User login
FDA: Clozapine REMS modified
The Food and Drug Administration has modified the Risk Evaluation and Mitigation Strategy (REMS) Program for clozapine, a second-generation antipsychotic used for patients who do not respond adequately to standard antipsychotic treatment. Use of clozapine comes with the risk of neutropenia, which can make patients vulnerable to serious infections, so routine monitoring of absolute neutrophil counts is a must.
The new requirements, including one that requires both prescribers and pharmacies to be certified in the clozapine REMS program, take effect Feb. 28.
More information about clozapine and this change can be found on the FDA web page for the drug.
The Food and Drug Administration has modified the Risk Evaluation and Mitigation Strategy (REMS) Program for clozapine, a second-generation antipsychotic used for patients who do not respond adequately to standard antipsychotic treatment. Use of clozapine comes with the risk of neutropenia, which can make patients vulnerable to serious infections, so routine monitoring of absolute neutrophil counts is a must.
The new requirements, including one that requires both prescribers and pharmacies to be certified in the clozapine REMS program, take effect Feb. 28.
More information about clozapine and this change can be found on the FDA web page for the drug.
The Food and Drug Administration has modified the Risk Evaluation and Mitigation Strategy (REMS) Program for clozapine, a second-generation antipsychotic used for patients who do not respond adequately to standard antipsychotic treatment. Use of clozapine comes with the risk of neutropenia, which can make patients vulnerable to serious infections, so routine monitoring of absolute neutrophil counts is a must.
The new requirements, including one that requires both prescribers and pharmacies to be certified in the clozapine REMS program, take effect Feb. 28.
More information about clozapine and this change can be found on the FDA web page for the drug.
Medicaid youth suicides include more females, younger kids, hanging deaths
Young people enrolled in Medicaid who commit suicide are disproportionately female, younger, and more likely to die by hanging, compared with non-Medicaid youth, results of a large, observational, population-based study suggest.
Nearly 40% of young people in the study who died by suicide were covered by Medicaid, according to study lead author Cynthia A. Fontanella, PhD, of the department of psychiatry and behavioral health at the Ohio State University, Columbus. Those findings, in addition to those of other studies indicating that youth enrolled in Medicaid endure more maltreatment and poverty-related adversity, suggest a need for health care delivery systems to develop “trauma-informed approaches” and implement them, Dr. Fontanella and her coauthors reported in the American Journal of Preventive Medicine.
“Effective suicide screening of enrollees could substantially decrease suicide mortality in the United States,” they wrote.
Dr. Fontanella and her coauthors reviewed death certificate data from the 16 most populous states to identify all youth aged 10-18 who committed suicide during 2009-2013. They identified 4,045 deaths from suicide based on state death certificate data in California, Florida, Georgia, Illinois, Indiana, Massachusetts, Michigan, Minnesota, New York, North Carolina, Ohio, Oregon, Texas, Virginia, Washington, and Wisconsin. To identify the subset of youth who were enrolled in Medicaid, they used Social Security numbers to link the death certificate data to data from a Medicaid database.
Out of 4,045 youth suicide deaths that occurred during that time period, 39% were among youth enrolled in Medicaid, the investigators found.
Although the overall suicide rate did not differ significantly between the Medicaid and non-Medicaid groups, investigators said they did identify significant differences in age and sex subgroups. Specifically, those in the Medicaid group had a 28% increased risk of suicide among the 10- to 14-year age subgroup, and a 14% increased risk of suicide among females, the findings showed. Moreover, the risk of death by hanging was 26% greater among the Medicare youth.
Dr. Fontanella and her coauthors reported several limitations. One is that the findings might not be generalizable to all 50 states. Also, they said, because suicide is underreported as a cause of death, the prevalence of suicide found in the study might have been underreported.
Nevertheless, , Dr. Fontanella and her associates wrote. Boundaried populations are those defined by a service setting or organizational function. In other words, they wrote, findings based on an analysis of service use patterns captured in Medicaid claims “could prove helpful in identifying periods known to be associated with heightened suicide risk, such as that immediately following discharge from inpatient psychiatric care.”
The National Action Alliance for Suicide Prevention’s Research Prioritization Task Force has recommended that those populations be targeted for research on interventions designed to reduce suicide deaths, Dr. Fontanella and her coauthors wrote.
This is the first-ever study to evaluate suicide-related mortality among Medicaid-covered youth, the investigators said. Previous studies of suicide in Medicaid have focused on adults – specifically those in the Veterans Health Administration, specific state Medicaid programs, or health maintenance organization networks.
The American Foundation for Suicide Prevention and the National Institutes of Health funded the study. Dr. Fontanella and her coauthors reported no other financial conflicts of interest.
SOURCE: Fontanella CA et al. Am J Prev Med. 2019 Jan 17. doi: 10.1016/j.amepre.2018.10.008.
Young people enrolled in Medicaid who commit suicide are disproportionately female, younger, and more likely to die by hanging, compared with non-Medicaid youth, results of a large, observational, population-based study suggest.
Nearly 40% of young people in the study who died by suicide were covered by Medicaid, according to study lead author Cynthia A. Fontanella, PhD, of the department of psychiatry and behavioral health at the Ohio State University, Columbus. Those findings, in addition to those of other studies indicating that youth enrolled in Medicaid endure more maltreatment and poverty-related adversity, suggest a need for health care delivery systems to develop “trauma-informed approaches” and implement them, Dr. Fontanella and her coauthors reported in the American Journal of Preventive Medicine.
“Effective suicide screening of enrollees could substantially decrease suicide mortality in the United States,” they wrote.
Dr. Fontanella and her coauthors reviewed death certificate data from the 16 most populous states to identify all youth aged 10-18 who committed suicide during 2009-2013. They identified 4,045 deaths from suicide based on state death certificate data in California, Florida, Georgia, Illinois, Indiana, Massachusetts, Michigan, Minnesota, New York, North Carolina, Ohio, Oregon, Texas, Virginia, Washington, and Wisconsin. To identify the subset of youth who were enrolled in Medicaid, they used Social Security numbers to link the death certificate data to data from a Medicaid database.
Out of 4,045 youth suicide deaths that occurred during that time period, 39% were among youth enrolled in Medicaid, the investigators found.
Although the overall suicide rate did not differ significantly between the Medicaid and non-Medicaid groups, investigators said they did identify significant differences in age and sex subgroups. Specifically, those in the Medicaid group had a 28% increased risk of suicide among the 10- to 14-year age subgroup, and a 14% increased risk of suicide among females, the findings showed. Moreover, the risk of death by hanging was 26% greater among the Medicare youth.
Dr. Fontanella and her coauthors reported several limitations. One is that the findings might not be generalizable to all 50 states. Also, they said, because suicide is underreported as a cause of death, the prevalence of suicide found in the study might have been underreported.
Nevertheless, , Dr. Fontanella and her associates wrote. Boundaried populations are those defined by a service setting or organizational function. In other words, they wrote, findings based on an analysis of service use patterns captured in Medicaid claims “could prove helpful in identifying periods known to be associated with heightened suicide risk, such as that immediately following discharge from inpatient psychiatric care.”
The National Action Alliance for Suicide Prevention’s Research Prioritization Task Force has recommended that those populations be targeted for research on interventions designed to reduce suicide deaths, Dr. Fontanella and her coauthors wrote.
This is the first-ever study to evaluate suicide-related mortality among Medicaid-covered youth, the investigators said. Previous studies of suicide in Medicaid have focused on adults – specifically those in the Veterans Health Administration, specific state Medicaid programs, or health maintenance organization networks.
The American Foundation for Suicide Prevention and the National Institutes of Health funded the study. Dr. Fontanella and her coauthors reported no other financial conflicts of interest.
SOURCE: Fontanella CA et al. Am J Prev Med. 2019 Jan 17. doi: 10.1016/j.amepre.2018.10.008.
Young people enrolled in Medicaid who commit suicide are disproportionately female, younger, and more likely to die by hanging, compared with non-Medicaid youth, results of a large, observational, population-based study suggest.
Nearly 40% of young people in the study who died by suicide were covered by Medicaid, according to study lead author Cynthia A. Fontanella, PhD, of the department of psychiatry and behavioral health at the Ohio State University, Columbus. Those findings, in addition to those of other studies indicating that youth enrolled in Medicaid endure more maltreatment and poverty-related adversity, suggest a need for health care delivery systems to develop “trauma-informed approaches” and implement them, Dr. Fontanella and her coauthors reported in the American Journal of Preventive Medicine.
“Effective suicide screening of enrollees could substantially decrease suicide mortality in the United States,” they wrote.
Dr. Fontanella and her coauthors reviewed death certificate data from the 16 most populous states to identify all youth aged 10-18 who committed suicide during 2009-2013. They identified 4,045 deaths from suicide based on state death certificate data in California, Florida, Georgia, Illinois, Indiana, Massachusetts, Michigan, Minnesota, New York, North Carolina, Ohio, Oregon, Texas, Virginia, Washington, and Wisconsin. To identify the subset of youth who were enrolled in Medicaid, they used Social Security numbers to link the death certificate data to data from a Medicaid database.
Out of 4,045 youth suicide deaths that occurred during that time period, 39% were among youth enrolled in Medicaid, the investigators found.
Although the overall suicide rate did not differ significantly between the Medicaid and non-Medicaid groups, investigators said they did identify significant differences in age and sex subgroups. Specifically, those in the Medicaid group had a 28% increased risk of suicide among the 10- to 14-year age subgroup, and a 14% increased risk of suicide among females, the findings showed. Moreover, the risk of death by hanging was 26% greater among the Medicare youth.
Dr. Fontanella and her coauthors reported several limitations. One is that the findings might not be generalizable to all 50 states. Also, they said, because suicide is underreported as a cause of death, the prevalence of suicide found in the study might have been underreported.
Nevertheless, , Dr. Fontanella and her associates wrote. Boundaried populations are those defined by a service setting or organizational function. In other words, they wrote, findings based on an analysis of service use patterns captured in Medicaid claims “could prove helpful in identifying periods known to be associated with heightened suicide risk, such as that immediately following discharge from inpatient psychiatric care.”
The National Action Alliance for Suicide Prevention’s Research Prioritization Task Force has recommended that those populations be targeted for research on interventions designed to reduce suicide deaths, Dr. Fontanella and her coauthors wrote.
This is the first-ever study to evaluate suicide-related mortality among Medicaid-covered youth, the investigators said. Previous studies of suicide in Medicaid have focused on adults – specifically those in the Veterans Health Administration, specific state Medicaid programs, or health maintenance organization networks.
The American Foundation for Suicide Prevention and the National Institutes of Health funded the study. Dr. Fontanella and her coauthors reported no other financial conflicts of interest.
SOURCE: Fontanella CA et al. Am J Prev Med. 2019 Jan 17. doi: 10.1016/j.amepre.2018.10.008.
FROM THE AMERICAN JOURNAL OF PREVENTIVE MEDICINE
Key clinical point: Youth enrolled in Medicaid who commit suicide are disproportionately female, younger, and more likely to die by hanging, compared with non-Medicaid youth.
Major finding: The Medicaid group had a 28% increased risk of suicide among the 10- to 14-year age subgroup, a 14% increased risk of suicide among females, and a 26% greater risk of death by hanging.
Study details: An observational study from the 16 most populous states that includes 4,045 youth who committed suicide during 2009-2013.
Disclosures: The authors reported no financial conflicts. The study was funded by the American Foundation for Suicide Prevention and the National Institutes of Health.
Source: Fontanella CA et al. Am J Prev Med. 2019 Jan 17. doi: 10.1016/j.amepre.2018.10.008.
Sleep: Too much, too little both tied to atherosclerosis
; dabigatran matches aspirin for second stroke prevention; HDL particle subfractions may be prognostic in heart failure; and a novel drug safely reduced LDL cholesterol in statin-intolerant patients.
Subscribe to Cardiocast wherever you get your podcasts.
Amazon Alexa
Apple Podcasts
; dabigatran matches aspirin for second stroke prevention; HDL particle subfractions may be prognostic in heart failure; and a novel drug safely reduced LDL cholesterol in statin-intolerant patients.
Subscribe to Cardiocast wherever you get your podcasts.
Amazon Alexa
Apple Podcasts
; dabigatran matches aspirin for second stroke prevention; HDL particle subfractions may be prognostic in heart failure; and a novel drug safely reduced LDL cholesterol in statin-intolerant patients.
Subscribe to Cardiocast wherever you get your podcasts.
Amazon Alexa
Apple Podcasts
Survey: Government shutdown is affecting patient health
A majority of U.S. health care professionals report that their patients have been negatively affected by the federal government’s partial shutdown, according to a survey conducted Jan. 11 by health care market research company InCrowd.
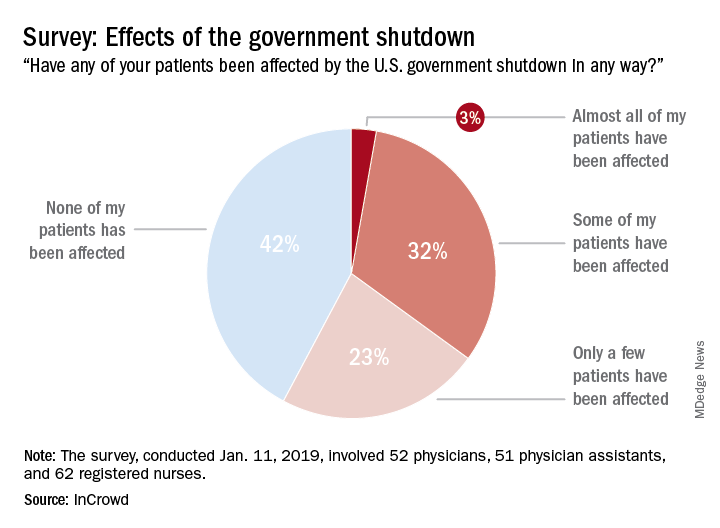
The results showed that 58% of the 165 respondents (52 primary care physicians, 51 physician assistants, and 63 registered nurses) surveyed believe that their patents have been affected in some way by the shutdown: Three percent said that almost all of their patients have been affected, 32% said that some have been affected, and 23% said that only a few patients have been affected. The largest share of clinicians (42%), however, believes that none of their patients have experienced any effects from the shutdown, InCrowd reported Jan. 17.
That distribution changes considerably, however, when looking at the physicians only: 4% (almost all), 39% (some), 31% (a few), and 26% (none). Registered nurses (50%) and physician assistants (45%) were much more likely to say that none of their patients had been affected, InCrowd reported.
“Patient access to care and compliance issues due to financial concerns and loss of benefits are already being observed by respondents. Forty percent of respondents reported a high degree of both issues with patients affording medicine and incidences where patient avoided treatments and appointments all together,” the InCrowd investigators said.
This article was updated 1/18/19.
A majority of U.S. health care professionals report that their patients have been negatively affected by the federal government’s partial shutdown, according to a survey conducted Jan. 11 by health care market research company InCrowd.
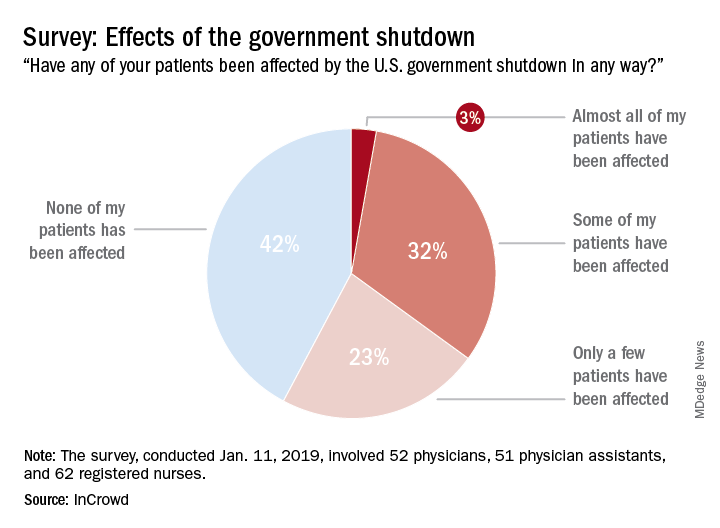
The results showed that 58% of the 165 respondents (52 primary care physicians, 51 physician assistants, and 63 registered nurses) surveyed believe that their patents have been affected in some way by the shutdown: Three percent said that almost all of their patients have been affected, 32% said that some have been affected, and 23% said that only a few patients have been affected. The largest share of clinicians (42%), however, believes that none of their patients have experienced any effects from the shutdown, InCrowd reported Jan. 17.
That distribution changes considerably, however, when looking at the physicians only: 4% (almost all), 39% (some), 31% (a few), and 26% (none). Registered nurses (50%) and physician assistants (45%) were much more likely to say that none of their patients had been affected, InCrowd reported.
“Patient access to care and compliance issues due to financial concerns and loss of benefits are already being observed by respondents. Forty percent of respondents reported a high degree of both issues with patients affording medicine and incidences where patient avoided treatments and appointments all together,” the InCrowd investigators said.
This article was updated 1/18/19.
A majority of U.S. health care professionals report that their patients have been negatively affected by the federal government’s partial shutdown, according to a survey conducted Jan. 11 by health care market research company InCrowd.
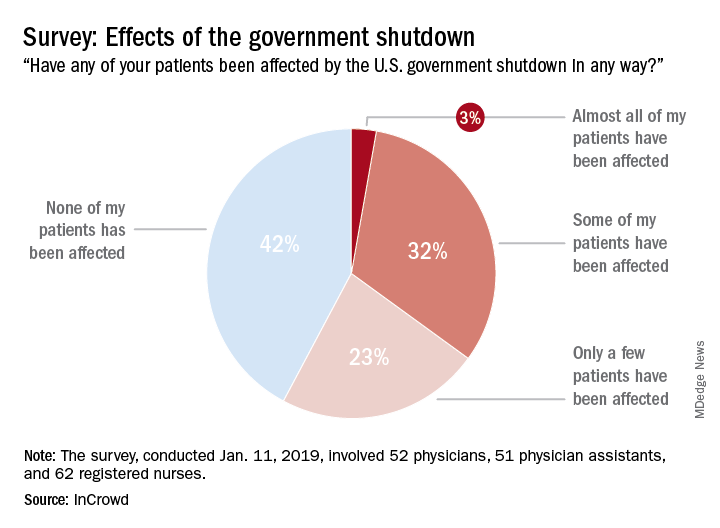
The results showed that 58% of the 165 respondents (52 primary care physicians, 51 physician assistants, and 63 registered nurses) surveyed believe that their patents have been affected in some way by the shutdown: Three percent said that almost all of their patients have been affected, 32% said that some have been affected, and 23% said that only a few patients have been affected. The largest share of clinicians (42%), however, believes that none of their patients have experienced any effects from the shutdown, InCrowd reported Jan. 17.
That distribution changes considerably, however, when looking at the physicians only: 4% (almost all), 39% (some), 31% (a few), and 26% (none). Registered nurses (50%) and physician assistants (45%) were much more likely to say that none of their patients had been affected, InCrowd reported.
“Patient access to care and compliance issues due to financial concerns and loss of benefits are already being observed by respondents. Forty percent of respondents reported a high degree of both issues with patients affording medicine and incidences where patient avoided treatments and appointments all together,” the InCrowd investigators said.
This article was updated 1/18/19.
Patient-centric pain management decision aid reduces opioid use posthysterectomy
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.
GoFundMe CEO: ‘Gigantic gaps’ in health system showing up in crowdfunding
Scrolling through the GoFundMe website reveals seemingly an endless number of people who need help or community support. A common theme: the cost of health care.
It didn’t start out this way. Back in 2010, when the crowdfunding website began, it suggested fundraisers for “ideas and dreams,” “wedding donations and honeymoon registry” or “special occasions.” A spokeswoman said the bulk of collection efforts from the first year were “related to charities and foundations.” A category for medical needs existed, but it was farther down the list.
In the 9 years since, campaigns to pay for health care have reaped the most cash. Of the $5 billion the company says it has raised, about a third has been for medical expenses from more than 250,000 medical campaigns conducted annually.
Take, for instance, the 25-year-old California woman who had a stroke and “needs financial support for rehabilitation, home nursing, medical equipment, and uncovered medical expenses.” Or the Tennessee couple who want to get pregnant, but whose insurance doesn’t cover the $20,000 worth of “medications, surgeries, scans, lab monitoring, and appointments [that] will need to be paid for upfront and out-of-pocket” for in vitro fertilization.
The prominence of the medical category is the symptom of a broken system, according to CEO Rob Solomon, 51, who has a long tech résumé as an executive at places like Groupon and Yahoo. He said he never realized how hard it was for some people to pay their bills: “I needed to understand the gigantic gaps in the system.”
This year, Time Magazine named Mr. Solomon one of the 50 most influential people in health care.
“We didn’t build the platform to focus on medical expenses,” Mr. Solomon said. But it turned out, he said, to be one of those “categories of need” with which many people struggle.
Mr. Solomon talked to Kaiser Health News’ Rachel Bluth about his company’s role in financing health care and what it says about the system when so many people rely on the kindness of strangers to get treatment. The conversation has been edited for length and clarity.
Q: KHN and other news outlets have reported that hospitals often advise patients to crowdfund their transplants. It’s become almost institutionalized to use GoFundMe. How do you feel about that?
It saddens me that this is a reality. Every single day on GoFundMe we see the huge challenges people face. Their stories are heartbreaking.
Some progress has been made here and there with the Affordable Care Act, and it’s under fire, but there’s ever-widening gaps in coverage for treatment, for prescriptions, for everything related to health care costs. Even patients who have insurance and supposedly decent insurance [come up short]. We’ve become an indispensable institution, indispensable technology, and indispensable platform for anyone who finds themselves needing help because there just isn’t adequate coverage or assistance.
I would love nothing more than for “medical” to not be a category on GoFundMe. The reality is, though, that access to health care is connected to the ability to pay for it. If you can’t do that, people die. People suffer. We feel good that our platform is there when people need it.
Q: Did anyone expect medical funding would become such a big part of GoFundMe?
I don’t think anyone anticipated it. What we realized early on is that medical need is a gigantic category.
A lot of insurance doesn’t cover clinical trials and research and things like that, where people need access to leading-edge potential treatments. We strive to fill these gaps until the institutions that are supposed to handle this handle it properly. There has to be a renaissance, a dramatic change in public policy, in how the government focuses on this and how the health care companies solve this.
This is very interesting. In the places like the United Kingdom, Canada, and other European countries that have some form of universal or government-sponsored health coverage, medical [costs] are still the largest category. So it’s not just medical bills for treatment. There’s travel and accommodations for families who have to support people when they fall ill.
Q: What have you learned that you didn’t know before?
I guess what I realized [when I came] to this job is that I had no notion of how severe the problem is. You read about the debate about single-payer health care and all the issues, the partisan politics. What I really learned is the health care system in the United States is really broken. Way too many people fall through the cracks.
The government is supposed to be there, and sometimes they are. The health care companies are supposed to be there, and sometimes they are. But for literally millions of people they’re not. The only thing you can really do is rely on the kindness of friends and family and community. That’s where GoFundMe comes in.
I was not ready for that at all when I started at the company. When you live and breathe it every day and you see the need that exists, when you realize there are many people with rare diseases but they aren’t diseases a drug company can make money from, they’re just left with nothing.
Q: But what does this say about the system?
The system is terrible. It needs to be rethought and retooled. Politicians are failing us. Health care companies are failing us. Those are realities. I don’t want to mince words here. We are facing a huge potential tragedy. We provide relief for a lot of people. But there are people who are not getting relief from us or from the institutions that are supposed to be there. We shouldn’t be the solution to a complex set of systemic problems. They should be solved by the government working properly, and by health care companies working with their constituents. We firmly believe that access to comprehensive health care is a right and things have to be fixed at the local, state, and federal levels of government to make this a reality.
Q: Do you ever worry that medical fundraising on your site is taking away from other causes or other things that need to be funded?
We have billions being raised on our platform on an annual basis. Everything from medical, memorial, and emergency to people funding Little League teams and community projects.
Another thing that’s happened in the last few years is we’ve really become the “take action button.” Whenever there’s a news cycle on something where people want to help, they create GoFundMe campaigns. This government shutdown, for example: We have over a thousand campaigns right now for people who have been affected by it – they’re raising money for people to pay rent, mortgages, car payments while the government isn’t.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Scrolling through the GoFundMe website reveals seemingly an endless number of people who need help or community support. A common theme: the cost of health care.
It didn’t start out this way. Back in 2010, when the crowdfunding website began, it suggested fundraisers for “ideas and dreams,” “wedding donations and honeymoon registry” or “special occasions.” A spokeswoman said the bulk of collection efforts from the first year were “related to charities and foundations.” A category for medical needs existed, but it was farther down the list.
In the 9 years since, campaigns to pay for health care have reaped the most cash. Of the $5 billion the company says it has raised, about a third has been for medical expenses from more than 250,000 medical campaigns conducted annually.
Take, for instance, the 25-year-old California woman who had a stroke and “needs financial support for rehabilitation, home nursing, medical equipment, and uncovered medical expenses.” Or the Tennessee couple who want to get pregnant, but whose insurance doesn’t cover the $20,000 worth of “medications, surgeries, scans, lab monitoring, and appointments [that] will need to be paid for upfront and out-of-pocket” for in vitro fertilization.
The prominence of the medical category is the symptom of a broken system, according to CEO Rob Solomon, 51, who has a long tech résumé as an executive at places like Groupon and Yahoo. He said he never realized how hard it was for some people to pay their bills: “I needed to understand the gigantic gaps in the system.”
This year, Time Magazine named Mr. Solomon one of the 50 most influential people in health care.
“We didn’t build the platform to focus on medical expenses,” Mr. Solomon said. But it turned out, he said, to be one of those “categories of need” with which many people struggle.
Mr. Solomon talked to Kaiser Health News’ Rachel Bluth about his company’s role in financing health care and what it says about the system when so many people rely on the kindness of strangers to get treatment. The conversation has been edited for length and clarity.
Q: KHN and other news outlets have reported that hospitals often advise patients to crowdfund their transplants. It’s become almost institutionalized to use GoFundMe. How do you feel about that?
It saddens me that this is a reality. Every single day on GoFundMe we see the huge challenges people face. Their stories are heartbreaking.
Some progress has been made here and there with the Affordable Care Act, and it’s under fire, but there’s ever-widening gaps in coverage for treatment, for prescriptions, for everything related to health care costs. Even patients who have insurance and supposedly decent insurance [come up short]. We’ve become an indispensable institution, indispensable technology, and indispensable platform for anyone who finds themselves needing help because there just isn’t adequate coverage or assistance.
I would love nothing more than for “medical” to not be a category on GoFundMe. The reality is, though, that access to health care is connected to the ability to pay for it. If you can’t do that, people die. People suffer. We feel good that our platform is there when people need it.
Q: Did anyone expect medical funding would become such a big part of GoFundMe?
I don’t think anyone anticipated it. What we realized early on is that medical need is a gigantic category.
A lot of insurance doesn’t cover clinical trials and research and things like that, where people need access to leading-edge potential treatments. We strive to fill these gaps until the institutions that are supposed to handle this handle it properly. There has to be a renaissance, a dramatic change in public policy, in how the government focuses on this and how the health care companies solve this.
This is very interesting. In the places like the United Kingdom, Canada, and other European countries that have some form of universal or government-sponsored health coverage, medical [costs] are still the largest category. So it’s not just medical bills for treatment. There’s travel and accommodations for families who have to support people when they fall ill.
Q: What have you learned that you didn’t know before?
I guess what I realized [when I came] to this job is that I had no notion of how severe the problem is. You read about the debate about single-payer health care and all the issues, the partisan politics. What I really learned is the health care system in the United States is really broken. Way too many people fall through the cracks.
The government is supposed to be there, and sometimes they are. The health care companies are supposed to be there, and sometimes they are. But for literally millions of people they’re not. The only thing you can really do is rely on the kindness of friends and family and community. That’s where GoFundMe comes in.
I was not ready for that at all when I started at the company. When you live and breathe it every day and you see the need that exists, when you realize there are many people with rare diseases but they aren’t diseases a drug company can make money from, they’re just left with nothing.
Q: But what does this say about the system?
The system is terrible. It needs to be rethought and retooled. Politicians are failing us. Health care companies are failing us. Those are realities. I don’t want to mince words here. We are facing a huge potential tragedy. We provide relief for a lot of people. But there are people who are not getting relief from us or from the institutions that are supposed to be there. We shouldn’t be the solution to a complex set of systemic problems. They should be solved by the government working properly, and by health care companies working with their constituents. We firmly believe that access to comprehensive health care is a right and things have to be fixed at the local, state, and federal levels of government to make this a reality.
Q: Do you ever worry that medical fundraising on your site is taking away from other causes or other things that need to be funded?
We have billions being raised on our platform on an annual basis. Everything from medical, memorial, and emergency to people funding Little League teams and community projects.
Another thing that’s happened in the last few years is we’ve really become the “take action button.” Whenever there’s a news cycle on something where people want to help, they create GoFundMe campaigns. This government shutdown, for example: We have over a thousand campaigns right now for people who have been affected by it – they’re raising money for people to pay rent, mortgages, car payments while the government isn’t.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Scrolling through the GoFundMe website reveals seemingly an endless number of people who need help or community support. A common theme: the cost of health care.
It didn’t start out this way. Back in 2010, when the crowdfunding website began, it suggested fundraisers for “ideas and dreams,” “wedding donations and honeymoon registry” or “special occasions.” A spokeswoman said the bulk of collection efforts from the first year were “related to charities and foundations.” A category for medical needs existed, but it was farther down the list.
In the 9 years since, campaigns to pay for health care have reaped the most cash. Of the $5 billion the company says it has raised, about a third has been for medical expenses from more than 250,000 medical campaigns conducted annually.
Take, for instance, the 25-year-old California woman who had a stroke and “needs financial support for rehabilitation, home nursing, medical equipment, and uncovered medical expenses.” Or the Tennessee couple who want to get pregnant, but whose insurance doesn’t cover the $20,000 worth of “medications, surgeries, scans, lab monitoring, and appointments [that] will need to be paid for upfront and out-of-pocket” for in vitro fertilization.
The prominence of the medical category is the symptom of a broken system, according to CEO Rob Solomon, 51, who has a long tech résumé as an executive at places like Groupon and Yahoo. He said he never realized how hard it was for some people to pay their bills: “I needed to understand the gigantic gaps in the system.”
This year, Time Magazine named Mr. Solomon one of the 50 most influential people in health care.
“We didn’t build the platform to focus on medical expenses,” Mr. Solomon said. But it turned out, he said, to be one of those “categories of need” with which many people struggle.
Mr. Solomon talked to Kaiser Health News’ Rachel Bluth about his company’s role in financing health care and what it says about the system when so many people rely on the kindness of strangers to get treatment. The conversation has been edited for length and clarity.
Q: KHN and other news outlets have reported that hospitals often advise patients to crowdfund their transplants. It’s become almost institutionalized to use GoFundMe. How do you feel about that?
It saddens me that this is a reality. Every single day on GoFundMe we see the huge challenges people face. Their stories are heartbreaking.
Some progress has been made here and there with the Affordable Care Act, and it’s under fire, but there’s ever-widening gaps in coverage for treatment, for prescriptions, for everything related to health care costs. Even patients who have insurance and supposedly decent insurance [come up short]. We’ve become an indispensable institution, indispensable technology, and indispensable platform for anyone who finds themselves needing help because there just isn’t adequate coverage or assistance.
I would love nothing more than for “medical” to not be a category on GoFundMe. The reality is, though, that access to health care is connected to the ability to pay for it. If you can’t do that, people die. People suffer. We feel good that our platform is there when people need it.
Q: Did anyone expect medical funding would become such a big part of GoFundMe?
I don’t think anyone anticipated it. What we realized early on is that medical need is a gigantic category.
A lot of insurance doesn’t cover clinical trials and research and things like that, where people need access to leading-edge potential treatments. We strive to fill these gaps until the institutions that are supposed to handle this handle it properly. There has to be a renaissance, a dramatic change in public policy, in how the government focuses on this and how the health care companies solve this.
This is very interesting. In the places like the United Kingdom, Canada, and other European countries that have some form of universal or government-sponsored health coverage, medical [costs] are still the largest category. So it’s not just medical bills for treatment. There’s travel and accommodations for families who have to support people when they fall ill.
Q: What have you learned that you didn’t know before?
I guess what I realized [when I came] to this job is that I had no notion of how severe the problem is. You read about the debate about single-payer health care and all the issues, the partisan politics. What I really learned is the health care system in the United States is really broken. Way too many people fall through the cracks.
The government is supposed to be there, and sometimes they are. The health care companies are supposed to be there, and sometimes they are. But for literally millions of people they’re not. The only thing you can really do is rely on the kindness of friends and family and community. That’s where GoFundMe comes in.
I was not ready for that at all when I started at the company. When you live and breathe it every day and you see the need that exists, when you realize there are many people with rare diseases but they aren’t diseases a drug company can make money from, they’re just left with nothing.
Q: But what does this say about the system?
The system is terrible. It needs to be rethought and retooled. Politicians are failing us. Health care companies are failing us. Those are realities. I don’t want to mince words here. We are facing a huge potential tragedy. We provide relief for a lot of people. But there are people who are not getting relief from us or from the institutions that are supposed to be there. We shouldn’t be the solution to a complex set of systemic problems. They should be solved by the government working properly, and by health care companies working with their constituents. We firmly believe that access to comprehensive health care is a right and things have to be fixed at the local, state, and federal levels of government to make this a reality.
Q: Do you ever worry that medical fundraising on your site is taking away from other causes or other things that need to be funded?
We have billions being raised on our platform on an annual basis. Everything from medical, memorial, and emergency to people funding Little League teams and community projects.
Another thing that’s happened in the last few years is we’ve really become the “take action button.” Whenever there’s a news cycle on something where people want to help, they create GoFundMe campaigns. This government shutdown, for example: We have over a thousand campaigns right now for people who have been affected by it – they’re raising money for people to pay rent, mortgages, car payments while the government isn’t.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Mandatory reporting laws
Question: You are moonlighting in the emergency department and have just finished treating a 5-year-old boy with an apparent Colles’ fracture, who was accompanied by his mother with bruises on her face. Her exam revealed additional bruises over her abdominal wall. The mother said they accidentally tripped and fell down the stairs, and spontaneously denied any acts of violence in the family.
Given this scenario, which of the following is best?
A. You suspect both child and spousal abuse, but lack sufficient evidence to report the incident.
B. Failure to report based on reasonable suspicion alone may amount to a criminal offense punishable by possible imprisonment.
C. You may face a potential malpractice lawsuit if subsequent injuries caused by abuse could have been prevented had you reported.
D. Mandatory reporting laws apply not only to abuse of children and spouses, but also of the elderly and other vulnerable adults.
E. All are correct except A.
Answer: E. All doctors, especially those working in emergency departments, treat injuries on a regular basis. Accidents probably account for the majority of these injuries, but the most pernicious are those caused by willful abuse or neglect. Such conduct, believed to be widespread and underrecognized, victimizes children, women, the elderly, and other vulnerable groups.
Mandatory reporting laws arose from the need to identify and prevent these activities that cause serious harm and loss of lives. Physicians and other health care workers are in a prime position to diagnose or raise the suspicion of abuse and neglect. This article focuses on laws that mandate physician reporting of such behavior. Not addressed are other reportable situations such as certain infectious diseases, gunshot wounds, threats to third parties, and so on.
Child abuse
The best-known example of a mandatory reporting law relates to child abuse, which is broadly defined as when a parent or caretaker emotionally, physically, or sexually abuses, neglects, or abandons a child. Child abuse laws are intended to protect children from serious harm without abridging parental discipline of their children.
Cases of child abuse are pervasive; four or five children are tragically killed by abuse or neglect every day, and each year, some 6 million children are reported as victims of child abuse. Henry Kempe’s studies on the “battered child syndrome” in 1962 served to underscore the physician’s role in exposing child maltreatment, and 1973 saw the enactment of the Child Abuse Prevention and Treatment Act, which set standards for mandatory reporting as a condition for federal funding.
All U.S. states have statutes identifying persons who are required to report suspected child maltreatment to an appropriate agency, such as child protective services. Reasonable suspicion, without need for proof, is sufficient to trigger the mandatory reporting duty. A summary of the general reporting requirements, as well as each state’s key statutory features, are available at Child Welfare Information Gateway.1
Bruises, fractures, and burns are recurring examples of injuries resulting from child abuse, but there are many others, including severe emotional harm, which is an important consequence. Clues to abuse include a child’s fearful and anxious demeanor, wearing clothes to hide injuries, and inappropriate sexual conduct.2 The perpetrators and/or complicit parties typically blame an innocent home accident for the victim’s injuries to mislead the health care provider.
Elder abuse
Elder abuse is broadly construed to include physical, sexual, and psychological abuse, as well as financial exploitation and caregiver neglect.3 It is a serious problem in the United States, estimated in 2008 to affect 1 in 10 elders. The figure is likely an underestimate, because many elderly victims are afraid or unwilling to lodge a complaint against the abuser whom they love and may depend upon.4
The law, which protects the “elderly” (e.g., those aged 62 years or older in Hawaii), may also be extended to other younger vulnerable adults, who because of an impairment, are unable to 1) communicate or make responsible decisions to manage one’s own care or resources, 2) carry out or arrange for essential activities of daily living, or 3) protect one’s self from abuse.5
The law mandates reporting where there is reason to believe abuse has occurred or the vulnerable adult is in danger of abuse if immediate action is not taken. Reporting statutes for elder abuse vary somewhat on the identity of mandated reporters (health care providers are always included), the victim’s mental capacity, dwelling place (home or in an assisted-living facility), and type of purported activity that warrants reporting.
Domestic violence
As defined by the National Coalition Against Domestic Violence, “Domestic violence is the willful intimidation, physical assault, battery, sexual assault, and/or other abusive behavior as part of a systematic pattern of power and control perpetrated by one intimate partner against another. ... The frequency and severity of domestic violence can vary dramatically; however, the one constant component of domestic violence is one partner’s consistent efforts to maintain power and control over the other.”6 Domestic violence is said to have reached epidemic proportions, with one in four women experiencing it at some point in her life.
Virtually all states mandate the reporting of domestic violence by health care providers if there is a reasonable suspicion that observed patient injuries are the result of physical abuse.7 California, for example, requires the provider to call local law enforcement as soon as possible or to send in a written report within 48 hours.
There may be exceptions to required reporting, as when an adult victim withholds consent but accepts victim referral services. State laws encourage but do not always require that the health care provider inform the patient about the report, but federal law dictates otherwise unless this puts the patient at risk. Hawaii’s domestic violence laws were originally enacted to deter spousal abuse, but they now also protect other household members.8
Any individual who assumes a duty or responsibility pursuant to all of these reporting laws is immunized from criminal or civil liability. On the other hand, a mandated reporter who knowingly fails to report an incident or who willfully prevents another person from reporting such an incident commits a criminal offence.
In the case of a physician, there is the added risk of a malpractice lawsuit based on “violation of statute” (breach of a legal duty), should another injury occur down the road that was arguably preventable by his or her failure to report.
Experts generally believe that mandatory reporting laws are important in identifying child maltreatment. However, it has been asserted that despite a 5-decade history of mandatory reporting, no clear endpoints attest to the efficacy of this approach, and it is argued that no data exist to demonstrate that incremental increases in reporting have contributed to child safety.
Particularly challenging are attempts at impact comparisons between states with different policies. A number of countries, including the United Kingdom, do not have mandatory reporting laws and regulate reporting by professional societies.9
In addition, some critics of mandatory reporting raise concerns surrounding law enforcement showing up at the victim’s house to question the family about abuse, or to make an arrest or issue warnings. They posit that when the behavior of an abuser is under scrutiny, this can paradoxically create a potentially more dangerous environment for the patient-victim, whom the perpetrator now considers to have betrayed his or her trust. Others bemoan that revealing patient confidences violates the physician’s ethical code.
However, the intolerable incidence of violence against the vulnerable has properly made mandatory reporting the law of the land. Although the criminal penalty is currently light for failure to report, there is a move toward increasing its severity. Hawaii, for example, recently introduced Senate Bill 2477 that makes nonreporting by those required to do so a Class C felony punishable by up to 5 years in prison. The offense currently is a petty misdemeanor punishable by up to 30 days in jail.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. Child Welfare Information Gateway (2016). Mandatory reporters of child abuse and neglect. Washington, D.C.: U.S. Department of Health and Human Services, Children’s Bureau. Available at www.childwelfare.gov; email: info@childwelfare.gov; phone: 800-394-3366.
2. Available at www.childwelfare.gov/topics/can.
3. Available at www.justice.gov/elderjustice/elder-justice-statutes-0.
4. Available at www.cdc.gov/violenceprevention/elderabuse/index.html.
5. Hawaii Revised Statutes, Sec. 346-222, 346-224, 346-250, 412:3-114.5.
6. Available at ncadv.org.
7. Ann Emerg Med. 2002 Jan;39(1):56-60.
8. Hawaii Revised Statutes, Sec. 709-906.
9. Pediatrics. 2017 Apr;139(4). pii: e20163511.
Question: You are moonlighting in the emergency department and have just finished treating a 5-year-old boy with an apparent Colles’ fracture, who was accompanied by his mother with bruises on her face. Her exam revealed additional bruises over her abdominal wall. The mother said they accidentally tripped and fell down the stairs, and spontaneously denied any acts of violence in the family.
Given this scenario, which of the following is best?
A. You suspect both child and spousal abuse, but lack sufficient evidence to report the incident.
B. Failure to report based on reasonable suspicion alone may amount to a criminal offense punishable by possible imprisonment.
C. You may face a potential malpractice lawsuit if subsequent injuries caused by abuse could have been prevented had you reported.
D. Mandatory reporting laws apply not only to abuse of children and spouses, but also of the elderly and other vulnerable adults.
E. All are correct except A.
Answer: E. All doctors, especially those working in emergency departments, treat injuries on a regular basis. Accidents probably account for the majority of these injuries, but the most pernicious are those caused by willful abuse or neglect. Such conduct, believed to be widespread and underrecognized, victimizes children, women, the elderly, and other vulnerable groups.
Mandatory reporting laws arose from the need to identify and prevent these activities that cause serious harm and loss of lives. Physicians and other health care workers are in a prime position to diagnose or raise the suspicion of abuse and neglect. This article focuses on laws that mandate physician reporting of such behavior. Not addressed are other reportable situations such as certain infectious diseases, gunshot wounds, threats to third parties, and so on.
Child abuse
The best-known example of a mandatory reporting law relates to child abuse, which is broadly defined as when a parent or caretaker emotionally, physically, or sexually abuses, neglects, or abandons a child. Child abuse laws are intended to protect children from serious harm without abridging parental discipline of their children.
Cases of child abuse are pervasive; four or five children are tragically killed by abuse or neglect every day, and each year, some 6 million children are reported as victims of child abuse. Henry Kempe’s studies on the “battered child syndrome” in 1962 served to underscore the physician’s role in exposing child maltreatment, and 1973 saw the enactment of the Child Abuse Prevention and Treatment Act, which set standards for mandatory reporting as a condition for federal funding.
All U.S. states have statutes identifying persons who are required to report suspected child maltreatment to an appropriate agency, such as child protective services. Reasonable suspicion, without need for proof, is sufficient to trigger the mandatory reporting duty. A summary of the general reporting requirements, as well as each state’s key statutory features, are available at Child Welfare Information Gateway.1
Bruises, fractures, and burns are recurring examples of injuries resulting from child abuse, but there are many others, including severe emotional harm, which is an important consequence. Clues to abuse include a child’s fearful and anxious demeanor, wearing clothes to hide injuries, and inappropriate sexual conduct.2 The perpetrators and/or complicit parties typically blame an innocent home accident for the victim’s injuries to mislead the health care provider.
Elder abuse
Elder abuse is broadly construed to include physical, sexual, and psychological abuse, as well as financial exploitation and caregiver neglect.3 It is a serious problem in the United States, estimated in 2008 to affect 1 in 10 elders. The figure is likely an underestimate, because many elderly victims are afraid or unwilling to lodge a complaint against the abuser whom they love and may depend upon.4
The law, which protects the “elderly” (e.g., those aged 62 years or older in Hawaii), may also be extended to other younger vulnerable adults, who because of an impairment, are unable to 1) communicate or make responsible decisions to manage one’s own care or resources, 2) carry out or arrange for essential activities of daily living, or 3) protect one’s self from abuse.5
The law mandates reporting where there is reason to believe abuse has occurred or the vulnerable adult is in danger of abuse if immediate action is not taken. Reporting statutes for elder abuse vary somewhat on the identity of mandated reporters (health care providers are always included), the victim’s mental capacity, dwelling place (home or in an assisted-living facility), and type of purported activity that warrants reporting.
Domestic violence
As defined by the National Coalition Against Domestic Violence, “Domestic violence is the willful intimidation, physical assault, battery, sexual assault, and/or other abusive behavior as part of a systematic pattern of power and control perpetrated by one intimate partner against another. ... The frequency and severity of domestic violence can vary dramatically; however, the one constant component of domestic violence is one partner’s consistent efforts to maintain power and control over the other.”6 Domestic violence is said to have reached epidemic proportions, with one in four women experiencing it at some point in her life.
Virtually all states mandate the reporting of domestic violence by health care providers if there is a reasonable suspicion that observed patient injuries are the result of physical abuse.7 California, for example, requires the provider to call local law enforcement as soon as possible or to send in a written report within 48 hours.
There may be exceptions to required reporting, as when an adult victim withholds consent but accepts victim referral services. State laws encourage but do not always require that the health care provider inform the patient about the report, but federal law dictates otherwise unless this puts the patient at risk. Hawaii’s domestic violence laws were originally enacted to deter spousal abuse, but they now also protect other household members.8
Any individual who assumes a duty or responsibility pursuant to all of these reporting laws is immunized from criminal or civil liability. On the other hand, a mandated reporter who knowingly fails to report an incident or who willfully prevents another person from reporting such an incident commits a criminal offence.
In the case of a physician, there is the added risk of a malpractice lawsuit based on “violation of statute” (breach of a legal duty), should another injury occur down the road that was arguably preventable by his or her failure to report.
Experts generally believe that mandatory reporting laws are important in identifying child maltreatment. However, it has been asserted that despite a 5-decade history of mandatory reporting, no clear endpoints attest to the efficacy of this approach, and it is argued that no data exist to demonstrate that incremental increases in reporting have contributed to child safety.
Particularly challenging are attempts at impact comparisons between states with different policies. A number of countries, including the United Kingdom, do not have mandatory reporting laws and regulate reporting by professional societies.9
In addition, some critics of mandatory reporting raise concerns surrounding law enforcement showing up at the victim’s house to question the family about abuse, or to make an arrest or issue warnings. They posit that when the behavior of an abuser is under scrutiny, this can paradoxically create a potentially more dangerous environment for the patient-victim, whom the perpetrator now considers to have betrayed his or her trust. Others bemoan that revealing patient confidences violates the physician’s ethical code.
However, the intolerable incidence of violence against the vulnerable has properly made mandatory reporting the law of the land. Although the criminal penalty is currently light for failure to report, there is a move toward increasing its severity. Hawaii, for example, recently introduced Senate Bill 2477 that makes nonreporting by those required to do so a Class C felony punishable by up to 5 years in prison. The offense currently is a petty misdemeanor punishable by up to 30 days in jail.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. Child Welfare Information Gateway (2016). Mandatory reporters of child abuse and neglect. Washington, D.C.: U.S. Department of Health and Human Services, Children’s Bureau. Available at www.childwelfare.gov; email: info@childwelfare.gov; phone: 800-394-3366.
2. Available at www.childwelfare.gov/topics/can.
3. Available at www.justice.gov/elderjustice/elder-justice-statutes-0.
4. Available at www.cdc.gov/violenceprevention/elderabuse/index.html.
5. Hawaii Revised Statutes, Sec. 346-222, 346-224, 346-250, 412:3-114.5.
6. Available at ncadv.org.
7. Ann Emerg Med. 2002 Jan;39(1):56-60.
8. Hawaii Revised Statutes, Sec. 709-906.
9. Pediatrics. 2017 Apr;139(4). pii: e20163511.
Question: You are moonlighting in the emergency department and have just finished treating a 5-year-old boy with an apparent Colles’ fracture, who was accompanied by his mother with bruises on her face. Her exam revealed additional bruises over her abdominal wall. The mother said they accidentally tripped and fell down the stairs, and spontaneously denied any acts of violence in the family.
Given this scenario, which of the following is best?
A. You suspect both child and spousal abuse, but lack sufficient evidence to report the incident.
B. Failure to report based on reasonable suspicion alone may amount to a criminal offense punishable by possible imprisonment.
C. You may face a potential malpractice lawsuit if subsequent injuries caused by abuse could have been prevented had you reported.
D. Mandatory reporting laws apply not only to abuse of children and spouses, but also of the elderly and other vulnerable adults.
E. All are correct except A.
Answer: E. All doctors, especially those working in emergency departments, treat injuries on a regular basis. Accidents probably account for the majority of these injuries, but the most pernicious are those caused by willful abuse or neglect. Such conduct, believed to be widespread and underrecognized, victimizes children, women, the elderly, and other vulnerable groups.
Mandatory reporting laws arose from the need to identify and prevent these activities that cause serious harm and loss of lives. Physicians and other health care workers are in a prime position to diagnose or raise the suspicion of abuse and neglect. This article focuses on laws that mandate physician reporting of such behavior. Not addressed are other reportable situations such as certain infectious diseases, gunshot wounds, threats to third parties, and so on.
Child abuse
The best-known example of a mandatory reporting law relates to child abuse, which is broadly defined as when a parent or caretaker emotionally, physically, or sexually abuses, neglects, or abandons a child. Child abuse laws are intended to protect children from serious harm without abridging parental discipline of their children.
Cases of child abuse are pervasive; four or five children are tragically killed by abuse or neglect every day, and each year, some 6 million children are reported as victims of child abuse. Henry Kempe’s studies on the “battered child syndrome” in 1962 served to underscore the physician’s role in exposing child maltreatment, and 1973 saw the enactment of the Child Abuse Prevention and Treatment Act, which set standards for mandatory reporting as a condition for federal funding.
All U.S. states have statutes identifying persons who are required to report suspected child maltreatment to an appropriate agency, such as child protective services. Reasonable suspicion, without need for proof, is sufficient to trigger the mandatory reporting duty. A summary of the general reporting requirements, as well as each state’s key statutory features, are available at Child Welfare Information Gateway.1
Bruises, fractures, and burns are recurring examples of injuries resulting from child abuse, but there are many others, including severe emotional harm, which is an important consequence. Clues to abuse include a child’s fearful and anxious demeanor, wearing clothes to hide injuries, and inappropriate sexual conduct.2 The perpetrators and/or complicit parties typically blame an innocent home accident for the victim’s injuries to mislead the health care provider.
Elder abuse
Elder abuse is broadly construed to include physical, sexual, and psychological abuse, as well as financial exploitation and caregiver neglect.3 It is a serious problem in the United States, estimated in 2008 to affect 1 in 10 elders. The figure is likely an underestimate, because many elderly victims are afraid or unwilling to lodge a complaint against the abuser whom they love and may depend upon.4
The law, which protects the “elderly” (e.g., those aged 62 years or older in Hawaii), may also be extended to other younger vulnerable adults, who because of an impairment, are unable to 1) communicate or make responsible decisions to manage one’s own care or resources, 2) carry out or arrange for essential activities of daily living, or 3) protect one’s self from abuse.5
The law mandates reporting where there is reason to believe abuse has occurred or the vulnerable adult is in danger of abuse if immediate action is not taken. Reporting statutes for elder abuse vary somewhat on the identity of mandated reporters (health care providers are always included), the victim’s mental capacity, dwelling place (home or in an assisted-living facility), and type of purported activity that warrants reporting.
Domestic violence
As defined by the National Coalition Against Domestic Violence, “Domestic violence is the willful intimidation, physical assault, battery, sexual assault, and/or other abusive behavior as part of a systematic pattern of power and control perpetrated by one intimate partner against another. ... The frequency and severity of domestic violence can vary dramatically; however, the one constant component of domestic violence is one partner’s consistent efforts to maintain power and control over the other.”6 Domestic violence is said to have reached epidemic proportions, with one in four women experiencing it at some point in her life.
Virtually all states mandate the reporting of domestic violence by health care providers if there is a reasonable suspicion that observed patient injuries are the result of physical abuse.7 California, for example, requires the provider to call local law enforcement as soon as possible or to send in a written report within 48 hours.
There may be exceptions to required reporting, as when an adult victim withholds consent but accepts victim referral services. State laws encourage but do not always require that the health care provider inform the patient about the report, but federal law dictates otherwise unless this puts the patient at risk. Hawaii’s domestic violence laws were originally enacted to deter spousal abuse, but they now also protect other household members.8
Any individual who assumes a duty or responsibility pursuant to all of these reporting laws is immunized from criminal or civil liability. On the other hand, a mandated reporter who knowingly fails to report an incident or who willfully prevents another person from reporting such an incident commits a criminal offence.
In the case of a physician, there is the added risk of a malpractice lawsuit based on “violation of statute” (breach of a legal duty), should another injury occur down the road that was arguably preventable by his or her failure to report.
Experts generally believe that mandatory reporting laws are important in identifying child maltreatment. However, it has been asserted that despite a 5-decade history of mandatory reporting, no clear endpoints attest to the efficacy of this approach, and it is argued that no data exist to demonstrate that incremental increases in reporting have contributed to child safety.
Particularly challenging are attempts at impact comparisons between states with different policies. A number of countries, including the United Kingdom, do not have mandatory reporting laws and regulate reporting by professional societies.9
In addition, some critics of mandatory reporting raise concerns surrounding law enforcement showing up at the victim’s house to question the family about abuse, or to make an arrest or issue warnings. They posit that when the behavior of an abuser is under scrutiny, this can paradoxically create a potentially more dangerous environment for the patient-victim, whom the perpetrator now considers to have betrayed his or her trust. Others bemoan that revealing patient confidences violates the physician’s ethical code.
However, the intolerable incidence of violence against the vulnerable has properly made mandatory reporting the law of the land. Although the criminal penalty is currently light for failure to report, there is a move toward increasing its severity. Hawaii, for example, recently introduced Senate Bill 2477 that makes nonreporting by those required to do so a Class C felony punishable by up to 5 years in prison. The offense currently is a petty misdemeanor punishable by up to 30 days in jail.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. Child Welfare Information Gateway (2016). Mandatory reporters of child abuse and neglect. Washington, D.C.: U.S. Department of Health and Human Services, Children’s Bureau. Available at www.childwelfare.gov; email: info@childwelfare.gov; phone: 800-394-3366.
2. Available at www.childwelfare.gov/topics/can.
3. Available at www.justice.gov/elderjustice/elder-justice-statutes-0.
4. Available at www.cdc.gov/violenceprevention/elderabuse/index.html.
5. Hawaii Revised Statutes, Sec. 346-222, 346-224, 346-250, 412:3-114.5.
6. Available at ncadv.org.
7. Ann Emerg Med. 2002 Jan;39(1):56-60.
8. Hawaii Revised Statutes, Sec. 709-906.
9. Pediatrics. 2017 Apr;139(4). pii: e20163511.
Obesity paradox applies to post-stroke mortality
CHICAGO – Overweight and obese military veterans who experienced an in-hospital stroke had a lower 30-day and 1-year all-cause mortality than did those who were normal weight in a large national study, Lauren Costa reported at the American Heart Association scientific sessions.
Underweight patients had a significantly increased mortality risk, added Ms. Costa of the VA Boston Healthcare System.
It’s yet another instance of what is known as the obesity paradox, which has also been described in patients with heart failure, acute coronary syndrome, MI, chronic obstructive pulmonary disease, and other conditions.
Ms. Costa presented a retrospective study of 26,267 patients in the Veterans Health Administration database who had a first stroke in-hospital during 2002-2012. There were subsequently 14,166 deaths, including 2,473 within the first 30 days and 5,854 in the first year post stroke.
Each patient’s body mass index was calculated based on the average of all BMI measurements obtained 1-24 months prior to the stroke. The analysis of the relationship between BMI and poststroke mortality included extensive statistical adjustment for potential confounders, including age, sex, smoking, cancer, dementia, peripheral artery disease, diabetes, coronary heart disease, atrial fibrillation, chronic kidney disease, use of statins, and antihypertensive therapy.
Breaking down the study population into eight BMI categories, Ms. Costa found that the adjusted risk of 30-day all-cause mortality post stroke was reduced by 22%-38% in patients in the overweight or obese groupings, compared with the reference population with a normal-weight BMI of 22.5 to less than 25 kg/m2.
One-year, all-cause mortality showed the same pattern of BMI-based significant differences.
Of deaths within 30 days post stroke, 34% were stroke-related. In an analysis restricted to that group, the evidence of an obesity paradox was attenuated. Indeed, the only BMI group with an adjusted 30-day stroke-related mortality significantly different from the normal-weight reference group were patients with Class III obesity, defined as a BMI of 40 or more. Their risk was reduced by 45%.
The obesity paradox remains a controversial issue among epidemiologists. The increased mortality associated with being underweight among patients with diseases where the obesity paradox has been documented is widely thought to be caused by frailty and/or an underlying illness not adjusted for in analyses. But the mechanism for the reduced mortality risk in overweight and obese patients seen in the VA stroke study and other studies remains unknown despite much speculation.
Ms. Costa reported having no financial conflicts regarding her study, which was supported by the Department of Veterans Affairs.
SOURCE: Costa L. Circulation. 2018;138(suppl 1): Abstract 14288.
CHICAGO – Overweight and obese military veterans who experienced an in-hospital stroke had a lower 30-day and 1-year all-cause mortality than did those who were normal weight in a large national study, Lauren Costa reported at the American Heart Association scientific sessions.
Underweight patients had a significantly increased mortality risk, added Ms. Costa of the VA Boston Healthcare System.
It’s yet another instance of what is known as the obesity paradox, which has also been described in patients with heart failure, acute coronary syndrome, MI, chronic obstructive pulmonary disease, and other conditions.
Ms. Costa presented a retrospective study of 26,267 patients in the Veterans Health Administration database who had a first stroke in-hospital during 2002-2012. There were subsequently 14,166 deaths, including 2,473 within the first 30 days and 5,854 in the first year post stroke.
Each patient’s body mass index was calculated based on the average of all BMI measurements obtained 1-24 months prior to the stroke. The analysis of the relationship between BMI and poststroke mortality included extensive statistical adjustment for potential confounders, including age, sex, smoking, cancer, dementia, peripheral artery disease, diabetes, coronary heart disease, atrial fibrillation, chronic kidney disease, use of statins, and antihypertensive therapy.
Breaking down the study population into eight BMI categories, Ms. Costa found that the adjusted risk of 30-day all-cause mortality post stroke was reduced by 22%-38% in patients in the overweight or obese groupings, compared with the reference population with a normal-weight BMI of 22.5 to less than 25 kg/m2.
One-year, all-cause mortality showed the same pattern of BMI-based significant differences.
Of deaths within 30 days post stroke, 34% were stroke-related. In an analysis restricted to that group, the evidence of an obesity paradox was attenuated. Indeed, the only BMI group with an adjusted 30-day stroke-related mortality significantly different from the normal-weight reference group were patients with Class III obesity, defined as a BMI of 40 or more. Their risk was reduced by 45%.
The obesity paradox remains a controversial issue among epidemiologists. The increased mortality associated with being underweight among patients with diseases where the obesity paradox has been documented is widely thought to be caused by frailty and/or an underlying illness not adjusted for in analyses. But the mechanism for the reduced mortality risk in overweight and obese patients seen in the VA stroke study and other studies remains unknown despite much speculation.
Ms. Costa reported having no financial conflicts regarding her study, which was supported by the Department of Veterans Affairs.
SOURCE: Costa L. Circulation. 2018;138(suppl 1): Abstract 14288.
CHICAGO – Overweight and obese military veterans who experienced an in-hospital stroke had a lower 30-day and 1-year all-cause mortality than did those who were normal weight in a large national study, Lauren Costa reported at the American Heart Association scientific sessions.
Underweight patients had a significantly increased mortality risk, added Ms. Costa of the VA Boston Healthcare System.
It’s yet another instance of what is known as the obesity paradox, which has also been described in patients with heart failure, acute coronary syndrome, MI, chronic obstructive pulmonary disease, and other conditions.
Ms. Costa presented a retrospective study of 26,267 patients in the Veterans Health Administration database who had a first stroke in-hospital during 2002-2012. There were subsequently 14,166 deaths, including 2,473 within the first 30 days and 5,854 in the first year post stroke.
Each patient’s body mass index was calculated based on the average of all BMI measurements obtained 1-24 months prior to the stroke. The analysis of the relationship between BMI and poststroke mortality included extensive statistical adjustment for potential confounders, including age, sex, smoking, cancer, dementia, peripheral artery disease, diabetes, coronary heart disease, atrial fibrillation, chronic kidney disease, use of statins, and antihypertensive therapy.
Breaking down the study population into eight BMI categories, Ms. Costa found that the adjusted risk of 30-day all-cause mortality post stroke was reduced by 22%-38% in patients in the overweight or obese groupings, compared with the reference population with a normal-weight BMI of 22.5 to less than 25 kg/m2.
One-year, all-cause mortality showed the same pattern of BMI-based significant differences.
Of deaths within 30 days post stroke, 34% were stroke-related. In an analysis restricted to that group, the evidence of an obesity paradox was attenuated. Indeed, the only BMI group with an adjusted 30-day stroke-related mortality significantly different from the normal-weight reference group were patients with Class III obesity, defined as a BMI of 40 or more. Their risk was reduced by 45%.
The obesity paradox remains a controversial issue among epidemiologists. The increased mortality associated with being underweight among patients with diseases where the obesity paradox has been documented is widely thought to be caused by frailty and/or an underlying illness not adjusted for in analyses. But the mechanism for the reduced mortality risk in overweight and obese patients seen in the VA stroke study and other studies remains unknown despite much speculation.
Ms. Costa reported having no financial conflicts regarding her study, which was supported by the Department of Veterans Affairs.
SOURCE: Costa L. Circulation. 2018;138(suppl 1): Abstract 14288.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: Heavier stroke patients have lower 30-day and 1-year all-cause mortality.
Major finding: The 30-day stroke-related mortality rate after in-hospital stroke was reduced by 45% in VA patients with Class III obesity.
Study details: This retrospective study looked at the relationship between body mass index and post-stroke mortality in more than 26,000 veterans who had an inpatient stroke, with extensive adjustments made for potential confounders.
Disclosures: The presenter reported having no financial conflicts regarding the study, which was sponsored by the Department of Veterans Affairs.
Source: Costa L. Circulation. 2018;138(suppl 1): Abstract 14288.
Participate in a Retirement Plan
"Tranche" dates -- for completing all the paperwork for the Kai-Zen retirement accelerator program offered through the SVS Affinity Program of expanded benefits -- have been set for 2019. The first dates are Jan. 28, March 11 and May 6. Generally, paperwork can take approximately 30 or more days, but someone who has already started could meet the Jan. 28 date. Kai-Zen combines financing and life insurance, with premiums jointly funded by lenders and the participant (or an employer). It can help members speed investment growth in their life insurance policies, using leverage that provides up to 60 percent more death benefit protection and 60 percent more supplemental retirement income. See a video of how Kai-Zen works here. For more information contact Mark Blocker at mark@nationalaffinity.net or at 312-291-4472.
"Tranche" dates -- for completing all the paperwork for the Kai-Zen retirement accelerator program offered through the SVS Affinity Program of expanded benefits -- have been set for 2019. The first dates are Jan. 28, March 11 and May 6. Generally, paperwork can take approximately 30 or more days, but someone who has already started could meet the Jan. 28 date. Kai-Zen combines financing and life insurance, with premiums jointly funded by lenders and the participant (or an employer). It can help members speed investment growth in their life insurance policies, using leverage that provides up to 60 percent more death benefit protection and 60 percent more supplemental retirement income. See a video of how Kai-Zen works here. For more information contact Mark Blocker at mark@nationalaffinity.net or at 312-291-4472.
"Tranche" dates -- for completing all the paperwork for the Kai-Zen retirement accelerator program offered through the SVS Affinity Program of expanded benefits -- have been set for 2019. The first dates are Jan. 28, March 11 and May 6. Generally, paperwork can take approximately 30 or more days, but someone who has already started could meet the Jan. 28 date. Kai-Zen combines financing and life insurance, with premiums jointly funded by lenders and the participant (or an employer). It can help members speed investment growth in their life insurance policies, using leverage that provides up to 60 percent more death benefit protection and 60 percent more supplemental retirement income. See a video of how Kai-Zen works here. For more information contact Mark Blocker at mark@nationalaffinity.net or at 312-291-4472.
Emerging Roles of Social Media in Dermatology
As the residents on the podium ran through case presentations at the Texas Dermatological Society meeting this past fall (September 21-22, 2018; Galveston, Texas), I discretely surveyed the room. To no surprise, perhaps half of the attendees at some point during the hour-long presentation glanced down at their smartphones, and 2018 statistics suggest that approximately 74% of these Internet glances were made by engagers of social media sites.1 My FOMO (fear of missing out) kicked in. What was everyone looking at? I opened Instagram on my smartphone and plastered at the top of my home page were Texas Dermatological Society–related “stories” posted by other dermatology residents from across the state, one story featuring the very presentation I was attending. I peeked 2 rows ahead to find the social media “influencer” I have been following on Instagram for months in real life for the first time.
It is not just the younger population glued to their social media accounts. In fact, Facebook boasted a more than 80% increase in users 55 years and older between 2011 and 2014 and a 41% increase in users aged 35 to 54 years.2 In total, there were 3.2 billion social media users globally in 2018.3 With such a large portion of the population engaged in social media, it is no wonder that it has become a rapidly emerging presence within the field of dermatology.
#Ad
Social media has become a powerful marketing tool for the practicing dermatologist. In a recent survey, 41% of social media users reported that social media influenced their choice of a particular physician, facility, or medical practice.4 Corresponding to this behavior, dermatology practices also have used social media to educate patients on services offered, acquire new patients, engage existing patients, create brand loyalty, become a trusted source of medical information in a sea of digital misinformation, and facilitate positive word-of-mouth opportunities.5 In fact, 53% of physician practices in the United States operate a Facebook page.6 For these physicians, marketing through social media carries the advantages of low cost and rapid transmission of information to a wide audience.7 Furthermore, the development of business insights and statistics by some social media platforms, such as those available to users on business profiles on Instagram, enables practices and marketers to target their audiences and optimize reach.
#DermLife
The role of social media in dermatology extends far beyond marketing. Lifestyle blogs centered on daily life as a medical provider, even within the field of dermatology, are gaining popularity. Dermatology-centered lifestyle blogs often incorporate the root derm in their handle, enabling other users to identify the account holder and interact in meaningful ways. According to a post from one popular Instagram influencer Dr. Audrey Sue Cruz (@dr.audreyxsue), such profiles may serve to prevent burnout, provide a creative outlet, share life as a resident, develop a supportive community, provide mentorship, and spread inspiration.
#Hashtag
Another interesting utility of social media is the use of standardized hashtags to facilitate scientific and clinical dialogue among medical professionals. Standardization of hashtag ontology on Twitter and Instagram has been adopted by the urology and gastroenterology fields to filter out “noise” by individuals not intending to join academic discussion.8 In dermatology, standardized hashtags have not been adopted, to my knowledge; however, a search for esoteric dermatologic terms such as #dermatopathology or #mohssurgery directs users to specialty-specific discussions.
#DontFryDay
Another role of social media in dermatology is dissemination of information. One notable example is the reach on Twitter of the “Don’t Fry Day” campaign, an annual campaign by the National Council on Skin Cancer Prevention to promote sun safety awareness and sun protection behaviors. In a recent study by Nguyen et al,9 the hashtag #DontFryDay was tracked on Twitter to assess the reach of the campaign. They found that this campaign had an impressive reach of approximately 1200 contributors, resulting in more than 16.5 million impressions; 18 celebrities and verified individuals accounted for 8,735,549 impressions.9
Despite the large potential for dissemination of information on social media, in 2014 none of the top 10 dermatologic journals or professional dermatologic organizations maintained an Instagram account. Only one of the top 10 patient advocate groups related to dermatology conditions—the Melanoma Research Foundation—was found on Instagram as of 2014.10 Furthermore, none of the top 10 most popular dermatology journals, professional dermatology organizations, or dermatology-related patient advocate groups could be found on Tumblr as of 2014.11 Although some of the aforementioned organizations have since adopted social media accounts, such as Cutis and Dermatology News (@mdedgederm) on Instagram in 2018, these social media platforms remain largely untapped outlets for dissemination of information to the public by reputable sources.
#VerifyHealthcare
Although social media has offered many advantages to the field of dermatology, it also has brought about unique challenges such as blind authorship, lack of source citation, and presentation of opinion as fact.7 To compound the challenge, 90% of millennials aged 18 to 24 years reportedly trust health care information shared by others on social media.12 Do we, as dermatologists, have a duty to take to social media to provide reputable health information? In an effort to address this emerging problem, popular Instagram influencer Dr. Austin Chiang (@austinchiangmd) initiated the #VerifyHealthcare movement, which called for physicians active on social media to practice transparency by providing users with their credentials.13 The goal of the movement is to help users differentiate medical information disseminated by trained medical professionals from misinformation by disreputable sources.
Final Thoughts
Despite its shortcomings, the emerging roles of social media in dermatology have proven to be a prominent force here to stay, providing new and innovative opportunities to dermatologists for social networking, dissemination of health information, motivation and inspiration, and marketing.
- Warden C. 30 statistics on social media and healthcare. Referral MD website. https://getreferralmd.com/2017/01/30-facts-statistics-on-social-media-and-healthcare/. Accessed January 16, 2019.
- Saul DJ. 3 million teens leave Facebook in 3 years: the Facebook demographic report. ISL website. https://isl.co/2014/01/3-million-teens-leave-facebook-in-3-years-the-2014-facebook-demographic-report/. Published January 15, 2014. Accessed January 9, 2019.
- Chaffey D. Global social media research summary 2018. Smart Insights website. https://www.smartinsights.com/social-media-marketing/social-media-strategy/new-global-social-media-research/. Published November 23, 2018. Accessed January 3, 2019.
- Ottenhoff M. Infographic: rising use of social and mobile in healthcare. The Spark Report. December 17, 2012. http://thesparkreport.com/infographic-social-mobile-healthcare/. Accessed January 9, 2019.
- Benabio J. The value of social media for dermatologists. Cutis. 2013;91:269-270.
- The healthcare social media shakeup. CDW Healthcare website. http://www.cdwcommunit.com/resources/infographic/social-media/. Accessed January 9, 2019.
- Vance K, Howe W, Dellavelle RP. Social internet sites as a source of public health information. Dermatol Clin. 2009;27:133-136.
- Chang AL, Vartabedian B, Spiegel B. Harnessing the hashtag: a standard approach to GI dialogue on social media. Am J Gastroeneterol. 2016;111:1082-1084.
- Nguyen JL, Heckman C, Perna F. Analysis of the Twitter “Don’t Fry Day” campaign. JAMA Dermatol. 2018;154:961-962.
- Karimkhani C, Connett J, Boyars L, et al. Dermatology on Instagram. Dermatol Online J. 2014;20. pii:13030/qt71g178w9.
- Correnti C, Boyars L, Karimkhani C, et al. Dermatology on Tumblr. Dermatol Online J. 2014;20:22642.
- Honigman B. 24 outstanding statistics on how social media has impacted healthcare. Referral MD website. https://getreferralmd.com/2013/09/healthcare-social-media-statistics. Accessed January 16, 2019.
- Oliver E. #VerifyHealthcare campaign seeks to increase social media transparency—5 insights. Becker’s GI & Endoscopy website. https://www.beckersasc.com/gastroenterology-and-endoscopy/verifyhealthcare-campaign-seeks-to-increase-social-media-transparency-5-insights.html. Published September 24, 2018. Accessed January 16, 2019.
As the residents on the podium ran through case presentations at the Texas Dermatological Society meeting this past fall (September 21-22, 2018; Galveston, Texas), I discretely surveyed the room. To no surprise, perhaps half of the attendees at some point during the hour-long presentation glanced down at their smartphones, and 2018 statistics suggest that approximately 74% of these Internet glances were made by engagers of social media sites.1 My FOMO (fear of missing out) kicked in. What was everyone looking at? I opened Instagram on my smartphone and plastered at the top of my home page were Texas Dermatological Society–related “stories” posted by other dermatology residents from across the state, one story featuring the very presentation I was attending. I peeked 2 rows ahead to find the social media “influencer” I have been following on Instagram for months in real life for the first time.
It is not just the younger population glued to their social media accounts. In fact, Facebook boasted a more than 80% increase in users 55 years and older between 2011 and 2014 and a 41% increase in users aged 35 to 54 years.2 In total, there were 3.2 billion social media users globally in 2018.3 With such a large portion of the population engaged in social media, it is no wonder that it has become a rapidly emerging presence within the field of dermatology.
#Ad
Social media has become a powerful marketing tool for the practicing dermatologist. In a recent survey, 41% of social media users reported that social media influenced their choice of a particular physician, facility, or medical practice.4 Corresponding to this behavior, dermatology practices also have used social media to educate patients on services offered, acquire new patients, engage existing patients, create brand loyalty, become a trusted source of medical information in a sea of digital misinformation, and facilitate positive word-of-mouth opportunities.5 In fact, 53% of physician practices in the United States operate a Facebook page.6 For these physicians, marketing through social media carries the advantages of low cost and rapid transmission of information to a wide audience.7 Furthermore, the development of business insights and statistics by some social media platforms, such as those available to users on business profiles on Instagram, enables practices and marketers to target their audiences and optimize reach.
#DermLife
The role of social media in dermatology extends far beyond marketing. Lifestyle blogs centered on daily life as a medical provider, even within the field of dermatology, are gaining popularity. Dermatology-centered lifestyle blogs often incorporate the root derm in their handle, enabling other users to identify the account holder and interact in meaningful ways. According to a post from one popular Instagram influencer Dr. Audrey Sue Cruz (@dr.audreyxsue), such profiles may serve to prevent burnout, provide a creative outlet, share life as a resident, develop a supportive community, provide mentorship, and spread inspiration.
#Hashtag
Another interesting utility of social media is the use of standardized hashtags to facilitate scientific and clinical dialogue among medical professionals. Standardization of hashtag ontology on Twitter and Instagram has been adopted by the urology and gastroenterology fields to filter out “noise” by individuals not intending to join academic discussion.8 In dermatology, standardized hashtags have not been adopted, to my knowledge; however, a search for esoteric dermatologic terms such as #dermatopathology or #mohssurgery directs users to specialty-specific discussions.
#DontFryDay
Another role of social media in dermatology is dissemination of information. One notable example is the reach on Twitter of the “Don’t Fry Day” campaign, an annual campaign by the National Council on Skin Cancer Prevention to promote sun safety awareness and sun protection behaviors. In a recent study by Nguyen et al,9 the hashtag #DontFryDay was tracked on Twitter to assess the reach of the campaign. They found that this campaign had an impressive reach of approximately 1200 contributors, resulting in more than 16.5 million impressions; 18 celebrities and verified individuals accounted for 8,735,549 impressions.9
Despite the large potential for dissemination of information on social media, in 2014 none of the top 10 dermatologic journals or professional dermatologic organizations maintained an Instagram account. Only one of the top 10 patient advocate groups related to dermatology conditions—the Melanoma Research Foundation—was found on Instagram as of 2014.10 Furthermore, none of the top 10 most popular dermatology journals, professional dermatology organizations, or dermatology-related patient advocate groups could be found on Tumblr as of 2014.11 Although some of the aforementioned organizations have since adopted social media accounts, such as Cutis and Dermatology News (@mdedgederm) on Instagram in 2018, these social media platforms remain largely untapped outlets for dissemination of information to the public by reputable sources.
#VerifyHealthcare
Although social media has offered many advantages to the field of dermatology, it also has brought about unique challenges such as blind authorship, lack of source citation, and presentation of opinion as fact.7 To compound the challenge, 90% of millennials aged 18 to 24 years reportedly trust health care information shared by others on social media.12 Do we, as dermatologists, have a duty to take to social media to provide reputable health information? In an effort to address this emerging problem, popular Instagram influencer Dr. Austin Chiang (@austinchiangmd) initiated the #VerifyHealthcare movement, which called for physicians active on social media to practice transparency by providing users with their credentials.13 The goal of the movement is to help users differentiate medical information disseminated by trained medical professionals from misinformation by disreputable sources.
Final Thoughts
Despite its shortcomings, the emerging roles of social media in dermatology have proven to be a prominent force here to stay, providing new and innovative opportunities to dermatologists for social networking, dissemination of health information, motivation and inspiration, and marketing.
As the residents on the podium ran through case presentations at the Texas Dermatological Society meeting this past fall (September 21-22, 2018; Galveston, Texas), I discretely surveyed the room. To no surprise, perhaps half of the attendees at some point during the hour-long presentation glanced down at their smartphones, and 2018 statistics suggest that approximately 74% of these Internet glances were made by engagers of social media sites.1 My FOMO (fear of missing out) kicked in. What was everyone looking at? I opened Instagram on my smartphone and plastered at the top of my home page were Texas Dermatological Society–related “stories” posted by other dermatology residents from across the state, one story featuring the very presentation I was attending. I peeked 2 rows ahead to find the social media “influencer” I have been following on Instagram for months in real life for the first time.
It is not just the younger population glued to their social media accounts. In fact, Facebook boasted a more than 80% increase in users 55 years and older between 2011 and 2014 and a 41% increase in users aged 35 to 54 years.2 In total, there were 3.2 billion social media users globally in 2018.3 With such a large portion of the population engaged in social media, it is no wonder that it has become a rapidly emerging presence within the field of dermatology.
#Ad
Social media has become a powerful marketing tool for the practicing dermatologist. In a recent survey, 41% of social media users reported that social media influenced their choice of a particular physician, facility, or medical practice.4 Corresponding to this behavior, dermatology practices also have used social media to educate patients on services offered, acquire new patients, engage existing patients, create brand loyalty, become a trusted source of medical information in a sea of digital misinformation, and facilitate positive word-of-mouth opportunities.5 In fact, 53% of physician practices in the United States operate a Facebook page.6 For these physicians, marketing through social media carries the advantages of low cost and rapid transmission of information to a wide audience.7 Furthermore, the development of business insights and statistics by some social media platforms, such as those available to users on business profiles on Instagram, enables practices and marketers to target their audiences and optimize reach.
#DermLife
The role of social media in dermatology extends far beyond marketing. Lifestyle blogs centered on daily life as a medical provider, even within the field of dermatology, are gaining popularity. Dermatology-centered lifestyle blogs often incorporate the root derm in their handle, enabling other users to identify the account holder and interact in meaningful ways. According to a post from one popular Instagram influencer Dr. Audrey Sue Cruz (@dr.audreyxsue), such profiles may serve to prevent burnout, provide a creative outlet, share life as a resident, develop a supportive community, provide mentorship, and spread inspiration.
#Hashtag
Another interesting utility of social media is the use of standardized hashtags to facilitate scientific and clinical dialogue among medical professionals. Standardization of hashtag ontology on Twitter and Instagram has been adopted by the urology and gastroenterology fields to filter out “noise” by individuals not intending to join academic discussion.8 In dermatology, standardized hashtags have not been adopted, to my knowledge; however, a search for esoteric dermatologic terms such as #dermatopathology or #mohssurgery directs users to specialty-specific discussions.
#DontFryDay
Another role of social media in dermatology is dissemination of information. One notable example is the reach on Twitter of the “Don’t Fry Day” campaign, an annual campaign by the National Council on Skin Cancer Prevention to promote sun safety awareness and sun protection behaviors. In a recent study by Nguyen et al,9 the hashtag #DontFryDay was tracked on Twitter to assess the reach of the campaign. They found that this campaign had an impressive reach of approximately 1200 contributors, resulting in more than 16.5 million impressions; 18 celebrities and verified individuals accounted for 8,735,549 impressions.9
Despite the large potential for dissemination of information on social media, in 2014 none of the top 10 dermatologic journals or professional dermatologic organizations maintained an Instagram account. Only one of the top 10 patient advocate groups related to dermatology conditions—the Melanoma Research Foundation—was found on Instagram as of 2014.10 Furthermore, none of the top 10 most popular dermatology journals, professional dermatology organizations, or dermatology-related patient advocate groups could be found on Tumblr as of 2014.11 Although some of the aforementioned organizations have since adopted social media accounts, such as Cutis and Dermatology News (@mdedgederm) on Instagram in 2018, these social media platforms remain largely untapped outlets for dissemination of information to the public by reputable sources.
#VerifyHealthcare
Although social media has offered many advantages to the field of dermatology, it also has brought about unique challenges such as blind authorship, lack of source citation, and presentation of opinion as fact.7 To compound the challenge, 90% of millennials aged 18 to 24 years reportedly trust health care information shared by others on social media.12 Do we, as dermatologists, have a duty to take to social media to provide reputable health information? In an effort to address this emerging problem, popular Instagram influencer Dr. Austin Chiang (@austinchiangmd) initiated the #VerifyHealthcare movement, which called for physicians active on social media to practice transparency by providing users with their credentials.13 The goal of the movement is to help users differentiate medical information disseminated by trained medical professionals from misinformation by disreputable sources.
Final Thoughts
Despite its shortcomings, the emerging roles of social media in dermatology have proven to be a prominent force here to stay, providing new and innovative opportunities to dermatologists for social networking, dissemination of health information, motivation and inspiration, and marketing.
- Warden C. 30 statistics on social media and healthcare. Referral MD website. https://getreferralmd.com/2017/01/30-facts-statistics-on-social-media-and-healthcare/. Accessed January 16, 2019.
- Saul DJ. 3 million teens leave Facebook in 3 years: the Facebook demographic report. ISL website. https://isl.co/2014/01/3-million-teens-leave-facebook-in-3-years-the-2014-facebook-demographic-report/. Published January 15, 2014. Accessed January 9, 2019.
- Chaffey D. Global social media research summary 2018. Smart Insights website. https://www.smartinsights.com/social-media-marketing/social-media-strategy/new-global-social-media-research/. Published November 23, 2018. Accessed January 3, 2019.
- Ottenhoff M. Infographic: rising use of social and mobile in healthcare. The Spark Report. December 17, 2012. http://thesparkreport.com/infographic-social-mobile-healthcare/. Accessed January 9, 2019.
- Benabio J. The value of social media for dermatologists. Cutis. 2013;91:269-270.
- The healthcare social media shakeup. CDW Healthcare website. http://www.cdwcommunit.com/resources/infographic/social-media/. Accessed January 9, 2019.
- Vance K, Howe W, Dellavelle RP. Social internet sites as a source of public health information. Dermatol Clin. 2009;27:133-136.
- Chang AL, Vartabedian B, Spiegel B. Harnessing the hashtag: a standard approach to GI dialogue on social media. Am J Gastroeneterol. 2016;111:1082-1084.
- Nguyen JL, Heckman C, Perna F. Analysis of the Twitter “Don’t Fry Day” campaign. JAMA Dermatol. 2018;154:961-962.
- Karimkhani C, Connett J, Boyars L, et al. Dermatology on Instagram. Dermatol Online J. 2014;20. pii:13030/qt71g178w9.
- Correnti C, Boyars L, Karimkhani C, et al. Dermatology on Tumblr. Dermatol Online J. 2014;20:22642.
- Honigman B. 24 outstanding statistics on how social media has impacted healthcare. Referral MD website. https://getreferralmd.com/2013/09/healthcare-social-media-statistics. Accessed January 16, 2019.
- Oliver E. #VerifyHealthcare campaign seeks to increase social media transparency—5 insights. Becker’s GI & Endoscopy website. https://www.beckersasc.com/gastroenterology-and-endoscopy/verifyhealthcare-campaign-seeks-to-increase-social-media-transparency-5-insights.html. Published September 24, 2018. Accessed January 16, 2019.
- Warden C. 30 statistics on social media and healthcare. Referral MD website. https://getreferralmd.com/2017/01/30-facts-statistics-on-social-media-and-healthcare/. Accessed January 16, 2019.
- Saul DJ. 3 million teens leave Facebook in 3 years: the Facebook demographic report. ISL website. https://isl.co/2014/01/3-million-teens-leave-facebook-in-3-years-the-2014-facebook-demographic-report/. Published January 15, 2014. Accessed January 9, 2019.
- Chaffey D. Global social media research summary 2018. Smart Insights website. https://www.smartinsights.com/social-media-marketing/social-media-strategy/new-global-social-media-research/. Published November 23, 2018. Accessed January 3, 2019.
- Ottenhoff M. Infographic: rising use of social and mobile in healthcare. The Spark Report. December 17, 2012. http://thesparkreport.com/infographic-social-mobile-healthcare/. Accessed January 9, 2019.
- Benabio J. The value of social media for dermatologists. Cutis. 2013;91:269-270.
- The healthcare social media shakeup. CDW Healthcare website. http://www.cdwcommunit.com/resources/infographic/social-media/. Accessed January 9, 2019.
- Vance K, Howe W, Dellavelle RP. Social internet sites as a source of public health information. Dermatol Clin. 2009;27:133-136.
- Chang AL, Vartabedian B, Spiegel B. Harnessing the hashtag: a standard approach to GI dialogue on social media. Am J Gastroeneterol. 2016;111:1082-1084.
- Nguyen JL, Heckman C, Perna F. Analysis of the Twitter “Don’t Fry Day” campaign. JAMA Dermatol. 2018;154:961-962.
- Karimkhani C, Connett J, Boyars L, et al. Dermatology on Instagram. Dermatol Online J. 2014;20. pii:13030/qt71g178w9.
- Correnti C, Boyars L, Karimkhani C, et al. Dermatology on Tumblr. Dermatol Online J. 2014;20:22642.
- Honigman B. 24 outstanding statistics on how social media has impacted healthcare. Referral MD website. https://getreferralmd.com/2013/09/healthcare-social-media-statistics. Accessed January 16, 2019.
- Oliver E. #VerifyHealthcare campaign seeks to increase social media transparency—5 insights. Becker’s GI & Endoscopy website. https://www.beckersasc.com/gastroenterology-and-endoscopy/verifyhealthcare-campaign-seeks-to-increase-social-media-transparency-5-insights.html. Published September 24, 2018. Accessed January 16, 2019.
Resident Pearl
- The emerging presence of social media in dermatology provides opportunities for dermatologists to participate in dissemination and consumption of reliable health information, marketing, social networking among colleagues, and motivation and inspiration. It has been proposed that participation may serve to prevent resident burnout.



