User login
Elagolix with add-back therapy appears efficacious despite uterine and fibroid factors
PHILADELPHIA – according to results presented at the annual meeting of the American Society for Reproductive Medicine.
Ayman Al-Hendy, MD, PhD, director of translational research at the University of Illinois at Chicago, and associates, analyzed a pooled subgroup of 790 patients from the Elaris UF-1 and UF-2 trials who received elagolix twice daily at a dose of 300 mg (199 patients), elagolix 300 mg twice daily with add-back therapy (1 mg of estradiol plus 0.5 mg of norethindrone acetate; 395 patients), and a placebo group (196 patients) for treatment of heavy menstrual bleeding. Patients were premenopausal women aged 18-51 years with more than 80 mL of menstrual blood loss per cycle. The study design included a washout period, followed by a 2.5-month to 3.5-month screening period, and patients were randomized to 6 months of treatment with placebo, elagolix alone, or elagolix with add-back therapy in a 1:1:2 ratio. Researchers evaluated whether patients had less than 80 mL of menstrual blood loss per cycle and a 50% or more reduction in menstrual blood loss per cycle by the end of the study.
In a subgroup analysis, they also analyzed primary fibroid volume, fibroid stage, and uterine volume. The median primary fibroid volume was 36.2 cm3 (range, 1.0-1,081.5 cm3). Fibroid location was classified using the International Federation of Gynecology and Obstetrics (FIGO) staging system, and researchers placed fibroids into FIGO 0-3, FIGO 4, and FIGO 5-8 groups. At baseline, characteristics between groups were similar, but the patients who received elagolix alone had a lower number of fibroids classified as FIGO 0-3 and had a greater percentage of fibroids less than 36.2 cm3. The median uterine volume was 356.5 cm3 (range, 71.6-3,347.9 cm3).
At final follow-up, 81% of patients receiving elagolix alone and 72% of patients receiving elagolix with add-back therapy responded to treatment, compared with placebo (9%).
Patients receiving elagolix plus add-back therapy responded to treatment better than placebo, and there were no significant differences in outcomes in terms of FIGO stage: Response was as follows for patients with FIGO 0-3 classified fibroids (78% of 47 patients vs. 9% of 25 patients), FIGO 4 fibroids (68% of 177 patients vs. 15% of 85 patients) and FIGO 5-8 fibroids (74% of 165 patients vs. 4% of 82 patients). The same was true in terms of both primary fibroid volume and uterine volume in patients who received elagolix plus add-back therapy, compared with those who received placebo: Patients with a primary fibroid volume of less than 36.2 cm3 (74% of 189 patients vs. 15% of 92 patients) responded similarly to elagolix plus add-back therapy as did patients with a primary fibroid volume greater than 36.2 cm3 (70% of 200 patients vs. 5% of 100 patients), and there were no significant differences between the treatment response of patients with a uterine volume less than 365.5 cm3 (75% of 203 patients vs. 15% of 88 patients) and a uterine volume greater than 365.5 cm3 (70% of 192 patients vs. 5% of 108 patients).
“These really are very encouraging results and suggests that, in women with different fibroids, elagolix with add-back therapy would be an effective treatment option despite uterine and fibroid volume and location of fibroids,” said Dr. Al-Hendy.
Dr. Al-Hendy noted there are ongoing studies analyzing elagolix with add-back in women with fibroids, in women with endometriosis, and elagolix in women with polycystic ovary syndrome.
AbbVie recently submitted a new drug application to the Food and Drug Administration for elagolix based on results from these two trials. Elagolix, an oral GnRh receptor antagonist, is an FDA-approved oral medication for the management of endometriosis with associated moderate to severe pain.
This study was funded by AbbVie, and the company was involved in the study design, research, data collection, analysis and interpretation of the data, as well as the writing, reviewing and approving of the study for publication. The authors reported various relationships with industry, pharmaceutical companies, government entities, and other organizations.
SOURCE: Al-Hendy A et al. ASRM 2019, Abstract O-205.
PHILADELPHIA – according to results presented at the annual meeting of the American Society for Reproductive Medicine.
Ayman Al-Hendy, MD, PhD, director of translational research at the University of Illinois at Chicago, and associates, analyzed a pooled subgroup of 790 patients from the Elaris UF-1 and UF-2 trials who received elagolix twice daily at a dose of 300 mg (199 patients), elagolix 300 mg twice daily with add-back therapy (1 mg of estradiol plus 0.5 mg of norethindrone acetate; 395 patients), and a placebo group (196 patients) for treatment of heavy menstrual bleeding. Patients were premenopausal women aged 18-51 years with more than 80 mL of menstrual blood loss per cycle. The study design included a washout period, followed by a 2.5-month to 3.5-month screening period, and patients were randomized to 6 months of treatment with placebo, elagolix alone, or elagolix with add-back therapy in a 1:1:2 ratio. Researchers evaluated whether patients had less than 80 mL of menstrual blood loss per cycle and a 50% or more reduction in menstrual blood loss per cycle by the end of the study.
In a subgroup analysis, they also analyzed primary fibroid volume, fibroid stage, and uterine volume. The median primary fibroid volume was 36.2 cm3 (range, 1.0-1,081.5 cm3). Fibroid location was classified using the International Federation of Gynecology and Obstetrics (FIGO) staging system, and researchers placed fibroids into FIGO 0-3, FIGO 4, and FIGO 5-8 groups. At baseline, characteristics between groups were similar, but the patients who received elagolix alone had a lower number of fibroids classified as FIGO 0-3 and had a greater percentage of fibroids less than 36.2 cm3. The median uterine volume was 356.5 cm3 (range, 71.6-3,347.9 cm3).
At final follow-up, 81% of patients receiving elagolix alone and 72% of patients receiving elagolix with add-back therapy responded to treatment, compared with placebo (9%).
Patients receiving elagolix plus add-back therapy responded to treatment better than placebo, and there were no significant differences in outcomes in terms of FIGO stage: Response was as follows for patients with FIGO 0-3 classified fibroids (78% of 47 patients vs. 9% of 25 patients), FIGO 4 fibroids (68% of 177 patients vs. 15% of 85 patients) and FIGO 5-8 fibroids (74% of 165 patients vs. 4% of 82 patients). The same was true in terms of both primary fibroid volume and uterine volume in patients who received elagolix plus add-back therapy, compared with those who received placebo: Patients with a primary fibroid volume of less than 36.2 cm3 (74% of 189 patients vs. 15% of 92 patients) responded similarly to elagolix plus add-back therapy as did patients with a primary fibroid volume greater than 36.2 cm3 (70% of 200 patients vs. 5% of 100 patients), and there were no significant differences between the treatment response of patients with a uterine volume less than 365.5 cm3 (75% of 203 patients vs. 15% of 88 patients) and a uterine volume greater than 365.5 cm3 (70% of 192 patients vs. 5% of 108 patients).
“These really are very encouraging results and suggests that, in women with different fibroids, elagolix with add-back therapy would be an effective treatment option despite uterine and fibroid volume and location of fibroids,” said Dr. Al-Hendy.
Dr. Al-Hendy noted there are ongoing studies analyzing elagolix with add-back in women with fibroids, in women with endometriosis, and elagolix in women with polycystic ovary syndrome.
AbbVie recently submitted a new drug application to the Food and Drug Administration for elagolix based on results from these two trials. Elagolix, an oral GnRh receptor antagonist, is an FDA-approved oral medication for the management of endometriosis with associated moderate to severe pain.
This study was funded by AbbVie, and the company was involved in the study design, research, data collection, analysis and interpretation of the data, as well as the writing, reviewing and approving of the study for publication. The authors reported various relationships with industry, pharmaceutical companies, government entities, and other organizations.
SOURCE: Al-Hendy A et al. ASRM 2019, Abstract O-205.
PHILADELPHIA – according to results presented at the annual meeting of the American Society for Reproductive Medicine.
Ayman Al-Hendy, MD, PhD, director of translational research at the University of Illinois at Chicago, and associates, analyzed a pooled subgroup of 790 patients from the Elaris UF-1 and UF-2 trials who received elagolix twice daily at a dose of 300 mg (199 patients), elagolix 300 mg twice daily with add-back therapy (1 mg of estradiol plus 0.5 mg of norethindrone acetate; 395 patients), and a placebo group (196 patients) for treatment of heavy menstrual bleeding. Patients were premenopausal women aged 18-51 years with more than 80 mL of menstrual blood loss per cycle. The study design included a washout period, followed by a 2.5-month to 3.5-month screening period, and patients were randomized to 6 months of treatment with placebo, elagolix alone, or elagolix with add-back therapy in a 1:1:2 ratio. Researchers evaluated whether patients had less than 80 mL of menstrual blood loss per cycle and a 50% or more reduction in menstrual blood loss per cycle by the end of the study.
In a subgroup analysis, they also analyzed primary fibroid volume, fibroid stage, and uterine volume. The median primary fibroid volume was 36.2 cm3 (range, 1.0-1,081.5 cm3). Fibroid location was classified using the International Federation of Gynecology and Obstetrics (FIGO) staging system, and researchers placed fibroids into FIGO 0-3, FIGO 4, and FIGO 5-8 groups. At baseline, characteristics between groups were similar, but the patients who received elagolix alone had a lower number of fibroids classified as FIGO 0-3 and had a greater percentage of fibroids less than 36.2 cm3. The median uterine volume was 356.5 cm3 (range, 71.6-3,347.9 cm3).
At final follow-up, 81% of patients receiving elagolix alone and 72% of patients receiving elagolix with add-back therapy responded to treatment, compared with placebo (9%).
Patients receiving elagolix plus add-back therapy responded to treatment better than placebo, and there were no significant differences in outcomes in terms of FIGO stage: Response was as follows for patients with FIGO 0-3 classified fibroids (78% of 47 patients vs. 9% of 25 patients), FIGO 4 fibroids (68% of 177 patients vs. 15% of 85 patients) and FIGO 5-8 fibroids (74% of 165 patients vs. 4% of 82 patients). The same was true in terms of both primary fibroid volume and uterine volume in patients who received elagolix plus add-back therapy, compared with those who received placebo: Patients with a primary fibroid volume of less than 36.2 cm3 (74% of 189 patients vs. 15% of 92 patients) responded similarly to elagolix plus add-back therapy as did patients with a primary fibroid volume greater than 36.2 cm3 (70% of 200 patients vs. 5% of 100 patients), and there were no significant differences between the treatment response of patients with a uterine volume less than 365.5 cm3 (75% of 203 patients vs. 15% of 88 patients) and a uterine volume greater than 365.5 cm3 (70% of 192 patients vs. 5% of 108 patients).
“These really are very encouraging results and suggests that, in women with different fibroids, elagolix with add-back therapy would be an effective treatment option despite uterine and fibroid volume and location of fibroids,” said Dr. Al-Hendy.
Dr. Al-Hendy noted there are ongoing studies analyzing elagolix with add-back in women with fibroids, in women with endometriosis, and elagolix in women with polycystic ovary syndrome.
AbbVie recently submitted a new drug application to the Food and Drug Administration for elagolix based on results from these two trials. Elagolix, an oral GnRh receptor antagonist, is an FDA-approved oral medication for the management of endometriosis with associated moderate to severe pain.
This study was funded by AbbVie, and the company was involved in the study design, research, data collection, analysis and interpretation of the data, as well as the writing, reviewing and approving of the study for publication. The authors reported various relationships with industry, pharmaceutical companies, government entities, and other organizations.
SOURCE: Al-Hendy A et al. ASRM 2019, Abstract O-205.
REPORTING FROM ASRM 2019
Yoga life lessons
I love empty storefronts. The realtor headshot in the window is a sign of hope. What was here is no more. What is coming will be better.
I’ve waited a year for one such sign to come down and scaffolding to go up. Just one block from my condo, my curiosity has been slaked: a yoga studio! At first, disappointment; so many potentials unrealized: a coffee shop, cleaners, speakeasy! Yet, I decided to make the best of it. I bought Rainbow sandals, a Lululemon mat, and a pack of 10 classes. As it turns out, yoga can transform your life.
I didn’t realize how beautifully yoga combines physical exertion, meditation, and spirituality. It is both a model for understanding and a ritualistic training for life. Take resting pigeon for example. (Yogis reading this will forgive my imperfect explanation.) This moderately difficult pose opens your hip and stretches your glutes. Imagine doing a split but with your front knee bent and your forehead and arms resting on the floor in front of you. Done correctly, it puts a stretch deep into the hip of the forward leg. It is uncomfortable. Holding it for a minute or 2 is hard. But rather than just focusing on releasing, with each breath you find yourself deepening the stretch. Sweat streams down your arms and the discomfort builds as you hold. All you can think about is your breath. Then, it’s over. You feel freer, lighter than you were before. The deeper the discomfort, the deeper the delight that arises afterward. You are wise, yogis would say, to have chosen “the good over the pleasant.”
We have many opportunities for resting pigeon in everyday life. The patient to be added to your Monday morning clinic – which already had added patients. The Friday afternoon Mohs case that went to periosteum and still needs a flap to close. The “yet another” GI bleed patient that needs to be scoped tonight. These are all deep stretches, uncomfortable hip openings. Rather, when you must be uncomfortable, breathe and lean into it. Choosing the good sometimes means choosing suffering, but it isn’t the pain that makes it hard to bear. It is a lack of significance for that difficulty. By choosing what is good, you answer the question: “Who am I?” I am the one able and willing to endure inconvenience or disquiet to help others. This is my job, what I’m here to do. The pose, the call, the case will be over quickly. The freedom you feel after, along with the satisfaction you have served your purpose, will sustain you.
There are many poses and endless lessons from yoga. In fact, doing yoga is called “practicing.” Each time you learn and try. Each time you are imperfect and uncomfortable and reemerge sweaty and satisfied, just a little better human than you were before.
Dr. Benabio is director of health care transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
I love empty storefronts. The realtor headshot in the window is a sign of hope. What was here is no more. What is coming will be better.
I’ve waited a year for one such sign to come down and scaffolding to go up. Just one block from my condo, my curiosity has been slaked: a yoga studio! At first, disappointment; so many potentials unrealized: a coffee shop, cleaners, speakeasy! Yet, I decided to make the best of it. I bought Rainbow sandals, a Lululemon mat, and a pack of 10 classes. As it turns out, yoga can transform your life.
I didn’t realize how beautifully yoga combines physical exertion, meditation, and spirituality. It is both a model for understanding and a ritualistic training for life. Take resting pigeon for example. (Yogis reading this will forgive my imperfect explanation.) This moderately difficult pose opens your hip and stretches your glutes. Imagine doing a split but with your front knee bent and your forehead and arms resting on the floor in front of you. Done correctly, it puts a stretch deep into the hip of the forward leg. It is uncomfortable. Holding it for a minute or 2 is hard. But rather than just focusing on releasing, with each breath you find yourself deepening the stretch. Sweat streams down your arms and the discomfort builds as you hold. All you can think about is your breath. Then, it’s over. You feel freer, lighter than you were before. The deeper the discomfort, the deeper the delight that arises afterward. You are wise, yogis would say, to have chosen “the good over the pleasant.”
We have many opportunities for resting pigeon in everyday life. The patient to be added to your Monday morning clinic – which already had added patients. The Friday afternoon Mohs case that went to periosteum and still needs a flap to close. The “yet another” GI bleed patient that needs to be scoped tonight. These are all deep stretches, uncomfortable hip openings. Rather, when you must be uncomfortable, breathe and lean into it. Choosing the good sometimes means choosing suffering, but it isn’t the pain that makes it hard to bear. It is a lack of significance for that difficulty. By choosing what is good, you answer the question: “Who am I?” I am the one able and willing to endure inconvenience or disquiet to help others. This is my job, what I’m here to do. The pose, the call, the case will be over quickly. The freedom you feel after, along with the satisfaction you have served your purpose, will sustain you.
There are many poses and endless lessons from yoga. In fact, doing yoga is called “practicing.” Each time you learn and try. Each time you are imperfect and uncomfortable and reemerge sweaty and satisfied, just a little better human than you were before.
Dr. Benabio is director of health care transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
I love empty storefronts. The realtor headshot in the window is a sign of hope. What was here is no more. What is coming will be better.
I’ve waited a year for one such sign to come down and scaffolding to go up. Just one block from my condo, my curiosity has been slaked: a yoga studio! At first, disappointment; so many potentials unrealized: a coffee shop, cleaners, speakeasy! Yet, I decided to make the best of it. I bought Rainbow sandals, a Lululemon mat, and a pack of 10 classes. As it turns out, yoga can transform your life.
I didn’t realize how beautifully yoga combines physical exertion, meditation, and spirituality. It is both a model for understanding and a ritualistic training for life. Take resting pigeon for example. (Yogis reading this will forgive my imperfect explanation.) This moderately difficult pose opens your hip and stretches your glutes. Imagine doing a split but with your front knee bent and your forehead and arms resting on the floor in front of you. Done correctly, it puts a stretch deep into the hip of the forward leg. It is uncomfortable. Holding it for a minute or 2 is hard. But rather than just focusing on releasing, with each breath you find yourself deepening the stretch. Sweat streams down your arms and the discomfort builds as you hold. All you can think about is your breath. Then, it’s over. You feel freer, lighter than you were before. The deeper the discomfort, the deeper the delight that arises afterward. You are wise, yogis would say, to have chosen “the good over the pleasant.”
We have many opportunities for resting pigeon in everyday life. The patient to be added to your Monday morning clinic – which already had added patients. The Friday afternoon Mohs case that went to periosteum and still needs a flap to close. The “yet another” GI bleed patient that needs to be scoped tonight. These are all deep stretches, uncomfortable hip openings. Rather, when you must be uncomfortable, breathe and lean into it. Choosing the good sometimes means choosing suffering, but it isn’t the pain that makes it hard to bear. It is a lack of significance for that difficulty. By choosing what is good, you answer the question: “Who am I?” I am the one able and willing to endure inconvenience or disquiet to help others. This is my job, what I’m here to do. The pose, the call, the case will be over quickly. The freedom you feel after, along with the satisfaction you have served your purpose, will sustain you.
There are many poses and endless lessons from yoga. In fact, doing yoga is called “practicing.” Each time you learn and try. Each time you are imperfect and uncomfortable and reemerge sweaty and satisfied, just a little better human than you were before.
Dr. Benabio is director of health care transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Consider treating ovarian torsion with conservative surgery in young women
PHILADELPHIA – Women with ovarian torsion had a lower rate of perioperative complications when treated with conservative surgery, compared with oophorectomy, according to results from a retrospective study presented at the annual meeting of the American Society for Reproductive Medicine.
The effectiveness of laparoscopy and conservative surgery has increased in recent years, but over 75% of women with ovarian torsion in the study were treated with oophorectomy and 60% underwent a laparotomy, said Rachel S. Mandelbaum, MD, of the department of obstetrics & gynecology at the University of Southern California, Los Angeles.
“We believe that conservative surgery should be performed whenever possible in young women with ovarian torsion regardless of the appearance of the ovary intraoperatively,” said Dr. Mandelbaum.
The researchers performed a retrospective, observational study of 89,801 women in the Nationwide Inpatient Sample who were younger than age 50 years, were diagnosed with ovarian torsion during Jan. 2001–Sept. 2015, and were treated with conservative surgery or oophorectomy. Patients were excluded if they had malignancy, were older than 50 years of age, or their surgery information was unavailable. The majority of patients in the study were white (46%), nonobese (91%), without comorbidities, privately insured (59%), and were seen at a large (61%) urban hospital (51% teaching; 38% nonteaching).
Dr. Mandelbaum and colleagues found 78% of patients received a cystectomy, 19% had cyst drainage, 11% had detorsion alone, and 0.5% had an oophoropexy, with less than 10% of patients having a combination of cystectomy, cyst drainage, and oophoropexy. According to a multivariable analysis, patients who were treated with conservative surgery were more likely to be young, have a high income, live in the northeastern United States, be treated with laparoscopy, and be seen at a large hospital or teaching hospital (P less than .001). Oophorectomy was more common in patients with a high number of comorbidities and in patients with morbid obesity (P less than .001).
Between 2001 and 2015, the rate of conservative surgery increased from 19% to 25% (P less than .001); however, the rate of conservative surgery by age was nearly 40% in pediatric patients up to 15 years old, while the rate of conservative surgery declined by almost half until 35 years, followed by a further decline until age 50 years, said Dr. Mandelbaum. Use of laparoscopy also increased from 31% in 2001 to 42% in 2015 (P less than .001).
Overall, 20,643 patients underwent conservative surgery and 69,157 patients received an oophorectomy. Patients in the conservative surgery group were more likely to undergo a conservative surgery with a laparoscopic surgical approach (51%) than a laparotomy (41%), while patients receiving an oophorectomy were more likely to have a laparotomy (67%) than a laparoscopic surgical approach (33%). In 1,663 conservative surgeries (8%), the approach was unknown.
(odds ratio, 0.57; 95% confidence interval, 0.57-0.78; P less than .001), but there was a similar rate of venous thromboembolism (0.3% vs. 0.2%; P equals .568) and sepsis (0.3% vs. 0.3%; P equals .865) in each group.
Dr. Mandelbaum attributed the high rate of oophorectomies in the study to “differential uptake of evidence” in different areas of the United States, fear of complications from leaving an infected ovary in situ, or the surgeon’s belief that the ovary is not viable because of its color intraoperatively. “We know from animal and human studies that the intraoperative appearance of the ovary does not correlate to viability, and that 90% of black or blue ovaries regain function and subsequently appear normal on both transvaginal ultrasound or on a second look grossly,” she said. Oophorectomy rates also vary by surgeon, and gynecologists are more likely to perform conservative surgery, she added.
The researchers said they were unable to obtain data on specific surgical variables such as the size of the mass, time to surgery, intraoperative appearance, laterality, fertility wishes of the patient, and surgeon type. There were also no postdischarge data, or information on the timing of complications.
Dr. Mandelbaum reported no relevant conflicts of interest.
SOURCE: Mandelbaum RS et al. ASRM 2019. Abstract O-96.
PHILADELPHIA – Women with ovarian torsion had a lower rate of perioperative complications when treated with conservative surgery, compared with oophorectomy, according to results from a retrospective study presented at the annual meeting of the American Society for Reproductive Medicine.
The effectiveness of laparoscopy and conservative surgery has increased in recent years, but over 75% of women with ovarian torsion in the study were treated with oophorectomy and 60% underwent a laparotomy, said Rachel S. Mandelbaum, MD, of the department of obstetrics & gynecology at the University of Southern California, Los Angeles.
“We believe that conservative surgery should be performed whenever possible in young women with ovarian torsion regardless of the appearance of the ovary intraoperatively,” said Dr. Mandelbaum.
The researchers performed a retrospective, observational study of 89,801 women in the Nationwide Inpatient Sample who were younger than age 50 years, were diagnosed with ovarian torsion during Jan. 2001–Sept. 2015, and were treated with conservative surgery or oophorectomy. Patients were excluded if they had malignancy, were older than 50 years of age, or their surgery information was unavailable. The majority of patients in the study were white (46%), nonobese (91%), without comorbidities, privately insured (59%), and were seen at a large (61%) urban hospital (51% teaching; 38% nonteaching).
Dr. Mandelbaum and colleagues found 78% of patients received a cystectomy, 19% had cyst drainage, 11% had detorsion alone, and 0.5% had an oophoropexy, with less than 10% of patients having a combination of cystectomy, cyst drainage, and oophoropexy. According to a multivariable analysis, patients who were treated with conservative surgery were more likely to be young, have a high income, live in the northeastern United States, be treated with laparoscopy, and be seen at a large hospital or teaching hospital (P less than .001). Oophorectomy was more common in patients with a high number of comorbidities and in patients with morbid obesity (P less than .001).
Between 2001 and 2015, the rate of conservative surgery increased from 19% to 25% (P less than .001); however, the rate of conservative surgery by age was nearly 40% in pediatric patients up to 15 years old, while the rate of conservative surgery declined by almost half until 35 years, followed by a further decline until age 50 years, said Dr. Mandelbaum. Use of laparoscopy also increased from 31% in 2001 to 42% in 2015 (P less than .001).
Overall, 20,643 patients underwent conservative surgery and 69,157 patients received an oophorectomy. Patients in the conservative surgery group were more likely to undergo a conservative surgery with a laparoscopic surgical approach (51%) than a laparotomy (41%), while patients receiving an oophorectomy were more likely to have a laparotomy (67%) than a laparoscopic surgical approach (33%). In 1,663 conservative surgeries (8%), the approach was unknown.
(odds ratio, 0.57; 95% confidence interval, 0.57-0.78; P less than .001), but there was a similar rate of venous thromboembolism (0.3% vs. 0.2%; P equals .568) and sepsis (0.3% vs. 0.3%; P equals .865) in each group.
Dr. Mandelbaum attributed the high rate of oophorectomies in the study to “differential uptake of evidence” in different areas of the United States, fear of complications from leaving an infected ovary in situ, or the surgeon’s belief that the ovary is not viable because of its color intraoperatively. “We know from animal and human studies that the intraoperative appearance of the ovary does not correlate to viability, and that 90% of black or blue ovaries regain function and subsequently appear normal on both transvaginal ultrasound or on a second look grossly,” she said. Oophorectomy rates also vary by surgeon, and gynecologists are more likely to perform conservative surgery, she added.
The researchers said they were unable to obtain data on specific surgical variables such as the size of the mass, time to surgery, intraoperative appearance, laterality, fertility wishes of the patient, and surgeon type. There were also no postdischarge data, or information on the timing of complications.
Dr. Mandelbaum reported no relevant conflicts of interest.
SOURCE: Mandelbaum RS et al. ASRM 2019. Abstract O-96.
PHILADELPHIA – Women with ovarian torsion had a lower rate of perioperative complications when treated with conservative surgery, compared with oophorectomy, according to results from a retrospective study presented at the annual meeting of the American Society for Reproductive Medicine.
The effectiveness of laparoscopy and conservative surgery has increased in recent years, but over 75% of women with ovarian torsion in the study were treated with oophorectomy and 60% underwent a laparotomy, said Rachel S. Mandelbaum, MD, of the department of obstetrics & gynecology at the University of Southern California, Los Angeles.
“We believe that conservative surgery should be performed whenever possible in young women with ovarian torsion regardless of the appearance of the ovary intraoperatively,” said Dr. Mandelbaum.
The researchers performed a retrospective, observational study of 89,801 women in the Nationwide Inpatient Sample who were younger than age 50 years, were diagnosed with ovarian torsion during Jan. 2001–Sept. 2015, and were treated with conservative surgery or oophorectomy. Patients were excluded if they had malignancy, were older than 50 years of age, or their surgery information was unavailable. The majority of patients in the study were white (46%), nonobese (91%), without comorbidities, privately insured (59%), and were seen at a large (61%) urban hospital (51% teaching; 38% nonteaching).
Dr. Mandelbaum and colleagues found 78% of patients received a cystectomy, 19% had cyst drainage, 11% had detorsion alone, and 0.5% had an oophoropexy, with less than 10% of patients having a combination of cystectomy, cyst drainage, and oophoropexy. According to a multivariable analysis, patients who were treated with conservative surgery were more likely to be young, have a high income, live in the northeastern United States, be treated with laparoscopy, and be seen at a large hospital or teaching hospital (P less than .001). Oophorectomy was more common in patients with a high number of comorbidities and in patients with morbid obesity (P less than .001).
Between 2001 and 2015, the rate of conservative surgery increased from 19% to 25% (P less than .001); however, the rate of conservative surgery by age was nearly 40% in pediatric patients up to 15 years old, while the rate of conservative surgery declined by almost half until 35 years, followed by a further decline until age 50 years, said Dr. Mandelbaum. Use of laparoscopy also increased from 31% in 2001 to 42% in 2015 (P less than .001).
Overall, 20,643 patients underwent conservative surgery and 69,157 patients received an oophorectomy. Patients in the conservative surgery group were more likely to undergo a conservative surgery with a laparoscopic surgical approach (51%) than a laparotomy (41%), while patients receiving an oophorectomy were more likely to have a laparotomy (67%) than a laparoscopic surgical approach (33%). In 1,663 conservative surgeries (8%), the approach was unknown.
(odds ratio, 0.57; 95% confidence interval, 0.57-0.78; P less than .001), but there was a similar rate of venous thromboembolism (0.3% vs. 0.2%; P equals .568) and sepsis (0.3% vs. 0.3%; P equals .865) in each group.
Dr. Mandelbaum attributed the high rate of oophorectomies in the study to “differential uptake of evidence” in different areas of the United States, fear of complications from leaving an infected ovary in situ, or the surgeon’s belief that the ovary is not viable because of its color intraoperatively. “We know from animal and human studies that the intraoperative appearance of the ovary does not correlate to viability, and that 90% of black or blue ovaries regain function and subsequently appear normal on both transvaginal ultrasound or on a second look grossly,” she said. Oophorectomy rates also vary by surgeon, and gynecologists are more likely to perform conservative surgery, she added.
The researchers said they were unable to obtain data on specific surgical variables such as the size of the mass, time to surgery, intraoperative appearance, laterality, fertility wishes of the patient, and surgeon type. There were also no postdischarge data, or information on the timing of complications.
Dr. Mandelbaum reported no relevant conflicts of interest.
SOURCE: Mandelbaum RS et al. ASRM 2019. Abstract O-96.
REPORTING FROM ASRM 2019
Placebo response in negative rituximab BeatMG trial provides important lessons
AUSTIN, TEX. – Among patients with acetylcholine receptor (AChR) antibody-positive generalized myasthenia gravis, rituximab and placebo may have a similar glucocorticoid-sparing effect regardless of disease severity, according to research presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
B Cell Targeted Treatment In Myasthenia Gravis (BeatMG) was a 52-week, randomized, double-blind, placebo-controlled clinical trial. The phase 2 study’s primary outcomes were safety and the glucocorticoid-sparing effect assessed by the percentage of patients who reduced their mean daily prednisone dose by at least 75% and maintained clinical stability. Secondary outcomes were change in Myasthenia Gravis Composite (MGC) score and change in Quantitative Myasthenia Gravis (QMG) score from baseline to 52 weeks.
Investigators randomized 52 participants 1:1 to rituximab (Rituxan) or placebo. Patients were taking at least 15 mg/day of prednisone and were a mean of about age 50 years. About two-thirds were treated with glucocorticoids alone at baseline, and nearly two-thirds had a Myasthenia Gravis Foundation of America (MGFA) clinical classification of II. “It was a mildly symptomatic group of individuals in terms of disease severity,” said Richard Nowak, MD, assistant professor of neurology and director of the Yale Myasthenia Gravis Clinic in New Haven, Conn.
During the study, 60% of patients who received rituximab had a 75% or greater reduction in their mean daily prednisone dose and maintained clinical stability. “However, what surprised us is that we had a significantly high placebo response rate of 56%,” he said. The difference between groups was not significant.
Patients who received rituximab had “directionally favorable reductions” in MGC and QMG scores over 52 weeks, compared with patients who received placebo. Nevertheless, “after correcting for baseline differences, there was no significant difference between the two groups,” Dr. Nowak said.
Rituximab had good safety and tolerability, and the placebo group had a threefold higher rate of clinical relapse requiring IV immunoglobulin or plasmapheresis. “While the placebo arm did achieve a similar rate of reduction in their steroid dose, at 52 weeks the patients may have been doing less well, reflected by the higher rate of relapse,” he said.
Subgroup analysis
To explore whether rituximab might benefit patients who were treatment resistant or had more symptomatic disease, Dr. Nowak and his colleagues conducted a post hoc subgroup analysis of 20 participants – 10 in the rituximab arm and 10 in the placebo arm – who were MGFA class III-IV. In each group, 70% were on glucocorticoid treatment alone, and 90% were MGFA class III.
As in the overall study, the glucocorticoid-sparing effect was not significant (60% of the rituximab group vs. 50% of the placebo group).
Mean change in QMG score was –3.9 in the rituximab group and –0.5 in the placebo group, and mean change in MGC score was –7.0 in the rituximab group and –4.8 in the placebo group. These secondary outcomes again show “directional favorability” with rituximab, Dr. Nowak said. The researchers saw similar trends for scores that assess quality of life and activities of daily living.
In the subgroup analysis, myasthenia gravis relapses requiring rescue therapy occurred in 20% of patients in the rituximab arm and in 30% of the placebo arm. Overall, the researchers did not see a difference in treatment response between those with moderate to severe disease and those with mild disease, Dr. Nowak said.
Suggestions from the data
The post hoc subgroup analysis should be interpreted with caution, and the study does not provide firm conclusions, Dr. Nowak noted. In addition, the trial population does not reflect all patients with myasthenia gravis. Dr. Nowak routinely uses rituximab in patients with muscle-specific kinase antibody-positive disease, he said. For acetylcholine receptor antibody-positive generalized myasthenia gravis, which has approved therapies available, Dr. Nowak presents rituximab as an option for some patients. Further research may clarify where B-cell depletion therapy may fit into the treatment paradigm.
Nonetheless, BeatMG and the subgroup analysis may help physicians better understand the disease and the role of various therapies. Investigators successfully lowered prednisone dose “at a pretty high rate in the placebo arm,” he said. “It suggests that many of our patients potentially may be on higher than required prednisone doses.”
Finally, the BeatMG findings emphasize the need for placebo-controlled trials to understand potential therapies. “We need to pause when we see a lot of retrospective and uncontrolled studies that are very promising,” Dr. Nowak said.
The study was supported by the National Institute of Neurological Disorders and Stroke. Genentech provided the study drug and placebo through an investigator-sponsored study agreement. Dr. Nowak has received research support from Alexion Pharmaceuticals, Genentech, Grifols, and Ra Pharmaceuticals. He has served as a paid consultant for Alexion, Momenta, Ra, Roivant, Shire, Grifols, and CSL Behring.
SOURCE: Nowak R et al. AANEM 2019. Unnumbered Abstract: Rituximab in patients with moderate to severe myasthenia gravis: a subgroup analysis of the BeatMG study
AUSTIN, TEX. – Among patients with acetylcholine receptor (AChR) antibody-positive generalized myasthenia gravis, rituximab and placebo may have a similar glucocorticoid-sparing effect regardless of disease severity, according to research presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
B Cell Targeted Treatment In Myasthenia Gravis (BeatMG) was a 52-week, randomized, double-blind, placebo-controlled clinical trial. The phase 2 study’s primary outcomes were safety and the glucocorticoid-sparing effect assessed by the percentage of patients who reduced their mean daily prednisone dose by at least 75% and maintained clinical stability. Secondary outcomes were change in Myasthenia Gravis Composite (MGC) score and change in Quantitative Myasthenia Gravis (QMG) score from baseline to 52 weeks.
Investigators randomized 52 participants 1:1 to rituximab (Rituxan) or placebo. Patients were taking at least 15 mg/day of prednisone and were a mean of about age 50 years. About two-thirds were treated with glucocorticoids alone at baseline, and nearly two-thirds had a Myasthenia Gravis Foundation of America (MGFA) clinical classification of II. “It was a mildly symptomatic group of individuals in terms of disease severity,” said Richard Nowak, MD, assistant professor of neurology and director of the Yale Myasthenia Gravis Clinic in New Haven, Conn.
During the study, 60% of patients who received rituximab had a 75% or greater reduction in their mean daily prednisone dose and maintained clinical stability. “However, what surprised us is that we had a significantly high placebo response rate of 56%,” he said. The difference between groups was not significant.
Patients who received rituximab had “directionally favorable reductions” in MGC and QMG scores over 52 weeks, compared with patients who received placebo. Nevertheless, “after correcting for baseline differences, there was no significant difference between the two groups,” Dr. Nowak said.
Rituximab had good safety and tolerability, and the placebo group had a threefold higher rate of clinical relapse requiring IV immunoglobulin or plasmapheresis. “While the placebo arm did achieve a similar rate of reduction in their steroid dose, at 52 weeks the patients may have been doing less well, reflected by the higher rate of relapse,” he said.
Subgroup analysis
To explore whether rituximab might benefit patients who were treatment resistant or had more symptomatic disease, Dr. Nowak and his colleagues conducted a post hoc subgroup analysis of 20 participants – 10 in the rituximab arm and 10 in the placebo arm – who were MGFA class III-IV. In each group, 70% were on glucocorticoid treatment alone, and 90% were MGFA class III.
As in the overall study, the glucocorticoid-sparing effect was not significant (60% of the rituximab group vs. 50% of the placebo group).
Mean change in QMG score was –3.9 in the rituximab group and –0.5 in the placebo group, and mean change in MGC score was –7.0 in the rituximab group and –4.8 in the placebo group. These secondary outcomes again show “directional favorability” with rituximab, Dr. Nowak said. The researchers saw similar trends for scores that assess quality of life and activities of daily living.
In the subgroup analysis, myasthenia gravis relapses requiring rescue therapy occurred in 20% of patients in the rituximab arm and in 30% of the placebo arm. Overall, the researchers did not see a difference in treatment response between those with moderate to severe disease and those with mild disease, Dr. Nowak said.
Suggestions from the data
The post hoc subgroup analysis should be interpreted with caution, and the study does not provide firm conclusions, Dr. Nowak noted. In addition, the trial population does not reflect all patients with myasthenia gravis. Dr. Nowak routinely uses rituximab in patients with muscle-specific kinase antibody-positive disease, he said. For acetylcholine receptor antibody-positive generalized myasthenia gravis, which has approved therapies available, Dr. Nowak presents rituximab as an option for some patients. Further research may clarify where B-cell depletion therapy may fit into the treatment paradigm.
Nonetheless, BeatMG and the subgroup analysis may help physicians better understand the disease and the role of various therapies. Investigators successfully lowered prednisone dose “at a pretty high rate in the placebo arm,” he said. “It suggests that many of our patients potentially may be on higher than required prednisone doses.”
Finally, the BeatMG findings emphasize the need for placebo-controlled trials to understand potential therapies. “We need to pause when we see a lot of retrospective and uncontrolled studies that are very promising,” Dr. Nowak said.
The study was supported by the National Institute of Neurological Disorders and Stroke. Genentech provided the study drug and placebo through an investigator-sponsored study agreement. Dr. Nowak has received research support from Alexion Pharmaceuticals, Genentech, Grifols, and Ra Pharmaceuticals. He has served as a paid consultant for Alexion, Momenta, Ra, Roivant, Shire, Grifols, and CSL Behring.
SOURCE: Nowak R et al. AANEM 2019. Unnumbered Abstract: Rituximab in patients with moderate to severe myasthenia gravis: a subgroup analysis of the BeatMG study
AUSTIN, TEX. – Among patients with acetylcholine receptor (AChR) antibody-positive generalized myasthenia gravis, rituximab and placebo may have a similar glucocorticoid-sparing effect regardless of disease severity, according to research presented at the annual meeting of the American Association of Neuromuscular and Electrodiagnostic Medicine.
B Cell Targeted Treatment In Myasthenia Gravis (BeatMG) was a 52-week, randomized, double-blind, placebo-controlled clinical trial. The phase 2 study’s primary outcomes were safety and the glucocorticoid-sparing effect assessed by the percentage of patients who reduced their mean daily prednisone dose by at least 75% and maintained clinical stability. Secondary outcomes were change in Myasthenia Gravis Composite (MGC) score and change in Quantitative Myasthenia Gravis (QMG) score from baseline to 52 weeks.
Investigators randomized 52 participants 1:1 to rituximab (Rituxan) or placebo. Patients were taking at least 15 mg/day of prednisone and were a mean of about age 50 years. About two-thirds were treated with glucocorticoids alone at baseline, and nearly two-thirds had a Myasthenia Gravis Foundation of America (MGFA) clinical classification of II. “It was a mildly symptomatic group of individuals in terms of disease severity,” said Richard Nowak, MD, assistant professor of neurology and director of the Yale Myasthenia Gravis Clinic in New Haven, Conn.
During the study, 60% of patients who received rituximab had a 75% or greater reduction in their mean daily prednisone dose and maintained clinical stability. “However, what surprised us is that we had a significantly high placebo response rate of 56%,” he said. The difference between groups was not significant.
Patients who received rituximab had “directionally favorable reductions” in MGC and QMG scores over 52 weeks, compared with patients who received placebo. Nevertheless, “after correcting for baseline differences, there was no significant difference between the two groups,” Dr. Nowak said.
Rituximab had good safety and tolerability, and the placebo group had a threefold higher rate of clinical relapse requiring IV immunoglobulin or plasmapheresis. “While the placebo arm did achieve a similar rate of reduction in their steroid dose, at 52 weeks the patients may have been doing less well, reflected by the higher rate of relapse,” he said.
Subgroup analysis
To explore whether rituximab might benefit patients who were treatment resistant or had more symptomatic disease, Dr. Nowak and his colleagues conducted a post hoc subgroup analysis of 20 participants – 10 in the rituximab arm and 10 in the placebo arm – who were MGFA class III-IV. In each group, 70% were on glucocorticoid treatment alone, and 90% were MGFA class III.
As in the overall study, the glucocorticoid-sparing effect was not significant (60% of the rituximab group vs. 50% of the placebo group).
Mean change in QMG score was –3.9 in the rituximab group and –0.5 in the placebo group, and mean change in MGC score was –7.0 in the rituximab group and –4.8 in the placebo group. These secondary outcomes again show “directional favorability” with rituximab, Dr. Nowak said. The researchers saw similar trends for scores that assess quality of life and activities of daily living.
In the subgroup analysis, myasthenia gravis relapses requiring rescue therapy occurred in 20% of patients in the rituximab arm and in 30% of the placebo arm. Overall, the researchers did not see a difference in treatment response between those with moderate to severe disease and those with mild disease, Dr. Nowak said.
Suggestions from the data
The post hoc subgroup analysis should be interpreted with caution, and the study does not provide firm conclusions, Dr. Nowak noted. In addition, the trial population does not reflect all patients with myasthenia gravis. Dr. Nowak routinely uses rituximab in patients with muscle-specific kinase antibody-positive disease, he said. For acetylcholine receptor antibody-positive generalized myasthenia gravis, which has approved therapies available, Dr. Nowak presents rituximab as an option for some patients. Further research may clarify where B-cell depletion therapy may fit into the treatment paradigm.
Nonetheless, BeatMG and the subgroup analysis may help physicians better understand the disease and the role of various therapies. Investigators successfully lowered prednisone dose “at a pretty high rate in the placebo arm,” he said. “It suggests that many of our patients potentially may be on higher than required prednisone doses.”
Finally, the BeatMG findings emphasize the need for placebo-controlled trials to understand potential therapies. “We need to pause when we see a lot of retrospective and uncontrolled studies that are very promising,” Dr. Nowak said.
The study was supported by the National Institute of Neurological Disorders and Stroke. Genentech provided the study drug and placebo through an investigator-sponsored study agreement. Dr. Nowak has received research support from Alexion Pharmaceuticals, Genentech, Grifols, and Ra Pharmaceuticals. He has served as a paid consultant for Alexion, Momenta, Ra, Roivant, Shire, Grifols, and CSL Behring.
SOURCE: Nowak R et al. AANEM 2019. Unnumbered Abstract: Rituximab in patients with moderate to severe myasthenia gravis: a subgroup analysis of the BeatMG study
REPORTING FROM AANEM 2019
America’s peas problem and freshly grated tattoos
Hold the peas, pass the spiders
There’s an old saying – and by “old,” we mean that we just made it up – in the medical-humor business: When in doubt, find a survey.
Some group is always surveying somebody about something and coming up with a wacky assumption or misguided opinion held by a minority of the respondents. It’s a classic go-to move for the desperate writer.
And look, here’s one now. According to a recent survey conducted by OnePoll for VeggieTracker.com, 83% of Americans like – and this makes us feel oogie just thinking about it – peas. Blecch. Even more amazing? About a quarter of the 2,000 respondents said that they had never even eaten a vegetable. That might explain a good bit of the country’s obesity problem.
And then there’s the survey that OnePoll did for Mattress Advisor, which questioned 2,000 Americans about sleep science and myth. Among the results: 23% believe that an hour of sleep before midnight is worth more than two after, 25% think that sleeping on your left side helps digestion, and 15% said that circadian rhythm was the proper term for the body’s blood flow.
Our favorite, though, was the myth that you swallow eight spiders a year while you sleep. We’ve never heard that one, but 20% of respondents thought it was true.
We’re glad that it’s just a myth, but even spiders would be better than peas.
The politics of pretty
It’s an age-old political question: Did a majority of U.S. voters back Martin Van Buren in the 1836 presidential election because he pushed the popular policies of his boss, fellow Democrat Andrew Jackson? Or was it the suave sideburns of Jackson’s stylish vice president that trumped (see what we did there?) the clean-shaven Whig William Henry Harrison?
The evidence-backed answer: Probably both.
Researchers at the University of Freiburg in Germany conducted two style-or-substance studies to determine how much political advantage a pretty face confers. The first study examined the impact attractive looks and the ability to appear competent riding atop an Abrams tank (ooooh, sorry, Dukakis fans), er, the ability to look competent in photos had in Germany’s 2017 Bundestag elections.
The study’s precise answer: 3.8 percentage points. That’s the polling advantage candidates gained by being judged more attractive than their competitors. Admittedly, the researchers also found it helped to be more than just a pretty face – the unaesthetic quality of relative competence also played a positive role.
The second study took the same approach to U.S. House of Representatives races. In that research beauty contest, America’s aesthetically attuned voters delivered up to an 11-point advantage to the prettiest person.
Now, as anyone will tell you who’s watched congressional TMZ – a.k.a. C-SPAN – beauty in politics is a relative matter. As one of our colleagues noted after visiting the Bureau of LOTME’s Washington hometown and seeing several political stars up close and personal: “Washington is Hollywood for the not so good lookin’.”
Grate idea, or greatest idea?
Tattoo removal is a big part of business for quite a few dermatologists out there. In 2011, more than 100,000 tattoo removal procedures were performed, according to the American Society for Dermatologic Surgery.
But dermatologists beware, because an Argentinian man may have found a far cheaper method for getting rid of unwanted tattoos, one that would make all those fancy lasers obsolete.
And it all hinges on a humble kitchen utensil: the cheese grater.
The story began when our intrepid hero found out that he wouldn’t be able to work as airport police with a visible tattoo. Simultaneously, he decided that the detail on the week-old tattoo was not up to his standard. So, the man took to the Internet, searching for a cheap way to remove the offending mark. He tried a pumice stone but had no luck. So, next came the cheese grater.
And credit where credit’s due – he did get rid of the tattoo. He washed the wound, applied disinfectant, and everything was good.
Okay, he MAY have required a trip to his local emergency department because he needed a tetanus shot. And while the man isn’t sorry that he did what he did, he wouldn’t recommend the procedure to anyone else.
But consider yourselves on notice, dermatologists. There are always new ways to innovate.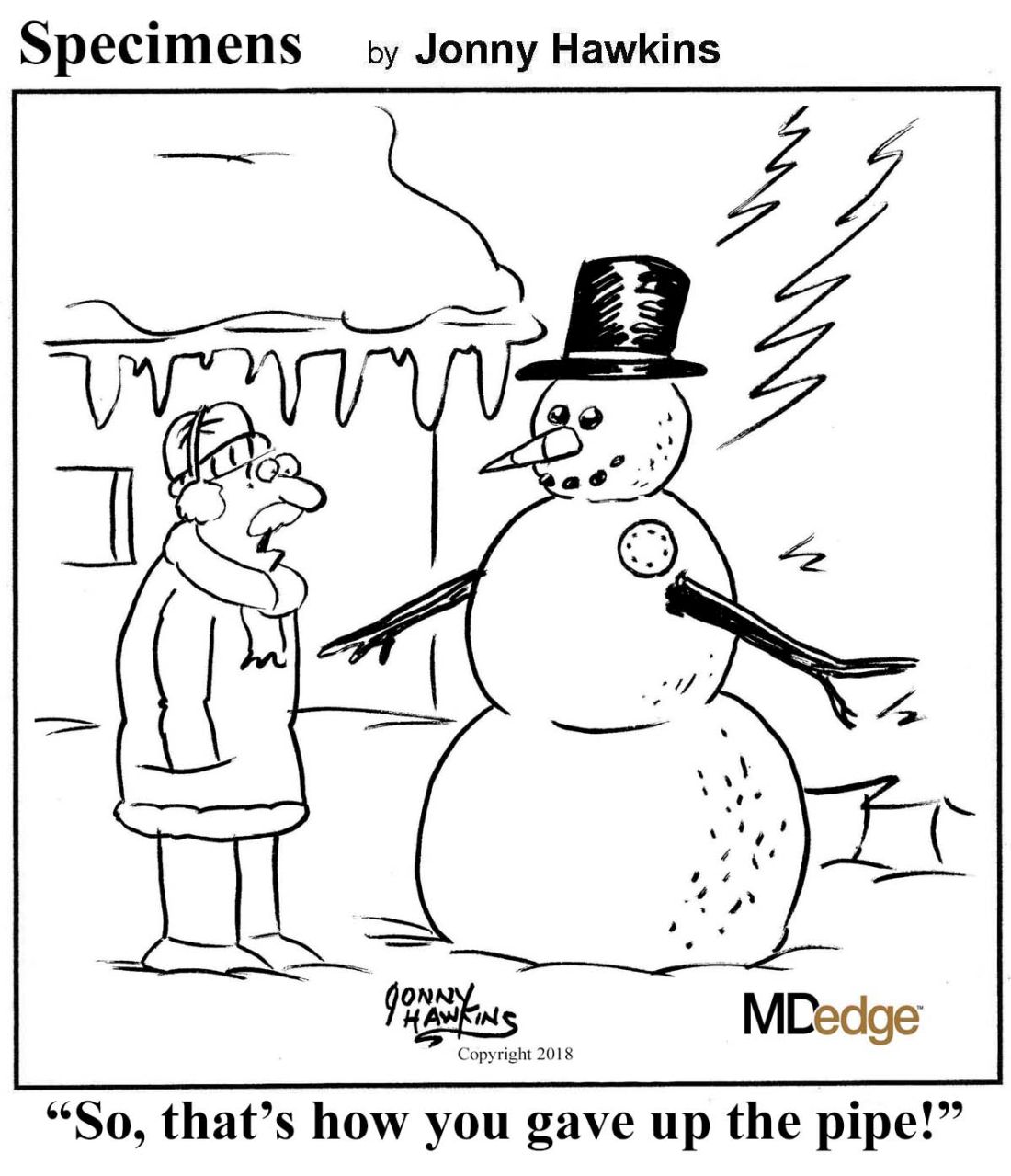
Hold the peas, pass the spiders
There’s an old saying – and by “old,” we mean that we just made it up – in the medical-humor business: When in doubt, find a survey.
Some group is always surveying somebody about something and coming up with a wacky assumption or misguided opinion held by a minority of the respondents. It’s a classic go-to move for the desperate writer.
And look, here’s one now. According to a recent survey conducted by OnePoll for VeggieTracker.com, 83% of Americans like – and this makes us feel oogie just thinking about it – peas. Blecch. Even more amazing? About a quarter of the 2,000 respondents said that they had never even eaten a vegetable. That might explain a good bit of the country’s obesity problem.
And then there’s the survey that OnePoll did for Mattress Advisor, which questioned 2,000 Americans about sleep science and myth. Among the results: 23% believe that an hour of sleep before midnight is worth more than two after, 25% think that sleeping on your left side helps digestion, and 15% said that circadian rhythm was the proper term for the body’s blood flow.
Our favorite, though, was the myth that you swallow eight spiders a year while you sleep. We’ve never heard that one, but 20% of respondents thought it was true.
We’re glad that it’s just a myth, but even spiders would be better than peas.
The politics of pretty
It’s an age-old political question: Did a majority of U.S. voters back Martin Van Buren in the 1836 presidential election because he pushed the popular policies of his boss, fellow Democrat Andrew Jackson? Or was it the suave sideburns of Jackson’s stylish vice president that trumped (see what we did there?) the clean-shaven Whig William Henry Harrison?
The evidence-backed answer: Probably both.
Researchers at the University of Freiburg in Germany conducted two style-or-substance studies to determine how much political advantage a pretty face confers. The first study examined the impact attractive looks and the ability to appear competent riding atop an Abrams tank (ooooh, sorry, Dukakis fans), er, the ability to look competent in photos had in Germany’s 2017 Bundestag elections.
The study’s precise answer: 3.8 percentage points. That’s the polling advantage candidates gained by being judged more attractive than their competitors. Admittedly, the researchers also found it helped to be more than just a pretty face – the unaesthetic quality of relative competence also played a positive role.
The second study took the same approach to U.S. House of Representatives races. In that research beauty contest, America’s aesthetically attuned voters delivered up to an 11-point advantage to the prettiest person.
Now, as anyone will tell you who’s watched congressional TMZ – a.k.a. C-SPAN – beauty in politics is a relative matter. As one of our colleagues noted after visiting the Bureau of LOTME’s Washington hometown and seeing several political stars up close and personal: “Washington is Hollywood for the not so good lookin’.”
Grate idea, or greatest idea?
Tattoo removal is a big part of business for quite a few dermatologists out there. In 2011, more than 100,000 tattoo removal procedures were performed, according to the American Society for Dermatologic Surgery.
But dermatologists beware, because an Argentinian man may have found a far cheaper method for getting rid of unwanted tattoos, one that would make all those fancy lasers obsolete.
And it all hinges on a humble kitchen utensil: the cheese grater.
The story began when our intrepid hero found out that he wouldn’t be able to work as airport police with a visible tattoo. Simultaneously, he decided that the detail on the week-old tattoo was not up to his standard. So, the man took to the Internet, searching for a cheap way to remove the offending mark. He tried a pumice stone but had no luck. So, next came the cheese grater.
And credit where credit’s due – he did get rid of the tattoo. He washed the wound, applied disinfectant, and everything was good.
Okay, he MAY have required a trip to his local emergency department because he needed a tetanus shot. And while the man isn’t sorry that he did what he did, he wouldn’t recommend the procedure to anyone else.
But consider yourselves on notice, dermatologists. There are always new ways to innovate.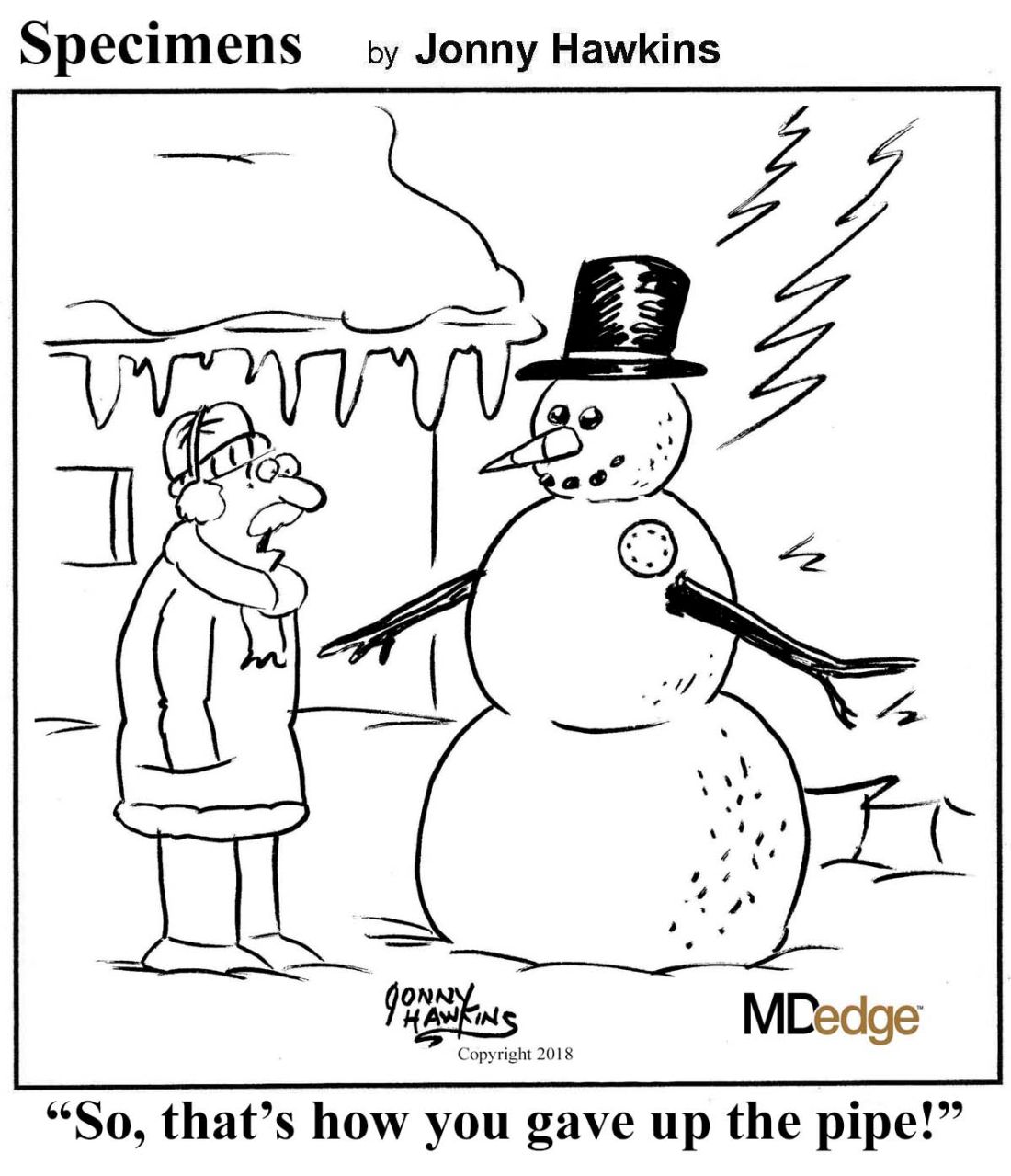
Hold the peas, pass the spiders
There’s an old saying – and by “old,” we mean that we just made it up – in the medical-humor business: When in doubt, find a survey.
Some group is always surveying somebody about something and coming up with a wacky assumption or misguided opinion held by a minority of the respondents. It’s a classic go-to move for the desperate writer.
And look, here’s one now. According to a recent survey conducted by OnePoll for VeggieTracker.com, 83% of Americans like – and this makes us feel oogie just thinking about it – peas. Blecch. Even more amazing? About a quarter of the 2,000 respondents said that they had never even eaten a vegetable. That might explain a good bit of the country’s obesity problem.
And then there’s the survey that OnePoll did for Mattress Advisor, which questioned 2,000 Americans about sleep science and myth. Among the results: 23% believe that an hour of sleep before midnight is worth more than two after, 25% think that sleeping on your left side helps digestion, and 15% said that circadian rhythm was the proper term for the body’s blood flow.
Our favorite, though, was the myth that you swallow eight spiders a year while you sleep. We’ve never heard that one, but 20% of respondents thought it was true.
We’re glad that it’s just a myth, but even spiders would be better than peas.
The politics of pretty
It’s an age-old political question: Did a majority of U.S. voters back Martin Van Buren in the 1836 presidential election because he pushed the popular policies of his boss, fellow Democrat Andrew Jackson? Or was it the suave sideburns of Jackson’s stylish vice president that trumped (see what we did there?) the clean-shaven Whig William Henry Harrison?
The evidence-backed answer: Probably both.
Researchers at the University of Freiburg in Germany conducted two style-or-substance studies to determine how much political advantage a pretty face confers. The first study examined the impact attractive looks and the ability to appear competent riding atop an Abrams tank (ooooh, sorry, Dukakis fans), er, the ability to look competent in photos had in Germany’s 2017 Bundestag elections.
The study’s precise answer: 3.8 percentage points. That’s the polling advantage candidates gained by being judged more attractive than their competitors. Admittedly, the researchers also found it helped to be more than just a pretty face – the unaesthetic quality of relative competence also played a positive role.
The second study took the same approach to U.S. House of Representatives races. In that research beauty contest, America’s aesthetically attuned voters delivered up to an 11-point advantage to the prettiest person.
Now, as anyone will tell you who’s watched congressional TMZ – a.k.a. C-SPAN – beauty in politics is a relative matter. As one of our colleagues noted after visiting the Bureau of LOTME’s Washington hometown and seeing several political stars up close and personal: “Washington is Hollywood for the not so good lookin’.”
Grate idea, or greatest idea?
Tattoo removal is a big part of business for quite a few dermatologists out there. In 2011, more than 100,000 tattoo removal procedures were performed, according to the American Society for Dermatologic Surgery.
But dermatologists beware, because an Argentinian man may have found a far cheaper method for getting rid of unwanted tattoos, one that would make all those fancy lasers obsolete.
And it all hinges on a humble kitchen utensil: the cheese grater.
The story began when our intrepid hero found out that he wouldn’t be able to work as airport police with a visible tattoo. Simultaneously, he decided that the detail on the week-old tattoo was not up to his standard. So, the man took to the Internet, searching for a cheap way to remove the offending mark. He tried a pumice stone but had no luck. So, next came the cheese grater.
And credit where credit’s due – he did get rid of the tattoo. He washed the wound, applied disinfectant, and everything was good.
Okay, he MAY have required a trip to his local emergency department because he needed a tetanus shot. And while the man isn’t sorry that he did what he did, he wouldn’t recommend the procedure to anyone else.
But consider yourselves on notice, dermatologists. There are always new ways to innovate.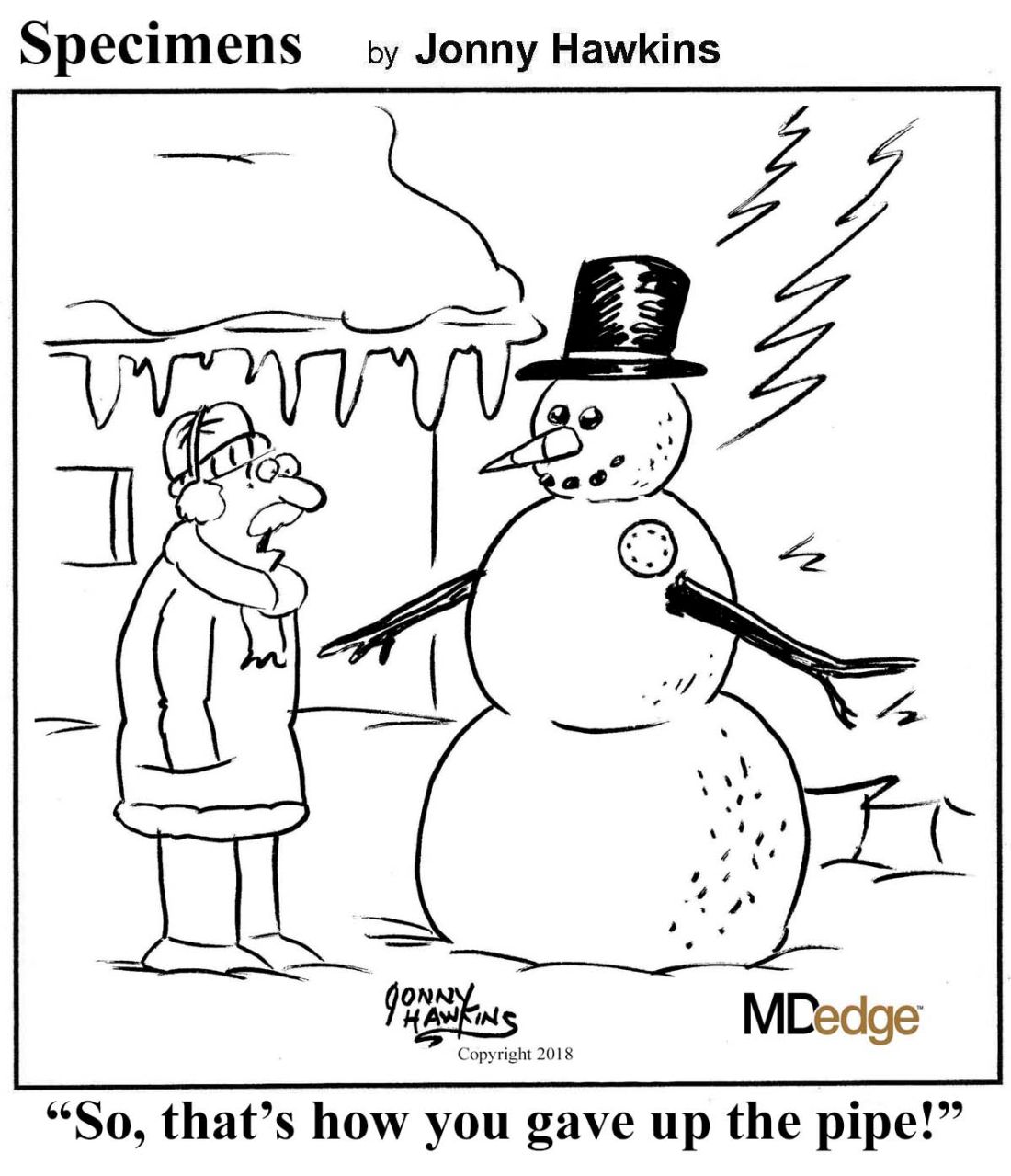
Congenital myasthenic syndrome diagnosed best with repetitive stimulation and jitter analysis
AUSTIN, TEX. – suggests newly presented research.
“In case RS is negative, SFEMG [single fiber electromyography] alone is not very specific and cannot distinguish CMS from mitochondrial myopathies, even in the presence of impulse blocking,” Vitor Marques Caldas, MD, a neurologist at the Syrian Libanes Hospital in Brasilia, Brazil, and a PhD student at the University of São Paulo, told attendees at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine. “An isolated SFEMG test can lead to a misdiagnosis of myasthenia syndrome if not interpreted in the right clinical context.”
The researchers sought to understand the relative sensitivity and specificity of low-frequency RS versus jitter analysis using disposable concentric needle electrodes (CNE).
The study involved 69 patients, of whom 19 had mitochondrial myopathy, 18 had congenital myopathy, 18 had CMS, and 14 were asymptomatic controls. The control group all tested normal with both RS and jitter analysis.
The 18 participants with CMS, average age 24 years, received low-frequency RS in at least six different muscles: two distal muscles (abductor digiti minimi and tibialis anterior), two proximal muscles (deltoid and trapezius) and two facial muscles (nasalis and orbicularis oculi). They also underwent jitter analysis of their orbicularis oculi muscle under voluntary activation using CNE.
These patients had heterogeneous genetic profiles: 11 had the CHRNE gene mutation, 2 had the RAPSN gene mutation, 2 had the COLQ gene mutation, 2 had the DOK-7 gene mutation, and 1 had the COL13A1 mutation.
All but two patients with congenital CMS tested positive (88.9%) with RS: one female with CHRNE mutation and one male with RAPSN mutation. Using mean jitter, all but one patient tested positive (94.4%): a female with DOK-7 mutation who had tested abnormal on RS.
All patients with CMS tested positive with at least one of the two tests, but only 83.3% tested positive with both tests, resulting in a sensitivity of 83.3%, a specificity of 100%, and overall accuracy of 95.6% using both tests.
Among the 19 patients with mitochondrial myopathy, 5 had abnormal jitter analysis.
When the researchers looked only at participants with abnormal jitter analysis but normal RS, two of these were patients with CMS, but another seven had congenital or mitochondrial myopathies. Using abnormal jitter alone therefore resulted in a sensitivity of 100% but a specificity of only 86%, for overall 86.5% accuracy.
“It’s important to notice that if you have an abnormal jitter, we have to look at the clinical symptoms of the patients,” Dr. Marques Caldas said in an interview. “Jitter abnormalities are not enough to distinguish between myasthenic disorder and a myopathic disorder.”
The research used no external funding, and Dr. Marques Caldas had no disclosures.
SOURCE: Caldas VM et al. AANEM 2019. Unnumbered Abstract: Sensitivity of neurophysiologic tests regarding the neuromuscular junction in patients with congenital myasthenic syndromes.
AUSTIN, TEX. – suggests newly presented research.
“In case RS is negative, SFEMG [single fiber electromyography] alone is not very specific and cannot distinguish CMS from mitochondrial myopathies, even in the presence of impulse blocking,” Vitor Marques Caldas, MD, a neurologist at the Syrian Libanes Hospital in Brasilia, Brazil, and a PhD student at the University of São Paulo, told attendees at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine. “An isolated SFEMG test can lead to a misdiagnosis of myasthenia syndrome if not interpreted in the right clinical context.”
The researchers sought to understand the relative sensitivity and specificity of low-frequency RS versus jitter analysis using disposable concentric needle electrodes (CNE).
The study involved 69 patients, of whom 19 had mitochondrial myopathy, 18 had congenital myopathy, 18 had CMS, and 14 were asymptomatic controls. The control group all tested normal with both RS and jitter analysis.
The 18 participants with CMS, average age 24 years, received low-frequency RS in at least six different muscles: two distal muscles (abductor digiti minimi and tibialis anterior), two proximal muscles (deltoid and trapezius) and two facial muscles (nasalis and orbicularis oculi). They also underwent jitter analysis of their orbicularis oculi muscle under voluntary activation using CNE.
These patients had heterogeneous genetic profiles: 11 had the CHRNE gene mutation, 2 had the RAPSN gene mutation, 2 had the COLQ gene mutation, 2 had the DOK-7 gene mutation, and 1 had the COL13A1 mutation.
All but two patients with congenital CMS tested positive (88.9%) with RS: one female with CHRNE mutation and one male with RAPSN mutation. Using mean jitter, all but one patient tested positive (94.4%): a female with DOK-7 mutation who had tested abnormal on RS.
All patients with CMS tested positive with at least one of the two tests, but only 83.3% tested positive with both tests, resulting in a sensitivity of 83.3%, a specificity of 100%, and overall accuracy of 95.6% using both tests.
Among the 19 patients with mitochondrial myopathy, 5 had abnormal jitter analysis.
When the researchers looked only at participants with abnormal jitter analysis but normal RS, two of these were patients with CMS, but another seven had congenital or mitochondrial myopathies. Using abnormal jitter alone therefore resulted in a sensitivity of 100% but a specificity of only 86%, for overall 86.5% accuracy.
“It’s important to notice that if you have an abnormal jitter, we have to look at the clinical symptoms of the patients,” Dr. Marques Caldas said in an interview. “Jitter abnormalities are not enough to distinguish between myasthenic disorder and a myopathic disorder.”
The research used no external funding, and Dr. Marques Caldas had no disclosures.
SOURCE: Caldas VM et al. AANEM 2019. Unnumbered Abstract: Sensitivity of neurophysiologic tests regarding the neuromuscular junction in patients with congenital myasthenic syndromes.
AUSTIN, TEX. – suggests newly presented research.
“In case RS is negative, SFEMG [single fiber electromyography] alone is not very specific and cannot distinguish CMS from mitochondrial myopathies, even in the presence of impulse blocking,” Vitor Marques Caldas, MD, a neurologist at the Syrian Libanes Hospital in Brasilia, Brazil, and a PhD student at the University of São Paulo, told attendees at the annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine. “An isolated SFEMG test can lead to a misdiagnosis of myasthenia syndrome if not interpreted in the right clinical context.”
The researchers sought to understand the relative sensitivity and specificity of low-frequency RS versus jitter analysis using disposable concentric needle electrodes (CNE).
The study involved 69 patients, of whom 19 had mitochondrial myopathy, 18 had congenital myopathy, 18 had CMS, and 14 were asymptomatic controls. The control group all tested normal with both RS and jitter analysis.
The 18 participants with CMS, average age 24 years, received low-frequency RS in at least six different muscles: two distal muscles (abductor digiti minimi and tibialis anterior), two proximal muscles (deltoid and trapezius) and two facial muscles (nasalis and orbicularis oculi). They also underwent jitter analysis of their orbicularis oculi muscle under voluntary activation using CNE.
These patients had heterogeneous genetic profiles: 11 had the CHRNE gene mutation, 2 had the RAPSN gene mutation, 2 had the COLQ gene mutation, 2 had the DOK-7 gene mutation, and 1 had the COL13A1 mutation.
All but two patients with congenital CMS tested positive (88.9%) with RS: one female with CHRNE mutation and one male with RAPSN mutation. Using mean jitter, all but one patient tested positive (94.4%): a female with DOK-7 mutation who had tested abnormal on RS.
All patients with CMS tested positive with at least one of the two tests, but only 83.3% tested positive with both tests, resulting in a sensitivity of 83.3%, a specificity of 100%, and overall accuracy of 95.6% using both tests.
Among the 19 patients with mitochondrial myopathy, 5 had abnormal jitter analysis.
When the researchers looked only at participants with abnormal jitter analysis but normal RS, two of these were patients with CMS, but another seven had congenital or mitochondrial myopathies. Using abnormal jitter alone therefore resulted in a sensitivity of 100% but a specificity of only 86%, for overall 86.5% accuracy.
“It’s important to notice that if you have an abnormal jitter, we have to look at the clinical symptoms of the patients,” Dr. Marques Caldas said in an interview. “Jitter abnormalities are not enough to distinguish between myasthenic disorder and a myopathic disorder.”
The research used no external funding, and Dr. Marques Caldas had no disclosures.
SOURCE: Caldas VM et al. AANEM 2019. Unnumbered Abstract: Sensitivity of neurophysiologic tests regarding the neuromuscular junction in patients with congenital myasthenic syndromes.
REPORTING FROM AANEM 2019
Veliparib improves PFS in high-grade serous epithelial ovarian cancer
BARCELONA – (HGSC) in the phase 3 VELIA/GOG-3005 trial.
The benefit associated with the oral poly (ADP-ribose) polymerase (PARP) inhibitor was seen in all women with newly diagnosed HGSC included in the randomized, placebo-controlled trial, regardless of BRCA mutation (BRCAm) status or homologous recombination deficiency (HRD) status, Robert L. Coleman, MD, reported at the European Society for Medical Oncology Congress.
Of 1,140 patients enrolled in the international, multicenter trial, 26% had a BRCAm and 55% were HRD positive. In the intent-to-treat population, median progression-free survival (PFS) was 23.5 months in 382 patients who received carboplatin/paclitaxel (CP) plus veliparib followed by veliparib maintenance (veliparib group 1) versus 17.3 months in 375 patients treated with CP alone followed by placebo maintenance (the control group) (hazard ratio, 0.68), according to Dr. Coleman, professor and Ann Rife Cox Chair in Gynecology in the department of gynecologic oncology and reproductive medicine in the division of surgery at the University of Texas MD Anderson Cancer Center, Houston.
Among 200 patients with a deleterious BRCAm, including 108 in the veliparib 1 group and 92 in the control group, median PFS was 34.7 and 22.0 months, respectively (HR, 0.44), and among 421 patients with HRD and BRCAm, including 214 in the veliparib 1 group and 207 in the control group, median PFS was 31.9 versus 20.5 months (HR, 0.57).
In the non-HRD population of 249 patients (125 in the veliparib 1 arm and 124 in the control arm), median PFS was 15.0 and 11.5 months, respectively.
The PFS for an additional group of 383 patients treated with CP plus veliparib followed by placebo maintenance (veliparib group 2) didn’t differ significantly from either the veliparib 1 or the control group (HR, 1.07 vs. the control group in the intent-to-treat population), and the PFS rates were also similar for the BRCAm and HRD-positive patients in the veliparib 2 group and control group, he noted, explaining that the main focus of his presentation was the primary study endpoint of median PFS in the veliparib 1 versus control group.
The overall response rates at the end of treatment in the intent-to-treat populations were 84% in the veliparib 1 group, 74% in the control group, and 79% in the veliparib 2 group, Dr. Coleman said, adding that response rates were numerically higher in both veliparib-containing arms.
Additional analyses, including overall survival, will be reported at a future date, he noted.
Study participants were adults with a mean age of 62 years who had previously untreated stage III-IV HGSC. Treatment included six cycles of CP at 21-day intervals, with paclitaxel given either weekly or every 3 weeks following primary cytoreduction or neoadjuvant chemotherapy with interval cytoreduction. The veliparib dose when given with CP was 150 mg twice daily, and the veliparib maintenance dose was 400 mg twice daily for 30 cycles.
Relative CP dose intensities were similar between arms, and grade 3-4 adverse events were similar in the veliparib 1 and control groups during CP – with the exception of thrombocytopenia, which occurred in 27% and 8% of patients in the groups, respectively. During maintenance, the rates of any grade 3-4 adverse events were higher in the veliparib 1 group versus the control group (45% vs. 32%), but serious adverse event rates were similar in the groups (17% and 19%).
Observed toxicities were consistent with the known veliparib safety profile, Dr. Coleman said.
The findings are notable, as PARP inhibitors have proven effective in ovarian cancer, but their use in combination with chemotherapy has been challenging because of hematologic toxicity, he added, explaining, however, that veliparib has not only been shown to have single agent activity in germline BRCAm recurrent ovarian cancer patients, but also has binding characteristics – namely increased protein poly ADP-ribosylation and decreased PARP trapping – that could allow for its use in combination with chemotherapy.
VELIA/GOG-3005 is the first randomized trial designed to enroll only untreated patients with advanced-stage HGSC regardless of BRCA status, surgical management, or response to treatment, and the findings suggest that veliparib can be safely administered with CP and should be considered a new treatment option for women with newly diagnosed, advanced-stage serous ovarian cancer, he concluded.
In an ESMO press release, Ana Oaknin, MD, PhD, head of the gynecologic cancer program at Vall d’Hebron Institute of Oncology, Vall d’Hebron University Hospital, Barcelona, said that this trial, along with others such as the SOLO-1 trial, the PAOLA-1/ENGOT-Ov25 trial, and the PRIMA/ENGOT-OV26/GOG-3012 trial, which each looked at integrating PARP inhibitors into first-line treatment, represents “a milestone for patients.”
“After decades studying different chemotherapy approaches, it is the first time we have meaningfully prolonged progression free survival and hopefully we will improve long-term outcome,” she said.
The study was sponsored by AbbVie. Dr. Coleman and Dr. Oaknin reported relationships with numerous pharmaceutical companies.
SOURCE: Coleman RL et al. ESMO 2019, Abstract LBA3-PR.
BARCELONA – (HGSC) in the phase 3 VELIA/GOG-3005 trial.
The benefit associated with the oral poly (ADP-ribose) polymerase (PARP) inhibitor was seen in all women with newly diagnosed HGSC included in the randomized, placebo-controlled trial, regardless of BRCA mutation (BRCAm) status or homologous recombination deficiency (HRD) status, Robert L. Coleman, MD, reported at the European Society for Medical Oncology Congress.
Of 1,140 patients enrolled in the international, multicenter trial, 26% had a BRCAm and 55% were HRD positive. In the intent-to-treat population, median progression-free survival (PFS) was 23.5 months in 382 patients who received carboplatin/paclitaxel (CP) plus veliparib followed by veliparib maintenance (veliparib group 1) versus 17.3 months in 375 patients treated with CP alone followed by placebo maintenance (the control group) (hazard ratio, 0.68), according to Dr. Coleman, professor and Ann Rife Cox Chair in Gynecology in the department of gynecologic oncology and reproductive medicine in the division of surgery at the University of Texas MD Anderson Cancer Center, Houston.
Among 200 patients with a deleterious BRCAm, including 108 in the veliparib 1 group and 92 in the control group, median PFS was 34.7 and 22.0 months, respectively (HR, 0.44), and among 421 patients with HRD and BRCAm, including 214 in the veliparib 1 group and 207 in the control group, median PFS was 31.9 versus 20.5 months (HR, 0.57).
In the non-HRD population of 249 patients (125 in the veliparib 1 arm and 124 in the control arm), median PFS was 15.0 and 11.5 months, respectively.
The PFS for an additional group of 383 patients treated with CP plus veliparib followed by placebo maintenance (veliparib group 2) didn’t differ significantly from either the veliparib 1 or the control group (HR, 1.07 vs. the control group in the intent-to-treat population), and the PFS rates were also similar for the BRCAm and HRD-positive patients in the veliparib 2 group and control group, he noted, explaining that the main focus of his presentation was the primary study endpoint of median PFS in the veliparib 1 versus control group.
The overall response rates at the end of treatment in the intent-to-treat populations were 84% in the veliparib 1 group, 74% in the control group, and 79% in the veliparib 2 group, Dr. Coleman said, adding that response rates were numerically higher in both veliparib-containing arms.
Additional analyses, including overall survival, will be reported at a future date, he noted.
Study participants were adults with a mean age of 62 years who had previously untreated stage III-IV HGSC. Treatment included six cycles of CP at 21-day intervals, with paclitaxel given either weekly or every 3 weeks following primary cytoreduction or neoadjuvant chemotherapy with interval cytoreduction. The veliparib dose when given with CP was 150 mg twice daily, and the veliparib maintenance dose was 400 mg twice daily for 30 cycles.
Relative CP dose intensities were similar between arms, and grade 3-4 adverse events were similar in the veliparib 1 and control groups during CP – with the exception of thrombocytopenia, which occurred in 27% and 8% of patients in the groups, respectively. During maintenance, the rates of any grade 3-4 adverse events were higher in the veliparib 1 group versus the control group (45% vs. 32%), but serious adverse event rates were similar in the groups (17% and 19%).
Observed toxicities were consistent with the known veliparib safety profile, Dr. Coleman said.
The findings are notable, as PARP inhibitors have proven effective in ovarian cancer, but their use in combination with chemotherapy has been challenging because of hematologic toxicity, he added, explaining, however, that veliparib has not only been shown to have single agent activity in germline BRCAm recurrent ovarian cancer patients, but also has binding characteristics – namely increased protein poly ADP-ribosylation and decreased PARP trapping – that could allow for its use in combination with chemotherapy.
VELIA/GOG-3005 is the first randomized trial designed to enroll only untreated patients with advanced-stage HGSC regardless of BRCA status, surgical management, or response to treatment, and the findings suggest that veliparib can be safely administered with CP and should be considered a new treatment option for women with newly diagnosed, advanced-stage serous ovarian cancer, he concluded.
In an ESMO press release, Ana Oaknin, MD, PhD, head of the gynecologic cancer program at Vall d’Hebron Institute of Oncology, Vall d’Hebron University Hospital, Barcelona, said that this trial, along with others such as the SOLO-1 trial, the PAOLA-1/ENGOT-Ov25 trial, and the PRIMA/ENGOT-OV26/GOG-3012 trial, which each looked at integrating PARP inhibitors into first-line treatment, represents “a milestone for patients.”
“After decades studying different chemotherapy approaches, it is the first time we have meaningfully prolonged progression free survival and hopefully we will improve long-term outcome,” she said.
The study was sponsored by AbbVie. Dr. Coleman and Dr. Oaknin reported relationships with numerous pharmaceutical companies.
SOURCE: Coleman RL et al. ESMO 2019, Abstract LBA3-PR.
BARCELONA – (HGSC) in the phase 3 VELIA/GOG-3005 trial.
The benefit associated with the oral poly (ADP-ribose) polymerase (PARP) inhibitor was seen in all women with newly diagnosed HGSC included in the randomized, placebo-controlled trial, regardless of BRCA mutation (BRCAm) status or homologous recombination deficiency (HRD) status, Robert L. Coleman, MD, reported at the European Society for Medical Oncology Congress.
Of 1,140 patients enrolled in the international, multicenter trial, 26% had a BRCAm and 55% were HRD positive. In the intent-to-treat population, median progression-free survival (PFS) was 23.5 months in 382 patients who received carboplatin/paclitaxel (CP) plus veliparib followed by veliparib maintenance (veliparib group 1) versus 17.3 months in 375 patients treated with CP alone followed by placebo maintenance (the control group) (hazard ratio, 0.68), according to Dr. Coleman, professor and Ann Rife Cox Chair in Gynecology in the department of gynecologic oncology and reproductive medicine in the division of surgery at the University of Texas MD Anderson Cancer Center, Houston.
Among 200 patients with a deleterious BRCAm, including 108 in the veliparib 1 group and 92 in the control group, median PFS was 34.7 and 22.0 months, respectively (HR, 0.44), and among 421 patients with HRD and BRCAm, including 214 in the veliparib 1 group and 207 in the control group, median PFS was 31.9 versus 20.5 months (HR, 0.57).
In the non-HRD population of 249 patients (125 in the veliparib 1 arm and 124 in the control arm), median PFS was 15.0 and 11.5 months, respectively.
The PFS for an additional group of 383 patients treated with CP plus veliparib followed by placebo maintenance (veliparib group 2) didn’t differ significantly from either the veliparib 1 or the control group (HR, 1.07 vs. the control group in the intent-to-treat population), and the PFS rates were also similar for the BRCAm and HRD-positive patients in the veliparib 2 group and control group, he noted, explaining that the main focus of his presentation was the primary study endpoint of median PFS in the veliparib 1 versus control group.
The overall response rates at the end of treatment in the intent-to-treat populations were 84% in the veliparib 1 group, 74% in the control group, and 79% in the veliparib 2 group, Dr. Coleman said, adding that response rates were numerically higher in both veliparib-containing arms.
Additional analyses, including overall survival, will be reported at a future date, he noted.
Study participants were adults with a mean age of 62 years who had previously untreated stage III-IV HGSC. Treatment included six cycles of CP at 21-day intervals, with paclitaxel given either weekly or every 3 weeks following primary cytoreduction or neoadjuvant chemotherapy with interval cytoreduction. The veliparib dose when given with CP was 150 mg twice daily, and the veliparib maintenance dose was 400 mg twice daily for 30 cycles.
Relative CP dose intensities were similar between arms, and grade 3-4 adverse events were similar in the veliparib 1 and control groups during CP – with the exception of thrombocytopenia, which occurred in 27% and 8% of patients in the groups, respectively. During maintenance, the rates of any grade 3-4 adverse events were higher in the veliparib 1 group versus the control group (45% vs. 32%), but serious adverse event rates were similar in the groups (17% and 19%).
Observed toxicities were consistent with the known veliparib safety profile, Dr. Coleman said.
The findings are notable, as PARP inhibitors have proven effective in ovarian cancer, but their use in combination with chemotherapy has been challenging because of hematologic toxicity, he added, explaining, however, that veliparib has not only been shown to have single agent activity in germline BRCAm recurrent ovarian cancer patients, but also has binding characteristics – namely increased protein poly ADP-ribosylation and decreased PARP trapping – that could allow for its use in combination with chemotherapy.
VELIA/GOG-3005 is the first randomized trial designed to enroll only untreated patients with advanced-stage HGSC regardless of BRCA status, surgical management, or response to treatment, and the findings suggest that veliparib can be safely administered with CP and should be considered a new treatment option for women with newly diagnosed, advanced-stage serous ovarian cancer, he concluded.
In an ESMO press release, Ana Oaknin, MD, PhD, head of the gynecologic cancer program at Vall d’Hebron Institute of Oncology, Vall d’Hebron University Hospital, Barcelona, said that this trial, along with others such as the SOLO-1 trial, the PAOLA-1/ENGOT-Ov25 trial, and the PRIMA/ENGOT-OV26/GOG-3012 trial, which each looked at integrating PARP inhibitors into first-line treatment, represents “a milestone for patients.”
“After decades studying different chemotherapy approaches, it is the first time we have meaningfully prolonged progression free survival and hopefully we will improve long-term outcome,” she said.
The study was sponsored by AbbVie. Dr. Coleman and Dr. Oaknin reported relationships with numerous pharmaceutical companies.
SOURCE: Coleman RL et al. ESMO 2019, Abstract LBA3-PR.
REPORTING FROM ESMO 2019
Low P values shouldn’t always impress you
SAN DIEGO – Even if a P value hints at statistical significance by dipping under .05, it might not tell you anything worthwhile. Effect sizes are hugely important – as long as accompanying P values measure up. And pharmaceutical companies often keep revealing numbers under wraps unless you know what – and whom – to ask.
Those lessons come courtesy of Leslie Citrome, MD, MPH, who spoke to colleagues about study numbers at Psych Congress 2019.
Dr. Citrome, clinical professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, offered several tips about interpreting medical statistics as you make clinical decisions.
Don’t get hung up on the P value.
The P value helps you understand how likely it is that a difference in a study is statistically significant. In medical research, P values under .05 are considered especially desirable. They suggest that an outcome – drug A performed better than drug B, for example – didn’t happen purely by chance.
Here’s the hitch: The P value might not matter at all. “Clinicians often assume that if the P value is less than.05, the result must be important. But even a P value of less than .05 is meaningless outside of the context of how big the treatment effect is,” Dr. Citrome said. “If a clinical trial result shows us a small effect size, then who cares?”
Understand what effect sizes tell you.
Effect size measurements evaluate clinical impact and include number needed to treat (NNT) and number needed to harm (NNH). NNT refers to the number of patients needed to treat with an intervention in order to get a positive effect in one additional patient; NNH is the reverse and examines negative effects that can range from the minor (mild dry mouth) to the devastating (death).
What’s a good size for an NNT? “I respect any NNT versus placebo of less than 10,” Dr. Citrome said. “It’s something I’ll probably consider in day-to-day practice.” Double-digit and triple-digit NNTs “are usually irrelevant unless we’re dealing with very specific outcomes that have long-term consequences.”
As for the opposite side of the picture – NNH – values higher than 10 are ideal.
He cautioned that NNT and NNH, like P values, cannot stand alone. In fact, they work together. In order to have value, NNT or NNH must be statistically significant, and P values provide this crucial insight.
Consider Dr. Citrome’s blood pressure.
As Dr. Citrome noted, research suggests that, among patients with diastolic BP from 90 to 109 mm Hg, 1 additional person will avoid death, stroke, or heart attack for every 141 people who take an antihypertensive medication, compared to those who do not, over a 5-year period. That’s a lot of people taking medication for a long time, with potential side effects, for a fairly small effect size. However, the outcomes are dire, so it is still worth it.
Then there’s Dr. Citrome himself, who has had diastolic BP in the range of 115 to 129 mm Hg. The NNT is 3. For every 3 people who take an antihypertensive vs. not over a 5-year period, 1 additional person will avoid a potentially catastrophic cardiovascular event.
“Guess who’s pretty adherent to taking his antihypertensive medication?” he asked. “I am.”
Ask for effect sizes if you don’t see them.
It’s not unusual for pharmaceutical representatives to avoid providing information about medication effect sizes. “The sales representatives as well as speakers at [Food and Drug Administration]–regulated promotional speaking events can only speak to basically what’s on the label. NNT and NNH are not currently found on product labels. But they are very relevant, and we need to know this information.”
What to do? “There is a workaround here,” he said. “Ask the sales rep to talk to a medical science liaison, who is free to come to your office and talk about all the data that they have.”
Dr. Citrome reported multiple disclosures, including various relationships with pharmaceutical companies.
SAN DIEGO – Even if a P value hints at statistical significance by dipping under .05, it might not tell you anything worthwhile. Effect sizes are hugely important – as long as accompanying P values measure up. And pharmaceutical companies often keep revealing numbers under wraps unless you know what – and whom – to ask.
Those lessons come courtesy of Leslie Citrome, MD, MPH, who spoke to colleagues about study numbers at Psych Congress 2019.
Dr. Citrome, clinical professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, offered several tips about interpreting medical statistics as you make clinical decisions.
Don’t get hung up on the P value.
The P value helps you understand how likely it is that a difference in a study is statistically significant. In medical research, P values under .05 are considered especially desirable. They suggest that an outcome – drug A performed better than drug B, for example – didn’t happen purely by chance.
Here’s the hitch: The P value might not matter at all. “Clinicians often assume that if the P value is less than.05, the result must be important. But even a P value of less than .05 is meaningless outside of the context of how big the treatment effect is,” Dr. Citrome said. “If a clinical trial result shows us a small effect size, then who cares?”
Understand what effect sizes tell you.
Effect size measurements evaluate clinical impact and include number needed to treat (NNT) and number needed to harm (NNH). NNT refers to the number of patients needed to treat with an intervention in order to get a positive effect in one additional patient; NNH is the reverse and examines negative effects that can range from the minor (mild dry mouth) to the devastating (death).
What’s a good size for an NNT? “I respect any NNT versus placebo of less than 10,” Dr. Citrome said. “It’s something I’ll probably consider in day-to-day practice.” Double-digit and triple-digit NNTs “are usually irrelevant unless we’re dealing with very specific outcomes that have long-term consequences.”
As for the opposite side of the picture – NNH – values higher than 10 are ideal.
He cautioned that NNT and NNH, like P values, cannot stand alone. In fact, they work together. In order to have value, NNT or NNH must be statistically significant, and P values provide this crucial insight.
Consider Dr. Citrome’s blood pressure.
As Dr. Citrome noted, research suggests that, among patients with diastolic BP from 90 to 109 mm Hg, 1 additional person will avoid death, stroke, or heart attack for every 141 people who take an antihypertensive medication, compared to those who do not, over a 5-year period. That’s a lot of people taking medication for a long time, with potential side effects, for a fairly small effect size. However, the outcomes are dire, so it is still worth it.
Then there’s Dr. Citrome himself, who has had diastolic BP in the range of 115 to 129 mm Hg. The NNT is 3. For every 3 people who take an antihypertensive vs. not over a 5-year period, 1 additional person will avoid a potentially catastrophic cardiovascular event.
“Guess who’s pretty adherent to taking his antihypertensive medication?” he asked. “I am.”
Ask for effect sizes if you don’t see them.
It’s not unusual for pharmaceutical representatives to avoid providing information about medication effect sizes. “The sales representatives as well as speakers at [Food and Drug Administration]–regulated promotional speaking events can only speak to basically what’s on the label. NNT and NNH are not currently found on product labels. But they are very relevant, and we need to know this information.”
What to do? “There is a workaround here,” he said. “Ask the sales rep to talk to a medical science liaison, who is free to come to your office and talk about all the data that they have.”
Dr. Citrome reported multiple disclosures, including various relationships with pharmaceutical companies.
SAN DIEGO – Even if a P value hints at statistical significance by dipping under .05, it might not tell you anything worthwhile. Effect sizes are hugely important – as long as accompanying P values measure up. And pharmaceutical companies often keep revealing numbers under wraps unless you know what – and whom – to ask.
Those lessons come courtesy of Leslie Citrome, MD, MPH, who spoke to colleagues about study numbers at Psych Congress 2019.
Dr. Citrome, clinical professor of psychiatry and behavioral sciences at New York Medical College, Valhalla, offered several tips about interpreting medical statistics as you make clinical decisions.
Don’t get hung up on the P value.
The P value helps you understand how likely it is that a difference in a study is statistically significant. In medical research, P values under .05 are considered especially desirable. They suggest that an outcome – drug A performed better than drug B, for example – didn’t happen purely by chance.
Here’s the hitch: The P value might not matter at all. “Clinicians often assume that if the P value is less than.05, the result must be important. But even a P value of less than .05 is meaningless outside of the context of how big the treatment effect is,” Dr. Citrome said. “If a clinical trial result shows us a small effect size, then who cares?”
Understand what effect sizes tell you.
Effect size measurements evaluate clinical impact and include number needed to treat (NNT) and number needed to harm (NNH). NNT refers to the number of patients needed to treat with an intervention in order to get a positive effect in one additional patient; NNH is the reverse and examines negative effects that can range from the minor (mild dry mouth) to the devastating (death).
What’s a good size for an NNT? “I respect any NNT versus placebo of less than 10,” Dr. Citrome said. “It’s something I’ll probably consider in day-to-day practice.” Double-digit and triple-digit NNTs “are usually irrelevant unless we’re dealing with very specific outcomes that have long-term consequences.”
As for the opposite side of the picture – NNH – values higher than 10 are ideal.
He cautioned that NNT and NNH, like P values, cannot stand alone. In fact, they work together. In order to have value, NNT or NNH must be statistically significant, and P values provide this crucial insight.
Consider Dr. Citrome’s blood pressure.
As Dr. Citrome noted, research suggests that, among patients with diastolic BP from 90 to 109 mm Hg, 1 additional person will avoid death, stroke, or heart attack for every 141 people who take an antihypertensive medication, compared to those who do not, over a 5-year period. That’s a lot of people taking medication for a long time, with potential side effects, for a fairly small effect size. However, the outcomes are dire, so it is still worth it.
Then there’s Dr. Citrome himself, who has had diastolic BP in the range of 115 to 129 mm Hg. The NNT is 3. For every 3 people who take an antihypertensive vs. not over a 5-year period, 1 additional person will avoid a potentially catastrophic cardiovascular event.
“Guess who’s pretty adherent to taking his antihypertensive medication?” he asked. “I am.”
Ask for effect sizes if you don’t see them.
It’s not unusual for pharmaceutical representatives to avoid providing information about medication effect sizes. “The sales representatives as well as speakers at [Food and Drug Administration]–regulated promotional speaking events can only speak to basically what’s on the label. NNT and NNH are not currently found on product labels. But they are very relevant, and we need to know this information.”
What to do? “There is a workaround here,” he said. “Ask the sales rep to talk to a medical science liaison, who is free to come to your office and talk about all the data that they have.”
Dr. Citrome reported multiple disclosures, including various relationships with pharmaceutical companies.
REPORTING FROM PSYCH CONGRESS 2019
Rituximab bests mycophenolate in pemphigus vulgaris
MADRID – Pascal Joly, MD, PhD, reported at the annual congress of the European Academy of Dermatology and Venereology.
Not only did rituximab prove superior in terms of efficacy in the PEMPHIX trial, with a five times greater likelihood of achieving a complete remission lasting for at least 16 weeks while off oral corticosteroids than with mycophenolate mofetil in the 52-week study, but the total number of disease flares in the mycophenolate mofetil group was five times higher. Moreover, rituximab-treated patients received a markedly lower cumulative dose of prednisone as well.
“Rituximab has a superior overall benefit-risk profile, compared to mycophenolate mofetil, in patients with moderate to severe pemphigus vulgaris,” concluded Dr. Joly, professor of dermatology at the University of Rouen (France) and president of the French Society of Dermatology.
The study was undertaken because mycophenolate mofetil is commonly used as a corticosteroid-sparing drug in patients with pemphigus vulgaris, even though its efficacy for the treatment of this rare, severe autoimmune blistering disease is unproven, he explained.
In contrast, rituximab was approved by the Food and Drug Administration and European regulators for treatment of pemphigus vulgaris on the strength of the pivotal phase 3 Ritux 3 trial – also led by Dr. Joly – which demonstrated the superiority of this intravenously administered anti-CD20 monoclonal antibody plus short-term prednisone over high-dose corticosteroid monotherapy, which for decades had been the standard treatment despite its considerable toxicity burden (Lancet. 2017 May 20;389[10083]:2031-40).
An independently conducted analysis of Ritux 3 recently concluded that rituximab plus short-term prednisone was more effective than prednisone alone, with a lower risk of life-threatening, corticosteroid-related adverse events and less cumulative corticosteroid exposure (Br J Dermatol. 2019 Sep 5. doi: 10.1111/bjd.18482).
Also, an international panel of 93 pemphigus experts has declared that rituximab should be considered an evidence-based first-line therapy for moderate to-severe pemphigus (J Am Acad Dermatol. 2018 Feb 10. doi: 10.1016/j.jaad.2018.02.021).
The phase 3, placebo-controlled PEMPHIX trial randomized 135 patients with moderate or severe pemphigus at 49 academic medical centers in the United States and nine other countries to double-blind rituximab or mycophenolate mofetil on top of background oral prednisone at 1.0-1.5 mg/kg per day, with the steroid to be tapered and discontinued within 4-6 months.
The primary endpoint of the study was the proportion of patients in each study arm at week 52 who had achieved a sustained complete remission lasting for at least 16 weeks while off prednisone. The rate was 40.3% in the rituximab group and 9.5% with mycophenolate mofetil, for a 383% increased likelihood of sustained complete remission in the rituximab group.
In addition, all of the study’s secondary endpoints significantly favored rituximab. The median cumulative dose of corticosteroid was 2.7 g through 52 weeks in the rituximab arm, compared with 4 g with mycophenolate mofetil. The total number of disease flares over 52 weeks was 6 in the rituximab group and 44 in the mycophenolate arm. Five rituximab-treated patients experienced disease flares, as did 26 on mycophenolate. Thus, the likelihood of a flare was seven times lower with rituximab.
Scores on the Dermatology Life Quality Index improved by an average of 8.87 points from baseline to week 52 in the rituximab group versus 6 points with mycophenolate. And 62.7% of rituximab-treated patients had a week-52 Dermatology Life Quality Index score of 0, meaning no impact of the disease on their quality of life, compared with 25% of the mycophenolate group.
Dr. Joly characterized the safety profile of rituximab as “manageable, with acceptable tolerability.” About 9% of the rituximab group and 7.4% of mycophenolate-treated patients had one or more treatment-related adverse events, a nonsignificant difference. The rate of treatment-related serious infections was 3.0% with rituximab and 2.9% with mycophenolate. Serious infusion reactions leading to study withdrawal occurred in three patients on rituximab and one on mycophenolate. The rate of grade 3 or worse corticosteroid-related adverse events was 1.5% with rituximab and significantly greater at 7.4% with mycophenolate.
An additional 48-week safety assessment beyond the 52-week primary outcome is ongoing.
Asked what future role he sees for mycophenolate in pemphigus vulgaris, Dr. Joly replied that the only study in the literature that shows the drug outperforms placebo was seriously flawed. “In the future, it’s very likely that the indications for use of mycophenolate in pemphigus vulgaris will be fewer and fewer,” the dermatologist added.
In reply to a question about the merits of routine antibiotic prophylaxis against pneumocystis carinii pneumonia in patients taking rituximab for pemphigus vulgaris, Dr. Joly said the incidence isn’t sufficiently high to justify such practice. After all, he noted, there were no cases of pneumocystis carinii pneumonia in rituximab-treated patients in PEMPHIX and only one in Ritux 3.
EADV Scientific Programming Committee Chair Brigitte Dreno, MD, PhD, professor and head of dermatology at University Hospital in Nantes, France, inquired as to whether there’s a role for maintenance therapy in a potent rituximab-based treatment strategy such as utilized in PEMPHIX.
Definitely, Dr. Joly replied. However, further study is required to work out the best maintenance program.
“There are many arguments for maintenance therapy in these patients. For one, the frequency of relapses increases with the length of follow-up. Also, anti–desmoglein-specific T cells can still be detected after rituximab therapy, even in patients in complete remission. So there is a need for maintenance therapy, perhaps at months 6, 12, and 18, but the optimal regimen isn’t determined yet,” according to Dr. Joly.
PEMPHIX was sponsored by F. Hoffmann-La Roche. Dr. Joly reported serving as a consultant to Roche, Amgen, Principia Biopharma, and Argenx.
MADRID – Pascal Joly, MD, PhD, reported at the annual congress of the European Academy of Dermatology and Venereology.
Not only did rituximab prove superior in terms of efficacy in the PEMPHIX trial, with a five times greater likelihood of achieving a complete remission lasting for at least 16 weeks while off oral corticosteroids than with mycophenolate mofetil in the 52-week study, but the total number of disease flares in the mycophenolate mofetil group was five times higher. Moreover, rituximab-treated patients received a markedly lower cumulative dose of prednisone as well.
“Rituximab has a superior overall benefit-risk profile, compared to mycophenolate mofetil, in patients with moderate to severe pemphigus vulgaris,” concluded Dr. Joly, professor of dermatology at the University of Rouen (France) and president of the French Society of Dermatology.
The study was undertaken because mycophenolate mofetil is commonly used as a corticosteroid-sparing drug in patients with pemphigus vulgaris, even though its efficacy for the treatment of this rare, severe autoimmune blistering disease is unproven, he explained.
In contrast, rituximab was approved by the Food and Drug Administration and European regulators for treatment of pemphigus vulgaris on the strength of the pivotal phase 3 Ritux 3 trial – also led by Dr. Joly – which demonstrated the superiority of this intravenously administered anti-CD20 monoclonal antibody plus short-term prednisone over high-dose corticosteroid monotherapy, which for decades had been the standard treatment despite its considerable toxicity burden (Lancet. 2017 May 20;389[10083]:2031-40).
An independently conducted analysis of Ritux 3 recently concluded that rituximab plus short-term prednisone was more effective than prednisone alone, with a lower risk of life-threatening, corticosteroid-related adverse events and less cumulative corticosteroid exposure (Br J Dermatol. 2019 Sep 5. doi: 10.1111/bjd.18482).
Also, an international panel of 93 pemphigus experts has declared that rituximab should be considered an evidence-based first-line therapy for moderate to-severe pemphigus (J Am Acad Dermatol. 2018 Feb 10. doi: 10.1016/j.jaad.2018.02.021).
The phase 3, placebo-controlled PEMPHIX trial randomized 135 patients with moderate or severe pemphigus at 49 academic medical centers in the United States and nine other countries to double-blind rituximab or mycophenolate mofetil on top of background oral prednisone at 1.0-1.5 mg/kg per day, with the steroid to be tapered and discontinued within 4-6 months.
The primary endpoint of the study was the proportion of patients in each study arm at week 52 who had achieved a sustained complete remission lasting for at least 16 weeks while off prednisone. The rate was 40.3% in the rituximab group and 9.5% with mycophenolate mofetil, for a 383% increased likelihood of sustained complete remission in the rituximab group.
In addition, all of the study’s secondary endpoints significantly favored rituximab. The median cumulative dose of corticosteroid was 2.7 g through 52 weeks in the rituximab arm, compared with 4 g with mycophenolate mofetil. The total number of disease flares over 52 weeks was 6 in the rituximab group and 44 in the mycophenolate arm. Five rituximab-treated patients experienced disease flares, as did 26 on mycophenolate. Thus, the likelihood of a flare was seven times lower with rituximab.
Scores on the Dermatology Life Quality Index improved by an average of 8.87 points from baseline to week 52 in the rituximab group versus 6 points with mycophenolate. And 62.7% of rituximab-treated patients had a week-52 Dermatology Life Quality Index score of 0, meaning no impact of the disease on their quality of life, compared with 25% of the mycophenolate group.
Dr. Joly characterized the safety profile of rituximab as “manageable, with acceptable tolerability.” About 9% of the rituximab group and 7.4% of mycophenolate-treated patients had one or more treatment-related adverse events, a nonsignificant difference. The rate of treatment-related serious infections was 3.0% with rituximab and 2.9% with mycophenolate. Serious infusion reactions leading to study withdrawal occurred in three patients on rituximab and one on mycophenolate. The rate of grade 3 or worse corticosteroid-related adverse events was 1.5% with rituximab and significantly greater at 7.4% with mycophenolate.
An additional 48-week safety assessment beyond the 52-week primary outcome is ongoing.
Asked what future role he sees for mycophenolate in pemphigus vulgaris, Dr. Joly replied that the only study in the literature that shows the drug outperforms placebo was seriously flawed. “In the future, it’s very likely that the indications for use of mycophenolate in pemphigus vulgaris will be fewer and fewer,” the dermatologist added.
In reply to a question about the merits of routine antibiotic prophylaxis against pneumocystis carinii pneumonia in patients taking rituximab for pemphigus vulgaris, Dr. Joly said the incidence isn’t sufficiently high to justify such practice. After all, he noted, there were no cases of pneumocystis carinii pneumonia in rituximab-treated patients in PEMPHIX and only one in Ritux 3.
EADV Scientific Programming Committee Chair Brigitte Dreno, MD, PhD, professor and head of dermatology at University Hospital in Nantes, France, inquired as to whether there’s a role for maintenance therapy in a potent rituximab-based treatment strategy such as utilized in PEMPHIX.
Definitely, Dr. Joly replied. However, further study is required to work out the best maintenance program.
“There are many arguments for maintenance therapy in these patients. For one, the frequency of relapses increases with the length of follow-up. Also, anti–desmoglein-specific T cells can still be detected after rituximab therapy, even in patients in complete remission. So there is a need for maintenance therapy, perhaps at months 6, 12, and 18, but the optimal regimen isn’t determined yet,” according to Dr. Joly.
PEMPHIX was sponsored by F. Hoffmann-La Roche. Dr. Joly reported serving as a consultant to Roche, Amgen, Principia Biopharma, and Argenx.
MADRID – Pascal Joly, MD, PhD, reported at the annual congress of the European Academy of Dermatology and Venereology.
Not only did rituximab prove superior in terms of efficacy in the PEMPHIX trial, with a five times greater likelihood of achieving a complete remission lasting for at least 16 weeks while off oral corticosteroids than with mycophenolate mofetil in the 52-week study, but the total number of disease flares in the mycophenolate mofetil group was five times higher. Moreover, rituximab-treated patients received a markedly lower cumulative dose of prednisone as well.
“Rituximab has a superior overall benefit-risk profile, compared to mycophenolate mofetil, in patients with moderate to severe pemphigus vulgaris,” concluded Dr. Joly, professor of dermatology at the University of Rouen (France) and president of the French Society of Dermatology.
The study was undertaken because mycophenolate mofetil is commonly used as a corticosteroid-sparing drug in patients with pemphigus vulgaris, even though its efficacy for the treatment of this rare, severe autoimmune blistering disease is unproven, he explained.
In contrast, rituximab was approved by the Food and Drug Administration and European regulators for treatment of pemphigus vulgaris on the strength of the pivotal phase 3 Ritux 3 trial – also led by Dr. Joly – which demonstrated the superiority of this intravenously administered anti-CD20 monoclonal antibody plus short-term prednisone over high-dose corticosteroid monotherapy, which for decades had been the standard treatment despite its considerable toxicity burden (Lancet. 2017 May 20;389[10083]:2031-40).
An independently conducted analysis of Ritux 3 recently concluded that rituximab plus short-term prednisone was more effective than prednisone alone, with a lower risk of life-threatening, corticosteroid-related adverse events and less cumulative corticosteroid exposure (Br J Dermatol. 2019 Sep 5. doi: 10.1111/bjd.18482).
Also, an international panel of 93 pemphigus experts has declared that rituximab should be considered an evidence-based first-line therapy for moderate to-severe pemphigus (J Am Acad Dermatol. 2018 Feb 10. doi: 10.1016/j.jaad.2018.02.021).
The phase 3, placebo-controlled PEMPHIX trial randomized 135 patients with moderate or severe pemphigus at 49 academic medical centers in the United States and nine other countries to double-blind rituximab or mycophenolate mofetil on top of background oral prednisone at 1.0-1.5 mg/kg per day, with the steroid to be tapered and discontinued within 4-6 months.
The primary endpoint of the study was the proportion of patients in each study arm at week 52 who had achieved a sustained complete remission lasting for at least 16 weeks while off prednisone. The rate was 40.3% in the rituximab group and 9.5% with mycophenolate mofetil, for a 383% increased likelihood of sustained complete remission in the rituximab group.
In addition, all of the study’s secondary endpoints significantly favored rituximab. The median cumulative dose of corticosteroid was 2.7 g through 52 weeks in the rituximab arm, compared with 4 g with mycophenolate mofetil. The total number of disease flares over 52 weeks was 6 in the rituximab group and 44 in the mycophenolate arm. Five rituximab-treated patients experienced disease flares, as did 26 on mycophenolate. Thus, the likelihood of a flare was seven times lower with rituximab.
Scores on the Dermatology Life Quality Index improved by an average of 8.87 points from baseline to week 52 in the rituximab group versus 6 points with mycophenolate. And 62.7% of rituximab-treated patients had a week-52 Dermatology Life Quality Index score of 0, meaning no impact of the disease on their quality of life, compared with 25% of the mycophenolate group.
Dr. Joly characterized the safety profile of rituximab as “manageable, with acceptable tolerability.” About 9% of the rituximab group and 7.4% of mycophenolate-treated patients had one or more treatment-related adverse events, a nonsignificant difference. The rate of treatment-related serious infections was 3.0% with rituximab and 2.9% with mycophenolate. Serious infusion reactions leading to study withdrawal occurred in three patients on rituximab and one on mycophenolate. The rate of grade 3 or worse corticosteroid-related adverse events was 1.5% with rituximab and significantly greater at 7.4% with mycophenolate.
An additional 48-week safety assessment beyond the 52-week primary outcome is ongoing.
Asked what future role he sees for mycophenolate in pemphigus vulgaris, Dr. Joly replied that the only study in the literature that shows the drug outperforms placebo was seriously flawed. “In the future, it’s very likely that the indications for use of mycophenolate in pemphigus vulgaris will be fewer and fewer,” the dermatologist added.
In reply to a question about the merits of routine antibiotic prophylaxis against pneumocystis carinii pneumonia in patients taking rituximab for pemphigus vulgaris, Dr. Joly said the incidence isn’t sufficiently high to justify such practice. After all, he noted, there were no cases of pneumocystis carinii pneumonia in rituximab-treated patients in PEMPHIX and only one in Ritux 3.
EADV Scientific Programming Committee Chair Brigitte Dreno, MD, PhD, professor and head of dermatology at University Hospital in Nantes, France, inquired as to whether there’s a role for maintenance therapy in a potent rituximab-based treatment strategy such as utilized in PEMPHIX.
Definitely, Dr. Joly replied. However, further study is required to work out the best maintenance program.
“There are many arguments for maintenance therapy in these patients. For one, the frequency of relapses increases with the length of follow-up. Also, anti–desmoglein-specific T cells can still be detected after rituximab therapy, even in patients in complete remission. So there is a need for maintenance therapy, perhaps at months 6, 12, and 18, but the optimal regimen isn’t determined yet,” according to Dr. Joly.
PEMPHIX was sponsored by F. Hoffmann-La Roche. Dr. Joly reported serving as a consultant to Roche, Amgen, Principia Biopharma, and Argenx.
REPORTING FROM THE EADV CONGRESS
Making and using guidelines
Modern medicine increasingly relies on the adoption and use of guidelines.
Forty years ago, medicine was like free-form, rhythmic gymnastics in which physicians would develop an artisanal treatment plan for each patient. Now, medicine frequently involves recognizing when we need to do a triple-twisting, double-back somersault (the Biles II) and then performing it. The belief is that better outcomes flow from reduced variability in diagnostic and treatment plans, based on guidelines developed from evidence-based medicine from large meta-analyses. This dogma, still unproven in real life, probably works best for 95% of patients. The physician must not omit a step of deciding whether their particular patient is one of the 5% of patients to whom the guideline does not apply.
To be useful, the guidelines must be based on accurate science, produce a significantly positive cost-benefit-risk analysis, be wisely constructed, and be clearly written.
Alas, many guidelines fall far short of this ideal, and when they fail, they impugn all of medical care, they lower the credibility of the organizations that issue them, and they lower the public’s trust in medicine, which thereby impedes improving the public health. Don’t sweat the small stuff for public health guidelines.
The science matters. Nutritional guidelines have been particularly rickety, as John P.A. Ioannidis, MD, wrote in a JAMA op-ed 1 year ago.1 For instance, previous dietary recommendations to reduce cholesterol by avoiding eggs have since been shown to be wrong. The recommendation for reducing salt intake has been heavily criticized. Now the decades-long condemnation of red meat has been challenged. New “guidelines,” suggested by one group (let’s view it as a minority report that contradicts many official guidelines) in the October 1, 2019, issue of Annals of Internal Medicine, say that red meat and processed meats aren’t the boogeyman.2 The authors of the accompanying editorial are from the Center for Pediatric and Adolescent Comparative Effectiveness Research at Indiana University, Indianapolis.3 The editorial supports the new study, criticizing past recommendations because “the field of nutritional epidemiology is plagued by observational studies that have conducted inappropriate analyses, accompanied by likely erroneous conclusions.”
Clarity also matters. One factor in the current opiate epidemic was guidance in the mid-1990s making pain the “fifth vital sign.” This certainly was not the only factor nor was it necessarily the primary one. Most disasters, like most codes on the ward, proceed from multiple smaller failures and missteps. An emphasis on assessing pain in hospitalized patients did not intend to be interpreted as requiring that all pain be eliminated with strong medication, but that was the practical consequence. In response to the epidemic of overdose deaths, guidelines were promulgated in 2016 recommending reducing doses used for chronic opiate regimens. Some patients with chronic pain feared, and soon experienced, the consequences of those changes. In October 2019, those guidelines were revised telling physicians to go slower.4 In explaining the revision, one government official is quoted as saying: “Clearly we believe that there has been misinterpretation of the guidelines, which were very clear.”5 F. Scott Fitzgerald once wrote that “the test of a first-rate intelligence is the ability to hold two opposed ideas in mind at the same time and still retain the ability to function.” I reread that governmental doublespeak three times and my brain broke.
Clinical practice guidelines are an important part of modern medicine. But we need to be wiser about their creation. The science needs to be rigorous. The committees need to contain skeptics rather than just research scientists and clinicians with a vested interest in the field. The purported benefits of the guideline must be weighed against costs, risks, and unintended consequences. Humility is important. All physicians are taught the principle: “First, do no harm.” In explaining medical ethics to students, I rephrase that principle as: “Be cautious and humble. You are not as smart as you think you are.” Consider this food for thought the next time you read or create a guideline.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
References
1. JAMA. 2018;320(10):969-70.
2. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-1621.
3. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-2620.
4. U.S. Department of Health & Human Services. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of opioid analgesics. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf.
5. “New guidelines on opioid tapering tell doctors to go slow.” Washington Post. 2019 Oct 10.
Modern medicine increasingly relies on the adoption and use of guidelines.
Forty years ago, medicine was like free-form, rhythmic gymnastics in which physicians would develop an artisanal treatment plan for each patient. Now, medicine frequently involves recognizing when we need to do a triple-twisting, double-back somersault (the Biles II) and then performing it. The belief is that better outcomes flow from reduced variability in diagnostic and treatment plans, based on guidelines developed from evidence-based medicine from large meta-analyses. This dogma, still unproven in real life, probably works best for 95% of patients. The physician must not omit a step of deciding whether their particular patient is one of the 5% of patients to whom the guideline does not apply.
To be useful, the guidelines must be based on accurate science, produce a significantly positive cost-benefit-risk analysis, be wisely constructed, and be clearly written.
Alas, many guidelines fall far short of this ideal, and when they fail, they impugn all of medical care, they lower the credibility of the organizations that issue them, and they lower the public’s trust in medicine, which thereby impedes improving the public health. Don’t sweat the small stuff for public health guidelines.
The science matters. Nutritional guidelines have been particularly rickety, as John P.A. Ioannidis, MD, wrote in a JAMA op-ed 1 year ago.1 For instance, previous dietary recommendations to reduce cholesterol by avoiding eggs have since been shown to be wrong. The recommendation for reducing salt intake has been heavily criticized. Now the decades-long condemnation of red meat has been challenged. New “guidelines,” suggested by one group (let’s view it as a minority report that contradicts many official guidelines) in the October 1, 2019, issue of Annals of Internal Medicine, say that red meat and processed meats aren’t the boogeyman.2 The authors of the accompanying editorial are from the Center for Pediatric and Adolescent Comparative Effectiveness Research at Indiana University, Indianapolis.3 The editorial supports the new study, criticizing past recommendations because “the field of nutritional epidemiology is plagued by observational studies that have conducted inappropriate analyses, accompanied by likely erroneous conclusions.”
Clarity also matters. One factor in the current opiate epidemic was guidance in the mid-1990s making pain the “fifth vital sign.” This certainly was not the only factor nor was it necessarily the primary one. Most disasters, like most codes on the ward, proceed from multiple smaller failures and missteps. An emphasis on assessing pain in hospitalized patients did not intend to be interpreted as requiring that all pain be eliminated with strong medication, but that was the practical consequence. In response to the epidemic of overdose deaths, guidelines were promulgated in 2016 recommending reducing doses used for chronic opiate regimens. Some patients with chronic pain feared, and soon experienced, the consequences of those changes. In October 2019, those guidelines were revised telling physicians to go slower.4 In explaining the revision, one government official is quoted as saying: “Clearly we believe that there has been misinterpretation of the guidelines, which were very clear.”5 F. Scott Fitzgerald once wrote that “the test of a first-rate intelligence is the ability to hold two opposed ideas in mind at the same time and still retain the ability to function.” I reread that governmental doublespeak three times and my brain broke.
Clinical practice guidelines are an important part of modern medicine. But we need to be wiser about their creation. The science needs to be rigorous. The committees need to contain skeptics rather than just research scientists and clinicians with a vested interest in the field. The purported benefits of the guideline must be weighed against costs, risks, and unintended consequences. Humility is important. All physicians are taught the principle: “First, do no harm.” In explaining medical ethics to students, I rephrase that principle as: “Be cautious and humble. You are not as smart as you think you are.” Consider this food for thought the next time you read or create a guideline.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
References
1. JAMA. 2018;320(10):969-70.
2. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-1621.
3. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-2620.
4. U.S. Department of Health & Human Services. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of opioid analgesics. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf.
5. “New guidelines on opioid tapering tell doctors to go slow.” Washington Post. 2019 Oct 10.
Modern medicine increasingly relies on the adoption and use of guidelines.
Forty years ago, medicine was like free-form, rhythmic gymnastics in which physicians would develop an artisanal treatment plan for each patient. Now, medicine frequently involves recognizing when we need to do a triple-twisting, double-back somersault (the Biles II) and then performing it. The belief is that better outcomes flow from reduced variability in diagnostic and treatment plans, based on guidelines developed from evidence-based medicine from large meta-analyses. This dogma, still unproven in real life, probably works best for 95% of patients. The physician must not omit a step of deciding whether their particular patient is one of the 5% of patients to whom the guideline does not apply.
To be useful, the guidelines must be based on accurate science, produce a significantly positive cost-benefit-risk analysis, be wisely constructed, and be clearly written.
Alas, many guidelines fall far short of this ideal, and when they fail, they impugn all of medical care, they lower the credibility of the organizations that issue them, and they lower the public’s trust in medicine, which thereby impedes improving the public health. Don’t sweat the small stuff for public health guidelines.
The science matters. Nutritional guidelines have been particularly rickety, as John P.A. Ioannidis, MD, wrote in a JAMA op-ed 1 year ago.1 For instance, previous dietary recommendations to reduce cholesterol by avoiding eggs have since been shown to be wrong. The recommendation for reducing salt intake has been heavily criticized. Now the decades-long condemnation of red meat has been challenged. New “guidelines,” suggested by one group (let’s view it as a minority report that contradicts many official guidelines) in the October 1, 2019, issue of Annals of Internal Medicine, say that red meat and processed meats aren’t the boogeyman.2 The authors of the accompanying editorial are from the Center for Pediatric and Adolescent Comparative Effectiveness Research at Indiana University, Indianapolis.3 The editorial supports the new study, criticizing past recommendations because “the field of nutritional epidemiology is plagued by observational studies that have conducted inappropriate analyses, accompanied by likely erroneous conclusions.”
Clarity also matters. One factor in the current opiate epidemic was guidance in the mid-1990s making pain the “fifth vital sign.” This certainly was not the only factor nor was it necessarily the primary one. Most disasters, like most codes on the ward, proceed from multiple smaller failures and missteps. An emphasis on assessing pain in hospitalized patients did not intend to be interpreted as requiring that all pain be eliminated with strong medication, but that was the practical consequence. In response to the epidemic of overdose deaths, guidelines were promulgated in 2016 recommending reducing doses used for chronic opiate regimens. Some patients with chronic pain feared, and soon experienced, the consequences of those changes. In October 2019, those guidelines were revised telling physicians to go slower.4 In explaining the revision, one government official is quoted as saying: “Clearly we believe that there has been misinterpretation of the guidelines, which were very clear.”5 F. Scott Fitzgerald once wrote that “the test of a first-rate intelligence is the ability to hold two opposed ideas in mind at the same time and still retain the ability to function.” I reread that governmental doublespeak three times and my brain broke.
Clinical practice guidelines are an important part of modern medicine. But we need to be wiser about their creation. The science needs to be rigorous. The committees need to contain skeptics rather than just research scientists and clinicians with a vested interest in the field. The purported benefits of the guideline must be weighed against costs, risks, and unintended consequences. Humility is important. All physicians are taught the principle: “First, do no harm.” In explaining medical ethics to students, I rephrase that principle as: “Be cautious and humble. You are not as smart as you think you are.” Consider this food for thought the next time you read or create a guideline.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
References
1. JAMA. 2018;320(10):969-70.
2. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-1621.
3. Ann Intern Med. 2019 Oct 1. doi: 10.7326/M19-2620.
4. U.S. Department of Health & Human Services. HHS guide for clinicians on the appropriate dosage reduction or discontinuation of opioid analgesics. https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf.
5. “New guidelines on opioid tapering tell doctors to go slow.” Washington Post. 2019 Oct 10.