User login
Cellulitis ranks as top reason for skin-related pediatric inpatient admissions
AUSTIN, TEX. – showed.
“Skin conditions significantly affect pediatric inpatients, and dermatologists ought be accessible for consultation to enhance care and costs,” the study’s first author, Marcus L. Elias, said in an interview prior to the annual meeting of the Society for Pediatric Dermatology.
According to Mr. Elias, who is a 4th-year medical student at Rutgers New Jersey Medical School–Newark, few national studies on skin diseases for pediatric inpatients have been published in the medical literature. Earlier this year, researchers examined inpatient dermatologic conditions in patients aged 18 years and older (J Am Acad Dermatol 2019;80[2]:425-32), but Mr. Elias and associates set out to analyze the burden of inpatient pediatric dermatologic conditions on a national basis. “We wanted to see if the same conditions that were hospitalizing adults were also hospitalizing kids,” he said. “We found that this was indeed the case.”
The researchers queried the National Inpatient Sample database for all cases involving patients aged 18 years and younger during 2001-2013. The search yielded a sample of 16,837,857 patients. From this, the researchers analyzed diagnosis-related groups for dermatologic conditions denoting the principal diagnosis at discharge, which left a final sample of 84,090 patients. Frequency and chi-squared tests were used to analyze categorical variables.
More than half of patients (54%) were male, 36% were white, 48% had Medicaid insurance, and 43% had private insurance. Mr. Elias reported that the median length of stay for patients was 2 days and the median cost of care was $6,289.50 for each case. More than three-quarters of pediatric inpatients with dermatologic diagnoses were treated for “cellulitis” (66,147 cases, or 79%), with most cases involving the legs (16,875 cases, or 20%). Other pediatric inpatients were admitted for “minor skin disorder without complications” (5,458 cases, or 7%), and “minor skin disorder with complications” (2,822 cases, or 3%). A total of 64 patients died during the study period. Of these, 31 cases (50%) involved “skin graft and/or debridement of skin ulcer or cellulitis without complications,” the study found.
“We were surprised that the major cause of mortality for our patients was classified as ‘skin graft and/or debridement of skin ulcer or cellulitis without complications,’ as a similar diagnosis-related groupings exist denoting that complications did arise,” Mr. Elias said. “Still, it is not possible for us to determine if the mortality was from the skin graft/debridement or another cause entirely. It is possible that the procedure was without complications, only to have the patient succumb to an ancillary process.”
He acknowledged certain limitations of the study, including the fact that the function of dermatologic consults for hospitalized patients was not examined. “We also cannot draw conclusions as to whether improved outpatient therapy reduces the need for hospitalization,” he said. Mr. Elias reported having no financial disclosures.
AUSTIN, TEX. – showed.
“Skin conditions significantly affect pediatric inpatients, and dermatologists ought be accessible for consultation to enhance care and costs,” the study’s first author, Marcus L. Elias, said in an interview prior to the annual meeting of the Society for Pediatric Dermatology.
According to Mr. Elias, who is a 4th-year medical student at Rutgers New Jersey Medical School–Newark, few national studies on skin diseases for pediatric inpatients have been published in the medical literature. Earlier this year, researchers examined inpatient dermatologic conditions in patients aged 18 years and older (J Am Acad Dermatol 2019;80[2]:425-32), but Mr. Elias and associates set out to analyze the burden of inpatient pediatric dermatologic conditions on a national basis. “We wanted to see if the same conditions that were hospitalizing adults were also hospitalizing kids,” he said. “We found that this was indeed the case.”
The researchers queried the National Inpatient Sample database for all cases involving patients aged 18 years and younger during 2001-2013. The search yielded a sample of 16,837,857 patients. From this, the researchers analyzed diagnosis-related groups for dermatologic conditions denoting the principal diagnosis at discharge, which left a final sample of 84,090 patients. Frequency and chi-squared tests were used to analyze categorical variables.
More than half of patients (54%) were male, 36% were white, 48% had Medicaid insurance, and 43% had private insurance. Mr. Elias reported that the median length of stay for patients was 2 days and the median cost of care was $6,289.50 for each case. More than three-quarters of pediatric inpatients with dermatologic diagnoses were treated for “cellulitis” (66,147 cases, or 79%), with most cases involving the legs (16,875 cases, or 20%). Other pediatric inpatients were admitted for “minor skin disorder without complications” (5,458 cases, or 7%), and “minor skin disorder with complications” (2,822 cases, or 3%). A total of 64 patients died during the study period. Of these, 31 cases (50%) involved “skin graft and/or debridement of skin ulcer or cellulitis without complications,” the study found.
“We were surprised that the major cause of mortality for our patients was classified as ‘skin graft and/or debridement of skin ulcer or cellulitis without complications,’ as a similar diagnosis-related groupings exist denoting that complications did arise,” Mr. Elias said. “Still, it is not possible for us to determine if the mortality was from the skin graft/debridement or another cause entirely. It is possible that the procedure was without complications, only to have the patient succumb to an ancillary process.”
He acknowledged certain limitations of the study, including the fact that the function of dermatologic consults for hospitalized patients was not examined. “We also cannot draw conclusions as to whether improved outpatient therapy reduces the need for hospitalization,” he said. Mr. Elias reported having no financial disclosures.
AUSTIN, TEX. – showed.
“Skin conditions significantly affect pediatric inpatients, and dermatologists ought be accessible for consultation to enhance care and costs,” the study’s first author, Marcus L. Elias, said in an interview prior to the annual meeting of the Society for Pediatric Dermatology.
According to Mr. Elias, who is a 4th-year medical student at Rutgers New Jersey Medical School–Newark, few national studies on skin diseases for pediatric inpatients have been published in the medical literature. Earlier this year, researchers examined inpatient dermatologic conditions in patients aged 18 years and older (J Am Acad Dermatol 2019;80[2]:425-32), but Mr. Elias and associates set out to analyze the burden of inpatient pediatric dermatologic conditions on a national basis. “We wanted to see if the same conditions that were hospitalizing adults were also hospitalizing kids,” he said. “We found that this was indeed the case.”
The researchers queried the National Inpatient Sample database for all cases involving patients aged 18 years and younger during 2001-2013. The search yielded a sample of 16,837,857 patients. From this, the researchers analyzed diagnosis-related groups for dermatologic conditions denoting the principal diagnosis at discharge, which left a final sample of 84,090 patients. Frequency and chi-squared tests were used to analyze categorical variables.
More than half of patients (54%) were male, 36% were white, 48% had Medicaid insurance, and 43% had private insurance. Mr. Elias reported that the median length of stay for patients was 2 days and the median cost of care was $6,289.50 for each case. More than three-quarters of pediatric inpatients with dermatologic diagnoses were treated for “cellulitis” (66,147 cases, or 79%), with most cases involving the legs (16,875 cases, or 20%). Other pediatric inpatients were admitted for “minor skin disorder without complications” (5,458 cases, or 7%), and “minor skin disorder with complications” (2,822 cases, or 3%). A total of 64 patients died during the study period. Of these, 31 cases (50%) involved “skin graft and/or debridement of skin ulcer or cellulitis without complications,” the study found.
“We were surprised that the major cause of mortality for our patients was classified as ‘skin graft and/or debridement of skin ulcer or cellulitis without complications,’ as a similar diagnosis-related groupings exist denoting that complications did arise,” Mr. Elias said. “Still, it is not possible for us to determine if the mortality was from the skin graft/debridement or another cause entirely. It is possible that the procedure was without complications, only to have the patient succumb to an ancillary process.”
He acknowledged certain limitations of the study, including the fact that the function of dermatologic consults for hospitalized patients was not examined. “We also cannot draw conclusions as to whether improved outpatient therapy reduces the need for hospitalization,” he said. Mr. Elias reported having no financial disclosures.
REPORTING FROM SPD 2019
Key clinical point: Cellulitis is the cause of the majority of skin-related pediatric inpatient admissions in the United States.
Major finding: In all, 79% of pediatric inpatients with dermatologic diagnoses were treated for cellulitis.
Study details: An analysis of data from 84,090 patients younger than age 18 in the National Inpatient Sample.
Disclosures: The researchers reported having no financial disclosures.
Neonatal ICU stay found ‘protective’ against risk for developing atopic dermatitis
AUSTIN – The
“While more time in the NICU is associated with a lesser risk of developing atopic dermatitis, we certainly do not want to keep infants in the NICU longer in order to lower their risk of atopic dermatitis,” the study’s first author, Jennifer J. Schoch, MD, said in an interview prior to the annual meeting of the Society for Pediatric Dermatology. “Instead, we need to work on understanding the mechanisms behind this relationship. For example, are there certain exposures in the NICU that influence the cutaneous immunity to ultimately reduce the risk of atopic dermatitis?”
According to Dr. Schoch, a pediatric dermatologist at the University of Florida, Gainesville, the medical literature has been conflicted regarding the relationship between prematurity and eczema. A recent meta-analysis of 18 studies found an association between very preterm birth and a decreased risk of eczema, yet the risk became insignificant among children born moderately preterm (J Am Acad Dermatol. 2018;78[6]:1142-8). However, the factors contributing to this relationship are not well understood.
In an effort to explore the infant, maternal, and environmental factors of infants who developed AD, compared with infants who did not, Dr. Schoch and colleagues evaluated infants who were born at University of Florida Health from June 1, 2011, to April 30, 2017; had at least two well-child visits; and had at least one visit at 300 days old or later. The researchers included 4,016 mother-infant dyads in the study. Atopic dermatitis was diagnosed in 26.5% of the infants. Factors significantly associated with the incidence of AD were delivery mode (P = .0127), NICU stay (P = .0001), gestational age (P = .0006), and birth weight (P = .0020). Specifically, infants had a higher risk of developing AD if they were delivered vaginally, did not stay in the NICU, had a higher gestational age, or had a higher birth weight. Extremely preterm (less than 28 weeks’ gestation) and very preterm (28 to less than 32 weeks’ gestation) infants had the lowest rates of AD, at 10.9% and 19%, respectively.
When the researchers adjusted for other variables to their model, only length of stay in the NICU was related to the development of AD. Specifically, infants who spent more time in the NICU had a lower risk of developing atopic dermatitis (P = .0039).
“We were surprised to find that the length of stay in the neonatal intensive care unit was the strongest protective factor against the future development of eczema,” Dr. Schoch said. “Instead of this relationship being mediated by gestational age or birth weight, it was how much time the infants spent in the NICU that seemed to ‘protect’ from future eczema.”
She acknowledged certain limitations of the study, including its retrospective design with data gathered from electronic medical records. Also, “diagnosis was determined by ICD-9 or ICD-10 code, and not confirmed by dermatologists,” she said.
In their abstract, the researchers wrote that the finding highlights “the importance of early life interactions between the microbiome, developing cutaneous immunity, and the evolving skin barrier of the preterm infant. The skin microbiome of premature infants differs from full-term infants, in that the premature infant cutaneous microbiome is dominated by Staphylococcus species” (Microbiome. 2018;6[1]:98). They added that “the early presence of Staphylococcus on the skin may confer protection.”
Dr. Schoch reported having no relevant financial disclosures.
SOURCE: Schoch J et al. SPD 2019, Poster 2.
AUSTIN – The
“While more time in the NICU is associated with a lesser risk of developing atopic dermatitis, we certainly do not want to keep infants in the NICU longer in order to lower their risk of atopic dermatitis,” the study’s first author, Jennifer J. Schoch, MD, said in an interview prior to the annual meeting of the Society for Pediatric Dermatology. “Instead, we need to work on understanding the mechanisms behind this relationship. For example, are there certain exposures in the NICU that influence the cutaneous immunity to ultimately reduce the risk of atopic dermatitis?”
According to Dr. Schoch, a pediatric dermatologist at the University of Florida, Gainesville, the medical literature has been conflicted regarding the relationship between prematurity and eczema. A recent meta-analysis of 18 studies found an association between very preterm birth and a decreased risk of eczema, yet the risk became insignificant among children born moderately preterm (J Am Acad Dermatol. 2018;78[6]:1142-8). However, the factors contributing to this relationship are not well understood.
In an effort to explore the infant, maternal, and environmental factors of infants who developed AD, compared with infants who did not, Dr. Schoch and colleagues evaluated infants who were born at University of Florida Health from June 1, 2011, to April 30, 2017; had at least two well-child visits; and had at least one visit at 300 days old or later. The researchers included 4,016 mother-infant dyads in the study. Atopic dermatitis was diagnosed in 26.5% of the infants. Factors significantly associated with the incidence of AD were delivery mode (P = .0127), NICU stay (P = .0001), gestational age (P = .0006), and birth weight (P = .0020). Specifically, infants had a higher risk of developing AD if they were delivered vaginally, did not stay in the NICU, had a higher gestational age, or had a higher birth weight. Extremely preterm (less than 28 weeks’ gestation) and very preterm (28 to less than 32 weeks’ gestation) infants had the lowest rates of AD, at 10.9% and 19%, respectively.
When the researchers adjusted for other variables to their model, only length of stay in the NICU was related to the development of AD. Specifically, infants who spent more time in the NICU had a lower risk of developing atopic dermatitis (P = .0039).
“We were surprised to find that the length of stay in the neonatal intensive care unit was the strongest protective factor against the future development of eczema,” Dr. Schoch said. “Instead of this relationship being mediated by gestational age or birth weight, it was how much time the infants spent in the NICU that seemed to ‘protect’ from future eczema.”
She acknowledged certain limitations of the study, including its retrospective design with data gathered from electronic medical records. Also, “diagnosis was determined by ICD-9 or ICD-10 code, and not confirmed by dermatologists,” she said.
In their abstract, the researchers wrote that the finding highlights “the importance of early life interactions between the microbiome, developing cutaneous immunity, and the evolving skin barrier of the preterm infant. The skin microbiome of premature infants differs from full-term infants, in that the premature infant cutaneous microbiome is dominated by Staphylococcus species” (Microbiome. 2018;6[1]:98). They added that “the early presence of Staphylococcus on the skin may confer protection.”
Dr. Schoch reported having no relevant financial disclosures.
SOURCE: Schoch J et al. SPD 2019, Poster 2.
AUSTIN – The
“While more time in the NICU is associated with a lesser risk of developing atopic dermatitis, we certainly do not want to keep infants in the NICU longer in order to lower their risk of atopic dermatitis,” the study’s first author, Jennifer J. Schoch, MD, said in an interview prior to the annual meeting of the Society for Pediatric Dermatology. “Instead, we need to work on understanding the mechanisms behind this relationship. For example, are there certain exposures in the NICU that influence the cutaneous immunity to ultimately reduce the risk of atopic dermatitis?”
According to Dr. Schoch, a pediatric dermatologist at the University of Florida, Gainesville, the medical literature has been conflicted regarding the relationship between prematurity and eczema. A recent meta-analysis of 18 studies found an association between very preterm birth and a decreased risk of eczema, yet the risk became insignificant among children born moderately preterm (J Am Acad Dermatol. 2018;78[6]:1142-8). However, the factors contributing to this relationship are not well understood.
In an effort to explore the infant, maternal, and environmental factors of infants who developed AD, compared with infants who did not, Dr. Schoch and colleagues evaluated infants who were born at University of Florida Health from June 1, 2011, to April 30, 2017; had at least two well-child visits; and had at least one visit at 300 days old or later. The researchers included 4,016 mother-infant dyads in the study. Atopic dermatitis was diagnosed in 26.5% of the infants. Factors significantly associated with the incidence of AD were delivery mode (P = .0127), NICU stay (P = .0001), gestational age (P = .0006), and birth weight (P = .0020). Specifically, infants had a higher risk of developing AD if they were delivered vaginally, did not stay in the NICU, had a higher gestational age, or had a higher birth weight. Extremely preterm (less than 28 weeks’ gestation) and very preterm (28 to less than 32 weeks’ gestation) infants had the lowest rates of AD, at 10.9% and 19%, respectively.
When the researchers adjusted for other variables to their model, only length of stay in the NICU was related to the development of AD. Specifically, infants who spent more time in the NICU had a lower risk of developing atopic dermatitis (P = .0039).
“We were surprised to find that the length of stay in the neonatal intensive care unit was the strongest protective factor against the future development of eczema,” Dr. Schoch said. “Instead of this relationship being mediated by gestational age or birth weight, it was how much time the infants spent in the NICU that seemed to ‘protect’ from future eczema.”
She acknowledged certain limitations of the study, including its retrospective design with data gathered from electronic medical records. Also, “diagnosis was determined by ICD-9 or ICD-10 code, and not confirmed by dermatologists,” she said.
In their abstract, the researchers wrote that the finding highlights “the importance of early life interactions between the microbiome, developing cutaneous immunity, and the evolving skin barrier of the preterm infant. The skin microbiome of premature infants differs from full-term infants, in that the premature infant cutaneous microbiome is dominated by Staphylococcus species” (Microbiome. 2018;6[1]:98). They added that “the early presence of Staphylococcus on the skin may confer protection.”
Dr. Schoch reported having no relevant financial disclosures.
SOURCE: Schoch J et al. SPD 2019, Poster 2.
REPORTING FROM SPD 2019
Key clinical point: Preterm infants develop atopic dermatitis less often than full term infants.
Major finding: Infants that spent more time in the neonatal ICU had a lower risk of developing atopic dermatitis (P = .0039).
Study details: A single-center study of 4,016 mother-infant dyads.
Disclosures: Dr. Schoch reported having no relevant financial disclosures.
Source: Schoch J et al. SPD 2019, Poster 2.
Migraine comorbidities rise with increased headache days
PHILADELPHIA – The more days per month a person reported experiencing migraine headaches the greater their prevalence of various comorbidities associated with migraine headaches, including insomnia, depression, anxiety, and gastric ulcer disease, according to results from a survey of more than 92,000 U.S. residents.
“Increasing monthly headache day [MHD] frequency was associated with an increased risk of other health conditions in people with migraine,” Richard B. Lipton, MD, and his associates reported in a poster at the annual meeting of the American Headache Society. “The findings may be due to direct causality, reverse causality, shared risk factors, or detection bias.”
Additional analysis of the association with gastric ulcer disease (GUD) showed that it also linked with the number of days per month when a person with migraine used an NSAID. Migraineurs who self-reported having GUD averaged 10.5 days a month using an NSAID, compared with an average NSAID usage of just over 6 days a month among migraineurs without GUD, Dr. Lipton, a professor and vice-chair of neurology at Albert Einstein College of Medicine, New York, reported in a separate poster at the meeting.
The Migraine in America Symptoms and Treatment (MAST) study enrolled more than 90,000 U.S. residents starting in 2016. Using a validated diagnostic screening tool, the MAST researchers identified 15,133 of these people as having at least one day with a migraine headache during the 3 months prior to the survey and 77,453 who reported no migraine history (Headache. 2018 Oct;58[9]: 1408-26). The people with migraine averaged 43 years old, compared with an average of 52 years for those without migraine; 73% of the migraineurs were women.
Analysis of the prevalence of various self-reported, physician-diagnosed comorbidities showed a strong correlation between the relative odds of having a comorbidity and the self-reported number of MHDs. For example, the odds ratio for having insomnia, compared with the people without migraine, was nearly 200% among people reporting 1-4 MHDs, more than 300% higher among those reporting 5-9 MHDs, 500% higher with MHDs of 10-14, and nearly 700% higher among people reporting 20 or more MHDs. The researchers saw roughly similar patterns of rising comorbidity prevalence with higher numbers of MHDs for depression, anxiety, and GUD. The prevalence of a history of stroke or transient ischemic attack also increased with increasing numbers of MHDs but less steeply than for the other comorbidities. And while the prevalence of peripheral artery disease and epilepsy was consistently more than 100% greater among the migraineurs, compared with those with no recent migraine history, the prevalence of each of these two comorbidities showed no clear pattern of increasing prevalence as MHDs increased.
The analysis looked specifically at the relationship between GUD and NSAID use among people reporting migraine. Overall, the migraineurs had a greater than 200% increased prevalence of GUD than those without migraine. The odds ratio for GUD among migraineurs with 1-4 MHDs was 2.6, compared with those without migraine, and the odds ratio steadily rose with increasing MHDs to a peak of 490% higher among those who averaged 21 or more MHDs.
This link between the number of MHDs and prevalence of GUD may have some relationship to oral NSAID use, as overall NSAID use was higher among people with recent migraines than in those without migraines. However, the number of days per month of oral NSAID use appeared to plateau at an average of about 19 days once people reported having at least 10 MHDs, the researchers said. Even when people reported having more than twice as many MHDs their NSAID use remained at an average of about 19 days per month.
MAST was sponsored by Dr. Reddy’s Laboratories. Dr. Lipton had been a consultant to Dr. Reddy’s and to several other companies.
SOURCE: Lipton RB et al. Headache. 2019 June;59[S1]:1-208, P54.
PHILADELPHIA – The more days per month a person reported experiencing migraine headaches the greater their prevalence of various comorbidities associated with migraine headaches, including insomnia, depression, anxiety, and gastric ulcer disease, according to results from a survey of more than 92,000 U.S. residents.
“Increasing monthly headache day [MHD] frequency was associated with an increased risk of other health conditions in people with migraine,” Richard B. Lipton, MD, and his associates reported in a poster at the annual meeting of the American Headache Society. “The findings may be due to direct causality, reverse causality, shared risk factors, or detection bias.”
Additional analysis of the association with gastric ulcer disease (GUD) showed that it also linked with the number of days per month when a person with migraine used an NSAID. Migraineurs who self-reported having GUD averaged 10.5 days a month using an NSAID, compared with an average NSAID usage of just over 6 days a month among migraineurs without GUD, Dr. Lipton, a professor and vice-chair of neurology at Albert Einstein College of Medicine, New York, reported in a separate poster at the meeting.
The Migraine in America Symptoms and Treatment (MAST) study enrolled more than 90,000 U.S. residents starting in 2016. Using a validated diagnostic screening tool, the MAST researchers identified 15,133 of these people as having at least one day with a migraine headache during the 3 months prior to the survey and 77,453 who reported no migraine history (Headache. 2018 Oct;58[9]: 1408-26). The people with migraine averaged 43 years old, compared with an average of 52 years for those without migraine; 73% of the migraineurs were women.
Analysis of the prevalence of various self-reported, physician-diagnosed comorbidities showed a strong correlation between the relative odds of having a comorbidity and the self-reported number of MHDs. For example, the odds ratio for having insomnia, compared with the people without migraine, was nearly 200% among people reporting 1-4 MHDs, more than 300% higher among those reporting 5-9 MHDs, 500% higher with MHDs of 10-14, and nearly 700% higher among people reporting 20 or more MHDs. The researchers saw roughly similar patterns of rising comorbidity prevalence with higher numbers of MHDs for depression, anxiety, and GUD. The prevalence of a history of stroke or transient ischemic attack also increased with increasing numbers of MHDs but less steeply than for the other comorbidities. And while the prevalence of peripheral artery disease and epilepsy was consistently more than 100% greater among the migraineurs, compared with those with no recent migraine history, the prevalence of each of these two comorbidities showed no clear pattern of increasing prevalence as MHDs increased.
The analysis looked specifically at the relationship between GUD and NSAID use among people reporting migraine. Overall, the migraineurs had a greater than 200% increased prevalence of GUD than those without migraine. The odds ratio for GUD among migraineurs with 1-4 MHDs was 2.6, compared with those without migraine, and the odds ratio steadily rose with increasing MHDs to a peak of 490% higher among those who averaged 21 or more MHDs.
This link between the number of MHDs and prevalence of GUD may have some relationship to oral NSAID use, as overall NSAID use was higher among people with recent migraines than in those without migraines. However, the number of days per month of oral NSAID use appeared to plateau at an average of about 19 days once people reported having at least 10 MHDs, the researchers said. Even when people reported having more than twice as many MHDs their NSAID use remained at an average of about 19 days per month.
MAST was sponsored by Dr. Reddy’s Laboratories. Dr. Lipton had been a consultant to Dr. Reddy’s and to several other companies.
SOURCE: Lipton RB et al. Headache. 2019 June;59[S1]:1-208, P54.
PHILADELPHIA – The more days per month a person reported experiencing migraine headaches the greater their prevalence of various comorbidities associated with migraine headaches, including insomnia, depression, anxiety, and gastric ulcer disease, according to results from a survey of more than 92,000 U.S. residents.
“Increasing monthly headache day [MHD] frequency was associated with an increased risk of other health conditions in people with migraine,” Richard B. Lipton, MD, and his associates reported in a poster at the annual meeting of the American Headache Society. “The findings may be due to direct causality, reverse causality, shared risk factors, or detection bias.”
Additional analysis of the association with gastric ulcer disease (GUD) showed that it also linked with the number of days per month when a person with migraine used an NSAID. Migraineurs who self-reported having GUD averaged 10.5 days a month using an NSAID, compared with an average NSAID usage of just over 6 days a month among migraineurs without GUD, Dr. Lipton, a professor and vice-chair of neurology at Albert Einstein College of Medicine, New York, reported in a separate poster at the meeting.
The Migraine in America Symptoms and Treatment (MAST) study enrolled more than 90,000 U.S. residents starting in 2016. Using a validated diagnostic screening tool, the MAST researchers identified 15,133 of these people as having at least one day with a migraine headache during the 3 months prior to the survey and 77,453 who reported no migraine history (Headache. 2018 Oct;58[9]: 1408-26). The people with migraine averaged 43 years old, compared with an average of 52 years for those without migraine; 73% of the migraineurs were women.
Analysis of the prevalence of various self-reported, physician-diagnosed comorbidities showed a strong correlation between the relative odds of having a comorbidity and the self-reported number of MHDs. For example, the odds ratio for having insomnia, compared with the people without migraine, was nearly 200% among people reporting 1-4 MHDs, more than 300% higher among those reporting 5-9 MHDs, 500% higher with MHDs of 10-14, and nearly 700% higher among people reporting 20 or more MHDs. The researchers saw roughly similar patterns of rising comorbidity prevalence with higher numbers of MHDs for depression, anxiety, and GUD. The prevalence of a history of stroke or transient ischemic attack also increased with increasing numbers of MHDs but less steeply than for the other comorbidities. And while the prevalence of peripheral artery disease and epilepsy was consistently more than 100% greater among the migraineurs, compared with those with no recent migraine history, the prevalence of each of these two comorbidities showed no clear pattern of increasing prevalence as MHDs increased.
The analysis looked specifically at the relationship between GUD and NSAID use among people reporting migraine. Overall, the migraineurs had a greater than 200% increased prevalence of GUD than those without migraine. The odds ratio for GUD among migraineurs with 1-4 MHDs was 2.6, compared with those without migraine, and the odds ratio steadily rose with increasing MHDs to a peak of 490% higher among those who averaged 21 or more MHDs.
This link between the number of MHDs and prevalence of GUD may have some relationship to oral NSAID use, as overall NSAID use was higher among people with recent migraines than in those without migraines. However, the number of days per month of oral NSAID use appeared to plateau at an average of about 19 days once people reported having at least 10 MHDs, the researchers said. Even when people reported having more than twice as many MHDs their NSAID use remained at an average of about 19 days per month.
MAST was sponsored by Dr. Reddy’s Laboratories. Dr. Lipton had been a consultant to Dr. Reddy’s and to several other companies.
SOURCE: Lipton RB et al. Headache. 2019 June;59[S1]:1-208, P54.
REPORTING FROM AHS 2019
A third of serious malpractice claims due to diagnostic error
A third of medical malpractice cases associated with patient death or permanent disability result from diagnostic errors by health providers, an analysis finds.
Lead investigator David E. Newman-Toker, MD, PhD, of Johns Hopkins University, Baltimore, and colleagues reviewed malpractice claims during 2006-2015 from medical liability insurer CRICO’s Comparative Benchmarking System database, which represents 30% of all malpractice claims in the United States.
Investigators sought to identify diseases accounting for the majority of serious diagnosis-related harms associated with the claims. Of 55,377 closed claims, researchers identified 11,592 diagnostic error cases, of which 7,379 resulted in high-severity harm.
Of the high-severity claims, 34% stemmed from inaccurate or delayed diagnosis (Diagnosis 2019 Jul 11. doi. org/10.1515/dx-2019-0019).
The majority of diagnostic mistakes (74%) causing the most severe harm were attributable to cancer (38%), vascular events (23%), and infection (14%). These cases resulted in nearly $2 billion in malpractice payouts over a 10-year period, investigators found.
Clinical judgment factors were the primary reason behind the alleged errors, specifically: failure or delay in ordering a diagnostic test, narrow diagnostic focus with failure to establish a differential diagnosis, failure to appreciate and reconcile relevant symptoms or test results, and failure or delay in obtaining consultation or referral and misinterpretation of diagnostic studies.
“Diagnostic errors are the most common, the most catastrophic, and the most costly of medical errors,” Dr. Newman-Toker said at a press conference July 11. “We know that this is a major problem, at an individual, personal level, but also at a societal level and something we really have to take action toward fixing.”
This study breaks new ground by drilling into the major diseases most commonly associated with diagnostic errors, Dr. Newman-Toker said. In the cancer category, the most common cancers linked to severe harm were lung, breast, colorectal, prostate, and melanoma. In the vascular category, the most common conditions were stroke; myocardial infarction; venous thromboembolism; aortic aneurysm and dissection; and arterial thromboembolism. In the area of infection, sepsis; meningitis and encephalitis; spinal abscess; pneumonia; and endocarditis were the most common infections identified.
The findings provide a starting point to make improvements in the area of medical errors, said Dr. Newman-Toker, president of the Society to Improve Diagnosis in Medicine, an organization that aims to improve diagnosis and eliminate harm from diagnostic error.
“Although diagnostic errors happen everywhere, across all of medicine in every discipline with every disease, we might be able to take a big chunk out of this problem if we save a lot of lives and prevent a lot disability and if we focus some energy on tackling these problems,” he said. “It at least gives us a starting place and a roadmap for how to move the ball forward in this regard.”
The Society to Improve Diagnosis in Medicine has called on Congress to invest more funding into research to address diagnostic errors. Society CEO and cofounder Paul L. Epner noted that the 2019 House appropriations bill proposes not less than $4 million for diagnostic safety and quality research, which is up from $2 million last year.
“It’s a small step, but in the right direction,” Mr. Epner said. “[However,] the federal investment in research remains trivially small in relation to the public burden. That’s why we urge Congress to commit to research funding levels proportionate to the societal cost, in both human lives and in dollars.”
agallegos@mdedge.com
A third of medical malpractice cases associated with patient death or permanent disability result from diagnostic errors by health providers, an analysis finds.
Lead investigator David E. Newman-Toker, MD, PhD, of Johns Hopkins University, Baltimore, and colleagues reviewed malpractice claims during 2006-2015 from medical liability insurer CRICO’s Comparative Benchmarking System database, which represents 30% of all malpractice claims in the United States.
Investigators sought to identify diseases accounting for the majority of serious diagnosis-related harms associated with the claims. Of 55,377 closed claims, researchers identified 11,592 diagnostic error cases, of which 7,379 resulted in high-severity harm.
Of the high-severity claims, 34% stemmed from inaccurate or delayed diagnosis (Diagnosis 2019 Jul 11. doi. org/10.1515/dx-2019-0019).
The majority of diagnostic mistakes (74%) causing the most severe harm were attributable to cancer (38%), vascular events (23%), and infection (14%). These cases resulted in nearly $2 billion in malpractice payouts over a 10-year period, investigators found.
Clinical judgment factors were the primary reason behind the alleged errors, specifically: failure or delay in ordering a diagnostic test, narrow diagnostic focus with failure to establish a differential diagnosis, failure to appreciate and reconcile relevant symptoms or test results, and failure or delay in obtaining consultation or referral and misinterpretation of diagnostic studies.
“Diagnostic errors are the most common, the most catastrophic, and the most costly of medical errors,” Dr. Newman-Toker said at a press conference July 11. “We know that this is a major problem, at an individual, personal level, but also at a societal level and something we really have to take action toward fixing.”
This study breaks new ground by drilling into the major diseases most commonly associated with diagnostic errors, Dr. Newman-Toker said. In the cancer category, the most common cancers linked to severe harm were lung, breast, colorectal, prostate, and melanoma. In the vascular category, the most common conditions were stroke; myocardial infarction; venous thromboembolism; aortic aneurysm and dissection; and arterial thromboembolism. In the area of infection, sepsis; meningitis and encephalitis; spinal abscess; pneumonia; and endocarditis were the most common infections identified.
The findings provide a starting point to make improvements in the area of medical errors, said Dr. Newman-Toker, president of the Society to Improve Diagnosis in Medicine, an organization that aims to improve diagnosis and eliminate harm from diagnostic error.
“Although diagnostic errors happen everywhere, across all of medicine in every discipline with every disease, we might be able to take a big chunk out of this problem if we save a lot of lives and prevent a lot disability and if we focus some energy on tackling these problems,” he said. “It at least gives us a starting place and a roadmap for how to move the ball forward in this regard.”
The Society to Improve Diagnosis in Medicine has called on Congress to invest more funding into research to address diagnostic errors. Society CEO and cofounder Paul L. Epner noted that the 2019 House appropriations bill proposes not less than $4 million for diagnostic safety and quality research, which is up from $2 million last year.
“It’s a small step, but in the right direction,” Mr. Epner said. “[However,] the federal investment in research remains trivially small in relation to the public burden. That’s why we urge Congress to commit to research funding levels proportionate to the societal cost, in both human lives and in dollars.”
agallegos@mdedge.com
A third of medical malpractice cases associated with patient death or permanent disability result from diagnostic errors by health providers, an analysis finds.
Lead investigator David E. Newman-Toker, MD, PhD, of Johns Hopkins University, Baltimore, and colleagues reviewed malpractice claims during 2006-2015 from medical liability insurer CRICO’s Comparative Benchmarking System database, which represents 30% of all malpractice claims in the United States.
Investigators sought to identify diseases accounting for the majority of serious diagnosis-related harms associated with the claims. Of 55,377 closed claims, researchers identified 11,592 diagnostic error cases, of which 7,379 resulted in high-severity harm.
Of the high-severity claims, 34% stemmed from inaccurate or delayed diagnosis (Diagnosis 2019 Jul 11. doi. org/10.1515/dx-2019-0019).
The majority of diagnostic mistakes (74%) causing the most severe harm were attributable to cancer (38%), vascular events (23%), and infection (14%). These cases resulted in nearly $2 billion in malpractice payouts over a 10-year period, investigators found.
Clinical judgment factors were the primary reason behind the alleged errors, specifically: failure or delay in ordering a diagnostic test, narrow diagnostic focus with failure to establish a differential diagnosis, failure to appreciate and reconcile relevant symptoms or test results, and failure or delay in obtaining consultation or referral and misinterpretation of diagnostic studies.
“Diagnostic errors are the most common, the most catastrophic, and the most costly of medical errors,” Dr. Newman-Toker said at a press conference July 11. “We know that this is a major problem, at an individual, personal level, but also at a societal level and something we really have to take action toward fixing.”
This study breaks new ground by drilling into the major diseases most commonly associated with diagnostic errors, Dr. Newman-Toker said. In the cancer category, the most common cancers linked to severe harm were lung, breast, colorectal, prostate, and melanoma. In the vascular category, the most common conditions were stroke; myocardial infarction; venous thromboembolism; aortic aneurysm and dissection; and arterial thromboembolism. In the area of infection, sepsis; meningitis and encephalitis; spinal abscess; pneumonia; and endocarditis were the most common infections identified.
The findings provide a starting point to make improvements in the area of medical errors, said Dr. Newman-Toker, president of the Society to Improve Diagnosis in Medicine, an organization that aims to improve diagnosis and eliminate harm from diagnostic error.
“Although diagnostic errors happen everywhere, across all of medicine in every discipline with every disease, we might be able to take a big chunk out of this problem if we save a lot of lives and prevent a lot disability and if we focus some energy on tackling these problems,” he said. “It at least gives us a starting place and a roadmap for how to move the ball forward in this regard.”
The Society to Improve Diagnosis in Medicine has called on Congress to invest more funding into research to address diagnostic errors. Society CEO and cofounder Paul L. Epner noted that the 2019 House appropriations bill proposes not less than $4 million for diagnostic safety and quality research, which is up from $2 million last year.
“It’s a small step, but in the right direction,” Mr. Epner said. “[However,] the federal investment in research remains trivially small in relation to the public burden. That’s why we urge Congress to commit to research funding levels proportionate to the societal cost, in both human lives and in dollars.”
agallegos@mdedge.com
FDA pushes for more diversity in clinical trials in draft guidance
Officials at the Food and Drug Administration have issued draft guidance aimed at increasing the diversity of clinical trial populations, including adding children and adolescents earlier in drug development and making trial participation less burdensome for patients.
Despite efforts to enroll clinical trial participants who better reflect a real-world population, “challenges to participation in clinical trials remain, and certain groups continue to be unnecessarily underrepresented in many clinical trials,” the FDA noted in the document’s introduction.
The FDA noted that these challenges could have a significant impact on trial outcomes.
For example, the failure to include complex patients in a clinical trial “may lead to a failure to discover important safety information about the use of the investigational drug in patients who will take the drug after approval.”
In its draft recommendations, the FDA calls on trial sponsors to conduct a closer examination of exclusion criteria and to make it as narrow as possible; consider whether criteria from phase 2 studies, which are restrictive but often transferred to phase 3 protocols, can be eliminated or modified; and consider including children and adolescents when appropriate.
Recommendations related to trial design include characterizing early on the drug metabolism and clearance across populations that may metabolize or clear the drug differently, such as elderly or patients with liver or kidney dysfunction. The agency also called on trial sponsors to use “adaptive clinical trials,” which allow for prespecified trial design changes during the trial, and an early pediatric development program.
Another set of draft recommendations relates to ensuring trial participation is less burdensome for patients by reducing the frequency of study visits and making participants more aware of reimbursement for travel and lodging associated with the trial.
Additionally, the agency is recommending that trial sponsors adopt enrollment and retention practices that enhance inclusiveness, such as ensuring that trial sites include geographic locations with a higher concentration of racial and ethnic minority patients, and holding recruitment events on nights and weekends and in nonclinical locations.
Finally, the FDA issued a set of recommendations to trial sponsors aimed at broadening eligibility criteria when evaluating drugs intended for the treatment of rare diseases. In those trials, the FDA recommended reenrolling participants from early-phase trials in later-phase trials if it can be done safely.
“Because rare diseases often affect small, geographically dispersed patient populations with disease-related travel limitations, special efforts may be necessary to enroll and retain these participants to ensure that a broad spectrum of the patient population is represented,” the agency stated.
At first blush, the draft recommendations are being greeted with a positive response.
“We certainly need more diversity in clinical trial populations, so I think anything that FDA can say that will help encourage that is a good thing,” Richard Schilsky, MD, senior vice president and chief medical officer at the American Society of Clinical Oncology, said in an interview, noting that this new guidance builds off the work that ASCO and Friends of Cancer Research did with the FDA on previous efforts to expand clinical trial populations.
“I think that this new guidance, as best as I can tell, builds off of that, generalizes it across all therapeutic areas and goes a little bit beyond eligibility criteria to other features of clinical trials that may be impediments to patient participation and thereby limit the diversity of the populations in the studies,” he added.
That said, Dr. Schilsky said he welcomed the draft document as a step toward getting broader participation from patients who are more representative of the ultimate users of these treatments.
“All people who could potentially benefit from the trial should have the opportunity to participate as long as it’s safe for them to do so, and they should not be excluded based upon some of these arbitrary structural things,” he said.
“More importantly, we need data on how these new interventions perform in the patients who are seen and treated by doctors every day. We don’t want data just on patients who have no comorbid illnesses, patients who are otherwise perfectly well, patients who could run a marathon before they go to the doctor’s office. Those are generally not the patients that most doctors are seeing. If they are not represented in the trial population, then we are left with having to extrapolate from the trial data to a population for whom there is no information on how to use the treatment,” he added.
Public comments on the draft document are due on Aug. 6.
Officials at the Food and Drug Administration have issued draft guidance aimed at increasing the diversity of clinical trial populations, including adding children and adolescents earlier in drug development and making trial participation less burdensome for patients.
Despite efforts to enroll clinical trial participants who better reflect a real-world population, “challenges to participation in clinical trials remain, and certain groups continue to be unnecessarily underrepresented in many clinical trials,” the FDA noted in the document’s introduction.
The FDA noted that these challenges could have a significant impact on trial outcomes.
For example, the failure to include complex patients in a clinical trial “may lead to a failure to discover important safety information about the use of the investigational drug in patients who will take the drug after approval.”
In its draft recommendations, the FDA calls on trial sponsors to conduct a closer examination of exclusion criteria and to make it as narrow as possible; consider whether criteria from phase 2 studies, which are restrictive but often transferred to phase 3 protocols, can be eliminated or modified; and consider including children and adolescents when appropriate.
Recommendations related to trial design include characterizing early on the drug metabolism and clearance across populations that may metabolize or clear the drug differently, such as elderly or patients with liver or kidney dysfunction. The agency also called on trial sponsors to use “adaptive clinical trials,” which allow for prespecified trial design changes during the trial, and an early pediatric development program.
Another set of draft recommendations relates to ensuring trial participation is less burdensome for patients by reducing the frequency of study visits and making participants more aware of reimbursement for travel and lodging associated with the trial.
Additionally, the agency is recommending that trial sponsors adopt enrollment and retention practices that enhance inclusiveness, such as ensuring that trial sites include geographic locations with a higher concentration of racial and ethnic minority patients, and holding recruitment events on nights and weekends and in nonclinical locations.
Finally, the FDA issued a set of recommendations to trial sponsors aimed at broadening eligibility criteria when evaluating drugs intended for the treatment of rare diseases. In those trials, the FDA recommended reenrolling participants from early-phase trials in later-phase trials if it can be done safely.
“Because rare diseases often affect small, geographically dispersed patient populations with disease-related travel limitations, special efforts may be necessary to enroll and retain these participants to ensure that a broad spectrum of the patient population is represented,” the agency stated.
At first blush, the draft recommendations are being greeted with a positive response.
“We certainly need more diversity in clinical trial populations, so I think anything that FDA can say that will help encourage that is a good thing,” Richard Schilsky, MD, senior vice president and chief medical officer at the American Society of Clinical Oncology, said in an interview, noting that this new guidance builds off the work that ASCO and Friends of Cancer Research did with the FDA on previous efforts to expand clinical trial populations.
“I think that this new guidance, as best as I can tell, builds off of that, generalizes it across all therapeutic areas and goes a little bit beyond eligibility criteria to other features of clinical trials that may be impediments to patient participation and thereby limit the diversity of the populations in the studies,” he added.
That said, Dr. Schilsky said he welcomed the draft document as a step toward getting broader participation from patients who are more representative of the ultimate users of these treatments.
“All people who could potentially benefit from the trial should have the opportunity to participate as long as it’s safe for them to do so, and they should not be excluded based upon some of these arbitrary structural things,” he said.
“More importantly, we need data on how these new interventions perform in the patients who are seen and treated by doctors every day. We don’t want data just on patients who have no comorbid illnesses, patients who are otherwise perfectly well, patients who could run a marathon before they go to the doctor’s office. Those are generally not the patients that most doctors are seeing. If they are not represented in the trial population, then we are left with having to extrapolate from the trial data to a population for whom there is no information on how to use the treatment,” he added.
Public comments on the draft document are due on Aug. 6.
Officials at the Food and Drug Administration have issued draft guidance aimed at increasing the diversity of clinical trial populations, including adding children and adolescents earlier in drug development and making trial participation less burdensome for patients.
Despite efforts to enroll clinical trial participants who better reflect a real-world population, “challenges to participation in clinical trials remain, and certain groups continue to be unnecessarily underrepresented in many clinical trials,” the FDA noted in the document’s introduction.
The FDA noted that these challenges could have a significant impact on trial outcomes.
For example, the failure to include complex patients in a clinical trial “may lead to a failure to discover important safety information about the use of the investigational drug in patients who will take the drug after approval.”
In its draft recommendations, the FDA calls on trial sponsors to conduct a closer examination of exclusion criteria and to make it as narrow as possible; consider whether criteria from phase 2 studies, which are restrictive but often transferred to phase 3 protocols, can be eliminated or modified; and consider including children and adolescents when appropriate.
Recommendations related to trial design include characterizing early on the drug metabolism and clearance across populations that may metabolize or clear the drug differently, such as elderly or patients with liver or kidney dysfunction. The agency also called on trial sponsors to use “adaptive clinical trials,” which allow for prespecified trial design changes during the trial, and an early pediatric development program.
Another set of draft recommendations relates to ensuring trial participation is less burdensome for patients by reducing the frequency of study visits and making participants more aware of reimbursement for travel and lodging associated with the trial.
Additionally, the agency is recommending that trial sponsors adopt enrollment and retention practices that enhance inclusiveness, such as ensuring that trial sites include geographic locations with a higher concentration of racial and ethnic minority patients, and holding recruitment events on nights and weekends and in nonclinical locations.
Finally, the FDA issued a set of recommendations to trial sponsors aimed at broadening eligibility criteria when evaluating drugs intended for the treatment of rare diseases. In those trials, the FDA recommended reenrolling participants from early-phase trials in later-phase trials if it can be done safely.
“Because rare diseases often affect small, geographically dispersed patient populations with disease-related travel limitations, special efforts may be necessary to enroll and retain these participants to ensure that a broad spectrum of the patient population is represented,” the agency stated.
At first blush, the draft recommendations are being greeted with a positive response.
“We certainly need more diversity in clinical trial populations, so I think anything that FDA can say that will help encourage that is a good thing,” Richard Schilsky, MD, senior vice president and chief medical officer at the American Society of Clinical Oncology, said in an interview, noting that this new guidance builds off the work that ASCO and Friends of Cancer Research did with the FDA on previous efforts to expand clinical trial populations.
“I think that this new guidance, as best as I can tell, builds off of that, generalizes it across all therapeutic areas and goes a little bit beyond eligibility criteria to other features of clinical trials that may be impediments to patient participation and thereby limit the diversity of the populations in the studies,” he added.
That said, Dr. Schilsky said he welcomed the draft document as a step toward getting broader participation from patients who are more representative of the ultimate users of these treatments.
“All people who could potentially benefit from the trial should have the opportunity to participate as long as it’s safe for them to do so, and they should not be excluded based upon some of these arbitrary structural things,” he said.
“More importantly, we need data on how these new interventions perform in the patients who are seen and treated by doctors every day. We don’t want data just on patients who have no comorbid illnesses, patients who are otherwise perfectly well, patients who could run a marathon before they go to the doctor’s office. Those are generally not the patients that most doctors are seeing. If they are not represented in the trial population, then we are left with having to extrapolate from the trial data to a population for whom there is no information on how to use the treatment,” he added.
Public comments on the draft document are due on Aug. 6.
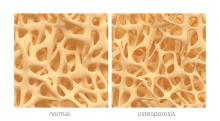
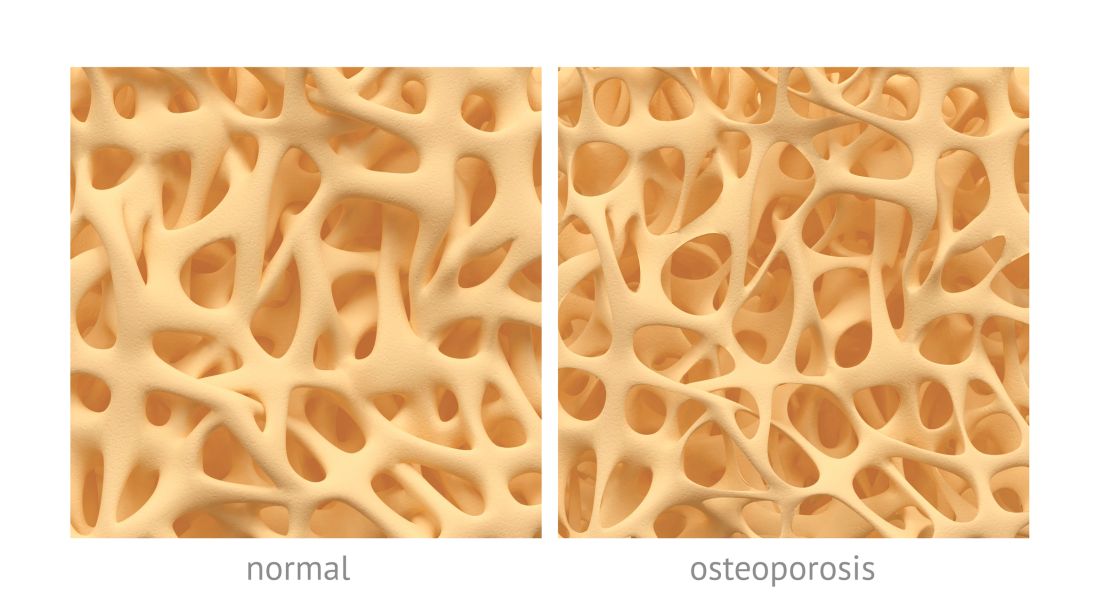
Osteoporosis, osteoarthritis risk high among cerebral palsy patients
compared with adults without the disorder, according to a study published in Bone.
Neil E. O’Connell, PhD, of Brunel University London, and colleagues assessed the risks of osteoporosis, osteoarthritis, and inflammatory musculoskeletal diseases in a population-based cohort study that used data collected by the U.K. Clinical Practice Research Datalink during 1987-2015. The study included 1,705 patients with CP and 5,115 patients matched for age, sex, and general practices; data on smoking status and alcohol consumption for many of the patients also were gathered.
After adjustment for smoking status, alcohol consumption, and mean yearly general practice visits, investigators found evidence of significantly increased risk for osteoarthritis (hazard ratio, 1.54; 95% confidence interval, 1.17-2.02; P = .002) and osteoporosis (HR, 6.19; 95% CI, 3.37-11.39; P less than .001); they did not see increased risk for inflammatory musculoskeletal diseases (HR, 0.89; 95% CI, 0.45-1.75; P = .731).
One limitation of the study is the risk for residual confounding given the investigators could not account for mobility status or physical activity. Other limitations include potential incompleteness of diagnostic code lists, how identification of cases is depending on quality of original recording in the database, and that data regarding smoking status and alcohol consumption were missing for a substantial proportion of patients.
“Despite previous studies identifying a high prevalence of joint pain and functional deterioration among people with CP, there is a dearth of literature on the burden of musculoskeletal disorders in this population,” they wrote. “Further research is required into effective management of these conditions in adults with CP.”
This study was supported by an interdisciplinary award from Brunel University London’s Research Catalyst Fund. The authors declared no competing interests.
SOURCE: O’Connell NE et al. Bone. 2019 Aug;125:30-5.
compared with adults without the disorder, according to a study published in Bone.
Neil E. O’Connell, PhD, of Brunel University London, and colleagues assessed the risks of osteoporosis, osteoarthritis, and inflammatory musculoskeletal diseases in a population-based cohort study that used data collected by the U.K. Clinical Practice Research Datalink during 1987-2015. The study included 1,705 patients with CP and 5,115 patients matched for age, sex, and general practices; data on smoking status and alcohol consumption for many of the patients also were gathered.
After adjustment for smoking status, alcohol consumption, and mean yearly general practice visits, investigators found evidence of significantly increased risk for osteoarthritis (hazard ratio, 1.54; 95% confidence interval, 1.17-2.02; P = .002) and osteoporosis (HR, 6.19; 95% CI, 3.37-11.39; P less than .001); they did not see increased risk for inflammatory musculoskeletal diseases (HR, 0.89; 95% CI, 0.45-1.75; P = .731).
One limitation of the study is the risk for residual confounding given the investigators could not account for mobility status or physical activity. Other limitations include potential incompleteness of diagnostic code lists, how identification of cases is depending on quality of original recording in the database, and that data regarding smoking status and alcohol consumption were missing for a substantial proportion of patients.
“Despite previous studies identifying a high prevalence of joint pain and functional deterioration among people with CP, there is a dearth of literature on the burden of musculoskeletal disorders in this population,” they wrote. “Further research is required into effective management of these conditions in adults with CP.”
This study was supported by an interdisciplinary award from Brunel University London’s Research Catalyst Fund. The authors declared no competing interests.
SOURCE: O’Connell NE et al. Bone. 2019 Aug;125:30-5.
compared with adults without the disorder, according to a study published in Bone.
Neil E. O’Connell, PhD, of Brunel University London, and colleagues assessed the risks of osteoporosis, osteoarthritis, and inflammatory musculoskeletal diseases in a population-based cohort study that used data collected by the U.K. Clinical Practice Research Datalink during 1987-2015. The study included 1,705 patients with CP and 5,115 patients matched for age, sex, and general practices; data on smoking status and alcohol consumption for many of the patients also were gathered.
After adjustment for smoking status, alcohol consumption, and mean yearly general practice visits, investigators found evidence of significantly increased risk for osteoarthritis (hazard ratio, 1.54; 95% confidence interval, 1.17-2.02; P = .002) and osteoporosis (HR, 6.19; 95% CI, 3.37-11.39; P less than .001); they did not see increased risk for inflammatory musculoskeletal diseases (HR, 0.89; 95% CI, 0.45-1.75; P = .731).
One limitation of the study is the risk for residual confounding given the investigators could not account for mobility status or physical activity. Other limitations include potential incompleteness of diagnostic code lists, how identification of cases is depending on quality of original recording in the database, and that data regarding smoking status and alcohol consumption were missing for a substantial proportion of patients.
“Despite previous studies identifying a high prevalence of joint pain and functional deterioration among people with CP, there is a dearth of literature on the burden of musculoskeletal disorders in this population,” they wrote. “Further research is required into effective management of these conditions in adults with CP.”
This study was supported by an interdisciplinary award from Brunel University London’s Research Catalyst Fund. The authors declared no competing interests.
SOURCE: O’Connell NE et al. Bone. 2019 Aug;125:30-5.
FROM BONE
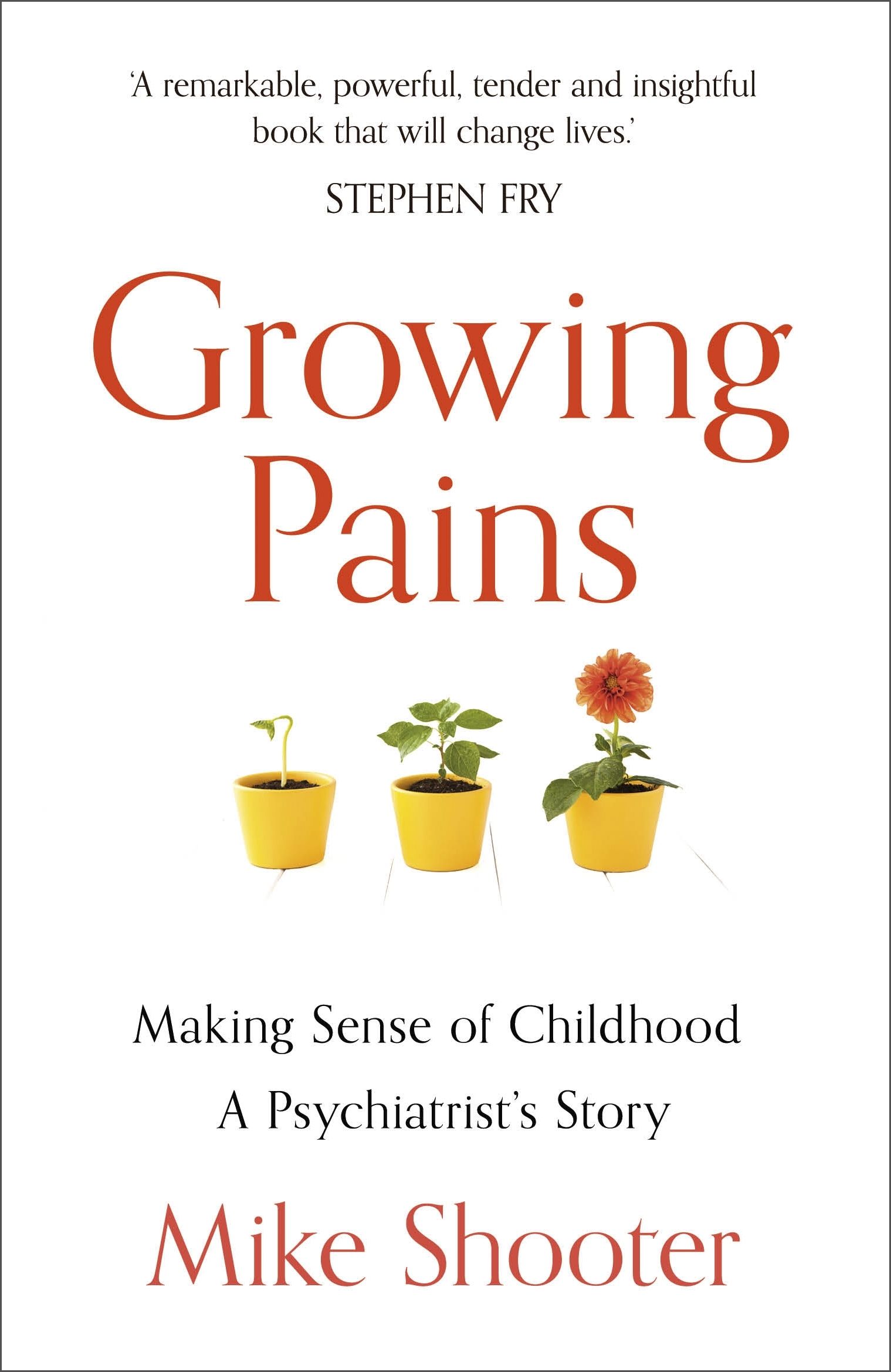
Book Review: The hope that comes from ‘Growing Pains’
You might be surprised by child psychiatrist’s Mike Shooter’s response revealed in his book, “Growing Pains: Making Sense of Childhood: A Psychiatrist’s Story”(London: Hodder & Stoughton, 2018). Rather than hospitalizing this patient, as was done many times before, he makes a bold decision to listen to the group members, who help the patient develop a plan that ultimately leads to greater resiliency.
Dr. Shooter shares many stories about the power of therapy to heal, often visiting patients at their homes to better understand the dynamics of their distress. Stories themselves heal: “It is the job of the therapist to encourage them to reveal their story, to listen to it, and to help them find a better outcome.”
From these stories, we learn about Dr. Shooter’s passion and commitment to his relationship with the child – listening, fostering autonomy, recognizing the power of family systems, working with a multidisciplinary team, and using his own experiences with depression to better help his patients.
Dr. Shooter closes the distance between himself and readers by sharing his own story – his difficult relationship with his strict father, his own uncertainty about his future profession, the deep depression that could have derailed his family life and career, and the treatment that got him back on track.
This book is an excellent read for psychiatrists and other mental health professionals, whether they work with children or adults. It is especially valuable to psychiatrists like me who work with college students – transitional-age youth at the border between childhood and adulthood. Dr. Shooter beautifully describes the societal ills that have contributed to a global rise in child and adolescent mental health problems:
“We live in an ever-more competitive world. To the normal pressures of growing up are added the educational demands to pass more and more exams, a gloominess about the future, and a loss of faith in political processes to put it right; private catastrophes at home and global catastrophes beamed in from all over the world; and a media that’s in love with how to be popular, how to look attractive, and how to be a success.”
The general public would also find this book an interesting glimpse into the world of child psychiatry. The public as well as politicians would benefit from knowing the value child psychiatry can provide at a time when services are underfunded in many countries, including the United States.
This book uses the words of children to highlight the challenges young people face – from bereavement to bullying to abuse. He writes about children on the “margins of margins.” As I read the book, Dr. Shooter reminded me of psychiatrist and author Robert Coles, who taught my favorite college class and wrote about children in crisis from the Appalachians to Africa.
Not surprisingly, Dr. Shooter describes spending time with Dr. Coles at a conference on bereavement. He adheres to the advice Dr. Coles offered, which was to “Listen to what the children say, not what the adults say about them. ... Follow what your gut tells you, not your head.”
In addition to listening to the patient and your gut, Dr. Shooter describes offering hope as another essential element to treatment. He describes giving hope to children of parents who die by suicide, as these children often fear they will meet their parents’ fate. “And they need to know, too, that suicide is not inevitable. … Help is ready and available to stop the children and young people ever getting to that state.”
One element of treatment Dr. Shooter minimally addresses is psychopharmacology, and mostly in a negative way. While he acknowledges that some children genuinely do have attention-deficit/hyperactivity disorder or depression, he feels they are overdiagnosed and thus overtreated with medication. I would have liked to hear more about the times he prescribed medication and how it was integrated into comprehensive care that included therapy and lifestyle changes. I would not want parents reading this book to feel badly if they have supported having their child take medication for a mental health disorder.
Dr. Shooter does make the important point that therapy is often left on the sidelines in current medical systems. Therapy can benefit people of all ages as we face our own “growing pains.” He highlights the “opportunity for growth” that challenges provide, and indeed gives us a great sense of hope in our lives and our work as psychiatrists.
Dr. Morris is an associate professor of psychiatry and associate program director for student health psychiatry at the University of Florida, Gainesville. She is the author of “The Campus Cure: A Parent’s Guide to Mental Health and Wellness for College Students” (Lanham, Md.: Rowman & Littlefield of Lanham, 2018).
You might be surprised by child psychiatrist’s Mike Shooter’s response revealed in his book, “Growing Pains: Making Sense of Childhood: A Psychiatrist’s Story”(London: Hodder & Stoughton, 2018). Rather than hospitalizing this patient, as was done many times before, he makes a bold decision to listen to the group members, who help the patient develop a plan that ultimately leads to greater resiliency.
Dr. Shooter shares many stories about the power of therapy to heal, often visiting patients at their homes to better understand the dynamics of their distress. Stories themselves heal: “It is the job of the therapist to encourage them to reveal their story, to listen to it, and to help them find a better outcome.”
From these stories, we learn about Dr. Shooter’s passion and commitment to his relationship with the child – listening, fostering autonomy, recognizing the power of family systems, working with a multidisciplinary team, and using his own experiences with depression to better help his patients.
Dr. Shooter closes the distance between himself and readers by sharing his own story – his difficult relationship with his strict father, his own uncertainty about his future profession, the deep depression that could have derailed his family life and career, and the treatment that got him back on track.
This book is an excellent read for psychiatrists and other mental health professionals, whether they work with children or adults. It is especially valuable to psychiatrists like me who work with college students – transitional-age youth at the border between childhood and adulthood. Dr. Shooter beautifully describes the societal ills that have contributed to a global rise in child and adolescent mental health problems:
“We live in an ever-more competitive world. To the normal pressures of growing up are added the educational demands to pass more and more exams, a gloominess about the future, and a loss of faith in political processes to put it right; private catastrophes at home and global catastrophes beamed in from all over the world; and a media that’s in love with how to be popular, how to look attractive, and how to be a success.”
The general public would also find this book an interesting glimpse into the world of child psychiatry. The public as well as politicians would benefit from knowing the value child psychiatry can provide at a time when services are underfunded in many countries, including the United States.
This book uses the words of children to highlight the challenges young people face – from bereavement to bullying to abuse. He writes about children on the “margins of margins.” As I read the book, Dr. Shooter reminded me of psychiatrist and author Robert Coles, who taught my favorite college class and wrote about children in crisis from the Appalachians to Africa.
Not surprisingly, Dr. Shooter describes spending time with Dr. Coles at a conference on bereavement. He adheres to the advice Dr. Coles offered, which was to “Listen to what the children say, not what the adults say about them. ... Follow what your gut tells you, not your head.”
In addition to listening to the patient and your gut, Dr. Shooter describes offering hope as another essential element to treatment. He describes giving hope to children of parents who die by suicide, as these children often fear they will meet their parents’ fate. “And they need to know, too, that suicide is not inevitable. … Help is ready and available to stop the children and young people ever getting to that state.”
One element of treatment Dr. Shooter minimally addresses is psychopharmacology, and mostly in a negative way. While he acknowledges that some children genuinely do have attention-deficit/hyperactivity disorder or depression, he feels they are overdiagnosed and thus overtreated with medication. I would have liked to hear more about the times he prescribed medication and how it was integrated into comprehensive care that included therapy and lifestyle changes. I would not want parents reading this book to feel badly if they have supported having their child take medication for a mental health disorder.
Dr. Shooter does make the important point that therapy is often left on the sidelines in current medical systems. Therapy can benefit people of all ages as we face our own “growing pains.” He highlights the “opportunity for growth” that challenges provide, and indeed gives us a great sense of hope in our lives and our work as psychiatrists.
Dr. Morris is an associate professor of psychiatry and associate program director for student health psychiatry at the University of Florida, Gainesville. She is the author of “The Campus Cure: A Parent’s Guide to Mental Health and Wellness for College Students” (Lanham, Md.: Rowman & Littlefield of Lanham, 2018).
You might be surprised by child psychiatrist’s Mike Shooter’s response revealed in his book, “Growing Pains: Making Sense of Childhood: A Psychiatrist’s Story”(London: Hodder & Stoughton, 2018). Rather than hospitalizing this patient, as was done many times before, he makes a bold decision to listen to the group members, who help the patient develop a plan that ultimately leads to greater resiliency.
Dr. Shooter shares many stories about the power of therapy to heal, often visiting patients at their homes to better understand the dynamics of their distress. Stories themselves heal: “It is the job of the therapist to encourage them to reveal their story, to listen to it, and to help them find a better outcome.”
From these stories, we learn about Dr. Shooter’s passion and commitment to his relationship with the child – listening, fostering autonomy, recognizing the power of family systems, working with a multidisciplinary team, and using his own experiences with depression to better help his patients.
Dr. Shooter closes the distance between himself and readers by sharing his own story – his difficult relationship with his strict father, his own uncertainty about his future profession, the deep depression that could have derailed his family life and career, and the treatment that got him back on track.
This book is an excellent read for psychiatrists and other mental health professionals, whether they work with children or adults. It is especially valuable to psychiatrists like me who work with college students – transitional-age youth at the border between childhood and adulthood. Dr. Shooter beautifully describes the societal ills that have contributed to a global rise in child and adolescent mental health problems:
“We live in an ever-more competitive world. To the normal pressures of growing up are added the educational demands to pass more and more exams, a gloominess about the future, and a loss of faith in political processes to put it right; private catastrophes at home and global catastrophes beamed in from all over the world; and a media that’s in love with how to be popular, how to look attractive, and how to be a success.”
The general public would also find this book an interesting glimpse into the world of child psychiatry. The public as well as politicians would benefit from knowing the value child psychiatry can provide at a time when services are underfunded in many countries, including the United States.
This book uses the words of children to highlight the challenges young people face – from bereavement to bullying to abuse. He writes about children on the “margins of margins.” As I read the book, Dr. Shooter reminded me of psychiatrist and author Robert Coles, who taught my favorite college class and wrote about children in crisis from the Appalachians to Africa.
Not surprisingly, Dr. Shooter describes spending time with Dr. Coles at a conference on bereavement. He adheres to the advice Dr. Coles offered, which was to “Listen to what the children say, not what the adults say about them. ... Follow what your gut tells you, not your head.”
In addition to listening to the patient and your gut, Dr. Shooter describes offering hope as another essential element to treatment. He describes giving hope to children of parents who die by suicide, as these children often fear they will meet their parents’ fate. “And they need to know, too, that suicide is not inevitable. … Help is ready and available to stop the children and young people ever getting to that state.”
One element of treatment Dr. Shooter minimally addresses is psychopharmacology, and mostly in a negative way. While he acknowledges that some children genuinely do have attention-deficit/hyperactivity disorder or depression, he feels they are overdiagnosed and thus overtreated with medication. I would have liked to hear more about the times he prescribed medication and how it was integrated into comprehensive care that included therapy and lifestyle changes. I would not want parents reading this book to feel badly if they have supported having their child take medication for a mental health disorder.
Dr. Shooter does make the important point that therapy is often left on the sidelines in current medical systems. Therapy can benefit people of all ages as we face our own “growing pains.” He highlights the “opportunity for growth” that challenges provide, and indeed gives us a great sense of hope in our lives and our work as psychiatrists.
Dr. Morris is an associate professor of psychiatry and associate program director for student health psychiatry at the University of Florida, Gainesville. She is the author of “The Campus Cure: A Parent’s Guide to Mental Health and Wellness for College Students” (Lanham, Md.: Rowman & Littlefield of Lanham, 2018).
Perinatal depression screening improves screening, treatment for postpartum depression
A policy of universal screening of perinatal depression for women receiving prenatal care at an academic medical center led to more regular screening of depression, and made it more likely that women with postpartum depression would be referred for treatment, according to recent research published in Obstetrics & Gynecology.
Emily S. Miller, MD, MPH, at Northwestern University, Chicago, and colleagues performed a retrospective study of 5,127 women receiving prenatal care at the center between 2008 and 2015. They divided the group into those who were at the center before (n = 1,122) and after (n = 4,005) initiation of a policy on universal perinatal depression screening, which consisted of two antenatal screenings at the first prenatal visit and third trimester, and one postpartum screening.
After initiation of the policy, screening increased during the first trimester (0.1% vs. 66%; P less than .001), the third trimester (0% vs. 43%; P less than .001), and at the postpartum visit (70% vs. 90%; P less than .001). Screening continued to increase at both prenatal visits, while screening prevalence remained the same for the postpartum visit. in the post-policy group (30% vs. 65%).
Katrina S. Mark, MD, associate professor of the department of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, said in an interview that the study “brings attention to an incredibly important topic.
“The researchers in this study found that, after implementation of a new policy regarding antenatal and postpartum depression screening, there was a significant increase in women who were screened during and after pregnancy as well as an increase in those who were appropriately treated,” she said. “Importantly, however, their intervention was not only a policy, but also provided education and resources to providers to increase awareness and knowledge surrounding the subject of depression and how to screen and treat this common condition.”
Dr. Miller and colleagues noted their study was limited because they were unable to determine whether prescriptions were filled or if referrals led to actual provider visits. Other obstacles to mental health care in the perinatal period also exist in the form of logistic barriers to appointments and stigma about mental health treatment.
“Depression is common, and screening and treatment during pregnancy and the postpartum period are extremely important to improve maternal and child health. As the authors point out, there has historically been a hesitation among obstetric providers to screen for depression,” Dr. Mark said. “My suspicion is that this hesitation is not because of a lack of awareness, but rather due to a lack of knowledge of what to do when a woman has a positive screen. In my opinion, the take-home message from this study is that implementation of a policy is possible and can lead to real change if it is accompanied by the appropriate resources and education.”
This study was funded by the Maternal-Fetal Medicine/Lumara Health Policy Award, and grants from the Eunice Kennedy Shriver National Institute of Child and Human Development and from the National Institutes of Health’s National Center for Advancing Translational Sciences. The authors reported no conflicts of interest.
SOURCE: Miller ES et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003369.
A policy of universal screening of perinatal depression for women receiving prenatal care at an academic medical center led to more regular screening of depression, and made it more likely that women with postpartum depression would be referred for treatment, according to recent research published in Obstetrics & Gynecology.
Emily S. Miller, MD, MPH, at Northwestern University, Chicago, and colleagues performed a retrospective study of 5,127 women receiving prenatal care at the center between 2008 and 2015. They divided the group into those who were at the center before (n = 1,122) and after (n = 4,005) initiation of a policy on universal perinatal depression screening, which consisted of two antenatal screenings at the first prenatal visit and third trimester, and one postpartum screening.
After initiation of the policy, screening increased during the first trimester (0.1% vs. 66%; P less than .001), the third trimester (0% vs. 43%; P less than .001), and at the postpartum visit (70% vs. 90%; P less than .001). Screening continued to increase at both prenatal visits, while screening prevalence remained the same for the postpartum visit. in the post-policy group (30% vs. 65%).
Katrina S. Mark, MD, associate professor of the department of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, said in an interview that the study “brings attention to an incredibly important topic.
“The researchers in this study found that, after implementation of a new policy regarding antenatal and postpartum depression screening, there was a significant increase in women who were screened during and after pregnancy as well as an increase in those who were appropriately treated,” she said. “Importantly, however, their intervention was not only a policy, but also provided education and resources to providers to increase awareness and knowledge surrounding the subject of depression and how to screen and treat this common condition.”
Dr. Miller and colleagues noted their study was limited because they were unable to determine whether prescriptions were filled or if referrals led to actual provider visits. Other obstacles to mental health care in the perinatal period also exist in the form of logistic barriers to appointments and stigma about mental health treatment.
“Depression is common, and screening and treatment during pregnancy and the postpartum period are extremely important to improve maternal and child health. As the authors point out, there has historically been a hesitation among obstetric providers to screen for depression,” Dr. Mark said. “My suspicion is that this hesitation is not because of a lack of awareness, but rather due to a lack of knowledge of what to do when a woman has a positive screen. In my opinion, the take-home message from this study is that implementation of a policy is possible and can lead to real change if it is accompanied by the appropriate resources and education.”
This study was funded by the Maternal-Fetal Medicine/Lumara Health Policy Award, and grants from the Eunice Kennedy Shriver National Institute of Child and Human Development and from the National Institutes of Health’s National Center for Advancing Translational Sciences. The authors reported no conflicts of interest.
SOURCE: Miller ES et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003369.
A policy of universal screening of perinatal depression for women receiving prenatal care at an academic medical center led to more regular screening of depression, and made it more likely that women with postpartum depression would be referred for treatment, according to recent research published in Obstetrics & Gynecology.
Emily S. Miller, MD, MPH, at Northwestern University, Chicago, and colleagues performed a retrospective study of 5,127 women receiving prenatal care at the center between 2008 and 2015. They divided the group into those who were at the center before (n = 1,122) and after (n = 4,005) initiation of a policy on universal perinatal depression screening, which consisted of two antenatal screenings at the first prenatal visit and third trimester, and one postpartum screening.
After initiation of the policy, screening increased during the first trimester (0.1% vs. 66%; P less than .001), the third trimester (0% vs. 43%; P less than .001), and at the postpartum visit (70% vs. 90%; P less than .001). Screening continued to increase at both prenatal visits, while screening prevalence remained the same for the postpartum visit. in the post-policy group (30% vs. 65%).
Katrina S. Mark, MD, associate professor of the department of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, said in an interview that the study “brings attention to an incredibly important topic.
“The researchers in this study found that, after implementation of a new policy regarding antenatal and postpartum depression screening, there was a significant increase in women who were screened during and after pregnancy as well as an increase in those who were appropriately treated,” she said. “Importantly, however, their intervention was not only a policy, but also provided education and resources to providers to increase awareness and knowledge surrounding the subject of depression and how to screen and treat this common condition.”
Dr. Miller and colleagues noted their study was limited because they were unable to determine whether prescriptions were filled or if referrals led to actual provider visits. Other obstacles to mental health care in the perinatal period also exist in the form of logistic barriers to appointments and stigma about mental health treatment.
“Depression is common, and screening and treatment during pregnancy and the postpartum period are extremely important to improve maternal and child health. As the authors point out, there has historically been a hesitation among obstetric providers to screen for depression,” Dr. Mark said. “My suspicion is that this hesitation is not because of a lack of awareness, but rather due to a lack of knowledge of what to do when a woman has a positive screen. In my opinion, the take-home message from this study is that implementation of a policy is possible and can lead to real change if it is accompanied by the appropriate resources and education.”
This study was funded by the Maternal-Fetal Medicine/Lumara Health Policy Award, and grants from the Eunice Kennedy Shriver National Institute of Child and Human Development and from the National Institutes of Health’s National Center for Advancing Translational Sciences. The authors reported no conflicts of interest.
SOURCE: Miller ES et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003369.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: A policy of universal perinatal screening improved adherence to screening and treatment for women with postpartum depression.
Major finding: After initiation of the policy, screening increased during the first prenatal visit (0.1% vs. 66%), the third trimester (0% vs. 43%), and at a postpartum visit (70% vs. 90%). Women who had a positive result after postpartum depression screening were more than twice as likely to receive treatment or a referral for their depression in the post-policy group (30% vs. 65%).
Study details: A retrospective cohort study of 5,127 women at a single academic center undergoing perinatal care before and after an institutional policy for perinatal depression screening between 2008 and 2015.
Disclosures: This study was funded by the Maternal-Fetal Medicine/Lumara Health Policy Award, and grants from the Eunice Kennedy Shriver National Institute of Child and Human Development and from the National Institutes of Health’s National Center for Advancing Translational Sciences. The authors reported no conflicts of interest.
Source: Miller ES et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003369.
Medication abortion with telemedicine is comparable to in-person visit
Patients who underwent medication abortion under the care of a clinician through a telemedicine service did not have any difference in outcomes, compared with patients who saw a clinician in person, according to a study in Obstetrics & Gynecology.
“To the extent that state bans on telemedicine for abortion rest on arguments of improved patient safety, the findings of this and previous studies do not support such contentions,” Julia E. Kohn, PhD, MPA, from Planned Parenthood Federation of America in New York and colleagues wrote.
Dr. Kohn, with colleagues from Ibis Reproductive Health, Bixby Center for Global Reproductive Health, and the University of California, San Francisco, assessed the outcomes of 5,952 patients who underwent medication abortion either through a telemedicine visit (738 patients) or in-person visit (5,214 patients). In the telemedicine group, the patients took mifepristone in view of the clinician over a secure videoconference platform followed by misoprostol 48 hours later as dispensed by a health center. Patients in the telemedicine group had a slightly older gestational age (50 days), compared with patients in the standard-care group (49 days).
Telemedicine patients received the same on-site care as those patients who saw a clinician in person, including informed consent, lab testing, and ultrasound scans. Patients who received care over telemedicine also received the same follow-up instructions as those who received standard of care, which consisted of an ultrasound evaluation 1-2 weeks after the visit, or human chorionic gonadotropin (hCG) testing.
While telemedicine patients were less likely to follow up at 45 days than were patients who received standard care (60% vs. 77%; prevalence ratio, 0.83; 95% confidence interval, 0.78-0.88), they also were less likely to have an ongoing pregnancy at follow-up (0.5% vs. 1.8%; adjusted odds ratio, 0.23; 95% CI, 0.14–0.39) or undergo an aspiration procedure (1% vs. 5%; aOR, 0.28; 95% CI, 0.17–0.46) than were standard-of-care patients. With regard to adverse events, the rate was less than 1% for each group, and the researchers reported no maternal deaths in either group.
Eve Espey, MD, MPH, professor and chair of the department of obstetrics and gynecology and director of the family planning fellowship at the University of New Mexico, Albuquerque, commented that this study expands the evidence of positive outcomes of telemedicine abortion to four new states: Alaska, Idaho, Nevada, and Washington.
“Abortion access is limited in the large rural states in which the study was conducted; across the country, abortion access is increasingly limited by restrictive legislation including telemedicine abortion bans,” she said in an interview. “This reassuring study helps demonstrate the safety of telemedicine medication abortion and highlights the role of telemedicine in improving health equity by increasing access to a critical health care service.”
The researchers said the results were limited in that most telemedicine care was centered in one state, Nevada, and the sample size was inadequate to do per-state comparisons of in-person visits and telemedicine. In addition, follow-up data was available for 75% of patients, which meant approximately one-fourth of patients did not follow up with the health center.
The Susan T. Buffett Foundation provided a grant for this study. Dr. Grossman receives consulting payments from Planned Parenthood Federation of America for work related to telemedicine for medication abortion. The other authors reported no relevant conflicts of interest.
SOURCE: Kohn JE et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003357.
Patients who underwent medication abortion under the care of a clinician through a telemedicine service did not have any difference in outcomes, compared with patients who saw a clinician in person, according to a study in Obstetrics & Gynecology.
“To the extent that state bans on telemedicine for abortion rest on arguments of improved patient safety, the findings of this and previous studies do not support such contentions,” Julia E. Kohn, PhD, MPA, from Planned Parenthood Federation of America in New York and colleagues wrote.
Dr. Kohn, with colleagues from Ibis Reproductive Health, Bixby Center for Global Reproductive Health, and the University of California, San Francisco, assessed the outcomes of 5,952 patients who underwent medication abortion either through a telemedicine visit (738 patients) or in-person visit (5,214 patients). In the telemedicine group, the patients took mifepristone in view of the clinician over a secure videoconference platform followed by misoprostol 48 hours later as dispensed by a health center. Patients in the telemedicine group had a slightly older gestational age (50 days), compared with patients in the standard-care group (49 days).
Telemedicine patients received the same on-site care as those patients who saw a clinician in person, including informed consent, lab testing, and ultrasound scans. Patients who received care over telemedicine also received the same follow-up instructions as those who received standard of care, which consisted of an ultrasound evaluation 1-2 weeks after the visit, or human chorionic gonadotropin (hCG) testing.
While telemedicine patients were less likely to follow up at 45 days than were patients who received standard care (60% vs. 77%; prevalence ratio, 0.83; 95% confidence interval, 0.78-0.88), they also were less likely to have an ongoing pregnancy at follow-up (0.5% vs. 1.8%; adjusted odds ratio, 0.23; 95% CI, 0.14–0.39) or undergo an aspiration procedure (1% vs. 5%; aOR, 0.28; 95% CI, 0.17–0.46) than were standard-of-care patients. With regard to adverse events, the rate was less than 1% for each group, and the researchers reported no maternal deaths in either group.
Eve Espey, MD, MPH, professor and chair of the department of obstetrics and gynecology and director of the family planning fellowship at the University of New Mexico, Albuquerque, commented that this study expands the evidence of positive outcomes of telemedicine abortion to four new states: Alaska, Idaho, Nevada, and Washington.
“Abortion access is limited in the large rural states in which the study was conducted; across the country, abortion access is increasingly limited by restrictive legislation including telemedicine abortion bans,” she said in an interview. “This reassuring study helps demonstrate the safety of telemedicine medication abortion and highlights the role of telemedicine in improving health equity by increasing access to a critical health care service.”
The researchers said the results were limited in that most telemedicine care was centered in one state, Nevada, and the sample size was inadequate to do per-state comparisons of in-person visits and telemedicine. In addition, follow-up data was available for 75% of patients, which meant approximately one-fourth of patients did not follow up with the health center.
The Susan T. Buffett Foundation provided a grant for this study. Dr. Grossman receives consulting payments from Planned Parenthood Federation of America for work related to telemedicine for medication abortion. The other authors reported no relevant conflicts of interest.
SOURCE: Kohn JE et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003357.
Patients who underwent medication abortion under the care of a clinician through a telemedicine service did not have any difference in outcomes, compared with patients who saw a clinician in person, according to a study in Obstetrics & Gynecology.
“To the extent that state bans on telemedicine for abortion rest on arguments of improved patient safety, the findings of this and previous studies do not support such contentions,” Julia E. Kohn, PhD, MPA, from Planned Parenthood Federation of America in New York and colleagues wrote.
Dr. Kohn, with colleagues from Ibis Reproductive Health, Bixby Center for Global Reproductive Health, and the University of California, San Francisco, assessed the outcomes of 5,952 patients who underwent medication abortion either through a telemedicine visit (738 patients) or in-person visit (5,214 patients). In the telemedicine group, the patients took mifepristone in view of the clinician over a secure videoconference platform followed by misoprostol 48 hours later as dispensed by a health center. Patients in the telemedicine group had a slightly older gestational age (50 days), compared with patients in the standard-care group (49 days).
Telemedicine patients received the same on-site care as those patients who saw a clinician in person, including informed consent, lab testing, and ultrasound scans. Patients who received care over telemedicine also received the same follow-up instructions as those who received standard of care, which consisted of an ultrasound evaluation 1-2 weeks after the visit, or human chorionic gonadotropin (hCG) testing.
While telemedicine patients were less likely to follow up at 45 days than were patients who received standard care (60% vs. 77%; prevalence ratio, 0.83; 95% confidence interval, 0.78-0.88), they also were less likely to have an ongoing pregnancy at follow-up (0.5% vs. 1.8%; adjusted odds ratio, 0.23; 95% CI, 0.14–0.39) or undergo an aspiration procedure (1% vs. 5%; aOR, 0.28; 95% CI, 0.17–0.46) than were standard-of-care patients. With regard to adverse events, the rate was less than 1% for each group, and the researchers reported no maternal deaths in either group.
Eve Espey, MD, MPH, professor and chair of the department of obstetrics and gynecology and director of the family planning fellowship at the University of New Mexico, Albuquerque, commented that this study expands the evidence of positive outcomes of telemedicine abortion to four new states: Alaska, Idaho, Nevada, and Washington.
“Abortion access is limited in the large rural states in which the study was conducted; across the country, abortion access is increasingly limited by restrictive legislation including telemedicine abortion bans,” she said in an interview. “This reassuring study helps demonstrate the safety of telemedicine medication abortion and highlights the role of telemedicine in improving health equity by increasing access to a critical health care service.”
The researchers said the results were limited in that most telemedicine care was centered in one state, Nevada, and the sample size was inadequate to do per-state comparisons of in-person visits and telemedicine. In addition, follow-up data was available for 75% of patients, which meant approximately one-fourth of patients did not follow up with the health center.
The Susan T. Buffett Foundation provided a grant for this study. Dr. Grossman receives consulting payments from Planned Parenthood Federation of America for work related to telemedicine for medication abortion. The other authors reported no relevant conflicts of interest.
SOURCE: Kohn JE et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003357.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: Telemedicine patients were less likely to have an ongoing pregnancy at follow-up (0.5% vs. 1.8%; adjusted odds ratio, 0.23; 95% confidence interval, 0.14–0.39) or undergo an aspiration procedure (1% vs. 5%; aOR, 0.28; 95% CI, 0.17–0.46) than standard-of-care patients.
Study details: A retrospective cohort study of 5,932 patients who underwent medical abortion at Planned Parenthood health centers in Alaska, Idaho, Nevada, and Washington.
Disclosures: The Susan T. Buffett Foundation provided a grant for this study. Dr. Grossman receives consulting payments from Planned Parenthood Federation of America for work related to telemedicine for medication abortion. The other authors reported no relevant conflicts of interest.
Source: Kohn JE et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003357.
Endoscopic treatment effective in T1b esophageal cancer
Findings from a systematic review may help guide treatment of patients with T1b esophageal cancer.
The review suggests that endoscopic submucosal dissection and endoscopic mucosal resection are appropriate for T1b esophageal cancers with a low risk of metastasis. The authors identified several factors associated with a higher risk of lymph node metastasis and said patients with these risk factors may benefit from adjuvant chemotherapy and radiation.
Mohamed O. Othman, MD, of Baylor College of Medicine, Houston, and colleagues conducted the review. Their report is in Clinical Gastroenterology and Hepatology.
The authors cited studies suggesting that survival rates are not significantly different among early-stage esophageal cancer patients who undergo esophagectomy and those who receive endoscopic treatment (Am J Gastroenterol. 2008;103:1340-5, Gastric Cancer. 2017;20:84-91).
However, studies have indicated that patients with submucosal invasion and an increased risk of metastasis may fare better when endoscopic treatment is combined with chemoradiation (Clin Transl Gastroenterol. 2017;8:e110, Radiat Oncol. 2015;10:31).
With that in mind, the authors described several factors associated with a higher risk of lymph node metastasis in T1b tumors.
First, the risk of lymph node metastasis is higher in esophageal squamous cell carcinoma (ESCC) than in esophageal adenocarcinoma (EAC). The risk is also higher in patients with deeper submucosal invasion (greater than 200 mcm for ESCC or greater than 500 mcm for EAC).
In fact, research suggested the risk of lymph node metastasis is:
- 27% in SM1 ESCC and 6% in SM1 EAC
- 36% in SM2 ESCC and 23% in SM2 EAC
- 55% in SM3 ESCC and 58% in SM3 EAC (Expert Rev Gastroenterol Hepatol. 2011;5:371-84).
Patients also have a higher risk of lymph node metastasis if they have Paris type 0-I protruded lesions or Paris type 0-III excavated lesions. Research suggested that, in ESCC, these lesions confer the highest risk of deep mucosal invasion — 79% for type 0-I protruded lesions and 84% for type 0-III excavated lesions (Surgery 1998;123:432-9).
An additional factor associated with a higher risk of lymph node metastasis in ESCC is type B microvessels. Researchers found that type B vessels could estimate the depth of invasion with 90.5% accuracy (Esophagus 2017;14:105-112).
Patients with poorly differentiated tumors, tumors larger than 2 cm, or lymphovascular invasion have a higher risk of lymph node metastasis as well.
In a study of 782 patients who underwent esophagectomy, those with poorly differentiated tumors and/or tumors larger than 2 cm had a higher rate of lymph node metastasis (Ann Surg Oncol 2018;25:318-25). And in a study of 90 patients with resected T1 EAC, lymphovascular invasion was significantly associated with tumor recurrence and overall survival (Am J Surg Pathol 2005;29:1079-85).
Research has also suggested that immunohistochemistry markers, such as E-cadherin and cyclin D1, are associated with a higher risk of lymph node metastasis (J Surg Oncol 2002;79:166-73).
“Future research should focus on novel biological and immunohistochemistry markers which can aid in the prediction of tumor behavior and lymph node metastasis status in T1b esophageal cancer,” Dr. Othman and colleagues concluded.
The authors disclosed relationships with Olympus, Boston Scientific, Lumendi, Aries Pharmaceutical, and Fujinon.
SOURCE: Othman MO et al. Clin Gastroenterol Hepatol 2019. doi: 10.1016/j.cgh.2019.05.045.
Findings from a systematic review may help guide treatment of patients with T1b esophageal cancer.
The review suggests that endoscopic submucosal dissection and endoscopic mucosal resection are appropriate for T1b esophageal cancers with a low risk of metastasis. The authors identified several factors associated with a higher risk of lymph node metastasis and said patients with these risk factors may benefit from adjuvant chemotherapy and radiation.
Mohamed O. Othman, MD, of Baylor College of Medicine, Houston, and colleagues conducted the review. Their report is in Clinical Gastroenterology and Hepatology.
The authors cited studies suggesting that survival rates are not significantly different among early-stage esophageal cancer patients who undergo esophagectomy and those who receive endoscopic treatment (Am J Gastroenterol. 2008;103:1340-5, Gastric Cancer. 2017;20:84-91).
However, studies have indicated that patients with submucosal invasion and an increased risk of metastasis may fare better when endoscopic treatment is combined with chemoradiation (Clin Transl Gastroenterol. 2017;8:e110, Radiat Oncol. 2015;10:31).
With that in mind, the authors described several factors associated with a higher risk of lymph node metastasis in T1b tumors.
First, the risk of lymph node metastasis is higher in esophageal squamous cell carcinoma (ESCC) than in esophageal adenocarcinoma (EAC). The risk is also higher in patients with deeper submucosal invasion (greater than 200 mcm for ESCC or greater than 500 mcm for EAC).
In fact, research suggested the risk of lymph node metastasis is:
- 27% in SM1 ESCC and 6% in SM1 EAC
- 36% in SM2 ESCC and 23% in SM2 EAC
- 55% in SM3 ESCC and 58% in SM3 EAC (Expert Rev Gastroenterol Hepatol. 2011;5:371-84).
Patients also have a higher risk of lymph node metastasis if they have Paris type 0-I protruded lesions or Paris type 0-III excavated lesions. Research suggested that, in ESCC, these lesions confer the highest risk of deep mucosal invasion — 79% for type 0-I protruded lesions and 84% for type 0-III excavated lesions (Surgery 1998;123:432-9).
An additional factor associated with a higher risk of lymph node metastasis in ESCC is type B microvessels. Researchers found that type B vessels could estimate the depth of invasion with 90.5% accuracy (Esophagus 2017;14:105-112).
Patients with poorly differentiated tumors, tumors larger than 2 cm, or lymphovascular invasion have a higher risk of lymph node metastasis as well.
In a study of 782 patients who underwent esophagectomy, those with poorly differentiated tumors and/or tumors larger than 2 cm had a higher rate of lymph node metastasis (Ann Surg Oncol 2018;25:318-25). And in a study of 90 patients with resected T1 EAC, lymphovascular invasion was significantly associated with tumor recurrence and overall survival (Am J Surg Pathol 2005;29:1079-85).
Research has also suggested that immunohistochemistry markers, such as E-cadherin and cyclin D1, are associated with a higher risk of lymph node metastasis (J Surg Oncol 2002;79:166-73).
“Future research should focus on novel biological and immunohistochemistry markers which can aid in the prediction of tumor behavior and lymph node metastasis status in T1b esophageal cancer,” Dr. Othman and colleagues concluded.
The authors disclosed relationships with Olympus, Boston Scientific, Lumendi, Aries Pharmaceutical, and Fujinon.
SOURCE: Othman MO et al. Clin Gastroenterol Hepatol 2019. doi: 10.1016/j.cgh.2019.05.045.
Findings from a systematic review may help guide treatment of patients with T1b esophageal cancer.
The review suggests that endoscopic submucosal dissection and endoscopic mucosal resection are appropriate for T1b esophageal cancers with a low risk of metastasis. The authors identified several factors associated with a higher risk of lymph node metastasis and said patients with these risk factors may benefit from adjuvant chemotherapy and radiation.
Mohamed O. Othman, MD, of Baylor College of Medicine, Houston, and colleagues conducted the review. Their report is in Clinical Gastroenterology and Hepatology.
The authors cited studies suggesting that survival rates are not significantly different among early-stage esophageal cancer patients who undergo esophagectomy and those who receive endoscopic treatment (Am J Gastroenterol. 2008;103:1340-5, Gastric Cancer. 2017;20:84-91).
However, studies have indicated that patients with submucosal invasion and an increased risk of metastasis may fare better when endoscopic treatment is combined with chemoradiation (Clin Transl Gastroenterol. 2017;8:e110, Radiat Oncol. 2015;10:31).
With that in mind, the authors described several factors associated with a higher risk of lymph node metastasis in T1b tumors.
First, the risk of lymph node metastasis is higher in esophageal squamous cell carcinoma (ESCC) than in esophageal adenocarcinoma (EAC). The risk is also higher in patients with deeper submucosal invasion (greater than 200 mcm for ESCC or greater than 500 mcm for EAC).
In fact, research suggested the risk of lymph node metastasis is:
- 27% in SM1 ESCC and 6% in SM1 EAC
- 36% in SM2 ESCC and 23% in SM2 EAC
- 55% in SM3 ESCC and 58% in SM3 EAC (Expert Rev Gastroenterol Hepatol. 2011;5:371-84).
Patients also have a higher risk of lymph node metastasis if they have Paris type 0-I protruded lesions or Paris type 0-III excavated lesions. Research suggested that, in ESCC, these lesions confer the highest risk of deep mucosal invasion — 79% for type 0-I protruded lesions and 84% for type 0-III excavated lesions (Surgery 1998;123:432-9).
An additional factor associated with a higher risk of lymph node metastasis in ESCC is type B microvessels. Researchers found that type B vessels could estimate the depth of invasion with 90.5% accuracy (Esophagus 2017;14:105-112).
Patients with poorly differentiated tumors, tumors larger than 2 cm, or lymphovascular invasion have a higher risk of lymph node metastasis as well.
In a study of 782 patients who underwent esophagectomy, those with poorly differentiated tumors and/or tumors larger than 2 cm had a higher rate of lymph node metastasis (Ann Surg Oncol 2018;25:318-25). And in a study of 90 patients with resected T1 EAC, lymphovascular invasion was significantly associated with tumor recurrence and overall survival (Am J Surg Pathol 2005;29:1079-85).
Research has also suggested that immunohistochemistry markers, such as E-cadherin and cyclin D1, are associated with a higher risk of lymph node metastasis (J Surg Oncol 2002;79:166-73).
“Future research should focus on novel biological and immunohistochemistry markers which can aid in the prediction of tumor behavior and lymph node metastasis status in T1b esophageal cancer,” Dr. Othman and colleagues concluded.
The authors disclosed relationships with Olympus, Boston Scientific, Lumendi, Aries Pharmaceutical, and Fujinon.
SOURCE: Othman MO et al. Clin Gastroenterol Hepatol 2019. doi: 10.1016/j.cgh.2019.05.045.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY