User login
Consider caffeine effects on children and adolescents
Less clinical attention has been paid to caffeine lately as the medical community works to overcome the negative effects of substances such as opiates and cannabis. Quietly, however, caffeine continues to be widely consumed among children and adolescents, and its use often flies under the radar for pediatricians who have so many other topics to address. To help clinicians decide whether more focus on caffeine use is needed, a review was published in the Journal of the American Academy of Child & Adolescent Psychiatry (2019;58[1]:36-45). A synopsis of this paper which summarizes 90 individual studies on caffeine use in children and adolescents is provided here.
Caffeine usage in children and adolescents
Caffeine continues to be one of the most commonly used substances in youth, with about 75% of older children and adolescents consuming it regularly, often at an average dose of about 25 mg/day for children aged 6-11 years and 50 mg/day for adolescents. Because most people have trouble quickly converting commonly used products into milligrams of caffeine, the following guide can be useful:
- Soda (12 oz). About 40 mg caffeine.
- Coffee (8 oz). About 100 mg caffeine.
- Tea (8 oz). About 48 mg caffeine.
- Energy drinks (12 oz). About 150 mg caffeine plus, with 5-Hour Energy being around 215 mg caffeine, according to a Consumer Reports study.
It is important to pay attention to the serving size, as the actual volume consumed of products like coffee or soft drinks often are much higher.
With regards to caffeine trends over time, a surprising observation is that total caffeine consumption among youth over the past decade or so looks relatively flat and may even be decreasing. This trend has occurred despite the aggressive marketing to youth of many energy drinks that contain high amounts of caffeine. In many ways, the pattern of caffeine use fits with what we know about substance use in general in adolescents, with rates dropping for many commonly used substances – with the exception of cannabis.
Effects of caffeine
As many know, caffeine is a stimulant and is known to increase arousal, alertness, and amount of motor behavior. While many youth drink caffeine in an effort to improve cognitive performance, the evidence that it does so directly is modest. There are some studies that show improvements on some cognitive tests when children take moderate doses of caffeine, but these effects tend to be most pronounced for kids who are more naive to caffeine at baseline. Of course, caffeine also can temporarily reduce feelings of fatigue and sleepiness.
Anecdotally, many youth and parents will report that caffeine is a way to “self-medicate” various symptoms of ADHD. While many will report some benefit, there is a surprising lack of rigorous data about the effects of caffeine for youth who meet criteria for ADHD, according to this review.
There also are some well-known negative effects of caffeine use. One of the most important ones is that caffeine can interfere with sleep onset, thereby inducing a cycle that reinforces more caffeine use in the day in an effort to compensate for poor sleep at night. A less obvious negative effect that has been documented is that caffeine added to sweetened beverages can increase consumption of similar sugary foods, even if they don’t have caffeine.
A number of adverse effects have been observed when youth consume caffeine at excessive doses, which tend to be around a threshold of 400 mg/day for teens and about 100 mg/day for younger children. These can include both behavioral and nonbehavioral changes such as agitation or irritability, anxiety, heart arrhythmias, and hypertension. Concern over high caffeine intake also was raised in relation to a number of cases of sudden death, although these events fortunately are rare. The review mentions that one factor that could increase the risk of a serious medical event related to caffeine use is the presence of an underlying cardiac problem which may go undetected until a negative outcome occurs. In thinking about these risks associated with “excessive” caffeine consumption, it can be important to go back to the guides and see just how easily an adolescent can get to a level of 400 mg or more. A couple large cups of coffee per day or two to three specific “energy-boosting” products can be all that it takes.
There also are a few large longitudinal studies that have shown a significant association between increased caffeine consumption and future problems with anger, aggression, risky sexual behavior, and substance use. Energy drinks, which can deliver a lot of caffeine quickly, were singled out as particularly problematic in some of these studies, although these naturalistic studies are unable to determine causation, and it also is possible that teens who are already prone towards behavioral problems tend to consume more caffeine. However, the review also mentions animal studies that have demonstrated that caffeine may prime the brain to use other substances like amphetamines or cocaine. Finally, another concern raised about energy drinks in particular is that they also often contain other substances which may have similar physiological effects but are relatively untested when it comes to safety.
Conclusions
This review, like the current position of the Food and Drug Administration, considers caffeine as generally safe at low doses because there does not appear to be much evidence that low or moderate use in youth leads to significant problems. The conclusion changes, however, with higher levels of consumption, as more frequent and more serious risks are encountered. The article recommends that both parents and doctors be more vigilant in monitoring the amount of caffeine that a child consumes as well as the timing of that use during the day. Some quick calculations can be done to give adolescents and their parents an estimate of their caffeine use in milligrams. And while caffeine may not rise to the level of public health concern as substances like opiates or alcohol, there is evidence that it can cause some real problems in children and teens, especially in higher amounts, and thus shouldn’t be given a total pass by parents and doctors alike.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at pdnews@mdedge.com. Follow him on Twitter @PediPsych. Looking for more mental health training? Attend the 13th annual Child Psychiatry in Primary Care conference in Burlington, Vt., May 3, 2019 (http://www.med.uvm.edu/cme/conferences).
Less clinical attention has been paid to caffeine lately as the medical community works to overcome the negative effects of substances such as opiates and cannabis. Quietly, however, caffeine continues to be widely consumed among children and adolescents, and its use often flies under the radar for pediatricians who have so many other topics to address. To help clinicians decide whether more focus on caffeine use is needed, a review was published in the Journal of the American Academy of Child & Adolescent Psychiatry (2019;58[1]:36-45). A synopsis of this paper which summarizes 90 individual studies on caffeine use in children and adolescents is provided here.
Caffeine usage in children and adolescents
Caffeine continues to be one of the most commonly used substances in youth, with about 75% of older children and adolescents consuming it regularly, often at an average dose of about 25 mg/day for children aged 6-11 years and 50 mg/day for adolescents. Because most people have trouble quickly converting commonly used products into milligrams of caffeine, the following guide can be useful:
- Soda (12 oz). About 40 mg caffeine.
- Coffee (8 oz). About 100 mg caffeine.
- Tea (8 oz). About 48 mg caffeine.
- Energy drinks (12 oz). About 150 mg caffeine plus, with 5-Hour Energy being around 215 mg caffeine, according to a Consumer Reports study.
It is important to pay attention to the serving size, as the actual volume consumed of products like coffee or soft drinks often are much higher.
With regards to caffeine trends over time, a surprising observation is that total caffeine consumption among youth over the past decade or so looks relatively flat and may even be decreasing. This trend has occurred despite the aggressive marketing to youth of many energy drinks that contain high amounts of caffeine. In many ways, the pattern of caffeine use fits with what we know about substance use in general in adolescents, with rates dropping for many commonly used substances – with the exception of cannabis.
Effects of caffeine
As many know, caffeine is a stimulant and is known to increase arousal, alertness, and amount of motor behavior. While many youth drink caffeine in an effort to improve cognitive performance, the evidence that it does so directly is modest. There are some studies that show improvements on some cognitive tests when children take moderate doses of caffeine, but these effects tend to be most pronounced for kids who are more naive to caffeine at baseline. Of course, caffeine also can temporarily reduce feelings of fatigue and sleepiness.
Anecdotally, many youth and parents will report that caffeine is a way to “self-medicate” various symptoms of ADHD. While many will report some benefit, there is a surprising lack of rigorous data about the effects of caffeine for youth who meet criteria for ADHD, according to this review.
There also are some well-known negative effects of caffeine use. One of the most important ones is that caffeine can interfere with sleep onset, thereby inducing a cycle that reinforces more caffeine use in the day in an effort to compensate for poor sleep at night. A less obvious negative effect that has been documented is that caffeine added to sweetened beverages can increase consumption of similar sugary foods, even if they don’t have caffeine.
A number of adverse effects have been observed when youth consume caffeine at excessive doses, which tend to be around a threshold of 400 mg/day for teens and about 100 mg/day for younger children. These can include both behavioral and nonbehavioral changes such as agitation or irritability, anxiety, heart arrhythmias, and hypertension. Concern over high caffeine intake also was raised in relation to a number of cases of sudden death, although these events fortunately are rare. The review mentions that one factor that could increase the risk of a serious medical event related to caffeine use is the presence of an underlying cardiac problem which may go undetected until a negative outcome occurs. In thinking about these risks associated with “excessive” caffeine consumption, it can be important to go back to the guides and see just how easily an adolescent can get to a level of 400 mg or more. A couple large cups of coffee per day or two to three specific “energy-boosting” products can be all that it takes.
There also are a few large longitudinal studies that have shown a significant association between increased caffeine consumption and future problems with anger, aggression, risky sexual behavior, and substance use. Energy drinks, which can deliver a lot of caffeine quickly, were singled out as particularly problematic in some of these studies, although these naturalistic studies are unable to determine causation, and it also is possible that teens who are already prone towards behavioral problems tend to consume more caffeine. However, the review also mentions animal studies that have demonstrated that caffeine may prime the brain to use other substances like amphetamines or cocaine. Finally, another concern raised about energy drinks in particular is that they also often contain other substances which may have similar physiological effects but are relatively untested when it comes to safety.
Conclusions
This review, like the current position of the Food and Drug Administration, considers caffeine as generally safe at low doses because there does not appear to be much evidence that low or moderate use in youth leads to significant problems. The conclusion changes, however, with higher levels of consumption, as more frequent and more serious risks are encountered. The article recommends that both parents and doctors be more vigilant in monitoring the amount of caffeine that a child consumes as well as the timing of that use during the day. Some quick calculations can be done to give adolescents and their parents an estimate of their caffeine use in milligrams. And while caffeine may not rise to the level of public health concern as substances like opiates or alcohol, there is evidence that it can cause some real problems in children and teens, especially in higher amounts, and thus shouldn’t be given a total pass by parents and doctors alike.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at pdnews@mdedge.com. Follow him on Twitter @PediPsych. Looking for more mental health training? Attend the 13th annual Child Psychiatry in Primary Care conference in Burlington, Vt., May 3, 2019 (http://www.med.uvm.edu/cme/conferences).
Less clinical attention has been paid to caffeine lately as the medical community works to overcome the negative effects of substances such as opiates and cannabis. Quietly, however, caffeine continues to be widely consumed among children and adolescents, and its use often flies under the radar for pediatricians who have so many other topics to address. To help clinicians decide whether more focus on caffeine use is needed, a review was published in the Journal of the American Academy of Child & Adolescent Psychiatry (2019;58[1]:36-45). A synopsis of this paper which summarizes 90 individual studies on caffeine use in children and adolescents is provided here.
Caffeine usage in children and adolescents
Caffeine continues to be one of the most commonly used substances in youth, with about 75% of older children and adolescents consuming it regularly, often at an average dose of about 25 mg/day for children aged 6-11 years and 50 mg/day for adolescents. Because most people have trouble quickly converting commonly used products into milligrams of caffeine, the following guide can be useful:
- Soda (12 oz). About 40 mg caffeine.
- Coffee (8 oz). About 100 mg caffeine.
- Tea (8 oz). About 48 mg caffeine.
- Energy drinks (12 oz). About 150 mg caffeine plus, with 5-Hour Energy being around 215 mg caffeine, according to a Consumer Reports study.
It is important to pay attention to the serving size, as the actual volume consumed of products like coffee or soft drinks often are much higher.
With regards to caffeine trends over time, a surprising observation is that total caffeine consumption among youth over the past decade or so looks relatively flat and may even be decreasing. This trend has occurred despite the aggressive marketing to youth of many energy drinks that contain high amounts of caffeine. In many ways, the pattern of caffeine use fits with what we know about substance use in general in adolescents, with rates dropping for many commonly used substances – with the exception of cannabis.
Effects of caffeine
As many know, caffeine is a stimulant and is known to increase arousal, alertness, and amount of motor behavior. While many youth drink caffeine in an effort to improve cognitive performance, the evidence that it does so directly is modest. There are some studies that show improvements on some cognitive tests when children take moderate doses of caffeine, but these effects tend to be most pronounced for kids who are more naive to caffeine at baseline. Of course, caffeine also can temporarily reduce feelings of fatigue and sleepiness.
Anecdotally, many youth and parents will report that caffeine is a way to “self-medicate” various symptoms of ADHD. While many will report some benefit, there is a surprising lack of rigorous data about the effects of caffeine for youth who meet criteria for ADHD, according to this review.
There also are some well-known negative effects of caffeine use. One of the most important ones is that caffeine can interfere with sleep onset, thereby inducing a cycle that reinforces more caffeine use in the day in an effort to compensate for poor sleep at night. A less obvious negative effect that has been documented is that caffeine added to sweetened beverages can increase consumption of similar sugary foods, even if they don’t have caffeine.
A number of adverse effects have been observed when youth consume caffeine at excessive doses, which tend to be around a threshold of 400 mg/day for teens and about 100 mg/day for younger children. These can include both behavioral and nonbehavioral changes such as agitation or irritability, anxiety, heart arrhythmias, and hypertension. Concern over high caffeine intake also was raised in relation to a number of cases of sudden death, although these events fortunately are rare. The review mentions that one factor that could increase the risk of a serious medical event related to caffeine use is the presence of an underlying cardiac problem which may go undetected until a negative outcome occurs. In thinking about these risks associated with “excessive” caffeine consumption, it can be important to go back to the guides and see just how easily an adolescent can get to a level of 400 mg or more. A couple large cups of coffee per day or two to three specific “energy-boosting” products can be all that it takes.
There also are a few large longitudinal studies that have shown a significant association between increased caffeine consumption and future problems with anger, aggression, risky sexual behavior, and substance use. Energy drinks, which can deliver a lot of caffeine quickly, were singled out as particularly problematic in some of these studies, although these naturalistic studies are unable to determine causation, and it also is possible that teens who are already prone towards behavioral problems tend to consume more caffeine. However, the review also mentions animal studies that have demonstrated that caffeine may prime the brain to use other substances like amphetamines or cocaine. Finally, another concern raised about energy drinks in particular is that they also often contain other substances which may have similar physiological effects but are relatively untested when it comes to safety.
Conclusions
This review, like the current position of the Food and Drug Administration, considers caffeine as generally safe at low doses because there does not appear to be much evidence that low or moderate use in youth leads to significant problems. The conclusion changes, however, with higher levels of consumption, as more frequent and more serious risks are encountered. The article recommends that both parents and doctors be more vigilant in monitoring the amount of caffeine that a child consumes as well as the timing of that use during the day. Some quick calculations can be done to give adolescents and their parents an estimate of their caffeine use in milligrams. And while caffeine may not rise to the level of public health concern as substances like opiates or alcohol, there is evidence that it can cause some real problems in children and teens, especially in higher amounts, and thus shouldn’t be given a total pass by parents and doctors alike.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at pdnews@mdedge.com. Follow him on Twitter @PediPsych. Looking for more mental health training? Attend the 13th annual Child Psychiatry in Primary Care conference in Burlington, Vt., May 3, 2019 (http://www.med.uvm.edu/cme/conferences).
Meth’s resurgence spotlights lack of meds to combat the addiction
In 2016, news reports warned the public of an opioid epidemic gripping the nation.
But Madeline Vaughn, then a lead clinical intake coordinator at the Houston-based addiction treatment organization Council on Recovery, sensed something different was going on with the patients she checked in from the street.
Their behavior, marked by twitchy suspicion, a poor memory, and the feeling that someone was following them, signaled that the people coming through the center’s doors were increasingly hooked on a different drug: methamphetamine.
“When you’re in the boots on the ground,” Ms. Vaughn said, “what you see may surprise you, because it’s not in the headlines.”
In the time since, it’s become increasingly clear that, even as the opioid epidemic continues, the toll of methamphetamine use, also known as meth or crystal meth, is on the rise, too.
The rate of overdose deaths involving the stimulant more than tripled from 2011 to 2016, the Centers for Disease Control and Prevention reported.
But unlike the opioid epidemic – for which medications exist to help combat addiction – medical providers have few such tools to help methamphetamine users survive and recover. A drug such as naloxone, which can reverse an opioid overdose, does not exist for meth. And there are no drugs approved by the Food and Drug Administration that can treat a meth addiction.
“We’re realizing that we don’t have everything we might wish we had to address these different kinds of drugs,” said Margaret Jarvis, MD, a psychiatrist and distinguished fellow for the American Society of Addiction Medicine.
Meth revs up the human body, causing euphoria, elevated blood pressure, and energy that enables users to go for days without sleeping or eating. In some cases, long-term use alters the user’s brain and causes psychotic symptoms that can take up to one year after the person has stopped using it to dissipate.
Overdosing can trigger heart attacks, strokes, and seizures, which can make pinpointing the drug’s involvement difficult.
Meth users also tend to abuse other substances, which complicates first responders’ efforts to treat a patient in the event of an overdose, said David Persse, MD, EMS physician director for Houston. With multiple drugs in a patient’s system, overdose symptoms may not neatly fit under the description for one substance.
“If we had five or six miracle drugs,” Dr. Persse said, to use immediately on the scene of the overdose, “it’s still gonna be difficult to know which one that patient needs.”
Research is underway to develop a medication that helps those with methamphetamine addiction overcome their condition. The National Institute on Drug Abuse Clinical Trials Network is testing a combination of naltrexone, a medication typically used to treat opioid and alcohol use disorders, and an antidepressant called bupropion.
And a team from the Universities of Kentucky and Arkansas created a molecule called lobeline that shows promise in blocking meth’s effects in the brain.
For now, though, existing treatments, such as the Matrix Model, a drug counseling technique, and contingency management, which offers patients incentives to stay away from drugs, are key options for what appears to be a meth resurgence, said Dr. Jarvis.
Illegal drugs never disappear from the street, she said. Their popularity waxes and wanes with demand. And as the demand for methamphetamine use increases, the gaps in treatment become more apparent.
Dr. Persse said he hasn’t seen a rise in the number of calls related to methamphetamine overdoses in his area. However, the death toll in Texas from meth now exceeds that of heroin.
Provisional death counts for 2017 showed methamphetamine claimed 813 lives in the Lone Star State. By comparison, 591 people died because of heroin.
The Drug Enforcement Administration reported that the price of meth is the lowest the agency has seen in years. It is increasingly available in the eastern region of the United States. Primary suppliers are Mexican drug cartels. And the meth on the streets is now more than 90% pure.
“The new methods [of making methamphetamine] have really altered the potency,” said Jane Maxwell, PhD, research professor at the University of Texas at Austin’s social work school. “So the meth we’re looking at today is much more potent than it was 10 years ago.”
For Ms. Vaughn, who works as an outpatient therapist and treatment coordinator, these variables are a regular part of her daily challenge. So until the research arms her with something new, her go-to strategy is to use the available tools to tackle her patients’ methamphetamine addiction in layers.
She starts with writing assignments, then coping skills until they are capable of unpacking their trauma. Addiction is rarely the sole demon patients wrestle with, Ms. Vaughn said.
“Substance use is often a symptom for what’s really going on with someone,” she said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
In 2016, news reports warned the public of an opioid epidemic gripping the nation.
But Madeline Vaughn, then a lead clinical intake coordinator at the Houston-based addiction treatment organization Council on Recovery, sensed something different was going on with the patients she checked in from the street.
Their behavior, marked by twitchy suspicion, a poor memory, and the feeling that someone was following them, signaled that the people coming through the center’s doors were increasingly hooked on a different drug: methamphetamine.
“When you’re in the boots on the ground,” Ms. Vaughn said, “what you see may surprise you, because it’s not in the headlines.”
In the time since, it’s become increasingly clear that, even as the opioid epidemic continues, the toll of methamphetamine use, also known as meth or crystal meth, is on the rise, too.
The rate of overdose deaths involving the stimulant more than tripled from 2011 to 2016, the Centers for Disease Control and Prevention reported.
But unlike the opioid epidemic – for which medications exist to help combat addiction – medical providers have few such tools to help methamphetamine users survive and recover. A drug such as naloxone, which can reverse an opioid overdose, does not exist for meth. And there are no drugs approved by the Food and Drug Administration that can treat a meth addiction.
“We’re realizing that we don’t have everything we might wish we had to address these different kinds of drugs,” said Margaret Jarvis, MD, a psychiatrist and distinguished fellow for the American Society of Addiction Medicine.
Meth revs up the human body, causing euphoria, elevated blood pressure, and energy that enables users to go for days without sleeping or eating. In some cases, long-term use alters the user’s brain and causes psychotic symptoms that can take up to one year after the person has stopped using it to dissipate.
Overdosing can trigger heart attacks, strokes, and seizures, which can make pinpointing the drug’s involvement difficult.
Meth users also tend to abuse other substances, which complicates first responders’ efforts to treat a patient in the event of an overdose, said David Persse, MD, EMS physician director for Houston. With multiple drugs in a patient’s system, overdose symptoms may not neatly fit under the description for one substance.
“If we had five or six miracle drugs,” Dr. Persse said, to use immediately on the scene of the overdose, “it’s still gonna be difficult to know which one that patient needs.”
Research is underway to develop a medication that helps those with methamphetamine addiction overcome their condition. The National Institute on Drug Abuse Clinical Trials Network is testing a combination of naltrexone, a medication typically used to treat opioid and alcohol use disorders, and an antidepressant called bupropion.
And a team from the Universities of Kentucky and Arkansas created a molecule called lobeline that shows promise in blocking meth’s effects in the brain.
For now, though, existing treatments, such as the Matrix Model, a drug counseling technique, and contingency management, which offers patients incentives to stay away from drugs, are key options for what appears to be a meth resurgence, said Dr. Jarvis.
Illegal drugs never disappear from the street, she said. Their popularity waxes and wanes with demand. And as the demand for methamphetamine use increases, the gaps in treatment become more apparent.
Dr. Persse said he hasn’t seen a rise in the number of calls related to methamphetamine overdoses in his area. However, the death toll in Texas from meth now exceeds that of heroin.
Provisional death counts for 2017 showed methamphetamine claimed 813 lives in the Lone Star State. By comparison, 591 people died because of heroin.
The Drug Enforcement Administration reported that the price of meth is the lowest the agency has seen in years. It is increasingly available in the eastern region of the United States. Primary suppliers are Mexican drug cartels. And the meth on the streets is now more than 90% pure.
“The new methods [of making methamphetamine] have really altered the potency,” said Jane Maxwell, PhD, research professor at the University of Texas at Austin’s social work school. “So the meth we’re looking at today is much more potent than it was 10 years ago.”
For Ms. Vaughn, who works as an outpatient therapist and treatment coordinator, these variables are a regular part of her daily challenge. So until the research arms her with something new, her go-to strategy is to use the available tools to tackle her patients’ methamphetamine addiction in layers.
She starts with writing assignments, then coping skills until they are capable of unpacking their trauma. Addiction is rarely the sole demon patients wrestle with, Ms. Vaughn said.
“Substance use is often a symptom for what’s really going on with someone,” she said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
In 2016, news reports warned the public of an opioid epidemic gripping the nation.
But Madeline Vaughn, then a lead clinical intake coordinator at the Houston-based addiction treatment organization Council on Recovery, sensed something different was going on with the patients she checked in from the street.
Their behavior, marked by twitchy suspicion, a poor memory, and the feeling that someone was following them, signaled that the people coming through the center’s doors were increasingly hooked on a different drug: methamphetamine.
“When you’re in the boots on the ground,” Ms. Vaughn said, “what you see may surprise you, because it’s not in the headlines.”
In the time since, it’s become increasingly clear that, even as the opioid epidemic continues, the toll of methamphetamine use, also known as meth or crystal meth, is on the rise, too.
The rate of overdose deaths involving the stimulant more than tripled from 2011 to 2016, the Centers for Disease Control and Prevention reported.
But unlike the opioid epidemic – for which medications exist to help combat addiction – medical providers have few such tools to help methamphetamine users survive and recover. A drug such as naloxone, which can reverse an opioid overdose, does not exist for meth. And there are no drugs approved by the Food and Drug Administration that can treat a meth addiction.
“We’re realizing that we don’t have everything we might wish we had to address these different kinds of drugs,” said Margaret Jarvis, MD, a psychiatrist and distinguished fellow for the American Society of Addiction Medicine.
Meth revs up the human body, causing euphoria, elevated blood pressure, and energy that enables users to go for days without sleeping or eating. In some cases, long-term use alters the user’s brain and causes psychotic symptoms that can take up to one year after the person has stopped using it to dissipate.
Overdosing can trigger heart attacks, strokes, and seizures, which can make pinpointing the drug’s involvement difficult.
Meth users also tend to abuse other substances, which complicates first responders’ efforts to treat a patient in the event of an overdose, said David Persse, MD, EMS physician director for Houston. With multiple drugs in a patient’s system, overdose symptoms may not neatly fit under the description for one substance.
“If we had five or six miracle drugs,” Dr. Persse said, to use immediately on the scene of the overdose, “it’s still gonna be difficult to know which one that patient needs.”
Research is underway to develop a medication that helps those with methamphetamine addiction overcome their condition. The National Institute on Drug Abuse Clinical Trials Network is testing a combination of naltrexone, a medication typically used to treat opioid and alcohol use disorders, and an antidepressant called bupropion.
And a team from the Universities of Kentucky and Arkansas created a molecule called lobeline that shows promise in blocking meth’s effects in the brain.
For now, though, existing treatments, such as the Matrix Model, a drug counseling technique, and contingency management, which offers patients incentives to stay away from drugs, are key options for what appears to be a meth resurgence, said Dr. Jarvis.
Illegal drugs never disappear from the street, she said. Their popularity waxes and wanes with demand. And as the demand for methamphetamine use increases, the gaps in treatment become more apparent.
Dr. Persse said he hasn’t seen a rise in the number of calls related to methamphetamine overdoses in his area. However, the death toll in Texas from meth now exceeds that of heroin.
Provisional death counts for 2017 showed methamphetamine claimed 813 lives in the Lone Star State. By comparison, 591 people died because of heroin.
The Drug Enforcement Administration reported that the price of meth is the lowest the agency has seen in years. It is increasingly available in the eastern region of the United States. Primary suppliers are Mexican drug cartels. And the meth on the streets is now more than 90% pure.
“The new methods [of making methamphetamine] have really altered the potency,” said Jane Maxwell, PhD, research professor at the University of Texas at Austin’s social work school. “So the meth we’re looking at today is much more potent than it was 10 years ago.”
For Ms. Vaughn, who works as an outpatient therapist and treatment coordinator, these variables are a regular part of her daily challenge. So until the research arms her with something new, her go-to strategy is to use the available tools to tackle her patients’ methamphetamine addiction in layers.
She starts with writing assignments, then coping skills until they are capable of unpacking their trauma. Addiction is rarely the sole demon patients wrestle with, Ms. Vaughn said.
“Substance use is often a symptom for what’s really going on with someone,” she said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Cardiac failure due to left atrial angiosarcoma
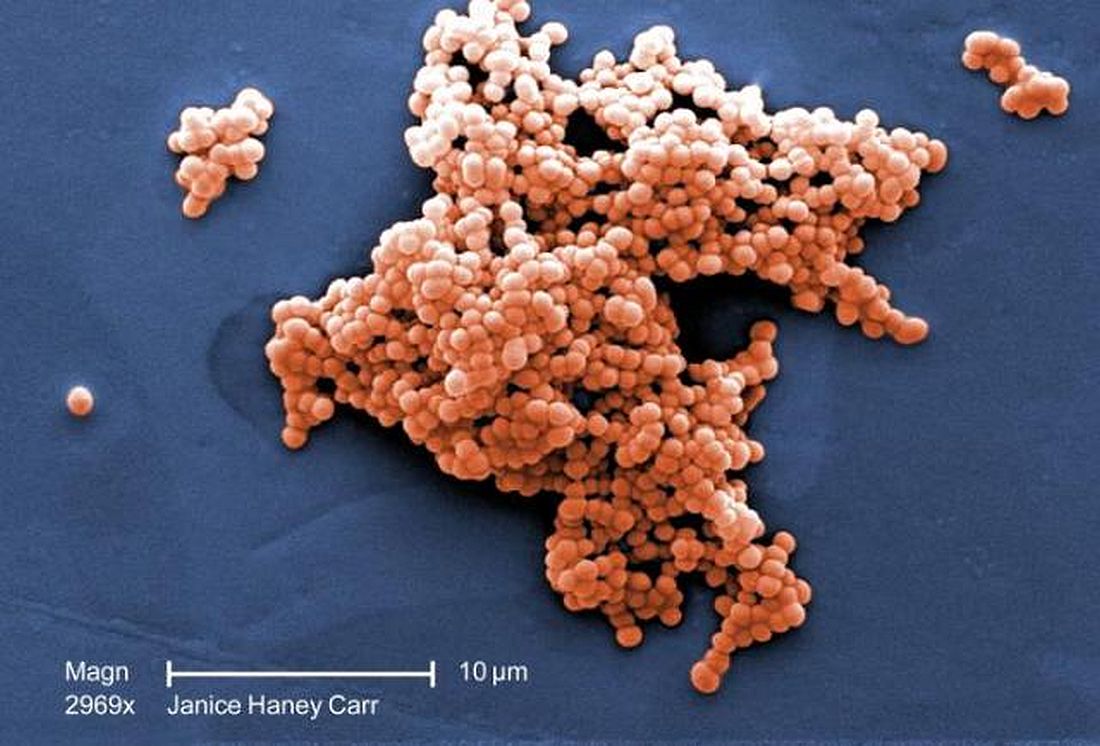
Incidence of late-onset GBS cases are higher than early-onset disease
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
Perinatal group B Streptococcus (GBS) disease prevention guidelines are credited for the low rate of early-onset disease (EOD) cases of GBS in the United States, but the practice of intrapartum antibiotic prophylaxis (IAP) remains controversial in places like the United Kingdom where the National Health Service does not recommend screening-based IAP for GBS, Sagori Mukhopadhyay, MD, MMSc, and Karen M. Puopolo, MD, PhD, wrote in a related editorial.
One reason for concern about GBS IAP policies is that, despite the decreased number of EOD cases after implementation of IAP, the rate of late-onset disease (LOD) cases remain the same, the authors wrote. And implementation of IAP is not perfect: In some cases IAP was used for less than the recommended duration, used less effective drugs, or given too late so fetal infections were already established.
In addition, some may be uncomfortable with increased perinatal exposure to antibiotics – “a long-held concern about the extent to which widespread perinatal antibiotic use may contribute to the emergence and expansion of antibiotic-resistant GBS,” they added. However, despite the concern, the fatality ratio for EOD was 7% in the study by Nanduri et al., and one complication of GBS in survivors is neurodevelopmental impairment, according to a meta-analysis of 18 studies.
One solution that could address both EOD and LOD cases of GBS is the development of a GBS vaccine. Although there is reluctance to vaccinate pregnant women, recent studies have shown success in vaccinating women for influenza, tetanus, diphtheria, and pertussis; these recent efforts have “reinvigorated” academia’s interest in vaccine research for this population.
“Vaccination certainly could be a first step to eliminating neonatal GBS disease in the United States and may be the only available approach to addressing the substantial international burden of GBS-associated stillbirth, preterm birth, and neonatal disease morbidity and mortality,” the authors wrote. “But for now, while GBS IAP may be imperfect, it is the success we have.”
Dr. Mukhopadhyay and Dr. Puopolo are from the division of neonatology at the Children’s Hospital of Philadelphia. Dr. Mukhopadhyay and Dr. Puopolo commented on the study by Nanduri et al. in an accompanying editorial (Mukhopadhyay et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2018.4824). They reported no relevant conflicts of interest.
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
according to a multistate study of invasive group B streptococcal disease published in JAMA Pediatrics.
Using data from the Active Bacterial Core surveillance (ABCs) program, Srinivas Acharya Nanduri, MD, MPH, at the Centers for Disease Control and Prevention, and colleagues performed an analysis of early-onset disease (EOD) and late-onset disease (LOD) cases of group B Streptococcus (GBS) in infants from 10 different states between 2006 and 2015, and whether mothers of infants with EOD received intrapartum antibiotic prophylaxis (IAP). EOD was defined as between 0 and 6 days old, while LOD occurred between 7 days and 89 days old.
They found 1,277 cases of EOD and 1,387 cases of LOD in total, with a decrease in incidence of EOD from 0.37 per 1,000 live births in 2006 to 0.23 per 1,000 live births in 2015 (P less than .001); LOD incidence remained stable at a mean 0.31 per 1,000 live births during the same time period.
In 2015, the national burden for EOD and LOD was estimated at 840 and 1,265 cases, respectively. Mothers of infants with EOD did not have indications for and did not receive IAP in 617 cases (48%) and did not receive IAP despite indications in 278 (22%) cases.
“While the current culture-based screening strategy has been highly successful in reducing EOD burden, our data show that almost half of remaining infants with EOD were born to mothers with no indication for receiving IAP,” Dr. Nanduri and colleagues wrote.
Because there currently is no effective prevention strategy against LOS GBS, the investigators wrote that a maternal vaccine against the most common serotypes “holds promise to prevent a substantial portion of this remaining burden,” and noted several GBS candidate vaccines were in advanced stages of development.
The researchers also looked at GBS serotype data in 1,743 patients from seven different centers. The most commonly found serotype isolates of 887 EOD cases were Ia (242 cases, 27%) and III (242 cases, 27%) overall. Serotype III was most common for LOD cases (481 cases, 56%) and increased in incidence from 0.12 per 1,000 live births to 0.20 per 1,000 live births during the study period (P less than .001), while serotype IV was responsible for 53 cases (6%) of both EOD and LOD.
Dr. Nanduri and associates wrote that over 99% of the serotyped EOD (881 cases) and serotyped LOD (853 cases) cases were caused by serotypes Ia, Ib, II, III, IV, and V. With regard to antimicrobial resistance, there were no cases of beta-lactam resistance, but there was constitutive clindamycin resistance in 359 isolate test results (21%).
The researchers noted that they were limited in the study by 1 year of whole-genome sequencing data, the ABCs capturing only 10% of live birth data in the United States, and conclusions on EOD prevention restricted to data from labor and delivery records.
This study was funded in part by the CDC. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
SOURCE: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
FROM JAMA PEDIATRICS
Key clinical point: Between 2006 and 2015, early-onset disease cases of group B Streptococcus (GBS) declined, while the incidence of late-onset cases did not change.
Major finding: The rate of early-onset GBS declined from 0.37 to 0.23 per 1,000 live births and the rate of late-onset GBS cases remained at a mean 0.31 per 1,000 live births.
Study details: A population-based study of infants with early-onset disease and late-onset disease GBS from 10 different states in the Active Bacterial Core surveillance program between 2006 and 2015.
Disclosures: This study was funded in part by the Centers for Disease Control and Prevention. Paula S. Vagnone received grants from the CDC, while William S. Schaffner, MD, received grants from the CDC and personal fees from Pfizer, Merck, SutroVax, Shionogi, Dynavax, and Seqirus outside of the study. The other authors reported no relevant disclosures.
Source: Nanduri SA et al. JAMA Pediatr. 2019 Jan 14. doi: 10.1001/jamapediatrics.2018.4826.
VTE prophylaxis often overused in low-risk patients
Background: Per Chest guidelines, VTE prophylaxis is recommended for hospitalized patients at increased risk for VTE but is not recommended for low-risk patients. Risk stratification can be guided by the Padua Prediction Score to categorize patients.
Study design: Multicenter observational study.
Setting: A total of 52 U.S. hospitals (Michigan Hospital Medicine Safety Consortium database).
Synopsis: Patients admitted during Jan. 1, 2015–Dec. 21, 2016, to 52 non–intensive care medical units for 2 or more days were analyzed and stratified as high or low risk for VTE using the Padua Prediction Score. Excessive VTE prophylaxis was defined as low-risk patients prescribed pharmacologic or mechanical prophylaxis, high-risk patients receiving therapy despite a contraindication to prophylaxis, or any patient who received both mechanical and pharmacologic therapy. Underuse of VTE prophylaxis included high-risk patients who did not receive pharmacologic or mechanical prophylaxis. Of the 44,775 patients included in the study, 32,549 were low risk, and 77.9% (25,369 patients) received excessive VTE prophylaxis. Overtreatment also was present in high-risk patients with and without a contraindication to VTE prophylaxis (26.9% and 32.3%, respectively). Underuse of VTE prophylaxis occurred in 2,693 high-risk patients (22%).
Bottom line: Patients who are at low risk for VTE by Padua Prediction Score often are prescribed pharmacologic or mechanical prophylaxis that may be unnecessary. Overuse of VTE prophylaxis was more common than is underuse.
Citation: Grant PJ et al. Use of venous thromboembolism prophylaxis in hospitalized patients. JAMA Intern Med. 2018 Aug 1;178(8):1122-4. Published online May 21, 2018.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Background: Per Chest guidelines, VTE prophylaxis is recommended for hospitalized patients at increased risk for VTE but is not recommended for low-risk patients. Risk stratification can be guided by the Padua Prediction Score to categorize patients.
Study design: Multicenter observational study.
Setting: A total of 52 U.S. hospitals (Michigan Hospital Medicine Safety Consortium database).
Synopsis: Patients admitted during Jan. 1, 2015–Dec. 21, 2016, to 52 non–intensive care medical units for 2 or more days were analyzed and stratified as high or low risk for VTE using the Padua Prediction Score. Excessive VTE prophylaxis was defined as low-risk patients prescribed pharmacologic or mechanical prophylaxis, high-risk patients receiving therapy despite a contraindication to prophylaxis, or any patient who received both mechanical and pharmacologic therapy. Underuse of VTE prophylaxis included high-risk patients who did not receive pharmacologic or mechanical prophylaxis. Of the 44,775 patients included in the study, 32,549 were low risk, and 77.9% (25,369 patients) received excessive VTE prophylaxis. Overtreatment also was present in high-risk patients with and without a contraindication to VTE prophylaxis (26.9% and 32.3%, respectively). Underuse of VTE prophylaxis occurred in 2,693 high-risk patients (22%).
Bottom line: Patients who are at low risk for VTE by Padua Prediction Score often are prescribed pharmacologic or mechanical prophylaxis that may be unnecessary. Overuse of VTE prophylaxis was more common than is underuse.
Citation: Grant PJ et al. Use of venous thromboembolism prophylaxis in hospitalized patients. JAMA Intern Med. 2018 Aug 1;178(8):1122-4. Published online May 21, 2018.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Background: Per Chest guidelines, VTE prophylaxis is recommended for hospitalized patients at increased risk for VTE but is not recommended for low-risk patients. Risk stratification can be guided by the Padua Prediction Score to categorize patients.
Study design: Multicenter observational study.
Setting: A total of 52 U.S. hospitals (Michigan Hospital Medicine Safety Consortium database).
Synopsis: Patients admitted during Jan. 1, 2015–Dec. 21, 2016, to 52 non–intensive care medical units for 2 or more days were analyzed and stratified as high or low risk for VTE using the Padua Prediction Score. Excessive VTE prophylaxis was defined as low-risk patients prescribed pharmacologic or mechanical prophylaxis, high-risk patients receiving therapy despite a contraindication to prophylaxis, or any patient who received both mechanical and pharmacologic therapy. Underuse of VTE prophylaxis included high-risk patients who did not receive pharmacologic or mechanical prophylaxis. Of the 44,775 patients included in the study, 32,549 were low risk, and 77.9% (25,369 patients) received excessive VTE prophylaxis. Overtreatment also was present in high-risk patients with and without a contraindication to VTE prophylaxis (26.9% and 32.3%, respectively). Underuse of VTE prophylaxis occurred in 2,693 high-risk patients (22%).
Bottom line: Patients who are at low risk for VTE by Padua Prediction Score often are prescribed pharmacologic or mechanical prophylaxis that may be unnecessary. Overuse of VTE prophylaxis was more common than is underuse.
Citation: Grant PJ et al. Use of venous thromboembolism prophylaxis in hospitalized patients. JAMA Intern Med. 2018 Aug 1;178(8):1122-4. Published online May 21, 2018.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Phone etiquette, part 2
My recent column on proper telephone technique for front office employees triggered some interesting commentary. “What about the calls we take?” someone asked. “.”
How true! Haven’t we all answered a call from another physician, only to hear, “Please hold for Dr. ___________”?
Let’s begin with that, since it’s one of my major pet peeves: Long tradition, and common courtesy, dictate that the person initiating a call be on the line when the recipient picks up the receiver. So don’t ask an assistant to dial calls for you. Is it really that much bother to do it yourself? A peer should never answer and then be expected to wait while your employee tracks you down. It is impolite, and implies that you consider your time much more valuable than his or hers.
Speaking of common courtesy: Always give callers your undivided attention; they can tell if you are distracted. If it’s not a good time for you, say so honestly, at the outset. “Listen, I can give you a couple of minutes, but I’m right in the middle of office hours ...” That’s much more polite than abruptly cutting someone off, mid-conversation. If the caller needs more time, offer to call back.
By the same token, if you are the caller, be sure to ask, “Is this a good time for you?” Then, be aware of how long you keep the other person on the line. We all have a finite amount of time, and not everyone knows how to end a phone conversation gracefully. Respect others’ time and get to your point quickly.
When you reach an answering machine or voice mail, talk clearly and distinctly. Few things are more frustrating than a mumbled message that no one can decipher. I always repeat my name and phone number for clarity’s sake. And please don’t leave a callback number that no one answers, or that automatically rejects all unidentified callers.
Mobile phones have become so ubiquitous, it is hard to believe that they were relatively scarce only 15 years ago. A distinct set of faux pas has evolved around them; for example, few things are less professional than a loud, indiscreet, annoying, or profane ring tone. Your recorded voice mail message needs to sound professional too – especially if patients will be hearing it.
It should be obvious that cell phones be turned off in theaters and during meetings, but many still remain on. Vibrate mode doesn’t count; anyone close by will still hear it, and you’ll be tempted to answer it. If you get a call during a movie or show, or at a meeting, and you absolutely have to answer it, quietly excuse yourself, and don’t take the call until you are alone. If you miss the call, you can always call the person back.
Answering phone calls in a restaurant is my wife’s biggest pet peeve. She says it is rude and inappropriate, and she’s right – yet it is now, arguably, the most common etiquette mistake. Never take calls (or worse, answer texts or emails) while seated at the table – which leads to another issue: Don’t put your phone on the table! You can hear it just fine from your purse or pocket; and putting it on the table implies to your companions that you are looking for something – anything – more interesting than their company. If you must take a call or read a message, excuse yourself and go to a private area.
In fact, you shouldn’t answer any nonemergent calls or texts when you are with others; it makes your friends and colleagues feel unimportant and ignored. The people you are with should always take precedence over your phone, unless it is a medical emergency or otherwise extremely urgent. On those rare occasions when it is, be polite: “Do you mind if I take this call? It’s important.” Then, once again, excuse yourself to answer privately.
One final thought: Don’t walk around wearing one of those wireless Bluetooth earpieces on your ear, as if the Governor might call at any moment. Everyone around you has to guess whether you’re addressing them or some unseen caller; and frankly – with all respect – it looks ridiculous. And pretentious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
My recent column on proper telephone technique for front office employees triggered some interesting commentary. “What about the calls we take?” someone asked. “.”
How true! Haven’t we all answered a call from another physician, only to hear, “Please hold for Dr. ___________”?
Let’s begin with that, since it’s one of my major pet peeves: Long tradition, and common courtesy, dictate that the person initiating a call be on the line when the recipient picks up the receiver. So don’t ask an assistant to dial calls for you. Is it really that much bother to do it yourself? A peer should never answer and then be expected to wait while your employee tracks you down. It is impolite, and implies that you consider your time much more valuable than his or hers.
Speaking of common courtesy: Always give callers your undivided attention; they can tell if you are distracted. If it’s not a good time for you, say so honestly, at the outset. “Listen, I can give you a couple of minutes, but I’m right in the middle of office hours ...” That’s much more polite than abruptly cutting someone off, mid-conversation. If the caller needs more time, offer to call back.
By the same token, if you are the caller, be sure to ask, “Is this a good time for you?” Then, be aware of how long you keep the other person on the line. We all have a finite amount of time, and not everyone knows how to end a phone conversation gracefully. Respect others’ time and get to your point quickly.
When you reach an answering machine or voice mail, talk clearly and distinctly. Few things are more frustrating than a mumbled message that no one can decipher. I always repeat my name and phone number for clarity’s sake. And please don’t leave a callback number that no one answers, or that automatically rejects all unidentified callers.
Mobile phones have become so ubiquitous, it is hard to believe that they were relatively scarce only 15 years ago. A distinct set of faux pas has evolved around them; for example, few things are less professional than a loud, indiscreet, annoying, or profane ring tone. Your recorded voice mail message needs to sound professional too – especially if patients will be hearing it.
It should be obvious that cell phones be turned off in theaters and during meetings, but many still remain on. Vibrate mode doesn’t count; anyone close by will still hear it, and you’ll be tempted to answer it. If you get a call during a movie or show, or at a meeting, and you absolutely have to answer it, quietly excuse yourself, and don’t take the call until you are alone. If you miss the call, you can always call the person back.
Answering phone calls in a restaurant is my wife’s biggest pet peeve. She says it is rude and inappropriate, and she’s right – yet it is now, arguably, the most common etiquette mistake. Never take calls (or worse, answer texts or emails) while seated at the table – which leads to another issue: Don’t put your phone on the table! You can hear it just fine from your purse or pocket; and putting it on the table implies to your companions that you are looking for something – anything – more interesting than their company. If you must take a call or read a message, excuse yourself and go to a private area.
In fact, you shouldn’t answer any nonemergent calls or texts when you are with others; it makes your friends and colleagues feel unimportant and ignored. The people you are with should always take precedence over your phone, unless it is a medical emergency or otherwise extremely urgent. On those rare occasions when it is, be polite: “Do you mind if I take this call? It’s important.” Then, once again, excuse yourself to answer privately.
One final thought: Don’t walk around wearing one of those wireless Bluetooth earpieces on your ear, as if the Governor might call at any moment. Everyone around you has to guess whether you’re addressing them or some unseen caller; and frankly – with all respect – it looks ridiculous. And pretentious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
My recent column on proper telephone technique for front office employees triggered some interesting commentary. “What about the calls we take?” someone asked. “.”
How true! Haven’t we all answered a call from another physician, only to hear, “Please hold for Dr. ___________”?
Let’s begin with that, since it’s one of my major pet peeves: Long tradition, and common courtesy, dictate that the person initiating a call be on the line when the recipient picks up the receiver. So don’t ask an assistant to dial calls for you. Is it really that much bother to do it yourself? A peer should never answer and then be expected to wait while your employee tracks you down. It is impolite, and implies that you consider your time much more valuable than his or hers.
Speaking of common courtesy: Always give callers your undivided attention; they can tell if you are distracted. If it’s not a good time for you, say so honestly, at the outset. “Listen, I can give you a couple of minutes, but I’m right in the middle of office hours ...” That’s much more polite than abruptly cutting someone off, mid-conversation. If the caller needs more time, offer to call back.
By the same token, if you are the caller, be sure to ask, “Is this a good time for you?” Then, be aware of how long you keep the other person on the line. We all have a finite amount of time, and not everyone knows how to end a phone conversation gracefully. Respect others’ time and get to your point quickly.
When you reach an answering machine or voice mail, talk clearly and distinctly. Few things are more frustrating than a mumbled message that no one can decipher. I always repeat my name and phone number for clarity’s sake. And please don’t leave a callback number that no one answers, or that automatically rejects all unidentified callers.
Mobile phones have become so ubiquitous, it is hard to believe that they were relatively scarce only 15 years ago. A distinct set of faux pas has evolved around them; for example, few things are less professional than a loud, indiscreet, annoying, or profane ring tone. Your recorded voice mail message needs to sound professional too – especially if patients will be hearing it.
It should be obvious that cell phones be turned off in theaters and during meetings, but many still remain on. Vibrate mode doesn’t count; anyone close by will still hear it, and you’ll be tempted to answer it. If you get a call during a movie or show, or at a meeting, and you absolutely have to answer it, quietly excuse yourself, and don’t take the call until you are alone. If you miss the call, you can always call the person back.
Answering phone calls in a restaurant is my wife’s biggest pet peeve. She says it is rude and inappropriate, and she’s right – yet it is now, arguably, the most common etiquette mistake. Never take calls (or worse, answer texts or emails) while seated at the table – which leads to another issue: Don’t put your phone on the table! You can hear it just fine from your purse or pocket; and putting it on the table implies to your companions that you are looking for something – anything – more interesting than their company. If you must take a call or read a message, excuse yourself and go to a private area.
In fact, you shouldn’t answer any nonemergent calls or texts when you are with others; it makes your friends and colleagues feel unimportant and ignored. The people you are with should always take precedence over your phone, unless it is a medical emergency or otherwise extremely urgent. On those rare occasions when it is, be polite: “Do you mind if I take this call? It’s important.” Then, once again, excuse yourself to answer privately.
One final thought: Don’t walk around wearing one of those wireless Bluetooth earpieces on your ear, as if the Governor might call at any moment. Everyone around you has to guess whether you’re addressing them or some unseen caller; and frankly – with all respect – it looks ridiculous. And pretentious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Dietary aluminum may trigger IBS
Aluminum ingested in small amounts causes visceral hypersensitivity in rats, suggesting that dietary levels of aluminum may trigger irritable bowel syndrome (IBS) in humans, according to a study published in Cellular and Molecular Gastroenterology and Hepatology.
Rats given oral aluminum exhibited dose-dependent visceral pain along with activation of proteinase-activated receptor-2 (PAR2) and mast cell degranulation, a combination of events that mirror clinical signs and molecular mechanisms of IBS in humans, reported lead author, Nicolas Esquerre, PhD, of Lille Inflammation Research International Center at Université Lille in France, and his colleagues. The study contributes to ongoing research surrounding causes and mechanisms of IBS, which may vary among patients because of disease subsets. These findings suggest that some patients with IBS may benefit from dietary aluminum restriction or chelation therapy.
“[T]he question of the initial trigger [of IBS] still remains unresolved,” the investigators wrote. “A more precise link between food and IBS has been demonstrated for gluten and other wheat proteins, lactose, and nickel, highlighting particular subsets of IBS patients now diagnosed as nonceliac gluten/wheat sensitivity, lactose intolerance, and nickel-allergic contact mucositis,” they added. “Here, we evaluated the effect of aluminum, a common contaminant of food and water, on abdominal pain.”
Aluminum may enter the diet as a food additive, or it may contaminate foods grown in aluminum-rich soil. Other sources of oral exposure include packaging and kitchenware. A previous study showed that most Americans ingest 0.01-1.4 mg/kg of aluminum daily, and 5% ingest 1.58 mg/kg daily (i.e., 95 mg per day for a 60-kg person).
Based on these statistics, rats in the present study received oral aluminum citrate (AlCi) corresponding with three doses of aluminum: 0.5 mg/kg, 1.5 mg/kg, or 3.0 mg/kg. Treatment continued for 30 days, with colorectal distension (CRD) measured on days 2, 4, 8, 15, and 30.
Results showed a dose-dependent relationship between aluminum ingestion and visceral hypersensitivity. Within 2 days, rats receiving 3.0 mg/kg of aluminum exhibited a significantly lower pain threshold, and within 8 days, rats receiving 0.5 mg/kg and 1.5 mg/kg also showed increased visceral hypersensitivity.
After 1 month of treatment, rats receiving 1.5 mg/kg per day demonstrated a 30% increase in pain compared with control animals. In the same group, visceral hypersensitivity began to wane 7 days after cessation of treatment; 4 more weeks were needed to return to baseline. When treatment was restarted, visceral hypersensitivity occurred within 2 days, compared with 8 days upon initial administration. These findings are particularly relevant to some people, as the 1.5-mg/kg dose corresponds with the daily amount of aluminum ingested by 5% of Americans. Similar patterns of response and sensitization were observed in rats ingesting 0.5 mg/kg and 3.0 mg/kg. Female rats were more sensitive to aluminum than were male rats, a sex pattern that mimics human IBS.
Further testing showed that rats treated with zinc citrate (ZnCi) did not exhibit changes to pain threshold, thereby excluding citrate as an aggravating factor. Rat models of noninflammatory and inflammatory colonic hypersensitivity (butyrate enema or intrathecal injection of 25%-50% ethanol in combination with 2,4,6-trinitrobenzenesulfonic acid, respectively) had visceral hypersensitivity similar to that of rats in the 1.5-mg/kg AlCi group.
Testing of colonic tissue from AlCi-treated rats did not reveal inflammatory changes according to a variety of qualifiers, including histology, myeloperoxidase activity, mRNA expression of several inflammatory cytokines, or infiltration of eosinophils or macrophages. Noninflammatory effects of aluminum, however, were found. For instance, treated rats had lower serotonin levels in enteroendocrine cells.
“Enteroendocrine cells are specialized epithelial cells that respond to luminal stimuli by releasing various biologically active compounds,” the investigators wrote. “They regulate several physiological and homeostatic functions of the gastrointestinal tract, such as postprandial secretion, motility, immune responses, and sensory functions. A reduced number of enteroendocrine cells has been observed in the duodenum, ileum, and colon of some patients with IBS.”
In addition to changes in enteroendocrine cells, AlCi-treated rats had greater colonic mast cell degranulation and histamine with upregulation of histidine decarboxylase transcripts, suggesting that aluminum activated mast cells.
To determine the role of mast cell activation in visceral hypersensitivity, rats were given AlCi with cromoglycate, an inhibitor of mast cell degranulation. This treatment reduced mast cell degranulation and visceral pain threshold, compared with AlCi-treated rats not receiving cromoglycate, suggesting that mast cell degranulation is a primary driver of visceral hypersensitivity. This observation was confirmed by a mast cell–deficient mouse strain (Kit W-sh/W-sh), that had a normal number of mast cells incapable of degranulation. Treating the mast cell–deficient mice with AlCi did not induce visceral hypersensitivity, thereby confirming the role of mast cell degranulation.
Along with mast cell degranulation, AlCi treatment led to PAR2 activation. Investigators explored the significance of this finding with PAR2 knockout mice. When treated with AlCi, PAR2 knockout mice showed no increase in visceral hypersensitivity, suggesting that hypersensitivity is dependent on PAR2 activation. Further testing revealed that mast cell–deficient mice (Kit W-sh/W-sh) did not have PAR2 upregulation either, connecting a sequence in which aluminum triggers mast cell degranulation, mast cell degranulation drives PAR2 upregulation, and PAR2 upregulation causes visceral hypersensitivity. The latter two events in this chain – mast cell degranulation and PAR2 upregulation – mirror molecular mechanisms of IBS in humans.
“We speculate that aluminum activates mast cells to release mediators that can increase excitability of nociceptive afferences contributing to the visceral pain phenotype,” the investigators wrote. “Taken together, our results linked aluminum to several mechanisms implicated in IBS pathophysiology, highlighting a possible role for aluminum as a triggering factor in IBS development.”
The investigators suggested that these findings could influence preventive or therapeutic strategies: “Aluminum might be the first identified dietary risk factor for IBS, implying that measures to limit aluminum dietary consumption or to chelate aluminum may represent novel pathways of prevention and treatment of IBS in some susceptible patients,” they wrote.
The study was funded by the European Fund for Regional Economic Development; the Hauts de France Region, Ministère de l’Enseignement Supérieur et de la Recherche (CPER IRENI); and Digestscience (European Research Foundation on Intestinal Diseases and Nutrition).
SOURCE: Esquerre N et al. Cell Mol Gastroenterol Hepatol. 2019 Sep 20. doi: 10.1016/j.jcmgh.2018.09.012.
Irritable bowel syndrome is a chronic functional gastrointestinal disorder, characterized by relapsing/remitting diarrhea, constipation, and visceral pain. IBS afflicts 10%-25% of the population in developed countries.
Despite histologically normal intestinal biopsy specimens, biological signatures of IBS include alterations in intestinal gene expression, increased gut permeability, and changes in gut microbiota composition. Thus, although the cause or causes of IBS are not defined, these and other data highlight the enormous breadth of factors that might play a role in this disorder. Similar alterations also are associated with inflammatory bowel disease (IBD), although the magnitude of changes is typically greater in IBD. Nevertheless, these data suggest that IBS and IBD may share triggers and pathogenetic mechanisms. That prevalence of both IBS and IBD have shown marked increases in incidence, roughly paralleling the modernization of society that accelerated in the mid-20th century, raises the possibility that environmental factors associated with human activity may be a driver of both diseases. Recent findings suggest that aluminum may be one such trigger. While humans have always been exposed to aluminum, the most abundant metal on earth, industrialization has increased the magnitude of exposure owing to the use of aluminum salts as stabilizers in processed foods and the concentration of ground water aluminum in agricultural products. Mimicking estimated average human ingestion of aluminum via administering it orally to rats increases their perception of visceral pain. These results suggest a possible role for increased exposure to aluminum in driving the post–mid-20th-century increased incidence of IBS. Unfortunately, only broad societal estimates of aluminum exposure are available, and aluminum levels are difficult to measure in individuals, making it difficult to epidemiologically investigate the role of aluminum in promoting GI disease in humans. Hence, I submit that levels of aluminum ingestion by humans should be more closely monitored and the potential of aluminum to promote GI disease carefully scrutinized.
Andrew Ted Gewirtz, PhD, distinguished university center professor, Georgia State University’s Institute for Biomedical Sciences’ Center for Inflammation, Immunity and Infection, Atlanta.
Irritable bowel syndrome is a chronic functional gastrointestinal disorder, characterized by relapsing/remitting diarrhea, constipation, and visceral pain. IBS afflicts 10%-25% of the population in developed countries.
Despite histologically normal intestinal biopsy specimens, biological signatures of IBS include alterations in intestinal gene expression, increased gut permeability, and changes in gut microbiota composition. Thus, although the cause or causes of IBS are not defined, these and other data highlight the enormous breadth of factors that might play a role in this disorder. Similar alterations also are associated with inflammatory bowel disease (IBD), although the magnitude of changes is typically greater in IBD. Nevertheless, these data suggest that IBS and IBD may share triggers and pathogenetic mechanisms. That prevalence of both IBS and IBD have shown marked increases in incidence, roughly paralleling the modernization of society that accelerated in the mid-20th century, raises the possibility that environmental factors associated with human activity may be a driver of both diseases. Recent findings suggest that aluminum may be one such trigger. While humans have always been exposed to aluminum, the most abundant metal on earth, industrialization has increased the magnitude of exposure owing to the use of aluminum salts as stabilizers in processed foods and the concentration of ground water aluminum in agricultural products. Mimicking estimated average human ingestion of aluminum via administering it orally to rats increases their perception of visceral pain. These results suggest a possible role for increased exposure to aluminum in driving the post–mid-20th-century increased incidence of IBS. Unfortunately, only broad societal estimates of aluminum exposure are available, and aluminum levels are difficult to measure in individuals, making it difficult to epidemiologically investigate the role of aluminum in promoting GI disease in humans. Hence, I submit that levels of aluminum ingestion by humans should be more closely monitored and the potential of aluminum to promote GI disease carefully scrutinized.
Andrew Ted Gewirtz, PhD, distinguished university center professor, Georgia State University’s Institute for Biomedical Sciences’ Center for Inflammation, Immunity and Infection, Atlanta.
Irritable bowel syndrome is a chronic functional gastrointestinal disorder, characterized by relapsing/remitting diarrhea, constipation, and visceral pain. IBS afflicts 10%-25% of the population in developed countries.
Despite histologically normal intestinal biopsy specimens, biological signatures of IBS include alterations in intestinal gene expression, increased gut permeability, and changes in gut microbiota composition. Thus, although the cause or causes of IBS are not defined, these and other data highlight the enormous breadth of factors that might play a role in this disorder. Similar alterations also are associated with inflammatory bowel disease (IBD), although the magnitude of changes is typically greater in IBD. Nevertheless, these data suggest that IBS and IBD may share triggers and pathogenetic mechanisms. That prevalence of both IBS and IBD have shown marked increases in incidence, roughly paralleling the modernization of society that accelerated in the mid-20th century, raises the possibility that environmental factors associated with human activity may be a driver of both diseases. Recent findings suggest that aluminum may be one such trigger. While humans have always been exposed to aluminum, the most abundant metal on earth, industrialization has increased the magnitude of exposure owing to the use of aluminum salts as stabilizers in processed foods and the concentration of ground water aluminum in agricultural products. Mimicking estimated average human ingestion of aluminum via administering it orally to rats increases their perception of visceral pain. These results suggest a possible role for increased exposure to aluminum in driving the post–mid-20th-century increased incidence of IBS. Unfortunately, only broad societal estimates of aluminum exposure are available, and aluminum levels are difficult to measure in individuals, making it difficult to epidemiologically investigate the role of aluminum in promoting GI disease in humans. Hence, I submit that levels of aluminum ingestion by humans should be more closely monitored and the potential of aluminum to promote GI disease carefully scrutinized.
Andrew Ted Gewirtz, PhD, distinguished university center professor, Georgia State University’s Institute for Biomedical Sciences’ Center for Inflammation, Immunity and Infection, Atlanta.
Aluminum ingested in small amounts causes visceral hypersensitivity in rats, suggesting that dietary levels of aluminum may trigger irritable bowel syndrome (IBS) in humans, according to a study published in Cellular and Molecular Gastroenterology and Hepatology.
Rats given oral aluminum exhibited dose-dependent visceral pain along with activation of proteinase-activated receptor-2 (PAR2) and mast cell degranulation, a combination of events that mirror clinical signs and molecular mechanisms of IBS in humans, reported lead author, Nicolas Esquerre, PhD, of Lille Inflammation Research International Center at Université Lille in France, and his colleagues. The study contributes to ongoing research surrounding causes and mechanisms of IBS, which may vary among patients because of disease subsets. These findings suggest that some patients with IBS may benefit from dietary aluminum restriction or chelation therapy.
“[T]he question of the initial trigger [of IBS] still remains unresolved,” the investigators wrote. “A more precise link between food and IBS has been demonstrated for gluten and other wheat proteins, lactose, and nickel, highlighting particular subsets of IBS patients now diagnosed as nonceliac gluten/wheat sensitivity, lactose intolerance, and nickel-allergic contact mucositis,” they added. “Here, we evaluated the effect of aluminum, a common contaminant of food and water, on abdominal pain.”
Aluminum may enter the diet as a food additive, or it may contaminate foods grown in aluminum-rich soil. Other sources of oral exposure include packaging and kitchenware. A previous study showed that most Americans ingest 0.01-1.4 mg/kg of aluminum daily, and 5% ingest 1.58 mg/kg daily (i.e., 95 mg per day for a 60-kg person).
Based on these statistics, rats in the present study received oral aluminum citrate (AlCi) corresponding with three doses of aluminum: 0.5 mg/kg, 1.5 mg/kg, or 3.0 mg/kg. Treatment continued for 30 days, with colorectal distension (CRD) measured on days 2, 4, 8, 15, and 30.
Results showed a dose-dependent relationship between aluminum ingestion and visceral hypersensitivity. Within 2 days, rats receiving 3.0 mg/kg of aluminum exhibited a significantly lower pain threshold, and within 8 days, rats receiving 0.5 mg/kg and 1.5 mg/kg also showed increased visceral hypersensitivity.
After 1 month of treatment, rats receiving 1.5 mg/kg per day demonstrated a 30% increase in pain compared with control animals. In the same group, visceral hypersensitivity began to wane 7 days after cessation of treatment; 4 more weeks were needed to return to baseline. When treatment was restarted, visceral hypersensitivity occurred within 2 days, compared with 8 days upon initial administration. These findings are particularly relevant to some people, as the 1.5-mg/kg dose corresponds with the daily amount of aluminum ingested by 5% of Americans. Similar patterns of response and sensitization were observed in rats ingesting 0.5 mg/kg and 3.0 mg/kg. Female rats were more sensitive to aluminum than were male rats, a sex pattern that mimics human IBS.
Further testing showed that rats treated with zinc citrate (ZnCi) did not exhibit changes to pain threshold, thereby excluding citrate as an aggravating factor. Rat models of noninflammatory and inflammatory colonic hypersensitivity (butyrate enema or intrathecal injection of 25%-50% ethanol in combination with 2,4,6-trinitrobenzenesulfonic acid, respectively) had visceral hypersensitivity similar to that of rats in the 1.5-mg/kg AlCi group.
Testing of colonic tissue from AlCi-treated rats did not reveal inflammatory changes according to a variety of qualifiers, including histology, myeloperoxidase activity, mRNA expression of several inflammatory cytokines, or infiltration of eosinophils or macrophages. Noninflammatory effects of aluminum, however, were found. For instance, treated rats had lower serotonin levels in enteroendocrine cells.
“Enteroendocrine cells are specialized epithelial cells that respond to luminal stimuli by releasing various biologically active compounds,” the investigators wrote. “They regulate several physiological and homeostatic functions of the gastrointestinal tract, such as postprandial secretion, motility, immune responses, and sensory functions. A reduced number of enteroendocrine cells has been observed in the duodenum, ileum, and colon of some patients with IBS.”
In addition to changes in enteroendocrine cells, AlCi-treated rats had greater colonic mast cell degranulation and histamine with upregulation of histidine decarboxylase transcripts, suggesting that aluminum activated mast cells.
To determine the role of mast cell activation in visceral hypersensitivity, rats were given AlCi with cromoglycate, an inhibitor of mast cell degranulation. This treatment reduced mast cell degranulation and visceral pain threshold, compared with AlCi-treated rats not receiving cromoglycate, suggesting that mast cell degranulation is a primary driver of visceral hypersensitivity. This observation was confirmed by a mast cell–deficient mouse strain (Kit W-sh/W-sh), that had a normal number of mast cells incapable of degranulation. Treating the mast cell–deficient mice with AlCi did not induce visceral hypersensitivity, thereby confirming the role of mast cell degranulation.
Along with mast cell degranulation, AlCi treatment led to PAR2 activation. Investigators explored the significance of this finding with PAR2 knockout mice. When treated with AlCi, PAR2 knockout mice showed no increase in visceral hypersensitivity, suggesting that hypersensitivity is dependent on PAR2 activation. Further testing revealed that mast cell–deficient mice (Kit W-sh/W-sh) did not have PAR2 upregulation either, connecting a sequence in which aluminum triggers mast cell degranulation, mast cell degranulation drives PAR2 upregulation, and PAR2 upregulation causes visceral hypersensitivity. The latter two events in this chain – mast cell degranulation and PAR2 upregulation – mirror molecular mechanisms of IBS in humans.
“We speculate that aluminum activates mast cells to release mediators that can increase excitability of nociceptive afferences contributing to the visceral pain phenotype,” the investigators wrote. “Taken together, our results linked aluminum to several mechanisms implicated in IBS pathophysiology, highlighting a possible role for aluminum as a triggering factor in IBS development.”
The investigators suggested that these findings could influence preventive or therapeutic strategies: “Aluminum might be the first identified dietary risk factor for IBS, implying that measures to limit aluminum dietary consumption or to chelate aluminum may represent novel pathways of prevention and treatment of IBS in some susceptible patients,” they wrote.
The study was funded by the European Fund for Regional Economic Development; the Hauts de France Region, Ministère de l’Enseignement Supérieur et de la Recherche (CPER IRENI); and Digestscience (European Research Foundation on Intestinal Diseases and Nutrition).
SOURCE: Esquerre N et al. Cell Mol Gastroenterol Hepatol. 2019 Sep 20. doi: 10.1016/j.jcmgh.2018.09.012.
Aluminum ingested in small amounts causes visceral hypersensitivity in rats, suggesting that dietary levels of aluminum may trigger irritable bowel syndrome (IBS) in humans, according to a study published in Cellular and Molecular Gastroenterology and Hepatology.
Rats given oral aluminum exhibited dose-dependent visceral pain along with activation of proteinase-activated receptor-2 (PAR2) and mast cell degranulation, a combination of events that mirror clinical signs and molecular mechanisms of IBS in humans, reported lead author, Nicolas Esquerre, PhD, of Lille Inflammation Research International Center at Université Lille in France, and his colleagues. The study contributes to ongoing research surrounding causes and mechanisms of IBS, which may vary among patients because of disease subsets. These findings suggest that some patients with IBS may benefit from dietary aluminum restriction or chelation therapy.
“[T]he question of the initial trigger [of IBS] still remains unresolved,” the investigators wrote. “A more precise link between food and IBS has been demonstrated for gluten and other wheat proteins, lactose, and nickel, highlighting particular subsets of IBS patients now diagnosed as nonceliac gluten/wheat sensitivity, lactose intolerance, and nickel-allergic contact mucositis,” they added. “Here, we evaluated the effect of aluminum, a common contaminant of food and water, on abdominal pain.”
Aluminum may enter the diet as a food additive, or it may contaminate foods grown in aluminum-rich soil. Other sources of oral exposure include packaging and kitchenware. A previous study showed that most Americans ingest 0.01-1.4 mg/kg of aluminum daily, and 5% ingest 1.58 mg/kg daily (i.e., 95 mg per day for a 60-kg person).
Based on these statistics, rats in the present study received oral aluminum citrate (AlCi) corresponding with three doses of aluminum: 0.5 mg/kg, 1.5 mg/kg, or 3.0 mg/kg. Treatment continued for 30 days, with colorectal distension (CRD) measured on days 2, 4, 8, 15, and 30.
Results showed a dose-dependent relationship between aluminum ingestion and visceral hypersensitivity. Within 2 days, rats receiving 3.0 mg/kg of aluminum exhibited a significantly lower pain threshold, and within 8 days, rats receiving 0.5 mg/kg and 1.5 mg/kg also showed increased visceral hypersensitivity.
After 1 month of treatment, rats receiving 1.5 mg/kg per day demonstrated a 30% increase in pain compared with control animals. In the same group, visceral hypersensitivity began to wane 7 days after cessation of treatment; 4 more weeks were needed to return to baseline. When treatment was restarted, visceral hypersensitivity occurred within 2 days, compared with 8 days upon initial administration. These findings are particularly relevant to some people, as the 1.5-mg/kg dose corresponds with the daily amount of aluminum ingested by 5% of Americans. Similar patterns of response and sensitization were observed in rats ingesting 0.5 mg/kg and 3.0 mg/kg. Female rats were more sensitive to aluminum than were male rats, a sex pattern that mimics human IBS.
Further testing showed that rats treated with zinc citrate (ZnCi) did not exhibit changes to pain threshold, thereby excluding citrate as an aggravating factor. Rat models of noninflammatory and inflammatory colonic hypersensitivity (butyrate enema or intrathecal injection of 25%-50% ethanol in combination with 2,4,6-trinitrobenzenesulfonic acid, respectively) had visceral hypersensitivity similar to that of rats in the 1.5-mg/kg AlCi group.
Testing of colonic tissue from AlCi-treated rats did not reveal inflammatory changes according to a variety of qualifiers, including histology, myeloperoxidase activity, mRNA expression of several inflammatory cytokines, or infiltration of eosinophils or macrophages. Noninflammatory effects of aluminum, however, were found. For instance, treated rats had lower serotonin levels in enteroendocrine cells.
“Enteroendocrine cells are specialized epithelial cells that respond to luminal stimuli by releasing various biologically active compounds,” the investigators wrote. “They regulate several physiological and homeostatic functions of the gastrointestinal tract, such as postprandial secretion, motility, immune responses, and sensory functions. A reduced number of enteroendocrine cells has been observed in the duodenum, ileum, and colon of some patients with IBS.”
In addition to changes in enteroendocrine cells, AlCi-treated rats had greater colonic mast cell degranulation and histamine with upregulation of histidine decarboxylase transcripts, suggesting that aluminum activated mast cells.
To determine the role of mast cell activation in visceral hypersensitivity, rats were given AlCi with cromoglycate, an inhibitor of mast cell degranulation. This treatment reduced mast cell degranulation and visceral pain threshold, compared with AlCi-treated rats not receiving cromoglycate, suggesting that mast cell degranulation is a primary driver of visceral hypersensitivity. This observation was confirmed by a mast cell–deficient mouse strain (Kit W-sh/W-sh), that had a normal number of mast cells incapable of degranulation. Treating the mast cell–deficient mice with AlCi did not induce visceral hypersensitivity, thereby confirming the role of mast cell degranulation.
Along with mast cell degranulation, AlCi treatment led to PAR2 activation. Investigators explored the significance of this finding with PAR2 knockout mice. When treated with AlCi, PAR2 knockout mice showed no increase in visceral hypersensitivity, suggesting that hypersensitivity is dependent on PAR2 activation. Further testing revealed that mast cell–deficient mice (Kit W-sh/W-sh) did not have PAR2 upregulation either, connecting a sequence in which aluminum triggers mast cell degranulation, mast cell degranulation drives PAR2 upregulation, and PAR2 upregulation causes visceral hypersensitivity. The latter two events in this chain – mast cell degranulation and PAR2 upregulation – mirror molecular mechanisms of IBS in humans.
“We speculate that aluminum activates mast cells to release mediators that can increase excitability of nociceptive afferences contributing to the visceral pain phenotype,” the investigators wrote. “Taken together, our results linked aluminum to several mechanisms implicated in IBS pathophysiology, highlighting a possible role for aluminum as a triggering factor in IBS development.”
The investigators suggested that these findings could influence preventive or therapeutic strategies: “Aluminum might be the first identified dietary risk factor for IBS, implying that measures to limit aluminum dietary consumption or to chelate aluminum may represent novel pathways of prevention and treatment of IBS in some susceptible patients,” they wrote.
The study was funded by the European Fund for Regional Economic Development; the Hauts de France Region, Ministère de l’Enseignement Supérieur et de la Recherche (CPER IRENI); and Digestscience (European Research Foundation on Intestinal Diseases and Nutrition).
SOURCE: Esquerre N et al. Cell Mol Gastroenterol Hepatol. 2019 Sep 20. doi: 10.1016/j.jcmgh.2018.09.012.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Aluminum ingestion triggers visceral hypersensitivity in rats, suggesting that dietary levels of aluminum may contribute to development of irritable bowel syndrome in humans.
Major finding: In rodents, 1 month of oral aluminum administration led to a 30% increase in pain during colorectal distension, compared with control subjects.
Study details: A rodent study including noninflammatory and inflammatory IBS rat models, mast cell–deficient mice, and PAR2 knockout mice.
Disclosures: The study was funded by the European Fund for Regional Economic Development; the Hauts de France Region, Ministère de l’Enseignement Supérieur et de la Recherche (CPER IRENI); and Digestscience (European Research Foundation on Intestinal Diseases and Nutrition).
Source: Esquerre N et al. Cell Mol Gastroenterol Hepatol. 2019 Sep 20. doi: 10.1016/j.jcmgh.2018.09.012.
Anti-TNFs slow SIJ damage in early axial spondyloarthritis
Long-term anti–tumor necrosis factor therapy seemed to slow progression of sacroiliac joint damage in early axial spondyloarthritis in a German study of 42 patients.
They were all part of the ESTHER trial, which found that in early axial spondyloarthritis (axSpA), active inflammatory lesions on MRI improved significantly more with etanercept (Enbrel) than with sulfasalazine-treated patients (Ann Rheum Dis. 2011 Apr 1;70[4]:590-6).
In the new work, published in the Arthritis & Rheumatology, investigators reviewed 42 ESTHER subjects who were on etanercept for up to 6 years and who also had baseline and at least one bilateral sacroiliac joint (SIJ) x-ray at 2-, 4-, or 6-year follow-up. Two blinded readers scored the x-rays, and a sacroiliitis sum score was assigned to each subject. The sum score ranged from 0, meaning no signs of sacroiliitis, to 8, meaning total ankylosis of both SIJs.
The mean progression in sacroiliitis sum score was 0.13 points from baseline to 2 years; followed by a regression of –0.27 points during years 2-4, and –0.09 points from years 4-6. There was no comparator group of untreated patients, but the authors noted that previous work would suggest a slight, but detectable, progression in joint damage over that time.
Elevated C-reactive protein and the presence of osteitis on MRI, meanwhile, were independently associated with progression.
“This is the first study to analyze the long-term (up to 6 years) progression of radiographic sacroiliitis in patients with axSpA treated with an anti-TNF agent, in this case with etanercept. Our results suggest that long-term treatment with a potent anti-inflammatory drug like a TNF inhibitor may influence the evolution of the disease by decelerating the radiographic progression of SIJ [damage] in patients with” early axSpA, wrote the investigators, led by Valeria Rios Rodriguez, MD, of the Charité Universitätsmedizin, Berlin.
Progression from nonradiographic to radiographic axSpA occurred only in the first 2 years of treatment, among 5 of 27 patients, while 2 of 15 patients who started with radiographic disease regressed to nonradiographic axSpA, yielding a net progression of 7.1%.
Although that’s higher than what’s been reported in previous studies, it might be related to greater inflammation in the SIJ at baseline in ESTHER, since active osteitis on MRI was an inclusion criteria. Also, “treatment with a TNF inhibitor ... might have triggered a faster bone repair visible on x-rays as a progression of structural damage,” the investigators said.
The results seem “congruent with the retardation of the spine progression seen in [ankylosing spondylitis] patients treated long-term with TNF inhibitors. ... Long-term treatment with TNF inhibitors could reduce ... new bone formation by preventing the development of new inflammatory lesions resulting in structural damage” of the SIJ, they said, which, in turn, “might have an impact on the functional status and spinal mobility in patients with axSpA, independently of structural damage of the spine.”
Two-thirds of the trial participants were men; the mean age was 34 years, and mean duration of symptoms 3.1 years at baseline. No information was reported on adverse events.
The work was funded by Pfizer, a marketer of etanercept. Some of the investigators disclosed consulting and other payments from the company, as well as other companies involved in marketing and/or development of drugs for axSpA. One investigator was an employee of Pfizer.
SOURCE: Rios Rodriguez V et al. Arthritis Rheumatol. 2019 Jan 9. doi: 10.1002/art.40786
Long-term anti–tumor necrosis factor therapy seemed to slow progression of sacroiliac joint damage in early axial spondyloarthritis in a German study of 42 patients.
They were all part of the ESTHER trial, which found that in early axial spondyloarthritis (axSpA), active inflammatory lesions on MRI improved significantly more with etanercept (Enbrel) than with sulfasalazine-treated patients (Ann Rheum Dis. 2011 Apr 1;70[4]:590-6).
In the new work, published in the Arthritis & Rheumatology, investigators reviewed 42 ESTHER subjects who were on etanercept for up to 6 years and who also had baseline and at least one bilateral sacroiliac joint (SIJ) x-ray at 2-, 4-, or 6-year follow-up. Two blinded readers scored the x-rays, and a sacroiliitis sum score was assigned to each subject. The sum score ranged from 0, meaning no signs of sacroiliitis, to 8, meaning total ankylosis of both SIJs.
The mean progression in sacroiliitis sum score was 0.13 points from baseline to 2 years; followed by a regression of –0.27 points during years 2-4, and –0.09 points from years 4-6. There was no comparator group of untreated patients, but the authors noted that previous work would suggest a slight, but detectable, progression in joint damage over that time.
Elevated C-reactive protein and the presence of osteitis on MRI, meanwhile, were independently associated with progression.
“This is the first study to analyze the long-term (up to 6 years) progression of radiographic sacroiliitis in patients with axSpA treated with an anti-TNF agent, in this case with etanercept. Our results suggest that long-term treatment with a potent anti-inflammatory drug like a TNF inhibitor may influence the evolution of the disease by decelerating the radiographic progression of SIJ [damage] in patients with” early axSpA, wrote the investigators, led by Valeria Rios Rodriguez, MD, of the Charité Universitätsmedizin, Berlin.
Progression from nonradiographic to radiographic axSpA occurred only in the first 2 years of treatment, among 5 of 27 patients, while 2 of 15 patients who started with radiographic disease regressed to nonradiographic axSpA, yielding a net progression of 7.1%.
Although that’s higher than what’s been reported in previous studies, it might be related to greater inflammation in the SIJ at baseline in ESTHER, since active osteitis on MRI was an inclusion criteria. Also, “treatment with a TNF inhibitor ... might have triggered a faster bone repair visible on x-rays as a progression of structural damage,” the investigators said.
The results seem “congruent with the retardation of the spine progression seen in [ankylosing spondylitis] patients treated long-term with TNF inhibitors. ... Long-term treatment with TNF inhibitors could reduce ... new bone formation by preventing the development of new inflammatory lesions resulting in structural damage” of the SIJ, they said, which, in turn, “might have an impact on the functional status and spinal mobility in patients with axSpA, independently of structural damage of the spine.”
Two-thirds of the trial participants were men; the mean age was 34 years, and mean duration of symptoms 3.1 years at baseline. No information was reported on adverse events.
The work was funded by Pfizer, a marketer of etanercept. Some of the investigators disclosed consulting and other payments from the company, as well as other companies involved in marketing and/or development of drugs for axSpA. One investigator was an employee of Pfizer.
SOURCE: Rios Rodriguez V et al. Arthritis Rheumatol. 2019 Jan 9. doi: 10.1002/art.40786
Long-term anti–tumor necrosis factor therapy seemed to slow progression of sacroiliac joint damage in early axial spondyloarthritis in a German study of 42 patients.
They were all part of the ESTHER trial, which found that in early axial spondyloarthritis (axSpA), active inflammatory lesions on MRI improved significantly more with etanercept (Enbrel) than with sulfasalazine-treated patients (Ann Rheum Dis. 2011 Apr 1;70[4]:590-6).
In the new work, published in the Arthritis & Rheumatology, investigators reviewed 42 ESTHER subjects who were on etanercept for up to 6 years and who also had baseline and at least one bilateral sacroiliac joint (SIJ) x-ray at 2-, 4-, or 6-year follow-up. Two blinded readers scored the x-rays, and a sacroiliitis sum score was assigned to each subject. The sum score ranged from 0, meaning no signs of sacroiliitis, to 8, meaning total ankylosis of both SIJs.
The mean progression in sacroiliitis sum score was 0.13 points from baseline to 2 years; followed by a regression of –0.27 points during years 2-4, and –0.09 points from years 4-6. There was no comparator group of untreated patients, but the authors noted that previous work would suggest a slight, but detectable, progression in joint damage over that time.
Elevated C-reactive protein and the presence of osteitis on MRI, meanwhile, were independently associated with progression.
“This is the first study to analyze the long-term (up to 6 years) progression of radiographic sacroiliitis in patients with axSpA treated with an anti-TNF agent, in this case with etanercept. Our results suggest that long-term treatment with a potent anti-inflammatory drug like a TNF inhibitor may influence the evolution of the disease by decelerating the radiographic progression of SIJ [damage] in patients with” early axSpA, wrote the investigators, led by Valeria Rios Rodriguez, MD, of the Charité Universitätsmedizin, Berlin.
Progression from nonradiographic to radiographic axSpA occurred only in the first 2 years of treatment, among 5 of 27 patients, while 2 of 15 patients who started with radiographic disease regressed to nonradiographic axSpA, yielding a net progression of 7.1%.
Although that’s higher than what’s been reported in previous studies, it might be related to greater inflammation in the SIJ at baseline in ESTHER, since active osteitis on MRI was an inclusion criteria. Also, “treatment with a TNF inhibitor ... might have triggered a faster bone repair visible on x-rays as a progression of structural damage,” the investigators said.
The results seem “congruent with the retardation of the spine progression seen in [ankylosing spondylitis] patients treated long-term with TNF inhibitors. ... Long-term treatment with TNF inhibitors could reduce ... new bone formation by preventing the development of new inflammatory lesions resulting in structural damage” of the SIJ, they said, which, in turn, “might have an impact on the functional status and spinal mobility in patients with axSpA, independently of structural damage of the spine.”
Two-thirds of the trial participants were men; the mean age was 34 years, and mean duration of symptoms 3.1 years at baseline. No information was reported on adverse events.
The work was funded by Pfizer, a marketer of etanercept. Some of the investigators disclosed consulting and other payments from the company, as well as other companies involved in marketing and/or development of drugs for axSpA. One investigator was an employee of Pfizer.
SOURCE: Rios Rodriguez V et al. Arthritis Rheumatol. 2019 Jan 9. doi: 10.1002/art.40786
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Major finding: The mean progression in sacroiliitis sum score was 0.13 points from baseline to 2 years; followed by a regression of –0.27 points during years 2-4, and –0.09 points from years 4-6.
Study details: Review of 42 patients with early disease.
Disclosures: The work was funded by Pfizer, a marketer of etanercept. Some of the investigators disclosed consulting and other payments from the company, as well as other companies involved in marketing and/or development of drugs for axSpA. One investigator was an employee of Pfizer.
Source: Rios Rodriguez V et al. Arthritis Rheumatol. 2019 Jan 9. doi: 10.1002/art.40786
Clinical trial: AVATaR studies pulmonary complications following robotic surgery
A trial is underway to assess the incidence of postoperative pulmonary complications in patients undergoing and to study current practices of mechanical ventilation and the potential link between ventilatory parameters and postoperative pulmonary complications.
The Assessment of Ventilatory Management During General Anesthesia for Robotic Surgery (AVATaR) trial is an international observational, prospective study involving more than a dozen institutions in the United States and elsewhere, with the goal of eventually recruiting 40-50 institutions worldwide. Enrollment of consecutive patients undergoing mechanical ventilation for robotic surgery is ongoing. Exclusions are pregnant patients and those procedures not carried out in the OR.
A predefined composite of pulmonary complications was the primary outcome measured. These predefined complications are recorded regularly from medical chart until the first 5 postoperative days, discharge from hospital, or death, whatever comes first.
For full details and recruitment information on the AVATaR study (NCT02989415), go to clinicaltrials.gov.
A trial is underway to assess the incidence of postoperative pulmonary complications in patients undergoing and to study current practices of mechanical ventilation and the potential link between ventilatory parameters and postoperative pulmonary complications.
The Assessment of Ventilatory Management During General Anesthesia for Robotic Surgery (AVATaR) trial is an international observational, prospective study involving more than a dozen institutions in the United States and elsewhere, with the goal of eventually recruiting 40-50 institutions worldwide. Enrollment of consecutive patients undergoing mechanical ventilation for robotic surgery is ongoing. Exclusions are pregnant patients and those procedures not carried out in the OR.
A predefined composite of pulmonary complications was the primary outcome measured. These predefined complications are recorded regularly from medical chart until the first 5 postoperative days, discharge from hospital, or death, whatever comes first.
For full details and recruitment information on the AVATaR study (NCT02989415), go to clinicaltrials.gov.
A trial is underway to assess the incidence of postoperative pulmonary complications in patients undergoing and to study current practices of mechanical ventilation and the potential link between ventilatory parameters and postoperative pulmonary complications.
The Assessment of Ventilatory Management During General Anesthesia for Robotic Surgery (AVATaR) trial is an international observational, prospective study involving more than a dozen institutions in the United States and elsewhere, with the goal of eventually recruiting 40-50 institutions worldwide. Enrollment of consecutive patients undergoing mechanical ventilation for robotic surgery is ongoing. Exclusions are pregnant patients and those procedures not carried out in the OR.
A predefined composite of pulmonary complications was the primary outcome measured. These predefined complications are recorded regularly from medical chart until the first 5 postoperative days, discharge from hospital, or death, whatever comes first.
For full details and recruitment information on the AVATaR study (NCT02989415), go to clinicaltrials.gov.
HDL-P subfractions may be prognostic in heart failure
In heart failure, derangements in HDL cholesterol particle (HDL-P) subfractions have prognostic implications beyond those of conventional cardiovascular risk factors, according to investigators who analyzed plasma samples from more than 6,500 patients.
The study revealed derangements that were shared and more severe in heart failure with reduced ejection fraction (HFrEF) as compared to heart failure with preserved ejection fraction (HFpEF), according to the researchers, who said their study is the largest to date of HDL-P subfractions in heart failure.
Both total HDL-P and small HDL-P had a strong inverse association with adverse outcomes, consistent with the conclusions of previous studies, they said in a report on their study in the Journal of the American College of Cardiology.
“Altogether, our findings support total and small HDL-P as important markers of residual risk in both HFrEF and HFpEF,” said the investigators, led by Wynn G. Hunter, MD, of Duke University, Durham, N.C.
Dr. Hunter and colleagues used the CATHGEN (Catheterization Genetics) biorepository to identify plasma samples obtained at catheterization for 782 patients with HFrEF, 1,004 with HFpEF, and 4,742 with no heart failure.
Lipoprotein profiling of the samples revealed that mean HDL-P size was greater in HFrEF than in HFpEF, and in both of those cases, mean HDL-P size was greater than in patients with no heart failure (P less than .0001), investigators reported.
Concentrations of small HDL-P and total HDL-P were by contrast lower in HFrEF versus HFpEF, and again, the values for both HFrEF and HFpEF were lower than in patients without heart failure (P less than .0001), they added.
Small HDL-P and total HDL-P had an inverse association with time to adverse events and all-cause mortality for both the HFrEF and HFpEF groups, according to investigators, who said those links remained robust even after multivariate adjustment for 14 cardiovascular risk factors, including diabetes, LDL particle, and GlycA, a marker of inflammation.
For example, small HDL-P and total HDL-P were inversely associated with all-cause mortality risk, with adjusted hazard ratios of 0.69-0.79 (P less than .0001), they reported. Similarly, a greater mean HDL-P size was associated with increased risk of all-cause mortality, yielding adjusted hazard ratios of 1.23-1.46 (P less than .0001).
Further studies are needed to clarify the role of HDL-P in the pathophysiology of heart failure, and to identify treatments that might increase total and small HDL-P in heart failure patients, Dr. Hunter and coauthors concluded.
Dr. Hunter reported no disclosures related to the study. Coauthors provided disclosures related to Amgen, Ostuka, Roche Diagnostics, Novartis, Trevena, Singulex, Medtronic, AstraZeneca, Bristol-Myers Squibb, Janssen, Portola, Boston Scientific, Gilead, GlaxoSmithKline, Merck, Alnylam, Ikaria Pharmaceuticals, Pfizer, Philips, LipoScience, and Pfizer, among others.
SOURCE: Hunter WG et al. J Am Coll Cardiol. 2019 Jan 22;73(2):177-86.
Although the study by Dr. Hunter and colleagues confirms the role of HDL cholesterol and HDL-P subfractions in heart failure, the immediate clinical implications of their findings are uncertain.
However, clinical use as a biomarker remains a “distant vision,” in part because a useful biomarker must be proven to provide an incremental benefit in terms of reducing disease-associated morbidity or mortality.
Even so, the present study could begin to inform future therapeutic studies looking at increasing specific HDL-P subfractions, rather than increasing HDL cholesterol across the board.
“Perhaps, this study will possibly serve to spur investigation into therapies designed to reduce derangements of [HDL cholesterol] metabolism and primarily target HDL-P as a regulator molecule, a promise that may keep the HDL story alive into the near future of scientific excursion.”
These comments were taken from an accompanying editorial by Hector O. Ventura, MD, and Carl J. Lavie, MD, of the University of Queensland Ochsner Clinical School, Brisbane, Australia, and New Orleans; and Mandeep R. Mehra, MD, of the Center of Advanced Heart Disease, Harvard University, Boston (J Am Coll Cardiol 2019 Jan 22;73[2]:187-9). Dr. Mehra reported that he is a consultant for Abbott, Medtronic, nupulseCV, Portola, Bayer, and FineHeart.
Although the study by Dr. Hunter and colleagues confirms the role of HDL cholesterol and HDL-P subfractions in heart failure, the immediate clinical implications of their findings are uncertain.
However, clinical use as a biomarker remains a “distant vision,” in part because a useful biomarker must be proven to provide an incremental benefit in terms of reducing disease-associated morbidity or mortality.
Even so, the present study could begin to inform future therapeutic studies looking at increasing specific HDL-P subfractions, rather than increasing HDL cholesterol across the board.
“Perhaps, this study will possibly serve to spur investigation into therapies designed to reduce derangements of [HDL cholesterol] metabolism and primarily target HDL-P as a regulator molecule, a promise that may keep the HDL story alive into the near future of scientific excursion.”
These comments were taken from an accompanying editorial by Hector O. Ventura, MD, and Carl J. Lavie, MD, of the University of Queensland Ochsner Clinical School, Brisbane, Australia, and New Orleans; and Mandeep R. Mehra, MD, of the Center of Advanced Heart Disease, Harvard University, Boston (J Am Coll Cardiol 2019 Jan 22;73[2]:187-9). Dr. Mehra reported that he is a consultant for Abbott, Medtronic, nupulseCV, Portola, Bayer, and FineHeart.
Although the study by Dr. Hunter and colleagues confirms the role of HDL cholesterol and HDL-P subfractions in heart failure, the immediate clinical implications of their findings are uncertain.
However, clinical use as a biomarker remains a “distant vision,” in part because a useful biomarker must be proven to provide an incremental benefit in terms of reducing disease-associated morbidity or mortality.
Even so, the present study could begin to inform future therapeutic studies looking at increasing specific HDL-P subfractions, rather than increasing HDL cholesterol across the board.
“Perhaps, this study will possibly serve to spur investigation into therapies designed to reduce derangements of [HDL cholesterol] metabolism and primarily target HDL-P as a regulator molecule, a promise that may keep the HDL story alive into the near future of scientific excursion.”
These comments were taken from an accompanying editorial by Hector O. Ventura, MD, and Carl J. Lavie, MD, of the University of Queensland Ochsner Clinical School, Brisbane, Australia, and New Orleans; and Mandeep R. Mehra, MD, of the Center of Advanced Heart Disease, Harvard University, Boston (J Am Coll Cardiol 2019 Jan 22;73[2]:187-9). Dr. Mehra reported that he is a consultant for Abbott, Medtronic, nupulseCV, Portola, Bayer, and FineHeart.
In heart failure, derangements in HDL cholesterol particle (HDL-P) subfractions have prognostic implications beyond those of conventional cardiovascular risk factors, according to investigators who analyzed plasma samples from more than 6,500 patients.
The study revealed derangements that were shared and more severe in heart failure with reduced ejection fraction (HFrEF) as compared to heart failure with preserved ejection fraction (HFpEF), according to the researchers, who said their study is the largest to date of HDL-P subfractions in heart failure.
Both total HDL-P and small HDL-P had a strong inverse association with adverse outcomes, consistent with the conclusions of previous studies, they said in a report on their study in the Journal of the American College of Cardiology.
“Altogether, our findings support total and small HDL-P as important markers of residual risk in both HFrEF and HFpEF,” said the investigators, led by Wynn G. Hunter, MD, of Duke University, Durham, N.C.
Dr. Hunter and colleagues used the CATHGEN (Catheterization Genetics) biorepository to identify plasma samples obtained at catheterization for 782 patients with HFrEF, 1,004 with HFpEF, and 4,742 with no heart failure.
Lipoprotein profiling of the samples revealed that mean HDL-P size was greater in HFrEF than in HFpEF, and in both of those cases, mean HDL-P size was greater than in patients with no heart failure (P less than .0001), investigators reported.
Concentrations of small HDL-P and total HDL-P were by contrast lower in HFrEF versus HFpEF, and again, the values for both HFrEF and HFpEF were lower than in patients without heart failure (P less than .0001), they added.
Small HDL-P and total HDL-P had an inverse association with time to adverse events and all-cause mortality for both the HFrEF and HFpEF groups, according to investigators, who said those links remained robust even after multivariate adjustment for 14 cardiovascular risk factors, including diabetes, LDL particle, and GlycA, a marker of inflammation.
For example, small HDL-P and total HDL-P were inversely associated with all-cause mortality risk, with adjusted hazard ratios of 0.69-0.79 (P less than .0001), they reported. Similarly, a greater mean HDL-P size was associated with increased risk of all-cause mortality, yielding adjusted hazard ratios of 1.23-1.46 (P less than .0001).
Further studies are needed to clarify the role of HDL-P in the pathophysiology of heart failure, and to identify treatments that might increase total and small HDL-P in heart failure patients, Dr. Hunter and coauthors concluded.
Dr. Hunter reported no disclosures related to the study. Coauthors provided disclosures related to Amgen, Ostuka, Roche Diagnostics, Novartis, Trevena, Singulex, Medtronic, AstraZeneca, Bristol-Myers Squibb, Janssen, Portola, Boston Scientific, Gilead, GlaxoSmithKline, Merck, Alnylam, Ikaria Pharmaceuticals, Pfizer, Philips, LipoScience, and Pfizer, among others.
SOURCE: Hunter WG et al. J Am Coll Cardiol. 2019 Jan 22;73(2):177-86.
In heart failure, derangements in HDL cholesterol particle (HDL-P) subfractions have prognostic implications beyond those of conventional cardiovascular risk factors, according to investigators who analyzed plasma samples from more than 6,500 patients.
The study revealed derangements that were shared and more severe in heart failure with reduced ejection fraction (HFrEF) as compared to heart failure with preserved ejection fraction (HFpEF), according to the researchers, who said their study is the largest to date of HDL-P subfractions in heart failure.
Both total HDL-P and small HDL-P had a strong inverse association with adverse outcomes, consistent with the conclusions of previous studies, they said in a report on their study in the Journal of the American College of Cardiology.
“Altogether, our findings support total and small HDL-P as important markers of residual risk in both HFrEF and HFpEF,” said the investigators, led by Wynn G. Hunter, MD, of Duke University, Durham, N.C.
Dr. Hunter and colleagues used the CATHGEN (Catheterization Genetics) biorepository to identify plasma samples obtained at catheterization for 782 patients with HFrEF, 1,004 with HFpEF, and 4,742 with no heart failure.
Lipoprotein profiling of the samples revealed that mean HDL-P size was greater in HFrEF than in HFpEF, and in both of those cases, mean HDL-P size was greater than in patients with no heart failure (P less than .0001), investigators reported.
Concentrations of small HDL-P and total HDL-P were by contrast lower in HFrEF versus HFpEF, and again, the values for both HFrEF and HFpEF were lower than in patients without heart failure (P less than .0001), they added.
Small HDL-P and total HDL-P had an inverse association with time to adverse events and all-cause mortality for both the HFrEF and HFpEF groups, according to investigators, who said those links remained robust even after multivariate adjustment for 14 cardiovascular risk factors, including diabetes, LDL particle, and GlycA, a marker of inflammation.
For example, small HDL-P and total HDL-P were inversely associated with all-cause mortality risk, with adjusted hazard ratios of 0.69-0.79 (P less than .0001), they reported. Similarly, a greater mean HDL-P size was associated with increased risk of all-cause mortality, yielding adjusted hazard ratios of 1.23-1.46 (P less than .0001).
Further studies are needed to clarify the role of HDL-P in the pathophysiology of heart failure, and to identify treatments that might increase total and small HDL-P in heart failure patients, Dr. Hunter and coauthors concluded.
Dr. Hunter reported no disclosures related to the study. Coauthors provided disclosures related to Amgen, Ostuka, Roche Diagnostics, Novartis, Trevena, Singulex, Medtronic, AstraZeneca, Bristol-Myers Squibb, Janssen, Portola, Boston Scientific, Gilead, GlaxoSmithKline, Merck, Alnylam, Ikaria Pharmaceuticals, Pfizer, Philips, LipoScience, and Pfizer, among others.
SOURCE: Hunter WG et al. J Am Coll Cardiol. 2019 Jan 22;73(2):177-86.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Derangements in HDL particle (HDL-P) subfractions may have prognostic implications in patients with heart failure with reduced or preserved ejection fraction.
Major finding: (P less than .0001).
Study details: Study based on lipid profiling of more than 6,500 plasma samples obtained at catheterization.
Disclosures: Study authors provided disclosures related to Amgen, Ostuka, Roche Diagnostics, Novartis, Medtronic, and others.
Source: Hunter WG et al. J Am Coll Cardiol. 2019 Jan 22;73(2):177-86.