User login
Psoriasis comorbidities: Biologics may help
SEATTLE – Psoriasis is a complex condition, made more difficult by comorbidities. Psoriatic arthritis is the most common and is frequently discussed. But mental health issues and cardiovascular events also co-occur and can present major complications, according to Jashin Wu, MD, founder and CEO of the Dermatology Research and Education Foundation, who discussed psoriasis comorbidities at the annual Coastal Dermatology Symposium.
Mental health–related issues associated with psoriasis (Psychiatr Danub. 2017 Dec;29[4]:401-6) include sleep disorders (prevalence, 62%), sexual dysfunction (46%), personality disorder (35%), anxiety (30%), adjustment (29%), and depressive disorders (28%); 25% of patients have an accompanying substance abuse disorder. Suicidal ideation and suicidal depression are particularly concerning, and a meta-analysis (J Am Acad Dermatol. 2017 Sep;77[3]:425-40.e2) showed a 44% increased risk of suicidal ideation associated with psoriasis.
Such problems aren’t surprising, since psoriasis is a lifelong disease, and many patients’ symptoms aren’t adequately controlled. “A lot of these patients get topical therapies, which is probably not enough, especially if they have severe disease,” said Dr. Wu in an interview.
Dermatologists can sometimes be nervous about biologics because of concerns over increased risk of infection or cancer. That can lead to conservative, topical treatment. Dr. Wu feels that rare side effects shouldn’t deter from aggressive treatment, when appropriate. “It’s better to treat the patient to make sure they’re clear, which may improve their comorbidities as well. In general, if you’re worried, you can send them to other specialists to do monitoring,” Dr. Wu said in the interview.
Different treatment methods may influence mental health outcomes, according to the PSOLAR study (J Am Acad Dermatol. 2018 Jan;78[1]:70-80). It examined the issue prospectively with over 12,000 psoriasis patients, and found a depression incidence of 3.01 per 100-patient years when treated with biologics, compared with 5.85 for phototherapy and 5.70 for conventional therapy. Put another way, exposure to biologics was associated with a reduced risk of depression, compared with conventional therapies (hazard ratio, 0.76; P = .0367). “It seems to show that biologics have a better improvement of depression symptoms, compared to phototherapy or oral therapy,” said Dr. Wu.
Those results suggest that dermatologists should be on the lookout for mental health issues, though that is a challenge for someone not trained in the field. Dr. Wu takes a simple approach. “I like just asking open-ended questions, like how they’re doing, and if you get a sense that maybe they’re depressed, ask more specific questions about their mood, how they’re feeling, how things are at work, how things are at home.” When things aren’t right, “the key is to try to get them on something that’s going to clear them very quickly. If it’s severe disease, use a biologic that’s going to clear it very quickly,” he added.
Unfortunately, just being clear isn’t a complete guarantee of improved mental health. Dr. Wu had two patients who committed suicide despite significant skin improvement. Patients may have between-visit flare-ups, or regular injections may be a reminder that psoriasis is an ongoing health struggle. Or patients may have other psychological concerns. That underlines the importance of awareness of mental health issues. “You don’t need to refer everyone [to a mental health specialist], but you should have a rolodex where you have someone you can send a patient to if you’re worried,” said Dr. Wu.
As with mental health issues, psoriasis patients are also at elevated risk for a wide range of cardiovascular comorbidities, such as diabetes, dyslipidemia, and high blood pressure. “As a dermatologist, you may not want to screen for these things, but you can send them to their primary care doctor or a cardiologist,” Dr. Wu said in the interview.
Also like mental health issues, there is evidence that treatment with biologics may have an outsized protective effect. One study (J Eur Acad Dermatol Venereol. 2018 Mar 24. doi: 10.1111/jdv.14951) led by Dr. Wu showed that treatment with a tumor necrosis factor (TNF)–alpha inhibitor led to a significant reduction in major adverse cardiac events, compared with topical therapy (propensity score–adjusted HR, 0.80; 95% CI, 0.66-0.98), while phototherapy or oral therapy trended towards an increased risk (adjusted HR, 1.13; 95% CI, 1.00-1.28). Another analysis (J Am Acad Dermatol. 2017 Jan;76[1]:81-90) from Dr. Wu’s group that included about 380,000 psoriasis patients found that treatment with TNF-alpha inhibitors was associated with fewer major cardiovascular events, compared with treatment with methotrexate (adjusted HR, 0.55; P less than .0001). Individual analyses showed associated reductions in stroke or transient ischemic attack (aHR, 0.55; P less than .0001), unstable angina (aHR, 0.58; P = .0024), and MI (aHR, 0.49; P = .0002). TNF-alpha inhibitors also seem to beat out phototherapy with respect to major cardiovascular events (aHR, 0.77; P = .046. J Am Acad Dermatol. 2018 Jul;79[1]:60-6).
More direct evidence of the benefit of biologics comes from the CANTOS trial (N Engl J Med. 2017 Sep 21;377[12]:1119-31), which randomized more than 10,000 patients with cryopyrin-associated periodic syndromes to receive the IL-1 beta-blocker canakinumab or placebo. Canakinumab was associated with significant reductions in nonfatal MI, nonfatal stroke, or cardiovascular death at 150 mg (HR, 0.85; P = .021) and 300 mg (HR, 0.86; P = .031), but not at 50 mg.
The bottom line, said Dr. Wu, is that psoriasis and psoriatic arthritis should be treated early with TNF-alpha inhibitors or IL-17 inhibitors in an effort to improve mental health, cardiovascular, and psoriatic arthritis outcomes.
Dr. Wu has been a consultant or speaker for, or done research on behalf of, AbbVie, Almirall, Amgen, Bristol-Myers Squibb, Celgene, Dermira, Dr. Reddy’s Laboratories, Eli Lilly, Janssen, LEO Pharma, Novartis, Regeneron, Sun Pharmaceutical, UCB, and Valeant Pharmaceuticals North America.
The meeting is jointly presented by the University of Louisville and Global Academy for Medical Education. This publication and Global Academy for Medical Education are owned by the same parent company.
SEATTLE – Psoriasis is a complex condition, made more difficult by comorbidities. Psoriatic arthritis is the most common and is frequently discussed. But mental health issues and cardiovascular events also co-occur and can present major complications, according to Jashin Wu, MD, founder and CEO of the Dermatology Research and Education Foundation, who discussed psoriasis comorbidities at the annual Coastal Dermatology Symposium.
Mental health–related issues associated with psoriasis (Psychiatr Danub. 2017 Dec;29[4]:401-6) include sleep disorders (prevalence, 62%), sexual dysfunction (46%), personality disorder (35%), anxiety (30%), adjustment (29%), and depressive disorders (28%); 25% of patients have an accompanying substance abuse disorder. Suicidal ideation and suicidal depression are particularly concerning, and a meta-analysis (J Am Acad Dermatol. 2017 Sep;77[3]:425-40.e2) showed a 44% increased risk of suicidal ideation associated with psoriasis.
Such problems aren’t surprising, since psoriasis is a lifelong disease, and many patients’ symptoms aren’t adequately controlled. “A lot of these patients get topical therapies, which is probably not enough, especially if they have severe disease,” said Dr. Wu in an interview.
Dermatologists can sometimes be nervous about biologics because of concerns over increased risk of infection or cancer. That can lead to conservative, topical treatment. Dr. Wu feels that rare side effects shouldn’t deter from aggressive treatment, when appropriate. “It’s better to treat the patient to make sure they’re clear, which may improve their comorbidities as well. In general, if you’re worried, you can send them to other specialists to do monitoring,” Dr. Wu said in the interview.
Different treatment methods may influence mental health outcomes, according to the PSOLAR study (J Am Acad Dermatol. 2018 Jan;78[1]:70-80). It examined the issue prospectively with over 12,000 psoriasis patients, and found a depression incidence of 3.01 per 100-patient years when treated with biologics, compared with 5.85 for phototherapy and 5.70 for conventional therapy. Put another way, exposure to biologics was associated with a reduced risk of depression, compared with conventional therapies (hazard ratio, 0.76; P = .0367). “It seems to show that biologics have a better improvement of depression symptoms, compared to phototherapy or oral therapy,” said Dr. Wu.
Those results suggest that dermatologists should be on the lookout for mental health issues, though that is a challenge for someone not trained in the field. Dr. Wu takes a simple approach. “I like just asking open-ended questions, like how they’re doing, and if you get a sense that maybe they’re depressed, ask more specific questions about their mood, how they’re feeling, how things are at work, how things are at home.” When things aren’t right, “the key is to try to get them on something that’s going to clear them very quickly. If it’s severe disease, use a biologic that’s going to clear it very quickly,” he added.
Unfortunately, just being clear isn’t a complete guarantee of improved mental health. Dr. Wu had two patients who committed suicide despite significant skin improvement. Patients may have between-visit flare-ups, or regular injections may be a reminder that psoriasis is an ongoing health struggle. Or patients may have other psychological concerns. That underlines the importance of awareness of mental health issues. “You don’t need to refer everyone [to a mental health specialist], but you should have a rolodex where you have someone you can send a patient to if you’re worried,” said Dr. Wu.
As with mental health issues, psoriasis patients are also at elevated risk for a wide range of cardiovascular comorbidities, such as diabetes, dyslipidemia, and high blood pressure. “As a dermatologist, you may not want to screen for these things, but you can send them to their primary care doctor or a cardiologist,” Dr. Wu said in the interview.
Also like mental health issues, there is evidence that treatment with biologics may have an outsized protective effect. One study (J Eur Acad Dermatol Venereol. 2018 Mar 24. doi: 10.1111/jdv.14951) led by Dr. Wu showed that treatment with a tumor necrosis factor (TNF)–alpha inhibitor led to a significant reduction in major adverse cardiac events, compared with topical therapy (propensity score–adjusted HR, 0.80; 95% CI, 0.66-0.98), while phototherapy or oral therapy trended towards an increased risk (adjusted HR, 1.13; 95% CI, 1.00-1.28). Another analysis (J Am Acad Dermatol. 2017 Jan;76[1]:81-90) from Dr. Wu’s group that included about 380,000 psoriasis patients found that treatment with TNF-alpha inhibitors was associated with fewer major cardiovascular events, compared with treatment with methotrexate (adjusted HR, 0.55; P less than .0001). Individual analyses showed associated reductions in stroke or transient ischemic attack (aHR, 0.55; P less than .0001), unstable angina (aHR, 0.58; P = .0024), and MI (aHR, 0.49; P = .0002). TNF-alpha inhibitors also seem to beat out phototherapy with respect to major cardiovascular events (aHR, 0.77; P = .046. J Am Acad Dermatol. 2018 Jul;79[1]:60-6).
More direct evidence of the benefit of biologics comes from the CANTOS trial (N Engl J Med. 2017 Sep 21;377[12]:1119-31), which randomized more than 10,000 patients with cryopyrin-associated periodic syndromes to receive the IL-1 beta-blocker canakinumab or placebo. Canakinumab was associated with significant reductions in nonfatal MI, nonfatal stroke, or cardiovascular death at 150 mg (HR, 0.85; P = .021) and 300 mg (HR, 0.86; P = .031), but not at 50 mg.
The bottom line, said Dr. Wu, is that psoriasis and psoriatic arthritis should be treated early with TNF-alpha inhibitors or IL-17 inhibitors in an effort to improve mental health, cardiovascular, and psoriatic arthritis outcomes.
Dr. Wu has been a consultant or speaker for, or done research on behalf of, AbbVie, Almirall, Amgen, Bristol-Myers Squibb, Celgene, Dermira, Dr. Reddy’s Laboratories, Eli Lilly, Janssen, LEO Pharma, Novartis, Regeneron, Sun Pharmaceutical, UCB, and Valeant Pharmaceuticals North America.
The meeting is jointly presented by the University of Louisville and Global Academy for Medical Education. This publication and Global Academy for Medical Education are owned by the same parent company.
SEATTLE – Psoriasis is a complex condition, made more difficult by comorbidities. Psoriatic arthritis is the most common and is frequently discussed. But mental health issues and cardiovascular events also co-occur and can present major complications, according to Jashin Wu, MD, founder and CEO of the Dermatology Research and Education Foundation, who discussed psoriasis comorbidities at the annual Coastal Dermatology Symposium.
Mental health–related issues associated with psoriasis (Psychiatr Danub. 2017 Dec;29[4]:401-6) include sleep disorders (prevalence, 62%), sexual dysfunction (46%), personality disorder (35%), anxiety (30%), adjustment (29%), and depressive disorders (28%); 25% of patients have an accompanying substance abuse disorder. Suicidal ideation and suicidal depression are particularly concerning, and a meta-analysis (J Am Acad Dermatol. 2017 Sep;77[3]:425-40.e2) showed a 44% increased risk of suicidal ideation associated with psoriasis.
Such problems aren’t surprising, since psoriasis is a lifelong disease, and many patients’ symptoms aren’t adequately controlled. “A lot of these patients get topical therapies, which is probably not enough, especially if they have severe disease,” said Dr. Wu in an interview.
Dermatologists can sometimes be nervous about biologics because of concerns over increased risk of infection or cancer. That can lead to conservative, topical treatment. Dr. Wu feels that rare side effects shouldn’t deter from aggressive treatment, when appropriate. “It’s better to treat the patient to make sure they’re clear, which may improve their comorbidities as well. In general, if you’re worried, you can send them to other specialists to do monitoring,” Dr. Wu said in the interview.
Different treatment methods may influence mental health outcomes, according to the PSOLAR study (J Am Acad Dermatol. 2018 Jan;78[1]:70-80). It examined the issue prospectively with over 12,000 psoriasis patients, and found a depression incidence of 3.01 per 100-patient years when treated with biologics, compared with 5.85 for phototherapy and 5.70 for conventional therapy. Put another way, exposure to biologics was associated with a reduced risk of depression, compared with conventional therapies (hazard ratio, 0.76; P = .0367). “It seems to show that biologics have a better improvement of depression symptoms, compared to phototherapy or oral therapy,” said Dr. Wu.
Those results suggest that dermatologists should be on the lookout for mental health issues, though that is a challenge for someone not trained in the field. Dr. Wu takes a simple approach. “I like just asking open-ended questions, like how they’re doing, and if you get a sense that maybe they’re depressed, ask more specific questions about their mood, how they’re feeling, how things are at work, how things are at home.” When things aren’t right, “the key is to try to get them on something that’s going to clear them very quickly. If it’s severe disease, use a biologic that’s going to clear it very quickly,” he added.
Unfortunately, just being clear isn’t a complete guarantee of improved mental health. Dr. Wu had two patients who committed suicide despite significant skin improvement. Patients may have between-visit flare-ups, or regular injections may be a reminder that psoriasis is an ongoing health struggle. Or patients may have other psychological concerns. That underlines the importance of awareness of mental health issues. “You don’t need to refer everyone [to a mental health specialist], but you should have a rolodex where you have someone you can send a patient to if you’re worried,” said Dr. Wu.
As with mental health issues, psoriasis patients are also at elevated risk for a wide range of cardiovascular comorbidities, such as diabetes, dyslipidemia, and high blood pressure. “As a dermatologist, you may not want to screen for these things, but you can send them to their primary care doctor or a cardiologist,” Dr. Wu said in the interview.
Also like mental health issues, there is evidence that treatment with biologics may have an outsized protective effect. One study (J Eur Acad Dermatol Venereol. 2018 Mar 24. doi: 10.1111/jdv.14951) led by Dr. Wu showed that treatment with a tumor necrosis factor (TNF)–alpha inhibitor led to a significant reduction in major adverse cardiac events, compared with topical therapy (propensity score–adjusted HR, 0.80; 95% CI, 0.66-0.98), while phototherapy or oral therapy trended towards an increased risk (adjusted HR, 1.13; 95% CI, 1.00-1.28). Another analysis (J Am Acad Dermatol. 2017 Jan;76[1]:81-90) from Dr. Wu’s group that included about 380,000 psoriasis patients found that treatment with TNF-alpha inhibitors was associated with fewer major cardiovascular events, compared with treatment with methotrexate (adjusted HR, 0.55; P less than .0001). Individual analyses showed associated reductions in stroke or transient ischemic attack (aHR, 0.55; P less than .0001), unstable angina (aHR, 0.58; P = .0024), and MI (aHR, 0.49; P = .0002). TNF-alpha inhibitors also seem to beat out phototherapy with respect to major cardiovascular events (aHR, 0.77; P = .046. J Am Acad Dermatol. 2018 Jul;79[1]:60-6).
More direct evidence of the benefit of biologics comes from the CANTOS trial (N Engl J Med. 2017 Sep 21;377[12]:1119-31), which randomized more than 10,000 patients with cryopyrin-associated periodic syndromes to receive the IL-1 beta-blocker canakinumab or placebo. Canakinumab was associated with significant reductions in nonfatal MI, nonfatal stroke, or cardiovascular death at 150 mg (HR, 0.85; P = .021) and 300 mg (HR, 0.86; P = .031), but not at 50 mg.
The bottom line, said Dr. Wu, is that psoriasis and psoriatic arthritis should be treated early with TNF-alpha inhibitors or IL-17 inhibitors in an effort to improve mental health, cardiovascular, and psoriatic arthritis outcomes.
Dr. Wu has been a consultant or speaker for, or done research on behalf of, AbbVie, Almirall, Amgen, Bristol-Myers Squibb, Celgene, Dermira, Dr. Reddy’s Laboratories, Eli Lilly, Janssen, LEO Pharma, Novartis, Regeneron, Sun Pharmaceutical, UCB, and Valeant Pharmaceuticals North America.
The meeting is jointly presented by the University of Louisville and Global Academy for Medical Education. This publication and Global Academy for Medical Education are owned by the same parent company.
EXPERT ANALYSIS FROM COASTAL DERM
Oral beta-lactams provide noninferior postdischarge pyelonephritis treatment
WASHINGTON – Patients hospitalized for pyelonephritis and discharged after receiving intravenous antibiotic treatment who then received step-down treatment with an oral beta-lactam had 30-day outcomes that were noninferior to patients who received an oral fluoroquinolone or trimethoprim-sulfamethoxazole as their discharge regimen, in a retrospective study of 211 patients managed at either of two U.S. hospitals.
This was the largest comparison reported on oral beta-lactam drugs for postdischarge treatment of pyelonephritis relative to the standard oral agents, fluoroquinolones and trimethoprim-sulfamethoxazole (Bactrim), Athena Hobbs, PharmD, said at an annual scientific meeting on infectious diseases. The superiority of an oral fluoroquinolone or trimethoprim-sulfamethoxazole and inferiority of oral beta-lactam drugs were cited in 2010 guidelines for managing pyelonephritis from the Infectious Diseases Society of America (Clin Infect Dis. 2011 March 1;52 [5]: e103-20).
Although limited as a nonrandomized, retrospective comparison, the finding of at least similar efficacy by beta-lactam agents “opens new treatment options” that avoid issues with drug resistance and adverse effects from treatment with fluoroquinolones or trimethoprim-sulfamethoxazole, Dr. Hobbs said in a video interview. Beta-lactams have already been embraced for this indication by some hospitalists, demonstrated by their use of beta-lactam antibiotics for 122 (58%) of the 211 patients included in the study. Among the 89 patients discharged on a non–beta-lactam, 69 (78%) had fluoroquinolone treatment and the remaining 20 patients went home taking trimethoprim-sulfamethoxazole. The new finding “confirms that we are not doing harm to patients,” with this existing practice of mostly prescribing an oral beta-lactam drug, noted Dr. Hobbs, an infectious diseases pharmacy specialist at Baptist Memorial Hospital in Memphis.
The study included patients aged 18-89 years hospitalized during 2014-2017 for a primary diagnosis of pyelonephritis at Baptist or at a second Hospital in Austin, Tex. The study excluded patients in intensive care, with a urologic abnormality, pregnant women, and patients treated with an intravenous antibiotic other than a beta-lactam for more than 24 hours. The most commonly used intravenous drugs were cefazolin and ceftriaxone. The enrolled patients averaged just over 40 years old, and more than 90% were women.
The study’s primary outcome was the 30-day rate of either hospital readmission or an ED visit for pyelonephritis or a urinary tract infection. This occurred in 4.9% of the patients discharged on an oral course of a beta-lactam drug, and in 5.6% of those discharged on either a fluoroquinolone or trimethoprim-sulfamethoxazole, a difference that was not statistically significant and that met the prespecified criteria for noninferiority, Dr. Hobbs reported. The most commonly prescribed oral beta-lactam was cefuroxime in about half the patients, followed by cephalexin or cefadroxil in about a quarter of patients, and amoxicillin with clavulanate in 19%. The two arms of the study also showed no significant difference in infection recurrences during 90-day follow-up.
The study received no commercial funding. Dr. Hobbs had no relevant disclosures.
WASHINGTON – Patients hospitalized for pyelonephritis and discharged after receiving intravenous antibiotic treatment who then received step-down treatment with an oral beta-lactam had 30-day outcomes that were noninferior to patients who received an oral fluoroquinolone or trimethoprim-sulfamethoxazole as their discharge regimen, in a retrospective study of 211 patients managed at either of two U.S. hospitals.
This was the largest comparison reported on oral beta-lactam drugs for postdischarge treatment of pyelonephritis relative to the standard oral agents, fluoroquinolones and trimethoprim-sulfamethoxazole (Bactrim), Athena Hobbs, PharmD, said at an annual scientific meeting on infectious diseases. The superiority of an oral fluoroquinolone or trimethoprim-sulfamethoxazole and inferiority of oral beta-lactam drugs were cited in 2010 guidelines for managing pyelonephritis from the Infectious Diseases Society of America (Clin Infect Dis. 2011 March 1;52 [5]: e103-20).
Although limited as a nonrandomized, retrospective comparison, the finding of at least similar efficacy by beta-lactam agents “opens new treatment options” that avoid issues with drug resistance and adverse effects from treatment with fluoroquinolones or trimethoprim-sulfamethoxazole, Dr. Hobbs said in a video interview. Beta-lactams have already been embraced for this indication by some hospitalists, demonstrated by their use of beta-lactam antibiotics for 122 (58%) of the 211 patients included in the study. Among the 89 patients discharged on a non–beta-lactam, 69 (78%) had fluoroquinolone treatment and the remaining 20 patients went home taking trimethoprim-sulfamethoxazole. The new finding “confirms that we are not doing harm to patients,” with this existing practice of mostly prescribing an oral beta-lactam drug, noted Dr. Hobbs, an infectious diseases pharmacy specialist at Baptist Memorial Hospital in Memphis.
The study included patients aged 18-89 years hospitalized during 2014-2017 for a primary diagnosis of pyelonephritis at Baptist or at a second Hospital in Austin, Tex. The study excluded patients in intensive care, with a urologic abnormality, pregnant women, and patients treated with an intravenous antibiotic other than a beta-lactam for more than 24 hours. The most commonly used intravenous drugs were cefazolin and ceftriaxone. The enrolled patients averaged just over 40 years old, and more than 90% were women.
The study’s primary outcome was the 30-day rate of either hospital readmission or an ED visit for pyelonephritis or a urinary tract infection. This occurred in 4.9% of the patients discharged on an oral course of a beta-lactam drug, and in 5.6% of those discharged on either a fluoroquinolone or trimethoprim-sulfamethoxazole, a difference that was not statistically significant and that met the prespecified criteria for noninferiority, Dr. Hobbs reported. The most commonly prescribed oral beta-lactam was cefuroxime in about half the patients, followed by cephalexin or cefadroxil in about a quarter of patients, and amoxicillin with clavulanate in 19%. The two arms of the study also showed no significant difference in infection recurrences during 90-day follow-up.
The study received no commercial funding. Dr. Hobbs had no relevant disclosures.
WASHINGTON – Patients hospitalized for pyelonephritis and discharged after receiving intravenous antibiotic treatment who then received step-down treatment with an oral beta-lactam had 30-day outcomes that were noninferior to patients who received an oral fluoroquinolone or trimethoprim-sulfamethoxazole as their discharge regimen, in a retrospective study of 211 patients managed at either of two U.S. hospitals.
This was the largest comparison reported on oral beta-lactam drugs for postdischarge treatment of pyelonephritis relative to the standard oral agents, fluoroquinolones and trimethoprim-sulfamethoxazole (Bactrim), Athena Hobbs, PharmD, said at an annual scientific meeting on infectious diseases. The superiority of an oral fluoroquinolone or trimethoprim-sulfamethoxazole and inferiority of oral beta-lactam drugs were cited in 2010 guidelines for managing pyelonephritis from the Infectious Diseases Society of America (Clin Infect Dis. 2011 March 1;52 [5]: e103-20).
Although limited as a nonrandomized, retrospective comparison, the finding of at least similar efficacy by beta-lactam agents “opens new treatment options” that avoid issues with drug resistance and adverse effects from treatment with fluoroquinolones or trimethoprim-sulfamethoxazole, Dr. Hobbs said in a video interview. Beta-lactams have already been embraced for this indication by some hospitalists, demonstrated by their use of beta-lactam antibiotics for 122 (58%) of the 211 patients included in the study. Among the 89 patients discharged on a non–beta-lactam, 69 (78%) had fluoroquinolone treatment and the remaining 20 patients went home taking trimethoprim-sulfamethoxazole. The new finding “confirms that we are not doing harm to patients,” with this existing practice of mostly prescribing an oral beta-lactam drug, noted Dr. Hobbs, an infectious diseases pharmacy specialist at Baptist Memorial Hospital in Memphis.
The study included patients aged 18-89 years hospitalized during 2014-2017 for a primary diagnosis of pyelonephritis at Baptist or at a second Hospital in Austin, Tex. The study excluded patients in intensive care, with a urologic abnormality, pregnant women, and patients treated with an intravenous antibiotic other than a beta-lactam for more than 24 hours. The most commonly used intravenous drugs were cefazolin and ceftriaxone. The enrolled patients averaged just over 40 years old, and more than 90% were women.
The study’s primary outcome was the 30-day rate of either hospital readmission or an ED visit for pyelonephritis or a urinary tract infection. This occurred in 4.9% of the patients discharged on an oral course of a beta-lactam drug, and in 5.6% of those discharged on either a fluoroquinolone or trimethoprim-sulfamethoxazole, a difference that was not statistically significant and that met the prespecified criteria for noninferiority, Dr. Hobbs reported. The most commonly prescribed oral beta-lactam was cefuroxime in about half the patients, followed by cephalexin or cefadroxil in about a quarter of patients, and amoxicillin with clavulanate in 19%. The two arms of the study also showed no significant difference in infection recurrences during 90-day follow-up.
The study received no commercial funding. Dr. Hobbs had no relevant disclosures.
REPORTING FROM IDWEEK 2019
Lithium drug interactions not quite as bad as imagined
SAN DIEGO – You don’t have to stop prescribing lithium when patients go on ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure treatment.
Some might opt to do that, but there’s no need to worry. In fact, the reason both classes are known to protect the kidneys is that they were tested with lithium; it was used to measure the drug’s effects on renal clearance, according to Stephen R. Saklad, PharmD, director of psychiatric pharmacy and clinical professor at the University of Texas at Austin.
There is interaction, but “lithium is not toxic in the presence of an ACE or an RB. You just have to adjust the dose,” he said at the annual Psych Congress.
Dr. Saklad shared lithium drug interaction pearls during a video interview at the meeting, including also using lithium with diuretics and NSAIDs. “The worst offender is probably my favorite of the NSAIDs, which is ibuprofen,” he said.
Most of the time with lithium, all that’s needed is a dose adjustment up or down of either it or the coadministered medication.
The overall guiding principle, he said, is that “lithium follows sodium. Anything that alters sodium in the body is going to alter sodium.”
SAN DIEGO – You don’t have to stop prescribing lithium when patients go on ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure treatment.
Some might opt to do that, but there’s no need to worry. In fact, the reason both classes are known to protect the kidneys is that they were tested with lithium; it was used to measure the drug’s effects on renal clearance, according to Stephen R. Saklad, PharmD, director of psychiatric pharmacy and clinical professor at the University of Texas at Austin.
There is interaction, but “lithium is not toxic in the presence of an ACE or an RB. You just have to adjust the dose,” he said at the annual Psych Congress.
Dr. Saklad shared lithium drug interaction pearls during a video interview at the meeting, including also using lithium with diuretics and NSAIDs. “The worst offender is probably my favorite of the NSAIDs, which is ibuprofen,” he said.
Most of the time with lithium, all that’s needed is a dose adjustment up or down of either it or the coadministered medication.
The overall guiding principle, he said, is that “lithium follows sodium. Anything that alters sodium in the body is going to alter sodium.”
SAN DIEGO – You don’t have to stop prescribing lithium when patients go on ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure treatment.
Some might opt to do that, but there’s no need to worry. In fact, the reason both classes are known to protect the kidneys is that they were tested with lithium; it was used to measure the drug’s effects on renal clearance, according to Stephen R. Saklad, PharmD, director of psychiatric pharmacy and clinical professor at the University of Texas at Austin.
There is interaction, but “lithium is not toxic in the presence of an ACE or an RB. You just have to adjust the dose,” he said at the annual Psych Congress.
Dr. Saklad shared lithium drug interaction pearls during a video interview at the meeting, including also using lithium with diuretics and NSAIDs. “The worst offender is probably my favorite of the NSAIDs, which is ibuprofen,” he said.
Most of the time with lithium, all that’s needed is a dose adjustment up or down of either it or the coadministered medication.
The overall guiding principle, he said, is that “lithium follows sodium. Anything that alters sodium in the body is going to alter sodium.”
REPORTING FROM PSYCH CONGRESS 2019
How to use lofexidine for quick opioid withdrawal
SAN DIEGO – Lofexidine (Lucemyra), the new kid on the block in the United States for opioid withdrawal, can help patients get through the process in a few days, instead of a week or more, according to Thomas Kosten, MD, a psychiatry professor and director of the division of addictions at Baylor College of Medicine, Houston.
Lofexidine relieves symptom withdrawal and has significant advantages over clonidine, a similar drug, including easier dosing and no orthostatic hypertension.
In a video interview at the annual Psych Congress, Dr. Kosten went into the nuts and bolts of how to use lofexidine with buprenorphine and naltrexone – plus benzodiazepines when needed – to help people safely go through withdrawal and in just a few days.
Once chronic pain patients are off opioids, the next question is what to do for their pain. In a presentation before the interview, Dr. Kosten said he favors tricyclic antidepressants, especially desipramine because it has the fewest side effects. The effect size with tricyclic antidepressants is larger than with gabapentin and other options. They take a few weeks to kick in, however, so he’s thinking about a unique approach: using ketamine – either infusions or the new nasal spray esketamine (Spravato) – to tide people over in the meantime. It’s becoming well known that ketamine works amazingly fast for depression and suicidality, and there is emerging support that it might do the same for chronic pain. Dr. Kosten is a consultant for US Worldmeds, maker of lofexidine.
SAN DIEGO – Lofexidine (Lucemyra), the new kid on the block in the United States for opioid withdrawal, can help patients get through the process in a few days, instead of a week or more, according to Thomas Kosten, MD, a psychiatry professor and director of the division of addictions at Baylor College of Medicine, Houston.
Lofexidine relieves symptom withdrawal and has significant advantages over clonidine, a similar drug, including easier dosing and no orthostatic hypertension.
In a video interview at the annual Psych Congress, Dr. Kosten went into the nuts and bolts of how to use lofexidine with buprenorphine and naltrexone – plus benzodiazepines when needed – to help people safely go through withdrawal and in just a few days.
Once chronic pain patients are off opioids, the next question is what to do for their pain. In a presentation before the interview, Dr. Kosten said he favors tricyclic antidepressants, especially desipramine because it has the fewest side effects. The effect size with tricyclic antidepressants is larger than with gabapentin and other options. They take a few weeks to kick in, however, so he’s thinking about a unique approach: using ketamine – either infusions or the new nasal spray esketamine (Spravato) – to tide people over in the meantime. It’s becoming well known that ketamine works amazingly fast for depression and suicidality, and there is emerging support that it might do the same for chronic pain. Dr. Kosten is a consultant for US Worldmeds, maker of lofexidine.
SAN DIEGO – Lofexidine (Lucemyra), the new kid on the block in the United States for opioid withdrawal, can help patients get through the process in a few days, instead of a week or more, according to Thomas Kosten, MD, a psychiatry professor and director of the division of addictions at Baylor College of Medicine, Houston.
Lofexidine relieves symptom withdrawal and has significant advantages over clonidine, a similar drug, including easier dosing and no orthostatic hypertension.
In a video interview at the annual Psych Congress, Dr. Kosten went into the nuts and bolts of how to use lofexidine with buprenorphine and naltrexone – plus benzodiazepines when needed – to help people safely go through withdrawal and in just a few days.
Once chronic pain patients are off opioids, the next question is what to do for their pain. In a presentation before the interview, Dr. Kosten said he favors tricyclic antidepressants, especially desipramine because it has the fewest side effects. The effect size with tricyclic antidepressants is larger than with gabapentin and other options. They take a few weeks to kick in, however, so he’s thinking about a unique approach: using ketamine – either infusions or the new nasal spray esketamine (Spravato) – to tide people over in the meantime. It’s becoming well known that ketamine works amazingly fast for depression and suicidality, and there is emerging support that it might do the same for chronic pain. Dr. Kosten is a consultant for US Worldmeds, maker of lofexidine.
REPORTING FROM PSYCH CONGRESS 2019
FDA approves benralizumab autoinjector for eosinophilic asthma
according to a press release from AstraZeneca. Benralizumab is already approved as add-on maintenance for this form of asthma, but not for other eosinophilic conditions or for acute bronchospasm or status asthmaticus.
The autoinjector “pen” was tested for usability and pharmacokinetic exposure in two studies, the phase 3 GRECO trial and the phase 1 AMES trial, respectively. The multicenter, open-label GRECO trial was designed to assess patient- or caregiver-reported functionality, and it found that 97% of at-home administrations were successful at week 12 and week 16. The multicenter, randomized, open-label, parallel-group AMES trial compared pharmacokinetic exposure with the subcutaneous administration using either prefilled syringe or prefilled autoinjector; it found that the eosinophils were rapidly depleted in patients with use of either device.
The safety profiles in both trials were comparable to those seen in previous trials. Hypersensitivity reactions have been sometimes observed in the hours following administration of benralizumab; discontinuation is advised in case of any hypersensitivity reaction. The therapy should not be used to treat acute asthma symptoms, such as exacerbations, or bronchospasm, and any reduction in corticosteroid therapy should be gradual and performed under careful supervision of a health care professional. Although benralizumab’s effects on helminth infections are currently unknown, care should be taken with preexisting or incident infections.
Full prescribing information can be found on the AstraZeneca website.
according to a press release from AstraZeneca. Benralizumab is already approved as add-on maintenance for this form of asthma, but not for other eosinophilic conditions or for acute bronchospasm or status asthmaticus.
The autoinjector “pen” was tested for usability and pharmacokinetic exposure in two studies, the phase 3 GRECO trial and the phase 1 AMES trial, respectively. The multicenter, open-label GRECO trial was designed to assess patient- or caregiver-reported functionality, and it found that 97% of at-home administrations were successful at week 12 and week 16. The multicenter, randomized, open-label, parallel-group AMES trial compared pharmacokinetic exposure with the subcutaneous administration using either prefilled syringe or prefilled autoinjector; it found that the eosinophils were rapidly depleted in patients with use of either device.
The safety profiles in both trials were comparable to those seen in previous trials. Hypersensitivity reactions have been sometimes observed in the hours following administration of benralizumab; discontinuation is advised in case of any hypersensitivity reaction. The therapy should not be used to treat acute asthma symptoms, such as exacerbations, or bronchospasm, and any reduction in corticosteroid therapy should be gradual and performed under careful supervision of a health care professional. Although benralizumab’s effects on helminth infections are currently unknown, care should be taken with preexisting or incident infections.
Full prescribing information can be found on the AstraZeneca website.
according to a press release from AstraZeneca. Benralizumab is already approved as add-on maintenance for this form of asthma, but not for other eosinophilic conditions or for acute bronchospasm or status asthmaticus.
The autoinjector “pen” was tested for usability and pharmacokinetic exposure in two studies, the phase 3 GRECO trial and the phase 1 AMES trial, respectively. The multicenter, open-label GRECO trial was designed to assess patient- or caregiver-reported functionality, and it found that 97% of at-home administrations were successful at week 12 and week 16. The multicenter, randomized, open-label, parallel-group AMES trial compared pharmacokinetic exposure with the subcutaneous administration using either prefilled syringe or prefilled autoinjector; it found that the eosinophils were rapidly depleted in patients with use of either device.
The safety profiles in both trials were comparable to those seen in previous trials. Hypersensitivity reactions have been sometimes observed in the hours following administration of benralizumab; discontinuation is advised in case of any hypersensitivity reaction. The therapy should not be used to treat acute asthma symptoms, such as exacerbations, or bronchospasm, and any reduction in corticosteroid therapy should be gradual and performed under careful supervision of a health care professional. Although benralizumab’s effects on helminth infections are currently unknown, care should be taken with preexisting or incident infections.
Full prescribing information can be found on the AstraZeneca website.
Hospitalist comanagement reduced odds of MI, shortened vascular surgery stays
CHICAGO – A care model that uses hospitalists to comanage vascular surgery patients cut myocardial infarction rates by more than half and reduced hospital stays by about 12%, according to results of a study of the hospitalist comanagement model from Loyola University Chicago, Maywood, Ill., presented at the annual meeting of the Midwestern Vascular Surgery Society.
“Hospitalist comanagement was associated with decreased length of stay without affecting readmission for patients undergoing amputation, embolectomy, and infected graft,” said Kaavya Adam, a third-year medical student at Loyola University Chicago. “In the overall population, there was a reduction in cases of MI, 30-day readmissions, and overall length of stay.”
In 2014, Loyola implemented a program that used 11 hospitalists to rotate through the vascular surgery service. The hospitalists call on any patient who stays more than 24 hours on the non-ICU floors. Adam said hospitalist duties include evaluating patient comorbidities, adjusting medication, talking with family about medical management, seeing patients on the day of surgery, ordering preoperative labs, and meeting with the anesthesiology and vascular surgery teams.
The study compared outcomes in 866 patients admitted during 2007-2013, before the comanagement model was put into place, and 572 admitted during 2014-2017.
Rates of diabetes, hypertension, chronic kidney disease, coronary artery disease, hyperlipidemia, and malnutrition were similar between the groups. However, the pre-comanagement group had significantly higher rates of ischemic pain (27.8% vs. 10.7%), gangrene (21.3% vs. 13.6%) and ulceration (30.6% vs. 21.9%), while the comanaged group had significantly higher rates of claudication (34.3% vs. 13.2%). The statistical analysis accounted for these variations, Adam said.
“We did find significant results for the reduction in the odds of MI at 30 days; there was a 61% reduction,” he said.
The reduction in hospital stay was even more pronounced for patients with complex cases, Adam said. In amputation, the length of stay was reduced by 3.77 days (P = .01); in embolectomy, by 7.35 (P = .004); and in infected graft, by 8.35 (P = .007).
Continuing research will evaluate the cost effectiveness of the hospitalist model and define a comanagement model that is most beneficial, Mr. Adam said. He had no relevant financial disclosures.
SOURCE: Adam K et al. Midwestern Vascular 2019, Abstract 14.
CHICAGO – A care model that uses hospitalists to comanage vascular surgery patients cut myocardial infarction rates by more than half and reduced hospital stays by about 12%, according to results of a study of the hospitalist comanagement model from Loyola University Chicago, Maywood, Ill., presented at the annual meeting of the Midwestern Vascular Surgery Society.
“Hospitalist comanagement was associated with decreased length of stay without affecting readmission for patients undergoing amputation, embolectomy, and infected graft,” said Kaavya Adam, a third-year medical student at Loyola University Chicago. “In the overall population, there was a reduction in cases of MI, 30-day readmissions, and overall length of stay.”
In 2014, Loyola implemented a program that used 11 hospitalists to rotate through the vascular surgery service. The hospitalists call on any patient who stays more than 24 hours on the non-ICU floors. Adam said hospitalist duties include evaluating patient comorbidities, adjusting medication, talking with family about medical management, seeing patients on the day of surgery, ordering preoperative labs, and meeting with the anesthesiology and vascular surgery teams.
The study compared outcomes in 866 patients admitted during 2007-2013, before the comanagement model was put into place, and 572 admitted during 2014-2017.
Rates of diabetes, hypertension, chronic kidney disease, coronary artery disease, hyperlipidemia, and malnutrition were similar between the groups. However, the pre-comanagement group had significantly higher rates of ischemic pain (27.8% vs. 10.7%), gangrene (21.3% vs. 13.6%) and ulceration (30.6% vs. 21.9%), while the comanaged group had significantly higher rates of claudication (34.3% vs. 13.2%). The statistical analysis accounted for these variations, Adam said.
“We did find significant results for the reduction in the odds of MI at 30 days; there was a 61% reduction,” he said.
The reduction in hospital stay was even more pronounced for patients with complex cases, Adam said. In amputation, the length of stay was reduced by 3.77 days (P = .01); in embolectomy, by 7.35 (P = .004); and in infected graft, by 8.35 (P = .007).
Continuing research will evaluate the cost effectiveness of the hospitalist model and define a comanagement model that is most beneficial, Mr. Adam said. He had no relevant financial disclosures.
SOURCE: Adam K et al. Midwestern Vascular 2019, Abstract 14.
CHICAGO – A care model that uses hospitalists to comanage vascular surgery patients cut myocardial infarction rates by more than half and reduced hospital stays by about 12%, according to results of a study of the hospitalist comanagement model from Loyola University Chicago, Maywood, Ill., presented at the annual meeting of the Midwestern Vascular Surgery Society.
“Hospitalist comanagement was associated with decreased length of stay without affecting readmission for patients undergoing amputation, embolectomy, and infected graft,” said Kaavya Adam, a third-year medical student at Loyola University Chicago. “In the overall population, there was a reduction in cases of MI, 30-day readmissions, and overall length of stay.”
In 2014, Loyola implemented a program that used 11 hospitalists to rotate through the vascular surgery service. The hospitalists call on any patient who stays more than 24 hours on the non-ICU floors. Adam said hospitalist duties include evaluating patient comorbidities, adjusting medication, talking with family about medical management, seeing patients on the day of surgery, ordering preoperative labs, and meeting with the anesthesiology and vascular surgery teams.
The study compared outcomes in 866 patients admitted during 2007-2013, before the comanagement model was put into place, and 572 admitted during 2014-2017.
Rates of diabetes, hypertension, chronic kidney disease, coronary artery disease, hyperlipidemia, and malnutrition were similar between the groups. However, the pre-comanagement group had significantly higher rates of ischemic pain (27.8% vs. 10.7%), gangrene (21.3% vs. 13.6%) and ulceration (30.6% vs. 21.9%), while the comanaged group had significantly higher rates of claudication (34.3% vs. 13.2%). The statistical analysis accounted for these variations, Adam said.
“We did find significant results for the reduction in the odds of MI at 30 days; there was a 61% reduction,” he said.
The reduction in hospital stay was even more pronounced for patients with complex cases, Adam said. In amputation, the length of stay was reduced by 3.77 days (P = .01); in embolectomy, by 7.35 (P = .004); and in infected graft, by 8.35 (P = .007).
Continuing research will evaluate the cost effectiveness of the hospitalist model and define a comanagement model that is most beneficial, Mr. Adam said. He had no relevant financial disclosures.
SOURCE: Adam K et al. Midwestern Vascular 2019, Abstract 14.
REPORTING FROM MIDWESTERN VASCULAR 2019
Key clinical point: Hospitalist comanagement of vascular surgery patients reduced hospital stays.
Major finding: Hospitalist comanagement significantly reduced the odds of MI at 30 days; a 61% reduction.
Study details: Database query of 1,438 vascular surgery admissions during 2007-2017.
Disclosures: Mr. Adam had no relevant financial disclosures.
Source: Adam K et al. Midwestern Vascular 2019, Abstract 14.
Guide to the guidelines: Biologics for psoriasis
SEATTLE – The availability of biologics for treating psoriasis and psoriatic arthritis has exploded in recent years, with 11 biologics now approved by the Food and Drug Administration. Targets include four separate mechanisms: inhibition of tumor necrosis factor (TNF), interleukin (IL) 23, IL-12/23, and IL-17. The surfeit of treatment options can be a little overwhelming.
“It can be confusing. We have a lot of choices, but the good news is that most of our choices are excellent, and they treat both psoriasis and psoriatic arthritis. That’s very important because, when we think of our psoriasis patients, we need to think not only about their skin but also their joint involvement. Assessment of psoriatic arthritis will drive some of our therapeutic [decisions],” April Armstrong, MD, professor of dermatology at the University of Southern California, Los Angeles, said at the annual Coastal Dermatology Symposium.
In April, the American Academy of Dermatology came to the rescue with comprehensive guidelines. Aside from general advice, the guidelines “provide tips for monitoring as well as dose escalation, which will be very helpful in daily practice,” Dr. Armstrong said in an interview.
The best studied of the biologics with respect to psoriasis and psoriatic arthritis are the IL-17 inhibitors and TNF inhibitors, she said. While TNF inhibitors have traditionally been the treatment of choice for both conditions, “I think these days, people realize that IL-17 inhibitors can be just as good.”
A head-to-head study of the IL-17 inhibitor ixekizumab and the TNF inhibitor adalimumab, presented at the EULAR Congress, looked at a combined outcome of skin and joints and found ixekizumab to be superior, though the study design’s inclusion of a skin outcome may have favored ixekizumab (Ann Rheum Dis. 2019 Jun. doi: 10.1136/annrheumdis-2019-eular.8709).
A few other head-to-head studies have been performed, but properly ranking all 11 biologics would require dozens of clinical trials. At the American Academy of Dermatology meeting last March, Dr. Armstrong presented the results of a network meta-analysis of anti-TNF agents, anti-interleukin agents, anti–phosphodiesterase 4 agents, and fumaric acid esters (J Am Acad Dermatol. doi: 10.1016/j.jaad.2019.06.488). That study, funded by AbbVie, compared the individual agents to a collective placebo group and concluded that anti-interleukin agents generate the highest level of PASI 90/100 response rate. Risankizumab, ixekizumab, brodalumab, and guselkumab, all IL inhibitors, achieved the best marks over the primary response period.
The AAD guidelines include recommendations for tests to be done upon initiation of a biologic, including a tuberculosis test, complete blood count, comprehensive metabolic panel, and tests for hepatitis B and C. TB testing should be performed annually during treatment.
The guidelines also include recommendations for dose escalation, which can provide leverage for getting coverage approved. “One can use those guidelines to show payers how dose escalation can be done, so that [physicians] can potentially get more access to medications for their patients,” Dr. Armstrong said at the meeting jointly presented by the University of Louisville and Global Academy for Medical Education.
The guideline also ranks the existing evidence supporting individual biologics for the treatment of psoriasis subtypes. For example, for the treatment of moderate to severe scalp psoriasis, etanercept and guselkumab have consistent and good-quality patient-oriented evidence supporting them; infliximab, adalimumab, secukinumab, and ixekizumab are recommended based on inconsistent or limited quality patient-oriented evidence; and ustekinumab is supported only by consensus opinion, case studies, or disease-oriented evidence. The guidelines provide similar categorization of biologics for the treatment of moderate to severe plaque type palmoplantar psoriasis, moderate to severe psoriasis affecting the nails, adults with pustular or erythrodermic psoriasis, and adults with psoriatic arthritis.
Dr. Armstrong is a research investigator and/or advisor to AbbVie, Janssen, Lily, LEO Pharma, Novartis, UCB, Ortho Dermatologics, Dermera, Regeneron, BMS, Dermavant, and KHK. This publication and Global Academy for Medical Education are owned by the same parent company.
SEATTLE – The availability of biologics for treating psoriasis and psoriatic arthritis has exploded in recent years, with 11 biologics now approved by the Food and Drug Administration. Targets include four separate mechanisms: inhibition of tumor necrosis factor (TNF), interleukin (IL) 23, IL-12/23, and IL-17. The surfeit of treatment options can be a little overwhelming.
“It can be confusing. We have a lot of choices, but the good news is that most of our choices are excellent, and they treat both psoriasis and psoriatic arthritis. That’s very important because, when we think of our psoriasis patients, we need to think not only about their skin but also their joint involvement. Assessment of psoriatic arthritis will drive some of our therapeutic [decisions],” April Armstrong, MD, professor of dermatology at the University of Southern California, Los Angeles, said at the annual Coastal Dermatology Symposium.
In April, the American Academy of Dermatology came to the rescue with comprehensive guidelines. Aside from general advice, the guidelines “provide tips for monitoring as well as dose escalation, which will be very helpful in daily practice,” Dr. Armstrong said in an interview.
The best studied of the biologics with respect to psoriasis and psoriatic arthritis are the IL-17 inhibitors and TNF inhibitors, she said. While TNF inhibitors have traditionally been the treatment of choice for both conditions, “I think these days, people realize that IL-17 inhibitors can be just as good.”
A head-to-head study of the IL-17 inhibitor ixekizumab and the TNF inhibitor adalimumab, presented at the EULAR Congress, looked at a combined outcome of skin and joints and found ixekizumab to be superior, though the study design’s inclusion of a skin outcome may have favored ixekizumab (Ann Rheum Dis. 2019 Jun. doi: 10.1136/annrheumdis-2019-eular.8709).
A few other head-to-head studies have been performed, but properly ranking all 11 biologics would require dozens of clinical trials. At the American Academy of Dermatology meeting last March, Dr. Armstrong presented the results of a network meta-analysis of anti-TNF agents, anti-interleukin agents, anti–phosphodiesterase 4 agents, and fumaric acid esters (J Am Acad Dermatol. doi: 10.1016/j.jaad.2019.06.488). That study, funded by AbbVie, compared the individual agents to a collective placebo group and concluded that anti-interleukin agents generate the highest level of PASI 90/100 response rate. Risankizumab, ixekizumab, brodalumab, and guselkumab, all IL inhibitors, achieved the best marks over the primary response period.
The AAD guidelines include recommendations for tests to be done upon initiation of a biologic, including a tuberculosis test, complete blood count, comprehensive metabolic panel, and tests for hepatitis B and C. TB testing should be performed annually during treatment.
The guidelines also include recommendations for dose escalation, which can provide leverage for getting coverage approved. “One can use those guidelines to show payers how dose escalation can be done, so that [physicians] can potentially get more access to medications for their patients,” Dr. Armstrong said at the meeting jointly presented by the University of Louisville and Global Academy for Medical Education.
The guideline also ranks the existing evidence supporting individual biologics for the treatment of psoriasis subtypes. For example, for the treatment of moderate to severe scalp psoriasis, etanercept and guselkumab have consistent and good-quality patient-oriented evidence supporting them; infliximab, adalimumab, secukinumab, and ixekizumab are recommended based on inconsistent or limited quality patient-oriented evidence; and ustekinumab is supported only by consensus opinion, case studies, or disease-oriented evidence. The guidelines provide similar categorization of biologics for the treatment of moderate to severe plaque type palmoplantar psoriasis, moderate to severe psoriasis affecting the nails, adults with pustular or erythrodermic psoriasis, and adults with psoriatic arthritis.
Dr. Armstrong is a research investigator and/or advisor to AbbVie, Janssen, Lily, LEO Pharma, Novartis, UCB, Ortho Dermatologics, Dermera, Regeneron, BMS, Dermavant, and KHK. This publication and Global Academy for Medical Education are owned by the same parent company.
SEATTLE – The availability of biologics for treating psoriasis and psoriatic arthritis has exploded in recent years, with 11 biologics now approved by the Food and Drug Administration. Targets include four separate mechanisms: inhibition of tumor necrosis factor (TNF), interleukin (IL) 23, IL-12/23, and IL-17. The surfeit of treatment options can be a little overwhelming.
“It can be confusing. We have a lot of choices, but the good news is that most of our choices are excellent, and they treat both psoriasis and psoriatic arthritis. That’s very important because, when we think of our psoriasis patients, we need to think not only about their skin but also their joint involvement. Assessment of psoriatic arthritis will drive some of our therapeutic [decisions],” April Armstrong, MD, professor of dermatology at the University of Southern California, Los Angeles, said at the annual Coastal Dermatology Symposium.
In April, the American Academy of Dermatology came to the rescue with comprehensive guidelines. Aside from general advice, the guidelines “provide tips for monitoring as well as dose escalation, which will be very helpful in daily practice,” Dr. Armstrong said in an interview.
The best studied of the biologics with respect to psoriasis and psoriatic arthritis are the IL-17 inhibitors and TNF inhibitors, she said. While TNF inhibitors have traditionally been the treatment of choice for both conditions, “I think these days, people realize that IL-17 inhibitors can be just as good.”
A head-to-head study of the IL-17 inhibitor ixekizumab and the TNF inhibitor adalimumab, presented at the EULAR Congress, looked at a combined outcome of skin and joints and found ixekizumab to be superior, though the study design’s inclusion of a skin outcome may have favored ixekizumab (Ann Rheum Dis. 2019 Jun. doi: 10.1136/annrheumdis-2019-eular.8709).
A few other head-to-head studies have been performed, but properly ranking all 11 biologics would require dozens of clinical trials. At the American Academy of Dermatology meeting last March, Dr. Armstrong presented the results of a network meta-analysis of anti-TNF agents, anti-interleukin agents, anti–phosphodiesterase 4 agents, and fumaric acid esters (J Am Acad Dermatol. doi: 10.1016/j.jaad.2019.06.488). That study, funded by AbbVie, compared the individual agents to a collective placebo group and concluded that anti-interleukin agents generate the highest level of PASI 90/100 response rate. Risankizumab, ixekizumab, brodalumab, and guselkumab, all IL inhibitors, achieved the best marks over the primary response period.
The AAD guidelines include recommendations for tests to be done upon initiation of a biologic, including a tuberculosis test, complete blood count, comprehensive metabolic panel, and tests for hepatitis B and C. TB testing should be performed annually during treatment.
The guidelines also include recommendations for dose escalation, which can provide leverage for getting coverage approved. “One can use those guidelines to show payers how dose escalation can be done, so that [physicians] can potentially get more access to medications for their patients,” Dr. Armstrong said at the meeting jointly presented by the University of Louisville and Global Academy for Medical Education.
The guideline also ranks the existing evidence supporting individual biologics for the treatment of psoriasis subtypes. For example, for the treatment of moderate to severe scalp psoriasis, etanercept and guselkumab have consistent and good-quality patient-oriented evidence supporting them; infliximab, adalimumab, secukinumab, and ixekizumab are recommended based on inconsistent or limited quality patient-oriented evidence; and ustekinumab is supported only by consensus opinion, case studies, or disease-oriented evidence. The guidelines provide similar categorization of biologics for the treatment of moderate to severe plaque type palmoplantar psoriasis, moderate to severe psoriasis affecting the nails, adults with pustular or erythrodermic psoriasis, and adults with psoriatic arthritis.
Dr. Armstrong is a research investigator and/or advisor to AbbVie, Janssen, Lily, LEO Pharma, Novartis, UCB, Ortho Dermatologics, Dermera, Regeneron, BMS, Dermavant, and KHK. This publication and Global Academy for Medical Education are owned by the same parent company.
EXPERT ANALYSIS FROM COASTAL DERM
Histologic analysis of vaping-associated lung injury suggests chemical pneumonitis
Vaping-associated lung injury is likely a form of airway-centered chemical pneumonitis, not exogenous lipoid pneumonia, according to Yasmeen M. Butt, MD, of the University of Texas Southwestern Medical Center, Dallas, and associates.
Dr. Butt and associates performed a review of lung biopsies from 17 patients (13 men; median age, 35 years) with a history of vaping and either suspected or confirmed vaping-associated lung injury. All cases showed patterns of acute lung injury, including acute fibrinous pneumonitis, diffuse alveolar damage, or organizing pneumonia, the authors noted in a letter to the editor published in the New England Journal of Medicine.
While no histologic findings were specific, foamy macrophages and pneumocyte vacuolization were seen in all cases, the authors added. Pigmented macrophages were occasionally present but not dominant, neutrophils were often prominent, eosinophils were rare, and granulomas were not seen. Two patients eventually died, despite treatment with glucocorticoids and maximum supportive care.
“None of our cases showed histologic evidence of exogenous lipoid pneumonia and no radiologic evidence thereof has been found; this calls into question the diagnostic utility of identifying lipid-laden macrophages or performing oil red O staining on bronchioloalveolar lavage fluid as a marker of vaping-associated lung injury, as has been proposed,” Dr. Butt and associates wrote.
No conflicts of interest were reported.
SOURCE: Butt YM et al. N Engl J Med. 2019 Oct 2. doi: 10.1056/NEJMc1913069.
Vaping-associated lung injury is likely a form of airway-centered chemical pneumonitis, not exogenous lipoid pneumonia, according to Yasmeen M. Butt, MD, of the University of Texas Southwestern Medical Center, Dallas, and associates.
Dr. Butt and associates performed a review of lung biopsies from 17 patients (13 men; median age, 35 years) with a history of vaping and either suspected or confirmed vaping-associated lung injury. All cases showed patterns of acute lung injury, including acute fibrinous pneumonitis, diffuse alveolar damage, or organizing pneumonia, the authors noted in a letter to the editor published in the New England Journal of Medicine.
While no histologic findings were specific, foamy macrophages and pneumocyte vacuolization were seen in all cases, the authors added. Pigmented macrophages were occasionally present but not dominant, neutrophils were often prominent, eosinophils were rare, and granulomas were not seen. Two patients eventually died, despite treatment with glucocorticoids and maximum supportive care.
“None of our cases showed histologic evidence of exogenous lipoid pneumonia and no radiologic evidence thereof has been found; this calls into question the diagnostic utility of identifying lipid-laden macrophages or performing oil red O staining on bronchioloalveolar lavage fluid as a marker of vaping-associated lung injury, as has been proposed,” Dr. Butt and associates wrote.
No conflicts of interest were reported.
SOURCE: Butt YM et al. N Engl J Med. 2019 Oct 2. doi: 10.1056/NEJMc1913069.
Vaping-associated lung injury is likely a form of airway-centered chemical pneumonitis, not exogenous lipoid pneumonia, according to Yasmeen M. Butt, MD, of the University of Texas Southwestern Medical Center, Dallas, and associates.
Dr. Butt and associates performed a review of lung biopsies from 17 patients (13 men; median age, 35 years) with a history of vaping and either suspected or confirmed vaping-associated lung injury. All cases showed patterns of acute lung injury, including acute fibrinous pneumonitis, diffuse alveolar damage, or organizing pneumonia, the authors noted in a letter to the editor published in the New England Journal of Medicine.
While no histologic findings were specific, foamy macrophages and pneumocyte vacuolization were seen in all cases, the authors added. Pigmented macrophages were occasionally present but not dominant, neutrophils were often prominent, eosinophils were rare, and granulomas were not seen. Two patients eventually died, despite treatment with glucocorticoids and maximum supportive care.
“None of our cases showed histologic evidence of exogenous lipoid pneumonia and no radiologic evidence thereof has been found; this calls into question the diagnostic utility of identifying lipid-laden macrophages or performing oil red O staining on bronchioloalveolar lavage fluid as a marker of vaping-associated lung injury, as has been proposed,” Dr. Butt and associates wrote.
No conflicts of interest were reported.
SOURCE: Butt YM et al. N Engl J Med. 2019 Oct 2. doi: 10.1056/NEJMc1913069.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
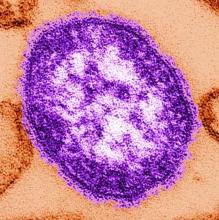
Measles 2019: Most cases occurred in close-knit, undervaccinated communities
While 22 outbreaks were reported in 17 states during 2019, the majority of measles cases occurred in a pair of outbreaks that started in late 2018, one in New York City and the other in New York state. Theses two outbreaks, which occurred in underimmunized, close-knit communities, accounted for 934 (75%) of the 2019 total. An additional six outbreaks in similar communities accounted for nearly half of the remaining reported cases.
The overall median patient age was 6 years, with 31% being children aged 1-4 years, 27% being school-age children aged 5-17 years, and 29% were adults aged at least 18 years. However, when excluding the New York City (NYC) and New York state outbreaks, the median patient age was 19 years. Outbreak length also differed significantly between the NYC and New York state outbreaks, compared with all other outbreaks; the NYC outbreak lasted for 9.5 months, involving 702 patients from start to finish, the New York state outbreak lasted for 10.5 months and involved 412 cases.
The rate of patients who were either unvaccinated or had unknown vaccination status was similar in the New York outbreaks and in the other U.S. outbreaks, ranging from 87% to 91%. A total of 119 patients were hospitalized, 20% of whom were younger than 1 year; no deaths were reported. A total of 81 cases were internationally imported; the rate of patients who were unvaccinated or had unknown status in this group was 90%.
While most outbreaks in 2019 were similar to those previously seen, the outbreaks in NYC and New York state were more sustained for three reasons, the CDC investigators said: pockets of low vaccination coverage and variable vaccine acceptance, relatively high population density and closed social nature of the community, and repeated importations of measles cases among unvaccinated persons traveling internationally and returning to or visiting the affected communities.
“Public health authorities need to identify pockets of undervaccinated persons to prevent these outbreaks, which require substantial resources to control. A preventive strategy to build vaccine confidence is important, especially one that uses culturally appropriate communication strategies to offset misinformation and disseminate accurate information about the safety and importance of vaccination in advance of outbreaks,” the CDC investigators concluded.
The CDC investigators reported that they had no conflicts of interest.
lfranki@mdedge.com
SOURCE: Patel M et al. MMWR Morb Mortal Wkly Rep. 2019 Oct 4. doi: 10.15585/mmwr.mm6840e2.
While 22 outbreaks were reported in 17 states during 2019, the majority of measles cases occurred in a pair of outbreaks that started in late 2018, one in New York City and the other in New York state. Theses two outbreaks, which occurred in underimmunized, close-knit communities, accounted for 934 (75%) of the 2019 total. An additional six outbreaks in similar communities accounted for nearly half of the remaining reported cases.
The overall median patient age was 6 years, with 31% being children aged 1-4 years, 27% being school-age children aged 5-17 years, and 29% were adults aged at least 18 years. However, when excluding the New York City (NYC) and New York state outbreaks, the median patient age was 19 years. Outbreak length also differed significantly between the NYC and New York state outbreaks, compared with all other outbreaks; the NYC outbreak lasted for 9.5 months, involving 702 patients from start to finish, the New York state outbreak lasted for 10.5 months and involved 412 cases.
The rate of patients who were either unvaccinated or had unknown vaccination status was similar in the New York outbreaks and in the other U.S. outbreaks, ranging from 87% to 91%. A total of 119 patients were hospitalized, 20% of whom were younger than 1 year; no deaths were reported. A total of 81 cases were internationally imported; the rate of patients who were unvaccinated or had unknown status in this group was 90%.
While most outbreaks in 2019 were similar to those previously seen, the outbreaks in NYC and New York state were more sustained for three reasons, the CDC investigators said: pockets of low vaccination coverage and variable vaccine acceptance, relatively high population density and closed social nature of the community, and repeated importations of measles cases among unvaccinated persons traveling internationally and returning to or visiting the affected communities.
“Public health authorities need to identify pockets of undervaccinated persons to prevent these outbreaks, which require substantial resources to control. A preventive strategy to build vaccine confidence is important, especially one that uses culturally appropriate communication strategies to offset misinformation and disseminate accurate information about the safety and importance of vaccination in advance of outbreaks,” the CDC investigators concluded.
The CDC investigators reported that they had no conflicts of interest.
lfranki@mdedge.com
SOURCE: Patel M et al. MMWR Morb Mortal Wkly Rep. 2019 Oct 4. doi: 10.15585/mmwr.mm6840e2.
While 22 outbreaks were reported in 17 states during 2019, the majority of measles cases occurred in a pair of outbreaks that started in late 2018, one in New York City and the other in New York state. Theses two outbreaks, which occurred in underimmunized, close-knit communities, accounted for 934 (75%) of the 2019 total. An additional six outbreaks in similar communities accounted for nearly half of the remaining reported cases.
The overall median patient age was 6 years, with 31% being children aged 1-4 years, 27% being school-age children aged 5-17 years, and 29% were adults aged at least 18 years. However, when excluding the New York City (NYC) and New York state outbreaks, the median patient age was 19 years. Outbreak length also differed significantly between the NYC and New York state outbreaks, compared with all other outbreaks; the NYC outbreak lasted for 9.5 months, involving 702 patients from start to finish, the New York state outbreak lasted for 10.5 months and involved 412 cases.
The rate of patients who were either unvaccinated or had unknown vaccination status was similar in the New York outbreaks and in the other U.S. outbreaks, ranging from 87% to 91%. A total of 119 patients were hospitalized, 20% of whom were younger than 1 year; no deaths were reported. A total of 81 cases were internationally imported; the rate of patients who were unvaccinated or had unknown status in this group was 90%.
While most outbreaks in 2019 were similar to those previously seen, the outbreaks in NYC and New York state were more sustained for three reasons, the CDC investigators said: pockets of low vaccination coverage and variable vaccine acceptance, relatively high population density and closed social nature of the community, and repeated importations of measles cases among unvaccinated persons traveling internationally and returning to or visiting the affected communities.
“Public health authorities need to identify pockets of undervaccinated persons to prevent these outbreaks, which require substantial resources to control. A preventive strategy to build vaccine confidence is important, especially one that uses culturally appropriate communication strategies to offset misinformation and disseminate accurate information about the safety and importance of vaccination in advance of outbreaks,” the CDC investigators concluded.
The CDC investigators reported that they had no conflicts of interest.
lfranki@mdedge.com
SOURCE: Patel M et al. MMWR Morb Mortal Wkly Rep. 2019 Oct 4. doi: 10.15585/mmwr.mm6840e2.
FROM THE MMWR
Oral drug cut viral respiratory tract infections in elderly
WASHINGTON – An investigational, oral, small molecule designed to boost innate antiviral immunity safely cut the incidence of various viral respiratory infections in elderly people during a winter season by nearly a third when administered once daily in a placebo-controlled, multicenter, phase 2 study of 952 patients. Based on these and other findings the drug, RTB101, is now undergoing testing in a phase 3 study, Joan Mannick, MD, said at an annual scientific meeting on infectious diseases.
At a dosage of 10 mg once daily, RTB101 was “well tolerated, upregulated innate antiviral gene expression, and reduced the incidence” of laboratory-confirmed respiratory tract infections caused by several different viruses, said Dr. Mannick, who disclosed that she is a cofounder and chief medical officer of resTORbio, a Boston-based company that’s developing the drug.
During 16 weeks of treatment during the winter virus season, once-daily dosing led to cuts in the rates of respiratory infections compared with placebo by rhinovirus and enterovirus, respiratory syncytial virus, coronavirus, influenza virus, metapneuomovirus, and parainfluenza virus, especially in patients whom the results identified as having the best drug responses: those who were at least 85 years old, and those who were at least 65 years old and also had asthma. Enrolled patients who were at least 65 years old and had other risk factors – current smoking, chronic obstructive pulmonary disease, or diabetes – had notably less robust responses to treatment, and the phase 3 study is not enrolling elderly people who currently smoke or have chronic obstructive pulmonary disease, Dr. Mannick said in an interview.
RTB101 inhibits the active site of the “mechanistic target of rapamycin” (mTOR) protein, the key player of the TORC1 protein complex that appears to downregulate innate antiviral immunity when active. Hence inhibiting mTOR and TORC1 activity should boost innate antiviral immunity. Once-daily dosing with 10 mg of RTB101 appears to mimic the normal daily cycle of high and low levels of TORC1 activity seen in younger adults but which is missing the elderly who generally have persistently elevated levels of TORC1 activity, Dr. Mannick explained.
The study she reported enrolled a total of 952 people at any of 10 sites in the Southern Hemisphere or 17 Northern Hemisphere study sites. The researchers randomized patients to receive either RTB101 or placebo at either of two once-daily dosages or either of two twice-daily regimens. The best drug performance was among the 356 patients treated with 10 mg once daily or placebo. Those who received the active drug at this level had a 19% incidence of any laboratory-confirmed respiratory tract infection, while those who received placebo had a 28% incidence, a 30.6% relative risk reduction with RTB101 treatment that was statistically significant.
The actively-treated patients showed upregulation for 19 of 20 “antiviral” genes assessed in the study compared with upregulation of just five of these genes in the those who received placebo. Two post hoc analyses showed that the people who received 10 mg once daily had about half the rate of all-cause hospitalizations compared with those on placebo, and among those who had respiratory infections treated patients had alleviation of their moderate or severe symptoms in about half the time compared with patients on placebo.
The 10-mg daily dosage of RTB101 is less than 1% of the maximum-tolerated dose in people, and the safety data collected in the current study showed adverse events occurring at similar rates in the patients who received the active drug and those who got placebo. Discontinuations because of adverse events occurred in 5% of people who received RTB101 and in 6% of those on placebo.
The researchers are planning to run a cost-effectiveness study to see whether the observed prevention of respiratory tract infections and their consequences can offset the cost of taking RTB101 daily for 16 weeks, Dr. Mannick said.
WASHINGTON – An investigational, oral, small molecule designed to boost innate antiviral immunity safely cut the incidence of various viral respiratory infections in elderly people during a winter season by nearly a third when administered once daily in a placebo-controlled, multicenter, phase 2 study of 952 patients. Based on these and other findings the drug, RTB101, is now undergoing testing in a phase 3 study, Joan Mannick, MD, said at an annual scientific meeting on infectious diseases.
At a dosage of 10 mg once daily, RTB101 was “well tolerated, upregulated innate antiviral gene expression, and reduced the incidence” of laboratory-confirmed respiratory tract infections caused by several different viruses, said Dr. Mannick, who disclosed that she is a cofounder and chief medical officer of resTORbio, a Boston-based company that’s developing the drug.
During 16 weeks of treatment during the winter virus season, once-daily dosing led to cuts in the rates of respiratory infections compared with placebo by rhinovirus and enterovirus, respiratory syncytial virus, coronavirus, influenza virus, metapneuomovirus, and parainfluenza virus, especially in patients whom the results identified as having the best drug responses: those who were at least 85 years old, and those who were at least 65 years old and also had asthma. Enrolled patients who were at least 65 years old and had other risk factors – current smoking, chronic obstructive pulmonary disease, or diabetes – had notably less robust responses to treatment, and the phase 3 study is not enrolling elderly people who currently smoke or have chronic obstructive pulmonary disease, Dr. Mannick said in an interview.
RTB101 inhibits the active site of the “mechanistic target of rapamycin” (mTOR) protein, the key player of the TORC1 protein complex that appears to downregulate innate antiviral immunity when active. Hence inhibiting mTOR and TORC1 activity should boost innate antiviral immunity. Once-daily dosing with 10 mg of RTB101 appears to mimic the normal daily cycle of high and low levels of TORC1 activity seen in younger adults but which is missing the elderly who generally have persistently elevated levels of TORC1 activity, Dr. Mannick explained.
The study she reported enrolled a total of 952 people at any of 10 sites in the Southern Hemisphere or 17 Northern Hemisphere study sites. The researchers randomized patients to receive either RTB101 or placebo at either of two once-daily dosages or either of two twice-daily regimens. The best drug performance was among the 356 patients treated with 10 mg once daily or placebo. Those who received the active drug at this level had a 19% incidence of any laboratory-confirmed respiratory tract infection, while those who received placebo had a 28% incidence, a 30.6% relative risk reduction with RTB101 treatment that was statistically significant.
The actively-treated patients showed upregulation for 19 of 20 “antiviral” genes assessed in the study compared with upregulation of just five of these genes in the those who received placebo. Two post hoc analyses showed that the people who received 10 mg once daily had about half the rate of all-cause hospitalizations compared with those on placebo, and among those who had respiratory infections treated patients had alleviation of their moderate or severe symptoms in about half the time compared with patients on placebo.
The 10-mg daily dosage of RTB101 is less than 1% of the maximum-tolerated dose in people, and the safety data collected in the current study showed adverse events occurring at similar rates in the patients who received the active drug and those who got placebo. Discontinuations because of adverse events occurred in 5% of people who received RTB101 and in 6% of those on placebo.
The researchers are planning to run a cost-effectiveness study to see whether the observed prevention of respiratory tract infections and their consequences can offset the cost of taking RTB101 daily for 16 weeks, Dr. Mannick said.
WASHINGTON – An investigational, oral, small molecule designed to boost innate antiviral immunity safely cut the incidence of various viral respiratory infections in elderly people during a winter season by nearly a third when administered once daily in a placebo-controlled, multicenter, phase 2 study of 952 patients. Based on these and other findings the drug, RTB101, is now undergoing testing in a phase 3 study, Joan Mannick, MD, said at an annual scientific meeting on infectious diseases.
At a dosage of 10 mg once daily, RTB101 was “well tolerated, upregulated innate antiviral gene expression, and reduced the incidence” of laboratory-confirmed respiratory tract infections caused by several different viruses, said Dr. Mannick, who disclosed that she is a cofounder and chief medical officer of resTORbio, a Boston-based company that’s developing the drug.
During 16 weeks of treatment during the winter virus season, once-daily dosing led to cuts in the rates of respiratory infections compared with placebo by rhinovirus and enterovirus, respiratory syncytial virus, coronavirus, influenza virus, metapneuomovirus, and parainfluenza virus, especially in patients whom the results identified as having the best drug responses: those who were at least 85 years old, and those who were at least 65 years old and also had asthma. Enrolled patients who were at least 65 years old and had other risk factors – current smoking, chronic obstructive pulmonary disease, or diabetes – had notably less robust responses to treatment, and the phase 3 study is not enrolling elderly people who currently smoke or have chronic obstructive pulmonary disease, Dr. Mannick said in an interview.
RTB101 inhibits the active site of the “mechanistic target of rapamycin” (mTOR) protein, the key player of the TORC1 protein complex that appears to downregulate innate antiviral immunity when active. Hence inhibiting mTOR and TORC1 activity should boost innate antiviral immunity. Once-daily dosing with 10 mg of RTB101 appears to mimic the normal daily cycle of high and low levels of TORC1 activity seen in younger adults but which is missing the elderly who generally have persistently elevated levels of TORC1 activity, Dr. Mannick explained.
The study she reported enrolled a total of 952 people at any of 10 sites in the Southern Hemisphere or 17 Northern Hemisphere study sites. The researchers randomized patients to receive either RTB101 or placebo at either of two once-daily dosages or either of two twice-daily regimens. The best drug performance was among the 356 patients treated with 10 mg once daily or placebo. Those who received the active drug at this level had a 19% incidence of any laboratory-confirmed respiratory tract infection, while those who received placebo had a 28% incidence, a 30.6% relative risk reduction with RTB101 treatment that was statistically significant.
The actively-treated patients showed upregulation for 19 of 20 “antiviral” genes assessed in the study compared with upregulation of just five of these genes in the those who received placebo. Two post hoc analyses showed that the people who received 10 mg once daily had about half the rate of all-cause hospitalizations compared with those on placebo, and among those who had respiratory infections treated patients had alleviation of their moderate or severe symptoms in about half the time compared with patients on placebo.
The 10-mg daily dosage of RTB101 is less than 1% of the maximum-tolerated dose in people, and the safety data collected in the current study showed adverse events occurring at similar rates in the patients who received the active drug and those who got placebo. Discontinuations because of adverse events occurred in 5% of people who received RTB101 and in 6% of those on placebo.
The researchers are planning to run a cost-effectiveness study to see whether the observed prevention of respiratory tract infections and their consequences can offset the cost of taking RTB101 daily for 16 weeks, Dr. Mannick said.
REPORTING FROM IDWEEK 2019