User login
Factor IX expression stable at up to 8 years with gene therapy
SAN DIEGO – according to interim follow-up data from a phase 1/2 dose-escalation study.
The therapy – a self-complementary adeno-associated virus vector containing a codon-optimized factor IX gene, under control of a synthetic liver specific promoter and pseudotyped with serotype 8 capsid (scAAV2/8-LP1-hFIXco) – was previously shown to result in a dose-dependent increase in plasma factor IX levels in all 10 patients enrolled in the study, and an earlier update showed stable factor IX activity for at least 3 years, Ulrike M. Reiss, MD, reported at the annual meeting of the American Society of Hematology.
However, declining factor IX expression over time remains a concern, because AAV-mediated transgene expression is mediated mainly by episomally retained viral genomes, which may be lost with natural turnover of hepatocytes, noted Dr. Reiss, director of the clinical hematology division and the Hemophilia Treatment Center at St. Jude Children’s Research Hospital in Memphis.
At the “halfway mark,” with a median follow-up of 6.7 years in 10 patients aged 18-64 years who were treated with doses of either 2 x 1011, 6 x 1011, or 2 x 1012 vector genomes per kg (in 2, 2, and 6 patients, respectively), “factor IX expression has been persistent and stable in all participants after vector infusion,” she said.
“Factor IX expression was vector-dose dependent, achieving average levels of 1.9%-2.3% at the lower doses, and 5.1% at the high vector dose. All patients converted from having severe hemophilia to mild-moderate hemophilia,” she added.
The single significant adverse event observed during annual follow-up evaluations in the patients was a vector-related, immune-mediated liver inflammation occurring within 2-3 months of infusion in four of the six high-dose participants.
“There was complete resolution in all cases after a short course of corticosteroids over 8-12 weeks, including the taper. There were no late sequelae or any recurrence of transaminitis over time,” Dr. Reiss said. “We did not observe any new factor IX inhibitor or any late toxicity in any of these participants.”
Additionally, a comparison of average data across 3 years prior to gene therapy with the average data at 6.7 years after gene therapy showed that the annualized bleed rate decreased by 82% in the 10 participants and factor IX use decreased by 66%. In the high-dose group, the bleed rate decreased from 21 bleeds to 2 bleeds per year, and vector consumption was markedly reduced to a mean of 500 IU/kg per year from a mean of more than 2800 IU/kg per year. “Only one of the six patients in the high-dose group currently continues on prophylaxis treatment, whereas three in the low- and mid-dose groups are currently on prophylaxis,” she said. “In all [patients], the interval between prophylactic infusions has lengthened.”
Of note, Dr. Reiss and her colleagues explored the ability of using a modified, empty capsid-reduced vector preparation of the gene therapy to prevent the transaminitis seen in the 2-3 months after infusion. A new clinical preparation of scAAV2/8-LP1-hFIXco was manufactured with most of the empty particles removed by cesium chloride density centrifugation, but this approach provided no benefit in that regard.
“This further supports the observation that the anticapsid immune response is vector-dose dependent,” she said.
Additionally, the pattern of humoral response to AAV8 capsid was consistent with the primary immune response in participants.
“High IgG antibody titers have persisted for over 6 years; this finding is important because it will preclude these patients from any retreatment with the same vector or even potentially alternative AAV vectors of other serotypes with cross-reactive antigenicity,” she said.
Dr. Reiss reported having no relevant disclosures
SOURCE: Reiss UM et al. ASH 2018, Abstract 491.
SAN DIEGO – according to interim follow-up data from a phase 1/2 dose-escalation study.
The therapy – a self-complementary adeno-associated virus vector containing a codon-optimized factor IX gene, under control of a synthetic liver specific promoter and pseudotyped with serotype 8 capsid (scAAV2/8-LP1-hFIXco) – was previously shown to result in a dose-dependent increase in plasma factor IX levels in all 10 patients enrolled in the study, and an earlier update showed stable factor IX activity for at least 3 years, Ulrike M. Reiss, MD, reported at the annual meeting of the American Society of Hematology.
However, declining factor IX expression over time remains a concern, because AAV-mediated transgene expression is mediated mainly by episomally retained viral genomes, which may be lost with natural turnover of hepatocytes, noted Dr. Reiss, director of the clinical hematology division and the Hemophilia Treatment Center at St. Jude Children’s Research Hospital in Memphis.
At the “halfway mark,” with a median follow-up of 6.7 years in 10 patients aged 18-64 years who were treated with doses of either 2 x 1011, 6 x 1011, or 2 x 1012 vector genomes per kg (in 2, 2, and 6 patients, respectively), “factor IX expression has been persistent and stable in all participants after vector infusion,” she said.
“Factor IX expression was vector-dose dependent, achieving average levels of 1.9%-2.3% at the lower doses, and 5.1% at the high vector dose. All patients converted from having severe hemophilia to mild-moderate hemophilia,” she added.
The single significant adverse event observed during annual follow-up evaluations in the patients was a vector-related, immune-mediated liver inflammation occurring within 2-3 months of infusion in four of the six high-dose participants.
“There was complete resolution in all cases after a short course of corticosteroids over 8-12 weeks, including the taper. There were no late sequelae or any recurrence of transaminitis over time,” Dr. Reiss said. “We did not observe any new factor IX inhibitor or any late toxicity in any of these participants.”
Additionally, a comparison of average data across 3 years prior to gene therapy with the average data at 6.7 years after gene therapy showed that the annualized bleed rate decreased by 82% in the 10 participants and factor IX use decreased by 66%. In the high-dose group, the bleed rate decreased from 21 bleeds to 2 bleeds per year, and vector consumption was markedly reduced to a mean of 500 IU/kg per year from a mean of more than 2800 IU/kg per year. “Only one of the six patients in the high-dose group currently continues on prophylaxis treatment, whereas three in the low- and mid-dose groups are currently on prophylaxis,” she said. “In all [patients], the interval between prophylactic infusions has lengthened.”
Of note, Dr. Reiss and her colleagues explored the ability of using a modified, empty capsid-reduced vector preparation of the gene therapy to prevent the transaminitis seen in the 2-3 months after infusion. A new clinical preparation of scAAV2/8-LP1-hFIXco was manufactured with most of the empty particles removed by cesium chloride density centrifugation, but this approach provided no benefit in that regard.
“This further supports the observation that the anticapsid immune response is vector-dose dependent,” she said.
Additionally, the pattern of humoral response to AAV8 capsid was consistent with the primary immune response in participants.
“High IgG antibody titers have persisted for over 6 years; this finding is important because it will preclude these patients from any retreatment with the same vector or even potentially alternative AAV vectors of other serotypes with cross-reactive antigenicity,” she said.
Dr. Reiss reported having no relevant disclosures
SOURCE: Reiss UM et al. ASH 2018, Abstract 491.
SAN DIEGO – according to interim follow-up data from a phase 1/2 dose-escalation study.
The therapy – a self-complementary adeno-associated virus vector containing a codon-optimized factor IX gene, under control of a synthetic liver specific promoter and pseudotyped with serotype 8 capsid (scAAV2/8-LP1-hFIXco) – was previously shown to result in a dose-dependent increase in plasma factor IX levels in all 10 patients enrolled in the study, and an earlier update showed stable factor IX activity for at least 3 years, Ulrike M. Reiss, MD, reported at the annual meeting of the American Society of Hematology.
However, declining factor IX expression over time remains a concern, because AAV-mediated transgene expression is mediated mainly by episomally retained viral genomes, which may be lost with natural turnover of hepatocytes, noted Dr. Reiss, director of the clinical hematology division and the Hemophilia Treatment Center at St. Jude Children’s Research Hospital in Memphis.
At the “halfway mark,” with a median follow-up of 6.7 years in 10 patients aged 18-64 years who were treated with doses of either 2 x 1011, 6 x 1011, or 2 x 1012 vector genomes per kg (in 2, 2, and 6 patients, respectively), “factor IX expression has been persistent and stable in all participants after vector infusion,” she said.
“Factor IX expression was vector-dose dependent, achieving average levels of 1.9%-2.3% at the lower doses, and 5.1% at the high vector dose. All patients converted from having severe hemophilia to mild-moderate hemophilia,” she added.
The single significant adverse event observed during annual follow-up evaluations in the patients was a vector-related, immune-mediated liver inflammation occurring within 2-3 months of infusion in four of the six high-dose participants.
“There was complete resolution in all cases after a short course of corticosteroids over 8-12 weeks, including the taper. There were no late sequelae or any recurrence of transaminitis over time,” Dr. Reiss said. “We did not observe any new factor IX inhibitor or any late toxicity in any of these participants.”
Additionally, a comparison of average data across 3 years prior to gene therapy with the average data at 6.7 years after gene therapy showed that the annualized bleed rate decreased by 82% in the 10 participants and factor IX use decreased by 66%. In the high-dose group, the bleed rate decreased from 21 bleeds to 2 bleeds per year, and vector consumption was markedly reduced to a mean of 500 IU/kg per year from a mean of more than 2800 IU/kg per year. “Only one of the six patients in the high-dose group currently continues on prophylaxis treatment, whereas three in the low- and mid-dose groups are currently on prophylaxis,” she said. “In all [patients], the interval between prophylactic infusions has lengthened.”
Of note, Dr. Reiss and her colleagues explored the ability of using a modified, empty capsid-reduced vector preparation of the gene therapy to prevent the transaminitis seen in the 2-3 months after infusion. A new clinical preparation of scAAV2/8-LP1-hFIXco was manufactured with most of the empty particles removed by cesium chloride density centrifugation, but this approach provided no benefit in that regard.
“This further supports the observation that the anticapsid immune response is vector-dose dependent,” she said.
Additionally, the pattern of humoral response to AAV8 capsid was consistent with the primary immune response in participants.
“High IgG antibody titers have persisted for over 6 years; this finding is important because it will preclude these patients from any retreatment with the same vector or even potentially alternative AAV vectors of other serotypes with cross-reactive antigenicity,” she said.
Dr. Reiss reported having no relevant disclosures
SOURCE: Reiss UM et al. ASH 2018, Abstract 491.
REPORTING FROM ASH 2018
Key clinical point: With a median follow-up of 6.7 years in 10 patients aged 18-64 years who were treated with scAAV2/8-LP1-hFIX–comediated gene therapy, factor IX expression has been persistent and stable.
Major finding: Factor IX expression averaged 1.9%-2.3% at the lower doses, and 5.1% at the high dose at up to 8.6 years.
Study details: An interim follow-up data for 10 patients in a phase 1/2 study.
Disclosures: Dr. Reiss reported having no disclosures.
Source: Reiss UM et al. ASH 2018, Abstract 491.
Similarity of CT-P6 and trastuzumab remain with longer follow-up
SAN ANTONIO –
Similarity in safety and efficacy at 1 year was previously demonstrated in the phase 3 trial, as well as similarity in cardiac toxicity at a median of 19 months. Updated disease-free survival, overall survival, and cardiac toxicity with a median follow-up of 2 years will be presented by Francisco J. Esteva, MD, PhD, of the Laura & Isaac Perlmutter Cancer Center at NYU Langone Health, New York, in a poster presentation at the San Antonio Breast Cancer Symposium.
For the trial, 549 patients with HER2-positive early breast cancer were randomized to receive CT-P6 (n = 271) or trastuzumab (n = 278) in combination with docetaxel (cycles 1-4) and 5-fluorouracil, epirubicin, and cyclophosphamide (cycles 5-8). CT-P6 or trastuzumab was administered at 8 mg/kg (cycle 1 only) followed by 6 mg/kg every 3 weeks. After surgery, patients received CT-P6 or trastuzumab monotherapy and then entered the follow-up period.
A total of 528 patients entered the follow-up period, with a median duration of 27 months. Disease-free and overall survival were similar in the two arms in both the per-protocol set and the intention-to-treat set. In the intention-to-treat set, the 2-year disease-free survival was 86% (95% confidence interval, 80%-90%) in the CT-P6 arm and 90% (95% CI, 85%-93%) in the trastuzumab arm. Two-year overall survival was 97% (95% CI, 93%-98%) in the CT-P6 arm and 98% (95% CI, 96%-99%) in the trastuzumab arm. Median disease-free and overall survival have not been reached, according to the abstract.
No new cases of heart failure were reported during the follow-up period. Left ventricular ejection fraction was similar in both arms. The efficacy and cardiac toxicity profile between CT-P6 and trastuzumab were consistent with published data.
“CT-P6 was consistently well tolerated with a similar cardiotoxicity profile to that of trastuzumab through a long duration of follow-up,” Dr. Esteva and authors said.
The study sponsor is Celltrion, maker of CT-P6. Dr. Esteva disclosed a consulting or advisory role with Celltrion, as well as relationships with various other pharmaceutical companies.
SOURCE: Esteva FJ et al. SABCS 2018, Abstract P6-17-03.
SAN ANTONIO –
Similarity in safety and efficacy at 1 year was previously demonstrated in the phase 3 trial, as well as similarity in cardiac toxicity at a median of 19 months. Updated disease-free survival, overall survival, and cardiac toxicity with a median follow-up of 2 years will be presented by Francisco J. Esteva, MD, PhD, of the Laura & Isaac Perlmutter Cancer Center at NYU Langone Health, New York, in a poster presentation at the San Antonio Breast Cancer Symposium.
For the trial, 549 patients with HER2-positive early breast cancer were randomized to receive CT-P6 (n = 271) or trastuzumab (n = 278) in combination with docetaxel (cycles 1-4) and 5-fluorouracil, epirubicin, and cyclophosphamide (cycles 5-8). CT-P6 or trastuzumab was administered at 8 mg/kg (cycle 1 only) followed by 6 mg/kg every 3 weeks. After surgery, patients received CT-P6 or trastuzumab monotherapy and then entered the follow-up period.
A total of 528 patients entered the follow-up period, with a median duration of 27 months. Disease-free and overall survival were similar in the two arms in both the per-protocol set and the intention-to-treat set. In the intention-to-treat set, the 2-year disease-free survival was 86% (95% confidence interval, 80%-90%) in the CT-P6 arm and 90% (95% CI, 85%-93%) in the trastuzumab arm. Two-year overall survival was 97% (95% CI, 93%-98%) in the CT-P6 arm and 98% (95% CI, 96%-99%) in the trastuzumab arm. Median disease-free and overall survival have not been reached, according to the abstract.
No new cases of heart failure were reported during the follow-up period. Left ventricular ejection fraction was similar in both arms. The efficacy and cardiac toxicity profile between CT-P6 and trastuzumab were consistent with published data.
“CT-P6 was consistently well tolerated with a similar cardiotoxicity profile to that of trastuzumab through a long duration of follow-up,” Dr. Esteva and authors said.
The study sponsor is Celltrion, maker of CT-P6. Dr. Esteva disclosed a consulting or advisory role with Celltrion, as well as relationships with various other pharmaceutical companies.
SOURCE: Esteva FJ et al. SABCS 2018, Abstract P6-17-03.
SAN ANTONIO –
Similarity in safety and efficacy at 1 year was previously demonstrated in the phase 3 trial, as well as similarity in cardiac toxicity at a median of 19 months. Updated disease-free survival, overall survival, and cardiac toxicity with a median follow-up of 2 years will be presented by Francisco J. Esteva, MD, PhD, of the Laura & Isaac Perlmutter Cancer Center at NYU Langone Health, New York, in a poster presentation at the San Antonio Breast Cancer Symposium.
For the trial, 549 patients with HER2-positive early breast cancer were randomized to receive CT-P6 (n = 271) or trastuzumab (n = 278) in combination with docetaxel (cycles 1-4) and 5-fluorouracil, epirubicin, and cyclophosphamide (cycles 5-8). CT-P6 or trastuzumab was administered at 8 mg/kg (cycle 1 only) followed by 6 mg/kg every 3 weeks. After surgery, patients received CT-P6 or trastuzumab monotherapy and then entered the follow-up period.
A total of 528 patients entered the follow-up period, with a median duration of 27 months. Disease-free and overall survival were similar in the two arms in both the per-protocol set and the intention-to-treat set. In the intention-to-treat set, the 2-year disease-free survival was 86% (95% confidence interval, 80%-90%) in the CT-P6 arm and 90% (95% CI, 85%-93%) in the trastuzumab arm. Two-year overall survival was 97% (95% CI, 93%-98%) in the CT-P6 arm and 98% (95% CI, 96%-99%) in the trastuzumab arm. Median disease-free and overall survival have not been reached, according to the abstract.
No new cases of heart failure were reported during the follow-up period. Left ventricular ejection fraction was similar in both arms. The efficacy and cardiac toxicity profile between CT-P6 and trastuzumab were consistent with published data.
“CT-P6 was consistently well tolerated with a similar cardiotoxicity profile to that of trastuzumab through a long duration of follow-up,” Dr. Esteva and authors said.
The study sponsor is Celltrion, maker of CT-P6. Dr. Esteva disclosed a consulting or advisory role with Celltrion, as well as relationships with various other pharmaceutical companies.
SOURCE: Esteva FJ et al. SABCS 2018, Abstract P6-17-03.
REPORTING FROM SABCS 2018
Key clinical point: Trastuzumab biosimilar candidate CT-P6 and trastuzumab, as neoadjuvant and then adjuvant therapy for patients with early HER2-positive breast cancer, have similar efficacy and cardiac toxicity profiles after 2 years.
Major finding: The number of DFS events (32 [12.4%] in CT-P6 and 26 [10.0%] in trastuzumab) and OS events (14 [5.2%] in CT-P6 and 12 [4.3%] in trastuzumab) were comparable in the intention-to-treat group.
Study details: Phase 3 trial of 549 patients with HER2-positive early breast cancer.
Disclosures: The study sponsor is Celltrion, maker of CT-P6. Dr. Esteva disclosed a consulting or advisory role with Celltrion, as well as relationships with various other pharmaceutical companies.
Source: Esteva FJ et al. SABCS 2018, Abstract P6-17-03.
PAD guidelines: Consensus needed between U.S. and Europe
Recent advances in the management of peripheral artery disease (PAD) have resulted in new guideline creation in both the United States and Europe.
While there is considerable consensus between the guidelines, there are multiple differences in emphasis and a differing approach to the types and quality of evidence used to back recommendations, according to a comparative review published in the Journal of the American College of Cardiology. The American Heart Association and American College of Cardiology, together with other organizations, issued an update to their previous guidelines on the management and diagnosis of lower extremity PAD in 2016. In 2017, the European Society of Cardiology in conjunction with the European Society for Vascular Surgery updated their own comprehensive guidelines.
Both the U.S. and the European guidelines stress the importance of lowering risk factors for PAD. This includes stopping smoking, lipid and blood pressure management, and controlling glucose, according to Aaron P. Kithcart, MD, of Brigham and Women’s Hospital, Boston, and Joshua A. Beckman, MD, of Vanderbilt University, Nashville, Tenn.
However, the U.S. guidelines focus more on moderating lifestyle factors, including the pursuit of regular physical activity and the use of supervised exercise, whereas the European guidelines focus considerable attention on recommendations for revascularization in patients with limb-threatening ischemia.
Perhaps the major source of variation between the two sets of guidelines, according to the reviewers, are based upon the intended audiences: “The American document limits its focus to PAD but is applicable to practitioners of every background, whereas the European guideline extends the discussion to all PADs to include carotid and vertebral, upper extremities, mesenteric, and renal arteries in addition to lower-extremity artery disease; but is designed to be a source for cardiologists.”
Accordingly, the ESC/ESVS guidelines approach medical therapy with a more holistic flavor, whereas the ACC/AHA guidelines are specific to the lower-extremity complications of atherosclerosis, according to the reviewers.
Both sets of guidelines come to the conclusion that there is a need for more evidence to identify patients who are at the greatest risk of tissue loss, but overall they differ in their approach to available data. The ACC/AHA is more inclusive of smaller, well-done nonrandomized studies, whereas the ESC/ESVS relegates small studies to Level of Evidence: C. “We believe this difference drives the variation of therapeutic recommendations more than any other factor,” the authors note.
More randomized studies would align recommendations across both organizations, according to Dr. Kithcart and Dr. Beckman (JACC 2018;72:2789-801).
“The management of PAD has progressed a great deal over the last decade. ... Several clinical trials over the coming years should help clarify how revascularization should be approached, and which patients are most likely to benefit. Until then, maintaining good cardiovascular health, including regular physical activity, smoking cessation, lipid-lowering therapy, blood pressure management, and glucose control have the most benefit in patients with PAD,” the researchers concluded.
Dr. Beckman served as a consultant for several pharmaceutical companies, and on the data and safety monitoring board for Bayer and Novartis. Dr. Kithcart reported that he has no relevant conflicts.
SOURCE: Kithcart, AP et al. JACC 2018;72:2789-801.
Recent advances in the management of peripheral artery disease (PAD) have resulted in new guideline creation in both the United States and Europe.
While there is considerable consensus between the guidelines, there are multiple differences in emphasis and a differing approach to the types and quality of evidence used to back recommendations, according to a comparative review published in the Journal of the American College of Cardiology. The American Heart Association and American College of Cardiology, together with other organizations, issued an update to their previous guidelines on the management and diagnosis of lower extremity PAD in 2016. In 2017, the European Society of Cardiology in conjunction with the European Society for Vascular Surgery updated their own comprehensive guidelines.
Both the U.S. and the European guidelines stress the importance of lowering risk factors for PAD. This includes stopping smoking, lipid and blood pressure management, and controlling glucose, according to Aaron P. Kithcart, MD, of Brigham and Women’s Hospital, Boston, and Joshua A. Beckman, MD, of Vanderbilt University, Nashville, Tenn.
However, the U.S. guidelines focus more on moderating lifestyle factors, including the pursuit of regular physical activity and the use of supervised exercise, whereas the European guidelines focus considerable attention on recommendations for revascularization in patients with limb-threatening ischemia.
Perhaps the major source of variation between the two sets of guidelines, according to the reviewers, are based upon the intended audiences: “The American document limits its focus to PAD but is applicable to practitioners of every background, whereas the European guideline extends the discussion to all PADs to include carotid and vertebral, upper extremities, mesenteric, and renal arteries in addition to lower-extremity artery disease; but is designed to be a source for cardiologists.”
Accordingly, the ESC/ESVS guidelines approach medical therapy with a more holistic flavor, whereas the ACC/AHA guidelines are specific to the lower-extremity complications of atherosclerosis, according to the reviewers.
Both sets of guidelines come to the conclusion that there is a need for more evidence to identify patients who are at the greatest risk of tissue loss, but overall they differ in their approach to available data. The ACC/AHA is more inclusive of smaller, well-done nonrandomized studies, whereas the ESC/ESVS relegates small studies to Level of Evidence: C. “We believe this difference drives the variation of therapeutic recommendations more than any other factor,” the authors note.
More randomized studies would align recommendations across both organizations, according to Dr. Kithcart and Dr. Beckman (JACC 2018;72:2789-801).
“The management of PAD has progressed a great deal over the last decade. ... Several clinical trials over the coming years should help clarify how revascularization should be approached, and which patients are most likely to benefit. Until then, maintaining good cardiovascular health, including regular physical activity, smoking cessation, lipid-lowering therapy, blood pressure management, and glucose control have the most benefit in patients with PAD,” the researchers concluded.
Dr. Beckman served as a consultant for several pharmaceutical companies, and on the data and safety monitoring board for Bayer and Novartis. Dr. Kithcart reported that he has no relevant conflicts.
SOURCE: Kithcart, AP et al. JACC 2018;72:2789-801.
Recent advances in the management of peripheral artery disease (PAD) have resulted in new guideline creation in both the United States and Europe.
While there is considerable consensus between the guidelines, there are multiple differences in emphasis and a differing approach to the types and quality of evidence used to back recommendations, according to a comparative review published in the Journal of the American College of Cardiology. The American Heart Association and American College of Cardiology, together with other organizations, issued an update to their previous guidelines on the management and diagnosis of lower extremity PAD in 2016. In 2017, the European Society of Cardiology in conjunction with the European Society for Vascular Surgery updated their own comprehensive guidelines.
Both the U.S. and the European guidelines stress the importance of lowering risk factors for PAD. This includes stopping smoking, lipid and blood pressure management, and controlling glucose, according to Aaron P. Kithcart, MD, of Brigham and Women’s Hospital, Boston, and Joshua A. Beckman, MD, of Vanderbilt University, Nashville, Tenn.
However, the U.S. guidelines focus more on moderating lifestyle factors, including the pursuit of regular physical activity and the use of supervised exercise, whereas the European guidelines focus considerable attention on recommendations for revascularization in patients with limb-threatening ischemia.
Perhaps the major source of variation between the two sets of guidelines, according to the reviewers, are based upon the intended audiences: “The American document limits its focus to PAD but is applicable to practitioners of every background, whereas the European guideline extends the discussion to all PADs to include carotid and vertebral, upper extremities, mesenteric, and renal arteries in addition to lower-extremity artery disease; but is designed to be a source for cardiologists.”
Accordingly, the ESC/ESVS guidelines approach medical therapy with a more holistic flavor, whereas the ACC/AHA guidelines are specific to the lower-extremity complications of atherosclerosis, according to the reviewers.
Both sets of guidelines come to the conclusion that there is a need for more evidence to identify patients who are at the greatest risk of tissue loss, but overall they differ in their approach to available data. The ACC/AHA is more inclusive of smaller, well-done nonrandomized studies, whereas the ESC/ESVS relegates small studies to Level of Evidence: C. “We believe this difference drives the variation of therapeutic recommendations more than any other factor,” the authors note.
More randomized studies would align recommendations across both organizations, according to Dr. Kithcart and Dr. Beckman (JACC 2018;72:2789-801).
“The management of PAD has progressed a great deal over the last decade. ... Several clinical trials over the coming years should help clarify how revascularization should be approached, and which patients are most likely to benefit. Until then, maintaining good cardiovascular health, including regular physical activity, smoking cessation, lipid-lowering therapy, blood pressure management, and glucose control have the most benefit in patients with PAD,” the researchers concluded.
Dr. Beckman served as a consultant for several pharmaceutical companies, and on the data and safety monitoring board for Bayer and Novartis. Dr. Kithcart reported that he has no relevant conflicts.
SOURCE: Kithcart, AP et al. JACC 2018;72:2789-801.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
CLL resistance mechanism to venetoclax identified
SAN DIEGO – A recurrent mutation in BCL2, the therapeutic target of venetoclax (Venclexta), appears to be a major contributor to drug resistance in patients with chronic lymphocytic leukemia (CLL), investigators reported.
The mutation has been detected in some patients with CLL up to 2 years before resistance to venetoclax actually develops, said lead author Piers Blombery, MBBS, from the Peter MacCallum Cancer Center in Melbourne.
“We have identified the first acquired BCL2 mutation developed in patients clinically treated with venetoclax,” he said in a late-breaking oral abstract session at the annual meeting of the American Society of Hematology.
The mutation, which the investigators have labeled BCL2 Gly101Val, “is a recurrent and frequent mediator of resistance and may be detected years before clinical relapse occurs,” he added.
The paper was published online in Cancer Discovery (2018 Dec 4. doi: 10.1158/2159-8290.CD-18-1119) to coincide with the presentation at ASH.
Despite the demonstrated efficacy of venetoclax as continuous therapy in patients with relapsed or refractory CLL, the majority of patients experience disease progression, prompting the investigators to explore molecular mechanisms of secondary resistance.
To do this, they analyzed paired samples from 15 patients with CLL, enrolled in clinical trials of venetoclax, collected both before the start of venetoclax therapy and at the time of disease progression.
In seven of the patients, they identified a novel mutation that showed up at the time of progression, but was absent from the pre-venetoclax samples. The mutation first became detectable from about 19 to 42 months after the start of therapy and preceded clinical progression by as much as 25 months, the investigators found.
They pinned the mutation down to the BH3-binding groove on BCL2, the same molecular site targeted by venetoclax. They found that the mutation was not present in samples from 96 patients with venetoclax-naive CLL nor in any other B-cell malignancies. Searches for references to the mutation in both a cancer database (COSMIC) and a population database (gnomAD) came up empty.
In other experiments, they determined that cell lines overexpressing BCL2 Gly101Val are resistant to venetoclax, and that in the presence of venetoclax in vitro, BCL2 Gly101Val-expressing cells have a growth advantage, compared with wild type cells.
Additionally, they showed that the mutation results in impaired venetoclax binding in vitro.
“BCL2 Gly101Val is observed subclonally, implicating multiple mechanisms of venetoclax resistance in the same patient,” Dr. Blombery said.
In an interview, Dr. Blombery said that the identification of the resistance mutation is a strong rationale for using combination therapy to treat patients with relapsed or refractory CLL to help prevent or attenuate selection pressures that lead to resistance.
The investigators were supported by the Wilson Center for Lymphoma Genomics, Snowdome Foundation, National Health Medical Research Council, Leukemia and Lymphoma Society, Leukemia Foundation, Cancer Council of Victoria, and Australian Cancer Research Foundation. Dr. Blombery reported having no relevant disclosures.
SOURCE: Blombery P et al. ASH 2018, Abstract LBA-7.
SAN DIEGO – A recurrent mutation in BCL2, the therapeutic target of venetoclax (Venclexta), appears to be a major contributor to drug resistance in patients with chronic lymphocytic leukemia (CLL), investigators reported.
The mutation has been detected in some patients with CLL up to 2 years before resistance to venetoclax actually develops, said lead author Piers Blombery, MBBS, from the Peter MacCallum Cancer Center in Melbourne.
“We have identified the first acquired BCL2 mutation developed in patients clinically treated with venetoclax,” he said in a late-breaking oral abstract session at the annual meeting of the American Society of Hematology.
The mutation, which the investigators have labeled BCL2 Gly101Val, “is a recurrent and frequent mediator of resistance and may be detected years before clinical relapse occurs,” he added.
The paper was published online in Cancer Discovery (2018 Dec 4. doi: 10.1158/2159-8290.CD-18-1119) to coincide with the presentation at ASH.
Despite the demonstrated efficacy of venetoclax as continuous therapy in patients with relapsed or refractory CLL, the majority of patients experience disease progression, prompting the investigators to explore molecular mechanisms of secondary resistance.
To do this, they analyzed paired samples from 15 patients with CLL, enrolled in clinical trials of venetoclax, collected both before the start of venetoclax therapy and at the time of disease progression.
In seven of the patients, they identified a novel mutation that showed up at the time of progression, but was absent from the pre-venetoclax samples. The mutation first became detectable from about 19 to 42 months after the start of therapy and preceded clinical progression by as much as 25 months, the investigators found.
They pinned the mutation down to the BH3-binding groove on BCL2, the same molecular site targeted by venetoclax. They found that the mutation was not present in samples from 96 patients with venetoclax-naive CLL nor in any other B-cell malignancies. Searches for references to the mutation in both a cancer database (COSMIC) and a population database (gnomAD) came up empty.
In other experiments, they determined that cell lines overexpressing BCL2 Gly101Val are resistant to venetoclax, and that in the presence of venetoclax in vitro, BCL2 Gly101Val-expressing cells have a growth advantage, compared with wild type cells.
Additionally, they showed that the mutation results in impaired venetoclax binding in vitro.
“BCL2 Gly101Val is observed subclonally, implicating multiple mechanisms of venetoclax resistance in the same patient,” Dr. Blombery said.
In an interview, Dr. Blombery said that the identification of the resistance mutation is a strong rationale for using combination therapy to treat patients with relapsed or refractory CLL to help prevent or attenuate selection pressures that lead to resistance.
The investigators were supported by the Wilson Center for Lymphoma Genomics, Snowdome Foundation, National Health Medical Research Council, Leukemia and Lymphoma Society, Leukemia Foundation, Cancer Council of Victoria, and Australian Cancer Research Foundation. Dr. Blombery reported having no relevant disclosures.
SOURCE: Blombery P et al. ASH 2018, Abstract LBA-7.
SAN DIEGO – A recurrent mutation in BCL2, the therapeutic target of venetoclax (Venclexta), appears to be a major contributor to drug resistance in patients with chronic lymphocytic leukemia (CLL), investigators reported.
The mutation has been detected in some patients with CLL up to 2 years before resistance to venetoclax actually develops, said lead author Piers Blombery, MBBS, from the Peter MacCallum Cancer Center in Melbourne.
“We have identified the first acquired BCL2 mutation developed in patients clinically treated with venetoclax,” he said in a late-breaking oral abstract session at the annual meeting of the American Society of Hematology.
The mutation, which the investigators have labeled BCL2 Gly101Val, “is a recurrent and frequent mediator of resistance and may be detected years before clinical relapse occurs,” he added.
The paper was published online in Cancer Discovery (2018 Dec 4. doi: 10.1158/2159-8290.CD-18-1119) to coincide with the presentation at ASH.
Despite the demonstrated efficacy of venetoclax as continuous therapy in patients with relapsed or refractory CLL, the majority of patients experience disease progression, prompting the investigators to explore molecular mechanisms of secondary resistance.
To do this, they analyzed paired samples from 15 patients with CLL, enrolled in clinical trials of venetoclax, collected both before the start of venetoclax therapy and at the time of disease progression.
In seven of the patients, they identified a novel mutation that showed up at the time of progression, but was absent from the pre-venetoclax samples. The mutation first became detectable from about 19 to 42 months after the start of therapy and preceded clinical progression by as much as 25 months, the investigators found.
They pinned the mutation down to the BH3-binding groove on BCL2, the same molecular site targeted by venetoclax. They found that the mutation was not present in samples from 96 patients with venetoclax-naive CLL nor in any other B-cell malignancies. Searches for references to the mutation in both a cancer database (COSMIC) and a population database (gnomAD) came up empty.
In other experiments, they determined that cell lines overexpressing BCL2 Gly101Val are resistant to venetoclax, and that in the presence of venetoclax in vitro, BCL2 Gly101Val-expressing cells have a growth advantage, compared with wild type cells.
Additionally, they showed that the mutation results in impaired venetoclax binding in vitro.
“BCL2 Gly101Val is observed subclonally, implicating multiple mechanisms of venetoclax resistance in the same patient,” Dr. Blombery said.
In an interview, Dr. Blombery said that the identification of the resistance mutation is a strong rationale for using combination therapy to treat patients with relapsed or refractory CLL to help prevent or attenuate selection pressures that lead to resistance.
The investigators were supported by the Wilson Center for Lymphoma Genomics, Snowdome Foundation, National Health Medical Research Council, Leukemia and Lymphoma Society, Leukemia Foundation, Cancer Council of Victoria, and Australian Cancer Research Foundation. Dr. Blombery reported having no relevant disclosures.
SOURCE: Blombery P et al. ASH 2018, Abstract LBA-7.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: The mutation was identified in samples from seven patients after venetoclax therapy, but not in any of the pretherapy samples.
Study details: Genetic analysis of CLL mutations in 15 patients enrolled in clinical trials of venetoclax.
Disclosures: The investigators were supported by the Wilson Center for Lymphoma Genomics, Snowdome Foundation, National Health Medical Research Council, Leukemia and Lymphoma Society, Leukemia Foundation, Cancer Council of Victoria, and Australian Cancer Research Foundation. Dr. Blombery reported having no relevant disclosures.
Source: Blombery P et al. ASH 2018, Abstract LBA-7.
KATHERINE: T-DM1 doubles HER2-positive invasive disease-free survival
SAN ANTONIO – Swapping trastuzumab out for the drug-antibody conjugate trastuzumab emtansine (T-DM1; Kadcyla) as adjuvant therapy resulted in a halving in the risk of invasive disease or death in patients with HER2-positive early breast cancer with residual invasive disease after neoadjuvant chemotherapy and HER2-targeted therapy, including trastuzumab.
For the primary endpoint in the KATHERINE trial of invasive disease-free survival – defined as freedom from ipsilateral invasive breast tumor recurrence, ipsilateral locoregional invasive breast cancer recurrence, contralateral invasive breast cancer, distant recurrence, or death from any cause – T-DM1 was associated with a hazard ratio of 0.50 (P less than .001).
The 3-year invasive disease-free survival rate for 743 patients treated with T-DMI 1 was 88.3%, compared with 77% for 743 patients treated with trastuzumab, reported Charles E. Geyer Jr., MD, from Virginia Commonwealth University, Richmond, at the San Antonio Breast Cancer Symposium.
In a video interview, Dr. Geyer discussed results of KATHERINE, which suggest that T-DM1 should be considered as a new standard of care in this patient population.
Dr. Geyer reported travel support from Roche and AstraZeneca, medical writing support from AbbVie and Roche, and honoraria from Celgene.
SAN ANTONIO – Swapping trastuzumab out for the drug-antibody conjugate trastuzumab emtansine (T-DM1; Kadcyla) as adjuvant therapy resulted in a halving in the risk of invasive disease or death in patients with HER2-positive early breast cancer with residual invasive disease after neoadjuvant chemotherapy and HER2-targeted therapy, including trastuzumab.
For the primary endpoint in the KATHERINE trial of invasive disease-free survival – defined as freedom from ipsilateral invasive breast tumor recurrence, ipsilateral locoregional invasive breast cancer recurrence, contralateral invasive breast cancer, distant recurrence, or death from any cause – T-DM1 was associated with a hazard ratio of 0.50 (P less than .001).
The 3-year invasive disease-free survival rate for 743 patients treated with T-DMI 1 was 88.3%, compared with 77% for 743 patients treated with trastuzumab, reported Charles E. Geyer Jr., MD, from Virginia Commonwealth University, Richmond, at the San Antonio Breast Cancer Symposium.
In a video interview, Dr. Geyer discussed results of KATHERINE, which suggest that T-DM1 should be considered as a new standard of care in this patient population.
Dr. Geyer reported travel support from Roche and AstraZeneca, medical writing support from AbbVie and Roche, and honoraria from Celgene.
SAN ANTONIO – Swapping trastuzumab out for the drug-antibody conjugate trastuzumab emtansine (T-DM1; Kadcyla) as adjuvant therapy resulted in a halving in the risk of invasive disease or death in patients with HER2-positive early breast cancer with residual invasive disease after neoadjuvant chemotherapy and HER2-targeted therapy, including trastuzumab.
For the primary endpoint in the KATHERINE trial of invasive disease-free survival – defined as freedom from ipsilateral invasive breast tumor recurrence, ipsilateral locoregional invasive breast cancer recurrence, contralateral invasive breast cancer, distant recurrence, or death from any cause – T-DM1 was associated with a hazard ratio of 0.50 (P less than .001).
The 3-year invasive disease-free survival rate for 743 patients treated with T-DMI 1 was 88.3%, compared with 77% for 743 patients treated with trastuzumab, reported Charles E. Geyer Jr., MD, from Virginia Commonwealth University, Richmond, at the San Antonio Breast Cancer Symposium.
In a video interview, Dr. Geyer discussed results of KATHERINE, which suggest that T-DM1 should be considered as a new standard of care in this patient population.
Dr. Geyer reported travel support from Roche and AstraZeneca, medical writing support from AbbVie and Roche, and honoraria from Celgene.
REPORTING FROM SABCS 2018
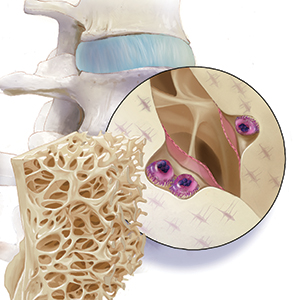
2018 Update on bone health
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
As ObGyns, we are the first-line health care providers for our menopausal patients in terms of identifying, preventing, and initiating treatment for women at risk for fragility fractures. Osteoporosis is probably the most important risk factor for bone health, although sarcopenia, frailty, poor eyesight, and falls also play a significant role in bone health and fragility fracture.
In 2005, more than 2 million incident fractures were reported in the United States, with a total cost of $17 billion.1 By 2025, annual fractures and costs are expected to rise by almost 50%. People who are 65 to 74 years of age will likely experience the largest increase in fracture—greater than 87%.1
Findings from the Women’s Health Initiative study showed that the number of women who had a clinical fracture in 1 year exceeded all the cases of myocardial infarction, stroke, and breast cancer combined.2 Furthermore, the morbidity and mortality rates for fractures are staggering. Thirty percent of women with a hip fracture will be dead within 1 year.3 So, although many patients fear developing breast cancer, and cardiovascular disease remains the number 1 cause of death, the impact of maintaining and protecting bone health cannot be emphasized enough.

_
WHI incidental findings: Hormone-treated menopausal women had decreased hip fracture rate
Manson JE, Aragaki AK, Rossouw JE, et al; WHI Investigators. Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA. 2017;318:927-938.
Manson and colleagues examined the total and cause-specific cumulative mortality of the 2 Women’s Health Initiative (WHI) hormone therapy trials. This was an observational follow-up of US multiethnic postmenopausal women aged 50 to 79 years (mean age at baseline, 63.4 years) enrolled in 2 randomized clinical trials between 1993 and 1998 and followed up through December 31, 2014. A total of 27,347 women were randomly assigned to treatment.
Treatment groups
Depending on the presence or absence of a uterus, women received conjugated equine estrogens (CEE, 0.625 mg/d) plus medroxyprogesterone acetate (MPA, 2.5 mg/d) (n = 8,506) or placebo (n = 8,102) for a median of 5.6 years or CEE alone (n = 5,310) versus placebo (n = 5,429) for a median of 7.2 years. All-cause mortality (the primary outcome) and cause-specific mortality (cardiovascular disease mortality, cancer mortality, and other major causes of mortality) were analyzed in the 2 trials pooled and in each trial individually.
All-cause and cause-specific mortality findings
Mortality follow-up was available for more than 98% of participants. During the cumulative 18-year follow-up, 7,489 deaths occurred. In the overall pooled cohort, all-cause mortality in the hormone therapy group was 27.1% compared with 27.6% in the placebo group (hazard ratio [HR], 0.99 [95% confidence interval (CI), 0.94–1.03]). In the CEE plus MPA group, the HR was 1.02 (95% CI, 0.96–1.08). For those in the CEE-alone group, the HR was 0.94 (95% CI, 0.88–1.01).
In the pooled cohort for cardiovascular mortality, the HR was 1.00 (95% CI, 0.92–1.08 [8.9% with hormone therapy vs 9.0% with placebo]). For total cancer mortality, the HR was 1.03 (95% CI, 0.95–1.12 [8.2% with hormone therapy vs 8.0% with placebo]). For other causes, the HR was 0.95 (95% CI, 0.88–1.02 [10.0% with hormone therapy vs 10.7% with placebo]). Results did not differ significantly between trials.
Key takeaway
The study authors concluded that among postmenopausal women, hormone therapy with CEE plus MPA for a median of 5.6 years or with CEE alone for a median of 7.2 years was not associated with risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years.
Postmenopausal hormone therapy is arguably the most effective “bone drug” available. While all other antiresorptive agents show hip fracture efficacy only in subgroup analyses of the highest-risk patients (women with established osteoporosis, who often already have pre-existing vertebral fractures), the hormone-treated women in the WHI—who were not chosen for having low bone mass (in fact, dual-energy x-ray absorptiometry [DXA] scores were not even recorded)—still had a statistically significant decrease in hip fracture as an adverse event when compared with placebo-treated women. Increasing data on the long-term safety of hormone therapy in menopausal patients will perhaps encourage its greater use from a bone health perspective.
Continue to: Appropriate to defer DXA testing to age 65...
Appropriate to defer DXA testing to age 65 when baseline FRAX score is below treatment level
Gourlay ML, Overman RA, Fine JP, et al; Women’s Health Initiative Investigators. Time to clinically relevant fracture risk scores in postmenopausal women. Am J Med. 2017;130:862.e15-862.e23.
Gourlay ML, Fine JP, Preisser JS, et al; Study of Osteoporotic Fractures Research Group. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225-233.
Many clinicians used to (and still do) order bone mineral density (BMD) testing at 23-month intervals because that was what insurance would allow. Gourlay and colleagues previously published a study on BMD testing intervals and the time it takes to develop osteoporosis. I covered that information in previous Updates.4,5
To recap, Gourlay and colleagues studied 4,957 women, 67 years of age or older, with normal BMD or osteopenia and with no history of hip or clinical vertebral fracture or of treatment for osteoporosis; the women were followed prospectively for up to 15 years. The estimated time for 10% of women to make the transition to osteoporosis was 16.8 years for those with normal BMD, 4.7 years for those with moderate osteopenia, and 1.1 years for women with advanced osteopenia.
Today, FRAX is recommended to assess need for treatment
Older treatment recommendations involved determining various osteopenic BMD levels and the presence or absence of certain risk factors. More recently, the National Osteoporosis Foundation and many medical societies, including the American College of Obstetricians and Gynecologists, have recommended using the FRAX fracture prediction algorithm (available at https://www.sheffield.ac.uk/FRAX/) instead of T-scores to consider initiating pharmacotherapy.
The FRAX calculation tool uses information such as the country where the patient lives, age, sex, height, weight, history of previous fracture, parental fracture, current smoking, glucocorticoid use, rheumatoid arthritis, secondary osteoporosis, alcohol use of 3 or more units per day, and, if available, BMD determination at the femoral neck. It then yields the 10-year absolute risk of hip fracture and any major osteoporotic fracture for that individual or, more precisely, for an individual like that.
In the United States, accepted levels for cost-effective pharmacotherapy are a 10-year absolute risk of hip fracture of 3% or major osteoporotic fracture of 20%.
Continue to: Age also is a key factor in fracture risk assessment
Age also is a key factor in fracture risk assessment
Gourlay and colleagues more recently conducted a retrospective analysis of new occurrence of treatment-level fracture risk scores in postmenopausal women (50 years of age and older) before they received pharmacologic treatment and before they experienced a first hip or clinical vertebral fracture.
In 54,280 postmenopausal women aged 50 to 64 without a BMD test, the time for 10% to develop a treatment-level FRAX score could not be estimated accurately because of the rarity of treatment-level scores. In 6,096 women who had FRAX scores calculated with their BMD score, the estimated time to treatment-level FRAX was 7.6 years for those 65 to 69 and 5.1 years for 75 to 79 year olds. Furthermore, of 17,967 women aged 50 to 64 with a screening-level FRAX at baseline, only 100 (0.6%) experienced a hip or clinical vertebral fracture by age 65.
The investigators concluded that, “Postmenopausal women with sub-threshold fracture risk scores at baseline were unlikely to develop a treatment-level FRAX score between ages 50 and 64 years. After age 65, the increased incidence of treatment-level fracture risk scores, osteoporosis, and major osteoporotic fracture supports more frequent consideration of FRAX and bone mineral density testing.”
Many health care providers begin BMD testing early in menopause. Bone mass results may motivate patients to initiate healthy lifestyle choices, such as adequate dietary calcium, vitamin D supplementation, exercise, moderate alcohol use, smoking cessation, and fall prevention strategies. However, providers and their patients should be aware that if the fracture risk is beneath the threshold score at baseline, the risk of experiencing an osteoporotic fracture prior to age 65 is extremely low, and this should be taken into account before prescribing pharmacotherapy. Furthermore, as stated, FRAX can be performed without a DXA score. When the result is beneath a treatment level in a woman under 65, DXA testing may be deferred until age 65.
Continue to: USPSTF offers updated recommendations for osteoporosis screening
USPSTF offers updated recommendations for osteoporosis screening
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:2521-2531.
The 2018 updated osteoporosis screening recommendations from the United States Preventative Services Task Force (USPSTF) may seem contradictory to the conclusions of Gourlay and colleagues discussed above. They are not.
The USPSTF authors point out that by 2020, about 12.3 million US individuals older than 50 years are expected to have osteoporosis. Osteoporotic fractures (especially hip fractures) are associated with limitations in ambulation, chronic pain and disability, loss of independence, and decreased quality of life. In fact, 21% to 30% of people who sustain a hip fracture die within 1 year. As the US population continues to age, the potential preventable burden will likely increase.
_
Evidence on bone measurement tests, risk assessment tools, and drug therapy efficacy
The USPSTF conducted an evidence review on screening for and treatment of osteoporotic fractures in women as well as risk assessment tools. The task force found the evidence convincing that bone measurement tests are accurate for detecting osteoporosis and predicting osteoporotic fractures. In addition, there is adequate evidence that clinical risk assessment tools are moderately accurate in identifying risk of osteoporosis and osteoporotic fractures. Furthermore, there is convincing evidence that drug therapies reduce subsequent fracture rates in postmenopausal women.
The USPSTF recommends the following:
- For women aged 65 and older, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
- For women younger than 65 who are at increased risk for osteoporosis based on formal clinical risk assessment tools, screen for osteoporosis with bone measurement testing to prevent osteoporotic fractures.
We all agree that women older than 65 years of age should be screened with DXA measurements of bone mass. The USPSTF says that in women under 65, a fracture assessment tool like FRAX, which does not require bone density testing to yield an individual’s absolute 10-year fracture risk, should be used to determine if bone mass measurement by DXA is, in fact, warranted. This recommendation is further supported by the article by Gourlay and colleagues, in which women aged 50 to 64 with subthreshold FRAX scores had a very low risk of fracture prior to age 65.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
- Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- Cauley JA, Wampler NS, Barnhart JM, et al; Women’s Health Initiative Observational Study. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717-1723.
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573-1579.
- Goldstein SR. Update on osteoporosis. OBG Manag. 2012;24:16-21.
- Goldstein SR. 2017 update on bone health. OBG Manag. 2017;29-32, 48.
Large cohort study IDs prognostic factors in thromboangiitis obliterans
CHICAGO – Nonwhite ethnicity and limb infection at diagnosis predict vascular events in patients with thromboangiitis obliterans (TAO), and the latter also predicts amputation, which occurs within 10 years of diagnosis in nearly a third of patients, according to findings from a large retrospective French cohort study.
After a mean follow-up of 5.7 years, 58.9% of 224 patients with TAO – also known as Buerger’s disease – experienced a vascular event, 21.4% experienced at least one amputation, and 1.3% died, Alexandre Le Joncour, MD, reported at the annual meeting of the American College of Rheumatology.
The 5- and 15-year vascular event-free survival rates were 45% and 28%, respectively, and the 10- and 15-year amputation-free survival rates were 74%, and 66%, respectively, said Dr. Le Joncour of Sorbonne University, Paris.
Of note, no significant difference was seen in the vascular event-free survival rates based on tobacco use levels (more than 22 pack-years vs. 22 or fewer pack-years; HR, 1.2), he said.
Patient characteristics and clinical factors found to independently predict vascular events included nonwhite ethnicity (hazard ratio, 2.35; P = .005) and limb infection at diagnosis (HR, 3.29; P = .045). Limb infection at diagnosis also independently predicted amputation (HR, 12.1; P less than .001), he said.
“But there was no significant [association with amputation] in patients who had claudication, critical ischemia, or ischemic ulcers/necrosis,” he noted, adding that a comparison of white and nonwhite patients showed that the groups were similar with respect to epidemiologic and cardiovascular factors, clinical symptom distribution, and rates of addiction to tobacco, alcohol, and illicit drugs.
It was also clear that patients who quit using tobacco had a significantly lower risk of amputation than did those who continued using tobacco (P = .001), he said, explaining that 43 of the 48 patients who experienced amputation were current smokers, and 5 were ex-smokers at the time of amputation.
Dr. Le Joncour and his colleagues included TAO patients diagnosed between 1967 and 2016 at a median age of 36 years at the time of first symptoms, with a median of 12 months from symptom onset until diagnosis. About 76% were men, and about 83% were white. Patients with diabetes, atherosclerosis, arterial emboli, connective tissue disease, and/or thrombophilia were excluded.
Vascular events in this study were defined as “an acute worsening of the disease course requiring treatment modifications,” and included critical ischemia (35% of cases), ulcers/necrosis (33%), claudication worsening (16%), deep vein thrombosis (3%), superficial phlebitis (7%), limb infection (4%), and “other” events (2%).
Major amputation was defined as “an amputation involving the tibio-tarsian articulation for lower limbs and the metacarpophalangeal articulation for upper limbs,” he explained.
The median time to amputation was 4 years, and patients who experienced amputation had a median age of 39 years. Half of the 48 patients who experienced amputation had one amputation, nearly a third had two amputations, and 19% had three amputations. About two-thirds had minor amputations and a third had major amputations.
The findings provide important prognostic information regarding TAO, Dr. Le Joncour said, noting that long-term data on outcomes in TAO patients have been lacking.
“We found specific characteristics that identified those at highest risk for subsequent vascular complications, and these factors are not only important predictors of vascular complications or relapse, but may also serve to adjust more aggressive management and close follow-up of these patients,” he concluded.
Dr. Le Joncour reported having no disclosures.
SOURCE: Le Joncour A et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 1885.
CHICAGO – Nonwhite ethnicity and limb infection at diagnosis predict vascular events in patients with thromboangiitis obliterans (TAO), and the latter also predicts amputation, which occurs within 10 years of diagnosis in nearly a third of patients, according to findings from a large retrospective French cohort study.
After a mean follow-up of 5.7 years, 58.9% of 224 patients with TAO – also known as Buerger’s disease – experienced a vascular event, 21.4% experienced at least one amputation, and 1.3% died, Alexandre Le Joncour, MD, reported at the annual meeting of the American College of Rheumatology.
The 5- and 15-year vascular event-free survival rates were 45% and 28%, respectively, and the 10- and 15-year amputation-free survival rates were 74%, and 66%, respectively, said Dr. Le Joncour of Sorbonne University, Paris.
Of note, no significant difference was seen in the vascular event-free survival rates based on tobacco use levels (more than 22 pack-years vs. 22 or fewer pack-years; HR, 1.2), he said.
Patient characteristics and clinical factors found to independently predict vascular events included nonwhite ethnicity (hazard ratio, 2.35; P = .005) and limb infection at diagnosis (HR, 3.29; P = .045). Limb infection at diagnosis also independently predicted amputation (HR, 12.1; P less than .001), he said.
“But there was no significant [association with amputation] in patients who had claudication, critical ischemia, or ischemic ulcers/necrosis,” he noted, adding that a comparison of white and nonwhite patients showed that the groups were similar with respect to epidemiologic and cardiovascular factors, clinical symptom distribution, and rates of addiction to tobacco, alcohol, and illicit drugs.
It was also clear that patients who quit using tobacco had a significantly lower risk of amputation than did those who continued using tobacco (P = .001), he said, explaining that 43 of the 48 patients who experienced amputation were current smokers, and 5 were ex-smokers at the time of amputation.
Dr. Le Joncour and his colleagues included TAO patients diagnosed between 1967 and 2016 at a median age of 36 years at the time of first symptoms, with a median of 12 months from symptom onset until diagnosis. About 76% were men, and about 83% were white. Patients with diabetes, atherosclerosis, arterial emboli, connective tissue disease, and/or thrombophilia were excluded.
Vascular events in this study were defined as “an acute worsening of the disease course requiring treatment modifications,” and included critical ischemia (35% of cases), ulcers/necrosis (33%), claudication worsening (16%), deep vein thrombosis (3%), superficial phlebitis (7%), limb infection (4%), and “other” events (2%).
Major amputation was defined as “an amputation involving the tibio-tarsian articulation for lower limbs and the metacarpophalangeal articulation for upper limbs,” he explained.
The median time to amputation was 4 years, and patients who experienced amputation had a median age of 39 years. Half of the 48 patients who experienced amputation had one amputation, nearly a third had two amputations, and 19% had three amputations. About two-thirds had minor amputations and a third had major amputations.
The findings provide important prognostic information regarding TAO, Dr. Le Joncour said, noting that long-term data on outcomes in TAO patients have been lacking.
“We found specific characteristics that identified those at highest risk for subsequent vascular complications, and these factors are not only important predictors of vascular complications or relapse, but may also serve to adjust more aggressive management and close follow-up of these patients,” he concluded.
Dr. Le Joncour reported having no disclosures.
SOURCE: Le Joncour A et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 1885.
CHICAGO – Nonwhite ethnicity and limb infection at diagnosis predict vascular events in patients with thromboangiitis obliterans (TAO), and the latter also predicts amputation, which occurs within 10 years of diagnosis in nearly a third of patients, according to findings from a large retrospective French cohort study.
After a mean follow-up of 5.7 years, 58.9% of 224 patients with TAO – also known as Buerger’s disease – experienced a vascular event, 21.4% experienced at least one amputation, and 1.3% died, Alexandre Le Joncour, MD, reported at the annual meeting of the American College of Rheumatology.
The 5- and 15-year vascular event-free survival rates were 45% and 28%, respectively, and the 10- and 15-year amputation-free survival rates were 74%, and 66%, respectively, said Dr. Le Joncour of Sorbonne University, Paris.
Of note, no significant difference was seen in the vascular event-free survival rates based on tobacco use levels (more than 22 pack-years vs. 22 or fewer pack-years; HR, 1.2), he said.
Patient characteristics and clinical factors found to independently predict vascular events included nonwhite ethnicity (hazard ratio, 2.35; P = .005) and limb infection at diagnosis (HR, 3.29; P = .045). Limb infection at diagnosis also independently predicted amputation (HR, 12.1; P less than .001), he said.
“But there was no significant [association with amputation] in patients who had claudication, critical ischemia, or ischemic ulcers/necrosis,” he noted, adding that a comparison of white and nonwhite patients showed that the groups were similar with respect to epidemiologic and cardiovascular factors, clinical symptom distribution, and rates of addiction to tobacco, alcohol, and illicit drugs.
It was also clear that patients who quit using tobacco had a significantly lower risk of amputation than did those who continued using tobacco (P = .001), he said, explaining that 43 of the 48 patients who experienced amputation were current smokers, and 5 were ex-smokers at the time of amputation.
Dr. Le Joncour and his colleagues included TAO patients diagnosed between 1967 and 2016 at a median age of 36 years at the time of first symptoms, with a median of 12 months from symptom onset until diagnosis. About 76% were men, and about 83% were white. Patients with diabetes, atherosclerosis, arterial emboli, connective tissue disease, and/or thrombophilia were excluded.
Vascular events in this study were defined as “an acute worsening of the disease course requiring treatment modifications,” and included critical ischemia (35% of cases), ulcers/necrosis (33%), claudication worsening (16%), deep vein thrombosis (3%), superficial phlebitis (7%), limb infection (4%), and “other” events (2%).
Major amputation was defined as “an amputation involving the tibio-tarsian articulation for lower limbs and the metacarpophalangeal articulation for upper limbs,” he explained.
The median time to amputation was 4 years, and patients who experienced amputation had a median age of 39 years. Half of the 48 patients who experienced amputation had one amputation, nearly a third had two amputations, and 19% had three amputations. About two-thirds had minor amputations and a third had major amputations.
The findings provide important prognostic information regarding TAO, Dr. Le Joncour said, noting that long-term data on outcomes in TAO patients have been lacking.
“We found specific characteristics that identified those at highest risk for subsequent vascular complications, and these factors are not only important predictors of vascular complications or relapse, but may also serve to adjust more aggressive management and close follow-up of these patients,” he concluded.
Dr. Le Joncour reported having no disclosures.
SOURCE: Le Joncour A et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 1885.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: Nonwhite ethnicity and limb infection predict poor prognosis in TAO.
Major finding: Ethnicity predicts vascular events (HR, 2.35); limb infection at diagnosis predicts vascular events and amputation (HR, 3.29 and 12.1, respectively).
Study details: A retrospective cohort study of 224 patients.
Disclosures: Dr. Le Joncour reported having no disclosures.
Source: Le Joncour A et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 1885.
RCC research has opened door to the future, but “much work remains to be done”
Recent research on the genetic basis of renal cell carcinoma has expanded and improved treatment options; however, personalized medicine is still largely unavailable, so future efforts should aim to link genetic knowledge with prognosis and treatment selection, according to the authors of a recent review article.
The article, written by Christopher D’Avella, MD, of the Fox Chase Cancer Center in Philadelphia, and his colleagues provides an overview of renal cell carcinoma (RCC) mutations and associated therapies, with updates of ongoing trials and a look at future directions.
“The expansion of treatment options for patients with advanced RCC over the past 15 years is a testament to enhanced understanding of the genetics and genomics of RCC and the ability to apply this knowledge to drug development,” the authors wrote in Urologic Oncology. “However, much work remains to be done as there are still no validated biomarkers to select patient treatment, and in only rare cases, the knowledge of particular mutations in RCC can lead to rational treatment selection.”
RCC accounts for approximately 80%-85% of renal tumors. About three out of four RCC patients have clear cell disease, of which about 30% develop metastases and need systemic therapy. The authors pointed out that vascular endothelial growth factor tyrosine kinase inhibitors (TKIs) have been standard first-line care for these patients since the mid-2000s, based on improved molecular understanding. Still, responses to TKIs are limited and patients eventually develop resistance. Several agents are in development to overcome this obstacle, including inhibitors of hypoxia inducible factor, which have recently shown promise. Among biomarkers for ccRCC, PBRM1 mutations may be associated with susceptibility to checkpoint inhibitors, and TSC1 could predict response to mTOR (mammalian target of rapamycin) inhibition.
Along with clear cell RCC, the review article addressed topics in papillary and sarcomatoid subtypes.
Patients with papillary RCC often have MET mutations, and ongoing research is focused on associated targeted therapies. For example, savolitinib is a highly selective MET inhibitor that has shown promise in this patient subgroup.
Sarcomatoid features remain characteristic of large and aggressive tumors. Unfortunately, treatment options are currently limited in this area. Recent studies suggest that TP53 and NF2 mutations are associated with sarcomatoid differentiation.
“Future studies should explore linking genetics to prognosis, resistance to targeted therapies, and the identification of future therapeutic targets,” the authors concluded.
SOURCE: D’Avella C et al. Urol Oncol. 2018 Nov 23. doi: 10.1016/j.urolonc.2018.10.027.
Recent research on the genetic basis of renal cell carcinoma has expanded and improved treatment options; however, personalized medicine is still largely unavailable, so future efforts should aim to link genetic knowledge with prognosis and treatment selection, according to the authors of a recent review article.
The article, written by Christopher D’Avella, MD, of the Fox Chase Cancer Center in Philadelphia, and his colleagues provides an overview of renal cell carcinoma (RCC) mutations and associated therapies, with updates of ongoing trials and a look at future directions.
“The expansion of treatment options for patients with advanced RCC over the past 15 years is a testament to enhanced understanding of the genetics and genomics of RCC and the ability to apply this knowledge to drug development,” the authors wrote in Urologic Oncology. “However, much work remains to be done as there are still no validated biomarkers to select patient treatment, and in only rare cases, the knowledge of particular mutations in RCC can lead to rational treatment selection.”
RCC accounts for approximately 80%-85% of renal tumors. About three out of four RCC patients have clear cell disease, of which about 30% develop metastases and need systemic therapy. The authors pointed out that vascular endothelial growth factor tyrosine kinase inhibitors (TKIs) have been standard first-line care for these patients since the mid-2000s, based on improved molecular understanding. Still, responses to TKIs are limited and patients eventually develop resistance. Several agents are in development to overcome this obstacle, including inhibitors of hypoxia inducible factor, which have recently shown promise. Among biomarkers for ccRCC, PBRM1 mutations may be associated with susceptibility to checkpoint inhibitors, and TSC1 could predict response to mTOR (mammalian target of rapamycin) inhibition.
Along with clear cell RCC, the review article addressed topics in papillary and sarcomatoid subtypes.
Patients with papillary RCC often have MET mutations, and ongoing research is focused on associated targeted therapies. For example, savolitinib is a highly selective MET inhibitor that has shown promise in this patient subgroup.
Sarcomatoid features remain characteristic of large and aggressive tumors. Unfortunately, treatment options are currently limited in this area. Recent studies suggest that TP53 and NF2 mutations are associated with sarcomatoid differentiation.
“Future studies should explore linking genetics to prognosis, resistance to targeted therapies, and the identification of future therapeutic targets,” the authors concluded.
SOURCE: D’Avella C et al. Urol Oncol. 2018 Nov 23. doi: 10.1016/j.urolonc.2018.10.027.
Recent research on the genetic basis of renal cell carcinoma has expanded and improved treatment options; however, personalized medicine is still largely unavailable, so future efforts should aim to link genetic knowledge with prognosis and treatment selection, according to the authors of a recent review article.
The article, written by Christopher D’Avella, MD, of the Fox Chase Cancer Center in Philadelphia, and his colleagues provides an overview of renal cell carcinoma (RCC) mutations and associated therapies, with updates of ongoing trials and a look at future directions.
“The expansion of treatment options for patients with advanced RCC over the past 15 years is a testament to enhanced understanding of the genetics and genomics of RCC and the ability to apply this knowledge to drug development,” the authors wrote in Urologic Oncology. “However, much work remains to be done as there are still no validated biomarkers to select patient treatment, and in only rare cases, the knowledge of particular mutations in RCC can lead to rational treatment selection.”
RCC accounts for approximately 80%-85% of renal tumors. About three out of four RCC patients have clear cell disease, of which about 30% develop metastases and need systemic therapy. The authors pointed out that vascular endothelial growth factor tyrosine kinase inhibitors (TKIs) have been standard first-line care for these patients since the mid-2000s, based on improved molecular understanding. Still, responses to TKIs are limited and patients eventually develop resistance. Several agents are in development to overcome this obstacle, including inhibitors of hypoxia inducible factor, which have recently shown promise. Among biomarkers for ccRCC, PBRM1 mutations may be associated with susceptibility to checkpoint inhibitors, and TSC1 could predict response to mTOR (mammalian target of rapamycin) inhibition.
Along with clear cell RCC, the review article addressed topics in papillary and sarcomatoid subtypes.
Patients with papillary RCC often have MET mutations, and ongoing research is focused on associated targeted therapies. For example, savolitinib is a highly selective MET inhibitor that has shown promise in this patient subgroup.
Sarcomatoid features remain characteristic of large and aggressive tumors. Unfortunately, treatment options are currently limited in this area. Recent studies suggest that TP53 and NF2 mutations are associated with sarcomatoid differentiation.
“Future studies should explore linking genetics to prognosis, resistance to targeted therapies, and the identification of future therapeutic targets,” the authors concluded.
SOURCE: D’Avella C et al. Urol Oncol. 2018 Nov 23. doi: 10.1016/j.urolonc.2018.10.027.
FROM UROLOGIC ONCOLOGY
Key clinical point: Recent research on the genetic basis of renal cell carcinoma has expanded and improved treatment options but personalized medicine is still largely unavailable.
Major finding: There are still no validated biomarkers to select patient treatment, and in only rare cases does the knowledge of particular mutations in renal cell carcinoma lead to rational treatment selection.
Study details: A review article of mutations in renal cell carcinoma and associated treatment options.
Disclosures: This work was supported by the Canadian Cancer Society and the Canadian Institutes of Health.
Source: D’Avella C et al. Urol Oncol. 2018 Nov 23. doi: 10.1016/j.urolonc.2018.10.027.
In IDH-mutated AML, first-line IDH inhibitors plus chemo may boost remission
SAN DIEGO – In patients with newly diagnosed acute myeloid leukemia (AML) bearing IDH1 or IDH2 mutations, combinations of either ivosidenib (Tibsovo, for IDH1) or enasidenib (Idhifa, for IDH2) with standard induction and consolidation regimens are safe and well tolerated and are associated with encouraging remission rates, results of a phase 1 trial indicate.
In the open-label, phase 1 trial, ivosidenib plus chemotherapy was associated with elimination of minimal residual disease (MRD) by flow cytometry in 88% of treated patients and with IDH1-mutation clearance in 41% of patients.
Enasidenib plus chemotherapy was associated with elimination of MRD in 45% of patients and with IDH2-mutation clearance in 25% of patients, said Eytan M. Stein, MD, from Memorial Sloan Kettering Cancer Center in New York.
“The overall survival rates are robust, with greater than 75% 1-year survival in both ivosidenib- and enasidenib-treated patients,” he said at the annual meeting of the American Society of Hematology.
Both ivosidenib and enasidenib are approved in the United States for treatment of patients with relapsed or refractory AML bearing either IDH1 or IDH2 mutations, respectively. In this trial, the investigators explored the therapeutic potential of the IDH inhibitors in patients with previously untreated disease.
Dr. Stein and his colleagues investigated combining each of the agents with standard induction therapy with either daunorubicin 60 mg/m2 per day or idarubicin 12 mg/m2 per day for 3 days, plus cytarabine 200 mg/m2 per day for 7 days. Patients with IDH1 mutations received ivosidenib 500 mg once daily, and those with IDH2 mutations received enasidenib 100 mg once daily.
After induction, patients with a complete remission (CR), CR with incomplete recovery of hematologic counts (CRi), or CR with incomplete recovery of platelets (CRp) could receive up to four cycles of consolidation therapy while continuing the IDH inhibitor. Patients who completed consolidation or were ineligible for consolidation could continue on maintenance therapy with their assigned drug until the end of the study.
The drugs were discontinued in patients who went on to hematopoietic stem cell transplant.
The most frequent co-occurring baseline mutations were DNMT3A, NPM1, and NRAS for patients with IDH1 mutations, and DNMT3A, SRSF2, and ASXL1 for patients with IDH2 mutations.
A total of 60 patients were assigned to ivosidenib and chemotherapy and 93 were assigned to enasidenib/chemotherapy. The median patient age was about 63 years in each arm.
All patients in each arm received a least one induction dose and about 48% in each arm received at least some consolidation dosing. In all, 18% of patients in the ivosidenib arm and 19% in the enasidenib arm went on to maintenance.
Treatment discontinuations occurred in 55% of patients in the ivosidenib group and 84% in the enasidenib group. The primary reason for discontinuation included HSCT, adverse events, progressive disease, and death (one and four patients in the respective arms).
Adverse events of interest, regardless of attribution, included the IDH differentiation syndrome in two patients on ivosidenib and one on enasidenib, leukocytosis, QT interval prolongation, and increased blood bilirubin.
The 30-day and 60-day mortality rates were 5% and 8% in the ivosidenib arm and 5% and 9% in the enasidenib arm, respectively.
Best overall response rates (CR+CRi+CRp) among all patients were 80% in the ivosidenib arm and 72% in the enasidenib arm. In each trial arm, the response rates were higher among patients with de novo AML, compared with secondary AML.
Of 12 ivosidenib-treated patients who had IDH1-mutation clearance, 10 had clearance at the end of induction therapy, and 2 achieved clearance during or after consolidation. Of 15 ivosidenib-treated patients who became MRD negative, 12 had achieved it by the end of induction, and 3 became MRD negative during consolidation.
In the enasidenib arm, 15 patients had IDH2 mutation clearance (11 after induction, 4 during consolidation) and 9 became MRD negative (7 after induction and 2 during or after consolidation).
The probability of surviving to 1 year after the start of induction among ivosidenib-treated patients was 79%; the median overall survival had not been reached and was not estimable at the time of data cutoff. The probability of surviving to 1 year among patients in the enasidenib arm was 75%. In this group, too, median overall survival had not been reached.
The clinical benefit of adding either IDH inhibitor to induction, consolidation, and maintenance therapy for patients with newly diagnosed AML with IDH mutations will be further evaluated in a randomized, phase 3 trial, Dr. Stein said.
The study was funded by Agios Pharmaceuticals and Celgene. Dr. Stein reported consulting with those companies and others.
SOURCE: Stein EM et al. ASH 2018, Abstract 560.
SAN DIEGO – In patients with newly diagnosed acute myeloid leukemia (AML) bearing IDH1 or IDH2 mutations, combinations of either ivosidenib (Tibsovo, for IDH1) or enasidenib (Idhifa, for IDH2) with standard induction and consolidation regimens are safe and well tolerated and are associated with encouraging remission rates, results of a phase 1 trial indicate.
In the open-label, phase 1 trial, ivosidenib plus chemotherapy was associated with elimination of minimal residual disease (MRD) by flow cytometry in 88% of treated patients and with IDH1-mutation clearance in 41% of patients.
Enasidenib plus chemotherapy was associated with elimination of MRD in 45% of patients and with IDH2-mutation clearance in 25% of patients, said Eytan M. Stein, MD, from Memorial Sloan Kettering Cancer Center in New York.
“The overall survival rates are robust, with greater than 75% 1-year survival in both ivosidenib- and enasidenib-treated patients,” he said at the annual meeting of the American Society of Hematology.
Both ivosidenib and enasidenib are approved in the United States for treatment of patients with relapsed or refractory AML bearing either IDH1 or IDH2 mutations, respectively. In this trial, the investigators explored the therapeutic potential of the IDH inhibitors in patients with previously untreated disease.
Dr. Stein and his colleagues investigated combining each of the agents with standard induction therapy with either daunorubicin 60 mg/m2 per day or idarubicin 12 mg/m2 per day for 3 days, plus cytarabine 200 mg/m2 per day for 7 days. Patients with IDH1 mutations received ivosidenib 500 mg once daily, and those with IDH2 mutations received enasidenib 100 mg once daily.
After induction, patients with a complete remission (CR), CR with incomplete recovery of hematologic counts (CRi), or CR with incomplete recovery of platelets (CRp) could receive up to four cycles of consolidation therapy while continuing the IDH inhibitor. Patients who completed consolidation or were ineligible for consolidation could continue on maintenance therapy with their assigned drug until the end of the study.
The drugs were discontinued in patients who went on to hematopoietic stem cell transplant.
The most frequent co-occurring baseline mutations were DNMT3A, NPM1, and NRAS for patients with IDH1 mutations, and DNMT3A, SRSF2, and ASXL1 for patients with IDH2 mutations.
A total of 60 patients were assigned to ivosidenib and chemotherapy and 93 were assigned to enasidenib/chemotherapy. The median patient age was about 63 years in each arm.
All patients in each arm received a least one induction dose and about 48% in each arm received at least some consolidation dosing. In all, 18% of patients in the ivosidenib arm and 19% in the enasidenib arm went on to maintenance.
Treatment discontinuations occurred in 55% of patients in the ivosidenib group and 84% in the enasidenib group. The primary reason for discontinuation included HSCT, adverse events, progressive disease, and death (one and four patients in the respective arms).
Adverse events of interest, regardless of attribution, included the IDH differentiation syndrome in two patients on ivosidenib and one on enasidenib, leukocytosis, QT interval prolongation, and increased blood bilirubin.
The 30-day and 60-day mortality rates were 5% and 8% in the ivosidenib arm and 5% and 9% in the enasidenib arm, respectively.
Best overall response rates (CR+CRi+CRp) among all patients were 80% in the ivosidenib arm and 72% in the enasidenib arm. In each trial arm, the response rates were higher among patients with de novo AML, compared with secondary AML.
Of 12 ivosidenib-treated patients who had IDH1-mutation clearance, 10 had clearance at the end of induction therapy, and 2 achieved clearance during or after consolidation. Of 15 ivosidenib-treated patients who became MRD negative, 12 had achieved it by the end of induction, and 3 became MRD negative during consolidation.
In the enasidenib arm, 15 patients had IDH2 mutation clearance (11 after induction, 4 during consolidation) and 9 became MRD negative (7 after induction and 2 during or after consolidation).
The probability of surviving to 1 year after the start of induction among ivosidenib-treated patients was 79%; the median overall survival had not been reached and was not estimable at the time of data cutoff. The probability of surviving to 1 year among patients in the enasidenib arm was 75%. In this group, too, median overall survival had not been reached.
The clinical benefit of adding either IDH inhibitor to induction, consolidation, and maintenance therapy for patients with newly diagnosed AML with IDH mutations will be further evaluated in a randomized, phase 3 trial, Dr. Stein said.
The study was funded by Agios Pharmaceuticals and Celgene. Dr. Stein reported consulting with those companies and others.
SOURCE: Stein EM et al. ASH 2018, Abstract 560.
SAN DIEGO – In patients with newly diagnosed acute myeloid leukemia (AML) bearing IDH1 or IDH2 mutations, combinations of either ivosidenib (Tibsovo, for IDH1) or enasidenib (Idhifa, for IDH2) with standard induction and consolidation regimens are safe and well tolerated and are associated with encouraging remission rates, results of a phase 1 trial indicate.
In the open-label, phase 1 trial, ivosidenib plus chemotherapy was associated with elimination of minimal residual disease (MRD) by flow cytometry in 88% of treated patients and with IDH1-mutation clearance in 41% of patients.
Enasidenib plus chemotherapy was associated with elimination of MRD in 45% of patients and with IDH2-mutation clearance in 25% of patients, said Eytan M. Stein, MD, from Memorial Sloan Kettering Cancer Center in New York.
“The overall survival rates are robust, with greater than 75% 1-year survival in both ivosidenib- and enasidenib-treated patients,” he said at the annual meeting of the American Society of Hematology.
Both ivosidenib and enasidenib are approved in the United States for treatment of patients with relapsed or refractory AML bearing either IDH1 or IDH2 mutations, respectively. In this trial, the investigators explored the therapeutic potential of the IDH inhibitors in patients with previously untreated disease.
Dr. Stein and his colleagues investigated combining each of the agents with standard induction therapy with either daunorubicin 60 mg/m2 per day or idarubicin 12 mg/m2 per day for 3 days, plus cytarabine 200 mg/m2 per day for 7 days. Patients with IDH1 mutations received ivosidenib 500 mg once daily, and those with IDH2 mutations received enasidenib 100 mg once daily.
After induction, patients with a complete remission (CR), CR with incomplete recovery of hematologic counts (CRi), or CR with incomplete recovery of platelets (CRp) could receive up to four cycles of consolidation therapy while continuing the IDH inhibitor. Patients who completed consolidation or were ineligible for consolidation could continue on maintenance therapy with their assigned drug until the end of the study.
The drugs were discontinued in patients who went on to hematopoietic stem cell transplant.
The most frequent co-occurring baseline mutations were DNMT3A, NPM1, and NRAS for patients with IDH1 mutations, and DNMT3A, SRSF2, and ASXL1 for patients with IDH2 mutations.
A total of 60 patients were assigned to ivosidenib and chemotherapy and 93 were assigned to enasidenib/chemotherapy. The median patient age was about 63 years in each arm.
All patients in each arm received a least one induction dose and about 48% in each arm received at least some consolidation dosing. In all, 18% of patients in the ivosidenib arm and 19% in the enasidenib arm went on to maintenance.
Treatment discontinuations occurred in 55% of patients in the ivosidenib group and 84% in the enasidenib group. The primary reason for discontinuation included HSCT, adverse events, progressive disease, and death (one and four patients in the respective arms).
Adverse events of interest, regardless of attribution, included the IDH differentiation syndrome in two patients on ivosidenib and one on enasidenib, leukocytosis, QT interval prolongation, and increased blood bilirubin.
The 30-day and 60-day mortality rates were 5% and 8% in the ivosidenib arm and 5% and 9% in the enasidenib arm, respectively.
Best overall response rates (CR+CRi+CRp) among all patients were 80% in the ivosidenib arm and 72% in the enasidenib arm. In each trial arm, the response rates were higher among patients with de novo AML, compared with secondary AML.
Of 12 ivosidenib-treated patients who had IDH1-mutation clearance, 10 had clearance at the end of induction therapy, and 2 achieved clearance during or after consolidation. Of 15 ivosidenib-treated patients who became MRD negative, 12 had achieved it by the end of induction, and 3 became MRD negative during consolidation.
In the enasidenib arm, 15 patients had IDH2 mutation clearance (11 after induction, 4 during consolidation) and 9 became MRD negative (7 after induction and 2 during or after consolidation).
The probability of surviving to 1 year after the start of induction among ivosidenib-treated patients was 79%; the median overall survival had not been reached and was not estimable at the time of data cutoff. The probability of surviving to 1 year among patients in the enasidenib arm was 75%. In this group, too, median overall survival had not been reached.
The clinical benefit of adding either IDH inhibitor to induction, consolidation, and maintenance therapy for patients with newly diagnosed AML with IDH mutations will be further evaluated in a randomized, phase 3 trial, Dr. Stein said.
The study was funded by Agios Pharmaceuticals and Celgene. Dr. Stein reported consulting with those companies and others.
SOURCE: Stein EM et al. ASH 2018, Abstract 560.
REPORTING FROM ASH 2018
Key clinical point: The IDH1 inhibitor ivosidenib and IDH2 inhibitor enasidenib combined with induction and consolidation therapy showed promising efficacy against newly diagnosed acute myeloid leukemia.
Major finding: The 1-year survival rates were greater than 75% for patients with previously untreated acute myeloid leukemia who received either of the IDH-mutated inhibitors.
Study details: An open-label, prospective trial in 153 patients with newly diagnosed acute myeloid leukemia.
Disclosures: The study was funded by Agios Pharmaceuticals and Celgene. Dr. Stein reported consulting with those companies and others.
Source: Stein EM et al. ASH 2018, Abstract 560.
Hepatitis C debrief: Therapy has matured, access issues remain
SAN FRANCISCO – Hepatitis C therapy has matured and now offers excellent sustained viral response (SVR) in the vast majority of cases, but key challenges remain in getting the therapy to those who need it.
“Unfortunately, we’re not making some of the progress we might have hoped to see, particularly in North America,” said Jordan Feld, MD, MPH, who gave a debrief of hepatitis C abstracts during a wrap-up session at the annual meeting of the American Association for the Study of Liver Diseases.
The problem is particularly acute in young adults aged 18-39 years – only about 9% of those who tested positive for HCV RNA saw a specialist, and about 23% of those who saw a specialist went on to receive treatment, according to an analysis of over 17 million patients in the United States (abstract 1567). The numbers were better for older adults but still far from optimal, with 23% who tested positive seeing a specialist, and just 32% of those patients getting treatment.
Another study (abstract 0147) looked state by state at the percentage of Medicaid patients who received a prescription for direct-acting antiviral (DAA) medication and then went on to fill the prescription. The rates ranged from 0% in Alaska to 96% in Connecticut. Eight states were higher than 70%, six were between 50% and 70%, and 15 states were below 50%.
“Despite our efforts, there continue to be major access barriers across the U.S., particularly for Medicaid individuals,” said Dr. Feld, who is a clinician-scientist at the Toronto Western Hospital Liver Clinic and the McLaughlin-Rotman Centre for Global Health.
A study examining the Chronic Hepatitis (CHeCS) cohort (abstract 0585) described a big spike in treatment uptake shortly after approvals of the new HCV regimens, but by 2016, only about one-third of individuals who required treatment actually began treatment. Factors associated with nontreatment largely reflected marginalization, including low income, being on Medicaid, and lack of long-term follow-up.
Even as health systems struggle to get treatment to those who need it, new studies are showing how to expand existing treatments into new populations.
Results from the EXPEDITION 8 study (abstract LB-7) showed efficacy of an 8-week regimen of the glecaprevir/pibrentasvir combination in patients with compensated cirrhosis. It looked at genotypes 1, 2, and 4-6. In an intention-to-treat analysis, 98% attained SVR and there were no viral failures or safety concerns. A follow-up trial is ongoing that includes patients with genotype 3. “This is exciting to be able to shorten therapy in patients with cirrhosis,” said Dr. Feld.
Although first-line DAAs are extremely effective, there are a few patients who do not achieve a cure. One study (abstract 0227) examined the combination of sofosbuvir, velpatasvir, and voxilaprevir in retreatment of these patients. The drugs resulted in SVR rates similar to those in registration trials, but the regimen was somewhat less effective in patients previously treated with sofosbuvir and velpatasvir. “I think we need to investigate that further,” said Dr. Feld.
The combination of glecaprevir and pibrentasvir also proved effective for retreatment in patients with genotype 1/1A who had failed treatment with an NS5A inhibitor plus sofosbuvir with or without ribavirin (abstract 226). SVR rates at 16 weeks were quite good, but lower in genotype 1a patients at 12 weeks (87% week 12 versus 94% week 16).”I think this is a really good regimen for genotype 1b. For 1a, serum definitely needs 16 weeks [to clear],” said Dr. Feld.
Other abstracts presented at the meeting detailed some of the benefits of SVR, not all of which are broadly appreciated. An analysis of the Hepatitis Testers Cohort in British Columbia (abstract 145), which includes over 7,000 patients who were followed for a median of 2 years (DAA) or 9.5 years (interferon-based), showed survival advantages to SVR in both cirrhotic (adjusted hazard ratio, 0.14) and noncirrhotic patients (aHR, 0.13). Other benefits include lower risk of diabetes (aHR, 0.53), chronic kidney disease/endstage renal disease (aHR, 0.48), stroke (aHR, 0.67), and mood and anxiety disorders (aHR, 0.53) (abstract 148).
As is generally accepted, SVR reduces the risk of hepatocellular cancer (HCC), according to analyses of VA and Gilead data (abstract 635), with a benefit in both cirrhotic and noncirrhotic patients. The risk almost disappears in patients without cirrhosis (incidence rate 0.07 per 100 person-years and is curbed in cirrhotic patients (incidence rate 1.30 in compensated, 4.05 in decompensated cirrhosis).
“There is really very significantly high incidence in cancer in decompensated cirrhosis, which just highlights that these patients continue to need ongoing surveillance. Although there have been efforts at developing strategies to risk stratify patients with cirrhosis, at least for now we’re stuck with surveillance, but I think for patients without cirrhosis there are now enough data showing a low enough incidence of primary HCC that we can probably avoid surveillance in that group,” said Dr. Feld.
Injectable drug users represent a special challenge in hepatitis C treatment, but new studies show cause for optimism in this population. These patients are harder to reach, and they may be less medication compliant, but one study (abstract 1632) found that imperfect adherence doesn’t necessarily undermine results – in a 12-week regimen, patients who didn’t finish until 14 weeks had no significant difference in SVR rates.
“So these therapies have a bit of forgiveness. We probably shouldn’t tell that to the patients, but it’s reassuring that we can use these therapies even in tough-to-reach populations,” said Dr. Feld.
In the GI Patient Center, AGA offers resources to help ensure patients are receiving the best possible care and living their best life.
SAN FRANCISCO – Hepatitis C therapy has matured and now offers excellent sustained viral response (SVR) in the vast majority of cases, but key challenges remain in getting the therapy to those who need it.
“Unfortunately, we’re not making some of the progress we might have hoped to see, particularly in North America,” said Jordan Feld, MD, MPH, who gave a debrief of hepatitis C abstracts during a wrap-up session at the annual meeting of the American Association for the Study of Liver Diseases.
The problem is particularly acute in young adults aged 18-39 years – only about 9% of those who tested positive for HCV RNA saw a specialist, and about 23% of those who saw a specialist went on to receive treatment, according to an analysis of over 17 million patients in the United States (abstract 1567). The numbers were better for older adults but still far from optimal, with 23% who tested positive seeing a specialist, and just 32% of those patients getting treatment.
Another study (abstract 0147) looked state by state at the percentage of Medicaid patients who received a prescription for direct-acting antiviral (DAA) medication and then went on to fill the prescription. The rates ranged from 0% in Alaska to 96% in Connecticut. Eight states were higher than 70%, six were between 50% and 70%, and 15 states were below 50%.
“Despite our efforts, there continue to be major access barriers across the U.S., particularly for Medicaid individuals,” said Dr. Feld, who is a clinician-scientist at the Toronto Western Hospital Liver Clinic and the McLaughlin-Rotman Centre for Global Health.
A study examining the Chronic Hepatitis (CHeCS) cohort (abstract 0585) described a big spike in treatment uptake shortly after approvals of the new HCV regimens, but by 2016, only about one-third of individuals who required treatment actually began treatment. Factors associated with nontreatment largely reflected marginalization, including low income, being on Medicaid, and lack of long-term follow-up.
Even as health systems struggle to get treatment to those who need it, new studies are showing how to expand existing treatments into new populations.
Results from the EXPEDITION 8 study (abstract LB-7) showed efficacy of an 8-week regimen of the glecaprevir/pibrentasvir combination in patients with compensated cirrhosis. It looked at genotypes 1, 2, and 4-6. In an intention-to-treat analysis, 98% attained SVR and there were no viral failures or safety concerns. A follow-up trial is ongoing that includes patients with genotype 3. “This is exciting to be able to shorten therapy in patients with cirrhosis,” said Dr. Feld.
Although first-line DAAs are extremely effective, there are a few patients who do not achieve a cure. One study (abstract 0227) examined the combination of sofosbuvir, velpatasvir, and voxilaprevir in retreatment of these patients. The drugs resulted in SVR rates similar to those in registration trials, but the regimen was somewhat less effective in patients previously treated with sofosbuvir and velpatasvir. “I think we need to investigate that further,” said Dr. Feld.
The combination of glecaprevir and pibrentasvir also proved effective for retreatment in patients with genotype 1/1A who had failed treatment with an NS5A inhibitor plus sofosbuvir with or without ribavirin (abstract 226). SVR rates at 16 weeks were quite good, but lower in genotype 1a patients at 12 weeks (87% week 12 versus 94% week 16).”I think this is a really good regimen for genotype 1b. For 1a, serum definitely needs 16 weeks [to clear],” said Dr. Feld.
Other abstracts presented at the meeting detailed some of the benefits of SVR, not all of which are broadly appreciated. An analysis of the Hepatitis Testers Cohort in British Columbia (abstract 145), which includes over 7,000 patients who were followed for a median of 2 years (DAA) or 9.5 years (interferon-based), showed survival advantages to SVR in both cirrhotic (adjusted hazard ratio, 0.14) and noncirrhotic patients (aHR, 0.13). Other benefits include lower risk of diabetes (aHR, 0.53), chronic kidney disease/endstage renal disease (aHR, 0.48), stroke (aHR, 0.67), and mood and anxiety disorders (aHR, 0.53) (abstract 148).
As is generally accepted, SVR reduces the risk of hepatocellular cancer (HCC), according to analyses of VA and Gilead data (abstract 635), with a benefit in both cirrhotic and noncirrhotic patients. The risk almost disappears in patients without cirrhosis (incidence rate 0.07 per 100 person-years and is curbed in cirrhotic patients (incidence rate 1.30 in compensated, 4.05 in decompensated cirrhosis).
“There is really very significantly high incidence in cancer in decompensated cirrhosis, which just highlights that these patients continue to need ongoing surveillance. Although there have been efforts at developing strategies to risk stratify patients with cirrhosis, at least for now we’re stuck with surveillance, but I think for patients without cirrhosis there are now enough data showing a low enough incidence of primary HCC that we can probably avoid surveillance in that group,” said Dr. Feld.
Injectable drug users represent a special challenge in hepatitis C treatment, but new studies show cause for optimism in this population. These patients are harder to reach, and they may be less medication compliant, but one study (abstract 1632) found that imperfect adherence doesn’t necessarily undermine results – in a 12-week regimen, patients who didn’t finish until 14 weeks had no significant difference in SVR rates.
“So these therapies have a bit of forgiveness. We probably shouldn’t tell that to the patients, but it’s reassuring that we can use these therapies even in tough-to-reach populations,” said Dr. Feld.
In the GI Patient Center, AGA offers resources to help ensure patients are receiving the best possible care and living their best life.
SAN FRANCISCO – Hepatitis C therapy has matured and now offers excellent sustained viral response (SVR) in the vast majority of cases, but key challenges remain in getting the therapy to those who need it.
“Unfortunately, we’re not making some of the progress we might have hoped to see, particularly in North America,” said Jordan Feld, MD, MPH, who gave a debrief of hepatitis C abstracts during a wrap-up session at the annual meeting of the American Association for the Study of Liver Diseases.
The problem is particularly acute in young adults aged 18-39 years – only about 9% of those who tested positive for HCV RNA saw a specialist, and about 23% of those who saw a specialist went on to receive treatment, according to an analysis of over 17 million patients in the United States (abstract 1567). The numbers were better for older adults but still far from optimal, with 23% who tested positive seeing a specialist, and just 32% of those patients getting treatment.
Another study (abstract 0147) looked state by state at the percentage of Medicaid patients who received a prescription for direct-acting antiviral (DAA) medication and then went on to fill the prescription. The rates ranged from 0% in Alaska to 96% in Connecticut. Eight states were higher than 70%, six were between 50% and 70%, and 15 states were below 50%.
“Despite our efforts, there continue to be major access barriers across the U.S., particularly for Medicaid individuals,” said Dr. Feld, who is a clinician-scientist at the Toronto Western Hospital Liver Clinic and the McLaughlin-Rotman Centre for Global Health.
A study examining the Chronic Hepatitis (CHeCS) cohort (abstract 0585) described a big spike in treatment uptake shortly after approvals of the new HCV regimens, but by 2016, only about one-third of individuals who required treatment actually began treatment. Factors associated with nontreatment largely reflected marginalization, including low income, being on Medicaid, and lack of long-term follow-up.
Even as health systems struggle to get treatment to those who need it, new studies are showing how to expand existing treatments into new populations.
Results from the EXPEDITION 8 study (abstract LB-7) showed efficacy of an 8-week regimen of the glecaprevir/pibrentasvir combination in patients with compensated cirrhosis. It looked at genotypes 1, 2, and 4-6. In an intention-to-treat analysis, 98% attained SVR and there were no viral failures or safety concerns. A follow-up trial is ongoing that includes patients with genotype 3. “This is exciting to be able to shorten therapy in patients with cirrhosis,” said Dr. Feld.
Although first-line DAAs are extremely effective, there are a few patients who do not achieve a cure. One study (abstract 0227) examined the combination of sofosbuvir, velpatasvir, and voxilaprevir in retreatment of these patients. The drugs resulted in SVR rates similar to those in registration trials, but the regimen was somewhat less effective in patients previously treated with sofosbuvir and velpatasvir. “I think we need to investigate that further,” said Dr. Feld.
The combination of glecaprevir and pibrentasvir also proved effective for retreatment in patients with genotype 1/1A who had failed treatment with an NS5A inhibitor plus sofosbuvir with or without ribavirin (abstract 226). SVR rates at 16 weeks were quite good, but lower in genotype 1a patients at 12 weeks (87% week 12 versus 94% week 16).”I think this is a really good regimen for genotype 1b. For 1a, serum definitely needs 16 weeks [to clear],” said Dr. Feld.
Other abstracts presented at the meeting detailed some of the benefits of SVR, not all of which are broadly appreciated. An analysis of the Hepatitis Testers Cohort in British Columbia (abstract 145), which includes over 7,000 patients who were followed for a median of 2 years (DAA) or 9.5 years (interferon-based), showed survival advantages to SVR in both cirrhotic (adjusted hazard ratio, 0.14) and noncirrhotic patients (aHR, 0.13). Other benefits include lower risk of diabetes (aHR, 0.53), chronic kidney disease/endstage renal disease (aHR, 0.48), stroke (aHR, 0.67), and mood and anxiety disorders (aHR, 0.53) (abstract 148).
As is generally accepted, SVR reduces the risk of hepatocellular cancer (HCC), according to analyses of VA and Gilead data (abstract 635), with a benefit in both cirrhotic and noncirrhotic patients. The risk almost disappears in patients without cirrhosis (incidence rate 0.07 per 100 person-years and is curbed in cirrhotic patients (incidence rate 1.30 in compensated, 4.05 in decompensated cirrhosis).
“There is really very significantly high incidence in cancer in decompensated cirrhosis, which just highlights that these patients continue to need ongoing surveillance. Although there have been efforts at developing strategies to risk stratify patients with cirrhosis, at least for now we’re stuck with surveillance, but I think for patients without cirrhosis there are now enough data showing a low enough incidence of primary HCC that we can probably avoid surveillance in that group,” said Dr. Feld.
Injectable drug users represent a special challenge in hepatitis C treatment, but new studies show cause for optimism in this population. These patients are harder to reach, and they may be less medication compliant, but one study (abstract 1632) found that imperfect adherence doesn’t necessarily undermine results – in a 12-week regimen, patients who didn’t finish until 14 weeks had no significant difference in SVR rates.
“So these therapies have a bit of forgiveness. We probably shouldn’t tell that to the patients, but it’s reassuring that we can use these therapies even in tough-to-reach populations,” said Dr. Feld.
In the GI Patient Center, AGA offers resources to help ensure patients are receiving the best possible care and living their best life.
REPORTING FROM THE LIVER MEETING 2018