User login
Registry data favor CHOEP regimen for PTCL
LA JOLLA, CALIF. – Data from the Czech National Lymphoma Registry (NiHiL) suggest the CHOEP regimen (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisone) prolongs survival in newly diagnosed patients with peripheral T-cell lymphoma (PTCL), but consolidation with autologous stem cell transplant (ASCT) does not.
“We failed to show that there is a real benefit for the patient to undergo autologous stem cell consolidation, so, nowadays, in the majority of the centers in our group, CHOEP is the chemotherapy of choice, and the patients are not consolidated,” said Marek Trneny, MD, of Charles University General Hospital in Prague.
Dr. Trneny presented results from NiHiL on behalf of the Czech Lymphoma Study Group at the annual T-cell Lymphoma Forum.
The NiHiL project is a prospective, observational study (NCT03199066) of patients newly diagnosed with non-Hodgkin lymphoma in the Czech Republic.
Dr. Trneny presented data on 838 PTCL patients who were diagnosed between 1999 and 2018, 462 of whom were included in a survival analysis (1999-2016).
The 462 patients had a median age of 61 years and more than half were men.
Patients had PTCL not otherwise specified (NOS, 43.9%), Anaplastic lymphoma kinase (ALK)–negative Anaplastic large-cell lymphoma (ALCL, 20.8%), ALK-positive ALCL (7.6%), unclassified ALCL (0.9%), angioimmunoblastic T-cell lymphoma (AITL, 10.6%), and other subtypes (16.2%).
Most patients (79.1%) had tumors measuring less than 7.5 cm, about half of patients (52.3%) had B symptoms, most (70.5%) had a performance status of 0-1, and most (68.5%) had stage III-IV disease. Half of patients were low or low/intermediate risk according to the International Prognostic Index.
For the entire cohort, the median progression-free survival (PFS) was 1.15 years, and the 5-year PFS rate was 34.2%. The median overall survival (OS) was 2.83 years, and the 5-year OS rate was 43.3%.
There was no significant difference in PFS or OS for patients diagnosed from 1999 to 2007 and those diagnosed from 2008 to 2016. The median PFS was 1.05 years and 1.23 years, respectively (P= .4487), and the median OS was 2.15 years and 3.39 years, respectively (P = .176).
Patients with ALK-positive ALCL had superior PFS and OS when compared to patients with the other disease subtypes (P = .0002 for PFS and P = .0009 for OS).
Treatment comparison
When Dr. Trneny and his colleagues compared the 223 patients who received CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) and the 65 patients who received CHOEP, the researchers found that patients who received CHOEP had superior PFS and OS.
In the CHOP group, the median PFS was 1.18 years and the 5-year PFS rate was 34.2%. In the CHOEP group, the median PFS was 3.67 years and the 5-year PFS rate was 49.0% (hazard ratio, 0.6781; P = .0373).
In the CHOP group, the median OS was 3.74 years and the 5-year OS was 45.5%. In the CHOEP group, the median OS was 7.46 years and the 5-year OS was 56.4% (HR, 0.6475; P = .0381).
Dr. Trneny noted that patients who received CHOP were significantly younger (P less than .0001), more likely to have AITL or ALK-positive ALCL (P = .0152), and more likely to have a performance status of 2-4 (P = .0385).
Dr. Trneny and his colleagues also compared survival in 56 ASCT recipients and 189 patients who received chemotherapy alone (either CHOP or CHOEP).
Patients who underwent ASCT were significantly younger (P less than .0001) and more likely to have stage III or IV disease (P = .0345).
However, the researchers found no significant survival differences between patients who underwent ASCT and those who did not.
ASCT recipients had a median PFS of 7.50 years and a 5-year PFS rate of 56.0%, while patients who received chemotherapy alone had a median PFS of 4.69 years and a 5-year PFS rate of 47.3% (P = .6537).
In ASCT recipients, the median OS was not reached, and the 5-year OS rate was 63.3%. Among patients who received chemotherapy alone, the median OS was 6.78 years, and the 5-year OS was 63.0% (P = .6201).
“For those patients who are eligible for a CHOP-like regimen, CHOEP gives a higher chance for longer progression-free survival and overall survival, at least in our ... analysis,” Dr. Trneny said. “Autologous stem cell transplant, on the other hand, doesn’t seem to prolong PFS or overall survival.”
This research is sponsored by the Czech Lymphoma Study Group. Dr. Trneny did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – Data from the Czech National Lymphoma Registry (NiHiL) suggest the CHOEP regimen (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisone) prolongs survival in newly diagnosed patients with peripheral T-cell lymphoma (PTCL), but consolidation with autologous stem cell transplant (ASCT) does not.
“We failed to show that there is a real benefit for the patient to undergo autologous stem cell consolidation, so, nowadays, in the majority of the centers in our group, CHOEP is the chemotherapy of choice, and the patients are not consolidated,” said Marek Trneny, MD, of Charles University General Hospital in Prague.
Dr. Trneny presented results from NiHiL on behalf of the Czech Lymphoma Study Group at the annual T-cell Lymphoma Forum.
The NiHiL project is a prospective, observational study (NCT03199066) of patients newly diagnosed with non-Hodgkin lymphoma in the Czech Republic.
Dr. Trneny presented data on 838 PTCL patients who were diagnosed between 1999 and 2018, 462 of whom were included in a survival analysis (1999-2016).
The 462 patients had a median age of 61 years and more than half were men.
Patients had PTCL not otherwise specified (NOS, 43.9%), Anaplastic lymphoma kinase (ALK)–negative Anaplastic large-cell lymphoma (ALCL, 20.8%), ALK-positive ALCL (7.6%), unclassified ALCL (0.9%), angioimmunoblastic T-cell lymphoma (AITL, 10.6%), and other subtypes (16.2%).
Most patients (79.1%) had tumors measuring less than 7.5 cm, about half of patients (52.3%) had B symptoms, most (70.5%) had a performance status of 0-1, and most (68.5%) had stage III-IV disease. Half of patients were low or low/intermediate risk according to the International Prognostic Index.
For the entire cohort, the median progression-free survival (PFS) was 1.15 years, and the 5-year PFS rate was 34.2%. The median overall survival (OS) was 2.83 years, and the 5-year OS rate was 43.3%.
There was no significant difference in PFS or OS for patients diagnosed from 1999 to 2007 and those diagnosed from 2008 to 2016. The median PFS was 1.05 years and 1.23 years, respectively (P= .4487), and the median OS was 2.15 years and 3.39 years, respectively (P = .176).
Patients with ALK-positive ALCL had superior PFS and OS when compared to patients with the other disease subtypes (P = .0002 for PFS and P = .0009 for OS).
Treatment comparison
When Dr. Trneny and his colleagues compared the 223 patients who received CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) and the 65 patients who received CHOEP, the researchers found that patients who received CHOEP had superior PFS and OS.
In the CHOP group, the median PFS was 1.18 years and the 5-year PFS rate was 34.2%. In the CHOEP group, the median PFS was 3.67 years and the 5-year PFS rate was 49.0% (hazard ratio, 0.6781; P = .0373).
In the CHOP group, the median OS was 3.74 years and the 5-year OS was 45.5%. In the CHOEP group, the median OS was 7.46 years and the 5-year OS was 56.4% (HR, 0.6475; P = .0381).
Dr. Trneny noted that patients who received CHOP were significantly younger (P less than .0001), more likely to have AITL or ALK-positive ALCL (P = .0152), and more likely to have a performance status of 2-4 (P = .0385).
Dr. Trneny and his colleagues also compared survival in 56 ASCT recipients and 189 patients who received chemotherapy alone (either CHOP or CHOEP).
Patients who underwent ASCT were significantly younger (P less than .0001) and more likely to have stage III or IV disease (P = .0345).
However, the researchers found no significant survival differences between patients who underwent ASCT and those who did not.
ASCT recipients had a median PFS of 7.50 years and a 5-year PFS rate of 56.0%, while patients who received chemotherapy alone had a median PFS of 4.69 years and a 5-year PFS rate of 47.3% (P = .6537).
In ASCT recipients, the median OS was not reached, and the 5-year OS rate was 63.3%. Among patients who received chemotherapy alone, the median OS was 6.78 years, and the 5-year OS was 63.0% (P = .6201).
“For those patients who are eligible for a CHOP-like regimen, CHOEP gives a higher chance for longer progression-free survival and overall survival, at least in our ... analysis,” Dr. Trneny said. “Autologous stem cell transplant, on the other hand, doesn’t seem to prolong PFS or overall survival.”
This research is sponsored by the Czech Lymphoma Study Group. Dr. Trneny did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
LA JOLLA, CALIF. – Data from the Czech National Lymphoma Registry (NiHiL) suggest the CHOEP regimen (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisone) prolongs survival in newly diagnosed patients with peripheral T-cell lymphoma (PTCL), but consolidation with autologous stem cell transplant (ASCT) does not.
“We failed to show that there is a real benefit for the patient to undergo autologous stem cell consolidation, so, nowadays, in the majority of the centers in our group, CHOEP is the chemotherapy of choice, and the patients are not consolidated,” said Marek Trneny, MD, of Charles University General Hospital in Prague.
Dr. Trneny presented results from NiHiL on behalf of the Czech Lymphoma Study Group at the annual T-cell Lymphoma Forum.
The NiHiL project is a prospective, observational study (NCT03199066) of patients newly diagnosed with non-Hodgkin lymphoma in the Czech Republic.
Dr. Trneny presented data on 838 PTCL patients who were diagnosed between 1999 and 2018, 462 of whom were included in a survival analysis (1999-2016).
The 462 patients had a median age of 61 years and more than half were men.
Patients had PTCL not otherwise specified (NOS, 43.9%), Anaplastic lymphoma kinase (ALK)–negative Anaplastic large-cell lymphoma (ALCL, 20.8%), ALK-positive ALCL (7.6%), unclassified ALCL (0.9%), angioimmunoblastic T-cell lymphoma (AITL, 10.6%), and other subtypes (16.2%).
Most patients (79.1%) had tumors measuring less than 7.5 cm, about half of patients (52.3%) had B symptoms, most (70.5%) had a performance status of 0-1, and most (68.5%) had stage III-IV disease. Half of patients were low or low/intermediate risk according to the International Prognostic Index.
For the entire cohort, the median progression-free survival (PFS) was 1.15 years, and the 5-year PFS rate was 34.2%. The median overall survival (OS) was 2.83 years, and the 5-year OS rate was 43.3%.
There was no significant difference in PFS or OS for patients diagnosed from 1999 to 2007 and those diagnosed from 2008 to 2016. The median PFS was 1.05 years and 1.23 years, respectively (P= .4487), and the median OS was 2.15 years and 3.39 years, respectively (P = .176).
Patients with ALK-positive ALCL had superior PFS and OS when compared to patients with the other disease subtypes (P = .0002 for PFS and P = .0009 for OS).
Treatment comparison
When Dr. Trneny and his colleagues compared the 223 patients who received CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) and the 65 patients who received CHOEP, the researchers found that patients who received CHOEP had superior PFS and OS.
In the CHOP group, the median PFS was 1.18 years and the 5-year PFS rate was 34.2%. In the CHOEP group, the median PFS was 3.67 years and the 5-year PFS rate was 49.0% (hazard ratio, 0.6781; P = .0373).
In the CHOP group, the median OS was 3.74 years and the 5-year OS was 45.5%. In the CHOEP group, the median OS was 7.46 years and the 5-year OS was 56.4% (HR, 0.6475; P = .0381).
Dr. Trneny noted that patients who received CHOP were significantly younger (P less than .0001), more likely to have AITL or ALK-positive ALCL (P = .0152), and more likely to have a performance status of 2-4 (P = .0385).
Dr. Trneny and his colleagues also compared survival in 56 ASCT recipients and 189 patients who received chemotherapy alone (either CHOP or CHOEP).
Patients who underwent ASCT were significantly younger (P less than .0001) and more likely to have stage III or IV disease (P = .0345).
However, the researchers found no significant survival differences between patients who underwent ASCT and those who did not.
ASCT recipients had a median PFS of 7.50 years and a 5-year PFS rate of 56.0%, while patients who received chemotherapy alone had a median PFS of 4.69 years and a 5-year PFS rate of 47.3% (P = .6537).
In ASCT recipients, the median OS was not reached, and the 5-year OS rate was 63.3%. Among patients who received chemotherapy alone, the median OS was 6.78 years, and the 5-year OS was 63.0% (P = .6201).
“For those patients who are eligible for a CHOP-like regimen, CHOEP gives a higher chance for longer progression-free survival and overall survival, at least in our ... analysis,” Dr. Trneny said. “Autologous stem cell transplant, on the other hand, doesn’t seem to prolong PFS or overall survival.”
This research is sponsored by the Czech Lymphoma Study Group. Dr. Trneny did not disclose any conflicts of interest.
The T-cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
REPORTING FROM TCLF 2019
Key clinical point:
Major finding: The 5-year progression free survival rate was 49.0% in the group receiving CHOEP, compared with 34.2% in the group receiving CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone).
Study details: A survival analysis of 462 patients with PTCL who were part of the Czech National Lymphoma Registry.
Disclosures: This research is sponsored by the Czech Lymphoma Study Group. Dr. Trneny did not disclose any conflicts of interest.
Impact of carbs vs. fats on CVD risk becoming better understood
LOS ANGELES – When it comes to understanding the impact of diet on cardiovascular disease, mounting evidence suggests that a high carbohydrate diet is associated with a higher risk of mortality, while consumption of fats, including saturated and unsaturated fats, is associated with a lower risk of mortality.
Ronald M. Krauss, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “There are various categories of evidence that we all consider. Randomized clinical trials are the most robust, but, in this field, there are few and, of these, a number have been subject to criticism. Observational cohort studies provide much of the data on which we base our dietary recommendations. This is a problem, because dietary information can be flawed, it’s challenging to adjust for all the covariates in an observational trial, and you can’t determine causation.”
Dr. Krauss, senior scientist and director of atherosclerosis research at Children’s Hospital Oakland (Calif.) Research Institute, emphasized that current dietary recommendations are often not based on food context. Meta-analyses may be used to make dietary recommendations, “but you have to be careful,” he said. “There is quite a bit of subjectivity in the criteria used to select the studies. Finally, there is individual variability in dietary effects. You lose that when you do statistical analysis in large study populations.”
An analysis of prospective observational cohort studies over the past several years showed that there is no significant effect of saturated fat intake on all-cause mortality, cardiovascular disease (CVD), coronary heart disease (CHD), ischemic stroke, or type 2 diabetes mellitus (BMJ. 2015 Aug 12. doi: 10.1136/bmj.h3978). However, it found that trans fats are associated with all-cause mortality, total CHD, and CHD mortality. A more recent meta-analysis of randomized, controlled trials of saturated fat intake and coronary heart disease in the past 5 years yielded similar findings.
“Saturated fat intake per se is not associated with all-cause mortality, CVD, CHD, stroke, or type 2 diabetes,” said Dr. Krauss, who was an author of a recent analysis on dietary fat and cardiometabolic health (BMJ. 2018 Jun 13. doi: 10.1136/bmj.k2139). “The replacement nutrient is important, but there has been controversy as to whether replacing saturated fat with n-6 (omega-6) polyunsaturated fatty acids reduced CHD events, CHD mortality, or total mortality.”
Other research has demonstrated differences in the relationship of saturated fat from meat sources vs. that from dairy sources. An analysis of 5,209 subjects who participated in the Multi-Ethnic Study of Atherosclerosis (MESA) study over 10 years found that a higher intake of dairy saturated fat was associated with lower CVD risk (Am J Clin Nutr. 2012;96[2]:397-404). In contrast, a higher intake of saturated fat from meat was associated with greater CVD risk.
In what Dr. Krauss said is the most extensive prospective cohort study of its kind to date, researchers led by Mahshid Dehghan, PhD, collected self-reported dietary data from 135,335 people aged 35-70 years in 18 countries, and grouped them according to the amount of carbohydrate, fat, and protein they consumed (Lancet. 2017 Aug 29. doi: 10.1016/S0140-6736[17]32252-3). Outcomes for the study, known as PURE, were major CVD and total mortality.
Over a median follow-up of 7.4 years, the researchers documented 5,796 deaths and 4,784 major cardiovascular disease events. Higher carbohydrate intake was associated with an increased risk of total mortality (highest [quintile 5] vs. lowest quintile [quintile 1] category, hazard ratio 1.28; P = .0001) but not with the risk of CVD or CVD mortality. Intake of total fat and each type of fat was associated with lower risk of total mortality (quintile 5 vs. quintile 1, total fat: HR, 0.77, P less than .0001; saturated fat, HR, 0.86, P = .0088; monounsaturated fat: HR 0.81, P less than .0001; and polyunsaturated fat: HR 0.80, P less than .0001). Higher saturated fat intake was associated with lower risk of stroke (quintile 5 vs. quintile 1, HR, 0.79; P = .0498). Total fat and saturated and unsaturated fats were not significantly associated with risk of myocardial infarction or cardiovascular disease mortality.
“The fat intake becomes a protective factor, while carbohydrates are the bad guys,” said Dr. Krauss, who also holds faculty positions at the University of California, San Francisco, and the University of California, Berkeley. He acknowledged certain limitations of PURE, including the fact that the random measurement used in the assessment of diet may dilute real associations, that high carbohydrate and low-fat diets may be a proxy for poverty, and that data on vegetable oil use were not included.
Dr. Krauss went on to note that work from other studies has shown that the Apo B/Apo A-1 ratio and its association with small – but not large – LDL particles is a stronger marker than is LDL cholesterol for predicting dietary effects on CVD risk (Lancet. 2004;364[9438]:937-52 and Arterioscler Thromb Vasc Biol. 2014;34[5]:1069-77). “These risk measures can be improved by lowering dietary carbohydrates, and not by lowering saturated fats,” he said.
Dr. Krauss disclosed that he has received grants from the National Institutes of Health and Dairy Management Inc. He is a member of the scientific advisory board for Virta Health and DayTwo and holds a patent related to lipoprotein particle analysis.
LOS ANGELES – When it comes to understanding the impact of diet on cardiovascular disease, mounting evidence suggests that a high carbohydrate diet is associated with a higher risk of mortality, while consumption of fats, including saturated and unsaturated fats, is associated with a lower risk of mortality.
Ronald M. Krauss, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “There are various categories of evidence that we all consider. Randomized clinical trials are the most robust, but, in this field, there are few and, of these, a number have been subject to criticism. Observational cohort studies provide much of the data on which we base our dietary recommendations. This is a problem, because dietary information can be flawed, it’s challenging to adjust for all the covariates in an observational trial, and you can’t determine causation.”
Dr. Krauss, senior scientist and director of atherosclerosis research at Children’s Hospital Oakland (Calif.) Research Institute, emphasized that current dietary recommendations are often not based on food context. Meta-analyses may be used to make dietary recommendations, “but you have to be careful,” he said. “There is quite a bit of subjectivity in the criteria used to select the studies. Finally, there is individual variability in dietary effects. You lose that when you do statistical analysis in large study populations.”
An analysis of prospective observational cohort studies over the past several years showed that there is no significant effect of saturated fat intake on all-cause mortality, cardiovascular disease (CVD), coronary heart disease (CHD), ischemic stroke, or type 2 diabetes mellitus (BMJ. 2015 Aug 12. doi: 10.1136/bmj.h3978). However, it found that trans fats are associated with all-cause mortality, total CHD, and CHD mortality. A more recent meta-analysis of randomized, controlled trials of saturated fat intake and coronary heart disease in the past 5 years yielded similar findings.
“Saturated fat intake per se is not associated with all-cause mortality, CVD, CHD, stroke, or type 2 diabetes,” said Dr. Krauss, who was an author of a recent analysis on dietary fat and cardiometabolic health (BMJ. 2018 Jun 13. doi: 10.1136/bmj.k2139). “The replacement nutrient is important, but there has been controversy as to whether replacing saturated fat with n-6 (omega-6) polyunsaturated fatty acids reduced CHD events, CHD mortality, or total mortality.”
Other research has demonstrated differences in the relationship of saturated fat from meat sources vs. that from dairy sources. An analysis of 5,209 subjects who participated in the Multi-Ethnic Study of Atherosclerosis (MESA) study over 10 years found that a higher intake of dairy saturated fat was associated with lower CVD risk (Am J Clin Nutr. 2012;96[2]:397-404). In contrast, a higher intake of saturated fat from meat was associated with greater CVD risk.
In what Dr. Krauss said is the most extensive prospective cohort study of its kind to date, researchers led by Mahshid Dehghan, PhD, collected self-reported dietary data from 135,335 people aged 35-70 years in 18 countries, and grouped them according to the amount of carbohydrate, fat, and protein they consumed (Lancet. 2017 Aug 29. doi: 10.1016/S0140-6736[17]32252-3). Outcomes for the study, known as PURE, were major CVD and total mortality.
Over a median follow-up of 7.4 years, the researchers documented 5,796 deaths and 4,784 major cardiovascular disease events. Higher carbohydrate intake was associated with an increased risk of total mortality (highest [quintile 5] vs. lowest quintile [quintile 1] category, hazard ratio 1.28; P = .0001) but not with the risk of CVD or CVD mortality. Intake of total fat and each type of fat was associated with lower risk of total mortality (quintile 5 vs. quintile 1, total fat: HR, 0.77, P less than .0001; saturated fat, HR, 0.86, P = .0088; monounsaturated fat: HR 0.81, P less than .0001; and polyunsaturated fat: HR 0.80, P less than .0001). Higher saturated fat intake was associated with lower risk of stroke (quintile 5 vs. quintile 1, HR, 0.79; P = .0498). Total fat and saturated and unsaturated fats were not significantly associated with risk of myocardial infarction or cardiovascular disease mortality.
“The fat intake becomes a protective factor, while carbohydrates are the bad guys,” said Dr. Krauss, who also holds faculty positions at the University of California, San Francisco, and the University of California, Berkeley. He acknowledged certain limitations of PURE, including the fact that the random measurement used in the assessment of diet may dilute real associations, that high carbohydrate and low-fat diets may be a proxy for poverty, and that data on vegetable oil use were not included.
Dr. Krauss went on to note that work from other studies has shown that the Apo B/Apo A-1 ratio and its association with small – but not large – LDL particles is a stronger marker than is LDL cholesterol for predicting dietary effects on CVD risk (Lancet. 2004;364[9438]:937-52 and Arterioscler Thromb Vasc Biol. 2014;34[5]:1069-77). “These risk measures can be improved by lowering dietary carbohydrates, and not by lowering saturated fats,” he said.
Dr. Krauss disclosed that he has received grants from the National Institutes of Health and Dairy Management Inc. He is a member of the scientific advisory board for Virta Health and DayTwo and holds a patent related to lipoprotein particle analysis.
LOS ANGELES – When it comes to understanding the impact of diet on cardiovascular disease, mounting evidence suggests that a high carbohydrate diet is associated with a higher risk of mortality, while consumption of fats, including saturated and unsaturated fats, is associated with a lower risk of mortality.
Ronald M. Krauss, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “There are various categories of evidence that we all consider. Randomized clinical trials are the most robust, but, in this field, there are few and, of these, a number have been subject to criticism. Observational cohort studies provide much of the data on which we base our dietary recommendations. This is a problem, because dietary information can be flawed, it’s challenging to adjust for all the covariates in an observational trial, and you can’t determine causation.”
Dr. Krauss, senior scientist and director of atherosclerosis research at Children’s Hospital Oakland (Calif.) Research Institute, emphasized that current dietary recommendations are often not based on food context. Meta-analyses may be used to make dietary recommendations, “but you have to be careful,” he said. “There is quite a bit of subjectivity in the criteria used to select the studies. Finally, there is individual variability in dietary effects. You lose that when you do statistical analysis in large study populations.”
An analysis of prospective observational cohort studies over the past several years showed that there is no significant effect of saturated fat intake on all-cause mortality, cardiovascular disease (CVD), coronary heart disease (CHD), ischemic stroke, or type 2 diabetes mellitus (BMJ. 2015 Aug 12. doi: 10.1136/bmj.h3978). However, it found that trans fats are associated with all-cause mortality, total CHD, and CHD mortality. A more recent meta-analysis of randomized, controlled trials of saturated fat intake and coronary heart disease in the past 5 years yielded similar findings.
“Saturated fat intake per se is not associated with all-cause mortality, CVD, CHD, stroke, or type 2 diabetes,” said Dr. Krauss, who was an author of a recent analysis on dietary fat and cardiometabolic health (BMJ. 2018 Jun 13. doi: 10.1136/bmj.k2139). “The replacement nutrient is important, but there has been controversy as to whether replacing saturated fat with n-6 (omega-6) polyunsaturated fatty acids reduced CHD events, CHD mortality, or total mortality.”
Other research has demonstrated differences in the relationship of saturated fat from meat sources vs. that from dairy sources. An analysis of 5,209 subjects who participated in the Multi-Ethnic Study of Atherosclerosis (MESA) study over 10 years found that a higher intake of dairy saturated fat was associated with lower CVD risk (Am J Clin Nutr. 2012;96[2]:397-404). In contrast, a higher intake of saturated fat from meat was associated with greater CVD risk.
In what Dr. Krauss said is the most extensive prospective cohort study of its kind to date, researchers led by Mahshid Dehghan, PhD, collected self-reported dietary data from 135,335 people aged 35-70 years in 18 countries, and grouped them according to the amount of carbohydrate, fat, and protein they consumed (Lancet. 2017 Aug 29. doi: 10.1016/S0140-6736[17]32252-3). Outcomes for the study, known as PURE, were major CVD and total mortality.
Over a median follow-up of 7.4 years, the researchers documented 5,796 deaths and 4,784 major cardiovascular disease events. Higher carbohydrate intake was associated with an increased risk of total mortality (highest [quintile 5] vs. lowest quintile [quintile 1] category, hazard ratio 1.28; P = .0001) but not with the risk of CVD or CVD mortality. Intake of total fat and each type of fat was associated with lower risk of total mortality (quintile 5 vs. quintile 1, total fat: HR, 0.77, P less than .0001; saturated fat, HR, 0.86, P = .0088; monounsaturated fat: HR 0.81, P less than .0001; and polyunsaturated fat: HR 0.80, P less than .0001). Higher saturated fat intake was associated with lower risk of stroke (quintile 5 vs. quintile 1, HR, 0.79; P = .0498). Total fat and saturated and unsaturated fats were not significantly associated with risk of myocardial infarction or cardiovascular disease mortality.
“The fat intake becomes a protective factor, while carbohydrates are the bad guys,” said Dr. Krauss, who also holds faculty positions at the University of California, San Francisco, and the University of California, Berkeley. He acknowledged certain limitations of PURE, including the fact that the random measurement used in the assessment of diet may dilute real associations, that high carbohydrate and low-fat diets may be a proxy for poverty, and that data on vegetable oil use were not included.
Dr. Krauss went on to note that work from other studies has shown that the Apo B/Apo A-1 ratio and its association with small – but not large – LDL particles is a stronger marker than is LDL cholesterol for predicting dietary effects on CVD risk (Lancet. 2004;364[9438]:937-52 and Arterioscler Thromb Vasc Biol. 2014;34[5]:1069-77). “These risk measures can be improved by lowering dietary carbohydrates, and not by lowering saturated fats,” he said.
Dr. Krauss disclosed that he has received grants from the National Institutes of Health and Dairy Management Inc. He is a member of the scientific advisory board for Virta Health and DayTwo and holds a patent related to lipoprotein particle analysis.
EXPERT ANALYSIS FROM WCIRDC 2018
Brazilian study finds oral tranexamic acid effective for facial melasma
of patients from a public dermatology clinic in Brazil.
“Our study was one of the few to compare the use of oral TA isolated against a control group using a placebo and to evaluate the results by four different methods,” wrote lead author Mariana Morais Tavares Colferai, MD, of the Universidade de Mogi das Cruzes (Brazil), and her coauthors. The study was published online in the Journal of Cosmetic Dermatology.TA is a plasmin inhibitor, first described as a treatment for melasma in 1979. It is approved in the United States for treating menorrhagia.
In the randomized, double-blind, controlled trial of 47 patients with facial melasma – 37 completed the study – participants were assigned to one of two groups: Group A received 250 mg of tranexamic acid twice daily (n = 20) while group B received a placebo twice daily (n = 17). All patients were advised to use sunscreen. Before treatment and after 12 weeks, the researchers evaluated patients with four methods: the Melasma Area Severity Index (MASI), photographic records, patient evaluation with questionnaire (MELASQoL), and colorimetry assessed via a colorimeter.
Per evaluation of all tests, melasma improved in 50% of patients in group A, compared with 5.9% of patients in group B (P less than .005). Group A saw improvements in the mean MASI score (20.9 at pretreatment vs. 10.8 after treatment, P less than .001), mean MELASQoL value (55.4 vs. 38.2, P less than .001), and colorimetry (55.0 vs. 56.1, with higher values indicating lighter pigmentation, P = .033).
The most common side effects among those who received TA were gastrointestinal effects, such as nausea and diarrhea (5%); changes in menstrual flow (10%); and headache (14%). No serious side effects were reported.
The authors acknowledged several potential limitations in their study, including a lack of intermediate evaluations between pretreatment and 12 weeks. They also noted that the photographs were dichotomously classified as either “yes for improvement” or “no for the lack of improvement or worsening,” which may “limit the accuracy of our results” for that particular method.
The tranexamic acid and placebo for the study was provided by U.SK Dermatology/Brazil. No conflicts of interest were reported.
SOURCE: Colferai MMT et al. J Cosmet Dermatol. 2018 Dec 9. doi: 10.1111/jocd.12830.
of patients from a public dermatology clinic in Brazil.
“Our study was one of the few to compare the use of oral TA isolated against a control group using a placebo and to evaluate the results by four different methods,” wrote lead author Mariana Morais Tavares Colferai, MD, of the Universidade de Mogi das Cruzes (Brazil), and her coauthors. The study was published online in the Journal of Cosmetic Dermatology.TA is a plasmin inhibitor, first described as a treatment for melasma in 1979. It is approved in the United States for treating menorrhagia.
In the randomized, double-blind, controlled trial of 47 patients with facial melasma – 37 completed the study – participants were assigned to one of two groups: Group A received 250 mg of tranexamic acid twice daily (n = 20) while group B received a placebo twice daily (n = 17). All patients were advised to use sunscreen. Before treatment and after 12 weeks, the researchers evaluated patients with four methods: the Melasma Area Severity Index (MASI), photographic records, patient evaluation with questionnaire (MELASQoL), and colorimetry assessed via a colorimeter.
Per evaluation of all tests, melasma improved in 50% of patients in group A, compared with 5.9% of patients in group B (P less than .005). Group A saw improvements in the mean MASI score (20.9 at pretreatment vs. 10.8 after treatment, P less than .001), mean MELASQoL value (55.4 vs. 38.2, P less than .001), and colorimetry (55.0 vs. 56.1, with higher values indicating lighter pigmentation, P = .033).
The most common side effects among those who received TA were gastrointestinal effects, such as nausea and diarrhea (5%); changes in menstrual flow (10%); and headache (14%). No serious side effects were reported.
The authors acknowledged several potential limitations in their study, including a lack of intermediate evaluations between pretreatment and 12 weeks. They also noted that the photographs were dichotomously classified as either “yes for improvement” or “no for the lack of improvement or worsening,” which may “limit the accuracy of our results” for that particular method.
The tranexamic acid and placebo for the study was provided by U.SK Dermatology/Brazil. No conflicts of interest were reported.
SOURCE: Colferai MMT et al. J Cosmet Dermatol. 2018 Dec 9. doi: 10.1111/jocd.12830.
of patients from a public dermatology clinic in Brazil.
“Our study was one of the few to compare the use of oral TA isolated against a control group using a placebo and to evaluate the results by four different methods,” wrote lead author Mariana Morais Tavares Colferai, MD, of the Universidade de Mogi das Cruzes (Brazil), and her coauthors. The study was published online in the Journal of Cosmetic Dermatology.TA is a plasmin inhibitor, first described as a treatment for melasma in 1979. It is approved in the United States for treating menorrhagia.
In the randomized, double-blind, controlled trial of 47 patients with facial melasma – 37 completed the study – participants were assigned to one of two groups: Group A received 250 mg of tranexamic acid twice daily (n = 20) while group B received a placebo twice daily (n = 17). All patients were advised to use sunscreen. Before treatment and after 12 weeks, the researchers evaluated patients with four methods: the Melasma Area Severity Index (MASI), photographic records, patient evaluation with questionnaire (MELASQoL), and colorimetry assessed via a colorimeter.
Per evaluation of all tests, melasma improved in 50% of patients in group A, compared with 5.9% of patients in group B (P less than .005). Group A saw improvements in the mean MASI score (20.9 at pretreatment vs. 10.8 after treatment, P less than .001), mean MELASQoL value (55.4 vs. 38.2, P less than .001), and colorimetry (55.0 vs. 56.1, with higher values indicating lighter pigmentation, P = .033).
The most common side effects among those who received TA were gastrointestinal effects, such as nausea and diarrhea (5%); changes in menstrual flow (10%); and headache (14%). No serious side effects were reported.
The authors acknowledged several potential limitations in their study, including a lack of intermediate evaluations between pretreatment and 12 weeks. They also noted that the photographs were dichotomously classified as either “yes for improvement” or “no for the lack of improvement or worsening,” which may “limit the accuracy of our results” for that particular method.
The tranexamic acid and placebo for the study was provided by U.SK Dermatology/Brazil. No conflicts of interest were reported.
SOURCE: Colferai MMT et al. J Cosmet Dermatol. 2018 Dec 9. doi: 10.1111/jocd.12830.
FROM THE JOURNAL OF COSMETIC DERMATOLOGY
Key clinical point: After 12 weeks and according to four methods of evaluation, oral tranexamic acid was effective in 50% of patients with melasma.
Major finding: Melasma improved in 50% of patients who received oral tranexamic acid, compared with 5.9% of patients who received placebo (P less than .005).
Study details: A randomized, double-blind, controlled trial of 37 patients who received oral tranexamic acid or placebo twice a day for 12 weeks.
Disclosures: The tranexamic acid and placebo were provided by U.SK Dermatology/Brazil. No conflicts of interest were reported.
Source: Colferai MMT et al. J Cosmet Dermatol. 2018 Dec 9. doi: 10.1111/jocd.12830.
Anaerobically prepared donor FMT led to steroid-free remission of ulcerative colitis
For patients with mild to moderate ulcerative colitis, a three-dose, 1-week induction course of anaerobically prepared donor fecal microbiota transplantation (FMT) produced steroid-free remission in 32% of patients, compared with 9% of those who received autologous aerobically prepared FMT in a randomized, double-blind, clinical trial.
Eight weeks after FMT, the odds of steroid-free remission were fivefold higher with anaerobically prepared donor versus aerobically prepared autologous FMT (odds ratio, 5; 95% confidence interval, 1.2-20.1; P = .03), reported Samuel P. Costello, MD, of the Queen Elizabeth Hospital in Woodville, Australia, and his associates. Donor FMT also significantly increased the likelihood of clinical remission and clinical response, the researchers said. “Further research is needed to assess longer-term maintenance of remission and safety,” they wrote in JAMA.
In prior studies, high-intensity FMT with aerobically prepared donor material remitted some cases of mild to moderate ulcerative colitis. However, anaerobic processing has been found to improve microbial viability, which might allow patients to remit with less intensive FMT, the researchers wrote. In their multicenter study, 73 adults with mildly to moderately active ulcerative colitis (total Mayo score, 3-10 points, with endoscopic subscore of at least 2) received either anaerobically prepared stool pooled from three to four highly screened donors or aerobically processed autologous stool. Patients in both arms received two enemas in the 7 days after FMT – a less dose-intensive treatment protocol than in prior FMT trials of patients with ulcerative colitis.
Among 38 patients in the intervention group, 12 (32%) achieved remission, defined as total Mayo score no greater than 2 with an endoscopic score no greater than 1. Strikingly, five (42%) of these patients remained in remission at 12 months, the researchers said. Additionally, 55% of the intervention group but only 23% of the comparator group (P = .007) achieved clinical response at 8 weeks, defined as at least a 3-point decrease in total Mayo score. Rates of clinical remission (Simple Colitis Activity Index score no greater than 2) were 47% and 17%, respectively (P = .01).
The study population averaged 39 years of age, 45% were women, and 95% completed the trial. Serious adverse events included one case each of worsening colitis, Clostridium difficile colitis requiring colectomy, and pneumonia in the donor FMT group, and two cases of worsening colitis in the comparator group. However, the study “was not powered to assess safety, and and thus further larger studies are required to assess this,” the researchers said. The study also suffered from a significant loss to follow-up at 12 months, so additional studies should assess long-term remission, they added.
The National Health and Medical Research Council and the Gutsy Foundation provided funding. Dr. Costello disclosed ties to Janssen, Shire, Ferring, Microbiotica, and Pfizer.
SOURCE: Costello SP et al. JAMA. 2019;321(2):156-64. doi: 10.1001/jama.2018.20046.
This is the fourth randomized clinical trial of fecal microbiota transplantation (FMT) in ulcerative colitis, and despite their differing methodologies, all four trials reported remission rates of 24%-32%, wrote Colleen R. Kelly, MD, and Ashwin N. Ananthakrishnan, MD, in an editorial accompanying the study.
Using pooled stool from multiple donors increases bacterial diversity and the likelihood that the sample will include a donor with optimal bacterial composition in the stool, the experts said. Based on studies to date, this approach works in about one-third of patients with ulcerative colitis, which resembles the rate of efficacy of systemic immunosuppression. Thus, FMT is likely to work best in combination with therapies such as immunomodulators and biologics, which target underlying immune dysregulation, they said.
Large multicenter trials are needed to answer questions on mechanism of action, optimal patient population and delivery methods, durability, and the use of FMT monotherapy versus combination regimens in patients with mild or severe ulcerative colitis, the experts wrote. “Finally, regulatory agencies must provide a reasonable pathway for approval of microbial-based therapeutics,” they added. “[The] therapeutic manipulation of the intestinal microbiota, whether by full-spectrum FMT or a more targeted approach using synthetic cultured consortia of bacterial species, is likely to be a component of therapy for [inflammatory bowel disease] and others in the not-so-distant future.”
Dr. Kelly is with Brown University in Providence, R.I. She disclosed ties to Finch Therapeutics and Openbiome. Dr. Ananthakrishnan is with Harvard Medical School, Boston. He disclosed ties to Pfizer and Gilead (JAMA. 2019;321[2]:151-2).
This is the fourth randomized clinical trial of fecal microbiota transplantation (FMT) in ulcerative colitis, and despite their differing methodologies, all four trials reported remission rates of 24%-32%, wrote Colleen R. Kelly, MD, and Ashwin N. Ananthakrishnan, MD, in an editorial accompanying the study.
Using pooled stool from multiple donors increases bacterial diversity and the likelihood that the sample will include a donor with optimal bacterial composition in the stool, the experts said. Based on studies to date, this approach works in about one-third of patients with ulcerative colitis, which resembles the rate of efficacy of systemic immunosuppression. Thus, FMT is likely to work best in combination with therapies such as immunomodulators and biologics, which target underlying immune dysregulation, they said.
Large multicenter trials are needed to answer questions on mechanism of action, optimal patient population and delivery methods, durability, and the use of FMT monotherapy versus combination regimens in patients with mild or severe ulcerative colitis, the experts wrote. “Finally, regulatory agencies must provide a reasonable pathway for approval of microbial-based therapeutics,” they added. “[The] therapeutic manipulation of the intestinal microbiota, whether by full-spectrum FMT or a more targeted approach using synthetic cultured consortia of bacterial species, is likely to be a component of therapy for [inflammatory bowel disease] and others in the not-so-distant future.”
Dr. Kelly is with Brown University in Providence, R.I. She disclosed ties to Finch Therapeutics and Openbiome. Dr. Ananthakrishnan is with Harvard Medical School, Boston. He disclosed ties to Pfizer and Gilead (JAMA. 2019;321[2]:151-2).
This is the fourth randomized clinical trial of fecal microbiota transplantation (FMT) in ulcerative colitis, and despite their differing methodologies, all four trials reported remission rates of 24%-32%, wrote Colleen R. Kelly, MD, and Ashwin N. Ananthakrishnan, MD, in an editorial accompanying the study.
Using pooled stool from multiple donors increases bacterial diversity and the likelihood that the sample will include a donor with optimal bacterial composition in the stool, the experts said. Based on studies to date, this approach works in about one-third of patients with ulcerative colitis, which resembles the rate of efficacy of systemic immunosuppression. Thus, FMT is likely to work best in combination with therapies such as immunomodulators and biologics, which target underlying immune dysregulation, they said.
Large multicenter trials are needed to answer questions on mechanism of action, optimal patient population and delivery methods, durability, and the use of FMT monotherapy versus combination regimens in patients with mild or severe ulcerative colitis, the experts wrote. “Finally, regulatory agencies must provide a reasonable pathway for approval of microbial-based therapeutics,” they added. “[The] therapeutic manipulation of the intestinal microbiota, whether by full-spectrum FMT or a more targeted approach using synthetic cultured consortia of bacterial species, is likely to be a component of therapy for [inflammatory bowel disease] and others in the not-so-distant future.”
Dr. Kelly is with Brown University in Providence, R.I. She disclosed ties to Finch Therapeutics and Openbiome. Dr. Ananthakrishnan is with Harvard Medical School, Boston. He disclosed ties to Pfizer and Gilead (JAMA. 2019;321[2]:151-2).
For patients with mild to moderate ulcerative colitis, a three-dose, 1-week induction course of anaerobically prepared donor fecal microbiota transplantation (FMT) produced steroid-free remission in 32% of patients, compared with 9% of those who received autologous aerobically prepared FMT in a randomized, double-blind, clinical trial.
Eight weeks after FMT, the odds of steroid-free remission were fivefold higher with anaerobically prepared donor versus aerobically prepared autologous FMT (odds ratio, 5; 95% confidence interval, 1.2-20.1; P = .03), reported Samuel P. Costello, MD, of the Queen Elizabeth Hospital in Woodville, Australia, and his associates. Donor FMT also significantly increased the likelihood of clinical remission and clinical response, the researchers said. “Further research is needed to assess longer-term maintenance of remission and safety,” they wrote in JAMA.
In prior studies, high-intensity FMT with aerobically prepared donor material remitted some cases of mild to moderate ulcerative colitis. However, anaerobic processing has been found to improve microbial viability, which might allow patients to remit with less intensive FMT, the researchers wrote. In their multicenter study, 73 adults with mildly to moderately active ulcerative colitis (total Mayo score, 3-10 points, with endoscopic subscore of at least 2) received either anaerobically prepared stool pooled from three to four highly screened donors or aerobically processed autologous stool. Patients in both arms received two enemas in the 7 days after FMT – a less dose-intensive treatment protocol than in prior FMT trials of patients with ulcerative colitis.
Among 38 patients in the intervention group, 12 (32%) achieved remission, defined as total Mayo score no greater than 2 with an endoscopic score no greater than 1. Strikingly, five (42%) of these patients remained in remission at 12 months, the researchers said. Additionally, 55% of the intervention group but only 23% of the comparator group (P = .007) achieved clinical response at 8 weeks, defined as at least a 3-point decrease in total Mayo score. Rates of clinical remission (Simple Colitis Activity Index score no greater than 2) were 47% and 17%, respectively (P = .01).
The study population averaged 39 years of age, 45% were women, and 95% completed the trial. Serious adverse events included one case each of worsening colitis, Clostridium difficile colitis requiring colectomy, and pneumonia in the donor FMT group, and two cases of worsening colitis in the comparator group. However, the study “was not powered to assess safety, and and thus further larger studies are required to assess this,” the researchers said. The study also suffered from a significant loss to follow-up at 12 months, so additional studies should assess long-term remission, they added.
The National Health and Medical Research Council and the Gutsy Foundation provided funding. Dr. Costello disclosed ties to Janssen, Shire, Ferring, Microbiotica, and Pfizer.
SOURCE: Costello SP et al. JAMA. 2019;321(2):156-64. doi: 10.1001/jama.2018.20046.
For patients with mild to moderate ulcerative colitis, a three-dose, 1-week induction course of anaerobically prepared donor fecal microbiota transplantation (FMT) produced steroid-free remission in 32% of patients, compared with 9% of those who received autologous aerobically prepared FMT in a randomized, double-blind, clinical trial.
Eight weeks after FMT, the odds of steroid-free remission were fivefold higher with anaerobically prepared donor versus aerobically prepared autologous FMT (odds ratio, 5; 95% confidence interval, 1.2-20.1; P = .03), reported Samuel P. Costello, MD, of the Queen Elizabeth Hospital in Woodville, Australia, and his associates. Donor FMT also significantly increased the likelihood of clinical remission and clinical response, the researchers said. “Further research is needed to assess longer-term maintenance of remission and safety,” they wrote in JAMA.
In prior studies, high-intensity FMT with aerobically prepared donor material remitted some cases of mild to moderate ulcerative colitis. However, anaerobic processing has been found to improve microbial viability, which might allow patients to remit with less intensive FMT, the researchers wrote. In their multicenter study, 73 adults with mildly to moderately active ulcerative colitis (total Mayo score, 3-10 points, with endoscopic subscore of at least 2) received either anaerobically prepared stool pooled from three to four highly screened donors or aerobically processed autologous stool. Patients in both arms received two enemas in the 7 days after FMT – a less dose-intensive treatment protocol than in prior FMT trials of patients with ulcerative colitis.
Among 38 patients in the intervention group, 12 (32%) achieved remission, defined as total Mayo score no greater than 2 with an endoscopic score no greater than 1. Strikingly, five (42%) of these patients remained in remission at 12 months, the researchers said. Additionally, 55% of the intervention group but only 23% of the comparator group (P = .007) achieved clinical response at 8 weeks, defined as at least a 3-point decrease in total Mayo score. Rates of clinical remission (Simple Colitis Activity Index score no greater than 2) were 47% and 17%, respectively (P = .01).
The study population averaged 39 years of age, 45% were women, and 95% completed the trial. Serious adverse events included one case each of worsening colitis, Clostridium difficile colitis requiring colectomy, and pneumonia in the donor FMT group, and two cases of worsening colitis in the comparator group. However, the study “was not powered to assess safety, and and thus further larger studies are required to assess this,” the researchers said. The study also suffered from a significant loss to follow-up at 12 months, so additional studies should assess long-term remission, they added.
The National Health and Medical Research Council and the Gutsy Foundation provided funding. Dr. Costello disclosed ties to Janssen, Shire, Ferring, Microbiotica, and Pfizer.
SOURCE: Costello SP et al. JAMA. 2019;321(2):156-64. doi: 10.1001/jama.2018.20046.
FROM JAMA
Key clinical point: Anaerobically prepared donor fecal microbiota transplantation (FMT) significantly increased the likelihood of steroid-free remission, compared with autologous FMT in patients with mild to moderately active ulcerative colitis.
Major finding: Eight weeks after FMT, 32% of the donor group achieved steroid-free remission, compared with 9% of the autologous FMT group (odds ratio, 5; P = .03).
Study details: Randomized, double-blind, multicenter trial of 73 patients with mild to moderate ulcerative colitis.
Disclosures: The National Health and Medical Research Council and the Gutsy Foundation provided funding. Dr. Costello disclosed ties to Janssen, Shire, Ferring, Microbiotica, and Pfizer.
Source: Costello SP et al. JAMA. 2019;321(2):156-64.
Getting the Right Numbers for Native American Drug-Overdose Deaths
More Native Americans have died of a drug overdose than members of any other racial or ethnic group in the US—which as a whole has seen drug overdose deaths triple since 1999. But little is known about the regional impact of opioids in tribal and urban American Indian/Alaska Native (AI/AN) communities, according to Indian Health Service (IHS) researchers from Portland, Oregon. They examined death records from the Washington State Center for Health Statistics to identify trends and disparities in drug, opioid-involved, and heroin-involved overdose deaths for AI/AN and non-Hispanic whites in Washington.
AI/AN and whites had similar overdose-related death rates during 1999 and 2001, but then the deaths began to multiply faster among Native Americans: Between 2013 and 2015, Native Americans were dying at nearly 3 times the rate of drug and opioid-related overdose. Heroin-related deaths were 4 times higher.
During 2013-2015, 184 AI/AN people died of a drug overdose in Washington; 126 from opioids. Most of the deaths were in urban communities (both Native American and white). Men were nearly twice as likely as women to die of overdose. Adults aged 25 to 54 years had the highest rates. Age-specific drug overdose mortality rates among AI/AN were almost twice those among whites.
The death rates are disturbing enough, but the researchers also found that death certificates that were not corrected for misclassification of AI/AN race underestimated the mortality rates among AI/AN by about 40%. For example, the uncorrected data showed 28.7 drug-overdose deaths in Washington. The corrected number was 40.9. In contrast, the uncorrected number for whites was 15.7, vs 15.1.
Even before correction for misclassification, AI/AN in Washington had higher drug-opioid-involved, and heroin-involved overdose mortality rates than did whites in Washington and AI/AN in the US.
The researchers note that misclassification of AI/AN in public health data can obscure the prevalence of disease and result in suppression of health statistics because of small numbers. That, in turn, can affect the ability of state and federal programs to direct resources needed for a “robust public health response to this epidemic.”
More Native Americans have died of a drug overdose than members of any other racial or ethnic group in the US—which as a whole has seen drug overdose deaths triple since 1999. But little is known about the regional impact of opioids in tribal and urban American Indian/Alaska Native (AI/AN) communities, according to Indian Health Service (IHS) researchers from Portland, Oregon. They examined death records from the Washington State Center for Health Statistics to identify trends and disparities in drug, opioid-involved, and heroin-involved overdose deaths for AI/AN and non-Hispanic whites in Washington.
AI/AN and whites had similar overdose-related death rates during 1999 and 2001, but then the deaths began to multiply faster among Native Americans: Between 2013 and 2015, Native Americans were dying at nearly 3 times the rate of drug and opioid-related overdose. Heroin-related deaths were 4 times higher.
During 2013-2015, 184 AI/AN people died of a drug overdose in Washington; 126 from opioids. Most of the deaths were in urban communities (both Native American and white). Men were nearly twice as likely as women to die of overdose. Adults aged 25 to 54 years had the highest rates. Age-specific drug overdose mortality rates among AI/AN were almost twice those among whites.
The death rates are disturbing enough, but the researchers also found that death certificates that were not corrected for misclassification of AI/AN race underestimated the mortality rates among AI/AN by about 40%. For example, the uncorrected data showed 28.7 drug-overdose deaths in Washington. The corrected number was 40.9. In contrast, the uncorrected number for whites was 15.7, vs 15.1.
Even before correction for misclassification, AI/AN in Washington had higher drug-opioid-involved, and heroin-involved overdose mortality rates than did whites in Washington and AI/AN in the US.
The researchers note that misclassification of AI/AN in public health data can obscure the prevalence of disease and result in suppression of health statistics because of small numbers. That, in turn, can affect the ability of state and federal programs to direct resources needed for a “robust public health response to this epidemic.”
More Native Americans have died of a drug overdose than members of any other racial or ethnic group in the US—which as a whole has seen drug overdose deaths triple since 1999. But little is known about the regional impact of opioids in tribal and urban American Indian/Alaska Native (AI/AN) communities, according to Indian Health Service (IHS) researchers from Portland, Oregon. They examined death records from the Washington State Center for Health Statistics to identify trends and disparities in drug, opioid-involved, and heroin-involved overdose deaths for AI/AN and non-Hispanic whites in Washington.
AI/AN and whites had similar overdose-related death rates during 1999 and 2001, but then the deaths began to multiply faster among Native Americans: Between 2013 and 2015, Native Americans were dying at nearly 3 times the rate of drug and opioid-related overdose. Heroin-related deaths were 4 times higher.
During 2013-2015, 184 AI/AN people died of a drug overdose in Washington; 126 from opioids. Most of the deaths were in urban communities (both Native American and white). Men were nearly twice as likely as women to die of overdose. Adults aged 25 to 54 years had the highest rates. Age-specific drug overdose mortality rates among AI/AN were almost twice those among whites.
The death rates are disturbing enough, but the researchers also found that death certificates that were not corrected for misclassification of AI/AN race underestimated the mortality rates among AI/AN by about 40%. For example, the uncorrected data showed 28.7 drug-overdose deaths in Washington. The corrected number was 40.9. In contrast, the uncorrected number for whites was 15.7, vs 15.1.
Even before correction for misclassification, AI/AN in Washington had higher drug-opioid-involved, and heroin-involved overdose mortality rates than did whites in Washington and AI/AN in the US.
The researchers note that misclassification of AI/AN in public health data can obscure the prevalence of disease and result in suppression of health statistics because of small numbers. That, in turn, can affect the ability of state and federal programs to direct resources needed for a “robust public health response to this epidemic.”
SMFM and ACOG team up for interpregnancy care guidance
A new consensus statement places renewed focus on maternal interpregnancy care, with a goal of extending care past the postpartum period to provide a wellness-maximizing continuum of care.
The document, developed by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (SMFM), recognizes that pregnancy is part of the lifelong continuum of health and wellness. Although not all women will go on to have another pregnancy, the concept of interpregnancy care recognizes that ob.gyns. have a vital role that extends past the postpartum period.
“This is a shift in what we used to think was our job. We used to think that our job ended when the baby came out,” said the first author of the obstetric care consensus statement, Judette Marie Louis, MD, an ob.gyn. faculty member at the University of South Florida, Tampa, and a SMFM board member. “For too long, our focus was just the baby; we need to tell women, ‘You’re important too,’ ” she said in an interview.
“The interpregnancy period is an opportunity to address these complications of medical issues that have developed during pregnancy, to assess a woman’s mental and physical well-being, and to optimize her health along her life course,” Dr. Louis and her coauthors wrote in Obstetrics & Gynecology.
Conceptually, the opportunity for interpregnancy care arises after any pregnancy, no matter the outcome, and is part of the continuum of care for women of reproductive age. For women who do not intend a future pregnancy, well-woman care is the focus, while women who currently intend to become pregnant again receive interpregnancy care. Women may move from one arm of the continuum to the other if their intentions change or if they become pregnant, explained Dr. Louis and her coauthors.
Birth spacing
The new consensus document includes an emphasis on long-term health outcomes as well as maternal and neonatal outcomes in future pregnancies. Although the evidence is of no more than moderate quality, women should be advised to have an interpregnancy interval of at least 6 months and offered counseling about family planning before delivery. Risks and benefits of an interpregnancy interval of less than 18 months should be reviewed as well.
For women with a history of preterm birth and those who have had a prior cesarean delivery and desire a subsequent trial of labor, birth spacing is particularly important, noted Dr. Louis and her colleagues. There is higher-risk evidence for uterine rupture after cesarean delivery if delivery-to-delivery intervals are 18-24 months or less.
Recommendations regarding the length of the interpregnancy interval generally should not be affected by a history of prior infertility.
Other recommendations
High-quality evidence supports breast feeding’s salutary effects on maternal and child health, so women should receive anticipatory support and guidance to enable breastfeeding, according to the document.
In accordance with other guidelines, the document recommends that all women be screened for depression post partum and as part of well-woman care in the interpregnancy interval. Procedures for effective diagnosis, treatment, and follow-up should accompany the screening.
Best practices dictate that women are asked about alcohol, prescription, and nonprescription drug use as a routine matter. High-quality evidence supports offering smoking cessation support to women who smoke and giving specific advice about nutrition and physical activity that’s based on “proven behavioral techniques.”
Evidence is of moderate quality that women should be encouraged to reach their prepregnancy weight by a year after delivery, with the ultimate goal of having a body mass index of 18.5-24.9.
High-quality evidence backs encouragement to engage in safe sex practices, with care providers also advised to facilitate partner screening and treatment for STIs.
Screening for STIs should follow guidance put forward by the Centers for Disease Control and Prevention and should be offered to women at high risk for STIs; those with a history of STI should have a careful history taken to determine risks for current or repeat infections, wrote Dr. Louis and her coauthors. These strong recommendations have high-quality evidence behind them.
The consensus statement recommends screening women for intimate partner violence, with moderate-quality evidence to support the recommendation. Patient navigators, expert medical interpretation, and other health educators can be offered to women with health literacy or language and communication challenges, but the evidence backing the recommendation is of low quality.
A subset of the interpregnancy care recommendations gives additional guidance regarding women with a history of high-risk pregnancy. All women planning pregnancy – or who could become pregnant – should take 500 mcg of folic acid daily beginning 1 month before fertilization and continuing through the 12th week of pregnancy. Folic acid supplementation for women who have had children with neural tube defects should begin at least 3 months before fertilization and continue through 12 weeks of pregnancy, at a dose of 400 mg.
All prescription and nonprescription medications, as well as potential environmental teratogens, should be reviewed before a repeat pregnancy. This, as well as the folic acid recommendations, are strong recommendations backed by high-quality evidence.
When appropriate, genetic counseling should be offered to women who have had prior pregnancies with genetic disorders or congenital anomalies. Asymptomatic genitourinary infections should not be treated in women with a history of preterm birth during the interpregnancy interval. These are strong recommendations, but are backed by low to moderate quality evidence, wrote Dr. Louis and her colleagues.
Another section of the consensus document specifically addresses specific health conditions, including diabetes, gestational diabetes, gestational and chronic hypertension, and preeclampsia, as well as mental health disorders and overweight or obesity.
For each, Dr. Louis and her coauthors recommend counseling that reviews complications and risk for future disease; for example, not only does prior preeclampsia increase risk for that complication in future pregnancies, risk for later cardiovascular disease is also doubled. The document outlines recommended interpregnancy testing, management considerations and medications of concern for health care providers caring for women with these conditions, and condition-specific goals.
Of the association between gestational diabetes, hypertension, and preeclampsia with later disease, Dr. Louis said in the interview, “We don’t know. ... It may be that pregnancy accelerates these diseases. We do know that normal changes in pregnancy stress your body, and that preeclampsia damages your vessels. Pregnancy can give you a warning, but we don’t have enough information to predict the outcome” in later life. “We do know there is some advice we can give: stop smoking and maintain a normal body weight.”
Other conditions such as HIV, renal disease, epilepsy, autoimmune and thyroid disease, and thrombophilias and antiphospholipid antibody syndrome are also addressed in this section of the consensus document.
Specific attention also is given to psychosocial risks, such as socioeconomic disadvantages and being a member of a racial or ethnic minority. Social determinants of health are complex, said Dr. Louis, but socioeconomic and racial stressors can include the added burden of caring for loved ones with constrained resources. Additionally, there can be access issues: Women can get emergent care by presenting to the ED but receiving continued primary and specialty care can be much more of a challenge.
Regarding racism, Dr. Louis said, “We all come into caring for these women with certain ideas.” For example, it’s not enough to say of a patient, “She’s noncompliant. You need to ask why.” When the “why” question is asked, then you may discover, “there’s something you can help the patient with,” she said. “We need to ask why, and then take steps to help our patients.”
Document building
The working group for the consensus document felt it was important to include nonphysicians who care for women, Dr. Louis said, so drafts were reviewed by and input received from the American College of Nurse-Midwives and the National Association of Nurse Practitioners in Women’s Health. Both groups endorsed the document.
The collaborative process of putting drafts together and then reviewing and revising the document was a big part of the reason it took 2 years to produce the interpregnancy care consensus statement. “It was the equivalent of two full gestations with a short interpregnancy interval!” said Dr. Louis, laughing. But seeking input from all stakeholders strengthened the final product.
Dr. Louis reported no conflicts of interest and no outside sources of funding were reported.
SOURCE: Louis JM et al. Obstet Gynecol. 2019;133:e51-72.
A new consensus statement places renewed focus on maternal interpregnancy care, with a goal of extending care past the postpartum period to provide a wellness-maximizing continuum of care.
The document, developed by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (SMFM), recognizes that pregnancy is part of the lifelong continuum of health and wellness. Although not all women will go on to have another pregnancy, the concept of interpregnancy care recognizes that ob.gyns. have a vital role that extends past the postpartum period.
“This is a shift in what we used to think was our job. We used to think that our job ended when the baby came out,” said the first author of the obstetric care consensus statement, Judette Marie Louis, MD, an ob.gyn. faculty member at the University of South Florida, Tampa, and a SMFM board member. “For too long, our focus was just the baby; we need to tell women, ‘You’re important too,’ ” she said in an interview.
“The interpregnancy period is an opportunity to address these complications of medical issues that have developed during pregnancy, to assess a woman’s mental and physical well-being, and to optimize her health along her life course,” Dr. Louis and her coauthors wrote in Obstetrics & Gynecology.
Conceptually, the opportunity for interpregnancy care arises after any pregnancy, no matter the outcome, and is part of the continuum of care for women of reproductive age. For women who do not intend a future pregnancy, well-woman care is the focus, while women who currently intend to become pregnant again receive interpregnancy care. Women may move from one arm of the continuum to the other if their intentions change or if they become pregnant, explained Dr. Louis and her coauthors.
Birth spacing
The new consensus document includes an emphasis on long-term health outcomes as well as maternal and neonatal outcomes in future pregnancies. Although the evidence is of no more than moderate quality, women should be advised to have an interpregnancy interval of at least 6 months and offered counseling about family planning before delivery. Risks and benefits of an interpregnancy interval of less than 18 months should be reviewed as well.
For women with a history of preterm birth and those who have had a prior cesarean delivery and desire a subsequent trial of labor, birth spacing is particularly important, noted Dr. Louis and her colleagues. There is higher-risk evidence for uterine rupture after cesarean delivery if delivery-to-delivery intervals are 18-24 months or less.
Recommendations regarding the length of the interpregnancy interval generally should not be affected by a history of prior infertility.
Other recommendations
High-quality evidence supports breast feeding’s salutary effects on maternal and child health, so women should receive anticipatory support and guidance to enable breastfeeding, according to the document.
In accordance with other guidelines, the document recommends that all women be screened for depression post partum and as part of well-woman care in the interpregnancy interval. Procedures for effective diagnosis, treatment, and follow-up should accompany the screening.
Best practices dictate that women are asked about alcohol, prescription, and nonprescription drug use as a routine matter. High-quality evidence supports offering smoking cessation support to women who smoke and giving specific advice about nutrition and physical activity that’s based on “proven behavioral techniques.”
Evidence is of moderate quality that women should be encouraged to reach their prepregnancy weight by a year after delivery, with the ultimate goal of having a body mass index of 18.5-24.9.
High-quality evidence backs encouragement to engage in safe sex practices, with care providers also advised to facilitate partner screening and treatment for STIs.
Screening for STIs should follow guidance put forward by the Centers for Disease Control and Prevention and should be offered to women at high risk for STIs; those with a history of STI should have a careful history taken to determine risks for current or repeat infections, wrote Dr. Louis and her coauthors. These strong recommendations have high-quality evidence behind them.
The consensus statement recommends screening women for intimate partner violence, with moderate-quality evidence to support the recommendation. Patient navigators, expert medical interpretation, and other health educators can be offered to women with health literacy or language and communication challenges, but the evidence backing the recommendation is of low quality.
A subset of the interpregnancy care recommendations gives additional guidance regarding women with a history of high-risk pregnancy. All women planning pregnancy – or who could become pregnant – should take 500 mcg of folic acid daily beginning 1 month before fertilization and continuing through the 12th week of pregnancy. Folic acid supplementation for women who have had children with neural tube defects should begin at least 3 months before fertilization and continue through 12 weeks of pregnancy, at a dose of 400 mg.
All prescription and nonprescription medications, as well as potential environmental teratogens, should be reviewed before a repeat pregnancy. This, as well as the folic acid recommendations, are strong recommendations backed by high-quality evidence.
When appropriate, genetic counseling should be offered to women who have had prior pregnancies with genetic disorders or congenital anomalies. Asymptomatic genitourinary infections should not be treated in women with a history of preterm birth during the interpregnancy interval. These are strong recommendations, but are backed by low to moderate quality evidence, wrote Dr. Louis and her colleagues.
Another section of the consensus document specifically addresses specific health conditions, including diabetes, gestational diabetes, gestational and chronic hypertension, and preeclampsia, as well as mental health disorders and overweight or obesity.
For each, Dr. Louis and her coauthors recommend counseling that reviews complications and risk for future disease; for example, not only does prior preeclampsia increase risk for that complication in future pregnancies, risk for later cardiovascular disease is also doubled. The document outlines recommended interpregnancy testing, management considerations and medications of concern for health care providers caring for women with these conditions, and condition-specific goals.
Of the association between gestational diabetes, hypertension, and preeclampsia with later disease, Dr. Louis said in the interview, “We don’t know. ... It may be that pregnancy accelerates these diseases. We do know that normal changes in pregnancy stress your body, and that preeclampsia damages your vessels. Pregnancy can give you a warning, but we don’t have enough information to predict the outcome” in later life. “We do know there is some advice we can give: stop smoking and maintain a normal body weight.”
Other conditions such as HIV, renal disease, epilepsy, autoimmune and thyroid disease, and thrombophilias and antiphospholipid antibody syndrome are also addressed in this section of the consensus document.
Specific attention also is given to psychosocial risks, such as socioeconomic disadvantages and being a member of a racial or ethnic minority. Social determinants of health are complex, said Dr. Louis, but socioeconomic and racial stressors can include the added burden of caring for loved ones with constrained resources. Additionally, there can be access issues: Women can get emergent care by presenting to the ED but receiving continued primary and specialty care can be much more of a challenge.
Regarding racism, Dr. Louis said, “We all come into caring for these women with certain ideas.” For example, it’s not enough to say of a patient, “She’s noncompliant. You need to ask why.” When the “why” question is asked, then you may discover, “there’s something you can help the patient with,” she said. “We need to ask why, and then take steps to help our patients.”
Document building
The working group for the consensus document felt it was important to include nonphysicians who care for women, Dr. Louis said, so drafts were reviewed by and input received from the American College of Nurse-Midwives and the National Association of Nurse Practitioners in Women’s Health. Both groups endorsed the document.
The collaborative process of putting drafts together and then reviewing and revising the document was a big part of the reason it took 2 years to produce the interpregnancy care consensus statement. “It was the equivalent of two full gestations with a short interpregnancy interval!” said Dr. Louis, laughing. But seeking input from all stakeholders strengthened the final product.
Dr. Louis reported no conflicts of interest and no outside sources of funding were reported.
SOURCE: Louis JM et al. Obstet Gynecol. 2019;133:e51-72.
A new consensus statement places renewed focus on maternal interpregnancy care, with a goal of extending care past the postpartum period to provide a wellness-maximizing continuum of care.
The document, developed by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (SMFM), recognizes that pregnancy is part of the lifelong continuum of health and wellness. Although not all women will go on to have another pregnancy, the concept of interpregnancy care recognizes that ob.gyns. have a vital role that extends past the postpartum period.
“This is a shift in what we used to think was our job. We used to think that our job ended when the baby came out,” said the first author of the obstetric care consensus statement, Judette Marie Louis, MD, an ob.gyn. faculty member at the University of South Florida, Tampa, and a SMFM board member. “For too long, our focus was just the baby; we need to tell women, ‘You’re important too,’ ” she said in an interview.
“The interpregnancy period is an opportunity to address these complications of medical issues that have developed during pregnancy, to assess a woman’s mental and physical well-being, and to optimize her health along her life course,” Dr. Louis and her coauthors wrote in Obstetrics & Gynecology.
Conceptually, the opportunity for interpregnancy care arises after any pregnancy, no matter the outcome, and is part of the continuum of care for women of reproductive age. For women who do not intend a future pregnancy, well-woman care is the focus, while women who currently intend to become pregnant again receive interpregnancy care. Women may move from one arm of the continuum to the other if their intentions change or if they become pregnant, explained Dr. Louis and her coauthors.
Birth spacing
The new consensus document includes an emphasis on long-term health outcomes as well as maternal and neonatal outcomes in future pregnancies. Although the evidence is of no more than moderate quality, women should be advised to have an interpregnancy interval of at least 6 months and offered counseling about family planning before delivery. Risks and benefits of an interpregnancy interval of less than 18 months should be reviewed as well.
For women with a history of preterm birth and those who have had a prior cesarean delivery and desire a subsequent trial of labor, birth spacing is particularly important, noted Dr. Louis and her colleagues. There is higher-risk evidence for uterine rupture after cesarean delivery if delivery-to-delivery intervals are 18-24 months or less.
Recommendations regarding the length of the interpregnancy interval generally should not be affected by a history of prior infertility.
Other recommendations
High-quality evidence supports breast feeding’s salutary effects on maternal and child health, so women should receive anticipatory support and guidance to enable breastfeeding, according to the document.
In accordance with other guidelines, the document recommends that all women be screened for depression post partum and as part of well-woman care in the interpregnancy interval. Procedures for effective diagnosis, treatment, and follow-up should accompany the screening.
Best practices dictate that women are asked about alcohol, prescription, and nonprescription drug use as a routine matter. High-quality evidence supports offering smoking cessation support to women who smoke and giving specific advice about nutrition and physical activity that’s based on “proven behavioral techniques.”
Evidence is of moderate quality that women should be encouraged to reach their prepregnancy weight by a year after delivery, with the ultimate goal of having a body mass index of 18.5-24.9.
High-quality evidence backs encouragement to engage in safe sex practices, with care providers also advised to facilitate partner screening and treatment for STIs.
Screening for STIs should follow guidance put forward by the Centers for Disease Control and Prevention and should be offered to women at high risk for STIs; those with a history of STI should have a careful history taken to determine risks for current or repeat infections, wrote Dr. Louis and her coauthors. These strong recommendations have high-quality evidence behind them.
The consensus statement recommends screening women for intimate partner violence, with moderate-quality evidence to support the recommendation. Patient navigators, expert medical interpretation, and other health educators can be offered to women with health literacy or language and communication challenges, but the evidence backing the recommendation is of low quality.
A subset of the interpregnancy care recommendations gives additional guidance regarding women with a history of high-risk pregnancy. All women planning pregnancy – or who could become pregnant – should take 500 mcg of folic acid daily beginning 1 month before fertilization and continuing through the 12th week of pregnancy. Folic acid supplementation for women who have had children with neural tube defects should begin at least 3 months before fertilization and continue through 12 weeks of pregnancy, at a dose of 400 mg.
All prescription and nonprescription medications, as well as potential environmental teratogens, should be reviewed before a repeat pregnancy. This, as well as the folic acid recommendations, are strong recommendations backed by high-quality evidence.
When appropriate, genetic counseling should be offered to women who have had prior pregnancies with genetic disorders or congenital anomalies. Asymptomatic genitourinary infections should not be treated in women with a history of preterm birth during the interpregnancy interval. These are strong recommendations, but are backed by low to moderate quality evidence, wrote Dr. Louis and her colleagues.
Another section of the consensus document specifically addresses specific health conditions, including diabetes, gestational diabetes, gestational and chronic hypertension, and preeclampsia, as well as mental health disorders and overweight or obesity.
For each, Dr. Louis and her coauthors recommend counseling that reviews complications and risk for future disease; for example, not only does prior preeclampsia increase risk for that complication in future pregnancies, risk for later cardiovascular disease is also doubled. The document outlines recommended interpregnancy testing, management considerations and medications of concern for health care providers caring for women with these conditions, and condition-specific goals.
Of the association between gestational diabetes, hypertension, and preeclampsia with later disease, Dr. Louis said in the interview, “We don’t know. ... It may be that pregnancy accelerates these diseases. We do know that normal changes in pregnancy stress your body, and that preeclampsia damages your vessels. Pregnancy can give you a warning, but we don’t have enough information to predict the outcome” in later life. “We do know there is some advice we can give: stop smoking and maintain a normal body weight.”
Other conditions such as HIV, renal disease, epilepsy, autoimmune and thyroid disease, and thrombophilias and antiphospholipid antibody syndrome are also addressed in this section of the consensus document.
Specific attention also is given to psychosocial risks, such as socioeconomic disadvantages and being a member of a racial or ethnic minority. Social determinants of health are complex, said Dr. Louis, but socioeconomic and racial stressors can include the added burden of caring for loved ones with constrained resources. Additionally, there can be access issues: Women can get emergent care by presenting to the ED but receiving continued primary and specialty care can be much more of a challenge.
Regarding racism, Dr. Louis said, “We all come into caring for these women with certain ideas.” For example, it’s not enough to say of a patient, “She’s noncompliant. You need to ask why.” When the “why” question is asked, then you may discover, “there’s something you can help the patient with,” she said. “We need to ask why, and then take steps to help our patients.”
Document building
The working group for the consensus document felt it was important to include nonphysicians who care for women, Dr. Louis said, so drafts were reviewed by and input received from the American College of Nurse-Midwives and the National Association of Nurse Practitioners in Women’s Health. Both groups endorsed the document.
The collaborative process of putting drafts together and then reviewing and revising the document was a big part of the reason it took 2 years to produce the interpregnancy care consensus statement. “It was the equivalent of two full gestations with a short interpregnancy interval!” said Dr. Louis, laughing. But seeking input from all stakeholders strengthened the final product.
Dr. Louis reported no conflicts of interest and no outside sources of funding were reported.
SOURCE: Louis JM et al. Obstet Gynecol. 2019;133:e51-72.
FROM OBSTETRICS & GYNECOLOGY
INPULSIS-ON: Nintedanib shows manageable long-term safety for IPF
For patients with showed acceptable safety and tolerability and might have slowed disease progression, according to the results of the open-label INPULSIS-ON trial.
No new safety signals were identified among patients who continued nintedanib or switched from placebo to the medication after completing one of the two 52-week phase 3 INPULSIS trials, reported Bruno Crestani, MD, of H
Idiopathic pulmonary fibrosis has had a poor prognosis – before antifibrotic therapy became available in the United States, median survival after diagnosis was estimated at 3-5 years, the researchers noted. Patients often die or deteriorate because of acute declines in respiratory function, often from unknown causes. Nintedanib (Ofev) is an intracellular tyrosine kinase inhibitor first approved for idiopathic pulmonary fibrosis in the United States in 2014, based on the results of the replicate randomized, placebo-controlled, double-blind, phase 3 INPULSIS trials, in which nintedanib (150 mg twice daily) was usually tolerable, showed an acceptable overall toxicity profile, and significantly lessened the annual rate of decline in forced vital capacity (FVC), compared with placebo.
Because idiopathic pulmonary fibrosis has a chronic trajectory, data on long-term safety and efficacy were clearly desirable. “Results from the open-label extension of the [foundational] phase 2 TOMORROW trial [also] identified no new safety signals and suggested an effect of nintedanib on slowing the progression of idiopathic pulmonary fibrosis beyond 52 weeks; however, only 35 patients treated with nintedanib 150 mg twice daily entered the extension study,” Dr. Crestani and his associates noted.
The open-label INPULSIS-ON extension trial included 734 patients, which was 91% of the population that completed the INPULSIS trials. A total of 59% patients in the open-label trial continued nintedanib while the rest switched to nintedanib from placebo. When considering both cohorts, the median duration of exposure to nintedanib was 44.7 months (range, 1.9-68.3 months).
Rates of major adverse cardiovascular events were 2.4 per 100 person-years of drug exposure among treatment initiators and 3.6 per 100 person-years among continuers, the researchers reported. Rates of bleeding were 6.7 and 8.4 events per 100 person-years, respectively, while rates of myocardial infarction, using the broadest possible definition, were 0.7 and 1.3 events per 100 person-years, respectively. The most common adverse event was diarrhea, with 60.1 and 71.2 events per 100 person-years among treatment initiators and continuers, respectively. In all, 10% of treatment initiators and 5% of continuers stopped nintedanib because of diarrhea. A total of 14% of treatment initiators and 12% of continuers stopped treatment because they experienced progression of idiopathic pulmonary fibrosis, making this adverse event the most common reason to stop treatment.
The adjusted annual rate of decline in FVC was −135.1 mL overall, –145 mL in nintedanib continuers, and –119.7 mL in nintedanib initiators, which resembled the findings of the INPULSIS trials, the researcher said. They added that the difference in FVC decline between INPULSIS-ON nintedanib initiators and continuers does not seem clinically meaningful, especially given that the average FVC decline in the INPULSIS placebo group was −223.5 mL per year, and the minimal clinically important difference in FVC is thought to be 2%-6% predicted, a difference of at least 75 mL-80 mL.
Boehringer Ingelheim funded the study. Dr. Crestani disclosed grants and personal fees from Boehringer Ingelheim and Roche, grants from Apellis and MedImmune, and personal fees from AstraZeneca and Sanofi.
SOURCE: Crestani B et al. Lancet Respir Med. 2018 Sep 14. doi: 10.1016/S2213-2600(18)30339-4.
The study provides “invaluable safety data, including a very low incidence of cardiovascular events” among patients who received long-term nintedanib therapy for idiopathic pulmonary fibrosis, wrote Athol U. Wells, MD, in an editorial published alongside the study.
But the efficacy data were substantially more problematic, he said. “At first sight, the data seem to show that treatment benefits are sustained during long-term follow-up. However, this finding applied to patients completing 4 years of treatment. Approximately 70% of patients discontinued nintedanib [during the open-label extension trial].”
Death, probable treatment failure, or adverse events unrelated to idiopathic pulmonary fibrosis accounted for 62% of withdrawals from this study, and the investigators did not present FVC trends for these patients, he noted. This makes it difficult to know whether bias affected the efficacy results. Long-term stability or slow progression was seen in 30%-40% of patients, exceeding results from previous IPF cohorts, but “this finding, although encouraging, is clearly non-definitive.”
The mortality data also were problematic because the trial excluded patients with major comorbidities and severe disease, and the researchers only tracked vital status for 6 weeks after patients withdrew from INPULSIS-ON, he said. “One cannot help but feel that a major opportunity was lost in this study and, equally, in the pirfenidone extension study. An intention-to-treat study design would have provided invaluable long-term efficacy data and should be prioritized in future.”
Dr. Wells is with Royal Brompton Hospital in London. He disclosed personal fees from Boehringer Ingelheim, Intermune/Roche, Bayer, Actelion, and Raffo, outside the submitted work (Lancet Respir Med. 2018 Sep 14. doi: 10.1016/S2213-2600[18]30385-0).
The study provides “invaluable safety data, including a very low incidence of cardiovascular events” among patients who received long-term nintedanib therapy for idiopathic pulmonary fibrosis, wrote Athol U. Wells, MD, in an editorial published alongside the study.
But the efficacy data were substantially more problematic, he said. “At first sight, the data seem to show that treatment benefits are sustained during long-term follow-up. However, this finding applied to patients completing 4 years of treatment. Approximately 70% of patients discontinued nintedanib [during the open-label extension trial].”
Death, probable treatment failure, or adverse events unrelated to idiopathic pulmonary fibrosis accounted for 62% of withdrawals from this study, and the investigators did not present FVC trends for these patients, he noted. This makes it difficult to know whether bias affected the efficacy results. Long-term stability or slow progression was seen in 30%-40% of patients, exceeding results from previous IPF cohorts, but “this finding, although encouraging, is clearly non-definitive.”
The mortality data also were problematic because the trial excluded patients with major comorbidities and severe disease, and the researchers only tracked vital status for 6 weeks after patients withdrew from INPULSIS-ON, he said. “One cannot help but feel that a major opportunity was lost in this study and, equally, in the pirfenidone extension study. An intention-to-treat study design would have provided invaluable long-term efficacy data and should be prioritized in future.”
Dr. Wells is with Royal Brompton Hospital in London. He disclosed personal fees from Boehringer Ingelheim, Intermune/Roche, Bayer, Actelion, and Raffo, outside the submitted work (Lancet Respir Med. 2018 Sep 14. doi: 10.1016/S2213-2600[18]30385-0).
The study provides “invaluable safety data, including a very low incidence of cardiovascular events” among patients who received long-term nintedanib therapy for idiopathic pulmonary fibrosis, wrote Athol U. Wells, MD, in an editorial published alongside the study.
But the efficacy data were substantially more problematic, he said. “At first sight, the data seem to show that treatment benefits are sustained during long-term follow-up. However, this finding applied to patients completing 4 years of treatment. Approximately 70% of patients discontinued nintedanib [during the open-label extension trial].”
Death, probable treatment failure, or adverse events unrelated to idiopathic pulmonary fibrosis accounted for 62% of withdrawals from this study, and the investigators did not present FVC trends for these patients, he noted. This makes it difficult to know whether bias affected the efficacy results. Long-term stability or slow progression was seen in 30%-40% of patients, exceeding results from previous IPF cohorts, but “this finding, although encouraging, is clearly non-definitive.”
The mortality data also were problematic because the trial excluded patients with major comorbidities and severe disease, and the researchers only tracked vital status for 6 weeks after patients withdrew from INPULSIS-ON, he said. “One cannot help but feel that a major opportunity was lost in this study and, equally, in the pirfenidone extension study. An intention-to-treat study design would have provided invaluable long-term efficacy data and should be prioritized in future.”
Dr. Wells is with Royal Brompton Hospital in London. He disclosed personal fees from Boehringer Ingelheim, Intermune/Roche, Bayer, Actelion, and Raffo, outside the submitted work (Lancet Respir Med. 2018 Sep 14. doi: 10.1016/S2213-2600[18]30385-0).
For patients with showed acceptable safety and tolerability and might have slowed disease progression, according to the results of the open-label INPULSIS-ON trial.
No new safety signals were identified among patients who continued nintedanib or switched from placebo to the medication after completing one of the two 52-week phase 3 INPULSIS trials, reported Bruno Crestani, MD, of H
Idiopathic pulmonary fibrosis has had a poor prognosis – before antifibrotic therapy became available in the United States, median survival after diagnosis was estimated at 3-5 years, the researchers noted. Patients often die or deteriorate because of acute declines in respiratory function, often from unknown causes. Nintedanib (Ofev) is an intracellular tyrosine kinase inhibitor first approved for idiopathic pulmonary fibrosis in the United States in 2014, based on the results of the replicate randomized, placebo-controlled, double-blind, phase 3 INPULSIS trials, in which nintedanib (150 mg twice daily) was usually tolerable, showed an acceptable overall toxicity profile, and significantly lessened the annual rate of decline in forced vital capacity (FVC), compared with placebo.
Because idiopathic pulmonary fibrosis has a chronic trajectory, data on long-term safety and efficacy were clearly desirable. “Results from the open-label extension of the [foundational] phase 2 TOMORROW trial [also] identified no new safety signals and suggested an effect of nintedanib on slowing the progression of idiopathic pulmonary fibrosis beyond 52 weeks; however, only 35 patients treated with nintedanib 150 mg twice daily entered the extension study,” Dr. Crestani and his associates noted.
The open-label INPULSIS-ON extension trial included 734 patients, which was 91% of the population that completed the INPULSIS trials. A total of 59% patients in the open-label trial continued nintedanib while the rest switched to nintedanib from placebo. When considering both cohorts, the median duration of exposure to nintedanib was 44.7 months (range, 1.9-68.3 months).
Rates of major adverse cardiovascular events were 2.4 per 100 person-years of drug exposure among treatment initiators and 3.6 per 100 person-years among continuers, the researchers reported. Rates of bleeding were 6.7 and 8.4 events per 100 person-years, respectively, while rates of myocardial infarction, using the broadest possible definition, were 0.7 and 1.3 events per 100 person-years, respectively. The most common adverse event was diarrhea, with 60.1 and 71.2 events per 100 person-years among treatment initiators and continuers, respectively. In all, 10% of treatment initiators and 5% of continuers stopped nintedanib because of diarrhea. A total of 14% of treatment initiators and 12% of continuers stopped treatment because they experienced progression of idiopathic pulmonary fibrosis, making this adverse event the most common reason to stop treatment.
The adjusted annual rate of decline in FVC was −135.1 mL overall, –145 mL in nintedanib continuers, and –119.7 mL in nintedanib initiators, which resembled the findings of the INPULSIS trials, the researcher said. They added that the difference in FVC decline between INPULSIS-ON nintedanib initiators and continuers does not seem clinically meaningful, especially given that the average FVC decline in the INPULSIS placebo group was −223.5 mL per year, and the minimal clinically important difference in FVC is thought to be 2%-6% predicted, a difference of at least 75 mL-80 mL.
Boehringer Ingelheim funded the study. Dr. Crestani disclosed grants and personal fees from Boehringer Ingelheim and Roche, grants from Apellis and MedImmune, and personal fees from AstraZeneca and Sanofi.
SOURCE: Crestani B et al. Lancet Respir Med. 2018 Sep 14. doi: 10.1016/S2213-2600(18)30339-4.
For patients with showed acceptable safety and tolerability and might have slowed disease progression, according to the results of the open-label INPULSIS-ON trial.
No new safety signals were identified among patients who continued nintedanib or switched from placebo to the medication after completing one of the two 52-week phase 3 INPULSIS trials, reported Bruno Crestani, MD, of H
Idiopathic pulmonary fibrosis has had a poor prognosis – before antifibrotic therapy became available in the United States, median survival after diagnosis was estimated at 3-5 years, the researchers noted. Patients often die or deteriorate because of acute declines in respiratory function, often from unknown causes. Nintedanib (Ofev) is an intracellular tyrosine kinase inhibitor first approved for idiopathic pulmonary fibrosis in the United States in 2014, based on the results of the replicate randomized, placebo-controlled, double-blind, phase 3 INPULSIS trials, in which nintedanib (150 mg twice daily) was usually tolerable, showed an acceptable overall toxicity profile, and significantly lessened the annual rate of decline in forced vital capacity (FVC), compared with placebo.
Because idiopathic pulmonary fibrosis has a chronic trajectory, data on long-term safety and efficacy were clearly desirable. “Results from the open-label extension of the [foundational] phase 2 TOMORROW trial [also] identified no new safety signals and suggested an effect of nintedanib on slowing the progression of idiopathic pulmonary fibrosis beyond 52 weeks; however, only 35 patients treated with nintedanib 150 mg twice daily entered the extension study,” Dr. Crestani and his associates noted.
The open-label INPULSIS-ON extension trial included 734 patients, which was 91% of the population that completed the INPULSIS trials. A total of 59% patients in the open-label trial continued nintedanib while the rest switched to nintedanib from placebo. When considering both cohorts, the median duration of exposure to nintedanib was 44.7 months (range, 1.9-68.3 months).
Rates of major adverse cardiovascular events were 2.4 per 100 person-years of drug exposure among treatment initiators and 3.6 per 100 person-years among continuers, the researchers reported. Rates of bleeding were 6.7 and 8.4 events per 100 person-years, respectively, while rates of myocardial infarction, using the broadest possible definition, were 0.7 and 1.3 events per 100 person-years, respectively. The most common adverse event was diarrhea, with 60.1 and 71.2 events per 100 person-years among treatment initiators and continuers, respectively. In all, 10% of treatment initiators and 5% of continuers stopped nintedanib because of diarrhea. A total of 14% of treatment initiators and 12% of continuers stopped treatment because they experienced progression of idiopathic pulmonary fibrosis, making this adverse event the most common reason to stop treatment.
The adjusted annual rate of decline in FVC was −135.1 mL overall, –145 mL in nintedanib continuers, and –119.7 mL in nintedanib initiators, which resembled the findings of the INPULSIS trials, the researcher said. They added that the difference in FVC decline between INPULSIS-ON nintedanib initiators and continuers does not seem clinically meaningful, especially given that the average FVC decline in the INPULSIS placebo group was −223.5 mL per year, and the minimal clinically important difference in FVC is thought to be 2%-6% predicted, a difference of at least 75 mL-80 mL.
Boehringer Ingelheim funded the study. Dr. Crestani disclosed grants and personal fees from Boehringer Ingelheim and Roche, grants from Apellis and MedImmune, and personal fees from AstraZeneca and Sanofi.
SOURCE: Crestani B et al. Lancet Respir Med. 2018 Sep 14. doi: 10.1016/S2213-2600(18)30339-4.
FROM THE LANCET RESPIRATORY MEDICINE
Key clinical point: Nintedanib showed manageable safety and tolerability and might have helped conserve forced vital capacity during long-term use for the treatment of IPF.
Major finding: No new safety signals were found over up to 68 months of treatment.
Study details: Open-label extension study of nintedanib initiation or continuation in 734 patients with idiopathic pulmonary fibrosis (median drug exposure 44.7 months; range, 11.9-68.3 months).
Disclosures: Boehringer Ingelheim funded the study. Dr. Crestani disclosed grants and personal fees from Boehringer Ingelheim and Roche, grants from Apellis and MedImmune, and personal fees from AstraZeneca and Sanofi.
Source: Crestani B et al. Lancet Respir Med. 2018 Sep 14.
Breast cancer study: No link between soy, all-cause mortality
Also today there is more benefit to chemoradiation earlier in small cell lung cancer, traditional jet nebulizers beat breath-enhanced nebulizers in pediatric asthma, and both new and existing drugs are fueling price inflation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today there is more benefit to chemoradiation earlier in small cell lung cancer, traditional jet nebulizers beat breath-enhanced nebulizers in pediatric asthma, and both new and existing drugs are fueling price inflation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today there is more benefit to chemoradiation earlier in small cell lung cancer, traditional jet nebulizers beat breath-enhanced nebulizers in pediatric asthma, and both new and existing drugs are fueling price inflation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Beer Before Liquor Affects the Ticker
ANSWER
The correct interpretation is atrial flutter with 2:1 conduction. In the absence of exercise, a tachycardia in a range of 130-150 beats/min with a regular rate should raise suspicion for atrial flutter. The presence of 2:1 conduction implies an atrial rate of 310 beats/min, within the range of an atrial macro-reentrant tachycardia.
There are two P waves for each QRS complex. One is hidden in the T wave in lead II, and the other occurs immediately before the QRS complex in leads II and aVF. Note that the P wave immediately preceding the QRS complex is not representative of a short PR interval with preexcitation, as seen in Wolff-Parkinson-White syndrome.
In this otherwise healthy male with no history of arrhythmia, the most likely cause of atrial flutter is alcohol consumption.
The patient was cardioverted to normal sinus rhythm and has had no further episodes.
ANSWER
The correct interpretation is atrial flutter with 2:1 conduction. In the absence of exercise, a tachycardia in a range of 130-150 beats/min with a regular rate should raise suspicion for atrial flutter. The presence of 2:1 conduction implies an atrial rate of 310 beats/min, within the range of an atrial macro-reentrant tachycardia.
There are two P waves for each QRS complex. One is hidden in the T wave in lead II, and the other occurs immediately before the QRS complex in leads II and aVF. Note that the P wave immediately preceding the QRS complex is not representative of a short PR interval with preexcitation, as seen in Wolff-Parkinson-White syndrome.
In this otherwise healthy male with no history of arrhythmia, the most likely cause of atrial flutter is alcohol consumption.
The patient was cardioverted to normal sinus rhythm and has had no further episodes.
ANSWER
The correct interpretation is atrial flutter with 2:1 conduction. In the absence of exercise, a tachycardia in a range of 130-150 beats/min with a regular rate should raise suspicion for atrial flutter. The presence of 2:1 conduction implies an atrial rate of 310 beats/min, within the range of an atrial macro-reentrant tachycardia.
There are two P waves for each QRS complex. One is hidden in the T wave in lead II, and the other occurs immediately before the QRS complex in leads II and aVF. Note that the P wave immediately preceding the QRS complex is not representative of a short PR interval with preexcitation, as seen in Wolff-Parkinson-White syndrome.
In this otherwise healthy male with no history of arrhythmia, the most likely cause of atrial flutter is alcohol consumption.
The patient was cardioverted to normal sinus rhythm and has had no further episodes.
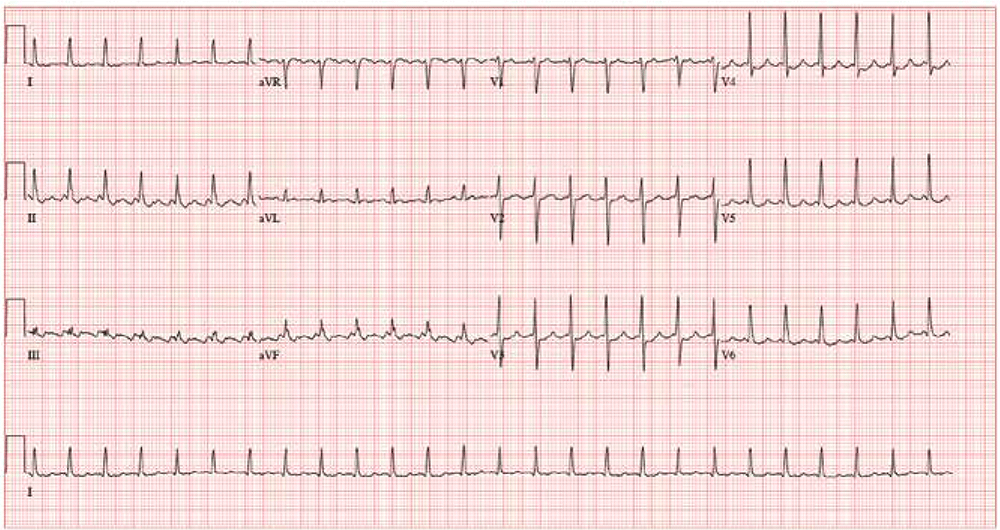
After a night of heavy drinking, a 34-year-old man awakens with a rapid heart rate and a fluttering sensation in his chest, which radiates up to his neck. By the time he arrives to your emergency department, he has had these symptoms for about 2 hours. He denies chest pain but reports having difficulty catching his breath. He says this is the first time he’s experienced these symptoms. He has no prior cardiac or pulmonary history.
The patient had been out with 4 old college friends, and they had between them consumed a case of beer and a fifth of whiskey. He cannot remember going home, but they all had ordered cabs ahead of time, knowing they would be drinking heavily. He denies taking any recreational drugs.
Past medical and surgical histories are remarkable only for a left tibial fracture sustained when the patient played high school football. He has no allergies and takes no medications. Although he doesn’t smoke tobacco, he admits to using marijuana sparingly; however, he says he hasn’t used it in the past 3 months. He works as a store manager at a local grocery chain. He isn’t married, has no children, and isn’t in a relationship.
Family history reveals the patient is an only child. His father has hypothyroidism, and his mother has type 2 diabetes, which is controlled with metformin. His maternal grandparents both have hypertension, which is managed with β-blockers.
The review of systems shows a recent increase in alcohol consumption following a breakup with his girlfriend 3 months ago. A 12-point review of systems is noncontributory.
Vital signs include a blood pressure of 118/62 mm Hg; pulse, 150 beats/min; and O2 saturation, 98% on room air. He is afebrile.
Physical exam reveals a thin, healthy but anxious man. His height is 72 in and his weight, 188 lb. The HEENT exam is normal. The neck is supple without thyromegaly and no jugular venous distention. The lungs are clear in all fields without wheezes, rales, or rhonchi.
Cardiac exam reveals tachycardia with a regular rate of 150 beats/min and no murmurs, extra heart sounds, or rubs. The abdomen is soft and nontender, with no palpable organomegaly. Peripheral pulses are equal bilaterally, with no palpable bruits. There is no peripheral edema, and the neurologic exam is intact.
An ECG reveals the following: a ventricular rate of 155 beats/min; PR interval, unmeasured, QRS duration, 78 ms; QT/QTc interval, 272/437 ms; P axis, unmeasured; R axis, +34°; and T axis, –50°. What is your interpretation?
Courts block Trump from eroding contraceptive mandate
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.