User login
Hospitalist Business Drivers
As physicians, including hospitalists, focus on the now—getting the patient in front of them better—they may lose sight of the trends shaping their professional lives. Those trends, called “business drivers” occupy CEOs, CFOs, and other top managers who build strategies by understanding what drivers make organizations successful.
It’s not an easy job. Even the Delphic Oracle might have trouble divining which of the myriad competing drivers will make a hospital better and more profitable than its rivals. Take your pick: Sluggish inpatient volumes, shifts to outpatient procedures, high construction costs, expensive new technologies, an aging population, and consumer-driven care are among the business drivers currently on managers’ minds. (See “Trend Spotters,” p. 48.)
Michael Guthrie, MD, MBA, an executive-in-residence at the University of Colorado, School of Business (Boulder), Health Administration and a presenter at SHM’s September 2005 Leadership Conference in Vail, Colo., sees our aging population as a key business driver shaping hospital and physician livelihoods.
“The aging population and the shift to consumerism in healthcare are definitely on the hospital CEO’s mind,” he says. “Hospitalists need to understand how patient satisfaction drives market share and is highly correlated with the hospital’s business objectives.” By extension, hospitalists’ key metrics, such as compliance with Medicare core measures, reducing length of stay (LOS), and costs per case, mesh well with administration’s.
Keeping the CEO’s need to enhance the organization’s reputation and growth in mind, Dr. Guthrie suggests that hospitalists have their hands full. By focusing on measuring quality, providing the 24/7 coverage that patients want and the hospital needs and finding ways to decrease LOS and costs per case, their interests and those of the hospital’s align.
“Based on their conversations and observations of the hospital’s senior managers, hospitalists can figure out what business drivers are preoccupying them,” adds Dr. Guthrie.
Smart hospitalists can significantly boost their hospital’s bottom line according to Tom Hochhausler, Deloitte & Touche USA LLP’s partner of Life Sciences and Health Care Practice and director of the firm’s biennial survey on trends concerning hospital CEOs. Hochhausler says that with hospitals operating on razor-thin margins, hospitalists can increase their value to hospital CEOs and CFOs by improving communication among clinical staff, better adherence to guidelines, and shortening LOS. “They also have some of the best insights into improving quality in hospitals and are powerful teachers of interns and residents,” he adds. (See “What Worries Hospital CEOs,” at left.)
The difficult part for hospitalists is keeping focused on the hospital’s big picture while doing their jobs. For example, Michael Freed, CFO of Grand Rapids, Mich.-based Spectrum Health, ponders the financial aspects of a huge integrated delivery system with seven hospitals, 12,000 employees, a medical staff of 1,400 and a $2.1 billion budget. Rather than day-to-day concerns he focuses on the future—not one year, but five to 10 years ahead.
“Since the hospitalist team’s job is to cover the hospital 24/7, they don’t always connect the dots of what’s happening throughout the system,” says Ford. That’s why top managers must focus on the future. “If management has the right road map and vision for the future, a lot of good things happen for hospitalists: Patients get better care, which leads to better outcomes, [and] we lower costs and pass the savings along to payers. That, in turn, drives higher market share and increases the hospital’s value proposition.”
Hospital medicine groups rather than individual physicians may be best suited to track the hospital’s business drivers, and align incentives accordingly. Davin Juckett, CPA, MBA, of the Charlotte, N.C., Piedmont Healthcare Management Group, a physician-owned consultancy to more than 100 hospitalists in the southeast, advises hospitalists to use their billing and encounter data to improve their decision-making.
“Hospitalists tend to be very focused on their LOS and quality indicators but there’s a lot more out there,” says Juckett. “Business drivers such as consumer-directed care and P4P [pay for performance] make quantifiable data extremely important. Some MCOs have started star ratings of hospitalist and ER groups, and some doctors are up in arms because they feel it’s subjective. But that’s the future.”
Juckett sees another key business driver for 2006 and 2007: an increasingly competitive business environment for hospitalists. “Hospital medicine groups will have to defend their contracts,” he says. “True, the newness of the specialty makes recruitment an issue, but supply will eventually catch up with demand, and P4P will happen.”
Hospitalists might examine how another major business driver—aggressive competition for payer dollars—can put them at odds with office-based colleagues. By competing with hospitals for lucrative procedures in orthopedics, gynecology, cardiology, and other specialties, community physicians can lure market share away. Hospitalists are well positioned to mediate the conflict, although a report by VHA of Irving, Texas, says hospitalists often don’t keep community doctors informed of issues facing their hospitals. That report adds that hospitalists do a poor job of bringing hospital administrators and physicians together to forge common solutions.
Bricks and Mortar
Balancing soaring construction costs with the need to give picky consumers and physicians the latest technology in gleaming new buildings is another trend. Big-ticket items keep Joann Marqusee, MPP, senior vice-president of operations and facilities at Boston-based Beth Israel Deaconess Medical Center occupied. Her job—prioritizing capital projects, keeping facilities up to date, and tailoring spending to reduce future maintenance needs—got even more challenging with Hurricane Katrina. “Things are always difficult, but now the price of oil and steel are rising,” says Marqusee. “And we can’t find dehumidifiers to help with our little floods; they’re all in New Orleans.”
She has capital-spending decisions down to a disciplined process: Match projects with the strategic plan (e.g., neurosurgery ahead of ob/gyn), assess impact on patient volume and return on investment, and improve patient safety and quality. Explaining those decisions to physicians who get feisty when a favored project is delayed or cancelled is the tough part.
To gain doctors’ support for management’s spending priorities, Marqusee has a PowerPoint presentation for them: “Space: The Final Frontier.” She raves about hospitalists’ response: ”The hospitalists’ input has been fantastic because of their analytic training. For example, they understand ED throughput, and we use their expertise to improve design. And when we tell them that the new ICU can’t open as soon as they’d like because it’s being built above the bone marrow transplant center, and we need a new HVAC system installed first, they get it. They care about patients and when we introduce bottom line issues as well, we strengthen our working relationship.”
Where the (Aging) Consumer Is King
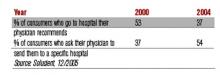
Consumerism is another business driver that hospitals can’t ignore. Individuals are increasingly willing to push their physicians to send them to the hospitals the consumers prefer, according to Solucient, a healthcare market intelligence firm in Evanston, Ill. In a survey of nearly 20,000 households Solucient identified a group of “responsive consumers,” (i.e., those proactive about managing their healthcare). Slightly older than the average consumer surveyed, the respondents have between 20% and 80% higher incidence of chronic diseases, and increasingly choose where they’re hospitalized rather than accept their physician’s recommendation:
Solucient’s data also show that responsive consumers heavily research and utilize hospital and physician ratings.
Homegrown Effort
While consultants are oracles of healthcare trends, some physician administrators rely on themselves instead. Akram Boutrous, MD, executive vice-president and CMO of South Nassau Community Hospital (Oceanside, N.Y.), turned the hospital around with an eight-year business improvement program based on understanding business trends. Some achievements: a 73% increase in patient revenues, 57% jump in outpatient services, and 27% increase in inpatient discharges.
Dr. Boutros considered using consultants, but disliked their high fees and lack of ongoing involvement. Instead he read stacks of books and articles on business drivers and strategies before selecting General Electric’s Accelerated Action Approach to Success. The method uses teams to solve problems that make organizations non-competitive.
“Hospitals face incredibly complex problems and competing demands from different departments,” says Dr. Boutros. “As a physician administrator I felt I could translate for all sides.”
He cites consumer-directed care as a key trend blindsiding most doctors. “They are completely unprepared for the changing market dynamics of consumer choice,” he says.
Consultants, administrators, and physicians agree: Hospitalists need to avoid the tunnel vision when it comes to their own metrics and pay attention to the business drivers changing healthcare. If they learn to spot key trends, they’re perfectly situated to work with hospital administrators and their office-based colleagues on using that knowledge to increase market share, and to have better and more profitable hospitals. TH
Writer Marlene Piturro covered SHM’s Leadership Conference in Vail for The Hospitalist.
As physicians, including hospitalists, focus on the now—getting the patient in front of them better—they may lose sight of the trends shaping their professional lives. Those trends, called “business drivers” occupy CEOs, CFOs, and other top managers who build strategies by understanding what drivers make organizations successful.
It’s not an easy job. Even the Delphic Oracle might have trouble divining which of the myriad competing drivers will make a hospital better and more profitable than its rivals. Take your pick: Sluggish inpatient volumes, shifts to outpatient procedures, high construction costs, expensive new technologies, an aging population, and consumer-driven care are among the business drivers currently on managers’ minds. (See “Trend Spotters,” p. 48.)
Michael Guthrie, MD, MBA, an executive-in-residence at the University of Colorado, School of Business (Boulder), Health Administration and a presenter at SHM’s September 2005 Leadership Conference in Vail, Colo., sees our aging population as a key business driver shaping hospital and physician livelihoods.
“The aging population and the shift to consumerism in healthcare are definitely on the hospital CEO’s mind,” he says. “Hospitalists need to understand how patient satisfaction drives market share and is highly correlated with the hospital’s business objectives.” By extension, hospitalists’ key metrics, such as compliance with Medicare core measures, reducing length of stay (LOS), and costs per case, mesh well with administration’s.
Keeping the CEO’s need to enhance the organization’s reputation and growth in mind, Dr. Guthrie suggests that hospitalists have their hands full. By focusing on measuring quality, providing the 24/7 coverage that patients want and the hospital needs and finding ways to decrease LOS and costs per case, their interests and those of the hospital’s align.
“Based on their conversations and observations of the hospital’s senior managers, hospitalists can figure out what business drivers are preoccupying them,” adds Dr. Guthrie.
Smart hospitalists can significantly boost their hospital’s bottom line according to Tom Hochhausler, Deloitte & Touche USA LLP’s partner of Life Sciences and Health Care Practice and director of the firm’s biennial survey on trends concerning hospital CEOs. Hochhausler says that with hospitals operating on razor-thin margins, hospitalists can increase their value to hospital CEOs and CFOs by improving communication among clinical staff, better adherence to guidelines, and shortening LOS. “They also have some of the best insights into improving quality in hospitals and are powerful teachers of interns and residents,” he adds. (See “What Worries Hospital CEOs,” at left.)
The difficult part for hospitalists is keeping focused on the hospital’s big picture while doing their jobs. For example, Michael Freed, CFO of Grand Rapids, Mich.-based Spectrum Health, ponders the financial aspects of a huge integrated delivery system with seven hospitals, 12,000 employees, a medical staff of 1,400 and a $2.1 billion budget. Rather than day-to-day concerns he focuses on the future—not one year, but five to 10 years ahead.
“Since the hospitalist team’s job is to cover the hospital 24/7, they don’t always connect the dots of what’s happening throughout the system,” says Ford. That’s why top managers must focus on the future. “If management has the right road map and vision for the future, a lot of good things happen for hospitalists: Patients get better care, which leads to better outcomes, [and] we lower costs and pass the savings along to payers. That, in turn, drives higher market share and increases the hospital’s value proposition.”
Hospital medicine groups rather than individual physicians may be best suited to track the hospital’s business drivers, and align incentives accordingly. Davin Juckett, CPA, MBA, of the Charlotte, N.C., Piedmont Healthcare Management Group, a physician-owned consultancy to more than 100 hospitalists in the southeast, advises hospitalists to use their billing and encounter data to improve their decision-making.
“Hospitalists tend to be very focused on their LOS and quality indicators but there’s a lot more out there,” says Juckett. “Business drivers such as consumer-directed care and P4P [pay for performance] make quantifiable data extremely important. Some MCOs have started star ratings of hospitalist and ER groups, and some doctors are up in arms because they feel it’s subjective. But that’s the future.”
Juckett sees another key business driver for 2006 and 2007: an increasingly competitive business environment for hospitalists. “Hospital medicine groups will have to defend their contracts,” he says. “True, the newness of the specialty makes recruitment an issue, but supply will eventually catch up with demand, and P4P will happen.”
Hospitalists might examine how another major business driver—aggressive competition for payer dollars—can put them at odds with office-based colleagues. By competing with hospitals for lucrative procedures in orthopedics, gynecology, cardiology, and other specialties, community physicians can lure market share away. Hospitalists are well positioned to mediate the conflict, although a report by VHA of Irving, Texas, says hospitalists often don’t keep community doctors informed of issues facing their hospitals. That report adds that hospitalists do a poor job of bringing hospital administrators and physicians together to forge common solutions.
Bricks and Mortar
Balancing soaring construction costs with the need to give picky consumers and physicians the latest technology in gleaming new buildings is another trend. Big-ticket items keep Joann Marqusee, MPP, senior vice-president of operations and facilities at Boston-based Beth Israel Deaconess Medical Center occupied. Her job—prioritizing capital projects, keeping facilities up to date, and tailoring spending to reduce future maintenance needs—got even more challenging with Hurricane Katrina. “Things are always difficult, but now the price of oil and steel are rising,” says Marqusee. “And we can’t find dehumidifiers to help with our little floods; they’re all in New Orleans.”
She has capital-spending decisions down to a disciplined process: Match projects with the strategic plan (e.g., neurosurgery ahead of ob/gyn), assess impact on patient volume and return on investment, and improve patient safety and quality. Explaining those decisions to physicians who get feisty when a favored project is delayed or cancelled is the tough part.
To gain doctors’ support for management’s spending priorities, Marqusee has a PowerPoint presentation for them: “Space: The Final Frontier.” She raves about hospitalists’ response: ”The hospitalists’ input has been fantastic because of their analytic training. For example, they understand ED throughput, and we use their expertise to improve design. And when we tell them that the new ICU can’t open as soon as they’d like because it’s being built above the bone marrow transplant center, and we need a new HVAC system installed first, they get it. They care about patients and when we introduce bottom line issues as well, we strengthen our working relationship.”
Where the (Aging) Consumer Is King
Consumerism is another business driver that hospitals can’t ignore. Individuals are increasingly willing to push their physicians to send them to the hospitals the consumers prefer, according to Solucient, a healthcare market intelligence firm in Evanston, Ill. In a survey of nearly 20,000 households Solucient identified a group of “responsive consumers,” (i.e., those proactive about managing their healthcare). Slightly older than the average consumer surveyed, the respondents have between 20% and 80% higher incidence of chronic diseases, and increasingly choose where they’re hospitalized rather than accept their physician’s recommendation:
Solucient’s data also show that responsive consumers heavily research and utilize hospital and physician ratings.
Homegrown Effort
While consultants are oracles of healthcare trends, some physician administrators rely on themselves instead. Akram Boutrous, MD, executive vice-president and CMO of South Nassau Community Hospital (Oceanside, N.Y.), turned the hospital around with an eight-year business improvement program based on understanding business trends. Some achievements: a 73% increase in patient revenues, 57% jump in outpatient services, and 27% increase in inpatient discharges.
Dr. Boutros considered using consultants, but disliked their high fees and lack of ongoing involvement. Instead he read stacks of books and articles on business drivers and strategies before selecting General Electric’s Accelerated Action Approach to Success. The method uses teams to solve problems that make organizations non-competitive.
“Hospitals face incredibly complex problems and competing demands from different departments,” says Dr. Boutros. “As a physician administrator I felt I could translate for all sides.”
He cites consumer-directed care as a key trend blindsiding most doctors. “They are completely unprepared for the changing market dynamics of consumer choice,” he says.
Consultants, administrators, and physicians agree: Hospitalists need to avoid the tunnel vision when it comes to their own metrics and pay attention to the business drivers changing healthcare. If they learn to spot key trends, they’re perfectly situated to work with hospital administrators and their office-based colleagues on using that knowledge to increase market share, and to have better and more profitable hospitals. TH
Writer Marlene Piturro covered SHM’s Leadership Conference in Vail for The Hospitalist.
As physicians, including hospitalists, focus on the now—getting the patient in front of them better—they may lose sight of the trends shaping their professional lives. Those trends, called “business drivers” occupy CEOs, CFOs, and other top managers who build strategies by understanding what drivers make organizations successful.
It’s not an easy job. Even the Delphic Oracle might have trouble divining which of the myriad competing drivers will make a hospital better and more profitable than its rivals. Take your pick: Sluggish inpatient volumes, shifts to outpatient procedures, high construction costs, expensive new technologies, an aging population, and consumer-driven care are among the business drivers currently on managers’ minds. (See “Trend Spotters,” p. 48.)
Michael Guthrie, MD, MBA, an executive-in-residence at the University of Colorado, School of Business (Boulder), Health Administration and a presenter at SHM’s September 2005 Leadership Conference in Vail, Colo., sees our aging population as a key business driver shaping hospital and physician livelihoods.
“The aging population and the shift to consumerism in healthcare are definitely on the hospital CEO’s mind,” he says. “Hospitalists need to understand how patient satisfaction drives market share and is highly correlated with the hospital’s business objectives.” By extension, hospitalists’ key metrics, such as compliance with Medicare core measures, reducing length of stay (LOS), and costs per case, mesh well with administration’s.
Keeping the CEO’s need to enhance the organization’s reputation and growth in mind, Dr. Guthrie suggests that hospitalists have their hands full. By focusing on measuring quality, providing the 24/7 coverage that patients want and the hospital needs and finding ways to decrease LOS and costs per case, their interests and those of the hospital’s align.
“Based on their conversations and observations of the hospital’s senior managers, hospitalists can figure out what business drivers are preoccupying them,” adds Dr. Guthrie.
Smart hospitalists can significantly boost their hospital’s bottom line according to Tom Hochhausler, Deloitte & Touche USA LLP’s partner of Life Sciences and Health Care Practice and director of the firm’s biennial survey on trends concerning hospital CEOs. Hochhausler says that with hospitals operating on razor-thin margins, hospitalists can increase their value to hospital CEOs and CFOs by improving communication among clinical staff, better adherence to guidelines, and shortening LOS. “They also have some of the best insights into improving quality in hospitals and are powerful teachers of interns and residents,” he adds. (See “What Worries Hospital CEOs,” at left.)
The difficult part for hospitalists is keeping focused on the hospital’s big picture while doing their jobs. For example, Michael Freed, CFO of Grand Rapids, Mich.-based Spectrum Health, ponders the financial aspects of a huge integrated delivery system with seven hospitals, 12,000 employees, a medical staff of 1,400 and a $2.1 billion budget. Rather than day-to-day concerns he focuses on the future—not one year, but five to 10 years ahead.
“Since the hospitalist team’s job is to cover the hospital 24/7, they don’t always connect the dots of what’s happening throughout the system,” says Ford. That’s why top managers must focus on the future. “If management has the right road map and vision for the future, a lot of good things happen for hospitalists: Patients get better care, which leads to better outcomes, [and] we lower costs and pass the savings along to payers. That, in turn, drives higher market share and increases the hospital’s value proposition.”
Hospital medicine groups rather than individual physicians may be best suited to track the hospital’s business drivers, and align incentives accordingly. Davin Juckett, CPA, MBA, of the Charlotte, N.C., Piedmont Healthcare Management Group, a physician-owned consultancy to more than 100 hospitalists in the southeast, advises hospitalists to use their billing and encounter data to improve their decision-making.
“Hospitalists tend to be very focused on their LOS and quality indicators but there’s a lot more out there,” says Juckett. “Business drivers such as consumer-directed care and P4P [pay for performance] make quantifiable data extremely important. Some MCOs have started star ratings of hospitalist and ER groups, and some doctors are up in arms because they feel it’s subjective. But that’s the future.”
Juckett sees another key business driver for 2006 and 2007: an increasingly competitive business environment for hospitalists. “Hospital medicine groups will have to defend their contracts,” he says. “True, the newness of the specialty makes recruitment an issue, but supply will eventually catch up with demand, and P4P will happen.”
Hospitalists might examine how another major business driver—aggressive competition for payer dollars—can put them at odds with office-based colleagues. By competing with hospitals for lucrative procedures in orthopedics, gynecology, cardiology, and other specialties, community physicians can lure market share away. Hospitalists are well positioned to mediate the conflict, although a report by VHA of Irving, Texas, says hospitalists often don’t keep community doctors informed of issues facing their hospitals. That report adds that hospitalists do a poor job of bringing hospital administrators and physicians together to forge common solutions.
Bricks and Mortar
Balancing soaring construction costs with the need to give picky consumers and physicians the latest technology in gleaming new buildings is another trend. Big-ticket items keep Joann Marqusee, MPP, senior vice-president of operations and facilities at Boston-based Beth Israel Deaconess Medical Center occupied. Her job—prioritizing capital projects, keeping facilities up to date, and tailoring spending to reduce future maintenance needs—got even more challenging with Hurricane Katrina. “Things are always difficult, but now the price of oil and steel are rising,” says Marqusee. “And we can’t find dehumidifiers to help with our little floods; they’re all in New Orleans.”
She has capital-spending decisions down to a disciplined process: Match projects with the strategic plan (e.g., neurosurgery ahead of ob/gyn), assess impact on patient volume and return on investment, and improve patient safety and quality. Explaining those decisions to physicians who get feisty when a favored project is delayed or cancelled is the tough part.
To gain doctors’ support for management’s spending priorities, Marqusee has a PowerPoint presentation for them: “Space: The Final Frontier.” She raves about hospitalists’ response: ”The hospitalists’ input has been fantastic because of their analytic training. For example, they understand ED throughput, and we use their expertise to improve design. And when we tell them that the new ICU can’t open as soon as they’d like because it’s being built above the bone marrow transplant center, and we need a new HVAC system installed first, they get it. They care about patients and when we introduce bottom line issues as well, we strengthen our working relationship.”
Where the (Aging) Consumer Is King
Consumerism is another business driver that hospitals can’t ignore. Individuals are increasingly willing to push their physicians to send them to the hospitals the consumers prefer, according to Solucient, a healthcare market intelligence firm in Evanston, Ill. In a survey of nearly 20,000 households Solucient identified a group of “responsive consumers,” (i.e., those proactive about managing their healthcare). Slightly older than the average consumer surveyed, the respondents have between 20% and 80% higher incidence of chronic diseases, and increasingly choose where they’re hospitalized rather than accept their physician’s recommendation:
Solucient’s data also show that responsive consumers heavily research and utilize hospital and physician ratings.
Homegrown Effort
While consultants are oracles of healthcare trends, some physician administrators rely on themselves instead. Akram Boutrous, MD, executive vice-president and CMO of South Nassau Community Hospital (Oceanside, N.Y.), turned the hospital around with an eight-year business improvement program based on understanding business trends. Some achievements: a 73% increase in patient revenues, 57% jump in outpatient services, and 27% increase in inpatient discharges.
Dr. Boutros considered using consultants, but disliked their high fees and lack of ongoing involvement. Instead he read stacks of books and articles on business drivers and strategies before selecting General Electric’s Accelerated Action Approach to Success. The method uses teams to solve problems that make organizations non-competitive.
“Hospitals face incredibly complex problems and competing demands from different departments,” says Dr. Boutros. “As a physician administrator I felt I could translate for all sides.”
He cites consumer-directed care as a key trend blindsiding most doctors. “They are completely unprepared for the changing market dynamics of consumer choice,” he says.
Consultants, administrators, and physicians agree: Hospitalists need to avoid the tunnel vision when it comes to their own metrics and pay attention to the business drivers changing healthcare. If they learn to spot key trends, they’re perfectly situated to work with hospital administrators and their office-based colleagues on using that knowledge to increase market share, and to have better and more profitable hospitals. TH
Writer Marlene Piturro covered SHM’s Leadership Conference in Vail for The Hospitalist.
Family Affairs
I started as a skeptic. In the middle of my residency at Cincinnati Children’s Hospital Medical Center (CCHMC), one of our general pediatric inpatient units piloted a different way to do rounds focusing on “family-centered care.” Initiated by a core group of nurses, physicians, and families working together, the program became a central piece of an institution-wide effort to successfully garner a “Pursuing Perfection” grant from the Robert Wood Johnson Foundation. The grant was based on the Institute of Medicine’s 2001 report, “Crossing the Quality Chasm,” that included patient-centeredness as one of six key principles to guide health-system reform.1
I was skeptical about family-centered rounds because the change didn’t seem that radical to me: I prided myself on keeping my patients’ families informed about the plan of care. I did not appreciate how fundamental a shift “family-centeredness” required.
In 2003, the Committee on Hospital Care of the American Academy of Pediatrics (AAP) published in Pediatrics a policy statement about family-centered care. Included in the statement was the following sentence: “[C]onducting attending physician rounds (i.e., patient presentations and rounds discussions) in the patients rooms with the family present should be standard practice.”2
It seemed straightforward, but it has required a significant and fundamental shift. In this article I discuss my experience and perceptions as a resident and hospitalist at CCHMC as it implemented the Institute of Medicine and AAP goal of family-centered rounds (FCRs).
What FCRs Look Like
Preparation for FCRs begins at admission. Ideally, at that time families are informed by both residents and nurses that during the following morning rounds will take place in the patient’s room. The family’s permission/preference is sought, but the team’s preference to round in the room is explained. Given published literature that some patients are upset by bedside rounds, it seems imperative to give the family a choice in how rounds are conducted.3 In practice, most families (more than 90%) choose to have rounds in the room.
On rounds the next day, the admitting intern or medical student enters the room to verify the family’s preference, and then the whole team enters the room. Team structure varies, but at a minimum a team includes interns, a senior resident, an attending, and a nursing representative.
The team starts by introducing themselves by name and role to the family. The intern or medical student then presents the history and physical, and the plan for the day is discussed with the family (if confidentiality is an issue—e.g., adolescent issues—the relevant information and discussion of how that information will be shared with the family is reviewed before entering the room).
In my transition from early skepticism to passionate advocacy for FCRs, the fundamental shift in my understanding has been how care changes when the plan is discussed and formulated with a family as opposed to simply being told to a family. Further, as an attending, I have learned the power of real-time verification of the information that the residents give me. In FCRs, families are encouraged to interject when the information is incomplete or inaccurate. Because the attending physician is more fully informed when decisions are being made on rounds, plans don’t routinely need to be altered later in the morning/afternoon.
Additional benefits include the fact that most orders and discharge paperwork are clarified and written on rounds, which has been an invaluable efficiency in the resident work-hours era. The most significant benefit of this process, though, is how much more reliable and sophisticated our plans have become. With nurse, family, and physician all communicating at the same time on rounds, there is exponentially less confusion about the plan of care. Discharge planning starts at admission, and each party acknowledges progression toward the well-defined goals. Residents (particularly cross-covering residents) get afternoon phone calls that a patient is ready to go, and can reliably just sign the order, knowing that follow-up plans, prescriptions, and criteria for discharge have been well defined that morning on rounds. Those calls from nurses that all physicians remember from training, “So and so needs a script, needs a note, needs home care orders signed ... ” occur less frequently because nurses are clarifying those needs on rounds.
What Participants Think About FCRs
We have learned much from data regarding participants’ perceptions of FCRs. Most of this early data was collected as part of routine customer service and staff satisfaction surveys, but some has been developed through more formal focus groups.
Some brief highlights of what we have learned to date: Family satisfaction, particularly in regard to their perception of involvement in their children’s care, is very high.4 More recently, in regard to units that do not use FCRs routinely, we have received critical comments from families about the difference in the quality of communication. Nurses comment that the discharge planning process has been greatly enhanced by FCRs. Echoing some of our family feedback, nurses noticed a void in discharge planning when rounds did not include families.
In addition, nurses indicate nurse-to-nurse communication at change of shift is better when nurses are included in rounds. Resident feedback is generally positive, particularly in regard to the enhanced efficiency and communication of FCRs. A vocal minority make it clear that FCRs need to be “done right” to balance resident’s educational needs with patient care. Participating attendings are nearly unanimous in the opinion that FCRs provide better care.5 Most also feel FCRs provide new, important educational opportunities, allowing for daily direct observation of trainees’ interactions with families. Echoing residents, attendings acknowledge it takes time to learn how to do FCRs well.
Further, ongoing quality assurance and improvement work has demonstrated decreased length of stay and increased discharge timeliness on units where FCRs are used extensively.
Barriers to FCRs
Probably the biggest barrier at CCHMC has been and continues to be attending physician buy-in. As I see it, at the core of attending physician reluctance is concern with sharing uncertainty in front of the family. The uncertainty issue cuts to the core of what family-centered means: The patient or family is in control of the decision-making process—not the physician. In practice at CCHMC, this concern has not been substantiated among the attendings participating in FCRs.5
Nurse-physician collaboration has been an intermittent barrier. For FCRs to reach their full potential, nurse and physician both need to actively participate and take responsibility for the process. A care plan truly comes together and becomes maximally effective when family, nurse, and physician can listen to each other’s points-of-view.
Many of the logistical barriers likely vary among institutions around issues like private rooms, computerized order entry, resident and nurse staffing, communication with referring or consulting physicians, and so on. While seeking for standardization across units, FCRs do look a little different within our institution depending on the logistical issues on specific units or with specific resident teams.
Final Thoughts
I am no longer a skeptic. While I have much to learn about how to make FCRs better, most days I feel FCRs enable me to be the doctor I hope to be: Families are informed, active participants in their children’s care; nurses are informed and empowered to make care more effective and efficient; residents get “work” done on rounds; and I get to consistently observe and model history taking, physical exam, and communication skills with physician trainees.
Fundamentally, FCRs have changed my appreciation of how to develop and teach a medical plan. I deliver better care when families are at the center of the presentation of information, the discussion of options, and the choice of plan for their children. TH
Dr. Simmons is an instructor in pediatrics at Cincinnati Children’s Hospital Medical Center, University of Cincinnati School of Medicine
References
- Crossing the Quality Chasm: A New Health System for the 21st Century, Committee on Quality of Health Care in America of the Institute of Medicine, National Academy Press, Washington, D.C., 2001.
- Family-Centered Care and the Pediatrician’s Role. Pediatrics. 2003;112(3):691-697.
- Lehmann LS, Brancati FL, Chen MC, et al. The effect of bedside case presentation on patients’ perceptions of their medical care. N Eng J Med. 1997;336(16):1150-1155.
- Muething SE, Britto MT, Gerhardt WE, et al. Using Patient-Centered Care Principles To Improve Discharge Timeliness. Presented at: Pediatric Academic Societies Meeting. May 1-4, 2004. San Francisco.
- Brinkman W, Pandzik G, Muething SE. Family-Centered Rounds: Lessons learned implementing a new care delivery process. Presented at: Pediatric Academic Societies Meeting. May 14-17, 2005. Washington, D.C.
I started as a skeptic. In the middle of my residency at Cincinnati Children’s Hospital Medical Center (CCHMC), one of our general pediatric inpatient units piloted a different way to do rounds focusing on “family-centered care.” Initiated by a core group of nurses, physicians, and families working together, the program became a central piece of an institution-wide effort to successfully garner a “Pursuing Perfection” grant from the Robert Wood Johnson Foundation. The grant was based on the Institute of Medicine’s 2001 report, “Crossing the Quality Chasm,” that included patient-centeredness as one of six key principles to guide health-system reform.1
I was skeptical about family-centered rounds because the change didn’t seem that radical to me: I prided myself on keeping my patients’ families informed about the plan of care. I did not appreciate how fundamental a shift “family-centeredness” required.
In 2003, the Committee on Hospital Care of the American Academy of Pediatrics (AAP) published in Pediatrics a policy statement about family-centered care. Included in the statement was the following sentence: “[C]onducting attending physician rounds (i.e., patient presentations and rounds discussions) in the patients rooms with the family present should be standard practice.”2
It seemed straightforward, but it has required a significant and fundamental shift. In this article I discuss my experience and perceptions as a resident and hospitalist at CCHMC as it implemented the Institute of Medicine and AAP goal of family-centered rounds (FCRs).
What FCRs Look Like
Preparation for FCRs begins at admission. Ideally, at that time families are informed by both residents and nurses that during the following morning rounds will take place in the patient’s room. The family’s permission/preference is sought, but the team’s preference to round in the room is explained. Given published literature that some patients are upset by bedside rounds, it seems imperative to give the family a choice in how rounds are conducted.3 In practice, most families (more than 90%) choose to have rounds in the room.
On rounds the next day, the admitting intern or medical student enters the room to verify the family’s preference, and then the whole team enters the room. Team structure varies, but at a minimum a team includes interns, a senior resident, an attending, and a nursing representative.
The team starts by introducing themselves by name and role to the family. The intern or medical student then presents the history and physical, and the plan for the day is discussed with the family (if confidentiality is an issue—e.g., adolescent issues—the relevant information and discussion of how that information will be shared with the family is reviewed before entering the room).
In my transition from early skepticism to passionate advocacy for FCRs, the fundamental shift in my understanding has been how care changes when the plan is discussed and formulated with a family as opposed to simply being told to a family. Further, as an attending, I have learned the power of real-time verification of the information that the residents give me. In FCRs, families are encouraged to interject when the information is incomplete or inaccurate. Because the attending physician is more fully informed when decisions are being made on rounds, plans don’t routinely need to be altered later in the morning/afternoon.
Additional benefits include the fact that most orders and discharge paperwork are clarified and written on rounds, which has been an invaluable efficiency in the resident work-hours era. The most significant benefit of this process, though, is how much more reliable and sophisticated our plans have become. With nurse, family, and physician all communicating at the same time on rounds, there is exponentially less confusion about the plan of care. Discharge planning starts at admission, and each party acknowledges progression toward the well-defined goals. Residents (particularly cross-covering residents) get afternoon phone calls that a patient is ready to go, and can reliably just sign the order, knowing that follow-up plans, prescriptions, and criteria for discharge have been well defined that morning on rounds. Those calls from nurses that all physicians remember from training, “So and so needs a script, needs a note, needs home care orders signed ... ” occur less frequently because nurses are clarifying those needs on rounds.
What Participants Think About FCRs
We have learned much from data regarding participants’ perceptions of FCRs. Most of this early data was collected as part of routine customer service and staff satisfaction surveys, but some has been developed through more formal focus groups.
Some brief highlights of what we have learned to date: Family satisfaction, particularly in regard to their perception of involvement in their children’s care, is very high.4 More recently, in regard to units that do not use FCRs routinely, we have received critical comments from families about the difference in the quality of communication. Nurses comment that the discharge planning process has been greatly enhanced by FCRs. Echoing some of our family feedback, nurses noticed a void in discharge planning when rounds did not include families.
In addition, nurses indicate nurse-to-nurse communication at change of shift is better when nurses are included in rounds. Resident feedback is generally positive, particularly in regard to the enhanced efficiency and communication of FCRs. A vocal minority make it clear that FCRs need to be “done right” to balance resident’s educational needs with patient care. Participating attendings are nearly unanimous in the opinion that FCRs provide better care.5 Most also feel FCRs provide new, important educational opportunities, allowing for daily direct observation of trainees’ interactions with families. Echoing residents, attendings acknowledge it takes time to learn how to do FCRs well.
Further, ongoing quality assurance and improvement work has demonstrated decreased length of stay and increased discharge timeliness on units where FCRs are used extensively.
Barriers to FCRs
Probably the biggest barrier at CCHMC has been and continues to be attending physician buy-in. As I see it, at the core of attending physician reluctance is concern with sharing uncertainty in front of the family. The uncertainty issue cuts to the core of what family-centered means: The patient or family is in control of the decision-making process—not the physician. In practice at CCHMC, this concern has not been substantiated among the attendings participating in FCRs.5
Nurse-physician collaboration has been an intermittent barrier. For FCRs to reach their full potential, nurse and physician both need to actively participate and take responsibility for the process. A care plan truly comes together and becomes maximally effective when family, nurse, and physician can listen to each other’s points-of-view.
Many of the logistical barriers likely vary among institutions around issues like private rooms, computerized order entry, resident and nurse staffing, communication with referring or consulting physicians, and so on. While seeking for standardization across units, FCRs do look a little different within our institution depending on the logistical issues on specific units or with specific resident teams.
Final Thoughts
I am no longer a skeptic. While I have much to learn about how to make FCRs better, most days I feel FCRs enable me to be the doctor I hope to be: Families are informed, active participants in their children’s care; nurses are informed and empowered to make care more effective and efficient; residents get “work” done on rounds; and I get to consistently observe and model history taking, physical exam, and communication skills with physician trainees.
Fundamentally, FCRs have changed my appreciation of how to develop and teach a medical plan. I deliver better care when families are at the center of the presentation of information, the discussion of options, and the choice of plan for their children. TH
Dr. Simmons is an instructor in pediatrics at Cincinnati Children’s Hospital Medical Center, University of Cincinnati School of Medicine
References
- Crossing the Quality Chasm: A New Health System for the 21st Century, Committee on Quality of Health Care in America of the Institute of Medicine, National Academy Press, Washington, D.C., 2001.
- Family-Centered Care and the Pediatrician’s Role. Pediatrics. 2003;112(3):691-697.
- Lehmann LS, Brancati FL, Chen MC, et al. The effect of bedside case presentation on patients’ perceptions of their medical care. N Eng J Med. 1997;336(16):1150-1155.
- Muething SE, Britto MT, Gerhardt WE, et al. Using Patient-Centered Care Principles To Improve Discharge Timeliness. Presented at: Pediatric Academic Societies Meeting. May 1-4, 2004. San Francisco.
- Brinkman W, Pandzik G, Muething SE. Family-Centered Rounds: Lessons learned implementing a new care delivery process. Presented at: Pediatric Academic Societies Meeting. May 14-17, 2005. Washington, D.C.
I started as a skeptic. In the middle of my residency at Cincinnati Children’s Hospital Medical Center (CCHMC), one of our general pediatric inpatient units piloted a different way to do rounds focusing on “family-centered care.” Initiated by a core group of nurses, physicians, and families working together, the program became a central piece of an institution-wide effort to successfully garner a “Pursuing Perfection” grant from the Robert Wood Johnson Foundation. The grant was based on the Institute of Medicine’s 2001 report, “Crossing the Quality Chasm,” that included patient-centeredness as one of six key principles to guide health-system reform.1
I was skeptical about family-centered rounds because the change didn’t seem that radical to me: I prided myself on keeping my patients’ families informed about the plan of care. I did not appreciate how fundamental a shift “family-centeredness” required.
In 2003, the Committee on Hospital Care of the American Academy of Pediatrics (AAP) published in Pediatrics a policy statement about family-centered care. Included in the statement was the following sentence: “[C]onducting attending physician rounds (i.e., patient presentations and rounds discussions) in the patients rooms with the family present should be standard practice.”2
It seemed straightforward, but it has required a significant and fundamental shift. In this article I discuss my experience and perceptions as a resident and hospitalist at CCHMC as it implemented the Institute of Medicine and AAP goal of family-centered rounds (FCRs).
What FCRs Look Like
Preparation for FCRs begins at admission. Ideally, at that time families are informed by both residents and nurses that during the following morning rounds will take place in the patient’s room. The family’s permission/preference is sought, but the team’s preference to round in the room is explained. Given published literature that some patients are upset by bedside rounds, it seems imperative to give the family a choice in how rounds are conducted.3 In practice, most families (more than 90%) choose to have rounds in the room.
On rounds the next day, the admitting intern or medical student enters the room to verify the family’s preference, and then the whole team enters the room. Team structure varies, but at a minimum a team includes interns, a senior resident, an attending, and a nursing representative.
The team starts by introducing themselves by name and role to the family. The intern or medical student then presents the history and physical, and the plan for the day is discussed with the family (if confidentiality is an issue—e.g., adolescent issues—the relevant information and discussion of how that information will be shared with the family is reviewed before entering the room).
In my transition from early skepticism to passionate advocacy for FCRs, the fundamental shift in my understanding has been how care changes when the plan is discussed and formulated with a family as opposed to simply being told to a family. Further, as an attending, I have learned the power of real-time verification of the information that the residents give me. In FCRs, families are encouraged to interject when the information is incomplete or inaccurate. Because the attending physician is more fully informed when decisions are being made on rounds, plans don’t routinely need to be altered later in the morning/afternoon.
Additional benefits include the fact that most orders and discharge paperwork are clarified and written on rounds, which has been an invaluable efficiency in the resident work-hours era. The most significant benefit of this process, though, is how much more reliable and sophisticated our plans have become. With nurse, family, and physician all communicating at the same time on rounds, there is exponentially less confusion about the plan of care. Discharge planning starts at admission, and each party acknowledges progression toward the well-defined goals. Residents (particularly cross-covering residents) get afternoon phone calls that a patient is ready to go, and can reliably just sign the order, knowing that follow-up plans, prescriptions, and criteria for discharge have been well defined that morning on rounds. Those calls from nurses that all physicians remember from training, “So and so needs a script, needs a note, needs home care orders signed ... ” occur less frequently because nurses are clarifying those needs on rounds.
What Participants Think About FCRs
We have learned much from data regarding participants’ perceptions of FCRs. Most of this early data was collected as part of routine customer service and staff satisfaction surveys, but some has been developed through more formal focus groups.
Some brief highlights of what we have learned to date: Family satisfaction, particularly in regard to their perception of involvement in their children’s care, is very high.4 More recently, in regard to units that do not use FCRs routinely, we have received critical comments from families about the difference in the quality of communication. Nurses comment that the discharge planning process has been greatly enhanced by FCRs. Echoing some of our family feedback, nurses noticed a void in discharge planning when rounds did not include families.
In addition, nurses indicate nurse-to-nurse communication at change of shift is better when nurses are included in rounds. Resident feedback is generally positive, particularly in regard to the enhanced efficiency and communication of FCRs. A vocal minority make it clear that FCRs need to be “done right” to balance resident’s educational needs with patient care. Participating attendings are nearly unanimous in the opinion that FCRs provide better care.5 Most also feel FCRs provide new, important educational opportunities, allowing for daily direct observation of trainees’ interactions with families. Echoing residents, attendings acknowledge it takes time to learn how to do FCRs well.
Further, ongoing quality assurance and improvement work has demonstrated decreased length of stay and increased discharge timeliness on units where FCRs are used extensively.
Barriers to FCRs
Probably the biggest barrier at CCHMC has been and continues to be attending physician buy-in. As I see it, at the core of attending physician reluctance is concern with sharing uncertainty in front of the family. The uncertainty issue cuts to the core of what family-centered means: The patient or family is in control of the decision-making process—not the physician. In practice at CCHMC, this concern has not been substantiated among the attendings participating in FCRs.5
Nurse-physician collaboration has been an intermittent barrier. For FCRs to reach their full potential, nurse and physician both need to actively participate and take responsibility for the process. A care plan truly comes together and becomes maximally effective when family, nurse, and physician can listen to each other’s points-of-view.
Many of the logistical barriers likely vary among institutions around issues like private rooms, computerized order entry, resident and nurse staffing, communication with referring or consulting physicians, and so on. While seeking for standardization across units, FCRs do look a little different within our institution depending on the logistical issues on specific units or with specific resident teams.
Final Thoughts
I am no longer a skeptic. While I have much to learn about how to make FCRs better, most days I feel FCRs enable me to be the doctor I hope to be: Families are informed, active participants in their children’s care; nurses are informed and empowered to make care more effective and efficient; residents get “work” done on rounds; and I get to consistently observe and model history taking, physical exam, and communication skills with physician trainees.
Fundamentally, FCRs have changed my appreciation of how to develop and teach a medical plan. I deliver better care when families are at the center of the presentation of information, the discussion of options, and the choice of plan for their children. TH
Dr. Simmons is an instructor in pediatrics at Cincinnati Children’s Hospital Medical Center, University of Cincinnati School of Medicine
References
- Crossing the Quality Chasm: A New Health System for the 21st Century, Committee on Quality of Health Care in America of the Institute of Medicine, National Academy Press, Washington, D.C., 2001.
- Family-Centered Care and the Pediatrician’s Role. Pediatrics. 2003;112(3):691-697.
- Lehmann LS, Brancati FL, Chen MC, et al. The effect of bedside case presentation on patients’ perceptions of their medical care. N Eng J Med. 1997;336(16):1150-1155.
- Muething SE, Britto MT, Gerhardt WE, et al. Using Patient-Centered Care Principles To Improve Discharge Timeliness. Presented at: Pediatric Academic Societies Meeting. May 1-4, 2004. San Francisco.
- Brinkman W, Pandzik G, Muething SE. Family-Centered Rounds: Lessons learned implementing a new care delivery process. Presented at: Pediatric Academic Societies Meeting. May 14-17, 2005. Washington, D.C.
Hospitalist Tracks
Five years ago, a medical resident interested in pursuing a career as a hospitalist had few opportunities to receive specialized training. Five years from now, residents likely will have numerous hospitalist training tracks and electives from which to choose. This is partly thanks to a small group of pioneers who have seen the value of specialized hospitalist training for residents. These individuals have carefully considered what skills, information, and experience residents need to practice as confident and competent hospitalists, and they have developed programs and courses that meet these needs.
Sharpening Residents’ Focus
“Actually, we don’t call them ‘tracks,’ ” says Andrew Rudmann, MD, assistant professor of medicine and chief of the Hospital Medicine Division at the University of Rochester Medical Center. “We don’t want students to think that they’re stuck in an area once they choose it.”
Nonetheless, he notes, students increasingly are choosing careers as hospitalists, and they are expressing an interest in gaining skills and knowledge to help them become hospitalists.
Dr. Rudmann adds that his students “are sorting out their career plans earlier,” so it is important to offer specialized focus area programs. He has divided these into three areas: general medicine inpatient (hospitalist), general medicine outpatient (primary care), and subspecialty (other specialties).
The focus area programs are still in the developmental stage, Dr. Rudmann stresses. “We are in the process of developing the curricula for these programs, all of which will be elective experiences,” he says. Determining course options will be a challenge because there are a limited number of hours available for these electives. Nonetheless, Dr. Rudmann has identified several activities essential to producing effective hospitalists. These include:
- Rotation at a community hospital. “This program will focus on communication issues with primary care physicians,” explains Dr. Rudmann. “The students also will spend time in primary care offices to focus on the transition of patients from hospital to community care.”
- Quality improvement (QI) project. Residents will work one-on-one with hospitalists and develop a QI project from their work that they will present at the end of the rotation. As hospitalists, says Dr. Rudmann, these individuals frequently will be involved in QI initiatives and committees, and it is important that residents be prepared for these activities.
- Billing, coding, documentation mentorship. Each student will have a mentor, who will be required to instruct residents (either one-on-one or in small groups) about these issues. While billing, coding, and documentation are not glamorous, they are important components of a hospitalist practice, so Dr. Rudmann wants to ensure that residents are comfortable handling these activities.
Hospitalist students also will have the opportunity to spend time shadowing healthcare professionals in other areas such as the detox unit and bronchoscopy suite.
“It’s useful for a resident to spend time learning what these people do and what happens in these areas,” says Dr. Rudmann. “Our current healthcare system tends to be fragmented, and this experience will help physicians ensure smooth transitions for patients from one site to the next.”
Dr. Rudmann says he will suggest that residents interested in being hospitalists spend time in the ED observation unit. Additionally, these residents will be exposed to patient safety and medico-legal issues through active participation in morbidity/mortality conferences.
Residents also will have the opportunity to take a research elective course. However, Dr. Rudmann notes that students will need a real interest or passion for research to participate in this option, as it will consume one-half of their elective hours.
Day in the Life
Providing exposure to many of the day-to-day aspects of hospitalist practice is a key component of the hospitalist elective program at Emory University in Georgia.
“We wanted to provide residents with an opportunity to get some clinical exposure that they don’t necessarily get during general residency training and give them a better sense of what hospital medicine is—aside from taking care of patients in the hospital,” says Dan Dressler, MD, MSc, director of hospitalist medicine at the Emory University School of Medicine (Atlanta).
Emory’s hospitalist electives also give residents an opportunity to “pick the brains” of hospitalists. “They get to ask about things like schedules, committee involvement, research activities, and so on,” explains Dr. Dressler. “Residents really like this opportunity. They can feel isolated in the academic setting, and this really broadens their horizons.”
Building a Hospitalist Track from the Ground Up
In developing Emory’s hospitalist elective program, Dr. Dressler sought guidance from colleagues at the University of California at San Francisco and the Mayo Clinic (Rochester, Minn.) who already had established specialized hospitalist education opportunities.
Still, developing a good program is not as easy as copying someone else’s efforts. In fact, Dr. Rudmann says that most of the ideas for Rochester’s program came from “a thorough self-examination process.”
“You don’t have to look far,” he explains. “Just look at your own program and talk to your own residents.”
One of the challenges of developing a hospitalist track is the limited time available for elective programs. Dr. Dressler suggests starting by “assessing what you already are doing in your general residency program. You don’t want to duplicate efforts. Determine what is being done well at your program already and what could be done additionally—either based on what others are doing or what should be considered core competencies in hospital medicine. Then implement the missing pieces.”
Even after all of these planning and self-examination efforts, Dr. Dressler cautions, “you probably won’t have enough time to do everything you want to do.” At this point, he suggests concentrating on those issues or skills for which “you have someone who is able and willing to teach and teach well.” For example, he suggested, “if you want to include training on QI but don’t have anyone who can teach this well, you might want to keep this as a goal for down the road.”
Problem-Solving as a Goal
Sometimes, hospitalist training programs can help solve a specific problem. For example, Jason Gundersen, MD, director of the Family Medicine Hospitalist Service at the University of Massachusetts Medical Center, saw that “facilities often don’t want to hire family physicians as hospitalists because they lack hospital experience. [So I] wanted to give family practice residents extra training and experience in hospital medicine.”
The result was a hospitalist fellowship program, the goal of which “is to help improve employment opportunities. It enables graduates to go to employers with specific hospital medicine training,” says Dr. Gundersen. “This gives family physicians more experiences and abilities so they can navigate an uncertain market more successfully. There is a growing interest in hospitalist opportunities on the part of family physicians, and we need to prepare them to fill these roles.”
Despite the growing popularity of hospitalist training tracks and the enthusiasm many express about them, there are people who do not believe these programs are important or necessary. John Ford, MD, MPH, assistant professor of medicine at University of California at Los Angeles’ (UCLA) David Geffen School of Medicine, agrees.
“The first thing you have to understand is that internal medicine residency programs involve a tremendous amount of inpatient care anyway,” says Dr. Ford. “And a lot of what residents do is take care of hospital patients, so this training is adequate for a career choice as a hospitalist.”
“With the rise of hospitalists, people think that we need to emphasize hospital training more. But our residents already do a tremendous amount of hospital training,” he explains. “They do wards, ICU, and CCU; and even many of their electives—infectious disease and cardiology, for example—involve inpatient care. In addition, all of our residents have night float responsibilities, so they cover overflow patients and are in the hospital all night. We are training people pretty solidly for hospital practice.”
Dr. Ford believes it would a mistake for a resident to replace an ambulatory care rotation with a hospitalist track because he or she wants to be a hospitalist. “There is no question that hospitalists save money, lower lengths of stay, and improve patient outcomes and satisfaction,” he says. “But anyone can be a hospitalist. We aren’t an elite group of people.”
It is best to give hospitalists broad training, insists Dr. Ford, because “they still will need the actual job experience of working as a hospitalist to be effective in that role.” He adds that lack of a hospitalist program at UCLA in no way hurts his residents: “We are conventional here, but we do a superb job of education and training. Our residents are not at a disadvantage.”
His advice to residents who want to be hospitalists? “Pay attention—learn to do ambulatory medicine really well. This will help you tremendously when you perform as a hospitalist,” he explains. “You will have better sense of when someone can be discharged and who doesn’t need to come into hospital in the first place.”
Does Hospitalist Training Make a Difference?
“The feedback we’ve received so far makes it clear that this type of training helps people understand hospital medicine and better determine where they want to practice,” says Dr. Dressler. “Residents also have said that they like the variety of exposure to community settings. They said that they learned about activities and issues that they didn’t realize were part of physicians’ responsibilities, such as quality improvement and committee work.”
Dr. Dressler says that his health system has benefited from the program as well. “We have had some good residents stay to practice at one of our hospitals because their hospitalist training was such a positive experience,” he states.
Emory’s program has been in existence for only a few years. And while the number of participants remains small, Dr. Dressler says interest is growing: “We get about 5%-10% of residents in any given year. We are pleased with the turnout, and it has become more popular.”
Way of the Future
“We feel that all of this additional preparation is in our residents’ best interest,” states Dr. Rudmann. “We think it will be popular. Our residents are excited about it already.” He predicts that before long there will be many such programs around the nation. “Residency training programs will use these to gain a competitive edge to attract the best students.” TH
Writer Joanne Kaldy is based in Maryland.
Five years ago, a medical resident interested in pursuing a career as a hospitalist had few opportunities to receive specialized training. Five years from now, residents likely will have numerous hospitalist training tracks and electives from which to choose. This is partly thanks to a small group of pioneers who have seen the value of specialized hospitalist training for residents. These individuals have carefully considered what skills, information, and experience residents need to practice as confident and competent hospitalists, and they have developed programs and courses that meet these needs.
Sharpening Residents’ Focus
“Actually, we don’t call them ‘tracks,’ ” says Andrew Rudmann, MD, assistant professor of medicine and chief of the Hospital Medicine Division at the University of Rochester Medical Center. “We don’t want students to think that they’re stuck in an area once they choose it.”
Nonetheless, he notes, students increasingly are choosing careers as hospitalists, and they are expressing an interest in gaining skills and knowledge to help them become hospitalists.
Dr. Rudmann adds that his students “are sorting out their career plans earlier,” so it is important to offer specialized focus area programs. He has divided these into three areas: general medicine inpatient (hospitalist), general medicine outpatient (primary care), and subspecialty (other specialties).
The focus area programs are still in the developmental stage, Dr. Rudmann stresses. “We are in the process of developing the curricula for these programs, all of which will be elective experiences,” he says. Determining course options will be a challenge because there are a limited number of hours available for these electives. Nonetheless, Dr. Rudmann has identified several activities essential to producing effective hospitalists. These include:
- Rotation at a community hospital. “This program will focus on communication issues with primary care physicians,” explains Dr. Rudmann. “The students also will spend time in primary care offices to focus on the transition of patients from hospital to community care.”
- Quality improvement (QI) project. Residents will work one-on-one with hospitalists and develop a QI project from their work that they will present at the end of the rotation. As hospitalists, says Dr. Rudmann, these individuals frequently will be involved in QI initiatives and committees, and it is important that residents be prepared for these activities.
- Billing, coding, documentation mentorship. Each student will have a mentor, who will be required to instruct residents (either one-on-one or in small groups) about these issues. While billing, coding, and documentation are not glamorous, they are important components of a hospitalist practice, so Dr. Rudmann wants to ensure that residents are comfortable handling these activities.
Hospitalist students also will have the opportunity to spend time shadowing healthcare professionals in other areas such as the detox unit and bronchoscopy suite.
“It’s useful for a resident to spend time learning what these people do and what happens in these areas,” says Dr. Rudmann. “Our current healthcare system tends to be fragmented, and this experience will help physicians ensure smooth transitions for patients from one site to the next.”
Dr. Rudmann says he will suggest that residents interested in being hospitalists spend time in the ED observation unit. Additionally, these residents will be exposed to patient safety and medico-legal issues through active participation in morbidity/mortality conferences.
Residents also will have the opportunity to take a research elective course. However, Dr. Rudmann notes that students will need a real interest or passion for research to participate in this option, as it will consume one-half of their elective hours.
Day in the Life
Providing exposure to many of the day-to-day aspects of hospitalist practice is a key component of the hospitalist elective program at Emory University in Georgia.
“We wanted to provide residents with an opportunity to get some clinical exposure that they don’t necessarily get during general residency training and give them a better sense of what hospital medicine is—aside from taking care of patients in the hospital,” says Dan Dressler, MD, MSc, director of hospitalist medicine at the Emory University School of Medicine (Atlanta).
Emory’s hospitalist electives also give residents an opportunity to “pick the brains” of hospitalists. “They get to ask about things like schedules, committee involvement, research activities, and so on,” explains Dr. Dressler. “Residents really like this opportunity. They can feel isolated in the academic setting, and this really broadens their horizons.”
Building a Hospitalist Track from the Ground Up
In developing Emory’s hospitalist elective program, Dr. Dressler sought guidance from colleagues at the University of California at San Francisco and the Mayo Clinic (Rochester, Minn.) who already had established specialized hospitalist education opportunities.
Still, developing a good program is not as easy as copying someone else’s efforts. In fact, Dr. Rudmann says that most of the ideas for Rochester’s program came from “a thorough self-examination process.”
“You don’t have to look far,” he explains. “Just look at your own program and talk to your own residents.”
One of the challenges of developing a hospitalist track is the limited time available for elective programs. Dr. Dressler suggests starting by “assessing what you already are doing in your general residency program. You don’t want to duplicate efforts. Determine what is being done well at your program already and what could be done additionally—either based on what others are doing or what should be considered core competencies in hospital medicine. Then implement the missing pieces.”
Even after all of these planning and self-examination efforts, Dr. Dressler cautions, “you probably won’t have enough time to do everything you want to do.” At this point, he suggests concentrating on those issues or skills for which “you have someone who is able and willing to teach and teach well.” For example, he suggested, “if you want to include training on QI but don’t have anyone who can teach this well, you might want to keep this as a goal for down the road.”
Problem-Solving as a Goal
Sometimes, hospitalist training programs can help solve a specific problem. For example, Jason Gundersen, MD, director of the Family Medicine Hospitalist Service at the University of Massachusetts Medical Center, saw that “facilities often don’t want to hire family physicians as hospitalists because they lack hospital experience. [So I] wanted to give family practice residents extra training and experience in hospital medicine.”
The result was a hospitalist fellowship program, the goal of which “is to help improve employment opportunities. It enables graduates to go to employers with specific hospital medicine training,” says Dr. Gundersen. “This gives family physicians more experiences and abilities so they can navigate an uncertain market more successfully. There is a growing interest in hospitalist opportunities on the part of family physicians, and we need to prepare them to fill these roles.”
Despite the growing popularity of hospitalist training tracks and the enthusiasm many express about them, there are people who do not believe these programs are important or necessary. John Ford, MD, MPH, assistant professor of medicine at University of California at Los Angeles’ (UCLA) David Geffen School of Medicine, agrees.
“The first thing you have to understand is that internal medicine residency programs involve a tremendous amount of inpatient care anyway,” says Dr. Ford. “And a lot of what residents do is take care of hospital patients, so this training is adequate for a career choice as a hospitalist.”
“With the rise of hospitalists, people think that we need to emphasize hospital training more. But our residents already do a tremendous amount of hospital training,” he explains. “They do wards, ICU, and CCU; and even many of their electives—infectious disease and cardiology, for example—involve inpatient care. In addition, all of our residents have night float responsibilities, so they cover overflow patients and are in the hospital all night. We are training people pretty solidly for hospital practice.”
Dr. Ford believes it would a mistake for a resident to replace an ambulatory care rotation with a hospitalist track because he or she wants to be a hospitalist. “There is no question that hospitalists save money, lower lengths of stay, and improve patient outcomes and satisfaction,” he says. “But anyone can be a hospitalist. We aren’t an elite group of people.”
It is best to give hospitalists broad training, insists Dr. Ford, because “they still will need the actual job experience of working as a hospitalist to be effective in that role.” He adds that lack of a hospitalist program at UCLA in no way hurts his residents: “We are conventional here, but we do a superb job of education and training. Our residents are not at a disadvantage.”
His advice to residents who want to be hospitalists? “Pay attention—learn to do ambulatory medicine really well. This will help you tremendously when you perform as a hospitalist,” he explains. “You will have better sense of when someone can be discharged and who doesn’t need to come into hospital in the first place.”
Does Hospitalist Training Make a Difference?
“The feedback we’ve received so far makes it clear that this type of training helps people understand hospital medicine and better determine where they want to practice,” says Dr. Dressler. “Residents also have said that they like the variety of exposure to community settings. They said that they learned about activities and issues that they didn’t realize were part of physicians’ responsibilities, such as quality improvement and committee work.”
Dr. Dressler says that his health system has benefited from the program as well. “We have had some good residents stay to practice at one of our hospitals because their hospitalist training was such a positive experience,” he states.
Emory’s program has been in existence for only a few years. And while the number of participants remains small, Dr. Dressler says interest is growing: “We get about 5%-10% of residents in any given year. We are pleased with the turnout, and it has become more popular.”
Way of the Future
“We feel that all of this additional preparation is in our residents’ best interest,” states Dr. Rudmann. “We think it will be popular. Our residents are excited about it already.” He predicts that before long there will be many such programs around the nation. “Residency training programs will use these to gain a competitive edge to attract the best students.” TH
Writer Joanne Kaldy is based in Maryland.
Five years ago, a medical resident interested in pursuing a career as a hospitalist had few opportunities to receive specialized training. Five years from now, residents likely will have numerous hospitalist training tracks and electives from which to choose. This is partly thanks to a small group of pioneers who have seen the value of specialized hospitalist training for residents. These individuals have carefully considered what skills, information, and experience residents need to practice as confident and competent hospitalists, and they have developed programs and courses that meet these needs.
Sharpening Residents’ Focus
“Actually, we don’t call them ‘tracks,’ ” says Andrew Rudmann, MD, assistant professor of medicine and chief of the Hospital Medicine Division at the University of Rochester Medical Center. “We don’t want students to think that they’re stuck in an area once they choose it.”
Nonetheless, he notes, students increasingly are choosing careers as hospitalists, and they are expressing an interest in gaining skills and knowledge to help them become hospitalists.
Dr. Rudmann adds that his students “are sorting out their career plans earlier,” so it is important to offer specialized focus area programs. He has divided these into three areas: general medicine inpatient (hospitalist), general medicine outpatient (primary care), and subspecialty (other specialties).
The focus area programs are still in the developmental stage, Dr. Rudmann stresses. “We are in the process of developing the curricula for these programs, all of which will be elective experiences,” he says. Determining course options will be a challenge because there are a limited number of hours available for these electives. Nonetheless, Dr. Rudmann has identified several activities essential to producing effective hospitalists. These include:
- Rotation at a community hospital. “This program will focus on communication issues with primary care physicians,” explains Dr. Rudmann. “The students also will spend time in primary care offices to focus on the transition of patients from hospital to community care.”
- Quality improvement (QI) project. Residents will work one-on-one with hospitalists and develop a QI project from their work that they will present at the end of the rotation. As hospitalists, says Dr. Rudmann, these individuals frequently will be involved in QI initiatives and committees, and it is important that residents be prepared for these activities.
- Billing, coding, documentation mentorship. Each student will have a mentor, who will be required to instruct residents (either one-on-one or in small groups) about these issues. While billing, coding, and documentation are not glamorous, they are important components of a hospitalist practice, so Dr. Rudmann wants to ensure that residents are comfortable handling these activities.
Hospitalist students also will have the opportunity to spend time shadowing healthcare professionals in other areas such as the detox unit and bronchoscopy suite.
“It’s useful for a resident to spend time learning what these people do and what happens in these areas,” says Dr. Rudmann. “Our current healthcare system tends to be fragmented, and this experience will help physicians ensure smooth transitions for patients from one site to the next.”
Dr. Rudmann says he will suggest that residents interested in being hospitalists spend time in the ED observation unit. Additionally, these residents will be exposed to patient safety and medico-legal issues through active participation in morbidity/mortality conferences.
Residents also will have the opportunity to take a research elective course. However, Dr. Rudmann notes that students will need a real interest or passion for research to participate in this option, as it will consume one-half of their elective hours.
Day in the Life
Providing exposure to many of the day-to-day aspects of hospitalist practice is a key component of the hospitalist elective program at Emory University in Georgia.
“We wanted to provide residents with an opportunity to get some clinical exposure that they don’t necessarily get during general residency training and give them a better sense of what hospital medicine is—aside from taking care of patients in the hospital,” says Dan Dressler, MD, MSc, director of hospitalist medicine at the Emory University School of Medicine (Atlanta).
Emory’s hospitalist electives also give residents an opportunity to “pick the brains” of hospitalists. “They get to ask about things like schedules, committee involvement, research activities, and so on,” explains Dr. Dressler. “Residents really like this opportunity. They can feel isolated in the academic setting, and this really broadens their horizons.”
Building a Hospitalist Track from the Ground Up
In developing Emory’s hospitalist elective program, Dr. Dressler sought guidance from colleagues at the University of California at San Francisco and the Mayo Clinic (Rochester, Minn.) who already had established specialized hospitalist education opportunities.
Still, developing a good program is not as easy as copying someone else’s efforts. In fact, Dr. Rudmann says that most of the ideas for Rochester’s program came from “a thorough self-examination process.”
“You don’t have to look far,” he explains. “Just look at your own program and talk to your own residents.”
One of the challenges of developing a hospitalist track is the limited time available for elective programs. Dr. Dressler suggests starting by “assessing what you already are doing in your general residency program. You don’t want to duplicate efforts. Determine what is being done well at your program already and what could be done additionally—either based on what others are doing or what should be considered core competencies in hospital medicine. Then implement the missing pieces.”
Even after all of these planning and self-examination efforts, Dr. Dressler cautions, “you probably won’t have enough time to do everything you want to do.” At this point, he suggests concentrating on those issues or skills for which “you have someone who is able and willing to teach and teach well.” For example, he suggested, “if you want to include training on QI but don’t have anyone who can teach this well, you might want to keep this as a goal for down the road.”
Problem-Solving as a Goal
Sometimes, hospitalist training programs can help solve a specific problem. For example, Jason Gundersen, MD, director of the Family Medicine Hospitalist Service at the University of Massachusetts Medical Center, saw that “facilities often don’t want to hire family physicians as hospitalists because they lack hospital experience. [So I] wanted to give family practice residents extra training and experience in hospital medicine.”
The result was a hospitalist fellowship program, the goal of which “is to help improve employment opportunities. It enables graduates to go to employers with specific hospital medicine training,” says Dr. Gundersen. “This gives family physicians more experiences and abilities so they can navigate an uncertain market more successfully. There is a growing interest in hospitalist opportunities on the part of family physicians, and we need to prepare them to fill these roles.”
Despite the growing popularity of hospitalist training tracks and the enthusiasm many express about them, there are people who do not believe these programs are important or necessary. John Ford, MD, MPH, assistant professor of medicine at University of California at Los Angeles’ (UCLA) David Geffen School of Medicine, agrees.
“The first thing you have to understand is that internal medicine residency programs involve a tremendous amount of inpatient care anyway,” says Dr. Ford. “And a lot of what residents do is take care of hospital patients, so this training is adequate for a career choice as a hospitalist.”
“With the rise of hospitalists, people think that we need to emphasize hospital training more. But our residents already do a tremendous amount of hospital training,” he explains. “They do wards, ICU, and CCU; and even many of their electives—infectious disease and cardiology, for example—involve inpatient care. In addition, all of our residents have night float responsibilities, so they cover overflow patients and are in the hospital all night. We are training people pretty solidly for hospital practice.”
Dr. Ford believes it would a mistake for a resident to replace an ambulatory care rotation with a hospitalist track because he or she wants to be a hospitalist. “There is no question that hospitalists save money, lower lengths of stay, and improve patient outcomes and satisfaction,” he says. “But anyone can be a hospitalist. We aren’t an elite group of people.”
It is best to give hospitalists broad training, insists Dr. Ford, because “they still will need the actual job experience of working as a hospitalist to be effective in that role.” He adds that lack of a hospitalist program at UCLA in no way hurts his residents: “We are conventional here, but we do a superb job of education and training. Our residents are not at a disadvantage.”
His advice to residents who want to be hospitalists? “Pay attention—learn to do ambulatory medicine really well. This will help you tremendously when you perform as a hospitalist,” he explains. “You will have better sense of when someone can be discharged and who doesn’t need to come into hospital in the first place.”
Does Hospitalist Training Make a Difference?
“The feedback we’ve received so far makes it clear that this type of training helps people understand hospital medicine and better determine where they want to practice,” says Dr. Dressler. “Residents also have said that they like the variety of exposure to community settings. They said that they learned about activities and issues that they didn’t realize were part of physicians’ responsibilities, such as quality improvement and committee work.”
Dr. Dressler says that his health system has benefited from the program as well. “We have had some good residents stay to practice at one of our hospitals because their hospitalist training was such a positive experience,” he states.
Emory’s program has been in existence for only a few years. And while the number of participants remains small, Dr. Dressler says interest is growing: “We get about 5%-10% of residents in any given year. We are pleased with the turnout, and it has become more popular.”
Way of the Future
“We feel that all of this additional preparation is in our residents’ best interest,” states Dr. Rudmann. “We think it will be popular. Our residents are excited about it already.” He predicts that before long there will be many such programs around the nation. “Residency training programs will use these to gain a competitive edge to attract the best students.” TH
Writer Joanne Kaldy is based in Maryland.
The Dutch Medical Education
Editors’ note: During 2006 we will publish coverage of hospital practices in other countries. This is the second article in that effort. Our first article, on the state of hospital medicine in Afghanistan, was published in the Jan. issue on p. 1.
For the first time in the Netherlands, the Free University of Amsterdam has appointed three professors in two non-university hospitals with a specific assignment for teaching. Until now, professors in such hospitals were appointed only for a specific research task that they perform in—or in close collaboration with—the university. In this article we describe the reasons and expectations for these appointments.
Medical Training in the Netherlands
Both undergraduate and postgraduate training in the Netherlands takes place in eight university medical centers. Although preclinical teaching is mainly a university domain, around two-thirds of the clinical training for interns and residents takes place in “affiliated” non-university teaching hospitals.
Until recently, medical education consisted of four years of preclinical studies and two years of clinical training. Now students are gradually admitted into the clinic during their first or second year of medical education. Further, the Dutch government has ruled that the number of first-year medical students must increase by 40. Both measures will result in a significant increase in the number of interns in the coming years.
Because university hospitals presently accommodate the maximum number of interns they can take, the participation of non-university hospitals will rise considerably. However, their role must take into consideration not only quantity, but also quality. Because more than 90% of care in the Netherlands is delivered in non-university hospitals, these institutions provide the most proper setting for contextual learning. Adequate training is a prime barrier against accidents, so more resources must be invested in the quality of training programs in non-university hospitals to ensure the quality of future health care in the Netherlands.1,2 (See “Barriers Against Accidents,” p. 41.)
Teaching in Non-University Hospitals
By definition, medical education should be a core objective for teaching hospitals. (See “Requirements for Teaching Hospitals,” at right) This requires wide involvement by hospitals. Doctors in university hospitals generally have a contractual obligation to participate in teaching as part of their appointment. For most doctors in non-university hospitals, teaching is not part of their contract. Yet many of them do so on a voluntary basis. The advantage is that they are intrinsically motivated; however, the consequence is that they are not professional teachers, but rather well-meaning amateurs. This problem was recently addressed by the Central College for Medical Specialists, the ruling committee for specialist training in the Netherlands. Program directors and other specialists involved in teaching now take special courses to develop their teaching abilities.
Another issue involves defining end goals and planning curricula.3 For interns the goals are outlined in the “Blueprint for the Training of Medical Doctors in the Netherlands”; however, in practice, most internships are not structured, and learning opportunities depend on patient availability.4 It’s even questionable to what extent the precise curricular goals are known to interns and doctors alike.
For specialists, the end goals used to be inferred from practice, leaving lots of room for individual interpretation in the local institutions. These end goals are only now being defined. Many practical dilemmas, such as the relative weight we award to the various competencies, remain. For example, how much time should a surgical resident spend inside and outside the operating room? And what is the relative importance of experience? A key problem is that instruments that reliably measure the acquired competencies and the efficiency and efficacy of clinical training programs are still in their infancy.
Evidence-based teaching methods are now being demanded by the Central College for Medical Specialists. Methods include a modular-structured, competency-based curriculum, including regular skills, lab activities, and other training sessions, and the use of portfolios and mini clinical-evaluation exercises for formative and cumulative assessment.5,6
There are also practical problems on the working floor. In contrast to the preclinical teaching setting, which should be student-centered, the clinical environment of the hospital is primarily patient-centered. Interns and residents therefore have a double role: that of learner and care provider. These activities sometimes conflict, and the time allotted to each one is not clearly defined.
This became a greater problem after the restriction of resident working hours to 48 hours weekly in 1997. An attempt to divide these already strongly reduced hours to 36 “white-coat” hours and 12 “jacket” hours—purely dedicated to learning activities—has been abandoned.
In addition, the number of different parties on the working floor is sizable, and patients, nurses, medical staff, paramedics, and management often have different priorities, of which teaching is not always No. 1. Obviously such problems interfere with a structured, competency-based curriculum.
The Role of the Teaching Professor
In the Netherlands there is much work to do in the affiliated teaching hospitals, and a more professional approach is urgently needed. Professionalism, learning goals, curricula planning, evidence-based teaching methods, and solutions for practical problems that interfere with the proper implementation of evidence-based learning should all be addressed. The ruling committee and the professional organizations have set outlines that meet the requirements of modern times, but the elaboration and implementation have yet to be realized.
The Free University Medical Centre has taken the lead by appointing medical specialists as full professors with a specific assignment for teaching in non-university hospitals in order to develop and promote the teaching facilities in those institutions. They elected practicing non-university medical specialists with a demonstrable record in the field of education and an academic background comparable to that of university professors. Their assignment is to teach for one day a week. By doing so, they are not only putting teaching more prominently on the agenda, but also opening career perspectives that will promote a broader involvement in the development of educational programs.
The teaching professors develop and implement modern medical curricula and collaborate on research projects to evaluate the effectiveness of the new curricula in clinical teaching. Teaching professors also form a bridge between the university and the affiliated hospitals by transferring knowledge and ideas on medical education from the university to the non-university teaching hospitals—and vice versa. They also have input in the development of preclinical and clinical education programs from the point of view of the non-university hospital. For instance, they take part in the curriculum committee that advises on the bachelor’s and master’s programs, and they help create tests for the assessment of knowledge.
Summary
Non-university teaching hospitals have an essential place in the clinical phase of the medical curriculum in the Netherlands. A paradigm shift from the old master-mate relationship toward a structured, competency-based curriculum is taking place. Nomination of teaching professors in these institutions helps to create the professional structure that is mandatory for quality improvement in clinical teaching, and it also promotes the required interaction between university and non-university hospitals. TH
A.B. Bijnen works at the Foreest Institute, Medical Centre Almaar, the Netherlands; F. Scheele works at Sint Lucas Andreas Ziekenhuis, Amsterdam, the Netherlands, and the Institute for Medical Education, Free University Medical Centre, Amsterdam, the Netherlands; A.E.R. Arnold also works at the Foreest Institute, as well as the Institute for Medical Education, Free University Medical Centre; A.M.J.J. Verweij works at the Sint Lucas Andreas Ziekenhuis, as well as the Institute for Medical Education at Free University Medical Centre; and H.J.M. van Rossum and J.A.A.M. van Diemen-Steenvoorde work at the Institute for Medical Education at Free University Medical Centre.
References
- Reason J. Human error: models and management. BMJ. 2000;320:768-770.
- Willems R. Sneller Beter—Hier werk je veilig, of je werkt hier niet. De veiligheid in de zorg. Eindrapportage Shell Nederland. November 2004.
- AMEE Education Guide No 14. Outcome-based education. 1999. ISBN: 1-903934-15-X.
- Metz JCM, Verbeek-Weel AMM, Huisjes HJ. Blueprint 2001: Training of doctors in The Netherlands. Adjusted objectives of undergraduate medical education in The Netherlands. Nijmegen: University Publication Office. 2001
- O’Connor HM, McGraw RC. Clinical skills training: developing objective assessment instruments. Med Educ. 1997;31:359-363.
- Davis MH, Harden RM. Competency-based assessment: making it a reality [editorial]. Med Teach. 2003;25:565-568.
Editors’ note: During 2006 we will publish coverage of hospital practices in other countries. This is the second article in that effort. Our first article, on the state of hospital medicine in Afghanistan, was published in the Jan. issue on p. 1.
For the first time in the Netherlands, the Free University of Amsterdam has appointed three professors in two non-university hospitals with a specific assignment for teaching. Until now, professors in such hospitals were appointed only for a specific research task that they perform in—or in close collaboration with—the university. In this article we describe the reasons and expectations for these appointments.
Medical Training in the Netherlands
Both undergraduate and postgraduate training in the Netherlands takes place in eight university medical centers. Although preclinical teaching is mainly a university domain, around two-thirds of the clinical training for interns and residents takes place in “affiliated” non-university teaching hospitals.
Until recently, medical education consisted of four years of preclinical studies and two years of clinical training. Now students are gradually admitted into the clinic during their first or second year of medical education. Further, the Dutch government has ruled that the number of first-year medical students must increase by 40. Both measures will result in a significant increase in the number of interns in the coming years.
Because university hospitals presently accommodate the maximum number of interns they can take, the participation of non-university hospitals will rise considerably. However, their role must take into consideration not only quantity, but also quality. Because more than 90% of care in the Netherlands is delivered in non-university hospitals, these institutions provide the most proper setting for contextual learning. Adequate training is a prime barrier against accidents, so more resources must be invested in the quality of training programs in non-university hospitals to ensure the quality of future health care in the Netherlands.1,2 (See “Barriers Against Accidents,” p. 41.)
Teaching in Non-University Hospitals
By definition, medical education should be a core objective for teaching hospitals. (See “Requirements for Teaching Hospitals,” at right) This requires wide involvement by hospitals. Doctors in university hospitals generally have a contractual obligation to participate in teaching as part of their appointment. For most doctors in non-university hospitals, teaching is not part of their contract. Yet many of them do so on a voluntary basis. The advantage is that they are intrinsically motivated; however, the consequence is that they are not professional teachers, but rather well-meaning amateurs. This problem was recently addressed by the Central College for Medical Specialists, the ruling committee for specialist training in the Netherlands. Program directors and other specialists involved in teaching now take special courses to develop their teaching abilities.
Another issue involves defining end goals and planning curricula.3 For interns the goals are outlined in the “Blueprint for the Training of Medical Doctors in the Netherlands”; however, in practice, most internships are not structured, and learning opportunities depend on patient availability.4 It’s even questionable to what extent the precise curricular goals are known to interns and doctors alike.
For specialists, the end goals used to be inferred from practice, leaving lots of room for individual interpretation in the local institutions. These end goals are only now being defined. Many practical dilemmas, such as the relative weight we award to the various competencies, remain. For example, how much time should a surgical resident spend inside and outside the operating room? And what is the relative importance of experience? A key problem is that instruments that reliably measure the acquired competencies and the efficiency and efficacy of clinical training programs are still in their infancy.
Evidence-based teaching methods are now being demanded by the Central College for Medical Specialists. Methods include a modular-structured, competency-based curriculum, including regular skills, lab activities, and other training sessions, and the use of portfolios and mini clinical-evaluation exercises for formative and cumulative assessment.5,6
There are also practical problems on the working floor. In contrast to the preclinical teaching setting, which should be student-centered, the clinical environment of the hospital is primarily patient-centered. Interns and residents therefore have a double role: that of learner and care provider. These activities sometimes conflict, and the time allotted to each one is not clearly defined.
This became a greater problem after the restriction of resident working hours to 48 hours weekly in 1997. An attempt to divide these already strongly reduced hours to 36 “white-coat” hours and 12 “jacket” hours—purely dedicated to learning activities—has been abandoned.
In addition, the number of different parties on the working floor is sizable, and patients, nurses, medical staff, paramedics, and management often have different priorities, of which teaching is not always No. 1. Obviously such problems interfere with a structured, competency-based curriculum.
The Role of the Teaching Professor
In the Netherlands there is much work to do in the affiliated teaching hospitals, and a more professional approach is urgently needed. Professionalism, learning goals, curricula planning, evidence-based teaching methods, and solutions for practical problems that interfere with the proper implementation of evidence-based learning should all be addressed. The ruling committee and the professional organizations have set outlines that meet the requirements of modern times, but the elaboration and implementation have yet to be realized.
The Free University Medical Centre has taken the lead by appointing medical specialists as full professors with a specific assignment for teaching in non-university hospitals in order to develop and promote the teaching facilities in those institutions. They elected practicing non-university medical specialists with a demonstrable record in the field of education and an academic background comparable to that of university professors. Their assignment is to teach for one day a week. By doing so, they are not only putting teaching more prominently on the agenda, but also opening career perspectives that will promote a broader involvement in the development of educational programs.
The teaching professors develop and implement modern medical curricula and collaborate on research projects to evaluate the effectiveness of the new curricula in clinical teaching. Teaching professors also form a bridge between the university and the affiliated hospitals by transferring knowledge and ideas on medical education from the university to the non-university teaching hospitals—and vice versa. They also have input in the development of preclinical and clinical education programs from the point of view of the non-university hospital. For instance, they take part in the curriculum committee that advises on the bachelor’s and master’s programs, and they help create tests for the assessment of knowledge.
Summary
Non-university teaching hospitals have an essential place in the clinical phase of the medical curriculum in the Netherlands. A paradigm shift from the old master-mate relationship toward a structured, competency-based curriculum is taking place. Nomination of teaching professors in these institutions helps to create the professional structure that is mandatory for quality improvement in clinical teaching, and it also promotes the required interaction between university and non-university hospitals. TH
A.B. Bijnen works at the Foreest Institute, Medical Centre Almaar, the Netherlands; F. Scheele works at Sint Lucas Andreas Ziekenhuis, Amsterdam, the Netherlands, and the Institute for Medical Education, Free University Medical Centre, Amsterdam, the Netherlands; A.E.R. Arnold also works at the Foreest Institute, as well as the Institute for Medical Education, Free University Medical Centre; A.M.J.J. Verweij works at the Sint Lucas Andreas Ziekenhuis, as well as the Institute for Medical Education at Free University Medical Centre; and H.J.M. van Rossum and J.A.A.M. van Diemen-Steenvoorde work at the Institute for Medical Education at Free University Medical Centre.
References
- Reason J. Human error: models and management. BMJ. 2000;320:768-770.
- Willems R. Sneller Beter—Hier werk je veilig, of je werkt hier niet. De veiligheid in de zorg. Eindrapportage Shell Nederland. November 2004.
- AMEE Education Guide No 14. Outcome-based education. 1999. ISBN: 1-903934-15-X.
- Metz JCM, Verbeek-Weel AMM, Huisjes HJ. Blueprint 2001: Training of doctors in The Netherlands. Adjusted objectives of undergraduate medical education in The Netherlands. Nijmegen: University Publication Office. 2001
- O’Connor HM, McGraw RC. Clinical skills training: developing objective assessment instruments. Med Educ. 1997;31:359-363.
- Davis MH, Harden RM. Competency-based assessment: making it a reality [editorial]. Med Teach. 2003;25:565-568.
Editors’ note: During 2006 we will publish coverage of hospital practices in other countries. This is the second article in that effort. Our first article, on the state of hospital medicine in Afghanistan, was published in the Jan. issue on p. 1.
For the first time in the Netherlands, the Free University of Amsterdam has appointed three professors in two non-university hospitals with a specific assignment for teaching. Until now, professors in such hospitals were appointed only for a specific research task that they perform in—or in close collaboration with—the university. In this article we describe the reasons and expectations for these appointments.
Medical Training in the Netherlands
Both undergraduate and postgraduate training in the Netherlands takes place in eight university medical centers. Although preclinical teaching is mainly a university domain, around two-thirds of the clinical training for interns and residents takes place in “affiliated” non-university teaching hospitals.
Until recently, medical education consisted of four years of preclinical studies and two years of clinical training. Now students are gradually admitted into the clinic during their first or second year of medical education. Further, the Dutch government has ruled that the number of first-year medical students must increase by 40. Both measures will result in a significant increase in the number of interns in the coming years.
Because university hospitals presently accommodate the maximum number of interns they can take, the participation of non-university hospitals will rise considerably. However, their role must take into consideration not only quantity, but also quality. Because more than 90% of care in the Netherlands is delivered in non-university hospitals, these institutions provide the most proper setting for contextual learning. Adequate training is a prime barrier against accidents, so more resources must be invested in the quality of training programs in non-university hospitals to ensure the quality of future health care in the Netherlands.1,2 (See “Barriers Against Accidents,” p. 41.)
Teaching in Non-University Hospitals
By definition, medical education should be a core objective for teaching hospitals. (See “Requirements for Teaching Hospitals,” at right) This requires wide involvement by hospitals. Doctors in university hospitals generally have a contractual obligation to participate in teaching as part of their appointment. For most doctors in non-university hospitals, teaching is not part of their contract. Yet many of them do so on a voluntary basis. The advantage is that they are intrinsically motivated; however, the consequence is that they are not professional teachers, but rather well-meaning amateurs. This problem was recently addressed by the Central College for Medical Specialists, the ruling committee for specialist training in the Netherlands. Program directors and other specialists involved in teaching now take special courses to develop their teaching abilities.
Another issue involves defining end goals and planning curricula.3 For interns the goals are outlined in the “Blueprint for the Training of Medical Doctors in the Netherlands”; however, in practice, most internships are not structured, and learning opportunities depend on patient availability.4 It’s even questionable to what extent the precise curricular goals are known to interns and doctors alike.
For specialists, the end goals used to be inferred from practice, leaving lots of room for individual interpretation in the local institutions. These end goals are only now being defined. Many practical dilemmas, such as the relative weight we award to the various competencies, remain. For example, how much time should a surgical resident spend inside and outside the operating room? And what is the relative importance of experience? A key problem is that instruments that reliably measure the acquired competencies and the efficiency and efficacy of clinical training programs are still in their infancy.
Evidence-based teaching methods are now being demanded by the Central College for Medical Specialists. Methods include a modular-structured, competency-based curriculum, including regular skills, lab activities, and other training sessions, and the use of portfolios and mini clinical-evaluation exercises for formative and cumulative assessment.5,6
There are also practical problems on the working floor. In contrast to the preclinical teaching setting, which should be student-centered, the clinical environment of the hospital is primarily patient-centered. Interns and residents therefore have a double role: that of learner and care provider. These activities sometimes conflict, and the time allotted to each one is not clearly defined.
This became a greater problem after the restriction of resident working hours to 48 hours weekly in 1997. An attempt to divide these already strongly reduced hours to 36 “white-coat” hours and 12 “jacket” hours—purely dedicated to learning activities—has been abandoned.
In addition, the number of different parties on the working floor is sizable, and patients, nurses, medical staff, paramedics, and management often have different priorities, of which teaching is not always No. 1. Obviously such problems interfere with a structured, competency-based curriculum.
The Role of the Teaching Professor
In the Netherlands there is much work to do in the affiliated teaching hospitals, and a more professional approach is urgently needed. Professionalism, learning goals, curricula planning, evidence-based teaching methods, and solutions for practical problems that interfere with the proper implementation of evidence-based learning should all be addressed. The ruling committee and the professional organizations have set outlines that meet the requirements of modern times, but the elaboration and implementation have yet to be realized.
The Free University Medical Centre has taken the lead by appointing medical specialists as full professors with a specific assignment for teaching in non-university hospitals in order to develop and promote the teaching facilities in those institutions. They elected practicing non-university medical specialists with a demonstrable record in the field of education and an academic background comparable to that of university professors. Their assignment is to teach for one day a week. By doing so, they are not only putting teaching more prominently on the agenda, but also opening career perspectives that will promote a broader involvement in the development of educational programs.
The teaching professors develop and implement modern medical curricula and collaborate on research projects to evaluate the effectiveness of the new curricula in clinical teaching. Teaching professors also form a bridge between the university and the affiliated hospitals by transferring knowledge and ideas on medical education from the university to the non-university teaching hospitals—and vice versa. They also have input in the development of preclinical and clinical education programs from the point of view of the non-university hospital. For instance, they take part in the curriculum committee that advises on the bachelor’s and master’s programs, and they help create tests for the assessment of knowledge.
Summary
Non-university teaching hospitals have an essential place in the clinical phase of the medical curriculum in the Netherlands. A paradigm shift from the old master-mate relationship toward a structured, competency-based curriculum is taking place. Nomination of teaching professors in these institutions helps to create the professional structure that is mandatory for quality improvement in clinical teaching, and it also promotes the required interaction between university and non-university hospitals. TH
A.B. Bijnen works at the Foreest Institute, Medical Centre Almaar, the Netherlands; F. Scheele works at Sint Lucas Andreas Ziekenhuis, Amsterdam, the Netherlands, and the Institute for Medical Education, Free University Medical Centre, Amsterdam, the Netherlands; A.E.R. Arnold also works at the Foreest Institute, as well as the Institute for Medical Education, Free University Medical Centre; A.M.J.J. Verweij works at the Sint Lucas Andreas Ziekenhuis, as well as the Institute for Medical Education at Free University Medical Centre; and H.J.M. van Rossum and J.A.A.M. van Diemen-Steenvoorde work at the Institute for Medical Education at Free University Medical Centre.
References
- Reason J. Human error: models and management. BMJ. 2000;320:768-770.
- Willems R. Sneller Beter—Hier werk je veilig, of je werkt hier niet. De veiligheid in de zorg. Eindrapportage Shell Nederland. November 2004.
- AMEE Education Guide No 14. Outcome-based education. 1999. ISBN: 1-903934-15-X.
- Metz JCM, Verbeek-Weel AMM, Huisjes HJ. Blueprint 2001: Training of doctors in The Netherlands. Adjusted objectives of undergraduate medical education in The Netherlands. Nijmegen: University Publication Office. 2001
- O’Connor HM, McGraw RC. Clinical skills training: developing objective assessment instruments. Med Educ. 1997;31:359-363.
- Davis MH, Harden RM. Competency-based assessment: making it a reality [editorial]. Med Teach. 2003;25:565-568.
A Trace of Improvement
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) has dramatically redesigned and improved the value of its accreditation process. The new process includes revised standards, a periodic performance review (PPR), new survey techniques, and a revised decision process.
Known as Shared Visions-New Pathways and implemented in 2004, this transformation of the accreditation process has shifted the emphasis from survey preparation to continuous improvement of operational systems that contribute directly to the delivery of safe, high-quality care. The emphasis of the revised accreditation process is on how healthcare organizations normally provide care and use JCAHO standards as a framework to deliver safe care on a daily basis. There is a significant focus on clinical care.
This article explores the two major parts of this revised accreditation process: the patient tracer methodology that guides the on-site survey and the PPR, a self-assessment tool that results in corrective action plans. (These are particularly relevant for the hospitalist.)
Patient Tracer Methodology and the Hospitalist
The patient tracer methodology provides a framework for JCAHO surveyors to assess standards compliance and patient safety during on-site surveys. The process involves interviewing the caregivers to evaluate the quality and safety of the patient care process. By evaluating the actual delivery of care services, less time is devoted to examining written policies and procedures. Surveyors use 50%-60% of their time tracing the care of randomly selected patients to learn how staff from various disciplines work together and communicate across departments to provide safe, high-quality care.
One way surveyors look at how hospitals deliver safe, high-quality care is to interview hospitalists and other staff physicians. In the patient tracer methodology, the surveyor selects a patient and uses that patient’s care record as a roadmap to assess and evaluate the services that the healthcare organization provides. This type of interaction, coupled with an emphasis on continual compliance with standards such as infection control and medication management (which address issues crucial to good outcomes for patients), is exactly what physicians have told JCAHO they desire from the accreditation process.
The goal is not for the hospitalist to memorize JCAHO standards, but instead to be able to discuss patient care systems and processes. This is already an area with which hospitalists are familiar. Hospitalists are a vital part of the organizational structure and play a large role within the care systems. Hospitalists can help surveyors understand processes used within their healthcare organizations.
How Patient Tracers Work
Surveyors begin the patient tracer by starting where the patient is currently located. They then move to where the patient first entered the organization, and to any areas in the organization where the patient received care. Each tracer takes from one hour to three hours to complete. A three-day survey includes an average of 11 individual tracers.
For example, a surveyor might select a patient admitted to a hospital’s emergency department with cardiac disease. The patient went to cardiac cath, to the operating room for a CABG, and then to the intensive care unit. The patient had complications and ventilator-associated pneumonia. The surveyor would trace the patient’s path through the emergency department, cardiac cath area, operating room, post-anesthesia care unit, and intensive care unit.
The surveyor might focus on how each of these departments assessed the patient, obtained a medical history, developed the care plan, provided treatment, and addressed issues related to infection control. The surveyor also would return to the unit where the patient resides to discuss the findings as they explore the care processes. It may be that a new theme or area of focus—such as assessment and care/services—emerges from this tracer process. The surveyor would then explore this new area more thoroughly and ask other surveyors at the hospital to explore assessment and care/services in their tracers to determine if similar findings exist in other tracer patients.
Surveyors also may use the tracer methodology to examine how National Patient Safety Goals are addressed. On the surgical unit, a surveyor may observe a nurse giving medications ordered by the hospitalist. The surveyor would spend time talking with the nurse and hospitalist about the patient selected for the tracer, perhaps asking for the unique identifiers used for the patient. Other queries may include: What is the patient’s diagnosis? How is the hospitalist caring for this patient? What was the admission date? The surveyor would note whether any of the “do not use” abbreviations related to medications are used and talk with the hospitalist about this issue. How are healthcare-acquired infections addressed?
The patient tracer process takes surveyors across a wide variety of departments and involves practitioners and other caregivers in the accreditation process, asking them to describe how they carried out their work. Instead of asking the hospitalist about particular standards, surveyors explain the purpose of the tracer and engage in an educational as well as an evaluative process. This approach moves the on-site survey away from high-level conferences with administrators about policies and procedures to focused discussions with those actually delivering care. The idea is to create an atmosphere that allows for an open exchange of information and ideas between surveyors and the hospitalist and other staff.
These discussions with hospitalists, other staff, and patients—combined with review of clinical charts and the observations of surveyors—make for a dynamic survey process that provides a complete picture of an organization’s processes and services. In other words, the tracers allow surveyors to “see” care or services through the eyes of patients and staff and then analyze the systems for providing that care, treatment, or services.
As surveyors use the tracer methodology to determine standards of compliance as they relate to care delivered to individual patients, they also assess organizational systems by conducting patient-system tracers. The concept behind the patient-system tracers methodology, which focuses on high-risk processes across an organization, is to test the strength of the chain of operations and processes. By examining a set of components that work together toward a common goal, the surveyor can evaluate its level of efficiency and the ways in which an organization’s systems function. This approach addresses the interrelationships of the many elements that go into delivering safe, high-quality care and translates standards compliance issues into potential organization-wide vulnerabilities.
The system tracers provide a forum for discussion of important topics related to the safety and quality of care at the organization level. Surveyors use the system tracers to understand organization findings and to facilitate an exchange of educational information on key topics such as data use for infection control and medication management.
While some of the patient system tracer activities consist of formal interviews, an interactive session, which involves a surveyor and relevant staff members, is an important component of the process. Discussions in this interactive session with the hospitalist and other staff include:
- The flow of the processes, including identification and management of risk points, integration of key activities, and communication among staff/units involved in the process;
- Strengths in the processes and possible actions to be taken in areas needing improvement;
- Issues requiring further exploration in other survey activities; and
- A baseline assessment of standards compliance.
PPR and the Hospitalist
Beyond the onsite survey, JCAHO’s accreditation process is designed to help organizations maintain continuous compliance with the standards and use them as a daily management tool for improving patient care and safety. This represents a paradigm shift for the hospitalist, who may be more accustomed to organizations ramping up before an on-site survey. This frenzy of activity prior to an on-site survey did not meet the goals of JCAHO accreditation in that it drew physicians and staff away from providing care and managing performance improvement over time.
The PPR is a new form of evaluation conducted by the organization to assess its level of compliance with standards. This comprehensive, self-directed review provides the framework for continuous standards compliance and focuses on the critical systems and processes that affect patient care and safety. By conducting the PPR annually, organizations can self-evaluate their compliance with all Accreditation Participation Requirements, Standards and Evidence of Performance; develop plans of action to address any identified opportunities for improvement; and implement those plans to improve care.
JCAHO requires that physicians at accredited hospitals be involved in the self-assessment component of the PPR and in developing plans of action. Each hospital must make its own determinations about how involved hospitalists and other physicians are with the PPR. JCAHO recognizes that hospitalists have limited time for performance improvement activities, but believes that their participation is crucial because of their commitment to providing care that results in positive outcomes for patients and reduces risk.
Patient Tracer Methodology and PPR in 2006
As part of changes to the accreditation process, JCAHO will shift from scheduled to unannounced on-site surveys. The transition to unannounced surveys began this year:
- To enhance the credibility of the accreditation process by ensuring that surveyors observe organization performance under normal circumstances;
- To help healthcare organizations focus on providing safe, high quality care at all times, and not just when preparing for survey;
- To reduce the unnecessary costs that healthcare organizations incur to prepare for survey; and
- To address public concerns that JCAHO receive an accurate reflection of the quality and safety of care.
The new accreditation process supports this transition by considering the information generated by the PPR. Organizations will be able to update the PPR, available on each organization’s extranet site, annually to support continuous performance improvement efforts.
JCAHO conducted pilot testing of the unannounced survey process in volunteer organizations during 2004 and 2005, giving its staff insight into real-life issues and concerns at accreditation organizations. JCAHO also worked closely with its various advisory groups, accredited organizations and other stakeholder groups to gain their input and smooth the transition to unannounced surveys.
Conclusion
The participation of the hospitalist in the JCAHO accreditation process is dependent upon common interests in improving healthcare quality and safety. JCAHO accreditation can be used to help the hospitalist and healthcare organizations meet their goals and responsibilities to individual patients. Accreditation activities can help to focus physician involvement in patient safety and other important areas, thus bringing increased relevance to the accreditation process.
In conclusion, the importance of the hospitalist to the JCAHO accreditation process on a continuous basis, not just during the on-site survey, is crucial. TH
Dr. Jacott was appointed a special advisor for professional relations to the Joint Commission in January 2002. As special advisor for professional relations, Dr. Jacott serves as the Joint Commission’s liaison to SHM.
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) has dramatically redesigned and improved the value of its accreditation process. The new process includes revised standards, a periodic performance review (PPR), new survey techniques, and a revised decision process.
Known as Shared Visions-New Pathways and implemented in 2004, this transformation of the accreditation process has shifted the emphasis from survey preparation to continuous improvement of operational systems that contribute directly to the delivery of safe, high-quality care. The emphasis of the revised accreditation process is on how healthcare organizations normally provide care and use JCAHO standards as a framework to deliver safe care on a daily basis. There is a significant focus on clinical care.
This article explores the two major parts of this revised accreditation process: the patient tracer methodology that guides the on-site survey and the PPR, a self-assessment tool that results in corrective action plans. (These are particularly relevant for the hospitalist.)
Patient Tracer Methodology and the Hospitalist
The patient tracer methodology provides a framework for JCAHO surveyors to assess standards compliance and patient safety during on-site surveys. The process involves interviewing the caregivers to evaluate the quality and safety of the patient care process. By evaluating the actual delivery of care services, less time is devoted to examining written policies and procedures. Surveyors use 50%-60% of their time tracing the care of randomly selected patients to learn how staff from various disciplines work together and communicate across departments to provide safe, high-quality care.
One way surveyors look at how hospitals deliver safe, high-quality care is to interview hospitalists and other staff physicians. In the patient tracer methodology, the surveyor selects a patient and uses that patient’s care record as a roadmap to assess and evaluate the services that the healthcare organization provides. This type of interaction, coupled with an emphasis on continual compliance with standards such as infection control and medication management (which address issues crucial to good outcomes for patients), is exactly what physicians have told JCAHO they desire from the accreditation process.
The goal is not for the hospitalist to memorize JCAHO standards, but instead to be able to discuss patient care systems and processes. This is already an area with which hospitalists are familiar. Hospitalists are a vital part of the organizational structure and play a large role within the care systems. Hospitalists can help surveyors understand processes used within their healthcare organizations.
How Patient Tracers Work
Surveyors begin the patient tracer by starting where the patient is currently located. They then move to where the patient first entered the organization, and to any areas in the organization where the patient received care. Each tracer takes from one hour to three hours to complete. A three-day survey includes an average of 11 individual tracers.
For example, a surveyor might select a patient admitted to a hospital’s emergency department with cardiac disease. The patient went to cardiac cath, to the operating room for a CABG, and then to the intensive care unit. The patient had complications and ventilator-associated pneumonia. The surveyor would trace the patient’s path through the emergency department, cardiac cath area, operating room, post-anesthesia care unit, and intensive care unit.
The surveyor might focus on how each of these departments assessed the patient, obtained a medical history, developed the care plan, provided treatment, and addressed issues related to infection control. The surveyor also would return to the unit where the patient resides to discuss the findings as they explore the care processes. It may be that a new theme or area of focus—such as assessment and care/services—emerges from this tracer process. The surveyor would then explore this new area more thoroughly and ask other surveyors at the hospital to explore assessment and care/services in their tracers to determine if similar findings exist in other tracer patients.
Surveyors also may use the tracer methodology to examine how National Patient Safety Goals are addressed. On the surgical unit, a surveyor may observe a nurse giving medications ordered by the hospitalist. The surveyor would spend time talking with the nurse and hospitalist about the patient selected for the tracer, perhaps asking for the unique identifiers used for the patient. Other queries may include: What is the patient’s diagnosis? How is the hospitalist caring for this patient? What was the admission date? The surveyor would note whether any of the “do not use” abbreviations related to medications are used and talk with the hospitalist about this issue. How are healthcare-acquired infections addressed?
The patient tracer process takes surveyors across a wide variety of departments and involves practitioners and other caregivers in the accreditation process, asking them to describe how they carried out their work. Instead of asking the hospitalist about particular standards, surveyors explain the purpose of the tracer and engage in an educational as well as an evaluative process. This approach moves the on-site survey away from high-level conferences with administrators about policies and procedures to focused discussions with those actually delivering care. The idea is to create an atmosphere that allows for an open exchange of information and ideas between surveyors and the hospitalist and other staff.
These discussions with hospitalists, other staff, and patients—combined with review of clinical charts and the observations of surveyors—make for a dynamic survey process that provides a complete picture of an organization’s processes and services. In other words, the tracers allow surveyors to “see” care or services through the eyes of patients and staff and then analyze the systems for providing that care, treatment, or services.
As surveyors use the tracer methodology to determine standards of compliance as they relate to care delivered to individual patients, they also assess organizational systems by conducting patient-system tracers. The concept behind the patient-system tracers methodology, which focuses on high-risk processes across an organization, is to test the strength of the chain of operations and processes. By examining a set of components that work together toward a common goal, the surveyor can evaluate its level of efficiency and the ways in which an organization’s systems function. This approach addresses the interrelationships of the many elements that go into delivering safe, high-quality care and translates standards compliance issues into potential organization-wide vulnerabilities.
The system tracers provide a forum for discussion of important topics related to the safety and quality of care at the organization level. Surveyors use the system tracers to understand organization findings and to facilitate an exchange of educational information on key topics such as data use for infection control and medication management.
While some of the patient system tracer activities consist of formal interviews, an interactive session, which involves a surveyor and relevant staff members, is an important component of the process. Discussions in this interactive session with the hospitalist and other staff include:
- The flow of the processes, including identification and management of risk points, integration of key activities, and communication among staff/units involved in the process;
- Strengths in the processes and possible actions to be taken in areas needing improvement;
- Issues requiring further exploration in other survey activities; and
- A baseline assessment of standards compliance.
PPR and the Hospitalist
Beyond the onsite survey, JCAHO’s accreditation process is designed to help organizations maintain continuous compliance with the standards and use them as a daily management tool for improving patient care and safety. This represents a paradigm shift for the hospitalist, who may be more accustomed to organizations ramping up before an on-site survey. This frenzy of activity prior to an on-site survey did not meet the goals of JCAHO accreditation in that it drew physicians and staff away from providing care and managing performance improvement over time.
The PPR is a new form of evaluation conducted by the organization to assess its level of compliance with standards. This comprehensive, self-directed review provides the framework for continuous standards compliance and focuses on the critical systems and processes that affect patient care and safety. By conducting the PPR annually, organizations can self-evaluate their compliance with all Accreditation Participation Requirements, Standards and Evidence of Performance; develop plans of action to address any identified opportunities for improvement; and implement those plans to improve care.
JCAHO requires that physicians at accredited hospitals be involved in the self-assessment component of the PPR and in developing plans of action. Each hospital must make its own determinations about how involved hospitalists and other physicians are with the PPR. JCAHO recognizes that hospitalists have limited time for performance improvement activities, but believes that their participation is crucial because of their commitment to providing care that results in positive outcomes for patients and reduces risk.
Patient Tracer Methodology and PPR in 2006
As part of changes to the accreditation process, JCAHO will shift from scheduled to unannounced on-site surveys. The transition to unannounced surveys began this year:
- To enhance the credibility of the accreditation process by ensuring that surveyors observe organization performance under normal circumstances;
- To help healthcare organizations focus on providing safe, high quality care at all times, and not just when preparing for survey;
- To reduce the unnecessary costs that healthcare organizations incur to prepare for survey; and
- To address public concerns that JCAHO receive an accurate reflection of the quality and safety of care.
The new accreditation process supports this transition by considering the information generated by the PPR. Organizations will be able to update the PPR, available on each organization’s extranet site, annually to support continuous performance improvement efforts.
JCAHO conducted pilot testing of the unannounced survey process in volunteer organizations during 2004 and 2005, giving its staff insight into real-life issues and concerns at accreditation organizations. JCAHO also worked closely with its various advisory groups, accredited organizations and other stakeholder groups to gain their input and smooth the transition to unannounced surveys.
Conclusion
The participation of the hospitalist in the JCAHO accreditation process is dependent upon common interests in improving healthcare quality and safety. JCAHO accreditation can be used to help the hospitalist and healthcare organizations meet their goals and responsibilities to individual patients. Accreditation activities can help to focus physician involvement in patient safety and other important areas, thus bringing increased relevance to the accreditation process.
In conclusion, the importance of the hospitalist to the JCAHO accreditation process on a continuous basis, not just during the on-site survey, is crucial. TH
Dr. Jacott was appointed a special advisor for professional relations to the Joint Commission in January 2002. As special advisor for professional relations, Dr. Jacott serves as the Joint Commission’s liaison to SHM.
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) has dramatically redesigned and improved the value of its accreditation process. The new process includes revised standards, a periodic performance review (PPR), new survey techniques, and a revised decision process.
Known as Shared Visions-New Pathways and implemented in 2004, this transformation of the accreditation process has shifted the emphasis from survey preparation to continuous improvement of operational systems that contribute directly to the delivery of safe, high-quality care. The emphasis of the revised accreditation process is on how healthcare organizations normally provide care and use JCAHO standards as a framework to deliver safe care on a daily basis. There is a significant focus on clinical care.
This article explores the two major parts of this revised accreditation process: the patient tracer methodology that guides the on-site survey and the PPR, a self-assessment tool that results in corrective action plans. (These are particularly relevant for the hospitalist.)
Patient Tracer Methodology and the Hospitalist
The patient tracer methodology provides a framework for JCAHO surveyors to assess standards compliance and patient safety during on-site surveys. The process involves interviewing the caregivers to evaluate the quality and safety of the patient care process. By evaluating the actual delivery of care services, less time is devoted to examining written policies and procedures. Surveyors use 50%-60% of their time tracing the care of randomly selected patients to learn how staff from various disciplines work together and communicate across departments to provide safe, high-quality care.
One way surveyors look at how hospitals deliver safe, high-quality care is to interview hospitalists and other staff physicians. In the patient tracer methodology, the surveyor selects a patient and uses that patient’s care record as a roadmap to assess and evaluate the services that the healthcare organization provides. This type of interaction, coupled with an emphasis on continual compliance with standards such as infection control and medication management (which address issues crucial to good outcomes for patients), is exactly what physicians have told JCAHO they desire from the accreditation process.
The goal is not for the hospitalist to memorize JCAHO standards, but instead to be able to discuss patient care systems and processes. This is already an area with which hospitalists are familiar. Hospitalists are a vital part of the organizational structure and play a large role within the care systems. Hospitalists can help surveyors understand processes used within their healthcare organizations.
How Patient Tracers Work
Surveyors begin the patient tracer by starting where the patient is currently located. They then move to where the patient first entered the organization, and to any areas in the organization where the patient received care. Each tracer takes from one hour to three hours to complete. A three-day survey includes an average of 11 individual tracers.
For example, a surveyor might select a patient admitted to a hospital’s emergency department with cardiac disease. The patient went to cardiac cath, to the operating room for a CABG, and then to the intensive care unit. The patient had complications and ventilator-associated pneumonia. The surveyor would trace the patient’s path through the emergency department, cardiac cath area, operating room, post-anesthesia care unit, and intensive care unit.
The surveyor might focus on how each of these departments assessed the patient, obtained a medical history, developed the care plan, provided treatment, and addressed issues related to infection control. The surveyor also would return to the unit where the patient resides to discuss the findings as they explore the care processes. It may be that a new theme or area of focus—such as assessment and care/services—emerges from this tracer process. The surveyor would then explore this new area more thoroughly and ask other surveyors at the hospital to explore assessment and care/services in their tracers to determine if similar findings exist in other tracer patients.
Surveyors also may use the tracer methodology to examine how National Patient Safety Goals are addressed. On the surgical unit, a surveyor may observe a nurse giving medications ordered by the hospitalist. The surveyor would spend time talking with the nurse and hospitalist about the patient selected for the tracer, perhaps asking for the unique identifiers used for the patient. Other queries may include: What is the patient’s diagnosis? How is the hospitalist caring for this patient? What was the admission date? The surveyor would note whether any of the “do not use” abbreviations related to medications are used and talk with the hospitalist about this issue. How are healthcare-acquired infections addressed?
The patient tracer process takes surveyors across a wide variety of departments and involves practitioners and other caregivers in the accreditation process, asking them to describe how they carried out their work. Instead of asking the hospitalist about particular standards, surveyors explain the purpose of the tracer and engage in an educational as well as an evaluative process. This approach moves the on-site survey away from high-level conferences with administrators about policies and procedures to focused discussions with those actually delivering care. The idea is to create an atmosphere that allows for an open exchange of information and ideas between surveyors and the hospitalist and other staff.
These discussions with hospitalists, other staff, and patients—combined with review of clinical charts and the observations of surveyors—make for a dynamic survey process that provides a complete picture of an organization’s processes and services. In other words, the tracers allow surveyors to “see” care or services through the eyes of patients and staff and then analyze the systems for providing that care, treatment, or services.
As surveyors use the tracer methodology to determine standards of compliance as they relate to care delivered to individual patients, they also assess organizational systems by conducting patient-system tracers. The concept behind the patient-system tracers methodology, which focuses on high-risk processes across an organization, is to test the strength of the chain of operations and processes. By examining a set of components that work together toward a common goal, the surveyor can evaluate its level of efficiency and the ways in which an organization’s systems function. This approach addresses the interrelationships of the many elements that go into delivering safe, high-quality care and translates standards compliance issues into potential organization-wide vulnerabilities.
The system tracers provide a forum for discussion of important topics related to the safety and quality of care at the organization level. Surveyors use the system tracers to understand organization findings and to facilitate an exchange of educational information on key topics such as data use for infection control and medication management.
While some of the patient system tracer activities consist of formal interviews, an interactive session, which involves a surveyor and relevant staff members, is an important component of the process. Discussions in this interactive session with the hospitalist and other staff include:
- The flow of the processes, including identification and management of risk points, integration of key activities, and communication among staff/units involved in the process;
- Strengths in the processes and possible actions to be taken in areas needing improvement;
- Issues requiring further exploration in other survey activities; and
- A baseline assessment of standards compliance.
PPR and the Hospitalist
Beyond the onsite survey, JCAHO’s accreditation process is designed to help organizations maintain continuous compliance with the standards and use them as a daily management tool for improving patient care and safety. This represents a paradigm shift for the hospitalist, who may be more accustomed to organizations ramping up before an on-site survey. This frenzy of activity prior to an on-site survey did not meet the goals of JCAHO accreditation in that it drew physicians and staff away from providing care and managing performance improvement over time.
The PPR is a new form of evaluation conducted by the organization to assess its level of compliance with standards. This comprehensive, self-directed review provides the framework for continuous standards compliance and focuses on the critical systems and processes that affect patient care and safety. By conducting the PPR annually, organizations can self-evaluate their compliance with all Accreditation Participation Requirements, Standards and Evidence of Performance; develop plans of action to address any identified opportunities for improvement; and implement those plans to improve care.
JCAHO requires that physicians at accredited hospitals be involved in the self-assessment component of the PPR and in developing plans of action. Each hospital must make its own determinations about how involved hospitalists and other physicians are with the PPR. JCAHO recognizes that hospitalists have limited time for performance improvement activities, but believes that their participation is crucial because of their commitment to providing care that results in positive outcomes for patients and reduces risk.
Patient Tracer Methodology and PPR in 2006
As part of changes to the accreditation process, JCAHO will shift from scheduled to unannounced on-site surveys. The transition to unannounced surveys began this year:
- To enhance the credibility of the accreditation process by ensuring that surveyors observe organization performance under normal circumstances;
- To help healthcare organizations focus on providing safe, high quality care at all times, and not just when preparing for survey;
- To reduce the unnecessary costs that healthcare organizations incur to prepare for survey; and
- To address public concerns that JCAHO receive an accurate reflection of the quality and safety of care.
The new accreditation process supports this transition by considering the information generated by the PPR. Organizations will be able to update the PPR, available on each organization’s extranet site, annually to support continuous performance improvement efforts.
JCAHO conducted pilot testing of the unannounced survey process in volunteer organizations during 2004 and 2005, giving its staff insight into real-life issues and concerns at accreditation organizations. JCAHO also worked closely with its various advisory groups, accredited organizations and other stakeholder groups to gain their input and smooth the transition to unannounced surveys.
Conclusion
The participation of the hospitalist in the JCAHO accreditation process is dependent upon common interests in improving healthcare quality and safety. JCAHO accreditation can be used to help the hospitalist and healthcare organizations meet their goals and responsibilities to individual patients. Accreditation activities can help to focus physician involvement in patient safety and other important areas, thus bringing increased relevance to the accreditation process.
In conclusion, the importance of the hospitalist to the JCAHO accreditation process on a continuous basis, not just during the on-site survey, is crucial. TH
Dr. Jacott was appointed a special advisor for professional relations to the Joint Commission in January 2002. As special advisor for professional relations, Dr. Jacott serves as the Joint Commission’s liaison to SHM.
A Midwest Partnership
Quite likely things are different in Minnesota than they are on either coast. People are polite, know how to work together, and are respectful about consuming resources. Or as Tom Anderson, MD, a HealthPartners Medical Group (HPMG) hospitalist says: “In Minnesota affable usually beats good.” Fortunately, the 25 physician members of the hospitalist team who belong to the 580-member HPMG, are beyond affable and good. By many measures they are excellent, and they are shaping the field of hospital medicine.
At the heart of the HPMG hospitalist program’s quality are its people. Burke Kealey, MD, HPMG’s assistant medical director, helped start the program in 1997, recruiting young, energetic, and personable physicians who liked practicing big city hospital medicine, Midwestern style. “Our hospitalist program was one of the early ones operating before the term ‘hospitalist’ was well-known,” says Dr. Kealey.
The hospitalists are employed neither by an academic medical nor a community hospital. Instead, they are members of a 580-multispecialty physician group that anchors HealthPartners Network, an organization that consistently ranks among The National Committee for Quality Assurance’s (NCQA) top five health plans regionally and top 10 nationally. Yet excellence has its price, as the perverse incentives of the U.S. healthcare system reveal. Mary Brainerd, HealthPartner’s CEO, comments that although the company consistently ranks high, it gets paid thousands of dollars less per patient by Medicare than poor performing plans.
“The way Medicare is set up, it actually punishes you for being good,” says Brainerd, referring to Medicare’s rules that qualify hospitals to receive additional payments each time a patient returns for more treatment—even if their return was caused by sub-par diagnosis and treatment. Under Medicare’s incentives, hospitals and doctors who order unnecessary tests, provide poor care, or even make patients worse often receive higher payments than those who provide efficient, high-quality care. That doesn’t stop HPMG from doing things correctly.
With the physician group employing both clinic and inpatient physicians, it’s more straightforward getting metrics and incentives aligned than in a healthcare environment where the outpatient physician’s loss may be the hospitalist’s gain—or vice versa. “Working closely with clinic and ER doctors decreases length of stay, improves clinical outcomes, and decreases costs,” says Dr. Kealey. “That helps the whole medical group.”
Another major contributor to clinical excellence goes beyond HPMG. Using the Minnesota mindset, HPMG’s physicians work with the area’s other medical heavyweights, the Mayo Clinic (Rochester, Minn.) and the Allina Medical Group (Minneapolis), forging a consensus on best practices and evidence-based guidelines (www.icsi.org). An example of HPMG’s outpatient and inpatient physician collaboration is their approach to CHF. After both groups tackled the job of operationalizing “perfect” CHF care in a one-day Rapid Design Workshop, “perfect treatment” outcomes rose from 22% in January 2005 to 50% in March 2005.
Nuts and Bolts
Scheduling logistics is among the challenges a hospitalist program’s manager faces, and Dr. Kealey and his colleagues have—through experience—done well. Each hospitalist selects a block schedule (either one week on, one week off or 14 days straight for 24 weeks). They also serve two night shift weeks (6 p.m.—8 a.m.), although residents run things at night. Hospitalists reconfigure their schedules every six months, helping to avoid burnout. Geographic deployment is another energy saver. Each hospitalist works in one or two units, allowing them to know patients, family, and the nursing staff well. It also cuts the nine-story hospital down to a size.
To communicate effectively, physicians use electronic technology. Voice pagers connect all HPMG physicians. Other devices sound alerts, allow for co-management of patients with chronic diseases, quick referrals to specialists within the group, in-box messaging, and a discharge summary to the primary physician in six to eight hours.
As for compensation, physicians receive a base salary, set at 80% of SHM’s annual average for the Midwest, accounting for 65% of pay. Of the balance, productivity as measured by relative value units (RVUs) accounts for 40%, with 20% each for high marks on patient and provider satisfaction surveys, and the medical director’s discretion.
Myriad Opportunities
The HPMG hospitalist program offers opportunities to pursue many professional paths, as its SHM award roster shows. SHM’s Award for Outstanding Service in Clinical Medicine to HPMG Hospitalists have included:
- 2002 Rusty Holman, Outstanding Service in Hospital Medicine;
- 2003 Burke Kealey, Clinical Excellence; and
- 2005 Shaun Frost, Clinical Excellence.
Adding depth to the program involves embracing physicians on unusual career paths, such as Tom Anderson, MD, one of HPMG’s family practice hospitalists. After finishing training at Ramsey County Hospital of St. Paul, Minn., which became Regions Hospital in 1997 (and where Dr. Kealey also trained), Dr. Anderson joined a seven-doctor rural practice in Iron Range, Wis.
“It was in a hard-working blue collar town, and we were throwbacks,” says Dr. Anderson, “doing all our own obstetrics, covering the ER, helping surgeons. I was a real person in that community. Everyone knew each other from the church or hardware store.” If the doctors wanted to change anything, they talked over doughnuts and coffee, deciding how it would affect them and their patients. Dr. Anderson loved the work, but wanted more family time than the all-consuming rural practice allowed.
A recruiting call from Dr. Kealey changed everything. Dr. Kealey calls Dr. Anderson “a bright and shining star, someone who sits in the front row and asks all the questions.”
Dr. Anderson joined HPMG’s hospitalist team in 2004, enjoying the one-week-on/one-week-off schedule and the continuity of care afforded by a large team. “This is a big busy hospital,” he says. “The patients are really sick, and we plan our 12-hour shift around them.” He starts with a 7 a.m. huddle of nurses and physicians to plan the day by prioritizing patient needs, reviewing orders, arranging time to talk to specialists, and visiting all patients. “By 9 a.m. we’ve planned the day, including 3 p.m. patient discharges. I like prioritizing what has to be done, and defining what has to be fixed.”
Rick Hilger, MD, board certified in internal medicine and pediatrics, is on another mission. After residency at the University of Minnesota Medical School (Duluth), he became Regions Hospital’s chief resident and then stayed on. He wanted a pediatrics hospitalist practice, which proved impractical because 95% of Regions’ pediatric cases now go to another hospital. “Down the line I’d like a 50/50 adult/peds mix, but that’s hard to accomplish in a hospitalist program,” he says.
Still looking for a challenge, Dr. Hilger chose the Institute for Healthcare Improvement’s “100K Lives” initiative, becoming the lead physician for Region’s rapid response team to prevent unnecessary code-blue calls. With the hospitalists’ geographic deployment to specific units that meant planning who would respond to codes and how that would be communicated. Dr. Hilger encouraged administration to hire full-time employees to field a rapid response team and created a pre-code team.
“At least 30%-40% of patients code outside the ICU,” he says. “We’ve observed that they often have unstable vital signs six to eight hours before coding. We’ve cut through administrative minutiae and red tape so that patients don’t sit there with unstable vitals for long.”
The pre-code team—an ICU trained nurse and respiratory therapist—are alerted to those signs and respond in five minutes or less, 24/7. The rest of the team is alerted via pagers, with hospitalists fielding an average of three calls per day.
Other hospitalists find their special niches. Shaun Frost, MD, is breaking ground in peri-surgical care in orthopedics, urology and neurology, and is active in process improvement teams. Howard Epstein, MD, leads the palliative care team, while John Degelau, MD, chief of hospital medical at North Memorial, pursues his interest in geriatrics. Rich Mahr, MD, is the physician champion for electronic health records.
So being an HPMG hospitalist allows physicians to pursue many avenues of clinical and process improvement, including national initiatives and teaching. Dr. Anderson sums up what HPMG is about: “I joined this group because of its passion for medicine. When we get older we’ll look back and say that we had our moment, our time to give it 100%.”
Dr. Kealey calls them “an energized creative group. Everyone wants to go to national meetings and to keep ahead of the pack, to ask what’s next to learn?” TH
Writer Marlene Piturro regularly writes practice profiles for The Hospitalist.
Quite likely things are different in Minnesota than they are on either coast. People are polite, know how to work together, and are respectful about consuming resources. Or as Tom Anderson, MD, a HealthPartners Medical Group (HPMG) hospitalist says: “In Minnesota affable usually beats good.” Fortunately, the 25 physician members of the hospitalist team who belong to the 580-member HPMG, are beyond affable and good. By many measures they are excellent, and they are shaping the field of hospital medicine.
At the heart of the HPMG hospitalist program’s quality are its people. Burke Kealey, MD, HPMG’s assistant medical director, helped start the program in 1997, recruiting young, energetic, and personable physicians who liked practicing big city hospital medicine, Midwestern style. “Our hospitalist program was one of the early ones operating before the term ‘hospitalist’ was well-known,” says Dr. Kealey.
The hospitalists are employed neither by an academic medical nor a community hospital. Instead, they are members of a 580-multispecialty physician group that anchors HealthPartners Network, an organization that consistently ranks among The National Committee for Quality Assurance’s (NCQA) top five health plans regionally and top 10 nationally. Yet excellence has its price, as the perverse incentives of the U.S. healthcare system reveal. Mary Brainerd, HealthPartner’s CEO, comments that although the company consistently ranks high, it gets paid thousands of dollars less per patient by Medicare than poor performing plans.
“The way Medicare is set up, it actually punishes you for being good,” says Brainerd, referring to Medicare’s rules that qualify hospitals to receive additional payments each time a patient returns for more treatment—even if their return was caused by sub-par diagnosis and treatment. Under Medicare’s incentives, hospitals and doctors who order unnecessary tests, provide poor care, or even make patients worse often receive higher payments than those who provide efficient, high-quality care. That doesn’t stop HPMG from doing things correctly.
With the physician group employing both clinic and inpatient physicians, it’s more straightforward getting metrics and incentives aligned than in a healthcare environment where the outpatient physician’s loss may be the hospitalist’s gain—or vice versa. “Working closely with clinic and ER doctors decreases length of stay, improves clinical outcomes, and decreases costs,” says Dr. Kealey. “That helps the whole medical group.”
Another major contributor to clinical excellence goes beyond HPMG. Using the Minnesota mindset, HPMG’s physicians work with the area’s other medical heavyweights, the Mayo Clinic (Rochester, Minn.) and the Allina Medical Group (Minneapolis), forging a consensus on best practices and evidence-based guidelines (www.icsi.org). An example of HPMG’s outpatient and inpatient physician collaboration is their approach to CHF. After both groups tackled the job of operationalizing “perfect” CHF care in a one-day Rapid Design Workshop, “perfect treatment” outcomes rose from 22% in January 2005 to 50% in March 2005.
Nuts and Bolts
Scheduling logistics is among the challenges a hospitalist program’s manager faces, and Dr. Kealey and his colleagues have—through experience—done well. Each hospitalist selects a block schedule (either one week on, one week off or 14 days straight for 24 weeks). They also serve two night shift weeks (6 p.m.—8 a.m.), although residents run things at night. Hospitalists reconfigure their schedules every six months, helping to avoid burnout. Geographic deployment is another energy saver. Each hospitalist works in one or two units, allowing them to know patients, family, and the nursing staff well. It also cuts the nine-story hospital down to a size.
To communicate effectively, physicians use electronic technology. Voice pagers connect all HPMG physicians. Other devices sound alerts, allow for co-management of patients with chronic diseases, quick referrals to specialists within the group, in-box messaging, and a discharge summary to the primary physician in six to eight hours.
As for compensation, physicians receive a base salary, set at 80% of SHM’s annual average for the Midwest, accounting for 65% of pay. Of the balance, productivity as measured by relative value units (RVUs) accounts for 40%, with 20% each for high marks on patient and provider satisfaction surveys, and the medical director’s discretion.
Myriad Opportunities
The HPMG hospitalist program offers opportunities to pursue many professional paths, as its SHM award roster shows. SHM’s Award for Outstanding Service in Clinical Medicine to HPMG Hospitalists have included:
- 2002 Rusty Holman, Outstanding Service in Hospital Medicine;
- 2003 Burke Kealey, Clinical Excellence; and
- 2005 Shaun Frost, Clinical Excellence.
Adding depth to the program involves embracing physicians on unusual career paths, such as Tom Anderson, MD, one of HPMG’s family practice hospitalists. After finishing training at Ramsey County Hospital of St. Paul, Minn., which became Regions Hospital in 1997 (and where Dr. Kealey also trained), Dr. Anderson joined a seven-doctor rural practice in Iron Range, Wis.
“It was in a hard-working blue collar town, and we were throwbacks,” says Dr. Anderson, “doing all our own obstetrics, covering the ER, helping surgeons. I was a real person in that community. Everyone knew each other from the church or hardware store.” If the doctors wanted to change anything, they talked over doughnuts and coffee, deciding how it would affect them and their patients. Dr. Anderson loved the work, but wanted more family time than the all-consuming rural practice allowed.
A recruiting call from Dr. Kealey changed everything. Dr. Kealey calls Dr. Anderson “a bright and shining star, someone who sits in the front row and asks all the questions.”
Dr. Anderson joined HPMG’s hospitalist team in 2004, enjoying the one-week-on/one-week-off schedule and the continuity of care afforded by a large team. “This is a big busy hospital,” he says. “The patients are really sick, and we plan our 12-hour shift around them.” He starts with a 7 a.m. huddle of nurses and physicians to plan the day by prioritizing patient needs, reviewing orders, arranging time to talk to specialists, and visiting all patients. “By 9 a.m. we’ve planned the day, including 3 p.m. patient discharges. I like prioritizing what has to be done, and defining what has to be fixed.”
Rick Hilger, MD, board certified in internal medicine and pediatrics, is on another mission. After residency at the University of Minnesota Medical School (Duluth), he became Regions Hospital’s chief resident and then stayed on. He wanted a pediatrics hospitalist practice, which proved impractical because 95% of Regions’ pediatric cases now go to another hospital. “Down the line I’d like a 50/50 adult/peds mix, but that’s hard to accomplish in a hospitalist program,” he says.
Still looking for a challenge, Dr. Hilger chose the Institute for Healthcare Improvement’s “100K Lives” initiative, becoming the lead physician for Region’s rapid response team to prevent unnecessary code-blue calls. With the hospitalists’ geographic deployment to specific units that meant planning who would respond to codes and how that would be communicated. Dr. Hilger encouraged administration to hire full-time employees to field a rapid response team and created a pre-code team.
“At least 30%-40% of patients code outside the ICU,” he says. “We’ve observed that they often have unstable vital signs six to eight hours before coding. We’ve cut through administrative minutiae and red tape so that patients don’t sit there with unstable vitals for long.”
The pre-code team—an ICU trained nurse and respiratory therapist—are alerted to those signs and respond in five minutes or less, 24/7. The rest of the team is alerted via pagers, with hospitalists fielding an average of three calls per day.
Other hospitalists find their special niches. Shaun Frost, MD, is breaking ground in peri-surgical care in orthopedics, urology and neurology, and is active in process improvement teams. Howard Epstein, MD, leads the palliative care team, while John Degelau, MD, chief of hospital medical at North Memorial, pursues his interest in geriatrics. Rich Mahr, MD, is the physician champion for electronic health records.
So being an HPMG hospitalist allows physicians to pursue many avenues of clinical and process improvement, including national initiatives and teaching. Dr. Anderson sums up what HPMG is about: “I joined this group because of its passion for medicine. When we get older we’ll look back and say that we had our moment, our time to give it 100%.”
Dr. Kealey calls them “an energized creative group. Everyone wants to go to national meetings and to keep ahead of the pack, to ask what’s next to learn?” TH
Writer Marlene Piturro regularly writes practice profiles for The Hospitalist.
Quite likely things are different in Minnesota than they are on either coast. People are polite, know how to work together, and are respectful about consuming resources. Or as Tom Anderson, MD, a HealthPartners Medical Group (HPMG) hospitalist says: “In Minnesota affable usually beats good.” Fortunately, the 25 physician members of the hospitalist team who belong to the 580-member HPMG, are beyond affable and good. By many measures they are excellent, and they are shaping the field of hospital medicine.
At the heart of the HPMG hospitalist program’s quality are its people. Burke Kealey, MD, HPMG’s assistant medical director, helped start the program in 1997, recruiting young, energetic, and personable physicians who liked practicing big city hospital medicine, Midwestern style. “Our hospitalist program was one of the early ones operating before the term ‘hospitalist’ was well-known,” says Dr. Kealey.
The hospitalists are employed neither by an academic medical nor a community hospital. Instead, they are members of a 580-multispecialty physician group that anchors HealthPartners Network, an organization that consistently ranks among The National Committee for Quality Assurance’s (NCQA) top five health plans regionally and top 10 nationally. Yet excellence has its price, as the perverse incentives of the U.S. healthcare system reveal. Mary Brainerd, HealthPartner’s CEO, comments that although the company consistently ranks high, it gets paid thousands of dollars less per patient by Medicare than poor performing plans.
“The way Medicare is set up, it actually punishes you for being good,” says Brainerd, referring to Medicare’s rules that qualify hospitals to receive additional payments each time a patient returns for more treatment—even if their return was caused by sub-par diagnosis and treatment. Under Medicare’s incentives, hospitals and doctors who order unnecessary tests, provide poor care, or even make patients worse often receive higher payments than those who provide efficient, high-quality care. That doesn’t stop HPMG from doing things correctly.
With the physician group employing both clinic and inpatient physicians, it’s more straightforward getting metrics and incentives aligned than in a healthcare environment where the outpatient physician’s loss may be the hospitalist’s gain—or vice versa. “Working closely with clinic and ER doctors decreases length of stay, improves clinical outcomes, and decreases costs,” says Dr. Kealey. “That helps the whole medical group.”
Another major contributor to clinical excellence goes beyond HPMG. Using the Minnesota mindset, HPMG’s physicians work with the area’s other medical heavyweights, the Mayo Clinic (Rochester, Minn.) and the Allina Medical Group (Minneapolis), forging a consensus on best practices and evidence-based guidelines (www.icsi.org). An example of HPMG’s outpatient and inpatient physician collaboration is their approach to CHF. After both groups tackled the job of operationalizing “perfect” CHF care in a one-day Rapid Design Workshop, “perfect treatment” outcomes rose from 22% in January 2005 to 50% in March 2005.
Nuts and Bolts
Scheduling logistics is among the challenges a hospitalist program’s manager faces, and Dr. Kealey and his colleagues have—through experience—done well. Each hospitalist selects a block schedule (either one week on, one week off or 14 days straight for 24 weeks). They also serve two night shift weeks (6 p.m.—8 a.m.), although residents run things at night. Hospitalists reconfigure their schedules every six months, helping to avoid burnout. Geographic deployment is another energy saver. Each hospitalist works in one or two units, allowing them to know patients, family, and the nursing staff well. It also cuts the nine-story hospital down to a size.
To communicate effectively, physicians use electronic technology. Voice pagers connect all HPMG physicians. Other devices sound alerts, allow for co-management of patients with chronic diseases, quick referrals to specialists within the group, in-box messaging, and a discharge summary to the primary physician in six to eight hours.
As for compensation, physicians receive a base salary, set at 80% of SHM’s annual average for the Midwest, accounting for 65% of pay. Of the balance, productivity as measured by relative value units (RVUs) accounts for 40%, with 20% each for high marks on patient and provider satisfaction surveys, and the medical director’s discretion.
Myriad Opportunities
The HPMG hospitalist program offers opportunities to pursue many professional paths, as its SHM award roster shows. SHM’s Award for Outstanding Service in Clinical Medicine to HPMG Hospitalists have included:
- 2002 Rusty Holman, Outstanding Service in Hospital Medicine;
- 2003 Burke Kealey, Clinical Excellence; and
- 2005 Shaun Frost, Clinical Excellence.
Adding depth to the program involves embracing physicians on unusual career paths, such as Tom Anderson, MD, one of HPMG’s family practice hospitalists. After finishing training at Ramsey County Hospital of St. Paul, Minn., which became Regions Hospital in 1997 (and where Dr. Kealey also trained), Dr. Anderson joined a seven-doctor rural practice in Iron Range, Wis.
“It was in a hard-working blue collar town, and we were throwbacks,” says Dr. Anderson, “doing all our own obstetrics, covering the ER, helping surgeons. I was a real person in that community. Everyone knew each other from the church or hardware store.” If the doctors wanted to change anything, they talked over doughnuts and coffee, deciding how it would affect them and their patients. Dr. Anderson loved the work, but wanted more family time than the all-consuming rural practice allowed.
A recruiting call from Dr. Kealey changed everything. Dr. Kealey calls Dr. Anderson “a bright and shining star, someone who sits in the front row and asks all the questions.”
Dr. Anderson joined HPMG’s hospitalist team in 2004, enjoying the one-week-on/one-week-off schedule and the continuity of care afforded by a large team. “This is a big busy hospital,” he says. “The patients are really sick, and we plan our 12-hour shift around them.” He starts with a 7 a.m. huddle of nurses and physicians to plan the day by prioritizing patient needs, reviewing orders, arranging time to talk to specialists, and visiting all patients. “By 9 a.m. we’ve planned the day, including 3 p.m. patient discharges. I like prioritizing what has to be done, and defining what has to be fixed.”
Rick Hilger, MD, board certified in internal medicine and pediatrics, is on another mission. After residency at the University of Minnesota Medical School (Duluth), he became Regions Hospital’s chief resident and then stayed on. He wanted a pediatrics hospitalist practice, which proved impractical because 95% of Regions’ pediatric cases now go to another hospital. “Down the line I’d like a 50/50 adult/peds mix, but that’s hard to accomplish in a hospitalist program,” he says.
Still looking for a challenge, Dr. Hilger chose the Institute for Healthcare Improvement’s “100K Lives” initiative, becoming the lead physician for Region’s rapid response team to prevent unnecessary code-blue calls. With the hospitalists’ geographic deployment to specific units that meant planning who would respond to codes and how that would be communicated. Dr. Hilger encouraged administration to hire full-time employees to field a rapid response team and created a pre-code team.
“At least 30%-40% of patients code outside the ICU,” he says. “We’ve observed that they often have unstable vital signs six to eight hours before coding. We’ve cut through administrative minutiae and red tape so that patients don’t sit there with unstable vitals for long.”
The pre-code team—an ICU trained nurse and respiratory therapist—are alerted to those signs and respond in five minutes or less, 24/7. The rest of the team is alerted via pagers, with hospitalists fielding an average of three calls per day.
Other hospitalists find their special niches. Shaun Frost, MD, is breaking ground in peri-surgical care in orthopedics, urology and neurology, and is active in process improvement teams. Howard Epstein, MD, leads the palliative care team, while John Degelau, MD, chief of hospital medical at North Memorial, pursues his interest in geriatrics. Rich Mahr, MD, is the physician champion for electronic health records.
So being an HPMG hospitalist allows physicians to pursue many avenues of clinical and process improvement, including national initiatives and teaching. Dr. Anderson sums up what HPMG is about: “I joined this group because of its passion for medicine. When we get older we’ll look back and say that we had our moment, our time to give it 100%.”
Dr. Kealey calls them “an energized creative group. Everyone wants to go to national meetings and to keep ahead of the pack, to ask what’s next to learn?” TH
Writer Marlene Piturro regularly writes practice profiles for The Hospitalist.
Information Overload
Physicians have struggled with the management of patient data for a long time. The struggle intensifies as we attempt to juggle increasingly large and complicated volumes of information during a 24-hour day. As the number and acuity of patients increase in parallel, our abilities to sift critical information and prioritize data are key.
Alarms or alerts to abnormal parameters are of limited benefit and may be counterproductive. The techniques of data display and information visualization hold great promise for revolutionizing how we manage this data overload. Other industries have realized such benefits, and healthcare (especially in the hospital) has good reason to want to catch up. In the meantime, before we can say management of clinical data in the hospital is optimal, there remains much work to do.
Physicians have struggled with the management of patient data for a long time. Such information used to be relatively simple—heart rate, respiratory rate, skin color and temperature, and so on. The limits of technology fundamentally limited what physicians could observe and record.
As our ability to gather information became more sophisticated, so did the data we could acquire. Still, the physician remained the primary collector, assessor, and interpreter of tests and their results. Individual physicians would spin urine and examine the sediment, perform blood smears, and even examine tissue samples for pathology. This was a manageable task for the physician because the number of tests was small, and the interpretation of results was fairly straightforward.
Today tests and the ways we can interpret them are both more numerous and more complicated. This has resulted in a significant issue for clinicians: How can we manage all of this information?
Too Much Data
The quantity of data available for the busy clinician is always increasing. This data explosion is happening for three reasons:
- Increased number of sophisticated tests. We test for more diseases, traits, and conditions than ever before. Example: Troponin I, T, and beta natriuretic peptide—all in widespread use today—were not available 10 years ago. Advanced genetic testing will continue this trend;
- Increased archival capability. The cost of data storage continues to decrease, making it inexpensive to archive data that might have been purged in the past; and
- Increased sophistication of data delivery methods. Computers and the networks that connect them are faster than ever. This allows for efficient transfer of data from the archive to the user. It also allows the user to access the data from a variety of geographic locations, including an outpatient office or home.
Patient care in the ICU provides a perfect example of the volumes of data that we generate in the course of clinical care. Monitors capture moment-by-moment readings of heart rate, blood pressure, respirations, oxygen saturation, temperature, electrocardiographic tracings, and more. In addition to capturing the patient’s physiologic signals, we also measure the interventions we perform on patients. We record intravenous fluid and medication rates, artificial ventilation parameters, and so on. A decade ago, East estimated the number of information categories in the ICU to have been in excess of 236.1 Certainly that number has only increased.
Increasingly Complicated Data
As the number of tests has increased, interpretation of the results has become more complex. In many institutions samples are obtained by highly qualified personnel—not the primary physician. Depending on the test, the sample may be sent to a lab (sometimes in a different area of the country) where another individual may perform the test. Finally, a trained observer reviews the results, may make an interpretation of those results, and then records that interpretation—together with the objective data—in the patient’s medical record. These data are then available for the physician to review.
A hospitalist is unlikely to collect the sample or run the test. How many of us centrifuge urine or examine blood smears? How many could read a complicated MRI or a PET scan? The busy clinical workflow coupled with the complexity of these tests demands that someone other than the primary caregiver interpret these tests. This also means that we are removed from the primary data and must rely on another practitioner’s interpretation. Even with this separation in the process, we are presented with more clinical data for each patient than ever before.
Too Much Information
Of course, the availability of these data is not without problems. An individual can review, assess, and act upon only so many data points.2 As the volume of data increases, so does the likelihood that a piece of important data will be missed. This setting can make things difficult for the busy hospitalist.
We need to quickly prioritize our time in the hospital. A first step in this process involves a quick review of physiologic studies that suggest levels of patient acuity. This information helps us to see the most critical patients first, and to identify other important issues that need to be addressed (although less urgently).
As more data are collected, this task gets more complicated. Certainly not all of the data collected are equally important for determining patient acuity. Given this, the volume of data contributes to the overall “noise” of the sample and—in some cases—the important data may be overlooked. Critical values (signals) become more likely to get lost in a sea of less important data (noise). More noise means more uncertainty and requires better evidence to make a clinical judgment.3
Information systems developers use various techniques to get around these problems. One way to manage the vast amount of information is to alert practitioners to outliers. Some have proposed that alarms may be the answer to our noise problem.
Alarms Don’t Work
Unfortunately, alerts and alarms can actually add to the noise, especially in ICU monitors. Anyone who has spent time in an ICU knows that alarms are constantly sounding. It has been estimated that false positive alarm rates range from 64%-87% in airway management situations.4
Alarms are often meaningless. Monitors can be so sensitive that they pick up background noise in their measurements, causing false alarms that increase the noise (both literally and figuratively). Anesthetists, recognizing that alarms are non-specific, frequently work without them.5 This is paralleled in the ICU because caregivers seem to ignore many alarms. (Most hospitalists who have spent time in the ICU can attest to this.) Specific problems with alarms include:
- They seldom localize the problem;
- They do not provide predictive information; and
- The diagnostic process is still left to the practitioner.5
Alarms also vary in importance. An intravenous pump that sounds because the fluid bag is empty may not be as important as an apnea alarm on a mechanical ventilator. A single alarm may not be as concerning as multiple simultaneous alarms for a patient with low blood pressure, high heart rate, and apnea. The goal in these cases is to signal a problem and to transmit that signal appropriately. But until this can be done reliably, alarms do not seem to be the answer.
On the other hand, presenting all the data (rather than just the important data) to a clinician may obscure important elements. This can result in missed diagnosis, delayed treatment, or incorrect treatment. So we don’t want to overwhelm the hospitalist with all the data; we just need to highlight and present important data. But how?
How Can We Manage All This Information?
To tackle this problem, we can look to work that has been done in other fields, specifically human-computer interaction. Norman, in his discussion of user experience, describes the complexity curve in technology, with technologies starting off simply and growing more complex until they peak.6 At this point, they get simpler to use as the technology matures. He points to airplane instrumentation that peaked with the Concorde in the 1970s. Since then instruments have gotten much simpler, with cockpit automation and better displays and controls. This has made the user experience easier, more efficient, and more effective.
There is a parallel with Norman’s observations and our information management problem in medicine. Our display technologies (paper, computer screen) are actually quite mature and powerful. However, our ability to detect and measure physiologic data continues to rise and may be outpacing our display technologies. Are there techniques from our display technologies that can make this problem easier to deal with?
Here, it’s worth clarifying two terms: data display and information visualization. Data display is a method for arranging and presenting information in a way that is easily reviewed and assessed, such as tables and charts. Information visualization describes the manipulation of the data to make it more easily understood by humans. Specifically it has been described as “the process of transforming data, information and knowledge into visual form making use of humans’ natural visual capabilities.”7
Data Displays
The simplest way to present data is the data display. Data displays can be very simple (a paper report with a glucose value), or extremely complex. (Think of bus schedules or the stock price pages in a business newspaper.) A complex data display in the clinical arena (which doubles as a data collection tool) is the clinical flow sheet. Nurses use a combination of graphing (heart rate, blood pressure) and numerical entry (intravenous fluid rate, pain scale) to record data. The flow sheet is particularly useful in the ICU. A large amount of data can be scanned quickly and examined for trends and outliers.
An example of a useful clinical data display is Pocket Rounds, a paper clinical summary report developed at the Regenstrief Institute in Indianapolis, Ind. Pocket Rounds is a high-density display designed to present clinical information including allergies, lab results, vitals, imaging, and other diagnostic studies from inpatients on a single 8.5" by 11" page. It is printed in very small type that allows for two logical pages on one landscape-oriented sheet of paper. It is called Pocket Rounds because, when folded in half, the sheet of reports fits perfectly into a white coat pocket.
The strength of Pocket Rounds seems to be the richness of the content displayed all at once, allowing the user to focus on specific areas of the report by following visual formatting clues. Of course, a significant disadvantage of Pocket Rounds is that it is static, with data only as current as the time of printing. Both authors used Pocket Rounds during their training and wish it were a more widely available tool.
Powsner and Tufte proposed a much more sophisticated display of clinical data.8 Their display is really a hybrid of data display and visualization, as processing of the data points (normalization) improves the layout of the display. It is easy to examine the report and pick out important trends and outliers. Additionally, with some thought as to the arrangement of the data elements, different results are easy to compare (for instance, white count, gentamycin dosage, and serum creatinine.) Unfortunately, this display has not been tested to compare its effectiveness with that of any other display.
Lessons for Medicine from Information Visualization
Information visualization is an area of increasing research and development, both in the scientific and business communities. It is closely linked with data mining: a method for knowledge discovery from extremely large, complex data sets. The goals of information visualization specifically germane to medicine include aiding the “discovery of details and relations” and “supporting the recognition of relevant patterns.”9 These relations and patterns may offer new knowledge or understanding that the individual data points do not adequately convey.
Visualization has been important in medical imaging for some time; however, less attention has been given to analysis of numeric and time series data on an individual patient. One example that is widely used is the pediatric growth chart, where the height, weight, and head circumference are mapped to percentages and plotted on a normalized curve to assess the child’s development. This task goes beyond simple display, as data synthesis is used (conversion to a percentage of normal). There are two tasks being performed as well. The first is the initial assessment of the patient in relation to the rest of the population. The second is a longitudinal trajectory of growth, where the points should follow the same line (population percentile growth) even though the actual data points (height, weight, head circumference) changes.
There are numerous examples of information visualization across non-medical disciplines. Taken together, many of these insights can provide a framework for creating improved data displays for clinicians. However, these concepts have not been tested in the clinical setting to determine whether they will increase efficiency of routines, such as acuity ranking. Further, we may need to support hospitalists’ common tasks with separate approaches. The acuity ranking activity might be supported by a summary page showing key outliers and critical values for each patient. The rest of the report could show all abnormal data and (as needed) the details for closer review.
Unfortunately, there has not been much direction in solving this problem from a scientific standpoint. In a review of the literature on the presentation of medical data, Starren and Johnson noted that, “there is a paucity of methods for developing new presentations” in the medical setting.10 Further, they observe that clinical data displays are rarely evaluated quantitatively. Rather they are shown to users to assess acceptance. We need to alleviate that shortcoming.
Next Steps
We believe that a significant amount of research needs to be performed in this area. We also believe that this research should focus on hospital-based specialties—especially hospitalist medicine. Why? Because hospitalists are charged with quickly assessing lots of information on lots of patients, and anything we can do to make that process more efficient will result in better patient care and hopefully, happier hospitalists. So what are next steps?
We can break up the research agenda into two arms: what needs to be displayed, and how do we display it? Although it may seem intuitive, we think it is important to decide the what before the how because the content will really drive the improvements in care.
There has been some emphasis on determining what clinical data are important for physicians. Work on prediction algorithms and scores has led to some estimations of what numbers are important for determining patient acuity and severity. However, an accurate and dependable determination of who is sick, how sick, and who will get sicker is some time off.
For now, it would be helpful to know what data physicians want to see. This will vary by provider and may not always lead directly to a specific outcome, but it is a start. It would be helpful to identify the values that most clinicians would want to know most of the time: high or low white counts, decrease in hemoglobin, decrease in platelets, normalization of creatinine, or other. This would provide the basis for experimenting with how best to display these items.
We then could move on to explore how these data should be displayed. What should be presented as discrete numbers? What would be better to summarize graphically? How can we highlight important trends? A significant amount of work has been done in fields with so-called “knowledge workers”—professionals who need to review and act on large amounts of data. Work also has been done with other data-intensive professionals such as airplane pilots, air traffic controllers, and stockbrokers. We should be able to glean valuable insights into solutions from these investigations and use them to improve our data management problem.
Finally, these displays need to be prototyped and tested on the wards. Does the new display help make the hospitalist more efficient? Can they pick out the important data faster? Do they improve length of stay, morbidity and mortality, or patient satisfaction? It is this critical evaluation that is dearly lacking as we work to improve how hospitalists do their jobs.
Healthcare providers generally are capable, hard-working professionals with the best intentions. Inefficient, overwhelmed data management systems ultimately make us equally inefficient and overwhelmed providers. In an age when abundant scientific study and complex healthcare delivery systems are generating volumes of new information, we have a lot to learn about what to do with it all. TH
Dr. Thomas is a hospitalist and assistant medical director, Clinical Informatics, The Queen’s Medical Center, Honolulu, Hawaii. He’s also assistant professor and chief, Division of Medical Informatics, Department of Medicine, John A. Burns School of Medicine, University of Hawaii at Manoa. Dr. Rosenman is senior associate consultant, Section of Hospital Medicine, Department of Internal Medicine, Mayo Clinic, and instructor of medicine, Mayo Clinic College of Medicine, Rochester, Minn.
References
- East TD, Morris AH, Wallace CJ, et al. A strategy for development of computerized critical care decision support systems. Int J Clin Monit Comput. 1992;8(4):263-269.
- Miller GA. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychol Rev. 1956;63(2):81-97.
- Morris AH, East TD, Wallace CJ, et al. Standardization of clinical decision making for the conduct of credible clinical research in complicated medical environments. Proc AMIA Annu Fall Symp. 1996;418-422.
- Xiao Y, Mackenzie CF, Spencer R, et al. Intrusiveness of auditory alarms during airway management. Anesthesiology. 1998 Sep;89(3AS):1224A.
- Lowe A, Jones RW, Harrison MJ. The graphical presentation of decision support in formation in an intelligent anaesthesia monitor. Artif Intell Med. 2001;22:173-191.
- Norman DA. The Invisible Computer. Cambridge, Mass.: The MIT Press; 1999.
- Gershon N, Eick SG, Card S. Information visualization. ACM Interactions. 1998;5(2):9-15.
- Powsner SM, Tufte ER. Graphical summary of patient status. Lancet. 1994; Aug 6:344(8919);386-389.
- Chittaro L. Information visualization and its application to medicine. Artif Intell Med. 2000;22:81-88.
- Starren J, Johnson SB. An object-oriented taxonomy of medical data presentations. J Am Med Inform Assoc. 2000 Jan;7(1):1-20.
Physicians have struggled with the management of patient data for a long time. The struggle intensifies as we attempt to juggle increasingly large and complicated volumes of information during a 24-hour day. As the number and acuity of patients increase in parallel, our abilities to sift critical information and prioritize data are key.
Alarms or alerts to abnormal parameters are of limited benefit and may be counterproductive. The techniques of data display and information visualization hold great promise for revolutionizing how we manage this data overload. Other industries have realized such benefits, and healthcare (especially in the hospital) has good reason to want to catch up. In the meantime, before we can say management of clinical data in the hospital is optimal, there remains much work to do.
Physicians have struggled with the management of patient data for a long time. Such information used to be relatively simple—heart rate, respiratory rate, skin color and temperature, and so on. The limits of technology fundamentally limited what physicians could observe and record.
As our ability to gather information became more sophisticated, so did the data we could acquire. Still, the physician remained the primary collector, assessor, and interpreter of tests and their results. Individual physicians would spin urine and examine the sediment, perform blood smears, and even examine tissue samples for pathology. This was a manageable task for the physician because the number of tests was small, and the interpretation of results was fairly straightforward.
Today tests and the ways we can interpret them are both more numerous and more complicated. This has resulted in a significant issue for clinicians: How can we manage all of this information?
Too Much Data
The quantity of data available for the busy clinician is always increasing. This data explosion is happening for three reasons:
- Increased number of sophisticated tests. We test for more diseases, traits, and conditions than ever before. Example: Troponin I, T, and beta natriuretic peptide—all in widespread use today—were not available 10 years ago. Advanced genetic testing will continue this trend;
- Increased archival capability. The cost of data storage continues to decrease, making it inexpensive to archive data that might have been purged in the past; and
- Increased sophistication of data delivery methods. Computers and the networks that connect them are faster than ever. This allows for efficient transfer of data from the archive to the user. It also allows the user to access the data from a variety of geographic locations, including an outpatient office or home.
Patient care in the ICU provides a perfect example of the volumes of data that we generate in the course of clinical care. Monitors capture moment-by-moment readings of heart rate, blood pressure, respirations, oxygen saturation, temperature, electrocardiographic tracings, and more. In addition to capturing the patient’s physiologic signals, we also measure the interventions we perform on patients. We record intravenous fluid and medication rates, artificial ventilation parameters, and so on. A decade ago, East estimated the number of information categories in the ICU to have been in excess of 236.1 Certainly that number has only increased.
Increasingly Complicated Data
As the number of tests has increased, interpretation of the results has become more complex. In many institutions samples are obtained by highly qualified personnel—not the primary physician. Depending on the test, the sample may be sent to a lab (sometimes in a different area of the country) where another individual may perform the test. Finally, a trained observer reviews the results, may make an interpretation of those results, and then records that interpretation—together with the objective data—in the patient’s medical record. These data are then available for the physician to review.
A hospitalist is unlikely to collect the sample or run the test. How many of us centrifuge urine or examine blood smears? How many could read a complicated MRI or a PET scan? The busy clinical workflow coupled with the complexity of these tests demands that someone other than the primary caregiver interpret these tests. This also means that we are removed from the primary data and must rely on another practitioner’s interpretation. Even with this separation in the process, we are presented with more clinical data for each patient than ever before.
Too Much Information
Of course, the availability of these data is not without problems. An individual can review, assess, and act upon only so many data points.2 As the volume of data increases, so does the likelihood that a piece of important data will be missed. This setting can make things difficult for the busy hospitalist.
We need to quickly prioritize our time in the hospital. A first step in this process involves a quick review of physiologic studies that suggest levels of patient acuity. This information helps us to see the most critical patients first, and to identify other important issues that need to be addressed (although less urgently).
As more data are collected, this task gets more complicated. Certainly not all of the data collected are equally important for determining patient acuity. Given this, the volume of data contributes to the overall “noise” of the sample and—in some cases—the important data may be overlooked. Critical values (signals) become more likely to get lost in a sea of less important data (noise). More noise means more uncertainty and requires better evidence to make a clinical judgment.3
Information systems developers use various techniques to get around these problems. One way to manage the vast amount of information is to alert practitioners to outliers. Some have proposed that alarms may be the answer to our noise problem.
Alarms Don’t Work
Unfortunately, alerts and alarms can actually add to the noise, especially in ICU monitors. Anyone who has spent time in an ICU knows that alarms are constantly sounding. It has been estimated that false positive alarm rates range from 64%-87% in airway management situations.4
Alarms are often meaningless. Monitors can be so sensitive that they pick up background noise in their measurements, causing false alarms that increase the noise (both literally and figuratively). Anesthetists, recognizing that alarms are non-specific, frequently work without them.5 This is paralleled in the ICU because caregivers seem to ignore many alarms. (Most hospitalists who have spent time in the ICU can attest to this.) Specific problems with alarms include:
- They seldom localize the problem;
- They do not provide predictive information; and
- The diagnostic process is still left to the practitioner.5
Alarms also vary in importance. An intravenous pump that sounds because the fluid bag is empty may not be as important as an apnea alarm on a mechanical ventilator. A single alarm may not be as concerning as multiple simultaneous alarms for a patient with low blood pressure, high heart rate, and apnea. The goal in these cases is to signal a problem and to transmit that signal appropriately. But until this can be done reliably, alarms do not seem to be the answer.
On the other hand, presenting all the data (rather than just the important data) to a clinician may obscure important elements. This can result in missed diagnosis, delayed treatment, or incorrect treatment. So we don’t want to overwhelm the hospitalist with all the data; we just need to highlight and present important data. But how?
How Can We Manage All This Information?
To tackle this problem, we can look to work that has been done in other fields, specifically human-computer interaction. Norman, in his discussion of user experience, describes the complexity curve in technology, with technologies starting off simply and growing more complex until they peak.6 At this point, they get simpler to use as the technology matures. He points to airplane instrumentation that peaked with the Concorde in the 1970s. Since then instruments have gotten much simpler, with cockpit automation and better displays and controls. This has made the user experience easier, more efficient, and more effective.
There is a parallel with Norman’s observations and our information management problem in medicine. Our display technologies (paper, computer screen) are actually quite mature and powerful. However, our ability to detect and measure physiologic data continues to rise and may be outpacing our display technologies. Are there techniques from our display technologies that can make this problem easier to deal with?
Here, it’s worth clarifying two terms: data display and information visualization. Data display is a method for arranging and presenting information in a way that is easily reviewed and assessed, such as tables and charts. Information visualization describes the manipulation of the data to make it more easily understood by humans. Specifically it has been described as “the process of transforming data, information and knowledge into visual form making use of humans’ natural visual capabilities.”7
Data Displays
The simplest way to present data is the data display. Data displays can be very simple (a paper report with a glucose value), or extremely complex. (Think of bus schedules or the stock price pages in a business newspaper.) A complex data display in the clinical arena (which doubles as a data collection tool) is the clinical flow sheet. Nurses use a combination of graphing (heart rate, blood pressure) and numerical entry (intravenous fluid rate, pain scale) to record data. The flow sheet is particularly useful in the ICU. A large amount of data can be scanned quickly and examined for trends and outliers.
An example of a useful clinical data display is Pocket Rounds, a paper clinical summary report developed at the Regenstrief Institute in Indianapolis, Ind. Pocket Rounds is a high-density display designed to present clinical information including allergies, lab results, vitals, imaging, and other diagnostic studies from inpatients on a single 8.5" by 11" page. It is printed in very small type that allows for two logical pages on one landscape-oriented sheet of paper. It is called Pocket Rounds because, when folded in half, the sheet of reports fits perfectly into a white coat pocket.
The strength of Pocket Rounds seems to be the richness of the content displayed all at once, allowing the user to focus on specific areas of the report by following visual formatting clues. Of course, a significant disadvantage of Pocket Rounds is that it is static, with data only as current as the time of printing. Both authors used Pocket Rounds during their training and wish it were a more widely available tool.
Powsner and Tufte proposed a much more sophisticated display of clinical data.8 Their display is really a hybrid of data display and visualization, as processing of the data points (normalization) improves the layout of the display. It is easy to examine the report and pick out important trends and outliers. Additionally, with some thought as to the arrangement of the data elements, different results are easy to compare (for instance, white count, gentamycin dosage, and serum creatinine.) Unfortunately, this display has not been tested to compare its effectiveness with that of any other display.
Lessons for Medicine from Information Visualization
Information visualization is an area of increasing research and development, both in the scientific and business communities. It is closely linked with data mining: a method for knowledge discovery from extremely large, complex data sets. The goals of information visualization specifically germane to medicine include aiding the “discovery of details and relations” and “supporting the recognition of relevant patterns.”9 These relations and patterns may offer new knowledge or understanding that the individual data points do not adequately convey.
Visualization has been important in medical imaging for some time; however, less attention has been given to analysis of numeric and time series data on an individual patient. One example that is widely used is the pediatric growth chart, where the height, weight, and head circumference are mapped to percentages and plotted on a normalized curve to assess the child’s development. This task goes beyond simple display, as data synthesis is used (conversion to a percentage of normal). There are two tasks being performed as well. The first is the initial assessment of the patient in relation to the rest of the population. The second is a longitudinal trajectory of growth, where the points should follow the same line (population percentile growth) even though the actual data points (height, weight, head circumference) changes.
There are numerous examples of information visualization across non-medical disciplines. Taken together, many of these insights can provide a framework for creating improved data displays for clinicians. However, these concepts have not been tested in the clinical setting to determine whether they will increase efficiency of routines, such as acuity ranking. Further, we may need to support hospitalists’ common tasks with separate approaches. The acuity ranking activity might be supported by a summary page showing key outliers and critical values for each patient. The rest of the report could show all abnormal data and (as needed) the details for closer review.
Unfortunately, there has not been much direction in solving this problem from a scientific standpoint. In a review of the literature on the presentation of medical data, Starren and Johnson noted that, “there is a paucity of methods for developing new presentations” in the medical setting.10 Further, they observe that clinical data displays are rarely evaluated quantitatively. Rather they are shown to users to assess acceptance. We need to alleviate that shortcoming.
Next Steps
We believe that a significant amount of research needs to be performed in this area. We also believe that this research should focus on hospital-based specialties—especially hospitalist medicine. Why? Because hospitalists are charged with quickly assessing lots of information on lots of patients, and anything we can do to make that process more efficient will result in better patient care and hopefully, happier hospitalists. So what are next steps?
We can break up the research agenda into two arms: what needs to be displayed, and how do we display it? Although it may seem intuitive, we think it is important to decide the what before the how because the content will really drive the improvements in care.
There has been some emphasis on determining what clinical data are important for physicians. Work on prediction algorithms and scores has led to some estimations of what numbers are important for determining patient acuity and severity. However, an accurate and dependable determination of who is sick, how sick, and who will get sicker is some time off.
For now, it would be helpful to know what data physicians want to see. This will vary by provider and may not always lead directly to a specific outcome, but it is a start. It would be helpful to identify the values that most clinicians would want to know most of the time: high or low white counts, decrease in hemoglobin, decrease in platelets, normalization of creatinine, or other. This would provide the basis for experimenting with how best to display these items.
We then could move on to explore how these data should be displayed. What should be presented as discrete numbers? What would be better to summarize graphically? How can we highlight important trends? A significant amount of work has been done in fields with so-called “knowledge workers”—professionals who need to review and act on large amounts of data. Work also has been done with other data-intensive professionals such as airplane pilots, air traffic controllers, and stockbrokers. We should be able to glean valuable insights into solutions from these investigations and use them to improve our data management problem.
Finally, these displays need to be prototyped and tested on the wards. Does the new display help make the hospitalist more efficient? Can they pick out the important data faster? Do they improve length of stay, morbidity and mortality, or patient satisfaction? It is this critical evaluation that is dearly lacking as we work to improve how hospitalists do their jobs.
Healthcare providers generally are capable, hard-working professionals with the best intentions. Inefficient, overwhelmed data management systems ultimately make us equally inefficient and overwhelmed providers. In an age when abundant scientific study and complex healthcare delivery systems are generating volumes of new information, we have a lot to learn about what to do with it all. TH
Dr. Thomas is a hospitalist and assistant medical director, Clinical Informatics, The Queen’s Medical Center, Honolulu, Hawaii. He’s also assistant professor and chief, Division of Medical Informatics, Department of Medicine, John A. Burns School of Medicine, University of Hawaii at Manoa. Dr. Rosenman is senior associate consultant, Section of Hospital Medicine, Department of Internal Medicine, Mayo Clinic, and instructor of medicine, Mayo Clinic College of Medicine, Rochester, Minn.
References
- East TD, Morris AH, Wallace CJ, et al. A strategy for development of computerized critical care decision support systems. Int J Clin Monit Comput. 1992;8(4):263-269.
- Miller GA. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychol Rev. 1956;63(2):81-97.
- Morris AH, East TD, Wallace CJ, et al. Standardization of clinical decision making for the conduct of credible clinical research in complicated medical environments. Proc AMIA Annu Fall Symp. 1996;418-422.
- Xiao Y, Mackenzie CF, Spencer R, et al. Intrusiveness of auditory alarms during airway management. Anesthesiology. 1998 Sep;89(3AS):1224A.
- Lowe A, Jones RW, Harrison MJ. The graphical presentation of decision support in formation in an intelligent anaesthesia monitor. Artif Intell Med. 2001;22:173-191.
- Norman DA. The Invisible Computer. Cambridge, Mass.: The MIT Press; 1999.
- Gershon N, Eick SG, Card S. Information visualization. ACM Interactions. 1998;5(2):9-15.
- Powsner SM, Tufte ER. Graphical summary of patient status. Lancet. 1994; Aug 6:344(8919);386-389.
- Chittaro L. Information visualization and its application to medicine. Artif Intell Med. 2000;22:81-88.
- Starren J, Johnson SB. An object-oriented taxonomy of medical data presentations. J Am Med Inform Assoc. 2000 Jan;7(1):1-20.
Physicians have struggled with the management of patient data for a long time. The struggle intensifies as we attempt to juggle increasingly large and complicated volumes of information during a 24-hour day. As the number and acuity of patients increase in parallel, our abilities to sift critical information and prioritize data are key.
Alarms or alerts to abnormal parameters are of limited benefit and may be counterproductive. The techniques of data display and information visualization hold great promise for revolutionizing how we manage this data overload. Other industries have realized such benefits, and healthcare (especially in the hospital) has good reason to want to catch up. In the meantime, before we can say management of clinical data in the hospital is optimal, there remains much work to do.
Physicians have struggled with the management of patient data for a long time. Such information used to be relatively simple—heart rate, respiratory rate, skin color and temperature, and so on. The limits of technology fundamentally limited what physicians could observe and record.
As our ability to gather information became more sophisticated, so did the data we could acquire. Still, the physician remained the primary collector, assessor, and interpreter of tests and their results. Individual physicians would spin urine and examine the sediment, perform blood smears, and even examine tissue samples for pathology. This was a manageable task for the physician because the number of tests was small, and the interpretation of results was fairly straightforward.
Today tests and the ways we can interpret them are both more numerous and more complicated. This has resulted in a significant issue for clinicians: How can we manage all of this information?
Too Much Data
The quantity of data available for the busy clinician is always increasing. This data explosion is happening for three reasons:
- Increased number of sophisticated tests. We test for more diseases, traits, and conditions than ever before. Example: Troponin I, T, and beta natriuretic peptide—all in widespread use today—were not available 10 years ago. Advanced genetic testing will continue this trend;
- Increased archival capability. The cost of data storage continues to decrease, making it inexpensive to archive data that might have been purged in the past; and
- Increased sophistication of data delivery methods. Computers and the networks that connect them are faster than ever. This allows for efficient transfer of data from the archive to the user. It also allows the user to access the data from a variety of geographic locations, including an outpatient office or home.
Patient care in the ICU provides a perfect example of the volumes of data that we generate in the course of clinical care. Monitors capture moment-by-moment readings of heart rate, blood pressure, respirations, oxygen saturation, temperature, electrocardiographic tracings, and more. In addition to capturing the patient’s physiologic signals, we also measure the interventions we perform on patients. We record intravenous fluid and medication rates, artificial ventilation parameters, and so on. A decade ago, East estimated the number of information categories in the ICU to have been in excess of 236.1 Certainly that number has only increased.
Increasingly Complicated Data
As the number of tests has increased, interpretation of the results has become more complex. In many institutions samples are obtained by highly qualified personnel—not the primary physician. Depending on the test, the sample may be sent to a lab (sometimes in a different area of the country) where another individual may perform the test. Finally, a trained observer reviews the results, may make an interpretation of those results, and then records that interpretation—together with the objective data—in the patient’s medical record. These data are then available for the physician to review.
A hospitalist is unlikely to collect the sample or run the test. How many of us centrifuge urine or examine blood smears? How many could read a complicated MRI or a PET scan? The busy clinical workflow coupled with the complexity of these tests demands that someone other than the primary caregiver interpret these tests. This also means that we are removed from the primary data and must rely on another practitioner’s interpretation. Even with this separation in the process, we are presented with more clinical data for each patient than ever before.
Too Much Information
Of course, the availability of these data is not without problems. An individual can review, assess, and act upon only so many data points.2 As the volume of data increases, so does the likelihood that a piece of important data will be missed. This setting can make things difficult for the busy hospitalist.
We need to quickly prioritize our time in the hospital. A first step in this process involves a quick review of physiologic studies that suggest levels of patient acuity. This information helps us to see the most critical patients first, and to identify other important issues that need to be addressed (although less urgently).
As more data are collected, this task gets more complicated. Certainly not all of the data collected are equally important for determining patient acuity. Given this, the volume of data contributes to the overall “noise” of the sample and—in some cases—the important data may be overlooked. Critical values (signals) become more likely to get lost in a sea of less important data (noise). More noise means more uncertainty and requires better evidence to make a clinical judgment.3
Information systems developers use various techniques to get around these problems. One way to manage the vast amount of information is to alert practitioners to outliers. Some have proposed that alarms may be the answer to our noise problem.
Alarms Don’t Work
Unfortunately, alerts and alarms can actually add to the noise, especially in ICU monitors. Anyone who has spent time in an ICU knows that alarms are constantly sounding. It has been estimated that false positive alarm rates range from 64%-87% in airway management situations.4
Alarms are often meaningless. Monitors can be so sensitive that they pick up background noise in their measurements, causing false alarms that increase the noise (both literally and figuratively). Anesthetists, recognizing that alarms are non-specific, frequently work without them.5 This is paralleled in the ICU because caregivers seem to ignore many alarms. (Most hospitalists who have spent time in the ICU can attest to this.) Specific problems with alarms include:
- They seldom localize the problem;
- They do not provide predictive information; and
- The diagnostic process is still left to the practitioner.5
Alarms also vary in importance. An intravenous pump that sounds because the fluid bag is empty may not be as important as an apnea alarm on a mechanical ventilator. A single alarm may not be as concerning as multiple simultaneous alarms for a patient with low blood pressure, high heart rate, and apnea. The goal in these cases is to signal a problem and to transmit that signal appropriately. But until this can be done reliably, alarms do not seem to be the answer.
On the other hand, presenting all the data (rather than just the important data) to a clinician may obscure important elements. This can result in missed diagnosis, delayed treatment, or incorrect treatment. So we don’t want to overwhelm the hospitalist with all the data; we just need to highlight and present important data. But how?
How Can We Manage All This Information?
To tackle this problem, we can look to work that has been done in other fields, specifically human-computer interaction. Norman, in his discussion of user experience, describes the complexity curve in technology, with technologies starting off simply and growing more complex until they peak.6 At this point, they get simpler to use as the technology matures. He points to airplane instrumentation that peaked with the Concorde in the 1970s. Since then instruments have gotten much simpler, with cockpit automation and better displays and controls. This has made the user experience easier, more efficient, and more effective.
There is a parallel with Norman’s observations and our information management problem in medicine. Our display technologies (paper, computer screen) are actually quite mature and powerful. However, our ability to detect and measure physiologic data continues to rise and may be outpacing our display technologies. Are there techniques from our display technologies that can make this problem easier to deal with?
Here, it’s worth clarifying two terms: data display and information visualization. Data display is a method for arranging and presenting information in a way that is easily reviewed and assessed, such as tables and charts. Information visualization describes the manipulation of the data to make it more easily understood by humans. Specifically it has been described as “the process of transforming data, information and knowledge into visual form making use of humans’ natural visual capabilities.”7
Data Displays
The simplest way to present data is the data display. Data displays can be very simple (a paper report with a glucose value), or extremely complex. (Think of bus schedules or the stock price pages in a business newspaper.) A complex data display in the clinical arena (which doubles as a data collection tool) is the clinical flow sheet. Nurses use a combination of graphing (heart rate, blood pressure) and numerical entry (intravenous fluid rate, pain scale) to record data. The flow sheet is particularly useful in the ICU. A large amount of data can be scanned quickly and examined for trends and outliers.
An example of a useful clinical data display is Pocket Rounds, a paper clinical summary report developed at the Regenstrief Institute in Indianapolis, Ind. Pocket Rounds is a high-density display designed to present clinical information including allergies, lab results, vitals, imaging, and other diagnostic studies from inpatients on a single 8.5" by 11" page. It is printed in very small type that allows for two logical pages on one landscape-oriented sheet of paper. It is called Pocket Rounds because, when folded in half, the sheet of reports fits perfectly into a white coat pocket.
The strength of Pocket Rounds seems to be the richness of the content displayed all at once, allowing the user to focus on specific areas of the report by following visual formatting clues. Of course, a significant disadvantage of Pocket Rounds is that it is static, with data only as current as the time of printing. Both authors used Pocket Rounds during their training and wish it were a more widely available tool.
Powsner and Tufte proposed a much more sophisticated display of clinical data.8 Their display is really a hybrid of data display and visualization, as processing of the data points (normalization) improves the layout of the display. It is easy to examine the report and pick out important trends and outliers. Additionally, with some thought as to the arrangement of the data elements, different results are easy to compare (for instance, white count, gentamycin dosage, and serum creatinine.) Unfortunately, this display has not been tested to compare its effectiveness with that of any other display.
Lessons for Medicine from Information Visualization
Information visualization is an area of increasing research and development, both in the scientific and business communities. It is closely linked with data mining: a method for knowledge discovery from extremely large, complex data sets. The goals of information visualization specifically germane to medicine include aiding the “discovery of details and relations” and “supporting the recognition of relevant patterns.”9 These relations and patterns may offer new knowledge or understanding that the individual data points do not adequately convey.
Visualization has been important in medical imaging for some time; however, less attention has been given to analysis of numeric and time series data on an individual patient. One example that is widely used is the pediatric growth chart, where the height, weight, and head circumference are mapped to percentages and plotted on a normalized curve to assess the child’s development. This task goes beyond simple display, as data synthesis is used (conversion to a percentage of normal). There are two tasks being performed as well. The first is the initial assessment of the patient in relation to the rest of the population. The second is a longitudinal trajectory of growth, where the points should follow the same line (population percentile growth) even though the actual data points (height, weight, head circumference) changes.
There are numerous examples of information visualization across non-medical disciplines. Taken together, many of these insights can provide a framework for creating improved data displays for clinicians. However, these concepts have not been tested in the clinical setting to determine whether they will increase efficiency of routines, such as acuity ranking. Further, we may need to support hospitalists’ common tasks with separate approaches. The acuity ranking activity might be supported by a summary page showing key outliers and critical values for each patient. The rest of the report could show all abnormal data and (as needed) the details for closer review.
Unfortunately, there has not been much direction in solving this problem from a scientific standpoint. In a review of the literature on the presentation of medical data, Starren and Johnson noted that, “there is a paucity of methods for developing new presentations” in the medical setting.10 Further, they observe that clinical data displays are rarely evaluated quantitatively. Rather they are shown to users to assess acceptance. We need to alleviate that shortcoming.
Next Steps
We believe that a significant amount of research needs to be performed in this area. We also believe that this research should focus on hospital-based specialties—especially hospitalist medicine. Why? Because hospitalists are charged with quickly assessing lots of information on lots of patients, and anything we can do to make that process more efficient will result in better patient care and hopefully, happier hospitalists. So what are next steps?
We can break up the research agenda into two arms: what needs to be displayed, and how do we display it? Although it may seem intuitive, we think it is important to decide the what before the how because the content will really drive the improvements in care.
There has been some emphasis on determining what clinical data are important for physicians. Work on prediction algorithms and scores has led to some estimations of what numbers are important for determining patient acuity and severity. However, an accurate and dependable determination of who is sick, how sick, and who will get sicker is some time off.
For now, it would be helpful to know what data physicians want to see. This will vary by provider and may not always lead directly to a specific outcome, but it is a start. It would be helpful to identify the values that most clinicians would want to know most of the time: high or low white counts, decrease in hemoglobin, decrease in platelets, normalization of creatinine, or other. This would provide the basis for experimenting with how best to display these items.
We then could move on to explore how these data should be displayed. What should be presented as discrete numbers? What would be better to summarize graphically? How can we highlight important trends? A significant amount of work has been done in fields with so-called “knowledge workers”—professionals who need to review and act on large amounts of data. Work also has been done with other data-intensive professionals such as airplane pilots, air traffic controllers, and stockbrokers. We should be able to glean valuable insights into solutions from these investigations and use them to improve our data management problem.
Finally, these displays need to be prototyped and tested on the wards. Does the new display help make the hospitalist more efficient? Can they pick out the important data faster? Do they improve length of stay, morbidity and mortality, or patient satisfaction? It is this critical evaluation that is dearly lacking as we work to improve how hospitalists do their jobs.
Healthcare providers generally are capable, hard-working professionals with the best intentions. Inefficient, overwhelmed data management systems ultimately make us equally inefficient and overwhelmed providers. In an age when abundant scientific study and complex healthcare delivery systems are generating volumes of new information, we have a lot to learn about what to do with it all. TH
Dr. Thomas is a hospitalist and assistant medical director, Clinical Informatics, The Queen’s Medical Center, Honolulu, Hawaii. He’s also assistant professor and chief, Division of Medical Informatics, Department of Medicine, John A. Burns School of Medicine, University of Hawaii at Manoa. Dr. Rosenman is senior associate consultant, Section of Hospital Medicine, Department of Internal Medicine, Mayo Clinic, and instructor of medicine, Mayo Clinic College of Medicine, Rochester, Minn.
References
- East TD, Morris AH, Wallace CJ, et al. A strategy for development of computerized critical care decision support systems. Int J Clin Monit Comput. 1992;8(4):263-269.
- Miller GA. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychol Rev. 1956;63(2):81-97.
- Morris AH, East TD, Wallace CJ, et al. Standardization of clinical decision making for the conduct of credible clinical research in complicated medical environments. Proc AMIA Annu Fall Symp. 1996;418-422.
- Xiao Y, Mackenzie CF, Spencer R, et al. Intrusiveness of auditory alarms during airway management. Anesthesiology. 1998 Sep;89(3AS):1224A.
- Lowe A, Jones RW, Harrison MJ. The graphical presentation of decision support in formation in an intelligent anaesthesia monitor. Artif Intell Med. 2001;22:173-191.
- Norman DA. The Invisible Computer. Cambridge, Mass.: The MIT Press; 1999.
- Gershon N, Eick SG, Card S. Information visualization. ACM Interactions. 1998;5(2):9-15.
- Powsner SM, Tufte ER. Graphical summary of patient status. Lancet. 1994; Aug 6:344(8919);386-389.
- Chittaro L. Information visualization and its application to medicine. Artif Intell Med. 2000;22:81-88.
- Starren J, Johnson SB. An object-oriented taxonomy of medical data presentations. J Am Med Inform Assoc. 2000 Jan;7(1):1-20.
Partners in Performance & Quality Care
As hospitalists become more prevalent in facilities nationwide, administrators and others increasingly seek out these practitioners to take a clinical leadership role. More than ever, this includes implementing clinical practice guidelines to maximize outcomes and standardize care processes. Guidelines may be called pathways, order sets, or protocols, but these evidence-based tools are being embraced by hospitals; and facilities leaders are encouraging physicians to jump on the bandwagon.
Why Use Guidelines?
Studies already show that hospitalists have a positive effect on lengths of stay and efficiency of care, and some have documented a correlation between hospitalist programs and outcomes. So why are guidelines necessary?
Guidelines use a foundation of evidence-based medicine, which promotes the use of proven practices and interventions. “Evidence-based medicine is tough to refute,” says Ken Simone, DO, founder and president of Hospitalist and Practice Solutions in Brewer, Maine. “Typically, when you see evidence-based medicine within a guideline, you can assume that you are improving medicine if you use the tool accurately.”
There are two reasons to employ guidelines, according to Richard Rubin, MD, MBA, chief medical officer, Seton Health Systems, Troy, N.Y. One is to ensure efficiency in providing care that is clinically based. The second reason is to ensure consistent quality by preventing variations in care from practitioner to practitioner.
“These tools serve as a road map, giving you an idea of where to go and how to get there,” says Dr. Rubin.
There are limited data from the literature documenting the value of guidelines in the hospital setting. However, one study looked at the effect of a clinical pathway on six outcomes of care in patients hospitalized for community-acquired pneumonia.1 The authors found that those patients managed by using a pathway were significantly less likely to die in-hospital compared with non-pathway patients. Pathway patients also were more likely to receive blood cultures and appropriate antibiotic therapy.
In patients with the most severe pneumonia, those managed via pathway had an 80% reduction in the odds of respiratory therapy requiring mechanical ventilation. Overall, the authors concluded that patients who were managed using a clinical pathway for pneumonia were more likely to experience positive outcomes than patients treated without these tools.
Another study looked a multidisciplinary approach to creating “templated” order sets for chemotherapy. The authors concluded that such tools reduced the duplication of effort by significantly lowering the number of changes made during the order verification process.2
Dr. Rubin undertook an internal study at his facility that found that using order sets was linked to shorter lengths of stay. He discovered that pathways were used 18% of the time for cases with the longest lengths of stays and 54% of the time with the shortest.
“There’s not much I don’t like about order sets,” says Dr. Rubin.
Todd Popp, MD, clinical partner, Critical Care and Pulmonary Consultants, Denver, agrees. “Of course, we want to use tools that help patients, and effective order sets help improve quality and efficiency,” he says.
Dr. Popp adds that guideline use has an added advantage for hospitalists. Those practitioners, he notes, who have a demonstrated ability to develop and implement order sets increasingly will be in demand.
“There is a fair amount of competition between hospitalist groups. If you can prove that you can develop, implement, and use these standards,” he says, “it helps hospitals and their patients, and it helps hospitalists get better contracts and have solid relationships with their facilities.”
In fact, says Dr. Simone, hospitalists who have experience and knowledge about guideline development and implementation will be considered tremendous assets by hospitals. “If the nationwide use of guidelines in hospitals isn’t common yet, it will be in the coming years. And hospitalists are perfectly positioned to take the lead on the effective development and use of these tools,” he offers.
Tools that Teach
Guidelines encourage standardization of care and help physicians and other clinicians quickly select appropriate assessments and interventions for various conditions. They also help prescribers make appropriate medication and dosage selections quickly and accurately. For example, an order set for admissions to a coronary care unit (CCU) for acute coronary syndrome likely will address considerations such as nursing orders, IVs, medications, diagnostic tests, consults, discharge planning, and primary care follow-up.
Used properly, these tools do not promote “cookbook” or “cookie cutter” medicine—as some opponents suggest; instead, they guide decision-making and enable practical, evidence-based choices for each patient.
Hospitals and hospitalists most frequently employ guidelines regarding the clinical conditions that most commonly lead to ED visits or hospital stays. These include community-acquired pneumonia, COPD, CHF, chest pain, MI, and stroke.
In choosing topics on which to implement guidelines, Dr. Simone suggests considering the demographics, needs, and challenges of the particular facility. For example, “if you have guidelines addressing diagnoses for which patients generally are put on 24-hour observation prior to hospital admission, you can ferret out who needs to be admitted and who doesn’t,” he says, adding, “and you can make these decisions in a consistent manner.”
Buy-in and Barriers
Hospitalists who use guidelines agree that they are natural leaders when it comes to the development, implementation, and use of these tools.
“As a hospitalist, I am employed by the hospital and have more of a stake in overall quality and cost-effectiveness of care,” says Justin Psaila, MD, of St. Luke’s Hospital in Bethlehem, Pa. “Some of the private attendings are doing their own thing and just see guidelines as creating more work.”
“Hospitals are looking for more standardized approaches to medical care via guidelines and order sets, and hospitalists can deliver this,” says Alex Strachan, Jr., MD, medical director for the Hospitalist Program at St. Joseph Hospital in Eureka, Calif., and medical director of Team Health West Hospital Medicine Programs. “There is a tremendous amount of teamwork involved in guideline implementation and use, and hospitalists are natural team players.”
In addition to working with facilities to develop and implement guidelines, hospitalists can help increase buy-in from other clinicians. This may involve working with facility leadership to develop materials to promote the guidelines to stakeholders, such as letters to attending physicians that outline how the guidelines will work, where they can obtain copies, how they can obtain electronic versions (if available), the advantages of using these tools, what to do if they don’t follow a step in the guideline (e.g., document the patient’s refusal to receive a particular treatment), and who to contact if they have questions about the guideline.
Despite all of the positives about guidelines and the growing number of physicians who use and embrace them, there continues to be some resistance to guideline use. “Many physicians still are hesitant to use guidelines,” explains Dr. Simone. “They feel as if they will lose some creativity and that it may obligate them to go in a particular direction.”
Even when a facility’s hospitalists are on board with guidelines, attending physicians—who usually are in the majority—who resist can prevent the documents from having a positive impact. Dr. Strachan offers an example: “If you have 50-100 medical staff admitting, they will use the antibiotics that they are most comfortable with—regardless of cost, staff time involved in medication administration, and so on. If even half of these buy into a guideline addressing antibiotic use, it can streamline medication management, administration, and costs considerably.”
Some physicians worry that guidelines put them at risk for lawsuits. “One physician said, ‘You put my back to the wall if I don’t do these things,’” says Dr. Simone. “However, good guidelines don’t set you up; they protect you. If you don’t follow a step or recommendation, you just need to document why.”
Often, some basic revisions can help overcome objections to guideline use. As Dr. Simone explains, “We had an order set that was five pages in length, and physicians balked at using it. They said that it was too complicated. So we winnowed it down to two to three concise pages, and now they all use it.”
He cautions that if guidelines are too confusing, complex, or long, they seem overwhelming and are less likely to be used.
Birth of a Hospitalist Guideline
While there are many clinical practice guidelines in existence that address a range of clinical issues and conditions, hospitalists and other physicians are more likely to use a tool they have helped create. Arun Tewari, MD, program director of the Hospitalist Program, Ball Memorial Hospital Medical Consultants, Muncie, Ind., has experienced this first-hand and has been involved in guideline development at his facility for the past three years.
“We’re just starting to track data, but we’ve already realized a reduced length of stay for all the pathways we use, including stroke, CHF, COPD, pneumonia, chest pains, MI, and GI bleed,” he says. “To date, the numbers are only statistically significant for pneumonia. However, we expect to see significant results in the other areas over time.”
Dr. Tewari and his group use a multidisciplinary approach to pathway development. “We invite key individuals from different disciplines and specialties to serve on a committee that is run by a physician and a nurse leader. These individuals are responsible for reviewing articles and other information and performing specific assigned tasks,” he explains.
The group starts with a tremendous amount of information. In addition to articles from the literature, they review national guidelines on the topic being addressed, as well as pathways used by other facilities or organizations.
The group takes the best clinical evidence and information they find, and they incorporate it into a tool that is useful and practical for the hospital.
“To be truly effective, these tools have to be institutionalized to your facility and practical in terms of what can be done or handled in this setting,” suggests Dr. Tewari.
Once the group reaches consensus on a completed draft, the document goes to several hospital committees for review. The original group then compiles the comments, makes any revisions or additions deemed necessary, and produces a final pathway. “This isn’t a short process,” cautions Dr. Tewari. On average it takes six months to a year from start to finish.
The final pathways are posted online, and physicians can print copies. Elsewhere, the pathways are available on the floors and in the emergency department as well. Currently, the pathways aren’t available for electronic applications such as PDAs. However, Dr. Tewari doesn’t rule this out as a possibility for the future.
Of course, Dr. Tewari emphasizes, just publishing a pathway or making it available to clinical staff isn’t enough. “You have to educate people about the pathways and gain their buy-in,” he notes. At his facility, each clinical department staff meeting involves a representative who will talk about pathways and spell out how to use them. This also presents another opportunity for practitioners and team leaders to have input on the tools.
The pathways aren’t mandatory, Dr. Tewari emphasizes, but they are strongly encouraged. “We don’t have statistics yet, but throughout the hospital, utilization probably is at about 50%. Within our hospitalist group, utilization is close to 100%. We hope to have some hard numbers soon to back this up.”
No Crystal Balls Needed: Guidelines Have a Future
Guidelines soundly rooted in evidence-based medicine have a future, predicts Dr. Simone.
“I think these are essential for the Medicare pay-for-performance measures that are coming down the pike. Medicare is likely to identify three to five different diagnoses to look at and may want hospitals to develop guidelines for these. Hospitals—as well as hospitalists and other physicians—will be rewarded if their performance is good in these areas based on these guidelines.”
Some hospitals already are using guidelines or order sets to prove quality. “We put our order sets together partly because we are part of a CMS [Centers for Medicare and Medicaid Services] pay-for-performance project,” says Dr. Psaila.
Guidelines that are commonly available via laptop or PDA also are coming. “Hospitalists tend to use technology more than other physicians, and they increasingly will want guideline applications for handheld devices,” notes Dr. Strachan.
There already are several companies offering such products. “Some of these are really useful tools,” he continues. “They allow you to pull up an order set for a particular illness and use it. You can click on medications and check the evidence basis for their use. You then can print out this information or transmit it electronically.”
The real future is to have electronic medical record solutions that interface with orders, predicts Dr. Strachan. However, he suggests that current availability and use of such systems is less than 10% of hospitals and hospitalists.
“I feel that it is essential that we develop various guidelines and use them in the hospital setting,” concludes Dr. Strachan. “We need to standardize our practice so that we can measure outcomes and quality of care doesn’t vary from one practitioner to another.” TH
Writer Joanne Kaldy also writes about hospitalist programs in this issue.
References
- Hauck LD, Adler LM, Mulla ZD. Clinical pathway care improves outcomes among patients hospitalized for community-acquired pneumonia. Ann Epidemiol. 2004;14(9):669-675.
- Dinning C, Branowicki P, O’Neill JB, et al. Chemotherapy error reduction: a multidisciplinary approach to create templated order sets. J Pediatr Oncol Nurs. 2005;22(1):20-30.
As hospitalists become more prevalent in facilities nationwide, administrators and others increasingly seek out these practitioners to take a clinical leadership role. More than ever, this includes implementing clinical practice guidelines to maximize outcomes and standardize care processes. Guidelines may be called pathways, order sets, or protocols, but these evidence-based tools are being embraced by hospitals; and facilities leaders are encouraging physicians to jump on the bandwagon.
Why Use Guidelines?
Studies already show that hospitalists have a positive effect on lengths of stay and efficiency of care, and some have documented a correlation between hospitalist programs and outcomes. So why are guidelines necessary?
Guidelines use a foundation of evidence-based medicine, which promotes the use of proven practices and interventions. “Evidence-based medicine is tough to refute,” says Ken Simone, DO, founder and president of Hospitalist and Practice Solutions in Brewer, Maine. “Typically, when you see evidence-based medicine within a guideline, you can assume that you are improving medicine if you use the tool accurately.”
There are two reasons to employ guidelines, according to Richard Rubin, MD, MBA, chief medical officer, Seton Health Systems, Troy, N.Y. One is to ensure efficiency in providing care that is clinically based. The second reason is to ensure consistent quality by preventing variations in care from practitioner to practitioner.
“These tools serve as a road map, giving you an idea of where to go and how to get there,” says Dr. Rubin.
There are limited data from the literature documenting the value of guidelines in the hospital setting. However, one study looked at the effect of a clinical pathway on six outcomes of care in patients hospitalized for community-acquired pneumonia.1 The authors found that those patients managed by using a pathway were significantly less likely to die in-hospital compared with non-pathway patients. Pathway patients also were more likely to receive blood cultures and appropriate antibiotic therapy.
In patients with the most severe pneumonia, those managed via pathway had an 80% reduction in the odds of respiratory therapy requiring mechanical ventilation. Overall, the authors concluded that patients who were managed using a clinical pathway for pneumonia were more likely to experience positive outcomes than patients treated without these tools.
Another study looked a multidisciplinary approach to creating “templated” order sets for chemotherapy. The authors concluded that such tools reduced the duplication of effort by significantly lowering the number of changes made during the order verification process.2
Dr. Rubin undertook an internal study at his facility that found that using order sets was linked to shorter lengths of stay. He discovered that pathways were used 18% of the time for cases with the longest lengths of stays and 54% of the time with the shortest.
“There’s not much I don’t like about order sets,” says Dr. Rubin.
Todd Popp, MD, clinical partner, Critical Care and Pulmonary Consultants, Denver, agrees. “Of course, we want to use tools that help patients, and effective order sets help improve quality and efficiency,” he says.
Dr. Popp adds that guideline use has an added advantage for hospitalists. Those practitioners, he notes, who have a demonstrated ability to develop and implement order sets increasingly will be in demand.
“There is a fair amount of competition between hospitalist groups. If you can prove that you can develop, implement, and use these standards,” he says, “it helps hospitals and their patients, and it helps hospitalists get better contracts and have solid relationships with their facilities.”
In fact, says Dr. Simone, hospitalists who have experience and knowledge about guideline development and implementation will be considered tremendous assets by hospitals. “If the nationwide use of guidelines in hospitals isn’t common yet, it will be in the coming years. And hospitalists are perfectly positioned to take the lead on the effective development and use of these tools,” he offers.
Tools that Teach
Guidelines encourage standardization of care and help physicians and other clinicians quickly select appropriate assessments and interventions for various conditions. They also help prescribers make appropriate medication and dosage selections quickly and accurately. For example, an order set for admissions to a coronary care unit (CCU) for acute coronary syndrome likely will address considerations such as nursing orders, IVs, medications, diagnostic tests, consults, discharge planning, and primary care follow-up.
Used properly, these tools do not promote “cookbook” or “cookie cutter” medicine—as some opponents suggest; instead, they guide decision-making and enable practical, evidence-based choices for each patient.
Hospitals and hospitalists most frequently employ guidelines regarding the clinical conditions that most commonly lead to ED visits or hospital stays. These include community-acquired pneumonia, COPD, CHF, chest pain, MI, and stroke.
In choosing topics on which to implement guidelines, Dr. Simone suggests considering the demographics, needs, and challenges of the particular facility. For example, “if you have guidelines addressing diagnoses for which patients generally are put on 24-hour observation prior to hospital admission, you can ferret out who needs to be admitted and who doesn’t,” he says, adding, “and you can make these decisions in a consistent manner.”
Buy-in and Barriers
Hospitalists who use guidelines agree that they are natural leaders when it comes to the development, implementation, and use of these tools.
“As a hospitalist, I am employed by the hospital and have more of a stake in overall quality and cost-effectiveness of care,” says Justin Psaila, MD, of St. Luke’s Hospital in Bethlehem, Pa. “Some of the private attendings are doing their own thing and just see guidelines as creating more work.”
“Hospitals are looking for more standardized approaches to medical care via guidelines and order sets, and hospitalists can deliver this,” says Alex Strachan, Jr., MD, medical director for the Hospitalist Program at St. Joseph Hospital in Eureka, Calif., and medical director of Team Health West Hospital Medicine Programs. “There is a tremendous amount of teamwork involved in guideline implementation and use, and hospitalists are natural team players.”
In addition to working with facilities to develop and implement guidelines, hospitalists can help increase buy-in from other clinicians. This may involve working with facility leadership to develop materials to promote the guidelines to stakeholders, such as letters to attending physicians that outline how the guidelines will work, where they can obtain copies, how they can obtain electronic versions (if available), the advantages of using these tools, what to do if they don’t follow a step in the guideline (e.g., document the patient’s refusal to receive a particular treatment), and who to contact if they have questions about the guideline.
Despite all of the positives about guidelines and the growing number of physicians who use and embrace them, there continues to be some resistance to guideline use. “Many physicians still are hesitant to use guidelines,” explains Dr. Simone. “They feel as if they will lose some creativity and that it may obligate them to go in a particular direction.”
Even when a facility’s hospitalists are on board with guidelines, attending physicians—who usually are in the majority—who resist can prevent the documents from having a positive impact. Dr. Strachan offers an example: “If you have 50-100 medical staff admitting, they will use the antibiotics that they are most comfortable with—regardless of cost, staff time involved in medication administration, and so on. If even half of these buy into a guideline addressing antibiotic use, it can streamline medication management, administration, and costs considerably.”
Some physicians worry that guidelines put them at risk for lawsuits. “One physician said, ‘You put my back to the wall if I don’t do these things,’” says Dr. Simone. “However, good guidelines don’t set you up; they protect you. If you don’t follow a step or recommendation, you just need to document why.”
Often, some basic revisions can help overcome objections to guideline use. As Dr. Simone explains, “We had an order set that was five pages in length, and physicians balked at using it. They said that it was too complicated. So we winnowed it down to two to three concise pages, and now they all use it.”
He cautions that if guidelines are too confusing, complex, or long, they seem overwhelming and are less likely to be used.
Birth of a Hospitalist Guideline
While there are many clinical practice guidelines in existence that address a range of clinical issues and conditions, hospitalists and other physicians are more likely to use a tool they have helped create. Arun Tewari, MD, program director of the Hospitalist Program, Ball Memorial Hospital Medical Consultants, Muncie, Ind., has experienced this first-hand and has been involved in guideline development at his facility for the past three years.
“We’re just starting to track data, but we’ve already realized a reduced length of stay for all the pathways we use, including stroke, CHF, COPD, pneumonia, chest pains, MI, and GI bleed,” he says. “To date, the numbers are only statistically significant for pneumonia. However, we expect to see significant results in the other areas over time.”
Dr. Tewari and his group use a multidisciplinary approach to pathway development. “We invite key individuals from different disciplines and specialties to serve on a committee that is run by a physician and a nurse leader. These individuals are responsible for reviewing articles and other information and performing specific assigned tasks,” he explains.
The group starts with a tremendous amount of information. In addition to articles from the literature, they review national guidelines on the topic being addressed, as well as pathways used by other facilities or organizations.
The group takes the best clinical evidence and information they find, and they incorporate it into a tool that is useful and practical for the hospital.
“To be truly effective, these tools have to be institutionalized to your facility and practical in terms of what can be done or handled in this setting,” suggests Dr. Tewari.
Once the group reaches consensus on a completed draft, the document goes to several hospital committees for review. The original group then compiles the comments, makes any revisions or additions deemed necessary, and produces a final pathway. “This isn’t a short process,” cautions Dr. Tewari. On average it takes six months to a year from start to finish.
The final pathways are posted online, and physicians can print copies. Elsewhere, the pathways are available on the floors and in the emergency department as well. Currently, the pathways aren’t available for electronic applications such as PDAs. However, Dr. Tewari doesn’t rule this out as a possibility for the future.
Of course, Dr. Tewari emphasizes, just publishing a pathway or making it available to clinical staff isn’t enough. “You have to educate people about the pathways and gain their buy-in,” he notes. At his facility, each clinical department staff meeting involves a representative who will talk about pathways and spell out how to use them. This also presents another opportunity for practitioners and team leaders to have input on the tools.
The pathways aren’t mandatory, Dr. Tewari emphasizes, but they are strongly encouraged. “We don’t have statistics yet, but throughout the hospital, utilization probably is at about 50%. Within our hospitalist group, utilization is close to 100%. We hope to have some hard numbers soon to back this up.”
No Crystal Balls Needed: Guidelines Have a Future
Guidelines soundly rooted in evidence-based medicine have a future, predicts Dr. Simone.
“I think these are essential for the Medicare pay-for-performance measures that are coming down the pike. Medicare is likely to identify three to five different diagnoses to look at and may want hospitals to develop guidelines for these. Hospitals—as well as hospitalists and other physicians—will be rewarded if their performance is good in these areas based on these guidelines.”
Some hospitals already are using guidelines or order sets to prove quality. “We put our order sets together partly because we are part of a CMS [Centers for Medicare and Medicaid Services] pay-for-performance project,” says Dr. Psaila.
Guidelines that are commonly available via laptop or PDA also are coming. “Hospitalists tend to use technology more than other physicians, and they increasingly will want guideline applications for handheld devices,” notes Dr. Strachan.
There already are several companies offering such products. “Some of these are really useful tools,” he continues. “They allow you to pull up an order set for a particular illness and use it. You can click on medications and check the evidence basis for their use. You then can print out this information or transmit it electronically.”
The real future is to have electronic medical record solutions that interface with orders, predicts Dr. Strachan. However, he suggests that current availability and use of such systems is less than 10% of hospitals and hospitalists.
“I feel that it is essential that we develop various guidelines and use them in the hospital setting,” concludes Dr. Strachan. “We need to standardize our practice so that we can measure outcomes and quality of care doesn’t vary from one practitioner to another.” TH
Writer Joanne Kaldy also writes about hospitalist programs in this issue.
References
- Hauck LD, Adler LM, Mulla ZD. Clinical pathway care improves outcomes among patients hospitalized for community-acquired pneumonia. Ann Epidemiol. 2004;14(9):669-675.
- Dinning C, Branowicki P, O’Neill JB, et al. Chemotherapy error reduction: a multidisciplinary approach to create templated order sets. J Pediatr Oncol Nurs. 2005;22(1):20-30.
As hospitalists become more prevalent in facilities nationwide, administrators and others increasingly seek out these practitioners to take a clinical leadership role. More than ever, this includes implementing clinical practice guidelines to maximize outcomes and standardize care processes. Guidelines may be called pathways, order sets, or protocols, but these evidence-based tools are being embraced by hospitals; and facilities leaders are encouraging physicians to jump on the bandwagon.
Why Use Guidelines?
Studies already show that hospitalists have a positive effect on lengths of stay and efficiency of care, and some have documented a correlation between hospitalist programs and outcomes. So why are guidelines necessary?
Guidelines use a foundation of evidence-based medicine, which promotes the use of proven practices and interventions. “Evidence-based medicine is tough to refute,” says Ken Simone, DO, founder and president of Hospitalist and Practice Solutions in Brewer, Maine. “Typically, when you see evidence-based medicine within a guideline, you can assume that you are improving medicine if you use the tool accurately.”
There are two reasons to employ guidelines, according to Richard Rubin, MD, MBA, chief medical officer, Seton Health Systems, Troy, N.Y. One is to ensure efficiency in providing care that is clinically based. The second reason is to ensure consistent quality by preventing variations in care from practitioner to practitioner.
“These tools serve as a road map, giving you an idea of where to go and how to get there,” says Dr. Rubin.
There are limited data from the literature documenting the value of guidelines in the hospital setting. However, one study looked at the effect of a clinical pathway on six outcomes of care in patients hospitalized for community-acquired pneumonia.1 The authors found that those patients managed by using a pathway were significantly less likely to die in-hospital compared with non-pathway patients. Pathway patients also were more likely to receive blood cultures and appropriate antibiotic therapy.
In patients with the most severe pneumonia, those managed via pathway had an 80% reduction in the odds of respiratory therapy requiring mechanical ventilation. Overall, the authors concluded that patients who were managed using a clinical pathway for pneumonia were more likely to experience positive outcomes than patients treated without these tools.
Another study looked a multidisciplinary approach to creating “templated” order sets for chemotherapy. The authors concluded that such tools reduced the duplication of effort by significantly lowering the number of changes made during the order verification process.2
Dr. Rubin undertook an internal study at his facility that found that using order sets was linked to shorter lengths of stay. He discovered that pathways were used 18% of the time for cases with the longest lengths of stays and 54% of the time with the shortest.
“There’s not much I don’t like about order sets,” says Dr. Rubin.
Todd Popp, MD, clinical partner, Critical Care and Pulmonary Consultants, Denver, agrees. “Of course, we want to use tools that help patients, and effective order sets help improve quality and efficiency,” he says.
Dr. Popp adds that guideline use has an added advantage for hospitalists. Those practitioners, he notes, who have a demonstrated ability to develop and implement order sets increasingly will be in demand.
“There is a fair amount of competition between hospitalist groups. If you can prove that you can develop, implement, and use these standards,” he says, “it helps hospitals and their patients, and it helps hospitalists get better contracts and have solid relationships with their facilities.”
In fact, says Dr. Simone, hospitalists who have experience and knowledge about guideline development and implementation will be considered tremendous assets by hospitals. “If the nationwide use of guidelines in hospitals isn’t common yet, it will be in the coming years. And hospitalists are perfectly positioned to take the lead on the effective development and use of these tools,” he offers.
Tools that Teach
Guidelines encourage standardization of care and help physicians and other clinicians quickly select appropriate assessments and interventions for various conditions. They also help prescribers make appropriate medication and dosage selections quickly and accurately. For example, an order set for admissions to a coronary care unit (CCU) for acute coronary syndrome likely will address considerations such as nursing orders, IVs, medications, diagnostic tests, consults, discharge planning, and primary care follow-up.
Used properly, these tools do not promote “cookbook” or “cookie cutter” medicine—as some opponents suggest; instead, they guide decision-making and enable practical, evidence-based choices for each patient.
Hospitals and hospitalists most frequently employ guidelines regarding the clinical conditions that most commonly lead to ED visits or hospital stays. These include community-acquired pneumonia, COPD, CHF, chest pain, MI, and stroke.
In choosing topics on which to implement guidelines, Dr. Simone suggests considering the demographics, needs, and challenges of the particular facility. For example, “if you have guidelines addressing diagnoses for which patients generally are put on 24-hour observation prior to hospital admission, you can ferret out who needs to be admitted and who doesn’t,” he says, adding, “and you can make these decisions in a consistent manner.”
Buy-in and Barriers
Hospitalists who use guidelines agree that they are natural leaders when it comes to the development, implementation, and use of these tools.
“As a hospitalist, I am employed by the hospital and have more of a stake in overall quality and cost-effectiveness of care,” says Justin Psaila, MD, of St. Luke’s Hospital in Bethlehem, Pa. “Some of the private attendings are doing their own thing and just see guidelines as creating more work.”
“Hospitals are looking for more standardized approaches to medical care via guidelines and order sets, and hospitalists can deliver this,” says Alex Strachan, Jr., MD, medical director for the Hospitalist Program at St. Joseph Hospital in Eureka, Calif., and medical director of Team Health West Hospital Medicine Programs. “There is a tremendous amount of teamwork involved in guideline implementation and use, and hospitalists are natural team players.”
In addition to working with facilities to develop and implement guidelines, hospitalists can help increase buy-in from other clinicians. This may involve working with facility leadership to develop materials to promote the guidelines to stakeholders, such as letters to attending physicians that outline how the guidelines will work, where they can obtain copies, how they can obtain electronic versions (if available), the advantages of using these tools, what to do if they don’t follow a step in the guideline (e.g., document the patient’s refusal to receive a particular treatment), and who to contact if they have questions about the guideline.
Despite all of the positives about guidelines and the growing number of physicians who use and embrace them, there continues to be some resistance to guideline use. “Many physicians still are hesitant to use guidelines,” explains Dr. Simone. “They feel as if they will lose some creativity and that it may obligate them to go in a particular direction.”
Even when a facility’s hospitalists are on board with guidelines, attending physicians—who usually are in the majority—who resist can prevent the documents from having a positive impact. Dr. Strachan offers an example: “If you have 50-100 medical staff admitting, they will use the antibiotics that they are most comfortable with—regardless of cost, staff time involved in medication administration, and so on. If even half of these buy into a guideline addressing antibiotic use, it can streamline medication management, administration, and costs considerably.”
Some physicians worry that guidelines put them at risk for lawsuits. “One physician said, ‘You put my back to the wall if I don’t do these things,’” says Dr. Simone. “However, good guidelines don’t set you up; they protect you. If you don’t follow a step or recommendation, you just need to document why.”
Often, some basic revisions can help overcome objections to guideline use. As Dr. Simone explains, “We had an order set that was five pages in length, and physicians balked at using it. They said that it was too complicated. So we winnowed it down to two to three concise pages, and now they all use it.”
He cautions that if guidelines are too confusing, complex, or long, they seem overwhelming and are less likely to be used.
Birth of a Hospitalist Guideline
While there are many clinical practice guidelines in existence that address a range of clinical issues and conditions, hospitalists and other physicians are more likely to use a tool they have helped create. Arun Tewari, MD, program director of the Hospitalist Program, Ball Memorial Hospital Medical Consultants, Muncie, Ind., has experienced this first-hand and has been involved in guideline development at his facility for the past three years.
“We’re just starting to track data, but we’ve already realized a reduced length of stay for all the pathways we use, including stroke, CHF, COPD, pneumonia, chest pains, MI, and GI bleed,” he says. “To date, the numbers are only statistically significant for pneumonia. However, we expect to see significant results in the other areas over time.”
Dr. Tewari and his group use a multidisciplinary approach to pathway development. “We invite key individuals from different disciplines and specialties to serve on a committee that is run by a physician and a nurse leader. These individuals are responsible for reviewing articles and other information and performing specific assigned tasks,” he explains.
The group starts with a tremendous amount of information. In addition to articles from the literature, they review national guidelines on the topic being addressed, as well as pathways used by other facilities or organizations.
The group takes the best clinical evidence and information they find, and they incorporate it into a tool that is useful and practical for the hospital.
“To be truly effective, these tools have to be institutionalized to your facility and practical in terms of what can be done or handled in this setting,” suggests Dr. Tewari.
Once the group reaches consensus on a completed draft, the document goes to several hospital committees for review. The original group then compiles the comments, makes any revisions or additions deemed necessary, and produces a final pathway. “This isn’t a short process,” cautions Dr. Tewari. On average it takes six months to a year from start to finish.
The final pathways are posted online, and physicians can print copies. Elsewhere, the pathways are available on the floors and in the emergency department as well. Currently, the pathways aren’t available for electronic applications such as PDAs. However, Dr. Tewari doesn’t rule this out as a possibility for the future.
Of course, Dr. Tewari emphasizes, just publishing a pathway or making it available to clinical staff isn’t enough. “You have to educate people about the pathways and gain their buy-in,” he notes. At his facility, each clinical department staff meeting involves a representative who will talk about pathways and spell out how to use them. This also presents another opportunity for practitioners and team leaders to have input on the tools.
The pathways aren’t mandatory, Dr. Tewari emphasizes, but they are strongly encouraged. “We don’t have statistics yet, but throughout the hospital, utilization probably is at about 50%. Within our hospitalist group, utilization is close to 100%. We hope to have some hard numbers soon to back this up.”
No Crystal Balls Needed: Guidelines Have a Future
Guidelines soundly rooted in evidence-based medicine have a future, predicts Dr. Simone.
“I think these are essential for the Medicare pay-for-performance measures that are coming down the pike. Medicare is likely to identify three to five different diagnoses to look at and may want hospitals to develop guidelines for these. Hospitals—as well as hospitalists and other physicians—will be rewarded if their performance is good in these areas based on these guidelines.”
Some hospitals already are using guidelines or order sets to prove quality. “We put our order sets together partly because we are part of a CMS [Centers for Medicare and Medicaid Services] pay-for-performance project,” says Dr. Psaila.
Guidelines that are commonly available via laptop or PDA also are coming. “Hospitalists tend to use technology more than other physicians, and they increasingly will want guideline applications for handheld devices,” notes Dr. Strachan.
There already are several companies offering such products. “Some of these are really useful tools,” he continues. “They allow you to pull up an order set for a particular illness and use it. You can click on medications and check the evidence basis for their use. You then can print out this information or transmit it electronically.”
The real future is to have electronic medical record solutions that interface with orders, predicts Dr. Strachan. However, he suggests that current availability and use of such systems is less than 10% of hospitals and hospitalists.
“I feel that it is essential that we develop various guidelines and use them in the hospital setting,” concludes Dr. Strachan. “We need to standardize our practice so that we can measure outcomes and quality of care doesn’t vary from one practitioner to another.” TH
Writer Joanne Kaldy also writes about hospitalist programs in this issue.
References
- Hauck LD, Adler LM, Mulla ZD. Clinical pathway care improves outcomes among patients hospitalized for community-acquired pneumonia. Ann Epidemiol. 2004;14(9):669-675.
- Dinning C, Branowicki P, O’Neill JB, et al. Chemotherapy error reduction: a multidisciplinary approach to create templated order sets. J Pediatr Oncol Nurs. 2005;22(1):20-30.
Like Mortar and Pestle
Editors’ note: “Alliances” is a series written about the relationships that hospitalists have with members of the clinical care team, from the team members’ points of view. Each installment of “Alliances” provides valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
At the bedside or in committee, hospitalists are earning high marks from their pharmacist colleagues for their flexibility, approachability, and availability. By most accounts, hospitalists make the job of hospital pharmacists much easier, say the clinical pharmacists whom The Hospitalist recently interviewed—two from large university teaching hospitals and one from a community-based for-profit facility. In fact, attempts to extricate even constructive recommendations for hospitalists from these PharmDs proved fruitless.
“I think they do just about everything right,” says Tom Bookwalter, PharmD, clinical pharmacist on the General Medicine Service at the University of California San Francisco Medical Center and a clinical professor of pharmacy at the UCSF School of Medicine. “I don’t find any fault with them.”
On the unit and in policy and procedure committee meetings, say the sources interviewed for this article, hospitalists develop good rapport with other staff members, address problems promptly, and are committed to improving processes for staff and patients alike.
Strengths of Hospitalists
As a clinical pharmacy specialist in general medicine on floor 15 at Brigham and Women’s Hospital (BWH) (Boston), Stephanie A. Wahlstrom, PharmD BCPS, begins rounds with the clinical team at 8 a.m. The group—typically consisting of Dr. Wahlstrom, a pharmacy student under her supervision, two or three physician assistants, a hospitalist, a nurse and a care coordinator—“runs the list” of patients to be seen until about 10:30 a.m. On floor 15, a general medicine unit, Dr. Wahlstrom and the clinical team usually care for 15 patients.
Most of Dr.Wahlstrom’s dealings with attending physicians in her four years at BWH have involved hospitalists. “Our team does accept other patients from Harvard Vanguard Medical Associates, so I do see those attending physicians, but I always round with the hospitalist from BWH.
“One of their major strengths is that they get to know the system so well, and they are committed to improving the hospital system,” she explains. “They know its efficiencies—and its inefficiencies—and they are familiar with processes and how long they take.”
For instance, a physician unfamiliar with the workings of the hospital laboratory timing might not know how long it would take to obtain lab results. A patient on enoxaparin who is being monitored would have an anti-Xa level drawn, and an attending physician from outside the hospital system would have to call the lab to find out when results would appear.
A hospitalist, on the other hand, “has an intuition about how long that lab [result] would take to come back,” says Dr. Wahlstrom, and times his or her return visit to the unit to review results with the pharmacist.
Robert Quinn, PharmD, is director of pharmacy services at Sierra Vista Regional Hospital, a 182-bed acute care facility owned by Tenet Healthcare Corporation and located in California. He is especially appreciative of hospitalists’ availability to staff.
“In ‘the old days,’ before hospitalists, one could feel disconnected from the medical staff. They didn’t always know or understand procedures,” says Dr. Quinn. In addition, “reaching community-based attending physicians was much more difficult. Now, [the hospitalists] know the ins and outs of the hospital system, and they know who to speak with in certain departments.
“Another physician not familiar with our system may call and ask for a pharmacist, but our hospitalists will know when they need to speak with the director of pharmacy services or when they should talk with a clinical pharmacist,” he continues. “They really do know the inner workings of the hospital on a much more intimate level.”
For instance, says Dr. Quinn, when hospitalists want a certain medication to be added to the hospital’s medication formulary, they know that their request should be routed to the director of pharmacy services. Direct patient care, including monitoring for blood levels of medications, drug information, and the like are the bailiwick of the clinical pharmacists.
“In my experience here at UCSF,” says Dr. Bookwalter, “[hospitalists] are very concerned about making the hospital work, which is one of their major missions. They’re also very collaborative. We really do work together—not just pharmacy and hospitalists—but with everybody.”
As an example of that collaborative approach, Dr. Bookwalter points to a palliative care program developed under the leadership of Hospitalist and SHM President Steve Pantilat, MD. The program has garnered Palliative Care Leadership Center status for the UCSF Medical Center.

—Robert Quinn, PharmD
Collaboration Is Primary
Dr. Bookwalter does have comparisons to his current situation on the General Medicine Service because he previously worked in the Intensive Care Nursery and with the General Surgery Service at UCSF. The latter, he says, “was very hierarchical. The team I was on included some very famous surgeons. They were all very personable and certainly knew what they were doing—they were really great. But, if you made a suggestion to them, chances were it would be rejected, since they insisted on ‘caring for their patients themselves.’”
At BWH Dr. Wahlstrom has also observed that hospitalists are very inclusive.
“When we do rounds, they ask the nurse to join us, so that we can have all points of care in our meetings,” she says. “If I recommend a change in a patient’s medication regimen, such as adding basal insulin for a patient, the hospitalist generally includes that in the patient’s plan immediately, and an order is written when we are on rounds. Then I approve it, and the patient can be started on medication promptly. We discuss what is going to happen and the care plan is made right there on the spot.”
Hospitalists with whom Dr. Wahlstrom works are comfortable with collaboration and open to ideas. “You’re not worried about suggesting ideas, or that your ideas might be rejected,” she explains. For instance, suggesting a change from IV to PO antibiotics would be welcomely discussed. “The hospitalists make the environment for presenting ideas regarding patient care open and encouraging.”
Communication a Plus
Availability of hospitalists is enhanced by their communication skills, says Dr. Quinn. “Once hospitalists get to know us, and we get to know them, the communication is just absolutely great,” he says. “Although I don’t get out as much as my clinicians do, if I have an issue I can go to the unit anytime and discuss it.”
The hospitalists with whom Dr. Quinn deals are interested in process issues as well as patient issues. For instance, if medication-administration records are not being placed in patients’ charts in a timely manner, hospital staff have the ability to quickly set up meetings with department managers and hospitalists to devise ways to improve procedures.
Meeting with other attending physicians is not as easy, says Dr. Quinn because they usually have very little time after making rounds and may have to be contacted at their practice office. “That’s one of the main advantages of having hospitalists,” he says. “They’re available. If anything happens, they’re there.”
During orientation at the UCSF Medical Center with new hospitalists, the General Medicine Service hospitalist residents take their teams on a tour of the pharmacy guided by Dr. Bookwalter. He explains the configuration of his department, which includes clinical pharmacists, pharmacy students, and a pharmacy practice resident. During the tour, he demonstrates how a medication order is processed, following it from the time the physician writes the prescription until the patient receives it. This contributes to both the residents’ and medical students’ understanding of how the hospital works.
If hospitalists have a concern about hospital policies, Dr. Bookwalter is there to aid them. “We promote rational drug therapy while the patient is in the hospital, smooth transitions in care, with the admit and discharge interviews, and we also follow up after patients leave to make sure they had no problems getting the medications they needed,” says Dr. Bookwalter.
During these contacts with patients, pharmacists also perform triage by asking patients how they feel at home. If they uncover problems during these interviews, “we first go to the team that took care of them in the hospital, and then to their primary physician,” he says.
A Boon for Patients, Staff
Are patients less comfortable with a new physician taking over their care? Dr. Quinn does not think this is a drawback. While the primary care physician may have a long-standing relationship with his or her patients, Dr. Quinn believes the availability of hospitalists can be very comforting to the patient.
“When a physician makes rounds and then leaves, patients may have a little bit of anxiety about whether they asked all their questions,” he speculates. It can be very comforting, he says, for the patient to know that the hospitalist is still on site.
Dr. Wahlstrom admits that sometimes she observes that patients may initially be uncomfortable meeting a physician other than their primary care physician. Again, building patient rapport seems to be no problem with the hospitalists with whom she works. “Patients seem to warm up to them right away,” she enthuses.
Dr. Quinn appreciates the fact that hospitalists are able and willing to participate in committees. “As a director of pharmacy services, I notice that their participation really helps—they understand the inner workings of the hospital and are able to look at situations in a different way.”
The hospital’s monthly hospitalist meeting is very well attended, Dr. Quinn reports: “[Our pharmacists] show up because we know that this is a tremendous forum for us to interact with physicians.”
Dr. Bookwalter also praises hospitalists’ interest in hospital safety and continuity of care. An innovative training program begun at UCSF Medical Center last year to address these issues entails sending pairs of pharmacy and medical students to patients’ homes after their hospital release.
“This has been very well received by both the pharmacy and medical students,” says Dr. Bookwalter. While at the patient’s home, the pharmacy student checks whether the patient has everything he or she needs, whether the patient understands how to take the medication, and whether it is being stored properly. If there are problems, the students can call the patient’s pharmacy, obtain special authorizations for third-party insurance coverage if needed, and help the patients obtain the care they need.
The program is designed to help students understand the change between hospital and home. “It’s a huge transition,” emphasizes Dr. Bookwalter. “Here in the hospital, the nurse is giving them their medicine every day, and then when they get home—and most of our patients are elderly—they get confused. Ultimately, we don’t want any discontinuities in care.”
High Ratings
It is their attention to innovation and collaboration among members of the multidisciplinary that our sources repeatedly praised about their hospitalist colleagues. Dr. Bookwalter doesn’t think there are any areas where hospitalists needed improvement.
“They all take it seriously, and they all perform well. You can really tell when you have someone on rotation who is not a hospitalist,” he says. “There are MDs who do research, are very well known, and are very familiar with the hospital, but it’s not the same collaborative experience. It’s like day and night.”
When pressed for recommendations he would give to hospitalists for improvement, Dr. Quinn admits he has one complaint: “I wish we had more. I’d like to see dozens of them!” TH
Writer Gretchen Henkel regularly writes “Alliances” for The Hospitalist.
Editors’ note: “Alliances” is a series written about the relationships that hospitalists have with members of the clinical care team, from the team members’ points of view. Each installment of “Alliances” provides valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
At the bedside or in committee, hospitalists are earning high marks from their pharmacist colleagues for their flexibility, approachability, and availability. By most accounts, hospitalists make the job of hospital pharmacists much easier, say the clinical pharmacists whom The Hospitalist recently interviewed—two from large university teaching hospitals and one from a community-based for-profit facility. In fact, attempts to extricate even constructive recommendations for hospitalists from these PharmDs proved fruitless.
“I think they do just about everything right,” says Tom Bookwalter, PharmD, clinical pharmacist on the General Medicine Service at the University of California San Francisco Medical Center and a clinical professor of pharmacy at the UCSF School of Medicine. “I don’t find any fault with them.”
On the unit and in policy and procedure committee meetings, say the sources interviewed for this article, hospitalists develop good rapport with other staff members, address problems promptly, and are committed to improving processes for staff and patients alike.
Strengths of Hospitalists
As a clinical pharmacy specialist in general medicine on floor 15 at Brigham and Women’s Hospital (BWH) (Boston), Stephanie A. Wahlstrom, PharmD BCPS, begins rounds with the clinical team at 8 a.m. The group—typically consisting of Dr. Wahlstrom, a pharmacy student under her supervision, two or three physician assistants, a hospitalist, a nurse and a care coordinator—“runs the list” of patients to be seen until about 10:30 a.m. On floor 15, a general medicine unit, Dr. Wahlstrom and the clinical team usually care for 15 patients.
Most of Dr.Wahlstrom’s dealings with attending physicians in her four years at BWH have involved hospitalists. “Our team does accept other patients from Harvard Vanguard Medical Associates, so I do see those attending physicians, but I always round with the hospitalist from BWH.
“One of their major strengths is that they get to know the system so well, and they are committed to improving the hospital system,” she explains. “They know its efficiencies—and its inefficiencies—and they are familiar with processes and how long they take.”
For instance, a physician unfamiliar with the workings of the hospital laboratory timing might not know how long it would take to obtain lab results. A patient on enoxaparin who is being monitored would have an anti-Xa level drawn, and an attending physician from outside the hospital system would have to call the lab to find out when results would appear.
A hospitalist, on the other hand, “has an intuition about how long that lab [result] would take to come back,” says Dr. Wahlstrom, and times his or her return visit to the unit to review results with the pharmacist.
Robert Quinn, PharmD, is director of pharmacy services at Sierra Vista Regional Hospital, a 182-bed acute care facility owned by Tenet Healthcare Corporation and located in California. He is especially appreciative of hospitalists’ availability to staff.
“In ‘the old days,’ before hospitalists, one could feel disconnected from the medical staff. They didn’t always know or understand procedures,” says Dr. Quinn. In addition, “reaching community-based attending physicians was much more difficult. Now, [the hospitalists] know the ins and outs of the hospital system, and they know who to speak with in certain departments.
“Another physician not familiar with our system may call and ask for a pharmacist, but our hospitalists will know when they need to speak with the director of pharmacy services or when they should talk with a clinical pharmacist,” he continues. “They really do know the inner workings of the hospital on a much more intimate level.”
For instance, says Dr. Quinn, when hospitalists want a certain medication to be added to the hospital’s medication formulary, they know that their request should be routed to the director of pharmacy services. Direct patient care, including monitoring for blood levels of medications, drug information, and the like are the bailiwick of the clinical pharmacists.
“In my experience here at UCSF,” says Dr. Bookwalter, “[hospitalists] are very concerned about making the hospital work, which is one of their major missions. They’re also very collaborative. We really do work together—not just pharmacy and hospitalists—but with everybody.”
As an example of that collaborative approach, Dr. Bookwalter points to a palliative care program developed under the leadership of Hospitalist and SHM President Steve Pantilat, MD. The program has garnered Palliative Care Leadership Center status for the UCSF Medical Center.

—Robert Quinn, PharmD
Collaboration Is Primary
Dr. Bookwalter does have comparisons to his current situation on the General Medicine Service because he previously worked in the Intensive Care Nursery and with the General Surgery Service at UCSF. The latter, he says, “was very hierarchical. The team I was on included some very famous surgeons. They were all very personable and certainly knew what they were doing—they were really great. But, if you made a suggestion to them, chances were it would be rejected, since they insisted on ‘caring for their patients themselves.’”
At BWH Dr. Wahlstrom has also observed that hospitalists are very inclusive.
“When we do rounds, they ask the nurse to join us, so that we can have all points of care in our meetings,” she says. “If I recommend a change in a patient’s medication regimen, such as adding basal insulin for a patient, the hospitalist generally includes that in the patient’s plan immediately, and an order is written when we are on rounds. Then I approve it, and the patient can be started on medication promptly. We discuss what is going to happen and the care plan is made right there on the spot.”
Hospitalists with whom Dr. Wahlstrom works are comfortable with collaboration and open to ideas. “You’re not worried about suggesting ideas, or that your ideas might be rejected,” she explains. For instance, suggesting a change from IV to PO antibiotics would be welcomely discussed. “The hospitalists make the environment for presenting ideas regarding patient care open and encouraging.”
Communication a Plus
Availability of hospitalists is enhanced by their communication skills, says Dr. Quinn. “Once hospitalists get to know us, and we get to know them, the communication is just absolutely great,” he says. “Although I don’t get out as much as my clinicians do, if I have an issue I can go to the unit anytime and discuss it.”
The hospitalists with whom Dr. Quinn deals are interested in process issues as well as patient issues. For instance, if medication-administration records are not being placed in patients’ charts in a timely manner, hospital staff have the ability to quickly set up meetings with department managers and hospitalists to devise ways to improve procedures.
Meeting with other attending physicians is not as easy, says Dr. Quinn because they usually have very little time after making rounds and may have to be contacted at their practice office. “That’s one of the main advantages of having hospitalists,” he says. “They’re available. If anything happens, they’re there.”
During orientation at the UCSF Medical Center with new hospitalists, the General Medicine Service hospitalist residents take their teams on a tour of the pharmacy guided by Dr. Bookwalter. He explains the configuration of his department, which includes clinical pharmacists, pharmacy students, and a pharmacy practice resident. During the tour, he demonstrates how a medication order is processed, following it from the time the physician writes the prescription until the patient receives it. This contributes to both the residents’ and medical students’ understanding of how the hospital works.
If hospitalists have a concern about hospital policies, Dr. Bookwalter is there to aid them. “We promote rational drug therapy while the patient is in the hospital, smooth transitions in care, with the admit and discharge interviews, and we also follow up after patients leave to make sure they had no problems getting the medications they needed,” says Dr. Bookwalter.
During these contacts with patients, pharmacists also perform triage by asking patients how they feel at home. If they uncover problems during these interviews, “we first go to the team that took care of them in the hospital, and then to their primary physician,” he says.
A Boon for Patients, Staff
Are patients less comfortable with a new physician taking over their care? Dr. Quinn does not think this is a drawback. While the primary care physician may have a long-standing relationship with his or her patients, Dr. Quinn believes the availability of hospitalists can be very comforting to the patient.
“When a physician makes rounds and then leaves, patients may have a little bit of anxiety about whether they asked all their questions,” he speculates. It can be very comforting, he says, for the patient to know that the hospitalist is still on site.
Dr. Wahlstrom admits that sometimes she observes that patients may initially be uncomfortable meeting a physician other than their primary care physician. Again, building patient rapport seems to be no problem with the hospitalists with whom she works. “Patients seem to warm up to them right away,” she enthuses.
Dr. Quinn appreciates the fact that hospitalists are able and willing to participate in committees. “As a director of pharmacy services, I notice that their participation really helps—they understand the inner workings of the hospital and are able to look at situations in a different way.”
The hospital’s monthly hospitalist meeting is very well attended, Dr. Quinn reports: “[Our pharmacists] show up because we know that this is a tremendous forum for us to interact with physicians.”
Dr. Bookwalter also praises hospitalists’ interest in hospital safety and continuity of care. An innovative training program begun at UCSF Medical Center last year to address these issues entails sending pairs of pharmacy and medical students to patients’ homes after their hospital release.
“This has been very well received by both the pharmacy and medical students,” says Dr. Bookwalter. While at the patient’s home, the pharmacy student checks whether the patient has everything he or she needs, whether the patient understands how to take the medication, and whether it is being stored properly. If there are problems, the students can call the patient’s pharmacy, obtain special authorizations for third-party insurance coverage if needed, and help the patients obtain the care they need.
The program is designed to help students understand the change between hospital and home. “It’s a huge transition,” emphasizes Dr. Bookwalter. “Here in the hospital, the nurse is giving them their medicine every day, and then when they get home—and most of our patients are elderly—they get confused. Ultimately, we don’t want any discontinuities in care.”
High Ratings
It is their attention to innovation and collaboration among members of the multidisciplinary that our sources repeatedly praised about their hospitalist colleagues. Dr. Bookwalter doesn’t think there are any areas where hospitalists needed improvement.
“They all take it seriously, and they all perform well. You can really tell when you have someone on rotation who is not a hospitalist,” he says. “There are MDs who do research, are very well known, and are very familiar with the hospital, but it’s not the same collaborative experience. It’s like day and night.”
When pressed for recommendations he would give to hospitalists for improvement, Dr. Quinn admits he has one complaint: “I wish we had more. I’d like to see dozens of them!” TH
Writer Gretchen Henkel regularly writes “Alliances” for The Hospitalist.
Editors’ note: “Alliances” is a series written about the relationships that hospitalists have with members of the clinical care team, from the team members’ points of view. Each installment of “Alliances” provides valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
At the bedside or in committee, hospitalists are earning high marks from their pharmacist colleagues for their flexibility, approachability, and availability. By most accounts, hospitalists make the job of hospital pharmacists much easier, say the clinical pharmacists whom The Hospitalist recently interviewed—two from large university teaching hospitals and one from a community-based for-profit facility. In fact, attempts to extricate even constructive recommendations for hospitalists from these PharmDs proved fruitless.
“I think they do just about everything right,” says Tom Bookwalter, PharmD, clinical pharmacist on the General Medicine Service at the University of California San Francisco Medical Center and a clinical professor of pharmacy at the UCSF School of Medicine. “I don’t find any fault with them.”
On the unit and in policy and procedure committee meetings, say the sources interviewed for this article, hospitalists develop good rapport with other staff members, address problems promptly, and are committed to improving processes for staff and patients alike.
Strengths of Hospitalists
As a clinical pharmacy specialist in general medicine on floor 15 at Brigham and Women’s Hospital (BWH) (Boston), Stephanie A. Wahlstrom, PharmD BCPS, begins rounds with the clinical team at 8 a.m. The group—typically consisting of Dr. Wahlstrom, a pharmacy student under her supervision, two or three physician assistants, a hospitalist, a nurse and a care coordinator—“runs the list” of patients to be seen until about 10:30 a.m. On floor 15, a general medicine unit, Dr. Wahlstrom and the clinical team usually care for 15 patients.
Most of Dr.Wahlstrom’s dealings with attending physicians in her four years at BWH have involved hospitalists. “Our team does accept other patients from Harvard Vanguard Medical Associates, so I do see those attending physicians, but I always round with the hospitalist from BWH.
“One of their major strengths is that they get to know the system so well, and they are committed to improving the hospital system,” she explains. “They know its efficiencies—and its inefficiencies—and they are familiar with processes and how long they take.”
For instance, a physician unfamiliar with the workings of the hospital laboratory timing might not know how long it would take to obtain lab results. A patient on enoxaparin who is being monitored would have an anti-Xa level drawn, and an attending physician from outside the hospital system would have to call the lab to find out when results would appear.
A hospitalist, on the other hand, “has an intuition about how long that lab [result] would take to come back,” says Dr. Wahlstrom, and times his or her return visit to the unit to review results with the pharmacist.
Robert Quinn, PharmD, is director of pharmacy services at Sierra Vista Regional Hospital, a 182-bed acute care facility owned by Tenet Healthcare Corporation and located in California. He is especially appreciative of hospitalists’ availability to staff.
“In ‘the old days,’ before hospitalists, one could feel disconnected from the medical staff. They didn’t always know or understand procedures,” says Dr. Quinn. In addition, “reaching community-based attending physicians was much more difficult. Now, [the hospitalists] know the ins and outs of the hospital system, and they know who to speak with in certain departments.
“Another physician not familiar with our system may call and ask for a pharmacist, but our hospitalists will know when they need to speak with the director of pharmacy services or when they should talk with a clinical pharmacist,” he continues. “They really do know the inner workings of the hospital on a much more intimate level.”
For instance, says Dr. Quinn, when hospitalists want a certain medication to be added to the hospital’s medication formulary, they know that their request should be routed to the director of pharmacy services. Direct patient care, including monitoring for blood levels of medications, drug information, and the like are the bailiwick of the clinical pharmacists.
“In my experience here at UCSF,” says Dr. Bookwalter, “[hospitalists] are very concerned about making the hospital work, which is one of their major missions. They’re also very collaborative. We really do work together—not just pharmacy and hospitalists—but with everybody.”
As an example of that collaborative approach, Dr. Bookwalter points to a palliative care program developed under the leadership of Hospitalist and SHM President Steve Pantilat, MD. The program has garnered Palliative Care Leadership Center status for the UCSF Medical Center.

—Robert Quinn, PharmD
Collaboration Is Primary
Dr. Bookwalter does have comparisons to his current situation on the General Medicine Service because he previously worked in the Intensive Care Nursery and with the General Surgery Service at UCSF. The latter, he says, “was very hierarchical. The team I was on included some very famous surgeons. They were all very personable and certainly knew what they were doing—they were really great. But, if you made a suggestion to them, chances were it would be rejected, since they insisted on ‘caring for their patients themselves.’”
At BWH Dr. Wahlstrom has also observed that hospitalists are very inclusive.
“When we do rounds, they ask the nurse to join us, so that we can have all points of care in our meetings,” she says. “If I recommend a change in a patient’s medication regimen, such as adding basal insulin for a patient, the hospitalist generally includes that in the patient’s plan immediately, and an order is written when we are on rounds. Then I approve it, and the patient can be started on medication promptly. We discuss what is going to happen and the care plan is made right there on the spot.”
Hospitalists with whom Dr. Wahlstrom works are comfortable with collaboration and open to ideas. “You’re not worried about suggesting ideas, or that your ideas might be rejected,” she explains. For instance, suggesting a change from IV to PO antibiotics would be welcomely discussed. “The hospitalists make the environment for presenting ideas regarding patient care open and encouraging.”
Communication a Plus
Availability of hospitalists is enhanced by their communication skills, says Dr. Quinn. “Once hospitalists get to know us, and we get to know them, the communication is just absolutely great,” he says. “Although I don’t get out as much as my clinicians do, if I have an issue I can go to the unit anytime and discuss it.”
The hospitalists with whom Dr. Quinn deals are interested in process issues as well as patient issues. For instance, if medication-administration records are not being placed in patients’ charts in a timely manner, hospital staff have the ability to quickly set up meetings with department managers and hospitalists to devise ways to improve procedures.
Meeting with other attending physicians is not as easy, says Dr. Quinn because they usually have very little time after making rounds and may have to be contacted at their practice office. “That’s one of the main advantages of having hospitalists,” he says. “They’re available. If anything happens, they’re there.”
During orientation at the UCSF Medical Center with new hospitalists, the General Medicine Service hospitalist residents take their teams on a tour of the pharmacy guided by Dr. Bookwalter. He explains the configuration of his department, which includes clinical pharmacists, pharmacy students, and a pharmacy practice resident. During the tour, he demonstrates how a medication order is processed, following it from the time the physician writes the prescription until the patient receives it. This contributes to both the residents’ and medical students’ understanding of how the hospital works.
If hospitalists have a concern about hospital policies, Dr. Bookwalter is there to aid them. “We promote rational drug therapy while the patient is in the hospital, smooth transitions in care, with the admit and discharge interviews, and we also follow up after patients leave to make sure they had no problems getting the medications they needed,” says Dr. Bookwalter.
During these contacts with patients, pharmacists also perform triage by asking patients how they feel at home. If they uncover problems during these interviews, “we first go to the team that took care of them in the hospital, and then to their primary physician,” he says.
A Boon for Patients, Staff
Are patients less comfortable with a new physician taking over their care? Dr. Quinn does not think this is a drawback. While the primary care physician may have a long-standing relationship with his or her patients, Dr. Quinn believes the availability of hospitalists can be very comforting to the patient.
“When a physician makes rounds and then leaves, patients may have a little bit of anxiety about whether they asked all their questions,” he speculates. It can be very comforting, he says, for the patient to know that the hospitalist is still on site.
Dr. Wahlstrom admits that sometimes she observes that patients may initially be uncomfortable meeting a physician other than their primary care physician. Again, building patient rapport seems to be no problem with the hospitalists with whom she works. “Patients seem to warm up to them right away,” she enthuses.
Dr. Quinn appreciates the fact that hospitalists are able and willing to participate in committees. “As a director of pharmacy services, I notice that their participation really helps—they understand the inner workings of the hospital and are able to look at situations in a different way.”
The hospital’s monthly hospitalist meeting is very well attended, Dr. Quinn reports: “[Our pharmacists] show up because we know that this is a tremendous forum for us to interact with physicians.”
Dr. Bookwalter also praises hospitalists’ interest in hospital safety and continuity of care. An innovative training program begun at UCSF Medical Center last year to address these issues entails sending pairs of pharmacy and medical students to patients’ homes after their hospital release.
“This has been very well received by both the pharmacy and medical students,” says Dr. Bookwalter. While at the patient’s home, the pharmacy student checks whether the patient has everything he or she needs, whether the patient understands how to take the medication, and whether it is being stored properly. If there are problems, the students can call the patient’s pharmacy, obtain special authorizations for third-party insurance coverage if needed, and help the patients obtain the care they need.
The program is designed to help students understand the change between hospital and home. “It’s a huge transition,” emphasizes Dr. Bookwalter. “Here in the hospital, the nurse is giving them their medicine every day, and then when they get home—and most of our patients are elderly—they get confused. Ultimately, we don’t want any discontinuities in care.”
High Ratings
It is their attention to innovation and collaboration among members of the multidisciplinary that our sources repeatedly praised about their hospitalist colleagues. Dr. Bookwalter doesn’t think there are any areas where hospitalists needed improvement.
“They all take it seriously, and they all perform well. You can really tell when you have someone on rotation who is not a hospitalist,” he says. “There are MDs who do research, are very well known, and are very familiar with the hospital, but it’s not the same collaborative experience. It’s like day and night.”
When pressed for recommendations he would give to hospitalists for improvement, Dr. Quinn admits he has one complaint: “I wish we had more. I’d like to see dozens of them!” TH
Writer Gretchen Henkel regularly writes “Alliances” for The Hospitalist.
11 Steps to a Successful Transition
A65-lb., 25-year-old, male cerebral palsy (CP) patient with pneumonia arrives at your Children’s Hospital via ambulance. Although chronologically this patient is an adult, in many ways he’s still a child, and the parents told the paramedics that they’ve always taken their son to Children’s. You’ve been the treating physician during the patient’s frequent hospital stays. Is Children’s Hospital still the best destination for this patient? Will the family’s insurance still cover an admission at Children’s?
During the hospital stay, the patient has complications. He has to be intubated. IV antibiotics need to be continued for a course after hospital discharge. A long recovery is expected. Is it time for the family to consider discharge to a long-term care facility rather than home? Are there any long-term care facilities in the area that accept young adult CP patients?
As the treating pediatric hospitalist, what is your role in helping this patient and his family transition from pediatric care to an adult-care medical home?
Introduction
Approximately 8.6 million children in the United States age 10–17 have a disability, according to the Adolescent Health Transition Project, which is housed at the Center on Human Development and Disability (CHDD) at the University of Washington, Seattle. Of these, 16% (or 1.4 million) experience limitations in their activities and will likely have difficulty making the transition to adult healthcare.1
Given enough time in the profession, every pediatric hospitalist will face the challenge of transitioning patients from child-centered to adult-oriented healthcare systems. The good news: Medical advances have made it increasingly possible for children who once would have died in childhood to survive into adulthood.
Example: One in 2,500 children is born with cystic fibrosis (CF); however, with the recent, unprecedented increase in the success of diagnosis and treatment modalities for the pulmonary component of CF, the estimated median survival age for those born in the 1990s is now 40.2 As of the year 2004, 41.8% of the 22,301 patients with CF were 18 or older.3 In fact, each year nearly 500,000 children with special healthcare needs reach adulthood, and 90% of children with a chronic illness and/or disability now survive to adulthood.4,5
The bad news: Many physicians whose practices focus on adults aren’t familiar with disease processes, such as CF, that have historically been considered pediatric illnesses.
For patients with chronic physical and medical conditions—particularly for those who are medically fragile and/or technology-dependent—the transition can prove especially difficult. And pediatric hospitalists in children’s hospitals face different challenges than those in facilities that admit patients of all ages. One thing remains the same, though, the goal: to provide uninterrupted, coordinated, developmentally appropriate healthcare.
Why Transition?
There are several good reasons for patients to be transitioned from pediatric care to adult care. First, as patients age medical issues develop that are beyond the sphere of pediatricians. In CF, for example, diabetes and biliary tract problems occur with greater frequency in adults. However, because so few CF patients historically survived to adulthood, few physicians who care for adults learned about the disease. Thus, the pediatricians who cared for CF patients continued to do so, leading to situations in which 30- and 40-year-olds have been hospitalized with children. But is that truly appropriate?
Adult patients may have high blood pressure, gynecologic issues, osteoporosis, or other problems the pediatrician may not be prepared to deal with. Example: A primary care pediatrician has been the “medical home” for a small, cerebral palsy patient since she was 10. She’s now 25. If she presents with a breast mass, will the pediatrician pick up on the condition adequately? Will they know where to send the patient?
“Adult providers know those systems better,” says Brett Pickering, MD, director of the Special Needs Clinic at San Diego’s UCSD Medical Center, Department of Pediatrics.
The adult patient has different emotional needs than the pediatric patient, and the pediatric hospitalist may not be in tune with adult needs. “Pediatricians do a lot of handholding,” says Dr. Pickering. “Adult providers are more matter of fact.”
Age restrictions on admissions, insurance, and funding issues also affect transition. For example, funding under the Social Security Act’s Title V Children with Special Health Care Needs typically ends at 21 despite a patient’s education or employment status.
Given these factors, what is the appropriate age to transition care from a pediatric floor or facility to an adult-oriented unit? According to the American Academy of Pediatrics, the responsibility of pediatrics continues through age 21, but there’s no hard-and-fast rule.
Challenges
The transition to adult-care facilities is typically a lengthy process involving multiple specialties and possibly joint care during a transition period—and a process that should ideally be coordinated by the patient’s primary care pediatrician. But hospitalists know that circumstances are typically far from ideal.
First, during a transition, the patient may feel abandoned by the medical team they’ve known for most of their lives. It takes time to develop trust and confidence in a new doctor. In this respect, pediatric hospitalists in facilities that care for patients of all ages have an advantage over hospitalists in children’s hospitals. They can call on their adult-care colleagues in other areas of the hospital for consultations and transfer care over time.
“The pediatric hospitalist must make bridges with their adult colleagues who are comfortable [with the issues] and willing to take on this patient population,” says Dr. Pickering.
Second, parents may feel an emotional dependency on the pediatric team and can feel threatened by the adult environment as they lose some control. To the parents, the patient will always be their child, Dr. Pickering notes.
Third, pediatric hospitalists may be reluctant to let go, particularly if they feel adult services are inferior to those they have provided, which brings us to the fourth major challenge: To whom do you transition care?
Many adult healthcare providers receive only limited training in disorders associated with pediatrics (e.g., CF, spina bifida). The Cystic Fibrosis Foundation is leading the way in educating physicians in what have historically been considered pediatric problems. In the 1980s, the foundation launched an educational program to train physicians already involved in adult pulmonary care in CF. Unfortunately, education in other areas has lagged. And finding a physician with both an interest in and knowledge of such disorders can prove challenging.
“It’s incumbent on our adult colleagues to take these patients on, but they need training,” says Dr. Pickering. “Long-term issues require long-term solutions.
How do you jazz people up to take care of this population?” she asks. Physicians must have at least a little bit of desire to learn about these special patient populations, but academic institutions also need to identify core knowledge and skills and make them part of training and certification requirements for primary care residents and physicians in practice. Continuing medical education for physicians, nurses, and allied healthcare professionals should include drug dosing, medical complications seen in transition populations, and related developmental, psychosocial, and behavioral issues.
Steps to a Successful Transition
So what should hospitalists do? In an April 2005 presentation at the SHM Annual Meeting, Joseph M. Geskey, DO, assistant professor of pediatrics and medicine, and director of inpatient pediatrics at Penn State College of Medicine, Hershey, Penn., recommended that pediatric hospitalists take the following steps:
- Identify the key aspects of transition;
- Bring stakeholders together;
- Identify transitional needs;
- Identify and provide resources;
- Create an audit and evaluation process;
- Decide who will hand off care of these patients when they are admitted to the hospital (the hospitalist or the disease-specific specialist);
- Create an up-to-date medical summary that is portable and accessible. It should include important historic information, such as diagnostic data, procedures, operations, and medications;
- Upon patient discharge, include specific instructions on who to call if the patient develops a problem after leaving the hospital;
- Create a working group in your area that represents pediatric and adult hospitalists to examine transition issues in the hospitalized patient; and
- Facilitate effective communication between patients and their families, primary care physicians and specialists; and
- Know when to transfer care to a center with more expertise in caring for specific conditions.
Conclusion
Just as every patient is different and every patient’s circumstances are unique, every transition needs to be individualized. “It’s hard to set policy,” says Dr. Pickering. Open, direct communication, specific discharge instructions, an up-to-date medical summary and knowledge of the adult resources in your area can make any transition a success. TH
Keri Losavio regularly writes for “Pediatric Special Section.”
References
- Adolescent Health Transition Project, Center on Human Development and Disability (CHDD) at the University of Washington, Seattle. Available at http://depts.washington.edu/healthtr/Providers/intro.htm. Last accessed January 16, 2006.
- Bufi PL. Cystic fibrosis: therapeutic options for co-management. Available at www.thorne.com/altmedrev/fulltext/cystic.html. Last accessed January 16, 2006.
- Cystic Fibrosis Foundation: 2004 Patient Registry Report. Available at www.cff.org/living_with_cf/. Last accessed Jan. 26, 2006
- Newacheck PW, Taylor WR. Childhood chronic illness: prevalence, severity, and impact. Am J Pub Health. 1992;82(3):364-371.
- Committee on Children with Disabilities and Committee on Adolescence, American Academy of Pediatrics. Transition of care provided for adolescents with special health care needs. Pediatrics. 1996;98(6):1203–1206.
Pediatric Special Section
In the Literature
By Mary Ann Queen, MD, and Amita Amonker, MD
Utilization of a Clinical Pathway Improves Care for Bronchiolitis
Cheney J, Barber S, Altamirano L, et al. A Clinical Pathway for Bronchiolitis is Effective in Reducing Readmission Rates. J Pediatr. 2005;147(5):622-626.
Bronchiolitis is the most common respiratory illness in infants that results in hospitalization. Many hospitals have developed clinical pathways to assist clinicians in managing this common infection; however, the effectiveness of such pathways has not been fully studied. Of those clinical practice guidelines analyzed, varying results have been identified.
To determine the effectiveness of a bronchiolitis pathway, this study compared infants managed prospectively using a pathway protocol with a retrospective analysis of infants managed without a pathway. Infants from a tertiary care children’s hospital and three regional hospitals were enrolled prospectively from May 2000 to August 2001. (One must note this study was completed in Australia, hence the difference from the typical Northern Hemisphere winter months.) The historical control group was admitted between May 1998 and August 1999 at the same four institutions. Two-hundred-twenty-nine patients admitted with bronchiolitis were treated using the pathway protocol. These patients were compared with 207 randomly selected control patients who were admitted prior to the institution of the bronchiolitis pathway. All patients were less than 12 months of age with their first episode of wheezing necessitating hospitalization.
These particular guidelines were developed and used to promote consistency of nursing management during a separate study on bronchiolitis. The pathway included an initial admission assessment. It also stated parameters for initiating and stopping both oxygen therapy and intravenous fluid therapy along with discharge guidelines.
The authors found no significant difference in length of stay or time in oxygen. Fifteen infants (7.2%) in the control group required readmission within two weeks of discharge compared with two infants (0.9%) in the pathway group (p=.001). Of the control group 33.8% received intravenous fluids (IVFs) compared with 19.2% of the pathway infants (p=.001). There was also greater steroid use in the control group but no difference in antibiotic usage. Specific data regarding steroids and antibiotics is not included.
The clinical pathway appears a useful tool for discharge planning with a decreased incidence of hospital readmission when specific discharge goals are utilized. The authors also reported a decreased use of IVFs in the pathway group. This was attributed to having specific parameters (O2 required, RR>60/min or inadequate oral feeding) for when to initiate them. It is unclear from the article whether meeting a single parameter or all three parameters triggered the initiation of IVFs.
The authors also point out the limitation of using a historical control given annual variations in severity sometimes seen with bronchiolitis. They attempted to minimize this by collecting data for each group over two consecutive winters.
Preprinted Paper Orders Reduce Medication Errors
Kozer E, Scolnik D, MacPherson A, et al. Using a preprinted order sheet to reduce prescription errors in a pediatric emergency department: A randomized, controlled trial. Pediatrics. 2005(116):1299-1302.
Medical errors, including medication errors, are common and are written about with increasing frequency in the lay press. Accreditation bodies and individual hospitals are striving for ways to decrease these errors. In some instances potential solutions include purchasing new computer systems for electronic physician order entry. This study looks at whether implementing a preprinted paper order sheet can decrease the incidence of medication errors in a pediatric ED.
This randomized, prospective study occurred during 18 days in July 2001 with nine days randomly assigned into each arm. The first arm used the hospital’s regular blank order sheets for all medication orders. The second arm used the experimental preprinted order sheet. This sheet required the staff to specify the dose, weight-adjusted dose, total daily dose, route of administration, and frequency for each medication ordered. Two medical students entered the data into a database that included information about patients’ demographics, diagnosis, acuity, details on the prescribing physician, the form used, and all medications prescribed and given to the patient. This information was subsequently reviewed by two blinded pediatric emergency physicians who determined if an error occurred and, if so, the degree of the error.
During the study period there were 2,157 visits to the ED with 95.4% charts available for review. Seven-hundred-ninety-five medications were prescribed with 376 ordered on the new form. Drug errors were identified in 68 (16.6%) orders when the regular form was used and in 37 (9.8%) orders on the new form. There was one severe error and 13 significant errors using the new form and 36 significant errors on the regular form. The new form was associated with a twofold decrease in the risk for a medication error even after accounting for the level of training of the ordering practitioner. There was an even greater reduction in the risk for a severe or significant error.
The literature has shown that computerized physician order entry can reduce the number of medication errors in the inpatient setting; however, it is not available in many hospitals and its effectiveness has not been shown in EDs. The authors point out that most medications ordered in the ED are prepared and given by nurses. The benefits of a computerized system in this setting is unclear.
This study occurred over an 18-day period with the new form only used for nine days outside of an earlier pilot period. One could speculate that the novelty of the form encouraged the physicians to examine orders more carefully, leading to decreased errors. It is unknown if the decrease in errors would be sustained over time.
Also important to note is that the definition of an error was limited to a mistake in dose, interval between doses, dose unit, and/or route. Errors such as legibility, medication allergy, or drug interactions are not discussed. However, as hospitals strive to implement technologies aimed at reducing errors this simple, economical solution may be of benefit.
No Association between Kawasaki Disease and Adenovirus
Shike H, Shimizu C, Kanegaye J, et al. Adenovirus, adeno-associated virus and Kawasaki disease. Pediatr Infect Dis J. 2005;24:1011-1014.
Kawasaki disease is a self-limited acute vasculitis of children with a suspected infectious etiology and defined seasonality. In an attempt to find a clue for a possible infectious cause of Kawasaki disease this study examined the seasonality of different viruses. The study recognized a similar bimodal seasonality for some serotypes of adenovirus. Adenovirus accounts for 5%-10% of respiratory tract infections in children and can mimic the clinical manifestations and laboratory abnormalities seen in Kawasaki disease.
This study postulated that infection with a non-cultivatable adenovirus or antecedent adenovirus infection might be a trigger for Kawasaki disease. The study analyzed patient samples using polymerase chain reaction primers for all 51 adenovirus serotypes, viral culture, and neutralization assay for the most common adenovirus serotypes. This study also investigated possible involvement of adeno-associated viruses (AAVs), because AAVs depend on helper viruses, such as adenovirus.
Kawasaki disease patients were enrolled during a 25-month period from February 2002 to February 2004 at Children’s Hospital and Health Center in San Diego. Illness day one was defined as the first day of fever. Clinical samples used in this study were collected within the first 14 days of fever onset and before intravenous immunoglobulin (IVIG) therapy.
Nasopharyngeal swabs were cultured for adenovirus. Standard adenoviral neutralization assays for the five most common serotypes were performed with the use of patient sera. Sera with a titer of 1/10 or greater were scored as positive. At least two clinical samples from each patient, including throat swabs, sera or urine, were tested by quantitative polymerase chain reaction (PCR) for adenovirus and AAV.
Nasopharyngeal viral cultures were collected before IVIG administration on illness day three—14 from 70 Kawasaki disease patients. Of the 70 patients, 52 patients fulfilled four of the five classic criteria or three of the five criteria with abnormal coronary arteries by echocardiogram. Of the remaining 18 patients with atypical Kawasaki disease, six had coronary artery abnormalities. Overall, seven patients had coronary artery aneurysms and 22 patients had coronary artery dilatation. Viral cultures were negative in 66 of the 70 Kawasaki disease patients. The viral isolates in four patients were respiratory syncytial (one), parainfluenza virus 3 (one) and adenovirus (two). Therefore adenovirus culture was negative in 97% of patients.
Fifteen Kawasaki disease patients with negative adenovirus cultures were evaluated by PCR assay on at least two clinical samples. Fourteen patients had a negative PCR result. The throat swab from one patient collected on illness day seven contained 800 adenovirus genome copies.
Results of the adenovirus neutralization assays from 26 Kawasaki disease patients revealed that neutralization titers against any of the five most common adenovirus serotypes were undetectable in four of 26 patients.
None of the 36 samples from the same 15 acute Kawasaki disease patients described for the PCR assay was positive for AAV.
This study concluded that despite the striking similarities between Kawasaki disease and adenovirus infection there is no evidence to suggest a link between the two.
Epidemiology and Clinical Description of Severe, Multifocal Staphylococcus aureus Infection
Miles F, Voss L, Segedin E, et al. Review of Staphylococcus aureus infections requiring admission to a paediatric intensive care unit. Arch Dis Child. 2005;90(12):1274-1278.
Staphylococcus aureus is a recognized cause of multifocal infection with a high mortality rate. Children with community acquired S. aureus bacteremia (SAB) have higher frequencies of unknown foci compared with hospital-acquired SAB. Those children with S. aureus sepsis (SAS) presenting to the pediatric intensive care unit tend to have multisystemic disease—either by direct invasion or toxin production—before the diagnosis is made and treatment is initiated.
This study evaluates the clinical features and mortality from SAS in those children who required intensive care management. A retrospective review of clinical notes from all children with SAS admitted from October 1993 to April 2004 to the PICU in Auckland Children’s Hospital in New Zealand was undertaken. Children coded for SAS were identified from the PICU database.
All clinical notes were reviewed by one investigator using a standardized questionnaire that sought information on patient demographics, clinical findings, investigations, microbiology, and management in the PICU. Cases were included if blood or an isolate from a site that is normally sterile was positive for S. aureus. Hospital-acquired infection was defined by an isolate obtained at least 48 hours after hospital admission; community acquired infection was defined by an isolate obtained within 48 hours of admission.
Fifty-eight patients were identified with SAS over the 10-year study period; 55 were community acquired. Children with staphylococcal illness comprised 1% of all admission to the PICU. Musculoskeletal symptoms (79%) dominated presentation rather than isolated pneumonia (10%). An aggressive search for foci and surgical drainage of infective foci was required in 50% of children.
Most children (67%) either presented with multiple site involvement or secondary sites developed during their hospital stay. These pathologies included pneumonia, septic arthritis, osteomyelitis, and soft tissue involvement (cellulitis, fasciitis, abscess). A transthoracic echocardiogram detected valve abnormalities in only 5% of children, and these children were known to have pre-existing cardiac lesions. Few children (12%) presenting with methicillin-resistant S. aureus (MRSA) had community-acquired infection. The median length of stay in the PICU was three (mean 5.8, range one-44) days. Mortality due to SAS was 8.6%. Ten children had significant morbidity after discharge; these morbidities included renal failure requiring dialysis (three), an ongoing oxygen requirement at three months follow-up (two), and problems relating to limb movement and function (eight). Two children with epidural abscesses were paraplegic.
Community-acquired SAS affects healthy children, is multifocal, and has a high morbidity and mortality. It is imperative to look for sites of dissemination and to drain and debride foci. Routine echocardiography had a low yield in the absence of pre-existing cardiac lesions, persisting fever, or persisting bacteremia.
Long-Term Outcomes for Childhood Headache
Brna P, Dooley J, Gordon K Dewan T. The prognosis of childhood headache. Arch Pediatr Adolesc Med. 2005;159(12):1157-1160.
Headaches affect most children and rank third among illness-related causes of school absenteeism. Although the short-term outcome for most children appears favorable, few studies have reported long-term outcome. The objective of this study was to evaluate the long-term prognosis of childhood headaches 20 years after initial diagnosis in a cohort of Atlantic Canadian children who had headaches diagnosed in 1983.
Ninety-five patients with headaches who consulted one of the authors in 1983 were subsequently studied in 1993. The 77 patients contacted in 1993 were followed up in 2003. A standard telephone interview was used. Data were collected regarding headache symptoms, severity, frequency, treatment, and precipitants. Headache severity was simply classified as mild, moderate, or severe.
Sixty (78%) of 77 patients responded (60 of the 95 in the original cohort). At 20 years 16 (27%) were headache free, 20 (33%) had tension-type headaches, 10 (17%) had migraine, 14 (23%) had migraine and tension-type headaches. Having more than one headache type was more than at diagnosis or initial follow-up, and headache type varied across time. Of those who had headaches at follow-up, 80% (35/44) described their headaches as moderate or severe, although improvement in headaches was reported by 29 (66%). Tension-type headaches were more likely than migraine to resolve. During the month before follow-up, non-prescription medications were used by six (14%). However, 20 (45%) felt that non-pharmacological methods were most effective. Medication use increased during the 10 years since the last follow-up. No patient used selective serotonin receptor agonists.
This study concluded that 20 years after the diagnosis of pediatric headache, most patients continue to have headache, although the headache classification often changed across time. Most patients report moderate or severe headache and increasingly choose to care for their headaches pharmacologically. TH
A65-lb., 25-year-old, male cerebral palsy (CP) patient with pneumonia arrives at your Children’s Hospital via ambulance. Although chronologically this patient is an adult, in many ways he’s still a child, and the parents told the paramedics that they’ve always taken their son to Children’s. You’ve been the treating physician during the patient’s frequent hospital stays. Is Children’s Hospital still the best destination for this patient? Will the family’s insurance still cover an admission at Children’s?
During the hospital stay, the patient has complications. He has to be intubated. IV antibiotics need to be continued for a course after hospital discharge. A long recovery is expected. Is it time for the family to consider discharge to a long-term care facility rather than home? Are there any long-term care facilities in the area that accept young adult CP patients?
As the treating pediatric hospitalist, what is your role in helping this patient and his family transition from pediatric care to an adult-care medical home?
Introduction
Approximately 8.6 million children in the United States age 10–17 have a disability, according to the Adolescent Health Transition Project, which is housed at the Center on Human Development and Disability (CHDD) at the University of Washington, Seattle. Of these, 16% (or 1.4 million) experience limitations in their activities and will likely have difficulty making the transition to adult healthcare.1
Given enough time in the profession, every pediatric hospitalist will face the challenge of transitioning patients from child-centered to adult-oriented healthcare systems. The good news: Medical advances have made it increasingly possible for children who once would have died in childhood to survive into adulthood.
Example: One in 2,500 children is born with cystic fibrosis (CF); however, with the recent, unprecedented increase in the success of diagnosis and treatment modalities for the pulmonary component of CF, the estimated median survival age for those born in the 1990s is now 40.2 As of the year 2004, 41.8% of the 22,301 patients with CF were 18 or older.3 In fact, each year nearly 500,000 children with special healthcare needs reach adulthood, and 90% of children with a chronic illness and/or disability now survive to adulthood.4,5
The bad news: Many physicians whose practices focus on adults aren’t familiar with disease processes, such as CF, that have historically been considered pediatric illnesses.
For patients with chronic physical and medical conditions—particularly for those who are medically fragile and/or technology-dependent—the transition can prove especially difficult. And pediatric hospitalists in children’s hospitals face different challenges than those in facilities that admit patients of all ages. One thing remains the same, though, the goal: to provide uninterrupted, coordinated, developmentally appropriate healthcare.
Why Transition?
There are several good reasons for patients to be transitioned from pediatric care to adult care. First, as patients age medical issues develop that are beyond the sphere of pediatricians. In CF, for example, diabetes and biliary tract problems occur with greater frequency in adults. However, because so few CF patients historically survived to adulthood, few physicians who care for adults learned about the disease. Thus, the pediatricians who cared for CF patients continued to do so, leading to situations in which 30- and 40-year-olds have been hospitalized with children. But is that truly appropriate?
Adult patients may have high blood pressure, gynecologic issues, osteoporosis, or other problems the pediatrician may not be prepared to deal with. Example: A primary care pediatrician has been the “medical home” for a small, cerebral palsy patient since she was 10. She’s now 25. If she presents with a breast mass, will the pediatrician pick up on the condition adequately? Will they know where to send the patient?
“Adult providers know those systems better,” says Brett Pickering, MD, director of the Special Needs Clinic at San Diego’s UCSD Medical Center, Department of Pediatrics.
The adult patient has different emotional needs than the pediatric patient, and the pediatric hospitalist may not be in tune with adult needs. “Pediatricians do a lot of handholding,” says Dr. Pickering. “Adult providers are more matter of fact.”
Age restrictions on admissions, insurance, and funding issues also affect transition. For example, funding under the Social Security Act’s Title V Children with Special Health Care Needs typically ends at 21 despite a patient’s education or employment status.
Given these factors, what is the appropriate age to transition care from a pediatric floor or facility to an adult-oriented unit? According to the American Academy of Pediatrics, the responsibility of pediatrics continues through age 21, but there’s no hard-and-fast rule.
Challenges
The transition to adult-care facilities is typically a lengthy process involving multiple specialties and possibly joint care during a transition period—and a process that should ideally be coordinated by the patient’s primary care pediatrician. But hospitalists know that circumstances are typically far from ideal.
First, during a transition, the patient may feel abandoned by the medical team they’ve known for most of their lives. It takes time to develop trust and confidence in a new doctor. In this respect, pediatric hospitalists in facilities that care for patients of all ages have an advantage over hospitalists in children’s hospitals. They can call on their adult-care colleagues in other areas of the hospital for consultations and transfer care over time.
“The pediatric hospitalist must make bridges with their adult colleagues who are comfortable [with the issues] and willing to take on this patient population,” says Dr. Pickering.
Second, parents may feel an emotional dependency on the pediatric team and can feel threatened by the adult environment as they lose some control. To the parents, the patient will always be their child, Dr. Pickering notes.
Third, pediatric hospitalists may be reluctant to let go, particularly if they feel adult services are inferior to those they have provided, which brings us to the fourth major challenge: To whom do you transition care?
Many adult healthcare providers receive only limited training in disorders associated with pediatrics (e.g., CF, spina bifida). The Cystic Fibrosis Foundation is leading the way in educating physicians in what have historically been considered pediatric problems. In the 1980s, the foundation launched an educational program to train physicians already involved in adult pulmonary care in CF. Unfortunately, education in other areas has lagged. And finding a physician with both an interest in and knowledge of such disorders can prove challenging.
“It’s incumbent on our adult colleagues to take these patients on, but they need training,” says Dr. Pickering. “Long-term issues require long-term solutions.
How do you jazz people up to take care of this population?” she asks. Physicians must have at least a little bit of desire to learn about these special patient populations, but academic institutions also need to identify core knowledge and skills and make them part of training and certification requirements for primary care residents and physicians in practice. Continuing medical education for physicians, nurses, and allied healthcare professionals should include drug dosing, medical complications seen in transition populations, and related developmental, psychosocial, and behavioral issues.
Steps to a Successful Transition
So what should hospitalists do? In an April 2005 presentation at the SHM Annual Meeting, Joseph M. Geskey, DO, assistant professor of pediatrics and medicine, and director of inpatient pediatrics at Penn State College of Medicine, Hershey, Penn., recommended that pediatric hospitalists take the following steps:
- Identify the key aspects of transition;
- Bring stakeholders together;
- Identify transitional needs;
- Identify and provide resources;
- Create an audit and evaluation process;
- Decide who will hand off care of these patients when they are admitted to the hospital (the hospitalist or the disease-specific specialist);
- Create an up-to-date medical summary that is portable and accessible. It should include important historic information, such as diagnostic data, procedures, operations, and medications;
- Upon patient discharge, include specific instructions on who to call if the patient develops a problem after leaving the hospital;
- Create a working group in your area that represents pediatric and adult hospitalists to examine transition issues in the hospitalized patient; and
- Facilitate effective communication between patients and their families, primary care physicians and specialists; and
- Know when to transfer care to a center with more expertise in caring for specific conditions.
Conclusion
Just as every patient is different and every patient’s circumstances are unique, every transition needs to be individualized. “It’s hard to set policy,” says Dr. Pickering. Open, direct communication, specific discharge instructions, an up-to-date medical summary and knowledge of the adult resources in your area can make any transition a success. TH
Keri Losavio regularly writes for “Pediatric Special Section.”
References
- Adolescent Health Transition Project, Center on Human Development and Disability (CHDD) at the University of Washington, Seattle. Available at http://depts.washington.edu/healthtr/Providers/intro.htm. Last accessed January 16, 2006.
- Bufi PL. Cystic fibrosis: therapeutic options for co-management. Available at www.thorne.com/altmedrev/fulltext/cystic.html. Last accessed January 16, 2006.
- Cystic Fibrosis Foundation: 2004 Patient Registry Report. Available at www.cff.org/living_with_cf/. Last accessed Jan. 26, 2006
- Newacheck PW, Taylor WR. Childhood chronic illness: prevalence, severity, and impact. Am J Pub Health. 1992;82(3):364-371.
- Committee on Children with Disabilities and Committee on Adolescence, American Academy of Pediatrics. Transition of care provided for adolescents with special health care needs. Pediatrics. 1996;98(6):1203–1206.
Pediatric Special Section
In the Literature
By Mary Ann Queen, MD, and Amita Amonker, MD
Utilization of a Clinical Pathway Improves Care for Bronchiolitis
Cheney J, Barber S, Altamirano L, et al. A Clinical Pathway for Bronchiolitis is Effective in Reducing Readmission Rates. J Pediatr. 2005;147(5):622-626.
Bronchiolitis is the most common respiratory illness in infants that results in hospitalization. Many hospitals have developed clinical pathways to assist clinicians in managing this common infection; however, the effectiveness of such pathways has not been fully studied. Of those clinical practice guidelines analyzed, varying results have been identified.
To determine the effectiveness of a bronchiolitis pathway, this study compared infants managed prospectively using a pathway protocol with a retrospective analysis of infants managed without a pathway. Infants from a tertiary care children’s hospital and three regional hospitals were enrolled prospectively from May 2000 to August 2001. (One must note this study was completed in Australia, hence the difference from the typical Northern Hemisphere winter months.) The historical control group was admitted between May 1998 and August 1999 at the same four institutions. Two-hundred-twenty-nine patients admitted with bronchiolitis were treated using the pathway protocol. These patients were compared with 207 randomly selected control patients who were admitted prior to the institution of the bronchiolitis pathway. All patients were less than 12 months of age with their first episode of wheezing necessitating hospitalization.
These particular guidelines were developed and used to promote consistency of nursing management during a separate study on bronchiolitis. The pathway included an initial admission assessment. It also stated parameters for initiating and stopping both oxygen therapy and intravenous fluid therapy along with discharge guidelines.
The authors found no significant difference in length of stay or time in oxygen. Fifteen infants (7.2%) in the control group required readmission within two weeks of discharge compared with two infants (0.9%) in the pathway group (p=.001). Of the control group 33.8% received intravenous fluids (IVFs) compared with 19.2% of the pathway infants (p=.001). There was also greater steroid use in the control group but no difference in antibiotic usage. Specific data regarding steroids and antibiotics is not included.
The clinical pathway appears a useful tool for discharge planning with a decreased incidence of hospital readmission when specific discharge goals are utilized. The authors also reported a decreased use of IVFs in the pathway group. This was attributed to having specific parameters (O2 required, RR>60/min or inadequate oral feeding) for when to initiate them. It is unclear from the article whether meeting a single parameter or all three parameters triggered the initiation of IVFs.
The authors also point out the limitation of using a historical control given annual variations in severity sometimes seen with bronchiolitis. They attempted to minimize this by collecting data for each group over two consecutive winters.
Preprinted Paper Orders Reduce Medication Errors
Kozer E, Scolnik D, MacPherson A, et al. Using a preprinted order sheet to reduce prescription errors in a pediatric emergency department: A randomized, controlled trial. Pediatrics. 2005(116):1299-1302.
Medical errors, including medication errors, are common and are written about with increasing frequency in the lay press. Accreditation bodies and individual hospitals are striving for ways to decrease these errors. In some instances potential solutions include purchasing new computer systems for electronic physician order entry. This study looks at whether implementing a preprinted paper order sheet can decrease the incidence of medication errors in a pediatric ED.
This randomized, prospective study occurred during 18 days in July 2001 with nine days randomly assigned into each arm. The first arm used the hospital’s regular blank order sheets for all medication orders. The second arm used the experimental preprinted order sheet. This sheet required the staff to specify the dose, weight-adjusted dose, total daily dose, route of administration, and frequency for each medication ordered. Two medical students entered the data into a database that included information about patients’ demographics, diagnosis, acuity, details on the prescribing physician, the form used, and all medications prescribed and given to the patient. This information was subsequently reviewed by two blinded pediatric emergency physicians who determined if an error occurred and, if so, the degree of the error.
During the study period there were 2,157 visits to the ED with 95.4% charts available for review. Seven-hundred-ninety-five medications were prescribed with 376 ordered on the new form. Drug errors were identified in 68 (16.6%) orders when the regular form was used and in 37 (9.8%) orders on the new form. There was one severe error and 13 significant errors using the new form and 36 significant errors on the regular form. The new form was associated with a twofold decrease in the risk for a medication error even after accounting for the level of training of the ordering practitioner. There was an even greater reduction in the risk for a severe or significant error.
The literature has shown that computerized physician order entry can reduce the number of medication errors in the inpatient setting; however, it is not available in many hospitals and its effectiveness has not been shown in EDs. The authors point out that most medications ordered in the ED are prepared and given by nurses. The benefits of a computerized system in this setting is unclear.
This study occurred over an 18-day period with the new form only used for nine days outside of an earlier pilot period. One could speculate that the novelty of the form encouraged the physicians to examine orders more carefully, leading to decreased errors. It is unknown if the decrease in errors would be sustained over time.
Also important to note is that the definition of an error was limited to a mistake in dose, interval between doses, dose unit, and/or route. Errors such as legibility, medication allergy, or drug interactions are not discussed. However, as hospitals strive to implement technologies aimed at reducing errors this simple, economical solution may be of benefit.
No Association between Kawasaki Disease and Adenovirus
Shike H, Shimizu C, Kanegaye J, et al. Adenovirus, adeno-associated virus and Kawasaki disease. Pediatr Infect Dis J. 2005;24:1011-1014.
Kawasaki disease is a self-limited acute vasculitis of children with a suspected infectious etiology and defined seasonality. In an attempt to find a clue for a possible infectious cause of Kawasaki disease this study examined the seasonality of different viruses. The study recognized a similar bimodal seasonality for some serotypes of adenovirus. Adenovirus accounts for 5%-10% of respiratory tract infections in children and can mimic the clinical manifestations and laboratory abnormalities seen in Kawasaki disease.
This study postulated that infection with a non-cultivatable adenovirus or antecedent adenovirus infection might be a trigger for Kawasaki disease. The study analyzed patient samples using polymerase chain reaction primers for all 51 adenovirus serotypes, viral culture, and neutralization assay for the most common adenovirus serotypes. This study also investigated possible involvement of adeno-associated viruses (AAVs), because AAVs depend on helper viruses, such as adenovirus.
Kawasaki disease patients were enrolled during a 25-month period from February 2002 to February 2004 at Children’s Hospital and Health Center in San Diego. Illness day one was defined as the first day of fever. Clinical samples used in this study were collected within the first 14 days of fever onset and before intravenous immunoglobulin (IVIG) therapy.
Nasopharyngeal swabs were cultured for adenovirus. Standard adenoviral neutralization assays for the five most common serotypes were performed with the use of patient sera. Sera with a titer of 1/10 or greater were scored as positive. At least two clinical samples from each patient, including throat swabs, sera or urine, were tested by quantitative polymerase chain reaction (PCR) for adenovirus and AAV.
Nasopharyngeal viral cultures were collected before IVIG administration on illness day three—14 from 70 Kawasaki disease patients. Of the 70 patients, 52 patients fulfilled four of the five classic criteria or three of the five criteria with abnormal coronary arteries by echocardiogram. Of the remaining 18 patients with atypical Kawasaki disease, six had coronary artery abnormalities. Overall, seven patients had coronary artery aneurysms and 22 patients had coronary artery dilatation. Viral cultures were negative in 66 of the 70 Kawasaki disease patients. The viral isolates in four patients were respiratory syncytial (one), parainfluenza virus 3 (one) and adenovirus (two). Therefore adenovirus culture was negative in 97% of patients.
Fifteen Kawasaki disease patients with negative adenovirus cultures were evaluated by PCR assay on at least two clinical samples. Fourteen patients had a negative PCR result. The throat swab from one patient collected on illness day seven contained 800 adenovirus genome copies.
Results of the adenovirus neutralization assays from 26 Kawasaki disease patients revealed that neutralization titers against any of the five most common adenovirus serotypes were undetectable in four of 26 patients.
None of the 36 samples from the same 15 acute Kawasaki disease patients described for the PCR assay was positive for AAV.
This study concluded that despite the striking similarities between Kawasaki disease and adenovirus infection there is no evidence to suggest a link between the two.
Epidemiology and Clinical Description of Severe, Multifocal Staphylococcus aureus Infection
Miles F, Voss L, Segedin E, et al. Review of Staphylococcus aureus infections requiring admission to a paediatric intensive care unit. Arch Dis Child. 2005;90(12):1274-1278.
Staphylococcus aureus is a recognized cause of multifocal infection with a high mortality rate. Children with community acquired S. aureus bacteremia (SAB) have higher frequencies of unknown foci compared with hospital-acquired SAB. Those children with S. aureus sepsis (SAS) presenting to the pediatric intensive care unit tend to have multisystemic disease—either by direct invasion or toxin production—before the diagnosis is made and treatment is initiated.
This study evaluates the clinical features and mortality from SAS in those children who required intensive care management. A retrospective review of clinical notes from all children with SAS admitted from October 1993 to April 2004 to the PICU in Auckland Children’s Hospital in New Zealand was undertaken. Children coded for SAS were identified from the PICU database.
All clinical notes were reviewed by one investigator using a standardized questionnaire that sought information on patient demographics, clinical findings, investigations, microbiology, and management in the PICU. Cases were included if blood or an isolate from a site that is normally sterile was positive for S. aureus. Hospital-acquired infection was defined by an isolate obtained at least 48 hours after hospital admission; community acquired infection was defined by an isolate obtained within 48 hours of admission.
Fifty-eight patients were identified with SAS over the 10-year study period; 55 were community acquired. Children with staphylococcal illness comprised 1% of all admission to the PICU. Musculoskeletal symptoms (79%) dominated presentation rather than isolated pneumonia (10%). An aggressive search for foci and surgical drainage of infective foci was required in 50% of children.
Most children (67%) either presented with multiple site involvement or secondary sites developed during their hospital stay. These pathologies included pneumonia, septic arthritis, osteomyelitis, and soft tissue involvement (cellulitis, fasciitis, abscess). A transthoracic echocardiogram detected valve abnormalities in only 5% of children, and these children were known to have pre-existing cardiac lesions. Few children (12%) presenting with methicillin-resistant S. aureus (MRSA) had community-acquired infection. The median length of stay in the PICU was three (mean 5.8, range one-44) days. Mortality due to SAS was 8.6%. Ten children had significant morbidity after discharge; these morbidities included renal failure requiring dialysis (three), an ongoing oxygen requirement at three months follow-up (two), and problems relating to limb movement and function (eight). Two children with epidural abscesses were paraplegic.
Community-acquired SAS affects healthy children, is multifocal, and has a high morbidity and mortality. It is imperative to look for sites of dissemination and to drain and debride foci. Routine echocardiography had a low yield in the absence of pre-existing cardiac lesions, persisting fever, or persisting bacteremia.
Long-Term Outcomes for Childhood Headache
Brna P, Dooley J, Gordon K Dewan T. The prognosis of childhood headache. Arch Pediatr Adolesc Med. 2005;159(12):1157-1160.
Headaches affect most children and rank third among illness-related causes of school absenteeism. Although the short-term outcome for most children appears favorable, few studies have reported long-term outcome. The objective of this study was to evaluate the long-term prognosis of childhood headaches 20 years after initial diagnosis in a cohort of Atlantic Canadian children who had headaches diagnosed in 1983.
Ninety-five patients with headaches who consulted one of the authors in 1983 were subsequently studied in 1993. The 77 patients contacted in 1993 were followed up in 2003. A standard telephone interview was used. Data were collected regarding headache symptoms, severity, frequency, treatment, and precipitants. Headache severity was simply classified as mild, moderate, or severe.
Sixty (78%) of 77 patients responded (60 of the 95 in the original cohort). At 20 years 16 (27%) were headache free, 20 (33%) had tension-type headaches, 10 (17%) had migraine, 14 (23%) had migraine and tension-type headaches. Having more than one headache type was more than at diagnosis or initial follow-up, and headache type varied across time. Of those who had headaches at follow-up, 80% (35/44) described their headaches as moderate or severe, although improvement in headaches was reported by 29 (66%). Tension-type headaches were more likely than migraine to resolve. During the month before follow-up, non-prescription medications were used by six (14%). However, 20 (45%) felt that non-pharmacological methods were most effective. Medication use increased during the 10 years since the last follow-up. No patient used selective serotonin receptor agonists.
This study concluded that 20 years after the diagnosis of pediatric headache, most patients continue to have headache, although the headache classification often changed across time. Most patients report moderate or severe headache and increasingly choose to care for their headaches pharmacologically. TH
A65-lb., 25-year-old, male cerebral palsy (CP) patient with pneumonia arrives at your Children’s Hospital via ambulance. Although chronologically this patient is an adult, in many ways he’s still a child, and the parents told the paramedics that they’ve always taken their son to Children’s. You’ve been the treating physician during the patient’s frequent hospital stays. Is Children’s Hospital still the best destination for this patient? Will the family’s insurance still cover an admission at Children’s?
During the hospital stay, the patient has complications. He has to be intubated. IV antibiotics need to be continued for a course after hospital discharge. A long recovery is expected. Is it time for the family to consider discharge to a long-term care facility rather than home? Are there any long-term care facilities in the area that accept young adult CP patients?
As the treating pediatric hospitalist, what is your role in helping this patient and his family transition from pediatric care to an adult-care medical home?
Introduction
Approximately 8.6 million children in the United States age 10–17 have a disability, according to the Adolescent Health Transition Project, which is housed at the Center on Human Development and Disability (CHDD) at the University of Washington, Seattle. Of these, 16% (or 1.4 million) experience limitations in their activities and will likely have difficulty making the transition to adult healthcare.1
Given enough time in the profession, every pediatric hospitalist will face the challenge of transitioning patients from child-centered to adult-oriented healthcare systems. The good news: Medical advances have made it increasingly possible for children who once would have died in childhood to survive into adulthood.
Example: One in 2,500 children is born with cystic fibrosis (CF); however, with the recent, unprecedented increase in the success of diagnosis and treatment modalities for the pulmonary component of CF, the estimated median survival age for those born in the 1990s is now 40.2 As of the year 2004, 41.8% of the 22,301 patients with CF were 18 or older.3 In fact, each year nearly 500,000 children with special healthcare needs reach adulthood, and 90% of children with a chronic illness and/or disability now survive to adulthood.4,5
The bad news: Many physicians whose practices focus on adults aren’t familiar with disease processes, such as CF, that have historically been considered pediatric illnesses.
For patients with chronic physical and medical conditions—particularly for those who are medically fragile and/or technology-dependent—the transition can prove especially difficult. And pediatric hospitalists in children’s hospitals face different challenges than those in facilities that admit patients of all ages. One thing remains the same, though, the goal: to provide uninterrupted, coordinated, developmentally appropriate healthcare.
Why Transition?
There are several good reasons for patients to be transitioned from pediatric care to adult care. First, as patients age medical issues develop that are beyond the sphere of pediatricians. In CF, for example, diabetes and biliary tract problems occur with greater frequency in adults. However, because so few CF patients historically survived to adulthood, few physicians who care for adults learned about the disease. Thus, the pediatricians who cared for CF patients continued to do so, leading to situations in which 30- and 40-year-olds have been hospitalized with children. But is that truly appropriate?
Adult patients may have high blood pressure, gynecologic issues, osteoporosis, or other problems the pediatrician may not be prepared to deal with. Example: A primary care pediatrician has been the “medical home” for a small, cerebral palsy patient since she was 10. She’s now 25. If she presents with a breast mass, will the pediatrician pick up on the condition adequately? Will they know where to send the patient?
“Adult providers know those systems better,” says Brett Pickering, MD, director of the Special Needs Clinic at San Diego’s UCSD Medical Center, Department of Pediatrics.
The adult patient has different emotional needs than the pediatric patient, and the pediatric hospitalist may not be in tune with adult needs. “Pediatricians do a lot of handholding,” says Dr. Pickering. “Adult providers are more matter of fact.”
Age restrictions on admissions, insurance, and funding issues also affect transition. For example, funding under the Social Security Act’s Title V Children with Special Health Care Needs typically ends at 21 despite a patient’s education or employment status.
Given these factors, what is the appropriate age to transition care from a pediatric floor or facility to an adult-oriented unit? According to the American Academy of Pediatrics, the responsibility of pediatrics continues through age 21, but there’s no hard-and-fast rule.
Challenges
The transition to adult-care facilities is typically a lengthy process involving multiple specialties and possibly joint care during a transition period—and a process that should ideally be coordinated by the patient’s primary care pediatrician. But hospitalists know that circumstances are typically far from ideal.
First, during a transition, the patient may feel abandoned by the medical team they’ve known for most of their lives. It takes time to develop trust and confidence in a new doctor. In this respect, pediatric hospitalists in facilities that care for patients of all ages have an advantage over hospitalists in children’s hospitals. They can call on their adult-care colleagues in other areas of the hospital for consultations and transfer care over time.
“The pediatric hospitalist must make bridges with their adult colleagues who are comfortable [with the issues] and willing to take on this patient population,” says Dr. Pickering.
Second, parents may feel an emotional dependency on the pediatric team and can feel threatened by the adult environment as they lose some control. To the parents, the patient will always be their child, Dr. Pickering notes.
Third, pediatric hospitalists may be reluctant to let go, particularly if they feel adult services are inferior to those they have provided, which brings us to the fourth major challenge: To whom do you transition care?
Many adult healthcare providers receive only limited training in disorders associated with pediatrics (e.g., CF, spina bifida). The Cystic Fibrosis Foundation is leading the way in educating physicians in what have historically been considered pediatric problems. In the 1980s, the foundation launched an educational program to train physicians already involved in adult pulmonary care in CF. Unfortunately, education in other areas has lagged. And finding a physician with both an interest in and knowledge of such disorders can prove challenging.
“It’s incumbent on our adult colleagues to take these patients on, but they need training,” says Dr. Pickering. “Long-term issues require long-term solutions.
How do you jazz people up to take care of this population?” she asks. Physicians must have at least a little bit of desire to learn about these special patient populations, but academic institutions also need to identify core knowledge and skills and make them part of training and certification requirements for primary care residents and physicians in practice. Continuing medical education for physicians, nurses, and allied healthcare professionals should include drug dosing, medical complications seen in transition populations, and related developmental, psychosocial, and behavioral issues.
Steps to a Successful Transition
So what should hospitalists do? In an April 2005 presentation at the SHM Annual Meeting, Joseph M. Geskey, DO, assistant professor of pediatrics and medicine, and director of inpatient pediatrics at Penn State College of Medicine, Hershey, Penn., recommended that pediatric hospitalists take the following steps:
- Identify the key aspects of transition;
- Bring stakeholders together;
- Identify transitional needs;
- Identify and provide resources;
- Create an audit and evaluation process;
- Decide who will hand off care of these patients when they are admitted to the hospital (the hospitalist or the disease-specific specialist);
- Create an up-to-date medical summary that is portable and accessible. It should include important historic information, such as diagnostic data, procedures, operations, and medications;
- Upon patient discharge, include specific instructions on who to call if the patient develops a problem after leaving the hospital;
- Create a working group in your area that represents pediatric and adult hospitalists to examine transition issues in the hospitalized patient; and
- Facilitate effective communication between patients and their families, primary care physicians and specialists; and
- Know when to transfer care to a center with more expertise in caring for specific conditions.
Conclusion
Just as every patient is different and every patient’s circumstances are unique, every transition needs to be individualized. “It’s hard to set policy,” says Dr. Pickering. Open, direct communication, specific discharge instructions, an up-to-date medical summary and knowledge of the adult resources in your area can make any transition a success. TH
Keri Losavio regularly writes for “Pediatric Special Section.”
References
- Adolescent Health Transition Project, Center on Human Development and Disability (CHDD) at the University of Washington, Seattle. Available at http://depts.washington.edu/healthtr/Providers/intro.htm. Last accessed January 16, 2006.
- Bufi PL. Cystic fibrosis: therapeutic options for co-management. Available at www.thorne.com/altmedrev/fulltext/cystic.html. Last accessed January 16, 2006.
- Cystic Fibrosis Foundation: 2004 Patient Registry Report. Available at www.cff.org/living_with_cf/. Last accessed Jan. 26, 2006
- Newacheck PW, Taylor WR. Childhood chronic illness: prevalence, severity, and impact. Am J Pub Health. 1992;82(3):364-371.
- Committee on Children with Disabilities and Committee on Adolescence, American Academy of Pediatrics. Transition of care provided for adolescents with special health care needs. Pediatrics. 1996;98(6):1203–1206.
Pediatric Special Section
In the Literature
By Mary Ann Queen, MD, and Amita Amonker, MD
Utilization of a Clinical Pathway Improves Care for Bronchiolitis
Cheney J, Barber S, Altamirano L, et al. A Clinical Pathway for Bronchiolitis is Effective in Reducing Readmission Rates. J Pediatr. 2005;147(5):622-626.
Bronchiolitis is the most common respiratory illness in infants that results in hospitalization. Many hospitals have developed clinical pathways to assist clinicians in managing this common infection; however, the effectiveness of such pathways has not been fully studied. Of those clinical practice guidelines analyzed, varying results have been identified.
To determine the effectiveness of a bronchiolitis pathway, this study compared infants managed prospectively using a pathway protocol with a retrospective analysis of infants managed without a pathway. Infants from a tertiary care children’s hospital and three regional hospitals were enrolled prospectively from May 2000 to August 2001. (One must note this study was completed in Australia, hence the difference from the typical Northern Hemisphere winter months.) The historical control group was admitted between May 1998 and August 1999 at the same four institutions. Two-hundred-twenty-nine patients admitted with bronchiolitis were treated using the pathway protocol. These patients were compared with 207 randomly selected control patients who were admitted prior to the institution of the bronchiolitis pathway. All patients were less than 12 months of age with their first episode of wheezing necessitating hospitalization.
These particular guidelines were developed and used to promote consistency of nursing management during a separate study on bronchiolitis. The pathway included an initial admission assessment. It also stated parameters for initiating and stopping both oxygen therapy and intravenous fluid therapy along with discharge guidelines.
The authors found no significant difference in length of stay or time in oxygen. Fifteen infants (7.2%) in the control group required readmission within two weeks of discharge compared with two infants (0.9%) in the pathway group (p=.001). Of the control group 33.8% received intravenous fluids (IVFs) compared with 19.2% of the pathway infants (p=.001). There was also greater steroid use in the control group but no difference in antibiotic usage. Specific data regarding steroids and antibiotics is not included.
The clinical pathway appears a useful tool for discharge planning with a decreased incidence of hospital readmission when specific discharge goals are utilized. The authors also reported a decreased use of IVFs in the pathway group. This was attributed to having specific parameters (O2 required, RR>60/min or inadequate oral feeding) for when to initiate them. It is unclear from the article whether meeting a single parameter or all three parameters triggered the initiation of IVFs.
The authors also point out the limitation of using a historical control given annual variations in severity sometimes seen with bronchiolitis. They attempted to minimize this by collecting data for each group over two consecutive winters.
Preprinted Paper Orders Reduce Medication Errors
Kozer E, Scolnik D, MacPherson A, et al. Using a preprinted order sheet to reduce prescription errors in a pediatric emergency department: A randomized, controlled trial. Pediatrics. 2005(116):1299-1302.
Medical errors, including medication errors, are common and are written about with increasing frequency in the lay press. Accreditation bodies and individual hospitals are striving for ways to decrease these errors. In some instances potential solutions include purchasing new computer systems for electronic physician order entry. This study looks at whether implementing a preprinted paper order sheet can decrease the incidence of medication errors in a pediatric ED.
This randomized, prospective study occurred during 18 days in July 2001 with nine days randomly assigned into each arm. The first arm used the hospital’s regular blank order sheets for all medication orders. The second arm used the experimental preprinted order sheet. This sheet required the staff to specify the dose, weight-adjusted dose, total daily dose, route of administration, and frequency for each medication ordered. Two medical students entered the data into a database that included information about patients’ demographics, diagnosis, acuity, details on the prescribing physician, the form used, and all medications prescribed and given to the patient. This information was subsequently reviewed by two blinded pediatric emergency physicians who determined if an error occurred and, if so, the degree of the error.
During the study period there were 2,157 visits to the ED with 95.4% charts available for review. Seven-hundred-ninety-five medications were prescribed with 376 ordered on the new form. Drug errors were identified in 68 (16.6%) orders when the regular form was used and in 37 (9.8%) orders on the new form. There was one severe error and 13 significant errors using the new form and 36 significant errors on the regular form. The new form was associated with a twofold decrease in the risk for a medication error even after accounting for the level of training of the ordering practitioner. There was an even greater reduction in the risk for a severe or significant error.
The literature has shown that computerized physician order entry can reduce the number of medication errors in the inpatient setting; however, it is not available in many hospitals and its effectiveness has not been shown in EDs. The authors point out that most medications ordered in the ED are prepared and given by nurses. The benefits of a computerized system in this setting is unclear.
This study occurred over an 18-day period with the new form only used for nine days outside of an earlier pilot period. One could speculate that the novelty of the form encouraged the physicians to examine orders more carefully, leading to decreased errors. It is unknown if the decrease in errors would be sustained over time.
Also important to note is that the definition of an error was limited to a mistake in dose, interval between doses, dose unit, and/or route. Errors such as legibility, medication allergy, or drug interactions are not discussed. However, as hospitals strive to implement technologies aimed at reducing errors this simple, economical solution may be of benefit.
No Association between Kawasaki Disease and Adenovirus
Shike H, Shimizu C, Kanegaye J, et al. Adenovirus, adeno-associated virus and Kawasaki disease. Pediatr Infect Dis J. 2005;24:1011-1014.
Kawasaki disease is a self-limited acute vasculitis of children with a suspected infectious etiology and defined seasonality. In an attempt to find a clue for a possible infectious cause of Kawasaki disease this study examined the seasonality of different viruses. The study recognized a similar bimodal seasonality for some serotypes of adenovirus. Adenovirus accounts for 5%-10% of respiratory tract infections in children and can mimic the clinical manifestations and laboratory abnormalities seen in Kawasaki disease.
This study postulated that infection with a non-cultivatable adenovirus or antecedent adenovirus infection might be a trigger for Kawasaki disease. The study analyzed patient samples using polymerase chain reaction primers for all 51 adenovirus serotypes, viral culture, and neutralization assay for the most common adenovirus serotypes. This study also investigated possible involvement of adeno-associated viruses (AAVs), because AAVs depend on helper viruses, such as adenovirus.
Kawasaki disease patients were enrolled during a 25-month period from February 2002 to February 2004 at Children’s Hospital and Health Center in San Diego. Illness day one was defined as the first day of fever. Clinical samples used in this study were collected within the first 14 days of fever onset and before intravenous immunoglobulin (IVIG) therapy.
Nasopharyngeal swabs were cultured for adenovirus. Standard adenoviral neutralization assays for the five most common serotypes were performed with the use of patient sera. Sera with a titer of 1/10 or greater were scored as positive. At least two clinical samples from each patient, including throat swabs, sera or urine, were tested by quantitative polymerase chain reaction (PCR) for adenovirus and AAV.
Nasopharyngeal viral cultures were collected before IVIG administration on illness day three—14 from 70 Kawasaki disease patients. Of the 70 patients, 52 patients fulfilled four of the five classic criteria or three of the five criteria with abnormal coronary arteries by echocardiogram. Of the remaining 18 patients with atypical Kawasaki disease, six had coronary artery abnormalities. Overall, seven patients had coronary artery aneurysms and 22 patients had coronary artery dilatation. Viral cultures were negative in 66 of the 70 Kawasaki disease patients. The viral isolates in four patients were respiratory syncytial (one), parainfluenza virus 3 (one) and adenovirus (two). Therefore adenovirus culture was negative in 97% of patients.
Fifteen Kawasaki disease patients with negative adenovirus cultures were evaluated by PCR assay on at least two clinical samples. Fourteen patients had a negative PCR result. The throat swab from one patient collected on illness day seven contained 800 adenovirus genome copies.
Results of the adenovirus neutralization assays from 26 Kawasaki disease patients revealed that neutralization titers against any of the five most common adenovirus serotypes were undetectable in four of 26 patients.
None of the 36 samples from the same 15 acute Kawasaki disease patients described for the PCR assay was positive for AAV.
This study concluded that despite the striking similarities between Kawasaki disease and adenovirus infection there is no evidence to suggest a link between the two.
Epidemiology and Clinical Description of Severe, Multifocal Staphylococcus aureus Infection
Miles F, Voss L, Segedin E, et al. Review of Staphylococcus aureus infections requiring admission to a paediatric intensive care unit. Arch Dis Child. 2005;90(12):1274-1278.
Staphylococcus aureus is a recognized cause of multifocal infection with a high mortality rate. Children with community acquired S. aureus bacteremia (SAB) have higher frequencies of unknown foci compared with hospital-acquired SAB. Those children with S. aureus sepsis (SAS) presenting to the pediatric intensive care unit tend to have multisystemic disease—either by direct invasion or toxin production—before the diagnosis is made and treatment is initiated.
This study evaluates the clinical features and mortality from SAS in those children who required intensive care management. A retrospective review of clinical notes from all children with SAS admitted from October 1993 to April 2004 to the PICU in Auckland Children’s Hospital in New Zealand was undertaken. Children coded for SAS were identified from the PICU database.
All clinical notes were reviewed by one investigator using a standardized questionnaire that sought information on patient demographics, clinical findings, investigations, microbiology, and management in the PICU. Cases were included if blood or an isolate from a site that is normally sterile was positive for S. aureus. Hospital-acquired infection was defined by an isolate obtained at least 48 hours after hospital admission; community acquired infection was defined by an isolate obtained within 48 hours of admission.
Fifty-eight patients were identified with SAS over the 10-year study period; 55 were community acquired. Children with staphylococcal illness comprised 1% of all admission to the PICU. Musculoskeletal symptoms (79%) dominated presentation rather than isolated pneumonia (10%). An aggressive search for foci and surgical drainage of infective foci was required in 50% of children.
Most children (67%) either presented with multiple site involvement or secondary sites developed during their hospital stay. These pathologies included pneumonia, septic arthritis, osteomyelitis, and soft tissue involvement (cellulitis, fasciitis, abscess). A transthoracic echocardiogram detected valve abnormalities in only 5% of children, and these children were known to have pre-existing cardiac lesions. Few children (12%) presenting with methicillin-resistant S. aureus (MRSA) had community-acquired infection. The median length of stay in the PICU was three (mean 5.8, range one-44) days. Mortality due to SAS was 8.6%. Ten children had significant morbidity after discharge; these morbidities included renal failure requiring dialysis (three), an ongoing oxygen requirement at three months follow-up (two), and problems relating to limb movement and function (eight). Two children with epidural abscesses were paraplegic.
Community-acquired SAS affects healthy children, is multifocal, and has a high morbidity and mortality. It is imperative to look for sites of dissemination and to drain and debride foci. Routine echocardiography had a low yield in the absence of pre-existing cardiac lesions, persisting fever, or persisting bacteremia.
Long-Term Outcomes for Childhood Headache
Brna P, Dooley J, Gordon K Dewan T. The prognosis of childhood headache. Arch Pediatr Adolesc Med. 2005;159(12):1157-1160.
Headaches affect most children and rank third among illness-related causes of school absenteeism. Although the short-term outcome for most children appears favorable, few studies have reported long-term outcome. The objective of this study was to evaluate the long-term prognosis of childhood headaches 20 years after initial diagnosis in a cohort of Atlantic Canadian children who had headaches diagnosed in 1983.
Ninety-five patients with headaches who consulted one of the authors in 1983 were subsequently studied in 1993. The 77 patients contacted in 1993 were followed up in 2003. A standard telephone interview was used. Data were collected regarding headache symptoms, severity, frequency, treatment, and precipitants. Headache severity was simply classified as mild, moderate, or severe.
Sixty (78%) of 77 patients responded (60 of the 95 in the original cohort). At 20 years 16 (27%) were headache free, 20 (33%) had tension-type headaches, 10 (17%) had migraine, 14 (23%) had migraine and tension-type headaches. Having more than one headache type was more than at diagnosis or initial follow-up, and headache type varied across time. Of those who had headaches at follow-up, 80% (35/44) described their headaches as moderate or severe, although improvement in headaches was reported by 29 (66%). Tension-type headaches were more likely than migraine to resolve. During the month before follow-up, non-prescription medications were used by six (14%). However, 20 (45%) felt that non-pharmacological methods were most effective. Medication use increased during the 10 years since the last follow-up. No patient used selective serotonin receptor agonists.
This study concluded that 20 years after the diagnosis of pediatric headache, most patients continue to have headache, although the headache classification often changed across time. Most patients report moderate or severe headache and increasingly choose to care for their headaches pharmacologically. TH