User login
White Concretions on the Hair Shaft
The Diagnosis: White Piedra
A fungal culture demonstrated a filamentous fungus that was identified as Trichosporon inkin via DNA sequencing, which confirmed the diagnosis of white piedra (WP).
Piedra refers to a group of fungal infections presenting as gritty nodules adherent to the hair shaft.1 It is further categorized into black piedra, which occurs more commonly in tropical climates and is caused by Piedraia hortae, and WP, which occurs in tropical and temperate climates and is caused by the Trichosporon genus.1-3 Among the Trichosporon genus, clinical manifestations have varied based on species; for example, T inkin commonly causes genital WP, Trichosporon ovoides commonly causes scalp WP, and Trichosporon asahii and Trichosporon mucoides have been described to cause systemic fungal infections in immunocompromised hosts.1,4 Scalp WP most commonly occurs in children and young adults, and females are at greater risk than males.1,2,5,6
Clinically, WP presents with pale irregular nodules along the hair shaft that are not fluorescent on Wood lamp examination.1,6,7 Nodules are soft and easily detached from the hair shaft, unlike the hard, tightly adherent nodules seen in black piedra.1,7 White piedra affects hair in a variety of areas including the scalp, beard, eyebrows, eyelashes, axillae, and genitals.1,7 Affected hair may become brittle and break at points of invasion.1 Alternatively, WP may resemble tinea capitis with scalp hyperkeratosis and alopecia, though tinea typically affects the base of the hair shaft.1 Immunocompromised patients can develop disseminated WP, and cases of progressive pneumonia, lung abscess, peritonitis, vascular access infection, and endocarditis have been reported.2
Diagnosis of WP is made through a combination of clinical findings and culture of infected hair. Potassium hydroxide preparation demonstrates sleevelike concretions formed of masses of septate hyphae with dense zones of arthrospores and blastospores.1,2 Culture on Sabouraud agar demonstrates creamy colonies that develop a dull, gray, wrinkled surface.1,2 Differential diagnosis includes pediculosis; however, the concretions of WP are circumferential around the hair shaft on microscopy.1 Notably, a case of concomitant WP and pediculosis has been reported.8 In cases of potential pediculosis resistant to therapy, consider hair casts, which are asymptomatic, white, cylindrical concretions that encircle the hair without adherence and can therefore be differentiated from pediculosis via dermoscopy.9 Because this phenomenon is more commonly observed in preadolescent girls, it is hypothesized that scalp inflammation due to traction from hairstyles or atopic dermatitis contributes to the development of hair casts.9,10 Thus, when a potassium hydroxide mount is equivocal for nits and dermoscopy demonstrates concretions that completely encircle the hair shaft, it is important to perform a microbiologic culture to rule out piedra of the hair or scalp. Other differential diagnoses include tinea capitis, black piedra, trichobacteriosis, and hair shaft abnormalities.
Transmission of WP is thought to result from a combination of poor hygiene; humidity due to climate; personal care practices such as habitually tying wet hair, applying hair oils and conditioners, or covering hair according to social customs; and close contact with an infected individual.1,3,6 Long scalp hair potentially correlates with increased risk.1,6 Finally, WP has been described in animals and has been isolated from soil, vegetable matter, and water.3,10
Treatment of WP generally involves removal of infected hair, antifungal agents, and improved hygienic habits to avoid relapses. The American Academy of Dermatology’s Guidelines/Outcomes Committee recommends complete removal of infected hair; however, patients may desire hair-preserving treatments.11 Kiken et al1 reported success with the combination of an oral azole antifungal agent for 3 weeks to 1 month and an antifungal shampoo for 2 to 3 months. The authors proposed that oral medication eliminates scalp carriage while antifungal shampoo eliminates hair shaft concretions.1
1. Kiken DA, Sekaran A, Antaya RJ, et al. White piedra in children. J Am Acad Dermatol. 2006;55:956-961.
2. Bonifaz A, Gómez-Daza F, Paredes V, et al. Tinea versicolor, tinea nigra, white piedra, and black piedra. Clin Dermatol. 2010;28:140-145.
3. Shivaprakash MR, Singh G, Gupta P, et al. Extensive white piedra of the scalp caused by Trichosporon inkin: a case report and review of literature. Mycopathologia. 2011;172:481-486.
4. Goldberg LJ, Wise EM, Miller NS. White piedra caused by Trichosporon inkin: a report of two cases in a northern climate. Br J Dermatol. 2015;173:866-868.
5. Schwartz RA. Superficial fungal infections. Lancet. 2004;364:1173-1182.
6. Fischman O, Bezerra FC, Francisco EC, et al. Trichosporon inkin: an uncommon agent of scalp white piedra. report of four cases in Brazilian children. Mycopathologia. 2014;178:85-89.
7. Pontes ZB, Ramos AL, Lima Ede O, et al. Clinical and mycological study of scalp white piedra in the State of Paraíba, Brazil. Mem Inst Oswaldo Cruz. 2002;97:747-750.
8. Marques SA, Richini-Pereira VB, Camargo RM. White piedra and pediculosis capitis in the same patient. An Bras Dermatol. 2012;87:786-787.
9. Gnarra M, Saraceni P, Rossi A, et al. Challenging diagnosis of peripillous sheaths. Pediatr Dermatol. 2014;31:E112-E113.
10. França K, Villa RT, Silva IR, et al. Hair casts or pseudonits. Int J Trichology. 2011;3:121-122.
11. Guidelines of care for superficial mycotic infections of the skin: piedra. Guidelines/Outcomes Committee. American Academy of Dermatology. J Am Acad Dermatol. 1996;34:122-124.
The Diagnosis: White Piedra
A fungal culture demonstrated a filamentous fungus that was identified as Trichosporon inkin via DNA sequencing, which confirmed the diagnosis of white piedra (WP).
Piedra refers to a group of fungal infections presenting as gritty nodules adherent to the hair shaft.1 It is further categorized into black piedra, which occurs more commonly in tropical climates and is caused by Piedraia hortae, and WP, which occurs in tropical and temperate climates and is caused by the Trichosporon genus.1-3 Among the Trichosporon genus, clinical manifestations have varied based on species; for example, T inkin commonly causes genital WP, Trichosporon ovoides commonly causes scalp WP, and Trichosporon asahii and Trichosporon mucoides have been described to cause systemic fungal infections in immunocompromised hosts.1,4 Scalp WP most commonly occurs in children and young adults, and females are at greater risk than males.1,2,5,6
Clinically, WP presents with pale irregular nodules along the hair shaft that are not fluorescent on Wood lamp examination.1,6,7 Nodules are soft and easily detached from the hair shaft, unlike the hard, tightly adherent nodules seen in black piedra.1,7 White piedra affects hair in a variety of areas including the scalp, beard, eyebrows, eyelashes, axillae, and genitals.1,7 Affected hair may become brittle and break at points of invasion.1 Alternatively, WP may resemble tinea capitis with scalp hyperkeratosis and alopecia, though tinea typically affects the base of the hair shaft.1 Immunocompromised patients can develop disseminated WP, and cases of progressive pneumonia, lung abscess, peritonitis, vascular access infection, and endocarditis have been reported.2
Diagnosis of WP is made through a combination of clinical findings and culture of infected hair. Potassium hydroxide preparation demonstrates sleevelike concretions formed of masses of septate hyphae with dense zones of arthrospores and blastospores.1,2 Culture on Sabouraud agar demonstrates creamy colonies that develop a dull, gray, wrinkled surface.1,2 Differential diagnosis includes pediculosis; however, the concretions of WP are circumferential around the hair shaft on microscopy.1 Notably, a case of concomitant WP and pediculosis has been reported.8 In cases of potential pediculosis resistant to therapy, consider hair casts, which are asymptomatic, white, cylindrical concretions that encircle the hair without adherence and can therefore be differentiated from pediculosis via dermoscopy.9 Because this phenomenon is more commonly observed in preadolescent girls, it is hypothesized that scalp inflammation due to traction from hairstyles or atopic dermatitis contributes to the development of hair casts.9,10 Thus, when a potassium hydroxide mount is equivocal for nits and dermoscopy demonstrates concretions that completely encircle the hair shaft, it is important to perform a microbiologic culture to rule out piedra of the hair or scalp. Other differential diagnoses include tinea capitis, black piedra, trichobacteriosis, and hair shaft abnormalities.
Transmission of WP is thought to result from a combination of poor hygiene; humidity due to climate; personal care practices such as habitually tying wet hair, applying hair oils and conditioners, or covering hair according to social customs; and close contact with an infected individual.1,3,6 Long scalp hair potentially correlates with increased risk.1,6 Finally, WP has been described in animals and has been isolated from soil, vegetable matter, and water.3,10
Treatment of WP generally involves removal of infected hair, antifungal agents, and improved hygienic habits to avoid relapses. The American Academy of Dermatology’s Guidelines/Outcomes Committee recommends complete removal of infected hair; however, patients may desire hair-preserving treatments.11 Kiken et al1 reported success with the combination of an oral azole antifungal agent for 3 weeks to 1 month and an antifungal shampoo for 2 to 3 months. The authors proposed that oral medication eliminates scalp carriage while antifungal shampoo eliminates hair shaft concretions.1
The Diagnosis: White Piedra
A fungal culture demonstrated a filamentous fungus that was identified as Trichosporon inkin via DNA sequencing, which confirmed the diagnosis of white piedra (WP).
Piedra refers to a group of fungal infections presenting as gritty nodules adherent to the hair shaft.1 It is further categorized into black piedra, which occurs more commonly in tropical climates and is caused by Piedraia hortae, and WP, which occurs in tropical and temperate climates and is caused by the Trichosporon genus.1-3 Among the Trichosporon genus, clinical manifestations have varied based on species; for example, T inkin commonly causes genital WP, Trichosporon ovoides commonly causes scalp WP, and Trichosporon asahii and Trichosporon mucoides have been described to cause systemic fungal infections in immunocompromised hosts.1,4 Scalp WP most commonly occurs in children and young adults, and females are at greater risk than males.1,2,5,6
Clinically, WP presents with pale irregular nodules along the hair shaft that are not fluorescent on Wood lamp examination.1,6,7 Nodules are soft and easily detached from the hair shaft, unlike the hard, tightly adherent nodules seen in black piedra.1,7 White piedra affects hair in a variety of areas including the scalp, beard, eyebrows, eyelashes, axillae, and genitals.1,7 Affected hair may become brittle and break at points of invasion.1 Alternatively, WP may resemble tinea capitis with scalp hyperkeratosis and alopecia, though tinea typically affects the base of the hair shaft.1 Immunocompromised patients can develop disseminated WP, and cases of progressive pneumonia, lung abscess, peritonitis, vascular access infection, and endocarditis have been reported.2
Diagnosis of WP is made through a combination of clinical findings and culture of infected hair. Potassium hydroxide preparation demonstrates sleevelike concretions formed of masses of septate hyphae with dense zones of arthrospores and blastospores.1,2 Culture on Sabouraud agar demonstrates creamy colonies that develop a dull, gray, wrinkled surface.1,2 Differential diagnosis includes pediculosis; however, the concretions of WP are circumferential around the hair shaft on microscopy.1 Notably, a case of concomitant WP and pediculosis has been reported.8 In cases of potential pediculosis resistant to therapy, consider hair casts, which are asymptomatic, white, cylindrical concretions that encircle the hair without adherence and can therefore be differentiated from pediculosis via dermoscopy.9 Because this phenomenon is more commonly observed in preadolescent girls, it is hypothesized that scalp inflammation due to traction from hairstyles or atopic dermatitis contributes to the development of hair casts.9,10 Thus, when a potassium hydroxide mount is equivocal for nits and dermoscopy demonstrates concretions that completely encircle the hair shaft, it is important to perform a microbiologic culture to rule out piedra of the hair or scalp. Other differential diagnoses include tinea capitis, black piedra, trichobacteriosis, and hair shaft abnormalities.
Transmission of WP is thought to result from a combination of poor hygiene; humidity due to climate; personal care practices such as habitually tying wet hair, applying hair oils and conditioners, or covering hair according to social customs; and close contact with an infected individual.1,3,6 Long scalp hair potentially correlates with increased risk.1,6 Finally, WP has been described in animals and has been isolated from soil, vegetable matter, and water.3,10
Treatment of WP generally involves removal of infected hair, antifungal agents, and improved hygienic habits to avoid relapses. The American Academy of Dermatology’s Guidelines/Outcomes Committee recommends complete removal of infected hair; however, patients may desire hair-preserving treatments.11 Kiken et al1 reported success with the combination of an oral azole antifungal agent for 3 weeks to 1 month and an antifungal shampoo for 2 to 3 months. The authors proposed that oral medication eliminates scalp carriage while antifungal shampoo eliminates hair shaft concretions.1
1. Kiken DA, Sekaran A, Antaya RJ, et al. White piedra in children. J Am Acad Dermatol. 2006;55:956-961.
2. Bonifaz A, Gómez-Daza F, Paredes V, et al. Tinea versicolor, tinea nigra, white piedra, and black piedra. Clin Dermatol. 2010;28:140-145.
3. Shivaprakash MR, Singh G, Gupta P, et al. Extensive white piedra of the scalp caused by Trichosporon inkin: a case report and review of literature. Mycopathologia. 2011;172:481-486.
4. Goldberg LJ, Wise EM, Miller NS. White piedra caused by Trichosporon inkin: a report of two cases in a northern climate. Br J Dermatol. 2015;173:866-868.
5. Schwartz RA. Superficial fungal infections. Lancet. 2004;364:1173-1182.
6. Fischman O, Bezerra FC, Francisco EC, et al. Trichosporon inkin: an uncommon agent of scalp white piedra. report of four cases in Brazilian children. Mycopathologia. 2014;178:85-89.
7. Pontes ZB, Ramos AL, Lima Ede O, et al. Clinical and mycological study of scalp white piedra in the State of Paraíba, Brazil. Mem Inst Oswaldo Cruz. 2002;97:747-750.
8. Marques SA, Richini-Pereira VB, Camargo RM. White piedra and pediculosis capitis in the same patient. An Bras Dermatol. 2012;87:786-787.
9. Gnarra M, Saraceni P, Rossi A, et al. Challenging diagnosis of peripillous sheaths. Pediatr Dermatol. 2014;31:E112-E113.
10. França K, Villa RT, Silva IR, et al. Hair casts or pseudonits. Int J Trichology. 2011;3:121-122.
11. Guidelines of care for superficial mycotic infections of the skin: piedra. Guidelines/Outcomes Committee. American Academy of Dermatology. J Am Acad Dermatol. 1996;34:122-124.
1. Kiken DA, Sekaran A, Antaya RJ, et al. White piedra in children. J Am Acad Dermatol. 2006;55:956-961.
2. Bonifaz A, Gómez-Daza F, Paredes V, et al. Tinea versicolor, tinea nigra, white piedra, and black piedra. Clin Dermatol. 2010;28:140-145.
3. Shivaprakash MR, Singh G, Gupta P, et al. Extensive white piedra of the scalp caused by Trichosporon inkin: a case report and review of literature. Mycopathologia. 2011;172:481-486.
4. Goldberg LJ, Wise EM, Miller NS. White piedra caused by Trichosporon inkin: a report of two cases in a northern climate. Br J Dermatol. 2015;173:866-868.
5. Schwartz RA. Superficial fungal infections. Lancet. 2004;364:1173-1182.
6. Fischman O, Bezerra FC, Francisco EC, et al. Trichosporon inkin: an uncommon agent of scalp white piedra. report of four cases in Brazilian children. Mycopathologia. 2014;178:85-89.
7. Pontes ZB, Ramos AL, Lima Ede O, et al. Clinical and mycological study of scalp white piedra in the State of Paraíba, Brazil. Mem Inst Oswaldo Cruz. 2002;97:747-750.
8. Marques SA, Richini-Pereira VB, Camargo RM. White piedra and pediculosis capitis in the same patient. An Bras Dermatol. 2012;87:786-787.
9. Gnarra M, Saraceni P, Rossi A, et al. Challenging diagnosis of peripillous sheaths. Pediatr Dermatol. 2014;31:E112-E113.
10. França K, Villa RT, Silva IR, et al. Hair casts or pseudonits. Int J Trichology. 2011;3:121-122.
11. Guidelines of care for superficial mycotic infections of the skin: piedra. Guidelines/Outcomes Committee. American Academy of Dermatology. J Am Acad Dermatol. 1996;34:122-124.
A 35-year-old woman presented with possible nits on the hair of 1 year’s duration. She was previously evaluated by several outside medical providers and was unsuccessfully treated with topical and systemic medications for pediculosis. She reported sporadic scalp pruritus but denied hair loss, breakage, close contacts with similar symptoms, or recent travel outside the United States. She was otherwise healthy and was not taking any medications. Physical examination revealed small 1- to 2-mm, generalized, somewhat detachable, white concretions randomly distributed on the hair shafts. No broken hairs were observed. The eyebrows, eyelash hairs, and surrounding skin were normal. Potassium hydroxide mount was equivocal for nits.
Next-generation anti-BCMA CAR T shows promise for RRMM
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
SAN DIEGO – The next-generation anti–B-cell maturation antigen (BCMA) chimeric antigen receptor (CAR) T-cell therapy bb21217 shows encouraging efficacy for relapsed/refractory multiple myeloma, according to early findings from the phase 1 CRB-402 study.
At a median follow-up of 26 weeks, an objective response was seen in 10 of 12 patients (83%) treated with bb21217 at a dose of 150 x 106 CAR+ T cells, Nina Shah, MD, reported at the annual meeting of the American Society of Hematology.
Immunomodulatory CAR T-cell therapy directed against BCMA has shown promising results for the treatment of relapsed/refractory multiple myeloma (RRMM) in several phase 1 clinical studies in patients with advanced disease; bb21217 is based on the investigational therapy bb2121, said Dr. Shah, a hematologist-oncologist at the University of California, San Francisco.
“It uses the same CAR construct design as bb2121. However, it is cultured in the presence of a pan-[phosphoinositide] 3 kinase inhibitor known as bb007 to enrich for T cells displaying a memory-like phenotype,” she said. “CAR T cells enriched with this phenotype may persist and function longer than nonenriched CAR T cells, and the persistence of functional CAR T cells after infusion may be one determinant of the duration of response.”
Preclinical data have supported this approach and CRB-402 – a first-in-human dose-ranging study – was designed to assess the safety, pharmacokinetics, efficacy, and duration of effect of bb21217, Dr. Shah said.
She presented only the data for the 150 x 106 cell dose.
Study subjects were adults with RRMM who had received at least three prior treatment regimens, including a proteasome inhibitor and an immunomodulatory agent, and who had at least 50% expression of BCMA on the plasma cells in bone marrow samples at screening. They had a median age of 63 years, and 58% had high-risk cytogenetic features.
“Patients tended to be pretty heavily pretreated with a median number of lines of treatment of seven,” Dr. Shah said, noting that almost all patients had prior autologous stem cell transplantation, 58% had been exposed to all five available therapies for RRMM, and 17% were refractory to all five therapies.
The patients underwent collection of peripheral blood mononuclear cells via leukapheresis and underwent lymphodepletion with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) daily for 3 days prior to receiving the single bb21217 infusion.
Grade 3 or higher adverse events occurring in more than one patient were predominantly cytopenias, which is to be expected in a clinical trial such as this, Dr. Shah said, adding that some hypophosphatemia also occurred.
In those with cytopenias, 58% recovered their absolute neutrophil count (ANC) to greater than 1,000 by day 32, and of the remaining five patients, four of them recovered by day 65.
“Therefore, 11 out of 12 had full ANC recovery by day 65,” she said.
Thrombocytopenia was seen in half of the patients, and in those six patients, two recovered platelet counts to more than 50,000 by day 32, and two more by day 65.
Overall, 10 out of 12 patients had platelet recovery to greater than 50,000 by day 65, she said.
Other adverse events of clinical interest included cytokine release syndrome (CRS) and neurotoxicity.
CRS was usually grade 1 or 2 and occurred in 8 of the 12 patients (67%). One grade 3 CRS event occurred.
“The median time to onset of the CRS was 4.5 days, and this was fairly manageable with or without tocilizumab,” she said.
Neurotoxicity occurred in 3 of 12 patients (25%), and a dose-limiting grade 4 encephalopathy and prolonged grade 3 CRS occurred in one patient with a high tumor burden and rapidly accelerating disease at baseline.
“Because of this, the dose level was expanded and we included patients equally who had high tumor burden and low tumor burden to further understand the contribution of this to this phenomenon. However, no other [dose-limiting toxicities] occurred,” she noted.
Additionally, one patient experienced a grade 3 catheter-related infection, but no other severe infections have been reported, Dr. Shah said, adding that four patients experienced one or more serious adverse events, but no deaths have occurred to date.
Of the 10 patients who achieved an objective response to bb21217, 3 had a complete response (CR) or stringent CR, and 6 patients achieved at least a very good partial response or better.
Some responses deepened over time, therefore some CRs were achieved as late as month 10. Responses are ongoing in all but one responding patient, and the first patient who was dosed continues to respond more than 1 year after treatment.
Of those with good minimal residual disease (MRD) samples available, four were responders, and all four were MRD negative. In contrast, both nonresponders who had tissue available for MRD analysis were MRD positive.
Correlative data show that bone marrow plasma cell clearance was observed early, by day 15, in these representative samples, Dr. Shah said.
“There was a dramatic decline in serum free light chain and serum BCMA ... in all responders by month 1. However, the M protein decline did have some delay, which we would expect based on the half-life, and this resulted in an evolving International Myeloma Working Group response over time,” she said.
Sustained serum BCMA suppression was observed up to month 9, which is likely consistent with ongoing plasma cell aplasia resulting from functional CAR T cell persistence, she explained.
An in vivo examination of the phenotype of the infused CAR T cells showed that while the numbers are small, “so far there seems to be an enrichment for memorylike T cells within the CAR T cell population in the blood post infusion – at least by looking at CD62-ligand T cells.”
There also was a robust and consistent CAR T cell expansion post infusion, which was independent of tumor burden.
“CAR T cells have been detectable up to 9 months post infusion,” she said.
However, the follow-up so far has been very short, she noted. “This action may be underrepresenting the true persistence of these T cells,” she added, explaining that there is only one patient at month 9, whereas all three at month 6 were positive for vector copy.
CRB-402 is ongoing with plans to enroll up to 50 patients. A 300 x 106 dosing cohort has been opened, and doses of 450, 800, and 1200 x 106 CAR+ T cells are planned.
“But longer-term follow-up in a larger patient population will further clarify the depth and durability of the bb21217 tumor response and dose response,” she said.
This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
SOURCE: Shah N et al. ASH 2018, Abstract 488.
REPORTING FROM ASH 2018
Key clinical point:
Major finding: Objective response rate was 83% in the first 12 treated patients.
Study details: The CRB-402 phase 1 dose-escalation of 12 patients (up to 50 planned).
Disclosures: This study is sponsored by Bluebird Bio. Dr. Shah reported research funding from Bluebird Bio and equity ownership in Indapta Therapeutics, as well as research funding and consulting relationships with other companies.
Source: Shah N et al. ASH 2018, Abstract 488.
Chidamide may be more effective in PTCL than previously thought
LA JOLLA, CALIF. – Real-world data suggest chidamide may be more effective against relapsed or refractory peripheral T-cell lymphoma (PTCL) than a pivotal study indicated.
Single-agent chidamide produced an overall response rate of 47.0% in a real-world study of more than 1,000 patients, compared with the 28.0% overall response rate that was observed in the phase 2 study of chidamide (Ann Oncol. 2015 Aug;26[8]:1766-71).
Yuqin Song, MD, PhD, of Peking University Cancer Hospital and Institute in Beijing, China, presented data from the real-world study at the annual T-cell Lymphoma Forum.
Dr. Song said this study is the largest cohort of real-world patients with relapsed or refractory PTCL. She and her colleagues analyzed data on 1,064 patients treated at 216 sites across China between February 2015 and December 2017.
The patients had a median age of 54 years, 63.9% were male, and 88.1% had stage III-IV disease.
Disease subtypes included PTCL not otherwise specified (NOS, 38.0%), angioimmunoblastic T-cell lymphoma (AITL, 29.1%), extranodal natural killer T-cell lymphoma (ENKTL, 13.4%), anaplastic large-cell lymphoma (ALCL, 9.1%), and others (10.3%), including cutaneous T-cell lymphoma (CTCL).
Fifty-two percent of patients (n = 553) received chidamide as a single agent, and 48% (n = 511) received the drug with other agents. The most common treatment regimens combined with chidamide were the following
- Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP, 20.7%).
- Gemcitabine, dexamethasone, and cisplatin (GDP, 11.8%).
- Etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (EPOCH, 9.8%).
- Patients with ENKTL received chidamide with L-asparaginase (35.4%) or without it (64.5%).
The median follow-up was 4.9 months (range, 0-36.2 months). Across disease subtypes, the overall response rate was 47.0% with single-agent chidamide and 65.4% when chidamide was given in combination with other agents (P less than .01).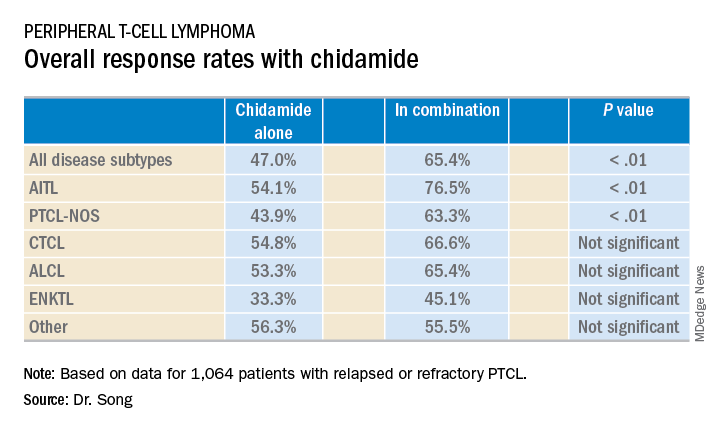
The median overall survival was 400 days for all patients, 342 days for patients treated with chidamide alone, and 457 days for patients who received combination therapy. The 1-year overall survival rates were 52%, 48%, and 56%, respectively.
Dr. Song said these data verify the efficacy of chidamide as a single agent and suggest chidamide might lead to improved survival in refractory or relapsed PTCLs.
Chidamide was generally well tolerated in this study, Dr. Song said. There were no unexpected adverse events (AEs) and most were grade 1 or 2.
The most common AEs (of any grade) observed with single-agent chidamide were neutropenia (42.9%), thrombocytopenia (40.5%), fatigue (38.3%), anemia (31.6%), and nausea/vomiting (21.0%).
The most common AEs observed with chidamide in combination were neutropenia (61.4%), thrombocytopenia (58.5%), fatigue (56.2%), anemia (54.2%), nausea/vomiting (30.7%), and fever (22.1%).
This study was supported by the Union for China Lymphoma Investigators and the Chinese Society of Clinical Oncology. Dr. Song did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – Real-world data suggest chidamide may be more effective against relapsed or refractory peripheral T-cell lymphoma (PTCL) than a pivotal study indicated.
Single-agent chidamide produced an overall response rate of 47.0% in a real-world study of more than 1,000 patients, compared with the 28.0% overall response rate that was observed in the phase 2 study of chidamide (Ann Oncol. 2015 Aug;26[8]:1766-71).
Yuqin Song, MD, PhD, of Peking University Cancer Hospital and Institute in Beijing, China, presented data from the real-world study at the annual T-cell Lymphoma Forum.
Dr. Song said this study is the largest cohort of real-world patients with relapsed or refractory PTCL. She and her colleagues analyzed data on 1,064 patients treated at 216 sites across China between February 2015 and December 2017.
The patients had a median age of 54 years, 63.9% were male, and 88.1% had stage III-IV disease.
Disease subtypes included PTCL not otherwise specified (NOS, 38.0%), angioimmunoblastic T-cell lymphoma (AITL, 29.1%), extranodal natural killer T-cell lymphoma (ENKTL, 13.4%), anaplastic large-cell lymphoma (ALCL, 9.1%), and others (10.3%), including cutaneous T-cell lymphoma (CTCL).
Fifty-two percent of patients (n = 553) received chidamide as a single agent, and 48% (n = 511) received the drug with other agents. The most common treatment regimens combined with chidamide were the following
- Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP, 20.7%).
- Gemcitabine, dexamethasone, and cisplatin (GDP, 11.8%).
- Etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (EPOCH, 9.8%).
- Patients with ENKTL received chidamide with L-asparaginase (35.4%) or without it (64.5%).
The median follow-up was 4.9 months (range, 0-36.2 months). Across disease subtypes, the overall response rate was 47.0% with single-agent chidamide and 65.4% when chidamide was given in combination with other agents (P less than .01).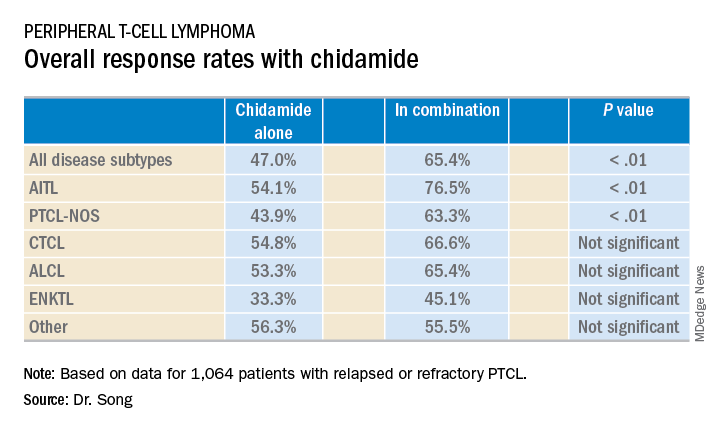
The median overall survival was 400 days for all patients, 342 days for patients treated with chidamide alone, and 457 days for patients who received combination therapy. The 1-year overall survival rates were 52%, 48%, and 56%, respectively.
Dr. Song said these data verify the efficacy of chidamide as a single agent and suggest chidamide might lead to improved survival in refractory or relapsed PTCLs.
Chidamide was generally well tolerated in this study, Dr. Song said. There were no unexpected adverse events (AEs) and most were grade 1 or 2.
The most common AEs (of any grade) observed with single-agent chidamide were neutropenia (42.9%), thrombocytopenia (40.5%), fatigue (38.3%), anemia (31.6%), and nausea/vomiting (21.0%).
The most common AEs observed with chidamide in combination were neutropenia (61.4%), thrombocytopenia (58.5%), fatigue (56.2%), anemia (54.2%), nausea/vomiting (30.7%), and fever (22.1%).
This study was supported by the Union for China Lymphoma Investigators and the Chinese Society of Clinical Oncology. Dr. Song did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – Real-world data suggest chidamide may be more effective against relapsed or refractory peripheral T-cell lymphoma (PTCL) than a pivotal study indicated.
Single-agent chidamide produced an overall response rate of 47.0% in a real-world study of more than 1,000 patients, compared with the 28.0% overall response rate that was observed in the phase 2 study of chidamide (Ann Oncol. 2015 Aug;26[8]:1766-71).
Yuqin Song, MD, PhD, of Peking University Cancer Hospital and Institute in Beijing, China, presented data from the real-world study at the annual T-cell Lymphoma Forum.
Dr. Song said this study is the largest cohort of real-world patients with relapsed or refractory PTCL. She and her colleagues analyzed data on 1,064 patients treated at 216 sites across China between February 2015 and December 2017.
The patients had a median age of 54 years, 63.9% were male, and 88.1% had stage III-IV disease.
Disease subtypes included PTCL not otherwise specified (NOS, 38.0%), angioimmunoblastic T-cell lymphoma (AITL, 29.1%), extranodal natural killer T-cell lymphoma (ENKTL, 13.4%), anaplastic large-cell lymphoma (ALCL, 9.1%), and others (10.3%), including cutaneous T-cell lymphoma (CTCL).
Fifty-two percent of patients (n = 553) received chidamide as a single agent, and 48% (n = 511) received the drug with other agents. The most common treatment regimens combined with chidamide were the following
- Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP, 20.7%).
- Gemcitabine, dexamethasone, and cisplatin (GDP, 11.8%).
- Etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (EPOCH, 9.8%).
- Patients with ENKTL received chidamide with L-asparaginase (35.4%) or without it (64.5%).
The median follow-up was 4.9 months (range, 0-36.2 months). Across disease subtypes, the overall response rate was 47.0% with single-agent chidamide and 65.4% when chidamide was given in combination with other agents (P less than .01).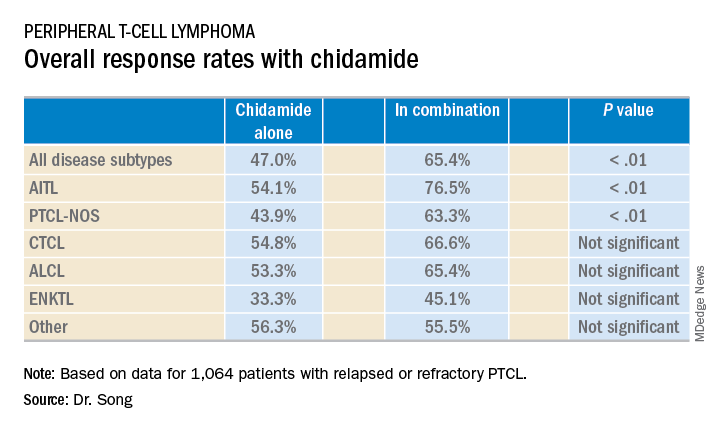
The median overall survival was 400 days for all patients, 342 days for patients treated with chidamide alone, and 457 days for patients who received combination therapy. The 1-year overall survival rates were 52%, 48%, and 56%, respectively.
Dr. Song said these data verify the efficacy of chidamide as a single agent and suggest chidamide might lead to improved survival in refractory or relapsed PTCLs.
Chidamide was generally well tolerated in this study, Dr. Song said. There were no unexpected adverse events (AEs) and most were grade 1 or 2.
The most common AEs (of any grade) observed with single-agent chidamide were neutropenia (42.9%), thrombocytopenia (40.5%), fatigue (38.3%), anemia (31.6%), and nausea/vomiting (21.0%).
The most common AEs observed with chidamide in combination were neutropenia (61.4%), thrombocytopenia (58.5%), fatigue (56.2%), anemia (54.2%), nausea/vomiting (30.7%), and fever (22.1%).
This study was supported by the Union for China Lymphoma Investigators and the Chinese Society of Clinical Oncology. Dr. Song did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is organized by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: Single-agent chidamide had an overall response rate of 47.0% among relapsed/refractory PTCL patients, compared with 65.4% when used in combination with other agents (P less than .01).
Study details: A real-world cohort of 1,064 relapsed/refractory PTCL patients treated at 216 sites across China between February 2015 and December 2017.
Disclosures: The study was supported by the Union for China Lymphoma Investigators and the Chinese Society of Clinical Oncology. Dr. Song did not disclose any conflicts of interest.
Warmth and moisture help keep preterm neonates’ skin healthy
The skin of premature infants is very fragile and can take up to 4 weeks to become cornified. Until then, it’s apt to rapidly lose water and heat, putting babies at risk of hypothermia, dehydration, and electrolyte imbalances, Ayan Kusari and his colleagues wrote in Pediatric Dermatology.
The team examined evidence-based skin care in these tiny patients, extracting recommendations from a meta-analysis of 68 studies.
“There are a number of unifying features that distinguish preterm skin from term skin,” wrote Mr. Kusari, a clinical research associate at the Rady Children’s Hospital–San Diego, and his associates. “Preterm skin is thinner, making preterm neonates more susceptible to skin infections and caustic agents. The vernix caseosa is typically thicker in preterm neonates [though thinner in extremely preterm neonates]. Accordingly, there are a number of general principles that can guide skin care for most preterm neonates.”
Bathing
The team identified eight studies of bathing preterm neonates and concluded that a daily bath isn’t necessary.
“Colonization by pathogenic bacterial strains, size of the total bacterial population, and incidence of skin infection do not vary between preterm infants bathed every 2 days and preterm infants bathed every 4 days in all studies,” the authors wrote.
These less frequent baths appear to decrease the risk of temperature variability, and tub baths are preferable to sponge baths. “In sponge bathing, wet skin is more exposed to ambient air, which is typically colder than body temperature. Physiological and behavioral parameters in preterm infants are often disrupted during sponge bathing. In contrast, tub bathing results in less variability in body temperature and warmer temperatures after bathing,” Mr. Kusari and his associates found.
However, premoistened baby wipes appeared beneficial, lowering skin pH, which might help “facilitate acid mantle development, infection control, and barrier repair,” they wrote.
Emollients
Seven studies and one meta-analysis examined the use of emollients in preterm infants; there was agreement that emollients do improve skin condition. Plant-based emollients appeared superior to petrolatum-based products.
“In developing countries where oil massage of infants and children is traditional, there appears to be a clear benefit to massage with some oils. In developed countries, research has emphasized petrolatum-based creams and ointments, whose benefits are tempered by the increased risk of serious infections with some products,” Mr. Kusari and his colleagues wrote.
Sunflower seed oil was particularly beneficial in studies carried out in developing countries. A mixture of 70% lanolin and 30% olive oil proved better than olive oil alone. Coconut oil also displayed positive impact on skin condition.
“In contrast, multiple studies show an increased risk of sepsis with the application of petrolatum ointment to preterm neonates,” they noted.
In one study, following the adoption of a new skin care protocol involving regular application of petrolatum‐based ointments for extremely low-birth-weight neonates, researchers in Texas observed a significant, 200% increase in the incidence of systemic candidiasis. A study in Saudi Arabia replicated this finding. The largest study of a petrolatum-based ointment on premature babies was conducted in Vermont and found a statistically significant increase in infection with coagulase-negative staphylococcus (CoNS). “This ... study appears to be the driving force in a Cochrane Database meta-analysis, which concludes that topical emollients are associated with increased CoNS infection in preterm neonates,” the authors wrote.
Temperature regulation
It’s notoriously tough to maintain core temperature in preterm newborns. Six studies in the meta-analysis tackled this issue using impermeable plastic wraps or garments after birth and semipermeable barriers in the weeks after.
“Plastic wraps or bags can help neonates to retain their body heat, and greater skin coverage with plastic devices appears to be associated with a better outcome. In infants less than 28 weeks’ gestational age, the use of polyethylene occlusive wraps prevents heat loss after delivery and results in higher NICU admission temperatures and a lower incidence of hypothermia,” Mr Kusari and his associates wrote.
Semipermeable wraps can be used for an extended period after birth to reduce transepidermal water loss. Seven studies examined this technique, using both adhesive and nonadhesive polyurethane dressings.
“These studies show that semipermeable adhesive membranes decrease water loss, reduce skin breakdown, and decrease erythema while applied, but may strip superficial skin layers when they are removed, leading to a transient post-removal increase in transepidermal water loss. Furthermore, due to their semipermeable design, application of these adhesive membranes does not appear to decrease fluid requirement or affect electrolyte status in preterm neonates; however, skin barrier function is disrupted following removal of plastic tape, with increased transepidermal water loss at sites of tape removal,” the investigators wrote.
Pectin-based dressings and those containing hydrocolloid or acrylate can damage preterm neonatal skin by inflicting medical adhesive-related skin injury, the team wrote; this can involve epidermal stripping, tension injury, shearing, maceration, folliculitis, or contact dermatitis.
Skin sterilization
There’s little consensus when it comes to sterilization choices for preterm neonatal skin about to undergo a venipuncture or other procedure. Popular methods are povidone-iodine and chlorhexidine, with gestational age affecting choice. Iodine-based antiseptics have been associated with thyroid disruption and chlorhexidine with chemical burns.
“Some studies suggest 0.2% chlorhexidine gluconate may be an attractive alternative to povidone-iodine for the very and extremely preterm,” the authors wrote. One study they examined compared chlorhexidine gluconate 0.2% and 0.5% in extremely preterm infants, showing a significant decrease in skin irritation in the lower-concentration group.
But a randomized trial following this finding, which compared 0.2% chlorhexidine gluconate with 10% aqueous povidone-iodine, found no differences in any infection outcome or skin irritation, but there was more thyroid suppression in the povidone-iodine group.
More research is needed, the team concluded.
Cord care
Tincture of time may be the best alternative here.
The investigators examined a meta-analysis of 21 umbilical cord care studies and found that cleaning the cord with antiseptic prolonged the time to cord separation, compared with simple air drying.
“Interestingly, one study does suggest that one-time cleansing with chlorhexidine reduces neonatal mortality when compared to dry cord care; however, most of the existing evidence suggests that antiseptic treatment does not offer a benefit over dry cord care,” they wrote.
“Further studies, particularly in the very preterm and extremely preterm neonates, with an emphasis placed on subclassifying the preterm patient population based on gestational age, are needed to further examine and validate the real‐world utility of these interventions,” Mr. Kusari and his associates concluded. “In the meantime, it may be useful to establish practice guidelines based on the evidence we have presented here.”
The authors reported no relevant financial disclosures.
SOURCE: Kusari A et al. Pediatr Dermatol. 2018 Dec 12. doi: 10.1111/pde.13725.
The skin of premature infants is very fragile and can take up to 4 weeks to become cornified. Until then, it’s apt to rapidly lose water and heat, putting babies at risk of hypothermia, dehydration, and electrolyte imbalances, Ayan Kusari and his colleagues wrote in Pediatric Dermatology.
The team examined evidence-based skin care in these tiny patients, extracting recommendations from a meta-analysis of 68 studies.
“There are a number of unifying features that distinguish preterm skin from term skin,” wrote Mr. Kusari, a clinical research associate at the Rady Children’s Hospital–San Diego, and his associates. “Preterm skin is thinner, making preterm neonates more susceptible to skin infections and caustic agents. The vernix caseosa is typically thicker in preterm neonates [though thinner in extremely preterm neonates]. Accordingly, there are a number of general principles that can guide skin care for most preterm neonates.”
Bathing
The team identified eight studies of bathing preterm neonates and concluded that a daily bath isn’t necessary.
“Colonization by pathogenic bacterial strains, size of the total bacterial population, and incidence of skin infection do not vary between preterm infants bathed every 2 days and preterm infants bathed every 4 days in all studies,” the authors wrote.
These less frequent baths appear to decrease the risk of temperature variability, and tub baths are preferable to sponge baths. “In sponge bathing, wet skin is more exposed to ambient air, which is typically colder than body temperature. Physiological and behavioral parameters in preterm infants are often disrupted during sponge bathing. In contrast, tub bathing results in less variability in body temperature and warmer temperatures after bathing,” Mr. Kusari and his associates found.
However, premoistened baby wipes appeared beneficial, lowering skin pH, which might help “facilitate acid mantle development, infection control, and barrier repair,” they wrote.
Emollients
Seven studies and one meta-analysis examined the use of emollients in preterm infants; there was agreement that emollients do improve skin condition. Plant-based emollients appeared superior to petrolatum-based products.
“In developing countries where oil massage of infants and children is traditional, there appears to be a clear benefit to massage with some oils. In developed countries, research has emphasized petrolatum-based creams and ointments, whose benefits are tempered by the increased risk of serious infections with some products,” Mr. Kusari and his colleagues wrote.
Sunflower seed oil was particularly beneficial in studies carried out in developing countries. A mixture of 70% lanolin and 30% olive oil proved better than olive oil alone. Coconut oil also displayed positive impact on skin condition.
“In contrast, multiple studies show an increased risk of sepsis with the application of petrolatum ointment to preterm neonates,” they noted.
In one study, following the adoption of a new skin care protocol involving regular application of petrolatum‐based ointments for extremely low-birth-weight neonates, researchers in Texas observed a significant, 200% increase in the incidence of systemic candidiasis. A study in Saudi Arabia replicated this finding. The largest study of a petrolatum-based ointment on premature babies was conducted in Vermont and found a statistically significant increase in infection with coagulase-negative staphylococcus (CoNS). “This ... study appears to be the driving force in a Cochrane Database meta-analysis, which concludes that topical emollients are associated with increased CoNS infection in preterm neonates,” the authors wrote.
Temperature regulation
It’s notoriously tough to maintain core temperature in preterm newborns. Six studies in the meta-analysis tackled this issue using impermeable plastic wraps or garments after birth and semipermeable barriers in the weeks after.
“Plastic wraps or bags can help neonates to retain their body heat, and greater skin coverage with plastic devices appears to be associated with a better outcome. In infants less than 28 weeks’ gestational age, the use of polyethylene occlusive wraps prevents heat loss after delivery and results in higher NICU admission temperatures and a lower incidence of hypothermia,” Mr Kusari and his associates wrote.
Semipermeable wraps can be used for an extended period after birth to reduce transepidermal water loss. Seven studies examined this technique, using both adhesive and nonadhesive polyurethane dressings.
“These studies show that semipermeable adhesive membranes decrease water loss, reduce skin breakdown, and decrease erythema while applied, but may strip superficial skin layers when they are removed, leading to a transient post-removal increase in transepidermal water loss. Furthermore, due to their semipermeable design, application of these adhesive membranes does not appear to decrease fluid requirement or affect electrolyte status in preterm neonates; however, skin barrier function is disrupted following removal of plastic tape, with increased transepidermal water loss at sites of tape removal,” the investigators wrote.
Pectin-based dressings and those containing hydrocolloid or acrylate can damage preterm neonatal skin by inflicting medical adhesive-related skin injury, the team wrote; this can involve epidermal stripping, tension injury, shearing, maceration, folliculitis, or contact dermatitis.
Skin sterilization
There’s little consensus when it comes to sterilization choices for preterm neonatal skin about to undergo a venipuncture or other procedure. Popular methods are povidone-iodine and chlorhexidine, with gestational age affecting choice. Iodine-based antiseptics have been associated with thyroid disruption and chlorhexidine with chemical burns.
“Some studies suggest 0.2% chlorhexidine gluconate may be an attractive alternative to povidone-iodine for the very and extremely preterm,” the authors wrote. One study they examined compared chlorhexidine gluconate 0.2% and 0.5% in extremely preterm infants, showing a significant decrease in skin irritation in the lower-concentration group.
But a randomized trial following this finding, which compared 0.2% chlorhexidine gluconate with 10% aqueous povidone-iodine, found no differences in any infection outcome or skin irritation, but there was more thyroid suppression in the povidone-iodine group.
More research is needed, the team concluded.
Cord care
Tincture of time may be the best alternative here.
The investigators examined a meta-analysis of 21 umbilical cord care studies and found that cleaning the cord with antiseptic prolonged the time to cord separation, compared with simple air drying.
“Interestingly, one study does suggest that one-time cleansing with chlorhexidine reduces neonatal mortality when compared to dry cord care; however, most of the existing evidence suggests that antiseptic treatment does not offer a benefit over dry cord care,” they wrote.
“Further studies, particularly in the very preterm and extremely preterm neonates, with an emphasis placed on subclassifying the preterm patient population based on gestational age, are needed to further examine and validate the real‐world utility of these interventions,” Mr. Kusari and his associates concluded. “In the meantime, it may be useful to establish practice guidelines based on the evidence we have presented here.”
The authors reported no relevant financial disclosures.
SOURCE: Kusari A et al. Pediatr Dermatol. 2018 Dec 12. doi: 10.1111/pde.13725.
The skin of premature infants is very fragile and can take up to 4 weeks to become cornified. Until then, it’s apt to rapidly lose water and heat, putting babies at risk of hypothermia, dehydration, and electrolyte imbalances, Ayan Kusari and his colleagues wrote in Pediatric Dermatology.
The team examined evidence-based skin care in these tiny patients, extracting recommendations from a meta-analysis of 68 studies.
“There are a number of unifying features that distinguish preterm skin from term skin,” wrote Mr. Kusari, a clinical research associate at the Rady Children’s Hospital–San Diego, and his associates. “Preterm skin is thinner, making preterm neonates more susceptible to skin infections and caustic agents. The vernix caseosa is typically thicker in preterm neonates [though thinner in extremely preterm neonates]. Accordingly, there are a number of general principles that can guide skin care for most preterm neonates.”
Bathing
The team identified eight studies of bathing preterm neonates and concluded that a daily bath isn’t necessary.
“Colonization by pathogenic bacterial strains, size of the total bacterial population, and incidence of skin infection do not vary between preterm infants bathed every 2 days and preterm infants bathed every 4 days in all studies,” the authors wrote.
These less frequent baths appear to decrease the risk of temperature variability, and tub baths are preferable to sponge baths. “In sponge bathing, wet skin is more exposed to ambient air, which is typically colder than body temperature. Physiological and behavioral parameters in preterm infants are often disrupted during sponge bathing. In contrast, tub bathing results in less variability in body temperature and warmer temperatures after bathing,” Mr. Kusari and his associates found.
However, premoistened baby wipes appeared beneficial, lowering skin pH, which might help “facilitate acid mantle development, infection control, and barrier repair,” they wrote.
Emollients
Seven studies and one meta-analysis examined the use of emollients in preterm infants; there was agreement that emollients do improve skin condition. Plant-based emollients appeared superior to petrolatum-based products.
“In developing countries where oil massage of infants and children is traditional, there appears to be a clear benefit to massage with some oils. In developed countries, research has emphasized petrolatum-based creams and ointments, whose benefits are tempered by the increased risk of serious infections with some products,” Mr. Kusari and his colleagues wrote.
Sunflower seed oil was particularly beneficial in studies carried out in developing countries. A mixture of 70% lanolin and 30% olive oil proved better than olive oil alone. Coconut oil also displayed positive impact on skin condition.
“In contrast, multiple studies show an increased risk of sepsis with the application of petrolatum ointment to preterm neonates,” they noted.
In one study, following the adoption of a new skin care protocol involving regular application of petrolatum‐based ointments for extremely low-birth-weight neonates, researchers in Texas observed a significant, 200% increase in the incidence of systemic candidiasis. A study in Saudi Arabia replicated this finding. The largest study of a petrolatum-based ointment on premature babies was conducted in Vermont and found a statistically significant increase in infection with coagulase-negative staphylococcus (CoNS). “This ... study appears to be the driving force in a Cochrane Database meta-analysis, which concludes that topical emollients are associated with increased CoNS infection in preterm neonates,” the authors wrote.
Temperature regulation
It’s notoriously tough to maintain core temperature in preterm newborns. Six studies in the meta-analysis tackled this issue using impermeable plastic wraps or garments after birth and semipermeable barriers in the weeks after.
“Plastic wraps or bags can help neonates to retain their body heat, and greater skin coverage with plastic devices appears to be associated with a better outcome. In infants less than 28 weeks’ gestational age, the use of polyethylene occlusive wraps prevents heat loss after delivery and results in higher NICU admission temperatures and a lower incidence of hypothermia,” Mr Kusari and his associates wrote.
Semipermeable wraps can be used for an extended period after birth to reduce transepidermal water loss. Seven studies examined this technique, using both adhesive and nonadhesive polyurethane dressings.
“These studies show that semipermeable adhesive membranes decrease water loss, reduce skin breakdown, and decrease erythema while applied, but may strip superficial skin layers when they are removed, leading to a transient post-removal increase in transepidermal water loss. Furthermore, due to their semipermeable design, application of these adhesive membranes does not appear to decrease fluid requirement or affect electrolyte status in preterm neonates; however, skin barrier function is disrupted following removal of plastic tape, with increased transepidermal water loss at sites of tape removal,” the investigators wrote.
Pectin-based dressings and those containing hydrocolloid or acrylate can damage preterm neonatal skin by inflicting medical adhesive-related skin injury, the team wrote; this can involve epidermal stripping, tension injury, shearing, maceration, folliculitis, or contact dermatitis.
Skin sterilization
There’s little consensus when it comes to sterilization choices for preterm neonatal skin about to undergo a venipuncture or other procedure. Popular methods are povidone-iodine and chlorhexidine, with gestational age affecting choice. Iodine-based antiseptics have been associated with thyroid disruption and chlorhexidine with chemical burns.
“Some studies suggest 0.2% chlorhexidine gluconate may be an attractive alternative to povidone-iodine for the very and extremely preterm,” the authors wrote. One study they examined compared chlorhexidine gluconate 0.2% and 0.5% in extremely preterm infants, showing a significant decrease in skin irritation in the lower-concentration group.
But a randomized trial following this finding, which compared 0.2% chlorhexidine gluconate with 10% aqueous povidone-iodine, found no differences in any infection outcome or skin irritation, but there was more thyroid suppression in the povidone-iodine group.
More research is needed, the team concluded.
Cord care
Tincture of time may be the best alternative here.
The investigators examined a meta-analysis of 21 umbilical cord care studies and found that cleaning the cord with antiseptic prolonged the time to cord separation, compared with simple air drying.
“Interestingly, one study does suggest that one-time cleansing with chlorhexidine reduces neonatal mortality when compared to dry cord care; however, most of the existing evidence suggests that antiseptic treatment does not offer a benefit over dry cord care,” they wrote.
“Further studies, particularly in the very preterm and extremely preterm neonates, with an emphasis placed on subclassifying the preterm patient population based on gestational age, are needed to further examine and validate the real‐world utility of these interventions,” Mr. Kusari and his associates concluded. “In the meantime, it may be useful to establish practice guidelines based on the evidence we have presented here.”
The authors reported no relevant financial disclosures.
SOURCE: Kusari A et al. Pediatr Dermatol. 2018 Dec 12. doi: 10.1111/pde.13725.
FROM PEDIATRIC DERMATOLOGY
Key clinical point: Limiting baths, using plant-based emollients, and using plastic wraps benefit preterm neonates’ skin early in life.
Major finding: The team identified eight studies of bathing preterm neonates and concluded that a daily bath isn’t necessary.
Study details: A meta-analysis of 68 studies.
Disclosures: The authors reported no relevant financial disclosures.
Source: Kusari A et al. Pediatr Dermatol. 2018 Dec 12. doi: 10.1111/pde.13725.
High postpartum breast cancer metastasis risk may persist for a decade
Increased risk of metastasis associated with postpartum breast cancer (PPBC) in women 45 years or younger may persist for 10 years after childbirth, a finding that may give reason to extend the 5-year window currently defining PPBC.
Analysis of more than 700 patients showed that risk of metastasis was approximately twofold higher for a decade after childbirth, with risks about 3.5- to fivefold higher in women diagnosed with stage I or II disease, reported lead author Erica Goddard, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, and her colleagues. Regardless of parity status, patients diagnosed with stage III disease had poor outcomes.
“The high risk for metastasis is independent of poor prognostic indicators, including biological subtype, stage, age, or year of diagnosis,” the investigators wrote in JAMA Network Open. “Yet, PPBC is an underrecognized subset of breast cancer, and few studies address the associated high risk for metastasis.”
The cohort study involved 701 women 45 years or younger who were diagnosed with breast cancer between 1981 and 2014. Early cases were retrospective, until the study switched to a prospective method in 2004. The investigators analyzed rates of distant metastasis and looked for associations with tumor cell proliferation, lymphovascular invasion, lymph node involvement, and other clinical attributes. Distant metastasis was defined by spread beyond the ipsilateral breast or local draining lymph node, as detected by physical exam, imaging, and/or pathological testing. The investigators also stained available tumor samples for Ki67 positivity, which is used for prognostic purposes, and to distinguish between ER-positive luminal A versus ER-positive luminal B disease.
Compared with nulliparous patients, women under 45 who were diagnosed with PPBC within 5 years of childbirth were 2.13 times as likely to develop metastasis (P = .009). This risk persisted for 5 more years. Women diagnosed within 5-10 years of childbirth showed a similar hazard ratio, of 2.23 (P = .006). After 10 years, the hazard ratio dropped to 1.6, but this value was statistically insignificant (P = .13). Patients identified with stage I or II disease had more dramatic risk profiles, with hazard ratios of 3.5 and 5.2, for diagnoses up to 5 years postpartum, and diagnoses 5-10 years postpartum, respectively. These findings suggest that, for some patients, the 5- to 10-year window may be the riskiest time for metastasis, and, incidentally, one that has historically been excluded from the definition of PPBC.
In addition, patients diagnosed with estrogen receptor–positive breast cancer within 10 years of childbirth had outcomes similar to those of nulliparous women with estrogen receptor–negative breast cancer, and postpartum women with estrogen receptor–negative breast cancer had worse outcomes than did nulliparous women with the same subtype. Furthermore, PPBC was associated with higher rates of lymph node involvement and lymphovascular invasion. Collectively, these findings suggest that PPBC is generally more aggressive than nulliparous breast cancer. In contrast, Ki67 positivity, identifying the luminal B subtype, was associated with worse outcome regardless of parity status, but this finding was statistically insignificant.
“[T]hese data suggest that stages I and II breast cancer in patients with PPBC diagnosed within 10 years of parturition may be underestimated in their risk for metastasis, as parity status is not currently factored into clinical decision-making algorithms, such as the National Comprehensive Cancer Network guidelines,” the investigators concluded. “In sum, we suggest that poor-prognostic PPBC is an increasing problem that merits more dedicated research.”
The study was funded by the National Cancer Institute, the National Institutes of Health, the U.S. Department of Defense, and other organizations. Dr. Goddard reported funding from the NCI and NIH. Dr. Mori reported financial support from the Department of Defense.
SOURCE: Goddard et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.
Increased risk of metastasis associated with postpartum breast cancer (PPBC) in women 45 years or younger may persist for 10 years after childbirth, a finding that may give reason to extend the 5-year window currently defining PPBC.
Analysis of more than 700 patients showed that risk of metastasis was approximately twofold higher for a decade after childbirth, with risks about 3.5- to fivefold higher in women diagnosed with stage I or II disease, reported lead author Erica Goddard, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, and her colleagues. Regardless of parity status, patients diagnosed with stage III disease had poor outcomes.
“The high risk for metastasis is independent of poor prognostic indicators, including biological subtype, stage, age, or year of diagnosis,” the investigators wrote in JAMA Network Open. “Yet, PPBC is an underrecognized subset of breast cancer, and few studies address the associated high risk for metastasis.”
The cohort study involved 701 women 45 years or younger who were diagnosed with breast cancer between 1981 and 2014. Early cases were retrospective, until the study switched to a prospective method in 2004. The investigators analyzed rates of distant metastasis and looked for associations with tumor cell proliferation, lymphovascular invasion, lymph node involvement, and other clinical attributes. Distant metastasis was defined by spread beyond the ipsilateral breast or local draining lymph node, as detected by physical exam, imaging, and/or pathological testing. The investigators also stained available tumor samples for Ki67 positivity, which is used for prognostic purposes, and to distinguish between ER-positive luminal A versus ER-positive luminal B disease.
Compared with nulliparous patients, women under 45 who were diagnosed with PPBC within 5 years of childbirth were 2.13 times as likely to develop metastasis (P = .009). This risk persisted for 5 more years. Women diagnosed within 5-10 years of childbirth showed a similar hazard ratio, of 2.23 (P = .006). After 10 years, the hazard ratio dropped to 1.6, but this value was statistically insignificant (P = .13). Patients identified with stage I or II disease had more dramatic risk profiles, with hazard ratios of 3.5 and 5.2, for diagnoses up to 5 years postpartum, and diagnoses 5-10 years postpartum, respectively. These findings suggest that, for some patients, the 5- to 10-year window may be the riskiest time for metastasis, and, incidentally, one that has historically been excluded from the definition of PPBC.
In addition, patients diagnosed with estrogen receptor–positive breast cancer within 10 years of childbirth had outcomes similar to those of nulliparous women with estrogen receptor–negative breast cancer, and postpartum women with estrogen receptor–negative breast cancer had worse outcomes than did nulliparous women with the same subtype. Furthermore, PPBC was associated with higher rates of lymph node involvement and lymphovascular invasion. Collectively, these findings suggest that PPBC is generally more aggressive than nulliparous breast cancer. In contrast, Ki67 positivity, identifying the luminal B subtype, was associated with worse outcome regardless of parity status, but this finding was statistically insignificant.
“[T]hese data suggest that stages I and II breast cancer in patients with PPBC diagnosed within 10 years of parturition may be underestimated in their risk for metastasis, as parity status is not currently factored into clinical decision-making algorithms, such as the National Comprehensive Cancer Network guidelines,” the investigators concluded. “In sum, we suggest that poor-prognostic PPBC is an increasing problem that merits more dedicated research.”
The study was funded by the National Cancer Institute, the National Institutes of Health, the U.S. Department of Defense, and other organizations. Dr. Goddard reported funding from the NCI and NIH. Dr. Mori reported financial support from the Department of Defense.
SOURCE: Goddard et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.
Increased risk of metastasis associated with postpartum breast cancer (PPBC) in women 45 years or younger may persist for 10 years after childbirth, a finding that may give reason to extend the 5-year window currently defining PPBC.
Analysis of more than 700 patients showed that risk of metastasis was approximately twofold higher for a decade after childbirth, with risks about 3.5- to fivefold higher in women diagnosed with stage I or II disease, reported lead author Erica Goddard, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, and her colleagues. Regardless of parity status, patients diagnosed with stage III disease had poor outcomes.
“The high risk for metastasis is independent of poor prognostic indicators, including biological subtype, stage, age, or year of diagnosis,” the investigators wrote in JAMA Network Open. “Yet, PPBC is an underrecognized subset of breast cancer, and few studies address the associated high risk for metastasis.”
The cohort study involved 701 women 45 years or younger who were diagnosed with breast cancer between 1981 and 2014. Early cases were retrospective, until the study switched to a prospective method in 2004. The investigators analyzed rates of distant metastasis and looked for associations with tumor cell proliferation, lymphovascular invasion, lymph node involvement, and other clinical attributes. Distant metastasis was defined by spread beyond the ipsilateral breast or local draining lymph node, as detected by physical exam, imaging, and/or pathological testing. The investigators also stained available tumor samples for Ki67 positivity, which is used for prognostic purposes, and to distinguish between ER-positive luminal A versus ER-positive luminal B disease.
Compared with nulliparous patients, women under 45 who were diagnosed with PPBC within 5 years of childbirth were 2.13 times as likely to develop metastasis (P = .009). This risk persisted for 5 more years. Women diagnosed within 5-10 years of childbirth showed a similar hazard ratio, of 2.23 (P = .006). After 10 years, the hazard ratio dropped to 1.6, but this value was statistically insignificant (P = .13). Patients identified with stage I or II disease had more dramatic risk profiles, with hazard ratios of 3.5 and 5.2, for diagnoses up to 5 years postpartum, and diagnoses 5-10 years postpartum, respectively. These findings suggest that, for some patients, the 5- to 10-year window may be the riskiest time for metastasis, and, incidentally, one that has historically been excluded from the definition of PPBC.
In addition, patients diagnosed with estrogen receptor–positive breast cancer within 10 years of childbirth had outcomes similar to those of nulliparous women with estrogen receptor–negative breast cancer, and postpartum women with estrogen receptor–negative breast cancer had worse outcomes than did nulliparous women with the same subtype. Furthermore, PPBC was associated with higher rates of lymph node involvement and lymphovascular invasion. Collectively, these findings suggest that PPBC is generally more aggressive than nulliparous breast cancer. In contrast, Ki67 positivity, identifying the luminal B subtype, was associated with worse outcome regardless of parity status, but this finding was statistically insignificant.
“[T]hese data suggest that stages I and II breast cancer in patients with PPBC diagnosed within 10 years of parturition may be underestimated in their risk for metastasis, as parity status is not currently factored into clinical decision-making algorithms, such as the National Comprehensive Cancer Network guidelines,” the investigators concluded. “In sum, we suggest that poor-prognostic PPBC is an increasing problem that merits more dedicated research.”
The study was funded by the National Cancer Institute, the National Institutes of Health, the U.S. Department of Defense, and other organizations. Dr. Goddard reported funding from the NCI and NIH. Dr. Mori reported financial support from the Department of Defense.
SOURCE: Goddard et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.
FROM JAMA NETWORK OPEN
Key clinical point: Increased risk of metastasis associated with postpartum breast cancer in women 45 years or younger may persist for 10 years after childbirth, instead of 5 years, as previously reported.
Major finding: Compared with nulliparous breast cancer patients, women 45 years or younger diagnosed with breast cancer within 5-10 years of childbirth were 2.23 times as likely to develop metastasis.
Study details: A retrospective and prospective cohort study involving 701 women with stage I, II, or III breast cancer who were 45 years or younger at time of diagnosis.
Disclosures: The study was funded by the National Cancer Institute, the National Institutes of Health, the U.S. Department of Defense, and other organizations. Dr. Goddard reported funding from the NCI and NIH. Dr. Mori reported financial support from the Department of Defense.
Source: Goddard et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.6997.
Acute Kwashiorkor in the Setting of Cerebral Palsy and Pancreatic Insufficiency
To the Editor:
Kwashiorkor, or protein-calorie malnutrition, is a common issue in developing countries subject to starvation. In economically advanced nations, however, kwashiorkor is extremely rare and may appear in children placed on restrictive diets instituted by well-meaning guardians. Kwashiorkor also may occur because of gastrointestinal malabsorption. We present a unique case of kwashiorkor that revealed an underlying diagnosis of pancreatic insufficiency.
A 12-year-old girl presented to the hospital with 4 days of watery nonbloody diarrhea occurring with every feeding as well as new onset of presumed diaper dermatitis that had not responded to nystatin cream. Facial swelling also was noted the day prior to admission. Her medical history was notable for cerebral palsy secondary to nonaccidental trauma, leaving the patient nonverbal and quadriplegic. She had numerous prior admissions for sepsis with marked hypotension and more recently was diagnosed with insulin-dependent type 2 diabetes mellitus. She had never lived outside the United States and resided at home with her adoptive parents.
Physical examination revealed a nonverbal underweight girl (weight, 25 kg). Large areas of denudation with surrounding desquamated skin resembling flaking enamel paint covered the buttocks and posterior legs bilaterally (Figure). She had linear hyperpigmented patches on the dorsal hands with one superficial erosion on the left wrist. Marked periorbital edema as well as nonpitting edema of the face, arms, and legs were present.
Upon additional questioning, the patient’s adoptive parent reported a diet of formula containing 1.0 cal/mL with 200-mL feedings 3 times daily through a Geiger-Müller tube, providing a daily protein intake of approximately 17.7 g per day (0.7 g/kg per day). On the day of admission, abnormal laboratory findings included low protein and albumin levels at 4.6 g/dL (reference range, 5.7–8.2 g/dL) and 2.1 g/dL (reference range, 3.2–4.8 g/dL), respectively; an elevated aspartate aminotransferase level of 73 U/L (reference range, 10–34 U/L); and an elevated alanine aminotransferase level of 80 U/L (reference range, 10–40 U/L). Based on the patient’s characteristic clinical findings and abnormal laboratory values, a diagnosis of acute kwashiorkor was made. Although the zinc level was low at 0.29 µg/mL (reference range, 0.66–1.10 µg/mL), the patient did not have any periorificial involvement to support a diagnosis of acrodermatitis enteropathica.
Upon further workup, stool elastase was measured at less than 50 µg per gram of stool (reference range, >200 µg pancreatic elastase per gram of stool), confirming a diagnosis of severe pancreatic insufficiency. Pancreatic enzyme supplementation was initiated along with an increase in protein intake to 1.5 g/kg per day. The patient’s hospital course was complicated by respiratory distress and sepsis, leading to a prolonged hospital stay. A component of refeeding syndrome may have contributed to the patient’s respiratory distress.
Kwashiorkor, a form of protein malnutrition, is caused by inadequate protein intake and usually is seen in developing countries when children are weaned from breastmilk to a diet high in starch and low in protein. It is characterized by edema, growth retardation, a characteristic dermatosis, depigmentation of hair, lethargy, and irritability.1 If left untreated, kwashiorkor can be fatal. Skin changes associated with kwashiorkor first occur in areas of friction or pressure. The skin develops patches of hyperpigmentation that subsequently desquamate in a pattern likened to flaky paint. In the current case of a nonmobile child with diarrhea, prominent involvement of the buttocks and thighs would be expected. This dermatosis does not appear in marasmus and is pathognomonic for kwashiorkor when seen in a child with edema.2
Children in the United States developing kwashiorkor secondary to severely restrictive diets has been reported.3 However, kwashiorkor also may occur due to underlying chronic malabsorptive disease. There have been rare reports of children with cystic fibrosis presenting with kwashiorkor,4 as well as a case of kwashiorkor secondary to underlying infantile Crohn disease.5
Cerebral palsy is associated with multiple different risk factors for malnutrition. Musculoskeletal deformities, oral-motor difficulties, medication side effects, limited communication skills, compromised pulmonary status, and poor muscle tone can all contribute to energy and nutrient deprivation.6 A 2018 study including 728 children registered into the Bangladesh Cerebral Palsy Register between January 2015 and December 2016 demonstrated that more than two-thirds were underweight (70.0%) and stunted (73.1%) and that children with tri/quadriplegic cerebral palsy presented with the highest proportion of severe malnutrition.7 In another report (N=142), up to 85% of children with spastic quadriplegia had severe feeding problems,8 making this population particularly high risk for poor nutritional status.
Pancreatic exocrine insufficiency is characterized by reduced secretion of amylase, lipase, and protease, and it may result in diarrhea, weight loss, malabsorption of essential nutrients, and malnutrition. Pancreatic exocrine insufficiency may occur in the setting of chronic pancreatitis, pancreatic surgery, and cystic fibrosis. Our patient had numerous hospitalizations for sepsis marked by hypotension, and in the absence of more typical causes, we postulate that both endocrine and exocrine pancreatic damage resulted from prolonged hypotension. A sweat chloride test was not performed, as the patient had not experienced frequent pulmonary infections or other signs of cystic fibrosis.
According to a report from the Food and Agriculture Organization of the United Nations/World Health Organization/United Nations University (FAO/WHO/UNU), protein should provide at least 10% of the total caloric intake in a child.9 Although the adoptive parent approximated that our patient received 12% of her daily calories in the form of protein, the amount that she absorbed in the context of pancreatic insufficiency was undoubtedly much lower.
In this case, the diagnosis of kwashiorkor led to the discovery of underlying pancreatic exocrine insufficiency. Low stool elastase confirmed the diagnosis. Because kwashiorkor is rare in developed countries, the classic signs and symptoms may go unrecognized, which can lead to delayed diagnosis and notable morbidity and mortality. New-onset edema and desquamative rash in a child, especially a child with cerebral palsy, should alert physicians to the possibility of acute kwashiorkor and prompt investigation into underlying medical issues that may have contributed to its development.
1. Trowell HC, Davies JN, Dean RF. Kwashiorkor. II. clinical picture, pathology, and differential diagnosis. Br Med J. 1952;2:798-801.
2. Latham MC. The dermatosis of kwashiorkor in young children. Semin Dermatol. 1991;10:270-272.
3. Liu T, Howard RM, Mancini AJ, et al. Kwashiorkor in the United States: fad diets, perceived and true milk allergy, and nutritional ignorance. Arch Dermatol. 2001;137:630-636.
4. Phillips RJ, Crock CM, Dillon MJ, et al. Cystic fibrosis presenting as kwashiorkor with florid skin rash. Arch Dis Childhood. 1993;69:446-448.
5. Al-Mubarak L, Al-Khenaizan S, Al Goufi T. Cutaneous presentation of kwashiorkor due to infantile Crohn’s disease. Eur J Pediatr. 2010;169:117-119.
6. Wittenbrook W. Nutritional assessment and intervention in cerebral palsy. Practical Gastroenterol. Feb 2011;92:16-32. http://www.practicalgastro.com/pdf/February11/WittenbrookArticle.pdf.
7. Jahan I, Muhit M, Karim T, et al. What makes children with cerebral palsy vulnerable to malnutrition? findings from the Bangladesh cerebral palsy register (BCPR)[published online April 16, 2018]. Disabil Rehabil. doi:10.1080/09638288.2018.1461260.
8. Stallings VA, Charney EB, Davies JC, et al. Nutrition-related growth failure of children with quadriplegic cerebral palsy. Dev Med Child Neurol. 1993;35:126-138.
9. World Health Organization. Energy and Protein Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation. Geneva, Switzerland: World Health Organization; 1985. Technical Report Series 724.
To the Editor:
Kwashiorkor, or protein-calorie malnutrition, is a common issue in developing countries subject to starvation. In economically advanced nations, however, kwashiorkor is extremely rare and may appear in children placed on restrictive diets instituted by well-meaning guardians. Kwashiorkor also may occur because of gastrointestinal malabsorption. We present a unique case of kwashiorkor that revealed an underlying diagnosis of pancreatic insufficiency.
A 12-year-old girl presented to the hospital with 4 days of watery nonbloody diarrhea occurring with every feeding as well as new onset of presumed diaper dermatitis that had not responded to nystatin cream. Facial swelling also was noted the day prior to admission. Her medical history was notable for cerebral palsy secondary to nonaccidental trauma, leaving the patient nonverbal and quadriplegic. She had numerous prior admissions for sepsis with marked hypotension and more recently was diagnosed with insulin-dependent type 2 diabetes mellitus. She had never lived outside the United States and resided at home with her adoptive parents.
Physical examination revealed a nonverbal underweight girl (weight, 25 kg). Large areas of denudation with surrounding desquamated skin resembling flaking enamel paint covered the buttocks and posterior legs bilaterally (Figure). She had linear hyperpigmented patches on the dorsal hands with one superficial erosion on the left wrist. Marked periorbital edema as well as nonpitting edema of the face, arms, and legs were present.
Upon additional questioning, the patient’s adoptive parent reported a diet of formula containing 1.0 cal/mL with 200-mL feedings 3 times daily through a Geiger-Müller tube, providing a daily protein intake of approximately 17.7 g per day (0.7 g/kg per day). On the day of admission, abnormal laboratory findings included low protein and albumin levels at 4.6 g/dL (reference range, 5.7–8.2 g/dL) and 2.1 g/dL (reference range, 3.2–4.8 g/dL), respectively; an elevated aspartate aminotransferase level of 73 U/L (reference range, 10–34 U/L); and an elevated alanine aminotransferase level of 80 U/L (reference range, 10–40 U/L). Based on the patient’s characteristic clinical findings and abnormal laboratory values, a diagnosis of acute kwashiorkor was made. Although the zinc level was low at 0.29 µg/mL (reference range, 0.66–1.10 µg/mL), the patient did not have any periorificial involvement to support a diagnosis of acrodermatitis enteropathica.
Upon further workup, stool elastase was measured at less than 50 µg per gram of stool (reference range, >200 µg pancreatic elastase per gram of stool), confirming a diagnosis of severe pancreatic insufficiency. Pancreatic enzyme supplementation was initiated along with an increase in protein intake to 1.5 g/kg per day. The patient’s hospital course was complicated by respiratory distress and sepsis, leading to a prolonged hospital stay. A component of refeeding syndrome may have contributed to the patient’s respiratory distress.
Kwashiorkor, a form of protein malnutrition, is caused by inadequate protein intake and usually is seen in developing countries when children are weaned from breastmilk to a diet high in starch and low in protein. It is characterized by edema, growth retardation, a characteristic dermatosis, depigmentation of hair, lethargy, and irritability.1 If left untreated, kwashiorkor can be fatal. Skin changes associated with kwashiorkor first occur in areas of friction or pressure. The skin develops patches of hyperpigmentation that subsequently desquamate in a pattern likened to flaky paint. In the current case of a nonmobile child with diarrhea, prominent involvement of the buttocks and thighs would be expected. This dermatosis does not appear in marasmus and is pathognomonic for kwashiorkor when seen in a child with edema.2
Children in the United States developing kwashiorkor secondary to severely restrictive diets has been reported.3 However, kwashiorkor also may occur due to underlying chronic malabsorptive disease. There have been rare reports of children with cystic fibrosis presenting with kwashiorkor,4 as well as a case of kwashiorkor secondary to underlying infantile Crohn disease.5
Cerebral palsy is associated with multiple different risk factors for malnutrition. Musculoskeletal deformities, oral-motor difficulties, medication side effects, limited communication skills, compromised pulmonary status, and poor muscle tone can all contribute to energy and nutrient deprivation.6 A 2018 study including 728 children registered into the Bangladesh Cerebral Palsy Register between January 2015 and December 2016 demonstrated that more than two-thirds were underweight (70.0%) and stunted (73.1%) and that children with tri/quadriplegic cerebral palsy presented with the highest proportion of severe malnutrition.7 In another report (N=142), up to 85% of children with spastic quadriplegia had severe feeding problems,8 making this population particularly high risk for poor nutritional status.
Pancreatic exocrine insufficiency is characterized by reduced secretion of amylase, lipase, and protease, and it may result in diarrhea, weight loss, malabsorption of essential nutrients, and malnutrition. Pancreatic exocrine insufficiency may occur in the setting of chronic pancreatitis, pancreatic surgery, and cystic fibrosis. Our patient had numerous hospitalizations for sepsis marked by hypotension, and in the absence of more typical causes, we postulate that both endocrine and exocrine pancreatic damage resulted from prolonged hypotension. A sweat chloride test was not performed, as the patient had not experienced frequent pulmonary infections or other signs of cystic fibrosis.
According to a report from the Food and Agriculture Organization of the United Nations/World Health Organization/United Nations University (FAO/WHO/UNU), protein should provide at least 10% of the total caloric intake in a child.9 Although the adoptive parent approximated that our patient received 12% of her daily calories in the form of protein, the amount that she absorbed in the context of pancreatic insufficiency was undoubtedly much lower.
In this case, the diagnosis of kwashiorkor led to the discovery of underlying pancreatic exocrine insufficiency. Low stool elastase confirmed the diagnosis. Because kwashiorkor is rare in developed countries, the classic signs and symptoms may go unrecognized, which can lead to delayed diagnosis and notable morbidity and mortality. New-onset edema and desquamative rash in a child, especially a child with cerebral palsy, should alert physicians to the possibility of acute kwashiorkor and prompt investigation into underlying medical issues that may have contributed to its development.
To the Editor:
Kwashiorkor, or protein-calorie malnutrition, is a common issue in developing countries subject to starvation. In economically advanced nations, however, kwashiorkor is extremely rare and may appear in children placed on restrictive diets instituted by well-meaning guardians. Kwashiorkor also may occur because of gastrointestinal malabsorption. We present a unique case of kwashiorkor that revealed an underlying diagnosis of pancreatic insufficiency.
A 12-year-old girl presented to the hospital with 4 days of watery nonbloody diarrhea occurring with every feeding as well as new onset of presumed diaper dermatitis that had not responded to nystatin cream. Facial swelling also was noted the day prior to admission. Her medical history was notable for cerebral palsy secondary to nonaccidental trauma, leaving the patient nonverbal and quadriplegic. She had numerous prior admissions for sepsis with marked hypotension and more recently was diagnosed with insulin-dependent type 2 diabetes mellitus. She had never lived outside the United States and resided at home with her adoptive parents.
Physical examination revealed a nonverbal underweight girl (weight, 25 kg). Large areas of denudation with surrounding desquamated skin resembling flaking enamel paint covered the buttocks and posterior legs bilaterally (Figure). She had linear hyperpigmented patches on the dorsal hands with one superficial erosion on the left wrist. Marked periorbital edema as well as nonpitting edema of the face, arms, and legs were present.
Upon additional questioning, the patient’s adoptive parent reported a diet of formula containing 1.0 cal/mL with 200-mL feedings 3 times daily through a Geiger-Müller tube, providing a daily protein intake of approximately 17.7 g per day (0.7 g/kg per day). On the day of admission, abnormal laboratory findings included low protein and albumin levels at 4.6 g/dL (reference range, 5.7–8.2 g/dL) and 2.1 g/dL (reference range, 3.2–4.8 g/dL), respectively; an elevated aspartate aminotransferase level of 73 U/L (reference range, 10–34 U/L); and an elevated alanine aminotransferase level of 80 U/L (reference range, 10–40 U/L). Based on the patient’s characteristic clinical findings and abnormal laboratory values, a diagnosis of acute kwashiorkor was made. Although the zinc level was low at 0.29 µg/mL (reference range, 0.66–1.10 µg/mL), the patient did not have any periorificial involvement to support a diagnosis of acrodermatitis enteropathica.
Upon further workup, stool elastase was measured at less than 50 µg per gram of stool (reference range, >200 µg pancreatic elastase per gram of stool), confirming a diagnosis of severe pancreatic insufficiency. Pancreatic enzyme supplementation was initiated along with an increase in protein intake to 1.5 g/kg per day. The patient’s hospital course was complicated by respiratory distress and sepsis, leading to a prolonged hospital stay. A component of refeeding syndrome may have contributed to the patient’s respiratory distress.
Kwashiorkor, a form of protein malnutrition, is caused by inadequate protein intake and usually is seen in developing countries when children are weaned from breastmilk to a diet high in starch and low in protein. It is characterized by edema, growth retardation, a characteristic dermatosis, depigmentation of hair, lethargy, and irritability.1 If left untreated, kwashiorkor can be fatal. Skin changes associated with kwashiorkor first occur in areas of friction or pressure. The skin develops patches of hyperpigmentation that subsequently desquamate in a pattern likened to flaky paint. In the current case of a nonmobile child with diarrhea, prominent involvement of the buttocks and thighs would be expected. This dermatosis does not appear in marasmus and is pathognomonic for kwashiorkor when seen in a child with edema.2
Children in the United States developing kwashiorkor secondary to severely restrictive diets has been reported.3 However, kwashiorkor also may occur due to underlying chronic malabsorptive disease. There have been rare reports of children with cystic fibrosis presenting with kwashiorkor,4 as well as a case of kwashiorkor secondary to underlying infantile Crohn disease.5
Cerebral palsy is associated with multiple different risk factors for malnutrition. Musculoskeletal deformities, oral-motor difficulties, medication side effects, limited communication skills, compromised pulmonary status, and poor muscle tone can all contribute to energy and nutrient deprivation.6 A 2018 study including 728 children registered into the Bangladesh Cerebral Palsy Register between January 2015 and December 2016 demonstrated that more than two-thirds were underweight (70.0%) and stunted (73.1%) and that children with tri/quadriplegic cerebral palsy presented with the highest proportion of severe malnutrition.7 In another report (N=142), up to 85% of children with spastic quadriplegia had severe feeding problems,8 making this population particularly high risk for poor nutritional status.
Pancreatic exocrine insufficiency is characterized by reduced secretion of amylase, lipase, and protease, and it may result in diarrhea, weight loss, malabsorption of essential nutrients, and malnutrition. Pancreatic exocrine insufficiency may occur in the setting of chronic pancreatitis, pancreatic surgery, and cystic fibrosis. Our patient had numerous hospitalizations for sepsis marked by hypotension, and in the absence of more typical causes, we postulate that both endocrine and exocrine pancreatic damage resulted from prolonged hypotension. A sweat chloride test was not performed, as the patient had not experienced frequent pulmonary infections or other signs of cystic fibrosis.
According to a report from the Food and Agriculture Organization of the United Nations/World Health Organization/United Nations University (FAO/WHO/UNU), protein should provide at least 10% of the total caloric intake in a child.9 Although the adoptive parent approximated that our patient received 12% of her daily calories in the form of protein, the amount that she absorbed in the context of pancreatic insufficiency was undoubtedly much lower.
In this case, the diagnosis of kwashiorkor led to the discovery of underlying pancreatic exocrine insufficiency. Low stool elastase confirmed the diagnosis. Because kwashiorkor is rare in developed countries, the classic signs and symptoms may go unrecognized, which can lead to delayed diagnosis and notable morbidity and mortality. New-onset edema and desquamative rash in a child, especially a child with cerebral palsy, should alert physicians to the possibility of acute kwashiorkor and prompt investigation into underlying medical issues that may have contributed to its development.
1. Trowell HC, Davies JN, Dean RF. Kwashiorkor. II. clinical picture, pathology, and differential diagnosis. Br Med J. 1952;2:798-801.
2. Latham MC. The dermatosis of kwashiorkor in young children. Semin Dermatol. 1991;10:270-272.
3. Liu T, Howard RM, Mancini AJ, et al. Kwashiorkor in the United States: fad diets, perceived and true milk allergy, and nutritional ignorance. Arch Dermatol. 2001;137:630-636.
4. Phillips RJ, Crock CM, Dillon MJ, et al. Cystic fibrosis presenting as kwashiorkor with florid skin rash. Arch Dis Childhood. 1993;69:446-448.
5. Al-Mubarak L, Al-Khenaizan S, Al Goufi T. Cutaneous presentation of kwashiorkor due to infantile Crohn’s disease. Eur J Pediatr. 2010;169:117-119.
6. Wittenbrook W. Nutritional assessment and intervention in cerebral palsy. Practical Gastroenterol. Feb 2011;92:16-32. http://www.practicalgastro.com/pdf/February11/WittenbrookArticle.pdf.
7. Jahan I, Muhit M, Karim T, et al. What makes children with cerebral palsy vulnerable to malnutrition? findings from the Bangladesh cerebral palsy register (BCPR)[published online April 16, 2018]. Disabil Rehabil. doi:10.1080/09638288.2018.1461260.
8. Stallings VA, Charney EB, Davies JC, et al. Nutrition-related growth failure of children with quadriplegic cerebral palsy. Dev Med Child Neurol. 1993;35:126-138.
9. World Health Organization. Energy and Protein Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation. Geneva, Switzerland: World Health Organization; 1985. Technical Report Series 724.
1. Trowell HC, Davies JN, Dean RF. Kwashiorkor. II. clinical picture, pathology, and differential diagnosis. Br Med J. 1952;2:798-801.
2. Latham MC. The dermatosis of kwashiorkor in young children. Semin Dermatol. 1991;10:270-272.
3. Liu T, Howard RM, Mancini AJ, et al. Kwashiorkor in the United States: fad diets, perceived and true milk allergy, and nutritional ignorance. Arch Dermatol. 2001;137:630-636.
4. Phillips RJ, Crock CM, Dillon MJ, et al. Cystic fibrosis presenting as kwashiorkor with florid skin rash. Arch Dis Childhood. 1993;69:446-448.
5. Al-Mubarak L, Al-Khenaizan S, Al Goufi T. Cutaneous presentation of kwashiorkor due to infantile Crohn’s disease. Eur J Pediatr. 2010;169:117-119.
6. Wittenbrook W. Nutritional assessment and intervention in cerebral palsy. Practical Gastroenterol. Feb 2011;92:16-32. http://www.practicalgastro.com/pdf/February11/WittenbrookArticle.pdf.
7. Jahan I, Muhit M, Karim T, et al. What makes children with cerebral palsy vulnerable to malnutrition? findings from the Bangladesh cerebral palsy register (BCPR)[published online April 16, 2018]. Disabil Rehabil. doi:10.1080/09638288.2018.1461260.
8. Stallings VA, Charney EB, Davies JC, et al. Nutrition-related growth failure of children with quadriplegic cerebral palsy. Dev Med Child Neurol. 1993;35:126-138.
9. World Health Organization. Energy and Protein Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation. Geneva, Switzerland: World Health Organization; 1985. Technical Report Series 724.
Practice Points
• Pancreatic exocrine deficiency, confirmed by low stool elastase, can lead to kwashiorkor and requires a high index of suspicion for diagnosis.
• Kwashiorkor is not only seen in developing countries but also in certain at-risk populations in economically advantaged countries.
• For multiple reasons, patients with cerebral palsy are at particular risk for nutritional deficiencies including kwashiorkor.
External Trigeminal Neurostimulation Offers Relief
One-hour treatment with external trigeminal nerve stimulation resulted in significant headache pain relief compared to sham stimulation and was well tolerated, according to a recent double-blind, randomized, sham-controlled study conducted across 3 headache centers in the United States. Adult patients who were experiencing an acute migraine attack, with or without aura, were recruited on site and randomly assigned 1:1 to receive either verum or sham external trigeminal nerve stimulation treatment for 1 hour. Pain intensity was scored using a visual analog scale. Researchers found:
- One hundred and six patients were randomized and included in the intention-to-treat analysis (verum: n=52; sham: n=54).
- The primary outcome measure was significantly more reduced in the verum group than in the sham group: −3.46 ± 2.32 vs −1.78 ± 1.89, or −59% vs −30%.
- With regards to migraine subgroups, there was a significant difference in pain reduction between verum and sham for “migraine without aura” attacks.
- For “migraine with aura” attacks, pain reduction was numerically greater for verum vs sham, but did not reach significance: mean visual analog scale reduction at 1 hour was −4.3 ± 1.8 for the verum group vs −2.6 ± 1.9 for the sham group.
Chou DE, Yugrakh MS, Winegarner D, Rowe V, Kuruvilla D, Schoenen. Acute migraine therapy with external trigeminal neurostimulation (ACME): A randomized controlled trial. [Published online ahead of print November 17, 2018]. Cephalalgia. doi:10.1177%2F0333102418811573.
One-hour treatment with external trigeminal nerve stimulation resulted in significant headache pain relief compared to sham stimulation and was well tolerated, according to a recent double-blind, randomized, sham-controlled study conducted across 3 headache centers in the United States. Adult patients who were experiencing an acute migraine attack, with or without aura, were recruited on site and randomly assigned 1:1 to receive either verum or sham external trigeminal nerve stimulation treatment for 1 hour. Pain intensity was scored using a visual analog scale. Researchers found:
- One hundred and six patients were randomized and included in the intention-to-treat analysis (verum: n=52; sham: n=54).
- The primary outcome measure was significantly more reduced in the verum group than in the sham group: −3.46 ± 2.32 vs −1.78 ± 1.89, or −59% vs −30%.
- With regards to migraine subgroups, there was a significant difference in pain reduction between verum and sham for “migraine without aura” attacks.
- For “migraine with aura” attacks, pain reduction was numerically greater for verum vs sham, but did not reach significance: mean visual analog scale reduction at 1 hour was −4.3 ± 1.8 for the verum group vs −2.6 ± 1.9 for the sham group.
Chou DE, Yugrakh MS, Winegarner D, Rowe V, Kuruvilla D, Schoenen. Acute migraine therapy with external trigeminal neurostimulation (ACME): A randomized controlled trial. [Published online ahead of print November 17, 2018]. Cephalalgia. doi:10.1177%2F0333102418811573.
One-hour treatment with external trigeminal nerve stimulation resulted in significant headache pain relief compared to sham stimulation and was well tolerated, according to a recent double-blind, randomized, sham-controlled study conducted across 3 headache centers in the United States. Adult patients who were experiencing an acute migraine attack, with or without aura, were recruited on site and randomly assigned 1:1 to receive either verum or sham external trigeminal nerve stimulation treatment for 1 hour. Pain intensity was scored using a visual analog scale. Researchers found:
- One hundred and six patients were randomized and included in the intention-to-treat analysis (verum: n=52; sham: n=54).
- The primary outcome measure was significantly more reduced in the verum group than in the sham group: −3.46 ± 2.32 vs −1.78 ± 1.89, or −59% vs −30%.
- With regards to migraine subgroups, there was a significant difference in pain reduction between verum and sham for “migraine without aura” attacks.
- For “migraine with aura” attacks, pain reduction was numerically greater for verum vs sham, but did not reach significance: mean visual analog scale reduction at 1 hour was −4.3 ± 1.8 for the verum group vs −2.6 ± 1.9 for the sham group.
Chou DE, Yugrakh MS, Winegarner D, Rowe V, Kuruvilla D, Schoenen. Acute migraine therapy with external trigeminal neurostimulation (ACME): A randomized controlled trial. [Published online ahead of print November 17, 2018]. Cephalalgia. doi:10.1177%2F0333102418811573.
Alcoholic Beverages Recognized as Migraine Trigger
Alcoholic beverages, especially red wine, are recognized as a migraine trigger factor by patients with migraine and have a substantial effect on alcohol consumption behavior, according to a recent study. Researchers conducted a cross‐sectional, web‐based, questionnaire study among 2197 patients with migraine from the well‐defined Leiden University MIgraine Neuro‐Analysis (LUMINA) study population. They assessed alcoholic beverage consumption and self‐reported trigger potential, reasons behind alcohol abstinence, and time between alcohol consumption and migraine attack onset. They found:
- Alcoholic beverages were reported as a trigger by 35.6% of participants with migraine.
- In addition, more than 25% of patients with migraine who had stopped consuming or never consumed alcoholic beverages did so because of presumed trigger effects.
- Wine, especially red wine (77.8% of participants), was recognized as the most common trigger among the alcoholic beverages.
- However, red wine consistently led to an attack in only 8.8% of participants.
- Time of onset was rapid (<3 hours) in one‐third of patients and almost 90% had an onset of less than 10 hours independent of beverage type.
Onderwater GLC, van Oosterhaut WPJ, Schoonman GG, Ferrari MD, Terwindt GM. Alcoholic beverages as trigger factor and the effect on alcohol consumption behavior in patients with migraine. [Published online ahead of print December 18, 2018]. Eur J Neurol. doi:10.1111/ene.13861.
Alcoholic beverages, especially red wine, are recognized as a migraine trigger factor by patients with migraine and have a substantial effect on alcohol consumption behavior, according to a recent study. Researchers conducted a cross‐sectional, web‐based, questionnaire study among 2197 patients with migraine from the well‐defined Leiden University MIgraine Neuro‐Analysis (LUMINA) study population. They assessed alcoholic beverage consumption and self‐reported trigger potential, reasons behind alcohol abstinence, and time between alcohol consumption and migraine attack onset. They found:
- Alcoholic beverages were reported as a trigger by 35.6% of participants with migraine.
- In addition, more than 25% of patients with migraine who had stopped consuming or never consumed alcoholic beverages did so because of presumed trigger effects.
- Wine, especially red wine (77.8% of participants), was recognized as the most common trigger among the alcoholic beverages.
- However, red wine consistently led to an attack in only 8.8% of participants.
- Time of onset was rapid (<3 hours) in one‐third of patients and almost 90% had an onset of less than 10 hours independent of beverage type.
Onderwater GLC, van Oosterhaut WPJ, Schoonman GG, Ferrari MD, Terwindt GM. Alcoholic beverages as trigger factor and the effect on alcohol consumption behavior in patients with migraine. [Published online ahead of print December 18, 2018]. Eur J Neurol. doi:10.1111/ene.13861.
Alcoholic beverages, especially red wine, are recognized as a migraine trigger factor by patients with migraine and have a substantial effect on alcohol consumption behavior, according to a recent study. Researchers conducted a cross‐sectional, web‐based, questionnaire study among 2197 patients with migraine from the well‐defined Leiden University MIgraine Neuro‐Analysis (LUMINA) study population. They assessed alcoholic beverage consumption and self‐reported trigger potential, reasons behind alcohol abstinence, and time between alcohol consumption and migraine attack onset. They found:
- Alcoholic beverages were reported as a trigger by 35.6% of participants with migraine.
- In addition, more than 25% of patients with migraine who had stopped consuming or never consumed alcoholic beverages did so because of presumed trigger effects.
- Wine, especially red wine (77.8% of participants), was recognized as the most common trigger among the alcoholic beverages.
- However, red wine consistently led to an attack in only 8.8% of participants.
- Time of onset was rapid (<3 hours) in one‐third of patients and almost 90% had an onset of less than 10 hours independent of beverage type.
Onderwater GLC, van Oosterhaut WPJ, Schoonman GG, Ferrari MD, Terwindt GM. Alcoholic beverages as trigger factor and the effect on alcohol consumption behavior in patients with migraine. [Published online ahead of print December 18, 2018]. Eur J Neurol. doi:10.1111/ene.13861.
Inhibitory Pain Modulation in Adolescents Assessed
Adolescents with migraine and healthy adolescents have similar inhibitory pain modulation capability despite having marked differences in pain sensitivity, according to a recent study. Although participants with a family history of migraine (Fam-His) were asymptomatic, they demonstrated alterations in pain processing, which may serve as markers for prediction of migraine development. In order to determine if inhibitory pain modulation occurs in youth as it does in adults, researchers performed a quantitative sensory testing investigation in adolescents with migraine (n=19). These patients were compared to healthy adolescents with (n=20) or without (n=29) Fam-His of migraine (eg, first degree relative with migraine). They found:
- In response to graded heat stimuli, Fam-His participants reported higher pain intensity ratings compared to migraine patients, who in turn, reported higher pain intensity ratings than the healthy controls.
- For heat- and pressure- conditioned pain modulation (CPM), there was no significant group difference in the magnitude of CPM responses.
Nahman-Averbuch H, Leon E, Hunter BM, et al. Increased pain sensitivity but normal pain modulation in adolescents with migraine. [Published online ahead of print January 7, 2019]. Pain. doi:10.1097/j.pain.0000000000001477.
Adolescents with migraine and healthy adolescents have similar inhibitory pain modulation capability despite having marked differences in pain sensitivity, according to a recent study. Although participants with a family history of migraine (Fam-His) were asymptomatic, they demonstrated alterations in pain processing, which may serve as markers for prediction of migraine development. In order to determine if inhibitory pain modulation occurs in youth as it does in adults, researchers performed a quantitative sensory testing investigation in adolescents with migraine (n=19). These patients were compared to healthy adolescents with (n=20) or without (n=29) Fam-His of migraine (eg, first degree relative with migraine). They found:
- In response to graded heat stimuli, Fam-His participants reported higher pain intensity ratings compared to migraine patients, who in turn, reported higher pain intensity ratings than the healthy controls.
- For heat- and pressure- conditioned pain modulation (CPM), there was no significant group difference in the magnitude of CPM responses.
Nahman-Averbuch H, Leon E, Hunter BM, et al. Increased pain sensitivity but normal pain modulation in adolescents with migraine. [Published online ahead of print January 7, 2019]. Pain. doi:10.1097/j.pain.0000000000001477.
Adolescents with migraine and healthy adolescents have similar inhibitory pain modulation capability despite having marked differences in pain sensitivity, according to a recent study. Although participants with a family history of migraine (Fam-His) were asymptomatic, they demonstrated alterations in pain processing, which may serve as markers for prediction of migraine development. In order to determine if inhibitory pain modulation occurs in youth as it does in adults, researchers performed a quantitative sensory testing investigation in adolescents with migraine (n=19). These patients were compared to healthy adolescents with (n=20) or without (n=29) Fam-His of migraine (eg, first degree relative with migraine). They found:
- In response to graded heat stimuli, Fam-His participants reported higher pain intensity ratings compared to migraine patients, who in turn, reported higher pain intensity ratings than the healthy controls.
- For heat- and pressure- conditioned pain modulation (CPM), there was no significant group difference in the magnitude of CPM responses.
Nahman-Averbuch H, Leon E, Hunter BM, et al. Increased pain sensitivity but normal pain modulation in adolescents with migraine. [Published online ahead of print January 7, 2019]. Pain. doi:10.1097/j.pain.0000000000001477.
AAP infantile hemangioma guideline should empower primary care clinicians
given the dramatic increase in information available over the past decade. 
The aim in providing an evidence-based approach to evaluating, triaging, and managing IH cases is to arm primary care providers with the confidence needed to successfully treat high-risk cases, reported Daniel P. Krowchuk, MD, of the department of pediatrics and dermatology, Wake Forest University, Winston-Salem, N.C., and his associates who are members of the AAP subcommittee on the management of IHs.
With an occurrence rate of 4%-5%, IHs are the most common benign tumor presenting in childhood, especially occurring in girls, twins, preterm or low-birth-weight infants, and white neonates.
The AAP’s guideline “provides a framework for clinical decision-making” – it should not be considered a sole source of guidance. It also should not be used to replace clinical judgment or as a protocol for managing all patients with IHs, explained Dr. Krowchuk and his associates.
Clinicians, especially, are encouraged to consult promptly with a hemangioma specialist if they are not experienced in managing IHs.
According to one study cited by the authors, the mean age of examination by a dermatologist is 5 months, when most growth has already been completed. Lesions are first noticed, on average, at 2 weeks; 4 weeks has been recommended as the ideal time for professional consultation. It is important for clinicians to recognize the difficulty families are likely to face in obtaining an appointment, which makes caregiver and clinician advocacy on behalf of infants affected critical, urged Dr. Krowchuk and his colleagues. In cases or locations where hemangioma specialists are in short supply, telemedicine triage or photographic consultation is especially helpful.
Dr. Krowchuk and his associates noted several possible challenges in implementing this clinical practice guideline (CPG) published in Pediatrics. The growth of individual IHs is difficult to predict, especially in young infants, and there are no markers or imaging studies to correct this challenge. For this reason, they advised: “Prompt evaluation, either in-person or via photographs, is warranted for any infant reported by parents to have a changing birthmark during the first 2 months of life.”
Wide heterogeneity in terms of size, location, patterns, of distribution, and depth, when coupled with unpredictable growth, makes management of IHs unpredictable. Thus, there can be no one-size-fits-all treatment approach.
Further complicating implementation of the CPG is the long-held myth that IHs are benign and resolve spontaneously. While this may accurately describe the vast majority of outcomes, “ample evidence” demonstrates what can happen when family and/or caregivers yield to such “false reassurance.” According to Dr. Krowchuk and his associates, hemangioma specialists have seen their share of “examples of lost opportunities to intervene and prevent poor outcomes because of lack of or delayed referral.”
The paucity of data on high-risk cases in primary care and referral care settings should be the subject of future research, the authors noted. Scorings systems, such as the Hemangioma Severity Score, are growing in popularity as a triage tool, but more research is needed to demonstrate that primary care physicians are accurately interpreting findings and that high-risk cases are accurately identified to avoid over-referral to specialists.
Dr. Krowchuk and his colleagues did call attention to important evidence gaps that may be answered by research currently underway, or that may require further research in the future by asking the following questions: How safe is treatment with topical timolol in early infancy, and what proportion of patients can be observed without referral? For healthy infants 5 weeks or older, to what extent, if any, is cardiovascular monitoring for propranolol necessary? How should pediatricians be involved in beta-blocker management of infants and when should specialty reevaluation be made? What is the accuracy of primary care identification of high-risk IH cases using many of the parameters offered within this CPG? Are pediatric trainees being sufficiently trained in stratifying and managing IH risk?
One noteworthy barrier to improved management and outcomes noted by the authors is the “imprecision of current diagnostic codes.” At present, the existing coding in the International Classification of Diseases, 10th Revision does not include specific reference to IH but rather describes “hemangioma of the skin and subcutaneous tissues” and can include congenital as well as verrucous hemangioma. The codes also do not address the details characteristic of IHs or the higher risk aspects of IH, such as location or multifocality. Advocacy, in this instance, would be appropriate, advised Dr. Krowchuk and his associates.
In an interview, Dr. Krowchuk provided additional insight into what sets the AAP’s CPG apart from consensus statements published previously by European and Australasian expert groups. Although these might appear to be similar documents with analogous content at first glance, there are important differences, he said.
The consensus statements were based on expert opinion, while “the academy’s CPG was founded on an extensive review of the medical literature (1982-2017) regarding the potential benefits and harms of diagnostic modalities and pharmacologic and surgical treatments,” Dr. Krowchuk explained. The information that came out of this extensive review is what members of the subcommittee used to develop key action statements that pediatricians can use to evaluate and manage infants with IHs.
“The scope of the consensus statements was more limited, focusing primarily on the treatment of IH with propranolol. While the benefits of propranolol, its use and dosing, and potential adverse effects were addressed in depth in the academy’s CPG, the document went well beyond this,” he clarified.
The AAP also previously published a clinical report that provides a comprehensive evaluation of the pathogenesis, clinical features, and treatment of IH (Pediatrics. 2015 Oct. doi: 10.1542/peds.2015-2485).
There was no external funding for the CPG, and the authors said there were no potential conflicts of interest. Ilona J. Frieden, MD, is a member of the data monitoring safety board for Pfizer and the scientific advisory board for Venthera/Bridge Bio; Anthony J. Mancini, MD, said he has advisory board relationships with Verrica, Valeant, and Pfizer.
SOURCE: Krowchuk, DP et al. Pediatrics 2019;143(1):e20183475.
given the dramatic increase in information available over the past decade. 
The aim in providing an evidence-based approach to evaluating, triaging, and managing IH cases is to arm primary care providers with the confidence needed to successfully treat high-risk cases, reported Daniel P. Krowchuk, MD, of the department of pediatrics and dermatology, Wake Forest University, Winston-Salem, N.C., and his associates who are members of the AAP subcommittee on the management of IHs.
With an occurrence rate of 4%-5%, IHs are the most common benign tumor presenting in childhood, especially occurring in girls, twins, preterm or low-birth-weight infants, and white neonates.
The AAP’s guideline “provides a framework for clinical decision-making” – it should not be considered a sole source of guidance. It also should not be used to replace clinical judgment or as a protocol for managing all patients with IHs, explained Dr. Krowchuk and his associates.
Clinicians, especially, are encouraged to consult promptly with a hemangioma specialist if they are not experienced in managing IHs.
According to one study cited by the authors, the mean age of examination by a dermatologist is 5 months, when most growth has already been completed. Lesions are first noticed, on average, at 2 weeks; 4 weeks has been recommended as the ideal time for professional consultation. It is important for clinicians to recognize the difficulty families are likely to face in obtaining an appointment, which makes caregiver and clinician advocacy on behalf of infants affected critical, urged Dr. Krowchuk and his colleagues. In cases or locations where hemangioma specialists are in short supply, telemedicine triage or photographic consultation is especially helpful.
Dr. Krowchuk and his associates noted several possible challenges in implementing this clinical practice guideline (CPG) published in Pediatrics. The growth of individual IHs is difficult to predict, especially in young infants, and there are no markers or imaging studies to correct this challenge. For this reason, they advised: “Prompt evaluation, either in-person or via photographs, is warranted for any infant reported by parents to have a changing birthmark during the first 2 months of life.”
Wide heterogeneity in terms of size, location, patterns, of distribution, and depth, when coupled with unpredictable growth, makes management of IHs unpredictable. Thus, there can be no one-size-fits-all treatment approach.
Further complicating implementation of the CPG is the long-held myth that IHs are benign and resolve spontaneously. While this may accurately describe the vast majority of outcomes, “ample evidence” demonstrates what can happen when family and/or caregivers yield to such “false reassurance.” According to Dr. Krowchuk and his associates, hemangioma specialists have seen their share of “examples of lost opportunities to intervene and prevent poor outcomes because of lack of or delayed referral.”
The paucity of data on high-risk cases in primary care and referral care settings should be the subject of future research, the authors noted. Scorings systems, such as the Hemangioma Severity Score, are growing in popularity as a triage tool, but more research is needed to demonstrate that primary care physicians are accurately interpreting findings and that high-risk cases are accurately identified to avoid over-referral to specialists.
Dr. Krowchuk and his colleagues did call attention to important evidence gaps that may be answered by research currently underway, or that may require further research in the future by asking the following questions: How safe is treatment with topical timolol in early infancy, and what proportion of patients can be observed without referral? For healthy infants 5 weeks or older, to what extent, if any, is cardiovascular monitoring for propranolol necessary? How should pediatricians be involved in beta-blocker management of infants and when should specialty reevaluation be made? What is the accuracy of primary care identification of high-risk IH cases using many of the parameters offered within this CPG? Are pediatric trainees being sufficiently trained in stratifying and managing IH risk?
One noteworthy barrier to improved management and outcomes noted by the authors is the “imprecision of current diagnostic codes.” At present, the existing coding in the International Classification of Diseases, 10th Revision does not include specific reference to IH but rather describes “hemangioma of the skin and subcutaneous tissues” and can include congenital as well as verrucous hemangioma. The codes also do not address the details characteristic of IHs or the higher risk aspects of IH, such as location or multifocality. Advocacy, in this instance, would be appropriate, advised Dr. Krowchuk and his associates.
In an interview, Dr. Krowchuk provided additional insight into what sets the AAP’s CPG apart from consensus statements published previously by European and Australasian expert groups. Although these might appear to be similar documents with analogous content at first glance, there are important differences, he said.
The consensus statements were based on expert opinion, while “the academy’s CPG was founded on an extensive review of the medical literature (1982-2017) regarding the potential benefits and harms of diagnostic modalities and pharmacologic and surgical treatments,” Dr. Krowchuk explained. The information that came out of this extensive review is what members of the subcommittee used to develop key action statements that pediatricians can use to evaluate and manage infants with IHs.
“The scope of the consensus statements was more limited, focusing primarily on the treatment of IH with propranolol. While the benefits of propranolol, its use and dosing, and potential adverse effects were addressed in depth in the academy’s CPG, the document went well beyond this,” he clarified.
The AAP also previously published a clinical report that provides a comprehensive evaluation of the pathogenesis, clinical features, and treatment of IH (Pediatrics. 2015 Oct. doi: 10.1542/peds.2015-2485).
There was no external funding for the CPG, and the authors said there were no potential conflicts of interest. Ilona J. Frieden, MD, is a member of the data monitoring safety board for Pfizer and the scientific advisory board for Venthera/Bridge Bio; Anthony J. Mancini, MD, said he has advisory board relationships with Verrica, Valeant, and Pfizer.
SOURCE: Krowchuk, DP et al. Pediatrics 2019;143(1):e20183475.
given the dramatic increase in information available over the past decade. 
The aim in providing an evidence-based approach to evaluating, triaging, and managing IH cases is to arm primary care providers with the confidence needed to successfully treat high-risk cases, reported Daniel P. Krowchuk, MD, of the department of pediatrics and dermatology, Wake Forest University, Winston-Salem, N.C., and his associates who are members of the AAP subcommittee on the management of IHs.
With an occurrence rate of 4%-5%, IHs are the most common benign tumor presenting in childhood, especially occurring in girls, twins, preterm or low-birth-weight infants, and white neonates.
The AAP’s guideline “provides a framework for clinical decision-making” – it should not be considered a sole source of guidance. It also should not be used to replace clinical judgment or as a protocol for managing all patients with IHs, explained Dr. Krowchuk and his associates.
Clinicians, especially, are encouraged to consult promptly with a hemangioma specialist if they are not experienced in managing IHs.
According to one study cited by the authors, the mean age of examination by a dermatologist is 5 months, when most growth has already been completed. Lesions are first noticed, on average, at 2 weeks; 4 weeks has been recommended as the ideal time for professional consultation. It is important for clinicians to recognize the difficulty families are likely to face in obtaining an appointment, which makes caregiver and clinician advocacy on behalf of infants affected critical, urged Dr. Krowchuk and his colleagues. In cases or locations where hemangioma specialists are in short supply, telemedicine triage or photographic consultation is especially helpful.
Dr. Krowchuk and his associates noted several possible challenges in implementing this clinical practice guideline (CPG) published in Pediatrics. The growth of individual IHs is difficult to predict, especially in young infants, and there are no markers or imaging studies to correct this challenge. For this reason, they advised: “Prompt evaluation, either in-person or via photographs, is warranted for any infant reported by parents to have a changing birthmark during the first 2 months of life.”
Wide heterogeneity in terms of size, location, patterns, of distribution, and depth, when coupled with unpredictable growth, makes management of IHs unpredictable. Thus, there can be no one-size-fits-all treatment approach.
Further complicating implementation of the CPG is the long-held myth that IHs are benign and resolve spontaneously. While this may accurately describe the vast majority of outcomes, “ample evidence” demonstrates what can happen when family and/or caregivers yield to such “false reassurance.” According to Dr. Krowchuk and his associates, hemangioma specialists have seen their share of “examples of lost opportunities to intervene and prevent poor outcomes because of lack of or delayed referral.”
The paucity of data on high-risk cases in primary care and referral care settings should be the subject of future research, the authors noted. Scorings systems, such as the Hemangioma Severity Score, are growing in popularity as a triage tool, but more research is needed to demonstrate that primary care physicians are accurately interpreting findings and that high-risk cases are accurately identified to avoid over-referral to specialists.
Dr. Krowchuk and his colleagues did call attention to important evidence gaps that may be answered by research currently underway, or that may require further research in the future by asking the following questions: How safe is treatment with topical timolol in early infancy, and what proportion of patients can be observed without referral? For healthy infants 5 weeks or older, to what extent, if any, is cardiovascular monitoring for propranolol necessary? How should pediatricians be involved in beta-blocker management of infants and when should specialty reevaluation be made? What is the accuracy of primary care identification of high-risk IH cases using many of the parameters offered within this CPG? Are pediatric trainees being sufficiently trained in stratifying and managing IH risk?
One noteworthy barrier to improved management and outcomes noted by the authors is the “imprecision of current diagnostic codes.” At present, the existing coding in the International Classification of Diseases, 10th Revision does not include specific reference to IH but rather describes “hemangioma of the skin and subcutaneous tissues” and can include congenital as well as verrucous hemangioma. The codes also do not address the details characteristic of IHs or the higher risk aspects of IH, such as location or multifocality. Advocacy, in this instance, would be appropriate, advised Dr. Krowchuk and his associates.
In an interview, Dr. Krowchuk provided additional insight into what sets the AAP’s CPG apart from consensus statements published previously by European and Australasian expert groups. Although these might appear to be similar documents with analogous content at first glance, there are important differences, he said.
The consensus statements were based on expert opinion, while “the academy’s CPG was founded on an extensive review of the medical literature (1982-2017) regarding the potential benefits and harms of diagnostic modalities and pharmacologic and surgical treatments,” Dr. Krowchuk explained. The information that came out of this extensive review is what members of the subcommittee used to develop key action statements that pediatricians can use to evaluate and manage infants with IHs.
“The scope of the consensus statements was more limited, focusing primarily on the treatment of IH with propranolol. While the benefits of propranolol, its use and dosing, and potential adverse effects were addressed in depth in the academy’s CPG, the document went well beyond this,” he clarified.
The AAP also previously published a clinical report that provides a comprehensive evaluation of the pathogenesis, clinical features, and treatment of IH (Pediatrics. 2015 Oct. doi: 10.1542/peds.2015-2485).
There was no external funding for the CPG, and the authors said there were no potential conflicts of interest. Ilona J. Frieden, MD, is a member of the data monitoring safety board for Pfizer and the scientific advisory board for Venthera/Bridge Bio; Anthony J. Mancini, MD, said he has advisory board relationships with Verrica, Valeant, and Pfizer.
SOURCE: Krowchuk, DP et al. Pediatrics 2019;143(1):e20183475.
FROM PEDIATRICS