User login
Hypoglycemia in the elderly: Watch for atypical symptoms
We read with interest the review article by Keber and Fiebert, “Diabetes in the elderly: Matching meds to needs” (J Fam Pract. 2018;67:408-410,412-415). The authors have provided a timely overview of antidiabetes medications for elderly people with type 2 diabetes mellitus (T2DM) and their relative risks for hypoglycemia.
We’d like to add to this important conversation.
Aging, per se, modifies the glycemic thresholds for autonomic symptoms and cognitive impairment; in older nondiabetic men (mean + SD: age 65 ± 3 years), autonomic symptoms and cognitive dysfunction commence at identical glycemic thresholds (3 ± 0.2 mmol/L [54 ± 4 mg/dL]). By contrast, in younger men (age 23 ± 2 years), a significant gap is observed between the glycemic threshold for symptom generation (3.6 mmol/L [65 mg/dL]) and the onset of cognitive dysfunction (2.6 mmol/L [47 mg/dL]).1,2 The simultaneous occurrence of symptoms and cognitive impairment in older people may adversely affect their ability to recognize and treat hypoglycemia promptly.
In addition, hypoglycemia in older T2DM patients often presents with atypical neurologic symptoms, including incoordination and ataxia, slurring of speech, and visual disturbances, which either are not identified as hypoglycemia or are misdiagnosed as other medical disorders (eg, transient ischemic attack).3 Knowledge about hypoglycemia symptoms is poor, in both elderly people with diabetes and their relatives and caregivers, which compromises the ability to identify hypoglycemia and provide effective treatment.4 Education about the possible presentations of hypoglycemia and its effective treatment is essential for older patients and their relatives.
Jan Brož, MD
Prague, Czech Republic
1. Meneilly GS, Elahi D. Physiological importance of first-phase insulin release in elderly patients with diabetes. Diabetes Care. 1998;21:1326-1329.
2. Matyka K, Evans M, Lomas J, et al. Altered hierarchy of protective responses against severe hypoglycemia in normal aging in healthy men. Diabetes Care. 1997;20:135-141.
3. Jaap AJ, Jones GC, McCrimmon RJ, et al. Perceived symptoms of hypoglycaemia in elderly type 2 diabetic patients treated with insulin. Diabet Med. 1998;15:398-401.
4. Thomson FJ, Masson EA, Leeming JT, et al. Lack of knowledge of symptoms of hypoglycaemia by elderly diabetic patients. Age Ageing. 1991;20:404-406.
We read with interest the review article by Keber and Fiebert, “Diabetes in the elderly: Matching meds to needs” (J Fam Pract. 2018;67:408-410,412-415). The authors have provided a timely overview of antidiabetes medications for elderly people with type 2 diabetes mellitus (T2DM) and their relative risks for hypoglycemia.
We’d like to add to this important conversation.
Aging, per se, modifies the glycemic thresholds for autonomic symptoms and cognitive impairment; in older nondiabetic men (mean + SD: age 65 ± 3 years), autonomic symptoms and cognitive dysfunction commence at identical glycemic thresholds (3 ± 0.2 mmol/L [54 ± 4 mg/dL]). By contrast, in younger men (age 23 ± 2 years), a significant gap is observed between the glycemic threshold for symptom generation (3.6 mmol/L [65 mg/dL]) and the onset of cognitive dysfunction (2.6 mmol/L [47 mg/dL]).1,2 The simultaneous occurrence of symptoms and cognitive impairment in older people may adversely affect their ability to recognize and treat hypoglycemia promptly.
In addition, hypoglycemia in older T2DM patients often presents with atypical neurologic symptoms, including incoordination and ataxia, slurring of speech, and visual disturbances, which either are not identified as hypoglycemia or are misdiagnosed as other medical disorders (eg, transient ischemic attack).3 Knowledge about hypoglycemia symptoms is poor, in both elderly people with diabetes and their relatives and caregivers, which compromises the ability to identify hypoglycemia and provide effective treatment.4 Education about the possible presentations of hypoglycemia and its effective treatment is essential for older patients and their relatives.
Jan Brož, MD
Prague, Czech Republic
We read with interest the review article by Keber and Fiebert, “Diabetes in the elderly: Matching meds to needs” (J Fam Pract. 2018;67:408-410,412-415). The authors have provided a timely overview of antidiabetes medications for elderly people with type 2 diabetes mellitus (T2DM) and their relative risks for hypoglycemia.
We’d like to add to this important conversation.
Aging, per se, modifies the glycemic thresholds for autonomic symptoms and cognitive impairment; in older nondiabetic men (mean + SD: age 65 ± 3 years), autonomic symptoms and cognitive dysfunction commence at identical glycemic thresholds (3 ± 0.2 mmol/L [54 ± 4 mg/dL]). By contrast, in younger men (age 23 ± 2 years), a significant gap is observed between the glycemic threshold for symptom generation (3.6 mmol/L [65 mg/dL]) and the onset of cognitive dysfunction (2.6 mmol/L [47 mg/dL]).1,2 The simultaneous occurrence of symptoms and cognitive impairment in older people may adversely affect their ability to recognize and treat hypoglycemia promptly.
In addition, hypoglycemia in older T2DM patients often presents with atypical neurologic symptoms, including incoordination and ataxia, slurring of speech, and visual disturbances, which either are not identified as hypoglycemia or are misdiagnosed as other medical disorders (eg, transient ischemic attack).3 Knowledge about hypoglycemia symptoms is poor, in both elderly people with diabetes and their relatives and caregivers, which compromises the ability to identify hypoglycemia and provide effective treatment.4 Education about the possible presentations of hypoglycemia and its effective treatment is essential for older patients and their relatives.
Jan Brož, MD
Prague, Czech Republic
1. Meneilly GS, Elahi D. Physiological importance of first-phase insulin release in elderly patients with diabetes. Diabetes Care. 1998;21:1326-1329.
2. Matyka K, Evans M, Lomas J, et al. Altered hierarchy of protective responses against severe hypoglycemia in normal aging in healthy men. Diabetes Care. 1997;20:135-141.
3. Jaap AJ, Jones GC, McCrimmon RJ, et al. Perceived symptoms of hypoglycaemia in elderly type 2 diabetic patients treated with insulin. Diabet Med. 1998;15:398-401.
4. Thomson FJ, Masson EA, Leeming JT, et al. Lack of knowledge of symptoms of hypoglycaemia by elderly diabetic patients. Age Ageing. 1991;20:404-406.
1. Meneilly GS, Elahi D. Physiological importance of first-phase insulin release in elderly patients with diabetes. Diabetes Care. 1998;21:1326-1329.
2. Matyka K, Evans M, Lomas J, et al. Altered hierarchy of protective responses against severe hypoglycemia in normal aging in healthy men. Diabetes Care. 1997;20:135-141.
3. Jaap AJ, Jones GC, McCrimmon RJ, et al. Perceived symptoms of hypoglycaemia in elderly type 2 diabetic patients treated with insulin. Diabet Med. 1998;15:398-401.
4. Thomson FJ, Masson EA, Leeming JT, et al. Lack of knowledge of symptoms of hypoglycaemia by elderly diabetic patients. Age Ageing. 1991;20:404-406.
Another practice’s experiences in “dialing back opioids”
It is with much enthusiasm that we read the article “Dialing back opioids for chronic pain one conversation at a time” (J Fam Pract. 2018;67:753-757) about the author’s approach to opioid tapering. We have implemented a similar process in our own medical home practice, based on the continuity relationship and the Ecological Systems Theory.
The use of the human resources within the medical home—care coordinator, pharmacist, community health worker, etc— distributes the responsibility and lessens the burden of care for the family physician. The Ecological Systems Theory provides a structure for understanding the interaction between proximal influencers (eg, the team) and more distal influences (eg, national guidelines and institutional mandates).
Recently, we presented our findings at the 2018 North American Primary Care Research Group (NAPCRG) Annual Meeting. Our results showed a 50% decline in per capita medication use over an almost 14-month period.
We feel that opioid tapering provides both a counterpoint and a complementary method to medication-assisted therapies (MAT). A counterpoint, because MAT involves the diagnosis and treatment of opioid misuse disorder. At the core of that diagnosis is the question of whether all chronic opioid use should be labelled as “misuse.” Tapering involves no such diagnosis and focuses on the safety of minimal opioid use, which, when MAT is used appropriately, is also a primary concern.
We appreciate the approach that the authors took in their project and look forward to seeing further iterations.
Bharat Gopal, MD
Cristina Capannolo, DO
Corvallis, Ore
It is with much enthusiasm that we read the article “Dialing back opioids for chronic pain one conversation at a time” (J Fam Pract. 2018;67:753-757) about the author’s approach to opioid tapering. We have implemented a similar process in our own medical home practice, based on the continuity relationship and the Ecological Systems Theory.
The use of the human resources within the medical home—care coordinator, pharmacist, community health worker, etc— distributes the responsibility and lessens the burden of care for the family physician. The Ecological Systems Theory provides a structure for understanding the interaction between proximal influencers (eg, the team) and more distal influences (eg, national guidelines and institutional mandates).
Recently, we presented our findings at the 2018 North American Primary Care Research Group (NAPCRG) Annual Meeting. Our results showed a 50% decline in per capita medication use over an almost 14-month period.
We feel that opioid tapering provides both a counterpoint and a complementary method to medication-assisted therapies (MAT). A counterpoint, because MAT involves the diagnosis and treatment of opioid misuse disorder. At the core of that diagnosis is the question of whether all chronic opioid use should be labelled as “misuse.” Tapering involves no such diagnosis and focuses on the safety of minimal opioid use, which, when MAT is used appropriately, is also a primary concern.
We appreciate the approach that the authors took in their project and look forward to seeing further iterations.
Bharat Gopal, MD
Cristina Capannolo, DO
Corvallis, Ore
It is with much enthusiasm that we read the article “Dialing back opioids for chronic pain one conversation at a time” (J Fam Pract. 2018;67:753-757) about the author’s approach to opioid tapering. We have implemented a similar process in our own medical home practice, based on the continuity relationship and the Ecological Systems Theory.
The use of the human resources within the medical home—care coordinator, pharmacist, community health worker, etc— distributes the responsibility and lessens the burden of care for the family physician. The Ecological Systems Theory provides a structure for understanding the interaction between proximal influencers (eg, the team) and more distal influences (eg, national guidelines and institutional mandates).
Recently, we presented our findings at the 2018 North American Primary Care Research Group (NAPCRG) Annual Meeting. Our results showed a 50% decline in per capita medication use over an almost 14-month period.
We feel that opioid tapering provides both a counterpoint and a complementary method to medication-assisted therapies (MAT). A counterpoint, because MAT involves the diagnosis and treatment of opioid misuse disorder. At the core of that diagnosis is the question of whether all chronic opioid use should be labelled as “misuse.” Tapering involves no such diagnosis and focuses on the safety of minimal opioid use, which, when MAT is used appropriately, is also a primary concern.
We appreciate the approach that the authors took in their project and look forward to seeing further iterations.
Bharat Gopal, MD
Cristina Capannolo, DO
Corvallis, Ore
FDA approves new valsartan generic
In response to a medication shortage, the Food and Drug Administration has approved a new generic of valsartan (Diovan), produced by Alkem Laboratories, for the treatment of high blood pressure and heart failure, the regulatory agency announced in a statement.
The FDA conducted an investigation into generic angiotensin II receptor blocker (ARB) products following reports of N-nitrosodimethylamine impurities being found in a separate valsartan product in the summer of 2018. Since that time, nitrosamine impurities have been detected in multiple ARBs, and as of March 1, 2019, hundreds of lots of ARBs produced by several companies have been recalled. The FDA has implemented new rules to prevent further contamination, but the ongoing recalls have caused a significant shortage.
“[To] address the public health consequences of these shortages, we’ve prioritized the review of generic applications for these valsartan products,” FDA commissioner Scott Gottlieb, MD, said in the statement.
For the new generic’s approval, the FDA assessed Alkem Laboratories’ manufacturing process and ensured that the company used proper testing methods to rule out the presence of nitrosamine impurities.
“We hope that today’s approval of this new generic will help reduce the valsartan shortage, and we remain committed to implementing measures to prevent the formation of these impurities during drug manufacturing processes for existing and future products,” Dr. Gottlieb said.
In response to a medication shortage, the Food and Drug Administration has approved a new generic of valsartan (Diovan), produced by Alkem Laboratories, for the treatment of high blood pressure and heart failure, the regulatory agency announced in a statement.
The FDA conducted an investigation into generic angiotensin II receptor blocker (ARB) products following reports of N-nitrosodimethylamine impurities being found in a separate valsartan product in the summer of 2018. Since that time, nitrosamine impurities have been detected in multiple ARBs, and as of March 1, 2019, hundreds of lots of ARBs produced by several companies have been recalled. The FDA has implemented new rules to prevent further contamination, but the ongoing recalls have caused a significant shortage.
“[To] address the public health consequences of these shortages, we’ve prioritized the review of generic applications for these valsartan products,” FDA commissioner Scott Gottlieb, MD, said in the statement.
For the new generic’s approval, the FDA assessed Alkem Laboratories’ manufacturing process and ensured that the company used proper testing methods to rule out the presence of nitrosamine impurities.
“We hope that today’s approval of this new generic will help reduce the valsartan shortage, and we remain committed to implementing measures to prevent the formation of these impurities during drug manufacturing processes for existing and future products,” Dr. Gottlieb said.
In response to a medication shortage, the Food and Drug Administration has approved a new generic of valsartan (Diovan), produced by Alkem Laboratories, for the treatment of high blood pressure and heart failure, the regulatory agency announced in a statement.
The FDA conducted an investigation into generic angiotensin II receptor blocker (ARB) products following reports of N-nitrosodimethylamine impurities being found in a separate valsartan product in the summer of 2018. Since that time, nitrosamine impurities have been detected in multiple ARBs, and as of March 1, 2019, hundreds of lots of ARBs produced by several companies have been recalled. The FDA has implemented new rules to prevent further contamination, but the ongoing recalls have caused a significant shortage.
“[To] address the public health consequences of these shortages, we’ve prioritized the review of generic applications for these valsartan products,” FDA commissioner Scott Gottlieb, MD, said in the statement.
For the new generic’s approval, the FDA assessed Alkem Laboratories’ manufacturing process and ensured that the company used proper testing methods to rule out the presence of nitrosamine impurities.
“We hope that today’s approval of this new generic will help reduce the valsartan shortage, and we remain committed to implementing measures to prevent the formation of these impurities during drug manufacturing processes for existing and future products,” Dr. Gottlieb said.
Raltegravir safe, effective in late pregnancy
SEATTLE – In HIV-positive pregnant women, an antiretroviral therapy (ART) regimen that included the integrase inhibitor raltegravir (RAL-ART) led to faster viral load (VL) reduction and a greater proportion of women with a VL of less than 200 copies/mL at delivery, compared with patients treated with an efavirenz-based ART (EFV-ART). There were no statistically significant differences between the two arms with respect to percentage of stillbirths, preterm delivery, or rates of HIV infection in the newborn.
“There are lots of advantages of these [integrase inhibitor] drugs, and we’d like to have pregnant women take advantage of them. The problem is, there’s no requirement of drug manufacturers to study the drugs in pregnancy. So these studies are put off until after the drug is licensed, and we’re playing catch-up,” Mark Mirochnick, MD, professor of pediatrics at Boston University, said in an interview. Dr. Mirochnick presented the results at the Conference on Retroviruses and Opportunistic Infections.
Another integrase inhibitor, dolutegravir, has a better resistance profile than that of raltegravir, but concerns over neural tube defects observed during a study in Botswana led both the Food and Drug Administration and the European Medicines Agency to issue safety warnings for that drug. The current study did not raise concern, since it began at 20 weeks’ gestation, well after the period when neural tube defects might occur. “I think it just demonstrates that [integrase inhibitors] are safe in mid- to late-pregnancy,” said Dr. Mirochnick.
It remains to be seen whether a potential link to neural tube defects, if it is a real effect, is due to a specific drug or the mechanism of action of integrase inhibitors more generally. “It’s a question we don’t have an answer to. So you have to balance the potential benefits and potential risks, and that’s probably a decision best made by an individual woman and her care provider. Some women do very well on a particular regimen and they don’t want to change, and you run the risk when you change that you’ll get a viral rebound. What do you tell women who are on dolutegravir and are thinking about becoming pregnant? That’s a controversial question. There are risks with both courses,” said Dr. Mirochnick.
The study comprised 408 patients recruited from centers in Brazil, Tanzania, South Africa, Thailand, Argentina, and the United States. The patients were between 20 and 37 weeks’ gestation and had not previously received ART. They were randomized to RAL-ART or EFV-ART. About 12% of patients were Asian, 36% were black, 52% were Hispanic, and 1% were white.
Overall, 94% of patients on RAL-ART had a VL less than 200 copies/mL at delivery, compared to 84% of EFV-ART patients (P = .001). The effect appeared to be driven by patients who enrolled later in pregnancy: There was no significant difference in those enrolled in weeks 20-28, but suppression occurred in 93% of the RAL-ART group versus 71% of the EFV-ART group among those enrolled in weeks 29-37 (P = .04).
Tolerability was slightly better in the RAL-ART group, with 99% versus 97% of patients staying on their assigned therapy (P = .05). In both groups, 30% of women experienced an adverse event of grade 3 or higher, as did 25% of live-born infants in both groups.
A total of 92% of women in the RAL-ART group had a sustained VL response through delivery, compared with 64% in the EFV-ART group (P less than .001). The median time to achieving a VL less than 200 copies/mL was 8 days in the RAL-ART group and 15 days in the EFV-ART group (generalized log-rank test P less than .001).
There was one stillbirth in the EFV-ART arm and three in the RAL-ART arm, with 11% in the EFV-ART group having preterm delivery compared with 12% in the RAL-ART group. In addition, the proportion of HIV-infected infants was lower in the RAL-ART arm (1% versus 3%). These differences were not significant.
The National Institutes of Health funded the study. Glaxo/ViiV, Merck, and Bristol-Myers Squibb supplied study drugs. Dr. Mirochnick has received research funding from those companies.
SOURCE: Mark Mirochnick et al. CROI 2019, Abstract 39 LB.
SEATTLE – In HIV-positive pregnant women, an antiretroviral therapy (ART) regimen that included the integrase inhibitor raltegravir (RAL-ART) led to faster viral load (VL) reduction and a greater proportion of women with a VL of less than 200 copies/mL at delivery, compared with patients treated with an efavirenz-based ART (EFV-ART). There were no statistically significant differences between the two arms with respect to percentage of stillbirths, preterm delivery, or rates of HIV infection in the newborn.
“There are lots of advantages of these [integrase inhibitor] drugs, and we’d like to have pregnant women take advantage of them. The problem is, there’s no requirement of drug manufacturers to study the drugs in pregnancy. So these studies are put off until after the drug is licensed, and we’re playing catch-up,” Mark Mirochnick, MD, professor of pediatrics at Boston University, said in an interview. Dr. Mirochnick presented the results at the Conference on Retroviruses and Opportunistic Infections.
Another integrase inhibitor, dolutegravir, has a better resistance profile than that of raltegravir, but concerns over neural tube defects observed during a study in Botswana led both the Food and Drug Administration and the European Medicines Agency to issue safety warnings for that drug. The current study did not raise concern, since it began at 20 weeks’ gestation, well after the period when neural tube defects might occur. “I think it just demonstrates that [integrase inhibitors] are safe in mid- to late-pregnancy,” said Dr. Mirochnick.
It remains to be seen whether a potential link to neural tube defects, if it is a real effect, is due to a specific drug or the mechanism of action of integrase inhibitors more generally. “It’s a question we don’t have an answer to. So you have to balance the potential benefits and potential risks, and that’s probably a decision best made by an individual woman and her care provider. Some women do very well on a particular regimen and they don’t want to change, and you run the risk when you change that you’ll get a viral rebound. What do you tell women who are on dolutegravir and are thinking about becoming pregnant? That’s a controversial question. There are risks with both courses,” said Dr. Mirochnick.
The study comprised 408 patients recruited from centers in Brazil, Tanzania, South Africa, Thailand, Argentina, and the United States. The patients were between 20 and 37 weeks’ gestation and had not previously received ART. They were randomized to RAL-ART or EFV-ART. About 12% of patients were Asian, 36% were black, 52% were Hispanic, and 1% were white.
Overall, 94% of patients on RAL-ART had a VL less than 200 copies/mL at delivery, compared to 84% of EFV-ART patients (P = .001). The effect appeared to be driven by patients who enrolled later in pregnancy: There was no significant difference in those enrolled in weeks 20-28, but suppression occurred in 93% of the RAL-ART group versus 71% of the EFV-ART group among those enrolled in weeks 29-37 (P = .04).
Tolerability was slightly better in the RAL-ART group, with 99% versus 97% of patients staying on their assigned therapy (P = .05). In both groups, 30% of women experienced an adverse event of grade 3 or higher, as did 25% of live-born infants in both groups.
A total of 92% of women in the RAL-ART group had a sustained VL response through delivery, compared with 64% in the EFV-ART group (P less than .001). The median time to achieving a VL less than 200 copies/mL was 8 days in the RAL-ART group and 15 days in the EFV-ART group (generalized log-rank test P less than .001).
There was one stillbirth in the EFV-ART arm and three in the RAL-ART arm, with 11% in the EFV-ART group having preterm delivery compared with 12% in the RAL-ART group. In addition, the proportion of HIV-infected infants was lower in the RAL-ART arm (1% versus 3%). These differences were not significant.
The National Institutes of Health funded the study. Glaxo/ViiV, Merck, and Bristol-Myers Squibb supplied study drugs. Dr. Mirochnick has received research funding from those companies.
SOURCE: Mark Mirochnick et al. CROI 2019, Abstract 39 LB.
SEATTLE – In HIV-positive pregnant women, an antiretroviral therapy (ART) regimen that included the integrase inhibitor raltegravir (RAL-ART) led to faster viral load (VL) reduction and a greater proportion of women with a VL of less than 200 copies/mL at delivery, compared with patients treated with an efavirenz-based ART (EFV-ART). There were no statistically significant differences between the two arms with respect to percentage of stillbirths, preterm delivery, or rates of HIV infection in the newborn.
“There are lots of advantages of these [integrase inhibitor] drugs, and we’d like to have pregnant women take advantage of them. The problem is, there’s no requirement of drug manufacturers to study the drugs in pregnancy. So these studies are put off until after the drug is licensed, and we’re playing catch-up,” Mark Mirochnick, MD, professor of pediatrics at Boston University, said in an interview. Dr. Mirochnick presented the results at the Conference on Retroviruses and Opportunistic Infections.
Another integrase inhibitor, dolutegravir, has a better resistance profile than that of raltegravir, but concerns over neural tube defects observed during a study in Botswana led both the Food and Drug Administration and the European Medicines Agency to issue safety warnings for that drug. The current study did not raise concern, since it began at 20 weeks’ gestation, well after the period when neural tube defects might occur. “I think it just demonstrates that [integrase inhibitors] are safe in mid- to late-pregnancy,” said Dr. Mirochnick.
It remains to be seen whether a potential link to neural tube defects, if it is a real effect, is due to a specific drug or the mechanism of action of integrase inhibitors more generally. “It’s a question we don’t have an answer to. So you have to balance the potential benefits and potential risks, and that’s probably a decision best made by an individual woman and her care provider. Some women do very well on a particular regimen and they don’t want to change, and you run the risk when you change that you’ll get a viral rebound. What do you tell women who are on dolutegravir and are thinking about becoming pregnant? That’s a controversial question. There are risks with both courses,” said Dr. Mirochnick.
The study comprised 408 patients recruited from centers in Brazil, Tanzania, South Africa, Thailand, Argentina, and the United States. The patients were between 20 and 37 weeks’ gestation and had not previously received ART. They were randomized to RAL-ART or EFV-ART. About 12% of patients were Asian, 36% were black, 52% were Hispanic, and 1% were white.
Overall, 94% of patients on RAL-ART had a VL less than 200 copies/mL at delivery, compared to 84% of EFV-ART patients (P = .001). The effect appeared to be driven by patients who enrolled later in pregnancy: There was no significant difference in those enrolled in weeks 20-28, but suppression occurred in 93% of the RAL-ART group versus 71% of the EFV-ART group among those enrolled in weeks 29-37 (P = .04).
Tolerability was slightly better in the RAL-ART group, with 99% versus 97% of patients staying on their assigned therapy (P = .05). In both groups, 30% of women experienced an adverse event of grade 3 or higher, as did 25% of live-born infants in both groups.
A total of 92% of women in the RAL-ART group had a sustained VL response through delivery, compared with 64% in the EFV-ART group (P less than .001). The median time to achieving a VL less than 200 copies/mL was 8 days in the RAL-ART group and 15 days in the EFV-ART group (generalized log-rank test P less than .001).
There was one stillbirth in the EFV-ART arm and three in the RAL-ART arm, with 11% in the EFV-ART group having preterm delivery compared with 12% in the RAL-ART group. In addition, the proportion of HIV-infected infants was lower in the RAL-ART arm (1% versus 3%). These differences were not significant.
The National Institutes of Health funded the study. Glaxo/ViiV, Merck, and Bristol-Myers Squibb supplied study drugs. Dr. Mirochnick has received research funding from those companies.
SOURCE: Mark Mirochnick et al. CROI 2019, Abstract 39 LB.
REPORTING FROM CROI 2019
Should we upend health care? Yes! (But how?)
In his guest editorial, “Upending this country’s approach to health care” (J Fam Pract. 2018;67:744-745), T. R. Reid makes a number of good points. However, I disagree with his opinion that “This disgraceful state of affairs is not the fault of the nation’s physicians. Rather, the problems with health care in the United States stem from the system that American providers have to work in.”
Through our choices, we have helped create this current system. I started as a family practice attending physician in 1994 and worked in 2 community hospitals. One of these hospitals closed its doors in 2012 and the other merged with a large health care system in 2015. During my 25 years of practice, I watched all of my outstanding primary care colleagues (family medicine, internal medicine, and pediatrics; 25 to 30 in total) stop their practice of combined outpatient and inpatient work. I currently do not see any primary care physicians (who do outpatient work) during my hospital patient care. Yes, it’s lonely.
I believe this significant change in practice across the United States has led to unintended consequences. First, the administrative burdens (and likely costs) for hospitals and health care systems have risen. Newborn, pediatric, and adult hospitalist services had to be built or bolstered, and then maintained, and the growing number of employed physicians had to be managed. Second, primary care’s attractiveness to some medical students has declined. Should students want a practice where they will likely never take care of their patients in the office and the hospital?
I agree we have a “disgraceful state of affairs,” and we need to work together for the tough solutions. However, as health care leaders, we must take responsibility for our roles in creating the current system. We must acknowledge these roles and learn from them.
Chris Noah, MD
Middleville, Mich
As a longtime family medicine practitioner, I can’t agree more with Mr. Reid’s assessments of the state of our health care system. I have experienced health care from my practice as part of an HMO in Wisconsin, and in a hospital system in Raleigh, NC. Our “system” has done such a poor job of allocating its resources and has sacrificed so much to generate profit for the insurance and pharmaceutical corporations. The question is: How do we develop the political will to overcome these deep pockets to change the system? Victor Fuch’s article in the November issue of JAMA makes a very compelling case for a national health plan.1
Jeff Keil, MD
Cary, NC
1. Fuchs VR. How to make US health care more equitable and less costly: begin by replacing employment-based insurance. JAMA. 2018;320:2071-2072.
In his guest editorial, “Upending this country’s approach to health care” (J Fam Pract. 2018;67:744-745), T. R. Reid makes a number of good points. However, I disagree with his opinion that “This disgraceful state of affairs is not the fault of the nation’s physicians. Rather, the problems with health care in the United States stem from the system that American providers have to work in.”
Through our choices, we have helped create this current system. I started as a family practice attending physician in 1994 and worked in 2 community hospitals. One of these hospitals closed its doors in 2012 and the other merged with a large health care system in 2015. During my 25 years of practice, I watched all of my outstanding primary care colleagues (family medicine, internal medicine, and pediatrics; 25 to 30 in total) stop their practice of combined outpatient and inpatient work. I currently do not see any primary care physicians (who do outpatient work) during my hospital patient care. Yes, it’s lonely.
I believe this significant change in practice across the United States has led to unintended consequences. First, the administrative burdens (and likely costs) for hospitals and health care systems have risen. Newborn, pediatric, and adult hospitalist services had to be built or bolstered, and then maintained, and the growing number of employed physicians had to be managed. Second, primary care’s attractiveness to some medical students has declined. Should students want a practice where they will likely never take care of their patients in the office and the hospital?
I agree we have a “disgraceful state of affairs,” and we need to work together for the tough solutions. However, as health care leaders, we must take responsibility for our roles in creating the current system. We must acknowledge these roles and learn from them.
Chris Noah, MD
Middleville, Mich
As a longtime family medicine practitioner, I can’t agree more with Mr. Reid’s assessments of the state of our health care system. I have experienced health care from my practice as part of an HMO in Wisconsin, and in a hospital system in Raleigh, NC. Our “system” has done such a poor job of allocating its resources and has sacrificed so much to generate profit for the insurance and pharmaceutical corporations. The question is: How do we develop the political will to overcome these deep pockets to change the system? Victor Fuch’s article in the November issue of JAMA makes a very compelling case for a national health plan.1
Jeff Keil, MD
Cary, NC
In his guest editorial, “Upending this country’s approach to health care” (J Fam Pract. 2018;67:744-745), T. R. Reid makes a number of good points. However, I disagree with his opinion that “This disgraceful state of affairs is not the fault of the nation’s physicians. Rather, the problems with health care in the United States stem from the system that American providers have to work in.”
Through our choices, we have helped create this current system. I started as a family practice attending physician in 1994 and worked in 2 community hospitals. One of these hospitals closed its doors in 2012 and the other merged with a large health care system in 2015. During my 25 years of practice, I watched all of my outstanding primary care colleagues (family medicine, internal medicine, and pediatrics; 25 to 30 in total) stop their practice of combined outpatient and inpatient work. I currently do not see any primary care physicians (who do outpatient work) during my hospital patient care. Yes, it’s lonely.
I believe this significant change in practice across the United States has led to unintended consequences. First, the administrative burdens (and likely costs) for hospitals and health care systems have risen. Newborn, pediatric, and adult hospitalist services had to be built or bolstered, and then maintained, and the growing number of employed physicians had to be managed. Second, primary care’s attractiveness to some medical students has declined. Should students want a practice where they will likely never take care of their patients in the office and the hospital?
I agree we have a “disgraceful state of affairs,” and we need to work together for the tough solutions. However, as health care leaders, we must take responsibility for our roles in creating the current system. We must acknowledge these roles and learn from them.
Chris Noah, MD
Middleville, Mich
As a longtime family medicine practitioner, I can’t agree more with Mr. Reid’s assessments of the state of our health care system. I have experienced health care from my practice as part of an HMO in Wisconsin, and in a hospital system in Raleigh, NC. Our “system” has done such a poor job of allocating its resources and has sacrificed so much to generate profit for the insurance and pharmaceutical corporations. The question is: How do we develop the political will to overcome these deep pockets to change the system? Victor Fuch’s article in the November issue of JAMA makes a very compelling case for a national health plan.1
Jeff Keil, MD
Cary, NC
1. Fuchs VR. How to make US health care more equitable and less costly: begin by replacing employment-based insurance. JAMA. 2018;320:2071-2072.
1. Fuchs VR. How to make US health care more equitable and less costly: begin by replacing employment-based insurance. JAMA. 2018;320:2071-2072.
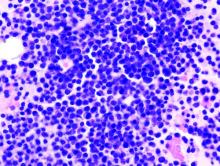
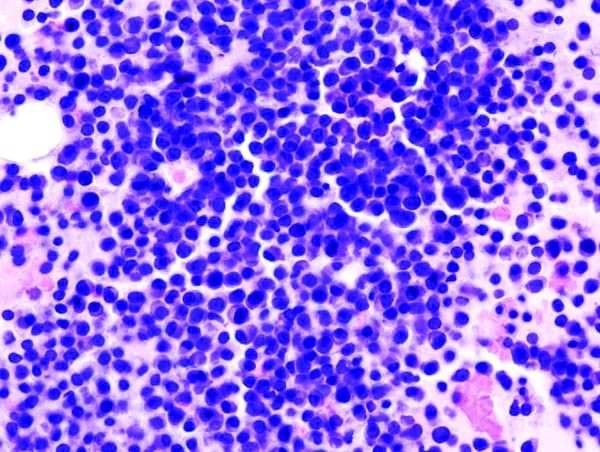
Oral triplet deemed effective in relapsed/refractory myeloma
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
FROM BLOOD ADVANCES
Consider individualized testosterone protocol for transgender acne
but patient compatibility will depend upon several factors, advised Jason A. Park and his associates in a research letter to the editor of the Journal of the American Academy of Dermatology.
In a multivariate logistic regression analysis, Mr. Park and his colleagues at Boston University sought to determine the timing of onset of acne in female-to-male transgender patients.
A total of 55 patients undergoing hormone therapy at the Center for Transgender Medicine and Surgery at Boston Medical Center between January 1, 2010, and December 31, 2017 were selected following a systematic chart review. Patients were excluded who were under the age of 18 years, who had been receiving testosterone therapy for less than 2 years, who presented with acne before start of treatment, or whose medical records were incomplete.
Given evidence in prior studies reporting on an association between elevated androgen levels and increased incidence of acne in this patient group, a median serum testosterone level of 630 ng/dL “was used to differentiate between higher and lower levels.”
Acne was found to develop in 9% of transgender men after 3 months and in 18% after 6 months; 38% of the subjects were found to have developed acne at some point during the study after 24 months of treatment. The authors found that acne was “significantly associated with serum testosterone levels higher than 630 ng/dL.” Increased body mass index (BMI), especially in those with positive smoking status, also was associated with an increased incidence of acne, the authors said.
According to several existing studies, transgender men undergoing testosterone therapy tend to develop increased sebum production and acne. Because the systemic and dermatologic virilization effects of testosterone are unpredictable once treatment has started, and because individual goals also are varied (from maximum virilization to only suppressing feminine secondary sex characteristics), Mr. Park and his colleagues suggested that customization may be ideal, provided they do not clash with individual patient transition goals, priorities, risk factors, and other comorbidities that may be present.
The study was funded by the Medical Student Summer Research Program at Boston University. The authors had no conflicts of interest to report.
SOURCE: Park JA et al. J Am Acad Dermatol. 2019. doi: 10.1016/j.jaad.2018.12.040.
but patient compatibility will depend upon several factors, advised Jason A. Park and his associates in a research letter to the editor of the Journal of the American Academy of Dermatology.
In a multivariate logistic regression analysis, Mr. Park and his colleagues at Boston University sought to determine the timing of onset of acne in female-to-male transgender patients.
A total of 55 patients undergoing hormone therapy at the Center for Transgender Medicine and Surgery at Boston Medical Center between January 1, 2010, and December 31, 2017 were selected following a systematic chart review. Patients were excluded who were under the age of 18 years, who had been receiving testosterone therapy for less than 2 years, who presented with acne before start of treatment, or whose medical records were incomplete.
Given evidence in prior studies reporting on an association between elevated androgen levels and increased incidence of acne in this patient group, a median serum testosterone level of 630 ng/dL “was used to differentiate between higher and lower levels.”
Acne was found to develop in 9% of transgender men after 3 months and in 18% after 6 months; 38% of the subjects were found to have developed acne at some point during the study after 24 months of treatment. The authors found that acne was “significantly associated with serum testosterone levels higher than 630 ng/dL.” Increased body mass index (BMI), especially in those with positive smoking status, also was associated with an increased incidence of acne, the authors said.
According to several existing studies, transgender men undergoing testosterone therapy tend to develop increased sebum production and acne. Because the systemic and dermatologic virilization effects of testosterone are unpredictable once treatment has started, and because individual goals also are varied (from maximum virilization to only suppressing feminine secondary sex characteristics), Mr. Park and his colleagues suggested that customization may be ideal, provided they do not clash with individual patient transition goals, priorities, risk factors, and other comorbidities that may be present.
The study was funded by the Medical Student Summer Research Program at Boston University. The authors had no conflicts of interest to report.
SOURCE: Park JA et al. J Am Acad Dermatol. 2019. doi: 10.1016/j.jaad.2018.12.040.
but patient compatibility will depend upon several factors, advised Jason A. Park and his associates in a research letter to the editor of the Journal of the American Academy of Dermatology.
In a multivariate logistic regression analysis, Mr. Park and his colleagues at Boston University sought to determine the timing of onset of acne in female-to-male transgender patients.
A total of 55 patients undergoing hormone therapy at the Center for Transgender Medicine and Surgery at Boston Medical Center between January 1, 2010, and December 31, 2017 were selected following a systematic chart review. Patients were excluded who were under the age of 18 years, who had been receiving testosterone therapy for less than 2 years, who presented with acne before start of treatment, or whose medical records were incomplete.
Given evidence in prior studies reporting on an association between elevated androgen levels and increased incidence of acne in this patient group, a median serum testosterone level of 630 ng/dL “was used to differentiate between higher and lower levels.”
Acne was found to develop in 9% of transgender men after 3 months and in 18% after 6 months; 38% of the subjects were found to have developed acne at some point during the study after 24 months of treatment. The authors found that acne was “significantly associated with serum testosterone levels higher than 630 ng/dL.” Increased body mass index (BMI), especially in those with positive smoking status, also was associated with an increased incidence of acne, the authors said.
According to several existing studies, transgender men undergoing testosterone therapy tend to develop increased sebum production and acne. Because the systemic and dermatologic virilization effects of testosterone are unpredictable once treatment has started, and because individual goals also are varied (from maximum virilization to only suppressing feminine secondary sex characteristics), Mr. Park and his colleagues suggested that customization may be ideal, provided they do not clash with individual patient transition goals, priorities, risk factors, and other comorbidities that may be present.
The study was funded by the Medical Student Summer Research Program at Boston University. The authors had no conflicts of interest to report.
SOURCE: Park JA et al. J Am Acad Dermatol. 2019. doi: 10.1016/j.jaad.2018.12.040.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Developing clinical mastery at HM19
Boosting your bedside diagnostic skills
A new three-session minitrack devoted to the clinical mastery of diagnostic and treatment skills at the hospitalized patient’s bedside should be a highlight of the Society of Hospital Medicine’s 2019 annual conference.
The “Clinical Mastery” track is designed to help hospitalists enhance their skills in making expert diagnoses at the bedside, said Dustin T. Smith, MD, SFHM, course director for HM19, and associate professor of medicine at Emory University, Atlanta. “We feel that all of the didactic sessions offered at HM19 are highly useful for hospitalists, but there is growing interest in having sessions devoted to learning clinical pearls that can aid in practicing medicine and acquiring the skill set of a master clinician.”
The three clinical mastery sessions at HM19 will address neurologic symptoms, ECG interpretation, and the role of point-of-care ultrasound (POCUS), currently a hot topic in hospital medicine. Recent advances in ultrasound technology have resulted in probes that can cost as little as $2,000, fit inside a lab coat pocket, and be read from a smartphone – making ultrasound far easier to bring to the bedside of hospitalized patients, said Ria Dancel, MD, FHM, associate professor of internal medicine and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Dancel will copresent the POCUS clinical mastery track at HM19. “Our focus will be on how POCUS and the physical exam relate to each other. These are not competing technologies but complementary, reflecting the evolution in bedside medicine. Because these new devices will soon be in the pockets of your colleagues, residents, physician assistants, and others, you should at least have the knowledge and vocabulary to communicate with them,” she said.
POCUS is a new technology that is not yet in wide use at the hospital bedside, but clearly a wave is building, said Dr. Dancel’s copresenter, Michael Janjigian, MD, associate professor in the department of medicine at NYU Langone Health in New York City.
“We’re at the inflection point where the cost of the machine and the availability of training means that hospitals need to decide if it’s time to embrace it,” he said. Hospitalists may also consider petitioning their hospital’s leadership to offer the machines and training.
“Hospitalists’ competencies and strengths lie primarily in making diagnoses,” Dr. Janjigian said. “We like to think of ourselves as master diagnosticians. Our session at HM19 will explore the strengths and weaknesses of both the physical exam and POCUS, presenting clinical scenarios common to hospital medicine. This course is designed for those who have never picked up an ultrasound probe and want to better understand why they should, and for those who want a better sense of how they might integrate it into their practice.”
While radiology and cardiology have been using ultrasound for decades, internists are finding uses at the bedside to speed diagnosis or focus their next diagnostic steps, Dr. Dancel noted. For certain diagnoses, the physical exam is still the tool of choice. But when looking for fluid around the heart or ascites buildup in the abdomen or when looking at the heart itself, she said, there is no better tool at the bedside than ultrasound.
In January 2019, the SHM issued a position statement on POCUS1, which is intended to inform hospitalists about the technology and its uses, encourage them to be more integrally involved in decision making processes surrounding POCUS program management for their hospitals, and promote development of standards for hospitalists in POCUS training and assessment. The SHM has also developed a pathway to teach the use of ultrasound, the Point-of-Care Ultrasound Certificate of Completion.
In order to qualify, clinicians complete online training modules, attend two live learning courses, compile a portfolio of ultrasound video clips on the job that are reviewed by a panel of experts, and then pass a final exam. The exam will be offered at HM19 for clinicians who have completed preliminary work for this new certificate – as well as precourses devoted to ultrasound and other procedures – and another workshop on POCUS.
Earning the POCUS certificate of completion requires a lot of effort, Dr. Dancel acknowledged. “It is a big commitment, and we don’t want hospitalists thinking that just because they have completed the certificate that they have fully mastered ultrasound. We encourage hospitalists to find a proctor in their own hospitals and to work with them to continue to refine their skills.”
Dr. Dancel and Dr. Janjigian reported no relevant disclosures.
References
1. Soni NJ et al. Point-of-care ultrasound for hospitalists: A position statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2. doi: 10.12788/jhm.3079.
Boosting your bedside diagnostic skills
Boosting your bedside diagnostic skills
A new three-session minitrack devoted to the clinical mastery of diagnostic and treatment skills at the hospitalized patient’s bedside should be a highlight of the Society of Hospital Medicine’s 2019 annual conference.
The “Clinical Mastery” track is designed to help hospitalists enhance their skills in making expert diagnoses at the bedside, said Dustin T. Smith, MD, SFHM, course director for HM19, and associate professor of medicine at Emory University, Atlanta. “We feel that all of the didactic sessions offered at HM19 are highly useful for hospitalists, but there is growing interest in having sessions devoted to learning clinical pearls that can aid in practicing medicine and acquiring the skill set of a master clinician.”
The three clinical mastery sessions at HM19 will address neurologic symptoms, ECG interpretation, and the role of point-of-care ultrasound (POCUS), currently a hot topic in hospital medicine. Recent advances in ultrasound technology have resulted in probes that can cost as little as $2,000, fit inside a lab coat pocket, and be read from a smartphone – making ultrasound far easier to bring to the bedside of hospitalized patients, said Ria Dancel, MD, FHM, associate professor of internal medicine and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Dancel will copresent the POCUS clinical mastery track at HM19. “Our focus will be on how POCUS and the physical exam relate to each other. These are not competing technologies but complementary, reflecting the evolution in bedside medicine. Because these new devices will soon be in the pockets of your colleagues, residents, physician assistants, and others, you should at least have the knowledge and vocabulary to communicate with them,” she said.
POCUS is a new technology that is not yet in wide use at the hospital bedside, but clearly a wave is building, said Dr. Dancel’s copresenter, Michael Janjigian, MD, associate professor in the department of medicine at NYU Langone Health in New York City.
“We’re at the inflection point where the cost of the machine and the availability of training means that hospitals need to decide if it’s time to embrace it,” he said. Hospitalists may also consider petitioning their hospital’s leadership to offer the machines and training.
“Hospitalists’ competencies and strengths lie primarily in making diagnoses,” Dr. Janjigian said. “We like to think of ourselves as master diagnosticians. Our session at HM19 will explore the strengths and weaknesses of both the physical exam and POCUS, presenting clinical scenarios common to hospital medicine. This course is designed for those who have never picked up an ultrasound probe and want to better understand why they should, and for those who want a better sense of how they might integrate it into their practice.”
While radiology and cardiology have been using ultrasound for decades, internists are finding uses at the bedside to speed diagnosis or focus their next diagnostic steps, Dr. Dancel noted. For certain diagnoses, the physical exam is still the tool of choice. But when looking for fluid around the heart or ascites buildup in the abdomen or when looking at the heart itself, she said, there is no better tool at the bedside than ultrasound.
In January 2019, the SHM issued a position statement on POCUS1, which is intended to inform hospitalists about the technology and its uses, encourage them to be more integrally involved in decision making processes surrounding POCUS program management for their hospitals, and promote development of standards for hospitalists in POCUS training and assessment. The SHM has also developed a pathway to teach the use of ultrasound, the Point-of-Care Ultrasound Certificate of Completion.
In order to qualify, clinicians complete online training modules, attend two live learning courses, compile a portfolio of ultrasound video clips on the job that are reviewed by a panel of experts, and then pass a final exam. The exam will be offered at HM19 for clinicians who have completed preliminary work for this new certificate – as well as precourses devoted to ultrasound and other procedures – and another workshop on POCUS.
Earning the POCUS certificate of completion requires a lot of effort, Dr. Dancel acknowledged. “It is a big commitment, and we don’t want hospitalists thinking that just because they have completed the certificate that they have fully mastered ultrasound. We encourage hospitalists to find a proctor in their own hospitals and to work with them to continue to refine their skills.”
Dr. Dancel and Dr. Janjigian reported no relevant disclosures.
References
1. Soni NJ et al. Point-of-care ultrasound for hospitalists: A position statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2. doi: 10.12788/jhm.3079.
A new three-session minitrack devoted to the clinical mastery of diagnostic and treatment skills at the hospitalized patient’s bedside should be a highlight of the Society of Hospital Medicine’s 2019 annual conference.
The “Clinical Mastery” track is designed to help hospitalists enhance their skills in making expert diagnoses at the bedside, said Dustin T. Smith, MD, SFHM, course director for HM19, and associate professor of medicine at Emory University, Atlanta. “We feel that all of the didactic sessions offered at HM19 are highly useful for hospitalists, but there is growing interest in having sessions devoted to learning clinical pearls that can aid in practicing medicine and acquiring the skill set of a master clinician.”
The three clinical mastery sessions at HM19 will address neurologic symptoms, ECG interpretation, and the role of point-of-care ultrasound (POCUS), currently a hot topic in hospital medicine. Recent advances in ultrasound technology have resulted in probes that can cost as little as $2,000, fit inside a lab coat pocket, and be read from a smartphone – making ultrasound far easier to bring to the bedside of hospitalized patients, said Ria Dancel, MD, FHM, associate professor of internal medicine and pediatrics at the University of North Carolina at Chapel Hill.
Dr. Dancel will copresent the POCUS clinical mastery track at HM19. “Our focus will be on how POCUS and the physical exam relate to each other. These are not competing technologies but complementary, reflecting the evolution in bedside medicine. Because these new devices will soon be in the pockets of your colleagues, residents, physician assistants, and others, you should at least have the knowledge and vocabulary to communicate with them,” she said.
POCUS is a new technology that is not yet in wide use at the hospital bedside, but clearly a wave is building, said Dr. Dancel’s copresenter, Michael Janjigian, MD, associate professor in the department of medicine at NYU Langone Health in New York City.
“We’re at the inflection point where the cost of the machine and the availability of training means that hospitals need to decide if it’s time to embrace it,” he said. Hospitalists may also consider petitioning their hospital’s leadership to offer the machines and training.
“Hospitalists’ competencies and strengths lie primarily in making diagnoses,” Dr. Janjigian said. “We like to think of ourselves as master diagnosticians. Our session at HM19 will explore the strengths and weaknesses of both the physical exam and POCUS, presenting clinical scenarios common to hospital medicine. This course is designed for those who have never picked up an ultrasound probe and want to better understand why they should, and for those who want a better sense of how they might integrate it into their practice.”
While radiology and cardiology have been using ultrasound for decades, internists are finding uses at the bedside to speed diagnosis or focus their next diagnostic steps, Dr. Dancel noted. For certain diagnoses, the physical exam is still the tool of choice. But when looking for fluid around the heart or ascites buildup in the abdomen or when looking at the heart itself, she said, there is no better tool at the bedside than ultrasound.
In January 2019, the SHM issued a position statement on POCUS1, which is intended to inform hospitalists about the technology and its uses, encourage them to be more integrally involved in decision making processes surrounding POCUS program management for their hospitals, and promote development of standards for hospitalists in POCUS training and assessment. The SHM has also developed a pathway to teach the use of ultrasound, the Point-of-Care Ultrasound Certificate of Completion.
In order to qualify, clinicians complete online training modules, attend two live learning courses, compile a portfolio of ultrasound video clips on the job that are reviewed by a panel of experts, and then pass a final exam. The exam will be offered at HM19 for clinicians who have completed preliminary work for this new certificate – as well as precourses devoted to ultrasound and other procedures – and another workshop on POCUS.
Earning the POCUS certificate of completion requires a lot of effort, Dr. Dancel acknowledged. “It is a big commitment, and we don’t want hospitalists thinking that just because they have completed the certificate that they have fully mastered ultrasound. We encourage hospitalists to find a proctor in their own hospitals and to work with them to continue to refine their skills.”
Dr. Dancel and Dr. Janjigian reported no relevant disclosures.
References
1. Soni NJ et al. Point-of-care ultrasound for hospitalists: A position statement of the Society of Hospital Medicine. J Hosp Med. 2019 Jan 2. doi: 10.12788/jhm.3079.
Prior authorization an increasing burden
The use of prior authorization for prescriptions and medical services has continued to increase in recent years, despite the consequences to continuity of care, according to a survey by the American Medical Association.

and 41% said that PA for medical services has done the same. The corresponding numbers for 5-year decreases in PAs were 2% and 1%, the AMA reported March 12.
Results of the survey, conducted in December 2018, also show that 85% of physicians believe that prior authorization sometimes, often, or always has a negative effect on the continuity of patients’ care. Almost 70% of respondents said that it is somewhat or extremely difficult to determine when PA is required for a prescription or medical service, and only 8% reported contracting with a health plan that offers programs to exempt physicians from the PA process, the AMA said.
“Physicians follow insurance protocols for prior authorization that require faxing recurring paperwork, multiple phone calls, and hours spent on hold. At the same time, patients’ lives can hang in the balance until health plans decide if needed care will qualify for insurance coverage,” AMA President Barbara L. McAneny, MD, said in a statement.
In January 2018, two organizations representing insurers – America’s Health Insurance Plans and the Blue Cross Blue Shield Association – signed onto a joint consensus statement with the AMA and other health care groups that provided five areas for improvement of the PA process. The current survey results show that “most health plans are not making meaningful progress on reforming the cumbersome prior authorization process,” the AMA said.
The use of prior authorization for prescriptions and medical services has continued to increase in recent years, despite the consequences to continuity of care, according to a survey by the American Medical Association.

and 41% said that PA for medical services has done the same. The corresponding numbers for 5-year decreases in PAs were 2% and 1%, the AMA reported March 12.
Results of the survey, conducted in December 2018, also show that 85% of physicians believe that prior authorization sometimes, often, or always has a negative effect on the continuity of patients’ care. Almost 70% of respondents said that it is somewhat or extremely difficult to determine when PA is required for a prescription or medical service, and only 8% reported contracting with a health plan that offers programs to exempt physicians from the PA process, the AMA said.
“Physicians follow insurance protocols for prior authorization that require faxing recurring paperwork, multiple phone calls, and hours spent on hold. At the same time, patients’ lives can hang in the balance until health plans decide if needed care will qualify for insurance coverage,” AMA President Barbara L. McAneny, MD, said in a statement.
In January 2018, two organizations representing insurers – America’s Health Insurance Plans and the Blue Cross Blue Shield Association – signed onto a joint consensus statement with the AMA and other health care groups that provided five areas for improvement of the PA process. The current survey results show that “most health plans are not making meaningful progress on reforming the cumbersome prior authorization process,” the AMA said.
The use of prior authorization for prescriptions and medical services has continued to increase in recent years, despite the consequences to continuity of care, according to a survey by the American Medical Association.

and 41% said that PA for medical services has done the same. The corresponding numbers for 5-year decreases in PAs were 2% and 1%, the AMA reported March 12.
Results of the survey, conducted in December 2018, also show that 85% of physicians believe that prior authorization sometimes, often, or always has a negative effect on the continuity of patients’ care. Almost 70% of respondents said that it is somewhat or extremely difficult to determine when PA is required for a prescription or medical service, and only 8% reported contracting with a health plan that offers programs to exempt physicians from the PA process, the AMA said.
“Physicians follow insurance protocols for prior authorization that require faxing recurring paperwork, multiple phone calls, and hours spent on hold. At the same time, patients’ lives can hang in the balance until health plans decide if needed care will qualify for insurance coverage,” AMA President Barbara L. McAneny, MD, said in a statement.
In January 2018, two organizations representing insurers – America’s Health Insurance Plans and the Blue Cross Blue Shield Association – signed onto a joint consensus statement with the AMA and other health care groups that provided five areas for improvement of the PA process. The current survey results show that “most health plans are not making meaningful progress on reforming the cumbersome prior authorization process,” the AMA said.
Crafting a “well-rounded” program
New tracks, interactive programs highlight HM19
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”
New tracks, interactive programs highlight HM19
New tracks, interactive programs highlight HM19
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”
As course director for the Society of Hospital Medicine’s 2019 annual conference – Hospital Medicine 2019 (HM19) – to be held March 24-27 in National Harbor, Md., Dustin T. Smith, MD, SFHM, hospitalist and associate professor of medicine at Emory University, Atlanta, tried his best to apply democratic processes to the work of the annual conference committee.
“We created numerous email surveys to go out to the 20 committee members for their vote. So many great topics were proposed for HM19, with so many great faculty, that we had to make hard choices – although we see that as a good problem. It was my job to make sure that we had a process that works,” Dr. Smith explained. “We have planned what we believe will be another well-attended and well-received hospital medicine conference. Every year it’s been great, but every year we try something to make it a little better.”
The SHM annual conference committee meets in person at the conference to kick off planning for the following year’s conference, then holds weekly conference calls for the next 4-5 months, Dr. Smith said. “These are all highly creative leaders in hospital medicine, with voices to be heard and taken under consideration.”
Committee members wear badges at the annual meeting to encourage attendees to offer them feedback and suggestions. “We have our ears to the ground. We look at the session ratings from prior years, speaker ratings, and all of the feedback we have received, and we take all of that into account to come up with new ideas for educational tracks,” Dr. Smith said. New for 2019 are “Between the Guidelines” and “Clinical Mastery”. “We went around the table at our meeting and asked everybody for their ideas for new tracks, and then we voted in the most popular ones.”
One change for 2019 was to “completely open” the call for submission of proposals – and for nominations of content to be covered and who should present it – for all sessions at HM19, not just for the workshop tracks. Dr. Smith said all submissions were peer reviewed by committee members and scored with objective ratings.
“For example, there was a lot of interest in emergency and disaster preparedness for hospitalists in a number of the submissions. Whether we’re talking about wildfires or mass shootings, it affects hospitals, and we are among the frontline practitioners for whatever happens in those hospitals. So we may need to be able to respond to large-scale emergencies,” he said. “But most of us haven’t been trained for that.”
A love of teaching
Dr. Smith’s preparation for being the HM19 course director includes his work teaching medical students, residents, and physicians at Emory University where he also attended medical school. He chairs the Emory division of hospital medicine’s education council, directs hospital medicine grand rounds at Emory, and serves as associate program director for the J. Willis Hurst Internal Medicine Residency Program at Emory as well as a section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center. Dr. Smith has also codirected, since 2012, the annual Southern Hospital Medicine regional conference.
“I have long had an interest in medical education for medical students, trainees, and faculty and I wanted to do more of it – with a number of mentors encouraging me along the way,” he said. “I have planned and coordinated teaching sessions needed for maintenance of board certification, which is similar to what we will present at HM19. Based on that experience, I applied to be on SHM’s annual conference committee, starting in 2012 for the planning of Hospital Medicine 2013. I believe I have been preparing myself all along to take on this role.”
A well-rounded program
The HM19 educational program will be well rounded, Dr. Smith said, offering clinical updates on topics such as sepsis, heart failure, and new clinical practice guidelines.
“You will see a big focus on wellness and how to avoid burnout, as well as other sessions on how to develop and sustain a career in hospital medicine,” he said. Another important HM19 theme will be the delivery of new models of population health and accountable care and their impact on both patients and hospital operations.
The 2019 agenda emphasizes other interactive formats, such as the “Great Debates,” where experts in the field are paired to debate clinical conundrums in hospital medicine. The number of Great Debates has grown from one on perioperative medicine at the 2017 annual conference, to three in 2018, and now to seven planned for 2019. “This format is very popular. We’re also planning ‘Medical Jeopardy,’ with three brilliant master clinicians in a quiz show format, and two ‘Stump the Professor’ sessions with expert diagnosticians,” Dr. Smith said.
It’s important to make every session at the conference interactive to engage attendees in learning from, and talking to, experts in the field, he said. “But it’s also important for some of them to be more entertaining in approach as a way to encourage learning. We know that this actually increases retention of information.”
The annual conference course director typically is selected several years in advance, in order to plan for the time commitment that will be required, and spends the year before this term as assistant course director. “It is a big honor to serve as course director. It’s fun and exciting to work with such a talented and diverse committee, but it’s also a lot of work,” Dr. Smith acknowledged. “I reviewed all 450 session proposals from this year’s open call for course content. The volume of emails is pretty outstanding, and I was extremely busy with conference planning for a season.”
Dr. Smith has continued to pursue his full-time commitments at Emory, without getting dedicated time off for planning the SHM conference. “But as a parent of three young children, I already feel busy all the time,” he said. “I put in a lot of late nights, but I found a way to make it work.”