User login
New Take on Elder Care
Families often note that after older relatives return home from the hospital, something is wrong with them.
While the acute condition that brought a relative into the hospital has been remedied, major functional and cognitive deficits such as confusion, falls, and difficulty with basic activities of daily living remain.
This post-hospital decline may not be appreciated by hospital clinicians, perhaps because the problems do not become visible until the patient is home. However, these problems place significant burdens on patients and families.
Following discharge for an acute hospitalization, about a third of older patients will have a major new disability that threatens their ability to live independently.1 Among community-dwelling elders, half of all new disability occurs within a month of hospitalization.2 It isn’t surprising that nursing home placement has grown more common for medical hospitalizations, even for seemingly reversible medical problems.
Older adults will make up an increasing number of the patients cared for by hospitalists. The Acute Care for Elders (ACE) unit model of care focuses on preventing functional decline and increasing discharges to home.
In 2005, leadership of the San Francisco General Hospital Medical Center (SFGHMC) committed to improving care for hospitalized elders by adopting the ACE model.3
The ACE model combats hospital-acquired disability by improving care processes for older patients.
Major motivating factors for the change included demographic and quality-of-care imperatives. After a nine-month planning process, the SFGHMC ACE unit opened in February.
Rationale
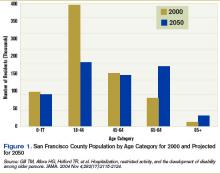
Largely driven by the baby boom, the number of California seniors older than 65 will double from 3.5 million to 7 million over the next 40 years, and those older than 85 will triple from about 500,000 to 1.5 million. In San Francisco, changes will be even more dramatic as the number of residents over 65 increases from 14% of the population to 32%.4 (See Figure 1, right).
In California, people 65 to 84 are almost three times as likely to be hospitalized as those between 45 and 64. If rates of hospitalization do not change, an increase in hospitalized older adults will occur as the baby boom generation ages.
In addition, hospitalization can be hazardous for older adults, with increased risk for functional and cognitive disability and adverse events.5-7 As a result, hospitalization-associated disability represents a growing threat to the independence of the older population. A variety of changes to usual care have been adopted in an effort to reduce the hazards of hospitalization in the elderly.8-11
ACE Model
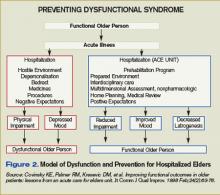
The ACE unit model, proven to reduce the risk of hospital-acquired disability in the elderly, is based on the Model of Dysfunction for Hospitalized Elders.12 (See Figure 2, p. 23)
This model outlines how processes of hospital care for the elderly promote physical impairment and depressed mood, leading to dysfunction. Counterproduc-tive factors in older adults include a hostile environment (lack of natural sunlight, high-glare floors, poor way-finding cues, high noise levels), depersonalization (lack of personal effects, clothing, and usual daily routines), bed rest through multiple tethers or inattention, medicines inappropriate in the elderly or given at inappropriate doses, procedures, and negative expectations (usually that the patient will require nursing home placement after admission).
These processes are the targets of the ACE intervention. The idea is to improve quality of care for the elderly by promoting rehabilitation and preventing disability.
The ACE unit addresses these issues through a “prehabilitation program.” The ACE unit is a physical location in the hospital with 10 beds. Care is redesigned by placing the patient at the center of restorative efforts of an interdisciplinary team consisting of an advanced practice nurse, a social worker, an occupational and a physical therapist, a nutritionist, a pharmacist, and a medical director. This ACE Unit team meets daily to review and plan care for all patients. Recommendations for nursing care and rehabilitation evaluation are implemented by the ACE team directly. Other recommendations, such as changing medications or considering alternative approaches to common geriatric syndromes are communicated to the primary team, which maintains overall responsibility for the care of the patient.
Each patient’s assessment is multidimensional, with an emphasis on nonpharmacologic interventions where practical. For example, an emphasis is placed on after-dinner exercise such as walking and socializing to promote sleep and reduce medication use. Nursing-care plans were revised to promote mobility, discourage inappropriate Foley use, and encourage adequate hydration and nutrition.
Recommendations are communicated to the primary team via a recommendation form placed in the physician-order section and text pages. The unit’s medical director and pharmacist review medications. Recommendations that involve medication changes are discussed with the primary team, which write all medication orders. Home planning begins on the day of admission.
Prior to opening the unit, the ACE unit social worker met with key city and county agencies including Aging and Adult Services, the Public Guardian, In-Home Supportive Services, and community nursing homes to introduce the unit and plan for an effective and safe transition.
All staff expect patients to maintain prehospital physical functioning. When possible, patients are expected to wear their own clothes, eat all their meals in a common dining room, and ambulate or exercise daily.
We considered establishing criteria for admission.13 We have not adopted formal criteria for patients 65 or older, presence of medical non-surgical condition(s) that require(s) acute hospitalization, and no need for telemetry or chemotherapy. As we learn how best to serve our hospitalized older adult population with the resources of the unit, we will re-evaluate targeting criteria. Most of our admissions are from the emergency department (ED), and the remainder are from other units in the hospital.
Challenges
Key challenges in opening the new service include securing commitment and resources from organizational leaders and key stakeholders; incorporation of the ACE unit concept in an academic training center; hiring key staff, especially the geriatric clinical nurse specialist and pharmacist positions; and completing the environmental rehabilitation on a limited budget.
While gaps in the care of the geriatric patient population were well identified at SFGHMC as far back as 1996 by a multidisciplinary task force, no actions on recommendations were taken, for several key reasons.
First, an executive level administrator or physician champion was not a member of the task force. Second, the organization did not have a department or regulatory mandate to address the gaps in the care of the elderly patients. Third, there was no link between the hospital strategic plan and the recommendations.
By 2004, these issues were largely addressed. A new chief nursing officer with a background in quality improvement understood the demographic and quality imperatives to improve care for hospitalized older adults.
That same year, the Hospital Executive Committee incorporated patient safety into the hospital strategic plan. This resulted in a successful business plan for an ACE Unit and geriatric consultation service linked to organizational strategy.
Funding was allocated for a medical director and a clinical nurse specialist in fiscal year 2005-2006. In addition, a grant was obtained from the SFGH Foundation to fund equipment, renovations, and staff education/training.
The original ACE unit concept involved expert, interdisciplinary geriatric assessment and communication of suggestions via a paper-based chart.
Initially, we felt the primary medical team should round with the ACE team, preferably at the bedside. However, informal focus groups held with the residents suggested this would happen infrequently.
The demands on the medical teams of completing patient rounds before morning attending rounds were cited as the main reason that model wouldn’t work.
We have implemented the following methods to promote communication between the ACE unit team and the primary medical team:
- Medical teams are encouraged to attend ACE unit rounds while on bedside rounds. This provides an opportunity to model the team-delivered care for house staff and medical students, an ACGME requirement;
- Suggestions to change medications are directly text-paged to the house staff; and
- Recommendations are summarized in a communication sheet left in the chart (this not a permanent part of the medical record).
We plan on using the text-paging more widely once the unit has wireless computer capability. Despite this, there are occasions where a team is not aware of a recommendation or new emphasis in the care plan. We are considering additional ways to improve communication such as attending the primary team attending rounds.
In California and other states there is a shortage of clinical pharmacists and masters-prepared nurses with expertise in geriatrics.14-16 The advanced practice nurse performs a vital role in raising the level of knowledge, skills, and attitudes for the nursing staff on the ACE unit.
In addition, we see the ACE unit as a drop in the pond; we feel a responsibility to expand nursing geriatric competency throughout appropriate hospital areas. Thus, this nursing role is at the center of preparing the hospital to care for an older patient population.
This position remained unfilled for almost a year despite an intensive national search. This prompted us to incorporate the geriatric resource nurse model into our unit while we continued our recruitment.
Although we have successfully concluded our search for a nursing leader for the ACE unit, we have yet to hire a clinical pharmacist.
The rehabilitation of the unit would not have been possible without foundation support. As a public hospital with many competing demands, monies are limited for the rehabilitation required to create a more welcoming, safer environment for the older patient. In this case, the hospital foundation and a local foundation made grants to the ACE unit to allow us to change the environment.
These grants have allowed for significant changes to the unit, including elevated toilet seats, high-backed chairs, handrails, unit-based physical therapy equipment, and activities to promote non-pharmacological approaches to agitation.
Readiness for Change
All levels of hospital staff embraced the ACE unit concept. Department leaders in rehabilitation, nutrition, social work, and pharmacy felt ACE unit principles would improve care delivery over usual care.
Early on, department leaders and medical staff enthusiastically participated on a steering committee to help guide implementation efforts. In addition, when we offered geriatric resource nurse training to our nursing staff, more than 20 out of 50 unit nurses expressed interest.
Staff from all departments represented on the ACE unit team also expressed interest in and attended the three days of training. This provided baseline knowledge of common geriatric syndromes in hospitalized older patients for all team members. This been helpful during ACE team discussions.
Although medical residents felt they could not consistently attend ACE rounds, they appreciated potential benefits of the unit:
- Different perspectives could provide a wider range of evaluation and treatment recommendations for their patients;
- The co-location of key disciplines could result in overall time savings in calling for and ordering evaluations;
- The reduced likelihood that key interventions such as mobilization, feeding, catheter removal, and medication review would be missed; and
- The opportunity to learn principles of geriatric care through attending ACE rounds (when possible).
Medical staff in other departments immediately accepted the rationale for the unit.
Many expressed interest in expanding the concept to their departments, especially orthopedics, general surgery, and the ED. Although unfamiliar with specific interventions to improve care for hospitalized elders, the underlying concepts of patient-centered, team-delivered care with a focus on function resonated with most medical staff.
Next Steps
The unit is still in startup mode. Our major areas of focus are:
- Evaluating and improving team dynamics: We have engaged with researchers to evaluate our team dynamics and intervene where necessary to promote a high-functioning team.17
- Developing a culture of performance improvement: One of the hallmarks of high-functioning teams are measures of performance that are team-derived and reflect work product that the team can control.17
We are putting into place processes to measure key quality parameters including length of stay; nursing home placement; readmission rate, inappropriate catheter use; inappropriate medication prescribing; incidence of delirium, falls, and pressure ulcers; functional and cognitive status at admission and discharge; and patient satisfaction.
The orders set used by admitting residents are the standard general medical ward admission set and need revision for the ACE unit.
- Developing a research program: Our goal is to develop a research program evaluating interventions to prevent post-hospital degeneration of elders’ health. There is a dearth of research on improving hospital care for older, vulnerable adults.
- Expanding philanthropy support: The unit has benefited tremendously from philanthropy. In a relatively resource-poor setting, this allowed for rapid engagement with designers and vendors to remake the environment. We plan to expand our outreach efforts to interested philanthropists.
Summary
The ACE unit model can improve care for hospitalized older adults.
It requires a sustained level of commitment from hospital leaders, a focus on patient-centered, team-delivered care, sensitivity to communication modalities with primary caregivers, an awareness of the market for key professionals required, and flexibility to respond effectively to the many challenges that will emerge in implementing this model locally. TH
Dr. Pierluissi is medical director of the ACE unit at the San Francisco General Hospital. Susan Currin is the hospital’s chief nursing officer.
References
- Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451-458.
- Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004 Nov 3;292(17):2115-2124
- Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995 May 18;332(20):1338-1344.
- State of California, Department of Finance. Race/Ethnic Population with Age and Sex Detail, 2000–2050; 2004: Sacramento, Calif.
- Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993 Feb 1;118(3):219-223.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006 Jun 8;354(23):2509-2511; author reply 2509-11. Comment on: N Engl J Med. 2006 Mar 16;354(11):1157-1165.
- Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991 Feb 7;324(6):370-376. Comment in: N Engl J Med. 1991 Jul 18;325(3):210.
- Cohen HJ, Feussner JR, Weinberger M, et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002 Mar 21;346(12):905-912. Comment in: Curr Surg. 2004 May-Jun;61(3):266-74. N Engl J Med. 2002 Aug 1;347(5):371-373; author reply 371-373; author reply 371-3: N Engl J Med. 2002 Mar 21;346(12):874.
- Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999 Mar 4;340(9):669-676. Comment in: N Engl J Med. 1999 Jul 29;341(5):369-370; author reply 370. N Engl J Med. 1999 Mar 4;340(9):720-721.
- Reuben DB, Borok GM, Wolde-Tsadik G, et al. A randomized trial of comprehensive geriatric assessment in the care of hospitalized patients. N Engl J Med. 1995 May 18;332(20):1345-1350. Comment in: N Engl J Med. 1995 May 18;332(20):1376-1378.
- Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec 6;143(11):798-808. Comment in: Ann Intern Med. 2005 Dec 6;143(11):840-1. Ann Intern Med. 2006 Mar 21;144(6):456. Summary for patients in:Ann Intern Med. 2005 Dec 6;143(11):I56.
- Covinsky KE, Palmer RM, Kresevic DM, et. al. Improving functional outcomes in older patients: lessons from an acute care for elders unit. Jt Comm J Qual Improv. 1998 Feb;24(2):63-76.
- Wieland D, Rubenstein LZ. What do we know about patient targeting in geriatric evaluation and management (GEM) programs? Aging (Milano). 1996 Oct; 8(5):297-310.
- Spetz J, Dyer W. Forecasts of the Registered Nurse Workforce in California. 2005, University of California, San Francisco: San Francisco.
- Fleming KC, Evans JM, Chutka DS. Caregiver and clinician shortages in an aging nation. Mayo Clin Proc. 2003 Aug;78(8):1026-1040.
- Knapp KK, Quist RM, Walton SM, et al. Update on the pharmacist shortage: National and state data through 2003. Am J Health Syst Pharm. 2005 Mar 1;62(5):492-499.
- Katzenbach JR, Smith DK. The Discipline of Teams. Harv Bus Rev. July-August 2005:1-9.
Families often note that after older relatives return home from the hospital, something is wrong with them.
While the acute condition that brought a relative into the hospital has been remedied, major functional and cognitive deficits such as confusion, falls, and difficulty with basic activities of daily living remain.
This post-hospital decline may not be appreciated by hospital clinicians, perhaps because the problems do not become visible until the patient is home. However, these problems place significant burdens on patients and families.
Following discharge for an acute hospitalization, about a third of older patients will have a major new disability that threatens their ability to live independently.1 Among community-dwelling elders, half of all new disability occurs within a month of hospitalization.2 It isn’t surprising that nursing home placement has grown more common for medical hospitalizations, even for seemingly reversible medical problems.
Older adults will make up an increasing number of the patients cared for by hospitalists. The Acute Care for Elders (ACE) unit model of care focuses on preventing functional decline and increasing discharges to home.
In 2005, leadership of the San Francisco General Hospital Medical Center (SFGHMC) committed to improving care for hospitalized elders by adopting the ACE model.3
The ACE model combats hospital-acquired disability by improving care processes for older patients.
Major motivating factors for the change included demographic and quality-of-care imperatives. After a nine-month planning process, the SFGHMC ACE unit opened in February.
Rationale
Largely driven by the baby boom, the number of California seniors older than 65 will double from 3.5 million to 7 million over the next 40 years, and those older than 85 will triple from about 500,000 to 1.5 million. In San Francisco, changes will be even more dramatic as the number of residents over 65 increases from 14% of the population to 32%.4 (See Figure 1, right).
In California, people 65 to 84 are almost three times as likely to be hospitalized as those between 45 and 64. If rates of hospitalization do not change, an increase in hospitalized older adults will occur as the baby boom generation ages.
In addition, hospitalization can be hazardous for older adults, with increased risk for functional and cognitive disability and adverse events.5-7 As a result, hospitalization-associated disability represents a growing threat to the independence of the older population. A variety of changes to usual care have been adopted in an effort to reduce the hazards of hospitalization in the elderly.8-11
ACE Model
The ACE unit model, proven to reduce the risk of hospital-acquired disability in the elderly, is based on the Model of Dysfunction for Hospitalized Elders.12 (See Figure 2, p. 23)
This model outlines how processes of hospital care for the elderly promote physical impairment and depressed mood, leading to dysfunction. Counterproduc-tive factors in older adults include a hostile environment (lack of natural sunlight, high-glare floors, poor way-finding cues, high noise levels), depersonalization (lack of personal effects, clothing, and usual daily routines), bed rest through multiple tethers or inattention, medicines inappropriate in the elderly or given at inappropriate doses, procedures, and negative expectations (usually that the patient will require nursing home placement after admission).
These processes are the targets of the ACE intervention. The idea is to improve quality of care for the elderly by promoting rehabilitation and preventing disability.
The ACE unit addresses these issues through a “prehabilitation program.” The ACE unit is a physical location in the hospital with 10 beds. Care is redesigned by placing the patient at the center of restorative efforts of an interdisciplinary team consisting of an advanced practice nurse, a social worker, an occupational and a physical therapist, a nutritionist, a pharmacist, and a medical director. This ACE Unit team meets daily to review and plan care for all patients. Recommendations for nursing care and rehabilitation evaluation are implemented by the ACE team directly. Other recommendations, such as changing medications or considering alternative approaches to common geriatric syndromes are communicated to the primary team, which maintains overall responsibility for the care of the patient.
Each patient’s assessment is multidimensional, with an emphasis on nonpharmacologic interventions where practical. For example, an emphasis is placed on after-dinner exercise such as walking and socializing to promote sleep and reduce medication use. Nursing-care plans were revised to promote mobility, discourage inappropriate Foley use, and encourage adequate hydration and nutrition.
Recommendations are communicated to the primary team via a recommendation form placed in the physician-order section and text pages. The unit’s medical director and pharmacist review medications. Recommendations that involve medication changes are discussed with the primary team, which write all medication orders. Home planning begins on the day of admission.
Prior to opening the unit, the ACE unit social worker met with key city and county agencies including Aging and Adult Services, the Public Guardian, In-Home Supportive Services, and community nursing homes to introduce the unit and plan for an effective and safe transition.
All staff expect patients to maintain prehospital physical functioning. When possible, patients are expected to wear their own clothes, eat all their meals in a common dining room, and ambulate or exercise daily.
We considered establishing criteria for admission.13 We have not adopted formal criteria for patients 65 or older, presence of medical non-surgical condition(s) that require(s) acute hospitalization, and no need for telemetry or chemotherapy. As we learn how best to serve our hospitalized older adult population with the resources of the unit, we will re-evaluate targeting criteria. Most of our admissions are from the emergency department (ED), and the remainder are from other units in the hospital.
Challenges
Key challenges in opening the new service include securing commitment and resources from organizational leaders and key stakeholders; incorporation of the ACE unit concept in an academic training center; hiring key staff, especially the geriatric clinical nurse specialist and pharmacist positions; and completing the environmental rehabilitation on a limited budget.
While gaps in the care of the geriatric patient population were well identified at SFGHMC as far back as 1996 by a multidisciplinary task force, no actions on recommendations were taken, for several key reasons.
First, an executive level administrator or physician champion was not a member of the task force. Second, the organization did not have a department or regulatory mandate to address the gaps in the care of the elderly patients. Third, there was no link between the hospital strategic plan and the recommendations.
By 2004, these issues were largely addressed. A new chief nursing officer with a background in quality improvement understood the demographic and quality imperatives to improve care for hospitalized older adults.
That same year, the Hospital Executive Committee incorporated patient safety into the hospital strategic plan. This resulted in a successful business plan for an ACE Unit and geriatric consultation service linked to organizational strategy.
Funding was allocated for a medical director and a clinical nurse specialist in fiscal year 2005-2006. In addition, a grant was obtained from the SFGH Foundation to fund equipment, renovations, and staff education/training.
The original ACE unit concept involved expert, interdisciplinary geriatric assessment and communication of suggestions via a paper-based chart.
Initially, we felt the primary medical team should round with the ACE team, preferably at the bedside. However, informal focus groups held with the residents suggested this would happen infrequently.
The demands on the medical teams of completing patient rounds before morning attending rounds were cited as the main reason that model wouldn’t work.
We have implemented the following methods to promote communication between the ACE unit team and the primary medical team:
- Medical teams are encouraged to attend ACE unit rounds while on bedside rounds. This provides an opportunity to model the team-delivered care for house staff and medical students, an ACGME requirement;
- Suggestions to change medications are directly text-paged to the house staff; and
- Recommendations are summarized in a communication sheet left in the chart (this not a permanent part of the medical record).
We plan on using the text-paging more widely once the unit has wireless computer capability. Despite this, there are occasions where a team is not aware of a recommendation or new emphasis in the care plan. We are considering additional ways to improve communication such as attending the primary team attending rounds.
In California and other states there is a shortage of clinical pharmacists and masters-prepared nurses with expertise in geriatrics.14-16 The advanced practice nurse performs a vital role in raising the level of knowledge, skills, and attitudes for the nursing staff on the ACE unit.
In addition, we see the ACE unit as a drop in the pond; we feel a responsibility to expand nursing geriatric competency throughout appropriate hospital areas. Thus, this nursing role is at the center of preparing the hospital to care for an older patient population.
This position remained unfilled for almost a year despite an intensive national search. This prompted us to incorporate the geriatric resource nurse model into our unit while we continued our recruitment.
Although we have successfully concluded our search for a nursing leader for the ACE unit, we have yet to hire a clinical pharmacist.
The rehabilitation of the unit would not have been possible without foundation support. As a public hospital with many competing demands, monies are limited for the rehabilitation required to create a more welcoming, safer environment for the older patient. In this case, the hospital foundation and a local foundation made grants to the ACE unit to allow us to change the environment.
These grants have allowed for significant changes to the unit, including elevated toilet seats, high-backed chairs, handrails, unit-based physical therapy equipment, and activities to promote non-pharmacological approaches to agitation.
Readiness for Change
All levels of hospital staff embraced the ACE unit concept. Department leaders in rehabilitation, nutrition, social work, and pharmacy felt ACE unit principles would improve care delivery over usual care.
Early on, department leaders and medical staff enthusiastically participated on a steering committee to help guide implementation efforts. In addition, when we offered geriatric resource nurse training to our nursing staff, more than 20 out of 50 unit nurses expressed interest.
Staff from all departments represented on the ACE unit team also expressed interest in and attended the three days of training. This provided baseline knowledge of common geriatric syndromes in hospitalized older patients for all team members. This been helpful during ACE team discussions.
Although medical residents felt they could not consistently attend ACE rounds, they appreciated potential benefits of the unit:
- Different perspectives could provide a wider range of evaluation and treatment recommendations for their patients;
- The co-location of key disciplines could result in overall time savings in calling for and ordering evaluations;
- The reduced likelihood that key interventions such as mobilization, feeding, catheter removal, and medication review would be missed; and
- The opportunity to learn principles of geriatric care through attending ACE rounds (when possible).
Medical staff in other departments immediately accepted the rationale for the unit.
Many expressed interest in expanding the concept to their departments, especially orthopedics, general surgery, and the ED. Although unfamiliar with specific interventions to improve care for hospitalized elders, the underlying concepts of patient-centered, team-delivered care with a focus on function resonated with most medical staff.
Next Steps
The unit is still in startup mode. Our major areas of focus are:
- Evaluating and improving team dynamics: We have engaged with researchers to evaluate our team dynamics and intervene where necessary to promote a high-functioning team.17
- Developing a culture of performance improvement: One of the hallmarks of high-functioning teams are measures of performance that are team-derived and reflect work product that the team can control.17
We are putting into place processes to measure key quality parameters including length of stay; nursing home placement; readmission rate, inappropriate catheter use; inappropriate medication prescribing; incidence of delirium, falls, and pressure ulcers; functional and cognitive status at admission and discharge; and patient satisfaction.
The orders set used by admitting residents are the standard general medical ward admission set and need revision for the ACE unit.
- Developing a research program: Our goal is to develop a research program evaluating interventions to prevent post-hospital degeneration of elders’ health. There is a dearth of research on improving hospital care for older, vulnerable adults.
- Expanding philanthropy support: The unit has benefited tremendously from philanthropy. In a relatively resource-poor setting, this allowed for rapid engagement with designers and vendors to remake the environment. We plan to expand our outreach efforts to interested philanthropists.
Summary
The ACE unit model can improve care for hospitalized older adults.
It requires a sustained level of commitment from hospital leaders, a focus on patient-centered, team-delivered care, sensitivity to communication modalities with primary caregivers, an awareness of the market for key professionals required, and flexibility to respond effectively to the many challenges that will emerge in implementing this model locally. TH
Dr. Pierluissi is medical director of the ACE unit at the San Francisco General Hospital. Susan Currin is the hospital’s chief nursing officer.
References
- Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451-458.
- Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004 Nov 3;292(17):2115-2124
- Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995 May 18;332(20):1338-1344.
- State of California, Department of Finance. Race/Ethnic Population with Age and Sex Detail, 2000–2050; 2004: Sacramento, Calif.
- Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993 Feb 1;118(3):219-223.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006 Jun 8;354(23):2509-2511; author reply 2509-11. Comment on: N Engl J Med. 2006 Mar 16;354(11):1157-1165.
- Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991 Feb 7;324(6):370-376. Comment in: N Engl J Med. 1991 Jul 18;325(3):210.
- Cohen HJ, Feussner JR, Weinberger M, et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002 Mar 21;346(12):905-912. Comment in: Curr Surg. 2004 May-Jun;61(3):266-74. N Engl J Med. 2002 Aug 1;347(5):371-373; author reply 371-373; author reply 371-3: N Engl J Med. 2002 Mar 21;346(12):874.
- Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999 Mar 4;340(9):669-676. Comment in: N Engl J Med. 1999 Jul 29;341(5):369-370; author reply 370. N Engl J Med. 1999 Mar 4;340(9):720-721.
- Reuben DB, Borok GM, Wolde-Tsadik G, et al. A randomized trial of comprehensive geriatric assessment in the care of hospitalized patients. N Engl J Med. 1995 May 18;332(20):1345-1350. Comment in: N Engl J Med. 1995 May 18;332(20):1376-1378.
- Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec 6;143(11):798-808. Comment in: Ann Intern Med. 2005 Dec 6;143(11):840-1. Ann Intern Med. 2006 Mar 21;144(6):456. Summary for patients in:Ann Intern Med. 2005 Dec 6;143(11):I56.
- Covinsky KE, Palmer RM, Kresevic DM, et. al. Improving functional outcomes in older patients: lessons from an acute care for elders unit. Jt Comm J Qual Improv. 1998 Feb;24(2):63-76.
- Wieland D, Rubenstein LZ. What do we know about patient targeting in geriatric evaluation and management (GEM) programs? Aging (Milano). 1996 Oct; 8(5):297-310.
- Spetz J, Dyer W. Forecasts of the Registered Nurse Workforce in California. 2005, University of California, San Francisco: San Francisco.
- Fleming KC, Evans JM, Chutka DS. Caregiver and clinician shortages in an aging nation. Mayo Clin Proc. 2003 Aug;78(8):1026-1040.
- Knapp KK, Quist RM, Walton SM, et al. Update on the pharmacist shortage: National and state data through 2003. Am J Health Syst Pharm. 2005 Mar 1;62(5):492-499.
- Katzenbach JR, Smith DK. The Discipline of Teams. Harv Bus Rev. July-August 2005:1-9.
Families often note that after older relatives return home from the hospital, something is wrong with them.
While the acute condition that brought a relative into the hospital has been remedied, major functional and cognitive deficits such as confusion, falls, and difficulty with basic activities of daily living remain.
This post-hospital decline may not be appreciated by hospital clinicians, perhaps because the problems do not become visible until the patient is home. However, these problems place significant burdens on patients and families.
Following discharge for an acute hospitalization, about a third of older patients will have a major new disability that threatens their ability to live independently.1 Among community-dwelling elders, half of all new disability occurs within a month of hospitalization.2 It isn’t surprising that nursing home placement has grown more common for medical hospitalizations, even for seemingly reversible medical problems.
Older adults will make up an increasing number of the patients cared for by hospitalists. The Acute Care for Elders (ACE) unit model of care focuses on preventing functional decline and increasing discharges to home.
In 2005, leadership of the San Francisco General Hospital Medical Center (SFGHMC) committed to improving care for hospitalized elders by adopting the ACE model.3
The ACE model combats hospital-acquired disability by improving care processes for older patients.
Major motivating factors for the change included demographic and quality-of-care imperatives. After a nine-month planning process, the SFGHMC ACE unit opened in February.
Rationale
Largely driven by the baby boom, the number of California seniors older than 65 will double from 3.5 million to 7 million over the next 40 years, and those older than 85 will triple from about 500,000 to 1.5 million. In San Francisco, changes will be even more dramatic as the number of residents over 65 increases from 14% of the population to 32%.4 (See Figure 1, right).
In California, people 65 to 84 are almost three times as likely to be hospitalized as those between 45 and 64. If rates of hospitalization do not change, an increase in hospitalized older adults will occur as the baby boom generation ages.
In addition, hospitalization can be hazardous for older adults, with increased risk for functional and cognitive disability and adverse events.5-7 As a result, hospitalization-associated disability represents a growing threat to the independence of the older population. A variety of changes to usual care have been adopted in an effort to reduce the hazards of hospitalization in the elderly.8-11
ACE Model
The ACE unit model, proven to reduce the risk of hospital-acquired disability in the elderly, is based on the Model of Dysfunction for Hospitalized Elders.12 (See Figure 2, p. 23)
This model outlines how processes of hospital care for the elderly promote physical impairment and depressed mood, leading to dysfunction. Counterproduc-tive factors in older adults include a hostile environment (lack of natural sunlight, high-glare floors, poor way-finding cues, high noise levels), depersonalization (lack of personal effects, clothing, and usual daily routines), bed rest through multiple tethers or inattention, medicines inappropriate in the elderly or given at inappropriate doses, procedures, and negative expectations (usually that the patient will require nursing home placement after admission).
These processes are the targets of the ACE intervention. The idea is to improve quality of care for the elderly by promoting rehabilitation and preventing disability.
The ACE unit addresses these issues through a “prehabilitation program.” The ACE unit is a physical location in the hospital with 10 beds. Care is redesigned by placing the patient at the center of restorative efforts of an interdisciplinary team consisting of an advanced practice nurse, a social worker, an occupational and a physical therapist, a nutritionist, a pharmacist, and a medical director. This ACE Unit team meets daily to review and plan care for all patients. Recommendations for nursing care and rehabilitation evaluation are implemented by the ACE team directly. Other recommendations, such as changing medications or considering alternative approaches to common geriatric syndromes are communicated to the primary team, which maintains overall responsibility for the care of the patient.
Each patient’s assessment is multidimensional, with an emphasis on nonpharmacologic interventions where practical. For example, an emphasis is placed on after-dinner exercise such as walking and socializing to promote sleep and reduce medication use. Nursing-care plans were revised to promote mobility, discourage inappropriate Foley use, and encourage adequate hydration and nutrition.
Recommendations are communicated to the primary team via a recommendation form placed in the physician-order section and text pages. The unit’s medical director and pharmacist review medications. Recommendations that involve medication changes are discussed with the primary team, which write all medication orders. Home planning begins on the day of admission.
Prior to opening the unit, the ACE unit social worker met with key city and county agencies including Aging and Adult Services, the Public Guardian, In-Home Supportive Services, and community nursing homes to introduce the unit and plan for an effective and safe transition.
All staff expect patients to maintain prehospital physical functioning. When possible, patients are expected to wear their own clothes, eat all their meals in a common dining room, and ambulate or exercise daily.
We considered establishing criteria for admission.13 We have not adopted formal criteria for patients 65 or older, presence of medical non-surgical condition(s) that require(s) acute hospitalization, and no need for telemetry or chemotherapy. As we learn how best to serve our hospitalized older adult population with the resources of the unit, we will re-evaluate targeting criteria. Most of our admissions are from the emergency department (ED), and the remainder are from other units in the hospital.
Challenges
Key challenges in opening the new service include securing commitment and resources from organizational leaders and key stakeholders; incorporation of the ACE unit concept in an academic training center; hiring key staff, especially the geriatric clinical nurse specialist and pharmacist positions; and completing the environmental rehabilitation on a limited budget.
While gaps in the care of the geriatric patient population were well identified at SFGHMC as far back as 1996 by a multidisciplinary task force, no actions on recommendations were taken, for several key reasons.
First, an executive level administrator or physician champion was not a member of the task force. Second, the organization did not have a department or regulatory mandate to address the gaps in the care of the elderly patients. Third, there was no link between the hospital strategic plan and the recommendations.
By 2004, these issues were largely addressed. A new chief nursing officer with a background in quality improvement understood the demographic and quality imperatives to improve care for hospitalized older adults.
That same year, the Hospital Executive Committee incorporated patient safety into the hospital strategic plan. This resulted in a successful business plan for an ACE Unit and geriatric consultation service linked to organizational strategy.
Funding was allocated for a medical director and a clinical nurse specialist in fiscal year 2005-2006. In addition, a grant was obtained from the SFGH Foundation to fund equipment, renovations, and staff education/training.
The original ACE unit concept involved expert, interdisciplinary geriatric assessment and communication of suggestions via a paper-based chart.
Initially, we felt the primary medical team should round with the ACE team, preferably at the bedside. However, informal focus groups held with the residents suggested this would happen infrequently.
The demands on the medical teams of completing patient rounds before morning attending rounds were cited as the main reason that model wouldn’t work.
We have implemented the following methods to promote communication between the ACE unit team and the primary medical team:
- Medical teams are encouraged to attend ACE unit rounds while on bedside rounds. This provides an opportunity to model the team-delivered care for house staff and medical students, an ACGME requirement;
- Suggestions to change medications are directly text-paged to the house staff; and
- Recommendations are summarized in a communication sheet left in the chart (this not a permanent part of the medical record).
We plan on using the text-paging more widely once the unit has wireless computer capability. Despite this, there are occasions where a team is not aware of a recommendation or new emphasis in the care plan. We are considering additional ways to improve communication such as attending the primary team attending rounds.
In California and other states there is a shortage of clinical pharmacists and masters-prepared nurses with expertise in geriatrics.14-16 The advanced practice nurse performs a vital role in raising the level of knowledge, skills, and attitudes for the nursing staff on the ACE unit.
In addition, we see the ACE unit as a drop in the pond; we feel a responsibility to expand nursing geriatric competency throughout appropriate hospital areas. Thus, this nursing role is at the center of preparing the hospital to care for an older patient population.
This position remained unfilled for almost a year despite an intensive national search. This prompted us to incorporate the geriatric resource nurse model into our unit while we continued our recruitment.
Although we have successfully concluded our search for a nursing leader for the ACE unit, we have yet to hire a clinical pharmacist.
The rehabilitation of the unit would not have been possible without foundation support. As a public hospital with many competing demands, monies are limited for the rehabilitation required to create a more welcoming, safer environment for the older patient. In this case, the hospital foundation and a local foundation made grants to the ACE unit to allow us to change the environment.
These grants have allowed for significant changes to the unit, including elevated toilet seats, high-backed chairs, handrails, unit-based physical therapy equipment, and activities to promote non-pharmacological approaches to agitation.
Readiness for Change
All levels of hospital staff embraced the ACE unit concept. Department leaders in rehabilitation, nutrition, social work, and pharmacy felt ACE unit principles would improve care delivery over usual care.
Early on, department leaders and medical staff enthusiastically participated on a steering committee to help guide implementation efforts. In addition, when we offered geriatric resource nurse training to our nursing staff, more than 20 out of 50 unit nurses expressed interest.
Staff from all departments represented on the ACE unit team also expressed interest in and attended the three days of training. This provided baseline knowledge of common geriatric syndromes in hospitalized older patients for all team members. This been helpful during ACE team discussions.
Although medical residents felt they could not consistently attend ACE rounds, they appreciated potential benefits of the unit:
- Different perspectives could provide a wider range of evaluation and treatment recommendations for their patients;
- The co-location of key disciplines could result in overall time savings in calling for and ordering evaluations;
- The reduced likelihood that key interventions such as mobilization, feeding, catheter removal, and medication review would be missed; and
- The opportunity to learn principles of geriatric care through attending ACE rounds (when possible).
Medical staff in other departments immediately accepted the rationale for the unit.
Many expressed interest in expanding the concept to their departments, especially orthopedics, general surgery, and the ED. Although unfamiliar with specific interventions to improve care for hospitalized elders, the underlying concepts of patient-centered, team-delivered care with a focus on function resonated with most medical staff.
Next Steps
The unit is still in startup mode. Our major areas of focus are:
- Evaluating and improving team dynamics: We have engaged with researchers to evaluate our team dynamics and intervene where necessary to promote a high-functioning team.17
- Developing a culture of performance improvement: One of the hallmarks of high-functioning teams are measures of performance that are team-derived and reflect work product that the team can control.17
We are putting into place processes to measure key quality parameters including length of stay; nursing home placement; readmission rate, inappropriate catheter use; inappropriate medication prescribing; incidence of delirium, falls, and pressure ulcers; functional and cognitive status at admission and discharge; and patient satisfaction.
The orders set used by admitting residents are the standard general medical ward admission set and need revision for the ACE unit.
- Developing a research program: Our goal is to develop a research program evaluating interventions to prevent post-hospital degeneration of elders’ health. There is a dearth of research on improving hospital care for older, vulnerable adults.
- Expanding philanthropy support: The unit has benefited tremendously from philanthropy. In a relatively resource-poor setting, this allowed for rapid engagement with designers and vendors to remake the environment. We plan to expand our outreach efforts to interested philanthropists.
Summary
The ACE unit model can improve care for hospitalized older adults.
It requires a sustained level of commitment from hospital leaders, a focus on patient-centered, team-delivered care, sensitivity to communication modalities with primary caregivers, an awareness of the market for key professionals required, and flexibility to respond effectively to the many challenges that will emerge in implementing this model locally. TH
Dr. Pierluissi is medical director of the ACE unit at the San Francisco General Hospital. Susan Currin is the hospital’s chief nursing officer.
References
- Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451-458.
- Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004 Nov 3;292(17):2115-2124
- Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995 May 18;332(20):1338-1344.
- State of California, Department of Finance. Race/Ethnic Population with Age and Sex Detail, 2000–2050; 2004: Sacramento, Calif.
- Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993 Feb 1;118(3):219-223.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006 Jun 8;354(23):2509-2511; author reply 2509-11. Comment on: N Engl J Med. 2006 Mar 16;354(11):1157-1165.
- Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991 Feb 7;324(6):370-376. Comment in: N Engl J Med. 1991 Jul 18;325(3):210.
- Cohen HJ, Feussner JR, Weinberger M, et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002 Mar 21;346(12):905-912. Comment in: Curr Surg. 2004 May-Jun;61(3):266-74. N Engl J Med. 2002 Aug 1;347(5):371-373; author reply 371-373; author reply 371-3: N Engl J Med. 2002 Mar 21;346(12):874.
- Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999 Mar 4;340(9):669-676. Comment in: N Engl J Med. 1999 Jul 29;341(5):369-370; author reply 370. N Engl J Med. 1999 Mar 4;340(9):720-721.
- Reuben DB, Borok GM, Wolde-Tsadik G, et al. A randomized trial of comprehensive geriatric assessment in the care of hospitalized patients. N Engl J Med. 1995 May 18;332(20):1345-1350. Comment in: N Engl J Med. 1995 May 18;332(20):1376-1378.
- Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec 6;143(11):798-808. Comment in: Ann Intern Med. 2005 Dec 6;143(11):840-1. Ann Intern Med. 2006 Mar 21;144(6):456. Summary for patients in:Ann Intern Med. 2005 Dec 6;143(11):I56.
- Covinsky KE, Palmer RM, Kresevic DM, et. al. Improving functional outcomes in older patients: lessons from an acute care for elders unit. Jt Comm J Qual Improv. 1998 Feb;24(2):63-76.
- Wieland D, Rubenstein LZ. What do we know about patient targeting in geriatric evaluation and management (GEM) programs? Aging (Milano). 1996 Oct; 8(5):297-310.
- Spetz J, Dyer W. Forecasts of the Registered Nurse Workforce in California. 2005, University of California, San Francisco: San Francisco.
- Fleming KC, Evans JM, Chutka DS. Caregiver and clinician shortages in an aging nation. Mayo Clin Proc. 2003 Aug;78(8):1026-1040.
- Knapp KK, Quist RM, Walton SM, et al. Update on the pharmacist shortage: National and state data through 2003. Am J Health Syst Pharm. 2005 Mar 1;62(5):492-499.
- Katzenbach JR, Smith DK. The Discipline of Teams. Harv Bus Rev. July-August 2005:1-9.
The Power of “Sorry”
Like many people, we like to sing while secure in the anonymity of our cars. This morning, one of us was wailing along with Elton John as he sang “Sorry Seems to Be the Hardest Word”:
It’s sad, so sad
Why can’t we talk it over
Oh, it seems to me
That sorry seems to be the hardest word.
That verse frames a critical legal question physicians regularly encounter: how to communicate with patients after an unexpected outcome. More precisely, should a physician apologize to a patient who suffers complications because of that physician’s treatment?
Traditionally, after a patient suffered a complication, defense lawyers were reluctant to allow the physician to express apologies or regret. The defense lawyer feared the apology would be treated as an “admission against interest.” In other words, the defense lawyer wanted to prevent a plaintiff’s lawyer from someday arguing that the physician’s apology was an admission of negligence or wrongdoing.
But the lawyer’s strategy fails. The patient wants the physician to apologize for an error. In fact, the patient distrusts a physician who does not admit errors.
‘‘Although a physician may wish to tell a patient when he has made a mistake, lawyers often order doctors to say nothing,’’ wrote University of Florida law professor Jonathan R. Cohen in the Southern California Law Review.1 “The physician’s silence may then trigger the patient’s anger. This alienation may then prompt the patient to sue.”
These observations are consistent with studies demonstrating that patients are far less to sue when provided with a full explanation and apology.2
Certainly no physician wants to make a statement that a plaintiff’s lawyer will use against him in court. But the same physician rationally wants to take any steps that might prevent the patient from feeling as though he or she needs to consult with a plaintiff’s lawyer. So, what’s a physician to do when caught between the hospital’s lawsuit-fearing attorney and a patient who expects his doctor to communicate with her honestly and forthrightly?
Fortunately, several state legislatures have recognized this tension and passed legislation that encourages physicians to apologize without facing the prospect that a plaintiff’s lawyer will argue that the physician apologized only because he knew he did something wrong. An example best illustrates how such “I’m sorry” statutes work.
Dr. Smith is treating a 22-year-old patient, John Elway, for a fractured fibula. Dr. Smith sees no signs of neurological compromise while the patient is in a cast. After the cast is removed, it appears the patient has lost function in the leg because the cast was too tight. The patient was a star college athlete who was expected to be drafted into the NFL, but now likely won’t be drafted. Dr. Smith tells the patient: “It’s my fault this happened. I’m really sorry that I didn’t pick up on this sooner.”
Does Dr. Smith’s statement come into evidence in court? Does part of it? The answers probably depend upon which state’s apology statute is applied. Massachusetts was one of the first states to pass an apology statute. It reads:
Statements, writings, or benevolent gestures expressing sympathy or a general sense of benevolence relating to the pain, suffering or death of a person involved in an accident and made to the person or to the family of such a person shall be inadmissible as evidence of an admission of liability in a civil action.
Significantly, the Massachusetts statute applies to people “involved in an accident,” which might imply that it is limited to automobile accidents or workplace accidents. The Massachusetts statute prevents this limited construction by providing a broad definition of “accident,” including any “occurrence resulting in injury or death to one or more persons which is not the result of a willful action by a party.” This definition would encompass ordinary medical negligence.
It would seem clear that the statute would protect Dr. Smith if he simply stated: “I want you to know how sorry I am this happened. I feel awful that you experienced this complication.”
But if Dr. Smith said, “It’s my fault this happened,” would the Massachusetts statute protect Dr. Smith? That’s a much harder call. Saying “It’s my fault” is technically not an expression of “sympathy or a general act of benevolence.” There no clear answer under Massachusetts law. But we believe the result would probably depend on whether the judge hearing the case thought this statement occurred during an overall act of apology.
The answer is clearer in California. That state’s apology statute reads:
The portion of statements, writings, or benevolent gestures expressing sympathy or a general sense of benevolence relating to the pain, suffering or death of a person involved in an accident and made to that person or to the family of that person shall be inadmissible as evidence of an admission of liability in a civil action. A statement of fault, however, which is part of, or in addition to, any of the above shall not be inadmissible pursuant to this section.
California draws a clear distinction between “the portion of statements ... expressing sympathy or a general sense of benevolence” and “a statement of fault.”
In our scenario, the jury would almost certainly be able to hear Dr. Smith’s statement, “It’s my fault this happened.” Critics of California’s law believe it creates too narrow a window for physicians to believe that plaintiff’s lawyers will not use their apology against them in a lawsuit.3
While Dr. Smith’s statement is likely to come into evidence in California, it’s also clear the opposite would occur in Colorado. Colorado’s apology statute, which specifically applies to medical malpractice actions, reads:
In any civil action brought by an alleged victim of an unanticipated outcome of medical care ... any and all statements … expressing apology, fault, sympathy, commiseration, condolence, compassion or a general sense of benevolence ... shall be inadmissible as evidence of an admission of liability or as evidence of an admission against interest.
Because Colorado’s statute specifically renders statements of “fault” inadmissible, a jury would not be able to consider any of Dr. Smith’s statements made during the course of his apology. Colorado’s law provides the physician with the most protection. Critics of Colorado’s law believe it’s unfair for physicians to admit fault to their patients in the hospital, then deny liability after the patient files a lawsuit.
Twenty-six other states have passed apology statutes; each works a bit differently. The choice of words matters. Legally, there is a big difference between a physician telling a patient, “I’m sorry about your pain” or saying, “It’s my fault you’re in pain.”
While apologies are valuable and important in relationships of trust—including the relationship between physicians and patients—we suggest you consult an experienced lawyer when crafting an apology to make sure it conveys your sympathies without opening a door to liability. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, Denver.
References
- Cohen JR. Advising clients to apologize. Southern California Law Review. 1999;72:1009-1131.
- Hickson GB, Clayton EW, Githens PB, et al. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992 Mar;267(10):1359-1363.
- Eisenberg D. When doctors say, “We’re sorry.” Time. 2005 Aug 15;166(7):50-52.
Like many people, we like to sing while secure in the anonymity of our cars. This morning, one of us was wailing along with Elton John as he sang “Sorry Seems to Be the Hardest Word”:
It’s sad, so sad
Why can’t we talk it over
Oh, it seems to me
That sorry seems to be the hardest word.
That verse frames a critical legal question physicians regularly encounter: how to communicate with patients after an unexpected outcome. More precisely, should a physician apologize to a patient who suffers complications because of that physician’s treatment?
Traditionally, after a patient suffered a complication, defense lawyers were reluctant to allow the physician to express apologies or regret. The defense lawyer feared the apology would be treated as an “admission against interest.” In other words, the defense lawyer wanted to prevent a plaintiff’s lawyer from someday arguing that the physician’s apology was an admission of negligence or wrongdoing.
But the lawyer’s strategy fails. The patient wants the physician to apologize for an error. In fact, the patient distrusts a physician who does not admit errors.
‘‘Although a physician may wish to tell a patient when he has made a mistake, lawyers often order doctors to say nothing,’’ wrote University of Florida law professor Jonathan R. Cohen in the Southern California Law Review.1 “The physician’s silence may then trigger the patient’s anger. This alienation may then prompt the patient to sue.”
These observations are consistent with studies demonstrating that patients are far less to sue when provided with a full explanation and apology.2
Certainly no physician wants to make a statement that a plaintiff’s lawyer will use against him in court. But the same physician rationally wants to take any steps that might prevent the patient from feeling as though he or she needs to consult with a plaintiff’s lawyer. So, what’s a physician to do when caught between the hospital’s lawsuit-fearing attorney and a patient who expects his doctor to communicate with her honestly and forthrightly?
Fortunately, several state legislatures have recognized this tension and passed legislation that encourages physicians to apologize without facing the prospect that a plaintiff’s lawyer will argue that the physician apologized only because he knew he did something wrong. An example best illustrates how such “I’m sorry” statutes work.
Dr. Smith is treating a 22-year-old patient, John Elway, for a fractured fibula. Dr. Smith sees no signs of neurological compromise while the patient is in a cast. After the cast is removed, it appears the patient has lost function in the leg because the cast was too tight. The patient was a star college athlete who was expected to be drafted into the NFL, but now likely won’t be drafted. Dr. Smith tells the patient: “It’s my fault this happened. I’m really sorry that I didn’t pick up on this sooner.”
Does Dr. Smith’s statement come into evidence in court? Does part of it? The answers probably depend upon which state’s apology statute is applied. Massachusetts was one of the first states to pass an apology statute. It reads:
Statements, writings, or benevolent gestures expressing sympathy or a general sense of benevolence relating to the pain, suffering or death of a person involved in an accident and made to the person or to the family of such a person shall be inadmissible as evidence of an admission of liability in a civil action.
Significantly, the Massachusetts statute applies to people “involved in an accident,” which might imply that it is limited to automobile accidents or workplace accidents. The Massachusetts statute prevents this limited construction by providing a broad definition of “accident,” including any “occurrence resulting in injury or death to one or more persons which is not the result of a willful action by a party.” This definition would encompass ordinary medical negligence.
It would seem clear that the statute would protect Dr. Smith if he simply stated: “I want you to know how sorry I am this happened. I feel awful that you experienced this complication.”
But if Dr. Smith said, “It’s my fault this happened,” would the Massachusetts statute protect Dr. Smith? That’s a much harder call. Saying “It’s my fault” is technically not an expression of “sympathy or a general act of benevolence.” There no clear answer under Massachusetts law. But we believe the result would probably depend on whether the judge hearing the case thought this statement occurred during an overall act of apology.
The answer is clearer in California. That state’s apology statute reads:
The portion of statements, writings, or benevolent gestures expressing sympathy or a general sense of benevolence relating to the pain, suffering or death of a person involved in an accident and made to that person or to the family of that person shall be inadmissible as evidence of an admission of liability in a civil action. A statement of fault, however, which is part of, or in addition to, any of the above shall not be inadmissible pursuant to this section.
California draws a clear distinction between “the portion of statements ... expressing sympathy or a general sense of benevolence” and “a statement of fault.”
In our scenario, the jury would almost certainly be able to hear Dr. Smith’s statement, “It’s my fault this happened.” Critics of California’s law believe it creates too narrow a window for physicians to believe that plaintiff’s lawyers will not use their apology against them in a lawsuit.3
While Dr. Smith’s statement is likely to come into evidence in California, it’s also clear the opposite would occur in Colorado. Colorado’s apology statute, which specifically applies to medical malpractice actions, reads:
In any civil action brought by an alleged victim of an unanticipated outcome of medical care ... any and all statements … expressing apology, fault, sympathy, commiseration, condolence, compassion or a general sense of benevolence ... shall be inadmissible as evidence of an admission of liability or as evidence of an admission against interest.
Because Colorado’s statute specifically renders statements of “fault” inadmissible, a jury would not be able to consider any of Dr. Smith’s statements made during the course of his apology. Colorado’s law provides the physician with the most protection. Critics of Colorado’s law believe it’s unfair for physicians to admit fault to their patients in the hospital, then deny liability after the patient files a lawsuit.
Twenty-six other states have passed apology statutes; each works a bit differently. The choice of words matters. Legally, there is a big difference between a physician telling a patient, “I’m sorry about your pain” or saying, “It’s my fault you’re in pain.”
While apologies are valuable and important in relationships of trust—including the relationship between physicians and patients—we suggest you consult an experienced lawyer when crafting an apology to make sure it conveys your sympathies without opening a door to liability. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, Denver.
References
- Cohen JR. Advising clients to apologize. Southern California Law Review. 1999;72:1009-1131.
- Hickson GB, Clayton EW, Githens PB, et al. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992 Mar;267(10):1359-1363.
- Eisenberg D. When doctors say, “We’re sorry.” Time. 2005 Aug 15;166(7):50-52.
Like many people, we like to sing while secure in the anonymity of our cars. This morning, one of us was wailing along with Elton John as he sang “Sorry Seems to Be the Hardest Word”:
It’s sad, so sad
Why can’t we talk it over
Oh, it seems to me
That sorry seems to be the hardest word.
That verse frames a critical legal question physicians regularly encounter: how to communicate with patients after an unexpected outcome. More precisely, should a physician apologize to a patient who suffers complications because of that physician’s treatment?
Traditionally, after a patient suffered a complication, defense lawyers were reluctant to allow the physician to express apologies or regret. The defense lawyer feared the apology would be treated as an “admission against interest.” In other words, the defense lawyer wanted to prevent a plaintiff’s lawyer from someday arguing that the physician’s apology was an admission of negligence or wrongdoing.
But the lawyer’s strategy fails. The patient wants the physician to apologize for an error. In fact, the patient distrusts a physician who does not admit errors.
‘‘Although a physician may wish to tell a patient when he has made a mistake, lawyers often order doctors to say nothing,’’ wrote University of Florida law professor Jonathan R. Cohen in the Southern California Law Review.1 “The physician’s silence may then trigger the patient’s anger. This alienation may then prompt the patient to sue.”
These observations are consistent with studies demonstrating that patients are far less to sue when provided with a full explanation and apology.2
Certainly no physician wants to make a statement that a plaintiff’s lawyer will use against him in court. But the same physician rationally wants to take any steps that might prevent the patient from feeling as though he or she needs to consult with a plaintiff’s lawyer. So, what’s a physician to do when caught between the hospital’s lawsuit-fearing attorney and a patient who expects his doctor to communicate with her honestly and forthrightly?
Fortunately, several state legislatures have recognized this tension and passed legislation that encourages physicians to apologize without facing the prospect that a plaintiff’s lawyer will argue that the physician apologized only because he knew he did something wrong. An example best illustrates how such “I’m sorry” statutes work.
Dr. Smith is treating a 22-year-old patient, John Elway, for a fractured fibula. Dr. Smith sees no signs of neurological compromise while the patient is in a cast. After the cast is removed, it appears the patient has lost function in the leg because the cast was too tight. The patient was a star college athlete who was expected to be drafted into the NFL, but now likely won’t be drafted. Dr. Smith tells the patient: “It’s my fault this happened. I’m really sorry that I didn’t pick up on this sooner.”
Does Dr. Smith’s statement come into evidence in court? Does part of it? The answers probably depend upon which state’s apology statute is applied. Massachusetts was one of the first states to pass an apology statute. It reads:
Statements, writings, or benevolent gestures expressing sympathy or a general sense of benevolence relating to the pain, suffering or death of a person involved in an accident and made to the person or to the family of such a person shall be inadmissible as evidence of an admission of liability in a civil action.
Significantly, the Massachusetts statute applies to people “involved in an accident,” which might imply that it is limited to automobile accidents or workplace accidents. The Massachusetts statute prevents this limited construction by providing a broad definition of “accident,” including any “occurrence resulting in injury or death to one or more persons which is not the result of a willful action by a party.” This definition would encompass ordinary medical negligence.
It would seem clear that the statute would protect Dr. Smith if he simply stated: “I want you to know how sorry I am this happened. I feel awful that you experienced this complication.”
But if Dr. Smith said, “It’s my fault this happened,” would the Massachusetts statute protect Dr. Smith? That’s a much harder call. Saying “It’s my fault” is technically not an expression of “sympathy or a general act of benevolence.” There no clear answer under Massachusetts law. But we believe the result would probably depend on whether the judge hearing the case thought this statement occurred during an overall act of apology.
The answer is clearer in California. That state’s apology statute reads:
The portion of statements, writings, or benevolent gestures expressing sympathy or a general sense of benevolence relating to the pain, suffering or death of a person involved in an accident and made to that person or to the family of that person shall be inadmissible as evidence of an admission of liability in a civil action. A statement of fault, however, which is part of, or in addition to, any of the above shall not be inadmissible pursuant to this section.
California draws a clear distinction between “the portion of statements ... expressing sympathy or a general sense of benevolence” and “a statement of fault.”
In our scenario, the jury would almost certainly be able to hear Dr. Smith’s statement, “It’s my fault this happened.” Critics of California’s law believe it creates too narrow a window for physicians to believe that plaintiff’s lawyers will not use their apology against them in a lawsuit.3
While Dr. Smith’s statement is likely to come into evidence in California, it’s also clear the opposite would occur in Colorado. Colorado’s apology statute, which specifically applies to medical malpractice actions, reads:
In any civil action brought by an alleged victim of an unanticipated outcome of medical care ... any and all statements … expressing apology, fault, sympathy, commiseration, condolence, compassion or a general sense of benevolence ... shall be inadmissible as evidence of an admission of liability or as evidence of an admission against interest.
Because Colorado’s statute specifically renders statements of “fault” inadmissible, a jury would not be able to consider any of Dr. Smith’s statements made during the course of his apology. Colorado’s law provides the physician with the most protection. Critics of Colorado’s law believe it’s unfair for physicians to admit fault to their patients in the hospital, then deny liability after the patient files a lawsuit.
Twenty-six other states have passed apology statutes; each works a bit differently. The choice of words matters. Legally, there is a big difference between a physician telling a patient, “I’m sorry about your pain” or saying, “It’s my fault you’re in pain.”
While apologies are valuable and important in relationships of trust—including the relationship between physicians and patients—we suggest you consult an experienced lawyer when crafting an apology to make sure it conveys your sympathies without opening a door to liability. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, Denver.
References
- Cohen JR. Advising clients to apologize. Southern California Law Review. 1999;72:1009-1131.
- Hickson GB, Clayton EW, Githens PB, et al. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992 Mar;267(10):1359-1363.
- Eisenberg D. When doctors say, “We’re sorry.” Time. 2005 Aug 15;166(7):50-52.
Is P4P Paying off?
Pay for performance (P4P) has been the hottest topic among physicians for quite a while. Perhaps the time has come to ask: Is it worth the hype?
“In terms of organized pay-for-performance programs, we’re at the very beginning of seeing pay for performance in action,” says Patrick J. Torcson, MD, MMM, FACP, member of SHM’s Public Policy Committee and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
Although P4P is still in its infancy, one major demonstration trial is complete, and researchers have begun to mine results for indications of success.
The largest national P4P trial to date is the Centers for Medicare and Medicaid (CMS)/Premier Hospital Quality Incentive Demonstration Project, which involved more than 260 hospitals reporting on 34 quality measures from October 2003 through September 2006. The measures were grouped in five clinical areas: acute myocardial infarction, heart failure, coronary artery bypass graft, pneumonia, and hip and knee replacement.
Hospitals in the top 10% for each of the quality measures received a 2% bonus of their Medicare payments for the measured condition; hospitals in the top 20% received a 1% bonus; and hospitals in the bottom 20% returned 1% to 2% of their diagnosis-related group (DRG) payments.
CMS has paid $17.55 million in incentives to the top-tier, participating hospitals and reported savings of $1.4 billion in terms of avoidable deaths, complications and readmissions prevented, and shortened lengths of stay.
As for quality improvements, results from the first two years of the demonstration project show proven improvement across all five clinical focus areas. The average improvement of the composite quality scores (CQS), an aggregate of all quality measures within each clinical area, in the project’s second year was 6.7%, for total gains of 11.8% over the project’s first two years.
The CQS improved significantly between the start date and the end of the second year in all five clinical focus areas:
- From 87.5% to 94.4% for patients with acute myocardial infarction;
- From 64.5% to 82.4% for patients with heart failure;
- From 69.3% to 85.8% for patients with community acquired pneumonia;
- From 84.8% to 93.8% for patients with coronary artery bypass graft; and
- From 84.6% to 93.4% for patients with hip and knee replacement.
“In many circles, this is proof positive that pay for performance works,” Dr. Torcson says of the results of the Premier demo. “However, this was hospital-level P4P and involves a different methodology than physician-level P4P. I don’t think it’s safe or accurate to extrapolate these results.”
What the Research Says
Various researchers have examined available P4P data to see if incentives improve care.
Recent studies include one led by hospitalist Peter Lindenauer, MD, MSc, FACP, medical director, clinical and quality informatics, Baystate Health in Springfield, Mass., and assistant professor of medicine at Tufts University School of Medicine in Boston.1 Dr. Lindenauer and his colleagues examined data from the CMS data warehouse gathered as part of the Hospital Quality Alliance (Hospital Compare) project. Specifically, they compared P4P CMS Premier hospitals with 408 hospitals that participated only in public reporting, with no compensation.
They found that the P4P hospitals showed modestly greater improvement in all composite measures of quality than hospitals that simply reported on measures. Specifically, improvements in the P4P hospitals ranged from 2.6% to 4.1% over two years. “The small gains in process of care measures observed in the study are unlikely to have translated into meaningful improvements in outcomes,” Dr. Lindenauer says.
Other studies of P4P are inconclusive. A literature review on the subject finds “little evidence to support the effectiveness of paying for quality.”2
A second literature review out of the Baylor College of Medicine in Houston based on 17 studies “suggests some positive effects of financial incentives at the physician level, the provider group level, and the healthcare payment system level. The findings also suggest that ongoing monitoring of incentive programs is critical to determine whether incentives are having unintended effects on quality of care.”3
Finally, a study of P4P programs for family practices in the United Kingdom revealed that serious financial incentives for physicians resulted in 83.4% achieving goals for 10 chronic diseases in a year.4
“There is no conclusive evidence that physician-level P4P works to improve quality of care and reduce cost of care,” concludes Dr. Torcson. “The U.K. experience demonstrates that given a sufficient incentive, physicians will adhere to and report on performance measures. Further study is being done to see if this translates into quality improvement for patients.”
The next phase of P4P is pay for reporting—which may help pin down the true value of P4P.
The Physician Quality Reporting Initiative (PQRI), now well under way, “is the first nationwide pay-for-performance program, and one of the first to include hospitalists,” says Dr. Torcson. “This is the first taste we’re all having of physician-level pay-for-performance since the PQRI started on July 1.”
The incentives for participating in the trial aren’t high. “Based on projections of PQRI reporting, hospitalists can earn a bonus of $807,” says Dr. Torcson. “This may not be a strong motivator to participate in PQRI. However, it’s a beginning. If you’re going to fail [at reporting], this is the time to do it.”
The PQRI trial is short; it will end Dec. 31. And early next year, it’s guaranteed that all eyes will be on outcomes from this program. “Private payers are watching this very closely; they’re ready to jump into the game,” says Dr. Torcson. Healthcare organizations and professionals should be ready to jump as well, because next steps for P4P and other payment factors are still unknown.
“What happens after Dec. 31 is wide open,” Dr. Torcson says. “We don’t know what to expect from Congress. Right now we’re looking at a proposed 9.8% cut to physician fees. Will this cut be made up by pay-for-performance bonuses? Congress determines what will happen, and the [2008] election could change everything.”
To date, P4P has not lived up to its hype; however, the use of incentives to improve quality is in the early stages. Time will tell if P4P pays off in improved care—but CMS and many physicians seem committed to the idea.
“I think there’s a lot to be said for the concept of providing incentives that encourage hospitals to invest in quality of care,” says Dr. Lindenauer. “Our current system of healthcare hasn’t done that.”
Dr. Lindenauer’s advice for moving ahead with P4P? “We need to proceed cautiously and be mindful of some of the unintended consequences,” he concludes. TH
Jane Jerrard has been writing for The Hospitalist since 2005.
References
- Lindenauer PK, Remus D, Roman S, et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007 Feb 1;356(5):486-496.
- Rosenthal MB, Frank RG. What is the empirical basis for paying for quality in health care? Med Care Res Rev. 2006;63(2):135-137.
- Petersen LA, Woodard LD, Urech T, et al. Does pay-for-performance improve the quality of health care? Ann Intern Med. 2006;145(4):265-272.
- Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355(4):375-384.
Pay for performance (P4P) has been the hottest topic among physicians for quite a while. Perhaps the time has come to ask: Is it worth the hype?
“In terms of organized pay-for-performance programs, we’re at the very beginning of seeing pay for performance in action,” says Patrick J. Torcson, MD, MMM, FACP, member of SHM’s Public Policy Committee and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
Although P4P is still in its infancy, one major demonstration trial is complete, and researchers have begun to mine results for indications of success.
The largest national P4P trial to date is the Centers for Medicare and Medicaid (CMS)/Premier Hospital Quality Incentive Demonstration Project, which involved more than 260 hospitals reporting on 34 quality measures from October 2003 through September 2006. The measures were grouped in five clinical areas: acute myocardial infarction, heart failure, coronary artery bypass graft, pneumonia, and hip and knee replacement.
Hospitals in the top 10% for each of the quality measures received a 2% bonus of their Medicare payments for the measured condition; hospitals in the top 20% received a 1% bonus; and hospitals in the bottom 20% returned 1% to 2% of their diagnosis-related group (DRG) payments.
CMS has paid $17.55 million in incentives to the top-tier, participating hospitals and reported savings of $1.4 billion in terms of avoidable deaths, complications and readmissions prevented, and shortened lengths of stay.
As for quality improvements, results from the first two years of the demonstration project show proven improvement across all five clinical focus areas. The average improvement of the composite quality scores (CQS), an aggregate of all quality measures within each clinical area, in the project’s second year was 6.7%, for total gains of 11.8% over the project’s first two years.
The CQS improved significantly between the start date and the end of the second year in all five clinical focus areas:
- From 87.5% to 94.4% for patients with acute myocardial infarction;
- From 64.5% to 82.4% for patients with heart failure;
- From 69.3% to 85.8% for patients with community acquired pneumonia;
- From 84.8% to 93.8% for patients with coronary artery bypass graft; and
- From 84.6% to 93.4% for patients with hip and knee replacement.
“In many circles, this is proof positive that pay for performance works,” Dr. Torcson says of the results of the Premier demo. “However, this was hospital-level P4P and involves a different methodology than physician-level P4P. I don’t think it’s safe or accurate to extrapolate these results.”
What the Research Says
Various researchers have examined available P4P data to see if incentives improve care.
Recent studies include one led by hospitalist Peter Lindenauer, MD, MSc, FACP, medical director, clinical and quality informatics, Baystate Health in Springfield, Mass., and assistant professor of medicine at Tufts University School of Medicine in Boston.1 Dr. Lindenauer and his colleagues examined data from the CMS data warehouse gathered as part of the Hospital Quality Alliance (Hospital Compare) project. Specifically, they compared P4P CMS Premier hospitals with 408 hospitals that participated only in public reporting, with no compensation.
They found that the P4P hospitals showed modestly greater improvement in all composite measures of quality than hospitals that simply reported on measures. Specifically, improvements in the P4P hospitals ranged from 2.6% to 4.1% over two years. “The small gains in process of care measures observed in the study are unlikely to have translated into meaningful improvements in outcomes,” Dr. Lindenauer says.
Other studies of P4P are inconclusive. A literature review on the subject finds “little evidence to support the effectiveness of paying for quality.”2
A second literature review out of the Baylor College of Medicine in Houston based on 17 studies “suggests some positive effects of financial incentives at the physician level, the provider group level, and the healthcare payment system level. The findings also suggest that ongoing monitoring of incentive programs is critical to determine whether incentives are having unintended effects on quality of care.”3
Finally, a study of P4P programs for family practices in the United Kingdom revealed that serious financial incentives for physicians resulted in 83.4% achieving goals for 10 chronic diseases in a year.4
“There is no conclusive evidence that physician-level P4P works to improve quality of care and reduce cost of care,” concludes Dr. Torcson. “The U.K. experience demonstrates that given a sufficient incentive, physicians will adhere to and report on performance measures. Further study is being done to see if this translates into quality improvement for patients.”
The next phase of P4P is pay for reporting—which may help pin down the true value of P4P.
The Physician Quality Reporting Initiative (PQRI), now well under way, “is the first nationwide pay-for-performance program, and one of the first to include hospitalists,” says Dr. Torcson. “This is the first taste we’re all having of physician-level pay-for-performance since the PQRI started on July 1.”
The incentives for participating in the trial aren’t high. “Based on projections of PQRI reporting, hospitalists can earn a bonus of $807,” says Dr. Torcson. “This may not be a strong motivator to participate in PQRI. However, it’s a beginning. If you’re going to fail [at reporting], this is the time to do it.”
The PQRI trial is short; it will end Dec. 31. And early next year, it’s guaranteed that all eyes will be on outcomes from this program. “Private payers are watching this very closely; they’re ready to jump into the game,” says Dr. Torcson. Healthcare organizations and professionals should be ready to jump as well, because next steps for P4P and other payment factors are still unknown.
“What happens after Dec. 31 is wide open,” Dr. Torcson says. “We don’t know what to expect from Congress. Right now we’re looking at a proposed 9.8% cut to physician fees. Will this cut be made up by pay-for-performance bonuses? Congress determines what will happen, and the [2008] election could change everything.”
To date, P4P has not lived up to its hype; however, the use of incentives to improve quality is in the early stages. Time will tell if P4P pays off in improved care—but CMS and many physicians seem committed to the idea.
“I think there’s a lot to be said for the concept of providing incentives that encourage hospitals to invest in quality of care,” says Dr. Lindenauer. “Our current system of healthcare hasn’t done that.”
Dr. Lindenauer’s advice for moving ahead with P4P? “We need to proceed cautiously and be mindful of some of the unintended consequences,” he concludes. TH
Jane Jerrard has been writing for The Hospitalist since 2005.
References
- Lindenauer PK, Remus D, Roman S, et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007 Feb 1;356(5):486-496.
- Rosenthal MB, Frank RG. What is the empirical basis for paying for quality in health care? Med Care Res Rev. 2006;63(2):135-137.
- Petersen LA, Woodard LD, Urech T, et al. Does pay-for-performance improve the quality of health care? Ann Intern Med. 2006;145(4):265-272.
- Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355(4):375-384.
Pay for performance (P4P) has been the hottest topic among physicians for quite a while. Perhaps the time has come to ask: Is it worth the hype?
“In terms of organized pay-for-performance programs, we’re at the very beginning of seeing pay for performance in action,” says Patrick J. Torcson, MD, MMM, FACP, member of SHM’s Public Policy Committee and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
Although P4P is still in its infancy, one major demonstration trial is complete, and researchers have begun to mine results for indications of success.
The largest national P4P trial to date is the Centers for Medicare and Medicaid (CMS)/Premier Hospital Quality Incentive Demonstration Project, which involved more than 260 hospitals reporting on 34 quality measures from October 2003 through September 2006. The measures were grouped in five clinical areas: acute myocardial infarction, heart failure, coronary artery bypass graft, pneumonia, and hip and knee replacement.
Hospitals in the top 10% for each of the quality measures received a 2% bonus of their Medicare payments for the measured condition; hospitals in the top 20% received a 1% bonus; and hospitals in the bottom 20% returned 1% to 2% of their diagnosis-related group (DRG) payments.
CMS has paid $17.55 million in incentives to the top-tier, participating hospitals and reported savings of $1.4 billion in terms of avoidable deaths, complications and readmissions prevented, and shortened lengths of stay.
As for quality improvements, results from the first two years of the demonstration project show proven improvement across all five clinical focus areas. The average improvement of the composite quality scores (CQS), an aggregate of all quality measures within each clinical area, in the project’s second year was 6.7%, for total gains of 11.8% over the project’s first two years.
The CQS improved significantly between the start date and the end of the second year in all five clinical focus areas:
- From 87.5% to 94.4% for patients with acute myocardial infarction;
- From 64.5% to 82.4% for patients with heart failure;
- From 69.3% to 85.8% for patients with community acquired pneumonia;
- From 84.8% to 93.8% for patients with coronary artery bypass graft; and
- From 84.6% to 93.4% for patients with hip and knee replacement.
“In many circles, this is proof positive that pay for performance works,” Dr. Torcson says of the results of the Premier demo. “However, this was hospital-level P4P and involves a different methodology than physician-level P4P. I don’t think it’s safe or accurate to extrapolate these results.”
What the Research Says
Various researchers have examined available P4P data to see if incentives improve care.
Recent studies include one led by hospitalist Peter Lindenauer, MD, MSc, FACP, medical director, clinical and quality informatics, Baystate Health in Springfield, Mass., and assistant professor of medicine at Tufts University School of Medicine in Boston.1 Dr. Lindenauer and his colleagues examined data from the CMS data warehouse gathered as part of the Hospital Quality Alliance (Hospital Compare) project. Specifically, they compared P4P CMS Premier hospitals with 408 hospitals that participated only in public reporting, with no compensation.
They found that the P4P hospitals showed modestly greater improvement in all composite measures of quality than hospitals that simply reported on measures. Specifically, improvements in the P4P hospitals ranged from 2.6% to 4.1% over two years. “The small gains in process of care measures observed in the study are unlikely to have translated into meaningful improvements in outcomes,” Dr. Lindenauer says.
Other studies of P4P are inconclusive. A literature review on the subject finds “little evidence to support the effectiveness of paying for quality.”2
A second literature review out of the Baylor College of Medicine in Houston based on 17 studies “suggests some positive effects of financial incentives at the physician level, the provider group level, and the healthcare payment system level. The findings also suggest that ongoing monitoring of incentive programs is critical to determine whether incentives are having unintended effects on quality of care.”3
Finally, a study of P4P programs for family practices in the United Kingdom revealed that serious financial incentives for physicians resulted in 83.4% achieving goals for 10 chronic diseases in a year.4
“There is no conclusive evidence that physician-level P4P works to improve quality of care and reduce cost of care,” concludes Dr. Torcson. “The U.K. experience demonstrates that given a sufficient incentive, physicians will adhere to and report on performance measures. Further study is being done to see if this translates into quality improvement for patients.”
The next phase of P4P is pay for reporting—which may help pin down the true value of P4P.
The Physician Quality Reporting Initiative (PQRI), now well under way, “is the first nationwide pay-for-performance program, and one of the first to include hospitalists,” says Dr. Torcson. “This is the first taste we’re all having of physician-level pay-for-performance since the PQRI started on July 1.”
The incentives for participating in the trial aren’t high. “Based on projections of PQRI reporting, hospitalists can earn a bonus of $807,” says Dr. Torcson. “This may not be a strong motivator to participate in PQRI. However, it’s a beginning. If you’re going to fail [at reporting], this is the time to do it.”
The PQRI trial is short; it will end Dec. 31. And early next year, it’s guaranteed that all eyes will be on outcomes from this program. “Private payers are watching this very closely; they’re ready to jump into the game,” says Dr. Torcson. Healthcare organizations and professionals should be ready to jump as well, because next steps for P4P and other payment factors are still unknown.
“What happens after Dec. 31 is wide open,” Dr. Torcson says. “We don’t know what to expect from Congress. Right now we’re looking at a proposed 9.8% cut to physician fees. Will this cut be made up by pay-for-performance bonuses? Congress determines what will happen, and the [2008] election could change everything.”
To date, P4P has not lived up to its hype; however, the use of incentives to improve quality is in the early stages. Time will tell if P4P pays off in improved care—but CMS and many physicians seem committed to the idea.
“I think there’s a lot to be said for the concept of providing incentives that encourage hospitals to invest in quality of care,” says Dr. Lindenauer. “Our current system of healthcare hasn’t done that.”
Dr. Lindenauer’s advice for moving ahead with P4P? “We need to proceed cautiously and be mindful of some of the unintended consequences,” he concludes. TH
Jane Jerrard has been writing for The Hospitalist since 2005.
References
- Lindenauer PK, Remus D, Roman S, et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007 Feb 1;356(5):486-496.
- Rosenthal MB, Frank RG. What is the empirical basis for paying for quality in health care? Med Care Res Rev. 2006;63(2):135-137.
- Petersen LA, Woodard LD, Urech T, et al. Does pay-for-performance improve the quality of health care? Ann Intern Med. 2006;145(4):265-272.
- Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355(4):375-384.
Group Growth
Ambitious hospitalists may be eager to add an MBA or a PhD to their credentials, in the belief those magic letters will open doors to leadership positions or higher compensation. But before you fork over tuition for an advanced degree program, consider whether that degree will pay off.
Choose Your Career Path
If you’re considering pursuing a Master of Business Administration (MBA), Master of Public Health (MPH), Master of Health Administration (MPH), or even a doctorate degree, the first thing you should consider is which career path within hospital medicine you’re interested in. What position would you ultimately like to hold? And which, if any, advanced degree can help you get there?
“Explore the idea [of earning an advanced degree], but the most important steps are to try to get some work experience and set some goals,” says Mary Jo Gorman, MD, MBA, the CEO of Advanced ICU Care, St. Louis, Mo. “Along the way, find out what you have an aptitude for.” Once you know your general or specific career goals, you can consider whether to earn an advanced degree.
“It’s a significant monetary and time commitment, so make sure it makes sense for where you want to go,” advises Dr. Gorman. “I’d also advise career counseling to help with this. Great people to talk to are recruiters. They’ll tell you what you need in order to apply for certain positions.”
It should be obvious that some positions will require certain degrees beyond an MD or a DO. Look at the next—or final—job you want. Is the job held by someone with an MBA, a PhD, or another degree? Is that person’s successor likely to need specific education?
“If you want to be the chief operating officer of a hospital, or the CEO of a large medical group, you’re not getting that without an MBA,” Dr. Gorman says. “In fact, if you’re planning to apply for a position that requires strong financial expertise, they’re not going to accept you without [an MBA] unless you’re of a certain age and have a great track record that shows you can do the job.”
On the other hand, many experienced hospitalist leaders don’t have an MBA and won’t need one. “A lot of community-based hospitalists are already doing these things and don’t need the degree,” Dr. Gorman points out. “They created the job, or they created the group.”
A New Way of Thinking
Perhaps the most valuable aspect of any higher degree is the training one receives, which can provide new ways to approach one’s work, problem solving and general thought processes.
“The degree alone won’t help if you haven’t learned while getting it,” explains Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine, Ann Arbor Veterans Affairs (VA) Medical Center and University of Michigan Medical School. “That’s the real value: Learn the material and it will alter how you approach things.”
Fred A. McCurdy, MD, who holds a PhD and an MBA, was recently promoted from pediatric department chair at Texas Tech University Health Sciences Center at Amarillo to associate dean for faculty development. He earned his MBA with an eye on becoming department chair and says that the MBA program “gave me a background in thought process. From there, I could build on that foundation.”
As for his PhD, Dr. McCurdy says the degree “has its place. The program taught me methodology and scientific process. It taught me how to break down a problem into researchable questions, and I can apply that to areas like education. If your job calls for thinking logically and critically, a PhD gives experience in using scientific methods.”
Earning an MPH also bears fruit.
“Having an MPH is helpful,” says Dr. Saint. “In addition to helping you learn how to research, how to be a better user of literature, it helps prepare someone for taking a leadership role.”

—Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine, Ann Arbor VA Medical Center and University of Michigan Medical School, Ann Arbor
Your Dream Job
While an additional degree can improve your knowledge and skills, it’s no guarantee you’ll move to the top of a list for a promotion or new job.
“It’s not a given that it will necessarily help your career,” warns Dr. Gorman. “You need to first do an analysis about what you want to achieve, then work toward that goal. A lot of doctors don’t really realize that they need to think in terms of their total career plan.”
Dr. Saint agrees, saying of an MPH, “It may open the door, but you still have to walk through it. You still have to do the work yourself. You cannot hide behind the MPH. You have to be productive and even be an overperformer. But it does give you the tools you need, and it can help you get that first job.”
Dr. McCurdy believes a degree such as an MBA can be helpful for today’s hospitalists: “For a hospitalist with a strong interest in rising up through the hospital administrative ranks, having an MBA early in their career could definitely be beneficial,” speculates Dr. McCurdy. “Holding an MBA [in academia] is becoming the norm rather than the exception. There’s an increasing awareness in academics that this is a business.”
Does an advanced degree make a new hospitalist more hirable? “That depends,” says Dr. McCurdy. “For hospitalists working in a large hospital system, it becomes a matter of choice. I don’t think you’d be hired based on an advanced degree [such as a PhD] unless the job has something to do with a scholarly pursuit such as research or teaching. If you’re competing for a job in an academic health science center, a PhD degree can help if it has to do with scholarship.”
The Final Answer
Follow this sound advice: Chart your hospital medicine career path, and then work backward to see whether you’ll benefit from obtaining a specific degree.
“It has to do with what you intend to do in a five- or 10-year timeframe, with the course direction of your career,” says Dr. McCurdy. “If you plan to pursue academic scholarship, a PhD can be very helpful. If you aspire to become medical director at Maryland Shock Trauma, an MBA is the ticket you’re definitely going to need to punch.” TH
Jane Jerrard has been writing for The Hospitalist since 2005.
Ambitious hospitalists may be eager to add an MBA or a PhD to their credentials, in the belief those magic letters will open doors to leadership positions or higher compensation. But before you fork over tuition for an advanced degree program, consider whether that degree will pay off.
Choose Your Career Path
If you’re considering pursuing a Master of Business Administration (MBA), Master of Public Health (MPH), Master of Health Administration (MPH), or even a doctorate degree, the first thing you should consider is which career path within hospital medicine you’re interested in. What position would you ultimately like to hold? And which, if any, advanced degree can help you get there?
“Explore the idea [of earning an advanced degree], but the most important steps are to try to get some work experience and set some goals,” says Mary Jo Gorman, MD, MBA, the CEO of Advanced ICU Care, St. Louis, Mo. “Along the way, find out what you have an aptitude for.” Once you know your general or specific career goals, you can consider whether to earn an advanced degree.
“It’s a significant monetary and time commitment, so make sure it makes sense for where you want to go,” advises Dr. Gorman. “I’d also advise career counseling to help with this. Great people to talk to are recruiters. They’ll tell you what you need in order to apply for certain positions.”
It should be obvious that some positions will require certain degrees beyond an MD or a DO. Look at the next—or final—job you want. Is the job held by someone with an MBA, a PhD, or another degree? Is that person’s successor likely to need specific education?
“If you want to be the chief operating officer of a hospital, or the CEO of a large medical group, you’re not getting that without an MBA,” Dr. Gorman says. “In fact, if you’re planning to apply for a position that requires strong financial expertise, they’re not going to accept you without [an MBA] unless you’re of a certain age and have a great track record that shows you can do the job.”
On the other hand, many experienced hospitalist leaders don’t have an MBA and won’t need one. “A lot of community-based hospitalists are already doing these things and don’t need the degree,” Dr. Gorman points out. “They created the job, or they created the group.”
A New Way of Thinking
Perhaps the most valuable aspect of any higher degree is the training one receives, which can provide new ways to approach one’s work, problem solving and general thought processes.
“The degree alone won’t help if you haven’t learned while getting it,” explains Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine, Ann Arbor Veterans Affairs (VA) Medical Center and University of Michigan Medical School. “That’s the real value: Learn the material and it will alter how you approach things.”
Fred A. McCurdy, MD, who holds a PhD and an MBA, was recently promoted from pediatric department chair at Texas Tech University Health Sciences Center at Amarillo to associate dean for faculty development. He earned his MBA with an eye on becoming department chair and says that the MBA program “gave me a background in thought process. From there, I could build on that foundation.”
As for his PhD, Dr. McCurdy says the degree “has its place. The program taught me methodology and scientific process. It taught me how to break down a problem into researchable questions, and I can apply that to areas like education. If your job calls for thinking logically and critically, a PhD gives experience in using scientific methods.”
Earning an MPH also bears fruit.
“Having an MPH is helpful,” says Dr. Saint. “In addition to helping you learn how to research, how to be a better user of literature, it helps prepare someone for taking a leadership role.”

—Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine, Ann Arbor VA Medical Center and University of Michigan Medical School, Ann Arbor
Your Dream Job
While an additional degree can improve your knowledge and skills, it’s no guarantee you’ll move to the top of a list for a promotion or new job.
“It’s not a given that it will necessarily help your career,” warns Dr. Gorman. “You need to first do an analysis about what you want to achieve, then work toward that goal. A lot of doctors don’t really realize that they need to think in terms of their total career plan.”
Dr. Saint agrees, saying of an MPH, “It may open the door, but you still have to walk through it. You still have to do the work yourself. You cannot hide behind the MPH. You have to be productive and even be an overperformer. But it does give you the tools you need, and it can help you get that first job.”
Dr. McCurdy believes a degree such as an MBA can be helpful for today’s hospitalists: “For a hospitalist with a strong interest in rising up through the hospital administrative ranks, having an MBA early in their career could definitely be beneficial,” speculates Dr. McCurdy. “Holding an MBA [in academia] is becoming the norm rather than the exception. There’s an increasing awareness in academics that this is a business.”
Does an advanced degree make a new hospitalist more hirable? “That depends,” says Dr. McCurdy. “For hospitalists working in a large hospital system, it becomes a matter of choice. I don’t think you’d be hired based on an advanced degree [such as a PhD] unless the job has something to do with a scholarly pursuit such as research or teaching. If you’re competing for a job in an academic health science center, a PhD degree can help if it has to do with scholarship.”
The Final Answer
Follow this sound advice: Chart your hospital medicine career path, and then work backward to see whether you’ll benefit from obtaining a specific degree.
“It has to do with what you intend to do in a five- or 10-year timeframe, with the course direction of your career,” says Dr. McCurdy. “If you plan to pursue academic scholarship, a PhD can be very helpful. If you aspire to become medical director at Maryland Shock Trauma, an MBA is the ticket you’re definitely going to need to punch.” TH
Jane Jerrard has been writing for The Hospitalist since 2005.
Ambitious hospitalists may be eager to add an MBA or a PhD to their credentials, in the belief those magic letters will open doors to leadership positions or higher compensation. But before you fork over tuition for an advanced degree program, consider whether that degree will pay off.
Choose Your Career Path
If you’re considering pursuing a Master of Business Administration (MBA), Master of Public Health (MPH), Master of Health Administration (MPH), or even a doctorate degree, the first thing you should consider is which career path within hospital medicine you’re interested in. What position would you ultimately like to hold? And which, if any, advanced degree can help you get there?
“Explore the idea [of earning an advanced degree], but the most important steps are to try to get some work experience and set some goals,” says Mary Jo Gorman, MD, MBA, the CEO of Advanced ICU Care, St. Louis, Mo. “Along the way, find out what you have an aptitude for.” Once you know your general or specific career goals, you can consider whether to earn an advanced degree.
“It’s a significant monetary and time commitment, so make sure it makes sense for where you want to go,” advises Dr. Gorman. “I’d also advise career counseling to help with this. Great people to talk to are recruiters. They’ll tell you what you need in order to apply for certain positions.”
It should be obvious that some positions will require certain degrees beyond an MD or a DO. Look at the next—or final—job you want. Is the job held by someone with an MBA, a PhD, or another degree? Is that person’s successor likely to need specific education?
“If you want to be the chief operating officer of a hospital, or the CEO of a large medical group, you’re not getting that without an MBA,” Dr. Gorman says. “In fact, if you’re planning to apply for a position that requires strong financial expertise, they’re not going to accept you without [an MBA] unless you’re of a certain age and have a great track record that shows you can do the job.”
On the other hand, many experienced hospitalist leaders don’t have an MBA and won’t need one. “A lot of community-based hospitalists are already doing these things and don’t need the degree,” Dr. Gorman points out. “They created the job, or they created the group.”
A New Way of Thinking
Perhaps the most valuable aspect of any higher degree is the training one receives, which can provide new ways to approach one’s work, problem solving and general thought processes.
“The degree alone won’t help if you haven’t learned while getting it,” explains Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine, Ann Arbor Veterans Affairs (VA) Medical Center and University of Michigan Medical School. “That’s the real value: Learn the material and it will alter how you approach things.”
Fred A. McCurdy, MD, who holds a PhD and an MBA, was recently promoted from pediatric department chair at Texas Tech University Health Sciences Center at Amarillo to associate dean for faculty development. He earned his MBA with an eye on becoming department chair and says that the MBA program “gave me a background in thought process. From there, I could build on that foundation.”
As for his PhD, Dr. McCurdy says the degree “has its place. The program taught me methodology and scientific process. It taught me how to break down a problem into researchable questions, and I can apply that to areas like education. If your job calls for thinking logically and critically, a PhD gives experience in using scientific methods.”
Earning an MPH also bears fruit.
“Having an MPH is helpful,” says Dr. Saint. “In addition to helping you learn how to research, how to be a better user of literature, it helps prepare someone for taking a leadership role.”

—Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine, Ann Arbor VA Medical Center and University of Michigan Medical School, Ann Arbor
Your Dream Job
While an additional degree can improve your knowledge and skills, it’s no guarantee you’ll move to the top of a list for a promotion or new job.
“It’s not a given that it will necessarily help your career,” warns Dr. Gorman. “You need to first do an analysis about what you want to achieve, then work toward that goal. A lot of doctors don’t really realize that they need to think in terms of their total career plan.”
Dr. Saint agrees, saying of an MPH, “It may open the door, but you still have to walk through it. You still have to do the work yourself. You cannot hide behind the MPH. You have to be productive and even be an overperformer. But it does give you the tools you need, and it can help you get that first job.”
Dr. McCurdy believes a degree such as an MBA can be helpful for today’s hospitalists: “For a hospitalist with a strong interest in rising up through the hospital administrative ranks, having an MBA early in their career could definitely be beneficial,” speculates Dr. McCurdy. “Holding an MBA [in academia] is becoming the norm rather than the exception. There’s an increasing awareness in academics that this is a business.”
Does an advanced degree make a new hospitalist more hirable? “That depends,” says Dr. McCurdy. “For hospitalists working in a large hospital system, it becomes a matter of choice. I don’t think you’d be hired based on an advanced degree [such as a PhD] unless the job has something to do with a scholarly pursuit such as research or teaching. If you’re competing for a job in an academic health science center, a PhD degree can help if it has to do with scholarship.”
The Final Answer
Follow this sound advice: Chart your hospital medicine career path, and then work backward to see whether you’ll benefit from obtaining a specific degree.
“It has to do with what you intend to do in a five- or 10-year timeframe, with the course direction of your career,” says Dr. McCurdy. “If you plan to pursue academic scholarship, a PhD can be very helpful. If you aspire to become medical director at Maryland Shock Trauma, an MBA is the ticket you’re definitely going to need to punch.” TH
Jane Jerrard has been writing for The Hospitalist since 2005.
When Discharge Fails
A significant percentage of patients do not remember or understand the instructions they receive before leaving the hospital, according to a study in this month’s Journal of Hospital Medicine.
“Anyone who’s taken care of patients or put together a discharge plan only to have things not work out knows how frustrating that can be,” says lead author Jonathan Flacker, MD.
Dr. Flacker, assistant professor of medicine in the Division of Geriatric Medicine and Gerontology, Emory University School of Medicine, Atlanta, and coauthors Wansoo Park, PhD, and Addie Sims, MSW, surveyed a group of elderly patients shortly after discharge to determine their recall and comprehension of their pre-discharge instructions. Dr. Park is an assistant professor of social work at the University of Windsor in Ontario, Canada. Dr. Sims is director of Senior Services at Grady Health System in Atlanta.
They conducted telephone interviews with 269 patients 70 or older, or their caregivers, within 10 days of discharge from Grady Memorial Hospital in Atlanta. Most interviews were conducted within a mean of three days of discharge and lasted 20 to 30 minutes. No effort was made to determine the patients’ cognitive status or degree of health literacy.
The survey was an offshoot of Aging Atlanta, a project funded by the Robert Wood Johnson Foundation to study the overall care of older adults in the community. It asked 37 questions covering patients’ financial resources and activities of daily living as well as the nature of their discharge instructions.
The authors found the survey “feasible and easily administered,” but its results were somewhat discouraging. In 52% of the cases, respondents claimed no one spoke to them prior to discharge about caring for themselves at home. Almost as many (47%) says they were not given a phone number or the name of a person to call if they experienced problems at home. “Yet the number was on the discharge papers; 100% of the people received it,” says Dr. Flacker.
Also, 41% says they were not told what to do if they experienced problems at home. On a more positive note, only 13% of the patients had to call concerning problems, and 84% felt they had received enough help after returning home.
Of the 115 (43%) patients who said the received instructions prior to discharge, 103 (90%) remembered how they were delivered: verbally in 68 cases (63%), written in 11 cases (11%), and both ways in 24 cases (23%).
“Patients receiving instructions both verbally and in writing were more likely to report that they understood care instruction ‘very well’ versus ‘somewhat’ or ‘very little,’ ” the authors wrote. Of those who recalled being instructed on how to take their medication, 86% says they took their medicine correctly, compared with 62% who had no such recollection.
To those who can’t understand how someone might completely forget receiving discharge instructions, Dr. Flacker suggests thinking back to the first day of residency or medical school when “you’re handed a whole pile of stuff” while trying to acclimate to unfamiliar surroundings. “Add to that being uncomfortable, sick, and uncertain about the future, and a lot of what is said goes untransferred,” he says.
In an elderly population, cognitive status and poor health literacy are certainly important potential confounders, but “based on my experience, our results are not a whole lot different than those of other investigators who accounted for those factors,” says Dr. Flacker.
These findings suggest that merely transmitting information is not sufficient. Some follow-up is needed to ensure that patients understand the information as their healthcare providers intend, Dr. Flacker and his colleagues wrote. Anything less might violate the spirit of Joint Commission on Accreditation of Healthcare Organization (JCAHO) standards requiring the clear and routine provision of information to patients.
Because of this study, Grady has revised its discharge sheet so information concerning telephone numbers, medication, and other important details are displayed more prominently. The hospital has retrained its nurses to deliver the information more effectively. Follow-up studies will assess how these changes affect patient comprehension and outcomes.
If hospitalists perceive their responsibility to the patient ending not at hospital discharge, but when the patient resumes seeing his or her primary care physician, then “their job is to ensure that the patient understands the discharge instructions,” Dr. Flacker points out.
He suggests they have a social worker or other staff member call patients within a few days after discharge to see how they’re doing and nip any problems in the bud. Admittedly, “a lot depends on where you want to put your resources,” he says. Time and budgets can be stretched only so far. Nevertheless, he maintains, “Post discharge contact is a critically important piece of the process.” TH
Norra MacReady is a medical writer based in California.
A significant percentage of patients do not remember or understand the instructions they receive before leaving the hospital, according to a study in this month’s Journal of Hospital Medicine.
“Anyone who’s taken care of patients or put together a discharge plan only to have things not work out knows how frustrating that can be,” says lead author Jonathan Flacker, MD.
Dr. Flacker, assistant professor of medicine in the Division of Geriatric Medicine and Gerontology, Emory University School of Medicine, Atlanta, and coauthors Wansoo Park, PhD, and Addie Sims, MSW, surveyed a group of elderly patients shortly after discharge to determine their recall and comprehension of their pre-discharge instructions. Dr. Park is an assistant professor of social work at the University of Windsor in Ontario, Canada. Dr. Sims is director of Senior Services at Grady Health System in Atlanta.
They conducted telephone interviews with 269 patients 70 or older, or their caregivers, within 10 days of discharge from Grady Memorial Hospital in Atlanta. Most interviews were conducted within a mean of three days of discharge and lasted 20 to 30 minutes. No effort was made to determine the patients’ cognitive status or degree of health literacy.
The survey was an offshoot of Aging Atlanta, a project funded by the Robert Wood Johnson Foundation to study the overall care of older adults in the community. It asked 37 questions covering patients’ financial resources and activities of daily living as well as the nature of their discharge instructions.
The authors found the survey “feasible and easily administered,” but its results were somewhat discouraging. In 52% of the cases, respondents claimed no one spoke to them prior to discharge about caring for themselves at home. Almost as many (47%) says they were not given a phone number or the name of a person to call if they experienced problems at home. “Yet the number was on the discharge papers; 100% of the people received it,” says Dr. Flacker.
Also, 41% says they were not told what to do if they experienced problems at home. On a more positive note, only 13% of the patients had to call concerning problems, and 84% felt they had received enough help after returning home.
Of the 115 (43%) patients who said the received instructions prior to discharge, 103 (90%) remembered how they were delivered: verbally in 68 cases (63%), written in 11 cases (11%), and both ways in 24 cases (23%).
“Patients receiving instructions both verbally and in writing were more likely to report that they understood care instruction ‘very well’ versus ‘somewhat’ or ‘very little,’ ” the authors wrote. Of those who recalled being instructed on how to take their medication, 86% says they took their medicine correctly, compared with 62% who had no such recollection.
To those who can’t understand how someone might completely forget receiving discharge instructions, Dr. Flacker suggests thinking back to the first day of residency or medical school when “you’re handed a whole pile of stuff” while trying to acclimate to unfamiliar surroundings. “Add to that being uncomfortable, sick, and uncertain about the future, and a lot of what is said goes untransferred,” he says.
In an elderly population, cognitive status and poor health literacy are certainly important potential confounders, but “based on my experience, our results are not a whole lot different than those of other investigators who accounted for those factors,” says Dr. Flacker.
These findings suggest that merely transmitting information is not sufficient. Some follow-up is needed to ensure that patients understand the information as their healthcare providers intend, Dr. Flacker and his colleagues wrote. Anything less might violate the spirit of Joint Commission on Accreditation of Healthcare Organization (JCAHO) standards requiring the clear and routine provision of information to patients.
Because of this study, Grady has revised its discharge sheet so information concerning telephone numbers, medication, and other important details are displayed more prominently. The hospital has retrained its nurses to deliver the information more effectively. Follow-up studies will assess how these changes affect patient comprehension and outcomes.
If hospitalists perceive their responsibility to the patient ending not at hospital discharge, but when the patient resumes seeing his or her primary care physician, then “their job is to ensure that the patient understands the discharge instructions,” Dr. Flacker points out.
He suggests they have a social worker or other staff member call patients within a few days after discharge to see how they’re doing and nip any problems in the bud. Admittedly, “a lot depends on where you want to put your resources,” he says. Time and budgets can be stretched only so far. Nevertheless, he maintains, “Post discharge contact is a critically important piece of the process.” TH
Norra MacReady is a medical writer based in California.
A significant percentage of patients do not remember or understand the instructions they receive before leaving the hospital, according to a study in this month’s Journal of Hospital Medicine.
“Anyone who’s taken care of patients or put together a discharge plan only to have things not work out knows how frustrating that can be,” says lead author Jonathan Flacker, MD.
Dr. Flacker, assistant professor of medicine in the Division of Geriatric Medicine and Gerontology, Emory University School of Medicine, Atlanta, and coauthors Wansoo Park, PhD, and Addie Sims, MSW, surveyed a group of elderly patients shortly after discharge to determine their recall and comprehension of their pre-discharge instructions. Dr. Park is an assistant professor of social work at the University of Windsor in Ontario, Canada. Dr. Sims is director of Senior Services at Grady Health System in Atlanta.
They conducted telephone interviews with 269 patients 70 or older, or their caregivers, within 10 days of discharge from Grady Memorial Hospital in Atlanta. Most interviews were conducted within a mean of three days of discharge and lasted 20 to 30 minutes. No effort was made to determine the patients’ cognitive status or degree of health literacy.
The survey was an offshoot of Aging Atlanta, a project funded by the Robert Wood Johnson Foundation to study the overall care of older adults in the community. It asked 37 questions covering patients’ financial resources and activities of daily living as well as the nature of their discharge instructions.
The authors found the survey “feasible and easily administered,” but its results were somewhat discouraging. In 52% of the cases, respondents claimed no one spoke to them prior to discharge about caring for themselves at home. Almost as many (47%) says they were not given a phone number or the name of a person to call if they experienced problems at home. “Yet the number was on the discharge papers; 100% of the people received it,” says Dr. Flacker.
Also, 41% says they were not told what to do if they experienced problems at home. On a more positive note, only 13% of the patients had to call concerning problems, and 84% felt they had received enough help after returning home.
Of the 115 (43%) patients who said the received instructions prior to discharge, 103 (90%) remembered how they were delivered: verbally in 68 cases (63%), written in 11 cases (11%), and both ways in 24 cases (23%).
“Patients receiving instructions both verbally and in writing were more likely to report that they understood care instruction ‘very well’ versus ‘somewhat’ or ‘very little,’ ” the authors wrote. Of those who recalled being instructed on how to take their medication, 86% says they took their medicine correctly, compared with 62% who had no such recollection.
To those who can’t understand how someone might completely forget receiving discharge instructions, Dr. Flacker suggests thinking back to the first day of residency or medical school when “you’re handed a whole pile of stuff” while trying to acclimate to unfamiliar surroundings. “Add to that being uncomfortable, sick, and uncertain about the future, and a lot of what is said goes untransferred,” he says.
In an elderly population, cognitive status and poor health literacy are certainly important potential confounders, but “based on my experience, our results are not a whole lot different than those of other investigators who accounted for those factors,” says Dr. Flacker.
These findings suggest that merely transmitting information is not sufficient. Some follow-up is needed to ensure that patients understand the information as their healthcare providers intend, Dr. Flacker and his colleagues wrote. Anything less might violate the spirit of Joint Commission on Accreditation of Healthcare Organization (JCAHO) standards requiring the clear and routine provision of information to patients.
Because of this study, Grady has revised its discharge sheet so information concerning telephone numbers, medication, and other important details are displayed more prominently. The hospital has retrained its nurses to deliver the information more effectively. Follow-up studies will assess how these changes affect patient comprehension and outcomes.
If hospitalists perceive their responsibility to the patient ending not at hospital discharge, but when the patient resumes seeing his or her primary care physician, then “their job is to ensure that the patient understands the discharge instructions,” Dr. Flacker points out.
He suggests they have a social worker or other staff member call patients within a few days after discharge to see how they’re doing and nip any problems in the bud. Admittedly, “a lot depends on where you want to put your resources,” he says. Time and budgets can be stretched only so far. Nevertheless, he maintains, “Post discharge contact is a critically important piece of the process.” TH
Norra MacReady is a medical writer based in California.
Stress Ulcer Agents
An article published this year in the American Journal of Health-Systems Pharmacy defined stress ulcers as “acute superficial inflammatory lesions of the gastric mucosa induced when an individual is subjected to abnormally high physiologic demands.”1
These stress ulcers are believed to be caused by an imbalance between gastric acid production and the normal physiologic protective mucosal mechanisms in the gastrointestinal (GI) tract. Reduction of blood flow to the gastric mucosa may also lead to ischemic damage to the GI mucosa.
The development of stress ulcers, or stress-related mucosal disease (SRMD), occurs in 75% to 100% of critically ill patients within 24 hours of intensive care unit (ICU) admission. Although bleeding risk has decreased over the years, mortality from stress-related bleeding nears 50%. According a peer-reviewed guideline from the American Society of Health-System Pharmacists (ASHP), indications for SRMD in the ICU setting include:2
- Coagulopathy;
- Mechanical ventilation longer than 48 hours;
- History of GI ulceration or bleeding within one year of the current admission;
- Glasgow Coma score of 10 or less (or if unable to obey simple commands);
- Thermal injury to more than 35% of the body surface area;
- Partial hepatectomy;
- Multiple trauma;
- Transplantation perioperatively in the ICU;
- Spinal cord injury;
- Hepatic failure; and
- Two or more of the following risk factors: sepsis, ICU stay of a week or longer, occult bleeding for more than six days, or high-dose corticosteroids (more than 250 mg a day of hydrocortisone or the equivalent).
Other risk factors for SRMD in ICU patients include multiorgan failure, chronic renal failure, major surgical procedures, shock, and tetraplegia.3,4
Recommended SRMD prophylaxis agents should be institution-based, taking into account the administration route (e.g., functioning GI tract), daily dosing regimens, adverse effect profile, drug interactions, and total costs. Classes that can be used include sucralfate, antacids, H2 receptor antagonists (H2RA), and proton-pump inhibitors (PPIs).
Some patients may prefer the oral route. Some agents can be given in solution or suspension and administered via a nasogastric tube—but be aware of drug interactions. There are limited comparative data for preventing SRMD with these classes. The H2RA and PPI classes of agents are available in intravenous forms, which may be preferable in critically ill patients. However, none of the PPIs are FDA-approved for SRMD prophylaxis.
In the general patient population, SRMD prophylaxis with H2RAs or PPIs is common in 30% to 50% of patients without clear evidence of benefit. Qadeer, et al., identified a 0.4% bleeding rate in their retrospective case-control study of nearly 18,000 patients over a four-year period. In their study, the key risk factor for development of nosocomial GI bleeding was treatment with full-dose anticoagulation or clopidogrel.
Another concern they identified is that when a patient commences an SRMD prophylaxis agent in the hospital, they continue on it post-discharge when it is not needed. This creates an unnecessary cost burden and risks adverse drug interactions.
Todd Janicki, MD, and Scott Stewart, MD, both with the department of medicine at the State University of New York at Buffalo, this year reported on a review of evidence for SRMD prophylaxis in general medicine patients from the peer-reviewed literature.5 They found limited data, identifying only five citations meeting their evaluation criteria. Two of these studies noted only a 3% to 6% reduction in clinically significant bleeding utilizing SRMD prophylaxis. TH
Michele Kaufman is a clinical/managed care consultant and medical writer based in New York City.
References
- Grube RRA, May DB. Stress ulcer prophylaxis in hospitalized patients not in intensive care units. Am J Health-Syst Pharm. 2007;64:1396-400.
- ASHP Commission on Therapeutics. ASHP therapeutic guidelines on stress ulcer prophylaxis. Am J Health-Syst Pharm. 1999;56:347-379.
- Qadeer MA, Richter JE, Brotman DJ. Hospital-acquired gastrointestinal bleeding outside the critical care unit: risk factors, role of acid suppression, and endoscopy findings. J Hosp Med. 2006;1(1):13-20.
- Weinhouse GL, Manaker S. Stress ulcer prophylaxis in the intensive care unit. In: UpToDate, Rose, BD (Ed), UpToDate, Waltham, Mass. 2007.
- Janicki T, Stewart S. Stress-ulcer prophylaxis for general medical patients: a review of the evidence. J Hosp Med. 2007;2(2):86-92.
An article published this year in the American Journal of Health-Systems Pharmacy defined stress ulcers as “acute superficial inflammatory lesions of the gastric mucosa induced when an individual is subjected to abnormally high physiologic demands.”1
These stress ulcers are believed to be caused by an imbalance between gastric acid production and the normal physiologic protective mucosal mechanisms in the gastrointestinal (GI) tract. Reduction of blood flow to the gastric mucosa may also lead to ischemic damage to the GI mucosa.
The development of stress ulcers, or stress-related mucosal disease (SRMD), occurs in 75% to 100% of critically ill patients within 24 hours of intensive care unit (ICU) admission. Although bleeding risk has decreased over the years, mortality from stress-related bleeding nears 50%. According a peer-reviewed guideline from the American Society of Health-System Pharmacists (ASHP), indications for SRMD in the ICU setting include:2
- Coagulopathy;
- Mechanical ventilation longer than 48 hours;
- History of GI ulceration or bleeding within one year of the current admission;
- Glasgow Coma score of 10 or less (or if unable to obey simple commands);
- Thermal injury to more than 35% of the body surface area;
- Partial hepatectomy;
- Multiple trauma;
- Transplantation perioperatively in the ICU;
- Spinal cord injury;
- Hepatic failure; and
- Two or more of the following risk factors: sepsis, ICU stay of a week or longer, occult bleeding for more than six days, or high-dose corticosteroids (more than 250 mg a day of hydrocortisone or the equivalent).
Other risk factors for SRMD in ICU patients include multiorgan failure, chronic renal failure, major surgical procedures, shock, and tetraplegia.3,4
Recommended SRMD prophylaxis agents should be institution-based, taking into account the administration route (e.g., functioning GI tract), daily dosing regimens, adverse effect profile, drug interactions, and total costs. Classes that can be used include sucralfate, antacids, H2 receptor antagonists (H2RA), and proton-pump inhibitors (PPIs).
Some patients may prefer the oral route. Some agents can be given in solution or suspension and administered via a nasogastric tube—but be aware of drug interactions. There are limited comparative data for preventing SRMD with these classes. The H2RA and PPI classes of agents are available in intravenous forms, which may be preferable in critically ill patients. However, none of the PPIs are FDA-approved for SRMD prophylaxis.
In the general patient population, SRMD prophylaxis with H2RAs or PPIs is common in 30% to 50% of patients without clear evidence of benefit. Qadeer, et al., identified a 0.4% bleeding rate in their retrospective case-control study of nearly 18,000 patients over a four-year period. In their study, the key risk factor for development of nosocomial GI bleeding was treatment with full-dose anticoagulation or clopidogrel.
Another concern they identified is that when a patient commences an SRMD prophylaxis agent in the hospital, they continue on it post-discharge when it is not needed. This creates an unnecessary cost burden and risks adverse drug interactions.
Todd Janicki, MD, and Scott Stewart, MD, both with the department of medicine at the State University of New York at Buffalo, this year reported on a review of evidence for SRMD prophylaxis in general medicine patients from the peer-reviewed literature.5 They found limited data, identifying only five citations meeting their evaluation criteria. Two of these studies noted only a 3% to 6% reduction in clinically significant bleeding utilizing SRMD prophylaxis. TH
Michele Kaufman is a clinical/managed care consultant and medical writer based in New York City.
References
- Grube RRA, May DB. Stress ulcer prophylaxis in hospitalized patients not in intensive care units. Am J Health-Syst Pharm. 2007;64:1396-400.
- ASHP Commission on Therapeutics. ASHP therapeutic guidelines on stress ulcer prophylaxis. Am J Health-Syst Pharm. 1999;56:347-379.
- Qadeer MA, Richter JE, Brotman DJ. Hospital-acquired gastrointestinal bleeding outside the critical care unit: risk factors, role of acid suppression, and endoscopy findings. J Hosp Med. 2006;1(1):13-20.
- Weinhouse GL, Manaker S. Stress ulcer prophylaxis in the intensive care unit. In: UpToDate, Rose, BD (Ed), UpToDate, Waltham, Mass. 2007.
- Janicki T, Stewart S. Stress-ulcer prophylaxis for general medical patients: a review of the evidence. J Hosp Med. 2007;2(2):86-92.
An article published this year in the American Journal of Health-Systems Pharmacy defined stress ulcers as “acute superficial inflammatory lesions of the gastric mucosa induced when an individual is subjected to abnormally high physiologic demands.”1
These stress ulcers are believed to be caused by an imbalance between gastric acid production and the normal physiologic protective mucosal mechanisms in the gastrointestinal (GI) tract. Reduction of blood flow to the gastric mucosa may also lead to ischemic damage to the GI mucosa.
The development of stress ulcers, or stress-related mucosal disease (SRMD), occurs in 75% to 100% of critically ill patients within 24 hours of intensive care unit (ICU) admission. Although bleeding risk has decreased over the years, mortality from stress-related bleeding nears 50%. According a peer-reviewed guideline from the American Society of Health-System Pharmacists (ASHP), indications for SRMD in the ICU setting include:2
- Coagulopathy;
- Mechanical ventilation longer than 48 hours;
- History of GI ulceration or bleeding within one year of the current admission;
- Glasgow Coma score of 10 or less (or if unable to obey simple commands);
- Thermal injury to more than 35% of the body surface area;
- Partial hepatectomy;
- Multiple trauma;
- Transplantation perioperatively in the ICU;
- Spinal cord injury;
- Hepatic failure; and
- Two or more of the following risk factors: sepsis, ICU stay of a week or longer, occult bleeding for more than six days, or high-dose corticosteroids (more than 250 mg a day of hydrocortisone or the equivalent).
Other risk factors for SRMD in ICU patients include multiorgan failure, chronic renal failure, major surgical procedures, shock, and tetraplegia.3,4
Recommended SRMD prophylaxis agents should be institution-based, taking into account the administration route (e.g., functioning GI tract), daily dosing regimens, adverse effect profile, drug interactions, and total costs. Classes that can be used include sucralfate, antacids, H2 receptor antagonists (H2RA), and proton-pump inhibitors (PPIs).
Some patients may prefer the oral route. Some agents can be given in solution or suspension and administered via a nasogastric tube—but be aware of drug interactions. There are limited comparative data for preventing SRMD with these classes. The H2RA and PPI classes of agents are available in intravenous forms, which may be preferable in critically ill patients. However, none of the PPIs are FDA-approved for SRMD prophylaxis.
In the general patient population, SRMD prophylaxis with H2RAs or PPIs is common in 30% to 50% of patients without clear evidence of benefit. Qadeer, et al., identified a 0.4% bleeding rate in their retrospective case-control study of nearly 18,000 patients over a four-year period. In their study, the key risk factor for development of nosocomial GI bleeding was treatment with full-dose anticoagulation or clopidogrel.
Another concern they identified is that when a patient commences an SRMD prophylaxis agent in the hospital, they continue on it post-discharge when it is not needed. This creates an unnecessary cost burden and risks adverse drug interactions.
Todd Janicki, MD, and Scott Stewart, MD, both with the department of medicine at the State University of New York at Buffalo, this year reported on a review of evidence for SRMD prophylaxis in general medicine patients from the peer-reviewed literature.5 They found limited data, identifying only five citations meeting their evaluation criteria. Two of these studies noted only a 3% to 6% reduction in clinically significant bleeding utilizing SRMD prophylaxis. TH
Michele Kaufman is a clinical/managed care consultant and medical writer based in New York City.
References
- Grube RRA, May DB. Stress ulcer prophylaxis in hospitalized patients not in intensive care units. Am J Health-Syst Pharm. 2007;64:1396-400.
- ASHP Commission on Therapeutics. ASHP therapeutic guidelines on stress ulcer prophylaxis. Am J Health-Syst Pharm. 1999;56:347-379.
- Qadeer MA, Richter JE, Brotman DJ. Hospital-acquired gastrointestinal bleeding outside the critical care unit: risk factors, role of acid suppression, and endoscopy findings. J Hosp Med. 2006;1(1):13-20.
- Weinhouse GL, Manaker S. Stress ulcer prophylaxis in the intensive care unit. In: UpToDate, Rose, BD (Ed), UpToDate, Waltham, Mass. 2007.
- Janicki T, Stewart S. Stress-ulcer prophylaxis for general medical patients: a review of the evidence. J Hosp Med. 2007;2(2):86-92.
In the Literature
In This Edition
- Pay-for-performance associated with limited benefits on quality in acute myocardial infarction patients.
- Meta-analysis finds increased risk of acute myocardial infarction with use of rosiglitazone.
- Rosiglitazone increases risk of heart failure, but not acute myocardial infarction or death, interim analysis shows.
- Surgery versus prolonged conservative treatment for severe sciatica.
- Predicting poor outcomes in upper gastrointestinal bleeds.
- Discharging patients with unresolved medical issues.
Does Pay for Performance Improve Hospital Quality?
Background: In 2003, the Centers for Medicare and Medicaid Services (CMS) instituted a pay-for-performance (P4P) pilot program in which participating hospitals would be reimbursed more if they met specific quality standards of care for patients with certain conditions, including acute myocardial infarction (AMI). It is unknown if this type of financial incentive produces improvements in the processes or outcomes of care.
Study design: Observational cohort.
Setting: 500 hospitals across the U.S.
Synopsis: This study compared compliance with CMS quality indicators in the treatment of more than 100,000 patients with acute non-ST-elevation myocardial infarction at 54 participating and 446 non-participating hospitals in the P4P pilot. They found no significant difference in mortality or in a composite measure of the six quality indicators but a slight improvement in two of the six quality indicators (aspirin at discharge and smoking cessation counseling). They did not find that P4P adversely affected indicators not subject to financial incentives.
Bottom line: P4P is associated with limited improvements in compliance with CMS quality indicators in patients with AMI.
Citation: Glickman SW, Ou F-S, DeLong ER, et al. Pay for performance, quality of care, and outcomes in acute myocardial infarction. JAMA. 2007 Jun;297(21):2373-2380.
Is Rosiglitazone Associated with Adverse Cardiovascular Outcomes in a Meta-analysis?
Background: Rosiglitazone (Avandia) is one of two approved oral thiazolidinedione drugs used for diabetic control. Muraglitazar, another thiazolidinedione drug, was not approved for market due to adverse cardiovascular outcomes. The cardiovascular effects of rosiglitazone had not previously been evaluated.
Study design: Meta-analysis.
Setting: All clinical trials (published and unpublished) involving rosiglitazone.
Synopsis: The authors reviewed data from all randomized trials of rosiglitazone versus placebo or other drugs for at least 24 weeks. From the 42 included trials (including more than 28,000 patients) researchers found a statistically significant increased risk of the odds of AMI (odds ratio 1.43, confidence interval 1.03-1.98) in the rosiglitazone group, and a non-significant risk of death from any cardiovascular cause (odds ratio 1.64, confidence interval 0.98-2.74) and all-cause mortality (odds ratio 1.18, confidence interval 0.89-1.55). The meta-analysis was criticized due to the small number of events (fewer than 100 acute AMIs in each group) and lack of patient-level data, but one expert wrote that “in view of the potential cardiovascular risks and in the absence of evidence of other health advantages ... the rationale for prescribing rosiglitazone at this time is unclear.”
The study raised larger concerns regarding Food and Drug Administration drug approvals, because the drug was approved due to its effect on lowering blood sugar levels (a surrogate outcome) without enough scrutiny of other patient outcomes.
Bottom line: Rosiglitazone is associated with increased risk of AMI. Alternative oral agents should be considered first for blood sugar control in diabetics.
Citation: Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007 Jun;356(24):2457-2471.
Editorial: Psaty BM, Furberg CD. Rosiglitazone and cardiovascular risk. N Engl J Med. 2007 Jun;356(24):2522-2524.
Is Rosiglitazone Associated with Adverse Cardiovascular Outcomes in Interim Analysis?
Background: In response to a meta-analysis, an interim analysis of an ongoing open-label manufacturer-sponsored trial was undertaken to determine the cardiovascular risks of rosiglitazone.
Study design: Unplanned interim analysis of a randomized, multicenter, open-label, non-inferiority trial.
Subjects: Outpatient, inadequately controlled type 2 diabetics.
Synopsis: This was an unplanned interim analysis of an open-label manufacturer-sponsored trial. There were 4,447 inadequately controlled type 2 diabetics on either metformin or sulfonylurea. The patients were randomized to receive both drugs (controls) or add-on rosiglitazone. After a mean follow up of 3.75 years, there was no statistically significant difference between the groups in the primary end point (hospitalization or death from cardiovascular causes), or other end points (MI and death from cardiovascular causes or any cause). However, rosiglitazone was associated with an increased risk of heart failure (hazard ratio 2.15, confidence interval 1.30-3.57). Because this was an unplanned interim analysis for a trial expected to continue for six years, experts caution that the results are inconclusive due to low statistical significance and small event rates.
Bottom line: Rosiglitazone is associated with an increased risk of heart failure, but the risks of hospitalization, death, and acute MI remain unclear.
Citation: Home PD, Phil D, Pockock SJ, et al. Rosiglitazone evaluated for cardiovascular outcomes—an interim analysis. N Engl J Med. 2007 Jul;357(1):28-38.
How Often do Discharged Patients with Unresolved Medical Issues Require Outpatient Workups?
Background: Patients are often discharged from the hospital with incomplete workups, but it is unknown how often and what factors affect the completion of the intended workup.
Study design: Retrospective cohort.
Setting: Single institution teaching hospital.
Synopsis: The authors evaluated the inpatient and outpatient medical records of all patients discharged from the medicine or geriatric service over 18 months. Of almost 700 discharges, 28% of the patients had outpatient workups recommended (48% diagnostic procedures, 35% referrals, and 17% lab tests) by the discharging physician. Completion of the workup did not occur 36% of the time, and the likelihood of non-completion increased with time to the first follow-up appointment and lack of availability of the discharge summary.
Bottom line: Outpatient workups are intended in almost a third of discharged patient, the completion of which can likely be enhanced by timely follow-up and discharge summary availability.
Citation: Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305-1311.
Can We Predict Patients at Low Risk for Compli-cations from Acute Upper Gastrointestinal Bleeds?
Background: Although multiple risk-prediction scales exist for patients with upper gastrointestinal (UGI) bleeds, few have been prospectively validated or widely used in clinical practice.
Study design: Prospective cohort.
Setting: Veterans Affairs (VA) hospitals.
Synopsis: VA researchers created and validated a risk predictor in 391 patients with acute upper gastrointestinal bleeding. Data from the derivation set (two-thirds of the patients) was used to create the model tested on the validation set (one-third of the patients). Outcome one (re-bleeding, need for intervention to stop bleeding, or all-cause hospital mortality) was predicted by an APACHE score >11, stigmata of recent bleeding, or varices. Outcome two (outcome one plus new/worsening co-morbidity) was predicted by the above three factors plus an unstable co-morbidity at admission. In the validation group, outcome one occurred in 1%, 5%, and 25% of patients with zero, one, and two or more factors. Outcome two occurred in 6%, 18%, and 49%, respectively. A score of zero accurately identified 93% and 91% of patients for outcomes one and two. The authors speculated that these patients could be safely treated as outpatients. The study excluded patients on anticoagulation, and this VA cohort (99% male) may not be generalizable to other populations.
Bottom line: This validated prediction model can accurately predict more than 90% of patients at low-risk of poor outcomes with UGI bleeding, which could be used to stratify patients in need of hospital admission.
Citation: Imperiale TF, Dominitz JA, Provenzale DT, et al. Predicting poor outcome from acute upper gastrointestinal hemorrhage. Arch Intern Med. 2007 Jun;167(12):1291-1296.
Does Surgery or Conservative Therapy Improve Symptoms of Sciatica Faster?
Background: The optimal timing and benefit of lumbar-disk surgery in patients with symptomatic lumbar disk herniation is unknown.
Study design: Multicenter randomized trial.
Setting: Netherlands.
Synopsis: 283 patients with severe sciatica were randomly chosen to receive early surgery or conservative treatment (with surgery as needed) for six to 12 weeks. The methods for determining the three primary outcomes were: score on the Roland Disability Questionnaire, leg pain score, and self-report of perceived recovery. At one year, 89% of the surgery group and 39% of the control group underwent surgery after a mean of 2.2 and 18.7 weeks, respectively. There was no difference between the groups in the disability score, but time to relief of leg pain and recovery was faster in the surgery group. At one year, 95% in each group reported perceived recovery.
Bottom line: Rates of pain relief and perceived recovery are faster with early surgery than conservative treatment in patients with severe sciatica, but one-year recovery rates are the same. TH
Citation: Peul WC, Van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. NEJM. 2007 May;356(22):2245-2256.
In This Edition
- Pay-for-performance associated with limited benefits on quality in acute myocardial infarction patients.
- Meta-analysis finds increased risk of acute myocardial infarction with use of rosiglitazone.
- Rosiglitazone increases risk of heart failure, but not acute myocardial infarction or death, interim analysis shows.
- Surgery versus prolonged conservative treatment for severe sciatica.
- Predicting poor outcomes in upper gastrointestinal bleeds.
- Discharging patients with unresolved medical issues.
Does Pay for Performance Improve Hospital Quality?
Background: In 2003, the Centers for Medicare and Medicaid Services (CMS) instituted a pay-for-performance (P4P) pilot program in which participating hospitals would be reimbursed more if they met specific quality standards of care for patients with certain conditions, including acute myocardial infarction (AMI). It is unknown if this type of financial incentive produces improvements in the processes or outcomes of care.
Study design: Observational cohort.
Setting: 500 hospitals across the U.S.
Synopsis: This study compared compliance with CMS quality indicators in the treatment of more than 100,000 patients with acute non-ST-elevation myocardial infarction at 54 participating and 446 non-participating hospitals in the P4P pilot. They found no significant difference in mortality or in a composite measure of the six quality indicators but a slight improvement in two of the six quality indicators (aspirin at discharge and smoking cessation counseling). They did not find that P4P adversely affected indicators not subject to financial incentives.
Bottom line: P4P is associated with limited improvements in compliance with CMS quality indicators in patients with AMI.
Citation: Glickman SW, Ou F-S, DeLong ER, et al. Pay for performance, quality of care, and outcomes in acute myocardial infarction. JAMA. 2007 Jun;297(21):2373-2380.
Is Rosiglitazone Associated with Adverse Cardiovascular Outcomes in a Meta-analysis?
Background: Rosiglitazone (Avandia) is one of two approved oral thiazolidinedione drugs used for diabetic control. Muraglitazar, another thiazolidinedione drug, was not approved for market due to adverse cardiovascular outcomes. The cardiovascular effects of rosiglitazone had not previously been evaluated.
Study design: Meta-analysis.
Setting: All clinical trials (published and unpublished) involving rosiglitazone.
Synopsis: The authors reviewed data from all randomized trials of rosiglitazone versus placebo or other drugs for at least 24 weeks. From the 42 included trials (including more than 28,000 patients) researchers found a statistically significant increased risk of the odds of AMI (odds ratio 1.43, confidence interval 1.03-1.98) in the rosiglitazone group, and a non-significant risk of death from any cardiovascular cause (odds ratio 1.64, confidence interval 0.98-2.74) and all-cause mortality (odds ratio 1.18, confidence interval 0.89-1.55). The meta-analysis was criticized due to the small number of events (fewer than 100 acute AMIs in each group) and lack of patient-level data, but one expert wrote that “in view of the potential cardiovascular risks and in the absence of evidence of other health advantages ... the rationale for prescribing rosiglitazone at this time is unclear.”
The study raised larger concerns regarding Food and Drug Administration drug approvals, because the drug was approved due to its effect on lowering blood sugar levels (a surrogate outcome) without enough scrutiny of other patient outcomes.
Bottom line: Rosiglitazone is associated with increased risk of AMI. Alternative oral agents should be considered first for blood sugar control in diabetics.
Citation: Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007 Jun;356(24):2457-2471.
Editorial: Psaty BM, Furberg CD. Rosiglitazone and cardiovascular risk. N Engl J Med. 2007 Jun;356(24):2522-2524.
Is Rosiglitazone Associated with Adverse Cardiovascular Outcomes in Interim Analysis?
Background: In response to a meta-analysis, an interim analysis of an ongoing open-label manufacturer-sponsored trial was undertaken to determine the cardiovascular risks of rosiglitazone.
Study design: Unplanned interim analysis of a randomized, multicenter, open-label, non-inferiority trial.
Subjects: Outpatient, inadequately controlled type 2 diabetics.
Synopsis: This was an unplanned interim analysis of an open-label manufacturer-sponsored trial. There were 4,447 inadequately controlled type 2 diabetics on either metformin or sulfonylurea. The patients were randomized to receive both drugs (controls) or add-on rosiglitazone. After a mean follow up of 3.75 years, there was no statistically significant difference between the groups in the primary end point (hospitalization or death from cardiovascular causes), or other end points (MI and death from cardiovascular causes or any cause). However, rosiglitazone was associated with an increased risk of heart failure (hazard ratio 2.15, confidence interval 1.30-3.57). Because this was an unplanned interim analysis for a trial expected to continue for six years, experts caution that the results are inconclusive due to low statistical significance and small event rates.
Bottom line: Rosiglitazone is associated with an increased risk of heart failure, but the risks of hospitalization, death, and acute MI remain unclear.
Citation: Home PD, Phil D, Pockock SJ, et al. Rosiglitazone evaluated for cardiovascular outcomes—an interim analysis. N Engl J Med. 2007 Jul;357(1):28-38.
How Often do Discharged Patients with Unresolved Medical Issues Require Outpatient Workups?
Background: Patients are often discharged from the hospital with incomplete workups, but it is unknown how often and what factors affect the completion of the intended workup.
Study design: Retrospective cohort.
Setting: Single institution teaching hospital.
Synopsis: The authors evaluated the inpatient and outpatient medical records of all patients discharged from the medicine or geriatric service over 18 months. Of almost 700 discharges, 28% of the patients had outpatient workups recommended (48% diagnostic procedures, 35% referrals, and 17% lab tests) by the discharging physician. Completion of the workup did not occur 36% of the time, and the likelihood of non-completion increased with time to the first follow-up appointment and lack of availability of the discharge summary.
Bottom line: Outpatient workups are intended in almost a third of discharged patient, the completion of which can likely be enhanced by timely follow-up and discharge summary availability.
Citation: Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305-1311.
Can We Predict Patients at Low Risk for Compli-cations from Acute Upper Gastrointestinal Bleeds?
Background: Although multiple risk-prediction scales exist for patients with upper gastrointestinal (UGI) bleeds, few have been prospectively validated or widely used in clinical practice.
Study design: Prospective cohort.
Setting: Veterans Affairs (VA) hospitals.
Synopsis: VA researchers created and validated a risk predictor in 391 patients with acute upper gastrointestinal bleeding. Data from the derivation set (two-thirds of the patients) was used to create the model tested on the validation set (one-third of the patients). Outcome one (re-bleeding, need for intervention to stop bleeding, or all-cause hospital mortality) was predicted by an APACHE score >11, stigmata of recent bleeding, or varices. Outcome two (outcome one plus new/worsening co-morbidity) was predicted by the above three factors plus an unstable co-morbidity at admission. In the validation group, outcome one occurred in 1%, 5%, and 25% of patients with zero, one, and two or more factors. Outcome two occurred in 6%, 18%, and 49%, respectively. A score of zero accurately identified 93% and 91% of patients for outcomes one and two. The authors speculated that these patients could be safely treated as outpatients. The study excluded patients on anticoagulation, and this VA cohort (99% male) may not be generalizable to other populations.
Bottom line: This validated prediction model can accurately predict more than 90% of patients at low-risk of poor outcomes with UGI bleeding, which could be used to stratify patients in need of hospital admission.
Citation: Imperiale TF, Dominitz JA, Provenzale DT, et al. Predicting poor outcome from acute upper gastrointestinal hemorrhage. Arch Intern Med. 2007 Jun;167(12):1291-1296.
Does Surgery or Conservative Therapy Improve Symptoms of Sciatica Faster?
Background: The optimal timing and benefit of lumbar-disk surgery in patients with symptomatic lumbar disk herniation is unknown.
Study design: Multicenter randomized trial.
Setting: Netherlands.
Synopsis: 283 patients with severe sciatica were randomly chosen to receive early surgery or conservative treatment (with surgery as needed) for six to 12 weeks. The methods for determining the three primary outcomes were: score on the Roland Disability Questionnaire, leg pain score, and self-report of perceived recovery. At one year, 89% of the surgery group and 39% of the control group underwent surgery after a mean of 2.2 and 18.7 weeks, respectively. There was no difference between the groups in the disability score, but time to relief of leg pain and recovery was faster in the surgery group. At one year, 95% in each group reported perceived recovery.
Bottom line: Rates of pain relief and perceived recovery are faster with early surgery than conservative treatment in patients with severe sciatica, but one-year recovery rates are the same. TH
Citation: Peul WC, Van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. NEJM. 2007 May;356(22):2245-2256.
In This Edition
- Pay-for-performance associated with limited benefits on quality in acute myocardial infarction patients.
- Meta-analysis finds increased risk of acute myocardial infarction with use of rosiglitazone.
- Rosiglitazone increases risk of heart failure, but not acute myocardial infarction or death, interim analysis shows.
- Surgery versus prolonged conservative treatment for severe sciatica.
- Predicting poor outcomes in upper gastrointestinal bleeds.
- Discharging patients with unresolved medical issues.
Does Pay for Performance Improve Hospital Quality?
Background: In 2003, the Centers for Medicare and Medicaid Services (CMS) instituted a pay-for-performance (P4P) pilot program in which participating hospitals would be reimbursed more if they met specific quality standards of care for patients with certain conditions, including acute myocardial infarction (AMI). It is unknown if this type of financial incentive produces improvements in the processes or outcomes of care.
Study design: Observational cohort.
Setting: 500 hospitals across the U.S.
Synopsis: This study compared compliance with CMS quality indicators in the treatment of more than 100,000 patients with acute non-ST-elevation myocardial infarction at 54 participating and 446 non-participating hospitals in the P4P pilot. They found no significant difference in mortality or in a composite measure of the six quality indicators but a slight improvement in two of the six quality indicators (aspirin at discharge and smoking cessation counseling). They did not find that P4P adversely affected indicators not subject to financial incentives.
Bottom line: P4P is associated with limited improvements in compliance with CMS quality indicators in patients with AMI.
Citation: Glickman SW, Ou F-S, DeLong ER, et al. Pay for performance, quality of care, and outcomes in acute myocardial infarction. JAMA. 2007 Jun;297(21):2373-2380.
Is Rosiglitazone Associated with Adverse Cardiovascular Outcomes in a Meta-analysis?
Background: Rosiglitazone (Avandia) is one of two approved oral thiazolidinedione drugs used for diabetic control. Muraglitazar, another thiazolidinedione drug, was not approved for market due to adverse cardiovascular outcomes. The cardiovascular effects of rosiglitazone had not previously been evaluated.
Study design: Meta-analysis.
Setting: All clinical trials (published and unpublished) involving rosiglitazone.
Synopsis: The authors reviewed data from all randomized trials of rosiglitazone versus placebo or other drugs for at least 24 weeks. From the 42 included trials (including more than 28,000 patients) researchers found a statistically significant increased risk of the odds of AMI (odds ratio 1.43, confidence interval 1.03-1.98) in the rosiglitazone group, and a non-significant risk of death from any cardiovascular cause (odds ratio 1.64, confidence interval 0.98-2.74) and all-cause mortality (odds ratio 1.18, confidence interval 0.89-1.55). The meta-analysis was criticized due to the small number of events (fewer than 100 acute AMIs in each group) and lack of patient-level data, but one expert wrote that “in view of the potential cardiovascular risks and in the absence of evidence of other health advantages ... the rationale for prescribing rosiglitazone at this time is unclear.”
The study raised larger concerns regarding Food and Drug Administration drug approvals, because the drug was approved due to its effect on lowering blood sugar levels (a surrogate outcome) without enough scrutiny of other patient outcomes.
Bottom line: Rosiglitazone is associated with increased risk of AMI. Alternative oral agents should be considered first for blood sugar control in diabetics.
Citation: Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007 Jun;356(24):2457-2471.
Editorial: Psaty BM, Furberg CD. Rosiglitazone and cardiovascular risk. N Engl J Med. 2007 Jun;356(24):2522-2524.
Is Rosiglitazone Associated with Adverse Cardiovascular Outcomes in Interim Analysis?
Background: In response to a meta-analysis, an interim analysis of an ongoing open-label manufacturer-sponsored trial was undertaken to determine the cardiovascular risks of rosiglitazone.
Study design: Unplanned interim analysis of a randomized, multicenter, open-label, non-inferiority trial.
Subjects: Outpatient, inadequately controlled type 2 diabetics.
Synopsis: This was an unplanned interim analysis of an open-label manufacturer-sponsored trial. There were 4,447 inadequately controlled type 2 diabetics on either metformin or sulfonylurea. The patients were randomized to receive both drugs (controls) or add-on rosiglitazone. After a mean follow up of 3.75 years, there was no statistically significant difference between the groups in the primary end point (hospitalization or death from cardiovascular causes), or other end points (MI and death from cardiovascular causes or any cause). However, rosiglitazone was associated with an increased risk of heart failure (hazard ratio 2.15, confidence interval 1.30-3.57). Because this was an unplanned interim analysis for a trial expected to continue for six years, experts caution that the results are inconclusive due to low statistical significance and small event rates.
Bottom line: Rosiglitazone is associated with an increased risk of heart failure, but the risks of hospitalization, death, and acute MI remain unclear.
Citation: Home PD, Phil D, Pockock SJ, et al. Rosiglitazone evaluated for cardiovascular outcomes—an interim analysis. N Engl J Med. 2007 Jul;357(1):28-38.
How Often do Discharged Patients with Unresolved Medical Issues Require Outpatient Workups?
Background: Patients are often discharged from the hospital with incomplete workups, but it is unknown how often and what factors affect the completion of the intended workup.
Study design: Retrospective cohort.
Setting: Single institution teaching hospital.
Synopsis: The authors evaluated the inpatient and outpatient medical records of all patients discharged from the medicine or geriatric service over 18 months. Of almost 700 discharges, 28% of the patients had outpatient workups recommended (48% diagnostic procedures, 35% referrals, and 17% lab tests) by the discharging physician. Completion of the workup did not occur 36% of the time, and the likelihood of non-completion increased with time to the first follow-up appointment and lack of availability of the discharge summary.
Bottom line: Outpatient workups are intended in almost a third of discharged patient, the completion of which can likely be enhanced by timely follow-up and discharge summary availability.
Citation: Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305-1311.
Can We Predict Patients at Low Risk for Compli-cations from Acute Upper Gastrointestinal Bleeds?
Background: Although multiple risk-prediction scales exist for patients with upper gastrointestinal (UGI) bleeds, few have been prospectively validated or widely used in clinical practice.
Study design: Prospective cohort.
Setting: Veterans Affairs (VA) hospitals.
Synopsis: VA researchers created and validated a risk predictor in 391 patients with acute upper gastrointestinal bleeding. Data from the derivation set (two-thirds of the patients) was used to create the model tested on the validation set (one-third of the patients). Outcome one (re-bleeding, need for intervention to stop bleeding, or all-cause hospital mortality) was predicted by an APACHE score >11, stigmata of recent bleeding, or varices. Outcome two (outcome one plus new/worsening co-morbidity) was predicted by the above three factors plus an unstable co-morbidity at admission. In the validation group, outcome one occurred in 1%, 5%, and 25% of patients with zero, one, and two or more factors. Outcome two occurred in 6%, 18%, and 49%, respectively. A score of zero accurately identified 93% and 91% of patients for outcomes one and two. The authors speculated that these patients could be safely treated as outpatients. The study excluded patients on anticoagulation, and this VA cohort (99% male) may not be generalizable to other populations.
Bottom line: This validated prediction model can accurately predict more than 90% of patients at low-risk of poor outcomes with UGI bleeding, which could be used to stratify patients in need of hospital admission.
Citation: Imperiale TF, Dominitz JA, Provenzale DT, et al. Predicting poor outcome from acute upper gastrointestinal hemorrhage. Arch Intern Med. 2007 Jun;167(12):1291-1296.
Does Surgery or Conservative Therapy Improve Symptoms of Sciatica Faster?
Background: The optimal timing and benefit of lumbar-disk surgery in patients with symptomatic lumbar disk herniation is unknown.
Study design: Multicenter randomized trial.
Setting: Netherlands.
Synopsis: 283 patients with severe sciatica were randomly chosen to receive early surgery or conservative treatment (with surgery as needed) for six to 12 weeks. The methods for determining the three primary outcomes were: score on the Roland Disability Questionnaire, leg pain score, and self-report of perceived recovery. At one year, 89% of the surgery group and 39% of the control group underwent surgery after a mean of 2.2 and 18.7 weeks, respectively. There was no difference between the groups in the disability score, but time to relief of leg pain and recovery was faster in the surgery group. At one year, 95% in each group reported perceived recovery.
Bottom line: Rates of pain relief and perceived recovery are faster with early surgery than conservative treatment in patients with severe sciatica, but one-year recovery rates are the same. TH
Citation: Peul WC, Van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. NEJM. 2007 May;356(22):2245-2256.
The Life of a Task Force
The Performance and Standards Task Force (PSTF) was formed a little more than a year ago after SHM leadership recognized the need for a coordinated approach to working with external organizations in the performance and standards quality arena.
As SHM’s senior adviser for quality standards and compliance, I work with PSTF Chairman Patrick Torcson, MD, (medical director of hospital medicine at the St. Tammany Parish Hospital in Covington, La.) along with senior staff and leadership of the Public Policy Committee (PPC). We monitor the performance and quality landscape at national organizations charged with measuring development and building consensus. We also develop relationships with other professional medical societies and organizations.
Since its inception in spring 2006, the PSTF has become engaged in the American Medical Association’s (AMA) Physician Consortium for Performance Improvement (PCPI) and the National Quality Forum (NQF). The NQF is a nonprofit organization instructed by Congress to endorse consensus-based national standards for measurement and public reporting of healthcare performance data. Specifically, NQF aims to influence the development of physician-level performance measures as part of the Centers for Medicare and Medicaid Service’s (CMS) Physician Quality Reporting Initiative (PQRI).
By joining the PCPI, SHM has aligned with other medical specialties to develop performance measures in geriatrics, emergency medicine, outpatient parenteral antimicrobial therapy, and facets of anesthesiology such as perioperative normothermia and critical care.
Additionally, SHM has given feedback during public comment periods on perioperative care, chronic kidney disease, and other measures. The task force continues to evaluate which workgroups it should appoint members to participate in, depending on the topic.
SHM leadership has continued to foster relationships with CMS by sending letters in support of the 2007 PQRI. SHM was able to influence changes to the 2007 measure specifications so hospitalists would have measures to report. Of the 74 measures included in the PQRI, 11 have specifications allowing reporting by hospitalists, underscoring the importance of SHM’s influence and participation in the PCPI process.
Dr. Torcson and Eric Siegal, MD, (regional medical director, Cogent Healthcare, Madison, Wis.) co-chaired a CMS-led SHM member conference call focused on PQRI and how it affects hospitalists. The program was well received by SHM members.
When SHM became a member of the NQF last summer, it nominated several members who were selected to participate on various technical advisory panels overseeing work on the development of consensus standards for hospital care. This project, sponsored by the Agency for Healthcare Research and Quality (AHRQ), is addressing patient safety, pediatrics, and inpatient care.
Last fall, SHM sent Mark Williams, MD (professor of medicine at Emory University School of Medicine in Atlanta and editor of The Journal of Hospital Medicine) to the NQF’s 7th Annual Meeting, a National Policy Conference on Quality. The meeting featured plenary sessions that focused on issues at the forefront of policy discussions, including incentivizing healthcare quality improvement, the role of policymakers, leading professional and trade associations in improving healthcare quality, and efforts under way in the federal government to foster healthcare improvements.
This fall, Greg Seymann, MD, will attend the 8th Annual Meeting. Dr. Seymann is an assistant professor with the Department of Medicine, Hospital Medicine Program, at the University of California San Diego Medical Center.
Goals for 2008, Beyond
By taking an active role in the performance and standard arena, SHM senior staff and leadership have been able to build key relationships. This has paved the way for influencing the current physician reporting program and taking the lead on developing measures that will most reflect hospital medicine in the future.
The task force intends to be at the helm of the development of performance measures that more accurately reflect services provided by hospitalists. Senior staff and leadership have discussed this goal with several national stakeholders including the PCPI and the NQF, whose senior staff have supported its agenda.
In July, SHM, along with the American College of Physicians (ACP), the Society of General Internal Medicine (SGIM), and the American Geriatrics Society (AGS), formed a steering committee to convene a transitions of care consensus conference. This multispecialty, multidisciplinary group reviewed the principles and standards that came from the ABIM Foundation’s Stepping Up to the Plate (SUTTP) Alliance, which met this spring. SHM and PCPI are working to form an expert workgroup that will develop six to eight care transitions measures for inclusion in the 2009 PQRI.
SHM also is exploring collaboration with the American Hospital Association and its Hospital Quality Alliance (HQA), which coordinates the promotion of quality measurement, transparency, and improvement in the hospital setting.
In addition to its work with these external national groups, task force members would also like to start a resource room on the SHM Web site, www.hospitalmedicine.org, which would be devoted to member efforts in research related to quality and performance standards, as well as the member go-to place for tools and references on best practices in performance standards and pay for reporting initiatives.
Finally, Dr. Torcson hopes to shape and disseminate a national research agenda for hospitalist performance measurement and reporting. TH
SHM Behind the Scenes
Quality is our Middle Name
By Geri Barnes
The Education and Quality Initiatives Department’s (EQID) mission is to lead and manage an integrative program that brings resources to improve patient care. With the help of many individuals and partner organizations, SHM is working toward improved care for inpatients. Let’s review our progress as we begin the second quarter of SHM’s fiscal year.
Educational Programs
Our focus over the past few months has been the development of “Hospital Medicine 2008,” which will be held April 3-5 in San Diego. Under the leadership of Sylvia McKean, MD, head of the hospitalist service at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School in Boston, the Annual Meeting Committee has developed an innovative program. The session will include a new evidence-based rapid fire track and a new teaching skills pre-course for academic and clinical educators. EQID obtains CMEs, communicates with faculty, and fine-tunes logistical efforts.
Leadership Academy Level I is a mainstay of SHM’s educational efforts. EQID supports Eric Howell, MD, chair of the Leadership Committee, as it focuses on addressing attendee input and encouraging the revision of the program in a continuous quality improvement effort. Dr. Howell is director of the Collaborative Inpatient Medicine Service and director of the Zieve Medical Services for Johns Hopkins Bayview Medical Center in Baltimore.
Along with Level I, Leadership Academy Level II will be presented again this year Nov. 5-8 in San Antonio. It builds on the success of last fall’s first offering by expanding on the concepts presented in the Level I academy.
A new educational initiative, supported by Sanofi-Aventis, provides three training sessions at regional chapters or other designated meetings across the country. The meetings educate hospitalists on best practices for glycemic control, prevention of venous thromboembolism, and transitions of care. Meetings will highlight successful interventions as outlined in the respective quality improvement (QI) implementation guides and resource rooms. Meetings will aim to include 20 to 50 participants.
The last piece of the SHM Heart Failure Quality Improvement Initiative is in its final planning stages, and a third CME module for Team Communications as it relates to the heart failure patient will be developed in the coming months. This initiative is supported in part by Scios Inc. and led by Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.
Quality Initiatives
Over the past several years, SHM has developed initiatives that range from convening a panel to assess the state of the art of a QI intervention to developing a Web-based resource room. Projects EQID is involved with:
- SHM is in the early stages of a three-year effort to develop resources and programs for improving hospital care transitions for older adults. This is supported through a major grant from the John A. Hartford Foundation in New York City, under the leadership of Mark Williams, MD, and Eric Coleman, MD, MPH. Dr. Williams is chief of the new Division of Hospital Medicine at Northwestern Memorial Hospital in Chicago and editor of the Journal of Hospital Medicine. Dr. Coleman is associate professor of medicine within the divisions of healthcare policy and research and geriatric medicine at the University of Colorado Health Sciences Center in Aurora.
- “The Heart Failure Quality Improvement Implementation Guide” has been updated. The Heart Failure Resource Room on SHM’s Web site has been redesigned to make it easier for visitors who wish to follow the process of developing a QI intervention related to care of the hospitalized heart failure patient. We are communicating these changes to the hospital medicine community. Supported in part by Scios Inc., based in Mountain View, Calif., this effort includes presentations at regional meetings. This project was led by Nurcan Ilksoy, MD, assistant professor of Medicine at Emory University School of Medicine in Atlanta.
- The VTE Prevention Collaborative is open to all members implementing a QI program to combat venous thromboembolism in the hospitalized patient. The Sanofi-Aventis-supported collaborative uses seasoned QI leaders as mentors. Greg Maynard, MD, MS, and Jason Stein, MD, lead the enrollees through the QI process. The mentees have the benefit of regularly scheduled calls to ask questions and receive instant feedback on their process and progress. An add-on to this program, funded by the Kettering Foundation of Dayton, Ohio, provides the opportunity for on-site consultations. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of Medicine at Emory University School of Medicine, and director of Quality Improvement for the Emory Hospital Medicine Unit.
- An expert panel convened in July to kick off development of an Acute Coronary Syndrome Resource Room and determine the content the resource room will cover. Content address diagnosis and risk stratification, medication, interventional procedures, patient education, transitions, and care coordination. This initiative is being led by Chad Whelan, MD, and is supported in part by Bristol-Myers Squibb Company, New York City. Dr. Whelan is an academic hospitalist and an assistant professor of medicine at University of Chicago in the Section of General Internal Medicine.
- SHM often studies strategies to improve patient satisfaction, outcomes, length of stay, and other important metrics. An expert panel assesses observation units as they contribute to improved treatment of patients with acute decompensated heart failure, chest pain, and other clinical conditions such as asthma. A white paper is pending on the use and value of observation units. Support for the meeting and development and distribution of the white paper was provided by Scios Inc.
Committee Support
A major staff role is the support of the Education and Hospital Quality and Patient Safety (HQPS) committees, the groups that direct and drive SHM in these important areas. The Education Committee, led by Chairman Bill Rifkin, MD, assistant professor of medicine at Yale University School of Medicine in New Haven, Conn., is focusing on:
- Developing the teaching skills pre-course that will be presented at the 2008 Annual Meeting;
- Defining a workable strategy to promote The Core Competencies in Hospital Medicine;
- Developing educational and/or communication modalities that support maintenance of certification; and
- Further defining the direction of the committee to meet members’ educational needs.
Janet Nagamine, MD, leads the HQPS Committee in the following priorities:
- Planning and holding a quality summit to define goals and priorities for the next three to five years;
- Submitting a grant application to AHRQ to support a multidisciplinary conference in the area of medication reconciliation;
- Developing SHM’s role in care transitions;
- Reviewing quality pre-course information and determining the curriculum for ‘‘Hospital Medicine 2008”; and
- Developing the Quality track for ‘‘Hospital Medicine 2008.”
The Performance and Standards Task Force (PSTF) was formed a little more than a year ago after SHM leadership recognized the need for a coordinated approach to working with external organizations in the performance and standards quality arena.
As SHM’s senior adviser for quality standards and compliance, I work with PSTF Chairman Patrick Torcson, MD, (medical director of hospital medicine at the St. Tammany Parish Hospital in Covington, La.) along with senior staff and leadership of the Public Policy Committee (PPC). We monitor the performance and quality landscape at national organizations charged with measuring development and building consensus. We also develop relationships with other professional medical societies and organizations.
Since its inception in spring 2006, the PSTF has become engaged in the American Medical Association’s (AMA) Physician Consortium for Performance Improvement (PCPI) and the National Quality Forum (NQF). The NQF is a nonprofit organization instructed by Congress to endorse consensus-based national standards for measurement and public reporting of healthcare performance data. Specifically, NQF aims to influence the development of physician-level performance measures as part of the Centers for Medicare and Medicaid Service’s (CMS) Physician Quality Reporting Initiative (PQRI).
By joining the PCPI, SHM has aligned with other medical specialties to develop performance measures in geriatrics, emergency medicine, outpatient parenteral antimicrobial therapy, and facets of anesthesiology such as perioperative normothermia and critical care.
Additionally, SHM has given feedback during public comment periods on perioperative care, chronic kidney disease, and other measures. The task force continues to evaluate which workgroups it should appoint members to participate in, depending on the topic.
SHM leadership has continued to foster relationships with CMS by sending letters in support of the 2007 PQRI. SHM was able to influence changes to the 2007 measure specifications so hospitalists would have measures to report. Of the 74 measures included in the PQRI, 11 have specifications allowing reporting by hospitalists, underscoring the importance of SHM’s influence and participation in the PCPI process.
Dr. Torcson and Eric Siegal, MD, (regional medical director, Cogent Healthcare, Madison, Wis.) co-chaired a CMS-led SHM member conference call focused on PQRI and how it affects hospitalists. The program was well received by SHM members.
When SHM became a member of the NQF last summer, it nominated several members who were selected to participate on various technical advisory panels overseeing work on the development of consensus standards for hospital care. This project, sponsored by the Agency for Healthcare Research and Quality (AHRQ), is addressing patient safety, pediatrics, and inpatient care.
Last fall, SHM sent Mark Williams, MD (professor of medicine at Emory University School of Medicine in Atlanta and editor of The Journal of Hospital Medicine) to the NQF’s 7th Annual Meeting, a National Policy Conference on Quality. The meeting featured plenary sessions that focused on issues at the forefront of policy discussions, including incentivizing healthcare quality improvement, the role of policymakers, leading professional and trade associations in improving healthcare quality, and efforts under way in the federal government to foster healthcare improvements.
This fall, Greg Seymann, MD, will attend the 8th Annual Meeting. Dr. Seymann is an assistant professor with the Department of Medicine, Hospital Medicine Program, at the University of California San Diego Medical Center.
Goals for 2008, Beyond
By taking an active role in the performance and standard arena, SHM senior staff and leadership have been able to build key relationships. This has paved the way for influencing the current physician reporting program and taking the lead on developing measures that will most reflect hospital medicine in the future.
The task force intends to be at the helm of the development of performance measures that more accurately reflect services provided by hospitalists. Senior staff and leadership have discussed this goal with several national stakeholders including the PCPI and the NQF, whose senior staff have supported its agenda.
In July, SHM, along with the American College of Physicians (ACP), the Society of General Internal Medicine (SGIM), and the American Geriatrics Society (AGS), formed a steering committee to convene a transitions of care consensus conference. This multispecialty, multidisciplinary group reviewed the principles and standards that came from the ABIM Foundation’s Stepping Up to the Plate (SUTTP) Alliance, which met this spring. SHM and PCPI are working to form an expert workgroup that will develop six to eight care transitions measures for inclusion in the 2009 PQRI.
SHM also is exploring collaboration with the American Hospital Association and its Hospital Quality Alliance (HQA), which coordinates the promotion of quality measurement, transparency, and improvement in the hospital setting.
In addition to its work with these external national groups, task force members would also like to start a resource room on the SHM Web site, www.hospitalmedicine.org, which would be devoted to member efforts in research related to quality and performance standards, as well as the member go-to place for tools and references on best practices in performance standards and pay for reporting initiatives.
Finally, Dr. Torcson hopes to shape and disseminate a national research agenda for hospitalist performance measurement and reporting. TH
SHM Behind the Scenes
Quality is our Middle Name
By Geri Barnes
The Education and Quality Initiatives Department’s (EQID) mission is to lead and manage an integrative program that brings resources to improve patient care. With the help of many individuals and partner organizations, SHM is working toward improved care for inpatients. Let’s review our progress as we begin the second quarter of SHM’s fiscal year.
Educational Programs
Our focus over the past few months has been the development of “Hospital Medicine 2008,” which will be held April 3-5 in San Diego. Under the leadership of Sylvia McKean, MD, head of the hospitalist service at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School in Boston, the Annual Meeting Committee has developed an innovative program. The session will include a new evidence-based rapid fire track and a new teaching skills pre-course for academic and clinical educators. EQID obtains CMEs, communicates with faculty, and fine-tunes logistical efforts.
Leadership Academy Level I is a mainstay of SHM’s educational efforts. EQID supports Eric Howell, MD, chair of the Leadership Committee, as it focuses on addressing attendee input and encouraging the revision of the program in a continuous quality improvement effort. Dr. Howell is director of the Collaborative Inpatient Medicine Service and director of the Zieve Medical Services for Johns Hopkins Bayview Medical Center in Baltimore.
Along with Level I, Leadership Academy Level II will be presented again this year Nov. 5-8 in San Antonio. It builds on the success of last fall’s first offering by expanding on the concepts presented in the Level I academy.
A new educational initiative, supported by Sanofi-Aventis, provides three training sessions at regional chapters or other designated meetings across the country. The meetings educate hospitalists on best practices for glycemic control, prevention of venous thromboembolism, and transitions of care. Meetings will highlight successful interventions as outlined in the respective quality improvement (QI) implementation guides and resource rooms. Meetings will aim to include 20 to 50 participants.
The last piece of the SHM Heart Failure Quality Improvement Initiative is in its final planning stages, and a third CME module for Team Communications as it relates to the heart failure patient will be developed in the coming months. This initiative is supported in part by Scios Inc. and led by Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.
Quality Initiatives
Over the past several years, SHM has developed initiatives that range from convening a panel to assess the state of the art of a QI intervention to developing a Web-based resource room. Projects EQID is involved with:
- SHM is in the early stages of a three-year effort to develop resources and programs for improving hospital care transitions for older adults. This is supported through a major grant from the John A. Hartford Foundation in New York City, under the leadership of Mark Williams, MD, and Eric Coleman, MD, MPH. Dr. Williams is chief of the new Division of Hospital Medicine at Northwestern Memorial Hospital in Chicago and editor of the Journal of Hospital Medicine. Dr. Coleman is associate professor of medicine within the divisions of healthcare policy and research and geriatric medicine at the University of Colorado Health Sciences Center in Aurora.
- “The Heart Failure Quality Improvement Implementation Guide” has been updated. The Heart Failure Resource Room on SHM’s Web site has been redesigned to make it easier for visitors who wish to follow the process of developing a QI intervention related to care of the hospitalized heart failure patient. We are communicating these changes to the hospital medicine community. Supported in part by Scios Inc., based in Mountain View, Calif., this effort includes presentations at regional meetings. This project was led by Nurcan Ilksoy, MD, assistant professor of Medicine at Emory University School of Medicine in Atlanta.
- The VTE Prevention Collaborative is open to all members implementing a QI program to combat venous thromboembolism in the hospitalized patient. The Sanofi-Aventis-supported collaborative uses seasoned QI leaders as mentors. Greg Maynard, MD, MS, and Jason Stein, MD, lead the enrollees through the QI process. The mentees have the benefit of regularly scheduled calls to ask questions and receive instant feedback on their process and progress. An add-on to this program, funded by the Kettering Foundation of Dayton, Ohio, provides the opportunity for on-site consultations. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of Medicine at Emory University School of Medicine, and director of Quality Improvement for the Emory Hospital Medicine Unit.
- An expert panel convened in July to kick off development of an Acute Coronary Syndrome Resource Room and determine the content the resource room will cover. Content address diagnosis and risk stratification, medication, interventional procedures, patient education, transitions, and care coordination. This initiative is being led by Chad Whelan, MD, and is supported in part by Bristol-Myers Squibb Company, New York City. Dr. Whelan is an academic hospitalist and an assistant professor of medicine at University of Chicago in the Section of General Internal Medicine.
- SHM often studies strategies to improve patient satisfaction, outcomes, length of stay, and other important metrics. An expert panel assesses observation units as they contribute to improved treatment of patients with acute decompensated heart failure, chest pain, and other clinical conditions such as asthma. A white paper is pending on the use and value of observation units. Support for the meeting and development and distribution of the white paper was provided by Scios Inc.
Committee Support
A major staff role is the support of the Education and Hospital Quality and Patient Safety (HQPS) committees, the groups that direct and drive SHM in these important areas. The Education Committee, led by Chairman Bill Rifkin, MD, assistant professor of medicine at Yale University School of Medicine in New Haven, Conn., is focusing on:
- Developing the teaching skills pre-course that will be presented at the 2008 Annual Meeting;
- Defining a workable strategy to promote The Core Competencies in Hospital Medicine;
- Developing educational and/or communication modalities that support maintenance of certification; and
- Further defining the direction of the committee to meet members’ educational needs.
Janet Nagamine, MD, leads the HQPS Committee in the following priorities:
- Planning and holding a quality summit to define goals and priorities for the next three to five years;
- Submitting a grant application to AHRQ to support a multidisciplinary conference in the area of medication reconciliation;
- Developing SHM’s role in care transitions;
- Reviewing quality pre-course information and determining the curriculum for ‘‘Hospital Medicine 2008”; and
- Developing the Quality track for ‘‘Hospital Medicine 2008.”
The Performance and Standards Task Force (PSTF) was formed a little more than a year ago after SHM leadership recognized the need for a coordinated approach to working with external organizations in the performance and standards quality arena.
As SHM’s senior adviser for quality standards and compliance, I work with PSTF Chairman Patrick Torcson, MD, (medical director of hospital medicine at the St. Tammany Parish Hospital in Covington, La.) along with senior staff and leadership of the Public Policy Committee (PPC). We monitor the performance and quality landscape at national organizations charged with measuring development and building consensus. We also develop relationships with other professional medical societies and organizations.
Since its inception in spring 2006, the PSTF has become engaged in the American Medical Association’s (AMA) Physician Consortium for Performance Improvement (PCPI) and the National Quality Forum (NQF). The NQF is a nonprofit organization instructed by Congress to endorse consensus-based national standards for measurement and public reporting of healthcare performance data. Specifically, NQF aims to influence the development of physician-level performance measures as part of the Centers for Medicare and Medicaid Service’s (CMS) Physician Quality Reporting Initiative (PQRI).
By joining the PCPI, SHM has aligned with other medical specialties to develop performance measures in geriatrics, emergency medicine, outpatient parenteral antimicrobial therapy, and facets of anesthesiology such as perioperative normothermia and critical care.
Additionally, SHM has given feedback during public comment periods on perioperative care, chronic kidney disease, and other measures. The task force continues to evaluate which workgroups it should appoint members to participate in, depending on the topic.
SHM leadership has continued to foster relationships with CMS by sending letters in support of the 2007 PQRI. SHM was able to influence changes to the 2007 measure specifications so hospitalists would have measures to report. Of the 74 measures included in the PQRI, 11 have specifications allowing reporting by hospitalists, underscoring the importance of SHM’s influence and participation in the PCPI process.
Dr. Torcson and Eric Siegal, MD, (regional medical director, Cogent Healthcare, Madison, Wis.) co-chaired a CMS-led SHM member conference call focused on PQRI and how it affects hospitalists. The program was well received by SHM members.
When SHM became a member of the NQF last summer, it nominated several members who were selected to participate on various technical advisory panels overseeing work on the development of consensus standards for hospital care. This project, sponsored by the Agency for Healthcare Research and Quality (AHRQ), is addressing patient safety, pediatrics, and inpatient care.
Last fall, SHM sent Mark Williams, MD (professor of medicine at Emory University School of Medicine in Atlanta and editor of The Journal of Hospital Medicine) to the NQF’s 7th Annual Meeting, a National Policy Conference on Quality. The meeting featured plenary sessions that focused on issues at the forefront of policy discussions, including incentivizing healthcare quality improvement, the role of policymakers, leading professional and trade associations in improving healthcare quality, and efforts under way in the federal government to foster healthcare improvements.
This fall, Greg Seymann, MD, will attend the 8th Annual Meeting. Dr. Seymann is an assistant professor with the Department of Medicine, Hospital Medicine Program, at the University of California San Diego Medical Center.
Goals for 2008, Beyond
By taking an active role in the performance and standard arena, SHM senior staff and leadership have been able to build key relationships. This has paved the way for influencing the current physician reporting program and taking the lead on developing measures that will most reflect hospital medicine in the future.
The task force intends to be at the helm of the development of performance measures that more accurately reflect services provided by hospitalists. Senior staff and leadership have discussed this goal with several national stakeholders including the PCPI and the NQF, whose senior staff have supported its agenda.
In July, SHM, along with the American College of Physicians (ACP), the Society of General Internal Medicine (SGIM), and the American Geriatrics Society (AGS), formed a steering committee to convene a transitions of care consensus conference. This multispecialty, multidisciplinary group reviewed the principles and standards that came from the ABIM Foundation’s Stepping Up to the Plate (SUTTP) Alliance, which met this spring. SHM and PCPI are working to form an expert workgroup that will develop six to eight care transitions measures for inclusion in the 2009 PQRI.
SHM also is exploring collaboration with the American Hospital Association and its Hospital Quality Alliance (HQA), which coordinates the promotion of quality measurement, transparency, and improvement in the hospital setting.
In addition to its work with these external national groups, task force members would also like to start a resource room on the SHM Web site, www.hospitalmedicine.org, which would be devoted to member efforts in research related to quality and performance standards, as well as the member go-to place for tools and references on best practices in performance standards and pay for reporting initiatives.
Finally, Dr. Torcson hopes to shape and disseminate a national research agenda for hospitalist performance measurement and reporting. TH
SHM Behind the Scenes
Quality is our Middle Name
By Geri Barnes
The Education and Quality Initiatives Department’s (EQID) mission is to lead and manage an integrative program that brings resources to improve patient care. With the help of many individuals and partner organizations, SHM is working toward improved care for inpatients. Let’s review our progress as we begin the second quarter of SHM’s fiscal year.
Educational Programs
Our focus over the past few months has been the development of “Hospital Medicine 2008,” which will be held April 3-5 in San Diego. Under the leadership of Sylvia McKean, MD, head of the hospitalist service at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School in Boston, the Annual Meeting Committee has developed an innovative program. The session will include a new evidence-based rapid fire track and a new teaching skills pre-course for academic and clinical educators. EQID obtains CMEs, communicates with faculty, and fine-tunes logistical efforts.
Leadership Academy Level I is a mainstay of SHM’s educational efforts. EQID supports Eric Howell, MD, chair of the Leadership Committee, as it focuses on addressing attendee input and encouraging the revision of the program in a continuous quality improvement effort. Dr. Howell is director of the Collaborative Inpatient Medicine Service and director of the Zieve Medical Services for Johns Hopkins Bayview Medical Center in Baltimore.
Along with Level I, Leadership Academy Level II will be presented again this year Nov. 5-8 in San Antonio. It builds on the success of last fall’s first offering by expanding on the concepts presented in the Level I academy.
A new educational initiative, supported by Sanofi-Aventis, provides three training sessions at regional chapters or other designated meetings across the country. The meetings educate hospitalists on best practices for glycemic control, prevention of venous thromboembolism, and transitions of care. Meetings will highlight successful interventions as outlined in the respective quality improvement (QI) implementation guides and resource rooms. Meetings will aim to include 20 to 50 participants.
The last piece of the SHM Heart Failure Quality Improvement Initiative is in its final planning stages, and a third CME module for Team Communications as it relates to the heart failure patient will be developed in the coming months. This initiative is supported in part by Scios Inc. and led by Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.
Quality Initiatives
Over the past several years, SHM has developed initiatives that range from convening a panel to assess the state of the art of a QI intervention to developing a Web-based resource room. Projects EQID is involved with:
- SHM is in the early stages of a three-year effort to develop resources and programs for improving hospital care transitions for older adults. This is supported through a major grant from the John A. Hartford Foundation in New York City, under the leadership of Mark Williams, MD, and Eric Coleman, MD, MPH. Dr. Williams is chief of the new Division of Hospital Medicine at Northwestern Memorial Hospital in Chicago and editor of the Journal of Hospital Medicine. Dr. Coleman is associate professor of medicine within the divisions of healthcare policy and research and geriatric medicine at the University of Colorado Health Sciences Center in Aurora.
- “The Heart Failure Quality Improvement Implementation Guide” has been updated. The Heart Failure Resource Room on SHM’s Web site has been redesigned to make it easier for visitors who wish to follow the process of developing a QI intervention related to care of the hospitalized heart failure patient. We are communicating these changes to the hospital medicine community. Supported in part by Scios Inc., based in Mountain View, Calif., this effort includes presentations at regional meetings. This project was led by Nurcan Ilksoy, MD, assistant professor of Medicine at Emory University School of Medicine in Atlanta.
- The VTE Prevention Collaborative is open to all members implementing a QI program to combat venous thromboembolism in the hospitalized patient. The Sanofi-Aventis-supported collaborative uses seasoned QI leaders as mentors. Greg Maynard, MD, MS, and Jason Stein, MD, lead the enrollees through the QI process. The mentees have the benefit of regularly scheduled calls to ask questions and receive instant feedback on their process and progress. An add-on to this program, funded by the Kettering Foundation of Dayton, Ohio, provides the opportunity for on-site consultations. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of Medicine at Emory University School of Medicine, and director of Quality Improvement for the Emory Hospital Medicine Unit.
- An expert panel convened in July to kick off development of an Acute Coronary Syndrome Resource Room and determine the content the resource room will cover. Content address diagnosis and risk stratification, medication, interventional procedures, patient education, transitions, and care coordination. This initiative is being led by Chad Whelan, MD, and is supported in part by Bristol-Myers Squibb Company, New York City. Dr. Whelan is an academic hospitalist and an assistant professor of medicine at University of Chicago in the Section of General Internal Medicine.
- SHM often studies strategies to improve patient satisfaction, outcomes, length of stay, and other important metrics. An expert panel assesses observation units as they contribute to improved treatment of patients with acute decompensated heart failure, chest pain, and other clinical conditions such as asthma. A white paper is pending on the use and value of observation units. Support for the meeting and development and distribution of the white paper was provided by Scios Inc.
Committee Support
A major staff role is the support of the Education and Hospital Quality and Patient Safety (HQPS) committees, the groups that direct and drive SHM in these important areas. The Education Committee, led by Chairman Bill Rifkin, MD, assistant professor of medicine at Yale University School of Medicine in New Haven, Conn., is focusing on:
- Developing the teaching skills pre-course that will be presented at the 2008 Annual Meeting;
- Defining a workable strategy to promote The Core Competencies in Hospital Medicine;
- Developing educational and/or communication modalities that support maintenance of certification; and
- Further defining the direction of the committee to meet members’ educational needs.
Janet Nagamine, MD, leads the HQPS Committee in the following priorities:
- Planning and holding a quality summit to define goals and priorities for the next three to five years;
- Submitting a grant application to AHRQ to support a multidisciplinary conference in the area of medication reconciliation;
- Developing SHM’s role in care transitions;
- Reviewing quality pre-course information and determining the curriculum for ‘‘Hospital Medicine 2008”; and
- Developing the Quality track for ‘‘Hospital Medicine 2008.”
Psychiatric hospitalists diagnose, treat mental illness
Within hospital medicine lives a small subspecialty that addresses a specific and real need in today’s hospitals: psychiatric hospitalists. These physicians provide medical and psychiatric care to hospitalized patients, negating the need for a referral to a psychiatrist.
“There’s little or no compensation for a psychiatrist consultation on a medical patient, so they don’t want to do it,” says Robert P. Albanese, MD, associate professor of psychiatry and medicine at Medical University of South Carolina (MUSC) in Charleston. A psychiatric hospitalist can diagnose and treat medical conditions as well as often overlooked or untreated conditions, such as schizophrenia, major depression, and delirium, as well as substance abuse issues.
Many hospitalized patients with these problems are either on Medicare or uninsured; some are homeless. Because these patients seek emergency care for advanced diseases, general hospitalists are likely to treat their medical problems.
A small percentage of medical facilities across the U.S. have hired psychiatric hospitalists to screen patients, provide psychiatric consults, and take pressure off other hospital staff, including general hospitalists. This summer, St. Luke’s Episcopal Hospital in Houston added a psychiatric hospitalist to its team of five hospitalists and plans to hire a second.
While the job market for psychiatric hospitalists will never come close to the meteoric rise in general hospitalist positions, Dr. Albanese says: “I think we’re on the threshold of some growth. We’ll see more small, community-based hospitals starting psychiatric programs.”
Built-In Roadblocks
Psychiatric hospitalists are limited partly because hospitals don’t have the patient load to necessitate hiring them.
“Back in the ’50s, there were around 650,000 hospital beds for patients with mental illness,” says Dr. Albanese. “Today, it’s estimated that there are between 25,000 and 45,000, according to the National Alliance on Mental Illness [NAMI].”
That drastic reduction is in state psychiatric facilities. Across the U.S., state budget cuts have resulted in mass closings of public psychiatric hospitals over the past 40 years—and the so-called “deinstitutionalization” of patients—while remaining state facilities have suffered significant cuts in funding. According to NAMI, there were 50,000 mentally ill homeless people in California because of deinstitutionalization between 1957 and 1988.
“There’s not a lot out there on psychiatric hospitalists because there aren’t many beds—they’ve kicked out [the patients],” explains Dr. Albanese. “Time’s arrow points to no major increase in the number of beds any time soon. This is a big problem everywhere because there are still a lot of psychiatric patients out there.”
Another factor keeping the number of psychiatric hospitalists fairly static is that most psychiatric medical students aren’t interested in inpatient care, says Dr. Albanese.
Dual-Boarded Specialists
According to the Accreditation Council for Graduate Medical Education, 29 universities offer a combined residency program in internal medicine and psychiatry or family medicine and psychiatry. Dr. Albanese’s university, MUSC, is one of them.
“Our focus is on training young physicians who are interested in becoming dual-boarded to work in a psychiatric setting,” he says. “We’re looking at hospital psychiatry as a special area within our expertise.”
MUSC’s program is highly selective. “We have a five-year residency, and we take two medical students each year,” says Dr. Albanese. “I believe that Rush-Presbyterian in Chicago has the largest program. They take four students per year.”
Despite the lack of beds for mentally ill patients, Dr. Albanese hopes for more psychiatric hospitalists to address those patients’ needs.
“These patients have such a shortened life expectancy, I think there will be increased focus on meeting their needs,” he says. He points to an article in USA Today from May 3, “Mentally ill die 25 year earlier on average,” that documented the trend. TH
Jane Jerrard is a frequent contributor to The Hospitalist.
Within hospital medicine lives a small subspecialty that addresses a specific and real need in today’s hospitals: psychiatric hospitalists. These physicians provide medical and psychiatric care to hospitalized patients, negating the need for a referral to a psychiatrist.
“There’s little or no compensation for a psychiatrist consultation on a medical patient, so they don’t want to do it,” says Robert P. Albanese, MD, associate professor of psychiatry and medicine at Medical University of South Carolina (MUSC) in Charleston. A psychiatric hospitalist can diagnose and treat medical conditions as well as often overlooked or untreated conditions, such as schizophrenia, major depression, and delirium, as well as substance abuse issues.
Many hospitalized patients with these problems are either on Medicare or uninsured; some are homeless. Because these patients seek emergency care for advanced diseases, general hospitalists are likely to treat their medical problems.
A small percentage of medical facilities across the U.S. have hired psychiatric hospitalists to screen patients, provide psychiatric consults, and take pressure off other hospital staff, including general hospitalists. This summer, St. Luke’s Episcopal Hospital in Houston added a psychiatric hospitalist to its team of five hospitalists and plans to hire a second.
While the job market for psychiatric hospitalists will never come close to the meteoric rise in general hospitalist positions, Dr. Albanese says: “I think we’re on the threshold of some growth. We’ll see more small, community-based hospitals starting psychiatric programs.”
Built-In Roadblocks
Psychiatric hospitalists are limited partly because hospitals don’t have the patient load to necessitate hiring them.
“Back in the ’50s, there were around 650,000 hospital beds for patients with mental illness,” says Dr. Albanese. “Today, it’s estimated that there are between 25,000 and 45,000, according to the National Alliance on Mental Illness [NAMI].”
That drastic reduction is in state psychiatric facilities. Across the U.S., state budget cuts have resulted in mass closings of public psychiatric hospitals over the past 40 years—and the so-called “deinstitutionalization” of patients—while remaining state facilities have suffered significant cuts in funding. According to NAMI, there were 50,000 mentally ill homeless people in California because of deinstitutionalization between 1957 and 1988.
“There’s not a lot out there on psychiatric hospitalists because there aren’t many beds—they’ve kicked out [the patients],” explains Dr. Albanese. “Time’s arrow points to no major increase in the number of beds any time soon. This is a big problem everywhere because there are still a lot of psychiatric patients out there.”
Another factor keeping the number of psychiatric hospitalists fairly static is that most psychiatric medical students aren’t interested in inpatient care, says Dr. Albanese.
Dual-Boarded Specialists
According to the Accreditation Council for Graduate Medical Education, 29 universities offer a combined residency program in internal medicine and psychiatry or family medicine and psychiatry. Dr. Albanese’s university, MUSC, is one of them.
“Our focus is on training young physicians who are interested in becoming dual-boarded to work in a psychiatric setting,” he says. “We’re looking at hospital psychiatry as a special area within our expertise.”
MUSC’s program is highly selective. “We have a five-year residency, and we take two medical students each year,” says Dr. Albanese. “I believe that Rush-Presbyterian in Chicago has the largest program. They take four students per year.”
Despite the lack of beds for mentally ill patients, Dr. Albanese hopes for more psychiatric hospitalists to address those patients’ needs.
“These patients have such a shortened life expectancy, I think there will be increased focus on meeting their needs,” he says. He points to an article in USA Today from May 3, “Mentally ill die 25 year earlier on average,” that documented the trend. TH
Jane Jerrard is a frequent contributor to The Hospitalist.
Within hospital medicine lives a small subspecialty that addresses a specific and real need in today’s hospitals: psychiatric hospitalists. These physicians provide medical and psychiatric care to hospitalized patients, negating the need for a referral to a psychiatrist.
“There’s little or no compensation for a psychiatrist consultation on a medical patient, so they don’t want to do it,” says Robert P. Albanese, MD, associate professor of psychiatry and medicine at Medical University of South Carolina (MUSC) in Charleston. A psychiatric hospitalist can diagnose and treat medical conditions as well as often overlooked or untreated conditions, such as schizophrenia, major depression, and delirium, as well as substance abuse issues.
Many hospitalized patients with these problems are either on Medicare or uninsured; some are homeless. Because these patients seek emergency care for advanced diseases, general hospitalists are likely to treat their medical problems.
A small percentage of medical facilities across the U.S. have hired psychiatric hospitalists to screen patients, provide psychiatric consults, and take pressure off other hospital staff, including general hospitalists. This summer, St. Luke’s Episcopal Hospital in Houston added a psychiatric hospitalist to its team of five hospitalists and plans to hire a second.
While the job market for psychiatric hospitalists will never come close to the meteoric rise in general hospitalist positions, Dr. Albanese says: “I think we’re on the threshold of some growth. We’ll see more small, community-based hospitals starting psychiatric programs.”
Built-In Roadblocks
Psychiatric hospitalists are limited partly because hospitals don’t have the patient load to necessitate hiring them.
“Back in the ’50s, there were around 650,000 hospital beds for patients with mental illness,” says Dr. Albanese. “Today, it’s estimated that there are between 25,000 and 45,000, according to the National Alliance on Mental Illness [NAMI].”
That drastic reduction is in state psychiatric facilities. Across the U.S., state budget cuts have resulted in mass closings of public psychiatric hospitals over the past 40 years—and the so-called “deinstitutionalization” of patients—while remaining state facilities have suffered significant cuts in funding. According to NAMI, there were 50,000 mentally ill homeless people in California because of deinstitutionalization between 1957 and 1988.
“There’s not a lot out there on psychiatric hospitalists because there aren’t many beds—they’ve kicked out [the patients],” explains Dr. Albanese. “Time’s arrow points to no major increase in the number of beds any time soon. This is a big problem everywhere because there are still a lot of psychiatric patients out there.”
Another factor keeping the number of psychiatric hospitalists fairly static is that most psychiatric medical students aren’t interested in inpatient care, says Dr. Albanese.
Dual-Boarded Specialists
According to the Accreditation Council for Graduate Medical Education, 29 universities offer a combined residency program in internal medicine and psychiatry or family medicine and psychiatry. Dr. Albanese’s university, MUSC, is one of them.
“Our focus is on training young physicians who are interested in becoming dual-boarded to work in a psychiatric setting,” he says. “We’re looking at hospital psychiatry as a special area within our expertise.”
MUSC’s program is highly selective. “We have a five-year residency, and we take two medical students each year,” says Dr. Albanese. “I believe that Rush-Presbyterian in Chicago has the largest program. They take four students per year.”
Despite the lack of beds for mentally ill patients, Dr. Albanese hopes for more psychiatric hospitalists to address those patients’ needs.
“These patients have such a shortened life expectancy, I think there will be increased focus on meeting their needs,” he says. He points to an article in USA Today from May 3, “Mentally ill die 25 year earlier on average,” that documented the trend. TH
Jane Jerrard is a frequent contributor to The Hospitalist.
Flexibility Is Key
When Manjusha Gupte, MD, had her second child, she realized that parenting and working full-time as a hospitalist was going to be too much.
“My husband is a hospitalist as well, so since there’s two in the family, we needed to get our time a little better situated with the kids,” she says.
She and another hospitalist, also a mother, approached their program director at Gaston Memorial Hospital, a busy community hospital in Gastonia, N.C., about going part-time.
Since then, the two physicians have shared a full-time job. Dr. Gupte works three or four consecutive shifts a week, two weeks a month. She still sees a full complement of patients—about 20 at a time—and she gets to spend more time with her daughter, 4, and her son, almost 2.
“Most hospitalist programs are scared,” Dr. Gupte says. “They think there won’t be continuity of care for patients, or it’s going to be disruptive to other doctors who are full-time. I have not yet heard of anybody complaining about continuity of care.”
Even though hiring part-timers and job-sharers raises these and other concerns, it’s increasingly important to offer this kind of scheduling flexibility, industry experts say.
“Hospital medicine, more than many other specialty, tends to attract people who care a lot about lifestyle,” says Leslie Flores, MHA, Nelson/Flores Associates. “A practice that isn’t willing to be flexible and consider part-time is sort of shooting itself in the foot.”
Before deciding whether to hire part-time or job-sharing hospitalists, there are many factors to consider, such as how to handle benefits and malpractice insurance and how to make sure a part-timer with a private practice doesn’t draw patients away from the hospital’s crew of referring doctors—intentionally or not.
There are benefits to the hospital: It’s easier to provide vacation and gap coverage, it’s less likely the full-time hospitalists will burn out, and in some cases, a part-time specialist can provide services the hospital didn’t offer.
“We’re real advocates of part-time hospitalists,” Flores says. “I think the benefits really outweigh the risks.”
The Benefits
A part-time hospitalist can be anyone from a physician who cuts back to 75% of her hours so she can spend more time with her kids, to a resident or fellow who signs up for a few shifts a month. A job-sharer splits a full-time job with another physician, sometimes sharing office space and even a malpractice insurance policy.
Part-timers can free full-time hospitalists to participate on committees, conduct research, teach, attend a conference or seminar, take a sabbatical, or simply pursue outside interests, says Kenneth Simone, DO, who founded and served as director for 10 years of a hospitalist program in Maine. He is now president of Hospitalist and Practice Solutions, a consultancy, in Brewer, Maine.
“Also, they’re extremely helpful when the practice is in an expansion mode,” Dr. Simone says. “If they want to bring in two or three more referring providers’ practices, you can utilize the part-timers to help with the extra work so you don’t overwork your staff.”
Though it’s less common these days, a new hospitalist program may meet with resistance from local doctors. Offering those doctors part-time shifts can help ease the transition.
“They’re worried about what’s going to happen to their inpatient skills, what their patients may think, and their income,” says Steven Nahm, vice president of the Camden Group, a hospitalist consultancy and management company with offices in Chicago and El Segundo, Calif. As part-timers, these doctors keep current with inpatient care and can gauge the impact of the program on their practices.
A respected local physician who comes in part-time also lends credibility and gives medical staff a greater sense of confidence in the program, Nahm says. Dr. Simone calls these part-timers ambassadors.
One Example
The hospitalist program at Hudson Valley Hospital Center in Cortlandt Manor, N.Y., began in July 2005 at the request of local doctors. The program, Hospital Medicine Associates, contracts with the hospital and has its own billing system. It has eight full-time hospitalists, and as of about six months ago, four hospitalists sharing two full-time positions. They even share malpractice insurance because New York state law allows for half-policies. The part-timers work under pro-rated policies because they work fewer hours.
Allowing doctors to job-share seemed like common sense, says Richard Becker, MD, who leads the program.
“If you have good physicians, you want to keep them,” he says. “Having two doctors share shifts gives you flexibility. If one is sick or ill or on vacation, the other can come in and take care of it. You never have to worry about that position.”
While most programs have a few part-time physicians, it’s rare to see a program fully staffed by part-timers or job-sharers, Nahm says.
“Generally, they’re transition steps toward a program staffed by full-time hospitalists,” he says.
It can take more than a year to staff a program, especially for medical centers that aren’t in a city with a medical school. Now that more hospitals want to start hospitalist programs—and quickly—it helps to bring in part-timers to support an incomplete team, says Betty Abbott, chief operating officer of Eagle Hospital Physicians in Atlanta, Ga., a hospitalist consultancy that serves the southeast and Atlantic states.
“It used to be you had three to nine months to start a program, and now many people are saying, ‘We’d like to have it next Monday,’ ” Abbott says.
Some smaller or rural hospitals run part-time-only hospitalist programs because it’s the only option that makes economic sense, or because they have trouble recruiting full-time hospitalists. In these cases, part-timers can give a much-needed boost to admissions.
“The doctors typically in the community don’t want to work on weekends,” says Alan Himmelstein, FACMPE, president of Hospital Care Consultants Inc. (HCC) in San Antonio, Texas. “So if they see a patient in their office on a Thursday that has pneumonia, they will opt to either transfer to a bigger city, or treat the patient in an outpatient setting, which is not optimal. With the hospitalist there, the hospital can take that patient.”
Competition, Commitment
Two of the major concerns about part-time and job-sharing hospitalists are that they won’t be as committed to the program as other hospitalists, or that they’ll attract patients to their own private practice—away from referring physicians.
“This is a big factor,” Nahm says. “You should have a policy that a part-timer who has an outpatient practice cannot accept hospitalist patients into their practice for a period of at least one year. That’s the biggest concern for using part-timers, because they are a potentially competitive threat.” Even the suspicion that it might happen can be enough to persuade local physicians to refer their patients elsewhere. To ward off concerns, the hospital can implement a policy to instruct patients upon discharge to make an appointment with their primary physician. Some hospitals go so far as to book the appointments on behalf of patients.
“It gets tricky sometimes because patients may really like their hospitalist,” Flores acknowledges. Some programs bring in only part-time hospitalists who don’t have a private practice, or hire specialists who want to keep up their general medicine skills but aren’t a threat to primary care physicians. But what about levels of commitment?
“Part-timers, just by the nature of being part-time, aren’t as emotionally connected to the practice,” Flores says. “You don’t get the same level of buy-in, or maybe the same kinds of camaraderie.”
Dr. Gupte, the job-sharing physician at Gaston Memorial, says she and her partner may be even more focused and intense than full-time hospitalists because they know they have just three or four days to care for their patients.
“We just kind of go in and say, ‘Now I need to know this [and] this; this needs to be done,’” Dr. Gupte says. “I need to get them discharged in two or three days, what’s the plan? The weekend’s coming.”
To encourage commitment to the program, Nahm suggests including dedicated part-timers—those who work a significant number of shifts per month—in your productivity and quality compensation plan. Part-timers should also have the same orientation and training as full-timers, and be required to attend all hospitalist group meetings, Nahm says.
“One of the benefits of the hospitalist is that they know the ins and outs, the ups and downs of the hospital,” Dr. Simone says. “If I’m not going to the medical staff meetings and to my committee meetings, I’m not going to have adequate information—and that may make me less effective as a hospitalist.”
Continuity of Care
Job-sharing works well for Hudson Valley Hospital Center, but allowing physicians to come in for just a few shifts a month doesn’t sound as appealing, Dr. Becker says.
If a hospital uses part-timers only sporadically, “that opens the chances for errors and for patient dissatisfaction,” he says.
To counter this, a hospital might hire only part-timers who can work consecutive shifts. Or it might use doctors who are available sporadically to support the program other ways.
“Dr. A is willing to provide 12 shifts per month but only wants to work two or three days a week,” Dr. Simone says. “You probably want to utilize him or her as an admitting doctor or a float, not a rounder, since patient continuity may be negatively affected.
“Dr. B is willing to provide 12 shifts per month and doesn’t mind working several days in a row; for example, six or 10 or 12 consecutive days. That schedule offers wonderful continuity, and this provider can be utilized as a rounder, following patients from admission through discharge.”
Even physicians who fill in only when volume is high—perhaps in four- or six-hour shifts in the evenings or on weekends—can benefit some hospitals, Abbott says; that support might make it easier to recruit full-timers.
Johns Hopkins Medicine in Baltimore supplements its nine full-time hospitalists with part-timers.
“The nature of our job is such that it’s fairly easy to coordinate that,” says Daniel J. Brotman, MD, FACP, director of the hospitalist program there. “It creates sort of auxiliary staffing.”
The hospitalist program at Johns Hopkins started in 2002. Part-timers tend to work nights and weekends and get a lot of flexibility; they sign up for shifts instead of working a guaranteed schedule. Continuity of care is rarely an issue because full-time staff provides that, Dr. Brotman says.
“We divide labor into somebody who’s doing admissions and someone who’s taking care of the patients day to day,” he says. “The person who’s doing admissions can be anybody who’s competent to do so and doesn’t need to be someone who’s available the next day to take care of the patients.”
So far, hand-offs have been smooth, Dr. Brotman says, partly because the transfer of information about Hopkins’ complex tertiary-care patients is thorough by necessity. While good communication is important for all hospitalists, it’s especially important for part-timers and job-sharers, Dr. Simone says. In addition to requiring thorough notes and communication, he suggests finding out ahead of time whether a part-timer will be available to answer questions during off hours.
“Are they flexible so they can come in a heartbeat if you need them?” Dr. Simone says. By the same token, referring physicians have to commit to doing a verbal hand-off to the hospitalists, and hospitalists have to commit to sending a report when the patients are handed back, Abbott says.
When HCC tried establishing a hospitalist program that covered only weekend shifts, Himmelstein says, tight turnarounds on Monday mornings and spotty cell phone service in rural areas made it too hard to coordinate hand-offs.
Other Issues
There are other factors to consider before bringing in full-time hospitalists or job-shares, such as billing.
“They’re working as a hospitalist for a week, and one of their private patients comes in to be admitted,” Nahm says. “Are they seeing that patient as a hospitalist or are they seeing that patient outside of the program, as their own patient?”
The same issue can come up with a pulmonary or infectious disease specialist, for example. If she consults on other patients during her shift, is she doing so as a hospitalist or in her private practice?
“I find it best if you just take the philosophy that you’re buying this physician’s time, and anything this physician does on the clock for you is considered a service of the hospitalist group—and all billing and collection and revenue, in other words, go back to the hospitalist group,” Nahm says.
Also, a part-time hospitalist may face competing demands for his or her time.
“Sometimes they come in and they’re lacking focus because they’re tired—they’ve been up all night moonlighting in the ED,” Dr. Simone says. “Or they pace themselves because they know tomorrow and for the next four days, they’re on call for their private practice.”
Despite the practical issues part-timers bring, Dr. Simone points out, they tend to increase a program’s flexibility and efficiency, allow the hospital to offer more value, lower burnout, and increase job satisfaction.
Dr. Gupte wants more programs to start hiring part-time hospitalists—especially to help families like hers, where both parents are busy physicians.
“I think that makes a big difference in family care,” she says. “People sometimes think that we won’t be as intense or as focused when you’re doing the part-time thing. I don’t think that’s true.” TH
Liz Tascio is a freelance journalist based in New York City.
When Manjusha Gupte, MD, had her second child, she realized that parenting and working full-time as a hospitalist was going to be too much.
“My husband is a hospitalist as well, so since there’s two in the family, we needed to get our time a little better situated with the kids,” she says.
She and another hospitalist, also a mother, approached their program director at Gaston Memorial Hospital, a busy community hospital in Gastonia, N.C., about going part-time.
Since then, the two physicians have shared a full-time job. Dr. Gupte works three or four consecutive shifts a week, two weeks a month. She still sees a full complement of patients—about 20 at a time—and she gets to spend more time with her daughter, 4, and her son, almost 2.
“Most hospitalist programs are scared,” Dr. Gupte says. “They think there won’t be continuity of care for patients, or it’s going to be disruptive to other doctors who are full-time. I have not yet heard of anybody complaining about continuity of care.”
Even though hiring part-timers and job-sharers raises these and other concerns, it’s increasingly important to offer this kind of scheduling flexibility, industry experts say.
“Hospital medicine, more than many other specialty, tends to attract people who care a lot about lifestyle,” says Leslie Flores, MHA, Nelson/Flores Associates. “A practice that isn’t willing to be flexible and consider part-time is sort of shooting itself in the foot.”
Before deciding whether to hire part-time or job-sharing hospitalists, there are many factors to consider, such as how to handle benefits and malpractice insurance and how to make sure a part-timer with a private practice doesn’t draw patients away from the hospital’s crew of referring doctors—intentionally or not.
There are benefits to the hospital: It’s easier to provide vacation and gap coverage, it’s less likely the full-time hospitalists will burn out, and in some cases, a part-time specialist can provide services the hospital didn’t offer.
“We’re real advocates of part-time hospitalists,” Flores says. “I think the benefits really outweigh the risks.”
The Benefits
A part-time hospitalist can be anyone from a physician who cuts back to 75% of her hours so she can spend more time with her kids, to a resident or fellow who signs up for a few shifts a month. A job-sharer splits a full-time job with another physician, sometimes sharing office space and even a malpractice insurance policy.
Part-timers can free full-time hospitalists to participate on committees, conduct research, teach, attend a conference or seminar, take a sabbatical, or simply pursue outside interests, says Kenneth Simone, DO, who founded and served as director for 10 years of a hospitalist program in Maine. He is now president of Hospitalist and Practice Solutions, a consultancy, in Brewer, Maine.
“Also, they’re extremely helpful when the practice is in an expansion mode,” Dr. Simone says. “If they want to bring in two or three more referring providers’ practices, you can utilize the part-timers to help with the extra work so you don’t overwork your staff.”
Though it’s less common these days, a new hospitalist program may meet with resistance from local doctors. Offering those doctors part-time shifts can help ease the transition.
“They’re worried about what’s going to happen to their inpatient skills, what their patients may think, and their income,” says Steven Nahm, vice president of the Camden Group, a hospitalist consultancy and management company with offices in Chicago and El Segundo, Calif. As part-timers, these doctors keep current with inpatient care and can gauge the impact of the program on their practices.
A respected local physician who comes in part-time also lends credibility and gives medical staff a greater sense of confidence in the program, Nahm says. Dr. Simone calls these part-timers ambassadors.
One Example
The hospitalist program at Hudson Valley Hospital Center in Cortlandt Manor, N.Y., began in July 2005 at the request of local doctors. The program, Hospital Medicine Associates, contracts with the hospital and has its own billing system. It has eight full-time hospitalists, and as of about six months ago, four hospitalists sharing two full-time positions. They even share malpractice insurance because New York state law allows for half-policies. The part-timers work under pro-rated policies because they work fewer hours.
Allowing doctors to job-share seemed like common sense, says Richard Becker, MD, who leads the program.
“If you have good physicians, you want to keep them,” he says. “Having two doctors share shifts gives you flexibility. If one is sick or ill or on vacation, the other can come in and take care of it. You never have to worry about that position.”
While most programs have a few part-time physicians, it’s rare to see a program fully staffed by part-timers or job-sharers, Nahm says.
“Generally, they’re transition steps toward a program staffed by full-time hospitalists,” he says.
It can take more than a year to staff a program, especially for medical centers that aren’t in a city with a medical school. Now that more hospitals want to start hospitalist programs—and quickly—it helps to bring in part-timers to support an incomplete team, says Betty Abbott, chief operating officer of Eagle Hospital Physicians in Atlanta, Ga., a hospitalist consultancy that serves the southeast and Atlantic states.
“It used to be you had three to nine months to start a program, and now many people are saying, ‘We’d like to have it next Monday,’ ” Abbott says.
Some smaller or rural hospitals run part-time-only hospitalist programs because it’s the only option that makes economic sense, or because they have trouble recruiting full-time hospitalists. In these cases, part-timers can give a much-needed boost to admissions.
“The doctors typically in the community don’t want to work on weekends,” says Alan Himmelstein, FACMPE, president of Hospital Care Consultants Inc. (HCC) in San Antonio, Texas. “So if they see a patient in their office on a Thursday that has pneumonia, they will opt to either transfer to a bigger city, or treat the patient in an outpatient setting, which is not optimal. With the hospitalist there, the hospital can take that patient.”
Competition, Commitment
Two of the major concerns about part-time and job-sharing hospitalists are that they won’t be as committed to the program as other hospitalists, or that they’ll attract patients to their own private practice—away from referring physicians.
“This is a big factor,” Nahm says. “You should have a policy that a part-timer who has an outpatient practice cannot accept hospitalist patients into their practice for a period of at least one year. That’s the biggest concern for using part-timers, because they are a potentially competitive threat.” Even the suspicion that it might happen can be enough to persuade local physicians to refer their patients elsewhere. To ward off concerns, the hospital can implement a policy to instruct patients upon discharge to make an appointment with their primary physician. Some hospitals go so far as to book the appointments on behalf of patients.
“It gets tricky sometimes because patients may really like their hospitalist,” Flores acknowledges. Some programs bring in only part-time hospitalists who don’t have a private practice, or hire specialists who want to keep up their general medicine skills but aren’t a threat to primary care physicians. But what about levels of commitment?
“Part-timers, just by the nature of being part-time, aren’t as emotionally connected to the practice,” Flores says. “You don’t get the same level of buy-in, or maybe the same kinds of camaraderie.”
Dr. Gupte, the job-sharing physician at Gaston Memorial, says she and her partner may be even more focused and intense than full-time hospitalists because they know they have just three or four days to care for their patients.
“We just kind of go in and say, ‘Now I need to know this [and] this; this needs to be done,’” Dr. Gupte says. “I need to get them discharged in two or three days, what’s the plan? The weekend’s coming.”
To encourage commitment to the program, Nahm suggests including dedicated part-timers—those who work a significant number of shifts per month—in your productivity and quality compensation plan. Part-timers should also have the same orientation and training as full-timers, and be required to attend all hospitalist group meetings, Nahm says.
“One of the benefits of the hospitalist is that they know the ins and outs, the ups and downs of the hospital,” Dr. Simone says. “If I’m not going to the medical staff meetings and to my committee meetings, I’m not going to have adequate information—and that may make me less effective as a hospitalist.”
Continuity of Care
Job-sharing works well for Hudson Valley Hospital Center, but allowing physicians to come in for just a few shifts a month doesn’t sound as appealing, Dr. Becker says.
If a hospital uses part-timers only sporadically, “that opens the chances for errors and for patient dissatisfaction,” he says.
To counter this, a hospital might hire only part-timers who can work consecutive shifts. Or it might use doctors who are available sporadically to support the program other ways.
“Dr. A is willing to provide 12 shifts per month but only wants to work two or three days a week,” Dr. Simone says. “You probably want to utilize him or her as an admitting doctor or a float, not a rounder, since patient continuity may be negatively affected.
“Dr. B is willing to provide 12 shifts per month and doesn’t mind working several days in a row; for example, six or 10 or 12 consecutive days. That schedule offers wonderful continuity, and this provider can be utilized as a rounder, following patients from admission through discharge.”
Even physicians who fill in only when volume is high—perhaps in four- or six-hour shifts in the evenings or on weekends—can benefit some hospitals, Abbott says; that support might make it easier to recruit full-timers.
Johns Hopkins Medicine in Baltimore supplements its nine full-time hospitalists with part-timers.
“The nature of our job is such that it’s fairly easy to coordinate that,” says Daniel J. Brotman, MD, FACP, director of the hospitalist program there. “It creates sort of auxiliary staffing.”
The hospitalist program at Johns Hopkins started in 2002. Part-timers tend to work nights and weekends and get a lot of flexibility; they sign up for shifts instead of working a guaranteed schedule. Continuity of care is rarely an issue because full-time staff provides that, Dr. Brotman says.
“We divide labor into somebody who’s doing admissions and someone who’s taking care of the patients day to day,” he says. “The person who’s doing admissions can be anybody who’s competent to do so and doesn’t need to be someone who’s available the next day to take care of the patients.”
So far, hand-offs have been smooth, Dr. Brotman says, partly because the transfer of information about Hopkins’ complex tertiary-care patients is thorough by necessity. While good communication is important for all hospitalists, it’s especially important for part-timers and job-sharers, Dr. Simone says. In addition to requiring thorough notes and communication, he suggests finding out ahead of time whether a part-timer will be available to answer questions during off hours.
“Are they flexible so they can come in a heartbeat if you need them?” Dr. Simone says. By the same token, referring physicians have to commit to doing a verbal hand-off to the hospitalists, and hospitalists have to commit to sending a report when the patients are handed back, Abbott says.
When HCC tried establishing a hospitalist program that covered only weekend shifts, Himmelstein says, tight turnarounds on Monday mornings and spotty cell phone service in rural areas made it too hard to coordinate hand-offs.
Other Issues
There are other factors to consider before bringing in full-time hospitalists or job-shares, such as billing.
“They’re working as a hospitalist for a week, and one of their private patients comes in to be admitted,” Nahm says. “Are they seeing that patient as a hospitalist or are they seeing that patient outside of the program, as their own patient?”
The same issue can come up with a pulmonary or infectious disease specialist, for example. If she consults on other patients during her shift, is she doing so as a hospitalist or in her private practice?
“I find it best if you just take the philosophy that you’re buying this physician’s time, and anything this physician does on the clock for you is considered a service of the hospitalist group—and all billing and collection and revenue, in other words, go back to the hospitalist group,” Nahm says.
Also, a part-time hospitalist may face competing demands for his or her time.
“Sometimes they come in and they’re lacking focus because they’re tired—they’ve been up all night moonlighting in the ED,” Dr. Simone says. “Or they pace themselves because they know tomorrow and for the next four days, they’re on call for their private practice.”
Despite the practical issues part-timers bring, Dr. Simone points out, they tend to increase a program’s flexibility and efficiency, allow the hospital to offer more value, lower burnout, and increase job satisfaction.
Dr. Gupte wants more programs to start hiring part-time hospitalists—especially to help families like hers, where both parents are busy physicians.
“I think that makes a big difference in family care,” she says. “People sometimes think that we won’t be as intense or as focused when you’re doing the part-time thing. I don’t think that’s true.” TH
Liz Tascio is a freelance journalist based in New York City.
When Manjusha Gupte, MD, had her second child, she realized that parenting and working full-time as a hospitalist was going to be too much.
“My husband is a hospitalist as well, so since there’s two in the family, we needed to get our time a little better situated with the kids,” she says.
She and another hospitalist, also a mother, approached their program director at Gaston Memorial Hospital, a busy community hospital in Gastonia, N.C., about going part-time.
Since then, the two physicians have shared a full-time job. Dr. Gupte works three or four consecutive shifts a week, two weeks a month. She still sees a full complement of patients—about 20 at a time—and she gets to spend more time with her daughter, 4, and her son, almost 2.
“Most hospitalist programs are scared,” Dr. Gupte says. “They think there won’t be continuity of care for patients, or it’s going to be disruptive to other doctors who are full-time. I have not yet heard of anybody complaining about continuity of care.”
Even though hiring part-timers and job-sharers raises these and other concerns, it’s increasingly important to offer this kind of scheduling flexibility, industry experts say.
“Hospital medicine, more than many other specialty, tends to attract people who care a lot about lifestyle,” says Leslie Flores, MHA, Nelson/Flores Associates. “A practice that isn’t willing to be flexible and consider part-time is sort of shooting itself in the foot.”
Before deciding whether to hire part-time or job-sharing hospitalists, there are many factors to consider, such as how to handle benefits and malpractice insurance and how to make sure a part-timer with a private practice doesn’t draw patients away from the hospital’s crew of referring doctors—intentionally or not.
There are benefits to the hospital: It’s easier to provide vacation and gap coverage, it’s less likely the full-time hospitalists will burn out, and in some cases, a part-time specialist can provide services the hospital didn’t offer.
“We’re real advocates of part-time hospitalists,” Flores says. “I think the benefits really outweigh the risks.”
The Benefits
A part-time hospitalist can be anyone from a physician who cuts back to 75% of her hours so she can spend more time with her kids, to a resident or fellow who signs up for a few shifts a month. A job-sharer splits a full-time job with another physician, sometimes sharing office space and even a malpractice insurance policy.
Part-timers can free full-time hospitalists to participate on committees, conduct research, teach, attend a conference or seminar, take a sabbatical, or simply pursue outside interests, says Kenneth Simone, DO, who founded and served as director for 10 years of a hospitalist program in Maine. He is now president of Hospitalist and Practice Solutions, a consultancy, in Brewer, Maine.
“Also, they’re extremely helpful when the practice is in an expansion mode,” Dr. Simone says. “If they want to bring in two or three more referring providers’ practices, you can utilize the part-timers to help with the extra work so you don’t overwork your staff.”
Though it’s less common these days, a new hospitalist program may meet with resistance from local doctors. Offering those doctors part-time shifts can help ease the transition.
“They’re worried about what’s going to happen to their inpatient skills, what their patients may think, and their income,” says Steven Nahm, vice president of the Camden Group, a hospitalist consultancy and management company with offices in Chicago and El Segundo, Calif. As part-timers, these doctors keep current with inpatient care and can gauge the impact of the program on their practices.
A respected local physician who comes in part-time also lends credibility and gives medical staff a greater sense of confidence in the program, Nahm says. Dr. Simone calls these part-timers ambassadors.
One Example
The hospitalist program at Hudson Valley Hospital Center in Cortlandt Manor, N.Y., began in July 2005 at the request of local doctors. The program, Hospital Medicine Associates, contracts with the hospital and has its own billing system. It has eight full-time hospitalists, and as of about six months ago, four hospitalists sharing two full-time positions. They even share malpractice insurance because New York state law allows for half-policies. The part-timers work under pro-rated policies because they work fewer hours.
Allowing doctors to job-share seemed like common sense, says Richard Becker, MD, who leads the program.
“If you have good physicians, you want to keep them,” he says. “Having two doctors share shifts gives you flexibility. If one is sick or ill or on vacation, the other can come in and take care of it. You never have to worry about that position.”
While most programs have a few part-time physicians, it’s rare to see a program fully staffed by part-timers or job-sharers, Nahm says.
“Generally, they’re transition steps toward a program staffed by full-time hospitalists,” he says.
It can take more than a year to staff a program, especially for medical centers that aren’t in a city with a medical school. Now that more hospitals want to start hospitalist programs—and quickly—it helps to bring in part-timers to support an incomplete team, says Betty Abbott, chief operating officer of Eagle Hospital Physicians in Atlanta, Ga., a hospitalist consultancy that serves the southeast and Atlantic states.
“It used to be you had three to nine months to start a program, and now many people are saying, ‘We’d like to have it next Monday,’ ” Abbott says.
Some smaller or rural hospitals run part-time-only hospitalist programs because it’s the only option that makes economic sense, or because they have trouble recruiting full-time hospitalists. In these cases, part-timers can give a much-needed boost to admissions.
“The doctors typically in the community don’t want to work on weekends,” says Alan Himmelstein, FACMPE, president of Hospital Care Consultants Inc. (HCC) in San Antonio, Texas. “So if they see a patient in their office on a Thursday that has pneumonia, they will opt to either transfer to a bigger city, or treat the patient in an outpatient setting, which is not optimal. With the hospitalist there, the hospital can take that patient.”
Competition, Commitment
Two of the major concerns about part-time and job-sharing hospitalists are that they won’t be as committed to the program as other hospitalists, or that they’ll attract patients to their own private practice—away from referring physicians.
“This is a big factor,” Nahm says. “You should have a policy that a part-timer who has an outpatient practice cannot accept hospitalist patients into their practice for a period of at least one year. That’s the biggest concern for using part-timers, because they are a potentially competitive threat.” Even the suspicion that it might happen can be enough to persuade local physicians to refer their patients elsewhere. To ward off concerns, the hospital can implement a policy to instruct patients upon discharge to make an appointment with their primary physician. Some hospitals go so far as to book the appointments on behalf of patients.
“It gets tricky sometimes because patients may really like their hospitalist,” Flores acknowledges. Some programs bring in only part-time hospitalists who don’t have a private practice, or hire specialists who want to keep up their general medicine skills but aren’t a threat to primary care physicians. But what about levels of commitment?
“Part-timers, just by the nature of being part-time, aren’t as emotionally connected to the practice,” Flores says. “You don’t get the same level of buy-in, or maybe the same kinds of camaraderie.”
Dr. Gupte, the job-sharing physician at Gaston Memorial, says she and her partner may be even more focused and intense than full-time hospitalists because they know they have just three or four days to care for their patients.
“We just kind of go in and say, ‘Now I need to know this [and] this; this needs to be done,’” Dr. Gupte says. “I need to get them discharged in two or three days, what’s the plan? The weekend’s coming.”
To encourage commitment to the program, Nahm suggests including dedicated part-timers—those who work a significant number of shifts per month—in your productivity and quality compensation plan. Part-timers should also have the same orientation and training as full-timers, and be required to attend all hospitalist group meetings, Nahm says.
“One of the benefits of the hospitalist is that they know the ins and outs, the ups and downs of the hospital,” Dr. Simone says. “If I’m not going to the medical staff meetings and to my committee meetings, I’m not going to have adequate information—and that may make me less effective as a hospitalist.”
Continuity of Care
Job-sharing works well for Hudson Valley Hospital Center, but allowing physicians to come in for just a few shifts a month doesn’t sound as appealing, Dr. Becker says.
If a hospital uses part-timers only sporadically, “that opens the chances for errors and for patient dissatisfaction,” he says.
To counter this, a hospital might hire only part-timers who can work consecutive shifts. Or it might use doctors who are available sporadically to support the program other ways.
“Dr. A is willing to provide 12 shifts per month but only wants to work two or three days a week,” Dr. Simone says. “You probably want to utilize him or her as an admitting doctor or a float, not a rounder, since patient continuity may be negatively affected.
“Dr. B is willing to provide 12 shifts per month and doesn’t mind working several days in a row; for example, six or 10 or 12 consecutive days. That schedule offers wonderful continuity, and this provider can be utilized as a rounder, following patients from admission through discharge.”
Even physicians who fill in only when volume is high—perhaps in four- or six-hour shifts in the evenings or on weekends—can benefit some hospitals, Abbott says; that support might make it easier to recruit full-timers.
Johns Hopkins Medicine in Baltimore supplements its nine full-time hospitalists with part-timers.
“The nature of our job is such that it’s fairly easy to coordinate that,” says Daniel J. Brotman, MD, FACP, director of the hospitalist program there. “It creates sort of auxiliary staffing.”
The hospitalist program at Johns Hopkins started in 2002. Part-timers tend to work nights and weekends and get a lot of flexibility; they sign up for shifts instead of working a guaranteed schedule. Continuity of care is rarely an issue because full-time staff provides that, Dr. Brotman says.
“We divide labor into somebody who’s doing admissions and someone who’s taking care of the patients day to day,” he says. “The person who’s doing admissions can be anybody who’s competent to do so and doesn’t need to be someone who’s available the next day to take care of the patients.”
So far, hand-offs have been smooth, Dr. Brotman says, partly because the transfer of information about Hopkins’ complex tertiary-care patients is thorough by necessity. While good communication is important for all hospitalists, it’s especially important for part-timers and job-sharers, Dr. Simone says. In addition to requiring thorough notes and communication, he suggests finding out ahead of time whether a part-timer will be available to answer questions during off hours.
“Are they flexible so they can come in a heartbeat if you need them?” Dr. Simone says. By the same token, referring physicians have to commit to doing a verbal hand-off to the hospitalists, and hospitalists have to commit to sending a report when the patients are handed back, Abbott says.
When HCC tried establishing a hospitalist program that covered only weekend shifts, Himmelstein says, tight turnarounds on Monday mornings and spotty cell phone service in rural areas made it too hard to coordinate hand-offs.
Other Issues
There are other factors to consider before bringing in full-time hospitalists or job-shares, such as billing.
“They’re working as a hospitalist for a week, and one of their private patients comes in to be admitted,” Nahm says. “Are they seeing that patient as a hospitalist or are they seeing that patient outside of the program, as their own patient?”
The same issue can come up with a pulmonary or infectious disease specialist, for example. If she consults on other patients during her shift, is she doing so as a hospitalist or in her private practice?
“I find it best if you just take the philosophy that you’re buying this physician’s time, and anything this physician does on the clock for you is considered a service of the hospitalist group—and all billing and collection and revenue, in other words, go back to the hospitalist group,” Nahm says.
Also, a part-time hospitalist may face competing demands for his or her time.
“Sometimes they come in and they’re lacking focus because they’re tired—they’ve been up all night moonlighting in the ED,” Dr. Simone says. “Or they pace themselves because they know tomorrow and for the next four days, they’re on call for their private practice.”
Despite the practical issues part-timers bring, Dr. Simone points out, they tend to increase a program’s flexibility and efficiency, allow the hospital to offer more value, lower burnout, and increase job satisfaction.
Dr. Gupte wants more programs to start hiring part-time hospitalists—especially to help families like hers, where both parents are busy physicians.
“I think that makes a big difference in family care,” she says. “People sometimes think that we won’t be as intense or as focused when you’re doing the part-time thing. I don’t think that’s true.” TH
Liz Tascio is a freelance journalist based in New York City.