User login
ECHO rheumatology programs increase access, improve care
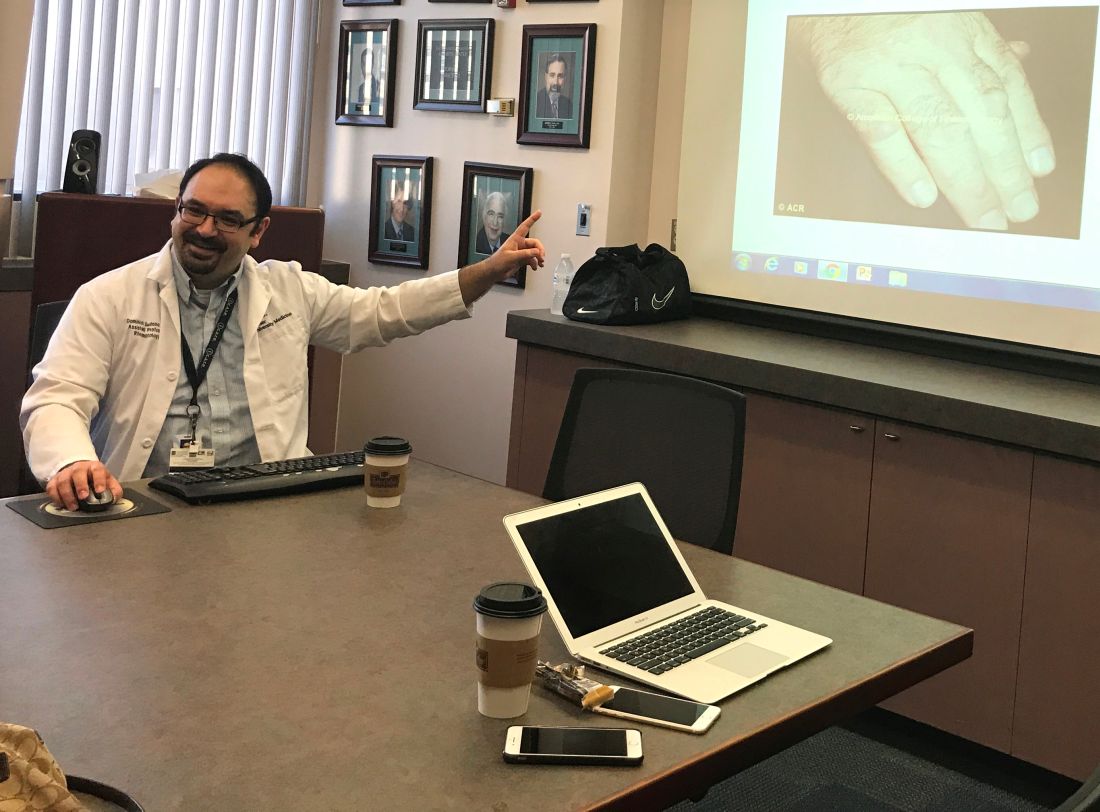
As in many places throughout the country, rheumatologists are in short supply in southern Arizona. Patients frequently wait up to 6 months to visit a rheumatologist at Banner University Medical Center (BUMC) in Tucson, and many drive between 3 and 4 hours for the appointment, said Dominick G. Sudano, MD, a rheumatologist at BUMC, which is affiliated with the University of Arizona.
[polldaddy:9823712]
The high demand for rheumatologists and lack of timely access led the University of Arizona to develop a program that will train primary care providers at remote sites to treat rheumatic diseases. The program, a partnership between the university’s Arizona Telemedicine Program and the University of Arizona Center for Rural Health, will use the popular ECHO (Extension for Community Healthcare Outcomes) model, founded by the University of New Mexico in Albuquerque, which aims to increase workforce capacity by sharing medical knowledge.
A unique model of care
As part of the program, set to launch this month, Dr. Sudano will hold rheumatology training sessions via telemedicine for primary care physicians and other nonphysicians at four remote sites around Arizona. Participating sites include Canyonlands Healthcare, North County Healthcare, and Northern Arizona Healthcare – all located in the northern part of the state – and Copper Queen Community Hospital in southern Arizona.
The virtual sessions will include both educational topics and the opportunity for local doctors and health professionals to present patient cases to Dr. Sudano for guidance. The local doctors and health professionals will eventually treat rheumatic cases in their communities, while cases identified as severe will still be referred to rheumatologists.
The university’s Arizona Telemedicine Program was fortunate to receive a $17,700 grant from Lilly to launch the 1-year rheumatology ECHO pilot program, Dr. Sudano noted. The grant will enable the program to get off the ground, while administrators search for additional funding sources to become sustainable, he said.
Dr. Sudano credits the assistance and support of the University of New Mexico and its ECHO leaders for helping the University of Arizona build its ECHO rheumatology program and helping administrators address the details of setting up the program.
“[The University of New Mexico] was immensely helpful,” he said. “They have immersion sessions about once a month and you spend [time] working with their team. They work with you to get the logistics ironed out.”
A spreading movement
The University of New Mexico (UNM) has good reason to assist other health and academic medical centers in launching their own ECHO programs. UNM’s mission is to continue building the ECHO movement and accomplish its goal of “touching 1 billion lives” by 2025, said Sanjeev Arora, MD, a gastroenterologist at UNM and founder/director of the university’s Project ECHO.
“There was a great shortage of specialists to treat hepatitis C so I came up with this idea of ECHO to bring access to care to everyone in New Mexico who needed care,” he said. “The second part of the idea was, if we could do that for hepatitis C, we could do that for a lot of other problems like rheumatoid arthritis, like addiction, like diabetes.”
Project ECHO has now spread to medical centers and hospitals across the country, with programs that center on asthma, HIV infection, cardiac risk reduction, chronic pain management, geriatrics, palliative care, substance abuse, and obesity, among others. The model is now in 139 academic hubs in 24 countries with more than 65 health conditions targeted, according to Dr. Arora. Replication sites focus on four key principles of ECHO: technology used to leverage scarce health care expertise and resources; best practices shared to standardize care across disparate health care delivery systems; case-based learning used as the primary modality to build knowledge, confidence, and expertise; and evaluations conducted to monitor outcomes.
Data show the care patients receive via the ECHO model is equal to that of care provided by university-based specialists. A 2011 report published in the New England Journal of Medicine, for example, found that a sustained viral response to treatment for hepatitis C was achieved in 58% of patients managed at the university and by 58% of patients managed by primary care physicians at rural and prison sites who participated in Project ECHO (N Engl J Med. 2011;364:2199-2207). Response rates to different subtypes of hepatitis C also did not differ significantly between the two groups.
The ECHO model has also greatly improved access and outcomes for hepatitis C patients in Northern Arizona, said Colleen Hopkins, telehealth coordinator at North Country Healthcare in Flagstaff. North Country Healthcare has participated in a hepatitis C ECHO program since 2012, linking its chain of 14 community health centers with a hepatologist-educator at St. Joseph’s Hospital and Medical Center in Phoenix, 140 miles to the south.
“In 2011, more than 950 patients in the health system’s network had a hepatitis C diagnosis, but the majority did not have access to care,” Ms. Hopkins said in an interview.
“To date, over 500 patients have received care for their liver disease in rural Northern Arizona,” she said. “These numbers continue to climb as our awareness has caused an increase in screening and various outreach efforts ... Overall, our providers and patients are empowered by having access to specialty care; they are living longer healthier lives as well as keeping money in our communities.”
Rheumatology and the ECHO model
The volume of rheumatic conditions encountered by primary care physicians and the shortage of specialists make rheumatology a logical fit for the ECHO model, Dr. Arora said. Rheumatoid arthritis, osteoarthritis, osteoporosis, fibromyalgia, and joint pain account for as many as one in five visits to primary care doctors, he noted.
“Osteoporosis and rheumatoid arthritis produce massive disability in the world,” he said. “Treatment exists, but it’s not getting to patients. ECHO can fundamentally transform the field of rheumatology if it’s adopted widely.”
However, compared with other specialty ECHO models, there are not many rheumatology ECHO programs in operation. Dr. Arora is hopeful that as word spreads about how well rheumatology fits into the ECHO structure, more programs will develop, he said.
“We have found over the years that with our training these providers – both physicians and nonphysician – are able to function as well as a specially trained [rheumatologist],” Dr. Bankhurst said. “We help them as needed by our weekly teleconference where they present cases to us and those cases which appear to be most difficult, we see immediately in our clinics.”
The program has led to decreased referrals to the university from outlying areas and more care access for patients in rural areas, Dr. Bankhurst said. A university study is underway to analyze clinical outcomes for rheumatoid arthritis as conducted by distant provider sites compared with treatment at the university clinic.
“It’s my perspective, based on 12 years of experience, that they’ll be identical,” he said.
Setting up such ECHO programs is not without challenges. Financial support for telecommunication equipment in all needed areas can be difficult, Dr. Bankhurst said. Recruiting individuals who are well motivated to participate in the program can also be a challenge.
“It needs a commitment by the administration,” he said. “It does take time from other activities. It requires dedicated time away from a busy clinic.”
agallegos@frontlinemedcom.com
On Twitter @legal_med
As in many places throughout the country, rheumatologists are in short supply in southern Arizona. Patients frequently wait up to 6 months to visit a rheumatologist at Banner University Medical Center (BUMC) in Tucson, and many drive between 3 and 4 hours for the appointment, said Dominick G. Sudano, MD, a rheumatologist at BUMC, which is affiliated with the University of Arizona.
[polldaddy:9823712]
The high demand for rheumatologists and lack of timely access led the University of Arizona to develop a program that will train primary care providers at remote sites to treat rheumatic diseases. The program, a partnership between the university’s Arizona Telemedicine Program and the University of Arizona Center for Rural Health, will use the popular ECHO (Extension for Community Healthcare Outcomes) model, founded by the University of New Mexico in Albuquerque, which aims to increase workforce capacity by sharing medical knowledge.
A unique model of care
As part of the program, set to launch this month, Dr. Sudano will hold rheumatology training sessions via telemedicine for primary care physicians and other nonphysicians at four remote sites around Arizona. Participating sites include Canyonlands Healthcare, North County Healthcare, and Northern Arizona Healthcare – all located in the northern part of the state – and Copper Queen Community Hospital in southern Arizona.
The virtual sessions will include both educational topics and the opportunity for local doctors and health professionals to present patient cases to Dr. Sudano for guidance. The local doctors and health professionals will eventually treat rheumatic cases in their communities, while cases identified as severe will still be referred to rheumatologists.
The university’s Arizona Telemedicine Program was fortunate to receive a $17,700 grant from Lilly to launch the 1-year rheumatology ECHO pilot program, Dr. Sudano noted. The grant will enable the program to get off the ground, while administrators search for additional funding sources to become sustainable, he said.
Dr. Sudano credits the assistance and support of the University of New Mexico and its ECHO leaders for helping the University of Arizona build its ECHO rheumatology program and helping administrators address the details of setting up the program.
“[The University of New Mexico] was immensely helpful,” he said. “They have immersion sessions about once a month and you spend [time] working with their team. They work with you to get the logistics ironed out.”
A spreading movement
The University of New Mexico (UNM) has good reason to assist other health and academic medical centers in launching their own ECHO programs. UNM’s mission is to continue building the ECHO movement and accomplish its goal of “touching 1 billion lives” by 2025, said Sanjeev Arora, MD, a gastroenterologist at UNM and founder/director of the university’s Project ECHO.
“There was a great shortage of specialists to treat hepatitis C so I came up with this idea of ECHO to bring access to care to everyone in New Mexico who needed care,” he said. “The second part of the idea was, if we could do that for hepatitis C, we could do that for a lot of other problems like rheumatoid arthritis, like addiction, like diabetes.”
Project ECHO has now spread to medical centers and hospitals across the country, with programs that center on asthma, HIV infection, cardiac risk reduction, chronic pain management, geriatrics, palliative care, substance abuse, and obesity, among others. The model is now in 139 academic hubs in 24 countries with more than 65 health conditions targeted, according to Dr. Arora. Replication sites focus on four key principles of ECHO: technology used to leverage scarce health care expertise and resources; best practices shared to standardize care across disparate health care delivery systems; case-based learning used as the primary modality to build knowledge, confidence, and expertise; and evaluations conducted to monitor outcomes.
Data show the care patients receive via the ECHO model is equal to that of care provided by university-based specialists. A 2011 report published in the New England Journal of Medicine, for example, found that a sustained viral response to treatment for hepatitis C was achieved in 58% of patients managed at the university and by 58% of patients managed by primary care physicians at rural and prison sites who participated in Project ECHO (N Engl J Med. 2011;364:2199-2207). Response rates to different subtypes of hepatitis C also did not differ significantly between the two groups.
The ECHO model has also greatly improved access and outcomes for hepatitis C patients in Northern Arizona, said Colleen Hopkins, telehealth coordinator at North Country Healthcare in Flagstaff. North Country Healthcare has participated in a hepatitis C ECHO program since 2012, linking its chain of 14 community health centers with a hepatologist-educator at St. Joseph’s Hospital and Medical Center in Phoenix, 140 miles to the south.
“In 2011, more than 950 patients in the health system’s network had a hepatitis C diagnosis, but the majority did not have access to care,” Ms. Hopkins said in an interview.
“To date, over 500 patients have received care for their liver disease in rural Northern Arizona,” she said. “These numbers continue to climb as our awareness has caused an increase in screening and various outreach efforts ... Overall, our providers and patients are empowered by having access to specialty care; they are living longer healthier lives as well as keeping money in our communities.”
Rheumatology and the ECHO model
The volume of rheumatic conditions encountered by primary care physicians and the shortage of specialists make rheumatology a logical fit for the ECHO model, Dr. Arora said. Rheumatoid arthritis, osteoarthritis, osteoporosis, fibromyalgia, and joint pain account for as many as one in five visits to primary care doctors, he noted.
“Osteoporosis and rheumatoid arthritis produce massive disability in the world,” he said. “Treatment exists, but it’s not getting to patients. ECHO can fundamentally transform the field of rheumatology if it’s adopted widely.”
However, compared with other specialty ECHO models, there are not many rheumatology ECHO programs in operation. Dr. Arora is hopeful that as word spreads about how well rheumatology fits into the ECHO structure, more programs will develop, he said.
“We have found over the years that with our training these providers – both physicians and nonphysician – are able to function as well as a specially trained [rheumatologist],” Dr. Bankhurst said. “We help them as needed by our weekly teleconference where they present cases to us and those cases which appear to be most difficult, we see immediately in our clinics.”
The program has led to decreased referrals to the university from outlying areas and more care access for patients in rural areas, Dr. Bankhurst said. A university study is underway to analyze clinical outcomes for rheumatoid arthritis as conducted by distant provider sites compared with treatment at the university clinic.
“It’s my perspective, based on 12 years of experience, that they’ll be identical,” he said.
Setting up such ECHO programs is not without challenges. Financial support for telecommunication equipment in all needed areas can be difficult, Dr. Bankhurst said. Recruiting individuals who are well motivated to participate in the program can also be a challenge.
“It needs a commitment by the administration,” he said. “It does take time from other activities. It requires dedicated time away from a busy clinic.”
agallegos@frontlinemedcom.com
On Twitter @legal_med
As in many places throughout the country, rheumatologists are in short supply in southern Arizona. Patients frequently wait up to 6 months to visit a rheumatologist at Banner University Medical Center (BUMC) in Tucson, and many drive between 3 and 4 hours for the appointment, said Dominick G. Sudano, MD, a rheumatologist at BUMC, which is affiliated with the University of Arizona.
[polldaddy:9823712]
The high demand for rheumatologists and lack of timely access led the University of Arizona to develop a program that will train primary care providers at remote sites to treat rheumatic diseases. The program, a partnership between the university’s Arizona Telemedicine Program and the University of Arizona Center for Rural Health, will use the popular ECHO (Extension for Community Healthcare Outcomes) model, founded by the University of New Mexico in Albuquerque, which aims to increase workforce capacity by sharing medical knowledge.
A unique model of care
As part of the program, set to launch this month, Dr. Sudano will hold rheumatology training sessions via telemedicine for primary care physicians and other nonphysicians at four remote sites around Arizona. Participating sites include Canyonlands Healthcare, North County Healthcare, and Northern Arizona Healthcare – all located in the northern part of the state – and Copper Queen Community Hospital in southern Arizona.
The virtual sessions will include both educational topics and the opportunity for local doctors and health professionals to present patient cases to Dr. Sudano for guidance. The local doctors and health professionals will eventually treat rheumatic cases in their communities, while cases identified as severe will still be referred to rheumatologists.
The university’s Arizona Telemedicine Program was fortunate to receive a $17,700 grant from Lilly to launch the 1-year rheumatology ECHO pilot program, Dr. Sudano noted. The grant will enable the program to get off the ground, while administrators search for additional funding sources to become sustainable, he said.
Dr. Sudano credits the assistance and support of the University of New Mexico and its ECHO leaders for helping the University of Arizona build its ECHO rheumatology program and helping administrators address the details of setting up the program.
“[The University of New Mexico] was immensely helpful,” he said. “They have immersion sessions about once a month and you spend [time] working with their team. They work with you to get the logistics ironed out.”
A spreading movement
The University of New Mexico (UNM) has good reason to assist other health and academic medical centers in launching their own ECHO programs. UNM’s mission is to continue building the ECHO movement and accomplish its goal of “touching 1 billion lives” by 2025, said Sanjeev Arora, MD, a gastroenterologist at UNM and founder/director of the university’s Project ECHO.
“There was a great shortage of specialists to treat hepatitis C so I came up with this idea of ECHO to bring access to care to everyone in New Mexico who needed care,” he said. “The second part of the idea was, if we could do that for hepatitis C, we could do that for a lot of other problems like rheumatoid arthritis, like addiction, like diabetes.”
Project ECHO has now spread to medical centers and hospitals across the country, with programs that center on asthma, HIV infection, cardiac risk reduction, chronic pain management, geriatrics, palliative care, substance abuse, and obesity, among others. The model is now in 139 academic hubs in 24 countries with more than 65 health conditions targeted, according to Dr. Arora. Replication sites focus on four key principles of ECHO: technology used to leverage scarce health care expertise and resources; best practices shared to standardize care across disparate health care delivery systems; case-based learning used as the primary modality to build knowledge, confidence, and expertise; and evaluations conducted to monitor outcomes.
Data show the care patients receive via the ECHO model is equal to that of care provided by university-based specialists. A 2011 report published in the New England Journal of Medicine, for example, found that a sustained viral response to treatment for hepatitis C was achieved in 58% of patients managed at the university and by 58% of patients managed by primary care physicians at rural and prison sites who participated in Project ECHO (N Engl J Med. 2011;364:2199-2207). Response rates to different subtypes of hepatitis C also did not differ significantly between the two groups.
The ECHO model has also greatly improved access and outcomes for hepatitis C patients in Northern Arizona, said Colleen Hopkins, telehealth coordinator at North Country Healthcare in Flagstaff. North Country Healthcare has participated in a hepatitis C ECHO program since 2012, linking its chain of 14 community health centers with a hepatologist-educator at St. Joseph’s Hospital and Medical Center in Phoenix, 140 miles to the south.
“In 2011, more than 950 patients in the health system’s network had a hepatitis C diagnosis, but the majority did not have access to care,” Ms. Hopkins said in an interview.
“To date, over 500 patients have received care for their liver disease in rural Northern Arizona,” she said. “These numbers continue to climb as our awareness has caused an increase in screening and various outreach efforts ... Overall, our providers and patients are empowered by having access to specialty care; they are living longer healthier lives as well as keeping money in our communities.”
Rheumatology and the ECHO model
The volume of rheumatic conditions encountered by primary care physicians and the shortage of specialists make rheumatology a logical fit for the ECHO model, Dr. Arora said. Rheumatoid arthritis, osteoarthritis, osteoporosis, fibromyalgia, and joint pain account for as many as one in five visits to primary care doctors, he noted.
“Osteoporosis and rheumatoid arthritis produce massive disability in the world,” he said. “Treatment exists, but it’s not getting to patients. ECHO can fundamentally transform the field of rheumatology if it’s adopted widely.”
However, compared with other specialty ECHO models, there are not many rheumatology ECHO programs in operation. Dr. Arora is hopeful that as word spreads about how well rheumatology fits into the ECHO structure, more programs will develop, he said.
“We have found over the years that with our training these providers – both physicians and nonphysician – are able to function as well as a specially trained [rheumatologist],” Dr. Bankhurst said. “We help them as needed by our weekly teleconference where they present cases to us and those cases which appear to be most difficult, we see immediately in our clinics.”
The program has led to decreased referrals to the university from outlying areas and more care access for patients in rural areas, Dr. Bankhurst said. A university study is underway to analyze clinical outcomes for rheumatoid arthritis as conducted by distant provider sites compared with treatment at the university clinic.
“It’s my perspective, based on 12 years of experience, that they’ll be identical,” he said.
Setting up such ECHO programs is not without challenges. Financial support for telecommunication equipment in all needed areas can be difficult, Dr. Bankhurst said. Recruiting individuals who are well motivated to participate in the program can also be a challenge.
“It needs a commitment by the administration,” he said. “It does take time from other activities. It requires dedicated time away from a busy clinic.”
agallegos@frontlinemedcom.com
On Twitter @legal_med
How would you treat ... recurrent pre-B ALL in a 24-year-old woman?
Welcome to our new online feature, "How would you treat?"
This new item seeks to stimulate a lively conversation around cases that address the "art of medicine," in which there are no right or wrong ways to treat a specific patient. Instead, we posit to you "if this was your patient, how would you treat her?" The goal is to offer each other our thoughts on how we view treatment options from the perspectives of potential for cure and quality of life for a specific patient given his or her unique treatment history.
Our first case for your consideration will examine perspectives on the treatment of recurrent acute lymphoblastic leukemia, a condition with increasing therapeutic options.
A 24-year-old female was diagnosed with pre-B Acute Lymphoblastic Leukemia. She achieved complete remission on a standard chemotherapy protocol that included L-asparaginase and completed maintenance therapy 1 year ago, but no tests for MRD were performed. Routine surveillance blood counts worsened and a bone marrow biopsy confirms relapse. She feels well. There is no detectable BCR/ABL, but the leukemic blasts express CD19, CD20, and CD22. She has an HLA-matched sibling donor. Her exam is normal with WBC 23,000 (76% Blasts), Hgb 10.3, Plt 32K.
Welcome to our new online feature, "How would you treat?"
This new item seeks to stimulate a lively conversation around cases that address the "art of medicine," in which there are no right or wrong ways to treat a specific patient. Instead, we posit to you "if this was your patient, how would you treat her?" The goal is to offer each other our thoughts on how we view treatment options from the perspectives of potential for cure and quality of life for a specific patient given his or her unique treatment history.
Our first case for your consideration will examine perspectives on the treatment of recurrent acute lymphoblastic leukemia, a condition with increasing therapeutic options.
A 24-year-old female was diagnosed with pre-B Acute Lymphoblastic Leukemia. She achieved complete remission on a standard chemotherapy protocol that included L-asparaginase and completed maintenance therapy 1 year ago, but no tests for MRD were performed. Routine surveillance blood counts worsened and a bone marrow biopsy confirms relapse. She feels well. There is no detectable BCR/ABL, but the leukemic blasts express CD19, CD20, and CD22. She has an HLA-matched sibling donor. Her exam is normal with WBC 23,000 (76% Blasts), Hgb 10.3, Plt 32K.
Welcome to our new online feature, "How would you treat?"
This new item seeks to stimulate a lively conversation around cases that address the "art of medicine," in which there are no right or wrong ways to treat a specific patient. Instead, we posit to you "if this was your patient, how would you treat her?" The goal is to offer each other our thoughts on how we view treatment options from the perspectives of potential for cure and quality of life for a specific patient given his or her unique treatment history.
Our first case for your consideration will examine perspectives on the treatment of recurrent acute lymphoblastic leukemia, a condition with increasing therapeutic options.
A 24-year-old female was diagnosed with pre-B Acute Lymphoblastic Leukemia. She achieved complete remission on a standard chemotherapy protocol that included L-asparaginase and completed maintenance therapy 1 year ago, but no tests for MRD were performed. Routine surveillance blood counts worsened and a bone marrow biopsy confirms relapse. She feels well. There is no detectable BCR/ABL, but the leukemic blasts express CD19, CD20, and CD22. She has an HLA-matched sibling donor. Her exam is normal with WBC 23,000 (76% Blasts), Hgb 10.3, Plt 32K.
Never too old
What are the age parameters for your practice? I suspect that at one end of the spectrum, you feel that a child is never too young to come to your practice. In fact you may even go out of your way to encourage expectant mothers to make a get-acquainted visit before they deliver because you know that a face-to-face encounter is very likely to make your job easier for the next decade or two.
On the other hand, I suspect that you have set an upper age limit above which you suggest that your patients transition to a physician whose practice is focused on adult care. Is this limit stated as a number – 18? 19? 21? Or are you so uncomfortable with the challenges of adolescent medicine that you urge the teenagers in your practice to find another medical home?
In my practice, I had a very simple and seldom-enforced upper age limit. A patient who was still a student, not even a full-time student, was welcome to keep coming to see me. This made us very popular with college students who knew that we would be there for them when they came home between semesters with a sore throat or needed a refill for their anxiety medicine. No long waits to see a customer-unfriendly internist. Of course, this meant that it was not unusual for me to see patients who were working on their master’s degree or just a few months short of their doctoral dissertation.
One of our exam rooms had large plywood cutouts of the number 1-10 on the walls, but otherwise I avoided large murals of jungle figures or cartoon characters. A checked shirt and a muted wine-red knit tie were about as wild and crazy as my professional wardrobe ever got. I never really bought into the notion that I could put a nervous young child at ease by dressing like a clown. In my experience, it was the personality and warmth radiating from the caregiver that set the tone of the visit, not what he or she was wearing.
Recently, the American Academy of Pediatrics published a recommendation discouraging pediatricians from setting upper age limits for their patients (Pediatrics. 2017;140[3]:e20172151). As someone who practiced most of his career with a very lenient age limit policy, I think this is an excellent and long overdue recommendation.
Patients in their older teens and early twenties seldom present with problems that are beyond our professional competency. Furthermore, one cannot underestimate the value that comes from the years of continuity we can fall back on, particularly for those patients with chronic and multiorgan system disease. But most of all, the chance to spend a few quiet minutes having an adult conversation and catching up with someone you have known since infancy can be a pleasant oasis in an otherwise hectic day spent seeing unappreciative, inarticulate infants and whining toddlers.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/never-too-old?iframe=1"}]
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
What are the age parameters for your practice? I suspect that at one end of the spectrum, you feel that a child is never too young to come to your practice. In fact you may even go out of your way to encourage expectant mothers to make a get-acquainted visit before they deliver because you know that a face-to-face encounter is very likely to make your job easier for the next decade or two.
On the other hand, I suspect that you have set an upper age limit above which you suggest that your patients transition to a physician whose practice is focused on adult care. Is this limit stated as a number – 18? 19? 21? Or are you so uncomfortable with the challenges of adolescent medicine that you urge the teenagers in your practice to find another medical home?
In my practice, I had a very simple and seldom-enforced upper age limit. A patient who was still a student, not even a full-time student, was welcome to keep coming to see me. This made us very popular with college students who knew that we would be there for them when they came home between semesters with a sore throat or needed a refill for their anxiety medicine. No long waits to see a customer-unfriendly internist. Of course, this meant that it was not unusual for me to see patients who were working on their master’s degree or just a few months short of their doctoral dissertation.
One of our exam rooms had large plywood cutouts of the number 1-10 on the walls, but otherwise I avoided large murals of jungle figures or cartoon characters. A checked shirt and a muted wine-red knit tie were about as wild and crazy as my professional wardrobe ever got. I never really bought into the notion that I could put a nervous young child at ease by dressing like a clown. In my experience, it was the personality and warmth radiating from the caregiver that set the tone of the visit, not what he or she was wearing.
Recently, the American Academy of Pediatrics published a recommendation discouraging pediatricians from setting upper age limits for their patients (Pediatrics. 2017;140[3]:e20172151). As someone who practiced most of his career with a very lenient age limit policy, I think this is an excellent and long overdue recommendation.
Patients in their older teens and early twenties seldom present with problems that are beyond our professional competency. Furthermore, one cannot underestimate the value that comes from the years of continuity we can fall back on, particularly for those patients with chronic and multiorgan system disease. But most of all, the chance to spend a few quiet minutes having an adult conversation and catching up with someone you have known since infancy can be a pleasant oasis in an otherwise hectic day spent seeing unappreciative, inarticulate infants and whining toddlers.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/never-too-old?iframe=1"}]
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
What are the age parameters for your practice? I suspect that at one end of the spectrum, you feel that a child is never too young to come to your practice. In fact you may even go out of your way to encourage expectant mothers to make a get-acquainted visit before they deliver because you know that a face-to-face encounter is very likely to make your job easier for the next decade or two.
On the other hand, I suspect that you have set an upper age limit above which you suggest that your patients transition to a physician whose practice is focused on adult care. Is this limit stated as a number – 18? 19? 21? Or are you so uncomfortable with the challenges of adolescent medicine that you urge the teenagers in your practice to find another medical home?
In my practice, I had a very simple and seldom-enforced upper age limit. A patient who was still a student, not even a full-time student, was welcome to keep coming to see me. This made us very popular with college students who knew that we would be there for them when they came home between semesters with a sore throat or needed a refill for their anxiety medicine. No long waits to see a customer-unfriendly internist. Of course, this meant that it was not unusual for me to see patients who were working on their master’s degree or just a few months short of their doctoral dissertation.
One of our exam rooms had large plywood cutouts of the number 1-10 on the walls, but otherwise I avoided large murals of jungle figures or cartoon characters. A checked shirt and a muted wine-red knit tie were about as wild and crazy as my professional wardrobe ever got. I never really bought into the notion that I could put a nervous young child at ease by dressing like a clown. In my experience, it was the personality and warmth radiating from the caregiver that set the tone of the visit, not what he or she was wearing.
Recently, the American Academy of Pediatrics published a recommendation discouraging pediatricians from setting upper age limits for their patients (Pediatrics. 2017;140[3]:e20172151). As someone who practiced most of his career with a very lenient age limit policy, I think this is an excellent and long overdue recommendation.
Patients in their older teens and early twenties seldom present with problems that are beyond our professional competency. Furthermore, one cannot underestimate the value that comes from the years of continuity we can fall back on, particularly for those patients with chronic and multiorgan system disease. But most of all, the chance to spend a few quiet minutes having an adult conversation and catching up with someone you have known since infancy can be a pleasant oasis in an otherwise hectic day spent seeing unappreciative, inarticulate infants and whining toddlers.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/never-too-old?iframe=1"}]
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Recommendations for infant sleep position are not being followed
Despite the American Academy of Pediatrics recommendation that parents place infants supine for sleeping, many mothers do not do so, according to the results of the Study of Attitudes and Factors Affecting Infant Care.
In 32 hospitals, 3,297 mothers were surveyed to determine their intentions, the actual infant sleeping position used, and the factors that affected their behaviors. Of those, 2,491 (77%) reported that they usually place their infants in supine position, but only 49% reported that they exclusively place their infants supine. In addition, 14% reported that they place infants on their sides and 8% prone, reported Eve R. Colson, MD, of the department of pediatrics at Yale University, New Haven, Conn., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-0596).
Several other discrepancies in compliance with the AAP recommendation also were noted. African American mothers were more likely to intend to use prone position, compared with white mothers (adjusted odds ratio, 2.5; 95% confidence interval, 1.57-3.85). Those who did not complete high school were also more likely to intend to use the prone position (aOR, 2.1; 95% CI, 1.16-3.73). On the other hand, those who received recommendation-compliant advice from a doctor were less likely to place their infants in the prone (aOR, 0.6; 95% CI, 0.39-0.93) or side (aOR, 0.5; 95% CI, 0.36-0.67) positions.
“Of particular note, those who reported that their social norms supported placing the infant in the prone position were much more likely to do so, compared with those who felt that their social norms supported using only the supine position (aOR, 11.6; 95% CI, 7.24-18.7). And, most remarkably, those who had positive attitudes about the prone sleep position ... were more likely to choose the prone position (aOR, 130; 95% CI, 71.8-236),” the researchers wrote. These findings indicate that choices in infant sleeping position are directly influenced by attitudes toward the choice, subjective social norms, and perceptions about control.
“These beliefs persist and are potentially modifiable, so they should be considered an important part of any intervention to change practice,” Dr. Colson and her colleagues wrote.
The study was a nationally representative sample of mothers of infants aged 2-6 months. Although the data were taken from patient surveys, which could have been misreported, they are supported by the findings of other studies.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/recommendations-for-infant-sleep-position-are-not-being-followed?iframe=1"}]
“Maternal race and education continue to be factors associated with choice of infant sleeping position as does advice from a doctor. Factors that appear to be of equal or greater importance are those related to attitudes, subjective social norms, and perceived control, all of which can potentially be altered through educational interventions,” Dr. Colson and her colleagues concluded.
The Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institutes of Health funded the study. The authors reported no financial disclosures.
Over the 10 years spanning 1994-2004, the sudden infant death syndrome rate in the United States fell by 53%, correlating with an increase in exclusive supine sleep from less than 10% to 78%. However, since then, rates of both supine sleep and SIDS death have remained stagnant.
To make progress in these areas, current data are needed on supine sleep to enhance understanding of how families make these decisions. Colson et al. provide exactly the kind of information we need to guide providers and public health officials in their efforts to help families maintain the safest sleep environments for their infants.
As a start, mothers who want to practice safe sleep need to be empowered to insist that other caregivers in their lives support their parenting decisions, because the study shows that mothers who feel that they have more control are more likely to use the recommended position. We also must look at how we can help change personal attitudes and societal norms in favor of supine sleep because these issues were found to be some of the strongest predictors of prone sleep position.
We, as health care providers, need to provide clear and consistent messaging in both word and behavior to help mothers make safe decisions for their infants.
Michael H. Goodstein, MD, is a neonatologist at WellSpan York (Pa.) Hospital. Barbara M. Ostfeld, PhD, is the program director of the SIDS Center of New Jersey at Rutgers University, New Brunswick. Their remarks accompanied the article by Colson et al. (Pediatrics 2017 Aug 21. doi: 10.1542/peds.2017-2068). Neither author reported any financial disclosures.
Over the 10 years spanning 1994-2004, the sudden infant death syndrome rate in the United States fell by 53%, correlating with an increase in exclusive supine sleep from less than 10% to 78%. However, since then, rates of both supine sleep and SIDS death have remained stagnant.
To make progress in these areas, current data are needed on supine sleep to enhance understanding of how families make these decisions. Colson et al. provide exactly the kind of information we need to guide providers and public health officials in their efforts to help families maintain the safest sleep environments for their infants.
As a start, mothers who want to practice safe sleep need to be empowered to insist that other caregivers in their lives support their parenting decisions, because the study shows that mothers who feel that they have more control are more likely to use the recommended position. We also must look at how we can help change personal attitudes and societal norms in favor of supine sleep because these issues were found to be some of the strongest predictors of prone sleep position.
We, as health care providers, need to provide clear and consistent messaging in both word and behavior to help mothers make safe decisions for their infants.
Michael H. Goodstein, MD, is a neonatologist at WellSpan York (Pa.) Hospital. Barbara M. Ostfeld, PhD, is the program director of the SIDS Center of New Jersey at Rutgers University, New Brunswick. Their remarks accompanied the article by Colson et al. (Pediatrics 2017 Aug 21. doi: 10.1542/peds.2017-2068). Neither author reported any financial disclosures.
Over the 10 years spanning 1994-2004, the sudden infant death syndrome rate in the United States fell by 53%, correlating with an increase in exclusive supine sleep from less than 10% to 78%. However, since then, rates of both supine sleep and SIDS death have remained stagnant.
To make progress in these areas, current data are needed on supine sleep to enhance understanding of how families make these decisions. Colson et al. provide exactly the kind of information we need to guide providers and public health officials in their efforts to help families maintain the safest sleep environments for their infants.
As a start, mothers who want to practice safe sleep need to be empowered to insist that other caregivers in their lives support their parenting decisions, because the study shows that mothers who feel that they have more control are more likely to use the recommended position. We also must look at how we can help change personal attitudes and societal norms in favor of supine sleep because these issues were found to be some of the strongest predictors of prone sleep position.
We, as health care providers, need to provide clear and consistent messaging in both word and behavior to help mothers make safe decisions for their infants.
Michael H. Goodstein, MD, is a neonatologist at WellSpan York (Pa.) Hospital. Barbara M. Ostfeld, PhD, is the program director of the SIDS Center of New Jersey at Rutgers University, New Brunswick. Their remarks accompanied the article by Colson et al. (Pediatrics 2017 Aug 21. doi: 10.1542/peds.2017-2068). Neither author reported any financial disclosures.
Despite the American Academy of Pediatrics recommendation that parents place infants supine for sleeping, many mothers do not do so, according to the results of the Study of Attitudes and Factors Affecting Infant Care.
In 32 hospitals, 3,297 mothers were surveyed to determine their intentions, the actual infant sleeping position used, and the factors that affected their behaviors. Of those, 2,491 (77%) reported that they usually place their infants in supine position, but only 49% reported that they exclusively place their infants supine. In addition, 14% reported that they place infants on their sides and 8% prone, reported Eve R. Colson, MD, of the department of pediatrics at Yale University, New Haven, Conn., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-0596).
Several other discrepancies in compliance with the AAP recommendation also were noted. African American mothers were more likely to intend to use prone position, compared with white mothers (adjusted odds ratio, 2.5; 95% confidence interval, 1.57-3.85). Those who did not complete high school were also more likely to intend to use the prone position (aOR, 2.1; 95% CI, 1.16-3.73). On the other hand, those who received recommendation-compliant advice from a doctor were less likely to place their infants in the prone (aOR, 0.6; 95% CI, 0.39-0.93) or side (aOR, 0.5; 95% CI, 0.36-0.67) positions.
“Of particular note, those who reported that their social norms supported placing the infant in the prone position were much more likely to do so, compared with those who felt that their social norms supported using only the supine position (aOR, 11.6; 95% CI, 7.24-18.7). And, most remarkably, those who had positive attitudes about the prone sleep position ... were more likely to choose the prone position (aOR, 130; 95% CI, 71.8-236),” the researchers wrote. These findings indicate that choices in infant sleeping position are directly influenced by attitudes toward the choice, subjective social norms, and perceptions about control.
“These beliefs persist and are potentially modifiable, so they should be considered an important part of any intervention to change practice,” Dr. Colson and her colleagues wrote.
The study was a nationally representative sample of mothers of infants aged 2-6 months. Although the data were taken from patient surveys, which could have been misreported, they are supported by the findings of other studies.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/recommendations-for-infant-sleep-position-are-not-being-followed?iframe=1"}]
“Maternal race and education continue to be factors associated with choice of infant sleeping position as does advice from a doctor. Factors that appear to be of equal or greater importance are those related to attitudes, subjective social norms, and perceived control, all of which can potentially be altered through educational interventions,” Dr. Colson and her colleagues concluded.
The Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institutes of Health funded the study. The authors reported no financial disclosures.
Despite the American Academy of Pediatrics recommendation that parents place infants supine for sleeping, many mothers do not do so, according to the results of the Study of Attitudes and Factors Affecting Infant Care.
In 32 hospitals, 3,297 mothers were surveyed to determine their intentions, the actual infant sleeping position used, and the factors that affected their behaviors. Of those, 2,491 (77%) reported that they usually place their infants in supine position, but only 49% reported that they exclusively place their infants supine. In addition, 14% reported that they place infants on their sides and 8% prone, reported Eve R. Colson, MD, of the department of pediatrics at Yale University, New Haven, Conn., and her coauthors (Pediatrics. 2017. doi: 10.1542/peds.2017-0596).
Several other discrepancies in compliance with the AAP recommendation also were noted. African American mothers were more likely to intend to use prone position, compared with white mothers (adjusted odds ratio, 2.5; 95% confidence interval, 1.57-3.85). Those who did not complete high school were also more likely to intend to use the prone position (aOR, 2.1; 95% CI, 1.16-3.73). On the other hand, those who received recommendation-compliant advice from a doctor were less likely to place their infants in the prone (aOR, 0.6; 95% CI, 0.39-0.93) or side (aOR, 0.5; 95% CI, 0.36-0.67) positions.
“Of particular note, those who reported that their social norms supported placing the infant in the prone position were much more likely to do so, compared with those who felt that their social norms supported using only the supine position (aOR, 11.6; 95% CI, 7.24-18.7). And, most remarkably, those who had positive attitudes about the prone sleep position ... were more likely to choose the prone position (aOR, 130; 95% CI, 71.8-236),” the researchers wrote. These findings indicate that choices in infant sleeping position are directly influenced by attitudes toward the choice, subjective social norms, and perceptions about control.
“These beliefs persist and are potentially modifiable, so they should be considered an important part of any intervention to change practice,” Dr. Colson and her colleagues wrote.
The study was a nationally representative sample of mothers of infants aged 2-6 months. Although the data were taken from patient surveys, which could have been misreported, they are supported by the findings of other studies.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/recommendations-for-infant-sleep-position-are-not-being-followed?iframe=1"}]
“Maternal race and education continue to be factors associated with choice of infant sleeping position as does advice from a doctor. Factors that appear to be of equal or greater importance are those related to attitudes, subjective social norms, and perceived control, all of which can potentially be altered through educational interventions,” Dr. Colson and her colleagues concluded.
The Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institutes of Health funded the study. The authors reported no financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: Of the 3,297 mothers surveyed, 2,491 (77%) reported that they usually place their infants in supine position, but only 49% reported that they exclusively place their infants supine.
Data source: The Study of Attitudes and Factors Affecting Infant Care, involving 3,297 mothers.
Disclosures: The Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institutes of Health funded the study. The authors reported no financial disclosures.
POLL: Draft classification criteria for SLE stir controversy
[polldaddy:9802068]
[polldaddy:9802068]
[polldaddy:9802068]
How would you handle predictions of Alzheimer’s disease?
We love to try and predict the future. Some of it is scientific, like checking the weather forecast to see what we’re in for. (Here in Phoenix, it’s always hot, hotter, or melting.)
On the other hand, some of it is just for entertainment, like checking a horoscope or seeing what a fortune cookie says.
The breakthroughs in biomarkers for Alzheimer’s disease are accelerating. Although still experimental, we’re getting pretty close to predicting the disease many years before it develops. At the same time, we aren’t nearly as close to a treatment that will have a meaningful impact on the course of the disease.
In 1993, the genetic marker for Huntington’s disease was identified, quickly leading to a blood test with high accuracy to know if you were – or were not – going to develop the fatal disorder down the road.
Some wanted to know and used the information to decide if they wanted to have families. Others, understandably fearful, decided not to and let their lives play out as they will. Sadly, either way we have nothing close to a cure for the disease.
Now, we come to Alzheimer’s disease, many times more common than Huntington’s. Close to predicting its coming and not really close to a cure.
What would you do?
[polldaddy:9778279]
In “Back to the Future,” Doc Brown said “no man should know too much about their own destiny” (though later changed his mind). But, for Doc Brown, a bulletproof vest was all he needed. In Alzheimer’s disease, it’s not that simple.
I’m sure some would see it as a way to have their affairs in order long in advance, to spare themselves and their loved ones the frantic scramble that often comes after a diagnosis. Others would be afraid to know what the future holds, with every misplaced set of keys or iPhone becoming a reason to panic.
Obviously, if we had a true cure for the disorder, the decision would be easy. Then, it becomes a preventive measure in the same category as mammograms and colonoscopies. Early detection saves lives.
What would you do? And how will you guide the patients who ask your opinion?
For better or worse, these questions are coming. All of us need to think about how we’ll handle them.
Dr. Block has a solo neurology private practice in Scottsdale, Ariz.
We love to try and predict the future. Some of it is scientific, like checking the weather forecast to see what we’re in for. (Here in Phoenix, it’s always hot, hotter, or melting.)
On the other hand, some of it is just for entertainment, like checking a horoscope or seeing what a fortune cookie says.
The breakthroughs in biomarkers for Alzheimer’s disease are accelerating. Although still experimental, we’re getting pretty close to predicting the disease many years before it develops. At the same time, we aren’t nearly as close to a treatment that will have a meaningful impact on the course of the disease.
In 1993, the genetic marker for Huntington’s disease was identified, quickly leading to a blood test with high accuracy to know if you were – or were not – going to develop the fatal disorder down the road.
Some wanted to know and used the information to decide if they wanted to have families. Others, understandably fearful, decided not to and let their lives play out as they will. Sadly, either way we have nothing close to a cure for the disease.
Now, we come to Alzheimer’s disease, many times more common than Huntington’s. Close to predicting its coming and not really close to a cure.
What would you do?
[polldaddy:9778279]
In “Back to the Future,” Doc Brown said “no man should know too much about their own destiny” (though later changed his mind). But, for Doc Brown, a bulletproof vest was all he needed. In Alzheimer’s disease, it’s not that simple.
I’m sure some would see it as a way to have their affairs in order long in advance, to spare themselves and their loved ones the frantic scramble that often comes after a diagnosis. Others would be afraid to know what the future holds, with every misplaced set of keys or iPhone becoming a reason to panic.
Obviously, if we had a true cure for the disorder, the decision would be easy. Then, it becomes a preventive measure in the same category as mammograms and colonoscopies. Early detection saves lives.
What would you do? And how will you guide the patients who ask your opinion?
For better or worse, these questions are coming. All of us need to think about how we’ll handle them.
Dr. Block has a solo neurology private practice in Scottsdale, Ariz.
We love to try and predict the future. Some of it is scientific, like checking the weather forecast to see what we’re in for. (Here in Phoenix, it’s always hot, hotter, or melting.)
On the other hand, some of it is just for entertainment, like checking a horoscope or seeing what a fortune cookie says.
The breakthroughs in biomarkers for Alzheimer’s disease are accelerating. Although still experimental, we’re getting pretty close to predicting the disease many years before it develops. At the same time, we aren’t nearly as close to a treatment that will have a meaningful impact on the course of the disease.
In 1993, the genetic marker for Huntington’s disease was identified, quickly leading to a blood test with high accuracy to know if you were – or were not – going to develop the fatal disorder down the road.
Some wanted to know and used the information to decide if they wanted to have families. Others, understandably fearful, decided not to and let their lives play out as they will. Sadly, either way we have nothing close to a cure for the disease.
Now, we come to Alzheimer’s disease, many times more common than Huntington’s. Close to predicting its coming and not really close to a cure.
What would you do?
[polldaddy:9778279]
In “Back to the Future,” Doc Brown said “no man should know too much about their own destiny” (though later changed his mind). But, for Doc Brown, a bulletproof vest was all he needed. In Alzheimer’s disease, it’s not that simple.
I’m sure some would see it as a way to have their affairs in order long in advance, to spare themselves and their loved ones the frantic scramble that often comes after a diagnosis. Others would be afraid to know what the future holds, with every misplaced set of keys or iPhone becoming a reason to panic.
Obviously, if we had a true cure for the disorder, the decision would be easy. Then, it becomes a preventive measure in the same category as mammograms and colonoscopies. Early detection saves lives.
What would you do? And how will you guide the patients who ask your opinion?
For better or worse, these questions are coming. All of us need to think about how we’ll handle them.
Dr. Block has a solo neurology private practice in Scottsdale, Ariz.
VIDEO: Tocilizumab tested in children with sJIA under 2 years old
MADRID – The results of the first trial of a biologic agent in children less than 2 years of age with systemic juvenile idiopathic arthritis (sJIA) suggest that tocilizumab is likely to be effective in this age group.
“sJIA is the most severe form of childhood arthritis, and as you are aware, it’s the most difficult to treat as well,” said Navita L. Mallalieu, PhD, director of clinical pharmacology at Roche Innovation Center New York, the company that funded the study.
Tocilizumab (Actemra) has been available for the treatment of sJIA, both in the United States and the European Union since 2011, she observed at the European Congress of Rheumatology, but only for children aged 2 years or older at the current time.
Because of this prior history of use in sJIA, “we have confidence in the safety profile, and so we were able to go to the next step of testing children who were even younger than 2 years of age,” Dr. Mallalieu said in a video interview.
[polldaddy:9771949]
Dr. Mallalieu presented findings from an open-label, single-arm, phase I trial that evaluated a 12 mg/kg dosing regimen of tocilizumab, which was given intravenously every 2 weeks for 12 weeks. Eleven children were studied who had a mean age of 1.3 years and active disease for at least 1 month despite treatment with glucocorticoids or nonsteroidal anti-inflammatory drugs.
The primary endpoint was the pharmacokinetics of tocilizumab in this younger patient population, and secondary endpoints were safety, pharmacodynamics, and exploring the efficacy over 12 weeks on top of stable background therapy, she explained.
Results showed that tocilizumab in children under 2 years of age could achieve pharmacokinetics similar to those seen in older children in the TENDER trial (N Engl J Med. 2012;367:2385-95), which is the trial that helped the biologic get licensed for use in the older sJIA population. Reductions in soluble interleukin-6 receptor, C-reactive protein, and the erythrocyte sedimentation rate were seen, again to a similar extent as seen in the TENDER trial. There was also an indication that similar reductions in the Juvenile Arthritis Disease Activity Score (JADAS)-71 score could be achieved, Dr. Mallalieu reported.
While the pattern and nature of adverse events were similar to those seen in the TENDER trial, there were more cases of hypersensitivity in this phase I study. Four cases of hypersensitivity were clinically confirmed, three of which were deemed serious. The three serious cases were observed at day 15, with two of the cases associated with multiple signs and symptoms that were confounded by either subclinical macrophage activation syndrome (MAS) or a faster infusion rate. One patient had urticaria and was hospitalized for observation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MADRID – The results of the first trial of a biologic agent in children less than 2 years of age with systemic juvenile idiopathic arthritis (sJIA) suggest that tocilizumab is likely to be effective in this age group.
“sJIA is the most severe form of childhood arthritis, and as you are aware, it’s the most difficult to treat as well,” said Navita L. Mallalieu, PhD, director of clinical pharmacology at Roche Innovation Center New York, the company that funded the study.
Tocilizumab (Actemra) has been available for the treatment of sJIA, both in the United States and the European Union since 2011, she observed at the European Congress of Rheumatology, but only for children aged 2 years or older at the current time.
Because of this prior history of use in sJIA, “we have confidence in the safety profile, and so we were able to go to the next step of testing children who were even younger than 2 years of age,” Dr. Mallalieu said in a video interview.
[polldaddy:9771949]
Dr. Mallalieu presented findings from an open-label, single-arm, phase I trial that evaluated a 12 mg/kg dosing regimen of tocilizumab, which was given intravenously every 2 weeks for 12 weeks. Eleven children were studied who had a mean age of 1.3 years and active disease for at least 1 month despite treatment with glucocorticoids or nonsteroidal anti-inflammatory drugs.
The primary endpoint was the pharmacokinetics of tocilizumab in this younger patient population, and secondary endpoints were safety, pharmacodynamics, and exploring the efficacy over 12 weeks on top of stable background therapy, she explained.
Results showed that tocilizumab in children under 2 years of age could achieve pharmacokinetics similar to those seen in older children in the TENDER trial (N Engl J Med. 2012;367:2385-95), which is the trial that helped the biologic get licensed for use in the older sJIA population. Reductions in soluble interleukin-6 receptor, C-reactive protein, and the erythrocyte sedimentation rate were seen, again to a similar extent as seen in the TENDER trial. There was also an indication that similar reductions in the Juvenile Arthritis Disease Activity Score (JADAS)-71 score could be achieved, Dr. Mallalieu reported.
While the pattern and nature of adverse events were similar to those seen in the TENDER trial, there were more cases of hypersensitivity in this phase I study. Four cases of hypersensitivity were clinically confirmed, three of which were deemed serious. The three serious cases were observed at day 15, with two of the cases associated with multiple signs and symptoms that were confounded by either subclinical macrophage activation syndrome (MAS) or a faster infusion rate. One patient had urticaria and was hospitalized for observation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MADRID – The results of the first trial of a biologic agent in children less than 2 years of age with systemic juvenile idiopathic arthritis (sJIA) suggest that tocilizumab is likely to be effective in this age group.
“sJIA is the most severe form of childhood arthritis, and as you are aware, it’s the most difficult to treat as well,” said Navita L. Mallalieu, PhD, director of clinical pharmacology at Roche Innovation Center New York, the company that funded the study.
Tocilizumab (Actemra) has been available for the treatment of sJIA, both in the United States and the European Union since 2011, she observed at the European Congress of Rheumatology, but only for children aged 2 years or older at the current time.
Because of this prior history of use in sJIA, “we have confidence in the safety profile, and so we were able to go to the next step of testing children who were even younger than 2 years of age,” Dr. Mallalieu said in a video interview.
[polldaddy:9771949]
Dr. Mallalieu presented findings from an open-label, single-arm, phase I trial that evaluated a 12 mg/kg dosing regimen of tocilizumab, which was given intravenously every 2 weeks for 12 weeks. Eleven children were studied who had a mean age of 1.3 years and active disease for at least 1 month despite treatment with glucocorticoids or nonsteroidal anti-inflammatory drugs.
The primary endpoint was the pharmacokinetics of tocilizumab in this younger patient population, and secondary endpoints were safety, pharmacodynamics, and exploring the efficacy over 12 weeks on top of stable background therapy, she explained.
Results showed that tocilizumab in children under 2 years of age could achieve pharmacokinetics similar to those seen in older children in the TENDER trial (N Engl J Med. 2012;367:2385-95), which is the trial that helped the biologic get licensed for use in the older sJIA population. Reductions in soluble interleukin-6 receptor, C-reactive protein, and the erythrocyte sedimentation rate were seen, again to a similar extent as seen in the TENDER trial. There was also an indication that similar reductions in the Juvenile Arthritis Disease Activity Score (JADAS)-71 score could be achieved, Dr. Mallalieu reported.
While the pattern and nature of adverse events were similar to those seen in the TENDER trial, there were more cases of hypersensitivity in this phase I study. Four cases of hypersensitivity were clinically confirmed, three of which were deemed serious. The three serious cases were observed at day 15, with two of the cases associated with multiple signs and symptoms that were confounded by either subclinical macrophage activation syndrome (MAS) or a faster infusion rate. One patient had urticaria and was hospitalized for observation.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: Similar pharmacokinetics were observed in children under 2 years of age as those seen in a prior study of older children.
Data source: Open-label, single-arm, phase I trial that evaluated a 12-mg/kg dosing regimen of tocilizumab given intravenously every 2 weeks for 12 weeks.
Disclosures: Roche funded the study. The presenter is an employee of Roche.
Want to take action on health care legislation? Here’s how
The U.S. House of Representatives recently passed a revised version of the American Health Care Act (AHCA), which the nonpartisan Congressional Budget Office concluded would result in 14 million people losing coverage by 2018 and 23 million people losing coverage by 2026.
The American Congress of Obstetricians and Gynecologists is opposed to this bill and has stated that it will leave Americans “worse off than they are today” by cutting Medicaid, eliminating Medicaid expansion, allowing states to opt out of covering essential benefits like maternity care, and weakening protections for people with preexisting conditions.
[polldaddy:9770191]
State level
At the state level, the best person to contact is your ACOG section chairman, who can then direct you to your state’s legislative chairman. The legislative chairman will provide you with information on legislative actions that have been taken by the section. If you are interested in women’s health legislation, there may be an advocacy list to join that will provide legislative alerts. You may even choose to tweet about the alerts.
Often the state legislative chairman will send out information about an upcoming bill and ask for ACOG members to provide testimony. If there is a bill of particular interest, you can offer to testify either in person or submit written testimony. Often talking points are made available to help in the preparation of testimony.
Many states also have a Lobby Day, a day when members of the ob.gyn. community meet at the state house to advocate for or oppose legislation. This action can be easier than providing testimony because the time and date are predictable, while legislative hearings may not be.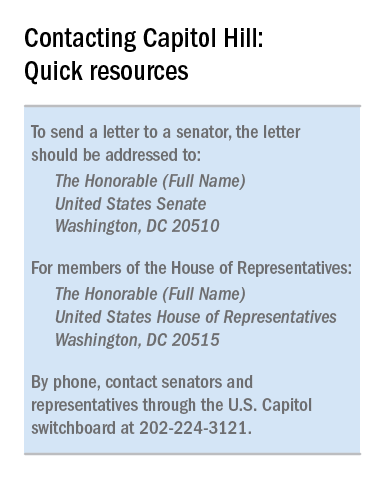
There is a great deal that can be done at the state level in support of women’s health. Perhaps your state does not have a maternal mortality committee, perhaps there needs to be funding for vaccinations, or perhaps you want to support legislation that continues to provide health care for women even if the AHCA becomes law.
National action
Legislative action at the national level mirrors that at the state level, but it is coordinated by the ACOG Government Affairs Department. Contact this department via acog.org. One option is to become an advocate and receive legislative alerts. This alert system informs ACOG members about congressional actions and gives you the option to directly contact your members of Congress through email with a specific message. Some physicians may prefer to send an email different than the one provided by ACOG, while others may tweet using hashtags like #obgynaction or #docs4coverage.
You may prefer to contact your member of Congress by phone. The U.S. Capitol Switchboard number is 202-224-3121. Phone calls typically are taken by staff members. It is reasonable to ask for a staff member who handles the issue you wish to discuss. This person may be referred to as the L.A. (legislative assistant). Inform the staff member that you are a constituent and you would like to leave a brief message for the Senator or Representative. Your comments may be as brief as stating that you support or oppose a particular piece of legislation. As with the letter, you should state the reasons for your opinion and may include a short personal story. If you do not already know it, you should ask for the lawmaker’s position on the bill.
An ideal method of interacting with members of Congress is through town hall meetings. These meetings typically are posted on the member’s website and hearing from constituents in person can have a tremendous impact on legislators. Letters to the Editor, interviews with journalists, and advocating for candidates are also options to consider. In such cases, consider contacting the ACOG Government Affairs Department. They can provide helpful dos and don’ts before an interview is scheduled or an article is written.
Health care policymaking that is not based on scientific or medical evidence is dangerous for our patients. We, as their physicians, need to advocate on their behalf. Stay or get involved to help ensure that our patients can get the health care they need when they need it.
Dr. Bohon is an ob.gyn. in private practice in Washington, and an ACOG state legislative chair from the District of Columbia. She is a member of the Ob.Gyn. News Editorial Advisory Board. Dr. Bohon reported having no relevant financial disclosures.
The U.S. House of Representatives recently passed a revised version of the American Health Care Act (AHCA), which the nonpartisan Congressional Budget Office concluded would result in 14 million people losing coverage by 2018 and 23 million people losing coverage by 2026.
The American Congress of Obstetricians and Gynecologists is opposed to this bill and has stated that it will leave Americans “worse off than they are today” by cutting Medicaid, eliminating Medicaid expansion, allowing states to opt out of covering essential benefits like maternity care, and weakening protections for people with preexisting conditions.
[polldaddy:9770191]
State level
At the state level, the best person to contact is your ACOG section chairman, who can then direct you to your state’s legislative chairman. The legislative chairman will provide you with information on legislative actions that have been taken by the section. If you are interested in women’s health legislation, there may be an advocacy list to join that will provide legislative alerts. You may even choose to tweet about the alerts.
Often the state legislative chairman will send out information about an upcoming bill and ask for ACOG members to provide testimony. If there is a bill of particular interest, you can offer to testify either in person or submit written testimony. Often talking points are made available to help in the preparation of testimony.
Many states also have a Lobby Day, a day when members of the ob.gyn. community meet at the state house to advocate for or oppose legislation. This action can be easier than providing testimony because the time and date are predictable, while legislative hearings may not be.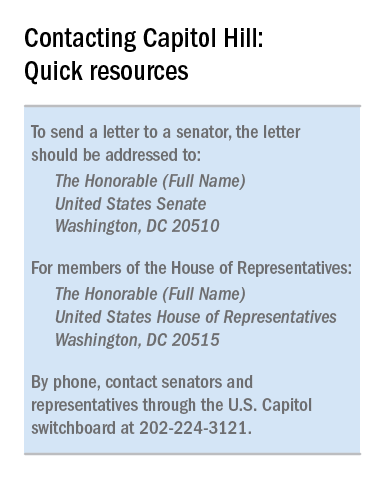
There is a great deal that can be done at the state level in support of women’s health. Perhaps your state does not have a maternal mortality committee, perhaps there needs to be funding for vaccinations, or perhaps you want to support legislation that continues to provide health care for women even if the AHCA becomes law.
National action
Legislative action at the national level mirrors that at the state level, but it is coordinated by the ACOG Government Affairs Department. Contact this department via acog.org. One option is to become an advocate and receive legislative alerts. This alert system informs ACOG members about congressional actions and gives you the option to directly contact your members of Congress through email with a specific message. Some physicians may prefer to send an email different than the one provided by ACOG, while others may tweet using hashtags like #obgynaction or #docs4coverage.
You may prefer to contact your member of Congress by phone. The U.S. Capitol Switchboard number is 202-224-3121. Phone calls typically are taken by staff members. It is reasonable to ask for a staff member who handles the issue you wish to discuss. This person may be referred to as the L.A. (legislative assistant). Inform the staff member that you are a constituent and you would like to leave a brief message for the Senator or Representative. Your comments may be as brief as stating that you support or oppose a particular piece of legislation. As with the letter, you should state the reasons for your opinion and may include a short personal story. If you do not already know it, you should ask for the lawmaker’s position on the bill.
An ideal method of interacting with members of Congress is through town hall meetings. These meetings typically are posted on the member’s website and hearing from constituents in person can have a tremendous impact on legislators. Letters to the Editor, interviews with journalists, and advocating for candidates are also options to consider. In such cases, consider contacting the ACOG Government Affairs Department. They can provide helpful dos and don’ts before an interview is scheduled or an article is written.
Health care policymaking that is not based on scientific or medical evidence is dangerous for our patients. We, as their physicians, need to advocate on their behalf. Stay or get involved to help ensure that our patients can get the health care they need when they need it.
Dr. Bohon is an ob.gyn. in private practice in Washington, and an ACOG state legislative chair from the District of Columbia. She is a member of the Ob.Gyn. News Editorial Advisory Board. Dr. Bohon reported having no relevant financial disclosures.
The U.S. House of Representatives recently passed a revised version of the American Health Care Act (AHCA), which the nonpartisan Congressional Budget Office concluded would result in 14 million people losing coverage by 2018 and 23 million people losing coverage by 2026.
The American Congress of Obstetricians and Gynecologists is opposed to this bill and has stated that it will leave Americans “worse off than they are today” by cutting Medicaid, eliminating Medicaid expansion, allowing states to opt out of covering essential benefits like maternity care, and weakening protections for people with preexisting conditions.
[polldaddy:9770191]
State level
At the state level, the best person to contact is your ACOG section chairman, who can then direct you to your state’s legislative chairman. The legislative chairman will provide you with information on legislative actions that have been taken by the section. If you are interested in women’s health legislation, there may be an advocacy list to join that will provide legislative alerts. You may even choose to tweet about the alerts.
Often the state legislative chairman will send out information about an upcoming bill and ask for ACOG members to provide testimony. If there is a bill of particular interest, you can offer to testify either in person or submit written testimony. Often talking points are made available to help in the preparation of testimony.
Many states also have a Lobby Day, a day when members of the ob.gyn. community meet at the state house to advocate for or oppose legislation. This action can be easier than providing testimony because the time and date are predictable, while legislative hearings may not be.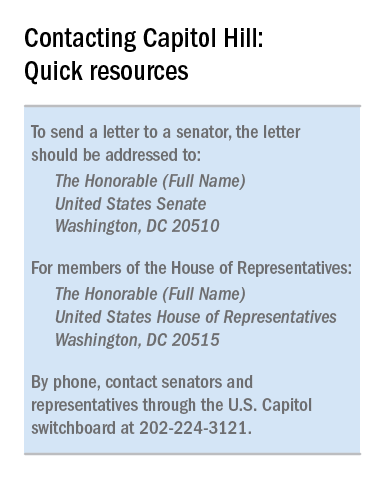
There is a great deal that can be done at the state level in support of women’s health. Perhaps your state does not have a maternal mortality committee, perhaps there needs to be funding for vaccinations, or perhaps you want to support legislation that continues to provide health care for women even if the AHCA becomes law.
National action
Legislative action at the national level mirrors that at the state level, but it is coordinated by the ACOG Government Affairs Department. Contact this department via acog.org. One option is to become an advocate and receive legislative alerts. This alert system informs ACOG members about congressional actions and gives you the option to directly contact your members of Congress through email with a specific message. Some physicians may prefer to send an email different than the one provided by ACOG, while others may tweet using hashtags like #obgynaction or #docs4coverage.
You may prefer to contact your member of Congress by phone. The U.S. Capitol Switchboard number is 202-224-3121. Phone calls typically are taken by staff members. It is reasonable to ask for a staff member who handles the issue you wish to discuss. This person may be referred to as the L.A. (legislative assistant). Inform the staff member that you are a constituent and you would like to leave a brief message for the Senator or Representative. Your comments may be as brief as stating that you support or oppose a particular piece of legislation. As with the letter, you should state the reasons for your opinion and may include a short personal story. If you do not already know it, you should ask for the lawmaker’s position on the bill.
An ideal method of interacting with members of Congress is through town hall meetings. These meetings typically are posted on the member’s website and hearing from constituents in person can have a tremendous impact on legislators. Letters to the Editor, interviews with journalists, and advocating for candidates are also options to consider. In such cases, consider contacting the ACOG Government Affairs Department. They can provide helpful dos and don’ts before an interview is scheduled or an article is written.
Health care policymaking that is not based on scientific or medical evidence is dangerous for our patients. We, as their physicians, need to advocate on their behalf. Stay or get involved to help ensure that our patients can get the health care they need when they need it.
Dr. Bohon is an ob.gyn. in private practice in Washington, and an ACOG state legislative chair from the District of Columbia. She is a member of the Ob.Gyn. News Editorial Advisory Board. Dr. Bohon reported having no relevant financial disclosures.
Mild OSA linked to hypertension
BOSTON – Sleep apnea doesn’t have to be severe or even symptomatic to increase the risk of hypertension and diabetes, according to a pair of new studies.
“We found that even mild sleep apnea was strongly associated with increased risk of developing hypertension by four times, compared to individuals without sleep apnea,” said principal investigator and top sleep researcher Alexandros N. Vgontzas, MD, of Pennsylvania State University College of Medicine in a SLEEP press release. “Similarly, moderate sleep apnea was associated with increased risk of developing diabetes by almost three times, compared to individuals without sleep apnea.”
Dr. Vgontzas presented his team’s results on the link between mild to moderate OSA and hypertension at the annual meeting of the American Academy of Sleep Medicine. In a separate session, his colleague at Penn State, Yun Li, MD, presented the diabetes-related findings of the same study.
After multivariate adjustment, including controlling for change in body mass index over time, both mild and moderate OSA were significantly associated with increased odds for developing hypertension, compared with controls without OSA (odds ratios, 4.36 and 3.46, respectively.).
The researchers found their test for an age interaction was also significant, indicating that younger adults with nonsevere OSA were at increased risk of hypertension, while those over 60 years of age were not.
[polldaddy:9792720]
“In young and middle-aged adults, our findings suggest that early detection and treatment of mild to moderate sleep apnea is warranted in order to prevent future cardiometabolic disease,” said Dr. Li in a press release. “Given the stronger association of sleep apnea with metabolic abnormalities in this age group, emphasis should be placed on yearly monitoring of indices of metabolic symptoms and lifestyle interventions, such as weight control, healthy diet, regular exercise, and stress management.”
For diabetes, moderate OSA was significantly associated with an almost threefold increased odds for developing diabetes after adjusting for a range of baseline and follow-up variables (OR, 2.78), but mild OSA was not associated with incident diabetes (OR, 0.47).
Both studies utilized data from the Penn State Adult Cohort, a random general population sample of 1,741 adults who underwent an overnight polysomnography sleep study and had a detailed medical history interview at baseline. Mild and moderate OSA were defined as an apnea hypopnea index from 5 to 14.9 and from 15 to 29.9, respectively. The presence of hypertension or diabetes at baseline and follow-up was defined by a self-report of receiving treatment for or having a physician diagnosis of either condition.
The age range of the studied population was wide (20-84 years), with a mean age of about 47 years. The incidence of diabetes was 10.2% at follow-up, while hypertension was found in 34.2% of patients. Dr. Vgontzas said the percentage of patients with hypertension was roughly what he had expected for this population.
“Our conclusion is that, the younger a person is, the stronger is the need for detection and treatment of sleep apnea,” said Dr. Vgontzas, though he acknowledged that putting these millions of people on continuous positive airway pressure therapy is not an easy proposition.
The study was supported by National Institutes of Health grants. Dr. Vgontzas reported no conflicts of interest.
BOSTON – Sleep apnea doesn’t have to be severe or even symptomatic to increase the risk of hypertension and diabetes, according to a pair of new studies.
“We found that even mild sleep apnea was strongly associated with increased risk of developing hypertension by four times, compared to individuals without sleep apnea,” said principal investigator and top sleep researcher Alexandros N. Vgontzas, MD, of Pennsylvania State University College of Medicine in a SLEEP press release. “Similarly, moderate sleep apnea was associated with increased risk of developing diabetes by almost three times, compared to individuals without sleep apnea.”
Dr. Vgontzas presented his team’s results on the link between mild to moderate OSA and hypertension at the annual meeting of the American Academy of Sleep Medicine. In a separate session, his colleague at Penn State, Yun Li, MD, presented the diabetes-related findings of the same study.
After multivariate adjustment, including controlling for change in body mass index over time, both mild and moderate OSA were significantly associated with increased odds for developing hypertension, compared with controls without OSA (odds ratios, 4.36 and 3.46, respectively.).
The researchers found their test for an age interaction was also significant, indicating that younger adults with nonsevere OSA were at increased risk of hypertension, while those over 60 years of age were not.
[polldaddy:9792720]
“In young and middle-aged adults, our findings suggest that early detection and treatment of mild to moderate sleep apnea is warranted in order to prevent future cardiometabolic disease,” said Dr. Li in a press release. “Given the stronger association of sleep apnea with metabolic abnormalities in this age group, emphasis should be placed on yearly monitoring of indices of metabolic symptoms and lifestyle interventions, such as weight control, healthy diet, regular exercise, and stress management.”
For diabetes, moderate OSA was significantly associated with an almost threefold increased odds for developing diabetes after adjusting for a range of baseline and follow-up variables (OR, 2.78), but mild OSA was not associated with incident diabetes (OR, 0.47).
Both studies utilized data from the Penn State Adult Cohort, a random general population sample of 1,741 adults who underwent an overnight polysomnography sleep study and had a detailed medical history interview at baseline. Mild and moderate OSA were defined as an apnea hypopnea index from 5 to 14.9 and from 15 to 29.9, respectively. The presence of hypertension or diabetes at baseline and follow-up was defined by a self-report of receiving treatment for or having a physician diagnosis of either condition.
The age range of the studied population was wide (20-84 years), with a mean age of about 47 years. The incidence of diabetes was 10.2% at follow-up, while hypertension was found in 34.2% of patients. Dr. Vgontzas said the percentage of patients with hypertension was roughly what he had expected for this population.
“Our conclusion is that, the younger a person is, the stronger is the need for detection and treatment of sleep apnea,” said Dr. Vgontzas, though he acknowledged that putting these millions of people on continuous positive airway pressure therapy is not an easy proposition.
The study was supported by National Institutes of Health grants. Dr. Vgontzas reported no conflicts of interest.
BOSTON – Sleep apnea doesn’t have to be severe or even symptomatic to increase the risk of hypertension and diabetes, according to a pair of new studies.
“We found that even mild sleep apnea was strongly associated with increased risk of developing hypertension by four times, compared to individuals without sleep apnea,” said principal investigator and top sleep researcher Alexandros N. Vgontzas, MD, of Pennsylvania State University College of Medicine in a SLEEP press release. “Similarly, moderate sleep apnea was associated with increased risk of developing diabetes by almost three times, compared to individuals without sleep apnea.”
Dr. Vgontzas presented his team’s results on the link between mild to moderate OSA and hypertension at the annual meeting of the American Academy of Sleep Medicine. In a separate session, his colleague at Penn State, Yun Li, MD, presented the diabetes-related findings of the same study.
After multivariate adjustment, including controlling for change in body mass index over time, both mild and moderate OSA were significantly associated with increased odds for developing hypertension, compared with controls without OSA (odds ratios, 4.36 and 3.46, respectively.).
The researchers found their test for an age interaction was also significant, indicating that younger adults with nonsevere OSA were at increased risk of hypertension, while those over 60 years of age were not.
[polldaddy:9792720]
“In young and middle-aged adults, our findings suggest that early detection and treatment of mild to moderate sleep apnea is warranted in order to prevent future cardiometabolic disease,” said Dr. Li in a press release. “Given the stronger association of sleep apnea with metabolic abnormalities in this age group, emphasis should be placed on yearly monitoring of indices of metabolic symptoms and lifestyle interventions, such as weight control, healthy diet, regular exercise, and stress management.”
For diabetes, moderate OSA was significantly associated with an almost threefold increased odds for developing diabetes after adjusting for a range of baseline and follow-up variables (OR, 2.78), but mild OSA was not associated with incident diabetes (OR, 0.47).
Both studies utilized data from the Penn State Adult Cohort, a random general population sample of 1,741 adults who underwent an overnight polysomnography sleep study and had a detailed medical history interview at baseline. Mild and moderate OSA were defined as an apnea hypopnea index from 5 to 14.9 and from 15 to 29.9, respectively. The presence of hypertension or diabetes at baseline and follow-up was defined by a self-report of receiving treatment for or having a physician diagnosis of either condition.
The age range of the studied population was wide (20-84 years), with a mean age of about 47 years. The incidence of diabetes was 10.2% at follow-up, while hypertension was found in 34.2% of patients. Dr. Vgontzas said the percentage of patients with hypertension was roughly what he had expected for this population.
“Our conclusion is that, the younger a person is, the stronger is the need for detection and treatment of sleep apnea,” said Dr. Vgontzas, though he acknowledged that putting these millions of people on continuous positive airway pressure therapy is not an easy proposition.
The study was supported by National Institutes of Health grants. Dr. Vgontzas reported no conflicts of interest.
AT SLEEP 2017
Key clinical point: In a random sample of adults, the presence of mild to moderate OSA was associated with a significantly higher risk of hypertension and diabetes.
Major finding: Individuals with mild to moderate OSA had more than a fourfold increased risk of hypertension over 10 years of follow-up (OR, 4.36). Moderate OSA was significantly associated with incident diabetes risk (OR, 2.78), but mild OSA was not.
Data source: An observational study including a random sample of 1,741 adults between the ages of 20 and 84 years.
Disclosures: The study was supported by National Institutes of Health grants. Dr. Vgontzas reported no conflicts of interest.
NIH releases COPD National Action Plan
WASHINGTON – The National Institutes of Health on Monday released its first COPD National Action Plan, a five-point initiative to reduce the burden of chronic obstructive pulmonary disease and increase research into prevention and treatment.
On the same day, the National Heart, Lung, and Blood Institute and other supporters of the plan described its evolution and why they thought the plan’s implementation was important.
The plan’s five goals are:
- Empower people with COPD, their families, and caregivers to recognize and reduce the burden of COPD.
- Improve the prevention, diagnosis, treatment, and management of COPD by increasing the quality of care delivered across the health care continuum.
- Collect, analyze, report, and disseminate COPD-related public health data that drive change and track progress.
- Increase and sustain research to better understand the prevention, pathogenesis, diagnosis, treatment, and management of COPD.
- Translate national policy, educational, and program recommendations into research and public health care actions.
“Chronic obstructive pulmonary disease is the third-leading cause of death in this country; it’s just behind heart disease and cancer,” Dr. Kiley noted. “What’s really disappointing and discouraging is it’s the only cause of death in this country where the numbers are not declining.”
COPD “got the attention of Congress a number of years ago,” he added. “They encouraged the National Institutes of Health to work with the community stakeholders and other federal agencies to develop a national action plan to respond to the growing burden of this disease.”
COPD’s stakeholder community, the federal government, and other partners worked together to develop a set of core goals that the National Action Plan would address, Dr. Kiley continued. “It was meant to obtain the broadest amount of input possible so that we could get it right from the start.”
Another of the plan’s advocates, MeiLan Han, MD, medical director of the women’s respiratory health program at the University of Michigan, Ann Arbor, illustrated the need to increase and sustain COPD research related to the disease.
[polldaddy:9806142]
“I see the suffering and disease toll that this takes on my patients, and I can’t convince you enough of the level of frustration that I have as a physician in not being able to provide the level of care that I want to be able to provide,” said Dr. Han, who served as a panelist at the press conference.
“We face some serious barriers to being able to provide adequate care for patients,” she added. Those barriers include lack of access to providers who are knowledgeable about COPD, as well as lack of access to affordable and conveniently located pulmonology rehabilitation and education materials. From a research standpoint, Dr. Han added, medicine still doesn’t know enough about the disease. “We certainly have good treatments, but we need better treatments,” she said.
“What’s clear is that we as society can no longer afford to brush this under the table and ignore this problem,” Dr. Han added.
The National Action Plan and information about how to get involved are available at copd.nih.gov.
WASHINGTON – The National Institutes of Health on Monday released its first COPD National Action Plan, a five-point initiative to reduce the burden of chronic obstructive pulmonary disease and increase research into prevention and treatment.
On the same day, the National Heart, Lung, and Blood Institute and other supporters of the plan described its evolution and why they thought the plan’s implementation was important.
The plan’s five goals are:
- Empower people with COPD, their families, and caregivers to recognize and reduce the burden of COPD.
- Improve the prevention, diagnosis, treatment, and management of COPD by increasing the quality of care delivered across the health care continuum.
- Collect, analyze, report, and disseminate COPD-related public health data that drive change and track progress.
- Increase and sustain research to better understand the prevention, pathogenesis, diagnosis, treatment, and management of COPD.
- Translate national policy, educational, and program recommendations into research and public health care actions.
“Chronic obstructive pulmonary disease is the third-leading cause of death in this country; it’s just behind heart disease and cancer,” Dr. Kiley noted. “What’s really disappointing and discouraging is it’s the only cause of death in this country where the numbers are not declining.”
COPD “got the attention of Congress a number of years ago,” he added. “They encouraged the National Institutes of Health to work with the community stakeholders and other federal agencies to develop a national action plan to respond to the growing burden of this disease.”
COPD’s stakeholder community, the federal government, and other partners worked together to develop a set of core goals that the National Action Plan would address, Dr. Kiley continued. “It was meant to obtain the broadest amount of input possible so that we could get it right from the start.”
Another of the plan’s advocates, MeiLan Han, MD, medical director of the women’s respiratory health program at the University of Michigan, Ann Arbor, illustrated the need to increase and sustain COPD research related to the disease.
[polldaddy:9806142]
“I see the suffering and disease toll that this takes on my patients, and I can’t convince you enough of the level of frustration that I have as a physician in not being able to provide the level of care that I want to be able to provide,” said Dr. Han, who served as a panelist at the press conference.
“We face some serious barriers to being able to provide adequate care for patients,” she added. Those barriers include lack of access to providers who are knowledgeable about COPD, as well as lack of access to affordable and conveniently located pulmonology rehabilitation and education materials. From a research standpoint, Dr. Han added, medicine still doesn’t know enough about the disease. “We certainly have good treatments, but we need better treatments,” she said.
“What’s clear is that we as society can no longer afford to brush this under the table and ignore this problem,” Dr. Han added.
The National Action Plan and information about how to get involved are available at copd.nih.gov.
WASHINGTON – The National Institutes of Health on Monday released its first COPD National Action Plan, a five-point initiative to reduce the burden of chronic obstructive pulmonary disease and increase research into prevention and treatment.
On the same day, the National Heart, Lung, and Blood Institute and other supporters of the plan described its evolution and why they thought the plan’s implementation was important.
The plan’s five goals are:
- Empower people with COPD, their families, and caregivers to recognize and reduce the burden of COPD.
- Improve the prevention, diagnosis, treatment, and management of COPD by increasing the quality of care delivered across the health care continuum.
- Collect, analyze, report, and disseminate COPD-related public health data that drive change and track progress.
- Increase and sustain research to better understand the prevention, pathogenesis, diagnosis, treatment, and management of COPD.
- Translate national policy, educational, and program recommendations into research and public health care actions.
“Chronic obstructive pulmonary disease is the third-leading cause of death in this country; it’s just behind heart disease and cancer,” Dr. Kiley noted. “What’s really disappointing and discouraging is it’s the only cause of death in this country where the numbers are not declining.”
COPD “got the attention of Congress a number of years ago,” he added. “They encouraged the National Institutes of Health to work with the community stakeholders and other federal agencies to develop a national action plan to respond to the growing burden of this disease.”
COPD’s stakeholder community, the federal government, and other partners worked together to develop a set of core goals that the National Action Plan would address, Dr. Kiley continued. “It was meant to obtain the broadest amount of input possible so that we could get it right from the start.”
Another of the plan’s advocates, MeiLan Han, MD, medical director of the women’s respiratory health program at the University of Michigan, Ann Arbor, illustrated the need to increase and sustain COPD research related to the disease.
[polldaddy:9806142]
“I see the suffering and disease toll that this takes on my patients, and I can’t convince you enough of the level of frustration that I have as a physician in not being able to provide the level of care that I want to be able to provide,” said Dr. Han, who served as a panelist at the press conference.
“We face some serious barriers to being able to provide adequate care for patients,” she added. Those barriers include lack of access to providers who are knowledgeable about COPD, as well as lack of access to affordable and conveniently located pulmonology rehabilitation and education materials. From a research standpoint, Dr. Han added, medicine still doesn’t know enough about the disease. “We certainly have good treatments, but we need better treatments,” she said.
“What’s clear is that we as society can no longer afford to brush this under the table and ignore this problem,” Dr. Han added.
The National Action Plan and information about how to get involved are available at copd.nih.gov.
AT ATS 2017