User login
EHR default order slashes unnecessary imaging during palliative RT
Simply adding a default order to the electronic health record that automatically opts patients out of commonly used but unnecessary radiation oncology procedures can dramatically curtail their use, suggests a stepped-wedge, cluster-randomized, controlled trial.
Daily x-ray or CT imaging is often used to better reproducibly position patients during curative radiotherapy, but guidelines consider it unnecessary during palliative radiotherapy because of limited clinical benefit, according to the investigators, led by Sonam Sharma, MD, of the Icahn School of Medicine at Mount Sinai, New York, and the Abramson Cancer Center at the University of Pennsylvania, Philadelphia. “Unnecessary imaging can increase treatment time and expense for patients in distress,” they noted.
The investigators conducted a 2-year trial among 21 radiation oncologists from five practices (one university, four community) in which they added to the EHR a default order that specified no daily imaging during palliative radiation therapy. (Radiation oncologists could select another imaging frequency if they preferred.) The default order was first rolled out in the university practice and subsequently in the community practices.
Study analyses were based on 1,019 adult patients with bone, soft tissue, or brain metastases who received 1,188 courses of palliative three-dimensional conformal radiotherapy during the trial.
Results reported in a JAMA Oncology research letter showed that the proportion of patients receiving daily imaging during their palliative radiotherapy (imaging during 80% or more of treatments) fell from 68.2% during the combined preintervention periods to 32.4% during the combined intervention periods.
After potential confounders were taken into account, implementation of the default order in the EHR was associated with a more than halving of the odds of daily imaging during palliative radiotherapy (adjusted odds ratio, 0.37; P = .003), with an adjusted percentage point reduction of –18.8.
Findings were similar in the university practice alone (aOR, 0.33; P = .01; –22.3 percentage points) and in the community practices alone (aOR, 0.45; P = .02; –27.5 percentage points).
“In a network of five radiation oncology practices, introducing a default order in the EHR reduced unnecessary daily imaging during palliative radiotherapy,” Dr. Sharma and colleagues concluded. “Our findings suggest that simple nudges, such as setting default orders, can meaningfully reduce unnecessary care.”
Dr. Sharma reported that she had no relevant conflicts of interest. The study was funded in part by the National Cancer Institute and the University of Pennsylvania Health System through the Penn Medicine Nudge Unit and the department of radiation oncology.
SOURCE: Sharma S et al. JAMA Oncol. 2019 Jun 27. doi: 10.1001/jamaoncol.2019.1432.
Simply adding a default order to the electronic health record that automatically opts patients out of commonly used but unnecessary radiation oncology procedures can dramatically curtail their use, suggests a stepped-wedge, cluster-randomized, controlled trial.
Daily x-ray or CT imaging is often used to better reproducibly position patients during curative radiotherapy, but guidelines consider it unnecessary during palliative radiotherapy because of limited clinical benefit, according to the investigators, led by Sonam Sharma, MD, of the Icahn School of Medicine at Mount Sinai, New York, and the Abramson Cancer Center at the University of Pennsylvania, Philadelphia. “Unnecessary imaging can increase treatment time and expense for patients in distress,” they noted.
The investigators conducted a 2-year trial among 21 radiation oncologists from five practices (one university, four community) in which they added to the EHR a default order that specified no daily imaging during palliative radiation therapy. (Radiation oncologists could select another imaging frequency if they preferred.) The default order was first rolled out in the university practice and subsequently in the community practices.
Study analyses were based on 1,019 adult patients with bone, soft tissue, or brain metastases who received 1,188 courses of palliative three-dimensional conformal radiotherapy during the trial.
Results reported in a JAMA Oncology research letter showed that the proportion of patients receiving daily imaging during their palliative radiotherapy (imaging during 80% or more of treatments) fell from 68.2% during the combined preintervention periods to 32.4% during the combined intervention periods.
After potential confounders were taken into account, implementation of the default order in the EHR was associated with a more than halving of the odds of daily imaging during palliative radiotherapy (adjusted odds ratio, 0.37; P = .003), with an adjusted percentage point reduction of –18.8.
Findings were similar in the university practice alone (aOR, 0.33; P = .01; –22.3 percentage points) and in the community practices alone (aOR, 0.45; P = .02; –27.5 percentage points).
“In a network of five radiation oncology practices, introducing a default order in the EHR reduced unnecessary daily imaging during palliative radiotherapy,” Dr. Sharma and colleagues concluded. “Our findings suggest that simple nudges, such as setting default orders, can meaningfully reduce unnecessary care.”
Dr. Sharma reported that she had no relevant conflicts of interest. The study was funded in part by the National Cancer Institute and the University of Pennsylvania Health System through the Penn Medicine Nudge Unit and the department of radiation oncology.
SOURCE: Sharma S et al. JAMA Oncol. 2019 Jun 27. doi: 10.1001/jamaoncol.2019.1432.
Simply adding a default order to the electronic health record that automatically opts patients out of commonly used but unnecessary radiation oncology procedures can dramatically curtail their use, suggests a stepped-wedge, cluster-randomized, controlled trial.
Daily x-ray or CT imaging is often used to better reproducibly position patients during curative radiotherapy, but guidelines consider it unnecessary during palliative radiotherapy because of limited clinical benefit, according to the investigators, led by Sonam Sharma, MD, of the Icahn School of Medicine at Mount Sinai, New York, and the Abramson Cancer Center at the University of Pennsylvania, Philadelphia. “Unnecessary imaging can increase treatment time and expense for patients in distress,” they noted.
The investigators conducted a 2-year trial among 21 radiation oncologists from five practices (one university, four community) in which they added to the EHR a default order that specified no daily imaging during palliative radiation therapy. (Radiation oncologists could select another imaging frequency if they preferred.) The default order was first rolled out in the university practice and subsequently in the community practices.
Study analyses were based on 1,019 adult patients with bone, soft tissue, or brain metastases who received 1,188 courses of palliative three-dimensional conformal radiotherapy during the trial.
Results reported in a JAMA Oncology research letter showed that the proportion of patients receiving daily imaging during their palliative radiotherapy (imaging during 80% or more of treatments) fell from 68.2% during the combined preintervention periods to 32.4% during the combined intervention periods.
After potential confounders were taken into account, implementation of the default order in the EHR was associated with a more than halving of the odds of daily imaging during palliative radiotherapy (adjusted odds ratio, 0.37; P = .003), with an adjusted percentage point reduction of –18.8.
Findings were similar in the university practice alone (aOR, 0.33; P = .01; –22.3 percentage points) and in the community practices alone (aOR, 0.45; P = .02; –27.5 percentage points).
“In a network of five radiation oncology practices, introducing a default order in the EHR reduced unnecessary daily imaging during palliative radiotherapy,” Dr. Sharma and colleagues concluded. “Our findings suggest that simple nudges, such as setting default orders, can meaningfully reduce unnecessary care.”
Dr. Sharma reported that she had no relevant conflicts of interest. The study was funded in part by the National Cancer Institute and the University of Pennsylvania Health System through the Penn Medicine Nudge Unit and the department of radiation oncology.
SOURCE: Sharma S et al. JAMA Oncol. 2019 Jun 27. doi: 10.1001/jamaoncol.2019.1432.
FROM JAMA ONCOLOGY
Eculizumab Cuts Relapse Risk in NMO Spectrum Disorder
Key clinical point: Treatment with eculizumab substantially reduced risk of relapse versus placebo in patients with aquaporin-4 positive neuromyelitis optica spectrum disorder.
Major finding: Time to first adjudicated relapse on trial, the primary endpoint of the study, showed a significant (P less than .0001) effect in favor of monoclonal antibody treatment over placebo, with a 94.2% reduction in risk of relapse.
Study details: A phase 3, randomized, double-blind, placebo-controlled, multicenter trial (PREVENT) including 143 adult patients.
Disclosures: The study was supported by Alexion Pharmaceuticals. Dr. Pittock provided disclosures related to Alexion Pharmaceuticals, MedImmune, and Grifols, along with patents related to administration of eculizumab and cancer markers in neuromyelitis optica.
Citation: Pittock SJ et al. AAN 2019, Emerging Science Abstract 009.
Key clinical point: Treatment with eculizumab substantially reduced risk of relapse versus placebo in patients with aquaporin-4 positive neuromyelitis optica spectrum disorder.
Major finding: Time to first adjudicated relapse on trial, the primary endpoint of the study, showed a significant (P less than .0001) effect in favor of monoclonal antibody treatment over placebo, with a 94.2% reduction in risk of relapse.
Study details: A phase 3, randomized, double-blind, placebo-controlled, multicenter trial (PREVENT) including 143 adult patients.
Disclosures: The study was supported by Alexion Pharmaceuticals. Dr. Pittock provided disclosures related to Alexion Pharmaceuticals, MedImmune, and Grifols, along with patents related to administration of eculizumab and cancer markers in neuromyelitis optica.
Citation: Pittock SJ et al. AAN 2019, Emerging Science Abstract 009.
Key clinical point: Treatment with eculizumab substantially reduced risk of relapse versus placebo in patients with aquaporin-4 positive neuromyelitis optica spectrum disorder.
Major finding: Time to first adjudicated relapse on trial, the primary endpoint of the study, showed a significant (P less than .0001) effect in favor of monoclonal antibody treatment over placebo, with a 94.2% reduction in risk of relapse.
Study details: A phase 3, randomized, double-blind, placebo-controlled, multicenter trial (PREVENT) including 143 adult patients.
Disclosures: The study was supported by Alexion Pharmaceuticals. Dr. Pittock provided disclosures related to Alexion Pharmaceuticals, MedImmune, and Grifols, along with patents related to administration of eculizumab and cancer markers in neuromyelitis optica.
Citation: Pittock SJ et al. AAN 2019, Emerging Science Abstract 009.
Pediatric MS May Go Untreated in Year After Diagnosis
Key clinical point: Physicians face considerable uncertainty regarding how to treat pediatric patients with MS.
Major finding: About 65% of pediatric patients with multiple sclerosis do not receive disease-modifying therapy within 1 year of diagnosis.
Study details: Retrospective, observational study of claims data from 288 patients with pediatric MS.
Disclosures: Novartis funded the study, and Dr. Deshpande, who presented the findings, and a coauthor are employees of Novartis. Other coauthors reported consulting fees from Novartis, as well as consulting fees and grant funding from other pharmaceutical companies.
Citation: Greenberg B et al. CMSC 2019, Abstract DXM02.
Key clinical point: Physicians face considerable uncertainty regarding how to treat pediatric patients with MS.
Major finding: About 65% of pediatric patients with multiple sclerosis do not receive disease-modifying therapy within 1 year of diagnosis.
Study details: Retrospective, observational study of claims data from 288 patients with pediatric MS.
Disclosures: Novartis funded the study, and Dr. Deshpande, who presented the findings, and a coauthor are employees of Novartis. Other coauthors reported consulting fees from Novartis, as well as consulting fees and grant funding from other pharmaceutical companies.
Citation: Greenberg B et al. CMSC 2019, Abstract DXM02.
Key clinical point: Physicians face considerable uncertainty regarding how to treat pediatric patients with MS.
Major finding: About 65% of pediatric patients with multiple sclerosis do not receive disease-modifying therapy within 1 year of diagnosis.
Study details: Retrospective, observational study of claims data from 288 patients with pediatric MS.
Disclosures: Novartis funded the study, and Dr. Deshpande, who presented the findings, and a coauthor are employees of Novartis. Other coauthors reported consulting fees from Novartis, as well as consulting fees and grant funding from other pharmaceutical companies.
Citation: Greenberg B et al. CMSC 2019, Abstract DXM02.
What is your diagnosis? - July 2019
The diagnosis
von Hippel-Lindau disease
The diagnosis is von Hippel-Lindau disease (VHL). Subsequent brain and renal magnetic resonance imaging showed features suggestive of a 5-mm right cerebellar hemangioblastoma and right renal cell carcinoma (RCC), respectively. Fundoscopy showed bilateral small retinal angiomas. Plasma and 24-hour urinary metenephrine levels were normal. Genetic testing confirmed a germline VHL mutation.
VHL is a rare autosomal-dominant hereditary multicancer condition characterized by germline mutations of the VHL tumor suppressor gene, with an incidence of 1 in 36,000 live births. The commonest associated tumors are retinal and central nervous system hemangioblastomas, RCC, pheochromocytoma, pancreatic islet cell tumors, and endolymphatic sac tumors.1 Cystic lesions may also be seen in other viscera such as the liver and ovaries. Clinical diagnostic criteria require the presence of any of these tumors in a patient with a positive family history, or alternatively, at least 2 retinal or cerebellar hemangioblastomas, or 1 hemangioblastoma plus 1 visceral tumor.2
Pancreatic involvement occurs in 65%–77% of patients with VHL, and may be the sole manifestation in 7.6%. Findings include multiple true cysts (91%), microcystic serous cystadenomas (12%), solid pancreatic neuroendocrine tumors (5%–10%), or a combination (11.5%). Most lesions are asymptomatic, but may present with vague symptoms of epigastric pain, diarrhea, dyspepsia, obstructive jaundice, or endocrine and/or exocrine pancreatic insufficiency. Surgery is required for symptomatic cysts or large pancreatic neuroendocrine tumors. The main causes of death are RCC and central nervous system hemangioblastomas.3 Our patient underwent laser therapy for her retinal angiomas, and is currently undergoing close regular surveillance. Clinicians should have a high index of suspicion for diagnosing VHL in patients with multiple pancreatic cysts. Because EUS is now widely used for the evaluation of pancreatic cysts, gastroenterologists may be first in making the diagnosis, as in this patient.
References
1. Lonser R.R., Glenn G.M., Walther M. et al. von Hippel-Lindau disease. Lancet. 2003;361:2059-67.
2. Melmon K., Rosen S. Lindau’s disease. Am J Med. 1964;36:595-617
3. Hammel P.R., Vilgrain V., Terris B. et al. Pancreatic involvement in von Hippel-Lindau disease. The Groupe Francophone d’Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000;119:1087-95.
The diagnosis
von Hippel-Lindau disease
The diagnosis is von Hippel-Lindau disease (VHL). Subsequent brain and renal magnetic resonance imaging showed features suggestive of a 5-mm right cerebellar hemangioblastoma and right renal cell carcinoma (RCC), respectively. Fundoscopy showed bilateral small retinal angiomas. Plasma and 24-hour urinary metenephrine levels were normal. Genetic testing confirmed a germline VHL mutation.
VHL is a rare autosomal-dominant hereditary multicancer condition characterized by germline mutations of the VHL tumor suppressor gene, with an incidence of 1 in 36,000 live births. The commonest associated tumors are retinal and central nervous system hemangioblastomas, RCC, pheochromocytoma, pancreatic islet cell tumors, and endolymphatic sac tumors.1 Cystic lesions may also be seen in other viscera such as the liver and ovaries. Clinical diagnostic criteria require the presence of any of these tumors in a patient with a positive family history, or alternatively, at least 2 retinal or cerebellar hemangioblastomas, or 1 hemangioblastoma plus 1 visceral tumor.2
Pancreatic involvement occurs in 65%–77% of patients with VHL, and may be the sole manifestation in 7.6%. Findings include multiple true cysts (91%), microcystic serous cystadenomas (12%), solid pancreatic neuroendocrine tumors (5%–10%), or a combination (11.5%). Most lesions are asymptomatic, but may present with vague symptoms of epigastric pain, diarrhea, dyspepsia, obstructive jaundice, or endocrine and/or exocrine pancreatic insufficiency. Surgery is required for symptomatic cysts or large pancreatic neuroendocrine tumors. The main causes of death are RCC and central nervous system hemangioblastomas.3 Our patient underwent laser therapy for her retinal angiomas, and is currently undergoing close regular surveillance. Clinicians should have a high index of suspicion for diagnosing VHL in patients with multiple pancreatic cysts. Because EUS is now widely used for the evaluation of pancreatic cysts, gastroenterologists may be first in making the diagnosis, as in this patient.
References
1. Lonser R.R., Glenn G.M., Walther M. et al. von Hippel-Lindau disease. Lancet. 2003;361:2059-67.
2. Melmon K., Rosen S. Lindau’s disease. Am J Med. 1964;36:595-617
3. Hammel P.R., Vilgrain V., Terris B. et al. Pancreatic involvement in von Hippel-Lindau disease. The Groupe Francophone d’Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000;119:1087-95.
The diagnosis
von Hippel-Lindau disease
The diagnosis is von Hippel-Lindau disease (VHL). Subsequent brain and renal magnetic resonance imaging showed features suggestive of a 5-mm right cerebellar hemangioblastoma and right renal cell carcinoma (RCC), respectively. Fundoscopy showed bilateral small retinal angiomas. Plasma and 24-hour urinary metenephrine levels were normal. Genetic testing confirmed a germline VHL mutation.
VHL is a rare autosomal-dominant hereditary multicancer condition characterized by germline mutations of the VHL tumor suppressor gene, with an incidence of 1 in 36,000 live births. The commonest associated tumors are retinal and central nervous system hemangioblastomas, RCC, pheochromocytoma, pancreatic islet cell tumors, and endolymphatic sac tumors.1 Cystic lesions may also be seen in other viscera such as the liver and ovaries. Clinical diagnostic criteria require the presence of any of these tumors in a patient with a positive family history, or alternatively, at least 2 retinal or cerebellar hemangioblastomas, or 1 hemangioblastoma plus 1 visceral tumor.2
Pancreatic involvement occurs in 65%–77% of patients with VHL, and may be the sole manifestation in 7.6%. Findings include multiple true cysts (91%), microcystic serous cystadenomas (12%), solid pancreatic neuroendocrine tumors (5%–10%), or a combination (11.5%). Most lesions are asymptomatic, but may present with vague symptoms of epigastric pain, diarrhea, dyspepsia, obstructive jaundice, or endocrine and/or exocrine pancreatic insufficiency. Surgery is required for symptomatic cysts or large pancreatic neuroendocrine tumors. The main causes of death are RCC and central nervous system hemangioblastomas.3 Our patient underwent laser therapy for her retinal angiomas, and is currently undergoing close regular surveillance. Clinicians should have a high index of suspicion for diagnosing VHL in patients with multiple pancreatic cysts. Because EUS is now widely used for the evaluation of pancreatic cysts, gastroenterologists may be first in making the diagnosis, as in this patient.
References
1. Lonser R.R., Glenn G.M., Walther M. et al. von Hippel-Lindau disease. Lancet. 2003;361:2059-67.
2. Melmon K., Rosen S. Lindau’s disease. Am J Med. 1964;36:595-617
3. Hammel P.R., Vilgrain V., Terris B. et al. Pancreatic involvement in von Hippel-Lindau disease. The Groupe Francophone d’Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000;119:1087-95.
A 32-year-old Filipino woman was referred for endoscopic ultrasound (EUS) imaging of the pancreas from another hospital where she had presented with a history of intermittent abdominal pain with radiation to the back precipitated by alcohol, and recurrent palpitations. During outpatient review before EUS, she gave a background history of previous laparoscopic ovarian cystectomy, as well as multiple previous admissions with supraventricular tachycardia requiring cardioversion on 1 occasion. One of her brothers had undergone brain surgery to remove a cyst, and another had died of an unspecified brain tumor at 25 years of age. Her mother had died of ovarian cancer.
Physical examination was unremarkable, with a normal pulse rate and blood pressure and no anemia, jaundice, or lymphadenopathy. Laboratory investigations including a full blood count, urea and electrolytes, liver function tests, thyroid function tests, and serum lipase were all normal. Abdominal computed tomography and ultrasound imaging revealed multiple cysts of varying sizes throughout the pancreas (Figure A), as well as multiple small benign-looking cysts in the liver.
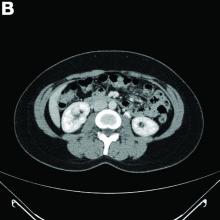
In addition, there was a 17-mm hyperdense solid lesion in the midpole of her right kidney visualized on computed tomography scan (Figure B). EUS revealed multiple thinly septated anechoic cysts throughout the pancreas, the largest measuring 36 mm located in the body, with no associated masses (Figure C).
What is the likely diagnosis? What other investigations would you do for confirmation?
Daratumumab wins new indication for newly diagnosed myeloma patients
Janssen’s daratumumab (Darzalex) has picked up a sixth adult multiple myeloma indication, this time in combination with lenalidomide (Revlimid) and dexamethasone in newly diagnosed patients ineligible for autologous stem cell transplants.
The phase 3 MAIA trial found that 97 of 368 patients (26.4%) treated with the combination – dubbed DRd – progressed or died at a median follow-up of 28 months, versus 143 of 269 (38.8%) treated with lenalidomide and dexamethasone alone (Rd). An estimated 55.6% of patients on lenalidomide and dexamethasone, versus 70.6% with the daratumumab add-on, were alive without progression at 30 months (N Engl J Med. 2019 May 30;380[22]:2104-15).
Previously approved indications for daratumumab include relapsed or refractory disease after at least one other therapy; and combination treatment with bortezomib, melphalan, and prednisone, also in newly diagnosed patients who are ineligible for transplant.
The most common grade 3 and 4 adverse events reported in the MAIA trial were neutropenia (50.0% for the DRd group versus 35.3% for the Rd group), anemia (11.8% vs. 19.7%), lymphopenia (15.1% vs. 10.7%), and pneumonia (13.7% vs. 7.9%).
Janssen’s daratumumab (Darzalex) has picked up a sixth adult multiple myeloma indication, this time in combination with lenalidomide (Revlimid) and dexamethasone in newly diagnosed patients ineligible for autologous stem cell transplants.
The phase 3 MAIA trial found that 97 of 368 patients (26.4%) treated with the combination – dubbed DRd – progressed or died at a median follow-up of 28 months, versus 143 of 269 (38.8%) treated with lenalidomide and dexamethasone alone (Rd). An estimated 55.6% of patients on lenalidomide and dexamethasone, versus 70.6% with the daratumumab add-on, were alive without progression at 30 months (N Engl J Med. 2019 May 30;380[22]:2104-15).
Previously approved indications for daratumumab include relapsed or refractory disease after at least one other therapy; and combination treatment with bortezomib, melphalan, and prednisone, also in newly diagnosed patients who are ineligible for transplant.
The most common grade 3 and 4 adverse events reported in the MAIA trial were neutropenia (50.0% for the DRd group versus 35.3% for the Rd group), anemia (11.8% vs. 19.7%), lymphopenia (15.1% vs. 10.7%), and pneumonia (13.7% vs. 7.9%).
Janssen’s daratumumab (Darzalex) has picked up a sixth adult multiple myeloma indication, this time in combination with lenalidomide (Revlimid) and dexamethasone in newly diagnosed patients ineligible for autologous stem cell transplants.
The phase 3 MAIA trial found that 97 of 368 patients (26.4%) treated with the combination – dubbed DRd – progressed or died at a median follow-up of 28 months, versus 143 of 269 (38.8%) treated with lenalidomide and dexamethasone alone (Rd). An estimated 55.6% of patients on lenalidomide and dexamethasone, versus 70.6% with the daratumumab add-on, were alive without progression at 30 months (N Engl J Med. 2019 May 30;380[22]:2104-15).
Previously approved indications for daratumumab include relapsed or refractory disease after at least one other therapy; and combination treatment with bortezomib, melphalan, and prednisone, also in newly diagnosed patients who are ineligible for transplant.
The most common grade 3 and 4 adverse events reported in the MAIA trial were neutropenia (50.0% for the DRd group versus 35.3% for the Rd group), anemia (11.8% vs. 19.7%), lymphopenia (15.1% vs. 10.7%), and pneumonia (13.7% vs. 7.9%).
Allergic Contact Dermatitis With Sparing of Exposed Psoriasis Plaques
To the Editor:
Allergic contact dermatitis (ACD) is a delayed-type hypersensitivity reaction against antigens to which the skin’s immune system was previously sensitized. The initial sensitization requires penetration of the antigen through the stratum corneum. Thus, the ability of a particle to cause ACD is related to its molecular structure and size, lipophilicity, and protein-binding affinity, as well as the dose and duration of exposure.1 Psoriasis typically presents as well-demarcated areas of skin that may be erythematous, indurated, and scaly to variable degrees. Histologically, psoriasis plaques are characterized by epidermal hyperplasia in the presence of a T-cell infiltrate and neutrophilic microabscesses. We report a case of a patient with plaque-type psoriasis who experienced ACD with sparing of exposed psoriatic plaques.
A 45-year-old man with a 5-year history of generalized moderate to severe psoriasis undergoing therapy with ustekinumab 45 mg subcutaneously once every 12 weeks presented to the emergency department with intensely erythematous, pruritic, vesicular lesions on the trunk, arms, and legs within 24 hours of exposure to poison oak while hiking. The patient reported pruritus, pain, and swelling of the affected areas. On physical examination, he was afebrile. Widespread erythematous vesicular lesions were noted on the face, trunk, arms, and legs, sparing the well-demarcated scaly psoriatic plaques on the arms and legs (Figure). The patient was given intravenous fluids and intravenous diphenhydramine. After responding to initial treatment, the patient was discharged with ibuprofen and a tapering dose of oral prednisone from 60 mg 5 times daily, to 40 mg 5 times daily, to 20 mg 5 times daily over 15 days.
star), with a linear border demarcating the ACD lesion and the unaffected psoriatic plaque (black arrow).
Allergic contact dermatitis occurs after sensitization to environmental allergens or haptens. Clinically, ACD is characterized by pruritic, erythematous, vesicular papules and plaques. The predominant effector cells in ACD are CD8+ T cells, along with contributions from helper T cells (TH2). Together, these cell types produce an environment enriched in IFN-γ, IL-2, IL-4, IL-10, IL-17, and tumor necrosis factor α.2 Ultimately, the ACD response induces keratinocyte apoptosis via cytotoxic effects.3,4
Plaque psoriasis is a chronic, immune-mediated, inflammatory disease that presents clinically as erythematous well-demarcated plaques with a micaceous scale. The immunologic environment of psoriasis plaques is characterized by infiltration of CD4+ TH17 cells and elevated levels of IL-17, IL-23, tumor necrosis factor α, and IL-1β, which induce keratinocyte hyperproliferation through a complex mechanism resulting in hyperkeratosis composed of orthokeratosis and parakeratosis, a neutrophilic infiltrate, and Munro microabscesses.5
The predominant effector cells and the final effects on keratinocyte survival are divergent in psoriasis and ACD. The possibly antagonistic relationship between these immunologic processes is further supported by epidemiologic studies demonstrating a decreased incidence of ACD in patients with psoriasis.6,7
Our patient demonstrated a typical ACD reaction in response to exposure to urushiol, the allergen present in poison oak, in areas unaffected by psoriasis plaques. Interestingly, the patient displayed this response even while undergoing therapy with ustekinumab, a fully humanized antibody that binds IL-12 and IL-23 and ultimately downregulates TH17 cell-mediated release of IL-17 in the treatment of psoriasis. Although IL-17 also has been implicated in ACD, the lack of inhibition of ACD with ustekinumab treatment was previously demonstrated in a small retrospective study, indicating a potentially different source of IL-17 in ACD.8
Our patient did not demonstrate a typical ACD response in areas of active psoriasis plaques. This phenomenon was of great interest to us. It is possible that the presence of hyperkeratosis, manifested clinically as scaling, served as a mechanical barrier preventing the diffusion and exposure of cutaneous immune cells to urushiol. On the other hand, it is possible that the immunologic environment of the active psoriasis plaque was altered in such a way that it did not demonstrate the typical response to allergen exposure.
We hypothesize that the lack of a typical ACD response at sites of psoriatic plaques in our patient may be attributed to the intensity and duration of exposure to the allergen. Quaranta et al9 reported a typical ACD clinical response and a mixed immunohistologic response to nickel patch testing at sites of active plaques in nickel-sensitized psoriasis patients. Patch testing involves 48 hours of direct contact with an allergen, while our patient experienced an estimated 8 to 10 hours of exposure to the allergen prior to removal via washing. Supporting this line of reasoning, a proportion of patients who are responsive to nickel patch testing do not exhibit clinical symptoms in response to casual nickel exposure.10 Although a physical barrier effect due to hyperkeratosis may have contributed to the lack of ACD response in sites of psoriasis plaques in our patient, it remains possible that a more limited duration of exposure to the allergen is not sufficient to overcome the native immunologic milieu of the psoriasis plaque and induce the immunologic cascade resulting in ACD. Further research into the potentially antagonistic relationship of psoriasis and ACD should be performed to elucidate the interaction between these two common conditions.
- Kimber I, Basketter DA, Gerberick GF, et al. Allergic contact dermatitis. Int Immunopharmacol. 2002;2:201-211.
- Vocanson M, Hennino A, Cluzel-Tailhardat M, et al. CD8+ T cells are effector cells of contact dermatitis to common skin allergens in mice. J Invest Dermatol. 2006;126:815-820.
- Akiba H, Kehren J, Ducluzeau MT, et al. Skin inflammation during contact hypersensitivity is mediated by early recruitment of CD8+ T cytotoxic 1 cells inducing keratinocyte apoptosis. J Immunol. 2002;168:3079-3087.
- Trautmann A, Akdis M, Kleemann D, et al. T cell-mediated Fas-induced keratinocyte apoptosis plays a key pathogenetic role in eczematous dermatitis. J Clin Invest. 2000;106:25-35.
- Lynde CW, Poulin Y, Vender R, et al. Interleukin 17A: toward a new understanding of psoriasis pathogenesis. J Am Acad Dermatol. 2014;71:141-150.
- Bangsgaard N, Engkilde K, Thyssen JP, et al. Inverse relationship between contact allergy and psoriasis: results from a patient- and a population-based study. Br J Dermatol. 2009;161:1119-1123.
- Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32:982-986.
- Bangsgaard N, Zachariae C, Menne T, et al. Lack of effect of ustekinumab in treatment of allergic contact dermatitis. Contact Dermatitis. 2011;65:227-230.
- Quaranta M, Eyerich S, Knapp B, et al. Allergic contact dermatitis in psoriasis patients: typical, delayed, and non-interacting. PLoS One. 2014;9:e101814.
- Kimber I, Basketter DA, Gerberick GF, et al. Allergic contact dermatitis. Int Immunopharmacol. 2002;2:201-211.
To the Editor:
Allergic contact dermatitis (ACD) is a delayed-type hypersensitivity reaction against antigens to which the skin’s immune system was previously sensitized. The initial sensitization requires penetration of the antigen through the stratum corneum. Thus, the ability of a particle to cause ACD is related to its molecular structure and size, lipophilicity, and protein-binding affinity, as well as the dose and duration of exposure.1 Psoriasis typically presents as well-demarcated areas of skin that may be erythematous, indurated, and scaly to variable degrees. Histologically, psoriasis plaques are characterized by epidermal hyperplasia in the presence of a T-cell infiltrate and neutrophilic microabscesses. We report a case of a patient with plaque-type psoriasis who experienced ACD with sparing of exposed psoriatic plaques.
A 45-year-old man with a 5-year history of generalized moderate to severe psoriasis undergoing therapy with ustekinumab 45 mg subcutaneously once every 12 weeks presented to the emergency department with intensely erythematous, pruritic, vesicular lesions on the trunk, arms, and legs within 24 hours of exposure to poison oak while hiking. The patient reported pruritus, pain, and swelling of the affected areas. On physical examination, he was afebrile. Widespread erythematous vesicular lesions were noted on the face, trunk, arms, and legs, sparing the well-demarcated scaly psoriatic plaques on the arms and legs (Figure). The patient was given intravenous fluids and intravenous diphenhydramine. After responding to initial treatment, the patient was discharged with ibuprofen and a tapering dose of oral prednisone from 60 mg 5 times daily, to 40 mg 5 times daily, to 20 mg 5 times daily over 15 days.
star), with a linear border demarcating the ACD lesion and the unaffected psoriatic plaque (black arrow).
Allergic contact dermatitis occurs after sensitization to environmental allergens or haptens. Clinically, ACD is characterized by pruritic, erythematous, vesicular papules and plaques. The predominant effector cells in ACD are CD8+ T cells, along with contributions from helper T cells (TH2). Together, these cell types produce an environment enriched in IFN-γ, IL-2, IL-4, IL-10, IL-17, and tumor necrosis factor α.2 Ultimately, the ACD response induces keratinocyte apoptosis via cytotoxic effects.3,4
Plaque psoriasis is a chronic, immune-mediated, inflammatory disease that presents clinically as erythematous well-demarcated plaques with a micaceous scale. The immunologic environment of psoriasis plaques is characterized by infiltration of CD4+ TH17 cells and elevated levels of IL-17, IL-23, tumor necrosis factor α, and IL-1β, which induce keratinocyte hyperproliferation through a complex mechanism resulting in hyperkeratosis composed of orthokeratosis and parakeratosis, a neutrophilic infiltrate, and Munro microabscesses.5
The predominant effector cells and the final effects on keratinocyte survival are divergent in psoriasis and ACD. The possibly antagonistic relationship between these immunologic processes is further supported by epidemiologic studies demonstrating a decreased incidence of ACD in patients with psoriasis.6,7
Our patient demonstrated a typical ACD reaction in response to exposure to urushiol, the allergen present in poison oak, in areas unaffected by psoriasis plaques. Interestingly, the patient displayed this response even while undergoing therapy with ustekinumab, a fully humanized antibody that binds IL-12 and IL-23 and ultimately downregulates TH17 cell-mediated release of IL-17 in the treatment of psoriasis. Although IL-17 also has been implicated in ACD, the lack of inhibition of ACD with ustekinumab treatment was previously demonstrated in a small retrospective study, indicating a potentially different source of IL-17 in ACD.8
Our patient did not demonstrate a typical ACD response in areas of active psoriasis plaques. This phenomenon was of great interest to us. It is possible that the presence of hyperkeratosis, manifested clinically as scaling, served as a mechanical barrier preventing the diffusion and exposure of cutaneous immune cells to urushiol. On the other hand, it is possible that the immunologic environment of the active psoriasis plaque was altered in such a way that it did not demonstrate the typical response to allergen exposure.
We hypothesize that the lack of a typical ACD response at sites of psoriatic plaques in our patient may be attributed to the intensity and duration of exposure to the allergen. Quaranta et al9 reported a typical ACD clinical response and a mixed immunohistologic response to nickel patch testing at sites of active plaques in nickel-sensitized psoriasis patients. Patch testing involves 48 hours of direct contact with an allergen, while our patient experienced an estimated 8 to 10 hours of exposure to the allergen prior to removal via washing. Supporting this line of reasoning, a proportion of patients who are responsive to nickel patch testing do not exhibit clinical symptoms in response to casual nickel exposure.10 Although a physical barrier effect due to hyperkeratosis may have contributed to the lack of ACD response in sites of psoriasis plaques in our patient, it remains possible that a more limited duration of exposure to the allergen is not sufficient to overcome the native immunologic milieu of the psoriasis plaque and induce the immunologic cascade resulting in ACD. Further research into the potentially antagonistic relationship of psoriasis and ACD should be performed to elucidate the interaction between these two common conditions.
To the Editor:
Allergic contact dermatitis (ACD) is a delayed-type hypersensitivity reaction against antigens to which the skin’s immune system was previously sensitized. The initial sensitization requires penetration of the antigen through the stratum corneum. Thus, the ability of a particle to cause ACD is related to its molecular structure and size, lipophilicity, and protein-binding affinity, as well as the dose and duration of exposure.1 Psoriasis typically presents as well-demarcated areas of skin that may be erythematous, indurated, and scaly to variable degrees. Histologically, psoriasis plaques are characterized by epidermal hyperplasia in the presence of a T-cell infiltrate and neutrophilic microabscesses. We report a case of a patient with plaque-type psoriasis who experienced ACD with sparing of exposed psoriatic plaques.
A 45-year-old man with a 5-year history of generalized moderate to severe psoriasis undergoing therapy with ustekinumab 45 mg subcutaneously once every 12 weeks presented to the emergency department with intensely erythematous, pruritic, vesicular lesions on the trunk, arms, and legs within 24 hours of exposure to poison oak while hiking. The patient reported pruritus, pain, and swelling of the affected areas. On physical examination, he was afebrile. Widespread erythematous vesicular lesions were noted on the face, trunk, arms, and legs, sparing the well-demarcated scaly psoriatic plaques on the arms and legs (Figure). The patient was given intravenous fluids and intravenous diphenhydramine. After responding to initial treatment, the patient was discharged with ibuprofen and a tapering dose of oral prednisone from 60 mg 5 times daily, to 40 mg 5 times daily, to 20 mg 5 times daily over 15 days.
star), with a linear border demarcating the ACD lesion and the unaffected psoriatic plaque (black arrow).
Allergic contact dermatitis occurs after sensitization to environmental allergens or haptens. Clinically, ACD is characterized by pruritic, erythematous, vesicular papules and plaques. The predominant effector cells in ACD are CD8+ T cells, along with contributions from helper T cells (TH2). Together, these cell types produce an environment enriched in IFN-γ, IL-2, IL-4, IL-10, IL-17, and tumor necrosis factor α.2 Ultimately, the ACD response induces keratinocyte apoptosis via cytotoxic effects.3,4
Plaque psoriasis is a chronic, immune-mediated, inflammatory disease that presents clinically as erythematous well-demarcated plaques with a micaceous scale. The immunologic environment of psoriasis plaques is characterized by infiltration of CD4+ TH17 cells and elevated levels of IL-17, IL-23, tumor necrosis factor α, and IL-1β, which induce keratinocyte hyperproliferation through a complex mechanism resulting in hyperkeratosis composed of orthokeratosis and parakeratosis, a neutrophilic infiltrate, and Munro microabscesses.5
The predominant effector cells and the final effects on keratinocyte survival are divergent in psoriasis and ACD. The possibly antagonistic relationship between these immunologic processes is further supported by epidemiologic studies demonstrating a decreased incidence of ACD in patients with psoriasis.6,7
Our patient demonstrated a typical ACD reaction in response to exposure to urushiol, the allergen present in poison oak, in areas unaffected by psoriasis plaques. Interestingly, the patient displayed this response even while undergoing therapy with ustekinumab, a fully humanized antibody that binds IL-12 and IL-23 and ultimately downregulates TH17 cell-mediated release of IL-17 in the treatment of psoriasis. Although IL-17 also has been implicated in ACD, the lack of inhibition of ACD with ustekinumab treatment was previously demonstrated in a small retrospective study, indicating a potentially different source of IL-17 in ACD.8
Our patient did not demonstrate a typical ACD response in areas of active psoriasis plaques. This phenomenon was of great interest to us. It is possible that the presence of hyperkeratosis, manifested clinically as scaling, served as a mechanical barrier preventing the diffusion and exposure of cutaneous immune cells to urushiol. On the other hand, it is possible that the immunologic environment of the active psoriasis plaque was altered in such a way that it did not demonstrate the typical response to allergen exposure.
We hypothesize that the lack of a typical ACD response at sites of psoriatic plaques in our patient may be attributed to the intensity and duration of exposure to the allergen. Quaranta et al9 reported a typical ACD clinical response and a mixed immunohistologic response to nickel patch testing at sites of active plaques in nickel-sensitized psoriasis patients. Patch testing involves 48 hours of direct contact with an allergen, while our patient experienced an estimated 8 to 10 hours of exposure to the allergen prior to removal via washing. Supporting this line of reasoning, a proportion of patients who are responsive to nickel patch testing do not exhibit clinical symptoms in response to casual nickel exposure.10 Although a physical barrier effect due to hyperkeratosis may have contributed to the lack of ACD response in sites of psoriasis plaques in our patient, it remains possible that a more limited duration of exposure to the allergen is not sufficient to overcome the native immunologic milieu of the psoriasis plaque and induce the immunologic cascade resulting in ACD. Further research into the potentially antagonistic relationship of psoriasis and ACD should be performed to elucidate the interaction between these two common conditions.
- Kimber I, Basketter DA, Gerberick GF, et al. Allergic contact dermatitis. Int Immunopharmacol. 2002;2:201-211.
- Vocanson M, Hennino A, Cluzel-Tailhardat M, et al. CD8+ T cells are effector cells of contact dermatitis to common skin allergens in mice. J Invest Dermatol. 2006;126:815-820.
- Akiba H, Kehren J, Ducluzeau MT, et al. Skin inflammation during contact hypersensitivity is mediated by early recruitment of CD8+ T cytotoxic 1 cells inducing keratinocyte apoptosis. J Immunol. 2002;168:3079-3087.
- Trautmann A, Akdis M, Kleemann D, et al. T cell-mediated Fas-induced keratinocyte apoptosis plays a key pathogenetic role in eczematous dermatitis. J Clin Invest. 2000;106:25-35.
- Lynde CW, Poulin Y, Vender R, et al. Interleukin 17A: toward a new understanding of psoriasis pathogenesis. J Am Acad Dermatol. 2014;71:141-150.
- Bangsgaard N, Engkilde K, Thyssen JP, et al. Inverse relationship between contact allergy and psoriasis: results from a patient- and a population-based study. Br J Dermatol. 2009;161:1119-1123.
- Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32:982-986.
- Bangsgaard N, Zachariae C, Menne T, et al. Lack of effect of ustekinumab in treatment of allergic contact dermatitis. Contact Dermatitis. 2011;65:227-230.
- Quaranta M, Eyerich S, Knapp B, et al. Allergic contact dermatitis in psoriasis patients: typical, delayed, and non-interacting. PLoS One. 2014;9:e101814.
- Kimber I, Basketter DA, Gerberick GF, et al. Allergic contact dermatitis. Int Immunopharmacol. 2002;2:201-211.
- Kimber I, Basketter DA, Gerberick GF, et al. Allergic contact dermatitis. Int Immunopharmacol. 2002;2:201-211.
- Vocanson M, Hennino A, Cluzel-Tailhardat M, et al. CD8+ T cells are effector cells of contact dermatitis to common skin allergens in mice. J Invest Dermatol. 2006;126:815-820.
- Akiba H, Kehren J, Ducluzeau MT, et al. Skin inflammation during contact hypersensitivity is mediated by early recruitment of CD8+ T cytotoxic 1 cells inducing keratinocyte apoptosis. J Immunol. 2002;168:3079-3087.
- Trautmann A, Akdis M, Kleemann D, et al. T cell-mediated Fas-induced keratinocyte apoptosis plays a key pathogenetic role in eczematous dermatitis. J Clin Invest. 2000;106:25-35.
- Lynde CW, Poulin Y, Vender R, et al. Interleukin 17A: toward a new understanding of psoriasis pathogenesis. J Am Acad Dermatol. 2014;71:141-150.
- Bangsgaard N, Engkilde K, Thyssen JP, et al. Inverse relationship between contact allergy and psoriasis: results from a patient- and a population-based study. Br J Dermatol. 2009;161:1119-1123.
- Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32:982-986.
- Bangsgaard N, Zachariae C, Menne T, et al. Lack of effect of ustekinumab in treatment of allergic contact dermatitis. Contact Dermatitis. 2011;65:227-230.
- Quaranta M, Eyerich S, Knapp B, et al. Allergic contact dermatitis in psoriasis patients: typical, delayed, and non-interacting. PLoS One. 2014;9:e101814.
- Kimber I, Basketter DA, Gerberick GF, et al. Allergic contact dermatitis. Int Immunopharmacol. 2002;2:201-211.
Practice Points
- Patients with plaque-type psoriasis who experience allergic contact dermatitis (ACD) may present with sparing of exposed psoriatic plaques.
- The divergent immunologic milieus present in ACD and psoriasis likely underly the decreased incidence of ACD in patients with psoriasis.
Atypical food allergies common in IBS
, with accompanying changes in epithelial tight junction proteins and eosinophils.
Among 108 patients who completed the study, 61% showed this atypical allergic response to wheat, wrote Annette Fritscher-Ravens, MD, PhD, of University Hospital Schleswig-Holstein in Kiel, Germany, and her associates. Strikingly, almost 70% of patients with atypical food allergies to wheat, yeast, milk, soy, or egg white who eliminated these foods from their diets showed at least an 80% improvement in IBS symptoms after 3 months. These findings were published in Gastroenterology.
Confocal laser endomicroscopy (CLE) “permits real-time detection and quantification of changes in intestinal tissues and cells, including increases in intraepithelial lymphocytes and fluid extravasation through epithelial leaks,” the investigators wrote. This approach helps clinicians objectively detect and measure gastrointestinal pathology in response to specific foods, potentially freeing IBS patients from highly restrictive diets that ease symptoms but are hard to follow, and are not meant for long-term use.
For the study, the researchers enrolled patients meeting Rome III IBS criteria who tested negative for common food antigens on immunoglobulin E serology and skin tests. During endoscopy, each patient underwent sequential duodenal challenges with 20-mL suspensions of wheat, yeast, milk, soy, and egg white, followed by CLE with biopsy.
Among 108 patients who finished the study, 76 (70%) were CLE positive. They and their first-degree relatives were significantly more likely to have atopic disorders than were CLE-negative patients (P = .001). The most common allergen was wheat (61% of patients), followed by yeast (20%), milk (9%), soy (7%), and egg white (4%). Also, nine patients reacted to two of the tested food antigens.
Compared with CLE-negative patients or controls, CLE-positive patients also had significantly more intraepithelial lymphocytes (P = .001) and postchallenge expression of claudin-2 (P = .023), which contributes to tight junction permeability and is known to be upregulated in intestinal barrier dysfunction, IBS, and inflammatory bowel disease. Conversely, levels of the tight junction protein occludin were significantly lower in duodenal biopsies from CLE-positive patients versus controls (P = .022). “Levels of mRNAs encoding inflammatory cytokines were unchanged in duodenal tissues after CLE challenge, but eosinophil degranulation increased,” the researchers wrote.
In a double-blind, randomized, crossover study, patients then excluded from their diet the antigen to which they had tested positive or consumed a sham (placebo) diet that excluded only some foods containing the antigen, with a 2-week washout period in between. The CLE-positive patients showed a 70% average improvement in Francis IBS severity score after 3 months of the intervention diet and a 76% improvement at 6 months. Strikingly, 68% of CLE-positive patients showed at least an 80% improvement in symptoms, while only 4% did not respond at all.
“Since we do not observe a histological mast cell/basophil increase or activation, and [we] do not find increased mast cell mediators (tryptase) in the duodenal fluid after positive challenge, we assume a nonclassical or atypical food allergy as cause of the mucosal reaction observed by CLE,” the researchers wrote. Other immune cell parameters remained unchanged, but additional studies are needed to see if these changes are truly absent or occur later after challenge. The researchers are conducting murine studies of eosinophilic food allergy to shed more light on these nonclassical food allergies.
Funders included the Rashid Hussein Charity Trust, the German Research Foundation, and the Leibniz Foundation. The researchers reported having no conflicts of interest.
SOURCE: Fritscher-Ravens A et al. Gastroenterology. 2019 May 14. doi: 10.1053/j.gastro.2019.03.046.
, with accompanying changes in epithelial tight junction proteins and eosinophils.
Among 108 patients who completed the study, 61% showed this atypical allergic response to wheat, wrote Annette Fritscher-Ravens, MD, PhD, of University Hospital Schleswig-Holstein in Kiel, Germany, and her associates. Strikingly, almost 70% of patients with atypical food allergies to wheat, yeast, milk, soy, or egg white who eliminated these foods from their diets showed at least an 80% improvement in IBS symptoms after 3 months. These findings were published in Gastroenterology.
Confocal laser endomicroscopy (CLE) “permits real-time detection and quantification of changes in intestinal tissues and cells, including increases in intraepithelial lymphocytes and fluid extravasation through epithelial leaks,” the investigators wrote. This approach helps clinicians objectively detect and measure gastrointestinal pathology in response to specific foods, potentially freeing IBS patients from highly restrictive diets that ease symptoms but are hard to follow, and are not meant for long-term use.
For the study, the researchers enrolled patients meeting Rome III IBS criteria who tested negative for common food antigens on immunoglobulin E serology and skin tests. During endoscopy, each patient underwent sequential duodenal challenges with 20-mL suspensions of wheat, yeast, milk, soy, and egg white, followed by CLE with biopsy.
Among 108 patients who finished the study, 76 (70%) were CLE positive. They and their first-degree relatives were significantly more likely to have atopic disorders than were CLE-negative patients (P = .001). The most common allergen was wheat (61% of patients), followed by yeast (20%), milk (9%), soy (7%), and egg white (4%). Also, nine patients reacted to two of the tested food antigens.
Compared with CLE-negative patients or controls, CLE-positive patients also had significantly more intraepithelial lymphocytes (P = .001) and postchallenge expression of claudin-2 (P = .023), which contributes to tight junction permeability and is known to be upregulated in intestinal barrier dysfunction, IBS, and inflammatory bowel disease. Conversely, levels of the tight junction protein occludin were significantly lower in duodenal biopsies from CLE-positive patients versus controls (P = .022). “Levels of mRNAs encoding inflammatory cytokines were unchanged in duodenal tissues after CLE challenge, but eosinophil degranulation increased,” the researchers wrote.
In a double-blind, randomized, crossover study, patients then excluded from their diet the antigen to which they had tested positive or consumed a sham (placebo) diet that excluded only some foods containing the antigen, with a 2-week washout period in between. The CLE-positive patients showed a 70% average improvement in Francis IBS severity score after 3 months of the intervention diet and a 76% improvement at 6 months. Strikingly, 68% of CLE-positive patients showed at least an 80% improvement in symptoms, while only 4% did not respond at all.
“Since we do not observe a histological mast cell/basophil increase or activation, and [we] do not find increased mast cell mediators (tryptase) in the duodenal fluid after positive challenge, we assume a nonclassical or atypical food allergy as cause of the mucosal reaction observed by CLE,” the researchers wrote. Other immune cell parameters remained unchanged, but additional studies are needed to see if these changes are truly absent or occur later after challenge. The researchers are conducting murine studies of eosinophilic food allergy to shed more light on these nonclassical food allergies.
Funders included the Rashid Hussein Charity Trust, the German Research Foundation, and the Leibniz Foundation. The researchers reported having no conflicts of interest.
SOURCE: Fritscher-Ravens A et al. Gastroenterology. 2019 May 14. doi: 10.1053/j.gastro.2019.03.046.
, with accompanying changes in epithelial tight junction proteins and eosinophils.
Among 108 patients who completed the study, 61% showed this atypical allergic response to wheat, wrote Annette Fritscher-Ravens, MD, PhD, of University Hospital Schleswig-Holstein in Kiel, Germany, and her associates. Strikingly, almost 70% of patients with atypical food allergies to wheat, yeast, milk, soy, or egg white who eliminated these foods from their diets showed at least an 80% improvement in IBS symptoms after 3 months. These findings were published in Gastroenterology.
Confocal laser endomicroscopy (CLE) “permits real-time detection and quantification of changes in intestinal tissues and cells, including increases in intraepithelial lymphocytes and fluid extravasation through epithelial leaks,” the investigators wrote. This approach helps clinicians objectively detect and measure gastrointestinal pathology in response to specific foods, potentially freeing IBS patients from highly restrictive diets that ease symptoms but are hard to follow, and are not meant for long-term use.
For the study, the researchers enrolled patients meeting Rome III IBS criteria who tested negative for common food antigens on immunoglobulin E serology and skin tests. During endoscopy, each patient underwent sequential duodenal challenges with 20-mL suspensions of wheat, yeast, milk, soy, and egg white, followed by CLE with biopsy.
Among 108 patients who finished the study, 76 (70%) were CLE positive. They and their first-degree relatives were significantly more likely to have atopic disorders than were CLE-negative patients (P = .001). The most common allergen was wheat (61% of patients), followed by yeast (20%), milk (9%), soy (7%), and egg white (4%). Also, nine patients reacted to two of the tested food antigens.
Compared with CLE-negative patients or controls, CLE-positive patients also had significantly more intraepithelial lymphocytes (P = .001) and postchallenge expression of claudin-2 (P = .023), which contributes to tight junction permeability and is known to be upregulated in intestinal barrier dysfunction, IBS, and inflammatory bowel disease. Conversely, levels of the tight junction protein occludin were significantly lower in duodenal biopsies from CLE-positive patients versus controls (P = .022). “Levels of mRNAs encoding inflammatory cytokines were unchanged in duodenal tissues after CLE challenge, but eosinophil degranulation increased,” the researchers wrote.
In a double-blind, randomized, crossover study, patients then excluded from their diet the antigen to which they had tested positive or consumed a sham (placebo) diet that excluded only some foods containing the antigen, with a 2-week washout period in between. The CLE-positive patients showed a 70% average improvement in Francis IBS severity score after 3 months of the intervention diet and a 76% improvement at 6 months. Strikingly, 68% of CLE-positive patients showed at least an 80% improvement in symptoms, while only 4% did not respond at all.
“Since we do not observe a histological mast cell/basophil increase or activation, and [we] do not find increased mast cell mediators (tryptase) in the duodenal fluid after positive challenge, we assume a nonclassical or atypical food allergy as cause of the mucosal reaction observed by CLE,” the researchers wrote. Other immune cell parameters remained unchanged, but additional studies are needed to see if these changes are truly absent or occur later after challenge. The researchers are conducting murine studies of eosinophilic food allergy to shed more light on these nonclassical food allergies.
Funders included the Rashid Hussein Charity Trust, the German Research Foundation, and the Leibniz Foundation. The researchers reported having no conflicts of interest.
SOURCE: Fritscher-Ravens A et al. Gastroenterology. 2019 May 14. doi: 10.1053/j.gastro.2019.03.046.
FROM GASTROENTEROLOGY
Total margin control surgery warranted for high-risk keratinocyte carcinomas
MILAN – A recent meta-analysis found that total margin control surgery substantially cut the risk of recurrence in patients with high-risk keratinocyte carcinomas, Chrysalyne Schmults, MD, said at the World Congress of Dermatology.
While standard excision will cure the vast majority of low-risk basal cell carcinoma (BCC) or squamous cell carcinoma (SCC), those classified as high risk are best treated with the advanced surgical procedure, also referred to as circumferential peripheral and deep margin assessment (CCPDMA), said Dr. Schmults, director of the Mohs and Dermatologic Surgery Center at Brigham and Women’s Hospital in Boston.
For high-risk cases, CCPDMA has superior outcomes, compared with standard excision, according to results of the meta-analysis conducted by Dr. Schmults and colleagues. The meta-analysis has not yet been published.
The in the meta-analysis of medical literature from 1993 to 2017.
“This is a really big drop,” Dr. Schmults said. “If you do total margin control surgery on your perineural invasive cases, you’re going to drop your recurrence rate by two-thirds, and that’s a really big difference.”
For carcinomas without perineural invasion, the recurrence rate is about 4.5% for standard excision and about 2.0% for CCPDMA, the analysis showed. “That’s a difference, but it’s not a big enough difference that we’re going to start doing total margin control surgery on every single basal cell and squamous cell carcinoma that comes to us,” Dr. Schmults commented.
Using techniques such as Mohs surgery that allow for CCPDMA, nearly 100% of the surgical margin can be seen; by contrast, standard histology allows for visualization of only about 1% of the marginal surface, according to Dr. Schmults.
While CCPDMA may have superior outcomes for high-risk keratinocyte carcinomas, defining what constitutes high risk remains a challenge, particularly for patients with BCCs. “We don’t have good literature on which are the rare, bad basal cells,” she said.
But more clarity may be on the way. In a paper under review for publication on Brigham and Women’s Hospital (BWH) staging criteria for BCC, Dr. Schmults and colleagues describe a subset of patients with BCC at higher risk of metastasis and death based on specific high-risk tumor characteristics.
High risk is better defined for SCCs. According to the BWH classification system for cutaneous SCCs, developed by Dr. Schmults and colleagues, high-risk features include larger tumor diameter, poorly differentiated histology, perineural invasion, and tumor invasion beyond subcutaneous fat or to bone.
Patients with SCC classified as high stage by the BWH system have about a 25% risk of metastasis or death. “These patients really need that total margin control surgery,” Dr. Schmults said.
High-stage SCC patients who did not get Mohs surgery in a study (J Clin Oncol. 2014 Feb 1;32[4]:327-34) conducted by Dr. Schmults and her associates, had a quadrupling in risk of death from disease, compared with those who did get the procedure in a more recent study (J Am Acad Dermatol. 2019 Mar;80[3]:633-8).
“These are fairly small studies,” she pointed out. But the large meta-analysis she presented at the meeting showed the same result, “that the higher the stage, the worse your tumor is, and whether it’s basal cell or squamous cell, the greater the advantage for total margin control surgery.”
Dr. Schmults reported that she is the panel chair for the National Comprehensive Cancer Network guidelines on nonmelanoma skin cancer, and that she was a cutaneous SCC committee member for the 8th edition of the American Joint Committee on Cancer cancer staging system. She also participated in the development of the BWH staging system for SCC.
MILAN – A recent meta-analysis found that total margin control surgery substantially cut the risk of recurrence in patients with high-risk keratinocyte carcinomas, Chrysalyne Schmults, MD, said at the World Congress of Dermatology.
While standard excision will cure the vast majority of low-risk basal cell carcinoma (BCC) or squamous cell carcinoma (SCC), those classified as high risk are best treated with the advanced surgical procedure, also referred to as circumferential peripheral and deep margin assessment (CCPDMA), said Dr. Schmults, director of the Mohs and Dermatologic Surgery Center at Brigham and Women’s Hospital in Boston.
For high-risk cases, CCPDMA has superior outcomes, compared with standard excision, according to results of the meta-analysis conducted by Dr. Schmults and colleagues. The meta-analysis has not yet been published.
The in the meta-analysis of medical literature from 1993 to 2017.
“This is a really big drop,” Dr. Schmults said. “If you do total margin control surgery on your perineural invasive cases, you’re going to drop your recurrence rate by two-thirds, and that’s a really big difference.”
For carcinomas without perineural invasion, the recurrence rate is about 4.5% for standard excision and about 2.0% for CCPDMA, the analysis showed. “That’s a difference, but it’s not a big enough difference that we’re going to start doing total margin control surgery on every single basal cell and squamous cell carcinoma that comes to us,” Dr. Schmults commented.
Using techniques such as Mohs surgery that allow for CCPDMA, nearly 100% of the surgical margin can be seen; by contrast, standard histology allows for visualization of only about 1% of the marginal surface, according to Dr. Schmults.
While CCPDMA may have superior outcomes for high-risk keratinocyte carcinomas, defining what constitutes high risk remains a challenge, particularly for patients with BCCs. “We don’t have good literature on which are the rare, bad basal cells,” she said.
But more clarity may be on the way. In a paper under review for publication on Brigham and Women’s Hospital (BWH) staging criteria for BCC, Dr. Schmults and colleagues describe a subset of patients with BCC at higher risk of metastasis and death based on specific high-risk tumor characteristics.
High risk is better defined for SCCs. According to the BWH classification system for cutaneous SCCs, developed by Dr. Schmults and colleagues, high-risk features include larger tumor diameter, poorly differentiated histology, perineural invasion, and tumor invasion beyond subcutaneous fat or to bone.
Patients with SCC classified as high stage by the BWH system have about a 25% risk of metastasis or death. “These patients really need that total margin control surgery,” Dr. Schmults said.
High-stage SCC patients who did not get Mohs surgery in a study (J Clin Oncol. 2014 Feb 1;32[4]:327-34) conducted by Dr. Schmults and her associates, had a quadrupling in risk of death from disease, compared with those who did get the procedure in a more recent study (J Am Acad Dermatol. 2019 Mar;80[3]:633-8).
“These are fairly small studies,” she pointed out. But the large meta-analysis she presented at the meeting showed the same result, “that the higher the stage, the worse your tumor is, and whether it’s basal cell or squamous cell, the greater the advantage for total margin control surgery.”
Dr. Schmults reported that she is the panel chair for the National Comprehensive Cancer Network guidelines on nonmelanoma skin cancer, and that she was a cutaneous SCC committee member for the 8th edition of the American Joint Committee on Cancer cancer staging system. She also participated in the development of the BWH staging system for SCC.
MILAN – A recent meta-analysis found that total margin control surgery substantially cut the risk of recurrence in patients with high-risk keratinocyte carcinomas, Chrysalyne Schmults, MD, said at the World Congress of Dermatology.
While standard excision will cure the vast majority of low-risk basal cell carcinoma (BCC) or squamous cell carcinoma (SCC), those classified as high risk are best treated with the advanced surgical procedure, also referred to as circumferential peripheral and deep margin assessment (CCPDMA), said Dr. Schmults, director of the Mohs and Dermatologic Surgery Center at Brigham and Women’s Hospital in Boston.
For high-risk cases, CCPDMA has superior outcomes, compared with standard excision, according to results of the meta-analysis conducted by Dr. Schmults and colleagues. The meta-analysis has not yet been published.
The in the meta-analysis of medical literature from 1993 to 2017.
“This is a really big drop,” Dr. Schmults said. “If you do total margin control surgery on your perineural invasive cases, you’re going to drop your recurrence rate by two-thirds, and that’s a really big difference.”
For carcinomas without perineural invasion, the recurrence rate is about 4.5% for standard excision and about 2.0% for CCPDMA, the analysis showed. “That’s a difference, but it’s not a big enough difference that we’re going to start doing total margin control surgery on every single basal cell and squamous cell carcinoma that comes to us,” Dr. Schmults commented.
Using techniques such as Mohs surgery that allow for CCPDMA, nearly 100% of the surgical margin can be seen; by contrast, standard histology allows for visualization of only about 1% of the marginal surface, according to Dr. Schmults.
While CCPDMA may have superior outcomes for high-risk keratinocyte carcinomas, defining what constitutes high risk remains a challenge, particularly for patients with BCCs. “We don’t have good literature on which are the rare, bad basal cells,” she said.
But more clarity may be on the way. In a paper under review for publication on Brigham and Women’s Hospital (BWH) staging criteria for BCC, Dr. Schmults and colleagues describe a subset of patients with BCC at higher risk of metastasis and death based on specific high-risk tumor characteristics.
High risk is better defined for SCCs. According to the BWH classification system for cutaneous SCCs, developed by Dr. Schmults and colleagues, high-risk features include larger tumor diameter, poorly differentiated histology, perineural invasion, and tumor invasion beyond subcutaneous fat or to bone.
Patients with SCC classified as high stage by the BWH system have about a 25% risk of metastasis or death. “These patients really need that total margin control surgery,” Dr. Schmults said.
High-stage SCC patients who did not get Mohs surgery in a study (J Clin Oncol. 2014 Feb 1;32[4]:327-34) conducted by Dr. Schmults and her associates, had a quadrupling in risk of death from disease, compared with those who did get the procedure in a more recent study (J Am Acad Dermatol. 2019 Mar;80[3]:633-8).
“These are fairly small studies,” she pointed out. But the large meta-analysis she presented at the meeting showed the same result, “that the higher the stage, the worse your tumor is, and whether it’s basal cell or squamous cell, the greater the advantage for total margin control surgery.”
Dr. Schmults reported that she is the panel chair for the National Comprehensive Cancer Network guidelines on nonmelanoma skin cancer, and that she was a cutaneous SCC committee member for the 8th edition of the American Joint Committee on Cancer cancer staging system. She also participated in the development of the BWH staging system for SCC.
REPORTING FROM WCD2019
Cryptosporidiosis infections spike during summer swim season
Outbreaks of cryptosporidiosis increased in the United States by an average of 13% each year between 2009 and 2017, based on data from the Centers for Disease Control and Prevention.
In a study published in the CDC’s Morbidity and Mortality Weekly Report, researchers reviewed data from 444 reported outbreaks submitted to the CDC’s National Outbreak Reporting System totaling 7,465 cases, including 287 hospitalizations and one death.
The outbreaks during this period were most commonly associated with pools and water parks (35%), exposure to cattle (15%), and child care settings (13%). Another 3% of outbreaks were associated with drinking unpasteurized milk or apple cider. An outbreak was defined as two or more cases linked to a common source.
The profuse, watery diarrhea associated with infection from the cryptosporidium parasite can last for 3 weeks in healthy individuals and can cause life-threatening malnutrition in the immunocompromised, wrote Radhika Gharpure, DVM, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and colleagues.
The overall number of outbreaks peaked during July and August each year; the number associated with pools and water parks peaked between June and August, the number associated with cattle peaked between March and May, and the number associated with child care settings peaked between July and September.
The results were limited by several factors including likely underestimation of the number of outbreaks, the use of multipathogen testing panels that could have inflated the number of outbreaks, and the variation in the ability of jurisdictions to detect, investigate, and report outbreaks, the researchers noted. CryptoNet, a molecularly-based surveillance system, has shown potential to track disease transmission, they said.
However, primary prevention is important to prevent the spread of disease, and strategies include refraining from swimming when one has diarrhea and for 2 weeks after resolution of diarrhea, not sending children to child care when they have diarrhea, and washing hands thoroughly after contact with animals, the researchers said.
“If a cryptosporidiosis outbreak occurs, substantial decontamination measures are needed, including hyperchlorinating public treated recreational water venues (e.g., swimming pools at a hotel, apartment complex, or water park) and using hydrogen peroxide to disinfect surfaces in child care settings to inactivate Cryptosporidium oocysts,” they emphasized.
The researchers had no financial conflicts to disclose.
SOURCE: Gharpure R et al. MMWR. 2019 June 28. 68:568-72.
Outbreaks of cryptosporidiosis increased in the United States by an average of 13% each year between 2009 and 2017, based on data from the Centers for Disease Control and Prevention.
In a study published in the CDC’s Morbidity and Mortality Weekly Report, researchers reviewed data from 444 reported outbreaks submitted to the CDC’s National Outbreak Reporting System totaling 7,465 cases, including 287 hospitalizations and one death.
The outbreaks during this period were most commonly associated with pools and water parks (35%), exposure to cattle (15%), and child care settings (13%). Another 3% of outbreaks were associated with drinking unpasteurized milk or apple cider. An outbreak was defined as two or more cases linked to a common source.
The profuse, watery diarrhea associated with infection from the cryptosporidium parasite can last for 3 weeks in healthy individuals and can cause life-threatening malnutrition in the immunocompromised, wrote Radhika Gharpure, DVM, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and colleagues.
The overall number of outbreaks peaked during July and August each year; the number associated with pools and water parks peaked between June and August, the number associated with cattle peaked between March and May, and the number associated with child care settings peaked between July and September.
The results were limited by several factors including likely underestimation of the number of outbreaks, the use of multipathogen testing panels that could have inflated the number of outbreaks, and the variation in the ability of jurisdictions to detect, investigate, and report outbreaks, the researchers noted. CryptoNet, a molecularly-based surveillance system, has shown potential to track disease transmission, they said.
However, primary prevention is important to prevent the spread of disease, and strategies include refraining from swimming when one has diarrhea and for 2 weeks after resolution of diarrhea, not sending children to child care when they have diarrhea, and washing hands thoroughly after contact with animals, the researchers said.
“If a cryptosporidiosis outbreak occurs, substantial decontamination measures are needed, including hyperchlorinating public treated recreational water venues (e.g., swimming pools at a hotel, apartment complex, or water park) and using hydrogen peroxide to disinfect surfaces in child care settings to inactivate Cryptosporidium oocysts,” they emphasized.
The researchers had no financial conflicts to disclose.
SOURCE: Gharpure R et al. MMWR. 2019 June 28. 68:568-72.
Outbreaks of cryptosporidiosis increased in the United States by an average of 13% each year between 2009 and 2017, based on data from the Centers for Disease Control and Prevention.
In a study published in the CDC’s Morbidity and Mortality Weekly Report, researchers reviewed data from 444 reported outbreaks submitted to the CDC’s National Outbreak Reporting System totaling 7,465 cases, including 287 hospitalizations and one death.
The outbreaks during this period were most commonly associated with pools and water parks (35%), exposure to cattle (15%), and child care settings (13%). Another 3% of outbreaks were associated with drinking unpasteurized milk or apple cider. An outbreak was defined as two or more cases linked to a common source.
The profuse, watery diarrhea associated with infection from the cryptosporidium parasite can last for 3 weeks in healthy individuals and can cause life-threatening malnutrition in the immunocompromised, wrote Radhika Gharpure, DVM, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and colleagues.
The overall number of outbreaks peaked during July and August each year; the number associated with pools and water parks peaked between June and August, the number associated with cattle peaked between March and May, and the number associated with child care settings peaked between July and September.
The results were limited by several factors including likely underestimation of the number of outbreaks, the use of multipathogen testing panels that could have inflated the number of outbreaks, and the variation in the ability of jurisdictions to detect, investigate, and report outbreaks, the researchers noted. CryptoNet, a molecularly-based surveillance system, has shown potential to track disease transmission, they said.
However, primary prevention is important to prevent the spread of disease, and strategies include refraining from swimming when one has diarrhea and for 2 weeks after resolution of diarrhea, not sending children to child care when they have diarrhea, and washing hands thoroughly after contact with animals, the researchers said.
“If a cryptosporidiosis outbreak occurs, substantial decontamination measures are needed, including hyperchlorinating public treated recreational water venues (e.g., swimming pools at a hotel, apartment complex, or water park) and using hydrogen peroxide to disinfect surfaces in child care settings to inactivate Cryptosporidium oocysts,” they emphasized.
The researchers had no financial conflicts to disclose.
SOURCE: Gharpure R et al. MMWR. 2019 June 28. 68:568-72.
FROM MMWR
July 2019 - Question 2
Q2. Correct answer: C
Rationale
Oral iron, and not infusions, are associated with peptic ulcer disease. Sumatriptan alone, or tamoxifen, are not known to cause ulcers.
Reference:
Miyake K., Kusunoki M., Shinji Y., et al. Bisphosphonate increases risk of gastroduodenal ulcer in rheumatoid arthritis patients on long-term nonsteroidal anti-inflammatory drug therapy. J Gastroenterol. 2009;44(2):113.
ginews@gastro.org
Q2. Correct answer: C
Rationale
Oral iron, and not infusions, are associated with peptic ulcer disease. Sumatriptan alone, or tamoxifen, are not known to cause ulcers.
Reference:
Miyake K., Kusunoki M., Shinji Y., et al. Bisphosphonate increases risk of gastroduodenal ulcer in rheumatoid arthritis patients on long-term nonsteroidal anti-inflammatory drug therapy. J Gastroenterol. 2009;44(2):113.
ginews@gastro.org
Q2. Correct answer: C
Rationale
Oral iron, and not infusions, are associated with peptic ulcer disease. Sumatriptan alone, or tamoxifen, are not known to cause ulcers.
Reference:
Miyake K., Kusunoki M., Shinji Y., et al. Bisphosphonate increases risk of gastroduodenal ulcer in rheumatoid arthritis patients on long-term nonsteroidal anti-inflammatory drug therapy. J Gastroenterol. 2009;44(2):113.
ginews@gastro.org
Q2. A 63-year-old woman is admitted with abdominal pain and iron deficiency anemia. She reports long-standing anemia and a negative workup in the past year including an upper endoscopy, colonoscopy, and video capsule endoscopy. She was started on iron infusions with a modest improvement in her anemia. Her other medical history includes osteoporosis; osteoarthritis, for which she takes over the counter NSAIDs, breast cancer (20 years ago treated with lumpectomy and local radiation); and migraines for which she takes sumatriptan once or twice a month.