User login
Potential new role for FFR
Paris – Fractional flow reserve is under study for a potential major application: guidance on percutaneous coronary intervention (PCI) optimization immediately after stent placement, Roberto Diletti, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
At the end of the procedure, FFR measurement using a novel monorail optical pressure sensor catheter revealed that 43% of the lesions had a suboptimal FFR value of 0.90 or less.
“Just this year, two meta-analyses showed that a cutoff of 0.90 is important to define a group of patients at high risk for major adverse cardiovascular events and revascularization,” noted Dr. Diletti of Erasmus University Medical Center in Rotterdam, the Netherlands.
Using the older, more conservative cutoff of an FFR of 0.85 or less, 20% of the lesions would potentially benefit from further action to optimize the physiologic result, most often in the form of additional expansion of the stent.
“We are used to thinking of FFR as a tool to understand whether a lesion has to be treated or not. Now we can also start thinking about FFR as a tool to guide PCI optimization,” the cardiologist said.
Optimization wasn’t actually performed in this observational registry. That will be the focus of FFR-REACT, a planned randomized trial investigating the clinical impact of intravascular ultrasound (IVUS)-directed FFR optimization of PCI.
In a per-patient analysis, 48% of FFR-SEARCH participants had a poststent FFR of 0.90 or less in one or more treated lesions. Another 22% had a postprocedure FFR of 0.85 or less in at least one treated lesion, while 8.9% had an FFR of 0.80, which is below the threshold for ischemia.
The primary endpoint in the ongoing FFR-SEARCH study is the 2-year composite rate of major adverse cardiovascular events, defined as MI, any revascularization, or all-cause mortality. Only the 30-day MACE rate was available at the time of Dr. Diletti’s presentation in Paris. The rate was 1.5% in patients with a postprocedure FFR greater than 0.90, 2.0% in those with an FFR of 0.86-0.90, 2.6% with an FFR of 0.81-0.85, and 2.8% with a poststent FFR of 0.80 or less. While those early between-group differences weren’t statistically significant, the trend is encouraging, he noted.
Postprocedure FFR measurement took an average of 5 minutes. The procedure was simple and safe, according to Dr. Diletti. There were no complications related to the use of the Navvus MicroCatheter technology. He explained that the device profile is comparable to a 0.022-inch diameter at the lesion site. Wire access to the vessel was maintained throughout. The rapid-exchange monorail microcatheter was inserted over the previously used standard 0.014-inch coronary guidewire. The optical pressure sensor was positioned roughly 20 mm distal to the distal stent edge. Manual pullback with measurements obtained at various locations in the vicinity of the stented lesion was repeated as necessary in order to identify where optimization, if appropriate, should be focused.
Operators were unable to crossover the microcatheter in 3.5% of cases, mostly because of vessel tortuosity or calcification.
Audience members commented that many of the low FFRs after stenting may reflect diffuse coronary disease, which can be corrected only by placing numerous additional stents, creating its own problems. Dr. Diletti offered reassurance on that score. He explained that in an IVUS substudy of FFR-SEARCH, an unstented physiologically important focal lesion or stent underexpansion was identified in 86% of the cases of low FFR.
“That means you can do something about it. In the other 14% of cases, in my opinion, you cannot do a lot because of very diffuse disease distally,” he said.
He reported having no financial conflicts of interest in connection with the study, supported by ACIST Medical Systems. The Navvus MicroCatheter is approved by both the Food and Drug Administration and the European regulatory agency.
Paris – Fractional flow reserve is under study for a potential major application: guidance on percutaneous coronary intervention (PCI) optimization immediately after stent placement, Roberto Diletti, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
At the end of the procedure, FFR measurement using a novel monorail optical pressure sensor catheter revealed that 43% of the lesions had a suboptimal FFR value of 0.90 or less.
“Just this year, two meta-analyses showed that a cutoff of 0.90 is important to define a group of patients at high risk for major adverse cardiovascular events and revascularization,” noted Dr. Diletti of Erasmus University Medical Center in Rotterdam, the Netherlands.
Using the older, more conservative cutoff of an FFR of 0.85 or less, 20% of the lesions would potentially benefit from further action to optimize the physiologic result, most often in the form of additional expansion of the stent.
“We are used to thinking of FFR as a tool to understand whether a lesion has to be treated or not. Now we can also start thinking about FFR as a tool to guide PCI optimization,” the cardiologist said.
Optimization wasn’t actually performed in this observational registry. That will be the focus of FFR-REACT, a planned randomized trial investigating the clinical impact of intravascular ultrasound (IVUS)-directed FFR optimization of PCI.
In a per-patient analysis, 48% of FFR-SEARCH participants had a poststent FFR of 0.90 or less in one or more treated lesions. Another 22% had a postprocedure FFR of 0.85 or less in at least one treated lesion, while 8.9% had an FFR of 0.80, which is below the threshold for ischemia.
The primary endpoint in the ongoing FFR-SEARCH study is the 2-year composite rate of major adverse cardiovascular events, defined as MI, any revascularization, or all-cause mortality. Only the 30-day MACE rate was available at the time of Dr. Diletti’s presentation in Paris. The rate was 1.5% in patients with a postprocedure FFR greater than 0.90, 2.0% in those with an FFR of 0.86-0.90, 2.6% with an FFR of 0.81-0.85, and 2.8% with a poststent FFR of 0.80 or less. While those early between-group differences weren’t statistically significant, the trend is encouraging, he noted.
Postprocedure FFR measurement took an average of 5 minutes. The procedure was simple and safe, according to Dr. Diletti. There were no complications related to the use of the Navvus MicroCatheter technology. He explained that the device profile is comparable to a 0.022-inch diameter at the lesion site. Wire access to the vessel was maintained throughout. The rapid-exchange monorail microcatheter was inserted over the previously used standard 0.014-inch coronary guidewire. The optical pressure sensor was positioned roughly 20 mm distal to the distal stent edge. Manual pullback with measurements obtained at various locations in the vicinity of the stented lesion was repeated as necessary in order to identify where optimization, if appropriate, should be focused.
Operators were unable to crossover the microcatheter in 3.5% of cases, mostly because of vessel tortuosity or calcification.
Audience members commented that many of the low FFRs after stenting may reflect diffuse coronary disease, which can be corrected only by placing numerous additional stents, creating its own problems. Dr. Diletti offered reassurance on that score. He explained that in an IVUS substudy of FFR-SEARCH, an unstented physiologically important focal lesion or stent underexpansion was identified in 86% of the cases of low FFR.
“That means you can do something about it. In the other 14% of cases, in my opinion, you cannot do a lot because of very diffuse disease distally,” he said.
He reported having no financial conflicts of interest in connection with the study, supported by ACIST Medical Systems. The Navvus MicroCatheter is approved by both the Food and Drug Administration and the European regulatory agency.
Paris – Fractional flow reserve is under study for a potential major application: guidance on percutaneous coronary intervention (PCI) optimization immediately after stent placement, Roberto Diletti, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
At the end of the procedure, FFR measurement using a novel monorail optical pressure sensor catheter revealed that 43% of the lesions had a suboptimal FFR value of 0.90 or less.
“Just this year, two meta-analyses showed that a cutoff of 0.90 is important to define a group of patients at high risk for major adverse cardiovascular events and revascularization,” noted Dr. Diletti of Erasmus University Medical Center in Rotterdam, the Netherlands.
Using the older, more conservative cutoff of an FFR of 0.85 or less, 20% of the lesions would potentially benefit from further action to optimize the physiologic result, most often in the form of additional expansion of the stent.
“We are used to thinking of FFR as a tool to understand whether a lesion has to be treated or not. Now we can also start thinking about FFR as a tool to guide PCI optimization,” the cardiologist said.
Optimization wasn’t actually performed in this observational registry. That will be the focus of FFR-REACT, a planned randomized trial investigating the clinical impact of intravascular ultrasound (IVUS)-directed FFR optimization of PCI.
In a per-patient analysis, 48% of FFR-SEARCH participants had a poststent FFR of 0.90 or less in one or more treated lesions. Another 22% had a postprocedure FFR of 0.85 or less in at least one treated lesion, while 8.9% had an FFR of 0.80, which is below the threshold for ischemia.
The primary endpoint in the ongoing FFR-SEARCH study is the 2-year composite rate of major adverse cardiovascular events, defined as MI, any revascularization, or all-cause mortality. Only the 30-day MACE rate was available at the time of Dr. Diletti’s presentation in Paris. The rate was 1.5% in patients with a postprocedure FFR greater than 0.90, 2.0% in those with an FFR of 0.86-0.90, 2.6% with an FFR of 0.81-0.85, and 2.8% with a poststent FFR of 0.80 or less. While those early between-group differences weren’t statistically significant, the trend is encouraging, he noted.
Postprocedure FFR measurement took an average of 5 minutes. The procedure was simple and safe, according to Dr. Diletti. There were no complications related to the use of the Navvus MicroCatheter technology. He explained that the device profile is comparable to a 0.022-inch diameter at the lesion site. Wire access to the vessel was maintained throughout. The rapid-exchange monorail microcatheter was inserted over the previously used standard 0.014-inch coronary guidewire. The optical pressure sensor was positioned roughly 20 mm distal to the distal stent edge. Manual pullback with measurements obtained at various locations in the vicinity of the stented lesion was repeated as necessary in order to identify where optimization, if appropriate, should be focused.
Operators were unable to crossover the microcatheter in 3.5% of cases, mostly because of vessel tortuosity or calcification.
Audience members commented that many of the low FFRs after stenting may reflect diffuse coronary disease, which can be corrected only by placing numerous additional stents, creating its own problems. Dr. Diletti offered reassurance on that score. He explained that in an IVUS substudy of FFR-SEARCH, an unstented physiologically important focal lesion or stent underexpansion was identified in 86% of the cases of low FFR.
“That means you can do something about it. In the other 14% of cases, in my opinion, you cannot do a lot because of very diffuse disease distally,” he said.
He reported having no financial conflicts of interest in connection with the study, supported by ACIST Medical Systems. The Navvus MicroCatheter is approved by both the Food and Drug Administration and the European regulatory agency.
EXPERT ANALYSIS FROM EuroPCR
Genetic predisposition to hypercalcemia linked to CAD, MI
in a large mendelian randomization study published online July 25 in JAMA.
Each 0.5-mg rise in genetically predicted serum calcium concentration increased the odds of coronary artery disease (CAD) and myocardial infarction by about 25%, reported Susanna C. Larsson, Ph.D., of Karolinska Institutet in Stockholm, Sweden, and her associates. It remains unclear whether short- or medium-term calcium supplementation also increases the risk of these outcomes, they added.
Observational studies have linked high serum calcium with cardiovascular disease, but such studies are subject to confounding, the researchers noted. Randomized trials indicate that calcium supplementation might contribute to MI, but the trials are not designed to quantify long-term risks. Therefore, the investigators evaluated a proxy for lifelong hypercalcemia – six single nucleotide polymorphisms (SNPs) that have been linked to high serum calcium, but not to other CAD risk factors such as type 2 diabetes, fasting glucose and insulin levels, body mass index, waist-to-hip ratio, major lipids, or hypertension (JAMA. 2017 Jul 25;318[4]:371-80. doi: 10.1001/jama.2017.8981).
To examine how these SNPs affect the risk of CAD and MI, the researchers analyzed summary statistics for 184,305 individuals from a meta-analysis of CAD genome-wide association studies (Nat Genet. 2015;47:1121-30), including 60,801 cases (of whom about 70% also had MI) and 123,504 controls.
Together, these six SNPs explained about 0.8% of variations in serum calcium levels. Each 0.5-mg/dL (about one standard deviation) increase in genetically predicted serum calcium level significantly increased the risk of CAD (odds ratio, 1.25; 95% confidence interval, 1.08-1.45; P = .003) and MI (OR, 1.24; 95% CI, 1.05-1.46; P = .009). The genetic variant rs1801725 exerted the greatest effect on serum calcium levels, the investigators noted. This SNP affects the CASR gene, which encodes a calcium-sensing receptor that “plays a key role in calcium homeostasis.” However, four of the other five variants also had odds ratios above 1.0, and three had odds ratios above 1.25. A sensitivity analysis that excluded the CASR variant generated an identical odds ratio, although the confidence interval was wider. Studies of other risk factors for CAD have yielded odds ratios between 1.3 (triglyceride levels) and 1.7 (LDL cholesterol levels), the researchers noted.
A link between calcium supplementation and MI remains debatable. However, supplementation can lead to hypercalcemia and greater formation of insoluble calciprotein particles, the investigators said. Coronary artery disease might result from downstream effects on vascular calcification, vascular cells, blood coagulation pathways, or gene expression, but such mechanisms need more study, they added.
This analysis included men and women from the United States, Canada, the United Kingdom, Germany, Sweden, Ireland, the Netherlands, Finland, Iceland, Italy, Estonia, Lebanon, China, Korea, India, Pakistan and Greece. Participants tended to be men in their 50s and 60s, but more than half of studies lacked data on age and sex. Nearly all participants were of white European ancestry.
Karolinska Institutet supported Dr. Larsson. The investigators reported having no relevant conflicts of interest.
in a large mendelian randomization study published online July 25 in JAMA.
Each 0.5-mg rise in genetically predicted serum calcium concentration increased the odds of coronary artery disease (CAD) and myocardial infarction by about 25%, reported Susanna C. Larsson, Ph.D., of Karolinska Institutet in Stockholm, Sweden, and her associates. It remains unclear whether short- or medium-term calcium supplementation also increases the risk of these outcomes, they added.
Observational studies have linked high serum calcium with cardiovascular disease, but such studies are subject to confounding, the researchers noted. Randomized trials indicate that calcium supplementation might contribute to MI, but the trials are not designed to quantify long-term risks. Therefore, the investigators evaluated a proxy for lifelong hypercalcemia – six single nucleotide polymorphisms (SNPs) that have been linked to high serum calcium, but not to other CAD risk factors such as type 2 diabetes, fasting glucose and insulin levels, body mass index, waist-to-hip ratio, major lipids, or hypertension (JAMA. 2017 Jul 25;318[4]:371-80. doi: 10.1001/jama.2017.8981).
To examine how these SNPs affect the risk of CAD and MI, the researchers analyzed summary statistics for 184,305 individuals from a meta-analysis of CAD genome-wide association studies (Nat Genet. 2015;47:1121-30), including 60,801 cases (of whom about 70% also had MI) and 123,504 controls.
Together, these six SNPs explained about 0.8% of variations in serum calcium levels. Each 0.5-mg/dL (about one standard deviation) increase in genetically predicted serum calcium level significantly increased the risk of CAD (odds ratio, 1.25; 95% confidence interval, 1.08-1.45; P = .003) and MI (OR, 1.24; 95% CI, 1.05-1.46; P = .009). The genetic variant rs1801725 exerted the greatest effect on serum calcium levels, the investigators noted. This SNP affects the CASR gene, which encodes a calcium-sensing receptor that “plays a key role in calcium homeostasis.” However, four of the other five variants also had odds ratios above 1.0, and three had odds ratios above 1.25. A sensitivity analysis that excluded the CASR variant generated an identical odds ratio, although the confidence interval was wider. Studies of other risk factors for CAD have yielded odds ratios between 1.3 (triglyceride levels) and 1.7 (LDL cholesterol levels), the researchers noted.
A link between calcium supplementation and MI remains debatable. However, supplementation can lead to hypercalcemia and greater formation of insoluble calciprotein particles, the investigators said. Coronary artery disease might result from downstream effects on vascular calcification, vascular cells, blood coagulation pathways, or gene expression, but such mechanisms need more study, they added.
This analysis included men and women from the United States, Canada, the United Kingdom, Germany, Sweden, Ireland, the Netherlands, Finland, Iceland, Italy, Estonia, Lebanon, China, Korea, India, Pakistan and Greece. Participants tended to be men in their 50s and 60s, but more than half of studies lacked data on age and sex. Nearly all participants were of white European ancestry.
Karolinska Institutet supported Dr. Larsson. The investigators reported having no relevant conflicts of interest.
in a large mendelian randomization study published online July 25 in JAMA.
Each 0.5-mg rise in genetically predicted serum calcium concentration increased the odds of coronary artery disease (CAD) and myocardial infarction by about 25%, reported Susanna C. Larsson, Ph.D., of Karolinska Institutet in Stockholm, Sweden, and her associates. It remains unclear whether short- or medium-term calcium supplementation also increases the risk of these outcomes, they added.
Observational studies have linked high serum calcium with cardiovascular disease, but such studies are subject to confounding, the researchers noted. Randomized trials indicate that calcium supplementation might contribute to MI, but the trials are not designed to quantify long-term risks. Therefore, the investigators evaluated a proxy for lifelong hypercalcemia – six single nucleotide polymorphisms (SNPs) that have been linked to high serum calcium, but not to other CAD risk factors such as type 2 diabetes, fasting glucose and insulin levels, body mass index, waist-to-hip ratio, major lipids, or hypertension (JAMA. 2017 Jul 25;318[4]:371-80. doi: 10.1001/jama.2017.8981).
To examine how these SNPs affect the risk of CAD and MI, the researchers analyzed summary statistics for 184,305 individuals from a meta-analysis of CAD genome-wide association studies (Nat Genet. 2015;47:1121-30), including 60,801 cases (of whom about 70% also had MI) and 123,504 controls.
Together, these six SNPs explained about 0.8% of variations in serum calcium levels. Each 0.5-mg/dL (about one standard deviation) increase in genetically predicted serum calcium level significantly increased the risk of CAD (odds ratio, 1.25; 95% confidence interval, 1.08-1.45; P = .003) and MI (OR, 1.24; 95% CI, 1.05-1.46; P = .009). The genetic variant rs1801725 exerted the greatest effect on serum calcium levels, the investigators noted. This SNP affects the CASR gene, which encodes a calcium-sensing receptor that “plays a key role in calcium homeostasis.” However, four of the other five variants also had odds ratios above 1.0, and three had odds ratios above 1.25. A sensitivity analysis that excluded the CASR variant generated an identical odds ratio, although the confidence interval was wider. Studies of other risk factors for CAD have yielded odds ratios between 1.3 (triglyceride levels) and 1.7 (LDL cholesterol levels), the researchers noted.
A link between calcium supplementation and MI remains debatable. However, supplementation can lead to hypercalcemia and greater formation of insoluble calciprotein particles, the investigators said. Coronary artery disease might result from downstream effects on vascular calcification, vascular cells, blood coagulation pathways, or gene expression, but such mechanisms need more study, they added.
This analysis included men and women from the United States, Canada, the United Kingdom, Germany, Sweden, Ireland, the Netherlands, Finland, Iceland, Italy, Estonia, Lebanon, China, Korea, India, Pakistan and Greece. Participants tended to be men in their 50s and 60s, but more than half of studies lacked data on age and sex. Nearly all participants were of white European ancestry.
Karolinska Institutet supported Dr. Larsson. The investigators reported having no relevant conflicts of interest.
FROM JAMA
Key clinical point: Genetic predisposition to higher serum calcium levels was significantly associated with coronary artery disease and myocardial infarction.
Major finding: Each 0.5-mg per dL rise in serum calcium increased the odds of these outcomes by about 25% (odds ratios, 1.25 and 1.24, respectively).
Data source: A mendelian randomization study of 60,801 cases of coronary artery disease, 123,504 controls, and six single nucleotide polymorphisms linked to serum calcium but not to other risk factors for coronary artery disease.
Disclosures: Karolinska Institutet supported Dr. Larsson. The investigators reported having no relevant conflicts of interest.
Blocking a lipoprotein lipase inhibitor improves lipid profiles
Two different approaches to shutting down the function of a human liver protein that inhibits lipoprotein lipase showed preliminary evidence of safely producing favorable lipid changes in healthy volunteers in two separate, phase 1 studies.
These findings, coupled with promising observational data from people who carry loss-of-function mutations in the gene for this protein, angiopoietin-like 3 (ANGPTL3), have raised hopes that interventions that interfere with the function of the ANGPTL3 protein may provide new and effective ways to improve lipid levels and cut the incidence of cardiovascular disease events.
“There is now a growing body of epidemiologic, genetic, and genomewide association studies supporting the hypothesis that lowering levels of ANGPTL3 in plasma by inhibiting hepatic ANGPTL3 synthesis will be beneficial in terms of reducing plasma levels of atherogenic apolipoprotein B and in improving metabolic measures associated with dyslipidemia,” wrote Mark J. Graham and his associates in a recently published article (N Engl J Med. 2017 Jul 20;377[3]:222-32).
The phase 1 study results reported by this group came from 44 healthy adults aged 18-65 years who received varying doses of a commercially developed antisense drug, ANGPTL3-LRX, as either single or serial subcutaneous injections. ANGPTL3-LRX is an oligonucleotide designed to inhibit production of messenger RNA for the ANGPTL3 protein.
Six people received the highest ANGPTL3-LRX dosage administered, 60 mg given as a weekly injection for 6 weeks, and after this regimen they showed an average 50% cut in triglycerides levels, compared with baseline, and an average 33% drop in their low LDL cholesterol levels from baseline. None of the 33 people treated with ANGPTL3-LRX in the trial had a documented serious adverse event, and the only treatment dropout was a patient who was lost to follow-up during the treatment phase, reported Mr. Graham, a researcher at Ionis Pharmaceuticals, the sponsor of the study and the company developing the antisense drug, and his associates.
The second phase 1 study examined a different way to block ANGPTL3 activity, with a human monoclonal antibody to this protein. The study involved 83 healthy adults aged 18-65 years with fasting triglyceride levels of 150-450 mg/dL and fasting LDL cholesterol levels of at least 100 mg/dL. Each participant received a single subcutaneous injection or intravenous dose of the antibody, evinacumab, at varying amounts or placebo. The maximum observed lipid changes seen was a drop in triglycerides of 76% and a fall in LDL cholesterol by 23%. Treatment also produced a maximum drop in HDL cholesterol of 18%. No person left the study because of an adverse event. The most common adverse event was headache, in seven people (11% of evinacumab recipients), reported Frederick E. Dewey, MD, a researcher at Regeneron Pharmaceuticals, the company developing evinacumab, and his associates (N Engl J Med. 2017 Jul 20;377[3]:211-21).
The Regeneron report also included results from population studies they ran. They reported performing genome sequencing on specimens from 58,335 adults enrolled in the DiscovEHR study, and identified 13 distinct loss-of-function variants in the ANGPTL3 genes that occurred individually in a small number of these people.
They then ran analyses of lipid levels and coronary artery disease prevalence rates in people who carry one of these 13 loss-of-function genetic signatures in one of their ANGTPL3 genes. Among 45,226 of the people in DiscovEHR those with a variant had on average a 27% lower triglyceride level, a 9% lower LDL cholesterol level, and a 4% lower HDL cholesterol level than noncarriers, after adjustment for covariates. Analysis of coronary artery disease prevalence showed that, after adjusting for age, sex, and ancestry, carrying a loss-of-function variant was linked with a statistically significant 41% lower prevalence of all coronary artery disease, and a 34% lower prevalence of myocardial infarction that fell short of statistical significance.
A second population study looked at links between loss-of-function variants and coronary artery disease in more than 130,000 Danish people. This showed a nonsignificant 37% lower prevalence of coronary artery disease in people with a variant. Two different types of meta-analyses of the data from both the DiscovEHR and Danish studies showed coronary disease rates reduced by either 31% or 39% in variant carriers depending on which meta-analysis approach the researchers used, both statistically significant reductions.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
The findings from these two studies together with other recent study results open a new therapeutic window for reducing elevated levels of triglyceride-rich lipoproteins by activating lipoprotein lipase.
The findings also suggest that inhibition of the ANGPTL3 gene or protein is potentially an effective way to treat patients with familial hypercholesterolemia because of a deficiency in the receptor for low density lipoprotein. It is likely that lowering triglyceride levels with an agent that boosts the activity of lipoprotein lipase will result in a different spectrum of benefits and adverse effects, compared with agents that boost the number of LDL receptors.
New approaches to boost lipoprotein lipase activity, such as inhibiting ANGPTL3 function as was done in these two reports, represents a fresh frontier for treatment of hypertriglyceridemia and coronary artery disease.
Alan R. Tall, MD , professor of medicine at Columbia University, New York, made these comments in an editorial ( N Engl J Med. 2017 Jul 20;377[3]:280-3 ).
The findings from these two studies together with other recent study results open a new therapeutic window for reducing elevated levels of triglyceride-rich lipoproteins by activating lipoprotein lipase.
The findings also suggest that inhibition of the ANGPTL3 gene or protein is potentially an effective way to treat patients with familial hypercholesterolemia because of a deficiency in the receptor for low density lipoprotein. It is likely that lowering triglyceride levels with an agent that boosts the activity of lipoprotein lipase will result in a different spectrum of benefits and adverse effects, compared with agents that boost the number of LDL receptors.
New approaches to boost lipoprotein lipase activity, such as inhibiting ANGPTL3 function as was done in these two reports, represents a fresh frontier for treatment of hypertriglyceridemia and coronary artery disease.
Alan R. Tall, MD , professor of medicine at Columbia University, New York, made these comments in an editorial ( N Engl J Med. 2017 Jul 20;377[3]:280-3 ).
The findings from these two studies together with other recent study results open a new therapeutic window for reducing elevated levels of triglyceride-rich lipoproteins by activating lipoprotein lipase.
The findings also suggest that inhibition of the ANGPTL3 gene or protein is potentially an effective way to treat patients with familial hypercholesterolemia because of a deficiency in the receptor for low density lipoprotein. It is likely that lowering triglyceride levels with an agent that boosts the activity of lipoprotein lipase will result in a different spectrum of benefits and adverse effects, compared with agents that boost the number of LDL receptors.
New approaches to boost lipoprotein lipase activity, such as inhibiting ANGPTL3 function as was done in these two reports, represents a fresh frontier for treatment of hypertriglyceridemia and coronary artery disease.
Alan R. Tall, MD , professor of medicine at Columbia University, New York, made these comments in an editorial ( N Engl J Med. 2017 Jul 20;377[3]:280-3 ).
Two different approaches to shutting down the function of a human liver protein that inhibits lipoprotein lipase showed preliminary evidence of safely producing favorable lipid changes in healthy volunteers in two separate, phase 1 studies.
These findings, coupled with promising observational data from people who carry loss-of-function mutations in the gene for this protein, angiopoietin-like 3 (ANGPTL3), have raised hopes that interventions that interfere with the function of the ANGPTL3 protein may provide new and effective ways to improve lipid levels and cut the incidence of cardiovascular disease events.
“There is now a growing body of epidemiologic, genetic, and genomewide association studies supporting the hypothesis that lowering levels of ANGPTL3 in plasma by inhibiting hepatic ANGPTL3 synthesis will be beneficial in terms of reducing plasma levels of atherogenic apolipoprotein B and in improving metabolic measures associated with dyslipidemia,” wrote Mark J. Graham and his associates in a recently published article (N Engl J Med. 2017 Jul 20;377[3]:222-32).
The phase 1 study results reported by this group came from 44 healthy adults aged 18-65 years who received varying doses of a commercially developed antisense drug, ANGPTL3-LRX, as either single or serial subcutaneous injections. ANGPTL3-LRX is an oligonucleotide designed to inhibit production of messenger RNA for the ANGPTL3 protein.
Six people received the highest ANGPTL3-LRX dosage administered, 60 mg given as a weekly injection for 6 weeks, and after this regimen they showed an average 50% cut in triglycerides levels, compared with baseline, and an average 33% drop in their low LDL cholesterol levels from baseline. None of the 33 people treated with ANGPTL3-LRX in the trial had a documented serious adverse event, and the only treatment dropout was a patient who was lost to follow-up during the treatment phase, reported Mr. Graham, a researcher at Ionis Pharmaceuticals, the sponsor of the study and the company developing the antisense drug, and his associates.
The second phase 1 study examined a different way to block ANGPTL3 activity, with a human monoclonal antibody to this protein. The study involved 83 healthy adults aged 18-65 years with fasting triglyceride levels of 150-450 mg/dL and fasting LDL cholesterol levels of at least 100 mg/dL. Each participant received a single subcutaneous injection or intravenous dose of the antibody, evinacumab, at varying amounts or placebo. The maximum observed lipid changes seen was a drop in triglycerides of 76% and a fall in LDL cholesterol by 23%. Treatment also produced a maximum drop in HDL cholesterol of 18%. No person left the study because of an adverse event. The most common adverse event was headache, in seven people (11% of evinacumab recipients), reported Frederick E. Dewey, MD, a researcher at Regeneron Pharmaceuticals, the company developing evinacumab, and his associates (N Engl J Med. 2017 Jul 20;377[3]:211-21).
The Regeneron report also included results from population studies they ran. They reported performing genome sequencing on specimens from 58,335 adults enrolled in the DiscovEHR study, and identified 13 distinct loss-of-function variants in the ANGPTL3 genes that occurred individually in a small number of these people.
They then ran analyses of lipid levels and coronary artery disease prevalence rates in people who carry one of these 13 loss-of-function genetic signatures in one of their ANGTPL3 genes. Among 45,226 of the people in DiscovEHR those with a variant had on average a 27% lower triglyceride level, a 9% lower LDL cholesterol level, and a 4% lower HDL cholesterol level than noncarriers, after adjustment for covariates. Analysis of coronary artery disease prevalence showed that, after adjusting for age, sex, and ancestry, carrying a loss-of-function variant was linked with a statistically significant 41% lower prevalence of all coronary artery disease, and a 34% lower prevalence of myocardial infarction that fell short of statistical significance.
A second population study looked at links between loss-of-function variants and coronary artery disease in more than 130,000 Danish people. This showed a nonsignificant 37% lower prevalence of coronary artery disease in people with a variant. Two different types of meta-analyses of the data from both the DiscovEHR and Danish studies showed coronary disease rates reduced by either 31% or 39% in variant carriers depending on which meta-analysis approach the researchers used, both statistically significant reductions.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
Two different approaches to shutting down the function of a human liver protein that inhibits lipoprotein lipase showed preliminary evidence of safely producing favorable lipid changes in healthy volunteers in two separate, phase 1 studies.
These findings, coupled with promising observational data from people who carry loss-of-function mutations in the gene for this protein, angiopoietin-like 3 (ANGPTL3), have raised hopes that interventions that interfere with the function of the ANGPTL3 protein may provide new and effective ways to improve lipid levels and cut the incidence of cardiovascular disease events.
“There is now a growing body of epidemiologic, genetic, and genomewide association studies supporting the hypothesis that lowering levels of ANGPTL3 in plasma by inhibiting hepatic ANGPTL3 synthesis will be beneficial in terms of reducing plasma levels of atherogenic apolipoprotein B and in improving metabolic measures associated with dyslipidemia,” wrote Mark J. Graham and his associates in a recently published article (N Engl J Med. 2017 Jul 20;377[3]:222-32).
The phase 1 study results reported by this group came from 44 healthy adults aged 18-65 years who received varying doses of a commercially developed antisense drug, ANGPTL3-LRX, as either single or serial subcutaneous injections. ANGPTL3-LRX is an oligonucleotide designed to inhibit production of messenger RNA for the ANGPTL3 protein.
Six people received the highest ANGPTL3-LRX dosage administered, 60 mg given as a weekly injection for 6 weeks, and after this regimen they showed an average 50% cut in triglycerides levels, compared with baseline, and an average 33% drop in their low LDL cholesterol levels from baseline. None of the 33 people treated with ANGPTL3-LRX in the trial had a documented serious adverse event, and the only treatment dropout was a patient who was lost to follow-up during the treatment phase, reported Mr. Graham, a researcher at Ionis Pharmaceuticals, the sponsor of the study and the company developing the antisense drug, and his associates.
The second phase 1 study examined a different way to block ANGPTL3 activity, with a human monoclonal antibody to this protein. The study involved 83 healthy adults aged 18-65 years with fasting triglyceride levels of 150-450 mg/dL and fasting LDL cholesterol levels of at least 100 mg/dL. Each participant received a single subcutaneous injection or intravenous dose of the antibody, evinacumab, at varying amounts or placebo. The maximum observed lipid changes seen was a drop in triglycerides of 76% and a fall in LDL cholesterol by 23%. Treatment also produced a maximum drop in HDL cholesterol of 18%. No person left the study because of an adverse event. The most common adverse event was headache, in seven people (11% of evinacumab recipients), reported Frederick E. Dewey, MD, a researcher at Regeneron Pharmaceuticals, the company developing evinacumab, and his associates (N Engl J Med. 2017 Jul 20;377[3]:211-21).
The Regeneron report also included results from population studies they ran. They reported performing genome sequencing on specimens from 58,335 adults enrolled in the DiscovEHR study, and identified 13 distinct loss-of-function variants in the ANGPTL3 genes that occurred individually in a small number of these people.
They then ran analyses of lipid levels and coronary artery disease prevalence rates in people who carry one of these 13 loss-of-function genetic signatures in one of their ANGTPL3 genes. Among 45,226 of the people in DiscovEHR those with a variant had on average a 27% lower triglyceride level, a 9% lower LDL cholesterol level, and a 4% lower HDL cholesterol level than noncarriers, after adjustment for covariates. Analysis of coronary artery disease prevalence showed that, after adjusting for age, sex, and ancestry, carrying a loss-of-function variant was linked with a statistically significant 41% lower prevalence of all coronary artery disease, and a 34% lower prevalence of myocardial infarction that fell short of statistical significance.
A second population study looked at links between loss-of-function variants and coronary artery disease in more than 130,000 Danish people. This showed a nonsignificant 37% lower prevalence of coronary artery disease in people with a variant. Two different types of meta-analyses of the data from both the DiscovEHR and Danish studies showed coronary disease rates reduced by either 31% or 39% in variant carriers depending on which meta-analysis approach the researchers used, both statistically significant reductions.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Serial doses of the antisense oligonucleotide ANGPTL3-LRX produced an average 50% cut in triglycerides and 33% cut in LDL cholesterol.
Data source: The ANGPTL3-LRX phase 1 trial enrolled 44 healthy adults. The evinacumab phase 1 trial enrolled 83 healthy adults.
Disclosures: The ANGPTL3-LRX study was funded by Ionis. Mr. Graham is an employee of Ionis. The evinacumab study was funded by Regeneron. Dr. Dewey is an employee of Regeneron.
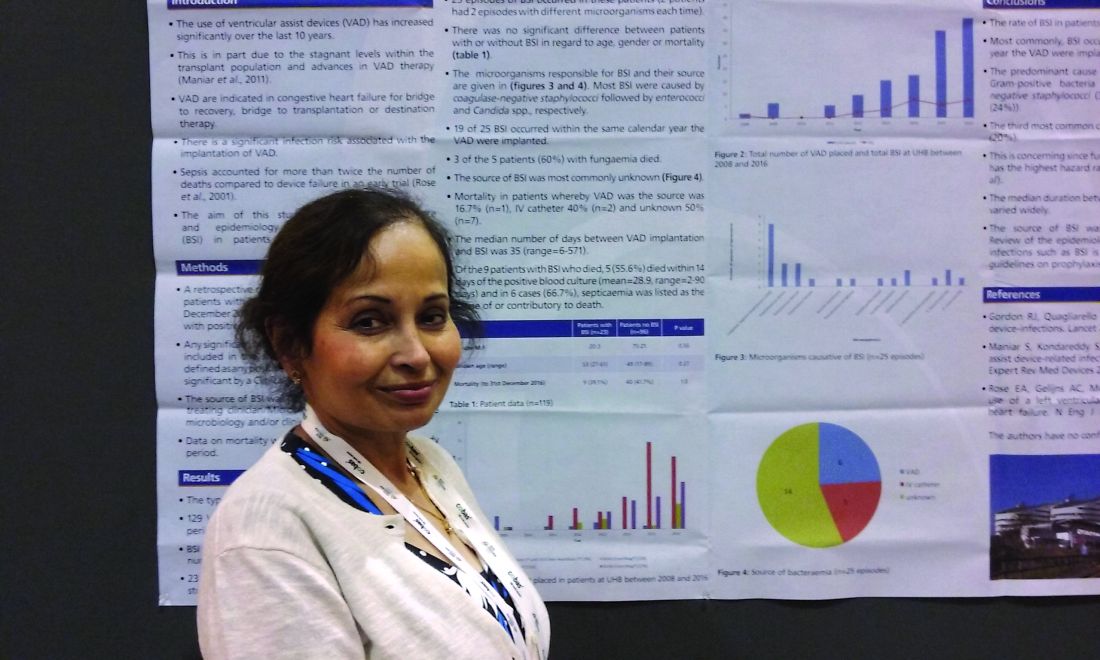
Ventricular assist devices linked to sepsis
NEW ORLEANS – Back in 2008, there was only one case.
Since then, however, the number of patients with ventricular assist devices who developed sepsis while being treated in the cardiac unit at Queen Elizabeth Hospital in Birmingham, England, appeared to be noticeably growing. So, investigators launched a study to confirm their suspicions and to learn more about the underlying causes.
“Bloodstream infection is a serious infection, so I thought, ‘Let’s see what’s happening,’ ” explained Ira Das, MD, a consultant microbiologist at Queen Elizabeth Hospital.
Coagulase-negative staphylococci were the most common cause, present in 32% of the 25 cases. Sepsis was caused by Enterococcus faecium in 12%, Candida parapsilosis in 8%, and Staphylococcus aureus in 2%. Another 4% were either Enterococcus faecalis, Serratia marcescens, Pseudomonas aeruginosa, C. guilliermondii, or C. orthopsilosis. The remaining 16% of bloodstream infections were polymicrobial.
Less certain was the source of these infections.
“In the majority of cases, we didn’t know where it was coming from,” Dr. Das said at the annual meeting of the American Society for Microbiology. In 6 of the 25 cases, VAD was confirmed to be the focus of infection, either through imaging or because a failing component of the explanted device was examined later. An intravascular catheter was the source in another 5 patients, and in 14 cases, the source remained a mystery.
“Some of these infections just might have been hard to see,” Dr. Das said. “If the infection is inside the device, it’s not always easy to visualize.”
The study supports earlier findings from a review article that points to a significant infection risk associated with the implantation of VADs (Expert Rev Med Devices. 2011 Sep;8[5]:627-34). That article’s authors noted, “Despite recent improvements in outcomes, device-related infections remain a significant complication of LVAD [left ventricular assist device] therapy.”
In a previous study of people with end-stage heart failure, other investigators noted that, “despite the substantial survival benefit, the morbidity and mortality associated with the use of the left ventricular assist device were considerable. In particular, infection and mechanical failure of the device were major factors in the 2-year survival rate of only 23%” (N Engl J Med. 2001 Nov 15;345[20]:1435-43).
Similarly, in the current study, mortality was higher among those with sepsis and a VAD. Mortality was 39% – including eight patients who died with a VAD in situ and one following cardiac transplantation. However, Dr. Das cautioned, “It’s a small number, and there are other factors that could have contributed. They all go on anticoagulants so they have bleeding tendencies, and many of the patients are in the ICU with multiorgan failure.”
Infection prevention remains paramount to minimize mortality and other adverse events associated with a patient’s having a VAD. “We have to make sure that infection control procedures and our treatments are up to the optimal standard,” Dr. Das said. “It’s not easy to remove the device.”
Of the 129 VADs implanted, 68 were long-term LVADs, 11 were short-term LVADs, 15 were right ventricular devices, and 35 were biventricular devices.
The study is ongoing. The data presented at the meeting were collected up until December 2016.
“Since then, I’ve seen two more cases, and – very interestingly – one was Haemophilus influenzae,” Dr. Das said. “The patient was on the device, he was at home, and he came in with bacteremia.” Again, the source of infection proved elusive. “With H. influenzae, you would think it was coming from his chest, but the chest x-ray was normal.”
The second case, a patient with a coagulase-negative staphylococci bloodstream infection, was scheduled for a PET scan at the time of Dr. Das’ presentation to try to identify the source of infection.
Dr. Das had no relevant disclosures.
Modern technology saves our patients' lives, but there is always another side to the coin. Reports that LVAD devices are associated with a high incidence of bloodstream infections is important for future clinical practice. The fact that the causes and risk factors for these infections are unknown make this phenomena one of high interest.
Modern technology saves our patients' lives, but there is always another side to the coin. Reports that LVAD devices are associated with a high incidence of bloodstream infections is important for future clinical practice. The fact that the causes and risk factors for these infections are unknown make this phenomena one of high interest.
Modern technology saves our patients' lives, but there is always another side to the coin. Reports that LVAD devices are associated with a high incidence of bloodstream infections is important for future clinical practice. The fact that the causes and risk factors for these infections are unknown make this phenomena one of high interest.
NEW ORLEANS – Back in 2008, there was only one case.
Since then, however, the number of patients with ventricular assist devices who developed sepsis while being treated in the cardiac unit at Queen Elizabeth Hospital in Birmingham, England, appeared to be noticeably growing. So, investigators launched a study to confirm their suspicions and to learn more about the underlying causes.
“Bloodstream infection is a serious infection, so I thought, ‘Let’s see what’s happening,’ ” explained Ira Das, MD, a consultant microbiologist at Queen Elizabeth Hospital.
Coagulase-negative staphylococci were the most common cause, present in 32% of the 25 cases. Sepsis was caused by Enterococcus faecium in 12%, Candida parapsilosis in 8%, and Staphylococcus aureus in 2%. Another 4% were either Enterococcus faecalis, Serratia marcescens, Pseudomonas aeruginosa, C. guilliermondii, or C. orthopsilosis. The remaining 16% of bloodstream infections were polymicrobial.
Less certain was the source of these infections.
“In the majority of cases, we didn’t know where it was coming from,” Dr. Das said at the annual meeting of the American Society for Microbiology. In 6 of the 25 cases, VAD was confirmed to be the focus of infection, either through imaging or because a failing component of the explanted device was examined later. An intravascular catheter was the source in another 5 patients, and in 14 cases, the source remained a mystery.
“Some of these infections just might have been hard to see,” Dr. Das said. “If the infection is inside the device, it’s not always easy to visualize.”
The study supports earlier findings from a review article that points to a significant infection risk associated with the implantation of VADs (Expert Rev Med Devices. 2011 Sep;8[5]:627-34). That article’s authors noted, “Despite recent improvements in outcomes, device-related infections remain a significant complication of LVAD [left ventricular assist device] therapy.”
In a previous study of people with end-stage heart failure, other investigators noted that, “despite the substantial survival benefit, the morbidity and mortality associated with the use of the left ventricular assist device were considerable. In particular, infection and mechanical failure of the device were major factors in the 2-year survival rate of only 23%” (N Engl J Med. 2001 Nov 15;345[20]:1435-43).
Similarly, in the current study, mortality was higher among those with sepsis and a VAD. Mortality was 39% – including eight patients who died with a VAD in situ and one following cardiac transplantation. However, Dr. Das cautioned, “It’s a small number, and there are other factors that could have contributed. They all go on anticoagulants so they have bleeding tendencies, and many of the patients are in the ICU with multiorgan failure.”
Infection prevention remains paramount to minimize mortality and other adverse events associated with a patient’s having a VAD. “We have to make sure that infection control procedures and our treatments are up to the optimal standard,” Dr. Das said. “It’s not easy to remove the device.”
Of the 129 VADs implanted, 68 were long-term LVADs, 11 were short-term LVADs, 15 were right ventricular devices, and 35 were biventricular devices.
The study is ongoing. The data presented at the meeting were collected up until December 2016.
“Since then, I’ve seen two more cases, and – very interestingly – one was Haemophilus influenzae,” Dr. Das said. “The patient was on the device, he was at home, and he came in with bacteremia.” Again, the source of infection proved elusive. “With H. influenzae, you would think it was coming from his chest, but the chest x-ray was normal.”
The second case, a patient with a coagulase-negative staphylococci bloodstream infection, was scheduled for a PET scan at the time of Dr. Das’ presentation to try to identify the source of infection.
Dr. Das had no relevant disclosures.
NEW ORLEANS – Back in 2008, there was only one case.
Since then, however, the number of patients with ventricular assist devices who developed sepsis while being treated in the cardiac unit at Queen Elizabeth Hospital in Birmingham, England, appeared to be noticeably growing. So, investigators launched a study to confirm their suspicions and to learn more about the underlying causes.
“Bloodstream infection is a serious infection, so I thought, ‘Let’s see what’s happening,’ ” explained Ira Das, MD, a consultant microbiologist at Queen Elizabeth Hospital.
Coagulase-negative staphylococci were the most common cause, present in 32% of the 25 cases. Sepsis was caused by Enterococcus faecium in 12%, Candida parapsilosis in 8%, and Staphylococcus aureus in 2%. Another 4% were either Enterococcus faecalis, Serratia marcescens, Pseudomonas aeruginosa, C. guilliermondii, or C. orthopsilosis. The remaining 16% of bloodstream infections were polymicrobial.
Less certain was the source of these infections.
“In the majority of cases, we didn’t know where it was coming from,” Dr. Das said at the annual meeting of the American Society for Microbiology. In 6 of the 25 cases, VAD was confirmed to be the focus of infection, either through imaging or because a failing component of the explanted device was examined later. An intravascular catheter was the source in another 5 patients, and in 14 cases, the source remained a mystery.
“Some of these infections just might have been hard to see,” Dr. Das said. “If the infection is inside the device, it’s not always easy to visualize.”
The study supports earlier findings from a review article that points to a significant infection risk associated with the implantation of VADs (Expert Rev Med Devices. 2011 Sep;8[5]:627-34). That article’s authors noted, “Despite recent improvements in outcomes, device-related infections remain a significant complication of LVAD [left ventricular assist device] therapy.”
In a previous study of people with end-stage heart failure, other investigators noted that, “despite the substantial survival benefit, the morbidity and mortality associated with the use of the left ventricular assist device were considerable. In particular, infection and mechanical failure of the device were major factors in the 2-year survival rate of only 23%” (N Engl J Med. 2001 Nov 15;345[20]:1435-43).
Similarly, in the current study, mortality was higher among those with sepsis and a VAD. Mortality was 39% – including eight patients who died with a VAD in situ and one following cardiac transplantation. However, Dr. Das cautioned, “It’s a small number, and there are other factors that could have contributed. They all go on anticoagulants so they have bleeding tendencies, and many of the patients are in the ICU with multiorgan failure.”
Infection prevention remains paramount to minimize mortality and other adverse events associated with a patient’s having a VAD. “We have to make sure that infection control procedures and our treatments are up to the optimal standard,” Dr. Das said. “It’s not easy to remove the device.”
Of the 129 VADs implanted, 68 were long-term LVADs, 11 were short-term LVADs, 15 were right ventricular devices, and 35 were biventricular devices.
The study is ongoing. The data presented at the meeting were collected up until December 2016.
“Since then, I’ve seen two more cases, and – very interestingly – one was Haemophilus influenzae,” Dr. Das said. “The patient was on the device, he was at home, and he came in with bacteremia.” Again, the source of infection proved elusive. “With H. influenzae, you would think it was coming from his chest, but the chest x-ray was normal.”
The second case, a patient with a coagulase-negative staphylococci bloodstream infection, was scheduled for a PET scan at the time of Dr. Das’ presentation to try to identify the source of infection.
Dr. Das had no relevant disclosures.
AT ASM MICROBE 2017
Key clinical point: There may be a significant rate of bloodstream infections among people with a ventricular assist device.
Major finding: A total of 20% of the 118 people with a VAD had a bloodstream infection.
Data source: A retrospective study of 129 ventricular assist devices placed in 118 people between 2008 and 2016.
Disclosures: Dr. Das had no relevant disclosures.
Factory contamination seen as likely source of postop endocarditis outbreak
Since 2013, over 100 cases of Mycobacterium chimaera prosthetic valve endocarditis and disseminated disease were detected in Europe and the United States, and these were presumptively linked to contaminated heater-cooler units (HCUs) used during cardiac surgery. A molecular epidemiological analysis of microbial isolate genomes detected a “remarkable clonality of isolates” in almost all of the assessed patients with M. chimaera disease, which “strongly points to a common source of infection,” as reported online in The Lancet Infectious Diseases.
The analysis comprised 250 whole-genome sequencing datasets: 24 isolates from 21 cardiac surgery–related patients in Switzerland, Germany, the Netherlands, and the United Kingdom; 36 from 35 unrelated patients; 126 from LivaNova HCUs in use (85 water cultures, 41 air cultures); 13 from LivaNova HCUs returned to the production site in Germany for disinfection; 4 from the LivaNova production site (3 from newly produced HCUs, 1 from a water source); 2 from Maquet extracorporeal membrane oxygenation (ECMO) devices in use; 14 from Maquet HCUs in use; 15 from new Maquet HCUs sampled at the production site; and 7 from hospital water supplies in Switzerland, Germany, and the Netherlands, plus one M. chimaera DSM 44623–type strain, and eight M. intracellulare strains (from four unrelated patients from Germany and four published genomes).
Isolates were analyzed by next-generation whole-genome sequencing and compared with published M. chimaera genomes, according to Jakko van Ingen, PhD, Radboud University Medical Center, Nijmegen, the Netherlands, and his colleagues. Phylogenetic analysis of these 250 isolates revealed two major M. chimaera groups. They found that all cardiac surgery–related patient isolates could be classified into group 1. They then did a subgroup analysis.
“Three distinct strains of M. chimaera appear to have contaminated the water systems of LivaNova HCUs at the production site, belonging to subgroups 1.1, 1.8, and 2.1,” the authors stated. However, most M. chimaera isolates from air samples taken near operating LivaNova HCUs and those of 23 of the 24 related patients belonged to subgroup 1.1.
“This finding further supports the presumed airborne transmission pathway leading to endocarditis, aortic graft infection, disseminated disease, and surgical site infections in the affected patients,” according to the authors (doi: 10.1016/S1473-3099[17]30324-9).
The results suggest “the possibility that the vast majority of cases of cardiothoracic surgery–related severe M. chimaera infections diagnosed in Switzerland, Germany, the Netherlands, the United Kingdom, the United States, and Australia resulted from a single common source of infection: LivaNova HCUs that were most likely contaminated during production in Germany,” the researchers concluded.
The study was partly funded by the EU Horizon 2020 program, its FP7 program, the German Center for Infection Research (DZIF), the Swiss National Science Foundation, the Swiss Federal Office of Public Health, and National Institute of Health Research Oxford Health Protection Research Units on Healthcare Associated Infection and Antimicrobial Resistance. The authors reported having no relevant conflicts.
Since 2013, over 100 cases of Mycobacterium chimaera prosthetic valve endocarditis and disseminated disease were detected in Europe and the United States, and these were presumptively linked to contaminated heater-cooler units (HCUs) used during cardiac surgery. A molecular epidemiological analysis of microbial isolate genomes detected a “remarkable clonality of isolates” in almost all of the assessed patients with M. chimaera disease, which “strongly points to a common source of infection,” as reported online in The Lancet Infectious Diseases.
The analysis comprised 250 whole-genome sequencing datasets: 24 isolates from 21 cardiac surgery–related patients in Switzerland, Germany, the Netherlands, and the United Kingdom; 36 from 35 unrelated patients; 126 from LivaNova HCUs in use (85 water cultures, 41 air cultures); 13 from LivaNova HCUs returned to the production site in Germany for disinfection; 4 from the LivaNova production site (3 from newly produced HCUs, 1 from a water source); 2 from Maquet extracorporeal membrane oxygenation (ECMO) devices in use; 14 from Maquet HCUs in use; 15 from new Maquet HCUs sampled at the production site; and 7 from hospital water supplies in Switzerland, Germany, and the Netherlands, plus one M. chimaera DSM 44623–type strain, and eight M. intracellulare strains (from four unrelated patients from Germany and four published genomes).
Isolates were analyzed by next-generation whole-genome sequencing and compared with published M. chimaera genomes, according to Jakko van Ingen, PhD, Radboud University Medical Center, Nijmegen, the Netherlands, and his colleagues. Phylogenetic analysis of these 250 isolates revealed two major M. chimaera groups. They found that all cardiac surgery–related patient isolates could be classified into group 1. They then did a subgroup analysis.
“Three distinct strains of M. chimaera appear to have contaminated the water systems of LivaNova HCUs at the production site, belonging to subgroups 1.1, 1.8, and 2.1,” the authors stated. However, most M. chimaera isolates from air samples taken near operating LivaNova HCUs and those of 23 of the 24 related patients belonged to subgroup 1.1.
“This finding further supports the presumed airborne transmission pathway leading to endocarditis, aortic graft infection, disseminated disease, and surgical site infections in the affected patients,” according to the authors (doi: 10.1016/S1473-3099[17]30324-9).
The results suggest “the possibility that the vast majority of cases of cardiothoracic surgery–related severe M. chimaera infections diagnosed in Switzerland, Germany, the Netherlands, the United Kingdom, the United States, and Australia resulted from a single common source of infection: LivaNova HCUs that were most likely contaminated during production in Germany,” the researchers concluded.
The study was partly funded by the EU Horizon 2020 program, its FP7 program, the German Center for Infection Research (DZIF), the Swiss National Science Foundation, the Swiss Federal Office of Public Health, and National Institute of Health Research Oxford Health Protection Research Units on Healthcare Associated Infection and Antimicrobial Resistance. The authors reported having no relevant conflicts.
Since 2013, over 100 cases of Mycobacterium chimaera prosthetic valve endocarditis and disseminated disease were detected in Europe and the United States, and these were presumptively linked to contaminated heater-cooler units (HCUs) used during cardiac surgery. A molecular epidemiological analysis of microbial isolate genomes detected a “remarkable clonality of isolates” in almost all of the assessed patients with M. chimaera disease, which “strongly points to a common source of infection,” as reported online in The Lancet Infectious Diseases.
The analysis comprised 250 whole-genome sequencing datasets: 24 isolates from 21 cardiac surgery–related patients in Switzerland, Germany, the Netherlands, and the United Kingdom; 36 from 35 unrelated patients; 126 from LivaNova HCUs in use (85 water cultures, 41 air cultures); 13 from LivaNova HCUs returned to the production site in Germany for disinfection; 4 from the LivaNova production site (3 from newly produced HCUs, 1 from a water source); 2 from Maquet extracorporeal membrane oxygenation (ECMO) devices in use; 14 from Maquet HCUs in use; 15 from new Maquet HCUs sampled at the production site; and 7 from hospital water supplies in Switzerland, Germany, and the Netherlands, plus one M. chimaera DSM 44623–type strain, and eight M. intracellulare strains (from four unrelated patients from Germany and four published genomes).
Isolates were analyzed by next-generation whole-genome sequencing and compared with published M. chimaera genomes, according to Jakko van Ingen, PhD, Radboud University Medical Center, Nijmegen, the Netherlands, and his colleagues. Phylogenetic analysis of these 250 isolates revealed two major M. chimaera groups. They found that all cardiac surgery–related patient isolates could be classified into group 1. They then did a subgroup analysis.
“Three distinct strains of M. chimaera appear to have contaminated the water systems of LivaNova HCUs at the production site, belonging to subgroups 1.1, 1.8, and 2.1,” the authors stated. However, most M. chimaera isolates from air samples taken near operating LivaNova HCUs and those of 23 of the 24 related patients belonged to subgroup 1.1.
“This finding further supports the presumed airborne transmission pathway leading to endocarditis, aortic graft infection, disseminated disease, and surgical site infections in the affected patients,” according to the authors (doi: 10.1016/S1473-3099[17]30324-9).
The results suggest “the possibility that the vast majority of cases of cardiothoracic surgery–related severe M. chimaera infections diagnosed in Switzerland, Germany, the Netherlands, the United Kingdom, the United States, and Australia resulted from a single common source of infection: LivaNova HCUs that were most likely contaminated during production in Germany,” the researchers concluded.
The study was partly funded by the EU Horizon 2020 program, its FP7 program, the German Center for Infection Research (DZIF), the Swiss National Science Foundation, the Swiss Federal Office of Public Health, and National Institute of Health Research Oxford Health Protection Research Units on Healthcare Associated Infection and Antimicrobial Resistance. The authors reported having no relevant conflicts.
FROM THE LANCET INFECTIOUS DISEASES
Key clinical point:
Major finding: Cardiac surgery–related patient isolates were all classified into the same group, in which all, except one, formed a distinct subgroup of Mycobacterium chimaera, which also comprised most isolates from LivaNova HCUs, and one from the equipment production site.
Data source: Phylogenetic analysis based on whole-genome sequencing of 250 M. chimaera isolates obtained from cardiac surgery patients, hospitals, and other sources.
Disclosures: Partly funded by the EU Horizon 2020 program and several German, Swiss, and U.K. infectious disease–related NGOs. The authors reported having no disclosures.
Recovery: Where TAVR gains advantage over SAVR
A post hoc analysis of the first randomized clinical to show the superiority of an interventional technique for aortic valve repair over surgery in terms of postoperative death has found the period of 30 days to 4 months after the procedure to be the most perilous for surgery patients, when their risk of death was almost twice that of interventional patients, likely because surgery patients were more vulnerable to complications and were less likely to go home after the procedure.
“This mortality difference was largely driven by higher rates of technical failure, surgical complications, and lack of recovery following surgery,” said Vincent A. Gaudiani, MD, of El Camino Hospital, Mountain View, Calif., and his coauthors (J Thorac Cardiovasc Surg. 2017;153:1293-99). The analysis investigated causes and timing of death in the CoreValve US Pivotal High-Risk Trial, a randomized, high-risk trial of the CoreValve self-expanding bioprosthesis (Medtronic). The trial favored transcatheter aortic valve replacement (TAVR) over surgical aortic valve replacement (SAVR).
The post hoc analysis evaluated all-cause mortality through the first year based on three time periods: early, up to 30 days; recovery, 31-120 days; and late, 121-365 days. Death rates for the two procedures were similar in the early and late postoperative periods, but deviated significantly in the recovery period: 4% for TAVR vs. 7.9% for SAVR (P = .25). SAVR patients were more likely affected by the overall influence of physical stress associated with surgery, the study found, whereas rates of technical failure and complications were similar between the two groups. “This suggests that early TAVR results can improve with technical refinements and that high-risk surgical patients will benefit from reducing complications,” wrote Dr. Gaudiani and his coauthors.
They noted the CoreValve trial findings, in terms of the survival differences between TAVR and SAVR, are significant because previous trials that compared TAVR and SAVR, including the Placement of Aortic Transcatheter Valves A trial (Lancet. 2015;385:2477-84), showed equivalent survival between the two procedures at up to 5 years. “This unique finding is provocative and the reason for this survival difference is important to understanding TAVR and SAVR and improving both therapies,” said Dr. Gaudiani and his coauthors.
While SAVR patients had a higher overall death rate in the recovery period, TAVR patients had a larger proportion of cardiovascular deaths – 12 of 15 (80%) vs. 16 of 27 (59.3%) for SAVR. The leading noncardiovascular cause of death in the SAVR group was sepsis (six), followed by malignancy (one), chronic obstructive pulmonary disease (one) and other (three). “Although these deaths were adjudicated as noncardiovascular by the CEC [clinical events committee], our review showed that some of these patients had never really recovered from the initial procedure,” the researchers wrote.
In the early period, death rates were 3.3% for TAVR and 4.5% for SAVR, a nonsignificant difference. TAVR patients who died had higher rates of peripheral vascular disease and recent falls; SAVR patients who died were more likely to have had a pacemaker. In the late period, the death rates were 7.5% for TAVR and 7.7% for SAVR, and the researchers also found no significant difference in the number of cardiovascular deaths (4.4% and 4.2%, respectively). “Hierarchical causes of death were primarily due to other reasons deemed unrelated to the initial aortic valve replacement,” noted Dr. Gaudiani and his coauthors.
However, the study also found that TAVR patients were significantly more likely to go home after hospital discharge rather than to a rehabilitation facility or another hospital – 66.9% vs. 39.7% (P less than .001).
In the SAVR group, five cardiovascular deaths in the recovery period occurred because the operation failed to correct aortic stenosis – all related to placement of a valve too small for the patient. “Placing a valve appropriately sized to the patient should be a priority for surgeons if we are to improve our outcomes,” the researchers noted. “Most other deaths were the result of patients’ inability to cope with the physical trauma of surgery.”
Dr. Gaudiani disclosed that he is a consultant and paid instructor for Medtronic, St. Jude Medical, and Edwards Lifesciences. Coauthors disclosed relationships with Edwards Lifesciences, Terumo, Gore Medical, Medtronic, Boston Scientific, and other device companies.
In his invited discussion, Craig R. Smith, MD, of New York, noted that comparisons “are odious” and that comparing clinical trials requires caution. (J Thorac Cardiovasc Surg. 2017;153:1300-1) He also acknowledged that surgeons would hope for evidence that the findings of the CoreValve US Pivotal High-Risk Trial were somehow wrong.
Dr. Smith raised a question about the CoreValve trial, which was designed to enroll high-risk patients, “but actually enrolled at the upper end of the intermediate risk range with a Society of Thoracic Surgeons (STS) score of 7.4 versus 11.3 in the high-risk PARTNER 1.” However, he noted that it would not be fair to consider the self-expanding TAVR trial intermediate risk, because the intermediate risk PARTNER 2 trial had an STS score of 5.8. And while outcomes for SAVR in the CoreValve trial were within the expected variable of less than 1 using the STS Predicted Risk for Mortality, the “bulge” of deaths in the recovery phase raises “a whiff of concern.”
Dr. Smith said that the early technical mortalities with TAVR in the trial are already disappearing with experience. He also noted that Dr. Gaudiani and his coauthors pointed out the frequency of failure to repair and failure to recover. “Whether competing against TAVR in a randomized trial or operating on TAVR in eligible patients in the future, as the authors have emphasized, it behooves us to correct the problem as completely as possible and take the best possible care of our patients afterward,” Dr. Smith said. He also noted the difference in discharge rates home “illustrates a very significant advantage of TAVR.”
Dr. Smith disclosed he has received reimbursement for expenses in his leadership role in the Placement of Aortic Transcatheter Valves (PARTNER) trials.
In his invited discussion, Craig R. Smith, MD, of New York, noted that comparisons “are odious” and that comparing clinical trials requires caution. (J Thorac Cardiovasc Surg. 2017;153:1300-1) He also acknowledged that surgeons would hope for evidence that the findings of the CoreValve US Pivotal High-Risk Trial were somehow wrong.
Dr. Smith raised a question about the CoreValve trial, which was designed to enroll high-risk patients, “but actually enrolled at the upper end of the intermediate risk range with a Society of Thoracic Surgeons (STS) score of 7.4 versus 11.3 in the high-risk PARTNER 1.” However, he noted that it would not be fair to consider the self-expanding TAVR trial intermediate risk, because the intermediate risk PARTNER 2 trial had an STS score of 5.8. And while outcomes for SAVR in the CoreValve trial were within the expected variable of less than 1 using the STS Predicted Risk for Mortality, the “bulge” of deaths in the recovery phase raises “a whiff of concern.”
Dr. Smith said that the early technical mortalities with TAVR in the trial are already disappearing with experience. He also noted that Dr. Gaudiani and his coauthors pointed out the frequency of failure to repair and failure to recover. “Whether competing against TAVR in a randomized trial or operating on TAVR in eligible patients in the future, as the authors have emphasized, it behooves us to correct the problem as completely as possible and take the best possible care of our patients afterward,” Dr. Smith said. He also noted the difference in discharge rates home “illustrates a very significant advantage of TAVR.”
Dr. Smith disclosed he has received reimbursement for expenses in his leadership role in the Placement of Aortic Transcatheter Valves (PARTNER) trials.
In his invited discussion, Craig R. Smith, MD, of New York, noted that comparisons “are odious” and that comparing clinical trials requires caution. (J Thorac Cardiovasc Surg. 2017;153:1300-1) He also acknowledged that surgeons would hope for evidence that the findings of the CoreValve US Pivotal High-Risk Trial were somehow wrong.
Dr. Smith raised a question about the CoreValve trial, which was designed to enroll high-risk patients, “but actually enrolled at the upper end of the intermediate risk range with a Society of Thoracic Surgeons (STS) score of 7.4 versus 11.3 in the high-risk PARTNER 1.” However, he noted that it would not be fair to consider the self-expanding TAVR trial intermediate risk, because the intermediate risk PARTNER 2 trial had an STS score of 5.8. And while outcomes for SAVR in the CoreValve trial were within the expected variable of less than 1 using the STS Predicted Risk for Mortality, the “bulge” of deaths in the recovery phase raises “a whiff of concern.”
Dr. Smith said that the early technical mortalities with TAVR in the trial are already disappearing with experience. He also noted that Dr. Gaudiani and his coauthors pointed out the frequency of failure to repair and failure to recover. “Whether competing against TAVR in a randomized trial or operating on TAVR in eligible patients in the future, as the authors have emphasized, it behooves us to correct the problem as completely as possible and take the best possible care of our patients afterward,” Dr. Smith said. He also noted the difference in discharge rates home “illustrates a very significant advantage of TAVR.”
Dr. Smith disclosed he has received reimbursement for expenses in his leadership role in the Placement of Aortic Transcatheter Valves (PARTNER) trials.
A post hoc analysis of the first randomized clinical to show the superiority of an interventional technique for aortic valve repair over surgery in terms of postoperative death has found the period of 30 days to 4 months after the procedure to be the most perilous for surgery patients, when their risk of death was almost twice that of interventional patients, likely because surgery patients were more vulnerable to complications and were less likely to go home after the procedure.
“This mortality difference was largely driven by higher rates of technical failure, surgical complications, and lack of recovery following surgery,” said Vincent A. Gaudiani, MD, of El Camino Hospital, Mountain View, Calif., and his coauthors (J Thorac Cardiovasc Surg. 2017;153:1293-99). The analysis investigated causes and timing of death in the CoreValve US Pivotal High-Risk Trial, a randomized, high-risk trial of the CoreValve self-expanding bioprosthesis (Medtronic). The trial favored transcatheter aortic valve replacement (TAVR) over surgical aortic valve replacement (SAVR).
The post hoc analysis evaluated all-cause mortality through the first year based on three time periods: early, up to 30 days; recovery, 31-120 days; and late, 121-365 days. Death rates for the two procedures were similar in the early and late postoperative periods, but deviated significantly in the recovery period: 4% for TAVR vs. 7.9% for SAVR (P = .25). SAVR patients were more likely affected by the overall influence of physical stress associated with surgery, the study found, whereas rates of technical failure and complications were similar between the two groups. “This suggests that early TAVR results can improve with technical refinements and that high-risk surgical patients will benefit from reducing complications,” wrote Dr. Gaudiani and his coauthors.
They noted the CoreValve trial findings, in terms of the survival differences between TAVR and SAVR, are significant because previous trials that compared TAVR and SAVR, including the Placement of Aortic Transcatheter Valves A trial (Lancet. 2015;385:2477-84), showed equivalent survival between the two procedures at up to 5 years. “This unique finding is provocative and the reason for this survival difference is important to understanding TAVR and SAVR and improving both therapies,” said Dr. Gaudiani and his coauthors.
While SAVR patients had a higher overall death rate in the recovery period, TAVR patients had a larger proportion of cardiovascular deaths – 12 of 15 (80%) vs. 16 of 27 (59.3%) for SAVR. The leading noncardiovascular cause of death in the SAVR group was sepsis (six), followed by malignancy (one), chronic obstructive pulmonary disease (one) and other (three). “Although these deaths were adjudicated as noncardiovascular by the CEC [clinical events committee], our review showed that some of these patients had never really recovered from the initial procedure,” the researchers wrote.
In the early period, death rates were 3.3% for TAVR and 4.5% for SAVR, a nonsignificant difference. TAVR patients who died had higher rates of peripheral vascular disease and recent falls; SAVR patients who died were more likely to have had a pacemaker. In the late period, the death rates were 7.5% for TAVR and 7.7% for SAVR, and the researchers also found no significant difference in the number of cardiovascular deaths (4.4% and 4.2%, respectively). “Hierarchical causes of death were primarily due to other reasons deemed unrelated to the initial aortic valve replacement,” noted Dr. Gaudiani and his coauthors.
However, the study also found that TAVR patients were significantly more likely to go home after hospital discharge rather than to a rehabilitation facility or another hospital – 66.9% vs. 39.7% (P less than .001).
In the SAVR group, five cardiovascular deaths in the recovery period occurred because the operation failed to correct aortic stenosis – all related to placement of a valve too small for the patient. “Placing a valve appropriately sized to the patient should be a priority for surgeons if we are to improve our outcomes,” the researchers noted. “Most other deaths were the result of patients’ inability to cope with the physical trauma of surgery.”
Dr. Gaudiani disclosed that he is a consultant and paid instructor for Medtronic, St. Jude Medical, and Edwards Lifesciences. Coauthors disclosed relationships with Edwards Lifesciences, Terumo, Gore Medical, Medtronic, Boston Scientific, and other device companies.
A post hoc analysis of the first randomized clinical to show the superiority of an interventional technique for aortic valve repair over surgery in terms of postoperative death has found the period of 30 days to 4 months after the procedure to be the most perilous for surgery patients, when their risk of death was almost twice that of interventional patients, likely because surgery patients were more vulnerable to complications and were less likely to go home after the procedure.
“This mortality difference was largely driven by higher rates of technical failure, surgical complications, and lack of recovery following surgery,” said Vincent A. Gaudiani, MD, of El Camino Hospital, Mountain View, Calif., and his coauthors (J Thorac Cardiovasc Surg. 2017;153:1293-99). The analysis investigated causes and timing of death in the CoreValve US Pivotal High-Risk Trial, a randomized, high-risk trial of the CoreValve self-expanding bioprosthesis (Medtronic). The trial favored transcatheter aortic valve replacement (TAVR) over surgical aortic valve replacement (SAVR).
The post hoc analysis evaluated all-cause mortality through the first year based on three time periods: early, up to 30 days; recovery, 31-120 days; and late, 121-365 days. Death rates for the two procedures were similar in the early and late postoperative periods, but deviated significantly in the recovery period: 4% for TAVR vs. 7.9% for SAVR (P = .25). SAVR patients were more likely affected by the overall influence of physical stress associated with surgery, the study found, whereas rates of technical failure and complications were similar between the two groups. “This suggests that early TAVR results can improve with technical refinements and that high-risk surgical patients will benefit from reducing complications,” wrote Dr. Gaudiani and his coauthors.
They noted the CoreValve trial findings, in terms of the survival differences between TAVR and SAVR, are significant because previous trials that compared TAVR and SAVR, including the Placement of Aortic Transcatheter Valves A trial (Lancet. 2015;385:2477-84), showed equivalent survival between the two procedures at up to 5 years. “This unique finding is provocative and the reason for this survival difference is important to understanding TAVR and SAVR and improving both therapies,” said Dr. Gaudiani and his coauthors.
While SAVR patients had a higher overall death rate in the recovery period, TAVR patients had a larger proportion of cardiovascular deaths – 12 of 15 (80%) vs. 16 of 27 (59.3%) for SAVR. The leading noncardiovascular cause of death in the SAVR group was sepsis (six), followed by malignancy (one), chronic obstructive pulmonary disease (one) and other (three). “Although these deaths were adjudicated as noncardiovascular by the CEC [clinical events committee], our review showed that some of these patients had never really recovered from the initial procedure,” the researchers wrote.
In the early period, death rates were 3.3% for TAVR and 4.5% for SAVR, a nonsignificant difference. TAVR patients who died had higher rates of peripheral vascular disease and recent falls; SAVR patients who died were more likely to have had a pacemaker. In the late period, the death rates were 7.5% for TAVR and 7.7% for SAVR, and the researchers also found no significant difference in the number of cardiovascular deaths (4.4% and 4.2%, respectively). “Hierarchical causes of death were primarily due to other reasons deemed unrelated to the initial aortic valve replacement,” noted Dr. Gaudiani and his coauthors.
However, the study also found that TAVR patients were significantly more likely to go home after hospital discharge rather than to a rehabilitation facility or another hospital – 66.9% vs. 39.7% (P less than .001).
In the SAVR group, five cardiovascular deaths in the recovery period occurred because the operation failed to correct aortic stenosis – all related to placement of a valve too small for the patient. “Placing a valve appropriately sized to the patient should be a priority for surgeons if we are to improve our outcomes,” the researchers noted. “Most other deaths were the result of patients’ inability to cope with the physical trauma of surgery.”
Dr. Gaudiani disclosed that he is a consultant and paid instructor for Medtronic, St. Jude Medical, and Edwards Lifesciences. Coauthors disclosed relationships with Edwards Lifesciences, Terumo, Gore Medical, Medtronic, Boston Scientific, and other device companies.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Differences in survival between transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR) in high-risk patients appear to be driven primarily by issues with disease repair and patient recovery from SAVR.
Major finding: During the recovery period (31-120 days) the death rate was 4% for TAVR vs. 7.9% for SAVR (P = .025).
Data source: Post hoc analysis of CoreValve US Pivotal High-Risk Trial involving 750 patients and 45 sites with outcomes reported through 3 years.
Disclosures: Dr. Gaudiani disclosed that he is a consultant and paid instructor for Medtronic, St. Jude Medical, and Edwards Lifesciences. Coauthors disclosed relationships with Edwards Lifesciences, Terumo, Gore Medical, Medtronic, Boston Scientific, and other device companies.
CABG with arterial grafts provides excellent outcomes for CTO
PARIS – Eighty-eight percent of chronic total occlusions (CTOs) in a large series of patients undergoing coronary artery bypass graft surgery were successfully bypassed using arterial conduits with durable patency.
“Bypass graft surgery using arterial grafts is an acceptable modality of treatment for patients with CTOs and perhaps can be a benchmark against which PCI [percutaneous coronary intervention] for CTOs should be measured,” Teresa May Kieser, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“We have previously shown in another paper that arterial grafting mitigates the adverse effect of incomplete revascularization,” said Dr. Kieser, a cardiothoracic surgeon at the University of Calgary (Alt.).
In recent years, treatment of CTOs has increasingly drawn the attention of interventional cardiologists. Dr. Kieser presented what she thinks is the first study of coronary artery bypass graft (CABG) surgery for management of CTOs. It included 1,333 consecutive CABG patients with a total of 3,906 bypasses, a whopping 98% of which were arterial grafts, with a mean of 2.9 grafts per patient. Eleven percent of the CABGs were done emergently, 48% urgently, and 41% electively.
The key epidemiologic finding to emerge from the study is that CTOs are quite common in CABG patients. In this series, 47% of CABG patients had a mean of 1.35 chronically occluded coronary arteries.
Of 843 CTOs in three major territories, 88% were able to be bypassed. All of the 246 CTOs in the left anterior descending coronary artery were able to be bypassed, as were 84% of 415 CTOs in the right coronary artery and 85% in the circumflex system.
The CTO group as a whole had significantly greater impairment of left ventricular function. Thirty-seven percent of them had an ejection fraction of 30%-50%, compared with 22% of the non-CTO patients. The 10% prevalence of an left ventricular ejection fraction (LVEF) below 30% in the CTO group was twice that of the non-CTO group. The CTO group was also significantly more likely to undergo incomplete revascularization, by a margin of 21% versus 5.7%.
Operative mortality was 3.7% overall and just 0.55% in the elective CABG patients. In a multivariate logistic regression analysis controlled for surgical urgency, incomplete revascularization, and EuroSCORE risk, operative mortality didn’t differ significantly between the CTO and non-CTO groups.
However, in the presence of CTOs, incomplete revascularization was associated with an 11.6% operative mortality, compared with a 2.8% rate in fully revascularized CTO patients.
A total of 110 patients with bypassed CTOs underwent symptom-driven follow-up coronary angiography at a median of 3.6 years after CABG. Reassuringly, CTO graft patency was noted in 95% of the LAD grafts, 92% of the right coronary artery grafts, and 79% of the circumflex grafts.
Dr. Kieser’s audience of interventional cardiologists was clearly bowled over by her results, not only the high rate of successful surgical bypass of CTOs, but also by her use of arterial grafts 98% of the time.
“This is my personal practice,” she explained. “I just believe in arterial grafting so much. They perform best in CTO arteries because of their lack of competitive flow.”
Session chair Oliver Gämperli, MD, of University Hospital Zurich, commented, “We are very concerned about patency rates, and you showed us fantastic patency rates. This is much better than what we’re used to with saphenous vein grafts. I think we need to talk to our surgeons and try to get them to do more arterial grafts of CTOs.”
It’s worth noting that in the CTO subgroup from the landmark randomized SYNTAX trial, the complete revascularization rate was only about 50% in the PCI group, compared with nearly 65% in the CABG group, he added.
Asked why a cardiac surgeon wouldn’t bypass a CTO, Dr. Kieser rattled off several technical reasons, including a vessel size of less than 1 mm, diffuse disease, extensive scar, or an inaccessible location. But that’s not the whole story, she added. She has heard surgical colleagues say, “The patient doesn’t need that artery, he’s learned to live without it.” That burns her up.
“Patients need every artery in the heart, and the one with a CTO is the best one for an arterial graft because it almost cannot fail, especially to the left anterior descending artery. I think we have to change the mentality of the surgeons to ‘If it can be done, it should be done,’ ” Dr. Kieser said.
She reported having no financial conflicts of interest regarding her study.
PARIS – Eighty-eight percent of chronic total occlusions (CTOs) in a large series of patients undergoing coronary artery bypass graft surgery were successfully bypassed using arterial conduits with durable patency.
“Bypass graft surgery using arterial grafts is an acceptable modality of treatment for patients with CTOs and perhaps can be a benchmark against which PCI [percutaneous coronary intervention] for CTOs should be measured,” Teresa May Kieser, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“We have previously shown in another paper that arterial grafting mitigates the adverse effect of incomplete revascularization,” said Dr. Kieser, a cardiothoracic surgeon at the University of Calgary (Alt.).
In recent years, treatment of CTOs has increasingly drawn the attention of interventional cardiologists. Dr. Kieser presented what she thinks is the first study of coronary artery bypass graft (CABG) surgery for management of CTOs. It included 1,333 consecutive CABG patients with a total of 3,906 bypasses, a whopping 98% of which were arterial grafts, with a mean of 2.9 grafts per patient. Eleven percent of the CABGs were done emergently, 48% urgently, and 41% electively.
The key epidemiologic finding to emerge from the study is that CTOs are quite common in CABG patients. In this series, 47% of CABG patients had a mean of 1.35 chronically occluded coronary arteries.
Of 843 CTOs in three major territories, 88% were able to be bypassed. All of the 246 CTOs in the left anterior descending coronary artery were able to be bypassed, as were 84% of 415 CTOs in the right coronary artery and 85% in the circumflex system.
The CTO group as a whole had significantly greater impairment of left ventricular function. Thirty-seven percent of them had an ejection fraction of 30%-50%, compared with 22% of the non-CTO patients. The 10% prevalence of an left ventricular ejection fraction (LVEF) below 30% in the CTO group was twice that of the non-CTO group. The CTO group was also significantly more likely to undergo incomplete revascularization, by a margin of 21% versus 5.7%.
Operative mortality was 3.7% overall and just 0.55% in the elective CABG patients. In a multivariate logistic regression analysis controlled for surgical urgency, incomplete revascularization, and EuroSCORE risk, operative mortality didn’t differ significantly between the CTO and non-CTO groups.
However, in the presence of CTOs, incomplete revascularization was associated with an 11.6% operative mortality, compared with a 2.8% rate in fully revascularized CTO patients.
A total of 110 patients with bypassed CTOs underwent symptom-driven follow-up coronary angiography at a median of 3.6 years after CABG. Reassuringly, CTO graft patency was noted in 95% of the LAD grafts, 92% of the right coronary artery grafts, and 79% of the circumflex grafts.
Dr. Kieser’s audience of interventional cardiologists was clearly bowled over by her results, not only the high rate of successful surgical bypass of CTOs, but also by her use of arterial grafts 98% of the time.
“This is my personal practice,” she explained. “I just believe in arterial grafting so much. They perform best in CTO arteries because of their lack of competitive flow.”
Session chair Oliver Gämperli, MD, of University Hospital Zurich, commented, “We are very concerned about patency rates, and you showed us fantastic patency rates. This is much better than what we’re used to with saphenous vein grafts. I think we need to talk to our surgeons and try to get them to do more arterial grafts of CTOs.”
It’s worth noting that in the CTO subgroup from the landmark randomized SYNTAX trial, the complete revascularization rate was only about 50% in the PCI group, compared with nearly 65% in the CABG group, he added.
Asked why a cardiac surgeon wouldn’t bypass a CTO, Dr. Kieser rattled off several technical reasons, including a vessel size of less than 1 mm, diffuse disease, extensive scar, or an inaccessible location. But that’s not the whole story, she added. She has heard surgical colleagues say, “The patient doesn’t need that artery, he’s learned to live without it.” That burns her up.
“Patients need every artery in the heart, and the one with a CTO is the best one for an arterial graft because it almost cannot fail, especially to the left anterior descending artery. I think we have to change the mentality of the surgeons to ‘If it can be done, it should be done,’ ” Dr. Kieser said.
She reported having no financial conflicts of interest regarding her study.
PARIS – Eighty-eight percent of chronic total occlusions (CTOs) in a large series of patients undergoing coronary artery bypass graft surgery were successfully bypassed using arterial conduits with durable patency.
“Bypass graft surgery using arterial grafts is an acceptable modality of treatment for patients with CTOs and perhaps can be a benchmark against which PCI [percutaneous coronary intervention] for CTOs should be measured,” Teresa May Kieser, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“We have previously shown in another paper that arterial grafting mitigates the adverse effect of incomplete revascularization,” said Dr. Kieser, a cardiothoracic surgeon at the University of Calgary (Alt.).
In recent years, treatment of CTOs has increasingly drawn the attention of interventional cardiologists. Dr. Kieser presented what she thinks is the first study of coronary artery bypass graft (CABG) surgery for management of CTOs. It included 1,333 consecutive CABG patients with a total of 3,906 bypasses, a whopping 98% of which were arterial grafts, with a mean of 2.9 grafts per patient. Eleven percent of the CABGs were done emergently, 48% urgently, and 41% electively.
The key epidemiologic finding to emerge from the study is that CTOs are quite common in CABG patients. In this series, 47% of CABG patients had a mean of 1.35 chronically occluded coronary arteries.
Of 843 CTOs in three major territories, 88% were able to be bypassed. All of the 246 CTOs in the left anterior descending coronary artery were able to be bypassed, as were 84% of 415 CTOs in the right coronary artery and 85% in the circumflex system.
The CTO group as a whole had significantly greater impairment of left ventricular function. Thirty-seven percent of them had an ejection fraction of 30%-50%, compared with 22% of the non-CTO patients. The 10% prevalence of an left ventricular ejection fraction (LVEF) below 30% in the CTO group was twice that of the non-CTO group. The CTO group was also significantly more likely to undergo incomplete revascularization, by a margin of 21% versus 5.7%.
Operative mortality was 3.7% overall and just 0.55% in the elective CABG patients. In a multivariate logistic regression analysis controlled for surgical urgency, incomplete revascularization, and EuroSCORE risk, operative mortality didn’t differ significantly between the CTO and non-CTO groups.
However, in the presence of CTOs, incomplete revascularization was associated with an 11.6% operative mortality, compared with a 2.8% rate in fully revascularized CTO patients.
A total of 110 patients with bypassed CTOs underwent symptom-driven follow-up coronary angiography at a median of 3.6 years after CABG. Reassuringly, CTO graft patency was noted in 95% of the LAD grafts, 92% of the right coronary artery grafts, and 79% of the circumflex grafts.
Dr. Kieser’s audience of interventional cardiologists was clearly bowled over by her results, not only the high rate of successful surgical bypass of CTOs, but also by her use of arterial grafts 98% of the time.
“This is my personal practice,” she explained. “I just believe in arterial grafting so much. They perform best in CTO arteries because of their lack of competitive flow.”
Session chair Oliver Gämperli, MD, of University Hospital Zurich, commented, “We are very concerned about patency rates, and you showed us fantastic patency rates. This is much better than what we’re used to with saphenous vein grafts. I think we need to talk to our surgeons and try to get them to do more arterial grafts of CTOs.”
It’s worth noting that in the CTO subgroup from the landmark randomized SYNTAX trial, the complete revascularization rate was only about 50% in the PCI group, compared with nearly 65% in the CABG group, he added.
Asked why a cardiac surgeon wouldn’t bypass a CTO, Dr. Kieser rattled off several technical reasons, including a vessel size of less than 1 mm, diffuse disease, extensive scar, or an inaccessible location. But that’s not the whole story, she added. She has heard surgical colleagues say, “The patient doesn’t need that artery, he’s learned to live without it.” That burns her up.
“Patients need every artery in the heart, and the one with a CTO is the best one for an arterial graft because it almost cannot fail, especially to the left anterior descending artery. I think we have to change the mentality of the surgeons to ‘If it can be done, it should be done,’ ” Dr. Kieser said.
She reported having no financial conflicts of interest regarding her study.
AT EUROPCR
Key clinical point:
Major finding: Chronic total occlusions were present in 47% of 1,333 consecutive CABG patients, and 88% of the CTOs were successfully bypassed using arterial conduits.
Data source: A retrospective observational study of 1,333 consecutive CABG patients, 47% of whom had one or more chronic total occlusions.
Disclosures: The study presenter reported having no financial conflicts.
Plasma biomarker distinguishes ARDS, acute heart failure
WASHINGTON – Plasma levels of an interleukin-33 receptor that’s involved in inflammation regulation appeared able to discriminate between acute respiratory distress syndrome and acute decompensated heart failure in an analysis with 72 patients.
In a second study, high plasma levels of the same interleukin-33 receptor, known as soluble suppressor of tumorgenicity 2 (sST2), identified acute respiratory distress syndrome (ARDS) patients who were sicker and more responsive to conservative fluid management, Sean D. Levy, MD, said at an international conference of the American Thoracic Society.
In order to assess the ability of sST2 to reliably distinguish patients with ARDS from those with acute decompensated heart failure, he and his associates selected 72 patients seen at the Massachusetts General Hospital in Boston with an initial diagnosis of acute decompensated heart failure accompanied by bilateral lung infiltrates and acute hypoxemia respiratory failure requiring endotracheal intubation and mechanical ventilation. The investigators measured the sST2 level in a plasma specimen from each patient. In addition, after each patient either left the hospital or died, their case underwent review by two critical care physicians who retrospectively rediagnosed the patients as either having ARDS or acute decompensated heart failure. This divided the cohort into 30 patients with ARDS and 42 with true acute heart failure. The two subgroups matched up fairly closely for most clinical measures and comorbidities, but APACHE III (Acute Physiology and Chronic Health Evaluation III) scores averaged significantly higher in the ARDS patients.
The plasma levels of sST2 showed a dramatic split between the two subgroups. The 30 patients retrospectively diagnosed with ARDS had an average level of 386 ng/mL with an interquartile range of 318-611 ng/mL. The 42 acute decompensated heart failure patients averaged a sST2 level of 148 ng/mL, with an interquartile range of 84-225 ng/mL. The area under the receiver operator curve for discriminating between ARDS and acute heart failure using a cutpoint of 271 mg/mL was 0.86, showing “good” discrimination, Dr. Levy said. This cutpoint had a sensitivity of 83% and specificity of 88% for correctly distinguishing between ARDS and acute heart failure.
In a second analysis, Dr. Levy and his associates looked at the ability of sST2 levels to separate out patients with acute lung injury who had a more robust response to either the conservative or liberal fluid-management strategies tested in the Fluid and Catheter Treatment Trial (FACTT), run by the National Heart, Lung, and Blood Institute’s ARDS Clinical Trials Network. The primary outcome of FACTT was death from any cause 60 days after entry, and this showed no significant difference between conservative (restricted fluids and increased urine output) and liberal (the reverse) fluid management strategies in acute lung injury patients (N Engl J Med. 2006 Jun 15;354[14]:2564-75). From among the 1,001 patients enrolled in FACTT, 826 had specimens available for measuring sST2 (Crit Care Med. 2013 Nov;41[11]:2521-31),
The researchers applied the sST2 cut point they derived in the first analysis to the FACTT cohort and identified 133 (16%) patients with a low sST2 level and 693 (84%) with a high level. The patients with high sST2 were sicker, with significantly higher APACHE III scores, worse acidemia, and worse renal function.
Patients with high sST2 levels had a significant increase in ventilator-free days on conservative fluid management, compared with liberal management, while the two management strategies produced virtually identical results in the patients with low levels of sST2. Patients with high sST2 also had a significantly quicker time to extubation on a conservative strategy compared with the liberal strategy, and again this correlation did not exist among patients with low sST2. However, as in the overall trial a conservative strategy had no discernible impact on 60-day mortality, compared with the liberal strategy, even in the subgroup with high sST2.
Dr. Levy had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
WASHINGTON – Plasma levels of an interleukin-33 receptor that’s involved in inflammation regulation appeared able to discriminate between acute respiratory distress syndrome and acute decompensated heart failure in an analysis with 72 patients.
In a second study, high plasma levels of the same interleukin-33 receptor, known as soluble suppressor of tumorgenicity 2 (sST2), identified acute respiratory distress syndrome (ARDS) patients who were sicker and more responsive to conservative fluid management, Sean D. Levy, MD, said at an international conference of the American Thoracic Society.
In order to assess the ability of sST2 to reliably distinguish patients with ARDS from those with acute decompensated heart failure, he and his associates selected 72 patients seen at the Massachusetts General Hospital in Boston with an initial diagnosis of acute decompensated heart failure accompanied by bilateral lung infiltrates and acute hypoxemia respiratory failure requiring endotracheal intubation and mechanical ventilation. The investigators measured the sST2 level in a plasma specimen from each patient. In addition, after each patient either left the hospital or died, their case underwent review by two critical care physicians who retrospectively rediagnosed the patients as either having ARDS or acute decompensated heart failure. This divided the cohort into 30 patients with ARDS and 42 with true acute heart failure. The two subgroups matched up fairly closely for most clinical measures and comorbidities, but APACHE III (Acute Physiology and Chronic Health Evaluation III) scores averaged significantly higher in the ARDS patients.
The plasma levels of sST2 showed a dramatic split between the two subgroups. The 30 patients retrospectively diagnosed with ARDS had an average level of 386 ng/mL with an interquartile range of 318-611 ng/mL. The 42 acute decompensated heart failure patients averaged a sST2 level of 148 ng/mL, with an interquartile range of 84-225 ng/mL. The area under the receiver operator curve for discriminating between ARDS and acute heart failure using a cutpoint of 271 mg/mL was 0.86, showing “good” discrimination, Dr. Levy said. This cutpoint had a sensitivity of 83% and specificity of 88% for correctly distinguishing between ARDS and acute heart failure.
In a second analysis, Dr. Levy and his associates looked at the ability of sST2 levels to separate out patients with acute lung injury who had a more robust response to either the conservative or liberal fluid-management strategies tested in the Fluid and Catheter Treatment Trial (FACTT), run by the National Heart, Lung, and Blood Institute’s ARDS Clinical Trials Network. The primary outcome of FACTT was death from any cause 60 days after entry, and this showed no significant difference between conservative (restricted fluids and increased urine output) and liberal (the reverse) fluid management strategies in acute lung injury patients (N Engl J Med. 2006 Jun 15;354[14]:2564-75). From among the 1,001 patients enrolled in FACTT, 826 had specimens available for measuring sST2 (Crit Care Med. 2013 Nov;41[11]:2521-31),
The researchers applied the sST2 cut point they derived in the first analysis to the FACTT cohort and identified 133 (16%) patients with a low sST2 level and 693 (84%) with a high level. The patients with high sST2 were sicker, with significantly higher APACHE III scores, worse acidemia, and worse renal function.
Patients with high sST2 levels had a significant increase in ventilator-free days on conservative fluid management, compared with liberal management, while the two management strategies produced virtually identical results in the patients with low levels of sST2. Patients with high sST2 also had a significantly quicker time to extubation on a conservative strategy compared with the liberal strategy, and again this correlation did not exist among patients with low sST2. However, as in the overall trial a conservative strategy had no discernible impact on 60-day mortality, compared with the liberal strategy, even in the subgroup with high sST2.
Dr. Levy had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
WASHINGTON – Plasma levels of an interleukin-33 receptor that’s involved in inflammation regulation appeared able to discriminate between acute respiratory distress syndrome and acute decompensated heart failure in an analysis with 72 patients.
In a second study, high plasma levels of the same interleukin-33 receptor, known as soluble suppressor of tumorgenicity 2 (sST2), identified acute respiratory distress syndrome (ARDS) patients who were sicker and more responsive to conservative fluid management, Sean D. Levy, MD, said at an international conference of the American Thoracic Society.
In order to assess the ability of sST2 to reliably distinguish patients with ARDS from those with acute decompensated heart failure, he and his associates selected 72 patients seen at the Massachusetts General Hospital in Boston with an initial diagnosis of acute decompensated heart failure accompanied by bilateral lung infiltrates and acute hypoxemia respiratory failure requiring endotracheal intubation and mechanical ventilation. The investigators measured the sST2 level in a plasma specimen from each patient. In addition, after each patient either left the hospital or died, their case underwent review by two critical care physicians who retrospectively rediagnosed the patients as either having ARDS or acute decompensated heart failure. This divided the cohort into 30 patients with ARDS and 42 with true acute heart failure. The two subgroups matched up fairly closely for most clinical measures and comorbidities, but APACHE III (Acute Physiology and Chronic Health Evaluation III) scores averaged significantly higher in the ARDS patients.
The plasma levels of sST2 showed a dramatic split between the two subgroups. The 30 patients retrospectively diagnosed with ARDS had an average level of 386 ng/mL with an interquartile range of 318-611 ng/mL. The 42 acute decompensated heart failure patients averaged a sST2 level of 148 ng/mL, with an interquartile range of 84-225 ng/mL. The area under the receiver operator curve for discriminating between ARDS and acute heart failure using a cutpoint of 271 mg/mL was 0.86, showing “good” discrimination, Dr. Levy said. This cutpoint had a sensitivity of 83% and specificity of 88% for correctly distinguishing between ARDS and acute heart failure.
In a second analysis, Dr. Levy and his associates looked at the ability of sST2 levels to separate out patients with acute lung injury who had a more robust response to either the conservative or liberal fluid-management strategies tested in the Fluid and Catheter Treatment Trial (FACTT), run by the National Heart, Lung, and Blood Institute’s ARDS Clinical Trials Network. The primary outcome of FACTT was death from any cause 60 days after entry, and this showed no significant difference between conservative (restricted fluids and increased urine output) and liberal (the reverse) fluid management strategies in acute lung injury patients (N Engl J Med. 2006 Jun 15;354[14]:2564-75). From among the 1,001 patients enrolled in FACTT, 826 had specimens available for measuring sST2 (Crit Care Med. 2013 Nov;41[11]:2521-31),
The researchers applied the sST2 cut point they derived in the first analysis to the FACTT cohort and identified 133 (16%) patients with a low sST2 level and 693 (84%) with a high level. The patients with high sST2 were sicker, with significantly higher APACHE III scores, worse acidemia, and worse renal function.
Patients with high sST2 levels had a significant increase in ventilator-free days on conservative fluid management, compared with liberal management, while the two management strategies produced virtually identical results in the patients with low levels of sST2. Patients with high sST2 also had a significantly quicker time to extubation on a conservative strategy compared with the liberal strategy, and again this correlation did not exist among patients with low sST2. However, as in the overall trial a conservative strategy had no discernible impact on 60-day mortality, compared with the liberal strategy, even in the subgroup with high sST2.
Dr. Levy had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT ATS 2017
Key clinical point:
Major finding: An sST2 cutpoint of 271 ng/mL discriminated between ARDS and acute heart failure with 83% sensitivity and 88% specificity.
Data source: Review of 72 patients admitted for acute decompensated heart failure at one U.S. center.
Disclosures: Dr. Levy had no disclosures.
Evolute transcatheter valve, now FDA approved for intermediate-risk patients, impresses in real-world practice
PARIS – The Evolut R transcatheter aortic valve demonstrated excellent 30-day results in a real-world, mixed surgical risk population in the large Evolut R FORWARD study.
In this 1,038-patient observational study conducted at 53 sites in 20 countries, the Evolut R valve showed excellent forward hemodynamics and low 30-day rates of all-cause mortality and stroke that were unaffected by utilization of the device’s repositioning feature, Eberhard Grube, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The importance of the FORWARD study, Dr. Grube observed, is that it illustrates the clinical outcomes obtained in a large population drawn from routine clinical practice. Unlike in a randomized trial such as SURTAVI, the participating sites in the Evolut R Forward study weren’t all high-volume enrollment centers, and operators had widely varying degrees of experience with the valve.
Also, SURTAVI utilized the first generation of the self-expanding CoreValve, which lacked the repositioning feature introduced in the second-generation Evolut R. The FORWARD study is the first rigorous evaluation of Evolut R with centrally adjudicated outcomes.
The mean Society of Thoracic Surgeons predicted risk of mortality score in participants was 5.5%, and 47% had a low-risk score of less than 4%. However, the patients had a mean age of 82 years, one-third were deemed frail, 30% had diabetes, and 26% had chronic lung disease.
The primary study endpoint was 30-day all-cause mortality. The rate was 1.9%, compared with a predicted 5.5% rate based on STS score, for an impressive observed-to-expected ratio of 0.35.
Hemodynamically, the effective orifice area improved from 0.8 cm2 at baseline to 1.9 cm2 at 30 days, while the mean aortic valve gradient plunged from 41.7 to 8.5 mm Hg.
At baseline only 1.5% of patients were New York Heart Association functional class I and 26.5% were class II. At 30 days, 44.7% were class I and 43.4% were class II. The prevalence of NYHA class III status decreased from 63.8% to 11.3%.
There was no or only trace paravalvular leak at discharge in 67.2% of patients as adjudicated in a core laboratory, mild leak in 30.9%, moderate in 1.9%, and severe leak in just 0.1%.
The 30-day total stroke rate was 2.8%, including a 1.8% rate of disabling stroke. Major vascular complications occurred in 6.5% of patients, valve embolization in 0.7%, and life-threatening or disabling bleeding in 3.3%. There were no cases of coronary obstruction or annular rupture.
New pacemaker implantation was required within 30 days in 17.5% of patients. Three-quarters of the pacemakers were placed because of third-degree atrioventricular block.
The new valve ended up in proper anatomic position in 98.9% of patients.
The repositioning feature was utilized in 26% of participants. It had no impact on the rate of pacemaker implantation, mortality, stroke, or other safety endpoints.
“I think the ability to reposition this valve, which is a safety feature, is an important feature, particularly for centers that don’t have so much experience. If the valve is considered to be too high or too low, or you see, for example, a higher degree of paravalvular leak, you have the chance to correct that by using this feature. So it’s an important feature for the operator. It helps to get an optimal result. And the most important thing is there was no price in terms of safety that we paid for repositioning,” said Dr. Grube, professor of cardiology and head of the Center for Innovative Intervention in Cardiology at the University of Bonn in Siegberg, Germany.
Session cochair Alain Cribier, MD, famed for having performed the world’s first TAVR procedure, pronounced the FORWARD results “very impressive.”
“Less than 2% mortality, around a 2% disabling stroke rate, and the data on paravalvular leak are excellent as well. It’s very nice to see that what was a limited data set earlier, with a smaller number of patients, has now been replicated in 1,000 patients. So I think now we can confidently talk about the clinical outcomes – and they are excellent,” declared Dr. Cribier, professor of medicine at the University of Rouen (France) and chief of cardiology at Charles Nicolle Hospital.
The FORWARD study was sponsored by Medtronic. Dr. Grube reported serving as a consultant to that company as well as to Boston Scientific, Abbott, and Millipede Medical.
PARIS – The Evolut R transcatheter aortic valve demonstrated excellent 30-day results in a real-world, mixed surgical risk population in the large Evolut R FORWARD study.
In this 1,038-patient observational study conducted at 53 sites in 20 countries, the Evolut R valve showed excellent forward hemodynamics and low 30-day rates of all-cause mortality and stroke that were unaffected by utilization of the device’s repositioning feature, Eberhard Grube, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The importance of the FORWARD study, Dr. Grube observed, is that it illustrates the clinical outcomes obtained in a large population drawn from routine clinical practice. Unlike in a randomized trial such as SURTAVI, the participating sites in the Evolut R Forward study weren’t all high-volume enrollment centers, and operators had widely varying degrees of experience with the valve.
Also, SURTAVI utilized the first generation of the self-expanding CoreValve, which lacked the repositioning feature introduced in the second-generation Evolut R. The FORWARD study is the first rigorous evaluation of Evolut R with centrally adjudicated outcomes.
The mean Society of Thoracic Surgeons predicted risk of mortality score in participants was 5.5%, and 47% had a low-risk score of less than 4%. However, the patients had a mean age of 82 years, one-third were deemed frail, 30% had diabetes, and 26% had chronic lung disease.
The primary study endpoint was 30-day all-cause mortality. The rate was 1.9%, compared with a predicted 5.5% rate based on STS score, for an impressive observed-to-expected ratio of 0.35.
Hemodynamically, the effective orifice area improved from 0.8 cm2 at baseline to 1.9 cm2 at 30 days, while the mean aortic valve gradient plunged from 41.7 to 8.5 mm Hg.
At baseline only 1.5% of patients were New York Heart Association functional class I and 26.5% were class II. At 30 days, 44.7% were class I and 43.4% were class II. The prevalence of NYHA class III status decreased from 63.8% to 11.3%.
There was no or only trace paravalvular leak at discharge in 67.2% of patients as adjudicated in a core laboratory, mild leak in 30.9%, moderate in 1.9%, and severe leak in just 0.1%.
The 30-day total stroke rate was 2.8%, including a 1.8% rate of disabling stroke. Major vascular complications occurred in 6.5% of patients, valve embolization in 0.7%, and life-threatening or disabling bleeding in 3.3%. There were no cases of coronary obstruction or annular rupture.
New pacemaker implantation was required within 30 days in 17.5% of patients. Three-quarters of the pacemakers were placed because of third-degree atrioventricular block.
The new valve ended up in proper anatomic position in 98.9% of patients.
The repositioning feature was utilized in 26% of participants. It had no impact on the rate of pacemaker implantation, mortality, stroke, or other safety endpoints.
“I think the ability to reposition this valve, which is a safety feature, is an important feature, particularly for centers that don’t have so much experience. If the valve is considered to be too high or too low, or you see, for example, a higher degree of paravalvular leak, you have the chance to correct that by using this feature. So it’s an important feature for the operator. It helps to get an optimal result. And the most important thing is there was no price in terms of safety that we paid for repositioning,” said Dr. Grube, professor of cardiology and head of the Center for Innovative Intervention in Cardiology at the University of Bonn in Siegberg, Germany.
Session cochair Alain Cribier, MD, famed for having performed the world’s first TAVR procedure, pronounced the FORWARD results “very impressive.”
“Less than 2% mortality, around a 2% disabling stroke rate, and the data on paravalvular leak are excellent as well. It’s very nice to see that what was a limited data set earlier, with a smaller number of patients, has now been replicated in 1,000 patients. So I think now we can confidently talk about the clinical outcomes – and they are excellent,” declared Dr. Cribier, professor of medicine at the University of Rouen (France) and chief of cardiology at Charles Nicolle Hospital.
The FORWARD study was sponsored by Medtronic. Dr. Grube reported serving as a consultant to that company as well as to Boston Scientific, Abbott, and Millipede Medical.
PARIS – The Evolut R transcatheter aortic valve demonstrated excellent 30-day results in a real-world, mixed surgical risk population in the large Evolut R FORWARD study.
In this 1,038-patient observational study conducted at 53 sites in 20 countries, the Evolut R valve showed excellent forward hemodynamics and low 30-day rates of all-cause mortality and stroke that were unaffected by utilization of the device’s repositioning feature, Eberhard Grube, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The importance of the FORWARD study, Dr. Grube observed, is that it illustrates the clinical outcomes obtained in a large population drawn from routine clinical practice. Unlike in a randomized trial such as SURTAVI, the participating sites in the Evolut R Forward study weren’t all high-volume enrollment centers, and operators had widely varying degrees of experience with the valve.
Also, SURTAVI utilized the first generation of the self-expanding CoreValve, which lacked the repositioning feature introduced in the second-generation Evolut R. The FORWARD study is the first rigorous evaluation of Evolut R with centrally adjudicated outcomes.
The mean Society of Thoracic Surgeons predicted risk of mortality score in participants was 5.5%, and 47% had a low-risk score of less than 4%. However, the patients had a mean age of 82 years, one-third were deemed frail, 30% had diabetes, and 26% had chronic lung disease.
The primary study endpoint was 30-day all-cause mortality. The rate was 1.9%, compared with a predicted 5.5% rate based on STS score, for an impressive observed-to-expected ratio of 0.35.
Hemodynamically, the effective orifice area improved from 0.8 cm2 at baseline to 1.9 cm2 at 30 days, while the mean aortic valve gradient plunged from 41.7 to 8.5 mm Hg.
At baseline only 1.5% of patients were New York Heart Association functional class I and 26.5% were class II. At 30 days, 44.7% were class I and 43.4% were class II. The prevalence of NYHA class III status decreased from 63.8% to 11.3%.
There was no or only trace paravalvular leak at discharge in 67.2% of patients as adjudicated in a core laboratory, mild leak in 30.9%, moderate in 1.9%, and severe leak in just 0.1%.
The 30-day total stroke rate was 2.8%, including a 1.8% rate of disabling stroke. Major vascular complications occurred in 6.5% of patients, valve embolization in 0.7%, and life-threatening or disabling bleeding in 3.3%. There were no cases of coronary obstruction or annular rupture.
New pacemaker implantation was required within 30 days in 17.5% of patients. Three-quarters of the pacemakers were placed because of third-degree atrioventricular block.
The new valve ended up in proper anatomic position in 98.9% of patients.
The repositioning feature was utilized in 26% of participants. It had no impact on the rate of pacemaker implantation, mortality, stroke, or other safety endpoints.
“I think the ability to reposition this valve, which is a safety feature, is an important feature, particularly for centers that don’t have so much experience. If the valve is considered to be too high or too low, or you see, for example, a higher degree of paravalvular leak, you have the chance to correct that by using this feature. So it’s an important feature for the operator. It helps to get an optimal result. And the most important thing is there was no price in terms of safety that we paid for repositioning,” said Dr. Grube, professor of cardiology and head of the Center for Innovative Intervention in Cardiology at the University of Bonn in Siegberg, Germany.
Session cochair Alain Cribier, MD, famed for having performed the world’s first TAVR procedure, pronounced the FORWARD results “very impressive.”
“Less than 2% mortality, around a 2% disabling stroke rate, and the data on paravalvular leak are excellent as well. It’s very nice to see that what was a limited data set earlier, with a smaller number of patients, has now been replicated in 1,000 patients. So I think now we can confidently talk about the clinical outcomes – and they are excellent,” declared Dr. Cribier, professor of medicine at the University of Rouen (France) and chief of cardiology at Charles Nicolle Hospital.
The FORWARD study was sponsored by Medtronic. Dr. Grube reported serving as a consultant to that company as well as to Boston Scientific, Abbott, and Millipede Medical.
AT EUROPCR
Key clinical point:
Major finding: Thirty-day all-cause mortality was 1.9% with a 2.8% stroke rate in a large, real-world study of TAVR with the repositionable self-expanding Evolut R transcatheter aortic valve.
Data source: The Evolut R FORWARD study of 1,038 recipients of the Evolut R transcatheter aortic valve at 53 sites in 20 countries.
Disclosures: The FORWARD study was sponsored by Medtronic. The presenter reported serving as a consultant to that company as well as to Boston Scientific, Abbott, and Millipede Medical.
Watchman device for AF patients ineligible for oral anticoagulation gains support from 1-year registry outcomes
PARIS – Patients with atrial fibrillation at high stroke risk and a contraindication for oral anticoagulation experienced an 83% reduction in their risk of ischemic stroke and transient ischemic attack during their first year after receiving the Watchman left atrial appendage closure device backed by limited-duration dual-antiplatelet therapy, according to a report from the EWOLUTION registry.
Of 605 participants in the European registry who went on dual-antiplatelet treatment (DAPT) in conjunction with receiving the Watchman device, 39% discontinued DAPT within 3 months and 72% were off DAPT by 6 months. Yet the 1-year rate of ischemic stroke or TIA in the EWOLUTION group was just 1.8%, an 83% relative risk reduction compared with the expected 10.5% rate based on the participants’ mean CHA2DS2-VASc score of 4.6 in the absence of oral anticoagulation, Martin W. Bergmann, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Obviously this isn’t a randomized trial. This is just reassuring data that we are going in the right direction in terms of efficacy,” said Dr. Bergmann of Cardiologicum Hamburg, a large German group practice.
However, the ESC guidelines were largely based on randomized trials of the Watchman versus oral anticoagulation, including PREVAIL and PROTECT-AF, showing noninferiority. The safety and efficacy of the device in warfarin-ineligible patients was less well studied at the time the guidelines were formulated. And in fact, such patients are excluded from the Food and Drug Administration’s approved indication, which is specifically for patients judged “suitable for warfarin.”
“This gap is now filled by EWOLUTION. This is a registry that’s as good as it gets. We have all the things in place that you need these days to be able to rely on the outcome data,” according to the cardiologist.
EWOLUTION is a prospective, multicenter, all-comers registry. The EWOLUTION population of AF patients on DAPT was high risk: 89% had a CHA2DS2-VASc score of 3 or more, 31% were at least 80 years old, the mean HAS-BLED score was 2.4, and oral anticoagulation was contraindicated in 84% of participants.
Eighty-seven percent of subjects underwent follow-up transesophageal echocardiography. The imaging study showed the Watchman effectively sealed the left atrial appendage in 99.2% of patients as defined by no leak greater than 5 mm. The echo exam also showed the presence of thrombus on the device at follow-up in 4% of patients, although only 1 of the 22 patients with device thrombus experienced a stroke.
“We can conclude two things from this which are in line with earlier studies. First, the rate of thrombus on the device is equal to the rate reported in the randomized controlled trials, which was also 4%, even if the patients were on warfarin for the first 45 days. And second, these thrombi are not related to stroke,” Dr. Bergmann said.
At the 1-year mark, 71% of patients had switched to a single antiplatelet agent, while 17% remained on DAPT, mainly because of comorbid coronary disease for which DAPT is indicated. Seven percent of patients were on no antithrombotic medications. The remaining 5% were transiently on warfarin or a novel oral anticoagulant.
The 1-year cumulative rate of ischemic stroke or TIA was 1.8%, with no instances of systemic embolism. Of note, there were no hemorrhagic strokes. And of the 11 cases of ischemic stroke, none were fatal and only one was disabling.
“This is a sign that comes also from the PREVAIL trial, that if you have a stroke while on left atrial appendage–closure therapy, most of the time it’s not disabling. It’s much less severe on the modified Rankin Scale than if you’re on oral anticoagulation,” said Dr. Bergmann.
The 1.4% rate of ischemic stroke at 1 year in Watchman recipients represents an 81% reduction in risk compared with the expected 7.5% rate in patients with similar CHA2DS2-VASc scores not on oral anticoagulation. This level of stroke risk reduction is similar to that seen in the pivotal ARISTOTLE trial of apixaban (Eliquis) in a high-risk AF population (Lancet. 2012 Nov 17;380[9855]:1749-58).
Major bleeding occurred in 2.5% of patients. The rate of fatal bleeding was 0.5%. To put that in perspective, the 2.5% major bleeding rate was 52% lower than would be expected based upon similar HAS-BLED scores in patients on warfarin. Still, 2.5% is unacceptably high.
“The major serious adverse event is not pericardial effusion or late device embolization, it’s major bleeding occurring during the time the patient is on DAPT, mostly within the first 3 months. So I think we have to do something about this,” he said.
One possibility worthy of formal study is 3 months of periprocedural NOAC monotherapy. “Maybe even low-dose therapy, like 75 mg of dabigatran [Pradaxa] twice daily. We have an antidote that works nicely [idarucizumab, Praxbind] so I think maybe this is the way to go,” Dr. Bergmann observed.
The ongoing EWOLUTION registry is sponsored by Boston Scientific. Dr. Bergmann is a consultant to that company as well as Bayer AG, Daiichi Sankyo, Eli Lilly, and St. Jude Medical.
PARIS – Patients with atrial fibrillation at high stroke risk and a contraindication for oral anticoagulation experienced an 83% reduction in their risk of ischemic stroke and transient ischemic attack during their first year after receiving the Watchman left atrial appendage closure device backed by limited-duration dual-antiplatelet therapy, according to a report from the EWOLUTION registry.
Of 605 participants in the European registry who went on dual-antiplatelet treatment (DAPT) in conjunction with receiving the Watchman device, 39% discontinued DAPT within 3 months and 72% were off DAPT by 6 months. Yet the 1-year rate of ischemic stroke or TIA in the EWOLUTION group was just 1.8%, an 83% relative risk reduction compared with the expected 10.5% rate based on the participants’ mean CHA2DS2-VASc score of 4.6 in the absence of oral anticoagulation, Martin W. Bergmann, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Obviously this isn’t a randomized trial. This is just reassuring data that we are going in the right direction in terms of efficacy,” said Dr. Bergmann of Cardiologicum Hamburg, a large German group practice.
However, the ESC guidelines were largely based on randomized trials of the Watchman versus oral anticoagulation, including PREVAIL and PROTECT-AF, showing noninferiority. The safety and efficacy of the device in warfarin-ineligible patients was less well studied at the time the guidelines were formulated. And in fact, such patients are excluded from the Food and Drug Administration’s approved indication, which is specifically for patients judged “suitable for warfarin.”
“This gap is now filled by EWOLUTION. This is a registry that’s as good as it gets. We have all the things in place that you need these days to be able to rely on the outcome data,” according to the cardiologist.
EWOLUTION is a prospective, multicenter, all-comers registry. The EWOLUTION population of AF patients on DAPT was high risk: 89% had a CHA2DS2-VASc score of 3 or more, 31% were at least 80 years old, the mean HAS-BLED score was 2.4, and oral anticoagulation was contraindicated in 84% of participants.
Eighty-seven percent of subjects underwent follow-up transesophageal echocardiography. The imaging study showed the Watchman effectively sealed the left atrial appendage in 99.2% of patients as defined by no leak greater than 5 mm. The echo exam also showed the presence of thrombus on the device at follow-up in 4% of patients, although only 1 of the 22 patients with device thrombus experienced a stroke.
“We can conclude two things from this which are in line with earlier studies. First, the rate of thrombus on the device is equal to the rate reported in the randomized controlled trials, which was also 4%, even if the patients were on warfarin for the first 45 days. And second, these thrombi are not related to stroke,” Dr. Bergmann said.
At the 1-year mark, 71% of patients had switched to a single antiplatelet agent, while 17% remained on DAPT, mainly because of comorbid coronary disease for which DAPT is indicated. Seven percent of patients were on no antithrombotic medications. The remaining 5% were transiently on warfarin or a novel oral anticoagulant.
The 1-year cumulative rate of ischemic stroke or TIA was 1.8%, with no instances of systemic embolism. Of note, there were no hemorrhagic strokes. And of the 11 cases of ischemic stroke, none were fatal and only one was disabling.
“This is a sign that comes also from the PREVAIL trial, that if you have a stroke while on left atrial appendage–closure therapy, most of the time it’s not disabling. It’s much less severe on the modified Rankin Scale than if you’re on oral anticoagulation,” said Dr. Bergmann.
The 1.4% rate of ischemic stroke at 1 year in Watchman recipients represents an 81% reduction in risk compared with the expected 7.5% rate in patients with similar CHA2DS2-VASc scores not on oral anticoagulation. This level of stroke risk reduction is similar to that seen in the pivotal ARISTOTLE trial of apixaban (Eliquis) in a high-risk AF population (Lancet. 2012 Nov 17;380[9855]:1749-58).
Major bleeding occurred in 2.5% of patients. The rate of fatal bleeding was 0.5%. To put that in perspective, the 2.5% major bleeding rate was 52% lower than would be expected based upon similar HAS-BLED scores in patients on warfarin. Still, 2.5% is unacceptably high.
“The major serious adverse event is not pericardial effusion or late device embolization, it’s major bleeding occurring during the time the patient is on DAPT, mostly within the first 3 months. So I think we have to do something about this,” he said.
One possibility worthy of formal study is 3 months of periprocedural NOAC monotherapy. “Maybe even low-dose therapy, like 75 mg of dabigatran [Pradaxa] twice daily. We have an antidote that works nicely [idarucizumab, Praxbind] so I think maybe this is the way to go,” Dr. Bergmann observed.
The ongoing EWOLUTION registry is sponsored by Boston Scientific. Dr. Bergmann is a consultant to that company as well as Bayer AG, Daiichi Sankyo, Eli Lilly, and St. Jude Medical.
PARIS – Patients with atrial fibrillation at high stroke risk and a contraindication for oral anticoagulation experienced an 83% reduction in their risk of ischemic stroke and transient ischemic attack during their first year after receiving the Watchman left atrial appendage closure device backed by limited-duration dual-antiplatelet therapy, according to a report from the EWOLUTION registry.
Of 605 participants in the European registry who went on dual-antiplatelet treatment (DAPT) in conjunction with receiving the Watchman device, 39% discontinued DAPT within 3 months and 72% were off DAPT by 6 months. Yet the 1-year rate of ischemic stroke or TIA in the EWOLUTION group was just 1.8%, an 83% relative risk reduction compared with the expected 10.5% rate based on the participants’ mean CHA2DS2-VASc score of 4.6 in the absence of oral anticoagulation, Martin W. Bergmann, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“Obviously this isn’t a randomized trial. This is just reassuring data that we are going in the right direction in terms of efficacy,” said Dr. Bergmann of Cardiologicum Hamburg, a large German group practice.
However, the ESC guidelines were largely based on randomized trials of the Watchman versus oral anticoagulation, including PREVAIL and PROTECT-AF, showing noninferiority. The safety and efficacy of the device in warfarin-ineligible patients was less well studied at the time the guidelines were formulated. And in fact, such patients are excluded from the Food and Drug Administration’s approved indication, which is specifically for patients judged “suitable for warfarin.”
“This gap is now filled by EWOLUTION. This is a registry that’s as good as it gets. We have all the things in place that you need these days to be able to rely on the outcome data,” according to the cardiologist.
EWOLUTION is a prospective, multicenter, all-comers registry. The EWOLUTION population of AF patients on DAPT was high risk: 89% had a CHA2DS2-VASc score of 3 or more, 31% were at least 80 years old, the mean HAS-BLED score was 2.4, and oral anticoagulation was contraindicated in 84% of participants.
Eighty-seven percent of subjects underwent follow-up transesophageal echocardiography. The imaging study showed the Watchman effectively sealed the left atrial appendage in 99.2% of patients as defined by no leak greater than 5 mm. The echo exam also showed the presence of thrombus on the device at follow-up in 4% of patients, although only 1 of the 22 patients with device thrombus experienced a stroke.
“We can conclude two things from this which are in line with earlier studies. First, the rate of thrombus on the device is equal to the rate reported in the randomized controlled trials, which was also 4%, even if the patients were on warfarin for the first 45 days. And second, these thrombi are not related to stroke,” Dr. Bergmann said.
At the 1-year mark, 71% of patients had switched to a single antiplatelet agent, while 17% remained on DAPT, mainly because of comorbid coronary disease for which DAPT is indicated. Seven percent of patients were on no antithrombotic medications. The remaining 5% were transiently on warfarin or a novel oral anticoagulant.
The 1-year cumulative rate of ischemic stroke or TIA was 1.8%, with no instances of systemic embolism. Of note, there were no hemorrhagic strokes. And of the 11 cases of ischemic stroke, none were fatal and only one was disabling.
“This is a sign that comes also from the PREVAIL trial, that if you have a stroke while on left atrial appendage–closure therapy, most of the time it’s not disabling. It’s much less severe on the modified Rankin Scale than if you’re on oral anticoagulation,” said Dr. Bergmann.
The 1.4% rate of ischemic stroke at 1 year in Watchman recipients represents an 81% reduction in risk compared with the expected 7.5% rate in patients with similar CHA2DS2-VASc scores not on oral anticoagulation. This level of stroke risk reduction is similar to that seen in the pivotal ARISTOTLE trial of apixaban (Eliquis) in a high-risk AF population (Lancet. 2012 Nov 17;380[9855]:1749-58).
Major bleeding occurred in 2.5% of patients. The rate of fatal bleeding was 0.5%. To put that in perspective, the 2.5% major bleeding rate was 52% lower than would be expected based upon similar HAS-BLED scores in patients on warfarin. Still, 2.5% is unacceptably high.
“The major serious adverse event is not pericardial effusion or late device embolization, it’s major bleeding occurring during the time the patient is on DAPT, mostly within the first 3 months. So I think we have to do something about this,” he said.
One possibility worthy of formal study is 3 months of periprocedural NOAC monotherapy. “Maybe even low-dose therapy, like 75 mg of dabigatran [Pradaxa] twice daily. We have an antidote that works nicely [idarucizumab, Praxbind] so I think maybe this is the way to go,” Dr. Bergmann observed.
The ongoing EWOLUTION registry is sponsored by Boston Scientific. Dr. Bergmann is a consultant to that company as well as Bayer AG, Daiichi Sankyo, Eli Lilly, and St. Jude Medical.
AT EUROPCR
Key clinical point:
Major finding: Patients with AF at high stroke risk and ineligible for oral anticoagulation experienced an 81% reduction in their expected risk of ischemic stroke during their first year of LAA closure with the Watchman device backed by limited-duration dual-antiplatelet therapy
Data source: A prospective, multicenter, single-arm registry that includes 605 patients with AF who underwent left atrial appendage closure with the WATCHMAN device supported by limited-duration dual-antiplatelet therapy.
Disclosures: The ongoing EWOLUTION registry is sponsored by Boston Scientific. The presenter is a consultant to that company and several others.