User login
Treating the pregnant patient with opioid addiction
OBG Management : How has the opioid crisis affected women in general?
Mishka Terplan, MD: Everyone is aware that we are experiencing a massive opioid crisis in the United States, and from a historical perspective, this is at least the third or fourth significant opioid epidemic in our nation’s history.1 It is similar in some ways to the very first one, which also featured a large proportion of women and also was driven initially by physician prescribing practices. However, the magnitude of this crisis is unparalleled compared with prior opioid epidemics.
There are lots of reasons why women are overrepresented in this crisis. There are gender-based differences in pain—chronic pain syndromes are more common in women. In addition, we have a gender bias in prescribing opioids and prescribe more opioids to women (especially older women) than to men. Cultural differences also contribute. As providers, we tend not to think of women as people who use drugs or people who develop addictions the same way as we think of these risks and behaviors for men. Therefore, compared with men, we are less likely to screen, assess, or refer women for substance use, misuse, and addiction. All of this adds up to creating a crisis in which women are increasingly the face of the epidemic.
OBG Management : What are the concerns about opioid addiction and pregnant women specifically?
Dr. Terplan: Addiction is a chronic condition, just like diabetes or depression, and the same principles that we think of in terms of optimizing maternal and newborn health apply to addiction. Ideally, we want, for women with chronic diseases to have stable disease at the time of conception and through pregnancy. We know this maximizes birth outcomes.
Unfortunately, there is a massive treatment gap in the United States. Most people with addiction receive no treatment. Only 11% of people with a substance use disorder report receipt of treatment. By contrast, more than 70% of people with depression, hypertension, or diabetes receive care. This treatment gap is also present in pregnancy. Among use disorders, treatment receipt is highest for opioid use disorder; however, nationally, at best, 25% of pregnant women with opioid addiction receive any care.
In other words, when we encounter addiction clinically, it is often untreated addiction. Therefore, many times providers will have women presenting to care who are both pregnant and have untreated addiction. From both a public health and a clinical practice perspective, the salient distinction is not between people with addiction and those without but between people with treated disease and people with untreated disease.
Untreated addiction is a serious medical condition. It is associated with preterm delivery and low birth weight infants. It is associated with acquisition and transmission of HIV and hepatitis C. It is associated with overdose and overdose death. By contrast, treated addiction is associated with term delivery and normal weight infants. Pharmacotherapies for opioid use disorder stabilize the intrauterine environment and allow for normal fetal growth. Pharmacotherapies for opioid use disorder help to structure and stabilize the mom’s social circumstance, providing a platform to deliver prenatal care and essential social services. And pharmacotherapies for opioid use disorder protect women and their fetuses from overdose and from overdose deaths. The goal of management of addiction in pregnancy is treatment of the underlying condition, treating the addiction.
Continue to: OBG Management...
OBG Management : What should the ObGyn do when faced with a patient who might have an addiction?
Dr. Terplan: The good news is that there are lots of recently published guidance documents from the World Health Organization,2 the American College of Obstetricians and Gynecologists (ACOG),3 and the Substance Abuse and Mental Health Services Administration (SAMHSA),4 and there have been a whole series of trainings throughout the United States organized by both ACOG and SAMHSA.
There is also a collaboration between ACOG and the American Society of Addiction Medicine (ASAM) to provide buprenorphine waiver trainings specifically designed for ObGyns. Check both the ACOG and ASAM pages for details. I encourage every provider to get a waiver to prescribe buprenorphine. There are about 30 ObGyns who are also board certified in addiction medicine in the United States, and all of us are more than happy to help our colleagues in the clinical care of this population, a population that all of us really enjoy taking care of.
Although care in pregnancy is important, we must not forget about the postpartum period. Generally speaking, women do quite well during pregnancy in terms of treatment. Postpartum, however, is a vulnerable period, where relapse happens, where gaps in care happen, where child welfare involvement and sometimes child removal happens, which can be very stressful for anyone much less somebody with a substance use disorder. Recent data demonstrate that one of the leading causes of maternal mortality in the US in from overdose, and most of these deaths occur in the postpartum period.5 Regardless of what happens during pregnancy, it is essential that we be able to link and continue care for women with opioid use disorder throughout the postpartum period.
OBG Management : How do you treat opioid use disorder in pregnancy?
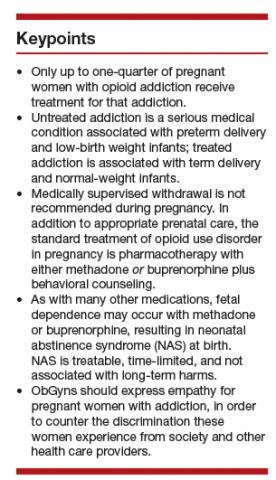
Dr. Terplan: The standard of care for treatment of opioid use disorder in pregnancy is pharmacotherapy with either methadone or buprenorphine (TABLE) plus behavioral counseling—ideally, co-located with prenatal care. The evidence base for pharmacotherapy for opioid use disorder in pregnancy is supported by every single professional society that has ever issued guidance on this, from the World Health Organization to ACOG, to ASAM, to the Royal College in the UK as well as Canadian and Australian obstetrics and gynecology societies; literally every single professional society supports medication.
The core principle of maternal fetal medicine rests upon the fact that chronic conditions need to be treated and that treated illness improves birth outcomes. For both maternal and fetal health, treated addiction is way better than untreated addiction. One concern people have regarding methadone and buprenorphine is the development of dependence. Dependence is a physiologic effect of medication and occurs with opioids, as well as with many other medications, such as antidepressants and most hypertensive agents. For the fetus, dependence means that at the time of delivery, the infant may go into withdrawal, which is also called neonatal abstinence syndrome. Neonatal abstinence syndrome is an expected outcome of in-utero opioid exposure. It is a time-limited and treatable condition. Prospective data do not demonstrate any long-term harms among infants whose mothers received pharmacotherapy for opioid use disorder during pregnancy.6
The treatment for neonatal abstinence syndrome is costly, especially when in a neonatal intensive care unit. It can be quite concerning to a new mother to have an infant that has to spend extra time in the hospital and sometimes be medicated for management of withdrawal.
There has been a renewed interest amongst ObGyns in investigating medically-supervised withdrawal during pregnancy. Although there are remaining questions, overall, the literature does not support withdrawal during pregnancy—mostly because withdrawal is associated with relapse, and relapse is associated with cessation of care (both prenatal care and addiction treatment), acquisition and transmission of HIV and Hepatitis C, and overdose and overdose death. The pertinent clinical and public health goal is the treatment of the chronic condition of addiction during pregnancy. The standard of care remains pharmacotherapy plus behavioral counseling for the treatment of opioid use disorder in pregnancy.
Clinical care, however, is both evidence-based and person-centered. All of us who have worked in this field, long before there was attention to the opioid crisis, all of us have provided medically-supervised withdrawal of a pregnant person, and that is because we understand the principles of care. When evidence-based care conflicts with person-centered care, the ethical course is the provision of person-centered care. Patients have the right of refusal. If someone wants to discontinue medication, I have tapered the medication during pregnancy, but continued to provide (and often increase) behavioral counseling and prenatal care.
Treated addiction is better for the fetus than untreated addiction. Untreated opioid addiction is associated with preterm birth and low birth weight. These obstetric risks are not because of the opioid per se, but because of the repeated cycles of withdrawal that an individual with untreated addiction experiences. People with untreated addiction are not getting “high” when they use, they are just becoming a little bit less sick. It is this repeated cycle of withdrawal that stresses the fetus, which leads to preterm delivery and low birth weight.
Medications for opioid use disorder are long-acting and dosed daily. In contrast to the repeated cycles of fetal withdrawal in untreated addiction, pharmacotherapy stabilizes the intrauterine environment. There is no cyclic, repeated, stressful withdrawal, and consequentially, the fetus grows normally and delivers at term. Obstetric risk is from repeated cyclic withdrawal more than from opioid exposure itself.
Continue to: OBG Management...
OBG Management : Research reports that women are not using all of the opioids that are prescribed to them after a cesarean delivery. What are the risks for addiction in this setting?
Dr. Terplan: I mark a distinction between use (ie, using something as prescribed) and misuse, which means using a prescribed medication not in the manner in which it was prescribed, or using somebody else’s medications, or using an illicit substance. And I differentiate use and misuse from addiction, which is a behavioral condition, a disease. There has been a lot of attention paid to opioid prescribing in general and in particular postdelivery and post–cesarean delivery, which is one of the most common operative procedures in the United States.
It seems clear from the literature that we have overprescribed opioids postdelivery, and a small number of women, about 1 in 300 will continue an opioid script.7 This means that 1 in 300 women who received an opioid prescription following delivery present for care and get another opioid prescription filled. Now, that is a small number at the level of the individual, but because we do so many cesarean deliveries, this is a large number of women at the level of the population. This does not mean, however, that 1 in 300 women who received opioids after cesarean delivery are going to become addicted to them. It just means that 1 in 300 will continue the prescription. Prescription continuation is a risk factor for opioid misuse, and opioid misuse is on the pathway toward addiction.
Most people who use substances do not develop an addiction to that substance. We know from the opioid literature that at most only 10% of people who receive chronic opioid therapy will meet criteria for opioid use disorder.8 Now 10% is not 100%, nor is it 0%, but because we prescribed so many opioids to so many people for so long, the absolute number of people with opioid use disorder from physician opioid prescribing is large, even though the risk at the level of the individual is not as large as people think.
OBG Management : From your experience in treating addiction during pregnancy, are there clinical pearls you would like to share with ObGyns?
Dr. Terplan: There are a couple of takeaways. One is that all women are motivated to maximize their health and that of their baby to be, and every pregnant woman engages in behavioral change; in fact most women quit or cutback substance use during pregnancy. But some can’t. Those that can’t likely have a substance use disorder. We think of addiction as a chronic condition, centered in the brain, but the primary symptoms of addiction are behaviors. The salient feature of addiction is continued use despite adverse consequences; using something that you know is harming yourself and others but you can’t stop using it. In other words, continuing substance use during pregnancy. When we see clinically a pregnant woman who is using a substance, 99% of the time we are seeing a pregnant woman who has the condition of addiction, and what she needs is treatment. She does not need to be told that injecting heroin is unsafe for her and her fetus, she knows that. What she needs is treatment.
The second point is that pregnant women who use drugs and pregnant women with addiction experience a real specific and strong form of discrimination by providers, by other people with addiction, by the legal system, and by their friends and families. Caring for people who have substance use disorder is grounded in human rights, which means treating people with dignity and respect. It is important for providers to have empathy, especially for pregnant people who use drugs, to counter the discrimination they experience from society and from other health care providers.
Continue to: OBG Management...
OBG Management : Are there specific ways in which ObGyns can show empathy when speaking with a pregnant woman who likely has addiction?
Dr. Terplan: In general when we talk to people about drug use, it is important to ask their permission to talk about it. For example, “Is it okay if I ask you some questions about smoking, drinking, and other drugs?” If someone says, “No, I don’t want you to ask those questions,” we have to respect that. Assessment of substance use should be a universal part of all medical care, as substance use, misuse, and addiction are essential domains of wellness, but I think we should ask permission before screening.
One of the really good things about prenatal care is that people come back; we have multiple visits across the gestational period. The behavioral work of addiction treatment rests upon a strong therapeutic alliance. If you do not respect your patient, then there is no way you can achieve a therapeutic alliance. Asking permission, and then respecting somebody’s answers, I think goes a really long way to establishing a strong therapeutic alliance, which is the basis of any medical care.
- Terplan M. Women and the opioid crisis: historical context and public health solutions. Fertil Steril. 2017;108:195-199.
- Management of substance abuse. World Health Organization website. https://www.who.int/substance_abuse/activities/treatment_opioid_dependence/en/. Accessed March 20, 2019.
- Committee on Obstetric Practice. Committee Opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
- Substance Abuse and Mental Health Services Administration. Clinical guidance for treating pregnant and parenting women with opioid use disorder and their infants. HHS Publication No. (SMA) 18-5054. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2018.
- Metz TD, Royner P, Hoffman MC, et al. Maternal deaths from suicide and overdose in Colorado, 2004-2012. Obstet Gynecol. 2016;128:1233-1240.
- Kaltenbach K, O’Grady E, Heil SH, et al. Prenatal exposure to methadone or buprenorphine: early childhood developmental outcomes. Drug Alcohol Depend. 2018;185:40-49.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naive women. Am J Obstet Gynecol. 2016;215:353.e1-353.e18.
OBG Management : How has the opioid crisis affected women in general?
Mishka Terplan, MD: Everyone is aware that we are experiencing a massive opioid crisis in the United States, and from a historical perspective, this is at least the third or fourth significant opioid epidemic in our nation’s history.1 It is similar in some ways to the very first one, which also featured a large proportion of women and also was driven initially by physician prescribing practices. However, the magnitude of this crisis is unparalleled compared with prior opioid epidemics.
There are lots of reasons why women are overrepresented in this crisis. There are gender-based differences in pain—chronic pain syndromes are more common in women. In addition, we have a gender bias in prescribing opioids and prescribe more opioids to women (especially older women) than to men. Cultural differences also contribute. As providers, we tend not to think of women as people who use drugs or people who develop addictions the same way as we think of these risks and behaviors for men. Therefore, compared with men, we are less likely to screen, assess, or refer women for substance use, misuse, and addiction. All of this adds up to creating a crisis in which women are increasingly the face of the epidemic.
OBG Management : What are the concerns about opioid addiction and pregnant women specifically?
Dr. Terplan: Addiction is a chronic condition, just like diabetes or depression, and the same principles that we think of in terms of optimizing maternal and newborn health apply to addiction. Ideally, we want, for women with chronic diseases to have stable disease at the time of conception and through pregnancy. We know this maximizes birth outcomes.
Unfortunately, there is a massive treatment gap in the United States. Most people with addiction receive no treatment. Only 11% of people with a substance use disorder report receipt of treatment. By contrast, more than 70% of people with depression, hypertension, or diabetes receive care. This treatment gap is also present in pregnancy. Among use disorders, treatment receipt is highest for opioid use disorder; however, nationally, at best, 25% of pregnant women with opioid addiction receive any care.
In other words, when we encounter addiction clinically, it is often untreated addiction. Therefore, many times providers will have women presenting to care who are both pregnant and have untreated addiction. From both a public health and a clinical practice perspective, the salient distinction is not between people with addiction and those without but between people with treated disease and people with untreated disease.
Untreated addiction is a serious medical condition. It is associated with preterm delivery and low birth weight infants. It is associated with acquisition and transmission of HIV and hepatitis C. It is associated with overdose and overdose death. By contrast, treated addiction is associated with term delivery and normal weight infants. Pharmacotherapies for opioid use disorder stabilize the intrauterine environment and allow for normal fetal growth. Pharmacotherapies for opioid use disorder help to structure and stabilize the mom’s social circumstance, providing a platform to deliver prenatal care and essential social services. And pharmacotherapies for opioid use disorder protect women and their fetuses from overdose and from overdose deaths. The goal of management of addiction in pregnancy is treatment of the underlying condition, treating the addiction.
Continue to: OBG Management...
OBG Management : What should the ObGyn do when faced with a patient who might have an addiction?
Dr. Terplan: The good news is that there are lots of recently published guidance documents from the World Health Organization,2 the American College of Obstetricians and Gynecologists (ACOG),3 and the Substance Abuse and Mental Health Services Administration (SAMHSA),4 and there have been a whole series of trainings throughout the United States organized by both ACOG and SAMHSA.
There is also a collaboration between ACOG and the American Society of Addiction Medicine (ASAM) to provide buprenorphine waiver trainings specifically designed for ObGyns. Check both the ACOG and ASAM pages for details. I encourage every provider to get a waiver to prescribe buprenorphine. There are about 30 ObGyns who are also board certified in addiction medicine in the United States, and all of us are more than happy to help our colleagues in the clinical care of this population, a population that all of us really enjoy taking care of.
Although care in pregnancy is important, we must not forget about the postpartum period. Generally speaking, women do quite well during pregnancy in terms of treatment. Postpartum, however, is a vulnerable period, where relapse happens, where gaps in care happen, where child welfare involvement and sometimes child removal happens, which can be very stressful for anyone much less somebody with a substance use disorder. Recent data demonstrate that one of the leading causes of maternal mortality in the US in from overdose, and most of these deaths occur in the postpartum period.5 Regardless of what happens during pregnancy, it is essential that we be able to link and continue care for women with opioid use disorder throughout the postpartum period.
OBG Management : How do you treat opioid use disorder in pregnancy?
Dr. Terplan: The standard of care for treatment of opioid use disorder in pregnancy is pharmacotherapy with either methadone or buprenorphine (TABLE) plus behavioral counseling—ideally, co-located with prenatal care. The evidence base for pharmacotherapy for opioid use disorder in pregnancy is supported by every single professional society that has ever issued guidance on this, from the World Health Organization to ACOG, to ASAM, to the Royal College in the UK as well as Canadian and Australian obstetrics and gynecology societies; literally every single professional society supports medication.
The core principle of maternal fetal medicine rests upon the fact that chronic conditions need to be treated and that treated illness improves birth outcomes. For both maternal and fetal health, treated addiction is way better than untreated addiction. One concern people have regarding methadone and buprenorphine is the development of dependence. Dependence is a physiologic effect of medication and occurs with opioids, as well as with many other medications, such as antidepressants and most hypertensive agents. For the fetus, dependence means that at the time of delivery, the infant may go into withdrawal, which is also called neonatal abstinence syndrome. Neonatal abstinence syndrome is an expected outcome of in-utero opioid exposure. It is a time-limited and treatable condition. Prospective data do not demonstrate any long-term harms among infants whose mothers received pharmacotherapy for opioid use disorder during pregnancy.6
The treatment for neonatal abstinence syndrome is costly, especially when in a neonatal intensive care unit. It can be quite concerning to a new mother to have an infant that has to spend extra time in the hospital and sometimes be medicated for management of withdrawal.
There has been a renewed interest amongst ObGyns in investigating medically-supervised withdrawal during pregnancy. Although there are remaining questions, overall, the literature does not support withdrawal during pregnancy—mostly because withdrawal is associated with relapse, and relapse is associated with cessation of care (both prenatal care and addiction treatment), acquisition and transmission of HIV and Hepatitis C, and overdose and overdose death. The pertinent clinical and public health goal is the treatment of the chronic condition of addiction during pregnancy. The standard of care remains pharmacotherapy plus behavioral counseling for the treatment of opioid use disorder in pregnancy.
Clinical care, however, is both evidence-based and person-centered. All of us who have worked in this field, long before there was attention to the opioid crisis, all of us have provided medically-supervised withdrawal of a pregnant person, and that is because we understand the principles of care. When evidence-based care conflicts with person-centered care, the ethical course is the provision of person-centered care. Patients have the right of refusal. If someone wants to discontinue medication, I have tapered the medication during pregnancy, but continued to provide (and often increase) behavioral counseling and prenatal care.
Treated addiction is better for the fetus than untreated addiction. Untreated opioid addiction is associated with preterm birth and low birth weight. These obstetric risks are not because of the opioid per se, but because of the repeated cycles of withdrawal that an individual with untreated addiction experiences. People with untreated addiction are not getting “high” when they use, they are just becoming a little bit less sick. It is this repeated cycle of withdrawal that stresses the fetus, which leads to preterm delivery and low birth weight.
Medications for opioid use disorder are long-acting and dosed daily. In contrast to the repeated cycles of fetal withdrawal in untreated addiction, pharmacotherapy stabilizes the intrauterine environment. There is no cyclic, repeated, stressful withdrawal, and consequentially, the fetus grows normally and delivers at term. Obstetric risk is from repeated cyclic withdrawal more than from opioid exposure itself.
Continue to: OBG Management...
OBG Management : Research reports that women are not using all of the opioids that are prescribed to them after a cesarean delivery. What are the risks for addiction in this setting?
Dr. Terplan: I mark a distinction between use (ie, using something as prescribed) and misuse, which means using a prescribed medication not in the manner in which it was prescribed, or using somebody else’s medications, or using an illicit substance. And I differentiate use and misuse from addiction, which is a behavioral condition, a disease. There has been a lot of attention paid to opioid prescribing in general and in particular postdelivery and post–cesarean delivery, which is one of the most common operative procedures in the United States.
It seems clear from the literature that we have overprescribed opioids postdelivery, and a small number of women, about 1 in 300 will continue an opioid script.7 This means that 1 in 300 women who received an opioid prescription following delivery present for care and get another opioid prescription filled. Now, that is a small number at the level of the individual, but because we do so many cesarean deliveries, this is a large number of women at the level of the population. This does not mean, however, that 1 in 300 women who received opioids after cesarean delivery are going to become addicted to them. It just means that 1 in 300 will continue the prescription. Prescription continuation is a risk factor for opioid misuse, and opioid misuse is on the pathway toward addiction.
Most people who use substances do not develop an addiction to that substance. We know from the opioid literature that at most only 10% of people who receive chronic opioid therapy will meet criteria for opioid use disorder.8 Now 10% is not 100%, nor is it 0%, but because we prescribed so many opioids to so many people for so long, the absolute number of people with opioid use disorder from physician opioid prescribing is large, even though the risk at the level of the individual is not as large as people think.
OBG Management : From your experience in treating addiction during pregnancy, are there clinical pearls you would like to share with ObGyns?
Dr. Terplan: There are a couple of takeaways. One is that all women are motivated to maximize their health and that of their baby to be, and every pregnant woman engages in behavioral change; in fact most women quit or cutback substance use during pregnancy. But some can’t. Those that can’t likely have a substance use disorder. We think of addiction as a chronic condition, centered in the brain, but the primary symptoms of addiction are behaviors. The salient feature of addiction is continued use despite adverse consequences; using something that you know is harming yourself and others but you can’t stop using it. In other words, continuing substance use during pregnancy. When we see clinically a pregnant woman who is using a substance, 99% of the time we are seeing a pregnant woman who has the condition of addiction, and what she needs is treatment. She does not need to be told that injecting heroin is unsafe for her and her fetus, she knows that. What she needs is treatment.
The second point is that pregnant women who use drugs and pregnant women with addiction experience a real specific and strong form of discrimination by providers, by other people with addiction, by the legal system, and by their friends and families. Caring for people who have substance use disorder is grounded in human rights, which means treating people with dignity and respect. It is important for providers to have empathy, especially for pregnant people who use drugs, to counter the discrimination they experience from society and from other health care providers.
Continue to: OBG Management...
OBG Management : Are there specific ways in which ObGyns can show empathy when speaking with a pregnant woman who likely has addiction?
Dr. Terplan: In general when we talk to people about drug use, it is important to ask their permission to talk about it. For example, “Is it okay if I ask you some questions about smoking, drinking, and other drugs?” If someone says, “No, I don’t want you to ask those questions,” we have to respect that. Assessment of substance use should be a universal part of all medical care, as substance use, misuse, and addiction are essential domains of wellness, but I think we should ask permission before screening.
One of the really good things about prenatal care is that people come back; we have multiple visits across the gestational period. The behavioral work of addiction treatment rests upon a strong therapeutic alliance. If you do not respect your patient, then there is no way you can achieve a therapeutic alliance. Asking permission, and then respecting somebody’s answers, I think goes a really long way to establishing a strong therapeutic alliance, which is the basis of any medical care.
OBG Management : How has the opioid crisis affected women in general?
Mishka Terplan, MD: Everyone is aware that we are experiencing a massive opioid crisis in the United States, and from a historical perspective, this is at least the third or fourth significant opioid epidemic in our nation’s history.1 It is similar in some ways to the very first one, which also featured a large proportion of women and also was driven initially by physician prescribing practices. However, the magnitude of this crisis is unparalleled compared with prior opioid epidemics.
There are lots of reasons why women are overrepresented in this crisis. There are gender-based differences in pain—chronic pain syndromes are more common in women. In addition, we have a gender bias in prescribing opioids and prescribe more opioids to women (especially older women) than to men. Cultural differences also contribute. As providers, we tend not to think of women as people who use drugs or people who develop addictions the same way as we think of these risks and behaviors for men. Therefore, compared with men, we are less likely to screen, assess, or refer women for substance use, misuse, and addiction. All of this adds up to creating a crisis in which women are increasingly the face of the epidemic.
OBG Management : What are the concerns about opioid addiction and pregnant women specifically?
Dr. Terplan: Addiction is a chronic condition, just like diabetes or depression, and the same principles that we think of in terms of optimizing maternal and newborn health apply to addiction. Ideally, we want, for women with chronic diseases to have stable disease at the time of conception and through pregnancy. We know this maximizes birth outcomes.
Unfortunately, there is a massive treatment gap in the United States. Most people with addiction receive no treatment. Only 11% of people with a substance use disorder report receipt of treatment. By contrast, more than 70% of people with depression, hypertension, or diabetes receive care. This treatment gap is also present in pregnancy. Among use disorders, treatment receipt is highest for opioid use disorder; however, nationally, at best, 25% of pregnant women with opioid addiction receive any care.
In other words, when we encounter addiction clinically, it is often untreated addiction. Therefore, many times providers will have women presenting to care who are both pregnant and have untreated addiction. From both a public health and a clinical practice perspective, the salient distinction is not between people with addiction and those without but between people with treated disease and people with untreated disease.
Untreated addiction is a serious medical condition. It is associated with preterm delivery and low birth weight infants. It is associated with acquisition and transmission of HIV and hepatitis C. It is associated with overdose and overdose death. By contrast, treated addiction is associated with term delivery and normal weight infants. Pharmacotherapies for opioid use disorder stabilize the intrauterine environment and allow for normal fetal growth. Pharmacotherapies for opioid use disorder help to structure and stabilize the mom’s social circumstance, providing a platform to deliver prenatal care and essential social services. And pharmacotherapies for opioid use disorder protect women and their fetuses from overdose and from overdose deaths. The goal of management of addiction in pregnancy is treatment of the underlying condition, treating the addiction.
Continue to: OBG Management...
OBG Management : What should the ObGyn do when faced with a patient who might have an addiction?
Dr. Terplan: The good news is that there are lots of recently published guidance documents from the World Health Organization,2 the American College of Obstetricians and Gynecologists (ACOG),3 and the Substance Abuse and Mental Health Services Administration (SAMHSA),4 and there have been a whole series of trainings throughout the United States organized by both ACOG and SAMHSA.
There is also a collaboration between ACOG and the American Society of Addiction Medicine (ASAM) to provide buprenorphine waiver trainings specifically designed for ObGyns. Check both the ACOG and ASAM pages for details. I encourage every provider to get a waiver to prescribe buprenorphine. There are about 30 ObGyns who are also board certified in addiction medicine in the United States, and all of us are more than happy to help our colleagues in the clinical care of this population, a population that all of us really enjoy taking care of.
Although care in pregnancy is important, we must not forget about the postpartum period. Generally speaking, women do quite well during pregnancy in terms of treatment. Postpartum, however, is a vulnerable period, where relapse happens, where gaps in care happen, where child welfare involvement and sometimes child removal happens, which can be very stressful for anyone much less somebody with a substance use disorder. Recent data demonstrate that one of the leading causes of maternal mortality in the US in from overdose, and most of these deaths occur in the postpartum period.5 Regardless of what happens during pregnancy, it is essential that we be able to link and continue care for women with opioid use disorder throughout the postpartum period.
OBG Management : How do you treat opioid use disorder in pregnancy?
Dr. Terplan: The standard of care for treatment of opioid use disorder in pregnancy is pharmacotherapy with either methadone or buprenorphine (TABLE) plus behavioral counseling—ideally, co-located with prenatal care. The evidence base for pharmacotherapy for opioid use disorder in pregnancy is supported by every single professional society that has ever issued guidance on this, from the World Health Organization to ACOG, to ASAM, to the Royal College in the UK as well as Canadian and Australian obstetrics and gynecology societies; literally every single professional society supports medication.
The core principle of maternal fetal medicine rests upon the fact that chronic conditions need to be treated and that treated illness improves birth outcomes. For both maternal and fetal health, treated addiction is way better than untreated addiction. One concern people have regarding methadone and buprenorphine is the development of dependence. Dependence is a physiologic effect of medication and occurs with opioids, as well as with many other medications, such as antidepressants and most hypertensive agents. For the fetus, dependence means that at the time of delivery, the infant may go into withdrawal, which is also called neonatal abstinence syndrome. Neonatal abstinence syndrome is an expected outcome of in-utero opioid exposure. It is a time-limited and treatable condition. Prospective data do not demonstrate any long-term harms among infants whose mothers received pharmacotherapy for opioid use disorder during pregnancy.6
The treatment for neonatal abstinence syndrome is costly, especially when in a neonatal intensive care unit. It can be quite concerning to a new mother to have an infant that has to spend extra time in the hospital and sometimes be medicated for management of withdrawal.
There has been a renewed interest amongst ObGyns in investigating medically-supervised withdrawal during pregnancy. Although there are remaining questions, overall, the literature does not support withdrawal during pregnancy—mostly because withdrawal is associated with relapse, and relapse is associated with cessation of care (both prenatal care and addiction treatment), acquisition and transmission of HIV and Hepatitis C, and overdose and overdose death. The pertinent clinical and public health goal is the treatment of the chronic condition of addiction during pregnancy. The standard of care remains pharmacotherapy plus behavioral counseling for the treatment of opioid use disorder in pregnancy.
Clinical care, however, is both evidence-based and person-centered. All of us who have worked in this field, long before there was attention to the opioid crisis, all of us have provided medically-supervised withdrawal of a pregnant person, and that is because we understand the principles of care. When evidence-based care conflicts with person-centered care, the ethical course is the provision of person-centered care. Patients have the right of refusal. If someone wants to discontinue medication, I have tapered the medication during pregnancy, but continued to provide (and often increase) behavioral counseling and prenatal care.
Treated addiction is better for the fetus than untreated addiction. Untreated opioid addiction is associated with preterm birth and low birth weight. These obstetric risks are not because of the opioid per se, but because of the repeated cycles of withdrawal that an individual with untreated addiction experiences. People with untreated addiction are not getting “high” when they use, they are just becoming a little bit less sick. It is this repeated cycle of withdrawal that stresses the fetus, which leads to preterm delivery and low birth weight.
Medications for opioid use disorder are long-acting and dosed daily. In contrast to the repeated cycles of fetal withdrawal in untreated addiction, pharmacotherapy stabilizes the intrauterine environment. There is no cyclic, repeated, stressful withdrawal, and consequentially, the fetus grows normally and delivers at term. Obstetric risk is from repeated cyclic withdrawal more than from opioid exposure itself.
Continue to: OBG Management...
OBG Management : Research reports that women are not using all of the opioids that are prescribed to them after a cesarean delivery. What are the risks for addiction in this setting?
Dr. Terplan: I mark a distinction between use (ie, using something as prescribed) and misuse, which means using a prescribed medication not in the manner in which it was prescribed, or using somebody else’s medications, or using an illicit substance. And I differentiate use and misuse from addiction, which is a behavioral condition, a disease. There has been a lot of attention paid to opioid prescribing in general and in particular postdelivery and post–cesarean delivery, which is one of the most common operative procedures in the United States.
It seems clear from the literature that we have overprescribed opioids postdelivery, and a small number of women, about 1 in 300 will continue an opioid script.7 This means that 1 in 300 women who received an opioid prescription following delivery present for care and get another opioid prescription filled. Now, that is a small number at the level of the individual, but because we do so many cesarean deliveries, this is a large number of women at the level of the population. This does not mean, however, that 1 in 300 women who received opioids after cesarean delivery are going to become addicted to them. It just means that 1 in 300 will continue the prescription. Prescription continuation is a risk factor for opioid misuse, and opioid misuse is on the pathway toward addiction.
Most people who use substances do not develop an addiction to that substance. We know from the opioid literature that at most only 10% of people who receive chronic opioid therapy will meet criteria for opioid use disorder.8 Now 10% is not 100%, nor is it 0%, but because we prescribed so many opioids to so many people for so long, the absolute number of people with opioid use disorder from physician opioid prescribing is large, even though the risk at the level of the individual is not as large as people think.
OBG Management : From your experience in treating addiction during pregnancy, are there clinical pearls you would like to share with ObGyns?
Dr. Terplan: There are a couple of takeaways. One is that all women are motivated to maximize their health and that of their baby to be, and every pregnant woman engages in behavioral change; in fact most women quit or cutback substance use during pregnancy. But some can’t. Those that can’t likely have a substance use disorder. We think of addiction as a chronic condition, centered in the brain, but the primary symptoms of addiction are behaviors. The salient feature of addiction is continued use despite adverse consequences; using something that you know is harming yourself and others but you can’t stop using it. In other words, continuing substance use during pregnancy. When we see clinically a pregnant woman who is using a substance, 99% of the time we are seeing a pregnant woman who has the condition of addiction, and what she needs is treatment. She does not need to be told that injecting heroin is unsafe for her and her fetus, she knows that. What she needs is treatment.
The second point is that pregnant women who use drugs and pregnant women with addiction experience a real specific and strong form of discrimination by providers, by other people with addiction, by the legal system, and by their friends and families. Caring for people who have substance use disorder is grounded in human rights, which means treating people with dignity and respect. It is important for providers to have empathy, especially for pregnant people who use drugs, to counter the discrimination they experience from society and from other health care providers.
Continue to: OBG Management...
OBG Management : Are there specific ways in which ObGyns can show empathy when speaking with a pregnant woman who likely has addiction?
Dr. Terplan: In general when we talk to people about drug use, it is important to ask their permission to talk about it. For example, “Is it okay if I ask you some questions about smoking, drinking, and other drugs?” If someone says, “No, I don’t want you to ask those questions,” we have to respect that. Assessment of substance use should be a universal part of all medical care, as substance use, misuse, and addiction are essential domains of wellness, but I think we should ask permission before screening.
One of the really good things about prenatal care is that people come back; we have multiple visits across the gestational period. The behavioral work of addiction treatment rests upon a strong therapeutic alliance. If you do not respect your patient, then there is no way you can achieve a therapeutic alliance. Asking permission, and then respecting somebody’s answers, I think goes a really long way to establishing a strong therapeutic alliance, which is the basis of any medical care.
- Terplan M. Women and the opioid crisis: historical context and public health solutions. Fertil Steril. 2017;108:195-199.
- Management of substance abuse. World Health Organization website. https://www.who.int/substance_abuse/activities/treatment_opioid_dependence/en/. Accessed March 20, 2019.
- Committee on Obstetric Practice. Committee Opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
- Substance Abuse and Mental Health Services Administration. Clinical guidance for treating pregnant and parenting women with opioid use disorder and their infants. HHS Publication No. (SMA) 18-5054. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2018.
- Metz TD, Royner P, Hoffman MC, et al. Maternal deaths from suicide and overdose in Colorado, 2004-2012. Obstet Gynecol. 2016;128:1233-1240.
- Kaltenbach K, O’Grady E, Heil SH, et al. Prenatal exposure to methadone or buprenorphine: early childhood developmental outcomes. Drug Alcohol Depend. 2018;185:40-49.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naive women. Am J Obstet Gynecol. 2016;215:353.e1-353.e18.
- Terplan M. Women and the opioid crisis: historical context and public health solutions. Fertil Steril. 2017;108:195-199.
- Management of substance abuse. World Health Organization website. https://www.who.int/substance_abuse/activities/treatment_opioid_dependence/en/. Accessed March 20, 2019.
- Committee on Obstetric Practice. Committee Opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
- Substance Abuse and Mental Health Services Administration. Clinical guidance for treating pregnant and parenting women with opioid use disorder and their infants. HHS Publication No. (SMA) 18-5054. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2018.
- Metz TD, Royner P, Hoffman MC, et al. Maternal deaths from suicide and overdose in Colorado, 2004-2012. Obstet Gynecol. 2016;128:1233-1240.
- Kaltenbach K, O’Grady E, Heil SH, et al. Prenatal exposure to methadone or buprenorphine: early childhood developmental outcomes. Drug Alcohol Depend. 2018;185:40-49.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naive women. Am J Obstet Gynecol. 2016;215:353.e1-353.e18.
Mortality rates higher in affiliates, compared with top-ranked hospitals
The sharing of a top-ranked cancer hospital brand across affiliate hospitals doesn’t necessarily guarantee the same quality of care, a new study suggests.
In a paper published in JAMA Network Open, researchers presented the outcomes of a cross-sectional study of 29,228 patients aged over 65 years who underwent complex cancer surgery at either 59 top-ranked hospitals or 343 affiliated hospitals.
The researchers saw a significant 40% higher 90-day mortality rate among patients who underwent complex cancer surgery at one of the affiliate hospitals, compared with those who were treated at the top-ranked hospitals (P less than .001), even after adjusting for factors such as age, comorbidity score, procedure type, and admission type.
“This is not entirely surprising, as affiliated hospitals are generally smaller, less likely to be teaching hospitals, and perform complex surgical procedures with less frequency (lower volume) when compared with top-ranked hospitals,” wrote Jessica R. Hoag, PhD, from the department of surgery at Yale University, New Haven, Conn., and her coauthors. However, including hospital characteristics in the models attenuated but did not eliminate the differences in mortality rates between top-ranked and affiliate hospitals.
The difference in 90-day mortality was particularly evident for gastrectomy, where there was a 100% higher 90-day mortality rate in affiliate hospitals, compared with top-ranked hospitals (P less than .001). The mortality rate for pancreaticoduodenectomy was 59% higher in affiliate hospitals, compared with top-ranked hospitals (P = .009); for colectomy it was 32% higher (P = .001), and for lobectomy it was 34% higher (P = .03).
The only procedure where the mortality rate was not statistically significantly different between top-ranked and affiliate hospitals was esophagectomy (odds ratio, 1.48; P = .06).
When the authors looked at standardized mortality ratios for the top-ranked and affiliate hospitals, they found that 41 of the 49 top-ranked hospitals had lower mortality ratios than their collective affiliates. In 37 cases, the difference in standardized mortality ratios between the top-ranked hospital and its affiliates was statistically significant.
Overall, 39 of the 49 top-ranked hospitals had better standardized mortality ratios than the national average, compared with 17 of the affiliated networks.
The authors wrote that their findings were important because previous studies showed affiliation status played a significant role in which hospital patients choose for their treatment.
“As a result, there is cause for concern that a proportion of the U.S. public could misinterpret brand sharing as indicating equivalent care,” they wrote, suggesting that one way to reduce mortality might therefore be to direct patients with the most risky and complex surgical requirements to top-ranked hospitals rather than affiliates, although acknowledged this might be challenging to implement.
One author reported receiving funding from the Centers for Medicare & Medicaid Services, one reported advisory board and steering committee positions with the private medical sector, and one reported receiving nonfinancial support from private industry outside the submitted work. No other conflicts of interest were reported.
SOURCE: Hoag JR et al. JAMA Netw Open. 2019 Apr 12. doi: 10.1001/jamanetworkopen.2019.1912.
Network affiliations with top-ranked hospitals could help expand access to high-quality cancer care and reduce travel times for patients who live too far away to access the top-ranked hospital itself. However, this study shows that the outcomes and quality of the flagship hospital do not necessarily translate to the affiliate hospitals in the network.
While affiliate hospitals are likely to deal with smaller numbers of complex patients and are less likely to be teaching hospitals, they do offer a way to potentially leverage their affiliation with top-ranked hospitals to improve the overall quality of care for cancer patients. The challenge is to work out how best to do this and to identify which patients are likely to do just as well at an affiliate hospital and which patients will be optimally treated at the flagship hospital.
Lesly A. Dossett, MD, MPH, is from the department of surgery at the University of Michigan, Ann Arbor. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Apr 12. doi:10.1001/jamanetworkopen.2019.1910). No conflicts of interest were reported.
Network affiliations with top-ranked hospitals could help expand access to high-quality cancer care and reduce travel times for patients who live too far away to access the top-ranked hospital itself. However, this study shows that the outcomes and quality of the flagship hospital do not necessarily translate to the affiliate hospitals in the network.
While affiliate hospitals are likely to deal with smaller numbers of complex patients and are less likely to be teaching hospitals, they do offer a way to potentially leverage their affiliation with top-ranked hospitals to improve the overall quality of care for cancer patients. The challenge is to work out how best to do this and to identify which patients are likely to do just as well at an affiliate hospital and which patients will be optimally treated at the flagship hospital.
Lesly A. Dossett, MD, MPH, is from the department of surgery at the University of Michigan, Ann Arbor. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Apr 12. doi:10.1001/jamanetworkopen.2019.1910). No conflicts of interest were reported.
Network affiliations with top-ranked hospitals could help expand access to high-quality cancer care and reduce travel times for patients who live too far away to access the top-ranked hospital itself. However, this study shows that the outcomes and quality of the flagship hospital do not necessarily translate to the affiliate hospitals in the network.
While affiliate hospitals are likely to deal with smaller numbers of complex patients and are less likely to be teaching hospitals, they do offer a way to potentially leverage their affiliation with top-ranked hospitals to improve the overall quality of care for cancer patients. The challenge is to work out how best to do this and to identify which patients are likely to do just as well at an affiliate hospital and which patients will be optimally treated at the flagship hospital.
Lesly A. Dossett, MD, MPH, is from the department of surgery at the University of Michigan, Ann Arbor. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Apr 12. doi:10.1001/jamanetworkopen.2019.1910). No conflicts of interest were reported.
The sharing of a top-ranked cancer hospital brand across affiliate hospitals doesn’t necessarily guarantee the same quality of care, a new study suggests.
In a paper published in JAMA Network Open, researchers presented the outcomes of a cross-sectional study of 29,228 patients aged over 65 years who underwent complex cancer surgery at either 59 top-ranked hospitals or 343 affiliated hospitals.
The researchers saw a significant 40% higher 90-day mortality rate among patients who underwent complex cancer surgery at one of the affiliate hospitals, compared with those who were treated at the top-ranked hospitals (P less than .001), even after adjusting for factors such as age, comorbidity score, procedure type, and admission type.
“This is not entirely surprising, as affiliated hospitals are generally smaller, less likely to be teaching hospitals, and perform complex surgical procedures with less frequency (lower volume) when compared with top-ranked hospitals,” wrote Jessica R. Hoag, PhD, from the department of surgery at Yale University, New Haven, Conn., and her coauthors. However, including hospital characteristics in the models attenuated but did not eliminate the differences in mortality rates between top-ranked and affiliate hospitals.
The difference in 90-day mortality was particularly evident for gastrectomy, where there was a 100% higher 90-day mortality rate in affiliate hospitals, compared with top-ranked hospitals (P less than .001). The mortality rate for pancreaticoduodenectomy was 59% higher in affiliate hospitals, compared with top-ranked hospitals (P = .009); for colectomy it was 32% higher (P = .001), and for lobectomy it was 34% higher (P = .03).
The only procedure where the mortality rate was not statistically significantly different between top-ranked and affiliate hospitals was esophagectomy (odds ratio, 1.48; P = .06).
When the authors looked at standardized mortality ratios for the top-ranked and affiliate hospitals, they found that 41 of the 49 top-ranked hospitals had lower mortality ratios than their collective affiliates. In 37 cases, the difference in standardized mortality ratios between the top-ranked hospital and its affiliates was statistically significant.
Overall, 39 of the 49 top-ranked hospitals had better standardized mortality ratios than the national average, compared with 17 of the affiliated networks.
The authors wrote that their findings were important because previous studies showed affiliation status played a significant role in which hospital patients choose for their treatment.
“As a result, there is cause for concern that a proportion of the U.S. public could misinterpret brand sharing as indicating equivalent care,” they wrote, suggesting that one way to reduce mortality might therefore be to direct patients with the most risky and complex surgical requirements to top-ranked hospitals rather than affiliates, although acknowledged this might be challenging to implement.
One author reported receiving funding from the Centers for Medicare & Medicaid Services, one reported advisory board and steering committee positions with the private medical sector, and one reported receiving nonfinancial support from private industry outside the submitted work. No other conflicts of interest were reported.
SOURCE: Hoag JR et al. JAMA Netw Open. 2019 Apr 12. doi: 10.1001/jamanetworkopen.2019.1912.
The sharing of a top-ranked cancer hospital brand across affiliate hospitals doesn’t necessarily guarantee the same quality of care, a new study suggests.
In a paper published in JAMA Network Open, researchers presented the outcomes of a cross-sectional study of 29,228 patients aged over 65 years who underwent complex cancer surgery at either 59 top-ranked hospitals or 343 affiliated hospitals.
The researchers saw a significant 40% higher 90-day mortality rate among patients who underwent complex cancer surgery at one of the affiliate hospitals, compared with those who were treated at the top-ranked hospitals (P less than .001), even after adjusting for factors such as age, comorbidity score, procedure type, and admission type.
“This is not entirely surprising, as affiliated hospitals are generally smaller, less likely to be teaching hospitals, and perform complex surgical procedures with less frequency (lower volume) when compared with top-ranked hospitals,” wrote Jessica R. Hoag, PhD, from the department of surgery at Yale University, New Haven, Conn., and her coauthors. However, including hospital characteristics in the models attenuated but did not eliminate the differences in mortality rates between top-ranked and affiliate hospitals.
The difference in 90-day mortality was particularly evident for gastrectomy, where there was a 100% higher 90-day mortality rate in affiliate hospitals, compared with top-ranked hospitals (P less than .001). The mortality rate for pancreaticoduodenectomy was 59% higher in affiliate hospitals, compared with top-ranked hospitals (P = .009); for colectomy it was 32% higher (P = .001), and for lobectomy it was 34% higher (P = .03).
The only procedure where the mortality rate was not statistically significantly different between top-ranked and affiliate hospitals was esophagectomy (odds ratio, 1.48; P = .06).
When the authors looked at standardized mortality ratios for the top-ranked and affiliate hospitals, they found that 41 of the 49 top-ranked hospitals had lower mortality ratios than their collective affiliates. In 37 cases, the difference in standardized mortality ratios between the top-ranked hospital and its affiliates was statistically significant.
Overall, 39 of the 49 top-ranked hospitals had better standardized mortality ratios than the national average, compared with 17 of the affiliated networks.
The authors wrote that their findings were important because previous studies showed affiliation status played a significant role in which hospital patients choose for their treatment.
“As a result, there is cause for concern that a proportion of the U.S. public could misinterpret brand sharing as indicating equivalent care,” they wrote, suggesting that one way to reduce mortality might therefore be to direct patients with the most risky and complex surgical requirements to top-ranked hospitals rather than affiliates, although acknowledged this might be challenging to implement.
One author reported receiving funding from the Centers for Medicare & Medicaid Services, one reported advisory board and steering committee positions with the private medical sector, and one reported receiving nonfinancial support from private industry outside the submitted work. No other conflicts of interest were reported.
SOURCE: Hoag JR et al. JAMA Netw Open. 2019 Apr 12. doi: 10.1001/jamanetworkopen.2019.1912.
FROM JAMA NETWORK OPEN
Leveraging consumer technology in gastroenterology practice
SAN FRANCISCO – Dr. Michael Docktor, a pediatric gastroenterologist at Boston Hospital, described myriad digital tools that physicians – especially gastroenterologists – as well as patients are now using. Some tools may be implemented to track stool output or diet for diseases like irritable bowel syndrome or Crohn’s disease, he said in an interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology.
There are patient-facing applications that provide data that can be used by both patients and their physicians to better understand the disease. These data can help in diagnosis and management and give the GI doctor a “window into the 99% of the time that they aren’t with the patient.” Other apps can build a timeline of the disease that can help the patient get a better understanding of their disease and learn to distinguish a flare from a bad day with poor food choices. Dr. Docktor described the AGA Tech Summit as a place to try out new ideas and work with like-minded doctors.
SAN FRANCISCO – Dr. Michael Docktor, a pediatric gastroenterologist at Boston Hospital, described myriad digital tools that physicians – especially gastroenterologists – as well as patients are now using. Some tools may be implemented to track stool output or diet for diseases like irritable bowel syndrome or Crohn’s disease, he said in an interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology.
There are patient-facing applications that provide data that can be used by both patients and their physicians to better understand the disease. These data can help in diagnosis and management and give the GI doctor a “window into the 99% of the time that they aren’t with the patient.” Other apps can build a timeline of the disease that can help the patient get a better understanding of their disease and learn to distinguish a flare from a bad day with poor food choices. Dr. Docktor described the AGA Tech Summit as a place to try out new ideas and work with like-minded doctors.
SAN FRANCISCO – Dr. Michael Docktor, a pediatric gastroenterologist at Boston Hospital, described myriad digital tools that physicians – especially gastroenterologists – as well as patients are now using. Some tools may be implemented to track stool output or diet for diseases like irritable bowel syndrome or Crohn’s disease, he said in an interview at the AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology.
There are patient-facing applications that provide data that can be used by both patients and their physicians to better understand the disease. These data can help in diagnosis and management and give the GI doctor a “window into the 99% of the time that they aren’t with the patient.” Other apps can build a timeline of the disease that can help the patient get a better understanding of their disease and learn to distinguish a flare from a bad day with poor food choices. Dr. Docktor described the AGA Tech Summit as a place to try out new ideas and work with like-minded doctors.
REPORTING FROM 2019 AGA TECH SUMMIT
Obeticholic acid reversed NASH liver fibrosis in phase 3 trial
VIENNA – making obeticholic acid the first agent proven to improve the course of this disease.
“There is no doubt that with these data we have changed the treatment” of nonalcoholic steatohepatitis (NASH), Zobair M. Younossi, MD, of Inova Fairfax Medical Campus in Falls Church, Va., said at the meeting sponsored by the European Association for the Study of the Liver. “We are at a watershed moment” in NASH treatment, Dr. Younossi added in a video interview.
Until now “we have had no effective treatments for NASH. This is the first success in a phase 3 trial; obeticholic acid looks very promising,” commented Philip N. Newsome, PhD, professor of experimental hepatology at the University of Birmingham (England).
Obeticholic acid (OCA), an agonist of the farnesoid X receptor, already has Food and Drug Administration marketing approval for the indication of primary biliary cholangitis, a much rarer disease than NASH.
The REGENERATE (Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment) trial has so far enrolled 931 patients at about 350 sites in 20 countries, including the United States, and followed them during 18 months of treatment, the prespecified time for an interim analysis. The study enrolled adults with biopsy-proven NASH and generally focused on patients with either stage 2 or 3 liver fibrosis and a nonalcoholic fatty liver disease activity score of at least 4. Enrolled patients averaged about 55 years old, slightly more than half the enrolled patients had type 2 diabetes, and more than half had stage 3 fibrosis.
The study design included two coprimary endpoints, and specified that a statistically significant finding for either outcome meant a positive trial result, but the design also prespecified that the benefit would need to meet a stringent definition of statistical significance, compared with placebo patients, with a P value of no more than .01. REGENERATE tested two different OCA dosages, 10 mg or 25 mg, once daily. The results showed a trend for benefit from the smaller dosage, but these effects did not achieve statistical significance.
For the primary endpoint of regression of liver fibrosis by at least one stage with no worsening of NASH the intention-to-treat analysis showed after 18 months a 13% rate with placebo, a 21% rate with the 10-mg dosage, and a 23% rate with the 25-mg dosage, a statistically significant improvement over placebo for the higher dosage.
The second primary endpoint was resolution of NASH without worsening liver fibrosis, which occurred in 8% of placebo patients, 11% of patients on 10 mg OCA/day and 12% of those on 25 mg/day. The differences between each of the active groups and the controls were not statistically significant for this endpoint.
Among the 931 enrolled patients 668 (72%) actually received treatment fully consistent with the study protocol, and among these per-protocol patients the benefit from 25 mg/day OCA was even more striking: a 28% rate of fibrosis regression, compared with 13% in the control patients. Regression by at least two fibrotic stages occurred in 5% of placebo patients and 13% of those on 25 mg/day OCA. Many treated patients also showed normalizations of liver enzyme levels.
Adverse events on OCA were mostly mild or moderate, with similar rates of serious adverse events in the OCA groups and in control patients. The most common adverse effect on OCA treatment was pruritus, a previously described effect, reported by 51% of patients on the 25 mg/day dosage and by 19% of control patients.
REGENERATE will continue until a goal level of endpoint events occur, and may eventually enroll as many as 2,400 patients and extend for a few more years. By then, Dr. Younossi said, he hopes that an analysis will be possible of “harder” endpoints than fibrosis, such as development of cirrhosis. He noted, however, that the FDA has designated fibrosis regression as a valid surrogate endpoint for assessing treatment efficacy for NASH.
Already on the U.S. market, a single 10-mg OCA pill currently retails for almost $230; a 25-mg formulation is not currently marketed. Dr. Younossi said that subsequent studies will assess the cost-effectiveness of OCA treatment for NASH. He also hopes that further study of patient characteristics will identify which NASH patients are most likely to respond to OCA. Eventually, OCA may be part of a multidrug strategy for treating this disease, Dr. Younossi said.
REGENERATE was sponsored by Intercept, the company that markets obeticholic acid (Ocaliva). Dr. Younossi is a consultant to and has received research funding from Intercept. He has also been a consultant to Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Novartis, Novo Nordisk, Quest, Siemens, Terns Pharmaceutical, and Viking Therapeutics. Dr. Newsome has been a consultant or speaker for Intercept as well as Boehringer Ingelheim, Dignity Sciences, Johnson & Johnson, Novo Nordisk, and Shire, and he has received research funding from Pharmaxis and Boehringer Ingelheim.
VIENNA – making obeticholic acid the first agent proven to improve the course of this disease.
“There is no doubt that with these data we have changed the treatment” of nonalcoholic steatohepatitis (NASH), Zobair M. Younossi, MD, of Inova Fairfax Medical Campus in Falls Church, Va., said at the meeting sponsored by the European Association for the Study of the Liver. “We are at a watershed moment” in NASH treatment, Dr. Younossi added in a video interview.
Until now “we have had no effective treatments for NASH. This is the first success in a phase 3 trial; obeticholic acid looks very promising,” commented Philip N. Newsome, PhD, professor of experimental hepatology at the University of Birmingham (England).
Obeticholic acid (OCA), an agonist of the farnesoid X receptor, already has Food and Drug Administration marketing approval for the indication of primary biliary cholangitis, a much rarer disease than NASH.
The REGENERATE (Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment) trial has so far enrolled 931 patients at about 350 sites in 20 countries, including the United States, and followed them during 18 months of treatment, the prespecified time for an interim analysis. The study enrolled adults with biopsy-proven NASH and generally focused on patients with either stage 2 or 3 liver fibrosis and a nonalcoholic fatty liver disease activity score of at least 4. Enrolled patients averaged about 55 years old, slightly more than half the enrolled patients had type 2 diabetes, and more than half had stage 3 fibrosis.
The study design included two coprimary endpoints, and specified that a statistically significant finding for either outcome meant a positive trial result, but the design also prespecified that the benefit would need to meet a stringent definition of statistical significance, compared with placebo patients, with a P value of no more than .01. REGENERATE tested two different OCA dosages, 10 mg or 25 mg, once daily. The results showed a trend for benefit from the smaller dosage, but these effects did not achieve statistical significance.
For the primary endpoint of regression of liver fibrosis by at least one stage with no worsening of NASH the intention-to-treat analysis showed after 18 months a 13% rate with placebo, a 21% rate with the 10-mg dosage, and a 23% rate with the 25-mg dosage, a statistically significant improvement over placebo for the higher dosage.
The second primary endpoint was resolution of NASH without worsening liver fibrosis, which occurred in 8% of placebo patients, 11% of patients on 10 mg OCA/day and 12% of those on 25 mg/day. The differences between each of the active groups and the controls were not statistically significant for this endpoint.
Among the 931 enrolled patients 668 (72%) actually received treatment fully consistent with the study protocol, and among these per-protocol patients the benefit from 25 mg/day OCA was even more striking: a 28% rate of fibrosis regression, compared with 13% in the control patients. Regression by at least two fibrotic stages occurred in 5% of placebo patients and 13% of those on 25 mg/day OCA. Many treated patients also showed normalizations of liver enzyme levels.
Adverse events on OCA were mostly mild or moderate, with similar rates of serious adverse events in the OCA groups and in control patients. The most common adverse effect on OCA treatment was pruritus, a previously described effect, reported by 51% of patients on the 25 mg/day dosage and by 19% of control patients.
REGENERATE will continue until a goal level of endpoint events occur, and may eventually enroll as many as 2,400 patients and extend for a few more years. By then, Dr. Younossi said, he hopes that an analysis will be possible of “harder” endpoints than fibrosis, such as development of cirrhosis. He noted, however, that the FDA has designated fibrosis regression as a valid surrogate endpoint for assessing treatment efficacy for NASH.
Already on the U.S. market, a single 10-mg OCA pill currently retails for almost $230; a 25-mg formulation is not currently marketed. Dr. Younossi said that subsequent studies will assess the cost-effectiveness of OCA treatment for NASH. He also hopes that further study of patient characteristics will identify which NASH patients are most likely to respond to OCA. Eventually, OCA may be part of a multidrug strategy for treating this disease, Dr. Younossi said.
REGENERATE was sponsored by Intercept, the company that markets obeticholic acid (Ocaliva). Dr. Younossi is a consultant to and has received research funding from Intercept. He has also been a consultant to Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Novartis, Novo Nordisk, Quest, Siemens, Terns Pharmaceutical, and Viking Therapeutics. Dr. Newsome has been a consultant or speaker for Intercept as well as Boehringer Ingelheim, Dignity Sciences, Johnson & Johnson, Novo Nordisk, and Shire, and he has received research funding from Pharmaxis and Boehringer Ingelheim.
VIENNA – making obeticholic acid the first agent proven to improve the course of this disease.
“There is no doubt that with these data we have changed the treatment” of nonalcoholic steatohepatitis (NASH), Zobair M. Younossi, MD, of Inova Fairfax Medical Campus in Falls Church, Va., said at the meeting sponsored by the European Association for the Study of the Liver. “We are at a watershed moment” in NASH treatment, Dr. Younossi added in a video interview.
Until now “we have had no effective treatments for NASH. This is the first success in a phase 3 trial; obeticholic acid looks very promising,” commented Philip N. Newsome, PhD, professor of experimental hepatology at the University of Birmingham (England).
Obeticholic acid (OCA), an agonist of the farnesoid X receptor, already has Food and Drug Administration marketing approval for the indication of primary biliary cholangitis, a much rarer disease than NASH.
The REGENERATE (Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment) trial has so far enrolled 931 patients at about 350 sites in 20 countries, including the United States, and followed them during 18 months of treatment, the prespecified time for an interim analysis. The study enrolled adults with biopsy-proven NASH and generally focused on patients with either stage 2 or 3 liver fibrosis and a nonalcoholic fatty liver disease activity score of at least 4. Enrolled patients averaged about 55 years old, slightly more than half the enrolled patients had type 2 diabetes, and more than half had stage 3 fibrosis.
The study design included two coprimary endpoints, and specified that a statistically significant finding for either outcome meant a positive trial result, but the design also prespecified that the benefit would need to meet a stringent definition of statistical significance, compared with placebo patients, with a P value of no more than .01. REGENERATE tested two different OCA dosages, 10 mg or 25 mg, once daily. The results showed a trend for benefit from the smaller dosage, but these effects did not achieve statistical significance.
For the primary endpoint of regression of liver fibrosis by at least one stage with no worsening of NASH the intention-to-treat analysis showed after 18 months a 13% rate with placebo, a 21% rate with the 10-mg dosage, and a 23% rate with the 25-mg dosage, a statistically significant improvement over placebo for the higher dosage.
The second primary endpoint was resolution of NASH without worsening liver fibrosis, which occurred in 8% of placebo patients, 11% of patients on 10 mg OCA/day and 12% of those on 25 mg/day. The differences between each of the active groups and the controls were not statistically significant for this endpoint.
Among the 931 enrolled patients 668 (72%) actually received treatment fully consistent with the study protocol, and among these per-protocol patients the benefit from 25 mg/day OCA was even more striking: a 28% rate of fibrosis regression, compared with 13% in the control patients. Regression by at least two fibrotic stages occurred in 5% of placebo patients and 13% of those on 25 mg/day OCA. Many treated patients also showed normalizations of liver enzyme levels.
Adverse events on OCA were mostly mild or moderate, with similar rates of serious adverse events in the OCA groups and in control patients. The most common adverse effect on OCA treatment was pruritus, a previously described effect, reported by 51% of patients on the 25 mg/day dosage and by 19% of control patients.
REGENERATE will continue until a goal level of endpoint events occur, and may eventually enroll as many as 2,400 patients and extend for a few more years. By then, Dr. Younossi said, he hopes that an analysis will be possible of “harder” endpoints than fibrosis, such as development of cirrhosis. He noted, however, that the FDA has designated fibrosis regression as a valid surrogate endpoint for assessing treatment efficacy for NASH.
Already on the U.S. market, a single 10-mg OCA pill currently retails for almost $230; a 25-mg formulation is not currently marketed. Dr. Younossi said that subsequent studies will assess the cost-effectiveness of OCA treatment for NASH. He also hopes that further study of patient characteristics will identify which NASH patients are most likely to respond to OCA. Eventually, OCA may be part of a multidrug strategy for treating this disease, Dr. Younossi said.
REGENERATE was sponsored by Intercept, the company that markets obeticholic acid (Ocaliva). Dr. Younossi is a consultant to and has received research funding from Intercept. He has also been a consultant to Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Novartis, Novo Nordisk, Quest, Siemens, Terns Pharmaceutical, and Viking Therapeutics. Dr. Newsome has been a consultant or speaker for Intercept as well as Boehringer Ingelheim, Dignity Sciences, Johnson & Johnson, Novo Nordisk, and Shire, and he has received research funding from Pharmaxis and Boehringer Ingelheim.
REPORTING FROM ILC 2019
Nontraditional specialty physicians supplement hospitalist staffing
More HMGs cover inpatient and ED settings
Our profession continues to experience steady growth, and demand for hospitalist physicians exceeds supply. In a recent article in The Hospitalist, Andrew White, MD, SFHM, highlighted the fact that most hospital medicine groups (HMGs) are constantly recruiting and open positions are not uncommon.
When we think about recruitment and staffing, I bet many of us think principally of physicians trained in the general medicine specialties of internal medicine, family medicine, and pediatrics. Yet, to help meet demand for hospital-based clinicians, HMGs sometimes turn to physicians certified in emergency medicine, critical care, geriatric medicine, palliative care, and other fields.
To gain a better understanding of the diversity within our profession, the Society of Hospital Medicine’s State of Hospital Medicine survey asked HMGs whether they employ at least one physician in these various specialties. Results published in the recently released 2018 State of Hospital Medicine (SoHM) Report show significant differences among groups, affected by location, group size, and type of employer.
At the core of our profession are physicians trained in internal medicine, present in 99.2% of adult medicine HMGs throughout the United States. No surprise given that our field was founded by internists and remains a popular career choice for IM residency graduates. Family physicians follow, with the highest percentage of groups employing at least one FP located in the southern United States at 70.3% and lowest in the west at 54.7%. Small-sized groups – fewer than 10 full-time equivalents (FTEs) – were also more likely to employ FPs.
This speaks to the challenge – often faced by smaller hospitals – of covering both adult and pediatric patient populations and limited workforce availability. Pediatrics- and internal medicine/pediatrics–trained physicians help meet this need and were prevalent within small-sized groups. Another distinction found in the report is that, while 92.1% of multistate hospitalist management companies employed family physicians, only 28.8% of academic university settings did so. Partly because of Accreditation Council for Graduate Medical Education requirements for IM-certified teaching attending for internal medicine residents, FP and other specialties are filling some non–teaching hospitalist positions within our academic programs.
What may be surprising is that emergency medicine and critical care had the largest increase in representation in hospital medicine. The two specialties showed similar growth trends, with a larger presence in the South and Midwest states and 56% of multistate hospitalist management companies employing them. Small- to medium-sized groups of up to 20 FTEs were also more likely to have physicians from these fields, with up to 44% of groups doing so. This is a significant change from 2016, when less than 3.4% of all HMGs overall had a physician certified in emergency or critical care medicine.
This finding seems to coincide with the growth in hospital medicine groups who are covering both ED and inpatient services. For small and rural hospitals, it has become necessary and beneficial to have physicians capable of covering both clinical settings.
Contrast this with geriatric medicine and palliative care. Here, we saw these two specialties to be present in our academic institutions at 26.8% and 22.5%, respectively. Large-sized HMGs were more likely to employ them, whereas their presence in multistate management groups or private multispecialty/primary care groups was quite low. Compared with our last survey in 2016, their overall prevalence in HMGs hasn’t changed significantly. Whether this will be different in the future with our aging population will be interesting to follow.
Published biannually, the SoHM report provides insight into these and other market-based dynamics that shape hospital medicine. The demand for hospital-based clinicians and the demands of acute inpatient care are leading to the broad and inclusive nature of hospital medicine. Our staffing will continue to be met not only by internal medicine and family medicine physicians but also through these other specialties joining our ranks and adding diversity to our profession.
Dr. Sites is the executive medical director of acute medicine at Providence St. Joseph Health, Oregon, and a member of SHM’s Practice Analysis Committee. She leads the hospital medicine programs and is involved in strategy development and alignment of acute inpatient medicine services at eight member hospitals. She has been a practicing hospitalist for 20 years and volunteers on medical mission trips to Guatemala annually.
More HMGs cover inpatient and ED settings
More HMGs cover inpatient and ED settings
Our profession continues to experience steady growth, and demand for hospitalist physicians exceeds supply. In a recent article in The Hospitalist, Andrew White, MD, SFHM, highlighted the fact that most hospital medicine groups (HMGs) are constantly recruiting and open positions are not uncommon.
When we think about recruitment and staffing, I bet many of us think principally of physicians trained in the general medicine specialties of internal medicine, family medicine, and pediatrics. Yet, to help meet demand for hospital-based clinicians, HMGs sometimes turn to physicians certified in emergency medicine, critical care, geriatric medicine, palliative care, and other fields.
To gain a better understanding of the diversity within our profession, the Society of Hospital Medicine’s State of Hospital Medicine survey asked HMGs whether they employ at least one physician in these various specialties. Results published in the recently released 2018 State of Hospital Medicine (SoHM) Report show significant differences among groups, affected by location, group size, and type of employer.
At the core of our profession are physicians trained in internal medicine, present in 99.2% of adult medicine HMGs throughout the United States. No surprise given that our field was founded by internists and remains a popular career choice for IM residency graduates. Family physicians follow, with the highest percentage of groups employing at least one FP located in the southern United States at 70.3% and lowest in the west at 54.7%. Small-sized groups – fewer than 10 full-time equivalents (FTEs) – were also more likely to employ FPs.
This speaks to the challenge – often faced by smaller hospitals – of covering both adult and pediatric patient populations and limited workforce availability. Pediatrics- and internal medicine/pediatrics–trained physicians help meet this need and were prevalent within small-sized groups. Another distinction found in the report is that, while 92.1% of multistate hospitalist management companies employed family physicians, only 28.8% of academic university settings did so. Partly because of Accreditation Council for Graduate Medical Education requirements for IM-certified teaching attending for internal medicine residents, FP and other specialties are filling some non–teaching hospitalist positions within our academic programs.
What may be surprising is that emergency medicine and critical care had the largest increase in representation in hospital medicine. The two specialties showed similar growth trends, with a larger presence in the South and Midwest states and 56% of multistate hospitalist management companies employing them. Small- to medium-sized groups of up to 20 FTEs were also more likely to have physicians from these fields, with up to 44% of groups doing so. This is a significant change from 2016, when less than 3.4% of all HMGs overall had a physician certified in emergency or critical care medicine.
This finding seems to coincide with the growth in hospital medicine groups who are covering both ED and inpatient services. For small and rural hospitals, it has become necessary and beneficial to have physicians capable of covering both clinical settings.
Contrast this with geriatric medicine and palliative care. Here, we saw these two specialties to be present in our academic institutions at 26.8% and 22.5%, respectively. Large-sized HMGs were more likely to employ them, whereas their presence in multistate management groups or private multispecialty/primary care groups was quite low. Compared with our last survey in 2016, their overall prevalence in HMGs hasn’t changed significantly. Whether this will be different in the future with our aging population will be interesting to follow.
Published biannually, the SoHM report provides insight into these and other market-based dynamics that shape hospital medicine. The demand for hospital-based clinicians and the demands of acute inpatient care are leading to the broad and inclusive nature of hospital medicine. Our staffing will continue to be met not only by internal medicine and family medicine physicians but also through these other specialties joining our ranks and adding diversity to our profession.
Dr. Sites is the executive medical director of acute medicine at Providence St. Joseph Health, Oregon, and a member of SHM’s Practice Analysis Committee. She leads the hospital medicine programs and is involved in strategy development and alignment of acute inpatient medicine services at eight member hospitals. She has been a practicing hospitalist for 20 years and volunteers on medical mission trips to Guatemala annually.
Our profession continues to experience steady growth, and demand for hospitalist physicians exceeds supply. In a recent article in The Hospitalist, Andrew White, MD, SFHM, highlighted the fact that most hospital medicine groups (HMGs) are constantly recruiting and open positions are not uncommon.
When we think about recruitment and staffing, I bet many of us think principally of physicians trained in the general medicine specialties of internal medicine, family medicine, and pediatrics. Yet, to help meet demand for hospital-based clinicians, HMGs sometimes turn to physicians certified in emergency medicine, critical care, geriatric medicine, palliative care, and other fields.
To gain a better understanding of the diversity within our profession, the Society of Hospital Medicine’s State of Hospital Medicine survey asked HMGs whether they employ at least one physician in these various specialties. Results published in the recently released 2018 State of Hospital Medicine (SoHM) Report show significant differences among groups, affected by location, group size, and type of employer.
At the core of our profession are physicians trained in internal medicine, present in 99.2% of adult medicine HMGs throughout the United States. No surprise given that our field was founded by internists and remains a popular career choice for IM residency graduates. Family physicians follow, with the highest percentage of groups employing at least one FP located in the southern United States at 70.3% and lowest in the west at 54.7%. Small-sized groups – fewer than 10 full-time equivalents (FTEs) – were also more likely to employ FPs.
This speaks to the challenge – often faced by smaller hospitals – of covering both adult and pediatric patient populations and limited workforce availability. Pediatrics- and internal medicine/pediatrics–trained physicians help meet this need and were prevalent within small-sized groups. Another distinction found in the report is that, while 92.1% of multistate hospitalist management companies employed family physicians, only 28.8% of academic university settings did so. Partly because of Accreditation Council for Graduate Medical Education requirements for IM-certified teaching attending for internal medicine residents, FP and other specialties are filling some non–teaching hospitalist positions within our academic programs.
What may be surprising is that emergency medicine and critical care had the largest increase in representation in hospital medicine. The two specialties showed similar growth trends, with a larger presence in the South and Midwest states and 56% of multistate hospitalist management companies employing them. Small- to medium-sized groups of up to 20 FTEs were also more likely to have physicians from these fields, with up to 44% of groups doing so. This is a significant change from 2016, when less than 3.4% of all HMGs overall had a physician certified in emergency or critical care medicine.
This finding seems to coincide with the growth in hospital medicine groups who are covering both ED and inpatient services. For small and rural hospitals, it has become necessary and beneficial to have physicians capable of covering both clinical settings.
Contrast this with geriatric medicine and palliative care. Here, we saw these two specialties to be present in our academic institutions at 26.8% and 22.5%, respectively. Large-sized HMGs were more likely to employ them, whereas their presence in multistate management groups or private multispecialty/primary care groups was quite low. Compared with our last survey in 2016, their overall prevalence in HMGs hasn’t changed significantly. Whether this will be different in the future with our aging population will be interesting to follow.
Published biannually, the SoHM report provides insight into these and other market-based dynamics that shape hospital medicine. The demand for hospital-based clinicians and the demands of acute inpatient care are leading to the broad and inclusive nature of hospital medicine. Our staffing will continue to be met not only by internal medicine and family medicine physicians but also through these other specialties joining our ranks and adding diversity to our profession.
Dr. Sites is the executive medical director of acute medicine at Providence St. Joseph Health, Oregon, and a member of SHM’s Practice Analysis Committee. She leads the hospital medicine programs and is involved in strategy development and alignment of acute inpatient medicine services at eight member hospitals. She has been a practicing hospitalist for 20 years and volunteers on medical mission trips to Guatemala annually.
FDA approves pembrolizumab for first-line stage III NSCLC
The who are not candidates for surgical resection or definitive chemoradiation, and for stage IV NSCLC.
Patients’ tumors must express programmed death-ligand 1 (PD-L1) as determined by an FDA-approved test (tumor proportion score ≥1%) and have no epidermal growth factor receptor or anaplastic lymphoma kinase mutations.
The checkpoint inhibitor was previously approved as a single agent for the first-line treatment of patients with metastatic disease with PD-L1 expression at a higher level (TPS ≥50%), the FDA said in a press statement.
Approval was based on statistically significant overall survival improvement with pembrolizumab, compared with investigator’s choice of a carboplatin-containing regimen with either pemetrexed or paclitaxel in KEYNOTE‑042. The trial enrolled 1,274 patients with stage III or IV NSCLC who had not received prior systemic treatment for metastatic NSCLC and whose tumors expressed PD-L1 (TPS ≥1%).
Overall survival was improved in all three subgroups for pembrolizumab, compared with chemotherapy: in the TPS ≥50% subgroup, the TPS ≥20% subgroup, and the overall population (TPS ≥1%). The median overall survival in the TPS ≥1% population was 16.7 for pembrolizumab and 12.1 months for the chemotherapy arms (hazard ratio, 0.81; 95% confidence interval, 0.71-0.93; P = .0036). For the TPS ≥50% subgroup, the estimated median overall survival was 20 months for pembrolizumab and 12.2 months for the chemotherapy arm (HR, 0.69; 95% CI, 0.56-0.85; P = .0006).
The most common adverse reactions reported for patients who received pembrolizumab included fatigue, decreased appetite, dyspnea, cough, rash, constipation, diarrhea, nausea, hypothyroidism, pneumonia, pyrexia, and weight loss, the FDA said.
The recommended dose for NSCLC is 200 mg as an IV infusion over 30 minutes every 3 weeks.
The who are not candidates for surgical resection or definitive chemoradiation, and for stage IV NSCLC.
Patients’ tumors must express programmed death-ligand 1 (PD-L1) as determined by an FDA-approved test (tumor proportion score ≥1%) and have no epidermal growth factor receptor or anaplastic lymphoma kinase mutations.
The checkpoint inhibitor was previously approved as a single agent for the first-line treatment of patients with metastatic disease with PD-L1 expression at a higher level (TPS ≥50%), the FDA said in a press statement.
Approval was based on statistically significant overall survival improvement with pembrolizumab, compared with investigator’s choice of a carboplatin-containing regimen with either pemetrexed or paclitaxel in KEYNOTE‑042. The trial enrolled 1,274 patients with stage III or IV NSCLC who had not received prior systemic treatment for metastatic NSCLC and whose tumors expressed PD-L1 (TPS ≥1%).
Overall survival was improved in all three subgroups for pembrolizumab, compared with chemotherapy: in the TPS ≥50% subgroup, the TPS ≥20% subgroup, and the overall population (TPS ≥1%). The median overall survival in the TPS ≥1% population was 16.7 for pembrolizumab and 12.1 months for the chemotherapy arms (hazard ratio, 0.81; 95% confidence interval, 0.71-0.93; P = .0036). For the TPS ≥50% subgroup, the estimated median overall survival was 20 months for pembrolizumab and 12.2 months for the chemotherapy arm (HR, 0.69; 95% CI, 0.56-0.85; P = .0006).
The most common adverse reactions reported for patients who received pembrolizumab included fatigue, decreased appetite, dyspnea, cough, rash, constipation, diarrhea, nausea, hypothyroidism, pneumonia, pyrexia, and weight loss, the FDA said.
The recommended dose for NSCLC is 200 mg as an IV infusion over 30 minutes every 3 weeks.
The who are not candidates for surgical resection or definitive chemoradiation, and for stage IV NSCLC.
Patients’ tumors must express programmed death-ligand 1 (PD-L1) as determined by an FDA-approved test (tumor proportion score ≥1%) and have no epidermal growth factor receptor or anaplastic lymphoma kinase mutations.
The checkpoint inhibitor was previously approved as a single agent for the first-line treatment of patients with metastatic disease with PD-L1 expression at a higher level (TPS ≥50%), the FDA said in a press statement.
Approval was based on statistically significant overall survival improvement with pembrolizumab, compared with investigator’s choice of a carboplatin-containing regimen with either pemetrexed or paclitaxel in KEYNOTE‑042. The trial enrolled 1,274 patients with stage III or IV NSCLC who had not received prior systemic treatment for metastatic NSCLC and whose tumors expressed PD-L1 (TPS ≥1%).
Overall survival was improved in all three subgroups for pembrolizumab, compared with chemotherapy: in the TPS ≥50% subgroup, the TPS ≥20% subgroup, and the overall population (TPS ≥1%). The median overall survival in the TPS ≥1% population was 16.7 for pembrolizumab and 12.1 months for the chemotherapy arms (hazard ratio, 0.81; 95% confidence interval, 0.71-0.93; P = .0036). For the TPS ≥50% subgroup, the estimated median overall survival was 20 months for pembrolizumab and 12.2 months for the chemotherapy arm (HR, 0.69; 95% CI, 0.56-0.85; P = .0006).
The most common adverse reactions reported for patients who received pembrolizumab included fatigue, decreased appetite, dyspnea, cough, rash, constipation, diarrhea, nausea, hypothyroidism, pneumonia, pyrexia, and weight loss, the FDA said.
The recommended dose for NSCLC is 200 mg as an IV infusion over 30 minutes every 3 weeks.
Low LDL cholesterol may increase women’s risk of hemorrhagic stroke
, according to research published in Neurology.
“Women with very low LDL cholesterol or low triglycerides should be monitored by their doctors for other stroke risk factors that can be modified, like high blood pressure and smoking, in order to reduce their risk of hemorrhagic stroke,” said Pamela M. Rist, ScD, instructor in epidemiology at Harvard Medical School, Boston. “Additional research is needed to determine how to lower the risk of hemorrhagic stroke in women with very low LDL and low triglycerides.”
Several meta-analyses have indicated that LDL cholesterol levels are inversely associated with the risk of hemorrhagic stroke. Because lipid-lowering treatments are used to prevent cardiovascular disease, this potential association has implications for clinical practice. Most of the studies included in these meta-analyses had low numbers of events among women, which prevented researchers from stratifying their results by sex. Because women are at greater risk of stroke than men, Dr. Rist and her colleagues sought to evaluate the association between lipid levels and risk of hemorrhagic stroke.
An analysis of the Women’s Health Study
The investigators examined data from the Women’s Health Study, a randomized, double-blind, placebo-controlled trial of low-dose aspirin and vitamin E for the primary prevention of cardiovascular disease and cancer among female American health professionals aged 45 years or older. The study ended in March 2004, but follow-up is ongoing. At regular intervals, the women complete a questionnaire about disease outcomes, including stroke. Some participants agreed to provide a fasting venous blood sample before randomization. With the subjects’ permission, a committee of physicians examined medical records for women who reported a stroke on a follow-up questionnaire.
Dr. Rist and her colleagues analyzed 27,937 samples for levels of LDL cholesterol, HDL cholesterol, total cholesterol, and triglycerides. They assigned each sample to one of five cholesterol level categories that were based on Adult Treatment Panel III guidelines. Cox proportional hazards models enabled the researchers to calculate the hazard ratio of incident hemorrhagic stroke events. They adjusted their results for covariates such as age, smoking status, menopausal status, body mass index, and alcohol consumption.
A U-shaped association
Women in the lowest category of LDL cholesterol level (less than 70 mg/dL) were younger, less likely to have a history of hypertension, and less likely to use cholesterol-lowering drugs than women in the reference group (100.0-129.9 mg/dL). Women with the lowest LDL cholesterol level were more likely to consume alcohol, have a normal weight, engage in physical activity, and be premenopausal than women in the reference group. The investigators confirmed 137 incident hemorrhagic stroke events during a mean 19.3 years of follow-up.
After data adjustment, the researchers found that women with the lowest level of LDL cholesterol had 2.17 times the risk of hemorrhagic stroke, compared with participants in the reference group. They found a trend toward increased risk among women with an LDL cholesterol level of 160 mg/dL or higher, but the result was not statistically significant. The highest risk for intracerebral hemorrhage (ICH) was among women with an LDL cholesterol level of less than 70 mg/dL (relative risk, 2.32), followed by women with a level of 160 mg/dL or higher (RR, 1.71).
In addition, after multivariable adjustment, women in the lowest quartile of triglycerides (less than or equal to 74 mg/dL for fasting and less than or equal to 85 mg/dL for nonfasting) had a significantly increased risk of hemorrhagic stroke, compared with women in the highest quartile (RR, 2.00). Low triglyceride levels were associated with an increased risk of subarachnoid hemorrhage, but not with an increased risk of ICH. Neither HDL cholesterol nor total cholesterol was associated with risk of hemorrhagic stroke, the researchers wrote.
Mechanism of increased risk unclear
The researchers do not yet know how low triglyceride and LDL cholesterol levels increase the risk of hemorrhagic stroke. One hypothesis is that low cholesterol promotes necrosis of the arterial medial layer’s smooth muscle cells. This impaired endothelium might be more susceptible to microaneurysms, which are common in patients with ICH, said the researchers.
The prospective design and the large sample size were two of the study’s strengths, but the study had important weaknesses as well, the researchers wrote. For example, few women were premenopausal at baseline, so the investigators could not evaluate whether menopausal status modifies the association between lipid levels and risk of hemorrhagic stroke. In addition, lipid levels were measured only at baseline, which prevented an analysis of whether change in lipid levels over time modifies the risk of hemorrhagic stroke.
Dr. Rist reported receiving a grant from the National Institutes of Health.
SOURCE: Rist PM et al. Neurology. 2019 April 10. doi: 10.1212/WNL.0000000000007454.
, according to research published in Neurology.
“Women with very low LDL cholesterol or low triglycerides should be monitored by their doctors for other stroke risk factors that can be modified, like high blood pressure and smoking, in order to reduce their risk of hemorrhagic stroke,” said Pamela M. Rist, ScD, instructor in epidemiology at Harvard Medical School, Boston. “Additional research is needed to determine how to lower the risk of hemorrhagic stroke in women with very low LDL and low triglycerides.”
Several meta-analyses have indicated that LDL cholesterol levels are inversely associated with the risk of hemorrhagic stroke. Because lipid-lowering treatments are used to prevent cardiovascular disease, this potential association has implications for clinical practice. Most of the studies included in these meta-analyses had low numbers of events among women, which prevented researchers from stratifying their results by sex. Because women are at greater risk of stroke than men, Dr. Rist and her colleagues sought to evaluate the association between lipid levels and risk of hemorrhagic stroke.
An analysis of the Women’s Health Study
The investigators examined data from the Women’s Health Study, a randomized, double-blind, placebo-controlled trial of low-dose aspirin and vitamin E for the primary prevention of cardiovascular disease and cancer among female American health professionals aged 45 years or older. The study ended in March 2004, but follow-up is ongoing. At regular intervals, the women complete a questionnaire about disease outcomes, including stroke. Some participants agreed to provide a fasting venous blood sample before randomization. With the subjects’ permission, a committee of physicians examined medical records for women who reported a stroke on a follow-up questionnaire.
Dr. Rist and her colleagues analyzed 27,937 samples for levels of LDL cholesterol, HDL cholesterol, total cholesterol, and triglycerides. They assigned each sample to one of five cholesterol level categories that were based on Adult Treatment Panel III guidelines. Cox proportional hazards models enabled the researchers to calculate the hazard ratio of incident hemorrhagic stroke events. They adjusted their results for covariates such as age, smoking status, menopausal status, body mass index, and alcohol consumption.
A U-shaped association
Women in the lowest category of LDL cholesterol level (less than 70 mg/dL) were younger, less likely to have a history of hypertension, and less likely to use cholesterol-lowering drugs than women in the reference group (100.0-129.9 mg/dL). Women with the lowest LDL cholesterol level were more likely to consume alcohol, have a normal weight, engage in physical activity, and be premenopausal than women in the reference group. The investigators confirmed 137 incident hemorrhagic stroke events during a mean 19.3 years of follow-up.
After data adjustment, the researchers found that women with the lowest level of LDL cholesterol had 2.17 times the risk of hemorrhagic stroke, compared with participants in the reference group. They found a trend toward increased risk among women with an LDL cholesterol level of 160 mg/dL or higher, but the result was not statistically significant. The highest risk for intracerebral hemorrhage (ICH) was among women with an LDL cholesterol level of less than 70 mg/dL (relative risk, 2.32), followed by women with a level of 160 mg/dL or higher (RR, 1.71).
In addition, after multivariable adjustment, women in the lowest quartile of triglycerides (less than or equal to 74 mg/dL for fasting and less than or equal to 85 mg/dL for nonfasting) had a significantly increased risk of hemorrhagic stroke, compared with women in the highest quartile (RR, 2.00). Low triglyceride levels were associated with an increased risk of subarachnoid hemorrhage, but not with an increased risk of ICH. Neither HDL cholesterol nor total cholesterol was associated with risk of hemorrhagic stroke, the researchers wrote.
Mechanism of increased risk unclear
The researchers do not yet know how low triglyceride and LDL cholesterol levels increase the risk of hemorrhagic stroke. One hypothesis is that low cholesterol promotes necrosis of the arterial medial layer’s smooth muscle cells. This impaired endothelium might be more susceptible to microaneurysms, which are common in patients with ICH, said the researchers.
The prospective design and the large sample size were two of the study’s strengths, but the study had important weaknesses as well, the researchers wrote. For example, few women were premenopausal at baseline, so the investigators could not evaluate whether menopausal status modifies the association between lipid levels and risk of hemorrhagic stroke. In addition, lipid levels were measured only at baseline, which prevented an analysis of whether change in lipid levels over time modifies the risk of hemorrhagic stroke.
Dr. Rist reported receiving a grant from the National Institutes of Health.
SOURCE: Rist PM et al. Neurology. 2019 April 10. doi: 10.1212/WNL.0000000000007454.
, according to research published in Neurology.
“Women with very low LDL cholesterol or low triglycerides should be monitored by their doctors for other stroke risk factors that can be modified, like high blood pressure and smoking, in order to reduce their risk of hemorrhagic stroke,” said Pamela M. Rist, ScD, instructor in epidemiology at Harvard Medical School, Boston. “Additional research is needed to determine how to lower the risk of hemorrhagic stroke in women with very low LDL and low triglycerides.”
Several meta-analyses have indicated that LDL cholesterol levels are inversely associated with the risk of hemorrhagic stroke. Because lipid-lowering treatments are used to prevent cardiovascular disease, this potential association has implications for clinical practice. Most of the studies included in these meta-analyses had low numbers of events among women, which prevented researchers from stratifying their results by sex. Because women are at greater risk of stroke than men, Dr. Rist and her colleagues sought to evaluate the association between lipid levels and risk of hemorrhagic stroke.
An analysis of the Women’s Health Study
The investigators examined data from the Women’s Health Study, a randomized, double-blind, placebo-controlled trial of low-dose aspirin and vitamin E for the primary prevention of cardiovascular disease and cancer among female American health professionals aged 45 years or older. The study ended in March 2004, but follow-up is ongoing. At regular intervals, the women complete a questionnaire about disease outcomes, including stroke. Some participants agreed to provide a fasting venous blood sample before randomization. With the subjects’ permission, a committee of physicians examined medical records for women who reported a stroke on a follow-up questionnaire.
Dr. Rist and her colleagues analyzed 27,937 samples for levels of LDL cholesterol, HDL cholesterol, total cholesterol, and triglycerides. They assigned each sample to one of five cholesterol level categories that were based on Adult Treatment Panel III guidelines. Cox proportional hazards models enabled the researchers to calculate the hazard ratio of incident hemorrhagic stroke events. They adjusted their results for covariates such as age, smoking status, menopausal status, body mass index, and alcohol consumption.
A U-shaped association
Women in the lowest category of LDL cholesterol level (less than 70 mg/dL) were younger, less likely to have a history of hypertension, and less likely to use cholesterol-lowering drugs than women in the reference group (100.0-129.9 mg/dL). Women with the lowest LDL cholesterol level were more likely to consume alcohol, have a normal weight, engage in physical activity, and be premenopausal than women in the reference group. The investigators confirmed 137 incident hemorrhagic stroke events during a mean 19.3 years of follow-up.
After data adjustment, the researchers found that women with the lowest level of LDL cholesterol had 2.17 times the risk of hemorrhagic stroke, compared with participants in the reference group. They found a trend toward increased risk among women with an LDL cholesterol level of 160 mg/dL or higher, but the result was not statistically significant. The highest risk for intracerebral hemorrhage (ICH) was among women with an LDL cholesterol level of less than 70 mg/dL (relative risk, 2.32), followed by women with a level of 160 mg/dL or higher (RR, 1.71).
In addition, after multivariable adjustment, women in the lowest quartile of triglycerides (less than or equal to 74 mg/dL for fasting and less than or equal to 85 mg/dL for nonfasting) had a significantly increased risk of hemorrhagic stroke, compared with women in the highest quartile (RR, 2.00). Low triglyceride levels were associated with an increased risk of subarachnoid hemorrhage, but not with an increased risk of ICH. Neither HDL cholesterol nor total cholesterol was associated with risk of hemorrhagic stroke, the researchers wrote.
Mechanism of increased risk unclear
The researchers do not yet know how low triglyceride and LDL cholesterol levels increase the risk of hemorrhagic stroke. One hypothesis is that low cholesterol promotes necrosis of the arterial medial layer’s smooth muscle cells. This impaired endothelium might be more susceptible to microaneurysms, which are common in patients with ICH, said the researchers.
The prospective design and the large sample size were two of the study’s strengths, but the study had important weaknesses as well, the researchers wrote. For example, few women were premenopausal at baseline, so the investigators could not evaluate whether menopausal status modifies the association between lipid levels and risk of hemorrhagic stroke. In addition, lipid levels were measured only at baseline, which prevented an analysis of whether change in lipid levels over time modifies the risk of hemorrhagic stroke.
Dr. Rist reported receiving a grant from the National Institutes of Health.
SOURCE: Rist PM et al. Neurology. 2019 April 10. doi: 10.1212/WNL.0000000000007454.
FROM NEUROLOGY
Proportion of women speaking at medical conferences rises over decade
The proportion of women speaking at medical conferences in the United States and Canada increased significantly between 2007 and 2017, while the proportion at surgical specialty conferences lagged noticeably behind, according to new research.
“Although female representation at academic meetings has been identified as an important gender equity issue, the proportion of conference speakers who are women has not yet been systematically measured across different medical subspecialties,” wrote Shannon M. Ruzycki, MD, and her colleagues from the University of Calgary (Alta.). The report is in JAMA Network Open.
Using the Web of Science Conference database, the investigators identified 181 conferences and 701 unique meetings (40 in 2007, 104 in 2013, 115 in 2014, 124 in 2015, 137 in 2016, and 181 in 2017). The list of names from each meeting program was analyzed by the Gender Balance Assessment Tool to identify the likely proportion of female speakers by assigning a probability of each name belonging to a gender, based on social media data.
In 2007, the proportion of female speakers was 24.6% , which increased to 34.1% by 2017, an average increase of 0.97% per year. The range of female speakers at each meeting ranged from 0% to 82.6%, with 82 (12%) of the 701 meetings having more than 50% female speakers. The proportion of female speakers was slightly less than the proportion of female doctors in the United States and Canada in 2007 (26.1%), but was slightly greater than the proportion of female doctors in 2015 (32.4%).
During the study period, the proportion of female speakers at surgical specialty conferences was significantly lower than that for medical specialty conferences (20.1% in 2007 and 28.4% in 2017 vs. 29.9% in 2007 and 38.8% in 2017). While the number of speakers at medical meetings in 2015 matched the proportion of doctors in the United States and Canada in that year, the proportion of speakers at surgical meetings was noticeably higher than the number of female surgeons.
“We hypothesize that the low proportion of female speakers at medical conferences reflects broader gender inequity within the medical profession, particularly in subspecialties where the majority of physicians are men. It has been shown that the presence of female role models in male-dominated career streams can increase engagement of young women,” the investigators wrote. “Exposure to female speakers at medical conferences may be a means of encouraging female medical students and residents to choose specialties that have historically been male dominated. Strategies to promote inclusivity of female speakers at academic conferences may therefore represent an important opportunity to influence gender equity within medicine,” they concluded.
The University of Calgary funded the study. The authors reported no conflicts of interest.
SOURCE: Ruzycki SM et al. JAMA Netw Open. 2019 Apr 12. doi: 10.1001/jamanetworkopen.2019.2103.
The proportion of women speaking at medical conferences in the United States and Canada increased significantly between 2007 and 2017, while the proportion at surgical specialty conferences lagged noticeably behind, according to new research.
“Although female representation at academic meetings has been identified as an important gender equity issue, the proportion of conference speakers who are women has not yet been systematically measured across different medical subspecialties,” wrote Shannon M. Ruzycki, MD, and her colleagues from the University of Calgary (Alta.). The report is in JAMA Network Open.
Using the Web of Science Conference database, the investigators identified 181 conferences and 701 unique meetings (40 in 2007, 104 in 2013, 115 in 2014, 124 in 2015, 137 in 2016, and 181 in 2017). The list of names from each meeting program was analyzed by the Gender Balance Assessment Tool to identify the likely proportion of female speakers by assigning a probability of each name belonging to a gender, based on social media data.
In 2007, the proportion of female speakers was 24.6% , which increased to 34.1% by 2017, an average increase of 0.97% per year. The range of female speakers at each meeting ranged from 0% to 82.6%, with 82 (12%) of the 701 meetings having more than 50% female speakers. The proportion of female speakers was slightly less than the proportion of female doctors in the United States and Canada in 2007 (26.1%), but was slightly greater than the proportion of female doctors in 2015 (32.4%).
During the study period, the proportion of female speakers at surgical specialty conferences was significantly lower than that for medical specialty conferences (20.1% in 2007 and 28.4% in 2017 vs. 29.9% in 2007 and 38.8% in 2017). While the number of speakers at medical meetings in 2015 matched the proportion of doctors in the United States and Canada in that year, the proportion of speakers at surgical meetings was noticeably higher than the number of female surgeons.
“We hypothesize that the low proportion of female speakers at medical conferences reflects broader gender inequity within the medical profession, particularly in subspecialties where the majority of physicians are men. It has been shown that the presence of female role models in male-dominated career streams can increase engagement of young women,” the investigators wrote. “Exposure to female speakers at medical conferences may be a means of encouraging female medical students and residents to choose specialties that have historically been male dominated. Strategies to promote inclusivity of female speakers at academic conferences may therefore represent an important opportunity to influence gender equity within medicine,” they concluded.
The University of Calgary funded the study. The authors reported no conflicts of interest.
SOURCE: Ruzycki SM et al. JAMA Netw Open. 2019 Apr 12. doi: 10.1001/jamanetworkopen.2019.2103.
The proportion of women speaking at medical conferences in the United States and Canada increased significantly between 2007 and 2017, while the proportion at surgical specialty conferences lagged noticeably behind, according to new research.
“Although female representation at academic meetings has been identified as an important gender equity issue, the proportion of conference speakers who are women has not yet been systematically measured across different medical subspecialties,” wrote Shannon M. Ruzycki, MD, and her colleagues from the University of Calgary (Alta.). The report is in JAMA Network Open.
Using the Web of Science Conference database, the investigators identified 181 conferences and 701 unique meetings (40 in 2007, 104 in 2013, 115 in 2014, 124 in 2015, 137 in 2016, and 181 in 2017). The list of names from each meeting program was analyzed by the Gender Balance Assessment Tool to identify the likely proportion of female speakers by assigning a probability of each name belonging to a gender, based on social media data.
In 2007, the proportion of female speakers was 24.6% , which increased to 34.1% by 2017, an average increase of 0.97% per year. The range of female speakers at each meeting ranged from 0% to 82.6%, with 82 (12%) of the 701 meetings having more than 50% female speakers. The proportion of female speakers was slightly less than the proportion of female doctors in the United States and Canada in 2007 (26.1%), but was slightly greater than the proportion of female doctors in 2015 (32.4%).
During the study period, the proportion of female speakers at surgical specialty conferences was significantly lower than that for medical specialty conferences (20.1% in 2007 and 28.4% in 2017 vs. 29.9% in 2007 and 38.8% in 2017). While the number of speakers at medical meetings in 2015 matched the proportion of doctors in the United States and Canada in that year, the proportion of speakers at surgical meetings was noticeably higher than the number of female surgeons.
“We hypothesize that the low proportion of female speakers at medical conferences reflects broader gender inequity within the medical profession, particularly in subspecialties where the majority of physicians are men. It has been shown that the presence of female role models in male-dominated career streams can increase engagement of young women,” the investigators wrote. “Exposure to female speakers at medical conferences may be a means of encouraging female medical students and residents to choose specialties that have historically been male dominated. Strategies to promote inclusivity of female speakers at academic conferences may therefore represent an important opportunity to influence gender equity within medicine,” they concluded.
The University of Calgary funded the study. The authors reported no conflicts of interest.
SOURCE: Ruzycki SM et al. JAMA Netw Open. 2019 Apr 12. doi: 10.1001/jamanetworkopen.2019.2103.
FROM JAMA NETWORK OPEN
Key clinical point: By 2015, the proportion of women presenting at medical conferences matched the proportion of women practicing medicine in the United States and Canada.
Major finding: Between 2007 and 2017, the proportion of women presenting at medical conferences rose from 24.60% to 34.10%, an average increase of 0.97% per year.
Study details: A review of presenters from 181 conferences and 701 unique meetings.
Disclosures: The University of Calgary funded the study. The authors reported no conflicts of interest.
Source: Ruzycki SM et al. JAMA Netw Open. 2019 Apr 12. doi: 10.1001/jamanetworkopen.2019.2103.
Negotiating an employment contract? Lawyer up
advised in a presentation at the annual meeting of the American College of Physicians.
In a presentation that outlined the essentials of reviewing an employment contract, Dr. Sinha of Harvard Medical School, Boston, advised hiring a lawyer with expertise in health care law and health care employment contracts once the letter of intent has been received. Understanding the contract process is helpful, “but ultimately the lawyer is going to be the one helping you with regional expertise. Perhaps they have already interacted with this employer and have a long-standing relationship. They are going to know state laws that are relevant to you. They are going to have a lot of insights that you are just not going to be able to bring to the table very easily.”
A lawyer also will have expertise in negotiation. “If you can form an alliance and negotiate as a team, you are much more likely to get the things you want out of a negotiation,” he said.
Dr. Sinha advised going into a contract knowing exactly what you want. He recommended coming up with six or seven things that matter to you, such as base pay and bonus structure, fringe benefits, relocation expenses, work hours and locations, terms, employee versus independent contractor, and no compete clauses. Even if you have only three key things you’re looking for out of the negotiations, still try to come up with six or seven items.
To get the best results, you need to do your homework. Find out starting salaries and use salary scales when available. Get a sense of who the prospective employer is, what their needs are, and who is competing with you for that contract. Talk to the staff to get a sense of what the work environment is like.
“And then, really speak to people in the community. ... I think this [factor] gets overlooked,” he said. “You can get a lot of valuable information, get a sense of public perception about a physician group, a hospital, a medical school. Those are important considerations as well.”
He also stressed understanding the economic viability of the organization and the growth opportunities for the organization, and recommended reading the contract multiple times. “Understanding the contract is the key to being able to negotiate the provisions.”
Finally, he emphasized that there is no need to accept the first offer made.
“There is always room for negotiating and the bottom line is both sides have to be happy with the contract they negotiated,” he said.
advised in a presentation at the annual meeting of the American College of Physicians.
In a presentation that outlined the essentials of reviewing an employment contract, Dr. Sinha of Harvard Medical School, Boston, advised hiring a lawyer with expertise in health care law and health care employment contracts once the letter of intent has been received. Understanding the contract process is helpful, “but ultimately the lawyer is going to be the one helping you with regional expertise. Perhaps they have already interacted with this employer and have a long-standing relationship. They are going to know state laws that are relevant to you. They are going to have a lot of insights that you are just not going to be able to bring to the table very easily.”
A lawyer also will have expertise in negotiation. “If you can form an alliance and negotiate as a team, you are much more likely to get the things you want out of a negotiation,” he said.
Dr. Sinha advised going into a contract knowing exactly what you want. He recommended coming up with six or seven things that matter to you, such as base pay and bonus structure, fringe benefits, relocation expenses, work hours and locations, terms, employee versus independent contractor, and no compete clauses. Even if you have only three key things you’re looking for out of the negotiations, still try to come up with six or seven items.
To get the best results, you need to do your homework. Find out starting salaries and use salary scales when available. Get a sense of who the prospective employer is, what their needs are, and who is competing with you for that contract. Talk to the staff to get a sense of what the work environment is like.
“And then, really speak to people in the community. ... I think this [factor] gets overlooked,” he said. “You can get a lot of valuable information, get a sense of public perception about a physician group, a hospital, a medical school. Those are important considerations as well.”
He also stressed understanding the economic viability of the organization and the growth opportunities for the organization, and recommended reading the contract multiple times. “Understanding the contract is the key to being able to negotiate the provisions.”
Finally, he emphasized that there is no need to accept the first offer made.
“There is always room for negotiating and the bottom line is both sides have to be happy with the contract they negotiated,” he said.
advised in a presentation at the annual meeting of the American College of Physicians.
In a presentation that outlined the essentials of reviewing an employment contract, Dr. Sinha of Harvard Medical School, Boston, advised hiring a lawyer with expertise in health care law and health care employment contracts once the letter of intent has been received. Understanding the contract process is helpful, “but ultimately the lawyer is going to be the one helping you with regional expertise. Perhaps they have already interacted with this employer and have a long-standing relationship. They are going to know state laws that are relevant to you. They are going to have a lot of insights that you are just not going to be able to bring to the table very easily.”
A lawyer also will have expertise in negotiation. “If you can form an alliance and negotiate as a team, you are much more likely to get the things you want out of a negotiation,” he said.
Dr. Sinha advised going into a contract knowing exactly what you want. He recommended coming up with six or seven things that matter to you, such as base pay and bonus structure, fringe benefits, relocation expenses, work hours and locations, terms, employee versus independent contractor, and no compete clauses. Even if you have only three key things you’re looking for out of the negotiations, still try to come up with six or seven items.
To get the best results, you need to do your homework. Find out starting salaries and use salary scales when available. Get a sense of who the prospective employer is, what their needs are, and who is competing with you for that contract. Talk to the staff to get a sense of what the work environment is like.
“And then, really speak to people in the community. ... I think this [factor] gets overlooked,” he said. “You can get a lot of valuable information, get a sense of public perception about a physician group, a hospital, a medical school. Those are important considerations as well.”
He also stressed understanding the economic viability of the organization and the growth opportunities for the organization, and recommended reading the contract multiple times. “Understanding the contract is the key to being able to negotiate the provisions.”
Finally, he emphasized that there is no need to accept the first offer made.
“There is always room for negotiating and the bottom line is both sides have to be happy with the contract they negotiated,” he said.
REPORTING FROM INTERNAL MEDICINE 2019
Updates in MS: Highlights From the ECTRIMS and ACTRIMS Annual Meetings
This supplement to Neurology Reviews compiles news briefs from the 2018 ECTRIMS annual meeting in Berlin and the 2019 annual ACTRIMS meeting in Dallas.
This supplement to Neurology Reviews compiles news briefs from the 2018 ECTRIMS annual meeting in Berlin and the 2019 annual ACTRIMS meeting in Dallas.
This supplement to Neurology Reviews compiles news briefs from the 2018 ECTRIMS annual meeting in Berlin and the 2019 annual ACTRIMS meeting in Dallas.