User login
HQPS Competencies
Healthcare quality is defined as the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.1 Delivering high quality care to patients in the hospital setting is especially challenging, given the rapid pace of clinical care, the severity and multitude of patient conditions, and the interdependence of complex processes within the hospital system. Research has shown that hospitalized patients do not consistently receive recommended care2 and are at risk for experiencing preventable harm.3 In an effort to stimulate improvement, stakeholders have called for increased accountability, including enhanced transparency and differential payment based on performance. A growing number of hospital process and outcome measures are readily available to the public via the Internet.46 The Joint Commission, which accredits US hospitals, requires the collection of core quality measure data7 and sets the expectation that National Patient Safety Goals be met to maintain accreditation.8 Moreover, the Center for Medicare and Medicaid Services (CMS) has developed a Value‐Based Purchasing (VBP) plan intended to adjust hospital payment based on quality measures and the occurrence of certain hospital‐acquired conditions.9, 10
Because of their clinical expertise, understanding of hospital clinical operations, leadership of multidisciplinary inpatient teams, and vested interest to improve the systems in which they work, hospitalists are perfectly positioned to collaborate with their institutions to improve the quality of care delivered to inpatients. However, many hospitalists are inadequately prepared to engage in efforts to improve quality, because medical schools and residency programs have not traditionally included or emphasized healthcare quality and patient safety in their curricula.1113 In a survey of 389 internal medicine‐trained hospitalists, significant educational deficiencies were identified in the area of systems‐based practice.14 Specifically, the topics of quality improvement, team management, practice guideline development, health information systems management, and coordination of care between healthcare settings were listed as essential skills for hospitalist practice but underemphasized in residency training. Recognizing the gap between the needs of practicing physicians and current medical education provided in healthcare quality, professional societies have recently published position papers calling for increased training in quality, safety, and systems, both in medical school11 and residency training.15, 16
The Society of Hospital Medicine (SHM) convened a Quality Summit in December 2008 to develop strategic plans related to healthcare quality. Summit attendees felt that most hospitalists lack the formal training necessary to evaluate, implement, and sustain system changes within the hospital. In response, the SHM Hospital Quality and Patient Safety (HQPS) Committee formed a Quality Improvement Education (QIE) subcommittee in 2009 to assess the needs of hospitalists with respect to hospital quality and patient safety, and to evaluate and expand upon existing educational programs in this area. Membership of the QIE subcommittee consisted of hospitalists with extensive experience in healthcare quality and medical education. The QIE subcommittee refined and expanded upon the healthcare quality and patient safety‐related competencies initially described in the Core Competencies in Hospital Medicine.17 The purpose of this report is to describe the development, provide definitions, and make recommendations on the use of the Hospital Quality and Patient Safety (HQPS) Competencies.
Development of The Hospital Quality and Patient Safety Competencies
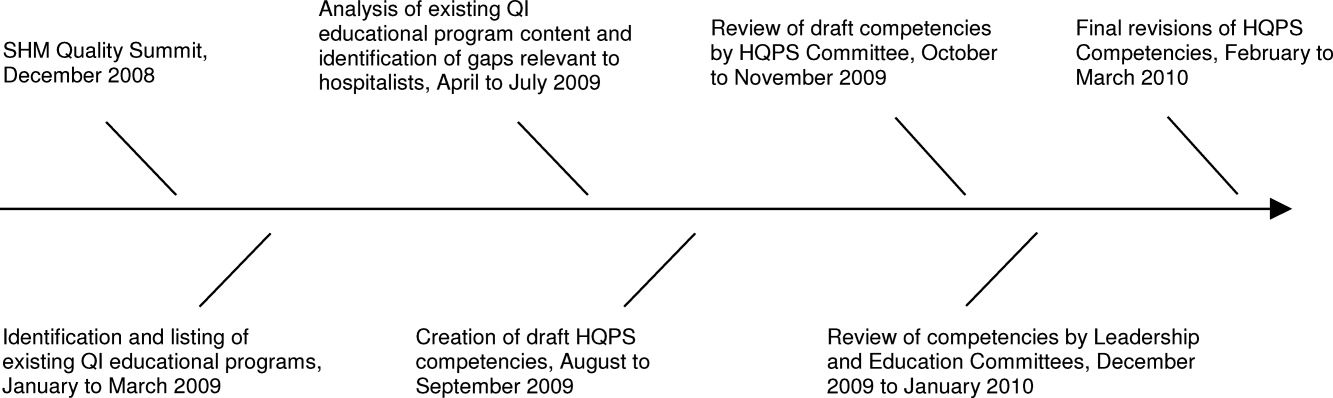
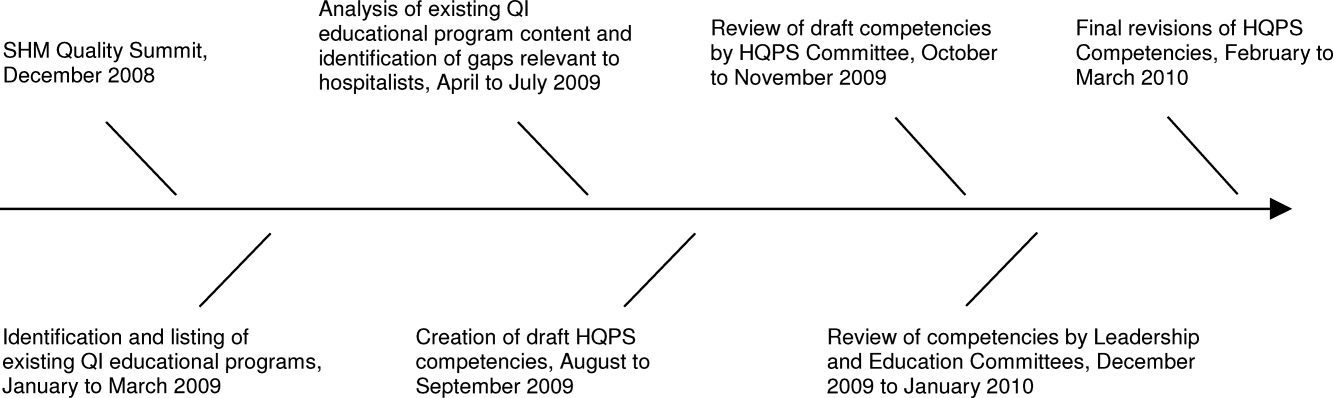
The multistep process used by the SHM QIE subcommittee to develop the HQPS Competencies is summarized in Figure 1. We performed an in‐depth evaluation of current educational materials and offerings, including a review of the Core Competencies in Hospital Medicine, past annual SHM Quality Improvement Pre‐Course objectives, and the content of training courses offered by other organizations.1722 Throughout our analysis, we emphasized the identification of gaps in content relevant to hospitalists. We then used the Institute of Medicine's (IOM) 6 aims for healthcare quality as a foundation for developing the HQPS Competencies.1 Specifically, the IOM states that healthcare should be safe, effective, patient‐centered, timely, efficient, and equitable. Additionally, we reviewed and integrated elements of the Practice‐Based Learning and Improvement (PBLI) and Systems‐Based Practice (SBP) competencies as defined by the Accreditation Council for Graduate Medical Education (ACGME).23 We defined general areas of competence and specific standards for knowledge, skills, and attitudes within each area. Subcommittee members reflected on their own experience, as clinicians, educators, and leaders in healthcare quality and patient safety, to inform and refine the competency definitions and standards. Acknowledging that some hospitalists may serve as collaborators or clinical content experts, while others may serve as leaders of hospital quality initiatives, 3 levels of expertise were established: basic, intermediate, and advanced.
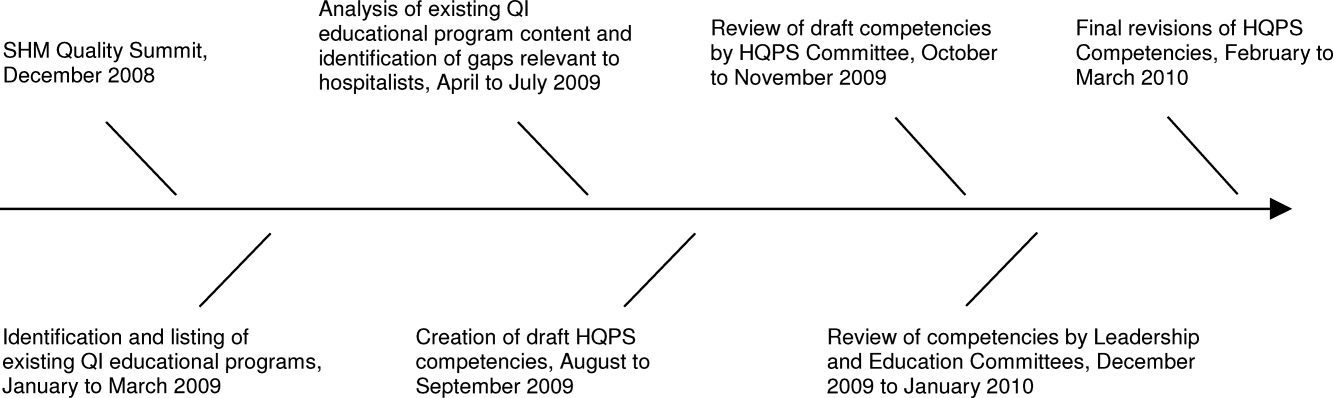
The QIE subcommittee presented a draft version of the HQPS Competencies to the HQPS Committee in the fall of 2009 and incorporated suggested revisions. The revised set of competencies was then reviewed by members of the Leadership and Education Committees during the winter of 2009‐2010, and additional recommendations were included in the final version now described.
Description of The Competencies
The 8 areas of competence include: Quality Measurement and Stakeholder Interests, Data Acquisition and Interpretation, Organizational Knowledge and Leadership Skills, Patient Safety Principles, Teamwork and Communication, Quality and Safety Improvement Methods, Health Information Systems, and Patient Centeredness. Three levels of competence and standards within each level and area are defined in Table 1. Standards use carefully selected action verbs to reflect educational goals for hospitalists at each level.24 The basic level represents a minimum level of competency for all practicing hospitalists. The intermediate level represents a hospitalist who is prepared to meaningfully engage and collaborate with his or her institution in quality improvement efforts. A hospitalist at this level may also lead uncomplicated improvement projects for his or her medical center and/or hospital medicine group. The advanced level represents a hospitalist prepared to lead quality improvement efforts for his or her institution and/or hospital medicine group. Many hospitalists at this level will have, or will be prepared to have, leadership positions in quality and patient safety at their institutions. Advanced level hospitalists will also have the expertise to teach and mentor other individuals in their quality improvement efforts.
| Competency | Basic | Intermediate | Advanced |
|---|---|---|---|
| |||
| Quality measurement and stakeholder interests | Define structure, process, and outcome measures | Compare and contrast relative benefits of using one type of measure vs another | Anticipate and respond to stakeholders' needs and interests |
| Define stakeholders and understand their interests related to healthcare quality | Explain measures as defined by stakeholders (Center for Medicare and Medicaid Services, Leapfrog, etc) | Anticipate and respond to changes in quality measures and incentive programs | |
| Identify measures as defined by stakeholders (Center for Medicare and Medicaid Services, Leapfrog, etc) | Appreciate variation in quality and utilization performance | Lead efforts to reduce variation in care delivery (see also quality improvement methods) | |
| Describe potential unintended consequences of quality measurement and incentive programs | Avoid unintended consequences of quality measurement and incentive programs | ||
| Data acquisition and interpretation | Interpret simple statistical methods to compare populations within a sample (chi‐square, t tests, etc) | Describe sources of data for quality measurement | Acquire data from internal and external sources |
| Define basic terms used to describe continuous and categorical data (mean, median, standard deviation, interquartile range, percentages, rates, etc) | Identify potential pitfalls in administrative data | Create visual representations of data (Bar, Pareto, and Control Charts) | |
| Summarize basic principles of statistical process control | Explain variation in data | Use simple statistical methods to compare populations within a sample (chi‐square, t tests, etc) | |
| Interpret data displayed in Pareto and Control Charts | Administer and interpret a survey | ||
| Summarize basic survey techniques (including methods to maximize response, minimize bias, and use of ordinal response scales) | |||
| Use appropriate terms to describe continuous and categorical data (mean, median, standard deviation, interquartile range, percentages, rates, etc) | |||
| Organizational knowledge and leadership skills | Describe the organizational structure of one's institution | Define interests of internal and external stakeholders | Effectively negotiate with stakeholders |
| Define leaders within the organization and describe their roles | Collaborate as an effective team member of a quality improvement project | Assemble a quality improvement project team and effectively lead meetings (setting agendas, hold members accountable, etc) | |
| Exemplify the importance of leading by example | Explain principles of change management and how it can positively or negatively impact quality improvement project implementation | Motivate change and create vision for ideal state | |
| Effectively communicate quality or safety issues identified during routine patient care to the appropriate parties | Communicate effectively in a variety of settings (lead a meeting, public speaking, etc) | ||
| Serve as a resource and/or mentor for less‐experienced team members | |||
| Patient safety principles | Identify potential sources of error encountered during routine patient care | Compare methods to measure errors and adverse events, including administrative data analysis, chart review, and incident reporting systems | Lead efforts to appropriately measure medical error and/or adverse events |
| Compare and contrast medical error with adverse event | Identify and explain how human factors can contribute to medical errors | Lead efforts to redesign systems to reduce errors from occurring; this may include the facilitation of a hospital, departmental, or divisional Root Cause Analysis | |
| Describe how the systems approach to medical error is more productive than assigning individual blame | Know the difference between a strong vs a weak action plan for improvement (ie, brief education intervention is weak; skills training with deliberate practice or physical changes are stronger) | Lead efforts to advance the culture of patient safety in the hospital | |
| Differentiate among types of error (knowledge/judgment vs systems vs procedural/technical; latent vs active) | |||
| Explain the role that incident reporting plays in quality improvement efforts and how reporting can foster a culture of safety | |||
| Describe principles of medical error disclosure | |||
| Teamwork and communication | Explain how poor teamwork and communication failures contribute to adverse events | Collaborate on administration and interpretation of teamwork and safety culture measures | Lead efforts to improve teamwork and safety culture |
| Identify the potential for errors during transitions within and between healthcare settings (handoffs, transfers, discharge) | Describe the principles of effective teamwork and identify behaviors consistent with effective teamwork | Lead efforts to improve teamwork in specific settings (intensive care, medical‐surgical unit, etc) | |
| Identify deficiencies in transitions within and between healthcare settings (handoffs, transfers, discharge) | Successfully improve the safety of transitions within and between healthcare settings (handoffs, transfers, discharge) | ||
| Quality and safety improvement methods and tools | Define the quality improvement methods used and infrastructure in place at one's hospital | Compare and contrast various quality improvement methods, including six sigma, lean, and PDSA | Lead a quality improvement project using six sigma, lean, or PDSA methodology |
| Summarize the basic principles and use of Root Cause Analysis as a tool to evaluate medical error | Collaborate on a quality improvement project using six sigma, lean, or PDSA | Use high level process mapping, fishbone diagrams, etc, to identify areas for opportunity in evaluating a process | |
| Describe and collaborate on Failure Mode and Effects Analysis | Lead the development and implementation of clinical protocols to standardize care delivery when appropriate | ||
| Actively participate in a Root Cause Analysis | Conduct Failure Mode and Effects Analysis | ||
| Conduct Root Cause Analysis | |||
| Health information systems | Identify the potential for information systems to reduce as well as contribute to medical error | Define types of clinical decision support | Lead or co‐lead efforts to leverage information systems in quality measurement |
| Describe how information systems fit into provider workflow and care delivery | Collaborate on the design of health information systems | Lead or co‐lead efforts to leverage information systems to reduce error and/or improve delivery of effective care | |
| Anticipate and prevent unintended consequences of implementation or revision of information systems | |||
| Lead or co‐lead efforts to leverage clinical decision support to improve quality and safety | |||
| Patient centeredness | Explain the clinical benefits of a patient‐centered approach | Explain benefits and potential limitations of patient satisfaction surveys | Interpret data from patient satisfaction surveys and lead efforts to improve patient satisfaction |
| Identify system barriers to effective and safe care from the patient's perspective | Identify clinical areas with suboptimal efficiency and/or timeliness from the patient's perspective | Lead effort to reduce inefficiency and/or improve timeliness from the patient's perspective | |
| Describe the value of patient satisfaction surveys and patient and family partnership in care | Promote patient and caregiver education including use of effective education tools | Lead efforts to eliminate system barriers to effective and safe care from the patient's perspective | |
| Lead efforts to improve patent and caregiver education including development or implementation of effective education tools | |||
| Lead efforts to actively involve patients and families in the redesign of healthcare delivery systems and processes | |||
Recommended Use of The Competencies
The HQPS Competencies provide a framework for curricula and other professional development experiences in healthcare quality and patient safety. We recommend a step‐wise approach to curriculum development which includes conducting a targeted needs assessment, defining goals and specific learning objectives, and evaluation of the curriculum.25 The HQPS Competencies can be used at each step and provide educational targets for learners across a range of interest and experience.
Professional Development
Since residency programs historically have not trained their graduates to achieve a basic level of competence, practicing hospitalists will need to seek out professional development opportunities. Some educational opportunities which already exist include the Quality Track sessions during the SHM Annual Meeting, and the SHM Quality Improvement Pre‐Course. Hospitalist leaders are currently using the HQPS Competencies to review and revise annual meeting and pre‐course objectives and content in an effort to meet the expected level of competence for SHM members. Similarly, local SHM Chapter and regional hospital medicine leaders should look to the competencies to help select topics and objectives for future presentations. Additionally, the SHM Web site offers tools to develop skills, including a resource room and quality improvement primer.26 Mentored‐implementation programs, supported by SHM, can help hospitalists' acquire more advanced experiential training in quality improvement.
New educational opportunities are being developed, including a comprehensive set of Internet‐based modules designed to help practicing hospitalists achieve a basic level of competence. Hospitalists will be able to achieve continuing medical education (CME) credit upon completion of individual modules. Plans are underway to provide Certification in Hospital Quality and Patient Safety, reflecting an advanced level of competence, upon completion of the entire set, and demonstration of knowledge and skill application through an approved quality improvement project. The certification process will leverage the success of the SHM Leadership Academies and Mentored Implementation projects to help hospitalists apply their new skills in a real world setting.
HQPS Competencies and Focused Practice in Hospital Medicine
Recently, the American Board of Internal Medicine (ABIM) has recognized the field of hospital medicine by developing a new program that provides hospitalists the opportunity to earn Maintenance of Certification (MOC) in Internal Medicine with a Focused Practice in Hospital Medicine.27 Appropriately, hospital quality and patient safety content is included among the knowledge questions on the secure exam, and completion of a practice improvement module (commonly known as PIM) is required for the certification. The SHM Education Committee has developed a Self‐Evaluation of Medical Knowledge module related to hospital quality and patient safety for use in the MOC process. ABIM recertification with Focused Practice in Hospital Medicine is an important and visible step for the Hospital Medicine movement; the content of both the secure exam and the MOC reaffirms the notion that the acquisition of knowledge, skills, and attitudes in hospital quality and patient safety is essential to the practice of hospital medicine.
Medical Education
Because teaching hospitalists frequently serve in important roles as educators and physician leaders in quality improvement, they are often responsible for medical student and resident training in healthcare quality and patient safety. Medical schools and residency programs have struggled to integrate healthcare quality and patient safety into their curricula.11, 12, 28 Hospitalists can play a major role in academic medical centers by helping to develop curricular materials and evaluations related to healthcare quality. Though intended primarily for future and current hospitalists, the HQPS Competencies and standards for the basic level may be adapted to provide educational targets for many learners in undergraduate and graduate medical education. Teaching hospitalists may use these standards to evaluate current educational efforts and design new curricula in collaboration with their medical school and residency program leaders.
Beyond the basic level of training in healthcare quality required for all, many residents will benefit from more advanced training experiences, including opportunities to apply knowledge and develop skills related to quality improvement. A recent report from the ACGME concluded that role models and mentors were essential for engaging residents in quality improvement efforts.29 Hospitalists are ideally suited to serve as role models during residents' experiential learning opportunities related to hospital quality. Several residency programs have begun to implement hospitalist tracks13 and quality improvement rotations.3032 Additionally, some academic medical centers have begun to develop and offer fellowship training in Hospital Medicine.33 These hospitalist‐led educational programs are an ideal opportunity to teach the intermediate and advanced training components, of healthcare quality and patient safety, to residents and fellows that wish to incorporate activity or leadership in quality improvement and patient safety science into their generalist or subspecialty careers. Teaching hospitalists should use the HQPS competency standards to define learning objectives for trainees at this stage of development.
To address the enormous educational needs in quality and safety for future physicians, a cadre of expert teachers in quality and safety will need to be developed. In collaboration with the Alliance for Academic Internal Medicine (AAIM), SHM is developing a Quality and Safety Educators Academy which will target academic hospitalists and other medical educators interested in developing advanced skills in quality improvement and patient safety education.
Assessment of Competence
An essential component of a rigorous faculty development program or medical education initiative is the assessment of whether these endeavors are achieving their stated aims. Published literature provides examples of useful assessment methods applicable to the HQPS Competencies. Knowledge in several areas of HQPS competence may be assessed with the use of multiple choice tests.34, 35 Knowledge of quality improvement methods may be assessed using the Quality Improvement Knowledge Application Tool (QIKAT), an instrument in which the learner responds to each of 3 scenarios with an aim, outcome and process measures, and ideas for changes which may result in improved performance.36 Teamwork and communication skills may be assessed using 360‐degree evaluations3739 and direct observation using behaviorally anchored rating scales.4043 Objective structured clinical examinations have been used to assess knowledge and skills related to patient safety principles.44, 45 Notably, few studies have rigorously assessed the validity and reliability of tools designed to evaluate competence related to healthcare quality.46 Additionally, to our knowledge, no prior research has evaluated assessment specifically for hospitalists. Thus, the development and validation of new assessment tools based on the HQPS Competencies for learners at each level is a crucial next step in the educational process. Additionally, evaluation of educational initiatives should include analyses of clinical benefit, as the ultimate goal of these efforts is to improve patient care.47, 48
Conclusion
Hospitalists are poised to have a tremendous impact on improving the quality of care for hospitalized patients. The lack of training in quality improvement in traditional medical education programs, in which most current hospitalists were trained, can be overcome through appropriate use of the HQPS Competencies. Formal incorporation of the HQPS Competencies into professional development programs, and innovative educational initiatives and curricula, will help provide current hospitalists and the next generations of hospitalists with the needed skills to be successful.
- Crossing the Quality Chasm: A New Health System for the Twenty‐first Century.Washington, DC:Institute of Medicine;2001.
- ,,,.Care in U.S. hospitals—the Hospital Quality Alliance program.N Engl J Med.2005;353(3):265–274.
- ,.Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization.JAMA.2003;290(14):1868–1874.
- Hospital Compare—A quality tool provided by Medicare. Available at: http://www.hospitalcompare.hhs.gov/. Accessed April 23,2010.
- The Leapfrog Group: Hospital Quality Ratings. Available at: http://www.leapfroggroup.org/cp. Accessed April 30,2010.
- Why Not the Best? A Healthcare Quality Improvement Resource. Available at: http://www.whynotthebest.org/. Accessed April 30,2010.
- The Joint Commission: Facts about ORYX for hospitals (National Hospital Quality Measures). Available at: http://www.jointcommission.org/accreditationprograms/hospitals/oryx/oryx_facts.htm. Accessed August 19,2010.
- The Joint Commission: National Patient Safety Goals. Available at: http://www.jointcommission.org/patientsafety/nationalpatientsafetygoals/. Accessed August 9,2010.
- Hospital Acquired Conditions: Overview. Available at: http://www.cms.gov/HospitalAcqCond/01_Overview.asp. Accessed April 30,2010.
- Report to Congress:Plan to Implement a Medicare Hospital Value‐based Purchasing Program. Washington, DC: US Department of Health and Human Services, Center for Medicare and Medicaid Services;2007.
- Unmet Needs: Teaching Physicians to Provide Safe Patient Care.Boston, MA:Lucian Leape Institute at the National Patient Safety Foundation;2010.
- ,,,,.Patient safety education at U.S. and Canadian medical schools: results from the 2006 Clerkship Directors in Internal Medicine survey.Acad Med.2009;84(12):1672–1676.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
- ,,,,.Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- ,,.Redesigning training for internal medicine.Ann Intern Med.2006;144(12):927–932.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- Intermountain Healthcare. 20‐Day Course for Executives 2001.
- ,,,.Curriculum Development for Medical Education: A Six‐step Approach.Baltimore, MD:Johns Hopkins Press;1998.
- Society of Hospital Medicine Quality Improvement Basics. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/QualityImprovement/QIPrimer/QI_Primer_Landing_Pa.htm. Accessed June 4,2010.
- American Board of Internal Medicine: Questions and Answers Regarding ABIM's Maintenance of Certification in Internal Medicine With a Focused Practice in Hospital Medicine Program. Available at: http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Accessed August 9,2010.
- ,,.Assessing the needs of residency program directors to meet the ACGME general competencies.Acad Med.2002;77(7):750.
- .Accreditation Council for Graduate Medical Education and Institute for Healthcare Improvement 90‐Day Project. Involving Residents in Quality Improvement: Contrasting “Top‐Down” and “Bottom‐Up” Approaches.Chicago, IL;ACGME;2008.
- ,,,.Teaching internal medicine residents quality improvement techniques using the ABIM's practice improvement modules.J Gen Intern Med.2008;23(7):927–930.
- ,,,,.A self‐instructional model to teach systems‐based practice and practice‐based learning and improvement.J Gen Intern Med.2008;23(7):931–936.
- ,,,,.Creating a quality improvement elective for medical house officers.J Gen Intern Med.2004;19(8):861–867.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119(1):72.e1‐e7.
- ,,,.Web‐based education in systems‐based practice: a randomized trial.Arch Intern Med.2007;167(4):361–366.
- ,,,,.A self‐instructional model to teach systems‐based practice and practice‐based learning and improvement.J Gen Intern Med.2008;23(7):931–936.
- ,,,.The quality improvement knowledge application tool: an instrument to assess knowledge application in practice‐based learning and improvement.J Gen Intern Med.2003;18(suppl 1):250.
- ,,, et al.Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial.Arch Pediatr Adolesc Med.2007;161(1):44–49.
- ,.Reliability of a 360‐degree evaluation to assess resident competence.Am J Phys Med Rehabil.2007;86(10):845–852.
- ,,,.Pilot study of a 360‐degree assessment instrument for physical medicine 82(5):394–402.
- ,,,,,.Anaesthetists' non‐technical skills (ANTS): evaluation of a behavioural marker system.Br J Anaesth.2003;90(5):580–588.
- ,,, et al.The Mayo high performance teamwork scale: reliability and validity for evaluating key crew resource management skills.Simul Healthc.2007;2(1):4–10.
- ,,,,,.Reliability of a revised NOTECHS scale for use in surgical teams.Am J Surg.2008;196(2):184–190.
- ,,,,,.Observational teamwork assessment for surgery: construct validation with expert versus novice raters.Ann Surg.2009;249(6):1047–1051.
- ,,,,,.A patient safety objective structured clinical examination.J Patient Saf.2009;5(2):55–60.
- ,.The Objective Structured Clinical Examination as an educational tool in patient safety.Jt Comm J Qual Patient Saf.2007;33(1):48–53.
- ,,.Measurement of the general competencies of the Accreditation Council for Graduate Medical Education: a systematic review.Acad Med.2009;84(3):301–309.
- ,,,,,.Effectiveness of teaching quality improvement to clinicians: a systematic review.JAMA.2007;298(9):1023–1037.
- ,,,,.Methodological rigor of quality improvement curricula for physician trainees: a systematic review and recommendations for change.Acad Med.2009;84(12):1677–1692.
Healthcare quality is defined as the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.1 Delivering high quality care to patients in the hospital setting is especially challenging, given the rapid pace of clinical care, the severity and multitude of patient conditions, and the interdependence of complex processes within the hospital system. Research has shown that hospitalized patients do not consistently receive recommended care2 and are at risk for experiencing preventable harm.3 In an effort to stimulate improvement, stakeholders have called for increased accountability, including enhanced transparency and differential payment based on performance. A growing number of hospital process and outcome measures are readily available to the public via the Internet.46 The Joint Commission, which accredits US hospitals, requires the collection of core quality measure data7 and sets the expectation that National Patient Safety Goals be met to maintain accreditation.8 Moreover, the Center for Medicare and Medicaid Services (CMS) has developed a Value‐Based Purchasing (VBP) plan intended to adjust hospital payment based on quality measures and the occurrence of certain hospital‐acquired conditions.9, 10
Because of their clinical expertise, understanding of hospital clinical operations, leadership of multidisciplinary inpatient teams, and vested interest to improve the systems in which they work, hospitalists are perfectly positioned to collaborate with their institutions to improve the quality of care delivered to inpatients. However, many hospitalists are inadequately prepared to engage in efforts to improve quality, because medical schools and residency programs have not traditionally included or emphasized healthcare quality and patient safety in their curricula.1113 In a survey of 389 internal medicine‐trained hospitalists, significant educational deficiencies were identified in the area of systems‐based practice.14 Specifically, the topics of quality improvement, team management, practice guideline development, health information systems management, and coordination of care between healthcare settings were listed as essential skills for hospitalist practice but underemphasized in residency training. Recognizing the gap between the needs of practicing physicians and current medical education provided in healthcare quality, professional societies have recently published position papers calling for increased training in quality, safety, and systems, both in medical school11 and residency training.15, 16
The Society of Hospital Medicine (SHM) convened a Quality Summit in December 2008 to develop strategic plans related to healthcare quality. Summit attendees felt that most hospitalists lack the formal training necessary to evaluate, implement, and sustain system changes within the hospital. In response, the SHM Hospital Quality and Patient Safety (HQPS) Committee formed a Quality Improvement Education (QIE) subcommittee in 2009 to assess the needs of hospitalists with respect to hospital quality and patient safety, and to evaluate and expand upon existing educational programs in this area. Membership of the QIE subcommittee consisted of hospitalists with extensive experience in healthcare quality and medical education. The QIE subcommittee refined and expanded upon the healthcare quality and patient safety‐related competencies initially described in the Core Competencies in Hospital Medicine.17 The purpose of this report is to describe the development, provide definitions, and make recommendations on the use of the Hospital Quality and Patient Safety (HQPS) Competencies.
Development of The Hospital Quality and Patient Safety Competencies
The multistep process used by the SHM QIE subcommittee to develop the HQPS Competencies is summarized in Figure 1. We performed an in‐depth evaluation of current educational materials and offerings, including a review of the Core Competencies in Hospital Medicine, past annual SHM Quality Improvement Pre‐Course objectives, and the content of training courses offered by other organizations.1722 Throughout our analysis, we emphasized the identification of gaps in content relevant to hospitalists. We then used the Institute of Medicine's (IOM) 6 aims for healthcare quality as a foundation for developing the HQPS Competencies.1 Specifically, the IOM states that healthcare should be safe, effective, patient‐centered, timely, efficient, and equitable. Additionally, we reviewed and integrated elements of the Practice‐Based Learning and Improvement (PBLI) and Systems‐Based Practice (SBP) competencies as defined by the Accreditation Council for Graduate Medical Education (ACGME).23 We defined general areas of competence and specific standards for knowledge, skills, and attitudes within each area. Subcommittee members reflected on their own experience, as clinicians, educators, and leaders in healthcare quality and patient safety, to inform and refine the competency definitions and standards. Acknowledging that some hospitalists may serve as collaborators or clinical content experts, while others may serve as leaders of hospital quality initiatives, 3 levels of expertise were established: basic, intermediate, and advanced.
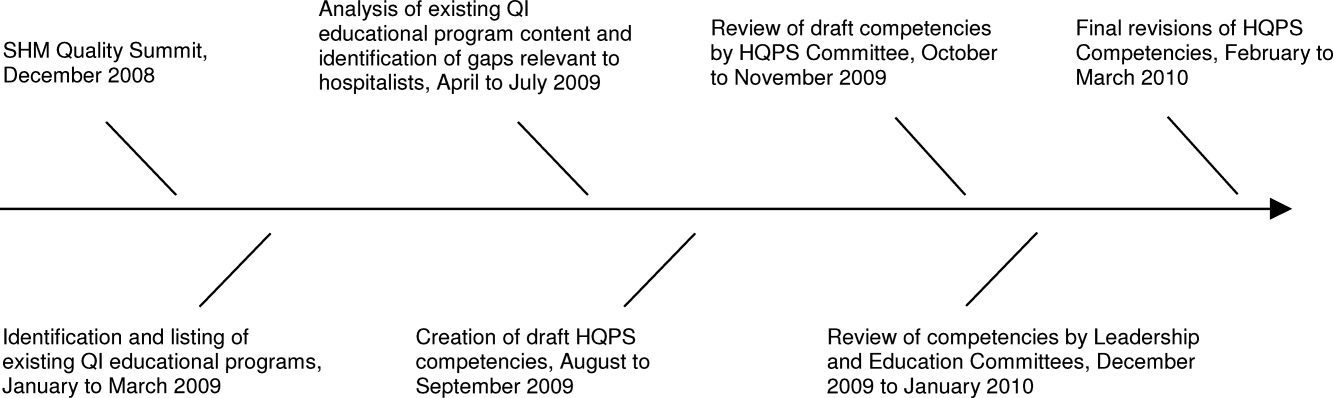
The QIE subcommittee presented a draft version of the HQPS Competencies to the HQPS Committee in the fall of 2009 and incorporated suggested revisions. The revised set of competencies was then reviewed by members of the Leadership and Education Committees during the winter of 2009‐2010, and additional recommendations were included in the final version now described.
Description of The Competencies
The 8 areas of competence include: Quality Measurement and Stakeholder Interests, Data Acquisition and Interpretation, Organizational Knowledge and Leadership Skills, Patient Safety Principles, Teamwork and Communication, Quality and Safety Improvement Methods, Health Information Systems, and Patient Centeredness. Three levels of competence and standards within each level and area are defined in Table 1. Standards use carefully selected action verbs to reflect educational goals for hospitalists at each level.24 The basic level represents a minimum level of competency for all practicing hospitalists. The intermediate level represents a hospitalist who is prepared to meaningfully engage and collaborate with his or her institution in quality improvement efforts. A hospitalist at this level may also lead uncomplicated improvement projects for his or her medical center and/or hospital medicine group. The advanced level represents a hospitalist prepared to lead quality improvement efforts for his or her institution and/or hospital medicine group. Many hospitalists at this level will have, or will be prepared to have, leadership positions in quality and patient safety at their institutions. Advanced level hospitalists will also have the expertise to teach and mentor other individuals in their quality improvement efforts.
| Competency | Basic | Intermediate | Advanced |
|---|---|---|---|
| |||
| Quality measurement and stakeholder interests | Define structure, process, and outcome measures | Compare and contrast relative benefits of using one type of measure vs another | Anticipate and respond to stakeholders' needs and interests |
| Define stakeholders and understand their interests related to healthcare quality | Explain measures as defined by stakeholders (Center for Medicare and Medicaid Services, Leapfrog, etc) | Anticipate and respond to changes in quality measures and incentive programs | |
| Identify measures as defined by stakeholders (Center for Medicare and Medicaid Services, Leapfrog, etc) | Appreciate variation in quality and utilization performance | Lead efforts to reduce variation in care delivery (see also quality improvement methods) | |
| Describe potential unintended consequences of quality measurement and incentive programs | Avoid unintended consequences of quality measurement and incentive programs | ||
| Data acquisition and interpretation | Interpret simple statistical methods to compare populations within a sample (chi‐square, t tests, etc) | Describe sources of data for quality measurement | Acquire data from internal and external sources |
| Define basic terms used to describe continuous and categorical data (mean, median, standard deviation, interquartile range, percentages, rates, etc) | Identify potential pitfalls in administrative data | Create visual representations of data (Bar, Pareto, and Control Charts) | |
| Summarize basic principles of statistical process control | Explain variation in data | Use simple statistical methods to compare populations within a sample (chi‐square, t tests, etc) | |
| Interpret data displayed in Pareto and Control Charts | Administer and interpret a survey | ||
| Summarize basic survey techniques (including methods to maximize response, minimize bias, and use of ordinal response scales) | |||
| Use appropriate terms to describe continuous and categorical data (mean, median, standard deviation, interquartile range, percentages, rates, etc) | |||
| Organizational knowledge and leadership skills | Describe the organizational structure of one's institution | Define interests of internal and external stakeholders | Effectively negotiate with stakeholders |
| Define leaders within the organization and describe their roles | Collaborate as an effective team member of a quality improvement project | Assemble a quality improvement project team and effectively lead meetings (setting agendas, hold members accountable, etc) | |
| Exemplify the importance of leading by example | Explain principles of change management and how it can positively or negatively impact quality improvement project implementation | Motivate change and create vision for ideal state | |
| Effectively communicate quality or safety issues identified during routine patient care to the appropriate parties | Communicate effectively in a variety of settings (lead a meeting, public speaking, etc) | ||
| Serve as a resource and/or mentor for less‐experienced team members | |||
| Patient safety principles | Identify potential sources of error encountered during routine patient care | Compare methods to measure errors and adverse events, including administrative data analysis, chart review, and incident reporting systems | Lead efforts to appropriately measure medical error and/or adverse events |
| Compare and contrast medical error with adverse event | Identify and explain how human factors can contribute to medical errors | Lead efforts to redesign systems to reduce errors from occurring; this may include the facilitation of a hospital, departmental, or divisional Root Cause Analysis | |
| Describe how the systems approach to medical error is more productive than assigning individual blame | Know the difference between a strong vs a weak action plan for improvement (ie, brief education intervention is weak; skills training with deliberate practice or physical changes are stronger) | Lead efforts to advance the culture of patient safety in the hospital | |
| Differentiate among types of error (knowledge/judgment vs systems vs procedural/technical; latent vs active) | |||
| Explain the role that incident reporting plays in quality improvement efforts and how reporting can foster a culture of safety | |||
| Describe principles of medical error disclosure | |||
| Teamwork and communication | Explain how poor teamwork and communication failures contribute to adverse events | Collaborate on administration and interpretation of teamwork and safety culture measures | Lead efforts to improve teamwork and safety culture |
| Identify the potential for errors during transitions within and between healthcare settings (handoffs, transfers, discharge) | Describe the principles of effective teamwork and identify behaviors consistent with effective teamwork | Lead efforts to improve teamwork in specific settings (intensive care, medical‐surgical unit, etc) | |
| Identify deficiencies in transitions within and between healthcare settings (handoffs, transfers, discharge) | Successfully improve the safety of transitions within and between healthcare settings (handoffs, transfers, discharge) | ||
| Quality and safety improvement methods and tools | Define the quality improvement methods used and infrastructure in place at one's hospital | Compare and contrast various quality improvement methods, including six sigma, lean, and PDSA | Lead a quality improvement project using six sigma, lean, or PDSA methodology |
| Summarize the basic principles and use of Root Cause Analysis as a tool to evaluate medical error | Collaborate on a quality improvement project using six sigma, lean, or PDSA | Use high level process mapping, fishbone diagrams, etc, to identify areas for opportunity in evaluating a process | |
| Describe and collaborate on Failure Mode and Effects Analysis | Lead the development and implementation of clinical protocols to standardize care delivery when appropriate | ||
| Actively participate in a Root Cause Analysis | Conduct Failure Mode and Effects Analysis | ||
| Conduct Root Cause Analysis | |||
| Health information systems | Identify the potential for information systems to reduce as well as contribute to medical error | Define types of clinical decision support | Lead or co‐lead efforts to leverage information systems in quality measurement |
| Describe how information systems fit into provider workflow and care delivery | Collaborate on the design of health information systems | Lead or co‐lead efforts to leverage information systems to reduce error and/or improve delivery of effective care | |
| Anticipate and prevent unintended consequences of implementation or revision of information systems | |||
| Lead or co‐lead efforts to leverage clinical decision support to improve quality and safety | |||
| Patient centeredness | Explain the clinical benefits of a patient‐centered approach | Explain benefits and potential limitations of patient satisfaction surveys | Interpret data from patient satisfaction surveys and lead efforts to improve patient satisfaction |
| Identify system barriers to effective and safe care from the patient's perspective | Identify clinical areas with suboptimal efficiency and/or timeliness from the patient's perspective | Lead effort to reduce inefficiency and/or improve timeliness from the patient's perspective | |
| Describe the value of patient satisfaction surveys and patient and family partnership in care | Promote patient and caregiver education including use of effective education tools | Lead efforts to eliminate system barriers to effective and safe care from the patient's perspective | |
| Lead efforts to improve patent and caregiver education including development or implementation of effective education tools | |||
| Lead efforts to actively involve patients and families in the redesign of healthcare delivery systems and processes | |||
Recommended Use of The Competencies
The HQPS Competencies provide a framework for curricula and other professional development experiences in healthcare quality and patient safety. We recommend a step‐wise approach to curriculum development which includes conducting a targeted needs assessment, defining goals and specific learning objectives, and evaluation of the curriculum.25 The HQPS Competencies can be used at each step and provide educational targets for learners across a range of interest and experience.
Professional Development
Since residency programs historically have not trained their graduates to achieve a basic level of competence, practicing hospitalists will need to seek out professional development opportunities. Some educational opportunities which already exist include the Quality Track sessions during the SHM Annual Meeting, and the SHM Quality Improvement Pre‐Course. Hospitalist leaders are currently using the HQPS Competencies to review and revise annual meeting and pre‐course objectives and content in an effort to meet the expected level of competence for SHM members. Similarly, local SHM Chapter and regional hospital medicine leaders should look to the competencies to help select topics and objectives for future presentations. Additionally, the SHM Web site offers tools to develop skills, including a resource room and quality improvement primer.26 Mentored‐implementation programs, supported by SHM, can help hospitalists' acquire more advanced experiential training in quality improvement.
New educational opportunities are being developed, including a comprehensive set of Internet‐based modules designed to help practicing hospitalists achieve a basic level of competence. Hospitalists will be able to achieve continuing medical education (CME) credit upon completion of individual modules. Plans are underway to provide Certification in Hospital Quality and Patient Safety, reflecting an advanced level of competence, upon completion of the entire set, and demonstration of knowledge and skill application through an approved quality improvement project. The certification process will leverage the success of the SHM Leadership Academies and Mentored Implementation projects to help hospitalists apply their new skills in a real world setting.
HQPS Competencies and Focused Practice in Hospital Medicine
Recently, the American Board of Internal Medicine (ABIM) has recognized the field of hospital medicine by developing a new program that provides hospitalists the opportunity to earn Maintenance of Certification (MOC) in Internal Medicine with a Focused Practice in Hospital Medicine.27 Appropriately, hospital quality and patient safety content is included among the knowledge questions on the secure exam, and completion of a practice improvement module (commonly known as PIM) is required for the certification. The SHM Education Committee has developed a Self‐Evaluation of Medical Knowledge module related to hospital quality and patient safety for use in the MOC process. ABIM recertification with Focused Practice in Hospital Medicine is an important and visible step for the Hospital Medicine movement; the content of both the secure exam and the MOC reaffirms the notion that the acquisition of knowledge, skills, and attitudes in hospital quality and patient safety is essential to the practice of hospital medicine.
Medical Education
Because teaching hospitalists frequently serve in important roles as educators and physician leaders in quality improvement, they are often responsible for medical student and resident training in healthcare quality and patient safety. Medical schools and residency programs have struggled to integrate healthcare quality and patient safety into their curricula.11, 12, 28 Hospitalists can play a major role in academic medical centers by helping to develop curricular materials and evaluations related to healthcare quality. Though intended primarily for future and current hospitalists, the HQPS Competencies and standards for the basic level may be adapted to provide educational targets for many learners in undergraduate and graduate medical education. Teaching hospitalists may use these standards to evaluate current educational efforts and design new curricula in collaboration with their medical school and residency program leaders.
Beyond the basic level of training in healthcare quality required for all, many residents will benefit from more advanced training experiences, including opportunities to apply knowledge and develop skills related to quality improvement. A recent report from the ACGME concluded that role models and mentors were essential for engaging residents in quality improvement efforts.29 Hospitalists are ideally suited to serve as role models during residents' experiential learning opportunities related to hospital quality. Several residency programs have begun to implement hospitalist tracks13 and quality improvement rotations.3032 Additionally, some academic medical centers have begun to develop and offer fellowship training in Hospital Medicine.33 These hospitalist‐led educational programs are an ideal opportunity to teach the intermediate and advanced training components, of healthcare quality and patient safety, to residents and fellows that wish to incorporate activity or leadership in quality improvement and patient safety science into their generalist or subspecialty careers. Teaching hospitalists should use the HQPS competency standards to define learning objectives for trainees at this stage of development.
To address the enormous educational needs in quality and safety for future physicians, a cadre of expert teachers in quality and safety will need to be developed. In collaboration with the Alliance for Academic Internal Medicine (AAIM), SHM is developing a Quality and Safety Educators Academy which will target academic hospitalists and other medical educators interested in developing advanced skills in quality improvement and patient safety education.
Assessment of Competence
An essential component of a rigorous faculty development program or medical education initiative is the assessment of whether these endeavors are achieving their stated aims. Published literature provides examples of useful assessment methods applicable to the HQPS Competencies. Knowledge in several areas of HQPS competence may be assessed with the use of multiple choice tests.34, 35 Knowledge of quality improvement methods may be assessed using the Quality Improvement Knowledge Application Tool (QIKAT), an instrument in which the learner responds to each of 3 scenarios with an aim, outcome and process measures, and ideas for changes which may result in improved performance.36 Teamwork and communication skills may be assessed using 360‐degree evaluations3739 and direct observation using behaviorally anchored rating scales.4043 Objective structured clinical examinations have been used to assess knowledge and skills related to patient safety principles.44, 45 Notably, few studies have rigorously assessed the validity and reliability of tools designed to evaluate competence related to healthcare quality.46 Additionally, to our knowledge, no prior research has evaluated assessment specifically for hospitalists. Thus, the development and validation of new assessment tools based on the HQPS Competencies for learners at each level is a crucial next step in the educational process. Additionally, evaluation of educational initiatives should include analyses of clinical benefit, as the ultimate goal of these efforts is to improve patient care.47, 48
Conclusion
Hospitalists are poised to have a tremendous impact on improving the quality of care for hospitalized patients. The lack of training in quality improvement in traditional medical education programs, in which most current hospitalists were trained, can be overcome through appropriate use of the HQPS Competencies. Formal incorporation of the HQPS Competencies into professional development programs, and innovative educational initiatives and curricula, will help provide current hospitalists and the next generations of hospitalists with the needed skills to be successful.
Healthcare quality is defined as the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.1 Delivering high quality care to patients in the hospital setting is especially challenging, given the rapid pace of clinical care, the severity and multitude of patient conditions, and the interdependence of complex processes within the hospital system. Research has shown that hospitalized patients do not consistently receive recommended care2 and are at risk for experiencing preventable harm.3 In an effort to stimulate improvement, stakeholders have called for increased accountability, including enhanced transparency and differential payment based on performance. A growing number of hospital process and outcome measures are readily available to the public via the Internet.46 The Joint Commission, which accredits US hospitals, requires the collection of core quality measure data7 and sets the expectation that National Patient Safety Goals be met to maintain accreditation.8 Moreover, the Center for Medicare and Medicaid Services (CMS) has developed a Value‐Based Purchasing (VBP) plan intended to adjust hospital payment based on quality measures and the occurrence of certain hospital‐acquired conditions.9, 10
Because of their clinical expertise, understanding of hospital clinical operations, leadership of multidisciplinary inpatient teams, and vested interest to improve the systems in which they work, hospitalists are perfectly positioned to collaborate with their institutions to improve the quality of care delivered to inpatients. However, many hospitalists are inadequately prepared to engage in efforts to improve quality, because medical schools and residency programs have not traditionally included or emphasized healthcare quality and patient safety in their curricula.1113 In a survey of 389 internal medicine‐trained hospitalists, significant educational deficiencies were identified in the area of systems‐based practice.14 Specifically, the topics of quality improvement, team management, practice guideline development, health information systems management, and coordination of care between healthcare settings were listed as essential skills for hospitalist practice but underemphasized in residency training. Recognizing the gap between the needs of practicing physicians and current medical education provided in healthcare quality, professional societies have recently published position papers calling for increased training in quality, safety, and systems, both in medical school11 and residency training.15, 16
The Society of Hospital Medicine (SHM) convened a Quality Summit in December 2008 to develop strategic plans related to healthcare quality. Summit attendees felt that most hospitalists lack the formal training necessary to evaluate, implement, and sustain system changes within the hospital. In response, the SHM Hospital Quality and Patient Safety (HQPS) Committee formed a Quality Improvement Education (QIE) subcommittee in 2009 to assess the needs of hospitalists with respect to hospital quality and patient safety, and to evaluate and expand upon existing educational programs in this area. Membership of the QIE subcommittee consisted of hospitalists with extensive experience in healthcare quality and medical education. The QIE subcommittee refined and expanded upon the healthcare quality and patient safety‐related competencies initially described in the Core Competencies in Hospital Medicine.17 The purpose of this report is to describe the development, provide definitions, and make recommendations on the use of the Hospital Quality and Patient Safety (HQPS) Competencies.
Development of The Hospital Quality and Patient Safety Competencies
The multistep process used by the SHM QIE subcommittee to develop the HQPS Competencies is summarized in Figure 1. We performed an in‐depth evaluation of current educational materials and offerings, including a review of the Core Competencies in Hospital Medicine, past annual SHM Quality Improvement Pre‐Course objectives, and the content of training courses offered by other organizations.1722 Throughout our analysis, we emphasized the identification of gaps in content relevant to hospitalists. We then used the Institute of Medicine's (IOM) 6 aims for healthcare quality as a foundation for developing the HQPS Competencies.1 Specifically, the IOM states that healthcare should be safe, effective, patient‐centered, timely, efficient, and equitable. Additionally, we reviewed and integrated elements of the Practice‐Based Learning and Improvement (PBLI) and Systems‐Based Practice (SBP) competencies as defined by the Accreditation Council for Graduate Medical Education (ACGME).23 We defined general areas of competence and specific standards for knowledge, skills, and attitudes within each area. Subcommittee members reflected on their own experience, as clinicians, educators, and leaders in healthcare quality and patient safety, to inform and refine the competency definitions and standards. Acknowledging that some hospitalists may serve as collaborators or clinical content experts, while others may serve as leaders of hospital quality initiatives, 3 levels of expertise were established: basic, intermediate, and advanced.
The QIE subcommittee presented a draft version of the HQPS Competencies to the HQPS Committee in the fall of 2009 and incorporated suggested revisions. The revised set of competencies was then reviewed by members of the Leadership and Education Committees during the winter of 2009‐2010, and additional recommendations were included in the final version now described.
Description of The Competencies
The 8 areas of competence include: Quality Measurement and Stakeholder Interests, Data Acquisition and Interpretation, Organizational Knowledge and Leadership Skills, Patient Safety Principles, Teamwork and Communication, Quality and Safety Improvement Methods, Health Information Systems, and Patient Centeredness. Three levels of competence and standards within each level and area are defined in Table 1. Standards use carefully selected action verbs to reflect educational goals for hospitalists at each level.24 The basic level represents a minimum level of competency for all practicing hospitalists. The intermediate level represents a hospitalist who is prepared to meaningfully engage and collaborate with his or her institution in quality improvement efforts. A hospitalist at this level may also lead uncomplicated improvement projects for his or her medical center and/or hospital medicine group. The advanced level represents a hospitalist prepared to lead quality improvement efforts for his or her institution and/or hospital medicine group. Many hospitalists at this level will have, or will be prepared to have, leadership positions in quality and patient safety at their institutions. Advanced level hospitalists will also have the expertise to teach and mentor other individuals in their quality improvement efforts.
| Competency | Basic | Intermediate | Advanced |
|---|---|---|---|
| |||
| Quality measurement and stakeholder interests | Define structure, process, and outcome measures | Compare and contrast relative benefits of using one type of measure vs another | Anticipate and respond to stakeholders' needs and interests |
| Define stakeholders and understand their interests related to healthcare quality | Explain measures as defined by stakeholders (Center for Medicare and Medicaid Services, Leapfrog, etc) | Anticipate and respond to changes in quality measures and incentive programs | |
| Identify measures as defined by stakeholders (Center for Medicare and Medicaid Services, Leapfrog, etc) | Appreciate variation in quality and utilization performance | Lead efforts to reduce variation in care delivery (see also quality improvement methods) | |
| Describe potential unintended consequences of quality measurement and incentive programs | Avoid unintended consequences of quality measurement and incentive programs | ||
| Data acquisition and interpretation | Interpret simple statistical methods to compare populations within a sample (chi‐square, t tests, etc) | Describe sources of data for quality measurement | Acquire data from internal and external sources |
| Define basic terms used to describe continuous and categorical data (mean, median, standard deviation, interquartile range, percentages, rates, etc) | Identify potential pitfalls in administrative data | Create visual representations of data (Bar, Pareto, and Control Charts) | |
| Summarize basic principles of statistical process control | Explain variation in data | Use simple statistical methods to compare populations within a sample (chi‐square, t tests, etc) | |
| Interpret data displayed in Pareto and Control Charts | Administer and interpret a survey | ||
| Summarize basic survey techniques (including methods to maximize response, minimize bias, and use of ordinal response scales) | |||
| Use appropriate terms to describe continuous and categorical data (mean, median, standard deviation, interquartile range, percentages, rates, etc) | |||
| Organizational knowledge and leadership skills | Describe the organizational structure of one's institution | Define interests of internal and external stakeholders | Effectively negotiate with stakeholders |
| Define leaders within the organization and describe their roles | Collaborate as an effective team member of a quality improvement project | Assemble a quality improvement project team and effectively lead meetings (setting agendas, hold members accountable, etc) | |
| Exemplify the importance of leading by example | Explain principles of change management and how it can positively or negatively impact quality improvement project implementation | Motivate change and create vision for ideal state | |
| Effectively communicate quality or safety issues identified during routine patient care to the appropriate parties | Communicate effectively in a variety of settings (lead a meeting, public speaking, etc) | ||
| Serve as a resource and/or mentor for less‐experienced team members | |||
| Patient safety principles | Identify potential sources of error encountered during routine patient care | Compare methods to measure errors and adverse events, including administrative data analysis, chart review, and incident reporting systems | Lead efforts to appropriately measure medical error and/or adverse events |
| Compare and contrast medical error with adverse event | Identify and explain how human factors can contribute to medical errors | Lead efforts to redesign systems to reduce errors from occurring; this may include the facilitation of a hospital, departmental, or divisional Root Cause Analysis | |
| Describe how the systems approach to medical error is more productive than assigning individual blame | Know the difference between a strong vs a weak action plan for improvement (ie, brief education intervention is weak; skills training with deliberate practice or physical changes are stronger) | Lead efforts to advance the culture of patient safety in the hospital | |
| Differentiate among types of error (knowledge/judgment vs systems vs procedural/technical; latent vs active) | |||
| Explain the role that incident reporting plays in quality improvement efforts and how reporting can foster a culture of safety | |||
| Describe principles of medical error disclosure | |||
| Teamwork and communication | Explain how poor teamwork and communication failures contribute to adverse events | Collaborate on administration and interpretation of teamwork and safety culture measures | Lead efforts to improve teamwork and safety culture |
| Identify the potential for errors during transitions within and between healthcare settings (handoffs, transfers, discharge) | Describe the principles of effective teamwork and identify behaviors consistent with effective teamwork | Lead efforts to improve teamwork in specific settings (intensive care, medical‐surgical unit, etc) | |
| Identify deficiencies in transitions within and between healthcare settings (handoffs, transfers, discharge) | Successfully improve the safety of transitions within and between healthcare settings (handoffs, transfers, discharge) | ||
| Quality and safety improvement methods and tools | Define the quality improvement methods used and infrastructure in place at one's hospital | Compare and contrast various quality improvement methods, including six sigma, lean, and PDSA | Lead a quality improvement project using six sigma, lean, or PDSA methodology |
| Summarize the basic principles and use of Root Cause Analysis as a tool to evaluate medical error | Collaborate on a quality improvement project using six sigma, lean, or PDSA | Use high level process mapping, fishbone diagrams, etc, to identify areas for opportunity in evaluating a process | |
| Describe and collaborate on Failure Mode and Effects Analysis | Lead the development and implementation of clinical protocols to standardize care delivery when appropriate | ||
| Actively participate in a Root Cause Analysis | Conduct Failure Mode and Effects Analysis | ||
| Conduct Root Cause Analysis | |||
| Health information systems | Identify the potential for information systems to reduce as well as contribute to medical error | Define types of clinical decision support | Lead or co‐lead efforts to leverage information systems in quality measurement |
| Describe how information systems fit into provider workflow and care delivery | Collaborate on the design of health information systems | Lead or co‐lead efforts to leverage information systems to reduce error and/or improve delivery of effective care | |
| Anticipate and prevent unintended consequences of implementation or revision of information systems | |||
| Lead or co‐lead efforts to leverage clinical decision support to improve quality and safety | |||
| Patient centeredness | Explain the clinical benefits of a patient‐centered approach | Explain benefits and potential limitations of patient satisfaction surveys | Interpret data from patient satisfaction surveys and lead efforts to improve patient satisfaction |
| Identify system barriers to effective and safe care from the patient's perspective | Identify clinical areas with suboptimal efficiency and/or timeliness from the patient's perspective | Lead effort to reduce inefficiency and/or improve timeliness from the patient's perspective | |
| Describe the value of patient satisfaction surveys and patient and family partnership in care | Promote patient and caregiver education including use of effective education tools | Lead efforts to eliminate system barriers to effective and safe care from the patient's perspective | |
| Lead efforts to improve patent and caregiver education including development or implementation of effective education tools | |||
| Lead efforts to actively involve patients and families in the redesign of healthcare delivery systems and processes | |||
Recommended Use of The Competencies
The HQPS Competencies provide a framework for curricula and other professional development experiences in healthcare quality and patient safety. We recommend a step‐wise approach to curriculum development which includes conducting a targeted needs assessment, defining goals and specific learning objectives, and evaluation of the curriculum.25 The HQPS Competencies can be used at each step and provide educational targets for learners across a range of interest and experience.
Professional Development
Since residency programs historically have not trained their graduates to achieve a basic level of competence, practicing hospitalists will need to seek out professional development opportunities. Some educational opportunities which already exist include the Quality Track sessions during the SHM Annual Meeting, and the SHM Quality Improvement Pre‐Course. Hospitalist leaders are currently using the HQPS Competencies to review and revise annual meeting and pre‐course objectives and content in an effort to meet the expected level of competence for SHM members. Similarly, local SHM Chapter and regional hospital medicine leaders should look to the competencies to help select topics and objectives for future presentations. Additionally, the SHM Web site offers tools to develop skills, including a resource room and quality improvement primer.26 Mentored‐implementation programs, supported by SHM, can help hospitalists' acquire more advanced experiential training in quality improvement.
New educational opportunities are being developed, including a comprehensive set of Internet‐based modules designed to help practicing hospitalists achieve a basic level of competence. Hospitalists will be able to achieve continuing medical education (CME) credit upon completion of individual modules. Plans are underway to provide Certification in Hospital Quality and Patient Safety, reflecting an advanced level of competence, upon completion of the entire set, and demonstration of knowledge and skill application through an approved quality improvement project. The certification process will leverage the success of the SHM Leadership Academies and Mentored Implementation projects to help hospitalists apply their new skills in a real world setting.
HQPS Competencies and Focused Practice in Hospital Medicine
Recently, the American Board of Internal Medicine (ABIM) has recognized the field of hospital medicine by developing a new program that provides hospitalists the opportunity to earn Maintenance of Certification (MOC) in Internal Medicine with a Focused Practice in Hospital Medicine.27 Appropriately, hospital quality and patient safety content is included among the knowledge questions on the secure exam, and completion of a practice improvement module (commonly known as PIM) is required for the certification. The SHM Education Committee has developed a Self‐Evaluation of Medical Knowledge module related to hospital quality and patient safety for use in the MOC process. ABIM recertification with Focused Practice in Hospital Medicine is an important and visible step for the Hospital Medicine movement; the content of both the secure exam and the MOC reaffirms the notion that the acquisition of knowledge, skills, and attitudes in hospital quality and patient safety is essential to the practice of hospital medicine.
Medical Education
Because teaching hospitalists frequently serve in important roles as educators and physician leaders in quality improvement, they are often responsible for medical student and resident training in healthcare quality and patient safety. Medical schools and residency programs have struggled to integrate healthcare quality and patient safety into their curricula.11, 12, 28 Hospitalists can play a major role in academic medical centers by helping to develop curricular materials and evaluations related to healthcare quality. Though intended primarily for future and current hospitalists, the HQPS Competencies and standards for the basic level may be adapted to provide educational targets for many learners in undergraduate and graduate medical education. Teaching hospitalists may use these standards to evaluate current educational efforts and design new curricula in collaboration with their medical school and residency program leaders.
Beyond the basic level of training in healthcare quality required for all, many residents will benefit from more advanced training experiences, including opportunities to apply knowledge and develop skills related to quality improvement. A recent report from the ACGME concluded that role models and mentors were essential for engaging residents in quality improvement efforts.29 Hospitalists are ideally suited to serve as role models during residents' experiential learning opportunities related to hospital quality. Several residency programs have begun to implement hospitalist tracks13 and quality improvement rotations.3032 Additionally, some academic medical centers have begun to develop and offer fellowship training in Hospital Medicine.33 These hospitalist‐led educational programs are an ideal opportunity to teach the intermediate and advanced training components, of healthcare quality and patient safety, to residents and fellows that wish to incorporate activity or leadership in quality improvement and patient safety science into their generalist or subspecialty careers. Teaching hospitalists should use the HQPS competency standards to define learning objectives for trainees at this stage of development.
To address the enormous educational needs in quality and safety for future physicians, a cadre of expert teachers in quality and safety will need to be developed. In collaboration with the Alliance for Academic Internal Medicine (AAIM), SHM is developing a Quality and Safety Educators Academy which will target academic hospitalists and other medical educators interested in developing advanced skills in quality improvement and patient safety education.
Assessment of Competence
An essential component of a rigorous faculty development program or medical education initiative is the assessment of whether these endeavors are achieving their stated aims. Published literature provides examples of useful assessment methods applicable to the HQPS Competencies. Knowledge in several areas of HQPS competence may be assessed with the use of multiple choice tests.34, 35 Knowledge of quality improvement methods may be assessed using the Quality Improvement Knowledge Application Tool (QIKAT), an instrument in which the learner responds to each of 3 scenarios with an aim, outcome and process measures, and ideas for changes which may result in improved performance.36 Teamwork and communication skills may be assessed using 360‐degree evaluations3739 and direct observation using behaviorally anchored rating scales.4043 Objective structured clinical examinations have been used to assess knowledge and skills related to patient safety principles.44, 45 Notably, few studies have rigorously assessed the validity and reliability of tools designed to evaluate competence related to healthcare quality.46 Additionally, to our knowledge, no prior research has evaluated assessment specifically for hospitalists. Thus, the development and validation of new assessment tools based on the HQPS Competencies for learners at each level is a crucial next step in the educational process. Additionally, evaluation of educational initiatives should include analyses of clinical benefit, as the ultimate goal of these efforts is to improve patient care.47, 48
Conclusion
Hospitalists are poised to have a tremendous impact on improving the quality of care for hospitalized patients. The lack of training in quality improvement in traditional medical education programs, in which most current hospitalists were trained, can be overcome through appropriate use of the HQPS Competencies. Formal incorporation of the HQPS Competencies into professional development programs, and innovative educational initiatives and curricula, will help provide current hospitalists and the next generations of hospitalists with the needed skills to be successful.
- Crossing the Quality Chasm: A New Health System for the Twenty‐first Century.Washington, DC:Institute of Medicine;2001.
- ,,,.Care in U.S. hospitals—the Hospital Quality Alliance program.N Engl J Med.2005;353(3):265–274.
- ,.Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization.JAMA.2003;290(14):1868–1874.
- Hospital Compare—A quality tool provided by Medicare. Available at: http://www.hospitalcompare.hhs.gov/. Accessed April 23,2010.
- The Leapfrog Group: Hospital Quality Ratings. Available at: http://www.leapfroggroup.org/cp. Accessed April 30,2010.
- Why Not the Best? A Healthcare Quality Improvement Resource. Available at: http://www.whynotthebest.org/. Accessed April 30,2010.
- The Joint Commission: Facts about ORYX for hospitals (National Hospital Quality Measures). Available at: http://www.jointcommission.org/accreditationprograms/hospitals/oryx/oryx_facts.htm. Accessed August 19,2010.
- The Joint Commission: National Patient Safety Goals. Available at: http://www.jointcommission.org/patientsafety/nationalpatientsafetygoals/. Accessed August 9,2010.
- Hospital Acquired Conditions: Overview. Available at: http://www.cms.gov/HospitalAcqCond/01_Overview.asp. Accessed April 30,2010.
- Report to Congress:Plan to Implement a Medicare Hospital Value‐based Purchasing Program. Washington, DC: US Department of Health and Human Services, Center for Medicare and Medicaid Services;2007.
- Unmet Needs: Teaching Physicians to Provide Safe Patient Care.Boston, MA:Lucian Leape Institute at the National Patient Safety Foundation;2010.
- ,,,,.Patient safety education at U.S. and Canadian medical schools: results from the 2006 Clerkship Directors in Internal Medicine survey.Acad Med.2009;84(12):1672–1676.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
- ,,,,.Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- ,,.Redesigning training for internal medicine.Ann Intern Med.2006;144(12):927–932.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- Intermountain Healthcare. 20‐Day Course for Executives 2001.
- ,,,.Curriculum Development for Medical Education: A Six‐step Approach.Baltimore, MD:Johns Hopkins Press;1998.
- Society of Hospital Medicine Quality Improvement Basics. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/QualityImprovement/QIPrimer/QI_Primer_Landing_Pa.htm. Accessed June 4,2010.
- American Board of Internal Medicine: Questions and Answers Regarding ABIM's Maintenance of Certification in Internal Medicine With a Focused Practice in Hospital Medicine Program. Available at: http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Accessed August 9,2010.
- ,,.Assessing the needs of residency program directors to meet the ACGME general competencies.Acad Med.2002;77(7):750.
- .Accreditation Council for Graduate Medical Education and Institute for Healthcare Improvement 90‐Day Project. Involving Residents in Quality Improvement: Contrasting “Top‐Down” and “Bottom‐Up” Approaches.Chicago, IL;ACGME;2008.
- ,,,.Teaching internal medicine residents quality improvement techniques using the ABIM's practice improvement modules.J Gen Intern Med.2008;23(7):927–930.
- ,,,,.A self‐instructional model to teach systems‐based practice and practice‐based learning and improvement.J Gen Intern Med.2008;23(7):931–936.
- ,,,,.Creating a quality improvement elective for medical house officers.J Gen Intern Med.2004;19(8):861–867.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119(1):72.e1‐e7.
- ,,,.Web‐based education in systems‐based practice: a randomized trial.Arch Intern Med.2007;167(4):361–366.
- ,,,,.A self‐instructional model to teach systems‐based practice and practice‐based learning and improvement.J Gen Intern Med.2008;23(7):931–936.
- ,,,.The quality improvement knowledge application tool: an instrument to assess knowledge application in practice‐based learning and improvement.J Gen Intern Med.2003;18(suppl 1):250.
- ,,, et al.Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial.Arch Pediatr Adolesc Med.2007;161(1):44–49.
- ,.Reliability of a 360‐degree evaluation to assess resident competence.Am J Phys Med Rehabil.2007;86(10):845–852.
- ,,,.Pilot study of a 360‐degree assessment instrument for physical medicine 82(5):394–402.
- ,,,,,.Anaesthetists' non‐technical skills (ANTS): evaluation of a behavioural marker system.Br J Anaesth.2003;90(5):580–588.
- ,,, et al.The Mayo high performance teamwork scale: reliability and validity for evaluating key crew resource management skills.Simul Healthc.2007;2(1):4–10.
- ,,,,,.Reliability of a revised NOTECHS scale for use in surgical teams.Am J Surg.2008;196(2):184–190.
- ,,,,,.Observational teamwork assessment for surgery: construct validation with expert versus novice raters.Ann Surg.2009;249(6):1047–1051.
- ,,,,,.A patient safety objective structured clinical examination.J Patient Saf.2009;5(2):55–60.
- ,.The Objective Structured Clinical Examination as an educational tool in patient safety.Jt Comm J Qual Patient Saf.2007;33(1):48–53.
- ,,.Measurement of the general competencies of the Accreditation Council for Graduate Medical Education: a systematic review.Acad Med.2009;84(3):301–309.
- ,,,,,.Effectiveness of teaching quality improvement to clinicians: a systematic review.JAMA.2007;298(9):1023–1037.
- ,,,,.Methodological rigor of quality improvement curricula for physician trainees: a systematic review and recommendations for change.Acad Med.2009;84(12):1677–1692.
- Crossing the Quality Chasm: A New Health System for the Twenty‐first Century.Washington, DC:Institute of Medicine;2001.
- ,,,.Care in U.S. hospitals—the Hospital Quality Alliance program.N Engl J Med.2005;353(3):265–274.
- ,.Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization.JAMA.2003;290(14):1868–1874.
- Hospital Compare—A quality tool provided by Medicare. Available at: http://www.hospitalcompare.hhs.gov/. Accessed April 23,2010.
- The Leapfrog Group: Hospital Quality Ratings. Available at: http://www.leapfroggroup.org/cp. Accessed April 30,2010.
- Why Not the Best? A Healthcare Quality Improvement Resource. Available at: http://www.whynotthebest.org/. Accessed April 30,2010.
- The Joint Commission: Facts about ORYX for hospitals (National Hospital Quality Measures). Available at: http://www.jointcommission.org/accreditationprograms/hospitals/oryx/oryx_facts.htm. Accessed August 19,2010.
- The Joint Commission: National Patient Safety Goals. Available at: http://www.jointcommission.org/patientsafety/nationalpatientsafetygoals/. Accessed August 9,2010.
- Hospital Acquired Conditions: Overview. Available at: http://www.cms.gov/HospitalAcqCond/01_Overview.asp. Accessed April 30,2010.
- Report to Congress:Plan to Implement a Medicare Hospital Value‐based Purchasing Program. Washington, DC: US Department of Health and Human Services, Center for Medicare and Medicaid Services;2007.
- Unmet Needs: Teaching Physicians to Provide Safe Patient Care.Boston, MA:Lucian Leape Institute at the National Patient Safety Foundation;2010.
- ,,,,.Patient safety education at U.S. and Canadian medical schools: results from the 2006 Clerkship Directors in Internal Medicine survey.Acad Med.2009;84(12):1672–1676.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
- ,,,,.Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- ,,.Redesigning training for internal medicine.Ann Intern Med.2006;144(12):927–932.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- Intermountain Healthcare. 20‐Day Course for Executives 2001.
- ,,,.Curriculum Development for Medical Education: A Six‐step Approach.Baltimore, MD:Johns Hopkins Press;1998.
- Society of Hospital Medicine Quality Improvement Basics. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/QualityImprovement/QIPrimer/QI_Primer_Landing_Pa.htm. Accessed June 4,2010.
- American Board of Internal Medicine: Questions and Answers Regarding ABIM's Maintenance of Certification in Internal Medicine With a Focused Practice in Hospital Medicine Program. Available at: http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Accessed August 9,2010.
- ,,.Assessing the needs of residency program directors to meet the ACGME general competencies.Acad Med.2002;77(7):750.
- .Accreditation Council for Graduate Medical Education and Institute for Healthcare Improvement 90‐Day Project. Involving Residents in Quality Improvement: Contrasting “Top‐Down” and “Bottom‐Up” Approaches.Chicago, IL;ACGME;2008.
- ,,,.Teaching internal medicine residents quality improvement techniques using the ABIM's practice improvement modules.J Gen Intern Med.2008;23(7):927–930.
- ,,,,.A self‐instructional model to teach systems‐based practice and practice‐based learning and improvement.J Gen Intern Med.2008;23(7):931–936.
- ,,,,.Creating a quality improvement elective for medical house officers.J Gen Intern Med.2004;19(8):861–867.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119(1):72.e1‐e7.
- ,,,.Web‐based education in systems‐based practice: a randomized trial.Arch Intern Med.2007;167(4):361–366.
- ,,,,.A self‐instructional model to teach systems‐based practice and practice‐based learning and improvement.J Gen Intern Med.2008;23(7):931–936.
- ,,,.The quality improvement knowledge application tool: an instrument to assess knowledge application in practice‐based learning and improvement.J Gen Intern Med.2003;18(suppl 1):250.
- ,,, et al.Effect of multisource feedback on resident communication skills and professionalism: a randomized controlled trial.Arch Pediatr Adolesc Med.2007;161(1):44–49.
- ,.Reliability of a 360‐degree evaluation to assess resident competence.Am J Phys Med Rehabil.2007;86(10):845–852.
- ,,,.Pilot study of a 360‐degree assessment instrument for physical medicine 82(5):394–402.
- ,,,,,.Anaesthetists' non‐technical skills (ANTS): evaluation of a behavioural marker system.Br J Anaesth.2003;90(5):580–588.
- ,,, et al.The Mayo high performance teamwork scale: reliability and validity for evaluating key crew resource management skills.Simul Healthc.2007;2(1):4–10.
- ,,,,,.Reliability of a revised NOTECHS scale for use in surgical teams.Am J Surg.2008;196(2):184–190.
- ,,,,,.Observational teamwork assessment for surgery: construct validation with expert versus novice raters.Ann Surg.2009;249(6):1047–1051.
- ,,,,,.A patient safety objective structured clinical examination.J Patient Saf.2009;5(2):55–60.
- ,.The Objective Structured Clinical Examination as an educational tool in patient safety.Jt Comm J Qual Patient Saf.2007;33(1):48–53.
- ,,.Measurement of the general competencies of the Accreditation Council for Graduate Medical Education: a systematic review.Acad Med.2009;84(3):301–309.
- ,,,,,.Effectiveness of teaching quality improvement to clinicians: a systematic review.JAMA.2007;298(9):1023–1037.
- ,,,,.Methodological rigor of quality improvement curricula for physician trainees: a systematic review and recommendations for change.Acad Med.2009;84(12):1677–1692.
Hospitalist Sedation Service
There is growing demand for safe and effective procedural sedation in pediatric facilities around the country. Multiple articles published in the last 10 years have addressed the shortage of pediatric anesthesiologists to meet this rising need.14 In 2005, Lalwani and Michel published results of a survey of North American children's hospitals that showed 87% of institutions reporting barriers to development of a pediatric sedation service, and that the most common barrier was shortage of anesthesiologists.5 In our hospital, the wait time for an outpatient sedated pediatric magnetic resonance imaging (MRI) grew to as long as 6 weeks. Many institutions have had to look for unique ways to solve this problem. Pediatric sedation programs have been developed which utilize intensivists, emergency medicine physicians, nurse anesthetists, or trained sedation nurses to provide safe pediatric sedation.611 Each of these programs has grown from the particular strengths and needs at each institution. In many institutions, hospitalists are the best candidates to meet this need because of their knowledge of patient needs and safety. They are accessible and receptive to obtaining additional training and, therefore, are a natural fit to provide this service.
As more non‐anesthesiologists are called upon to meet this growing need, the principles and practice of safe sedation must be followed. The Pediatric Sedation Research Consortium, a collaborative group of 37 locations that provide data on pediatric sedations, has published their findings on the safety of pediatric sedation/anesthesia outside of the operating room (OR) performed by anesthesiologists and non‐anesthesiologists.1213 This data has been very valuable, given that studies from single institutions will often lack the power to investigate the rare, but potentially devastating, adverse events which can occur in pediatric sedation/anesthesia.
Despite the widespread use of propofol by non‐anesthesiologists, the lack of substantial data regarding safety by these providers makes its use controversial. A search of the literature finds only 1 prior article that describes the use of propofol by general pediatricians. This was sedation for endoscopy, and the sedation was performed by specially trained pediatric residents in Italy.14 A recently published study from the Consortium regarding the use of propofol showed that the majority of propofol sedations were being performed by intensivists (49%), emergency medicine physicians (36%), or anesthesiologists (10%). General pediatricians or hospitalists performed just 2% of the cases in this series.13
In 2003, a large group of experienced pediatric hospitalists were already providing sedation in the Emergency Unit (EU) and Center for After‐hours Referrals for Emergency Services (CARES) at St Louis Children's Hospital. The Division of Hospital Medicine was approached to meet the demand for increased sedation services at our institution. The Division of Pediatric Anesthesia agreed to provide our physicians with the appropriate training to provide safe, effective, and efficient sedations for painful and non‐painful procedures outside of the OR. One of our sedation units, the Ambulatory Procedure Center (APC), has been described in detail in a prior publication by Strauser Sterni et al.15 Here, we will describe the operations of our sedation services, and specifically describe the training required for our hospitalists to provide sedation services.
METHODS
St Louis Children's Hospital is a 250‐bed tertiary‐care teaching hospital affiliated with Washington University School of Medicine. The Division of Hospitalist Medicine is today comprised of 43 physicians who provide care in the EU, CARES, inpatient units, Transport, and Sedation Services at St Louis Children's Hospital. Our division also provides pediatric care in the EU, inpatient units, newborn nursery, and labor and delivery at 3 affiliated hospitals. In 2003, we developed a dedicated program in our division to meet our institutional need for sedation, with training and oversight by the Division of Pediatric Anesthesia. We developed a structured 3‐tiered program of sedation providers to manage all of our sedation needs. We then designed a training program for these 3 tiers of sedation providers. The 3‐tired program is based on the level of sedation training of each member.
Current American Academy of Pediatrics (AAP) guidelines state:
The practitioner responsible for the treatment of the patient and/or the administration of drugs for sedation must be competent to use such techniques, provide the level of monitoring provided in these guidelines, and manage complications of these techniques (ie, to be able to rescue the patient). Because the level of intended sedation may be exceeded, the practitioner must be sufficiently skilled to provide rescue should the child progress to a level of deep sedation. The practitioner must be trained in, and capable of providing, at the minimum, bag‐valve‐mask ventilation to be able to oxygenate a child who develops airway obstruction or apnea. Training in, and maintenance of, advanced pediatric airway skills is required; regular skills reinforcement is strongly encouraged.16
Our first‐tier sedation providers are junior faculty who provide sedation in the EU and CARES, and in the EU at our community hospitals. The first tier completes sedation training as part of overall hospitalist orientation in order to provide this service. The second tier goes through an advanced sedation provider program to provide sedation in the APC, Pediatric Acute Wound Service (PAWS), inpatient units, and After Hours sedation call, as well as the locations from the first tier. The third tier completes a more complex advanced sedation training program, specifically using propofol, and provides propofol sedation in the APC only, as well as providing sedation in all of the units from the first and second tiers. The responsibilities of the hospitalist providing sedation are described in detail by tier below, including the specific training requirements necessary for each tier (Table 1).
|
| Tier One |
| Provides sedation services in the EU |
| Drugs: ketamine, nitrous oxide |
| Training consists of: |
| 1‐hr didactic hospitalist orientation |
| 4 days of shadowing a hospitalist on the sedation service |
| Continuing on‐the‐job training |
| Tier Two |
| Provides sedation throughout the hospital: EU, APC, PAWS, and night/weekend call for urgent needs |
| Drugs: ketamine, nitrous oxide, plus pentobarbital or dexmedetomidine for radiologic procedures for both inpatients and outpatients |
| Training consists of: |
| 1 yr of first tier experience |
| 2‐hr didactic session with anesthesia |
| 1‐hr advanced hospitalist sedation orientation |
| 5 days of operating room training with an anesthesiologist |
| Tier Three |
| Provides sedation throughout the hospital: EU, APC, PAWS, and night/weekend call |
| Drugs: ketamine, nitrous oxide, pentobarbital, dexmedetomidine, and propofol |
| Training consists of: |
| 1 yr of second tier experience |
| 3‐hr didactic lecture with anesthesia |
| 10 days of operating room training |
| 25 supervised propofol sedations |
| Maintenance of certification requires >75 propofol sedations every 2 yr |
Tier One
First‐tier hospitalist sedation providers perform sedation services in the EU and CARES. The staffing model in St Louis Children's Hospital EU is comprised of a pediatric emergency medicine‐trained attending or fellow and a pediatric hospitalist who both help to oversee care within the unit. The unit is also staffed by pediatric residents, emergency medicine residents, medical students, and nurse practitioners. One of the main responsibilities of the pediatric hospitalist, however, is sedation within the unit. In CARES, the pediatric hospitalist is the attending providing direct care to patients without trainees. Any procedure requiring sedation in CARES would be performed by the hospitalist. The hospitalist providing care in the EU at both of our community hospitals would also be the physician to perform procedural sedation within the unit. Procedural sedation in all of these units are primarily for fracture reduction, laceration repair, abscess incision and drainage, foreign body removal, lumbar puncture, joint aspiration, burn debridement, and radiology imaging. Sedations performed within these units are classified as moderate or deep sedation.16 Common medications used by Tier‐One sedation providers are intravenous ketamine, inhaled nitrous oxide in combination with oral oxycodone or oral/ intravenous midazolam, intravenous pentobarbital, and occasional intravenous fentanyl in combination with intravenous midazolam.
For a hospitalist to perform any pediatric sedation within the 4 hospitals in our program, the physician must be credentialed in accordance with the specific criteria of each institution. There are varied institutional policies across all hospitals nationally. At St Louis Children's Hospital, sedation credentialing criteria states that a sedation provider must review the specific institutional policies governing sedation and perform 25 supervised sedations, before any independent sedation is attempted. The type of procedure requiring sedation and the medications used for the sedation may vary among these 25 supervised sedations. Given the structure of our program, the majority of supervised sedations are for painful procedures utilizing ketamine or a combination of oxycodone and nitrous oxide.
Our division also requires the Tier‐One group to shadow at least 4 shifts with senior hospitalists in Tiers Two or Three providing sedation, in a unit where there is an average of 6 sedations performed per day. The Tier‐One sedation hospitalist must also attend a 1‐hour didactic orientation session where the principles and practice of sedation are taught. This didactic session provides the principles of pediatric sedation and defines the important skills necessary to provide safe sedation and recovery. In addition, hospitalists are trained to recognize which children can be safely sedated by a hospitalist, and manage common side effects and adverse events during and after sedation.
The Tier‐One hospitalist performing sedation in the EU/CARES is responsible for performing pre‐procedure sedation evaluation, developing a sedation plan, and delivering procedural sedation. A dedicated sedation‐trained nurse is available throughout the procedure to record vital signs, leaving the hospitalist free to monitor the patient directly, titrate sedation medications, and manage airway or adverse events as they arise. A separate provider is responsible for performing the actual procedure. The patient continues to be monitored by the sedation nurse during the recovery period, while the hospitalist remains immediately available in the unit to address any problems. At St Louis Children's Hospital, specific monitoring and documentation criteria, using standard forms and sedation scores, are strictly adhered to for every sedation, both during the sedation and throughout the recovery phase. These criteria are based upon the AAP guidelines for monitoring and management of pediatric sedation as described by Cot and Wilson.16 Hospital Medicine provides services in the EU 17 hours per day, 7 days a week. On average, 3 sedations are provided by the hospitalist per 8‐hour shift in the EU.
Tier Two
Second‐tier providers perform all services provided by Tier‐One providers, as well as expanded sedation services on the inpatient units, APC, and PAWS. Tier‐Two providers also provide on‐call services for urgent night, weekend, and holiday sedation needs.
APC and PAWS provide more specialized sedation care than that provided in the EU. PAWS is a separate and dedicated wound care unit housed on the surgical/post‐op floor where children are sedated for painful wound care, primarily burn debridement, abscess incision and drainage (I&D), and dressing changes. Sedation services are occasionally provided for other wound care issues or procedures. Both inpatients and outpatients are seen in this unit. The unit operates 10 hours per day, 7 days a week. The PAWS unit has 2 rooms specifically equipped for sedation, monitoring, and rescue, as well as 2 additional rooms for recovery or for patients not requiring sedation. Sedations in PAWS generally utilize intravenous ketamine or inhaled nitrous oxide coupled with premedication of oxycodone. Responsibilities of the hospitalist in the unit include completing and documenting the pre‐sedation evaluation, developing an appropriate sedation plan, delivering sedation medications, ongoing monitoring and documenting of vital signs throughout the case, and recovery of the patient. All nursing staff in this unit are sedation‐trained and are responsible for continued patient monitoring during the recovery period, until the patient has returned to baseline and is safe for discharge or transfer.
The APC has been described in a prior publication.15 Hospitalist sedations in the APC are performed primarily for radiology procedures, the majority of which are MRI but also include computed tomographic (CT) and nuclear medicine scans. Sedation is also provided for automated brainstem response (ABR), electromyogram (EMG), and peripherally inserted central catheter (PICC) placements. Like PAWS, APC serves both inpatients and outpatients. The APC is staffed 10 hours per day, 5 days per week. The primary sedation medications used in this unit are ketamine, dexmedetomidine, and occasionally fentanyl and midazolam. There are 11 patient beds, all equipped for patient monitoring and recovery. Hospitalists in the APC may provide direct patient care or supervise sedation‐trained nurses delivering sedation services after having a pre‐sedation evaluation performed by the hospitalist. If a sedation‐trained nurse is delivering sedation, the hospitalist may be doing other interruptible tasks, but is immediately available on the unit to respond to any concerns from the sedation nurse. All units are fully equipped with resuscitation equipment/crash carts, and an anesthesiologist is readily available to come to the unit from the OR in the event of an issue. A rapid response team that consists of a pediatric intensive care unit (ICU) fellow, respiratory therapist, and pediatric ICU charge nurse is also always on call.
Urgent sedations on the inpatient wards are common and can usually be accommodated in PAWS or APC. Rarely, however, an MRI, CT, joint aspiration, abscess drainage, or lumbar puncture must be completed urgently in the evenings, weekends, or holidays. In this situation, the hospitalist is responsible for performing the pre‐sedation evaluation, developing an appropriate sedation technique, delivering the sedation medications, monitoring and documenting during the procedure as well as throughout the recovery period, until the patient has returned to baseline. Sedation‐trained nursing staff are available to provide assistance. The sedation medications commonly used in these after‐hours sedations include ketamine for short or painful procedures and dexmedetomidine for longer radiology studies.
Training for second‐tier services consists of a minimum of 1 year of first‐tier sedation experience, a 2‐hour didactic lecture with Pediatric Anesthesia, a 1‐hour hospitalist orientation for advanced sedation providers, and 5 days of OR training with an anesthesiologist. Operating room training focuses on building skills in bag‐mask ventilation, intravenous (IV) placement, endotracheal intubation, and laryngeal mask airway (LMA) placement.
Tier Three
Third‐tier sedation providers have completed all of the training of a Tier‐Two provider and have had additional training to prepare them to deliver propofol for non‐painful procedures. Hospitalist‐delivered propofol sedation is provided exclusively in the APC for non‐painful procedures. The hospitalist is responsible for the pre‐sedation evaluation, induction and maintenance of sedation, and patient monitoring and documentation of vital signs. Monitoring for propofol sedation includes end‐tidal carbon dioxide monitoring in addition to electrocardiogram (EKG), respiratory rate (RR), pulse oximetry, and non‐invasive blood pressure (NIBP). A sedation‐trained nurse is present during induction and assists with patient positioning within the scanner. The nurse will then assume care of the patient at the completion of the procedure to continue patient monitoring during recovery.
Training for Tier‐Three providers consists of a 3‐hour didactic session with Anesthesia, 10 days of OR training, use of simulation scenarios, and a written exam. The hospitalist must then perform 25 supervised propofol sedations before being credentialed to provide propofol sedation independently. To maintain certification for Tier‐Three services, hospitalists must perform at least 75 propofol sedations every 2 years.
RESULTS
Utilizing this design and training method, we have developed a successful pediatric hospitalist sedation program. Based on fiscal year 2009 billing data, the Division of Hospital Medicine performed 2471 sedations. There were 2069 sedations performed in APC or PAWS; of those, 1017 were performed on inpatients and 1052 were performed on outpatients. Hospitalists performed 402 sedations on patients in the EU. The EU numbers are likely much larger given that, for over half the year, billing data was not collected from the EU. Unfortunately, we did not have billing data regarding night and weekend sedations, but our best estimate is 1 to 2 per week. The wait time for an outpatient sedated pediatric MRI has gone from 6 weeks to 2 days or less. As of July 2010, we have trained 90 providers at Tier One, 32 at Tier Two, and 11 at Tier Three. We currently have 43 hospitalists providing Tier‐One sedation, 18 providing Tier‐Two, and 6 providing Tier‐Three. Average cumulative hospitalist experience is 1 year for Tier One, 5 years for Tier Two, and 10 years for Tier Three.
DISCUSSION
We believe this is the first description of a pediatric hospitalist training program for a sedation service. However, it is clear that many other pediatric hospitalists are performing sedation and developing similar training programs. When starting a program such as this, there are many things to consider. First, patient volume/demand must allow for each hospitalist to perform sedations on a regular basis, both for training and Maintenance of Certification. Second, Anesthesia must be willing to provide training and oversight. Third, the hospital or university must be willing to support the cost associated with the training period. Finally, negotiating with third party payers for reimbursement is critical to financial sustainability.
The success of our program hinged upon the ability to develop a strong and collaborative relationship with Anesthesiology. Many factors played into making this relationship work. Initially, Anesthesia approached us to help them meet an unmet clinical need. Because of this, we were viewed as helpful and as problem solvers, rather than as a threat. Additionally, each division had a sedation service champion that pushed for the development of a hospitalist sedation service. Lastly, regular meetings with Anesthesia, and the intense training program itself, helped to develop a sense of collegiality between the divisions.
We have faced many challenges and learned many lessons while developing this program. There is a significant cost to training sedation providers; 47 hospitalists trained to provide Tier‐One sedation have left the program. Of those, 16 hospitalists completed training for Tier‐Two sedation, and 5 completed Tier Three. The Tier‐Two training described earlier requires approximately 50 hours of dedicated time away from other hospitalist duties, while Tier Three requires an additional 125 hours. The majority of our turnover occurred in the first few years of the program. From a financial perspective, we have had to reserve sedation training beyond Tier One to hospitalists who are able to demonstrate evidence of a long‐term commitment to our division. Every person providing Tier‐Three sedation has been with the division over 6 years. From a broader perspective, we are providing hospitalists with an important and useful skill that may enhance their careerssafe and effective sedation.
Balancing the volume of cases is another issue to consider. Our goal is to provide safe and timely sedation, therefore we need to have enough scheduled cases to maintain competency and financial viability, but we must also leave adequate flexibility in the schedule for urgent cases.
In addition to the operating room training, we are beginning to incorporate pediatric simulation as an adjunct to our training. We have designed simulation scenarios which address issues of obstruction, apnea, hypotension, bronchospasm, and aspiration. However, OR training remains a mandatory requirement for sedation training and, at times, can be challenging to schedule.
We complete a post‐sedation assessment on all patients; we are currently performing a chart review of over 1600 patients sedated with propofol, to look at the rate of planned and unplanned interventions. We believe this data will show that our training has been successful, and that with analysis of our Quality Improvement data, we can improve the safety and efficacy of our sedation program even further.
CONCLUSIONS
A pediatric hospitalist sedation service, with proper training and oversight, can successfully augment sedation services provided by anesthesiologists. As has been stated in prior publications, a defined system, and the use of a dedicated well‐trained team makes a sedation service a success.1719 A collegial and mutually respectful relationship between Anesthesia and non‐Anesthesia sedation providers is critical in developing and maintaining a successful sedation program.
- ,,,,.Anesthesia services outside of the operating room.Pediatr Nurs.2007;33(3):232,234,236–237.
- ,.Pediatric sedation/anesthesia outside the operating room.Curr Opin Anaesthesiol.2008;21(4):494–498.
- ,.Procedural sedation in the pediatric patient.Anesthesiol Clin North Am.2005;23(4):635–654, viii.
- .Pediatric sedation: can it be safely performed by non‐anesthesiologists?Curr Opin Anaesthesiol.2002;15(4):455–459.
- ,.Pediatric sedation in North American children's hospitals: a survey of anesthesia providers.Paediatr Anaesth.2005;15(3):209–213.
- ,,, et al.Safety of propofol sedation for pediatric outpatient procedures.Clin Pediatr (Phila).2009;48(8):819–823.
- ,,, et al.High dose dexmedetomidine as the sole sedative for pediatric MRI.Paediatr Anaesth.2008;18(5):403–411.
- ,.Successful implementation of a radiology sedation service staffed exclusively by pediatric emergency physicians.Pediatrics.2006;117(3):e413–e422.
- ,.Management of children undergoing painful procedures in the emergency department by non‐anesthesiologists.Isr Med Assoc J.2004;6(6):350–355.
- ,,,,.Development of a nurse‐led sedation service for paediatric magnetic resonance imaging.Lancet.1999;353(9165):1667–1671.
- ,,.Propofol sedation: intensivists' experience with 7304 cases in a children's hospital.Pediatrics.2007;120(6):e1411–e1417.
- .Risk and safety of pediatric sedation/anesthesia for procedures outside the operating room.Curr Opin Anaesthesiol.2009;22(4):509–513.
- ,,,,.The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: a report from the Pediatric Sedation Research Consortium.Anesth Analg.2009;108(3):795–804.
- ,,, et al.Deep sedation with propofol for upper gastrointestinal endoscopy in children, administered by specially trained pediatricians: a prospective case series with emphasis on side effects.Endoscopy.2006;38(4):368–375.
- ,,,,.A model for pediatric sedation centers using pharmacologic sedation for successful completion of radiologic and procedural studies.J Radiol Nurs2008;27(2):46–60.
- ,.Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: an update.Pediatrics.2006;118(6):2587–2602.
- ,.Non‐anesthesiologist‐provided pediatric procedural sedation: an update.Curr Opin Anaesthesiol.2007;20(4):365–372.
- ,,.Professional skills and competence for safe and effective procedural sedation in children: recommendations based on a systematic review of the literature.Int J Pediatr.2010; doi://10.1155/2010/934298.
- ,.Pediatric sedation outside the operating room: the year in review.Curr Opin Anaesthesiol.2005;18(4):442–446.
There is growing demand for safe and effective procedural sedation in pediatric facilities around the country. Multiple articles published in the last 10 years have addressed the shortage of pediatric anesthesiologists to meet this rising need.14 In 2005, Lalwani and Michel published results of a survey of North American children's hospitals that showed 87% of institutions reporting barriers to development of a pediatric sedation service, and that the most common barrier was shortage of anesthesiologists.5 In our hospital, the wait time for an outpatient sedated pediatric magnetic resonance imaging (MRI) grew to as long as 6 weeks. Many institutions have had to look for unique ways to solve this problem. Pediatric sedation programs have been developed which utilize intensivists, emergency medicine physicians, nurse anesthetists, or trained sedation nurses to provide safe pediatric sedation.611 Each of these programs has grown from the particular strengths and needs at each institution. In many institutions, hospitalists are the best candidates to meet this need because of their knowledge of patient needs and safety. They are accessible and receptive to obtaining additional training and, therefore, are a natural fit to provide this service.
As more non‐anesthesiologists are called upon to meet this growing need, the principles and practice of safe sedation must be followed. The Pediatric Sedation Research Consortium, a collaborative group of 37 locations that provide data on pediatric sedations, has published their findings on the safety of pediatric sedation/anesthesia outside of the operating room (OR) performed by anesthesiologists and non‐anesthesiologists.1213 This data has been very valuable, given that studies from single institutions will often lack the power to investigate the rare, but potentially devastating, adverse events which can occur in pediatric sedation/anesthesia.
Despite the widespread use of propofol by non‐anesthesiologists, the lack of substantial data regarding safety by these providers makes its use controversial. A search of the literature finds only 1 prior article that describes the use of propofol by general pediatricians. This was sedation for endoscopy, and the sedation was performed by specially trained pediatric residents in Italy.14 A recently published study from the Consortium regarding the use of propofol showed that the majority of propofol sedations were being performed by intensivists (49%), emergency medicine physicians (36%), or anesthesiologists (10%). General pediatricians or hospitalists performed just 2% of the cases in this series.13
In 2003, a large group of experienced pediatric hospitalists were already providing sedation in the Emergency Unit (EU) and Center for After‐hours Referrals for Emergency Services (CARES) at St Louis Children's Hospital. The Division of Hospital Medicine was approached to meet the demand for increased sedation services at our institution. The Division of Pediatric Anesthesia agreed to provide our physicians with the appropriate training to provide safe, effective, and efficient sedations for painful and non‐painful procedures outside of the OR. One of our sedation units, the Ambulatory Procedure Center (APC), has been described in detail in a prior publication by Strauser Sterni et al.15 Here, we will describe the operations of our sedation services, and specifically describe the training required for our hospitalists to provide sedation services.
METHODS
St Louis Children's Hospital is a 250‐bed tertiary‐care teaching hospital affiliated with Washington University School of Medicine. The Division of Hospitalist Medicine is today comprised of 43 physicians who provide care in the EU, CARES, inpatient units, Transport, and Sedation Services at St Louis Children's Hospital. Our division also provides pediatric care in the EU, inpatient units, newborn nursery, and labor and delivery at 3 affiliated hospitals. In 2003, we developed a dedicated program in our division to meet our institutional need for sedation, with training and oversight by the Division of Pediatric Anesthesia. We developed a structured 3‐tiered program of sedation providers to manage all of our sedation needs. We then designed a training program for these 3 tiers of sedation providers. The 3‐tired program is based on the level of sedation training of each member.
Current American Academy of Pediatrics (AAP) guidelines state:
The practitioner responsible for the treatment of the patient and/or the administration of drugs for sedation must be competent to use such techniques, provide the level of monitoring provided in these guidelines, and manage complications of these techniques (ie, to be able to rescue the patient). Because the level of intended sedation may be exceeded, the practitioner must be sufficiently skilled to provide rescue should the child progress to a level of deep sedation. The practitioner must be trained in, and capable of providing, at the minimum, bag‐valve‐mask ventilation to be able to oxygenate a child who develops airway obstruction or apnea. Training in, and maintenance of, advanced pediatric airway skills is required; regular skills reinforcement is strongly encouraged.16
Our first‐tier sedation providers are junior faculty who provide sedation in the EU and CARES, and in the EU at our community hospitals. The first tier completes sedation training as part of overall hospitalist orientation in order to provide this service. The second tier goes through an advanced sedation provider program to provide sedation in the APC, Pediatric Acute Wound Service (PAWS), inpatient units, and After Hours sedation call, as well as the locations from the first tier. The third tier completes a more complex advanced sedation training program, specifically using propofol, and provides propofol sedation in the APC only, as well as providing sedation in all of the units from the first and second tiers. The responsibilities of the hospitalist providing sedation are described in detail by tier below, including the specific training requirements necessary for each tier (Table 1).
|
| Tier One |
| Provides sedation services in the EU |
| Drugs: ketamine, nitrous oxide |
| Training consists of: |
| 1‐hr didactic hospitalist orientation |
| 4 days of shadowing a hospitalist on the sedation service |
| Continuing on‐the‐job training |
| Tier Two |
| Provides sedation throughout the hospital: EU, APC, PAWS, and night/weekend call for urgent needs |
| Drugs: ketamine, nitrous oxide, plus pentobarbital or dexmedetomidine for radiologic procedures for both inpatients and outpatients |
| Training consists of: |
| 1 yr of first tier experience |
| 2‐hr didactic session with anesthesia |
| 1‐hr advanced hospitalist sedation orientation |
| 5 days of operating room training with an anesthesiologist |
| Tier Three |
| Provides sedation throughout the hospital: EU, APC, PAWS, and night/weekend call |
| Drugs: ketamine, nitrous oxide, pentobarbital, dexmedetomidine, and propofol |
| Training consists of: |
| 1 yr of second tier experience |
| 3‐hr didactic lecture with anesthesia |
| 10 days of operating room training |
| 25 supervised propofol sedations |
| Maintenance of certification requires >75 propofol sedations every 2 yr |
Tier One
First‐tier hospitalist sedation providers perform sedation services in the EU and CARES. The staffing model in St Louis Children's Hospital EU is comprised of a pediatric emergency medicine‐trained attending or fellow and a pediatric hospitalist who both help to oversee care within the unit. The unit is also staffed by pediatric residents, emergency medicine residents, medical students, and nurse practitioners. One of the main responsibilities of the pediatric hospitalist, however, is sedation within the unit. In CARES, the pediatric hospitalist is the attending providing direct care to patients without trainees. Any procedure requiring sedation in CARES would be performed by the hospitalist. The hospitalist providing care in the EU at both of our community hospitals would also be the physician to perform procedural sedation within the unit. Procedural sedation in all of these units are primarily for fracture reduction, laceration repair, abscess incision and drainage, foreign body removal, lumbar puncture, joint aspiration, burn debridement, and radiology imaging. Sedations performed within these units are classified as moderate or deep sedation.16 Common medications used by Tier‐One sedation providers are intravenous ketamine, inhaled nitrous oxide in combination with oral oxycodone or oral/ intravenous midazolam, intravenous pentobarbital, and occasional intravenous fentanyl in combination with intravenous midazolam.
For a hospitalist to perform any pediatric sedation within the 4 hospitals in our program, the physician must be credentialed in accordance with the specific criteria of each institution. There are varied institutional policies across all hospitals nationally. At St Louis Children's Hospital, sedation credentialing criteria states that a sedation provider must review the specific institutional policies governing sedation and perform 25 supervised sedations, before any independent sedation is attempted. The type of procedure requiring sedation and the medications used for the sedation may vary among these 25 supervised sedations. Given the structure of our program, the majority of supervised sedations are for painful procedures utilizing ketamine or a combination of oxycodone and nitrous oxide.
Our division also requires the Tier‐One group to shadow at least 4 shifts with senior hospitalists in Tiers Two or Three providing sedation, in a unit where there is an average of 6 sedations performed per day. The Tier‐One sedation hospitalist must also attend a 1‐hour didactic orientation session where the principles and practice of sedation are taught. This didactic session provides the principles of pediatric sedation and defines the important skills necessary to provide safe sedation and recovery. In addition, hospitalists are trained to recognize which children can be safely sedated by a hospitalist, and manage common side effects and adverse events during and after sedation.
The Tier‐One hospitalist performing sedation in the EU/CARES is responsible for performing pre‐procedure sedation evaluation, developing a sedation plan, and delivering procedural sedation. A dedicated sedation‐trained nurse is available throughout the procedure to record vital signs, leaving the hospitalist free to monitor the patient directly, titrate sedation medications, and manage airway or adverse events as they arise. A separate provider is responsible for performing the actual procedure. The patient continues to be monitored by the sedation nurse during the recovery period, while the hospitalist remains immediately available in the unit to address any problems. At St Louis Children's Hospital, specific monitoring and documentation criteria, using standard forms and sedation scores, are strictly adhered to for every sedation, both during the sedation and throughout the recovery phase. These criteria are based upon the AAP guidelines for monitoring and management of pediatric sedation as described by Cot and Wilson.16 Hospital Medicine provides services in the EU 17 hours per day, 7 days a week. On average, 3 sedations are provided by the hospitalist per 8‐hour shift in the EU.
Tier Two
Second‐tier providers perform all services provided by Tier‐One providers, as well as expanded sedation services on the inpatient units, APC, and PAWS. Tier‐Two providers also provide on‐call services for urgent night, weekend, and holiday sedation needs.
APC and PAWS provide more specialized sedation care than that provided in the EU. PAWS is a separate and dedicated wound care unit housed on the surgical/post‐op floor where children are sedated for painful wound care, primarily burn debridement, abscess incision and drainage (I&D), and dressing changes. Sedation services are occasionally provided for other wound care issues or procedures. Both inpatients and outpatients are seen in this unit. The unit operates 10 hours per day, 7 days a week. The PAWS unit has 2 rooms specifically equipped for sedation, monitoring, and rescue, as well as 2 additional rooms for recovery or for patients not requiring sedation. Sedations in PAWS generally utilize intravenous ketamine or inhaled nitrous oxide coupled with premedication of oxycodone. Responsibilities of the hospitalist in the unit include completing and documenting the pre‐sedation evaluation, developing an appropriate sedation plan, delivering sedation medications, ongoing monitoring and documenting of vital signs throughout the case, and recovery of the patient. All nursing staff in this unit are sedation‐trained and are responsible for continued patient monitoring during the recovery period, until the patient has returned to baseline and is safe for discharge or transfer.
The APC has been described in a prior publication.15 Hospitalist sedations in the APC are performed primarily for radiology procedures, the majority of which are MRI but also include computed tomographic (CT) and nuclear medicine scans. Sedation is also provided for automated brainstem response (ABR), electromyogram (EMG), and peripherally inserted central catheter (PICC) placements. Like PAWS, APC serves both inpatients and outpatients. The APC is staffed 10 hours per day, 5 days per week. The primary sedation medications used in this unit are ketamine, dexmedetomidine, and occasionally fentanyl and midazolam. There are 11 patient beds, all equipped for patient monitoring and recovery. Hospitalists in the APC may provide direct patient care or supervise sedation‐trained nurses delivering sedation services after having a pre‐sedation evaluation performed by the hospitalist. If a sedation‐trained nurse is delivering sedation, the hospitalist may be doing other interruptible tasks, but is immediately available on the unit to respond to any concerns from the sedation nurse. All units are fully equipped with resuscitation equipment/crash carts, and an anesthesiologist is readily available to come to the unit from the OR in the event of an issue. A rapid response team that consists of a pediatric intensive care unit (ICU) fellow, respiratory therapist, and pediatric ICU charge nurse is also always on call.
Urgent sedations on the inpatient wards are common and can usually be accommodated in PAWS or APC. Rarely, however, an MRI, CT, joint aspiration, abscess drainage, or lumbar puncture must be completed urgently in the evenings, weekends, or holidays. In this situation, the hospitalist is responsible for performing the pre‐sedation evaluation, developing an appropriate sedation technique, delivering the sedation medications, monitoring and documenting during the procedure as well as throughout the recovery period, until the patient has returned to baseline. Sedation‐trained nursing staff are available to provide assistance. The sedation medications commonly used in these after‐hours sedations include ketamine for short or painful procedures and dexmedetomidine for longer radiology studies.
Training for second‐tier services consists of a minimum of 1 year of first‐tier sedation experience, a 2‐hour didactic lecture with Pediatric Anesthesia, a 1‐hour hospitalist orientation for advanced sedation providers, and 5 days of OR training with an anesthesiologist. Operating room training focuses on building skills in bag‐mask ventilation, intravenous (IV) placement, endotracheal intubation, and laryngeal mask airway (LMA) placement.
Tier Three
Third‐tier sedation providers have completed all of the training of a Tier‐Two provider and have had additional training to prepare them to deliver propofol for non‐painful procedures. Hospitalist‐delivered propofol sedation is provided exclusively in the APC for non‐painful procedures. The hospitalist is responsible for the pre‐sedation evaluation, induction and maintenance of sedation, and patient monitoring and documentation of vital signs. Monitoring for propofol sedation includes end‐tidal carbon dioxide monitoring in addition to electrocardiogram (EKG), respiratory rate (RR), pulse oximetry, and non‐invasive blood pressure (NIBP). A sedation‐trained nurse is present during induction and assists with patient positioning within the scanner. The nurse will then assume care of the patient at the completion of the procedure to continue patient monitoring during recovery.
Training for Tier‐Three providers consists of a 3‐hour didactic session with Anesthesia, 10 days of OR training, use of simulation scenarios, and a written exam. The hospitalist must then perform 25 supervised propofol sedations before being credentialed to provide propofol sedation independently. To maintain certification for Tier‐Three services, hospitalists must perform at least 75 propofol sedations every 2 years.
RESULTS
Utilizing this design and training method, we have developed a successful pediatric hospitalist sedation program. Based on fiscal year 2009 billing data, the Division of Hospital Medicine performed 2471 sedations. There were 2069 sedations performed in APC or PAWS; of those, 1017 were performed on inpatients and 1052 were performed on outpatients. Hospitalists performed 402 sedations on patients in the EU. The EU numbers are likely much larger given that, for over half the year, billing data was not collected from the EU. Unfortunately, we did not have billing data regarding night and weekend sedations, but our best estimate is 1 to 2 per week. The wait time for an outpatient sedated pediatric MRI has gone from 6 weeks to 2 days or less. As of July 2010, we have trained 90 providers at Tier One, 32 at Tier Two, and 11 at Tier Three. We currently have 43 hospitalists providing Tier‐One sedation, 18 providing Tier‐Two, and 6 providing Tier‐Three. Average cumulative hospitalist experience is 1 year for Tier One, 5 years for Tier Two, and 10 years for Tier Three.
DISCUSSION
We believe this is the first description of a pediatric hospitalist training program for a sedation service. However, it is clear that many other pediatric hospitalists are performing sedation and developing similar training programs. When starting a program such as this, there are many things to consider. First, patient volume/demand must allow for each hospitalist to perform sedations on a regular basis, both for training and Maintenance of Certification. Second, Anesthesia must be willing to provide training and oversight. Third, the hospital or university must be willing to support the cost associated with the training period. Finally, negotiating with third party payers for reimbursement is critical to financial sustainability.
The success of our program hinged upon the ability to develop a strong and collaborative relationship with Anesthesiology. Many factors played into making this relationship work. Initially, Anesthesia approached us to help them meet an unmet clinical need. Because of this, we were viewed as helpful and as problem solvers, rather than as a threat. Additionally, each division had a sedation service champion that pushed for the development of a hospitalist sedation service. Lastly, regular meetings with Anesthesia, and the intense training program itself, helped to develop a sense of collegiality between the divisions.
We have faced many challenges and learned many lessons while developing this program. There is a significant cost to training sedation providers; 47 hospitalists trained to provide Tier‐One sedation have left the program. Of those, 16 hospitalists completed training for Tier‐Two sedation, and 5 completed Tier Three. The Tier‐Two training described earlier requires approximately 50 hours of dedicated time away from other hospitalist duties, while Tier Three requires an additional 125 hours. The majority of our turnover occurred in the first few years of the program. From a financial perspective, we have had to reserve sedation training beyond Tier One to hospitalists who are able to demonstrate evidence of a long‐term commitment to our division. Every person providing Tier‐Three sedation has been with the division over 6 years. From a broader perspective, we are providing hospitalists with an important and useful skill that may enhance their careerssafe and effective sedation.
Balancing the volume of cases is another issue to consider. Our goal is to provide safe and timely sedation, therefore we need to have enough scheduled cases to maintain competency and financial viability, but we must also leave adequate flexibility in the schedule for urgent cases.
In addition to the operating room training, we are beginning to incorporate pediatric simulation as an adjunct to our training. We have designed simulation scenarios which address issues of obstruction, apnea, hypotension, bronchospasm, and aspiration. However, OR training remains a mandatory requirement for sedation training and, at times, can be challenging to schedule.
We complete a post‐sedation assessment on all patients; we are currently performing a chart review of over 1600 patients sedated with propofol, to look at the rate of planned and unplanned interventions. We believe this data will show that our training has been successful, and that with analysis of our Quality Improvement data, we can improve the safety and efficacy of our sedation program even further.
CONCLUSIONS
A pediatric hospitalist sedation service, with proper training and oversight, can successfully augment sedation services provided by anesthesiologists. As has been stated in prior publications, a defined system, and the use of a dedicated well‐trained team makes a sedation service a success.1719 A collegial and mutually respectful relationship between Anesthesia and non‐Anesthesia sedation providers is critical in developing and maintaining a successful sedation program.
There is growing demand for safe and effective procedural sedation in pediatric facilities around the country. Multiple articles published in the last 10 years have addressed the shortage of pediatric anesthesiologists to meet this rising need.14 In 2005, Lalwani and Michel published results of a survey of North American children's hospitals that showed 87% of institutions reporting barriers to development of a pediatric sedation service, and that the most common barrier was shortage of anesthesiologists.5 In our hospital, the wait time for an outpatient sedated pediatric magnetic resonance imaging (MRI) grew to as long as 6 weeks. Many institutions have had to look for unique ways to solve this problem. Pediatric sedation programs have been developed which utilize intensivists, emergency medicine physicians, nurse anesthetists, or trained sedation nurses to provide safe pediatric sedation.611 Each of these programs has grown from the particular strengths and needs at each institution. In many institutions, hospitalists are the best candidates to meet this need because of their knowledge of patient needs and safety. They are accessible and receptive to obtaining additional training and, therefore, are a natural fit to provide this service.
As more non‐anesthesiologists are called upon to meet this growing need, the principles and practice of safe sedation must be followed. The Pediatric Sedation Research Consortium, a collaborative group of 37 locations that provide data on pediatric sedations, has published their findings on the safety of pediatric sedation/anesthesia outside of the operating room (OR) performed by anesthesiologists and non‐anesthesiologists.1213 This data has been very valuable, given that studies from single institutions will often lack the power to investigate the rare, but potentially devastating, adverse events which can occur in pediatric sedation/anesthesia.
Despite the widespread use of propofol by non‐anesthesiologists, the lack of substantial data regarding safety by these providers makes its use controversial. A search of the literature finds only 1 prior article that describes the use of propofol by general pediatricians. This was sedation for endoscopy, and the sedation was performed by specially trained pediatric residents in Italy.14 A recently published study from the Consortium regarding the use of propofol showed that the majority of propofol sedations were being performed by intensivists (49%), emergency medicine physicians (36%), or anesthesiologists (10%). General pediatricians or hospitalists performed just 2% of the cases in this series.13
In 2003, a large group of experienced pediatric hospitalists were already providing sedation in the Emergency Unit (EU) and Center for After‐hours Referrals for Emergency Services (CARES) at St Louis Children's Hospital. The Division of Hospital Medicine was approached to meet the demand for increased sedation services at our institution. The Division of Pediatric Anesthesia agreed to provide our physicians with the appropriate training to provide safe, effective, and efficient sedations for painful and non‐painful procedures outside of the OR. One of our sedation units, the Ambulatory Procedure Center (APC), has been described in detail in a prior publication by Strauser Sterni et al.15 Here, we will describe the operations of our sedation services, and specifically describe the training required for our hospitalists to provide sedation services.
METHODS
St Louis Children's Hospital is a 250‐bed tertiary‐care teaching hospital affiliated with Washington University School of Medicine. The Division of Hospitalist Medicine is today comprised of 43 physicians who provide care in the EU, CARES, inpatient units, Transport, and Sedation Services at St Louis Children's Hospital. Our division also provides pediatric care in the EU, inpatient units, newborn nursery, and labor and delivery at 3 affiliated hospitals. In 2003, we developed a dedicated program in our division to meet our institutional need for sedation, with training and oversight by the Division of Pediatric Anesthesia. We developed a structured 3‐tiered program of sedation providers to manage all of our sedation needs. We then designed a training program for these 3 tiers of sedation providers. The 3‐tired program is based on the level of sedation training of each member.
Current American Academy of Pediatrics (AAP) guidelines state:
The practitioner responsible for the treatment of the patient and/or the administration of drugs for sedation must be competent to use such techniques, provide the level of monitoring provided in these guidelines, and manage complications of these techniques (ie, to be able to rescue the patient). Because the level of intended sedation may be exceeded, the practitioner must be sufficiently skilled to provide rescue should the child progress to a level of deep sedation. The practitioner must be trained in, and capable of providing, at the minimum, bag‐valve‐mask ventilation to be able to oxygenate a child who develops airway obstruction or apnea. Training in, and maintenance of, advanced pediatric airway skills is required; regular skills reinforcement is strongly encouraged.16
Our first‐tier sedation providers are junior faculty who provide sedation in the EU and CARES, and in the EU at our community hospitals. The first tier completes sedation training as part of overall hospitalist orientation in order to provide this service. The second tier goes through an advanced sedation provider program to provide sedation in the APC, Pediatric Acute Wound Service (PAWS), inpatient units, and After Hours sedation call, as well as the locations from the first tier. The third tier completes a more complex advanced sedation training program, specifically using propofol, and provides propofol sedation in the APC only, as well as providing sedation in all of the units from the first and second tiers. The responsibilities of the hospitalist providing sedation are described in detail by tier below, including the specific training requirements necessary for each tier (Table 1).
|
| Tier One |
| Provides sedation services in the EU |
| Drugs: ketamine, nitrous oxide |
| Training consists of: |
| 1‐hr didactic hospitalist orientation |
| 4 days of shadowing a hospitalist on the sedation service |
| Continuing on‐the‐job training |
| Tier Two |
| Provides sedation throughout the hospital: EU, APC, PAWS, and night/weekend call for urgent needs |
| Drugs: ketamine, nitrous oxide, plus pentobarbital or dexmedetomidine for radiologic procedures for both inpatients and outpatients |
| Training consists of: |
| 1 yr of first tier experience |
| 2‐hr didactic session with anesthesia |
| 1‐hr advanced hospitalist sedation orientation |
| 5 days of operating room training with an anesthesiologist |
| Tier Three |
| Provides sedation throughout the hospital: EU, APC, PAWS, and night/weekend call |
| Drugs: ketamine, nitrous oxide, pentobarbital, dexmedetomidine, and propofol |
| Training consists of: |
| 1 yr of second tier experience |
| 3‐hr didactic lecture with anesthesia |
| 10 days of operating room training |
| 25 supervised propofol sedations |
| Maintenance of certification requires >75 propofol sedations every 2 yr |
Tier One
First‐tier hospitalist sedation providers perform sedation services in the EU and CARES. The staffing model in St Louis Children's Hospital EU is comprised of a pediatric emergency medicine‐trained attending or fellow and a pediatric hospitalist who both help to oversee care within the unit. The unit is also staffed by pediatric residents, emergency medicine residents, medical students, and nurse practitioners. One of the main responsibilities of the pediatric hospitalist, however, is sedation within the unit. In CARES, the pediatric hospitalist is the attending providing direct care to patients without trainees. Any procedure requiring sedation in CARES would be performed by the hospitalist. The hospitalist providing care in the EU at both of our community hospitals would also be the physician to perform procedural sedation within the unit. Procedural sedation in all of these units are primarily for fracture reduction, laceration repair, abscess incision and drainage, foreign body removal, lumbar puncture, joint aspiration, burn debridement, and radiology imaging. Sedations performed within these units are classified as moderate or deep sedation.16 Common medications used by Tier‐One sedation providers are intravenous ketamine, inhaled nitrous oxide in combination with oral oxycodone or oral/ intravenous midazolam, intravenous pentobarbital, and occasional intravenous fentanyl in combination with intravenous midazolam.
For a hospitalist to perform any pediatric sedation within the 4 hospitals in our program, the physician must be credentialed in accordance with the specific criteria of each institution. There are varied institutional policies across all hospitals nationally. At St Louis Children's Hospital, sedation credentialing criteria states that a sedation provider must review the specific institutional policies governing sedation and perform 25 supervised sedations, before any independent sedation is attempted. The type of procedure requiring sedation and the medications used for the sedation may vary among these 25 supervised sedations. Given the structure of our program, the majority of supervised sedations are for painful procedures utilizing ketamine or a combination of oxycodone and nitrous oxide.
Our division also requires the Tier‐One group to shadow at least 4 shifts with senior hospitalists in Tiers Two or Three providing sedation, in a unit where there is an average of 6 sedations performed per day. The Tier‐One sedation hospitalist must also attend a 1‐hour didactic orientation session where the principles and practice of sedation are taught. This didactic session provides the principles of pediatric sedation and defines the important skills necessary to provide safe sedation and recovery. In addition, hospitalists are trained to recognize which children can be safely sedated by a hospitalist, and manage common side effects and adverse events during and after sedation.
The Tier‐One hospitalist performing sedation in the EU/CARES is responsible for performing pre‐procedure sedation evaluation, developing a sedation plan, and delivering procedural sedation. A dedicated sedation‐trained nurse is available throughout the procedure to record vital signs, leaving the hospitalist free to monitor the patient directly, titrate sedation medications, and manage airway or adverse events as they arise. A separate provider is responsible for performing the actual procedure. The patient continues to be monitored by the sedation nurse during the recovery period, while the hospitalist remains immediately available in the unit to address any problems. At St Louis Children's Hospital, specific monitoring and documentation criteria, using standard forms and sedation scores, are strictly adhered to for every sedation, both during the sedation and throughout the recovery phase. These criteria are based upon the AAP guidelines for monitoring and management of pediatric sedation as described by Cot and Wilson.16 Hospital Medicine provides services in the EU 17 hours per day, 7 days a week. On average, 3 sedations are provided by the hospitalist per 8‐hour shift in the EU.
Tier Two
Second‐tier providers perform all services provided by Tier‐One providers, as well as expanded sedation services on the inpatient units, APC, and PAWS. Tier‐Two providers also provide on‐call services for urgent night, weekend, and holiday sedation needs.
APC and PAWS provide more specialized sedation care than that provided in the EU. PAWS is a separate and dedicated wound care unit housed on the surgical/post‐op floor where children are sedated for painful wound care, primarily burn debridement, abscess incision and drainage (I&D), and dressing changes. Sedation services are occasionally provided for other wound care issues or procedures. Both inpatients and outpatients are seen in this unit. The unit operates 10 hours per day, 7 days a week. The PAWS unit has 2 rooms specifically equipped for sedation, monitoring, and rescue, as well as 2 additional rooms for recovery or for patients not requiring sedation. Sedations in PAWS generally utilize intravenous ketamine or inhaled nitrous oxide coupled with premedication of oxycodone. Responsibilities of the hospitalist in the unit include completing and documenting the pre‐sedation evaluation, developing an appropriate sedation plan, delivering sedation medications, ongoing monitoring and documenting of vital signs throughout the case, and recovery of the patient. All nursing staff in this unit are sedation‐trained and are responsible for continued patient monitoring during the recovery period, until the patient has returned to baseline and is safe for discharge or transfer.
The APC has been described in a prior publication.15 Hospitalist sedations in the APC are performed primarily for radiology procedures, the majority of which are MRI but also include computed tomographic (CT) and nuclear medicine scans. Sedation is also provided for automated brainstem response (ABR), electromyogram (EMG), and peripherally inserted central catheter (PICC) placements. Like PAWS, APC serves both inpatients and outpatients. The APC is staffed 10 hours per day, 5 days per week. The primary sedation medications used in this unit are ketamine, dexmedetomidine, and occasionally fentanyl and midazolam. There are 11 patient beds, all equipped for patient monitoring and recovery. Hospitalists in the APC may provide direct patient care or supervise sedation‐trained nurses delivering sedation services after having a pre‐sedation evaluation performed by the hospitalist. If a sedation‐trained nurse is delivering sedation, the hospitalist may be doing other interruptible tasks, but is immediately available on the unit to respond to any concerns from the sedation nurse. All units are fully equipped with resuscitation equipment/crash carts, and an anesthesiologist is readily available to come to the unit from the OR in the event of an issue. A rapid response team that consists of a pediatric intensive care unit (ICU) fellow, respiratory therapist, and pediatric ICU charge nurse is also always on call.
Urgent sedations on the inpatient wards are common and can usually be accommodated in PAWS or APC. Rarely, however, an MRI, CT, joint aspiration, abscess drainage, or lumbar puncture must be completed urgently in the evenings, weekends, or holidays. In this situation, the hospitalist is responsible for performing the pre‐sedation evaluation, developing an appropriate sedation technique, delivering the sedation medications, monitoring and documenting during the procedure as well as throughout the recovery period, until the patient has returned to baseline. Sedation‐trained nursing staff are available to provide assistance. The sedation medications commonly used in these after‐hours sedations include ketamine for short or painful procedures and dexmedetomidine for longer radiology studies.
Training for second‐tier services consists of a minimum of 1 year of first‐tier sedation experience, a 2‐hour didactic lecture with Pediatric Anesthesia, a 1‐hour hospitalist orientation for advanced sedation providers, and 5 days of OR training with an anesthesiologist. Operating room training focuses on building skills in bag‐mask ventilation, intravenous (IV) placement, endotracheal intubation, and laryngeal mask airway (LMA) placement.
Tier Three
Third‐tier sedation providers have completed all of the training of a Tier‐Two provider and have had additional training to prepare them to deliver propofol for non‐painful procedures. Hospitalist‐delivered propofol sedation is provided exclusively in the APC for non‐painful procedures. The hospitalist is responsible for the pre‐sedation evaluation, induction and maintenance of sedation, and patient monitoring and documentation of vital signs. Monitoring for propofol sedation includes end‐tidal carbon dioxide monitoring in addition to electrocardiogram (EKG), respiratory rate (RR), pulse oximetry, and non‐invasive blood pressure (NIBP). A sedation‐trained nurse is present during induction and assists with patient positioning within the scanner. The nurse will then assume care of the patient at the completion of the procedure to continue patient monitoring during recovery.
Training for Tier‐Three providers consists of a 3‐hour didactic session with Anesthesia, 10 days of OR training, use of simulation scenarios, and a written exam. The hospitalist must then perform 25 supervised propofol sedations before being credentialed to provide propofol sedation independently. To maintain certification for Tier‐Three services, hospitalists must perform at least 75 propofol sedations every 2 years.
RESULTS
Utilizing this design and training method, we have developed a successful pediatric hospitalist sedation program. Based on fiscal year 2009 billing data, the Division of Hospital Medicine performed 2471 sedations. There were 2069 sedations performed in APC or PAWS; of those, 1017 were performed on inpatients and 1052 were performed on outpatients. Hospitalists performed 402 sedations on patients in the EU. The EU numbers are likely much larger given that, for over half the year, billing data was not collected from the EU. Unfortunately, we did not have billing data regarding night and weekend sedations, but our best estimate is 1 to 2 per week. The wait time for an outpatient sedated pediatric MRI has gone from 6 weeks to 2 days or less. As of July 2010, we have trained 90 providers at Tier One, 32 at Tier Two, and 11 at Tier Three. We currently have 43 hospitalists providing Tier‐One sedation, 18 providing Tier‐Two, and 6 providing Tier‐Three. Average cumulative hospitalist experience is 1 year for Tier One, 5 years for Tier Two, and 10 years for Tier Three.
DISCUSSION
We believe this is the first description of a pediatric hospitalist training program for a sedation service. However, it is clear that many other pediatric hospitalists are performing sedation and developing similar training programs. When starting a program such as this, there are many things to consider. First, patient volume/demand must allow for each hospitalist to perform sedations on a regular basis, both for training and Maintenance of Certification. Second, Anesthesia must be willing to provide training and oversight. Third, the hospital or university must be willing to support the cost associated with the training period. Finally, negotiating with third party payers for reimbursement is critical to financial sustainability.
The success of our program hinged upon the ability to develop a strong and collaborative relationship with Anesthesiology. Many factors played into making this relationship work. Initially, Anesthesia approached us to help them meet an unmet clinical need. Because of this, we were viewed as helpful and as problem solvers, rather than as a threat. Additionally, each division had a sedation service champion that pushed for the development of a hospitalist sedation service. Lastly, regular meetings with Anesthesia, and the intense training program itself, helped to develop a sense of collegiality between the divisions.
We have faced many challenges and learned many lessons while developing this program. There is a significant cost to training sedation providers; 47 hospitalists trained to provide Tier‐One sedation have left the program. Of those, 16 hospitalists completed training for Tier‐Two sedation, and 5 completed Tier Three. The Tier‐Two training described earlier requires approximately 50 hours of dedicated time away from other hospitalist duties, while Tier Three requires an additional 125 hours. The majority of our turnover occurred in the first few years of the program. From a financial perspective, we have had to reserve sedation training beyond Tier One to hospitalists who are able to demonstrate evidence of a long‐term commitment to our division. Every person providing Tier‐Three sedation has been with the division over 6 years. From a broader perspective, we are providing hospitalists with an important and useful skill that may enhance their careerssafe and effective sedation.
Balancing the volume of cases is another issue to consider. Our goal is to provide safe and timely sedation, therefore we need to have enough scheduled cases to maintain competency and financial viability, but we must also leave adequate flexibility in the schedule for urgent cases.
In addition to the operating room training, we are beginning to incorporate pediatric simulation as an adjunct to our training. We have designed simulation scenarios which address issues of obstruction, apnea, hypotension, bronchospasm, and aspiration. However, OR training remains a mandatory requirement for sedation training and, at times, can be challenging to schedule.
We complete a post‐sedation assessment on all patients; we are currently performing a chart review of over 1600 patients sedated with propofol, to look at the rate of planned and unplanned interventions. We believe this data will show that our training has been successful, and that with analysis of our Quality Improvement data, we can improve the safety and efficacy of our sedation program even further.
CONCLUSIONS
A pediatric hospitalist sedation service, with proper training and oversight, can successfully augment sedation services provided by anesthesiologists. As has been stated in prior publications, a defined system, and the use of a dedicated well‐trained team makes a sedation service a success.1719 A collegial and mutually respectful relationship between Anesthesia and non‐Anesthesia sedation providers is critical in developing and maintaining a successful sedation program.
- ,,,,.Anesthesia services outside of the operating room.Pediatr Nurs.2007;33(3):232,234,236–237.
- ,.Pediatric sedation/anesthesia outside the operating room.Curr Opin Anaesthesiol.2008;21(4):494–498.
- ,.Procedural sedation in the pediatric patient.Anesthesiol Clin North Am.2005;23(4):635–654, viii.
- .Pediatric sedation: can it be safely performed by non‐anesthesiologists?Curr Opin Anaesthesiol.2002;15(4):455–459.
- ,.Pediatric sedation in North American children's hospitals: a survey of anesthesia providers.Paediatr Anaesth.2005;15(3):209–213.
- ,,, et al.Safety of propofol sedation for pediatric outpatient procedures.Clin Pediatr (Phila).2009;48(8):819–823.
- ,,, et al.High dose dexmedetomidine as the sole sedative for pediatric MRI.Paediatr Anaesth.2008;18(5):403–411.
- ,.Successful implementation of a radiology sedation service staffed exclusively by pediatric emergency physicians.Pediatrics.2006;117(3):e413–e422.
- ,.Management of children undergoing painful procedures in the emergency department by non‐anesthesiologists.Isr Med Assoc J.2004;6(6):350–355.
- ,,,,.Development of a nurse‐led sedation service for paediatric magnetic resonance imaging.Lancet.1999;353(9165):1667–1671.
- ,,.Propofol sedation: intensivists' experience with 7304 cases in a children's hospital.Pediatrics.2007;120(6):e1411–e1417.
- .Risk and safety of pediatric sedation/anesthesia for procedures outside the operating room.Curr Opin Anaesthesiol.2009;22(4):509–513.
- ,,,,.The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: a report from the Pediatric Sedation Research Consortium.Anesth Analg.2009;108(3):795–804.
- ,,, et al.Deep sedation with propofol for upper gastrointestinal endoscopy in children, administered by specially trained pediatricians: a prospective case series with emphasis on side effects.Endoscopy.2006;38(4):368–375.
- ,,,,.A model for pediatric sedation centers using pharmacologic sedation for successful completion of radiologic and procedural studies.J Radiol Nurs2008;27(2):46–60.
- ,.Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: an update.Pediatrics.2006;118(6):2587–2602.
- ,.Non‐anesthesiologist‐provided pediatric procedural sedation: an update.Curr Opin Anaesthesiol.2007;20(4):365–372.
- ,,.Professional skills and competence for safe and effective procedural sedation in children: recommendations based on a systematic review of the literature.Int J Pediatr.2010; doi://10.1155/2010/934298.
- ,.Pediatric sedation outside the operating room: the year in review.Curr Opin Anaesthesiol.2005;18(4):442–446.
- ,,,,.Anesthesia services outside of the operating room.Pediatr Nurs.2007;33(3):232,234,236–237.
- ,.Pediatric sedation/anesthesia outside the operating room.Curr Opin Anaesthesiol.2008;21(4):494–498.
- ,.Procedural sedation in the pediatric patient.Anesthesiol Clin North Am.2005;23(4):635–654, viii.
- .Pediatric sedation: can it be safely performed by non‐anesthesiologists?Curr Opin Anaesthesiol.2002;15(4):455–459.
- ,.Pediatric sedation in North American children's hospitals: a survey of anesthesia providers.Paediatr Anaesth.2005;15(3):209–213.
- ,,, et al.Safety of propofol sedation for pediatric outpatient procedures.Clin Pediatr (Phila).2009;48(8):819–823.
- ,,, et al.High dose dexmedetomidine as the sole sedative for pediatric MRI.Paediatr Anaesth.2008;18(5):403–411.
- ,.Successful implementation of a radiology sedation service staffed exclusively by pediatric emergency physicians.Pediatrics.2006;117(3):e413–e422.
- ,.Management of children undergoing painful procedures in the emergency department by non‐anesthesiologists.Isr Med Assoc J.2004;6(6):350–355.
- ,,,,.Development of a nurse‐led sedation service for paediatric magnetic resonance imaging.Lancet.1999;353(9165):1667–1671.
- ,,.Propofol sedation: intensivists' experience with 7304 cases in a children's hospital.Pediatrics.2007;120(6):e1411–e1417.
- .Risk and safety of pediatric sedation/anesthesia for procedures outside the operating room.Curr Opin Anaesthesiol.2009;22(4):509–513.
- ,,,,.The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: a report from the Pediatric Sedation Research Consortium.Anesth Analg.2009;108(3):795–804.
- ,,, et al.Deep sedation with propofol for upper gastrointestinal endoscopy in children, administered by specially trained pediatricians: a prospective case series with emphasis on side effects.Endoscopy.2006;38(4):368–375.
- ,,,,.A model for pediatric sedation centers using pharmacologic sedation for successful completion of radiologic and procedural studies.J Radiol Nurs2008;27(2):46–60.
- ,.Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: an update.Pediatrics.2006;118(6):2587–2602.
- ,.Non‐anesthesiologist‐provided pediatric procedural sedation: an update.Curr Opin Anaesthesiol.2007;20(4):365–372.
- ,,.Professional skills and competence for safe and effective procedural sedation in children: recommendations based on a systematic review of the literature.Int J Pediatr.2010; doi://10.1155/2010/934298.
- ,.Pediatric sedation outside the operating room: the year in review.Curr Opin Anaesthesiol.2005;18(4):442–446.
Incident Database
Recognition that healthcare carries considerable risks of patient injury has focused efforts on identifying problems before they occur, and understanding the root causes of those problems that do occur to prevent them from happening again.1 To further these efforts, a Joint Commission (JC) standard requires hospitals to review sentinel events (SE).2 Reviews must develop a timely, thorough, and credible root cause analysis (RCA), implement action plans to reduce risk, and monitor the effectiveness of implemented improvements.3
Ideally, hospitals would summarize their experiences with SE reviews, identify high‐risk activities and patients, institute system changes to prevent SE recurrences, and share their findings with other healthcare organizations to help them avoid similar patient injuries.1 In support of this last goal, the JC maintains a voluntary database system that allows hospitals to report their SE analyses for other facilities to review and institute preventative actions.
Unfortunately, the reality of SE reviews does not match their ideals for improving patient safety.4 Healthcare organizations often describe their review process as less than credible and note a need for ongoing oversight to maintain the reviews' effectiveness.5 The JC voluntary reporting system captures less than 1% of the SEs that occur nationally,2 because hospitals perceive barriers to external reporting.1 If healthcare organizations decide against reporting externally, they can create their own internal systems to aggregate and summarize SEs, but few such systems exist. A major impediment to designing internal systems is the absence of universally endorsed nomenclature for safety‐related events.6, 7 Poorly aligned terminology and subjective conceptualizations for safety incidents impede the aggregation of SEs, comparisons between facilities, and trend analyses for tracking SE patterns.
In 2005, the World Health Organization (WHO) World Alliance for Patient Safety, in collaboration with the JC, began developing an International Classification for Patient Safety (ICPS) to provide healthcare organizations a consistent conceptual model for safety incidents and promote their classification by a standardized taxonomy.810 Although this system has promise for allowing standardization, data aggregation, analysis, and learning between institutions,11 integration of the ICPS conceptual model into an SE decision support tool with summarizing and reporting features has not been reported.
This report describes our development of an intranet‐based SE reporting system, called Incident Tracker (I‐Tracker), based on the ICPS model. For our SE review groups from the 4 Providence Health Systems (PHS) Portland Service Area (PSA) hospitals, the I‐Tracker system offers a tool to guide efforts in developing RCAs and action plans in alignment with the ICPS framework. The system includes scripts that automatically generate and distribute standardized reports of individual and aggregated SEs. The objectives of this project were to report our experience with developing a flexible and accessible intranet‐based system that assists RCA participants in conforming to the ICPS framework and oversight safety staff in summarizing and reporting root cause analyses.
METHODS
The 4 PSA hospitals have 1083 licensed beds and perform SE reviews with a centralized process that reports results to a Community Governing Board. An ad hoc team for each SE performs the RCAs. The SE groups report RCAs and action plans in an unstructured format that varies for each event. A paper file is maintained for each SE report, but a system for aggregating reports to track trends, disseminating SE trends, or monitoring the completion or effectiveness of action plans is not available.
We designed a system to achieve the following objectives:
-
Apply the ICPS framework (Figure 1) and taxonomy of terms to SE analyses;
-
Provide a computer‐based tool to assist review groups and quality staff to perform their SE reviews and data collection in alignment with the ICPS framework;
-
Create an intranet‐based database that captures elements of the reviews, RCAs, and action plans with the use of drop‐down lists, help windows, windows with live access to Internet educational resources and tools, decision support tools, default entries, and audio prompts to streamline data entry;
-
Generate a suite of standardized reports customized for different audiences that can be accessed online and printed from the database with automated scripts;
-
Produce intranet‐based summaries of aggregated events to identify common causes and disseminate observed patterns and action plans to other PSA hospitals.
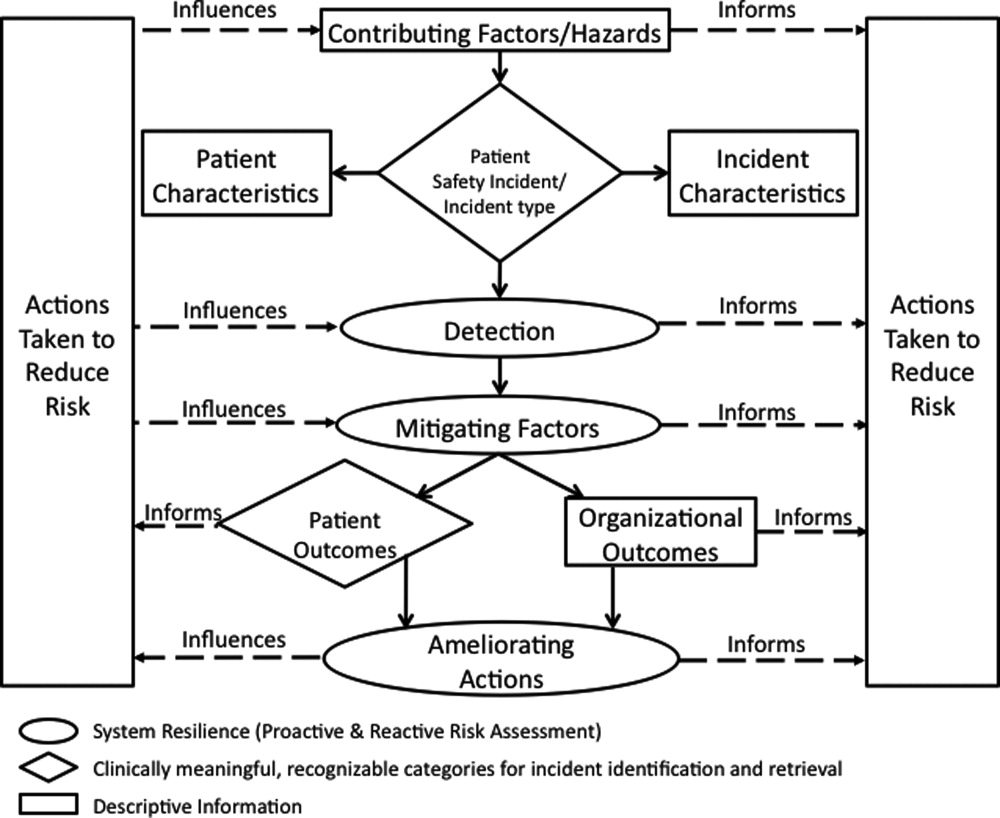
We selected FileMaker Pro 11 Advanced (FMP11) for authoring and maintaining the decision support tool and database, and FileMaker Pro Server 11 Advanced (FMPS11) (Filemaker, Inc, Santa Clara, CA) for hosting the system, because it provides intranet access and tools for updating the system by personnel with minimal programming experience. End users can view and enter data through layouts that display only the information allowed by the user's login password and access privileges, with external authentication by Active Directory and Open Directory technology. Staff who author and manage the database do so through client FMP11 software loaded on a computer that provides remote server access.
The I‐Tracker system was authored using the ICPS definitions for the 48 preferred terms for safety incidents and the ICPS conceptual framework.8 The conceptual framework consists of 10 major incident domains, that include incident type, patient outcomes, patient characteristics, incident characteristics, contributing factors and hazards, organizational outcomes, detection, mitigating factors, ameliorating actions, and actions taken to reduce risk (Figure 1).11 The framework is applicable to all hospital safety incidents, but we limited I‐Tracker to SEs because our hospitals had completed comprehensive reviews and action plans only for these more serious events. The literature on the ICPS framework812 was carefully reviewed to identify the specific data fields that were recommended by ICPS developers to be included under each of the 10 major classification domains. In most instances, data fields existed only in the body of these reports. Article texts, however, provided sufficient descriptions of these data fields to allow their translation into data entry fields in I‐Tracker with accompanying help windows and explanations to guide I‐Tracker users. Sixty ICPS data fields were programmed into I‐Tracker, with another 120 fields that allowed entry of descriptions and explanations of the ICPS data field entries. For instance, an entry of Yes into an ICPS data field that queried Was there a systems problem of an external organization other than a Providence entity opens a Describe field that allows a brief description of the problem, and an additional Details field that allows a longer explanation of the problem if necessary. The brief Describe field contents populate an automatically generated fishbone diagram.
The authors and quality staff translated the most recent 15 SE reviews into ICPS terms and classifications, and entered the results into I‐Tracker as it was being developed, to assist system design and programming of the system. The authors noted during data entry which of the 10 ICPS major domains had not been analyzed by the previous 15 reviews. Because existing reports were unstructured with considerable variation in style and usage of terms, the authors and quality staff made group decisions regarding how to cross‐walk existing information into the standardized ICPS data fields.
RESULTS
In developing I‐Tracker, the authors and quality staff observed that the ICPS framework and recommended data fields were logical and straightforward to learn. Although it was difficult to find the definitions of specific ICPS data fields within the 10 major domains in the text of retrieved articles, these fields could be readily cross‐walked into I‐Tracker data entry fields. Translating existing SE reports into I‐Tracker classifications, however, presented considerable challenges because of the unstructured, discursive, and variable nature of our SE review and reports. The authors and staff spent 1 to 2 hours conferring over each report to make judgments as to which elements of the review would be entered into which I‐Tracker data fields. Once the authors and staff translated existing reports into ICPS terms, actual data entry into I‐Tracker took typically less than 30 minutes for each review. We found that none of our 15 SE reviews included information on the following ICPS major domains: detection, mitigating factors, and ameliorating actions. We also observed that many ICPS data fields were not assessed, such as patient contributions to errors and external organization's contributions to a safety incident.
The latest version of I‐Tracker receives and displays information at the individual patient level. Records are shown onscreen with different screen layouts depending on the viewer's login security clearance. Hospital safety staff have full access to view and enter data on the initial layout, which displays patient demographic information and folder tabs that navigate when clicked to other database fields (Figure 2). Viewers with lower security clearance either view the same opening screen, but have limited access to other screens, or view a different opening screen designed to meet their specific needs. All screens provide definitions of terms and information to assist data entry, buttons that navigate to help pages, pop‐up windows that provide tips, and buttons that trigger brief audio explanations. Most fields use drop‐down lists to standardize data entry around the ICPS definitions, with default values entered into many fields to streamline data entry. A list view allows review of all patients and quick access to an individual patient's record. All fields and combinations of fields with Boolean rules are searchable within the database.
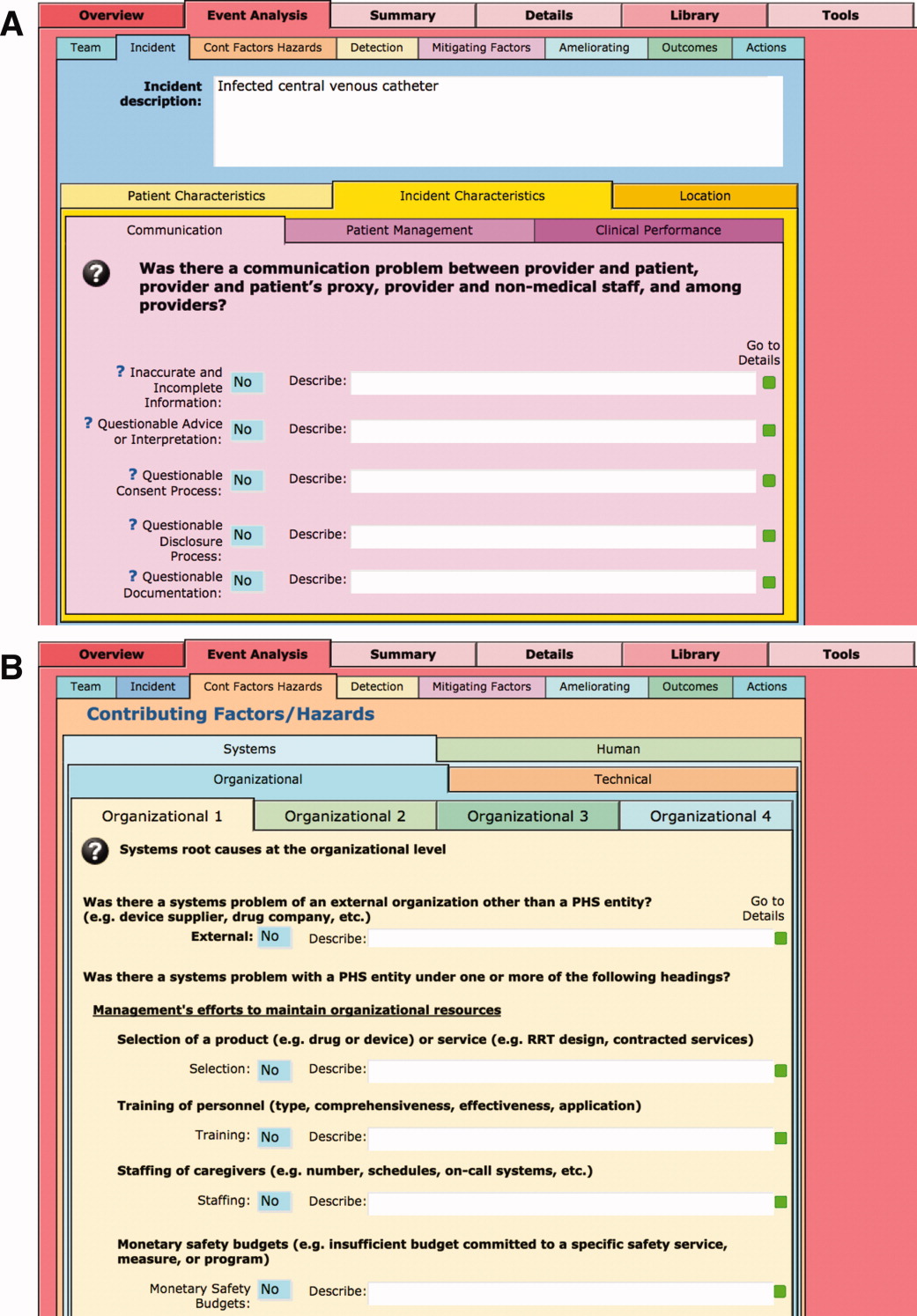
I‐Tracker has features that support SE review groups in beginning an SE review by providing them a paper form or electronic interface by way of a portable computer or tablet device, that guides their discussions and analyses toward providing conclusions that can be entered into the database fields, thereby aligning their deliberations with the ICPS conceptual framework. The same resource is available within the database online for those groups who would prefer to use computer prompts and enter data directly into the database as they proceed through their analyses. Some layouts contain windows that port live views from external Web sites (eg, JC RCA resources) that provide participants of RCA groups with tools to assist their work. FMP11 allows users to access the database by portable computers or handheld tablet devices using the hospitals' WiFi network.
A report screen allows automatic generation of different printouts of individual or aggregate summary reports. A Comprehensive Report includes all of the data fields included in the ICPS conceptual framework. Other reports present subsets of data depending on the user's needs and access privileges. The FMPS11 database allows printing the reports to paper or Portable Document Format (pdf), exporting data into an Excel spreadsheet, or e‐mailing reports to recipients from within I‐Tracker.
Additionally, I‐Tracker functionality facilitates follow‐up and monitoring of action items developed during the RCA process in a manner that conforms to the ICPS framework. We are now developing educational resources for RCA team members to investigate the implementation of I‐Tracker into future RCAs.
DISCUSSION
I‐Tracker provides an intranet‐based tool that met the objectives of the present project. The process of entering 15 existing SE reviews and action plans from our healthcare system into I‐Tracker allowed an incremental development of the database and identified gaps in our existing RCA process. For instance, none of the previous RCAs critically appraised detection, mitigating factors, or ameliorating actions; defined the specific nature or quantified severity of patient injuries using standardized terms; distinguished between human errors and negligence; or comprehensively reported the full spectrum of underlying causes of Tracker's use of standardized terms based on the ICPS conceptual framework provided a potential resource for focusing SE reviews and producing more comprehensive RCAs and action plans in the future. I‐Tracker has additional potential to facilitate dissemination of RCAs to other facilities, both as individual incident reports and aggregated summaries as recommended by experts in patient safety.13
The deficiencies in our existing RCA analyses, identified during data entry into I‐Tracker, represent common shortcomings experienced by other healthcare organizations and summarized in a report by the Agency for Healthcare Research and Quality.4 Considerable hindsight bias and prevailing concerns of the day taint the RCA process, which is time‐consuming and labor intensive, and thereby hinders comprehensive reviews. Also, our SE reviews, like others reviewed in the literature,14 focused on biologic injury to patients and omitted assessment of psychologic, organizational, social, and economic injury domains. Although SE review teams benefit from involvement of quality improvement staff who are trained in techniques and goals of RCA,15 many hospitals like ours have limited resources for fully staffing all SE reviews with trained facilitators. These SE reviews generate both quantitative and qualitative data, the latter of which hinders standardized data entry in the absence of a conceptual framework. A structured database with formative tools to guide RCAs in conformance with the ICPS framework in organizations without sufficient numbers of trained facilitators offers opportunities to produce more comprehensive, standardized, and actionable reports. To date, our quality staff and leadership have responded positively to presentations of the functional features of I‐Tracker (Table 1).
|
| Online availability of the system that allows access both from client database software loaded on Quality Office computers and through intranet browser software (Explorer, Safari, Firefox, etc) |
| Security features of encrypted software that allow full or limited views depending on the user's password security clearance and purpose for reviewing data |
| Software accessibility in authoring and managing the database, which do not require support from information technology data analysts |
| Decision support tools provided in the system to assist RCA analysis |
| System flexibility that allows scripted reporting of single SEs or multiple SE summaries within any selected timeframe |
Limitations of our report include its focus solely on the development and programming phase of I‐Tracker and the absence of information on its actual implementation. We believe, however, the development phase is important to report because it demonstrates that the ICPS framework and specific ICPS data fields are amenable to incorporation into a decision support and reporting tool, which to our knowledge has not been previously reported. We begin implementation of I‐Tracker within our organization this year and will have observations on its feasibility, acceptability, and staff training needs. As an additional limitation, we emphasize that we do not propose I‐Tracker as a solution for other organizations, because we have no plans for its commercial or public domain development. This report is intended to demonstrate, however, that commercially available software, such as FileMaker, can readily support the ICPS Framework and thereby has potential to assist RCAs and SE reporting. Other organizations may develop similar systems on other database platforms that incorporate the ICPS system into their reviews.
To implement I‐Tracker, we are now working with nursing and pharmacy leadership focus groups to develop formative tools, data collection forms, and other resources to assist their RCA efforts and data entry into the database. We also plan to apply the database tool to our residency training program to promote resident involvement in SE reviews by providing standardized, reproducible, and structured processes.16 Our 5‐state healthcare system has funded an evaluation of the implementation phase of I‐Tracker to other Providence facilities. Because the ICPS framework applies to all safety incidents beyond SEs (Table 2), a successful implementation of I‐Tracker for SEs will allow its eventual application to other types of critical incidents.
|
| Clinical administration |
| Clinical process/procedure |
| Documentation |
| Healthcare‐associated infection |
| Medication/IV fluids |
| Blood/blood products |
| Nutrition |
| Oxygen/gas/vapor |
| Medical device/equipment |
| Behavior |
| Patient accidents |
| Infrastructure/building/fixtures |
| Resources/organizational management |
The strength of this project derives from its innovative development of an intranet‐based tool that allows groups to conform their RCAs to the ICPS framework. Because the absence of a standardized classification for patient safety concepts has hindered advances in patient safety,11 we believe I‐Tracker, or decision support tools like it that use the ICPS framework, can standardize RCAs and promote dissemination and adoption of action plans.
Acknowledgements
We appreciate the support of Judy Stenstrom, Lynette Savage, and the Portland Service Area Quality Improvement Office.
- .Reporting of adverse events.N Engl J Med.2002;347:1633–1638.
- The Joint Commission's Sentinel Event Policy: ten years of improving the quality and safety of health care.Jt Comm Perspect.2005;25(1):3–5.
- ,.Root cause analysis and nursing management responsibilities in wrong‐site surgery.Dimens Crit Care Nurs.2006;25,221–225.
- ,.Root Cause Analysis.Making Health Care Safer. Available at: http://archive.ahrq.gov/clinic/ptsafety/chap5.htm. Accessed May 21,2010.
- Oversight group holds RCA teams accountable.Healthcare Benchmarks Qual Improv.2008;15:117–118.
- .Shared meanings: preferred terms and definitions for safety and quality concepts.Med J Aust.2006;184:S41–S43.
- ,,.What do family physicians consider an error? A comparison of definitions and physician perception.BMC Fam Pract.2006;7:73.
- ,,,,,.Towards an International Classification for Patient Safety: key concepts and terms.Int J Qual Health Care.2009;21:18–26.
- ,,,,.The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events.Int J Qual Health Care.2005;17:95–105.
- World Health Organization. 2009 Conceptual Framework for the International Classification for Patient Safety. Final Technical Report Version 1.1. Available at: http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf. Accessed April 25,2011.
- ,,, et al.Towards an International Classification for Patient Safety: the conceptual framework.Int J Qual Health Care.2009;21:2–8.
- ,,,,,.Towards an International Classification for Patient Safety: a Delphi survey.Int J Qual Health Care.2009;21:9–17.
- ,,.Effectiveness and efficiency of root cause analysis in medicine.JAMA.2008;299:685–687.
- ,,,,.How can clinicians measure safety and quality in acute care?Lancet.2004;363:1061–1067.
- ,,,,.Systematic root cause analysis of adverse drug events in a tertiary referral hospital.Jt Comm J Qual Improv.2000;26:563–575.
- ,,,,,.Educational quality improvement report: outcomes from a revised morbidity and mortality format that emphasised patient safety.Postgrad Med J.2008;84:211–216.
Recognition that healthcare carries considerable risks of patient injury has focused efforts on identifying problems before they occur, and understanding the root causes of those problems that do occur to prevent them from happening again.1 To further these efforts, a Joint Commission (JC) standard requires hospitals to review sentinel events (SE).2 Reviews must develop a timely, thorough, and credible root cause analysis (RCA), implement action plans to reduce risk, and monitor the effectiveness of implemented improvements.3
Ideally, hospitals would summarize their experiences with SE reviews, identify high‐risk activities and patients, institute system changes to prevent SE recurrences, and share their findings with other healthcare organizations to help them avoid similar patient injuries.1 In support of this last goal, the JC maintains a voluntary database system that allows hospitals to report their SE analyses for other facilities to review and institute preventative actions.
Unfortunately, the reality of SE reviews does not match their ideals for improving patient safety.4 Healthcare organizations often describe their review process as less than credible and note a need for ongoing oversight to maintain the reviews' effectiveness.5 The JC voluntary reporting system captures less than 1% of the SEs that occur nationally,2 because hospitals perceive barriers to external reporting.1 If healthcare organizations decide against reporting externally, they can create their own internal systems to aggregate and summarize SEs, but few such systems exist. A major impediment to designing internal systems is the absence of universally endorsed nomenclature for safety‐related events.6, 7 Poorly aligned terminology and subjective conceptualizations for safety incidents impede the aggregation of SEs, comparisons between facilities, and trend analyses for tracking SE patterns.
In 2005, the World Health Organization (WHO) World Alliance for Patient Safety, in collaboration with the JC, began developing an International Classification for Patient Safety (ICPS) to provide healthcare organizations a consistent conceptual model for safety incidents and promote their classification by a standardized taxonomy.810 Although this system has promise for allowing standardization, data aggregation, analysis, and learning between institutions,11 integration of the ICPS conceptual model into an SE decision support tool with summarizing and reporting features has not been reported.
This report describes our development of an intranet‐based SE reporting system, called Incident Tracker (I‐Tracker), based on the ICPS model. For our SE review groups from the 4 Providence Health Systems (PHS) Portland Service Area (PSA) hospitals, the I‐Tracker system offers a tool to guide efforts in developing RCAs and action plans in alignment with the ICPS framework. The system includes scripts that automatically generate and distribute standardized reports of individual and aggregated SEs. The objectives of this project were to report our experience with developing a flexible and accessible intranet‐based system that assists RCA participants in conforming to the ICPS framework and oversight safety staff in summarizing and reporting root cause analyses.
METHODS
The 4 PSA hospitals have 1083 licensed beds and perform SE reviews with a centralized process that reports results to a Community Governing Board. An ad hoc team for each SE performs the RCAs. The SE groups report RCAs and action plans in an unstructured format that varies for each event. A paper file is maintained for each SE report, but a system for aggregating reports to track trends, disseminating SE trends, or monitoring the completion or effectiveness of action plans is not available.
We designed a system to achieve the following objectives:
-
Apply the ICPS framework (Figure 1) and taxonomy of terms to SE analyses;
-
Provide a computer‐based tool to assist review groups and quality staff to perform their SE reviews and data collection in alignment with the ICPS framework;
-
Create an intranet‐based database that captures elements of the reviews, RCAs, and action plans with the use of drop‐down lists, help windows, windows with live access to Internet educational resources and tools, decision support tools, default entries, and audio prompts to streamline data entry;
-
Generate a suite of standardized reports customized for different audiences that can be accessed online and printed from the database with automated scripts;
-
Produce intranet‐based summaries of aggregated events to identify common causes and disseminate observed patterns and action plans to other PSA hospitals.
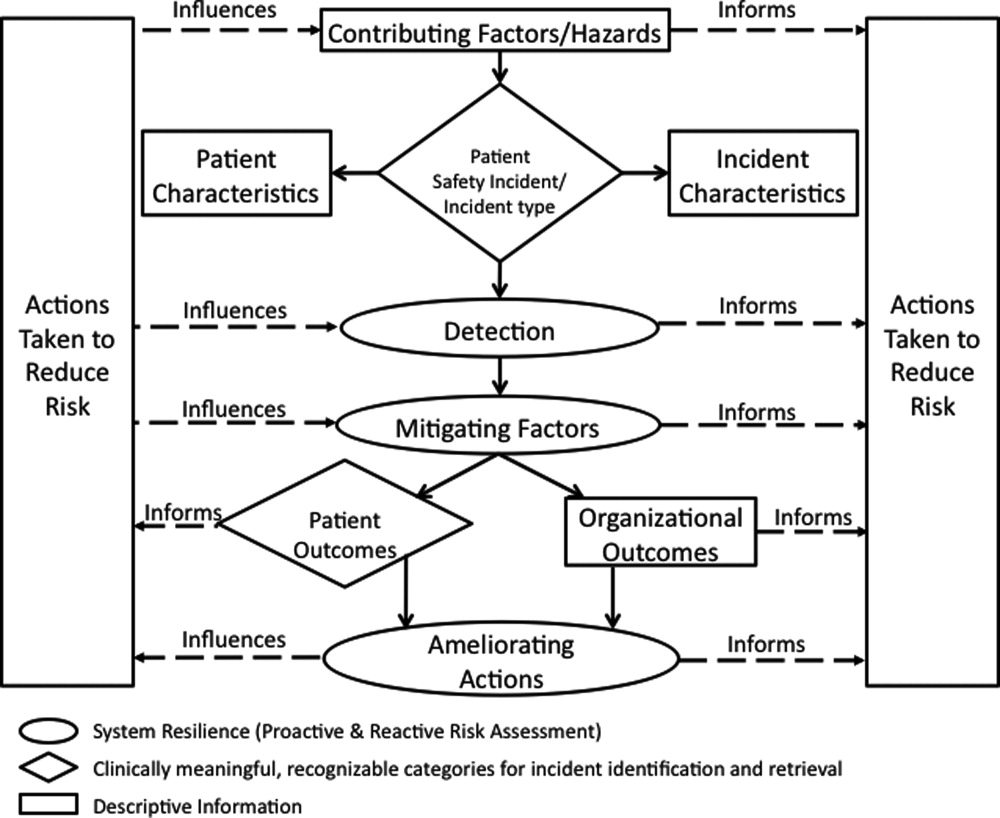
We selected FileMaker Pro 11 Advanced (FMP11) for authoring and maintaining the decision support tool and database, and FileMaker Pro Server 11 Advanced (FMPS11) (Filemaker, Inc, Santa Clara, CA) for hosting the system, because it provides intranet access and tools for updating the system by personnel with minimal programming experience. End users can view and enter data through layouts that display only the information allowed by the user's login password and access privileges, with external authentication by Active Directory and Open Directory technology. Staff who author and manage the database do so through client FMP11 software loaded on a computer that provides remote server access.
The I‐Tracker system was authored using the ICPS definitions for the 48 preferred terms for safety incidents and the ICPS conceptual framework.8 The conceptual framework consists of 10 major incident domains, that include incident type, patient outcomes, patient characteristics, incident characteristics, contributing factors and hazards, organizational outcomes, detection, mitigating factors, ameliorating actions, and actions taken to reduce risk (Figure 1).11 The framework is applicable to all hospital safety incidents, but we limited I‐Tracker to SEs because our hospitals had completed comprehensive reviews and action plans only for these more serious events. The literature on the ICPS framework812 was carefully reviewed to identify the specific data fields that were recommended by ICPS developers to be included under each of the 10 major classification domains. In most instances, data fields existed only in the body of these reports. Article texts, however, provided sufficient descriptions of these data fields to allow their translation into data entry fields in I‐Tracker with accompanying help windows and explanations to guide I‐Tracker users. Sixty ICPS data fields were programmed into I‐Tracker, with another 120 fields that allowed entry of descriptions and explanations of the ICPS data field entries. For instance, an entry of Yes into an ICPS data field that queried Was there a systems problem of an external organization other than a Providence entity opens a Describe field that allows a brief description of the problem, and an additional Details field that allows a longer explanation of the problem if necessary. The brief Describe field contents populate an automatically generated fishbone diagram.
The authors and quality staff translated the most recent 15 SE reviews into ICPS terms and classifications, and entered the results into I‐Tracker as it was being developed, to assist system design and programming of the system. The authors noted during data entry which of the 10 ICPS major domains had not been analyzed by the previous 15 reviews. Because existing reports were unstructured with considerable variation in style and usage of terms, the authors and quality staff made group decisions regarding how to cross‐walk existing information into the standardized ICPS data fields.
RESULTS
In developing I‐Tracker, the authors and quality staff observed that the ICPS framework and recommended data fields were logical and straightforward to learn. Although it was difficult to find the definitions of specific ICPS data fields within the 10 major domains in the text of retrieved articles, these fields could be readily cross‐walked into I‐Tracker data entry fields. Translating existing SE reports into I‐Tracker classifications, however, presented considerable challenges because of the unstructured, discursive, and variable nature of our SE review and reports. The authors and staff spent 1 to 2 hours conferring over each report to make judgments as to which elements of the review would be entered into which I‐Tracker data fields. Once the authors and staff translated existing reports into ICPS terms, actual data entry into I‐Tracker took typically less than 30 minutes for each review. We found that none of our 15 SE reviews included information on the following ICPS major domains: detection, mitigating factors, and ameliorating actions. We also observed that many ICPS data fields were not assessed, such as patient contributions to errors and external organization's contributions to a safety incident.
The latest version of I‐Tracker receives and displays information at the individual patient level. Records are shown onscreen with different screen layouts depending on the viewer's login security clearance. Hospital safety staff have full access to view and enter data on the initial layout, which displays patient demographic information and folder tabs that navigate when clicked to other database fields (Figure 2). Viewers with lower security clearance either view the same opening screen, but have limited access to other screens, or view a different opening screen designed to meet their specific needs. All screens provide definitions of terms and information to assist data entry, buttons that navigate to help pages, pop‐up windows that provide tips, and buttons that trigger brief audio explanations. Most fields use drop‐down lists to standardize data entry around the ICPS definitions, with default values entered into many fields to streamline data entry. A list view allows review of all patients and quick access to an individual patient's record. All fields and combinations of fields with Boolean rules are searchable within the database.
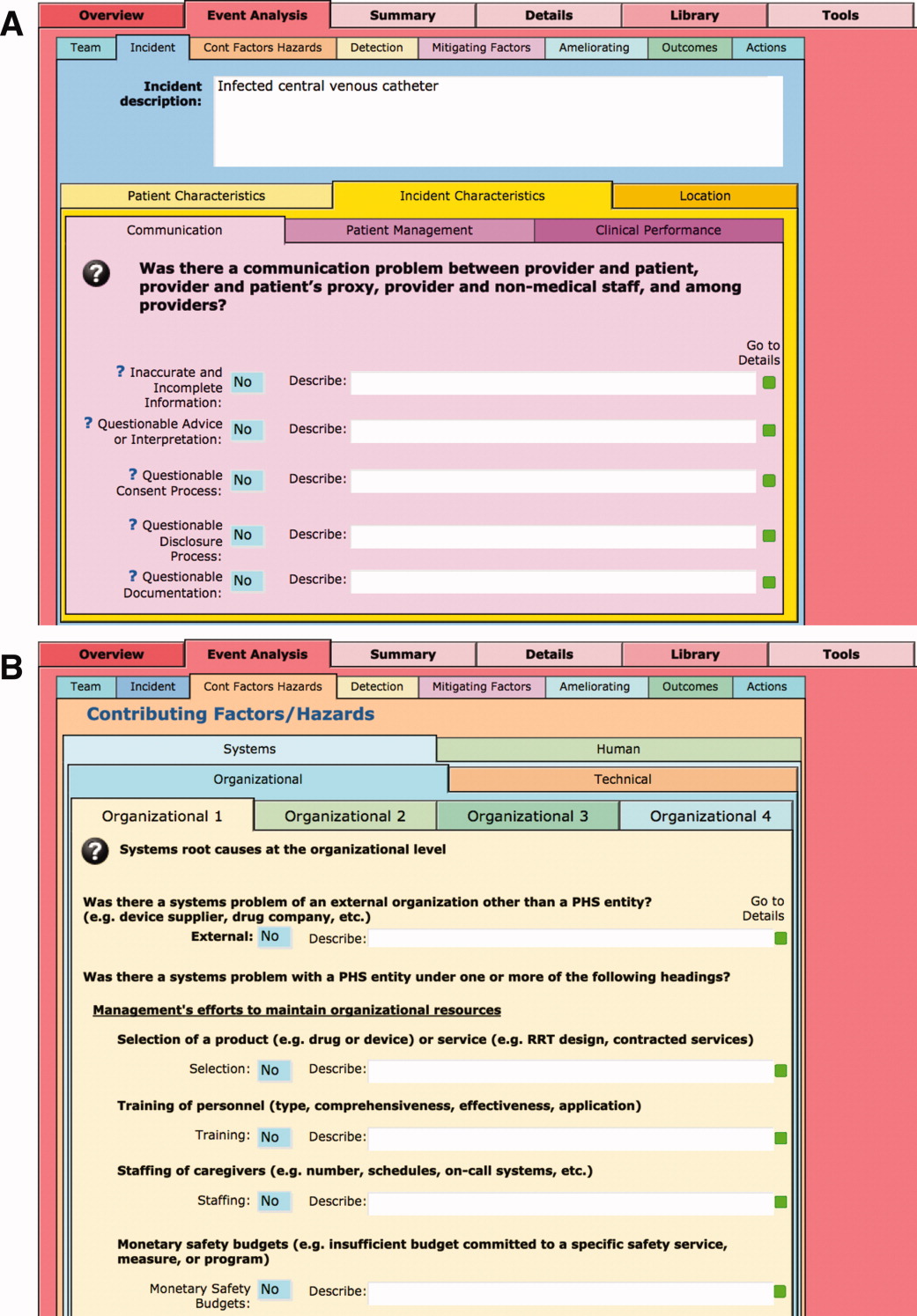
I‐Tracker has features that support SE review groups in beginning an SE review by providing them a paper form or electronic interface by way of a portable computer or tablet device, that guides their discussions and analyses toward providing conclusions that can be entered into the database fields, thereby aligning their deliberations with the ICPS conceptual framework. The same resource is available within the database online for those groups who would prefer to use computer prompts and enter data directly into the database as they proceed through their analyses. Some layouts contain windows that port live views from external Web sites (eg, JC RCA resources) that provide participants of RCA groups with tools to assist their work. FMP11 allows users to access the database by portable computers or handheld tablet devices using the hospitals' WiFi network.
A report screen allows automatic generation of different printouts of individual or aggregate summary reports. A Comprehensive Report includes all of the data fields included in the ICPS conceptual framework. Other reports present subsets of data depending on the user's needs and access privileges. The FMPS11 database allows printing the reports to paper or Portable Document Format (pdf), exporting data into an Excel spreadsheet, or e‐mailing reports to recipients from within I‐Tracker.
Additionally, I‐Tracker functionality facilitates follow‐up and monitoring of action items developed during the RCA process in a manner that conforms to the ICPS framework. We are now developing educational resources for RCA team members to investigate the implementation of I‐Tracker into future RCAs.
DISCUSSION
I‐Tracker provides an intranet‐based tool that met the objectives of the present project. The process of entering 15 existing SE reviews and action plans from our healthcare system into I‐Tracker allowed an incremental development of the database and identified gaps in our existing RCA process. For instance, none of the previous RCAs critically appraised detection, mitigating factors, or ameliorating actions; defined the specific nature or quantified severity of patient injuries using standardized terms; distinguished between human errors and negligence; or comprehensively reported the full spectrum of underlying causes of Tracker's use of standardized terms based on the ICPS conceptual framework provided a potential resource for focusing SE reviews and producing more comprehensive RCAs and action plans in the future. I‐Tracker has additional potential to facilitate dissemination of RCAs to other facilities, both as individual incident reports and aggregated summaries as recommended by experts in patient safety.13
The deficiencies in our existing RCA analyses, identified during data entry into I‐Tracker, represent common shortcomings experienced by other healthcare organizations and summarized in a report by the Agency for Healthcare Research and Quality.4 Considerable hindsight bias and prevailing concerns of the day taint the RCA process, which is time‐consuming and labor intensive, and thereby hinders comprehensive reviews. Also, our SE reviews, like others reviewed in the literature,14 focused on biologic injury to patients and omitted assessment of psychologic, organizational, social, and economic injury domains. Although SE review teams benefit from involvement of quality improvement staff who are trained in techniques and goals of RCA,15 many hospitals like ours have limited resources for fully staffing all SE reviews with trained facilitators. These SE reviews generate both quantitative and qualitative data, the latter of which hinders standardized data entry in the absence of a conceptual framework. A structured database with formative tools to guide RCAs in conformance with the ICPS framework in organizations without sufficient numbers of trained facilitators offers opportunities to produce more comprehensive, standardized, and actionable reports. To date, our quality staff and leadership have responded positively to presentations of the functional features of I‐Tracker (Table 1).
|
| Online availability of the system that allows access both from client database software loaded on Quality Office computers and through intranet browser software (Explorer, Safari, Firefox, etc) |
| Security features of encrypted software that allow full or limited views depending on the user's password security clearance and purpose for reviewing data |
| Software accessibility in authoring and managing the database, which do not require support from information technology data analysts |
| Decision support tools provided in the system to assist RCA analysis |
| System flexibility that allows scripted reporting of single SEs or multiple SE summaries within any selected timeframe |
Limitations of our report include its focus solely on the development and programming phase of I‐Tracker and the absence of information on its actual implementation. We believe, however, the development phase is important to report because it demonstrates that the ICPS framework and specific ICPS data fields are amenable to incorporation into a decision support and reporting tool, which to our knowledge has not been previously reported. We begin implementation of I‐Tracker within our organization this year and will have observations on its feasibility, acceptability, and staff training needs. As an additional limitation, we emphasize that we do not propose I‐Tracker as a solution for other organizations, because we have no plans for its commercial or public domain development. This report is intended to demonstrate, however, that commercially available software, such as FileMaker, can readily support the ICPS Framework and thereby has potential to assist RCAs and SE reporting. Other organizations may develop similar systems on other database platforms that incorporate the ICPS system into their reviews.
To implement I‐Tracker, we are now working with nursing and pharmacy leadership focus groups to develop formative tools, data collection forms, and other resources to assist their RCA efforts and data entry into the database. We also plan to apply the database tool to our residency training program to promote resident involvement in SE reviews by providing standardized, reproducible, and structured processes.16 Our 5‐state healthcare system has funded an evaluation of the implementation phase of I‐Tracker to other Providence facilities. Because the ICPS framework applies to all safety incidents beyond SEs (Table 2), a successful implementation of I‐Tracker for SEs will allow its eventual application to other types of critical incidents.
|
| Clinical administration |
| Clinical process/procedure |
| Documentation |
| Healthcare‐associated infection |
| Medication/IV fluids |
| Blood/blood products |
| Nutrition |
| Oxygen/gas/vapor |
| Medical device/equipment |
| Behavior |
| Patient accidents |
| Infrastructure/building/fixtures |
| Resources/organizational management |
The strength of this project derives from its innovative development of an intranet‐based tool that allows groups to conform their RCAs to the ICPS framework. Because the absence of a standardized classification for patient safety concepts has hindered advances in patient safety,11 we believe I‐Tracker, or decision support tools like it that use the ICPS framework, can standardize RCAs and promote dissemination and adoption of action plans.
Acknowledgements
We appreciate the support of Judy Stenstrom, Lynette Savage, and the Portland Service Area Quality Improvement Office.
Recognition that healthcare carries considerable risks of patient injury has focused efforts on identifying problems before they occur, and understanding the root causes of those problems that do occur to prevent them from happening again.1 To further these efforts, a Joint Commission (JC) standard requires hospitals to review sentinel events (SE).2 Reviews must develop a timely, thorough, and credible root cause analysis (RCA), implement action plans to reduce risk, and monitor the effectiveness of implemented improvements.3
Ideally, hospitals would summarize their experiences with SE reviews, identify high‐risk activities and patients, institute system changes to prevent SE recurrences, and share their findings with other healthcare organizations to help them avoid similar patient injuries.1 In support of this last goal, the JC maintains a voluntary database system that allows hospitals to report their SE analyses for other facilities to review and institute preventative actions.
Unfortunately, the reality of SE reviews does not match their ideals for improving patient safety.4 Healthcare organizations often describe their review process as less than credible and note a need for ongoing oversight to maintain the reviews' effectiveness.5 The JC voluntary reporting system captures less than 1% of the SEs that occur nationally,2 because hospitals perceive barriers to external reporting.1 If healthcare organizations decide against reporting externally, they can create their own internal systems to aggregate and summarize SEs, but few such systems exist. A major impediment to designing internal systems is the absence of universally endorsed nomenclature for safety‐related events.6, 7 Poorly aligned terminology and subjective conceptualizations for safety incidents impede the aggregation of SEs, comparisons between facilities, and trend analyses for tracking SE patterns.
In 2005, the World Health Organization (WHO) World Alliance for Patient Safety, in collaboration with the JC, began developing an International Classification for Patient Safety (ICPS) to provide healthcare organizations a consistent conceptual model for safety incidents and promote their classification by a standardized taxonomy.810 Although this system has promise for allowing standardization, data aggregation, analysis, and learning between institutions,11 integration of the ICPS conceptual model into an SE decision support tool with summarizing and reporting features has not been reported.
This report describes our development of an intranet‐based SE reporting system, called Incident Tracker (I‐Tracker), based on the ICPS model. For our SE review groups from the 4 Providence Health Systems (PHS) Portland Service Area (PSA) hospitals, the I‐Tracker system offers a tool to guide efforts in developing RCAs and action plans in alignment with the ICPS framework. The system includes scripts that automatically generate and distribute standardized reports of individual and aggregated SEs. The objectives of this project were to report our experience with developing a flexible and accessible intranet‐based system that assists RCA participants in conforming to the ICPS framework and oversight safety staff in summarizing and reporting root cause analyses.
METHODS
The 4 PSA hospitals have 1083 licensed beds and perform SE reviews with a centralized process that reports results to a Community Governing Board. An ad hoc team for each SE performs the RCAs. The SE groups report RCAs and action plans in an unstructured format that varies for each event. A paper file is maintained for each SE report, but a system for aggregating reports to track trends, disseminating SE trends, or monitoring the completion or effectiveness of action plans is not available.
We designed a system to achieve the following objectives:
-
Apply the ICPS framework (Figure 1) and taxonomy of terms to SE analyses;
-
Provide a computer‐based tool to assist review groups and quality staff to perform their SE reviews and data collection in alignment with the ICPS framework;
-
Create an intranet‐based database that captures elements of the reviews, RCAs, and action plans with the use of drop‐down lists, help windows, windows with live access to Internet educational resources and tools, decision support tools, default entries, and audio prompts to streamline data entry;
-
Generate a suite of standardized reports customized for different audiences that can be accessed online and printed from the database with automated scripts;
-
Produce intranet‐based summaries of aggregated events to identify common causes and disseminate observed patterns and action plans to other PSA hospitals.
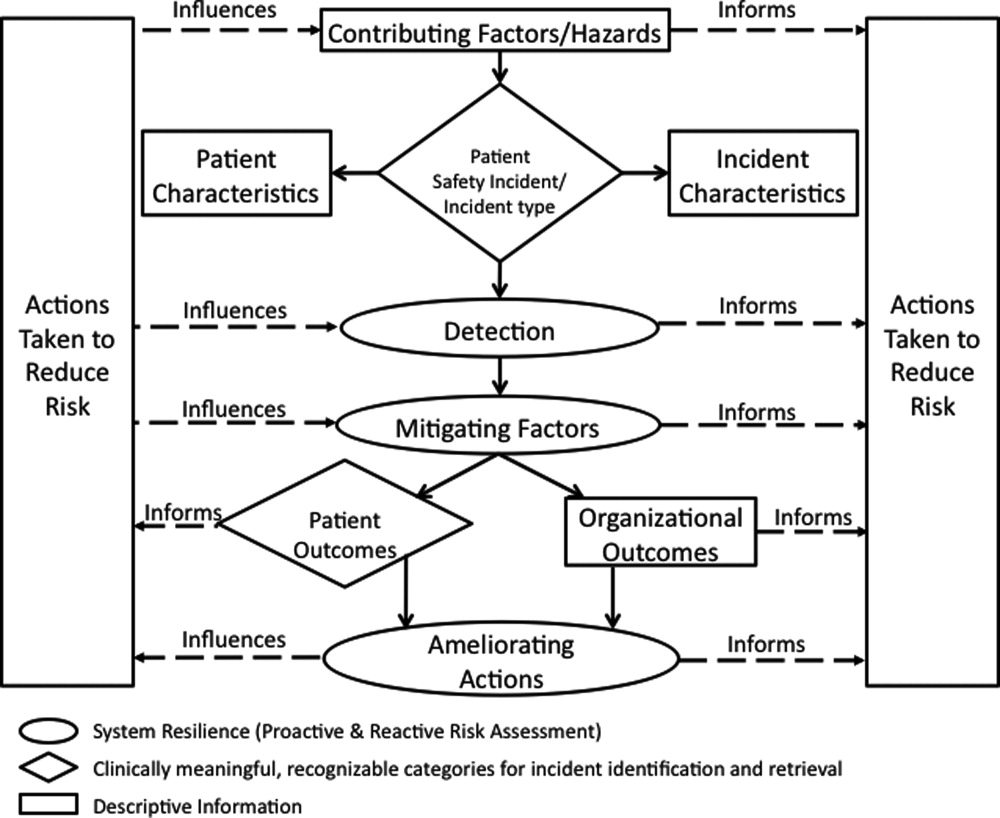
We selected FileMaker Pro 11 Advanced (FMP11) for authoring and maintaining the decision support tool and database, and FileMaker Pro Server 11 Advanced (FMPS11) (Filemaker, Inc, Santa Clara, CA) for hosting the system, because it provides intranet access and tools for updating the system by personnel with minimal programming experience. End users can view and enter data through layouts that display only the information allowed by the user's login password and access privileges, with external authentication by Active Directory and Open Directory technology. Staff who author and manage the database do so through client FMP11 software loaded on a computer that provides remote server access.
The I‐Tracker system was authored using the ICPS definitions for the 48 preferred terms for safety incidents and the ICPS conceptual framework.8 The conceptual framework consists of 10 major incident domains, that include incident type, patient outcomes, patient characteristics, incident characteristics, contributing factors and hazards, organizational outcomes, detection, mitigating factors, ameliorating actions, and actions taken to reduce risk (Figure 1).11 The framework is applicable to all hospital safety incidents, but we limited I‐Tracker to SEs because our hospitals had completed comprehensive reviews and action plans only for these more serious events. The literature on the ICPS framework812 was carefully reviewed to identify the specific data fields that were recommended by ICPS developers to be included under each of the 10 major classification domains. In most instances, data fields existed only in the body of these reports. Article texts, however, provided sufficient descriptions of these data fields to allow their translation into data entry fields in I‐Tracker with accompanying help windows and explanations to guide I‐Tracker users. Sixty ICPS data fields were programmed into I‐Tracker, with another 120 fields that allowed entry of descriptions and explanations of the ICPS data field entries. For instance, an entry of Yes into an ICPS data field that queried Was there a systems problem of an external organization other than a Providence entity opens a Describe field that allows a brief description of the problem, and an additional Details field that allows a longer explanation of the problem if necessary. The brief Describe field contents populate an automatically generated fishbone diagram.
The authors and quality staff translated the most recent 15 SE reviews into ICPS terms and classifications, and entered the results into I‐Tracker as it was being developed, to assist system design and programming of the system. The authors noted during data entry which of the 10 ICPS major domains had not been analyzed by the previous 15 reviews. Because existing reports were unstructured with considerable variation in style and usage of terms, the authors and quality staff made group decisions regarding how to cross‐walk existing information into the standardized ICPS data fields.
RESULTS
In developing I‐Tracker, the authors and quality staff observed that the ICPS framework and recommended data fields were logical and straightforward to learn. Although it was difficult to find the definitions of specific ICPS data fields within the 10 major domains in the text of retrieved articles, these fields could be readily cross‐walked into I‐Tracker data entry fields. Translating existing SE reports into I‐Tracker classifications, however, presented considerable challenges because of the unstructured, discursive, and variable nature of our SE review and reports. The authors and staff spent 1 to 2 hours conferring over each report to make judgments as to which elements of the review would be entered into which I‐Tracker data fields. Once the authors and staff translated existing reports into ICPS terms, actual data entry into I‐Tracker took typically less than 30 minutes for each review. We found that none of our 15 SE reviews included information on the following ICPS major domains: detection, mitigating factors, and ameliorating actions. We also observed that many ICPS data fields were not assessed, such as patient contributions to errors and external organization's contributions to a safety incident.
The latest version of I‐Tracker receives and displays information at the individual patient level. Records are shown onscreen with different screen layouts depending on the viewer's login security clearance. Hospital safety staff have full access to view and enter data on the initial layout, which displays patient demographic information and folder tabs that navigate when clicked to other database fields (Figure 2). Viewers with lower security clearance either view the same opening screen, but have limited access to other screens, or view a different opening screen designed to meet their specific needs. All screens provide definitions of terms and information to assist data entry, buttons that navigate to help pages, pop‐up windows that provide tips, and buttons that trigger brief audio explanations. Most fields use drop‐down lists to standardize data entry around the ICPS definitions, with default values entered into many fields to streamline data entry. A list view allows review of all patients and quick access to an individual patient's record. All fields and combinations of fields with Boolean rules are searchable within the database.
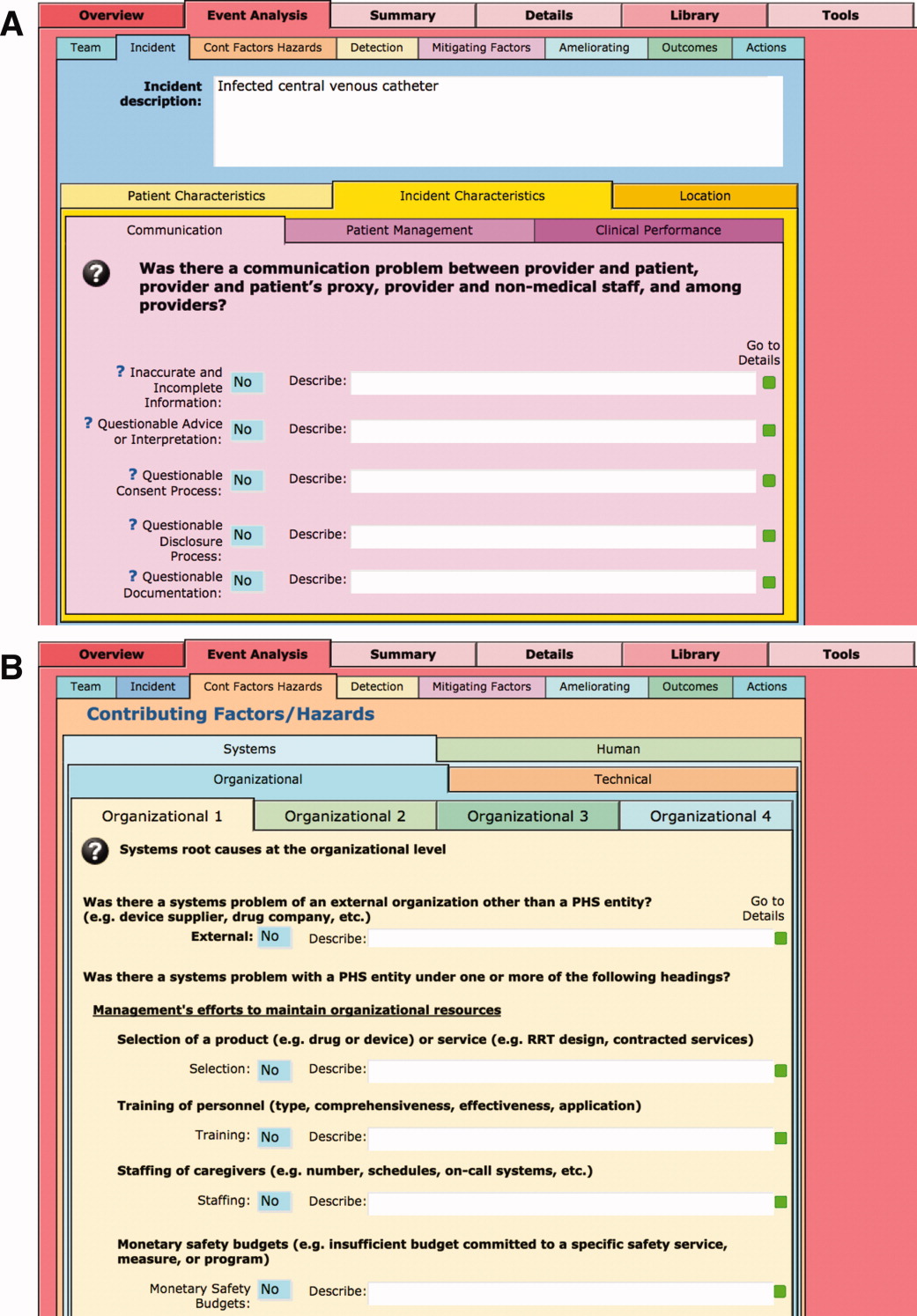
I‐Tracker has features that support SE review groups in beginning an SE review by providing them a paper form or electronic interface by way of a portable computer or tablet device, that guides their discussions and analyses toward providing conclusions that can be entered into the database fields, thereby aligning their deliberations with the ICPS conceptual framework. The same resource is available within the database online for those groups who would prefer to use computer prompts and enter data directly into the database as they proceed through their analyses. Some layouts contain windows that port live views from external Web sites (eg, JC RCA resources) that provide participants of RCA groups with tools to assist their work. FMP11 allows users to access the database by portable computers or handheld tablet devices using the hospitals' WiFi network.
A report screen allows automatic generation of different printouts of individual or aggregate summary reports. A Comprehensive Report includes all of the data fields included in the ICPS conceptual framework. Other reports present subsets of data depending on the user's needs and access privileges. The FMPS11 database allows printing the reports to paper or Portable Document Format (pdf), exporting data into an Excel spreadsheet, or e‐mailing reports to recipients from within I‐Tracker.
Additionally, I‐Tracker functionality facilitates follow‐up and monitoring of action items developed during the RCA process in a manner that conforms to the ICPS framework. We are now developing educational resources for RCA team members to investigate the implementation of I‐Tracker into future RCAs.
DISCUSSION
I‐Tracker provides an intranet‐based tool that met the objectives of the present project. The process of entering 15 existing SE reviews and action plans from our healthcare system into I‐Tracker allowed an incremental development of the database and identified gaps in our existing RCA process. For instance, none of the previous RCAs critically appraised detection, mitigating factors, or ameliorating actions; defined the specific nature or quantified severity of patient injuries using standardized terms; distinguished between human errors and negligence; or comprehensively reported the full spectrum of underlying causes of Tracker's use of standardized terms based on the ICPS conceptual framework provided a potential resource for focusing SE reviews and producing more comprehensive RCAs and action plans in the future. I‐Tracker has additional potential to facilitate dissemination of RCAs to other facilities, both as individual incident reports and aggregated summaries as recommended by experts in patient safety.13
The deficiencies in our existing RCA analyses, identified during data entry into I‐Tracker, represent common shortcomings experienced by other healthcare organizations and summarized in a report by the Agency for Healthcare Research and Quality.4 Considerable hindsight bias and prevailing concerns of the day taint the RCA process, which is time‐consuming and labor intensive, and thereby hinders comprehensive reviews. Also, our SE reviews, like others reviewed in the literature,14 focused on biologic injury to patients and omitted assessment of psychologic, organizational, social, and economic injury domains. Although SE review teams benefit from involvement of quality improvement staff who are trained in techniques and goals of RCA,15 many hospitals like ours have limited resources for fully staffing all SE reviews with trained facilitators. These SE reviews generate both quantitative and qualitative data, the latter of which hinders standardized data entry in the absence of a conceptual framework. A structured database with formative tools to guide RCAs in conformance with the ICPS framework in organizations without sufficient numbers of trained facilitators offers opportunities to produce more comprehensive, standardized, and actionable reports. To date, our quality staff and leadership have responded positively to presentations of the functional features of I‐Tracker (Table 1).
|
| Online availability of the system that allows access both from client database software loaded on Quality Office computers and through intranet browser software (Explorer, Safari, Firefox, etc) |
| Security features of encrypted software that allow full or limited views depending on the user's password security clearance and purpose for reviewing data |
| Software accessibility in authoring and managing the database, which do not require support from information technology data analysts |
| Decision support tools provided in the system to assist RCA analysis |
| System flexibility that allows scripted reporting of single SEs or multiple SE summaries within any selected timeframe |
Limitations of our report include its focus solely on the development and programming phase of I‐Tracker and the absence of information on its actual implementation. We believe, however, the development phase is important to report because it demonstrates that the ICPS framework and specific ICPS data fields are amenable to incorporation into a decision support and reporting tool, which to our knowledge has not been previously reported. We begin implementation of I‐Tracker within our organization this year and will have observations on its feasibility, acceptability, and staff training needs. As an additional limitation, we emphasize that we do not propose I‐Tracker as a solution for other organizations, because we have no plans for its commercial or public domain development. This report is intended to demonstrate, however, that commercially available software, such as FileMaker, can readily support the ICPS Framework and thereby has potential to assist RCAs and SE reporting. Other organizations may develop similar systems on other database platforms that incorporate the ICPS system into their reviews.
To implement I‐Tracker, we are now working with nursing and pharmacy leadership focus groups to develop formative tools, data collection forms, and other resources to assist their RCA efforts and data entry into the database. We also plan to apply the database tool to our residency training program to promote resident involvement in SE reviews by providing standardized, reproducible, and structured processes.16 Our 5‐state healthcare system has funded an evaluation of the implementation phase of I‐Tracker to other Providence facilities. Because the ICPS framework applies to all safety incidents beyond SEs (Table 2), a successful implementation of I‐Tracker for SEs will allow its eventual application to other types of critical incidents.
|
| Clinical administration |
| Clinical process/procedure |
| Documentation |
| Healthcare‐associated infection |
| Medication/IV fluids |
| Blood/blood products |
| Nutrition |
| Oxygen/gas/vapor |
| Medical device/equipment |
| Behavior |
| Patient accidents |
| Infrastructure/building/fixtures |
| Resources/organizational management |
The strength of this project derives from its innovative development of an intranet‐based tool that allows groups to conform their RCAs to the ICPS framework. Because the absence of a standardized classification for patient safety concepts has hindered advances in patient safety,11 we believe I‐Tracker, or decision support tools like it that use the ICPS framework, can standardize RCAs and promote dissemination and adoption of action plans.
Acknowledgements
We appreciate the support of Judy Stenstrom, Lynette Savage, and the Portland Service Area Quality Improvement Office.
- .Reporting of adverse events.N Engl J Med.2002;347:1633–1638.
- The Joint Commission's Sentinel Event Policy: ten years of improving the quality and safety of health care.Jt Comm Perspect.2005;25(1):3–5.
- ,.Root cause analysis and nursing management responsibilities in wrong‐site surgery.Dimens Crit Care Nurs.2006;25,221–225.
- ,.Root Cause Analysis.Making Health Care Safer. Available at: http://archive.ahrq.gov/clinic/ptsafety/chap5.htm. Accessed May 21,2010.
- Oversight group holds RCA teams accountable.Healthcare Benchmarks Qual Improv.2008;15:117–118.
- .Shared meanings: preferred terms and definitions for safety and quality concepts.Med J Aust.2006;184:S41–S43.
- ,,.What do family physicians consider an error? A comparison of definitions and physician perception.BMC Fam Pract.2006;7:73.
- ,,,,,.Towards an International Classification for Patient Safety: key concepts and terms.Int J Qual Health Care.2009;21:18–26.
- ,,,,.The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events.Int J Qual Health Care.2005;17:95–105.
- World Health Organization. 2009 Conceptual Framework for the International Classification for Patient Safety. Final Technical Report Version 1.1. Available at: http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf. Accessed April 25,2011.
- ,,, et al.Towards an International Classification for Patient Safety: the conceptual framework.Int J Qual Health Care.2009;21:2–8.
- ,,,,,.Towards an International Classification for Patient Safety: a Delphi survey.Int J Qual Health Care.2009;21:9–17.
- ,,.Effectiveness and efficiency of root cause analysis in medicine.JAMA.2008;299:685–687.
- ,,,,.How can clinicians measure safety and quality in acute care?Lancet.2004;363:1061–1067.
- ,,,,.Systematic root cause analysis of adverse drug events in a tertiary referral hospital.Jt Comm J Qual Improv.2000;26:563–575.
- ,,,,,.Educational quality improvement report: outcomes from a revised morbidity and mortality format that emphasised patient safety.Postgrad Med J.2008;84:211–216.
- .Reporting of adverse events.N Engl J Med.2002;347:1633–1638.
- The Joint Commission's Sentinel Event Policy: ten years of improving the quality and safety of health care.Jt Comm Perspect.2005;25(1):3–5.
- ,.Root cause analysis and nursing management responsibilities in wrong‐site surgery.Dimens Crit Care Nurs.2006;25,221–225.
- ,.Root Cause Analysis.Making Health Care Safer. Available at: http://archive.ahrq.gov/clinic/ptsafety/chap5.htm. Accessed May 21,2010.
- Oversight group holds RCA teams accountable.Healthcare Benchmarks Qual Improv.2008;15:117–118.
- .Shared meanings: preferred terms and definitions for safety and quality concepts.Med J Aust.2006;184:S41–S43.
- ,,.What do family physicians consider an error? A comparison of definitions and physician perception.BMC Fam Pract.2006;7:73.
- ,,,,,.Towards an International Classification for Patient Safety: key concepts and terms.Int J Qual Health Care.2009;21:18–26.
- ,,,,.The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events.Int J Qual Health Care.2005;17:95–105.
- World Health Organization. 2009 Conceptual Framework for the International Classification for Patient Safety. Final Technical Report Version 1.1. Available at: http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf. Accessed April 25,2011.
- ,,, et al.Towards an International Classification for Patient Safety: the conceptual framework.Int J Qual Health Care.2009;21:2–8.
- ,,,,,.Towards an International Classification for Patient Safety: a Delphi survey.Int J Qual Health Care.2009;21:9–17.
- ,,.Effectiveness and efficiency of root cause analysis in medicine.JAMA.2008;299:685–687.
- ,,,,.How can clinicians measure safety and quality in acute care?Lancet.2004;363:1061–1067.
- ,,,,.Systematic root cause analysis of adverse drug events in a tertiary referral hospital.Jt Comm J Qual Improv.2000;26:563–575.
- ,,,,,.Educational quality improvement report: outcomes from a revised morbidity and mortality format that emphasised patient safety.Postgrad Med J.2008;84:211–216.
PHM Strategic Planning Roundtable
Hospitalists are the fastest growing segment of physicians in the United States.1 Given the growing field of Pediatric Hospital Medicine (PHM) and the need to define strategic direction, the Society of Hospital Medicine (SHM), the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) sponsored a strategic planning meeting in February 2009 that brought together 22 PHM leaders to discuss the future of the field.
PHM is at a critical juncture in terms of clinical practice, research, workforce issues, and quality improvement. The field has developed sufficiently to produce leaders capable of setting an agenda and moving forward. A discussion with the American Board of Pediatrics (ABP) by PHM leaders from the AAP, APA, and SHM at the Pediatric Hospital Medicine 2007 Conference regarding subspecialty designation stimulated convening the PHM Strategic Planning Roundtable to address the task of coordinating further development of PHM (Table 1).
|
| Develop a strategic vision for the role of PHM in the future of children's health care |
| Describe the current gaps between the vision and today's reality |
| Develop a common understanding regarding current initiatives in PHM domains of clinical practice, quality, research, and workforce |
| Determine the method(s) by which participants can be organized to accomplish additional initiatives to implement the vision |
| Identify and prioritize key strategic initiatives |
| Assign accountability and determine next steps and timeline to implement the selected initiatives |
The objective of this article is to describe: (1) the Strategic Planning Roundtable's vision for the field of pediatric hospital medicine; (2) the generation and progress on specific initiatives in clinical practice, quality, research, and workforce identified by the Strategic Planning Roundtable; and (3) issues in the designation of PHM as a subspecialty.
METHODS
The PHM Strategic Planning Roundtable was conducted by a facilitator (S.M.) during a 2‐day retreat using established healthcare strategic planning methods.2
Participants were the existing PHM leaders from the AAP, APA, and SHM, as well as other national leaders in clinical practice, quality, research, and workforce. Development of the vision statement was a key step in which the participants developed a consensus‐based aspirational view of the future. The draft version of the vision statement was initially developed after extensive interviews with key stakeholders and experts in PHM, and was revised by the participants in the course of a facilitated group discussion during the retreat. Following creation of the vision statement, the group then defined the elements of transformation pertaining to PHM and detailed the components of the vision.
Analysis of internal and external environmental factors was critical in the strategic planning process. This type of analysis, detailing the current state of PHM practice, permitted the strategic planners to understand the gaps that existed between the aspirational vision statement and today's reality, and set the stage to identify and implement initiatives to achieve the vision. Several months before the meeting, 4 expert panels comprised of PHM specialists representing a variety of academic and clinical practice settings were brought together via e‐mail and conference calls to focus on 4 domains of PHM: clinical practice, quality of care, research, and workforce. These groups were asked to describe the current status, challenges, and opportunities in these areas. Combining literature review and key stakeholder interviews, their findings and recommendations were distilled into brief summaries that were presented at the Roundtable meeting. Following the presentations, the participants, working in small groups representing all areas of focus,provided additional feedback.
Following the creation of a consensus vision statement and review of internal and external factors, the participants worked to identify specific initiatives in the 4 domains that would advance the field towards the goals contained in the vision statement. These initiatives were grouped into categories. Initiatives by category were scored and prioritized according to predetermined criteria including potential impact, cost, operational complexity, and achievability.
For each initiative selected, the group developed targets and metrics that would be used to track progress. Assigning leadership, accountability, and a timeline to each of the selected projects completed the implementation plan. In addition, the group developed an organizational structure to provide oversight for the overall process, and designated individuals representing the sponsoring organizations into those roles. In conclusion, the group discussed potential structures to guide the future of PHM.
CLINICAL PRACTICE
The Roundtable defined clinical practice for PHM as the general medical care of the hospitalized child, including direct patient care and leadership of the inpatient service. Clinical practice is affected by a number of current national trends including: fewer primary care providers interested in, or with the time to provide, inpatient care; resident work hour restrictions; increasing complexity of clinical issues; and increasing availability of pediatric hospitalists. At the hospital level, clinical practice is affected by increasing need for quality and safety measures, electronic health records and computerized physician order entry, and mounting financial pressures on the hospital system. Hospitalists are assuming more roles in leading quality and safety initiatives, creating computerized systems that address children's needs, and creating financially viable systems of quality pediatric care.3 Hospitalists' clinical care and leadership roles are emerging, and therefore the field faces training and mentorship issues.
Progress to date in this area includes 2 textbooks that define a scope of knowledge and practice, and a newly developed journal in PHM. Core competencies in PHM have been published and provide further refinement of scope and a template for future training.4
Multiple opportunities exist for hospitalists to establish themselves as clinical leaders. Hospitalists can become the preferred providers for hospitalized chronically ill children, with specific initiatives to improve care coordination and multidisciplinary communication. In addition to care coordination and decreasing length of stay, hospitalists, with their intimate knowledge of hospital operations, can be leaders in hospital capacity management and patient flow to increase operational efficiency. Hospitalists can expand evidence‐based guidelines for, and data about, inpatient conditions, and explore the effect of workload and hours on patient care. In addition, there is an expanding role into administrative areas, as well as alternate care arenas, such as: intensive care support (pediatric and neonatal), transport, sedation, palliative care, and pain management. Activities in administrative and alternate care areas have profound direct affects on patient care, as well as providing value added services and additional revenue streams which can further support clinical needs. Finally, achieving quality targets will likely be increasingly linked to payment, so hospitalists may play a key role in the incentives paid to their hospitals. Meeting these challenges will further solidify the standing of hospitalists in the clinical realm.
QUALITY
National and governmental agencies have influenced quality and performance improvement measurements in adult healthcare, resulting in improvements in adult healthcare quality measurement.5 There is limited similar influence or measure development in pediatric medicine, so the quality chasm between adult and child healthcare has widened. Few resources are invested in improving quality and safety of pediatric inpatient care. Of the 18 private health insurance plans' quality and pay for performance programs identified by Leapfrog, only 17% developed pediatric‐specific inpatient measures.6 Only 5 of 40 controlled trials of quality improvement efforts for children published between 1980 and 1998 addressed inpatient problems.7
There have been recent efforts at the national level addressing these issues, highlighted by the introduction of The Children's Health Care Quality Act, in 2007. Early studies in PHM systems focused on overall operational efficiency, documenting 9% to 16% decreases in length of stay and cost compared to traditional models of care.8 Conway et al. identified higher reported adherence to evidence‐based care for hospitalists compared to community pediatricians.9 However, Landrigan et al. demonstrated that there is still large variation in care that exists in the management of common inpatient diagnoses, lacking strong evidence‐based guidelines even among pediatric hospitalists.10 Moreover, there have been no significant studies reviewing the impact of pediatric hospitalists on safety of inpatient care. Magnifying these challenges is the reality that our healthcare system is fragmented with various entities scrambling to define, measure, and compare the effectiveness and safety of pediatric healthcare.
These challenges create an opportunity for PHM to develop a model of how to deliver the highest quality and safest care to our patients. The solution is complex and will take cooperation at many levels of our healthcare system. Improving the safety and quality of care for children in all settings of inpatient care in the United States may best be accomplished via an effective collaborative. This collaborative should be comprehensive and inclusive, and focused on demonstrating and disseminating how standardized, evidence‐based care in both clinical and safety domains can lead to high‐value and high‐quality outcomes. The success of PHM will be measured by its ability to deliver a clear value proposition to all consumers and payers of healthcare. The creation of a robust national collaborative network is a first step towards meeting this goal and will take an extraordinary effort. A PHM Quality Improvement (QI) Collaborative workgroup was created in August 2009. Three collaboratives have been commissioned: (1) Reduction of patient identification errors; (2) Improving discharge communication to referring primary care providers for pediatric hospitalist programs, and (3) Reducing the misuse and overuse of bronchodilators for bronchiolitis. All the collaborative groups have effectively engaged key groups of stakeholders and utilized standard QI tools, demonstrating improvement by the fall of 2010 (unpublished data, S.N.).
RESEARCH
Despite being a relatively young field, there is a critical mass of pediatric hospitalist‐investigators who are establishing research career paths for themselves by securing external grant funding for their work, publishing, and receiving mentorship from largely non‐hospitalist mentors. Some hospitalists are now in a position to mentor junior investigators. These hospitalist‐investigators identified a collective goal of working together across multiple sites in a clinical research network. The goal is to conduct high‐quality studies and provide the necessary clinical information to allow practicing hospitalists to make better decisions regarding patient care. This new inpatient evidence‐base will have the added advantage of helping further define the field of PHM.
The Pediatric Research in Inpatient Settings Network (PRIS) was identified as the vehicle to accomplish these goals. A series of objectives were identified to redesign PRIS in order to accommodate and organize this new influx of hospitalist‐investigators. These objectives included having hospitalist‐investigators commit their time to the prioritization, design, and execution of multicenter studies, drafting new governance documents for PRIS, securing external funding, redefining the relationships of the 3 existing organizations that formed PRIS (AAP, APA, SHM), defining how new clinical sites could be added to PRIS, creating a pipeline for junior hospitalist‐investigators to transition to leadership roles, securing a data coordinating center with established expertise in conducting multicenter studies, and establishing an external research advisory committee of leaders in pediatric clinical research and QI.
Several critical issues were identified, but funding remained a priority for the sustainability of PRIS. Comparative effectiveness (CE) was recognized as a potential important source of future funding. Pediatric studies on CE (eg, surgery vs medical management) conducted by PRIS would provide important new data to allow hospitalists to practice evidence‐based medicine and to improve quality.
A Research Leadership Task Force was created with 4 members of the PHM Strategic Planning Roundtable to work on the identified issues. The APA leadership worked with PRIS to establish a new Executive Council (comprised of additional qualified hospitalist‐investigators). The Executive Council was charged with accomplishing the tasks outlined from the Strategic Planning Roundtable. They have created the governance documents and standard operating procedures necessary for PRIS to conduct multicenter studies, defined a strategic framework for PRIS including the mission, vision and values, and funding strategy. In February 2010, PRIS received a 3‐year award for over $1 million from the Child Health Corporation of America to both fund the infrastructure of PRIS and to conduct a Prioritization Project. The Prioritization Project seeks to identify the conditions that are costly, prevalent, and demonstrate high inter‐hospital variation in resource utilization, which signals either lack of high‐quality data upon which to base medical decisions, and/or an opportunity to standardize care across hospitals. Some of these conditions will warrant further investigation to define the evidence base, whereas other conditions may require implementation studies to reliably introduce evidence into practice. Members of the Executive Council received additional funding to investigate community settings, as most children are hospitalized outside of large children's hospitals. PRIS also reengaged all 3 societies (APA, AAP, and SHM) for support for the first face‐to‐face meeting of the Executive Council. PRIS applied for 2 Recovery Act stimulus grants, and received funding for both of approximately $12 million. The processes used to design, provide feedback, and shepherd these initial studies formed the basis for the standard operating procedures for the Network. PRIS is now reengaging its membership to establish how sites may be able to conduct research, and receive new ideas to be considered for study in PRIS.
Although much work remains to be done, the Executive Council is continuing the charge with quarterly face‐to‐face meetings, hiring of a full‐time PRIS Coordinator, and carrying out these initial projects, while maintaining the goal of meeting the needs of the membership and PHM. If PRIS is to accomplish its mission of improving the health of, and healthcare delivery to, hospitalized children and their families, then the types of studies undertaken will include not only original research questions, but also comparative implementation methods to better understand how hospitalists in a variety of settings can best translate research findings into clinical practice and ultimately improve patient outcomes.
WORKFORCE
The current number of pediatric hospitalists is difficult to gauge11; estimates range from 1500 to 3000 physicians. There are groups of pediatric hospitalists within several national organizations including the AAP, APA, and SHM, in addition to a very active listserve community. It is likely that only a portion of pediatric hospitalists are represented by membership in these organizations.
Most physicians entering the field of PHM come directly out of residency. A recent survey by Freed et al.12 reported that 3% of current pediatric residents are interested in PHM as a career. In another survey by Freed et al., about 6% of recent pediatric residency graduates reported currently practicing as pediatric hospitalists.13 This difference may indicate a number of pediatricians practicing transiently as pediatric hospitalists.
There are numerous issues that will affect the growth and sustainability of PHM. A large number of pediatric residents entering the field will be needed to maintain current numbers. With 45% of hospitalists in practice less than 3 years,11 the growth of PHM in both numbers and influence will require an increasing number of hospitalists with sustained careers in the field. Recognition as experts in inpatient care, as well as expansion of the role of hospitalists beyond the clinical realm to education, research, and hospital leadership, will foster long‐term career satisfaction. The increasingly common stature of hospital medicine as an independent division, equivalent to general pediatrics and subspecialty divisions within a department, may further bolster the perception of hospital medicine as a career.
The majority of pediatric hospitalists believe that current pediatric residency training does not provide all of the skills necessary to practice as a pediatric hospitalist,14 though there is disagreement regarding how additional training in pediatric hospital medicine should be achieved: a dedicated fellowship versus continuing medical education (CME). There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified. The Residency Review and Redesign Project indicates that pediatric residency is likely to be reformed to better meet the training demands of the individual resident's chosen career path. Changing residency to better prepare pediatric residents to take positions in pediatric hospital medicine will certainly affect the workforce emerging from residency programs and their subsequent training needs.15 The American Board of Internal Medicine and the American Board of Family Medicine have approved a Recognition of Focused Practice in Hospital Medicine. This recognition is gained through the Maintenance of Certification (MOC) Program of the respective boards after a minimum of 3 years of practice. SHM is offering fellow recognition in tiered designations of Fellow of Hospital Medicine (FHM), Senior Fellow of Hospital Medicine, and Master of Hospital Medicine. Five hundred hospitalists, including many pediatric hospitalists, received the inaugural FHM designation in 2009. Organizational recognition is a common process in many other medical fields, although previously limited in pediatrics to Fellow of the AAP. FHM is an important step, but cannot substitute for specific training and certification.
Academic fellowships in PHM will aid in the training of hospitalists with scholarly skills and will help produce more pediatric hospitalists with clinical, quality, administrative, and leadership skills. A model of subspecialty fellowship training and certification of all PHM physicians would require a several‐fold increase in available fellowships, currently approximately 15.
Ongoing CME offerings are also critical to sustaining and developing the workforce. The annual national meetings of the APA, AAP, and SHM all offer PHM‐dedicated content, and there is an annual PHM conference sponsored by these 3 organizations. There are now multiple additional national and regional meetings focused on PHM, reflecting the growing audience for PHM CME content. The AAP offers a PHM study guide and an Education in quality improvement for pediatric practice (eQIPP) module on inpatient asthma, specifically designed to facilitate the MOC process for pediatric hospitalists.
Some form of ABP recognition may be necessary to provide the status for PHM to be widely recognized as a viable academic career in the larger pediatric community. This would entail standardized fellowships that will ensure graduates have demonstrated proficiency in the core competencies. PHM leaders have engaged the ABP to better understand the subspecialty approval process and thoughtfully examine the ramifications of subspecialty status, specifically what subspecialty certification would mean for PHM providers and hospitals. Achieving ABP certification may create a new standard of care meaning that noncertified PHM providers will be at a disadvantage. It is unknown what the impact on pediatric inpatient care would be if a PHM standard was set without the supply of practitioners to provide that care.
STRUCTURE
The efforts of the Roundtable demonstrate the potential effectiveness of the current structure that guides the field: that of the cooperative interchange between the PHM leaders within the APA, AAP, and SHM. It may be that, similar to Pediatric Emergency Medicine (PEM), no formal, unifying structure is necessary. Alternatively, both Adolescent Medicine and Behavioral and Developmental Pediatrics (BDP) have their own organizations that guide their respective fields. A hybrid model is that of Pediatric Cardiology which has the Joint Council on Congenital Heart Disease. This structure assures that the leaders of the various organizations concerned with congenital heart disease meet at least annually to report on their activities and coordinate future efforts. Its makeup is similar to how the planning committee of the annual national PHM conference is constructed. Although PHM has largely succeeded with the current organizational structure, it is possible that a more formal structure is needed to continue forward.
CONCLUSION
The Roundtable members developed the following vision for PHM: Pediatric hospitalists will transform the delivery of hospital care for children. This will be done by achieving 7 goals (Table 2).
|
| We will ensure that care for hospitalized children is fully integrated and includes the medical home |
| We will design and support systems for children that eliminate harm associated with hospital care |
| We will develop a skilled and stable workforce that is the preferred provider of care for most hospitalized children |
| We will use collaborative research models to answer questions of clinical efficacy, comparative effectiveness, and quality improvement, and we will deliver care based on that knowledge |
| We will provide the expertise that supports continuing education in the care of the hospitalized child for pediatric hospitalists, trainees, midlevel providers, and hospital staff |
| We will create value for our patients and organizations in which we work based on our unique expertise in PHM clinical care, research, and education |
| We will be leaders and influential agents in national health care policies that impact hospital care |
Attaining this vision will take tremendous dedication, effort, and collaboration. As a starting point, the following initiatives were proposed and implemented as noted:
Clinical
-
Develop an educational plan supporting the PHM Core Competencies, addressing both hospitalist training needs and the role as formal educators.
-
Create a clinical practice monitoring dashboard template for use at PHM hospitals and practices (implemented July 2010).
Quality
-
Undertake environmental assessment of PHM participation on key quality and safety committees, societies, and agencies to ensure appropriate PHM representation in liaison and/or leadership positions.
-
Create a plan for a QI collaborative by assessing the needs and resources available; draft plans for 2 projects (1 safety and 1 quality) which will improve care for children hospitalized with common conditions (started July 2009).
Research
-
Create a collaborative research entity by restructuring the existing research network and formalizing relationships with affiliated networks.
-
Create a pipeline/mentorship system to increase the number of PHM researchers.
Workforce
-
Develop a descriptive statement that can be used by any PHM physician that defines the field of PHM and answers the question who are we?
-
Develop a communications tool describing value added of PHM.
-
Develop a tool to assess career satisfaction among PHM physicians, with links to current SHM work in this area.
Structure
-
Formalize an organizational infrastructure for oversight and guidance of PHM Strategic Planning Roundtable efforts, with clear delineation of the relationships with the AAP, APA, and SHM.
This review demonstrates the work that needs to be done to close the gaps between the current state of affairs and the full vision of the potential impact of PHM. Harm is still common in hospitalized children, and, as a group of physicians, we do not consistently provide evidence‐based care. Quality and safety activities are currently dispersed throughout multiple national entities often working in silos. Much of our PHM research is fragmented, with a lack of effective research networks and collaborative efforts. We also found that while our workforce has many strengths, it is not yet stable.
We believe the Roundtable was successful in describing the current state of PHM and laying a course for the future. We developed a series of deliverable products that have already seen success on many fronts, and that will serve as the foundation for further maturation of the field. We hope to engage the pediatric community, within and without PHM, to comment, advise, and foster PHM so that these efforts are not static but ongoing and evolving. Already, new challenges have arisen not addressed at the Roundtable, such as further resident work restrictions, and healthcare reform with its potential effects on hospital finances. This is truly an exciting and dynamic time, and we know that this is just the beginning.
Acknowledgements
The authors acknowledge the contribution of all members of the roundtable: Douglas Carlson, Vincent Chiang, Patrick Conway, Jennifer Daru, Matthew Garber, Christopher Landrigan, Patricia Lye, Sanjay Mahant, Jennifer Maniscalco, Sanford Melzer, Stephen Muething, Steve Narang, Mary Ottolini, Jack Percelay, Daniel Rauch, Mario Reyes, Beth Robbins, Jeff Sperring, Rajendu Srivastava, Erin Stucky, Lisa Zaoutis, and David Zipes. The authors thank David Zipes for his help in reviewing the manuscript.
- ,.The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,.The Physician Strategist: Setting Strategic Direction for Your Practice; Chicago, Irwin Professional Pub,1996.
- ,.Pediatric hospitalists: training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- The Pediatric Core Competencies Supplement.J Hosp Med.2010;5(suppl 2):1–114.
- ,,,.Reauthorizing SCHIP: Opportunities for Promoting Effective Health Coverage and High Quality Care for Children and Adolescents. Publication 1051.New York, NY:The Commonwealth Fund; August2007:4.
- ,.National Association of Children's Hospitals. Quality Performance Measurement in Medicaid and SCHIP: Result of a 2006 National Survey of State Officials.Lansing, MI:Health Management Associates; August2006.
- ,,,.A report card on quality improvement for children's health care.Pediatrics.2001;107:143–155.
- ,,, et al.Impact of a hospitalist system on length of stay and cost for children with common conditions.Pediatrics.2007;120(2):267–274.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics.2006;118:441–447.
- ,,,,.Variation in pediatric hospitalists' use of unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- ,,,.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(suppl 1):S26–S30.
- ,,,,.Recently trained general pediatricians: perspectives on residency training and scope of practice.Pediatrics.2009;123(suppl 1):S38–S43.
- ,,,.PRIS survey: pediatric hospitalist roles and training needs [abstract].Pediatr Res.2004(55):1.
- ,,.The Residency Review and Redesign in Pediatrics (R3P) Project: roots and branches.Pediatrics.2009;123(suppl 1):S8–S11.
Hospitalists are the fastest growing segment of physicians in the United States.1 Given the growing field of Pediatric Hospital Medicine (PHM) and the need to define strategic direction, the Society of Hospital Medicine (SHM), the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) sponsored a strategic planning meeting in February 2009 that brought together 22 PHM leaders to discuss the future of the field.
PHM is at a critical juncture in terms of clinical practice, research, workforce issues, and quality improvement. The field has developed sufficiently to produce leaders capable of setting an agenda and moving forward. A discussion with the American Board of Pediatrics (ABP) by PHM leaders from the AAP, APA, and SHM at the Pediatric Hospital Medicine 2007 Conference regarding subspecialty designation stimulated convening the PHM Strategic Planning Roundtable to address the task of coordinating further development of PHM (Table 1).
|
| Develop a strategic vision for the role of PHM in the future of children's health care |
| Describe the current gaps between the vision and today's reality |
| Develop a common understanding regarding current initiatives in PHM domains of clinical practice, quality, research, and workforce |
| Determine the method(s) by which participants can be organized to accomplish additional initiatives to implement the vision |
| Identify and prioritize key strategic initiatives |
| Assign accountability and determine next steps and timeline to implement the selected initiatives |
The objective of this article is to describe: (1) the Strategic Planning Roundtable's vision for the field of pediatric hospital medicine; (2) the generation and progress on specific initiatives in clinical practice, quality, research, and workforce identified by the Strategic Planning Roundtable; and (3) issues in the designation of PHM as a subspecialty.
METHODS
The PHM Strategic Planning Roundtable was conducted by a facilitator (S.M.) during a 2‐day retreat using established healthcare strategic planning methods.2
Participants were the existing PHM leaders from the AAP, APA, and SHM, as well as other national leaders in clinical practice, quality, research, and workforce. Development of the vision statement was a key step in which the participants developed a consensus‐based aspirational view of the future. The draft version of the vision statement was initially developed after extensive interviews with key stakeholders and experts in PHM, and was revised by the participants in the course of a facilitated group discussion during the retreat. Following creation of the vision statement, the group then defined the elements of transformation pertaining to PHM and detailed the components of the vision.
Analysis of internal and external environmental factors was critical in the strategic planning process. This type of analysis, detailing the current state of PHM practice, permitted the strategic planners to understand the gaps that existed between the aspirational vision statement and today's reality, and set the stage to identify and implement initiatives to achieve the vision. Several months before the meeting, 4 expert panels comprised of PHM specialists representing a variety of academic and clinical practice settings were brought together via e‐mail and conference calls to focus on 4 domains of PHM: clinical practice, quality of care, research, and workforce. These groups were asked to describe the current status, challenges, and opportunities in these areas. Combining literature review and key stakeholder interviews, their findings and recommendations were distilled into brief summaries that were presented at the Roundtable meeting. Following the presentations, the participants, working in small groups representing all areas of focus,provided additional feedback.
Following the creation of a consensus vision statement and review of internal and external factors, the participants worked to identify specific initiatives in the 4 domains that would advance the field towards the goals contained in the vision statement. These initiatives were grouped into categories. Initiatives by category were scored and prioritized according to predetermined criteria including potential impact, cost, operational complexity, and achievability.
For each initiative selected, the group developed targets and metrics that would be used to track progress. Assigning leadership, accountability, and a timeline to each of the selected projects completed the implementation plan. In addition, the group developed an organizational structure to provide oversight for the overall process, and designated individuals representing the sponsoring organizations into those roles. In conclusion, the group discussed potential structures to guide the future of PHM.
CLINICAL PRACTICE
The Roundtable defined clinical practice for PHM as the general medical care of the hospitalized child, including direct patient care and leadership of the inpatient service. Clinical practice is affected by a number of current national trends including: fewer primary care providers interested in, or with the time to provide, inpatient care; resident work hour restrictions; increasing complexity of clinical issues; and increasing availability of pediatric hospitalists. At the hospital level, clinical practice is affected by increasing need for quality and safety measures, electronic health records and computerized physician order entry, and mounting financial pressures on the hospital system. Hospitalists are assuming more roles in leading quality and safety initiatives, creating computerized systems that address children's needs, and creating financially viable systems of quality pediatric care.3 Hospitalists' clinical care and leadership roles are emerging, and therefore the field faces training and mentorship issues.
Progress to date in this area includes 2 textbooks that define a scope of knowledge and practice, and a newly developed journal in PHM. Core competencies in PHM have been published and provide further refinement of scope and a template for future training.4
Multiple opportunities exist for hospitalists to establish themselves as clinical leaders. Hospitalists can become the preferred providers for hospitalized chronically ill children, with specific initiatives to improve care coordination and multidisciplinary communication. In addition to care coordination and decreasing length of stay, hospitalists, with their intimate knowledge of hospital operations, can be leaders in hospital capacity management and patient flow to increase operational efficiency. Hospitalists can expand evidence‐based guidelines for, and data about, inpatient conditions, and explore the effect of workload and hours on patient care. In addition, there is an expanding role into administrative areas, as well as alternate care arenas, such as: intensive care support (pediatric and neonatal), transport, sedation, palliative care, and pain management. Activities in administrative and alternate care areas have profound direct affects on patient care, as well as providing value added services and additional revenue streams which can further support clinical needs. Finally, achieving quality targets will likely be increasingly linked to payment, so hospitalists may play a key role in the incentives paid to their hospitals. Meeting these challenges will further solidify the standing of hospitalists in the clinical realm.
QUALITY
National and governmental agencies have influenced quality and performance improvement measurements in adult healthcare, resulting in improvements in adult healthcare quality measurement.5 There is limited similar influence or measure development in pediatric medicine, so the quality chasm between adult and child healthcare has widened. Few resources are invested in improving quality and safety of pediatric inpatient care. Of the 18 private health insurance plans' quality and pay for performance programs identified by Leapfrog, only 17% developed pediatric‐specific inpatient measures.6 Only 5 of 40 controlled trials of quality improvement efforts for children published between 1980 and 1998 addressed inpatient problems.7
There have been recent efforts at the national level addressing these issues, highlighted by the introduction of The Children's Health Care Quality Act, in 2007. Early studies in PHM systems focused on overall operational efficiency, documenting 9% to 16% decreases in length of stay and cost compared to traditional models of care.8 Conway et al. identified higher reported adherence to evidence‐based care for hospitalists compared to community pediatricians.9 However, Landrigan et al. demonstrated that there is still large variation in care that exists in the management of common inpatient diagnoses, lacking strong evidence‐based guidelines even among pediatric hospitalists.10 Moreover, there have been no significant studies reviewing the impact of pediatric hospitalists on safety of inpatient care. Magnifying these challenges is the reality that our healthcare system is fragmented with various entities scrambling to define, measure, and compare the effectiveness and safety of pediatric healthcare.
These challenges create an opportunity for PHM to develop a model of how to deliver the highest quality and safest care to our patients. The solution is complex and will take cooperation at many levels of our healthcare system. Improving the safety and quality of care for children in all settings of inpatient care in the United States may best be accomplished via an effective collaborative. This collaborative should be comprehensive and inclusive, and focused on demonstrating and disseminating how standardized, evidence‐based care in both clinical and safety domains can lead to high‐value and high‐quality outcomes. The success of PHM will be measured by its ability to deliver a clear value proposition to all consumers and payers of healthcare. The creation of a robust national collaborative network is a first step towards meeting this goal and will take an extraordinary effort. A PHM Quality Improvement (QI) Collaborative workgroup was created in August 2009. Three collaboratives have been commissioned: (1) Reduction of patient identification errors; (2) Improving discharge communication to referring primary care providers for pediatric hospitalist programs, and (3) Reducing the misuse and overuse of bronchodilators for bronchiolitis. All the collaborative groups have effectively engaged key groups of stakeholders and utilized standard QI tools, demonstrating improvement by the fall of 2010 (unpublished data, S.N.).
RESEARCH
Despite being a relatively young field, there is a critical mass of pediatric hospitalist‐investigators who are establishing research career paths for themselves by securing external grant funding for their work, publishing, and receiving mentorship from largely non‐hospitalist mentors. Some hospitalists are now in a position to mentor junior investigators. These hospitalist‐investigators identified a collective goal of working together across multiple sites in a clinical research network. The goal is to conduct high‐quality studies and provide the necessary clinical information to allow practicing hospitalists to make better decisions regarding patient care. This new inpatient evidence‐base will have the added advantage of helping further define the field of PHM.
The Pediatric Research in Inpatient Settings Network (PRIS) was identified as the vehicle to accomplish these goals. A series of objectives were identified to redesign PRIS in order to accommodate and organize this new influx of hospitalist‐investigators. These objectives included having hospitalist‐investigators commit their time to the prioritization, design, and execution of multicenter studies, drafting new governance documents for PRIS, securing external funding, redefining the relationships of the 3 existing organizations that formed PRIS (AAP, APA, SHM), defining how new clinical sites could be added to PRIS, creating a pipeline for junior hospitalist‐investigators to transition to leadership roles, securing a data coordinating center with established expertise in conducting multicenter studies, and establishing an external research advisory committee of leaders in pediatric clinical research and QI.
Several critical issues were identified, but funding remained a priority for the sustainability of PRIS. Comparative effectiveness (CE) was recognized as a potential important source of future funding. Pediatric studies on CE (eg, surgery vs medical management) conducted by PRIS would provide important new data to allow hospitalists to practice evidence‐based medicine and to improve quality.
A Research Leadership Task Force was created with 4 members of the PHM Strategic Planning Roundtable to work on the identified issues. The APA leadership worked with PRIS to establish a new Executive Council (comprised of additional qualified hospitalist‐investigators). The Executive Council was charged with accomplishing the tasks outlined from the Strategic Planning Roundtable. They have created the governance documents and standard operating procedures necessary for PRIS to conduct multicenter studies, defined a strategic framework for PRIS including the mission, vision and values, and funding strategy. In February 2010, PRIS received a 3‐year award for over $1 million from the Child Health Corporation of America to both fund the infrastructure of PRIS and to conduct a Prioritization Project. The Prioritization Project seeks to identify the conditions that are costly, prevalent, and demonstrate high inter‐hospital variation in resource utilization, which signals either lack of high‐quality data upon which to base medical decisions, and/or an opportunity to standardize care across hospitals. Some of these conditions will warrant further investigation to define the evidence base, whereas other conditions may require implementation studies to reliably introduce evidence into practice. Members of the Executive Council received additional funding to investigate community settings, as most children are hospitalized outside of large children's hospitals. PRIS also reengaged all 3 societies (APA, AAP, and SHM) for support for the first face‐to‐face meeting of the Executive Council. PRIS applied for 2 Recovery Act stimulus grants, and received funding for both of approximately $12 million. The processes used to design, provide feedback, and shepherd these initial studies formed the basis for the standard operating procedures for the Network. PRIS is now reengaging its membership to establish how sites may be able to conduct research, and receive new ideas to be considered for study in PRIS.
Although much work remains to be done, the Executive Council is continuing the charge with quarterly face‐to‐face meetings, hiring of a full‐time PRIS Coordinator, and carrying out these initial projects, while maintaining the goal of meeting the needs of the membership and PHM. If PRIS is to accomplish its mission of improving the health of, and healthcare delivery to, hospitalized children and their families, then the types of studies undertaken will include not only original research questions, but also comparative implementation methods to better understand how hospitalists in a variety of settings can best translate research findings into clinical practice and ultimately improve patient outcomes.
WORKFORCE
The current number of pediatric hospitalists is difficult to gauge11; estimates range from 1500 to 3000 physicians. There are groups of pediatric hospitalists within several national organizations including the AAP, APA, and SHM, in addition to a very active listserve community. It is likely that only a portion of pediatric hospitalists are represented by membership in these organizations.
Most physicians entering the field of PHM come directly out of residency. A recent survey by Freed et al.12 reported that 3% of current pediatric residents are interested in PHM as a career. In another survey by Freed et al., about 6% of recent pediatric residency graduates reported currently practicing as pediatric hospitalists.13 This difference may indicate a number of pediatricians practicing transiently as pediatric hospitalists.
There are numerous issues that will affect the growth and sustainability of PHM. A large number of pediatric residents entering the field will be needed to maintain current numbers. With 45% of hospitalists in practice less than 3 years,11 the growth of PHM in both numbers and influence will require an increasing number of hospitalists with sustained careers in the field. Recognition as experts in inpatient care, as well as expansion of the role of hospitalists beyond the clinical realm to education, research, and hospital leadership, will foster long‐term career satisfaction. The increasingly common stature of hospital medicine as an independent division, equivalent to general pediatrics and subspecialty divisions within a department, may further bolster the perception of hospital medicine as a career.
The majority of pediatric hospitalists believe that current pediatric residency training does not provide all of the skills necessary to practice as a pediatric hospitalist,14 though there is disagreement regarding how additional training in pediatric hospital medicine should be achieved: a dedicated fellowship versus continuing medical education (CME). There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified. The Residency Review and Redesign Project indicates that pediatric residency is likely to be reformed to better meet the training demands of the individual resident's chosen career path. Changing residency to better prepare pediatric residents to take positions in pediatric hospital medicine will certainly affect the workforce emerging from residency programs and their subsequent training needs.15 The American Board of Internal Medicine and the American Board of Family Medicine have approved a Recognition of Focused Practice in Hospital Medicine. This recognition is gained through the Maintenance of Certification (MOC) Program of the respective boards after a minimum of 3 years of practice. SHM is offering fellow recognition in tiered designations of Fellow of Hospital Medicine (FHM), Senior Fellow of Hospital Medicine, and Master of Hospital Medicine. Five hundred hospitalists, including many pediatric hospitalists, received the inaugural FHM designation in 2009. Organizational recognition is a common process in many other medical fields, although previously limited in pediatrics to Fellow of the AAP. FHM is an important step, but cannot substitute for specific training and certification.
Academic fellowships in PHM will aid in the training of hospitalists with scholarly skills and will help produce more pediatric hospitalists with clinical, quality, administrative, and leadership skills. A model of subspecialty fellowship training and certification of all PHM physicians would require a several‐fold increase in available fellowships, currently approximately 15.
Ongoing CME offerings are also critical to sustaining and developing the workforce. The annual national meetings of the APA, AAP, and SHM all offer PHM‐dedicated content, and there is an annual PHM conference sponsored by these 3 organizations. There are now multiple additional national and regional meetings focused on PHM, reflecting the growing audience for PHM CME content. The AAP offers a PHM study guide and an Education in quality improvement for pediatric practice (eQIPP) module on inpatient asthma, specifically designed to facilitate the MOC process for pediatric hospitalists.
Some form of ABP recognition may be necessary to provide the status for PHM to be widely recognized as a viable academic career in the larger pediatric community. This would entail standardized fellowships that will ensure graduates have demonstrated proficiency in the core competencies. PHM leaders have engaged the ABP to better understand the subspecialty approval process and thoughtfully examine the ramifications of subspecialty status, specifically what subspecialty certification would mean for PHM providers and hospitals. Achieving ABP certification may create a new standard of care meaning that noncertified PHM providers will be at a disadvantage. It is unknown what the impact on pediatric inpatient care would be if a PHM standard was set without the supply of practitioners to provide that care.
STRUCTURE
The efforts of the Roundtable demonstrate the potential effectiveness of the current structure that guides the field: that of the cooperative interchange between the PHM leaders within the APA, AAP, and SHM. It may be that, similar to Pediatric Emergency Medicine (PEM), no formal, unifying structure is necessary. Alternatively, both Adolescent Medicine and Behavioral and Developmental Pediatrics (BDP) have their own organizations that guide their respective fields. A hybrid model is that of Pediatric Cardiology which has the Joint Council on Congenital Heart Disease. This structure assures that the leaders of the various organizations concerned with congenital heart disease meet at least annually to report on their activities and coordinate future efforts. Its makeup is similar to how the planning committee of the annual national PHM conference is constructed. Although PHM has largely succeeded with the current organizational structure, it is possible that a more formal structure is needed to continue forward.
CONCLUSION
The Roundtable members developed the following vision for PHM: Pediatric hospitalists will transform the delivery of hospital care for children. This will be done by achieving 7 goals (Table 2).
|
| We will ensure that care for hospitalized children is fully integrated and includes the medical home |
| We will design and support systems for children that eliminate harm associated with hospital care |
| We will develop a skilled and stable workforce that is the preferred provider of care for most hospitalized children |
| We will use collaborative research models to answer questions of clinical efficacy, comparative effectiveness, and quality improvement, and we will deliver care based on that knowledge |
| We will provide the expertise that supports continuing education in the care of the hospitalized child for pediatric hospitalists, trainees, midlevel providers, and hospital staff |
| We will create value for our patients and organizations in which we work based on our unique expertise in PHM clinical care, research, and education |
| We will be leaders and influential agents in national health care policies that impact hospital care |
Attaining this vision will take tremendous dedication, effort, and collaboration. As a starting point, the following initiatives were proposed and implemented as noted:
Clinical
-
Develop an educational plan supporting the PHM Core Competencies, addressing both hospitalist training needs and the role as formal educators.
-
Create a clinical practice monitoring dashboard template for use at PHM hospitals and practices (implemented July 2010).
Quality
-
Undertake environmental assessment of PHM participation on key quality and safety committees, societies, and agencies to ensure appropriate PHM representation in liaison and/or leadership positions.
-
Create a plan for a QI collaborative by assessing the needs and resources available; draft plans for 2 projects (1 safety and 1 quality) which will improve care for children hospitalized with common conditions (started July 2009).
Research
-
Create a collaborative research entity by restructuring the existing research network and formalizing relationships with affiliated networks.
-
Create a pipeline/mentorship system to increase the number of PHM researchers.
Workforce
-
Develop a descriptive statement that can be used by any PHM physician that defines the field of PHM and answers the question who are we?
-
Develop a communications tool describing value added of PHM.
-
Develop a tool to assess career satisfaction among PHM physicians, with links to current SHM work in this area.
Structure
-
Formalize an organizational infrastructure for oversight and guidance of PHM Strategic Planning Roundtable efforts, with clear delineation of the relationships with the AAP, APA, and SHM.
This review demonstrates the work that needs to be done to close the gaps between the current state of affairs and the full vision of the potential impact of PHM. Harm is still common in hospitalized children, and, as a group of physicians, we do not consistently provide evidence‐based care. Quality and safety activities are currently dispersed throughout multiple national entities often working in silos. Much of our PHM research is fragmented, with a lack of effective research networks and collaborative efforts. We also found that while our workforce has many strengths, it is not yet stable.
We believe the Roundtable was successful in describing the current state of PHM and laying a course for the future. We developed a series of deliverable products that have already seen success on many fronts, and that will serve as the foundation for further maturation of the field. We hope to engage the pediatric community, within and without PHM, to comment, advise, and foster PHM so that these efforts are not static but ongoing and evolving. Already, new challenges have arisen not addressed at the Roundtable, such as further resident work restrictions, and healthcare reform with its potential effects on hospital finances. This is truly an exciting and dynamic time, and we know that this is just the beginning.
Acknowledgements
The authors acknowledge the contribution of all members of the roundtable: Douglas Carlson, Vincent Chiang, Patrick Conway, Jennifer Daru, Matthew Garber, Christopher Landrigan, Patricia Lye, Sanjay Mahant, Jennifer Maniscalco, Sanford Melzer, Stephen Muething, Steve Narang, Mary Ottolini, Jack Percelay, Daniel Rauch, Mario Reyes, Beth Robbins, Jeff Sperring, Rajendu Srivastava, Erin Stucky, Lisa Zaoutis, and David Zipes. The authors thank David Zipes for his help in reviewing the manuscript.
Hospitalists are the fastest growing segment of physicians in the United States.1 Given the growing field of Pediatric Hospital Medicine (PHM) and the need to define strategic direction, the Society of Hospital Medicine (SHM), the American Academy of Pediatrics (AAP), and the Academic Pediatric Association (APA) sponsored a strategic planning meeting in February 2009 that brought together 22 PHM leaders to discuss the future of the field.
PHM is at a critical juncture in terms of clinical practice, research, workforce issues, and quality improvement. The field has developed sufficiently to produce leaders capable of setting an agenda and moving forward. A discussion with the American Board of Pediatrics (ABP) by PHM leaders from the AAP, APA, and SHM at the Pediatric Hospital Medicine 2007 Conference regarding subspecialty designation stimulated convening the PHM Strategic Planning Roundtable to address the task of coordinating further development of PHM (Table 1).
|
| Develop a strategic vision for the role of PHM in the future of children's health care |
| Describe the current gaps between the vision and today's reality |
| Develop a common understanding regarding current initiatives in PHM domains of clinical practice, quality, research, and workforce |
| Determine the method(s) by which participants can be organized to accomplish additional initiatives to implement the vision |
| Identify and prioritize key strategic initiatives |
| Assign accountability and determine next steps and timeline to implement the selected initiatives |
The objective of this article is to describe: (1) the Strategic Planning Roundtable's vision for the field of pediatric hospital medicine; (2) the generation and progress on specific initiatives in clinical practice, quality, research, and workforce identified by the Strategic Planning Roundtable; and (3) issues in the designation of PHM as a subspecialty.
METHODS
The PHM Strategic Planning Roundtable was conducted by a facilitator (S.M.) during a 2‐day retreat using established healthcare strategic planning methods.2
Participants were the existing PHM leaders from the AAP, APA, and SHM, as well as other national leaders in clinical practice, quality, research, and workforce. Development of the vision statement was a key step in which the participants developed a consensus‐based aspirational view of the future. The draft version of the vision statement was initially developed after extensive interviews with key stakeholders and experts in PHM, and was revised by the participants in the course of a facilitated group discussion during the retreat. Following creation of the vision statement, the group then defined the elements of transformation pertaining to PHM and detailed the components of the vision.
Analysis of internal and external environmental factors was critical in the strategic planning process. This type of analysis, detailing the current state of PHM practice, permitted the strategic planners to understand the gaps that existed between the aspirational vision statement and today's reality, and set the stage to identify and implement initiatives to achieve the vision. Several months before the meeting, 4 expert panels comprised of PHM specialists representing a variety of academic and clinical practice settings were brought together via e‐mail and conference calls to focus on 4 domains of PHM: clinical practice, quality of care, research, and workforce. These groups were asked to describe the current status, challenges, and opportunities in these areas. Combining literature review and key stakeholder interviews, their findings and recommendations were distilled into brief summaries that were presented at the Roundtable meeting. Following the presentations, the participants, working in small groups representing all areas of focus,provided additional feedback.
Following the creation of a consensus vision statement and review of internal and external factors, the participants worked to identify specific initiatives in the 4 domains that would advance the field towards the goals contained in the vision statement. These initiatives were grouped into categories. Initiatives by category were scored and prioritized according to predetermined criteria including potential impact, cost, operational complexity, and achievability.
For each initiative selected, the group developed targets and metrics that would be used to track progress. Assigning leadership, accountability, and a timeline to each of the selected projects completed the implementation plan. In addition, the group developed an organizational structure to provide oversight for the overall process, and designated individuals representing the sponsoring organizations into those roles. In conclusion, the group discussed potential structures to guide the future of PHM.
CLINICAL PRACTICE
The Roundtable defined clinical practice for PHM as the general medical care of the hospitalized child, including direct patient care and leadership of the inpatient service. Clinical practice is affected by a number of current national trends including: fewer primary care providers interested in, or with the time to provide, inpatient care; resident work hour restrictions; increasing complexity of clinical issues; and increasing availability of pediatric hospitalists. At the hospital level, clinical practice is affected by increasing need for quality and safety measures, electronic health records and computerized physician order entry, and mounting financial pressures on the hospital system. Hospitalists are assuming more roles in leading quality and safety initiatives, creating computerized systems that address children's needs, and creating financially viable systems of quality pediatric care.3 Hospitalists' clinical care and leadership roles are emerging, and therefore the field faces training and mentorship issues.
Progress to date in this area includes 2 textbooks that define a scope of knowledge and practice, and a newly developed journal in PHM. Core competencies in PHM have been published and provide further refinement of scope and a template for future training.4
Multiple opportunities exist for hospitalists to establish themselves as clinical leaders. Hospitalists can become the preferred providers for hospitalized chronically ill children, with specific initiatives to improve care coordination and multidisciplinary communication. In addition to care coordination and decreasing length of stay, hospitalists, with their intimate knowledge of hospital operations, can be leaders in hospital capacity management and patient flow to increase operational efficiency. Hospitalists can expand evidence‐based guidelines for, and data about, inpatient conditions, and explore the effect of workload and hours on patient care. In addition, there is an expanding role into administrative areas, as well as alternate care arenas, such as: intensive care support (pediatric and neonatal), transport, sedation, palliative care, and pain management. Activities in administrative and alternate care areas have profound direct affects on patient care, as well as providing value added services and additional revenue streams which can further support clinical needs. Finally, achieving quality targets will likely be increasingly linked to payment, so hospitalists may play a key role in the incentives paid to their hospitals. Meeting these challenges will further solidify the standing of hospitalists in the clinical realm.
QUALITY
National and governmental agencies have influenced quality and performance improvement measurements in adult healthcare, resulting in improvements in adult healthcare quality measurement.5 There is limited similar influence or measure development in pediatric medicine, so the quality chasm between adult and child healthcare has widened. Few resources are invested in improving quality and safety of pediatric inpatient care. Of the 18 private health insurance plans' quality and pay for performance programs identified by Leapfrog, only 17% developed pediatric‐specific inpatient measures.6 Only 5 of 40 controlled trials of quality improvement efforts for children published between 1980 and 1998 addressed inpatient problems.7
There have been recent efforts at the national level addressing these issues, highlighted by the introduction of The Children's Health Care Quality Act, in 2007. Early studies in PHM systems focused on overall operational efficiency, documenting 9% to 16% decreases in length of stay and cost compared to traditional models of care.8 Conway et al. identified higher reported adherence to evidence‐based care for hospitalists compared to community pediatricians.9 However, Landrigan et al. demonstrated that there is still large variation in care that exists in the management of common inpatient diagnoses, lacking strong evidence‐based guidelines even among pediatric hospitalists.10 Moreover, there have been no significant studies reviewing the impact of pediatric hospitalists on safety of inpatient care. Magnifying these challenges is the reality that our healthcare system is fragmented with various entities scrambling to define, measure, and compare the effectiveness and safety of pediatric healthcare.
These challenges create an opportunity for PHM to develop a model of how to deliver the highest quality and safest care to our patients. The solution is complex and will take cooperation at many levels of our healthcare system. Improving the safety and quality of care for children in all settings of inpatient care in the United States may best be accomplished via an effective collaborative. This collaborative should be comprehensive and inclusive, and focused on demonstrating and disseminating how standardized, evidence‐based care in both clinical and safety domains can lead to high‐value and high‐quality outcomes. The success of PHM will be measured by its ability to deliver a clear value proposition to all consumers and payers of healthcare. The creation of a robust national collaborative network is a first step towards meeting this goal and will take an extraordinary effort. A PHM Quality Improvement (QI) Collaborative workgroup was created in August 2009. Three collaboratives have been commissioned: (1) Reduction of patient identification errors; (2) Improving discharge communication to referring primary care providers for pediatric hospitalist programs, and (3) Reducing the misuse and overuse of bronchodilators for bronchiolitis. All the collaborative groups have effectively engaged key groups of stakeholders and utilized standard QI tools, demonstrating improvement by the fall of 2010 (unpublished data, S.N.).
RESEARCH
Despite being a relatively young field, there is a critical mass of pediatric hospitalist‐investigators who are establishing research career paths for themselves by securing external grant funding for their work, publishing, and receiving mentorship from largely non‐hospitalist mentors. Some hospitalists are now in a position to mentor junior investigators. These hospitalist‐investigators identified a collective goal of working together across multiple sites in a clinical research network. The goal is to conduct high‐quality studies and provide the necessary clinical information to allow practicing hospitalists to make better decisions regarding patient care. This new inpatient evidence‐base will have the added advantage of helping further define the field of PHM.
The Pediatric Research in Inpatient Settings Network (PRIS) was identified as the vehicle to accomplish these goals. A series of objectives were identified to redesign PRIS in order to accommodate and organize this new influx of hospitalist‐investigators. These objectives included having hospitalist‐investigators commit their time to the prioritization, design, and execution of multicenter studies, drafting new governance documents for PRIS, securing external funding, redefining the relationships of the 3 existing organizations that formed PRIS (AAP, APA, SHM), defining how new clinical sites could be added to PRIS, creating a pipeline for junior hospitalist‐investigators to transition to leadership roles, securing a data coordinating center with established expertise in conducting multicenter studies, and establishing an external research advisory committee of leaders in pediatric clinical research and QI.
Several critical issues were identified, but funding remained a priority for the sustainability of PRIS. Comparative effectiveness (CE) was recognized as a potential important source of future funding. Pediatric studies on CE (eg, surgery vs medical management) conducted by PRIS would provide important new data to allow hospitalists to practice evidence‐based medicine and to improve quality.
A Research Leadership Task Force was created with 4 members of the PHM Strategic Planning Roundtable to work on the identified issues. The APA leadership worked with PRIS to establish a new Executive Council (comprised of additional qualified hospitalist‐investigators). The Executive Council was charged with accomplishing the tasks outlined from the Strategic Planning Roundtable. They have created the governance documents and standard operating procedures necessary for PRIS to conduct multicenter studies, defined a strategic framework for PRIS including the mission, vision and values, and funding strategy. In February 2010, PRIS received a 3‐year award for over $1 million from the Child Health Corporation of America to both fund the infrastructure of PRIS and to conduct a Prioritization Project. The Prioritization Project seeks to identify the conditions that are costly, prevalent, and demonstrate high inter‐hospital variation in resource utilization, which signals either lack of high‐quality data upon which to base medical decisions, and/or an opportunity to standardize care across hospitals. Some of these conditions will warrant further investigation to define the evidence base, whereas other conditions may require implementation studies to reliably introduce evidence into practice. Members of the Executive Council received additional funding to investigate community settings, as most children are hospitalized outside of large children's hospitals. PRIS also reengaged all 3 societies (APA, AAP, and SHM) for support for the first face‐to‐face meeting of the Executive Council. PRIS applied for 2 Recovery Act stimulus grants, and received funding for both of approximately $12 million. The processes used to design, provide feedback, and shepherd these initial studies formed the basis for the standard operating procedures for the Network. PRIS is now reengaging its membership to establish how sites may be able to conduct research, and receive new ideas to be considered for study in PRIS.
Although much work remains to be done, the Executive Council is continuing the charge with quarterly face‐to‐face meetings, hiring of a full‐time PRIS Coordinator, and carrying out these initial projects, while maintaining the goal of meeting the needs of the membership and PHM. If PRIS is to accomplish its mission of improving the health of, and healthcare delivery to, hospitalized children and their families, then the types of studies undertaken will include not only original research questions, but also comparative implementation methods to better understand how hospitalists in a variety of settings can best translate research findings into clinical practice and ultimately improve patient outcomes.
WORKFORCE
The current number of pediatric hospitalists is difficult to gauge11; estimates range from 1500 to 3000 physicians. There are groups of pediatric hospitalists within several national organizations including the AAP, APA, and SHM, in addition to a very active listserve community. It is likely that only a portion of pediatric hospitalists are represented by membership in these organizations.
Most physicians entering the field of PHM come directly out of residency. A recent survey by Freed et al.12 reported that 3% of current pediatric residents are interested in PHM as a career. In another survey by Freed et al., about 6% of recent pediatric residency graduates reported currently practicing as pediatric hospitalists.13 This difference may indicate a number of pediatricians practicing transiently as pediatric hospitalists.
There are numerous issues that will affect the growth and sustainability of PHM. A large number of pediatric residents entering the field will be needed to maintain current numbers. With 45% of hospitalists in practice less than 3 years,11 the growth of PHM in both numbers and influence will require an increasing number of hospitalists with sustained careers in the field. Recognition as experts in inpatient care, as well as expansion of the role of hospitalists beyond the clinical realm to education, research, and hospital leadership, will foster long‐term career satisfaction. The increasingly common stature of hospital medicine as an independent division, equivalent to general pediatrics and subspecialty divisions within a department, may further bolster the perception of hospital medicine as a career.
The majority of pediatric hospitalists believe that current pediatric residency training does not provide all of the skills necessary to practice as a pediatric hospitalist,14 though there is disagreement regarding how additional training in pediatric hospital medicine should be achieved: a dedicated fellowship versus continuing medical education (CME). There are several initiatives with the potential to transform the way pediatric hospitalists are trained and certified. The Residency Review and Redesign Project indicates that pediatric residency is likely to be reformed to better meet the training demands of the individual resident's chosen career path. Changing residency to better prepare pediatric residents to take positions in pediatric hospital medicine will certainly affect the workforce emerging from residency programs and their subsequent training needs.15 The American Board of Internal Medicine and the American Board of Family Medicine have approved a Recognition of Focused Practice in Hospital Medicine. This recognition is gained through the Maintenance of Certification (MOC) Program of the respective boards after a minimum of 3 years of practice. SHM is offering fellow recognition in tiered designations of Fellow of Hospital Medicine (FHM), Senior Fellow of Hospital Medicine, and Master of Hospital Medicine. Five hundred hospitalists, including many pediatric hospitalists, received the inaugural FHM designation in 2009. Organizational recognition is a common process in many other medical fields, although previously limited in pediatrics to Fellow of the AAP. FHM is an important step, but cannot substitute for specific training and certification.
Academic fellowships in PHM will aid in the training of hospitalists with scholarly skills and will help produce more pediatric hospitalists with clinical, quality, administrative, and leadership skills. A model of subspecialty fellowship training and certification of all PHM physicians would require a several‐fold increase in available fellowships, currently approximately 15.
Ongoing CME offerings are also critical to sustaining and developing the workforce. The annual national meetings of the APA, AAP, and SHM all offer PHM‐dedicated content, and there is an annual PHM conference sponsored by these 3 organizations. There are now multiple additional national and regional meetings focused on PHM, reflecting the growing audience for PHM CME content. The AAP offers a PHM study guide and an Education in quality improvement for pediatric practice (eQIPP) module on inpatient asthma, specifically designed to facilitate the MOC process for pediatric hospitalists.
Some form of ABP recognition may be necessary to provide the status for PHM to be widely recognized as a viable academic career in the larger pediatric community. This would entail standardized fellowships that will ensure graduates have demonstrated proficiency in the core competencies. PHM leaders have engaged the ABP to better understand the subspecialty approval process and thoughtfully examine the ramifications of subspecialty status, specifically what subspecialty certification would mean for PHM providers and hospitals. Achieving ABP certification may create a new standard of care meaning that noncertified PHM providers will be at a disadvantage. It is unknown what the impact on pediatric inpatient care would be if a PHM standard was set without the supply of practitioners to provide that care.
STRUCTURE
The efforts of the Roundtable demonstrate the potential effectiveness of the current structure that guides the field: that of the cooperative interchange between the PHM leaders within the APA, AAP, and SHM. It may be that, similar to Pediatric Emergency Medicine (PEM), no formal, unifying structure is necessary. Alternatively, both Adolescent Medicine and Behavioral and Developmental Pediatrics (BDP) have their own organizations that guide their respective fields. A hybrid model is that of Pediatric Cardiology which has the Joint Council on Congenital Heart Disease. This structure assures that the leaders of the various organizations concerned with congenital heart disease meet at least annually to report on their activities and coordinate future efforts. Its makeup is similar to how the planning committee of the annual national PHM conference is constructed. Although PHM has largely succeeded with the current organizational structure, it is possible that a more formal structure is needed to continue forward.
CONCLUSION
The Roundtable members developed the following vision for PHM: Pediatric hospitalists will transform the delivery of hospital care for children. This will be done by achieving 7 goals (Table 2).
|
| We will ensure that care for hospitalized children is fully integrated and includes the medical home |
| We will design and support systems for children that eliminate harm associated with hospital care |
| We will develop a skilled and stable workforce that is the preferred provider of care for most hospitalized children |
| We will use collaborative research models to answer questions of clinical efficacy, comparative effectiveness, and quality improvement, and we will deliver care based on that knowledge |
| We will provide the expertise that supports continuing education in the care of the hospitalized child for pediatric hospitalists, trainees, midlevel providers, and hospital staff |
| We will create value for our patients and organizations in which we work based on our unique expertise in PHM clinical care, research, and education |
| We will be leaders and influential agents in national health care policies that impact hospital care |
Attaining this vision will take tremendous dedication, effort, and collaboration. As a starting point, the following initiatives were proposed and implemented as noted:
Clinical
-
Develop an educational plan supporting the PHM Core Competencies, addressing both hospitalist training needs and the role as formal educators.
-
Create a clinical practice monitoring dashboard template for use at PHM hospitals and practices (implemented July 2010).
Quality
-
Undertake environmental assessment of PHM participation on key quality and safety committees, societies, and agencies to ensure appropriate PHM representation in liaison and/or leadership positions.
-
Create a plan for a QI collaborative by assessing the needs and resources available; draft plans for 2 projects (1 safety and 1 quality) which will improve care for children hospitalized with common conditions (started July 2009).
Research
-
Create a collaborative research entity by restructuring the existing research network and formalizing relationships with affiliated networks.
-
Create a pipeline/mentorship system to increase the number of PHM researchers.
Workforce
-
Develop a descriptive statement that can be used by any PHM physician that defines the field of PHM and answers the question who are we?
-
Develop a communications tool describing value added of PHM.
-
Develop a tool to assess career satisfaction among PHM physicians, with links to current SHM work in this area.
Structure
-
Formalize an organizational infrastructure for oversight and guidance of PHM Strategic Planning Roundtable efforts, with clear delineation of the relationships with the AAP, APA, and SHM.
This review demonstrates the work that needs to be done to close the gaps between the current state of affairs and the full vision of the potential impact of PHM. Harm is still common in hospitalized children, and, as a group of physicians, we do not consistently provide evidence‐based care. Quality and safety activities are currently dispersed throughout multiple national entities often working in silos. Much of our PHM research is fragmented, with a lack of effective research networks and collaborative efforts. We also found that while our workforce has many strengths, it is not yet stable.
We believe the Roundtable was successful in describing the current state of PHM and laying a course for the future. We developed a series of deliverable products that have already seen success on many fronts, and that will serve as the foundation for further maturation of the field. We hope to engage the pediatric community, within and without PHM, to comment, advise, and foster PHM so that these efforts are not static but ongoing and evolving. Already, new challenges have arisen not addressed at the Roundtable, such as further resident work restrictions, and healthcare reform with its potential effects on hospital finances. This is truly an exciting and dynamic time, and we know that this is just the beginning.
Acknowledgements
The authors acknowledge the contribution of all members of the roundtable: Douglas Carlson, Vincent Chiang, Patrick Conway, Jennifer Daru, Matthew Garber, Christopher Landrigan, Patricia Lye, Sanjay Mahant, Jennifer Maniscalco, Sanford Melzer, Stephen Muething, Steve Narang, Mary Ottolini, Jack Percelay, Daniel Rauch, Mario Reyes, Beth Robbins, Jeff Sperring, Rajendu Srivastava, Erin Stucky, Lisa Zaoutis, and David Zipes. The authors thank David Zipes for his help in reviewing the manuscript.
- ,.The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,.The Physician Strategist: Setting Strategic Direction for Your Practice; Chicago, Irwin Professional Pub,1996.
- ,.Pediatric hospitalists: training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- The Pediatric Core Competencies Supplement.J Hosp Med.2010;5(suppl 2):1–114.
- ,,,.Reauthorizing SCHIP: Opportunities for Promoting Effective Health Coverage and High Quality Care for Children and Adolescents. Publication 1051.New York, NY:The Commonwealth Fund; August2007:4.
- ,.National Association of Children's Hospitals. Quality Performance Measurement in Medicaid and SCHIP: Result of a 2006 National Survey of State Officials.Lansing, MI:Health Management Associates; August2006.
- ,,,.A report card on quality improvement for children's health care.Pediatrics.2001;107:143–155.
- ,,, et al.Impact of a hospitalist system on length of stay and cost for children with common conditions.Pediatrics.2007;120(2):267–274.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics.2006;118:441–447.
- ,,,,.Variation in pediatric hospitalists' use of unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- ,,,.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(suppl 1):S26–S30.
- ,,,,.Recently trained general pediatricians: perspectives on residency training and scope of practice.Pediatrics.2009;123(suppl 1):S38–S43.
- ,,,.PRIS survey: pediatric hospitalist roles and training needs [abstract].Pediatr Res.2004(55):1.
- ,,.The Residency Review and Redesign in Pediatrics (R3P) Project: roots and branches.Pediatrics.2009;123(suppl 1):S8–S11.
- ,.The hospitalist movement 5 years later.JAMA.2002;287(4):487–494.
- ,,.The Physician Strategist: Setting Strategic Direction for Your Practice; Chicago, Irwin Professional Pub,1996.
- ,.Pediatric hospitalists: training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- The Pediatric Core Competencies Supplement.J Hosp Med.2010;5(suppl 2):1–114.
- ,,,.Reauthorizing SCHIP: Opportunities for Promoting Effective Health Coverage and High Quality Care for Children and Adolescents. Publication 1051.New York, NY:The Commonwealth Fund; August2007:4.
- ,.National Association of Children's Hospitals. Quality Performance Measurement in Medicaid and SCHIP: Result of a 2006 National Survey of State Officials.Lansing, MI:Health Management Associates; August2006.
- ,,,.A report card on quality improvement for children's health care.Pediatrics.2001;107:143–155.
- ,,, et al.Impact of a hospitalist system on length of stay and cost for children with common conditions.Pediatrics.2007;120(2):267–274.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics.2006;118:441–447.
- ,,,,.Variation in pediatric hospitalists' use of unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- ,,,.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(suppl 1):S26–S30.
- ,,,,.Recently trained general pediatricians: perspectives on residency training and scope of practice.Pediatrics.2009;123(suppl 1):S38–S43.
- ,,,.PRIS survey: pediatric hospitalist roles and training needs [abstract].Pediatr Res.2004(55):1.
- ,,.The Residency Review and Redesign in Pediatrics (R3P) Project: roots and branches.Pediatrics.2009;123(suppl 1):S8–S11.
Continuous Admission Model Reduces LOS
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
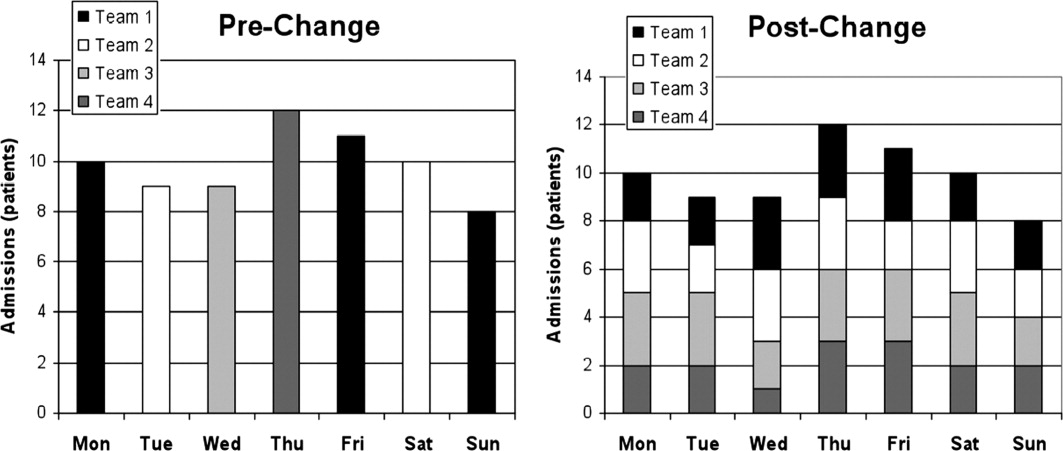
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (<7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
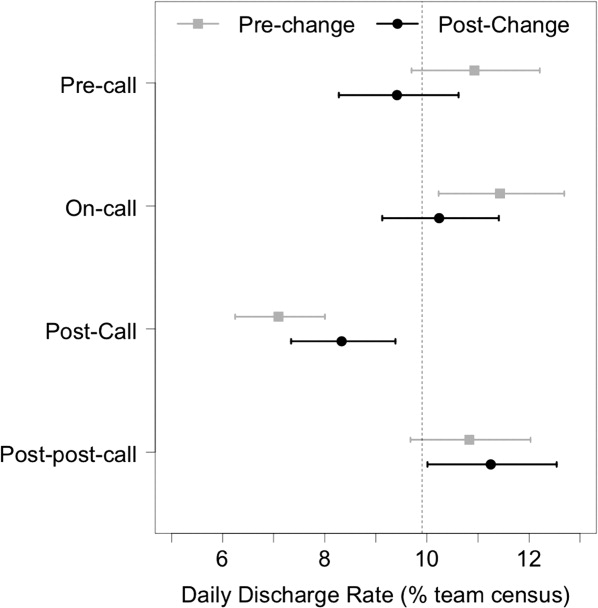
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P < 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
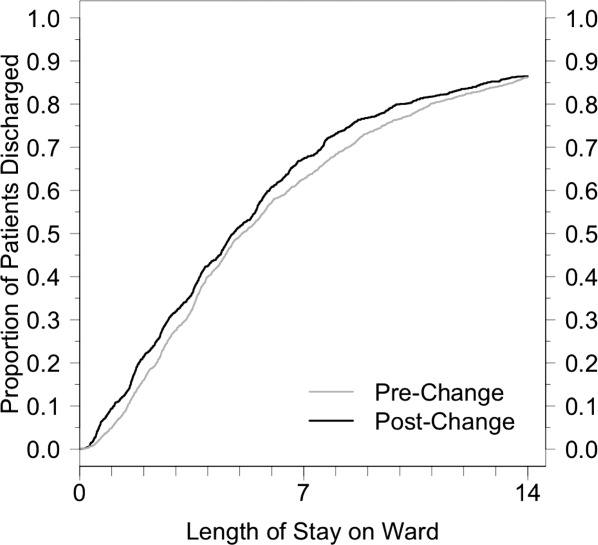
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
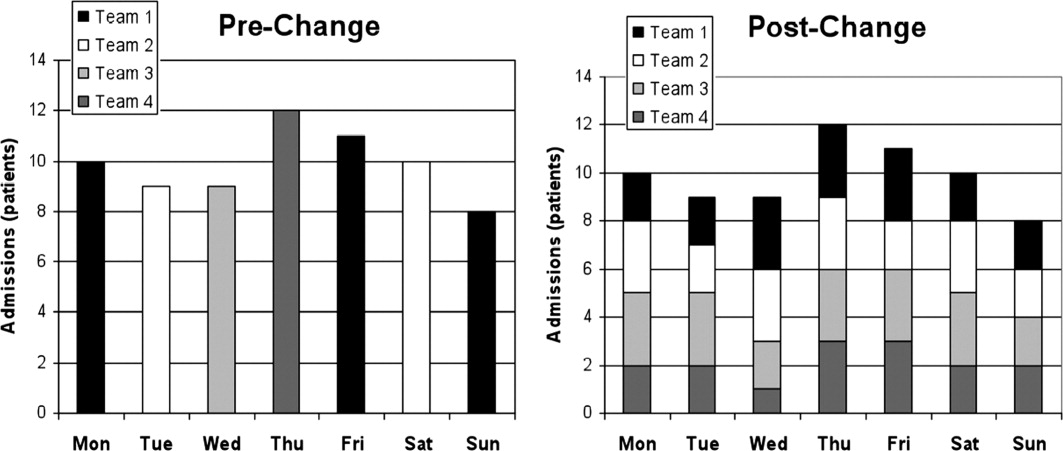
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (<7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
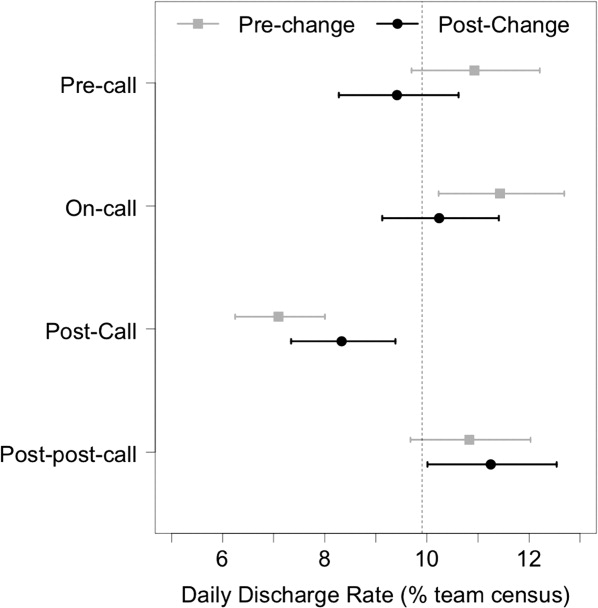
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P < 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
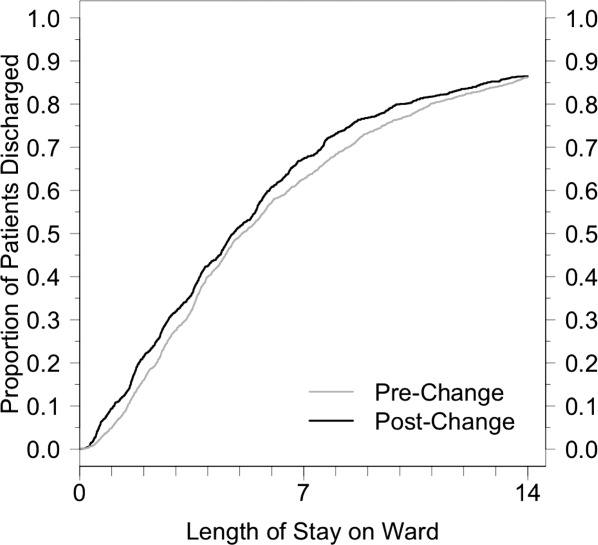
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
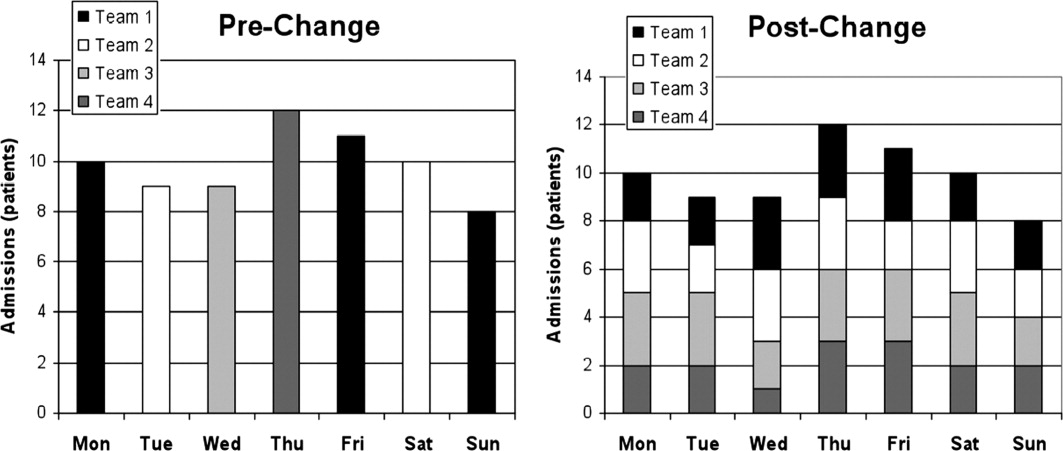
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (<7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
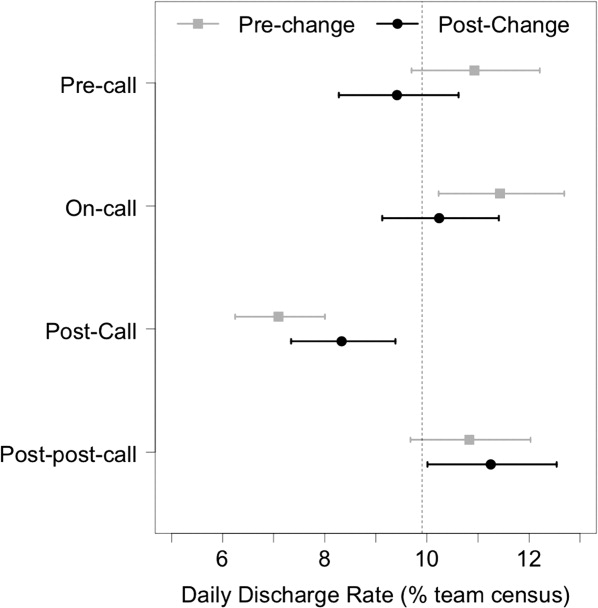
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P < 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
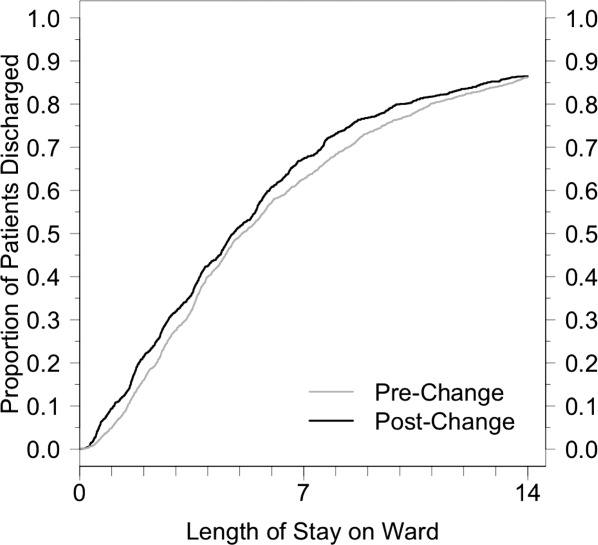
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.
Outcomes of a Mobile ACE Service
The traditional acute care for the elderly (ACE) unit has demonstrated improved functional outcomes without increased costs or changes in length of stay (LOS).15 It is, however, limited in scope to only those patients cared for on a fixed geographical unit. This structural limitation is of increasing relevance in times of high hospital bed occupancy rates, as during such times, many appropriate older patients are admitted elsewhere. In our experience with a traditional ACE unit‐based model, only 52% of our geriatrics practice patients were admitted to an ACE unit bed, while the remainder were admitted to various medical units throughout the hospital. We therefore abandoned our traditional unit‐based ACE service in July 2007 in favor of a mobile ACE (MACE) service, bringing the interdisciplinary, patient‐centered team approach to our hospitalized older adult patients admitted throughout the hospital.
The purpose of this study is to compare the operational and quality outcomes for patients cared for on the MACE service to those cared for on a unit‐based ACE service and matched controls cared for on other general medical services. We hypothesized that the MACE service would be associated with lower lengths of stay, reduced costs, and decreased rehospitalization rates.
METHODS
The MACE team was composed of a geriatrician‐hospitalist, geriatric medicine fellow, social worker, and nurse coordinator. The geriatric medicine attending on the MACE service was in the hospital providing patient care during regular working hours from Monday through Friday, while the weekends were covered by a rotating group of all geriatric medicine faculty. During the first and second years of MACE, there were 7 and 4 attendings, respectively; all fellowship‐trained geriatricians. Three of the 4 geriatric medicine hospitalists during year 2 had been in practice between 1 and 3 years postfellowship and also had training in palliative medicine, although were not board‐certified in the latter. The fourth hospitalist had been in practice for 5 years postfellowship. The interdisciplinary team met daily to discuss the care of all patients and used a transitional care model based on The Care Transitions Program6 adapted to our institution, with a focus on reducing the risks of hazards of hospitalization. Care coordination with the outpatient practice, early family meetings, discharge planning, patient and caregiver education, and postdischarge follow‐up phone calls were some of the key hallmarks of the service (Table 1).
| Team member(s) | Roles |
|---|---|
| |
| Team (MD, fellow, NC,SW) | Scheduled daily meetings at 8 am (or 8 am and 2 pm if needed) to discuss each patient's care and discharge plan |
| NC | Introduces the team to the patient/caregiver upon admission |
| Obtains prehospitalization information on cognitive and functional status | |
| Acts as a hospital coach educating the patient/caregiver | |
| Completes PRIs necessary for discharge to other institutions | |
| Completes medication reconciliation prior to discharge | |
| Initiates post‐discharge phone call and communicates with PCP via EMR | |
| Provides experiential one‐to‐one geriatric nursing education | |
| SW | Arranges family meeting, when indicated, with the team early in the hospitalization |
| Provides patient and family psychosocial support on an as needed basis | |
| Responsible for discharge planning | |
| MD | Attending physician of record |
| Communicates with PCP upon admission of the patient | |
| Assures discharge communiqu to PCP via EMR within 24 hours of discharge | |
We conducted a retrospective cohort study with propensity‐score matching in an urban academic medical center. Study subjects comprised 5 distinct groups. First were community‐dwelling older adults cared for at our outpatient geriatrics ambulatory practice who were discharged from our traditional ACE unit‐based acute care service at the Mount Sinai Hospital from July 1, 2006 through June 30, 2007 (N = 450). Second and third were patients from the same practice discharged from our MACE service during the first 2 years of operation (N = 556 from July 1, 2007 through June 30, 2008, and N = 501 from July 1, 2008 through June 30, 2009). Fourth and fifth were control cohorts of hospitalized older adults discharged from other medical services at the Mount Sinai Hospital during these same 2 years (N = 4863 and N = 4777, respectively). The average daily census on all services was 1012 patients.
Some patients on all 3 services are co‐managed with house staff, who are responsible for writing physician orders. Control cohort patients were cared for by a mix of private attendings (approximately 75%) or hospitalists (25%), and in contradistinction to MACE patients, their typical care did not include daily interdisciplinary team rounds, a nurse coordinator, or geriatrics fellow. Social work and case management were unit‐ as opposed to team‐based. Care on the ACE unit‐based service differed from care for matched control patients by having daily interdisciplinary team rounds, a prepared environment, and nursing‐led protocols for the patients on the ACE unit.
Because the ACE unit‐based service admitted both patients who were and were not cared for in our ambulatory practice, while the MACE service admitted only patients cared for in the ambulatory practice, we deleted from the study sample the patients who did not have a visit to our outpatient practice before the index hospitalization. This allowed us to isolate the effect of the model of care itself as opposed to the effect of simply changing the patient base for admissions. We then merged the files with the hospital's administrative database and electronic billing system to obtain demographic and claims data.
Additional demographic data were obtained through chart review of the MACE patients during year 1. The chart review process was standardized using a data abstraction instrument and by determining inter‐rater reliability of the individual data abstractors (comprised of author B.K. and 4 MACE team members).
Costs were assigned to individual admissions by the hospital's cost reporting system and include a combination of traceable costs (such as imaging, laboratory, and pharmacy) and applied costs (nursing; allocated based on geographic location in the hospital) to arrive at direct and total costs.
We made 3 distinct comparisons of operational and quality outcomes using the above 5 groups, first comparing patients cared for on our traditional ACE unit‐based service to those cared for on the MACE service, and second and third comparing patients on the MACE service to propensity score‐matched controls during the first and second year of operations. Specifically, we hypothesized that the MACE service would be associated with reduced LOS, costs, and readmission rates compared with the ACE unit‐based service and the matched control groups. We used multivariate logistic regression to estimate the association of binary quality outcomes (mortality during the hospital stay, 7‐ and 30‐day readmission rates) with the existence of MACE while adjusting for confounding variables which included patient demographic and clinical characteristics such as age, gender, race, total number of comorbidities (calculated by Elixhauser method that includes 30 categories of comorbid illnesses identified by secondary diagnosis codes and discharge diagnosis‐related groups [DRGs]).7 We considered the clustering effect due to the same attending physician into the model as well. While adjusting for the same covariates, we used generalized linear models with a gamma distribution and log link to estimate the association of continuous variables (costs and LOS) with the existence of MACE.
The same statistical methods were applied to the second and third comparisons between patients cared for on the MACE and the propensity score‐matched cohorts for the first and second year of the MACE service. First, 2 control cohorts (N = 6148 and 5803 of our hospital discharges from July 1, 2007 to June 30, 2008, and July 1, 2008 to June 30, 2009, respectively, with age > 64 and with the identical DRG and All Patient Refined DRG (APR DRG) Severity of Illness (SOI) score as those of the MACE groups were obtained from our hospital's administrative database to reduce the selection bias. Then, 4863 patients within the first cohort (N = 6148) and 4777 patients within the second cohort (N = 5,803) with the closest propensity score were matched to 545 of 556 MACE patients and 494 of 501 MACE patients, respectively, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score.
Propensity scores were determined by logistic regression on whether patients were admitted to the MACE. The covariates for the propensity model were the same as the previously stated adjusting variables. Usual care patients' data were weighted to account for the one‐to‐many propensity score‐matching algorithm.
We similarly conducted a post hoc analysis of MACE compared with a subgroup control cohort of patients cared for by medicine hospitalists in year 1 (N = 1175) and year 2 (N = 1564), with age > 64 and with the identical DRG and APR DRG SOI as those of the MACE group. We then matched 1012 of the 1175 discharges with the closest propensity score to 389 of the 411 MACE discharges who were cared for by 1 of the 4 geriatric medicine hospitalists in year 1 and 1308 of the 1564 discharges to 471 of the 501 MACE discharges in year 2, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score, using the same covariates described above.
All analyses were done using Stata software, version 9.2 (StataCorp LP, College Station, TX). This project was exempted by the Institutional Review Board at Mount Sinai School of Medicine, New York, New York.
RESULTS
Table 2 presents the characteristics of the study subjects in all 5 groups. Patients cared for on the ACE unit‐based service and the MACE service in years 1 and 2 were very similar, with a mean age of 82.6, 83.2, and 83.6 years; 74.4%, 75.9%, and 76.7% were female; and mean Elixhauser comorbidity scores were 3.4, 3.3, and 3.5, respectively. Patients in the 2 matched control groups were likewise very similar to those in the matched MACE groups with regard to all demographic variables.
| Demographics | ACE (N = 450) | Matched MACE year 1 (N = 545) | Matched controls year 1 (N = 4863) | Matched MACE year 2 (N = 494) | Matched controls year 2 (N = 4777) |
|---|---|---|---|---|---|
| |||||
| Age SD | 82.6 8.4 | 83.2 8.3 | 83.4 8.8 | 83.6 8.1 | 83.8 8.5 |
| Female, % | 74.4% | 75.9% | 74.7% | 76.7% | 77.4% |
| Race, % | |||||
| White | 35 | 37 | 36 | 43 | 42 |
| Black | 30 | 27 | 28 | 25 | 25 |
| Hispanic | 33 | 34 | 35 | 28 | 30 |
| Asian | 1 | 1 | 1 | 3 | 3 |
| Marital status, % | |||||
| Married | 20 | 20 | 21 | 23 | 23 |
| Widowed | 44 | 45 | 44 | 46 | 38 |
| Single | 25 | 22 | 27 | 21 | 28 |
| Elixhauser comorbidity index mean (SD) | 3.4 (1.8) | 3.4 (1.6) | 3.3 (1.7) | 3.5 (1.7) | 3.5 (1.7) |
| Hypertension, % | 61 | 54 | 54 | 49 | 49 |
| Heart Failure, % | 25 | 27 | 28 | 26 | 27 |
| Diabetes Mellitus, % | 26 | 25 | 25 | 24 | 25 |
| Atrial fibrillation, % | 22 | 23 | 23 | 28 | 27 |
| Chronic obstructive pulmonary disease, % | 15 | 15 | 15 | 15 | 14 |
Chart review of the year 1 MACE discharges revealed that 70% spoke English as their primary language and 46% had cognitive impairment. Most lived at home alone (49%) or with family members (41%) while receiving some paid caregiver help (59%). The remaining 10% were admitted from either an assisted living facility (5%) or subacute rehabilitation (5%). Only 12% were wheelchair or bed‐bound, while 21% ambulated without and 67% with an assistive device. Their functional status was limited, with 58% dependent for both ADLs and IADLs, 22% dependent for IADLs only, and 20% independent in both. They had relatively high prescription medication burdens, with 10% taking 05, 34% taking 610, 38% taking 1115, and 18% taking >15 medications.
Patients cared for by the MACE service had an adjusted 2.1 days shorter LOS (P < 0.001) when compared with patients cared for on the ACE unit service. Additionally, there was a net savings of $2872 in total costs per hospitalization (P = 0.002), $1094 in direct costs (P = 0.016), $849 in nursing costs (P < 0.001), and $237 in pharmacy costs (P = 0.002). Imaging and laboratory costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
| MACE to ACE | MACE to matched controls, year 1 | MACE to matched controls, year 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MACE (N = 556) | ACE (N = 450) | P value | MACE (N = 545) | Matched controls (N = 4863) | P value | MACE (N = 494) | Matched controls (N = 4777) | P value | |
| |||||||||
| LOS, days | 5.8 | 7.9 | <0.001 | 5.8 | 6.5 | 0.15 | 5.6 | 7.2 | <0.001 |
| Costs, $ | |||||||||
| Total | 10315 | 13187 | 0.002 | 10311 | 12764 | <0.001 | 10693 | 15636 | <0.001 |
| Direct | 4777 | 5871 | 0.016 | 4778 | 5620 | 0.03 | 4967 | 7048 | <0.001 |
| Nursing | 2361 | 3210 | <0.001 | 2356 | 2749 | 0.026 | 2143 | 3080 | <0.001 |
| Imaging | 342 | 332 | 0.61 | 344 | 349 | 0.73 | 382 | 471 | 0.06 |
| Laboratory | 206 | 243 | 0.079 | 206 | 245 | 0.029 | 213 | 281 | <0.001 |
| Pharmacy | 598 | 835 | 0.002 | 597 | 662 | 0.63 | 563 | 786 | 0.03 |
| In‐hospital mortality,% | 3.3 | 3.9 | 0.66 | 2.9 | 2.6 | 0.3 | 5.3 | 3.6 | 0.053 |
| 7‐day readmission,% | 9.3 | 10.2 | 0.55 | 9.7 | 11.8 | 0.3 | 4.8 | 5.5 | 0.71 |
| 30‐day readmission, % | 23.6 | 25.9 | 0.5 | 23.8 | 24.3 | 0.65 | 21.1 | 20.9 | 0.62 |
| 90‐day readmission, % | 40.9 | 38.7 | 0.1 | 41.3 | 38.4 | 0.005 | 38.0 | 36.5 | 0.74 |
There was no difference in LOS between the MACE patients during the first year of service compared with propensity score‐matched control patients (5.8 vs 6.5 days). There was, however, a net savings of $2453 in total costs per hospitalization (P < 0.001), $842 (P = 0.03) in direct costs, $393 in nursing costs (P = 0.026), and $39 in laboratory costs (P = 0.029). Imaging and pharmacy costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day or 30‐day readmission rates between the 2 groups. However, the 90‐day readmission rate was higher in MACE patients (Table 3).
During the second year of the MACE service, however, there was a significant reduction in LOS of 1.6 days (P < 0.001), a net savings of $4943 in total costs per hospitalization (P < 0.001), $2081 (P < 0.001) in direct costs, $937 in nursing costs (P < 0.001), $68 in laboratory costs (P < 0.001), and $223 in pharmacy costs (P = 0.03). There were no significant differences in imaging costs, in‐hospital mortality, and 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
A subgroup analysis of the first and second year comparisons including only those patients in the control groups cared for by medicine hospitalists demonstrated reductions in the MACE in total cost in year 1 and LOS, mortality, total, and nursing costs in year 2. However, in year 1, the 30‐day and 90‐day readmission rates were increased in the MACE compared with the control group (Table 4).
| MACE, year 1 (N = 389) | Matched controls, year 1 (N = 1012) | P Value | MACE, year 2 (N = 471) | Matched controls, year 2 (N = 1308) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| LOS, days | 6.0 | 6.0 | 0.34 | 5.7 | 6.9 | 0.001 |
| Costs, $ | ||||||
| Total | 10663 | 11599 | 0.049 | 10681 | 13493 | <0.001 |
| Direct | 4952 | 4704 | 0.98 | 4956 | 5618 | 0.055 |
| Nursing | 2394 | 2454 | 0.19 | 2124 | 2744 | <0.001 |
| Imaging | 349 | 322 | 0.63 | 387 | 390 | 0.82 |
| Laboratory | 213 | 199 | 0.49 | 212 | 225 | 0.47 |
| Pharmacy | 647 | 616 | 0.85 | 547 | 654 | 0.22 |
| In‐hospital mortality,% | 2.9 | 2.3 | 0.77 | 2.6 | 3.4 | 0.005 |
| 7‐Day readmission,% | 8.1 | 6.4 | 0.17 | 3.9 | 4.1 | 0.97 |
| 30‐Day readmission, % | 22.0 | 17.1 | 0.013 | 20.9 | 20.8 | 0.75 |
| 90‐Day readmission, % | 40.2 | 32.4 | 0.013 | 39.1 | 38.7 | 0.86 |
We found no differences in a separate post hoc subgroup analysis assessing whether a 3‐month nurse coordinator's leave of absence during year 1 affected year 1 results. The service size was unaffected by her absence, and all patients continued to receive daily visits by the attending and fellow. During this time, other team members took over many of the nurse coordinator roles, except for the postdischarge phone calls.
DISCUSSION
Older adults constitute a disproportionate share of hospital admissions and hospital days. They typically have multiple comorbid conditions, higher rates of cognitive impairment and functional dependence, and complex social situations that all increase their risk of adverse outcomes. Current efforts for national healthcare reform focus on the combined economic and quality imperatives to improve the care of hospitalized older adults. Given the increasing representation of this fastest growing segment of the population in the acute care setting, the geographical unit‐based model for care delivery is untenable in many circumstances. Therefore, we developed a mobile ACE service in an effort to provide the geriatric‐focused acute care found on ACE units to older adults admitted to any medical unit in the hospital.
Our study compared operational and quality outcomes for older patients cared for by our mobile ACE service to those cared for on the unit‐based ACE service and other general medical services. We found a significant reduction in both LOS and costs in all 3 comparisons, except for LOS during the first year of the mobile ACE service. This heightened efficiency was not associated with changes in the quality measures of in‐hospital mortality and 7‐ and 30‐day readmission rates, though the 90‐day readmission rate was slightly higher for the MACE in year 1.
The adjusted total cost savings per admission in years 1 and 2 of approximately $2400 ($12,764 vs $10,311) and $4900 ($15,636 vs $10,693), respectively, translate into an overall annual savings of roughly $1,200,000 (500 patients $2400/patient) in year 1 and $2,450,000 (500 patients $4,900/patient) in year 2. The only relevant cost of the MACE service model compared with the comparison groups is the nurse coordinator salary and benefits, which are paid for by the hospital (as job responsibilities include participation in nursing department quality improvement projects and nursing education) and would not meaningfully offset these savings. The team social worker is a re‐allocation of existing hospital resources, whose salary line is likewise paid for by the hospital.
Our study has several important limitations. First, we lack data on readmissions to other hospitals. Our readmission rates are high compared with the national 19.6% 30‐day Medicare readmission rate cited in a recent study, and we failed to show significant reductions in in‐hospital mortality or 7‐ or 30‐day readmission rates.10 This lack of benefit may be related to control group patients, some of whom receive their community care outside of our institution, being more likely to be readmitted to other hospitals compared with our MACE patients, who were all receiving their ambulatory care in our associated faculty practice. In addition, the high readmission rate on the MACE service may be driven by a relatively small number of patients who are frequently admitted. For example, of the 363 unique MACE patients from year 2, 22 had 3 and 11 had 4 or 5 admissions. We are currently evaluating these 33 patients who accounted for 22% of the admissions to better understand the causes.
A second limitation of the study is selection bias. While patients were very well‐matched through propensity scoring and had identical DRG and DRG‐SOI levels (the latter having been demonstrated in a previous study's regression analysis to be the leading correlate of LOS and cost),9 there may be unaccounted for differences between the patients cared for on the MACE and in the control group. A third limitation is the external validity of our study, which took place in a single large academic medical center in New York City. While the MACE model may very well be readily adaptable elsewhere, numerous studies have demonstrated wide variation in medical practice patterns and healthcare use which may influence the exportability of the model.11, 12 However, our LOS of 5.8 and 5.6 days in years 1 and 2 of the MACE service, respectively, are similar to national data of 5.6 days for hospitalized adults >74 years of age.13
Benefits in cost and LOS reductions may be, in part, due to the hospitalist nature of the model as hospital medicine literature has demonstrated similar reductions for Medicare patients of approximately $1000 and 0.5 days per admission.8, 9 Our findings support this hypothesis as the LOS reduction was not present during the first year of our MACE service during which the hospitalist model was not fully implemented. During this transition phase from the unit‐based ACE to the mobile ACE service, there were 4 physicians who covered more than 75% of on‐service time (10 of the 13 annual 4‐week rotations), while the remaining 25% was covered by 3 physicians (each working 1 block). The following year (July 2008 to June 2009), during which an LOS reduction was demonstrated, a full geriatric medicine hospitalist model was in effect, with patients on the MACE service cared for 100% of the time (excluding weekends) by 1 of 4 geriatric medicine hospitalists. By comparison, 22% and 29% of control group patients were cared for by medicine hospitalists during years 1 and 2, respectively. In addition to this transition to a hospitalist model, there may have been other undefined service improvements over the first year which contributed to the LOS and total cost reductions achieved in year 2 in the hospitalist subgroup analysis. Likewise, the increased 90‐day readmission rates seen in year 1 but not in year 2 in both the main and hospitalist subgroup analyses may be related to MACE service improvements over time. A more vigorous proactive intervention beyond the follow‐up phone call is likely needed to impact 90‐day readmissions.
LOS reductions may also have been related to the interdisciplinary team‐based approach in which a need for family meetings to address goals of care or assess and attempt to resolve complex family/living situations was identified early in the course of hospitalization. Likewise, in New York State, the application process for discharge to a postacute care setting begins with the completion of a Patient Review Instrument (PRI), which contains detailed information on the patient's physical, medical, and cognitive status. The MACE model circumvents the traditional case manager's role of completing the PRI by having the MACE nurse coordinator trained and certified to do so. The daily or twice daily MACE team meeting may have enabled more timely initiation of this early step in the discharge process for these patients, ultimately resulting in a reduced LOS.
An important concern this study is not able to address is whether LOS reductions are achieved at a price of impaired functional status. A prospective longitudinal study on the outcomes of patients cared for by a MACE service that includes detailed assessments of functional status based upon information gathered during admission and postdischarge during follow‐up phone calls is needed to properly evaluate this possibility.
Given the lack of wide‐spread adoption of the traditional ACE unit‐based model of care and its inherent limitations in the setting of high occupancy rates, a mobile ACE service may prove useful in providing high quality clinical care with reduced LOS and costs. This team‐based, as opposed to unit‐based, approach benefits from having low entry costs, as hospital administration can re‐allocate existing resources to fit the model and avoid costly capital investments in specialized unit design and outfitting. Further research should include metrics on functional status, all‐hospital readmission rates, and patient/caregiver satisfaction to better assess the feasibility of this acute care model.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.Do acute care for elders units increase hospital costs? A cost analysis using the hospital perspective.J Am Geriatr Soc.1997;45:729–734.
- ,,, et al.Effects of multicomponent intervention of functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of acute care for elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1578.
- ,,,.A medical unit for the acute care of the elderly.J Am Geriatr Soc.1994;42:545–552
- ,,, et al.A randomized trial of care in a hospital medicine unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1342.
- ,,,.The care transitions intervention.Arch Intern Med.2006;166:1822–1828.
- ,,,.Comorbidity measures for use with administrative data.Med Care.1998;36:8–27.
- ,,.The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- ,,,,,.The value of a hospitalist service.Chest.2001;19:580–589.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,.Slowing the growth of health care costs ‐ lessons from regional variation.N Engl J Med.2009;360:849–852.
- ,,, et al.Fostering accountable health care: moving forward in Medicare.Health Aff (Millwood).2009;28:w219–w231.
- Centers for Disease Control and Prevention. Health, United States, 2009. Table 102. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. Accessed June 10,2010.
The traditional acute care for the elderly (ACE) unit has demonstrated improved functional outcomes without increased costs or changes in length of stay (LOS).15 It is, however, limited in scope to only those patients cared for on a fixed geographical unit. This structural limitation is of increasing relevance in times of high hospital bed occupancy rates, as during such times, many appropriate older patients are admitted elsewhere. In our experience with a traditional ACE unit‐based model, only 52% of our geriatrics practice patients were admitted to an ACE unit bed, while the remainder were admitted to various medical units throughout the hospital. We therefore abandoned our traditional unit‐based ACE service in July 2007 in favor of a mobile ACE (MACE) service, bringing the interdisciplinary, patient‐centered team approach to our hospitalized older adult patients admitted throughout the hospital.
The purpose of this study is to compare the operational and quality outcomes for patients cared for on the MACE service to those cared for on a unit‐based ACE service and matched controls cared for on other general medical services. We hypothesized that the MACE service would be associated with lower lengths of stay, reduced costs, and decreased rehospitalization rates.
METHODS
The MACE team was composed of a geriatrician‐hospitalist, geriatric medicine fellow, social worker, and nurse coordinator. The geriatric medicine attending on the MACE service was in the hospital providing patient care during regular working hours from Monday through Friday, while the weekends were covered by a rotating group of all geriatric medicine faculty. During the first and second years of MACE, there were 7 and 4 attendings, respectively; all fellowship‐trained geriatricians. Three of the 4 geriatric medicine hospitalists during year 2 had been in practice between 1 and 3 years postfellowship and also had training in palliative medicine, although were not board‐certified in the latter. The fourth hospitalist had been in practice for 5 years postfellowship. The interdisciplinary team met daily to discuss the care of all patients and used a transitional care model based on The Care Transitions Program6 adapted to our institution, with a focus on reducing the risks of hazards of hospitalization. Care coordination with the outpatient practice, early family meetings, discharge planning, patient and caregiver education, and postdischarge follow‐up phone calls were some of the key hallmarks of the service (Table 1).
| Team member(s) | Roles |
|---|---|
| |
| Team (MD, fellow, NC,SW) | Scheduled daily meetings at 8 am (or 8 am and 2 pm if needed) to discuss each patient's care and discharge plan |
| NC | Introduces the team to the patient/caregiver upon admission |
| Obtains prehospitalization information on cognitive and functional status | |
| Acts as a hospital coach educating the patient/caregiver | |
| Completes PRIs necessary for discharge to other institutions | |
| Completes medication reconciliation prior to discharge | |
| Initiates post‐discharge phone call and communicates with PCP via EMR | |
| Provides experiential one‐to‐one geriatric nursing education | |
| SW | Arranges family meeting, when indicated, with the team early in the hospitalization |
| Provides patient and family psychosocial support on an as needed basis | |
| Responsible for discharge planning | |
| MD | Attending physician of record |
| Communicates with PCP upon admission of the patient | |
| Assures discharge communiqu to PCP via EMR within 24 hours of discharge | |
We conducted a retrospective cohort study with propensity‐score matching in an urban academic medical center. Study subjects comprised 5 distinct groups. First were community‐dwelling older adults cared for at our outpatient geriatrics ambulatory practice who were discharged from our traditional ACE unit‐based acute care service at the Mount Sinai Hospital from July 1, 2006 through June 30, 2007 (N = 450). Second and third were patients from the same practice discharged from our MACE service during the first 2 years of operation (N = 556 from July 1, 2007 through June 30, 2008, and N = 501 from July 1, 2008 through June 30, 2009). Fourth and fifth were control cohorts of hospitalized older adults discharged from other medical services at the Mount Sinai Hospital during these same 2 years (N = 4863 and N = 4777, respectively). The average daily census on all services was 1012 patients.
Some patients on all 3 services are co‐managed with house staff, who are responsible for writing physician orders. Control cohort patients were cared for by a mix of private attendings (approximately 75%) or hospitalists (25%), and in contradistinction to MACE patients, their typical care did not include daily interdisciplinary team rounds, a nurse coordinator, or geriatrics fellow. Social work and case management were unit‐ as opposed to team‐based. Care on the ACE unit‐based service differed from care for matched control patients by having daily interdisciplinary team rounds, a prepared environment, and nursing‐led protocols for the patients on the ACE unit.
Because the ACE unit‐based service admitted both patients who were and were not cared for in our ambulatory practice, while the MACE service admitted only patients cared for in the ambulatory practice, we deleted from the study sample the patients who did not have a visit to our outpatient practice before the index hospitalization. This allowed us to isolate the effect of the model of care itself as opposed to the effect of simply changing the patient base for admissions. We then merged the files with the hospital's administrative database and electronic billing system to obtain demographic and claims data.
Additional demographic data were obtained through chart review of the MACE patients during year 1. The chart review process was standardized using a data abstraction instrument and by determining inter‐rater reliability of the individual data abstractors (comprised of author B.K. and 4 MACE team members).
Costs were assigned to individual admissions by the hospital's cost reporting system and include a combination of traceable costs (such as imaging, laboratory, and pharmacy) and applied costs (nursing; allocated based on geographic location in the hospital) to arrive at direct and total costs.
We made 3 distinct comparisons of operational and quality outcomes using the above 5 groups, first comparing patients cared for on our traditional ACE unit‐based service to those cared for on the MACE service, and second and third comparing patients on the MACE service to propensity score‐matched controls during the first and second year of operations. Specifically, we hypothesized that the MACE service would be associated with reduced LOS, costs, and readmission rates compared with the ACE unit‐based service and the matched control groups. We used multivariate logistic regression to estimate the association of binary quality outcomes (mortality during the hospital stay, 7‐ and 30‐day readmission rates) with the existence of MACE while adjusting for confounding variables which included patient demographic and clinical characteristics such as age, gender, race, total number of comorbidities (calculated by Elixhauser method that includes 30 categories of comorbid illnesses identified by secondary diagnosis codes and discharge diagnosis‐related groups [DRGs]).7 We considered the clustering effect due to the same attending physician into the model as well. While adjusting for the same covariates, we used generalized linear models with a gamma distribution and log link to estimate the association of continuous variables (costs and LOS) with the existence of MACE.
The same statistical methods were applied to the second and third comparisons between patients cared for on the MACE and the propensity score‐matched cohorts for the first and second year of the MACE service. First, 2 control cohorts (N = 6148 and 5803 of our hospital discharges from July 1, 2007 to June 30, 2008, and July 1, 2008 to June 30, 2009, respectively, with age > 64 and with the identical DRG and All Patient Refined DRG (APR DRG) Severity of Illness (SOI) score as those of the MACE groups were obtained from our hospital's administrative database to reduce the selection bias. Then, 4863 patients within the first cohort (N = 6148) and 4777 patients within the second cohort (N = 5,803) with the closest propensity score were matched to 545 of 556 MACE patients and 494 of 501 MACE patients, respectively, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score.
Propensity scores were determined by logistic regression on whether patients were admitted to the MACE. The covariates for the propensity model were the same as the previously stated adjusting variables. Usual care patients' data were weighted to account for the one‐to‐many propensity score‐matching algorithm.
We similarly conducted a post hoc analysis of MACE compared with a subgroup control cohort of patients cared for by medicine hospitalists in year 1 (N = 1175) and year 2 (N = 1564), with age > 64 and with the identical DRG and APR DRG SOI as those of the MACE group. We then matched 1012 of the 1175 discharges with the closest propensity score to 389 of the 411 MACE discharges who were cared for by 1 of the 4 geriatric medicine hospitalists in year 1 and 1308 of the 1564 discharges to 471 of the 501 MACE discharges in year 2, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score, using the same covariates described above.
All analyses were done using Stata software, version 9.2 (StataCorp LP, College Station, TX). This project was exempted by the Institutional Review Board at Mount Sinai School of Medicine, New York, New York.
RESULTS
Table 2 presents the characteristics of the study subjects in all 5 groups. Patients cared for on the ACE unit‐based service and the MACE service in years 1 and 2 were very similar, with a mean age of 82.6, 83.2, and 83.6 years; 74.4%, 75.9%, and 76.7% were female; and mean Elixhauser comorbidity scores were 3.4, 3.3, and 3.5, respectively. Patients in the 2 matched control groups were likewise very similar to those in the matched MACE groups with regard to all demographic variables.
| Demographics | ACE (N = 450) | Matched MACE year 1 (N = 545) | Matched controls year 1 (N = 4863) | Matched MACE year 2 (N = 494) | Matched controls year 2 (N = 4777) |
|---|---|---|---|---|---|
| |||||
| Age SD | 82.6 8.4 | 83.2 8.3 | 83.4 8.8 | 83.6 8.1 | 83.8 8.5 |
| Female, % | 74.4% | 75.9% | 74.7% | 76.7% | 77.4% |
| Race, % | |||||
| White | 35 | 37 | 36 | 43 | 42 |
| Black | 30 | 27 | 28 | 25 | 25 |
| Hispanic | 33 | 34 | 35 | 28 | 30 |
| Asian | 1 | 1 | 1 | 3 | 3 |
| Marital status, % | |||||
| Married | 20 | 20 | 21 | 23 | 23 |
| Widowed | 44 | 45 | 44 | 46 | 38 |
| Single | 25 | 22 | 27 | 21 | 28 |
| Elixhauser comorbidity index mean (SD) | 3.4 (1.8) | 3.4 (1.6) | 3.3 (1.7) | 3.5 (1.7) | 3.5 (1.7) |
| Hypertension, % | 61 | 54 | 54 | 49 | 49 |
| Heart Failure, % | 25 | 27 | 28 | 26 | 27 |
| Diabetes Mellitus, % | 26 | 25 | 25 | 24 | 25 |
| Atrial fibrillation, % | 22 | 23 | 23 | 28 | 27 |
| Chronic obstructive pulmonary disease, % | 15 | 15 | 15 | 15 | 14 |
Chart review of the year 1 MACE discharges revealed that 70% spoke English as their primary language and 46% had cognitive impairment. Most lived at home alone (49%) or with family members (41%) while receiving some paid caregiver help (59%). The remaining 10% were admitted from either an assisted living facility (5%) or subacute rehabilitation (5%). Only 12% were wheelchair or bed‐bound, while 21% ambulated without and 67% with an assistive device. Their functional status was limited, with 58% dependent for both ADLs and IADLs, 22% dependent for IADLs only, and 20% independent in both. They had relatively high prescription medication burdens, with 10% taking 05, 34% taking 610, 38% taking 1115, and 18% taking >15 medications.
Patients cared for by the MACE service had an adjusted 2.1 days shorter LOS (P < 0.001) when compared with patients cared for on the ACE unit service. Additionally, there was a net savings of $2872 in total costs per hospitalization (P = 0.002), $1094 in direct costs (P = 0.016), $849 in nursing costs (P < 0.001), and $237 in pharmacy costs (P = 0.002). Imaging and laboratory costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
| MACE to ACE | MACE to matched controls, year 1 | MACE to matched controls, year 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MACE (N = 556) | ACE (N = 450) | P value | MACE (N = 545) | Matched controls (N = 4863) | P value | MACE (N = 494) | Matched controls (N = 4777) | P value | |
| |||||||||
| LOS, days | 5.8 | 7.9 | <0.001 | 5.8 | 6.5 | 0.15 | 5.6 | 7.2 | <0.001 |
| Costs, $ | |||||||||
| Total | 10315 | 13187 | 0.002 | 10311 | 12764 | <0.001 | 10693 | 15636 | <0.001 |
| Direct | 4777 | 5871 | 0.016 | 4778 | 5620 | 0.03 | 4967 | 7048 | <0.001 |
| Nursing | 2361 | 3210 | <0.001 | 2356 | 2749 | 0.026 | 2143 | 3080 | <0.001 |
| Imaging | 342 | 332 | 0.61 | 344 | 349 | 0.73 | 382 | 471 | 0.06 |
| Laboratory | 206 | 243 | 0.079 | 206 | 245 | 0.029 | 213 | 281 | <0.001 |
| Pharmacy | 598 | 835 | 0.002 | 597 | 662 | 0.63 | 563 | 786 | 0.03 |
| In‐hospital mortality,% | 3.3 | 3.9 | 0.66 | 2.9 | 2.6 | 0.3 | 5.3 | 3.6 | 0.053 |
| 7‐day readmission,% | 9.3 | 10.2 | 0.55 | 9.7 | 11.8 | 0.3 | 4.8 | 5.5 | 0.71 |
| 30‐day readmission, % | 23.6 | 25.9 | 0.5 | 23.8 | 24.3 | 0.65 | 21.1 | 20.9 | 0.62 |
| 90‐day readmission, % | 40.9 | 38.7 | 0.1 | 41.3 | 38.4 | 0.005 | 38.0 | 36.5 | 0.74 |
There was no difference in LOS between the MACE patients during the first year of service compared with propensity score‐matched control patients (5.8 vs 6.5 days). There was, however, a net savings of $2453 in total costs per hospitalization (P < 0.001), $842 (P = 0.03) in direct costs, $393 in nursing costs (P = 0.026), and $39 in laboratory costs (P = 0.029). Imaging and pharmacy costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day or 30‐day readmission rates between the 2 groups. However, the 90‐day readmission rate was higher in MACE patients (Table 3).
During the second year of the MACE service, however, there was a significant reduction in LOS of 1.6 days (P < 0.001), a net savings of $4943 in total costs per hospitalization (P < 0.001), $2081 (P < 0.001) in direct costs, $937 in nursing costs (P < 0.001), $68 in laboratory costs (P < 0.001), and $223 in pharmacy costs (P = 0.03). There were no significant differences in imaging costs, in‐hospital mortality, and 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
A subgroup analysis of the first and second year comparisons including only those patients in the control groups cared for by medicine hospitalists demonstrated reductions in the MACE in total cost in year 1 and LOS, mortality, total, and nursing costs in year 2. However, in year 1, the 30‐day and 90‐day readmission rates were increased in the MACE compared with the control group (Table 4).
| MACE, year 1 (N = 389) | Matched controls, year 1 (N = 1012) | P Value | MACE, year 2 (N = 471) | Matched controls, year 2 (N = 1308) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| LOS, days | 6.0 | 6.0 | 0.34 | 5.7 | 6.9 | 0.001 |
| Costs, $ | ||||||
| Total | 10663 | 11599 | 0.049 | 10681 | 13493 | <0.001 |
| Direct | 4952 | 4704 | 0.98 | 4956 | 5618 | 0.055 |
| Nursing | 2394 | 2454 | 0.19 | 2124 | 2744 | <0.001 |
| Imaging | 349 | 322 | 0.63 | 387 | 390 | 0.82 |
| Laboratory | 213 | 199 | 0.49 | 212 | 225 | 0.47 |
| Pharmacy | 647 | 616 | 0.85 | 547 | 654 | 0.22 |
| In‐hospital mortality,% | 2.9 | 2.3 | 0.77 | 2.6 | 3.4 | 0.005 |
| 7‐Day readmission,% | 8.1 | 6.4 | 0.17 | 3.9 | 4.1 | 0.97 |
| 30‐Day readmission, % | 22.0 | 17.1 | 0.013 | 20.9 | 20.8 | 0.75 |
| 90‐Day readmission, % | 40.2 | 32.4 | 0.013 | 39.1 | 38.7 | 0.86 |
We found no differences in a separate post hoc subgroup analysis assessing whether a 3‐month nurse coordinator's leave of absence during year 1 affected year 1 results. The service size was unaffected by her absence, and all patients continued to receive daily visits by the attending and fellow. During this time, other team members took over many of the nurse coordinator roles, except for the postdischarge phone calls.
DISCUSSION
Older adults constitute a disproportionate share of hospital admissions and hospital days. They typically have multiple comorbid conditions, higher rates of cognitive impairment and functional dependence, and complex social situations that all increase their risk of adverse outcomes. Current efforts for national healthcare reform focus on the combined economic and quality imperatives to improve the care of hospitalized older adults. Given the increasing representation of this fastest growing segment of the population in the acute care setting, the geographical unit‐based model for care delivery is untenable in many circumstances. Therefore, we developed a mobile ACE service in an effort to provide the geriatric‐focused acute care found on ACE units to older adults admitted to any medical unit in the hospital.
Our study compared operational and quality outcomes for older patients cared for by our mobile ACE service to those cared for on the unit‐based ACE service and other general medical services. We found a significant reduction in both LOS and costs in all 3 comparisons, except for LOS during the first year of the mobile ACE service. This heightened efficiency was not associated with changes in the quality measures of in‐hospital mortality and 7‐ and 30‐day readmission rates, though the 90‐day readmission rate was slightly higher for the MACE in year 1.
The adjusted total cost savings per admission in years 1 and 2 of approximately $2400 ($12,764 vs $10,311) and $4900 ($15,636 vs $10,693), respectively, translate into an overall annual savings of roughly $1,200,000 (500 patients $2400/patient) in year 1 and $2,450,000 (500 patients $4,900/patient) in year 2. The only relevant cost of the MACE service model compared with the comparison groups is the nurse coordinator salary and benefits, which are paid for by the hospital (as job responsibilities include participation in nursing department quality improvement projects and nursing education) and would not meaningfully offset these savings. The team social worker is a re‐allocation of existing hospital resources, whose salary line is likewise paid for by the hospital.
Our study has several important limitations. First, we lack data on readmissions to other hospitals. Our readmission rates are high compared with the national 19.6% 30‐day Medicare readmission rate cited in a recent study, and we failed to show significant reductions in in‐hospital mortality or 7‐ or 30‐day readmission rates.10 This lack of benefit may be related to control group patients, some of whom receive their community care outside of our institution, being more likely to be readmitted to other hospitals compared with our MACE patients, who were all receiving their ambulatory care in our associated faculty practice. In addition, the high readmission rate on the MACE service may be driven by a relatively small number of patients who are frequently admitted. For example, of the 363 unique MACE patients from year 2, 22 had 3 and 11 had 4 or 5 admissions. We are currently evaluating these 33 patients who accounted for 22% of the admissions to better understand the causes.
A second limitation of the study is selection bias. While patients were very well‐matched through propensity scoring and had identical DRG and DRG‐SOI levels (the latter having been demonstrated in a previous study's regression analysis to be the leading correlate of LOS and cost),9 there may be unaccounted for differences between the patients cared for on the MACE and in the control group. A third limitation is the external validity of our study, which took place in a single large academic medical center in New York City. While the MACE model may very well be readily adaptable elsewhere, numerous studies have demonstrated wide variation in medical practice patterns and healthcare use which may influence the exportability of the model.11, 12 However, our LOS of 5.8 and 5.6 days in years 1 and 2 of the MACE service, respectively, are similar to national data of 5.6 days for hospitalized adults >74 years of age.13
Benefits in cost and LOS reductions may be, in part, due to the hospitalist nature of the model as hospital medicine literature has demonstrated similar reductions for Medicare patients of approximately $1000 and 0.5 days per admission.8, 9 Our findings support this hypothesis as the LOS reduction was not present during the first year of our MACE service during which the hospitalist model was not fully implemented. During this transition phase from the unit‐based ACE to the mobile ACE service, there were 4 physicians who covered more than 75% of on‐service time (10 of the 13 annual 4‐week rotations), while the remaining 25% was covered by 3 physicians (each working 1 block). The following year (July 2008 to June 2009), during which an LOS reduction was demonstrated, a full geriatric medicine hospitalist model was in effect, with patients on the MACE service cared for 100% of the time (excluding weekends) by 1 of 4 geriatric medicine hospitalists. By comparison, 22% and 29% of control group patients were cared for by medicine hospitalists during years 1 and 2, respectively. In addition to this transition to a hospitalist model, there may have been other undefined service improvements over the first year which contributed to the LOS and total cost reductions achieved in year 2 in the hospitalist subgroup analysis. Likewise, the increased 90‐day readmission rates seen in year 1 but not in year 2 in both the main and hospitalist subgroup analyses may be related to MACE service improvements over time. A more vigorous proactive intervention beyond the follow‐up phone call is likely needed to impact 90‐day readmissions.
LOS reductions may also have been related to the interdisciplinary team‐based approach in which a need for family meetings to address goals of care or assess and attempt to resolve complex family/living situations was identified early in the course of hospitalization. Likewise, in New York State, the application process for discharge to a postacute care setting begins with the completion of a Patient Review Instrument (PRI), which contains detailed information on the patient's physical, medical, and cognitive status. The MACE model circumvents the traditional case manager's role of completing the PRI by having the MACE nurse coordinator trained and certified to do so. The daily or twice daily MACE team meeting may have enabled more timely initiation of this early step in the discharge process for these patients, ultimately resulting in a reduced LOS.
An important concern this study is not able to address is whether LOS reductions are achieved at a price of impaired functional status. A prospective longitudinal study on the outcomes of patients cared for by a MACE service that includes detailed assessments of functional status based upon information gathered during admission and postdischarge during follow‐up phone calls is needed to properly evaluate this possibility.
Given the lack of wide‐spread adoption of the traditional ACE unit‐based model of care and its inherent limitations in the setting of high occupancy rates, a mobile ACE service may prove useful in providing high quality clinical care with reduced LOS and costs. This team‐based, as opposed to unit‐based, approach benefits from having low entry costs, as hospital administration can re‐allocate existing resources to fit the model and avoid costly capital investments in specialized unit design and outfitting. Further research should include metrics on functional status, all‐hospital readmission rates, and patient/caregiver satisfaction to better assess the feasibility of this acute care model.
The traditional acute care for the elderly (ACE) unit has demonstrated improved functional outcomes without increased costs or changes in length of stay (LOS).15 It is, however, limited in scope to only those patients cared for on a fixed geographical unit. This structural limitation is of increasing relevance in times of high hospital bed occupancy rates, as during such times, many appropriate older patients are admitted elsewhere. In our experience with a traditional ACE unit‐based model, only 52% of our geriatrics practice patients were admitted to an ACE unit bed, while the remainder were admitted to various medical units throughout the hospital. We therefore abandoned our traditional unit‐based ACE service in July 2007 in favor of a mobile ACE (MACE) service, bringing the interdisciplinary, patient‐centered team approach to our hospitalized older adult patients admitted throughout the hospital.
The purpose of this study is to compare the operational and quality outcomes for patients cared for on the MACE service to those cared for on a unit‐based ACE service and matched controls cared for on other general medical services. We hypothesized that the MACE service would be associated with lower lengths of stay, reduced costs, and decreased rehospitalization rates.
METHODS
The MACE team was composed of a geriatrician‐hospitalist, geriatric medicine fellow, social worker, and nurse coordinator. The geriatric medicine attending on the MACE service was in the hospital providing patient care during regular working hours from Monday through Friday, while the weekends were covered by a rotating group of all geriatric medicine faculty. During the first and second years of MACE, there were 7 and 4 attendings, respectively; all fellowship‐trained geriatricians. Three of the 4 geriatric medicine hospitalists during year 2 had been in practice between 1 and 3 years postfellowship and also had training in palliative medicine, although were not board‐certified in the latter. The fourth hospitalist had been in practice for 5 years postfellowship. The interdisciplinary team met daily to discuss the care of all patients and used a transitional care model based on The Care Transitions Program6 adapted to our institution, with a focus on reducing the risks of hazards of hospitalization. Care coordination with the outpatient practice, early family meetings, discharge planning, patient and caregiver education, and postdischarge follow‐up phone calls were some of the key hallmarks of the service (Table 1).
| Team member(s) | Roles |
|---|---|
| |
| Team (MD, fellow, NC,SW) | Scheduled daily meetings at 8 am (or 8 am and 2 pm if needed) to discuss each patient's care and discharge plan |
| NC | Introduces the team to the patient/caregiver upon admission |
| Obtains prehospitalization information on cognitive and functional status | |
| Acts as a hospital coach educating the patient/caregiver | |
| Completes PRIs necessary for discharge to other institutions | |
| Completes medication reconciliation prior to discharge | |
| Initiates post‐discharge phone call and communicates with PCP via EMR | |
| Provides experiential one‐to‐one geriatric nursing education | |
| SW | Arranges family meeting, when indicated, with the team early in the hospitalization |
| Provides patient and family psychosocial support on an as needed basis | |
| Responsible for discharge planning | |
| MD | Attending physician of record |
| Communicates with PCP upon admission of the patient | |
| Assures discharge communiqu to PCP via EMR within 24 hours of discharge | |
We conducted a retrospective cohort study with propensity‐score matching in an urban academic medical center. Study subjects comprised 5 distinct groups. First were community‐dwelling older adults cared for at our outpatient geriatrics ambulatory practice who were discharged from our traditional ACE unit‐based acute care service at the Mount Sinai Hospital from July 1, 2006 through June 30, 2007 (N = 450). Second and third were patients from the same practice discharged from our MACE service during the first 2 years of operation (N = 556 from July 1, 2007 through June 30, 2008, and N = 501 from July 1, 2008 through June 30, 2009). Fourth and fifth were control cohorts of hospitalized older adults discharged from other medical services at the Mount Sinai Hospital during these same 2 years (N = 4863 and N = 4777, respectively). The average daily census on all services was 1012 patients.
Some patients on all 3 services are co‐managed with house staff, who are responsible for writing physician orders. Control cohort patients were cared for by a mix of private attendings (approximately 75%) or hospitalists (25%), and in contradistinction to MACE patients, their typical care did not include daily interdisciplinary team rounds, a nurse coordinator, or geriatrics fellow. Social work and case management were unit‐ as opposed to team‐based. Care on the ACE unit‐based service differed from care for matched control patients by having daily interdisciplinary team rounds, a prepared environment, and nursing‐led protocols for the patients on the ACE unit.
Because the ACE unit‐based service admitted both patients who were and were not cared for in our ambulatory practice, while the MACE service admitted only patients cared for in the ambulatory practice, we deleted from the study sample the patients who did not have a visit to our outpatient practice before the index hospitalization. This allowed us to isolate the effect of the model of care itself as opposed to the effect of simply changing the patient base for admissions. We then merged the files with the hospital's administrative database and electronic billing system to obtain demographic and claims data.
Additional demographic data were obtained through chart review of the MACE patients during year 1. The chart review process was standardized using a data abstraction instrument and by determining inter‐rater reliability of the individual data abstractors (comprised of author B.K. and 4 MACE team members).
Costs were assigned to individual admissions by the hospital's cost reporting system and include a combination of traceable costs (such as imaging, laboratory, and pharmacy) and applied costs (nursing; allocated based on geographic location in the hospital) to arrive at direct and total costs.
We made 3 distinct comparisons of operational and quality outcomes using the above 5 groups, first comparing patients cared for on our traditional ACE unit‐based service to those cared for on the MACE service, and second and third comparing patients on the MACE service to propensity score‐matched controls during the first and second year of operations. Specifically, we hypothesized that the MACE service would be associated with reduced LOS, costs, and readmission rates compared with the ACE unit‐based service and the matched control groups. We used multivariate logistic regression to estimate the association of binary quality outcomes (mortality during the hospital stay, 7‐ and 30‐day readmission rates) with the existence of MACE while adjusting for confounding variables which included patient demographic and clinical characteristics such as age, gender, race, total number of comorbidities (calculated by Elixhauser method that includes 30 categories of comorbid illnesses identified by secondary diagnosis codes and discharge diagnosis‐related groups [DRGs]).7 We considered the clustering effect due to the same attending physician into the model as well. While adjusting for the same covariates, we used generalized linear models with a gamma distribution and log link to estimate the association of continuous variables (costs and LOS) with the existence of MACE.
The same statistical methods were applied to the second and third comparisons between patients cared for on the MACE and the propensity score‐matched cohorts for the first and second year of the MACE service. First, 2 control cohorts (N = 6148 and 5803 of our hospital discharges from July 1, 2007 to June 30, 2008, and July 1, 2008 to June 30, 2009, respectively, with age > 64 and with the identical DRG and All Patient Refined DRG (APR DRG) Severity of Illness (SOI) score as those of the MACE groups were obtained from our hospital's administrative database to reduce the selection bias. Then, 4863 patients within the first cohort (N = 6148) and 4777 patients within the second cohort (N = 5,803) with the closest propensity score were matched to 545 of 556 MACE patients and 494 of 501 MACE patients, respectively, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score.
Propensity scores were determined by logistic regression on whether patients were admitted to the MACE. The covariates for the propensity model were the same as the previously stated adjusting variables. Usual care patients' data were weighted to account for the one‐to‐many propensity score‐matching algorithm.
We similarly conducted a post hoc analysis of MACE compared with a subgroup control cohort of patients cared for by medicine hospitalists in year 1 (N = 1175) and year 2 (N = 1564), with age > 64 and with the identical DRG and APR DRG SOI as those of the MACE group. We then matched 1012 of the 1175 discharges with the closest propensity score to 389 of the 411 MACE discharges who were cared for by 1 of the 4 geriatric medicine hospitalists in year 1 and 1308 of the 1564 discharges to 471 of the 501 MACE discharges in year 2, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score, using the same covariates described above.
All analyses were done using Stata software, version 9.2 (StataCorp LP, College Station, TX). This project was exempted by the Institutional Review Board at Mount Sinai School of Medicine, New York, New York.
RESULTS
Table 2 presents the characteristics of the study subjects in all 5 groups. Patients cared for on the ACE unit‐based service and the MACE service in years 1 and 2 were very similar, with a mean age of 82.6, 83.2, and 83.6 years; 74.4%, 75.9%, and 76.7% were female; and mean Elixhauser comorbidity scores were 3.4, 3.3, and 3.5, respectively. Patients in the 2 matched control groups were likewise very similar to those in the matched MACE groups with regard to all demographic variables.
| Demographics | ACE (N = 450) | Matched MACE year 1 (N = 545) | Matched controls year 1 (N = 4863) | Matched MACE year 2 (N = 494) | Matched controls year 2 (N = 4777) |
|---|---|---|---|---|---|
| |||||
| Age SD | 82.6 8.4 | 83.2 8.3 | 83.4 8.8 | 83.6 8.1 | 83.8 8.5 |
| Female, % | 74.4% | 75.9% | 74.7% | 76.7% | 77.4% |
| Race, % | |||||
| White | 35 | 37 | 36 | 43 | 42 |
| Black | 30 | 27 | 28 | 25 | 25 |
| Hispanic | 33 | 34 | 35 | 28 | 30 |
| Asian | 1 | 1 | 1 | 3 | 3 |
| Marital status, % | |||||
| Married | 20 | 20 | 21 | 23 | 23 |
| Widowed | 44 | 45 | 44 | 46 | 38 |
| Single | 25 | 22 | 27 | 21 | 28 |
| Elixhauser comorbidity index mean (SD) | 3.4 (1.8) | 3.4 (1.6) | 3.3 (1.7) | 3.5 (1.7) | 3.5 (1.7) |
| Hypertension, % | 61 | 54 | 54 | 49 | 49 |
| Heart Failure, % | 25 | 27 | 28 | 26 | 27 |
| Diabetes Mellitus, % | 26 | 25 | 25 | 24 | 25 |
| Atrial fibrillation, % | 22 | 23 | 23 | 28 | 27 |
| Chronic obstructive pulmonary disease, % | 15 | 15 | 15 | 15 | 14 |
Chart review of the year 1 MACE discharges revealed that 70% spoke English as their primary language and 46% had cognitive impairment. Most lived at home alone (49%) or with family members (41%) while receiving some paid caregiver help (59%). The remaining 10% were admitted from either an assisted living facility (5%) or subacute rehabilitation (5%). Only 12% were wheelchair or bed‐bound, while 21% ambulated without and 67% with an assistive device. Their functional status was limited, with 58% dependent for both ADLs and IADLs, 22% dependent for IADLs only, and 20% independent in both. They had relatively high prescription medication burdens, with 10% taking 05, 34% taking 610, 38% taking 1115, and 18% taking >15 medications.
Patients cared for by the MACE service had an adjusted 2.1 days shorter LOS (P < 0.001) when compared with patients cared for on the ACE unit service. Additionally, there was a net savings of $2872 in total costs per hospitalization (P = 0.002), $1094 in direct costs (P = 0.016), $849 in nursing costs (P < 0.001), and $237 in pharmacy costs (P = 0.002). Imaging and laboratory costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
| MACE to ACE | MACE to matched controls, year 1 | MACE to matched controls, year 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MACE (N = 556) | ACE (N = 450) | P value | MACE (N = 545) | Matched controls (N = 4863) | P value | MACE (N = 494) | Matched controls (N = 4777) | P value | |
| |||||||||
| LOS, days | 5.8 | 7.9 | <0.001 | 5.8 | 6.5 | 0.15 | 5.6 | 7.2 | <0.001 |
| Costs, $ | |||||||||
| Total | 10315 | 13187 | 0.002 | 10311 | 12764 | <0.001 | 10693 | 15636 | <0.001 |
| Direct | 4777 | 5871 | 0.016 | 4778 | 5620 | 0.03 | 4967 | 7048 | <0.001 |
| Nursing | 2361 | 3210 | <0.001 | 2356 | 2749 | 0.026 | 2143 | 3080 | <0.001 |
| Imaging | 342 | 332 | 0.61 | 344 | 349 | 0.73 | 382 | 471 | 0.06 |
| Laboratory | 206 | 243 | 0.079 | 206 | 245 | 0.029 | 213 | 281 | <0.001 |
| Pharmacy | 598 | 835 | 0.002 | 597 | 662 | 0.63 | 563 | 786 | 0.03 |
| In‐hospital mortality,% | 3.3 | 3.9 | 0.66 | 2.9 | 2.6 | 0.3 | 5.3 | 3.6 | 0.053 |
| 7‐day readmission,% | 9.3 | 10.2 | 0.55 | 9.7 | 11.8 | 0.3 | 4.8 | 5.5 | 0.71 |
| 30‐day readmission, % | 23.6 | 25.9 | 0.5 | 23.8 | 24.3 | 0.65 | 21.1 | 20.9 | 0.62 |
| 90‐day readmission, % | 40.9 | 38.7 | 0.1 | 41.3 | 38.4 | 0.005 | 38.0 | 36.5 | 0.74 |
There was no difference in LOS between the MACE patients during the first year of service compared with propensity score‐matched control patients (5.8 vs 6.5 days). There was, however, a net savings of $2453 in total costs per hospitalization (P < 0.001), $842 (P = 0.03) in direct costs, $393 in nursing costs (P = 0.026), and $39 in laboratory costs (P = 0.029). Imaging and pharmacy costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day or 30‐day readmission rates between the 2 groups. However, the 90‐day readmission rate was higher in MACE patients (Table 3).
During the second year of the MACE service, however, there was a significant reduction in LOS of 1.6 days (P < 0.001), a net savings of $4943 in total costs per hospitalization (P < 0.001), $2081 (P < 0.001) in direct costs, $937 in nursing costs (P < 0.001), $68 in laboratory costs (P < 0.001), and $223 in pharmacy costs (P = 0.03). There were no significant differences in imaging costs, in‐hospital mortality, and 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
A subgroup analysis of the first and second year comparisons including only those patients in the control groups cared for by medicine hospitalists demonstrated reductions in the MACE in total cost in year 1 and LOS, mortality, total, and nursing costs in year 2. However, in year 1, the 30‐day and 90‐day readmission rates were increased in the MACE compared with the control group (Table 4).
| MACE, year 1 (N = 389) | Matched controls, year 1 (N = 1012) | P Value | MACE, year 2 (N = 471) | Matched controls, year 2 (N = 1308) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| LOS, days | 6.0 | 6.0 | 0.34 | 5.7 | 6.9 | 0.001 |
| Costs, $ | ||||||
| Total | 10663 | 11599 | 0.049 | 10681 | 13493 | <0.001 |
| Direct | 4952 | 4704 | 0.98 | 4956 | 5618 | 0.055 |
| Nursing | 2394 | 2454 | 0.19 | 2124 | 2744 | <0.001 |
| Imaging | 349 | 322 | 0.63 | 387 | 390 | 0.82 |
| Laboratory | 213 | 199 | 0.49 | 212 | 225 | 0.47 |
| Pharmacy | 647 | 616 | 0.85 | 547 | 654 | 0.22 |
| In‐hospital mortality,% | 2.9 | 2.3 | 0.77 | 2.6 | 3.4 | 0.005 |
| 7‐Day readmission,% | 8.1 | 6.4 | 0.17 | 3.9 | 4.1 | 0.97 |
| 30‐Day readmission, % | 22.0 | 17.1 | 0.013 | 20.9 | 20.8 | 0.75 |
| 90‐Day readmission, % | 40.2 | 32.4 | 0.013 | 39.1 | 38.7 | 0.86 |
We found no differences in a separate post hoc subgroup analysis assessing whether a 3‐month nurse coordinator's leave of absence during year 1 affected year 1 results. The service size was unaffected by her absence, and all patients continued to receive daily visits by the attending and fellow. During this time, other team members took over many of the nurse coordinator roles, except for the postdischarge phone calls.
DISCUSSION
Older adults constitute a disproportionate share of hospital admissions and hospital days. They typically have multiple comorbid conditions, higher rates of cognitive impairment and functional dependence, and complex social situations that all increase their risk of adverse outcomes. Current efforts for national healthcare reform focus on the combined economic and quality imperatives to improve the care of hospitalized older adults. Given the increasing representation of this fastest growing segment of the population in the acute care setting, the geographical unit‐based model for care delivery is untenable in many circumstances. Therefore, we developed a mobile ACE service in an effort to provide the geriatric‐focused acute care found on ACE units to older adults admitted to any medical unit in the hospital.
Our study compared operational and quality outcomes for older patients cared for by our mobile ACE service to those cared for on the unit‐based ACE service and other general medical services. We found a significant reduction in both LOS and costs in all 3 comparisons, except for LOS during the first year of the mobile ACE service. This heightened efficiency was not associated with changes in the quality measures of in‐hospital mortality and 7‐ and 30‐day readmission rates, though the 90‐day readmission rate was slightly higher for the MACE in year 1.
The adjusted total cost savings per admission in years 1 and 2 of approximately $2400 ($12,764 vs $10,311) and $4900 ($15,636 vs $10,693), respectively, translate into an overall annual savings of roughly $1,200,000 (500 patients $2400/patient) in year 1 and $2,450,000 (500 patients $4,900/patient) in year 2. The only relevant cost of the MACE service model compared with the comparison groups is the nurse coordinator salary and benefits, which are paid for by the hospital (as job responsibilities include participation in nursing department quality improvement projects and nursing education) and would not meaningfully offset these savings. The team social worker is a re‐allocation of existing hospital resources, whose salary line is likewise paid for by the hospital.
Our study has several important limitations. First, we lack data on readmissions to other hospitals. Our readmission rates are high compared with the national 19.6% 30‐day Medicare readmission rate cited in a recent study, and we failed to show significant reductions in in‐hospital mortality or 7‐ or 30‐day readmission rates.10 This lack of benefit may be related to control group patients, some of whom receive their community care outside of our institution, being more likely to be readmitted to other hospitals compared with our MACE patients, who were all receiving their ambulatory care in our associated faculty practice. In addition, the high readmission rate on the MACE service may be driven by a relatively small number of patients who are frequently admitted. For example, of the 363 unique MACE patients from year 2, 22 had 3 and 11 had 4 or 5 admissions. We are currently evaluating these 33 patients who accounted for 22% of the admissions to better understand the causes.
A second limitation of the study is selection bias. While patients were very well‐matched through propensity scoring and had identical DRG and DRG‐SOI levels (the latter having been demonstrated in a previous study's regression analysis to be the leading correlate of LOS and cost),9 there may be unaccounted for differences between the patients cared for on the MACE and in the control group. A third limitation is the external validity of our study, which took place in a single large academic medical center in New York City. While the MACE model may very well be readily adaptable elsewhere, numerous studies have demonstrated wide variation in medical practice patterns and healthcare use which may influence the exportability of the model.11, 12 However, our LOS of 5.8 and 5.6 days in years 1 and 2 of the MACE service, respectively, are similar to national data of 5.6 days for hospitalized adults >74 years of age.13
Benefits in cost and LOS reductions may be, in part, due to the hospitalist nature of the model as hospital medicine literature has demonstrated similar reductions for Medicare patients of approximately $1000 and 0.5 days per admission.8, 9 Our findings support this hypothesis as the LOS reduction was not present during the first year of our MACE service during which the hospitalist model was not fully implemented. During this transition phase from the unit‐based ACE to the mobile ACE service, there were 4 physicians who covered more than 75% of on‐service time (10 of the 13 annual 4‐week rotations), while the remaining 25% was covered by 3 physicians (each working 1 block). The following year (July 2008 to June 2009), during which an LOS reduction was demonstrated, a full geriatric medicine hospitalist model was in effect, with patients on the MACE service cared for 100% of the time (excluding weekends) by 1 of 4 geriatric medicine hospitalists. By comparison, 22% and 29% of control group patients were cared for by medicine hospitalists during years 1 and 2, respectively. In addition to this transition to a hospitalist model, there may have been other undefined service improvements over the first year which contributed to the LOS and total cost reductions achieved in year 2 in the hospitalist subgroup analysis. Likewise, the increased 90‐day readmission rates seen in year 1 but not in year 2 in both the main and hospitalist subgroup analyses may be related to MACE service improvements over time. A more vigorous proactive intervention beyond the follow‐up phone call is likely needed to impact 90‐day readmissions.
LOS reductions may also have been related to the interdisciplinary team‐based approach in which a need for family meetings to address goals of care or assess and attempt to resolve complex family/living situations was identified early in the course of hospitalization. Likewise, in New York State, the application process for discharge to a postacute care setting begins with the completion of a Patient Review Instrument (PRI), which contains detailed information on the patient's physical, medical, and cognitive status. The MACE model circumvents the traditional case manager's role of completing the PRI by having the MACE nurse coordinator trained and certified to do so. The daily or twice daily MACE team meeting may have enabled more timely initiation of this early step in the discharge process for these patients, ultimately resulting in a reduced LOS.
An important concern this study is not able to address is whether LOS reductions are achieved at a price of impaired functional status. A prospective longitudinal study on the outcomes of patients cared for by a MACE service that includes detailed assessments of functional status based upon information gathered during admission and postdischarge during follow‐up phone calls is needed to properly evaluate this possibility.
Given the lack of wide‐spread adoption of the traditional ACE unit‐based model of care and its inherent limitations in the setting of high occupancy rates, a mobile ACE service may prove useful in providing high quality clinical care with reduced LOS and costs. This team‐based, as opposed to unit‐based, approach benefits from having low entry costs, as hospital administration can re‐allocate existing resources to fit the model and avoid costly capital investments in specialized unit design and outfitting. Further research should include metrics on functional status, all‐hospital readmission rates, and patient/caregiver satisfaction to better assess the feasibility of this acute care model.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.Do acute care for elders units increase hospital costs? A cost analysis using the hospital perspective.J Am Geriatr Soc.1997;45:729–734.
- ,,, et al.Effects of multicomponent intervention of functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of acute care for elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1578.
- ,,,.A medical unit for the acute care of the elderly.J Am Geriatr Soc.1994;42:545–552
- ,,, et al.A randomized trial of care in a hospital medicine unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1342.
- ,,,.The care transitions intervention.Arch Intern Med.2006;166:1822–1828.
- ,,,.Comorbidity measures for use with administrative data.Med Care.1998;36:8–27.
- ,,.The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- ,,,,,.The value of a hospitalist service.Chest.2001;19:580–589.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,.Slowing the growth of health care costs ‐ lessons from regional variation.N Engl J Med.2009;360:849–852.
- ,,, et al.Fostering accountable health care: moving forward in Medicare.Health Aff (Millwood).2009;28:w219–w231.
- Centers for Disease Control and Prevention. Health, United States, 2009. Table 102. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. Accessed June 10,2010.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.Do acute care for elders units increase hospital costs? A cost analysis using the hospital perspective.J Am Geriatr Soc.1997;45:729–734.
- ,,, et al.Effects of multicomponent intervention of functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of acute care for elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1578.
- ,,,.A medical unit for the acute care of the elderly.J Am Geriatr Soc.1994;42:545–552
- ,,, et al.A randomized trial of care in a hospital medicine unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1342.
- ,,,.The care transitions intervention.Arch Intern Med.2006;166:1822–1828.
- ,,,.Comorbidity measures for use with administrative data.Med Care.1998;36:8–27.
- ,,.The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- ,,,,,.The value of a hospitalist service.Chest.2001;19:580–589.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,.Slowing the growth of health care costs ‐ lessons from regional variation.N Engl J Med.2009;360:849–852.
- ,,, et al.Fostering accountable health care: moving forward in Medicare.Health Aff (Millwood).2009;28:w219–w231.
- Centers for Disease Control and Prevention. Health, United States, 2009. Table 102. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. Accessed June 10,2010.
Medication Reconciliation: A Consensus Statement From Stakeholders
Medication reconciliation is integral to reducing medication errors surrounding hospitalizations.1, 2 The practice of medication reconciliation requires a systematic and comprehensive review of all the medications a patient is currently taking to ensure that medications being added, changed, or discontinued are carefully evaluated with the goal of maintaining an accurate list; that this process is undertaken at every transition along the continuum of care; and that an accurate list of medications is available to the patient or family/caregiver and all providers involved in the patient's care, especially when a care handoff takes place. With regulators, payers and the public increasingly demanding action to reduce medication errors in hospitals, all health care providers must support efforts to achieve accurate medication reconciliation.1, 3
The Joint Commission's Definition of Medication
Any prescription medications, sample medications, herbal remedies, vitamins, nutraceuticals, vaccines, or over‐the‐counter drugs; diagnostic and contrast agents used on or administered to persons to diagnose, treat, or prevent disease or other abnormal conditions; radioactive medications, respiratory therapy treatments, parenteral nutrition, blood derivatives, and intravenous solutions (plain, with electrolytes and/or drugs); and any product designated by the Food and Drug Administration (FDA) as a drug. This definition of medication does not include enteral nutrition solutions (which are considered food products), oxygen, and other medical gases.
2010 Hospital Accreditation Standards,
The Joint Commission, 2010, p. GL19.
While conceptually straightforward, implementing medication reconciliation has proved to be very difficult in the myriad healthcare settings that exist. The disjointed nature of the American health care system and a conglomeration of paper and electronic systems for tracking medications synergize to thwart efforts to maintain an accurate, up‐to‐date medication list at every step along the care continuum. Although The Joint Commission defines medication for the purpose of its accreditation standards (see box), the healthcare community lacks a common understanding or agreement regarding what constitutes a medication. There is also confusion about who should ultimately be responsible for obtaining the patient's medication information, for performing the various steps in the reconciliation process, and for managing the multiple providers who alter the medication list but may not feel competent to perform reconciliation of medications outside their area of expertise safely. Importantly, there is also a lack of clarity around how patients and family/caregivers should be involved in the process.
Despite these challenges, medication reconciliation remains a critical patient safety activity that is supported by the organizations signing this consensus statement, (Table 1). Although medication reconciliation has an impact on medication safety in all care settings, this paper focuses on issues most germane to the continuum of care involving the hospital setting. The themes and issues discussed will likely apply to other care settings as well. In this paper, we also recommend several concrete steps that we believe should be initiated immediately to begin to reach the goal of optimizing the medication safety achievable through effective medication reconciliation.
Background
Medication reconciliation is intended to be a systematic extension of the medication history‐taking process that has been used by health care providers for decades. Its recent iteration was developed to ensure that medications were not added, omitted, or changed inadvertently during care transitions. It became codified, refined, and tested over the past decade through the efforts of a number of groups focused on medication safety including the Institute for Healthcare Improvement (IHI) and the Institute for Safe Medication Practices (ISMP). With the reinforcing adoption of medication reconciliation as National Patient Safety Goal (NPSG) No. 8 in 2005 by The Joint Commission, efforts to implement it became widespread in both hospital‐based and ambulatory settings.
Medication reconciliation has three steps, as described by IHI4:
-
Verification (collection of the patient's medication history);
-
Clarification (ensuring that the medications and doses are appropriate); and
-
Reconciliation (documentation of changes in the orders).
The details of the process vary by setting and by the availability of paper or electronic medical records. However, the essential steps remain the same, as does the need to perform reconciliation each time the patient transfers to a new setting or level of care. Table 2 lists the most common points at which medication reconciliation occurs in hospitalized patients.
|
| American Academy of Pediatrics |
| American Association of Critical‐Care Nurses |
| Consumers Advancing Patient Safety |
| Institute for Healthcare Improvement |
| Institute for Safe Medication Practices |
| The Joint Commission |
| Massachusetts Coalition for Prevention of Medical Errors |
| Microsoft Corporation |
| Northwestern Memorial Hospital and Northwestern University School of Medicine |
| Society of General Internal Medicine |
| Society of Hospital Medicine |
| University of California San Diego Medical Center |
Because of their complexity, organizations must take care to design their medication reconciliation processes systematically. IHI lists elements of a well‐designed medication reconciliation process as part of its 5 Million Lives Campaign How‐to Guide.4 Such a process:
-
Uses a patient centered approach.
-
Makes it easy to complete the process for all involved. Staff members recognize the what's‐in‐it‐for‐me aspect of the change.
-
Minimizes the opportunity for drug interactions and therapeutic duplications by making the patient's list of current medications available when clinicians prescribe new medications.
-
Provides the patient with an up‐to‐date list of medications.
-
Ensures that other providers who need to know have information about changes in a patient's medication plan.
Research on how adverse drug events (ADE) occur supports the need for tight control of medication orders at transitions in care. For instance:
-
In a study conducted at Mayo Health System in Wisconsin, poor communication of medical information at transition points was responsible for as many as 50% of all medication errors in the hospital and up to 20% of ADEs.5
-
Variances between the medications patients were taking prior to admission and their admission orders ranged from 30% to 70% in 2 literature reviews.1, 6
-
The largest study of medication reconciliation errors and risk factors at hospital admission documented that 36% of patients had errors in their admission orders.7
When The Joint Commission adopted medication reconciliation as NPSG No. 8 in 2005 it had 2 parts: Requirement 8Aa process must exist for comparing the patient's current medications with those ordered for the patient while under the care of the organization; and requirement 8Ba complete list of the patient's medications must be communicated to the next provider of service on transfer within or outside the organization and a complete list of medications must be provided to the patient on discharge.8
However, many hospitals found it difficult to implement medication reconciliation in a systematic way. There was also confusion among hospital staff and administration about the exact definition of medication reconciliation in terms of what it should entail.9 Given these difficulties, The Joint Commission announced that effective January 1, 2009, medication reconciliation would no longer be factored into an organization's accreditation decision or be considered for Requirements for Improvement. Additionally, The Joint Commission stated it is reviewing and revising the NPSG so that it will be ready to be released in January 2011 for implementation later that year.10
Recognizing the difficulty hospitals were having with meaningfully implementing medication reconciliation, the Society of Hospital Medicine convened a 1‐day conference on March 6, 2009, to obtain input from key stakeholders and focus on several critical domains relevant to the success of hospital‐based medication reconciliation. The Agency for Healthcare Research and Quality provided funding support for this conference through grant 1R13HS017520‐01.
An overarching theme emerged from the meeting: the need to reorient the focus of medication reconciliation away from that of an accreditation mandate and toward a broader view of patient safety. Forcing medication reconciliation via a requirement for accreditation tended to limit an organization's efforts to specific process measures. Addressing it as a more global patient safety issue takes into account the entire patient care experience and then opens the door to leverage nonclinical venues (e.g., medical home, family home, community, religious, and other social organizations, as well as social networking platforms) and engage the patient and family/caregivers to reinforce the importance of medication safety.
This white paper evolved from discussions at the March 2009 conference,11 and subsequent structured communication among attendees. Formal endorsement of this document was obtained from the organizations listed in Table 1. In this document, we explore several key issues in implementing clinically meaningful and patient‐centered medication reconciliation. We focus on building common language and understanding of the processes of and participants in medication reconciliation; consider issues of implementation and risk stratification; emphasize the need for research to identify best practices and discusses how to disseminate the findings; promote health information technology platforms that will support interoperable medication information exchange; support the formation of partnerships between patient care sites and nonclinical sites as well as utilizing social marketing opportunities to enhance opportunities for transmitting messages about medication safety; and reinforce the ongoing healthcare reform discussion which aims to align financial incentives with patient safety efforts. After each section, we offer concrete first steps to address the issues discussed.
| Admission: When clinicians reconcile the patient's medications taken at home or at a prior care setting with any new prescription orders to be prescribed by an admitting clinician. |
| Transfer (intra‐ or inter‐facility; with change of clinician or site of care): When clinicians review previous medication orders in light of the patient's clinical status, along with new orders or plans of care. |
| Discharge: When clinicians review all medications the patient was taking prior to being hospitalized, incorporating new prescriptions from the hospitalization and determining whether any medication should be added, discontinued, or modified while being mindful of therapeutic interchanges needed for formulary purposes. |
Methods
The invitation‐only meeting held on the Northwestern Medical Campus in Chicago, IL, brought together stakeholders representing professional, clinical, health care quality, consumer, and regulatory organizations (Table 3). The conference convened these participants with the goals of identifying barriers to meaningful implementation of medication reconciliation and developing a feasible plan toward its effective implementation in the hospital setting. At the meeting, all participants were divided into 1 of 4 groups, which held a facilitated discussion around 1 of 4 key relevant domains: (1) how to measure success in medication reconciliation; (2) key elements of successful strategies; (3) leveraging partnerships outside the hospital setting to support medication reconciliation; and (4) the roles of the patient and family/caregivers and health literacy. Individual group discussions were cofacilitated by experts in the content area. After each discussion, the small group then rotated to a different discussion. Ultimately, each group participated in all four discussions, which built iteratively on the content derived from the prior groups' insights. Key comments were then shared with the large group for further discussion. To help build consensus, these large group discussions were directed by professional facilitators.
| AACN American Association of Critical Care Nurses |
| AAFP American Academy of Family Physicians |
| AAP American Academy of Pediatrics |
| ACEP American College of Emergency Physicians |
| ACP American College of Physicians |
| AMA American Medical Association |
| AMSN Academy of Medical Surgical Nurses |
| ASHP American Society of Health‐System Pharmacists |
| ASHP Foundation American Society of Health‐System Pharmacists Foundation |
| CAPS Consumers Advancing Patient Safety |
| CMS Centers for Medicare and Medicaid Services |
| CMSA Case Management Society of America |
| HCI Hospitalist Consultants, Inc |
| IHI Institute for Healthcare Improvement |
| InCompass Health |
| ISMP Institute For Safe Medication Practice |
| JCR Joint Commission Resources |
| Massachusetts Coalition for Prevention of Medical Errors |
| Microsoft Corporation |
| Northwestern Memorial Hospital MATCH Program |
| NQF National Quality Forum |
| SGIM Society of General Internal Medicine |
| SHM Society of Hospital Medicine |
| The Joint Commission |
| UCSD Hospital Medicine |
| University of Oklahoma College of Pharmacy Tulsa |
After the meeting, attendees participated in 2 follow‐up conference calls to discuss issues raised at the conference and responses obtained from host organizations. They also subsequently participated in two focus groups with The Joint Commission, giving input on the revision of the medication reconciliation NPSG.
Results
Addressing Barriers to Medication Reconciliation
In order to implement successful medication reconciliation processes, one must build the steps with the patient and family/caregiver as the focus and demonstrate an understanding of the intent of these processes. At its roots, medication reconciliation was developed to ensure that clinicians do not inadvertently add, change, or omit medications and that changes made are communicated to all relevant caregivers.
A number of key issues with respect to successful medication reconciliation processes surfaced in discussions with stakeholders. We believe addressing these issues is necessary before meaningful and standardized implementation can be achieved. After each discussion below, we provide suggested first steps to address these issues.
1. Achieve Consensus on the Definition of Medication and Reconciliation
Despite proposed definitions of these terms by various organizations, there was little agreement about them in the healthcare community. This ambiguity contributed to general confusion about what actually constitutes medication reconciliation. There needs to be a single, clear, and broadly accepted definition of what constitutes a medication. For the purposes of medication reconciliation, the term medication should be broadly inclusive of substances that may have an impact on the patient's care and treatments as well as those substances that may interact with other therapies potentially used during the medical care episode. Illicit or recreational substances may also have impact on therapies considered and therefore may influence this definition.12 Concretely, this definition should encompass prescription and over‐the‐counter medications as well as herbal and dietary supplements.
The term reconciliation in its simplest form implies the process of verifying that a patient's current list of medications (including dose, route, and frequency) are correct and that the medications are currently medically necessary and safe. Reconciliation suggests a process which, by necessity, will vary based on clinical context and setting. Further defining this termand the process of reconciliation itselfshould be carried out using patient safety principles with a focus on patient‐ and family‐centeredness.
Designing hospital‐based medication reconciliation processes should:
-
Employ a multidisciplinary approach that involves nurses, pharmacists, and other appropriate personnel from the inpatient setting as well as ambulatory and community/retail areas, both ambulatory and inpatient physicians, and a patient/family representative;
-
Involve hospital leaders who support, provide guidance, and remove barriers for the multidisciplinary team working to implement the processes;
-
Clearly define the roles of each participant in the processes developed;
-
Include methods to assess and address any special needs due to the developmental stage, age, dependency, language or literacy levels of patients and their family/caregiver;
-
Use clinically relevant process measures (e.g., adherence to procedural steps) and outcome measures (e.g., change in the number of ADEs, unnecessary hospitalizations, or emergency department visits) where appropriate to assess the impact of the process;
-
Include feedback systems to allow for clinically significant process improvement.
Once a common understanding of the terms and intent of medication reconciliation is achieved, it will be important for accrediting organizations, medical societies, quality improvement organizations, and other interested parties to adopt the same language.
First Step
A consortium of clinical, quality, and regulatory stakeholders should work to achieve consensus on the definition for medication and the intent and expectations for the reconciliation process.
2. Clarify Roles and Responsibilities
Given the differences in organizational and practice structures in hospitals and the varying numbers of health professionals involved in a patient's care, no one process design will meet the needs of all sites. As it is clear that interdisciplinary teams are best suited to develop, implement, and carry out complex patient‐centered processes like medication reconciliation, it is crucial that all involved parties have clearly defined roles and responsibilities, including patients and their families/caregivers. It is also important to recognize that these responsibilities may change depending on the dependency or vulnerability of the patient (e.g., children or geriatric patients) or the transition of care being undertaken by the patient (i.e., admission, transfer, or discharge), thus requiring sites to develop clear policies about these roles and responsibilities and how they may change in various situations.
First Step
Individual sites must clearly define the roles and responsibilities of all parties directly involved in medication reconciliation as a part of designing local medication reconciliation processes.
3. Develop Measurement Tools
Ensuring that medication reconciliation processes result in clinically meaningful outcomes requires the development and standardization of a limited number of metrics that may be used by organizations and reported centrally for benchmarking. This core set of measures should be developed by clinical, quality, accreditation, and regulatory organizations (see #10 below) through a consensus building process utilizing multi‐stakeholder input. The set should be supplemented by additional site‐specific measures determined locally that focus on steps in the process itself and allow sites to perform continuous quality improvement. Sites should be encouraged to develop tools locally to support and facilitate organizational and professional adherence to medication reconciliation processes.
First Steps
Clinical, quality, accreditation, and regulatory organizations should develop reliable metrics to be assessed and reported.
The principles of patient‐centeredness and family/caregiver‐centeredness, the medical home, and clinical relevance must be central to the metrics chosen for quality and regulatory purposes.
4. Phased Implementation
Ultimately, comprehensive medication reconciliation processes need to be implemented in hospitals. However, to succeed in integrating complex processes like medication reconciliation into routine hospital practices, implementation may be facilitated by using a phased approach to allow for participants to adapt new processes and procedures to the local environment iteratively. While the most appropriate phased approach to implementation will vary by site and setting, options for phasing might include:
-
Starting with one clinical area or service.
-
Starting with either the admission or discharge reconciliation process.
-
Starting with a patient population at high risk for adverse events.
Irrespective of the phasing strategy employed, development of a clear and pragmatic schedule for the entire implementation process should be established. Phasing decisions should be made based on organizational resources and the clinical needs of the patient population within each clinical setting. As noted, the ultimate goal is to develop comprehensive reconciliation processes occurring during all significant care transitions (i.e., admission, service or site‐of‐care transfers, and discharge) for all hospitalized patients and involving all of their medications. Flexibility in design should be encouraged to ensure the processes can work within local workflow as long as progress toward this primary goal is made.
First Steps
Clinical sites should establish local, pragmatic priorities for a phased approach to implementation.
Tie the phased approach to a timeline or blueprint for programmatic expansion with ultimate plans for comprehensive implementation.
5. Develop Risk Stratification Systems
Medication‐related adverse events related to inadequate reconciliation are more likely to occur in hospitalized patients with certain identifiable risk factors. For example, the MATCH study documented that polypharmacy and age over 65 years were independently associated with increased risk for errors at the time of hospital admission.7 Other factors that may increase the likelihood of medication‐related adverse events at care transitions in the hospital might include: patients with multiple providers, developmental/cognitive impairment, dependency/vulnerability, multiple or high‐risk medications, or poor health literacy or limited English proficiency. Research is needed to elucidate these risk factors further.
An alert system for key risk factors for complications related to incompletely, inappropriately, or inaccurately completed medication reconciliation due to patient, clinician, or system factors should be developed, tested, and broadly implemented. Additionally, an alert system would help maintain vigilance toward this patient safety issue and, potentially, help focus additional resources on high‐risk patients. Such a tool has been tested in ambulatory settings.15
First Step
Additional research on inpatient predictors of failed medication reconciliation and ADE should be prioritized (see #6 below).
6. Study Interventions and Processes
Despite having been an NPSG since 2005, there is still a relative paucity of literature about broadly applicable and effective implementation strategies and demonstrated interventions that improve medication safety related to medication reconciliation. Some strategies that have shown to reduce medication errors at transitions include the involvement of pharmacist medication review on discharge16, 17 and the usefulness of planning by multidisciplinary groups.18 Other studies have outlined the continuing barriers to successful implementation of reconciliation, including the difficulty patients have in accurately recalling their current medications19 and the high cost in nurse and pharmacist time of tracking down a patient's ongoing prescriptions.20, 21 Studies evaluating potential solutions to overcome these and other common barriers are still needed.
Future research should focus on a comprehensive review of implementation strategies, (specifically including the role of health information technology‐based innovations) clinically relevant outcomes, and best practices, while being sensitive to the different needs of varying care settings (e.g., pediatric vs. adult centers, emergency departments vs. inpatient units, community hospital vs. academic medical center, etc.) as well as the resource requirements engendered in the interventions.
First Step
Funding agencies should explicitly prioritize outcomes‐focused medication reconciliation‐related projects (e.g., those which demonstrate a reduction in postdischarge ADE or reduced medication‐related emergency department visits). Previously identified successful strategies should be further investigated. Funded projects should explicitly partner with patients and family/caregivers and also include pediatric and adult patients, rural and urban locations of care, as well as academic and nonacademic hospital settings, to promote more broadly applicable results.
7. Disseminate Success
Best practices and lessons learned, especially those rigorously tested and driven by data, stratified by patient type, care setting (emergency department, intensive care, surgical ward, etc.) and institutional type (community, teaching, safety net, critical access, etc.) need to be disseminated so others can adopt and adapt them effectively. High‐quality case studies with clear explanations of successes, failures, and lessons learned may prove valuable sources of information. This knowledge should foster a learning community approach and accelerate implementation at new sites.
First Step
Hospitals, healthcare systems, as well as quality and regulatory agencies should develop mechanisms within reporting systems to track performance, identify notably successful sites, and publicly report and share methods and lessons learned from them.
8. Promote the Personal Health Record
A fully integrated and transferable personal health record should be accepted as the standard for health information storage and interoperability, giving both the patient (or family/caregiver) and clinical providers access and ownership. Both the HL7 Continuity of Care Document (CCD) and the Continuity of Care Record (CCR) meet these criteria. The CCR was endorsed by the American Society for Testing and Materials22 and a coalition of other medical societies.23 Notably, CCR and CCD were recently adopted as standards for structured electronic health record (EHR) exchange through the July 2010 publication of the Final Rule of the Health Information Technology for Economic and Clinical Health Act provision of the American Recovery and Reinvestment Act of 2009 (ARRA/HITECH) and is now part of the formal US Department of Health and Human Services certification criteria for EHR technologies.24
Mandating a content exchange standard such as the CCR or the CCD should also have the desired effect of ensuring that patients (and their caregivers) become increasingly involved in maintaining an accurate list of the medications they take. Additionally, systems must be sufficiently flexible to address the unique medication management needs of children and geriatric patients. An electronic version of a personal health record is a promising method for improving consistency across care platforms, but to be implemented effectively the record must be compatible across all settings, including, where possible, the patient's home. All health care organizations, pharmacy systems, and insurers, must make medication reconciliation‐related interoperability and accessibility a priority as they pursue information technology strategies.
First Step
Stakeholder organizations must send a clear and convincing message to legislators under the current atmosphere of health care reform, urging them to mandate that health information technology standards include interoperability and support platforms that are consistent with standards put forth in the 2009 HITECH Act Interim Final Rule for EHR certification.
9. Promote Partnerships
At a broader health care system level, leveraging existing partnerships and creating new ones among health care, public/private sector‐affiliated organizations (e.g., community and mail order pharmacies, pharmaceutical organizations and manufacturers, and insurers), and public health organizations are extremely important mechanisms for broader scale impact. This view recognizes the numerous opportunities to educate and influence patients about medication safety outside the dyadic relationship of the clinician and patient in traditional clinical settings. Partnerships between health care and public entities may capitalize on these opportunities to foster adoption of healthy medication practices (e.g., maintaining an accurate and updated medication list), thereby supporting medication reconciliation efforts when individuals encounter health care settings. Partnership and information sharing could be enhanced through the use of a central coordinating body or coalition. This body could generate a shared common vision and contribute expertise to the myriad issues in medication reconciliation.
Partnerships should utilize the following:
-
Social marketing techniques to engage the community. Included within this strategy must be a clear and compelling message that transmits the importance of safe medication practices. Current messages such as keep a list while important, do not offer enough of a sense of urgency or importance. A more powerful message could involve highly publicized medication errors or close calls that would resonate with a broad audience.
-
Local and national champions. Such individuals should be trusted for their health knowledge (e.g., television health care reporters) or be prominent, influential, and trusted figures in other circles (e.g., clergy, politicians, movie celebrities). Indeed, taking advantage of popular media by weaving a theme into a movie or television program about medication safety may prove effective.
Relevant partnerships would include:
-
Quality organizations partnering with other stakeholders to establish unambiguous and unified medication reconciliation standards across the care continuum.
-
Health systems partnering with community pharmacy providers to ensure an uninterrupted communication link in both the inpatient and outpatient settings.
-
Manufacturers and distributors of medications partnering with health care and public health organizations, the media, insurers and other constituents to promote the importance of maintaining and sharing an accurate list of medications.
-
Public health systems partnering with community‐based organizations to encourage and promote the established standards for medication safety through messaging and educational campaigns.
All partnerships must consider issues of patient language and literacy as well as the needs of vulnerable populations in the scope of their activities.
First Step
Public health agencies should partner with health care quality organizations and others to begin a national public campaign to increase the awareness of medication safety (the broader public health concept under which medication reconciliation would fall) and support the importance of the patient's role in maintaining an updated medication list at all times.
10. Align Financial Incentives With Newly Developed Regulatory and Accreditation Requirements
Implementing and performing medication reconciliation takes time, particularly at the outset of a new program. Time requirements and associated costs are major barriers to undertaking comprehensive medication reconciliation, despite its recognized importance for reducing avoidable injury to patients. At present, systems that impede efficiency and slow hospital throughput may be discouraged due to their potential for having an adverse impact on access, finances, and other aspects of care delivery. Moreover, the changed economic climate with reduced hospital fiscal margins limits resources for new initiatives. Currently, failed medication reconciliationand the related avoidable adverse events, culminating in readmission to the hospital or emergency departmentyields additional revenue for hospitals and other providers in some reimbursement models.
Alignment of financial incentives that ensured adequate time and resources for appropriate medication reconciliation processes would facilitate implementation. Additionally, start‐up funding to create and implement these processes needs to be made available.
One example illustrating efforts to align payment policy with medication safety efforts occurred when the Office of the National Coordinator (ONC), in publishing its Final Rule under the 2009 HITECH Act,24 endorsed the importance of financially supporting proper medication reconciliation, particularly at first encounter and transitions in care, by requiring EHR systems seeking certification under the rule to support the care team in the task of reconciliation. For example, vendors will have to support the ability to compare 2 or more medication lists electronically, create medication lists, drug allergy lists, perform drug formulary look‐ups, drug‐drug and drug‐allergy checks, and support creating patient summaries after each visit or post discharge that include medication lists. The ONC, in defining Meaningful Use for eligible health care organizations, included in that definition the goal of exchanging meaningful clinical information among the professional health care teams. This goal is demonstrated through organizations reporting that they performed medication reconciliation for at least 50% of transitions of care in which the patient is transitioned into the care of the eligible professional or admitted to the eligible hospital's or Critical Access Hospital's inpatient or emergency department. Organizations able to demonstrate this level of compliance, along with other Meaningful Use requirements, will be eligible to receive stimulus funds through 2015 and avoid financial penalties that begin after that period.
First Step
Future health care reform must address the misalignment of financial policies and structures, and provide financial incentives to support the development and implementation of better medication management systems and prevent avoidable rehospitalizations and emergency department visits resulting from medication‐related adverse events.
Conclusion
Medication reconciliation involves highly complex processes and is hampered by the disjointed nature of the American health care system. It is, however, a vital part of reducing ADE. If employed more broadly, it has the added benefits of enhancing communication among all providers of care and engaging patients and families/caregivers more consistently and meaningfully in their overall care.
Despite the difficulty of maintaining an accurate medication record in real time across disparate settings, reconciliation is a goal to which our organizations are committed. Given the wide range of healthcare organizations involved in providing medications to patients and the many agencies evaluating those efforts, we believed it would be helpful to provide an overarching set of goals to move medication reconciliation forward.
Our main message is this: Patient safety and patient/family‐centered care must be the principal drivers in the development and implementation of medication reconciliation systems. Ultimately this process is about ensuring that patients are receiving the most appropriate medications no matter where they are treated. With this document, we hope to bring to light the importance of creating and implementing a medication reconciliation program, addressing some barriers to success, and identifying potential solutions that will ensure utility and sustainability of this critical patient safety issue.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- .Prevention of medication errors in the pediatric inpatient setting. The American Academy of Pediatrics Policy Statement.Pediatrics.2003;112(2):431–436.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- Institute for Healthcare Improvement. 5 million lives getting started kit: preventing adverse drug events (medication reconciliation), how‐to guide. Available at: http://www.ihi.org/IHI/Programs/Campaign/ADEsMedReconciliation.htm. Published Oct. 1, 2008. Accessed September2010.
- ,.Medication safety: one organization's approach to the challenge.J Clin Outcomes Mana.2001;8(10):27–34.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Results of the Medications At Transitions and Clinical Handoffs (MATCH) Study: an analysis of medication reconciliation errors and risk factors at hospital admission.J Gen Intern Med.2010;25(5):441–447.
- Joint Commission on Accreditation of Healthcare Organizations.2005 Hospital Accreditation Standards, p.NPSG‐4.
- ,,,,.Brief communication: Results of a medication reconciliation survey from the 2006 Society of Hospital Medicine national meeting.J Hosp Med.2008;3(6):465–472.
- The Joint Commission.Approved: will not score medication reconciliation in 2009.Jt Comm Perspect.2009;29(3):1,3.
- Society of Hospital Medicine. Medication reconciliation: a team approach, conference summary. December 2009. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/QualityImprovement/QICurrentInitiativesandTrainingOpportunities/QI_Current_Initiativ.htm. Accessed September2010.
- The American Medical Association. The physician's role in medication reconciliation: issues, strategies and safety principles. 2007. Available at: http://www.ama‐assn.org/ama1/pub/upload/mm/370/med‐rec‐monograph.pdf. Accessed September2010.
- Institute of Safe Medication Practices. ISMP's list of high alert medications. 2008. Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed September2010.
- ,,,.Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147(11):755–765
- ,,, et al.Experience with a trigger tool for identifying adverse drug events among older adults in ambulatory primary care.Qual Saf Health Care.2009;18(3):199–204.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- ,,,,.Medication reconciliation at an academic medical center: implementation of a comprehensive program from admission to discharge.Am J Health Syst Pharm.2009;66(23):2126–2131.
- ,,,,,.Multidisciplinary approach to inpatient medication reconciliation in an academic setting.Am J Health Syst Pharm.2007;64(8):850–854.
- ,,.Lack of patient knowledge regarding hospital medications.J Hosp Med.2010;5(2):83–86.
- .The unexpected challenges of accurate medication reconciliation.Ann Emerg Med.2008;52(5):493–495.
- ,,,.Medication reconciliation in a rural trauma population.Ann Emerg Med.2008;52(5):483–491.
- ASTM International. ASTM E2369 ‐ 05e1 standard specification for continuity of care record (CCR). Available at: http://www.astm.org/Standards/E2369.htm. Accessed September2010.
- ,,.The continuity of care record.Am Fam Physician.2004;70(7):1220,1222–1223.
- Department of Health and Human Services. Health information technology: initial set of standards, implementation specifications, and certification criteria for electronic health record technology; final rule. Available at: http://edocket.access.gpo.gov/2010/pdf/2010–17210.pdf. Accessed September2010.
Medication reconciliation is integral to reducing medication errors surrounding hospitalizations.1, 2 The practice of medication reconciliation requires a systematic and comprehensive review of all the medications a patient is currently taking to ensure that medications being added, changed, or discontinued are carefully evaluated with the goal of maintaining an accurate list; that this process is undertaken at every transition along the continuum of care; and that an accurate list of medications is available to the patient or family/caregiver and all providers involved in the patient's care, especially when a care handoff takes place. With regulators, payers and the public increasingly demanding action to reduce medication errors in hospitals, all health care providers must support efforts to achieve accurate medication reconciliation.1, 3
The Joint Commission's Definition of Medication
Any prescription medications, sample medications, herbal remedies, vitamins, nutraceuticals, vaccines, or over‐the‐counter drugs; diagnostic and contrast agents used on or administered to persons to diagnose, treat, or prevent disease or other abnormal conditions; radioactive medications, respiratory therapy treatments, parenteral nutrition, blood derivatives, and intravenous solutions (plain, with electrolytes and/or drugs); and any product designated by the Food and Drug Administration (FDA) as a drug. This definition of medication does not include enteral nutrition solutions (which are considered food products), oxygen, and other medical gases.
2010 Hospital Accreditation Standards,
The Joint Commission, 2010, p. GL19.
While conceptually straightforward, implementing medication reconciliation has proved to be very difficult in the myriad healthcare settings that exist. The disjointed nature of the American health care system and a conglomeration of paper and electronic systems for tracking medications synergize to thwart efforts to maintain an accurate, up‐to‐date medication list at every step along the care continuum. Although The Joint Commission defines medication for the purpose of its accreditation standards (see box), the healthcare community lacks a common understanding or agreement regarding what constitutes a medication. There is also confusion about who should ultimately be responsible for obtaining the patient's medication information, for performing the various steps in the reconciliation process, and for managing the multiple providers who alter the medication list but may not feel competent to perform reconciliation of medications outside their area of expertise safely. Importantly, there is also a lack of clarity around how patients and family/caregivers should be involved in the process.
Despite these challenges, medication reconciliation remains a critical patient safety activity that is supported by the organizations signing this consensus statement, (Table 1). Although medication reconciliation has an impact on medication safety in all care settings, this paper focuses on issues most germane to the continuum of care involving the hospital setting. The themes and issues discussed will likely apply to other care settings as well. In this paper, we also recommend several concrete steps that we believe should be initiated immediately to begin to reach the goal of optimizing the medication safety achievable through effective medication reconciliation.
Background
Medication reconciliation is intended to be a systematic extension of the medication history‐taking process that has been used by health care providers for decades. Its recent iteration was developed to ensure that medications were not added, omitted, or changed inadvertently during care transitions. It became codified, refined, and tested over the past decade through the efforts of a number of groups focused on medication safety including the Institute for Healthcare Improvement (IHI) and the Institute for Safe Medication Practices (ISMP). With the reinforcing adoption of medication reconciliation as National Patient Safety Goal (NPSG) No. 8 in 2005 by The Joint Commission, efforts to implement it became widespread in both hospital‐based and ambulatory settings.
Medication reconciliation has three steps, as described by IHI4:
-
Verification (collection of the patient's medication history);
-
Clarification (ensuring that the medications and doses are appropriate); and
-
Reconciliation (documentation of changes in the orders).
The details of the process vary by setting and by the availability of paper or electronic medical records. However, the essential steps remain the same, as does the need to perform reconciliation each time the patient transfers to a new setting or level of care. Table 2 lists the most common points at which medication reconciliation occurs in hospitalized patients.
|
| American Academy of Pediatrics |
| American Association of Critical‐Care Nurses |
| Consumers Advancing Patient Safety |
| Institute for Healthcare Improvement |
| Institute for Safe Medication Practices |
| The Joint Commission |
| Massachusetts Coalition for Prevention of Medical Errors |
| Microsoft Corporation |
| Northwestern Memorial Hospital and Northwestern University School of Medicine |
| Society of General Internal Medicine |
| Society of Hospital Medicine |
| University of California San Diego Medical Center |
Because of their complexity, organizations must take care to design their medication reconciliation processes systematically. IHI lists elements of a well‐designed medication reconciliation process as part of its 5 Million Lives Campaign How‐to Guide.4 Such a process:
-
Uses a patient centered approach.
-
Makes it easy to complete the process for all involved. Staff members recognize the what's‐in‐it‐for‐me aspect of the change.
-
Minimizes the opportunity for drug interactions and therapeutic duplications by making the patient's list of current medications available when clinicians prescribe new medications.
-
Provides the patient with an up‐to‐date list of medications.
-
Ensures that other providers who need to know have information about changes in a patient's medication plan.
Research on how adverse drug events (ADE) occur supports the need for tight control of medication orders at transitions in care. For instance:
-
In a study conducted at Mayo Health System in Wisconsin, poor communication of medical information at transition points was responsible for as many as 50% of all medication errors in the hospital and up to 20% of ADEs.5
-
Variances between the medications patients were taking prior to admission and their admission orders ranged from 30% to 70% in 2 literature reviews.1, 6
-
The largest study of medication reconciliation errors and risk factors at hospital admission documented that 36% of patients had errors in their admission orders.7
When The Joint Commission adopted medication reconciliation as NPSG No. 8 in 2005 it had 2 parts: Requirement 8Aa process must exist for comparing the patient's current medications with those ordered for the patient while under the care of the organization; and requirement 8Ba complete list of the patient's medications must be communicated to the next provider of service on transfer within or outside the organization and a complete list of medications must be provided to the patient on discharge.8
However, many hospitals found it difficult to implement medication reconciliation in a systematic way. There was also confusion among hospital staff and administration about the exact definition of medication reconciliation in terms of what it should entail.9 Given these difficulties, The Joint Commission announced that effective January 1, 2009, medication reconciliation would no longer be factored into an organization's accreditation decision or be considered for Requirements for Improvement. Additionally, The Joint Commission stated it is reviewing and revising the NPSG so that it will be ready to be released in January 2011 for implementation later that year.10
Recognizing the difficulty hospitals were having with meaningfully implementing medication reconciliation, the Society of Hospital Medicine convened a 1‐day conference on March 6, 2009, to obtain input from key stakeholders and focus on several critical domains relevant to the success of hospital‐based medication reconciliation. The Agency for Healthcare Research and Quality provided funding support for this conference through grant 1R13HS017520‐01.
An overarching theme emerged from the meeting: the need to reorient the focus of medication reconciliation away from that of an accreditation mandate and toward a broader view of patient safety. Forcing medication reconciliation via a requirement for accreditation tended to limit an organization's efforts to specific process measures. Addressing it as a more global patient safety issue takes into account the entire patient care experience and then opens the door to leverage nonclinical venues (e.g., medical home, family home, community, religious, and other social organizations, as well as social networking platforms) and engage the patient and family/caregivers to reinforce the importance of medication safety.
This white paper evolved from discussions at the March 2009 conference,11 and subsequent structured communication among attendees. Formal endorsement of this document was obtained from the organizations listed in Table 1. In this document, we explore several key issues in implementing clinically meaningful and patient‐centered medication reconciliation. We focus on building common language and understanding of the processes of and participants in medication reconciliation; consider issues of implementation and risk stratification; emphasize the need for research to identify best practices and discusses how to disseminate the findings; promote health information technology platforms that will support interoperable medication information exchange; support the formation of partnerships between patient care sites and nonclinical sites as well as utilizing social marketing opportunities to enhance opportunities for transmitting messages about medication safety; and reinforce the ongoing healthcare reform discussion which aims to align financial incentives with patient safety efforts. After each section, we offer concrete first steps to address the issues discussed.
| Admission: When clinicians reconcile the patient's medications taken at home or at a prior care setting with any new prescription orders to be prescribed by an admitting clinician. |
| Transfer (intra‐ or inter‐facility; with change of clinician or site of care): When clinicians review previous medication orders in light of the patient's clinical status, along with new orders or plans of care. |
| Discharge: When clinicians review all medications the patient was taking prior to being hospitalized, incorporating new prescriptions from the hospitalization and determining whether any medication should be added, discontinued, or modified while being mindful of therapeutic interchanges needed for formulary purposes. |
Methods
The invitation‐only meeting held on the Northwestern Medical Campus in Chicago, IL, brought together stakeholders representing professional, clinical, health care quality, consumer, and regulatory organizations (Table 3). The conference convened these participants with the goals of identifying barriers to meaningful implementation of medication reconciliation and developing a feasible plan toward its effective implementation in the hospital setting. At the meeting, all participants were divided into 1 of 4 groups, which held a facilitated discussion around 1 of 4 key relevant domains: (1) how to measure success in medication reconciliation; (2) key elements of successful strategies; (3) leveraging partnerships outside the hospital setting to support medication reconciliation; and (4) the roles of the patient and family/caregivers and health literacy. Individual group discussions were cofacilitated by experts in the content area. After each discussion, the small group then rotated to a different discussion. Ultimately, each group participated in all four discussions, which built iteratively on the content derived from the prior groups' insights. Key comments were then shared with the large group for further discussion. To help build consensus, these large group discussions were directed by professional facilitators.
| AACN American Association of Critical Care Nurses |
| AAFP American Academy of Family Physicians |
| AAP American Academy of Pediatrics |
| ACEP American College of Emergency Physicians |
| ACP American College of Physicians |
| AMA American Medical Association |
| AMSN Academy of Medical Surgical Nurses |
| ASHP American Society of Health‐System Pharmacists |
| ASHP Foundation American Society of Health‐System Pharmacists Foundation |
| CAPS Consumers Advancing Patient Safety |
| CMS Centers for Medicare and Medicaid Services |
| CMSA Case Management Society of America |
| HCI Hospitalist Consultants, Inc |
| IHI Institute for Healthcare Improvement |
| InCompass Health |
| ISMP Institute For Safe Medication Practice |
| JCR Joint Commission Resources |
| Massachusetts Coalition for Prevention of Medical Errors |
| Microsoft Corporation |
| Northwestern Memorial Hospital MATCH Program |
| NQF National Quality Forum |
| SGIM Society of General Internal Medicine |
| SHM Society of Hospital Medicine |
| The Joint Commission |
| UCSD Hospital Medicine |
| University of Oklahoma College of Pharmacy Tulsa |
After the meeting, attendees participated in 2 follow‐up conference calls to discuss issues raised at the conference and responses obtained from host organizations. They also subsequently participated in two focus groups with The Joint Commission, giving input on the revision of the medication reconciliation NPSG.
Results
Addressing Barriers to Medication Reconciliation
In order to implement successful medication reconciliation processes, one must build the steps with the patient and family/caregiver as the focus and demonstrate an understanding of the intent of these processes. At its roots, medication reconciliation was developed to ensure that clinicians do not inadvertently add, change, or omit medications and that changes made are communicated to all relevant caregivers.
A number of key issues with respect to successful medication reconciliation processes surfaced in discussions with stakeholders. We believe addressing these issues is necessary before meaningful and standardized implementation can be achieved. After each discussion below, we provide suggested first steps to address these issues.
1. Achieve Consensus on the Definition of Medication and Reconciliation
Despite proposed definitions of these terms by various organizations, there was little agreement about them in the healthcare community. This ambiguity contributed to general confusion about what actually constitutes medication reconciliation. There needs to be a single, clear, and broadly accepted definition of what constitutes a medication. For the purposes of medication reconciliation, the term medication should be broadly inclusive of substances that may have an impact on the patient's care and treatments as well as those substances that may interact with other therapies potentially used during the medical care episode. Illicit or recreational substances may also have impact on therapies considered and therefore may influence this definition.12 Concretely, this definition should encompass prescription and over‐the‐counter medications as well as herbal and dietary supplements.
The term reconciliation in its simplest form implies the process of verifying that a patient's current list of medications (including dose, route, and frequency) are correct and that the medications are currently medically necessary and safe. Reconciliation suggests a process which, by necessity, will vary based on clinical context and setting. Further defining this termand the process of reconciliation itselfshould be carried out using patient safety principles with a focus on patient‐ and family‐centeredness.
Designing hospital‐based medication reconciliation processes should:
-
Employ a multidisciplinary approach that involves nurses, pharmacists, and other appropriate personnel from the inpatient setting as well as ambulatory and community/retail areas, both ambulatory and inpatient physicians, and a patient/family representative;
-
Involve hospital leaders who support, provide guidance, and remove barriers for the multidisciplinary team working to implement the processes;
-
Clearly define the roles of each participant in the processes developed;
-
Include methods to assess and address any special needs due to the developmental stage, age, dependency, language or literacy levels of patients and their family/caregiver;
-
Use clinically relevant process measures (e.g., adherence to procedural steps) and outcome measures (e.g., change in the number of ADEs, unnecessary hospitalizations, or emergency department visits) where appropriate to assess the impact of the process;
-
Include feedback systems to allow for clinically significant process improvement.
Once a common understanding of the terms and intent of medication reconciliation is achieved, it will be important for accrediting organizations, medical societies, quality improvement organizations, and other interested parties to adopt the same language.
First Step
A consortium of clinical, quality, and regulatory stakeholders should work to achieve consensus on the definition for medication and the intent and expectations for the reconciliation process.
2. Clarify Roles and Responsibilities
Given the differences in organizational and practice structures in hospitals and the varying numbers of health professionals involved in a patient's care, no one process design will meet the needs of all sites. As it is clear that interdisciplinary teams are best suited to develop, implement, and carry out complex patient‐centered processes like medication reconciliation, it is crucial that all involved parties have clearly defined roles and responsibilities, including patients and their families/caregivers. It is also important to recognize that these responsibilities may change depending on the dependency or vulnerability of the patient (e.g., children or geriatric patients) or the transition of care being undertaken by the patient (i.e., admission, transfer, or discharge), thus requiring sites to develop clear policies about these roles and responsibilities and how they may change in various situations.
First Step
Individual sites must clearly define the roles and responsibilities of all parties directly involved in medication reconciliation as a part of designing local medication reconciliation processes.
3. Develop Measurement Tools
Ensuring that medication reconciliation processes result in clinically meaningful outcomes requires the development and standardization of a limited number of metrics that may be used by organizations and reported centrally for benchmarking. This core set of measures should be developed by clinical, quality, accreditation, and regulatory organizations (see #10 below) through a consensus building process utilizing multi‐stakeholder input. The set should be supplemented by additional site‐specific measures determined locally that focus on steps in the process itself and allow sites to perform continuous quality improvement. Sites should be encouraged to develop tools locally to support and facilitate organizational and professional adherence to medication reconciliation processes.
First Steps
Clinical, quality, accreditation, and regulatory organizations should develop reliable metrics to be assessed and reported.
The principles of patient‐centeredness and family/caregiver‐centeredness, the medical home, and clinical relevance must be central to the metrics chosen for quality and regulatory purposes.
4. Phased Implementation
Ultimately, comprehensive medication reconciliation processes need to be implemented in hospitals. However, to succeed in integrating complex processes like medication reconciliation into routine hospital practices, implementation may be facilitated by using a phased approach to allow for participants to adapt new processes and procedures to the local environment iteratively. While the most appropriate phased approach to implementation will vary by site and setting, options for phasing might include:
-
Starting with one clinical area or service.
-
Starting with either the admission or discharge reconciliation process.
-
Starting with a patient population at high risk for adverse events.
Irrespective of the phasing strategy employed, development of a clear and pragmatic schedule for the entire implementation process should be established. Phasing decisions should be made based on organizational resources and the clinical needs of the patient population within each clinical setting. As noted, the ultimate goal is to develop comprehensive reconciliation processes occurring during all significant care transitions (i.e., admission, service or site‐of‐care transfers, and discharge) for all hospitalized patients and involving all of their medications. Flexibility in design should be encouraged to ensure the processes can work within local workflow as long as progress toward this primary goal is made.
First Steps
Clinical sites should establish local, pragmatic priorities for a phased approach to implementation.
Tie the phased approach to a timeline or blueprint for programmatic expansion with ultimate plans for comprehensive implementation.
5. Develop Risk Stratification Systems
Medication‐related adverse events related to inadequate reconciliation are more likely to occur in hospitalized patients with certain identifiable risk factors. For example, the MATCH study documented that polypharmacy and age over 65 years were independently associated with increased risk for errors at the time of hospital admission.7 Other factors that may increase the likelihood of medication‐related adverse events at care transitions in the hospital might include: patients with multiple providers, developmental/cognitive impairment, dependency/vulnerability, multiple or high‐risk medications, or poor health literacy or limited English proficiency. Research is needed to elucidate these risk factors further.
An alert system for key risk factors for complications related to incompletely, inappropriately, or inaccurately completed medication reconciliation due to patient, clinician, or system factors should be developed, tested, and broadly implemented. Additionally, an alert system would help maintain vigilance toward this patient safety issue and, potentially, help focus additional resources on high‐risk patients. Such a tool has been tested in ambulatory settings.15
First Step
Additional research on inpatient predictors of failed medication reconciliation and ADE should be prioritized (see #6 below).
6. Study Interventions and Processes
Despite having been an NPSG since 2005, there is still a relative paucity of literature about broadly applicable and effective implementation strategies and demonstrated interventions that improve medication safety related to medication reconciliation. Some strategies that have shown to reduce medication errors at transitions include the involvement of pharmacist medication review on discharge16, 17 and the usefulness of planning by multidisciplinary groups.18 Other studies have outlined the continuing barriers to successful implementation of reconciliation, including the difficulty patients have in accurately recalling their current medications19 and the high cost in nurse and pharmacist time of tracking down a patient's ongoing prescriptions.20, 21 Studies evaluating potential solutions to overcome these and other common barriers are still needed.
Future research should focus on a comprehensive review of implementation strategies, (specifically including the role of health information technology‐based innovations) clinically relevant outcomes, and best practices, while being sensitive to the different needs of varying care settings (e.g., pediatric vs. adult centers, emergency departments vs. inpatient units, community hospital vs. academic medical center, etc.) as well as the resource requirements engendered in the interventions.
First Step
Funding agencies should explicitly prioritize outcomes‐focused medication reconciliation‐related projects (e.g., those which demonstrate a reduction in postdischarge ADE or reduced medication‐related emergency department visits). Previously identified successful strategies should be further investigated. Funded projects should explicitly partner with patients and family/caregivers and also include pediatric and adult patients, rural and urban locations of care, as well as academic and nonacademic hospital settings, to promote more broadly applicable results.
7. Disseminate Success
Best practices and lessons learned, especially those rigorously tested and driven by data, stratified by patient type, care setting (emergency department, intensive care, surgical ward, etc.) and institutional type (community, teaching, safety net, critical access, etc.) need to be disseminated so others can adopt and adapt them effectively. High‐quality case studies with clear explanations of successes, failures, and lessons learned may prove valuable sources of information. This knowledge should foster a learning community approach and accelerate implementation at new sites.
First Step
Hospitals, healthcare systems, as well as quality and regulatory agencies should develop mechanisms within reporting systems to track performance, identify notably successful sites, and publicly report and share methods and lessons learned from them.
8. Promote the Personal Health Record
A fully integrated and transferable personal health record should be accepted as the standard for health information storage and interoperability, giving both the patient (or family/caregiver) and clinical providers access and ownership. Both the HL7 Continuity of Care Document (CCD) and the Continuity of Care Record (CCR) meet these criteria. The CCR was endorsed by the American Society for Testing and Materials22 and a coalition of other medical societies.23 Notably, CCR and CCD were recently adopted as standards for structured electronic health record (EHR) exchange through the July 2010 publication of the Final Rule of the Health Information Technology for Economic and Clinical Health Act provision of the American Recovery and Reinvestment Act of 2009 (ARRA/HITECH) and is now part of the formal US Department of Health and Human Services certification criteria for EHR technologies.24
Mandating a content exchange standard such as the CCR or the CCD should also have the desired effect of ensuring that patients (and their caregivers) become increasingly involved in maintaining an accurate list of the medications they take. Additionally, systems must be sufficiently flexible to address the unique medication management needs of children and geriatric patients. An electronic version of a personal health record is a promising method for improving consistency across care platforms, but to be implemented effectively the record must be compatible across all settings, including, where possible, the patient's home. All health care organizations, pharmacy systems, and insurers, must make medication reconciliation‐related interoperability and accessibility a priority as they pursue information technology strategies.
First Step
Stakeholder organizations must send a clear and convincing message to legislators under the current atmosphere of health care reform, urging them to mandate that health information technology standards include interoperability and support platforms that are consistent with standards put forth in the 2009 HITECH Act Interim Final Rule for EHR certification.
9. Promote Partnerships
At a broader health care system level, leveraging existing partnerships and creating new ones among health care, public/private sector‐affiliated organizations (e.g., community and mail order pharmacies, pharmaceutical organizations and manufacturers, and insurers), and public health organizations are extremely important mechanisms for broader scale impact. This view recognizes the numerous opportunities to educate and influence patients about medication safety outside the dyadic relationship of the clinician and patient in traditional clinical settings. Partnerships between health care and public entities may capitalize on these opportunities to foster adoption of healthy medication practices (e.g., maintaining an accurate and updated medication list), thereby supporting medication reconciliation efforts when individuals encounter health care settings. Partnership and information sharing could be enhanced through the use of a central coordinating body or coalition. This body could generate a shared common vision and contribute expertise to the myriad issues in medication reconciliation.
Partnerships should utilize the following:
-
Social marketing techniques to engage the community. Included within this strategy must be a clear and compelling message that transmits the importance of safe medication practices. Current messages such as keep a list while important, do not offer enough of a sense of urgency or importance. A more powerful message could involve highly publicized medication errors or close calls that would resonate with a broad audience.
-
Local and national champions. Such individuals should be trusted for their health knowledge (e.g., television health care reporters) or be prominent, influential, and trusted figures in other circles (e.g., clergy, politicians, movie celebrities). Indeed, taking advantage of popular media by weaving a theme into a movie or television program about medication safety may prove effective.
Relevant partnerships would include:
-
Quality organizations partnering with other stakeholders to establish unambiguous and unified medication reconciliation standards across the care continuum.
-
Health systems partnering with community pharmacy providers to ensure an uninterrupted communication link in both the inpatient and outpatient settings.
-
Manufacturers and distributors of medications partnering with health care and public health organizations, the media, insurers and other constituents to promote the importance of maintaining and sharing an accurate list of medications.
-
Public health systems partnering with community‐based organizations to encourage and promote the established standards for medication safety through messaging and educational campaigns.
All partnerships must consider issues of patient language and literacy as well as the needs of vulnerable populations in the scope of their activities.
First Step
Public health agencies should partner with health care quality organizations and others to begin a national public campaign to increase the awareness of medication safety (the broader public health concept under which medication reconciliation would fall) and support the importance of the patient's role in maintaining an updated medication list at all times.
10. Align Financial Incentives With Newly Developed Regulatory and Accreditation Requirements
Implementing and performing medication reconciliation takes time, particularly at the outset of a new program. Time requirements and associated costs are major barriers to undertaking comprehensive medication reconciliation, despite its recognized importance for reducing avoidable injury to patients. At present, systems that impede efficiency and slow hospital throughput may be discouraged due to their potential for having an adverse impact on access, finances, and other aspects of care delivery. Moreover, the changed economic climate with reduced hospital fiscal margins limits resources for new initiatives. Currently, failed medication reconciliationand the related avoidable adverse events, culminating in readmission to the hospital or emergency departmentyields additional revenue for hospitals and other providers in some reimbursement models.
Alignment of financial incentives that ensured adequate time and resources for appropriate medication reconciliation processes would facilitate implementation. Additionally, start‐up funding to create and implement these processes needs to be made available.
One example illustrating efforts to align payment policy with medication safety efforts occurred when the Office of the National Coordinator (ONC), in publishing its Final Rule under the 2009 HITECH Act,24 endorsed the importance of financially supporting proper medication reconciliation, particularly at first encounter and transitions in care, by requiring EHR systems seeking certification under the rule to support the care team in the task of reconciliation. For example, vendors will have to support the ability to compare 2 or more medication lists electronically, create medication lists, drug allergy lists, perform drug formulary look‐ups, drug‐drug and drug‐allergy checks, and support creating patient summaries after each visit or post discharge that include medication lists. The ONC, in defining Meaningful Use for eligible health care organizations, included in that definition the goal of exchanging meaningful clinical information among the professional health care teams. This goal is demonstrated through organizations reporting that they performed medication reconciliation for at least 50% of transitions of care in which the patient is transitioned into the care of the eligible professional or admitted to the eligible hospital's or Critical Access Hospital's inpatient or emergency department. Organizations able to demonstrate this level of compliance, along with other Meaningful Use requirements, will be eligible to receive stimulus funds through 2015 and avoid financial penalties that begin after that period.
First Step
Future health care reform must address the misalignment of financial policies and structures, and provide financial incentives to support the development and implementation of better medication management systems and prevent avoidable rehospitalizations and emergency department visits resulting from medication‐related adverse events.
Conclusion
Medication reconciliation involves highly complex processes and is hampered by the disjointed nature of the American health care system. It is, however, a vital part of reducing ADE. If employed more broadly, it has the added benefits of enhancing communication among all providers of care and engaging patients and families/caregivers more consistently and meaningfully in their overall care.
Despite the difficulty of maintaining an accurate medication record in real time across disparate settings, reconciliation is a goal to which our organizations are committed. Given the wide range of healthcare organizations involved in providing medications to patients and the many agencies evaluating those efforts, we believed it would be helpful to provide an overarching set of goals to move medication reconciliation forward.
Our main message is this: Patient safety and patient/family‐centered care must be the principal drivers in the development and implementation of medication reconciliation systems. Ultimately this process is about ensuring that patients are receiving the most appropriate medications no matter where they are treated. With this document, we hope to bring to light the importance of creating and implementing a medication reconciliation program, addressing some barriers to success, and identifying potential solutions that will ensure utility and sustainability of this critical patient safety issue.
Medication reconciliation is integral to reducing medication errors surrounding hospitalizations.1, 2 The practice of medication reconciliation requires a systematic and comprehensive review of all the medications a patient is currently taking to ensure that medications being added, changed, or discontinued are carefully evaluated with the goal of maintaining an accurate list; that this process is undertaken at every transition along the continuum of care; and that an accurate list of medications is available to the patient or family/caregiver and all providers involved in the patient's care, especially when a care handoff takes place. With regulators, payers and the public increasingly demanding action to reduce medication errors in hospitals, all health care providers must support efforts to achieve accurate medication reconciliation.1, 3
The Joint Commission's Definition of Medication
Any prescription medications, sample medications, herbal remedies, vitamins, nutraceuticals, vaccines, or over‐the‐counter drugs; diagnostic and contrast agents used on or administered to persons to diagnose, treat, or prevent disease or other abnormal conditions; radioactive medications, respiratory therapy treatments, parenteral nutrition, blood derivatives, and intravenous solutions (plain, with electrolytes and/or drugs); and any product designated by the Food and Drug Administration (FDA) as a drug. This definition of medication does not include enteral nutrition solutions (which are considered food products), oxygen, and other medical gases.
2010 Hospital Accreditation Standards,
The Joint Commission, 2010, p. GL19.
While conceptually straightforward, implementing medication reconciliation has proved to be very difficult in the myriad healthcare settings that exist. The disjointed nature of the American health care system and a conglomeration of paper and electronic systems for tracking medications synergize to thwart efforts to maintain an accurate, up‐to‐date medication list at every step along the care continuum. Although The Joint Commission defines medication for the purpose of its accreditation standards (see box), the healthcare community lacks a common understanding or agreement regarding what constitutes a medication. There is also confusion about who should ultimately be responsible for obtaining the patient's medication information, for performing the various steps in the reconciliation process, and for managing the multiple providers who alter the medication list but may not feel competent to perform reconciliation of medications outside their area of expertise safely. Importantly, there is also a lack of clarity around how patients and family/caregivers should be involved in the process.
Despite these challenges, medication reconciliation remains a critical patient safety activity that is supported by the organizations signing this consensus statement, (Table 1). Although medication reconciliation has an impact on medication safety in all care settings, this paper focuses on issues most germane to the continuum of care involving the hospital setting. The themes and issues discussed will likely apply to other care settings as well. In this paper, we also recommend several concrete steps that we believe should be initiated immediately to begin to reach the goal of optimizing the medication safety achievable through effective medication reconciliation.
Background
Medication reconciliation is intended to be a systematic extension of the medication history‐taking process that has been used by health care providers for decades. Its recent iteration was developed to ensure that medications were not added, omitted, or changed inadvertently during care transitions. It became codified, refined, and tested over the past decade through the efforts of a number of groups focused on medication safety including the Institute for Healthcare Improvement (IHI) and the Institute for Safe Medication Practices (ISMP). With the reinforcing adoption of medication reconciliation as National Patient Safety Goal (NPSG) No. 8 in 2005 by The Joint Commission, efforts to implement it became widespread in both hospital‐based and ambulatory settings.
Medication reconciliation has three steps, as described by IHI4:
-
Verification (collection of the patient's medication history);
-
Clarification (ensuring that the medications and doses are appropriate); and
-
Reconciliation (documentation of changes in the orders).
The details of the process vary by setting and by the availability of paper or electronic medical records. However, the essential steps remain the same, as does the need to perform reconciliation each time the patient transfers to a new setting or level of care. Table 2 lists the most common points at which medication reconciliation occurs in hospitalized patients.
|
| American Academy of Pediatrics |
| American Association of Critical‐Care Nurses |
| Consumers Advancing Patient Safety |
| Institute for Healthcare Improvement |
| Institute for Safe Medication Practices |
| The Joint Commission |
| Massachusetts Coalition for Prevention of Medical Errors |
| Microsoft Corporation |
| Northwestern Memorial Hospital and Northwestern University School of Medicine |
| Society of General Internal Medicine |
| Society of Hospital Medicine |
| University of California San Diego Medical Center |
Because of their complexity, organizations must take care to design their medication reconciliation processes systematically. IHI lists elements of a well‐designed medication reconciliation process as part of its 5 Million Lives Campaign How‐to Guide.4 Such a process:
-
Uses a patient centered approach.
-
Makes it easy to complete the process for all involved. Staff members recognize the what's‐in‐it‐for‐me aspect of the change.
-
Minimizes the opportunity for drug interactions and therapeutic duplications by making the patient's list of current medications available when clinicians prescribe new medications.
-
Provides the patient with an up‐to‐date list of medications.
-
Ensures that other providers who need to know have information about changes in a patient's medication plan.
Research on how adverse drug events (ADE) occur supports the need for tight control of medication orders at transitions in care. For instance:
-
In a study conducted at Mayo Health System in Wisconsin, poor communication of medical information at transition points was responsible for as many as 50% of all medication errors in the hospital and up to 20% of ADEs.5
-
Variances between the medications patients were taking prior to admission and their admission orders ranged from 30% to 70% in 2 literature reviews.1, 6
-
The largest study of medication reconciliation errors and risk factors at hospital admission documented that 36% of patients had errors in their admission orders.7
When The Joint Commission adopted medication reconciliation as NPSG No. 8 in 2005 it had 2 parts: Requirement 8Aa process must exist for comparing the patient's current medications with those ordered for the patient while under the care of the organization; and requirement 8Ba complete list of the patient's medications must be communicated to the next provider of service on transfer within or outside the organization and a complete list of medications must be provided to the patient on discharge.8
However, many hospitals found it difficult to implement medication reconciliation in a systematic way. There was also confusion among hospital staff and administration about the exact definition of medication reconciliation in terms of what it should entail.9 Given these difficulties, The Joint Commission announced that effective January 1, 2009, medication reconciliation would no longer be factored into an organization's accreditation decision or be considered for Requirements for Improvement. Additionally, The Joint Commission stated it is reviewing and revising the NPSG so that it will be ready to be released in January 2011 for implementation later that year.10
Recognizing the difficulty hospitals were having with meaningfully implementing medication reconciliation, the Society of Hospital Medicine convened a 1‐day conference on March 6, 2009, to obtain input from key stakeholders and focus on several critical domains relevant to the success of hospital‐based medication reconciliation. The Agency for Healthcare Research and Quality provided funding support for this conference through grant 1R13HS017520‐01.
An overarching theme emerged from the meeting: the need to reorient the focus of medication reconciliation away from that of an accreditation mandate and toward a broader view of patient safety. Forcing medication reconciliation via a requirement for accreditation tended to limit an organization's efforts to specific process measures. Addressing it as a more global patient safety issue takes into account the entire patient care experience and then opens the door to leverage nonclinical venues (e.g., medical home, family home, community, religious, and other social organizations, as well as social networking platforms) and engage the patient and family/caregivers to reinforce the importance of medication safety.
This white paper evolved from discussions at the March 2009 conference,11 and subsequent structured communication among attendees. Formal endorsement of this document was obtained from the organizations listed in Table 1. In this document, we explore several key issues in implementing clinically meaningful and patient‐centered medication reconciliation. We focus on building common language and understanding of the processes of and participants in medication reconciliation; consider issues of implementation and risk stratification; emphasize the need for research to identify best practices and discusses how to disseminate the findings; promote health information technology platforms that will support interoperable medication information exchange; support the formation of partnerships between patient care sites and nonclinical sites as well as utilizing social marketing opportunities to enhance opportunities for transmitting messages about medication safety; and reinforce the ongoing healthcare reform discussion which aims to align financial incentives with patient safety efforts. After each section, we offer concrete first steps to address the issues discussed.
| Admission: When clinicians reconcile the patient's medications taken at home or at a prior care setting with any new prescription orders to be prescribed by an admitting clinician. |
| Transfer (intra‐ or inter‐facility; with change of clinician or site of care): When clinicians review previous medication orders in light of the patient's clinical status, along with new orders or plans of care. |
| Discharge: When clinicians review all medications the patient was taking prior to being hospitalized, incorporating new prescriptions from the hospitalization and determining whether any medication should be added, discontinued, or modified while being mindful of therapeutic interchanges needed for formulary purposes. |
Methods
The invitation‐only meeting held on the Northwestern Medical Campus in Chicago, IL, brought together stakeholders representing professional, clinical, health care quality, consumer, and regulatory organizations (Table 3). The conference convened these participants with the goals of identifying barriers to meaningful implementation of medication reconciliation and developing a feasible plan toward its effective implementation in the hospital setting. At the meeting, all participants were divided into 1 of 4 groups, which held a facilitated discussion around 1 of 4 key relevant domains: (1) how to measure success in medication reconciliation; (2) key elements of successful strategies; (3) leveraging partnerships outside the hospital setting to support medication reconciliation; and (4) the roles of the patient and family/caregivers and health literacy. Individual group discussions were cofacilitated by experts in the content area. After each discussion, the small group then rotated to a different discussion. Ultimately, each group participated in all four discussions, which built iteratively on the content derived from the prior groups' insights. Key comments were then shared with the large group for further discussion. To help build consensus, these large group discussions were directed by professional facilitators.
| AACN American Association of Critical Care Nurses |
| AAFP American Academy of Family Physicians |
| AAP American Academy of Pediatrics |
| ACEP American College of Emergency Physicians |
| ACP American College of Physicians |
| AMA American Medical Association |
| AMSN Academy of Medical Surgical Nurses |
| ASHP American Society of Health‐System Pharmacists |
| ASHP Foundation American Society of Health‐System Pharmacists Foundation |
| CAPS Consumers Advancing Patient Safety |
| CMS Centers for Medicare and Medicaid Services |
| CMSA Case Management Society of America |
| HCI Hospitalist Consultants, Inc |
| IHI Institute for Healthcare Improvement |
| InCompass Health |
| ISMP Institute For Safe Medication Practice |
| JCR Joint Commission Resources |
| Massachusetts Coalition for Prevention of Medical Errors |
| Microsoft Corporation |
| Northwestern Memorial Hospital MATCH Program |
| NQF National Quality Forum |
| SGIM Society of General Internal Medicine |
| SHM Society of Hospital Medicine |
| The Joint Commission |
| UCSD Hospital Medicine |
| University of Oklahoma College of Pharmacy Tulsa |
After the meeting, attendees participated in 2 follow‐up conference calls to discuss issues raised at the conference and responses obtained from host organizations. They also subsequently participated in two focus groups with The Joint Commission, giving input on the revision of the medication reconciliation NPSG.
Results
Addressing Barriers to Medication Reconciliation
In order to implement successful medication reconciliation processes, one must build the steps with the patient and family/caregiver as the focus and demonstrate an understanding of the intent of these processes. At its roots, medication reconciliation was developed to ensure that clinicians do not inadvertently add, change, or omit medications and that changes made are communicated to all relevant caregivers.
A number of key issues with respect to successful medication reconciliation processes surfaced in discussions with stakeholders. We believe addressing these issues is necessary before meaningful and standardized implementation can be achieved. After each discussion below, we provide suggested first steps to address these issues.
1. Achieve Consensus on the Definition of Medication and Reconciliation
Despite proposed definitions of these terms by various organizations, there was little agreement about them in the healthcare community. This ambiguity contributed to general confusion about what actually constitutes medication reconciliation. There needs to be a single, clear, and broadly accepted definition of what constitutes a medication. For the purposes of medication reconciliation, the term medication should be broadly inclusive of substances that may have an impact on the patient's care and treatments as well as those substances that may interact with other therapies potentially used during the medical care episode. Illicit or recreational substances may also have impact on therapies considered and therefore may influence this definition.12 Concretely, this definition should encompass prescription and over‐the‐counter medications as well as herbal and dietary supplements.
The term reconciliation in its simplest form implies the process of verifying that a patient's current list of medications (including dose, route, and frequency) are correct and that the medications are currently medically necessary and safe. Reconciliation suggests a process which, by necessity, will vary based on clinical context and setting. Further defining this termand the process of reconciliation itselfshould be carried out using patient safety principles with a focus on patient‐ and family‐centeredness.
Designing hospital‐based medication reconciliation processes should:
-
Employ a multidisciplinary approach that involves nurses, pharmacists, and other appropriate personnel from the inpatient setting as well as ambulatory and community/retail areas, both ambulatory and inpatient physicians, and a patient/family representative;
-
Involve hospital leaders who support, provide guidance, and remove barriers for the multidisciplinary team working to implement the processes;
-
Clearly define the roles of each participant in the processes developed;
-
Include methods to assess and address any special needs due to the developmental stage, age, dependency, language or literacy levels of patients and their family/caregiver;
-
Use clinically relevant process measures (e.g., adherence to procedural steps) and outcome measures (e.g., change in the number of ADEs, unnecessary hospitalizations, or emergency department visits) where appropriate to assess the impact of the process;
-
Include feedback systems to allow for clinically significant process improvement.
Once a common understanding of the terms and intent of medication reconciliation is achieved, it will be important for accrediting organizations, medical societies, quality improvement organizations, and other interested parties to adopt the same language.
First Step
A consortium of clinical, quality, and regulatory stakeholders should work to achieve consensus on the definition for medication and the intent and expectations for the reconciliation process.
2. Clarify Roles and Responsibilities
Given the differences in organizational and practice structures in hospitals and the varying numbers of health professionals involved in a patient's care, no one process design will meet the needs of all sites. As it is clear that interdisciplinary teams are best suited to develop, implement, and carry out complex patient‐centered processes like medication reconciliation, it is crucial that all involved parties have clearly defined roles and responsibilities, including patients and their families/caregivers. It is also important to recognize that these responsibilities may change depending on the dependency or vulnerability of the patient (e.g., children or geriatric patients) or the transition of care being undertaken by the patient (i.e., admission, transfer, or discharge), thus requiring sites to develop clear policies about these roles and responsibilities and how they may change in various situations.
First Step
Individual sites must clearly define the roles and responsibilities of all parties directly involved in medication reconciliation as a part of designing local medication reconciliation processes.
3. Develop Measurement Tools
Ensuring that medication reconciliation processes result in clinically meaningful outcomes requires the development and standardization of a limited number of metrics that may be used by organizations and reported centrally for benchmarking. This core set of measures should be developed by clinical, quality, accreditation, and regulatory organizations (see #10 below) through a consensus building process utilizing multi‐stakeholder input. The set should be supplemented by additional site‐specific measures determined locally that focus on steps in the process itself and allow sites to perform continuous quality improvement. Sites should be encouraged to develop tools locally to support and facilitate organizational and professional adherence to medication reconciliation processes.
First Steps
Clinical, quality, accreditation, and regulatory organizations should develop reliable metrics to be assessed and reported.
The principles of patient‐centeredness and family/caregiver‐centeredness, the medical home, and clinical relevance must be central to the metrics chosen for quality and regulatory purposes.
4. Phased Implementation
Ultimately, comprehensive medication reconciliation processes need to be implemented in hospitals. However, to succeed in integrating complex processes like medication reconciliation into routine hospital practices, implementation may be facilitated by using a phased approach to allow for participants to adapt new processes and procedures to the local environment iteratively. While the most appropriate phased approach to implementation will vary by site and setting, options for phasing might include:
-
Starting with one clinical area or service.
-
Starting with either the admission or discharge reconciliation process.
-
Starting with a patient population at high risk for adverse events.
Irrespective of the phasing strategy employed, development of a clear and pragmatic schedule for the entire implementation process should be established. Phasing decisions should be made based on organizational resources and the clinical needs of the patient population within each clinical setting. As noted, the ultimate goal is to develop comprehensive reconciliation processes occurring during all significant care transitions (i.e., admission, service or site‐of‐care transfers, and discharge) for all hospitalized patients and involving all of their medications. Flexibility in design should be encouraged to ensure the processes can work within local workflow as long as progress toward this primary goal is made.
First Steps
Clinical sites should establish local, pragmatic priorities for a phased approach to implementation.
Tie the phased approach to a timeline or blueprint for programmatic expansion with ultimate plans for comprehensive implementation.
5. Develop Risk Stratification Systems
Medication‐related adverse events related to inadequate reconciliation are more likely to occur in hospitalized patients with certain identifiable risk factors. For example, the MATCH study documented that polypharmacy and age over 65 years were independently associated with increased risk for errors at the time of hospital admission.7 Other factors that may increase the likelihood of medication‐related adverse events at care transitions in the hospital might include: patients with multiple providers, developmental/cognitive impairment, dependency/vulnerability, multiple or high‐risk medications, or poor health literacy or limited English proficiency. Research is needed to elucidate these risk factors further.
An alert system for key risk factors for complications related to incompletely, inappropriately, or inaccurately completed medication reconciliation due to patient, clinician, or system factors should be developed, tested, and broadly implemented. Additionally, an alert system would help maintain vigilance toward this patient safety issue and, potentially, help focus additional resources on high‐risk patients. Such a tool has been tested in ambulatory settings.15
First Step
Additional research on inpatient predictors of failed medication reconciliation and ADE should be prioritized (see #6 below).
6. Study Interventions and Processes
Despite having been an NPSG since 2005, there is still a relative paucity of literature about broadly applicable and effective implementation strategies and demonstrated interventions that improve medication safety related to medication reconciliation. Some strategies that have shown to reduce medication errors at transitions include the involvement of pharmacist medication review on discharge16, 17 and the usefulness of planning by multidisciplinary groups.18 Other studies have outlined the continuing barriers to successful implementation of reconciliation, including the difficulty patients have in accurately recalling their current medications19 and the high cost in nurse and pharmacist time of tracking down a patient's ongoing prescriptions.20, 21 Studies evaluating potential solutions to overcome these and other common barriers are still needed.
Future research should focus on a comprehensive review of implementation strategies, (specifically including the role of health information technology‐based innovations) clinically relevant outcomes, and best practices, while being sensitive to the different needs of varying care settings (e.g., pediatric vs. adult centers, emergency departments vs. inpatient units, community hospital vs. academic medical center, etc.) as well as the resource requirements engendered in the interventions.
First Step
Funding agencies should explicitly prioritize outcomes‐focused medication reconciliation‐related projects (e.g., those which demonstrate a reduction in postdischarge ADE or reduced medication‐related emergency department visits). Previously identified successful strategies should be further investigated. Funded projects should explicitly partner with patients and family/caregivers and also include pediatric and adult patients, rural and urban locations of care, as well as academic and nonacademic hospital settings, to promote more broadly applicable results.
7. Disseminate Success
Best practices and lessons learned, especially those rigorously tested and driven by data, stratified by patient type, care setting (emergency department, intensive care, surgical ward, etc.) and institutional type (community, teaching, safety net, critical access, etc.) need to be disseminated so others can adopt and adapt them effectively. High‐quality case studies with clear explanations of successes, failures, and lessons learned may prove valuable sources of information. This knowledge should foster a learning community approach and accelerate implementation at new sites.
First Step
Hospitals, healthcare systems, as well as quality and regulatory agencies should develop mechanisms within reporting systems to track performance, identify notably successful sites, and publicly report and share methods and lessons learned from them.
8. Promote the Personal Health Record
A fully integrated and transferable personal health record should be accepted as the standard for health information storage and interoperability, giving both the patient (or family/caregiver) and clinical providers access and ownership. Both the HL7 Continuity of Care Document (CCD) and the Continuity of Care Record (CCR) meet these criteria. The CCR was endorsed by the American Society for Testing and Materials22 and a coalition of other medical societies.23 Notably, CCR and CCD were recently adopted as standards for structured electronic health record (EHR) exchange through the July 2010 publication of the Final Rule of the Health Information Technology for Economic and Clinical Health Act provision of the American Recovery and Reinvestment Act of 2009 (ARRA/HITECH) and is now part of the formal US Department of Health and Human Services certification criteria for EHR technologies.24
Mandating a content exchange standard such as the CCR or the CCD should also have the desired effect of ensuring that patients (and their caregivers) become increasingly involved in maintaining an accurate list of the medications they take. Additionally, systems must be sufficiently flexible to address the unique medication management needs of children and geriatric patients. An electronic version of a personal health record is a promising method for improving consistency across care platforms, but to be implemented effectively the record must be compatible across all settings, including, where possible, the patient's home. All health care organizations, pharmacy systems, and insurers, must make medication reconciliation‐related interoperability and accessibility a priority as they pursue information technology strategies.
First Step
Stakeholder organizations must send a clear and convincing message to legislators under the current atmosphere of health care reform, urging them to mandate that health information technology standards include interoperability and support platforms that are consistent with standards put forth in the 2009 HITECH Act Interim Final Rule for EHR certification.
9. Promote Partnerships
At a broader health care system level, leveraging existing partnerships and creating new ones among health care, public/private sector‐affiliated organizations (e.g., community and mail order pharmacies, pharmaceutical organizations and manufacturers, and insurers), and public health organizations are extremely important mechanisms for broader scale impact. This view recognizes the numerous opportunities to educate and influence patients about medication safety outside the dyadic relationship of the clinician and patient in traditional clinical settings. Partnerships between health care and public entities may capitalize on these opportunities to foster adoption of healthy medication practices (e.g., maintaining an accurate and updated medication list), thereby supporting medication reconciliation efforts when individuals encounter health care settings. Partnership and information sharing could be enhanced through the use of a central coordinating body or coalition. This body could generate a shared common vision and contribute expertise to the myriad issues in medication reconciliation.
Partnerships should utilize the following:
-
Social marketing techniques to engage the community. Included within this strategy must be a clear and compelling message that transmits the importance of safe medication practices. Current messages such as keep a list while important, do not offer enough of a sense of urgency or importance. A more powerful message could involve highly publicized medication errors or close calls that would resonate with a broad audience.
-
Local and national champions. Such individuals should be trusted for their health knowledge (e.g., television health care reporters) or be prominent, influential, and trusted figures in other circles (e.g., clergy, politicians, movie celebrities). Indeed, taking advantage of popular media by weaving a theme into a movie or television program about medication safety may prove effective.
Relevant partnerships would include:
-
Quality organizations partnering with other stakeholders to establish unambiguous and unified medication reconciliation standards across the care continuum.
-
Health systems partnering with community pharmacy providers to ensure an uninterrupted communication link in both the inpatient and outpatient settings.
-
Manufacturers and distributors of medications partnering with health care and public health organizations, the media, insurers and other constituents to promote the importance of maintaining and sharing an accurate list of medications.
-
Public health systems partnering with community‐based organizations to encourage and promote the established standards for medication safety through messaging and educational campaigns.
All partnerships must consider issues of patient language and literacy as well as the needs of vulnerable populations in the scope of their activities.
First Step
Public health agencies should partner with health care quality organizations and others to begin a national public campaign to increase the awareness of medication safety (the broader public health concept under which medication reconciliation would fall) and support the importance of the patient's role in maintaining an updated medication list at all times.
10. Align Financial Incentives With Newly Developed Regulatory and Accreditation Requirements
Implementing and performing medication reconciliation takes time, particularly at the outset of a new program. Time requirements and associated costs are major barriers to undertaking comprehensive medication reconciliation, despite its recognized importance for reducing avoidable injury to patients. At present, systems that impede efficiency and slow hospital throughput may be discouraged due to their potential for having an adverse impact on access, finances, and other aspects of care delivery. Moreover, the changed economic climate with reduced hospital fiscal margins limits resources for new initiatives. Currently, failed medication reconciliationand the related avoidable adverse events, culminating in readmission to the hospital or emergency departmentyields additional revenue for hospitals and other providers in some reimbursement models.
Alignment of financial incentives that ensured adequate time and resources for appropriate medication reconciliation processes would facilitate implementation. Additionally, start‐up funding to create and implement these processes needs to be made available.
One example illustrating efforts to align payment policy with medication safety efforts occurred when the Office of the National Coordinator (ONC), in publishing its Final Rule under the 2009 HITECH Act,24 endorsed the importance of financially supporting proper medication reconciliation, particularly at first encounter and transitions in care, by requiring EHR systems seeking certification under the rule to support the care team in the task of reconciliation. For example, vendors will have to support the ability to compare 2 or more medication lists electronically, create medication lists, drug allergy lists, perform drug formulary look‐ups, drug‐drug and drug‐allergy checks, and support creating patient summaries after each visit or post discharge that include medication lists. The ONC, in defining Meaningful Use for eligible health care organizations, included in that definition the goal of exchanging meaningful clinical information among the professional health care teams. This goal is demonstrated through organizations reporting that they performed medication reconciliation for at least 50% of transitions of care in which the patient is transitioned into the care of the eligible professional or admitted to the eligible hospital's or Critical Access Hospital's inpatient or emergency department. Organizations able to demonstrate this level of compliance, along with other Meaningful Use requirements, will be eligible to receive stimulus funds through 2015 and avoid financial penalties that begin after that period.
First Step
Future health care reform must address the misalignment of financial policies and structures, and provide financial incentives to support the development and implementation of better medication management systems and prevent avoidable rehospitalizations and emergency department visits resulting from medication‐related adverse events.
Conclusion
Medication reconciliation involves highly complex processes and is hampered by the disjointed nature of the American health care system. It is, however, a vital part of reducing ADE. If employed more broadly, it has the added benefits of enhancing communication among all providers of care and engaging patients and families/caregivers more consistently and meaningfully in their overall care.
Despite the difficulty of maintaining an accurate medication record in real time across disparate settings, reconciliation is a goal to which our organizations are committed. Given the wide range of healthcare organizations involved in providing medications to patients and the many agencies evaluating those efforts, we believed it would be helpful to provide an overarching set of goals to move medication reconciliation forward.
Our main message is this: Patient safety and patient/family‐centered care must be the principal drivers in the development and implementation of medication reconciliation systems. Ultimately this process is about ensuring that patients are receiving the most appropriate medications no matter where they are treated. With this document, we hope to bring to light the importance of creating and implementing a medication reconciliation program, addressing some barriers to success, and identifying potential solutions that will ensure utility and sustainability of this critical patient safety issue.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- .Prevention of medication errors in the pediatric inpatient setting. The American Academy of Pediatrics Policy Statement.Pediatrics.2003;112(2):431–436.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- Institute for Healthcare Improvement. 5 million lives getting started kit: preventing adverse drug events (medication reconciliation), how‐to guide. Available at: http://www.ihi.org/IHI/Programs/Campaign/ADEsMedReconciliation.htm. Published Oct. 1, 2008. Accessed September2010.
- ,.Medication safety: one organization's approach to the challenge.J Clin Outcomes Mana.2001;8(10):27–34.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Results of the Medications At Transitions and Clinical Handoffs (MATCH) Study: an analysis of medication reconciliation errors and risk factors at hospital admission.J Gen Intern Med.2010;25(5):441–447.
- Joint Commission on Accreditation of Healthcare Organizations.2005 Hospital Accreditation Standards, p.NPSG‐4.
- ,,,,.Brief communication: Results of a medication reconciliation survey from the 2006 Society of Hospital Medicine national meeting.J Hosp Med.2008;3(6):465–472.
- The Joint Commission.Approved: will not score medication reconciliation in 2009.Jt Comm Perspect.2009;29(3):1,3.
- Society of Hospital Medicine. Medication reconciliation: a team approach, conference summary. December 2009. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/QualityImprovement/QICurrentInitiativesandTrainingOpportunities/QI_Current_Initiativ.htm. Accessed September2010.
- The American Medical Association. The physician's role in medication reconciliation: issues, strategies and safety principles. 2007. Available at: http://www.ama‐assn.org/ama1/pub/upload/mm/370/med‐rec‐monograph.pdf. Accessed September2010.
- Institute of Safe Medication Practices. ISMP's list of high alert medications. 2008. Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed September2010.
- ,,,.Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147(11):755–765
- ,,, et al.Experience with a trigger tool for identifying adverse drug events among older adults in ambulatory primary care.Qual Saf Health Care.2009;18(3):199–204.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- ,,,,.Medication reconciliation at an academic medical center: implementation of a comprehensive program from admission to discharge.Am J Health Syst Pharm.2009;66(23):2126–2131.
- ,,,,,.Multidisciplinary approach to inpatient medication reconciliation in an academic setting.Am J Health Syst Pharm.2007;64(8):850–854.
- ,,.Lack of patient knowledge regarding hospital medications.J Hosp Med.2010;5(2):83–86.
- .The unexpected challenges of accurate medication reconciliation.Ann Emerg Med.2008;52(5):493–495.
- ,,,.Medication reconciliation in a rural trauma population.Ann Emerg Med.2008;52(5):483–491.
- ASTM International. ASTM E2369 ‐ 05e1 standard specification for continuity of care record (CCR). Available at: http://www.astm.org/Standards/E2369.htm. Accessed September2010.
- ,,.The continuity of care record.Am Fam Physician.2004;70(7):1220,1222–1223.
- Department of Health and Human Services. Health information technology: initial set of standards, implementation specifications, and certification criteria for electronic health record technology; final rule. Available at: http://edocket.access.gpo.gov/2010/pdf/2010–17210.pdf. Accessed September2010.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- .Prevention of medication errors in the pediatric inpatient setting. The American Academy of Pediatrics Policy Statement.Pediatrics.2003;112(2):431–436.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- Institute for Healthcare Improvement. 5 million lives getting started kit: preventing adverse drug events (medication reconciliation), how‐to guide. Available at: http://www.ihi.org/IHI/Programs/Campaign/ADEsMedReconciliation.htm. Published Oct. 1, 2008. Accessed September2010.
- ,.Medication safety: one organization's approach to the challenge.J Clin Outcomes Mana.2001;8(10):27–34.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Results of the Medications At Transitions and Clinical Handoffs (MATCH) Study: an analysis of medication reconciliation errors and risk factors at hospital admission.J Gen Intern Med.2010;25(5):441–447.
- Joint Commission on Accreditation of Healthcare Organizations.2005 Hospital Accreditation Standards, p.NPSG‐4.
- ,,,,.Brief communication: Results of a medication reconciliation survey from the 2006 Society of Hospital Medicine national meeting.J Hosp Med.2008;3(6):465–472.
- The Joint Commission.Approved: will not score medication reconciliation in 2009.Jt Comm Perspect.2009;29(3):1,3.
- Society of Hospital Medicine. Medication reconciliation: a team approach, conference summary. December 2009. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/QualityImprovement/QICurrentInitiativesandTrainingOpportunities/QI_Current_Initiativ.htm. Accessed September2010.
- The American Medical Association. The physician's role in medication reconciliation: issues, strategies and safety principles. 2007. Available at: http://www.ama‐assn.org/ama1/pub/upload/mm/370/med‐rec‐monograph.pdf. Accessed September2010.
- Institute of Safe Medication Practices. ISMP's list of high alert medications. 2008. Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed September2010.
- ,,,.Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147(11):755–765
- ,,, et al.Experience with a trigger tool for identifying adverse drug events among older adults in ambulatory primary care.Qual Saf Health Care.2009;18(3):199–204.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- ,,,,.Medication reconciliation at an academic medical center: implementation of a comprehensive program from admission to discharge.Am J Health Syst Pharm.2009;66(23):2126–2131.
- ,,,,,.Multidisciplinary approach to inpatient medication reconciliation in an academic setting.Am J Health Syst Pharm.2007;64(8):850–854.
- ,,.Lack of patient knowledge regarding hospital medications.J Hosp Med.2010;5(2):83–86.
- .The unexpected challenges of accurate medication reconciliation.Ann Emerg Med.2008;52(5):493–495.
- ,,,.Medication reconciliation in a rural trauma population.Ann Emerg Med.2008;52(5):483–491.
- ASTM International. ASTM E2369 ‐ 05e1 standard specification for continuity of care record (CCR). Available at: http://www.astm.org/Standards/E2369.htm. Accessed September2010.
- ,,.The continuity of care record.Am Fam Physician.2004;70(7):1220,1222–1223.
- Department of Health and Human Services. Health information technology: initial set of standards, implementation specifications, and certification criteria for electronic health record technology; final rule. Available at: http://edocket.access.gpo.gov/2010/pdf/2010–17210.pdf. Accessed September2010.
Business Case for an Electronic Discharge Summary
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
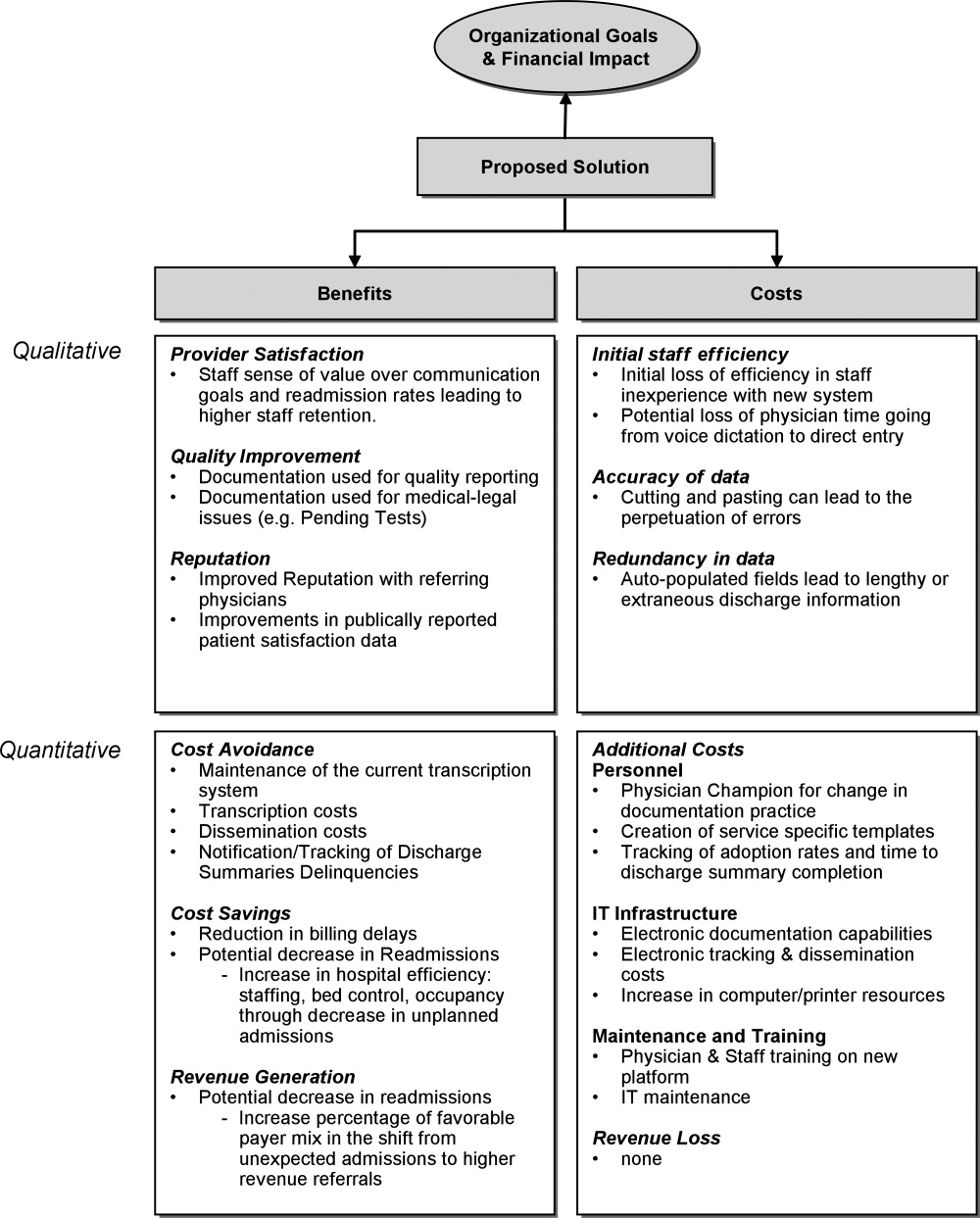
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
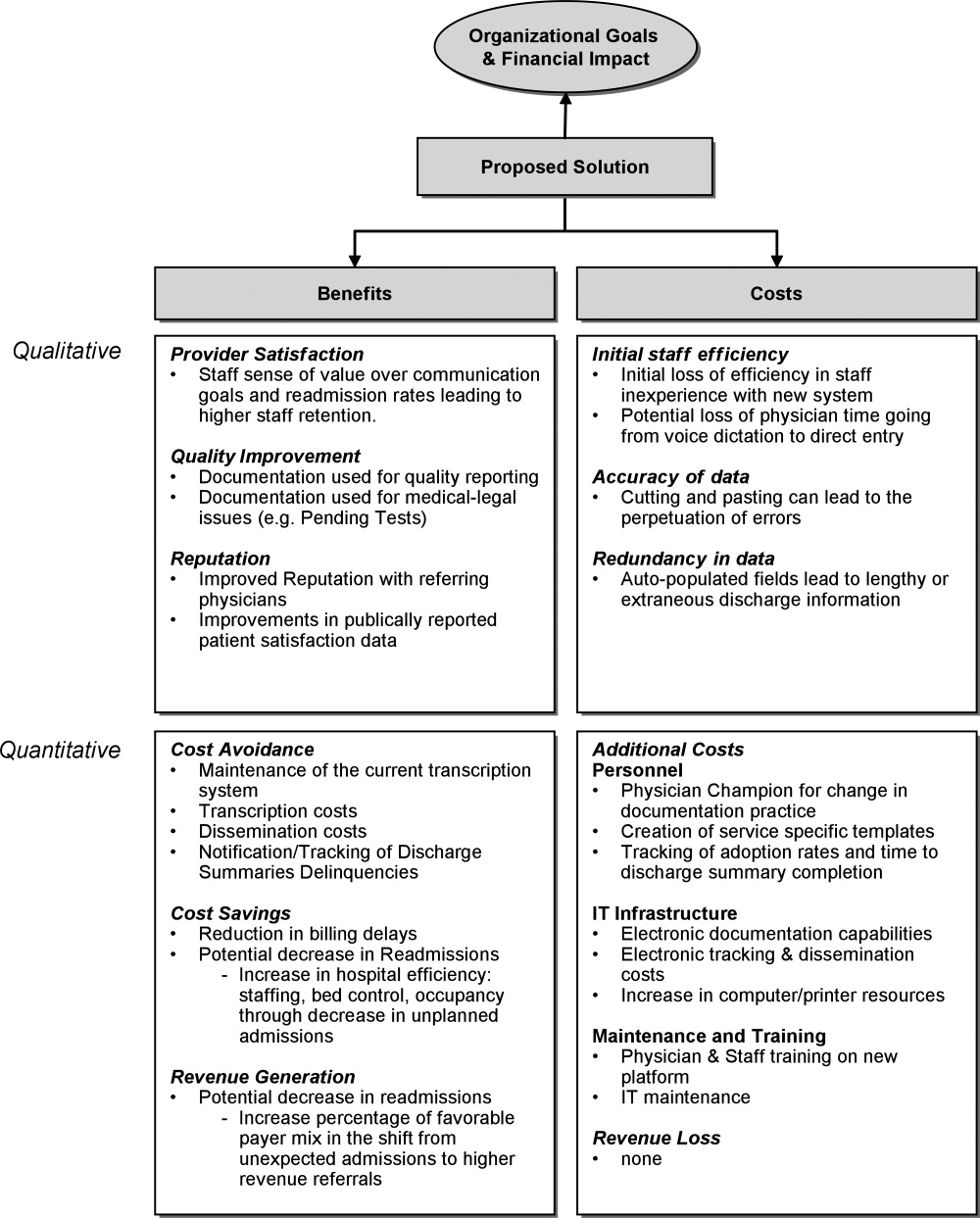
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
Delivering the highest possible quality of care is among the top priorities of all medical centers. That said, any quality innovation must be seen as adding value from a variety of perspectives. Especially in the current economic climate, a sound business case is paramount to the advancement of any quality innovation. Given the nature of their work, hospitalists are ideally suited to undertake system improvement innovations. To assist hospitalists in successfully implementing quality and safety initiatives, we have designed a framework of elements required for a business case. We describe our experience developing and implementing an electronic discharge summary and utilize a structured framework to articulate the business case for its implementation.
Defining a Business Case Framework
A business case is a structured proposal outlining the qualitative and quantitative factors that justify a course of action. An effective business case for a quality improvement initiative articulates how both factors are aligned with preexisting organizational goals. In modeling the business case framework for the electronic discharge summary, Figure 1 outlines the qualitative and quantitative costs and benefits that can affect institutional decision making.
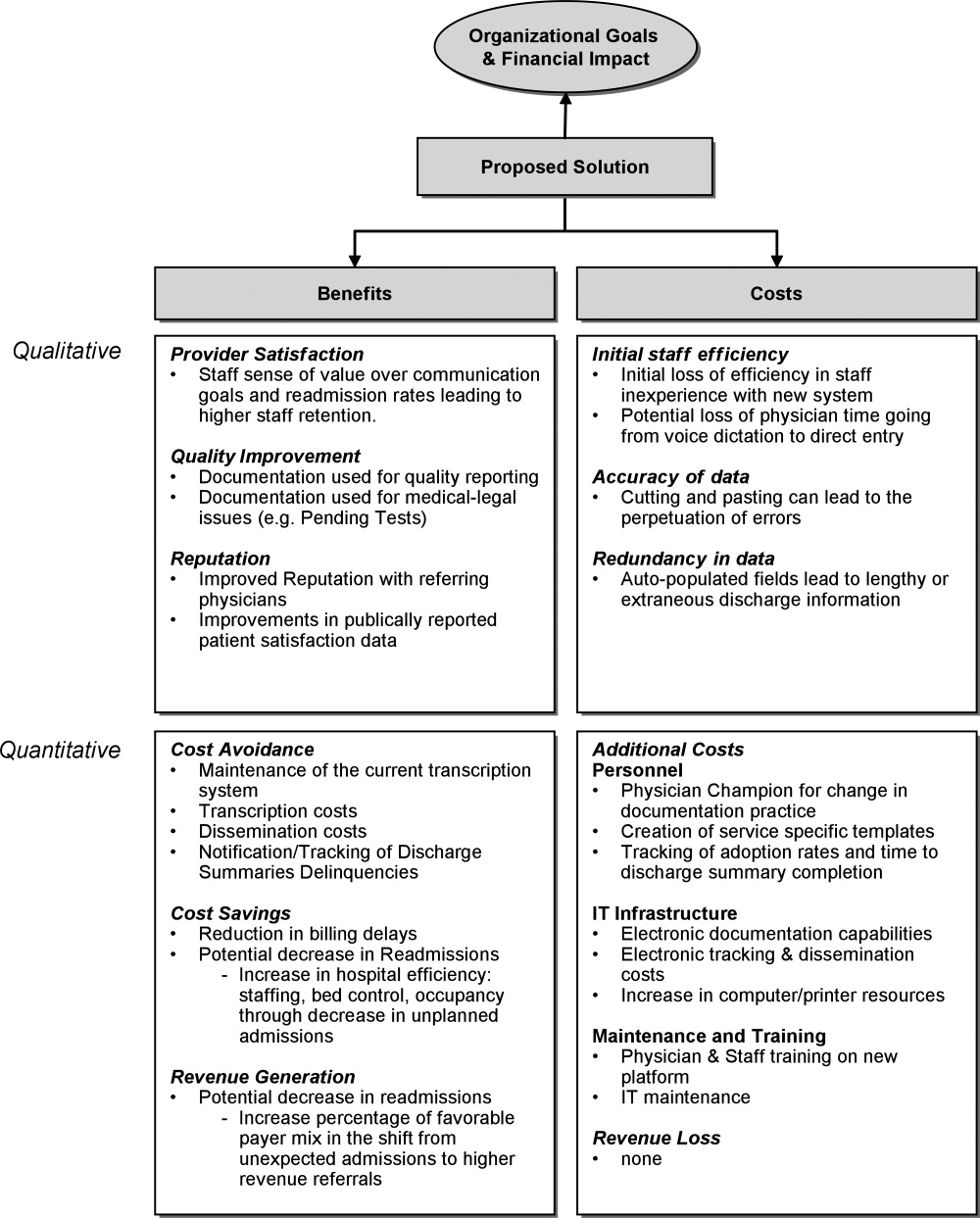
Organizational Aims and Financial Impact: Determining Costs and Benefits
Organizational goals drive decision making and resource allocation at all levels. As priorities change with time, understanding which predominate in an organization will be essential to building a business case. Institutions may be more willing to adopt expensive innovations if they are justified by progress toward the qualitative organizational goals. Figure 1 demonstrates several institutional goals both qualitative (provider satisfaction, quality improvement, and institutional reputation) and quantitative (cost avoidance, cost savings, and revenue generation) that could drive the decision making for an electronic discharge summary. After examining how an initiative aligns with institutional aims, the next step is to weigh the benefits against the potential costs. Costs in our example include not only the quantitative financial investment in information technology (IT) infrastructure, personnel and maintenance, but also may include qualitative costs such as loss of staff efficiency and redundant documentation. Costs and savings will be geographically variable and depend on the institutional framework, eg, the existing system for medical records, institutional patient payer mix, type of payment structure (global vs. utilization based*), and reimbursement rates. While it may be impractical to account for every cost and savings resulting from the project implementation, every effort should be made to account for the key variables that make up the cost‐benefit calculation.
The Business Case for an Electronic Discharge Summary at University of California San Francisco (UCSF)
Current State of Discharge Documentation a UCSF
UCSF Medical Center is a 600‐bed quaternary care academic institution that discharges approximately 100 patients per day. Our hospital discharge summary is used to document a patient's hospital course and post discharge plan, information necessary for continued care in the outpatient setting. Literature supports the potential for timely and relevant discharge summaries to improve care transitions, clinician satisfaction, and resource use.1 In 2008, however, the majority of our discharge summaries were completed greater than 14 days post discharge, in accordance with national practice.2 Despite Centers for Medicare & Medicaid Services (CMS) and the Joint Commission discharge summary standards regarding content,3, 4 most discharge summaries are composed using freeform dictation.2 Consequently, discharge summaries often lack critical information,57 and may not reach the correct outpatient provider in a timely manner.5, 811
Our Proposed Solution: E‐Discharge
As hospitals are increasingly implementing electronic medical records (EMR),12 there is a growing opportunity to efficiently and reliably incorporate information from the medical record into electronic or database assisted discharge materials. At UCSF the need to develop a system to document and communicate tests pending at discharge fueled the development of an electronic discharge summary. UCSF's vendor‐supplied EMR lacks the ability to integrate electronic patient data into a progress note or discharge summary in a manner usable for physicians. Instead physicians are required to use a telephone voice dictation system, which is subsequently transcribed to text within 1 to 3 days. A separate software platform tracks attending signature of the transcribed text and automatically triggers dissemination through computerized fax and campus mail. The turnaround time for a discharge summary can be as long as 3 weeks. With the time involved and high cost of implementing new or more sophisticated versions of EMR, we chose to design a solution that would improve care for our patients in a more immediate and cost neutral fashion. Our goal was to create an affordable, electronic, systematized solution to produce both timely and relevant discharge summaries, in the hopes of improving communications with providers and thus patient outcomes.
In earlier work, UCSF developed UCSF Note Writer, a template‐based documentation tool that uses web service to import data from the underlying database for provider documentation.13 As a standardized template has been shown to improve quality of communication to both patients and referring providers,1, 14, 15 we developed a template in UCSF Note Writer with both free text and auto‐populated fields for a discharge summary based on current guidelines.1619 We encouraged the documentation of medication changes, changes in functional status and pending tests.
The adoption of such an electronic format has also been shown to improve the efficiency of discharge documentation over conventional dictation and transcription.1, 2022 While this change may be institution dependent, we employed strategies such as allowing the discharge summary to be initiated and updated throughout the hospital admission and unifying the discharge summary with the last day's progress note to facilitate timeliness. To promote efficiency, we allowed providers to import pertinent labs, microbiology, and in the future, the importation of pending tests. While the electronic format in itself does not promote timeliness, it incorporates the discharge summary into physician daily workflow and enables efficiency in data gathering and transfer. For outpatient providers who can access the EMR, any delay or potential fault in the delivery of the discharge materials is eliminated, while outside providers can receive copies through other rapid and reliable modes of electronic delivery (eg, EMR inbox notification) with an appropriate infrastructure.
Application of the Business Framework to the Case for an Electronic Discharge
Considering the potential improvements in care delivery, the argument for an electronic discharge summary may seem self‐evident. To realize its implementation, however, it is necessary to consider other aspects of organizational decision making. We employed the following structure to articulate a robust and sound business case for e‐discharge.
Qualitative Benefits
Quality and Safety
Publically reported data are often derived from hospital chart abstraction and may impact accreditation, reputation, and pay for performance programs.18, 23, 24 The discharge summary is a readily available source of information regarding discharge medications, patient instruction, and communication regarding pending tests. As such, its quality should be a priority for hospital decision makers. Electronic discharge summaries have the potential to reduce adverse events in the high‐risk post‐hospitalization period.1, 25 As such they may improve outpatient physicians' ability to deliver relevant care, reduce preventable readmissions26 and reduce malpractice vulnerability27all key drivers in organizational decision making.
Patient Satisfaction
Patients want to feel prepared for discharge by understanding the continuity of their care from the hospital to the outpatient setting. Discharge preparedness, commonly queried and reported in national patient satisfaction surveys, is low.28 Many electronic discharge summary platforms allow for translation into tailored patient instructions available to the patient in real time, helping to ensure that patients receive quality discharge education.29
Referring Physician Satisfaction
Poor discharge communication reduces referring physicians' satisfaction, which may discourage them from referring patients to the hospital or organization, having broader financial implications.25, 30 Even for medical centers with a busy emergency department, outpatient physician referrals and recommendations make up over 50% of an institution's admissions.31 An electronic discharge summary available in the EMR at the time of discharge, electronically transmitted to referring providers can impact the referral patterns of community physicians.
Readmission
Now publicly reported, readmission rates are another benchmark by which to judge hospital care.32 Patients with discharge summaries that are unavailable to outpatient providers, a very common occurance,2 have a higher trend toward readmission.26 Improved quality of care at the time of discharge resulting in fewer readmissions will better position hospitals to contend with potential Medicare reforms.
Quantitative Benefits
IT Infrastructure: Transcription, Deficiency Tracking, Dissemination
Hospitals, including UCSF, use internal or external transcriptionists to transcribe dictated recordings into typed text at a substantial cost to large medical centers. Medical records staff also track both discharge summary completion and their dissemination to referring providers in compliance with regulatory mandates.4, 33 The use of electronic documentation that relies on physician‐direct entry and that automates dissemination and tracking of discharge documentation provides a potential cost savings to offset the costs of a new system. UCSF Medical Center discharges 100 patients per day and could conservatively avoid almost $500,000 in transcription costs annually (Text Box 1).34
Text Box 1
UCSF Transcription costs:
Average cost/line for transcribed text: $0.17
Average Lines in a discharge summary: 80
# pts discharged/day: 100
Yearly costs = $496,400
Billing
Delays in completion of discharge summaries result in billing delays when critical information required for coding is in the discharge summary. Deferred payment on long admissions can reach tens of thousands of dollars, representing a significant strain on medical center finances. Comprehensive electronic discharge materials may simplify coding through careful documentation and improve billing efficiency through rapid completion.
At our medical center, approximately 20% of billing is delayed due to incomplete discharge documentation. For a hospital that generates over $1.4 billion dollars in billing revenue per year, this can translate into significant financial losses. Hospitals may have to borrow money or draw from existing resources to cover operative deficits created by a delay in the receipt of large payment. Lenders charge approximately 1% to 2% annual interest rate, which translates into 0.2% to 0.4% in billed costs that the hospital gives away to their lenders. Hospitals would be well served by eliminating delays in billing to improve revenue flow (Text Box 2).
Text Box 2
UCSF Annual revenue: $1.4 Billion
Billing that requires discharge summary completion: 20%
Lender's interest rate: 12%
Lenders interest rate (12%) on delayed billing (20%) = 0.20.4% of total revenue
Assuming a 14 day delay in billing: 0.20.4% of total revenue ($1,400,000,000) for 14/365 days = $107,000$215,000
Qualitative Costs
Efficiency and Physician Time
Implementation of any new system is likely to result in initial diminished efficiency. If patient volume is stable, this may not translate into loss of revenue, but rather cause staff to change their workflow. For example, given the new inefficiency in charting, staff may spend less time on direct patient care tasks (Intravenous Catheter placement, FT placement, patient education, discharge instructions), thus increasing the qualitative costs to implementing the system.
To minimize these costs, we used a step wise phased role out starting with one pilot team, with a plan to expand to multiple teams prior to implementation on the entire medicine service. This allowed for the creation of one central and several ancillary physician champions to troubleshoot the new system to help minimize productivity losses. One of the largest concerns in the switch from voice dictation to physician‐direct entry into an electronic summary is the cost of physician time. System adjustments through several pilots helped ensure that the time investment of a novice user was not significantly greater than time previously spent dictating.
Quality of Documentation
Unanticipated consequences from a switch to an electronic platform must be considered, such as the possibility of longer more redundant discharge summaries. The amount of information available for automated import will vary by institutional preference, but the recipient's access to the EMR, primary physician preference, and technologic capabilities should be considered. At UCSF we made an effort to distill the information most important to subsequent care, disabling the importation of multiple days of radiology data and instead working to create a system for discharge medication importation. As with any electronic document, the medium also lends itself to cutting and pasting, which may lead to anachronistic information carried forward from hospital progress notes earlier in the stay.35, 36 The largest experience with this unintended consequence can be found in the Veteran's Affairs Health System EMR, which found that 9% of progress notes studied contained copied or duplicated text.37 The authors recommended that clear policies, programs to raise practitioner awareness, and the development of monitoring procedure be implemented coincident with electronic note‐writing capabilities.
Quantitative Costs
Quantitative Costs will be highly variable across institutions, geographical areas, and software platforms as the infrastructure of existing EMRs are highly variable. The cost of implementation depends heavily on whether inpatient documentation (and thus discharge documentation) is a feature of an institutional EMR, or whether a stand‐alone discharge documentation infrastructure is needed. An explanation of the differences between these types of EMRs and the importance to the cost of infrastructure implementation is further described in the following section. Rather than providing a direct accounting of costs, we have provided a tabular summary of costs that should be considered with the adoption of an electronic discharge summary based on the type of institutional EMR (Table 1).
| Voice Dictation | E‐Discharge in an EMR With Inpatient Documentation Abilities | E‐Discharge in an EMR Without Inpatient Documentation Abilities | |
|---|---|---|---|
| |||
| Infrastructure | |||
| Software | + | ||
| Hardware (sufficient computers and printers) | + | + | |
| Network connectivity | + | + | |
| Server capacity for system backup | + | + | |
| Interface with current EMR | + | ||
| Personnel | |||
| Physician champion | + | + | |
| Physician training | + | + | |
| Computer programmer | + | + | |
| Transcription | + | ||
| Deficiency tracking | + | ||
| Dissemination | + | ||
| Maintenance | |||
| Computer/printer maintenance | + | + | |
| Network maintenance | + | + | |
| Software add‐ons and updates | + | + | + |
Infrastructure
For most health care organizations, the transition to an EMR includes adoption of results reporting systems and computerized provider order entry; only a more select group of hospitals with a complete EMR electronically document inpatient care (eg, progress notes) through physician direct entry. While there is substantial literature regarding the benefits and pitfalls of adopting computerized order entry (CPOE),38, 39 there is less attention devoted to the costs of implementing large‐scale electronic documentation, including an electronic discharge summary, as opposed to paper notes or dictation.4042 Institutions using an EMR with electronic care documentation capability have already invested in the infrastructure to implement electronic discharge documentation, and can employ it at a modest cost. For these institutions, the infrastructure cost of the transition from paper charting or dictation to direct entry by physicians lies in ensuring sufficient computers and connectivity to handle the increased computer use. On the other hand, for those institutions where the EMR lacks this capability there are few freestanding documentation platforms available for purchase. The cost of implementing such a system is high, both for the purchase of additional software and the integration of that software in to the EMR supplied by the primary vendor. Other notable infrastructure costs to consider are ensuring sufficient network connectivity, computers and printers to accommodate increased use that will come with electronic note writing as well as server support for system backups.
Personnel
Engaging the right personnel will smooth the implementation of an electronic discharge summary. In addition to dedicated user training sessions, a physician champion who can promote and monitor user training on the new platform will facilitate prompt implementation. An IT support programmer should work with the physician champion to address concerns and troubleshoot problems. Additional personnel may also be needed to track progress in discharge summary adoption, quality and efficiency. Ideally these personnel can be funneled from those who work transcribing, disseminating and tracking completion of discharge summaries, positions that will be needed in a reduced capacity.
Maintenance
Increased IT infrastructure also means increased IT maintenance and upgrades of servers, network connectivity, computers and printers. Discussions with vendors regarding costs of maintenance, upgrades and add‐on features should be considered when adopting an electronic discharge summary platform.
Conclusion
While many QI initiatives have the potential to improve clinical care, resource limitations and competing priorities necessitate that hospital decision makers see the value of hospitalist driven improvements. A sound business case is the key to successfully influencing decision making and furthering necessary innovations. We have detailed the elements of a business case and applied them to a proposed innovationthe electronic discharge summary. While the cost of multifunctional EMR with full electronic care documentation may be impossible to implement given high initial costs and competing priorities, investing in an e‐discharge solution has real‐time benefits in the impact on patients, system improvements, qualitative benefits, and return on investment. Being able to articulate key qualitative and quantitative elements creates a sound business case that can be applied to QI initiatives in general, and assist hospitalists in garnering support and resources to continue to improve care.
Acknowledgements
The authors acknowledge Kathleen Kerr and the members of the BOOST collaborative for helping with background research and in creating the impetus for this work.
Global payments are fixed‐dollar payments for the care that patients may receive in a given time period, such as a month or year, whereas utilization based payments are payments based on the use of diagnostic and treatment modalities (eg, CT scans and blood cultures).
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.
- ,,, et al.Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary.J Hosp Med.2009;4(4):219–225.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- Standard IM.6.10Hospital Accredidation Standards. In: Oakbrook Terrace,IL:Joint Commission Resources;2006:338–340.
- .Medical Record Services, Section 482.24. In: MacDonald I, ed.The CMS Hospital Conditions of Participation.First edition.United States:Hc Pro Inc.;2005:24–25.
- .Hospital discharge and death communications.Br J Hosp Med.1989;42(1):59–61.
- ,,,.Hospital discharge reports: content and design.Br Med J.1975;4(5994):443–446.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- .Delayed communication between hospitals and general practitioners: where does the problem lie?BMJ.1988;297(6640):28–29.
- .Study of “discharge communications” from hospital.Br Med J (Clin Res Ed).1986;293(6557):1283–1284.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152(9):1437–1442.
- ,,,.General practitioner‐hospital communications: a review of discharge summaries.J Qual Clin Pract.2001;21(4):104–108.
- .Stimulus bill spurs plans for rapid IT progress.Manag Care.2009;18(2):5–6.
- ,,, et al. UCSF Notewriter. Copyright Regents of the University of California.2006–year="2010"2010.
- ,,,,.Assessing quality and efficiency of discharge summaries.Am J Med Qual.2005;20(6):337–343.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,.Are general practitioners satisfied with electronic discharge summaries?HIM J.2007;36(1):7–12.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160(3):319–326.
- ,,,.Evaluation of computer generated neonatal discharge summaries.Arch Dis Child.1991;66(4 Spec No):433–436.
- ,,,,,.Evaluation of a computer‐generated discharge summary for patients with acute coronary syndromes.Br J Gen Pract.1998;48(429):1163–1164.
- The Common Wealth Fund. Why not the best org. Available at: http/www.whynotthebest.org. Updated 2009. Accessed May2010.
- ,.Pay for performance: an overview of the literature.Am J Med Qual.2009;24(2):140–163.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170(3):345–349.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- ,,, et al.Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims.Ann Intern Med.2006;145(7):488–496.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20(4):317–323.
- ,,.Referring physician satisfaction: toward a better understanding of hospital referrals.J Hosp Mark.1998;12(2):95–111.
- U.S. Department of Health 7(3):269–272.
- .IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers.JAMA.2009;301(9):919–920.
- ,.Copy and paste: a remediable hazard of electronic health records.Am J Med.2009;122(6):495–496.
- ,,,.Are electronic medical records trustworthy? Observations on copying, pasting and duplication.AMIA Annu Symp Proc.2003:269–273.
- ,,, et al.Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review.JAMA.2005;293(10):1223–1238.
- ,,, et al.Role of computerized physician order entry systems in facilitating medication errors.JAMA.2005;293(10):1197–1203.
- ,,.The elements of electronic note style.J AHIMA.2003;74(2):68,70.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11(4):300–309.
- ,,,.The transition to electronic documentation on a teaching hospital medical service.AMIA Annu Symp Proc.2006:629–633.
Handoff Efficiency
Transfer of responsibility for patients, or handoff,1 occurs frequently in hospitalist services, requiring excellent and timely communication to ensure patient safety. Communication failure is a major contributor to medical errors.2, 3 Recognizing such findings, a growing body of literature addresses handoff techniques for learners.47
Vidyarthi described the handoff process as traditionally informal, unstructured, and idiosyncratic,4 and many believe efforts to formalize and structure this process are important for patient safety.8 Standardized handoff forms have improved accuracy of information.9 Web‐based sign‐out systems reportedly reduced the number of patients missed on rounds.10
Hospitalists also face challenges with effective communication during service change.11 The Society of Hospital Medicine identified the handoff skill as a core competency for hospitalists, and recommendations based on a systematic review of the literature were published.12 Inpatient medicine programs are increasingly using midlevel providers such as nurse practitioners (NPs) and physician assistants (PAs) along with hospitalists to accommodate workload while maintaining the scholarly enterprise in academic centers.13 To our knowledge there is no literature examining the hospitalist service handoffs involving NP/PAs.
We wished to study the effectiveness and timeliness of the morning handoff from the night coverage providers to the daytime teams consisting of one hospitalist and one NP/PA. Our objectives were to identify deficiencies and to evaluate the effectiveness of a restructured handoff process.
Methods
The Mayo Clinic Institutional Review Board reviewed and approved this study.
Setting
At the time of this study, the Division of Hospital Internal Medicine (HIM) at our institution consisted of 22 hospitalists, 11 NPs and 9 PAs (hereinafter NP/PAs), and 2 clinical assistants (CAs). The CAs assist with clerical duties not covered by Unit Secretaries:
-
Obtaining outside records
-
Clarifying referring physician contact information
-
Scheduling follow‐up outpatient appointments for tests, procedures, and visits
-
Attendance at morning handoff
Each CA can assist 3 or 4 daytime service teams.
Daytime Service Organization
Six HIM services, each managing up to 12 patients, are staffed by a partnership of 1 hospitalist and 1 NP/PA: Four services are primary general medicine services, and 2 consulting (orthopedic comanagement) services.
Night Coverage
Three of 4 primary daytime services and one consult service team transfer care to the (in‐house) night NP/PA. The night NP/PA addresses any acute‐care issues and reports at morning handoff to the 3 primary services and 1 consult service. In a designated conference room the morning handoff occurs, with at least 1 (day team) service representative present. This is usually the NP/PA, as the day team hospitalist concurrently receives a report on new admissions from the (in‐house) night hospitalist (who also covers one service and backs up the night NP/PA).
Improvement Process
An improvement team was formed within the Division of HIM consisting of 3 hospitalists, 3 NP/PAs, and 2 CAs to assess the existing handoff process at 7:45am between the Night NP/PA and daytime services. The improvement team met, reviewed evidence‐based literature on handoffs and discussed our local process. Four problems were identified by consensus:
-
Unpredictable start and finish times
-
Inefficiency (time wasted)
-
Poor environment (room noisy and distracting conversations)
-
Poor communication (overwrought and meandering narratives).
Intervention
The improvement team structured a new handoff process to address these deficiencies.
-
Environment: Moved to a smaller room (lower ceiling, less ambient noise).
-
Identification: table cards designating seats for participants (reduced queries regarding what service are you, today?).
-
Start Times: Each service team assigned a consistent start time (labeled on the table card) within a 15‐minute period, and although earlier reportage could occur, any service team present at their designated time has priority for the attention of the night NP/PA, and the opportunity to ask questions.
-
Quiet and Focus: HIM members were reminded to remain quiet in the handoff room, so the service receiving report has the floor and personal conversations must not impede the principals.
-
Visual Cue: Green Good to go sign placed on team table cards when no verbal was required.
-
Written e‐Material: The improvement team required elements of a brief written report in a specified column of our existing electronic service list (ESL). The ESL is a custom designed template importing laboratory, medication, and demographic data automatically but also capable of free text additions (Figure 1). All providers were instructed to update the ESL every 12 hours.
-
Admission and Progress Notes: After manual electronic medical record search, the CAs printed any notes generated in the preceding 12 hours and placed them by the team table card.
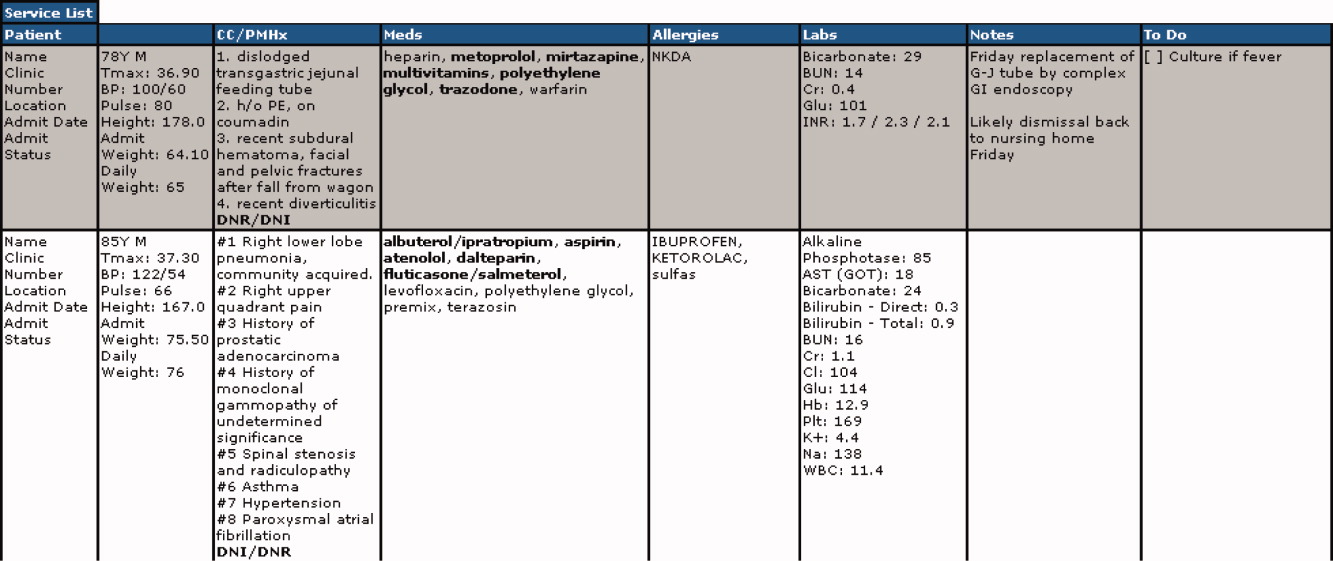
The improvement team provided education for the new process at a division meeting and through e‐mail. The recommended report sequence was night NP/PA reporting and day service teams asking questions and seeking clarifications. We discouraged editorial comments and chit‐chat.
A member of the improvement team monitored the new handoff process for 15 days, and 3 months later for 10 days.
Survey
An anonymous survey (Figure 2) concerning staff satisfaction with handoff was conducted immediately before and 15 days after the intervention. In the e‐mail containing the postintervention survey, providers were asked to respond only if they had been on service the preceding 15 days (and thus eligible to participate in handoff). To help insure this, the first question read, Have you been on service during the past 15 days?
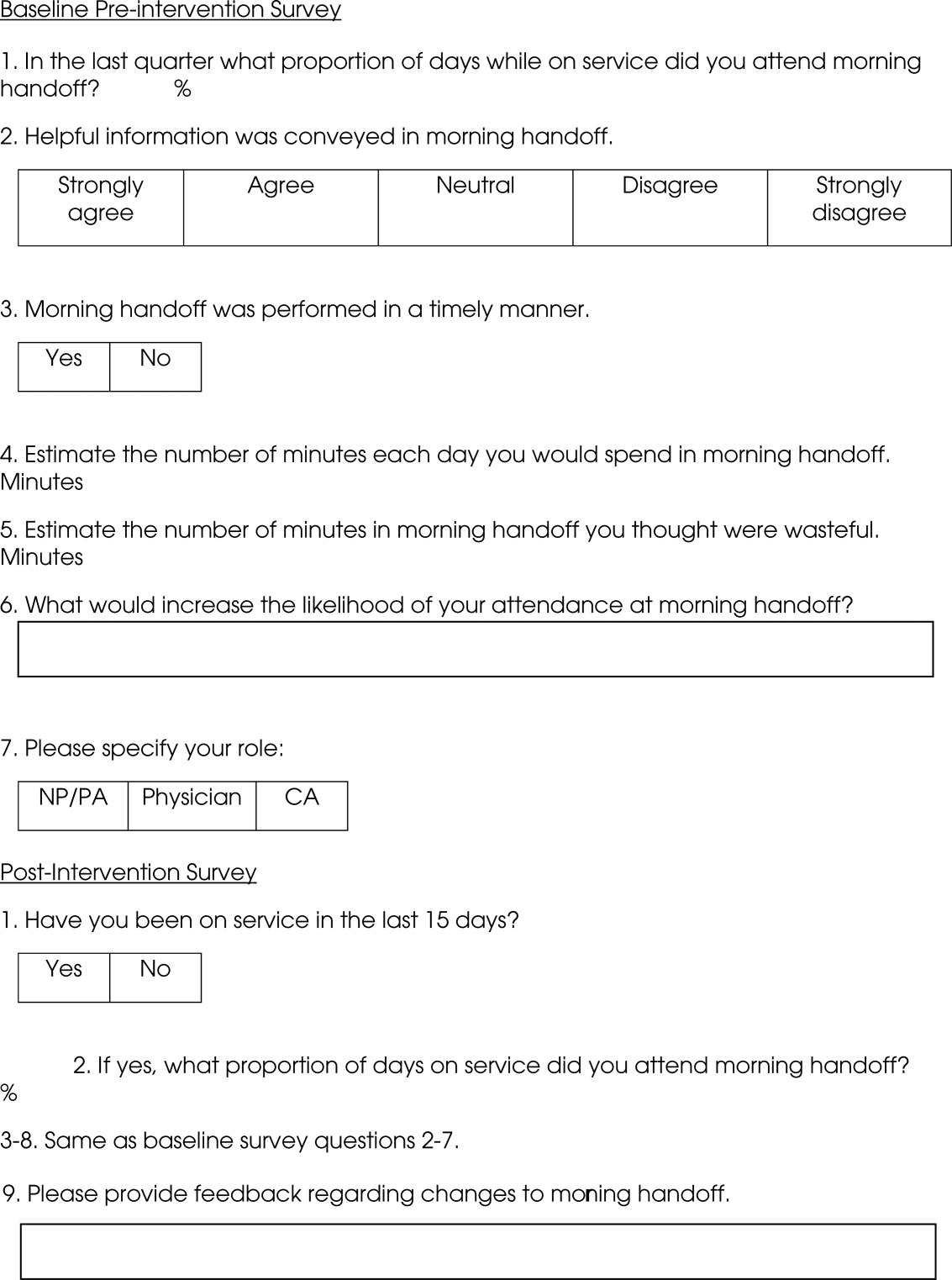
Statistics
To compare the relationship of preintervention and postintervention survey responses, Fisher's exact test was used to compare categorical variables and 2 sample t‐test and Wilcoxon rank sum test were used for continuous variables. Comparisons that adjusted for the possibility of someone responding to both the preintervention and postintervention surveys were not performed since the surveys were anonymous. A P value <0.05 was considered statistically significant. For the item concerning the percentage of days morning report was attended while on service, based on a common standard deviation estimate of 35.3, we had 80% power to detect a difference of 29.1 (pre vs. post). This computation assumes a 2‐sample t‐test of = 0.05 with sample sizes of 36 and 18. We have 59% power to detect a difference of 27% (67% pre vs. 94% post) for those who at least agree that helpful information was conveyed during handoff. This computation is based on a 2‐sided Pearson 2 test with = 0.05.
Qualitative data analysis of respondents' answers to the open‐ended survey questions What would increase the likelihood of your attending handoff? and What feedback do you have regarding the changes to handoff? was performed using the constant comparative method14 associated with grounded theory approaches to identify themes and categories.15 To establish interrater reliability, three investigators (MCB, DTK, LLK) independently identified coding categories for the data set, compared results, redefined coding categories as needed, and reanalyzed the data until 80% agreement was reached.
Results
Thirty‐six of the 44 providers (82%) answered the preintervention survey, including 18 of 22 hospitalists (82%), 17 of 20 NPs/PAs (85%), and 1 of 2 CAs (50%). During the intervention based on our staffing model, 21 providers had the opportunity to participate in handoff, and 18 (86%) answered the postintervention survey, including 5 of 6 hospitalists (83%), 9 of 14 NPs/PAs (64%), and 2 of 2 CAs (100%). All respondents to the postintervention survey reported being on service during the previous 15 days.
As summarized in Table 1, compared to 60.5% of survey participants (n = 38) who thought morning handoff was performed in a timely fashion preintervention, 100% (n = 15) felt it was performed in a timely fashion postintervention (P = 0.005). The average time spent in morning report before the intervention was 11 minutes, as compared to 5 minutes after the intervention (P < 0.0028). Prior to the intervention, 6.5 minutes of the handoff were viewed to be wasteful, as compared to 0.5 minutes of the handoff in the postintervention survey (P < 0.0001). Attendance and quality of information perceptions did not demonstrate statistically significant change.
| Survey Question | Preintervention | Postintervention | P |
|---|---|---|---|
| What proportion of days while on service did you attend morning report? (%) | 78 | 87 | 0.4119 |
| Helpful information was conveyed in morning report, n (%) | 0.112 | ||
| Strongly agree | 9 (25) | 9 (56) | |
| Agree | 15 (42) | 6 (38) | |
| Neutral | 8 (22) | 1 (6) | |
| Disagree | 4 (11) | 0 | |
| Strongly disagree | 0 | 0 | |
| Morning report was performed in a timely manner, #yes/#no | 23/15 | 15/0 | 0.005 |
| Estimate the number of minutes each day you would spend in morning report (minute) | 11 | 5 | <0.0028 |
| Estimate the number of minutes in morning report you thought were wasteful (minute) | 6.5 | 0.5 | <0.0001 |
During the 15‐day observation period, morning handoff started by 0745 on 14 of 15 (93%) of days and finished by 0800 on 15 of 15 (100%) of days. Table cards, ESL, and progress notes were on the table by 0745 on 15 of 15 (100%) of days following the intervention. Three months after the intervention, the following were observed: morning handoff started by 0745 on 10 of 10 (100%) of days; finished by 0800 on 10 of 10 (100%) of days; and table cards, ESL, and progress notes were on the table by 0745 on 10 of 10 (100%) of days.
Qualitative Data Analysis
Three themes were identified in both preintervention and postintervention surveys: timeliness, quality of report and environment (Table 2). In the preintervention survey, timeliness complaints involved inconsistent start time, prolonged duration of handoff, and inefficiency due to time wasted while teams waited for their handoff report. Comments about report quality mentioned the nonstandardized report process that included nonpertinent information and editorializing. Environmental concerns addressed noise from multiple service team members assembled in 1 large room and chatting while awaiting report. In the postintervention survey, respondents' comments noted improved efficiency, environment, and report quality.
| Deficiency | Pre‐Intervention | Post‐Intervention |
|---|---|---|
| Timeliness | Efficiency needed | I found the changes lead to more concise and valuable time spent in report |
| Timely, scheduled and efficient reports would help increase my attendance | I personally enjoyed having the times set so you are held accountable for a certain handoff | |
| Set report times so I don't have to listen to everyone else's report | More organized and efficient | |
| Too much time wasted | Love the good to go card! Can start on rounds | |
| Environment | Not having to listen to chit chat unrelated to patient carewould improve my attendance | There is less chit chat |
| Services should receive report in a quieter room | Seems less chaotic with less people overall in the room so less distraction | |
| Need a quieter and smaller room | Because the room is quieter, I did not have to repeat information | |
| Too noisy | Quiet and respectful | |
| Quality | I would like a more organized format More information isn't needed, just the correct information in a timely manner | I felt that the amount of information shared was only what was pertinent and important |
| If I first had the opportunity to review ESL and any notes generated in the last 12 hours, this would improve report | Written information on the ESL assured that I didn't forget something important | |
| Less editorializing about events and less adrenaline | I liked having the progress notes generated overnight available for review | |
| Need only meaningful information | Excellent report with prompt dissemination of information |
Discussion
We describe an intervention that set the expectation for formal, structured written and verbal communication in a focused environment involving outgoing and incoming clinicians, resulting in improved satisfaction. Before the intervention, the improvement team identified by consensus 4 problems: unpredictable start time, inefficiency, environment, and report quality. Formal structuring of our handoff process resulted in statistically significant improvement in handoff timeliness and efficiency in the view of the HIM division members. Process improvement included precise team specific start times within a 12‐minute window to improve reliability and predictability and eliminating nonproductive waiting. Additionally, receiving teams were clearly identified with table cards so that no time was wasted locating the appropriate service for report, and minimizing role‐identification challenges. The good to go sign signaled teams that no events had occurred overnight requiring verbal report. Handoff timeliness persisted 3 months after the intervention, suggesting that the process is easily sustainable.
Postintervention survey comments noted the improved environment: a smaller, quieter room with the door closed. Before the intervention, all day team providers, CAs and night provider met in a large, loud room where multiple conversations were commonplace. Previous study of the handoff process supports creating an environment free of distraction.4
Postintervention survey responses to the open‐ended questions suggested improved provider satisfaction with the quality of the report. We believe this occurred for several reasons. First, having a precise start time for each team within a 12‐minute window led to a more focused report. Second, the ESL provided a column for providers to suggest plans of care for anticipated overnight events to improve preparedness and avoid significant omissions. Third, hospital notes generated overnight were made available which allowed daytime providers to review events before handoff, for a more informed update, or just after verbal report to reinforce the information just received, a technique used in other high‐reliability organizations.16 This measure also provided an at‐a‐glance view of each patient, decreasing the complexity of handoff.17
This study has important limitations. We address the handoff process of 1 hospitalist group at a single academic center. NP/PAs are the clinicians with first‐call responsibility for the night coverage of our patients, and the handoff process between the night NP/PA and daytime provider was studied. The handoff between physicians for patients admitted overnight was not assessed. Another limitation is that the time spent in handoff is reported as a participant estimate. There was no objective measurement of time, and respondents may have been biased. An additional limitation of our study concerns the preintervention and postintervention surveys. Both surveys were anonymous, which makes discerning the absolute impact of the intervention difficult due to the lack of paired responses. Lastly, our institution has an ESL. This option may not be available in other hospital systems.
Several deficiencies in the handoff process were addressed by providing key clinical data verbally and in written format, enhancing the physical environment, and defining each team's handoff start time. Our process improvements are consistent with the handoff recommendations endorsed by the Society of Hospital Medicine.12 Subsequent direct observation, subjective reports, and survey results demonstrated improvement in the handoff process.
Future studies might measure the effectiveness of morning handoff by end‐shift interviews of the daytime clinicians. Similarly, a study of evening handoff could measure the efficiency and effectiveness of report given by day teams to night‐coverage colleagues. Furthermore, if the handoff report skill set can be more rigorously defined and measured, a hospitalist clinical competency for hospitalists and NP/PAs could be developed in this core process‐of‐care.12
Acknowledgements
The authors thank Lisa Boucher for preparation of this manuscript.
- , , , et al.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- , , .Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- , , .The human factor: the critical importance of effective teamwork and communication in providing safe care.Quality 13 Suppl 1:i85–90.
- , , , et al.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- , , .Development and implementation of an oral sign‐out skills curriculum.J Gen Intern Med.2007;22:1470–1474.
- , , , et al.The top 10 list for a safe and effective sign‐out.Arch Surg2008;143(10):1008–1010.
- , , , et al.Residents' and attending physicians' handoffs: a systematic review of the literature.Acad Med.2009;84(12):1775–1787.
- , , , et al.A structured handoff program for interns.Acad Med.2009;84:347–352.
- , , , et al.Simple standardized patient handoff system that increases accuracy and completeness.J Surg.2008;65:476–485.
- , , , et al.A randomized, controlled trial evaluation the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- , , , .Understanding communication during hospitalist service changes: A mixed methods study.J Hosp Med.2009;4(9):535–540.
- , , , , , .Hospitalist handoffs: a systematic review and task force recommendations.J of Hosp Med.2009;4(7):433–440.
- , , , et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3:361–368.
- , .Basics of Qualitiative Research: Grounded Theory Procedures and Techniques.Sage Publications, Inc.Newbury Park, CA.1990.
- , .Naturalistic Inquiry.Sage Publications, Inc.Newbury Park, CA.1985.
- .Communication strategies from high‐reliability organizations.Ann Surg.2007;245(2):170–172.
- , , , et al.Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125.
Transfer of responsibility for patients, or handoff,1 occurs frequently in hospitalist services, requiring excellent and timely communication to ensure patient safety. Communication failure is a major contributor to medical errors.2, 3 Recognizing such findings, a growing body of literature addresses handoff techniques for learners.47
Vidyarthi described the handoff process as traditionally informal, unstructured, and idiosyncratic,4 and many believe efforts to formalize and structure this process are important for patient safety.8 Standardized handoff forms have improved accuracy of information.9 Web‐based sign‐out systems reportedly reduced the number of patients missed on rounds.10
Hospitalists also face challenges with effective communication during service change.11 The Society of Hospital Medicine identified the handoff skill as a core competency for hospitalists, and recommendations based on a systematic review of the literature were published.12 Inpatient medicine programs are increasingly using midlevel providers such as nurse practitioners (NPs) and physician assistants (PAs) along with hospitalists to accommodate workload while maintaining the scholarly enterprise in academic centers.13 To our knowledge there is no literature examining the hospitalist service handoffs involving NP/PAs.
We wished to study the effectiveness and timeliness of the morning handoff from the night coverage providers to the daytime teams consisting of one hospitalist and one NP/PA. Our objectives were to identify deficiencies and to evaluate the effectiveness of a restructured handoff process.
Methods
The Mayo Clinic Institutional Review Board reviewed and approved this study.
Setting
At the time of this study, the Division of Hospital Internal Medicine (HIM) at our institution consisted of 22 hospitalists, 11 NPs and 9 PAs (hereinafter NP/PAs), and 2 clinical assistants (CAs). The CAs assist with clerical duties not covered by Unit Secretaries:
-
Obtaining outside records
-
Clarifying referring physician contact information
-
Scheduling follow‐up outpatient appointments for tests, procedures, and visits
-
Attendance at morning handoff
Each CA can assist 3 or 4 daytime service teams.
Daytime Service Organization
Six HIM services, each managing up to 12 patients, are staffed by a partnership of 1 hospitalist and 1 NP/PA: Four services are primary general medicine services, and 2 consulting (orthopedic comanagement) services.
Night Coverage
Three of 4 primary daytime services and one consult service team transfer care to the (in‐house) night NP/PA. The night NP/PA addresses any acute‐care issues and reports at morning handoff to the 3 primary services and 1 consult service. In a designated conference room the morning handoff occurs, with at least 1 (day team) service representative present. This is usually the NP/PA, as the day team hospitalist concurrently receives a report on new admissions from the (in‐house) night hospitalist (who also covers one service and backs up the night NP/PA).
Improvement Process
An improvement team was formed within the Division of HIM consisting of 3 hospitalists, 3 NP/PAs, and 2 CAs to assess the existing handoff process at 7:45am between the Night NP/PA and daytime services. The improvement team met, reviewed evidence‐based literature on handoffs and discussed our local process. Four problems were identified by consensus:
-
Unpredictable start and finish times
-
Inefficiency (time wasted)
-
Poor environment (room noisy and distracting conversations)
-
Poor communication (overwrought and meandering narratives).
Intervention
The improvement team structured a new handoff process to address these deficiencies.
-
Environment: Moved to a smaller room (lower ceiling, less ambient noise).
-
Identification: table cards designating seats for participants (reduced queries regarding what service are you, today?).
-
Start Times: Each service team assigned a consistent start time (labeled on the table card) within a 15‐minute period, and although earlier reportage could occur, any service team present at their designated time has priority for the attention of the night NP/PA, and the opportunity to ask questions.
-
Quiet and Focus: HIM members were reminded to remain quiet in the handoff room, so the service receiving report has the floor and personal conversations must not impede the principals.
-
Visual Cue: Green Good to go sign placed on team table cards when no verbal was required.
-
Written e‐Material: The improvement team required elements of a brief written report in a specified column of our existing electronic service list (ESL). The ESL is a custom designed template importing laboratory, medication, and demographic data automatically but also capable of free text additions (Figure 1). All providers were instructed to update the ESL every 12 hours.
-
Admission and Progress Notes: After manual electronic medical record search, the CAs printed any notes generated in the preceding 12 hours and placed them by the team table card.
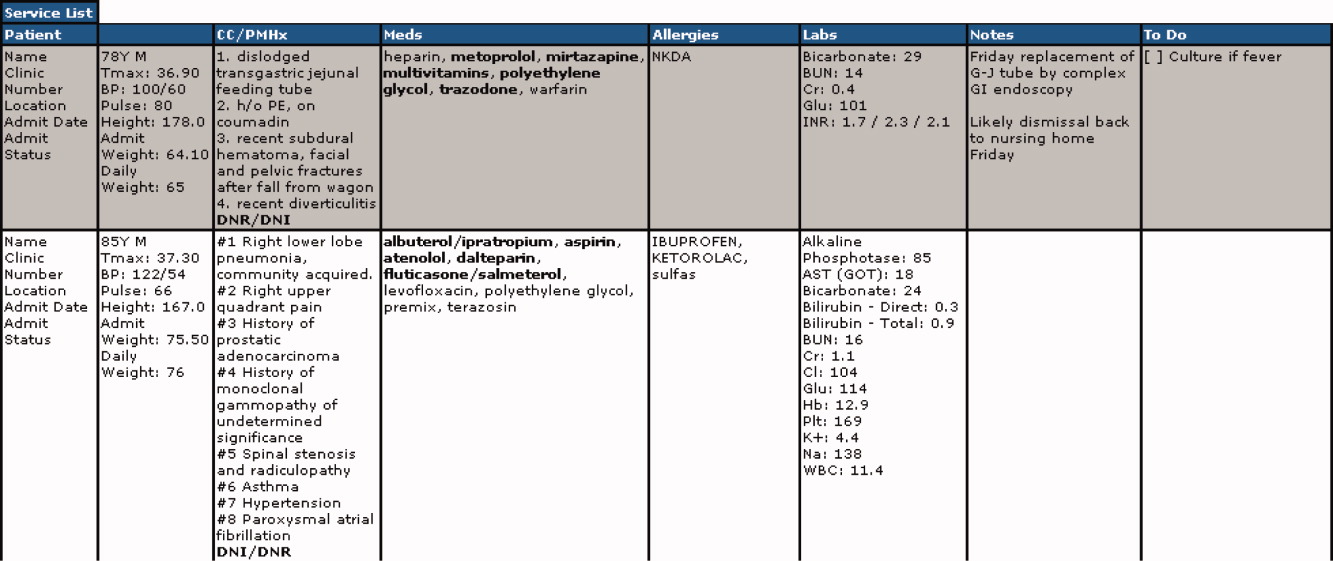
The improvement team provided education for the new process at a division meeting and through e‐mail. The recommended report sequence was night NP/PA reporting and day service teams asking questions and seeking clarifications. We discouraged editorial comments and chit‐chat.
A member of the improvement team monitored the new handoff process for 15 days, and 3 months later for 10 days.
Survey
An anonymous survey (Figure 2) concerning staff satisfaction with handoff was conducted immediately before and 15 days after the intervention. In the e‐mail containing the postintervention survey, providers were asked to respond only if they had been on service the preceding 15 days (and thus eligible to participate in handoff). To help insure this, the first question read, Have you been on service during the past 15 days?
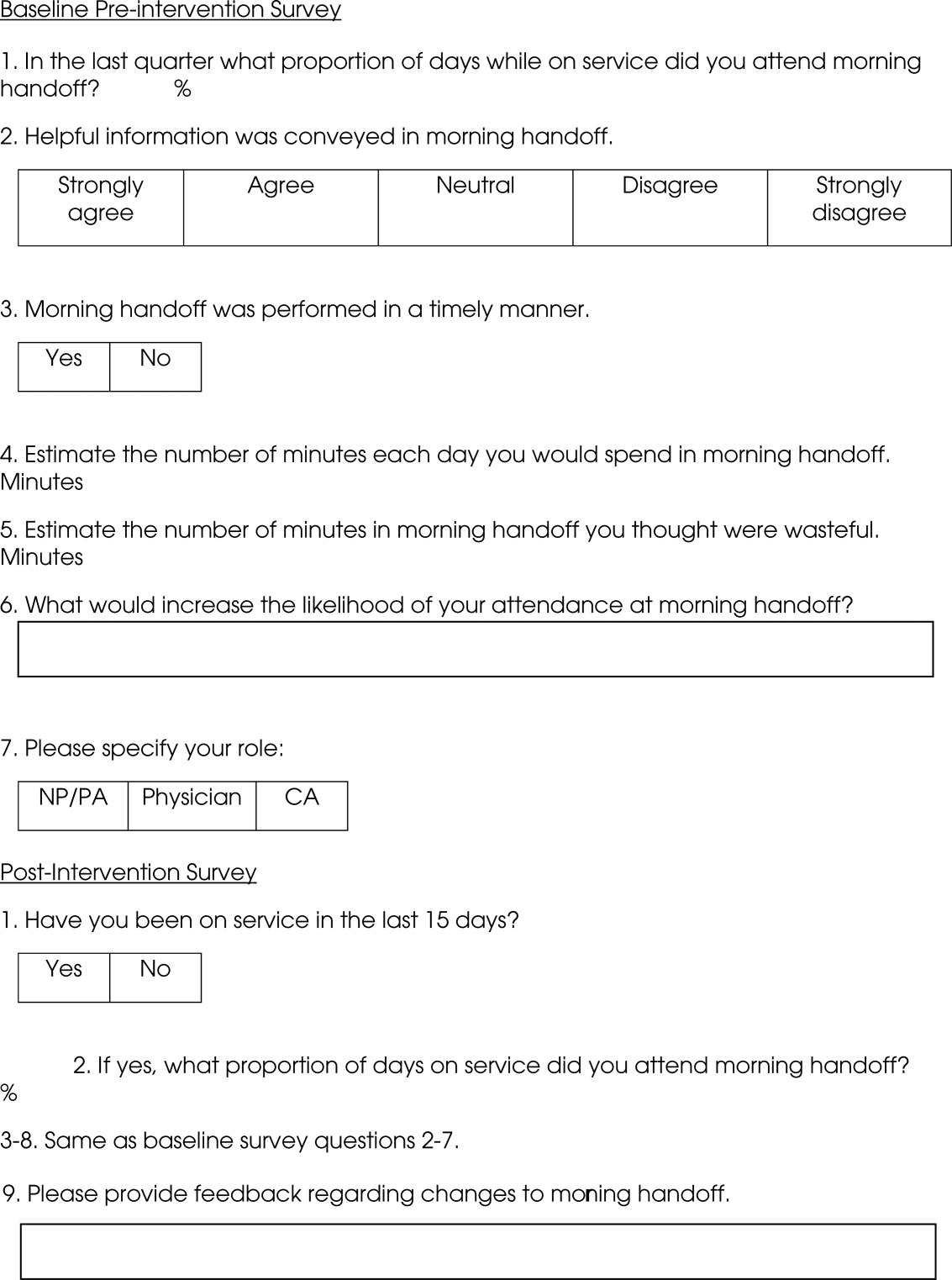
Statistics
To compare the relationship of preintervention and postintervention survey responses, Fisher's exact test was used to compare categorical variables and 2 sample t‐test and Wilcoxon rank sum test were used for continuous variables. Comparisons that adjusted for the possibility of someone responding to both the preintervention and postintervention surveys were not performed since the surveys were anonymous. A P value <0.05 was considered statistically significant. For the item concerning the percentage of days morning report was attended while on service, based on a common standard deviation estimate of 35.3, we had 80% power to detect a difference of 29.1 (pre vs. post). This computation assumes a 2‐sample t‐test of = 0.05 with sample sizes of 36 and 18. We have 59% power to detect a difference of 27% (67% pre vs. 94% post) for those who at least agree that helpful information was conveyed during handoff. This computation is based on a 2‐sided Pearson 2 test with = 0.05.
Qualitative data analysis of respondents' answers to the open‐ended survey questions What would increase the likelihood of your attending handoff? and What feedback do you have regarding the changes to handoff? was performed using the constant comparative method14 associated with grounded theory approaches to identify themes and categories.15 To establish interrater reliability, three investigators (MCB, DTK, LLK) independently identified coding categories for the data set, compared results, redefined coding categories as needed, and reanalyzed the data until 80% agreement was reached.
Results
Thirty‐six of the 44 providers (82%) answered the preintervention survey, including 18 of 22 hospitalists (82%), 17 of 20 NPs/PAs (85%), and 1 of 2 CAs (50%). During the intervention based on our staffing model, 21 providers had the opportunity to participate in handoff, and 18 (86%) answered the postintervention survey, including 5 of 6 hospitalists (83%), 9 of 14 NPs/PAs (64%), and 2 of 2 CAs (100%). All respondents to the postintervention survey reported being on service during the previous 15 days.
As summarized in Table 1, compared to 60.5% of survey participants (n = 38) who thought morning handoff was performed in a timely fashion preintervention, 100% (n = 15) felt it was performed in a timely fashion postintervention (P = 0.005). The average time spent in morning report before the intervention was 11 minutes, as compared to 5 minutes after the intervention (P < 0.0028). Prior to the intervention, 6.5 minutes of the handoff were viewed to be wasteful, as compared to 0.5 minutes of the handoff in the postintervention survey (P < 0.0001). Attendance and quality of information perceptions did not demonstrate statistically significant change.
| Survey Question | Preintervention | Postintervention | P |
|---|---|---|---|
| What proportion of days while on service did you attend morning report? (%) | 78 | 87 | 0.4119 |
| Helpful information was conveyed in morning report, n (%) | 0.112 | ||
| Strongly agree | 9 (25) | 9 (56) | |
| Agree | 15 (42) | 6 (38) | |
| Neutral | 8 (22) | 1 (6) | |
| Disagree | 4 (11) | 0 | |
| Strongly disagree | 0 | 0 | |
| Morning report was performed in a timely manner, #yes/#no | 23/15 | 15/0 | 0.005 |
| Estimate the number of minutes each day you would spend in morning report (minute) | 11 | 5 | <0.0028 |
| Estimate the number of minutes in morning report you thought were wasteful (minute) | 6.5 | 0.5 | <0.0001 |
During the 15‐day observation period, morning handoff started by 0745 on 14 of 15 (93%) of days and finished by 0800 on 15 of 15 (100%) of days. Table cards, ESL, and progress notes were on the table by 0745 on 15 of 15 (100%) of days following the intervention. Three months after the intervention, the following were observed: morning handoff started by 0745 on 10 of 10 (100%) of days; finished by 0800 on 10 of 10 (100%) of days; and table cards, ESL, and progress notes were on the table by 0745 on 10 of 10 (100%) of days.
Qualitative Data Analysis
Three themes were identified in both preintervention and postintervention surveys: timeliness, quality of report and environment (Table 2). In the preintervention survey, timeliness complaints involved inconsistent start time, prolonged duration of handoff, and inefficiency due to time wasted while teams waited for their handoff report. Comments about report quality mentioned the nonstandardized report process that included nonpertinent information and editorializing. Environmental concerns addressed noise from multiple service team members assembled in 1 large room and chatting while awaiting report. In the postintervention survey, respondents' comments noted improved efficiency, environment, and report quality.
| Deficiency | Pre‐Intervention | Post‐Intervention |
|---|---|---|
| Timeliness | Efficiency needed | I found the changes lead to more concise and valuable time spent in report |
| Timely, scheduled and efficient reports would help increase my attendance | I personally enjoyed having the times set so you are held accountable for a certain handoff | |
| Set report times so I don't have to listen to everyone else's report | More organized and efficient | |
| Too much time wasted | Love the good to go card! Can start on rounds | |
| Environment | Not having to listen to chit chat unrelated to patient carewould improve my attendance | There is less chit chat |
| Services should receive report in a quieter room | Seems less chaotic with less people overall in the room so less distraction | |
| Need a quieter and smaller room | Because the room is quieter, I did not have to repeat information | |
| Too noisy | Quiet and respectful | |
| Quality | I would like a more organized format More information isn't needed, just the correct information in a timely manner | I felt that the amount of information shared was only what was pertinent and important |
| If I first had the opportunity to review ESL and any notes generated in the last 12 hours, this would improve report | Written information on the ESL assured that I didn't forget something important | |
| Less editorializing about events and less adrenaline | I liked having the progress notes generated overnight available for review | |
| Need only meaningful information | Excellent report with prompt dissemination of information |
Discussion
We describe an intervention that set the expectation for formal, structured written and verbal communication in a focused environment involving outgoing and incoming clinicians, resulting in improved satisfaction. Before the intervention, the improvement team identified by consensus 4 problems: unpredictable start time, inefficiency, environment, and report quality. Formal structuring of our handoff process resulted in statistically significant improvement in handoff timeliness and efficiency in the view of the HIM division members. Process improvement included precise team specific start times within a 12‐minute window to improve reliability and predictability and eliminating nonproductive waiting. Additionally, receiving teams were clearly identified with table cards so that no time was wasted locating the appropriate service for report, and minimizing role‐identification challenges. The good to go sign signaled teams that no events had occurred overnight requiring verbal report. Handoff timeliness persisted 3 months after the intervention, suggesting that the process is easily sustainable.
Postintervention survey comments noted the improved environment: a smaller, quieter room with the door closed. Before the intervention, all day team providers, CAs and night provider met in a large, loud room where multiple conversations were commonplace. Previous study of the handoff process supports creating an environment free of distraction.4
Postintervention survey responses to the open‐ended questions suggested improved provider satisfaction with the quality of the report. We believe this occurred for several reasons. First, having a precise start time for each team within a 12‐minute window led to a more focused report. Second, the ESL provided a column for providers to suggest plans of care for anticipated overnight events to improve preparedness and avoid significant omissions. Third, hospital notes generated overnight were made available which allowed daytime providers to review events before handoff, for a more informed update, or just after verbal report to reinforce the information just received, a technique used in other high‐reliability organizations.16 This measure also provided an at‐a‐glance view of each patient, decreasing the complexity of handoff.17
This study has important limitations. We address the handoff process of 1 hospitalist group at a single academic center. NP/PAs are the clinicians with first‐call responsibility for the night coverage of our patients, and the handoff process between the night NP/PA and daytime provider was studied. The handoff between physicians for patients admitted overnight was not assessed. Another limitation is that the time spent in handoff is reported as a participant estimate. There was no objective measurement of time, and respondents may have been biased. An additional limitation of our study concerns the preintervention and postintervention surveys. Both surveys were anonymous, which makes discerning the absolute impact of the intervention difficult due to the lack of paired responses. Lastly, our institution has an ESL. This option may not be available in other hospital systems.
Several deficiencies in the handoff process were addressed by providing key clinical data verbally and in written format, enhancing the physical environment, and defining each team's handoff start time. Our process improvements are consistent with the handoff recommendations endorsed by the Society of Hospital Medicine.12 Subsequent direct observation, subjective reports, and survey results demonstrated improvement in the handoff process.
Future studies might measure the effectiveness of morning handoff by end‐shift interviews of the daytime clinicians. Similarly, a study of evening handoff could measure the efficiency and effectiveness of report given by day teams to night‐coverage colleagues. Furthermore, if the handoff report skill set can be more rigorously defined and measured, a hospitalist clinical competency for hospitalists and NP/PAs could be developed in this core process‐of‐care.12
Acknowledgements
The authors thank Lisa Boucher for preparation of this manuscript.
Transfer of responsibility for patients, or handoff,1 occurs frequently in hospitalist services, requiring excellent and timely communication to ensure patient safety. Communication failure is a major contributor to medical errors.2, 3 Recognizing such findings, a growing body of literature addresses handoff techniques for learners.47
Vidyarthi described the handoff process as traditionally informal, unstructured, and idiosyncratic,4 and many believe efforts to formalize and structure this process are important for patient safety.8 Standardized handoff forms have improved accuracy of information.9 Web‐based sign‐out systems reportedly reduced the number of patients missed on rounds.10
Hospitalists also face challenges with effective communication during service change.11 The Society of Hospital Medicine identified the handoff skill as a core competency for hospitalists, and recommendations based on a systematic review of the literature were published.12 Inpatient medicine programs are increasingly using midlevel providers such as nurse practitioners (NPs) and physician assistants (PAs) along with hospitalists to accommodate workload while maintaining the scholarly enterprise in academic centers.13 To our knowledge there is no literature examining the hospitalist service handoffs involving NP/PAs.
We wished to study the effectiveness and timeliness of the morning handoff from the night coverage providers to the daytime teams consisting of one hospitalist and one NP/PA. Our objectives were to identify deficiencies and to evaluate the effectiveness of a restructured handoff process.
Methods
The Mayo Clinic Institutional Review Board reviewed and approved this study.
Setting
At the time of this study, the Division of Hospital Internal Medicine (HIM) at our institution consisted of 22 hospitalists, 11 NPs and 9 PAs (hereinafter NP/PAs), and 2 clinical assistants (CAs). The CAs assist with clerical duties not covered by Unit Secretaries:
-
Obtaining outside records
-
Clarifying referring physician contact information
-
Scheduling follow‐up outpatient appointments for tests, procedures, and visits
-
Attendance at morning handoff
Each CA can assist 3 or 4 daytime service teams.
Daytime Service Organization
Six HIM services, each managing up to 12 patients, are staffed by a partnership of 1 hospitalist and 1 NP/PA: Four services are primary general medicine services, and 2 consulting (orthopedic comanagement) services.
Night Coverage
Three of 4 primary daytime services and one consult service team transfer care to the (in‐house) night NP/PA. The night NP/PA addresses any acute‐care issues and reports at morning handoff to the 3 primary services and 1 consult service. In a designated conference room the morning handoff occurs, with at least 1 (day team) service representative present. This is usually the NP/PA, as the day team hospitalist concurrently receives a report on new admissions from the (in‐house) night hospitalist (who also covers one service and backs up the night NP/PA).
Improvement Process
An improvement team was formed within the Division of HIM consisting of 3 hospitalists, 3 NP/PAs, and 2 CAs to assess the existing handoff process at 7:45am between the Night NP/PA and daytime services. The improvement team met, reviewed evidence‐based literature on handoffs and discussed our local process. Four problems were identified by consensus:
-
Unpredictable start and finish times
-
Inefficiency (time wasted)
-
Poor environment (room noisy and distracting conversations)
-
Poor communication (overwrought and meandering narratives).
Intervention
The improvement team structured a new handoff process to address these deficiencies.
-
Environment: Moved to a smaller room (lower ceiling, less ambient noise).
-
Identification: table cards designating seats for participants (reduced queries regarding what service are you, today?).
-
Start Times: Each service team assigned a consistent start time (labeled on the table card) within a 15‐minute period, and although earlier reportage could occur, any service team present at their designated time has priority for the attention of the night NP/PA, and the opportunity to ask questions.
-
Quiet and Focus: HIM members were reminded to remain quiet in the handoff room, so the service receiving report has the floor and personal conversations must not impede the principals.
-
Visual Cue: Green Good to go sign placed on team table cards when no verbal was required.
-
Written e‐Material: The improvement team required elements of a brief written report in a specified column of our existing electronic service list (ESL). The ESL is a custom designed template importing laboratory, medication, and demographic data automatically but also capable of free text additions (Figure 1). All providers were instructed to update the ESL every 12 hours.
-
Admission and Progress Notes: After manual electronic medical record search, the CAs printed any notes generated in the preceding 12 hours and placed them by the team table card.
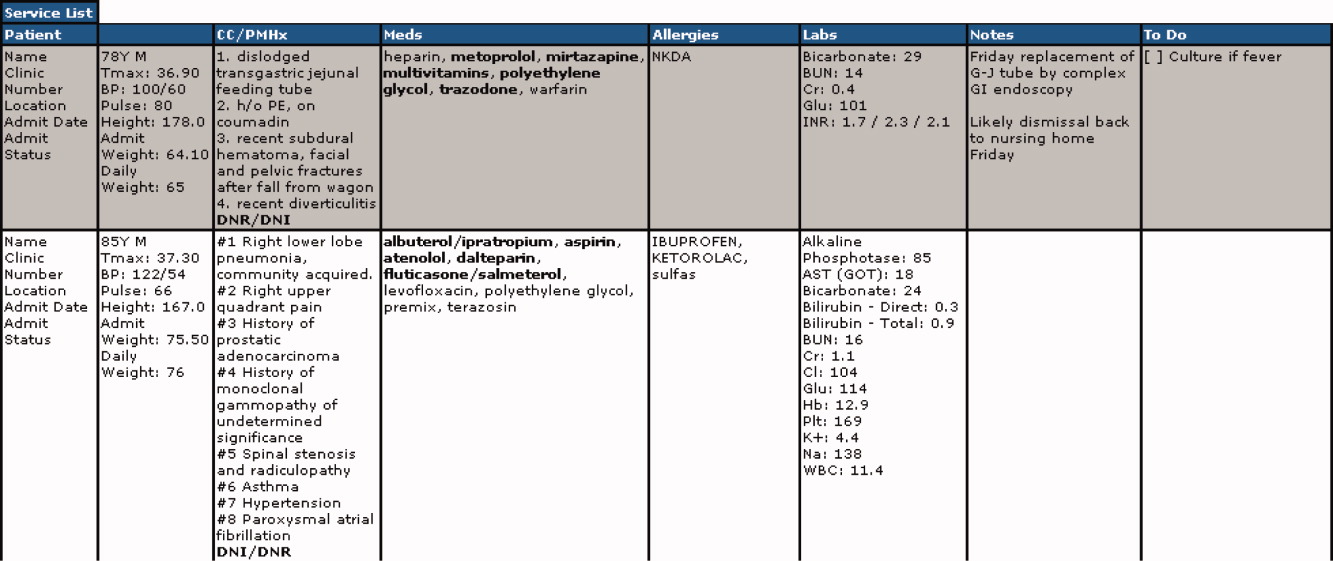
The improvement team provided education for the new process at a division meeting and through e‐mail. The recommended report sequence was night NP/PA reporting and day service teams asking questions and seeking clarifications. We discouraged editorial comments and chit‐chat.
A member of the improvement team monitored the new handoff process for 15 days, and 3 months later for 10 days.
Survey
An anonymous survey (Figure 2) concerning staff satisfaction with handoff was conducted immediately before and 15 days after the intervention. In the e‐mail containing the postintervention survey, providers were asked to respond only if they had been on service the preceding 15 days (and thus eligible to participate in handoff). To help insure this, the first question read, Have you been on service during the past 15 days?
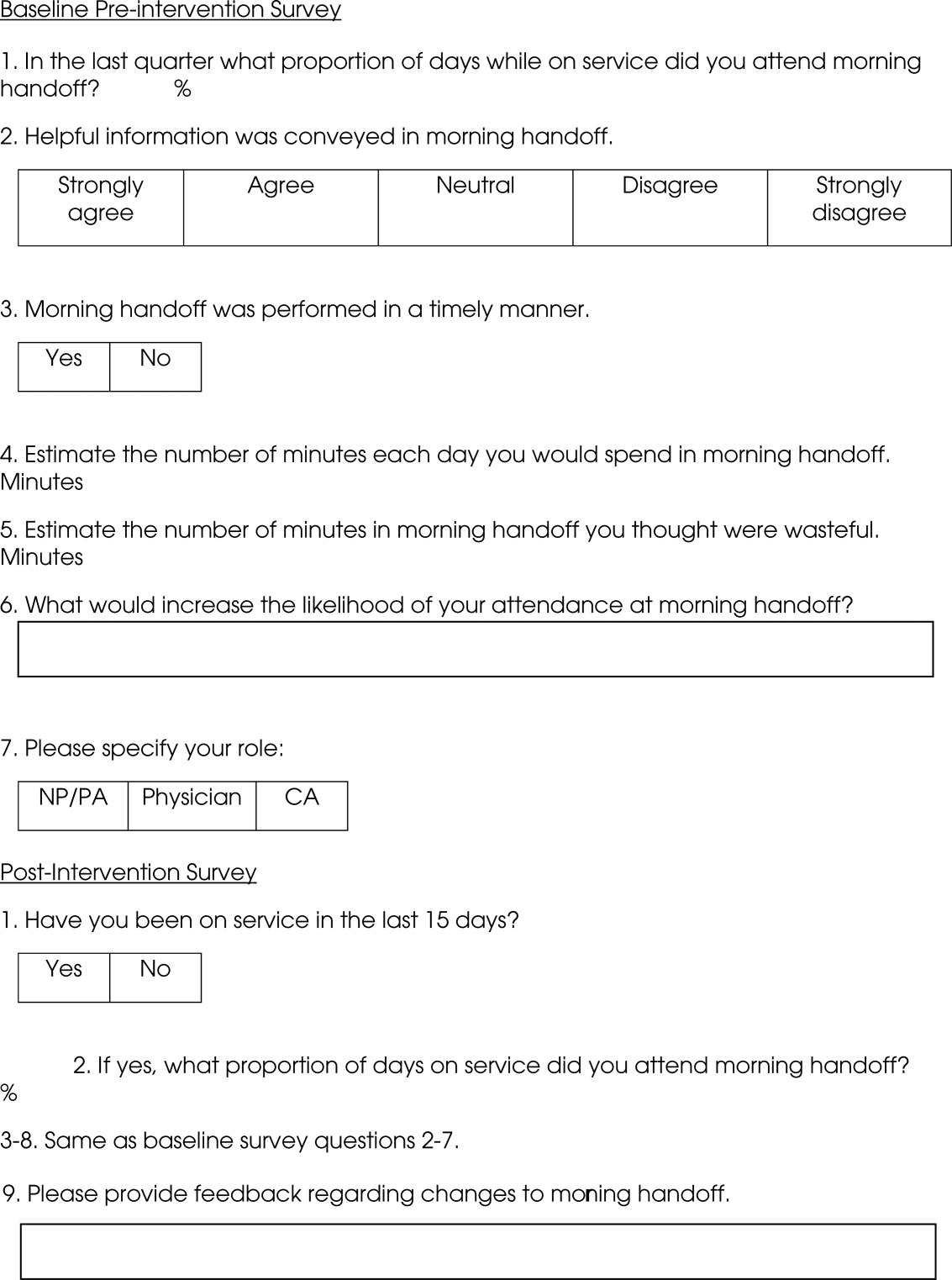
Statistics
To compare the relationship of preintervention and postintervention survey responses, Fisher's exact test was used to compare categorical variables and 2 sample t‐test and Wilcoxon rank sum test were used for continuous variables. Comparisons that adjusted for the possibility of someone responding to both the preintervention and postintervention surveys were not performed since the surveys were anonymous. A P value <0.05 was considered statistically significant. For the item concerning the percentage of days morning report was attended while on service, based on a common standard deviation estimate of 35.3, we had 80% power to detect a difference of 29.1 (pre vs. post). This computation assumes a 2‐sample t‐test of = 0.05 with sample sizes of 36 and 18. We have 59% power to detect a difference of 27% (67% pre vs. 94% post) for those who at least agree that helpful information was conveyed during handoff. This computation is based on a 2‐sided Pearson 2 test with = 0.05.
Qualitative data analysis of respondents' answers to the open‐ended survey questions What would increase the likelihood of your attending handoff? and What feedback do you have regarding the changes to handoff? was performed using the constant comparative method14 associated with grounded theory approaches to identify themes and categories.15 To establish interrater reliability, three investigators (MCB, DTK, LLK) independently identified coding categories for the data set, compared results, redefined coding categories as needed, and reanalyzed the data until 80% agreement was reached.
Results
Thirty‐six of the 44 providers (82%) answered the preintervention survey, including 18 of 22 hospitalists (82%), 17 of 20 NPs/PAs (85%), and 1 of 2 CAs (50%). During the intervention based on our staffing model, 21 providers had the opportunity to participate in handoff, and 18 (86%) answered the postintervention survey, including 5 of 6 hospitalists (83%), 9 of 14 NPs/PAs (64%), and 2 of 2 CAs (100%). All respondents to the postintervention survey reported being on service during the previous 15 days.
As summarized in Table 1, compared to 60.5% of survey participants (n = 38) who thought morning handoff was performed in a timely fashion preintervention, 100% (n = 15) felt it was performed in a timely fashion postintervention (P = 0.005). The average time spent in morning report before the intervention was 11 minutes, as compared to 5 minutes after the intervention (P < 0.0028). Prior to the intervention, 6.5 minutes of the handoff were viewed to be wasteful, as compared to 0.5 minutes of the handoff in the postintervention survey (P < 0.0001). Attendance and quality of information perceptions did not demonstrate statistically significant change.
| Survey Question | Preintervention | Postintervention | P |
|---|---|---|---|
| What proportion of days while on service did you attend morning report? (%) | 78 | 87 | 0.4119 |
| Helpful information was conveyed in morning report, n (%) | 0.112 | ||
| Strongly agree | 9 (25) | 9 (56) | |
| Agree | 15 (42) | 6 (38) | |
| Neutral | 8 (22) | 1 (6) | |
| Disagree | 4 (11) | 0 | |
| Strongly disagree | 0 | 0 | |
| Morning report was performed in a timely manner, #yes/#no | 23/15 | 15/0 | 0.005 |
| Estimate the number of minutes each day you would spend in morning report (minute) | 11 | 5 | <0.0028 |
| Estimate the number of minutes in morning report you thought were wasteful (minute) | 6.5 | 0.5 | <0.0001 |
During the 15‐day observation period, morning handoff started by 0745 on 14 of 15 (93%) of days and finished by 0800 on 15 of 15 (100%) of days. Table cards, ESL, and progress notes were on the table by 0745 on 15 of 15 (100%) of days following the intervention. Three months after the intervention, the following were observed: morning handoff started by 0745 on 10 of 10 (100%) of days; finished by 0800 on 10 of 10 (100%) of days; and table cards, ESL, and progress notes were on the table by 0745 on 10 of 10 (100%) of days.
Qualitative Data Analysis
Three themes were identified in both preintervention and postintervention surveys: timeliness, quality of report and environment (Table 2). In the preintervention survey, timeliness complaints involved inconsistent start time, prolonged duration of handoff, and inefficiency due to time wasted while teams waited for their handoff report. Comments about report quality mentioned the nonstandardized report process that included nonpertinent information and editorializing. Environmental concerns addressed noise from multiple service team members assembled in 1 large room and chatting while awaiting report. In the postintervention survey, respondents' comments noted improved efficiency, environment, and report quality.
| Deficiency | Pre‐Intervention | Post‐Intervention |
|---|---|---|
| Timeliness | Efficiency needed | I found the changes lead to more concise and valuable time spent in report |
| Timely, scheduled and efficient reports would help increase my attendance | I personally enjoyed having the times set so you are held accountable for a certain handoff | |
| Set report times so I don't have to listen to everyone else's report | More organized and efficient | |
| Too much time wasted | Love the good to go card! Can start on rounds | |
| Environment | Not having to listen to chit chat unrelated to patient carewould improve my attendance | There is less chit chat |
| Services should receive report in a quieter room | Seems less chaotic with less people overall in the room so less distraction | |
| Need a quieter and smaller room | Because the room is quieter, I did not have to repeat information | |
| Too noisy | Quiet and respectful | |
| Quality | I would like a more organized format More information isn't needed, just the correct information in a timely manner | I felt that the amount of information shared was only what was pertinent and important |
| If I first had the opportunity to review ESL and any notes generated in the last 12 hours, this would improve report | Written information on the ESL assured that I didn't forget something important | |
| Less editorializing about events and less adrenaline | I liked having the progress notes generated overnight available for review | |
| Need only meaningful information | Excellent report with prompt dissemination of information |
Discussion
We describe an intervention that set the expectation for formal, structured written and verbal communication in a focused environment involving outgoing and incoming clinicians, resulting in improved satisfaction. Before the intervention, the improvement team identified by consensus 4 problems: unpredictable start time, inefficiency, environment, and report quality. Formal structuring of our handoff process resulted in statistically significant improvement in handoff timeliness and efficiency in the view of the HIM division members. Process improvement included precise team specific start times within a 12‐minute window to improve reliability and predictability and eliminating nonproductive waiting. Additionally, receiving teams were clearly identified with table cards so that no time was wasted locating the appropriate service for report, and minimizing role‐identification challenges. The good to go sign signaled teams that no events had occurred overnight requiring verbal report. Handoff timeliness persisted 3 months after the intervention, suggesting that the process is easily sustainable.
Postintervention survey comments noted the improved environment: a smaller, quieter room with the door closed. Before the intervention, all day team providers, CAs and night provider met in a large, loud room where multiple conversations were commonplace. Previous study of the handoff process supports creating an environment free of distraction.4
Postintervention survey responses to the open‐ended questions suggested improved provider satisfaction with the quality of the report. We believe this occurred for several reasons. First, having a precise start time for each team within a 12‐minute window led to a more focused report. Second, the ESL provided a column for providers to suggest plans of care for anticipated overnight events to improve preparedness and avoid significant omissions. Third, hospital notes generated overnight were made available which allowed daytime providers to review events before handoff, for a more informed update, or just after verbal report to reinforce the information just received, a technique used in other high‐reliability organizations.16 This measure also provided an at‐a‐glance view of each patient, decreasing the complexity of handoff.17
This study has important limitations. We address the handoff process of 1 hospitalist group at a single academic center. NP/PAs are the clinicians with first‐call responsibility for the night coverage of our patients, and the handoff process between the night NP/PA and daytime provider was studied. The handoff between physicians for patients admitted overnight was not assessed. Another limitation is that the time spent in handoff is reported as a participant estimate. There was no objective measurement of time, and respondents may have been biased. An additional limitation of our study concerns the preintervention and postintervention surveys. Both surveys were anonymous, which makes discerning the absolute impact of the intervention difficult due to the lack of paired responses. Lastly, our institution has an ESL. This option may not be available in other hospital systems.
Several deficiencies in the handoff process were addressed by providing key clinical data verbally and in written format, enhancing the physical environment, and defining each team's handoff start time. Our process improvements are consistent with the handoff recommendations endorsed by the Society of Hospital Medicine.12 Subsequent direct observation, subjective reports, and survey results demonstrated improvement in the handoff process.
Future studies might measure the effectiveness of morning handoff by end‐shift interviews of the daytime clinicians. Similarly, a study of evening handoff could measure the efficiency and effectiveness of report given by day teams to night‐coverage colleagues. Furthermore, if the handoff report skill set can be more rigorously defined and measured, a hospitalist clinical competency for hospitalists and NP/PAs could be developed in this core process‐of‐care.12
Acknowledgements
The authors thank Lisa Boucher for preparation of this manuscript.
- , , , et al.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- , , .Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- , , .The human factor: the critical importance of effective teamwork and communication in providing safe care.Quality 13 Suppl 1:i85–90.
- , , , et al.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- , , .Development and implementation of an oral sign‐out skills curriculum.J Gen Intern Med.2007;22:1470–1474.
- , , , et al.The top 10 list for a safe and effective sign‐out.Arch Surg2008;143(10):1008–1010.
- , , , et al.Residents' and attending physicians' handoffs: a systematic review of the literature.Acad Med.2009;84(12):1775–1787.
- , , , et al.A structured handoff program for interns.Acad Med.2009;84:347–352.
- , , , et al.Simple standardized patient handoff system that increases accuracy and completeness.J Surg.2008;65:476–485.
- , , , et al.A randomized, controlled trial evaluation the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- , , , .Understanding communication during hospitalist service changes: A mixed methods study.J Hosp Med.2009;4(9):535–540.
- , , , , , .Hospitalist handoffs: a systematic review and task force recommendations.J of Hosp Med.2009;4(7):433–440.
- , , , et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3:361–368.
- , .Basics of Qualitiative Research: Grounded Theory Procedures and Techniques.Sage Publications, Inc.Newbury Park, CA.1990.
- , .Naturalistic Inquiry.Sage Publications, Inc.Newbury Park, CA.1985.
- .Communication strategies from high‐reliability organizations.Ann Surg.2007;245(2):170–172.
- , , , et al.Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125.
- , , , et al.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- , , .Communication failures: an insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- , , .The human factor: the critical importance of effective teamwork and communication in providing safe care.Quality 13 Suppl 1:i85–90.
- , , , et al.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- , , .Development and implementation of an oral sign‐out skills curriculum.J Gen Intern Med.2007;22:1470–1474.
- , , , et al.The top 10 list for a safe and effective sign‐out.Arch Surg2008;143(10):1008–1010.
- , , , et al.Residents' and attending physicians' handoffs: a systematic review of the literature.Acad Med.2009;84(12):1775–1787.
- , , , et al.A structured handoff program for interns.Acad Med.2009;84:347–352.
- , , , et al.Simple standardized patient handoff system that increases accuracy and completeness.J Surg.2008;65:476–485.
- , , , et al.A randomized, controlled trial evaluation the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- , , , .Understanding communication during hospitalist service changes: A mixed methods study.J Hosp Med.2009;4(9):535–540.
- , , , , , .Hospitalist handoffs: a systematic review and task force recommendations.J of Hosp Med.2009;4(7):433–440.
- , , , et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3:361–368.
- , .Basics of Qualitiative Research: Grounded Theory Procedures and Techniques.Sage Publications, Inc.Newbury Park, CA.1990.
- , .Naturalistic Inquiry.Sage Publications, Inc.Newbury Park, CA.1985.
- .Communication strategies from high‐reliability organizations.Ann Surg.2007;245(2):170–172.
- , , , et al.Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125.
Smartphones for Clinical Communication
The scope and importance of communication between clinicians in the delivery of health care is increasingly being recognized.1, 2 Poor communication is known to be a source of inefficiency and errors within healthcare.36 The major issues with communication include the frequent use of interruptive communication mechanisms and the difficulty of knowing who to contact.2 Traditional paging remains the primary method to contact a physician despite being disruptive, inefficient, and predisposing to errors.710 The identification of the responsible physician for a patient can also be complicated with the numerous call schedules, different coverage rules, vacations, and protected academic time for residents. In 1 observational study, 25% of calls in a hospital were attempts to identify a responsible individual for a specific role.11 A recent study revealed that 14% of pages went to the wrong physician and that 47% of these errant pages warranted an urgent response.12 In our institution, the process for a nurse to identify which physician to contact regarding a patient care issue can be complex (Figure 1).
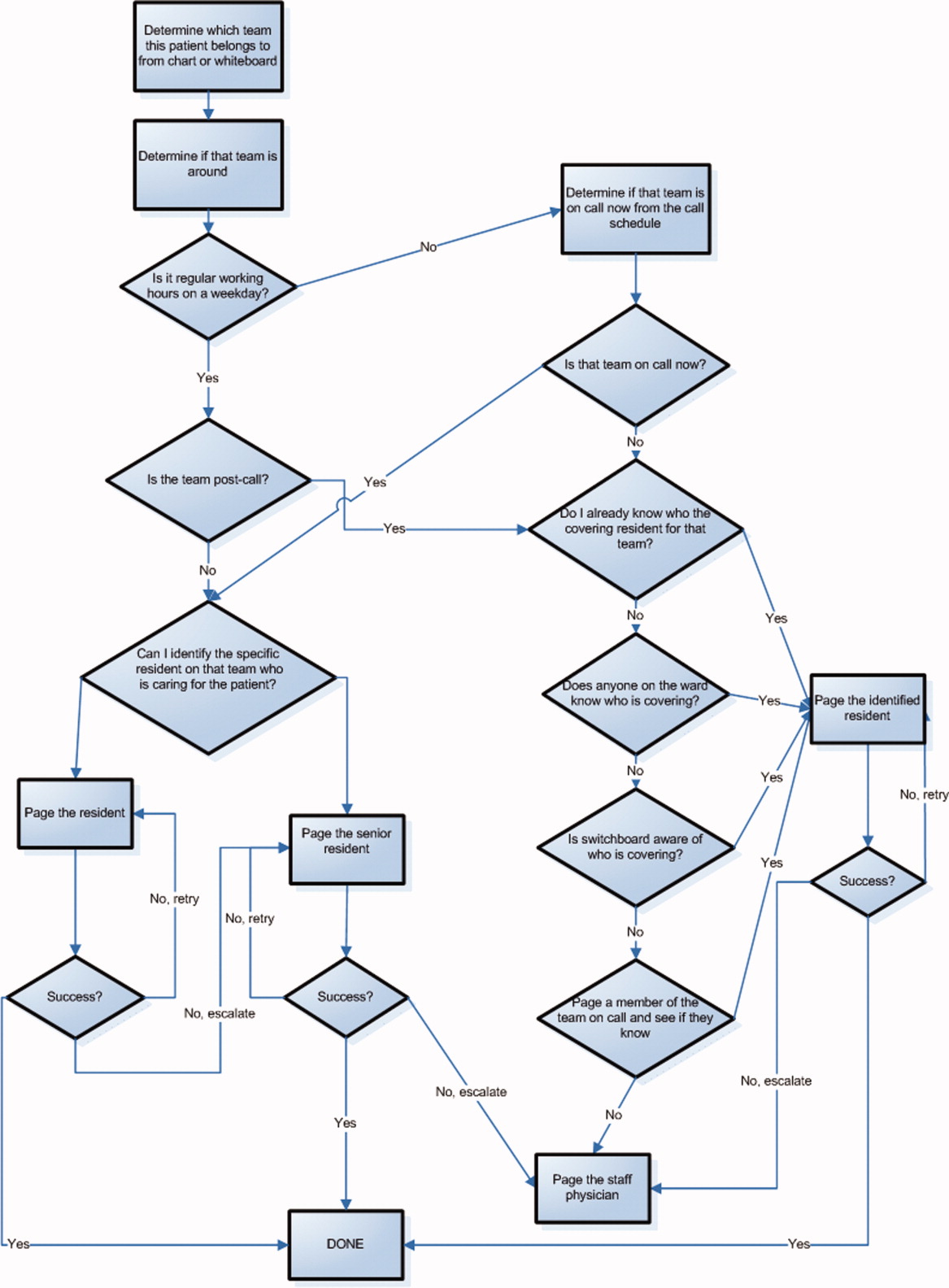
The use of email and mobile phone technology has been recommended as a method to improve communication.2 It can improve communication between clinicians by providing a method of triaging based on importance: instantly by telephone for urgent issues and less disruptively by email for nonurgent issues. There is limited literature on the use of email for improving communication between clinicians or on the use of smartphones. In a previous pilot study, we found that with minimal training, residents were able to use smartphones on general medical wards for clinical communication and that technical challenges were minimal.13 In an intensive care setting, the use of wireless emails using smartphones was perceived by staff to improve communication.14
Methods
Aim
To evaluate the use of smartphones to improve the communication processes on an academic general internal medicine service.
Setting
We conducted the study within the General Internal Medicine service at the Toronto General Hospital, an academic teaching hospital. The service is comprised of 4 teaching teams, each with 1 staff physician, 1 senior resident, 2 to 3 junior residents, and medical students. The environment is typically characterized by a high volume of medically complex patients and constant turnover of physicians with varying degrees of experience. Ethical review of the study was performed by the University Health Network Research Ethics Board.
Program Description
Recognizing the difficulty in implementing complex interventions within clinical care, we used a staged approach applying the standard Plan‐Do‐Study‐Act (PDSA) methodology for quality improvement.15 This involved developing a component of the system, releasing it to the users to learn from their experience, then taking this feedback to make changes and continuing with the next cycle. This allowed early identification and quicker resolution of issues.
Smartphones as Clinical Communication Tools
The first change implemented was to supplement the standard numeric pager with smartphones as the primary communication device for the residents. The BlackBerry device (Research in Motion, Ontario, Canada) was selected because it is an efficient, usable device with voice and secure email functionality that also happens to be the standard smartphone for our hospital administrators. Beginning in March 2008, all residents on the internal medicine service were equipped with a smartphone that they kept for their entire rotation. Contact lists of all devices were prepopulated with the hospital phone numbers that were important in coordinating patient care. These included numbers such as hospital flow coordinators, radiology reporting rooms, interventional radiology, and microbiology.
To facilitate reaching the most responsible resident for patients, we provided an additional smartphone, the Team BlackBerry, that was carried by the senior resident of each team during regular hours and then passed to the resident that was covering the team at night and on weekends. With the new process, a nurse would only require knowledge of which team the patient belonged to in order to contact the most responsible resident (Figure 2). The Team BlackBerry also received critical laboratory and medication alerts that contained clinical decision support. The laboratory and medication alerts were generated through the hospital rule‐based clinical decision support system (Misys Insight).
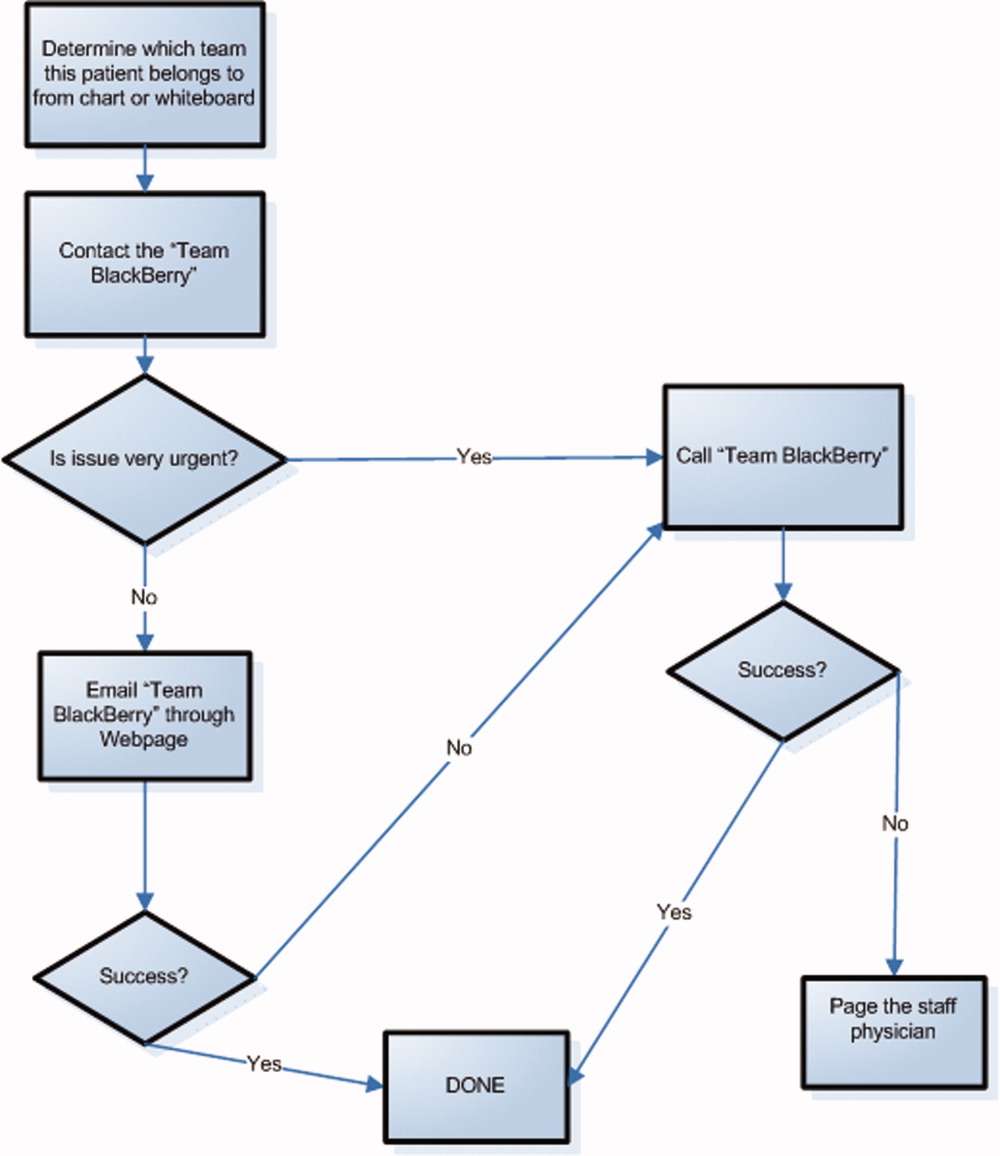
Web‐paging to Improve Nurse‐Physician Communication
In May 2008, we implemented a platform for text paging that we called web‐paging that allowed the nurses to efficiently send email messages securely through a hospital intranet page to the Team BlackBerry. A nurse would access the form from any computer on the wards, select the appropriate team, provide relevant information, and then send the message. Although the form would send an email, the term web‐paging was used to create familiarity with their previous process of contacting a resident, namely paging. This process reserved voice communication for urgent matters only while routing less urgent issues through the web‐paging form. Furthermore, emails were categorized into three priority levels:
-
Call back requested messages were for issues that were not life threatening but needed immediate action or required discussion with a physician.
-
E‐mail response requested messages were for issues that needed an action but could wait until the physician was available, such as cosigning an order.
-
Information only with no response necessary messages facilitated 1‐way communication, such as updating the team of recent vital signs for a patient.
Physicians would receive prompt notification of a new email on their smartphone, and they could reply to the email or call back using a link within the email. Nurses were able to view the physician's email responses from an email account that was shared amongst the nurses on each ward.
Program Evaluation
The outcome measures of the study were residents' use of smartphones and perceptions of residents and nurses on the new communication process. Resident use of the smartphones was measured by the volume and the frequency of phone calls and emails over a 3‐month period from September 2008 to November 2008. Residents' perceptions were measured by a survey administered prior to the start of their clinical rotation and at the end of their rotation (Table 1). Data collection for residents occurred between June 2008 and February 2009. Nurses' perceptions were measured by surveys administered to the nurses working on either day shifts or night shifts over a 1‐week period prior to the intervention in March 2008 and then 6 months after in September 2008 (Table 2).
| Pre‐Survey (n = 59) Median, (mode, mean) | Post‐Survey (n = 65) Median, (mode, mean) | P value | |
|---|---|---|---|
| Training level | |||
| Postgraduate Year 1 | 39 (66.1%) | 43 (66.2%) | |
| Postgraduate Year 2 | 17 (28.8%) | 19 (29.2%) | |
| Postgraduate Year 3 | 3 (5.1%) | 3 (4.6%) | |
| Currently own and use a personal digital assistant | 30 (55.6%) | 38 (62.3%) | |
| Currently own a BlackBerry | 6 (10.5%) | 5 (8.3%) | |
| The following questions used a Likert scale with 1 representing strongly disagree and 5 representing strongly agree | |||
| Q1. I never have issues accessing a phone to discuss patient care issues | 3 (2, 2.8) | 4 (5, 3.9) | <0.001 |
| Q2. I often waste a lot of time waiting for my pages to be answered | 4 (4, 4.1) | 4 (4, 3.3) | 0.004 |
| Q3. Communicating with my team often takes a lot of time | 4 (4, 3.5) | 2 (1, 2.5) | <0.001 |
| Q4. I have quick and easy access to contact information (eg, allied health, departments, consultants, etc) necessary for providing patient care | 3 (2, 2.6) | 4 (4, 3.7) | <0.001 |
| Q5. My primary communication device (pager/ BlackBerry) is non‐disruptive to my workflow | 3 (3, 2.7) | 4 (4, 3.4) | 0.002 |
| Q6. My primary communication device (pager/ BlackBerry) helps me prioritize my tasks | 3 (3, 2.9) | 4 (4, 3.7) | <0.001 |
| Q7. Email and/or text messaging is something I find useful for communication about patient care | 4 (3, 3.6) | 5 (5, 4.4) | <0.001 |
| Q8. Overall, I am satisfied with my primary communication device (pager/BlackBerry) | 3 (3, 2.9) | 4 (5, 4.2) | <0.001 |
| Q9. Overall, being phoned on the BlackBerry (instead of receiving a page) is disruptive to me | 3 (2, 3.0) | ||
| Q10. I consider Internet access on the BlackBerry useful for looking up information related to patient care. | 3 (3, 3.0) | ||
| Q11. I prefer not having a BlackBerry at all than having to deal with technical difficulties when I use it | 2 (1, 1.9) | ||
| Q12. I feel that overall a BlackBerry saves me time | 4 (5, 4.3) | ||
| Pre‐Survey (n = 27) Median, Mode | Post‐Survey (n = 35) Median, Mode | P Value | |
|---|---|---|---|
| Day shifts | 18 (66.7%) | 20 (57.1%) | |
| Total number of times you tried to page, email or telephone a resident or medical student in the shift just completed. | 3.70 | 2.51 | 0.16 |
| Did you need to repeatedly try to contact (page, email, or call) a resident at any time during the shift regarding the same issue? | 80% | 34.3% | 0.0012 |
| Total amount of time that you spent in the last shift trying to contact doctors or other health care providers (minutes). | 27.6 | 11.1 | <0.001 |
| The following questions used a Likert scale with 1 representing Strongly Disagree and 5 representing Strongly Agree: | |||
| Overall, it is straightforward to contact the resident taking care of my patients. | 4 (4) | 4 (4) | 0.27 |
| Overall, I am satisfied with physicians' response time when I need to contact them urgently. | 3 (4) | 4 (4) | 0.54 |
| I spend a lot of time away from the bedside just trying to contact physicians. | 3 (4) | 3 (3) | 0.17 |
| I like being able to call and reach the doctor directly. | 4 (5) | ||
| Overall I am satisfied with the BlackBerry/email communication system. | 4 (4) |
Data Analysis
We present utilization as the mean number of messages sent and received daily. We report survey responses as the mean scores on a 5‐point Likert scale. For ordinal data, we described the survey responses using median and mode, and the Mann Whitney U test was used to test for differences between before and after responses. For parametric data, unpaired t‐tests were used to look for differences in the perceptions before and after the intervention. All P values are 2‐sided.
Results
Smartphone Usage
Usage of emails and calls for the team devices over the three months is shown in Table 3. Most communications were through the Team BlackBerry devices with the individual devices showing less usage than the team device with 2.1 sent emails per day and 4.0 received emails per day. On the days with highest use, there were 7 calls received per hour and 6 emails received per hour at peak times through the day to a Team BlackBerry. Web‐paging was the largest source of emails sent to Team BlackBerrys (42%). Critical laboratory or medication alerts represented 17.1% and the remainder (40.9%) were other communications such as communication from residents, staff physicians, pharmacists, and allied health professionals. Of the web‐paging communications, 35.1% requested a call back, 22.6% requested email response, and 42.2% were informational items only that did not require a response.
| Phone Calls | Emails | |||
|---|---|---|---|---|
| Incoming | Outgoing | Received | Sent | |
| Average | 9.1 | 6.6 | 14.3 | 2.8 |
| Minimum | 0 | 0 | 0 | 0 |
| Maximum | 35 | 45 | 57 | 13 |
| Median | 8 | 4 | 13.5 | 2 |
Resident Perceptions
Of the 91 residents, 59 residents completed the presurveys (response rate 65%) and 65 completed the postsurveys (response rate 71%) (Table 1). There was a statistically significant improvement in all of the items measured. There were also 26 postsurvey comments with 22 describing positive aspects and 9 describing negative aspects. Specific positive attributes of the new communication system that were mentioned were: easier to communicate with other physicians within the team (n = 6), easier to communicate with other health care members of the team (nurses, allied health) (n = 3), and increased mobility (n = 2). The following are some examples:
-
Blackberrys are great for contacting team member, able to mobile in hospital instead of waiting by phone ‐ since we're so busy
-
Excellent for interpersonal communication. It definitely sped up patients care ie, consults, getting investigations done and discharges. Everyone should have one.
-
Text messaging, especially in group format so that all members participate in conversations is the primary communication tool of choice. Emailing is a necessity of the modern workforce.
The 2 predominant issues described were that the direct calling by nurses was disruptive (n = 6) and voice mail was not useful (n = 3):
-
I dislike the voicemail as it is like paging back but you also need to make a phone call to your phone list. Also we are always being interrupted which is disruptive to work but prefer BlackBerrys.
-
Helpful but often disruptive such as getting calls when seeing patients.
Nursing Perceptions
From the typical staff of 94 full‐time and part‐time nurses, 27 of 48 (56%) completed the preintervention survey, and 35 of 54 (65%) completed the postintervention survey. There was a perceived significant decrease in the need to repeatedly try to contact a physician for the same issue (80% vs. 34.3%, P = 0.001) and a significant decrease in the perceived amount of time spent trying to contact clinicians (27.6 minutes vs. 11.1 minutes, P < 0.001) (Table 2). On 5 point Likert scales, there was no perceived improvement in communication areas such as finding out who to reach and resident response time. Nurses appreciated the ability to call the physicians directly for urgent issues (median response 4, mode of 5).
Discussion
Principal Results
In this pilot study of using smartphones and email, residents perceived that it significantly improved their efficiency. Nurses perceived a reduction in the time spent trying to communicate with clinicians.
There were significant lessons learned. First, we found that residents readily utilized smartphones and felt that it improved their efficiency. Staff physicians and residents have outlined multiple concerns over increased workload, increasing patient complexity, and longer work hours. Therefore, interventions that improve physician productivity are essential in maintaining and improving patient care.16 From residents' comments, it appears their improved efficiency is derived not only from improved communication within the medical team, but also within the interprofessional team. Efficiency was also perceived to improve from the greater mobility of being able to walk while returning a page or while waiting for a page to be returned.
Second, we found that changing the communication process was complicated. While the number of calls and emails per day appeared manageable, the peak times had very high volumes and may actually be unmanageable. By facilitating the process of reaching the responsible physician, we may have lowered the threshold for contacting the physician and thus actually increased communication volumes. It is unclear whether the end result is beneficial as improved management of patients is balanced by the increased interruptions. Further study is required to understand the effect of increasing communication on patient outcomes.
Finally, residents indicated quite strongly that they did not want telephone calls to be the primary mode of contact as they found the frequent telephone calls too disruptive. A direct call to a physician created significant disruption to workflow requiring interrupting a task to answer the call or deferring the call to later review of a voice mail message. Accessing voice mail would typically take at least a minute, much more time than the few seconds it takes to review a numeric page or a text page. Residents quickly provided feedback that this process was unacceptable and reduced their ability to deliver care effectively. Furthermore, nurses were frustrated by the added time required to leave voice messages and the poor response rate. As information within voice mails was not acted upon, nurses quickly learned to just keep calling.
Costs of implementation were significantly more than the numeric paging system. With a cost of $5/month for a numeric pager, the cost of numeric pagers for 4 medical teams with 4 physicians each was $80/month (all costs in Canadian dollars). From our implementation, the approximate cost of an individual smartphone was $80/month while team‐based devices were $160/month due to much higher usage. With 4 individual smartphones and one team‐based smartphone per team, costs with the new system were approximately $1,600/month. While implementing smartphones creates a significantly greater expense, it may be worthwhile if improved communication leads to more efficient and higher quality care. Our current system is funded through the hospital to allow for further evaluation, and whether other hospitals provide smartphones for clinical communications likely would depend on whether they provided a cost effective alternative to numeric pagers. This would likely require some more tangible benefit than perceived improved efficiency.
Comparison With Prior Work
Similar to the study of wireless email using smartphones in the Intensive Care Unit, physicians in our study perceived an improvement in efficiency.14 Our study adds further information to the literature since we implemented on general medical wards in an academic teaching hospital. Our study is consistent with the previous studies have documented physicians' perceptions of improved performance with mobile phones.7, 17
Limitations
There are limitations to this study. In order to improve communication, we implemented a complex intervention with several components: (1) smartphones for residents, (2) Web‐paging for nurses, and (3) a new process of identifying the most responsible physician using Team BlackBerrys. From our surveys, it is difficult to know the relative impact of each individual component. Other interventions such as team‐based alphanumeric pagers may achieve similar improvements to nurses' perceptions of improved communication.
As this was a pilot study assessing new communication methods, we informally assessed perceptions using surveys which had not been validated. While the use of formally validated surveys would be more useful, we were unable to find any that specifically addressed the innovation in communication seen with smartphones. Validity issues with the instruments and the low response rates may have contributed to the incongruent result seen with nurses' surveys in that there was a perceived improvement in time to contact physicians but not in the ease of contact of physicians or the satisfaction of the communication method. This incongruent result may also reflect that in spite of the fact that the nurses were accustomed to the new system and that things may have improved, communication issues still remain and likely would benefit from further study.
It would have also been useful to determine the effect of this intervention on numeric pages sent to traditional pagers, which was not captured. It is also important to realize that we did not replace the pagers but instead supplemented residents with smartphones. To replace pagers may involve significant costs to upgrade reception within hospital walls to reduce areas of little or no reception. Finally, this study was completed at 1 academic health science center, and the generalizability of the findings may be limited.
Future Study
There is great opportunity to improve communication between clinicians, and the use of smartphones, email and improved identification of the most responsible physician are some methods to achieving this. Further research would be useful to determine the relative importance of each component. With smartphones, it is would be useful to know whether the benefits seen were primarily due to the mobile email or having another phone available or other features. Finally, the use of web‐paging and email to communicate increases the documentation of communications, but a further improvement could be providing acknowledgement to nurses that web‐pages were received and read. This would close the loop on communications, ensuring that there are no lost communications and that escalation occurs promptly for urgent communications.
In summary, we implemented and evaluated a system to route and prioritize clinical communications combining the use of phone calls and secure email messaging to smartphones. Residents strongly perceived an improvement in communication with smartphones. Further objective clinical evaluation is necessary to determine if this intervention improves efficiency and more importantly, the quality of care.
Acknowledgements
The investigators retained all control over study design, data collection, analysis and interpretation, and preparation of reports.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7(3):277–286.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I.N Engl J Med.1991;324(6):370–376.
- ,,, et al.Gaps in pediatric clinician communication and opportunities for improvement.J Healthc Qual.2008;30(5):43–54.
- ,,,,,.The quality in Australian Health Care Study.Med J Aust.1995;163(9):458–471.
- ,,,,.Quality in Australian Health Care Study.Med J Aust.1996;164(12):754.
- ,,,,.Communication in critical care environments: mobile telephones improve patient care.Anesth Analg.2006;102(2):535–541.
- ,.Interrupted care. The effects of paging on pediatric resident activities.Am J Dis Child.1992;146(7):806–808.
- ,,.Patterns of paging medical interns during night calls at two teaching hospitals.CMAJ.1994;151(3):307–311.
- ,.The sounds of the hospital. Paging patterns in three teaching hospitals.N Engl J Med.1988;319(24):1585–1589.
- ,.Communication behaviours in a hospital setting: an observational study.BMJ1998;316(7132):673–676.
- ,,, et al.Why isn't anyone returning my page? Frequency and clinical importance of pages sent to the wrong physician.Arch Intern Med.2009;169(11):1072–1073.
- ,,, et al.Demonstrating the BlackBerry as a clinical communication tool: a pilot study conducted through the centre for innovation in complex care.Healthc Q2008;11(4):94–98.
- ,,,.The use of wireless email to improve healthcare team communication.J Am Med Inform Assoc.2009;16(5):705–713.
- .A primer on leading the improvement of systems.BMJ.1996;312(7031):619–622.
- .An elusive balance—residents' work hours and the continuity of care.N Engl J Med.2007;356(26):2665–2667.
- ,,, et al.Use of mobile phones by medical staff at Queen Elizabeth Hospital, Barbados: evidence for both benefit and harm.J Hosp Infect.2008;70(2):160–165.
The scope and importance of communication between clinicians in the delivery of health care is increasingly being recognized.1, 2 Poor communication is known to be a source of inefficiency and errors within healthcare.36 The major issues with communication include the frequent use of interruptive communication mechanisms and the difficulty of knowing who to contact.2 Traditional paging remains the primary method to contact a physician despite being disruptive, inefficient, and predisposing to errors.710 The identification of the responsible physician for a patient can also be complicated with the numerous call schedules, different coverage rules, vacations, and protected academic time for residents. In 1 observational study, 25% of calls in a hospital were attempts to identify a responsible individual for a specific role.11 A recent study revealed that 14% of pages went to the wrong physician and that 47% of these errant pages warranted an urgent response.12 In our institution, the process for a nurse to identify which physician to contact regarding a patient care issue can be complex (Figure 1).
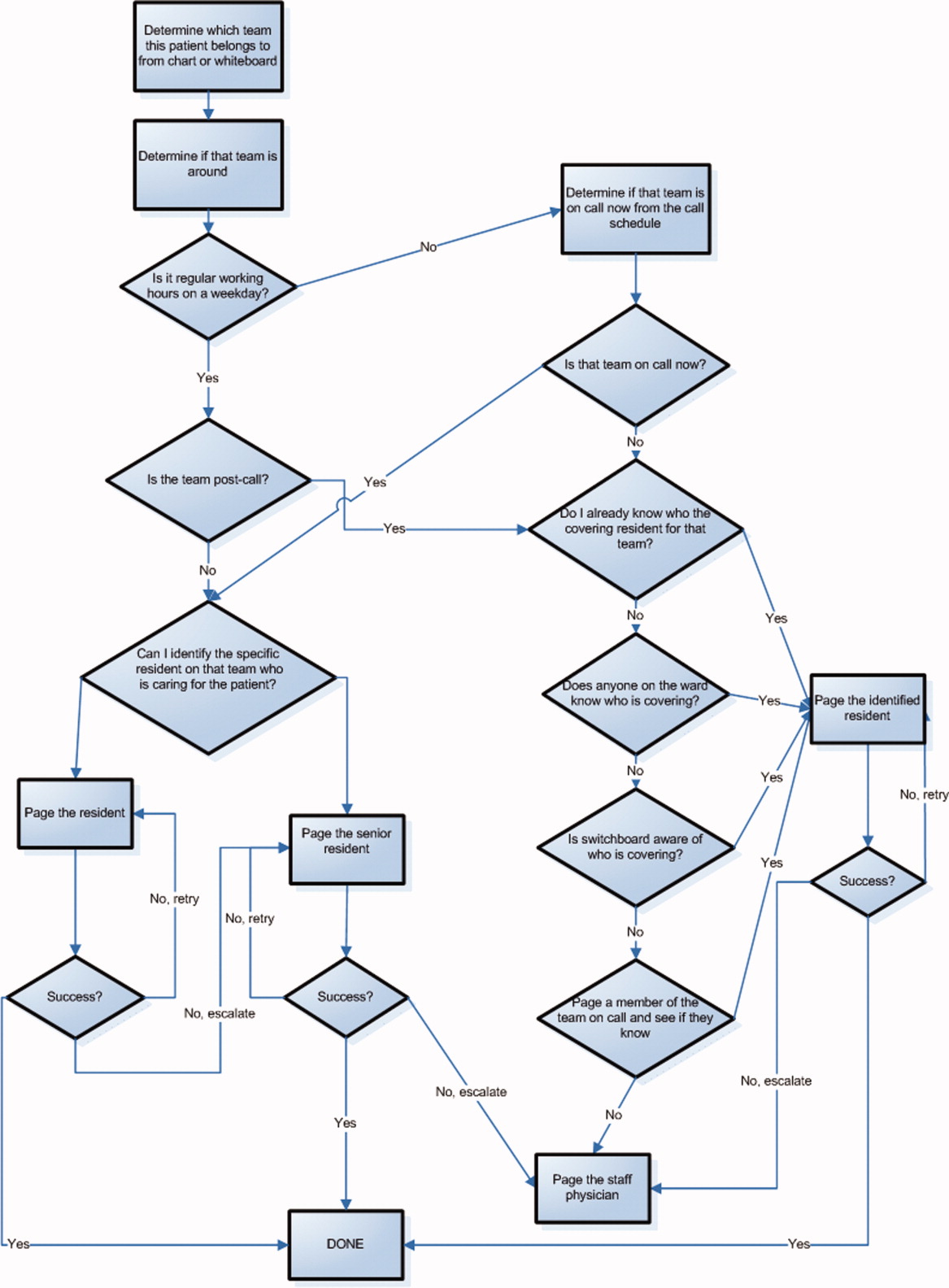
The use of email and mobile phone technology has been recommended as a method to improve communication.2 It can improve communication between clinicians by providing a method of triaging based on importance: instantly by telephone for urgent issues and less disruptively by email for nonurgent issues. There is limited literature on the use of email for improving communication between clinicians or on the use of smartphones. In a previous pilot study, we found that with minimal training, residents were able to use smartphones on general medical wards for clinical communication and that technical challenges were minimal.13 In an intensive care setting, the use of wireless emails using smartphones was perceived by staff to improve communication.14
Methods
Aim
To evaluate the use of smartphones to improve the communication processes on an academic general internal medicine service.
Setting
We conducted the study within the General Internal Medicine service at the Toronto General Hospital, an academic teaching hospital. The service is comprised of 4 teaching teams, each with 1 staff physician, 1 senior resident, 2 to 3 junior residents, and medical students. The environment is typically characterized by a high volume of medically complex patients and constant turnover of physicians with varying degrees of experience. Ethical review of the study was performed by the University Health Network Research Ethics Board.
Program Description
Recognizing the difficulty in implementing complex interventions within clinical care, we used a staged approach applying the standard Plan‐Do‐Study‐Act (PDSA) methodology for quality improvement.15 This involved developing a component of the system, releasing it to the users to learn from their experience, then taking this feedback to make changes and continuing with the next cycle. This allowed early identification and quicker resolution of issues.
Smartphones as Clinical Communication Tools
The first change implemented was to supplement the standard numeric pager with smartphones as the primary communication device for the residents. The BlackBerry device (Research in Motion, Ontario, Canada) was selected because it is an efficient, usable device with voice and secure email functionality that also happens to be the standard smartphone for our hospital administrators. Beginning in March 2008, all residents on the internal medicine service were equipped with a smartphone that they kept for their entire rotation. Contact lists of all devices were prepopulated with the hospital phone numbers that were important in coordinating patient care. These included numbers such as hospital flow coordinators, radiology reporting rooms, interventional radiology, and microbiology.
To facilitate reaching the most responsible resident for patients, we provided an additional smartphone, the Team BlackBerry, that was carried by the senior resident of each team during regular hours and then passed to the resident that was covering the team at night and on weekends. With the new process, a nurse would only require knowledge of which team the patient belonged to in order to contact the most responsible resident (Figure 2). The Team BlackBerry also received critical laboratory and medication alerts that contained clinical decision support. The laboratory and medication alerts were generated through the hospital rule‐based clinical decision support system (Misys Insight).
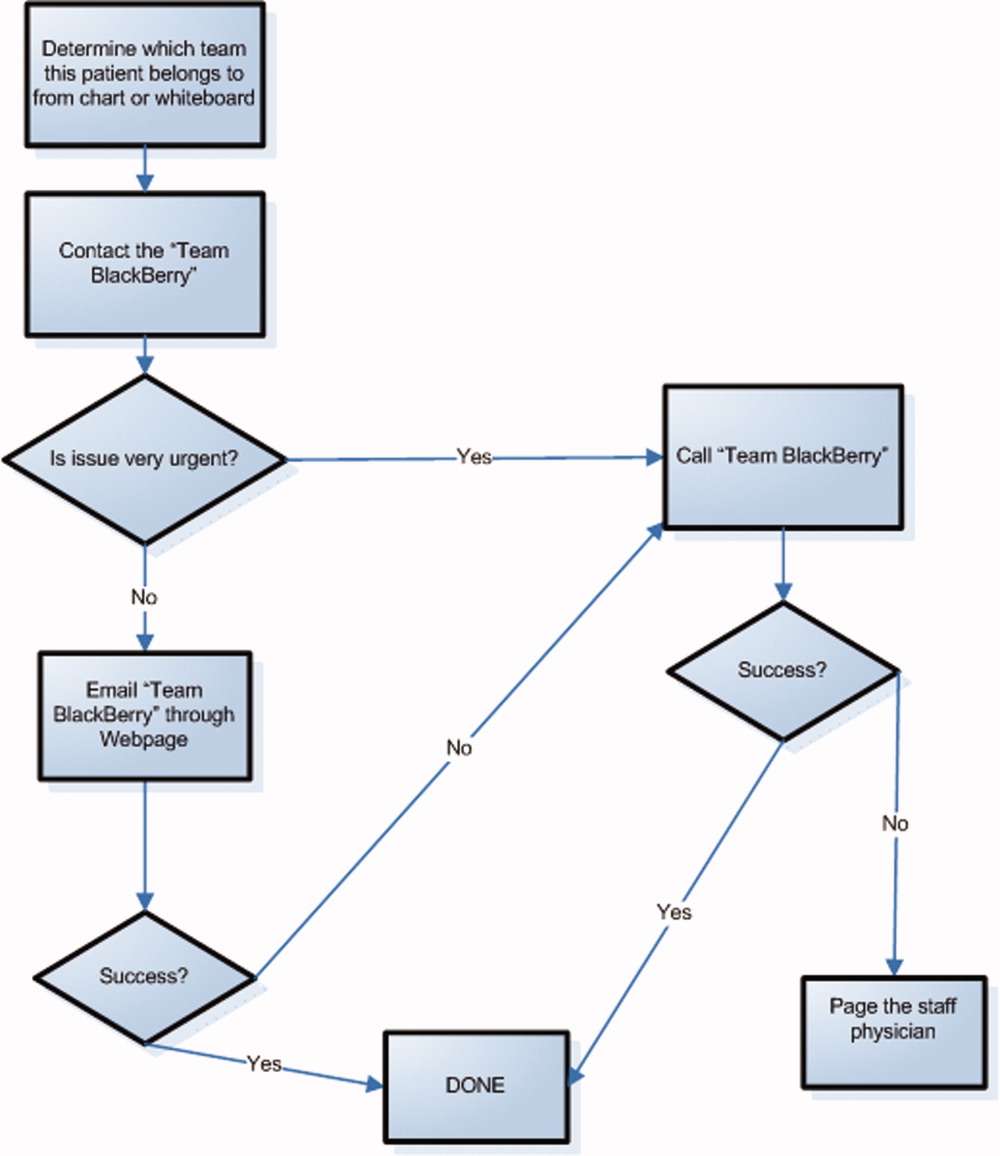
Web‐paging to Improve Nurse‐Physician Communication
In May 2008, we implemented a platform for text paging that we called web‐paging that allowed the nurses to efficiently send email messages securely through a hospital intranet page to the Team BlackBerry. A nurse would access the form from any computer on the wards, select the appropriate team, provide relevant information, and then send the message. Although the form would send an email, the term web‐paging was used to create familiarity with their previous process of contacting a resident, namely paging. This process reserved voice communication for urgent matters only while routing less urgent issues through the web‐paging form. Furthermore, emails were categorized into three priority levels:
-
Call back requested messages were for issues that were not life threatening but needed immediate action or required discussion with a physician.
-
E‐mail response requested messages were for issues that needed an action but could wait until the physician was available, such as cosigning an order.
-
Information only with no response necessary messages facilitated 1‐way communication, such as updating the team of recent vital signs for a patient.
Physicians would receive prompt notification of a new email on their smartphone, and they could reply to the email or call back using a link within the email. Nurses were able to view the physician's email responses from an email account that was shared amongst the nurses on each ward.
Program Evaluation
The outcome measures of the study were residents' use of smartphones and perceptions of residents and nurses on the new communication process. Resident use of the smartphones was measured by the volume and the frequency of phone calls and emails over a 3‐month period from September 2008 to November 2008. Residents' perceptions were measured by a survey administered prior to the start of their clinical rotation and at the end of their rotation (Table 1). Data collection for residents occurred between June 2008 and February 2009. Nurses' perceptions were measured by surveys administered to the nurses working on either day shifts or night shifts over a 1‐week period prior to the intervention in March 2008 and then 6 months after in September 2008 (Table 2).
| Pre‐Survey (n = 59) Median, (mode, mean) | Post‐Survey (n = 65) Median, (mode, mean) | P value | |
|---|---|---|---|
| Training level | |||
| Postgraduate Year 1 | 39 (66.1%) | 43 (66.2%) | |
| Postgraduate Year 2 | 17 (28.8%) | 19 (29.2%) | |
| Postgraduate Year 3 | 3 (5.1%) | 3 (4.6%) | |
| Currently own and use a personal digital assistant | 30 (55.6%) | 38 (62.3%) | |
| Currently own a BlackBerry | 6 (10.5%) | 5 (8.3%) | |
| The following questions used a Likert scale with 1 representing strongly disagree and 5 representing strongly agree | |||
| Q1. I never have issues accessing a phone to discuss patient care issues | 3 (2, 2.8) | 4 (5, 3.9) | <0.001 |
| Q2. I often waste a lot of time waiting for my pages to be answered | 4 (4, 4.1) | 4 (4, 3.3) | 0.004 |
| Q3. Communicating with my team often takes a lot of time | 4 (4, 3.5) | 2 (1, 2.5) | <0.001 |
| Q4. I have quick and easy access to contact information (eg, allied health, departments, consultants, etc) necessary for providing patient care | 3 (2, 2.6) | 4 (4, 3.7) | <0.001 |
| Q5. My primary communication device (pager/ BlackBerry) is non‐disruptive to my workflow | 3 (3, 2.7) | 4 (4, 3.4) | 0.002 |
| Q6. My primary communication device (pager/ BlackBerry) helps me prioritize my tasks | 3 (3, 2.9) | 4 (4, 3.7) | <0.001 |
| Q7. Email and/or text messaging is something I find useful for communication about patient care | 4 (3, 3.6) | 5 (5, 4.4) | <0.001 |
| Q8. Overall, I am satisfied with my primary communication device (pager/BlackBerry) | 3 (3, 2.9) | 4 (5, 4.2) | <0.001 |
| Q9. Overall, being phoned on the BlackBerry (instead of receiving a page) is disruptive to me | 3 (2, 3.0) | ||
| Q10. I consider Internet access on the BlackBerry useful for looking up information related to patient care. | 3 (3, 3.0) | ||
| Q11. I prefer not having a BlackBerry at all than having to deal with technical difficulties when I use it | 2 (1, 1.9) | ||
| Q12. I feel that overall a BlackBerry saves me time | 4 (5, 4.3) | ||
| Pre‐Survey (n = 27) Median, Mode | Post‐Survey (n = 35) Median, Mode | P Value | |
|---|---|---|---|
| Day shifts | 18 (66.7%) | 20 (57.1%) | |
| Total number of times you tried to page, email or telephone a resident or medical student in the shift just completed. | 3.70 | 2.51 | 0.16 |
| Did you need to repeatedly try to contact (page, email, or call) a resident at any time during the shift regarding the same issue? | 80% | 34.3% | 0.0012 |
| Total amount of time that you spent in the last shift trying to contact doctors or other health care providers (minutes). | 27.6 | 11.1 | <0.001 |
| The following questions used a Likert scale with 1 representing Strongly Disagree and 5 representing Strongly Agree: | |||
| Overall, it is straightforward to contact the resident taking care of my patients. | 4 (4) | 4 (4) | 0.27 |
| Overall, I am satisfied with physicians' response time when I need to contact them urgently. | 3 (4) | 4 (4) | 0.54 |
| I spend a lot of time away from the bedside just trying to contact physicians. | 3 (4) | 3 (3) | 0.17 |
| I like being able to call and reach the doctor directly. | 4 (5) | ||
| Overall I am satisfied with the BlackBerry/email communication system. | 4 (4) |
Data Analysis
We present utilization as the mean number of messages sent and received daily. We report survey responses as the mean scores on a 5‐point Likert scale. For ordinal data, we described the survey responses using median and mode, and the Mann Whitney U test was used to test for differences between before and after responses. For parametric data, unpaired t‐tests were used to look for differences in the perceptions before and after the intervention. All P values are 2‐sided.
Results
Smartphone Usage
Usage of emails and calls for the team devices over the three months is shown in Table 3. Most communications were through the Team BlackBerry devices with the individual devices showing less usage than the team device with 2.1 sent emails per day and 4.0 received emails per day. On the days with highest use, there were 7 calls received per hour and 6 emails received per hour at peak times through the day to a Team BlackBerry. Web‐paging was the largest source of emails sent to Team BlackBerrys (42%). Critical laboratory or medication alerts represented 17.1% and the remainder (40.9%) were other communications such as communication from residents, staff physicians, pharmacists, and allied health professionals. Of the web‐paging communications, 35.1% requested a call back, 22.6% requested email response, and 42.2% were informational items only that did not require a response.
| Phone Calls | Emails | |||
|---|---|---|---|---|
| Incoming | Outgoing | Received | Sent | |
| Average | 9.1 | 6.6 | 14.3 | 2.8 |
| Minimum | 0 | 0 | 0 | 0 |
| Maximum | 35 | 45 | 57 | 13 |
| Median | 8 | 4 | 13.5 | 2 |
Resident Perceptions
Of the 91 residents, 59 residents completed the presurveys (response rate 65%) and 65 completed the postsurveys (response rate 71%) (Table 1). There was a statistically significant improvement in all of the items measured. There were also 26 postsurvey comments with 22 describing positive aspects and 9 describing negative aspects. Specific positive attributes of the new communication system that were mentioned were: easier to communicate with other physicians within the team (n = 6), easier to communicate with other health care members of the team (nurses, allied health) (n = 3), and increased mobility (n = 2). The following are some examples:
-
Blackberrys are great for contacting team member, able to mobile in hospital instead of waiting by phone ‐ since we're so busy
-
Excellent for interpersonal communication. It definitely sped up patients care ie, consults, getting investigations done and discharges. Everyone should have one.
-
Text messaging, especially in group format so that all members participate in conversations is the primary communication tool of choice. Emailing is a necessity of the modern workforce.
The 2 predominant issues described were that the direct calling by nurses was disruptive (n = 6) and voice mail was not useful (n = 3):
-
I dislike the voicemail as it is like paging back but you also need to make a phone call to your phone list. Also we are always being interrupted which is disruptive to work but prefer BlackBerrys.
-
Helpful but often disruptive such as getting calls when seeing patients.
Nursing Perceptions
From the typical staff of 94 full‐time and part‐time nurses, 27 of 48 (56%) completed the preintervention survey, and 35 of 54 (65%) completed the postintervention survey. There was a perceived significant decrease in the need to repeatedly try to contact a physician for the same issue (80% vs. 34.3%, P = 0.001) and a significant decrease in the perceived amount of time spent trying to contact clinicians (27.6 minutes vs. 11.1 minutes, P < 0.001) (Table 2). On 5 point Likert scales, there was no perceived improvement in communication areas such as finding out who to reach and resident response time. Nurses appreciated the ability to call the physicians directly for urgent issues (median response 4, mode of 5).
Discussion
Principal Results
In this pilot study of using smartphones and email, residents perceived that it significantly improved their efficiency. Nurses perceived a reduction in the time spent trying to communicate with clinicians.
There were significant lessons learned. First, we found that residents readily utilized smartphones and felt that it improved their efficiency. Staff physicians and residents have outlined multiple concerns over increased workload, increasing patient complexity, and longer work hours. Therefore, interventions that improve physician productivity are essential in maintaining and improving patient care.16 From residents' comments, it appears their improved efficiency is derived not only from improved communication within the medical team, but also within the interprofessional team. Efficiency was also perceived to improve from the greater mobility of being able to walk while returning a page or while waiting for a page to be returned.
Second, we found that changing the communication process was complicated. While the number of calls and emails per day appeared manageable, the peak times had very high volumes and may actually be unmanageable. By facilitating the process of reaching the responsible physician, we may have lowered the threshold for contacting the physician and thus actually increased communication volumes. It is unclear whether the end result is beneficial as improved management of patients is balanced by the increased interruptions. Further study is required to understand the effect of increasing communication on patient outcomes.
Finally, residents indicated quite strongly that they did not want telephone calls to be the primary mode of contact as they found the frequent telephone calls too disruptive. A direct call to a physician created significant disruption to workflow requiring interrupting a task to answer the call or deferring the call to later review of a voice mail message. Accessing voice mail would typically take at least a minute, much more time than the few seconds it takes to review a numeric page or a text page. Residents quickly provided feedback that this process was unacceptable and reduced their ability to deliver care effectively. Furthermore, nurses were frustrated by the added time required to leave voice messages and the poor response rate. As information within voice mails was not acted upon, nurses quickly learned to just keep calling.
Costs of implementation were significantly more than the numeric paging system. With a cost of $5/month for a numeric pager, the cost of numeric pagers for 4 medical teams with 4 physicians each was $80/month (all costs in Canadian dollars). From our implementation, the approximate cost of an individual smartphone was $80/month while team‐based devices were $160/month due to much higher usage. With 4 individual smartphones and one team‐based smartphone per team, costs with the new system were approximately $1,600/month. While implementing smartphones creates a significantly greater expense, it may be worthwhile if improved communication leads to more efficient and higher quality care. Our current system is funded through the hospital to allow for further evaluation, and whether other hospitals provide smartphones for clinical communications likely would depend on whether they provided a cost effective alternative to numeric pagers. This would likely require some more tangible benefit than perceived improved efficiency.
Comparison With Prior Work
Similar to the study of wireless email using smartphones in the Intensive Care Unit, physicians in our study perceived an improvement in efficiency.14 Our study adds further information to the literature since we implemented on general medical wards in an academic teaching hospital. Our study is consistent with the previous studies have documented physicians' perceptions of improved performance with mobile phones.7, 17
Limitations
There are limitations to this study. In order to improve communication, we implemented a complex intervention with several components: (1) smartphones for residents, (2) Web‐paging for nurses, and (3) a new process of identifying the most responsible physician using Team BlackBerrys. From our surveys, it is difficult to know the relative impact of each individual component. Other interventions such as team‐based alphanumeric pagers may achieve similar improvements to nurses' perceptions of improved communication.
As this was a pilot study assessing new communication methods, we informally assessed perceptions using surveys which had not been validated. While the use of formally validated surveys would be more useful, we were unable to find any that specifically addressed the innovation in communication seen with smartphones. Validity issues with the instruments and the low response rates may have contributed to the incongruent result seen with nurses' surveys in that there was a perceived improvement in time to contact physicians but not in the ease of contact of physicians or the satisfaction of the communication method. This incongruent result may also reflect that in spite of the fact that the nurses were accustomed to the new system and that things may have improved, communication issues still remain and likely would benefit from further study.
It would have also been useful to determine the effect of this intervention on numeric pages sent to traditional pagers, which was not captured. It is also important to realize that we did not replace the pagers but instead supplemented residents with smartphones. To replace pagers may involve significant costs to upgrade reception within hospital walls to reduce areas of little or no reception. Finally, this study was completed at 1 academic health science center, and the generalizability of the findings may be limited.
Future Study
There is great opportunity to improve communication between clinicians, and the use of smartphones, email and improved identification of the most responsible physician are some methods to achieving this. Further research would be useful to determine the relative importance of each component. With smartphones, it is would be useful to know whether the benefits seen were primarily due to the mobile email or having another phone available or other features. Finally, the use of web‐paging and email to communicate increases the documentation of communications, but a further improvement could be providing acknowledgement to nurses that web‐pages were received and read. This would close the loop on communications, ensuring that there are no lost communications and that escalation occurs promptly for urgent communications.
In summary, we implemented and evaluated a system to route and prioritize clinical communications combining the use of phone calls and secure email messaging to smartphones. Residents strongly perceived an improvement in communication with smartphones. Further objective clinical evaluation is necessary to determine if this intervention improves efficiency and more importantly, the quality of care.
Acknowledgements
The investigators retained all control over study design, data collection, analysis and interpretation, and preparation of reports.
The scope and importance of communication between clinicians in the delivery of health care is increasingly being recognized.1, 2 Poor communication is known to be a source of inefficiency and errors within healthcare.36 The major issues with communication include the frequent use of interruptive communication mechanisms and the difficulty of knowing who to contact.2 Traditional paging remains the primary method to contact a physician despite being disruptive, inefficient, and predisposing to errors.710 The identification of the responsible physician for a patient can also be complicated with the numerous call schedules, different coverage rules, vacations, and protected academic time for residents. In 1 observational study, 25% of calls in a hospital were attempts to identify a responsible individual for a specific role.11 A recent study revealed that 14% of pages went to the wrong physician and that 47% of these errant pages warranted an urgent response.12 In our institution, the process for a nurse to identify which physician to contact regarding a patient care issue can be complex (Figure 1).
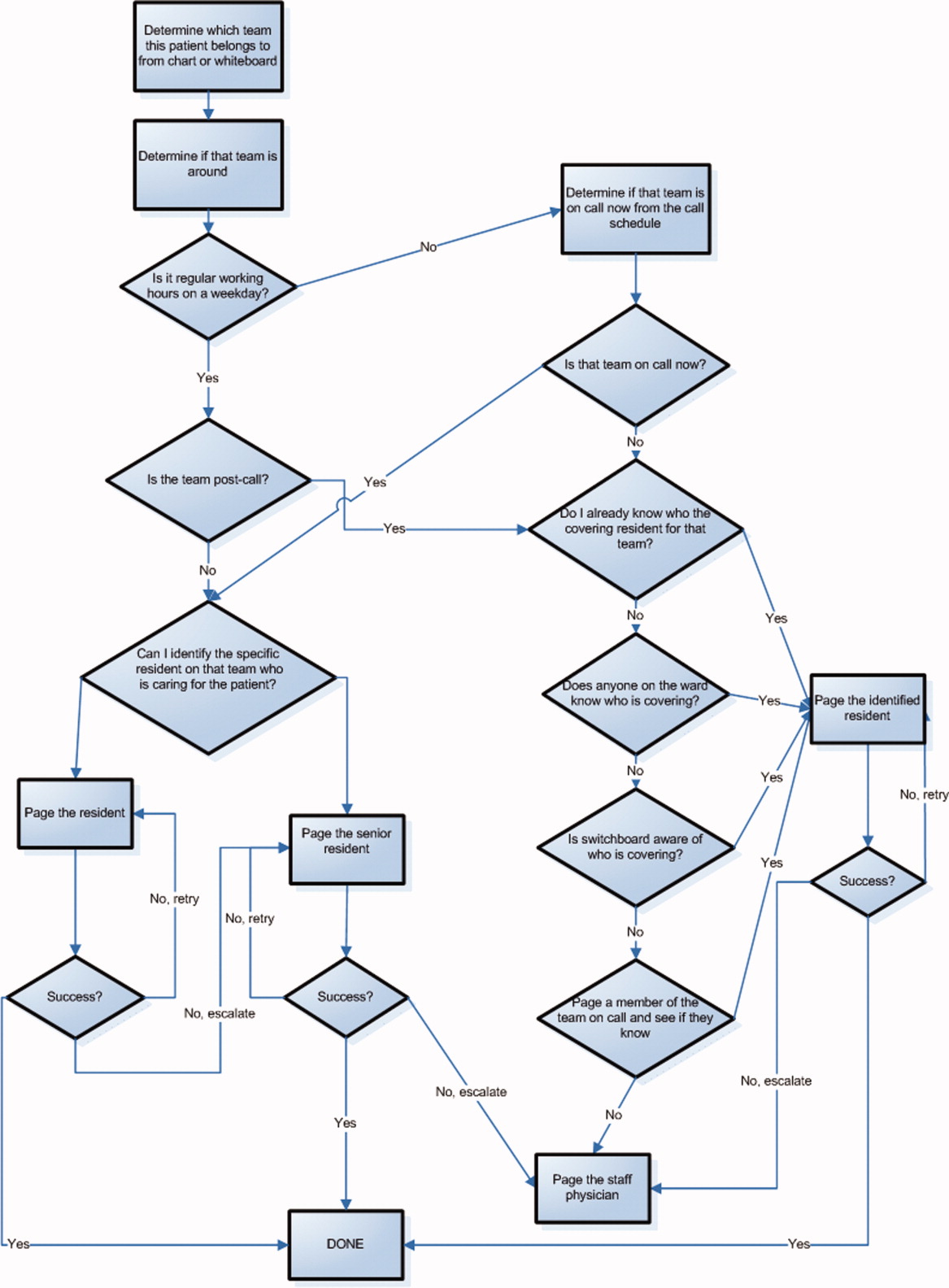
The use of email and mobile phone technology has been recommended as a method to improve communication.2 It can improve communication between clinicians by providing a method of triaging based on importance: instantly by telephone for urgent issues and less disruptively by email for nonurgent issues. There is limited literature on the use of email for improving communication between clinicians or on the use of smartphones. In a previous pilot study, we found that with minimal training, residents were able to use smartphones on general medical wards for clinical communication and that technical challenges were minimal.13 In an intensive care setting, the use of wireless emails using smartphones was perceived by staff to improve communication.14
Methods
Aim
To evaluate the use of smartphones to improve the communication processes on an academic general internal medicine service.
Setting
We conducted the study within the General Internal Medicine service at the Toronto General Hospital, an academic teaching hospital. The service is comprised of 4 teaching teams, each with 1 staff physician, 1 senior resident, 2 to 3 junior residents, and medical students. The environment is typically characterized by a high volume of medically complex patients and constant turnover of physicians with varying degrees of experience. Ethical review of the study was performed by the University Health Network Research Ethics Board.
Program Description
Recognizing the difficulty in implementing complex interventions within clinical care, we used a staged approach applying the standard Plan‐Do‐Study‐Act (PDSA) methodology for quality improvement.15 This involved developing a component of the system, releasing it to the users to learn from their experience, then taking this feedback to make changes and continuing with the next cycle. This allowed early identification and quicker resolution of issues.
Smartphones as Clinical Communication Tools
The first change implemented was to supplement the standard numeric pager with smartphones as the primary communication device for the residents. The BlackBerry device (Research in Motion, Ontario, Canada) was selected because it is an efficient, usable device with voice and secure email functionality that also happens to be the standard smartphone for our hospital administrators. Beginning in March 2008, all residents on the internal medicine service were equipped with a smartphone that they kept for their entire rotation. Contact lists of all devices were prepopulated with the hospital phone numbers that were important in coordinating patient care. These included numbers such as hospital flow coordinators, radiology reporting rooms, interventional radiology, and microbiology.
To facilitate reaching the most responsible resident for patients, we provided an additional smartphone, the Team BlackBerry, that was carried by the senior resident of each team during regular hours and then passed to the resident that was covering the team at night and on weekends. With the new process, a nurse would only require knowledge of which team the patient belonged to in order to contact the most responsible resident (Figure 2). The Team BlackBerry also received critical laboratory and medication alerts that contained clinical decision support. The laboratory and medication alerts were generated through the hospital rule‐based clinical decision support system (Misys Insight).
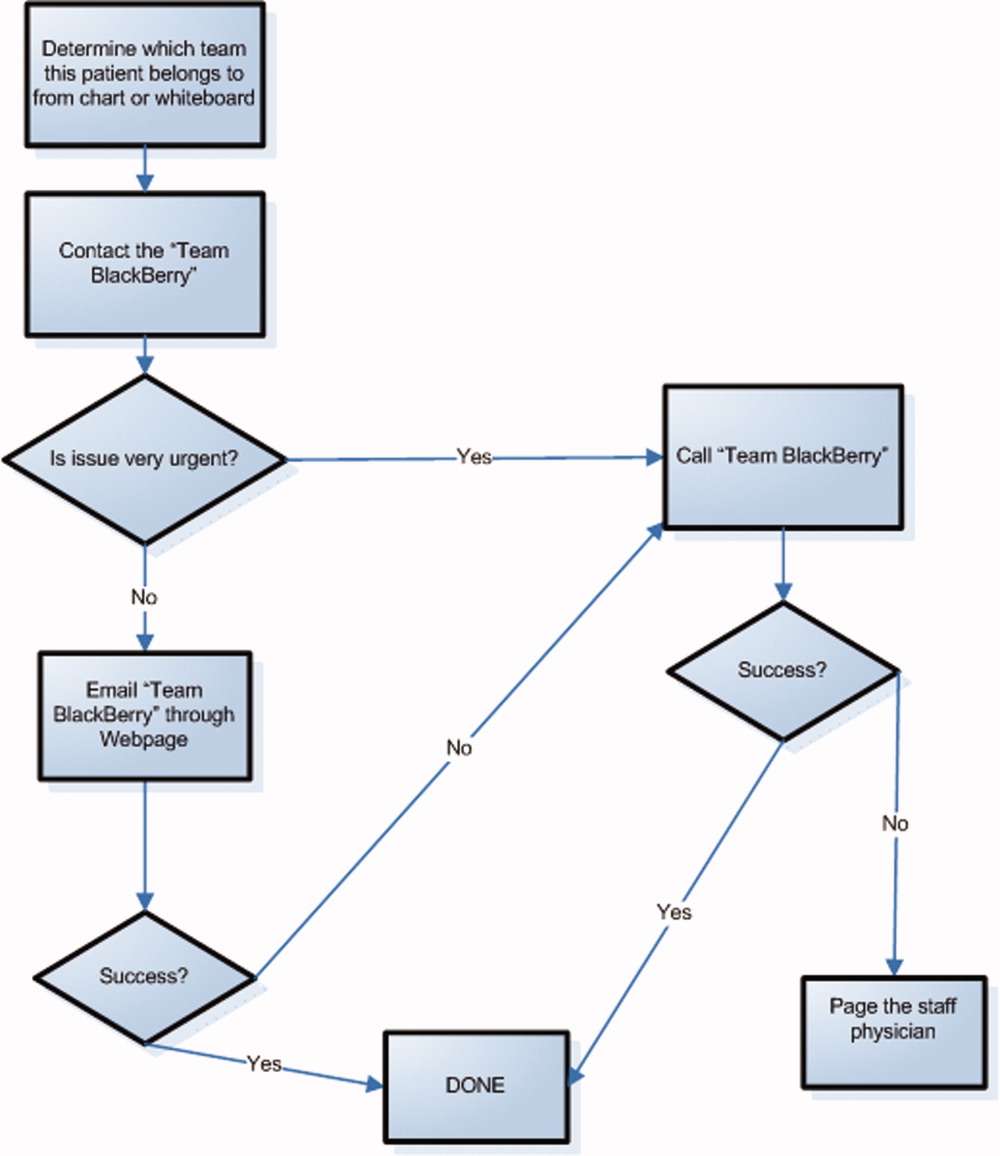
Web‐paging to Improve Nurse‐Physician Communication
In May 2008, we implemented a platform for text paging that we called web‐paging that allowed the nurses to efficiently send email messages securely through a hospital intranet page to the Team BlackBerry. A nurse would access the form from any computer on the wards, select the appropriate team, provide relevant information, and then send the message. Although the form would send an email, the term web‐paging was used to create familiarity with their previous process of contacting a resident, namely paging. This process reserved voice communication for urgent matters only while routing less urgent issues through the web‐paging form. Furthermore, emails were categorized into three priority levels:
-
Call back requested messages were for issues that were not life threatening but needed immediate action or required discussion with a physician.
-
E‐mail response requested messages were for issues that needed an action but could wait until the physician was available, such as cosigning an order.
-
Information only with no response necessary messages facilitated 1‐way communication, such as updating the team of recent vital signs for a patient.
Physicians would receive prompt notification of a new email on their smartphone, and they could reply to the email or call back using a link within the email. Nurses were able to view the physician's email responses from an email account that was shared amongst the nurses on each ward.
Program Evaluation
The outcome measures of the study were residents' use of smartphones and perceptions of residents and nurses on the new communication process. Resident use of the smartphones was measured by the volume and the frequency of phone calls and emails over a 3‐month period from September 2008 to November 2008. Residents' perceptions were measured by a survey administered prior to the start of their clinical rotation and at the end of their rotation (Table 1). Data collection for residents occurred between June 2008 and February 2009. Nurses' perceptions were measured by surveys administered to the nurses working on either day shifts or night shifts over a 1‐week period prior to the intervention in March 2008 and then 6 months after in September 2008 (Table 2).
| Pre‐Survey (n = 59) Median, (mode, mean) | Post‐Survey (n = 65) Median, (mode, mean) | P value | |
|---|---|---|---|
| Training level | |||
| Postgraduate Year 1 | 39 (66.1%) | 43 (66.2%) | |
| Postgraduate Year 2 | 17 (28.8%) | 19 (29.2%) | |
| Postgraduate Year 3 | 3 (5.1%) | 3 (4.6%) | |
| Currently own and use a personal digital assistant | 30 (55.6%) | 38 (62.3%) | |
| Currently own a BlackBerry | 6 (10.5%) | 5 (8.3%) | |
| The following questions used a Likert scale with 1 representing strongly disagree and 5 representing strongly agree | |||
| Q1. I never have issues accessing a phone to discuss patient care issues | 3 (2, 2.8) | 4 (5, 3.9) | <0.001 |
| Q2. I often waste a lot of time waiting for my pages to be answered | 4 (4, 4.1) | 4 (4, 3.3) | 0.004 |
| Q3. Communicating with my team often takes a lot of time | 4 (4, 3.5) | 2 (1, 2.5) | <0.001 |
| Q4. I have quick and easy access to contact information (eg, allied health, departments, consultants, etc) necessary for providing patient care | 3 (2, 2.6) | 4 (4, 3.7) | <0.001 |
| Q5. My primary communication device (pager/ BlackBerry) is non‐disruptive to my workflow | 3 (3, 2.7) | 4 (4, 3.4) | 0.002 |
| Q6. My primary communication device (pager/ BlackBerry) helps me prioritize my tasks | 3 (3, 2.9) | 4 (4, 3.7) | <0.001 |
| Q7. Email and/or text messaging is something I find useful for communication about patient care | 4 (3, 3.6) | 5 (5, 4.4) | <0.001 |
| Q8. Overall, I am satisfied with my primary communication device (pager/BlackBerry) | 3 (3, 2.9) | 4 (5, 4.2) | <0.001 |
| Q9. Overall, being phoned on the BlackBerry (instead of receiving a page) is disruptive to me | 3 (2, 3.0) | ||
| Q10. I consider Internet access on the BlackBerry useful for looking up information related to patient care. | 3 (3, 3.0) | ||
| Q11. I prefer not having a BlackBerry at all than having to deal with technical difficulties when I use it | 2 (1, 1.9) | ||
| Q12. I feel that overall a BlackBerry saves me time | 4 (5, 4.3) | ||
| Pre‐Survey (n = 27) Median, Mode | Post‐Survey (n = 35) Median, Mode | P Value | |
|---|---|---|---|
| Day shifts | 18 (66.7%) | 20 (57.1%) | |
| Total number of times you tried to page, email or telephone a resident or medical student in the shift just completed. | 3.70 | 2.51 | 0.16 |
| Did you need to repeatedly try to contact (page, email, or call) a resident at any time during the shift regarding the same issue? | 80% | 34.3% | 0.0012 |
| Total amount of time that you spent in the last shift trying to contact doctors or other health care providers (minutes). | 27.6 | 11.1 | <0.001 |
| The following questions used a Likert scale with 1 representing Strongly Disagree and 5 representing Strongly Agree: | |||
| Overall, it is straightforward to contact the resident taking care of my patients. | 4 (4) | 4 (4) | 0.27 |
| Overall, I am satisfied with physicians' response time when I need to contact them urgently. | 3 (4) | 4 (4) | 0.54 |
| I spend a lot of time away from the bedside just trying to contact physicians. | 3 (4) | 3 (3) | 0.17 |
| I like being able to call and reach the doctor directly. | 4 (5) | ||
| Overall I am satisfied with the BlackBerry/email communication system. | 4 (4) |
Data Analysis
We present utilization as the mean number of messages sent and received daily. We report survey responses as the mean scores on a 5‐point Likert scale. For ordinal data, we described the survey responses using median and mode, and the Mann Whitney U test was used to test for differences between before and after responses. For parametric data, unpaired t‐tests were used to look for differences in the perceptions before and after the intervention. All P values are 2‐sided.
Results
Smartphone Usage
Usage of emails and calls for the team devices over the three months is shown in Table 3. Most communications were through the Team BlackBerry devices with the individual devices showing less usage than the team device with 2.1 sent emails per day and 4.0 received emails per day. On the days with highest use, there were 7 calls received per hour and 6 emails received per hour at peak times through the day to a Team BlackBerry. Web‐paging was the largest source of emails sent to Team BlackBerrys (42%). Critical laboratory or medication alerts represented 17.1% and the remainder (40.9%) were other communications such as communication from residents, staff physicians, pharmacists, and allied health professionals. Of the web‐paging communications, 35.1% requested a call back, 22.6% requested email response, and 42.2% were informational items only that did not require a response.
| Phone Calls | Emails | |||
|---|---|---|---|---|
| Incoming | Outgoing | Received | Sent | |
| Average | 9.1 | 6.6 | 14.3 | 2.8 |
| Minimum | 0 | 0 | 0 | 0 |
| Maximum | 35 | 45 | 57 | 13 |
| Median | 8 | 4 | 13.5 | 2 |
Resident Perceptions
Of the 91 residents, 59 residents completed the presurveys (response rate 65%) and 65 completed the postsurveys (response rate 71%) (Table 1). There was a statistically significant improvement in all of the items measured. There were also 26 postsurvey comments with 22 describing positive aspects and 9 describing negative aspects. Specific positive attributes of the new communication system that were mentioned were: easier to communicate with other physicians within the team (n = 6), easier to communicate with other health care members of the team (nurses, allied health) (n = 3), and increased mobility (n = 2). The following are some examples:
-
Blackberrys are great for contacting team member, able to mobile in hospital instead of waiting by phone ‐ since we're so busy
-
Excellent for interpersonal communication. It definitely sped up patients care ie, consults, getting investigations done and discharges. Everyone should have one.
-
Text messaging, especially in group format so that all members participate in conversations is the primary communication tool of choice. Emailing is a necessity of the modern workforce.
The 2 predominant issues described were that the direct calling by nurses was disruptive (n = 6) and voice mail was not useful (n = 3):
-
I dislike the voicemail as it is like paging back but you also need to make a phone call to your phone list. Also we are always being interrupted which is disruptive to work but prefer BlackBerrys.
-
Helpful but often disruptive such as getting calls when seeing patients.
Nursing Perceptions
From the typical staff of 94 full‐time and part‐time nurses, 27 of 48 (56%) completed the preintervention survey, and 35 of 54 (65%) completed the postintervention survey. There was a perceived significant decrease in the need to repeatedly try to contact a physician for the same issue (80% vs. 34.3%, P = 0.001) and a significant decrease in the perceived amount of time spent trying to contact clinicians (27.6 minutes vs. 11.1 minutes, P < 0.001) (Table 2). On 5 point Likert scales, there was no perceived improvement in communication areas such as finding out who to reach and resident response time. Nurses appreciated the ability to call the physicians directly for urgent issues (median response 4, mode of 5).
Discussion
Principal Results
In this pilot study of using smartphones and email, residents perceived that it significantly improved their efficiency. Nurses perceived a reduction in the time spent trying to communicate with clinicians.
There were significant lessons learned. First, we found that residents readily utilized smartphones and felt that it improved their efficiency. Staff physicians and residents have outlined multiple concerns over increased workload, increasing patient complexity, and longer work hours. Therefore, interventions that improve physician productivity are essential in maintaining and improving patient care.16 From residents' comments, it appears their improved efficiency is derived not only from improved communication within the medical team, but also within the interprofessional team. Efficiency was also perceived to improve from the greater mobility of being able to walk while returning a page or while waiting for a page to be returned.
Second, we found that changing the communication process was complicated. While the number of calls and emails per day appeared manageable, the peak times had very high volumes and may actually be unmanageable. By facilitating the process of reaching the responsible physician, we may have lowered the threshold for contacting the physician and thus actually increased communication volumes. It is unclear whether the end result is beneficial as improved management of patients is balanced by the increased interruptions. Further study is required to understand the effect of increasing communication on patient outcomes.
Finally, residents indicated quite strongly that they did not want telephone calls to be the primary mode of contact as they found the frequent telephone calls too disruptive. A direct call to a physician created significant disruption to workflow requiring interrupting a task to answer the call or deferring the call to later review of a voice mail message. Accessing voice mail would typically take at least a minute, much more time than the few seconds it takes to review a numeric page or a text page. Residents quickly provided feedback that this process was unacceptable and reduced their ability to deliver care effectively. Furthermore, nurses were frustrated by the added time required to leave voice messages and the poor response rate. As information within voice mails was not acted upon, nurses quickly learned to just keep calling.
Costs of implementation were significantly more than the numeric paging system. With a cost of $5/month for a numeric pager, the cost of numeric pagers for 4 medical teams with 4 physicians each was $80/month (all costs in Canadian dollars). From our implementation, the approximate cost of an individual smartphone was $80/month while team‐based devices were $160/month due to much higher usage. With 4 individual smartphones and one team‐based smartphone per team, costs with the new system were approximately $1,600/month. While implementing smartphones creates a significantly greater expense, it may be worthwhile if improved communication leads to more efficient and higher quality care. Our current system is funded through the hospital to allow for further evaluation, and whether other hospitals provide smartphones for clinical communications likely would depend on whether they provided a cost effective alternative to numeric pagers. This would likely require some more tangible benefit than perceived improved efficiency.
Comparison With Prior Work
Similar to the study of wireless email using smartphones in the Intensive Care Unit, physicians in our study perceived an improvement in efficiency.14 Our study adds further information to the literature since we implemented on general medical wards in an academic teaching hospital. Our study is consistent with the previous studies have documented physicians' perceptions of improved performance with mobile phones.7, 17
Limitations
There are limitations to this study. In order to improve communication, we implemented a complex intervention with several components: (1) smartphones for residents, (2) Web‐paging for nurses, and (3) a new process of identifying the most responsible physician using Team BlackBerrys. From our surveys, it is difficult to know the relative impact of each individual component. Other interventions such as team‐based alphanumeric pagers may achieve similar improvements to nurses' perceptions of improved communication.
As this was a pilot study assessing new communication methods, we informally assessed perceptions using surveys which had not been validated. While the use of formally validated surveys would be more useful, we were unable to find any that specifically addressed the innovation in communication seen with smartphones. Validity issues with the instruments and the low response rates may have contributed to the incongruent result seen with nurses' surveys in that there was a perceived improvement in time to contact physicians but not in the ease of contact of physicians or the satisfaction of the communication method. This incongruent result may also reflect that in spite of the fact that the nurses were accustomed to the new system and that things may have improved, communication issues still remain and likely would benefit from further study.
It would have also been useful to determine the effect of this intervention on numeric pages sent to traditional pagers, which was not captured. It is also important to realize that we did not replace the pagers but instead supplemented residents with smartphones. To replace pagers may involve significant costs to upgrade reception within hospital walls to reduce areas of little or no reception. Finally, this study was completed at 1 academic health science center, and the generalizability of the findings may be limited.
Future Study
There is great opportunity to improve communication between clinicians, and the use of smartphones, email and improved identification of the most responsible physician are some methods to achieving this. Further research would be useful to determine the relative importance of each component. With smartphones, it is would be useful to know whether the benefits seen were primarily due to the mobile email or having another phone available or other features. Finally, the use of web‐paging and email to communicate increases the documentation of communications, but a further improvement could be providing acknowledgement to nurses that web‐pages were received and read. This would close the loop on communications, ensuring that there are no lost communications and that escalation occurs promptly for urgent communications.
In summary, we implemented and evaluated a system to route and prioritize clinical communications combining the use of phone calls and secure email messaging to smartphones. Residents strongly perceived an improvement in communication with smartphones. Further objective clinical evaluation is necessary to determine if this intervention improves efficiency and more importantly, the quality of care.
Acknowledgements
The investigators retained all control over study design, data collection, analysis and interpretation, and preparation of reports.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7(3):277–286.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I.N Engl J Med.1991;324(6):370–376.
- ,,, et al.Gaps in pediatric clinician communication and opportunities for improvement.J Healthc Qual.2008;30(5):43–54.
- ,,,,,.The quality in Australian Health Care Study.Med J Aust.1995;163(9):458–471.
- ,,,,.Quality in Australian Health Care Study.Med J Aust.1996;164(12):754.
- ,,,,.Communication in critical care environments: mobile telephones improve patient care.Anesth Analg.2006;102(2):535–541.
- ,.Interrupted care. The effects of paging on pediatric resident activities.Am J Dis Child.1992;146(7):806–808.
- ,,.Patterns of paging medical interns during night calls at two teaching hospitals.CMAJ.1994;151(3):307–311.
- ,.The sounds of the hospital. Paging patterns in three teaching hospitals.N Engl J Med.1988;319(24):1585–1589.
- ,.Communication behaviours in a hospital setting: an observational study.BMJ1998;316(7132):673–676.
- ,,, et al.Why isn't anyone returning my page? Frequency and clinical importance of pages sent to the wrong physician.Arch Intern Med.2009;169(11):1072–1073.
- ,,, et al.Demonstrating the BlackBerry as a clinical communication tool: a pilot study conducted through the centre for innovation in complex care.Healthc Q2008;11(4):94–98.
- ,,,.The use of wireless email to improve healthcare team communication.J Am Med Inform Assoc.2009;16(5):705–713.
- .A primer on leading the improvement of systems.BMJ.1996;312(7031):619–622.
- .An elusive balance—residents' work hours and the continuity of care.N Engl J Med.2007;356(26):2665–2667.
- ,,, et al.Use of mobile phones by medical staff at Queen Elizabeth Hospital, Barbados: evidence for both benefit and harm.J Hosp Infect.2008;70(2):160–165.
- ,,.How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7(3):277–286.
- ,,, et al.Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I.N Engl J Med.1991;324(6):370–376.
- ,,, et al.Gaps in pediatric clinician communication and opportunities for improvement.J Healthc Qual.2008;30(5):43–54.
- ,,,,,.The quality in Australian Health Care Study.Med J Aust.1995;163(9):458–471.
- ,,,,.Quality in Australian Health Care Study.Med J Aust.1996;164(12):754.
- ,,,,.Communication in critical care environments: mobile telephones improve patient care.Anesth Analg.2006;102(2):535–541.
- ,.Interrupted care. The effects of paging on pediatric resident activities.Am J Dis Child.1992;146(7):806–808.
- ,,.Patterns of paging medical interns during night calls at two teaching hospitals.CMAJ.1994;151(3):307–311.
- ,.The sounds of the hospital. Paging patterns in three teaching hospitals.N Engl J Med.1988;319(24):1585–1589.
- ,.Communication behaviours in a hospital setting: an observational study.BMJ1998;316(7132):673–676.
- ,,, et al.Why isn't anyone returning my page? Frequency and clinical importance of pages sent to the wrong physician.Arch Intern Med.2009;169(11):1072–1073.
- ,,, et al.Demonstrating the BlackBerry as a clinical communication tool: a pilot study conducted through the centre for innovation in complex care.Healthc Q2008;11(4):94–98.
- ,,,.The use of wireless email to improve healthcare team communication.J Am Med Inform Assoc.2009;16(5):705–713.
- .A primer on leading the improvement of systems.BMJ.1996;312(7031):619–622.
- .An elusive balance—residents' work hours and the continuity of care.N Engl J Med.2007;356(26):2665–2667.
- ,,, et al.Use of mobile phones by medical staff at Queen Elizabeth Hospital, Barbados: evidence for both benefit and harm.J Hosp Infect.2008;70(2):160–165.