User login
COVID-19: A guide to making telepsychiatry work
Changes prompted by social distancing could last beyond the pandemic
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
Changes prompted by social distancing could last beyond the pandemic
Changes prompted by social distancing could last beyond the pandemic
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
Cardiology groups push back on hydroxychloroquine, azithromycin for COVID-19
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
COVID-19: Are acute stroke patients avoiding emergency care?
(EDs).
Stroke specialists in New Orleans, Chicago, Seattle, and elsewhere told Medscape Medical News they are seeing a precipitous drop in the number of acute strokes at their institutions – and not just in the number of milder cases. Doctors on Twitter are sharing similar reports and are using social media to highlight this issue.
Gabriel Vidal, MD, a vascular and interventional neurologist at the Ochsner Medical Center, New Orleans, Louisiana, said there are “definitely” fewer patients with stroke and transient ischemic attack (TIA) seeking care at his facility and others throughout the New Orleans area, which has been hard hit by COVID-19.
“Even in Louisiana, we have a very large 53-hospital telestroke network, and the number of consults has diminished greatly,” Vidal added.
In Chicago, emergency medical service activations for patients with suspected strokes are down about 30%, Shyam Prabhakaran, MD, professor and chair of neurology at the University of Chicago Biological Sciences, Illinois, told Medscape Medical News.
“It appears to be that mild stroke and TIA patients may be more likely to stay at home and seek alternative care rather than come to the ED,” Prabhakaran said. However, “the severe strokes may be less affected and continue to come to emergency departments.”
“Getting the Word Out”
That may not be the whole story in Seattle, Washington, where a stroke specialist at Harborview Medical Center reported a drop in patients across the stroke-severity spectrum.
Some patients with milder strokes no longer come to Harborview for a comprehensive evaluation and workup, but that is only “a partial explanation,” said David Tirschwell, MD, medical director of comprehensive stroke care at the University of Washington (UW) Medicine Stroke Center at Harborview and a professor of neurology at UW.
“The thrombectomies are down also,” he added. “It’s hard to have great numbers in real time, but it’s probably safe to say it’s at least a 50% reduction in the number of admissions.”
As a stroke referral center, his institution is seeing fewer local cases and referrals from outside hospitals. “I think both of those sources for admissions of stroke cases are down,” Tirschwell said.
Recognizing the seriousness of forgoing essential care for acute stroke, neurologists, institutions, and medical groups are taking to social media to potentially save lives.
“Across our @FLStrokeReg we are seeing less patients with #stroke symptoms coming to our hospitals. We need to get the word out that our teams are working hard to safely provide care when needed during #COVID19,” tweeted Ralph Sacco, MD, chief and professor of neurology, University of Miami Miller School of Medicine in South Florida.
Although Florida Stroke Registry data are not publicly available, anecdotal reports suggest that stroke admissions are down among many hospitals, Sacco told Medscape Medical News.
Furthermore, this is not a phenomenon only in the United States. “This has also been reported in other nations hit by COVID-19,” he said.
China is a prime example. There, many stroke centers have shown reduced functioning “because of fear of in-hospital cross infection and lack of experienced stroke care experts,” Jing Zhao, MD, PhD, and colleagues write in an editorial published online March 31 in Stroke.
Preliminary data show that “thrombectomies in Shanghai decreased by 50% in the first month after the Spring Festival compared with the same period in 2019,” write the editorialists, who are from Kings College London and the University of Pennsylvania in Philadelphia.
“Although the control of the COVID-19 is very important, at the same time, the management of stroke must not be neglected,” they add.
“Over 9000 new stroke cases occur each day in China alone. It cannot be right that treatment for one potentially curable disease is euthanized at the expense of another.”
Fear Factor?
The reasons individuals who may have experienced a stroke are avoiding emergency care is unclear at the moment. “I’m not really sure anyone really understands why, quite honestly,” Tirschwell said.
Until survey data or other data emerge, many experts are assuming that fear of COVID-19 is trumping other medical concerns, including emergency treatment of stroke.
“We believe this could represent patients being fearful to come to medical facilities with stroke-like symptoms, given the COVID-19 pandemic,” said Sacco, who is also incoming editor-in-chief of Stroke.
The BBC has been getting the word out in the United Kingdom via social media, with a tweet to “Dial 999 for stroke emergencies despite coronavirus.”
The World Stroke Campaign is also using Twitter to emphasize the need for urgent stroke care when appropriate:
“Don’t let concerns about COVID19 prevent you from seeking emergency treatment for stroke. If you spot the signs of stroke act FAST. Get emergency medical assistance,” the group urged in a tweet.
Don’t Hesitate
The American Heart Association (AHA) has addressed this troubling trend as well.
“People with serious symptoms shouldn’t ignore them,” Sarah Perlman, MD, associate professor of emergency medicine at the University of Colorado School of Medicine, Denver, states in an article on the AHA website.
Perlman added that some individuals who have signs of stroke and heart disease may hesitate to seek care because of fear that they are adding to an overburdened healthcare staff and system. However, she dismissed those concerns outright.
“If you’re experiencing warning signs of a heart attack or stroke, call 911,” she said. “Clearly, if there’s an emergency, we are available and capable and eager to take care of you.”
This article first appeared on Medscape.com.
(EDs).
Stroke specialists in New Orleans, Chicago, Seattle, and elsewhere told Medscape Medical News they are seeing a precipitous drop in the number of acute strokes at their institutions – and not just in the number of milder cases. Doctors on Twitter are sharing similar reports and are using social media to highlight this issue.
Gabriel Vidal, MD, a vascular and interventional neurologist at the Ochsner Medical Center, New Orleans, Louisiana, said there are “definitely” fewer patients with stroke and transient ischemic attack (TIA) seeking care at his facility and others throughout the New Orleans area, which has been hard hit by COVID-19.
“Even in Louisiana, we have a very large 53-hospital telestroke network, and the number of consults has diminished greatly,” Vidal added.
In Chicago, emergency medical service activations for patients with suspected strokes are down about 30%, Shyam Prabhakaran, MD, professor and chair of neurology at the University of Chicago Biological Sciences, Illinois, told Medscape Medical News.
“It appears to be that mild stroke and TIA patients may be more likely to stay at home and seek alternative care rather than come to the ED,” Prabhakaran said. However, “the severe strokes may be less affected and continue to come to emergency departments.”
“Getting the Word Out”
That may not be the whole story in Seattle, Washington, where a stroke specialist at Harborview Medical Center reported a drop in patients across the stroke-severity spectrum.
Some patients with milder strokes no longer come to Harborview for a comprehensive evaluation and workup, but that is only “a partial explanation,” said David Tirschwell, MD, medical director of comprehensive stroke care at the University of Washington (UW) Medicine Stroke Center at Harborview and a professor of neurology at UW.
“The thrombectomies are down also,” he added. “It’s hard to have great numbers in real time, but it’s probably safe to say it’s at least a 50% reduction in the number of admissions.”
As a stroke referral center, his institution is seeing fewer local cases and referrals from outside hospitals. “I think both of those sources for admissions of stroke cases are down,” Tirschwell said.
Recognizing the seriousness of forgoing essential care for acute stroke, neurologists, institutions, and medical groups are taking to social media to potentially save lives.
“Across our @FLStrokeReg we are seeing less patients with #stroke symptoms coming to our hospitals. We need to get the word out that our teams are working hard to safely provide care when needed during #COVID19,” tweeted Ralph Sacco, MD, chief and professor of neurology, University of Miami Miller School of Medicine in South Florida.
Although Florida Stroke Registry data are not publicly available, anecdotal reports suggest that stroke admissions are down among many hospitals, Sacco told Medscape Medical News.
Furthermore, this is not a phenomenon only in the United States. “This has also been reported in other nations hit by COVID-19,” he said.
China is a prime example. There, many stroke centers have shown reduced functioning “because of fear of in-hospital cross infection and lack of experienced stroke care experts,” Jing Zhao, MD, PhD, and colleagues write in an editorial published online March 31 in Stroke.
Preliminary data show that “thrombectomies in Shanghai decreased by 50% in the first month after the Spring Festival compared with the same period in 2019,” write the editorialists, who are from Kings College London and the University of Pennsylvania in Philadelphia.
“Although the control of the COVID-19 is very important, at the same time, the management of stroke must not be neglected,” they add.
“Over 9000 new stroke cases occur each day in China alone. It cannot be right that treatment for one potentially curable disease is euthanized at the expense of another.”
Fear Factor?
The reasons individuals who may have experienced a stroke are avoiding emergency care is unclear at the moment. “I’m not really sure anyone really understands why, quite honestly,” Tirschwell said.
Until survey data or other data emerge, many experts are assuming that fear of COVID-19 is trumping other medical concerns, including emergency treatment of stroke.
“We believe this could represent patients being fearful to come to medical facilities with stroke-like symptoms, given the COVID-19 pandemic,” said Sacco, who is also incoming editor-in-chief of Stroke.
The BBC has been getting the word out in the United Kingdom via social media, with a tweet to “Dial 999 for stroke emergencies despite coronavirus.”
The World Stroke Campaign is also using Twitter to emphasize the need for urgent stroke care when appropriate:
“Don’t let concerns about COVID19 prevent you from seeking emergency treatment for stroke. If you spot the signs of stroke act FAST. Get emergency medical assistance,” the group urged in a tweet.
Don’t Hesitate
The American Heart Association (AHA) has addressed this troubling trend as well.
“People with serious symptoms shouldn’t ignore them,” Sarah Perlman, MD, associate professor of emergency medicine at the University of Colorado School of Medicine, Denver, states in an article on the AHA website.
Perlman added that some individuals who have signs of stroke and heart disease may hesitate to seek care because of fear that they are adding to an overburdened healthcare staff and system. However, she dismissed those concerns outright.
“If you’re experiencing warning signs of a heart attack or stroke, call 911,” she said. “Clearly, if there’s an emergency, we are available and capable and eager to take care of you.”
This article first appeared on Medscape.com.
(EDs).
Stroke specialists in New Orleans, Chicago, Seattle, and elsewhere told Medscape Medical News they are seeing a precipitous drop in the number of acute strokes at their institutions – and not just in the number of milder cases. Doctors on Twitter are sharing similar reports and are using social media to highlight this issue.
Gabriel Vidal, MD, a vascular and interventional neurologist at the Ochsner Medical Center, New Orleans, Louisiana, said there are “definitely” fewer patients with stroke and transient ischemic attack (TIA) seeking care at his facility and others throughout the New Orleans area, which has been hard hit by COVID-19.
“Even in Louisiana, we have a very large 53-hospital telestroke network, and the number of consults has diminished greatly,” Vidal added.
In Chicago, emergency medical service activations for patients with suspected strokes are down about 30%, Shyam Prabhakaran, MD, professor and chair of neurology at the University of Chicago Biological Sciences, Illinois, told Medscape Medical News.
“It appears to be that mild stroke and TIA patients may be more likely to stay at home and seek alternative care rather than come to the ED,” Prabhakaran said. However, “the severe strokes may be less affected and continue to come to emergency departments.”
“Getting the Word Out”
That may not be the whole story in Seattle, Washington, where a stroke specialist at Harborview Medical Center reported a drop in patients across the stroke-severity spectrum.
Some patients with milder strokes no longer come to Harborview for a comprehensive evaluation and workup, but that is only “a partial explanation,” said David Tirschwell, MD, medical director of comprehensive stroke care at the University of Washington (UW) Medicine Stroke Center at Harborview and a professor of neurology at UW.
“The thrombectomies are down also,” he added. “It’s hard to have great numbers in real time, but it’s probably safe to say it’s at least a 50% reduction in the number of admissions.”
As a stroke referral center, his institution is seeing fewer local cases and referrals from outside hospitals. “I think both of those sources for admissions of stroke cases are down,” Tirschwell said.
Recognizing the seriousness of forgoing essential care for acute stroke, neurologists, institutions, and medical groups are taking to social media to potentially save lives.
“Across our @FLStrokeReg we are seeing less patients with #stroke symptoms coming to our hospitals. We need to get the word out that our teams are working hard to safely provide care when needed during #COVID19,” tweeted Ralph Sacco, MD, chief and professor of neurology, University of Miami Miller School of Medicine in South Florida.
Although Florida Stroke Registry data are not publicly available, anecdotal reports suggest that stroke admissions are down among many hospitals, Sacco told Medscape Medical News.
Furthermore, this is not a phenomenon only in the United States. “This has also been reported in other nations hit by COVID-19,” he said.
China is a prime example. There, many stroke centers have shown reduced functioning “because of fear of in-hospital cross infection and lack of experienced stroke care experts,” Jing Zhao, MD, PhD, and colleagues write in an editorial published online March 31 in Stroke.
Preliminary data show that “thrombectomies in Shanghai decreased by 50% in the first month after the Spring Festival compared with the same period in 2019,” write the editorialists, who are from Kings College London and the University of Pennsylvania in Philadelphia.
“Although the control of the COVID-19 is very important, at the same time, the management of stroke must not be neglected,” they add.
“Over 9000 new stroke cases occur each day in China alone. It cannot be right that treatment for one potentially curable disease is euthanized at the expense of another.”
Fear Factor?
The reasons individuals who may have experienced a stroke are avoiding emergency care is unclear at the moment. “I’m not really sure anyone really understands why, quite honestly,” Tirschwell said.
Until survey data or other data emerge, many experts are assuming that fear of COVID-19 is trumping other medical concerns, including emergency treatment of stroke.
“We believe this could represent patients being fearful to come to medical facilities with stroke-like symptoms, given the COVID-19 pandemic,” said Sacco, who is also incoming editor-in-chief of Stroke.
The BBC has been getting the word out in the United Kingdom via social media, with a tweet to “Dial 999 for stroke emergencies despite coronavirus.”
The World Stroke Campaign is also using Twitter to emphasize the need for urgent stroke care when appropriate:
“Don’t let concerns about COVID19 prevent you from seeking emergency treatment for stroke. If you spot the signs of stroke act FAST. Get emergency medical assistance,” the group urged in a tweet.
Don’t Hesitate
The American Heart Association (AHA) has addressed this troubling trend as well.
“People with serious symptoms shouldn’t ignore them,” Sarah Perlman, MD, associate professor of emergency medicine at the University of Colorado School of Medicine, Denver, states in an article on the AHA website.
Perlman added that some individuals who have signs of stroke and heart disease may hesitate to seek care because of fear that they are adding to an overburdened healthcare staff and system. However, she dismissed those concerns outright.
“If you’re experiencing warning signs of a heart attack or stroke, call 911,” she said. “Clearly, if there’s an emergency, we are available and capable and eager to take care of you.”
This article first appeared on Medscape.com.
COVID-19: Dramatic changes to telepsychiatry rules and regs
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
FDA approves first generic albuterol inhaler
The Food and Drug Administration has approved the first generic of Proventil HFA (albuterol sulfate) metered-dose inhaler, 90 mcg/inhalation, according to a release from the agency. This inhaler is indicated for prevention of bronchospasm in patients aged 4 years and older. Specifically, these are patients with reversible obstructive airway disease or exercise-induced bronchospasm.
“The FDA recognizes the increased demand for albuterol products during the novel coronavirus pandemic,” said FDA Commissioner Stephen M. Hahn, MD.
The most common side effects include upper respiratory tract infection, rhinitis, nausea, vomiting, rapid heart rate, tremor, and nervousness.
This approval comes as part of FDA’s efforts to guide industry through the development process of generic products, according to the release. Complex combination products – such as this inhaler, which comprises both medication and a delivery system – can be more challenging to develop than solid oral dosage forms, such as tablets.
The FDA released a draft guidance in March 2020 specific to proposed generic albuterol sulfate metered-dose inhalers, including drug products referencing Proventil HFA. As with other similar guidances, it details the steps companies need to take in developing generics in order to submit complete applications for those products. The full news release regarding this approval is available on the FDA website.
This article was updated 4/8/20.
The Food and Drug Administration has approved the first generic of Proventil HFA (albuterol sulfate) metered-dose inhaler, 90 mcg/inhalation, according to a release from the agency. This inhaler is indicated for prevention of bronchospasm in patients aged 4 years and older. Specifically, these are patients with reversible obstructive airway disease or exercise-induced bronchospasm.
“The FDA recognizes the increased demand for albuterol products during the novel coronavirus pandemic,” said FDA Commissioner Stephen M. Hahn, MD.
The most common side effects include upper respiratory tract infection, rhinitis, nausea, vomiting, rapid heart rate, tremor, and nervousness.
This approval comes as part of FDA’s efforts to guide industry through the development process of generic products, according to the release. Complex combination products – such as this inhaler, which comprises both medication and a delivery system – can be more challenging to develop than solid oral dosage forms, such as tablets.
The FDA released a draft guidance in March 2020 specific to proposed generic albuterol sulfate metered-dose inhalers, including drug products referencing Proventil HFA. As with other similar guidances, it details the steps companies need to take in developing generics in order to submit complete applications for those products. The full news release regarding this approval is available on the FDA website.
This article was updated 4/8/20.
The Food and Drug Administration has approved the first generic of Proventil HFA (albuterol sulfate) metered-dose inhaler, 90 mcg/inhalation, according to a release from the agency. This inhaler is indicated for prevention of bronchospasm in patients aged 4 years and older. Specifically, these are patients with reversible obstructive airway disease or exercise-induced bronchospasm.
“The FDA recognizes the increased demand for albuterol products during the novel coronavirus pandemic,” said FDA Commissioner Stephen M. Hahn, MD.
The most common side effects include upper respiratory tract infection, rhinitis, nausea, vomiting, rapid heart rate, tremor, and nervousness.
This approval comes as part of FDA’s efforts to guide industry through the development process of generic products, according to the release. Complex combination products – such as this inhaler, which comprises both medication and a delivery system – can be more challenging to develop than solid oral dosage forms, such as tablets.
The FDA released a draft guidance in March 2020 specific to proposed generic albuterol sulfate metered-dose inhalers, including drug products referencing Proventil HFA. As with other similar guidances, it details the steps companies need to take in developing generics in order to submit complete applications for those products. The full news release regarding this approval is available on the FDA website.
This article was updated 4/8/20.
ACOG offers guidance on optimizing patient care in the midst of COVID-19
The American College of Obstetricians and Gynecologists (ACOG) posted a useful resource on its website on March 30 for clinicians practicing ambulatory gynecology. The guidance, “COVID-19 FAQs for Obstetrician–Gynecologists, Gynecology” (https://www.acog.org/), is based on expert opinion and is intended to supplement guidance from the Centers for Disease Control and Prevention as well as previously issued ACOG guidance.1
Which patients need to be seen, and when
The ACOG guidance provides examples of patients needing in-person appointments, video or telephone visits, or for whom deferral of a visit until after the COVID-19 outbreak would be appropriate. Highlights include:
In-person appointments
- suspected ectopic pregnancy
- profuse vaginal bleeding
Video or telephone visits
- contraceptive counseling and prescribing
- management of menopausal symptoms
Deferral of a visit until after the COVID-19 outbreak
- routine well-woman visits for average-risk patients.
Cervical screening
With respect to patients with abnormal cervical cancer screening results, ACOG recommends the ASCCP’s guidance that2:
- for patients with low-grade test results, colposcopy/cervical biopsies be deferred up to 6 to 12 months
- for patients with high-grade results, colposcopy/cervical biopsies be performed within 3 months.
Contraception
Regarding contraceptive services, the ACOG guidance suggests that placement of intrauterine devices (IUDs) and contraceptive implants should continue “where possible.” If initiation of long-acting reversible contraception (LARC) is not feasible, the guidance recommends that use of self-administered contraceptives (including subcutaneous injections, oral, transdermal patch, and vaginal ring contraception) be encouraged as a bridge to later initiation of LARC.
The guidance suggests that removal of IUDs and implants be postponed when possible.
Finally, the guidance suggests that patients with an existing IUD or implant who seek removal and replacement of their contraceptives be counseled regarding extended use of these devices.
Individualize your approach
ACOG emphasizes that no single solution applies to all situations and that each practice or clinic should evaluate the individual situation, including the availability of local and regional resources, staffing, and personal protective equipment; the prevalence of COVID-19 in the region; and the type of practice.
A roadmap for care
This guidance from ACOG should help clinicians caring for women during the COVID-19 outbreak to counsel and guide patients in a prudent manner.
- American College of Obstetricians and Gynecologists website. COVID-19 FAQs for obstetrician-gynecologists, gynecology. https://www.acog.org/clinical-information/physician-faqs/covid19-faqs-for-ob-gyns-gynecology. Accessed April 3, 2020.
- ASCCP website. ASCCP interim guidance for timing of diagnostic and treatment procedures for patients with abnormal cervical screening tests. https://www.asccp.org/covid-19. Accessed April 3, 2020.
The American College of Obstetricians and Gynecologists (ACOG) posted a useful resource on its website on March 30 for clinicians practicing ambulatory gynecology. The guidance, “COVID-19 FAQs for Obstetrician–Gynecologists, Gynecology” (https://www.acog.org/), is based on expert opinion and is intended to supplement guidance from the Centers for Disease Control and Prevention as well as previously issued ACOG guidance.1
Which patients need to be seen, and when
The ACOG guidance provides examples of patients needing in-person appointments, video or telephone visits, or for whom deferral of a visit until after the COVID-19 outbreak would be appropriate. Highlights include:
In-person appointments
- suspected ectopic pregnancy
- profuse vaginal bleeding
Video or telephone visits
- contraceptive counseling and prescribing
- management of menopausal symptoms
Deferral of a visit until after the COVID-19 outbreak
- routine well-woman visits for average-risk patients.
Cervical screening
With respect to patients with abnormal cervical cancer screening results, ACOG recommends the ASCCP’s guidance that2:
- for patients with low-grade test results, colposcopy/cervical biopsies be deferred up to 6 to 12 months
- for patients with high-grade results, colposcopy/cervical biopsies be performed within 3 months.
Contraception
Regarding contraceptive services, the ACOG guidance suggests that placement of intrauterine devices (IUDs) and contraceptive implants should continue “where possible.” If initiation of long-acting reversible contraception (LARC) is not feasible, the guidance recommends that use of self-administered contraceptives (including subcutaneous injections, oral, transdermal patch, and vaginal ring contraception) be encouraged as a bridge to later initiation of LARC.
The guidance suggests that removal of IUDs and implants be postponed when possible.
Finally, the guidance suggests that patients with an existing IUD or implant who seek removal and replacement of their contraceptives be counseled regarding extended use of these devices.
Individualize your approach
ACOG emphasizes that no single solution applies to all situations and that each practice or clinic should evaluate the individual situation, including the availability of local and regional resources, staffing, and personal protective equipment; the prevalence of COVID-19 in the region; and the type of practice.
A roadmap for care
This guidance from ACOG should help clinicians caring for women during the COVID-19 outbreak to counsel and guide patients in a prudent manner.
The American College of Obstetricians and Gynecologists (ACOG) posted a useful resource on its website on March 30 for clinicians practicing ambulatory gynecology. The guidance, “COVID-19 FAQs for Obstetrician–Gynecologists, Gynecology” (https://www.acog.org/), is based on expert opinion and is intended to supplement guidance from the Centers for Disease Control and Prevention as well as previously issued ACOG guidance.1
Which patients need to be seen, and when
The ACOG guidance provides examples of patients needing in-person appointments, video or telephone visits, or for whom deferral of a visit until after the COVID-19 outbreak would be appropriate. Highlights include:
In-person appointments
- suspected ectopic pregnancy
- profuse vaginal bleeding
Video or telephone visits
- contraceptive counseling and prescribing
- management of menopausal symptoms
Deferral of a visit until after the COVID-19 outbreak
- routine well-woman visits for average-risk patients.
Cervical screening
With respect to patients with abnormal cervical cancer screening results, ACOG recommends the ASCCP’s guidance that2:
- for patients with low-grade test results, colposcopy/cervical biopsies be deferred up to 6 to 12 months
- for patients with high-grade results, colposcopy/cervical biopsies be performed within 3 months.
Contraception
Regarding contraceptive services, the ACOG guidance suggests that placement of intrauterine devices (IUDs) and contraceptive implants should continue “where possible.” If initiation of long-acting reversible contraception (LARC) is not feasible, the guidance recommends that use of self-administered contraceptives (including subcutaneous injections, oral, transdermal patch, and vaginal ring contraception) be encouraged as a bridge to later initiation of LARC.
The guidance suggests that removal of IUDs and implants be postponed when possible.
Finally, the guidance suggests that patients with an existing IUD or implant who seek removal and replacement of their contraceptives be counseled regarding extended use of these devices.
Individualize your approach
ACOG emphasizes that no single solution applies to all situations and that each practice or clinic should evaluate the individual situation, including the availability of local and regional resources, staffing, and personal protective equipment; the prevalence of COVID-19 in the region; and the type of practice.
A roadmap for care
This guidance from ACOG should help clinicians caring for women during the COVID-19 outbreak to counsel and guide patients in a prudent manner.
- American College of Obstetricians and Gynecologists website. COVID-19 FAQs for obstetrician-gynecologists, gynecology. https://www.acog.org/clinical-information/physician-faqs/covid19-faqs-for-ob-gyns-gynecology. Accessed April 3, 2020.
- ASCCP website. ASCCP interim guidance for timing of diagnostic and treatment procedures for patients with abnormal cervical screening tests. https://www.asccp.org/covid-19. Accessed April 3, 2020.
- American College of Obstetricians and Gynecologists website. COVID-19 FAQs for obstetrician-gynecologists, gynecology. https://www.acog.org/clinical-information/physician-faqs/covid19-faqs-for-ob-gyns-gynecology. Accessed April 3, 2020.
- ASCCP website. ASCCP interim guidance for timing of diagnostic and treatment procedures for patients with abnormal cervical screening tests. https://www.asccp.org/covid-19. Accessed April 3, 2020.
Comorbidities the rule in New York’s COVID-19 deaths
In New York state, just over 86% of reported COVID-19 deaths involved at least one comorbidity, according to the state’s department of health.
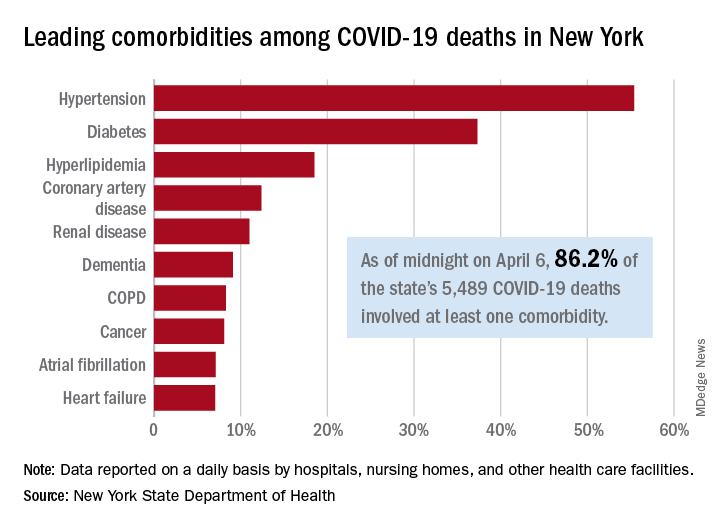
As of midnight on April 6, there had been 5,489 fatalities caused by COVID-19 in the state, of which 86.2% (4,732) had at least one underlying condition, the New York State Department of Health reported April 7 on its COVID-19 tracker.
The leading comorbidity, seen in 55.4% of all deaths, was hypertension. In comparison, a recent estimate from the U.S. Department of Health & Human Services put the prevalence of high blood pressure at about 45% in the overall adult population.
In New York, the rest of the 10 most common comorbidities in COVID-19 fatalities were diabetes (37.3%), hyperlipidemia (18.5%), coronary artery disease (12.4%), renal disease (11.0%), dementia (9.1%), chronic obstructive pulmonary disease (8.3%), cancer (8.1%), atrial fibrillation (7.1%), and heart failure (7.1%), the NYSDOH said.
Other data on the tracker site show that 63% of all deaths involved a patient who was aged 70 years or older and that 61% of COVID-19 patients who have died in New York were male and 38.8% were female (sex unknown for 0.2%). Among all individuals who have tested positive, 54.8% were male and 44.6% were female (sex unknown for 0.6%).
As of the end of day on April 6, a total of 340,058 persons had been tested in the state and 40.8% (138,863) were positive for the SARS-CoV-2 virus. By county, the highest positive rates are in New York City: Queens at 57.4%, Brooklyn at 52.4%, and the Bronx at 52.3%, according to the NYSDOH.
In New York state, just over 86% of reported COVID-19 deaths involved at least one comorbidity, according to the state’s department of health.
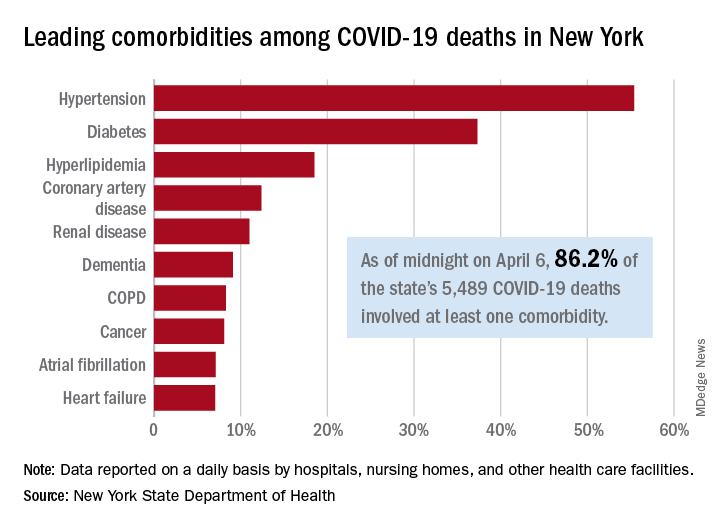
As of midnight on April 6, there had been 5,489 fatalities caused by COVID-19 in the state, of which 86.2% (4,732) had at least one underlying condition, the New York State Department of Health reported April 7 on its COVID-19 tracker.
The leading comorbidity, seen in 55.4% of all deaths, was hypertension. In comparison, a recent estimate from the U.S. Department of Health & Human Services put the prevalence of high blood pressure at about 45% in the overall adult population.
In New York, the rest of the 10 most common comorbidities in COVID-19 fatalities were diabetes (37.3%), hyperlipidemia (18.5%), coronary artery disease (12.4%), renal disease (11.0%), dementia (9.1%), chronic obstructive pulmonary disease (8.3%), cancer (8.1%), atrial fibrillation (7.1%), and heart failure (7.1%), the NYSDOH said.
Other data on the tracker site show that 63% of all deaths involved a patient who was aged 70 years or older and that 61% of COVID-19 patients who have died in New York were male and 38.8% were female (sex unknown for 0.2%). Among all individuals who have tested positive, 54.8% were male and 44.6% were female (sex unknown for 0.6%).
As of the end of day on April 6, a total of 340,058 persons had been tested in the state and 40.8% (138,863) were positive for the SARS-CoV-2 virus. By county, the highest positive rates are in New York City: Queens at 57.4%, Brooklyn at 52.4%, and the Bronx at 52.3%, according to the NYSDOH.
In New York state, just over 86% of reported COVID-19 deaths involved at least one comorbidity, according to the state’s department of health.
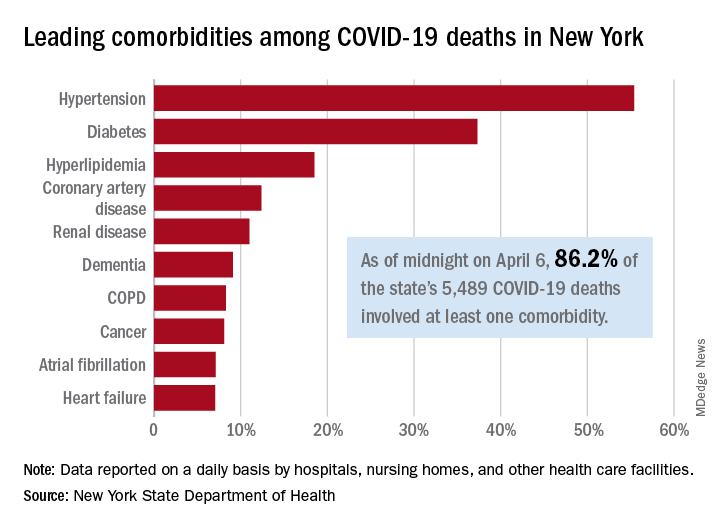
As of midnight on April 6, there had been 5,489 fatalities caused by COVID-19 in the state, of which 86.2% (4,732) had at least one underlying condition, the New York State Department of Health reported April 7 on its COVID-19 tracker.
The leading comorbidity, seen in 55.4% of all deaths, was hypertension. In comparison, a recent estimate from the U.S. Department of Health & Human Services put the prevalence of high blood pressure at about 45% in the overall adult population.
In New York, the rest of the 10 most common comorbidities in COVID-19 fatalities were diabetes (37.3%), hyperlipidemia (18.5%), coronary artery disease (12.4%), renal disease (11.0%), dementia (9.1%), chronic obstructive pulmonary disease (8.3%), cancer (8.1%), atrial fibrillation (7.1%), and heart failure (7.1%), the NYSDOH said.
Other data on the tracker site show that 63% of all deaths involved a patient who was aged 70 years or older and that 61% of COVID-19 patients who have died in New York were male and 38.8% were female (sex unknown for 0.2%). Among all individuals who have tested positive, 54.8% were male and 44.6% were female (sex unknown for 0.6%).
As of the end of day on April 6, a total of 340,058 persons had been tested in the state and 40.8% (138,863) were positive for the SARS-CoV-2 virus. By county, the highest positive rates are in New York City: Queens at 57.4%, Brooklyn at 52.4%, and the Bronx at 52.3%, according to the NYSDOH.
SARS-CoV-2 escapes cotton, surgical masks of infected
June 9, 2020 — Editor’s note: The study on which this news story is based has been retracted by the journal. The retraction notice can be found here.
according to Seongman Bae, MD, of the University of Ulsan College of Medicine in Seoul, South Korea, and associates.
The report was published in Annals of Internal Medicine.
Because the COVID-19 pandemic has caused a shortage of N95 and surgical masks, cotton masks have gained interest as a substitute, as surgical masks have been shown to effectively filter influenza virus, the researchers wrote. However, the size of and concentrations of SARS-CoV-2 in aerosols generated during coughing are unknown.
To compare the effectiveness of cotton and surgical masks, a group of patients infected with SARS-CoV-2 coughed into petri dishes while wearing no mask, a surgical mask, and a cotton mask. The mask surfaces were swabbed afterward to assess viral positivity on the mask itself.
The median nasopharyngeal and saliva viral load was 5.66 log copies/mL and 4.00 log copies/mL, respectively. The median viral loads after coughing was 2.56 log copies/mL without a mask, 2.42 log copies/mL with a surgical mask, and 1.85 log copies/mL with a cotton mask. All outer surfaces of the mask were positive for SARS-CoV-2, while most inner surfaces were negative.
The investigators acknowledged that the test did not include N95 masks and does not reflect the actual infection transmission, and that they didn’t know whether cotton or surgical masks shorten the travel distance of droplets while coughing.
“Further study is needed to recommend whether face masks decrease transmission of virus from asymptomatic individuals or those with suspected COVID-19 who are not coughing,” they added.
The study was funded by a grant from the government-wide R&D Fund Project for Infectious Disease Research. The investigators reported that they had no conflicts of interest.
SOURCE: Bae S et al. Ann Intern Med. 2020 Apr 6. doi: 10.7326/M20-1342.
Correction, 4/9/20: The headline of an earlier version of this article misstated a finding of this study. Whether cotton and surgical masks can block transmission was not investigated.
June 9, 2020 — Editor’s note: The study on which this news story is based has been retracted by the journal. The retraction notice can be found here.
according to Seongman Bae, MD, of the University of Ulsan College of Medicine in Seoul, South Korea, and associates.
The report was published in Annals of Internal Medicine.
Because the COVID-19 pandemic has caused a shortage of N95 and surgical masks, cotton masks have gained interest as a substitute, as surgical masks have been shown to effectively filter influenza virus, the researchers wrote. However, the size of and concentrations of SARS-CoV-2 in aerosols generated during coughing are unknown.
To compare the effectiveness of cotton and surgical masks, a group of patients infected with SARS-CoV-2 coughed into petri dishes while wearing no mask, a surgical mask, and a cotton mask. The mask surfaces were swabbed afterward to assess viral positivity on the mask itself.
The median nasopharyngeal and saliva viral load was 5.66 log copies/mL and 4.00 log copies/mL, respectively. The median viral loads after coughing was 2.56 log copies/mL without a mask, 2.42 log copies/mL with a surgical mask, and 1.85 log copies/mL with a cotton mask. All outer surfaces of the mask were positive for SARS-CoV-2, while most inner surfaces were negative.
The investigators acknowledged that the test did not include N95 masks and does not reflect the actual infection transmission, and that they didn’t know whether cotton or surgical masks shorten the travel distance of droplets while coughing.
“Further study is needed to recommend whether face masks decrease transmission of virus from asymptomatic individuals or those with suspected COVID-19 who are not coughing,” they added.
The study was funded by a grant from the government-wide R&D Fund Project for Infectious Disease Research. The investigators reported that they had no conflicts of interest.
SOURCE: Bae S et al. Ann Intern Med. 2020 Apr 6. doi: 10.7326/M20-1342.
Correction, 4/9/20: The headline of an earlier version of this article misstated a finding of this study. Whether cotton and surgical masks can block transmission was not investigated.
June 9, 2020 — Editor’s note: The study on which this news story is based has been retracted by the journal. The retraction notice can be found here.
according to Seongman Bae, MD, of the University of Ulsan College of Medicine in Seoul, South Korea, and associates.
The report was published in Annals of Internal Medicine.
Because the COVID-19 pandemic has caused a shortage of N95 and surgical masks, cotton masks have gained interest as a substitute, as surgical masks have been shown to effectively filter influenza virus, the researchers wrote. However, the size of and concentrations of SARS-CoV-2 in aerosols generated during coughing are unknown.
To compare the effectiveness of cotton and surgical masks, a group of patients infected with SARS-CoV-2 coughed into petri dishes while wearing no mask, a surgical mask, and a cotton mask. The mask surfaces were swabbed afterward to assess viral positivity on the mask itself.
The median nasopharyngeal and saliva viral load was 5.66 log copies/mL and 4.00 log copies/mL, respectively. The median viral loads after coughing was 2.56 log copies/mL without a mask, 2.42 log copies/mL with a surgical mask, and 1.85 log copies/mL with a cotton mask. All outer surfaces of the mask were positive for SARS-CoV-2, while most inner surfaces were negative.
The investigators acknowledged that the test did not include N95 masks and does not reflect the actual infection transmission, and that they didn’t know whether cotton or surgical masks shorten the travel distance of droplets while coughing.
“Further study is needed to recommend whether face masks decrease transmission of virus from asymptomatic individuals or those with suspected COVID-19 who are not coughing,” they added.
The study was funded by a grant from the government-wide R&D Fund Project for Infectious Disease Research. The investigators reported that they had no conflicts of interest.
SOURCE: Bae S et al. Ann Intern Med. 2020 Apr 6. doi: 10.7326/M20-1342.
Correction, 4/9/20: The headline of an earlier version of this article misstated a finding of this study. Whether cotton and surgical masks can block transmission was not investigated.
FROM ANNALS OF INTERNAL MEDICINE
Treating lung cancer in COVID-19 times: Update from experts
Lung cancer experts in Europe issued highly considered recommendations for the management of lung cancer during the COVID-19 crisis, the main intention of which is to minimize the risk of patients getting infected by SARS-CoV-2 while in hospital receiving treatment.
The recommendations were published online April 3 in ESMO Open.
“We know that having cancer increases the risk of dying of COVID-19, although not necessarily the risk of getting the virus, and we also know that having lung cancer could increase the risk of pulmonary complications from SARS-CoV-2,” lead author Alfredo Addeo, MD, University Hospital of Geneva, Switzerland, told Medscape Medical News.
“But patients who are often in the hospital have a higher risk of catching the virus. So this paper is not about not giving necessary treatment, it’s about treating patients the best you can based on the area where you live and the resources you have and keeping patients away from the hospital as much as possible,” he added.
“The main message is, try to personalize the care you deliver,” Addeo said. “Rather than remain rigid about how you’ve been treating patients thus far, try to think outside the box and find a way to minimize the risk of infection, and, if you have to limit treatment, discuss the pros and cons of your treatment plan with the patient and make sure the message is given clearly.”
How much benefit?
The first general concept to keep in mind is: How likely is a patient to benefit from treatment?
“All regimens with a survival benefit should be maintained and prioritised whenever possible,” Addeo and colleagues observe. The other co-authors of the paper are Giuseppe Banna, MD, Ospedale Cannizzaro, Catania, Italy; Alessandra Curioni-Fontecedro, MD, University Hospital Zurich, Switzerland; and Alex Friedlaender, MD, University Hospital of Geneva.
For non–small cell lung cancer (NSCLC), neoadjuvant chemotherapy for locally advanced resectable disease and sequential/concurrent chemotherapy/radiation therapy for patients with stage III lung cancer – provided they have adequate respiratory function – should be started when possible and should not be stopped without justification, the authors point out.
This is also true for first-line therapy in patients with metastatic disease. Treatment should also not be stopped without good reason among patients already receiving maintenance immune checkpoint inhibitor therapy.
For small cell lung cancer (SCLC), both first-line treatment for extensive-stage disease as well as concurrent chemotherapy/radiotherapy for patients with limited-stage disease should be started when possible, again provided they have adequate respiratory function.
Palliative or stereotactic body radiotherapy (SBRT) delivered outside the lung should also be initiated when possible in SCLC patients.
The authors caution, however, that if palliative or SBRT outside the lung requires multiple visits to the hospital, treatment to the lung should be limited to cases with compression of airways or bleeding.
Oncologists should also try to start radiotherapy on day 1 of chemotherapy because then only 2 cycles will be needed; if radiotherapy is started with cycle 2 or is given sequentially, 3 cycles of treatment will be required.
“Fractions of SBRT could be reduced, depending on organ at risk (8 fractions to 5 or 3) while palliative RT [given] as a single fraction or two (8-10 Gy or 17 Gy, respectively) should be used where possible,” the authors observe.
Concurrent chemotherapy with radiotherapy for limited-stage disease should not be stopped without justification and nor should first-line treatment for metastatic SCLC, the authors continue.
Again, however, patients must have adequate respiratory function to receive or continue with concurrent chemotherapy and radiotherapy, they add.
For patients with stage III NSCLC, concurrent chemotherapy plus radiotherapy may be considered and given preferentially or not.
Similarly, oral rather than intravenous chemotherapy may be preferred for elderly NSCLC patients or for those with an ECOG performance status of 2 as well as for SCLC patients.
Delaying surgery
As a general principle, the use of neoadjuvant chemotherapy instead of adjuvant therapy following surgery can delay the need for immediate surgery. If surgery can be delayed, “the risk of a patient catching the virus several months from now might be less,” Addeo noted. Thus, treating patients upfront with chemotherapy is one tactic to consider in appropriate patients.
For NSCLC patients at high risk for COVID-19, adjuvant chemotherapy should be discussed and potentially withheld, the authors observe.
NSCLC patients at high risk for COVID-19 include those with comorbidities, such as cardiovascular or pulmonary disease, as well as patients who are 70 years of age and older.
Immunotherapy should also be discussed and possibly delayed for stage III NSCLC patients following concurrent chemotherapy and radiation, they add.
Maintenance pemetrexed also may be withheld for NSCLC patients, and intervals of immunotherapy may be prolonged (e.g., nivolumab every 4 weeks and pembrolizumab every 6 weeks).
Intervals of immunotherapy should be similarly prolonged for SCLC patients, they continue.
“Shorter duration of chemotherapy (e.g., four cycles of chemotherapy instead of six) should be discussed with patients and maintenance chemotherapy can be withheld,” the authors note.
Furthermore, “given the pandemic, it is highly likely that metastatic cancer patients will be less likely to be intubated or to be heavily ventilated compared to patients without any comorbidity,” Addeo explained.
“So we have to acknowledge that metastatic lung cancer patients will be at higher risk of dying due to severe pulmonary COVID-19 complications,” he added.
Therefore, third and further lines of chemotherapy in both NSCLC and SCLC patients at significant COVID-19 risk should not be initiated without having a good reason to do so.
“Prophylactic cranial irradiation (PCI) is still a matter of debate [in SCLC patients],” Addeo noted. “So the reasonable alternative is to do surveillance MRI, and, in 6 or 8 months, we can probably offer PCI more safely at that point,” he suggested, adding that radiation therapy to the brain should only be considered if a patient develops brain metastases.
The authors also suggest that thoracic consolidation radiotherapy for extensive stage SCLC should not be initiated unless there is good reason to do so.
Patients with family members or caregivers who have tested positive for COVID-19 should themselves be tested before or during any cancer treatment.
If patients themselves then test positive and are asymptomatic, “28 days of delay should be considered before (re)starting the treatment,” the authors advise.
However, two negative tests done 1 week apart should be carried out before starting or restarting treatment, they note.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Lung cancer experts in Europe issued highly considered recommendations for the management of lung cancer during the COVID-19 crisis, the main intention of which is to minimize the risk of patients getting infected by SARS-CoV-2 while in hospital receiving treatment.
The recommendations were published online April 3 in ESMO Open.
“We know that having cancer increases the risk of dying of COVID-19, although not necessarily the risk of getting the virus, and we also know that having lung cancer could increase the risk of pulmonary complications from SARS-CoV-2,” lead author Alfredo Addeo, MD, University Hospital of Geneva, Switzerland, told Medscape Medical News.
“But patients who are often in the hospital have a higher risk of catching the virus. So this paper is not about not giving necessary treatment, it’s about treating patients the best you can based on the area where you live and the resources you have and keeping patients away from the hospital as much as possible,” he added.
“The main message is, try to personalize the care you deliver,” Addeo said. “Rather than remain rigid about how you’ve been treating patients thus far, try to think outside the box and find a way to minimize the risk of infection, and, if you have to limit treatment, discuss the pros and cons of your treatment plan with the patient and make sure the message is given clearly.”
How much benefit?
The first general concept to keep in mind is: How likely is a patient to benefit from treatment?
“All regimens with a survival benefit should be maintained and prioritised whenever possible,” Addeo and colleagues observe. The other co-authors of the paper are Giuseppe Banna, MD, Ospedale Cannizzaro, Catania, Italy; Alessandra Curioni-Fontecedro, MD, University Hospital Zurich, Switzerland; and Alex Friedlaender, MD, University Hospital of Geneva.
For non–small cell lung cancer (NSCLC), neoadjuvant chemotherapy for locally advanced resectable disease and sequential/concurrent chemotherapy/radiation therapy for patients with stage III lung cancer – provided they have adequate respiratory function – should be started when possible and should not be stopped without justification, the authors point out.
This is also true for first-line therapy in patients with metastatic disease. Treatment should also not be stopped without good reason among patients already receiving maintenance immune checkpoint inhibitor therapy.
For small cell lung cancer (SCLC), both first-line treatment for extensive-stage disease as well as concurrent chemotherapy/radiotherapy for patients with limited-stage disease should be started when possible, again provided they have adequate respiratory function.
Palliative or stereotactic body radiotherapy (SBRT) delivered outside the lung should also be initiated when possible in SCLC patients.
The authors caution, however, that if palliative or SBRT outside the lung requires multiple visits to the hospital, treatment to the lung should be limited to cases with compression of airways or bleeding.
Oncologists should also try to start radiotherapy on day 1 of chemotherapy because then only 2 cycles will be needed; if radiotherapy is started with cycle 2 or is given sequentially, 3 cycles of treatment will be required.
“Fractions of SBRT could be reduced, depending on organ at risk (8 fractions to 5 or 3) while palliative RT [given] as a single fraction or two (8-10 Gy or 17 Gy, respectively) should be used where possible,” the authors observe.
Concurrent chemotherapy with radiotherapy for limited-stage disease should not be stopped without justification and nor should first-line treatment for metastatic SCLC, the authors continue.
Again, however, patients must have adequate respiratory function to receive or continue with concurrent chemotherapy and radiotherapy, they add.
For patients with stage III NSCLC, concurrent chemotherapy plus radiotherapy may be considered and given preferentially or not.
Similarly, oral rather than intravenous chemotherapy may be preferred for elderly NSCLC patients or for those with an ECOG performance status of 2 as well as for SCLC patients.
Delaying surgery
As a general principle, the use of neoadjuvant chemotherapy instead of adjuvant therapy following surgery can delay the need for immediate surgery. If surgery can be delayed, “the risk of a patient catching the virus several months from now might be less,” Addeo noted. Thus, treating patients upfront with chemotherapy is one tactic to consider in appropriate patients.
For NSCLC patients at high risk for COVID-19, adjuvant chemotherapy should be discussed and potentially withheld, the authors observe.
NSCLC patients at high risk for COVID-19 include those with comorbidities, such as cardiovascular or pulmonary disease, as well as patients who are 70 years of age and older.
Immunotherapy should also be discussed and possibly delayed for stage III NSCLC patients following concurrent chemotherapy and radiation, they add.
Maintenance pemetrexed also may be withheld for NSCLC patients, and intervals of immunotherapy may be prolonged (e.g., nivolumab every 4 weeks and pembrolizumab every 6 weeks).
Intervals of immunotherapy should be similarly prolonged for SCLC patients, they continue.
“Shorter duration of chemotherapy (e.g., four cycles of chemotherapy instead of six) should be discussed with patients and maintenance chemotherapy can be withheld,” the authors note.
Furthermore, “given the pandemic, it is highly likely that metastatic cancer patients will be less likely to be intubated or to be heavily ventilated compared to patients without any comorbidity,” Addeo explained.
“So we have to acknowledge that metastatic lung cancer patients will be at higher risk of dying due to severe pulmonary COVID-19 complications,” he added.
Therefore, third and further lines of chemotherapy in both NSCLC and SCLC patients at significant COVID-19 risk should not be initiated without having a good reason to do so.
“Prophylactic cranial irradiation (PCI) is still a matter of debate [in SCLC patients],” Addeo noted. “So the reasonable alternative is to do surveillance MRI, and, in 6 or 8 months, we can probably offer PCI more safely at that point,” he suggested, adding that radiation therapy to the brain should only be considered if a patient develops brain metastases.
The authors also suggest that thoracic consolidation radiotherapy for extensive stage SCLC should not be initiated unless there is good reason to do so.
Patients with family members or caregivers who have tested positive for COVID-19 should themselves be tested before or during any cancer treatment.
If patients themselves then test positive and are asymptomatic, “28 days of delay should be considered before (re)starting the treatment,” the authors advise.
However, two negative tests done 1 week apart should be carried out before starting or restarting treatment, they note.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Lung cancer experts in Europe issued highly considered recommendations for the management of lung cancer during the COVID-19 crisis, the main intention of which is to minimize the risk of patients getting infected by SARS-CoV-2 while in hospital receiving treatment.
The recommendations were published online April 3 in ESMO Open.
“We know that having cancer increases the risk of dying of COVID-19, although not necessarily the risk of getting the virus, and we also know that having lung cancer could increase the risk of pulmonary complications from SARS-CoV-2,” lead author Alfredo Addeo, MD, University Hospital of Geneva, Switzerland, told Medscape Medical News.
“But patients who are often in the hospital have a higher risk of catching the virus. So this paper is not about not giving necessary treatment, it’s about treating patients the best you can based on the area where you live and the resources you have and keeping patients away from the hospital as much as possible,” he added.
“The main message is, try to personalize the care you deliver,” Addeo said. “Rather than remain rigid about how you’ve been treating patients thus far, try to think outside the box and find a way to minimize the risk of infection, and, if you have to limit treatment, discuss the pros and cons of your treatment plan with the patient and make sure the message is given clearly.”
How much benefit?
The first general concept to keep in mind is: How likely is a patient to benefit from treatment?
“All regimens with a survival benefit should be maintained and prioritised whenever possible,” Addeo and colleagues observe. The other co-authors of the paper are Giuseppe Banna, MD, Ospedale Cannizzaro, Catania, Italy; Alessandra Curioni-Fontecedro, MD, University Hospital Zurich, Switzerland; and Alex Friedlaender, MD, University Hospital of Geneva.
For non–small cell lung cancer (NSCLC), neoadjuvant chemotherapy for locally advanced resectable disease and sequential/concurrent chemotherapy/radiation therapy for patients with stage III lung cancer – provided they have adequate respiratory function – should be started when possible and should not be stopped without justification, the authors point out.
This is also true for first-line therapy in patients with metastatic disease. Treatment should also not be stopped without good reason among patients already receiving maintenance immune checkpoint inhibitor therapy.
For small cell lung cancer (SCLC), both first-line treatment for extensive-stage disease as well as concurrent chemotherapy/radiotherapy for patients with limited-stage disease should be started when possible, again provided they have adequate respiratory function.
Palliative or stereotactic body radiotherapy (SBRT) delivered outside the lung should also be initiated when possible in SCLC patients.
The authors caution, however, that if palliative or SBRT outside the lung requires multiple visits to the hospital, treatment to the lung should be limited to cases with compression of airways or bleeding.
Oncologists should also try to start radiotherapy on day 1 of chemotherapy because then only 2 cycles will be needed; if radiotherapy is started with cycle 2 or is given sequentially, 3 cycles of treatment will be required.
“Fractions of SBRT could be reduced, depending on organ at risk (8 fractions to 5 or 3) while palliative RT [given] as a single fraction or two (8-10 Gy or 17 Gy, respectively) should be used where possible,” the authors observe.
Concurrent chemotherapy with radiotherapy for limited-stage disease should not be stopped without justification and nor should first-line treatment for metastatic SCLC, the authors continue.
Again, however, patients must have adequate respiratory function to receive or continue with concurrent chemotherapy and radiotherapy, they add.
For patients with stage III NSCLC, concurrent chemotherapy plus radiotherapy may be considered and given preferentially or not.
Similarly, oral rather than intravenous chemotherapy may be preferred for elderly NSCLC patients or for those with an ECOG performance status of 2 as well as for SCLC patients.
Delaying surgery
As a general principle, the use of neoadjuvant chemotherapy instead of adjuvant therapy following surgery can delay the need for immediate surgery. If surgery can be delayed, “the risk of a patient catching the virus several months from now might be less,” Addeo noted. Thus, treating patients upfront with chemotherapy is one tactic to consider in appropriate patients.
For NSCLC patients at high risk for COVID-19, adjuvant chemotherapy should be discussed and potentially withheld, the authors observe.
NSCLC patients at high risk for COVID-19 include those with comorbidities, such as cardiovascular or pulmonary disease, as well as patients who are 70 years of age and older.
Immunotherapy should also be discussed and possibly delayed for stage III NSCLC patients following concurrent chemotherapy and radiation, they add.
Maintenance pemetrexed also may be withheld for NSCLC patients, and intervals of immunotherapy may be prolonged (e.g., nivolumab every 4 weeks and pembrolizumab every 6 weeks).
Intervals of immunotherapy should be similarly prolonged for SCLC patients, they continue.
“Shorter duration of chemotherapy (e.g., four cycles of chemotherapy instead of six) should be discussed with patients and maintenance chemotherapy can be withheld,” the authors note.
Furthermore, “given the pandemic, it is highly likely that metastatic cancer patients will be less likely to be intubated or to be heavily ventilated compared to patients without any comorbidity,” Addeo explained.
“So we have to acknowledge that metastatic lung cancer patients will be at higher risk of dying due to severe pulmonary COVID-19 complications,” he added.
Therefore, third and further lines of chemotherapy in both NSCLC and SCLC patients at significant COVID-19 risk should not be initiated without having a good reason to do so.
“Prophylactic cranial irradiation (PCI) is still a matter of debate [in SCLC patients],” Addeo noted. “So the reasonable alternative is to do surveillance MRI, and, in 6 or 8 months, we can probably offer PCI more safely at that point,” he suggested, adding that radiation therapy to the brain should only be considered if a patient develops brain metastases.
The authors also suggest that thoracic consolidation radiotherapy for extensive stage SCLC should not be initiated unless there is good reason to do so.
Patients with family members or caregivers who have tested positive for COVID-19 should themselves be tested before or during any cancer treatment.
If patients themselves then test positive and are asymptomatic, “28 days of delay should be considered before (re)starting the treatment,” the authors advise.
However, two negative tests done 1 week apart should be carried out before starting or restarting treatment, they note.
The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Treatment for RA, SpA may not affect COVID-19 severity
Patients being treated for RA or spondyloarthritis who develop symptoms of COVID-19 do not appear to be at higher risk of respiratory or life-threatening complications, results from a new study in Italy suggest.
Such patients, the study authors wrote, do not need to be taken off their immunosuppressive medications if they develop COVID-19 symptoms.
In a letter published in Annals of the Rheumatic Diseases, Sara Monti, MD, and colleagues in the rheumatology department of the Fondazione IRCCS Policlinico in San Matteo, Italy, described results from an observational cohort of 320 patients (68% women; mean age, 55 years) with RA or spondyloarthritis from a single outpatient clinic. The vast majority of subjects (92%) were taking biologic disease-modifying antirheumatic drugs (bDMARD), including tumor necrosis factor inhibitors, while the rest were taking targeted synthetic DMARDs (tsDMARD).
Four patients in the cohort developed laboratory-confirmed COVID-19; another four developed symptoms highly suggestive of the disease but did not receive confirmatory testing, and five had contact with a confirmed COVID-19 case but did not develop symptoms of COVID-19.
Among the eight confirmed and suspected COVID-19 patients, only one was hospitalized. All temporarily withdrew bDMARD or tsDMARD treatment at symptom onset.
“To date, there have been no significant relapses of the rheumatic disease,” Dr. Monti and colleagues reported. “None of the patients with a confirmed diagnosis of COVID-19 or with a highly suggestive clinical picture developed severe respiratory complications or died. Only one patient, aged 65, required admission to hospital and low-flow oxygen supplementation for a few days.”
The findings “do not allow any conclusions on the incidence rate of SARS-CoV-2 infection in patients with rheumatic diseases, nor on the overall outcome of immunocompromised patients affected by COVID-19,” the investigators cautioned, adding that such patients should receive careful attention and follow-up. “However, our preliminary experience shows that patients with chronic arthritis treated with bDMARDs or tsDMARDs do not seem to be at increased risk of respiratory or life-threatening complications from SARS-CoV-2, compared with the general population.”
Dr. Monti and colleagues noted that, during previous outbreaks of other coronaviruses, no increased mortality was reported for people taking immunosuppressive drugs for a range of conditions, including autoimmune diseases.
“These data can support rheumatologists [in] avoiding the unjustifiable preventive withdrawal of DMARDs, which could lead to an increased risk of relapses and morbidity from the chronic rheumatological condition,” the researchers concluded.
Dr. Monti and colleagues reported no outside funding or financial conflicts of interest.
SOURCE: Monti S et al. Ann Rheum Dis. 2020 April 2. doi: 10.1136/annrheumdis-2020-217424.
Patients being treated for RA or spondyloarthritis who develop symptoms of COVID-19 do not appear to be at higher risk of respiratory or life-threatening complications, results from a new study in Italy suggest.
Such patients, the study authors wrote, do not need to be taken off their immunosuppressive medications if they develop COVID-19 symptoms.
In a letter published in Annals of the Rheumatic Diseases, Sara Monti, MD, and colleagues in the rheumatology department of the Fondazione IRCCS Policlinico in San Matteo, Italy, described results from an observational cohort of 320 patients (68% women; mean age, 55 years) with RA or spondyloarthritis from a single outpatient clinic. The vast majority of subjects (92%) were taking biologic disease-modifying antirheumatic drugs (bDMARD), including tumor necrosis factor inhibitors, while the rest were taking targeted synthetic DMARDs (tsDMARD).
Four patients in the cohort developed laboratory-confirmed COVID-19; another four developed symptoms highly suggestive of the disease but did not receive confirmatory testing, and five had contact with a confirmed COVID-19 case but did not develop symptoms of COVID-19.
Among the eight confirmed and suspected COVID-19 patients, only one was hospitalized. All temporarily withdrew bDMARD or tsDMARD treatment at symptom onset.
“To date, there have been no significant relapses of the rheumatic disease,” Dr. Monti and colleagues reported. “None of the patients with a confirmed diagnosis of COVID-19 or with a highly suggestive clinical picture developed severe respiratory complications or died. Only one patient, aged 65, required admission to hospital and low-flow oxygen supplementation for a few days.”
The findings “do not allow any conclusions on the incidence rate of SARS-CoV-2 infection in patients with rheumatic diseases, nor on the overall outcome of immunocompromised patients affected by COVID-19,” the investigators cautioned, adding that such patients should receive careful attention and follow-up. “However, our preliminary experience shows that patients with chronic arthritis treated with bDMARDs or tsDMARDs do not seem to be at increased risk of respiratory or life-threatening complications from SARS-CoV-2, compared with the general population.”
Dr. Monti and colleagues noted that, during previous outbreaks of other coronaviruses, no increased mortality was reported for people taking immunosuppressive drugs for a range of conditions, including autoimmune diseases.
“These data can support rheumatologists [in] avoiding the unjustifiable preventive withdrawal of DMARDs, which could lead to an increased risk of relapses and morbidity from the chronic rheumatological condition,” the researchers concluded.
Dr. Monti and colleagues reported no outside funding or financial conflicts of interest.
SOURCE: Monti S et al. Ann Rheum Dis. 2020 April 2. doi: 10.1136/annrheumdis-2020-217424.
Patients being treated for RA or spondyloarthritis who develop symptoms of COVID-19 do not appear to be at higher risk of respiratory or life-threatening complications, results from a new study in Italy suggest.
Such patients, the study authors wrote, do not need to be taken off their immunosuppressive medications if they develop COVID-19 symptoms.
In a letter published in Annals of the Rheumatic Diseases, Sara Monti, MD, and colleagues in the rheumatology department of the Fondazione IRCCS Policlinico in San Matteo, Italy, described results from an observational cohort of 320 patients (68% women; mean age, 55 years) with RA or spondyloarthritis from a single outpatient clinic. The vast majority of subjects (92%) were taking biologic disease-modifying antirheumatic drugs (bDMARD), including tumor necrosis factor inhibitors, while the rest were taking targeted synthetic DMARDs (tsDMARD).
Four patients in the cohort developed laboratory-confirmed COVID-19; another four developed symptoms highly suggestive of the disease but did not receive confirmatory testing, and five had contact with a confirmed COVID-19 case but did not develop symptoms of COVID-19.
Among the eight confirmed and suspected COVID-19 patients, only one was hospitalized. All temporarily withdrew bDMARD or tsDMARD treatment at symptom onset.
“To date, there have been no significant relapses of the rheumatic disease,” Dr. Monti and colleagues reported. “None of the patients with a confirmed diagnosis of COVID-19 or with a highly suggestive clinical picture developed severe respiratory complications or died. Only one patient, aged 65, required admission to hospital and low-flow oxygen supplementation for a few days.”
The findings “do not allow any conclusions on the incidence rate of SARS-CoV-2 infection in patients with rheumatic diseases, nor on the overall outcome of immunocompromised patients affected by COVID-19,” the investigators cautioned, adding that such patients should receive careful attention and follow-up. “However, our preliminary experience shows that patients with chronic arthritis treated with bDMARDs or tsDMARDs do not seem to be at increased risk of respiratory or life-threatening complications from SARS-CoV-2, compared with the general population.”
Dr. Monti and colleagues noted that, during previous outbreaks of other coronaviruses, no increased mortality was reported for people taking immunosuppressive drugs for a range of conditions, including autoimmune diseases.
“These data can support rheumatologists [in] avoiding the unjustifiable preventive withdrawal of DMARDs, which could lead to an increased risk of relapses and morbidity from the chronic rheumatological condition,” the researchers concluded.
Dr. Monti and colleagues reported no outside funding or financial conflicts of interest.
SOURCE: Monti S et al. Ann Rheum Dis. 2020 April 2. doi: 10.1136/annrheumdis-2020-217424.
FROM ANNALS OF THE RHEUMATIC DISEASES







