User login
Treatment of Community‐Acquired Pneumonia
In the United States, community‐acquired pneumonia (CAP) leads to nearly 1 million hospitalizations annually, with aggregate costs of hospitalization approaching $9 billion.1, 2 In an effort to improve the appropriate, cost‐effective care for patients with CAP, several professional societies have developed clinical practice guidelines and pathways for pneumonia.37 Although the guidelines address all aspects of care, they devote substantial attention to antibiotic recommendations. Most U.S. guidelines recommend treatment of hospitalized patients with an intravenous beta‐lactam combined with a macrolide, or a fluoroquinolone with activity against Streptococcus pneumoniae. Of the major U.S. CAP practice guidelines, only one6 recommends doxycycline as an alternative to a macrolide for inpatients.
Doxycycline is an attractive alternative to macrolides. Similar to macrolides, doxycycline is active against a wide variety of organisms including atypical bacteria (Chlamydia pneumoniae, Legionella pneumophilus, and Mycoplasma pneumoniae) and is well tolerated.810 In addition, it is inexpensive (cost of $1.00/day [awp] for 100 mg p.o. bid), and rates of tetracycline/doxycycline resistance among S. pneumoniae isolates have remained low, in contrast to the increasing rates of resistance to macrolides and fluoroquinolones.11, 12 The most recent guidelines from the Infectious Diseases Society of America cited limited published clinical data on the effectiveness of doxycycline in CAP as a barrier to increased use.7 Only one study of hospitalized patients has been published in the era of penicillin‐resistant pneumococcus, and this study included only 43 low‐risk patients treated with doxycycline.13 At the university hospital affiliated with the University of California, San Francisco, ceftriaxone plus doxycycline is generally recommended as initial empiric antibiotic therapy for patients hospitalized with CAP, but significant variability in prescribing exists, allowing for comparisons between patients treated with different initial empiric antibiotic regimens. We compared outcomes of hospitalized patients with CAP treated with ceftriaxone plus doxycycline to those of patients treated with alternative initial empiric therapy at an academic medical center.
METHODS
Study Population
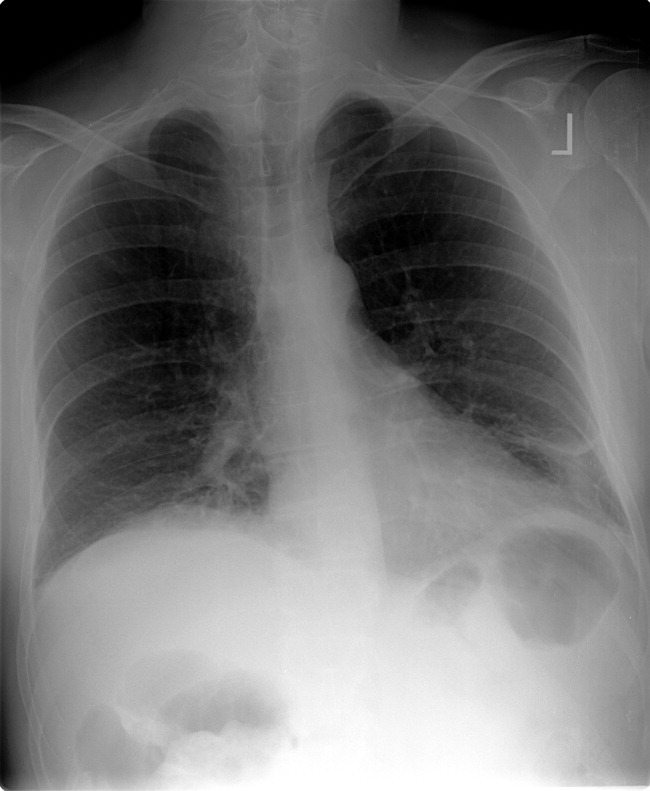
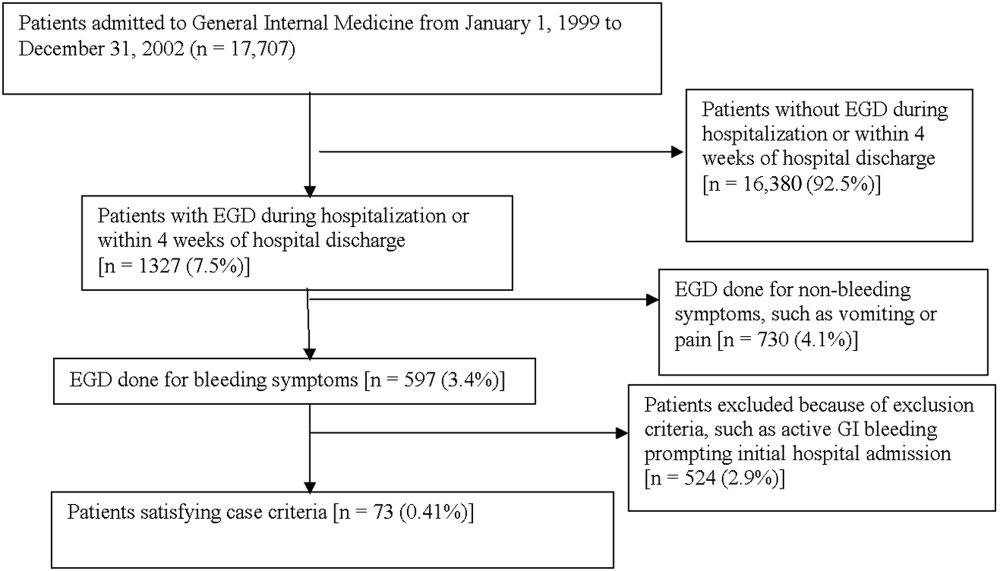
A retrospective cohort study of all adults (age 18 years) discharged from the inpatient general medicine service of Moffitt‐Long Hospital at the University of California, San Francisco, was conducted from January 1999 through July 2001. Eligibility criteria included a principal discharge diagnosis of CAP and a chest radiograph demonstrating an infiltrate within 48 hours of admission. Exclusion criteria included infection with the human immunodeficiency virus, history of organ transplantation or use of immunosuppressive therapy (including prednisone > 15 mg/day), cystic fibrosis, postobstructive pneumonia, active tuberculosis, recent hospitalization (within 10 days), or admission for comfort care. The study protocol and procedures were reviewed and approved by the UCSF Committee for Human Research.
Data Collection
Medical record review by trained research assistants blinded to the research question was used to gather demographic data, comorbid illnesses, physical examination findings on initial presentation, and laboratory or radiographic results on initial presentation. The pneumonia severity index (PSI) score was calculated for each patient using the above data.14 In addition, data were collected on antibiotic allergies, antibiotics used within the 30 days prior to admission, results of sputum or blood cultures, and admission location (intensive care unit [ICU] versus medical floor).
Data from TSI (Transition Systems Inc., Boston, MA), the hospital administrative database, were used to identify the initial empiric antibiotic regimen. All antibiotics prescribed within the first 48 hours of hospitalization were considered initial empiric therapy with few exceptions. Initial empiric therapy was classified as 1) ceftriaxone plus doxycycline (including patients treated with these agents alone in the first 48 hours, as well as patients treated with both agents in the first 24 hours who were switched to alternative therapy [broader coverage] on the second day), or 2) other appropriate therapy (treatment consistent with current national guideline recommendations including at least a beta‐lactam plus a macrolide or a beta‐lactam plus a fluoroquinolone, or fluoroquinolone monotherapy). Patients receiving therapy inconsistent with current national guideline recommendations were excluded.
Outcomes
TSI data were used to identify length of stay, death during the index hospitalization, and return to the emergency department or readmission within 30 days of discharge. The National Death Index was used to identify all deaths that occurred after hospital discharge. The 30‐day mortality data included deaths occurring during the index hospitalization and in the 30 days after the index hospitalization discharge.
Statistical Analysis
For the purposes of this analysis we compared patients treated with ceftriaxone plus doxycycline to patients treated with other appropriate therapy. To examine demographic and clinical differences between the two groups, statistical tests of comparison were performed using chi‐square tests for the dichotomous variables and t tests for the numeric variables, all of which were normally distributed (after log transformation in the case of length of stay).
To adjust for clinical variables that might contribute to differences in outcomes between the two groups, we used backward stepwise logistic regression analysis to construct a propensity score15 for the likelihood of ceftriaxone plus doxycycline use. The propensity score reflected the conditional probability of exposure to ceftriaxone plus doxycycline and allowed for stratification and, subsequently, comparisons by quintiles of propensity score. Propensity scores often have distinct advantages over direct adjustment for a large number of confounding variables and allow direct comparisons between groups with a similar propensity for receiving ceftriaxone plus doxycycline.15 Unlike random assignment of treatment, however, the propensity score cannot balance unmeasured variables that may affect treatment assignment. Thus, the possibility of bias remains. The variables used to build the score included age, presence of comorbid illness, admission from a nursing home or long‐term care facility, antibiotic allergy, prior antibiotic use, PSI score, PSI risk class, diagnosis of aspiration, admission to the ICU, and positive blood cultures. The propensity score was then stratified and used as an adjustment variable in comparisons between groups for in‐hospital mortality, 30‐day mortality, and 30‐day readmission rates. As expected, length of stay was highly skewed and was therefore log‐transformed and compared between groups with adjustment for the propensity score.
To further address issues related to potential selection bias, a separate analysis was performed on a subset of the original cohort that excluded patients for whom ceftriaxone plus doxycycline would not generally be recommended as first‐line therapy. For this analysis, patients admitted from a nursing home or long‐term care facility, patients admitted to the ICU, and patients with a principal diagnosis of aspiration pneumonia were excluded. A propensity score was rederived for this subset, which was used to adjust for differences in outcomes. All statistical procedures were performed using STATA (Ver. 7.0, Stata Corporation, College Station TX).
RESULTS
Patient Characteristics
A total of 341 patients were eligible for analysis. Of this group, 216 were treated with ceftriaxone plus doxycycline and 125 received other appropriate therapy. Both groups of patients were similar in age. Patients treated with ceftriaxone plus doxycycline had a lower median PSI score and fewer comorbid illnesses than did patients treated with other appropriate therapy (Table 1). Blood cultures were positive in 30 (8.8%) of the 341 patients included in the analysis, with S. pneumoniae the most commonly isolated organism (n = 17, 5.0%). Of S. pneumoniae isolates, 4 (24%) were resistant to penicillin (MIC 1 g/mL), and 2 (12%) were resistant to tetracycline (MIC 8 g/mL).
| Ceftriaxone/doxycycline | Other appropriate therapy | |
|---|---|---|
| ||
| Patients (n) | 216 | 125 |
| Age (median) | 76 | 74 |
| PSI Score (median)a | 97 | 108 |
| PSI Risk Class (%)a | ||
| Class I | 9.3 | 5.6 |
| Class II | 11.1 | 8.8 |
| Class III | 21.8 | 13.6 |
| Class IV | 40.7 | 40.0 |
| Class V | 17.1 | 32.0 |
| Comorbid Illness (%)a | 36.1 | 47.2 |
| Nursing Home/LCF (%)a | 5.1 | 14.4 |
| Aspiration (%)a | 3.2 | 20.0 |
| Admission to ICU (%)a | 6.0 | 28.0 |
Common antibiotic choices in patients receiving other appropriate therapy included a beta‐lactam/beta‐lactamase inhibitor plus doxycycline or a macrolide (n = 36, 29%), fluoroquinolone monotherapy (n = 16, 13%), and a variety of other antibiotic combinations with activity against S. pneumoniae and atypical bacteria (n = 52, 42%).
Clinical Outcomes
Analyses of unadjusted outcomes showed that patients treated with ceftriaxone plus doxycycline had significantly lower inpatient (2% vs. 14%, P < .001) and 30‐day (6% vs. 20%, P < .001) mortality compared to patients treated with other regimens (Table 2). Multivariable logistic regression analysis identified three variables (diagnosis of congestive heart failure, admission to the ICU, and the presence of comorbid illness) associated with initial antibiotic selection, which were used to build a propensity score. After adjustment for the propensity score, use of ceftriaxone plus doxycycline remained significantly associated with lower inpatient mortality (OR = 0.26, 95% CI: 0.080.81) and 30‐day mortality (OR = 0.37, 95% CI: 0.170.81). Differences in length of stay and 30‐day readmission rates between the treatment groups were not significant (Table 2).
| Ceftriaxone + doxycycline (n = 216) | Other appropriate therapy (n = 125) | Adjusted odds ratio (95% confidence interval) | |
|---|---|---|---|
| |||
| Inpatient Mortality | 2.3% | 14.4% | 0.26 (0.080.81) |
| 30‐day mortality | 6.0% | 20.0% | 0.37 (0.170.81) |
| Length of stay (median days) | 3.0 | 4.0 | 0.09 (0.250.06)a |
| 30‐day readmission | 10.7% | 12.0% | 0.87 (0.421.81) |
Subset Analysis
To address issues related to selection bias, we performed an analysis of a subset of the patients after excluding those admitted from a nursing home, diagnosed with aspiration, or admitted to the ICU, for whom ceftriaxone plus doxycycline would not be considered recommended (or first‐line) therapy. The two resulting groups were similar, except there were fewer patients with comorbid illness in the ceftriaxone plus doxycycline group (34% vs. 50%, P = .015). The propensity score was rederived for this subset and used for adjustment. Unadjusted and adjusted outcomes are shown in Table 3. Use of ceftriaxone plus doxycycline in this subset also was associated with reduced odds of inpatient mortality (OR = 0.17, 95% CI: 0.040.77). The odds of 30‐day mortality also were reduced but not significantly, as the confidence interval included 1.0 (OR = 0.43, 95% CI: 0.141.31). There were no differences between groups in length of stay or in 30‐day readmission rate.
| Ceftriaxone + doxycycline (n = 188) | Other appropriate therapy (n = 70) | Adjusted odds ratio (95% CI) | |
|---|---|---|---|
| |||
| Age (median years) | 75 | 71 | |
| PSI score (mean) | 95 | 98 | |
| Comorbid illness (%)a | 33.5 | 50.0 | |
| Inpatient mortality | 1.6% | 7.1% | 0.17 (0.040.77) |
| 30‐day mortality | 4.8% | 8.6% | 0.43 (0.141.31) |
| LOS (median days) | 3 | 3 | 0.06 (0.240.12)b |
| 30‐day readmission | 11.9% | 10.0% | 1.31 (0.523.28) |
DISCUSSION
In our hospital setting, the use of ceftriaxone plus doxycycline as the initial empiric antibiotic therapy for patients hospitalized with community‐acquired pneumonia was associated with significantly lower inpatient and 30‐day mortality, even after adjusting for clinical differences between groups. We did not find a difference between regimens in hospital length of stay or 30‐day readmission rate. In case the multivariable model was insufficient to account for the clinical differences (i.e., selection bias) between groups, we also performed an analysis of a subgroup of less severely ill patients by excluding those admitted from nursing homes, those admitted to the intensive care unit, and those with aspiration pneumonia. In this subset, use of ceftriaxone plus doxycycline remained associated with lower inpatient mortality but not with lower 30‐day mortality. Although, as an observational study, the results of our findings could still be a result of residual confounding, we believe the results provide valuable information regarding doxycycline.
Combination therapy with a macrolide, but not doxycycline, is advocated by the practice guidelines of several major U.S. professional societies,3, 4, 7 apparently because of a lack of data on the effectiveness of combination therapy with doxycycline.7 Only one randomized, unblinded study, in 87 low‐risk patients hospitalized with CAP, that compared monotherapy with IV doxycycline versus physician‐determined therapy has been conducted.13 This study found no differences between treatment groups in clinical outcomes but did find that use of doxycycline was associated with shorter hospital stays and reduced costs. Our results, achieved in a real‐world setting in relatively ill hospitalized patients (58% were in PSI risk class IV or V), provide further support for the use of combination therapy with doxycycline.
Hospitalized patients treated with a beta‐lactam in combination with a macrolide are often discharged on macrolide monotherapy. In our population most patients treated with ceftriaxone plus doxycycline were discharged on doxycycline if they required continued therapy (data not shown). In the current era of resistance of Streptococcus pneumoniae to antibiotics, there is good reason to believe doxycycline may perform as well, if not better, than macrolides when hospitalized patients with CAP are discharged on oral monotherapy. Macrolide resistance rates among invasive pneumococcal isolates in the United States doubled from 10% to 20% during a period in which prescriptions for macrolides increased by 13%.12 In addition, a large surveillance study of more than 1500 isolates collected in 1999 and 2000 found that 26% of the isolates were resistant to macrolides, whereas only 16% were resistant to tetracycline.16 In vitro testing against S. Pneumoniae has also suggested that tetracycline resistance overestimates doxycycline resistance.17, 18 More recently, Streptococcus pneumoniae susceptibility data from the SENTRY Antimicrobial Surveillance program reaffirmed doxycycline's in vitro superiority over macrolides.17
Our study had several limitations. The study design adopted precluded determining whether favorable results with the use of ceftriaxone plus doxycycline resulted from an effect unique to this combination of antibiotics, the possible anti‐inflammatory properties of doxycycline alone,19, 20 or unmeasured confounders. For example, processes of care that affect clinical outcomes for patients hospitalized with CAP, such as the timing of antibiotic delivery, the timing of blood cultures, and stability assessment on discharge were not measured in this study. To affect outcomes, these processes of care would need to be differentially distributed between our comparison groups. However, because this study was performed in a single institution during a single interval, it is likely that the performance of these processes of care would be similar for all patients.
In conclusion, ceftriaxone plus doxycycline appears to be an effective, and possibly superior, therapy for patients hospitalized with CAP. Randomized controlled trials of doxycycline‐containing regimens versus other regimens are warranted.
- ,,, et al.Hospitalized pneumonia. Outcomes, treatment patterns, and costs in urban and rural areas.J Gen Intern Med.1996;11:415–421.
- ,,, et al.The cost of treating community‐acquired pneumonia.Clin Ther.1998;20:820–837.
- ,,, et al.Practice guidelines for the management of community‐acquired pneumonia in adults. Infectious Diseases Society of America.Clin Infect Dis.2000;31:347–382.
- ,,, et al.Management of community‐acquired pneumonia in the era of pneumococcal resistance: a report from the Drug‐Resistant Streptococcus pneumoniae Therapeutic Working Group.Arch Intern Med.2000;160:1399–1408.
- ,,, et al.Canadian guidelines for the initial management of community‐acquired pneumonia: an evidence‐based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Canadian Community‐Acquired Pneumonia Working Group.Clin Infect Dis.2000;31:383–421.
- ,,, et al.Guidelines for the management of adults with community‐acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention.Am J Respir Crit Care Med.2001;163:1730–1754.
- ,,, et al.Update of practice guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433
- ,,.Doxycycline.Ther Drug Monit1982;4:115–135
- ,.Chloramphenicol and tetracyclines.Med Clin North Am.1987;71:1155–1168
- ,.Tetracyclines.Med Clin North Am.1995;79:789–801
- ,,, et al.Antibiotic resistance among gram‐negative bacilli in US intensive care units: implications for fluoroquinolone use.JAMA.2003;289:885–888
- ,,, et al.Macrolide resistance among invasive Streptococcus pneumoniae isolates.JAMA.2001;286:1857–1862.
- ,,, et al.Doxycycline is a cost‐effective therapy for hospitalized patients with community‐acquired pneumonia.Arch Intern Med.1999;159:266–270.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- .Reducing bias in observational studies using subclassification on the propensity score.J Am Stat Assoc.1984;79:516–524
- ,,, et al.Antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States during 1999—2000, including a comparison of resistance rates since 1994—1995.Antimicrob Agents Chemother.2001;45:1721–1729
- ,,.Doxycycline use for community‐acquired pneumonia: contemporary in vitro spectrum of activity against Streptococcus pneumoniae (1999–2002).Diagn Microbiol Infect Dis.2004;49:147–149
- ,,, et al.Doxycycline activity against Streptococcus pneumoniae.Chest.1995;108:1775–1776.
- ,,, et al.Inhibition of enzymatic activity of phospholipases A2 by minocycline and doxycycline.Biochem Pharmacol.1992;44:1165–1170.
- ,,, et al.Doxycycline reduces mortality to lethal endotoxemia by reducing nitric oxide synthesis via an interleukin‐10‐independent mechanism.J Infect Dis.1998;177:489–492.
In the United States, community‐acquired pneumonia (CAP) leads to nearly 1 million hospitalizations annually, with aggregate costs of hospitalization approaching $9 billion.1, 2 In an effort to improve the appropriate, cost‐effective care for patients with CAP, several professional societies have developed clinical practice guidelines and pathways for pneumonia.37 Although the guidelines address all aspects of care, they devote substantial attention to antibiotic recommendations. Most U.S. guidelines recommend treatment of hospitalized patients with an intravenous beta‐lactam combined with a macrolide, or a fluoroquinolone with activity against Streptococcus pneumoniae. Of the major U.S. CAP practice guidelines, only one6 recommends doxycycline as an alternative to a macrolide for inpatients.
Doxycycline is an attractive alternative to macrolides. Similar to macrolides, doxycycline is active against a wide variety of organisms including atypical bacteria (Chlamydia pneumoniae, Legionella pneumophilus, and Mycoplasma pneumoniae) and is well tolerated.810 In addition, it is inexpensive (cost of $1.00/day [awp] for 100 mg p.o. bid), and rates of tetracycline/doxycycline resistance among S. pneumoniae isolates have remained low, in contrast to the increasing rates of resistance to macrolides and fluoroquinolones.11, 12 The most recent guidelines from the Infectious Diseases Society of America cited limited published clinical data on the effectiveness of doxycycline in CAP as a barrier to increased use.7 Only one study of hospitalized patients has been published in the era of penicillin‐resistant pneumococcus, and this study included only 43 low‐risk patients treated with doxycycline.13 At the university hospital affiliated with the University of California, San Francisco, ceftriaxone plus doxycycline is generally recommended as initial empiric antibiotic therapy for patients hospitalized with CAP, but significant variability in prescribing exists, allowing for comparisons between patients treated with different initial empiric antibiotic regimens. We compared outcomes of hospitalized patients with CAP treated with ceftriaxone plus doxycycline to those of patients treated with alternative initial empiric therapy at an academic medical center.
METHODS
Study Population
A retrospective cohort study of all adults (age 18 years) discharged from the inpatient general medicine service of Moffitt‐Long Hospital at the University of California, San Francisco, was conducted from January 1999 through July 2001. Eligibility criteria included a principal discharge diagnosis of CAP and a chest radiograph demonstrating an infiltrate within 48 hours of admission. Exclusion criteria included infection with the human immunodeficiency virus, history of organ transplantation or use of immunosuppressive therapy (including prednisone > 15 mg/day), cystic fibrosis, postobstructive pneumonia, active tuberculosis, recent hospitalization (within 10 days), or admission for comfort care. The study protocol and procedures were reviewed and approved by the UCSF Committee for Human Research.
Data Collection
Medical record review by trained research assistants blinded to the research question was used to gather demographic data, comorbid illnesses, physical examination findings on initial presentation, and laboratory or radiographic results on initial presentation. The pneumonia severity index (PSI) score was calculated for each patient using the above data.14 In addition, data were collected on antibiotic allergies, antibiotics used within the 30 days prior to admission, results of sputum or blood cultures, and admission location (intensive care unit [ICU] versus medical floor).
Data from TSI (Transition Systems Inc., Boston, MA), the hospital administrative database, were used to identify the initial empiric antibiotic regimen. All antibiotics prescribed within the first 48 hours of hospitalization were considered initial empiric therapy with few exceptions. Initial empiric therapy was classified as 1) ceftriaxone plus doxycycline (including patients treated with these agents alone in the first 48 hours, as well as patients treated with both agents in the first 24 hours who were switched to alternative therapy [broader coverage] on the second day), or 2) other appropriate therapy (treatment consistent with current national guideline recommendations including at least a beta‐lactam plus a macrolide or a beta‐lactam plus a fluoroquinolone, or fluoroquinolone monotherapy). Patients receiving therapy inconsistent with current national guideline recommendations were excluded.
Outcomes
TSI data were used to identify length of stay, death during the index hospitalization, and return to the emergency department or readmission within 30 days of discharge. The National Death Index was used to identify all deaths that occurred after hospital discharge. The 30‐day mortality data included deaths occurring during the index hospitalization and in the 30 days after the index hospitalization discharge.
Statistical Analysis
For the purposes of this analysis we compared patients treated with ceftriaxone plus doxycycline to patients treated with other appropriate therapy. To examine demographic and clinical differences between the two groups, statistical tests of comparison were performed using chi‐square tests for the dichotomous variables and t tests for the numeric variables, all of which were normally distributed (after log transformation in the case of length of stay).
To adjust for clinical variables that might contribute to differences in outcomes between the two groups, we used backward stepwise logistic regression analysis to construct a propensity score15 for the likelihood of ceftriaxone plus doxycycline use. The propensity score reflected the conditional probability of exposure to ceftriaxone plus doxycycline and allowed for stratification and, subsequently, comparisons by quintiles of propensity score. Propensity scores often have distinct advantages over direct adjustment for a large number of confounding variables and allow direct comparisons between groups with a similar propensity for receiving ceftriaxone plus doxycycline.15 Unlike random assignment of treatment, however, the propensity score cannot balance unmeasured variables that may affect treatment assignment. Thus, the possibility of bias remains. The variables used to build the score included age, presence of comorbid illness, admission from a nursing home or long‐term care facility, antibiotic allergy, prior antibiotic use, PSI score, PSI risk class, diagnosis of aspiration, admission to the ICU, and positive blood cultures. The propensity score was then stratified and used as an adjustment variable in comparisons between groups for in‐hospital mortality, 30‐day mortality, and 30‐day readmission rates. As expected, length of stay was highly skewed and was therefore log‐transformed and compared between groups with adjustment for the propensity score.
To further address issues related to potential selection bias, a separate analysis was performed on a subset of the original cohort that excluded patients for whom ceftriaxone plus doxycycline would not generally be recommended as first‐line therapy. For this analysis, patients admitted from a nursing home or long‐term care facility, patients admitted to the ICU, and patients with a principal diagnosis of aspiration pneumonia were excluded. A propensity score was rederived for this subset, which was used to adjust for differences in outcomes. All statistical procedures were performed using STATA (Ver. 7.0, Stata Corporation, College Station TX).
RESULTS
Patient Characteristics
A total of 341 patients were eligible for analysis. Of this group, 216 were treated with ceftriaxone plus doxycycline and 125 received other appropriate therapy. Both groups of patients were similar in age. Patients treated with ceftriaxone plus doxycycline had a lower median PSI score and fewer comorbid illnesses than did patients treated with other appropriate therapy (Table 1). Blood cultures were positive in 30 (8.8%) of the 341 patients included in the analysis, with S. pneumoniae the most commonly isolated organism (n = 17, 5.0%). Of S. pneumoniae isolates, 4 (24%) were resistant to penicillin (MIC 1 g/mL), and 2 (12%) were resistant to tetracycline (MIC 8 g/mL).
| Ceftriaxone/doxycycline | Other appropriate therapy | |
|---|---|---|
| ||
| Patients (n) | 216 | 125 |
| Age (median) | 76 | 74 |
| PSI Score (median)a | 97 | 108 |
| PSI Risk Class (%)a | ||
| Class I | 9.3 | 5.6 |
| Class II | 11.1 | 8.8 |
| Class III | 21.8 | 13.6 |
| Class IV | 40.7 | 40.0 |
| Class V | 17.1 | 32.0 |
| Comorbid Illness (%)a | 36.1 | 47.2 |
| Nursing Home/LCF (%)a | 5.1 | 14.4 |
| Aspiration (%)a | 3.2 | 20.0 |
| Admission to ICU (%)a | 6.0 | 28.0 |
Common antibiotic choices in patients receiving other appropriate therapy included a beta‐lactam/beta‐lactamase inhibitor plus doxycycline or a macrolide (n = 36, 29%), fluoroquinolone monotherapy (n = 16, 13%), and a variety of other antibiotic combinations with activity against S. pneumoniae and atypical bacteria (n = 52, 42%).
Clinical Outcomes
Analyses of unadjusted outcomes showed that patients treated with ceftriaxone plus doxycycline had significantly lower inpatient (2% vs. 14%, P < .001) and 30‐day (6% vs. 20%, P < .001) mortality compared to patients treated with other regimens (Table 2). Multivariable logistic regression analysis identified three variables (diagnosis of congestive heart failure, admission to the ICU, and the presence of comorbid illness) associated with initial antibiotic selection, which were used to build a propensity score. After adjustment for the propensity score, use of ceftriaxone plus doxycycline remained significantly associated with lower inpatient mortality (OR = 0.26, 95% CI: 0.080.81) and 30‐day mortality (OR = 0.37, 95% CI: 0.170.81). Differences in length of stay and 30‐day readmission rates between the treatment groups were not significant (Table 2).
| Ceftriaxone + doxycycline (n = 216) | Other appropriate therapy (n = 125) | Adjusted odds ratio (95% confidence interval) | |
|---|---|---|---|
| |||
| Inpatient Mortality | 2.3% | 14.4% | 0.26 (0.080.81) |
| 30‐day mortality | 6.0% | 20.0% | 0.37 (0.170.81) |
| Length of stay (median days) | 3.0 | 4.0 | 0.09 (0.250.06)a |
| 30‐day readmission | 10.7% | 12.0% | 0.87 (0.421.81) |
Subset Analysis
To address issues related to selection bias, we performed an analysis of a subset of the patients after excluding those admitted from a nursing home, diagnosed with aspiration, or admitted to the ICU, for whom ceftriaxone plus doxycycline would not be considered recommended (or first‐line) therapy. The two resulting groups were similar, except there were fewer patients with comorbid illness in the ceftriaxone plus doxycycline group (34% vs. 50%, P = .015). The propensity score was rederived for this subset and used for adjustment. Unadjusted and adjusted outcomes are shown in Table 3. Use of ceftriaxone plus doxycycline in this subset also was associated with reduced odds of inpatient mortality (OR = 0.17, 95% CI: 0.040.77). The odds of 30‐day mortality also were reduced but not significantly, as the confidence interval included 1.0 (OR = 0.43, 95% CI: 0.141.31). There were no differences between groups in length of stay or in 30‐day readmission rate.
| Ceftriaxone + doxycycline (n = 188) | Other appropriate therapy (n = 70) | Adjusted odds ratio (95% CI) | |
|---|---|---|---|
| |||
| Age (median years) | 75 | 71 | |
| PSI score (mean) | 95 | 98 | |
| Comorbid illness (%)a | 33.5 | 50.0 | |
| Inpatient mortality | 1.6% | 7.1% | 0.17 (0.040.77) |
| 30‐day mortality | 4.8% | 8.6% | 0.43 (0.141.31) |
| LOS (median days) | 3 | 3 | 0.06 (0.240.12)b |
| 30‐day readmission | 11.9% | 10.0% | 1.31 (0.523.28) |
DISCUSSION
In our hospital setting, the use of ceftriaxone plus doxycycline as the initial empiric antibiotic therapy for patients hospitalized with community‐acquired pneumonia was associated with significantly lower inpatient and 30‐day mortality, even after adjusting for clinical differences between groups. We did not find a difference between regimens in hospital length of stay or 30‐day readmission rate. In case the multivariable model was insufficient to account for the clinical differences (i.e., selection bias) between groups, we also performed an analysis of a subgroup of less severely ill patients by excluding those admitted from nursing homes, those admitted to the intensive care unit, and those with aspiration pneumonia. In this subset, use of ceftriaxone plus doxycycline remained associated with lower inpatient mortality but not with lower 30‐day mortality. Although, as an observational study, the results of our findings could still be a result of residual confounding, we believe the results provide valuable information regarding doxycycline.
Combination therapy with a macrolide, but not doxycycline, is advocated by the practice guidelines of several major U.S. professional societies,3, 4, 7 apparently because of a lack of data on the effectiveness of combination therapy with doxycycline.7 Only one randomized, unblinded study, in 87 low‐risk patients hospitalized with CAP, that compared monotherapy with IV doxycycline versus physician‐determined therapy has been conducted.13 This study found no differences between treatment groups in clinical outcomes but did find that use of doxycycline was associated with shorter hospital stays and reduced costs. Our results, achieved in a real‐world setting in relatively ill hospitalized patients (58% were in PSI risk class IV or V), provide further support for the use of combination therapy with doxycycline.
Hospitalized patients treated with a beta‐lactam in combination with a macrolide are often discharged on macrolide monotherapy. In our population most patients treated with ceftriaxone plus doxycycline were discharged on doxycycline if they required continued therapy (data not shown). In the current era of resistance of Streptococcus pneumoniae to antibiotics, there is good reason to believe doxycycline may perform as well, if not better, than macrolides when hospitalized patients with CAP are discharged on oral monotherapy. Macrolide resistance rates among invasive pneumococcal isolates in the United States doubled from 10% to 20% during a period in which prescriptions for macrolides increased by 13%.12 In addition, a large surveillance study of more than 1500 isolates collected in 1999 and 2000 found that 26% of the isolates were resistant to macrolides, whereas only 16% were resistant to tetracycline.16 In vitro testing against S. Pneumoniae has also suggested that tetracycline resistance overestimates doxycycline resistance.17, 18 More recently, Streptococcus pneumoniae susceptibility data from the SENTRY Antimicrobial Surveillance program reaffirmed doxycycline's in vitro superiority over macrolides.17
Our study had several limitations. The study design adopted precluded determining whether favorable results with the use of ceftriaxone plus doxycycline resulted from an effect unique to this combination of antibiotics, the possible anti‐inflammatory properties of doxycycline alone,19, 20 or unmeasured confounders. For example, processes of care that affect clinical outcomes for patients hospitalized with CAP, such as the timing of antibiotic delivery, the timing of blood cultures, and stability assessment on discharge were not measured in this study. To affect outcomes, these processes of care would need to be differentially distributed between our comparison groups. However, because this study was performed in a single institution during a single interval, it is likely that the performance of these processes of care would be similar for all patients.
In conclusion, ceftriaxone plus doxycycline appears to be an effective, and possibly superior, therapy for patients hospitalized with CAP. Randomized controlled trials of doxycycline‐containing regimens versus other regimens are warranted.
In the United States, community‐acquired pneumonia (CAP) leads to nearly 1 million hospitalizations annually, with aggregate costs of hospitalization approaching $9 billion.1, 2 In an effort to improve the appropriate, cost‐effective care for patients with CAP, several professional societies have developed clinical practice guidelines and pathways for pneumonia.37 Although the guidelines address all aspects of care, they devote substantial attention to antibiotic recommendations. Most U.S. guidelines recommend treatment of hospitalized patients with an intravenous beta‐lactam combined with a macrolide, or a fluoroquinolone with activity against Streptococcus pneumoniae. Of the major U.S. CAP practice guidelines, only one6 recommends doxycycline as an alternative to a macrolide for inpatients.
Doxycycline is an attractive alternative to macrolides. Similar to macrolides, doxycycline is active against a wide variety of organisms including atypical bacteria (Chlamydia pneumoniae, Legionella pneumophilus, and Mycoplasma pneumoniae) and is well tolerated.810 In addition, it is inexpensive (cost of $1.00/day [awp] for 100 mg p.o. bid), and rates of tetracycline/doxycycline resistance among S. pneumoniae isolates have remained low, in contrast to the increasing rates of resistance to macrolides and fluoroquinolones.11, 12 The most recent guidelines from the Infectious Diseases Society of America cited limited published clinical data on the effectiveness of doxycycline in CAP as a barrier to increased use.7 Only one study of hospitalized patients has been published in the era of penicillin‐resistant pneumococcus, and this study included only 43 low‐risk patients treated with doxycycline.13 At the university hospital affiliated with the University of California, San Francisco, ceftriaxone plus doxycycline is generally recommended as initial empiric antibiotic therapy for patients hospitalized with CAP, but significant variability in prescribing exists, allowing for comparisons between patients treated with different initial empiric antibiotic regimens. We compared outcomes of hospitalized patients with CAP treated with ceftriaxone plus doxycycline to those of patients treated with alternative initial empiric therapy at an academic medical center.
METHODS
Study Population
A retrospective cohort study of all adults (age 18 years) discharged from the inpatient general medicine service of Moffitt‐Long Hospital at the University of California, San Francisco, was conducted from January 1999 through July 2001. Eligibility criteria included a principal discharge diagnosis of CAP and a chest radiograph demonstrating an infiltrate within 48 hours of admission. Exclusion criteria included infection with the human immunodeficiency virus, history of organ transplantation or use of immunosuppressive therapy (including prednisone > 15 mg/day), cystic fibrosis, postobstructive pneumonia, active tuberculosis, recent hospitalization (within 10 days), or admission for comfort care. The study protocol and procedures were reviewed and approved by the UCSF Committee for Human Research.
Data Collection
Medical record review by trained research assistants blinded to the research question was used to gather demographic data, comorbid illnesses, physical examination findings on initial presentation, and laboratory or radiographic results on initial presentation. The pneumonia severity index (PSI) score was calculated for each patient using the above data.14 In addition, data were collected on antibiotic allergies, antibiotics used within the 30 days prior to admission, results of sputum or blood cultures, and admission location (intensive care unit [ICU] versus medical floor).
Data from TSI (Transition Systems Inc., Boston, MA), the hospital administrative database, were used to identify the initial empiric antibiotic regimen. All antibiotics prescribed within the first 48 hours of hospitalization were considered initial empiric therapy with few exceptions. Initial empiric therapy was classified as 1) ceftriaxone plus doxycycline (including patients treated with these agents alone in the first 48 hours, as well as patients treated with both agents in the first 24 hours who were switched to alternative therapy [broader coverage] on the second day), or 2) other appropriate therapy (treatment consistent with current national guideline recommendations including at least a beta‐lactam plus a macrolide or a beta‐lactam plus a fluoroquinolone, or fluoroquinolone monotherapy). Patients receiving therapy inconsistent with current national guideline recommendations were excluded.
Outcomes
TSI data were used to identify length of stay, death during the index hospitalization, and return to the emergency department or readmission within 30 days of discharge. The National Death Index was used to identify all deaths that occurred after hospital discharge. The 30‐day mortality data included deaths occurring during the index hospitalization and in the 30 days after the index hospitalization discharge.
Statistical Analysis
For the purposes of this analysis we compared patients treated with ceftriaxone plus doxycycline to patients treated with other appropriate therapy. To examine demographic and clinical differences between the two groups, statistical tests of comparison were performed using chi‐square tests for the dichotomous variables and t tests for the numeric variables, all of which were normally distributed (after log transformation in the case of length of stay).
To adjust for clinical variables that might contribute to differences in outcomes between the two groups, we used backward stepwise logistic regression analysis to construct a propensity score15 for the likelihood of ceftriaxone plus doxycycline use. The propensity score reflected the conditional probability of exposure to ceftriaxone plus doxycycline and allowed for stratification and, subsequently, comparisons by quintiles of propensity score. Propensity scores often have distinct advantages over direct adjustment for a large number of confounding variables and allow direct comparisons between groups with a similar propensity for receiving ceftriaxone plus doxycycline.15 Unlike random assignment of treatment, however, the propensity score cannot balance unmeasured variables that may affect treatment assignment. Thus, the possibility of bias remains. The variables used to build the score included age, presence of comorbid illness, admission from a nursing home or long‐term care facility, antibiotic allergy, prior antibiotic use, PSI score, PSI risk class, diagnosis of aspiration, admission to the ICU, and positive blood cultures. The propensity score was then stratified and used as an adjustment variable in comparisons between groups for in‐hospital mortality, 30‐day mortality, and 30‐day readmission rates. As expected, length of stay was highly skewed and was therefore log‐transformed and compared between groups with adjustment for the propensity score.
To further address issues related to potential selection bias, a separate analysis was performed on a subset of the original cohort that excluded patients for whom ceftriaxone plus doxycycline would not generally be recommended as first‐line therapy. For this analysis, patients admitted from a nursing home or long‐term care facility, patients admitted to the ICU, and patients with a principal diagnosis of aspiration pneumonia were excluded. A propensity score was rederived for this subset, which was used to adjust for differences in outcomes. All statistical procedures were performed using STATA (Ver. 7.0, Stata Corporation, College Station TX).
RESULTS
Patient Characteristics
A total of 341 patients were eligible for analysis. Of this group, 216 were treated with ceftriaxone plus doxycycline and 125 received other appropriate therapy. Both groups of patients were similar in age. Patients treated with ceftriaxone plus doxycycline had a lower median PSI score and fewer comorbid illnesses than did patients treated with other appropriate therapy (Table 1). Blood cultures were positive in 30 (8.8%) of the 341 patients included in the analysis, with S. pneumoniae the most commonly isolated organism (n = 17, 5.0%). Of S. pneumoniae isolates, 4 (24%) were resistant to penicillin (MIC 1 g/mL), and 2 (12%) were resistant to tetracycline (MIC 8 g/mL).
| Ceftriaxone/doxycycline | Other appropriate therapy | |
|---|---|---|
| ||
| Patients (n) | 216 | 125 |
| Age (median) | 76 | 74 |
| PSI Score (median)a | 97 | 108 |
| PSI Risk Class (%)a | ||
| Class I | 9.3 | 5.6 |
| Class II | 11.1 | 8.8 |
| Class III | 21.8 | 13.6 |
| Class IV | 40.7 | 40.0 |
| Class V | 17.1 | 32.0 |
| Comorbid Illness (%)a | 36.1 | 47.2 |
| Nursing Home/LCF (%)a | 5.1 | 14.4 |
| Aspiration (%)a | 3.2 | 20.0 |
| Admission to ICU (%)a | 6.0 | 28.0 |
Common antibiotic choices in patients receiving other appropriate therapy included a beta‐lactam/beta‐lactamase inhibitor plus doxycycline or a macrolide (n = 36, 29%), fluoroquinolone monotherapy (n = 16, 13%), and a variety of other antibiotic combinations with activity against S. pneumoniae and atypical bacteria (n = 52, 42%).
Clinical Outcomes
Analyses of unadjusted outcomes showed that patients treated with ceftriaxone plus doxycycline had significantly lower inpatient (2% vs. 14%, P < .001) and 30‐day (6% vs. 20%, P < .001) mortality compared to patients treated with other regimens (Table 2). Multivariable logistic regression analysis identified three variables (diagnosis of congestive heart failure, admission to the ICU, and the presence of comorbid illness) associated with initial antibiotic selection, which were used to build a propensity score. After adjustment for the propensity score, use of ceftriaxone plus doxycycline remained significantly associated with lower inpatient mortality (OR = 0.26, 95% CI: 0.080.81) and 30‐day mortality (OR = 0.37, 95% CI: 0.170.81). Differences in length of stay and 30‐day readmission rates between the treatment groups were not significant (Table 2).
| Ceftriaxone + doxycycline (n = 216) | Other appropriate therapy (n = 125) | Adjusted odds ratio (95% confidence interval) | |
|---|---|---|---|
| |||
| Inpatient Mortality | 2.3% | 14.4% | 0.26 (0.080.81) |
| 30‐day mortality | 6.0% | 20.0% | 0.37 (0.170.81) |
| Length of stay (median days) | 3.0 | 4.0 | 0.09 (0.250.06)a |
| 30‐day readmission | 10.7% | 12.0% | 0.87 (0.421.81) |
Subset Analysis
To address issues related to selection bias, we performed an analysis of a subset of the patients after excluding those admitted from a nursing home, diagnosed with aspiration, or admitted to the ICU, for whom ceftriaxone plus doxycycline would not be considered recommended (or first‐line) therapy. The two resulting groups were similar, except there were fewer patients with comorbid illness in the ceftriaxone plus doxycycline group (34% vs. 50%, P = .015). The propensity score was rederived for this subset and used for adjustment. Unadjusted and adjusted outcomes are shown in Table 3. Use of ceftriaxone plus doxycycline in this subset also was associated with reduced odds of inpatient mortality (OR = 0.17, 95% CI: 0.040.77). The odds of 30‐day mortality also were reduced but not significantly, as the confidence interval included 1.0 (OR = 0.43, 95% CI: 0.141.31). There were no differences between groups in length of stay or in 30‐day readmission rate.
| Ceftriaxone + doxycycline (n = 188) | Other appropriate therapy (n = 70) | Adjusted odds ratio (95% CI) | |
|---|---|---|---|
| |||
| Age (median years) | 75 | 71 | |
| PSI score (mean) | 95 | 98 | |
| Comorbid illness (%)a | 33.5 | 50.0 | |
| Inpatient mortality | 1.6% | 7.1% | 0.17 (0.040.77) |
| 30‐day mortality | 4.8% | 8.6% | 0.43 (0.141.31) |
| LOS (median days) | 3 | 3 | 0.06 (0.240.12)b |
| 30‐day readmission | 11.9% | 10.0% | 1.31 (0.523.28) |
DISCUSSION
In our hospital setting, the use of ceftriaxone plus doxycycline as the initial empiric antibiotic therapy for patients hospitalized with community‐acquired pneumonia was associated with significantly lower inpatient and 30‐day mortality, even after adjusting for clinical differences between groups. We did not find a difference between regimens in hospital length of stay or 30‐day readmission rate. In case the multivariable model was insufficient to account for the clinical differences (i.e., selection bias) between groups, we also performed an analysis of a subgroup of less severely ill patients by excluding those admitted from nursing homes, those admitted to the intensive care unit, and those with aspiration pneumonia. In this subset, use of ceftriaxone plus doxycycline remained associated with lower inpatient mortality but not with lower 30‐day mortality. Although, as an observational study, the results of our findings could still be a result of residual confounding, we believe the results provide valuable information regarding doxycycline.
Combination therapy with a macrolide, but not doxycycline, is advocated by the practice guidelines of several major U.S. professional societies,3, 4, 7 apparently because of a lack of data on the effectiveness of combination therapy with doxycycline.7 Only one randomized, unblinded study, in 87 low‐risk patients hospitalized with CAP, that compared monotherapy with IV doxycycline versus physician‐determined therapy has been conducted.13 This study found no differences between treatment groups in clinical outcomes but did find that use of doxycycline was associated with shorter hospital stays and reduced costs. Our results, achieved in a real‐world setting in relatively ill hospitalized patients (58% were in PSI risk class IV or V), provide further support for the use of combination therapy with doxycycline.
Hospitalized patients treated with a beta‐lactam in combination with a macrolide are often discharged on macrolide monotherapy. In our population most patients treated with ceftriaxone plus doxycycline were discharged on doxycycline if they required continued therapy (data not shown). In the current era of resistance of Streptococcus pneumoniae to antibiotics, there is good reason to believe doxycycline may perform as well, if not better, than macrolides when hospitalized patients with CAP are discharged on oral monotherapy. Macrolide resistance rates among invasive pneumococcal isolates in the United States doubled from 10% to 20% during a period in which prescriptions for macrolides increased by 13%.12 In addition, a large surveillance study of more than 1500 isolates collected in 1999 and 2000 found that 26% of the isolates were resistant to macrolides, whereas only 16% were resistant to tetracycline.16 In vitro testing against S. Pneumoniae has also suggested that tetracycline resistance overestimates doxycycline resistance.17, 18 More recently, Streptococcus pneumoniae susceptibility data from the SENTRY Antimicrobial Surveillance program reaffirmed doxycycline's in vitro superiority over macrolides.17
Our study had several limitations. The study design adopted precluded determining whether favorable results with the use of ceftriaxone plus doxycycline resulted from an effect unique to this combination of antibiotics, the possible anti‐inflammatory properties of doxycycline alone,19, 20 or unmeasured confounders. For example, processes of care that affect clinical outcomes for patients hospitalized with CAP, such as the timing of antibiotic delivery, the timing of blood cultures, and stability assessment on discharge were not measured in this study. To affect outcomes, these processes of care would need to be differentially distributed between our comparison groups. However, because this study was performed in a single institution during a single interval, it is likely that the performance of these processes of care would be similar for all patients.
In conclusion, ceftriaxone plus doxycycline appears to be an effective, and possibly superior, therapy for patients hospitalized with CAP. Randomized controlled trials of doxycycline‐containing regimens versus other regimens are warranted.
- ,,, et al.Hospitalized pneumonia. Outcomes, treatment patterns, and costs in urban and rural areas.J Gen Intern Med.1996;11:415–421.
- ,,, et al.The cost of treating community‐acquired pneumonia.Clin Ther.1998;20:820–837.
- ,,, et al.Practice guidelines for the management of community‐acquired pneumonia in adults. Infectious Diseases Society of America.Clin Infect Dis.2000;31:347–382.
- ,,, et al.Management of community‐acquired pneumonia in the era of pneumococcal resistance: a report from the Drug‐Resistant Streptococcus pneumoniae Therapeutic Working Group.Arch Intern Med.2000;160:1399–1408.
- ,,, et al.Canadian guidelines for the initial management of community‐acquired pneumonia: an evidence‐based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Canadian Community‐Acquired Pneumonia Working Group.Clin Infect Dis.2000;31:383–421.
- ,,, et al.Guidelines for the management of adults with community‐acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention.Am J Respir Crit Care Med.2001;163:1730–1754.
- ,,, et al.Update of practice guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433
- ,,.Doxycycline.Ther Drug Monit1982;4:115–135
- ,.Chloramphenicol and tetracyclines.Med Clin North Am.1987;71:1155–1168
- ,.Tetracyclines.Med Clin North Am.1995;79:789–801
- ,,, et al.Antibiotic resistance among gram‐negative bacilli in US intensive care units: implications for fluoroquinolone use.JAMA.2003;289:885–888
- ,,, et al.Macrolide resistance among invasive Streptococcus pneumoniae isolates.JAMA.2001;286:1857–1862.
- ,,, et al.Doxycycline is a cost‐effective therapy for hospitalized patients with community‐acquired pneumonia.Arch Intern Med.1999;159:266–270.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- .Reducing bias in observational studies using subclassification on the propensity score.J Am Stat Assoc.1984;79:516–524
- ,,, et al.Antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States during 1999—2000, including a comparison of resistance rates since 1994—1995.Antimicrob Agents Chemother.2001;45:1721–1729
- ,,.Doxycycline use for community‐acquired pneumonia: contemporary in vitro spectrum of activity against Streptococcus pneumoniae (1999–2002).Diagn Microbiol Infect Dis.2004;49:147–149
- ,,, et al.Doxycycline activity against Streptococcus pneumoniae.Chest.1995;108:1775–1776.
- ,,, et al.Inhibition of enzymatic activity of phospholipases A2 by minocycline and doxycycline.Biochem Pharmacol.1992;44:1165–1170.
- ,,, et al.Doxycycline reduces mortality to lethal endotoxemia by reducing nitric oxide synthesis via an interleukin‐10‐independent mechanism.J Infect Dis.1998;177:489–492.
- ,,, et al.Hospitalized pneumonia. Outcomes, treatment patterns, and costs in urban and rural areas.J Gen Intern Med.1996;11:415–421.
- ,,, et al.The cost of treating community‐acquired pneumonia.Clin Ther.1998;20:820–837.
- ,,, et al.Practice guidelines for the management of community‐acquired pneumonia in adults. Infectious Diseases Society of America.Clin Infect Dis.2000;31:347–382.
- ,,, et al.Management of community‐acquired pneumonia in the era of pneumococcal resistance: a report from the Drug‐Resistant Streptococcus pneumoniae Therapeutic Working Group.Arch Intern Med.2000;160:1399–1408.
- ,,, et al.Canadian guidelines for the initial management of community‐acquired pneumonia: an evidence‐based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Canadian Community‐Acquired Pneumonia Working Group.Clin Infect Dis.2000;31:383–421.
- ,,, et al.Guidelines for the management of adults with community‐acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention.Am J Respir Crit Care Med.2001;163:1730–1754.
- ,,, et al.Update of practice guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433
- ,,.Doxycycline.Ther Drug Monit1982;4:115–135
- ,.Chloramphenicol and tetracyclines.Med Clin North Am.1987;71:1155–1168
- ,.Tetracyclines.Med Clin North Am.1995;79:789–801
- ,,, et al.Antibiotic resistance among gram‐negative bacilli in US intensive care units: implications for fluoroquinolone use.JAMA.2003;289:885–888
- ,,, et al.Macrolide resistance among invasive Streptococcus pneumoniae isolates.JAMA.2001;286:1857–1862.
- ,,, et al.Doxycycline is a cost‐effective therapy for hospitalized patients with community‐acquired pneumonia.Arch Intern Med.1999;159:266–270.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- .Reducing bias in observational studies using subclassification on the propensity score.J Am Stat Assoc.1984;79:516–524
- ,,, et al.Antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States during 1999—2000, including a comparison of resistance rates since 1994—1995.Antimicrob Agents Chemother.2001;45:1721–1729
- ,,.Doxycycline use for community‐acquired pneumonia: contemporary in vitro spectrum of activity against Streptococcus pneumoniae (1999–2002).Diagn Microbiol Infect Dis.2004;49:147–149
- ,,, et al.Doxycycline activity against Streptococcus pneumoniae.Chest.1995;108:1775–1776.
- ,,, et al.Inhibition of enzymatic activity of phospholipases A2 by minocycline and doxycycline.Biochem Pharmacol.1992;44:1165–1170.
- ,,, et al.Doxycycline reduces mortality to lethal endotoxemia by reducing nitric oxide synthesis via an interleukin‐10‐independent mechanism.J Infect Dis.1998;177:489–492.
Copyright © 2006 Society of Hospital Medicine
Editorial
You hold in your hands the inaugural issue of the Journal of Hospital Medicine (JHM). Our goal is for JHM to become the premier forum for peer‐reviewed research articles and evidence‐based reviews in the specialty of hospital medicine.
Yes, the specialty of hospital medicine. This official publication of the Society of Hospital Medicine signifies another step forward in the evolution of this specialty. With the publication of JHM the Society of Hospital Medicine continues its pivotal educational and leadership role in shaping the practice of hospital medicine. The Society is dedicated to promoting the highest‐quality care for all hospitalized patients and excellence in hospital medicine through education, advocacy, and research. As part of the Society's effort to improve care and standards, it is providing JHM to all members as part of their membership. We hope that our readership will grow to include individuals involved in all aspects of hospital care.
Packed with the results of new studies and state‐of‐the‐art reviews, JHM is not aimed solely at academicians and voracious readers of the medical literature. Rather, we hope that it fills a practical need to promote lifelong learning in both hospitalists and their hospital colleagues. For example, in this issue, national experts in palliative care and geriatrics summarize the pertinent literature and the important role of such care for hospitalized patients. JHM will also serve as a key venue for hospital medicine researchers to disseminate their findings and for educators to share their knowledge and techniques.
Why bother to create yet another journal? Given the stacks of journals that adorn many of our desks (and some of our chairs and windowsills), do we really need another to get lost among the mail that inundates us? We believe the field of hospital medicine involves a growing body of knowledge deserving of a journal focused solely on it. Hospital medicine evolved from efforts to fill a need identified by overstretched primary care physicians in the late 1980s. Physicians like the cofounders of SHM, John Nelson in Florida and Win Whitcomb in Massachusetts, began careers in a field that today numbers more than 12,000 physicians. Labeled with the moniker hospitalist given us by Bob Wachter and Lee Goldman,1 we now make up the fastest‐growing medical specialty in the United States.2 Yet, until now, no journal was devoted solely to this specialty.
The Journal of Hospital Medicine aims to provide physicians and other health care professionals with continuing insight into the basic and clinical sciences to support informed clinical decision making in the hospital. As hospitalists increasingly take an active role in the successful delivery of bench research discoveries to the bedside and become vigorous participants in the translational and clinical research sought by the National Institutes of Health,3 JHM will disseminate their findings. In addition, we hope to foster balanced debates on medical issues and health care trends that affect hospital medicine and patient care. Nonclinical aspects of hospital medicine also will be featured, including public health and the political, philosophic, ethical, legal, environmental, economic, historical, and cultural issues surrounding hospital care. We especially want to encourage submissions that evaluate projects involving the entire hospital care team: physicians and our colleagues in the hospitalnurses, pharmacists, administrators, physical and occupational therapists, social workers, and case managers.
Two articles (see pages 48 and 57) highlight this inaugural issue. One describes the development of The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (a supplement to this issue), and the other demonstrates how this document can be applied to curriculum development.4, 5 This milestone in the evolution of hospital medicine provides an initial structural framework to guide medical educators in developing curricula that incorporate these competencies into the training and evaluation of students, clinicians‐in‐training, and practicing hospitalists.4 The president and CEO of the American Board of Internal Medicine (ABIM), Christine Cassel, offers her perspective on this landmark document.6 Its timeliness is reflected by the current efforts of the American College of Physicians, the ABIM, and others to redesign the training and the certification requirements of internists. As this supplement demonstrates, the Society of Hospital Medicine will be intimately involved in this process.
After this auspicious start, subsequent issues will include articles in the following categories. Original research articles will report results of randomized controlled trials, evaluations of diagnostic tests, prospective cohort studies, casecontrol studies, and high‐quality observational studies. We are interested in publishing both quantitative and qualitative research. Review articles, especially those targeting the hospital medicine core competencies, are eagerly sought. We also seek descriptions of interventions that transform hospital care delivery in the hospital. For example, accounts of the implementation of quality‐improvement projects and outcomes, including barriers that were overcome or that blocked implementation, would be invaluable to hospitalists throughout the country. Clinical conundrums should describe clinical cases that present diagnostic dilemmas or involve issues of medical errors. To facilitate the professional development of hospitalists, we seek articles focused on their professional development in community, academic, and administrative settings. Examples of leadership topics are managing physician performance, leading and managing change, and self‐evaluation. Teaching tips or descriptions of educational programs or curricula also are desired. For researchers, potential topics include descriptions of specific techniques used for surveys, meta‐analyses, economic evaluations, and statistical analyses.Penetrating point manuscripts, those that go beyond the cutting edge to explain the next potential breakthrough or intervention in the developing field of hospital medicine, may be authored by thought leaders inside and outside the health care field as well as by hospitalists with novel ideas. Equally vital, I want to share the illuminating perspectives of physicians, patients, and families of patients as they reflect on the experience of being in the hospitalhospitalists can enlighten us through their handoffs, and patients and their families can inform us about their view from the hospital bed.
Finally, never forget that this is your journal. Let me know what you like and what changes you think can make it better. Please e‐mail your suggestions, comments, criticisms, and ideas to us at JHMeditor@ hospitalmedicine.org. This is your chance to help shape the practice of hospital medicine and the future of hospital care. I look forward to your guidance. Together we can expand our knowledge and continue to grow in our careers.
The more you see the less you know
The less you find out as you grow
I knew much more then than I do now.
U2, City of Blinding Lights,
How to Dismantle an Atomic Bomb
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- .Translational and clinical science—time for a new vision.N Engl J Med2005;35:1621‐1623.
- ,,,,, eds.The core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
- .Hospital medicine: early successes and challenges ahead.J Hosp Med.2006;1:3–4.
You hold in your hands the inaugural issue of the Journal of Hospital Medicine (JHM). Our goal is for JHM to become the premier forum for peer‐reviewed research articles and evidence‐based reviews in the specialty of hospital medicine.
Yes, the specialty of hospital medicine. This official publication of the Society of Hospital Medicine signifies another step forward in the evolution of this specialty. With the publication of JHM the Society of Hospital Medicine continues its pivotal educational and leadership role in shaping the practice of hospital medicine. The Society is dedicated to promoting the highest‐quality care for all hospitalized patients and excellence in hospital medicine through education, advocacy, and research. As part of the Society's effort to improve care and standards, it is providing JHM to all members as part of their membership. We hope that our readership will grow to include individuals involved in all aspects of hospital care.
Packed with the results of new studies and state‐of‐the‐art reviews, JHM is not aimed solely at academicians and voracious readers of the medical literature. Rather, we hope that it fills a practical need to promote lifelong learning in both hospitalists and their hospital colleagues. For example, in this issue, national experts in palliative care and geriatrics summarize the pertinent literature and the important role of such care for hospitalized patients. JHM will also serve as a key venue for hospital medicine researchers to disseminate their findings and for educators to share their knowledge and techniques.
Why bother to create yet another journal? Given the stacks of journals that adorn many of our desks (and some of our chairs and windowsills), do we really need another to get lost among the mail that inundates us? We believe the field of hospital medicine involves a growing body of knowledge deserving of a journal focused solely on it. Hospital medicine evolved from efforts to fill a need identified by overstretched primary care physicians in the late 1980s. Physicians like the cofounders of SHM, John Nelson in Florida and Win Whitcomb in Massachusetts, began careers in a field that today numbers more than 12,000 physicians. Labeled with the moniker hospitalist given us by Bob Wachter and Lee Goldman,1 we now make up the fastest‐growing medical specialty in the United States.2 Yet, until now, no journal was devoted solely to this specialty.
The Journal of Hospital Medicine aims to provide physicians and other health care professionals with continuing insight into the basic and clinical sciences to support informed clinical decision making in the hospital. As hospitalists increasingly take an active role in the successful delivery of bench research discoveries to the bedside and become vigorous participants in the translational and clinical research sought by the National Institutes of Health,3 JHM will disseminate their findings. In addition, we hope to foster balanced debates on medical issues and health care trends that affect hospital medicine and patient care. Nonclinical aspects of hospital medicine also will be featured, including public health and the political, philosophic, ethical, legal, environmental, economic, historical, and cultural issues surrounding hospital care. We especially want to encourage submissions that evaluate projects involving the entire hospital care team: physicians and our colleagues in the hospitalnurses, pharmacists, administrators, physical and occupational therapists, social workers, and case managers.
Two articles (see pages 48 and 57) highlight this inaugural issue. One describes the development of The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (a supplement to this issue), and the other demonstrates how this document can be applied to curriculum development.4, 5 This milestone in the evolution of hospital medicine provides an initial structural framework to guide medical educators in developing curricula that incorporate these competencies into the training and evaluation of students, clinicians‐in‐training, and practicing hospitalists.4 The president and CEO of the American Board of Internal Medicine (ABIM), Christine Cassel, offers her perspective on this landmark document.6 Its timeliness is reflected by the current efforts of the American College of Physicians, the ABIM, and others to redesign the training and the certification requirements of internists. As this supplement demonstrates, the Society of Hospital Medicine will be intimately involved in this process.
After this auspicious start, subsequent issues will include articles in the following categories. Original research articles will report results of randomized controlled trials, evaluations of diagnostic tests, prospective cohort studies, casecontrol studies, and high‐quality observational studies. We are interested in publishing both quantitative and qualitative research. Review articles, especially those targeting the hospital medicine core competencies, are eagerly sought. We also seek descriptions of interventions that transform hospital care delivery in the hospital. For example, accounts of the implementation of quality‐improvement projects and outcomes, including barriers that were overcome or that blocked implementation, would be invaluable to hospitalists throughout the country. Clinical conundrums should describe clinical cases that present diagnostic dilemmas or involve issues of medical errors. To facilitate the professional development of hospitalists, we seek articles focused on their professional development in community, academic, and administrative settings. Examples of leadership topics are managing physician performance, leading and managing change, and self‐evaluation. Teaching tips or descriptions of educational programs or curricula also are desired. For researchers, potential topics include descriptions of specific techniques used for surveys, meta‐analyses, economic evaluations, and statistical analyses.Penetrating point manuscripts, those that go beyond the cutting edge to explain the next potential breakthrough or intervention in the developing field of hospital medicine, may be authored by thought leaders inside and outside the health care field as well as by hospitalists with novel ideas. Equally vital, I want to share the illuminating perspectives of physicians, patients, and families of patients as they reflect on the experience of being in the hospitalhospitalists can enlighten us through their handoffs, and patients and their families can inform us about their view from the hospital bed.
Finally, never forget that this is your journal. Let me know what you like and what changes you think can make it better. Please e‐mail your suggestions, comments, criticisms, and ideas to us at JHMeditor@ hospitalmedicine.org. This is your chance to help shape the practice of hospital medicine and the future of hospital care. I look forward to your guidance. Together we can expand our knowledge and continue to grow in our careers.
The more you see the less you know
The less you find out as you grow
I knew much more then than I do now.
U2, City of Blinding Lights,
How to Dismantle an Atomic Bomb
You hold in your hands the inaugural issue of the Journal of Hospital Medicine (JHM). Our goal is for JHM to become the premier forum for peer‐reviewed research articles and evidence‐based reviews in the specialty of hospital medicine.
Yes, the specialty of hospital medicine. This official publication of the Society of Hospital Medicine signifies another step forward in the evolution of this specialty. With the publication of JHM the Society of Hospital Medicine continues its pivotal educational and leadership role in shaping the practice of hospital medicine. The Society is dedicated to promoting the highest‐quality care for all hospitalized patients and excellence in hospital medicine through education, advocacy, and research. As part of the Society's effort to improve care and standards, it is providing JHM to all members as part of their membership. We hope that our readership will grow to include individuals involved in all aspects of hospital care.
Packed with the results of new studies and state‐of‐the‐art reviews, JHM is not aimed solely at academicians and voracious readers of the medical literature. Rather, we hope that it fills a practical need to promote lifelong learning in both hospitalists and their hospital colleagues. For example, in this issue, national experts in palliative care and geriatrics summarize the pertinent literature and the important role of such care for hospitalized patients. JHM will also serve as a key venue for hospital medicine researchers to disseminate their findings and for educators to share their knowledge and techniques.
Why bother to create yet another journal? Given the stacks of journals that adorn many of our desks (and some of our chairs and windowsills), do we really need another to get lost among the mail that inundates us? We believe the field of hospital medicine involves a growing body of knowledge deserving of a journal focused solely on it. Hospital medicine evolved from efforts to fill a need identified by overstretched primary care physicians in the late 1980s. Physicians like the cofounders of SHM, John Nelson in Florida and Win Whitcomb in Massachusetts, began careers in a field that today numbers more than 12,000 physicians. Labeled with the moniker hospitalist given us by Bob Wachter and Lee Goldman,1 we now make up the fastest‐growing medical specialty in the United States.2 Yet, until now, no journal was devoted solely to this specialty.
The Journal of Hospital Medicine aims to provide physicians and other health care professionals with continuing insight into the basic and clinical sciences to support informed clinical decision making in the hospital. As hospitalists increasingly take an active role in the successful delivery of bench research discoveries to the bedside and become vigorous participants in the translational and clinical research sought by the National Institutes of Health,3 JHM will disseminate their findings. In addition, we hope to foster balanced debates on medical issues and health care trends that affect hospital medicine and patient care. Nonclinical aspects of hospital medicine also will be featured, including public health and the political, philosophic, ethical, legal, environmental, economic, historical, and cultural issues surrounding hospital care. We especially want to encourage submissions that evaluate projects involving the entire hospital care team: physicians and our colleagues in the hospitalnurses, pharmacists, administrators, physical and occupational therapists, social workers, and case managers.
Two articles (see pages 48 and 57) highlight this inaugural issue. One describes the development of The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (a supplement to this issue), and the other demonstrates how this document can be applied to curriculum development.4, 5 This milestone in the evolution of hospital medicine provides an initial structural framework to guide medical educators in developing curricula that incorporate these competencies into the training and evaluation of students, clinicians‐in‐training, and practicing hospitalists.4 The president and CEO of the American Board of Internal Medicine (ABIM), Christine Cassel, offers her perspective on this landmark document.6 Its timeliness is reflected by the current efforts of the American College of Physicians, the ABIM, and others to redesign the training and the certification requirements of internists. As this supplement demonstrates, the Society of Hospital Medicine will be intimately involved in this process.
After this auspicious start, subsequent issues will include articles in the following categories. Original research articles will report results of randomized controlled trials, evaluations of diagnostic tests, prospective cohort studies, casecontrol studies, and high‐quality observational studies. We are interested in publishing both quantitative and qualitative research. Review articles, especially those targeting the hospital medicine core competencies, are eagerly sought. We also seek descriptions of interventions that transform hospital care delivery in the hospital. For example, accounts of the implementation of quality‐improvement projects and outcomes, including barriers that were overcome or that blocked implementation, would be invaluable to hospitalists throughout the country. Clinical conundrums should describe clinical cases that present diagnostic dilemmas or involve issues of medical errors. To facilitate the professional development of hospitalists, we seek articles focused on their professional development in community, academic, and administrative settings. Examples of leadership topics are managing physician performance, leading and managing change, and self‐evaluation. Teaching tips or descriptions of educational programs or curricula also are desired. For researchers, potential topics include descriptions of specific techniques used for surveys, meta‐analyses, economic evaluations, and statistical analyses.Penetrating point manuscripts, those that go beyond the cutting edge to explain the next potential breakthrough or intervention in the developing field of hospital medicine, may be authored by thought leaders inside and outside the health care field as well as by hospitalists with novel ideas. Equally vital, I want to share the illuminating perspectives of physicians, patients, and families of patients as they reflect on the experience of being in the hospitalhospitalists can enlighten us through their handoffs, and patients and their families can inform us about their view from the hospital bed.
Finally, never forget that this is your journal. Let me know what you like and what changes you think can make it better. Please e‐mail your suggestions, comments, criticisms, and ideas to us at JHMeditor@ hospitalmedicine.org. This is your chance to help shape the practice of hospital medicine and the future of hospital care. I look forward to your guidance. Together we can expand our knowledge and continue to grow in our careers.
The more you see the less you know
The less you find out as you grow
I knew much more then than I do now.
U2, City of Blinding Lights,
How to Dismantle an Atomic Bomb
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- .Translational and clinical science—time for a new vision.N Engl J Med2005;35:1621‐1623.
- ,,,,, eds.The core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
- .Hospital medicine: early successes and challenges ahead.J Hosp Med.2006;1:3–4.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- .Translational and clinical science—time for a new vision.N Engl J Med2005;35:1621‐1623.
- ,,,,, eds.The core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
- .Hospital medicine: early successes and challenges ahead.J Hosp Med.2006;1:3–4.
Care of Hospitalized Older Patients
An emergency room resident once was instructing a medical student in how to place a nasogastric tube in order to evaluate a patient with melena and postural hypotension. When the tube came to a stop, the student connected a syringe to the tube and aspirated. Then, to the consternation of the resident, the student yanked out the tube as soon as he saw blood flowing into the syringe. Why'd you do that? the surprised resident asked. There's blood down there! came the quick reply.
Like that medical student, hospital‐based physicianshospitalists, geriatricians, and othersmay miss the boat when caring for hospitalized older patients. Hospitals are full, and they're filled largely with older patients. These patients, like those who are younger, generally want to be treated and sent home. Older patients, however, frequently pose specific challenges. They may talk and move more slowly, stay longer, and be more likely to die. They more often need help in caring for themselves, and many have lost the support necessary to remain at home, making it difficult for them to return there. In short, older patients often need more care and more time.
It may be tempting to ignore the challenges that arise in caring for older patients. An avoidance strategy is expedient, at least in the short term. Ultimately, however, ignoring the challenges of caring for older patients will prove no wiser than yanking the nasogastric tube. Instead, we can recognize the challenges and use this opportunity to learn to improve their care.
This article describes the state of the science in hospital care for older patients, opportunities awaiting those who care for these patients, and barriers to seizing those opportunities. I conclude with five recommendations for physicians who care for hospitalized older patients.
STATE OF THE SCIENCE
Older patients shape hospital medicine and will determine its future. In 2002 the 12% of the population age 65 years or older accounted for roughly 50% of all hospitalizations unrelated to childbirth.1, 2 Hospital admissions of older persons will balloon as the number of persons older than age 65 rises by a million a year, increasing from 13% of the population today to 21% by 2030.2
Older persons in hospitals pose substantial clinical challenges. Many have multiple comorbid diseases and virtually all have complex medical regimens.1, 35 Many have cognitive impairment or dementia, often accompanied by delirium, which hinder communication and can lead to behaviors that require extra attention and impede diagnostic tests and treatment.611 Some have difficulty walking and caring for themselves, and a third leave the hospital without having recovered to their baseline level of function, with those age 85 years or older at highest risk for this decline independent of the reason for admission.1215 These characteristics increase the care, resources, and staff time older patients need, prolong their stays, and increase their hospital costs beyond those expected for their diagnosis.16 They also are at higher risk for iatrogenic complications, death, and rehospitalization,1720 and the risk of errors may be increased by frequent transitions in providers and sites of care.2125 Older persons require greater assistance at home, and yet they have often lost much of the support needed to live at home.10, 13, 20
Despite the magnitude of these challenges, we know surprisingly little about how best to care for hospitalized older persons, especially those older than age 75. The evidence base for treatment of specific common diseases is inadequate. The very old are underrepresented in clinical trials,26, 27 and the majority of older patients with common conditions such as heart failure may not meet the enrollment criteria for clinical trials.28 Thus, what is known about treating diseases in younger patients may be extrapolated to determine treatments in older persons based only on a leap of faith, which may be misguided.29, 30 In fact, the efficacy of conventional treatments for common conditions (e.g., acute myocardial infarction and hypertension) may diminish with age,31, 32 indicating that clinical trials targeted specifically to older patients may be necessary.
Despite the dearth of evidence about the management of common diseases in hospitalized older patients, hospital‐based geriatricians have developed substantial high‐grade evidence about the prevention of two geriatric syndromes, functional disability and delirium. The incidence of both syndromes can be reduced (without increasing hospital or health care costs) by multicomponent interventions that include comprehensive assessment, targeted treatment, and environmental modification to promote independence and safety.3, 3335 Moreover, the randomized trials that evaluated these interventions have provided models for how other innovations by hospital‐based physicians can be evaluated. Despite the evidence that these approaches are effective and either cost saving or cost neutral, these models have not been widely adopted.36
Many challenges in the prevention and management of geriatric syndromes in the hospital remain. For example, sophisticated approaches to the management of delirium are disappointingonce delirium has developed, intensive state‐of‐the‐art approaches to its management are no more effective than standard care in shortening its duration or ameliorating its sequelae.37, 38 The indiscriminate use of indwelling urinary catheters is decried, but there is no evidence that their use is declining, even in patients without an indication for catheterization.3942 Malnutrition and falls can be prevented and depression treated in patients outside the hospital,4345 but it is unclear whether these maladies can be prevented or treated effectively in hospitalized elders. Finally, intriguing evidence suggests that geriatric syndromes and their sequelae may be prevented and outcomes improved by caring for patients at home whenever possible, bringing intensive nursing and physician care into the home without some of the adverse effects of hospitalization.46
The physician workforce is not prepared to provide optimal care to hospitalized older persons. Few hospitalists or other hospital‐based physicians have received more than minimal training in geriatric medicine, and few geriatricians practice extensively in the hospital. At the same time that the ranks of physicians who consider themselves hospitalists have been expanding by 1000 or more a year in the United States, the number of certified geriatricians has been decreasing as hundreds decide each year not to renew their certificates.47, 48 Fewer than 300 geriatricians complete training each year and enter the workforce, and most new geriatricians practice in ambulatory or long‐term‐care settings. Wald's study in this issue indicates the paucity of geriatricians in hospital medicine (with the apparently single exception of the Mayo Clinic's Hospital Internal Medicine Group) and a relative lack of interest among hospitalists in developing knowledge about the effective and efficient treatment of older persons, in particular.49
OPPORTUNITIES
Opportunities to improve the care of hospitalized older patients arise from the state of the science in their care and from the common ground that hospitalists and geriatricians share. The older patients of both hospitalists and geriatricians are seriously ill, with annual mortality rates of 20%30% for patients with common conditions such as myocardial infarction or colon cancer and mortality rates of 50% or higher for patients with dementia or severe disability.5, 5053 We should view the care of our patients in the context of their prognoses,5, 54 recognizing that patients' preferences for the goals, style, and site of care vary widely.55, 56 The substantial association of mortality with geriatric syndromes such as disability, dementia, delirium, and depressionan association that is independent of pathophysiologic indicators of disease severitysuggests that substantial benefits may accrue by targeting interventions to the prevention or amelioration of these syndromes.5, 9, 10, 53, 57, 58
Hospitalists and geriatricians also share the perspective of working in complex systems in which the effectiveness, efficiency, and safety of care depend on system functions as well as on their technical expertise as individuals.5961 Together, and with colleagues in other disciplines, they may redesign how hospitals and the systems around them work to reduce errors, increase attention to aspects of care that are easily overlooked, and improve patient outcomes.
BARRIERS
Hospitalists and geriatricians face barriers to improving care for hospitalized older patients. First, gaps in knowledge limit the capacity to provide the care and achieve the outcomes desired. Fundamental discoveries in clinical science are needed to prevent or treat geriatric syndromes, to treat common diseases in the very old, and to put into practice what is known. Addressing these gaps in knowledge will require a sustained effort that spans methods and disciplines.
Second, the dominant reductionist paradigm values discovery of the mechanism of disease over discovery of ways to manage illness effectively and efficiently.6267 Similarly, diagnostic tests and therapies based on beliefs about the mechanism of diseasefor example, PET scans in persons with memory disorders and chemotherapy in persons with refractory cancersare pursued aggressively and paid handsomely, whereas efforts to reduce errors or improve continuity of care receive little attention or reward. The challenges of caring for hospitalized older patients will require advances on both fronts: in our knowledge of the pathogenesis of disorders that have proven resistant to current therapies (such as delirium) and in our knowledge of how to structure clinical care that engages patients and families and achieves desired outcomes effectively, consistently, and efficiently.
The structure and styles of our practices provide the third challenge. Hospitalists pride themselves on their efficient management of patients while maintaining or improving patient outcomes. A focus on efficient management can, however, lead to an assembly‐line approach, turning each patient into a series of do‐order‐call‐check tasks to get the patient out of the hospital as quickly as possible. This approach has advantages but may also blind physicians to the scope and complexity of issues that arise in caring for the very old through the course of an illness that often extends beyond hospitalization.25 Geriatricians pride themselves on their comprehensive management of patients, gathering clinical information from many sources (especially in the many patients with cognitive impairment), exploring and articulating goals of care, and assessing self‐care and neurologic, psychological, and social domains in addition to conventional pathophysiology. Yet too often, geriatricians are not available in hospitals, and as Wald found, they have rarely been integrated into hospitalist groups.
FIVE RECOMMENDATIONS FOR HOSPITALISTS AND GERIATRICIANS
I conclude with five recommendations for hospital‐based physicians who care for older patients and for geriatricians. First, step back, look at your patients, and note their predicament in its full complexity. Once hospitalists start looking for cognitive impairment, weakness, and difficulty walking and the difficulty of finding a good situation after leaving the hospital, it will be easy to see these problems. And once geriatricians start looking at why their patients are going into the hospital and what happens to them, it will be easy to see the need to become engaged. Seeing the full range of patients' problems won't address them, but we certainly won't address them if we don't look.
Second, learn what is known about how best to care for the aged and integrate this learning into your hospital practice. For hospitalists, learning how to identify each patient's goals of care, what works to prevent delirium and promote mobility, which drugs to avoid and which doses to modify, and how to access resources to help patients and families achieve their goals after they leave the hospital will benefit older patients. Pocket and PDA resources to extend learning are readily available.68 For geriatricians, learning how to avoid hospitalization (especially when resources can be mobilized to provide a hospital at home), how to work within the timeframe of hospitalization, and what current disease‐specific management strategies have been shown to be effective in the aged will benefit their patients. Maintaining the distinction between what is believed and what is known on the basis of high‐quality evidence will enhance learning and decrease the risk of stubbornly pursuing harmful or wasteful practices. This is especially important in situations where the evidence is weak and opinions are strong.
Third, to provide the best care for our older patients, we must embrace aging, not deny it. Most hospitalized older patients, and most patients of geriatricians, will decline and die in a few years. The inevitability of these outcomes may tempt us either to abandon our incurable patients or to focus single‐mindedly on treatable problems one at a time, rather than on the interplay of multiple problems in an individual person. Either choice is mistaken. Although we are powerless to prevent decline and death in the long run, we have a tremendous capacity to delay and ameliorate decline, to enhance comfort and joy, to protect from harm, and, often, to delay death.
Fourth, ask questions about what you do not know or understand. The risk, of course, is that your curiosity will be sparked, possibly slowing you in completing the myriad tasks to be donea risk worth taking. Will ACE inhibitors and beta‐blockers benefit patients with heart failure without systolic dysfunction? Why do so many older patients become delirious, and are features of hospitalization catalyzing the effects of disease in causing delirium? Why do we continue to send cognitively impaired patients home without scheduled follow‐up and with instruction sheets they cannot read, and how can we change the system to prevent this? If you cannot find answers to your questions grounded in strong evidence, maintain your skepticism about answers given easily.
Finally, consider discovering the answers to some of your questions. Part of the excitement of caring for the very old is that we have so much to learn and that what we do learn can be so powerful.
- ,.Hospitalization in the United States, 2002. Publication 05‐056.Washington (DC):AHRQ,2005.
- .Improving health care for older persons.Ann Intern Med.2003;139:421–424.
- ,,, et al.A controlled trial of inpatient and outpatient geriatric evaluation and management.N Engl J Med.2002;346:905–912.
- ,,, et al.Hospital diagnoses, Medicare charges, and nursing home admissions in the year when older persons become severely disabled.JAMA.1997;277:728–734.
- ,,, et al.Development and validation of a prognostic index for 1‐year mortality in older adults after hospitalization.JAMA.2001;285:2987–2994.
- ,,,.Delirium is independently associated with poor functional recovery after hip fracture.J Am Geriatr Soc.2000;48:618–624.
- ,,, et al.The course of delirium in older medical inpatients: a prospective study.J Gen Intern Med.2003;18:696–704.
- ,,,.Does delirium increase hospital stay?J Am Geriatr Soc.2003;51:1539–1546.
- ,,, et al.Does delirium contribute to poor hospital outcomes? A three‐site epidemiologic study.J Gen Intern Med.1998;13:234–242.
- ,,, et al.A predictive index for functional decline in hospitalized elderly medical patients.J Gen Intern Med.1993;8:645–652.
- ,,.A prospective study of delirium in hospitalized elderly.JAMA.1990;263:1097–1101.
- ,,, et al.Unsteadiness reported by older hospitalized patients predicts functional decline.J Am Geriatr Soc.2003;51:621–626.
- ,,, et al.Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age.J Am Geriatr Soc.2003;51:451–458.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,, et al.Functional disability in the hospitalized elderly.JAMA.1982;248:847–850.
- ,,, et al.Diagnosis‐related group‐adjusted hospital costs are higher in older medical patients with lower functional status.J Am Geriatr Soc.2003;51:1729–1734.
- ,.Adverse events, negligence in hospitalized patients: results from the Harvard Medical Practice Study.Perspect Healthc Risk Manage.1991;11(2):2–8.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I.N Engl J Med.1991;324:370–376.
- ,,, et al.The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II.N Engl J Med.1991;324:377–384.
- ,,,.Effects of functional status changes before and during hospitalization on nursing home admission of older adults.J Gerontol A Biol Sci Med Sci.1999;54:M521–M526.
- ,,.Characterization of geriatric drug‐related hospital readmissions.Med Care.1991;29:989–1003.
- ,,,.The impact of clinical pharmacists' consultations on physicians' geriatric drug prescribing. A randomized controlled trial.Med Care.1992;30:646–658.
- ,,,.Posthospital medication discrepancies: prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,.A new tool for identifying discrepancies in postacute medications for community‐dwelling older adults.Am J Geriatr Pharmacother.2004;2(2):141–147.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141:533–536.
- ,,, et al.Enrollment of older persons in cancer trials after the medicare reimbursement policy change.Arch Intern Med.2005;165:1514–1520.
- ,,, et al.Underrepresentation of patients 65 years of age or older in cancer‐treatment trials.N Engl J Med.1999;341:2061–2067.
- ,,, et al.Most hospitalized older persons do not meet the enrollment criteria for clinical trials in heart failure.Am Heart J.2003;146(2):250–257.
- ,.Problems in the “evidence” of “evidence‐based medicine.”Am J Med.1997;103:529–535.
- .National initiatives in ageing research in the United Kingdom.Age Ageing.2002;31(2):93–95.
- .Embracing complexity: A consideration of hypertension in the very old.J Gerontol A Biol Sci Med Sci.2003;58:653–658.
- ,,, et al.Lack of benefit for intravenous thrombolysis in patients with myocardial infarction who are older than 75 years.Circulation.2000;101:2239–2246.
- ,,, et al.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,,.Dissemination and characteristics of acute care for elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19(1):220–227.
- ,.Treatment of delirium in older medical inpatients: a challenge for geriatric specialists.J Am Geriatr Soc.2002;50:2101–2103.
- ,,, et al.Systematic detection and multidisciplinary care of delirium in older medical inpatients: a randomized trial.CMAJ.2002;167:753–759.
- .Clinical and economic consequences of nosocomial catheter‐related bacteriuria.Am J Infect Control.2000;28(1):68–75.
- ,.Preventing catheter‐related bacteriuria: should we? Can we? How?Arch Intern Med.1999;159:800–808.
- ,,.Indwelling urinary catheters: a one‐point restraint?Ann Intern Med.2002;137(2):125–127.
- ,, et al.Risk factors for indwelling urinary catheterization among older hospitalized patients without a specific medical indication for catheterization.J Patient Saf.2005. In press.
- ,,.Protein and energy supplementation in elderly people at risk from malnutrition.Cochrane Database Syst Rev.2005(2):CD003288.
- .Clinical practice. Preventing falls in elderly persons.N Engl J Med.2003;348(1):42–49.
- ,,, et al.Collaborative care management of late‐life depression in the primary care setting: a randomized controlled trial.JAMA.2002;288:2836–2845.
- ,,,,,.Hospital in the home: a randomised controlled trial.Med J Aust.1999;170(4):156–160.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350:1935–1936.
- ,,,.Academic geriatric programs in US allopathic and osteopathic medical schools.JAMA.2002;288:2313–2319.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,, et al.The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care.Ann Intern Med.2003;138:273–287.
- ,,, et al.The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care.Ann Intern Med.2003;138:288–298.
- ,.Mortality from pneumonia and hip fractures in patients with advanced dementia.JAMA.2000;284:2447–2448.
- ,.Survival in end‐stage dementia following acute illness.JAMA.2000;284(1):47–52.
- ,.Cancer screening in elderly patients: a framework for individualized decision making.JAMA.2001;285:2750–2756.
- ,,,.Understanding the treatment preferences of seriously ill patients.N Engl J Med.2002;346:1061–1066.
- ,,, et al.Health values of hospitalized patients 80 years or older. HELP Investigators. Hospitalized Elderly Longitudinal Project.JAMA.1998;279:371–375.
- ,,, et al.Depressive symptoms and 3‐year mortality in older hospitalized medical patients.Ann Intern Med.1999;130:563–569.
- ,,, et al.Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons.Ann Intern Med.1997;126:417–425.
- ,,,.Five system barriers to achieving ultrasafe health care.Ann Intern Med.2005;142:756–764.
- .Specialized care for elderly patients.N Engl J Med.2002;346:874.
- .The end of the beginning: patient safety five years after ‘To Err Is Human.’Health Aff (Millwood).2004;Suppl Web Exclusives:W4–534–545.
- .An additional basic science for clinical medicine: II. The limitations of randomized trials.Ann Intern Med.1983;99:544–550.
- .An additional basic science for clinical medicine: III. The challenges of comparison and measurement.Ann Intern Med.1983;99:705–712.
- .An additional basic science for clinical medicine: IV. The development of clinimetrics.Ann Intern Med.1983;99:843–848.
- .An additional basic science for clinical medicine: I. The constraining fundamental paradigms.Ann Intern Med.1983;99:393–397.
- ,.The end of the disease era.Am J Med.2004;116(3):179–185.
- ,, Agostini JV. Potential pitfalls of disease‐specific guidelines for patients with multiple conditions.N Engl J Med.2004;351:2870–2874.
- ,,, et al.Geriatrics at your fingertips: 2005.7th ed.Malden (MA):Blackwell Publishing, for the American Geriatrics Society,2005.
An emergency room resident once was instructing a medical student in how to place a nasogastric tube in order to evaluate a patient with melena and postural hypotension. When the tube came to a stop, the student connected a syringe to the tube and aspirated. Then, to the consternation of the resident, the student yanked out the tube as soon as he saw blood flowing into the syringe. Why'd you do that? the surprised resident asked. There's blood down there! came the quick reply.
Like that medical student, hospital‐based physicianshospitalists, geriatricians, and othersmay miss the boat when caring for hospitalized older patients. Hospitals are full, and they're filled largely with older patients. These patients, like those who are younger, generally want to be treated and sent home. Older patients, however, frequently pose specific challenges. They may talk and move more slowly, stay longer, and be more likely to die. They more often need help in caring for themselves, and many have lost the support necessary to remain at home, making it difficult for them to return there. In short, older patients often need more care and more time.
It may be tempting to ignore the challenges that arise in caring for older patients. An avoidance strategy is expedient, at least in the short term. Ultimately, however, ignoring the challenges of caring for older patients will prove no wiser than yanking the nasogastric tube. Instead, we can recognize the challenges and use this opportunity to learn to improve their care.
This article describes the state of the science in hospital care for older patients, opportunities awaiting those who care for these patients, and barriers to seizing those opportunities. I conclude with five recommendations for physicians who care for hospitalized older patients.
STATE OF THE SCIENCE
Older patients shape hospital medicine and will determine its future. In 2002 the 12% of the population age 65 years or older accounted for roughly 50% of all hospitalizations unrelated to childbirth.1, 2 Hospital admissions of older persons will balloon as the number of persons older than age 65 rises by a million a year, increasing from 13% of the population today to 21% by 2030.2
Older persons in hospitals pose substantial clinical challenges. Many have multiple comorbid diseases and virtually all have complex medical regimens.1, 35 Many have cognitive impairment or dementia, often accompanied by delirium, which hinder communication and can lead to behaviors that require extra attention and impede diagnostic tests and treatment.611 Some have difficulty walking and caring for themselves, and a third leave the hospital without having recovered to their baseline level of function, with those age 85 years or older at highest risk for this decline independent of the reason for admission.1215 These characteristics increase the care, resources, and staff time older patients need, prolong their stays, and increase their hospital costs beyond those expected for their diagnosis.16 They also are at higher risk for iatrogenic complications, death, and rehospitalization,1720 and the risk of errors may be increased by frequent transitions in providers and sites of care.2125 Older persons require greater assistance at home, and yet they have often lost much of the support needed to live at home.10, 13, 20
Despite the magnitude of these challenges, we know surprisingly little about how best to care for hospitalized older persons, especially those older than age 75. The evidence base for treatment of specific common diseases is inadequate. The very old are underrepresented in clinical trials,26, 27 and the majority of older patients with common conditions such as heart failure may not meet the enrollment criteria for clinical trials.28 Thus, what is known about treating diseases in younger patients may be extrapolated to determine treatments in older persons based only on a leap of faith, which may be misguided.29, 30 In fact, the efficacy of conventional treatments for common conditions (e.g., acute myocardial infarction and hypertension) may diminish with age,31, 32 indicating that clinical trials targeted specifically to older patients may be necessary.
Despite the dearth of evidence about the management of common diseases in hospitalized older patients, hospital‐based geriatricians have developed substantial high‐grade evidence about the prevention of two geriatric syndromes, functional disability and delirium. The incidence of both syndromes can be reduced (without increasing hospital or health care costs) by multicomponent interventions that include comprehensive assessment, targeted treatment, and environmental modification to promote independence and safety.3, 3335 Moreover, the randomized trials that evaluated these interventions have provided models for how other innovations by hospital‐based physicians can be evaluated. Despite the evidence that these approaches are effective and either cost saving or cost neutral, these models have not been widely adopted.36
Many challenges in the prevention and management of geriatric syndromes in the hospital remain. For example, sophisticated approaches to the management of delirium are disappointingonce delirium has developed, intensive state‐of‐the‐art approaches to its management are no more effective than standard care in shortening its duration or ameliorating its sequelae.37, 38 The indiscriminate use of indwelling urinary catheters is decried, but there is no evidence that their use is declining, even in patients without an indication for catheterization.3942 Malnutrition and falls can be prevented and depression treated in patients outside the hospital,4345 but it is unclear whether these maladies can be prevented or treated effectively in hospitalized elders. Finally, intriguing evidence suggests that geriatric syndromes and their sequelae may be prevented and outcomes improved by caring for patients at home whenever possible, bringing intensive nursing and physician care into the home without some of the adverse effects of hospitalization.46
The physician workforce is not prepared to provide optimal care to hospitalized older persons. Few hospitalists or other hospital‐based physicians have received more than minimal training in geriatric medicine, and few geriatricians practice extensively in the hospital. At the same time that the ranks of physicians who consider themselves hospitalists have been expanding by 1000 or more a year in the United States, the number of certified geriatricians has been decreasing as hundreds decide each year not to renew their certificates.47, 48 Fewer than 300 geriatricians complete training each year and enter the workforce, and most new geriatricians practice in ambulatory or long‐term‐care settings. Wald's study in this issue indicates the paucity of geriatricians in hospital medicine (with the apparently single exception of the Mayo Clinic's Hospital Internal Medicine Group) and a relative lack of interest among hospitalists in developing knowledge about the effective and efficient treatment of older persons, in particular.49
OPPORTUNITIES
Opportunities to improve the care of hospitalized older patients arise from the state of the science in their care and from the common ground that hospitalists and geriatricians share. The older patients of both hospitalists and geriatricians are seriously ill, with annual mortality rates of 20%30% for patients with common conditions such as myocardial infarction or colon cancer and mortality rates of 50% or higher for patients with dementia or severe disability.5, 5053 We should view the care of our patients in the context of their prognoses,5, 54 recognizing that patients' preferences for the goals, style, and site of care vary widely.55, 56 The substantial association of mortality with geriatric syndromes such as disability, dementia, delirium, and depressionan association that is independent of pathophysiologic indicators of disease severitysuggests that substantial benefits may accrue by targeting interventions to the prevention or amelioration of these syndromes.5, 9, 10, 53, 57, 58
Hospitalists and geriatricians also share the perspective of working in complex systems in which the effectiveness, efficiency, and safety of care depend on system functions as well as on their technical expertise as individuals.5961 Together, and with colleagues in other disciplines, they may redesign how hospitals and the systems around them work to reduce errors, increase attention to aspects of care that are easily overlooked, and improve patient outcomes.
BARRIERS
Hospitalists and geriatricians face barriers to improving care for hospitalized older patients. First, gaps in knowledge limit the capacity to provide the care and achieve the outcomes desired. Fundamental discoveries in clinical science are needed to prevent or treat geriatric syndromes, to treat common diseases in the very old, and to put into practice what is known. Addressing these gaps in knowledge will require a sustained effort that spans methods and disciplines.
Second, the dominant reductionist paradigm values discovery of the mechanism of disease over discovery of ways to manage illness effectively and efficiently.6267 Similarly, diagnostic tests and therapies based on beliefs about the mechanism of diseasefor example, PET scans in persons with memory disorders and chemotherapy in persons with refractory cancersare pursued aggressively and paid handsomely, whereas efforts to reduce errors or improve continuity of care receive little attention or reward. The challenges of caring for hospitalized older patients will require advances on both fronts: in our knowledge of the pathogenesis of disorders that have proven resistant to current therapies (such as delirium) and in our knowledge of how to structure clinical care that engages patients and families and achieves desired outcomes effectively, consistently, and efficiently.
The structure and styles of our practices provide the third challenge. Hospitalists pride themselves on their efficient management of patients while maintaining or improving patient outcomes. A focus on efficient management can, however, lead to an assembly‐line approach, turning each patient into a series of do‐order‐call‐check tasks to get the patient out of the hospital as quickly as possible. This approach has advantages but may also blind physicians to the scope and complexity of issues that arise in caring for the very old through the course of an illness that often extends beyond hospitalization.25 Geriatricians pride themselves on their comprehensive management of patients, gathering clinical information from many sources (especially in the many patients with cognitive impairment), exploring and articulating goals of care, and assessing self‐care and neurologic, psychological, and social domains in addition to conventional pathophysiology. Yet too often, geriatricians are not available in hospitals, and as Wald found, they have rarely been integrated into hospitalist groups.
FIVE RECOMMENDATIONS FOR HOSPITALISTS AND GERIATRICIANS
I conclude with five recommendations for hospital‐based physicians who care for older patients and for geriatricians. First, step back, look at your patients, and note their predicament in its full complexity. Once hospitalists start looking for cognitive impairment, weakness, and difficulty walking and the difficulty of finding a good situation after leaving the hospital, it will be easy to see these problems. And once geriatricians start looking at why their patients are going into the hospital and what happens to them, it will be easy to see the need to become engaged. Seeing the full range of patients' problems won't address them, but we certainly won't address them if we don't look.
Second, learn what is known about how best to care for the aged and integrate this learning into your hospital practice. For hospitalists, learning how to identify each patient's goals of care, what works to prevent delirium and promote mobility, which drugs to avoid and which doses to modify, and how to access resources to help patients and families achieve their goals after they leave the hospital will benefit older patients. Pocket and PDA resources to extend learning are readily available.68 For geriatricians, learning how to avoid hospitalization (especially when resources can be mobilized to provide a hospital at home), how to work within the timeframe of hospitalization, and what current disease‐specific management strategies have been shown to be effective in the aged will benefit their patients. Maintaining the distinction between what is believed and what is known on the basis of high‐quality evidence will enhance learning and decrease the risk of stubbornly pursuing harmful or wasteful practices. This is especially important in situations where the evidence is weak and opinions are strong.
Third, to provide the best care for our older patients, we must embrace aging, not deny it. Most hospitalized older patients, and most patients of geriatricians, will decline and die in a few years. The inevitability of these outcomes may tempt us either to abandon our incurable patients or to focus single‐mindedly on treatable problems one at a time, rather than on the interplay of multiple problems in an individual person. Either choice is mistaken. Although we are powerless to prevent decline and death in the long run, we have a tremendous capacity to delay and ameliorate decline, to enhance comfort and joy, to protect from harm, and, often, to delay death.
Fourth, ask questions about what you do not know or understand. The risk, of course, is that your curiosity will be sparked, possibly slowing you in completing the myriad tasks to be donea risk worth taking. Will ACE inhibitors and beta‐blockers benefit patients with heart failure without systolic dysfunction? Why do so many older patients become delirious, and are features of hospitalization catalyzing the effects of disease in causing delirium? Why do we continue to send cognitively impaired patients home without scheduled follow‐up and with instruction sheets they cannot read, and how can we change the system to prevent this? If you cannot find answers to your questions grounded in strong evidence, maintain your skepticism about answers given easily.
Finally, consider discovering the answers to some of your questions. Part of the excitement of caring for the very old is that we have so much to learn and that what we do learn can be so powerful.
An emergency room resident once was instructing a medical student in how to place a nasogastric tube in order to evaluate a patient with melena and postural hypotension. When the tube came to a stop, the student connected a syringe to the tube and aspirated. Then, to the consternation of the resident, the student yanked out the tube as soon as he saw blood flowing into the syringe. Why'd you do that? the surprised resident asked. There's blood down there! came the quick reply.
Like that medical student, hospital‐based physicianshospitalists, geriatricians, and othersmay miss the boat when caring for hospitalized older patients. Hospitals are full, and they're filled largely with older patients. These patients, like those who are younger, generally want to be treated and sent home. Older patients, however, frequently pose specific challenges. They may talk and move more slowly, stay longer, and be more likely to die. They more often need help in caring for themselves, and many have lost the support necessary to remain at home, making it difficult for them to return there. In short, older patients often need more care and more time.
It may be tempting to ignore the challenges that arise in caring for older patients. An avoidance strategy is expedient, at least in the short term. Ultimately, however, ignoring the challenges of caring for older patients will prove no wiser than yanking the nasogastric tube. Instead, we can recognize the challenges and use this opportunity to learn to improve their care.
This article describes the state of the science in hospital care for older patients, opportunities awaiting those who care for these patients, and barriers to seizing those opportunities. I conclude with five recommendations for physicians who care for hospitalized older patients.
STATE OF THE SCIENCE
Older patients shape hospital medicine and will determine its future. In 2002 the 12% of the population age 65 years or older accounted for roughly 50% of all hospitalizations unrelated to childbirth.1, 2 Hospital admissions of older persons will balloon as the number of persons older than age 65 rises by a million a year, increasing from 13% of the population today to 21% by 2030.2
Older persons in hospitals pose substantial clinical challenges. Many have multiple comorbid diseases and virtually all have complex medical regimens.1, 35 Many have cognitive impairment or dementia, often accompanied by delirium, which hinder communication and can lead to behaviors that require extra attention and impede diagnostic tests and treatment.611 Some have difficulty walking and caring for themselves, and a third leave the hospital without having recovered to their baseline level of function, with those age 85 years or older at highest risk for this decline independent of the reason for admission.1215 These characteristics increase the care, resources, and staff time older patients need, prolong their stays, and increase their hospital costs beyond those expected for their diagnosis.16 They also are at higher risk for iatrogenic complications, death, and rehospitalization,1720 and the risk of errors may be increased by frequent transitions in providers and sites of care.2125 Older persons require greater assistance at home, and yet they have often lost much of the support needed to live at home.10, 13, 20
Despite the magnitude of these challenges, we know surprisingly little about how best to care for hospitalized older persons, especially those older than age 75. The evidence base for treatment of specific common diseases is inadequate. The very old are underrepresented in clinical trials,26, 27 and the majority of older patients with common conditions such as heart failure may not meet the enrollment criteria for clinical trials.28 Thus, what is known about treating diseases in younger patients may be extrapolated to determine treatments in older persons based only on a leap of faith, which may be misguided.29, 30 In fact, the efficacy of conventional treatments for common conditions (e.g., acute myocardial infarction and hypertension) may diminish with age,31, 32 indicating that clinical trials targeted specifically to older patients may be necessary.
Despite the dearth of evidence about the management of common diseases in hospitalized older patients, hospital‐based geriatricians have developed substantial high‐grade evidence about the prevention of two geriatric syndromes, functional disability and delirium. The incidence of both syndromes can be reduced (without increasing hospital or health care costs) by multicomponent interventions that include comprehensive assessment, targeted treatment, and environmental modification to promote independence and safety.3, 3335 Moreover, the randomized trials that evaluated these interventions have provided models for how other innovations by hospital‐based physicians can be evaluated. Despite the evidence that these approaches are effective and either cost saving or cost neutral, these models have not been widely adopted.36
Many challenges in the prevention and management of geriatric syndromes in the hospital remain. For example, sophisticated approaches to the management of delirium are disappointingonce delirium has developed, intensive state‐of‐the‐art approaches to its management are no more effective than standard care in shortening its duration or ameliorating its sequelae.37, 38 The indiscriminate use of indwelling urinary catheters is decried, but there is no evidence that their use is declining, even in patients without an indication for catheterization.3942 Malnutrition and falls can be prevented and depression treated in patients outside the hospital,4345 but it is unclear whether these maladies can be prevented or treated effectively in hospitalized elders. Finally, intriguing evidence suggests that geriatric syndromes and their sequelae may be prevented and outcomes improved by caring for patients at home whenever possible, bringing intensive nursing and physician care into the home without some of the adverse effects of hospitalization.46
The physician workforce is not prepared to provide optimal care to hospitalized older persons. Few hospitalists or other hospital‐based physicians have received more than minimal training in geriatric medicine, and few geriatricians practice extensively in the hospital. At the same time that the ranks of physicians who consider themselves hospitalists have been expanding by 1000 or more a year in the United States, the number of certified geriatricians has been decreasing as hundreds decide each year not to renew their certificates.47, 48 Fewer than 300 geriatricians complete training each year and enter the workforce, and most new geriatricians practice in ambulatory or long‐term‐care settings. Wald's study in this issue indicates the paucity of geriatricians in hospital medicine (with the apparently single exception of the Mayo Clinic's Hospital Internal Medicine Group) and a relative lack of interest among hospitalists in developing knowledge about the effective and efficient treatment of older persons, in particular.49
OPPORTUNITIES
Opportunities to improve the care of hospitalized older patients arise from the state of the science in their care and from the common ground that hospitalists and geriatricians share. The older patients of both hospitalists and geriatricians are seriously ill, with annual mortality rates of 20%30% for patients with common conditions such as myocardial infarction or colon cancer and mortality rates of 50% or higher for patients with dementia or severe disability.5, 5053 We should view the care of our patients in the context of their prognoses,5, 54 recognizing that patients' preferences for the goals, style, and site of care vary widely.55, 56 The substantial association of mortality with geriatric syndromes such as disability, dementia, delirium, and depressionan association that is independent of pathophysiologic indicators of disease severitysuggests that substantial benefits may accrue by targeting interventions to the prevention or amelioration of these syndromes.5, 9, 10, 53, 57, 58
Hospitalists and geriatricians also share the perspective of working in complex systems in which the effectiveness, efficiency, and safety of care depend on system functions as well as on their technical expertise as individuals.5961 Together, and with colleagues in other disciplines, they may redesign how hospitals and the systems around them work to reduce errors, increase attention to aspects of care that are easily overlooked, and improve patient outcomes.
BARRIERS
Hospitalists and geriatricians face barriers to improving care for hospitalized older patients. First, gaps in knowledge limit the capacity to provide the care and achieve the outcomes desired. Fundamental discoveries in clinical science are needed to prevent or treat geriatric syndromes, to treat common diseases in the very old, and to put into practice what is known. Addressing these gaps in knowledge will require a sustained effort that spans methods and disciplines.
Second, the dominant reductionist paradigm values discovery of the mechanism of disease over discovery of ways to manage illness effectively and efficiently.6267 Similarly, diagnostic tests and therapies based on beliefs about the mechanism of diseasefor example, PET scans in persons with memory disorders and chemotherapy in persons with refractory cancersare pursued aggressively and paid handsomely, whereas efforts to reduce errors or improve continuity of care receive little attention or reward. The challenges of caring for hospitalized older patients will require advances on both fronts: in our knowledge of the pathogenesis of disorders that have proven resistant to current therapies (such as delirium) and in our knowledge of how to structure clinical care that engages patients and families and achieves desired outcomes effectively, consistently, and efficiently.
The structure and styles of our practices provide the third challenge. Hospitalists pride themselves on their efficient management of patients while maintaining or improving patient outcomes. A focus on efficient management can, however, lead to an assembly‐line approach, turning each patient into a series of do‐order‐call‐check tasks to get the patient out of the hospital as quickly as possible. This approach has advantages but may also blind physicians to the scope and complexity of issues that arise in caring for the very old through the course of an illness that often extends beyond hospitalization.25 Geriatricians pride themselves on their comprehensive management of patients, gathering clinical information from many sources (especially in the many patients with cognitive impairment), exploring and articulating goals of care, and assessing self‐care and neurologic, psychological, and social domains in addition to conventional pathophysiology. Yet too often, geriatricians are not available in hospitals, and as Wald found, they have rarely been integrated into hospitalist groups.
FIVE RECOMMENDATIONS FOR HOSPITALISTS AND GERIATRICIANS
I conclude with five recommendations for hospital‐based physicians who care for older patients and for geriatricians. First, step back, look at your patients, and note their predicament in its full complexity. Once hospitalists start looking for cognitive impairment, weakness, and difficulty walking and the difficulty of finding a good situation after leaving the hospital, it will be easy to see these problems. And once geriatricians start looking at why their patients are going into the hospital and what happens to them, it will be easy to see the need to become engaged. Seeing the full range of patients' problems won't address them, but we certainly won't address them if we don't look.
Second, learn what is known about how best to care for the aged and integrate this learning into your hospital practice. For hospitalists, learning how to identify each patient's goals of care, what works to prevent delirium and promote mobility, which drugs to avoid and which doses to modify, and how to access resources to help patients and families achieve their goals after they leave the hospital will benefit older patients. Pocket and PDA resources to extend learning are readily available.68 For geriatricians, learning how to avoid hospitalization (especially when resources can be mobilized to provide a hospital at home), how to work within the timeframe of hospitalization, and what current disease‐specific management strategies have been shown to be effective in the aged will benefit their patients. Maintaining the distinction between what is believed and what is known on the basis of high‐quality evidence will enhance learning and decrease the risk of stubbornly pursuing harmful or wasteful practices. This is especially important in situations where the evidence is weak and opinions are strong.
Third, to provide the best care for our older patients, we must embrace aging, not deny it. Most hospitalized older patients, and most patients of geriatricians, will decline and die in a few years. The inevitability of these outcomes may tempt us either to abandon our incurable patients or to focus single‐mindedly on treatable problems one at a time, rather than on the interplay of multiple problems in an individual person. Either choice is mistaken. Although we are powerless to prevent decline and death in the long run, we have a tremendous capacity to delay and ameliorate decline, to enhance comfort and joy, to protect from harm, and, often, to delay death.
Fourth, ask questions about what you do not know or understand. The risk, of course, is that your curiosity will be sparked, possibly slowing you in completing the myriad tasks to be donea risk worth taking. Will ACE inhibitors and beta‐blockers benefit patients with heart failure without systolic dysfunction? Why do so many older patients become delirious, and are features of hospitalization catalyzing the effects of disease in causing delirium? Why do we continue to send cognitively impaired patients home without scheduled follow‐up and with instruction sheets they cannot read, and how can we change the system to prevent this? If you cannot find answers to your questions grounded in strong evidence, maintain your skepticism about answers given easily.
Finally, consider discovering the answers to some of your questions. Part of the excitement of caring for the very old is that we have so much to learn and that what we do learn can be so powerful.
- ,.Hospitalization in the United States, 2002. Publication 05‐056.Washington (DC):AHRQ,2005.
- .Improving health care for older persons.Ann Intern Med.2003;139:421–424.
- ,,, et al.A controlled trial of inpatient and outpatient geriatric evaluation and management.N Engl J Med.2002;346:905–912.
- ,,, et al.Hospital diagnoses, Medicare charges, and nursing home admissions in the year when older persons become severely disabled.JAMA.1997;277:728–734.
- ,,, et al.Development and validation of a prognostic index for 1‐year mortality in older adults after hospitalization.JAMA.2001;285:2987–2994.
- ,,,.Delirium is independently associated with poor functional recovery after hip fracture.J Am Geriatr Soc.2000;48:618–624.
- ,,, et al.The course of delirium in older medical inpatients: a prospective study.J Gen Intern Med.2003;18:696–704.
- ,,,.Does delirium increase hospital stay?J Am Geriatr Soc.2003;51:1539–1546.
- ,,, et al.Does delirium contribute to poor hospital outcomes? A three‐site epidemiologic study.J Gen Intern Med.1998;13:234–242.
- ,,, et al.A predictive index for functional decline in hospitalized elderly medical patients.J Gen Intern Med.1993;8:645–652.
- ,,.A prospective study of delirium in hospitalized elderly.JAMA.1990;263:1097–1101.
- ,,, et al.Unsteadiness reported by older hospitalized patients predicts functional decline.J Am Geriatr Soc.2003;51:621–626.
- ,,, et al.Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age.J Am Geriatr Soc.2003;51:451–458.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,, et al.Functional disability in the hospitalized elderly.JAMA.1982;248:847–850.
- ,,, et al.Diagnosis‐related group‐adjusted hospital costs are higher in older medical patients with lower functional status.J Am Geriatr Soc.2003;51:1729–1734.
- ,.Adverse events, negligence in hospitalized patients: results from the Harvard Medical Practice Study.Perspect Healthc Risk Manage.1991;11(2):2–8.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I.N Engl J Med.1991;324:370–376.
- ,,, et al.The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II.N Engl J Med.1991;324:377–384.
- ,,,.Effects of functional status changes before and during hospitalization on nursing home admission of older adults.J Gerontol A Biol Sci Med Sci.1999;54:M521–M526.
- ,,.Characterization of geriatric drug‐related hospital readmissions.Med Care.1991;29:989–1003.
- ,,,.The impact of clinical pharmacists' consultations on physicians' geriatric drug prescribing. A randomized controlled trial.Med Care.1992;30:646–658.
- ,,,.Posthospital medication discrepancies: prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,.A new tool for identifying discrepancies in postacute medications for community‐dwelling older adults.Am J Geriatr Pharmacother.2004;2(2):141–147.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141:533–536.
- ,,, et al.Enrollment of older persons in cancer trials after the medicare reimbursement policy change.Arch Intern Med.2005;165:1514–1520.
- ,,, et al.Underrepresentation of patients 65 years of age or older in cancer‐treatment trials.N Engl J Med.1999;341:2061–2067.
- ,,, et al.Most hospitalized older persons do not meet the enrollment criteria for clinical trials in heart failure.Am Heart J.2003;146(2):250–257.
- ,.Problems in the “evidence” of “evidence‐based medicine.”Am J Med.1997;103:529–535.
- .National initiatives in ageing research in the United Kingdom.Age Ageing.2002;31(2):93–95.
- .Embracing complexity: A consideration of hypertension in the very old.J Gerontol A Biol Sci Med Sci.2003;58:653–658.
- ,,, et al.Lack of benefit for intravenous thrombolysis in patients with myocardial infarction who are older than 75 years.Circulation.2000;101:2239–2246.
- ,,, et al.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,,.Dissemination and characteristics of acute care for elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19(1):220–227.
- ,.Treatment of delirium in older medical inpatients: a challenge for geriatric specialists.J Am Geriatr Soc.2002;50:2101–2103.
- ,,, et al.Systematic detection and multidisciplinary care of delirium in older medical inpatients: a randomized trial.CMAJ.2002;167:753–759.
- .Clinical and economic consequences of nosocomial catheter‐related bacteriuria.Am J Infect Control.2000;28(1):68–75.
- ,.Preventing catheter‐related bacteriuria: should we? Can we? How?Arch Intern Med.1999;159:800–808.
- ,,.Indwelling urinary catheters: a one‐point restraint?Ann Intern Med.2002;137(2):125–127.
- ,, et al.Risk factors for indwelling urinary catheterization among older hospitalized patients without a specific medical indication for catheterization.J Patient Saf.2005. In press.
- ,,.Protein and energy supplementation in elderly people at risk from malnutrition.Cochrane Database Syst Rev.2005(2):CD003288.
- .Clinical practice. Preventing falls in elderly persons.N Engl J Med.2003;348(1):42–49.
- ,,, et al.Collaborative care management of late‐life depression in the primary care setting: a randomized controlled trial.JAMA.2002;288:2836–2845.
- ,,,,,.Hospital in the home: a randomised controlled trial.Med J Aust.1999;170(4):156–160.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350:1935–1936.
- ,,,.Academic geriatric programs in US allopathic and osteopathic medical schools.JAMA.2002;288:2313–2319.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,, et al.The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care.Ann Intern Med.2003;138:273–287.
- ,,, et al.The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care.Ann Intern Med.2003;138:288–298.
- ,.Mortality from pneumonia and hip fractures in patients with advanced dementia.JAMA.2000;284:2447–2448.
- ,.Survival in end‐stage dementia following acute illness.JAMA.2000;284(1):47–52.
- ,.Cancer screening in elderly patients: a framework for individualized decision making.JAMA.2001;285:2750–2756.
- ,,,.Understanding the treatment preferences of seriously ill patients.N Engl J Med.2002;346:1061–1066.
- ,,, et al.Health values of hospitalized patients 80 years or older. HELP Investigators. Hospitalized Elderly Longitudinal Project.JAMA.1998;279:371–375.
- ,,, et al.Depressive symptoms and 3‐year mortality in older hospitalized medical patients.Ann Intern Med.1999;130:563–569.
- ,,, et al.Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons.Ann Intern Med.1997;126:417–425.
- ,,,.Five system barriers to achieving ultrasafe health care.Ann Intern Med.2005;142:756–764.
- .Specialized care for elderly patients.N Engl J Med.2002;346:874.
- .The end of the beginning: patient safety five years after ‘To Err Is Human.’Health Aff (Millwood).2004;Suppl Web Exclusives:W4–534–545.
- .An additional basic science for clinical medicine: II. The limitations of randomized trials.Ann Intern Med.1983;99:544–550.
- .An additional basic science for clinical medicine: III. The challenges of comparison and measurement.Ann Intern Med.1983;99:705–712.
- .An additional basic science for clinical medicine: IV. The development of clinimetrics.Ann Intern Med.1983;99:843–848.
- .An additional basic science for clinical medicine: I. The constraining fundamental paradigms.Ann Intern Med.1983;99:393–397.
- ,.The end of the disease era.Am J Med.2004;116(3):179–185.
- ,, Agostini JV. Potential pitfalls of disease‐specific guidelines for patients with multiple conditions.N Engl J Med.2004;351:2870–2874.
- ,,, et al.Geriatrics at your fingertips: 2005.7th ed.Malden (MA):Blackwell Publishing, for the American Geriatrics Society,2005.
- ,.Hospitalization in the United States, 2002. Publication 05‐056.Washington (DC):AHRQ,2005.
- .Improving health care for older persons.Ann Intern Med.2003;139:421–424.
- ,,, et al.A controlled trial of inpatient and outpatient geriatric evaluation and management.N Engl J Med.2002;346:905–912.
- ,,, et al.Hospital diagnoses, Medicare charges, and nursing home admissions in the year when older persons become severely disabled.JAMA.1997;277:728–734.
- ,,, et al.Development and validation of a prognostic index for 1‐year mortality in older adults after hospitalization.JAMA.2001;285:2987–2994.
- ,,,.Delirium is independently associated with poor functional recovery after hip fracture.J Am Geriatr Soc.2000;48:618–624.
- ,,, et al.The course of delirium in older medical inpatients: a prospective study.J Gen Intern Med.2003;18:696–704.
- ,,,.Does delirium increase hospital stay?J Am Geriatr Soc.2003;51:1539–1546.
- ,,, et al.Does delirium contribute to poor hospital outcomes? A three‐site epidemiologic study.J Gen Intern Med.1998;13:234–242.
- ,,, et al.A predictive index for functional decline in hospitalized elderly medical patients.J Gen Intern Med.1993;8:645–652.
- ,,.A prospective study of delirium in hospitalized elderly.JAMA.1990;263:1097–1101.
- ,,, et al.Unsteadiness reported by older hospitalized patients predicts functional decline.J Am Geriatr Soc.2003;51:621–626.
- ,,, et al.Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age.J Am Geriatr Soc.2003;51:451–458.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,, et al.Functional disability in the hospitalized elderly.JAMA.1982;248:847–850.
- ,,, et al.Diagnosis‐related group‐adjusted hospital costs are higher in older medical patients with lower functional status.J Am Geriatr Soc.2003;51:1729–1734.
- ,.Adverse events, negligence in hospitalized patients: results from the Harvard Medical Practice Study.Perspect Healthc Risk Manage.1991;11(2):2–8.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I.N Engl J Med.1991;324:370–376.
- ,,, et al.The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II.N Engl J Med.1991;324:377–384.
- ,,,.Effects of functional status changes before and during hospitalization on nursing home admission of older adults.J Gerontol A Biol Sci Med Sci.1999;54:M521–M526.
- ,,.Characterization of geriatric drug‐related hospital readmissions.Med Care.1991;29:989–1003.
- ,,,.The impact of clinical pharmacists' consultations on physicians' geriatric drug prescribing. A randomized controlled trial.Med Care.1992;30:646–658.
- ,,,.Posthospital medication discrepancies: prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,.A new tool for identifying discrepancies in postacute medications for community‐dwelling older adults.Am J Geriatr Pharmacother.2004;2(2):141–147.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141:533–536.
- ,,, et al.Enrollment of older persons in cancer trials after the medicare reimbursement policy change.Arch Intern Med.2005;165:1514–1520.
- ,,, et al.Underrepresentation of patients 65 years of age or older in cancer‐treatment trials.N Engl J Med.1999;341:2061–2067.
- ,,, et al.Most hospitalized older persons do not meet the enrollment criteria for clinical trials in heart failure.Am Heart J.2003;146(2):250–257.
- ,.Problems in the “evidence” of “evidence‐based medicine.”Am J Med.1997;103:529–535.
- .National initiatives in ageing research in the United Kingdom.Age Ageing.2002;31(2):93–95.
- .Embracing complexity: A consideration of hypertension in the very old.J Gerontol A Biol Sci Med Sci.2003;58:653–658.
- ,,, et al.Lack of benefit for intravenous thrombolysis in patients with myocardial infarction who are older than 75 years.Circulation.2000;101:2239–2246.
- ,,, et al.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,,.Dissemination and characteristics of acute care for elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19(1):220–227.
- ,.Treatment of delirium in older medical inpatients: a challenge for geriatric specialists.J Am Geriatr Soc.2002;50:2101–2103.
- ,,, et al.Systematic detection and multidisciplinary care of delirium in older medical inpatients: a randomized trial.CMAJ.2002;167:753–759.
- .Clinical and economic consequences of nosocomial catheter‐related bacteriuria.Am J Infect Control.2000;28(1):68–75.
- ,.Preventing catheter‐related bacteriuria: should we? Can we? How?Arch Intern Med.1999;159:800–808.
- ,,.Indwelling urinary catheters: a one‐point restraint?Ann Intern Med.2002;137(2):125–127.
- ,, et al.Risk factors for indwelling urinary catheterization among older hospitalized patients without a specific medical indication for catheterization.J Patient Saf.2005. In press.
- ,,.Protein and energy supplementation in elderly people at risk from malnutrition.Cochrane Database Syst Rev.2005(2):CD003288.
- .Clinical practice. Preventing falls in elderly persons.N Engl J Med.2003;348(1):42–49.
- ,,, et al.Collaborative care management of late‐life depression in the primary care setting: a randomized controlled trial.JAMA.2002;288:2836–2845.
- ,,,,,.Hospital in the home: a randomised controlled trial.Med J Aust.1999;170(4):156–160.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350:1935–1936.
- ,,,.Academic geriatric programs in US allopathic and osteopathic medical schools.JAMA.2002;288:2313–2319.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,, et al.The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care.Ann Intern Med.2003;138:273–287.
- ,,, et al.The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care.Ann Intern Med.2003;138:288–298.
- ,.Mortality from pneumonia and hip fractures in patients with advanced dementia.JAMA.2000;284:2447–2448.
- ,.Survival in end‐stage dementia following acute illness.JAMA.2000;284(1):47–52.
- ,.Cancer screening in elderly patients: a framework for individualized decision making.JAMA.2001;285:2750–2756.
- ,,,.Understanding the treatment preferences of seriously ill patients.N Engl J Med.2002;346:1061–1066.
- ,,, et al.Health values of hospitalized patients 80 years or older. HELP Investigators. Hospitalized Elderly Longitudinal Project.JAMA.1998;279:371–375.
- ,,, et al.Depressive symptoms and 3‐year mortality in older hospitalized medical patients.Ann Intern Med.1999;130:563–569.
- ,,, et al.Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons.Ann Intern Med.1997;126:417–425.
- ,,,.Five system barriers to achieving ultrasafe health care.Ann Intern Med.2005;142:756–764.
- .Specialized care for elderly patients.N Engl J Med.2002;346:874.
- .The end of the beginning: patient safety five years after ‘To Err Is Human.’Health Aff (Millwood).2004;Suppl Web Exclusives:W4–534–545.
- .An additional basic science for clinical medicine: II. The limitations of randomized trials.Ann Intern Med.1983;99:544–550.
- .An additional basic science for clinical medicine: III. The challenges of comparison and measurement.Ann Intern Med.1983;99:705–712.
- .An additional basic science for clinical medicine: IV. The development of clinimetrics.Ann Intern Med.1983;99:843–848.
- .An additional basic science for clinical medicine: I. The constraining fundamental paradigms.Ann Intern Med.1983;99:393–397.
- ,.The end of the disease era.Am J Med.2004;116(3):179–185.
- ,, Agostini JV. Potential pitfalls of disease‐specific guidelines for patients with multiple conditions.N Engl J Med.2004;351:2870–2874.
- ,,, et al.Geriatrics at your fingertips: 2005.7th ed.Malden (MA):Blackwell Publishing, for the American Geriatrics Society,2005.
View from the Hospital Bed
For many of you, the hospital has by now become your home away from home. You spend a great deal of time there. You know your way from the ER to the ICU and the morgue. You've learned the hierarchy of who can tell whom what to do, and when it's your turn to do so, you can rattle off an impressive string of acronyms and medspeak in rapid fire. And then, there's that white coat that gives you added stature and authority.
We, the patients, family members, and other concerned visitors, are babes in the woods in this setting. If we've been lucky in life heretofore, we find that visiting a hospital can be like stepping off a hijacked plane into a foreign country we never planned to visit. Few things look familiar. We don't fully understand what we're being made to do. We don't speak the language well enough to communicate with those surrounding us, and we're not certain how friendly they are or what might provoke them into hurting us or our loved ones.
The signs we see don't mean much to usthe few words we recognize tend to scare us more than anything else. We don't know how to interpret the various uniforms people are wearing, other than the white coats we're all familiar with. Quite a few of the busy people moving with confidence around us have the aura of authority figures, no matter what they're wearing. When it's our turn, they focus on us or our loved ones, freely taking samples of blood, attaching instruments, probing private body parts, and asking intensely personal questions. But they don't really say much at all directly to us, and they don't seem interested in a lot of what we try to tell them. We're left feeling confused, humiliated, and somewhat stupid. Obviously, we're not astute enough to figure out what they want us to tell them. Why couldn't we remember everything we'd eaten or taken in the last 24 hours? We failed the test, and the consequences could be life threatening.
I am not exaggerating the situation. Last winter, my husbandwho had some chronic health issues but was still able to hold down a demanding job and carry on a fairly normal lifewas taken down by a nasty anonymous virus that attacked several major organ systems. We thought it was a bad case of the flu. I only took him to the emergency room because his weakness failed to pass in a few days and listening to him struggle to breathe scared me badly. It was the doctor's answering service (not the doctor on call, who never returned my call) that advised me to take him to the ER.
Within the first 24 hours at the hospital, I lost all ability to communicate with my husband when he was sedated and hooked up to a ventilator. For the next three and a half weeks, he lay unconscious, struggling for survival, and I lived on what his doctors and nurses chose to tell me. And they weren't saying a lot that I could make sense of.
For one thing, as his condition worsened he was in the care of eight specialists. Each would tell me something different, and I wasn't equipped to put all these pieces of information together in a meaningful way. For example, early on, I heard the following statements from different doctors all in the same day: He has a virus. His lungs are in really bad shape, and he could die. There are some indications he had a heart attack. His kidneys are failing, and he's going to need dialysis.
I knew that viruses can kill people. I knew that my husband was considered a high risk for heart attacks and that his lungs had been compromised by years of smoking. But I could not fathom how all of these things were related, let alone what was causing the kidneys to fail at this particular time. It took a very long timedays, maybe a week or morebefore I had both the courage and opportunity to pester my husband's infectious disease specialist with so many questions that he explained that the virus had attacked the heart, lungs, and kidneys and that most of what we were seeing was the aftermath of that battle.
This same doctor also helped me by shedding light on why the brief reports I was receiving from different specialists often seemed, to my layman's ears, to contradict each other. (One day the cardiologist told me, His heart's basically in pretty good shape. Yet, a scant hour later, the pulmonary specialist informed me, He's getting worse. He could die.) Each specialist, he told me, tends to focus on the area of the body he or she specializes in, not the patient's overall condition, and their comments reflect that narrow focus. How long would it have taken me to figure that out, if not for this man?
A lot of the frustration I felt as I chased after valuable tidbits of information about my husband's condition could have been alleviated with just a few words. Some days it would have been enough just to have had my anguish acknowledged with something as simple as I know you're frustrated and tired of hearing that we have no clear answers. Believe me, we want a better understanding of what's happening to your husband, too.
Aside from having to assemble the comments my husband's many doctors gave me into a comprehensive picture, I grew very weary of trying to catch these men and women as they came through on their rounds. Some routinely came through the ICU before the start of visiting hours each day. A few had no discernable routine at allI was as likely to encounter them at 8:30 p.m. as at 3 p.m. or 10 a.m. Yet if I was not at my husband's bedside or in the ICU waiting room, I'd get no report from them that day. This system forces the family to forgo any semblance of a normal life. In my case, there were no other family members with which to trade off this vigil, so I missed doctors whenever I went home or out of the room for a bite to eat.
I do not believe that our local hospital is unusual in any of these respects. In talking to people in other parts of the country who've been through a hospital experience, I have heard similar complaints voiced over and over.
And I do not question the quality of the medical care my husband received. As far as I know, everyone involved did their best to save him. Sadly, they did not succeed. Doug died on March 16, 2005, after five and a half weeks in the ICU. Many very good‐hearted, caring people worked on him during that time.
But some, though pleasant, didn't go out of their way to help me one iota. The day my husband started waking up after 25 days in a comalike state, I was in a funk and had found excuses to stay home until midafternoon, figuring there'd be no change in his condition. When I finally dragged myself into his room and spoke to him, I was astonished to see him react with a very slight head movement. Overjoyed, I immediately informed his nurse that he had responded to me, and she replied with a smile, Yes, I know. He's been responsive all day!
Now, these people knew that I'd been hovering at his bedside for 25 days, anxiously waiting for him to wake up, pestering them about why he wasn't and asking what was wrong. Did no one think this development worth a phone call to me?
Since my husband's death, I have heard that some hospitals have patient advocates and hospitalists, but my impression is that a fairly small percentage of hospitals have invested in these types of positions. And I question how well one or two such people in a hospital full of sick patients can help everyone who needs their services. It was hard enough for me to connect with the one woman in our hospital who, during the short time my husband seemed to be on the way to recovering, could help to arrange his transfer to a long‐term care facility.
My point is, the system that is routinely followed in most hospitalsthe system that determines doctors' routines, the system that causes health care workers to tend to treat patients and their families more like objects than human beingsdoes not do service to those it was set up to serve.
My point is, when it's everyone's responsibility to communicate with a patient's family, it winds up being no one's responsibility. Hospitals need to assign this responsibility to a specific person when a critically ill patient is in the care of a team of specialists.
My point is, please think of us wandering lost and scared in that foreign land you call home the next time you encounter one of us there.
For many of you, the hospital has by now become your home away from home. You spend a great deal of time there. You know your way from the ER to the ICU and the morgue. You've learned the hierarchy of who can tell whom what to do, and when it's your turn to do so, you can rattle off an impressive string of acronyms and medspeak in rapid fire. And then, there's that white coat that gives you added stature and authority.
We, the patients, family members, and other concerned visitors, are babes in the woods in this setting. If we've been lucky in life heretofore, we find that visiting a hospital can be like stepping off a hijacked plane into a foreign country we never planned to visit. Few things look familiar. We don't fully understand what we're being made to do. We don't speak the language well enough to communicate with those surrounding us, and we're not certain how friendly they are or what might provoke them into hurting us or our loved ones.
The signs we see don't mean much to usthe few words we recognize tend to scare us more than anything else. We don't know how to interpret the various uniforms people are wearing, other than the white coats we're all familiar with. Quite a few of the busy people moving with confidence around us have the aura of authority figures, no matter what they're wearing. When it's our turn, they focus on us or our loved ones, freely taking samples of blood, attaching instruments, probing private body parts, and asking intensely personal questions. But they don't really say much at all directly to us, and they don't seem interested in a lot of what we try to tell them. We're left feeling confused, humiliated, and somewhat stupid. Obviously, we're not astute enough to figure out what they want us to tell them. Why couldn't we remember everything we'd eaten or taken in the last 24 hours? We failed the test, and the consequences could be life threatening.
I am not exaggerating the situation. Last winter, my husbandwho had some chronic health issues but was still able to hold down a demanding job and carry on a fairly normal lifewas taken down by a nasty anonymous virus that attacked several major organ systems. We thought it was a bad case of the flu. I only took him to the emergency room because his weakness failed to pass in a few days and listening to him struggle to breathe scared me badly. It was the doctor's answering service (not the doctor on call, who never returned my call) that advised me to take him to the ER.
Within the first 24 hours at the hospital, I lost all ability to communicate with my husband when he was sedated and hooked up to a ventilator. For the next three and a half weeks, he lay unconscious, struggling for survival, and I lived on what his doctors and nurses chose to tell me. And they weren't saying a lot that I could make sense of.
For one thing, as his condition worsened he was in the care of eight specialists. Each would tell me something different, and I wasn't equipped to put all these pieces of information together in a meaningful way. For example, early on, I heard the following statements from different doctors all in the same day: He has a virus. His lungs are in really bad shape, and he could die. There are some indications he had a heart attack. His kidneys are failing, and he's going to need dialysis.
I knew that viruses can kill people. I knew that my husband was considered a high risk for heart attacks and that his lungs had been compromised by years of smoking. But I could not fathom how all of these things were related, let alone what was causing the kidneys to fail at this particular time. It took a very long timedays, maybe a week or morebefore I had both the courage and opportunity to pester my husband's infectious disease specialist with so many questions that he explained that the virus had attacked the heart, lungs, and kidneys and that most of what we were seeing was the aftermath of that battle.
This same doctor also helped me by shedding light on why the brief reports I was receiving from different specialists often seemed, to my layman's ears, to contradict each other. (One day the cardiologist told me, His heart's basically in pretty good shape. Yet, a scant hour later, the pulmonary specialist informed me, He's getting worse. He could die.) Each specialist, he told me, tends to focus on the area of the body he or she specializes in, not the patient's overall condition, and their comments reflect that narrow focus. How long would it have taken me to figure that out, if not for this man?
A lot of the frustration I felt as I chased after valuable tidbits of information about my husband's condition could have been alleviated with just a few words. Some days it would have been enough just to have had my anguish acknowledged with something as simple as I know you're frustrated and tired of hearing that we have no clear answers. Believe me, we want a better understanding of what's happening to your husband, too.
Aside from having to assemble the comments my husband's many doctors gave me into a comprehensive picture, I grew very weary of trying to catch these men and women as they came through on their rounds. Some routinely came through the ICU before the start of visiting hours each day. A few had no discernable routine at allI was as likely to encounter them at 8:30 p.m. as at 3 p.m. or 10 a.m. Yet if I was not at my husband's bedside or in the ICU waiting room, I'd get no report from them that day. This system forces the family to forgo any semblance of a normal life. In my case, there were no other family members with which to trade off this vigil, so I missed doctors whenever I went home or out of the room for a bite to eat.
I do not believe that our local hospital is unusual in any of these respects. In talking to people in other parts of the country who've been through a hospital experience, I have heard similar complaints voiced over and over.
And I do not question the quality of the medical care my husband received. As far as I know, everyone involved did their best to save him. Sadly, they did not succeed. Doug died on March 16, 2005, after five and a half weeks in the ICU. Many very good‐hearted, caring people worked on him during that time.
But some, though pleasant, didn't go out of their way to help me one iota. The day my husband started waking up after 25 days in a comalike state, I was in a funk and had found excuses to stay home until midafternoon, figuring there'd be no change in his condition. When I finally dragged myself into his room and spoke to him, I was astonished to see him react with a very slight head movement. Overjoyed, I immediately informed his nurse that he had responded to me, and she replied with a smile, Yes, I know. He's been responsive all day!
Now, these people knew that I'd been hovering at his bedside for 25 days, anxiously waiting for him to wake up, pestering them about why he wasn't and asking what was wrong. Did no one think this development worth a phone call to me?
Since my husband's death, I have heard that some hospitals have patient advocates and hospitalists, but my impression is that a fairly small percentage of hospitals have invested in these types of positions. And I question how well one or two such people in a hospital full of sick patients can help everyone who needs their services. It was hard enough for me to connect with the one woman in our hospital who, during the short time my husband seemed to be on the way to recovering, could help to arrange his transfer to a long‐term care facility.
My point is, the system that is routinely followed in most hospitalsthe system that determines doctors' routines, the system that causes health care workers to tend to treat patients and their families more like objects than human beingsdoes not do service to those it was set up to serve.
My point is, when it's everyone's responsibility to communicate with a patient's family, it winds up being no one's responsibility. Hospitals need to assign this responsibility to a specific person when a critically ill patient is in the care of a team of specialists.
My point is, please think of us wandering lost and scared in that foreign land you call home the next time you encounter one of us there.
For many of you, the hospital has by now become your home away from home. You spend a great deal of time there. You know your way from the ER to the ICU and the morgue. You've learned the hierarchy of who can tell whom what to do, and when it's your turn to do so, you can rattle off an impressive string of acronyms and medspeak in rapid fire. And then, there's that white coat that gives you added stature and authority.
We, the patients, family members, and other concerned visitors, are babes in the woods in this setting. If we've been lucky in life heretofore, we find that visiting a hospital can be like stepping off a hijacked plane into a foreign country we never planned to visit. Few things look familiar. We don't fully understand what we're being made to do. We don't speak the language well enough to communicate with those surrounding us, and we're not certain how friendly they are or what might provoke them into hurting us or our loved ones.
The signs we see don't mean much to usthe few words we recognize tend to scare us more than anything else. We don't know how to interpret the various uniforms people are wearing, other than the white coats we're all familiar with. Quite a few of the busy people moving with confidence around us have the aura of authority figures, no matter what they're wearing. When it's our turn, they focus on us or our loved ones, freely taking samples of blood, attaching instruments, probing private body parts, and asking intensely personal questions. But they don't really say much at all directly to us, and they don't seem interested in a lot of what we try to tell them. We're left feeling confused, humiliated, and somewhat stupid. Obviously, we're not astute enough to figure out what they want us to tell them. Why couldn't we remember everything we'd eaten or taken in the last 24 hours? We failed the test, and the consequences could be life threatening.
I am not exaggerating the situation. Last winter, my husbandwho had some chronic health issues but was still able to hold down a demanding job and carry on a fairly normal lifewas taken down by a nasty anonymous virus that attacked several major organ systems. We thought it was a bad case of the flu. I only took him to the emergency room because his weakness failed to pass in a few days and listening to him struggle to breathe scared me badly. It was the doctor's answering service (not the doctor on call, who never returned my call) that advised me to take him to the ER.
Within the first 24 hours at the hospital, I lost all ability to communicate with my husband when he was sedated and hooked up to a ventilator. For the next three and a half weeks, he lay unconscious, struggling for survival, and I lived on what his doctors and nurses chose to tell me. And they weren't saying a lot that I could make sense of.
For one thing, as his condition worsened he was in the care of eight specialists. Each would tell me something different, and I wasn't equipped to put all these pieces of information together in a meaningful way. For example, early on, I heard the following statements from different doctors all in the same day: He has a virus. His lungs are in really bad shape, and he could die. There are some indications he had a heart attack. His kidneys are failing, and he's going to need dialysis.
I knew that viruses can kill people. I knew that my husband was considered a high risk for heart attacks and that his lungs had been compromised by years of smoking. But I could not fathom how all of these things were related, let alone what was causing the kidneys to fail at this particular time. It took a very long timedays, maybe a week or morebefore I had both the courage and opportunity to pester my husband's infectious disease specialist with so many questions that he explained that the virus had attacked the heart, lungs, and kidneys and that most of what we were seeing was the aftermath of that battle.
This same doctor also helped me by shedding light on why the brief reports I was receiving from different specialists often seemed, to my layman's ears, to contradict each other. (One day the cardiologist told me, His heart's basically in pretty good shape. Yet, a scant hour later, the pulmonary specialist informed me, He's getting worse. He could die.) Each specialist, he told me, tends to focus on the area of the body he or she specializes in, not the patient's overall condition, and their comments reflect that narrow focus. How long would it have taken me to figure that out, if not for this man?
A lot of the frustration I felt as I chased after valuable tidbits of information about my husband's condition could have been alleviated with just a few words. Some days it would have been enough just to have had my anguish acknowledged with something as simple as I know you're frustrated and tired of hearing that we have no clear answers. Believe me, we want a better understanding of what's happening to your husband, too.
Aside from having to assemble the comments my husband's many doctors gave me into a comprehensive picture, I grew very weary of trying to catch these men and women as they came through on their rounds. Some routinely came through the ICU before the start of visiting hours each day. A few had no discernable routine at allI was as likely to encounter them at 8:30 p.m. as at 3 p.m. or 10 a.m. Yet if I was not at my husband's bedside or in the ICU waiting room, I'd get no report from them that day. This system forces the family to forgo any semblance of a normal life. In my case, there were no other family members with which to trade off this vigil, so I missed doctors whenever I went home or out of the room for a bite to eat.
I do not believe that our local hospital is unusual in any of these respects. In talking to people in other parts of the country who've been through a hospital experience, I have heard similar complaints voiced over and over.
And I do not question the quality of the medical care my husband received. As far as I know, everyone involved did their best to save him. Sadly, they did not succeed. Doug died on March 16, 2005, after five and a half weeks in the ICU. Many very good‐hearted, caring people worked on him during that time.
But some, though pleasant, didn't go out of their way to help me one iota. The day my husband started waking up after 25 days in a comalike state, I was in a funk and had found excuses to stay home until midafternoon, figuring there'd be no change in his condition. When I finally dragged myself into his room and spoke to him, I was astonished to see him react with a very slight head movement. Overjoyed, I immediately informed his nurse that he had responded to me, and she replied with a smile, Yes, I know. He's been responsive all day!
Now, these people knew that I'd been hovering at his bedside for 25 days, anxiously waiting for him to wake up, pestering them about why he wasn't and asking what was wrong. Did no one think this development worth a phone call to me?
Since my husband's death, I have heard that some hospitals have patient advocates and hospitalists, but my impression is that a fairly small percentage of hospitals have invested in these types of positions. And I question how well one or two such people in a hospital full of sick patients can help everyone who needs their services. It was hard enough for me to connect with the one woman in our hospital who, during the short time my husband seemed to be on the way to recovering, could help to arrange his transfer to a long‐term care facility.
My point is, the system that is routinely followed in most hospitalsthe system that determines doctors' routines, the system that causes health care workers to tend to treat patients and their families more like objects than human beingsdoes not do service to those it was set up to serve.
My point is, when it's everyone's responsibility to communicate with a patient's family, it winds up being no one's responsibility. Hospitals need to assign this responsibility to a specific person when a critically ill patient is in the care of a team of specialists.
My point is, please think of us wandering lost and scared in that foreign land you call home the next time you encounter one of us there.
Clinical Conundrum
A 49‐year‐old man presented with 2 days of chills, fever, anorexia, and increased cough and dyspnea. The patient had a history of chronic obstructive pulmonary disease (COPD) and noted that his cough and dyspnea had increased above normal for several days. He was now dyspneic with minimal activity and had slept at a 45‐degree incline the night prior to evaluation due to dyspnea. He noted less improvement than usual with the use of his metered dose inhaler. His cough was occasionally productive of small amounts of white phlegm. He had vomited once. During a coughing episode the patient experienced a sudden onset of sharp right upper quadrant abdominal pain that worsened with coughing and sudden position changes. The patient denied a prior history of abdominal pain or surgery. The patient's last bowel movement was 2 days prior to admission. He denied melena or bright red blood per rectum.
My initial differential diagnosis for this patient's dyspnea and cough is pneumonia, acute exacerbation of COPD, or congestive heart failure. The presence of fever and anorexia increases the likelihood of infectious etiologies, whereas the presence of orthopnea points toward congestive heart failure. Noncardiac processessuch as a large pleural effusion or apical lung diseasecould also cause orthopnea. His abdominal pain could be a result of pneumonia alone (perhaps in the right lower lobe with diaphragmatic irritation), but I am also considering complications of pneumonia such as empyema. Although his abdominal pain, dyspnea, and cough could also be a result of hepatobiliary disease, a perforated viscus, or pancreatitis, we currently have little reason to suspect a direct abdominal etiology. My top diagnosis is community‐acquired pneumonia, perhaps accompanied by pleural effusion.
His medical history was significant for dilated cardiomyopathy and heavy alcohol use. His medications included various meter‐dosed inhalers, bupropion, digoxin, spironolactone, lisinopril, and metoprolol. He had never received corticosteroid therapy and had not previously been hospitalized for COPD‐related problems. He had smoked one pack of cigarettes daily for 40 years.
Heavy alcohol use is associated with an increased risk of several pulmonary infections such as gram‐negative necrotizing pneumonia (classically, Klebsiella pneumoniae), pneumococcal pneumonia, aspiration pneumonia, anaerobic lung abscesses, and tuberculosis. Given his right upper quadrant pain, acute alcoholic hepatitis and alcohol‐related pancreatitis enter the differential. His history of cardiomyopathy makes me consider congestive heart failure as more likely than before, and perhaps his abdominal pain is a result of hepatic congestion from right heart failure. His fever, however, cannot be attributed to cardiac failure. Less likely diagnoses include ischemic conditions related to his cardiomyopathy such as mesenteric ischemia from low perfusion or embolism from a cardiac thrombus. A pulmonary infection remains the most likely diagnosis.
He was an ill‐appearing man in moderate respiratory distress, looking older than his stated age. His temperature was 38.4C, heart rate 129 beats/minute, blood pressure 85/56 mm Hg, respiratory rate 24 breaths/minute, and oxygen saturation 92% on room air. A cardiovascular exam revealed no murmur, gallop, or rub. The jugular venous pulse was not elevated. His lungs were clear to auscultation. Abdominal exam revealed right‐sided abdominal tenderness that appeared to localize to the rectus sheath. Otherwise, the abdomen was soft, with normal bowel sounds and no organomegaly. Rectal examination revealed guaiac negative stool and no focal tenderness. His extremities were normal.
His vital signs are worrisome for impending cardiovascular collapse and shock, possibly due to sepsis. The relatively nonfocal cardiopulmonary exam is surprising given his initial symptoms and makes me wonder if his dyspnea is primarily related to an abdominal process leading to diaphragmatic irritation rather than to a thoracic process. Congestive heart failure seems unlikely given the lack of supportive physical examination findings. His abdominal exam findings are puzzling. Although his abdominal wall tenderness could be benignperhaps from muscular strain or a tear from coughingit could represent a more worrisome process such as infection or a hematoma in the abdominal wall muscles. Mesenteric ischemia is still possible, as the exam is often unimpressive. A hepatic abscess or subphrenic abscess should be considered, as physical exam findings in these conditions can be subtle.
My differential remains relatively unchanged, but I have now put consideration of a hepatic or subphrenic abscess higher on my list. Early empiric broad‐spectrum antibiotics seem necessary.
He had a white blood cell count of 26,700/mL with 92% neutrophils, a hemoglobin of 14.6 g/dL, and a platelet count of 312,000/mL. Sodium was 134 mmol/L, potassium was 4.3 mmol/L, chloride was 94 mmol/L, bicarbonate was 23 mmol/L, blood urea nitrogen was 23 mg/dL, and creatinine was 2.1 mg/dL. The results of the calcium, protein, albumin, and liver function tests were normal. Urinalysis was negative for protein and red blood cells. An electrocardiogram revealed sinus tachycardia. A chest radiograph at admission revealed mild opacities in both lower lobes and the right middle lobe consistent with either atelectasis or pneumonia (Fig. 1). A very small left effusion was also identified.
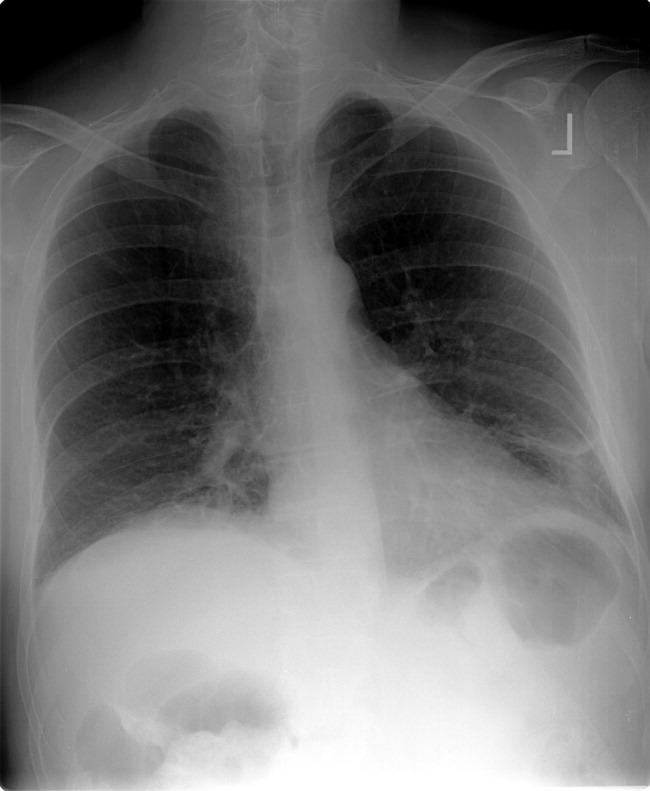
The additional data reinforce my clinical impression that this process is likely to be infectious. The chest radiograph is consistent with community‐acquired pneumonia, possibly from an atypical pathogen. Given his elevated creatinine, I am also considering a pulmonary‐renal syndrome such as vasculitis, though hematuria was not present. A subphrenic abscess, mesenteric ischemia, or an abdominal wall process (because his abdominal tenderness on exam still needs an explanation) remain possibilities; my suspicion would increase if he does not respond appropriately to therapy for community‐acquired pneumonia.
The clinical team's working diagnosis also was community‐acquired pneumonia. Blood and sputum cultures were obtained, and the patient was treated with intravenous ceftriaxone, azithromycin, and intravenous fluid. By the second day, his creatinine had normalized; however, his hypoxemia had worsened, and he now required supplemental oxygen. His temperature was 39.3C, and his heart rate was 150 beats/minute. The findings of an abdominal ultrasound of the kidneys, spleen, and right upper quadrant were normal.
It is too early to say the patient has failed therapy because a patient can get worse before getting better during the course of antibiotic therapy for community‐acquired pneumonia. Fever, for example, may take up to 7 days to resolve, depending on host factors and the pathogen. Though I typically wait about 72 hours before assuming a patient is not appropriately responding to therapy, the additional information has made me concerned. The degree of tachycardia is significant and warrants an EKG to exclude an arrthymia. I would also repeat the chest radiograph to evaluate for worsening infiltrates or increased pleural effusion.
On the third hospital day, the patient's abdominal pain had decreased with analgesia, but his fever, cough, and dyspnea remained largely unchanged. Antibiotics were changed to intravenous levofloxacin. A repeat chest radiograph revealed elevation of the right hemidiaphragm and bilateral effusions (Fig. 2). An electrocardiogram revealed sinus tachycardia. Blood cultures revealed no growth, and sputum cultures grew oral flora.
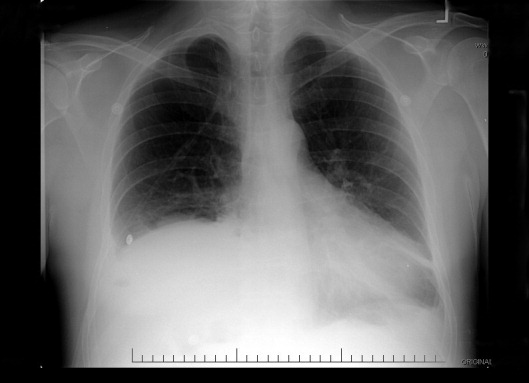
A significantly elevated right hemidiaphragm makes me reconsider the diagnosis of simple community‐acquired pneumonia. The differential diagnosis for an elevated hemidiaphragm is best considered by location in relation to the diaphragm. Causes above the diaphragm include rib fracture, atelectasis, pleural thickening, and volume loss of the lung for another reason (e.g., surgery, bronchial obstruction due to tumor or mucus plugging), as well as mimics such as a densely consolidated pneumonia, pulmonary infarction, or a subpulmonary effusion. Diaphragmatic causes include eventration, rupture, phrenic nerve weakness, and intrinsic weakness because of neuromuscular disease (usually bilateral). Causes below the diaphragm that must be considered are subphrenic or liver abscess, liver (and other abdominal) malignancy, pancreatic pseudocyst, and distended bowel. Given the clinical picture, I am focusing below the diaphragmespecially on a possible hepatic or subphrenic abscess (which could be missed on ultrasound) and mimics of it such as dense consolidation or a subpulmonary effusion. Given the lack of response to antibiotics, I need to consider an infection that is not being treated, either because of location (abscess, effusion) or microbiology (tuberculosis, a parasite, a fungus, resistant bacteria). After confirming that the patient has a substantive pleural effusion, he needs a thoracentesis.
On the fourth hospital day, his temperature was 38.8C, and his white blood cell count was 21,000/mL. A right‐sided thoracentesis was performed; approximately 250 cc of fluid was obtained. Pleural fluid analysis revealed bloody fluid, with a white blood cell count of 16,750/mL with 94% neutrophils, 40,000 red blood cells/mL, lactate dehydrogenase of 278 U/L (normal serum value 80200 U/L), protein of 3.7 g/dL, and glucose of 81 mg/dL. A pleural fluid pH was not obtained. A gram stain revealed many white blood cells with no organisms noted. Serum protein was 7.4 g/dL. These results were thought to represent an exudative parapneumonic effusion; levofloxacin and supplemental oxygen were continued.
The pleural fluid appears exudative, but I am not sure this man has a parapneumonic effusion because, despite clinical deterioration, an obvious infiltrate is not seen on interval chest radiography. We must look closely at the fluid because this is a bloody effusion and somewhat atypical for a parapneumonic effusion. Also, the effusion does not appear large enough to explain why he has not improved on the current antibiotics. We should thus reconsider our diagnosis and management. I would obtain additional imaging (such as an abdominal and chest computed tomography [CT]) and perhaps obtain a consultation from the pulmonary team regarding the postulated initial diagnosis of pneumonia with effusion.
On the fifth day of hospitalization, the patient's dyspnea and cough persisted but were improved. His abdominal pain was minimal and felt improved with flatus. Fever continued to 38.8C, and the white blood cell count was 20,000/mL. On examination the patient had decreased breath sounds at the right base and bibasilar crackles. His abdomen was soft, with tenderness in his right upper quadrant only with deep palpation; bowel sounds remained. An ultrasound of the chest was performed to look for a loculated effusion; however, no fluid was identified. The pulmonary consultant thought it likely that the patient had a subpulmonic effusion and recommended CT of the abdomen and chest.
His right upper quadrant tenderness is still unexplained. I would agree with the CT, primarily to evaluate other causes of his elevated diaphragm such as subphrenic or hepatic abscess. For now, I would make no change in antibiotic therapy.
On the sixth hospital day, the patient had an episode of bilious emesis. Chest and abdominal CT revealed collapse of the right middle and lower lobes with a small adjacent effusion, and a 6 6 16 cm abscess intimately opposed to the right lobe of the liver. Extending from the inferior extent of the abscess was a tubular thick‐walled structure connecting to the cecum that was suspicious of a thickened inflamed appendix. There was periappendiceal stranding suggesting inflammation. The small bowel was diffusely dilated up to 4.5 cm, suggesting a small bowel obstruction.
I suspect that his abscess is related to a perforated appendix and that the dilated small bowel is most likely a result of localized irritation of the bowel by the abscess and appendicitis. The collapsed lung is most likely due to local inflammation from the subdiaphragmatic abscess. Treatment should now be changed substantially. I would ask a surgeon to evaluate the patient because the most likely diagnosis is perforated appendicitis with abscess formation.
When the periappendiceal abscess was drained percutaneously, 190 mL of purulent fluid was removed. The cultures were positive for Klebsiella pneumonia, Enterococcus faecalis,and Streptococcus milleri. The patient was given 6 weeks of intravenous antibiotics with improvement in his clinical symptoms. During the interval the findings on his chest radiograph resolved completely. A laproscopic appendectomy 3 months later revealed significant right lower quadrant adhesions. The pathology specimen identified a distorted appendix with regeneration consistent with prior appendicitis. The patient was contacted 4 months after his surgery, and he reported that he was doing well, with no cardiopulmonary or gastrointestinal symptoms.
COMMENTARY
Community‐acquired pneumonia (CAP) is a common cause of acute illness and accounts for nearly 1 million admissions per year in the United States.1 The diagnosis of CAP is made when symptoms including dyspnea, fever, cough, or leukocytosis are present, with confirmation provided by a chest radiograph. Often the diagnosis is clear; however, there is no pathognomonic constellation of signs or symptoms that establish the diagnosis with certainty.2 Many physicians learn that pneumoniaespecially lower‐lobe pneumoniacan lead to abdominal findings such as upper quadrant pain, vomiting, and tenderness to palpation. Conversely, the patient discussed above illustrates that a primary abdominal process can also result in a symptom complex that mimics pneumonia.
The prevalence of CAP coupled with the inherent uncertainty of a clinical diagnosis of CAP leads to an important question: How long is too long before questioning the diagnosis? An analysis of the pneumonia Patient Outcomes Research Trial (PORT) limited to inpatients with CAP examined time to clinical stability. For the majority of patients, abnormal vital signs resolved within 23 days.3 In this study, 29% of patients had severe disease, and not surprisingly, these patients took longer to improve. Using the pneumonia severity index score, which accounts for age, comorbidity, abnormal vital signs, and laboratory data, the patient described in this article would be considered at high risk for death and complication with an estimated mortality of 9%.4 Using a combination of defervescence, resolution of tachycardia, tachypnea, and hypoxemia as markers of clinical stability, a patient like ours should respond within 4 days (with a range of 27 days). On the basis of these dataand the discrepancy between the patient's severe illness and relatively minor pulmonary infiltratesit seems reasonable to have considered this patient as failing CAP therapy as early as the fourth day of hospitalization.
In approximately 10% of hospitalized patients with CAP, the clinical course is protracted.5 When patients do not improve as quickly as expected, the reasons that could explain this should be investigated. In a cohort of 49 patients with CAP who failed therapy the most common reasons for failure to improve were severity of the pneumonia and drug resistance.6 A multicenter study found that the incidence of resistance to penicillin by Streptococcus pneumoniae, the most common bacterial pathogen in CAP, was 30%, with a 4% in vitro resistance rate to ceftriaxone.7 How well in vitro resistance predicts clinical response, however, is unclear. Risk factors for antibiotic resistance include close exposure to children, recent antibiotic use, and recent hospitalization. Immunosuppressive conditions should also be considered in patients who fail to improve. Suppurative complications of pneumoniasuch as empyema, parapneumonic effusion, and lung abscessalso delay recovery.
Another consideration in a patient with what appears to be a nonresolving pneumonia with pleural effusion is that the initial diagnosis is incorrect and the cause is extrathoracic. Pulmonary and cardiac diseases account for more than 90% of effusions, whereas less than 5% of pleural effusions result from intraabdominal causes.8 When should intraabdominal diseases be sought in patients with an effusion, fever, dyspnea, and cough? Light suggests that intraabdominal pathology should be investigated in patients who have pleural effusions without significant parenchymal disease.8 This point is underscored by the experience of our patient, whose chest radiographs showed, despite clinical decline, minimal airspace disease.
Several abdominal entities cause pleural effusion. Pancreatitis, either acute or chronic, with pseudocyst formation is the most common abdominal cause of exudative pleural effusions. Approximately 10% of patients with pancreatic disease will develop effusions, usually left‐sided.9 These left‐sided effusions are also seen in splenic abscesses, usually as a result of endocarditis. Intrahepatic abscess is associated with effusions in 20% of patients.10 A subphrenic abscess, as seen in our patient, is an uncommon cause of exudative pleural effusions. Historically, subphrenic abscesses resulted from a perforated viscus, with ruptured appendicitis the most common cause,11 followed by perforated peptic ulcers and biliary tract disease. With the advent of antibiotics, the causes of subphrenic abscess changed considerably, with the majority of current cases resulting from postsurgical complications.12 The findings of a chest radiograph are abnormal in 80% of patients with subphrenic abscess;1214 an elevated hemidiaphragm and pleural effusion are found in the majority of cases. The symptoms of a subphrenic abscess are nonspecific, and patient's complaints are equally split between predominantly thoracic and predomninantly abdominal complaints.15
Appendicitis, a common disease predominantly of the young, may lead to atypical presentations in older individuals. In a retrospective analysis of 113 patients older than 60 years with appendicitis, 70% presented in an atypical fashion.16 Typical symptoms include right lower quadrant pain, fever, anorexia and a white blood cell count greater than 10,000/mL. Fever was the most frequently absent symptom, seen in only 37% of older patients. In this cohort, approximately one third of older patients waited more than 48 hours prior to presentation. The time between symptom onset and clinical presentation is a strong predictor of perforation risk.17 As in this case, roughly 2% of patients with acute appendicitis will present with perforation and abscess formation.18 In such patients the management is initially conservative. Percutaneous drainage and broad spectrum antibiotics are the treatment of choice, followed by an interval appendectomy in 612 weeks.19 The rationale for delayed surgery is that earlier surgery may disseminate a localized inflammatory process.20
Community‐acquired pneumonia is a more frequent cause of hospital admission than is intraabdominal abscess. Physicians often face the dilemma of when to pursue alternative diagnoses after a patient who is thought to have an atypical presentation of a common disease (ie, CAP) fails to respond to conventional therapy. Although clinicians learn that right upper quadrant pain may be a symptom of pneumonia, our patient revealed that abdominal causes may mimic pneumonia and produce a pleural effusion. Determining whether the primary disease originates above or below the diaphragm is critical to guiding therapy. When patients fail to respond adequately to therapy, clinicians should set a low threshold for deciding to image the abdomen in a patient with modest pulmonary infiltrates, pleural effusion, and abdominal pain.
- ,,, et al.The cost of treating community‐acquired pneumonia.Clin Ther.1998;20:820–827.
- ,,.Does this patient have community‐acquired pneumonia? Diagnosing pneumonia by history and physical examination.JAMA.1997;278:1440–1445.
- ,,, et al.Time to clinical stability in patients hospitalized with community acquired pneumonia. Implications for practice guidelines.JAMA.1998;279:1452–1457.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,, et al.Utility of fiberoptic bronchoscopy in non resolving pneumonia.Chest.1990;98:1322–1326.
- ,,, et al.Antimicrobial treatment failures in patients with community acquired pneumonia. Causes and prognostic implications.Am J Respir Crit Care Med.2000;162:154–160.
- ,,, et al.Antimicrobial resistance with Streptococcus pneumoniae in the United States, 1997–98.Emerg Infect Dis.1999;5:757–765.
- ,.Pleural effusion. In:Murray JF,Nadel JA, eds.Textbook of respiratory medicine. 3rd ed.Philadelphia:WB Saunders,2000:2013–2041.
- ,,.Significance of pleural effusion in patients with acute pancreatitis.Am J Gastroenterol.1992;87:871–874.
- .Exudative pleural effusions secondary to gastrointestinal diseases.Clin Chest Med.1985;6(1):103–111.
- .Subphrenic abscess.Ann Surg.1963;158:240–248.
- ,,,.Upper abdominal abscess: a continuing and deadly problem.Am J Roentgenol.1980;134:759–765.
- .Subphrenic abscess. A clinical study of 101 cases.Acta Chir Scand.1959;117:388–408.
- ,,.Subphrenic abscess a continuing hazard.Am J Surg.1969:117–122.
- ,.Subphrenic abscess: a thoracoabdominal clinical complex. The changing picture with antibiotics.Am J Surg.1964;108:165–172.
- ,.What have we learned over the past 20 years about appendicitis in the elderly.Am J Surg.2003;185:198–201.
- ,,, et al.Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies.Am Surg.2000;66:548–554.
- ,,.Appendicitis with a palpable mass.Ann Surg.1981;193:227–229.
- ,,, et al.Nonoperative management of perforated appendicitis without periappendiceal mass.Am J Surg.2000;179:177–181.
- ,,.Appendix. In:Townsend CM, ed.Sabiston textbook of surgery. The biologic basis of modern surgical practice. 16th ed.Philadelphia:W. B. Saunders,2001:917–928.
A 49‐year‐old man presented with 2 days of chills, fever, anorexia, and increased cough and dyspnea. The patient had a history of chronic obstructive pulmonary disease (COPD) and noted that his cough and dyspnea had increased above normal for several days. He was now dyspneic with minimal activity and had slept at a 45‐degree incline the night prior to evaluation due to dyspnea. He noted less improvement than usual with the use of his metered dose inhaler. His cough was occasionally productive of small amounts of white phlegm. He had vomited once. During a coughing episode the patient experienced a sudden onset of sharp right upper quadrant abdominal pain that worsened with coughing and sudden position changes. The patient denied a prior history of abdominal pain or surgery. The patient's last bowel movement was 2 days prior to admission. He denied melena or bright red blood per rectum.
My initial differential diagnosis for this patient's dyspnea and cough is pneumonia, acute exacerbation of COPD, or congestive heart failure. The presence of fever and anorexia increases the likelihood of infectious etiologies, whereas the presence of orthopnea points toward congestive heart failure. Noncardiac processessuch as a large pleural effusion or apical lung diseasecould also cause orthopnea. His abdominal pain could be a result of pneumonia alone (perhaps in the right lower lobe with diaphragmatic irritation), but I am also considering complications of pneumonia such as empyema. Although his abdominal pain, dyspnea, and cough could also be a result of hepatobiliary disease, a perforated viscus, or pancreatitis, we currently have little reason to suspect a direct abdominal etiology. My top diagnosis is community‐acquired pneumonia, perhaps accompanied by pleural effusion.
His medical history was significant for dilated cardiomyopathy and heavy alcohol use. His medications included various meter‐dosed inhalers, bupropion, digoxin, spironolactone, lisinopril, and metoprolol. He had never received corticosteroid therapy and had not previously been hospitalized for COPD‐related problems. He had smoked one pack of cigarettes daily for 40 years.
Heavy alcohol use is associated with an increased risk of several pulmonary infections such as gram‐negative necrotizing pneumonia (classically, Klebsiella pneumoniae), pneumococcal pneumonia, aspiration pneumonia, anaerobic lung abscesses, and tuberculosis. Given his right upper quadrant pain, acute alcoholic hepatitis and alcohol‐related pancreatitis enter the differential. His history of cardiomyopathy makes me consider congestive heart failure as more likely than before, and perhaps his abdominal pain is a result of hepatic congestion from right heart failure. His fever, however, cannot be attributed to cardiac failure. Less likely diagnoses include ischemic conditions related to his cardiomyopathy such as mesenteric ischemia from low perfusion or embolism from a cardiac thrombus. A pulmonary infection remains the most likely diagnosis.
He was an ill‐appearing man in moderate respiratory distress, looking older than his stated age. His temperature was 38.4C, heart rate 129 beats/minute, blood pressure 85/56 mm Hg, respiratory rate 24 breaths/minute, and oxygen saturation 92% on room air. A cardiovascular exam revealed no murmur, gallop, or rub. The jugular venous pulse was not elevated. His lungs were clear to auscultation. Abdominal exam revealed right‐sided abdominal tenderness that appeared to localize to the rectus sheath. Otherwise, the abdomen was soft, with normal bowel sounds and no organomegaly. Rectal examination revealed guaiac negative stool and no focal tenderness. His extremities were normal.
His vital signs are worrisome for impending cardiovascular collapse and shock, possibly due to sepsis. The relatively nonfocal cardiopulmonary exam is surprising given his initial symptoms and makes me wonder if his dyspnea is primarily related to an abdominal process leading to diaphragmatic irritation rather than to a thoracic process. Congestive heart failure seems unlikely given the lack of supportive physical examination findings. His abdominal exam findings are puzzling. Although his abdominal wall tenderness could be benignperhaps from muscular strain or a tear from coughingit could represent a more worrisome process such as infection or a hematoma in the abdominal wall muscles. Mesenteric ischemia is still possible, as the exam is often unimpressive. A hepatic abscess or subphrenic abscess should be considered, as physical exam findings in these conditions can be subtle.
My differential remains relatively unchanged, but I have now put consideration of a hepatic or subphrenic abscess higher on my list. Early empiric broad‐spectrum antibiotics seem necessary.
He had a white blood cell count of 26,700/mL with 92% neutrophils, a hemoglobin of 14.6 g/dL, and a platelet count of 312,000/mL. Sodium was 134 mmol/L, potassium was 4.3 mmol/L, chloride was 94 mmol/L, bicarbonate was 23 mmol/L, blood urea nitrogen was 23 mg/dL, and creatinine was 2.1 mg/dL. The results of the calcium, protein, albumin, and liver function tests were normal. Urinalysis was negative for protein and red blood cells. An electrocardiogram revealed sinus tachycardia. A chest radiograph at admission revealed mild opacities in both lower lobes and the right middle lobe consistent with either atelectasis or pneumonia (Fig. 1). A very small left effusion was also identified.
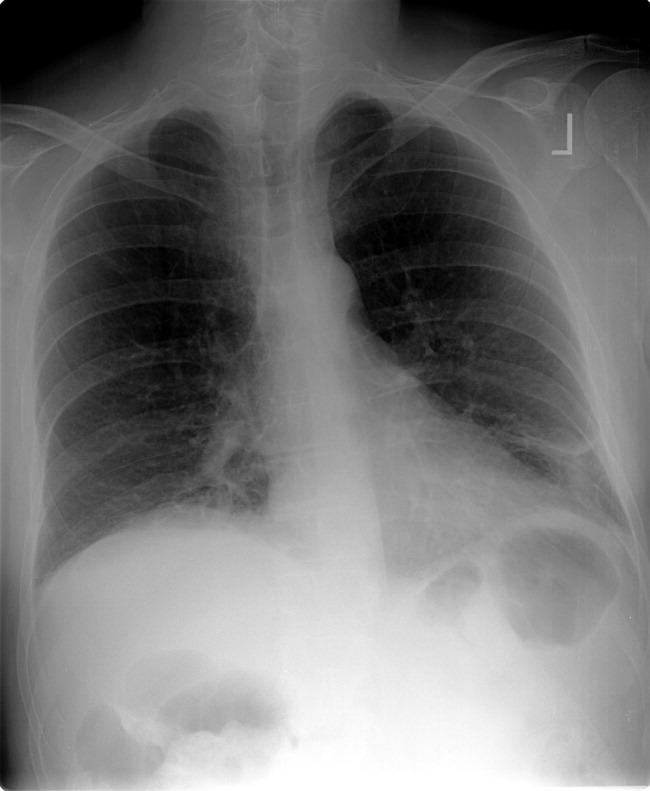
The additional data reinforce my clinical impression that this process is likely to be infectious. The chest radiograph is consistent with community‐acquired pneumonia, possibly from an atypical pathogen. Given his elevated creatinine, I am also considering a pulmonary‐renal syndrome such as vasculitis, though hematuria was not present. A subphrenic abscess, mesenteric ischemia, or an abdominal wall process (because his abdominal tenderness on exam still needs an explanation) remain possibilities; my suspicion would increase if he does not respond appropriately to therapy for community‐acquired pneumonia.
The clinical team's working diagnosis also was community‐acquired pneumonia. Blood and sputum cultures were obtained, and the patient was treated with intravenous ceftriaxone, azithromycin, and intravenous fluid. By the second day, his creatinine had normalized; however, his hypoxemia had worsened, and he now required supplemental oxygen. His temperature was 39.3C, and his heart rate was 150 beats/minute. The findings of an abdominal ultrasound of the kidneys, spleen, and right upper quadrant were normal.
It is too early to say the patient has failed therapy because a patient can get worse before getting better during the course of antibiotic therapy for community‐acquired pneumonia. Fever, for example, may take up to 7 days to resolve, depending on host factors and the pathogen. Though I typically wait about 72 hours before assuming a patient is not appropriately responding to therapy, the additional information has made me concerned. The degree of tachycardia is significant and warrants an EKG to exclude an arrthymia. I would also repeat the chest radiograph to evaluate for worsening infiltrates or increased pleural effusion.
On the third hospital day, the patient's abdominal pain had decreased with analgesia, but his fever, cough, and dyspnea remained largely unchanged. Antibiotics were changed to intravenous levofloxacin. A repeat chest radiograph revealed elevation of the right hemidiaphragm and bilateral effusions (Fig. 2). An electrocardiogram revealed sinus tachycardia. Blood cultures revealed no growth, and sputum cultures grew oral flora.
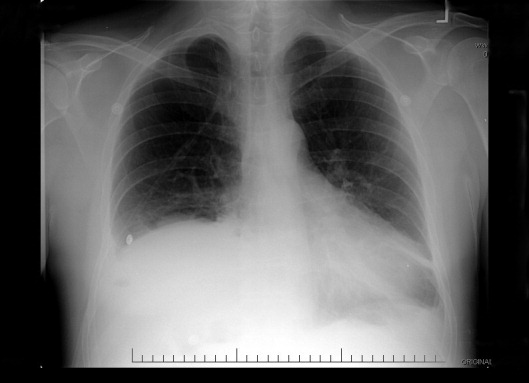
A significantly elevated right hemidiaphragm makes me reconsider the diagnosis of simple community‐acquired pneumonia. The differential diagnosis for an elevated hemidiaphragm is best considered by location in relation to the diaphragm. Causes above the diaphragm include rib fracture, atelectasis, pleural thickening, and volume loss of the lung for another reason (e.g., surgery, bronchial obstruction due to tumor or mucus plugging), as well as mimics such as a densely consolidated pneumonia, pulmonary infarction, or a subpulmonary effusion. Diaphragmatic causes include eventration, rupture, phrenic nerve weakness, and intrinsic weakness because of neuromuscular disease (usually bilateral). Causes below the diaphragm that must be considered are subphrenic or liver abscess, liver (and other abdominal) malignancy, pancreatic pseudocyst, and distended bowel. Given the clinical picture, I am focusing below the diaphragmespecially on a possible hepatic or subphrenic abscess (which could be missed on ultrasound) and mimics of it such as dense consolidation or a subpulmonary effusion. Given the lack of response to antibiotics, I need to consider an infection that is not being treated, either because of location (abscess, effusion) or microbiology (tuberculosis, a parasite, a fungus, resistant bacteria). After confirming that the patient has a substantive pleural effusion, he needs a thoracentesis.
On the fourth hospital day, his temperature was 38.8C, and his white blood cell count was 21,000/mL. A right‐sided thoracentesis was performed; approximately 250 cc of fluid was obtained. Pleural fluid analysis revealed bloody fluid, with a white blood cell count of 16,750/mL with 94% neutrophils, 40,000 red blood cells/mL, lactate dehydrogenase of 278 U/L (normal serum value 80200 U/L), protein of 3.7 g/dL, and glucose of 81 mg/dL. A pleural fluid pH was not obtained. A gram stain revealed many white blood cells with no organisms noted. Serum protein was 7.4 g/dL. These results were thought to represent an exudative parapneumonic effusion; levofloxacin and supplemental oxygen were continued.
The pleural fluid appears exudative, but I am not sure this man has a parapneumonic effusion because, despite clinical deterioration, an obvious infiltrate is not seen on interval chest radiography. We must look closely at the fluid because this is a bloody effusion and somewhat atypical for a parapneumonic effusion. Also, the effusion does not appear large enough to explain why he has not improved on the current antibiotics. We should thus reconsider our diagnosis and management. I would obtain additional imaging (such as an abdominal and chest computed tomography [CT]) and perhaps obtain a consultation from the pulmonary team regarding the postulated initial diagnosis of pneumonia with effusion.
On the fifth day of hospitalization, the patient's dyspnea and cough persisted but were improved. His abdominal pain was minimal and felt improved with flatus. Fever continued to 38.8C, and the white blood cell count was 20,000/mL. On examination the patient had decreased breath sounds at the right base and bibasilar crackles. His abdomen was soft, with tenderness in his right upper quadrant only with deep palpation; bowel sounds remained. An ultrasound of the chest was performed to look for a loculated effusion; however, no fluid was identified. The pulmonary consultant thought it likely that the patient had a subpulmonic effusion and recommended CT of the abdomen and chest.
His right upper quadrant tenderness is still unexplained. I would agree with the CT, primarily to evaluate other causes of his elevated diaphragm such as subphrenic or hepatic abscess. For now, I would make no change in antibiotic therapy.
On the sixth hospital day, the patient had an episode of bilious emesis. Chest and abdominal CT revealed collapse of the right middle and lower lobes with a small adjacent effusion, and a 6 6 16 cm abscess intimately opposed to the right lobe of the liver. Extending from the inferior extent of the abscess was a tubular thick‐walled structure connecting to the cecum that was suspicious of a thickened inflamed appendix. There was periappendiceal stranding suggesting inflammation. The small bowel was diffusely dilated up to 4.5 cm, suggesting a small bowel obstruction.
I suspect that his abscess is related to a perforated appendix and that the dilated small bowel is most likely a result of localized irritation of the bowel by the abscess and appendicitis. The collapsed lung is most likely due to local inflammation from the subdiaphragmatic abscess. Treatment should now be changed substantially. I would ask a surgeon to evaluate the patient because the most likely diagnosis is perforated appendicitis with abscess formation.
When the periappendiceal abscess was drained percutaneously, 190 mL of purulent fluid was removed. The cultures were positive for Klebsiella pneumonia, Enterococcus faecalis,and Streptococcus milleri. The patient was given 6 weeks of intravenous antibiotics with improvement in his clinical symptoms. During the interval the findings on his chest radiograph resolved completely. A laproscopic appendectomy 3 months later revealed significant right lower quadrant adhesions. The pathology specimen identified a distorted appendix with regeneration consistent with prior appendicitis. The patient was contacted 4 months after his surgery, and he reported that he was doing well, with no cardiopulmonary or gastrointestinal symptoms.
COMMENTARY
Community‐acquired pneumonia (CAP) is a common cause of acute illness and accounts for nearly 1 million admissions per year in the United States.1 The diagnosis of CAP is made when symptoms including dyspnea, fever, cough, or leukocytosis are present, with confirmation provided by a chest radiograph. Often the diagnosis is clear; however, there is no pathognomonic constellation of signs or symptoms that establish the diagnosis with certainty.2 Many physicians learn that pneumoniaespecially lower‐lobe pneumoniacan lead to abdominal findings such as upper quadrant pain, vomiting, and tenderness to palpation. Conversely, the patient discussed above illustrates that a primary abdominal process can also result in a symptom complex that mimics pneumonia.
The prevalence of CAP coupled with the inherent uncertainty of a clinical diagnosis of CAP leads to an important question: How long is too long before questioning the diagnosis? An analysis of the pneumonia Patient Outcomes Research Trial (PORT) limited to inpatients with CAP examined time to clinical stability. For the majority of patients, abnormal vital signs resolved within 23 days.3 In this study, 29% of patients had severe disease, and not surprisingly, these patients took longer to improve. Using the pneumonia severity index score, which accounts for age, comorbidity, abnormal vital signs, and laboratory data, the patient described in this article would be considered at high risk for death and complication with an estimated mortality of 9%.4 Using a combination of defervescence, resolution of tachycardia, tachypnea, and hypoxemia as markers of clinical stability, a patient like ours should respond within 4 days (with a range of 27 days). On the basis of these dataand the discrepancy between the patient's severe illness and relatively minor pulmonary infiltratesit seems reasonable to have considered this patient as failing CAP therapy as early as the fourth day of hospitalization.
In approximately 10% of hospitalized patients with CAP, the clinical course is protracted.5 When patients do not improve as quickly as expected, the reasons that could explain this should be investigated. In a cohort of 49 patients with CAP who failed therapy the most common reasons for failure to improve were severity of the pneumonia and drug resistance.6 A multicenter study found that the incidence of resistance to penicillin by Streptococcus pneumoniae, the most common bacterial pathogen in CAP, was 30%, with a 4% in vitro resistance rate to ceftriaxone.7 How well in vitro resistance predicts clinical response, however, is unclear. Risk factors for antibiotic resistance include close exposure to children, recent antibiotic use, and recent hospitalization. Immunosuppressive conditions should also be considered in patients who fail to improve. Suppurative complications of pneumoniasuch as empyema, parapneumonic effusion, and lung abscessalso delay recovery.
Another consideration in a patient with what appears to be a nonresolving pneumonia with pleural effusion is that the initial diagnosis is incorrect and the cause is extrathoracic. Pulmonary and cardiac diseases account for more than 90% of effusions, whereas less than 5% of pleural effusions result from intraabdominal causes.8 When should intraabdominal diseases be sought in patients with an effusion, fever, dyspnea, and cough? Light suggests that intraabdominal pathology should be investigated in patients who have pleural effusions without significant parenchymal disease.8 This point is underscored by the experience of our patient, whose chest radiographs showed, despite clinical decline, minimal airspace disease.
Several abdominal entities cause pleural effusion. Pancreatitis, either acute or chronic, with pseudocyst formation is the most common abdominal cause of exudative pleural effusions. Approximately 10% of patients with pancreatic disease will develop effusions, usually left‐sided.9 These left‐sided effusions are also seen in splenic abscesses, usually as a result of endocarditis. Intrahepatic abscess is associated with effusions in 20% of patients.10 A subphrenic abscess, as seen in our patient, is an uncommon cause of exudative pleural effusions. Historically, subphrenic abscesses resulted from a perforated viscus, with ruptured appendicitis the most common cause,11 followed by perforated peptic ulcers and biliary tract disease. With the advent of antibiotics, the causes of subphrenic abscess changed considerably, with the majority of current cases resulting from postsurgical complications.12 The findings of a chest radiograph are abnormal in 80% of patients with subphrenic abscess;1214 an elevated hemidiaphragm and pleural effusion are found in the majority of cases. The symptoms of a subphrenic abscess are nonspecific, and patient's complaints are equally split between predominantly thoracic and predomninantly abdominal complaints.15
Appendicitis, a common disease predominantly of the young, may lead to atypical presentations in older individuals. In a retrospective analysis of 113 patients older than 60 years with appendicitis, 70% presented in an atypical fashion.16 Typical symptoms include right lower quadrant pain, fever, anorexia and a white blood cell count greater than 10,000/mL. Fever was the most frequently absent symptom, seen in only 37% of older patients. In this cohort, approximately one third of older patients waited more than 48 hours prior to presentation. The time between symptom onset and clinical presentation is a strong predictor of perforation risk.17 As in this case, roughly 2% of patients with acute appendicitis will present with perforation and abscess formation.18 In such patients the management is initially conservative. Percutaneous drainage and broad spectrum antibiotics are the treatment of choice, followed by an interval appendectomy in 612 weeks.19 The rationale for delayed surgery is that earlier surgery may disseminate a localized inflammatory process.20
Community‐acquired pneumonia is a more frequent cause of hospital admission than is intraabdominal abscess. Physicians often face the dilemma of when to pursue alternative diagnoses after a patient who is thought to have an atypical presentation of a common disease (ie, CAP) fails to respond to conventional therapy. Although clinicians learn that right upper quadrant pain may be a symptom of pneumonia, our patient revealed that abdominal causes may mimic pneumonia and produce a pleural effusion. Determining whether the primary disease originates above or below the diaphragm is critical to guiding therapy. When patients fail to respond adequately to therapy, clinicians should set a low threshold for deciding to image the abdomen in a patient with modest pulmonary infiltrates, pleural effusion, and abdominal pain.
A 49‐year‐old man presented with 2 days of chills, fever, anorexia, and increased cough and dyspnea. The patient had a history of chronic obstructive pulmonary disease (COPD) and noted that his cough and dyspnea had increased above normal for several days. He was now dyspneic with minimal activity and had slept at a 45‐degree incline the night prior to evaluation due to dyspnea. He noted less improvement than usual with the use of his metered dose inhaler. His cough was occasionally productive of small amounts of white phlegm. He had vomited once. During a coughing episode the patient experienced a sudden onset of sharp right upper quadrant abdominal pain that worsened with coughing and sudden position changes. The patient denied a prior history of abdominal pain or surgery. The patient's last bowel movement was 2 days prior to admission. He denied melena or bright red blood per rectum.
My initial differential diagnosis for this patient's dyspnea and cough is pneumonia, acute exacerbation of COPD, or congestive heart failure. The presence of fever and anorexia increases the likelihood of infectious etiologies, whereas the presence of orthopnea points toward congestive heart failure. Noncardiac processessuch as a large pleural effusion or apical lung diseasecould also cause orthopnea. His abdominal pain could be a result of pneumonia alone (perhaps in the right lower lobe with diaphragmatic irritation), but I am also considering complications of pneumonia such as empyema. Although his abdominal pain, dyspnea, and cough could also be a result of hepatobiliary disease, a perforated viscus, or pancreatitis, we currently have little reason to suspect a direct abdominal etiology. My top diagnosis is community‐acquired pneumonia, perhaps accompanied by pleural effusion.
His medical history was significant for dilated cardiomyopathy and heavy alcohol use. His medications included various meter‐dosed inhalers, bupropion, digoxin, spironolactone, lisinopril, and metoprolol. He had never received corticosteroid therapy and had not previously been hospitalized for COPD‐related problems. He had smoked one pack of cigarettes daily for 40 years.
Heavy alcohol use is associated with an increased risk of several pulmonary infections such as gram‐negative necrotizing pneumonia (classically, Klebsiella pneumoniae), pneumococcal pneumonia, aspiration pneumonia, anaerobic lung abscesses, and tuberculosis. Given his right upper quadrant pain, acute alcoholic hepatitis and alcohol‐related pancreatitis enter the differential. His history of cardiomyopathy makes me consider congestive heart failure as more likely than before, and perhaps his abdominal pain is a result of hepatic congestion from right heart failure. His fever, however, cannot be attributed to cardiac failure. Less likely diagnoses include ischemic conditions related to his cardiomyopathy such as mesenteric ischemia from low perfusion or embolism from a cardiac thrombus. A pulmonary infection remains the most likely diagnosis.
He was an ill‐appearing man in moderate respiratory distress, looking older than his stated age. His temperature was 38.4C, heart rate 129 beats/minute, blood pressure 85/56 mm Hg, respiratory rate 24 breaths/minute, and oxygen saturation 92% on room air. A cardiovascular exam revealed no murmur, gallop, or rub. The jugular venous pulse was not elevated. His lungs were clear to auscultation. Abdominal exam revealed right‐sided abdominal tenderness that appeared to localize to the rectus sheath. Otherwise, the abdomen was soft, with normal bowel sounds and no organomegaly. Rectal examination revealed guaiac negative stool and no focal tenderness. His extremities were normal.
His vital signs are worrisome for impending cardiovascular collapse and shock, possibly due to sepsis. The relatively nonfocal cardiopulmonary exam is surprising given his initial symptoms and makes me wonder if his dyspnea is primarily related to an abdominal process leading to diaphragmatic irritation rather than to a thoracic process. Congestive heart failure seems unlikely given the lack of supportive physical examination findings. His abdominal exam findings are puzzling. Although his abdominal wall tenderness could be benignperhaps from muscular strain or a tear from coughingit could represent a more worrisome process such as infection or a hematoma in the abdominal wall muscles. Mesenteric ischemia is still possible, as the exam is often unimpressive. A hepatic abscess or subphrenic abscess should be considered, as physical exam findings in these conditions can be subtle.
My differential remains relatively unchanged, but I have now put consideration of a hepatic or subphrenic abscess higher on my list. Early empiric broad‐spectrum antibiotics seem necessary.
He had a white blood cell count of 26,700/mL with 92% neutrophils, a hemoglobin of 14.6 g/dL, and a platelet count of 312,000/mL. Sodium was 134 mmol/L, potassium was 4.3 mmol/L, chloride was 94 mmol/L, bicarbonate was 23 mmol/L, blood urea nitrogen was 23 mg/dL, and creatinine was 2.1 mg/dL. The results of the calcium, protein, albumin, and liver function tests were normal. Urinalysis was negative for protein and red blood cells. An electrocardiogram revealed sinus tachycardia. A chest radiograph at admission revealed mild opacities in both lower lobes and the right middle lobe consistent with either atelectasis or pneumonia (Fig. 1). A very small left effusion was also identified.
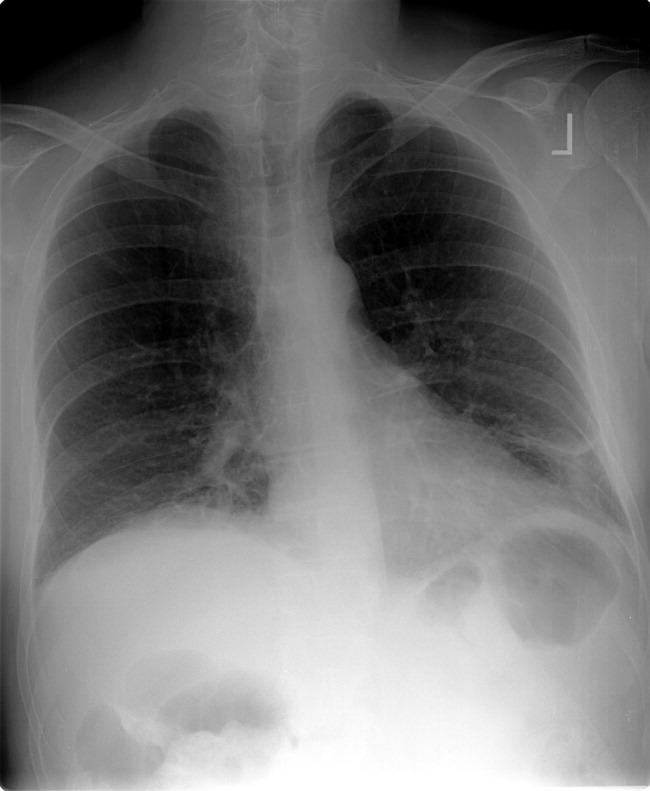
The additional data reinforce my clinical impression that this process is likely to be infectious. The chest radiograph is consistent with community‐acquired pneumonia, possibly from an atypical pathogen. Given his elevated creatinine, I am also considering a pulmonary‐renal syndrome such as vasculitis, though hematuria was not present. A subphrenic abscess, mesenteric ischemia, or an abdominal wall process (because his abdominal tenderness on exam still needs an explanation) remain possibilities; my suspicion would increase if he does not respond appropriately to therapy for community‐acquired pneumonia.
The clinical team's working diagnosis also was community‐acquired pneumonia. Blood and sputum cultures were obtained, and the patient was treated with intravenous ceftriaxone, azithromycin, and intravenous fluid. By the second day, his creatinine had normalized; however, his hypoxemia had worsened, and he now required supplemental oxygen. His temperature was 39.3C, and his heart rate was 150 beats/minute. The findings of an abdominal ultrasound of the kidneys, spleen, and right upper quadrant were normal.
It is too early to say the patient has failed therapy because a patient can get worse before getting better during the course of antibiotic therapy for community‐acquired pneumonia. Fever, for example, may take up to 7 days to resolve, depending on host factors and the pathogen. Though I typically wait about 72 hours before assuming a patient is not appropriately responding to therapy, the additional information has made me concerned. The degree of tachycardia is significant and warrants an EKG to exclude an arrthymia. I would also repeat the chest radiograph to evaluate for worsening infiltrates or increased pleural effusion.
On the third hospital day, the patient's abdominal pain had decreased with analgesia, but his fever, cough, and dyspnea remained largely unchanged. Antibiotics were changed to intravenous levofloxacin. A repeat chest radiograph revealed elevation of the right hemidiaphragm and bilateral effusions (Fig. 2). An electrocardiogram revealed sinus tachycardia. Blood cultures revealed no growth, and sputum cultures grew oral flora.
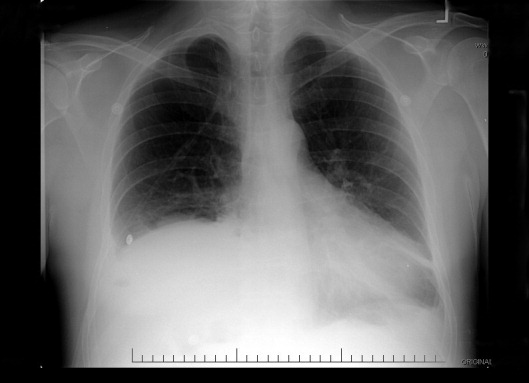
A significantly elevated right hemidiaphragm makes me reconsider the diagnosis of simple community‐acquired pneumonia. The differential diagnosis for an elevated hemidiaphragm is best considered by location in relation to the diaphragm. Causes above the diaphragm include rib fracture, atelectasis, pleural thickening, and volume loss of the lung for another reason (e.g., surgery, bronchial obstruction due to tumor or mucus plugging), as well as mimics such as a densely consolidated pneumonia, pulmonary infarction, or a subpulmonary effusion. Diaphragmatic causes include eventration, rupture, phrenic nerve weakness, and intrinsic weakness because of neuromuscular disease (usually bilateral). Causes below the diaphragm that must be considered are subphrenic or liver abscess, liver (and other abdominal) malignancy, pancreatic pseudocyst, and distended bowel. Given the clinical picture, I am focusing below the diaphragmespecially on a possible hepatic or subphrenic abscess (which could be missed on ultrasound) and mimics of it such as dense consolidation or a subpulmonary effusion. Given the lack of response to antibiotics, I need to consider an infection that is not being treated, either because of location (abscess, effusion) or microbiology (tuberculosis, a parasite, a fungus, resistant bacteria). After confirming that the patient has a substantive pleural effusion, he needs a thoracentesis.
On the fourth hospital day, his temperature was 38.8C, and his white blood cell count was 21,000/mL. A right‐sided thoracentesis was performed; approximately 250 cc of fluid was obtained. Pleural fluid analysis revealed bloody fluid, with a white blood cell count of 16,750/mL with 94% neutrophils, 40,000 red blood cells/mL, lactate dehydrogenase of 278 U/L (normal serum value 80200 U/L), protein of 3.7 g/dL, and glucose of 81 mg/dL. A pleural fluid pH was not obtained. A gram stain revealed many white blood cells with no organisms noted. Serum protein was 7.4 g/dL. These results were thought to represent an exudative parapneumonic effusion; levofloxacin and supplemental oxygen were continued.
The pleural fluid appears exudative, but I am not sure this man has a parapneumonic effusion because, despite clinical deterioration, an obvious infiltrate is not seen on interval chest radiography. We must look closely at the fluid because this is a bloody effusion and somewhat atypical for a parapneumonic effusion. Also, the effusion does not appear large enough to explain why he has not improved on the current antibiotics. We should thus reconsider our diagnosis and management. I would obtain additional imaging (such as an abdominal and chest computed tomography [CT]) and perhaps obtain a consultation from the pulmonary team regarding the postulated initial diagnosis of pneumonia with effusion.
On the fifth day of hospitalization, the patient's dyspnea and cough persisted but were improved. His abdominal pain was minimal and felt improved with flatus. Fever continued to 38.8C, and the white blood cell count was 20,000/mL. On examination the patient had decreased breath sounds at the right base and bibasilar crackles. His abdomen was soft, with tenderness in his right upper quadrant only with deep palpation; bowel sounds remained. An ultrasound of the chest was performed to look for a loculated effusion; however, no fluid was identified. The pulmonary consultant thought it likely that the patient had a subpulmonic effusion and recommended CT of the abdomen and chest.
His right upper quadrant tenderness is still unexplained. I would agree with the CT, primarily to evaluate other causes of his elevated diaphragm such as subphrenic or hepatic abscess. For now, I would make no change in antibiotic therapy.
On the sixth hospital day, the patient had an episode of bilious emesis. Chest and abdominal CT revealed collapse of the right middle and lower lobes with a small adjacent effusion, and a 6 6 16 cm abscess intimately opposed to the right lobe of the liver. Extending from the inferior extent of the abscess was a tubular thick‐walled structure connecting to the cecum that was suspicious of a thickened inflamed appendix. There was periappendiceal stranding suggesting inflammation. The small bowel was diffusely dilated up to 4.5 cm, suggesting a small bowel obstruction.
I suspect that his abscess is related to a perforated appendix and that the dilated small bowel is most likely a result of localized irritation of the bowel by the abscess and appendicitis. The collapsed lung is most likely due to local inflammation from the subdiaphragmatic abscess. Treatment should now be changed substantially. I would ask a surgeon to evaluate the patient because the most likely diagnosis is perforated appendicitis with abscess formation.
When the periappendiceal abscess was drained percutaneously, 190 mL of purulent fluid was removed. The cultures were positive for Klebsiella pneumonia, Enterococcus faecalis,and Streptococcus milleri. The patient was given 6 weeks of intravenous antibiotics with improvement in his clinical symptoms. During the interval the findings on his chest radiograph resolved completely. A laproscopic appendectomy 3 months later revealed significant right lower quadrant adhesions. The pathology specimen identified a distorted appendix with regeneration consistent with prior appendicitis. The patient was contacted 4 months after his surgery, and he reported that he was doing well, with no cardiopulmonary or gastrointestinal symptoms.
COMMENTARY
Community‐acquired pneumonia (CAP) is a common cause of acute illness and accounts for nearly 1 million admissions per year in the United States.1 The diagnosis of CAP is made when symptoms including dyspnea, fever, cough, or leukocytosis are present, with confirmation provided by a chest radiograph. Often the diagnosis is clear; however, there is no pathognomonic constellation of signs or symptoms that establish the diagnosis with certainty.2 Many physicians learn that pneumoniaespecially lower‐lobe pneumoniacan lead to abdominal findings such as upper quadrant pain, vomiting, and tenderness to palpation. Conversely, the patient discussed above illustrates that a primary abdominal process can also result in a symptom complex that mimics pneumonia.
The prevalence of CAP coupled with the inherent uncertainty of a clinical diagnosis of CAP leads to an important question: How long is too long before questioning the diagnosis? An analysis of the pneumonia Patient Outcomes Research Trial (PORT) limited to inpatients with CAP examined time to clinical stability. For the majority of patients, abnormal vital signs resolved within 23 days.3 In this study, 29% of patients had severe disease, and not surprisingly, these patients took longer to improve. Using the pneumonia severity index score, which accounts for age, comorbidity, abnormal vital signs, and laboratory data, the patient described in this article would be considered at high risk for death and complication with an estimated mortality of 9%.4 Using a combination of defervescence, resolution of tachycardia, tachypnea, and hypoxemia as markers of clinical stability, a patient like ours should respond within 4 days (with a range of 27 days). On the basis of these dataand the discrepancy between the patient's severe illness and relatively minor pulmonary infiltratesit seems reasonable to have considered this patient as failing CAP therapy as early as the fourth day of hospitalization.
In approximately 10% of hospitalized patients with CAP, the clinical course is protracted.5 When patients do not improve as quickly as expected, the reasons that could explain this should be investigated. In a cohort of 49 patients with CAP who failed therapy the most common reasons for failure to improve were severity of the pneumonia and drug resistance.6 A multicenter study found that the incidence of resistance to penicillin by Streptococcus pneumoniae, the most common bacterial pathogen in CAP, was 30%, with a 4% in vitro resistance rate to ceftriaxone.7 How well in vitro resistance predicts clinical response, however, is unclear. Risk factors for antibiotic resistance include close exposure to children, recent antibiotic use, and recent hospitalization. Immunosuppressive conditions should also be considered in patients who fail to improve. Suppurative complications of pneumoniasuch as empyema, parapneumonic effusion, and lung abscessalso delay recovery.
Another consideration in a patient with what appears to be a nonresolving pneumonia with pleural effusion is that the initial diagnosis is incorrect and the cause is extrathoracic. Pulmonary and cardiac diseases account for more than 90% of effusions, whereas less than 5% of pleural effusions result from intraabdominal causes.8 When should intraabdominal diseases be sought in patients with an effusion, fever, dyspnea, and cough? Light suggests that intraabdominal pathology should be investigated in patients who have pleural effusions without significant parenchymal disease.8 This point is underscored by the experience of our patient, whose chest radiographs showed, despite clinical decline, minimal airspace disease.
Several abdominal entities cause pleural effusion. Pancreatitis, either acute or chronic, with pseudocyst formation is the most common abdominal cause of exudative pleural effusions. Approximately 10% of patients with pancreatic disease will develop effusions, usually left‐sided.9 These left‐sided effusions are also seen in splenic abscesses, usually as a result of endocarditis. Intrahepatic abscess is associated with effusions in 20% of patients.10 A subphrenic abscess, as seen in our patient, is an uncommon cause of exudative pleural effusions. Historically, subphrenic abscesses resulted from a perforated viscus, with ruptured appendicitis the most common cause,11 followed by perforated peptic ulcers and biliary tract disease. With the advent of antibiotics, the causes of subphrenic abscess changed considerably, with the majority of current cases resulting from postsurgical complications.12 The findings of a chest radiograph are abnormal in 80% of patients with subphrenic abscess;1214 an elevated hemidiaphragm and pleural effusion are found in the majority of cases. The symptoms of a subphrenic abscess are nonspecific, and patient's complaints are equally split between predominantly thoracic and predomninantly abdominal complaints.15
Appendicitis, a common disease predominantly of the young, may lead to atypical presentations in older individuals. In a retrospective analysis of 113 patients older than 60 years with appendicitis, 70% presented in an atypical fashion.16 Typical symptoms include right lower quadrant pain, fever, anorexia and a white blood cell count greater than 10,000/mL. Fever was the most frequently absent symptom, seen in only 37% of older patients. In this cohort, approximately one third of older patients waited more than 48 hours prior to presentation. The time between symptom onset and clinical presentation is a strong predictor of perforation risk.17 As in this case, roughly 2% of patients with acute appendicitis will present with perforation and abscess formation.18 In such patients the management is initially conservative. Percutaneous drainage and broad spectrum antibiotics are the treatment of choice, followed by an interval appendectomy in 612 weeks.19 The rationale for delayed surgery is that earlier surgery may disseminate a localized inflammatory process.20
Community‐acquired pneumonia is a more frequent cause of hospital admission than is intraabdominal abscess. Physicians often face the dilemma of when to pursue alternative diagnoses after a patient who is thought to have an atypical presentation of a common disease (ie, CAP) fails to respond to conventional therapy. Although clinicians learn that right upper quadrant pain may be a symptom of pneumonia, our patient revealed that abdominal causes may mimic pneumonia and produce a pleural effusion. Determining whether the primary disease originates above or below the diaphragm is critical to guiding therapy. When patients fail to respond adequately to therapy, clinicians should set a low threshold for deciding to image the abdomen in a patient with modest pulmonary infiltrates, pleural effusion, and abdominal pain.
- ,,, et al.The cost of treating community‐acquired pneumonia.Clin Ther.1998;20:820–827.
- ,,.Does this patient have community‐acquired pneumonia? Diagnosing pneumonia by history and physical examination.JAMA.1997;278:1440–1445.
- ,,, et al.Time to clinical stability in patients hospitalized with community acquired pneumonia. Implications for practice guidelines.JAMA.1998;279:1452–1457.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,, et al.Utility of fiberoptic bronchoscopy in non resolving pneumonia.Chest.1990;98:1322–1326.
- ,,, et al.Antimicrobial treatment failures in patients with community acquired pneumonia. Causes and prognostic implications.Am J Respir Crit Care Med.2000;162:154–160.
- ,,, et al.Antimicrobial resistance with Streptococcus pneumoniae in the United States, 1997–98.Emerg Infect Dis.1999;5:757–765.
- ,.Pleural effusion. In:Murray JF,Nadel JA, eds.Textbook of respiratory medicine. 3rd ed.Philadelphia:WB Saunders,2000:2013–2041.
- ,,.Significance of pleural effusion in patients with acute pancreatitis.Am J Gastroenterol.1992;87:871–874.
- .Exudative pleural effusions secondary to gastrointestinal diseases.Clin Chest Med.1985;6(1):103–111.
- .Subphrenic abscess.Ann Surg.1963;158:240–248.
- ,,,.Upper abdominal abscess: a continuing and deadly problem.Am J Roentgenol.1980;134:759–765.
- .Subphrenic abscess. A clinical study of 101 cases.Acta Chir Scand.1959;117:388–408.
- ,,.Subphrenic abscess a continuing hazard.Am J Surg.1969:117–122.
- ,.Subphrenic abscess: a thoracoabdominal clinical complex. The changing picture with antibiotics.Am J Surg.1964;108:165–172.
- ,.What have we learned over the past 20 years about appendicitis in the elderly.Am J Surg.2003;185:198–201.
- ,,, et al.Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies.Am Surg.2000;66:548–554.
- ,,.Appendicitis with a palpable mass.Ann Surg.1981;193:227–229.
- ,,, et al.Nonoperative management of perforated appendicitis without periappendiceal mass.Am J Surg.2000;179:177–181.
- ,,.Appendix. In:Townsend CM, ed.Sabiston textbook of surgery. The biologic basis of modern surgical practice. 16th ed.Philadelphia:W. B. Saunders,2001:917–928.
- ,,, et al.The cost of treating community‐acquired pneumonia.Clin Ther.1998;20:820–827.
- ,,.Does this patient have community‐acquired pneumonia? Diagnosing pneumonia by history and physical examination.JAMA.1997;278:1440–1445.
- ,,, et al.Time to clinical stability in patients hospitalized with community acquired pneumonia. Implications for practice guidelines.JAMA.1998;279:1452–1457.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,,, et al.Utility of fiberoptic bronchoscopy in non resolving pneumonia.Chest.1990;98:1322–1326.
- ,,, et al.Antimicrobial treatment failures in patients with community acquired pneumonia. Causes and prognostic implications.Am J Respir Crit Care Med.2000;162:154–160.
- ,,, et al.Antimicrobial resistance with Streptococcus pneumoniae in the United States, 1997–98.Emerg Infect Dis.1999;5:757–765.
- ,.Pleural effusion. In:Murray JF,Nadel JA, eds.Textbook of respiratory medicine. 3rd ed.Philadelphia:WB Saunders,2000:2013–2041.
- ,,.Significance of pleural effusion in patients with acute pancreatitis.Am J Gastroenterol.1992;87:871–874.
- .Exudative pleural effusions secondary to gastrointestinal diseases.Clin Chest Med.1985;6(1):103–111.
- .Subphrenic abscess.Ann Surg.1963;158:240–248.
- ,,,.Upper abdominal abscess: a continuing and deadly problem.Am J Roentgenol.1980;134:759–765.
- .Subphrenic abscess. A clinical study of 101 cases.Acta Chir Scand.1959;117:388–408.
- ,,.Subphrenic abscess a continuing hazard.Am J Surg.1969:117–122.
- ,.Subphrenic abscess: a thoracoabdominal clinical complex. The changing picture with antibiotics.Am J Surg.1964;108:165–172.
- ,.What have we learned over the past 20 years about appendicitis in the elderly.Am J Surg.2003;185:198–201.
- ,,, et al.Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies.Am Surg.2000;66:548–554.
- ,,.Appendicitis with a palpable mass.Ann Surg.1981;193:227–229.
- ,,, et al.Nonoperative management of perforated appendicitis without periappendiceal mass.Am J Surg.2000;179:177–181.
- ,,.Appendix. In:Townsend CM, ed.Sabiston textbook of surgery. The biologic basis of modern surgical practice. 16th ed.Philadelphia:W. B. Saunders,2001:917–928.
Hospital‐Acquired Gastrointestinal Bleeding
Gastrointestinal bleeding occurring in hospitalized patients admitted for nongastrointestinal disorders has been extensively studied in intensive care unit patients. However, a systematic study in noncritically ill medical patients has not yet been done. In critically ill patients the incidence of hospital‐acquired gastrointestinal bleeding (GIB) varies from 0.17% to 5%, depending on its definition.16 These bleeding events significantly increase the morbidity and duration of hospitalization.1, 5, 79
Risk factors for bleeding in the intensive care unit include mechanical ventilation, coagulopathy, burns, chronic renal failure, and neurological insults.15 Several studies have found that stress ulcer prophylaxis with histamine‐2 (H2) receptor antagonists, sucralfate, or proton pump inhibitors (PPIs) decreases bleeding in this group of patients, with a relative risk reduction of 29%61%.10, 11 However, use of these drugs outside this high‐risk group has been questioned because of the low overall risk of bleeding.1, 11, 12 Despite their being an unproven benefit in the noncritically ill population, prophylactic H2 antagonists or PPIs are prescribed in an indiscriminant fashion to up to 30%50% of patients admitted to the hospital,13, 14 suggesting that physician preference dictates this practice. To shed light on this issue in noncritically ill patients, we conducted a retrospective casecontrol study in order to identify risk factors that predict hospital‐acquired gastrointestinal bleeding in this group of patients and to assess whether treatment with prophylactic acid suppression was associated with fewer bleeding events. We also sought to characterize the endoscopic lesions in these patients.
MATERIALS AND METHODS
Study Patients
The institutional review board of the Cleveland Clinic Foundation (Cleveland, OH) approved this study. All patients admitted to the General Internal Medicine service between January 1, 1999, and December 31, 2002, were eligible for inclusion. Two types of cases were included: 1) patients admitted for nongastrointestinal illnesses who developed bleeding at least 24 hours after admission and required esophagogastroduodenoscopy (EGD) during hospitalization (designated in‐hospital bleeding), and 2) patients admitted with gastrointestinal bleeding (requiring EGD) who had been hospitalized on the General Medical service during the preceding 4 weeks for a nongastrointestinal illness (designated out‐of‐hospital bleeding). This second group was included to identify risk factors for delayed bleeding that might not be obvious during hospitalization.
Medical records of all General Medicine patients who underwent EGD were reviewed in a standardized fashion (Fig. 1). We excluded patients with documented gastrointestinal complaints (including bleeding) at the time of the index admission or within 24 hours of admission, bleeding in the intensive care unit (ICU) or in another hospital prior to transfer to the General Medicine service, or a history of gastrointestinal bleeding during the month prior to admission. ICU stay prior to General Medicine admission, if not associated with GI bleeding, was not an exclusion criterion for our study.
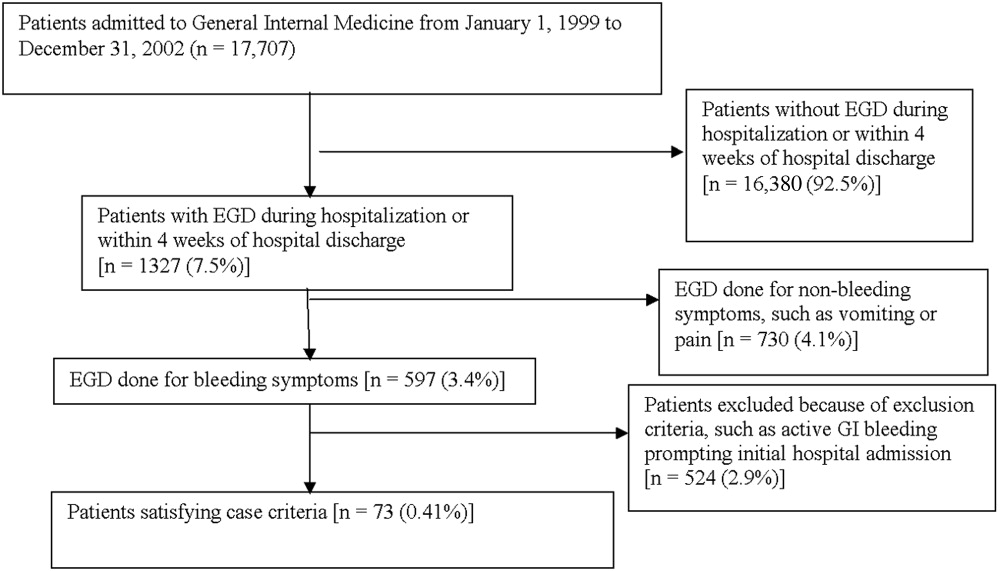
Controls, also without any acute gastrointestinal symptoms at admission, were randomly matched to cases in a 1:1 ratio by date of admission. We used this liberal matching strategy because any factors matched for would no longer be eligible to be risk factors for bleeding. If more than one control was admitted on the same day as a case, then a random number was used to select the control.
Definition of Prophylactic Acid Suppression
We defined prophylactic acid suppression as in‐hospital de novo treatment with histamine‐2 receptor antagonists and/or proton pump inhibitors received prior to the onset of any symptoms that would suggest GI bleeding (for cases) or any time during hospitalization (for controls). Patients taking these drugs prior to admission were deemed ineligible for in‐hospital prophylactic acid blockade and were excluded from the related analyses.
Data Collection
We extracted demographic information, medical history, medication usage, and laboratory data by chart review. For those patients readmitted for gastrointestinal bleeding following discharge, data from the initial (nongastrointestinal illnessassociated) hospitalization were recorded. Bleeding symptoms triggering endoscopy were grouped into four categories: 1) melena or hematochezia; 2) hematemesis (frank blood in vomitus or coffee‐grounds emesis); 3) melena or hematochezia plus hematemesis (both 1 and 2); 4) stool positivity for occult blood or unexplained drop in hemoglobin in the absence of overt bleeding. Endoscopic findings were categorized by the nature of the visualized lesions, and if multiple lesions were noted, the endoscopist's impression of the most likely bleeding site was used to define the source of bleeding. We recorded colonoscopy findings for patients undergoing this evaluation.
Statistical Analysis
We analyzed data utilizing JMP 5.1 (SAS Institute, Cary, NC). Random controls were chosen using computer‐generated random numbers. The proportions of patients with various categorical characteristics were compared using the chi‐square test or Fisher's exact test as appropriate. We used the Student t test or Wilcoxon's test to compare continuous variables. Odds ratios and adjusted odds ratios were calculated by logistic regression. Two‐tailed P values less than .05 were considered statistically significant.
RESULTS: Identification of Cases and Controls
Of 17,707 patients admitted to the General Medicine service, 1327 (7.5%) underwent EGD during hospitalization or within 1 month of discharge. Only 73 (0.41%) of the total number of patients met the case definition (Fig. 1). Of these cases, 62 (84.9%) had developed gastrointestinal bleeding during the index hospitalization, whereas 11 (15.1%) were readmitted for bleeding within 4 weeks of hospital discharge. The remaining 1254 patients who underwent EGD were excluded based on exclusion criteria, including an absence of documented bleeding prompting the EGD.
Clinical Risk Factors for Bleeding
In univariate analysis, as shown in Table 1, predictors of GIB included: 1) age (P = .02); 2) admission diagnosis (P = .01); 3) preexisting coronary artery disease (P = .004); 4) treatment with blood‐thinning medications, including warfarin (P = .0004), intravenous heparin (P = .0003), and clopidogrel (P = .02); and 5) treatment with PPIs (P = .02). After adjusting for the use of full‐dose anticoagulation and/or clopidogrel, the only of these risk factors that remained significantly associated with GIB was treatment with PPIs prior to hospitalization (adjusted OR = 2.1; 95% CI 1.17.0; P = .04), suggesting that PPI treatment in the outpatient setting may be a marker for GI vulnerability.
| Characteristic | Cases n = 73 | Controls n = 73 | Unadjusted | Adjusted for treatment with full‐dose anticoagulants or clopidogrel | ||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value (2‐tailed) | Odds ratio (95% CI) | P value (2‐tailed) | |||
| ||||||
| Demographics | ||||||
| Women | 36 (49.3%) | 29 (39.7%) | 1.5 (0.82.9) | .24 | 1.6 (0.83.3) | .19 |
| Age (years), mean (SD) | 71.6 (13.7) | 65.7 (17.2) | 1.5 (1.12.1)c | .02 | 1.3 (0.91.8) | .19 |
| Caucasian | 42 (58.3%) | 32 (44.4%) | 1.7 (0.93.4) | .09 | 1.3 (0.62.6) | .50 |
| Nursing home residents | 5 (6.9%) | 5 (6.9%) | 1.0 (0.33.7) | >.99 | 0.5 (0.12.2) | .35 |
| Admission diagnosisa | .01d | .30d | ||||
| Cardiovascular (non‐thrombotic) | 15 (20.5%) | 6 (8.2%) | 2.9 (1.18.5) | .04 | 2.1 (0.76.5) | .19 |
| Arterial or venous thrombosis | 13 (17.8%) | 2 (2.7%) | 7.9 (2.050.4) | .009 | 3.3 (0.822.1) | .15 |
| Infection | 21 (28.8%) | 24 (32.9%) | 0.8 (0.41.7) | .59 | 1.1 (0.52.3) | .86 |
| Pulmonary (noninfectious) | 4 (5.5%) | 10 (13.7%) | 0.4 (0.11.2) | .10 | 0.5 (0.11.7) | .31 |
| Altered level of consciousness | 7 (9.6%) | 10 (13.7%) | 0.7 (0.21.8) | .44 | 0.7 (0.22.2) | .59 |
| Other | 13 (17.8%) | 21 (28.8%) | 0.5 (0.21.2) | .12 | 0.6 (0.31.5) | .29 |
| Baseline medical conditions | ||||||
| Diabetes mellitus | 28 (38.4%) | 25 (34.3%) | 1.2 (0.62.4) | .61 | 1.3 (0.62.7) | .48 |
| Hypertension | 50 (68.5%) | 48 (65.8%) | 1.1 (0.62.3) | .72 | 1.2 (0.52.5) | .71 |
| Coronary artery disease | 36 (49.3%) | 19 (26.0%) | 2.8 (1.45.6) | .004 | 2.0 (1.04.3) | .06 |
| Atrial fibrillation | 18 (24.7%) | 10 (13.7%) | 2.1 (0.95.0) | .09 | 1.4 (0.53.6) | .49 |
| Congestive heart failure | 25 (34.3%) | 16 (21.9%) | 1.9 (0.93.9) | .10 | 1.5 (0.73.3) | .35 |
| Renal insufficiency (creatinine > 2) | 18 (24.7%) | 11 (15.1%) | 1.8 (0.84.4) | .14 | 1.9 (0.84.7) | .33 |
| Chronic obstructive pulmonary disease | 21 (28.8%) | 20 (27.4%) | 1.1 (0.52.2) | .85 | 1.5 (0.73.4) | .29 |
| Stroke | 13 (17.8%) | 16 (21.9%) | 0.8 (0.31.7) | .53 | 0.7 (0.31.6) | .39 |
| Active malignancy | 6 (8.2%) | 8 (11.0%) | 0.7 (0.32.2) | .57 | 1.0 (0.33.5) | .80 |
| Gastroesophageal reflux (GERD) | 10 (13.7%) | 10 (13.7%) | 1.0 (0.42.6) | >.99 | 1.0 (0.32.7) | .92 |
| Liver disease | 7 (9.6%) | 6 (8.2%) | 1.2 (0.43.9) | .77 | 1.4 (0.44.9) | .59 |
| Peptic ulcer disease | 13 (17.8%) | 5 (6.9%) | 2.9 (1.09.6) | .04 | 2.7 (0.99.4) | .09 |
| Colonic disease (diverticulosis, polyp, or AVM) | 7 (9.6%) | 4 (5.5%) | 1.8 (0.57.3) | .34 | 1.2 (0.35.2) | .79 |
| Prior gastrointestinal hemorrhage | 15 (20.1%) | 7 (9.6%) | 2.4 (1.06.8) | .06 | 2.0 (0.75.8) | .20 |
| Tobacco abuse (current smoking) | 9 (12.3%) | 18 (24.7%) | 0.4 (0.21.0) | .05 | 0.6 (0.21.5) | .26 |
| Heavy drinking (>8 drinks/day) | 2 (2.7%) | 2 (2.7%) | 1.0 (0.18.5) | >.99 | 1.3 (0.111.7) | .83 |
| Medication exposure prior to bleeding (excluding acid blockade)b | ||||||
| Aspirin (with or without NSAID) | 34 (46.6%) | 32 (43.8%) | 1.1 (0.62.1) | .74 | 0.7 (0.31.5) | .42 |
| Nonselective NSAID (without aspirin) | 3 (4.1%) | 5 (6.9%) | 0.6 (0.12.5) | .72 | 0.6 (0.12.6) | .44 |
| COX‐2 inhibitors | 3 (4.1%) | 7 (9.6%) | 0.4 (0.11.5) | .18 | 0.3 (0.11.4) | .15 |
| Glucocorticoids | 17 (23.3%) | 20 (27.4%) | 0.8 (0.41.7) | .57 | 0.9 (0.42.1) | .89 |
| Warfarin | 24 (32.9%) | 7 (9.6%) | 4.6 (1.912.4) | .004 | N/A | N/A |
| Unfractionated heparin, UFH (full‐dose intravenous | 23 (31.5%) | 6 (20.7%) | 5.1 (2.114.8) | .0003 | N/A | N/A |
| Full‐dose low‐molecular‐weight heparin (LMWH) | 2 (2.7%) | 0 (0%) | infinity | .50 | N/A | N/A |
| Clopidogrel | 9 (12.3%) | 2 (2.7%) | 5.0 (1.233.5) | .02 | N/A | N/A |
| Prophylactic LMWH or UFH (among 103 patients not on full‐dose anticoagulants) | 19 (47.5%) | 32 (50.8%) | 0.9 (0.41.9) | .74 | N/A | N/A |
| Any treatment with warfarin, full‐dose UFH, full‐ dose LMWH, and/or clopidogrel | 41 (56.2%) | 14 (19.2%) | 5.4 (2.611.7) | <.0001 | N/A | N/A |
| Gastric acid suppression (prior to any gastrointestinal hemorrhage) | ||||||
| H2‐receptor antagonists (H2RA) (total) | 11 (15.1%) | 19 (26.0%) | 0.5 (0.21.1) | .10 | 0.6 (0.31.5) | .31 |
| Taken prior to admission | 6 (8.2%) | 9 (12.3%) | 0.6 (0.21.9) | .41 | 0.6 (0.22.1) | .47 |
| Started de novo at admission | 5 (6.9%) | 10 (13.7%) | 0.5 (0.11.4) | .17 | 0.7 (0.22.2) | .53 |
| Proton‐pump inhibitor (PPI) (total) | 28 (38.6%) | 16 (21.9%) | 2.2 (1.14.7) | .03 | 2.1 (1.04.6) | .07 |
| Taken prior to admission | 20 (27.4%) | 9 (12.3%) | 2.2 (1.14.7) | .02 | 2.7 (1.17.0) | .04 |
| Started de novo at admission | 8 (11.0%) | 7 (9.6%) | 1.2 (0.43.5) | .79 | 1.0 (0.33.2) | .99 |
| Any treatment with PPI or H2RA prior to hemorrhage (total) | 39 (53.4%) | 33 (45.2%) | 1.4 (0.72.7) | .32 | 1.5 (0.73.0) | .28 |
| Taken prior to admission | 26 (35.6%) | 18 (24.7%) | 1.7 (0.83.5) | .15 | 1.7 (0.83.7) | .18 |
| Started de novo at admission (among the 102 patients not taking prior to admission) | 13 (27.7%) | 15 (27.3%) | 1.0 (0.42.4) | .97 | 1.1 (0.42.9) | .80 |
Among patients on warfarin, the peak international normalized ratio (median [IQR]) was 3.0 (1.25.0) for cases and 1.9 (1.64.8) for controls (P = .52). For those on heparin (23 cases and 6 controls), the median peak activated partial thromboplastin time (aPTT) was 67 (5082) and 128 (67180) seconds for cases and controls, respectively (P = .03), a surprising finding that was likely a result of type III error and small sample size.
Outcomes
We found no evidence of major complications from bleeding, as shown in Table 2. As expected, cases were more likely to receive blood transfusions than were controls, but clinically serious outcomes were uncommon in both groups.
| Characteristic | Cases n = 73 | Controls n = 73 | P value |
|---|---|---|---|
| |||
| Pulmonary complicationsa | 4 ( 5.5%) | 2 (2.7%) | .68 |
| Cardiac complicationsb | 4 ( 5.5%) | 3 (4.1%) | >.99 |
| Acute renal failure requiring dialysis | 0 ( 0.0%) | 1 (1.4%) | >.99 |
| Stroke or transient cerebral ischemia | 1 ( 1.4%) | 1 (1.4%) | >.99 |
| Transfer to intensive care unit | 9 (12.3%) | 4 (5.5%) | .14 |
| Blood transfusion required | 46 (63.0%) | 3 (4.1%) | <.0001 |
| All‐cause mortality | 3 ( 4.1%) | 2 (2.7%) | >.99 |
Gastrointestinal Symptoms and Endoscopic Findings
Bleeding symptoms prompting EGD and associated endoscopic findings are shown in Table 3. Findings on colonoscopy (performed in 34 patients) are included. Overall, 54 (74%) patients had a detected abnormality on EGD and/or colonoscopy that was believed to be a likely source of bleeding by the endoscopist, and 19 (26%) had no apparent culprit lesions. Melena and stool positivity for occult blood were the most common manifestations of gastrointestinal bleeding (77%) and also accounted for all the normal endoscopic evaluations. Of the 21 ulcers, 18 (85.7%) had a clean base, 1 (4.8%) had a red spot, and 2 (9.5%) had an adherent clot. None had a bleeding vessel. Endoscopic treatment was performed in one patient and angiography in one patient. A possible gastric stromal tumor (not the source of bleeding) was seen in one patient, but no mucosal malignant lesions were identified. Of the 73 cases, 41 (56.2% of cases and 0.2% of the total cohort of 17,707 patients) had culprit lesions that might have been preventable with gastric acid suppression (including peptic ulcers, esophagitis, and duodenitis).
| Most likely primary source of bleeding based on EGD with or without colonoscopya | Hematemesis only n = 10 (13.7% of cases) | Melena or hematochezia n = 33 (45.2% of cases) | Hematemesis plus either melena or hematochezia n = 4 (5.5% of cases) | Occult blood (+) and/or drop in hemoglobin (without overt bleeding) n = 26 (35.6% of cases) |
|---|---|---|---|---|
| ||||
| Normal (no lesions identified n = 19 (26.0% of cases) | 0 | 12 | 0 | 7 |
| Peptic ulcer n = 21 (28.8% of cases) | 4 | 10 | 0 | 7 |
| Esophagitis n = 8 (11.0% of cases) | 2 | 2 | 2 | 2 |
| Gastritis or duodenitis n = 12 (16.4% of cases) | 1 | 6 | 1 | 4 |
| Lower GI source only n = 1 (1.4% of cases) | 0 | 0 | 0 | 1 |
| Miscellaneous upper GI sourceb n = 12 (16.4% of cases) | 3 | 3 | 1 | 5 |
Prophylactic Gastric Acid Suppression
One hundred and two patients were not taking any acid‐suppressive prophylaxis on admission to the hospital. Of these patients, on admission 28 (27.5%) were prescribed either histamine‐2 receptor antagonists or proton pump inhibitors. We identified no clinical features associated with the prescriptions for these medications (Table 4), suggesting that physician preference, rather than perceived risk factors for bleeding, determined which patients received prophylactic acid blockade. There was no association between this prophylaxis and GI bleeding, but because of the small size of our sample, the confidence interval was wide (OR = 1.0; 95% CI 0.42.4; P = .97). In the analysis of the subgroup of patients receiving anticoagulation or clopidogrel, prophylaxis showed a nonsignificant trend toward benefit (OR = 0.71; 95% CI 0.23.9; P = .67). There was no significant interaction between the presence of anticoagulation or clopidogrel and prophylaxis (P = .61). Similarly, when we excluded those without prior GI bleeding from analysis, there was still no apparent protective effect of acid‐suppressive prophylaxis (OR = 1.0; 95% CI 0.42.5; P = .97). Finally, there was no significant association between the use of prophylaxis and lesions (theoretically) preventable by acid blockade (OR = 0.9; 95% CI 0.32.3; P = .84).
| Characteristic | Prophylaxis | |||
|---|---|---|---|---|
| Initiated n = 28 (27.5%) | Withheld n = 74 (72.5%) | Odds ratio (95% CI) | P value | |
| ||||
| Cases | ||||
| All lesions | 13 (46.4%) | 34 (46.0%) | 1.0 (0.42.4) | .97 |
| Lesions preventable with acid blockadeb | 8 (28.6%) | 20 (27.0%) | 1.1 (0.42.8) | .88 |
| Demographics | ||||
| Age, in years (SD) | 70.3 (18.6) | 66.9 (15.7) | 1.2 (0.81.9) | .40 |
| Female | 10 (35.7%) | 36 (48.7%) | 0.6 (0.21.4) | .24 |
| Medical history | ||||
| Prior gastrointestinal bleeding | 4 (14.3%) | 7 ( 9.5%) | 1.6 (0.45.8) | .49 |
| History of GERD | 1 ( 3.6%) | 4 ( 5.4%) | 0.6 (0.04.6) | >.99 |
| History of peptic ulcer disease | 3 (10.7%) | 5 ( 6.8%) | 1.7 (0.37.3) | .68 |
| Hospitalization variables | ||||
| Transferred from ICU | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Cardiovascular admission diagnosis | 7 (25.0%) | 21 (28.4%) | 0.8 (0.32.2) | .73 |
| Medication exposure | ||||
| Aspirin (with or without NSAID) | 13 (46.4%) | 30 (40.5%) | 1.3 (0.53.1) | .59 |
| NSAID alone (nonselective) | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Glucocorticoids | 6 (21.4%) | 19 (25.7%) | 0.8 (0.32.2) | .65 |
| Warfarin, clopidogrel, or IV heparin | 9 (32.1%) | 28 (37.8%) | 0.8 (0.31.9) | .59 |
DISCUSSION
Our data suggest that the incidence of hospital‐acquired gastrointestinal bleeding in noncritically ill medical patients is low (approximately 0.4%) and that treatment with anticoagulants or clopidogrel predisposes to this complication. Anticoagulation is a well‐known risk factor for gastrointestinal bleeding, with an estimated odds ratio of 2416; our study confirmed this risk.
Although some studies have questioned the utility of prophylactic acid blockade in the intensive care unit,15 the weight of current evidence supports prophylaxis in selected critically ill patients. In a randomized double‐blind study of 1200 mechanically ventilated patients, the relative risk of gastrointestinal bleeding in patients treated with ranitidine was 0.44 (95% CI 0.210.92 P = .02).11 Many experts discourage indiscriminant use of prophylaxes, even by patients in intensive care units, recommending that it be used only in patients with established risk factors for bleeding.1, 12
Despite the absence of evidence of any benefit of the use of prophylactic acid blockade outside the intensive care unit, this practice is common. In our study, 27.5% of patients who were not on outpatient acid suppression medications (PPIs or H2 antagonists) were started on them on admission to the hospital, presumably as prophylaxes, as we excluded patients admitted for acute gastrointestinal complaints. Other studies have reported prophylaxis rates of 30%50%.13, 14 Many patients started on this prophylaxis during hospitalization go on to take these drugs following discharge, creating an unnecessary economic burden.13, 14 In our study, GI prophylaxis did not appear to prevent hospital‐acquired gastrointestinal bleeding. However, the odds ratio associating the use of prophylactic acid suppression with gastrointestinal bleeding (1.0) was associated with a wide 95% confidence interval (0.42.4), so we cannot exclude the possibility that these medications might provide a relative risk reduction that we were unable to detect. Finally, although gastrointestinal bleeding in the intensive care unit is associated with significant morbidity and mortality,8, 9 we found no evidence to suggest that gastrointestinal bleeding in our patients was associated with poor outcomes.
In interpreting the data from this study, it is important to note that the definition of hospital‐acquired gastrointestinal bleeding in the literature has been inconsistent. Some studies have required that bleeding be hemodynamically significant1, 2, 5, 11a stringent criterion that may be present in only 10%15% of patients with bleeding16whereas other studies defined gastrointestinal bleeding on the basis of occult‐blood‐positive nasogastric aspirates or positive endoscopic findings.7, 15 Because the definition used in the present study required a hard clinical event (EGD), it excluded bleeding events that were considered clinically insignificant by treating physicians. We justified this definition on our belief that any bleeding that warrants invasive evaluation is clinically relevant because it is expensive and puts the patient at some physical risk. Even though some of our patients were diagnosed with GIB without obvious melena or hematemesis (ie, based on stool positivity for occult blood), many of these patients had significant drops in hemoglobin during hospitalization, which, accompanied by occult blood positivity, justified inpatient EGD. We do not believe our definition of GI bleeding was too restrictive, at least for our institution, as physicians at the Cleveland Clinic generally pursue inpatient EGD with clinically apparent gastrointestinal bleeding; we maintain that bleeding that is minor enough not to change management is of limited clinical relevance. Nevertheless, the threshold for EGD at a given institution could affect the rate of EGD for soft indications and the overall prevalence of nosocomial GI bleeding based on our definition.
It also is worth noting that our definition of nosocomial bleeding encompassed some patients with recent hospitalization on the medical service who bled following discharge (15% of cases in this study). This inclusion criterion was chosen because of our concern that the stress of hospitalization might lead to complications even after discharge. We chose an arbitrary postdischarge cutoff of 4 weeks. When we excluded these patients from analysis, the results were similar (data not shown). Although it is possible that we missed some patient who presented to other institutions with GI bleeding following discharge from the Cleveland Clinic, we suspect that the number of such patients was very small based on current referral patterns.
We do not have complete information to determine exactly why patients were on acid‐suppressive therapy prior to admission, but the available data suggest that many had gastroesophageal reflux disease (GERD), PUD, or prior GI bleeding. For this reason, we focused the investigation of the potential efficacy of prophylactic initiation of acid blockade among patients who at presentation were not taking these medications, as prior GERD (or undocumented GIB) leading to chronic use of acid blockade may predispose to subsequent GIB. Although we analyzed only those patients who had newly started taking acid‐suppressive medications, we acknowledge that a few of them may have been started on these medications for other reasons, like chest pain or GERD. However, the evidence suggests that an overwhelming number are started on these medications for the sole purpose of GI prophylaxis.13, 14
Our study was limited by its retrospective casecontrol design. However, because of the low prevalence of hospital‐acquired gastrointestinal bleeding outside the critical care unit, a prospective study would have to enroll thousands of patients in order to generate statistically meaningful results.
In summary, hospital‐acquired gastrointestinal bleeding outside the intensive care unit is uncommon, with an incidence of about 0.4% according to our definition of bleeding. We found no evidence that these bleeding episodes are associated with increased mortality or with occult malignancy. Furthermore, we found no evidence that prophylactic gastric acid suppression prevents these events, and only 41 patients (0.2% of the total cohort) had lesions that might be preventable with gastric acid blockade. We discourage the indiscriminant use of prophylactic acid suppressants in general medical patients.
Acknowledgements
The authors thank Donna M. Richey and Betty Lou Harrison for clerical support.
- ,,, et al.Risk factors for gastrointestinal bleeding in critically ill patients. Canadian Critical Care Trials Group.N Engl J Med.1994;330:377–381.
- ,,, et al.Risk factors for clinically important upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.Crit Care Med.1999;27:2812–2817.
- ,,,,.Prospective evaluation of the risk of upper gastrointestinal bleeding after admission to a medical intensive care unit.Am J Med.1984;76:623–630.
- ,,, et al.Risk factors for hospitalized gastrointestinal bleeding among older persons. Cardiovascular Health Study Investigators.J Am Geriatr Soc.2001;49:126–133.
- ,.Gastrointestinal bleeding in the hospitalized patient: a case–control study to assess risk factors, causes, and outcome.Am J Med.1998;104:349–354.
- ,,.Characterization of gastrointestinal bleeding in severely ill hospitalized patients.Crit Care Med.2000;28:46–50.
- ,,,,.Clinically significant gastrointestinal bleeding in critically ill patients in an era of prophylaxis.Am J Gastroenterol.2000;95:2801–2806.
- ,,, et al.The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients.Crit Care.2001;5:368–375.
- ,,,.Risks for developing critical illness with GI hemorrhage.Chest.2000;118:473–478.
- .Stress ulcer prophylaxis: gastrointestinal bleeding and nosocomial pneumonia. Best evidence synthesis.Scand J GastroenterolSuppl.1995;210:48–52.
- ,,, et al.A comparison of sucralfate and ranitidine for the prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.N Engl J Med.1998;338:791–797.
- ,.Stress ulcer: is routine prophylaxis necessary?Am J Gastroenterol.1995;90:708–712.
- ,,, et al.Hospital use of acid‐suppressive medications and its fall‐out on prescribing in general practice: a 1‐month survey.Aliment Pharmacol Ther.2003;17:1503–1506.
- ,,.Overuse of acid‐suppressive therapy in hospitalized patients.Am J Gastroenterol.2000;95:3118–122.
- ,,, et al.Prophylaxis for stress‐related gastric hemorrhage in the medical intensive care unit. A randomized, controlled, single‐blind study.Ann Intern Med.1994;121:568–575.
- .Low incidence of hemodynamic instability in patients with gastrointestinal hemorrhage.South Med J.1996;89:386–390.
Gastrointestinal bleeding occurring in hospitalized patients admitted for nongastrointestinal disorders has been extensively studied in intensive care unit patients. However, a systematic study in noncritically ill medical patients has not yet been done. In critically ill patients the incidence of hospital‐acquired gastrointestinal bleeding (GIB) varies from 0.17% to 5%, depending on its definition.16 These bleeding events significantly increase the morbidity and duration of hospitalization.1, 5, 79
Risk factors for bleeding in the intensive care unit include mechanical ventilation, coagulopathy, burns, chronic renal failure, and neurological insults.15 Several studies have found that stress ulcer prophylaxis with histamine‐2 (H2) receptor antagonists, sucralfate, or proton pump inhibitors (PPIs) decreases bleeding in this group of patients, with a relative risk reduction of 29%61%.10, 11 However, use of these drugs outside this high‐risk group has been questioned because of the low overall risk of bleeding.1, 11, 12 Despite their being an unproven benefit in the noncritically ill population, prophylactic H2 antagonists or PPIs are prescribed in an indiscriminant fashion to up to 30%50% of patients admitted to the hospital,13, 14 suggesting that physician preference dictates this practice. To shed light on this issue in noncritically ill patients, we conducted a retrospective casecontrol study in order to identify risk factors that predict hospital‐acquired gastrointestinal bleeding in this group of patients and to assess whether treatment with prophylactic acid suppression was associated with fewer bleeding events. We also sought to characterize the endoscopic lesions in these patients.
MATERIALS AND METHODS
Study Patients
The institutional review board of the Cleveland Clinic Foundation (Cleveland, OH) approved this study. All patients admitted to the General Internal Medicine service between January 1, 1999, and December 31, 2002, were eligible for inclusion. Two types of cases were included: 1) patients admitted for nongastrointestinal illnesses who developed bleeding at least 24 hours after admission and required esophagogastroduodenoscopy (EGD) during hospitalization (designated in‐hospital bleeding), and 2) patients admitted with gastrointestinal bleeding (requiring EGD) who had been hospitalized on the General Medical service during the preceding 4 weeks for a nongastrointestinal illness (designated out‐of‐hospital bleeding). This second group was included to identify risk factors for delayed bleeding that might not be obvious during hospitalization.
Medical records of all General Medicine patients who underwent EGD were reviewed in a standardized fashion (Fig. 1). We excluded patients with documented gastrointestinal complaints (including bleeding) at the time of the index admission or within 24 hours of admission, bleeding in the intensive care unit (ICU) or in another hospital prior to transfer to the General Medicine service, or a history of gastrointestinal bleeding during the month prior to admission. ICU stay prior to General Medicine admission, if not associated with GI bleeding, was not an exclusion criterion for our study.
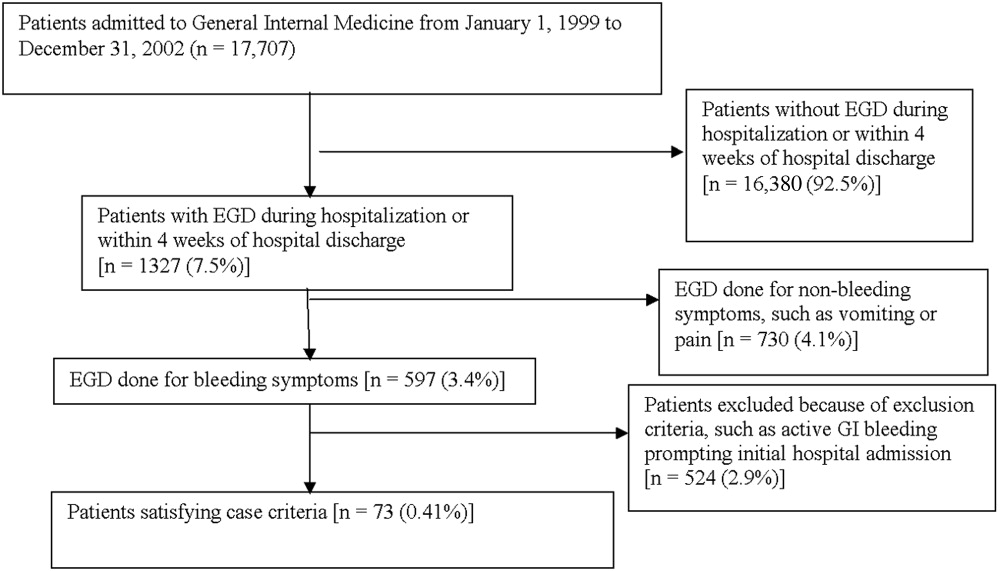
Controls, also without any acute gastrointestinal symptoms at admission, were randomly matched to cases in a 1:1 ratio by date of admission. We used this liberal matching strategy because any factors matched for would no longer be eligible to be risk factors for bleeding. If more than one control was admitted on the same day as a case, then a random number was used to select the control.
Definition of Prophylactic Acid Suppression
We defined prophylactic acid suppression as in‐hospital de novo treatment with histamine‐2 receptor antagonists and/or proton pump inhibitors received prior to the onset of any symptoms that would suggest GI bleeding (for cases) or any time during hospitalization (for controls). Patients taking these drugs prior to admission were deemed ineligible for in‐hospital prophylactic acid blockade and were excluded from the related analyses.
Data Collection
We extracted demographic information, medical history, medication usage, and laboratory data by chart review. For those patients readmitted for gastrointestinal bleeding following discharge, data from the initial (nongastrointestinal illnessassociated) hospitalization were recorded. Bleeding symptoms triggering endoscopy were grouped into four categories: 1) melena or hematochezia; 2) hematemesis (frank blood in vomitus or coffee‐grounds emesis); 3) melena or hematochezia plus hematemesis (both 1 and 2); 4) stool positivity for occult blood or unexplained drop in hemoglobin in the absence of overt bleeding. Endoscopic findings were categorized by the nature of the visualized lesions, and if multiple lesions were noted, the endoscopist's impression of the most likely bleeding site was used to define the source of bleeding. We recorded colonoscopy findings for patients undergoing this evaluation.
Statistical Analysis
We analyzed data utilizing JMP 5.1 (SAS Institute, Cary, NC). Random controls were chosen using computer‐generated random numbers. The proportions of patients with various categorical characteristics were compared using the chi‐square test or Fisher's exact test as appropriate. We used the Student t test or Wilcoxon's test to compare continuous variables. Odds ratios and adjusted odds ratios were calculated by logistic regression. Two‐tailed P values less than .05 were considered statistically significant.
RESULTS: Identification of Cases and Controls
Of 17,707 patients admitted to the General Medicine service, 1327 (7.5%) underwent EGD during hospitalization or within 1 month of discharge. Only 73 (0.41%) of the total number of patients met the case definition (Fig. 1). Of these cases, 62 (84.9%) had developed gastrointestinal bleeding during the index hospitalization, whereas 11 (15.1%) were readmitted for bleeding within 4 weeks of hospital discharge. The remaining 1254 patients who underwent EGD were excluded based on exclusion criteria, including an absence of documented bleeding prompting the EGD.
Clinical Risk Factors for Bleeding
In univariate analysis, as shown in Table 1, predictors of GIB included: 1) age (P = .02); 2) admission diagnosis (P = .01); 3) preexisting coronary artery disease (P = .004); 4) treatment with blood‐thinning medications, including warfarin (P = .0004), intravenous heparin (P = .0003), and clopidogrel (P = .02); and 5) treatment with PPIs (P = .02). After adjusting for the use of full‐dose anticoagulation and/or clopidogrel, the only of these risk factors that remained significantly associated with GIB was treatment with PPIs prior to hospitalization (adjusted OR = 2.1; 95% CI 1.17.0; P = .04), suggesting that PPI treatment in the outpatient setting may be a marker for GI vulnerability.
| Characteristic | Cases n = 73 | Controls n = 73 | Unadjusted | Adjusted for treatment with full‐dose anticoagulants or clopidogrel | ||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value (2‐tailed) | Odds ratio (95% CI) | P value (2‐tailed) | |||
| ||||||
| Demographics | ||||||
| Women | 36 (49.3%) | 29 (39.7%) | 1.5 (0.82.9) | .24 | 1.6 (0.83.3) | .19 |
| Age (years), mean (SD) | 71.6 (13.7) | 65.7 (17.2) | 1.5 (1.12.1)c | .02 | 1.3 (0.91.8) | .19 |
| Caucasian | 42 (58.3%) | 32 (44.4%) | 1.7 (0.93.4) | .09 | 1.3 (0.62.6) | .50 |
| Nursing home residents | 5 (6.9%) | 5 (6.9%) | 1.0 (0.33.7) | >.99 | 0.5 (0.12.2) | .35 |
| Admission diagnosisa | .01d | .30d | ||||
| Cardiovascular (non‐thrombotic) | 15 (20.5%) | 6 (8.2%) | 2.9 (1.18.5) | .04 | 2.1 (0.76.5) | .19 |
| Arterial or venous thrombosis | 13 (17.8%) | 2 (2.7%) | 7.9 (2.050.4) | .009 | 3.3 (0.822.1) | .15 |
| Infection | 21 (28.8%) | 24 (32.9%) | 0.8 (0.41.7) | .59 | 1.1 (0.52.3) | .86 |
| Pulmonary (noninfectious) | 4 (5.5%) | 10 (13.7%) | 0.4 (0.11.2) | .10 | 0.5 (0.11.7) | .31 |
| Altered level of consciousness | 7 (9.6%) | 10 (13.7%) | 0.7 (0.21.8) | .44 | 0.7 (0.22.2) | .59 |
| Other | 13 (17.8%) | 21 (28.8%) | 0.5 (0.21.2) | .12 | 0.6 (0.31.5) | .29 |
| Baseline medical conditions | ||||||
| Diabetes mellitus | 28 (38.4%) | 25 (34.3%) | 1.2 (0.62.4) | .61 | 1.3 (0.62.7) | .48 |
| Hypertension | 50 (68.5%) | 48 (65.8%) | 1.1 (0.62.3) | .72 | 1.2 (0.52.5) | .71 |
| Coronary artery disease | 36 (49.3%) | 19 (26.0%) | 2.8 (1.45.6) | .004 | 2.0 (1.04.3) | .06 |
| Atrial fibrillation | 18 (24.7%) | 10 (13.7%) | 2.1 (0.95.0) | .09 | 1.4 (0.53.6) | .49 |
| Congestive heart failure | 25 (34.3%) | 16 (21.9%) | 1.9 (0.93.9) | .10 | 1.5 (0.73.3) | .35 |
| Renal insufficiency (creatinine > 2) | 18 (24.7%) | 11 (15.1%) | 1.8 (0.84.4) | .14 | 1.9 (0.84.7) | .33 |
| Chronic obstructive pulmonary disease | 21 (28.8%) | 20 (27.4%) | 1.1 (0.52.2) | .85 | 1.5 (0.73.4) | .29 |
| Stroke | 13 (17.8%) | 16 (21.9%) | 0.8 (0.31.7) | .53 | 0.7 (0.31.6) | .39 |
| Active malignancy | 6 (8.2%) | 8 (11.0%) | 0.7 (0.32.2) | .57 | 1.0 (0.33.5) | .80 |
| Gastroesophageal reflux (GERD) | 10 (13.7%) | 10 (13.7%) | 1.0 (0.42.6) | >.99 | 1.0 (0.32.7) | .92 |
| Liver disease | 7 (9.6%) | 6 (8.2%) | 1.2 (0.43.9) | .77 | 1.4 (0.44.9) | .59 |
| Peptic ulcer disease | 13 (17.8%) | 5 (6.9%) | 2.9 (1.09.6) | .04 | 2.7 (0.99.4) | .09 |
| Colonic disease (diverticulosis, polyp, or AVM) | 7 (9.6%) | 4 (5.5%) | 1.8 (0.57.3) | .34 | 1.2 (0.35.2) | .79 |
| Prior gastrointestinal hemorrhage | 15 (20.1%) | 7 (9.6%) | 2.4 (1.06.8) | .06 | 2.0 (0.75.8) | .20 |
| Tobacco abuse (current smoking) | 9 (12.3%) | 18 (24.7%) | 0.4 (0.21.0) | .05 | 0.6 (0.21.5) | .26 |
| Heavy drinking (>8 drinks/day) | 2 (2.7%) | 2 (2.7%) | 1.0 (0.18.5) | >.99 | 1.3 (0.111.7) | .83 |
| Medication exposure prior to bleeding (excluding acid blockade)b | ||||||
| Aspirin (with or without NSAID) | 34 (46.6%) | 32 (43.8%) | 1.1 (0.62.1) | .74 | 0.7 (0.31.5) | .42 |
| Nonselective NSAID (without aspirin) | 3 (4.1%) | 5 (6.9%) | 0.6 (0.12.5) | .72 | 0.6 (0.12.6) | .44 |
| COX‐2 inhibitors | 3 (4.1%) | 7 (9.6%) | 0.4 (0.11.5) | .18 | 0.3 (0.11.4) | .15 |
| Glucocorticoids | 17 (23.3%) | 20 (27.4%) | 0.8 (0.41.7) | .57 | 0.9 (0.42.1) | .89 |
| Warfarin | 24 (32.9%) | 7 (9.6%) | 4.6 (1.912.4) | .004 | N/A | N/A |
| Unfractionated heparin, UFH (full‐dose intravenous | 23 (31.5%) | 6 (20.7%) | 5.1 (2.114.8) | .0003 | N/A | N/A |
| Full‐dose low‐molecular‐weight heparin (LMWH) | 2 (2.7%) | 0 (0%) | infinity | .50 | N/A | N/A |
| Clopidogrel | 9 (12.3%) | 2 (2.7%) | 5.0 (1.233.5) | .02 | N/A | N/A |
| Prophylactic LMWH or UFH (among 103 patients not on full‐dose anticoagulants) | 19 (47.5%) | 32 (50.8%) | 0.9 (0.41.9) | .74 | N/A | N/A |
| Any treatment with warfarin, full‐dose UFH, full‐ dose LMWH, and/or clopidogrel | 41 (56.2%) | 14 (19.2%) | 5.4 (2.611.7) | <.0001 | N/A | N/A |
| Gastric acid suppression (prior to any gastrointestinal hemorrhage) | ||||||
| H2‐receptor antagonists (H2RA) (total) | 11 (15.1%) | 19 (26.0%) | 0.5 (0.21.1) | .10 | 0.6 (0.31.5) | .31 |
| Taken prior to admission | 6 (8.2%) | 9 (12.3%) | 0.6 (0.21.9) | .41 | 0.6 (0.22.1) | .47 |
| Started de novo at admission | 5 (6.9%) | 10 (13.7%) | 0.5 (0.11.4) | .17 | 0.7 (0.22.2) | .53 |
| Proton‐pump inhibitor (PPI) (total) | 28 (38.6%) | 16 (21.9%) | 2.2 (1.14.7) | .03 | 2.1 (1.04.6) | .07 |
| Taken prior to admission | 20 (27.4%) | 9 (12.3%) | 2.2 (1.14.7) | .02 | 2.7 (1.17.0) | .04 |
| Started de novo at admission | 8 (11.0%) | 7 (9.6%) | 1.2 (0.43.5) | .79 | 1.0 (0.33.2) | .99 |
| Any treatment with PPI or H2RA prior to hemorrhage (total) | 39 (53.4%) | 33 (45.2%) | 1.4 (0.72.7) | .32 | 1.5 (0.73.0) | .28 |
| Taken prior to admission | 26 (35.6%) | 18 (24.7%) | 1.7 (0.83.5) | .15 | 1.7 (0.83.7) | .18 |
| Started de novo at admission (among the 102 patients not taking prior to admission) | 13 (27.7%) | 15 (27.3%) | 1.0 (0.42.4) | .97 | 1.1 (0.42.9) | .80 |
Among patients on warfarin, the peak international normalized ratio (median [IQR]) was 3.0 (1.25.0) for cases and 1.9 (1.64.8) for controls (P = .52). For those on heparin (23 cases and 6 controls), the median peak activated partial thromboplastin time (aPTT) was 67 (5082) and 128 (67180) seconds for cases and controls, respectively (P = .03), a surprising finding that was likely a result of type III error and small sample size.
Outcomes
We found no evidence of major complications from bleeding, as shown in Table 2. As expected, cases were more likely to receive blood transfusions than were controls, but clinically serious outcomes were uncommon in both groups.
| Characteristic | Cases n = 73 | Controls n = 73 | P value |
|---|---|---|---|
| |||
| Pulmonary complicationsa | 4 ( 5.5%) | 2 (2.7%) | .68 |
| Cardiac complicationsb | 4 ( 5.5%) | 3 (4.1%) | >.99 |
| Acute renal failure requiring dialysis | 0 ( 0.0%) | 1 (1.4%) | >.99 |
| Stroke or transient cerebral ischemia | 1 ( 1.4%) | 1 (1.4%) | >.99 |
| Transfer to intensive care unit | 9 (12.3%) | 4 (5.5%) | .14 |
| Blood transfusion required | 46 (63.0%) | 3 (4.1%) | <.0001 |
| All‐cause mortality | 3 ( 4.1%) | 2 (2.7%) | >.99 |
Gastrointestinal Symptoms and Endoscopic Findings
Bleeding symptoms prompting EGD and associated endoscopic findings are shown in Table 3. Findings on colonoscopy (performed in 34 patients) are included. Overall, 54 (74%) patients had a detected abnormality on EGD and/or colonoscopy that was believed to be a likely source of bleeding by the endoscopist, and 19 (26%) had no apparent culprit lesions. Melena and stool positivity for occult blood were the most common manifestations of gastrointestinal bleeding (77%) and also accounted for all the normal endoscopic evaluations. Of the 21 ulcers, 18 (85.7%) had a clean base, 1 (4.8%) had a red spot, and 2 (9.5%) had an adherent clot. None had a bleeding vessel. Endoscopic treatment was performed in one patient and angiography in one patient. A possible gastric stromal tumor (not the source of bleeding) was seen in one patient, but no mucosal malignant lesions were identified. Of the 73 cases, 41 (56.2% of cases and 0.2% of the total cohort of 17,707 patients) had culprit lesions that might have been preventable with gastric acid suppression (including peptic ulcers, esophagitis, and duodenitis).
| Most likely primary source of bleeding based on EGD with or without colonoscopya | Hematemesis only n = 10 (13.7% of cases) | Melena or hematochezia n = 33 (45.2% of cases) | Hematemesis plus either melena or hematochezia n = 4 (5.5% of cases) | Occult blood (+) and/or drop in hemoglobin (without overt bleeding) n = 26 (35.6% of cases) |
|---|---|---|---|---|
| ||||
| Normal (no lesions identified n = 19 (26.0% of cases) | 0 | 12 | 0 | 7 |
| Peptic ulcer n = 21 (28.8% of cases) | 4 | 10 | 0 | 7 |
| Esophagitis n = 8 (11.0% of cases) | 2 | 2 | 2 | 2 |
| Gastritis or duodenitis n = 12 (16.4% of cases) | 1 | 6 | 1 | 4 |
| Lower GI source only n = 1 (1.4% of cases) | 0 | 0 | 0 | 1 |
| Miscellaneous upper GI sourceb n = 12 (16.4% of cases) | 3 | 3 | 1 | 5 |
Prophylactic Gastric Acid Suppression
One hundred and two patients were not taking any acid‐suppressive prophylaxis on admission to the hospital. Of these patients, on admission 28 (27.5%) were prescribed either histamine‐2 receptor antagonists or proton pump inhibitors. We identified no clinical features associated with the prescriptions for these medications (Table 4), suggesting that physician preference, rather than perceived risk factors for bleeding, determined which patients received prophylactic acid blockade. There was no association between this prophylaxis and GI bleeding, but because of the small size of our sample, the confidence interval was wide (OR = 1.0; 95% CI 0.42.4; P = .97). In the analysis of the subgroup of patients receiving anticoagulation or clopidogrel, prophylaxis showed a nonsignificant trend toward benefit (OR = 0.71; 95% CI 0.23.9; P = .67). There was no significant interaction between the presence of anticoagulation or clopidogrel and prophylaxis (P = .61). Similarly, when we excluded those without prior GI bleeding from analysis, there was still no apparent protective effect of acid‐suppressive prophylaxis (OR = 1.0; 95% CI 0.42.5; P = .97). Finally, there was no significant association between the use of prophylaxis and lesions (theoretically) preventable by acid blockade (OR = 0.9; 95% CI 0.32.3; P = .84).
| Characteristic | Prophylaxis | |||
|---|---|---|---|---|
| Initiated n = 28 (27.5%) | Withheld n = 74 (72.5%) | Odds ratio (95% CI) | P value | |
| ||||
| Cases | ||||
| All lesions | 13 (46.4%) | 34 (46.0%) | 1.0 (0.42.4) | .97 |
| Lesions preventable with acid blockadeb | 8 (28.6%) | 20 (27.0%) | 1.1 (0.42.8) | .88 |
| Demographics | ||||
| Age, in years (SD) | 70.3 (18.6) | 66.9 (15.7) | 1.2 (0.81.9) | .40 |
| Female | 10 (35.7%) | 36 (48.7%) | 0.6 (0.21.4) | .24 |
| Medical history | ||||
| Prior gastrointestinal bleeding | 4 (14.3%) | 7 ( 9.5%) | 1.6 (0.45.8) | .49 |
| History of GERD | 1 ( 3.6%) | 4 ( 5.4%) | 0.6 (0.04.6) | >.99 |
| History of peptic ulcer disease | 3 (10.7%) | 5 ( 6.8%) | 1.7 (0.37.3) | .68 |
| Hospitalization variables | ||||
| Transferred from ICU | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Cardiovascular admission diagnosis | 7 (25.0%) | 21 (28.4%) | 0.8 (0.32.2) | .73 |
| Medication exposure | ||||
| Aspirin (with or without NSAID) | 13 (46.4%) | 30 (40.5%) | 1.3 (0.53.1) | .59 |
| NSAID alone (nonselective) | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Glucocorticoids | 6 (21.4%) | 19 (25.7%) | 0.8 (0.32.2) | .65 |
| Warfarin, clopidogrel, or IV heparin | 9 (32.1%) | 28 (37.8%) | 0.8 (0.31.9) | .59 |
DISCUSSION
Our data suggest that the incidence of hospital‐acquired gastrointestinal bleeding in noncritically ill medical patients is low (approximately 0.4%) and that treatment with anticoagulants or clopidogrel predisposes to this complication. Anticoagulation is a well‐known risk factor for gastrointestinal bleeding, with an estimated odds ratio of 2416; our study confirmed this risk.
Although some studies have questioned the utility of prophylactic acid blockade in the intensive care unit,15 the weight of current evidence supports prophylaxis in selected critically ill patients. In a randomized double‐blind study of 1200 mechanically ventilated patients, the relative risk of gastrointestinal bleeding in patients treated with ranitidine was 0.44 (95% CI 0.210.92 P = .02).11 Many experts discourage indiscriminant use of prophylaxes, even by patients in intensive care units, recommending that it be used only in patients with established risk factors for bleeding.1, 12
Despite the absence of evidence of any benefit of the use of prophylactic acid blockade outside the intensive care unit, this practice is common. In our study, 27.5% of patients who were not on outpatient acid suppression medications (PPIs or H2 antagonists) were started on them on admission to the hospital, presumably as prophylaxes, as we excluded patients admitted for acute gastrointestinal complaints. Other studies have reported prophylaxis rates of 30%50%.13, 14 Many patients started on this prophylaxis during hospitalization go on to take these drugs following discharge, creating an unnecessary economic burden.13, 14 In our study, GI prophylaxis did not appear to prevent hospital‐acquired gastrointestinal bleeding. However, the odds ratio associating the use of prophylactic acid suppression with gastrointestinal bleeding (1.0) was associated with a wide 95% confidence interval (0.42.4), so we cannot exclude the possibility that these medications might provide a relative risk reduction that we were unable to detect. Finally, although gastrointestinal bleeding in the intensive care unit is associated with significant morbidity and mortality,8, 9 we found no evidence to suggest that gastrointestinal bleeding in our patients was associated with poor outcomes.
In interpreting the data from this study, it is important to note that the definition of hospital‐acquired gastrointestinal bleeding in the literature has been inconsistent. Some studies have required that bleeding be hemodynamically significant1, 2, 5, 11a stringent criterion that may be present in only 10%15% of patients with bleeding16whereas other studies defined gastrointestinal bleeding on the basis of occult‐blood‐positive nasogastric aspirates or positive endoscopic findings.7, 15 Because the definition used in the present study required a hard clinical event (EGD), it excluded bleeding events that were considered clinically insignificant by treating physicians. We justified this definition on our belief that any bleeding that warrants invasive evaluation is clinically relevant because it is expensive and puts the patient at some physical risk. Even though some of our patients were diagnosed with GIB without obvious melena or hematemesis (ie, based on stool positivity for occult blood), many of these patients had significant drops in hemoglobin during hospitalization, which, accompanied by occult blood positivity, justified inpatient EGD. We do not believe our definition of GI bleeding was too restrictive, at least for our institution, as physicians at the Cleveland Clinic generally pursue inpatient EGD with clinically apparent gastrointestinal bleeding; we maintain that bleeding that is minor enough not to change management is of limited clinical relevance. Nevertheless, the threshold for EGD at a given institution could affect the rate of EGD for soft indications and the overall prevalence of nosocomial GI bleeding based on our definition.
It also is worth noting that our definition of nosocomial bleeding encompassed some patients with recent hospitalization on the medical service who bled following discharge (15% of cases in this study). This inclusion criterion was chosen because of our concern that the stress of hospitalization might lead to complications even after discharge. We chose an arbitrary postdischarge cutoff of 4 weeks. When we excluded these patients from analysis, the results were similar (data not shown). Although it is possible that we missed some patient who presented to other institutions with GI bleeding following discharge from the Cleveland Clinic, we suspect that the number of such patients was very small based on current referral patterns.
We do not have complete information to determine exactly why patients were on acid‐suppressive therapy prior to admission, but the available data suggest that many had gastroesophageal reflux disease (GERD), PUD, or prior GI bleeding. For this reason, we focused the investigation of the potential efficacy of prophylactic initiation of acid blockade among patients who at presentation were not taking these medications, as prior GERD (or undocumented GIB) leading to chronic use of acid blockade may predispose to subsequent GIB. Although we analyzed only those patients who had newly started taking acid‐suppressive medications, we acknowledge that a few of them may have been started on these medications for other reasons, like chest pain or GERD. However, the evidence suggests that an overwhelming number are started on these medications for the sole purpose of GI prophylaxis.13, 14
Our study was limited by its retrospective casecontrol design. However, because of the low prevalence of hospital‐acquired gastrointestinal bleeding outside the critical care unit, a prospective study would have to enroll thousands of patients in order to generate statistically meaningful results.
In summary, hospital‐acquired gastrointestinal bleeding outside the intensive care unit is uncommon, with an incidence of about 0.4% according to our definition of bleeding. We found no evidence that these bleeding episodes are associated with increased mortality or with occult malignancy. Furthermore, we found no evidence that prophylactic gastric acid suppression prevents these events, and only 41 patients (0.2% of the total cohort) had lesions that might be preventable with gastric acid blockade. We discourage the indiscriminant use of prophylactic acid suppressants in general medical patients.
Acknowledgements
The authors thank Donna M. Richey and Betty Lou Harrison for clerical support.
Gastrointestinal bleeding occurring in hospitalized patients admitted for nongastrointestinal disorders has been extensively studied in intensive care unit patients. However, a systematic study in noncritically ill medical patients has not yet been done. In critically ill patients the incidence of hospital‐acquired gastrointestinal bleeding (GIB) varies from 0.17% to 5%, depending on its definition.16 These bleeding events significantly increase the morbidity and duration of hospitalization.1, 5, 79
Risk factors for bleeding in the intensive care unit include mechanical ventilation, coagulopathy, burns, chronic renal failure, and neurological insults.15 Several studies have found that stress ulcer prophylaxis with histamine‐2 (H2) receptor antagonists, sucralfate, or proton pump inhibitors (PPIs) decreases bleeding in this group of patients, with a relative risk reduction of 29%61%.10, 11 However, use of these drugs outside this high‐risk group has been questioned because of the low overall risk of bleeding.1, 11, 12 Despite their being an unproven benefit in the noncritically ill population, prophylactic H2 antagonists or PPIs are prescribed in an indiscriminant fashion to up to 30%50% of patients admitted to the hospital,13, 14 suggesting that physician preference dictates this practice. To shed light on this issue in noncritically ill patients, we conducted a retrospective casecontrol study in order to identify risk factors that predict hospital‐acquired gastrointestinal bleeding in this group of patients and to assess whether treatment with prophylactic acid suppression was associated with fewer bleeding events. We also sought to characterize the endoscopic lesions in these patients.
MATERIALS AND METHODS
Study Patients
The institutional review board of the Cleveland Clinic Foundation (Cleveland, OH) approved this study. All patients admitted to the General Internal Medicine service between January 1, 1999, and December 31, 2002, were eligible for inclusion. Two types of cases were included: 1) patients admitted for nongastrointestinal illnesses who developed bleeding at least 24 hours after admission and required esophagogastroduodenoscopy (EGD) during hospitalization (designated in‐hospital bleeding), and 2) patients admitted with gastrointestinal bleeding (requiring EGD) who had been hospitalized on the General Medical service during the preceding 4 weeks for a nongastrointestinal illness (designated out‐of‐hospital bleeding). This second group was included to identify risk factors for delayed bleeding that might not be obvious during hospitalization.
Medical records of all General Medicine patients who underwent EGD were reviewed in a standardized fashion (Fig. 1). We excluded patients with documented gastrointestinal complaints (including bleeding) at the time of the index admission or within 24 hours of admission, bleeding in the intensive care unit (ICU) or in another hospital prior to transfer to the General Medicine service, or a history of gastrointestinal bleeding during the month prior to admission. ICU stay prior to General Medicine admission, if not associated with GI bleeding, was not an exclusion criterion for our study.
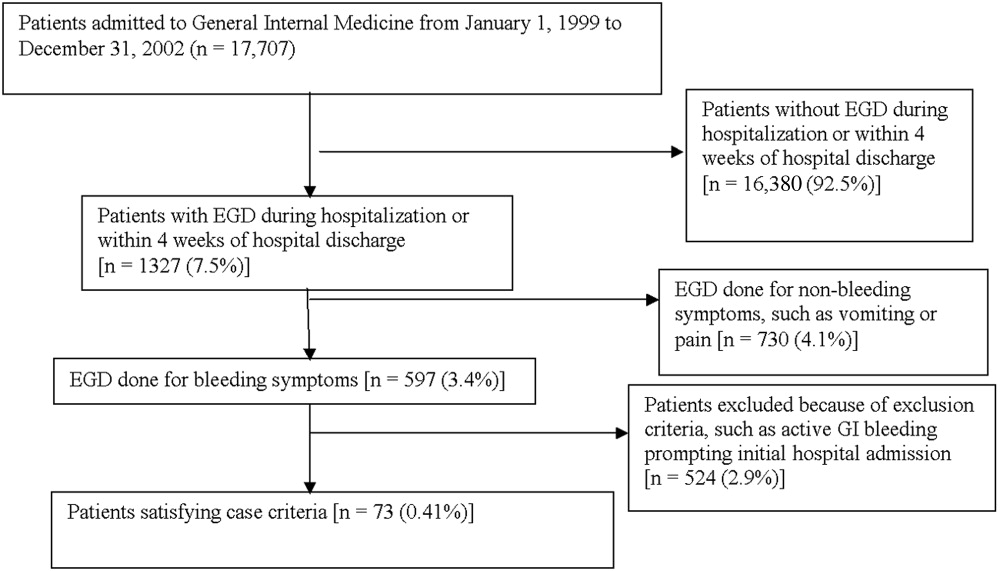
Controls, also without any acute gastrointestinal symptoms at admission, were randomly matched to cases in a 1:1 ratio by date of admission. We used this liberal matching strategy because any factors matched for would no longer be eligible to be risk factors for bleeding. If more than one control was admitted on the same day as a case, then a random number was used to select the control.
Definition of Prophylactic Acid Suppression
We defined prophylactic acid suppression as in‐hospital de novo treatment with histamine‐2 receptor antagonists and/or proton pump inhibitors received prior to the onset of any symptoms that would suggest GI bleeding (for cases) or any time during hospitalization (for controls). Patients taking these drugs prior to admission were deemed ineligible for in‐hospital prophylactic acid blockade and were excluded from the related analyses.
Data Collection
We extracted demographic information, medical history, medication usage, and laboratory data by chart review. For those patients readmitted for gastrointestinal bleeding following discharge, data from the initial (nongastrointestinal illnessassociated) hospitalization were recorded. Bleeding symptoms triggering endoscopy were grouped into four categories: 1) melena or hematochezia; 2) hematemesis (frank blood in vomitus or coffee‐grounds emesis); 3) melena or hematochezia plus hematemesis (both 1 and 2); 4) stool positivity for occult blood or unexplained drop in hemoglobin in the absence of overt bleeding. Endoscopic findings were categorized by the nature of the visualized lesions, and if multiple lesions were noted, the endoscopist's impression of the most likely bleeding site was used to define the source of bleeding. We recorded colonoscopy findings for patients undergoing this evaluation.
Statistical Analysis
We analyzed data utilizing JMP 5.1 (SAS Institute, Cary, NC). Random controls were chosen using computer‐generated random numbers. The proportions of patients with various categorical characteristics were compared using the chi‐square test or Fisher's exact test as appropriate. We used the Student t test or Wilcoxon's test to compare continuous variables. Odds ratios and adjusted odds ratios were calculated by logistic regression. Two‐tailed P values less than .05 were considered statistically significant.
RESULTS: Identification of Cases and Controls
Of 17,707 patients admitted to the General Medicine service, 1327 (7.5%) underwent EGD during hospitalization or within 1 month of discharge. Only 73 (0.41%) of the total number of patients met the case definition (Fig. 1). Of these cases, 62 (84.9%) had developed gastrointestinal bleeding during the index hospitalization, whereas 11 (15.1%) were readmitted for bleeding within 4 weeks of hospital discharge. The remaining 1254 patients who underwent EGD were excluded based on exclusion criteria, including an absence of documented bleeding prompting the EGD.
Clinical Risk Factors for Bleeding
In univariate analysis, as shown in Table 1, predictors of GIB included: 1) age (P = .02); 2) admission diagnosis (P = .01); 3) preexisting coronary artery disease (P = .004); 4) treatment with blood‐thinning medications, including warfarin (P = .0004), intravenous heparin (P = .0003), and clopidogrel (P = .02); and 5) treatment with PPIs (P = .02). After adjusting for the use of full‐dose anticoagulation and/or clopidogrel, the only of these risk factors that remained significantly associated with GIB was treatment with PPIs prior to hospitalization (adjusted OR = 2.1; 95% CI 1.17.0; P = .04), suggesting that PPI treatment in the outpatient setting may be a marker for GI vulnerability.
| Characteristic | Cases n = 73 | Controls n = 73 | Unadjusted | Adjusted for treatment with full‐dose anticoagulants or clopidogrel | ||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value (2‐tailed) | Odds ratio (95% CI) | P value (2‐tailed) | |||
| ||||||
| Demographics | ||||||
| Women | 36 (49.3%) | 29 (39.7%) | 1.5 (0.82.9) | .24 | 1.6 (0.83.3) | .19 |
| Age (years), mean (SD) | 71.6 (13.7) | 65.7 (17.2) | 1.5 (1.12.1)c | .02 | 1.3 (0.91.8) | .19 |
| Caucasian | 42 (58.3%) | 32 (44.4%) | 1.7 (0.93.4) | .09 | 1.3 (0.62.6) | .50 |
| Nursing home residents | 5 (6.9%) | 5 (6.9%) | 1.0 (0.33.7) | >.99 | 0.5 (0.12.2) | .35 |
| Admission diagnosisa | .01d | .30d | ||||
| Cardiovascular (non‐thrombotic) | 15 (20.5%) | 6 (8.2%) | 2.9 (1.18.5) | .04 | 2.1 (0.76.5) | .19 |
| Arterial or venous thrombosis | 13 (17.8%) | 2 (2.7%) | 7.9 (2.050.4) | .009 | 3.3 (0.822.1) | .15 |
| Infection | 21 (28.8%) | 24 (32.9%) | 0.8 (0.41.7) | .59 | 1.1 (0.52.3) | .86 |
| Pulmonary (noninfectious) | 4 (5.5%) | 10 (13.7%) | 0.4 (0.11.2) | .10 | 0.5 (0.11.7) | .31 |
| Altered level of consciousness | 7 (9.6%) | 10 (13.7%) | 0.7 (0.21.8) | .44 | 0.7 (0.22.2) | .59 |
| Other | 13 (17.8%) | 21 (28.8%) | 0.5 (0.21.2) | .12 | 0.6 (0.31.5) | .29 |
| Baseline medical conditions | ||||||
| Diabetes mellitus | 28 (38.4%) | 25 (34.3%) | 1.2 (0.62.4) | .61 | 1.3 (0.62.7) | .48 |
| Hypertension | 50 (68.5%) | 48 (65.8%) | 1.1 (0.62.3) | .72 | 1.2 (0.52.5) | .71 |
| Coronary artery disease | 36 (49.3%) | 19 (26.0%) | 2.8 (1.45.6) | .004 | 2.0 (1.04.3) | .06 |
| Atrial fibrillation | 18 (24.7%) | 10 (13.7%) | 2.1 (0.95.0) | .09 | 1.4 (0.53.6) | .49 |
| Congestive heart failure | 25 (34.3%) | 16 (21.9%) | 1.9 (0.93.9) | .10 | 1.5 (0.73.3) | .35 |
| Renal insufficiency (creatinine > 2) | 18 (24.7%) | 11 (15.1%) | 1.8 (0.84.4) | .14 | 1.9 (0.84.7) | .33 |
| Chronic obstructive pulmonary disease | 21 (28.8%) | 20 (27.4%) | 1.1 (0.52.2) | .85 | 1.5 (0.73.4) | .29 |
| Stroke | 13 (17.8%) | 16 (21.9%) | 0.8 (0.31.7) | .53 | 0.7 (0.31.6) | .39 |
| Active malignancy | 6 (8.2%) | 8 (11.0%) | 0.7 (0.32.2) | .57 | 1.0 (0.33.5) | .80 |
| Gastroesophageal reflux (GERD) | 10 (13.7%) | 10 (13.7%) | 1.0 (0.42.6) | >.99 | 1.0 (0.32.7) | .92 |
| Liver disease | 7 (9.6%) | 6 (8.2%) | 1.2 (0.43.9) | .77 | 1.4 (0.44.9) | .59 |
| Peptic ulcer disease | 13 (17.8%) | 5 (6.9%) | 2.9 (1.09.6) | .04 | 2.7 (0.99.4) | .09 |
| Colonic disease (diverticulosis, polyp, or AVM) | 7 (9.6%) | 4 (5.5%) | 1.8 (0.57.3) | .34 | 1.2 (0.35.2) | .79 |
| Prior gastrointestinal hemorrhage | 15 (20.1%) | 7 (9.6%) | 2.4 (1.06.8) | .06 | 2.0 (0.75.8) | .20 |
| Tobacco abuse (current smoking) | 9 (12.3%) | 18 (24.7%) | 0.4 (0.21.0) | .05 | 0.6 (0.21.5) | .26 |
| Heavy drinking (>8 drinks/day) | 2 (2.7%) | 2 (2.7%) | 1.0 (0.18.5) | >.99 | 1.3 (0.111.7) | .83 |
| Medication exposure prior to bleeding (excluding acid blockade)b | ||||||
| Aspirin (with or without NSAID) | 34 (46.6%) | 32 (43.8%) | 1.1 (0.62.1) | .74 | 0.7 (0.31.5) | .42 |
| Nonselective NSAID (without aspirin) | 3 (4.1%) | 5 (6.9%) | 0.6 (0.12.5) | .72 | 0.6 (0.12.6) | .44 |
| COX‐2 inhibitors | 3 (4.1%) | 7 (9.6%) | 0.4 (0.11.5) | .18 | 0.3 (0.11.4) | .15 |
| Glucocorticoids | 17 (23.3%) | 20 (27.4%) | 0.8 (0.41.7) | .57 | 0.9 (0.42.1) | .89 |
| Warfarin | 24 (32.9%) | 7 (9.6%) | 4.6 (1.912.4) | .004 | N/A | N/A |
| Unfractionated heparin, UFH (full‐dose intravenous | 23 (31.5%) | 6 (20.7%) | 5.1 (2.114.8) | .0003 | N/A | N/A |
| Full‐dose low‐molecular‐weight heparin (LMWH) | 2 (2.7%) | 0 (0%) | infinity | .50 | N/A | N/A |
| Clopidogrel | 9 (12.3%) | 2 (2.7%) | 5.0 (1.233.5) | .02 | N/A | N/A |
| Prophylactic LMWH or UFH (among 103 patients not on full‐dose anticoagulants) | 19 (47.5%) | 32 (50.8%) | 0.9 (0.41.9) | .74 | N/A | N/A |
| Any treatment with warfarin, full‐dose UFH, full‐ dose LMWH, and/or clopidogrel | 41 (56.2%) | 14 (19.2%) | 5.4 (2.611.7) | <.0001 | N/A | N/A |
| Gastric acid suppression (prior to any gastrointestinal hemorrhage) | ||||||
| H2‐receptor antagonists (H2RA) (total) | 11 (15.1%) | 19 (26.0%) | 0.5 (0.21.1) | .10 | 0.6 (0.31.5) | .31 |
| Taken prior to admission | 6 (8.2%) | 9 (12.3%) | 0.6 (0.21.9) | .41 | 0.6 (0.22.1) | .47 |
| Started de novo at admission | 5 (6.9%) | 10 (13.7%) | 0.5 (0.11.4) | .17 | 0.7 (0.22.2) | .53 |
| Proton‐pump inhibitor (PPI) (total) | 28 (38.6%) | 16 (21.9%) | 2.2 (1.14.7) | .03 | 2.1 (1.04.6) | .07 |
| Taken prior to admission | 20 (27.4%) | 9 (12.3%) | 2.2 (1.14.7) | .02 | 2.7 (1.17.0) | .04 |
| Started de novo at admission | 8 (11.0%) | 7 (9.6%) | 1.2 (0.43.5) | .79 | 1.0 (0.33.2) | .99 |
| Any treatment with PPI or H2RA prior to hemorrhage (total) | 39 (53.4%) | 33 (45.2%) | 1.4 (0.72.7) | .32 | 1.5 (0.73.0) | .28 |
| Taken prior to admission | 26 (35.6%) | 18 (24.7%) | 1.7 (0.83.5) | .15 | 1.7 (0.83.7) | .18 |
| Started de novo at admission (among the 102 patients not taking prior to admission) | 13 (27.7%) | 15 (27.3%) | 1.0 (0.42.4) | .97 | 1.1 (0.42.9) | .80 |
Among patients on warfarin, the peak international normalized ratio (median [IQR]) was 3.0 (1.25.0) for cases and 1.9 (1.64.8) for controls (P = .52). For those on heparin (23 cases and 6 controls), the median peak activated partial thromboplastin time (aPTT) was 67 (5082) and 128 (67180) seconds for cases and controls, respectively (P = .03), a surprising finding that was likely a result of type III error and small sample size.
Outcomes
We found no evidence of major complications from bleeding, as shown in Table 2. As expected, cases were more likely to receive blood transfusions than were controls, but clinically serious outcomes were uncommon in both groups.
| Characteristic | Cases n = 73 | Controls n = 73 | P value |
|---|---|---|---|
| |||
| Pulmonary complicationsa | 4 ( 5.5%) | 2 (2.7%) | .68 |
| Cardiac complicationsb | 4 ( 5.5%) | 3 (4.1%) | >.99 |
| Acute renal failure requiring dialysis | 0 ( 0.0%) | 1 (1.4%) | >.99 |
| Stroke or transient cerebral ischemia | 1 ( 1.4%) | 1 (1.4%) | >.99 |
| Transfer to intensive care unit | 9 (12.3%) | 4 (5.5%) | .14 |
| Blood transfusion required | 46 (63.0%) | 3 (4.1%) | <.0001 |
| All‐cause mortality | 3 ( 4.1%) | 2 (2.7%) | >.99 |
Gastrointestinal Symptoms and Endoscopic Findings
Bleeding symptoms prompting EGD and associated endoscopic findings are shown in Table 3. Findings on colonoscopy (performed in 34 patients) are included. Overall, 54 (74%) patients had a detected abnormality on EGD and/or colonoscopy that was believed to be a likely source of bleeding by the endoscopist, and 19 (26%) had no apparent culprit lesions. Melena and stool positivity for occult blood were the most common manifestations of gastrointestinal bleeding (77%) and also accounted for all the normal endoscopic evaluations. Of the 21 ulcers, 18 (85.7%) had a clean base, 1 (4.8%) had a red spot, and 2 (9.5%) had an adherent clot. None had a bleeding vessel. Endoscopic treatment was performed in one patient and angiography in one patient. A possible gastric stromal tumor (not the source of bleeding) was seen in one patient, but no mucosal malignant lesions were identified. Of the 73 cases, 41 (56.2% of cases and 0.2% of the total cohort of 17,707 patients) had culprit lesions that might have been preventable with gastric acid suppression (including peptic ulcers, esophagitis, and duodenitis).
| Most likely primary source of bleeding based on EGD with or without colonoscopya | Hematemesis only n = 10 (13.7% of cases) | Melena or hematochezia n = 33 (45.2% of cases) | Hematemesis plus either melena or hematochezia n = 4 (5.5% of cases) | Occult blood (+) and/or drop in hemoglobin (without overt bleeding) n = 26 (35.6% of cases) |
|---|---|---|---|---|
| ||||
| Normal (no lesions identified n = 19 (26.0% of cases) | 0 | 12 | 0 | 7 |
| Peptic ulcer n = 21 (28.8% of cases) | 4 | 10 | 0 | 7 |
| Esophagitis n = 8 (11.0% of cases) | 2 | 2 | 2 | 2 |
| Gastritis or duodenitis n = 12 (16.4% of cases) | 1 | 6 | 1 | 4 |
| Lower GI source only n = 1 (1.4% of cases) | 0 | 0 | 0 | 1 |
| Miscellaneous upper GI sourceb n = 12 (16.4% of cases) | 3 | 3 | 1 | 5 |
Prophylactic Gastric Acid Suppression
One hundred and two patients were not taking any acid‐suppressive prophylaxis on admission to the hospital. Of these patients, on admission 28 (27.5%) were prescribed either histamine‐2 receptor antagonists or proton pump inhibitors. We identified no clinical features associated with the prescriptions for these medications (Table 4), suggesting that physician preference, rather than perceived risk factors for bleeding, determined which patients received prophylactic acid blockade. There was no association between this prophylaxis and GI bleeding, but because of the small size of our sample, the confidence interval was wide (OR = 1.0; 95% CI 0.42.4; P = .97). In the analysis of the subgroup of patients receiving anticoagulation or clopidogrel, prophylaxis showed a nonsignificant trend toward benefit (OR = 0.71; 95% CI 0.23.9; P = .67). There was no significant interaction between the presence of anticoagulation or clopidogrel and prophylaxis (P = .61). Similarly, when we excluded those without prior GI bleeding from analysis, there was still no apparent protective effect of acid‐suppressive prophylaxis (OR = 1.0; 95% CI 0.42.5; P = .97). Finally, there was no significant association between the use of prophylaxis and lesions (theoretically) preventable by acid blockade (OR = 0.9; 95% CI 0.32.3; P = .84).
| Characteristic | Prophylaxis | |||
|---|---|---|---|---|
| Initiated n = 28 (27.5%) | Withheld n = 74 (72.5%) | Odds ratio (95% CI) | P value | |
| ||||
| Cases | ||||
| All lesions | 13 (46.4%) | 34 (46.0%) | 1.0 (0.42.4) | .97 |
| Lesions preventable with acid blockadeb | 8 (28.6%) | 20 (27.0%) | 1.1 (0.42.8) | .88 |
| Demographics | ||||
| Age, in years (SD) | 70.3 (18.6) | 66.9 (15.7) | 1.2 (0.81.9) | .40 |
| Female | 10 (35.7%) | 36 (48.7%) | 0.6 (0.21.4) | .24 |
| Medical history | ||||
| Prior gastrointestinal bleeding | 4 (14.3%) | 7 ( 9.5%) | 1.6 (0.45.8) | .49 |
| History of GERD | 1 ( 3.6%) | 4 ( 5.4%) | 0.6 (0.04.6) | >.99 |
| History of peptic ulcer disease | 3 (10.7%) | 5 ( 6.8%) | 1.7 (0.37.3) | .68 |
| Hospitalization variables | ||||
| Transferred from ICU | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Cardiovascular admission diagnosis | 7 (25.0%) | 21 (28.4%) | 0.8 (0.32.2) | .73 |
| Medication exposure | ||||
| Aspirin (with or without NSAID) | 13 (46.4%) | 30 (40.5%) | 1.3 (0.53.1) | .59 |
| NSAID alone (nonselective) | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Glucocorticoids | 6 (21.4%) | 19 (25.7%) | 0.8 (0.32.2) | .65 |
| Warfarin, clopidogrel, or IV heparin | 9 (32.1%) | 28 (37.8%) | 0.8 (0.31.9) | .59 |
DISCUSSION
Our data suggest that the incidence of hospital‐acquired gastrointestinal bleeding in noncritically ill medical patients is low (approximately 0.4%) and that treatment with anticoagulants or clopidogrel predisposes to this complication. Anticoagulation is a well‐known risk factor for gastrointestinal bleeding, with an estimated odds ratio of 2416; our study confirmed this risk.
Although some studies have questioned the utility of prophylactic acid blockade in the intensive care unit,15 the weight of current evidence supports prophylaxis in selected critically ill patients. In a randomized double‐blind study of 1200 mechanically ventilated patients, the relative risk of gastrointestinal bleeding in patients treated with ranitidine was 0.44 (95% CI 0.210.92 P = .02).11 Many experts discourage indiscriminant use of prophylaxes, even by patients in intensive care units, recommending that it be used only in patients with established risk factors for bleeding.1, 12
Despite the absence of evidence of any benefit of the use of prophylactic acid blockade outside the intensive care unit, this practice is common. In our study, 27.5% of patients who were not on outpatient acid suppression medications (PPIs or H2 antagonists) were started on them on admission to the hospital, presumably as prophylaxes, as we excluded patients admitted for acute gastrointestinal complaints. Other studies have reported prophylaxis rates of 30%50%.13, 14 Many patients started on this prophylaxis during hospitalization go on to take these drugs following discharge, creating an unnecessary economic burden.13, 14 In our study, GI prophylaxis did not appear to prevent hospital‐acquired gastrointestinal bleeding. However, the odds ratio associating the use of prophylactic acid suppression with gastrointestinal bleeding (1.0) was associated with a wide 95% confidence interval (0.42.4), so we cannot exclude the possibility that these medications might provide a relative risk reduction that we were unable to detect. Finally, although gastrointestinal bleeding in the intensive care unit is associated with significant morbidity and mortality,8, 9 we found no evidence to suggest that gastrointestinal bleeding in our patients was associated with poor outcomes.
In interpreting the data from this study, it is important to note that the definition of hospital‐acquired gastrointestinal bleeding in the literature has been inconsistent. Some studies have required that bleeding be hemodynamically significant1, 2, 5, 11a stringent criterion that may be present in only 10%15% of patients with bleeding16whereas other studies defined gastrointestinal bleeding on the basis of occult‐blood‐positive nasogastric aspirates or positive endoscopic findings.7, 15 Because the definition used in the present study required a hard clinical event (EGD), it excluded bleeding events that were considered clinically insignificant by treating physicians. We justified this definition on our belief that any bleeding that warrants invasive evaluation is clinically relevant because it is expensive and puts the patient at some physical risk. Even though some of our patients were diagnosed with GIB without obvious melena or hematemesis (ie, based on stool positivity for occult blood), many of these patients had significant drops in hemoglobin during hospitalization, which, accompanied by occult blood positivity, justified inpatient EGD. We do not believe our definition of GI bleeding was too restrictive, at least for our institution, as physicians at the Cleveland Clinic generally pursue inpatient EGD with clinically apparent gastrointestinal bleeding; we maintain that bleeding that is minor enough not to change management is of limited clinical relevance. Nevertheless, the threshold for EGD at a given institution could affect the rate of EGD for soft indications and the overall prevalence of nosocomial GI bleeding based on our definition.
It also is worth noting that our definition of nosocomial bleeding encompassed some patients with recent hospitalization on the medical service who bled following discharge (15% of cases in this study). This inclusion criterion was chosen because of our concern that the stress of hospitalization might lead to complications even after discharge. We chose an arbitrary postdischarge cutoff of 4 weeks. When we excluded these patients from analysis, the results were similar (data not shown). Although it is possible that we missed some patient who presented to other institutions with GI bleeding following discharge from the Cleveland Clinic, we suspect that the number of such patients was very small based on current referral patterns.
We do not have complete information to determine exactly why patients were on acid‐suppressive therapy prior to admission, but the available data suggest that many had gastroesophageal reflux disease (GERD), PUD, or prior GI bleeding. For this reason, we focused the investigation of the potential efficacy of prophylactic initiation of acid blockade among patients who at presentation were not taking these medications, as prior GERD (or undocumented GIB) leading to chronic use of acid blockade may predispose to subsequent GIB. Although we analyzed only those patients who had newly started taking acid‐suppressive medications, we acknowledge that a few of them may have been started on these medications for other reasons, like chest pain or GERD. However, the evidence suggests that an overwhelming number are started on these medications for the sole purpose of GI prophylaxis.13, 14
Our study was limited by its retrospective casecontrol design. However, because of the low prevalence of hospital‐acquired gastrointestinal bleeding outside the critical care unit, a prospective study would have to enroll thousands of patients in order to generate statistically meaningful results.
In summary, hospital‐acquired gastrointestinal bleeding outside the intensive care unit is uncommon, with an incidence of about 0.4% according to our definition of bleeding. We found no evidence that these bleeding episodes are associated with increased mortality or with occult malignancy. Furthermore, we found no evidence that prophylactic gastric acid suppression prevents these events, and only 41 patients (0.2% of the total cohort) had lesions that might be preventable with gastric acid blockade. We discourage the indiscriminant use of prophylactic acid suppressants in general medical patients.
Acknowledgements
The authors thank Donna M. Richey and Betty Lou Harrison for clerical support.
- ,,, et al.Risk factors for gastrointestinal bleeding in critically ill patients. Canadian Critical Care Trials Group.N Engl J Med.1994;330:377–381.
- ,,, et al.Risk factors for clinically important upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.Crit Care Med.1999;27:2812–2817.
- ,,,,.Prospective evaluation of the risk of upper gastrointestinal bleeding after admission to a medical intensive care unit.Am J Med.1984;76:623–630.
- ,,, et al.Risk factors for hospitalized gastrointestinal bleeding among older persons. Cardiovascular Health Study Investigators.J Am Geriatr Soc.2001;49:126–133.
- ,.Gastrointestinal bleeding in the hospitalized patient: a case–control study to assess risk factors, causes, and outcome.Am J Med.1998;104:349–354.
- ,,.Characterization of gastrointestinal bleeding in severely ill hospitalized patients.Crit Care Med.2000;28:46–50.
- ,,,,.Clinically significant gastrointestinal bleeding in critically ill patients in an era of prophylaxis.Am J Gastroenterol.2000;95:2801–2806.
- ,,, et al.The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients.Crit Care.2001;5:368–375.
- ,,,.Risks for developing critical illness with GI hemorrhage.Chest.2000;118:473–478.
- .Stress ulcer prophylaxis: gastrointestinal bleeding and nosocomial pneumonia. Best evidence synthesis.Scand J GastroenterolSuppl.1995;210:48–52.
- ,,, et al.A comparison of sucralfate and ranitidine for the prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.N Engl J Med.1998;338:791–797.
- ,.Stress ulcer: is routine prophylaxis necessary?Am J Gastroenterol.1995;90:708–712.
- ,,, et al.Hospital use of acid‐suppressive medications and its fall‐out on prescribing in general practice: a 1‐month survey.Aliment Pharmacol Ther.2003;17:1503–1506.
- ,,.Overuse of acid‐suppressive therapy in hospitalized patients.Am J Gastroenterol.2000;95:3118–122.
- ,,, et al.Prophylaxis for stress‐related gastric hemorrhage in the medical intensive care unit. A randomized, controlled, single‐blind study.Ann Intern Med.1994;121:568–575.
- .Low incidence of hemodynamic instability in patients with gastrointestinal hemorrhage.South Med J.1996;89:386–390.
- ,,, et al.Risk factors for gastrointestinal bleeding in critically ill patients. Canadian Critical Care Trials Group.N Engl J Med.1994;330:377–381.
- ,,, et al.Risk factors for clinically important upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.Crit Care Med.1999;27:2812–2817.
- ,,,,.Prospective evaluation of the risk of upper gastrointestinal bleeding after admission to a medical intensive care unit.Am J Med.1984;76:623–630.
- ,,, et al.Risk factors for hospitalized gastrointestinal bleeding among older persons. Cardiovascular Health Study Investigators.J Am Geriatr Soc.2001;49:126–133.
- ,.Gastrointestinal bleeding in the hospitalized patient: a case–control study to assess risk factors, causes, and outcome.Am J Med.1998;104:349–354.
- ,,.Characterization of gastrointestinal bleeding in severely ill hospitalized patients.Crit Care Med.2000;28:46–50.
- ,,,,.Clinically significant gastrointestinal bleeding in critically ill patients in an era of prophylaxis.Am J Gastroenterol.2000;95:2801–2806.
- ,,, et al.The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients.Crit Care.2001;5:368–375.
- ,,,.Risks for developing critical illness with GI hemorrhage.Chest.2000;118:473–478.
- .Stress ulcer prophylaxis: gastrointestinal bleeding and nosocomial pneumonia. Best evidence synthesis.Scand J GastroenterolSuppl.1995;210:48–52.
- ,,, et al.A comparison of sucralfate and ranitidine for the prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.N Engl J Med.1998;338:791–797.
- ,.Stress ulcer: is routine prophylaxis necessary?Am J Gastroenterol.1995;90:708–712.
- ,,, et al.Hospital use of acid‐suppressive medications and its fall‐out on prescribing in general practice: a 1‐month survey.Aliment Pharmacol Ther.2003;17:1503–1506.
- ,,.Overuse of acid‐suppressive therapy in hospitalized patients.Am J Gastroenterol.2000;95:3118–122.
- ,,, et al.Prophylaxis for stress‐related gastric hemorrhage in the medical intensive care unit. A randomized, controlled, single‐blind study.Ann Intern Med.1994;121:568–575.
- .Low incidence of hemodynamic instability in patients with gastrointestinal hemorrhage.South Med J.1996;89:386–390.
Copyright © 2006 Society of Hospital Medicine
Editorial
It is right and fitting that an article focused on palliative care appears in the inaugural issue of the Journal of Hospital Medicine (JHM).1 Both hospital medicine and palliative care are rapidly growing fields expanding in response to quality and economic imperatives. Both fields recognize the need to develop systems to care for seriously ill patients and to work within interdisciplinary teams. In fact, a natural and mutually beneficial relationship should exist between these two fields. For palliative care, hospital medicine and hospitalists offer the physicians and systems approach to care that could guarantee access to high‐quality palliative care for all hospitalized patients. In addition, hospitalists offer the promise of increasing the number of hospital‐based palliative care programs as the presence of a hospitalist program is strongly associated with having or starting such a program.2, 3 For hospital medicine and hospitalists, palliative care offers a compassionate and high‐quality response to the challenge of caring for seriously and terminally ill patients and their families. By each embracing the other, both fields could find willing and eager partners in the quest to provide the highest possible quality of care for hospitalized patients.
In this first issue of JHM, Dr. Meier offers hospitalists an intriguing and attractive picture of palliative care. She describes how the growth of palliative care is driven by the needs of an ever‐larger group of patients living with chronic and life‐threatening illness and evidence of high quality and satisfaction for these patients who have many physical, emotional, psychological, and spiritual concerns. Dr. Meier also demonstrates how hospital‐based palliative care can coordinate with hospices to provide the continuity of care for terminally ill patients that is often elusive at hospital discharge. Finally, Dr. Meier provides a practical list of resources for clinicians seeking further training in the field. No doubt hospitalists will appreciate this list as the core competencies in hospital medicine, published as a supplement to this issue of JHM, include palliative care, pain management, communication, and discharge planning.
As Dr. Meier states in her article Palliative Care in Hospitals, many types of clinicians can provide palliative care in hospitals, including general internists, nurses, geriatricians, oncologists, hospitalists, and others, yet hospitalists are likely to emerge as the predominant providers of palliative care to hospitalized patients.4 That 75% of Americans die in institutionalized settings, where hospitalists are becoming the dominant providers of care, will drive this prediction.5 In addition, hospitalists are increasingly leading efforts in quality improvement, patient satisfaction, and patient safety.6 Of necessity these initiatives will involve the sickest hospitalized patients and will look to palliative care as a proven response for improving quality and increasing satisfaction.
Hospital medicine and palliative care have other aspects in common that make a melding of the two fields beneficial. Both fields recognize and emphasize the need for interdisciplinary care; good communication between members of the health care team and between health care providers and patients; and timely, effective, and responsible discharge planning. Finally, both fields often rely on multiple sources of funding including professional fee billing and support from the hospital for the added value that programs provide. Sharing so many issues in common should help hospital medicine and palliative care form strong links.
For these links to take hold and for the benefits of this partnership to bear fruit, members of both fields, and especially those with a foot in each, need to reach out. For hospitalists this means getting educated in palliative care, an area for which hospitalists recognize they are underprepared.7 Each hospitalist must be able to provide primary, basic palliative care to each patient.8 Some hospitalists will discover the rewards of palliative care and seek further training and even board certification. These hospitalists can start or join palliative care teams in their institutions. Finally, some hospitalists will become experts in palliative care and join or lead palliative care programs at tertiary care centers. In turn, palliative care providers must reach out to hospitalists. Palliative care clinicians should seek out hospitalists at their institutions and hospices should contact hospitalists at their local hospitals. These programs need to invite hospitalists to participate in the palliative care team and suggest how their services can help the patients of hospitalists. This natural alliance can come about only if both sides reach out.
A partnership between palliative care and hospital medicine will be good for patients and their families as well as for each field, as hospitalists enable realization of the goal of providing palliative care to every patient in the United States. In addition, this partnership will be good for hospitalists who embrace this work. Palliative care can connect us to the humanism and compassion that brought so many of us to medicine and can serve as an antidote to burnout. Furthermore, by caring for patients with life‐threatening illnesses we remember that our time is limited and that each day is a gift. We recognize the importance of making the most of our time regardless of how long we have and of choosing carefully how and with whom we spend our time.
In this first issue of JHM, Dr. Meier makes a strong argument for the need and continued growth of palliative care in hospitals, lays out a strategy for achieving this growth through education and program development, and in doing so, opens the door to hope for the future. Through palliative care we can offer patients hope for healing when cure is not possible, for comfort in the face of suffering, and for what can still be despite all that cannot. The possibility that hospitalists could provide all patients access to palliative care is cause enough for hope. The knowledge that hospitalists will play a major role in making this possibility a reality and may become the predominant providers of palliative care can make that hope a reality.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,,,,,.Evaluation of the California Hospital Initiative in Palliative Services (CHIPS).Arch Intern Med. In press.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111:10S–14S.
- Field MJ,Cassell CK, Eds.Approaching death: improving care at the end of life.Washington, DC:National Academy Press,1997.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
- .Secondary and tertiary palliative care in US hospitals.JAMA.2002;287:875–881.
It is right and fitting that an article focused on palliative care appears in the inaugural issue of the Journal of Hospital Medicine (JHM).1 Both hospital medicine and palliative care are rapidly growing fields expanding in response to quality and economic imperatives. Both fields recognize the need to develop systems to care for seriously ill patients and to work within interdisciplinary teams. In fact, a natural and mutually beneficial relationship should exist between these two fields. For palliative care, hospital medicine and hospitalists offer the physicians and systems approach to care that could guarantee access to high‐quality palliative care for all hospitalized patients. In addition, hospitalists offer the promise of increasing the number of hospital‐based palliative care programs as the presence of a hospitalist program is strongly associated with having or starting such a program.2, 3 For hospital medicine and hospitalists, palliative care offers a compassionate and high‐quality response to the challenge of caring for seriously and terminally ill patients and their families. By each embracing the other, both fields could find willing and eager partners in the quest to provide the highest possible quality of care for hospitalized patients.
In this first issue of JHM, Dr. Meier offers hospitalists an intriguing and attractive picture of palliative care. She describes how the growth of palliative care is driven by the needs of an ever‐larger group of patients living with chronic and life‐threatening illness and evidence of high quality and satisfaction for these patients who have many physical, emotional, psychological, and spiritual concerns. Dr. Meier also demonstrates how hospital‐based palliative care can coordinate with hospices to provide the continuity of care for terminally ill patients that is often elusive at hospital discharge. Finally, Dr. Meier provides a practical list of resources for clinicians seeking further training in the field. No doubt hospitalists will appreciate this list as the core competencies in hospital medicine, published as a supplement to this issue of JHM, include palliative care, pain management, communication, and discharge planning.
As Dr. Meier states in her article Palliative Care in Hospitals, many types of clinicians can provide palliative care in hospitals, including general internists, nurses, geriatricians, oncologists, hospitalists, and others, yet hospitalists are likely to emerge as the predominant providers of palliative care to hospitalized patients.4 That 75% of Americans die in institutionalized settings, where hospitalists are becoming the dominant providers of care, will drive this prediction.5 In addition, hospitalists are increasingly leading efforts in quality improvement, patient satisfaction, and patient safety.6 Of necessity these initiatives will involve the sickest hospitalized patients and will look to palliative care as a proven response for improving quality and increasing satisfaction.
Hospital medicine and palliative care have other aspects in common that make a melding of the two fields beneficial. Both fields recognize and emphasize the need for interdisciplinary care; good communication between members of the health care team and between health care providers and patients; and timely, effective, and responsible discharge planning. Finally, both fields often rely on multiple sources of funding including professional fee billing and support from the hospital for the added value that programs provide. Sharing so many issues in common should help hospital medicine and palliative care form strong links.
For these links to take hold and for the benefits of this partnership to bear fruit, members of both fields, and especially those with a foot in each, need to reach out. For hospitalists this means getting educated in palliative care, an area for which hospitalists recognize they are underprepared.7 Each hospitalist must be able to provide primary, basic palliative care to each patient.8 Some hospitalists will discover the rewards of palliative care and seek further training and even board certification. These hospitalists can start or join palliative care teams in their institutions. Finally, some hospitalists will become experts in palliative care and join or lead palliative care programs at tertiary care centers. In turn, palliative care providers must reach out to hospitalists. Palliative care clinicians should seek out hospitalists at their institutions and hospices should contact hospitalists at their local hospitals. These programs need to invite hospitalists to participate in the palliative care team and suggest how their services can help the patients of hospitalists. This natural alliance can come about only if both sides reach out.
A partnership between palliative care and hospital medicine will be good for patients and their families as well as for each field, as hospitalists enable realization of the goal of providing palliative care to every patient in the United States. In addition, this partnership will be good for hospitalists who embrace this work. Palliative care can connect us to the humanism and compassion that brought so many of us to medicine and can serve as an antidote to burnout. Furthermore, by caring for patients with life‐threatening illnesses we remember that our time is limited and that each day is a gift. We recognize the importance of making the most of our time regardless of how long we have and of choosing carefully how and with whom we spend our time.
In this first issue of JHM, Dr. Meier makes a strong argument for the need and continued growth of palliative care in hospitals, lays out a strategy for achieving this growth through education and program development, and in doing so, opens the door to hope for the future. Through palliative care we can offer patients hope for healing when cure is not possible, for comfort in the face of suffering, and for what can still be despite all that cannot. The possibility that hospitalists could provide all patients access to palliative care is cause enough for hope. The knowledge that hospitalists will play a major role in making this possibility a reality and may become the predominant providers of palliative care can make that hope a reality.
It is right and fitting that an article focused on palliative care appears in the inaugural issue of the Journal of Hospital Medicine (JHM).1 Both hospital medicine and palliative care are rapidly growing fields expanding in response to quality and economic imperatives. Both fields recognize the need to develop systems to care for seriously ill patients and to work within interdisciplinary teams. In fact, a natural and mutually beneficial relationship should exist between these two fields. For palliative care, hospital medicine and hospitalists offer the physicians and systems approach to care that could guarantee access to high‐quality palliative care for all hospitalized patients. In addition, hospitalists offer the promise of increasing the number of hospital‐based palliative care programs as the presence of a hospitalist program is strongly associated with having or starting such a program.2, 3 For hospital medicine and hospitalists, palliative care offers a compassionate and high‐quality response to the challenge of caring for seriously and terminally ill patients and their families. By each embracing the other, both fields could find willing and eager partners in the quest to provide the highest possible quality of care for hospitalized patients.
In this first issue of JHM, Dr. Meier offers hospitalists an intriguing and attractive picture of palliative care. She describes how the growth of palliative care is driven by the needs of an ever‐larger group of patients living with chronic and life‐threatening illness and evidence of high quality and satisfaction for these patients who have many physical, emotional, psychological, and spiritual concerns. Dr. Meier also demonstrates how hospital‐based palliative care can coordinate with hospices to provide the continuity of care for terminally ill patients that is often elusive at hospital discharge. Finally, Dr. Meier provides a practical list of resources for clinicians seeking further training in the field. No doubt hospitalists will appreciate this list as the core competencies in hospital medicine, published as a supplement to this issue of JHM, include palliative care, pain management, communication, and discharge planning.
As Dr. Meier states in her article Palliative Care in Hospitals, many types of clinicians can provide palliative care in hospitals, including general internists, nurses, geriatricians, oncologists, hospitalists, and others, yet hospitalists are likely to emerge as the predominant providers of palliative care to hospitalized patients.4 That 75% of Americans die in institutionalized settings, where hospitalists are becoming the dominant providers of care, will drive this prediction.5 In addition, hospitalists are increasingly leading efforts in quality improvement, patient satisfaction, and patient safety.6 Of necessity these initiatives will involve the sickest hospitalized patients and will look to palliative care as a proven response for improving quality and increasing satisfaction.
Hospital medicine and palliative care have other aspects in common that make a melding of the two fields beneficial. Both fields recognize and emphasize the need for interdisciplinary care; good communication between members of the health care team and between health care providers and patients; and timely, effective, and responsible discharge planning. Finally, both fields often rely on multiple sources of funding including professional fee billing and support from the hospital for the added value that programs provide. Sharing so many issues in common should help hospital medicine and palliative care form strong links.
For these links to take hold and for the benefits of this partnership to bear fruit, members of both fields, and especially those with a foot in each, need to reach out. For hospitalists this means getting educated in palliative care, an area for which hospitalists recognize they are underprepared.7 Each hospitalist must be able to provide primary, basic palliative care to each patient.8 Some hospitalists will discover the rewards of palliative care and seek further training and even board certification. These hospitalists can start or join palliative care teams in their institutions. Finally, some hospitalists will become experts in palliative care and join or lead palliative care programs at tertiary care centers. In turn, palliative care providers must reach out to hospitalists. Palliative care clinicians should seek out hospitalists at their institutions and hospices should contact hospitalists at their local hospitals. These programs need to invite hospitalists to participate in the palliative care team and suggest how their services can help the patients of hospitalists. This natural alliance can come about only if both sides reach out.
A partnership between palliative care and hospital medicine will be good for patients and their families as well as for each field, as hospitalists enable realization of the goal of providing palliative care to every patient in the United States. In addition, this partnership will be good for hospitalists who embrace this work. Palliative care can connect us to the humanism and compassion that brought so many of us to medicine and can serve as an antidote to burnout. Furthermore, by caring for patients with life‐threatening illnesses we remember that our time is limited and that each day is a gift. We recognize the importance of making the most of our time regardless of how long we have and of choosing carefully how and with whom we spend our time.
In this first issue of JHM, Dr. Meier makes a strong argument for the need and continued growth of palliative care in hospitals, lays out a strategy for achieving this growth through education and program development, and in doing so, opens the door to hope for the future. Through palliative care we can offer patients hope for healing when cure is not possible, for comfort in the face of suffering, and for what can still be despite all that cannot. The possibility that hospitalists could provide all patients access to palliative care is cause enough for hope. The knowledge that hospitalists will play a major role in making this possibility a reality and may become the predominant providers of palliative care can make that hope a reality.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,,,,,.Evaluation of the California Hospital Initiative in Palliative Services (CHIPS).Arch Intern Med. In press.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111:10S–14S.
- Field MJ,Cassell CK, Eds.Approaching death: improving care at the end of life.Washington, DC:National Academy Press,1997.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
- .Secondary and tertiary palliative care in US hospitals.JAMA.2002;287:875–881.
- .Palliative care in hospitals.J Hosp Med.2006;1:21–28.
- ,.Prevalence and structure of palliative care services in California hospitals.Arch Intern Med.2003;163:1084–1088.
- ,,,,,.Evaluation of the California Hospital Initiative in Palliative Services (CHIPS).Arch Intern Med. In press.
- ,.Palliative care and the hospitalist: an opportunity for cross‐fertilization.Am J Med.2001;111:10S–14S.
- Field MJ,Cassell CK, Eds.Approaching death: improving care at the end of life.Washington, DC:National Academy Press,1997.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
- .Secondary and tertiary palliative care in US hospitals.JAMA.2002;287:875–881.
How to Use The Core Competencies
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
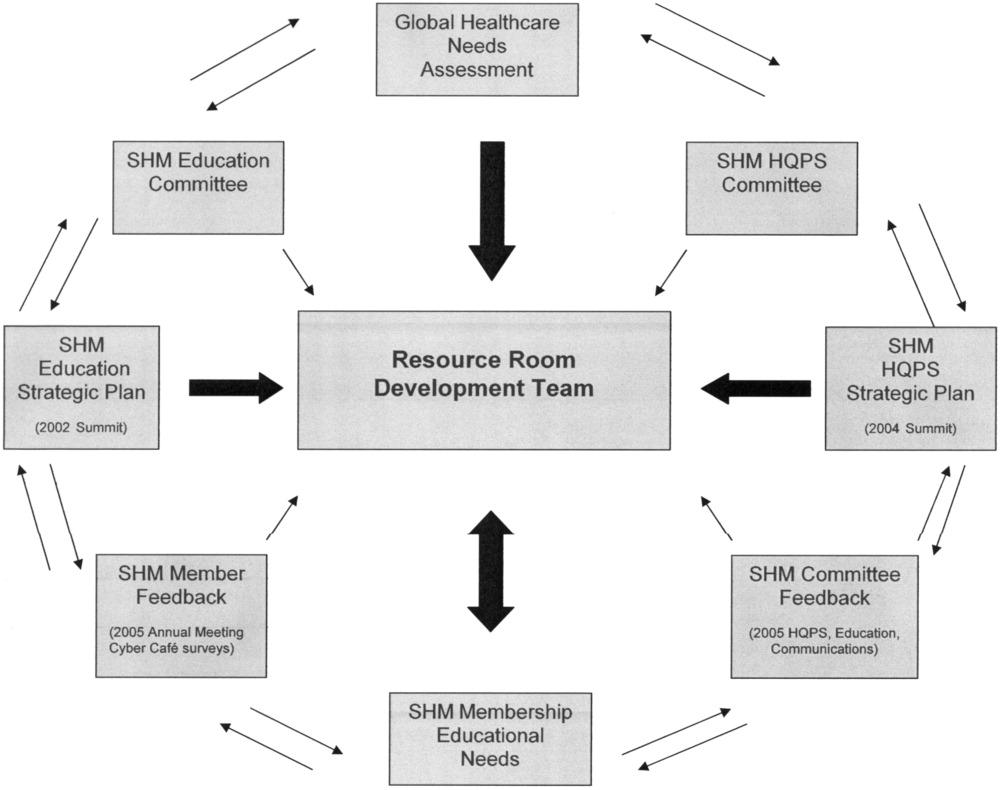
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other | The Current Approach: The focus of traditional medical education. |
| members of the inpatient team | How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. |
| Didactic lectures on the pathophysiology of VTE. rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional | Research Questions |
| research | Identifying barriers to VTE prophylaxis in the hospital setting. |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for | Quality issues in the transfer of care. |
| improvement | Failure to review radiographic study. |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other | The Current Approach: Inherent discontinuities of inpatient care. |
| embers of the inpatient team | ACGME legislated work hours: resident shifts. |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for | Research Questions |
| additional research | What are the key components of the sign‐out process? |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members | The Current Approach: Problems with the work environment |
| of the inpatient team | Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org[accessed November 2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org[accessed November 2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL:http://www.med‐ed‐online.org/pdf/f0000040.pdf[accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org[accessed November 2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
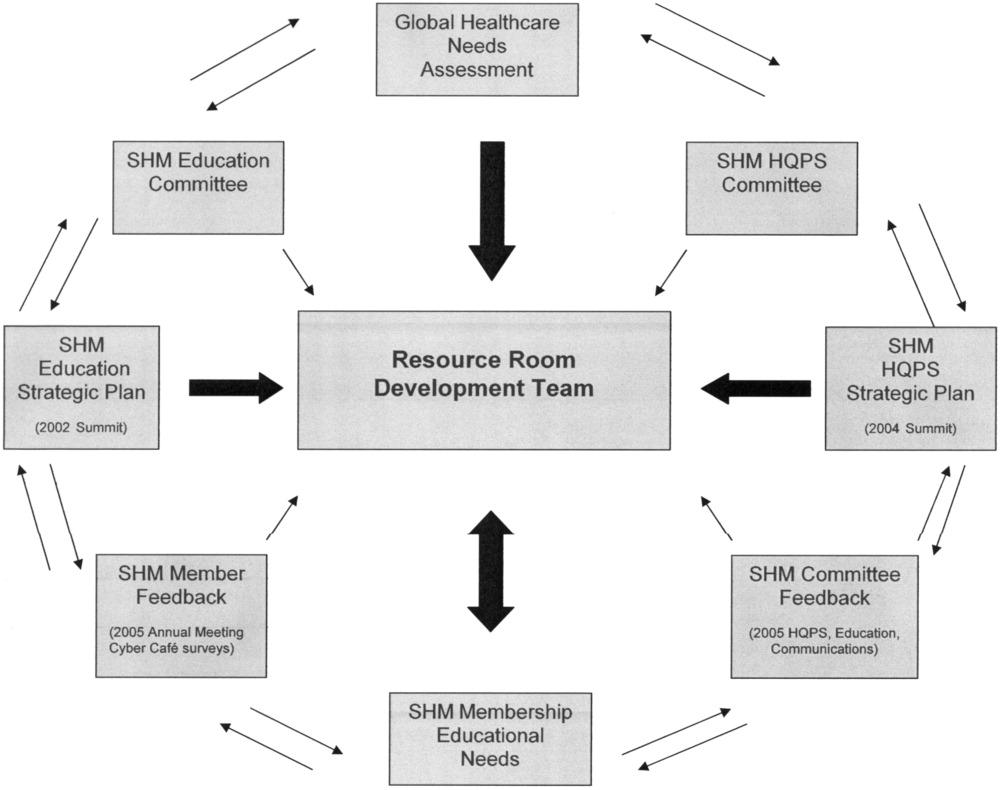
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other | The Current Approach: The focus of traditional medical education. |
| members of the inpatient team | How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. |
| Didactic lectures on the pathophysiology of VTE. rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional | Research Questions |
| research | Identifying barriers to VTE prophylaxis in the hospital setting. |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for | Quality issues in the transfer of care. |
| improvement | Failure to review radiographic study. |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other | The Current Approach: Inherent discontinuities of inpatient care. |
| embers of the inpatient team | ACGME legislated work hours: resident shifts. |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for | Research Questions |
| additional research | What are the key components of the sign‐out process? |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members | The Current Approach: Problems with the work environment |
| of the inpatient team | Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
The seminal article that coined the term hospitalist, in 1996, attributed the role of the hospitalist to enhancing throughput and cost reduction, primarily through reduction in length of stay, accomplished by having a dedicated clinician on site in the hospital.1 Since that time the role of the hospitalist has evolved to address the needs of multiple stakeholders at a time when traditional residency programs in inpatient adult medicine do not adequately train physicians to become effective agents of change in complex and potentially unsafe hospital systems. Continuing the trend of pediatrics, obstetrics, gynecology, and geriatrics, hospitalists have emerged as a distinct group of physicians who fill a needed clinical niche and are demonstrating the benefits of bringing a unique role and skill sets to the general hospital ward.2
The eligibility requirements for certification by the American Board of Internal Medicine specify that the discipline must 1) have a distinct and unique body of knowledge, 2) have clinical applicability sufficient to support a distinct clinical practice, 3) generate new information and research, 4) require a minimum training period of 12 months, and 5) have a substantial number of trainees and training programs nationwide.3 The Society of Hospital Medicine (SHM), the national professional organization of hospitalists, commissioned a task force to develop The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to from here on as the Core Competencies) to standardize the expectations of practicing hospitalists, serve as a foundation for curricula and other professional development experiences, prioritize educational scholarship and research strategies, and assess the adequacy and improvement opportunities for current training and accreditation of hospital medicine physicians.4 The preceding companion article The Core Competencies in Hospital Medicine: Development and Methodology, describes in detail the rationale for the development of the Core Competencies and the methods by which the document was created.5
PURPOSE
The purpose of this article is to illustrate how curriculum developers can apply the Core Competencies in Hospital Medicine to educate trainees and faculty, to prioritize educational scholarship and research strategies, and thus to improve the care of our patients.
TARGET AUDIENCE
The Core Competencies specifically targets directors of continuing medical education (CME), hospitalist programs and fellowships, residency programs, and medical school internal medicine clerkships. It is also intended for health educators, hospital administrators, potential employers, policy makers, and agencies funding quality‐improvement initiatives in the hospital setting. For residency program directors and clerkship directors, the chapters can guide in the development of curricula for inpatient medicine rotations or in meeting the Accreditation Council on Graduate Medical Education's Outcomes Project. For directors developing medical education curricula, The Core Competencies in Hospital Medicine can serve as a template for CME. For hospitalists, hospital administrators, and potential employers, the Core Competencies can be used to as the starting point in local program development and as a resource for refining the skills of all hospitalists, even very experienced practicing clinicians.
DEFINITION OF CORE COMPETENCIES IN HOSPITAL MEDICINE
The Core Competencies in Hospital Medicine provides a framework for curricular development based on a shared understanding of the essential knowledge, skills, and attitudes expected of physicians working as hospitalists. The development process will be ongoing, with revisions reflecting the evolving specialty of hospital medicine, the needs of practicing hospitalists, and feedback from users of the Core Competencies.
PROBLEM IDENTIFICATION AND GENERAL NEEDS ASSESSMENT
Delivery of health care has large gaps compared to ideal performance. Since the publication by the Institute of Medicine of To Err Is Human, in 1999, multiple agencies including the American Hospital Association, the National Quality Forum, and the U.S. Agency for Health Care Research and Quality (AHRQ) have reported on the incidence of medical errors in U.S. hospitals.6, 7 Recognizing that medical errors represent a major health concern in the United States, the Joint Commission on the Accreditation of Health Care Organizations (JCAHO) now requires patient safety initiatives for hospital accreditation.8 Problem‐based learning and improvement and systems based practice are now required competencies in medical residency curricula by the Accreditation Council for Graduate Medical Education (ACGME) and these requirements have led to the development of continuous quality techniques for preventing errors and a variety of patient safety initiatives.9
In 2002 the SHM recognized the need for identifying a distinct set of competencies in hospital medicine. The published competencies highlight the current gap in training of hospitalists and the imperative for revising curricula relating to inpatient care, hospital systems, and teaching.4 With adequate training and preparation, hospitalists can take the lead in implementing systems for best practices from admission through discharge and care transition, and they can direct the development of a safer, more patient‐centered, and cost‐efficient culture.
By defining the role of the hospitalist, the Core Competencies reflects the view of the SHM about what is possible but does not suggest how a training program might be modified to achieve desired outcomes or provide any content, resources, or teaching strategies. It will be up to curriculum developers to determine the scope of cognitive, psychomotor, and affective objectives that targeted learnershospitalists, residents, and other members of the multidisciplinary teamshould be required to acquire through lectures, discussions, syllabus material, clinical experience, and other venues. We agree with a broader definition of the term curriculum for graduate medical education, one that goes beyond curriculum as a plan and takes into account the learners' experiences, both planned and unplanned in the hospital setting.10 In contrast to the technologic theory of curriculum, in which lists of knowledge and skills represent final destinations, in the experiential model of curriculum, the lists provide only points of departure.11 The goal of the Core Competencies is to facilitate curriculum development using complex teaching environments as building blocks through which learning can occur.
CORE COMPETENCIES FOR HOSPITALISTS: OVERVIEW
The Core Competencies in Hospital Medicine is the first published competency‐based framework for professional development of hospitalists and provides the basis for accreditation in hospital medicine.12 The Core Competencies is organized into three sectionsClinical Conditions, Procedures, and Healthcare Systems. The supplement intentionally does not focus on content; rather, specific competencies describe unambiguous, measurable learning objectives. Each chapter can be used as a stand‐alone chapter to develop training and curricula for a particular topic area. Each chapter divides competencies into three domains of educational outcomes: cognitive (knowledge), affective (attitudes), and psychomotor (skills). Each domain has defined levels of proficiency going from knowledge, the lowest level, to evaluation, the highest.12, 13 A specific level of proficiency is articulated in the competencies through careful selection of corresponding action verbs, which clearly indicate how mastery could be assessed (see Table 1).
| GI Bleed ExampleLevels of Proficiency in the Cognitive Domain (Knowledge) | |
|---|---|
| UNDERSTAND the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | The first option, use of the verb understand gives little insight into level of proficiency. A patient could read a list on a pamphlet and truthfully claim to have achieved understanding of the advantages of each approach. An experienced gastroenterologist could make the same claim. Yet the two obviously differ in their level of comprehension. |
| LIST the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In the second option, use of the verb list indicates that the expectation for a learner is to be able to literally make a quick list of advantages, perhaps merely regurgitating what was read in a text, indicating the lowest level of learning outcome, or knowledge. |
| COMPARE the advantages and disadvantages of medical, endoscopic, and surgical treatments for patients with upper and lower GI bleeding | In this option, use of the verb compare indicates that a clinician must be able to grasp the meaning of material and consider all options, indicating a higher level of learning outcome, or comprehension. |
| Although the differences in these statements may seem subtle, they are essential to discerning a level of proficiency. Verbs that convey higher levels of proficiency in the cognitive domain include: | |
| Apply, or the ability to use learned material in new and concrete situations, | |
| Analyze, which requires an understanding of both content and its organizational structure, | |
| Synthesize, or the ability to create new patterns of structures, and | |
| Evaluate, or the ability to judge the value of material (statement, research) for a given purpose, the highest level. | |
| Learning outcomes in the evaluation category are the highest because they contain elements of all other categories plus conscious value judgments based on clearly defined criteria.13 | |
| Each competency in the Core Competencies was crafted to indicate the relevant concept, its level of proficiency, and how mastery could be evaluated. The teaching processes and learning experiences that must take place to achieve competency is left to the design of the curriculum developers and instructors. | |
In addition to specific competencies in these commonly accepted learning domains, the Clinical Conditions and Procedure sections of the Core Competencies articulate the proficiencies that hospitalists should possess in systems organization and improvement. The clinical topics were selected to set expectations of leading or participating in system improvements specific to a clinical area and to prevent predictable complications of acute illness. Competencies in the Systems Organization and Improvement section indicate mastery of multiple competencies across categories. The Core Competencies describes how the hospitalist approach facilitates coordination among all participants within the hospital system (clinical and nonclinical) and effects system changes that improve patient care processes. At the same time, the statements indicate a range of involvement from participation to leadership. For example, lead, coordination or participate in acknowledges the unique needs of different practice settings and suggests a potential professional evolution. The Systems Organization and Improvement competencies of each clinical and procedure chapter strive to capture the essence of hospitalists whose goals are to improve patient outcomes for a specific population of patients. Hospitalists do not solely focus on the care of the patient with x disease, but rather develop systems to provide the best and most efficient care for all patients with x disease, successfully transitioning these patients to outpatient care and avoiding readmission.
The third section of chapters in the Core Competencies, Healthcare Systems, distinguishes a hospitalist from others working in the inpatient setting whether practicing at academic medical centers, community hospitals, teaching hospitals, managed‐care settings, or for‐profit settings. The Healthcare Systems section identifies the integral components of the successful practice of hospital medicine and mastery of multiple competencies. This section highlights how hospitalists can facilitate coordination among all care providers within the hospital and with outpatient care providers. Hospitalists can effect system changes that improve complex care processes. It is likely that additional work experience and training beyond residency are required to attain global proficiency in the care of hospital medicine patients.
HOW TO USE THE CORE COMPETENCIES TO DEVELOP A CURRICULUM
The whole document, three sections and 51 chapters, develops expectations about the role of the hospitalist. Proficiency can be acquired through multiple means and should match the needs of the targeted learners in order to develop and maintain the necessary level of performance within the discipline of hospital medicine. Specific cases that hospitalists may encounter in their daily practice are used to illustrate how the Core Competencies can be applied to curriculum development.
The cases will employ the following six‐step approach described in Curriculum Development in Medical Education14:
A problem and a need for improvement (the actual case and quality gap)
Needs assessment of targeted learners (hospitalists, clinicians‐in‐training)
Goals and specific measurable objectives (with competencies bridging the gap between traditional roles and setting expectations about the hospitalist role)
Educational strategies (with competencies providing structure and guidance to educational efforts)
Implementation (applying competencies to a variety of training opportunities and curricula)
Evaluation and feedback (ongoing nationally, regionally, locally).
Like any quality‐improvement educational initiative, subsequent steps in curriculum development for hospitalists should include, after evaluation and feedback, dissemination of core competencies and promotion of rigorous ongoing evaluation and adaptation as needs and expectations evolve.
The first case example, failure to prevent and diagnose pulmonary embolism (see Table 2), illustrates quality issues relating to prevention of predictable complications of illness, clinical problem solving in complex conditions of uncertainty, repetitive and nondiagnostic testing, and triage of a critically ill patient between services. The Core Competencies sets expectations about the ideal role of the hospitalist that might lead to improved outcomes.
| A Common Problem That Seemed to Defy the Right Approach to Solving It |
|---|
| A 52‐year‐old female, status posthysterectomy for endometrial cancer, presents with shortness of breath. |
| High pretest probability of pulmonary embolism (PE): suggestive symptoms, major risk factors, and omission of appropriate perioperative venous thromboembolism (VTE) prophylaxis. |
| Her presentation complicated by emesis, hypotension, hypoxia after presumed aspiration, and likely PE. |
| Chest computed tomography (CT), PE protocol, reportedly negative for PE but positive for multilobar pneumonia. |
| Small bowel obstruction, 51% bandemia, and acute renal failure. |
| Subsequent emergency incarcerated hernia repair without VTE prophylaxis. |
| She is transferred to general medicine for hemodynamic monitoring and evaluation of hemoptysis and elevated troponin, presumably caused by a PE. |
| Transthoracic echocardiogram notable for right ventricular (RV) dilation and pulmonary hypertension. |
| Review of two chest CT scans, one PE protocol significant for an enlarged right ventricle and multilobar pneumonia but no PE. |
| Absence of confirmatory evidence of suspected PE by subsequent extensive testing, including beta‐natriuretic peptide (BNP) level, repeat PE protocol CT, repeat transthoracic echocardiogram, bilateral lower extremity ultrasound, persantine positron emission tomography (PET) scan, cardiac magnetic resonance imaging (MRI), and right heart catheterization. |
| Discharge plan: home on warfarin. |
| Repetitive testing did not alter management. |
| Retrospective review: Using the enlarged right atrium and ventricle as the radiographic clue to look more closely for PE, an experienced chest radiologist was able to diagnose the presence of acute PE on the first chest CT. |
Using this case example, the Evidence‐Based Medicine (EBM) chapter establishes explicit expectations for hospitalists in clinical problem solving, including 1) explaining how the tests help to verify a suspected diagnosis, 2) describing the human factor in test interpretation (e.g., technical limitations of the most recent multi‐detector‐row spiral CT), and 3) explaining how timing relative to the onset of symptoms affects test results. Rather than an overreliance on technology, leading to repeating the chest CT with PE protocol and subsequent excessive nondiagnostic testing, the hospitalist would use knowledge of pretest probability and test characteristics to determine the best diagnostic strategy. The hospitalist approach to patient care, articulated in the affective (attitudes) domains of each chapter, integrates the application of EBM principles to clinical problem solving with deliberation of cost effectiveness and efficiency.
Continuing with this case example, the Team Approach and Communication chapters establish explicit expectations for practicing hospitalists who would take the extra steps to communicate with multiple members of the care team. Knowledgeable about the hospital, the hospitalist would review the chest CT with a radiologist skilled in chest interpretation and specifically query about the significance of an enlarged right atrium and right ventricle in the setting of a high pretest clinical probability of PE. Together the radiologist and hospitalist would consider a different imaging modality if the patient flunked the chest CT when the pretest probability was high. Rather than simply deferring to the medical specialist who is consulting, the hospitalist would be expected to improve the efficiency of care and reduce cost by only ordering tests that would change clinical management, perhaps with improved outcomes.
The Hospitalist as Teacher chapter provides a frameworkcore competencies for impromptu learningbased on the patient encounter. Members of the multidisciplinary care team can be exposed to explicit clinical decision making, an approach made possible by hospitalists on site, who can provide teaching moments in real time when decisions have to be made and educational feedback is needed. Teaching expectations for hospitalists include unambiguous clinical problem solving at the bedside and possibly directing the education of residents, physician assistants, and nurses on how to initiate a quality improvement (QI) project in a hospital setting.
The Quality Improvement and Venous Thromboembolism chapters clarify the role of the hospitalist, who should direct therapy against predictable complications of serious illness, critically review prophylaxis, provide hospital‐specific data to clinicians, identify and lower barriers to prevention, devise strategies to bridge the gap between knowledge and practice, develop automated reminder systems, and participate in clinical research.
The SHM has used the Core Competencies to develop educational resources to better meet the needs of the healthcare system. Although patient safety initiatives are mandated by JCAHO for hospital accreditation and AHRQ has identified areas for safety improvement that lists venous thromboembolism (VTE) prevention as the number one priority, VTE prophylaxis is still underutilized in the United States. Although some mechanisms are in place to educate residents and hospitalists about how to manage a specific disease, traditional medical education does not focus on teaching students and residents how to manage complex patients with multiple comorbidities, to prevent predictable complications of illness, and to examine and improve care processes.15, 16 When it comes to leading quality improvement (QI), individual feedback and traditional curricula, which may include didactic lectures on the pathophysiology of VTE and morbidity and mortality conferences, have not demonstrated improved outcomes.17
The SHM QI Web‐based resource rooms offer support to any QI effort and raise collective awareness of a performance gap.18 Each resource room will describe the evidence‐based practices that should be put into effect and will leverage experience with the disease as well as with the improvement process. The underlying goal of the resource rooms is to enhance the ability of hospitalists to actually improve inpatient outcomes through self‐directed learning (see Fig. 1).
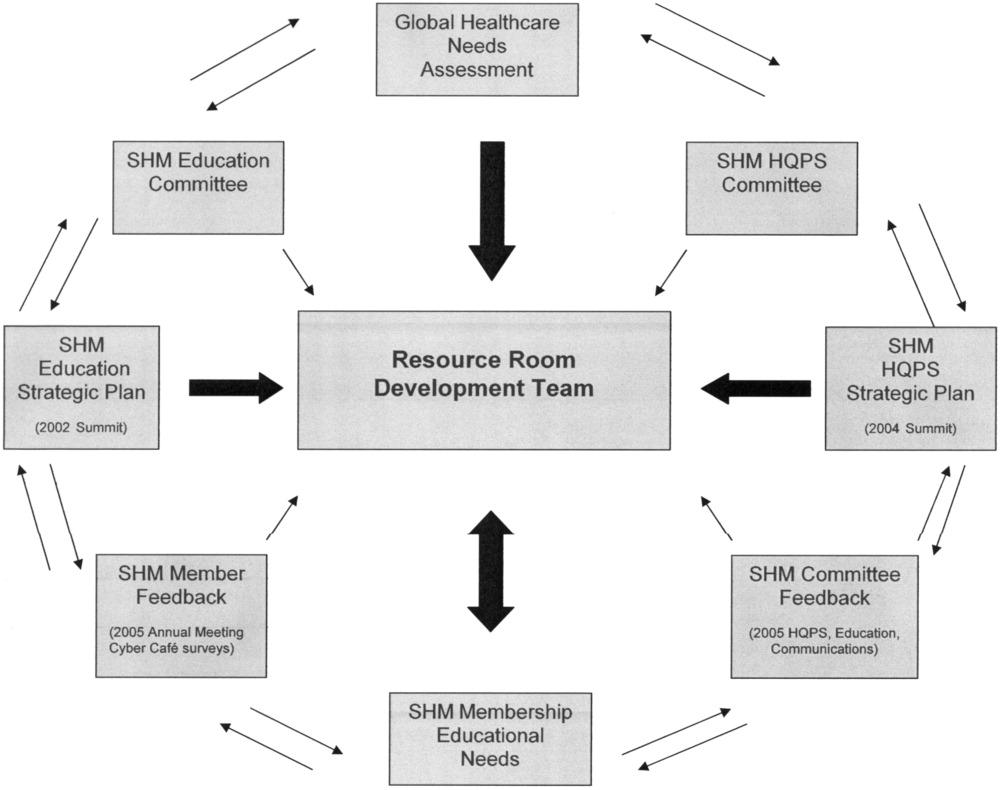
Hospitalists, residency directors, and directors of hospitalist fellowships and continuing education can use The Core Competencies in Hospital Medicine to develop curricula for their local hospitalist service and request that invited speakers develop learning objectives and content based on core competencies rather than giving a prepared lecture on a specific clinical condition. This case of PE illustrates that risk assessment, prophylaxis, EBM clinical problem solving, and QI are core topics that should be emphasized in the training of hospitalists and physicians in training.0
| STEP 1 The current problem and the need for improvement | Quality Issues |
| Prevention of predictable complications of illness: VTE still underutilized. | |
| Clinical problem‐solving in complex systems, cost‐effective, diagnostic testing. | |
| Triage of patients between services. | |
| STEP 2 Needs assessment of hospitalists and other | The Current Approach: The focus of traditional medical education. |
| members of the inpatient team | How to manage a specific disease rather than how to manage complex patients with multiple co‐morbidities. |
| Didactic lectures on the pathophysiology of VTE. rather than prevention, QI. | |
| Individual feedback, morbidity and mortality conferences | |
| STEP 3 Goals and specific measurable objectives | The Ideal Approach: Competencies as a framework for setting expectations about the role of the hospitalist |
| Direct therapy against predictable complications of serious illness. | |
| Critically review prophylaxis. | |
| Devise strategies to bridge the gap between knowledge and practice. | |
| STEP 4 Educational strategies | The first in a new online series: The VTE Resource Room, by SHM |
| Key knowledge, approaches, methods, and tools can be applied to improve performance despite variances due to particular systems and advances in medicine. | |
| Enhance the ability of hospitalists as self‐directed learners to improve inpatient outcomes. | |
| STEP 5 Implementation | The VTE Resource Room |
| A downloadable workbook and companion project outline for the improvement process. | |
| A slide set to disseminate valuable information about a safer system for VTE prevention. | |
| A moderated forum of VTE and QI experts to pose questions. | |
| STEP 6 Evaluation and feedback | Ongoing Evaluation and Feedback |
Continuous with other steps (see Fig. 1). | |
| STEP 7 Remaining questionsthe need for additional | Research Questions |
| research | Identifying barriers to VTE prophylaxis in the hospital setting. |
| Root cause analysis to determine prevention, process improvements, and training practices to encourage the safety of hospitalized patients. |
The second case example, the hand‐off (see Table 3), illustrates quality issues related to transfer of care from one physician to another. In this example, if the patient with moderate pleural effusion had been signed out, an earlier thoracentesis to drain a presumptive parapneumonic infection might have relieved this patient's shortness of breath and saved her from undergoing a subsequent VATS procedure. This case also demonstrates the importance of correlating imaging abnormalities with a patient's clinical presentation rather than using the traditional approach of just ruling out potential diagnoses to determine the cause of a problem. This case highlights elements of the process and system of care that can be modified to improve patient outcomes. Being proficient in transferring care of patients can save the hospitalist from error and prevent adverse events.
| The Hand‐Off: Avoiding Pitfalls in the Hospitalist System |
|---|
| A 30‐year‐old female, status postruptured uterus and caesarian section for pregnancy, presents with hypotension. |
| Shortness of breath postexploratory laparoscopy during fluid resuscitation. |
| Spiral CT performed to rule out pulmonary embolism, signed out as negative based on verbal report. |
| Estimated pulmonary arterial systolic pressure of 70 mmHg by transthoracic echocardiogram. |
| Extensive testing for underlying causes of pulmonary hypertension, hypercoagulable states. |
| Outpatient right heart catheterization scheduled by cardiology. |
| Sleep study advised to complete the workup of pulmonary hypertension. |
| After diuresis with a corresponding reduction in pulmonary capillary wedge pressure, her pulmonary hypertension resolves and her outpatient right heart catheterization is cancelled. |
| Final reading of chest CT (not signed out to receiving attending) reportedly notable for moderate right‐sided pleural effusion, small left‐sided effusion, and an apparent filling defect of right subclavian vein |
| Six days after the original spiral CT, unsuccessful thoracentesis attempted, with removal of 1 cc of fluid consistent with exudate. |
| Video‐assisted thorascopic surgery (VATS) procedure required to avoid chronic disability from trapped lung. |
| Retrospective review: Early drainage of a parapneumonic infection in the setting of sepsis might have avoided this complication. |
The Team Approach chapter establishes the need to acquire proficiencies not ordinarily obtained during residency in order to lead a multidisciplinary care team. This role requires a level of functioning beyond that of simply being the attending of record. The hospitalist must be able to synthesize information rather than simply defer to the consultant. Competencies specified in the Diagnostic Decision‐Making chapter can be used to identify the educational needs of hospitalists, who are expected to minimize diagnostic errors by knowing when to ask for help and where to get it, recognizing common diseases with uncommon presentations, and generating a broad differential diagnosis where there is uncertainty. The Patient Handoff chapter defines the proficiencies hospitalists need to facilitate the safe transfer of patients to other physicians on their service.0
| STEP 1 | |
| The current problem and the need for | Quality issues in the transfer of care. |
| improvement | Failure to review radiographic study. |
| Signing out pending test results. | |
| Failure to correlate imaging abnormalities with the patient's clinical presentation. | |
| STEP 2 | |
| Seeds assessment of hospitalists and other | The Current Approach: Inherent discontinuities of inpatient care. |
| embers of the inpatient team | ACGME legislated work hours: resident shifts. |
| Transfer of care to and from primary care physicians to hospitalists and between hospitalists. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Development of a standardized method of communication between hospitalists and between residents. |
| A hand‐off checklist would include pending tests, including final readings of radiographic studies. | |
| Systematic review of all films with a radiologist. | |
| STEP 4 | |
| Educational strategies | Critical examination of local practice for variability in sign‐outs. |
| Development of curricula with an agreed‐upon standard using the Core Competencies as a templatethe Patient Hand‐Offs chapter. | |
| Measure quality of hand‐off and provide feedback. | |
| STEP 5 | |
| Implementation | Dissemination of the expectations of the hand‐off. |
| Series of didactic talks for residents, physician assistants, and medical students by hospitalists based on specific cases.19 | |
| Using the core competencies as a framework; didactic lectures on hospital medicine topics can be revised to better reflect the continuing educational needs of hospitalists and their roles and responsibilities. | |
| STEP 6 | |
| Evaluation and feedback | A Framework for Educational Scholarship: the process of evaluation. |
| Innovative educational pilots, designed for members of the multidisciplinary care team | |
| Clear goals, adequate preparation, appropriate methods, significant results, effective presentation, and reflective critique. | |
| New curricular designs and materials development in topics not traditionally taught during medical school and residency such as patient hand‐offs20, 21 | |
| Not limited to publication; educational scholarship can be funded through risk management and hospital‐funded seed grants. | |
| STEP 7 | |
| Remaining questionsthe need for | Research Questions |
| additional research | What are the key components of the sign‐out process? |
| How can an electronic medical record or other system be utilized to standardize and improve the process? |
The third case example, which expands the responsibilities of hospitalist to include meeting important needs in the hospital (see Table 4), illustrates that hospitalist services cannot succeed by offering all things to all people, a distraction that that keeps the members of these services from concentrating on their goals. Always saying yes to whoever asks for help is a band‐aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems.
| No Problem |
|---|
| A proposal has been made that a new academic hospitalist service care for neurosurgical patients in order to meet the goals of the neurosurgical residency program to maximize the operating room exposure of surgeons in training. |
| Patients would be admitted to the hospitalist service, with subsequent neurosurgical consultation. |
| Another proposal has been made that the hospitalist service care for uncovered patients without residents in order to meet the goals of the medical residency program. |
| Hospital leaders assume the hospitalist service would have no problem with this proposal. |
| The hospitalists, who are not in‐house at night, are asked to handle off‐hours triage issues when there is disagreement between two services; their proposed role would be to support the medical residents who do not feel empowered to say no to the surgical team seeing patients in the emergency department. |
| The hospitalist service has the following concerns: |
| Assuming responsibility for a nonteaching service undermines the vision of this new hospitalist service in an academic tertiary care facility. |
| Assuming responsibility for a surgical specialty service increases medical legal risk and concerns about timely backup. |
| Setting a bad precedent sends the wrong message. |
| Hospitalists functioning as superresidents damages the reputation of the service. |
| The proposal comes with a price, namely, accelerating physician burnout, declining job satisfaction, and inevitable turnover. |
| The proposal would adversely affect future physician recruitment and promotion through the medical school clinician educator track. |
| Existing problems with the work environment of this new hospitalist service include: |
| The service already does not have time to meet the responsibilities of inpatient care expected of hospitalists because of rapid growth and the need for further recruitment. |
| Lack of advocacy by hospital administrators who may not understand the role of the hospitalist and entertain other solutions is an ongoing concern. |
| Lack of support for other missions of teaching and quality improvement research, coupled with a changing job description and the daily unpredictability of the work, promotes the view that hospital medicine may not be sustainable as a career. |
| The challenge and opportunity: Expertise in strategic planning and operations management is needed in order to effectively respond to conflicting pressures and focus on goals that will sustain the ability to change, grow, and continuously improve. |
The Core Competencies sets expectations about the roles of hospitalists, who serve as well‐informed clinicians and clinical opinion leaders; effective educators, mentors, and role models; empathetic and timely communicators; efficient caregivers; and creative problem solvers arriving at durable, longer‐term solutions. The competencies demonstrate the knowledge, skills, and attitudes required to be effective agents of change. Changing business as usual almost always requires significant improvements in the underlying system, however uncomfortable. The Leadership chapter articulates competencies that hospitalists need in order to define their roles within the hospital, promote group cohesiveness, expand their practices intelligently, and anticipate and respond to change. This chapter details the proficiencies that hospitalists need in order to develop personal, team, and program goals and to identify and resolve conflicts using specific negotiation techniques. The Business Practices chapter articulates the fundamental skills needed to enhance program development and growth. Hospitalists can use the Core Competencies to identify educational needs and develop curricula to enhance their leadership and business skill sets.0
| STEP 1 | |
| The current problem and the need for improvement | Hospitalist Services cannot succeed by attempting to offer all things to all people. |
| Distracting members from their work and from concentrating on their goals. | |
| Always saying yes to whoever asks for help as a Band‐Aid, a short‐term fix that impedes the effort and creativity required for durable long‐term solutions to problems. | |
| STEP 2 | |
| Needs assessment of hospitalists and other members | The Current Approach: Problems with the work environment |
| of the inpatient team | Hospital medicine, a new specialty, does not yet have a similar supportive infrastructure analogous to other well‐established specialties with most hospitalist programs within divisions of general medicine. |
| Multiple stakeholdersadministrators, primary care providers, residency and clerkship directors, specialty services. | |
| Leadership and administrative skills are not consistently acquired proficiencies during residency training. | |
| STEP 3 | |
| Goals and specific measurable objectives | The Ideal Approach: Hospitalists can proactively improve their work life by developing skills and knowledge in hospital systems. |
| Develop personal, team, and program goals. | |
| Identify and resolve conflicts using specific negotiation techniques | |
| Enhance program development and growth. | |
| Identify senior physician leaders as mentors and advocates. | |
| STEP 4 | |
| Educational strategies | Annual retreats to generate enthusiasm, establish a strategic plan, continue a trajectory of success. |
| Invite an outside expert in QI or professional development to facilitate discussion. | |
| Recruit hospitalists and colleagues with expertise in healthcare systems to mentor and educate other members of the hospitalist service how to lead QI and other initiatives. | |
| STEP 5 | |
| Implementation | Use the core competencies to advocate for resources to support professional goals. |
| Funding for leadership courses and further training in business. | |
| Directors of CME sponsored by SHM have begun the process of using the core competencies as the framework for the development of hospital medicine curricula in leadership and QI. | |
| STEP 6 | |
| Evaluation and feedback | Consider using the Core Competencies to develop an internal report card on performance. |
| A self‐assessment tool based on the core values and goals of the hospitalist program. | |
| A means to help identify areas for improvement, modifiable risk factors for turnover, and opportunities to provide incentives to measure interventions, reward success, and ultimately deliver on the mandate to improve inpatient care. | |
| STEP 7 | |
| Remaining questionsthe need for additional | Challenges facing hospitalists practicing in multiple settings. |
| research | How to make processes of care efficient by examining specific tasks that hospitalists do and determining what tools, technologies, organizational structure, and supporting staff need to be available to make the performance of these tasks efficient. |
| How to make hospital medicine a sustainable and satisfying career. |
Medical educators should examine the outcomes of current training practices and assess what modifications of objectives, content, and instructional strategies should be made to better prepare the current and next generations of physicians to practice hospital medicine and to improve the hospital setting. Given the scope of the field of hospital medicine, the Core Competencies should guide: 1) what to teach and how much to teach; 2) how to teach and assess trainees, and how to assess and compare faculty development programs; 3) how to design systems for improving quality of care and assuring patient safety; and 4) how to establish priorities for hospital medicine research.
TRANSLATING A SET OF COMPETENCIES INTO CURRICULA: POTENTIAL BENEFITS
The Core Competencies in Hospital Medicine transcends hospital type, size, and setting and standardizes what the expectations for and proficiencies of a practicing hospitalist should be. By defining the role of the hospitalist, the Core Competencies serves as a resource for refining inpatient skills and assists in program development at the local, regional, and national levels. In addition, by using the Core Competencies as the standard and framework for the development of preparatory curricula, hospital administrators and other employers can rely on hospitalists having had a common preparation.
The medical profession is constantly evolving. Internal medicine curricula address the challenges hospital medicine physicians faced yesterday but could improve the training and preparation of physicians to serve in their new and emerging roles as leaders of multidisciplinary healthcare teams working to improve patient outcomes and the system of inpatient care. Hospital medicine no longer represents a group of physicians merely supporting other specialists and primary care physicians; it is itself a specialty, composed of physicians leading, directing, and improving inpatient care. The competencies presented in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, by the Society of Hospital Medicine, should spark debate about the adequacy and appropriateness of current training and certification expectations and serve as a foundation for the development of curricula to improve hospital medicine education.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org[accessed November 2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org[accessed November 2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL:http://www.med‐ed‐online.org/pdf/f0000040.pdf[accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org[accessed November 2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1 (supplement 1).
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- Koh LT,Corrigan JM,Donaldson MS, eds.To err is human.Washington, DC:National Academy Press,2000.
- ,,,,.Making healthcare safer: a critical analysis of patient safety practices. AHRQ publication 01‐E058,2001.
- Joint Commission on the Accreditation of Health Care Organizations. Available at URL: http://www.jcaho.org[accessed November 2005].
- Accreditation Council for Graduate Medical Education. Available at URL: http://www.acgme.org[accessed November 2005].
- ,.What is a curriculum?Ann Intern Med.1992;116:1055–1056.
- ,.Conceptualizing curriculum for graduate medical education.Acad Med.1992;67:528–534.
- American Association for Health Education,National Commission for Health Education Credentialing, Inc.,Society for Public Health Education.A competency‐based framework for graduate‐level health educators.Allentown, PA:NCHEC,1999.
- .How to write and use instructional objectives.6th ed.Upper Saddle River, NJ:Prentice Hall,2000.
- ,,, et al.Curriculum development for medical education: a six‐step approach.Baltimore:Johns Hopkins University Press,1998.
- ,.Needs assessment in postgraduate medical education: a review.Med Educ Online [serial online].2002;7. Available at URL:http://www.med‐ed‐online.org/pdf/f0000040.pdf[accessed December 7, 2005].
- .Identifying, appraising, and implementing medical education curricula: a guide for medical educators.Ann Intern Med.2001;135:889–896.
- ,,, et al.A quality improvement initiative at Brigham and Women's Hospital.N Engl J Med.2005;352:969.
- The Society of Hospital Medicine. Available from URL: http://www.hospitalmedicine.org[accessed November 2005].
- ,,.Teaching and the case method.3rd ed.Cambridge, MA:Harvard Business School,1994.
- .Scholarship reconsidered: priorities of the professoriate.Princeton, NJ:Carnegie Foundation for the Advance of Teaching,1990.
- ,Scholarly activities of faculty promoted in a teacher–clinician ladder.Acad Med.2000;75:649–52.
Copyright © 2006 Society of Hospital Medicine
Core Competencies: Development and Methodology
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
|
|
|
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org[accessed July 22, 2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
|
|
|
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
Identification of the core competencies of a medical specialty provides the necessary framework for that specialty to develop, refine itself, and evolve. It also provides a structure from which training, testing, and curricula can be developed and effectively utilized. For nearly a decade, since the coining of the term hospitalist,1 the field of hospital medicine has been emerging as the next generation of site‐defined specialties, after emergency medicine and critical care medicine. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (referred to as the Core Competencies from this point on) introduces the expectations of hospitalists, helps to define their role, and suggests how knowledge, skill, and attitude acquisition might be evaluated. Furthermore, this document provides an initial structural framework from which curricula in adult hospital medicine may be developed.
The Core Competencies document, produced by the Society of Hospital Medicine (SHM) and published as a supplement to the first issue of the Journal of Hospital Medicine,2 is meant to serve as a framework for educators at all levels of medical education to develop curricula, training, and evaluations for students, clinicians‐in‐training, and practicing hospitalists. The Core Competencies document is not meant to contain a complete compilation of inpatient clinical topics or to re‐create what many residency training programs in adult inpatient care already provide. It should not limit and does not define every aspect of hospitalist practice. It includes the most common and fundamental elements of inpatient care without exhaustively listing every clinical entity that may be encountered by a hospitalist. Some of the more common clinical topics encountered by inpatient physicians are included, with an emphasis on subject areas that stress a systems‐based approach to health care, which is central to the practice of hospital medicine. This initial version of the Core Competencies document also focuses on potential areas of deficiency in the training of physicians to become hospitalists. It provides developers of curricula and content with a standardized set of measurable learning objectives, while allowing them the flexibility needed to address specific contexts and incorporate advances in medicine.
The SHM, the sole professional organization representing inpatient physicians, defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.3 An estimated 12,000 hospitalists are currently practicing in the United States, with a projected workforce need of an estimated 20,00030,000 practicing hospitalists in the United States in the next 510 years.4 Various factors have contributed to the rapid growth and expansion of hospital medicine, including factors related to care efficiency, care quality, and inpatient teaching.512 The pressures that have contributed to the development of and evolution toward the hospitalist model of care over the past decade are facilitating the transformation from a traditional model of inpatient care to the care of inpatients by hospitalist physicians dedicated primarily to the inpatient setting. As a result of this growth in hospital medicine, the SHM realized that core competencies were needed to help define the field.
The purpose of this article is to describe the developmental process and content structure of the Core Competencies document. It delineates the process from initial needs assessment to topic list development to chapter production to internal and external review and revisions of individual chapters and the complete document. The supplement to this first issue of the Journal of Hospital Medicine contains 1) the Core Competencies,2 2) a reprint of this article, and 3) a reprint of the article by McKean et al. in this issue detailing how to use the Core Competencies,13 with examples and suggestions related to curriculum development. The authors propose that this combined compilation may spur curriculum development in hospital medicine that will help to define the field and set expectations for practice.
PROCESS AND TIMELINE
Education Summit
Early in the growth of hospital medicine, the Society of Hospital Medicine identified a need to better define a common educational and practice framework for hospitalist physicians. Such a framework could help to define hospitalists as a distinct group of practicing physicians with common goals and a common set of competencies. The importance of identifying and delineating the common knowledge, skills, and attitudes of hospitalists was paramount. Figure 1 shows the details of the 4‐year process of developing the Core Competencies.
In 2002, the SHM drew together educational leaders in hospital medicine in its first educational summit. One of the primary charges that the SHM received from this summit was to develop the needed core curriculum in hospital medicine. After the summit, the SHM's Education Committee formed the Core Curriculum Task Force (CCTF), composed of approximately 15 member hospitalists, with representation from university and community hospitals, teaching and nonteaching programs, and for‐profit and not‐for‐profit settings from various geographic regions of the country. The selection process ensured that the task force was representative of practicing hospitalists and SHM membership throughout the United States.
The CCTF
The task force met through frequent conference‐call meetings and at least one in‐person meeting annually. The primary goal set forth by the task force was the initial development of a distinct set of core competencies in hospital medicine that could then guide curriculum development within the field.
Topic List
The task force determined that the topics (or chapters) should be divided into three sectionsClinical Conditions, Procedures, and Healthcare Systems (Table 1, Chapter List)all integral components of the practice of hospital medicine. For Clinical Conditions chapters, the task force decided that an exhaustive listing of all potential clinical entities that hospitalists might encounter during their clinical practice was not the goal of the Core Competencies. Rather, clinical topics were selected to reflect conditions in the hospital setting that are encountered with significant frequency, that might be significantly life‐threatening, or that are likely to have the significant involvement and impact of hospitalists in altering or refining care processes, leading to improvement in care quality and efficiency. The list of Clinical Condition chapters should not limit or rigidly define the scope of practice of hospitalist physicians. Instead, it should help those entering the field of hospital medicine better understand some of the core clinical topics on which hospitalists focus in the design of institutional or global quality initiatives.
| Clinical Conditions* | Procedures | Healthcare Systems |
|---|---|---|
| ||
|
|
|
Clinical Conditions Section
In an effort to both narrow and delineate the core Clinical Condition areas necessary for practicing hospital medicine, the task force elected first to draw from national data the most common diagnosis‐related groups (DRGs) discharged from U.S. hospitals. Utilizing the Medicare database, the top 15 nonsurgical discharge diagnoses were initially selected. Certain clinical conditions that the task force believed to be highly relevant to the practice of hospital medicine but that did not neatly fall into a specific DRG, such as pain management and perioperative medicine, were proposed for and then added to the list of Clinical Conditions chapters by the task force. Other chapters, such as that on venous thromboembolism, were added because a particular disease, although not necessarily a high‐ranked discharge DRG, showed high inpatient morbidity and mortality and reflected the role of the hospitalist in the prevention of predictable complications during hospitalization. When possible, some diagnoses were consolidated to better incorporate crosscutting competencies or to highlight opportunities for leadership in systems‐based improvements. For example, upper and lower gastrointestinal bleeding were consolidated into the chapter on gastrointestinal bleeding. Similarly, all relevant arrhythmias that a hospitalist might encounter were consolidated into a single chapter. For at least one clinical topic, pneumonia, the task force believed it necessary to have two distinct chapters, one on community‐acquired pneumonia and the other on hospital‐acquired pneumonia, because these two entities are significantly different and have distinct competencies. The final listing of Clinical Conditions chapters reflects 19 clinical areas that hospitalists encounter on a frequent basis and for which they can have an effect on systems and processes of care. These clinical chapters form a foundation of topics for which hospitalists have already begun quality and efficiency initiatives.
The task force further decided that symptom evaluation and management could be consolidated into a systems chapter dedicated to diagnostic decision making. A reasonably large constellation of symptoms, including but not limited to chest pain, shortness of breath, syncope, and altered mental status, are encountered by hospitalists daily. Although evaluation and management of these symptoms are extremely important parts of triage, subsequent testing, and hospital care, the ability to develop a differential diagnosis and proceed with the indicated testing and its interpretation is common to all symptom evaluation. Such evaluation and diagnostic decision making are therefore summarized in a single chapter in the Healthcare Systems section, and no symptom chapters are found in the Clinical section.
Procedures Section
The initial topic lists for the Procedures and Systems sections were developed through input from the broad representation of the Core Curriculum Task Force. The chapters in the Procedures section contain competencies expected for the inpatient procedures that hospitalists are most likely to perform or supervise in their day‐to‐day care of hospitalized patients. The presence of a procedural skill in the Core Competencies does not necessarily indicate that every hospitalist will perform or be proficient in that procedure. Similarly, the absence of a procedure from the Core Competencies should not exclude trained and experienced hospitalists from performing that procedure. The task force recognizes that the individual hospital setting, including local and regional variations, determines who might perform certain procedures depending on many factors, which may include whether there are trainees, specialty support including radiology, and procedure teams. The Procedures section outlines those procedures frequently performed in the everyday practice of hospital medicine and incorporates relevant competencies to afford proper performance, patient education and involvement, prevention of complications, and quality improvement for these procedures.
Healthcare Systems Section
Although many competencies delineated in the Clinical Conditions and Procedures sections of the supplement may be taught well during medical school and residency training, that is not true of the chapters and competencies in the Healthcare Systems section, many of which are not extensively taught in most undergraduate or graduate medical education programs. Therefore, many hospitalists must gain or supplant their knowledge, skills, and attitudes in system areas posttraining.
The Healthcare Systems section delineates themes integral to the successful practice of hospital medicine in diverse hospital settings. Many chapters in this section focus on processes and systems of care that typically span multiple disease entities and frequently require multidisciplinary input to create a coordinated effort for care quality and efficiency. The chapters and core competencies in the Healthcare Systems section direct hospitalists to lead and innovate in their own hospital practices and to convey the principles of evidence‐based inpatient medical care and systems‐based practice to medical students, physicians‐in‐training, other medical staff, colleagues, and patients. The task force expects that many new hospitalists will still be learning many of the competencies in the Healthcare Systems section during the early stages of their posttraining practice. However, as training of hospitalists during undergraduate and graduate medical education further evolves, we expect that more hospitalists will enter the workforce with more of the skills necessary to prepare them for their careers.
Some Healthcare Systems chapters have clinical themes but were included in this section because it is believed that the clinical approach always spans multiple clinical entities and always requires an organizational approach crossing several disciplines in medicine in order to optimize the hospital care. Such chapters include Care of the Elderly Patient, Prevention of Healthcare Associated Infections and Antimicrobial Resistance, Nutrition and the Hospitalized Patient, and Palliative Care. Other chapters in the Healthcare Systems section focus on educational themes that drive the practice of hospital medicine and the lifelong learning and teaching required of hospitalists. Some of these chapters include Evidence‐Based Medicine, Hospitalist as Teacher, Patient Education, and Practice‐Based Learning and Improvement. Still other chapters in the Healthcare Systems section identify much of the organizational approachboth from clinical practice and practice management standpointsthat must be adopted by hospitalists in order to provide high‐quality care while maintaining functional and sound practice. Examples of chapters focusing on clinical practice organization include Patient Safety, Quality Improvement, Team Approach and Multidisciplinary Care, Transitions of Care, and Patient Handoffs. Although the Transitions of Care chapter focuses on the processes and communication required for the safe transition of patients from one clinical setting to another; the Patient Handoffs (or sign‐out) chapter focuses on the hospitalist‐to‐hospitalist communication essential when one hospitalist assumes care of a patient from another (either from dayshift to nightshift on the same service or assuming care of service from a different service). Examples of chapters focusing on practice management organization include Business Practices, Equitable Allocation of Resources, Leadership, and Risk Management. Overall, the Healthcare Systems chapters help to characterize and delineate the practice and scope of hospital medicine, especially with topics not taught in detail during most residency training programs.
Editorial Board, Content Survey, and Topic List Refinement
Once the initial topic list was created, a five‐member editorial board was chosen from the CCTF membership, including the SHM CCTF chair, the Education Committee chair, two member hospitalists, and a health education specialist. The purpose of this board was to interpret survey feedback, solicit contributors to write competency chapters, review and revise the chapters submitted, and prepare the larger document for review and final publication. The Core Curriculum Task Force developed a survey to obtain feedback on the initial topic list. Face validity was established through a survey sent electronically in 2003 to the SHM Board of Directors and Education Committee, as well as to 10 representatives of each SHM regional council and local chapter. In all, more than 250 hospitalists representing diverse geographic and practice backgrounds were surveyed. Feedback from the survey was reviewed by the CCTF. The topic list was then revised with additions and modifications incorporated from survey feedback. The scope of individual topics also was modified in multiple iterations congruent with the internal and external review processes.
Contributors
Contributors were solicited by the task force, utilizing SHM databasesbelieved to be the most comprehensive registry of hospitalist physiciansand an electronic call for nominations to practicing hospitalists from around the United States. Other recognized content experts were solicited independently on the basis of chapter or content needs. Efforts were taken to identify hospitalists with expertise in specific topic areas, particularly those with a history of presentations or publications on individual chapter subject matter. Potential contributors submitted credentials, including curricula vitae and other supporting documents or information, when requesting to write a specific chapter for the Core Competencies compendium. Contributors were competitively selected on the basis of their submitted information compared to those of others requesting to write the same chapter. In some cases practicing hospitalists were paired with nonhospitalist expert contributors to create a chapter. Contributors were provided with guidelines with which to prepare their chapter.
Review and Revision
The editorial board reviewed all the chapters, rigorously evaluating each chapter through at least five stages of review and revision. First, chapters were reviewed by the editorial boardinitially by at least two physician members and then by the entire editorial board. Chapters were reviewed for the scope and completeness of concepts, adherence to educational theory, and consistency in chapter format. Changes in content and for consistency were extensive in some chapters, whereas others required only small or moderate changes. Significant editing was required to create chapters as a compilation of specific, measurable competencies as opposed to topic‐related content. All chapters required some level of modification to assist with consistency in style, language, and overall goals. Where appropriate, individual chapters were also reviewed by relevant SHM committees, task forces, or content experts, and initial feedback was provided. For example, the Leadership chapter was reviewed by the SHM Leadership Task Force. Other SHM committees and task forces involved in chapter reviews included the Education, Healthcare Quality and Patient Safety, and Ethics committees as well as the Geriatric Task Force. Changes recommended changes on the basis of committee and task force feedback were incorporated into the relevant chapters.
Second, revisions of individual chapters from the editorial board were sent back to contributors for final comment, revision, and approval. Third, the compilation of all chapters and sections was reviewed (as a whole) and underwent further revision by the editorial board based on feedback from the contributors and the relevant SHM committees. Fourth, the entire revised supplement was sent for an internal review by the SHM board and relevant SHM committees or committee representatives.
Fifth, final reviews were solicited from external reviewers of medical professional organizations and academic organizations. Feedback from the internal and external reviews were compiled and systematically evaluated by the CCTF editorial board. Recommended changes were incorporated into individual chapters or throughout the Core Competencies compendium on the basis of the evaluation and consensus approval of the editorial board. For example, one reviewer believed that quality improvement initiatives were necessary for all procedures that hospitalists perform in order to help reduce the risk of complications. Therefore, each procedure chapter was revised to reflect this competency. Similarly, another reviewer thought that in many chapters the involvement of nursing and other medical staff in the implementation of multidisciplinary teams was underemphasized. Therefore, efforts were taken to improve the emphasis of these key participants in multidisciplinary hospital care.
The efforts of many individuals and professional organizations have helped the CCTF to refine the expectations of a professional trained in the discipline of hospital medicine. Table 2 has a complete listing of those solicited to be internal and external reviewers. Although aggressive efforts were undertaken to encourage feedback from all solicited reviewers of the Core Competencies document, time or other constraints prevented some reviewers from responding to the review request (overall response or review rate: 52%). Nevertheless, the multiple review and revision process brought what was initially disparate content and organization together in a much more cohesive and consistent approach and structure to competencies in hospital medicine.
|
| Accreditation Council of Graduate Medical Education (ACGME) |
| Agency for Healthcare Research & Quality (AHRQ) |
| American Academy of Family Practice (AAFP) |
| American Association of Critical Care Nurses (AACCN) |
| American Association of Subspecialty Professors |
| American Board of Family Practice |
| American Board of Internal Medicine (ABIM) |
| American College of Chest Physicians (ACCP) |
| American College of Emergency Physicians (ACEP) |
| American College of Physicians (ACP) |
| American Geriatrics Society |
| American Hospital Association (AHA) |
| Association of American Medical Colleges (AAMC) |
| Institute for Healthcare Improvement (IHI) |
| John A. Hartford Foundation |
| Joint Commission on Accreditation of Healthcare Organizations (JCAHO) |
| Residency Review Committee Internal Medicine (RRC‐IM) |
| Reynolds Foundation |
| Robert Wood Johnson Foundation (RWJF) |
| Society of Critical Care Medicine (SCCM) |
| Society of General Internal Medicine (SGIM) |
| Society of Hospital Medicine |
| ○ Board of Directors (9 members solicited) |
| ○ CCTF Members (3 members solicited exclusive of editorial board) |
CHAPTER CONTENT DESCRIPTION
As previously delineated, the Core Competencies document has three sections: Clinical Conditions, Procedures, and Healthcare Systems. The chapters in the entire compendium and within each section have been designed to stand alone and to be used either individually or collectively to assist with curriculum development in hospital medicine. However, each chapter should be used in the context of the entire document because a particular issue may only be touched on in one chapter but may be more elaborately detailed in another. For example, all clinical conditions chapters include a competency on the issue of care transitions, but the specific competencies for care transitions are presented in a separate Transitions of Care chapter.
All chapters in each section begin with an introduction that provides brief background information and establishes the relevance of the topic to practicing hospitalists. Each chapter then utilizes the educational theory of learning domains. The learning domains include the cognitive domain (knowledge), the psychomotor domain (skills), and the affective domain (attitudes). The companion article How to Use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development13 describes in detail the educational theory guiding the development of the Core Competencies document and suggested methods for applying it to the development and revision of curricula and other training activities.
The task force further decided that each chapter in the Clinical Conditions and Procedures sections should include a subsection dedicated to system organization and improvement, an added domain that requires integration of knowledge, skills, and attitudes and the involvement of other medical services and disciplines for optimal patient care. The editorial board believed that system organization and improvement was already an intrinsic feature embedded in the chapters of the Healthcare Systems section. Therefore, this subsection was not included in those chapters.
Hospitalists subscribe to a systems organizational approach to clinical management and processes of care within the hospital. This systems approach, more than any level of knowledge or skill, is required to effectively and efficiently practice in the hospital setting. Practicing with a systems approach, with the interest of improving processes of care, is embedded throughout the Core Competencies document and is a practice method that all hospitalists may strive to achieve as they develop and improve their inpatient care. The competencies within the Systems Organization and Improvement section may contain a range of competency expectation (eg, lead, coordinate, or participate in) to acknowledge their uniqueness and variation according to practice settings and locally instituted responsibilities.
Each competency within a chapter details a level of proficiency, providing guidance on learning activities and potential evaluation strategies. Several overarching themes are followed in the chapters that help to define hospitalists as physicians who specialize in the care of hospitalized patients. First, hospitalists strive to support and adhere to a multidisciplinary approach for the patients under their care. Such an approach involves active interaction with and integration of other hospital medical staff (eg, nursing, rehabilitation therapies, social services) and of specialty medical or surgical services when indicated. Recognizing that hospitalists vary in experience and mastery of their field, the task force and editorial board believed that, at minimum, hospitalists would participate in multidisciplinary teams for improvement of the care and process related to the clinical conditions within their organization. However, they might also lead and/or coordinate teams in such efforts. Therefore, most chapters contain competencies that expect hospitalists to lead, coordinate, or participate in multidisciplinary teams or initiatives that will facilitate optimal care within their organization.
Second, because hospital medicine centers around the quality of inpatient care, participation in quality improvement (QI) initiatives, focusing on improving processes or systems of care in a local institution or organization, may be common in hospitalist practices. The level of involvement and role in QI initiatives may vary according to the particular system, the resources available, and a hospitalist's experience. Finally, because hospitalist care intrinsically involves an increase in the number of care transitions and handoffs, hospitalists need to remain sensitive to and focused on the care transitions that occur with their patients. Such transitions may occur as patients enter the hospital, move from one location to another within the hospital, or leave the hospital. This vulnerable time for patients requires hospitalists to be vigilant in their communication effortswith patients, with medical staff, and with outpatient clinicians.
Each competency was crafted to indicate the relevant concept, the level of proficiency expected, and a way to evaluate mastery. The teaching processes and learning experiences that must take place to achieve competency are left for curriculum developers and instructors to design. These core competencies represent an initial step in curriculum development, creating an identity and core set of expectations for hospitalists that we believe will lead to progress and maturity within the field.
SUMMARY AND FUTURE DIRECTIONS
The practice of hospital medicine requires proficiency of interrelated aspects of practiceclinical, procedural, and system‐based competencies. For practicing hospitalists, the Core Competencies document may serve as a resource to refine skills and assist in program development at individual institutions, both regionally and nationally. For residency program directors and clerkship directors, the Core Competencies document can function as a guide for developing the curriculum of inpatient medicine rotations or for meeting the requirements of the Outcomes Project of the Accreditation Council on Graduate Medical Education's. Last, for those developing continuing medical education programs, the Core Competencies document or individual chapters or topics within it may serve as an outline around which specific or broad‐based programs can be developed. Although the development of such curricula and the recipients of them should be evaluated, the actual evaluation is left to the curriculum developers.
Hospitalists are invested in making hospitals run better. They are positioned to take leadership roles in addressing quality, efficiency, and cost interests in both community and academic hospital settings. Their goals include improving care processes, hospital work life, and the setting in which they practice. The key core competencies described in this compendium define hospitalists as agents of change 1) to develop and implement systems to enable best practices to occur from admission through discharge, and 2) to promote the development of a safer culture within the hospital.
Hospital medicine remains an evolving specialty. Although great care was taken to construct these competencies so they would retain their relevance over time, SHM, the Core Curriculum Task Force, and the editorial board recognize the need for their continual reevaluation and modification in the context of advances and changes in the practice of hospital medicine. Our intent is that these competencies be a common reference and foundation for the creation of hospital medicine curricula and serve to standardize and improve training practices.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org[accessed July 22, 2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,, eds.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(supplement 1).
- Society of Hospital Medicine. About SHM: What is a hospitalist? Available from URL: http://www.hospitalmedicine.org[accessed July 22, 2005].
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,, et al.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137:866–874.
- ,,, et al.Making Healthcare aafer: a critical analysis of patient safety practices.Rockville, MD:U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality;2001. AHRQ publication 01‐E058. Available from URL: http://www.ahrq.gov.
- ,,, et al.Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79:78–82.
- ,,, et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- ,,, et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19:293–301.
- ,,, et al.Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1887.
- ,,,,.How to use The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1:57–67.
Copyright © 2006 Society of Hospital Medicine
Editorial
Congratulations to the Society of Hospital Medicine (SHM) for launching this important new journal. Congratulations as well to the SHM members, who have identified an important patient care need and moved to meet that need by defining the special competencies of the hospitalist. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (the Core Competencies), by the Society of Hospital Medicine, accompanies this inaugural issue of the Journal of Hospital Medicine.
As a geriatrician, I can personally attest to the need to have skilled physicians on‐site in the hospital to care for elderly patients. Older people with complex illnesses are susceptible to multiple hospital complications, which often present subtly but can quickly turn into life‐threateningbut potentially reversibleillnesses. Given the demography of hospitalized patients in the 21st century in the United States, every good hospitalist also has to be a good geriatrician.
As evidenced in the Core Competencies, the hospitalist community recognizes as well the importance of developing expertise in caring for both the medical and surgical conditions of patients. Providing attentive diagnostic and management skills to pre‐ and postoperative patients, especially those with preexisting chronic conditions, will surely improve outcomes.
Continuity and coordination within a single hospital episode and across multiple hospitalizations are major challenges for our fragmented and often chaotic health care system. The Core Competencies recognizes the centrality of systems‐based practice to the foundation of hospitalist skills. We at the American Board of Internal Medicine (ABIM) share the belief that every physician must understand the principles of quality improvement; accordingly, this competency is now demanded of every resident and is assessed in the maintenance of certification (MOC) of every internal medicine specialist. That hospitalists have grabbed the quality‐improvement mantle is a welcome development and shows that hospitalists are likely to become key teachers of systems‐based care and quality‐improvement competencies in teaching hospitals.
The growth of hospital medicine in the United States has raised many important issues concerning quality of care that cannot be totally solved by the creation of a hospital‐based practice discipline. The vexing issues of continuity of care, continuing relationships, and efficient management of resources over the entire trajectory of a patient's illness (not just during a hospitalization) are not fundamentally addressed by the existence of hospital medicine as a discipline. However, hospitalists can partner with others in the health care system to create a clinically meaningful continuum that truly would serve patients, especially those with the greatest need such as the elderly and the chronically ill. The ABIM has been in discussions with the Society of Hospital Medicine, the Society of General Internal Medicine, the American College of Physicians, and the Alliance of Academic Internal Medicine to develop a response to the important and evolving arenas of specific expertise in hospital and outpatient medicine. The Core Competencies in Hospital Medicine will significantly help to further these discussions.
Let me raise two concerns whose resolution will need the input of hospitalists as the discipline of hospital medicine becomes more mature. First, hospitalist models are quite variable. Many academic physicians who call themselves hospitalists attend on an inpatient service 2, 3, or 5 months a year and still see outpatients. Many physicians who consider themselves general internists (and not hospitalists) have a weekly half‐day clinic and attend on the wards 3 months a year. Which is a hospitalist? Does it matter? Will the definition of a hospitalist be based on achievement of the competencies described here, or will it be based primarily on the amount of time in hospital‐based practice? This will be an important question to resolve, especially as we embark on a path toward offering a hospitalist credential.
Second, general internal medicine is becoming an increasingly vital part of the continuum of care for patients with multiple complex chronic illnesses, at the same time that poor reimbursement has undermined its vitality and threatens its existence. (Family medicine is also suffering from reduced interest among medical students.) Because most institutions function on an each tub on its own bottom model, it is unrealistic to expect the practice of ambulatory general internal medicine to support itself. Generalist practices thrive in integrated group models. These practices recognize the importance of the physician who provides a coordinating function for all the specialists who care for a complex patient. Such an outpatient generalist thus reduces excess and unnecessary care while identifying gaps where relevant specialties could improve function or quality of life. Ambulatory practice also requires skill in systems and improvement, but few of the 80% of generalists who practice in small groups have sufficient infrastructure and resources to support practice redesign. Indeed, a new report from Mercer consultants coined the phrase ambulatory intensivists to identify practices with Medicare patients and recognizes that these practices are every bit as intense and complex and in need of systems management as an inpatient practice. What the complex patient needs is a seamless interface between the two.
The authors of the Core Competencies in Hospital Medicine hope that this document will stand the test of time as it evolves. I would urge that the document remain flexiblea living documentbecause the one thing about which we can be sure is that hospital practice will change. More and more critical care will be delivered throughout the hospital, more and more of all kinds of care will be performed outside the hospital, and the nature of hospitals will surely change with shifts in reimbursement that we cannot yet imagine but that might be right around the corner. If able to provide hands‐on care less expensively, physician assistants and nurse‐practitioners functioning according to protocols developed by systems thinkers, only some of whom will be physicians, may replace the physician in some settings. What will become of hospitalists as these systems change? I hope that hospitalists, together with other general internists, will be at the forefront of ensuring that the changes in practice that result from the combination of new technologies and financing structures will ultimately also serve the needs of patients. The patient is at the center of our discipline and, as articulated so clearly in the Core Competencies, should always be the focus of our future thinking.
- .Health care system chaos should spur innovation: summary of a report of the Society of General Internal Medicine Task Force on the Domain of General Internal Medicine.Ann Intern Med.2004;140:639–643.
Congratulations to the Society of Hospital Medicine (SHM) for launching this important new journal. Congratulations as well to the SHM members, who have identified an important patient care need and moved to meet that need by defining the special competencies of the hospitalist. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (the Core Competencies), by the Society of Hospital Medicine, accompanies this inaugural issue of the Journal of Hospital Medicine.
As a geriatrician, I can personally attest to the need to have skilled physicians on‐site in the hospital to care for elderly patients. Older people with complex illnesses are susceptible to multiple hospital complications, which often present subtly but can quickly turn into life‐threateningbut potentially reversibleillnesses. Given the demography of hospitalized patients in the 21st century in the United States, every good hospitalist also has to be a good geriatrician.
As evidenced in the Core Competencies, the hospitalist community recognizes as well the importance of developing expertise in caring for both the medical and surgical conditions of patients. Providing attentive diagnostic and management skills to pre‐ and postoperative patients, especially those with preexisting chronic conditions, will surely improve outcomes.
Continuity and coordination within a single hospital episode and across multiple hospitalizations are major challenges for our fragmented and often chaotic health care system. The Core Competencies recognizes the centrality of systems‐based practice to the foundation of hospitalist skills. We at the American Board of Internal Medicine (ABIM) share the belief that every physician must understand the principles of quality improvement; accordingly, this competency is now demanded of every resident and is assessed in the maintenance of certification (MOC) of every internal medicine specialist. That hospitalists have grabbed the quality‐improvement mantle is a welcome development and shows that hospitalists are likely to become key teachers of systems‐based care and quality‐improvement competencies in teaching hospitals.
The growth of hospital medicine in the United States has raised many important issues concerning quality of care that cannot be totally solved by the creation of a hospital‐based practice discipline. The vexing issues of continuity of care, continuing relationships, and efficient management of resources over the entire trajectory of a patient's illness (not just during a hospitalization) are not fundamentally addressed by the existence of hospital medicine as a discipline. However, hospitalists can partner with others in the health care system to create a clinically meaningful continuum that truly would serve patients, especially those with the greatest need such as the elderly and the chronically ill. The ABIM has been in discussions with the Society of Hospital Medicine, the Society of General Internal Medicine, the American College of Physicians, and the Alliance of Academic Internal Medicine to develop a response to the important and evolving arenas of specific expertise in hospital and outpatient medicine. The Core Competencies in Hospital Medicine will significantly help to further these discussions.
Let me raise two concerns whose resolution will need the input of hospitalists as the discipline of hospital medicine becomes more mature. First, hospitalist models are quite variable. Many academic physicians who call themselves hospitalists attend on an inpatient service 2, 3, or 5 months a year and still see outpatients. Many physicians who consider themselves general internists (and not hospitalists) have a weekly half‐day clinic and attend on the wards 3 months a year. Which is a hospitalist? Does it matter? Will the definition of a hospitalist be based on achievement of the competencies described here, or will it be based primarily on the amount of time in hospital‐based practice? This will be an important question to resolve, especially as we embark on a path toward offering a hospitalist credential.
Second, general internal medicine is becoming an increasingly vital part of the continuum of care for patients with multiple complex chronic illnesses, at the same time that poor reimbursement has undermined its vitality and threatens its existence. (Family medicine is also suffering from reduced interest among medical students.) Because most institutions function on an each tub on its own bottom model, it is unrealistic to expect the practice of ambulatory general internal medicine to support itself. Generalist practices thrive in integrated group models. These practices recognize the importance of the physician who provides a coordinating function for all the specialists who care for a complex patient. Such an outpatient generalist thus reduces excess and unnecessary care while identifying gaps where relevant specialties could improve function or quality of life. Ambulatory practice also requires skill in systems and improvement, but few of the 80% of generalists who practice in small groups have sufficient infrastructure and resources to support practice redesign. Indeed, a new report from Mercer consultants coined the phrase ambulatory intensivists to identify practices with Medicare patients and recognizes that these practices are every bit as intense and complex and in need of systems management as an inpatient practice. What the complex patient needs is a seamless interface between the two.
The authors of the Core Competencies in Hospital Medicine hope that this document will stand the test of time as it evolves. I would urge that the document remain flexiblea living documentbecause the one thing about which we can be sure is that hospital practice will change. More and more critical care will be delivered throughout the hospital, more and more of all kinds of care will be performed outside the hospital, and the nature of hospitals will surely change with shifts in reimbursement that we cannot yet imagine but that might be right around the corner. If able to provide hands‐on care less expensively, physician assistants and nurse‐practitioners functioning according to protocols developed by systems thinkers, only some of whom will be physicians, may replace the physician in some settings. What will become of hospitalists as these systems change? I hope that hospitalists, together with other general internists, will be at the forefront of ensuring that the changes in practice that result from the combination of new technologies and financing structures will ultimately also serve the needs of patients. The patient is at the center of our discipline and, as articulated so clearly in the Core Competencies, should always be the focus of our future thinking.
Congratulations to the Society of Hospital Medicine (SHM) for launching this important new journal. Congratulations as well to the SHM members, who have identified an important patient care need and moved to meet that need by defining the special competencies of the hospitalist. The Core Competencies in Hospital Medicine: A Framework for Curriculum Development (the Core Competencies), by the Society of Hospital Medicine, accompanies this inaugural issue of the Journal of Hospital Medicine.
As a geriatrician, I can personally attest to the need to have skilled physicians on‐site in the hospital to care for elderly patients. Older people with complex illnesses are susceptible to multiple hospital complications, which often present subtly but can quickly turn into life‐threateningbut potentially reversibleillnesses. Given the demography of hospitalized patients in the 21st century in the United States, every good hospitalist also has to be a good geriatrician.
As evidenced in the Core Competencies, the hospitalist community recognizes as well the importance of developing expertise in caring for both the medical and surgical conditions of patients. Providing attentive diagnostic and management skills to pre‐ and postoperative patients, especially those with preexisting chronic conditions, will surely improve outcomes.
Continuity and coordination within a single hospital episode and across multiple hospitalizations are major challenges for our fragmented and often chaotic health care system. The Core Competencies recognizes the centrality of systems‐based practice to the foundation of hospitalist skills. We at the American Board of Internal Medicine (ABIM) share the belief that every physician must understand the principles of quality improvement; accordingly, this competency is now demanded of every resident and is assessed in the maintenance of certification (MOC) of every internal medicine specialist. That hospitalists have grabbed the quality‐improvement mantle is a welcome development and shows that hospitalists are likely to become key teachers of systems‐based care and quality‐improvement competencies in teaching hospitals.
The growth of hospital medicine in the United States has raised many important issues concerning quality of care that cannot be totally solved by the creation of a hospital‐based practice discipline. The vexing issues of continuity of care, continuing relationships, and efficient management of resources over the entire trajectory of a patient's illness (not just during a hospitalization) are not fundamentally addressed by the existence of hospital medicine as a discipline. However, hospitalists can partner with others in the health care system to create a clinically meaningful continuum that truly would serve patients, especially those with the greatest need such as the elderly and the chronically ill. The ABIM has been in discussions with the Society of Hospital Medicine, the Society of General Internal Medicine, the American College of Physicians, and the Alliance of Academic Internal Medicine to develop a response to the important and evolving arenas of specific expertise in hospital and outpatient medicine. The Core Competencies in Hospital Medicine will significantly help to further these discussions.
Let me raise two concerns whose resolution will need the input of hospitalists as the discipline of hospital medicine becomes more mature. First, hospitalist models are quite variable. Many academic physicians who call themselves hospitalists attend on an inpatient service 2, 3, or 5 months a year and still see outpatients. Many physicians who consider themselves general internists (and not hospitalists) have a weekly half‐day clinic and attend on the wards 3 months a year. Which is a hospitalist? Does it matter? Will the definition of a hospitalist be based on achievement of the competencies described here, or will it be based primarily on the amount of time in hospital‐based practice? This will be an important question to resolve, especially as we embark on a path toward offering a hospitalist credential.
Second, general internal medicine is becoming an increasingly vital part of the continuum of care for patients with multiple complex chronic illnesses, at the same time that poor reimbursement has undermined its vitality and threatens its existence. (Family medicine is also suffering from reduced interest among medical students.) Because most institutions function on an each tub on its own bottom model, it is unrealistic to expect the practice of ambulatory general internal medicine to support itself. Generalist practices thrive in integrated group models. These practices recognize the importance of the physician who provides a coordinating function for all the specialists who care for a complex patient. Such an outpatient generalist thus reduces excess and unnecessary care while identifying gaps where relevant specialties could improve function or quality of life. Ambulatory practice also requires skill in systems and improvement, but few of the 80% of generalists who practice in small groups have sufficient infrastructure and resources to support practice redesign. Indeed, a new report from Mercer consultants coined the phrase ambulatory intensivists to identify practices with Medicare patients and recognizes that these practices are every bit as intense and complex and in need of systems management as an inpatient practice. What the complex patient needs is a seamless interface between the two.
The authors of the Core Competencies in Hospital Medicine hope that this document will stand the test of time as it evolves. I would urge that the document remain flexiblea living documentbecause the one thing about which we can be sure is that hospital practice will change. More and more critical care will be delivered throughout the hospital, more and more of all kinds of care will be performed outside the hospital, and the nature of hospitals will surely change with shifts in reimbursement that we cannot yet imagine but that might be right around the corner. If able to provide hands‐on care less expensively, physician assistants and nurse‐practitioners functioning according to protocols developed by systems thinkers, only some of whom will be physicians, may replace the physician in some settings. What will become of hospitalists as these systems change? I hope that hospitalists, together with other general internists, will be at the forefront of ensuring that the changes in practice that result from the combination of new technologies and financing structures will ultimately also serve the needs of patients. The patient is at the center of our discipline and, as articulated so clearly in the Core Competencies, should always be the focus of our future thinking.
- .Health care system chaos should spur innovation: summary of a report of the Society of General Internal Medicine Task Force on the Domain of General Internal Medicine.Ann Intern Med.2004;140:639–643.
- .Health care system chaos should spur innovation: summary of a report of the Society of General Internal Medicine Task Force on the Domain of General Internal Medicine.Ann Intern Med.2004;140:639–643.