User login
Tidying up a motley crew
It probably is buried in a box in your parents’ basement, but try to remember your soccer or football or track team picture from when you were in eighth grade. Tragically but predictably, most of your peers who were chubby in third grade are nowhere to be seen in the photo. But still it was a pretty motley crew. Some of you weren’t even up to the armpits of your taller teammates. Some guys were shaving. Others had little boys’ voices. Half the girls had reached menarche. Another third were still waiting impatiently for a breast bud.
The precocious and the late bloomers, you were all on the team. But it was pretty clear that those who had matured first generally were the more talented and successful athletes. By the time you were juniors in high school, many of those who matured late had quit the sport or been cut from the team, unable to catch up. Others may have been forced to give up the sport by their parents, who were concerned about the risk of injury when bodies of disparate size collide. A few of the early bloomers may have become depressed, older adolescents who had failed to match the hype and expectations that came when they were a head taller than their grade school teammates.
These natural consequences of biological variation are not small potatoes for the fragile egos of adolescents and preadolescents. The lead article in the November 2018 Pediatrics offers a partial solution for the issue of sports participation in a population with widely discrepant states of maturity (“Biobanding: A New Paradigm for Youth Sports and Training,” Pediatrics. 2018 Nov;142[5]:e20180423). The authors describe a system they call biobanding, in which “the percentage of predicted adult stature attained at the time of observation as the indicator of maturity status” is used to create groups or bands of participants with similar levels of maturity. They argue that this method is easy to use and report and that has been used with some success in Great Britain.
At first blush, biobanding sounds appealing, particularly for large communities. However, as someone who grew up in and practiced in a small town, I’m not sure how successfully it could be scaled down. There have been years when I could easily have disqualified a third of the high school football team were I to take into consideration the size and maturity of the competition they would be facing. But I didn’t. The fading interest in football in Maine has prompted some schools to consider moving to less-than-11-player competition or even to flag football. To some extent, the problem is taking care of itself.
How much tinkering should we be doing with something that is arguably a distorted natural selection process? With thoughtfully crafted rules, diligent supervision, and officiating, most of the issues of safety that one might attribute to discrepancies in maturity can be minimized. There always will be children who become discouraged and quit when they see the handwriting on the wall that reads “those who mature early win.” I’m certainly not wild about parents holding their children out of school to give them a jump on their peers. It can spiral out of control.
A more appealing solution is to do a better job of advertising the many successful late bloomers in professional sports ... and making sure that late-blooming children are given an abundance of active and competitive (if they wish) alternatives to sports dominated by their early maturing peers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
It probably is buried in a box in your parents’ basement, but try to remember your soccer or football or track team picture from when you were in eighth grade. Tragically but predictably, most of your peers who were chubby in third grade are nowhere to be seen in the photo. But still it was a pretty motley crew. Some of you weren’t even up to the armpits of your taller teammates. Some guys were shaving. Others had little boys’ voices. Half the girls had reached menarche. Another third were still waiting impatiently for a breast bud.
The precocious and the late bloomers, you were all on the team. But it was pretty clear that those who had matured first generally were the more talented and successful athletes. By the time you were juniors in high school, many of those who matured late had quit the sport or been cut from the team, unable to catch up. Others may have been forced to give up the sport by their parents, who were concerned about the risk of injury when bodies of disparate size collide. A few of the early bloomers may have become depressed, older adolescents who had failed to match the hype and expectations that came when they were a head taller than their grade school teammates.
These natural consequences of biological variation are not small potatoes for the fragile egos of adolescents and preadolescents. The lead article in the November 2018 Pediatrics offers a partial solution for the issue of sports participation in a population with widely discrepant states of maturity (“Biobanding: A New Paradigm for Youth Sports and Training,” Pediatrics. 2018 Nov;142[5]:e20180423). The authors describe a system they call biobanding, in which “the percentage of predicted adult stature attained at the time of observation as the indicator of maturity status” is used to create groups or bands of participants with similar levels of maturity. They argue that this method is easy to use and report and that has been used with some success in Great Britain.
At first blush, biobanding sounds appealing, particularly for large communities. However, as someone who grew up in and practiced in a small town, I’m not sure how successfully it could be scaled down. There have been years when I could easily have disqualified a third of the high school football team were I to take into consideration the size and maturity of the competition they would be facing. But I didn’t. The fading interest in football in Maine has prompted some schools to consider moving to less-than-11-player competition or even to flag football. To some extent, the problem is taking care of itself.
How much tinkering should we be doing with something that is arguably a distorted natural selection process? With thoughtfully crafted rules, diligent supervision, and officiating, most of the issues of safety that one might attribute to discrepancies in maturity can be minimized. There always will be children who become discouraged and quit when they see the handwriting on the wall that reads “those who mature early win.” I’m certainly not wild about parents holding their children out of school to give them a jump on their peers. It can spiral out of control.
A more appealing solution is to do a better job of advertising the many successful late bloomers in professional sports ... and making sure that late-blooming children are given an abundance of active and competitive (if they wish) alternatives to sports dominated by their early maturing peers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
It probably is buried in a box in your parents’ basement, but try to remember your soccer or football or track team picture from when you were in eighth grade. Tragically but predictably, most of your peers who were chubby in third grade are nowhere to be seen in the photo. But still it was a pretty motley crew. Some of you weren’t even up to the armpits of your taller teammates. Some guys were shaving. Others had little boys’ voices. Half the girls had reached menarche. Another third were still waiting impatiently for a breast bud.
The precocious and the late bloomers, you were all on the team. But it was pretty clear that those who had matured first generally were the more talented and successful athletes. By the time you were juniors in high school, many of those who matured late had quit the sport or been cut from the team, unable to catch up. Others may have been forced to give up the sport by their parents, who were concerned about the risk of injury when bodies of disparate size collide. A few of the early bloomers may have become depressed, older adolescents who had failed to match the hype and expectations that came when they were a head taller than their grade school teammates.
These natural consequences of biological variation are not small potatoes for the fragile egos of adolescents and preadolescents. The lead article in the November 2018 Pediatrics offers a partial solution for the issue of sports participation in a population with widely discrepant states of maturity (“Biobanding: A New Paradigm for Youth Sports and Training,” Pediatrics. 2018 Nov;142[5]:e20180423). The authors describe a system they call biobanding, in which “the percentage of predicted adult stature attained at the time of observation as the indicator of maturity status” is used to create groups or bands of participants with similar levels of maturity. They argue that this method is easy to use and report and that has been used with some success in Great Britain.
At first blush, biobanding sounds appealing, particularly for large communities. However, as someone who grew up in and practiced in a small town, I’m not sure how successfully it could be scaled down. There have been years when I could easily have disqualified a third of the high school football team were I to take into consideration the size and maturity of the competition they would be facing. But I didn’t. The fading interest in football in Maine has prompted some schools to consider moving to less-than-11-player competition or even to flag football. To some extent, the problem is taking care of itself.
How much tinkering should we be doing with something that is arguably a distorted natural selection process? With thoughtfully crafted rules, diligent supervision, and officiating, most of the issues of safety that one might attribute to discrepancies in maturity can be minimized. There always will be children who become discouraged and quit when they see the handwriting on the wall that reads “those who mature early win.” I’m certainly not wild about parents holding their children out of school to give them a jump on their peers. It can spiral out of control.
A more appealing solution is to do a better job of advertising the many successful late bloomers in professional sports ... and making sure that late-blooming children are given an abundance of active and competitive (if they wish) alternatives to sports dominated by their early maturing peers.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
Phase 3 study of novel pemphigus treatment is initiated
and will enroll about 120 patients with moderate to severe disease, according to Principia Biopharma, which is developing the drug.
In a press release, the company said that the randomized, double-blind PEGASYS study will compare PRN1008 with placebo, in about 120 patients with newly diagnosed or relapsing moderate to severe pemphigus.
The company also reported the results of an open label phase 2 study of patients with newly diagnosed or relapsing mild or moderate pemphigus, including pemphigus vulgaris and pemphigus foliaceus, which found that control of disease activity within 4 weeks of starting treatment – the primary efficacy endpoint – was achieved by more than 50% of patients taking PRN1008. Principia has extended the trial’s active treatment period from 12 to 24 weeks. The results also led the company to initiate the phase 3 trial.
PRN1008 is an inhibitor of BTK, an enzyme that “is present in the signaling pathways of most types of white blood cells except for T cells and plasma cells,” according to the company’s press release.
and will enroll about 120 patients with moderate to severe disease, according to Principia Biopharma, which is developing the drug.
In a press release, the company said that the randomized, double-blind PEGASYS study will compare PRN1008 with placebo, in about 120 patients with newly diagnosed or relapsing moderate to severe pemphigus.
The company also reported the results of an open label phase 2 study of patients with newly diagnosed or relapsing mild or moderate pemphigus, including pemphigus vulgaris and pemphigus foliaceus, which found that control of disease activity within 4 weeks of starting treatment – the primary efficacy endpoint – was achieved by more than 50% of patients taking PRN1008. Principia has extended the trial’s active treatment period from 12 to 24 weeks. The results also led the company to initiate the phase 3 trial.
PRN1008 is an inhibitor of BTK, an enzyme that “is present in the signaling pathways of most types of white blood cells except for T cells and plasma cells,” according to the company’s press release.
and will enroll about 120 patients with moderate to severe disease, according to Principia Biopharma, which is developing the drug.
In a press release, the company said that the randomized, double-blind PEGASYS study will compare PRN1008 with placebo, in about 120 patients with newly diagnosed or relapsing moderate to severe pemphigus.
The company also reported the results of an open label phase 2 study of patients with newly diagnosed or relapsing mild or moderate pemphigus, including pemphigus vulgaris and pemphigus foliaceus, which found that control of disease activity within 4 weeks of starting treatment – the primary efficacy endpoint – was achieved by more than 50% of patients taking PRN1008. Principia has extended the trial’s active treatment period from 12 to 24 weeks. The results also led the company to initiate the phase 3 trial.
PRN1008 is an inhibitor of BTK, an enzyme that “is present in the signaling pathways of most types of white blood cells except for T cells and plasma cells,” according to the company’s press release.
hTERT expression predicts RCC survival, tumor aggressiveness
Human telomerase reverse transcriptase (hTERT) protein expression is associated with clear cell renal carcinoma (ccRCC) tumor aggressiveness and disease-specific survival (DSS), according to investigators.
Associations between hTERT expression and clinicopathologic features and outcomes were less robust or nonexistent in papillary and chromophobe subtypes, reported Leili Saeednejad Zanjani, MD, of the Oncopathology Research Center at Iran University of Medical Sciences in Tehran, and colleagues.
“Evidence shows that telomerase is expressed in 85% of malignancies, and the level of its activity is higher in advanced and metastatic tumors,” the authors wrote in Pathology.
“A number of clinical studies have been performed to evaluate the association between telomerase activity and clinicopathological parameters in renal cancer showing that telomerase activity level correlates with progression of RCC,” Dr. Zanjani and associates wrote. As none of these specifically evaluated hTERT protein expression, the investigators conducted a study to learn more.
The investigators analyzed hTERT expression level in 176 cases of RCC, requiring that each tumor had three core biopsies because of concerns of heterogeneity. The population consisted of 113 clear cell, 12 type I papillary, 20 type II papillary, and 31 chromophobe subtypes. Patient and clinicopathologic features were compared with survival and hTERT expression. Median follow-up time was 42 months.
Correlations between hTERT expression and disease characteristics were pronounced in cases of ccRCC, compared with other subtypes. In ccRCC, hTERT expression was significantly associated with tumor stage, nucleolar grade, tumor size, microvascular invasion, lymph node invasion, renal pelvis involvement, renal sinus fat involvement, Gerota fascia invasion, and distant metastasis. Survival analysis showed that DSS of ccRCC patients with high hTERT expression was 58 months, compared with 68 months for those with low hTERT expression (P =.012). Other parameters associated with survival were nucleolar grade, tumor stage, and tumor size.
For type I and II papillary subtypes, associations were found between hTERT expression and tumor stage and distant metastasis. In contrast, chromophobe RCC revealed no such relationships. No associations were found between hTERT expression and survival in any of these three latter subtypes, for slightly different reasons; no patients with type I disease died of renal cancer, disallowing creation of a Kaplan-Meier survival curve, whereas type II and chromophobe survival curves revealed insignificant relationships with hTERT expression. Along the same lines, no clinicopathologic characteristics of these subtypes were tied with survival.
“From these findings we are able to conclude that hTERT protein expression may be a novel prognostic indicator of worse outcome in tumor biopsies of patients with ccRCC, if follow up time is more prolonged,” the authors wrote. They noted that “telomerase is an attractive and ideal target for therapy due to overexpression in the majority of malignancies and low or nonexpression in most somatic cells.”
The study was funded by the Iran National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Zanjani LS et al. Pathology. 2018 Nov 19. doi: 10.1016/j.pathol.2018.08.019.
Human telomerase reverse transcriptase (hTERT) protein expression is associated with clear cell renal carcinoma (ccRCC) tumor aggressiveness and disease-specific survival (DSS), according to investigators.
Associations between hTERT expression and clinicopathologic features and outcomes were less robust or nonexistent in papillary and chromophobe subtypes, reported Leili Saeednejad Zanjani, MD, of the Oncopathology Research Center at Iran University of Medical Sciences in Tehran, and colleagues.
“Evidence shows that telomerase is expressed in 85% of malignancies, and the level of its activity is higher in advanced and metastatic tumors,” the authors wrote in Pathology.
“A number of clinical studies have been performed to evaluate the association between telomerase activity and clinicopathological parameters in renal cancer showing that telomerase activity level correlates with progression of RCC,” Dr. Zanjani and associates wrote. As none of these specifically evaluated hTERT protein expression, the investigators conducted a study to learn more.
The investigators analyzed hTERT expression level in 176 cases of RCC, requiring that each tumor had three core biopsies because of concerns of heterogeneity. The population consisted of 113 clear cell, 12 type I papillary, 20 type II papillary, and 31 chromophobe subtypes. Patient and clinicopathologic features were compared with survival and hTERT expression. Median follow-up time was 42 months.
Correlations between hTERT expression and disease characteristics were pronounced in cases of ccRCC, compared with other subtypes. In ccRCC, hTERT expression was significantly associated with tumor stage, nucleolar grade, tumor size, microvascular invasion, lymph node invasion, renal pelvis involvement, renal sinus fat involvement, Gerota fascia invasion, and distant metastasis. Survival analysis showed that DSS of ccRCC patients with high hTERT expression was 58 months, compared with 68 months for those with low hTERT expression (P =.012). Other parameters associated with survival were nucleolar grade, tumor stage, and tumor size.
For type I and II papillary subtypes, associations were found between hTERT expression and tumor stage and distant metastasis. In contrast, chromophobe RCC revealed no such relationships. No associations were found between hTERT expression and survival in any of these three latter subtypes, for slightly different reasons; no patients with type I disease died of renal cancer, disallowing creation of a Kaplan-Meier survival curve, whereas type II and chromophobe survival curves revealed insignificant relationships with hTERT expression. Along the same lines, no clinicopathologic characteristics of these subtypes were tied with survival.
“From these findings we are able to conclude that hTERT protein expression may be a novel prognostic indicator of worse outcome in tumor biopsies of patients with ccRCC, if follow up time is more prolonged,” the authors wrote. They noted that “telomerase is an attractive and ideal target for therapy due to overexpression in the majority of malignancies and low or nonexpression in most somatic cells.”
The study was funded by the Iran National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Zanjani LS et al. Pathology. 2018 Nov 19. doi: 10.1016/j.pathol.2018.08.019.
Human telomerase reverse transcriptase (hTERT) protein expression is associated with clear cell renal carcinoma (ccRCC) tumor aggressiveness and disease-specific survival (DSS), according to investigators.
Associations between hTERT expression and clinicopathologic features and outcomes were less robust or nonexistent in papillary and chromophobe subtypes, reported Leili Saeednejad Zanjani, MD, of the Oncopathology Research Center at Iran University of Medical Sciences in Tehran, and colleagues.
“Evidence shows that telomerase is expressed in 85% of malignancies, and the level of its activity is higher in advanced and metastatic tumors,” the authors wrote in Pathology.
“A number of clinical studies have been performed to evaluate the association between telomerase activity and clinicopathological parameters in renal cancer showing that telomerase activity level correlates with progression of RCC,” Dr. Zanjani and associates wrote. As none of these specifically evaluated hTERT protein expression, the investigators conducted a study to learn more.
The investigators analyzed hTERT expression level in 176 cases of RCC, requiring that each tumor had three core biopsies because of concerns of heterogeneity. The population consisted of 113 clear cell, 12 type I papillary, 20 type II papillary, and 31 chromophobe subtypes. Patient and clinicopathologic features were compared with survival and hTERT expression. Median follow-up time was 42 months.
Correlations between hTERT expression and disease characteristics were pronounced in cases of ccRCC, compared with other subtypes. In ccRCC, hTERT expression was significantly associated with tumor stage, nucleolar grade, tumor size, microvascular invasion, lymph node invasion, renal pelvis involvement, renal sinus fat involvement, Gerota fascia invasion, and distant metastasis. Survival analysis showed that DSS of ccRCC patients with high hTERT expression was 58 months, compared with 68 months for those with low hTERT expression (P =.012). Other parameters associated with survival were nucleolar grade, tumor stage, and tumor size.
For type I and II papillary subtypes, associations were found between hTERT expression and tumor stage and distant metastasis. In contrast, chromophobe RCC revealed no such relationships. No associations were found between hTERT expression and survival in any of these three latter subtypes, for slightly different reasons; no patients with type I disease died of renal cancer, disallowing creation of a Kaplan-Meier survival curve, whereas type II and chromophobe survival curves revealed insignificant relationships with hTERT expression. Along the same lines, no clinicopathologic characteristics of these subtypes were tied with survival.
“From these findings we are able to conclude that hTERT protein expression may be a novel prognostic indicator of worse outcome in tumor biopsies of patients with ccRCC, if follow up time is more prolonged,” the authors wrote. They noted that “telomerase is an attractive and ideal target for therapy due to overexpression in the majority of malignancies and low or nonexpression in most somatic cells.”
The study was funded by the Iran National Science Foundation. The authors declared no conflicts of interest.
SOURCE: Zanjani LS et al. Pathology. 2018 Nov 19. doi: 10.1016/j.pathol.2018.08.019.
FROM PATHOLOGY
Key clinical point: Human telomerase reverse transcriptase (hTERT) protein expression is associated with clear cell renal carcinoma (ccRCC) tumor aggressiveness and disease-specific survival (DSS).
Major finding: DSS of ccRCC patients with high hTERT expression was 58 months, compared with 68 months for those with low hTERT expression (P equal to .012).
Study details: An analysis of hTERT protein expression and disease characteristics in 176 patients with RCC. The subtype population consisted of 113 clear cell, 12 type I papillary, 20 type II papillary, and 31 chromophobe cases.
Disclosures: The study was funded by the Iran National Science Foundation. The authors declared no conflicts of interest.
Source: Zanjani LS et al. Pathology. 2018 Nov 19. doi: 10.1016/j.pathol.2018.08.019.
Addressing Mental Health Needs of Patients with Epilepsy
A community-based program that helps patients with epilepsy self-manage their condition and related psychiatric problems has proven effective in reducing the severity of depression according to a study published in Epilepsy and Behavior.
- Community Targeted Self-Management for Epilepsy and Mental Illness (C-TIME), a behavioral program, consisted of ten 60 to 90-minute sessions conducted over 12 weeks.
- The program included outreach and engagement efforts to help patients suffering from both epilepsy and mental health conditions.
- Thirty patients were enrolled in the program; four months after participating in C-TIME, 66% of the enrolled patients were available for outcome evaluation.
- Researchers reported significant reduction in depression severity, and more than 90% of the group said they were satisfied with results.
Sajatovic M, Needham K, Colón-Zimmermann K, et al. The Community-targeted Self-management of Epilepsy and Mental Illness (C-TIME) initiative: A research, community, and healthcare administration partnership to reduce epilepsy burden [published online ahead of print October 29, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.10.004
A community-based program that helps patients with epilepsy self-manage their condition and related psychiatric problems has proven effective in reducing the severity of depression according to a study published in Epilepsy and Behavior.
- Community Targeted Self-Management for Epilepsy and Mental Illness (C-TIME), a behavioral program, consisted of ten 60 to 90-minute sessions conducted over 12 weeks.
- The program included outreach and engagement efforts to help patients suffering from both epilepsy and mental health conditions.
- Thirty patients were enrolled in the program; four months after participating in C-TIME, 66% of the enrolled patients were available for outcome evaluation.
- Researchers reported significant reduction in depression severity, and more than 90% of the group said they were satisfied with results.
Sajatovic M, Needham K, Colón-Zimmermann K, et al. The Community-targeted Self-management of Epilepsy and Mental Illness (C-TIME) initiative: A research, community, and healthcare administration partnership to reduce epilepsy burden [published online ahead of print October 29, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.10.004
A community-based program that helps patients with epilepsy self-manage their condition and related psychiatric problems has proven effective in reducing the severity of depression according to a study published in Epilepsy and Behavior.
- Community Targeted Self-Management for Epilepsy and Mental Illness (C-TIME), a behavioral program, consisted of ten 60 to 90-minute sessions conducted over 12 weeks.
- The program included outreach and engagement efforts to help patients suffering from both epilepsy and mental health conditions.
- Thirty patients were enrolled in the program; four months after participating in C-TIME, 66% of the enrolled patients were available for outcome evaluation.
- Researchers reported significant reduction in depression severity, and more than 90% of the group said they were satisfied with results.
Sajatovic M, Needham K, Colón-Zimmermann K, et al. The Community-targeted Self-management of Epilepsy and Mental Illness (C-TIME) initiative: A research, community, and healthcare administration partnership to reduce epilepsy burden [published online ahead of print October 29, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.10.004
Epilepsy Education That Reaches Underserved Communities
The Epilepsy Foundation, working with a pharmaceutical company, has launched an educational initiative to locate communities most in need of professional and consumer education. The program emphasizes the value of tailored and innovative approaches to reach underserved populations to improve their self-management skills for epilepsy.
- A data analysis conducted by The Connectors Project found 4 states in need of help: Michigan, Oklahoma, Nevada, and West Virginia, all of which have rural and/or underserved communities.
- The Foundation launched outreach and awareness programs in these states, as well as digital and in-person education for clinicians, patients, and families.
- The initiatives were designed to fill critical gaps in patients’ ability to self-manage epilepsy and gaps in their ability to get access to quality professional care.
Owens S, Sirven JI, Shafer PO, et al. Innovative approaches reaching underserved and rural communities to improve epilepsy care: A review of the methodology of the Connectors Project [published online ahead of print October 31, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.09.029
The Epilepsy Foundation, working with a pharmaceutical company, has launched an educational initiative to locate communities most in need of professional and consumer education. The program emphasizes the value of tailored and innovative approaches to reach underserved populations to improve their self-management skills for epilepsy.
- A data analysis conducted by The Connectors Project found 4 states in need of help: Michigan, Oklahoma, Nevada, and West Virginia, all of which have rural and/or underserved communities.
- The Foundation launched outreach and awareness programs in these states, as well as digital and in-person education for clinicians, patients, and families.
- The initiatives were designed to fill critical gaps in patients’ ability to self-manage epilepsy and gaps in their ability to get access to quality professional care.
Owens S, Sirven JI, Shafer PO, et al. Innovative approaches reaching underserved and rural communities to improve epilepsy care: A review of the methodology of the Connectors Project [published online ahead of print October 31, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.09.029
The Epilepsy Foundation, working with a pharmaceutical company, has launched an educational initiative to locate communities most in need of professional and consumer education. The program emphasizes the value of tailored and innovative approaches to reach underserved populations to improve their self-management skills for epilepsy.
- A data analysis conducted by The Connectors Project found 4 states in need of help: Michigan, Oklahoma, Nevada, and West Virginia, all of which have rural and/or underserved communities.
- The Foundation launched outreach and awareness programs in these states, as well as digital and in-person education for clinicians, patients, and families.
- The initiatives were designed to fill critical gaps in patients’ ability to self-manage epilepsy and gaps in their ability to get access to quality professional care.
Owens S, Sirven JI, Shafer PO, et al. Innovative approaches reaching underserved and rural communities to improve epilepsy care: A review of the methodology of the Connectors Project [published online ahead of print October 31, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.09.029
Should Neurologists Treat Psychiatric Problems in Patients with Epilepsy?
Giving neurologists the tools to diagnose and treat common psychiatric disorders can help meet the mental health needs of adults with epilepsy whose psychiatric comorbidities are being ignored, according to investigators from Wake Forest School of Medicine and Johns Hopkins University.
- There is a high prevalence of psychiatric disorders among adults with epilepsy.
- These comorbidities are often overlooked because patients have limited access to mental health services.
- Heidi Munger Clary and Jay Salpekar suggest that letting neurologists diagnose and manage common conditions like mood and anxiety disorders will help address this dilemma.
- The researchers suggest that validated screeners could help neurologists who do not have expertise in psychiatry to manage depression and anxiety.
- With such assistance, adult neurologists could be trained to effectively use selective serotonin reupdate inhibitors (SSRIs).
Munger Clary HM, Salpekar JA. Should adult neurologists play a role in the management of the most common psychiatric comorbidities? Practical considerations [published online ahead of print November 22, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.10.020
Giving neurologists the tools to diagnose and treat common psychiatric disorders can help meet the mental health needs of adults with epilepsy whose psychiatric comorbidities are being ignored, according to investigators from Wake Forest School of Medicine and Johns Hopkins University.
- There is a high prevalence of psychiatric disorders among adults with epilepsy.
- These comorbidities are often overlooked because patients have limited access to mental health services.
- Heidi Munger Clary and Jay Salpekar suggest that letting neurologists diagnose and manage common conditions like mood and anxiety disorders will help address this dilemma.
- The researchers suggest that validated screeners could help neurologists who do not have expertise in psychiatry to manage depression and anxiety.
- With such assistance, adult neurologists could be trained to effectively use selective serotonin reupdate inhibitors (SSRIs).
Munger Clary HM, Salpekar JA. Should adult neurologists play a role in the management of the most common psychiatric comorbidities? Practical considerations [published online ahead of print November 22, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.10.020
Giving neurologists the tools to diagnose and treat common psychiatric disorders can help meet the mental health needs of adults with epilepsy whose psychiatric comorbidities are being ignored, according to investigators from Wake Forest School of Medicine and Johns Hopkins University.
- There is a high prevalence of psychiatric disorders among adults with epilepsy.
- These comorbidities are often overlooked because patients have limited access to mental health services.
- Heidi Munger Clary and Jay Salpekar suggest that letting neurologists diagnose and manage common conditions like mood and anxiety disorders will help address this dilemma.
- The researchers suggest that validated screeners could help neurologists who do not have expertise in psychiatry to manage depression and anxiety.
- With such assistance, adult neurologists could be trained to effectively use selective serotonin reupdate inhibitors (SSRIs).
Munger Clary HM, Salpekar JA. Should adult neurologists play a role in the management of the most common psychiatric comorbidities? Practical considerations [published online ahead of print November 22, 2018]. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2018.10.020
Vitamin D–binding protein polymorphisms affect HCV susceptibility
Two specific polymorphisms within the vitamin D–binding protein (VDBP) gene may contribute to susceptibility to hepatitis C virus (HCV) infection in a high-risk Chinese Han population, according to the results of a case-control study published in Gene.
Previous research has indicated that vitamin D deficiency may have an impact on the antiviral response in chronic HCV, and VDBP has been shown to transport vitamin D and its metabolites, thereby influencing vitamin D status. This made VDBP a valid candidate for study as to its effects on HCV infection.
The current study initially recruited around 2,500 Chinese subjects over the period October 2008 to January 2016. The majority were women, and the average age of the subjects was 49-50 years.
The researchers genotyped seven genetic variants in the VDBP gene in 886 patients with HCV persistent infection, 539 subjects with spontaneous clearance, and 1,081 uninfected controls, according to Chao-Nan Xie of the department of epidemiology and biostatistics, Nanjing (China) Medical University, and colleagues.
The researchers found that two variants (rs7041-G and rs3733359-T alleles) were significantly associated with an increased susceptibility of HCV infection. In addition, the combined effect of having the two unfavorable alleles was related to an elevated risk of HCV infection in a locus-dosage manner (P = .000816).
Haplotype analysis suggested that the GT haplotype showed an increased risk effect of HCV infection (odds ratio, 1.464), compared with the most frequent TC haplotype.
“Taken together, polymorphisms within the VDBP gene (rs4588 and rs3733359) may contribute to susceptibility to HCV infection in a high-risk Chinese Han population, which implicates a role of VDR genetic polymorphisms and vitamin D levels in the immune regulation and course of HCV infection,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Xie C-N et al. Gene 2018;679:405-11.
Two specific polymorphisms within the vitamin D–binding protein (VDBP) gene may contribute to susceptibility to hepatitis C virus (HCV) infection in a high-risk Chinese Han population, according to the results of a case-control study published in Gene.
Previous research has indicated that vitamin D deficiency may have an impact on the antiviral response in chronic HCV, and VDBP has been shown to transport vitamin D and its metabolites, thereby influencing vitamin D status. This made VDBP a valid candidate for study as to its effects on HCV infection.
The current study initially recruited around 2,500 Chinese subjects over the period October 2008 to January 2016. The majority were women, and the average age of the subjects was 49-50 years.
The researchers genotyped seven genetic variants in the VDBP gene in 886 patients with HCV persistent infection, 539 subjects with spontaneous clearance, and 1,081 uninfected controls, according to Chao-Nan Xie of the department of epidemiology and biostatistics, Nanjing (China) Medical University, and colleagues.
The researchers found that two variants (rs7041-G and rs3733359-T alleles) were significantly associated with an increased susceptibility of HCV infection. In addition, the combined effect of having the two unfavorable alleles was related to an elevated risk of HCV infection in a locus-dosage manner (P = .000816).
Haplotype analysis suggested that the GT haplotype showed an increased risk effect of HCV infection (odds ratio, 1.464), compared with the most frequent TC haplotype.
“Taken together, polymorphisms within the VDBP gene (rs4588 and rs3733359) may contribute to susceptibility to HCV infection in a high-risk Chinese Han population, which implicates a role of VDR genetic polymorphisms and vitamin D levels in the immune regulation and course of HCV infection,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Xie C-N et al. Gene 2018;679:405-11.
Two specific polymorphisms within the vitamin D–binding protein (VDBP) gene may contribute to susceptibility to hepatitis C virus (HCV) infection in a high-risk Chinese Han population, according to the results of a case-control study published in Gene.
Previous research has indicated that vitamin D deficiency may have an impact on the antiviral response in chronic HCV, and VDBP has been shown to transport vitamin D and its metabolites, thereby influencing vitamin D status. This made VDBP a valid candidate for study as to its effects on HCV infection.
The current study initially recruited around 2,500 Chinese subjects over the period October 2008 to January 2016. The majority were women, and the average age of the subjects was 49-50 years.
The researchers genotyped seven genetic variants in the VDBP gene in 886 patients with HCV persistent infection, 539 subjects with spontaneous clearance, and 1,081 uninfected controls, according to Chao-Nan Xie of the department of epidemiology and biostatistics, Nanjing (China) Medical University, and colleagues.
The researchers found that two variants (rs7041-G and rs3733359-T alleles) were significantly associated with an increased susceptibility of HCV infection. In addition, the combined effect of having the two unfavorable alleles was related to an elevated risk of HCV infection in a locus-dosage manner (P = .000816).
Haplotype analysis suggested that the GT haplotype showed an increased risk effect of HCV infection (odds ratio, 1.464), compared with the most frequent TC haplotype.
“Taken together, polymorphisms within the VDBP gene (rs4588 and rs3733359) may contribute to susceptibility to HCV infection in a high-risk Chinese Han population, which implicates a role of VDR genetic polymorphisms and vitamin D levels in the immune regulation and course of HCV infection,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Xie C-N et al. Gene 2018;679:405-11.
FROM GENE
Key clinical point: VDBP alleles influence susceptibility to HCV infection in a Chinese population.
Major finding: The GT haplotype showed an increased risk effect of HCV infection (odds ratio 1.464) compared to the most frequent TC haplotype.
Study details: Case-control study of 886 HIV-infected, 539 spontaneously cleared, and 1,081 control patients.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Xie C-N et al. Gene. 2018;679:405-11.
What is an “early and accurate” diagnosis?
For the last few weeks, the eye-grabber at the top of the American Academy of Pediatrics shopAAP email has been “Early and Accurate Diagnosis.” The unstated claim is that a practitioner who subscribes to one of their continuing education products will improve his or her chances of making an early and accurate diagnosis that “Also Cures Missed School, Soccer Practice, and Music Lessons.” The tagline, Early and Accurate Diagnosis, got me ruminating.
What exactly is an accurate diagnosis? And how does one define an early diagnosis? These are not merely questions of semantics. An honest attempt to answer them scratches through the surface of some serious issues facing a primary care physician.
Who are the judges deciding whether a physician’s diagnosis is accurate? Should it be a panel of academic physicians, most of who are specialists and subspecialists, and who are most comfortable seeing patients with array of signs and symptoms that your patient has presented? Or, should it be a collection of your primary care peers working with limited resources miles away from a tertiary care center?
Is there such a thing as a diagnosis that is close enough? How often is it important that your diagnosis is spot on? Is it like a high school algebra problem in which you could get partial credit for showing how you arrived at the not-quite-right-answer? It really makes a difference only when you start acting (or, in some cases, not acting) on your diagnosis.
Let’s be honest. How often have you made the wrong diagnosis and the patient got better with your management plan? Your therapy may have worked for Diagnosis A even though you were targeting Diagnosis B. Or, more likely, the patient was going to get better without any intervention.
Don’t get me wrong. I think a correct diagnosis can be, and often is, extremely important, but it is really the patient who is the judge of whether you got it right. He doesn’t care what you called it. He is happy knowing that he got better and you didn’t hurt him.
Now, what about that “early” piece? Again, the patient might have something to say about this. You may have made the correct diagnosis but because your productivity is limited by a clunky EMR or your appointment desk does a poor job of triage, the patient was forced to wait an unconscionable amount of time to be seen.
A timely diagnosis certainly is important in many situations. But particularly, early in your career, you may not have the experience to make those quick one look and you’ve got it right diagnoses. These are times to come clean and tell the patient that you aren’t sure what they have. Of course, you might want to choose a better phrase than, “I don’t have clue.”
If I had been asked to write the AAP’s tag line, I would have chosen “efficient” instead of early. If you made the correct diagnosis and it was reasonably timely but you ordered a barrage of unnecessary and expensive tests that inconvenienced the patient, you should have done a better job.
Finally, if you make the correct and early diagnosis but deliver it to the patient poorly, your therapy may not work. Again, it boils down to being an artful and caring physician.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
For the last few weeks, the eye-grabber at the top of the American Academy of Pediatrics shopAAP email has been “Early and Accurate Diagnosis.” The unstated claim is that a practitioner who subscribes to one of their continuing education products will improve his or her chances of making an early and accurate diagnosis that “Also Cures Missed School, Soccer Practice, and Music Lessons.” The tagline, Early and Accurate Diagnosis, got me ruminating.
What exactly is an accurate diagnosis? And how does one define an early diagnosis? These are not merely questions of semantics. An honest attempt to answer them scratches through the surface of some serious issues facing a primary care physician.
Who are the judges deciding whether a physician’s diagnosis is accurate? Should it be a panel of academic physicians, most of who are specialists and subspecialists, and who are most comfortable seeing patients with array of signs and symptoms that your patient has presented? Or, should it be a collection of your primary care peers working with limited resources miles away from a tertiary care center?
Is there such a thing as a diagnosis that is close enough? How often is it important that your diagnosis is spot on? Is it like a high school algebra problem in which you could get partial credit for showing how you arrived at the not-quite-right-answer? It really makes a difference only when you start acting (or, in some cases, not acting) on your diagnosis.
Let’s be honest. How often have you made the wrong diagnosis and the patient got better with your management plan? Your therapy may have worked for Diagnosis A even though you were targeting Diagnosis B. Or, more likely, the patient was going to get better without any intervention.
Don’t get me wrong. I think a correct diagnosis can be, and often is, extremely important, but it is really the patient who is the judge of whether you got it right. He doesn’t care what you called it. He is happy knowing that he got better and you didn’t hurt him.
Now, what about that “early” piece? Again, the patient might have something to say about this. You may have made the correct diagnosis but because your productivity is limited by a clunky EMR or your appointment desk does a poor job of triage, the patient was forced to wait an unconscionable amount of time to be seen.
A timely diagnosis certainly is important in many situations. But particularly, early in your career, you may not have the experience to make those quick one look and you’ve got it right diagnoses. These are times to come clean and tell the patient that you aren’t sure what they have. Of course, you might want to choose a better phrase than, “I don’t have clue.”
If I had been asked to write the AAP’s tag line, I would have chosen “efficient” instead of early. If you made the correct diagnosis and it was reasonably timely but you ordered a barrage of unnecessary and expensive tests that inconvenienced the patient, you should have done a better job.
Finally, if you make the correct and early diagnosis but deliver it to the patient poorly, your therapy may not work. Again, it boils down to being an artful and caring physician.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
For the last few weeks, the eye-grabber at the top of the American Academy of Pediatrics shopAAP email has been “Early and Accurate Diagnosis.” The unstated claim is that a practitioner who subscribes to one of their continuing education products will improve his or her chances of making an early and accurate diagnosis that “Also Cures Missed School, Soccer Practice, and Music Lessons.” The tagline, Early and Accurate Diagnosis, got me ruminating.
What exactly is an accurate diagnosis? And how does one define an early diagnosis? These are not merely questions of semantics. An honest attempt to answer them scratches through the surface of some serious issues facing a primary care physician.
Who are the judges deciding whether a physician’s diagnosis is accurate? Should it be a panel of academic physicians, most of who are specialists and subspecialists, and who are most comfortable seeing patients with array of signs and symptoms that your patient has presented? Or, should it be a collection of your primary care peers working with limited resources miles away from a tertiary care center?
Is there such a thing as a diagnosis that is close enough? How often is it important that your diagnosis is spot on? Is it like a high school algebra problem in which you could get partial credit for showing how you arrived at the not-quite-right-answer? It really makes a difference only when you start acting (or, in some cases, not acting) on your diagnosis.
Let’s be honest. How often have you made the wrong diagnosis and the patient got better with your management plan? Your therapy may have worked for Diagnosis A even though you were targeting Diagnosis B. Or, more likely, the patient was going to get better without any intervention.
Don’t get me wrong. I think a correct diagnosis can be, and often is, extremely important, but it is really the patient who is the judge of whether you got it right. He doesn’t care what you called it. He is happy knowing that he got better and you didn’t hurt him.
Now, what about that “early” piece? Again, the patient might have something to say about this. You may have made the correct diagnosis but because your productivity is limited by a clunky EMR or your appointment desk does a poor job of triage, the patient was forced to wait an unconscionable amount of time to be seen.
A timely diagnosis certainly is important in many situations. But particularly, early in your career, you may not have the experience to make those quick one look and you’ve got it right diagnoses. These are times to come clean and tell the patient that you aren’t sure what they have. Of course, you might want to choose a better phrase than, “I don’t have clue.”
If I had been asked to write the AAP’s tag line, I would have chosen “efficient” instead of early. If you made the correct diagnosis and it was reasonably timely but you ordered a barrage of unnecessary and expensive tests that inconvenienced the patient, you should have done a better job.
Finally, if you make the correct and early diagnosis but deliver it to the patient poorly, your therapy may not work. Again, it boils down to being an artful and caring physician.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at pdnews@mdedge.com.
December 2018 Highlights
Nail Care: Survey of the Cutis Editorial Board
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on nail care. Here’s what we found.
Do you routinely perform diagnostic testing before treating for onychomycosis?
Ninety-five percent of dermatologists perform diagnostic testing before treating onychomycosis. Of them, nearly two-thirds only test before treating with systemic antifungals, while one-third test before starting systemic or topical antifungals.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
A laboratory diagnosis of onychomycosis is an absolute necessity before treating for onychomycosis, and the vast majority of our board members are testing routinely. Diagnosis should ideally be performed before initiating both oral and topical therapy. Failure to do so may lead to incorrect treatment with progression of disease and missed diagnoses of malignancy (Lipner and Scher, 2016; Lipner and Scher, 2016).
Next page: Nail fungus
What diagnostic tests do you use to confirm the presence of a nail fungus?
More than 70% of respondents use histopathology or fungal culture to confirm the presence of a nail fungus. Direct microscopy is used by 38% and only 5% use polymerase chain reaction.
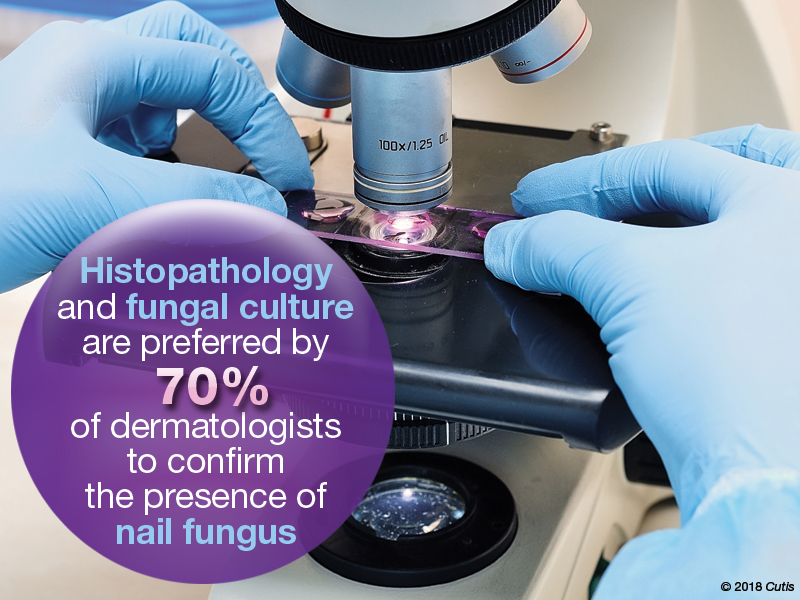
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Options for diagnosis are potassium hydroxide preparation with microscopy, fungal culture, or nail plate clipping with histopathology. Polymerase chain reaction is another option that is available and covered by many insurance plans. Many of our board members use histopathology and fungal culture more often than other methods. Histopathology is advantageous for its high sensitivity and capacity to detect other nail diseases, such as nail psoriasis. A disadvantage is that the identity and viability of the infecting organism cannot be determined. While fungal culture can detect both identity and viability, the organism may take several weeks to grow and there is a high false-negative rate (Lipner and Scher, 2018 [Part 1]).
Next page: Laboratory monitoring with terbinafine
Almost half (48%) of dermatologists monitor laboratory test results in onychomycosis patients taking terbinafine at both baseline and during therapy. Twenty-three percent monitor at baseline only; 14% at baseline and after therapy; 5% at baseline, during therapy, and after therapy; and 10% don’t monitor at all.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Almost half of board members perform laboratory monitoring for patients taking terbinafine, which was reasonable prior to any published data on blood count and liver function tests in patients taking this drug. However, a new study on this topic should make us reconsider our practices. This study analyzed the rate of laboratory test abnormalities in 4985 patients taking terbinafine or griseofulvin for dermatophyte infections. Elevated alanine aminotransferase, aspartate aminotransferase, anemia, lymphopenia, and neutropenia were uncommon and similar to the baseline rates. Therefore, routine interval laboratory monitoring may be unnecessary in healthy patients taking oral terbinafine for onychomycosis (Stolmeier et al).
Next page: Biotin recommendations
Do you routinely recommend biotin to your patients?
Approximately half (52%) of dermatologists do not recommend biotin to their patients. However, 29% do recommend it for hair and nail disorders.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Biotin is an essential cofactor for mammalian carboxylase enzymes that are involved in important metabolic pathways in humans. Biotin supplementation is likely unnecessary for most individuals, as biotin intake is likely sufficient in a Western diet. There are limited data on biotin supplementation to treat dermatologic conditions, especially in patients with normal biotin levels. In addition, a recent warning issued by the US Food and Drug Administration reported that consumption of biotin may interfere with laboratory tests. Therefore, biotin should not be routinely recommended to patients without sufficient evidence that it would benefit their condition (Lipner, 2018).
Next page: Medication for onychomycosis
Which medication(s) do you prescribe most often for onychomycosis?
The top medications prescribed by dermatologists for onychomycosis were oral terbinafine (62%) and topical ciclopirox (52%), followed by oral fluconazole (29%), topical efinaconazole (24%), oral itraconazole (14%), and topical tavaborole (5%).
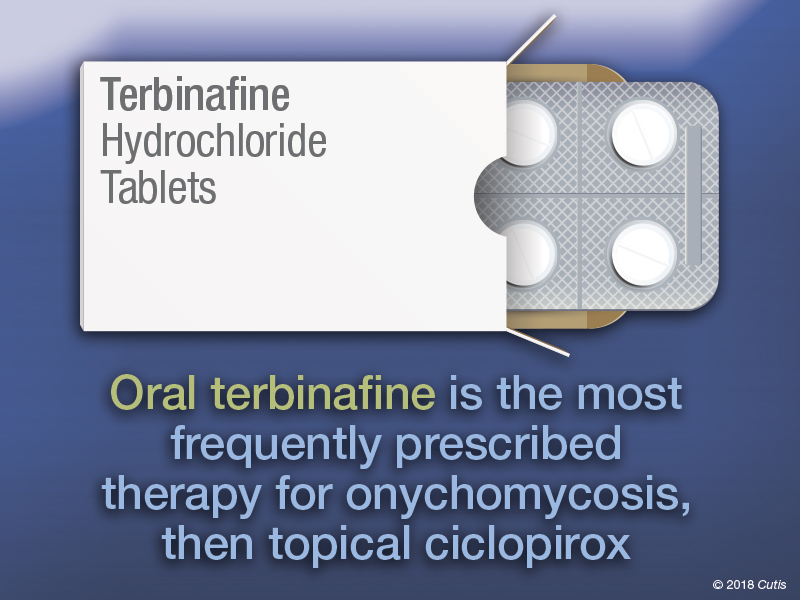
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Oral terbinafine is most frequently prescribed by our board, likely because it has the best efficacy, dosing regimen, and minimal potential for systemic side effects or drug-drug interactions. Efficacy with ciclopirox lacquer is quite low and the medication is difficult to apply. For toenail onychomycosis, application is daily with weekly clipping and removal and monthly debridement. Patients who are not candidates for terbinafine would likely benefit more from oral itraconazole, oral fluconazole (off label), efinaconazole, or tavaborole (Lipner and Scher, 2018 [Part II]).
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As with care in general in dermatology, the care and treatment of healthy nails and especially diseased nails is multifaceted and is optimized by using combination therapy. The combination of an oral antifungal and a topical that treats the local area and also provides protection and a healthy environment for nail growth and repair is ideal.—Fran E. Cook-Bolden, MD (New York, New York)
It’s important to culture for fungus before starting treatment. It seems many cultures turn out to be nondermatophytes, and terbinafine is not the best treatment.—Lawrence J. Green, MD (Washington, DC)
Nails do care. Diagnoses should be confirmed.—Richard K. Scher, MD (New York, New York)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from October 22, 2018, to November 14, 2018. A total of 21 usable responses were received.
- Lipner SR. Rethinking biotin therapy for hair, nail, and skin disorders. J Am Acad Dermatol. 2018;78:1236-1238.
- Lipner SR, Scher RK. Confirmatory testing for onychomycosis. JAMA Dermatol. 2016 Jul 1;152:847.
- Lipner SR, Scher RK. Onychomycosis–a small step for quality of care. Curr Med Res Opin. 2016;32:865-867.
- Lipner SR, Scher RK. Part I: onychomycosis: clinical overview and diagnosis [published online June 27, 2018]. J Am Acad Dermatol. pii:S0190-9622(18)32188-1.
- Lipner SR, Scher RK. Part II: onychomycosis: treatment and prevention of recurrence [published online June 27, 2018]. J Am Acad Dermatol. pii: S0190-9622(18)32187-X.)
- Stolmeier DA, Stratman HB, McIntee TJ, et al. Utility of laboratory test result monitoring in patients taking oral terbinafine or griseofulvin for dermatophyte infections [published online October 17, 2018]. JAMA Dermatol. doi:10.1001/jamadermatol.2018.3578.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on nail care. Here’s what we found.
Do you routinely perform diagnostic testing before treating for onychomycosis?
Ninety-five percent of dermatologists perform diagnostic testing before treating onychomycosis. Of them, nearly two-thirds only test before treating with systemic antifungals, while one-third test before starting systemic or topical antifungals.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
A laboratory diagnosis of onychomycosis is an absolute necessity before treating for onychomycosis, and the vast majority of our board members are testing routinely. Diagnosis should ideally be performed before initiating both oral and topical therapy. Failure to do so may lead to incorrect treatment with progression of disease and missed diagnoses of malignancy (Lipner and Scher, 2016; Lipner and Scher, 2016).
Next page: Nail fungus
What diagnostic tests do you use to confirm the presence of a nail fungus?
More than 70% of respondents use histopathology or fungal culture to confirm the presence of a nail fungus. Direct microscopy is used by 38% and only 5% use polymerase chain reaction.
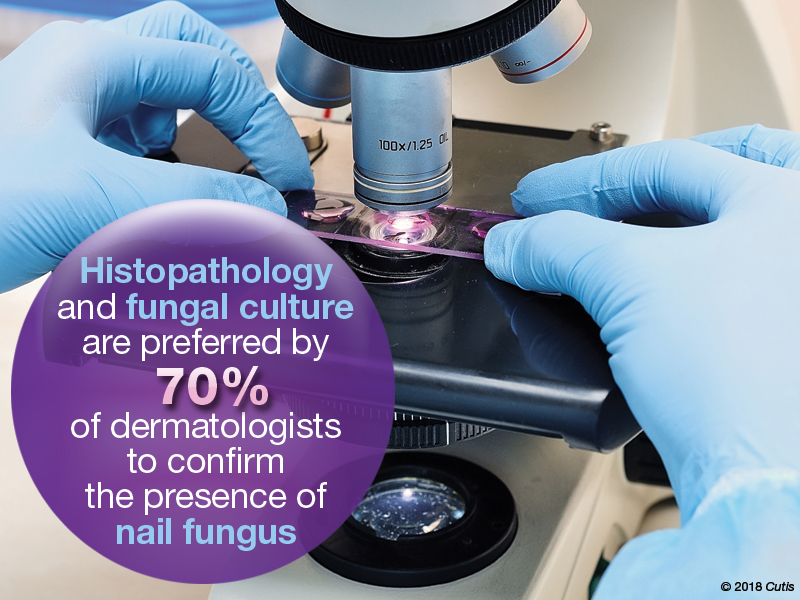
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Options for diagnosis are potassium hydroxide preparation with microscopy, fungal culture, or nail plate clipping with histopathology. Polymerase chain reaction is another option that is available and covered by many insurance plans. Many of our board members use histopathology and fungal culture more often than other methods. Histopathology is advantageous for its high sensitivity and capacity to detect other nail diseases, such as nail psoriasis. A disadvantage is that the identity and viability of the infecting organism cannot be determined. While fungal culture can detect both identity and viability, the organism may take several weeks to grow and there is a high false-negative rate (Lipner and Scher, 2018 [Part 1]).
Next page: Laboratory monitoring with terbinafine
Almost half (48%) of dermatologists monitor laboratory test results in onychomycosis patients taking terbinafine at both baseline and during therapy. Twenty-three percent monitor at baseline only; 14% at baseline and after therapy; 5% at baseline, during therapy, and after therapy; and 10% don’t monitor at all.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Almost half of board members perform laboratory monitoring for patients taking terbinafine, which was reasonable prior to any published data on blood count and liver function tests in patients taking this drug. However, a new study on this topic should make us reconsider our practices. This study analyzed the rate of laboratory test abnormalities in 4985 patients taking terbinafine or griseofulvin for dermatophyte infections. Elevated alanine aminotransferase, aspartate aminotransferase, anemia, lymphopenia, and neutropenia were uncommon and similar to the baseline rates. Therefore, routine interval laboratory monitoring may be unnecessary in healthy patients taking oral terbinafine for onychomycosis (Stolmeier et al).
Next page: Biotin recommendations
Do you routinely recommend biotin to your patients?
Approximately half (52%) of dermatologists do not recommend biotin to their patients. However, 29% do recommend it for hair and nail disorders.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Biotin is an essential cofactor for mammalian carboxylase enzymes that are involved in important metabolic pathways in humans. Biotin supplementation is likely unnecessary for most individuals, as biotin intake is likely sufficient in a Western diet. There are limited data on biotin supplementation to treat dermatologic conditions, especially in patients with normal biotin levels. In addition, a recent warning issued by the US Food and Drug Administration reported that consumption of biotin may interfere with laboratory tests. Therefore, biotin should not be routinely recommended to patients without sufficient evidence that it would benefit their condition (Lipner, 2018).
Next page: Medication for onychomycosis
Which medication(s) do you prescribe most often for onychomycosis?
The top medications prescribed by dermatologists for onychomycosis were oral terbinafine (62%) and topical ciclopirox (52%), followed by oral fluconazole (29%), topical efinaconazole (24%), oral itraconazole (14%), and topical tavaborole (5%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Oral terbinafine is most frequently prescribed by our board, likely because it has the best efficacy, dosing regimen, and minimal potential for systemic side effects or drug-drug interactions. Efficacy with ciclopirox lacquer is quite low and the medication is difficult to apply. For toenail onychomycosis, application is daily with weekly clipping and removal and monthly debridement. Patients who are not candidates for terbinafine would likely benefit more from oral itraconazole, oral fluconazole (off label), efinaconazole, or tavaborole (Lipner and Scher, 2018 [Part II]).
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As with care in general in dermatology, the care and treatment of healthy nails and especially diseased nails is multifaceted and is optimized by using combination therapy. The combination of an oral antifungal and a topical that treats the local area and also provides protection and a healthy environment for nail growth and repair is ideal.—Fran E. Cook-Bolden, MD (New York, New York)
It’s important to culture for fungus before starting treatment. It seems many cultures turn out to be nondermatophytes, and terbinafine is not the best treatment.—Lawrence J. Green, MD (Washington, DC)
Nails do care. Diagnoses should be confirmed.—Richard K. Scher, MD (New York, New York)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from October 22, 2018, to November 14, 2018. A total of 21 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on nail care. Here’s what we found.
Do you routinely perform diagnostic testing before treating for onychomycosis?
Ninety-five percent of dermatologists perform diagnostic testing before treating onychomycosis. Of them, nearly two-thirds only test before treating with systemic antifungals, while one-third test before starting systemic or topical antifungals.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
A laboratory diagnosis of onychomycosis is an absolute necessity before treating for onychomycosis, and the vast majority of our board members are testing routinely. Diagnosis should ideally be performed before initiating both oral and topical therapy. Failure to do so may lead to incorrect treatment with progression of disease and missed diagnoses of malignancy (Lipner and Scher, 2016; Lipner and Scher, 2016).
Next page: Nail fungus
What diagnostic tests do you use to confirm the presence of a nail fungus?
More than 70% of respondents use histopathology or fungal culture to confirm the presence of a nail fungus. Direct microscopy is used by 38% and only 5% use polymerase chain reaction.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Options for diagnosis are potassium hydroxide preparation with microscopy, fungal culture, or nail plate clipping with histopathology. Polymerase chain reaction is another option that is available and covered by many insurance plans. Many of our board members use histopathology and fungal culture more often than other methods. Histopathology is advantageous for its high sensitivity and capacity to detect other nail diseases, such as nail psoriasis. A disadvantage is that the identity and viability of the infecting organism cannot be determined. While fungal culture can detect both identity and viability, the organism may take several weeks to grow and there is a high false-negative rate (Lipner and Scher, 2018 [Part 1]).
Next page: Laboratory monitoring with terbinafine
Almost half (48%) of dermatologists monitor laboratory test results in onychomycosis patients taking terbinafine at both baseline and during therapy. Twenty-three percent monitor at baseline only; 14% at baseline and after therapy; 5% at baseline, during therapy, and after therapy; and 10% don’t monitor at all.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Almost half of board members perform laboratory monitoring for patients taking terbinafine, which was reasonable prior to any published data on blood count and liver function tests in patients taking this drug. However, a new study on this topic should make us reconsider our practices. This study analyzed the rate of laboratory test abnormalities in 4985 patients taking terbinafine or griseofulvin for dermatophyte infections. Elevated alanine aminotransferase, aspartate aminotransferase, anemia, lymphopenia, and neutropenia were uncommon and similar to the baseline rates. Therefore, routine interval laboratory monitoring may be unnecessary in healthy patients taking oral terbinafine for onychomycosis (Stolmeier et al).
Next page: Biotin recommendations
Do you routinely recommend biotin to your patients?
Approximately half (52%) of dermatologists do not recommend biotin to their patients. However, 29% do recommend it for hair and nail disorders.

Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Biotin is an essential cofactor for mammalian carboxylase enzymes that are involved in important metabolic pathways in humans. Biotin supplementation is likely unnecessary for most individuals, as biotin intake is likely sufficient in a Western diet. There are limited data on biotin supplementation to treat dermatologic conditions, especially in patients with normal biotin levels. In addition, a recent warning issued by the US Food and Drug Administration reported that consumption of biotin may interfere with laboratory tests. Therefore, biotin should not be routinely recommended to patients without sufficient evidence that it would benefit their condition (Lipner, 2018).
Next page: Medication for onychomycosis
Which medication(s) do you prescribe most often for onychomycosis?
The top medications prescribed by dermatologists for onychomycosis were oral terbinafine (62%) and topical ciclopirox (52%), followed by oral fluconazole (29%), topical efinaconazole (24%), oral itraconazole (14%), and topical tavaborole (5%).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Oral terbinafine is most frequently prescribed by our board, likely because it has the best efficacy, dosing regimen, and minimal potential for systemic side effects or drug-drug interactions. Efficacy with ciclopirox lacquer is quite low and the medication is difficult to apply. For toenail onychomycosis, application is daily with weekly clipping and removal and monthly debridement. Patients who are not candidates for terbinafine would likely benefit more from oral itraconazole, oral fluconazole (off label), efinaconazole, or tavaborole (Lipner and Scher, 2018 [Part II]).
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As with care in general in dermatology, the care and treatment of healthy nails and especially diseased nails is multifaceted and is optimized by using combination therapy. The combination of an oral antifungal and a topical that treats the local area and also provides protection and a healthy environment for nail growth and repair is ideal.—Fran E. Cook-Bolden, MD (New York, New York)
It’s important to culture for fungus before starting treatment. It seems many cultures turn out to be nondermatophytes, and terbinafine is not the best treatment.—Lawrence J. Green, MD (Washington, DC)
Nails do care. Diagnoses should be confirmed.—Richard K. Scher, MD (New York, New York)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from October 22, 2018, to November 14, 2018. A total of 21 usable responses were received.
- Lipner SR. Rethinking biotin therapy for hair, nail, and skin disorders. J Am Acad Dermatol. 2018;78:1236-1238.
- Lipner SR, Scher RK. Confirmatory testing for onychomycosis. JAMA Dermatol. 2016 Jul 1;152:847.
- Lipner SR, Scher RK. Onychomycosis–a small step for quality of care. Curr Med Res Opin. 2016;32:865-867.
- Lipner SR, Scher RK. Part I: onychomycosis: clinical overview and diagnosis [published online June 27, 2018]. J Am Acad Dermatol. pii:S0190-9622(18)32188-1.
- Lipner SR, Scher RK. Part II: onychomycosis: treatment and prevention of recurrence [published online June 27, 2018]. J Am Acad Dermatol. pii: S0190-9622(18)32187-X.)
- Stolmeier DA, Stratman HB, McIntee TJ, et al. Utility of laboratory test result monitoring in patients taking oral terbinafine or griseofulvin for dermatophyte infections [published online October 17, 2018]. JAMA Dermatol. doi:10.1001/jamadermatol.2018.3578.
- Lipner SR. Rethinking biotin therapy for hair, nail, and skin disorders. J Am Acad Dermatol. 2018;78:1236-1238.
- Lipner SR, Scher RK. Confirmatory testing for onychomycosis. JAMA Dermatol. 2016 Jul 1;152:847.
- Lipner SR, Scher RK. Onychomycosis–a small step for quality of care. Curr Med Res Opin. 2016;32:865-867.
- Lipner SR, Scher RK. Part I: onychomycosis: clinical overview and diagnosis [published online June 27, 2018]. J Am Acad Dermatol. pii:S0190-9622(18)32188-1.
- Lipner SR, Scher RK. Part II: onychomycosis: treatment and prevention of recurrence [published online June 27, 2018]. J Am Acad Dermatol. pii: S0190-9622(18)32187-X.)
- Stolmeier DA, Stratman HB, McIntee TJ, et al. Utility of laboratory test result monitoring in patients taking oral terbinafine or griseofulvin for dermatophyte infections [published online October 17, 2018]. JAMA Dermatol. doi:10.1001/jamadermatol.2018.3578.