User login
COVID-19 causes financial woes for GI practices
On a typical clinic day, Will Bulsiewicz, MD, a Charleston, S.C.–based gastroenterologist, used to see 22 patients, while other days were filled with up to 16 procedures.
Since COVID-19 however, things have vastly changed. Dr. Bulsiewicz now visits with all clinic patients through telehealth, and the volume has dipped to between zero and six patients per day. His three-doctor practice has also experienced a more than 90% reduction in endoscopy volume.
“Naturally, this has been devastating,” Dr. Bulsiewicz said in an interview. “Our practice was started in 1984, and we had a business model that we used for the history of our practice. That practice model was upended in a matter of 2 weeks.”
Dr. Bulsiewicz is far from alone. Community GI practices across the country are experiencing similar financial distress in the face of COVID-19. In addition to a decrease in patient referrals, the Centers for Medicare & Medicaid Services has requested that all elective esophagogastroduodenoscopies, colonoscopies, endoscopies, surgeries, and procedures be delayed during the coronavirus outbreak to conserve critical equipment and limit virus exposure. The guidance aligns with recent recommendations issued by American Gastroenterological Association, American Association for the Study of Liver Diseases, American College of Gastroenterology, and American Society for Gastrointestinal Endoscopy. The lack of patients has led to plummeting revenue for many GI practices and resulted in layoffs, reduced hours, and limited salaries in order to keep practices afloat.
“We’ve had to make drastic changes in the way we work,” said Rajeev Jain, MD, AGAF, a Dallas-based gastroenterologist. “The way private practices are economically set up, they don’t have large reserves of capital or liquidity. We’re not like Apple or these big companies that have these massive cushions. It’s one thing when you have a downturn in the economy and less people come to get care, but when you have a complete shutdown, your revenue stream to pay your bills is literally dried up.”
Dr. Jain’s practice is part of Texas Digestive Disease Consultants (TDDC), which provides GI care for patients in Texas and Louisiana. TDDC is part of GI Alliance, a private equity–based consolidation of practices that includes several states and more than 350 GIs. The management services organization is a collaboration between the PE firm and the partner physicians. Since the COVID-19 outbreak, Dr. Jain said his practice has seen a dramatic drop in patients. Normally, Dr. Jain would perform between 25 and 30 outpatient scopes over the course of 2 days, he said. On a recent Monday, he performed two procedures. To preserve cash flow, Dr. Jain said he and his senior partners are not taking an income right now. Some employees were recently furloughed and laid off.
“I never in my life thought that I would have to lay off people because of an economic issue,” Dr. Jain said. “That’s psychological strain that as a physician owner you feel because these are people that you work with on a day-to-day basis and you don’t want them suffering either. That’s been a tough thing.
James S. Leavitt, MD, said his 17-physician center in Miami, Fla., has furloughed about half its staff. The center is part of Gastro Health, a private equity firm–based medical group with more than 250 providers in four states. Dr. Leavitt, president and chief clinical officer for Gastro Health, said his center has gone from about 150 patients per day to 5 or fewer, while procedures have dropped from more than 100 a day to maybe 5.
Having partnered with a private equity firm, however, Dr. Leavitt believes his practice is bettered situated to manage the health crisis and address financial challenges.
“It’s made us better prepared to weather the storm. We have a very high-powered, sophisticated administration and much broader base and access to capital. [For example,] we had a lot of depth in management so that we could roll out a robust televisit program in a week in four states with over 250 doctors.”
From a business standpoint, however, certain goals for the company are on hold, he said, such as closing on potential acquisitions.
Telemedicine works well for many patients, particularly for follow-up patients and for patients who have an established relationship with Dr. Leavitt, he said. There are limitations of course, he noted.
“If I were a dermatologist, maybe I could see the skin rash, but you can’t examine the patient,” he said. “There are certain things you can’t do. If a patient has significant abdominal pain, a televisit isn’t the greatest.”
That’s why Dr. Leavitt’s care center remains open for the handful of patients who must be seen in-person, he said. Those patients are screened beforehand and their temperatures taken before treatment.
Dr. Bulsiewicz’s practice made the transition to telehealth after never having used the modality before COVID-19.
“This was a scramble,” said Dr. Bulsiewicz, who posts about COVID-19 on social media. “We started from zero knowledge to implementation in less than a week.”
Overall, the switch went smoothly, but Dr. Bulsiewicz said reimbursement challenges come with telehealth.
“The billing is not the same,” he said. “You’re doing the same work or more, and you’re taking a reduced fee because of the antiquated fee structure that is forcing you to apply the typical rules of an office encounter.”
He hopes CMS will alter the reimbursement schedule to temporarily pay on par with traditional evaluation and management codes based on medical complexity as opposed to documentation of physical exam. CMS has already expanded Medicare telehealth coverage to cover a wider range of health care services in light of the COVID-19 crisis and also broadened the range of communication tools that can be used, according to a March announcement.
In the meantime, many practices have applied for financial assistance programs. The AGA recently pushed the government for additional assistance to help struggling practices.
Dr. Jain hopes these assistance programs roll out quickly.
“If these don’t get out there quick enough and big enough, we are going to see a massive wave of loss of independent practices and/or consolidation,” he said. “I fear a death to small, independent practices because they’re not going to have the financial wherewithal to tolerate this for too long.”
On a typical clinic day, Will Bulsiewicz, MD, a Charleston, S.C.–based gastroenterologist, used to see 22 patients, while other days were filled with up to 16 procedures.
Since COVID-19 however, things have vastly changed. Dr. Bulsiewicz now visits with all clinic patients through telehealth, and the volume has dipped to between zero and six patients per day. His three-doctor practice has also experienced a more than 90% reduction in endoscopy volume.
“Naturally, this has been devastating,” Dr. Bulsiewicz said in an interview. “Our practice was started in 1984, and we had a business model that we used for the history of our practice. That practice model was upended in a matter of 2 weeks.”
Dr. Bulsiewicz is far from alone. Community GI practices across the country are experiencing similar financial distress in the face of COVID-19. In addition to a decrease in patient referrals, the Centers for Medicare & Medicaid Services has requested that all elective esophagogastroduodenoscopies, colonoscopies, endoscopies, surgeries, and procedures be delayed during the coronavirus outbreak to conserve critical equipment and limit virus exposure. The guidance aligns with recent recommendations issued by American Gastroenterological Association, American Association for the Study of Liver Diseases, American College of Gastroenterology, and American Society for Gastrointestinal Endoscopy. The lack of patients has led to plummeting revenue for many GI practices and resulted in layoffs, reduced hours, and limited salaries in order to keep practices afloat.
“We’ve had to make drastic changes in the way we work,” said Rajeev Jain, MD, AGAF, a Dallas-based gastroenterologist. “The way private practices are economically set up, they don’t have large reserves of capital or liquidity. We’re not like Apple or these big companies that have these massive cushions. It’s one thing when you have a downturn in the economy and less people come to get care, but when you have a complete shutdown, your revenue stream to pay your bills is literally dried up.”
Dr. Jain’s practice is part of Texas Digestive Disease Consultants (TDDC), which provides GI care for patients in Texas and Louisiana. TDDC is part of GI Alliance, a private equity–based consolidation of practices that includes several states and more than 350 GIs. The management services organization is a collaboration between the PE firm and the partner physicians. Since the COVID-19 outbreak, Dr. Jain said his practice has seen a dramatic drop in patients. Normally, Dr. Jain would perform between 25 and 30 outpatient scopes over the course of 2 days, he said. On a recent Monday, he performed two procedures. To preserve cash flow, Dr. Jain said he and his senior partners are not taking an income right now. Some employees were recently furloughed and laid off.
“I never in my life thought that I would have to lay off people because of an economic issue,” Dr. Jain said. “That’s psychological strain that as a physician owner you feel because these are people that you work with on a day-to-day basis and you don’t want them suffering either. That’s been a tough thing.
James S. Leavitt, MD, said his 17-physician center in Miami, Fla., has furloughed about half its staff. The center is part of Gastro Health, a private equity firm–based medical group with more than 250 providers in four states. Dr. Leavitt, president and chief clinical officer for Gastro Health, said his center has gone from about 150 patients per day to 5 or fewer, while procedures have dropped from more than 100 a day to maybe 5.
Having partnered with a private equity firm, however, Dr. Leavitt believes his practice is bettered situated to manage the health crisis and address financial challenges.
“It’s made us better prepared to weather the storm. We have a very high-powered, sophisticated administration and much broader base and access to capital. [For example,] we had a lot of depth in management so that we could roll out a robust televisit program in a week in four states with over 250 doctors.”
From a business standpoint, however, certain goals for the company are on hold, he said, such as closing on potential acquisitions.
Telemedicine works well for many patients, particularly for follow-up patients and for patients who have an established relationship with Dr. Leavitt, he said. There are limitations of course, he noted.
“If I were a dermatologist, maybe I could see the skin rash, but you can’t examine the patient,” he said. “There are certain things you can’t do. If a patient has significant abdominal pain, a televisit isn’t the greatest.”
That’s why Dr. Leavitt’s care center remains open for the handful of patients who must be seen in-person, he said. Those patients are screened beforehand and their temperatures taken before treatment.
Dr. Bulsiewicz’s practice made the transition to telehealth after never having used the modality before COVID-19.
“This was a scramble,” said Dr. Bulsiewicz, who posts about COVID-19 on social media. “We started from zero knowledge to implementation in less than a week.”
Overall, the switch went smoothly, but Dr. Bulsiewicz said reimbursement challenges come with telehealth.
“The billing is not the same,” he said. “You’re doing the same work or more, and you’re taking a reduced fee because of the antiquated fee structure that is forcing you to apply the typical rules of an office encounter.”
He hopes CMS will alter the reimbursement schedule to temporarily pay on par with traditional evaluation and management codes based on medical complexity as opposed to documentation of physical exam. CMS has already expanded Medicare telehealth coverage to cover a wider range of health care services in light of the COVID-19 crisis and also broadened the range of communication tools that can be used, according to a March announcement.
In the meantime, many practices have applied for financial assistance programs. The AGA recently pushed the government for additional assistance to help struggling practices.
Dr. Jain hopes these assistance programs roll out quickly.
“If these don’t get out there quick enough and big enough, we are going to see a massive wave of loss of independent practices and/or consolidation,” he said. “I fear a death to small, independent practices because they’re not going to have the financial wherewithal to tolerate this for too long.”
On a typical clinic day, Will Bulsiewicz, MD, a Charleston, S.C.–based gastroenterologist, used to see 22 patients, while other days were filled with up to 16 procedures.
Since COVID-19 however, things have vastly changed. Dr. Bulsiewicz now visits with all clinic patients through telehealth, and the volume has dipped to between zero and six patients per day. His three-doctor practice has also experienced a more than 90% reduction in endoscopy volume.
“Naturally, this has been devastating,” Dr. Bulsiewicz said in an interview. “Our practice was started in 1984, and we had a business model that we used for the history of our practice. That practice model was upended in a matter of 2 weeks.”
Dr. Bulsiewicz is far from alone. Community GI practices across the country are experiencing similar financial distress in the face of COVID-19. In addition to a decrease in patient referrals, the Centers for Medicare & Medicaid Services has requested that all elective esophagogastroduodenoscopies, colonoscopies, endoscopies, surgeries, and procedures be delayed during the coronavirus outbreak to conserve critical equipment and limit virus exposure. The guidance aligns with recent recommendations issued by American Gastroenterological Association, American Association for the Study of Liver Diseases, American College of Gastroenterology, and American Society for Gastrointestinal Endoscopy. The lack of patients has led to plummeting revenue for many GI practices and resulted in layoffs, reduced hours, and limited salaries in order to keep practices afloat.
“We’ve had to make drastic changes in the way we work,” said Rajeev Jain, MD, AGAF, a Dallas-based gastroenterologist. “The way private practices are economically set up, they don’t have large reserves of capital or liquidity. We’re not like Apple or these big companies that have these massive cushions. It’s one thing when you have a downturn in the economy and less people come to get care, but when you have a complete shutdown, your revenue stream to pay your bills is literally dried up.”
Dr. Jain’s practice is part of Texas Digestive Disease Consultants (TDDC), which provides GI care for patients in Texas and Louisiana. TDDC is part of GI Alliance, a private equity–based consolidation of practices that includes several states and more than 350 GIs. The management services organization is a collaboration between the PE firm and the partner physicians. Since the COVID-19 outbreak, Dr. Jain said his practice has seen a dramatic drop in patients. Normally, Dr. Jain would perform between 25 and 30 outpatient scopes over the course of 2 days, he said. On a recent Monday, he performed two procedures. To preserve cash flow, Dr. Jain said he and his senior partners are not taking an income right now. Some employees were recently furloughed and laid off.
“I never in my life thought that I would have to lay off people because of an economic issue,” Dr. Jain said. “That’s psychological strain that as a physician owner you feel because these are people that you work with on a day-to-day basis and you don’t want them suffering either. That’s been a tough thing.
James S. Leavitt, MD, said his 17-physician center in Miami, Fla., has furloughed about half its staff. The center is part of Gastro Health, a private equity firm–based medical group with more than 250 providers in four states. Dr. Leavitt, president and chief clinical officer for Gastro Health, said his center has gone from about 150 patients per day to 5 or fewer, while procedures have dropped from more than 100 a day to maybe 5.
Having partnered with a private equity firm, however, Dr. Leavitt believes his practice is bettered situated to manage the health crisis and address financial challenges.
“It’s made us better prepared to weather the storm. We have a very high-powered, sophisticated administration and much broader base and access to capital. [For example,] we had a lot of depth in management so that we could roll out a robust televisit program in a week in four states with over 250 doctors.”
From a business standpoint, however, certain goals for the company are on hold, he said, such as closing on potential acquisitions.
Telemedicine works well for many patients, particularly for follow-up patients and for patients who have an established relationship with Dr. Leavitt, he said. There are limitations of course, he noted.
“If I were a dermatologist, maybe I could see the skin rash, but you can’t examine the patient,” he said. “There are certain things you can’t do. If a patient has significant abdominal pain, a televisit isn’t the greatest.”
That’s why Dr. Leavitt’s care center remains open for the handful of patients who must be seen in-person, he said. Those patients are screened beforehand and their temperatures taken before treatment.
Dr. Bulsiewicz’s practice made the transition to telehealth after never having used the modality before COVID-19.
“This was a scramble,” said Dr. Bulsiewicz, who posts about COVID-19 on social media. “We started from zero knowledge to implementation in less than a week.”
Overall, the switch went smoothly, but Dr. Bulsiewicz said reimbursement challenges come with telehealth.
“The billing is not the same,” he said. “You’re doing the same work or more, and you’re taking a reduced fee because of the antiquated fee structure that is forcing you to apply the typical rules of an office encounter.”
He hopes CMS will alter the reimbursement schedule to temporarily pay on par with traditional evaluation and management codes based on medical complexity as opposed to documentation of physical exam. CMS has already expanded Medicare telehealth coverage to cover a wider range of health care services in light of the COVID-19 crisis and also broadened the range of communication tools that can be used, according to a March announcement.
In the meantime, many practices have applied for financial assistance programs. The AGA recently pushed the government for additional assistance to help struggling practices.
Dr. Jain hopes these assistance programs roll out quickly.
“If these don’t get out there quick enough and big enough, we are going to see a massive wave of loss of independent practices and/or consolidation,” he said. “I fear a death to small, independent practices because they’re not going to have the financial wherewithal to tolerate this for too long.”
Managing gynecologic cancers during the COVID-19 pandemic
To manage patients with gynecologic cancers, oncologists in the United States and Europe are recommending reducing outpatient visits, delaying surgeries, prolonging chemotherapy regimens, and generally trying to keep cancer patients away from those who have tested positive for COVID-19.
“We recognize that, in this special situation, we must continue to provide our gynecologic oncology patients with the highest quality of medical services,” Pedro T. Ramirez, MD, of the University of Texas MD Anderson Cancer Center in Houston and associates wrote in an editorial published in the International Journal of Gynecological Cancer.
At the same time, the authors added, the safety of patients, their families, and medical staff needs to be assured.
Dr. Ramirez and colleagues’ editorial includes recommendations on how to optimize the care of patients with gynecologic cancers while prioritizing safety and minimizing the burden to the healthcare system. The group’s recommendations outline when surgery, radiotherapy, and other treatments might be safely postponed and when they need to proceed out of urgency.
Some authors of the editorial also described their experiences with COVID-19 during a webinar on managing patients with advanced ovarian cancer, which was hosted by the European Society of Gynaecological Oncology (ESGO).
A lack of resources
In Spain, health resources “are collapsed” by the pandemic, editorial author Luis Chiva, MD, said during the webinar.
At his institution, the Clínica Universidad de Navarra in Madrid, 98% of the 1,500 intensive care beds were occupied by COVID-19 patients at the end of March. So the hope was to be able to refer their patients to other communities where there may still be some capacity.
Another problem in Spain is the high percentage of health workers infected with SARS-CoV-2, the virus behind COVID-19. More than 15,000 health workers were recently reported to be sick or self-isolating, which is around 14% of the health care workforce in the country.
Dr. Chiva noted that this puts those treating gynecologic cancers in a difficult position. On the one hand, surgery to remove a high-risk ovarian mass should not be delayed, but the majority of hospitals in Spain simply cannot perform this type of surgery during the pandemic.
“Unfortunately, due to this specific situation, almost, I would say in 80%-90% of hospitals, we are only able to carry out emergency surgical procedures,” Dr. Chiva said. That’s general emergency procedures such as appendectomies, removing blockages, and dealing with hemorrhages, not gynecologic surgeries. “It’s almost impossible to schedule the typical oncological cases,” he said.
Even with the Hospital IFEMA now set up at the Feria de Madrid, which is usually used to host large-scale events, there are “minimal options for performing standard oncological surgery,” Dr. Chiva said. He estimated that just 5% of hospitals in Spain are able to perform oncologic surgeries as normal, with maybe 15% able to offer surgery without the backup of postsurgical intensive care.
‘Ring-fencing’
“This is really an unusual time for us,” commented Jonathan Ledermann, MD, vice president of ESGO and a professor of medical oncology at University College London, who moderated the webinar.
“This is affecting the way in which we diagnose our patients and have access to care,” he said. “It compromises the way in which we treat patients. We have to adjust our treatment pathways. We have to look at the risks of coronavirus infection in cancer patients and how we manage patients in a socially distancing environment. We also need to think about managing gynecological oncology departments in the face of disease amongst staff, the risks of transmission, and the reduced clinical service.”
Dr. Ledermann noted that “ring-fencing” a few hospitals to deal only with patients free of COVID-19 might be a way forward. This approach has been used in Northern Italy and was recently started in London.
“We try to divide and have separate access between COVID-positive and -negative patients,” said Anna Fagotti, MD, an assistant professor at Fondazione Policlinico Universitario Agostino Gemelli IRCCS in Rome and another coauthor of the editorial.
“We are trying to divide the work flow of patients and try to ensure treatment to cancer patients as much as we can,” she explained. “This means that it’s a very difficult situation, and, every time, you have to deal with the number of places available as some places have been taken by other patients from the emergency room. We are still trying to have a number of beds and intensive care unit beds available for our patients.”
Setting up dedicated hospitals is a good idea, but it has to be done before the “tsunami” of cases hits and there are no more intensive care beds or ventilators, according to Antonio González-Martín, MD, of Clínica Universidad de Navarra in Madrid, another coauthor of the editorial.
Limiting hospital visits
Strategies to limit the number of times patients need to come into hospital for appointments and treatment is key to getting through the pandemic, Sandro Pignata, MD, of Instituto Nazionale Tumori IRCCS Fondazione G. Pascale in Naples, Italy, said during the webinar.
“It will be imperative to explore options that reduce the number of procedures or surgical interventions that may be associated with prolonged operative time, risk of major blood loss, necessitating blood products, risk of infection to the medical personnel, or admission to intensive care units,” Dr. Ramirez and colleagues wrote in their editorial.
“In considering management of disease, we must recognize that, in many centers, access to routine visits and surgery may be either completely restricted or significantly reduced. We must, therefore, consider options that may still offer our patients a treatment plan that addresses their disease while at the same time limiting risk of exposure,” the authors wrote.
The authors declared no competing interests or specific funding in relation to their work, and the webinar participants had no conflicts of interest.
SOURCE: Ramirez PT et al. Int J Gynecol Cancer. 2020 Mar 27. doi: 10.1136/ijgc-2020-001419.
To manage patients with gynecologic cancers, oncologists in the United States and Europe are recommending reducing outpatient visits, delaying surgeries, prolonging chemotherapy regimens, and generally trying to keep cancer patients away from those who have tested positive for COVID-19.
“We recognize that, in this special situation, we must continue to provide our gynecologic oncology patients with the highest quality of medical services,” Pedro T. Ramirez, MD, of the University of Texas MD Anderson Cancer Center in Houston and associates wrote in an editorial published in the International Journal of Gynecological Cancer.
At the same time, the authors added, the safety of patients, their families, and medical staff needs to be assured.
Dr. Ramirez and colleagues’ editorial includes recommendations on how to optimize the care of patients with gynecologic cancers while prioritizing safety and minimizing the burden to the healthcare system. The group’s recommendations outline when surgery, radiotherapy, and other treatments might be safely postponed and when they need to proceed out of urgency.
Some authors of the editorial also described their experiences with COVID-19 during a webinar on managing patients with advanced ovarian cancer, which was hosted by the European Society of Gynaecological Oncology (ESGO).
A lack of resources
In Spain, health resources “are collapsed” by the pandemic, editorial author Luis Chiva, MD, said during the webinar.
At his institution, the Clínica Universidad de Navarra in Madrid, 98% of the 1,500 intensive care beds were occupied by COVID-19 patients at the end of March. So the hope was to be able to refer their patients to other communities where there may still be some capacity.
Another problem in Spain is the high percentage of health workers infected with SARS-CoV-2, the virus behind COVID-19. More than 15,000 health workers were recently reported to be sick or self-isolating, which is around 14% of the health care workforce in the country.
Dr. Chiva noted that this puts those treating gynecologic cancers in a difficult position. On the one hand, surgery to remove a high-risk ovarian mass should not be delayed, but the majority of hospitals in Spain simply cannot perform this type of surgery during the pandemic.
“Unfortunately, due to this specific situation, almost, I would say in 80%-90% of hospitals, we are only able to carry out emergency surgical procedures,” Dr. Chiva said. That’s general emergency procedures such as appendectomies, removing blockages, and dealing with hemorrhages, not gynecologic surgeries. “It’s almost impossible to schedule the typical oncological cases,” he said.
Even with the Hospital IFEMA now set up at the Feria de Madrid, which is usually used to host large-scale events, there are “minimal options for performing standard oncological surgery,” Dr. Chiva said. He estimated that just 5% of hospitals in Spain are able to perform oncologic surgeries as normal, with maybe 15% able to offer surgery without the backup of postsurgical intensive care.
‘Ring-fencing’
“This is really an unusual time for us,” commented Jonathan Ledermann, MD, vice president of ESGO and a professor of medical oncology at University College London, who moderated the webinar.
“This is affecting the way in which we diagnose our patients and have access to care,” he said. “It compromises the way in which we treat patients. We have to adjust our treatment pathways. We have to look at the risks of coronavirus infection in cancer patients and how we manage patients in a socially distancing environment. We also need to think about managing gynecological oncology departments in the face of disease amongst staff, the risks of transmission, and the reduced clinical service.”
Dr. Ledermann noted that “ring-fencing” a few hospitals to deal only with patients free of COVID-19 might be a way forward. This approach has been used in Northern Italy and was recently started in London.
“We try to divide and have separate access between COVID-positive and -negative patients,” said Anna Fagotti, MD, an assistant professor at Fondazione Policlinico Universitario Agostino Gemelli IRCCS in Rome and another coauthor of the editorial.
“We are trying to divide the work flow of patients and try to ensure treatment to cancer patients as much as we can,” she explained. “This means that it’s a very difficult situation, and, every time, you have to deal with the number of places available as some places have been taken by other patients from the emergency room. We are still trying to have a number of beds and intensive care unit beds available for our patients.”
Setting up dedicated hospitals is a good idea, but it has to be done before the “tsunami” of cases hits and there are no more intensive care beds or ventilators, according to Antonio González-Martín, MD, of Clínica Universidad de Navarra in Madrid, another coauthor of the editorial.
Limiting hospital visits
Strategies to limit the number of times patients need to come into hospital for appointments and treatment is key to getting through the pandemic, Sandro Pignata, MD, of Instituto Nazionale Tumori IRCCS Fondazione G. Pascale in Naples, Italy, said during the webinar.
“It will be imperative to explore options that reduce the number of procedures or surgical interventions that may be associated with prolonged operative time, risk of major blood loss, necessitating blood products, risk of infection to the medical personnel, or admission to intensive care units,” Dr. Ramirez and colleagues wrote in their editorial.
“In considering management of disease, we must recognize that, in many centers, access to routine visits and surgery may be either completely restricted or significantly reduced. We must, therefore, consider options that may still offer our patients a treatment plan that addresses their disease while at the same time limiting risk of exposure,” the authors wrote.
The authors declared no competing interests or specific funding in relation to their work, and the webinar participants had no conflicts of interest.
SOURCE: Ramirez PT et al. Int J Gynecol Cancer. 2020 Mar 27. doi: 10.1136/ijgc-2020-001419.
To manage patients with gynecologic cancers, oncologists in the United States and Europe are recommending reducing outpatient visits, delaying surgeries, prolonging chemotherapy regimens, and generally trying to keep cancer patients away from those who have tested positive for COVID-19.
“We recognize that, in this special situation, we must continue to provide our gynecologic oncology patients with the highest quality of medical services,” Pedro T. Ramirez, MD, of the University of Texas MD Anderson Cancer Center in Houston and associates wrote in an editorial published in the International Journal of Gynecological Cancer.
At the same time, the authors added, the safety of patients, their families, and medical staff needs to be assured.
Dr. Ramirez and colleagues’ editorial includes recommendations on how to optimize the care of patients with gynecologic cancers while prioritizing safety and minimizing the burden to the healthcare system. The group’s recommendations outline when surgery, radiotherapy, and other treatments might be safely postponed and when they need to proceed out of urgency.
Some authors of the editorial also described their experiences with COVID-19 during a webinar on managing patients with advanced ovarian cancer, which was hosted by the European Society of Gynaecological Oncology (ESGO).
A lack of resources
In Spain, health resources “are collapsed” by the pandemic, editorial author Luis Chiva, MD, said during the webinar.
At his institution, the Clínica Universidad de Navarra in Madrid, 98% of the 1,500 intensive care beds were occupied by COVID-19 patients at the end of March. So the hope was to be able to refer their patients to other communities where there may still be some capacity.
Another problem in Spain is the high percentage of health workers infected with SARS-CoV-2, the virus behind COVID-19. More than 15,000 health workers were recently reported to be sick or self-isolating, which is around 14% of the health care workforce in the country.
Dr. Chiva noted that this puts those treating gynecologic cancers in a difficult position. On the one hand, surgery to remove a high-risk ovarian mass should not be delayed, but the majority of hospitals in Spain simply cannot perform this type of surgery during the pandemic.
“Unfortunately, due to this specific situation, almost, I would say in 80%-90% of hospitals, we are only able to carry out emergency surgical procedures,” Dr. Chiva said. That’s general emergency procedures such as appendectomies, removing blockages, and dealing with hemorrhages, not gynecologic surgeries. “It’s almost impossible to schedule the typical oncological cases,” he said.
Even with the Hospital IFEMA now set up at the Feria de Madrid, which is usually used to host large-scale events, there are “minimal options for performing standard oncological surgery,” Dr. Chiva said. He estimated that just 5% of hospitals in Spain are able to perform oncologic surgeries as normal, with maybe 15% able to offer surgery without the backup of postsurgical intensive care.
‘Ring-fencing’
“This is really an unusual time for us,” commented Jonathan Ledermann, MD, vice president of ESGO and a professor of medical oncology at University College London, who moderated the webinar.
“This is affecting the way in which we diagnose our patients and have access to care,” he said. “It compromises the way in which we treat patients. We have to adjust our treatment pathways. We have to look at the risks of coronavirus infection in cancer patients and how we manage patients in a socially distancing environment. We also need to think about managing gynecological oncology departments in the face of disease amongst staff, the risks of transmission, and the reduced clinical service.”
Dr. Ledermann noted that “ring-fencing” a few hospitals to deal only with patients free of COVID-19 might be a way forward. This approach has been used in Northern Italy and was recently started in London.
“We try to divide and have separate access between COVID-positive and -negative patients,” said Anna Fagotti, MD, an assistant professor at Fondazione Policlinico Universitario Agostino Gemelli IRCCS in Rome and another coauthor of the editorial.
“We are trying to divide the work flow of patients and try to ensure treatment to cancer patients as much as we can,” she explained. “This means that it’s a very difficult situation, and, every time, you have to deal with the number of places available as some places have been taken by other patients from the emergency room. We are still trying to have a number of beds and intensive care unit beds available for our patients.”
Setting up dedicated hospitals is a good idea, but it has to be done before the “tsunami” of cases hits and there are no more intensive care beds or ventilators, according to Antonio González-Martín, MD, of Clínica Universidad de Navarra in Madrid, another coauthor of the editorial.
Limiting hospital visits
Strategies to limit the number of times patients need to come into hospital for appointments and treatment is key to getting through the pandemic, Sandro Pignata, MD, of Instituto Nazionale Tumori IRCCS Fondazione G. Pascale in Naples, Italy, said during the webinar.
“It will be imperative to explore options that reduce the number of procedures or surgical interventions that may be associated with prolonged operative time, risk of major blood loss, necessitating blood products, risk of infection to the medical personnel, or admission to intensive care units,” Dr. Ramirez and colleagues wrote in their editorial.
“In considering management of disease, we must recognize that, in many centers, access to routine visits and surgery may be either completely restricted or significantly reduced. We must, therefore, consider options that may still offer our patients a treatment plan that addresses their disease while at the same time limiting risk of exposure,” the authors wrote.
The authors declared no competing interests or specific funding in relation to their work, and the webinar participants had no conflicts of interest.
SOURCE: Ramirez PT et al. Int J Gynecol Cancer. 2020 Mar 27. doi: 10.1136/ijgc-2020-001419.
FROM THE INTERNATIONAL JOURNAL OF GYNECOLOGICAL CANCER
CMS implements temporary regulatory changes to aid COVID-19 response
The Centers for Medicare & Medicaid Services has announced a wide range of temporary regulatory moves aimed at helping hospitals and health systems handle the surge of COVID-19 patients.
“We are waiving a wide and unprecedented range of regulatory requirements to equip the American health care system with maximum flexibility to deal with an influx of cases,” CMS Administrator Seema Verma said during a March 30 conference call with reporters. “Many health care systems may not need these waivers and they shouldn’t use them if the situation doesn’t warrant it. But the flexibilities are there if it does. At a time of crisis, no regulatory barriers should stand in the way of patient care.”
Among the changes is an expansion of the venues in which health care systems and hospitals can provide services.
Federal regulations call for hospitals to provide services within their own buildings, raising concerns as to whether there will be enough capacity to handle the anticipated COVID-19 caseload.
“Under CMS’s temporary new rules, hospitals will be able to transfer patients to outside facilities, such as ambulatory surgery centers, inpatient rehabilitation hospitals, hotels, and dormitories, while still receiving hospital payments under Medicare,” the CMS stated in a fact sheet highlighting the regulatory changes.
Ambulatory surgery centers will have the option to contract with local health care systems to provide hospital services or they can enroll and bill as hospitals during the emergency, the fact sheet noted. They will be able to perform hospital services such as cancer procedures, trauma surgeries, and other essential surgeries.
CMS also is waiving the limit on the number of beds a doctor-owned hospital can have.
For Medicare patients who may be homebound, CMS will now pay for a laboratory technician to make a home visit to collect a specimen for COVID-19 testing, and hospitals will be able to conduct testing in homes or other community-based settings under certain circumstances.
In addition, CMS is taking actions aimed at expanding the health care workforce.
For instance, the agency is issuing a “blanket waiver” that allows hospitals to provide benefits to medical staff, including multiple daily meals, laundry service for personal clothing, or child care services while the staff is at the hospital providing patient care, according to the fact sheet. Teaching hospitals will also receive more flexibility in using residents to provide health care services under the virtual direction of a teaching physician, who may be available through audio/video technology.
CMS also is temporarily eliminating paperwork requirements and allowing greater use of verbal orders so that clinicians can spend more time on direct patient care.
Another change announced deals with the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program. Clinicians affected by the pandemic can request reweighting of the MIPS performance categories for the 2019 performance year, which will allow clinicians who are unable to submit MIPS data in the current submission period to request reweighting and receive a neutral payment adjustment in the 2021 payment year.
CMS also added an option for calendar year 2020 in the improvement activity category. Clinicians will receive credit if they are participating in a clinical trial that uses a drug or biological product to treat a COVID-19 patient and they report the findings to a clinical trial repository or registry.
On the device/equipment side, Medicare will cover respiratory-related devices and equipment “for any medical reason determined by clinicians,” according to the fact sheet, rather than only under certain circumstances.
And on the telehealth side, CMS is expanding the number of services that it will pay for via telehealth by more than 80, including ED visits, initial nursing facility and discharge visits, and home visits, which must be provided by a clinician that is allowed to provide telehealth. CMS will allow the use of commonly available interactive apps with audio and video, as well as audio-only phones.
CMS noted that providers can report telehealth for new and established patients, even if the billing code is specific for established patients only. CMS also has removed requirements regarding documentation of medical history and/or physical examination in the medical records during the COVID-19 crisis to help facilitate the use of telehealth for evaluation and management visits.
To help practices financially, providers who participate in Medicare fee-for-service will be able to request up to a 100% advance on their Medicare payments for a 3-month period. Repayment begins 120 days after the advance payment is received and must be paid within 210 days of the payment. Repayment will be automatically deducted from claims processed.
The agency also included new exceptions to the Stark Law. Some examples include the ability for hospitals to pay above or below fair market value to rent equipment or receive services from physicians and the allowance of health care providers to provide financial assistance to each other to ensure continuity of operations.
*This story was updated on 4/17/2020.
The Centers for Medicare & Medicaid Services has announced a wide range of temporary regulatory moves aimed at helping hospitals and health systems handle the surge of COVID-19 patients.
“We are waiving a wide and unprecedented range of regulatory requirements to equip the American health care system with maximum flexibility to deal with an influx of cases,” CMS Administrator Seema Verma said during a March 30 conference call with reporters. “Many health care systems may not need these waivers and they shouldn’t use them if the situation doesn’t warrant it. But the flexibilities are there if it does. At a time of crisis, no regulatory barriers should stand in the way of patient care.”
Among the changes is an expansion of the venues in which health care systems and hospitals can provide services.
Federal regulations call for hospitals to provide services within their own buildings, raising concerns as to whether there will be enough capacity to handle the anticipated COVID-19 caseload.
“Under CMS’s temporary new rules, hospitals will be able to transfer patients to outside facilities, such as ambulatory surgery centers, inpatient rehabilitation hospitals, hotels, and dormitories, while still receiving hospital payments under Medicare,” the CMS stated in a fact sheet highlighting the regulatory changes.
Ambulatory surgery centers will have the option to contract with local health care systems to provide hospital services or they can enroll and bill as hospitals during the emergency, the fact sheet noted. They will be able to perform hospital services such as cancer procedures, trauma surgeries, and other essential surgeries.
CMS also is waiving the limit on the number of beds a doctor-owned hospital can have.
For Medicare patients who may be homebound, CMS will now pay for a laboratory technician to make a home visit to collect a specimen for COVID-19 testing, and hospitals will be able to conduct testing in homes or other community-based settings under certain circumstances.
In addition, CMS is taking actions aimed at expanding the health care workforce.
For instance, the agency is issuing a “blanket waiver” that allows hospitals to provide benefits to medical staff, including multiple daily meals, laundry service for personal clothing, or child care services while the staff is at the hospital providing patient care, according to the fact sheet. Teaching hospitals will also receive more flexibility in using residents to provide health care services under the virtual direction of a teaching physician, who may be available through audio/video technology.
CMS also is temporarily eliminating paperwork requirements and allowing greater use of verbal orders so that clinicians can spend more time on direct patient care.
Another change announced deals with the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program. Clinicians affected by the pandemic can request reweighting of the MIPS performance categories for the 2019 performance year, which will allow clinicians who are unable to submit MIPS data in the current submission period to request reweighting and receive a neutral payment adjustment in the 2021 payment year.
CMS also added an option for calendar year 2020 in the improvement activity category. Clinicians will receive credit if they are participating in a clinical trial that uses a drug or biological product to treat a COVID-19 patient and they report the findings to a clinical trial repository or registry.
On the device/equipment side, Medicare will cover respiratory-related devices and equipment “for any medical reason determined by clinicians,” according to the fact sheet, rather than only under certain circumstances.
And on the telehealth side, CMS is expanding the number of services that it will pay for via telehealth by more than 80, including ED visits, initial nursing facility and discharge visits, and home visits, which must be provided by a clinician that is allowed to provide telehealth. CMS will allow the use of commonly available interactive apps with audio and video, as well as audio-only phones.
CMS noted that providers can report telehealth for new and established patients, even if the billing code is specific for established patients only. CMS also has removed requirements regarding documentation of medical history and/or physical examination in the medical records during the COVID-19 crisis to help facilitate the use of telehealth for evaluation and management visits.
To help practices financially, providers who participate in Medicare fee-for-service will be able to request up to a 100% advance on their Medicare payments for a 3-month period. Repayment begins 120 days after the advance payment is received and must be paid within 210 days of the payment. Repayment will be automatically deducted from claims processed.
The agency also included new exceptions to the Stark Law. Some examples include the ability for hospitals to pay above or below fair market value to rent equipment or receive services from physicians and the allowance of health care providers to provide financial assistance to each other to ensure continuity of operations.
*This story was updated on 4/17/2020.
The Centers for Medicare & Medicaid Services has announced a wide range of temporary regulatory moves aimed at helping hospitals and health systems handle the surge of COVID-19 patients.
“We are waiving a wide and unprecedented range of regulatory requirements to equip the American health care system with maximum flexibility to deal with an influx of cases,” CMS Administrator Seema Verma said during a March 30 conference call with reporters. “Many health care systems may not need these waivers and they shouldn’t use them if the situation doesn’t warrant it. But the flexibilities are there if it does. At a time of crisis, no regulatory barriers should stand in the way of patient care.”
Among the changes is an expansion of the venues in which health care systems and hospitals can provide services.
Federal regulations call for hospitals to provide services within their own buildings, raising concerns as to whether there will be enough capacity to handle the anticipated COVID-19 caseload.
“Under CMS’s temporary new rules, hospitals will be able to transfer patients to outside facilities, such as ambulatory surgery centers, inpatient rehabilitation hospitals, hotels, and dormitories, while still receiving hospital payments under Medicare,” the CMS stated in a fact sheet highlighting the regulatory changes.
Ambulatory surgery centers will have the option to contract with local health care systems to provide hospital services or they can enroll and bill as hospitals during the emergency, the fact sheet noted. They will be able to perform hospital services such as cancer procedures, trauma surgeries, and other essential surgeries.
CMS also is waiving the limit on the number of beds a doctor-owned hospital can have.
For Medicare patients who may be homebound, CMS will now pay for a laboratory technician to make a home visit to collect a specimen for COVID-19 testing, and hospitals will be able to conduct testing in homes or other community-based settings under certain circumstances.
In addition, CMS is taking actions aimed at expanding the health care workforce.
For instance, the agency is issuing a “blanket waiver” that allows hospitals to provide benefits to medical staff, including multiple daily meals, laundry service for personal clothing, or child care services while the staff is at the hospital providing patient care, according to the fact sheet. Teaching hospitals will also receive more flexibility in using residents to provide health care services under the virtual direction of a teaching physician, who may be available through audio/video technology.
CMS also is temporarily eliminating paperwork requirements and allowing greater use of verbal orders so that clinicians can spend more time on direct patient care.
Another change announced deals with the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program. Clinicians affected by the pandemic can request reweighting of the MIPS performance categories for the 2019 performance year, which will allow clinicians who are unable to submit MIPS data in the current submission period to request reweighting and receive a neutral payment adjustment in the 2021 payment year.
CMS also added an option for calendar year 2020 in the improvement activity category. Clinicians will receive credit if they are participating in a clinical trial that uses a drug or biological product to treat a COVID-19 patient and they report the findings to a clinical trial repository or registry.
On the device/equipment side, Medicare will cover respiratory-related devices and equipment “for any medical reason determined by clinicians,” according to the fact sheet, rather than only under certain circumstances.
And on the telehealth side, CMS is expanding the number of services that it will pay for via telehealth by more than 80, including ED visits, initial nursing facility and discharge visits, and home visits, which must be provided by a clinician that is allowed to provide telehealth. CMS will allow the use of commonly available interactive apps with audio and video, as well as audio-only phones.
CMS noted that providers can report telehealth for new and established patients, even if the billing code is specific for established patients only. CMS also has removed requirements regarding documentation of medical history and/or physical examination in the medical records during the COVID-19 crisis to help facilitate the use of telehealth for evaluation and management visits.
To help practices financially, providers who participate in Medicare fee-for-service will be able to request up to a 100% advance on their Medicare payments for a 3-month period. Repayment begins 120 days after the advance payment is received and must be paid within 210 days of the payment. Repayment will be automatically deducted from claims processed.
The agency also included new exceptions to the Stark Law. Some examples include the ability for hospitals to pay above or below fair market value to rent equipment or receive services from physicians and the allowance of health care providers to provide financial assistance to each other to ensure continuity of operations.
*This story was updated on 4/17/2020.
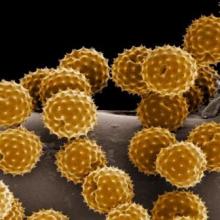
Ragweed SLIT tablets improve asthma outcome scores in patients with allergic rhinoconjunctivitis
during ragweed pollen season, compared with placebo, according to recent research that was to be presented as an abstract for the American Academy of Allergy, Asthma & Immunology annual meeting. The AAAAI canceled its annual meeting and provided abstracts and access to presenters for press coverage.
David I. Bernstein, MD, professor emeritus in the division of immunology, allergy and rheumatology at the University of Cincinnati and principal investigator at the Bernstein Clinical Research Center, examined exploratory endpoints of an international, double-blind, placebo-controlled trial evaluating ragweed SLIT tablets (Ragwitek; Merck) in 1,022 children with AR/C. The children enrolled were aged 5-17 years with ragweed AR/C, with 42.7% of the group having a history of asthma and the rest without asthma. Participants were included if they had a predicted first expiratory volume in 1 second (FEV1) of ≥ 80% and if they required high-dose inhaled corticosteroids (ICS) to control their asthma or had severe, unstable, or uncontrolled asthma. The children were randomized to receive a 12 Amb a 1-unit dose of the ragweed SLIT tablet or placebo each day for 28 weeks.
The primary outcome was the total combined score (TCS), which was the sum of the daily symptom score and medication scores during ragweed season, but researchers also examined three exploratory endpoints. All patients were evaluated for their average asthma daily symptom score at the peak of ragweed pollen season and during the entire season, which was measured on a 0-3 scale based on symptoms of cough, wheeze, and chest tightness or shortness of breath. Within a subgroup of 406 participants with asthma, Dr. Bernstein and colleagues examined use of average daily short-acting beta agonists (SABA), and the number of times per week a participant would use a SABA at night at the peak of ragweed season as well as across the whole season.
Researchers found the TCS improved by 38% during ragweed pollen season in the group receiving ragweed SLIT tablets (least-square [LS] mean TCS, 7.12), compared with placebo (LS mean TCS, 4.39; P < .001). Among the asthma exploratory outcomes, asthma daily symptom scores improved by 30.7% during the peak of the season (–46.9% vs. –9.6%; LS mean difference, –0.13) and by 23.1% during the whole season (–38.7% vs. –2.3%; LS mean difference, –0.09), compared with the placebo group. The mean number of daily puffs of rescue medication also decreased by 68.1% in the peak of ragweed season (–87.6% vs. –39.0%; LS mean difference, −0.14) and by 61.4% during the whole season (–80.9% vs. −32.9%; LS mean difference, –0.12) among participants taking ragweed SLIT tablets, compared with placebo. Participants in the group receiving ragweed SLIT tablets also had fewer nights awake using rescue medication, with a relative improvement of 75.1% during peak season (−99.3% vs. −35.2%; LS mean difference, −0.08) and 52.2% during the whole season (−80.4% vs. −3.7%; LS mean difference, −0.03), compared with the placebo group.
This magnitude of difference in the number of nocturnal awakenings in the treated group, compared with the placebo group, is similar to what researchers have seen in trials evaluating ICS or mometasone/formoterol, Dr. Bernstein said in an interview.
“Even though the magnitude in terms of difference in asthma symptoms and requirements for short-acting beta agonists was less than that of other studies of other drugs, it may reflect the fact these participants have less severe asthma,” said Dr. Bernstein. “But, there was an effect, and we did see some interesting differences between the placebo group and the treated group. This, I think, does generate at least a hypothesis that this could be an effective treatment for seasonal asthma, which would require future studies to determine that.”
Dr. Bernstein said that there were no adverse events from ragweed SLIT tablets unique to children with or without asthma, and although the data from this study cannot be compared directly to an adult population, there appeared to be a greater effect size for children than in trials evaluating adults. Compared with treatment options like subcutaneous immunotherapy, ragweed SLIT tablets may offer a relatively safer and more effective option for children and their parents, he said.
“The problem with kids is that they don’t particularly like the idea of getting injections. There’s a lot of needle-type injection phobia,” Dr. Bernstein said. “For a child who has maybe one or two major problem pollen seasons like during the ragweed and grass, they could do this.”
Ragwitek was approved by the Food and Drug Administration in 2014 for the treatment of adults with allergic rhinitis. Dr. Bernstein noted that Merck submitted this trial to the Food and Drug Administration as evidence of its effectiveness in children to secure a pediatric indication for the treatment.
This trial was funded by Merck, the developers of Ragwitek. The authors received medical writing and editing assistance from Scott Medical Communications, which was funded by ALK. Dr. Bernstein reports being on the advisory board for ALK America and GlaxoSmithKline; a consultant for Gerson-Lehman and Guidepoint Global; and received grant support from Aimmune, ALK, Amgen, AstraZeneca, Avillion, Biocryst, Boehringer Ingelheim, Cipla, Genentech, GlaxoSmithKline, Gossamer, Leo, Lupin, Menlo, Merck, Mylan, Novartis, Novum, Pearl, Regeneron, Shire, and TEVA. The other authors reported no relevant conflicts of interest.
SOURCE: Bernstein D et al. AAAAI 2020, Abstract 270.
during ragweed pollen season, compared with placebo, according to recent research that was to be presented as an abstract for the American Academy of Allergy, Asthma & Immunology annual meeting. The AAAAI canceled its annual meeting and provided abstracts and access to presenters for press coverage.
David I. Bernstein, MD, professor emeritus in the division of immunology, allergy and rheumatology at the University of Cincinnati and principal investigator at the Bernstein Clinical Research Center, examined exploratory endpoints of an international, double-blind, placebo-controlled trial evaluating ragweed SLIT tablets (Ragwitek; Merck) in 1,022 children with AR/C. The children enrolled were aged 5-17 years with ragweed AR/C, with 42.7% of the group having a history of asthma and the rest without asthma. Participants were included if they had a predicted first expiratory volume in 1 second (FEV1) of ≥ 80% and if they required high-dose inhaled corticosteroids (ICS) to control their asthma or had severe, unstable, or uncontrolled asthma. The children were randomized to receive a 12 Amb a 1-unit dose of the ragweed SLIT tablet or placebo each day for 28 weeks.
The primary outcome was the total combined score (TCS), which was the sum of the daily symptom score and medication scores during ragweed season, but researchers also examined three exploratory endpoints. All patients were evaluated for their average asthma daily symptom score at the peak of ragweed pollen season and during the entire season, which was measured on a 0-3 scale based on symptoms of cough, wheeze, and chest tightness or shortness of breath. Within a subgroup of 406 participants with asthma, Dr. Bernstein and colleagues examined use of average daily short-acting beta agonists (SABA), and the number of times per week a participant would use a SABA at night at the peak of ragweed season as well as across the whole season.
Researchers found the TCS improved by 38% during ragweed pollen season in the group receiving ragweed SLIT tablets (least-square [LS] mean TCS, 7.12), compared with placebo (LS mean TCS, 4.39; P < .001). Among the asthma exploratory outcomes, asthma daily symptom scores improved by 30.7% during the peak of the season (–46.9% vs. –9.6%; LS mean difference, –0.13) and by 23.1% during the whole season (–38.7% vs. –2.3%; LS mean difference, –0.09), compared with the placebo group. The mean number of daily puffs of rescue medication also decreased by 68.1% in the peak of ragweed season (–87.6% vs. –39.0%; LS mean difference, −0.14) and by 61.4% during the whole season (–80.9% vs. −32.9%; LS mean difference, –0.12) among participants taking ragweed SLIT tablets, compared with placebo. Participants in the group receiving ragweed SLIT tablets also had fewer nights awake using rescue medication, with a relative improvement of 75.1% during peak season (−99.3% vs. −35.2%; LS mean difference, −0.08) and 52.2% during the whole season (−80.4% vs. −3.7%; LS mean difference, −0.03), compared with the placebo group.
This magnitude of difference in the number of nocturnal awakenings in the treated group, compared with the placebo group, is similar to what researchers have seen in trials evaluating ICS or mometasone/formoterol, Dr. Bernstein said in an interview.
“Even though the magnitude in terms of difference in asthma symptoms and requirements for short-acting beta agonists was less than that of other studies of other drugs, it may reflect the fact these participants have less severe asthma,” said Dr. Bernstein. “But, there was an effect, and we did see some interesting differences between the placebo group and the treated group. This, I think, does generate at least a hypothesis that this could be an effective treatment for seasonal asthma, which would require future studies to determine that.”
Dr. Bernstein said that there were no adverse events from ragweed SLIT tablets unique to children with or without asthma, and although the data from this study cannot be compared directly to an adult population, there appeared to be a greater effect size for children than in trials evaluating adults. Compared with treatment options like subcutaneous immunotherapy, ragweed SLIT tablets may offer a relatively safer and more effective option for children and their parents, he said.
“The problem with kids is that they don’t particularly like the idea of getting injections. There’s a lot of needle-type injection phobia,” Dr. Bernstein said. “For a child who has maybe one or two major problem pollen seasons like during the ragweed and grass, they could do this.”
Ragwitek was approved by the Food and Drug Administration in 2014 for the treatment of adults with allergic rhinitis. Dr. Bernstein noted that Merck submitted this trial to the Food and Drug Administration as evidence of its effectiveness in children to secure a pediatric indication for the treatment.
This trial was funded by Merck, the developers of Ragwitek. The authors received medical writing and editing assistance from Scott Medical Communications, which was funded by ALK. Dr. Bernstein reports being on the advisory board for ALK America and GlaxoSmithKline; a consultant for Gerson-Lehman and Guidepoint Global; and received grant support from Aimmune, ALK, Amgen, AstraZeneca, Avillion, Biocryst, Boehringer Ingelheim, Cipla, Genentech, GlaxoSmithKline, Gossamer, Leo, Lupin, Menlo, Merck, Mylan, Novartis, Novum, Pearl, Regeneron, Shire, and TEVA. The other authors reported no relevant conflicts of interest.
SOURCE: Bernstein D et al. AAAAI 2020, Abstract 270.
during ragweed pollen season, compared with placebo, according to recent research that was to be presented as an abstract for the American Academy of Allergy, Asthma & Immunology annual meeting. The AAAAI canceled its annual meeting and provided abstracts and access to presenters for press coverage.
David I. Bernstein, MD, professor emeritus in the division of immunology, allergy and rheumatology at the University of Cincinnati and principal investigator at the Bernstein Clinical Research Center, examined exploratory endpoints of an international, double-blind, placebo-controlled trial evaluating ragweed SLIT tablets (Ragwitek; Merck) in 1,022 children with AR/C. The children enrolled were aged 5-17 years with ragweed AR/C, with 42.7% of the group having a history of asthma and the rest without asthma. Participants were included if they had a predicted first expiratory volume in 1 second (FEV1) of ≥ 80% and if they required high-dose inhaled corticosteroids (ICS) to control their asthma or had severe, unstable, or uncontrolled asthma. The children were randomized to receive a 12 Amb a 1-unit dose of the ragweed SLIT tablet or placebo each day for 28 weeks.
The primary outcome was the total combined score (TCS), which was the sum of the daily symptom score and medication scores during ragweed season, but researchers also examined three exploratory endpoints. All patients were evaluated for their average asthma daily symptom score at the peak of ragweed pollen season and during the entire season, which was measured on a 0-3 scale based on symptoms of cough, wheeze, and chest tightness or shortness of breath. Within a subgroup of 406 participants with asthma, Dr. Bernstein and colleagues examined use of average daily short-acting beta agonists (SABA), and the number of times per week a participant would use a SABA at night at the peak of ragweed season as well as across the whole season.
Researchers found the TCS improved by 38% during ragweed pollen season in the group receiving ragweed SLIT tablets (least-square [LS] mean TCS, 7.12), compared with placebo (LS mean TCS, 4.39; P < .001). Among the asthma exploratory outcomes, asthma daily symptom scores improved by 30.7% during the peak of the season (–46.9% vs. –9.6%; LS mean difference, –0.13) and by 23.1% during the whole season (–38.7% vs. –2.3%; LS mean difference, –0.09), compared with the placebo group. The mean number of daily puffs of rescue medication also decreased by 68.1% in the peak of ragweed season (–87.6% vs. –39.0%; LS mean difference, −0.14) and by 61.4% during the whole season (–80.9% vs. −32.9%; LS mean difference, –0.12) among participants taking ragweed SLIT tablets, compared with placebo. Participants in the group receiving ragweed SLIT tablets also had fewer nights awake using rescue medication, with a relative improvement of 75.1% during peak season (−99.3% vs. −35.2%; LS mean difference, −0.08) and 52.2% during the whole season (−80.4% vs. −3.7%; LS mean difference, −0.03), compared with the placebo group.
This magnitude of difference in the number of nocturnal awakenings in the treated group, compared with the placebo group, is similar to what researchers have seen in trials evaluating ICS or mometasone/formoterol, Dr. Bernstein said in an interview.
“Even though the magnitude in terms of difference in asthma symptoms and requirements for short-acting beta agonists was less than that of other studies of other drugs, it may reflect the fact these participants have less severe asthma,” said Dr. Bernstein. “But, there was an effect, and we did see some interesting differences between the placebo group and the treated group. This, I think, does generate at least a hypothesis that this could be an effective treatment for seasonal asthma, which would require future studies to determine that.”
Dr. Bernstein said that there were no adverse events from ragweed SLIT tablets unique to children with or without asthma, and although the data from this study cannot be compared directly to an adult population, there appeared to be a greater effect size for children than in trials evaluating adults. Compared with treatment options like subcutaneous immunotherapy, ragweed SLIT tablets may offer a relatively safer and more effective option for children and their parents, he said.
“The problem with kids is that they don’t particularly like the idea of getting injections. There’s a lot of needle-type injection phobia,” Dr. Bernstein said. “For a child who has maybe one or two major problem pollen seasons like during the ragweed and grass, they could do this.”
Ragwitek was approved by the Food and Drug Administration in 2014 for the treatment of adults with allergic rhinitis. Dr. Bernstein noted that Merck submitted this trial to the Food and Drug Administration as evidence of its effectiveness in children to secure a pediatric indication for the treatment.
This trial was funded by Merck, the developers of Ragwitek. The authors received medical writing and editing assistance from Scott Medical Communications, which was funded by ALK. Dr. Bernstein reports being on the advisory board for ALK America and GlaxoSmithKline; a consultant for Gerson-Lehman and Guidepoint Global; and received grant support from Aimmune, ALK, Amgen, AstraZeneca, Avillion, Biocryst, Boehringer Ingelheim, Cipla, Genentech, GlaxoSmithKline, Gossamer, Leo, Lupin, Menlo, Merck, Mylan, Novartis, Novum, Pearl, Regeneron, Shire, and TEVA. The other authors reported no relevant conflicts of interest.
SOURCE: Bernstein D et al. AAAAI 2020, Abstract 270.
FROM AAAAI
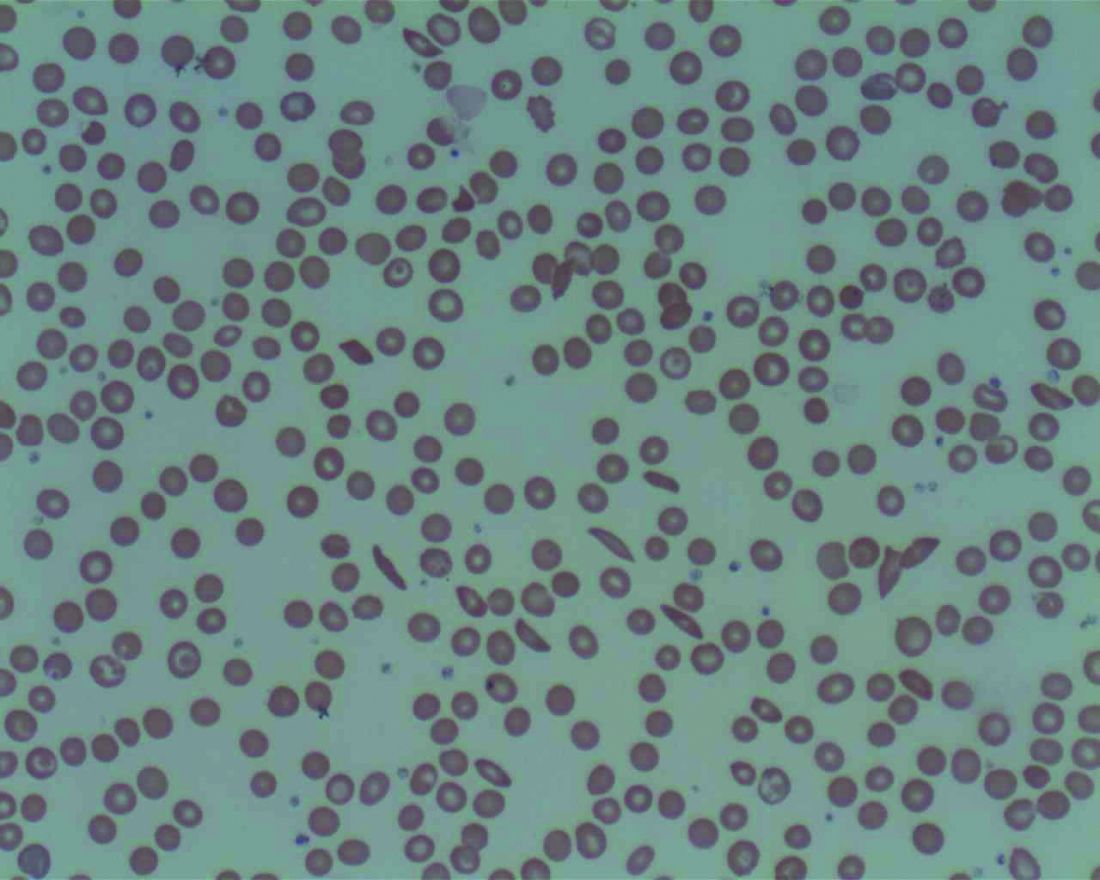
Low plasma sodium levels can predict complications in acute painful episodes of SCD
Although a low blood sodium level has been shown to be a prognostic factor for a number of disorders, it has not been reported on for sickle cell disease, according to French researchers Jean-Simon Rech, MD, and colleagues.
They found that hyponatremia at hospital admission was predictive of complications in initially uncomplicated episodes of painful episodes of sickle cell disease (SCD), according to their study published online in the American Journal of Medicine. Dr. Rech is with the department of internal medicine, Sickle Cell Disease Reference Center, Tenon Hospital, Assistance Publique-Hôpitaux de Paris.
The study assessed 1,218 stays (406 patients) admitted to a single center and the analyses were adjusted for age, sex, hemoglobin genotype and concentration, LDH concentration, and white blood cell count.
The researchers found that hyponatremia (defined as plasma sodium ≤ 135 mmol/L) was significantly associated with the primary endpoint of a composite criterion including acute chest syndrome, intensive care unit transfer, red blood cell transfusion, or inpatient death (P = .001).
With regard to the components of the primary endpoint, hyponatremia was significantly associated with acute chest syndrome (P = .008), as well as with receiving a red blood cell transfusion (P < .001) However, hyponatremia at admission was not significantly associated with intensive care unit transfer (P = .074) and there were no patient deaths.
In addition, hyponatremia was significantly associated with longer stays: 1.1 days adjusted mean length of stay (P < .001).
“Hyponatremia may lead to direct clinical consequences in the management of sickle cell disease patients. Indeed, a plasma sodium concentration ≤ 135mmol/L at admission or a decreasing natremia over the first days of an acute painful episode could be regarded as early signs of incipient acute chest syndrome, prompting clinicians to closely monitor the clinical status of their patients,” the researchers concluded.
The authors declared that they had no conflicts and that there was no funding source.
SOURCE: Rech JS et al. Am J Med. 2020 Mar 18. doi.org/10.1016/j.amjmed.2020.02.017.
Although a low blood sodium level has been shown to be a prognostic factor for a number of disorders, it has not been reported on for sickle cell disease, according to French researchers Jean-Simon Rech, MD, and colleagues.
They found that hyponatremia at hospital admission was predictive of complications in initially uncomplicated episodes of painful episodes of sickle cell disease (SCD), according to their study published online in the American Journal of Medicine. Dr. Rech is with the department of internal medicine, Sickle Cell Disease Reference Center, Tenon Hospital, Assistance Publique-Hôpitaux de Paris.
The study assessed 1,218 stays (406 patients) admitted to a single center and the analyses were adjusted for age, sex, hemoglobin genotype and concentration, LDH concentration, and white blood cell count.
The researchers found that hyponatremia (defined as plasma sodium ≤ 135 mmol/L) was significantly associated with the primary endpoint of a composite criterion including acute chest syndrome, intensive care unit transfer, red blood cell transfusion, or inpatient death (P = .001).
With regard to the components of the primary endpoint, hyponatremia was significantly associated with acute chest syndrome (P = .008), as well as with receiving a red blood cell transfusion (P < .001) However, hyponatremia at admission was not significantly associated with intensive care unit transfer (P = .074) and there were no patient deaths.
In addition, hyponatremia was significantly associated with longer stays: 1.1 days adjusted mean length of stay (P < .001).
“Hyponatremia may lead to direct clinical consequences in the management of sickle cell disease patients. Indeed, a plasma sodium concentration ≤ 135mmol/L at admission or a decreasing natremia over the first days of an acute painful episode could be regarded as early signs of incipient acute chest syndrome, prompting clinicians to closely monitor the clinical status of their patients,” the researchers concluded.
The authors declared that they had no conflicts and that there was no funding source.
SOURCE: Rech JS et al. Am J Med. 2020 Mar 18. doi.org/10.1016/j.amjmed.2020.02.017.
Although a low blood sodium level has been shown to be a prognostic factor for a number of disorders, it has not been reported on for sickle cell disease, according to French researchers Jean-Simon Rech, MD, and colleagues.
They found that hyponatremia at hospital admission was predictive of complications in initially uncomplicated episodes of painful episodes of sickle cell disease (SCD), according to their study published online in the American Journal of Medicine. Dr. Rech is with the department of internal medicine, Sickle Cell Disease Reference Center, Tenon Hospital, Assistance Publique-Hôpitaux de Paris.
The study assessed 1,218 stays (406 patients) admitted to a single center and the analyses were adjusted for age, sex, hemoglobin genotype and concentration, LDH concentration, and white blood cell count.
The researchers found that hyponatremia (defined as plasma sodium ≤ 135 mmol/L) was significantly associated with the primary endpoint of a composite criterion including acute chest syndrome, intensive care unit transfer, red blood cell transfusion, or inpatient death (P = .001).
With regard to the components of the primary endpoint, hyponatremia was significantly associated with acute chest syndrome (P = .008), as well as with receiving a red blood cell transfusion (P < .001) However, hyponatremia at admission was not significantly associated with intensive care unit transfer (P = .074) and there were no patient deaths.
In addition, hyponatremia was significantly associated with longer stays: 1.1 days adjusted mean length of stay (P < .001).
“Hyponatremia may lead to direct clinical consequences in the management of sickle cell disease patients. Indeed, a plasma sodium concentration ≤ 135mmol/L at admission or a decreasing natremia over the first days of an acute painful episode could be regarded as early signs of incipient acute chest syndrome, prompting clinicians to closely monitor the clinical status of their patients,” the researchers concluded.
The authors declared that they had no conflicts and that there was no funding source.
SOURCE: Rech JS et al. Am J Med. 2020 Mar 18. doi.org/10.1016/j.amjmed.2020.02.017.
FROM THE AMERICAN JOURNAL OF MEDICINE
Parents would avoid cognitive effects in children over better chance of cancer cure
Parents of children with cancer and their physicians are willing to opt for less effective treatment to avoid risk of neurocognitive disorders later in life, according to results from a new study.
While some 80% of children with cancer survive to adulthood, most will experience chronic health conditions related to treatment, and many pediatric oncologists will adjust treatment strategies to lessen the likelihood of later effects. For their research published in Pediatrics, Katie A. Greenzang, MD, of the Dana-Farber Cancer Institute in Boston and colleagues aimed to learn how both parents and physicians weighed the risks and benefits.
In a survey of 95 parents and 41 physicians at Dana-Farber, Dr. Greenzang and colleagues proposed hypothetical scenarios involving five common late effects of childhood cancer treatment: neurocognitive impairment, infertility, cardiac toxicity, second malignancies, and impaired development. The parents surveyed, all of whom had children diagnosed with cancer within the previous year, were asked to make decisions as though on behalf of their children, while physicians were asked to do so as on behalf of a newly diagnosed patient.
Avoiding severe cognitive impairment mattered more than an increased chance of a cure to both parents and physicians. Neurocognitive impairment was the risk that most affected treatment choices, with parents more likely to choose a treatment associated with no or mild neurocognitive impairment, compared with one that caused severe impairment (odds ratio, 2.83 for no impairment vs. severe impairment; P less than .001), which was also the case with physicians (OR, 4.01; P less than .001).
Parents would accept an 18% chance of another malignancy for a 10% greater chance of a cure, while physicians accepted a 15% risk. Parents were willing to tolerate a 31% risk of cardiac toxicity in exchange for the better chance of a cure, while physicians accepted a 22% higher risk.
The results, the researchers wrote in their analysis, offered a window into the level and type of later-life risks that parents can accept when making choices about cancer treatment and where those choices appear to differ from those made by physicians.
“Oncologists increasingly design clinical trials [for children with cancer] with dual goals of optimizing cure while minimizing late effects,” Dr. Greenzang and colleagues wrote. “In doing so, they make judgments about the relative value of short- and long-term outcomes in patients’ lives. Yet oncologists have largely done so in the absence of information about how parents prioritize avoidance of late effects relative to the chance of cure.”
In an editorial comment accompanying the study, Tara A. Brinkman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tenn., and James G. Gurney, PhD, of the University of Memphis noted that the findings “may have narrow clinical application” because many of the late-life effects presented in the survey will not present singly but will co-occur in survivors of childhood cancer. “Hypothetical scenarios that do not depict the full burden of late effects may not reflect a realistic understanding of the complexity of decisions to be made in a real-life diagnostic setting,” they said.
But the editorialists praised the study for revealing that many parents did not accurately perceive the true likelihood of late effects for their children. Parents in the survey tended to underestimate the risk for all the late effects besides infertility, which revealed a need for “better education about late effects early in the diagnostic and treatment process,” Dr. Brinkman and Dr. Gurney said, emphasizing that discussions should begin at diagnosis and continue beyond treatment “and long into the maintenance and surveillance period after the declaration of cure.”
Dr. Greenzang and colleagues’ study was funded by the National Institutes of Health and an Agency for Healthcare Research and Quality grant. The investigators declared no relevant financial disclosures. Dr. Brinkman and Dr. Gurney reported no relevant financial disclosures.
SOURCE: Greenzang et al. Pediatrics. 2020;145(5):e20193552.
Parents of children with cancer and their physicians are willing to opt for less effective treatment to avoid risk of neurocognitive disorders later in life, according to results from a new study.
While some 80% of children with cancer survive to adulthood, most will experience chronic health conditions related to treatment, and many pediatric oncologists will adjust treatment strategies to lessen the likelihood of later effects. For their research published in Pediatrics, Katie A. Greenzang, MD, of the Dana-Farber Cancer Institute in Boston and colleagues aimed to learn how both parents and physicians weighed the risks and benefits.
In a survey of 95 parents and 41 physicians at Dana-Farber, Dr. Greenzang and colleagues proposed hypothetical scenarios involving five common late effects of childhood cancer treatment: neurocognitive impairment, infertility, cardiac toxicity, second malignancies, and impaired development. The parents surveyed, all of whom had children diagnosed with cancer within the previous year, were asked to make decisions as though on behalf of their children, while physicians were asked to do so as on behalf of a newly diagnosed patient.
Avoiding severe cognitive impairment mattered more than an increased chance of a cure to both parents and physicians. Neurocognitive impairment was the risk that most affected treatment choices, with parents more likely to choose a treatment associated with no or mild neurocognitive impairment, compared with one that caused severe impairment (odds ratio, 2.83 for no impairment vs. severe impairment; P less than .001), which was also the case with physicians (OR, 4.01; P less than .001).
Parents would accept an 18% chance of another malignancy for a 10% greater chance of a cure, while physicians accepted a 15% risk. Parents were willing to tolerate a 31% risk of cardiac toxicity in exchange for the better chance of a cure, while physicians accepted a 22% higher risk.
The results, the researchers wrote in their analysis, offered a window into the level and type of later-life risks that parents can accept when making choices about cancer treatment and where those choices appear to differ from those made by physicians.
“Oncologists increasingly design clinical trials [for children with cancer] with dual goals of optimizing cure while minimizing late effects,” Dr. Greenzang and colleagues wrote. “In doing so, they make judgments about the relative value of short- and long-term outcomes in patients’ lives. Yet oncologists have largely done so in the absence of information about how parents prioritize avoidance of late effects relative to the chance of cure.”
In an editorial comment accompanying the study, Tara A. Brinkman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tenn., and James G. Gurney, PhD, of the University of Memphis noted that the findings “may have narrow clinical application” because many of the late-life effects presented in the survey will not present singly but will co-occur in survivors of childhood cancer. “Hypothetical scenarios that do not depict the full burden of late effects may not reflect a realistic understanding of the complexity of decisions to be made in a real-life diagnostic setting,” they said.
But the editorialists praised the study for revealing that many parents did not accurately perceive the true likelihood of late effects for their children. Parents in the survey tended to underestimate the risk for all the late effects besides infertility, which revealed a need for “better education about late effects early in the diagnostic and treatment process,” Dr. Brinkman and Dr. Gurney said, emphasizing that discussions should begin at diagnosis and continue beyond treatment “and long into the maintenance and surveillance period after the declaration of cure.”
Dr. Greenzang and colleagues’ study was funded by the National Institutes of Health and an Agency for Healthcare Research and Quality grant. The investigators declared no relevant financial disclosures. Dr. Brinkman and Dr. Gurney reported no relevant financial disclosures.
SOURCE: Greenzang et al. Pediatrics. 2020;145(5):e20193552.
Parents of children with cancer and their physicians are willing to opt for less effective treatment to avoid risk of neurocognitive disorders later in life, according to results from a new study.
While some 80% of children with cancer survive to adulthood, most will experience chronic health conditions related to treatment, and many pediatric oncologists will adjust treatment strategies to lessen the likelihood of later effects. For their research published in Pediatrics, Katie A. Greenzang, MD, of the Dana-Farber Cancer Institute in Boston and colleagues aimed to learn how both parents and physicians weighed the risks and benefits.
In a survey of 95 parents and 41 physicians at Dana-Farber, Dr. Greenzang and colleagues proposed hypothetical scenarios involving five common late effects of childhood cancer treatment: neurocognitive impairment, infertility, cardiac toxicity, second malignancies, and impaired development. The parents surveyed, all of whom had children diagnosed with cancer within the previous year, were asked to make decisions as though on behalf of their children, while physicians were asked to do so as on behalf of a newly diagnosed patient.
Avoiding severe cognitive impairment mattered more than an increased chance of a cure to both parents and physicians. Neurocognitive impairment was the risk that most affected treatment choices, with parents more likely to choose a treatment associated with no or mild neurocognitive impairment, compared with one that caused severe impairment (odds ratio, 2.83 for no impairment vs. severe impairment; P less than .001), which was also the case with physicians (OR, 4.01; P less than .001).
Parents would accept an 18% chance of another malignancy for a 10% greater chance of a cure, while physicians accepted a 15% risk. Parents were willing to tolerate a 31% risk of cardiac toxicity in exchange for the better chance of a cure, while physicians accepted a 22% higher risk.
The results, the researchers wrote in their analysis, offered a window into the level and type of later-life risks that parents can accept when making choices about cancer treatment and where those choices appear to differ from those made by physicians.
“Oncologists increasingly design clinical trials [for children with cancer] with dual goals of optimizing cure while minimizing late effects,” Dr. Greenzang and colleagues wrote. “In doing so, they make judgments about the relative value of short- and long-term outcomes in patients’ lives. Yet oncologists have largely done so in the absence of information about how parents prioritize avoidance of late effects relative to the chance of cure.”
In an editorial comment accompanying the study, Tara A. Brinkman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tenn., and James G. Gurney, PhD, of the University of Memphis noted that the findings “may have narrow clinical application” because many of the late-life effects presented in the survey will not present singly but will co-occur in survivors of childhood cancer. “Hypothetical scenarios that do not depict the full burden of late effects may not reflect a realistic understanding of the complexity of decisions to be made in a real-life diagnostic setting,” they said.
But the editorialists praised the study for revealing that many parents did not accurately perceive the true likelihood of late effects for their children. Parents in the survey tended to underestimate the risk for all the late effects besides infertility, which revealed a need for “better education about late effects early in the diagnostic and treatment process,” Dr. Brinkman and Dr. Gurney said, emphasizing that discussions should begin at diagnosis and continue beyond treatment “and long into the maintenance and surveillance period after the declaration of cure.”
Dr. Greenzang and colleagues’ study was funded by the National Institutes of Health and an Agency for Healthcare Research and Quality grant. The investigators declared no relevant financial disclosures. Dr. Brinkman and Dr. Gurney reported no relevant financial disclosures.
SOURCE: Greenzang et al. Pediatrics. 2020;145(5):e20193552.
FROM PEDIATRICS
Most endometrial cancers treated with minimally invasive procedures
Of 3,730 women with endometrial cancer in the Society of Gynecologic Oncology Clinical Outcomes Registry (SGO-COR), 88.8% underwent minimally invasive procedures, reported Amanda Nickles Fader, MD, of Johns Hopkins Hospital, Baltimore, and colleagues.
“When you have surgery with a gyn-oncologist who is specially trained in this type of surgery, we see that women have a very high likelihood of having the appropriate surgery, the minimally invasive surgery, and we thought that this benchmark of an 80% rate of minimally invasive surgery in these patients is very feasible and should be recognized as the standard of care,” Dr. Nickles Fader said in an interview.
Coinvestigator Summer B. Dewdney, MD, of Rush University Medical Center, Chicago, who was instrumental in creating and running the SGO-COR registry, said these findings are encouraging.
“We’re happy to see that rate. It’s the rate that it should be because minimally invasive surgery is the standard of care for endometrial cancer,” Dr. Dewdney said. She added, however, that data supplied to the registry come from gynecologic oncologists who are highly motivated to participate and follow best practice guidelines, which could skew the results slightly toward more favorable outcomes.
Results of the registry-based study are detailed in an abstract that was slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic.
Assessing adherence to guidelines
In 2015, the SGO Clinical Practice Committee and the American College of Obstetricians and Gynecologists issued a practice bulletin, which stated that “minimally invasive surgery should be embraced as the standard surgical approach for comprehensive surgical staging in women with endometrial cancer.”
Similarly, National Comprehensive Cancer Network guidelines for uterine cancer state that “minimally invasive surgery is the preferred approach when technically feasible” for treatment of endometrial cancer confined to the uterus.
Despite these recommendations, the overall rate of minimally invasive endometrial cancer surgery in the United States is reported be around to 60%, Dr. Nickles Fader and colleagues wrote.
With this in mind, the investigators set out to determine the rate of minimally invasive surgery in women with apparent stage I, II, or III endometrial cancer who underwent hysterectomy with or without staging from 2012 to 2017 at a center reporting to SGO-COR.
The team identified 3,730 women treated at 25 SGO-COR centers; 12 of which were university-affiliated centers and 13 of which were nonuniversity based. Most patients (83.2%) had stage I disease, 4.7% had stage II cancer, and 12.1% had stage III disease. The median patient age was 57 years. Most patients (88%) were white, and two-thirds (67.1%) were obese. In all, 80.4% of samples had endometrioid histology, and 77.7% were either grade 1 or 2.
Factors associated with minimally invasive surgery
The data showed that 88.8% of patients underwent a minimally invasive hysterectomy, composed of robotic-assisted procedures in 73.9% of cases, laparoscopy in 13.4%, and vaginal access in 1.6%.
The proportion of patients who underwent a minimally invasive procedure was significantly higher at nonuniversity centers, compared with academic centers (92.6% vs. 82.7%; P < .0001), but rates of minimally invasive procedures did not differ significantly across U.S. geographic regions.
Dr. Dewdney said that the higher proportion of open surgeries performed at university centers may be attributable to those centers treating patients with more advanced disease or rare aggressive cancers that may not be amenable to a minimally invasive approach.
In a multivariate analysis, factors associated with a failure to perform minimally invasive surgery were black race of the patient (adjusted odds ratio, 0.57), body mass index over 35 kg/m2 (aOR, 1.40), stage II disease (aOR, 0.49), stage III disease (aOR, 0.36), carcinosarcoma/leiomyosarcoma (aOR, 0.58), and university hospital (aOR, 3.46).
Looking at perioperative complications, the investigators found that laparotomy was associated with more in-hospital complications than minimally invasive procedures, including more unscheduled ICU stays (P < .001) and prolonged hospital stays (P = .0002).
Dr. Dewdney said that investigators are planning further registry-based studies focusing on ovarian cancer, uterine cancer, and cervical cancer.
Dr. Nickles Fader and Dr. Dewdney reported having no relevant conflicts of interest.
SOURCE: Nickles Fader A et al. SGO 2020, Abstract 63.
Of 3,730 women with endometrial cancer in the Society of Gynecologic Oncology Clinical Outcomes Registry (SGO-COR), 88.8% underwent minimally invasive procedures, reported Amanda Nickles Fader, MD, of Johns Hopkins Hospital, Baltimore, and colleagues.
“When you have surgery with a gyn-oncologist who is specially trained in this type of surgery, we see that women have a very high likelihood of having the appropriate surgery, the minimally invasive surgery, and we thought that this benchmark of an 80% rate of minimally invasive surgery in these patients is very feasible and should be recognized as the standard of care,” Dr. Nickles Fader said in an interview.
Coinvestigator Summer B. Dewdney, MD, of Rush University Medical Center, Chicago, who was instrumental in creating and running the SGO-COR registry, said these findings are encouraging.
“We’re happy to see that rate. It’s the rate that it should be because minimally invasive surgery is the standard of care for endometrial cancer,” Dr. Dewdney said. She added, however, that data supplied to the registry come from gynecologic oncologists who are highly motivated to participate and follow best practice guidelines, which could skew the results slightly toward more favorable outcomes.
Results of the registry-based study are detailed in an abstract that was slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic.
Assessing adherence to guidelines
In 2015, the SGO Clinical Practice Committee and the American College of Obstetricians and Gynecologists issued a practice bulletin, which stated that “minimally invasive surgery should be embraced as the standard surgical approach for comprehensive surgical staging in women with endometrial cancer.”
Similarly, National Comprehensive Cancer Network guidelines for uterine cancer state that “minimally invasive surgery is the preferred approach when technically feasible” for treatment of endometrial cancer confined to the uterus.
Despite these recommendations, the overall rate of minimally invasive endometrial cancer surgery in the United States is reported be around to 60%, Dr. Nickles Fader and colleagues wrote.
With this in mind, the investigators set out to determine the rate of minimally invasive surgery in women with apparent stage I, II, or III endometrial cancer who underwent hysterectomy with or without staging from 2012 to 2017 at a center reporting to SGO-COR.
The team identified 3,730 women treated at 25 SGO-COR centers; 12 of which were university-affiliated centers and 13 of which were nonuniversity based. Most patients (83.2%) had stage I disease, 4.7% had stage II cancer, and 12.1% had stage III disease. The median patient age was 57 years. Most patients (88%) were white, and two-thirds (67.1%) were obese. In all, 80.4% of samples had endometrioid histology, and 77.7% were either grade 1 or 2.
Factors associated with minimally invasive surgery
The data showed that 88.8% of patients underwent a minimally invasive hysterectomy, composed of robotic-assisted procedures in 73.9% of cases, laparoscopy in 13.4%, and vaginal access in 1.6%.
The proportion of patients who underwent a minimally invasive procedure was significantly higher at nonuniversity centers, compared with academic centers (92.6% vs. 82.7%; P < .0001), but rates of minimally invasive procedures did not differ significantly across U.S. geographic regions.
Dr. Dewdney said that the higher proportion of open surgeries performed at university centers may be attributable to those centers treating patients with more advanced disease or rare aggressive cancers that may not be amenable to a minimally invasive approach.
In a multivariate analysis, factors associated with a failure to perform minimally invasive surgery were black race of the patient (adjusted odds ratio, 0.57), body mass index over 35 kg/m2 (aOR, 1.40), stage II disease (aOR, 0.49), stage III disease (aOR, 0.36), carcinosarcoma/leiomyosarcoma (aOR, 0.58), and university hospital (aOR, 3.46).
Looking at perioperative complications, the investigators found that laparotomy was associated with more in-hospital complications than minimally invasive procedures, including more unscheduled ICU stays (P < .001) and prolonged hospital stays (P = .0002).
Dr. Dewdney said that investigators are planning further registry-based studies focusing on ovarian cancer, uterine cancer, and cervical cancer.
Dr. Nickles Fader and Dr. Dewdney reported having no relevant conflicts of interest.
SOURCE: Nickles Fader A et al. SGO 2020, Abstract 63.
Of 3,730 women with endometrial cancer in the Society of Gynecologic Oncology Clinical Outcomes Registry (SGO-COR), 88.8% underwent minimally invasive procedures, reported Amanda Nickles Fader, MD, of Johns Hopkins Hospital, Baltimore, and colleagues.
“When you have surgery with a gyn-oncologist who is specially trained in this type of surgery, we see that women have a very high likelihood of having the appropriate surgery, the minimally invasive surgery, and we thought that this benchmark of an 80% rate of minimally invasive surgery in these patients is very feasible and should be recognized as the standard of care,” Dr. Nickles Fader said in an interview.
Coinvestigator Summer B. Dewdney, MD, of Rush University Medical Center, Chicago, who was instrumental in creating and running the SGO-COR registry, said these findings are encouraging.
“We’re happy to see that rate. It’s the rate that it should be because minimally invasive surgery is the standard of care for endometrial cancer,” Dr. Dewdney said. She added, however, that data supplied to the registry come from gynecologic oncologists who are highly motivated to participate and follow best practice guidelines, which could skew the results slightly toward more favorable outcomes.
Results of the registry-based study are detailed in an abstract that was slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic.
Assessing adherence to guidelines
In 2015, the SGO Clinical Practice Committee and the American College of Obstetricians and Gynecologists issued a practice bulletin, which stated that “minimally invasive surgery should be embraced as the standard surgical approach for comprehensive surgical staging in women with endometrial cancer.”
Similarly, National Comprehensive Cancer Network guidelines for uterine cancer state that “minimally invasive surgery is the preferred approach when technically feasible” for treatment of endometrial cancer confined to the uterus.
Despite these recommendations, the overall rate of minimally invasive endometrial cancer surgery in the United States is reported be around to 60%, Dr. Nickles Fader and colleagues wrote.
With this in mind, the investigators set out to determine the rate of minimally invasive surgery in women with apparent stage I, II, or III endometrial cancer who underwent hysterectomy with or without staging from 2012 to 2017 at a center reporting to SGO-COR.
The team identified 3,730 women treated at 25 SGO-COR centers; 12 of which were university-affiliated centers and 13 of which were nonuniversity based. Most patients (83.2%) had stage I disease, 4.7% had stage II cancer, and 12.1% had stage III disease. The median patient age was 57 years. Most patients (88%) were white, and two-thirds (67.1%) were obese. In all, 80.4% of samples had endometrioid histology, and 77.7% were either grade 1 or 2.
Factors associated with minimally invasive surgery
The data showed that 88.8% of patients underwent a minimally invasive hysterectomy, composed of robotic-assisted procedures in 73.9% of cases, laparoscopy in 13.4%, and vaginal access in 1.6%.
The proportion of patients who underwent a minimally invasive procedure was significantly higher at nonuniversity centers, compared with academic centers (92.6% vs. 82.7%; P < .0001), but rates of minimally invasive procedures did not differ significantly across U.S. geographic regions.
Dr. Dewdney said that the higher proportion of open surgeries performed at university centers may be attributable to those centers treating patients with more advanced disease or rare aggressive cancers that may not be amenable to a minimally invasive approach.
In a multivariate analysis, factors associated with a failure to perform minimally invasive surgery were black race of the patient (adjusted odds ratio, 0.57), body mass index over 35 kg/m2 (aOR, 1.40), stage II disease (aOR, 0.49), stage III disease (aOR, 0.36), carcinosarcoma/leiomyosarcoma (aOR, 0.58), and university hospital (aOR, 3.46).
Looking at perioperative complications, the investigators found that laparotomy was associated with more in-hospital complications than minimally invasive procedures, including more unscheduled ICU stays (P < .001) and prolonged hospital stays (P = .0002).
Dr. Dewdney said that investigators are planning further registry-based studies focusing on ovarian cancer, uterine cancer, and cervical cancer.
Dr. Nickles Fader and Dr. Dewdney reported having no relevant conflicts of interest.
SOURCE: Nickles Fader A et al. SGO 2020, Abstract 63.
FROM SGO 2020
OSA increases odds of hospital readmission after COPD exacerbation
more than threefold, according to results from a single-center study published in CHEST.
Mario Naranjo, MD, and colleagues retrospectively examined data from Albert Einstein Medical Center in Philadelphia to assess the impact of OSA on hospital readmission within 30 days of discharge after treatment for a COPD exacerbation. Dr. Naranjo is affiliated with Johns Hopkins Medicine, Baltimore.
The researchers analyzed data from 238 patients admitted for COPD exacerbation between May 2017 and July 2018 who were screened for previously unrecognized and untreated OSA and underwent a high-resolution pulse-oximetry or portable sleep monitoring study. In all, 111 (46.6%) had OSA; 28.6% had mild OSA, 9.7% had moderate OSA, and 8.4% had severe OSA.
Most baseline characteristics were similar among patients with and without OSA, but patients with OSA had a greater mean body mass index (33.9 vs. 30.3 kg/m2) and were more likely to have comorbid heart failure (19.8% vs. 7.1%), compared with patients without OSA. In addition, the proportion of male patients was greater in the cohort with OSA (60.4% vs. 49.6%).
For patients with mild OSA (oxygen desaturation index [ODI] ≥ 5 and < 15/hour), the odds of 30-day readmission were 2.05 times higher, compared with patients without OSA (32.4% vs. 18.9%). With moderate OSA (ODI ≥ 15 and < 30/hour), the odds of 30-day readmission were 6.68 times higher (60.9% vs. 18.9%). For severe OSA (ODI ≥ 30/hour), the odds were 10.01 times higher (70.0% vs. 18.9%). “For combined OSA severity categories, the odds of 30-day readmission were 3.5 times higher,” said Dr. Naranjo and colleagues. In addition, 90- and 180-day readmission rates and 6-month mortality rates were higher among patients with OSA.
“These findings have important implications for the evaluation and care of patients admitted to the hospital for COPD exacerbations,” Dr. Naranjo and colleagues said. “Although the combination of COPD and OSA (also known as the “overlap syndrome”) in ambulatory settings has been shown to have worse outcomes in terms of COPD exacerbations and mortality, these findings have not been reported previously for hospitalized COPD patients.”
Greater degrees of nocturnal hypoxemia and hypercapnia, worse functional status, and daytime sleepiness and fatigue may contribute to the relationship between OSA and the likelihood of hospital readmission, according to the authors. A multicenter study is warranted to confirm the results, they said.
Dr. Naranjo had no conflicts of interest. Coauthors have received grants from ResMed, Dayzz, and the National Institutes of Health and consulted for Jazz Pharmaceuticals, Best Doctors, and ResMed. One author is a committee chair for the American Academy of Sleep Medicine.
SOURCE: Naranjo M et al. Chest. 2020 Apr 2. doi: 10.1016/j.chest.2020.03.036.
more than threefold, according to results from a single-center study published in CHEST.
Mario Naranjo, MD, and colleagues retrospectively examined data from Albert Einstein Medical Center in Philadelphia to assess the impact of OSA on hospital readmission within 30 days of discharge after treatment for a COPD exacerbation. Dr. Naranjo is affiliated with Johns Hopkins Medicine, Baltimore.
The researchers analyzed data from 238 patients admitted for COPD exacerbation between May 2017 and July 2018 who were screened for previously unrecognized and untreated OSA and underwent a high-resolution pulse-oximetry or portable sleep monitoring study. In all, 111 (46.6%) had OSA; 28.6% had mild OSA, 9.7% had moderate OSA, and 8.4% had severe OSA.
Most baseline characteristics were similar among patients with and without OSA, but patients with OSA had a greater mean body mass index (33.9 vs. 30.3 kg/m2) and were more likely to have comorbid heart failure (19.8% vs. 7.1%), compared with patients without OSA. In addition, the proportion of male patients was greater in the cohort with OSA (60.4% vs. 49.6%).
For patients with mild OSA (oxygen desaturation index [ODI] ≥ 5 and < 15/hour), the odds of 30-day readmission were 2.05 times higher, compared with patients without OSA (32.4% vs. 18.9%). With moderate OSA (ODI ≥ 15 and < 30/hour), the odds of 30-day readmission were 6.68 times higher (60.9% vs. 18.9%). For severe OSA (ODI ≥ 30/hour), the odds were 10.01 times higher (70.0% vs. 18.9%). “For combined OSA severity categories, the odds of 30-day readmission were 3.5 times higher,” said Dr. Naranjo and colleagues. In addition, 90- and 180-day readmission rates and 6-month mortality rates were higher among patients with OSA.
“These findings have important implications for the evaluation and care of patients admitted to the hospital for COPD exacerbations,” Dr. Naranjo and colleagues said. “Although the combination of COPD and OSA (also known as the “overlap syndrome”) in ambulatory settings has been shown to have worse outcomes in terms of COPD exacerbations and mortality, these findings have not been reported previously for hospitalized COPD patients.”
Greater degrees of nocturnal hypoxemia and hypercapnia, worse functional status, and daytime sleepiness and fatigue may contribute to the relationship between OSA and the likelihood of hospital readmission, according to the authors. A multicenter study is warranted to confirm the results, they said.
Dr. Naranjo had no conflicts of interest. Coauthors have received grants from ResMed, Dayzz, and the National Institutes of Health and consulted for Jazz Pharmaceuticals, Best Doctors, and ResMed. One author is a committee chair for the American Academy of Sleep Medicine.
SOURCE: Naranjo M et al. Chest. 2020 Apr 2. doi: 10.1016/j.chest.2020.03.036.
more than threefold, according to results from a single-center study published in CHEST.
Mario Naranjo, MD, and colleagues retrospectively examined data from Albert Einstein Medical Center in Philadelphia to assess the impact of OSA on hospital readmission within 30 days of discharge after treatment for a COPD exacerbation. Dr. Naranjo is affiliated with Johns Hopkins Medicine, Baltimore.
The researchers analyzed data from 238 patients admitted for COPD exacerbation between May 2017 and July 2018 who were screened for previously unrecognized and untreated OSA and underwent a high-resolution pulse-oximetry or portable sleep monitoring study. In all, 111 (46.6%) had OSA; 28.6% had mild OSA, 9.7% had moderate OSA, and 8.4% had severe OSA.
Most baseline characteristics were similar among patients with and without OSA, but patients with OSA had a greater mean body mass index (33.9 vs. 30.3 kg/m2) and were more likely to have comorbid heart failure (19.8% vs. 7.1%), compared with patients without OSA. In addition, the proportion of male patients was greater in the cohort with OSA (60.4% vs. 49.6%).
For patients with mild OSA (oxygen desaturation index [ODI] ≥ 5 and < 15/hour), the odds of 30-day readmission were 2.05 times higher, compared with patients without OSA (32.4% vs. 18.9%). With moderate OSA (ODI ≥ 15 and < 30/hour), the odds of 30-day readmission were 6.68 times higher (60.9% vs. 18.9%). For severe OSA (ODI ≥ 30/hour), the odds were 10.01 times higher (70.0% vs. 18.9%). “For combined OSA severity categories, the odds of 30-day readmission were 3.5 times higher,” said Dr. Naranjo and colleagues. In addition, 90- and 180-day readmission rates and 6-month mortality rates were higher among patients with OSA.
“These findings have important implications for the evaluation and care of patients admitted to the hospital for COPD exacerbations,” Dr. Naranjo and colleagues said. “Although the combination of COPD and OSA (also known as the “overlap syndrome”) in ambulatory settings has been shown to have worse outcomes in terms of COPD exacerbations and mortality, these findings have not been reported previously for hospitalized COPD patients.”
Greater degrees of nocturnal hypoxemia and hypercapnia, worse functional status, and daytime sleepiness and fatigue may contribute to the relationship between OSA and the likelihood of hospital readmission, according to the authors. A multicenter study is warranted to confirm the results, they said.
Dr. Naranjo had no conflicts of interest. Coauthors have received grants from ResMed, Dayzz, and the National Institutes of Health and consulted for Jazz Pharmaceuticals, Best Doctors, and ResMed. One author is a committee chair for the American Academy of Sleep Medicine.
SOURCE: Naranjo M et al. Chest. 2020 Apr 2. doi: 10.1016/j.chest.2020.03.036.
FROM CHEST
Erectile dysfunction: It’s worse than you think
Erectile dysfunction may be an early warning sign of broader health problems. That’s the suggestion from a new retrospective analysis of European men, which found that erectile dysfunction and other sexual symptoms were associated with a greater risk of death, independent of testosterone levels.
Similar studies have shown links between mortality and sexual dysfunction, or between mortality and testosterone level, but the current study is unique, Leen Antonio, MD, PhD, assistant professor of endocrinology at Katholieke Universiteit Leuven (Belgium), said during a virtual news conference held by the Endocrine Society. The study had been slated for presentation during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.
“It’s the first time we have put both together in the same group of people, and we can say that it’s mostly the sexual symptoms that are predicting the mortality risk, independent of the testosterone levels of these men,” Dr. Antonio said in an interview.
“We can regard sexual symptoms as a marker for adverse health status in general. It’s like a warning signal that you’re at risk for more severe problems,” Dr. Antonio added.
Dr. Antonio advised clinicians to test blood pressure and cholesterol levels in men presenting with sexual dysfunction and to counsel lifestyle changes, such as physical activity and weight management. “These can be beneficial for sexual symptoms and for general health and the risk for cardiovascular disease in the future.”
Although the study could not identify a reason for the relationship between sexual dysfunction and mortality, Dr. Antonio hypothesized that the narrow penile artery may be more likely to suffer noticeable effects in the early stages of atherosclerosis, before clinical effects occur in the coronary artery.
Michael Blaha, MD, professor of medicine and director of clinical research at the Ciccarone Center for the Prevention of Heart Disease at Johns Hopkins University, Baltimore, who has studied erectile dysfunction (ED) and its association with cardiovascular disease, said that the study is further evidence that ED is an important and independent risk factor for cardiovascular disease and other health risks. He would like to see a move toward establishing men’s health clinics, where risk factors can be identified and mitigated through lifestyle changes and therapies.
“There needs to be a complete rethink of the way we approach the whole group of patients who present with erectile dysfunction to various specialists,” he said in an interview, noting that middle-aged men often present to ED specialists after years of not having any contact with the health system. In that group, ED can be an early warning sign that could trigger broader interventions.
“This points to the need for more men’s health clinics that are focused on the early detection of risk factors, and treating erectile dysfunction and other risk factors in a more comprehensive way,” said Dr. Blaha, who was not associated with the study.
Dr. Antonio and colleagues studied 1,913 community-dwelling men, who participated in the European Male Ageing Study. Baseline information on sexual function and testosterone levels was collected between 2003 and 2005. The men were aged 40-79 years at study entry, and “because of the wide age range at study entry, age was used as time scale, instead of years since inclusion adjusting for age,” the researchers explained.
Over a mean follow-up of 12.4 years, 25.3% of participants died. Body mass index was higher in men who died (P = .002), but there was no significant difference in smoking status. Both groups had similar levels of total testosterone, but free testosterone was lower in the deceased population (270 pmol/L vs. 312 pmol/L; P < .001), whereas luteinizing hormone levels were higher (7.8 units/L vs. 5.7 units/L; P < .001).
The lowest quartile of free testosterone level was associated with higher mortality risk (hazard ratio, 1.43; P = .021), whereas the highest quartile of follicle-stimulating hormone was associated with greater mortality risk (HR, 1.38; P = .036). There was no association between mortality risk and total testosterone or estradiol.
Men reporting three sexual symptoms at baseline had a higher mortality risk than those reporting no symptoms (HR, 1.77; P < .001). There was an association between mortality risk and ED (HR, 1.40; P = .001) and poor morning erections (HR, 1.30; P = .012), but not low libido.
The associations were not affected after adjustment for total testosterone or free testosterone. Among men with normal total testosterone (>12 nmol/L), sexual symptoms were associated with heightened mortality risk (HR, 1.51; P = .003), and the same was true in men with total testosterone levels of less than 8 nmol, compared with men with normal total testosterone who reported no sexual symptoms (HR, 1.92; P = .035).
The European Male Ageing Study received support from the European Union. Dr. Antonio has no relevant financial disclosures. Dr. Blaha has received grants from Amgen and is on advisory boards for Amgen and other pharmaceutical firms.
Dr. Antonio and her team’s research will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
SOURCE: Antonio L et al. ENDO 2020, Abstract OR02-06.
This article was upadted on 4/17/2020.
Erectile dysfunction may be an early warning sign of broader health problems. That’s the suggestion from a new retrospective analysis of European men, which found that erectile dysfunction and other sexual symptoms were associated with a greater risk of death, independent of testosterone levels.
Similar studies have shown links between mortality and sexual dysfunction, or between mortality and testosterone level, but the current study is unique, Leen Antonio, MD, PhD, assistant professor of endocrinology at Katholieke Universiteit Leuven (Belgium), said during a virtual news conference held by the Endocrine Society. The study had been slated for presentation during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.
“It’s the first time we have put both together in the same group of people, and we can say that it’s mostly the sexual symptoms that are predicting the mortality risk, independent of the testosterone levels of these men,” Dr. Antonio said in an interview.
“We can regard sexual symptoms as a marker for adverse health status in general. It’s like a warning signal that you’re at risk for more severe problems,” Dr. Antonio added.
Dr. Antonio advised clinicians to test blood pressure and cholesterol levels in men presenting with sexual dysfunction and to counsel lifestyle changes, such as physical activity and weight management. “These can be beneficial for sexual symptoms and for general health and the risk for cardiovascular disease in the future.”
Although the study could not identify a reason for the relationship between sexual dysfunction and mortality, Dr. Antonio hypothesized that the narrow penile artery may be more likely to suffer noticeable effects in the early stages of atherosclerosis, before clinical effects occur in the coronary artery.
Michael Blaha, MD, professor of medicine and director of clinical research at the Ciccarone Center for the Prevention of Heart Disease at Johns Hopkins University, Baltimore, who has studied erectile dysfunction (ED) and its association with cardiovascular disease, said that the study is further evidence that ED is an important and independent risk factor for cardiovascular disease and other health risks. He would like to see a move toward establishing men’s health clinics, where risk factors can be identified and mitigated through lifestyle changes and therapies.
“There needs to be a complete rethink of the way we approach the whole group of patients who present with erectile dysfunction to various specialists,” he said in an interview, noting that middle-aged men often present to ED specialists after years of not having any contact with the health system. In that group, ED can be an early warning sign that could trigger broader interventions.
“This points to the need for more men’s health clinics that are focused on the early detection of risk factors, and treating erectile dysfunction and other risk factors in a more comprehensive way,” said Dr. Blaha, who was not associated with the study.
Dr. Antonio and colleagues studied 1,913 community-dwelling men, who participated in the European Male Ageing Study. Baseline information on sexual function and testosterone levels was collected between 2003 and 2005. The men were aged 40-79 years at study entry, and “because of the wide age range at study entry, age was used as time scale, instead of years since inclusion adjusting for age,” the researchers explained.
Over a mean follow-up of 12.4 years, 25.3% of participants died. Body mass index was higher in men who died (P = .002), but there was no significant difference in smoking status. Both groups had similar levels of total testosterone, but free testosterone was lower in the deceased population (270 pmol/L vs. 312 pmol/L; P < .001), whereas luteinizing hormone levels were higher (7.8 units/L vs. 5.7 units/L; P < .001).
The lowest quartile of free testosterone level was associated with higher mortality risk (hazard ratio, 1.43; P = .021), whereas the highest quartile of follicle-stimulating hormone was associated with greater mortality risk (HR, 1.38; P = .036). There was no association between mortality risk and total testosterone or estradiol.
Men reporting three sexual symptoms at baseline had a higher mortality risk than those reporting no symptoms (HR, 1.77; P < .001). There was an association between mortality risk and ED (HR, 1.40; P = .001) and poor morning erections (HR, 1.30; P = .012), but not low libido.
The associations were not affected after adjustment for total testosterone or free testosterone. Among men with normal total testosterone (>12 nmol/L), sexual symptoms were associated with heightened mortality risk (HR, 1.51; P = .003), and the same was true in men with total testosterone levels of less than 8 nmol, compared with men with normal total testosterone who reported no sexual symptoms (HR, 1.92; P = .035).
The European Male Ageing Study received support from the European Union. Dr. Antonio has no relevant financial disclosures. Dr. Blaha has received grants from Amgen and is on advisory boards for Amgen and other pharmaceutical firms.
Dr. Antonio and her team’s research will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
SOURCE: Antonio L et al. ENDO 2020, Abstract OR02-06.
This article was upadted on 4/17/2020.
Erectile dysfunction may be an early warning sign of broader health problems. That’s the suggestion from a new retrospective analysis of European men, which found that erectile dysfunction and other sexual symptoms were associated with a greater risk of death, independent of testosterone levels.
Similar studies have shown links between mortality and sexual dysfunction, or between mortality and testosterone level, but the current study is unique, Leen Antonio, MD, PhD, assistant professor of endocrinology at Katholieke Universiteit Leuven (Belgium), said during a virtual news conference held by the Endocrine Society. The study had been slated for presentation during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.
“It’s the first time we have put both together in the same group of people, and we can say that it’s mostly the sexual symptoms that are predicting the mortality risk, independent of the testosterone levels of these men,” Dr. Antonio said in an interview.
“We can regard sexual symptoms as a marker for adverse health status in general. It’s like a warning signal that you’re at risk for more severe problems,” Dr. Antonio added.
Dr. Antonio advised clinicians to test blood pressure and cholesterol levels in men presenting with sexual dysfunction and to counsel lifestyle changes, such as physical activity and weight management. “These can be beneficial for sexual symptoms and for general health and the risk for cardiovascular disease in the future.”
Although the study could not identify a reason for the relationship between sexual dysfunction and mortality, Dr. Antonio hypothesized that the narrow penile artery may be more likely to suffer noticeable effects in the early stages of atherosclerosis, before clinical effects occur in the coronary artery.
Michael Blaha, MD, professor of medicine and director of clinical research at the Ciccarone Center for the Prevention of Heart Disease at Johns Hopkins University, Baltimore, who has studied erectile dysfunction (ED) and its association with cardiovascular disease, said that the study is further evidence that ED is an important and independent risk factor for cardiovascular disease and other health risks. He would like to see a move toward establishing men’s health clinics, where risk factors can be identified and mitigated through lifestyle changes and therapies.
“There needs to be a complete rethink of the way we approach the whole group of patients who present with erectile dysfunction to various specialists,” he said in an interview, noting that middle-aged men often present to ED specialists after years of not having any contact with the health system. In that group, ED can be an early warning sign that could trigger broader interventions.
“This points to the need for more men’s health clinics that are focused on the early detection of risk factors, and treating erectile dysfunction and other risk factors in a more comprehensive way,” said Dr. Blaha, who was not associated with the study.
Dr. Antonio and colleagues studied 1,913 community-dwelling men, who participated in the European Male Ageing Study. Baseline information on sexual function and testosterone levels was collected between 2003 and 2005. The men were aged 40-79 years at study entry, and “because of the wide age range at study entry, age was used as time scale, instead of years since inclusion adjusting for age,” the researchers explained.
Over a mean follow-up of 12.4 years, 25.3% of participants died. Body mass index was higher in men who died (P = .002), but there was no significant difference in smoking status. Both groups had similar levels of total testosterone, but free testosterone was lower in the deceased population (270 pmol/L vs. 312 pmol/L; P < .001), whereas luteinizing hormone levels were higher (7.8 units/L vs. 5.7 units/L; P < .001).
The lowest quartile of free testosterone level was associated with higher mortality risk (hazard ratio, 1.43; P = .021), whereas the highest quartile of follicle-stimulating hormone was associated with greater mortality risk (HR, 1.38; P = .036). There was no association between mortality risk and total testosterone or estradiol.
Men reporting three sexual symptoms at baseline had a higher mortality risk than those reporting no symptoms (HR, 1.77; P < .001). There was an association between mortality risk and ED (HR, 1.40; P = .001) and poor morning erections (HR, 1.30; P = .012), but not low libido.
The associations were not affected after adjustment for total testosterone or free testosterone. Among men with normal total testosterone (>12 nmol/L), sexual symptoms were associated with heightened mortality risk (HR, 1.51; P = .003), and the same was true in men with total testosterone levels of less than 8 nmol, compared with men with normal total testosterone who reported no sexual symptoms (HR, 1.92; P = .035).
The European Male Ageing Study received support from the European Union. Dr. Antonio has no relevant financial disclosures. Dr. Blaha has received grants from Amgen and is on advisory boards for Amgen and other pharmaceutical firms.
Dr. Antonio and her team’s research will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
SOURCE: Antonio L et al. ENDO 2020, Abstract OR02-06.
This article was upadted on 4/17/2020.
FROM ENDO 2020
Drone flight launches first-ever insulin drop
After a year of planning, researchers sent a drone flight off the coast of western Ireland to the Aran Islands, delivering insulin and glucagon and retrieving a blood sample from the first patient to receive insulin successfully by autonomous drone delivery.
The nuts and bolts of arranging the drop and retrieval, which occurred in September 2019, were detailed by Spyridoula Maraka, MD, during a virtual news conference held by the Endocrine Society. The study had been slated for presentaion during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.
“There are multiple medical drone delivery opportunities that could be lifesaving during sentinel events such as hurricanes, earthquakes, and, of course, pandemics like the one we are currently experiencing,” said Dr. Maraka.
Drones, or unmanned aerial vehicles, are popular for recreational use and in some commercial applications – notably photography – but they are largely untapped as a medical resource, said Dr. Maraka, a collaborator on the project and an endocrinologist at the University of Arkansas for Medical Sciences, Little Rock.
Most of the exploration of drones for medical purposes has been in countries with emerging economies, such as Ghana and Rwanda in Africa, where the unmanned vehicles have been used by the U.S. medical product delivery company Zipline since 2016 to deliver blood.
The autonomous drone delivery of insulin originated in Galway, where the project’s lead investigator, Derek O’Keefe, MD, PhD, is an endocrinologist and professor of medical device technology at the National University of Ireland.
In 2017, Ireland was pummeled by Ophelia, a category 3 hurricane, and a year later by Storm Emma, a winter blizzard, said Dr. Maraka. Those extreme weather events trapped patients in their homes, made streets impassable for days on end, and interrupted the delivery of essential medical supplies, including insulin.
Until then, Ireland’s medical management plan had been passive and rested on the assumption that any weather-related interruptions would be relatively brief and not result in large-scale disruption of care and supply delivery for geographically isolated patients, said Dr. Maraka. But the two extreme and disruptive weather events in relatively quick succession prompted a reassessment of emergency medical management plans.
“We realized that [the prevailing plans were] not good enough,” said Dr. Maraka. “Medicine has a track record of practicing for emergencies before they actually happen,” to make sure that necessary resources are available and protocols in place in case of an emergency. The researchers extrapolated this preparedness mindset to medication delivery and realized that drones could be used both for a medication drop and to bring blood or other samples back from patients for testing.
Ireland’s Aran Islands came to mind as a location that was at risk of being cut off from services, but that was reachable by drone from Galway. “We quickly realized that this project would be very challenging, as no one in the developed world had done drone deliveries beyond the visual line of sight,” said Dr. Maraka, adding that flight operations had significant regulatory constraints.
The cross-disciplinary team that was pulled together to run the Diabetes Drone Mission, as the project was dubbed, included physicians and experts from pharmacies and pharmaceutical companies. To address drone operation specifically, a drone manufacturer, a flight operations firm, and a telecommunications company were also engaged. Drone pilots had to be licensed for beyond-the-visual-line-of-sight (BVLOS) operation, and Irish and European aviation regulators were consulted.
It took a full year to pull the pieces together for the inaugural flight. “One of the first challenges we faced was that we wanted to perform a civilian drone flight covering more than 40 kilometers,” said Dr. Maraka, whereas most drones flights are in the range of 1-10 km (0.6-6.2 miles). This long-range BVLOS flight required the drone to send live camera feed for the flight duration, which necessitated uninterrupted 4G wireless connectivity with satellite telecommunications as backup.
The Wingcopter 178 drone that was eventually chosen has a wingspan of 178 cm (about 70 inches) and can reach a top speed of 130 km/hr (about 81 mph) in fixed-wing mode.
“We had to comply with medication-dispensing legislation ... and we had to comply with medication transportation cold-chain legislation,” said Dr. Maraka. In other words, the insulin could not be loaded and delivered without the usual prescribing, dispensing, and chain-of-custody procedures being met.
In the end, the successful proof-of-concept flight saw the drone covering 43.3 km (26.9 miles) in a 32-minute flight to deliver insulin and glucagon and return a blood sample for hemoglobin A1c testing.
Dr. Maraka said she and her collaborators have an active collaboration with United Parcel Service and drone suppliers to expand into regular medical supply deliveries.
Dr. Maraka reported no conflicts of interest.
The report will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
SOURCE: Maraka S et al. ENDO 2020, Abstract OR30-04.
This article was updated on 4/17/2020.
After a year of planning, researchers sent a drone flight off the coast of western Ireland to the Aran Islands, delivering insulin and glucagon and retrieving a blood sample from the first patient to receive insulin successfully by autonomous drone delivery.
The nuts and bolts of arranging the drop and retrieval, which occurred in September 2019, were detailed by Spyridoula Maraka, MD, during a virtual news conference held by the Endocrine Society. The study had been slated for presentaion during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.
“There are multiple medical drone delivery opportunities that could be lifesaving during sentinel events such as hurricanes, earthquakes, and, of course, pandemics like the one we are currently experiencing,” said Dr. Maraka.
Drones, or unmanned aerial vehicles, are popular for recreational use and in some commercial applications – notably photography – but they are largely untapped as a medical resource, said Dr. Maraka, a collaborator on the project and an endocrinologist at the University of Arkansas for Medical Sciences, Little Rock.
Most of the exploration of drones for medical purposes has been in countries with emerging economies, such as Ghana and Rwanda in Africa, where the unmanned vehicles have been used by the U.S. medical product delivery company Zipline since 2016 to deliver blood.
The autonomous drone delivery of insulin originated in Galway, where the project’s lead investigator, Derek O’Keefe, MD, PhD, is an endocrinologist and professor of medical device technology at the National University of Ireland.
In 2017, Ireland was pummeled by Ophelia, a category 3 hurricane, and a year later by Storm Emma, a winter blizzard, said Dr. Maraka. Those extreme weather events trapped patients in their homes, made streets impassable for days on end, and interrupted the delivery of essential medical supplies, including insulin.
Until then, Ireland’s medical management plan had been passive and rested on the assumption that any weather-related interruptions would be relatively brief and not result in large-scale disruption of care and supply delivery for geographically isolated patients, said Dr. Maraka. But the two extreme and disruptive weather events in relatively quick succession prompted a reassessment of emergency medical management plans.
“We realized that [the prevailing plans were] not good enough,” said Dr. Maraka. “Medicine has a track record of practicing for emergencies before they actually happen,” to make sure that necessary resources are available and protocols in place in case of an emergency. The researchers extrapolated this preparedness mindset to medication delivery and realized that drones could be used both for a medication drop and to bring blood or other samples back from patients for testing.
Ireland’s Aran Islands came to mind as a location that was at risk of being cut off from services, but that was reachable by drone from Galway. “We quickly realized that this project would be very challenging, as no one in the developed world had done drone deliveries beyond the visual line of sight,” said Dr. Maraka, adding that flight operations had significant regulatory constraints.
The cross-disciplinary team that was pulled together to run the Diabetes Drone Mission, as the project was dubbed, included physicians and experts from pharmacies and pharmaceutical companies. To address drone operation specifically, a drone manufacturer, a flight operations firm, and a telecommunications company were also engaged. Drone pilots had to be licensed for beyond-the-visual-line-of-sight (BVLOS) operation, and Irish and European aviation regulators were consulted.
It took a full year to pull the pieces together for the inaugural flight. “One of the first challenges we faced was that we wanted to perform a civilian drone flight covering more than 40 kilometers,” said Dr. Maraka, whereas most drones flights are in the range of 1-10 km (0.6-6.2 miles). This long-range BVLOS flight required the drone to send live camera feed for the flight duration, which necessitated uninterrupted 4G wireless connectivity with satellite telecommunications as backup.
The Wingcopter 178 drone that was eventually chosen has a wingspan of 178 cm (about 70 inches) and can reach a top speed of 130 km/hr (about 81 mph) in fixed-wing mode.
“We had to comply with medication-dispensing legislation ... and we had to comply with medication transportation cold-chain legislation,” said Dr. Maraka. In other words, the insulin could not be loaded and delivered without the usual prescribing, dispensing, and chain-of-custody procedures being met.
In the end, the successful proof-of-concept flight saw the drone covering 43.3 km (26.9 miles) in a 32-minute flight to deliver insulin and glucagon and return a blood sample for hemoglobin A1c testing.
Dr. Maraka said she and her collaborators have an active collaboration with United Parcel Service and drone suppliers to expand into regular medical supply deliveries.
Dr. Maraka reported no conflicts of interest.
The report will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
SOURCE: Maraka S et al. ENDO 2020, Abstract OR30-04.
This article was updated on 4/17/2020.
After a year of planning, researchers sent a drone flight off the coast of western Ireland to the Aran Islands, delivering insulin and glucagon and retrieving a blood sample from the first patient to receive insulin successfully by autonomous drone delivery.
The nuts and bolts of arranging the drop and retrieval, which occurred in September 2019, were detailed by Spyridoula Maraka, MD, during a virtual news conference held by the Endocrine Society. The study had been slated for presentaion during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.
“There are multiple medical drone delivery opportunities that could be lifesaving during sentinel events such as hurricanes, earthquakes, and, of course, pandemics like the one we are currently experiencing,” said Dr. Maraka.
Drones, or unmanned aerial vehicles, are popular for recreational use and in some commercial applications – notably photography – but they are largely untapped as a medical resource, said Dr. Maraka, a collaborator on the project and an endocrinologist at the University of Arkansas for Medical Sciences, Little Rock.
Most of the exploration of drones for medical purposes has been in countries with emerging economies, such as Ghana and Rwanda in Africa, where the unmanned vehicles have been used by the U.S. medical product delivery company Zipline since 2016 to deliver blood.
The autonomous drone delivery of insulin originated in Galway, where the project’s lead investigator, Derek O’Keefe, MD, PhD, is an endocrinologist and professor of medical device technology at the National University of Ireland.
In 2017, Ireland was pummeled by Ophelia, a category 3 hurricane, and a year later by Storm Emma, a winter blizzard, said Dr. Maraka. Those extreme weather events trapped patients in their homes, made streets impassable for days on end, and interrupted the delivery of essential medical supplies, including insulin.
Until then, Ireland’s medical management plan had been passive and rested on the assumption that any weather-related interruptions would be relatively brief and not result in large-scale disruption of care and supply delivery for geographically isolated patients, said Dr. Maraka. But the two extreme and disruptive weather events in relatively quick succession prompted a reassessment of emergency medical management plans.
“We realized that [the prevailing plans were] not good enough,” said Dr. Maraka. “Medicine has a track record of practicing for emergencies before they actually happen,” to make sure that necessary resources are available and protocols in place in case of an emergency. The researchers extrapolated this preparedness mindset to medication delivery and realized that drones could be used both for a medication drop and to bring blood or other samples back from patients for testing.
Ireland’s Aran Islands came to mind as a location that was at risk of being cut off from services, but that was reachable by drone from Galway. “We quickly realized that this project would be very challenging, as no one in the developed world had done drone deliveries beyond the visual line of sight,” said Dr. Maraka, adding that flight operations had significant regulatory constraints.
The cross-disciplinary team that was pulled together to run the Diabetes Drone Mission, as the project was dubbed, included physicians and experts from pharmacies and pharmaceutical companies. To address drone operation specifically, a drone manufacturer, a flight operations firm, and a telecommunications company were also engaged. Drone pilots had to be licensed for beyond-the-visual-line-of-sight (BVLOS) operation, and Irish and European aviation regulators were consulted.
It took a full year to pull the pieces together for the inaugural flight. “One of the first challenges we faced was that we wanted to perform a civilian drone flight covering more than 40 kilometers,” said Dr. Maraka, whereas most drones flights are in the range of 1-10 km (0.6-6.2 miles). This long-range BVLOS flight required the drone to send live camera feed for the flight duration, which necessitated uninterrupted 4G wireless connectivity with satellite telecommunications as backup.
The Wingcopter 178 drone that was eventually chosen has a wingspan of 178 cm (about 70 inches) and can reach a top speed of 130 km/hr (about 81 mph) in fixed-wing mode.
“We had to comply with medication-dispensing legislation ... and we had to comply with medication transportation cold-chain legislation,” said Dr. Maraka. In other words, the insulin could not be loaded and delivered without the usual prescribing, dispensing, and chain-of-custody procedures being met.
In the end, the successful proof-of-concept flight saw the drone covering 43.3 km (26.9 miles) in a 32-minute flight to deliver insulin and glucagon and return a blood sample for hemoglobin A1c testing.
Dr. Maraka said she and her collaborators have an active collaboration with United Parcel Service and drone suppliers to expand into regular medical supply deliveries.
Dr. Maraka reported no conflicts of interest.
The report will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
SOURCE: Maraka S et al. ENDO 2020, Abstract OR30-04.
This article was updated on 4/17/2020.
FROM ENDO 2020