User login
Ventricular Arrhythmia Due to MS Treatment
Fingolimod, a sphingosine-1-phosphate receptor modulator, has been used to treat > 55,000 patients in the US, according to the manufacturer (Gilenya/Novartis). It is believed to work by keeping lymphocytes from migrating into the CNS, sequestering them in the lymph nodes.
Although it has been found effective in randomized controlled trials, fingolimod is also known to have a wide range of adverse effects (AEs), including some that are serious and even life-threatening, such as bradycardia and atrioventricular block. The drug is contraindicated for patients who have had myocardial infarction, unstable angina, or heart failure, among other conditions. Ventricular tachycardia has been reported only once, but clinicians from Hurley Medical Center in Flint, Michigan, suggest that it may actually be an underrecognized cause of sudden death.
They describe the case of their patient, a 63-year-old woman with relapsing-remitting multiple sclerosis and hypertension who was about to start fingolomod. She underwent a basal ECG to be cleared before starting treatment. She received her first dose of fingolimod at the cardiology office, was monitored for 6 hours, and went home with a surface-mounted Holter monitor.
Two weeks later, she was in the emergency department because the monitor had captured ventricular tachycardia, and she was reporting palpitations.
Lab work was normal; the echocardiogram was normal. Cardiac monitoring showed no other evidence of cardiac arrhythmias. Her only other medication was amlodipine. The fingolimod was held back. She was observed for4 days then discharged in a stable condition. Her clinicians followed her for 2 months but the arrhythmia did not return.
Although this patient had no further arrhythmias, the authors warn that serious outcomes are possible. They urge health care practitioners to let patients know of this potential AE and advise them to report symptoms such as palpitations immediately.
Fingolimod, a sphingosine-1-phosphate receptor modulator, has been used to treat > 55,000 patients in the US, according to the manufacturer (Gilenya/Novartis). It is believed to work by keeping lymphocytes from migrating into the CNS, sequestering them in the lymph nodes.
Although it has been found effective in randomized controlled trials, fingolimod is also known to have a wide range of adverse effects (AEs), including some that are serious and even life-threatening, such as bradycardia and atrioventricular block. The drug is contraindicated for patients who have had myocardial infarction, unstable angina, or heart failure, among other conditions. Ventricular tachycardia has been reported only once, but clinicians from Hurley Medical Center in Flint, Michigan, suggest that it may actually be an underrecognized cause of sudden death.
They describe the case of their patient, a 63-year-old woman with relapsing-remitting multiple sclerosis and hypertension who was about to start fingolomod. She underwent a basal ECG to be cleared before starting treatment. She received her first dose of fingolimod at the cardiology office, was monitored for 6 hours, and went home with a surface-mounted Holter monitor.
Two weeks later, she was in the emergency department because the monitor had captured ventricular tachycardia, and she was reporting palpitations.
Lab work was normal; the echocardiogram was normal. Cardiac monitoring showed no other evidence of cardiac arrhythmias. Her only other medication was amlodipine. The fingolimod was held back. She was observed for4 days then discharged in a stable condition. Her clinicians followed her for 2 months but the arrhythmia did not return.
Although this patient had no further arrhythmias, the authors warn that serious outcomes are possible. They urge health care practitioners to let patients know of this potential AE and advise them to report symptoms such as palpitations immediately.
Fingolimod, a sphingosine-1-phosphate receptor modulator, has been used to treat > 55,000 patients in the US, according to the manufacturer (Gilenya/Novartis). It is believed to work by keeping lymphocytes from migrating into the CNS, sequestering them in the lymph nodes.
Although it has been found effective in randomized controlled trials, fingolimod is also known to have a wide range of adverse effects (AEs), including some that are serious and even life-threatening, such as bradycardia and atrioventricular block. The drug is contraindicated for patients who have had myocardial infarction, unstable angina, or heart failure, among other conditions. Ventricular tachycardia has been reported only once, but clinicians from Hurley Medical Center in Flint, Michigan, suggest that it may actually be an underrecognized cause of sudden death.
They describe the case of their patient, a 63-year-old woman with relapsing-remitting multiple sclerosis and hypertension who was about to start fingolomod. She underwent a basal ECG to be cleared before starting treatment. She received her first dose of fingolimod at the cardiology office, was monitored for 6 hours, and went home with a surface-mounted Holter monitor.
Two weeks later, she was in the emergency department because the monitor had captured ventricular tachycardia, and she was reporting palpitations.
Lab work was normal; the echocardiogram was normal. Cardiac monitoring showed no other evidence of cardiac arrhythmias. Her only other medication was amlodipine. The fingolimod was held back. She was observed for4 days then discharged in a stable condition. Her clinicians followed her for 2 months but the arrhythmia did not return.
Although this patient had no further arrhythmias, the authors warn that serious outcomes are possible. They urge health care practitioners to let patients know of this potential AE and advise them to report symptoms such as palpitations immediately.
CMS plan will incentivize generic drug use
Patients will still be able to use drug manufacturer coupons and pay less at the pharmacy counter, but the money they spend won’t be applied to their out-of-pocket maximum if they choose the brand-name drug with coupon instead of the lower-cost generic.
The change will affect insurance plans offered in the individual market, small-group, large-group, and self-insured–group health plans.
The Centers for Medicare & Medicaid Services backed away from implementing two other generic drug provisions based on feedback on its draft proposal.
The provisions would have allowed insurers to remove brand-name drugs from a formulary midyear when a generic became available or move the drug to a higher tier, and allowed insurers to not count certain drug copayments toward the annual limits if the patient selected a brand-name drug when a generic was available.
“Based on issues raised by commenters, we are not finalizing these proposals,” CMS officials said.
Insurers “making mid-year formulary changes [should] only be permitted to move the brand-name drug to a different cost-sharing tier for the remainder of the plan year. [They] should not be allowed to remove a safe brand-name drug from the formulary until the time of plan renewal,” the American College of Physicians recommended in Feb. 12 comments on the proposal.
The final rule on Notice of Benefit and Payment Parameters for the 2020 benefit year also aims to provide more stability and lower premiums in the exchanges, according to CMS officials.
“The rule issued today will give consumers immediate premium relief by reducing the exchange user fees in the federally facilitated exchanges and state-based exchanges using the federal platform for 2020 thanks to successful efforts to improve the efficiency of the exchange,” CMS Administrator Seema Verma said in a statement.
CMS finalized a proposal to lower exchange user fees by 0.5%, fees that are generally passed on to consumers through premiums.
Other provisions cover exchange-related calculations, including how subsidies for exchange enrollees are calculated and how much enrollees are expected to contribute to benchmark plan premiums, which decreased slightly to 8.24%, down 0.07%, according to a CMS fact sheet.
For the out-of-pocket maximum, CMS said it “finalized a maximum annual limitation on cost sharing of $8,150 for self-only coverage and $16,300 for other than self-only coverage for the 2020 benefit year. This represents an approximately 3.16% increase above the 2019 parameters of $7,900 for self-only coverage and $15,800 for other than self-only coverage.”
Patients will still be able to use drug manufacturer coupons and pay less at the pharmacy counter, but the money they spend won’t be applied to their out-of-pocket maximum if they choose the brand-name drug with coupon instead of the lower-cost generic.
The change will affect insurance plans offered in the individual market, small-group, large-group, and self-insured–group health plans.
The Centers for Medicare & Medicaid Services backed away from implementing two other generic drug provisions based on feedback on its draft proposal.
The provisions would have allowed insurers to remove brand-name drugs from a formulary midyear when a generic became available or move the drug to a higher tier, and allowed insurers to not count certain drug copayments toward the annual limits if the patient selected a brand-name drug when a generic was available.
“Based on issues raised by commenters, we are not finalizing these proposals,” CMS officials said.
Insurers “making mid-year formulary changes [should] only be permitted to move the brand-name drug to a different cost-sharing tier for the remainder of the plan year. [They] should not be allowed to remove a safe brand-name drug from the formulary until the time of plan renewal,” the American College of Physicians recommended in Feb. 12 comments on the proposal.
The final rule on Notice of Benefit and Payment Parameters for the 2020 benefit year also aims to provide more stability and lower premiums in the exchanges, according to CMS officials.
“The rule issued today will give consumers immediate premium relief by reducing the exchange user fees in the federally facilitated exchanges and state-based exchanges using the federal platform for 2020 thanks to successful efforts to improve the efficiency of the exchange,” CMS Administrator Seema Verma said in a statement.
CMS finalized a proposal to lower exchange user fees by 0.5%, fees that are generally passed on to consumers through premiums.
Other provisions cover exchange-related calculations, including how subsidies for exchange enrollees are calculated and how much enrollees are expected to contribute to benchmark plan premiums, which decreased slightly to 8.24%, down 0.07%, according to a CMS fact sheet.
For the out-of-pocket maximum, CMS said it “finalized a maximum annual limitation on cost sharing of $8,150 for self-only coverage and $16,300 for other than self-only coverage for the 2020 benefit year. This represents an approximately 3.16% increase above the 2019 parameters of $7,900 for self-only coverage and $15,800 for other than self-only coverage.”
Patients will still be able to use drug manufacturer coupons and pay less at the pharmacy counter, but the money they spend won’t be applied to their out-of-pocket maximum if they choose the brand-name drug with coupon instead of the lower-cost generic.
The change will affect insurance plans offered in the individual market, small-group, large-group, and self-insured–group health plans.
The Centers for Medicare & Medicaid Services backed away from implementing two other generic drug provisions based on feedback on its draft proposal.
The provisions would have allowed insurers to remove brand-name drugs from a formulary midyear when a generic became available or move the drug to a higher tier, and allowed insurers to not count certain drug copayments toward the annual limits if the patient selected a brand-name drug when a generic was available.
“Based on issues raised by commenters, we are not finalizing these proposals,” CMS officials said.
Insurers “making mid-year formulary changes [should] only be permitted to move the brand-name drug to a different cost-sharing tier for the remainder of the plan year. [They] should not be allowed to remove a safe brand-name drug from the formulary until the time of plan renewal,” the American College of Physicians recommended in Feb. 12 comments on the proposal.
The final rule on Notice of Benefit and Payment Parameters for the 2020 benefit year also aims to provide more stability and lower premiums in the exchanges, according to CMS officials.
“The rule issued today will give consumers immediate premium relief by reducing the exchange user fees in the federally facilitated exchanges and state-based exchanges using the federal platform for 2020 thanks to successful efforts to improve the efficiency of the exchange,” CMS Administrator Seema Verma said in a statement.
CMS finalized a proposal to lower exchange user fees by 0.5%, fees that are generally passed on to consumers through premiums.
Other provisions cover exchange-related calculations, including how subsidies for exchange enrollees are calculated and how much enrollees are expected to contribute to benchmark plan premiums, which decreased slightly to 8.24%, down 0.07%, according to a CMS fact sheet.
For the out-of-pocket maximum, CMS said it “finalized a maximum annual limitation on cost sharing of $8,150 for self-only coverage and $16,300 for other than self-only coverage for the 2020 benefit year. This represents an approximately 3.16% increase above the 2019 parameters of $7,900 for self-only coverage and $15,800 for other than self-only coverage.”
Key clinical point: Patients will be able to use drug manufacturer coupons and pay less at the pharmacy counter, but the money they spend won’t be applied to their out-of-pocket maximum if they choose the brand-name drug with coupon instead of the lower-cost generic.
Major finding: The change will affect insurance plans offered in the individual market, small-group, large-group, and self-insured–group health plans.
Study details: Final rule for the Notice of Benefit and Payment Parameters for the 2020 benefit year
Disclosures: None.
Source: Patient Protection and Affordable Care Act; HHS Notice of Benefit and Payment Parameters for 2020. 45 CFR Parts 146, 147, 148, 153, 155, and 156.
Dr. Douglas Paauw gives updates on antihypertensives, statins, SGLT2 inhibitors
PHILADELPHIA – in a video interview at the annual meeting of the American College of Physicians.
Dr. Paauw, professor of medicine at the University of Washington, Seattle, began by discussing some of the issues that occurred with antihypertensive drugs in the past year. These included the link between hydrochlorothiazide use and the increased risk of nonmelanoma skin cancers, the recalls of many drug lots of angiotensin II receptor blockers, and a study that found an increased risk of lung cancer in people who were taking ACE inhibitors.
He then described the findings of studies that examined the links between statins and muscle pain and other new research on these drugs.
He also warned physicians to be particularity cautious about prescribing sodium-glucose cotransporter 2 inhibitors to certain kinds of patients.
Dr. Paauw concluded by explaining why clarithromycin is his most hated drug.
Dr. Paauw is also the Rathmann Family Foundation Endowed Chair for Patient-Centered Clinical Education and the medicine clerkship director at the University of Washington.
klennon@mdedge.com
PHILADELPHIA – in a video interview at the annual meeting of the American College of Physicians.
Dr. Paauw, professor of medicine at the University of Washington, Seattle, began by discussing some of the issues that occurred with antihypertensive drugs in the past year. These included the link between hydrochlorothiazide use and the increased risk of nonmelanoma skin cancers, the recalls of many drug lots of angiotensin II receptor blockers, and a study that found an increased risk of lung cancer in people who were taking ACE inhibitors.
He then described the findings of studies that examined the links between statins and muscle pain and other new research on these drugs.
He also warned physicians to be particularity cautious about prescribing sodium-glucose cotransporter 2 inhibitors to certain kinds of patients.
Dr. Paauw concluded by explaining why clarithromycin is his most hated drug.
Dr. Paauw is also the Rathmann Family Foundation Endowed Chair for Patient-Centered Clinical Education and the medicine clerkship director at the University of Washington.
klennon@mdedge.com
PHILADELPHIA – in a video interview at the annual meeting of the American College of Physicians.
Dr. Paauw, professor of medicine at the University of Washington, Seattle, began by discussing some of the issues that occurred with antihypertensive drugs in the past year. These included the link between hydrochlorothiazide use and the increased risk of nonmelanoma skin cancers, the recalls of many drug lots of angiotensin II receptor blockers, and a study that found an increased risk of lung cancer in people who were taking ACE inhibitors.
He then described the findings of studies that examined the links between statins and muscle pain and other new research on these drugs.
He also warned physicians to be particularity cautious about prescribing sodium-glucose cotransporter 2 inhibitors to certain kinds of patients.
Dr. Paauw concluded by explaining why clarithromycin is his most hated drug.
Dr. Paauw is also the Rathmann Family Foundation Endowed Chair for Patient-Centered Clinical Education and the medicine clerkship director at the University of Washington.
klennon@mdedge.com
REPORTING FROM INTERNAL MEDICINE 2019
Study highlights lack of data on transgender leukemia patients
NEWPORT BEACH, CALIF. – Researchers have shown they can identify transgender leukemia patients by detecting gender-karyotype mismatches, but some transgender patients may be overlooked with this method.
The researchers’ work also highlights how little we know about transgender patients with leukemia and other cancers.
Alison Alpert, MD, of the University of Rochester (N.Y.) Medical Center, and her colleagues conducted this research and presented their findings in a poster at the Acute Leukemia Forum of Hemedicus.
“There’s almost no data about transgender people with cancer ... in terms of prevalence or anything else,” Dr. Alpert noted. “And because we don’t know which patients with cancer are transgender, we can’t begin to answer any of the other big questions for patients.”
Specifically, it’s unclear what kinds of cancer transgender patients have, if there are health disparities among transgender patients, if it is safe to continue hormone therapy during cancer treatment, and if it is possible to do transition-related surgeries in the context of cancer care.
With this in mind, Dr. Alpert and her colleagues set out to identify transgender patients by detecting gender-karyotype mismatches. The team analyzed data on patients with acute myeloid leukemia (AML) or myelodysplastic syndromes enrolled in five Southwest Oncology Group (SWOG) trials.
Of the 1,748 patients analyzed, six (0.3%) had a gender-karyotype mismatch. Five patients had a 46,XY karyotype and identified as female, and one patient had a 46,XX karyotype and identified as male.
“Some transgender patients have their gender identity accurately reflected in the electronic medical record, [but] some transgender patients probably don’t,” Dr. Alpert noted. “So we identified some, but probably not all, and probably not even most, transgender patients with leukemia in this cohort.”
All six of the transgender patients identified had AML, and all were white. They ranged in age from 18 to 57 years. Four patients had achieved a complete response to therapy, and two had refractory disease.
Four patients, including one who was refractory, were still alive at last follow-up. The remaining two patients, including one who had achieved a complete response, had died.
The transgender patients identified in this analysis represent a very small percentage of the population studied, Dr. Alpert noted. Therefore, the researchers could not draw any conclusions about transgender patients with AML.
“Mostly, what we did was, we pointed out how little information we have,” Dr. Alpert said. “Oncologists don’t routinely collect gender identity information, and this information doesn’t exist in cooperative group databases either.”
“But going forward, what probably really needs to happen is that oncologists need to ask their patients whether they are transgender or not. And then, ideally, consent forms for large cooperative groups like SWOG would include gender identity data, and then we would be able to answer some of our other questions and better counsel our patients.”
Dr. Alpert and her colleagues are hoping to gain insights regarding transgender patients with lymphoma as well. The researchers are analyzing the lymphoma database at the University of Rochester Medical Center, which includes about 2,200 patients.
The team is attempting to identify transgender lymphoma patients using gender-karyotype mismatch as well as other methods, including assessing patients’ medication and surgical histories, determining whether patients have any aliases, and looking for the word “transgender” in patient charts.
“Given that the country is finally starting to talk about transgender patients, their health disparities, and their needs and experiences, it’s really time that we start collecting this data,” Dr. Alpert said.
“[I]f we are able to start to collect this data, it can help us build relationships with our patients, improve their care and outcomes, and, hopefully, be able to better counsel them about hormones and surgery.”
Dr. Alpert and her colleagues did not disclose any conflicts of interest.
The Acute Leukemia Forum is organized by Hemedicus, which is owned by the same company as this news organization.
NEWPORT BEACH, CALIF. – Researchers have shown they can identify transgender leukemia patients by detecting gender-karyotype mismatches, but some transgender patients may be overlooked with this method.
The researchers’ work also highlights how little we know about transgender patients with leukemia and other cancers.
Alison Alpert, MD, of the University of Rochester (N.Y.) Medical Center, and her colleagues conducted this research and presented their findings in a poster at the Acute Leukemia Forum of Hemedicus.
“There’s almost no data about transgender people with cancer ... in terms of prevalence or anything else,” Dr. Alpert noted. “And because we don’t know which patients with cancer are transgender, we can’t begin to answer any of the other big questions for patients.”
Specifically, it’s unclear what kinds of cancer transgender patients have, if there are health disparities among transgender patients, if it is safe to continue hormone therapy during cancer treatment, and if it is possible to do transition-related surgeries in the context of cancer care.
With this in mind, Dr. Alpert and her colleagues set out to identify transgender patients by detecting gender-karyotype mismatches. The team analyzed data on patients with acute myeloid leukemia (AML) or myelodysplastic syndromes enrolled in five Southwest Oncology Group (SWOG) trials.
Of the 1,748 patients analyzed, six (0.3%) had a gender-karyotype mismatch. Five patients had a 46,XY karyotype and identified as female, and one patient had a 46,XX karyotype and identified as male.
“Some transgender patients have their gender identity accurately reflected in the electronic medical record, [but] some transgender patients probably don’t,” Dr. Alpert noted. “So we identified some, but probably not all, and probably not even most, transgender patients with leukemia in this cohort.”
All six of the transgender patients identified had AML, and all were white. They ranged in age from 18 to 57 years. Four patients had achieved a complete response to therapy, and two had refractory disease.
Four patients, including one who was refractory, were still alive at last follow-up. The remaining two patients, including one who had achieved a complete response, had died.
The transgender patients identified in this analysis represent a very small percentage of the population studied, Dr. Alpert noted. Therefore, the researchers could not draw any conclusions about transgender patients with AML.
“Mostly, what we did was, we pointed out how little information we have,” Dr. Alpert said. “Oncologists don’t routinely collect gender identity information, and this information doesn’t exist in cooperative group databases either.”
“But going forward, what probably really needs to happen is that oncologists need to ask their patients whether they are transgender or not. And then, ideally, consent forms for large cooperative groups like SWOG would include gender identity data, and then we would be able to answer some of our other questions and better counsel our patients.”
Dr. Alpert and her colleagues are hoping to gain insights regarding transgender patients with lymphoma as well. The researchers are analyzing the lymphoma database at the University of Rochester Medical Center, which includes about 2,200 patients.
The team is attempting to identify transgender lymphoma patients using gender-karyotype mismatch as well as other methods, including assessing patients’ medication and surgical histories, determining whether patients have any aliases, and looking for the word “transgender” in patient charts.
“Given that the country is finally starting to talk about transgender patients, their health disparities, and their needs and experiences, it’s really time that we start collecting this data,” Dr. Alpert said.
“[I]f we are able to start to collect this data, it can help us build relationships with our patients, improve their care and outcomes, and, hopefully, be able to better counsel them about hormones and surgery.”
Dr. Alpert and her colleagues did not disclose any conflicts of interest.
The Acute Leukemia Forum is organized by Hemedicus, which is owned by the same company as this news organization.
NEWPORT BEACH, CALIF. – Researchers have shown they can identify transgender leukemia patients by detecting gender-karyotype mismatches, but some transgender patients may be overlooked with this method.
The researchers’ work also highlights how little we know about transgender patients with leukemia and other cancers.
Alison Alpert, MD, of the University of Rochester (N.Y.) Medical Center, and her colleagues conducted this research and presented their findings in a poster at the Acute Leukemia Forum of Hemedicus.
“There’s almost no data about transgender people with cancer ... in terms of prevalence or anything else,” Dr. Alpert noted. “And because we don’t know which patients with cancer are transgender, we can’t begin to answer any of the other big questions for patients.”
Specifically, it’s unclear what kinds of cancer transgender patients have, if there are health disparities among transgender patients, if it is safe to continue hormone therapy during cancer treatment, and if it is possible to do transition-related surgeries in the context of cancer care.
With this in mind, Dr. Alpert and her colleagues set out to identify transgender patients by detecting gender-karyotype mismatches. The team analyzed data on patients with acute myeloid leukemia (AML) or myelodysplastic syndromes enrolled in five Southwest Oncology Group (SWOG) trials.
Of the 1,748 patients analyzed, six (0.3%) had a gender-karyotype mismatch. Five patients had a 46,XY karyotype and identified as female, and one patient had a 46,XX karyotype and identified as male.
“Some transgender patients have their gender identity accurately reflected in the electronic medical record, [but] some transgender patients probably don’t,” Dr. Alpert noted. “So we identified some, but probably not all, and probably not even most, transgender patients with leukemia in this cohort.”
All six of the transgender patients identified had AML, and all were white. They ranged in age from 18 to 57 years. Four patients had achieved a complete response to therapy, and two had refractory disease.
Four patients, including one who was refractory, were still alive at last follow-up. The remaining two patients, including one who had achieved a complete response, had died.
The transgender patients identified in this analysis represent a very small percentage of the population studied, Dr. Alpert noted. Therefore, the researchers could not draw any conclusions about transgender patients with AML.
“Mostly, what we did was, we pointed out how little information we have,” Dr. Alpert said. “Oncologists don’t routinely collect gender identity information, and this information doesn’t exist in cooperative group databases either.”
“But going forward, what probably really needs to happen is that oncologists need to ask their patients whether they are transgender or not. And then, ideally, consent forms for large cooperative groups like SWOG would include gender identity data, and then we would be able to answer some of our other questions and better counsel our patients.”
Dr. Alpert and her colleagues are hoping to gain insights regarding transgender patients with lymphoma as well. The researchers are analyzing the lymphoma database at the University of Rochester Medical Center, which includes about 2,200 patients.
The team is attempting to identify transgender lymphoma patients using gender-karyotype mismatch as well as other methods, including assessing patients’ medication and surgical histories, determining whether patients have any aliases, and looking for the word “transgender” in patient charts.
“Given that the country is finally starting to talk about transgender patients, their health disparities, and their needs and experiences, it’s really time that we start collecting this data,” Dr. Alpert said.
“[I]f we are able to start to collect this data, it can help us build relationships with our patients, improve their care and outcomes, and, hopefully, be able to better counsel them about hormones and surgery.”
Dr. Alpert and her colleagues did not disclose any conflicts of interest.
The Acute Leukemia Forum is organized by Hemedicus, which is owned by the same company as this news organization.
REPORTING FROM ALF 2019
ALF 2019 showcases evolving treatment of AML
NEWPORT BEACH, CALIF. – The evolving treatment of acute myeloid leukemia (AML) was highlighted at the Acute Leukemia Forum of Hemedicus.
In a video interview, Martin Tallman, MD, of Memorial Sloan Kettering Cancer Center in New York, discussed several meeting presentations on the treatment of AML.
In his presentation, Craig Jordan, PhD, of the University of Colorado at Denver, Aurora, explained how the combination of venetoclax and azacitidine appears to target leukemic stem cells in AML.
Courtney DiNardo, MD, of the University of Texas MD Anderson Cancer Center, Houston, presented information on novel agents for AML, including antibody-drug conjugates; bispecific therapies; checkpoint inhibitors; and inhibitors of IDH1/2, MCL1, and MDM2.
Richard Larson, MD, of the University of Chicago, explored the possibility of an individualized approach to postremission therapy in AML.
Frederick Appelbaum, MD, of Fred Hutchinson Cancer Research Center in Seattle, showed that various maintenance therapies given after allogeneic hematopoietic stem cell transplant (HSCT) have not proven beneficial for AML patients.
Richard Jones, MD, of Johns Hopkins Medicine in Baltimore, presented data showing that post-HSCT cyclophosphamide has made haploidentical transplants safer and more effective for AML patients.
And James Ferrara, MD, of the Icahn School of Medicine at Mount Sinai, New York, detailed research showing that biomarkers of graft-versus-host disease can predict nonrelapse mortality after HSCT.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
NEWPORT BEACH, CALIF. – The evolving treatment of acute myeloid leukemia (AML) was highlighted at the Acute Leukemia Forum of Hemedicus.
In a video interview, Martin Tallman, MD, of Memorial Sloan Kettering Cancer Center in New York, discussed several meeting presentations on the treatment of AML.
In his presentation, Craig Jordan, PhD, of the University of Colorado at Denver, Aurora, explained how the combination of venetoclax and azacitidine appears to target leukemic stem cells in AML.
Courtney DiNardo, MD, of the University of Texas MD Anderson Cancer Center, Houston, presented information on novel agents for AML, including antibody-drug conjugates; bispecific therapies; checkpoint inhibitors; and inhibitors of IDH1/2, MCL1, and MDM2.
Richard Larson, MD, of the University of Chicago, explored the possibility of an individualized approach to postremission therapy in AML.
Frederick Appelbaum, MD, of Fred Hutchinson Cancer Research Center in Seattle, showed that various maintenance therapies given after allogeneic hematopoietic stem cell transplant (HSCT) have not proven beneficial for AML patients.
Richard Jones, MD, of Johns Hopkins Medicine in Baltimore, presented data showing that post-HSCT cyclophosphamide has made haploidentical transplants safer and more effective for AML patients.
And James Ferrara, MD, of the Icahn School of Medicine at Mount Sinai, New York, detailed research showing that biomarkers of graft-versus-host disease can predict nonrelapse mortality after HSCT.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
NEWPORT BEACH, CALIF. – The evolving treatment of acute myeloid leukemia (AML) was highlighted at the Acute Leukemia Forum of Hemedicus.
In a video interview, Martin Tallman, MD, of Memorial Sloan Kettering Cancer Center in New York, discussed several meeting presentations on the treatment of AML.
In his presentation, Craig Jordan, PhD, of the University of Colorado at Denver, Aurora, explained how the combination of venetoclax and azacitidine appears to target leukemic stem cells in AML.
Courtney DiNardo, MD, of the University of Texas MD Anderson Cancer Center, Houston, presented information on novel agents for AML, including antibody-drug conjugates; bispecific therapies; checkpoint inhibitors; and inhibitors of IDH1/2, MCL1, and MDM2.
Richard Larson, MD, of the University of Chicago, explored the possibility of an individualized approach to postremission therapy in AML.
Frederick Appelbaum, MD, of Fred Hutchinson Cancer Research Center in Seattle, showed that various maintenance therapies given after allogeneic hematopoietic stem cell transplant (HSCT) have not proven beneficial for AML patients.
Richard Jones, MD, of Johns Hopkins Medicine in Baltimore, presented data showing that post-HSCT cyclophosphamide has made haploidentical transplants safer and more effective for AML patients.
And James Ferrara, MD, of the Icahn School of Medicine at Mount Sinai, New York, detailed research showing that biomarkers of graft-versus-host disease can predict nonrelapse mortality after HSCT.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
REPORTING FROM ALF 2019
Medical societies endorse tiered certification for U.S. heart-valve care
The centerpiece of the integrated model is a certification process that would designate appropriate hospitals as “Comprehensive (Level I)” or “Primary (Level II)” valve centers to serve as the designated U.S. sites for performing repair or replacement of aortic and mitral valves by transcatheter or open-surgery procedures.
The consensus document, written by a panel of mostly interventional cardiologists or heart surgeons and published in Journal of the American College of Cardiology, cited the success of similar accreditation and tiered systems that have become fixtures in United States for the delivery of care for trauma, stroke, cancer, bariatric surgery, and percutaneous coronary intervention for acute ST-segment elevation MI.
The focus of the consensus document is to “initiate a discussion regarding whether a regionalized, tiered system of care for patients with [valvular heart disease (VHD)] that accounts for the differences in valve center expertise, experience, and resources constitutes a more rational delivery model than one left to expand continuously without direction,” the panel wrote.
Under the proposal, a key component of every designated valve center would be a multidisciplinary clinical team, staffed at minimum with an interventional cardiologist, a cardiac surgeon, echocardiographic and radiographic imaging specialists, a specialist in heart failure, a person with valve expertise, nurse practitioners, a cardiovascular anesthesiologist, a program navigator, and a data manager. Valve centers also would need to enroll patients in registries, perform research, education, and training, and collect data using carefully selected performance metrics.
The document addresses case-volume minimums, a topic that’s been tricky for leaders in the heart-valve field to reconcile as they try to balance volume thresholds against having valve procedures readily available and convenient for rural or remote patients.
“The primary motivation behind volume recommendations is not to exclude centers but rather to serve as one metric in the identification of centers that are most capable of providing certain services,” the consensus statement explained. “Volumes alone are not necessarily the best surrogate for quality, but a volume-outcome association does exist for many cardiac procedures.”
Recent proof of this relationship for transcatheter aortic valve replacement appeared in an article published earlier in April; the article reviewed 30-day mortality outcomes for more than 113,000 U.S. patients who underwent this procedure and showed that centers with the lowest procedure volumes also had the highest mortality rate (New Engl J Med. 2019 April 3. doi: 10.1056/NEJMsa1901109).
But the document also qualified its support of and the role for volume minimums, highlighting that case volume is an inadequate surrogate for program quality, especially when considered in isolation. “The proposed concept of system care for VHD patients is not conceived to deny individuals and institutions the opportunity to provide services, nor should it be perceived to impede the ability of a committed center to achieve its strategic goals. Rather, it is intended to focus more on outcomes and not simply on procedural volumes.”
The launch by the Joint Commission of a Comprehensive Cardiac Advanced Certification program in January 2017, which included VHD care, is a step toward that goal, but “there is a great deal of detailed work ahead to realize the goal of this proposal,” according to the consensus document.
The consensus statement was issued by the American Association for Thoracic Surgery, the American College of Cardiology, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons.
SOURCE: Nishimura RA et al. J Amer Coll Cardiol. 2019 April 19. doi: 10.1016/j.jacc.2018.10.007.
The centerpiece of the integrated model is a certification process that would designate appropriate hospitals as “Comprehensive (Level I)” or “Primary (Level II)” valve centers to serve as the designated U.S. sites for performing repair or replacement of aortic and mitral valves by transcatheter or open-surgery procedures.
The consensus document, written by a panel of mostly interventional cardiologists or heart surgeons and published in Journal of the American College of Cardiology, cited the success of similar accreditation and tiered systems that have become fixtures in United States for the delivery of care for trauma, stroke, cancer, bariatric surgery, and percutaneous coronary intervention for acute ST-segment elevation MI.
The focus of the consensus document is to “initiate a discussion regarding whether a regionalized, tiered system of care for patients with [valvular heart disease (VHD)] that accounts for the differences in valve center expertise, experience, and resources constitutes a more rational delivery model than one left to expand continuously without direction,” the panel wrote.
Under the proposal, a key component of every designated valve center would be a multidisciplinary clinical team, staffed at minimum with an interventional cardiologist, a cardiac surgeon, echocardiographic and radiographic imaging specialists, a specialist in heart failure, a person with valve expertise, nurse practitioners, a cardiovascular anesthesiologist, a program navigator, and a data manager. Valve centers also would need to enroll patients in registries, perform research, education, and training, and collect data using carefully selected performance metrics.
The document addresses case-volume minimums, a topic that’s been tricky for leaders in the heart-valve field to reconcile as they try to balance volume thresholds against having valve procedures readily available and convenient for rural or remote patients.
“The primary motivation behind volume recommendations is not to exclude centers but rather to serve as one metric in the identification of centers that are most capable of providing certain services,” the consensus statement explained. “Volumes alone are not necessarily the best surrogate for quality, but a volume-outcome association does exist for many cardiac procedures.”
Recent proof of this relationship for transcatheter aortic valve replacement appeared in an article published earlier in April; the article reviewed 30-day mortality outcomes for more than 113,000 U.S. patients who underwent this procedure and showed that centers with the lowest procedure volumes also had the highest mortality rate (New Engl J Med. 2019 April 3. doi: 10.1056/NEJMsa1901109).
But the document also qualified its support of and the role for volume minimums, highlighting that case volume is an inadequate surrogate for program quality, especially when considered in isolation. “The proposed concept of system care for VHD patients is not conceived to deny individuals and institutions the opportunity to provide services, nor should it be perceived to impede the ability of a committed center to achieve its strategic goals. Rather, it is intended to focus more on outcomes and not simply on procedural volumes.”
The launch by the Joint Commission of a Comprehensive Cardiac Advanced Certification program in January 2017, which included VHD care, is a step toward that goal, but “there is a great deal of detailed work ahead to realize the goal of this proposal,” according to the consensus document.
The consensus statement was issued by the American Association for Thoracic Surgery, the American College of Cardiology, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons.
SOURCE: Nishimura RA et al. J Amer Coll Cardiol. 2019 April 19. doi: 10.1016/j.jacc.2018.10.007.
The centerpiece of the integrated model is a certification process that would designate appropriate hospitals as “Comprehensive (Level I)” or “Primary (Level II)” valve centers to serve as the designated U.S. sites for performing repair or replacement of aortic and mitral valves by transcatheter or open-surgery procedures.
The consensus document, written by a panel of mostly interventional cardiologists or heart surgeons and published in Journal of the American College of Cardiology, cited the success of similar accreditation and tiered systems that have become fixtures in United States for the delivery of care for trauma, stroke, cancer, bariatric surgery, and percutaneous coronary intervention for acute ST-segment elevation MI.
The focus of the consensus document is to “initiate a discussion regarding whether a regionalized, tiered system of care for patients with [valvular heart disease (VHD)] that accounts for the differences in valve center expertise, experience, and resources constitutes a more rational delivery model than one left to expand continuously without direction,” the panel wrote.
Under the proposal, a key component of every designated valve center would be a multidisciplinary clinical team, staffed at minimum with an interventional cardiologist, a cardiac surgeon, echocardiographic and radiographic imaging specialists, a specialist in heart failure, a person with valve expertise, nurse practitioners, a cardiovascular anesthesiologist, a program navigator, and a data manager. Valve centers also would need to enroll patients in registries, perform research, education, and training, and collect data using carefully selected performance metrics.
The document addresses case-volume minimums, a topic that’s been tricky for leaders in the heart-valve field to reconcile as they try to balance volume thresholds against having valve procedures readily available and convenient for rural or remote patients.
“The primary motivation behind volume recommendations is not to exclude centers but rather to serve as one metric in the identification of centers that are most capable of providing certain services,” the consensus statement explained. “Volumes alone are not necessarily the best surrogate for quality, but a volume-outcome association does exist for many cardiac procedures.”
Recent proof of this relationship for transcatheter aortic valve replacement appeared in an article published earlier in April; the article reviewed 30-day mortality outcomes for more than 113,000 U.S. patients who underwent this procedure and showed that centers with the lowest procedure volumes also had the highest mortality rate (New Engl J Med. 2019 April 3. doi: 10.1056/NEJMsa1901109).
But the document also qualified its support of and the role for volume minimums, highlighting that case volume is an inadequate surrogate for program quality, especially when considered in isolation. “The proposed concept of system care for VHD patients is not conceived to deny individuals and institutions the opportunity to provide services, nor should it be perceived to impede the ability of a committed center to achieve its strategic goals. Rather, it is intended to focus more on outcomes and not simply on procedural volumes.”
The launch by the Joint Commission of a Comprehensive Cardiac Advanced Certification program in January 2017, which included VHD care, is a step toward that goal, but “there is a great deal of detailed work ahead to realize the goal of this proposal,” according to the consensus document.
The consensus statement was issued by the American Association for Thoracic Surgery, the American College of Cardiology, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons.
SOURCE: Nishimura RA et al. J Amer Coll Cardiol. 2019 April 19. doi: 10.1016/j.jacc.2018.10.007.
FROM JACC
Low-dose IL-2 found effective in SLE
SAN FRANCISCO – , according to the first randomized, double-blind, placebo-controlled clinical trial of the novel therapy.
Of note, more than half of the study participants with lupus nephritis experienced complete remission of their renal impairment, and another quarter had partial remission, Jing He, MD, PhD, reported at an international congress on systemic lupus erythematosus.
The mechanism of benefit appears to be the same as previously shown for low-dose interleukin-2 in patients with chronic graft versus host disease refractory to glucocorticoids (N Engl J Med. 2011 Dec 1;365[22]:2055-66): expansion of the deficient population of T regulatory cells, which is a hallmark of both inflammatory diseases.
“Low-dose IL-2 can reinstate the imbalance of T regulatory/T effector cells and improve immune homeostasis, which is critical in clinical remission of SLE,” said Dr. He of Peking University People’s Hospital in Beijing.
For nearly 20 years it has been known that SLE is characterized by very low levels of endogenous IL-2. Dr. He was lead author of the first proof-of-concept study, which showed low-dose subcutaneous IL-2 therapy resulted in markedly reduced SLE disease activity accompanied by expansion of the T regulatory cell population and suppression of follicular helper T cells and IL-17–producing helper T cells (Nat Med. 2016 Sep;22[9]:991-3). However, that was a small, single-center, uncontrolled study, so she and her coworkers have now carried out a 60-patient, double-blind, placebo-controlled randomized trial. In addition to hydroxychloroquine and other standard background medications, the patients in the active treatment arm received 1 million IU of IL-2 every other day for 2 weeks, followed by a 2-week hiatus, for a total of three courses.
At week 24 – 12 weeks after the last injection – the IL-2 recipients showed significantly greater improvement on numerous endpoints.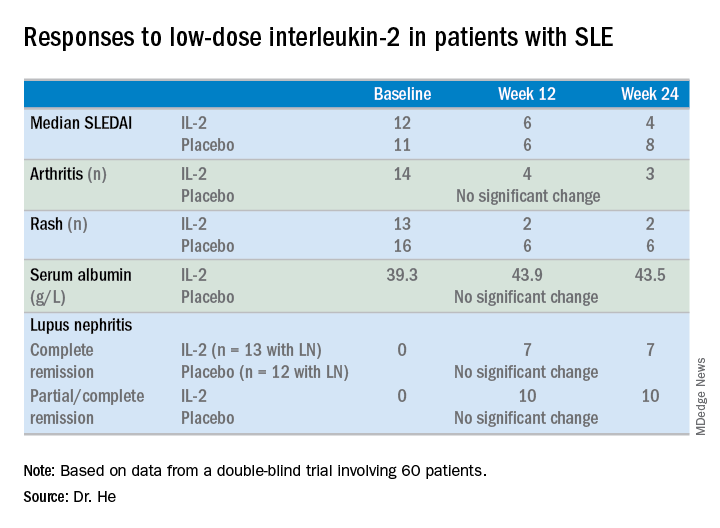
For example, the median SLE Disease Activity Index (SLEDAI) in the IL-2 group improved from 12 at baseline to 6 at week 12 and to 4 at week 24.
The marked improvement in renal impairment in the IL-2 recipients with lupus nephritis at baseline was accompanied by a significant increase in serum albumin and reduced 24-hour urinary protein, compared with controls.
The treatment was safe, with no increase in infections, severe or otherwise, and indeed with no serious adverse events of any kind, although nine patients in the IL-2 group experienced mild injection site reactions and three developed flu-like symptoms.
Dr. He reported having no financial conflicts regarding her study.
SAN FRANCISCO – , according to the first randomized, double-blind, placebo-controlled clinical trial of the novel therapy.
Of note, more than half of the study participants with lupus nephritis experienced complete remission of their renal impairment, and another quarter had partial remission, Jing He, MD, PhD, reported at an international congress on systemic lupus erythematosus.
The mechanism of benefit appears to be the same as previously shown for low-dose interleukin-2 in patients with chronic graft versus host disease refractory to glucocorticoids (N Engl J Med. 2011 Dec 1;365[22]:2055-66): expansion of the deficient population of T regulatory cells, which is a hallmark of both inflammatory diseases.
“Low-dose IL-2 can reinstate the imbalance of T regulatory/T effector cells and improve immune homeostasis, which is critical in clinical remission of SLE,” said Dr. He of Peking University People’s Hospital in Beijing.
For nearly 20 years it has been known that SLE is characterized by very low levels of endogenous IL-2. Dr. He was lead author of the first proof-of-concept study, which showed low-dose subcutaneous IL-2 therapy resulted in markedly reduced SLE disease activity accompanied by expansion of the T regulatory cell population and suppression of follicular helper T cells and IL-17–producing helper T cells (Nat Med. 2016 Sep;22[9]:991-3). However, that was a small, single-center, uncontrolled study, so she and her coworkers have now carried out a 60-patient, double-blind, placebo-controlled randomized trial. In addition to hydroxychloroquine and other standard background medications, the patients in the active treatment arm received 1 million IU of IL-2 every other day for 2 weeks, followed by a 2-week hiatus, for a total of three courses.
At week 24 – 12 weeks after the last injection – the IL-2 recipients showed significantly greater improvement on numerous endpoints.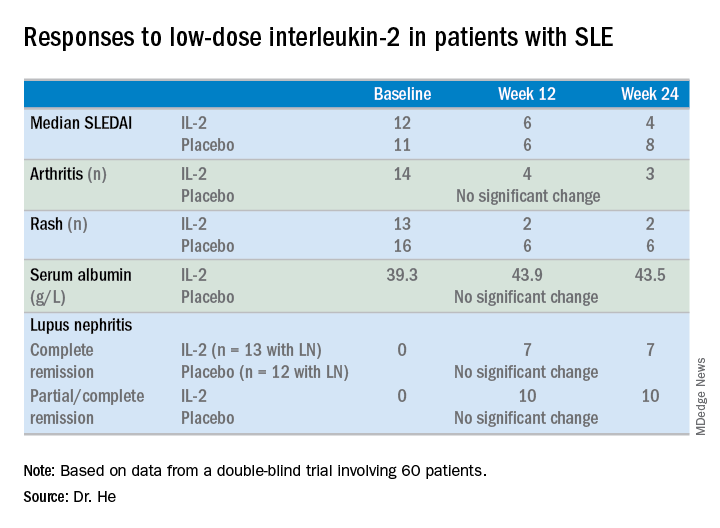
For example, the median SLE Disease Activity Index (SLEDAI) in the IL-2 group improved from 12 at baseline to 6 at week 12 and to 4 at week 24.
The marked improvement in renal impairment in the IL-2 recipients with lupus nephritis at baseline was accompanied by a significant increase in serum albumin and reduced 24-hour urinary protein, compared with controls.
The treatment was safe, with no increase in infections, severe or otherwise, and indeed with no serious adverse events of any kind, although nine patients in the IL-2 group experienced mild injection site reactions and three developed flu-like symptoms.
Dr. He reported having no financial conflicts regarding her study.
SAN FRANCISCO – , according to the first randomized, double-blind, placebo-controlled clinical trial of the novel therapy.
Of note, more than half of the study participants with lupus nephritis experienced complete remission of their renal impairment, and another quarter had partial remission, Jing He, MD, PhD, reported at an international congress on systemic lupus erythematosus.
The mechanism of benefit appears to be the same as previously shown for low-dose interleukin-2 in patients with chronic graft versus host disease refractory to glucocorticoids (N Engl J Med. 2011 Dec 1;365[22]:2055-66): expansion of the deficient population of T regulatory cells, which is a hallmark of both inflammatory diseases.
“Low-dose IL-2 can reinstate the imbalance of T regulatory/T effector cells and improve immune homeostasis, which is critical in clinical remission of SLE,” said Dr. He of Peking University People’s Hospital in Beijing.
For nearly 20 years it has been known that SLE is characterized by very low levels of endogenous IL-2. Dr. He was lead author of the first proof-of-concept study, which showed low-dose subcutaneous IL-2 therapy resulted in markedly reduced SLE disease activity accompanied by expansion of the T regulatory cell population and suppression of follicular helper T cells and IL-17–producing helper T cells (Nat Med. 2016 Sep;22[9]:991-3). However, that was a small, single-center, uncontrolled study, so she and her coworkers have now carried out a 60-patient, double-blind, placebo-controlled randomized trial. In addition to hydroxychloroquine and other standard background medications, the patients in the active treatment arm received 1 million IU of IL-2 every other day for 2 weeks, followed by a 2-week hiatus, for a total of three courses.
At week 24 – 12 weeks after the last injection – the IL-2 recipients showed significantly greater improvement on numerous endpoints.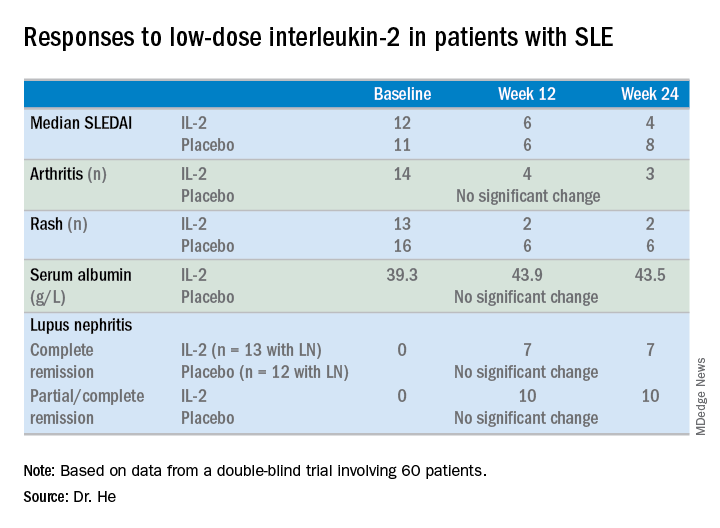
For example, the median SLE Disease Activity Index (SLEDAI) in the IL-2 group improved from 12 at baseline to 6 at week 12 and to 4 at week 24.
The marked improvement in renal impairment in the IL-2 recipients with lupus nephritis at baseline was accompanied by a significant increase in serum albumin and reduced 24-hour urinary protein, compared with controls.
The treatment was safe, with no increase in infections, severe or otherwise, and indeed with no serious adverse events of any kind, although nine patients in the IL-2 group experienced mild injection site reactions and three developed flu-like symptoms.
Dr. He reported having no financial conflicts regarding her study.
REPORTING FROM LUPUS 2019
LUPUS 2019 Congress: Top takeaways
Join us at #MDedgeChats on Tuesday, April 23, 2019, at 7:00 pm EST, for a Twitter discussion in Rheumatology on some of the top studies reported at the LUPUS 2019 Congress in San Francisco, April 5-8. Our special guests are two rheumatologists with expertise in lupus who attended the congress, Jinoos Yazdany, MD, and Gabriela Schmajuk, MD, both with the University of California, San Francisco. They will discuss the ins and outs of the study results presented.
We hope you can join us and invite a colleague, too.
We will discuss the results of the EMBRACE trial, which looks at the efficacy and safety of belimumab (Benlysta) in black patients with systemic lupus erythematosus (SLE); these patients have a higher prevalence of SLE and often higher disease severity but have been poorly represented in past belimumab studies.
We will also chat about the results of a phase 2 trial of baricitinib (Olumiant) in SLE patients.
Finally, we will look at the clinical utility of monitoring hydroxychloroquine levels in SLE patients and how well levels of the drug correlate with disease activity through the results of a meta-analysis of studies that examined these questions.
Topics of conversation
Q1: How does the methodology of the EMBRACE trial differ from past phase 3 belimumab trials?
Q2: How does the EMBRACE trial affect the way you prescribe belimumab?
Q3: Does the hydroxychloroquine level meta-analysis provide persuasive enough evidence to begin measuring it?
Q4: What kinds of interventions show the best evidence for improving hydroxychloroquine adherence?
Q5: Were concerns about the safety of baricitinib in SLE patients reduced by the trial results?
Resources
EMBRACE trial: Efficacy and Safety of Belimumab in Black Race Patients with Systemic Lupus Erythematosus.
LUPUS 2019 abstract | ClinicalTrials.gov listing
Phase 2 trial of baricitinib in SLE.
LUPUS 2019 abstract | ClinicalTrials.gov listing
Meta-analysis examining the clinical significance of monitoring of hydroxychloroquine levels in SLE.
LUPUS 2019 abstract
From LUPUS 2019:
Belimumab a bust for black SLE patients.
Here’s a top strategy for immunosuppressant discontinuation in SLE.
From EULAR 2018:
Baricitinib shows potential as lupus treatment.
About Dr. Yazdany
Dr. Yazdany is an associate professor in the division of rheumatology, department of medicine at UCSF (@UCSFMedicine). She is a rheumatologist and clinical researcher with expertise in systemic lupus erythematosus and health care quality measurement and improvement. Her clinical activities include seeing patients in the UCSF Lupus Clinic, where she serves as codirector, as well as at San Francisco General Hospital. Dr. Yazdany codirects the Quality and Informatics Lab (quil.ucsf.edu), which uses data to drive improvements in health care delivery and outcomes for people with rheumatic diseases. She also leads ongoing, longitudinal studies of lupus that are investigating health disparities and outcomes in the condition.
About Dr. Schmajuk
Dr. Schmajuk is an Associate Professor in the Division of Rheumatology, Department of Medicine at UCSF (@UCSFMedicine) and the San Francisco VA Medical Center. She is a rheumatologist and clinical researcher with expertise in systemic #lupus erythematosus, quality of care, and patient safety. Dr. Schmajuk also co-directs the Quality and Informatics Lab (quil.ucsf.edu), which uses data to drive improvements in health care delivery and outcomes for people with rheumatic diseases. She leads studies to develop patient-facing disease dashboards with the goal of improving patient-provider communication for patients with RA and SLE.
Are you new to Twitter chats? We have included simple steps below to help you join and participate in the conversation.
Join us at #MDedgeChats on Tuesday, April 23, 2019, at 7:00 pm EST, for a Twitter discussion in Rheumatology on some of the top studies reported at the LUPUS 2019 Congress in San Francisco, April 5-8. Our special guests are two rheumatologists with expertise in lupus who attended the congress, Jinoos Yazdany, MD, and Gabriela Schmajuk, MD, both with the University of California, San Francisco. They will discuss the ins and outs of the study results presented.
We hope you can join us and invite a colleague, too.
We will discuss the results of the EMBRACE trial, which looks at the efficacy and safety of belimumab (Benlysta) in black patients with systemic lupus erythematosus (SLE); these patients have a higher prevalence of SLE and often higher disease severity but have been poorly represented in past belimumab studies.
We will also chat about the results of a phase 2 trial of baricitinib (Olumiant) in SLE patients.
Finally, we will look at the clinical utility of monitoring hydroxychloroquine levels in SLE patients and how well levels of the drug correlate with disease activity through the results of a meta-analysis of studies that examined these questions.
Topics of conversation
Q1: How does the methodology of the EMBRACE trial differ from past phase 3 belimumab trials?
Q2: How does the EMBRACE trial affect the way you prescribe belimumab?
Q3: Does the hydroxychloroquine level meta-analysis provide persuasive enough evidence to begin measuring it?
Q4: What kinds of interventions show the best evidence for improving hydroxychloroquine adherence?
Q5: Were concerns about the safety of baricitinib in SLE patients reduced by the trial results?
Resources
EMBRACE trial: Efficacy and Safety of Belimumab in Black Race Patients with Systemic Lupus Erythematosus.
LUPUS 2019 abstract | ClinicalTrials.gov listing
Phase 2 trial of baricitinib in SLE.
LUPUS 2019 abstract | ClinicalTrials.gov listing
Meta-analysis examining the clinical significance of monitoring of hydroxychloroquine levels in SLE.
LUPUS 2019 abstract
From LUPUS 2019:
Belimumab a bust for black SLE patients.
Here’s a top strategy for immunosuppressant discontinuation in SLE.
From EULAR 2018:
Baricitinib shows potential as lupus treatment.
About Dr. Yazdany
Dr. Yazdany is an associate professor in the division of rheumatology, department of medicine at UCSF (@UCSFMedicine). She is a rheumatologist and clinical researcher with expertise in systemic lupus erythematosus and health care quality measurement and improvement. Her clinical activities include seeing patients in the UCSF Lupus Clinic, where she serves as codirector, as well as at San Francisco General Hospital. Dr. Yazdany codirects the Quality and Informatics Lab (quil.ucsf.edu), which uses data to drive improvements in health care delivery and outcomes for people with rheumatic diseases. She also leads ongoing, longitudinal studies of lupus that are investigating health disparities and outcomes in the condition.
About Dr. Schmajuk
Dr. Schmajuk is an Associate Professor in the Division of Rheumatology, Department of Medicine at UCSF (@UCSFMedicine) and the San Francisco VA Medical Center. She is a rheumatologist and clinical researcher with expertise in systemic #lupus erythematosus, quality of care, and patient safety. Dr. Schmajuk also co-directs the Quality and Informatics Lab (quil.ucsf.edu), which uses data to drive improvements in health care delivery and outcomes for people with rheumatic diseases. She leads studies to develop patient-facing disease dashboards with the goal of improving patient-provider communication for patients with RA and SLE.
Are you new to Twitter chats? We have included simple steps below to help you join and participate in the conversation.
Join us at #MDedgeChats on Tuesday, April 23, 2019, at 7:00 pm EST, for a Twitter discussion in Rheumatology on some of the top studies reported at the LUPUS 2019 Congress in San Francisco, April 5-8. Our special guests are two rheumatologists with expertise in lupus who attended the congress, Jinoos Yazdany, MD, and Gabriela Schmajuk, MD, both with the University of California, San Francisco. They will discuss the ins and outs of the study results presented.
We hope you can join us and invite a colleague, too.
We will discuss the results of the EMBRACE trial, which looks at the efficacy and safety of belimumab (Benlysta) in black patients with systemic lupus erythematosus (SLE); these patients have a higher prevalence of SLE and often higher disease severity but have been poorly represented in past belimumab studies.
We will also chat about the results of a phase 2 trial of baricitinib (Olumiant) in SLE patients.
Finally, we will look at the clinical utility of monitoring hydroxychloroquine levels in SLE patients and how well levels of the drug correlate with disease activity through the results of a meta-analysis of studies that examined these questions.
Topics of conversation
Q1: How does the methodology of the EMBRACE trial differ from past phase 3 belimumab trials?
Q2: How does the EMBRACE trial affect the way you prescribe belimumab?
Q3: Does the hydroxychloroquine level meta-analysis provide persuasive enough evidence to begin measuring it?
Q4: What kinds of interventions show the best evidence for improving hydroxychloroquine adherence?
Q5: Were concerns about the safety of baricitinib in SLE patients reduced by the trial results?
Resources
EMBRACE trial: Efficacy and Safety of Belimumab in Black Race Patients with Systemic Lupus Erythematosus.
LUPUS 2019 abstract | ClinicalTrials.gov listing
Phase 2 trial of baricitinib in SLE.
LUPUS 2019 abstract | ClinicalTrials.gov listing
Meta-analysis examining the clinical significance of monitoring of hydroxychloroquine levels in SLE.
LUPUS 2019 abstract
From LUPUS 2019:
Belimumab a bust for black SLE patients.
Here’s a top strategy for immunosuppressant discontinuation in SLE.
From EULAR 2018:
Baricitinib shows potential as lupus treatment.
About Dr. Yazdany
Dr. Yazdany is an associate professor in the division of rheumatology, department of medicine at UCSF (@UCSFMedicine). She is a rheumatologist and clinical researcher with expertise in systemic lupus erythematosus and health care quality measurement and improvement. Her clinical activities include seeing patients in the UCSF Lupus Clinic, where she serves as codirector, as well as at San Francisco General Hospital. Dr. Yazdany codirects the Quality and Informatics Lab (quil.ucsf.edu), which uses data to drive improvements in health care delivery and outcomes for people with rheumatic diseases. She also leads ongoing, longitudinal studies of lupus that are investigating health disparities and outcomes in the condition.
About Dr. Schmajuk
Dr. Schmajuk is an Associate Professor in the Division of Rheumatology, Department of Medicine at UCSF (@UCSFMedicine) and the San Francisco VA Medical Center. She is a rheumatologist and clinical researcher with expertise in systemic #lupus erythematosus, quality of care, and patient safety. Dr. Schmajuk also co-directs the Quality and Informatics Lab (quil.ucsf.edu), which uses data to drive improvements in health care delivery and outcomes for people with rheumatic diseases. She leads studies to develop patient-facing disease dashboards with the goal of improving patient-provider communication for patients with RA and SLE.
Are you new to Twitter chats? We have included simple steps below to help you join and participate in the conversation.
Dr. Joseph Vassalotti: Cancer risk minimal with ARBs
PHILADELPHIA – according to a senior officer of the National Kidney Foundation.
“I’ve been telling everyone not to stop on their own,” said Joseph A. Vassalotti, MD, chief medical officer for the National Kidney Foundation and associate clinical professor of medicine at Icahn School of Medicine at Mount Sinai, New York.
“The risk of cardiovascular events acutely and the long-term risk of kidney disease progression is much more concerning to me, if they self-discontinue the ARB, than the small risk of cancer,” Dr. Vassalotti said in a meet-the-professor session at the annual meeting of the American College of Physicians.
Put in perspective, the absolute risk of cancer according to the Food and Drug Administration is one new malignancy per 8,000 patients treated with 320 mg of valsartan daily – the highest ARB dose that contained N-Nitrosodimethylamine (NDMA), one of several impurities that led to the recent recalls.
Dr. Vassalotti said that so far, he’s been able to avoid switching patients from one ARB to another by working with pharmacies to get the same medication in a different generic brand not affected by the FDA recalls.
He advised caution in switching ARBs, noting a paucity of head-to-head comparative data between ARBs.
“There may be variable effects,” he said.
If switching is thought to be warranted, he said, some extra tests or visits might be needed to ensure avoidance of hyperkalemia, undertreated hypertension, or hypotension.
Dr. Vassalotti encouraged attendees to review a perspective piece in the New England Journal of Medicine (2019 Mar 13. doi: 10.1056/NEJMp1901657) describing this hypertension “hot potato” resulting from the large-scale voluntary recalls of products containing valsartan, losartan, and irbesartan due to nitrosamine contamination.
Patients may hear about recalls of hypertension drugs, but may not know what products or manufacturers are involved, leaving the burden on clinicians, pharmacies, and health care systems to respond to their concerns, said authors of that perspective piece, led by J. Brian Byrd, MD, of the University of Michigan, Ann Arbor.
“Recalls may trigger unnecessary concern among many people receiving antihypertensive therapy – and may be ignored by people who take ARBs for heart failure or chronic kidney disease,” wrote Dr. Byrd and his colleagues.
The FDA, which said it has worked with manufacturers to “swiftly” remove ARB drug products with impurity levels above acceptable limits, is now maintaining a list of other currently marketed ARB products that are being tested for impurities.
As of the latest update on April 4, the FDA listed more than 40 products with an overall nitrosamine impurity determination of “not present” and more than 300 additional products for which assessments are not yet complete.
“Essentially, we have a safe list now of ARBs that is being developed,” Dr. Vassalotti said. “So if a patient really wanted to change, I would consult that list, and consider picking one that’s been tested already on that list, and the FDA hopefully will complete testing on all the ARB drugs in the near future.”
Dr. Vassalotti is a consultant with Merck, Janssen, and the U.S. Nephrology Advisory Board.
PHILADELPHIA – according to a senior officer of the National Kidney Foundation.
“I’ve been telling everyone not to stop on their own,” said Joseph A. Vassalotti, MD, chief medical officer for the National Kidney Foundation and associate clinical professor of medicine at Icahn School of Medicine at Mount Sinai, New York.
“The risk of cardiovascular events acutely and the long-term risk of kidney disease progression is much more concerning to me, if they self-discontinue the ARB, than the small risk of cancer,” Dr. Vassalotti said in a meet-the-professor session at the annual meeting of the American College of Physicians.
Put in perspective, the absolute risk of cancer according to the Food and Drug Administration is one new malignancy per 8,000 patients treated with 320 mg of valsartan daily – the highest ARB dose that contained N-Nitrosodimethylamine (NDMA), one of several impurities that led to the recent recalls.
Dr. Vassalotti said that so far, he’s been able to avoid switching patients from one ARB to another by working with pharmacies to get the same medication in a different generic brand not affected by the FDA recalls.
He advised caution in switching ARBs, noting a paucity of head-to-head comparative data between ARBs.
“There may be variable effects,” he said.
If switching is thought to be warranted, he said, some extra tests or visits might be needed to ensure avoidance of hyperkalemia, undertreated hypertension, or hypotension.
Dr. Vassalotti encouraged attendees to review a perspective piece in the New England Journal of Medicine (2019 Mar 13. doi: 10.1056/NEJMp1901657) describing this hypertension “hot potato” resulting from the large-scale voluntary recalls of products containing valsartan, losartan, and irbesartan due to nitrosamine contamination.
Patients may hear about recalls of hypertension drugs, but may not know what products or manufacturers are involved, leaving the burden on clinicians, pharmacies, and health care systems to respond to their concerns, said authors of that perspective piece, led by J. Brian Byrd, MD, of the University of Michigan, Ann Arbor.
“Recalls may trigger unnecessary concern among many people receiving antihypertensive therapy – and may be ignored by people who take ARBs for heart failure or chronic kidney disease,” wrote Dr. Byrd and his colleagues.
The FDA, which said it has worked with manufacturers to “swiftly” remove ARB drug products with impurity levels above acceptable limits, is now maintaining a list of other currently marketed ARB products that are being tested for impurities.
As of the latest update on April 4, the FDA listed more than 40 products with an overall nitrosamine impurity determination of “not present” and more than 300 additional products for which assessments are not yet complete.
“Essentially, we have a safe list now of ARBs that is being developed,” Dr. Vassalotti said. “So if a patient really wanted to change, I would consult that list, and consider picking one that’s been tested already on that list, and the FDA hopefully will complete testing on all the ARB drugs in the near future.”
Dr. Vassalotti is a consultant with Merck, Janssen, and the U.S. Nephrology Advisory Board.
PHILADELPHIA – according to a senior officer of the National Kidney Foundation.
“I’ve been telling everyone not to stop on their own,” said Joseph A. Vassalotti, MD, chief medical officer for the National Kidney Foundation and associate clinical professor of medicine at Icahn School of Medicine at Mount Sinai, New York.
“The risk of cardiovascular events acutely and the long-term risk of kidney disease progression is much more concerning to me, if they self-discontinue the ARB, than the small risk of cancer,” Dr. Vassalotti said in a meet-the-professor session at the annual meeting of the American College of Physicians.
Put in perspective, the absolute risk of cancer according to the Food and Drug Administration is one new malignancy per 8,000 patients treated with 320 mg of valsartan daily – the highest ARB dose that contained N-Nitrosodimethylamine (NDMA), one of several impurities that led to the recent recalls.
Dr. Vassalotti said that so far, he’s been able to avoid switching patients from one ARB to another by working with pharmacies to get the same medication in a different generic brand not affected by the FDA recalls.
He advised caution in switching ARBs, noting a paucity of head-to-head comparative data between ARBs.
“There may be variable effects,” he said.
If switching is thought to be warranted, he said, some extra tests or visits might be needed to ensure avoidance of hyperkalemia, undertreated hypertension, or hypotension.
Dr. Vassalotti encouraged attendees to review a perspective piece in the New England Journal of Medicine (2019 Mar 13. doi: 10.1056/NEJMp1901657) describing this hypertension “hot potato” resulting from the large-scale voluntary recalls of products containing valsartan, losartan, and irbesartan due to nitrosamine contamination.
Patients may hear about recalls of hypertension drugs, but may not know what products or manufacturers are involved, leaving the burden on clinicians, pharmacies, and health care systems to respond to their concerns, said authors of that perspective piece, led by J. Brian Byrd, MD, of the University of Michigan, Ann Arbor.
“Recalls may trigger unnecessary concern among many people receiving antihypertensive therapy – and may be ignored by people who take ARBs for heart failure or chronic kidney disease,” wrote Dr. Byrd and his colleagues.
The FDA, which said it has worked with manufacturers to “swiftly” remove ARB drug products with impurity levels above acceptable limits, is now maintaining a list of other currently marketed ARB products that are being tested for impurities.
As of the latest update on April 4, the FDA listed more than 40 products with an overall nitrosamine impurity determination of “not present” and more than 300 additional products for which assessments are not yet complete.
“Essentially, we have a safe list now of ARBs that is being developed,” Dr. Vassalotti said. “So if a patient really wanted to change, I would consult that list, and consider picking one that’s been tested already on that list, and the FDA hopefully will complete testing on all the ARB drugs in the near future.”
Dr. Vassalotti is a consultant with Merck, Janssen, and the U.S. Nephrology Advisory Board.
FROM INTERNAL MEDICINE 2019
Malpractice: Diagnostic errors top allegation involving children
Diagnostic error is the most common allegation against pediatricians when sued by patients and their families, a study finds.
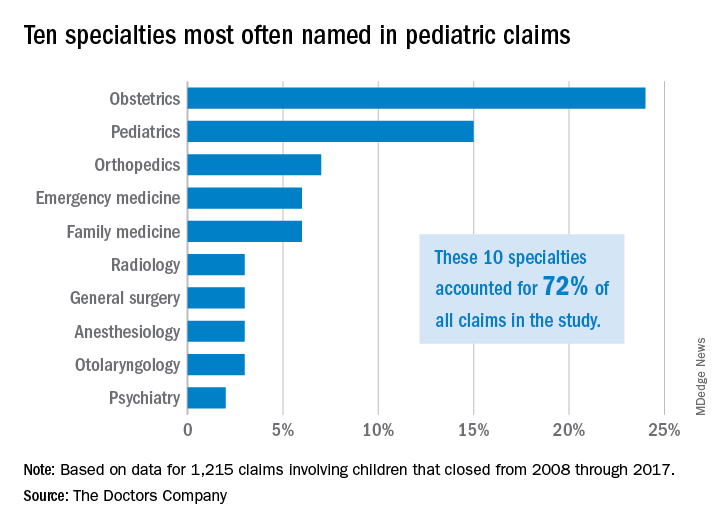
Investigators with The Doctors Company, a national medical liability insurer, examined 1,215 closed claims involving children from the company’s database between 2008 and 2017. Results showed that diagnostic mistakes, including delayed diagnosis, incorrect diagnosis, and failure to diagnose, were the most common accusations among claims that involved children ages 1 through 17. Poor medical treatment was the second most common allegation for claims that involved children aged 1-9, while surgical treatment-related error was the second most frequent accusation for children ages 10-17.
Pediatricians, orthopedic surgeons, and emergency medicine physicians were the most frequently named specialists in claims associated with children older than 1 month. Obstetricians were most frequently defendants in claims involving neonates. For these cases, errors during labor and delivery care were the most common complaints.
Of the 1,215 claims, obstetricians were named in 24% of the cases and pediatricians were named in 15% of the cases. The majority of claims were filed against physicians in the first 3 years following the medical incident alleged, according to the study, published by The Doctors Company.
The average patient payment in each case was $630,456, and the average expense to defend each claim was $157,502, according to the analysis. Claims that involved neonates had the highest average payment ($936,843) and the highest defense costs ($187,117), while claims involving children aged 10-17 years had the lowest average payment ($386,849) and cost the least to defend ($129,816).
For cases involving neonates, the type of therapy selected during labor and delivery and how it was managed were the most common factors contributing to the alleged injury, according to the analysis.
The most frequent factors contributing to patient harm for other age groups involved patient assessment issues and communication problems between the patient/family and the physician. Inadequate patient assessments were closely linked to incorrect diagnoses, while incomplete communication between patients/family members and providers impacted clinicians’ ability to make correct diagnoses, according to the study.
This analysis “shows that pediatric malpractice lawsuits impact nearly every area of medicine,” William F. Getman, MD, a pediatrician in Austin, Tex., said in an interview. “I was surprised to see that the most common age of a patient in a malpractice lawsuit was less than 1 month old. This age group also sustained the most severe injuries and had the highest indemnity paid.”
The study offers several key takeaways, including the importance of identifying system weaknesses in your medical practice and evaluating if improvements are needed, according to Darrell Ranum, vice president for patient safety and risk management for The Doctors Company.
Simple improvements, such as implementing tracking mechanisms for test results and referrals, can reduce the chance that important information falls through the cracks and delays diagnosis or treatment, Mr. Ranum said in an interview.
“When parents raise questions about their child’s complaints, this is the best opportunity to identify illnesses and conditions that represent a serious threat to children,” he said. “Prepare office staff members to know what complaints need to be evaluated by a clinician or require immediate care.”
In addition, the study findings point to the need to improve communication in all areas of the practice spectrum, Dr. Getman said.
“Many of the lawsuits could have been avoided by improvements in communication – doctor to patient, patient to doctor, doctor to nurse, doctor to doctor, nurse to patient, etc.,” he said. “Finding more effective and accurate ways to communicate will avoid mistakes, improve care, and improve outcomes. Examples of ways to improve communication include use of an interpreter when indicated, verbal and written explanations of instructions, and system improvements in tracking messages/labs/data. There are innumerable other ways to improve communication in health care.”
SOURCE: Ranum, D. The Doctor’s Advocate. First Quarter 2019.
Diagnostic error is the most common allegation against pediatricians when sued by patients and their families, a study finds.
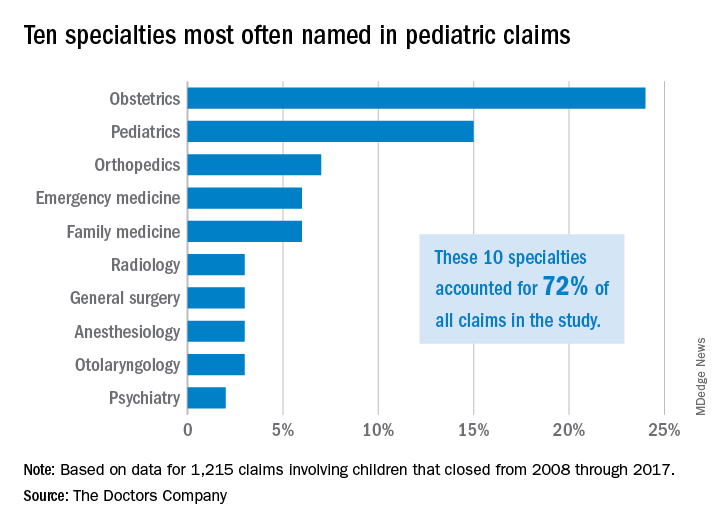
Investigators with The Doctors Company, a national medical liability insurer, examined 1,215 closed claims involving children from the company’s database between 2008 and 2017. Results showed that diagnostic mistakes, including delayed diagnosis, incorrect diagnosis, and failure to diagnose, were the most common accusations among claims that involved children ages 1 through 17. Poor medical treatment was the second most common allegation for claims that involved children aged 1-9, while surgical treatment-related error was the second most frequent accusation for children ages 10-17.
Pediatricians, orthopedic surgeons, and emergency medicine physicians were the most frequently named specialists in claims associated with children older than 1 month. Obstetricians were most frequently defendants in claims involving neonates. For these cases, errors during labor and delivery care were the most common complaints.
Of the 1,215 claims, obstetricians were named in 24% of the cases and pediatricians were named in 15% of the cases. The majority of claims were filed against physicians in the first 3 years following the medical incident alleged, according to the study, published by The Doctors Company.
The average patient payment in each case was $630,456, and the average expense to defend each claim was $157,502, according to the analysis. Claims that involved neonates had the highest average payment ($936,843) and the highest defense costs ($187,117), while claims involving children aged 10-17 years had the lowest average payment ($386,849) and cost the least to defend ($129,816).
For cases involving neonates, the type of therapy selected during labor and delivery and how it was managed were the most common factors contributing to the alleged injury, according to the analysis.
The most frequent factors contributing to patient harm for other age groups involved patient assessment issues and communication problems between the patient/family and the physician. Inadequate patient assessments were closely linked to incorrect diagnoses, while incomplete communication between patients/family members and providers impacted clinicians’ ability to make correct diagnoses, according to the study.
This analysis “shows that pediatric malpractice lawsuits impact nearly every area of medicine,” William F. Getman, MD, a pediatrician in Austin, Tex., said in an interview. “I was surprised to see that the most common age of a patient in a malpractice lawsuit was less than 1 month old. This age group also sustained the most severe injuries and had the highest indemnity paid.”
The study offers several key takeaways, including the importance of identifying system weaknesses in your medical practice and evaluating if improvements are needed, according to Darrell Ranum, vice president for patient safety and risk management for The Doctors Company.
Simple improvements, such as implementing tracking mechanisms for test results and referrals, can reduce the chance that important information falls through the cracks and delays diagnosis or treatment, Mr. Ranum said in an interview.
“When parents raise questions about their child’s complaints, this is the best opportunity to identify illnesses and conditions that represent a serious threat to children,” he said. “Prepare office staff members to know what complaints need to be evaluated by a clinician or require immediate care.”
In addition, the study findings point to the need to improve communication in all areas of the practice spectrum, Dr. Getman said.
“Many of the lawsuits could have been avoided by improvements in communication – doctor to patient, patient to doctor, doctor to nurse, doctor to doctor, nurse to patient, etc.,” he said. “Finding more effective and accurate ways to communicate will avoid mistakes, improve care, and improve outcomes. Examples of ways to improve communication include use of an interpreter when indicated, verbal and written explanations of instructions, and system improvements in tracking messages/labs/data. There are innumerable other ways to improve communication in health care.”
SOURCE: Ranum, D. The Doctor’s Advocate. First Quarter 2019.
Diagnostic error is the most common allegation against pediatricians when sued by patients and their families, a study finds.
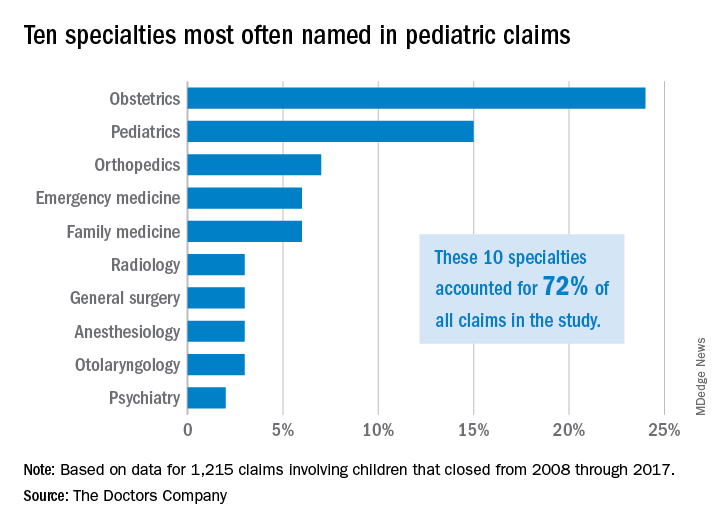
Investigators with The Doctors Company, a national medical liability insurer, examined 1,215 closed claims involving children from the company’s database between 2008 and 2017. Results showed that diagnostic mistakes, including delayed diagnosis, incorrect diagnosis, and failure to diagnose, were the most common accusations among claims that involved children ages 1 through 17. Poor medical treatment was the second most common allegation for claims that involved children aged 1-9, while surgical treatment-related error was the second most frequent accusation for children ages 10-17.
Pediatricians, orthopedic surgeons, and emergency medicine physicians were the most frequently named specialists in claims associated with children older than 1 month. Obstetricians were most frequently defendants in claims involving neonates. For these cases, errors during labor and delivery care were the most common complaints.
Of the 1,215 claims, obstetricians were named in 24% of the cases and pediatricians were named in 15% of the cases. The majority of claims were filed against physicians in the first 3 years following the medical incident alleged, according to the study, published by The Doctors Company.
The average patient payment in each case was $630,456, and the average expense to defend each claim was $157,502, according to the analysis. Claims that involved neonates had the highest average payment ($936,843) and the highest defense costs ($187,117), while claims involving children aged 10-17 years had the lowest average payment ($386,849) and cost the least to defend ($129,816).
For cases involving neonates, the type of therapy selected during labor and delivery and how it was managed were the most common factors contributing to the alleged injury, according to the analysis.
The most frequent factors contributing to patient harm for other age groups involved patient assessment issues and communication problems between the patient/family and the physician. Inadequate patient assessments were closely linked to incorrect diagnoses, while incomplete communication between patients/family members and providers impacted clinicians’ ability to make correct diagnoses, according to the study.
This analysis “shows that pediatric malpractice lawsuits impact nearly every area of medicine,” William F. Getman, MD, a pediatrician in Austin, Tex., said in an interview. “I was surprised to see that the most common age of a patient in a malpractice lawsuit was less than 1 month old. This age group also sustained the most severe injuries and had the highest indemnity paid.”
The study offers several key takeaways, including the importance of identifying system weaknesses in your medical practice and evaluating if improvements are needed, according to Darrell Ranum, vice president for patient safety and risk management for The Doctors Company.
Simple improvements, such as implementing tracking mechanisms for test results and referrals, can reduce the chance that important information falls through the cracks and delays diagnosis or treatment, Mr. Ranum said in an interview.
“When parents raise questions about their child’s complaints, this is the best opportunity to identify illnesses and conditions that represent a serious threat to children,” he said. “Prepare office staff members to know what complaints need to be evaluated by a clinician or require immediate care.”
In addition, the study findings point to the need to improve communication in all areas of the practice spectrum, Dr. Getman said.
“Many of the lawsuits could have been avoided by improvements in communication – doctor to patient, patient to doctor, doctor to nurse, doctor to doctor, nurse to patient, etc.,” he said. “Finding more effective and accurate ways to communicate will avoid mistakes, improve care, and improve outcomes. Examples of ways to improve communication include use of an interpreter when indicated, verbal and written explanations of instructions, and system improvements in tracking messages/labs/data. There are innumerable other ways to improve communication in health care.”
SOURCE: Ranum, D. The Doctor’s Advocate. First Quarter 2019.










