User login
Having unmet social needs ups cardiovascular risk
WASHINGTON – according to a study.
“Although there have been great medical interventions and our technology keeps improving, we can’t prevent the burden of cardiovascular disease. It’s the social factors that are playing this role,” said Ana Palacio, MD, MPH, of the University of Miami during her presentation of the study findings at the annual meeting of the Society of General Internal Medicine.
“We need to address issues at the patient’s home, such as food, isolation, and transportation, to help them prevent cardiovascular risk,” she added.
The study was designed to determine how patient-reported social determinants of health (SDH) had an effect on the Framingham risk score (FRS). Researchers also wanted to assess the relationship between the SDH score and individual risk factors for cardiovascular health, including blood pressure, hemoglobin A1c, LDL cholesterol, body mass index, tobacco use, and physical activity.
Results showed that several SDH factors significantly increase the FRS score, including being born outside of the United States, living alone, having a high social isolation score, and having a low geocoded-based median household income (P less than .01). The calculated SDH score ranged from 0 to 59.
Higher SDH scores were associated with high FRS scores in the areas of poor blood pressure and diabetes control. Additionally, those who had financial strain, poor health literacy, stress, lack of education, and a low median household income were more likely to have a sedentary lifestyle. Black or Hispanic patients who were born outside the United States and had low median household income were at a higher risk of obesity.
The retrospective cohort study originally involved 11,113 primary care patients who received care at the University of Miami Health System between Sept. 16, 2016 and Sept. 10, 2017 and answered an SDH survey. Of this group, 2,876 patients completed the electronic health record data to compile a score. This population had a mean age of 53.8 years and was 61% female; 38% were Hispanic and 9% were black. The mean household income was $53,677 and 87% reported speaking English.
The study examined a total of 11 self-reported and census-based SDH factors. The self-reported factors were race/ethnicity, education, financial strain, stress, tobacco use and physical activity, social isolation, years living in the United States, health literacy, and delayed care. The remaining factors were based on an area deprivation index and census-driven median household income.
“The most surprising finding was how much weight the social factors have in adding to the Framingham risk score, in taking a patient from a medium score to a higher score because of their social environment,” said Dr. Palacio.
The study was funded by the Precision Medicine and Health Disparities Collaborative and was supported by the National Institute on Minority Health and Health Disparities and National Human Genome Research Institute of the National Institutes of Health.
WASHINGTON – according to a study.
“Although there have been great medical interventions and our technology keeps improving, we can’t prevent the burden of cardiovascular disease. It’s the social factors that are playing this role,” said Ana Palacio, MD, MPH, of the University of Miami during her presentation of the study findings at the annual meeting of the Society of General Internal Medicine.
“We need to address issues at the patient’s home, such as food, isolation, and transportation, to help them prevent cardiovascular risk,” she added.
The study was designed to determine how patient-reported social determinants of health (SDH) had an effect on the Framingham risk score (FRS). Researchers also wanted to assess the relationship between the SDH score and individual risk factors for cardiovascular health, including blood pressure, hemoglobin A1c, LDL cholesterol, body mass index, tobacco use, and physical activity.
Results showed that several SDH factors significantly increase the FRS score, including being born outside of the United States, living alone, having a high social isolation score, and having a low geocoded-based median household income (P less than .01). The calculated SDH score ranged from 0 to 59.
Higher SDH scores were associated with high FRS scores in the areas of poor blood pressure and diabetes control. Additionally, those who had financial strain, poor health literacy, stress, lack of education, and a low median household income were more likely to have a sedentary lifestyle. Black or Hispanic patients who were born outside the United States and had low median household income were at a higher risk of obesity.
The retrospective cohort study originally involved 11,113 primary care patients who received care at the University of Miami Health System between Sept. 16, 2016 and Sept. 10, 2017 and answered an SDH survey. Of this group, 2,876 patients completed the electronic health record data to compile a score. This population had a mean age of 53.8 years and was 61% female; 38% were Hispanic and 9% were black. The mean household income was $53,677 and 87% reported speaking English.
The study examined a total of 11 self-reported and census-based SDH factors. The self-reported factors were race/ethnicity, education, financial strain, stress, tobacco use and physical activity, social isolation, years living in the United States, health literacy, and delayed care. The remaining factors were based on an area deprivation index and census-driven median household income.
“The most surprising finding was how much weight the social factors have in adding to the Framingham risk score, in taking a patient from a medium score to a higher score because of their social environment,” said Dr. Palacio.
The study was funded by the Precision Medicine and Health Disparities Collaborative and was supported by the National Institute on Minority Health and Health Disparities and National Human Genome Research Institute of the National Institutes of Health.
WASHINGTON – according to a study.
“Although there have been great medical interventions and our technology keeps improving, we can’t prevent the burden of cardiovascular disease. It’s the social factors that are playing this role,” said Ana Palacio, MD, MPH, of the University of Miami during her presentation of the study findings at the annual meeting of the Society of General Internal Medicine.
“We need to address issues at the patient’s home, such as food, isolation, and transportation, to help them prevent cardiovascular risk,” she added.
The study was designed to determine how patient-reported social determinants of health (SDH) had an effect on the Framingham risk score (FRS). Researchers also wanted to assess the relationship between the SDH score and individual risk factors for cardiovascular health, including blood pressure, hemoglobin A1c, LDL cholesterol, body mass index, tobacco use, and physical activity.
Results showed that several SDH factors significantly increase the FRS score, including being born outside of the United States, living alone, having a high social isolation score, and having a low geocoded-based median household income (P less than .01). The calculated SDH score ranged from 0 to 59.
Higher SDH scores were associated with high FRS scores in the areas of poor blood pressure and diabetes control. Additionally, those who had financial strain, poor health literacy, stress, lack of education, and a low median household income were more likely to have a sedentary lifestyle. Black or Hispanic patients who were born outside the United States and had low median household income were at a higher risk of obesity.
The retrospective cohort study originally involved 11,113 primary care patients who received care at the University of Miami Health System between Sept. 16, 2016 and Sept. 10, 2017 and answered an SDH survey. Of this group, 2,876 patients completed the electronic health record data to compile a score. This population had a mean age of 53.8 years and was 61% female; 38% were Hispanic and 9% were black. The mean household income was $53,677 and 87% reported speaking English.
The study examined a total of 11 self-reported and census-based SDH factors. The self-reported factors were race/ethnicity, education, financial strain, stress, tobacco use and physical activity, social isolation, years living in the United States, health literacy, and delayed care. The remaining factors were based on an area deprivation index and census-driven median household income.
“The most surprising finding was how much weight the social factors have in adding to the Framingham risk score, in taking a patient from a medium score to a higher score because of their social environment,” said Dr. Palacio.
The study was funded by the Precision Medicine and Health Disparities Collaborative and was supported by the National Institute on Minority Health and Health Disparities and National Human Genome Research Institute of the National Institutes of Health.
REPORTING FROM SGIM 2019
Upadacitinib monotherapy appears promising in RA patients with inadequate methotrexate response
The investigational oral Janus kinase (JAK) inhibitor upadacitinib has shown promise as a monotherapy treatment option for patients with active rheumatoid arthritis despite treatment with methotrexate, based on results from the phase 3 SELECT-MONOTHERAPY trial.
“The SELECT-MONOTHERAPY trial showed that patients who were having an inadequate response to methotrexate could be switched to oral upadacitinib monotherapy (15 mg or 30 mg) once a day, with improvements in clinical signs and symptoms, physical function, and quality of life measures, compared with patients who continued on their previous methotrexate dose,” Josef S. Smolen, MD, of the Medical University of Vienna, and his colleagues wrote in the Lancet.
The phase 3, double-blind, placebo-controlled trial randomized 648 RA patients with active disease despite methotrexate therapy from 138 sites in 24 countries.
Higher proportions of patients receiving upadacitinib 15 mg and 30 mg versus continued methotrexate achieved the primary endpoints of the proportion of patients achieving a 20% improvement in American College of Rheumatology (ACR 20) criteria at 14 weeks and the proportion achieving low disease activity defined as a 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) of 3.2 or lower.
An ACR 20 response was achieved by 89 (41%) of 216 patients (95% confidence interval, 35%-48%) in the continued methotrexate group, 147 (68%) of 217 patients (95% CI, 62%-74%) receiving upadacitinib 15 mg, and 153 (71%) of 215 patients (95% CI, 65%-77%) receiving upadacitinib 30 mg (P less than .0001 for both doses vs. continued methotrexate).
A DAS28-CRP score of 3.2 or lower was met by 42 (19%) of 216 (95% CI, 14%-25%) receiving methotrexate, 97 (45%) of 217 (95% CI, 38%-51%) receiving upadacitinib 15 mg, and 114 (53%) of 215 (95% CI, 46%-60%) receiving upadacitinib 30 mg (P less than .0001 for both doses vs. continued methotrexate).
The investigators noted that responses were observed with both 15-mg and 30-mg doses of upadacitinib, although numerically higher responses were seen with the 30-mg dose.
“Whether the 15-mg or the 30-mg dose is the more appropriate one for patients who switch from methotrexate to upadacitinib will have to be established in conjunction with data from the other phase 3 upadacitinib trials,” they wrote.
Treatment-emergent adverse events were reported at similar frequencies across the arms (n = 102 with methotrexate; n = 103 with upadacitinib 15 mg; n = 105 with upadacitinib 30 mg).
Serious adverse events were reported in 11 (5%) of 217 patients in the upadacitinib 15 mg arm, 6 (3%) of 216 patients in the continued methotrexate arm, and 6 (3%) of 215 patients in the upadacitinib 30 mg arm.
“This favorable benefit-risk profile of upadacitinib monotherapy has the potential to provide a treatment option for patients who are intolerant to methotrexate or who prefer a treatment without the need for concomitant [conventional synthetic] DMARDs,” the authors wrote.
The study was funded by AbbVie. Dr. Smolen and most authors reported financial ties to AbbVie and other companies marketing rheumatoid arthritis treatments. Five authors are employees of AbbVie.
SOURCE: Smolen JS et al. Lancet. 2019;393[10188]:2303-11. doi: 10.1016/S0140-6736(19)30419-2
Treatment recommendations for the management of RA do not currently include the use of novel disease-modifying antirheumatic drugs (DMARDs) as monotherapy. However, there is growing interest in this concept, most likely because of poor tolerability and contraindications to conventional synthetic DMARDs such as methotrexate.
The observed treatment effects of SELECT-NEXT and the current trial by Prof. Smolen and associates are similar for both control groups (responders: 36% vs. 41% on methotrexate plus placebo) and for the upadacitinib treatment groups, regardless of concomitant methotrexate status (64% on methotrexate plus upadacitinib 15 mg or 66% on methotrexate plus upadacitinib 30 mg vs. 68% on upadacitinib 15 mg or 71% on upadacitinib 30 mg).
Prof. Smolen and associates chose a trial design that assessed the continuation of methotrexate plus placebo versus switching from methotrexate to upadacitinib monotherapy, but does this research question adequately reflect the question often raised in clinical practice: Should a novel DMARD be added to methotrexate or should patients switch from methotrexate to a novel DMARD?
But we now need a trial that compares a switch versus an add-on strategy to adequately answer the question on the treatment of resistant RA.
These comments are adapted from an accompanying editorial by Anna Moltó, MD, and Maxime Dougados, MD, both with the rheumatology department at Cochin Hospital, Paris (Lancet. 2019;393[10188]:2277-8. doi: 10.1016/S0140-6736(19)30768-8). The rheumatology department at Cochin Hospital has received grants to do clinical studies and trials from AbbVie and other manufacturers of drugs for RA. Both Dr. Dougados and Dr. Moltó reported receiving personal fees for advisory boards and symposia from AbbVie and other manufacturers of drugs for RA outside the area of work commented on here.
Treatment recommendations for the management of RA do not currently include the use of novel disease-modifying antirheumatic drugs (DMARDs) as monotherapy. However, there is growing interest in this concept, most likely because of poor tolerability and contraindications to conventional synthetic DMARDs such as methotrexate.
The observed treatment effects of SELECT-NEXT and the current trial by Prof. Smolen and associates are similar for both control groups (responders: 36% vs. 41% on methotrexate plus placebo) and for the upadacitinib treatment groups, regardless of concomitant methotrexate status (64% on methotrexate plus upadacitinib 15 mg or 66% on methotrexate plus upadacitinib 30 mg vs. 68% on upadacitinib 15 mg or 71% on upadacitinib 30 mg).
Prof. Smolen and associates chose a trial design that assessed the continuation of methotrexate plus placebo versus switching from methotrexate to upadacitinib monotherapy, but does this research question adequately reflect the question often raised in clinical practice: Should a novel DMARD be added to methotrexate or should patients switch from methotrexate to a novel DMARD?
But we now need a trial that compares a switch versus an add-on strategy to adequately answer the question on the treatment of resistant RA.
These comments are adapted from an accompanying editorial by Anna Moltó, MD, and Maxime Dougados, MD, both with the rheumatology department at Cochin Hospital, Paris (Lancet. 2019;393[10188]:2277-8. doi: 10.1016/S0140-6736(19)30768-8). The rheumatology department at Cochin Hospital has received grants to do clinical studies and trials from AbbVie and other manufacturers of drugs for RA. Both Dr. Dougados and Dr. Moltó reported receiving personal fees for advisory boards and symposia from AbbVie and other manufacturers of drugs for RA outside the area of work commented on here.
Treatment recommendations for the management of RA do not currently include the use of novel disease-modifying antirheumatic drugs (DMARDs) as monotherapy. However, there is growing interest in this concept, most likely because of poor tolerability and contraindications to conventional synthetic DMARDs such as methotrexate.
The observed treatment effects of SELECT-NEXT and the current trial by Prof. Smolen and associates are similar for both control groups (responders: 36% vs. 41% on methotrexate plus placebo) and for the upadacitinib treatment groups, regardless of concomitant methotrexate status (64% on methotrexate plus upadacitinib 15 mg or 66% on methotrexate plus upadacitinib 30 mg vs. 68% on upadacitinib 15 mg or 71% on upadacitinib 30 mg).
Prof. Smolen and associates chose a trial design that assessed the continuation of methotrexate plus placebo versus switching from methotrexate to upadacitinib monotherapy, but does this research question adequately reflect the question often raised in clinical practice: Should a novel DMARD be added to methotrexate or should patients switch from methotrexate to a novel DMARD?
But we now need a trial that compares a switch versus an add-on strategy to adequately answer the question on the treatment of resistant RA.
These comments are adapted from an accompanying editorial by Anna Moltó, MD, and Maxime Dougados, MD, both with the rheumatology department at Cochin Hospital, Paris (Lancet. 2019;393[10188]:2277-8. doi: 10.1016/S0140-6736(19)30768-8). The rheumatology department at Cochin Hospital has received grants to do clinical studies and trials from AbbVie and other manufacturers of drugs for RA. Both Dr. Dougados and Dr. Moltó reported receiving personal fees for advisory boards and symposia from AbbVie and other manufacturers of drugs for RA outside the area of work commented on here.
The investigational oral Janus kinase (JAK) inhibitor upadacitinib has shown promise as a monotherapy treatment option for patients with active rheumatoid arthritis despite treatment with methotrexate, based on results from the phase 3 SELECT-MONOTHERAPY trial.
“The SELECT-MONOTHERAPY trial showed that patients who were having an inadequate response to methotrexate could be switched to oral upadacitinib monotherapy (15 mg or 30 mg) once a day, with improvements in clinical signs and symptoms, physical function, and quality of life measures, compared with patients who continued on their previous methotrexate dose,” Josef S. Smolen, MD, of the Medical University of Vienna, and his colleagues wrote in the Lancet.
The phase 3, double-blind, placebo-controlled trial randomized 648 RA patients with active disease despite methotrexate therapy from 138 sites in 24 countries.
Higher proportions of patients receiving upadacitinib 15 mg and 30 mg versus continued methotrexate achieved the primary endpoints of the proportion of patients achieving a 20% improvement in American College of Rheumatology (ACR 20) criteria at 14 weeks and the proportion achieving low disease activity defined as a 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) of 3.2 or lower.
An ACR 20 response was achieved by 89 (41%) of 216 patients (95% confidence interval, 35%-48%) in the continued methotrexate group, 147 (68%) of 217 patients (95% CI, 62%-74%) receiving upadacitinib 15 mg, and 153 (71%) of 215 patients (95% CI, 65%-77%) receiving upadacitinib 30 mg (P less than .0001 for both doses vs. continued methotrexate).
A DAS28-CRP score of 3.2 or lower was met by 42 (19%) of 216 (95% CI, 14%-25%) receiving methotrexate, 97 (45%) of 217 (95% CI, 38%-51%) receiving upadacitinib 15 mg, and 114 (53%) of 215 (95% CI, 46%-60%) receiving upadacitinib 30 mg (P less than .0001 for both doses vs. continued methotrexate).
The investigators noted that responses were observed with both 15-mg and 30-mg doses of upadacitinib, although numerically higher responses were seen with the 30-mg dose.
“Whether the 15-mg or the 30-mg dose is the more appropriate one for patients who switch from methotrexate to upadacitinib will have to be established in conjunction with data from the other phase 3 upadacitinib trials,” they wrote.
Treatment-emergent adverse events were reported at similar frequencies across the arms (n = 102 with methotrexate; n = 103 with upadacitinib 15 mg; n = 105 with upadacitinib 30 mg).
Serious adverse events were reported in 11 (5%) of 217 patients in the upadacitinib 15 mg arm, 6 (3%) of 216 patients in the continued methotrexate arm, and 6 (3%) of 215 patients in the upadacitinib 30 mg arm.
“This favorable benefit-risk profile of upadacitinib monotherapy has the potential to provide a treatment option for patients who are intolerant to methotrexate or who prefer a treatment without the need for concomitant [conventional synthetic] DMARDs,” the authors wrote.
The study was funded by AbbVie. Dr. Smolen and most authors reported financial ties to AbbVie and other companies marketing rheumatoid arthritis treatments. Five authors are employees of AbbVie.
SOURCE: Smolen JS et al. Lancet. 2019;393[10188]:2303-11. doi: 10.1016/S0140-6736(19)30419-2
The investigational oral Janus kinase (JAK) inhibitor upadacitinib has shown promise as a monotherapy treatment option for patients with active rheumatoid arthritis despite treatment with methotrexate, based on results from the phase 3 SELECT-MONOTHERAPY trial.
“The SELECT-MONOTHERAPY trial showed that patients who were having an inadequate response to methotrexate could be switched to oral upadacitinib monotherapy (15 mg or 30 mg) once a day, with improvements in clinical signs and symptoms, physical function, and quality of life measures, compared with patients who continued on their previous methotrexate dose,” Josef S. Smolen, MD, of the Medical University of Vienna, and his colleagues wrote in the Lancet.
The phase 3, double-blind, placebo-controlled trial randomized 648 RA patients with active disease despite methotrexate therapy from 138 sites in 24 countries.
Higher proportions of patients receiving upadacitinib 15 mg and 30 mg versus continued methotrexate achieved the primary endpoints of the proportion of patients achieving a 20% improvement in American College of Rheumatology (ACR 20) criteria at 14 weeks and the proportion achieving low disease activity defined as a 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) of 3.2 or lower.
An ACR 20 response was achieved by 89 (41%) of 216 patients (95% confidence interval, 35%-48%) in the continued methotrexate group, 147 (68%) of 217 patients (95% CI, 62%-74%) receiving upadacitinib 15 mg, and 153 (71%) of 215 patients (95% CI, 65%-77%) receiving upadacitinib 30 mg (P less than .0001 for both doses vs. continued methotrexate).
A DAS28-CRP score of 3.2 or lower was met by 42 (19%) of 216 (95% CI, 14%-25%) receiving methotrexate, 97 (45%) of 217 (95% CI, 38%-51%) receiving upadacitinib 15 mg, and 114 (53%) of 215 (95% CI, 46%-60%) receiving upadacitinib 30 mg (P less than .0001 for both doses vs. continued methotrexate).
The investigators noted that responses were observed with both 15-mg and 30-mg doses of upadacitinib, although numerically higher responses were seen with the 30-mg dose.
“Whether the 15-mg or the 30-mg dose is the more appropriate one for patients who switch from methotrexate to upadacitinib will have to be established in conjunction with data from the other phase 3 upadacitinib trials,” they wrote.
Treatment-emergent adverse events were reported at similar frequencies across the arms (n = 102 with methotrexate; n = 103 with upadacitinib 15 mg; n = 105 with upadacitinib 30 mg).
Serious adverse events were reported in 11 (5%) of 217 patients in the upadacitinib 15 mg arm, 6 (3%) of 216 patients in the continued methotrexate arm, and 6 (3%) of 215 patients in the upadacitinib 30 mg arm.
“This favorable benefit-risk profile of upadacitinib monotherapy has the potential to provide a treatment option for patients who are intolerant to methotrexate or who prefer a treatment without the need for concomitant [conventional synthetic] DMARDs,” the authors wrote.
The study was funded by AbbVie. Dr. Smolen and most authors reported financial ties to AbbVie and other companies marketing rheumatoid arthritis treatments. Five authors are employees of AbbVie.
SOURCE: Smolen JS et al. Lancet. 2019;393[10188]:2303-11. doi: 10.1016/S0140-6736(19)30419-2
FROM THE LANCET
Rituximab serious infection risk predicted by immunoglobulin levels
Monitoring immunoglobulin (Ig) levels at baseline and before each cycle of rituximab could reduce the risk of serious infection events (SIEs) in patients needing repeated treatment, according to research published in Arthritis & Rheumatology.
In a large, single-center, longitudinal study conducted at a tertiary referral center, having low IgG (less than 6 g/L) in particular was associated with a higher rate of SIEs, compared with having normal IgG levels (6-16 g/L). Considering 103 of 700 patients who had low levels of IgG before starting treatment with rituximab for various rheumatic and musculoskeletal diseases (RMDs), there were 16.4 SIEs per 100 patient-years. In those who developed low IgG during subsequent cycles of rituximab therapy, the SIE rate was even higher, at 21.3 per 100 patient-years. By comparison, the SIE rate for those with normal IgG levels was 9.7 per 100 patient-years.
“We really have to monitor immunoglobulins at baseline and also before we re-treat the patients, because higher IgG level is protective of serious infections,” study first author Md Yuzaiful Md Yusof, MBChB, PhD, said in an interview.
Low IgG has been linked to a higher risk of SIEs in the first 12 months of rituximab therapy but, until now, there have been limited data on infection predictors during repeated cycles of treatment. While IgG is a consistent marker of SIEs associated with repeated rituximab treatment, IgM and IgA should also be monitored to give a full picture of any hyperglobulinemia that may be present.
“There is no formal guidance on how to safely monitor patients on rituximab,” observed Dr. Md Yusof, who will present these data at the 2019 European Congress of Rheumatology in Madrid. The study’s findings could help to change that, however, as they offer a practical way to help predict and thus prevent SIEs. The study’s findings not only validate previous work, he noted, but also add new insights into why some patients treated with repeat rituximab cycles but not others may experience a higher rate of such infections.
Altogether, the investigators examined data on 700 patients with RMDs treated with rituximab who were consecutively seen during 2012-2017 at Dr. Md Yusof’s institution – the Leeds (England) Institute of Rheumatic and Musculoskeletal Medicine, which is part of the University of Leeds. Their immunoglobulin levels had been measured before starting rituximab therapy and every 4-6 months after each cycle of rituximab treatment.
Patients with any RMD being treated with at least one cycle of rituximab were eligible for inclusion in the retrospective study, with the majority (72%) taking it for rheumatoid arthritis and some for systemic lupus erythematosus (13%) or antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (7%).
One of the main aims of the study was to look for predictors of SIEs during the first 12 months and during repeated cycles of rituximab. Dr. Md Yusof and his associates also looked at how secondary hypogammaglobulinemia might affect SIE rates and the humoral response to vaccination challenge and its persistence following treatment discontinuation. Their ultimate aim was to see if these findings could then be used to develop a treatment algorithm for rituximab administration in RMDs.
Over a follow-up period encompassing 2,880 patient-years of treatment, 281 SIEs were recorded in 176 patients, giving a rate of 9.8 infections per 100 patient-years. Most (61%) of these were due to lower respiratory tract infections.
The proportion of patients experiencing their first SIE increased with time: 16% within 6 weeks of starting rituximab therapy, 35% at 12 weeks, 72% at 26 weeks, 83% at 38 weeks, and 100% by 1 year of repeated treatment.
Multivariable analysis showed that the presence of several comorbidities at baseline – notably chronic obstructive pulmonary disease, diabetes, heart failure, and prior cancer – raised the risk for SIEs with repeated rituximab therapy. The biggest factor, however, was a history of SIEs – with a sixfold increased risk of further serious infection.
Higher corticosteroid dose and factors specific to rituximab – low IgG, neutropenia, high IgM, and a longer time to retreatment – were also predictive of SIEs.
“Low IgG also results in poor humoral response to vaccination,” Dr. Md Yusof said, noting that the IgG level remains below the lower limit of normal for several years after rituximab is discontinued in most patients.
In the study, 5 of 8 (64%) patients had impaired humoral response to pneumococcal and haemophilus following vaccination challenge and 4 of 11 patients had IgG normalized after switching to another biologic disease-modifying antirheumatic drug (bDMARD).
Cyclophosphamide is commonly used as a first-line agent to induce remission in patients with severe and refractory systemic lupus erythematosus and ANCA-associated vasculitis, with patients switched to rituximab at relapse. The effect of this prior treatment was examined in 20 patients in the study, with a marked decline in almost all immunoglobulin classes seen up to 18 months. Prior treatment with immunosuppressants such as intravenous cyclophosphamide could be behind progressive reductions in Ig levels seen with repeated rituximab treatment rather than entirely because of rituximab, Dr. Md Yusof said.
Dr. Md Yusof, who is a National Institute for Health Research (NIHR) Academic Clinical Lecturer at the University of Leeds, said the value of the study, compared with others, is that hospital data for all patients treated with rituximab with at least 3 months follow-up were included, making it an almost complete data set.
“By carefully reviewing records of every patient to capture all infection episodes in the largest single-center cohort study to date, our findings provide insights on predictors of SIEs as well as a foundation for safety monitoring of rituximab,” he and his coauthors wrote.
They acknowledge reporting a higher rate of SIEs than seen in registry and clinical studies with rituximab, which may reflect a “channeling bias” as the patients comprised those with multiple comorbidities including those that represent a relative contraindication for bDMARD use. That said, the findings clearly show that Ig levels should be monitored before and after each rituximab cycle, especially in those with comorbid diseases and those with low IgG levels to start with.
They conclude that an “individualized benefit-risk assessment” is needed to determine whether rituximab should be repeated in those with low IgG as this is a “consistent predictor” of SIE and may “increase infection profiles when [rituximab] is switched to different bDMARDs.”
The research was supported by Octapharma, the National Institute for Health Research (NIHR), and NIHR Leeds Biomedical Research Centre based at Leeds Teaching Hospitals NHS Trust in England. Dr. Md Yusof had no conflicts of interest. Several coauthors disclosed financial ties to multiple pharmaceutical companies, including Roche.
SOURCE: Md Yusof MY et al. Arthritis Rheumatol. 2019 May 27. doi: 10.1002/art.40937.
Monitoring immunoglobulin (Ig) levels at baseline and before each cycle of rituximab could reduce the risk of serious infection events (SIEs) in patients needing repeated treatment, according to research published in Arthritis & Rheumatology.
In a large, single-center, longitudinal study conducted at a tertiary referral center, having low IgG (less than 6 g/L) in particular was associated with a higher rate of SIEs, compared with having normal IgG levels (6-16 g/L). Considering 103 of 700 patients who had low levels of IgG before starting treatment with rituximab for various rheumatic and musculoskeletal diseases (RMDs), there were 16.4 SIEs per 100 patient-years. In those who developed low IgG during subsequent cycles of rituximab therapy, the SIE rate was even higher, at 21.3 per 100 patient-years. By comparison, the SIE rate for those with normal IgG levels was 9.7 per 100 patient-years.
“We really have to monitor immunoglobulins at baseline and also before we re-treat the patients, because higher IgG level is protective of serious infections,” study first author Md Yuzaiful Md Yusof, MBChB, PhD, said in an interview.
Low IgG has been linked to a higher risk of SIEs in the first 12 months of rituximab therapy but, until now, there have been limited data on infection predictors during repeated cycles of treatment. While IgG is a consistent marker of SIEs associated with repeated rituximab treatment, IgM and IgA should also be monitored to give a full picture of any hyperglobulinemia that may be present.
“There is no formal guidance on how to safely monitor patients on rituximab,” observed Dr. Md Yusof, who will present these data at the 2019 European Congress of Rheumatology in Madrid. The study’s findings could help to change that, however, as they offer a practical way to help predict and thus prevent SIEs. The study’s findings not only validate previous work, he noted, but also add new insights into why some patients treated with repeat rituximab cycles but not others may experience a higher rate of such infections.
Altogether, the investigators examined data on 700 patients with RMDs treated with rituximab who were consecutively seen during 2012-2017 at Dr. Md Yusof’s institution – the Leeds (England) Institute of Rheumatic and Musculoskeletal Medicine, which is part of the University of Leeds. Their immunoglobulin levels had been measured before starting rituximab therapy and every 4-6 months after each cycle of rituximab treatment.
Patients with any RMD being treated with at least one cycle of rituximab were eligible for inclusion in the retrospective study, with the majority (72%) taking it for rheumatoid arthritis and some for systemic lupus erythematosus (13%) or antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (7%).
One of the main aims of the study was to look for predictors of SIEs during the first 12 months and during repeated cycles of rituximab. Dr. Md Yusof and his associates also looked at how secondary hypogammaglobulinemia might affect SIE rates and the humoral response to vaccination challenge and its persistence following treatment discontinuation. Their ultimate aim was to see if these findings could then be used to develop a treatment algorithm for rituximab administration in RMDs.
Over a follow-up period encompassing 2,880 patient-years of treatment, 281 SIEs were recorded in 176 patients, giving a rate of 9.8 infections per 100 patient-years. Most (61%) of these were due to lower respiratory tract infections.
The proportion of patients experiencing their first SIE increased with time: 16% within 6 weeks of starting rituximab therapy, 35% at 12 weeks, 72% at 26 weeks, 83% at 38 weeks, and 100% by 1 year of repeated treatment.
Multivariable analysis showed that the presence of several comorbidities at baseline – notably chronic obstructive pulmonary disease, diabetes, heart failure, and prior cancer – raised the risk for SIEs with repeated rituximab therapy. The biggest factor, however, was a history of SIEs – with a sixfold increased risk of further serious infection.
Higher corticosteroid dose and factors specific to rituximab – low IgG, neutropenia, high IgM, and a longer time to retreatment – were also predictive of SIEs.
“Low IgG also results in poor humoral response to vaccination,” Dr. Md Yusof said, noting that the IgG level remains below the lower limit of normal for several years after rituximab is discontinued in most patients.
In the study, 5 of 8 (64%) patients had impaired humoral response to pneumococcal and haemophilus following vaccination challenge and 4 of 11 patients had IgG normalized after switching to another biologic disease-modifying antirheumatic drug (bDMARD).
Cyclophosphamide is commonly used as a first-line agent to induce remission in patients with severe and refractory systemic lupus erythematosus and ANCA-associated vasculitis, with patients switched to rituximab at relapse. The effect of this prior treatment was examined in 20 patients in the study, with a marked decline in almost all immunoglobulin classes seen up to 18 months. Prior treatment with immunosuppressants such as intravenous cyclophosphamide could be behind progressive reductions in Ig levels seen with repeated rituximab treatment rather than entirely because of rituximab, Dr. Md Yusof said.
Dr. Md Yusof, who is a National Institute for Health Research (NIHR) Academic Clinical Lecturer at the University of Leeds, said the value of the study, compared with others, is that hospital data for all patients treated with rituximab with at least 3 months follow-up were included, making it an almost complete data set.
“By carefully reviewing records of every patient to capture all infection episodes in the largest single-center cohort study to date, our findings provide insights on predictors of SIEs as well as a foundation for safety monitoring of rituximab,” he and his coauthors wrote.
They acknowledge reporting a higher rate of SIEs than seen in registry and clinical studies with rituximab, which may reflect a “channeling bias” as the patients comprised those with multiple comorbidities including those that represent a relative contraindication for bDMARD use. That said, the findings clearly show that Ig levels should be monitored before and after each rituximab cycle, especially in those with comorbid diseases and those with low IgG levels to start with.
They conclude that an “individualized benefit-risk assessment” is needed to determine whether rituximab should be repeated in those with low IgG as this is a “consistent predictor” of SIE and may “increase infection profiles when [rituximab] is switched to different bDMARDs.”
The research was supported by Octapharma, the National Institute for Health Research (NIHR), and NIHR Leeds Biomedical Research Centre based at Leeds Teaching Hospitals NHS Trust in England. Dr. Md Yusof had no conflicts of interest. Several coauthors disclosed financial ties to multiple pharmaceutical companies, including Roche.
SOURCE: Md Yusof MY et al. Arthritis Rheumatol. 2019 May 27. doi: 10.1002/art.40937.
Monitoring immunoglobulin (Ig) levels at baseline and before each cycle of rituximab could reduce the risk of serious infection events (SIEs) in patients needing repeated treatment, according to research published in Arthritis & Rheumatology.
In a large, single-center, longitudinal study conducted at a tertiary referral center, having low IgG (less than 6 g/L) in particular was associated with a higher rate of SIEs, compared with having normal IgG levels (6-16 g/L). Considering 103 of 700 patients who had low levels of IgG before starting treatment with rituximab for various rheumatic and musculoskeletal diseases (RMDs), there were 16.4 SIEs per 100 patient-years. In those who developed low IgG during subsequent cycles of rituximab therapy, the SIE rate was even higher, at 21.3 per 100 patient-years. By comparison, the SIE rate for those with normal IgG levels was 9.7 per 100 patient-years.
“We really have to monitor immunoglobulins at baseline and also before we re-treat the patients, because higher IgG level is protective of serious infections,” study first author Md Yuzaiful Md Yusof, MBChB, PhD, said in an interview.
Low IgG has been linked to a higher risk of SIEs in the first 12 months of rituximab therapy but, until now, there have been limited data on infection predictors during repeated cycles of treatment. While IgG is a consistent marker of SIEs associated with repeated rituximab treatment, IgM and IgA should also be monitored to give a full picture of any hyperglobulinemia that may be present.
“There is no formal guidance on how to safely monitor patients on rituximab,” observed Dr. Md Yusof, who will present these data at the 2019 European Congress of Rheumatology in Madrid. The study’s findings could help to change that, however, as they offer a practical way to help predict and thus prevent SIEs. The study’s findings not only validate previous work, he noted, but also add new insights into why some patients treated with repeat rituximab cycles but not others may experience a higher rate of such infections.
Altogether, the investigators examined data on 700 patients with RMDs treated with rituximab who were consecutively seen during 2012-2017 at Dr. Md Yusof’s institution – the Leeds (England) Institute of Rheumatic and Musculoskeletal Medicine, which is part of the University of Leeds. Their immunoglobulin levels had been measured before starting rituximab therapy and every 4-6 months after each cycle of rituximab treatment.
Patients with any RMD being treated with at least one cycle of rituximab were eligible for inclusion in the retrospective study, with the majority (72%) taking it for rheumatoid arthritis and some for systemic lupus erythematosus (13%) or antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (7%).
One of the main aims of the study was to look for predictors of SIEs during the first 12 months and during repeated cycles of rituximab. Dr. Md Yusof and his associates also looked at how secondary hypogammaglobulinemia might affect SIE rates and the humoral response to vaccination challenge and its persistence following treatment discontinuation. Their ultimate aim was to see if these findings could then be used to develop a treatment algorithm for rituximab administration in RMDs.
Over a follow-up period encompassing 2,880 patient-years of treatment, 281 SIEs were recorded in 176 patients, giving a rate of 9.8 infections per 100 patient-years. Most (61%) of these were due to lower respiratory tract infections.
The proportion of patients experiencing their first SIE increased with time: 16% within 6 weeks of starting rituximab therapy, 35% at 12 weeks, 72% at 26 weeks, 83% at 38 weeks, and 100% by 1 year of repeated treatment.
Multivariable analysis showed that the presence of several comorbidities at baseline – notably chronic obstructive pulmonary disease, diabetes, heart failure, and prior cancer – raised the risk for SIEs with repeated rituximab therapy. The biggest factor, however, was a history of SIEs – with a sixfold increased risk of further serious infection.
Higher corticosteroid dose and factors specific to rituximab – low IgG, neutropenia, high IgM, and a longer time to retreatment – were also predictive of SIEs.
“Low IgG also results in poor humoral response to vaccination,” Dr. Md Yusof said, noting that the IgG level remains below the lower limit of normal for several years after rituximab is discontinued in most patients.
In the study, 5 of 8 (64%) patients had impaired humoral response to pneumococcal and haemophilus following vaccination challenge and 4 of 11 patients had IgG normalized after switching to another biologic disease-modifying antirheumatic drug (bDMARD).
Cyclophosphamide is commonly used as a first-line agent to induce remission in patients with severe and refractory systemic lupus erythematosus and ANCA-associated vasculitis, with patients switched to rituximab at relapse. The effect of this prior treatment was examined in 20 patients in the study, with a marked decline in almost all immunoglobulin classes seen up to 18 months. Prior treatment with immunosuppressants such as intravenous cyclophosphamide could be behind progressive reductions in Ig levels seen with repeated rituximab treatment rather than entirely because of rituximab, Dr. Md Yusof said.
Dr. Md Yusof, who is a National Institute for Health Research (NIHR) Academic Clinical Lecturer at the University of Leeds, said the value of the study, compared with others, is that hospital data for all patients treated with rituximab with at least 3 months follow-up were included, making it an almost complete data set.
“By carefully reviewing records of every patient to capture all infection episodes in the largest single-center cohort study to date, our findings provide insights on predictors of SIEs as well as a foundation for safety monitoring of rituximab,” he and his coauthors wrote.
They acknowledge reporting a higher rate of SIEs than seen in registry and clinical studies with rituximab, which may reflect a “channeling bias” as the patients comprised those with multiple comorbidities including those that represent a relative contraindication for bDMARD use. That said, the findings clearly show that Ig levels should be monitored before and after each rituximab cycle, especially in those with comorbid diseases and those with low IgG levels to start with.
They conclude that an “individualized benefit-risk assessment” is needed to determine whether rituximab should be repeated in those with low IgG as this is a “consistent predictor” of SIE and may “increase infection profiles when [rituximab] is switched to different bDMARDs.”
The research was supported by Octapharma, the National Institute for Health Research (NIHR), and NIHR Leeds Biomedical Research Centre based at Leeds Teaching Hospitals NHS Trust in England. Dr. Md Yusof had no conflicts of interest. Several coauthors disclosed financial ties to multiple pharmaceutical companies, including Roche.
SOURCE: Md Yusof MY et al. Arthritis Rheumatol. 2019 May 27. doi: 10.1002/art.40937.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Immunoglobulin should be monitored at baseline and before each rituximab cycle to identify patients at risk of serious infection events (SIEs).
Major finding: SIE rates per 100 patient-years were 16.4 and 21.3 in patients with low (less than 6 g/L) IgG at baseline and during rituximab cycles versus 9.7 for patients with normal (6–16 g/L) IgG levels.
Study details: A retrospective, single-center, longitudinal study involving 700 rituximab-treated patients with rheumatoid arthritis and other rheumatic and musculoskeletal diseases.
Disclosures: The research was supported by Octapharma, the National Institute for Health Research (NIHR), and NIHR Leeds Biomedical Research Centre based at Leeds Teaching Hospitals NHS Trust in the United Kingdom. Dr. Md Yusof had no conflicts of interest. Several coauthors disclosed financial ties to multiple pharmaceutical companies, including Roche.
Source: Md Yusof MY et al. Arthritis Rheumatol. 2019 May 27. doi: 10.1002/art.40937.
Discharge before noon: An appropriate metric for efficiency?
I first heard the term “discharge before noon” (DCBN) as a third-year medical student starting my internal medicine rotation. The basic idea made sense: Get patients out of the hospital early so rooms can be cleaned more quickly and new patients wouldn’t have to wait so long in the ED.
It quickly became apparent, however, that a lot of moving parts had to align perfectly for DCBN. Even if we prioritized rounding on dischargeable patients (starting 8-9 a.m. depending on the service/day), they still needed prescriptions filled, normal clothes to wear, and a way to get home, which wasn’t easy to coordinate while we were still trying to see all the other patients.
Fast forward through 5 years of residency/fellowship experience and DCBN seems even more unrealistic in hospitalized pediatric patients. As a simple example, discharge criteria for dehydration (one of the most common reasons for pediatric hospitalization) include demonstrating the ability to drink enough liquids to stay hydrated. Who’s going to force children to stay up all night sipping fluids (plus changing all those diapers or taking them to the bathroom)? If the child stays on intravenous fluids overnight, we have to monitor at least through breakfast, likely lunch, thus making DCBN nearly impossible.
In a January 2019 article in the Journal of Hospital Medicine, Hailey James, MHA, (@Haileyjms on Twitter) and her colleagues demonstrated an association between DCBN and decreased length of stay (LOS) for medical but not surgical pediatric discharges.1 This made them question if DCBN is an appropriate metric for discharge efficiency, as well as workflow differences between services. Many hospitals, however, still try to push DCBN as a goal (see Destino et al in the same January 2019 issue of JHM2), which could potentially lead to people trying to game the system.
How does your institution try to make discharge processes more efficient? Is it actually possible to do everything more quickly without sacrificing quality or trainee education? Whether your patients are kids, adults, or both, there are likely many issues in common where we could all learn from each other.
We discussed this topic in #JHMChat on April 15 on Twitter. New to Twitter or not familiar with #JHMChat? Since October 2015, JHM has reviewed and discussed dozens of articles spanning a wide variety of topics related to caring for hospitalized patients. All are welcome to join, including medical students, residents, nurses, practicing hospitalists, and more. It’s a great opportunity to virtually meet and learn from others while earning free CME.
To participate in future chats, type #JHMChat in the search box on the top right corner of your Twitter homepage, click on the “Latest” tab at the top left to see the most recent tweets, and join the conversation (don’t forget the hashtag)!
Dr. Chen is a pediatric hospital medicine fellow at Rady Children’s Hospital, University of California, San Diego. She is one of the cofounders/moderators of #PHMFellowJC, serves as a fellow district representative for the American Academy of Pediatrics, and is an active #tweetiatrician at @DrJenChen4kids. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
References
1. James HJ et al. The Association of Discharge Before Noon and Length of Stay in Hospitalized Pediatric Patients. J Hosp Med. 2019;14(1):28-32. doi: 10.12788/jhm.3111.
2. Destino L et al. Improving Patient Flow: Analysis of an Initiative to Improve Early Discharge. J Hosp Med. 2019;14(1):22-7. doi: 10.12788/jhm.3133.
I first heard the term “discharge before noon” (DCBN) as a third-year medical student starting my internal medicine rotation. The basic idea made sense: Get patients out of the hospital early so rooms can be cleaned more quickly and new patients wouldn’t have to wait so long in the ED.
It quickly became apparent, however, that a lot of moving parts had to align perfectly for DCBN. Even if we prioritized rounding on dischargeable patients (starting 8-9 a.m. depending on the service/day), they still needed prescriptions filled, normal clothes to wear, and a way to get home, which wasn’t easy to coordinate while we were still trying to see all the other patients.
Fast forward through 5 years of residency/fellowship experience and DCBN seems even more unrealistic in hospitalized pediatric patients. As a simple example, discharge criteria for dehydration (one of the most common reasons for pediatric hospitalization) include demonstrating the ability to drink enough liquids to stay hydrated. Who’s going to force children to stay up all night sipping fluids (plus changing all those diapers or taking them to the bathroom)? If the child stays on intravenous fluids overnight, we have to monitor at least through breakfast, likely lunch, thus making DCBN nearly impossible.
In a January 2019 article in the Journal of Hospital Medicine, Hailey James, MHA, (@Haileyjms on Twitter) and her colleagues demonstrated an association between DCBN and decreased length of stay (LOS) for medical but not surgical pediatric discharges.1 This made them question if DCBN is an appropriate metric for discharge efficiency, as well as workflow differences between services. Many hospitals, however, still try to push DCBN as a goal (see Destino et al in the same January 2019 issue of JHM2), which could potentially lead to people trying to game the system.
How does your institution try to make discharge processes more efficient? Is it actually possible to do everything more quickly without sacrificing quality or trainee education? Whether your patients are kids, adults, or both, there are likely many issues in common where we could all learn from each other.
We discussed this topic in #JHMChat on April 15 on Twitter. New to Twitter or not familiar with #JHMChat? Since October 2015, JHM has reviewed and discussed dozens of articles spanning a wide variety of topics related to caring for hospitalized patients. All are welcome to join, including medical students, residents, nurses, practicing hospitalists, and more. It’s a great opportunity to virtually meet and learn from others while earning free CME.
To participate in future chats, type #JHMChat in the search box on the top right corner of your Twitter homepage, click on the “Latest” tab at the top left to see the most recent tweets, and join the conversation (don’t forget the hashtag)!
Dr. Chen is a pediatric hospital medicine fellow at Rady Children’s Hospital, University of California, San Diego. She is one of the cofounders/moderators of #PHMFellowJC, serves as a fellow district representative for the American Academy of Pediatrics, and is an active #tweetiatrician at @DrJenChen4kids. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
References
1. James HJ et al. The Association of Discharge Before Noon and Length of Stay in Hospitalized Pediatric Patients. J Hosp Med. 2019;14(1):28-32. doi: 10.12788/jhm.3111.
2. Destino L et al. Improving Patient Flow: Analysis of an Initiative to Improve Early Discharge. J Hosp Med. 2019;14(1):22-7. doi: 10.12788/jhm.3133.
I first heard the term “discharge before noon” (DCBN) as a third-year medical student starting my internal medicine rotation. The basic idea made sense: Get patients out of the hospital early so rooms can be cleaned more quickly and new patients wouldn’t have to wait so long in the ED.
It quickly became apparent, however, that a lot of moving parts had to align perfectly for DCBN. Even if we prioritized rounding on dischargeable patients (starting 8-9 a.m. depending on the service/day), they still needed prescriptions filled, normal clothes to wear, and a way to get home, which wasn’t easy to coordinate while we were still trying to see all the other patients.
Fast forward through 5 years of residency/fellowship experience and DCBN seems even more unrealistic in hospitalized pediatric patients. As a simple example, discharge criteria for dehydration (one of the most common reasons for pediatric hospitalization) include demonstrating the ability to drink enough liquids to stay hydrated. Who’s going to force children to stay up all night sipping fluids (plus changing all those diapers or taking them to the bathroom)? If the child stays on intravenous fluids overnight, we have to monitor at least through breakfast, likely lunch, thus making DCBN nearly impossible.
In a January 2019 article in the Journal of Hospital Medicine, Hailey James, MHA, (@Haileyjms on Twitter) and her colleagues demonstrated an association between DCBN and decreased length of stay (LOS) for medical but not surgical pediatric discharges.1 This made them question if DCBN is an appropriate metric for discharge efficiency, as well as workflow differences between services. Many hospitals, however, still try to push DCBN as a goal (see Destino et al in the same January 2019 issue of JHM2), which could potentially lead to people trying to game the system.
How does your institution try to make discharge processes more efficient? Is it actually possible to do everything more quickly without sacrificing quality or trainee education? Whether your patients are kids, adults, or both, there are likely many issues in common where we could all learn from each other.
We discussed this topic in #JHMChat on April 15 on Twitter. New to Twitter or not familiar with #JHMChat? Since October 2015, JHM has reviewed and discussed dozens of articles spanning a wide variety of topics related to caring for hospitalized patients. All are welcome to join, including medical students, residents, nurses, practicing hospitalists, and more. It’s a great opportunity to virtually meet and learn from others while earning free CME.
To participate in future chats, type #JHMChat in the search box on the top right corner of your Twitter homepage, click on the “Latest” tab at the top left to see the most recent tweets, and join the conversation (don’t forget the hashtag)!
Dr. Chen is a pediatric hospital medicine fellow at Rady Children’s Hospital, University of California, San Diego. She is one of the cofounders/moderators of #PHMFellowJC, serves as a fellow district representative for the American Academy of Pediatrics, and is an active #tweetiatrician at @DrJenChen4kids. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
References
1. James HJ et al. The Association of Discharge Before Noon and Length of Stay in Hospitalized Pediatric Patients. J Hosp Med. 2019;14(1):28-32. doi: 10.12788/jhm.3111.
2. Destino L et al. Improving Patient Flow: Analysis of an Initiative to Improve Early Discharge. J Hosp Med. 2019;14(1):22-7. doi: 10.12788/jhm.3133.
Updated systematic review of aspirin primary prevention shows benefits, risks
Using daily aspirin treatment for the primary prevention of cardiovascular events remains an individualized decision that needs to balance a person’s risks for ischemic events and bleeding, according to results from a new systematic review of 15 randomized, aspirin-prevention trials, including results from 3 major trials that researchers reported during 2018.
“The findings suggest that the decision to use aspirin for primary prevention should be tailored to the individual patients based on estimated atherosclerotic cardiovascular disease risk and perceived bleeding risk, as well as patient preferences regarding the types of event prevented versus potential bleeding caused,” Jawahar L. Mehta, MD, and his associates wrote in an article published on June 10 in the Journal of the American College of Cardiology.
The authors also concluded that if a person decides to use aspirin for primary prevention, then a low dose of 100 mg/day or less is recommended.
This new systematic review follows two reviews published earlier in 2019 that reached roughly similar conclusions after analyzing largely the same randomized trial data, including the same three major trials from 2018. One of these prior reviews included data from 13 trials and a total of 164,225 people (JAMA. 2019 Jan 22;321[3]:277-87). The second review had data from 11 trials with 157,248 people (Eur Heart J. 2019 Feb 14;40[7]:607-17). The newly published review used data collected by 15 trials from 165,502 people.
The three 2018 trials that triggered the updated data assessments were the ARRIVE trial, with 12,546 people randomized (Lancet. 2018 Sep 22;392[10152]:1036-46), the ASPREE trial, with 19,114 people randomized (New Engl J Med. 2018 Oct 18;379[16]:1509-18), and the ASCEND trial, with 15,480 people randomized (New Engl J Med. 2018 Oct 18;379[16]:1529-39).
As stated in the new report from Dr. Mehta, a professor of medicine at the University of Arkansas for Medical Sciences in Little Rock, and his associates, the recent trial results from 2018 added new data from more than 45,000 additional subjects, a development that warranted a reappraisal of the evidence for aspirin’s efficacy and safety for primary prevention in contemporary practice.
The major findings from the analysis by Dr. Mehta and his associates were that in adults without a history of cardiovascular disease, daily aspirin use reduced the incidence of MIs, with a number needed to treat (NNT) of 357; reduced ischemic stroke (NNT, 500), reduced transient ischemic attack (NNT, 370), and reduced the overall, combined rate of all major adverse cardiovascular events (NNT, 263). But on the safety side, daily aspirin led to an increased rate of major bleeding episodes, with a number needed to harm (NNH) of 222, increased intracranial bleeds (NNH, 1,000), and an increase in gastrointestinal bleeds (NNH, 385).
The analysis “demonstrates a potential reduction of net benefit with aspirin in the contemporary era,” the authors concluded. They also noted that the benefits from aspirin prevention were, as expected, “more pronounced” among people with a higher estimated risk from atherosclerotic cardiovascular disease.
The systematic review findings came against the backdrop of a recently released primary prevention guideline from the American College of Cardiology and American Heart Association (J Am Coll Card. 2019 Mar. doi: 10.1016/j.jacc.2019.03.010). The guideline said that aspirin prophylaxis for primary prevention “might be considered” for adults aged 40-70 years, but should not be used for people who are older than 70, and also should not be given to people with an increased risk for bleeding. In general, the experts who produced this guideline said that aspirin prophylaxis should be infrequent.
The new analysis also found no reduction in the incidence of cancer or cancer-related death linked with aspirin use for primary prevention. The systematic review published earlier in 2019 in JAMA also found no link between aspirin use and cancer incidence or mortality. The review from the European Heart Journal did not report on the link between aspirin use and cancer incidence or mortality.
Dr. Mehta has been a consultant to AstraZeneca, Bayer, Boehringer Ingelheim, Medimmune, and Pfizer, and has received grant support from AstraZeneca, Bayer, and Boehringer Ingelheim.
On Twitter @mitchelzoler
SOURCE: Abdelaziz HK et al. J Am Coll Cardiol. 2019 Jun 10. doi: 10.1016/j.jacc.2019.03.501.
The three trials published in 2018 that added important new data on primary prevention for cardiovascular disease with aspirin must ideally be interpreted within the context of the totality of evidence on this subject. This was achieved in the analysis reported by Dr. Mehta and his associates, as well as in other more recent publications.
Making a decision about using aspirin for primary prevention in individuals based on trial data is very challenging because it requires weighing a modest potential benefit that people gain from daily aspirin for preventing a first cardiovascular event against the modest risk of an adverse bleeding event. It does not suffice simply to compare the number of cardiovascular and bleeding events, because those two types of events do not have the same immediate or long-term consequences. Each patient must make a personal choice between the risks and benefits.
The greatest potential benefit from aspirin prophylaxis seems to be in people with increased cardiovascular risk but with no increased bleeding risk. In general, this means people aged 50-59 years old, and also possibly those aged 60-69 years old if their estimated 10-year cardiovascular disease risk is more than 10%. It may make more sense to first focus on other risk-reducing steps, such as smoking cessation, blood pressure control, and statin treatment. After that, prophylactic aspirin may be reasonable for people who retain a 10-year cardiovascular disease risk of more than 10% who are also not at increased bleeding risk. That seems to make it prudent to avoid aspirin for primary prevention once people reach the age of 70 years, although people who have been taking aspirin safely for a period of time before reaching 70 might reasonably consider continuing the prophylaxis for a period of time.
This and similar reviews continue to have major limitations. The duration of the trials they reviewed, a mean of 6.4 years, is insufficient to understand the full effect from aspirin prophylaxis. Also, none of the recent reviews used a patient-level meta-analysis, which could better help us understand aspirin’s action in key subgroups, such as women, patients with diabetes, and patients on treatments such as statins that reduce their cardiovascular risk.
Michael Pignone, MD, is professor and chair of medicine at the University of Texas Dell Medical School in Austin. He had no disclosures. He made these comments in an editorial that accompanied the report (J Am Coll Cardiol. 2019 Jun 10. doi: 10.1016/j.jacc.2019.03.502).
The three trials published in 2018 that added important new data on primary prevention for cardiovascular disease with aspirin must ideally be interpreted within the context of the totality of evidence on this subject. This was achieved in the analysis reported by Dr. Mehta and his associates, as well as in other more recent publications.
Making a decision about using aspirin for primary prevention in individuals based on trial data is very challenging because it requires weighing a modest potential benefit that people gain from daily aspirin for preventing a first cardiovascular event against the modest risk of an adverse bleeding event. It does not suffice simply to compare the number of cardiovascular and bleeding events, because those two types of events do not have the same immediate or long-term consequences. Each patient must make a personal choice between the risks and benefits.
The greatest potential benefit from aspirin prophylaxis seems to be in people with increased cardiovascular risk but with no increased bleeding risk. In general, this means people aged 50-59 years old, and also possibly those aged 60-69 years old if their estimated 10-year cardiovascular disease risk is more than 10%. It may make more sense to first focus on other risk-reducing steps, such as smoking cessation, blood pressure control, and statin treatment. After that, prophylactic aspirin may be reasonable for people who retain a 10-year cardiovascular disease risk of more than 10% who are also not at increased bleeding risk. That seems to make it prudent to avoid aspirin for primary prevention once people reach the age of 70 years, although people who have been taking aspirin safely for a period of time before reaching 70 might reasonably consider continuing the prophylaxis for a period of time.
This and similar reviews continue to have major limitations. The duration of the trials they reviewed, a mean of 6.4 years, is insufficient to understand the full effect from aspirin prophylaxis. Also, none of the recent reviews used a patient-level meta-analysis, which could better help us understand aspirin’s action in key subgroups, such as women, patients with diabetes, and patients on treatments such as statins that reduce their cardiovascular risk.
Michael Pignone, MD, is professor and chair of medicine at the University of Texas Dell Medical School in Austin. He had no disclosures. He made these comments in an editorial that accompanied the report (J Am Coll Cardiol. 2019 Jun 10. doi: 10.1016/j.jacc.2019.03.502).
The three trials published in 2018 that added important new data on primary prevention for cardiovascular disease with aspirin must ideally be interpreted within the context of the totality of evidence on this subject. This was achieved in the analysis reported by Dr. Mehta and his associates, as well as in other more recent publications.
Making a decision about using aspirin for primary prevention in individuals based on trial data is very challenging because it requires weighing a modest potential benefit that people gain from daily aspirin for preventing a first cardiovascular event against the modest risk of an adverse bleeding event. It does not suffice simply to compare the number of cardiovascular and bleeding events, because those two types of events do not have the same immediate or long-term consequences. Each patient must make a personal choice between the risks and benefits.
The greatest potential benefit from aspirin prophylaxis seems to be in people with increased cardiovascular risk but with no increased bleeding risk. In general, this means people aged 50-59 years old, and also possibly those aged 60-69 years old if their estimated 10-year cardiovascular disease risk is more than 10%. It may make more sense to first focus on other risk-reducing steps, such as smoking cessation, blood pressure control, and statin treatment. After that, prophylactic aspirin may be reasonable for people who retain a 10-year cardiovascular disease risk of more than 10% who are also not at increased bleeding risk. That seems to make it prudent to avoid aspirin for primary prevention once people reach the age of 70 years, although people who have been taking aspirin safely for a period of time before reaching 70 might reasonably consider continuing the prophylaxis for a period of time.
This and similar reviews continue to have major limitations. The duration of the trials they reviewed, a mean of 6.4 years, is insufficient to understand the full effect from aspirin prophylaxis. Also, none of the recent reviews used a patient-level meta-analysis, which could better help us understand aspirin’s action in key subgroups, such as women, patients with diabetes, and patients on treatments such as statins that reduce their cardiovascular risk.
Michael Pignone, MD, is professor and chair of medicine at the University of Texas Dell Medical School in Austin. He had no disclosures. He made these comments in an editorial that accompanied the report (J Am Coll Cardiol. 2019 Jun 10. doi: 10.1016/j.jacc.2019.03.502).
Using daily aspirin treatment for the primary prevention of cardiovascular events remains an individualized decision that needs to balance a person’s risks for ischemic events and bleeding, according to results from a new systematic review of 15 randomized, aspirin-prevention trials, including results from 3 major trials that researchers reported during 2018.
“The findings suggest that the decision to use aspirin for primary prevention should be tailored to the individual patients based on estimated atherosclerotic cardiovascular disease risk and perceived bleeding risk, as well as patient preferences regarding the types of event prevented versus potential bleeding caused,” Jawahar L. Mehta, MD, and his associates wrote in an article published on June 10 in the Journal of the American College of Cardiology.
The authors also concluded that if a person decides to use aspirin for primary prevention, then a low dose of 100 mg/day or less is recommended.
This new systematic review follows two reviews published earlier in 2019 that reached roughly similar conclusions after analyzing largely the same randomized trial data, including the same three major trials from 2018. One of these prior reviews included data from 13 trials and a total of 164,225 people (JAMA. 2019 Jan 22;321[3]:277-87). The second review had data from 11 trials with 157,248 people (Eur Heart J. 2019 Feb 14;40[7]:607-17). The newly published review used data collected by 15 trials from 165,502 people.
The three 2018 trials that triggered the updated data assessments were the ARRIVE trial, with 12,546 people randomized (Lancet. 2018 Sep 22;392[10152]:1036-46), the ASPREE trial, with 19,114 people randomized (New Engl J Med. 2018 Oct 18;379[16]:1509-18), and the ASCEND trial, with 15,480 people randomized (New Engl J Med. 2018 Oct 18;379[16]:1529-39).
As stated in the new report from Dr. Mehta, a professor of medicine at the University of Arkansas for Medical Sciences in Little Rock, and his associates, the recent trial results from 2018 added new data from more than 45,000 additional subjects, a development that warranted a reappraisal of the evidence for aspirin’s efficacy and safety for primary prevention in contemporary practice.
The major findings from the analysis by Dr. Mehta and his associates were that in adults without a history of cardiovascular disease, daily aspirin use reduced the incidence of MIs, with a number needed to treat (NNT) of 357; reduced ischemic stroke (NNT, 500), reduced transient ischemic attack (NNT, 370), and reduced the overall, combined rate of all major adverse cardiovascular events (NNT, 263). But on the safety side, daily aspirin led to an increased rate of major bleeding episodes, with a number needed to harm (NNH) of 222, increased intracranial bleeds (NNH, 1,000), and an increase in gastrointestinal bleeds (NNH, 385).
The analysis “demonstrates a potential reduction of net benefit with aspirin in the contemporary era,” the authors concluded. They also noted that the benefits from aspirin prevention were, as expected, “more pronounced” among people with a higher estimated risk from atherosclerotic cardiovascular disease.
The systematic review findings came against the backdrop of a recently released primary prevention guideline from the American College of Cardiology and American Heart Association (J Am Coll Card. 2019 Mar. doi: 10.1016/j.jacc.2019.03.010). The guideline said that aspirin prophylaxis for primary prevention “might be considered” for adults aged 40-70 years, but should not be used for people who are older than 70, and also should not be given to people with an increased risk for bleeding. In general, the experts who produced this guideline said that aspirin prophylaxis should be infrequent.
The new analysis also found no reduction in the incidence of cancer or cancer-related death linked with aspirin use for primary prevention. The systematic review published earlier in 2019 in JAMA also found no link between aspirin use and cancer incidence or mortality. The review from the European Heart Journal did not report on the link between aspirin use and cancer incidence or mortality.
Dr. Mehta has been a consultant to AstraZeneca, Bayer, Boehringer Ingelheim, Medimmune, and Pfizer, and has received grant support from AstraZeneca, Bayer, and Boehringer Ingelheim.
On Twitter @mitchelzoler
SOURCE: Abdelaziz HK et al. J Am Coll Cardiol. 2019 Jun 10. doi: 10.1016/j.jacc.2019.03.501.
Using daily aspirin treatment for the primary prevention of cardiovascular events remains an individualized decision that needs to balance a person’s risks for ischemic events and bleeding, according to results from a new systematic review of 15 randomized, aspirin-prevention trials, including results from 3 major trials that researchers reported during 2018.
“The findings suggest that the decision to use aspirin for primary prevention should be tailored to the individual patients based on estimated atherosclerotic cardiovascular disease risk and perceived bleeding risk, as well as patient preferences regarding the types of event prevented versus potential bleeding caused,” Jawahar L. Mehta, MD, and his associates wrote in an article published on June 10 in the Journal of the American College of Cardiology.
The authors also concluded that if a person decides to use aspirin for primary prevention, then a low dose of 100 mg/day or less is recommended.
This new systematic review follows two reviews published earlier in 2019 that reached roughly similar conclusions after analyzing largely the same randomized trial data, including the same three major trials from 2018. One of these prior reviews included data from 13 trials and a total of 164,225 people (JAMA. 2019 Jan 22;321[3]:277-87). The second review had data from 11 trials with 157,248 people (Eur Heart J. 2019 Feb 14;40[7]:607-17). The newly published review used data collected by 15 trials from 165,502 people.
The three 2018 trials that triggered the updated data assessments were the ARRIVE trial, with 12,546 people randomized (Lancet. 2018 Sep 22;392[10152]:1036-46), the ASPREE trial, with 19,114 people randomized (New Engl J Med. 2018 Oct 18;379[16]:1509-18), and the ASCEND trial, with 15,480 people randomized (New Engl J Med. 2018 Oct 18;379[16]:1529-39).
As stated in the new report from Dr. Mehta, a professor of medicine at the University of Arkansas for Medical Sciences in Little Rock, and his associates, the recent trial results from 2018 added new data from more than 45,000 additional subjects, a development that warranted a reappraisal of the evidence for aspirin’s efficacy and safety for primary prevention in contemporary practice.
The major findings from the analysis by Dr. Mehta and his associates were that in adults without a history of cardiovascular disease, daily aspirin use reduced the incidence of MIs, with a number needed to treat (NNT) of 357; reduced ischemic stroke (NNT, 500), reduced transient ischemic attack (NNT, 370), and reduced the overall, combined rate of all major adverse cardiovascular events (NNT, 263). But on the safety side, daily aspirin led to an increased rate of major bleeding episodes, with a number needed to harm (NNH) of 222, increased intracranial bleeds (NNH, 1,000), and an increase in gastrointestinal bleeds (NNH, 385).
The analysis “demonstrates a potential reduction of net benefit with aspirin in the contemporary era,” the authors concluded. They also noted that the benefits from aspirin prevention were, as expected, “more pronounced” among people with a higher estimated risk from atherosclerotic cardiovascular disease.
The systematic review findings came against the backdrop of a recently released primary prevention guideline from the American College of Cardiology and American Heart Association (J Am Coll Card. 2019 Mar. doi: 10.1016/j.jacc.2019.03.010). The guideline said that aspirin prophylaxis for primary prevention “might be considered” for adults aged 40-70 years, but should not be used for people who are older than 70, and also should not be given to people with an increased risk for bleeding. In general, the experts who produced this guideline said that aspirin prophylaxis should be infrequent.
The new analysis also found no reduction in the incidence of cancer or cancer-related death linked with aspirin use for primary prevention. The systematic review published earlier in 2019 in JAMA also found no link between aspirin use and cancer incidence or mortality. The review from the European Heart Journal did not report on the link between aspirin use and cancer incidence or mortality.
Dr. Mehta has been a consultant to AstraZeneca, Bayer, Boehringer Ingelheim, Medimmune, and Pfizer, and has received grant support from AstraZeneca, Bayer, and Boehringer Ingelheim.
On Twitter @mitchelzoler
SOURCE: Abdelaziz HK et al. J Am Coll Cardiol. 2019 Jun 10. doi: 10.1016/j.jacc.2019.03.501.
FROM JACC
Key clinical point: Cumulative trial results continue to show that aspirin primary prevention cuts CVD events while boosting major bleeds.
Major finding: Aspirin prophylaxis cut cardiovascular events with an NNT of 263, but increased major bleeds with an NNH of 222.
Study details: Systematic review of data from 165,502 people enrolled in 15 randomized trials.
Disclosures: Dr. Mehta has been a consultant to AstraZeneca, Bayer, Boehringer Ingelheim, Medimmune, and Pfizer, and has received grant support from AstraZeneca, Bayer, and Boehringer Ingelheim.
Source: Abdelaziz HK et al. J Am Coll Cardiol. 2019 Jun 10. doi: 10.1016/j.jacc.2019.03.501.
VA Rolls Out New and Improved Veterans Community Care Program
Calling it a landmark initiative, the US Department of Veterans Affairs (VA) has launched its “new and improved” Veterans Community Care Program, implementing portions of the Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (MISSION Act). The initiative both ends the Veterans Choice Program, which expired June 6, and establishes a new Veterans Community Care Program. Senior VA leaders will visit > 30 VA hospitals across the country to support the rollout.
The MISSION Act is intended to provide veterans with more health care options. It also strengthens the VA’s ability to recruit and retain clinicians, authorizes “Anywhere to Anywhere” telehealth across state lines, gives veterans better access to community care, and establishes a new urgent care benefit.
“The changes not only improve our ability to provide the health care veterans need, but also when and where they need it,” said VA Secretary Robert Wilkie. “It will also put veterans at the center of their care and offer options, including expanded telehealth and urgent care, so they can find the balance in the system that is right for them.”
Eligibility for community care does not require veterans to receive that care in the community; they can still choose to have VA care. A veteran may elect to receive care in the community if he or she:
- needs a service not available at any VA medical facility;
- lives in a US state or territory without a full-service VA medical facility (applies to veterans living in Alaska, Hawaii, New Hampshire, Guam, American Samoa, the Northern Mariana Islands and the US Virgin Islands);
- qualifies under the “grandfather” provision related to distance eligibility under the Veterans Choice Program; and/or
- meets specific access standards for average drive time or appointment wait times.
The veteran also is eligible if he or she and the referring clinician agree that it is in the best medical interest of the veteran to receive community care based on defined factors, or if the VA has determined that a VA medical service line is not providing care in a manner that complies with VA’s standards for quality based on specific conditions.
In addition to the new eligibility rules, the VA says it has made a variety of improvements that will “make community care work better for veterans.”
One is that existing programs will be combined into a single community care program, to reduce complexity and the “likelihood of errors and problems.” The VA also is streamlining internal processes and modernizing IT systems, aiming to “speed up all aspects of community care—eligibility, authorizations, appointments, care coordination, claims, payments—while improving overall communication between veterans, community providers, and VA staff members.”
The VA has announced, as well, that 2 final regulations of the Veterans Community Care Program have been published in the Federal Register. One concerns the new urgent care benefit that provides eligible veterans with greater choice and access to timely, high-quality care for minor injuries and illnesses. The second regulation governs how eligible veterans receive necessary hospital care, medical services, and extended-care services from non-VA entities or providers in the community.
The VA will purchase most community care for veterans through its contracted network with third-party administrators (currently TriWest Healthcare Alliance and Optum Public). When the new Community Care Network of community providers is implemented, VA staff will work directly with veterans to schedule appointments and support care coordination.
A complete rollout of all 6 regions of the Community Care Network is expected by 2020. More detailed information is available at www.missionact.va.gov.
Calling it a landmark initiative, the US Department of Veterans Affairs (VA) has launched its “new and improved” Veterans Community Care Program, implementing portions of the Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (MISSION Act). The initiative both ends the Veterans Choice Program, which expired June 6, and establishes a new Veterans Community Care Program. Senior VA leaders will visit > 30 VA hospitals across the country to support the rollout.
The MISSION Act is intended to provide veterans with more health care options. It also strengthens the VA’s ability to recruit and retain clinicians, authorizes “Anywhere to Anywhere” telehealth across state lines, gives veterans better access to community care, and establishes a new urgent care benefit.
“The changes not only improve our ability to provide the health care veterans need, but also when and where they need it,” said VA Secretary Robert Wilkie. “It will also put veterans at the center of their care and offer options, including expanded telehealth and urgent care, so they can find the balance in the system that is right for them.”
Eligibility for community care does not require veterans to receive that care in the community; they can still choose to have VA care. A veteran may elect to receive care in the community if he or she:
- needs a service not available at any VA medical facility;
- lives in a US state or territory without a full-service VA medical facility (applies to veterans living in Alaska, Hawaii, New Hampshire, Guam, American Samoa, the Northern Mariana Islands and the US Virgin Islands);
- qualifies under the “grandfather” provision related to distance eligibility under the Veterans Choice Program; and/or
- meets specific access standards for average drive time or appointment wait times.
The veteran also is eligible if he or she and the referring clinician agree that it is in the best medical interest of the veteran to receive community care based on defined factors, or if the VA has determined that a VA medical service line is not providing care in a manner that complies with VA’s standards for quality based on specific conditions.
In addition to the new eligibility rules, the VA says it has made a variety of improvements that will “make community care work better for veterans.”
One is that existing programs will be combined into a single community care program, to reduce complexity and the “likelihood of errors and problems.” The VA also is streamlining internal processes and modernizing IT systems, aiming to “speed up all aspects of community care—eligibility, authorizations, appointments, care coordination, claims, payments—while improving overall communication between veterans, community providers, and VA staff members.”
The VA has announced, as well, that 2 final regulations of the Veterans Community Care Program have been published in the Federal Register. One concerns the new urgent care benefit that provides eligible veterans with greater choice and access to timely, high-quality care for minor injuries and illnesses. The second regulation governs how eligible veterans receive necessary hospital care, medical services, and extended-care services from non-VA entities or providers in the community.
The VA will purchase most community care for veterans through its contracted network with third-party administrators (currently TriWest Healthcare Alliance and Optum Public). When the new Community Care Network of community providers is implemented, VA staff will work directly with veterans to schedule appointments and support care coordination.
A complete rollout of all 6 regions of the Community Care Network is expected by 2020. More detailed information is available at www.missionact.va.gov.
Calling it a landmark initiative, the US Department of Veterans Affairs (VA) has launched its “new and improved” Veterans Community Care Program, implementing portions of the Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018 (MISSION Act). The initiative both ends the Veterans Choice Program, which expired June 6, and establishes a new Veterans Community Care Program. Senior VA leaders will visit > 30 VA hospitals across the country to support the rollout.
The MISSION Act is intended to provide veterans with more health care options. It also strengthens the VA’s ability to recruit and retain clinicians, authorizes “Anywhere to Anywhere” telehealth across state lines, gives veterans better access to community care, and establishes a new urgent care benefit.
“The changes not only improve our ability to provide the health care veterans need, but also when and where they need it,” said VA Secretary Robert Wilkie. “It will also put veterans at the center of their care and offer options, including expanded telehealth and urgent care, so they can find the balance in the system that is right for them.”
Eligibility for community care does not require veterans to receive that care in the community; they can still choose to have VA care. A veteran may elect to receive care in the community if he or she:
- needs a service not available at any VA medical facility;
- lives in a US state or territory without a full-service VA medical facility (applies to veterans living in Alaska, Hawaii, New Hampshire, Guam, American Samoa, the Northern Mariana Islands and the US Virgin Islands);
- qualifies under the “grandfather” provision related to distance eligibility under the Veterans Choice Program; and/or
- meets specific access standards for average drive time or appointment wait times.
The veteran also is eligible if he or she and the referring clinician agree that it is in the best medical interest of the veteran to receive community care based on defined factors, or if the VA has determined that a VA medical service line is not providing care in a manner that complies with VA’s standards for quality based on specific conditions.
In addition to the new eligibility rules, the VA says it has made a variety of improvements that will “make community care work better for veterans.”
One is that existing programs will be combined into a single community care program, to reduce complexity and the “likelihood of errors and problems.” The VA also is streamlining internal processes and modernizing IT systems, aiming to “speed up all aspects of community care—eligibility, authorizations, appointments, care coordination, claims, payments—while improving overall communication between veterans, community providers, and VA staff members.”
The VA has announced, as well, that 2 final regulations of the Veterans Community Care Program have been published in the Federal Register. One concerns the new urgent care benefit that provides eligible veterans with greater choice and access to timely, high-quality care for minor injuries and illnesses. The second regulation governs how eligible veterans receive necessary hospital care, medical services, and extended-care services from non-VA entities or providers in the community.
The VA will purchase most community care for veterans through its contracted network with third-party administrators (currently TriWest Healthcare Alliance and Optum Public). When the new Community Care Network of community providers is implemented, VA staff will work directly with veterans to schedule appointments and support care coordination.
A complete rollout of all 6 regions of the Community Care Network is expected by 2020. More detailed information is available at www.missionact.va.gov.
Medical community confronts physician depression, suicide
Many physicians work long hours and may ignore the fatigue and emotional toll that comes with those pressures. The stress cannot only lead to crippling depression but also to declined mental health and even thoughts of suicide.
Each year, an estimated 400 physicians take their own lives, mostly because of depression and stress, according to the West Journal of Emergency Medicine.
MDedge Internal Medicine recently hosted a Twitter conversation (#MDedgeChats) on how the health care community can address this emerging crisis and help their colleagues understand that they are not alone. Two primary care physicians — Sarah Candler, MD, and Elisabeth Poorman, MD — led the conversation, with guests Michael Rose, MD, Arghavan Salles, MD, Richard M. Wardrop III, MD, Jessica Gold, MD, and Janae Sharp.
Throughout the conversation, physicians encouraged other medical professionals to seek help if it is needed. “If you don’t feel comfortable sharing with your team, feel free to share with folks you met here,” Dr. Candler wrote. “Please seek professional solace with a therapist! That’s what this is about – the support to do what you need for yourself. Good doctors take care of themselves, too.”
These issues are not just important in the medical community “because everyone will get sick, and we are failing each other. We are failing our patients and our communities when we won’t fight for change. The center will not hold here,” said Dr. Elizabeth Poorman.
The following is an edited version of the discussion.
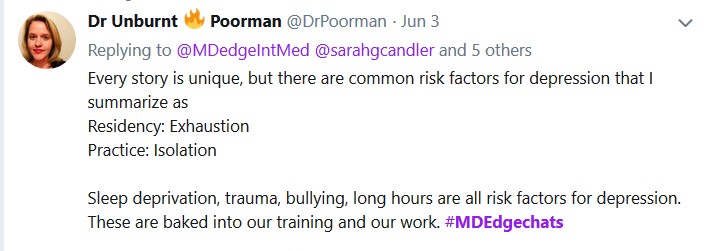
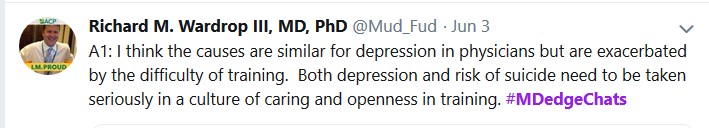
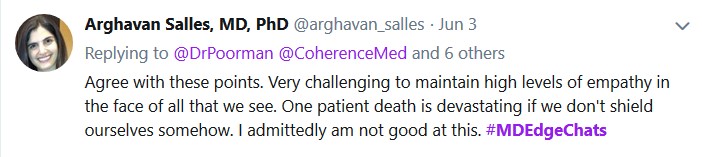
Question 2: "How can we end stigma against seeking mental health treatment among physicians?" is on the next page.

Question 3: "How can we prevent depression and suicide among medical students and physicians" is on the next page.


Question 4: "Which institutions or programs are exemplars in providing resources to improve mental health?" is on the next page.
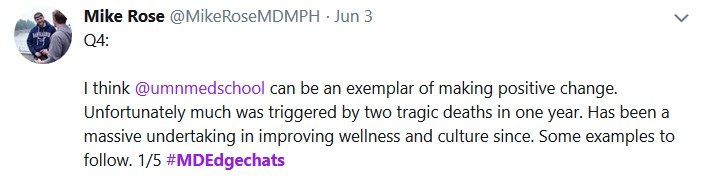
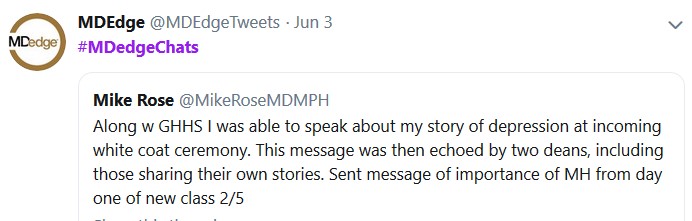
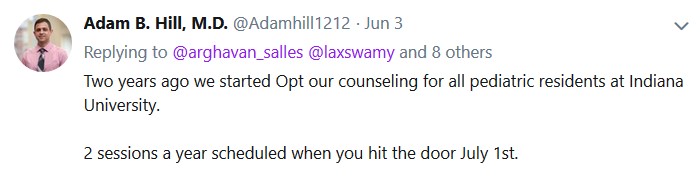


Question 5: "What organizational and political changes are likely to reduce physician suicides?" is on the next page.
Many physicians work long hours and may ignore the fatigue and emotional toll that comes with those pressures. The stress cannot only lead to crippling depression but also to declined mental health and even thoughts of suicide.
Each year, an estimated 400 physicians take their own lives, mostly because of depression and stress, according to the West Journal of Emergency Medicine.
MDedge Internal Medicine recently hosted a Twitter conversation (#MDedgeChats) on how the health care community can address this emerging crisis and help their colleagues understand that they are not alone. Two primary care physicians — Sarah Candler, MD, and Elisabeth Poorman, MD — led the conversation, with guests Michael Rose, MD, Arghavan Salles, MD, Richard M. Wardrop III, MD, Jessica Gold, MD, and Janae Sharp.
Throughout the conversation, physicians encouraged other medical professionals to seek help if it is needed. “If you don’t feel comfortable sharing with your team, feel free to share with folks you met here,” Dr. Candler wrote. “Please seek professional solace with a therapist! That’s what this is about – the support to do what you need for yourself. Good doctors take care of themselves, too.”
These issues are not just important in the medical community “because everyone will get sick, and we are failing each other. We are failing our patients and our communities when we won’t fight for change. The center will not hold here,” said Dr. Elizabeth Poorman.
The following is an edited version of the discussion.
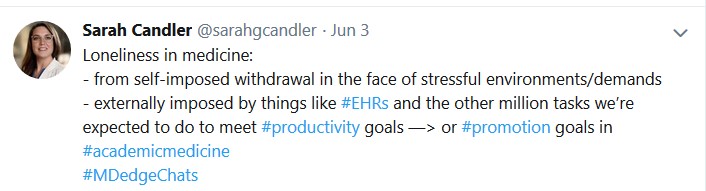
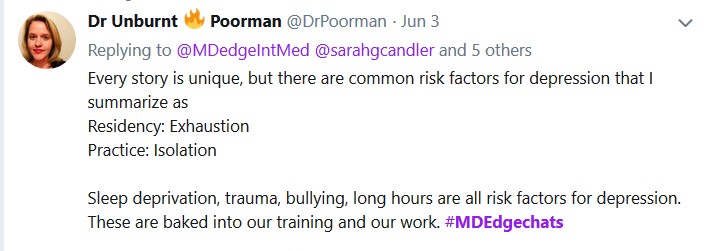
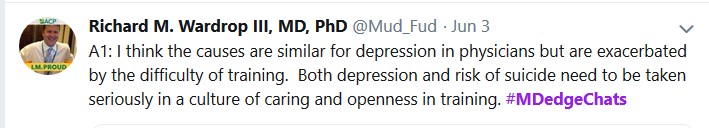
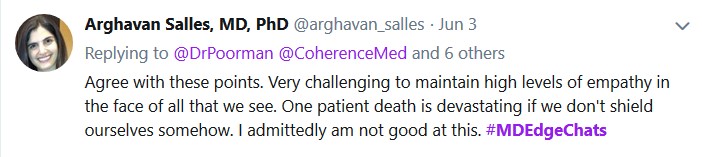
Question 2: "How can we end stigma against seeking mental health treatment among physicians?" is on the next page.
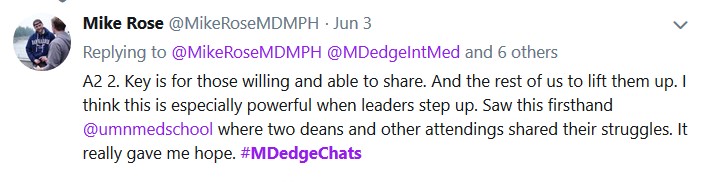

Question 3: "How can we prevent depression and suicide among medical students and physicians" is on the next page.


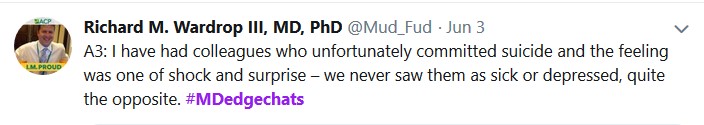
Question 4: "Which institutions or programs are exemplars in providing resources to improve mental health?" is on the next page.


Question 5: "What organizational and political changes are likely to reduce physician suicides?" is on the next page.
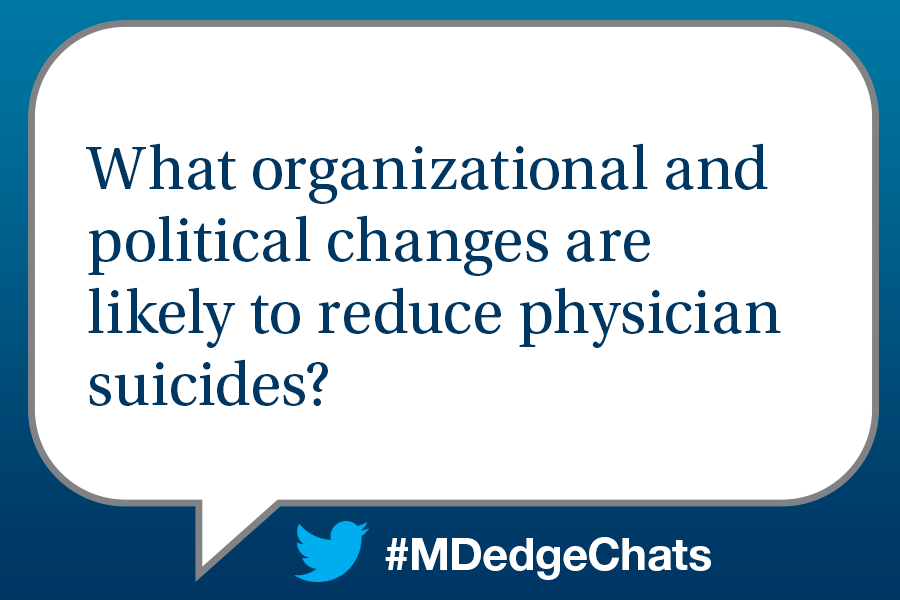
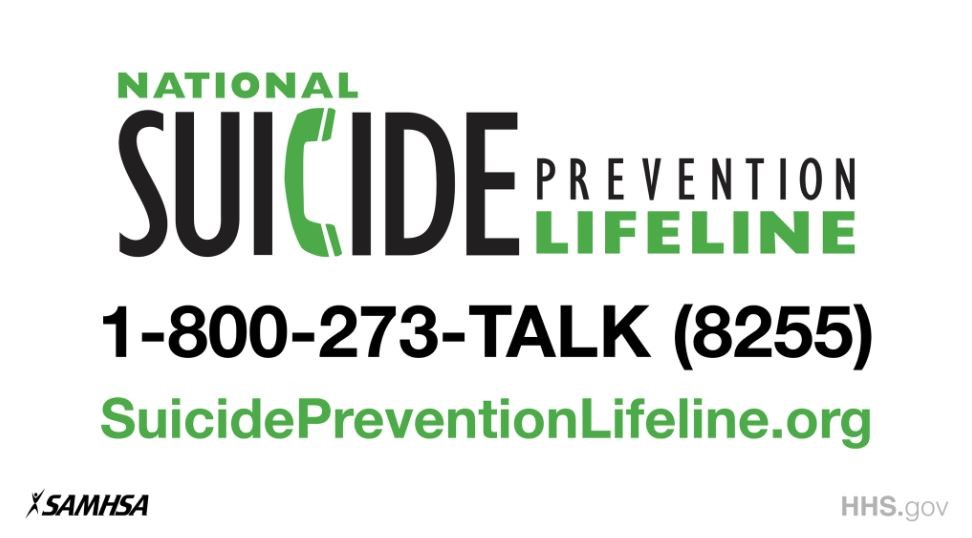
Many physicians work long hours and may ignore the fatigue and emotional toll that comes with those pressures. The stress cannot only lead to crippling depression but also to declined mental health and even thoughts of suicide.
Each year, an estimated 400 physicians take their own lives, mostly because of depression and stress, according to the West Journal of Emergency Medicine.
MDedge Internal Medicine recently hosted a Twitter conversation (#MDedgeChats) on how the health care community can address this emerging crisis and help their colleagues understand that they are not alone. Two primary care physicians — Sarah Candler, MD, and Elisabeth Poorman, MD — led the conversation, with guests Michael Rose, MD, Arghavan Salles, MD, Richard M. Wardrop III, MD, Jessica Gold, MD, and Janae Sharp.
Throughout the conversation, physicians encouraged other medical professionals to seek help if it is needed. “If you don’t feel comfortable sharing with your team, feel free to share with folks you met here,” Dr. Candler wrote. “Please seek professional solace with a therapist! That’s what this is about – the support to do what you need for yourself. Good doctors take care of themselves, too.”
These issues are not just important in the medical community “because everyone will get sick, and we are failing each other. We are failing our patients and our communities when we won’t fight for change. The center will not hold here,” said Dr. Elizabeth Poorman.
The following is an edited version of the discussion.
Question 2: "How can we end stigma against seeking mental health treatment among physicians?" is on the next page.
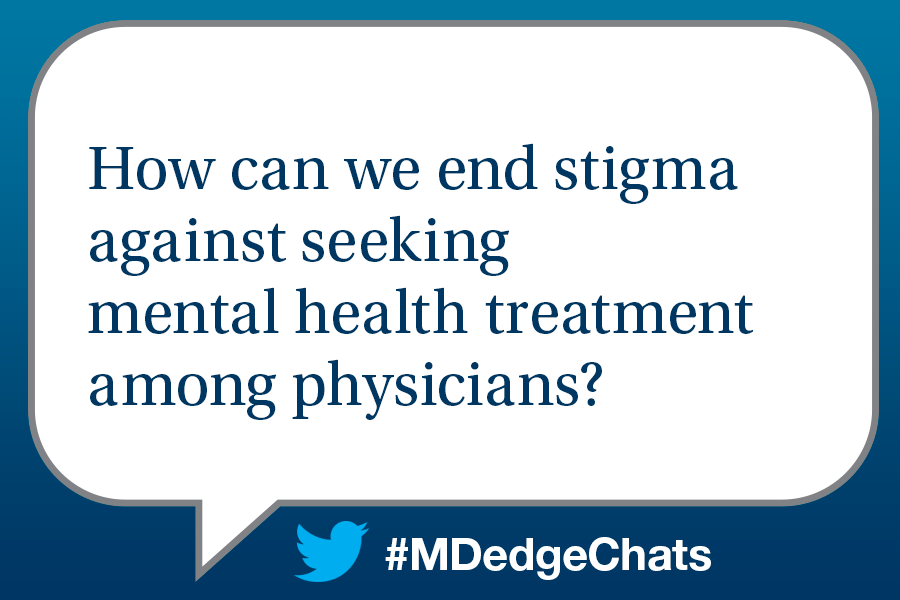
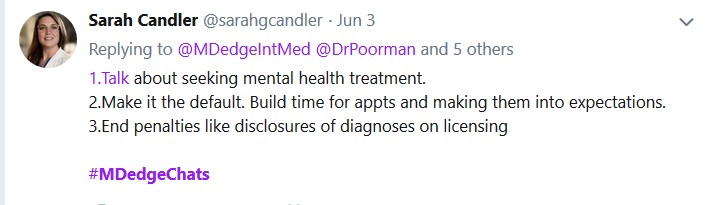
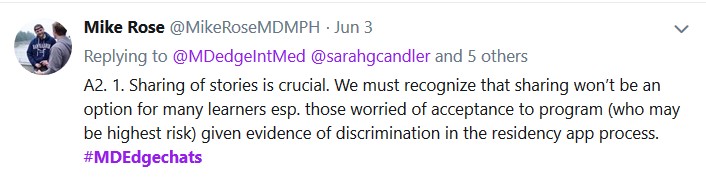
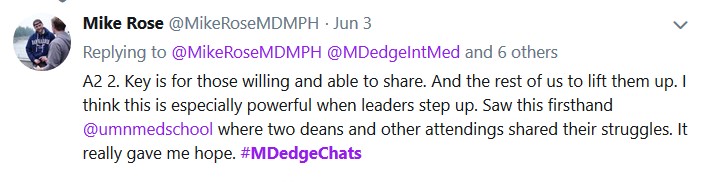

Question 3: "How can we prevent depression and suicide among medical students and physicians" is on the next page.


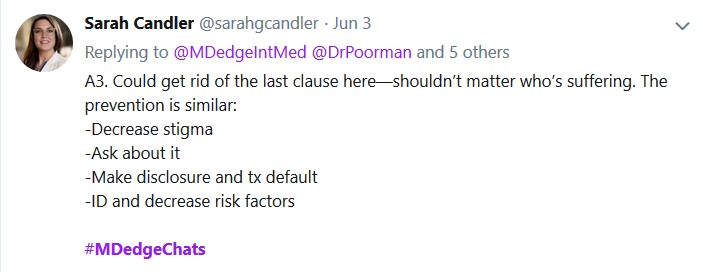
Question 4: "Which institutions or programs are exemplars in providing resources to improve mental health?" is on the next page.


Question 5: "What organizational and political changes are likely to reduce physician suicides?" is on the next page.
Excellence in Community Service Award to be Presented at Gala
In its inaugural year, the Excellence in Community service award will be presented this Friday at VAM during the ‘Vascular Spectacular’ Gala. This year’s winners are Drs. Richard Lynn, Carlo Dall’Olmo and Joseph Anain. These members have all exhibited outstanding leadership within their community as practicing vascular surgeons and are recognized for their sustained contributions to patients and their communities. Read more about the Excellence in Community Service award here.
In its inaugural year, the Excellence in Community service award will be presented this Friday at VAM during the ‘Vascular Spectacular’ Gala. This year’s winners are Drs. Richard Lynn, Carlo Dall’Olmo and Joseph Anain. These members have all exhibited outstanding leadership within their community as practicing vascular surgeons and are recognized for their sustained contributions to patients and their communities. Read more about the Excellence in Community Service award here.
In its inaugural year, the Excellence in Community service award will be presented this Friday at VAM during the ‘Vascular Spectacular’ Gala. This year’s winners are Drs. Richard Lynn, Carlo Dall’Olmo and Joseph Anain. These members have all exhibited outstanding leadership within their community as practicing vascular surgeons and are recognized for their sustained contributions to patients and their communities. Read more about the Excellence in Community Service award here.
Bidding for Silent Auction Open
Join others in placing bids on items available in the ‘Vascular Spectacular’ gala’s silent auction. Items include, but are not limited to, artwork, fine wines, travel experiences and sports memorabilia. Bidding will be open until this Friday, June 14, so be sure to bid early and often. The Gala will take place at the Vascular Annual Meeting and all proceeds benefit the work of the SVS Foundation. Sign up to participate here.
Join others in placing bids on items available in the ‘Vascular Spectacular’ gala’s silent auction. Items include, but are not limited to, artwork, fine wines, travel experiences and sports memorabilia. Bidding will be open until this Friday, June 14, so be sure to bid early and often. The Gala will take place at the Vascular Annual Meeting and all proceeds benefit the work of the SVS Foundation. Sign up to participate here.
Join others in placing bids on items available in the ‘Vascular Spectacular’ gala’s silent auction. Items include, but are not limited to, artwork, fine wines, travel experiences and sports memorabilia. Bidding will be open until this Friday, June 14, so be sure to bid early and often. The Gala will take place at the Vascular Annual Meeting and all proceeds benefit the work of the SVS Foundation. Sign up to participate here.
New CLTI Global Guidelines Available
On May 31, new global guidelines on the best ways to treat Chronic Limb-Threatening Ischemia were co-published in the Journal of Vascular Surgery and the European Journal of Vascular and Endovascular Surgery. This comes after four years of collaboration between vascular experts from around the world. According to the SVS’ own Dr. Conte, a co-editor, the group created a unique practice guideline that reflects the spectrum of the diseases and the approaches seen worldwide. Read the guidelines in the JVS here.
On May 31, new global guidelines on the best ways to treat Chronic Limb-Threatening Ischemia were co-published in the Journal of Vascular Surgery and the European Journal of Vascular and Endovascular Surgery. This comes after four years of collaboration between vascular experts from around the world. According to the SVS’ own Dr. Conte, a co-editor, the group created a unique practice guideline that reflects the spectrum of the diseases and the approaches seen worldwide. Read the guidelines in the JVS here.
On May 31, new global guidelines on the best ways to treat Chronic Limb-Threatening Ischemia were co-published in the Journal of Vascular Surgery and the European Journal of Vascular and Endovascular Surgery. This comes after four years of collaboration between vascular experts from around the world. According to the SVS’ own Dr. Conte, a co-editor, the group created a unique practice guideline that reflects the spectrum of the diseases and the approaches seen worldwide. Read the guidelines in the JVS here.