetic variables.
The researchers call for further investigation “to better elucidate underlying mechanisms and discover possible interventions targeting abdominal fat reduction as a strategy to maintain brain health.”
‘Helpful addition to the literature’
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, noted that “previous studies have linked obesity with cognitive decline and increased risk of dementia. Rather than using BMI as a proxy for body fat, the current study examined visceral and subcutaneous fat directly using imaging techniques.”
Dr. Sexton, who was not associated with this study, said the finding that increased body fat was associated with reduced brain volumes suggests “a possible mechanism to explain the previously reported associations between obesity and cognition.”
“Though some degree of atrophy and brain shrinkage is common with old age, awareness of this association is important because reduced brain volume may be associated with problems with thinking, memory, and performing everyday tasks, and because rates of obesity continue to rise in the United States, along with obesity-related conditions including heart disease, stroke, type 2 diabetes and certain types of cancer,” she added.
“While a helpful addition to the literature, the study does have important limitations. As an observational study, it cannot establish whether higher levels of body fat directly causes reduced brain volumes,” Dr. Sexton cautioned.
In addition, the study did not take into account important related factors like physical activity and diet, which may influence any relationship between body fat and brain volumes, she noted. “Overall, it is not just one factor that is important to consider when considering risk for cognitive decline and dementia, but multiple factors.
“Obesity and the location of body fat must be considered in combination with one’s total lived experience and habits, including physical activity, education, head injury, sleep, mental health, and the health of your heart/cardiovascular system and other key bodily systems,” Dr. Sexton said.
The Alzheimer’s Association is leading a 2-year clinical trial known as U.S. POINTER to see whether combining physical activity, healthy nutrition, social and intellectual challenges, and improved self-management of medical conditions can protect cognitive function in older adults who are at increased risk for cognitive decline.
This work was supported in part by Providence St. Joseph Health in Seattle; Saint John’s Health Center Foundation; Pacific Neuroscience Institute and Foundation; Will and Cary Singleton; and the McLoughlin family. Dr. Raji is a consultant for Brainreader, Apollo Health, Voxelwise, Neurevolution, Pacific Neuroscience Institute Foundation, and Icometrix. Dr. Sexton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AGING AND DISEASES
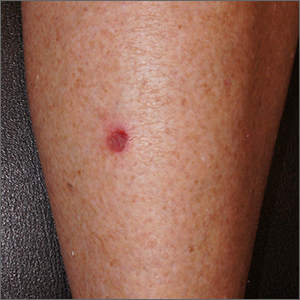
Small persistent leg wound

A leg ulcer may have many causes, including venous stasis, trauma, vasculitis, infection, or (as in this case) squamous cell carcinoma in situ (SCCis), aka Bowen’s Disease.
SCC and SCCis are common skin cancers that occur less frequently than basal cell carcinomas (BCCs).1 SCCis is normally scaly and hyperkeratotic, but it can manifest in rare cases as a chronic ulcer. Fair skin, long history of sun damage, and immunosuppression are significant risk factors for both SCCis and SCC.
While history and other clinical features may help narrow the diagnosis, a wound that does not heal despite treatments should be biopsied. Shave and punch biopsies are both excellent ways to diagnose an SCCis that has a classic appearance. However, ulcers and blisters can be caused by inflammatory processes (as in pyoderma gangrenosum or a fixed drug eruption) with characteristic findings deeper in the dermis; these lesions are better assessed with a punch biopsy.
In this case, a 4-mm punch biopsy was performed at the tissue edge and showed atypical keratinocytes limited to the epidermis. These atypical keratinocytes are associated with vesicle formation and ulcer, consistent with SCCis.
SCCis transforms into invasive disease in 3% to 5% of cases.2 Surgical treatment includes fusiform excision and electrodessication and curettage, both with cure rates that often exceed 90%.2,3 Nonsurgical options include topical 5-fluorouracil (67%-92% effective), topical imiquimod (75%-93%), and photodynamic therapy (52%-98%).4
Treatment choices depend on patient preference and provider capabilities. With surgical options there is the risk of bleeding and the need to care for a healing wound. Nonsurgical treatments can last longer and require topical treatment regimens and medications.
This patient opted for a fusiform excision and linear closure. She will continue to undergo serial skin evaluations twice a year for at least 2 years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.
1. Lukowiak TM, Aizman L, Perz A, et al. Association of age, sex, race, and geographic region with variation of the ratio of basal cell to cutaneous squamous cell carcinomas in the United States. JAMA Dermatol. 2020;156:1192-1198. doi:10.1001/jamadermatol.2020.2571
2. Morton CA, Birnie AJ, Eedy DJ. British Association of Dermatologists’ guidelines for the management of squamous cell carcinoma in situ (Bowen's disease). Br J Dermatol. 2014;170:245-246. doi: 10.1111/bjd.12766
3. Veverka KK, Stratman EJ. Electrodesiccation and curettage for squamous cell carcinoma in situ: the effect of anatomic location on local recurrence. Dermatol Surg. 2023;49:821-824. doi: 10.1097/DSS.0000000000003855
4. Algarin, YA, Jambusaria-Pahlajani A. Ruiz E, et al. Advances in topical treatments of cutaneous malignancies. Am J Clin Dermatol. 2023;24:69-80. doi: 10.1007/s40257-022-00731-x

A leg ulcer may have many causes, including venous stasis, trauma, vasculitis, infection, or (as in this case) squamous cell carcinoma in situ (SCCis), aka Bowen’s Disease.
SCC and SCCis are common skin cancers that occur less frequently than basal cell carcinomas (BCCs).1 SCCis is normally scaly and hyperkeratotic, but it can manifest in rare cases as a chronic ulcer. Fair skin, long history of sun damage, and immunosuppression are significant risk factors for both SCCis and SCC.
While history and other clinical features may help narrow the diagnosis, a wound that does not heal despite treatments should be biopsied. Shave and punch biopsies are both excellent ways to diagnose an SCCis that has a classic appearance. However, ulcers and blisters can be caused by inflammatory processes (as in pyoderma gangrenosum or a fixed drug eruption) with characteristic findings deeper in the dermis; these lesions are better assessed with a punch biopsy.
In this case, a 4-mm punch biopsy was performed at the tissue edge and showed atypical keratinocytes limited to the epidermis. These atypical keratinocytes are associated with vesicle formation and ulcer, consistent with SCCis.
SCCis transforms into invasive disease in 3% to 5% of cases.2 Surgical treatment includes fusiform excision and electrodessication and curettage, both with cure rates that often exceed 90%.2,3 Nonsurgical options include topical 5-fluorouracil (67%-92% effective), topical imiquimod (75%-93%), and photodynamic therapy (52%-98%).4
Treatment choices depend on patient preference and provider capabilities. With surgical options there is the risk of bleeding and the need to care for a healing wound. Nonsurgical treatments can last longer and require topical treatment regimens and medications.
This patient opted for a fusiform excision and linear closure. She will continue to undergo serial skin evaluations twice a year for at least 2 years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.

A leg ulcer may have many causes, including venous stasis, trauma, vasculitis, infection, or (as in this case) squamous cell carcinoma in situ (SCCis), aka Bowen’s Disease.
SCC and SCCis are common skin cancers that occur less frequently than basal cell carcinomas (BCCs).1 SCCis is normally scaly and hyperkeratotic, but it can manifest in rare cases as a chronic ulcer. Fair skin, long history of sun damage, and immunosuppression are significant risk factors for both SCCis and SCC.
While history and other clinical features may help narrow the diagnosis, a wound that does not heal despite treatments should be biopsied. Shave and punch biopsies are both excellent ways to diagnose an SCCis that has a classic appearance. However, ulcers and blisters can be caused by inflammatory processes (as in pyoderma gangrenosum or a fixed drug eruption) with characteristic findings deeper in the dermis; these lesions are better assessed with a punch biopsy.
In this case, a 4-mm punch biopsy was performed at the tissue edge and showed atypical keratinocytes limited to the epidermis. These atypical keratinocytes are associated with vesicle formation and ulcer, consistent with SCCis.
SCCis transforms into invasive disease in 3% to 5% of cases.2 Surgical treatment includes fusiform excision and electrodessication and curettage, both with cure rates that often exceed 90%.2,3 Nonsurgical options include topical 5-fluorouracil (67%-92% effective), topical imiquimod (75%-93%), and photodynamic therapy (52%-98%).4
Treatment choices depend on patient preference and provider capabilities. With surgical options there is the risk of bleeding and the need to care for a healing wound. Nonsurgical treatments can last longer and require topical treatment regimens and medications.
This patient opted for a fusiform excision and linear closure. She will continue to undergo serial skin evaluations twice a year for at least 2 years.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, Maine.
1. Lukowiak TM, Aizman L, Perz A, et al. Association of age, sex, race, and geographic region with variation of the ratio of basal cell to cutaneous squamous cell carcinomas in the United States. JAMA Dermatol. 2020;156:1192-1198. doi:10.1001/jamadermatol.2020.2571
2. Morton CA, Birnie AJ, Eedy DJ. British Association of Dermatologists’ guidelines for the management of squamous cell carcinoma in situ (Bowen's disease). Br J Dermatol. 2014;170:245-246. doi: 10.1111/bjd.12766
3. Veverka KK, Stratman EJ. Electrodesiccation and curettage for squamous cell carcinoma in situ: the effect of anatomic location on local recurrence. Dermatol Surg. 2023;49:821-824. doi: 10.1097/DSS.0000000000003855
4. Algarin, YA, Jambusaria-Pahlajani A. Ruiz E, et al. Advances in topical treatments of cutaneous malignancies. Am J Clin Dermatol. 2023;24:69-80. doi: 10.1007/s40257-022-00731-x
1. Lukowiak TM, Aizman L, Perz A, et al. Association of age, sex, race, and geographic region with variation of the ratio of basal cell to cutaneous squamous cell carcinomas in the United States. JAMA Dermatol. 2020;156:1192-1198. doi:10.1001/jamadermatol.2020.2571
2. Morton CA, Birnie AJ, Eedy DJ. British Association of Dermatologists’ guidelines for the management of squamous cell carcinoma in situ (Bowen's disease). Br J Dermatol. 2014;170:245-246. doi: 10.1111/bjd.12766
3. Veverka KK, Stratman EJ. Electrodesiccation and curettage for squamous cell carcinoma in situ: the effect of anatomic location on local recurrence. Dermatol Surg. 2023;49:821-824. doi: 10.1097/DSS.0000000000003855
4. Algarin, YA, Jambusaria-Pahlajani A. Ruiz E, et al. Advances in topical treatments of cutaneous malignancies. Am J Clin Dermatol. 2023;24:69-80. doi: 10.1007/s40257-022-00731-x
Underprescribed menopause relief: Women suffer needlessly
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
The result: Countless women grapple with the physical and emotional toll of this life transition.
These shortcomings have led to an influx of doctors moving from traditional practice to virtual startups that focus on women’s health issues, treating patients who come to them desperate and frustrated after years of unresolved issues.
The solution is often so simple it is almost maddening, specialists say: vaginal creams containing low-dose estrogen which can address the symptoms of menopause, from vaginal dryness to recurrent urinary tract infections.
“Hands down, this is one of the most meaningful interventions I’ve ever offered to a patient and yet it is underutilized,” said Ashley Winter, MD, chief medical officer and urologist at Odela Health, a digital women’s health clinic. “A lot of companies are blossoming in this menopause space because it is underserved by traditional health care – your gynecologist typically deals with reproduction, and typically when women are done with child-bearing, they’re kind of discharged from the care of their gynecologist.”
More than 1 million women in the United States go through menopause each year. According to a 2022 survey, 4 in 10 women report menopause symptoms that have been disruptive enough to interfere with their work performance on at least a weekly basis.
And yet, many women are not getting appropriate treatment.
Partially to blame is the harmful legacy of faulty data, doctors say. The early results of the federally funded Women’s Health Initiative, released in 2002, showed that hormone therapy (HT) led to increased risk for heart attacks, strokes, and breast cancer. But further analysis showed the opposite: Hormonal therapies have a helpful effect on cardiovascular and bone health and generally reduce risk of death in younger women or those in the early postmenopausal period.
Hormone therapy delivers estrogen, sometimes with progesterone, to the body through gels, creams, patches, pills, suppositories, or a device fitted inside the uterus. Systemic HT sends hormones into the bloodstream, while local HT – like vaginal estrogen cream – specifically treats vaginal symptoms of menopause.
Myths about the health risks linked to systemic and topical HT have long been debunked, and research on topical HT in particular shows it poses no risk for cancer or other chronic diseases.
Yet while 2 decades have passed since the misinformation first started to spread, people remain woefully uninformed about hormone treatments.
The FDA still requires that estrogen products carry a black-box warning on the early data, even though it has since been proven false.
“This is one of the most damaging PR misadventures of modern medicine in my opinion,” Dr. Winter said. “It has literally killed women, and it’s made them miserable.”
The public has a glaring lack of knowledge about menopause management, said Stephanie Faubion, MD, medical director for the North American Menopause Society and director of Mayo Clinic’s Center for Women’s Health.
Treating with low-dose estrogen isn’t a radical approach – in fact, it is the standard of care for women experiencing many menopause symptoms, Dr. Faubion said. But the topic does have nuance, and some people get lost in the specifics.
“I don’t think there’s a lot of knowledge on the risk-benefits of hormone therapy in general,” Dr. Faubion said. “New information comes out so frequently it’s difficult to keep track of. The answer is complicated and depends on dose, duration of treatment, what formulation you’re on. It’s difficult for a lot of people to understand.”
But Dr. Winter said the lack of public knowledge reflects a bigger problem: Knowledge gaps exist among doctors, too, stemming from insufficient training on menopause-related issues.
During her 6-year urology residency, she never learned the role of vaginal estrogen on urinary problems, Dr. Winter said. Only during a 1-year fellowship on sexual dysfunction did she hear about the treatment.
“Despite dealing with urinary issues, incontinence, blood in the urine – training to manage all those concerns – the role of local hormones in the vagina for managing all them was never taught, never discussed,” Dr. Winter said. “I never prescribed any of it.”
A year ago, Dr. Winter left her job at Kaiser Permanente to join Odela. After years of prescribing medications for overactive bladder with little to no results, she said, she now uses the knowledge she gained during her fellowship by helping women who have spent years battling debilitating symptoms.
Urologists are not the only clinicians who lack appropriate training. Obstetrics and gynecology residencies offer little knowledge on menopause treatments, said Ghazaleh Moayedi, DO, an ob.gyn. and complex family planning specialist for Texas-based Pegasus Health Justice Center.
The problem is partly a systems-based one, she said. Training programs often direct patients who are uninsured, or covered through public insurance, to medical residents. Patients who qualify for Medicaid or Medicare are often either pregnant or over 65, Dr. Moayedi said, so women actively going through the transition can slip through the cracks.
“What that means in a state like Texas where I’m based, where it is difficult to qualify for Medicaid, is that the people we see who do qualify are pregnant,” she said. “And you’re not on Medicare until you’re 65. So most ob.gyn. residents don’t graduate with expansive experience in menopause.”
According to Medicaid.gov, 80% of the national population covered by Medicaid is age 45 and younger.
When doctors have proper training and prescribe local hormones, patients don’t always follow the treatment plan, said Andrea Rapkin, MD, professor of obstetrics and gynecology at David Geffen School of Medicine at UCLA.
That failure to follow treatment is yet another example of remaining doubts from the misinformation spread through early research, Dr. Rapkin said.
“I’ll prescribe an estrogen product, and I’ll find out they didn’t take it even though I’ll reassure them,” she said. “I do think there are some lingering concerns, but I’m glad to see there is a growing interest in vaginal hormones.”
A version of this article first appeared on WebMD.com.
The most important study from ESC: FRAIL-AF
One of the hardest tasks of a clinician is applying evidence from trials to the person in your office. At the annual congress of the European Society of Cardiology, the surprising and unexpected results of the FRAIL-AF trial confirm the massive challenge of evidence translation.
FRAIL-AF investigators set out to study the question of whether frail, elderly patients with atrial fibrillation who were doing well with vitamin K antagonists (VKA) should be switched to direct-acting oral anticoagulants (DOAC).
Senior author Geert-Jan Geersing, MD, PhD, from the University Medical Center Utrecht (the Netherlands), told me that frustration led him to design this study. He was frustrated that colleagues assumed that evidence in nonfrail patients can always be translated to frail patients.
Dr. Geersing offered two reasons why common wisdom may be wrong. First was that the large DOAC versus warfarin trials included few elderly patients with frailty. Second, first author Linda Joosten, MD, made it clear in her presentation that frailty is a lot more than aging. It is a clinical syndrome, which entails a “high burden of comorbidities, dependency on others, and a reduced ability to resist stressors.”
The FRAIL-AF trial
The investigators recruited elderly, frail patients with fibrillation who were treated with VKAs and had stable international normalized ratios from outpatient clinics throughout the Netherlands. They screened about 2,600 patients and enrolled nearly 1,400. Most were excluded for not being frail.
Half the group was randomized to switching to a DOAC – drug choice was left to the treating clinician – and the other half remained on VKAs. Patients were 83 years of age on average with a mean CHA2DS2-VASc score of 4. All four classes of DOAC were used in the switching arm.
The primary endpoint was major or clinically relevant nonmajor bleeding, whichever came first, accounting for death as a competing risk. Follow-up was 1 year.
The results for switching to DOAC vs. VKA
Dr. Joosten started her presentation with this: “The results turned out to be different than we expected.” The authors designed the trial with the idea that switching to DOACs would be superior in safety to remaining on VKAs.
But the trial was halted after an interim analysis found a rate of major bleeding in the switching arm of 15.3% versus 9.4% in the arm staying on VKA (hazard ratio, 1.69; 95% confidence interval, 1.23-2.32; P = .0012).
The Kaplan-Meier event curves reveal that the excess risk of bleeding occurred after 100 days and increased with time. This argued against an early effect from transitioning the drugs.
An analysis looking at specific DOAC drugs revealed similar hazards for the two most common ones used – apixaban and rivaroxaban.
Thrombotic events were a secondary endpoint and were low in absolute numbers, 2.4% versus 2.0%, for remaining on VKA and switching to DOAC, respectively (HR, 1.26; 95% CI, 0.60-2.61).
The time in therapeutic range in FRAIL-AF was similar to that in the seminal DOAC trials.
Comments
Three reasons lead me to choose FRAIL-AF as the most important study from the 2023 ESC congress.
First is the specific lesson about switching drugs. Note that FRAIL-AF did not address the question of starting anticoagulation. The trial results show that if you have a frail older patient who is doing well on VKA, don’t change to a DOAC. That is important to know, but it is not what gives this study its heft.
The second reason centers on the investigators choice to do this trial. Dr. Geersing had a feeling that common wisdom was wrong. He did not try to persuade colleagues with anecdote or plausibility or meta-analyses of observational studies. He set out to answer a question in the correct way – with a randomized trial.
This is the path forward in medicine. I’ve often heard proponents of observational research declare that many topics in medicine cannot be studied with trials. I could hear people arguing that it’s not feasible to study mostly home-bound, elderly frail patients. And the fact that there exist so few trials in this space would support that argument.
But the FRAIL-AF authors showed that it is possible. This is the kind of science that medicine should celebrate. There were no soft endpoints, financial conflicts, or spin. If medical science had science as its incentive, rather than attention, FRAIL-AF easily wins top honors.
The third reason FRAIL-AF is so important is that it teaches us the humility required in translating evidence in our clinics. I like to say evidence is what separates doctors from palm readers. But using this evidence requires thinking hard about how average effects in trial environments apply to our patient.
Yes, of course, there is clear evidence from tens of thousands of patients in the DOAC versus warfarin trials, that, for those patients, on average, DOACs compare favorably with VKA. The average age of patients in these trials was 70-73 years; the average age in FRAIL-AF was 83 years. And that is just age. A substudy of the ENGAGE AF-TIMI 48 trial found that only 360 of more than 20,000 patients in the trial had severe frailty.
That lesson extends to nearly every common therapy in medicine today. It also casts great doubt on the soft-thinking idea of using evidence from trials to derive quality metrics. As if the nuance of evidence translation can be captured in an electronic health record.
The skillful use of evidence will be one of the main challenges of the next generation of clinicians. Thanks to advances in medical science, more patients will live long enough to become frail. And the so-called “guideline-directed” therapies may not apply to them.
Dr. Joosten, Dr. Geersing, and the FRAIL-AF team have taught us specific lessons about anticoagulation, but their greatest contribution has been to demonstrate the value of humility in science and the practice of evidence-based medicine.
If you treat patients, no trial at this meeting is more important.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
One of the hardest tasks of a clinician is applying evidence from trials to the person in your office. At the annual congress of the European Society of Cardiology, the surprising and unexpected results of the FRAIL-AF trial confirm the massive challenge of evidence translation.
FRAIL-AF investigators set out to study the question of whether frail, elderly patients with atrial fibrillation who were doing well with vitamin K antagonists (VKA) should be switched to direct-acting oral anticoagulants (DOAC).
Senior author Geert-Jan Geersing, MD, PhD, from the University Medical Center Utrecht (the Netherlands), told me that frustration led him to design this study. He was frustrated that colleagues assumed that evidence in nonfrail patients can always be translated to frail patients.
Dr. Geersing offered two reasons why common wisdom may be wrong. First was that the large DOAC versus warfarin trials included few elderly patients with frailty. Second, first author Linda Joosten, MD, made it clear in her presentation that frailty is a lot more than aging. It is a clinical syndrome, which entails a “high burden of comorbidities, dependency on others, and a reduced ability to resist stressors.”
The FRAIL-AF trial
The investigators recruited elderly, frail patients with fibrillation who were treated with VKAs and had stable international normalized ratios from outpatient clinics throughout the Netherlands. They screened about 2,600 patients and enrolled nearly 1,400. Most were excluded for not being frail.
Half the group was randomized to switching to a DOAC – drug choice was left to the treating clinician – and the other half remained on VKAs. Patients were 83 years of age on average with a mean CHA2DS2-VASc score of 4. All four classes of DOAC were used in the switching arm.
The primary endpoint was major or clinically relevant nonmajor bleeding, whichever came first, accounting for death as a competing risk. Follow-up was 1 year.
The results for switching to DOAC vs. VKA
Dr. Joosten started her presentation with this: “The results turned out to be different than we expected.” The authors designed the trial with the idea that switching to DOACs would be superior in safety to remaining on VKAs.
But the trial was halted after an interim analysis found a rate of major bleeding in the switching arm of 15.3% versus 9.4% in the arm staying on VKA (hazard ratio, 1.69; 95% confidence interval, 1.23-2.32; P = .0012).
The Kaplan-Meier event curves reveal that the excess risk of bleeding occurred after 100 days and increased with time. This argued against an early effect from transitioning the drugs.
An analysis looking at specific DOAC drugs revealed similar hazards for the two most common ones used – apixaban and rivaroxaban.
Thrombotic events were a secondary endpoint and were low in absolute numbers, 2.4% versus 2.0%, for remaining on VKA and switching to DOAC, respectively (HR, 1.26; 95% CI, 0.60-2.61).
The time in therapeutic range in FRAIL-AF was similar to that in the seminal DOAC trials.
Comments
Three reasons lead me to choose FRAIL-AF as the most important study from the 2023 ESC congress.
First is the specific lesson about switching drugs. Note that FRAIL-AF did not address the question of starting anticoagulation. The trial results show that if you have a frail older patient who is doing well on VKA, don’t change to a DOAC. That is important to know, but it is not what gives this study its heft.
The second reason centers on the investigators choice to do this trial. Dr. Geersing had a feeling that common wisdom was wrong. He did not try to persuade colleagues with anecdote or plausibility or meta-analyses of observational studies. He set out to answer a question in the correct way – with a randomized trial.
This is the path forward in medicine. I’ve often heard proponents of observational research declare that many topics in medicine cannot be studied with trials. I could hear people arguing that it’s not feasible to study mostly home-bound, elderly frail patients. And the fact that there exist so few trials in this space would support that argument.
But the FRAIL-AF authors showed that it is possible. This is the kind of science that medicine should celebrate. There were no soft endpoints, financial conflicts, or spin. If medical science had science as its incentive, rather than attention, FRAIL-AF easily wins top honors.
The third reason FRAIL-AF is so important is that it teaches us the humility required in translating evidence in our clinics. I like to say evidence is what separates doctors from palm readers. But using this evidence requires thinking hard about how average effects in trial environments apply to our patient.
Yes, of course, there is clear evidence from tens of thousands of patients in the DOAC versus warfarin trials, that, for those patients, on average, DOACs compare favorably with VKA. The average age of patients in these trials was 70-73 years; the average age in FRAIL-AF was 83 years. And that is just age. A substudy of the ENGAGE AF-TIMI 48 trial found that only 360 of more than 20,000 patients in the trial had severe frailty.
That lesson extends to nearly every common therapy in medicine today. It also casts great doubt on the soft-thinking idea of using evidence from trials to derive quality metrics. As if the nuance of evidence translation can be captured in an electronic health record.
The skillful use of evidence will be one of the main challenges of the next generation of clinicians. Thanks to advances in medical science, more patients will live long enough to become frail. And the so-called “guideline-directed” therapies may not apply to them.
Dr. Joosten, Dr. Geersing, and the FRAIL-AF team have taught us specific lessons about anticoagulation, but their greatest contribution has been to demonstrate the value of humility in science and the practice of evidence-based medicine.
If you treat patients, no trial at this meeting is more important.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
One of the hardest tasks of a clinician is applying evidence from trials to the person in your office. At the annual congress of the European Society of Cardiology, the surprising and unexpected results of the FRAIL-AF trial confirm the massive challenge of evidence translation.
FRAIL-AF investigators set out to study the question of whether frail, elderly patients with atrial fibrillation who were doing well with vitamin K antagonists (VKA) should be switched to direct-acting oral anticoagulants (DOAC).
Senior author Geert-Jan Geersing, MD, PhD, from the University Medical Center Utrecht (the Netherlands), told me that frustration led him to design this study. He was frustrated that colleagues assumed that evidence in nonfrail patients can always be translated to frail patients.
Dr. Geersing offered two reasons why common wisdom may be wrong. First was that the large DOAC versus warfarin trials included few elderly patients with frailty. Second, first author Linda Joosten, MD, made it clear in her presentation that frailty is a lot more than aging. It is a clinical syndrome, which entails a “high burden of comorbidities, dependency on others, and a reduced ability to resist stressors.”
The FRAIL-AF trial
The investigators recruited elderly, frail patients with fibrillation who were treated with VKAs and had stable international normalized ratios from outpatient clinics throughout the Netherlands. They screened about 2,600 patients and enrolled nearly 1,400. Most were excluded for not being frail.
Half the group was randomized to switching to a DOAC – drug choice was left to the treating clinician – and the other half remained on VKAs. Patients were 83 years of age on average with a mean CHA2DS2-VASc score of 4. All four classes of DOAC were used in the switching arm.
The primary endpoint was major or clinically relevant nonmajor bleeding, whichever came first, accounting for death as a competing risk. Follow-up was 1 year.
The results for switching to DOAC vs. VKA
Dr. Joosten started her presentation with this: “The results turned out to be different than we expected.” The authors designed the trial with the idea that switching to DOACs would be superior in safety to remaining on VKAs.
But the trial was halted after an interim analysis found a rate of major bleeding in the switching arm of 15.3% versus 9.4% in the arm staying on VKA (hazard ratio, 1.69; 95% confidence interval, 1.23-2.32; P = .0012).
The Kaplan-Meier event curves reveal that the excess risk of bleeding occurred after 100 days and increased with time. This argued against an early effect from transitioning the drugs.
An analysis looking at specific DOAC drugs revealed similar hazards for the two most common ones used – apixaban and rivaroxaban.
Thrombotic events were a secondary endpoint and were low in absolute numbers, 2.4% versus 2.0%, for remaining on VKA and switching to DOAC, respectively (HR, 1.26; 95% CI, 0.60-2.61).
The time in therapeutic range in FRAIL-AF was similar to that in the seminal DOAC trials.
Comments
Three reasons lead me to choose FRAIL-AF as the most important study from the 2023 ESC congress.
First is the specific lesson about switching drugs. Note that FRAIL-AF did not address the question of starting anticoagulation. The trial results show that if you have a frail older patient who is doing well on VKA, don’t change to a DOAC. That is important to know, but it is not what gives this study its heft.
The second reason centers on the investigators choice to do this trial. Dr. Geersing had a feeling that common wisdom was wrong. He did not try to persuade colleagues with anecdote or plausibility or meta-analyses of observational studies. He set out to answer a question in the correct way – with a randomized trial.
This is the path forward in medicine. I’ve often heard proponents of observational research declare that many topics in medicine cannot be studied with trials. I could hear people arguing that it’s not feasible to study mostly home-bound, elderly frail patients. And the fact that there exist so few trials in this space would support that argument.
But the FRAIL-AF authors showed that it is possible. This is the kind of science that medicine should celebrate. There were no soft endpoints, financial conflicts, or spin. If medical science had science as its incentive, rather than attention, FRAIL-AF easily wins top honors.
The third reason FRAIL-AF is so important is that it teaches us the humility required in translating evidence in our clinics. I like to say evidence is what separates doctors from palm readers. But using this evidence requires thinking hard about how average effects in trial environments apply to our patient.
Yes, of course, there is clear evidence from tens of thousands of patients in the DOAC versus warfarin trials, that, for those patients, on average, DOACs compare favorably with VKA. The average age of patients in these trials was 70-73 years; the average age in FRAIL-AF was 83 years. And that is just age. A substudy of the ENGAGE AF-TIMI 48 trial found that only 360 of more than 20,000 patients in the trial had severe frailty.
That lesson extends to nearly every common therapy in medicine today. It also casts great doubt on the soft-thinking idea of using evidence from trials to derive quality metrics. As if the nuance of evidence translation can be captured in an electronic health record.
The skillful use of evidence will be one of the main challenges of the next generation of clinicians. Thanks to advances in medical science, more patients will live long enough to become frail. And the so-called “guideline-directed” therapies may not apply to them.
Dr. Joosten, Dr. Geersing, and the FRAIL-AF team have taught us specific lessons about anticoagulation, but their greatest contribution has been to demonstrate the value of humility in science and the practice of evidence-based medicine.
If you treat patients, no trial at this meeting is more important.
Dr. Mandrola is a clinical electrophysiologist at Baptist Medical Associates, Louisville, Ky. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Low-dose aspirin cuts type 2 diabetes risk in over-65s
The data come from a secondary analysis of ASPREE, a double-blind, placebo-controlled trial of healthy adults aged 65 years or older, showing that 100 mg of aspirin taken daily for about 5 years did not provide a cardiovascular benefit but did significantly raise the risk for bleeding.
This new analysis shows that individuals taking aspirin had a 15% lower risk for developing type 2 diabetes and that the medication slowed the rate of increase in fasting plasma glucose, compared with placebo, during follow-up.
However, lead author Sophia Zoungas, MBBS, PhD, head of the School of Public Health and Preventive Medicine, Monash University, Melbourne, said: “Major prescribing guidelines now recommend older adults take daily aspirin only when there is a medical reason to do so, such as after a heart attack. ... Although these new findings are of interest, they do not change the clinical advice about aspirin use in older people at this time.”
Nonetheless, she said in an interview, “at this time, our findings are exploratory but ignite the debate of the important role that anti-inflammatory approaches may play in preventing diabetes. Further work is currently underway to understand which subpopulations may be better targeted and to understand the balance of risk versus benefit.”
The results are scheduled to be presented at the upcoming meeting of the European Association for the Study of Diabetes, taking place Oct. 2-6 in Hamburg, Germany.
New findings not robust enough to change current practice
Asked to comment, Debabrata Mukherjee, MD, said: “Given the post hoc secondary nature of the analysis, the findings should be considered hypothesis generating and not definitive… At this time, based on prospective randomized studies, the risks of aspirin outweigh the benefits for aspirin in older adults.”
Among those studies was an ASPREE substudy showing failure of low-dose aspirin to reduce fracture risk while increasing the risk for serious falls, and two other trials, ARRIVE and ASCEND, also showing that harms of aspirin outweigh the benefits in people with cardiovascular risk but not diabetes, and in those with diabetes, respectively, said Dr. Mukherjee, professor and chair of the department of internal medicine at Texas Tech University Health Sciences Center at El Paso.
And, Mukherjee noted, in 2019 the American College of Cardiology updated its practice guidelines to say that low-dose aspirin should not be administered on a routine basis for the primary prevention of atherosclerotic cardiovascular disease in adults over age 70. In 2021, the American Diabetes Association seconded that recommendation.
Asked whether these newest findings might change current practice for any higher-risk subgroup, such as people with prediabetes, Dr. Mukherjee replied: “Unless there is a prospective randomized trial that validates these findings in those with prediabetes, the findings should not change practice. There are also no data [showing] that another antiplatelet agent would be indicated or would be beneficial. Instead, I would recommend lifestyle changes including regular exercise and a healthy diet to minimize risk of diabetes.”
The 16,209 ASPREE participants were community dwelling and did not have diabetes, cardiovascular disease, or dementia at baseline. They were randomized in a 1:1 ratio to receive 100 mg/d of enteric-coated aspirin or placebo. Over a median follow-up of 4.7 years, the proportions developing type 2 diabetes were 5.7% with aspirin versus 6.6% with placebo (hazard ratio, 0.85; P = .01).
The annual rate of increase in fasting plasma glucose over the follow-up period was slowed by 0.006 mmol/L with aspirin, compared with placebo, also a significant difference (P = .004).
According to Dr. Zoungas, “the potential for anti-inflammatory agents like aspirin to prevent type 2 diabetes or improve glucose levels needs further study.”
The ASPREE trial was supported by the U.S. National Institutes of Health, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Dr. Zoungas and Dr. Mukherjee have no disclosures.
A version of this article first appeared on Medscape.com.
The data come from a secondary analysis of ASPREE, a double-blind, placebo-controlled trial of healthy adults aged 65 years or older, showing that 100 mg of aspirin taken daily for about 5 years did not provide a cardiovascular benefit but did significantly raise the risk for bleeding.
This new analysis shows that individuals taking aspirin had a 15% lower risk for developing type 2 diabetes and that the medication slowed the rate of increase in fasting plasma glucose, compared with placebo, during follow-up.
However, lead author Sophia Zoungas, MBBS, PhD, head of the School of Public Health and Preventive Medicine, Monash University, Melbourne, said: “Major prescribing guidelines now recommend older adults take daily aspirin only when there is a medical reason to do so, such as after a heart attack. ... Although these new findings are of interest, they do not change the clinical advice about aspirin use in older people at this time.”
Nonetheless, she said in an interview, “at this time, our findings are exploratory but ignite the debate of the important role that anti-inflammatory approaches may play in preventing diabetes. Further work is currently underway to understand which subpopulations may be better targeted and to understand the balance of risk versus benefit.”
The results are scheduled to be presented at the upcoming meeting of the European Association for the Study of Diabetes, taking place Oct. 2-6 in Hamburg, Germany.
New findings not robust enough to change current practice
Asked to comment, Debabrata Mukherjee, MD, said: “Given the post hoc secondary nature of the analysis, the findings should be considered hypothesis generating and not definitive… At this time, based on prospective randomized studies, the risks of aspirin outweigh the benefits for aspirin in older adults.”
Among those studies was an ASPREE substudy showing failure of low-dose aspirin to reduce fracture risk while increasing the risk for serious falls, and two other trials, ARRIVE and ASCEND, also showing that harms of aspirin outweigh the benefits in people with cardiovascular risk but not diabetes, and in those with diabetes, respectively, said Dr. Mukherjee, professor and chair of the department of internal medicine at Texas Tech University Health Sciences Center at El Paso.
And, Mukherjee noted, in 2019 the American College of Cardiology updated its practice guidelines to say that low-dose aspirin should not be administered on a routine basis for the primary prevention of atherosclerotic cardiovascular disease in adults over age 70. In 2021, the American Diabetes Association seconded that recommendation.
Asked whether these newest findings might change current practice for any higher-risk subgroup, such as people with prediabetes, Dr. Mukherjee replied: “Unless there is a prospective randomized trial that validates these findings in those with prediabetes, the findings should not change practice. There are also no data [showing] that another antiplatelet agent would be indicated or would be beneficial. Instead, I would recommend lifestyle changes including regular exercise and a healthy diet to minimize risk of diabetes.”
The 16,209 ASPREE participants were community dwelling and did not have diabetes, cardiovascular disease, or dementia at baseline. They were randomized in a 1:1 ratio to receive 100 mg/d of enteric-coated aspirin or placebo. Over a median follow-up of 4.7 years, the proportions developing type 2 diabetes were 5.7% with aspirin versus 6.6% with placebo (hazard ratio, 0.85; P = .01).
The annual rate of increase in fasting plasma glucose over the follow-up period was slowed by 0.006 mmol/L with aspirin, compared with placebo, also a significant difference (P = .004).
According to Dr. Zoungas, “the potential for anti-inflammatory agents like aspirin to prevent type 2 diabetes or improve glucose levels needs further study.”
The ASPREE trial was supported by the U.S. National Institutes of Health, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Dr. Zoungas and Dr. Mukherjee have no disclosures.
A version of this article first appeared on Medscape.com.
The data come from a secondary analysis of ASPREE, a double-blind, placebo-controlled trial of healthy adults aged 65 years or older, showing that 100 mg of aspirin taken daily for about 5 years did not provide a cardiovascular benefit but did significantly raise the risk for bleeding.
This new analysis shows that individuals taking aspirin had a 15% lower risk for developing type 2 diabetes and that the medication slowed the rate of increase in fasting plasma glucose, compared with placebo, during follow-up.
However, lead author Sophia Zoungas, MBBS, PhD, head of the School of Public Health and Preventive Medicine, Monash University, Melbourne, said: “Major prescribing guidelines now recommend older adults take daily aspirin only when there is a medical reason to do so, such as after a heart attack. ... Although these new findings are of interest, they do not change the clinical advice about aspirin use in older people at this time.”
Nonetheless, she said in an interview, “at this time, our findings are exploratory but ignite the debate of the important role that anti-inflammatory approaches may play in preventing diabetes. Further work is currently underway to understand which subpopulations may be better targeted and to understand the balance of risk versus benefit.”
The results are scheduled to be presented at the upcoming meeting of the European Association for the Study of Diabetes, taking place Oct. 2-6 in Hamburg, Germany.
New findings not robust enough to change current practice
Asked to comment, Debabrata Mukherjee, MD, said: “Given the post hoc secondary nature of the analysis, the findings should be considered hypothesis generating and not definitive… At this time, based on prospective randomized studies, the risks of aspirin outweigh the benefits for aspirin in older adults.”
Among those studies was an ASPREE substudy showing failure of low-dose aspirin to reduce fracture risk while increasing the risk for serious falls, and two other trials, ARRIVE and ASCEND, also showing that harms of aspirin outweigh the benefits in people with cardiovascular risk but not diabetes, and in those with diabetes, respectively, said Dr. Mukherjee, professor and chair of the department of internal medicine at Texas Tech University Health Sciences Center at El Paso.
And, Mukherjee noted, in 2019 the American College of Cardiology updated its practice guidelines to say that low-dose aspirin should not be administered on a routine basis for the primary prevention of atherosclerotic cardiovascular disease in adults over age 70. In 2021, the American Diabetes Association seconded that recommendation.
Asked whether these newest findings might change current practice for any higher-risk subgroup, such as people with prediabetes, Dr. Mukherjee replied: “Unless there is a prospective randomized trial that validates these findings in those with prediabetes, the findings should not change practice. There are also no data [showing] that another antiplatelet agent would be indicated or would be beneficial. Instead, I would recommend lifestyle changes including regular exercise and a healthy diet to minimize risk of diabetes.”
The 16,209 ASPREE participants were community dwelling and did not have diabetes, cardiovascular disease, or dementia at baseline. They were randomized in a 1:1 ratio to receive 100 mg/d of enteric-coated aspirin or placebo. Over a median follow-up of 4.7 years, the proportions developing type 2 diabetes were 5.7% with aspirin versus 6.6% with placebo (hazard ratio, 0.85; P = .01).
The annual rate of increase in fasting plasma glucose over the follow-up period was slowed by 0.006 mmol/L with aspirin, compared with placebo, also a significant difference (P = .004).
According to Dr. Zoungas, “the potential for anti-inflammatory agents like aspirin to prevent type 2 diabetes or improve glucose levels needs further study.”
The ASPREE trial was supported by the U.S. National Institutes of Health, the National Health and Medical Research Council of Australia, Monash University, and the Victorian Cancer Agency. Dr. Zoungas and Dr. Mukherjee have no disclosures.
A version of this article first appeared on Medscape.com.
FROM EASD 2023
One in five doctors with long COVID can no longer work: Survey
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
Crippling symptoms, lost careers, and eroded incomes: This is the harsh reality for doctors suffering with long COVID, according to the first major survey of physicians with the condition.
The survey, conducted by the British Medical Association and the Long COVID Doctors for Action support group, sheds light on the lingering effects of long COVID on more than 600 chronically ill and disabled doctors with the condition. It also spotlights what they describe as a lack of medical and financial support from their government and employers at the National Health Service.
“We feel betrayed and abandoned,” said Kelly Fearnley, MBChB, chair and cofounder of Long COVID Doctors for Action. “At a time of national crisis, when health care workers were asked to step up, we did. When the nation needed us, we stepped up. We put our lives on the line. We put our families’ lives on the line. And now that we are injured after knowingly being unprotected and deliberately and repeatedly exposed to a level 3 biohazard, we now find ourselves in this position.”
Dr. Fearnley fell ill while working in a hospital’s COVID ward in November 2020. She is one of an estimated 2 million people in the United Kingdom – including thousands of NHS employees – with long COVID. She hasn’t been able to return to work in nearly 3 years.
Long COVID affects more than 65 million people worldwide. It is estimated that 1 in 10 people infected with the virus develop long-term symptoms. In the United Kingdom, health care and social care workers are seven times more likely to have had severe COVID-19 than other types of employees.
Doctors responding to the BMA survey reported a wide range of long COVID symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, and respiratory problems.
Among the survey’s key findings, 60% of doctors said long COVID has affected their ability to carry out day-to-day tasks on a regular basis. Almost one in five (18%) said they were no longer able to work, while fewer than one in three (31%) were working full time. This compares with more than half (57%) of respondents working full time before the onset of their COVID illness – a decline of 46%.
Nearly half (48%) of respondents said they have experienced some form of loss of earnings as a result of long COVID, and almost half of the doctors were never referred to an NHS long COVID clinic. The survey included the following first-person accounts from doctors living with the condition.
- One doctor said: “I nearly lost my life, my home, my partner and my career. I have received little support to help keep these. The impact on my mental health nearly cost [me] my life again.”
- A senior consulting physician commented: “Life is absolutely miserable. Every day is a struggle. I wake up exhausted, the insomnia and night terrors are horrendous as I live through my worst fears every night. Any activity such as eating meals, washing, etc., will mean I have to go to bed for a few hours. I am unable to look after myself or my child, exercise or maintain social relationships. I have no financial security. Long COVID has totally destroyed my life.”
- A salaried general practitioner said: “I can no longer work, finances are ruined. I didn’t have employment protection so am now unemployed and penniless.”
Calls for action from the BMA include the following:
- Financial support for doctors and health care staff with long COVID.
- The recognition of long COVID as an occupational disease among health care workers, along with a definition of the condition that covers all of the debilitating disease’s symptoms.
- Improved access to physical and mental health services to help comprehensive assessment, investigations, and treatment.
- Greater workplace protection for health care staff who risk their lives for others.
- Better support for long COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
“One would think, given the circumstances under which we fell ill and current workforce shortages, NHS employers would be eager to do everything to facilitate the return to work of people with long COVID,” said Dr. Fearnley. “However, NHS employers are legally required to implement only ‘reasonable adjustments,’ and so things such as extended phased return or adjustments to shift patterns are not always being facilitated. Instead, an increasing number of employers are choosing to terminate contracts.”
Raymond Agius, the BMA’s occupational medicine committee cochair, also put the blame on inadequate safety measures for doctors. Those inadequate measures persist to this day, inasmuch as U.K. hospitals have dropped masking requirements.
“During the COVID-19 pandemic, doctors were left exposed and unprotected at work,” he said in a BMA press release. “They often did not have access to the right PPE. ... Too many risk assessments of workplaces and especially of vulnerable doctors were not undertaken.”
A small minority of doctors who were surveyed said they had access to respiratory protective equipment about the time they contracted COVID-19. Only 11% had access to an FFP2 respirator (the equivalent of an N95 mask); 16% had an FFP3 respirator (the equivalent of an N99 mask).
To date, the British government hasn’t issued much of a response to the survey, saying only that it has invested more than ₤50 million to better understand long COVID.
A version of this article first appeared on Medscape.com.
PPIs linked to long-term infection in kids
Researchers in France are warning against the overzealous use of acid-suppressing drugs in infants after finding that the medications are associated with an increase in risk of serious infections later in life.
The focus on the use of proton pump inhibitors (PPIs) during infancy comes as use of the drugs in young children is rising in France, New Zealand, Scandinavia, and the United States. Much of this use is not to manage confirmed cases of gastroesophageal reflux but rather to soothe the jangled nerves of parents of babies in discomfort, according to the researchers, who have studied national prescribing patterns. In addition to concerns about infection, inappropriate or prolonged use of the acid suppressants is also associated with an increase in the risk of such conditions as hospital-acquired acute kidney injury and inflammatory bowel diseases in children.
PPIs such as omeprazole are effective at reducing gastric acid in babies with gastroesophageal reflux disease. But the researchers warned against using the drugs to manage normal spitting up and dribbling that would have resolved of itself anyway.
“In this study, increased risk of serious infections was associated with PPI use in young children, overall and for various sites and pathogens. In this population, PPIs should not be used without a clear indication,” epidemiologist Marion Lassalle, PharmD, PhD, of EPI-PHARE in Saint-Denis, France, and colleagues reported in JAMA Pediatrics.
Drawing on data from a national birth registry, Dr. Lassalle and colleagues compared infection rates among more than 1.2 million infants who received a PPI at an average age of 88 days with infection rates among children who received another kind of acid suppressant (a histamine receptor blocker or antacid) at an average age of 82 days. More than 600,000 children made up each group.
Slightly over half of the participants were boys, and the study followed children to a maximum age of 9 years. Among children who used PPIs rather than another acid suppressant, there was an overall higher rate of serious infections that required hospitalization (adjusted hazard ratio, 1.34; 95% confidence interval, 1.32-1.36). There were higher rates of infections in the digestive tract; the ear, nose, and throat; the kidneys or urinary tract; the lower respiratory tract; and the nervous system.
Serious infections first appeared 9.7 (range, 3.9-21.3) months after a child stopped using a PPI – a date that Dr. Lassalle’s group determined on the basis of there being a delay of at least 90 days in filling a PPI prescription.
Possible confounders
“The study shows an association, it does not show causation,” said Rina Sanghavi, MD, a pediatric gastroenterologist at UT Southwestern Medical Center, Dallas. Dr. Sanghavi noted that the children who continued taking PPIs generally were sicker in their first year of life, as shown by the higher rates of respiratory ailments and corticosteroid use. This could mean that the infections they eventually experienced had many causes and not necessarily the PPI.
Similarly, pediatric gastroenterologist Sophia Patel, MD, of the Cleveland Clinic, pointed to the almost 10-month average lag time between stopping a PPI and developing a first serious infection. That interval is long enough that it is possible that the infection was caused by something else, Dr. Patel said.
Despite the limitations of the study, Dr. Sanghavi and Dr. Patel said the findings serve as a good reminder to clinicians to use PPIs only when needed and to limit their use once begun. The overall evidence base for limiting use of PPIs is strong, both physicians noted, even if this study does not show direct causation between PPI use and infection rates.
“Ask: Does this child need a PPI?” Dr. Sanghavi said. If so, she generally prescribes PPIs for a period of 2 weeks to a maximum of 2 months and she never authorizes automatic refills. Through this approach, a parent and child will come back to the clinic frequently, which in most cases allows faster tapering of the drugs.
Dr. Lassalle, Dr. Sanghavi, and Dr. Patel reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Researchers in France are warning against the overzealous use of acid-suppressing drugs in infants after finding that the medications are associated with an increase in risk of serious infections later in life.
The focus on the use of proton pump inhibitors (PPIs) during infancy comes as use of the drugs in young children is rising in France, New Zealand, Scandinavia, and the United States. Much of this use is not to manage confirmed cases of gastroesophageal reflux but rather to soothe the jangled nerves of parents of babies in discomfort, according to the researchers, who have studied national prescribing patterns. In addition to concerns about infection, inappropriate or prolonged use of the acid suppressants is also associated with an increase in the risk of such conditions as hospital-acquired acute kidney injury and inflammatory bowel diseases in children.
PPIs such as omeprazole are effective at reducing gastric acid in babies with gastroesophageal reflux disease. But the researchers warned against using the drugs to manage normal spitting up and dribbling that would have resolved of itself anyway.
“In this study, increased risk of serious infections was associated with PPI use in young children, overall and for various sites and pathogens. In this population, PPIs should not be used without a clear indication,” epidemiologist Marion Lassalle, PharmD, PhD, of EPI-PHARE in Saint-Denis, France, and colleagues reported in JAMA Pediatrics.
Drawing on data from a national birth registry, Dr. Lassalle and colleagues compared infection rates among more than 1.2 million infants who received a PPI at an average age of 88 days with infection rates among children who received another kind of acid suppressant (a histamine receptor blocker or antacid) at an average age of 82 days. More than 600,000 children made up each group.
Slightly over half of the participants were boys, and the study followed children to a maximum age of 9 years. Among children who used PPIs rather than another acid suppressant, there was an overall higher rate of serious infections that required hospitalization (adjusted hazard ratio, 1.34; 95% confidence interval, 1.32-1.36). There were higher rates of infections in the digestive tract; the ear, nose, and throat; the kidneys or urinary tract; the lower respiratory tract; and the nervous system.
Serious infections first appeared 9.7 (range, 3.9-21.3) months after a child stopped using a PPI – a date that Dr. Lassalle’s group determined on the basis of there being a delay of at least 90 days in filling a PPI prescription.
Possible confounders
“The study shows an association, it does not show causation,” said Rina Sanghavi, MD, a pediatric gastroenterologist at UT Southwestern Medical Center, Dallas. Dr. Sanghavi noted that the children who continued taking PPIs generally were sicker in their first year of life, as shown by the higher rates of respiratory ailments and corticosteroid use. This could mean that the infections they eventually experienced had many causes and not necessarily the PPI.
Similarly, pediatric gastroenterologist Sophia Patel, MD, of the Cleveland Clinic, pointed to the almost 10-month average lag time between stopping a PPI and developing a first serious infection. That interval is long enough that it is possible that the infection was caused by something else, Dr. Patel said.
Despite the limitations of the study, Dr. Sanghavi and Dr. Patel said the findings serve as a good reminder to clinicians to use PPIs only when needed and to limit their use once begun. The overall evidence base for limiting use of PPIs is strong, both physicians noted, even if this study does not show direct causation between PPI use and infection rates.
“Ask: Does this child need a PPI?” Dr. Sanghavi said. If so, she generally prescribes PPIs for a period of 2 weeks to a maximum of 2 months and she never authorizes automatic refills. Through this approach, a parent and child will come back to the clinic frequently, which in most cases allows faster tapering of the drugs.
Dr. Lassalle, Dr. Sanghavi, and Dr. Patel reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
Researchers in France are warning against the overzealous use of acid-suppressing drugs in infants after finding that the medications are associated with an increase in risk of serious infections later in life.
The focus on the use of proton pump inhibitors (PPIs) during infancy comes as use of the drugs in young children is rising in France, New Zealand, Scandinavia, and the United States. Much of this use is not to manage confirmed cases of gastroesophageal reflux but rather to soothe the jangled nerves of parents of babies in discomfort, according to the researchers, who have studied national prescribing patterns. In addition to concerns about infection, inappropriate or prolonged use of the acid suppressants is also associated with an increase in the risk of such conditions as hospital-acquired acute kidney injury and inflammatory bowel diseases in children.
PPIs such as omeprazole are effective at reducing gastric acid in babies with gastroesophageal reflux disease. But the researchers warned against using the drugs to manage normal spitting up and dribbling that would have resolved of itself anyway.
“In this study, increased risk of serious infections was associated with PPI use in young children, overall and for various sites and pathogens. In this population, PPIs should not be used without a clear indication,” epidemiologist Marion Lassalle, PharmD, PhD, of EPI-PHARE in Saint-Denis, France, and colleagues reported in JAMA Pediatrics.
Drawing on data from a national birth registry, Dr. Lassalle and colleagues compared infection rates among more than 1.2 million infants who received a PPI at an average age of 88 days with infection rates among children who received another kind of acid suppressant (a histamine receptor blocker or antacid) at an average age of 82 days. More than 600,000 children made up each group.
Slightly over half of the participants were boys, and the study followed children to a maximum age of 9 years. Among children who used PPIs rather than another acid suppressant, there was an overall higher rate of serious infections that required hospitalization (adjusted hazard ratio, 1.34; 95% confidence interval, 1.32-1.36). There were higher rates of infections in the digestive tract; the ear, nose, and throat; the kidneys or urinary tract; the lower respiratory tract; and the nervous system.
Serious infections first appeared 9.7 (range, 3.9-21.3) months after a child stopped using a PPI – a date that Dr. Lassalle’s group determined on the basis of there being a delay of at least 90 days in filling a PPI prescription.
Possible confounders
“The study shows an association, it does not show causation,” said Rina Sanghavi, MD, a pediatric gastroenterologist at UT Southwestern Medical Center, Dallas. Dr. Sanghavi noted that the children who continued taking PPIs generally were sicker in their first year of life, as shown by the higher rates of respiratory ailments and corticosteroid use. This could mean that the infections they eventually experienced had many causes and not necessarily the PPI.
Similarly, pediatric gastroenterologist Sophia Patel, MD, of the Cleveland Clinic, pointed to the almost 10-month average lag time between stopping a PPI and developing a first serious infection. That interval is long enough that it is possible that the infection was caused by something else, Dr. Patel said.
Despite the limitations of the study, Dr. Sanghavi and Dr. Patel said the findings serve as a good reminder to clinicians to use PPIs only when needed and to limit their use once begun. The overall evidence base for limiting use of PPIs is strong, both physicians noted, even if this study does not show direct causation between PPI use and infection rates.
“Ask: Does this child need a PPI?” Dr. Sanghavi said. If so, she generally prescribes PPIs for a period of 2 weeks to a maximum of 2 months and she never authorizes automatic refills. Through this approach, a parent and child will come back to the clinic frequently, which in most cases allows faster tapering of the drugs.
Dr. Lassalle, Dr. Sanghavi, and Dr. Patel reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM JAMA PEDIATRICS
Q&A: What to know about the new BA 2.86 COVID variant
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention and the World Health Organization have dubbed the BA 2.86 variant of COVID-19 as a variant to watch.
So far, only 26 cases of “Pirola,” as the new variant is being called, have been identified: 10 in Denmark, four each in Sweden and the United States, three in South Africa, two in Portugal, and one each the United Kingdom, Israel, and Canada. BA 2.86 is a subvariant of Omicron, but according to reports from the CDC, the strain has many more mutations than the ones that came before it.
With so many facts still unknown about this new variant, this news organization asked experts what people need to be aware of as it continues to spread.
What is unique about the BA 2.86 variant?
“It is unique in that it has more than three mutations on the spike protein,” said Purvi S. Parikh, MD, an infectious disease expert at New York University’s Langone Health. The virus uses the spike proteins to enter our cells.
This “may mean it will be more transmissible, cause more severe disease, and/or our vaccines and treatments may not work as well, as compared to other variants,” she said.
What do we need to watch with BA 2.86 going forward?
“We don’t know if this variant will be associated with a change in the disease severity. We currently see increased numbers of cases in general, even though we don’t yet see the BA.2.86 in our system,” said Heba Mostafa, PhD, director of the molecular virology laboratory at Johns Hopkins Hospital in Baltimore.
“It is important to monitor BA.2.86 (and other variants) and understand how its evolution impacts the number of cases and disease outcomes,” she said. “We should all be aware of the current increase in cases, though, and try to get tested and be treated as soon as possible, as antivirals should be effective against the circulating variants.”
What should doctors know?
Dr. Parikh said doctors should generally expect more COVID cases in their clinics and make sure to screen patients even if their symptoms are mild.
“We have tools that can be used – antivirals like Paxlovid are still efficacious with current dominant strains such as EG.5,” she said. “And encourage your patients to get their boosters, mask, wash hands, and social distance.”
How well can our vaccines fight BA 2.86?
“Vaccine coverage for the BA.2.86 is an area of uncertainty right now,” said Dr. Mostafa.
In its report, the CDC said scientists are still figuring out how well the updated COVID vaccine works. It’s expected to be available in the fall, and for now, they believe the new shot will still make infections less severe, new variants and all.
Prior vaccinations and infections have created antibodies in many people, and that will likely provide some protection, Dr. Mostafa said. “When we experienced the Omicron wave in December 2021, even though the variant was distant from what circulated before its emergence and was associated with a very large increase in the number of cases, vaccinations were still protective against severe disease.”
What is the most important thing to keep track of when it comes to this variant?
According to Dr. Parikh, “it’s most important to monitor how transmissible [BA 2.86] is, how severe it is, and if our current treatments and vaccines work.”
Dr. Mostafa said how well the new variants escape existing antibody protection should also be studied and watched closely.
What does this stage of the virus mutation tell us about where we are in the pandemic?
The history of the coronavirus over the past few years shows that variants with many changes evolve and can spread very quickly, Dr. Mostafa said. “Now that the virus is endemic, it is essential to monitor, update vaccinations if necessary, diagnose, treat, and implement infection control measures when necessary.”
With the limited data we have so far, experts seem to agree that while the variant’s makeup raises some red flags, it is too soon to jump to any conclusions about how easy it is to catch it and the ways it may change how the virus impacts those who contract it.
A version of this article first appeared on WebMD.com.
Young vapers and smokers beware: Eye problems abound
Adolescents and young adults who smoked and vaped were more likely to report ocular problems including dryness, redness, pain, blurry vision, light sensitivity, and headaches, according to an observational study published in JAMA Ophthalmology.
Eye symptoms were significantly worse among young people who reported using both cigarettes and e-cigarettes than for those who said they used only one of the products, according to researchers. Symptoms were particularly frequent and severe among those who had used both products in the prior week.
“In ophthalmology clinics, I’ve increasingly noticed patients, particularly adolescents and young adults, presenting with eye-related symptoms such as dryness, irritation, and even vision disturbances,” said Anne Xuan-Lan Nguyen, MDCM, an ophthalmology resident at the University of Toronto, who led the study.
Many of these patients said they did not use contact lenses or take medications associated with eye problems, but they did report a history of using e-cigarettes and cigarettes.
This “sparked my curiosity about the possible link between smoking or vaping and ocular symptoms,” Dr. Nguyen, who conducted the research as a medical student at McGill University in Montreal, told this news organization.
E-cigarettes are the most popular tobacco product among young people. Public health data show an increasing trend toward both vaping and smoking cigarettes, known as dual use. An estimated 40% of middle- and high school–aged tobacco users report using two or more tobacco products, according to the Centers for Disease Control and Prevention. Cigarette use has been linked to ocular damage, but the effects of e-cigarettes on eyesight and the combined effect with cigarettes are not as well known.
Dr. Nguyen and her colleagues surveyed more than 4,000 people aged 13-24 about their use of cigarettes or e-cigarettes in the last 30 days, the last 7 days, or ever. Half said they had never used any tobacco product and one quarter reported having used cigarettes, vapes, or both in the last month. More than 900 respondents said they had used one or both tobacco products in the last week.
Of the respondents who had ever vaped, 55.9% said they also used cigarettes. These dual users reported more severe and frequent eye symptoms compared with users of either product alone. Up to 4% of respondents who had ever been a dual user reported daily, severe, or very severe ocular symptoms – more than in the cigarette-only or e-cigarette-only groups.
More frequent tobacco use also was associated with more ocular symptoms. Young people who smoked or vaped in the previous week reported more symptoms than did the 30-day group, who reported more symptoms than the ever-user group (those who had taken at least a puff but not in the last month).
“All these conditions we know are worse as you get older,” said Laura B. Enyedi, MD, pediatric ophthalmologist at the Duke Eye Center in Durham, N.C., who was not associated with the study. “So if young people are having symptoms, it doesn’t bode well for them as they age.”
E-cigarette use alone did not appear to be linked to eye ailments, according to the findings. But to Dr. Nguyen’s surprise the survey results showed users of vaping products spent the most time worried about their eye health compared with all other participants. Users who smoked only cigarettes reported ocular symptoms, but not as severe or frequent as those of dual users.
The researchers hypothesized that ocular problems caused by vapes and cigarettes could be classified as oxidative damage. The combustion of the cigarette and the e-cigarette solvent (propylene glycol) potentially generates free radicals that can cause oxidative stress, damaging the ocular surface and film, Dr. Nguyen said.
Ophthalmologists are “always asking about contact lens use, lid hygiene, and screen time. Here’s another thing to consider when we get those common, nonspecific complaints of symptoms like dryness, redness, and burning,” Dr. Enyedi said.
Given the observational nature of the study, the researchers cannot confirm that dual use causes ocular symptoms. But given the public health challenge that tobacco use already presents for young people, the findings provide yet another reason to counsel against tobacco use and provide cessation options, Dr. Nguyen said.
“This study is just one of many, many studies showing a significant relationship among smoking, e-cigarette use, and health outcomes,” said Bonnie Halpern-Felsher, PhD, professor of pediatrics at Stanford (Calif.) University and a coauthor of the study. “We clearly need to help young people not use at all, or quit or cut back if using.”
This study was supported by the Taube Research Faculty Scholar Endowment; the National Heart, Lung, and Blood Institute; the Food and Drug Administration Center for Tobacco Products; the National Cancer Institute; the Stanford Maternal and Child Health Research Institute; and the Research to Prevent Blindness and National Eye Institute. Dr. Halpern-Felsher reported receiving personal fees as an expert scientist in litigation against some e-cigarette companies. The other study authors and Dr. Enyedi reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adolescents and young adults who smoked and vaped were more likely to report ocular problems including dryness, redness, pain, blurry vision, light sensitivity, and headaches, according to an observational study published in JAMA Ophthalmology.
Eye symptoms were significantly worse among young people who reported using both cigarettes and e-cigarettes than for those who said they used only one of the products, according to researchers. Symptoms were particularly frequent and severe among those who had used both products in the prior week.
“In ophthalmology clinics, I’ve increasingly noticed patients, particularly adolescents and young adults, presenting with eye-related symptoms such as dryness, irritation, and even vision disturbances,” said Anne Xuan-Lan Nguyen, MDCM, an ophthalmology resident at the University of Toronto, who led the study.
Many of these patients said they did not use contact lenses or take medications associated with eye problems, but they did report a history of using e-cigarettes and cigarettes.
This “sparked my curiosity about the possible link between smoking or vaping and ocular symptoms,” Dr. Nguyen, who conducted the research as a medical student at McGill University in Montreal, told this news organization.
E-cigarettes are the most popular tobacco product among young people. Public health data show an increasing trend toward both vaping and smoking cigarettes, known as dual use. An estimated 40% of middle- and high school–aged tobacco users report using two or more tobacco products, according to the Centers for Disease Control and Prevention. Cigarette use has been linked to ocular damage, but the effects of e-cigarettes on eyesight and the combined effect with cigarettes are not as well known.
Dr. Nguyen and her colleagues surveyed more than 4,000 people aged 13-24 about their use of cigarettes or e-cigarettes in the last 30 days, the last 7 days, or ever. Half said they had never used any tobacco product and one quarter reported having used cigarettes, vapes, or both in the last month. More than 900 respondents said they had used one or both tobacco products in the last week.
Of the respondents who had ever vaped, 55.9% said they also used cigarettes. These dual users reported more severe and frequent eye symptoms compared with users of either product alone. Up to 4% of respondents who had ever been a dual user reported daily, severe, or very severe ocular symptoms – more than in the cigarette-only or e-cigarette-only groups.
More frequent tobacco use also was associated with more ocular symptoms. Young people who smoked or vaped in the previous week reported more symptoms than did the 30-day group, who reported more symptoms than the ever-user group (those who had taken at least a puff but not in the last month).
“All these conditions we know are worse as you get older,” said Laura B. Enyedi, MD, pediatric ophthalmologist at the Duke Eye Center in Durham, N.C., who was not associated with the study. “So if young people are having symptoms, it doesn’t bode well for them as they age.”
E-cigarette use alone did not appear to be linked to eye ailments, according to the findings. But to Dr. Nguyen’s surprise the survey results showed users of vaping products spent the most time worried about their eye health compared with all other participants. Users who smoked only cigarettes reported ocular symptoms, but not as severe or frequent as those of dual users.
The researchers hypothesized that ocular problems caused by vapes and cigarettes could be classified as oxidative damage. The combustion of the cigarette and the e-cigarette solvent (propylene glycol) potentially generates free radicals that can cause oxidative stress, damaging the ocular surface and film, Dr. Nguyen said.
Ophthalmologists are “always asking about contact lens use, lid hygiene, and screen time. Here’s another thing to consider when we get those common, nonspecific complaints of symptoms like dryness, redness, and burning,” Dr. Enyedi said.
Given the observational nature of the study, the researchers cannot confirm that dual use causes ocular symptoms. But given the public health challenge that tobacco use already presents for young people, the findings provide yet another reason to counsel against tobacco use and provide cessation options, Dr. Nguyen said.
“This study is just one of many, many studies showing a significant relationship among smoking, e-cigarette use, and health outcomes,” said Bonnie Halpern-Felsher, PhD, professor of pediatrics at Stanford (Calif.) University and a coauthor of the study. “We clearly need to help young people not use at all, or quit or cut back if using.”
This study was supported by the Taube Research Faculty Scholar Endowment; the National Heart, Lung, and Blood Institute; the Food and Drug Administration Center for Tobacco Products; the National Cancer Institute; the Stanford Maternal and Child Health Research Institute; and the Research to Prevent Blindness and National Eye Institute. Dr. Halpern-Felsher reported receiving personal fees as an expert scientist in litigation against some e-cigarette companies. The other study authors and Dr. Enyedi reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adolescents and young adults who smoked and vaped were more likely to report ocular problems including dryness, redness, pain, blurry vision, light sensitivity, and headaches, according to an observational study published in JAMA Ophthalmology.
Eye symptoms were significantly worse among young people who reported using both cigarettes and e-cigarettes than for those who said they used only one of the products, according to researchers. Symptoms were particularly frequent and severe among those who had used both products in the prior week.
“In ophthalmology clinics, I’ve increasingly noticed patients, particularly adolescents and young adults, presenting with eye-related symptoms such as dryness, irritation, and even vision disturbances,” said Anne Xuan-Lan Nguyen, MDCM, an ophthalmology resident at the University of Toronto, who led the study.
Many of these patients said they did not use contact lenses or take medications associated with eye problems, but they did report a history of using e-cigarettes and cigarettes.
This “sparked my curiosity about the possible link between smoking or vaping and ocular symptoms,” Dr. Nguyen, who conducted the research as a medical student at McGill University in Montreal, told this news organization.
E-cigarettes are the most popular tobacco product among young people. Public health data show an increasing trend toward both vaping and smoking cigarettes, known as dual use. An estimated 40% of middle- and high school–aged tobacco users report using two or more tobacco products, according to the Centers for Disease Control and Prevention. Cigarette use has been linked to ocular damage, but the effects of e-cigarettes on eyesight and the combined effect with cigarettes are not as well known.
Dr. Nguyen and her colleagues surveyed more than 4,000 people aged 13-24 about their use of cigarettes or e-cigarettes in the last 30 days, the last 7 days, or ever. Half said they had never used any tobacco product and one quarter reported having used cigarettes, vapes, or both in the last month. More than 900 respondents said they had used one or both tobacco products in the last week.
Of the respondents who had ever vaped, 55.9% said they also used cigarettes. These dual users reported more severe and frequent eye symptoms compared with users of either product alone. Up to 4% of respondents who had ever been a dual user reported daily, severe, or very severe ocular symptoms – more than in the cigarette-only or e-cigarette-only groups.
More frequent tobacco use also was associated with more ocular symptoms. Young people who smoked or vaped in the previous week reported more symptoms than did the 30-day group, who reported more symptoms than the ever-user group (those who had taken at least a puff but not in the last month).
“All these conditions we know are worse as you get older,” said Laura B. Enyedi, MD, pediatric ophthalmologist at the Duke Eye Center in Durham, N.C., who was not associated with the study. “So if young people are having symptoms, it doesn’t bode well for them as they age.”
E-cigarette use alone did not appear to be linked to eye ailments, according to the findings. But to Dr. Nguyen’s surprise the survey results showed users of vaping products spent the most time worried about their eye health compared with all other participants. Users who smoked only cigarettes reported ocular symptoms, but not as severe or frequent as those of dual users.
The researchers hypothesized that ocular problems caused by vapes and cigarettes could be classified as oxidative damage. The combustion of the cigarette and the e-cigarette solvent (propylene glycol) potentially generates free radicals that can cause oxidative stress, damaging the ocular surface and film, Dr. Nguyen said.
Ophthalmologists are “always asking about contact lens use, lid hygiene, and screen time. Here’s another thing to consider when we get those common, nonspecific complaints of symptoms like dryness, redness, and burning,” Dr. Enyedi said.
Given the observational nature of the study, the researchers cannot confirm that dual use causes ocular symptoms. But given the public health challenge that tobacco use already presents for young people, the findings provide yet another reason to counsel against tobacco use and provide cessation options, Dr. Nguyen said.
“This study is just one of many, many studies showing a significant relationship among smoking, e-cigarette use, and health outcomes,” said Bonnie Halpern-Felsher, PhD, professor of pediatrics at Stanford (Calif.) University and a coauthor of the study. “We clearly need to help young people not use at all, or quit or cut back if using.”
This study was supported by the Taube Research Faculty Scholar Endowment; the National Heart, Lung, and Blood Institute; the Food and Drug Administration Center for Tobacco Products; the National Cancer Institute; the Stanford Maternal and Child Health Research Institute; and the Research to Prevent Blindness and National Eye Institute. Dr. Halpern-Felsher reported receiving personal fees as an expert scientist in litigation against some e-cigarette companies. The other study authors and Dr. Enyedi reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA OPHTHALMOLOGY