User login
In Memoriam
Decline in CIN2+ in younger women after HPV vaccine introduced
The introduction of human papillomavirus vaccination in the United States in 2006 was associated with a significant decrease in the rates of cervical intraepithelial neoplasia grades 2 and above (CIN2+) in younger women.
The overall rate of CIN2+ declined from an estimated 216,000 cases in 2008 – 55% of which were in women aged 18-29 years – to 196,000 cases in 2016, of which 36% were in women aged 18-29 years, according to analysis of data from the Human Papillomavirus Vaccine Impact Monitoring Program (MMWR. 2019 Apr 19;68:337-43.
In 2008, the highest rates of CIN2+ were seen in women aged 20-24 years and decreased with age, but in 2016, the highest rates were in women aged 25-29 years. The rates of CIN2+ declined significantly in women aged 18-19 years from 2008-2016, but increased in women aged 40-64 years.
In 2008 and 2016, around three-quarters of all CIN2+ cases were attributable to HPV types that are targeted by the HPV vaccine. However the rates of vaccine-preventable CIN2+ declined among women aged 18-24 years, from 52% in 2008 to 30% in 2016.
“Both the estimated number and rates of U.S. CIN2+ cases in this report must be interpreted in the context of cervical cancer prevention strategies, including HPV vaccination and cervical cancer screening,” wrote Nancy M. McClung, PhD, of the Epidemic Intelligence Service at the Centers for Disease Control and Prevention and coauthors.
Notably, the screening interval for cervical cancer was increased from yearly in 2008 to once in 3 years with cytology alone or once in 5 years with cytology plus HPV testing for women aged 30 or above in 2016.
“Older age at screening initiation, longer screening intervals, and more conservative management in young women might be expected to reduce the number of CIN2+ cases detected in younger age groups in whom lesions are most likely to regress and shift detection of some CIN2+ to older age groups, resulting in a transient increase in rates,” Dr. McClung and colleagues wrote.
However they noted that the decrease in HPV 16/18–attributable CIN2+ rates among younger age groups was likely a reflection of the impact of the introduction of the quadrivalent vaccine immunization program.
One author declared personal fees from Merck during the course of the study. No other conflicts of interest were declared.
SOURCE: McClung N et al. MMWR. 2019 Apr 19;68:337-43.
The introduction of human papillomavirus vaccination in the United States in 2006 was associated with a significant decrease in the rates of cervical intraepithelial neoplasia grades 2 and above (CIN2+) in younger women.
The overall rate of CIN2+ declined from an estimated 216,000 cases in 2008 – 55% of which were in women aged 18-29 years – to 196,000 cases in 2016, of which 36% were in women aged 18-29 years, according to analysis of data from the Human Papillomavirus Vaccine Impact Monitoring Program (MMWR. 2019 Apr 19;68:337-43.
In 2008, the highest rates of CIN2+ were seen in women aged 20-24 years and decreased with age, but in 2016, the highest rates were in women aged 25-29 years. The rates of CIN2+ declined significantly in women aged 18-19 years from 2008-2016, but increased in women aged 40-64 years.
In 2008 and 2016, around three-quarters of all CIN2+ cases were attributable to HPV types that are targeted by the HPV vaccine. However the rates of vaccine-preventable CIN2+ declined among women aged 18-24 years, from 52% in 2008 to 30% in 2016.
“Both the estimated number and rates of U.S. CIN2+ cases in this report must be interpreted in the context of cervical cancer prevention strategies, including HPV vaccination and cervical cancer screening,” wrote Nancy M. McClung, PhD, of the Epidemic Intelligence Service at the Centers for Disease Control and Prevention and coauthors.
Notably, the screening interval for cervical cancer was increased from yearly in 2008 to once in 3 years with cytology alone or once in 5 years with cytology plus HPV testing for women aged 30 or above in 2016.
“Older age at screening initiation, longer screening intervals, and more conservative management in young women might be expected to reduce the number of CIN2+ cases detected in younger age groups in whom lesions are most likely to regress and shift detection of some CIN2+ to older age groups, resulting in a transient increase in rates,” Dr. McClung and colleagues wrote.
However they noted that the decrease in HPV 16/18–attributable CIN2+ rates among younger age groups was likely a reflection of the impact of the introduction of the quadrivalent vaccine immunization program.
One author declared personal fees from Merck during the course of the study. No other conflicts of interest were declared.
SOURCE: McClung N et al. MMWR. 2019 Apr 19;68:337-43.
The introduction of human papillomavirus vaccination in the United States in 2006 was associated with a significant decrease in the rates of cervical intraepithelial neoplasia grades 2 and above (CIN2+) in younger women.
The overall rate of CIN2+ declined from an estimated 216,000 cases in 2008 – 55% of which were in women aged 18-29 years – to 196,000 cases in 2016, of which 36% were in women aged 18-29 years, according to analysis of data from the Human Papillomavirus Vaccine Impact Monitoring Program (MMWR. 2019 Apr 19;68:337-43.
In 2008, the highest rates of CIN2+ were seen in women aged 20-24 years and decreased with age, but in 2016, the highest rates were in women aged 25-29 years. The rates of CIN2+ declined significantly in women aged 18-19 years from 2008-2016, but increased in women aged 40-64 years.
In 2008 and 2016, around three-quarters of all CIN2+ cases were attributable to HPV types that are targeted by the HPV vaccine. However the rates of vaccine-preventable CIN2+ declined among women aged 18-24 years, from 52% in 2008 to 30% in 2016.
“Both the estimated number and rates of U.S. CIN2+ cases in this report must be interpreted in the context of cervical cancer prevention strategies, including HPV vaccination and cervical cancer screening,” wrote Nancy M. McClung, PhD, of the Epidemic Intelligence Service at the Centers for Disease Control and Prevention and coauthors.
Notably, the screening interval for cervical cancer was increased from yearly in 2008 to once in 3 years with cytology alone or once in 5 years with cytology plus HPV testing for women aged 30 or above in 2016.
“Older age at screening initiation, longer screening intervals, and more conservative management in young women might be expected to reduce the number of CIN2+ cases detected in younger age groups in whom lesions are most likely to regress and shift detection of some CIN2+ to older age groups, resulting in a transient increase in rates,” Dr. McClung and colleagues wrote.
However they noted that the decrease in HPV 16/18–attributable CIN2+ rates among younger age groups was likely a reflection of the impact of the introduction of the quadrivalent vaccine immunization program.
One author declared personal fees from Merck during the course of the study. No other conflicts of interest were declared.
SOURCE: McClung N et al. MMWR. 2019 Apr 19;68:337-43.
FROM MMWR
A Critical Review of Periodic Health Screening Using Specific Screening Criteria: Part 3: Selected Diseases of the Genitourinary System
Back to the drawing board for MPN combo
NEWPORT BEACH, CALIF. – The combination of ruxolitinib and decitabine will not proceed to a phase 3 trial in patients with accelerated or blast phase myeloproliferative neoplasms (MPNs).
The combination demonstrated activity and tolerability in a phase 2 trial, but outcomes were not optimal, according to Raajit K. Rampal, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
“[P]erhaps the outcomes might be favorable compared to standard induction chemotherapy regimens,” Dr. Rampal said. “Nonetheless, it’s clear that we still have a lot of work to do, and the outcomes are not optimal in these patients.”
However, Dr. Rampal and his colleagues are investigating the possibility of combining ruxolitinib and decitabine with other agents to treat patients with accelerated or blast phase MPNs.
Dr. Rampal and his colleagues presented results from the phase 2 trial in a poster at the Acute Leukemia Forum of Hemedicus.
The trial (NCT02076191) enrolled 25 patients, 10 with accelerated phase MPN (10%-19% blasts) and 15 with blast phase MPN (at least 20% blasts). The patients’ median age was 71 years.
Patients had a median disease duration of 72.9 months. Six patients (25%) had received prior ruxolitinib, and two (8.3%) had received prior decitabine.
Treatment and safety
For the first cycle, patients received decitabine at 20 mg/m2 per day on days 8-12 and ruxolitinib at 25 mg twice a day on days 1-35. For subsequent cycles, patients received the same dose of decitabine on days 1-5 and ruxolitinib at 10 mg twice a day on days 6-28. Patients were treated until progression, withdrawal, or unacceptable toxicity.
“The adverse events we saw in this study were typical for this population, including fevers, mostly neutropenic fevers, as well as anemia and thrombocytopenia,” Dr. Rampal said.
Nonhematologic adverse events (AEs) included fatigue, abdominal pain, pneumonia, diarrhea, dizziness, and constipation. Hematologic AEs included anemia, neutropenia, febrile neutropenia, and thrombocytopenia.
Response and survival
Eighteen patients were evaluable for response. Four patients were not evaluable because they withdrew from the study due to secondary AEs and completed one cycle of therapy or less, two patients did not have circulating blasts at baseline, and one patient refused further treatment.
Among the evaluable patients, nine (50%) achieved a partial response, including four patients with accelerated phase MPN and five with blast phase MPN.
Two patients (11.1%), one with accelerated phase MPN and one with blast phase MPN, achieved a complete response with incomplete count recovery.
The remaining seven patients (38.9%), five with blast phase MPN and two with accelerated phase MPN, did not respond.
The median overall survival was 7.6 months for the entire cohort, 9.7 months for patients with blast phase MPN, and 5.8 months for patients with accelerated phase MPN.
Based on these results, Dr. Rampal and his colleagues theorized that ruxolitinib plus decitabine might be improved by the addition of other agents. The researchers are currently investigating this possibility.
“The work for this trial really came out of preclinical work in the laboratory where we combined these drugs and saw efficacy in murine models,” Dr. Rampal said. “So we’re going back to the drawing board and looking at those again to see, ‘Can we come up with new rational combinations?’ ”
Dr. Rampal and his colleagues reported having no conflicts of interest. Their study was supported by the National Institutes of Health, the National Cancer Institute, and Incyte Corporation.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
NEWPORT BEACH, CALIF. – The combination of ruxolitinib and decitabine will not proceed to a phase 3 trial in patients with accelerated or blast phase myeloproliferative neoplasms (MPNs).
The combination demonstrated activity and tolerability in a phase 2 trial, but outcomes were not optimal, according to Raajit K. Rampal, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
“[P]erhaps the outcomes might be favorable compared to standard induction chemotherapy regimens,” Dr. Rampal said. “Nonetheless, it’s clear that we still have a lot of work to do, and the outcomes are not optimal in these patients.”
However, Dr. Rampal and his colleagues are investigating the possibility of combining ruxolitinib and decitabine with other agents to treat patients with accelerated or blast phase MPNs.
Dr. Rampal and his colleagues presented results from the phase 2 trial in a poster at the Acute Leukemia Forum of Hemedicus.
The trial (NCT02076191) enrolled 25 patients, 10 with accelerated phase MPN (10%-19% blasts) and 15 with blast phase MPN (at least 20% blasts). The patients’ median age was 71 years.
Patients had a median disease duration of 72.9 months. Six patients (25%) had received prior ruxolitinib, and two (8.3%) had received prior decitabine.
Treatment and safety
For the first cycle, patients received decitabine at 20 mg/m2 per day on days 8-12 and ruxolitinib at 25 mg twice a day on days 1-35. For subsequent cycles, patients received the same dose of decitabine on days 1-5 and ruxolitinib at 10 mg twice a day on days 6-28. Patients were treated until progression, withdrawal, or unacceptable toxicity.
“The adverse events we saw in this study were typical for this population, including fevers, mostly neutropenic fevers, as well as anemia and thrombocytopenia,” Dr. Rampal said.
Nonhematologic adverse events (AEs) included fatigue, abdominal pain, pneumonia, diarrhea, dizziness, and constipation. Hematologic AEs included anemia, neutropenia, febrile neutropenia, and thrombocytopenia.
Response and survival
Eighteen patients were evaluable for response. Four patients were not evaluable because they withdrew from the study due to secondary AEs and completed one cycle of therapy or less, two patients did not have circulating blasts at baseline, and one patient refused further treatment.
Among the evaluable patients, nine (50%) achieved a partial response, including four patients with accelerated phase MPN and five with blast phase MPN.
Two patients (11.1%), one with accelerated phase MPN and one with blast phase MPN, achieved a complete response with incomplete count recovery.
The remaining seven patients (38.9%), five with blast phase MPN and two with accelerated phase MPN, did not respond.
The median overall survival was 7.6 months for the entire cohort, 9.7 months for patients with blast phase MPN, and 5.8 months for patients with accelerated phase MPN.
Based on these results, Dr. Rampal and his colleagues theorized that ruxolitinib plus decitabine might be improved by the addition of other agents. The researchers are currently investigating this possibility.
“The work for this trial really came out of preclinical work in the laboratory where we combined these drugs and saw efficacy in murine models,” Dr. Rampal said. “So we’re going back to the drawing board and looking at those again to see, ‘Can we come up with new rational combinations?’ ”
Dr. Rampal and his colleagues reported having no conflicts of interest. Their study was supported by the National Institutes of Health, the National Cancer Institute, and Incyte Corporation.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
NEWPORT BEACH, CALIF. – The combination of ruxolitinib and decitabine will not proceed to a phase 3 trial in patients with accelerated or blast phase myeloproliferative neoplasms (MPNs).
The combination demonstrated activity and tolerability in a phase 2 trial, but outcomes were not optimal, according to Raajit K. Rampal, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
“[P]erhaps the outcomes might be favorable compared to standard induction chemotherapy regimens,” Dr. Rampal said. “Nonetheless, it’s clear that we still have a lot of work to do, and the outcomes are not optimal in these patients.”
However, Dr. Rampal and his colleagues are investigating the possibility of combining ruxolitinib and decitabine with other agents to treat patients with accelerated or blast phase MPNs.
Dr. Rampal and his colleagues presented results from the phase 2 trial in a poster at the Acute Leukemia Forum of Hemedicus.
The trial (NCT02076191) enrolled 25 patients, 10 with accelerated phase MPN (10%-19% blasts) and 15 with blast phase MPN (at least 20% blasts). The patients’ median age was 71 years.
Patients had a median disease duration of 72.9 months. Six patients (25%) had received prior ruxolitinib, and two (8.3%) had received prior decitabine.
Treatment and safety
For the first cycle, patients received decitabine at 20 mg/m2 per day on days 8-12 and ruxolitinib at 25 mg twice a day on days 1-35. For subsequent cycles, patients received the same dose of decitabine on days 1-5 and ruxolitinib at 10 mg twice a day on days 6-28. Patients were treated until progression, withdrawal, or unacceptable toxicity.
“The adverse events we saw in this study were typical for this population, including fevers, mostly neutropenic fevers, as well as anemia and thrombocytopenia,” Dr. Rampal said.
Nonhematologic adverse events (AEs) included fatigue, abdominal pain, pneumonia, diarrhea, dizziness, and constipation. Hematologic AEs included anemia, neutropenia, febrile neutropenia, and thrombocytopenia.
Response and survival
Eighteen patients were evaluable for response. Four patients were not evaluable because they withdrew from the study due to secondary AEs and completed one cycle of therapy or less, two patients did not have circulating blasts at baseline, and one patient refused further treatment.
Among the evaluable patients, nine (50%) achieved a partial response, including four patients with accelerated phase MPN and five with blast phase MPN.
Two patients (11.1%), one with accelerated phase MPN and one with blast phase MPN, achieved a complete response with incomplete count recovery.
The remaining seven patients (38.9%), five with blast phase MPN and two with accelerated phase MPN, did not respond.
The median overall survival was 7.6 months for the entire cohort, 9.7 months for patients with blast phase MPN, and 5.8 months for patients with accelerated phase MPN.
Based on these results, Dr. Rampal and his colleagues theorized that ruxolitinib plus decitabine might be improved by the addition of other agents. The researchers are currently investigating this possibility.
“The work for this trial really came out of preclinical work in the laboratory where we combined these drugs and saw efficacy in murine models,” Dr. Rampal said. “So we’re going back to the drawing board and looking at those again to see, ‘Can we come up with new rational combinations?’ ”
Dr. Rampal and his colleagues reported having no conflicts of interest. Their study was supported by the National Institutes of Health, the National Cancer Institute, and Incyte Corporation.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
REPORTING FROM ALF 2019
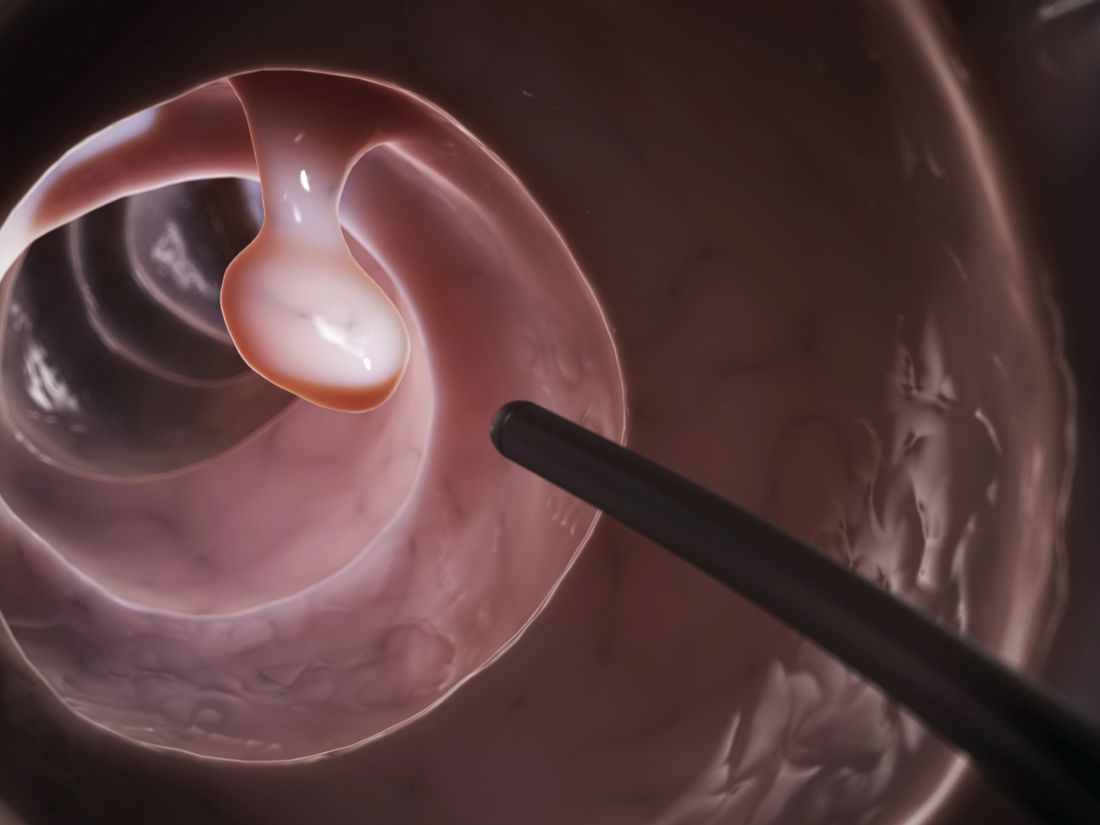
Polyp detection rates during colonoscopy similar among endoscopists
“We sought to assess the association between endoscopist characteristics and adenoma detection rates [ADRs] and proximal sessile serrated polyp detection rates [pSSPDRs],” wrote Shashank Sarvepalli, MD, MS, of the Cleveland Clinic along with his colleagues. The findings were reported in JAMA Surgery.
The researchers conducted a retrospective cohort study of 16,089 patients who underwent screening colonoscopies that were conducted by 56 endoscopists. Data were obtained from the Cleveland Clinic health system during 2015-2017.
Dr. Sarvepalli and his colleagues analyzed seven surgeon characteristics, including time since completion of training, number of colonoscopies performed annually, specialty, and practice setting. Subsequently, they examined the relationships between ADRs and pSSPDRs and these parameters.
“Only patients undergoing normal-risk screening colonoscopies and colonoscopies performed by clinicians who performed more than 100 normal-risk screening colonoscopies during the study period were included,” the researchers wrote.
After analysis, the researchers found that ADR was not significantly associated with any of the characteristics, while pSSPDR was significantly associated with number of years in practice (odds ratio per increment of 10 years, 0.86; 95% confidence interval, 0.83-0.89; P less than .001) and annual colonoscopies completed (OR per 50 colonoscopies annually, 1.05; 95% CI, 1.01-1.09; P = .02).
“After adjusting for additional factors, no difference in detection based on endoscopist characteristics was found,” they added.
The researchers acknowledged that a key limitation of the study was the retrospective design. As a result, the team reported that the findings could be prone to exclusions and misreporting.
No funding sources were reported, and the authors reported no conflicts of interest.
SOURCE: Sarvepalli S et al. JAMA Surg. 2019 Apr 17. doi: 10.1001/jamasurg.2019.0564.
“We sought to assess the association between endoscopist characteristics and adenoma detection rates [ADRs] and proximal sessile serrated polyp detection rates [pSSPDRs],” wrote Shashank Sarvepalli, MD, MS, of the Cleveland Clinic along with his colleagues. The findings were reported in JAMA Surgery.
The researchers conducted a retrospective cohort study of 16,089 patients who underwent screening colonoscopies that were conducted by 56 endoscopists. Data were obtained from the Cleveland Clinic health system during 2015-2017.
Dr. Sarvepalli and his colleagues analyzed seven surgeon characteristics, including time since completion of training, number of colonoscopies performed annually, specialty, and practice setting. Subsequently, they examined the relationships between ADRs and pSSPDRs and these parameters.
“Only patients undergoing normal-risk screening colonoscopies and colonoscopies performed by clinicians who performed more than 100 normal-risk screening colonoscopies during the study period were included,” the researchers wrote.
After analysis, the researchers found that ADR was not significantly associated with any of the characteristics, while pSSPDR was significantly associated with number of years in practice (odds ratio per increment of 10 years, 0.86; 95% confidence interval, 0.83-0.89; P less than .001) and annual colonoscopies completed (OR per 50 colonoscopies annually, 1.05; 95% CI, 1.01-1.09; P = .02).
“After adjusting for additional factors, no difference in detection based on endoscopist characteristics was found,” they added.
The researchers acknowledged that a key limitation of the study was the retrospective design. As a result, the team reported that the findings could be prone to exclusions and misreporting.
No funding sources were reported, and the authors reported no conflicts of interest.
SOURCE: Sarvepalli S et al. JAMA Surg. 2019 Apr 17. doi: 10.1001/jamasurg.2019.0564.
“We sought to assess the association between endoscopist characteristics and adenoma detection rates [ADRs] and proximal sessile serrated polyp detection rates [pSSPDRs],” wrote Shashank Sarvepalli, MD, MS, of the Cleveland Clinic along with his colleagues. The findings were reported in JAMA Surgery.
The researchers conducted a retrospective cohort study of 16,089 patients who underwent screening colonoscopies that were conducted by 56 endoscopists. Data were obtained from the Cleveland Clinic health system during 2015-2017.
Dr. Sarvepalli and his colleagues analyzed seven surgeon characteristics, including time since completion of training, number of colonoscopies performed annually, specialty, and practice setting. Subsequently, they examined the relationships between ADRs and pSSPDRs and these parameters.
“Only patients undergoing normal-risk screening colonoscopies and colonoscopies performed by clinicians who performed more than 100 normal-risk screening colonoscopies during the study period were included,” the researchers wrote.
After analysis, the researchers found that ADR was not significantly associated with any of the characteristics, while pSSPDR was significantly associated with number of years in practice (odds ratio per increment of 10 years, 0.86; 95% confidence interval, 0.83-0.89; P less than .001) and annual colonoscopies completed (OR per 50 colonoscopies annually, 1.05; 95% CI, 1.01-1.09; P = .02).
“After adjusting for additional factors, no difference in detection based on endoscopist characteristics was found,” they added.
The researchers acknowledged that a key limitation of the study was the retrospective design. As a result, the team reported that the findings could be prone to exclusions and misreporting.
No funding sources were reported, and the authors reported no conflicts of interest.
SOURCE: Sarvepalli S et al. JAMA Surg. 2019 Apr 17. doi: 10.1001/jamasurg.2019.0564.
FROM JAMA SURGERY
Reviews of Audiovisual Materials
Physicians discuss bringing cultural humility to medicine
PHILADELPHIA – during a panel discussion moderated by Sarah Candler, MD, an internist in Houston.
Dr. Candler, former chair, Council of Resident and Fellow Members, Board of Regents, American College of Physicians, began the discussion by asking Dr. DeLisser, to describe his role in teaching medical students about the social determinants of health, at the annual Internal Medicine meeting of the ACP.
Dr. DeLisser, associate dean for professionalism and humanism at the University of Pennsylvania, Philadelphia, said he focuses on a number of issues, including social medicine, cultural competency, and cultural humility.
“We look at health care disparities and try to do a lot of innovation around service learning that will bring our students into the community, one to learn about these determinants but more importantly to be able to see how these issues can be addressed both on a provider level but also on a more structural systemic level,” he noted.
Dr. Poorman, an internist at the University of Washington, later discussed the importance of practicing cultural humility as it related to her experience providing care to migrant workers while she was a medical school student.
Dr. Candler, an internist in Houston, concluded the discussion by describing some of the ACP’s newest resources designed to address the social determinants of health for specific groups of patients.
The full panel discussion was recorded as a video.
PHILADELPHIA – during a panel discussion moderated by Sarah Candler, MD, an internist in Houston.
Dr. Candler, former chair, Council of Resident and Fellow Members, Board of Regents, American College of Physicians, began the discussion by asking Dr. DeLisser, to describe his role in teaching medical students about the social determinants of health, at the annual Internal Medicine meeting of the ACP.
Dr. DeLisser, associate dean for professionalism and humanism at the University of Pennsylvania, Philadelphia, said he focuses on a number of issues, including social medicine, cultural competency, and cultural humility.
“We look at health care disparities and try to do a lot of innovation around service learning that will bring our students into the community, one to learn about these determinants but more importantly to be able to see how these issues can be addressed both on a provider level but also on a more structural systemic level,” he noted.
Dr. Poorman, an internist at the University of Washington, later discussed the importance of practicing cultural humility as it related to her experience providing care to migrant workers while she was a medical school student.
Dr. Candler, an internist in Houston, concluded the discussion by describing some of the ACP’s newest resources designed to address the social determinants of health for specific groups of patients.
The full panel discussion was recorded as a video.
PHILADELPHIA – during a panel discussion moderated by Sarah Candler, MD, an internist in Houston.
Dr. Candler, former chair, Council of Resident and Fellow Members, Board of Regents, American College of Physicians, began the discussion by asking Dr. DeLisser, to describe his role in teaching medical students about the social determinants of health, at the annual Internal Medicine meeting of the ACP.
Dr. DeLisser, associate dean for professionalism and humanism at the University of Pennsylvania, Philadelphia, said he focuses on a number of issues, including social medicine, cultural competency, and cultural humility.
“We look at health care disparities and try to do a lot of innovation around service learning that will bring our students into the community, one to learn about these determinants but more importantly to be able to see how these issues can be addressed both on a provider level but also on a more structural systemic level,” he noted.
Dr. Poorman, an internist at the University of Washington, later discussed the importance of practicing cultural humility as it related to her experience providing care to migrant workers while she was a medical school student.
Dr. Candler, an internist in Houston, concluded the discussion by describing some of the ACP’s newest resources designed to address the social determinants of health for specific groups of patients.
The full panel discussion was recorded as a video.
REPORTING FROM INTERNAL MEDICINE 2019
Reviews of Audiovisual Materials
The Future of Physician Extenders: An Emphatically Divergent View
ENCORE-601: Entinostat/pembrolizumab safe, active for melanoma
ATLANTA – Combined therapy with the class I selective histone deacetylase (HDAC) inhibitor entinostat and the programmed cell death 1 (PD-1) inhibitor pembrolizumab has significant clinical activity and acceptable safety in melanoma patients who progressed on prior PD-1 blockade, according to findings from the open-label ENCORE-601 trial.
Of 53 patients with recurrent or metastatic melanoma who were treated with 5 mg of oral entinostat weekly plus 200 mg of intravenous pembrolizumab every 3 weeks, 1 had a complete response, and 9 had a partial response, for an objective response rate of 19%, Ryan J. Sullivan, MD, reported at the annual meeting of the American Association for Cancer Research.
The median duration of response at the January 2018 data cut-off was 13 months, and four responders had ongoing responses. An additional nine patients had stable disease for at least 6 months at that time, for a clinical benefit rate of 36%, said Dr. Sullivan of Massachusetts General Hospital, Boston.
“At 1 year, 10 patients remained on therapy or in response,” he said, noting that, although one patient had received only a very short course of therapy before developing “significant hepatitis” and coming off therapy, but this patient still had a response at 1 year. Five others also went off therapy and continue to have a response, and four patients remain on active therapy and are being followed, he said.
Study participants are adults with Eastern Cooperative Oncology Group Performance Status of less than 2 who were previously treated with a PD-1–blocking antibody and experienced progression on or after therapy. The 23% of patients with a BRAF V600 mutation were required to have received BRAF/MEK therapy, and 70% of patients had received both a prior PD-1 inhibitor and ipilimumab, either in combination or in sequence.
The response rate to prior anti–PD-1 therapy was 13%, which was “much lower than you would imagine in all-comers,” Dr Sullivan said.
Inhibitors of PD-1 and its ligand (PD-L1) have improved outcomes in patients with advanced melanoma, but despite the progress, most patients develop resistance and most will still die from metastatic melanoma, he said.
“I think its always important to define what the unmet need is, and here it’s quite clear: Most patients are not receiving ultimate benefit, and as a result we need a better therapeutic approach,” he said, adding that “the front-line treatment setting is a critical place to be in terms of clinical trials ... but the most relevant and most unmet need now is what do we do in patients who have received anti–PD-1 therapy and need something else.”
Addressing the unmet need requires an improved understanding of the mechanisms of resistance and the development of more effective therapies, he said.
Dr. Sullivan and his colleagues previously reported preliminary data from the current cohort showing promising activity with entinostat in combination with pembrolizumab, which was found to alter the immunosuppressive tumor microenvironment. The rationale for using entinostat in this setting relates to its down-regulation of immunosuppressive cell types in the tumor microenvironment and its “quite robust” synergy with PD-1 inhibition as demonstrated in preclinical models, he explained.
Following those initial dose and safety findings, four phase 2 expansion cohorts were opened, including two non–small cell lung cancer cohorts, one mismatched-repair proficient colorectal cancer cohort, and the melanoma cohort. The current report, which focused on the latter, showed that the treatment-related adverse events (AEs) occurring in at least 15% of patients included nausea, fatigue, diarrhea, and myelosuppression.
“Six patients discontinued due to related AEs, and importantly, there were only five grade 3 or 4 immune-related AEs,” Dr. Sullivan said, adding that these included one case each of immune-related hepatitis, pneumonitis, and colitis and two cases of significant dermatitis.
The findings show that in this group of patients with limited treatment options, entinostat with pembrolizumab is “clearly safe and tolerable,” he said.
Additionally, “very preliminary biomarker analyses” in a small number of patients demonstrated findings consistent with the mechanism of action of entinostat, including a reduction in circulating myeloid-derived suppressor cells, he said.
Dr. Sullivan reported consulting or serving on an advisory board for Novartis, Amgen, Merck, Array, Syndax, Replimmune, and Bristol-Myers Squibb and receiving research sponsorship from Amgen and Merck & Co.
SOURCE: Sullivan R et al. AACR 2019, Abstract CT-072.
ATLANTA – Combined therapy with the class I selective histone deacetylase (HDAC) inhibitor entinostat and the programmed cell death 1 (PD-1) inhibitor pembrolizumab has significant clinical activity and acceptable safety in melanoma patients who progressed on prior PD-1 blockade, according to findings from the open-label ENCORE-601 trial.
Of 53 patients with recurrent or metastatic melanoma who were treated with 5 mg of oral entinostat weekly plus 200 mg of intravenous pembrolizumab every 3 weeks, 1 had a complete response, and 9 had a partial response, for an objective response rate of 19%, Ryan J. Sullivan, MD, reported at the annual meeting of the American Association for Cancer Research.
The median duration of response at the January 2018 data cut-off was 13 months, and four responders had ongoing responses. An additional nine patients had stable disease for at least 6 months at that time, for a clinical benefit rate of 36%, said Dr. Sullivan of Massachusetts General Hospital, Boston.
“At 1 year, 10 patients remained on therapy or in response,” he said, noting that, although one patient had received only a very short course of therapy before developing “significant hepatitis” and coming off therapy, but this patient still had a response at 1 year. Five others also went off therapy and continue to have a response, and four patients remain on active therapy and are being followed, he said.
Study participants are adults with Eastern Cooperative Oncology Group Performance Status of less than 2 who were previously treated with a PD-1–blocking antibody and experienced progression on or after therapy. The 23% of patients with a BRAF V600 mutation were required to have received BRAF/MEK therapy, and 70% of patients had received both a prior PD-1 inhibitor and ipilimumab, either in combination or in sequence.
The response rate to prior anti–PD-1 therapy was 13%, which was “much lower than you would imagine in all-comers,” Dr Sullivan said.
Inhibitors of PD-1 and its ligand (PD-L1) have improved outcomes in patients with advanced melanoma, but despite the progress, most patients develop resistance and most will still die from metastatic melanoma, he said.
“I think its always important to define what the unmet need is, and here it’s quite clear: Most patients are not receiving ultimate benefit, and as a result we need a better therapeutic approach,” he said, adding that “the front-line treatment setting is a critical place to be in terms of clinical trials ... but the most relevant and most unmet need now is what do we do in patients who have received anti–PD-1 therapy and need something else.”
Addressing the unmet need requires an improved understanding of the mechanisms of resistance and the development of more effective therapies, he said.
Dr. Sullivan and his colleagues previously reported preliminary data from the current cohort showing promising activity with entinostat in combination with pembrolizumab, which was found to alter the immunosuppressive tumor microenvironment. The rationale for using entinostat in this setting relates to its down-regulation of immunosuppressive cell types in the tumor microenvironment and its “quite robust” synergy with PD-1 inhibition as demonstrated in preclinical models, he explained.
Following those initial dose and safety findings, four phase 2 expansion cohorts were opened, including two non–small cell lung cancer cohorts, one mismatched-repair proficient colorectal cancer cohort, and the melanoma cohort. The current report, which focused on the latter, showed that the treatment-related adverse events (AEs) occurring in at least 15% of patients included nausea, fatigue, diarrhea, and myelosuppression.
“Six patients discontinued due to related AEs, and importantly, there were only five grade 3 or 4 immune-related AEs,” Dr. Sullivan said, adding that these included one case each of immune-related hepatitis, pneumonitis, and colitis and two cases of significant dermatitis.
The findings show that in this group of patients with limited treatment options, entinostat with pembrolizumab is “clearly safe and tolerable,” he said.
Additionally, “very preliminary biomarker analyses” in a small number of patients demonstrated findings consistent with the mechanism of action of entinostat, including a reduction in circulating myeloid-derived suppressor cells, he said.
Dr. Sullivan reported consulting or serving on an advisory board for Novartis, Amgen, Merck, Array, Syndax, Replimmune, and Bristol-Myers Squibb and receiving research sponsorship from Amgen and Merck & Co.
SOURCE: Sullivan R et al. AACR 2019, Abstract CT-072.
ATLANTA – Combined therapy with the class I selective histone deacetylase (HDAC) inhibitor entinostat and the programmed cell death 1 (PD-1) inhibitor pembrolizumab has significant clinical activity and acceptable safety in melanoma patients who progressed on prior PD-1 blockade, according to findings from the open-label ENCORE-601 trial.
Of 53 patients with recurrent or metastatic melanoma who were treated with 5 mg of oral entinostat weekly plus 200 mg of intravenous pembrolizumab every 3 weeks, 1 had a complete response, and 9 had a partial response, for an objective response rate of 19%, Ryan J. Sullivan, MD, reported at the annual meeting of the American Association for Cancer Research.
The median duration of response at the January 2018 data cut-off was 13 months, and four responders had ongoing responses. An additional nine patients had stable disease for at least 6 months at that time, for a clinical benefit rate of 36%, said Dr. Sullivan of Massachusetts General Hospital, Boston.
“At 1 year, 10 patients remained on therapy or in response,” he said, noting that, although one patient had received only a very short course of therapy before developing “significant hepatitis” and coming off therapy, but this patient still had a response at 1 year. Five others also went off therapy and continue to have a response, and four patients remain on active therapy and are being followed, he said.
Study participants are adults with Eastern Cooperative Oncology Group Performance Status of less than 2 who were previously treated with a PD-1–blocking antibody and experienced progression on or after therapy. The 23% of patients with a BRAF V600 mutation were required to have received BRAF/MEK therapy, and 70% of patients had received both a prior PD-1 inhibitor and ipilimumab, either in combination or in sequence.
The response rate to prior anti–PD-1 therapy was 13%, which was “much lower than you would imagine in all-comers,” Dr Sullivan said.
Inhibitors of PD-1 and its ligand (PD-L1) have improved outcomes in patients with advanced melanoma, but despite the progress, most patients develop resistance and most will still die from metastatic melanoma, he said.
“I think its always important to define what the unmet need is, and here it’s quite clear: Most patients are not receiving ultimate benefit, and as a result we need a better therapeutic approach,” he said, adding that “the front-line treatment setting is a critical place to be in terms of clinical trials ... but the most relevant and most unmet need now is what do we do in patients who have received anti–PD-1 therapy and need something else.”
Addressing the unmet need requires an improved understanding of the mechanisms of resistance and the development of more effective therapies, he said.
Dr. Sullivan and his colleagues previously reported preliminary data from the current cohort showing promising activity with entinostat in combination with pembrolizumab, which was found to alter the immunosuppressive tumor microenvironment. The rationale for using entinostat in this setting relates to its down-regulation of immunosuppressive cell types in the tumor microenvironment and its “quite robust” synergy with PD-1 inhibition as demonstrated in preclinical models, he explained.
Following those initial dose and safety findings, four phase 2 expansion cohorts were opened, including two non–small cell lung cancer cohorts, one mismatched-repair proficient colorectal cancer cohort, and the melanoma cohort. The current report, which focused on the latter, showed that the treatment-related adverse events (AEs) occurring in at least 15% of patients included nausea, fatigue, diarrhea, and myelosuppression.
“Six patients discontinued due to related AEs, and importantly, there were only five grade 3 or 4 immune-related AEs,” Dr. Sullivan said, adding that these included one case each of immune-related hepatitis, pneumonitis, and colitis and two cases of significant dermatitis.
The findings show that in this group of patients with limited treatment options, entinostat with pembrolizumab is “clearly safe and tolerable,” he said.
Additionally, “very preliminary biomarker analyses” in a small number of patients demonstrated findings consistent with the mechanism of action of entinostat, including a reduction in circulating myeloid-derived suppressor cells, he said.
Dr. Sullivan reported consulting or serving on an advisory board for Novartis, Amgen, Merck, Array, Syndax, Replimmune, and Bristol-Myers Squibb and receiving research sponsorship from Amgen and Merck & Co.
SOURCE: Sullivan R et al. AACR 2019, Abstract CT-072.
REPORTING FROM AACR 2019