User login
Are long-acting injectables the future of TB treatment?
Long-acting injectable (LAI) drug formulations represent a promising new strategy for the prevention and treatment of tuberculosis in women and children, according to an online presentation at the Conference on Retroviruses & Opportunistic Infections, held virtually.
“As a delivery strategy, LAIs hold the potential to unlock a vast chemical space of lipophilic compounds with very potent anti-TB activity that would otherwise not be developed due to poor predicted oral bioavailability,” explained presenter Eric Nuermberger, MD.
He summarized current preventive treatment options for TB and reviewed the potential impact of LAI formulations on TB therapy. In addition, he identified key challenges for future LAI development and proposed a new development path for clinical implementation.
Current TB preventive therapies
Despite widespread availability, the uptake of TB preventive therapy is poor and currently lags behind global targets. One key barrier to widespread uptake is the long duration of treatment, which may hinder patient adherence to therapy.
While shorter preventive regimens, such as 1 month of daily isoniazid plus rifapentine, show similar efficacy and higher completion rates, further shortening of therapy and reducing clinic visits are the most direct methods to increase adherence and treatment completion rates, Dr. Nuermberger said.
LAI drugs
LAI drug formulations allow for slow release of suitable drugs from a depot injected subcutaneously or intramuscularly.
The goal of LAI formulations is to free patients from the daily burden of oral administration. Other potential benefits include better adherence and efficacy, drug exposure, and the potential to overcome intrinsic poor oral bioavailability by bypassing the GI tract entirely.
Potential indications for LAIs include treatment of latent tuberculosis infection (LTBI), and as continuous therapy in people living with HIV in high-burden settings. There is also potential for treating younger children, such as household contacts, who have difficulty taking oral medications.
“We’ve already seen LAIs revolutionize other areas, such as psychiatry and contraception, and we appear to have another revolution in HIV prevention and treatment,” Dr. Nuermberger explained.
Not all existing TB drugs are suitable for LAI formulations, but drugs such as rifapentine, rifabutin, delamanid, and bedaquiline, show more promise than isoniazid or rifampin because of their physiochemical composition. Of all, bedaquiline may offer the best profile for LAI formulation, Dr. Nuermberger said.
Early proof-of-concept in vivo studies have shown potential use of LAI bedaquiline for TB prevention in both drug-sensitive and drug-resistant TB contacts. Translational PK modeling and simulation predicted that a 1-g intramuscular injection of LAI bedaquiline could maintain therapeutic plasma concentrations in humans for greater than 1 month.
Dr. Nuermberger noted that novel diarylquinoline-based therapies, currently in phase 1 studies, may be even better candidates for LAI-based TB preventive therapy. Early data suggests these compounds may be 10-20 times more potent and have a lower CV risk profile than that of bedaquiline.
Considerations for development and implementation
“Despite the promising potential of long-acting injectables for TB, we are still in the very early stages,” said Dr. Nuermberger.
Ensuring and optimizing acceptance of LAI formulations, especially in at-risk populations, will be very important, he explained. Early involvement of children and pregnant women in studies of who may benefit most from LAI drugs will also be essential.
Other important considerations include cost-effectiveness, particularly in at-risk and vulnerable populations. Furthermore, new dedicated research and development programs are needed to continue to develop more drug candidates suitable for LAI.
“Long-acting formulations hold enormous promise to be transformative for combating TB, through simplification of delivery and overcoming issues of adherence that can compromise success of current interventions,” said Andrew Owen, PhD, of the University of Liverpool (England).
“The ability to deliver an entire course of drug in a single visit promises to ensure missed doses don’t compromise outcomes or place unnecessary selective pressure in favor of drug resistance,” Dr. Owen said.
“Recent studies showing the value of one-month oral treatment regimens for LTBI make long-acting formulations seem more realistic and drugs such as long-acting bedaquiline put a one-shot regimen within reach,” Charles W. Flexner, MD, of Johns Hopkins University, Baltimore, said in an interview.
While no LAIs have been approved for TB, Dr. Nuermberger was optimistic that the recent success of LAI formulations for HIV treatment and prevention will catalyze further efforts in the TB landscape.
Dr. Nuermberger disclosed research support from Janssen Pharmaceuticals, TB Alliance, and the Gates Medical Research Institute. The presentation was sponsored by Janssen Pharmaceuticals, Johns Hopkins CFAR, NIH, Unitaid, and the TB Alliance.
Long-acting injectable (LAI) drug formulations represent a promising new strategy for the prevention and treatment of tuberculosis in women and children, according to an online presentation at the Conference on Retroviruses & Opportunistic Infections, held virtually.
“As a delivery strategy, LAIs hold the potential to unlock a vast chemical space of lipophilic compounds with very potent anti-TB activity that would otherwise not be developed due to poor predicted oral bioavailability,” explained presenter Eric Nuermberger, MD.
He summarized current preventive treatment options for TB and reviewed the potential impact of LAI formulations on TB therapy. In addition, he identified key challenges for future LAI development and proposed a new development path for clinical implementation.
Current TB preventive therapies
Despite widespread availability, the uptake of TB preventive therapy is poor and currently lags behind global targets. One key barrier to widespread uptake is the long duration of treatment, which may hinder patient adherence to therapy.
While shorter preventive regimens, such as 1 month of daily isoniazid plus rifapentine, show similar efficacy and higher completion rates, further shortening of therapy and reducing clinic visits are the most direct methods to increase adherence and treatment completion rates, Dr. Nuermberger said.
LAI drugs
LAI drug formulations allow for slow release of suitable drugs from a depot injected subcutaneously or intramuscularly.
The goal of LAI formulations is to free patients from the daily burden of oral administration. Other potential benefits include better adherence and efficacy, drug exposure, and the potential to overcome intrinsic poor oral bioavailability by bypassing the GI tract entirely.
Potential indications for LAIs include treatment of latent tuberculosis infection (LTBI), and as continuous therapy in people living with HIV in high-burden settings. There is also potential for treating younger children, such as household contacts, who have difficulty taking oral medications.
“We’ve already seen LAIs revolutionize other areas, such as psychiatry and contraception, and we appear to have another revolution in HIV prevention and treatment,” Dr. Nuermberger explained.
Not all existing TB drugs are suitable for LAI formulations, but drugs such as rifapentine, rifabutin, delamanid, and bedaquiline, show more promise than isoniazid or rifampin because of their physiochemical composition. Of all, bedaquiline may offer the best profile for LAI formulation, Dr. Nuermberger said.
Early proof-of-concept in vivo studies have shown potential use of LAI bedaquiline for TB prevention in both drug-sensitive and drug-resistant TB contacts. Translational PK modeling and simulation predicted that a 1-g intramuscular injection of LAI bedaquiline could maintain therapeutic plasma concentrations in humans for greater than 1 month.
Dr. Nuermberger noted that novel diarylquinoline-based therapies, currently in phase 1 studies, may be even better candidates for LAI-based TB preventive therapy. Early data suggests these compounds may be 10-20 times more potent and have a lower CV risk profile than that of bedaquiline.
Considerations for development and implementation
“Despite the promising potential of long-acting injectables for TB, we are still in the very early stages,” said Dr. Nuermberger.
Ensuring and optimizing acceptance of LAI formulations, especially in at-risk populations, will be very important, he explained. Early involvement of children and pregnant women in studies of who may benefit most from LAI drugs will also be essential.
Other important considerations include cost-effectiveness, particularly in at-risk and vulnerable populations. Furthermore, new dedicated research and development programs are needed to continue to develop more drug candidates suitable for LAI.
“Long-acting formulations hold enormous promise to be transformative for combating TB, through simplification of delivery and overcoming issues of adherence that can compromise success of current interventions,” said Andrew Owen, PhD, of the University of Liverpool (England).
“The ability to deliver an entire course of drug in a single visit promises to ensure missed doses don’t compromise outcomes or place unnecessary selective pressure in favor of drug resistance,” Dr. Owen said.
“Recent studies showing the value of one-month oral treatment regimens for LTBI make long-acting formulations seem more realistic and drugs such as long-acting bedaquiline put a one-shot regimen within reach,” Charles W. Flexner, MD, of Johns Hopkins University, Baltimore, said in an interview.
While no LAIs have been approved for TB, Dr. Nuermberger was optimistic that the recent success of LAI formulations for HIV treatment and prevention will catalyze further efforts in the TB landscape.
Dr. Nuermberger disclosed research support from Janssen Pharmaceuticals, TB Alliance, and the Gates Medical Research Institute. The presentation was sponsored by Janssen Pharmaceuticals, Johns Hopkins CFAR, NIH, Unitaid, and the TB Alliance.
Long-acting injectable (LAI) drug formulations represent a promising new strategy for the prevention and treatment of tuberculosis in women and children, according to an online presentation at the Conference on Retroviruses & Opportunistic Infections, held virtually.
“As a delivery strategy, LAIs hold the potential to unlock a vast chemical space of lipophilic compounds with very potent anti-TB activity that would otherwise not be developed due to poor predicted oral bioavailability,” explained presenter Eric Nuermberger, MD.
He summarized current preventive treatment options for TB and reviewed the potential impact of LAI formulations on TB therapy. In addition, he identified key challenges for future LAI development and proposed a new development path for clinical implementation.
Current TB preventive therapies
Despite widespread availability, the uptake of TB preventive therapy is poor and currently lags behind global targets. One key barrier to widespread uptake is the long duration of treatment, which may hinder patient adherence to therapy.
While shorter preventive regimens, such as 1 month of daily isoniazid plus rifapentine, show similar efficacy and higher completion rates, further shortening of therapy and reducing clinic visits are the most direct methods to increase adherence and treatment completion rates, Dr. Nuermberger said.
LAI drugs
LAI drug formulations allow for slow release of suitable drugs from a depot injected subcutaneously or intramuscularly.
The goal of LAI formulations is to free patients from the daily burden of oral administration. Other potential benefits include better adherence and efficacy, drug exposure, and the potential to overcome intrinsic poor oral bioavailability by bypassing the GI tract entirely.
Potential indications for LAIs include treatment of latent tuberculosis infection (LTBI), and as continuous therapy in people living with HIV in high-burden settings. There is also potential for treating younger children, such as household contacts, who have difficulty taking oral medications.
“We’ve already seen LAIs revolutionize other areas, such as psychiatry and contraception, and we appear to have another revolution in HIV prevention and treatment,” Dr. Nuermberger explained.
Not all existing TB drugs are suitable for LAI formulations, but drugs such as rifapentine, rifabutin, delamanid, and bedaquiline, show more promise than isoniazid or rifampin because of their physiochemical composition. Of all, bedaquiline may offer the best profile for LAI formulation, Dr. Nuermberger said.
Early proof-of-concept in vivo studies have shown potential use of LAI bedaquiline for TB prevention in both drug-sensitive and drug-resistant TB contacts. Translational PK modeling and simulation predicted that a 1-g intramuscular injection of LAI bedaquiline could maintain therapeutic plasma concentrations in humans for greater than 1 month.
Dr. Nuermberger noted that novel diarylquinoline-based therapies, currently in phase 1 studies, may be even better candidates for LAI-based TB preventive therapy. Early data suggests these compounds may be 10-20 times more potent and have a lower CV risk profile than that of bedaquiline.
Considerations for development and implementation
“Despite the promising potential of long-acting injectables for TB, we are still in the very early stages,” said Dr. Nuermberger.
Ensuring and optimizing acceptance of LAI formulations, especially in at-risk populations, will be very important, he explained. Early involvement of children and pregnant women in studies of who may benefit most from LAI drugs will also be essential.
Other important considerations include cost-effectiveness, particularly in at-risk and vulnerable populations. Furthermore, new dedicated research and development programs are needed to continue to develop more drug candidates suitable for LAI.
“Long-acting formulations hold enormous promise to be transformative for combating TB, through simplification of delivery and overcoming issues of adherence that can compromise success of current interventions,” said Andrew Owen, PhD, of the University of Liverpool (England).
“The ability to deliver an entire course of drug in a single visit promises to ensure missed doses don’t compromise outcomes or place unnecessary selective pressure in favor of drug resistance,” Dr. Owen said.
“Recent studies showing the value of one-month oral treatment regimens for LTBI make long-acting formulations seem more realistic and drugs such as long-acting bedaquiline put a one-shot regimen within reach,” Charles W. Flexner, MD, of Johns Hopkins University, Baltimore, said in an interview.
While no LAIs have been approved for TB, Dr. Nuermberger was optimistic that the recent success of LAI formulations for HIV treatment and prevention will catalyze further efforts in the TB landscape.
Dr. Nuermberger disclosed research support from Janssen Pharmaceuticals, TB Alliance, and the Gates Medical Research Institute. The presentation was sponsored by Janssen Pharmaceuticals, Johns Hopkins CFAR, NIH, Unitaid, and the TB Alliance.
FROM CROI 2021
Methotrexate users need tuberculosis tests in high-TB areas
People taking even low-dose methotrexate need tuberculosis screening and ongoing clinical care if they live in areas where TB is common, results of a study presented at the virtual annual meeting of the American College of Rheumatology suggest.
Coauthor Carol Hitchon, MD, MSc, a rheumatologist with the University of Manitoba in Winnipeg, who presented the findings, warned that methotrexate (MTX) users who also take corticosteroids or other immunosuppressants are at particular risk and need TB screening.
Current management guidelines for rheumatic disease address TB in relation to biologics, but not in relation to methotrexate, Dr. Hitchon said.
“We know that methotrexate is the foundational DMARD [disease-modifying antirheumatic drug] for many rheumatic diseases, especially rheumatoid arthritis,” Dr. Hitchon noted at a press conference. “It’s safe and effective when dosed properly. However, methotrexate does have the potential for significant liver toxicity as well as infection, particularly for infectious organisms that are targeted by cell-mediated immunity, and TB is one of those agents.”
Using multiple databases, researchers conducted a systematic review of the literature published from 1990 to 2018 on TB rates among people who take less than 30 mg of methotrexate a week. Of the 4,700 studies they examined, 31 fit the criteria for this analysis.
They collected data on tuberculosis incidence or new TB diagnoses vs. reactivation of latent TB infection as well as TB outcomes, such as pulmonary symptoms, dissemination, and mortality.
They found a modest increase in the risk of TB infections in the setting of low-dose methotrexate. In addition, rates of TB in people with rheumatic disease who are treated with either methotrexate or biologics are generally higher than in the general population.
They also found that methotrexate users had higher rates of the type of TB that spreads beyond a patient’s lungs, compared with the general population.
Safety of INH with methotrexate
Researchers also looked at the safety of isoniazid (INH), the antibiotic used to treat TB, and found that isoniazid-related liver toxicity and neutropenia were more common when people took the antibiotic along with methotrexate, but those effects were usually reversible.
TB is endemic in various regions around the world. Historically there hasn’t been much rheumatology capacity in many of these areas, but as that capacity increases more people who are at high risk for developing or reactivating TB will be receiving methotrexate for rheumatic diseases, Dr. Hitchon said.
“It’s prudent for people managing patients who may be at higher risk for TB either from where they live or from where they travel that we should have a high suspicion for TB and consider screening as part of our workup in the course of initiating treatment like methotrexate,” she said.
Narender Annapureddy, MD, a rheumatologist at Vanderbilt University, Nashville, Tenn., who was not involved in the research, pointed out that a limitation of the work is that only 27% of the studies are from developing countries, which are more likely to have endemic TB, and those studies had very few cases.
“This finding needs to be studied in larger populations in TB-endemic areas and in high-risk populations,” he said in an interview.
As for practice implications in the United States, Dr. Annapureddy noted that TB is rare in the United States and most of the cases occur in people born in other countries.
“This population may be at risk for TB and should probably be screened for TB before initiating methotrexate,” he said. “Since biologics are usually the next step, especially in RA after patients fail methotrexate, having information on TB status may also help guide management options after MTX failure.
“Since high-dose steroids are another important risk factor for TB activation,” Dr. Annapureddy continued, “rheumatologists should likely consider screening patients who are going to be on moderate to high doses of steroids with MTX.”
A version of this article originally appeared on Medscape.com.
People taking even low-dose methotrexate need tuberculosis screening and ongoing clinical care if they live in areas where TB is common, results of a study presented at the virtual annual meeting of the American College of Rheumatology suggest.
Coauthor Carol Hitchon, MD, MSc, a rheumatologist with the University of Manitoba in Winnipeg, who presented the findings, warned that methotrexate (MTX) users who also take corticosteroids or other immunosuppressants are at particular risk and need TB screening.
Current management guidelines for rheumatic disease address TB in relation to biologics, but not in relation to methotrexate, Dr. Hitchon said.
“We know that methotrexate is the foundational DMARD [disease-modifying antirheumatic drug] for many rheumatic diseases, especially rheumatoid arthritis,” Dr. Hitchon noted at a press conference. “It’s safe and effective when dosed properly. However, methotrexate does have the potential for significant liver toxicity as well as infection, particularly for infectious organisms that are targeted by cell-mediated immunity, and TB is one of those agents.”
Using multiple databases, researchers conducted a systematic review of the literature published from 1990 to 2018 on TB rates among people who take less than 30 mg of methotrexate a week. Of the 4,700 studies they examined, 31 fit the criteria for this analysis.
They collected data on tuberculosis incidence or new TB diagnoses vs. reactivation of latent TB infection as well as TB outcomes, such as pulmonary symptoms, dissemination, and mortality.
They found a modest increase in the risk of TB infections in the setting of low-dose methotrexate. In addition, rates of TB in people with rheumatic disease who are treated with either methotrexate or biologics are generally higher than in the general population.
They also found that methotrexate users had higher rates of the type of TB that spreads beyond a patient’s lungs, compared with the general population.
Safety of INH with methotrexate
Researchers also looked at the safety of isoniazid (INH), the antibiotic used to treat TB, and found that isoniazid-related liver toxicity and neutropenia were more common when people took the antibiotic along with methotrexate, but those effects were usually reversible.
TB is endemic in various regions around the world. Historically there hasn’t been much rheumatology capacity in many of these areas, but as that capacity increases more people who are at high risk for developing or reactivating TB will be receiving methotrexate for rheumatic diseases, Dr. Hitchon said.
“It’s prudent for people managing patients who may be at higher risk for TB either from where they live or from where they travel that we should have a high suspicion for TB and consider screening as part of our workup in the course of initiating treatment like methotrexate,” she said.
Narender Annapureddy, MD, a rheumatologist at Vanderbilt University, Nashville, Tenn., who was not involved in the research, pointed out that a limitation of the work is that only 27% of the studies are from developing countries, which are more likely to have endemic TB, and those studies had very few cases.
“This finding needs to be studied in larger populations in TB-endemic areas and in high-risk populations,” he said in an interview.
As for practice implications in the United States, Dr. Annapureddy noted that TB is rare in the United States and most of the cases occur in people born in other countries.
“This population may be at risk for TB and should probably be screened for TB before initiating methotrexate,” he said. “Since biologics are usually the next step, especially in RA after patients fail methotrexate, having information on TB status may also help guide management options after MTX failure.
“Since high-dose steroids are another important risk factor for TB activation,” Dr. Annapureddy continued, “rheumatologists should likely consider screening patients who are going to be on moderate to high doses of steroids with MTX.”
A version of this article originally appeared on Medscape.com.
People taking even low-dose methotrexate need tuberculosis screening and ongoing clinical care if they live in areas where TB is common, results of a study presented at the virtual annual meeting of the American College of Rheumatology suggest.
Coauthor Carol Hitchon, MD, MSc, a rheumatologist with the University of Manitoba in Winnipeg, who presented the findings, warned that methotrexate (MTX) users who also take corticosteroids or other immunosuppressants are at particular risk and need TB screening.
Current management guidelines for rheumatic disease address TB in relation to biologics, but not in relation to methotrexate, Dr. Hitchon said.
“We know that methotrexate is the foundational DMARD [disease-modifying antirheumatic drug] for many rheumatic diseases, especially rheumatoid arthritis,” Dr. Hitchon noted at a press conference. “It’s safe and effective when dosed properly. However, methotrexate does have the potential for significant liver toxicity as well as infection, particularly for infectious organisms that are targeted by cell-mediated immunity, and TB is one of those agents.”
Using multiple databases, researchers conducted a systematic review of the literature published from 1990 to 2018 on TB rates among people who take less than 30 mg of methotrexate a week. Of the 4,700 studies they examined, 31 fit the criteria for this analysis.
They collected data on tuberculosis incidence or new TB diagnoses vs. reactivation of latent TB infection as well as TB outcomes, such as pulmonary symptoms, dissemination, and mortality.
They found a modest increase in the risk of TB infections in the setting of low-dose methotrexate. In addition, rates of TB in people with rheumatic disease who are treated with either methotrexate or biologics are generally higher than in the general population.
They also found that methotrexate users had higher rates of the type of TB that spreads beyond a patient’s lungs, compared with the general population.
Safety of INH with methotrexate
Researchers also looked at the safety of isoniazid (INH), the antibiotic used to treat TB, and found that isoniazid-related liver toxicity and neutropenia were more common when people took the antibiotic along with methotrexate, but those effects were usually reversible.
TB is endemic in various regions around the world. Historically there hasn’t been much rheumatology capacity in many of these areas, but as that capacity increases more people who are at high risk for developing or reactivating TB will be receiving methotrexate for rheumatic diseases, Dr. Hitchon said.
“It’s prudent for people managing patients who may be at higher risk for TB either from where they live or from where they travel that we should have a high suspicion for TB and consider screening as part of our workup in the course of initiating treatment like methotrexate,” she said.
Narender Annapureddy, MD, a rheumatologist at Vanderbilt University, Nashville, Tenn., who was not involved in the research, pointed out that a limitation of the work is that only 27% of the studies are from developing countries, which are more likely to have endemic TB, and those studies had very few cases.
“This finding needs to be studied in larger populations in TB-endemic areas and in high-risk populations,” he said in an interview.
As for practice implications in the United States, Dr. Annapureddy noted that TB is rare in the United States and most of the cases occur in people born in other countries.
“This population may be at risk for TB and should probably be screened for TB before initiating methotrexate,” he said. “Since biologics are usually the next step, especially in RA after patients fail methotrexate, having information on TB status may also help guide management options after MTX failure.
“Since high-dose steroids are another important risk factor for TB activation,” Dr. Annapureddy continued, “rheumatologists should likely consider screening patients who are going to be on moderate to high doses of steroids with MTX.”
A version of this article originally appeared on Medscape.com.
Should ART for HIV be initiated prior to tuberculosis testing results?
Tuberculosis symptoms as defined by the World Health Organization were effective in identifying patients with TB for the purposes of same-day antiretroviral therapy (ART) initiation in patients diagnosed with HIV, according to a pooled study of patients in two clinical trials. Guidelines suggest that patients with one or more TB symptoms be investigated for active TB before initiation of ART.
However, more than 80% of patients with TB symptoms did not have the disease and faced a delay of ART initiation, despite the many benefits of same-day ART initiation, according to the study presented online at the Conference on Retroviruses & Opportunistic Infections. This year CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
In her presentation, Alana T. Brennan, PhD, of the Boston University School of Public Health discussed the pooled results of 834 patients in the SLATE (Simple Algorithm for Treatment Eligibility) I and SLATE II trials. These two trials, conducted in South Africa and Kenya, respectively, assessed two variations of a simplified algorithm for eligibility for same-day ART initiation.
A total of 834 patients at baseline reported any self-described symptoms of TB using the WHO four-symptom TB screen (cough, fever, weight loss, night sweats). Those patients with any TB symptoms were assessed by sputum samples. The outcomes were prevalence of TB symptoms, TB diagnosis, and treatment.
Among the 834 patients, 493 (60%) reported no symptoms; 215 (26%) reported one to two symptoms, and 120 (14%) reported three to four symptoms. Only 66% of the patients with one to two symptoms were tested for TB; 78% of the patients with three to four symptoms were tested. Of these, only 1% of the patients with one to two symptoms tested positive for TB, and only 2% of the patients with three to four symptoms tested positive, according to Dr. Brennan.
“More than 80% of patients with TB symptoms did not have TB, but faced delay in ART initiation. No same-day [ART] initiators reported adverse events, so we hope that there would be some reconsideration of the requirement of TB testing prior to ART initiation due to any symptom of TB. … A potential consideration of the severity of the symptoms a patient has is necessary,” Dr. Brennan concluded.
Dr. Brennan reported that there were no disclosures.
SOURCE: Brennan AT et al. CROI 2020, Abstract 720.
Tuberculosis symptoms as defined by the World Health Organization were effective in identifying patients with TB for the purposes of same-day antiretroviral therapy (ART) initiation in patients diagnosed with HIV, according to a pooled study of patients in two clinical trials. Guidelines suggest that patients with one or more TB symptoms be investigated for active TB before initiation of ART.
However, more than 80% of patients with TB symptoms did not have the disease and faced a delay of ART initiation, despite the many benefits of same-day ART initiation, according to the study presented online at the Conference on Retroviruses & Opportunistic Infections. This year CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
In her presentation, Alana T. Brennan, PhD, of the Boston University School of Public Health discussed the pooled results of 834 patients in the SLATE (Simple Algorithm for Treatment Eligibility) I and SLATE II trials. These two trials, conducted in South Africa and Kenya, respectively, assessed two variations of a simplified algorithm for eligibility for same-day ART initiation.
A total of 834 patients at baseline reported any self-described symptoms of TB using the WHO four-symptom TB screen (cough, fever, weight loss, night sweats). Those patients with any TB symptoms were assessed by sputum samples. The outcomes were prevalence of TB symptoms, TB diagnosis, and treatment.
Among the 834 patients, 493 (60%) reported no symptoms; 215 (26%) reported one to two symptoms, and 120 (14%) reported three to four symptoms. Only 66% of the patients with one to two symptoms were tested for TB; 78% of the patients with three to four symptoms were tested. Of these, only 1% of the patients with one to two symptoms tested positive for TB, and only 2% of the patients with three to four symptoms tested positive, according to Dr. Brennan.
“More than 80% of patients with TB symptoms did not have TB, but faced delay in ART initiation. No same-day [ART] initiators reported adverse events, so we hope that there would be some reconsideration of the requirement of TB testing prior to ART initiation due to any symptom of TB. … A potential consideration of the severity of the symptoms a patient has is necessary,” Dr. Brennan concluded.
Dr. Brennan reported that there were no disclosures.
SOURCE: Brennan AT et al. CROI 2020, Abstract 720.
Tuberculosis symptoms as defined by the World Health Organization were effective in identifying patients with TB for the purposes of same-day antiretroviral therapy (ART) initiation in patients diagnosed with HIV, according to a pooled study of patients in two clinical trials. Guidelines suggest that patients with one or more TB symptoms be investigated for active TB before initiation of ART.
However, more than 80% of patients with TB symptoms did not have the disease and faced a delay of ART initiation, despite the many benefits of same-day ART initiation, according to the study presented online at the Conference on Retroviruses & Opportunistic Infections. This year CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
In her presentation, Alana T. Brennan, PhD, of the Boston University School of Public Health discussed the pooled results of 834 patients in the SLATE (Simple Algorithm for Treatment Eligibility) I and SLATE II trials. These two trials, conducted in South Africa and Kenya, respectively, assessed two variations of a simplified algorithm for eligibility for same-day ART initiation.
A total of 834 patients at baseline reported any self-described symptoms of TB using the WHO four-symptom TB screen (cough, fever, weight loss, night sweats). Those patients with any TB symptoms were assessed by sputum samples. The outcomes were prevalence of TB symptoms, TB diagnosis, and treatment.
Among the 834 patients, 493 (60%) reported no symptoms; 215 (26%) reported one to two symptoms, and 120 (14%) reported three to four symptoms. Only 66% of the patients with one to two symptoms were tested for TB; 78% of the patients with three to four symptoms were tested. Of these, only 1% of the patients with one to two symptoms tested positive for TB, and only 2% of the patients with three to four symptoms tested positive, according to Dr. Brennan.
“More than 80% of patients with TB symptoms did not have TB, but faced delay in ART initiation. No same-day [ART] initiators reported adverse events, so we hope that there would be some reconsideration of the requirement of TB testing prior to ART initiation due to any symptom of TB. … A potential consideration of the severity of the symptoms a patient has is necessary,” Dr. Brennan concluded.
Dr. Brennan reported that there were no disclosures.
SOURCE: Brennan AT et al. CROI 2020, Abstract 720.
FROM CROI 2020
Antituberculosis drugs in pregnancy and lactation
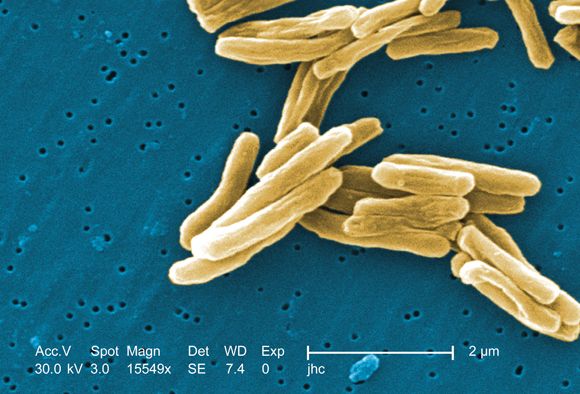
Tuberculosis is one of the top ten causes of death worldwide and the leading cause from a single infectious agent. In the 2012-2017 period, there were more than 9,000 cases of TB each year in the United States. The Centers for Disease Control and Prevention states that untreated TB is a greater hazard to a pregnant woman and her fetus than its treatment.
In the material below, the molecular weights, rounded to the nearest whole number, are shown in parentheses after the drug name. Those less than 1,000 or so suggest that the drug will cross the placenta throughout pregnancy. In the second half of pregnancy, especially in the third trimester, nearly all drugs will cross regardless of their molecular weight.
Para-aminosalicylic acid (Paser) (153) is most frequently used in combination with other agents for the treatment of multidrug-resistant tuberculosis; multidrug-resistant TB (MDR TB) is defined as being caused by TB bacteria that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. The drug has been associated with a marked increased risk of birth defects in some, but not all, studies. Because of this potential risk, the drug is best avoided in the first trimester. The drug is excreted into breast milk, but there are no reports of its use during breastfeeding.
Bedaquiline (Sirturo) (556) is used in combination therapy for patents with multidrug-resistant tuberculosis. One report describing the use of this drug during human pregnancy has been located. Treatment was started in the last 3 weeks of pregnancy and no abnormalities were noted in the child at birth and for 2 years after birth (Emerg Infect Dis. 2017. doi: 10.3201/eid2310.161398). The CDC states that the drug should be used only in a minimum four-drug treatment regimen and administered by direct observation (MMWR Recomm Rep. 2013 Oct 25;62[RR-09]:1-12). The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Capreomycin (Capastat) (653-669) is a polypeptide antibiotic isolated from Streptomyces capreolus that is given intramuscularly. The human pregnancy data are limited to three reports. The toxicity of capreomycin is similar to aminoglycosides (e.g., cranial nerve VIII and renal) and it should not be used with these agents. The CDC has classified the drug as contraindicated in pregnancy. The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Cycloserine (Seromycin) (102) is a broad spectrum antibiotic. The human pregnancy data are limited but have not shown embryo-fetal harm. Although the best course is to avoid the drug during gestation, it should not be withheld because of pregnancy if the maternal condition requires the antibiotic. The American Academy of Pediatrics classified cycloserine as compatible with breastfeeding.
Ethambutol (Myambutol) (205) should be used in conjunction with other antituberculosis drugs. The human pregnancy data do not suggest an embryo-fetal risk. A frequently used regimen is ethambutol + isoniazid + rifampin. The American Academy of Pediatrics classified ethambutol as compatible with breastfeeding.
Ethionamide (Trecator) (166) is indicated when Mycobacterium tuberculosis is resistant to isoniazid or rifampin, or when the patient is intolerant to other drugs. Although the animal reproductive data suggest risk, the limited human data suggest that the risk is probably low. If indicated, the drug should not be withheld because of pregnancy. Although the molecular weight suggests that the drug will be excreted into breast milk, no reports describing the amount in milk have been located.
Isoniazid (137) is compatible in pregnancy, even though the molecular weight suggests that it will cross the placenta, because the maternal benefit is much greater than the potential embryo-fetal risk. Although the human data are limited, the molecular weight also suggests that the drug will be excreted into breast milk, but it can be considered probably compatible during breastfeeding. No reports of isoniazid-induced effects in the nursing infant have been located, but the potential for interference with nucleic acid function and for hepatotoxicity may exist.
Pyrazinamide (123) is metabolized to an active metabolite. The molecular weight, low plasma protein binding (10%), and prolonged elimination half-life (9-10 hours) suggest that the drug will cross the placenta throughout pregnancy. The drug has been used in human pregnancy without causing embryo-fetal harm. Similar results, although limited, were reported when the drug was used during breastfeeding.
Rifabutin (Mycobutin) (847) has no reported human pregnancy data, but the animal data suggest low risk. The drug probably crosses the placenta throughout pregnancy. The maternal benefit appears to outweigh the unknown risk to the embryo-fetus, so therapy should not be withheld because of pregnancy. The drug probably is excreted into breast milk.
Rifampin (Rifadin) (823) appears to be compatible in pregnancy. Several reviews and reports have concluded that the drug was not a teratogen and recommended use of the drug with isoniazid and ethambutol. However, prophylactic vitamin K1 has been recommended to prevent drug-induced hemorrhagic disease of the newborn. There are no data regarding its use during breastfeeding, but it is probably compatible.
Rifapentine (Priftin) (877) was toxic and teratogenic in two animal species at doses close to those used in humans. In a 2018 study, however, the rates of fetal loss in pregnancies of less than 20 weeks (8/54, 15%) and congenital anomalies in live births (1/37, 3%) were within the expected background rates (Ann Am Thorac Soc. 2018 May;15[4]:570-80). There are no data regarding its use during breastfeeding, but it is probably compatible.
The CDC classifies four antituberculosis and one class of drugs as contraindicated in pregnancy. In addition to capreomycin mentioned above, they are amikacin, fluoroquinolones (ciprofloxacin, gemifloxacin, levofloxacin, lomefloxacin, moxifloxacin, ofloxacin), kanamycin, and streptomycin. These ten agents are discussed in the 11th edition of my book “Drugs in Pregnancy and Lactation,” (Wolters Kluwer Health: Riverwood, Il., 2017). If they have to be used, checking this source will provide information that has to be discussed with the patient.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs had no disclosures, except for his book. Email him at obnews@mdedge.com.
Tuberculosis is one of the top ten causes of death worldwide and the leading cause from a single infectious agent. In the 2012-2017 period, there were more than 9,000 cases of TB each year in the United States. The Centers for Disease Control and Prevention states that untreated TB is a greater hazard to a pregnant woman and her fetus than its treatment.
In the material below, the molecular weights, rounded to the nearest whole number, are shown in parentheses after the drug name. Those less than 1,000 or so suggest that the drug will cross the placenta throughout pregnancy. In the second half of pregnancy, especially in the third trimester, nearly all drugs will cross regardless of their molecular weight.
Para-aminosalicylic acid (Paser) (153) is most frequently used in combination with other agents for the treatment of multidrug-resistant tuberculosis; multidrug-resistant TB (MDR TB) is defined as being caused by TB bacteria that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. The drug has been associated with a marked increased risk of birth defects in some, but not all, studies. Because of this potential risk, the drug is best avoided in the first trimester. The drug is excreted into breast milk, but there are no reports of its use during breastfeeding.
Bedaquiline (Sirturo) (556) is used in combination therapy for patents with multidrug-resistant tuberculosis. One report describing the use of this drug during human pregnancy has been located. Treatment was started in the last 3 weeks of pregnancy and no abnormalities were noted in the child at birth and for 2 years after birth (Emerg Infect Dis. 2017. doi: 10.3201/eid2310.161398). The CDC states that the drug should be used only in a minimum four-drug treatment regimen and administered by direct observation (MMWR Recomm Rep. 2013 Oct 25;62[RR-09]:1-12). The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Capreomycin (Capastat) (653-669) is a polypeptide antibiotic isolated from Streptomyces capreolus that is given intramuscularly. The human pregnancy data are limited to three reports. The toxicity of capreomycin is similar to aminoglycosides (e.g., cranial nerve VIII and renal) and it should not be used with these agents. The CDC has classified the drug as contraindicated in pregnancy. The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Cycloserine (Seromycin) (102) is a broad spectrum antibiotic. The human pregnancy data are limited but have not shown embryo-fetal harm. Although the best course is to avoid the drug during gestation, it should not be withheld because of pregnancy if the maternal condition requires the antibiotic. The American Academy of Pediatrics classified cycloserine as compatible with breastfeeding.
Ethambutol (Myambutol) (205) should be used in conjunction with other antituberculosis drugs. The human pregnancy data do not suggest an embryo-fetal risk. A frequently used regimen is ethambutol + isoniazid + rifampin. The American Academy of Pediatrics classified ethambutol as compatible with breastfeeding.
Ethionamide (Trecator) (166) is indicated when Mycobacterium tuberculosis is resistant to isoniazid or rifampin, or when the patient is intolerant to other drugs. Although the animal reproductive data suggest risk, the limited human data suggest that the risk is probably low. If indicated, the drug should not be withheld because of pregnancy. Although the molecular weight suggests that the drug will be excreted into breast milk, no reports describing the amount in milk have been located.
Isoniazid (137) is compatible in pregnancy, even though the molecular weight suggests that it will cross the placenta, because the maternal benefit is much greater than the potential embryo-fetal risk. Although the human data are limited, the molecular weight also suggests that the drug will be excreted into breast milk, but it can be considered probably compatible during breastfeeding. No reports of isoniazid-induced effects in the nursing infant have been located, but the potential for interference with nucleic acid function and for hepatotoxicity may exist.
Pyrazinamide (123) is metabolized to an active metabolite. The molecular weight, low plasma protein binding (10%), and prolonged elimination half-life (9-10 hours) suggest that the drug will cross the placenta throughout pregnancy. The drug has been used in human pregnancy without causing embryo-fetal harm. Similar results, although limited, were reported when the drug was used during breastfeeding.
Rifabutin (Mycobutin) (847) has no reported human pregnancy data, but the animal data suggest low risk. The drug probably crosses the placenta throughout pregnancy. The maternal benefit appears to outweigh the unknown risk to the embryo-fetus, so therapy should not be withheld because of pregnancy. The drug probably is excreted into breast milk.
Rifampin (Rifadin) (823) appears to be compatible in pregnancy. Several reviews and reports have concluded that the drug was not a teratogen and recommended use of the drug with isoniazid and ethambutol. However, prophylactic vitamin K1 has been recommended to prevent drug-induced hemorrhagic disease of the newborn. There are no data regarding its use during breastfeeding, but it is probably compatible.
Rifapentine (Priftin) (877) was toxic and teratogenic in two animal species at doses close to those used in humans. In a 2018 study, however, the rates of fetal loss in pregnancies of less than 20 weeks (8/54, 15%) and congenital anomalies in live births (1/37, 3%) were within the expected background rates (Ann Am Thorac Soc. 2018 May;15[4]:570-80). There are no data regarding its use during breastfeeding, but it is probably compatible.
The CDC classifies four antituberculosis and one class of drugs as contraindicated in pregnancy. In addition to capreomycin mentioned above, they are amikacin, fluoroquinolones (ciprofloxacin, gemifloxacin, levofloxacin, lomefloxacin, moxifloxacin, ofloxacin), kanamycin, and streptomycin. These ten agents are discussed in the 11th edition of my book “Drugs in Pregnancy and Lactation,” (Wolters Kluwer Health: Riverwood, Il., 2017). If they have to be used, checking this source will provide information that has to be discussed with the patient.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs had no disclosures, except for his book. Email him at obnews@mdedge.com.
Tuberculosis is one of the top ten causes of death worldwide and the leading cause from a single infectious agent. In the 2012-2017 period, there were more than 9,000 cases of TB each year in the United States. The Centers for Disease Control and Prevention states that untreated TB is a greater hazard to a pregnant woman and her fetus than its treatment.
In the material below, the molecular weights, rounded to the nearest whole number, are shown in parentheses after the drug name. Those less than 1,000 or so suggest that the drug will cross the placenta throughout pregnancy. In the second half of pregnancy, especially in the third trimester, nearly all drugs will cross regardless of their molecular weight.
Para-aminosalicylic acid (Paser) (153) is most frequently used in combination with other agents for the treatment of multidrug-resistant tuberculosis; multidrug-resistant TB (MDR TB) is defined as being caused by TB bacteria that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. The drug has been associated with a marked increased risk of birth defects in some, but not all, studies. Because of this potential risk, the drug is best avoided in the first trimester. The drug is excreted into breast milk, but there are no reports of its use during breastfeeding.
Bedaquiline (Sirturo) (556) is used in combination therapy for patents with multidrug-resistant tuberculosis. One report describing the use of this drug during human pregnancy has been located. Treatment was started in the last 3 weeks of pregnancy and no abnormalities were noted in the child at birth and for 2 years after birth (Emerg Infect Dis. 2017. doi: 10.3201/eid2310.161398). The CDC states that the drug should be used only in a minimum four-drug treatment regimen and administered by direct observation (MMWR Recomm Rep. 2013 Oct 25;62[RR-09]:1-12). The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Capreomycin (Capastat) (653-669) is a polypeptide antibiotic isolated from Streptomyces capreolus that is given intramuscularly. The human pregnancy data are limited to three reports. The toxicity of capreomycin is similar to aminoglycosides (e.g., cranial nerve VIII and renal) and it should not be used with these agents. The CDC has classified the drug as contraindicated in pregnancy. The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Cycloserine (Seromycin) (102) is a broad spectrum antibiotic. The human pregnancy data are limited but have not shown embryo-fetal harm. Although the best course is to avoid the drug during gestation, it should not be withheld because of pregnancy if the maternal condition requires the antibiotic. The American Academy of Pediatrics classified cycloserine as compatible with breastfeeding.
Ethambutol (Myambutol) (205) should be used in conjunction with other antituberculosis drugs. The human pregnancy data do not suggest an embryo-fetal risk. A frequently used regimen is ethambutol + isoniazid + rifampin. The American Academy of Pediatrics classified ethambutol as compatible with breastfeeding.
Ethionamide (Trecator) (166) is indicated when Mycobacterium tuberculosis is resistant to isoniazid or rifampin, or when the patient is intolerant to other drugs. Although the animal reproductive data suggest risk, the limited human data suggest that the risk is probably low. If indicated, the drug should not be withheld because of pregnancy. Although the molecular weight suggests that the drug will be excreted into breast milk, no reports describing the amount in milk have been located.
Isoniazid (137) is compatible in pregnancy, even though the molecular weight suggests that it will cross the placenta, because the maternal benefit is much greater than the potential embryo-fetal risk. Although the human data are limited, the molecular weight also suggests that the drug will be excreted into breast milk, but it can be considered probably compatible during breastfeeding. No reports of isoniazid-induced effects in the nursing infant have been located, but the potential for interference with nucleic acid function and for hepatotoxicity may exist.
Pyrazinamide (123) is metabolized to an active metabolite. The molecular weight, low plasma protein binding (10%), and prolonged elimination half-life (9-10 hours) suggest that the drug will cross the placenta throughout pregnancy. The drug has been used in human pregnancy without causing embryo-fetal harm. Similar results, although limited, were reported when the drug was used during breastfeeding.
Rifabutin (Mycobutin) (847) has no reported human pregnancy data, but the animal data suggest low risk. The drug probably crosses the placenta throughout pregnancy. The maternal benefit appears to outweigh the unknown risk to the embryo-fetus, so therapy should not be withheld because of pregnancy. The drug probably is excreted into breast milk.
Rifampin (Rifadin) (823) appears to be compatible in pregnancy. Several reviews and reports have concluded that the drug was not a teratogen and recommended use of the drug with isoniazid and ethambutol. However, prophylactic vitamin K1 has been recommended to prevent drug-induced hemorrhagic disease of the newborn. There are no data regarding its use during breastfeeding, but it is probably compatible.
Rifapentine (Priftin) (877) was toxic and teratogenic in two animal species at doses close to those used in humans. In a 2018 study, however, the rates of fetal loss in pregnancies of less than 20 weeks (8/54, 15%) and congenital anomalies in live births (1/37, 3%) were within the expected background rates (Ann Am Thorac Soc. 2018 May;15[4]:570-80). There are no data regarding its use during breastfeeding, but it is probably compatible.
The CDC classifies four antituberculosis and one class of drugs as contraindicated in pregnancy. In addition to capreomycin mentioned above, they are amikacin, fluoroquinolones (ciprofloxacin, gemifloxacin, levofloxacin, lomefloxacin, moxifloxacin, ofloxacin), kanamycin, and streptomycin. These ten agents are discussed in the 11th edition of my book “Drugs in Pregnancy and Lactation,” (Wolters Kluwer Health: Riverwood, Il., 2017). If they have to be used, checking this source will provide information that has to be discussed with the patient.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs had no disclosures, except for his book. Email him at obnews@mdedge.com.
In vasculitis, the skin tells the story
MILAN – , Robert Micheletti, MD, said at the World Congress of Dermatology.
In granulomatous vasculitis, histiocytes and giant cells can play a significant role, explained Dr. Micheletti, director of the cutaneous vasculitis clinic at the University of Pennsylvania, Philadelphia. The condition may be secondary to an autoimmune disease such as lupus erythematosus or RA; a granulomatous disease such as Crohn’s disease or sarcoidosis; infections such as tuberculosis, a fungal disease, or herpes or zoster viruses, or lymphoma, Dr. Micheletti said.
However, a primary systemic vasculitis such as granulomatosis with polyangiitis (GPA; formerly known as Wegener’s polyangiitis) or eosinophilic granulomatosis with polyangiitis (EGPA; also known as Churg-Strauss vasculitis), giant cell arteritis, or Takayasu arteritis may also be responsible, he said. Occasionally, the culprit can also be a drug-induced vasculitis.
The physical examination gives clues to the size of involved vessels, which in turn helps to classify the vasculitis, Dr. Micheletti said.
When vasculitis affects small vessels, the skin findings will be palpable purpura, urticarial papules, vesicles, and petechiae, he said, adding that “The small vessel involvement accounts for the small size of the lesions, and complement cascade and inflammation account for the palpability of the lesions and the symptomatology.” As red blood cells extravasate from the affected vessels, nonblanching purpura develop, and gravity’s effect on the deposition of immune complex material dictates how lesions are distributed.
“Manifestations more typical of medium vessel vasculitis include subcutaneous nodules, livedo reticularis, retiform purpura, larger hemorrhagic bullae, and more significant ulceration and necrosis,” he said. “If such lesions are seen, suspect medium-vessel vasculitis or vasculitis overlapping small and medium vessels.” Cutaneous or systemic polyarteritis nodosa, antineutrophilic cytoplasmic autoantibody (ANCA)–associated vasculitis, and cryoglobulinemic vasculitis are examples, he added.
The particularities of renal manifestations of vasculitis also offer clues to the vessels involved. When a vasculitis patient has glomerulonephritis, suspect small-vessel involvement, Dr. Micheletti said. However, vasculitis affecting medium-sized vessels will cause renovascular hypertension and, potentially renal arterial aneurysms.
Nerves are typically spared in small-vessel vasculitis, while wrist or foot drop can be seen in mononeuritis multiplex.
Recently, the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS) looked at more than 6,800 patients at over 130 sites around the world, proposing new classification criteria for ANCA-associated vasculitis (AAV) and large-vessel vasculitis. The study found that skin findings are common in AAV, with 30%-50% of cases presenting initially with skin lesions. Petechiae and/or purpura are the most common of the skin manifestations, he said. By contrast, for EGPA, allergic and nonspecific findings were the most common findings.
Although skin biopsy can confirm the diagnosis in up to 94% of AAV cases, it’s underutilized and performed in less than half (24%-44%) of cases, Dr. Micheletti said. The study’s findings “demonstrate the importance of a good skin exam, as well as its utility for diagnosis” of vasculitis, he said.
An additional finding form the DCVAS study was that skin lesions can give clues to severity of vasculitis: “Among 1,184 patients with ANCA-associated vasculitis, those with cutaneous involvement were more likely to have systemic manifestations of disease, more likely to have such severe manifestations as glomerulonephritis, alveolar hemorrhage, and mononeuritis,” said Dr. Micheletti, with a hazard ratio of 2.0 among those individuals who had EGPA or GPA.
“Skin findings have diagnostic and, potentially, prognostic importance,” he said. “Use the physician exam and your clinical acumen to your advantage,” but always confirm vasculitis with a biopsy. “Clinicopathologic correlation is key.” A simple urinalysis will screen for renal involvement, and is of “paramount importance,” he added.
Dr. Micheletti reported that he had no relevant disclosures.
MILAN – , Robert Micheletti, MD, said at the World Congress of Dermatology.
In granulomatous vasculitis, histiocytes and giant cells can play a significant role, explained Dr. Micheletti, director of the cutaneous vasculitis clinic at the University of Pennsylvania, Philadelphia. The condition may be secondary to an autoimmune disease such as lupus erythematosus or RA; a granulomatous disease such as Crohn’s disease or sarcoidosis; infections such as tuberculosis, a fungal disease, or herpes or zoster viruses, or lymphoma, Dr. Micheletti said.
However, a primary systemic vasculitis such as granulomatosis with polyangiitis (GPA; formerly known as Wegener’s polyangiitis) or eosinophilic granulomatosis with polyangiitis (EGPA; also known as Churg-Strauss vasculitis), giant cell arteritis, or Takayasu arteritis may also be responsible, he said. Occasionally, the culprit can also be a drug-induced vasculitis.
The physical examination gives clues to the size of involved vessels, which in turn helps to classify the vasculitis, Dr. Micheletti said.
When vasculitis affects small vessels, the skin findings will be palpable purpura, urticarial papules, vesicles, and petechiae, he said, adding that “The small vessel involvement accounts for the small size of the lesions, and complement cascade and inflammation account for the palpability of the lesions and the symptomatology.” As red blood cells extravasate from the affected vessels, nonblanching purpura develop, and gravity’s effect on the deposition of immune complex material dictates how lesions are distributed.
“Manifestations more typical of medium vessel vasculitis include subcutaneous nodules, livedo reticularis, retiform purpura, larger hemorrhagic bullae, and more significant ulceration and necrosis,” he said. “If such lesions are seen, suspect medium-vessel vasculitis or vasculitis overlapping small and medium vessels.” Cutaneous or systemic polyarteritis nodosa, antineutrophilic cytoplasmic autoantibody (ANCA)–associated vasculitis, and cryoglobulinemic vasculitis are examples, he added.
The particularities of renal manifestations of vasculitis also offer clues to the vessels involved. When a vasculitis patient has glomerulonephritis, suspect small-vessel involvement, Dr. Micheletti said. However, vasculitis affecting medium-sized vessels will cause renovascular hypertension and, potentially renal arterial aneurysms.
Nerves are typically spared in small-vessel vasculitis, while wrist or foot drop can be seen in mononeuritis multiplex.
Recently, the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS) looked at more than 6,800 patients at over 130 sites around the world, proposing new classification criteria for ANCA-associated vasculitis (AAV) and large-vessel vasculitis. The study found that skin findings are common in AAV, with 30%-50% of cases presenting initially with skin lesions. Petechiae and/or purpura are the most common of the skin manifestations, he said. By contrast, for EGPA, allergic and nonspecific findings were the most common findings.
Although skin biopsy can confirm the diagnosis in up to 94% of AAV cases, it’s underutilized and performed in less than half (24%-44%) of cases, Dr. Micheletti said. The study’s findings “demonstrate the importance of a good skin exam, as well as its utility for diagnosis” of vasculitis, he said.
An additional finding form the DCVAS study was that skin lesions can give clues to severity of vasculitis: “Among 1,184 patients with ANCA-associated vasculitis, those with cutaneous involvement were more likely to have systemic manifestations of disease, more likely to have such severe manifestations as glomerulonephritis, alveolar hemorrhage, and mononeuritis,” said Dr. Micheletti, with a hazard ratio of 2.0 among those individuals who had EGPA or GPA.
“Skin findings have diagnostic and, potentially, prognostic importance,” he said. “Use the physician exam and your clinical acumen to your advantage,” but always confirm vasculitis with a biopsy. “Clinicopathologic correlation is key.” A simple urinalysis will screen for renal involvement, and is of “paramount importance,” he added.
Dr. Micheletti reported that he had no relevant disclosures.
MILAN – , Robert Micheletti, MD, said at the World Congress of Dermatology.
In granulomatous vasculitis, histiocytes and giant cells can play a significant role, explained Dr. Micheletti, director of the cutaneous vasculitis clinic at the University of Pennsylvania, Philadelphia. The condition may be secondary to an autoimmune disease such as lupus erythematosus or RA; a granulomatous disease such as Crohn’s disease or sarcoidosis; infections such as tuberculosis, a fungal disease, or herpes or zoster viruses, or lymphoma, Dr. Micheletti said.
However, a primary systemic vasculitis such as granulomatosis with polyangiitis (GPA; formerly known as Wegener’s polyangiitis) or eosinophilic granulomatosis with polyangiitis (EGPA; also known as Churg-Strauss vasculitis), giant cell arteritis, or Takayasu arteritis may also be responsible, he said. Occasionally, the culprit can also be a drug-induced vasculitis.
The physical examination gives clues to the size of involved vessels, which in turn helps to classify the vasculitis, Dr. Micheletti said.
When vasculitis affects small vessels, the skin findings will be palpable purpura, urticarial papules, vesicles, and petechiae, he said, adding that “The small vessel involvement accounts for the small size of the lesions, and complement cascade and inflammation account for the palpability of the lesions and the symptomatology.” As red blood cells extravasate from the affected vessels, nonblanching purpura develop, and gravity’s effect on the deposition of immune complex material dictates how lesions are distributed.
“Manifestations more typical of medium vessel vasculitis include subcutaneous nodules, livedo reticularis, retiform purpura, larger hemorrhagic bullae, and more significant ulceration and necrosis,” he said. “If such lesions are seen, suspect medium-vessel vasculitis or vasculitis overlapping small and medium vessels.” Cutaneous or systemic polyarteritis nodosa, antineutrophilic cytoplasmic autoantibody (ANCA)–associated vasculitis, and cryoglobulinemic vasculitis are examples, he added.
The particularities of renal manifestations of vasculitis also offer clues to the vessels involved. When a vasculitis patient has glomerulonephritis, suspect small-vessel involvement, Dr. Micheletti said. However, vasculitis affecting medium-sized vessels will cause renovascular hypertension and, potentially renal arterial aneurysms.
Nerves are typically spared in small-vessel vasculitis, while wrist or foot drop can be seen in mononeuritis multiplex.
Recently, the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS) looked at more than 6,800 patients at over 130 sites around the world, proposing new classification criteria for ANCA-associated vasculitis (AAV) and large-vessel vasculitis. The study found that skin findings are common in AAV, with 30%-50% of cases presenting initially with skin lesions. Petechiae and/or purpura are the most common of the skin manifestations, he said. By contrast, for EGPA, allergic and nonspecific findings were the most common findings.
Although skin biopsy can confirm the diagnosis in up to 94% of AAV cases, it’s underutilized and performed in less than half (24%-44%) of cases, Dr. Micheletti said. The study’s findings “demonstrate the importance of a good skin exam, as well as its utility for diagnosis” of vasculitis, he said.
An additional finding form the DCVAS study was that skin lesions can give clues to severity of vasculitis: “Among 1,184 patients with ANCA-associated vasculitis, those with cutaneous involvement were more likely to have systemic manifestations of disease, more likely to have such severe manifestations as glomerulonephritis, alveolar hemorrhage, and mononeuritis,” said Dr. Micheletti, with a hazard ratio of 2.0 among those individuals who had EGPA or GPA.
“Skin findings have diagnostic and, potentially, prognostic importance,” he said. “Use the physician exam and your clinical acumen to your advantage,” but always confirm vasculitis with a biopsy. “Clinicopathologic correlation is key.” A simple urinalysis will screen for renal involvement, and is of “paramount importance,” he added.
Dr. Micheletti reported that he had no relevant disclosures.
AT WCD2019
FDA approves drug combo to treat highly resistant TB
The U.S. Food and Drug Administration granted special approval to a new drug combo intended for the treatment of “a limited and specific population of adult patients with extensively drug resistant, treatment-intolerant or nonresponsive multidrug-resistant pulmonary” tuberculosis, according to an FDA news release.
The effectiveness of the combination treatment of pretomanid tablets with bedaquiline and linezolid was shown in a clinical study of patients with extensively drug-resistant, treatment-intolerant, or nonresponsive multidrug-resistant pulmonary tuberculosis of the lungs. Of 107 infected patients who were evaluated 6 months after the end of therapy, 95 (89%) were deemed successes, which significantly exceeded the historical success rates for treatment of extensively drug-resistant TB, the FDA reported. The trial is sponsored by the Global Alliance for TB Drug Development.
The most common adverse effects reported included peripheral neuropathy, anemia, nausea, vomiting, headache, increased liver enzymes, dyspepsia, rash, visual impairment, low blood sugar, and diarrhea, according to the release.
“Multidrug-resistant TB and extensively drug-resistant TB are public health threats due to limited treatment options. New treatments are important to meet patient national and global health needs,” stated FDA Principal Deputy Commissioner Amy Abernethy, MD, PhD, in the release. She also explained that the approval marked the second time a drug was approved under the “Limited Population Pathway for Antibacterial and Antifungal Drugs, a pathway advanced by Congress to spur development of drugs targeting infections that lack effective therapies.”
In 2016, the World Health Organization reported that there were an estimated 490,000 new cases of multidrug-resistant TB worldwide, with a smaller portion of cases of extensively drug-resistant TB, according to the release, demonstrating the need for new therapeutics.
SOURCE: U.S. Food and Drug Administration. Aug. 14, 2019. News release.
The U.S. Food and Drug Administration granted special approval to a new drug combo intended for the treatment of “a limited and specific population of adult patients with extensively drug resistant, treatment-intolerant or nonresponsive multidrug-resistant pulmonary” tuberculosis, according to an FDA news release.
The effectiveness of the combination treatment of pretomanid tablets with bedaquiline and linezolid was shown in a clinical study of patients with extensively drug-resistant, treatment-intolerant, or nonresponsive multidrug-resistant pulmonary tuberculosis of the lungs. Of 107 infected patients who were evaluated 6 months after the end of therapy, 95 (89%) were deemed successes, which significantly exceeded the historical success rates for treatment of extensively drug-resistant TB, the FDA reported. The trial is sponsored by the Global Alliance for TB Drug Development.
The most common adverse effects reported included peripheral neuropathy, anemia, nausea, vomiting, headache, increased liver enzymes, dyspepsia, rash, visual impairment, low blood sugar, and diarrhea, according to the release.
“Multidrug-resistant TB and extensively drug-resistant TB are public health threats due to limited treatment options. New treatments are important to meet patient national and global health needs,” stated FDA Principal Deputy Commissioner Amy Abernethy, MD, PhD, in the release. She also explained that the approval marked the second time a drug was approved under the “Limited Population Pathway for Antibacterial and Antifungal Drugs, a pathway advanced by Congress to spur development of drugs targeting infections that lack effective therapies.”
In 2016, the World Health Organization reported that there were an estimated 490,000 new cases of multidrug-resistant TB worldwide, with a smaller portion of cases of extensively drug-resistant TB, according to the release, demonstrating the need for new therapeutics.
SOURCE: U.S. Food and Drug Administration. Aug. 14, 2019. News release.
The U.S. Food and Drug Administration granted special approval to a new drug combo intended for the treatment of “a limited and specific population of adult patients with extensively drug resistant, treatment-intolerant or nonresponsive multidrug-resistant pulmonary” tuberculosis, according to an FDA news release.
The effectiveness of the combination treatment of pretomanid tablets with bedaquiline and linezolid was shown in a clinical study of patients with extensively drug-resistant, treatment-intolerant, or nonresponsive multidrug-resistant pulmonary tuberculosis of the lungs. Of 107 infected patients who were evaluated 6 months after the end of therapy, 95 (89%) were deemed successes, which significantly exceeded the historical success rates for treatment of extensively drug-resistant TB, the FDA reported. The trial is sponsored by the Global Alliance for TB Drug Development.
The most common adverse effects reported included peripheral neuropathy, anemia, nausea, vomiting, headache, increased liver enzymes, dyspepsia, rash, visual impairment, low blood sugar, and diarrhea, according to the release.
“Multidrug-resistant TB and extensively drug-resistant TB are public health threats due to limited treatment options. New treatments are important to meet patient national and global health needs,” stated FDA Principal Deputy Commissioner Amy Abernethy, MD, PhD, in the release. She also explained that the approval marked the second time a drug was approved under the “Limited Population Pathway for Antibacterial and Antifungal Drugs, a pathway advanced by Congress to spur development of drugs targeting infections that lack effective therapies.”
In 2016, the World Health Organization reported that there were an estimated 490,000 new cases of multidrug-resistant TB worldwide, with a smaller portion of cases of extensively drug-resistant TB, according to the release, demonstrating the need for new therapeutics.
SOURCE: U.S. Food and Drug Administration. Aug. 14, 2019. News release.
NEWS FROM THE FDA
New recommendations on TB screening for health care workers
U.S. health care personnel no longer need to undergo routine tuberculosis testing in the absence of known exposure, according to new screening guidelines from the National Tuberculosis Controllers Association and CDC.
The revised guidelines on tuberculosis screening, testing, and treatment of U.S. health care personnel, published in Morbidity and Mortality Weekly Report, are the first update since 2005. The new recommendations reflect a reduction in concern about U.S. health care personnel’s risk of occupational exposure to latent and active tuberculosis infection.
Lynn E. Sosa, MD, from the Connecticut Department of Public Health and National Tuberculosis Controllers Association, and coauthors wrote that rates of tuberculosis infection in the United States have declined by 73% since 1991, from 10.4/100,000 population in 1991 to 2.8/100,000 in 2017. This has been matched by similar declines among health care workers, which the authors said raised questions about the cost-effectiveness of the previously recommended routine serial occupational testing.
“In addition, a recent retrospective cohort study of approximately 40,000 health care personnel at a tertiary U.S. medical center in a low TB-incidence state found an extremely low rate of TST conversion (0.3%) during 1998-2014, with a limited proportion attributable to occupational exposure,” they wrote.
The new guidelines recommend health care personnel undergo baseline or preplacement tuberculosis testing with an interferon-gamma release assay (IGRA) or a tuberculin skin test (TST), as well as individual risk assessment and symptom evaluation.
The individual risk assessment considers whether the person has lived in a country with a high tuberculosis rate, whether they are immunosuppressed, or whether they have had close contact with someone with infectious tuberculosis.
This risk assessment can help decide how to interpret an initial positive test result, the authors said.
“For example, health care personnel with a positive test who are asymptomatic, unlikely to be infected with M. [Mycobacterium] tuberculosis, and at low risk for progression on the basis of their risk assessment should have a second test (either an IGRA or a TST) as recommended in the 2017 TB diagnostic guidelines of the American Thoracic Society, Infectious Diseases Society of America, and CDC,” they wrote. “In this example, the health care personnel should be considered infected with M. tuberculosis only if both the first and second tests are positive.”
After that baseline testing, personnel do not need to undergo routine serial testing except in the case of known exposure or ongoing transmission. The guideline authors suggested serial screening might be considered for health care workers whose work puts them at greater risk – for example, pulmonologists or respiratory therapists – or for those working in settings in which transmission has happened in the past.
For personnel with latent tuberculosis infection, the guidelines recommend “encouragement of treatment” unless it is contraindicated, and annual symptom screening in those not undergoing treatment.
The guideline committee also advocated for annual tuberculosis education for all health care workers.
The new recommendations were based on a systematic review of 36 studies of tuberculosis screening and testing among health care personnel, 16 of which were performed in the United States, and all but two of which were conducted in a hospital setting.
The authors stressed that recommendations from the 2005 CDC guidelines – which do not pertain to health care personnel screening, testing, treatment and education – remain unchanged.
One author declared personal fees from the National Tuberculosis Controllers Association during the conduct of the study. Two others reported unrelated grants and personal fees from private industry. No other conflicts of interest were disclosed.
SOURCE: Sosa L et al. MMWR. 2019;68:439-43.
U.S. health care personnel no longer need to undergo routine tuberculosis testing in the absence of known exposure, according to new screening guidelines from the National Tuberculosis Controllers Association and CDC.
The revised guidelines on tuberculosis screening, testing, and treatment of U.S. health care personnel, published in Morbidity and Mortality Weekly Report, are the first update since 2005. The new recommendations reflect a reduction in concern about U.S. health care personnel’s risk of occupational exposure to latent and active tuberculosis infection.
Lynn E. Sosa, MD, from the Connecticut Department of Public Health and National Tuberculosis Controllers Association, and coauthors wrote that rates of tuberculosis infection in the United States have declined by 73% since 1991, from 10.4/100,000 population in 1991 to 2.8/100,000 in 2017. This has been matched by similar declines among health care workers, which the authors said raised questions about the cost-effectiveness of the previously recommended routine serial occupational testing.
“In addition, a recent retrospective cohort study of approximately 40,000 health care personnel at a tertiary U.S. medical center in a low TB-incidence state found an extremely low rate of TST conversion (0.3%) during 1998-2014, with a limited proportion attributable to occupational exposure,” they wrote.
The new guidelines recommend health care personnel undergo baseline or preplacement tuberculosis testing with an interferon-gamma release assay (IGRA) or a tuberculin skin test (TST), as well as individual risk assessment and symptom evaluation.
The individual risk assessment considers whether the person has lived in a country with a high tuberculosis rate, whether they are immunosuppressed, or whether they have had close contact with someone with infectious tuberculosis.
This risk assessment can help decide how to interpret an initial positive test result, the authors said.
“For example, health care personnel with a positive test who are asymptomatic, unlikely to be infected with M. [Mycobacterium] tuberculosis, and at low risk for progression on the basis of their risk assessment should have a second test (either an IGRA or a TST) as recommended in the 2017 TB diagnostic guidelines of the American Thoracic Society, Infectious Diseases Society of America, and CDC,” they wrote. “In this example, the health care personnel should be considered infected with M. tuberculosis only if both the first and second tests are positive.”
After that baseline testing, personnel do not need to undergo routine serial testing except in the case of known exposure or ongoing transmission. The guideline authors suggested serial screening might be considered for health care workers whose work puts them at greater risk – for example, pulmonologists or respiratory therapists – or for those working in settings in which transmission has happened in the past.
For personnel with latent tuberculosis infection, the guidelines recommend “encouragement of treatment” unless it is contraindicated, and annual symptom screening in those not undergoing treatment.
The guideline committee also advocated for annual tuberculosis education for all health care workers.
The new recommendations were based on a systematic review of 36 studies of tuberculosis screening and testing among health care personnel, 16 of which were performed in the United States, and all but two of which were conducted in a hospital setting.
The authors stressed that recommendations from the 2005 CDC guidelines – which do not pertain to health care personnel screening, testing, treatment and education – remain unchanged.
One author declared personal fees from the National Tuberculosis Controllers Association during the conduct of the study. Two others reported unrelated grants and personal fees from private industry. No other conflicts of interest were disclosed.
SOURCE: Sosa L et al. MMWR. 2019;68:439-43.
U.S. health care personnel no longer need to undergo routine tuberculosis testing in the absence of known exposure, according to new screening guidelines from the National Tuberculosis Controllers Association and CDC.
The revised guidelines on tuberculosis screening, testing, and treatment of U.S. health care personnel, published in Morbidity and Mortality Weekly Report, are the first update since 2005. The new recommendations reflect a reduction in concern about U.S. health care personnel’s risk of occupational exposure to latent and active tuberculosis infection.
Lynn E. Sosa, MD, from the Connecticut Department of Public Health and National Tuberculosis Controllers Association, and coauthors wrote that rates of tuberculosis infection in the United States have declined by 73% since 1991, from 10.4/100,000 population in 1991 to 2.8/100,000 in 2017. This has been matched by similar declines among health care workers, which the authors said raised questions about the cost-effectiveness of the previously recommended routine serial occupational testing.
“In addition, a recent retrospective cohort study of approximately 40,000 health care personnel at a tertiary U.S. medical center in a low TB-incidence state found an extremely low rate of TST conversion (0.3%) during 1998-2014, with a limited proportion attributable to occupational exposure,” they wrote.
The new guidelines recommend health care personnel undergo baseline or preplacement tuberculosis testing with an interferon-gamma release assay (IGRA) or a tuberculin skin test (TST), as well as individual risk assessment and symptom evaluation.
The individual risk assessment considers whether the person has lived in a country with a high tuberculosis rate, whether they are immunosuppressed, or whether they have had close contact with someone with infectious tuberculosis.
This risk assessment can help decide how to interpret an initial positive test result, the authors said.
“For example, health care personnel with a positive test who are asymptomatic, unlikely to be infected with M. [Mycobacterium] tuberculosis, and at low risk for progression on the basis of their risk assessment should have a second test (either an IGRA or a TST) as recommended in the 2017 TB diagnostic guidelines of the American Thoracic Society, Infectious Diseases Society of America, and CDC,” they wrote. “In this example, the health care personnel should be considered infected with M. tuberculosis only if both the first and second tests are positive.”
After that baseline testing, personnel do not need to undergo routine serial testing except in the case of known exposure or ongoing transmission. The guideline authors suggested serial screening might be considered for health care workers whose work puts them at greater risk – for example, pulmonologists or respiratory therapists – or for those working in settings in which transmission has happened in the past.
For personnel with latent tuberculosis infection, the guidelines recommend “encouragement of treatment” unless it is contraindicated, and annual symptom screening in those not undergoing treatment.
The guideline committee also advocated for annual tuberculosis education for all health care workers.
The new recommendations were based on a systematic review of 36 studies of tuberculosis screening and testing among health care personnel, 16 of which were performed in the United States, and all but two of which were conducted in a hospital setting.
The authors stressed that recommendations from the 2005 CDC guidelines – which do not pertain to health care personnel screening, testing, treatment and education – remain unchanged.
One author declared personal fees from the National Tuberculosis Controllers Association during the conduct of the study. Two others reported unrelated grants and personal fees from private industry. No other conflicts of interest were disclosed.
SOURCE: Sosa L et al. MMWR. 2019;68:439-43.
FROM MMWR
ICYMI: Noninferior tuberculosis prevention in HIV has shorter duration
The primary endpoint – first case of tuberculosis or death from tuberculosis or unknown cause among patients with HIV – was reported in 2% of both arms in the open-label, phase 3, noninferiority trial BRIEF TB (NCT01404312).
In the New England Journal of Medicine (2019 Mar 14;380[11]:1001-11), 3,000 patients with HIV were randomized to receive either 1 month of rifapentine/isoniazid or 9 months of isoniazid monotherapy for prevention of tuberculosis. Although safety was also similar between arms, the completion rate was significantly higher in the combination treatment arm, compared with the monotherapy arm (97% vs. 90%; P less than .001).
We covered this story at the annual Conference on Retroviruses & Opportunistic Infections. See our coverage at the link below.
The primary endpoint – first case of tuberculosis or death from tuberculosis or unknown cause among patients with HIV – was reported in 2% of both arms in the open-label, phase 3, noninferiority trial BRIEF TB (NCT01404312).
In the New England Journal of Medicine (2019 Mar 14;380[11]:1001-11), 3,000 patients with HIV were randomized to receive either 1 month of rifapentine/isoniazid or 9 months of isoniazid monotherapy for prevention of tuberculosis. Although safety was also similar between arms, the completion rate was significantly higher in the combination treatment arm, compared with the monotherapy arm (97% vs. 90%; P less than .001).
We covered this story at the annual Conference on Retroviruses & Opportunistic Infections. See our coverage at the link below.
The primary endpoint – first case of tuberculosis or death from tuberculosis or unknown cause among patients with HIV – was reported in 2% of both arms in the open-label, phase 3, noninferiority trial BRIEF TB (NCT01404312).
In the New England Journal of Medicine (2019 Mar 14;380[11]:1001-11), 3,000 patients with HIV were randomized to receive either 1 month of rifapentine/isoniazid or 9 months of isoniazid monotherapy for prevention of tuberculosis. Although safety was also similar between arms, the completion rate was significantly higher in the combination treatment arm, compared with the monotherapy arm (97% vs. 90%; P less than .001).
We covered this story at the annual Conference on Retroviruses & Opportunistic Infections. See our coverage at the link below.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Variation in bacterial drug susceptibility tied to TB relapse risk
Higher pretreatment drug concentrations close to a resistance breakpoint for susceptibility were associated with greater relapse risk in TB, based on data from 54 patients who relapsed and 63 who were treated and cured.
“We postulated that drug-susceptible Mycobacterium tuberculosis might have a graded spectrum of susceptibilities that could be used to determine the risk of relapse,” wrote Roberto Colangeli, PhD, of Rutgers University, Newark, N.J., and his colleagues.
In a study published in the New England Journal of Medicine, the researchers examined pretreatment bacterial isolates from adults with TB who had experienced relapse and those who were cured. Using these isolates, they identified the minimum inhibitory concentration (MIC) – the lowest concentration of the drug that prevents visible bacterial growth in culture – for isoniazid and rifampin.
Overall, after controlling for other potential relapse risk factors, higher pretreatment MIC values for both isoniazid and rifampin were associated with an increased relapse risk. For isoniazid, the average MIC below the breakpoint was 0.0334 mcg/mL for relapsed patients and 0.0286 mcg/mL for cured patients. For rifampin, the average MIC below the breakpoint was 0.0695 mcg/mL for relapsed patients and 0.0453 mcg/mL for cured patients. The higher values for the relapsed versus cured patients were represented by factors of 1.17 and 1.53 for isoniazid and rifampin, respectively.
The average age of the patients was 41 years; 83% were men, and 35% were non-Hispanic white.
The study findings were limited by several factors, including the small sample size, retrospective design, and inability to test MIC values from primary cultures versus subcultures, the researchers wrote. However, the results suggest an impact of MIC values on treatment outcomes, and “additional studies that are performed in larger, well-defined prospective cohorts and that include MIC testing of pretreatment culture isolates will be useful to better validate these findings,”
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Colangeli reported no financial conflicts. Dr. Alland disclosed funding from Cepheid and several current and pending patents in the United States and Europe, with some royalties paid to Cepheid.
SOURCE: Colangeli R et al. N Engl J Med. 2018;379:823-33.
Although standard four-drug therapy has been shown to cure 90% of patients in several clinical trials, patients do relapse for reasons such as poor treatment adherence and “variations in the characteristics of the infected patients or the infecting pathogens,” wrote Eric J. Rubin, MD, in an accompanying editorial (N Engl J Med. 2018;379:882-3).
Current antibiotic susceptibility thresholds are often set by committees using models, said Dr. Rubin. “Given the uncertainties in modeling, as has been seen in clinical studies, these breakpoints can be imperfect predictors of treatment response.”
Dr. Rubin proposed that minimum inhibitory concentration (MIC) concentrations could be an alternative to in vitro testing as a predictor of treatment response.
“The clinical laboratory provides us not only with a breakpoint interpretation but also with raw data, a quantitative assessment of MIC values,” he noted. “These values can be thought of more as probabilities of successful therapy than as absolute thresholds, a change in attitude that may dispel a false sense of security about the choice of regimen in the treatment of patients with tuberculosis.”
Dr. Rubin is affiliated with the department of immunology and infectious diseases at the Harvard School of Public Health, Boston. He had no relevant financial conflicts to disclose.
Although standard four-drug therapy has been shown to cure 90% of patients in several clinical trials, patients do relapse for reasons such as poor treatment adherence and “variations in the characteristics of the infected patients or the infecting pathogens,” wrote Eric J. Rubin, MD, in an accompanying editorial (N Engl J Med. 2018;379:882-3).
Current antibiotic susceptibility thresholds are often set by committees using models, said Dr. Rubin. “Given the uncertainties in modeling, as has been seen in clinical studies, these breakpoints can be imperfect predictors of treatment response.”
Dr. Rubin proposed that minimum inhibitory concentration (MIC) concentrations could be an alternative to in vitro testing as a predictor of treatment response.
“The clinical laboratory provides us not only with a breakpoint interpretation but also with raw data, a quantitative assessment of MIC values,” he noted. “These values can be thought of more as probabilities of successful therapy than as absolute thresholds, a change in attitude that may dispel a false sense of security about the choice of regimen in the treatment of patients with tuberculosis.”
Dr. Rubin is affiliated with the department of immunology and infectious diseases at the Harvard School of Public Health, Boston. He had no relevant financial conflicts to disclose.
Although standard four-drug therapy has been shown to cure 90% of patients in several clinical trials, patients do relapse for reasons such as poor treatment adherence and “variations in the characteristics of the infected patients or the infecting pathogens,” wrote Eric J. Rubin, MD, in an accompanying editorial (N Engl J Med. 2018;379:882-3).
Current antibiotic susceptibility thresholds are often set by committees using models, said Dr. Rubin. “Given the uncertainties in modeling, as has been seen in clinical studies, these breakpoints can be imperfect predictors of treatment response.”
Dr. Rubin proposed that minimum inhibitory concentration (MIC) concentrations could be an alternative to in vitro testing as a predictor of treatment response.
“The clinical laboratory provides us not only with a breakpoint interpretation but also with raw data, a quantitative assessment of MIC values,” he noted. “These values can be thought of more as probabilities of successful therapy than as absolute thresholds, a change in attitude that may dispel a false sense of security about the choice of regimen in the treatment of patients with tuberculosis.”
Dr. Rubin is affiliated with the department of immunology and infectious diseases at the Harvard School of Public Health, Boston. He had no relevant financial conflicts to disclose.
Higher pretreatment drug concentrations close to a resistance breakpoint for susceptibility were associated with greater relapse risk in TB, based on data from 54 patients who relapsed and 63 who were treated and cured.
“We postulated that drug-susceptible Mycobacterium tuberculosis might have a graded spectrum of susceptibilities that could be used to determine the risk of relapse,” wrote Roberto Colangeli, PhD, of Rutgers University, Newark, N.J., and his colleagues.
In a study published in the New England Journal of Medicine, the researchers examined pretreatment bacterial isolates from adults with TB who had experienced relapse and those who were cured. Using these isolates, they identified the minimum inhibitory concentration (MIC) – the lowest concentration of the drug that prevents visible bacterial growth in culture – for isoniazid and rifampin.
Overall, after controlling for other potential relapse risk factors, higher pretreatment MIC values for both isoniazid and rifampin were associated with an increased relapse risk. For isoniazid, the average MIC below the breakpoint was 0.0334 mcg/mL for relapsed patients and 0.0286 mcg/mL for cured patients. For rifampin, the average MIC below the breakpoint was 0.0695 mcg/mL for relapsed patients and 0.0453 mcg/mL for cured patients. The higher values for the relapsed versus cured patients were represented by factors of 1.17 and 1.53 for isoniazid and rifampin, respectively.
The average age of the patients was 41 years; 83% were men, and 35% were non-Hispanic white.
The study findings were limited by several factors, including the small sample size, retrospective design, and inability to test MIC values from primary cultures versus subcultures, the researchers wrote. However, the results suggest an impact of MIC values on treatment outcomes, and “additional studies that are performed in larger, well-defined prospective cohorts and that include MIC testing of pretreatment culture isolates will be useful to better validate these findings,”
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Colangeli reported no financial conflicts. Dr. Alland disclosed funding from Cepheid and several current and pending patents in the United States and Europe, with some royalties paid to Cepheid.
SOURCE: Colangeli R et al. N Engl J Med. 2018;379:823-33.
Higher pretreatment drug concentrations close to a resistance breakpoint for susceptibility were associated with greater relapse risk in TB, based on data from 54 patients who relapsed and 63 who were treated and cured.
“We postulated that drug-susceptible Mycobacterium tuberculosis might have a graded spectrum of susceptibilities that could be used to determine the risk of relapse,” wrote Roberto Colangeli, PhD, of Rutgers University, Newark, N.J., and his colleagues.
In a study published in the New England Journal of Medicine, the researchers examined pretreatment bacterial isolates from adults with TB who had experienced relapse and those who were cured. Using these isolates, they identified the minimum inhibitory concentration (MIC) – the lowest concentration of the drug that prevents visible bacterial growth in culture – for isoniazid and rifampin.
Overall, after controlling for other potential relapse risk factors, higher pretreatment MIC values for both isoniazid and rifampin were associated with an increased relapse risk. For isoniazid, the average MIC below the breakpoint was 0.0334 mcg/mL for relapsed patients and 0.0286 mcg/mL for cured patients. For rifampin, the average MIC below the breakpoint was 0.0695 mcg/mL for relapsed patients and 0.0453 mcg/mL for cured patients. The higher values for the relapsed versus cured patients were represented by factors of 1.17 and 1.53 for isoniazid and rifampin, respectively.
The average age of the patients was 41 years; 83% were men, and 35% were non-Hispanic white.
The study findings were limited by several factors, including the small sample size, retrospective design, and inability to test MIC values from primary cultures versus subcultures, the researchers wrote. However, the results suggest an impact of MIC values on treatment outcomes, and “additional studies that are performed in larger, well-defined prospective cohorts and that include MIC testing of pretreatment culture isolates will be useful to better validate these findings,”
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Colangeli reported no financial conflicts. Dr. Alland disclosed funding from Cepheid and several current and pending patents in the United States and Europe, with some royalties paid to Cepheid.
SOURCE: Colangeli R et al. N Engl J Med. 2018;379:823-33.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Risk of TB relapse increased with higher pretreatment minimum inhibitory concentration values for either isoniazid or rifampin.
Major finding: The higher values for the relapsed versus cured patients were represented by factors of 1.17 and 1.53 for isoniazid and rifampin, respectively.
Study details: The data come from a retrospective study of isolates from 54 patients with TB who relapsed and 63 who were treated and cured.
Disclosures: The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Colangeli reported no financial conflicts. Dr. Alland disclosed funding from Cepheid and several current and pending patents in the United States and Europe, with some royalties paid to Cepheid.
Source: Colangeli R et al. N Engl J Med. 2018;379:823-33.
Better adherence, shorter course with rifampin for tuberculosis
Four months of rifampin is effective in prevention of active tuberculosis, with significantly higher adherence rates versus 9 months of isoniazid in adults and children, a pair of recent studies suggest.
In one randomized, open-label trial that included adults with latent Mycobacterium tuberculosis infection, the 4-month rifampin regimen was not inferior to the 9-month isoniazid regimen in preventing active tuberculosis, had better safety, and had a rate of treatment completion 15.1 percentage points higher than the comparator.
“This trial adds to the mounting evidence of benefits of rifamycin-containing regimens of 3 or 4 months’ duration,” investigators reported in the New England Journal of Medicine.
Similarly, in an open-label study in children with latent M. tuberculosis infection, the shorter rifampin regimen had comparable efficacy and safety, according to investigators, along with a rate of treatment completion 13.4 percentage points higher than the longer isoniazid regimen.
“Rifampin has the advantage of being a single-drug regimen with existing palatable formulations for children,” reported authors of this companion study, also published in the journal.
Treatment challenges
Treating latent tuberculosis infection is central to the World Health Organization End TB Strategy and other tuberculosis elimination plans. An estimated 1.7 billion individuals, or about one-quarter of the global population, harbor latent tuberculosis infection, according to one recent estimate.
The WHO recommends treatment of latent tuberculosis infection, as well as for children under 5 years of age who are household contacts of individuals with tuberculosis. The recommended treatment is 6 or 9 months of isoniazid, with the longer duration being associated with better efficacy, previous studies have shown.
However, isoniazid treatment has been associated with low rates of regimen completion because of the hepatotoxic effects, according to authors of the current studies comparing isoniazid to rifampin.
The 4-month daily rifampin regimen has been associated with superior treatment adherence rates and fewer hepatotoxic effects, compared with the 9-month isoniazid regimen in previous observational studies. Moreover, an earlier randomized trial including 679 men in Hong Kong demonstrated that 3 months of rifampin was superior to placebo and comparable to 6 months of isoniazid as tuberculosis prophylaxis.
Rifampin: Latest data
The adult trial just published in the New England Journal of Medicine demonstrates the efficacy and real-world effectiveness of the 4-month rifampin regimen versus the 9-month isoniazid regimen for prevention of active tuberculosis, according to lead author Dick Menzies, MD, of the Montreal Chest Institute at McGill University Health Centre.
The 4-month rifampin regimen is a “fundamental game-changer in TB prevention” based on its comparable efficacy is adults, along with improved safety and acceptability, Dr. Menzies said in a recent press release.
Dr. Menzies and his colleagues reported on 6,063 adults (aged 18 years or older) randomized to the 4-month rifampin or 9-month isoniazid regimen at trial sites in Australia, Benin, Brazil, Canada, Ghana, Guinea, Indonesia, Saudi Arabia, and South Korea.
Treatment was completed by 78.8% of individuals in the rifampin arm, compared with 63.2% of patients in the isoniazid arm, for a difference of 15.1 percentage points (95% confidence interval, 12.7-17.4; P less than .001), the researchers reported.
Rifampin was not inferior to isoniazid in preventing tuberculosis, according to the report. In the per-protocol analysis, there were a total of five confirmed or clinically diagnosed cases of active tuberculosis in each of the trial arms. All active cases were treated successfully, including two cases that had demonstrated drug resistance, investigators added.
The rifampin group had consistently lower rates of grade 3-grade 5 adverse events, particularly hepatotoxic events, versus the isoniazid group, according to analyses outlined in the report.
“We believe this 4-month rifampin treatment should replace the 9 months on isoniazid for most people who need therapy for latent tuberculosis,” said Dr. Menzies, a respirologist with the Montreal Chest Institute and a professor of medicine, epidemiology and biostatistics at McGill University, also in Montreal.
Experience in children
In the related study, reported by lead author Thierno Diallo, MD, of Hôpital National Ignace Deen, in Conakry, Guinea, along with Dr. Menzies, and their coauthors, 829 children were randomized to 4 months of rifampin or 9 months of isoniazid.
The study population included 79 children under 2 years, the age group that has the highest risk of life-threatening TB, Dr. Diallo and his colleagues wrote in their report.
Treatment was completed in 86.5% of all children randomized to rifampin, compared with 77.1% in the isoniazid arm (difference of 13.6 percentage points; 95% confidence interval, 7.9-19.3; P less than .001), according to the investigators.
Two active tuberculosis cases were diagnosed in the isoniazid group over 542 person-years of follow-up, versus no cases in the rifampin group over a similar follow-up period.
“Although the only cases of active tuberculosis were diagnosed in the isoniazid group, we cannot conclude that 4 months of rifampin was either superior or noninferior to 9 months of isoniazid for the prevention of active tuberculosis,” the authors wrote.
“However, since there were no cases of active tuberculosis in the rifampin group in our trial or among 434 children who received 3 months of once-weekly isoniazid plus rifapentine in another trial, we suggest that these shorter rifamycin containing regimens are effective,” they added.
In contrast to the adult trial, safety profiles in this study were similar for rifampin and isoniazid, investigators said.
The lack of difference is side effects was possibly because of the differences in the pharmacokinetic activity of rifampin in younger patients, a topic that deserves further study, they concluded.
No potential conflicts of interest relevant to the studies were reported by Dr. Menzies, Dr. Diallo, or their coauthors.
Both studies were supported by grants from the Canadian Institutes of Health Research. The adult study was supported in part by a grant from the Australian National Health and Medical Research Council, while the companion study in children was supported in part by a grant from the Conselho Nacional de Pesquisa in Brazil.
SOURCES: Menzies D et al. N Engl J Med. 2018 Aug 2;379(5):440-53; Diallo T et al. N Engl J Med. 2018 Aug 2;379(5):454-63.
Four months of rifampin is effective in prevention of active tuberculosis, with significantly higher adherence rates versus 9 months of isoniazid in adults and children, a pair of recent studies suggest.
In one randomized, open-label trial that included adults with latent Mycobacterium tuberculosis infection, the 4-month rifampin regimen was not inferior to the 9-month isoniazid regimen in preventing active tuberculosis, had better safety, and had a rate of treatment completion 15.1 percentage points higher than the comparator.
“This trial adds to the mounting evidence of benefits of rifamycin-containing regimens of 3 or 4 months’ duration,” investigators reported in the New England Journal of Medicine.
Similarly, in an open-label study in children with latent M. tuberculosis infection, the shorter rifampin regimen had comparable efficacy and safety, according to investigators, along with a rate of treatment completion 13.4 percentage points higher than the longer isoniazid regimen.
“Rifampin has the advantage of being a single-drug regimen with existing palatable formulations for children,” reported authors of this companion study, also published in the journal.
Treatment challenges
Treating latent tuberculosis infection is central to the World Health Organization End TB Strategy and other tuberculosis elimination plans. An estimated 1.7 billion individuals, or about one-quarter of the global population, harbor latent tuberculosis infection, according to one recent estimate.
The WHO recommends treatment of latent tuberculosis infection, as well as for children under 5 years of age who are household contacts of individuals with tuberculosis. The recommended treatment is 6 or 9 months of isoniazid, with the longer duration being associated with better efficacy, previous studies have shown.
However, isoniazid treatment has been associated with low rates of regimen completion because of the hepatotoxic effects, according to authors of the current studies comparing isoniazid to rifampin.
The 4-month daily rifampin regimen has been associated with superior treatment adherence rates and fewer hepatotoxic effects, compared with the 9-month isoniazid regimen in previous observational studies. Moreover, an earlier randomized trial including 679 men in Hong Kong demonstrated that 3 months of rifampin was superior to placebo and comparable to 6 months of isoniazid as tuberculosis prophylaxis.
Rifampin: Latest data
The adult trial just published in the New England Journal of Medicine demonstrates the efficacy and real-world effectiveness of the 4-month rifampin regimen versus the 9-month isoniazid regimen for prevention of active tuberculosis, according to lead author Dick Menzies, MD, of the Montreal Chest Institute at McGill University Health Centre.
The 4-month rifampin regimen is a “fundamental game-changer in TB prevention” based on its comparable efficacy is adults, along with improved safety and acceptability, Dr. Menzies said in a recent press release.
Dr. Menzies and his colleagues reported on 6,063 adults (aged 18 years or older) randomized to the 4-month rifampin or 9-month isoniazid regimen at trial sites in Australia, Benin, Brazil, Canada, Ghana, Guinea, Indonesia, Saudi Arabia, and South Korea.
Treatment was completed by 78.8% of individuals in the rifampin arm, compared with 63.2% of patients in the isoniazid arm, for a difference of 15.1 percentage points (95% confidence interval, 12.7-17.4; P less than .001), the researchers reported.
Rifampin was not inferior to isoniazid in preventing tuberculosis, according to the report. In the per-protocol analysis, there were a total of five confirmed or clinically diagnosed cases of active tuberculosis in each of the trial arms. All active cases were treated successfully, including two cases that had demonstrated drug resistance, investigators added.
The rifampin group had consistently lower rates of grade 3-grade 5 adverse events, particularly hepatotoxic events, versus the isoniazid group, according to analyses outlined in the report.
“We believe this 4-month rifampin treatment should replace the 9 months on isoniazid for most people who need therapy for latent tuberculosis,” said Dr. Menzies, a respirologist with the Montreal Chest Institute and a professor of medicine, epidemiology and biostatistics at McGill University, also in Montreal.
Experience in children
In the related study, reported by lead author Thierno Diallo, MD, of Hôpital National Ignace Deen, in Conakry, Guinea, along with Dr. Menzies, and their coauthors, 829 children were randomized to 4 months of rifampin or 9 months of isoniazid.
The study population included 79 children under 2 years, the age group that has the highest risk of life-threatening TB, Dr. Diallo and his colleagues wrote in their report.
Treatment was completed in 86.5% of all children randomized to rifampin, compared with 77.1% in the isoniazid arm (difference of 13.6 percentage points; 95% confidence interval, 7.9-19.3; P less than .001), according to the investigators.
Two active tuberculosis cases were diagnosed in the isoniazid group over 542 person-years of follow-up, versus no cases in the rifampin group over a similar follow-up period.
“Although the only cases of active tuberculosis were diagnosed in the isoniazid group, we cannot conclude that 4 months of rifampin was either superior or noninferior to 9 months of isoniazid for the prevention of active tuberculosis,” the authors wrote.
“However, since there were no cases of active tuberculosis in the rifampin group in our trial or among 434 children who received 3 months of once-weekly isoniazid plus rifapentine in another trial, we suggest that these shorter rifamycin containing regimens are effective,” they added.
In contrast to the adult trial, safety profiles in this study were similar for rifampin and isoniazid, investigators said.
The lack of difference is side effects was possibly because of the differences in the pharmacokinetic activity of rifampin in younger patients, a topic that deserves further study, they concluded.
No potential conflicts of interest relevant to the studies were reported by Dr. Menzies, Dr. Diallo, or their coauthors.
Both studies were supported by grants from the Canadian Institutes of Health Research. The adult study was supported in part by a grant from the Australian National Health and Medical Research Council, while the companion study in children was supported in part by a grant from the Conselho Nacional de Pesquisa in Brazil.
SOURCES: Menzies D et al. N Engl J Med. 2018 Aug 2;379(5):440-53; Diallo T et al. N Engl J Med. 2018 Aug 2;379(5):454-63.
Four months of rifampin is effective in prevention of active tuberculosis, with significantly higher adherence rates versus 9 months of isoniazid in adults and children, a pair of recent studies suggest.
In one randomized, open-label trial that included adults with latent Mycobacterium tuberculosis infection, the 4-month rifampin regimen was not inferior to the 9-month isoniazid regimen in preventing active tuberculosis, had better safety, and had a rate of treatment completion 15.1 percentage points higher than the comparator.
“This trial adds to the mounting evidence of benefits of rifamycin-containing regimens of 3 or 4 months’ duration,” investigators reported in the New England Journal of Medicine.
Similarly, in an open-label study in children with latent M. tuberculosis infection, the shorter rifampin regimen had comparable efficacy and safety, according to investigators, along with a rate of treatment completion 13.4 percentage points higher than the longer isoniazid regimen.
“Rifampin has the advantage of being a single-drug regimen with existing palatable formulations for children,” reported authors of this companion study, also published in the journal.
Treatment challenges
Treating latent tuberculosis infection is central to the World Health Organization End TB Strategy and other tuberculosis elimination plans. An estimated 1.7 billion individuals, or about one-quarter of the global population, harbor latent tuberculosis infection, according to one recent estimate.
The WHO recommends treatment of latent tuberculosis infection, as well as for children under 5 years of age who are household contacts of individuals with tuberculosis. The recommended treatment is 6 or 9 months of isoniazid, with the longer duration being associated with better efficacy, previous studies have shown.
However, isoniazid treatment has been associated with low rates of regimen completion because of the hepatotoxic effects, according to authors of the current studies comparing isoniazid to rifampin.
The 4-month daily rifampin regimen has been associated with superior treatment adherence rates and fewer hepatotoxic effects, compared with the 9-month isoniazid regimen in previous observational studies. Moreover, an earlier randomized trial including 679 men in Hong Kong demonstrated that 3 months of rifampin was superior to placebo and comparable to 6 months of isoniazid as tuberculosis prophylaxis.
Rifampin: Latest data
The adult trial just published in the New England Journal of Medicine demonstrates the efficacy and real-world effectiveness of the 4-month rifampin regimen versus the 9-month isoniazid regimen for prevention of active tuberculosis, according to lead author Dick Menzies, MD, of the Montreal Chest Institute at McGill University Health Centre.
The 4-month rifampin regimen is a “fundamental game-changer in TB prevention” based on its comparable efficacy is adults, along with improved safety and acceptability, Dr. Menzies said in a recent press release.
Dr. Menzies and his colleagues reported on 6,063 adults (aged 18 years or older) randomized to the 4-month rifampin or 9-month isoniazid regimen at trial sites in Australia, Benin, Brazil, Canada, Ghana, Guinea, Indonesia, Saudi Arabia, and South Korea.
Treatment was completed by 78.8% of individuals in the rifampin arm, compared with 63.2% of patients in the isoniazid arm, for a difference of 15.1 percentage points (95% confidence interval, 12.7-17.4; P less than .001), the researchers reported.
Rifampin was not inferior to isoniazid in preventing tuberculosis, according to the report. In the per-protocol analysis, there were a total of five confirmed or clinically diagnosed cases of active tuberculosis in each of the trial arms. All active cases were treated successfully, including two cases that had demonstrated drug resistance, investigators added.
The rifampin group had consistently lower rates of grade 3-grade 5 adverse events, particularly hepatotoxic events, versus the isoniazid group, according to analyses outlined in the report.
“We believe this 4-month rifampin treatment should replace the 9 months on isoniazid for most people who need therapy for latent tuberculosis,” said Dr. Menzies, a respirologist with the Montreal Chest Institute and a professor of medicine, epidemiology and biostatistics at McGill University, also in Montreal.
Experience in children
In the related study, reported by lead author Thierno Diallo, MD, of Hôpital National Ignace Deen, in Conakry, Guinea, along with Dr. Menzies, and their coauthors, 829 children were randomized to 4 months of rifampin or 9 months of isoniazid.
The study population included 79 children under 2 years, the age group that has the highest risk of life-threatening TB, Dr. Diallo and his colleagues wrote in their report.
Treatment was completed in 86.5% of all children randomized to rifampin, compared with 77.1% in the isoniazid arm (difference of 13.6 percentage points; 95% confidence interval, 7.9-19.3; P less than .001), according to the investigators.
Two active tuberculosis cases were diagnosed in the isoniazid group over 542 person-years of follow-up, versus no cases in the rifampin group over a similar follow-up period.
“Although the only cases of active tuberculosis were diagnosed in the isoniazid group, we cannot conclude that 4 months of rifampin was either superior or noninferior to 9 months of isoniazid for the prevention of active tuberculosis,” the authors wrote.
“However, since there were no cases of active tuberculosis in the rifampin group in our trial or among 434 children who received 3 months of once-weekly isoniazid plus rifapentine in another trial, we suggest that these shorter rifamycin containing regimens are effective,” they added.
In contrast to the adult trial, safety profiles in this study were similar for rifampin and isoniazid, investigators said.
The lack of difference is side effects was possibly because of the differences in the pharmacokinetic activity of rifampin in younger patients, a topic that deserves further study, they concluded.
No potential conflicts of interest relevant to the studies were reported by Dr. Menzies, Dr. Diallo, or their coauthors.
Both studies were supported by grants from the Canadian Institutes of Health Research. The adult study was supported in part by a grant from the Australian National Health and Medical Research Council, while the companion study in children was supported in part by a grant from the Conselho Nacional de Pesquisa in Brazil.
SOURCES: Menzies D et al. N Engl J Med. 2018 Aug 2;379(5):440-53; Diallo T et al. N Engl J Med. 2018 Aug 2;379(5):454-63.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Four months of rifampin is effective in prevention of active tuberculosis, with significantly higher adherence rates versus 9 months of isoniazid in adults and children.
Major finding: Treatment was completed by 78.8% and 63.2% of adults randomized to rifampin or isoniazid, respectively.
Study details: A randomized, open-label trial including 6,063 randomized adults, and a companion study including 829 children, with latent Mycobacterium tuberculosis infection.
Disclosures: Authors reported no potential conflicts of interest relevant to the research. Support for the research came from the Canadian Institutes of Health Research, the Australian National Health and Medical Research Council, and the Conselho Nacional de Pesquisa in Brazil.
Sources: Menzies D et al. N Engl J Med. 2018 Aug 2;379(5):440-53; Diallo T, et al. N Engl J Med. 2018 Aug 2;379(5):454-63.