User login
HFNC more comfortable for posthypercapnic patients with COPD
Following invasive ventilation for severe hypercapnic respiratory failure, patients with chronic obstructive pulmonary disease had similar levels of treatment failure if they received high-flow nasal cannula oxygen therapy or noninvasive ventilation, recent research in Critical Care has suggested.
However, for patients with COPD weaned off invasive ventilation, high-flow nasal cannula (HFNC) oxygen therapy was “more comfortable and better tolerated,” compared with noninvasive ventilation (NIV). In addition, “airway care interventions and the incidence of nasofacial skin breakdown associated with HFNC were significantly lower than in NIV,” according to Dingyu Tan of the Clinical Medical College of Yangzhou (China) University, Northern Jiangsu People’s Hospital, and colleagues. “HFNC appears to be an effective means of respiratory support for COPD patients extubated after severe hypercapnic respiratory failure,” they said.
The investigators screened patients with COPD and hypercapnic respiratory failure for enrollment, including those who met Global Initiative for Obstructive Lung Disease (GOLD) criteria, were 85 years old or younger and caring for themselves, had bronchopulmonary infection–induced respiratory failure, and had achieved pulmonary infection control criteria. Exclusion criteria were:
- Patients under age 18 years.
- Presence of oral or facial trauma.
- Poor sputum excretion ability.
- Hemodynamic instability that would contraindicate use of NIV.
- Poor cough during PIC window.
- Poor short-term prognosis.
- Failure of the heart, brain, liver or kidney.
- Patients who could not consent to treatment.
Patients were determined to have failed treatment if they returned to invasive mechanical ventilation or switched from one treatment to another (HFNC to NIV or NIV to HFNC). Investigators also performed an arterial blood gas analysis, recorded the number of duration of airway care interventions, and monitored vital signs at 1 hour, 24 hours, and 48 hours after extubation as secondary analyses.
Overall, 44 patients randomized to receive HFNC and 42 patients randomized for NIV were available for analysis. The investigators found 22.7% of patients in the HFNC group and 28.6% in the NIV group experienced treatment failure (risk difference, –5.8%; 95% confidence interval, −23.8 to 12.4%; P = .535), with patients in the HFNC group experiencing a significantly lower level of treatment intolerance, compared with patients in the NIV group (risk difference, –50.0%; 95% CI, −74.6 to −12.9%; P = .015). There were no significant differences between either group regarding intubation (−0.65%; 95% CI, −16.01 to 14.46%), while rate of switching treatments was lower in the HFNC group but not significant (−5.2%; 95% CI, −19.82 to 9.05%).
Patients in both the HFNC and NIV groups had faster mean respiratory rates 1 hour after extubation (P < .050). After 24 hours, the NIV group had higher-than-baseline respiratory rates, compared with the HFNC group, which had returned to normal (20 vs. 24.5 breaths per minute; P < .050). Both groups had returned to baseline by 48 hours after extubation. At 1 hour after extubation, patients in the HFNC group had lower PaO2/FiO2 (P < .050) and pH values (P < .050), and higher PaCO2 values (P less than .050), compared with baseline. There were no statistically significant differences in PaO2/FiO2, pH, and PaCO2 values in either group at 24 hours or 48 hours after extubation.
Daily airway care interventions were significantly higher on average in the NIV group, compared with the HFNC group (7 vs. 6; P = .0006), and the HFNC group also had significantly better comfort scores (7 vs. 5; P < .001) as measured by a modified visual analog scale, as well as incidence of nasal and facial skin breakdown (0 vs. 9.6%; P = .027), compared with the NIV group.
Results difficult to apply to North American patients
David L. Bowton, MD, FCCP, a professor specializing in critical care at Wake Forest University, Winston-Salem, N.C., said in an interview the results of this trial may not be applicable for patients with infection-related respiratory failure and COPD in North America “due to the differences in common weaning practices between North America and China.”
For example, the trial used the pulmonary infection control (PIC) window criteria for extubation, which requires a significant decrease in radiographic infiltrates, improvement in quality and quantity of sputum, normalizing of leukocyte count, a synchronized intermittent mandatory ventilation (SIMV) rate of 10-12 breaths per minute, and pressure support less than 10-12 cm/H2O (Int J Chron Obstruct Pulmon Dis. 2017;12:1255-67).
“The process used to achieve these measures is not standardized. In North America, daily awakening and screening for spontaneous breathing trials would be usual, but this was not reported in the current trial,” he explained.
Differences in patient population also make the application of the results difficult, Dr. Bowton said. “Only 60% of the patients had spirometrically confirmed COPD and fewer than half were on at least dual inhaled therapy prior to hospitalization with only one-third taking beta agonists or anticholinergic agents,” he noted. “The cause of respiratory failure was infectious, requiring an infiltrate on chest radiograph; thus, patients with hypercarbic respiratory failure without a new infiltrate were excluded from the study. On average, patients were hypercarbic, yet alkalemic at the time of extubation; the PaCO2 and pH at the time of intubation were not reported.
“This study suggests that in some patients with COPD and respiratory failure requiring invasive mechanical ventilation, HFO [high-flow oxygen] may be better tolerated and equally effective as NIPPV [noninvasive positive-pressure ventilation] at mitigating the need for reintubation following extubation. In this patient population where hypoxemia prior to extubation was not severe, the mechanisms by which HFO is beneficial remain speculative,” he said.
This study was funded by the Rui E special fund for emergency medicine research and the Yangzhou Science and Technology Development Plan. The authors report no relevant conflicts of interest. Dr. Bowton reports no relevant conflicts of interest.
SOURCE: Tan D et al. Crit Care. 2020 Aug 6. doi: 10.1186/s13054-020-03214-9.
Following invasive ventilation for severe hypercapnic respiratory failure, patients with chronic obstructive pulmonary disease had similar levels of treatment failure if they received high-flow nasal cannula oxygen therapy or noninvasive ventilation, recent research in Critical Care has suggested.
However, for patients with COPD weaned off invasive ventilation, high-flow nasal cannula (HFNC) oxygen therapy was “more comfortable and better tolerated,” compared with noninvasive ventilation (NIV). In addition, “airway care interventions and the incidence of nasofacial skin breakdown associated with HFNC were significantly lower than in NIV,” according to Dingyu Tan of the Clinical Medical College of Yangzhou (China) University, Northern Jiangsu People’s Hospital, and colleagues. “HFNC appears to be an effective means of respiratory support for COPD patients extubated after severe hypercapnic respiratory failure,” they said.
The investigators screened patients with COPD and hypercapnic respiratory failure for enrollment, including those who met Global Initiative for Obstructive Lung Disease (GOLD) criteria, were 85 years old or younger and caring for themselves, had bronchopulmonary infection–induced respiratory failure, and had achieved pulmonary infection control criteria. Exclusion criteria were:
- Patients under age 18 years.
- Presence of oral or facial trauma.
- Poor sputum excretion ability.
- Hemodynamic instability that would contraindicate use of NIV.
- Poor cough during PIC window.
- Poor short-term prognosis.
- Failure of the heart, brain, liver or kidney.
- Patients who could not consent to treatment.
Patients were determined to have failed treatment if they returned to invasive mechanical ventilation or switched from one treatment to another (HFNC to NIV or NIV to HFNC). Investigators also performed an arterial blood gas analysis, recorded the number of duration of airway care interventions, and monitored vital signs at 1 hour, 24 hours, and 48 hours after extubation as secondary analyses.
Overall, 44 patients randomized to receive HFNC and 42 patients randomized for NIV were available for analysis. The investigators found 22.7% of patients in the HFNC group and 28.6% in the NIV group experienced treatment failure (risk difference, –5.8%; 95% confidence interval, −23.8 to 12.4%; P = .535), with patients in the HFNC group experiencing a significantly lower level of treatment intolerance, compared with patients in the NIV group (risk difference, –50.0%; 95% CI, −74.6 to −12.9%; P = .015). There were no significant differences between either group regarding intubation (−0.65%; 95% CI, −16.01 to 14.46%), while rate of switching treatments was lower in the HFNC group but not significant (−5.2%; 95% CI, −19.82 to 9.05%).
Patients in both the HFNC and NIV groups had faster mean respiratory rates 1 hour after extubation (P < .050). After 24 hours, the NIV group had higher-than-baseline respiratory rates, compared with the HFNC group, which had returned to normal (20 vs. 24.5 breaths per minute; P < .050). Both groups had returned to baseline by 48 hours after extubation. At 1 hour after extubation, patients in the HFNC group had lower PaO2/FiO2 (P < .050) and pH values (P < .050), and higher PaCO2 values (P less than .050), compared with baseline. There were no statistically significant differences in PaO2/FiO2, pH, and PaCO2 values in either group at 24 hours or 48 hours after extubation.
Daily airway care interventions were significantly higher on average in the NIV group, compared with the HFNC group (7 vs. 6; P = .0006), and the HFNC group also had significantly better comfort scores (7 vs. 5; P < .001) as measured by a modified visual analog scale, as well as incidence of nasal and facial skin breakdown (0 vs. 9.6%; P = .027), compared with the NIV group.
Results difficult to apply to North American patients
David L. Bowton, MD, FCCP, a professor specializing in critical care at Wake Forest University, Winston-Salem, N.C., said in an interview the results of this trial may not be applicable for patients with infection-related respiratory failure and COPD in North America “due to the differences in common weaning practices between North America and China.”
For example, the trial used the pulmonary infection control (PIC) window criteria for extubation, which requires a significant decrease in radiographic infiltrates, improvement in quality and quantity of sputum, normalizing of leukocyte count, a synchronized intermittent mandatory ventilation (SIMV) rate of 10-12 breaths per minute, and pressure support less than 10-12 cm/H2O (Int J Chron Obstruct Pulmon Dis. 2017;12:1255-67).
“The process used to achieve these measures is not standardized. In North America, daily awakening and screening for spontaneous breathing trials would be usual, but this was not reported in the current trial,” he explained.
Differences in patient population also make the application of the results difficult, Dr. Bowton said. “Only 60% of the patients had spirometrically confirmed COPD and fewer than half were on at least dual inhaled therapy prior to hospitalization with only one-third taking beta agonists or anticholinergic agents,” he noted. “The cause of respiratory failure was infectious, requiring an infiltrate on chest radiograph; thus, patients with hypercarbic respiratory failure without a new infiltrate were excluded from the study. On average, patients were hypercarbic, yet alkalemic at the time of extubation; the PaCO2 and pH at the time of intubation were not reported.
“This study suggests that in some patients with COPD and respiratory failure requiring invasive mechanical ventilation, HFO [high-flow oxygen] may be better tolerated and equally effective as NIPPV [noninvasive positive-pressure ventilation] at mitigating the need for reintubation following extubation. In this patient population where hypoxemia prior to extubation was not severe, the mechanisms by which HFO is beneficial remain speculative,” he said.
This study was funded by the Rui E special fund for emergency medicine research and the Yangzhou Science and Technology Development Plan. The authors report no relevant conflicts of interest. Dr. Bowton reports no relevant conflicts of interest.
SOURCE: Tan D et al. Crit Care. 2020 Aug 6. doi: 10.1186/s13054-020-03214-9.
Following invasive ventilation for severe hypercapnic respiratory failure, patients with chronic obstructive pulmonary disease had similar levels of treatment failure if they received high-flow nasal cannula oxygen therapy or noninvasive ventilation, recent research in Critical Care has suggested.
However, for patients with COPD weaned off invasive ventilation, high-flow nasal cannula (HFNC) oxygen therapy was “more comfortable and better tolerated,” compared with noninvasive ventilation (NIV). In addition, “airway care interventions and the incidence of nasofacial skin breakdown associated with HFNC were significantly lower than in NIV,” according to Dingyu Tan of the Clinical Medical College of Yangzhou (China) University, Northern Jiangsu People’s Hospital, and colleagues. “HFNC appears to be an effective means of respiratory support for COPD patients extubated after severe hypercapnic respiratory failure,” they said.
The investigators screened patients with COPD and hypercapnic respiratory failure for enrollment, including those who met Global Initiative for Obstructive Lung Disease (GOLD) criteria, were 85 years old or younger and caring for themselves, had bronchopulmonary infection–induced respiratory failure, and had achieved pulmonary infection control criteria. Exclusion criteria were:
- Patients under age 18 years.
- Presence of oral or facial trauma.
- Poor sputum excretion ability.
- Hemodynamic instability that would contraindicate use of NIV.
- Poor cough during PIC window.
- Poor short-term prognosis.
- Failure of the heart, brain, liver or kidney.
- Patients who could not consent to treatment.
Patients were determined to have failed treatment if they returned to invasive mechanical ventilation or switched from one treatment to another (HFNC to NIV or NIV to HFNC). Investigators also performed an arterial blood gas analysis, recorded the number of duration of airway care interventions, and monitored vital signs at 1 hour, 24 hours, and 48 hours after extubation as secondary analyses.
Overall, 44 patients randomized to receive HFNC and 42 patients randomized for NIV were available for analysis. The investigators found 22.7% of patients in the HFNC group and 28.6% in the NIV group experienced treatment failure (risk difference, –5.8%; 95% confidence interval, −23.8 to 12.4%; P = .535), with patients in the HFNC group experiencing a significantly lower level of treatment intolerance, compared with patients in the NIV group (risk difference, –50.0%; 95% CI, −74.6 to −12.9%; P = .015). There were no significant differences between either group regarding intubation (−0.65%; 95% CI, −16.01 to 14.46%), while rate of switching treatments was lower in the HFNC group but not significant (−5.2%; 95% CI, −19.82 to 9.05%).
Patients in both the HFNC and NIV groups had faster mean respiratory rates 1 hour after extubation (P < .050). After 24 hours, the NIV group had higher-than-baseline respiratory rates, compared with the HFNC group, which had returned to normal (20 vs. 24.5 breaths per minute; P < .050). Both groups had returned to baseline by 48 hours after extubation. At 1 hour after extubation, patients in the HFNC group had lower PaO2/FiO2 (P < .050) and pH values (P < .050), and higher PaCO2 values (P less than .050), compared with baseline. There were no statistically significant differences in PaO2/FiO2, pH, and PaCO2 values in either group at 24 hours or 48 hours after extubation.
Daily airway care interventions were significantly higher on average in the NIV group, compared with the HFNC group (7 vs. 6; P = .0006), and the HFNC group also had significantly better comfort scores (7 vs. 5; P < .001) as measured by a modified visual analog scale, as well as incidence of nasal and facial skin breakdown (0 vs. 9.6%; P = .027), compared with the NIV group.
Results difficult to apply to North American patients
David L. Bowton, MD, FCCP, a professor specializing in critical care at Wake Forest University, Winston-Salem, N.C., said in an interview the results of this trial may not be applicable for patients with infection-related respiratory failure and COPD in North America “due to the differences in common weaning practices between North America and China.”
For example, the trial used the pulmonary infection control (PIC) window criteria for extubation, which requires a significant decrease in radiographic infiltrates, improvement in quality and quantity of sputum, normalizing of leukocyte count, a synchronized intermittent mandatory ventilation (SIMV) rate of 10-12 breaths per minute, and pressure support less than 10-12 cm/H2O (Int J Chron Obstruct Pulmon Dis. 2017;12:1255-67).
“The process used to achieve these measures is not standardized. In North America, daily awakening and screening for spontaneous breathing trials would be usual, but this was not reported in the current trial,” he explained.
Differences in patient population also make the application of the results difficult, Dr. Bowton said. “Only 60% of the patients had spirometrically confirmed COPD and fewer than half were on at least dual inhaled therapy prior to hospitalization with only one-third taking beta agonists or anticholinergic agents,” he noted. “The cause of respiratory failure was infectious, requiring an infiltrate on chest radiograph; thus, patients with hypercarbic respiratory failure without a new infiltrate were excluded from the study. On average, patients were hypercarbic, yet alkalemic at the time of extubation; the PaCO2 and pH at the time of intubation were not reported.
“This study suggests that in some patients with COPD and respiratory failure requiring invasive mechanical ventilation, HFO [high-flow oxygen] may be better tolerated and equally effective as NIPPV [noninvasive positive-pressure ventilation] at mitigating the need for reintubation following extubation. In this patient population where hypoxemia prior to extubation was not severe, the mechanisms by which HFO is beneficial remain speculative,” he said.
This study was funded by the Rui E special fund for emergency medicine research and the Yangzhou Science and Technology Development Plan. The authors report no relevant conflicts of interest. Dr. Bowton reports no relevant conflicts of interest.
SOURCE: Tan D et al. Crit Care. 2020 Aug 6. doi: 10.1186/s13054-020-03214-9.
FROM CRITICAL CARE
Patients with COPD plus sleep problems should be screened for mood disorders
A study has shown a strong link between sleeping disturbances and depression in patients with chronic obstructive pulmonary disease.
Adults with clinically stable COPD who reported sleep problems were significantly more likely to report depression or anxiety, poor self-efficacy, and poor health-related quality of life, compared with those not reporting sleep problems, according to the findings from a study of 245 patients.
Sleep problems are common in patients with COPD and have been associated with poor COPD-related outcomes, wrote Sang Hee Lee, MD, of Wonkwang University Sanbon Hospital, Gunpo-si, South Korea, and colleagues.
“However, there is a lack of research on factors associated with sleep disturbance in patients with COPD,” they wrote.
In a prospective, multicenter, cross-sectional study published in the Clinical Respiratory Journal, the researchers enrolled 245 adults with COPD who completed the COPD and Asthma Impact Scale (CASIS) to determine sleep impairment. The CASIS was developed to measure sleep-related problems associated with respiratory disease, and scored on a scale of 1-100, with higher scores indicating greater sleep impairment. The average CASIS score was 40.9. The average age of the patients was 67 years, and 92% were men.
Patients’ health-related quality of life, anxiety/depression, and self-efficacy were assessed using the St. George’s Respiratory Questionnaire (SGRQ), the 36-item Short-Form Health Survey (SF-36), Hospital Anxiety and Depression Scale (HADS), and the COPD Self-Efficacy Scale (CSES). The average scores on these measures were 36.0 for the SGRQ; 48.1 and 50.6, respectively, for the physical and mental components of the SF-36; 3.8 and 6.4, respectively, for the HADS-A and HADS-D measures of anxiety and depression; and 3.3 on the CSES.
Worse sleep in these patients was associated with worse scores on measures of mood. In a multivariate analysis, higher scores on all four measures of health-related quality of life were significantly associated with higher CASIS scores (P = .006 for SGRQ; P = .037 for SF-36, P < .001 for HADS, and P = .010 for CSES).
Although the CASIS did not allow for measurement of symptom severity and did not include many items related to breathing problems, the test “shows good internal consistency, test-retest reproducibility, and construct validity according to previous studies,” the researchers wrote. “The CASIS may be a good tool for evaluating sleep disturbances in COPD patients, and further study is needed,” they added.
The study findings were limited by several factors including the cross-sectional study design, lack of data on obstructive sleep apnea, and lack of information on specific treatments such as at-home oxygen use or high-dose steroid use, the researchers noted. However, the results were strengthened by the use of a disease-specific sleep measure, and the study is the first known to include self-efficacy in relation to sleep quality in COPD patients, they reported.
The results highlight the association between depression, poor quality of life, and self-efficacy in relation to poor sleep, and suggest that “Sleep quality could be improved by enhancing HRQL and self-efficacy,” the researchers said. “Screening for mood disorder in patients with COPD is also needed,” they concluded.
The study was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology. The researchers had no financial conflicts to disclose.
SOURCE: Lee SH et al. Clin Respir J. 2020 Jul 24. doi: 10.1111/crj.13235.
A study has shown a strong link between sleeping disturbances and depression in patients with chronic obstructive pulmonary disease.
Adults with clinically stable COPD who reported sleep problems were significantly more likely to report depression or anxiety, poor self-efficacy, and poor health-related quality of life, compared with those not reporting sleep problems, according to the findings from a study of 245 patients.
Sleep problems are common in patients with COPD and have been associated with poor COPD-related outcomes, wrote Sang Hee Lee, MD, of Wonkwang University Sanbon Hospital, Gunpo-si, South Korea, and colleagues.
“However, there is a lack of research on factors associated with sleep disturbance in patients with COPD,” they wrote.
In a prospective, multicenter, cross-sectional study published in the Clinical Respiratory Journal, the researchers enrolled 245 adults with COPD who completed the COPD and Asthma Impact Scale (CASIS) to determine sleep impairment. The CASIS was developed to measure sleep-related problems associated with respiratory disease, and scored on a scale of 1-100, with higher scores indicating greater sleep impairment. The average CASIS score was 40.9. The average age of the patients was 67 years, and 92% were men.
Patients’ health-related quality of life, anxiety/depression, and self-efficacy were assessed using the St. George’s Respiratory Questionnaire (SGRQ), the 36-item Short-Form Health Survey (SF-36), Hospital Anxiety and Depression Scale (HADS), and the COPD Self-Efficacy Scale (CSES). The average scores on these measures were 36.0 for the SGRQ; 48.1 and 50.6, respectively, for the physical and mental components of the SF-36; 3.8 and 6.4, respectively, for the HADS-A and HADS-D measures of anxiety and depression; and 3.3 on the CSES.
Worse sleep in these patients was associated with worse scores on measures of mood. In a multivariate analysis, higher scores on all four measures of health-related quality of life were significantly associated with higher CASIS scores (P = .006 for SGRQ; P = .037 for SF-36, P < .001 for HADS, and P = .010 for CSES).
Although the CASIS did not allow for measurement of symptom severity and did not include many items related to breathing problems, the test “shows good internal consistency, test-retest reproducibility, and construct validity according to previous studies,” the researchers wrote. “The CASIS may be a good tool for evaluating sleep disturbances in COPD patients, and further study is needed,” they added.
The study findings were limited by several factors including the cross-sectional study design, lack of data on obstructive sleep apnea, and lack of information on specific treatments such as at-home oxygen use or high-dose steroid use, the researchers noted. However, the results were strengthened by the use of a disease-specific sleep measure, and the study is the first known to include self-efficacy in relation to sleep quality in COPD patients, they reported.
The results highlight the association between depression, poor quality of life, and self-efficacy in relation to poor sleep, and suggest that “Sleep quality could be improved by enhancing HRQL and self-efficacy,” the researchers said. “Screening for mood disorder in patients with COPD is also needed,” they concluded.
The study was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology. The researchers had no financial conflicts to disclose.
SOURCE: Lee SH et al. Clin Respir J. 2020 Jul 24. doi: 10.1111/crj.13235.
A study has shown a strong link between sleeping disturbances and depression in patients with chronic obstructive pulmonary disease.
Adults with clinically stable COPD who reported sleep problems were significantly more likely to report depression or anxiety, poor self-efficacy, and poor health-related quality of life, compared with those not reporting sleep problems, according to the findings from a study of 245 patients.
Sleep problems are common in patients with COPD and have been associated with poor COPD-related outcomes, wrote Sang Hee Lee, MD, of Wonkwang University Sanbon Hospital, Gunpo-si, South Korea, and colleagues.
“However, there is a lack of research on factors associated with sleep disturbance in patients with COPD,” they wrote.
In a prospective, multicenter, cross-sectional study published in the Clinical Respiratory Journal, the researchers enrolled 245 adults with COPD who completed the COPD and Asthma Impact Scale (CASIS) to determine sleep impairment. The CASIS was developed to measure sleep-related problems associated with respiratory disease, and scored on a scale of 1-100, with higher scores indicating greater sleep impairment. The average CASIS score was 40.9. The average age of the patients was 67 years, and 92% were men.
Patients’ health-related quality of life, anxiety/depression, and self-efficacy were assessed using the St. George’s Respiratory Questionnaire (SGRQ), the 36-item Short-Form Health Survey (SF-36), Hospital Anxiety and Depression Scale (HADS), and the COPD Self-Efficacy Scale (CSES). The average scores on these measures were 36.0 for the SGRQ; 48.1 and 50.6, respectively, for the physical and mental components of the SF-36; 3.8 and 6.4, respectively, for the HADS-A and HADS-D measures of anxiety and depression; and 3.3 on the CSES.
Worse sleep in these patients was associated with worse scores on measures of mood. In a multivariate analysis, higher scores on all four measures of health-related quality of life were significantly associated with higher CASIS scores (P = .006 for SGRQ; P = .037 for SF-36, P < .001 for HADS, and P = .010 for CSES).
Although the CASIS did not allow for measurement of symptom severity and did not include many items related to breathing problems, the test “shows good internal consistency, test-retest reproducibility, and construct validity according to previous studies,” the researchers wrote. “The CASIS may be a good tool for evaluating sleep disturbances in COPD patients, and further study is needed,” they added.
The study findings were limited by several factors including the cross-sectional study design, lack of data on obstructive sleep apnea, and lack of information on specific treatments such as at-home oxygen use or high-dose steroid use, the researchers noted. However, the results were strengthened by the use of a disease-specific sleep measure, and the study is the first known to include self-efficacy in relation to sleep quality in COPD patients, they reported.
The results highlight the association between depression, poor quality of life, and self-efficacy in relation to poor sleep, and suggest that “Sleep quality could be improved by enhancing HRQL and self-efficacy,” the researchers said. “Screening for mood disorder in patients with COPD is also needed,” they concluded.
The study was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology. The researchers had no financial conflicts to disclose.
SOURCE: Lee SH et al. Clin Respir J. 2020 Jul 24. doi: 10.1111/crj.13235.
FROM THE CLINICAL RESPIRATORY JOURNAL
Even a few days of steroids may be risky, new study suggests
Extended use of corticosteroids for chronic inflammatory conditions puts patients at risk for serious adverse events (AEs), including cardiovascular disease, osteoporosis, cataracts, and diabetes. Now, a growing body of evidence suggests that even short bursts of these drugs are associated with serious risks.
Most recently, a population-based study of more than 2.6 million people found that taking corticosteroids for 14 days or less was associated with a substantially greater risk for gastrointestinal (GI) bleeding, sepsis, and heart failure, particularly within the first 30 days after therapy.
In the study, Tsung-Chieh Yao, MD, PhD, a professor in the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan, Taiwan, and colleagues used a self-controlled case series to analyze data from Taiwan’s National Health Insurance Research Database of medical claims. They compared patients’ conditions in the period from 5 to 90 days before treatment to conditions from the periods from 5 to 30 days and from 31 to 90 days after therapy.
With a median duration of 3 days of treatment, the incidence rate ratios (IRRs) were 1.80 (95% confidence interval, 1.75-1.84) for GI bleeding, 1.99 (95% CI, 1.70-2.32) for sepsis, and 2.37 (95% CI, 2.13-2.63) for heart failure.
Given the findings, physicians should weigh the benefits against the risks of rare but potentially serious consequences of these anti-inflammatory drugs, according to the authors.
“After initiating patients on oral steroid bursts, physicians should be on the lookout for these severe adverse events, particularly within the first month after initiation of steroid therapy,” Dr. Yao said in an interview.
The findings were published online July 6 in Annals of Internal Medicine.
Of the 15,859,129 adult Asians in the Taiwanese database, the study included 2,623,327 adults aged 20-64 years who received single steroid bursts (14 days or less) between Jan. 1, 2013, and Dec. 31, 2015.
Almost 60% of the indications were for skin disorders, such as eczema and urticaria, and for respiratory tract infections, such as sinusitis and acute pharyngitis. Among specialties, dermatology, otolaryngology, family practice, internal medicine, and pediatrics accounted for 88% of prescriptions.
“Our findings are important for physicians and guideline developers because short-term use of oral corticosteroids is common and the real-world safety of this approach remains unclear,” the authors wrote. They acknowledged that the database did not provide information on such potential confounders as disease severity and lifestyle factors, nor did it include children and vulnerable individuals, which may limit the generalizability of the results.
The findings echo those of a 2017 cohort study conducted by researchers at the University of Michigan in Ann Arbor. That study, by Akbar K. Waljee, MD, assistant professor of gastroenterology, University of Michigan, Ann Arbor, and colleagues, included data on more than 1.5 million privately insured U.S. adults. The researchers included somewhat longer steroid bursts of up to 30 days’ duration and found that use of the drugs was associated with a greater than fivefold increased risk for sepsis, a more than threefold increased risk for venous thromboembolism, and a nearly twofold increased risk for fracture within 30 days of starting treatment.
Furthermore, the elevated risk persisted at prednisone-equivalent doses of less than 20 mg/d (IRR, 4.02 for sepsis, 3.61 for venous thromboembolism, and 1.83 for fracture; all P < .001).
The U.S. study also found that during the 3-year period from 2012 to 2014, more than 20% of patients were prescribed short-term oral corticosteroids.
“Both studies indicate that these short-term regimens are more common in the real world than was previously thought and are not risk free,” Dr. Yao said.
Recognition that corticosteroids are associated with adverse events has been building for decades, according to the authors of an editorial that accompanies the new study.
“However, we commonly use short corticosteroid ‘bursts’ for minor ailments despite a lack of evidence for meaningful benefit. We are now learning that bursts as short as 3 days may increase risk for serious AEs, even in young and healthy people,” wrote editorialists Beth I. Wallace, MD, of the Center for Clinical Management Research at the VA Ann Arbor Healthcare System and the Institute for Healthcare Policy and Innovation at Michigan Medicine, Ann Arbor, and Dr. Waljee, who led the 2017 study.
Dr. Wallace and Dr. Waljee drew parallels between corticosteroid bursts and other short-term regimens, such as of antibiotics and opiates, in which prescriber preference and sometimes patient pressure play a role. “All of these treatments have well-defined indications but can cause net harm when used. We can thus conceive of a corticosteroid stewardship model of targeted interventions that aims to reduce inappropriate prescribing,” they wrote.
In an interview, Dr. Wallace, a rheumatologist who prescribes oral steroids fairly frequently, noted that the Taiwan study is the first to investigate steroid bursts. “Up till now, these very short courses have flown under the radar. Clinicians very commonly prescribe short courses to help relieve symptoms of self-limited conditions like bronchitis, and we assume that because the exposure duration is short, the risks are low, especially for patients who are otherwise healthy.”
She warned that the data in the current study indicate that these short bursts – even at the lower end of the 1- to 2-week courses American physicians prescribe most often – carry small but real increases in risk for serious AEs. “And these increases were seen in young, healthy people, not just in people with preexisting conditions,” she said. “So, we might need to start thinking harder about how we are prescribing even these very short courses of steroids and try to use steroids only when their meaningful benefits really outweigh the risk.”
She noted that a patient with a chronic inflammatory condition such as rheumatoid arthritis may benefit substantially from short-term steroids to treat a disease flare. In that specific case, the benefits of short-term steroids may outweigh the risks, Dr. Wallace said.
But not everyone thinks a new strategy is needed. For Whitney A. High, MD, associate professor of dermatology and pathology at the University of Colorado at Denver, Aurora, the overprescribing of short-term corticosteroids is not a problem, and dermatologists are already exercising caution.
“I only prescribe these drugs short term to, at a guess, about 1 in 40 patients and only when a patient is miserable and quality of life is being seriously affected,” he said in an interview. “And that’s something that can’t be measured in a database study like the one from Taiwan but only in a risk-benefit analysis,” he said.
Furthermore, dermatologists have other drugs and technologies in their armamentarium, including topical steroids with occlusion or with wet wraps, phototherapy, phosphodiesterase inhibitors, calcipotriene, methotrexate and other immunosuppressive agents, and biologics. “In fact, many of these agents are specifically referred to as steroid-sparing,” Dr. High said.
Nor does he experience much pressure from patients to prescribe these drugs. “While occasionally I may encounter a patient who places pressure on me for oral steroids, it’s probably not nearly as frequently as providers in other fields are pressured to prescribe antibiotics or narcotics,” he said.
According to the Taiwanese researchers, the next step is to conduct more studies, including clinical trials, to determine optimal use of corticosteroids by monitoring adverse events. In the meantime, for practitioners such as Dr. Wallace and Dr. High, there is ample evidence from several recent studies of the harms of short-term corticosteroids, whereas the benefits for patients with self-limiting conditions remain uncertain. “This and other studies like it quite appropriately remind providers to avoid oral steroids when they’re not necessary and to seek alternatives where possible,” Dr. High said.
The study was supported by the National Health Research Institutes of Taiwan, the Ministry of Science and Technology of Taiwan, the Chang Gung Medical Foundation, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (NIH). Dr. Yao has disclosed no relevant financial relationships. Dr. Wu has received grants from GlaxoSmithKline outside the submitted work. The editorialists and Dr. High have disclosed no relevant financial relationships. Dr. Wallace received an NIH grant during the writing of the editorial.
A version of this article originally appeared on Medscape.com.
Extended use of corticosteroids for chronic inflammatory conditions puts patients at risk for serious adverse events (AEs), including cardiovascular disease, osteoporosis, cataracts, and diabetes. Now, a growing body of evidence suggests that even short bursts of these drugs are associated with serious risks.
Most recently, a population-based study of more than 2.6 million people found that taking corticosteroids for 14 days or less was associated with a substantially greater risk for gastrointestinal (GI) bleeding, sepsis, and heart failure, particularly within the first 30 days after therapy.
In the study, Tsung-Chieh Yao, MD, PhD, a professor in the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan, Taiwan, and colleagues used a self-controlled case series to analyze data from Taiwan’s National Health Insurance Research Database of medical claims. They compared patients’ conditions in the period from 5 to 90 days before treatment to conditions from the periods from 5 to 30 days and from 31 to 90 days after therapy.
With a median duration of 3 days of treatment, the incidence rate ratios (IRRs) were 1.80 (95% confidence interval, 1.75-1.84) for GI bleeding, 1.99 (95% CI, 1.70-2.32) for sepsis, and 2.37 (95% CI, 2.13-2.63) for heart failure.
Given the findings, physicians should weigh the benefits against the risks of rare but potentially serious consequences of these anti-inflammatory drugs, according to the authors.
“After initiating patients on oral steroid bursts, physicians should be on the lookout for these severe adverse events, particularly within the first month after initiation of steroid therapy,” Dr. Yao said in an interview.
The findings were published online July 6 in Annals of Internal Medicine.
Of the 15,859,129 adult Asians in the Taiwanese database, the study included 2,623,327 adults aged 20-64 years who received single steroid bursts (14 days or less) between Jan. 1, 2013, and Dec. 31, 2015.
Almost 60% of the indications were for skin disorders, such as eczema and urticaria, and for respiratory tract infections, such as sinusitis and acute pharyngitis. Among specialties, dermatology, otolaryngology, family practice, internal medicine, and pediatrics accounted for 88% of prescriptions.
“Our findings are important for physicians and guideline developers because short-term use of oral corticosteroids is common and the real-world safety of this approach remains unclear,” the authors wrote. They acknowledged that the database did not provide information on such potential confounders as disease severity and lifestyle factors, nor did it include children and vulnerable individuals, which may limit the generalizability of the results.
The findings echo those of a 2017 cohort study conducted by researchers at the University of Michigan in Ann Arbor. That study, by Akbar K. Waljee, MD, assistant professor of gastroenterology, University of Michigan, Ann Arbor, and colleagues, included data on more than 1.5 million privately insured U.S. adults. The researchers included somewhat longer steroid bursts of up to 30 days’ duration and found that use of the drugs was associated with a greater than fivefold increased risk for sepsis, a more than threefold increased risk for venous thromboembolism, and a nearly twofold increased risk for fracture within 30 days of starting treatment.
Furthermore, the elevated risk persisted at prednisone-equivalent doses of less than 20 mg/d (IRR, 4.02 for sepsis, 3.61 for venous thromboembolism, and 1.83 for fracture; all P < .001).
The U.S. study also found that during the 3-year period from 2012 to 2014, more than 20% of patients were prescribed short-term oral corticosteroids.
“Both studies indicate that these short-term regimens are more common in the real world than was previously thought and are not risk free,” Dr. Yao said.
Recognition that corticosteroids are associated with adverse events has been building for decades, according to the authors of an editorial that accompanies the new study.
“However, we commonly use short corticosteroid ‘bursts’ for minor ailments despite a lack of evidence for meaningful benefit. We are now learning that bursts as short as 3 days may increase risk for serious AEs, even in young and healthy people,” wrote editorialists Beth I. Wallace, MD, of the Center for Clinical Management Research at the VA Ann Arbor Healthcare System and the Institute for Healthcare Policy and Innovation at Michigan Medicine, Ann Arbor, and Dr. Waljee, who led the 2017 study.
Dr. Wallace and Dr. Waljee drew parallels between corticosteroid bursts and other short-term regimens, such as of antibiotics and opiates, in which prescriber preference and sometimes patient pressure play a role. “All of these treatments have well-defined indications but can cause net harm when used. We can thus conceive of a corticosteroid stewardship model of targeted interventions that aims to reduce inappropriate prescribing,” they wrote.
In an interview, Dr. Wallace, a rheumatologist who prescribes oral steroids fairly frequently, noted that the Taiwan study is the first to investigate steroid bursts. “Up till now, these very short courses have flown under the radar. Clinicians very commonly prescribe short courses to help relieve symptoms of self-limited conditions like bronchitis, and we assume that because the exposure duration is short, the risks are low, especially for patients who are otherwise healthy.”
She warned that the data in the current study indicate that these short bursts – even at the lower end of the 1- to 2-week courses American physicians prescribe most often – carry small but real increases in risk for serious AEs. “And these increases were seen in young, healthy people, not just in people with preexisting conditions,” she said. “So, we might need to start thinking harder about how we are prescribing even these very short courses of steroids and try to use steroids only when their meaningful benefits really outweigh the risk.”
She noted that a patient with a chronic inflammatory condition such as rheumatoid arthritis may benefit substantially from short-term steroids to treat a disease flare. In that specific case, the benefits of short-term steroids may outweigh the risks, Dr. Wallace said.
But not everyone thinks a new strategy is needed. For Whitney A. High, MD, associate professor of dermatology and pathology at the University of Colorado at Denver, Aurora, the overprescribing of short-term corticosteroids is not a problem, and dermatologists are already exercising caution.
“I only prescribe these drugs short term to, at a guess, about 1 in 40 patients and only when a patient is miserable and quality of life is being seriously affected,” he said in an interview. “And that’s something that can’t be measured in a database study like the one from Taiwan but only in a risk-benefit analysis,” he said.
Furthermore, dermatologists have other drugs and technologies in their armamentarium, including topical steroids with occlusion or with wet wraps, phototherapy, phosphodiesterase inhibitors, calcipotriene, methotrexate and other immunosuppressive agents, and biologics. “In fact, many of these agents are specifically referred to as steroid-sparing,” Dr. High said.
Nor does he experience much pressure from patients to prescribe these drugs. “While occasionally I may encounter a patient who places pressure on me for oral steroids, it’s probably not nearly as frequently as providers in other fields are pressured to prescribe antibiotics or narcotics,” he said.
According to the Taiwanese researchers, the next step is to conduct more studies, including clinical trials, to determine optimal use of corticosteroids by monitoring adverse events. In the meantime, for practitioners such as Dr. Wallace and Dr. High, there is ample evidence from several recent studies of the harms of short-term corticosteroids, whereas the benefits for patients with self-limiting conditions remain uncertain. “This and other studies like it quite appropriately remind providers to avoid oral steroids when they’re not necessary and to seek alternatives where possible,” Dr. High said.
The study was supported by the National Health Research Institutes of Taiwan, the Ministry of Science and Technology of Taiwan, the Chang Gung Medical Foundation, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (NIH). Dr. Yao has disclosed no relevant financial relationships. Dr. Wu has received grants from GlaxoSmithKline outside the submitted work. The editorialists and Dr. High have disclosed no relevant financial relationships. Dr. Wallace received an NIH grant during the writing of the editorial.
A version of this article originally appeared on Medscape.com.
Extended use of corticosteroids for chronic inflammatory conditions puts patients at risk for serious adverse events (AEs), including cardiovascular disease, osteoporosis, cataracts, and diabetes. Now, a growing body of evidence suggests that even short bursts of these drugs are associated with serious risks.
Most recently, a population-based study of more than 2.6 million people found that taking corticosteroids for 14 days or less was associated with a substantially greater risk for gastrointestinal (GI) bleeding, sepsis, and heart failure, particularly within the first 30 days after therapy.
In the study, Tsung-Chieh Yao, MD, PhD, a professor in the division of allergy, asthma, and rheumatology in the department of pediatrics at Chang Gung Memorial Hospital in Taoyuan, Taiwan, and colleagues used a self-controlled case series to analyze data from Taiwan’s National Health Insurance Research Database of medical claims. They compared patients’ conditions in the period from 5 to 90 days before treatment to conditions from the periods from 5 to 30 days and from 31 to 90 days after therapy.
With a median duration of 3 days of treatment, the incidence rate ratios (IRRs) were 1.80 (95% confidence interval, 1.75-1.84) for GI bleeding, 1.99 (95% CI, 1.70-2.32) for sepsis, and 2.37 (95% CI, 2.13-2.63) for heart failure.
Given the findings, physicians should weigh the benefits against the risks of rare but potentially serious consequences of these anti-inflammatory drugs, according to the authors.
“After initiating patients on oral steroid bursts, physicians should be on the lookout for these severe adverse events, particularly within the first month after initiation of steroid therapy,” Dr. Yao said in an interview.
The findings were published online July 6 in Annals of Internal Medicine.
Of the 15,859,129 adult Asians in the Taiwanese database, the study included 2,623,327 adults aged 20-64 years who received single steroid bursts (14 days or less) between Jan. 1, 2013, and Dec. 31, 2015.
Almost 60% of the indications were for skin disorders, such as eczema and urticaria, and for respiratory tract infections, such as sinusitis and acute pharyngitis. Among specialties, dermatology, otolaryngology, family practice, internal medicine, and pediatrics accounted for 88% of prescriptions.
“Our findings are important for physicians and guideline developers because short-term use of oral corticosteroids is common and the real-world safety of this approach remains unclear,” the authors wrote. They acknowledged that the database did not provide information on such potential confounders as disease severity and lifestyle factors, nor did it include children and vulnerable individuals, which may limit the generalizability of the results.
The findings echo those of a 2017 cohort study conducted by researchers at the University of Michigan in Ann Arbor. That study, by Akbar K. Waljee, MD, assistant professor of gastroenterology, University of Michigan, Ann Arbor, and colleagues, included data on more than 1.5 million privately insured U.S. adults. The researchers included somewhat longer steroid bursts of up to 30 days’ duration and found that use of the drugs was associated with a greater than fivefold increased risk for sepsis, a more than threefold increased risk for venous thromboembolism, and a nearly twofold increased risk for fracture within 30 days of starting treatment.
Furthermore, the elevated risk persisted at prednisone-equivalent doses of less than 20 mg/d (IRR, 4.02 for sepsis, 3.61 for venous thromboembolism, and 1.83 for fracture; all P < .001).
The U.S. study also found that during the 3-year period from 2012 to 2014, more than 20% of patients were prescribed short-term oral corticosteroids.
“Both studies indicate that these short-term regimens are more common in the real world than was previously thought and are not risk free,” Dr. Yao said.
Recognition that corticosteroids are associated with adverse events has been building for decades, according to the authors of an editorial that accompanies the new study.
“However, we commonly use short corticosteroid ‘bursts’ for minor ailments despite a lack of evidence for meaningful benefit. We are now learning that bursts as short as 3 days may increase risk for serious AEs, even in young and healthy people,” wrote editorialists Beth I. Wallace, MD, of the Center for Clinical Management Research at the VA Ann Arbor Healthcare System and the Institute for Healthcare Policy and Innovation at Michigan Medicine, Ann Arbor, and Dr. Waljee, who led the 2017 study.
Dr. Wallace and Dr. Waljee drew parallels between corticosteroid bursts and other short-term regimens, such as of antibiotics and opiates, in which prescriber preference and sometimes patient pressure play a role. “All of these treatments have well-defined indications but can cause net harm when used. We can thus conceive of a corticosteroid stewardship model of targeted interventions that aims to reduce inappropriate prescribing,” they wrote.
In an interview, Dr. Wallace, a rheumatologist who prescribes oral steroids fairly frequently, noted that the Taiwan study is the first to investigate steroid bursts. “Up till now, these very short courses have flown under the radar. Clinicians very commonly prescribe short courses to help relieve symptoms of self-limited conditions like bronchitis, and we assume that because the exposure duration is short, the risks are low, especially for patients who are otherwise healthy.”
She warned that the data in the current study indicate that these short bursts – even at the lower end of the 1- to 2-week courses American physicians prescribe most often – carry small but real increases in risk for serious AEs. “And these increases were seen in young, healthy people, not just in people with preexisting conditions,” she said. “So, we might need to start thinking harder about how we are prescribing even these very short courses of steroids and try to use steroids only when their meaningful benefits really outweigh the risk.”
She noted that a patient with a chronic inflammatory condition such as rheumatoid arthritis may benefit substantially from short-term steroids to treat a disease flare. In that specific case, the benefits of short-term steroids may outweigh the risks, Dr. Wallace said.
But not everyone thinks a new strategy is needed. For Whitney A. High, MD, associate professor of dermatology and pathology at the University of Colorado at Denver, Aurora, the overprescribing of short-term corticosteroids is not a problem, and dermatologists are already exercising caution.
“I only prescribe these drugs short term to, at a guess, about 1 in 40 patients and only when a patient is miserable and quality of life is being seriously affected,” he said in an interview. “And that’s something that can’t be measured in a database study like the one from Taiwan but only in a risk-benefit analysis,” he said.
Furthermore, dermatologists have other drugs and technologies in their armamentarium, including topical steroids with occlusion or with wet wraps, phototherapy, phosphodiesterase inhibitors, calcipotriene, methotrexate and other immunosuppressive agents, and biologics. “In fact, many of these agents are specifically referred to as steroid-sparing,” Dr. High said.
Nor does he experience much pressure from patients to prescribe these drugs. “While occasionally I may encounter a patient who places pressure on me for oral steroids, it’s probably not nearly as frequently as providers in other fields are pressured to prescribe antibiotics or narcotics,” he said.
According to the Taiwanese researchers, the next step is to conduct more studies, including clinical trials, to determine optimal use of corticosteroids by monitoring adverse events. In the meantime, for practitioners such as Dr. Wallace and Dr. High, there is ample evidence from several recent studies of the harms of short-term corticosteroids, whereas the benefits for patients with self-limiting conditions remain uncertain. “This and other studies like it quite appropriately remind providers to avoid oral steroids when they’re not necessary and to seek alternatives where possible,” Dr. High said.
The study was supported by the National Health Research Institutes of Taiwan, the Ministry of Science and Technology of Taiwan, the Chang Gung Medical Foundation, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (NIH). Dr. Yao has disclosed no relevant financial relationships. Dr. Wu has received grants from GlaxoSmithKline outside the submitted work. The editorialists and Dr. High have disclosed no relevant financial relationships. Dr. Wallace received an NIH grant during the writing of the editorial.
A version of this article originally appeared on Medscape.com.
Triple inhaler combo quells COPD exacerbations
Phase 3 trial findings compared outcomes for COPD patients who had triple fixed-dose inhaled corticosteroid, long-acting muscarinic antagonist, and long-acting beta2 agonist with patients who received one of two dual-therapy combinations. The results were presented at the American Thoracic Society’s virtual clinical trial session.
A total of 8,509 patients were randomized on a 1:1:1:1 basis to receive twice daily:
- Single-inhaler combinations of the inhaled corticosteroid (ICS) budesonide at one of two doses, the long-acting muscarinic antagonist (LAMA) glycopyrrolate, and the long-acting beta2 agonist (LABA) formoterol.
- Dual-therapy combination glycopyrrolate and formoterol.
- Dual-therapy combination budesonide and formoterol.
The annual rate of moderate or severe COPD exacerbations was 1.08 and 1.07 for the triple combinations with 320 mcg and 180 mcg doses of budesonide, respectively, compared with 1.42 for glycopyrrolate-formoterol, and 1.24 for budesonide-formoterol.
Both triple combinations were significantly superior to the dual therapies for controlling exacerbations, reported Klaus F. Rabe, MD, PhD, from LungenClinic Grosshansdorf and Christian-Albrechts University Kiel (Germany), and colleagues in the ETHOS (Efficacy and Safety of Triple Therapy in Obstructive Lung Disease) trial (NCT02465567).
“Our findings show the benefits of triple therapy with a budesonide-glycopyrrolate-formoterol combination over dual therapy with a LAMA-LABA or an inhaled glucocorticoid-LABA combination with respect to the annual rate of moderate or severe COPD exacerbations, symptoms, and health-related quality of life in patients with moderate to very-severe COPD who are at risk of exacerbations,” they wrote in a study published online in the New England Journal of Medicine..
The trial showed for the first time that “triple therapy that has half the dose of steroid compared to a standard ICS/LABA combination has had greater efficacy for the exacerbation endpoint,” Dr. Rabe said during his presentation.
Triple-therapy combinations with an ICS, LAMA, and LABA are recommended for patients with COPD who remain symptomatic or experience further exacerbations on dual–ICS/LABA or –LAMA/LABA combinations. The triple combinations have been shown in several studies to lower risk of exacerbations and are associated with both better lung function and health-related quality of life, compared with dual therapies, the investigators noted.
However, concerns about adverse events associated with long-term ICS use – including pneumonia, cataracts, and increased fracture risk, possibly related to treatment duration, dose level, or type of corticosteroid used – spurred the ETHOS investigators to compare triple and dual fixed-dose combinations for efficacy and safety over 1 year.
Large study
They enrolled 8,509 adults aged 40-80 years with symptomatic COPD (defined as score of 10 or higher on the 40-point COPD Assessment Test). All patients were receiving at least two inhaled maintenance therapies at the time of screening, and had a postbronchodilator ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity of less than 0.7, with a postbronchodilator FEV1 of 25%-65% of the predicted normal value. The patients all had a smoking history of at least 10 pack-years and a documented history of at least one moderate or severe COPD exacerbation in the year before screening.
The patients were randomized in equal proportions to receive triple therapy with budesonide at 320- or 160-mcg doses plus glycopyrrolate 18 mcg, and formoterol 9.6 mcg twice daily, or to dual therapy with either glycopyrrolate plus formoterol at the same doses, or 320 mcg budesonide plus 9.6 mcg formoterol.
As noted, for the primary endpoint of the estimated annual rate of moderate or severe exacerbations, the triple combinations were associated with significantly lower rates, with a 24% lower rate (rate ratio, 0.76) with 320 mcg budesonide triple therapy, compared with glycopyrrolate-formoterol, and a 13% lower rate (RR, 0.87), compared with budesonide formoterol (P < .001 and P = .003, respectively).
The triple combination with the 160-mcg budesonide dose was associated with a 25% lower annual rate of exacerbations (RR, 0.75) vs. glycopyrrolate-formoterol, and a 14% lower rate (RR, 0.86) vs. budesonide-formoterol (P < .001 and P = .002, respectively).
Secondary efficacy endpoints also favored the triple combination, including a 20% lower rate ratio of severe exacerbations over 52 weeks for the 320-mcg budesonide group, compared with the budesonide-formoterol group (P = .02).
The 320-mcg dose combination was also associated with a 46% lower risk for all-cause mortality, compared with glycopyrrolate-formoterol (hazard ratio, 0.54; P = .0111).
Confirmed pneumonia was seen in 4.2% of patients on the 320-mcg budesonide dose, 3.5% of those in the 160-mcg group, and 4.5% of patients treated with budesonide-formoterol. The incidence of any adverse effect was similar across the treatment groups, ranging from 61.7% to 64.5%.
Balance exacerbation, pneumonia risk
In the question-and-answer session following his online presentation, Dr. Rabe was asked how the investigators reconciled their data showing increased incidence of pneumonia in budenoside-containing formulations with claims by the maker of the budesonide-formoterol (Symbicort, AstraZeneca) that budesonide is not associated with increased risk of pneumonia.
“We have to say that there are individuals that we have to balance the benefit of [less] exacerbation against the risk of pneumonia,” he replied, but noted that the size of the effect, observed both in ETHOS and in the KRONOS trial, was relatively small.
“This definitely adds some information for us to think about when we’re trying to do risk-benefit analysis,” commented MeiLan K. Han, MD, MS, from the University of Michigan, who moderated the session but was not involved in the study.
The ETHOS trial was funded by AstraZeneca. Dr. Rabe disclosed consulting/advisory board activity with that company and others. Dr. Han has previously disclosed consulting/advising and research funding relationships with other companies.
SOURCE: Rabe KF et al. N Engl J Med. 2020 Jun 24. doi: 10.1056/NEJMoa1916046.
Phase 3 trial findings compared outcomes for COPD patients who had triple fixed-dose inhaled corticosteroid, long-acting muscarinic antagonist, and long-acting beta2 agonist with patients who received one of two dual-therapy combinations. The results were presented at the American Thoracic Society’s virtual clinical trial session.
A total of 8,509 patients were randomized on a 1:1:1:1 basis to receive twice daily:
- Single-inhaler combinations of the inhaled corticosteroid (ICS) budesonide at one of two doses, the long-acting muscarinic antagonist (LAMA) glycopyrrolate, and the long-acting beta2 agonist (LABA) formoterol.
- Dual-therapy combination glycopyrrolate and formoterol.
- Dual-therapy combination budesonide and formoterol.
The annual rate of moderate or severe COPD exacerbations was 1.08 and 1.07 for the triple combinations with 320 mcg and 180 mcg doses of budesonide, respectively, compared with 1.42 for glycopyrrolate-formoterol, and 1.24 for budesonide-formoterol.
Both triple combinations were significantly superior to the dual therapies for controlling exacerbations, reported Klaus F. Rabe, MD, PhD, from LungenClinic Grosshansdorf and Christian-Albrechts University Kiel (Germany), and colleagues in the ETHOS (Efficacy and Safety of Triple Therapy in Obstructive Lung Disease) trial (NCT02465567).
“Our findings show the benefits of triple therapy with a budesonide-glycopyrrolate-formoterol combination over dual therapy with a LAMA-LABA or an inhaled glucocorticoid-LABA combination with respect to the annual rate of moderate or severe COPD exacerbations, symptoms, and health-related quality of life in patients with moderate to very-severe COPD who are at risk of exacerbations,” they wrote in a study published online in the New England Journal of Medicine..
The trial showed for the first time that “triple therapy that has half the dose of steroid compared to a standard ICS/LABA combination has had greater efficacy for the exacerbation endpoint,” Dr. Rabe said during his presentation.
Triple-therapy combinations with an ICS, LAMA, and LABA are recommended for patients with COPD who remain symptomatic or experience further exacerbations on dual–ICS/LABA or –LAMA/LABA combinations. The triple combinations have been shown in several studies to lower risk of exacerbations and are associated with both better lung function and health-related quality of life, compared with dual therapies, the investigators noted.
However, concerns about adverse events associated with long-term ICS use – including pneumonia, cataracts, and increased fracture risk, possibly related to treatment duration, dose level, or type of corticosteroid used – spurred the ETHOS investigators to compare triple and dual fixed-dose combinations for efficacy and safety over 1 year.
Large study
They enrolled 8,509 adults aged 40-80 years with symptomatic COPD (defined as score of 10 or higher on the 40-point COPD Assessment Test). All patients were receiving at least two inhaled maintenance therapies at the time of screening, and had a postbronchodilator ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity of less than 0.7, with a postbronchodilator FEV1 of 25%-65% of the predicted normal value. The patients all had a smoking history of at least 10 pack-years and a documented history of at least one moderate or severe COPD exacerbation in the year before screening.
The patients were randomized in equal proportions to receive triple therapy with budesonide at 320- or 160-mcg doses plus glycopyrrolate 18 mcg, and formoterol 9.6 mcg twice daily, or to dual therapy with either glycopyrrolate plus formoterol at the same doses, or 320 mcg budesonide plus 9.6 mcg formoterol.
As noted, for the primary endpoint of the estimated annual rate of moderate or severe exacerbations, the triple combinations were associated with significantly lower rates, with a 24% lower rate (rate ratio, 0.76) with 320 mcg budesonide triple therapy, compared with glycopyrrolate-formoterol, and a 13% lower rate (RR, 0.87), compared with budesonide formoterol (P < .001 and P = .003, respectively).
The triple combination with the 160-mcg budesonide dose was associated with a 25% lower annual rate of exacerbations (RR, 0.75) vs. glycopyrrolate-formoterol, and a 14% lower rate (RR, 0.86) vs. budesonide-formoterol (P < .001 and P = .002, respectively).
Secondary efficacy endpoints also favored the triple combination, including a 20% lower rate ratio of severe exacerbations over 52 weeks for the 320-mcg budesonide group, compared with the budesonide-formoterol group (P = .02).
The 320-mcg dose combination was also associated with a 46% lower risk for all-cause mortality, compared with glycopyrrolate-formoterol (hazard ratio, 0.54; P = .0111).
Confirmed pneumonia was seen in 4.2% of patients on the 320-mcg budesonide dose, 3.5% of those in the 160-mcg group, and 4.5% of patients treated with budesonide-formoterol. The incidence of any adverse effect was similar across the treatment groups, ranging from 61.7% to 64.5%.
Balance exacerbation, pneumonia risk
In the question-and-answer session following his online presentation, Dr. Rabe was asked how the investigators reconciled their data showing increased incidence of pneumonia in budenoside-containing formulations with claims by the maker of the budesonide-formoterol (Symbicort, AstraZeneca) that budesonide is not associated with increased risk of pneumonia.
“We have to say that there are individuals that we have to balance the benefit of [less] exacerbation against the risk of pneumonia,” he replied, but noted that the size of the effect, observed both in ETHOS and in the KRONOS trial, was relatively small.
“This definitely adds some information for us to think about when we’re trying to do risk-benefit analysis,” commented MeiLan K. Han, MD, MS, from the University of Michigan, who moderated the session but was not involved in the study.
The ETHOS trial was funded by AstraZeneca. Dr. Rabe disclosed consulting/advisory board activity with that company and others. Dr. Han has previously disclosed consulting/advising and research funding relationships with other companies.
SOURCE: Rabe KF et al. N Engl J Med. 2020 Jun 24. doi: 10.1056/NEJMoa1916046.
Phase 3 trial findings compared outcomes for COPD patients who had triple fixed-dose inhaled corticosteroid, long-acting muscarinic antagonist, and long-acting beta2 agonist with patients who received one of two dual-therapy combinations. The results were presented at the American Thoracic Society’s virtual clinical trial session.
A total of 8,509 patients were randomized on a 1:1:1:1 basis to receive twice daily:
- Single-inhaler combinations of the inhaled corticosteroid (ICS) budesonide at one of two doses, the long-acting muscarinic antagonist (LAMA) glycopyrrolate, and the long-acting beta2 agonist (LABA) formoterol.
- Dual-therapy combination glycopyrrolate and formoterol.
- Dual-therapy combination budesonide and formoterol.
The annual rate of moderate or severe COPD exacerbations was 1.08 and 1.07 for the triple combinations with 320 mcg and 180 mcg doses of budesonide, respectively, compared with 1.42 for glycopyrrolate-formoterol, and 1.24 for budesonide-formoterol.
Both triple combinations were significantly superior to the dual therapies for controlling exacerbations, reported Klaus F. Rabe, MD, PhD, from LungenClinic Grosshansdorf and Christian-Albrechts University Kiel (Germany), and colleagues in the ETHOS (Efficacy and Safety of Triple Therapy in Obstructive Lung Disease) trial (NCT02465567).
“Our findings show the benefits of triple therapy with a budesonide-glycopyrrolate-formoterol combination over dual therapy with a LAMA-LABA or an inhaled glucocorticoid-LABA combination with respect to the annual rate of moderate or severe COPD exacerbations, symptoms, and health-related quality of life in patients with moderate to very-severe COPD who are at risk of exacerbations,” they wrote in a study published online in the New England Journal of Medicine..
The trial showed for the first time that “triple therapy that has half the dose of steroid compared to a standard ICS/LABA combination has had greater efficacy for the exacerbation endpoint,” Dr. Rabe said during his presentation.
Triple-therapy combinations with an ICS, LAMA, and LABA are recommended for patients with COPD who remain symptomatic or experience further exacerbations on dual–ICS/LABA or –LAMA/LABA combinations. The triple combinations have been shown in several studies to lower risk of exacerbations and are associated with both better lung function and health-related quality of life, compared with dual therapies, the investigators noted.
However, concerns about adverse events associated with long-term ICS use – including pneumonia, cataracts, and increased fracture risk, possibly related to treatment duration, dose level, or type of corticosteroid used – spurred the ETHOS investigators to compare triple and dual fixed-dose combinations for efficacy and safety over 1 year.
Large study
They enrolled 8,509 adults aged 40-80 years with symptomatic COPD (defined as score of 10 or higher on the 40-point COPD Assessment Test). All patients were receiving at least two inhaled maintenance therapies at the time of screening, and had a postbronchodilator ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity of less than 0.7, with a postbronchodilator FEV1 of 25%-65% of the predicted normal value. The patients all had a smoking history of at least 10 pack-years and a documented history of at least one moderate or severe COPD exacerbation in the year before screening.
The patients were randomized in equal proportions to receive triple therapy with budesonide at 320- or 160-mcg doses plus glycopyrrolate 18 mcg, and formoterol 9.6 mcg twice daily, or to dual therapy with either glycopyrrolate plus formoterol at the same doses, or 320 mcg budesonide plus 9.6 mcg formoterol.
As noted, for the primary endpoint of the estimated annual rate of moderate or severe exacerbations, the triple combinations were associated with significantly lower rates, with a 24% lower rate (rate ratio, 0.76) with 320 mcg budesonide triple therapy, compared with glycopyrrolate-formoterol, and a 13% lower rate (RR, 0.87), compared with budesonide formoterol (P < .001 and P = .003, respectively).
The triple combination with the 160-mcg budesonide dose was associated with a 25% lower annual rate of exacerbations (RR, 0.75) vs. glycopyrrolate-formoterol, and a 14% lower rate (RR, 0.86) vs. budesonide-formoterol (P < .001 and P = .002, respectively).
Secondary efficacy endpoints also favored the triple combination, including a 20% lower rate ratio of severe exacerbations over 52 weeks for the 320-mcg budesonide group, compared with the budesonide-formoterol group (P = .02).
The 320-mcg dose combination was also associated with a 46% lower risk for all-cause mortality, compared with glycopyrrolate-formoterol (hazard ratio, 0.54; P = .0111).
Confirmed pneumonia was seen in 4.2% of patients on the 320-mcg budesonide dose, 3.5% of those in the 160-mcg group, and 4.5% of patients treated with budesonide-formoterol. The incidence of any adverse effect was similar across the treatment groups, ranging from 61.7% to 64.5%.
Balance exacerbation, pneumonia risk
In the question-and-answer session following his online presentation, Dr. Rabe was asked how the investigators reconciled their data showing increased incidence of pneumonia in budenoside-containing formulations with claims by the maker of the budesonide-formoterol (Symbicort, AstraZeneca) that budesonide is not associated with increased risk of pneumonia.
“We have to say that there are individuals that we have to balance the benefit of [less] exacerbation against the risk of pneumonia,” he replied, but noted that the size of the effect, observed both in ETHOS and in the KRONOS trial, was relatively small.
“This definitely adds some information for us to think about when we’re trying to do risk-benefit analysis,” commented MeiLan K. Han, MD, MS, from the University of Michigan, who moderated the session but was not involved in the study.
The ETHOS trial was funded by AstraZeneca. Dr. Rabe disclosed consulting/advisory board activity with that company and others. Dr. Han has previously disclosed consulting/advising and research funding relationships with other companies.
SOURCE: Rabe KF et al. N Engl J Med. 2020 Jun 24. doi: 10.1056/NEJMoa1916046.
FROM ATS 2020
Cost of preventable adult hospital stays topped $33 billion in 2017
according to the Agency for Healthcare Research and Quality.
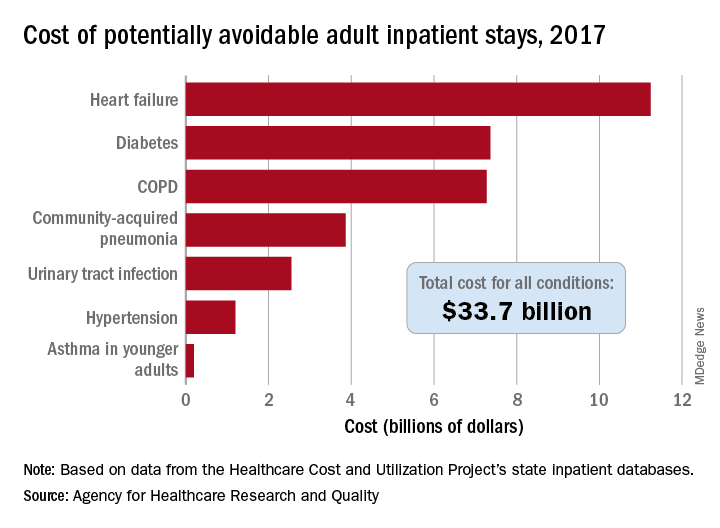
That year, there were 27.4 million inpatient visits by adults with a total cost of $380.1 billion, although obstetric stays were not included in the analysis. Of those inpatient admissions, 3.5 million (12.9%) were deemed to be “avoidable, in part, through timely and quality primary and preventive care,” Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, said in a recent AHRQ statistical brief.
The charges for those 3.5 million visits came to $33.7 billion, or 8.9% of aggregate hospital costs in 2017, based on data from the AHRQ Healthcare Cost and Utilization Project’s state inpatient databases.
“Determining the volume and costs of potentially preventable inpatient stays can identify where potential cost savings might be found associated with reducing these hospitalizations overall and among specific subpopulations,” the investigators pointed out.
Of the seven conditions that are potentially avoidable, heart failure was the most expensive, producing more than 1.1 million inpatient admissions at a cost of $11.2 billion. Diabetes was next with a cost of almost $7.4 billion, followed by chronic obstructive pulmonary disease (COPD) at nearly $7.3 billion, they said.
Those three conditions, along with hypertension and asthma in younger adults, brought the total cost of the preventable-stay equation’s chronic side to $27.3 billion in 2017, versus $6.4 billion for the two acute conditions, community-acquired pneumonia and urinary tract infections, said Dr. McDermott of IBM Watson Health and Dr. Jiang of the AHRQ.
The rate of potentially avoidable stays for chronic conditions was higher for men (1,112/100,000 population) than for women (954/100,000), but women had a higher rate for acute conditions, 346 vs. 257, which made the overall rates similar (1,369 for men and 1,300 for women), they reported.
Differences by race/ethnicity were more striking. The rate of potentially avoidable stays for blacks was 2,573/100,000 in 2017, compared with 1,315 for Hispanics, 1,173 for whites, and 581 for Asians/Pacific Islanders. The considerable margins between those figures, however, were far eclipsed by the “other” category, which had 4,911 stays per 100,000, the researchers said.
Large disparities also can be seen when looking at community-level income. Communities with income in the lowest quartile had a preventable-hospitalization rate of 2,013/100,000, and the rate dropped with each successive quartile until it reached 878/100,000 for the highest-income communities, according to the report.
“High hospital admission rates for these conditions may indicate areas where changes to the healthcare delivery system could be implemented to improve patient outcomes and lower costs,” Dr. McDermott and Dr. Jiang wrote.
SOURCE: McDermott KW and Jiang HJ. HCUP Statistical Brief #259. June 2020.
according to the Agency for Healthcare Research and Quality.
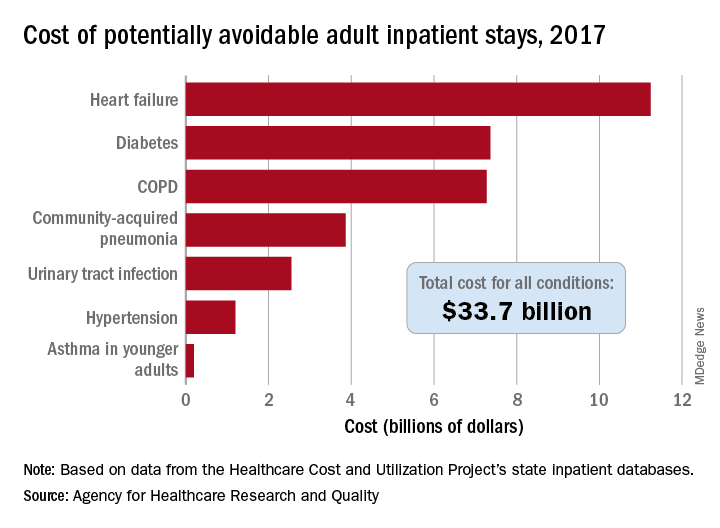
That year, there were 27.4 million inpatient visits by adults with a total cost of $380.1 billion, although obstetric stays were not included in the analysis. Of those inpatient admissions, 3.5 million (12.9%) were deemed to be “avoidable, in part, through timely and quality primary and preventive care,” Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, said in a recent AHRQ statistical brief.
The charges for those 3.5 million visits came to $33.7 billion, or 8.9% of aggregate hospital costs in 2017, based on data from the AHRQ Healthcare Cost and Utilization Project’s state inpatient databases.
“Determining the volume and costs of potentially preventable inpatient stays can identify where potential cost savings might be found associated with reducing these hospitalizations overall and among specific subpopulations,” the investigators pointed out.
Of the seven conditions that are potentially avoidable, heart failure was the most expensive, producing more than 1.1 million inpatient admissions at a cost of $11.2 billion. Diabetes was next with a cost of almost $7.4 billion, followed by chronic obstructive pulmonary disease (COPD) at nearly $7.3 billion, they said.
Those three conditions, along with hypertension and asthma in younger adults, brought the total cost of the preventable-stay equation’s chronic side to $27.3 billion in 2017, versus $6.4 billion for the two acute conditions, community-acquired pneumonia and urinary tract infections, said Dr. McDermott of IBM Watson Health and Dr. Jiang of the AHRQ.
The rate of potentially avoidable stays for chronic conditions was higher for men (1,112/100,000 population) than for women (954/100,000), but women had a higher rate for acute conditions, 346 vs. 257, which made the overall rates similar (1,369 for men and 1,300 for women), they reported.
Differences by race/ethnicity were more striking. The rate of potentially avoidable stays for blacks was 2,573/100,000 in 2017, compared with 1,315 for Hispanics, 1,173 for whites, and 581 for Asians/Pacific Islanders. The considerable margins between those figures, however, were far eclipsed by the “other” category, which had 4,911 stays per 100,000, the researchers said.
Large disparities also can be seen when looking at community-level income. Communities with income in the lowest quartile had a preventable-hospitalization rate of 2,013/100,000, and the rate dropped with each successive quartile until it reached 878/100,000 for the highest-income communities, according to the report.
“High hospital admission rates for these conditions may indicate areas where changes to the healthcare delivery system could be implemented to improve patient outcomes and lower costs,” Dr. McDermott and Dr. Jiang wrote.
SOURCE: McDermott KW and Jiang HJ. HCUP Statistical Brief #259. June 2020.
according to the Agency for Healthcare Research and Quality.
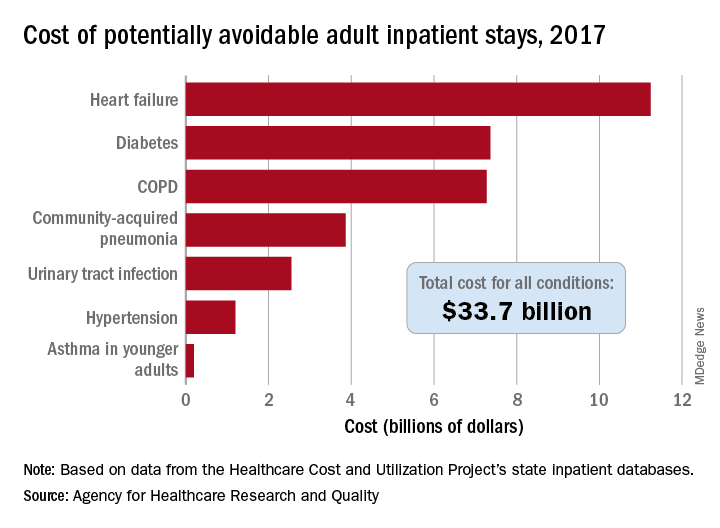
That year, there were 27.4 million inpatient visits by adults with a total cost of $380.1 billion, although obstetric stays were not included in the analysis. Of those inpatient admissions, 3.5 million (12.9%) were deemed to be “avoidable, in part, through timely and quality primary and preventive care,” Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, said in a recent AHRQ statistical brief.
The charges for those 3.5 million visits came to $33.7 billion, or 8.9% of aggregate hospital costs in 2017, based on data from the AHRQ Healthcare Cost and Utilization Project’s state inpatient databases.
“Determining the volume and costs of potentially preventable inpatient stays can identify where potential cost savings might be found associated with reducing these hospitalizations overall and among specific subpopulations,” the investigators pointed out.
Of the seven conditions that are potentially avoidable, heart failure was the most expensive, producing more than 1.1 million inpatient admissions at a cost of $11.2 billion. Diabetes was next with a cost of almost $7.4 billion, followed by chronic obstructive pulmonary disease (COPD) at nearly $7.3 billion, they said.
Those three conditions, along with hypertension and asthma in younger adults, brought the total cost of the preventable-stay equation’s chronic side to $27.3 billion in 2017, versus $6.4 billion for the two acute conditions, community-acquired pneumonia and urinary tract infections, said Dr. McDermott of IBM Watson Health and Dr. Jiang of the AHRQ.
The rate of potentially avoidable stays for chronic conditions was higher for men (1,112/100,000 population) than for women (954/100,000), but women had a higher rate for acute conditions, 346 vs. 257, which made the overall rates similar (1,369 for men and 1,300 for women), they reported.
Differences by race/ethnicity were more striking. The rate of potentially avoidable stays for blacks was 2,573/100,000 in 2017, compared with 1,315 for Hispanics, 1,173 for whites, and 581 for Asians/Pacific Islanders. The considerable margins between those figures, however, were far eclipsed by the “other” category, which had 4,911 stays per 100,000, the researchers said.
Large disparities also can be seen when looking at community-level income. Communities with income in the lowest quartile had a preventable-hospitalization rate of 2,013/100,000, and the rate dropped with each successive quartile until it reached 878/100,000 for the highest-income communities, according to the report.
“High hospital admission rates for these conditions may indicate areas where changes to the healthcare delivery system could be implemented to improve patient outcomes and lower costs,” Dr. McDermott and Dr. Jiang wrote.
SOURCE: McDermott KW and Jiang HJ. HCUP Statistical Brief #259. June 2020.
‘Collateral damage’: COVID-19 threatens patients with COPD
according to a commentary published in CHEST (2020 May 28. doi: 10.1016/j.chest.2020.05.549) by a group of physicians who study COPD.
Not only is COPD among the most prevalent underlying diseases among hospitalized COVID-19 patients (Clin Microbiol Infect. 2020 Jun 8. doi: 10.1016/j.cmi.2020.05.041), but other unanticipated factors of treatment put these patients at extra risk. Valerie Press, MD, assistant professor of medicine and pediatrics at the University of Chicago, and colleagues aimed to alert physicians to be aware of potential negative effects, or collateral damage, that the pandemic can have on their patients with COPD, even those without a COVID-19 diagnosis.
These concerns include that patients may delay presenting to the ED with acute exacerbations of COPD and once they present they may be at later stages of the exacerbation. Further, evaluation for COVID-19 as a possible trigger of acute exacerbations of COPD (AECOPD) is essential; however, implementing proven AECOPD therapies remains challenging. For instance, routine therapy with corticosteroids for AECOPD may be delayed due to diagnostic uncertainty and hesitation to treat COVID-19 with steroids while COVID-19 testing is pending,” Dr. Press and her colleagues stated.
Shortages and scarcity of medications such as albuterol inhalers to treat COPD have been reported. In addition, patients with COPD are currently less likely to access their health care providers because of fear of COVID-19 infection. This barrier to care and the current higher threshold for presenting to the hospital may to lead to more cases of AECOPD and worsening health in these patients, according to the authors.
Dr. Press said in an interview: “Access to medications delivered through inhalers is challenging even without the pandemic due to high cost of medications. Generic medications are key to improving access for patients with chronic lung disease, so once the generic albuterol becomes available, this should help with access. In the meantime, some companies help provide medications at reduced cost, but usually only on a short time basis. In addition, some pharmacies have lower-cost albuterol inhalers, but these are often not supplied with a full month of dosing.”
In addition to all these concerns is the economic toll this pandemic is taking on patients. The association between COPD and socioeconomic status has been studied in depth (Am J Respir Crit Care Med. 2019; 199[8]:961-69) and would indicate that low-income patients with COPD would face an increased burden during an economic downturn. The authors noted, “Historic rapid job loss and unemployment in the U.S., coupled with a health system of employment-integrated health insurance coverage, makes it more likely that people with COPD will not be able to afford their medication.”
Dr. Press stressed that the COVID pandemic has highlighted critically important disparities in access to health care and disparities in health. “Many of the recommendations regarding stay-at-home and other safety mechanisms to prevent contracting and spreading COVID-19 have not been feasible for all sub-populations in the United States. Those that were essential workers did not have the ability to stay home. Further, those that rely on public transportation had less opportunities to social distance. Finally, while telemedicine opportunities have advanced for clinical care, not all patients have equal access to these capabilities and health disparities could widen in this regard as well. Clinicians have a responsibility to identify social determinants of health that increase risks to our patients’ health and limit their safety.”*
The authors offer some concrete suggestions of how physicians can address some of these concerns, including the following:
- Be alert to potential barriers to accessing medication and be aware of generic albuterol inhaler recently approved by the FDA in response to COVID-19–related shortages.
- Use telemedicine to monitor patients and improvement of home self-management. Clinicians should help patients “seek care with worsening symptoms and have clear management guidelines regarding seeking phone/video visits; implementing therapy with corticosteroids, antibiotics, or inhalers and nebulizers; COVID-19 testing recommendations; and thresholds for seeking emergent, urgent, or outpatient care in person,” Dr. Press added, “Building on the work of nurse advice lines and case management and other support services for high-risk patients with COPD may continue via telehealth and telephone visits.”
- Ensure that untried therapy for COVID-19 “does not displace proven and necessary treatments for patients with COPD, hence placing them at increased risk for poor outcomes.”
Dr. Press is also concerned about the post–COVID-19 period for patients with COPD. “It is too early to know if there are specific after effects of the COVID infection on patients with COPD, but given the damage the virus does to even healthy lungs, there is reason to have concern that COVID could cause worsening damage to the lungs of individuals with COPD.”
She noted, “Post-ICU [PICU] syndrome has been recognized in patients with ARDS generally, and patients who recover from critical illness may have long-lasting (and permanent) effects on strength, cognition, disability, and pulmonary function. Whether the PICU syndrome in patients with ARDS due to COVID-19 specifically is different from the PICU syndrome due to other causes remains unknown. But clinicians whose patients with COPD survive COVID-19 may expect long-lasting effects and slow recovery in cases where COVID-19 led to severe ARDS and a prolonged ICU stay. Assessment of overall patient recovery and functional capacity (beyond lung function and dyspnea symptoms) including deconditioning, anxiety, PTSD, weakness, and malnutrition will need to be addressed. Additionally, clinicians may help patients and their families understand the expected recovery and help facilitate family conversations about residual effects of COVID-19.”
The authors had no disclosures.
SOURCE: Press V et al. Chest. 2020 May 28. doi:10.1016/j.chest.2020.05.549.
CORRECTION: *This story was updated with further comments and clarifications from Dr. Press. 6/23/2020
according to a commentary published in CHEST (2020 May 28. doi: 10.1016/j.chest.2020.05.549) by a group of physicians who study COPD.
Not only is COPD among the most prevalent underlying diseases among hospitalized COVID-19 patients (Clin Microbiol Infect. 2020 Jun 8. doi: 10.1016/j.cmi.2020.05.041), but other unanticipated factors of treatment put these patients at extra risk. Valerie Press, MD, assistant professor of medicine and pediatrics at the University of Chicago, and colleagues aimed to alert physicians to be aware of potential negative effects, or collateral damage, that the pandemic can have on their patients with COPD, even those without a COVID-19 diagnosis.
These concerns include that patients may delay presenting to the ED with acute exacerbations of COPD and once they present they may be at later stages of the exacerbation. Further, evaluation for COVID-19 as a possible trigger of acute exacerbations of COPD (AECOPD) is essential; however, implementing proven AECOPD therapies remains challenging. For instance, routine therapy with corticosteroids for AECOPD may be delayed due to diagnostic uncertainty and hesitation to treat COVID-19 with steroids while COVID-19 testing is pending,” Dr. Press and her colleagues stated.
Shortages and scarcity of medications such as albuterol inhalers to treat COPD have been reported. In addition, patients with COPD are currently less likely to access their health care providers because of fear of COVID-19 infection. This barrier to care and the current higher threshold for presenting to the hospital may to lead to more cases of AECOPD and worsening health in these patients, according to the authors.
Dr. Press said in an interview: “Access to medications delivered through inhalers is challenging even without the pandemic due to high cost of medications. Generic medications are key to improving access for patients with chronic lung disease, so once the generic albuterol becomes available, this should help with access. In the meantime, some companies help provide medications at reduced cost, but usually only on a short time basis. In addition, some pharmacies have lower-cost albuterol inhalers, but these are often not supplied with a full month of dosing.”
In addition to all these concerns is the economic toll this pandemic is taking on patients. The association between COPD and socioeconomic status has been studied in depth (Am J Respir Crit Care Med. 2019; 199[8]:961-69) and would indicate that low-income patients with COPD would face an increased burden during an economic downturn. The authors noted, “Historic rapid job loss and unemployment in the U.S., coupled with a health system of employment-integrated health insurance coverage, makes it more likely that people with COPD will not be able to afford their medication.”
Dr. Press stressed that the COVID pandemic has highlighted critically important disparities in access to health care and disparities in health. “Many of the recommendations regarding stay-at-home and other safety mechanisms to prevent contracting and spreading COVID-19 have not been feasible for all sub-populations in the United States. Those that were essential workers did not have the ability to stay home. Further, those that rely on public transportation had less opportunities to social distance. Finally, while telemedicine opportunities have advanced for clinical care, not all patients have equal access to these capabilities and health disparities could widen in this regard as well. Clinicians have a responsibility to identify social determinants of health that increase risks to our patients’ health and limit their safety.”*
The authors offer some concrete suggestions of how physicians can address some of these concerns, including the following:
- Be alert to potential barriers to accessing medication and be aware of generic albuterol inhaler recently approved by the FDA in response to COVID-19–related shortages.
- Use telemedicine to monitor patients and improvement of home self-management. Clinicians should help patients “seek care with worsening symptoms and have clear management guidelines regarding seeking phone/video visits; implementing therapy with corticosteroids, antibiotics, or inhalers and nebulizers; COVID-19 testing recommendations; and thresholds for seeking emergent, urgent, or outpatient care in person,” Dr. Press added, “Building on the work of nurse advice lines and case management and other support services for high-risk patients with COPD may continue via telehealth and telephone visits.”
- Ensure that untried therapy for COVID-19 “does not displace proven and necessary treatments for patients with COPD, hence placing them at increased risk for poor outcomes.”
Dr. Press is also concerned about the post–COVID-19 period for patients with COPD. “It is too early to know if there are specific after effects of the COVID infection on patients with COPD, but given the damage the virus does to even healthy lungs, there is reason to have concern that COVID could cause worsening damage to the lungs of individuals with COPD.”
She noted, “Post-ICU [PICU] syndrome has been recognized in patients with ARDS generally, and patients who recover from critical illness may have long-lasting (and permanent) effects on strength, cognition, disability, and pulmonary function. Whether the PICU syndrome in patients with ARDS due to COVID-19 specifically is different from the PICU syndrome due to other causes remains unknown. But clinicians whose patients with COPD survive COVID-19 may expect long-lasting effects and slow recovery in cases where COVID-19 led to severe ARDS and a prolonged ICU stay. Assessment of overall patient recovery and functional capacity (beyond lung function and dyspnea symptoms) including deconditioning, anxiety, PTSD, weakness, and malnutrition will need to be addressed. Additionally, clinicians may help patients and their families understand the expected recovery and help facilitate family conversations about residual effects of COVID-19.”
The authors had no disclosures.
SOURCE: Press V et al. Chest. 2020 May 28. doi:10.1016/j.chest.2020.05.549.
CORRECTION: *This story was updated with further comments and clarifications from Dr. Press. 6/23/2020
according to a commentary published in CHEST (2020 May 28. doi: 10.1016/j.chest.2020.05.549) by a group of physicians who study COPD.
Not only is COPD among the most prevalent underlying diseases among hospitalized COVID-19 patients (Clin Microbiol Infect. 2020 Jun 8. doi: 10.1016/j.cmi.2020.05.041), but other unanticipated factors of treatment put these patients at extra risk. Valerie Press, MD, assistant professor of medicine and pediatrics at the University of Chicago, and colleagues aimed to alert physicians to be aware of potential negative effects, or collateral damage, that the pandemic can have on their patients with COPD, even those without a COVID-19 diagnosis.
These concerns include that patients may delay presenting to the ED with acute exacerbations of COPD and once they present they may be at later stages of the exacerbation. Further, evaluation for COVID-19 as a possible trigger of acute exacerbations of COPD (AECOPD) is essential; however, implementing proven AECOPD therapies remains challenging. For instance, routine therapy with corticosteroids for AECOPD may be delayed due to diagnostic uncertainty and hesitation to treat COVID-19 with steroids while COVID-19 testing is pending,” Dr. Press and her colleagues stated.
Shortages and scarcity of medications such as albuterol inhalers to treat COPD have been reported. In addition, patients with COPD are currently less likely to access their health care providers because of fear of COVID-19 infection. This barrier to care and the current higher threshold for presenting to the hospital may to lead to more cases of AECOPD and worsening health in these patients, according to the authors.
Dr. Press said in an interview: “Access to medications delivered through inhalers is challenging even without the pandemic due to high cost of medications. Generic medications are key to improving access for patients with chronic lung disease, so once the generic albuterol becomes available, this should help with access. In the meantime, some companies help provide medications at reduced cost, but usually only on a short time basis. In addition, some pharmacies have lower-cost albuterol inhalers, but these are often not supplied with a full month of dosing.”
In addition to all these concerns is the economic toll this pandemic is taking on patients. The association between COPD and socioeconomic status has been studied in depth (Am J Respir Crit Care Med. 2019; 199[8]:961-69) and would indicate that low-income patients with COPD would face an increased burden during an economic downturn. The authors noted, “Historic rapid job loss and unemployment in the U.S., coupled with a health system of employment-integrated health insurance coverage, makes it more likely that people with COPD will not be able to afford their medication.”
Dr. Press stressed that the COVID pandemic has highlighted critically important disparities in access to health care and disparities in health. “Many of the recommendations regarding stay-at-home and other safety mechanisms to prevent contracting and spreading COVID-19 have not been feasible for all sub-populations in the United States. Those that were essential workers did not have the ability to stay home. Further, those that rely on public transportation had less opportunities to social distance. Finally, while telemedicine opportunities have advanced for clinical care, not all patients have equal access to these capabilities and health disparities could widen in this regard as well. Clinicians have a responsibility to identify social determinants of health that increase risks to our patients’ health and limit their safety.”*
The authors offer some concrete suggestions of how physicians can address some of these concerns, including the following:
- Be alert to potential barriers to accessing medication and be aware of generic albuterol inhaler recently approved by the FDA in response to COVID-19–related shortages.
- Use telemedicine to monitor patients and improvement of home self-management. Clinicians should help patients “seek care with worsening symptoms and have clear management guidelines regarding seeking phone/video visits; implementing therapy with corticosteroids, antibiotics, or inhalers and nebulizers; COVID-19 testing recommendations; and thresholds for seeking emergent, urgent, or outpatient care in person,” Dr. Press added, “Building on the work of nurse advice lines and case management and other support services for high-risk patients with COPD may continue via telehealth and telephone visits.”
- Ensure that untried therapy for COVID-19 “does not displace proven and necessary treatments for patients with COPD, hence placing them at increased risk for poor outcomes.”
Dr. Press is also concerned about the post–COVID-19 period for patients with COPD. “It is too early to know if there are specific after effects of the COVID infection on patients with COPD, but given the damage the virus does to even healthy lungs, there is reason to have concern that COVID could cause worsening damage to the lungs of individuals with COPD.”
She noted, “Post-ICU [PICU] syndrome has been recognized in patients with ARDS generally, and patients who recover from critical illness may have long-lasting (and permanent) effects on strength, cognition, disability, and pulmonary function. Whether the PICU syndrome in patients with ARDS due to COVID-19 specifically is different from the PICU syndrome due to other causes remains unknown. But clinicians whose patients with COPD survive COVID-19 may expect long-lasting effects and slow recovery in cases where COVID-19 led to severe ARDS and a prolonged ICU stay. Assessment of overall patient recovery and functional capacity (beyond lung function and dyspnea symptoms) including deconditioning, anxiety, PTSD, weakness, and malnutrition will need to be addressed. Additionally, clinicians may help patients and their families understand the expected recovery and help facilitate family conversations about residual effects of COVID-19.”
The authors had no disclosures.
SOURCE: Press V et al. Chest. 2020 May 28. doi:10.1016/j.chest.2020.05.549.
CORRECTION: *This story was updated with further comments and clarifications from Dr. Press. 6/23/2020
FROM CHEST
By the numbers: Asthma-COPD overlap deaths
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
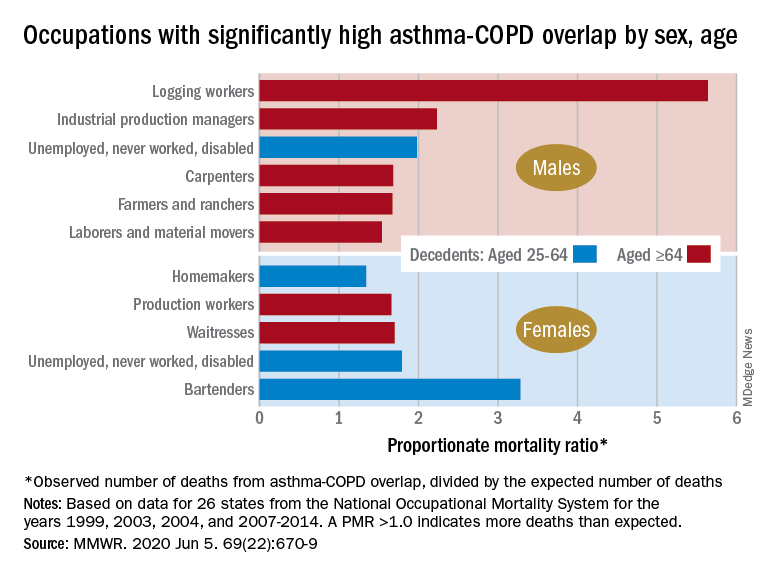
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
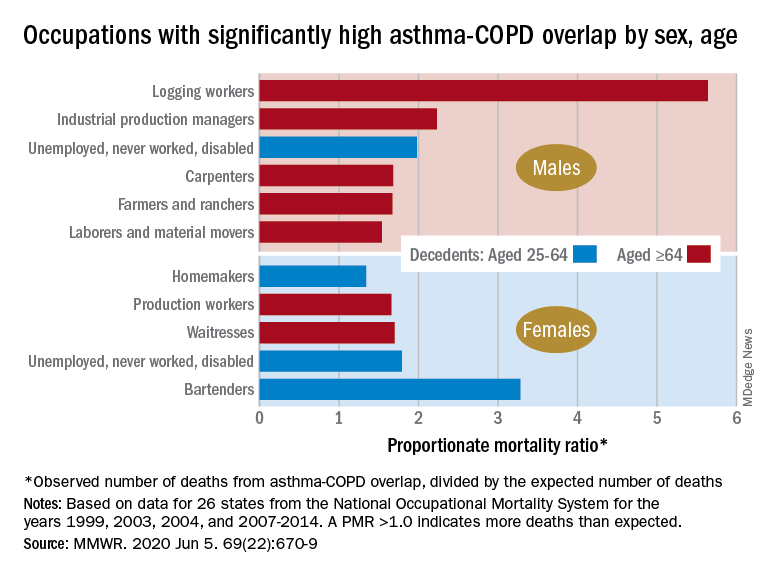
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
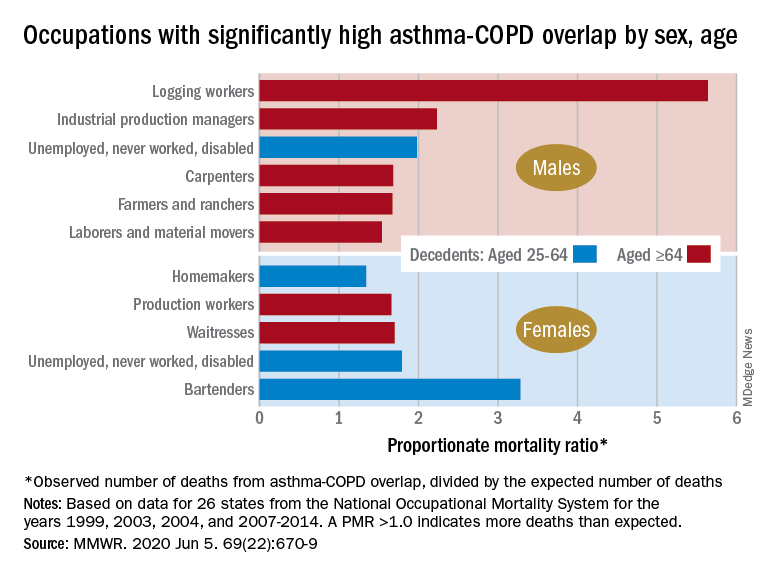
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
FROM MMWR
FLU/SAL inhalers for COPD carry greater pneumonia risk
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
FROM CHEST
Low IgG levels in COPD patients linked to increased risk of hospitalization
Among patients with COPD, the presence of hypogammaglobulinemia confers a nearly 30% increased risk of hospitalization, results from a pooled analysis of four studies showed.
“Mechanistic studies are still warranted to better elucidate how IgG and other immunoglobulins, in particular IgA, may contribute to the local airway host defense,” researchers led by Fernando Sergio Leitao Filho, MD, PhD, wrote in a study published in Chest (2020 May 18. doi: 10.1016/j.chest.2020.04.058). “Nevertheless, our results raise the possibility that, in select COPD patients, IgG replacement therapy may be effective in reducing the risk of COPD hospitalizations. Given the growing rate of COPD hospitalization in the U.S. and elsewhere, there is a pressing need for a large well-designed trial to test this hypothesis.”
In an effort to evaluate the effect of IgG levels on the cumulative incidence of COPD hospitalizations, Dr. Leitao Filho, of the University of British Columbia, Vancouver, and colleagues drew from 2,259 patients who participated in four different trials: Azithromycin for Prevention of Exacerbations of COPD (MACRO), Simvastatin for the Prevention of Exacerbations in Moderate and Severe COPD (STATCOPE), the Long-Term Oxygen Treatment Trial (LOTT), and COPD Activity: Serotonin Transporter, Cytokines and Depression (CASCADE). The mean baseline age of study participants was 66 years, and 641 (28.4%) had hypogammaglobulinemia, which was defined as having a serum IgG levels of less than 7.0 g/L, while the remainder had normal IgG levels.
The pooled meta-analysis, which is believed to be the largest of its kind, revealed that the presence of hypogammaglobulinemia was associated with an incidence of COPD hospitalizations that was 1.29-fold higher than that observed among participants who had normal IgG levels (P = .01). The incidence was even higher among patients with prior COPD admissions (pooled subdistribution hazard ratio, 1.58; P < .01), yet the risk of COPD admissions was similar between IgG groups in patients with no prior hospitalizations (pooled SHR, 1.15; P = .34). Patients with hypogammaglobulinemia also showed significantly higher rates of COPD hospitalizations per person-year, compared with their counterparts who had normal IgG levels (0.48 vs. 0.29, respectively; P < .001.)
The authors acknowledged certain limitations of the study, including the fact that they measured serum IgG levels only at baseline “when participants were clinically stable; thus, the variability of IgG levels in a given individual over time and during the course of an AECOPD [severe acute exacerbation of COPD] is uncertain. Secondly, clinical data on corticosteroid use (formulations, dose, and length of use) were not readily available. However, systemic steroid use (one or more courses due to AECOPD prior to study entry) was accounted for in our analyses.”
The MACRO, STATCOPE, LOTT trials, and the CASCADE cohort were supported by the National Heart, Lung, and Blood Institute; National Institutes of Health; and Department of Health & Human Services. The current study was funded by the Canadian Institutes of Health Research and BC Lung Association. The authors reported having no relevant disclosures.
SOURCE: Leitao Filho SF et al. Chest. 2020 May 18. doi: 10.1016/j.chest.2020.04.058.
Among patients with COPD, the presence of hypogammaglobulinemia confers a nearly 30% increased risk of hospitalization, results from a pooled analysis of four studies showed.
“Mechanistic studies are still warranted to better elucidate how IgG and other immunoglobulins, in particular IgA, may contribute to the local airway host defense,” researchers led by Fernando Sergio Leitao Filho, MD, PhD, wrote in a study published in Chest (2020 May 18. doi: 10.1016/j.chest.2020.04.058). “Nevertheless, our results raise the possibility that, in select COPD patients, IgG replacement therapy may be effective in reducing the risk of COPD hospitalizations. Given the growing rate of COPD hospitalization in the U.S. and elsewhere, there is a pressing need for a large well-designed trial to test this hypothesis.”
In an effort to evaluate the effect of IgG levels on the cumulative incidence of COPD hospitalizations, Dr. Leitao Filho, of the University of British Columbia, Vancouver, and colleagues drew from 2,259 patients who participated in four different trials: Azithromycin for Prevention of Exacerbations of COPD (MACRO), Simvastatin for the Prevention of Exacerbations in Moderate and Severe COPD (STATCOPE), the Long-Term Oxygen Treatment Trial (LOTT), and COPD Activity: Serotonin Transporter, Cytokines and Depression (CASCADE). The mean baseline age of study participants was 66 years, and 641 (28.4%) had hypogammaglobulinemia, which was defined as having a serum IgG levels of less than 7.0 g/L, while the remainder had normal IgG levels.
The pooled meta-analysis, which is believed to be the largest of its kind, revealed that the presence of hypogammaglobulinemia was associated with an incidence of COPD hospitalizations that was 1.29-fold higher than that observed among participants who had normal IgG levels (P = .01). The incidence was even higher among patients with prior COPD admissions (pooled subdistribution hazard ratio, 1.58; P < .01), yet the risk of COPD admissions was similar between IgG groups in patients with no prior hospitalizations (pooled SHR, 1.15; P = .34). Patients with hypogammaglobulinemia also showed significantly higher rates of COPD hospitalizations per person-year, compared with their counterparts who had normal IgG levels (0.48 vs. 0.29, respectively; P < .001.)
The authors acknowledged certain limitations of the study, including the fact that they measured serum IgG levels only at baseline “when participants were clinically stable; thus, the variability of IgG levels in a given individual over time and during the course of an AECOPD [severe acute exacerbation of COPD] is uncertain. Secondly, clinical data on corticosteroid use (formulations, dose, and length of use) were not readily available. However, systemic steroid use (one or more courses due to AECOPD prior to study entry) was accounted for in our analyses.”
The MACRO, STATCOPE, LOTT trials, and the CASCADE cohort were supported by the National Heart, Lung, and Blood Institute; National Institutes of Health; and Department of Health & Human Services. The current study was funded by the Canadian Institutes of Health Research and BC Lung Association. The authors reported having no relevant disclosures.
SOURCE: Leitao Filho SF et al. Chest. 2020 May 18. doi: 10.1016/j.chest.2020.04.058.
Among patients with COPD, the presence of hypogammaglobulinemia confers a nearly 30% increased risk of hospitalization, results from a pooled analysis of four studies showed.
“Mechanistic studies are still warranted to better elucidate how IgG and other immunoglobulins, in particular IgA, may contribute to the local airway host defense,” researchers led by Fernando Sergio Leitao Filho, MD, PhD, wrote in a study published in Chest (2020 May 18. doi: 10.1016/j.chest.2020.04.058). “Nevertheless, our results raise the possibility that, in select COPD patients, IgG replacement therapy may be effective in reducing the risk of COPD hospitalizations. Given the growing rate of COPD hospitalization in the U.S. and elsewhere, there is a pressing need for a large well-designed trial to test this hypothesis.”
In an effort to evaluate the effect of IgG levels on the cumulative incidence of COPD hospitalizations, Dr. Leitao Filho, of the University of British Columbia, Vancouver, and colleagues drew from 2,259 patients who participated in four different trials: Azithromycin for Prevention of Exacerbations of COPD (MACRO), Simvastatin for the Prevention of Exacerbations in Moderate and Severe COPD (STATCOPE), the Long-Term Oxygen Treatment Trial (LOTT), and COPD Activity: Serotonin Transporter, Cytokines and Depression (CASCADE). The mean baseline age of study participants was 66 years, and 641 (28.4%) had hypogammaglobulinemia, which was defined as having a serum IgG levels of less than 7.0 g/L, while the remainder had normal IgG levels.
The pooled meta-analysis, which is believed to be the largest of its kind, revealed that the presence of hypogammaglobulinemia was associated with an incidence of COPD hospitalizations that was 1.29-fold higher than that observed among participants who had normal IgG levels (P = .01). The incidence was even higher among patients with prior COPD admissions (pooled subdistribution hazard ratio, 1.58; P < .01), yet the risk of COPD admissions was similar between IgG groups in patients with no prior hospitalizations (pooled SHR, 1.15; P = .34). Patients with hypogammaglobulinemia also showed significantly higher rates of COPD hospitalizations per person-year, compared with their counterparts who had normal IgG levels (0.48 vs. 0.29, respectively; P < .001.)
The authors acknowledged certain limitations of the study, including the fact that they measured serum IgG levels only at baseline “when participants were clinically stable; thus, the variability of IgG levels in a given individual over time and during the course of an AECOPD [severe acute exacerbation of COPD] is uncertain. Secondly, clinical data on corticosteroid use (formulations, dose, and length of use) were not readily available. However, systemic steroid use (one or more courses due to AECOPD prior to study entry) was accounted for in our analyses.”
The MACRO, STATCOPE, LOTT trials, and the CASCADE cohort were supported by the National Heart, Lung, and Blood Institute; National Institutes of Health; and Department of Health & Human Services. The current study was funded by the Canadian Institutes of Health Research and BC Lung Association. The authors reported having no relevant disclosures.
SOURCE: Leitao Filho SF et al. Chest. 2020 May 18. doi: 10.1016/j.chest.2020.04.058.
FROM CHEST
Masks, fear, and loss of connection in the era of COVID-19
Over the din of the negative pressure machine, I shouted goodbye to my patient and zipped my way out of one of the little plastic enclosures in our ED and carefully shed my gloves, gown, and face shield, leaving on my precious mask. I discarded the rest with disgust and a bit of fear. I thought, “This is a whole new world, and I hate it.”
I feel as if I am constantly battling the fear of dying from COVID-19 but am doing the best I can, given the circumstances at hand. I have the proper equipment and use it well. My work still brings meaning: I serve those in need without hesitation. The problem is that deep feeling of connection with patients, which is such an important part of this work, feels like fraying threads moving further apart because of the havoc this virus has wrought. A few weeks ago, the intricate fabric of what it is to be human connected me to patients through the basics: touch, facial expressions, a physical proximity, and openhearted, honest dialogue. Much of that’s gone, and while I can carry on, I will surely burn out if I can’t figure out how to get at least some of that connection back.
Overwhelmed by the amount of information I need to process daily, I had not been thinking about the interpersonal side of the pandemic for the first weeks. I felt it leaving the ED that morning and later that day, and I felt it again with Ms. Z, who was not even suspected of having COVID. She is a 62-year-old I interviewed with the help of a translator phone. At the end of our encounter, she said “But doctor, will you make my tumor go away?” From across the room, I said, “I will try.” I saw her eyes dampen as I made a hasty exit, following protocol to limit time in the room of all patients.
Typically, leaving a patient’s room, I would feel a fullness associated with a sense of meaning. How did I feel after that? In that moment, mostly ashamed at my lack of compassion during my time with Ms. Z. Then, with further reflection, tense from all things COVID-19! Having an amped-up sympathetic nervous system is understandable, but it’s not where we want to be for our compassion to flow.
We connect best when our parasympathetic nervous system is predominant. So much of the stimuli we need to activate that part of the nervous system is gone. There is a virtuous cycle, much of it unconscious, where something positive leads to more positivity, which is crucial to meaningful patient encounters. We read each other’s facial expressions, hear the tone of voice, and as we pick up subtle cues from our patient, our nervous system is further engaged and our hearts opened.
The specter of COVID-19 has us battling a negative spiral of stress and fear. For the most part, I try to keep that from consuming me, but it clearly saps my energy during encounters. In the same way we need to marshal our resources to battle both the stress and the disease itself, we need to actively engage pro-social elements of providing care to maintain our compassion. Clearly, I needed a more concerted effort to kick start this virtuous cycle of compassion.
My next patient was Ms. J., a 55-year-old with advanced chronic obstructive pulmonary disease (COPD) who came in the night before with shortness of breath. Her slight frame shook from coughing as I entered the room. I did not think she had COVID-19, but we were ruling it out.
We reviewed how she felt since admission, and I performed a hasty exam and stepped back across the room. She coughed again and said, “I feel so weak, and the world feels so crazy; tell it to me straight.” Then looking in my eyes, “I am going to make it, doc?”
I took my cue from her; I walked back to the bedside, placed a gloved hand on her shoulder and with the other, I took her hand. I bent forward just a little. Making eye contact and attempting a comforting tone of voice, I said, “Everyone is a little scared, including me. We need each other more than ever these days. We will do our best for you. That means thoughtful medical care and a whole lot of love! And, truly, I don’t think you are dying; this is just one of your COPD flares.”
“God bless you!” she said, squeezing my hand as a tear rolled down her cheek.
“Bless you, too. We all need blessing with this madness going on,” I replied. Despite the mask, I am sure she saw the smile in my eyes. “Thanks for being the beautiful person you are and opening up to me. That’s the way we will make it through this. I will see you tomorrow.” Backing away, hands together in prayer, I gave a little bow and left the room.
With Ms. J.’s help, I began to figure it out. To tackle the stress of COVID, we need to be very direct – almost to the point of exaggeration – to make sure our words and actions convey what we need to express. William James, the father of psychology, believed that if you force a smile, your emotions would follow. The neural pathways could work backward in that way. He said, “If you want a quality, act as if you have it.” The modern translation would be, “Fake it ’til you make it.’ ” You may be feeling stressed, but with a deep breath and a moment’s reflection on the suffering of that patient you are about to see, you can turn the tide on anxiety and give those under your care what they need.
These are unprecedented times; anxiety abounds. While we can aspire to positivity, there are times when we simply can’t muster showing it. Alternatively, as I experienced with Ms. J., honesty and vulnerability can open the door to meaningful connection. This can be quite powerful when we, as physicians, open up to our patients.
People are yearning for deep connection, and we should attempt to deliver it with:
- Touch (as we can) to convey connection.
- Body language that adds emphasis to our message and our emotions that may go above and beyond what we are used to.
- Tone of voice that enhances our words.
- Talk that emphasizes the big stuff, such as love, fear, connection and community
With gloves, masks, distance, and fear between and us and our patients, we need to actively engage our pro-social tools to turn the negative spiral of fear into the virtuous cycle of positive emotions that promotes healing of our patients and emotional engagement for those providing their care.
Dr. Hass was trained in family medicine at University of California, San Francisco, after receiving his medical degree from the McGill University faculty of medicine, Montreal. He works as a hospitalist with Sutter Health in Oakland, Calif. He is an adviser on health and health care for the Greater Good Science Center at UC Berkeley and clinical faculty at UCSF School of Medicine. This article appeared initially at The Hospital Leader, the official blog of SHM.
Over the din of the negative pressure machine, I shouted goodbye to my patient and zipped my way out of one of the little plastic enclosures in our ED and carefully shed my gloves, gown, and face shield, leaving on my precious mask. I discarded the rest with disgust and a bit of fear. I thought, “This is a whole new world, and I hate it.”
I feel as if I am constantly battling the fear of dying from COVID-19 but am doing the best I can, given the circumstances at hand. I have the proper equipment and use it well. My work still brings meaning: I serve those in need without hesitation. The problem is that deep feeling of connection with patients, which is such an important part of this work, feels like fraying threads moving further apart because of the havoc this virus has wrought. A few weeks ago, the intricate fabric of what it is to be human connected me to patients through the basics: touch, facial expressions, a physical proximity, and openhearted, honest dialogue. Much of that’s gone, and while I can carry on, I will surely burn out if I can’t figure out how to get at least some of that connection back.
Overwhelmed by the amount of information I need to process daily, I had not been thinking about the interpersonal side of the pandemic for the first weeks. I felt it leaving the ED that morning and later that day, and I felt it again with Ms. Z, who was not even suspected of having COVID. She is a 62-year-old I interviewed with the help of a translator phone. At the end of our encounter, she said “But doctor, will you make my tumor go away?” From across the room, I said, “I will try.” I saw her eyes dampen as I made a hasty exit, following protocol to limit time in the room of all patients.
Typically, leaving a patient’s room, I would feel a fullness associated with a sense of meaning. How did I feel after that? In that moment, mostly ashamed at my lack of compassion during my time with Ms. Z. Then, with further reflection, tense from all things COVID-19! Having an amped-up sympathetic nervous system is understandable, but it’s not where we want to be for our compassion to flow.
We connect best when our parasympathetic nervous system is predominant. So much of the stimuli we need to activate that part of the nervous system is gone. There is a virtuous cycle, much of it unconscious, where something positive leads to more positivity, which is crucial to meaningful patient encounters. We read each other’s facial expressions, hear the tone of voice, and as we pick up subtle cues from our patient, our nervous system is further engaged and our hearts opened.
The specter of COVID-19 has us battling a negative spiral of stress and fear. For the most part, I try to keep that from consuming me, but it clearly saps my energy during encounters. In the same way we need to marshal our resources to battle both the stress and the disease itself, we need to actively engage pro-social elements of providing care to maintain our compassion. Clearly, I needed a more concerted effort to kick start this virtuous cycle of compassion.
My next patient was Ms. J., a 55-year-old with advanced chronic obstructive pulmonary disease (COPD) who came in the night before with shortness of breath. Her slight frame shook from coughing as I entered the room. I did not think she had COVID-19, but we were ruling it out.
We reviewed how she felt since admission, and I performed a hasty exam and stepped back across the room. She coughed again and said, “I feel so weak, and the world feels so crazy; tell it to me straight.” Then looking in my eyes, “I am going to make it, doc?”
I took my cue from her; I walked back to the bedside, placed a gloved hand on her shoulder and with the other, I took her hand. I bent forward just a little. Making eye contact and attempting a comforting tone of voice, I said, “Everyone is a little scared, including me. We need each other more than ever these days. We will do our best for you. That means thoughtful medical care and a whole lot of love! And, truly, I don’t think you are dying; this is just one of your COPD flares.”
“God bless you!” she said, squeezing my hand as a tear rolled down her cheek.
“Bless you, too. We all need blessing with this madness going on,” I replied. Despite the mask, I am sure she saw the smile in my eyes. “Thanks for being the beautiful person you are and opening up to me. That’s the way we will make it through this. I will see you tomorrow.” Backing away, hands together in prayer, I gave a little bow and left the room.
With Ms. J.’s help, I began to figure it out. To tackle the stress of COVID, we need to be very direct – almost to the point of exaggeration – to make sure our words and actions convey what we need to express. William James, the father of psychology, believed that if you force a smile, your emotions would follow. The neural pathways could work backward in that way. He said, “If you want a quality, act as if you have it.” The modern translation would be, “Fake it ’til you make it.’ ” You may be feeling stressed, but with a deep breath and a moment’s reflection on the suffering of that patient you are about to see, you can turn the tide on anxiety and give those under your care what they need.
These are unprecedented times; anxiety abounds. While we can aspire to positivity, there are times when we simply can’t muster showing it. Alternatively, as I experienced with Ms. J., honesty and vulnerability can open the door to meaningful connection. This can be quite powerful when we, as physicians, open up to our patients.
People are yearning for deep connection, and we should attempt to deliver it with:
- Touch (as we can) to convey connection.
- Body language that adds emphasis to our message and our emotions that may go above and beyond what we are used to.
- Tone of voice that enhances our words.
- Talk that emphasizes the big stuff, such as love, fear, connection and community
With gloves, masks, distance, and fear between and us and our patients, we need to actively engage our pro-social tools to turn the negative spiral of fear into the virtuous cycle of positive emotions that promotes healing of our patients and emotional engagement for those providing their care.
Dr. Hass was trained in family medicine at University of California, San Francisco, after receiving his medical degree from the McGill University faculty of medicine, Montreal. He works as a hospitalist with Sutter Health in Oakland, Calif. He is an adviser on health and health care for the Greater Good Science Center at UC Berkeley and clinical faculty at UCSF School of Medicine. This article appeared initially at The Hospital Leader, the official blog of SHM.
Over the din of the negative pressure machine, I shouted goodbye to my patient and zipped my way out of one of the little plastic enclosures in our ED and carefully shed my gloves, gown, and face shield, leaving on my precious mask. I discarded the rest with disgust and a bit of fear. I thought, “This is a whole new world, and I hate it.”
I feel as if I am constantly battling the fear of dying from COVID-19 but am doing the best I can, given the circumstances at hand. I have the proper equipment and use it well. My work still brings meaning: I serve those in need without hesitation. The problem is that deep feeling of connection with patients, which is such an important part of this work, feels like fraying threads moving further apart because of the havoc this virus has wrought. A few weeks ago, the intricate fabric of what it is to be human connected me to patients through the basics: touch, facial expressions, a physical proximity, and openhearted, honest dialogue. Much of that’s gone, and while I can carry on, I will surely burn out if I can’t figure out how to get at least some of that connection back.
Overwhelmed by the amount of information I need to process daily, I had not been thinking about the interpersonal side of the pandemic for the first weeks. I felt it leaving the ED that morning and later that day, and I felt it again with Ms. Z, who was not even suspected of having COVID. She is a 62-year-old I interviewed with the help of a translator phone. At the end of our encounter, she said “But doctor, will you make my tumor go away?” From across the room, I said, “I will try.” I saw her eyes dampen as I made a hasty exit, following protocol to limit time in the room of all patients.
Typically, leaving a patient’s room, I would feel a fullness associated with a sense of meaning. How did I feel after that? In that moment, mostly ashamed at my lack of compassion during my time with Ms. Z. Then, with further reflection, tense from all things COVID-19! Having an amped-up sympathetic nervous system is understandable, but it’s not where we want to be for our compassion to flow.
We connect best when our parasympathetic nervous system is predominant. So much of the stimuli we need to activate that part of the nervous system is gone. There is a virtuous cycle, much of it unconscious, where something positive leads to more positivity, which is crucial to meaningful patient encounters. We read each other’s facial expressions, hear the tone of voice, and as we pick up subtle cues from our patient, our nervous system is further engaged and our hearts opened.
The specter of COVID-19 has us battling a negative spiral of stress and fear. For the most part, I try to keep that from consuming me, but it clearly saps my energy during encounters. In the same way we need to marshal our resources to battle both the stress and the disease itself, we need to actively engage pro-social elements of providing care to maintain our compassion. Clearly, I needed a more concerted effort to kick start this virtuous cycle of compassion.
My next patient was Ms. J., a 55-year-old with advanced chronic obstructive pulmonary disease (COPD) who came in the night before with shortness of breath. Her slight frame shook from coughing as I entered the room. I did not think she had COVID-19, but we were ruling it out.
We reviewed how she felt since admission, and I performed a hasty exam and stepped back across the room. She coughed again and said, “I feel so weak, and the world feels so crazy; tell it to me straight.” Then looking in my eyes, “I am going to make it, doc?”
I took my cue from her; I walked back to the bedside, placed a gloved hand on her shoulder and with the other, I took her hand. I bent forward just a little. Making eye contact and attempting a comforting tone of voice, I said, “Everyone is a little scared, including me. We need each other more than ever these days. We will do our best for you. That means thoughtful medical care and a whole lot of love! And, truly, I don’t think you are dying; this is just one of your COPD flares.”
“God bless you!” she said, squeezing my hand as a tear rolled down her cheek.
“Bless you, too. We all need blessing with this madness going on,” I replied. Despite the mask, I am sure she saw the smile in my eyes. “Thanks for being the beautiful person you are and opening up to me. That’s the way we will make it through this. I will see you tomorrow.” Backing away, hands together in prayer, I gave a little bow and left the room.
With Ms. J.’s help, I began to figure it out. To tackle the stress of COVID, we need to be very direct – almost to the point of exaggeration – to make sure our words and actions convey what we need to express. William James, the father of psychology, believed that if you force a smile, your emotions would follow. The neural pathways could work backward in that way. He said, “If you want a quality, act as if you have it.” The modern translation would be, “Fake it ’til you make it.’ ” You may be feeling stressed, but with a deep breath and a moment’s reflection on the suffering of that patient you are about to see, you can turn the tide on anxiety and give those under your care what they need.
These are unprecedented times; anxiety abounds. While we can aspire to positivity, there are times when we simply can’t muster showing it. Alternatively, as I experienced with Ms. J., honesty and vulnerability can open the door to meaningful connection. This can be quite powerful when we, as physicians, open up to our patients.
People are yearning for deep connection, and we should attempt to deliver it with:
- Touch (as we can) to convey connection.
- Body language that adds emphasis to our message and our emotions that may go above and beyond what we are used to.
- Tone of voice that enhances our words.
- Talk that emphasizes the big stuff, such as love, fear, connection and community
With gloves, masks, distance, and fear between and us and our patients, we need to actively engage our pro-social tools to turn the negative spiral of fear into the virtuous cycle of positive emotions that promotes healing of our patients and emotional engagement for those providing their care.
Dr. Hass was trained in family medicine at University of California, San Francisco, after receiving his medical degree from the McGill University faculty of medicine, Montreal. He works as a hospitalist with Sutter Health in Oakland, Calif. He is an adviser on health and health care for the Greater Good Science Center at UC Berkeley and clinical faculty at UCSF School of Medicine. This article appeared initially at The Hospital Leader, the official blog of SHM.







