User login
PHS Message to Military Health Providers: Join Us
NATIONAL HARBOR, MD—As the Military Health System is undergoing significant structural and eventually manpower changes, ADM Brett P. Giroir, MD, the Assistant Secretary for Health in the US Department of Health and Human Services (HHS) and the US Food and Drug Administration acting commissioner, had one message: Come and join us. “Recruitment and retention are our top priorities,” ADM Giroir told the largely military health care provider audience, “If there is downsizing of any of the military health [system], we want you. If you touch health in any way…we need great people who are committed to our national goals in the Commissioned Corps.”
Not long ago, the US Public Health Service (PHS) was facing its own pressures to either reduce its workforce or to eliminate the PHS Commissioned Corps altogether. “The Corps’ mission assignments and functions have not evolved in step with the public health needs of the nation,” argued the fiscal year 2019 Office of Management and Budget, Budget of The U.S. Government. “It is time for that to change. HHS is committed to providing the best public health services and emergency response at the lowest cost and is undertaking a comprehensive look at how the Corps is structured.”
In response, PHS has undertaken a top-to-bottom audit and reevaluation of its mission, ADM Giroir noted, with the goal of defining the role for the PHS in the 21st century and beyond. As a result, the PHS recently completed the development of a modernization plan. The plan entails specifically managing the force to meet mission requirements, developing and training a Ready Reserve force, enhancing training and professional development for the Commissioned Corps, and updating and improving PHS systems and processes.
As a part of the modernization plan, ADM Giroir outlined projected growth plans for the Corps: an increase from the 6,400 regular Corps officers in FY 2018 to 7,725 by FY 2024 with an additional 2,500 Ready Reserve officers, to “minimally meet the mission requirements as we understand it,” ADM Giroir noted.
According to ADM Giroir, the goals for the Ready Reserve are an essential component in the PHS mission to meet any regional, national, or global public health emergency. The Ready Reserve would be a well-trained public health force that would be ready to deploy quickly. Whereas in the past, PHS officer deployments and specialties were tailored to the needs of the agencies in which they are embedded, this force would be more aligned with the needs for a rapid public health emergency response and would include specialized providers. In that context health care providers with military rapid response training would be highly valued.
Although the PHS has outlined its modernization plan, no budget has been allocated for it. Moreover, as ADM Giroir, has noted, PHS still remains dependent on the budgets of the embedding agencies to pay for the Commissioned Corps. “Right now our force structure is really determined by what federal agencies need,” he noted.
Currently, there are bills pending in both the House of Representatives and the Senate to codify the modernization effort.
NATIONAL HARBOR, MD—As the Military Health System is undergoing significant structural and eventually manpower changes, ADM Brett P. Giroir, MD, the Assistant Secretary for Health in the US Department of Health and Human Services (HHS) and the US Food and Drug Administration acting commissioner, had one message: Come and join us. “Recruitment and retention are our top priorities,” ADM Giroir told the largely military health care provider audience, “If there is downsizing of any of the military health [system], we want you. If you touch health in any way…we need great people who are committed to our national goals in the Commissioned Corps.”
Not long ago, the US Public Health Service (PHS) was facing its own pressures to either reduce its workforce or to eliminate the PHS Commissioned Corps altogether. “The Corps’ mission assignments and functions have not evolved in step with the public health needs of the nation,” argued the fiscal year 2019 Office of Management and Budget, Budget of The U.S. Government. “It is time for that to change. HHS is committed to providing the best public health services and emergency response at the lowest cost and is undertaking a comprehensive look at how the Corps is structured.”
In response, PHS has undertaken a top-to-bottom audit and reevaluation of its mission, ADM Giroir noted, with the goal of defining the role for the PHS in the 21st century and beyond. As a result, the PHS recently completed the development of a modernization plan. The plan entails specifically managing the force to meet mission requirements, developing and training a Ready Reserve force, enhancing training and professional development for the Commissioned Corps, and updating and improving PHS systems and processes.
As a part of the modernization plan, ADM Giroir outlined projected growth plans for the Corps: an increase from the 6,400 regular Corps officers in FY 2018 to 7,725 by FY 2024 with an additional 2,500 Ready Reserve officers, to “minimally meet the mission requirements as we understand it,” ADM Giroir noted.
According to ADM Giroir, the goals for the Ready Reserve are an essential component in the PHS mission to meet any regional, national, or global public health emergency. The Ready Reserve would be a well-trained public health force that would be ready to deploy quickly. Whereas in the past, PHS officer deployments and specialties were tailored to the needs of the agencies in which they are embedded, this force would be more aligned with the needs for a rapid public health emergency response and would include specialized providers. In that context health care providers with military rapid response training would be highly valued.
Although the PHS has outlined its modernization plan, no budget has been allocated for it. Moreover, as ADM Giroir, has noted, PHS still remains dependent on the budgets of the embedding agencies to pay for the Commissioned Corps. “Right now our force structure is really determined by what federal agencies need,” he noted.
Currently, there are bills pending in both the House of Representatives and the Senate to codify the modernization effort.
NATIONAL HARBOR, MD—As the Military Health System is undergoing significant structural and eventually manpower changes, ADM Brett P. Giroir, MD, the Assistant Secretary for Health in the US Department of Health and Human Services (HHS) and the US Food and Drug Administration acting commissioner, had one message: Come and join us. “Recruitment and retention are our top priorities,” ADM Giroir told the largely military health care provider audience, “If there is downsizing of any of the military health [system], we want you. If you touch health in any way…we need great people who are committed to our national goals in the Commissioned Corps.”
Not long ago, the US Public Health Service (PHS) was facing its own pressures to either reduce its workforce or to eliminate the PHS Commissioned Corps altogether. “The Corps’ mission assignments and functions have not evolved in step with the public health needs of the nation,” argued the fiscal year 2019 Office of Management and Budget, Budget of The U.S. Government. “It is time for that to change. HHS is committed to providing the best public health services and emergency response at the lowest cost and is undertaking a comprehensive look at how the Corps is structured.”
In response, PHS has undertaken a top-to-bottom audit and reevaluation of its mission, ADM Giroir noted, with the goal of defining the role for the PHS in the 21st century and beyond. As a result, the PHS recently completed the development of a modernization plan. The plan entails specifically managing the force to meet mission requirements, developing and training a Ready Reserve force, enhancing training and professional development for the Commissioned Corps, and updating and improving PHS systems and processes.
As a part of the modernization plan, ADM Giroir outlined projected growth plans for the Corps: an increase from the 6,400 regular Corps officers in FY 2018 to 7,725 by FY 2024 with an additional 2,500 Ready Reserve officers, to “minimally meet the mission requirements as we understand it,” ADM Giroir noted.
According to ADM Giroir, the goals for the Ready Reserve are an essential component in the PHS mission to meet any regional, national, or global public health emergency. The Ready Reserve would be a well-trained public health force that would be ready to deploy quickly. Whereas in the past, PHS officer deployments and specialties were tailored to the needs of the agencies in which they are embedded, this force would be more aligned with the needs for a rapid public health emergency response and would include specialized providers. In that context health care providers with military rapid response training would be highly valued.
Although the PHS has outlined its modernization plan, no budget has been allocated for it. Moreover, as ADM Giroir, has noted, PHS still remains dependent on the budgets of the embedding agencies to pay for the Commissioned Corps. “Right now our force structure is really determined by what federal agencies need,” he noted.
Currently, there are bills pending in both the House of Representatives and the Senate to codify the modernization effort.
Millennials in Medicine: Cross-Trained Physicians Not Valued in Medical Marketplace
Millennials, defined as those born between 1981 and 1996, currently comprise 15% of all active physicians in the US.1,2 A recent survey found that nearly 4 of 5 US millennial physicians have a desire for cross-sectional work in areas beyond patient care, such as academic research, health care consulting, entrepreneurship, and health care administration.3
For employers and educators, a better understanding of these preferences, through consideration of the unique education and skill set of the millennial physician workforce, may lead to more effective recruitment of young physicians and improved health systems, avoiding a mismatch between health care provider skills and available jobs that can be costly for both employers and employees.4
This article describes how US millennial physicians are choosing to cross-train (obtaining multiple degrees and/or completing combined medical residency training) throughout undergraduate, medical, and graduate medical education. We also outline ways in which the current physician marketplace may not match the skills of this population and suggest some ways that health care organizations could capitalize on this trend toward more cross-trained personnel in order to effectively recruit and retain the next generation of physicians.
Millennial Education
Undergraduates
The number of interdisciplinary undergraduate majors increased by almost 250% from 1975 to 2000.5 In 2010, nearly 20% of US college students graduated with 2 majors, representing a 70% increase in double majors between 2001 and 2011.6,7 One emerging category of interdisciplinary majors in US colleges is health humanities programs, which have quadrupled since 2000.8
Medical school applicants and matriculants reflect this trend. Whereas in 1994, only 19% of applicants to medical school held nonscience degrees, about one-third of applicants now hold such degrees.9,10 We have found no aggregated data on double majors entering US medical schools, but public class profiles suggest that medical school matriculants mirror their undergraduate counterparts in their tendency to hold double majors. In 2016, for example, 15% of the incoming class at the University of Michigan Medical School was composed of double majors, increasing to over 25% in 2017.11
Medical Students
Early dual-degree programs in undergraduate medical training were reserved for MD/PhD programs.12 Most US MD/PhD programs (90 out of 151) now offer doctorates in social sciences, humanities, or other nontraditional fields of graduate medical study, reflecting a shift in interests of those seeking dual-degree training in undergraduate medical education.13 While only 3 MD/PhD programs in the 1970s included trainees in the social sciences, 17 such programs exist today.14
Interest in dual-degree programs offering master’s level study has also increased over the past decade. In 2017, 87 medical schools offered programs for students to pursue a master of public health (MPH) and 41 offered master of science degrees in various fields, up from 52 and 37 institutions, respectively in 2006.15 The number of schools offering combined training in nonscience fields has also grown, with 63 institutions now offering a master of business administration (MBA), nearly double the number offered in 2006.15 At some institutions more than 20% of students are earning a master’s degree or doctorate in addition to their MD degree.16
Residents
The authors found no documentation of US residency training programs, outside of those in the specialty of preventive medicine, providing trainees with formal opportunities to obtain an MBA or MPH prior to 2001.17 However, of the 510 internal medicine residency programs listed on the American Medical Association residency and fellowship database (freida.ama-assn.org), 45 identified as having established a pathway for residents to pursue an MBA, MPH, or PhD during residency.18
Over the past 20 years, combined residency programs have increased 49% (from 128 to 191), which is triple the 16% rate (1,350 to 1,562) of increase in programs in internal medicine, pediatrics, family medicine, psychiatry, and emergency medicine.19,20 A 2009 moratorium on the creation of new combined residency programs in psychiatry and neurology was lifted in 2016and is likely to increase the rate of total combined programs.21
The Table shows the number of categorical and combined residency programs available in 1996 and in 2016. Over 2 decades, 17 new specialty combinations became available for residency training. While there were no combined training programs within these 17 new combinations in 1996,there were 66 programs with these combinations in 2016.19,20
Although surgical specialties are notably absent from the list of combined residency options, likely due to the duration of surgical training, some surgical training programs do offer pathways that culminate in combined degrees,22 and a high number of surgery program directors agree that residents should receive formal training in business and practice management.23
The Medical Job Market
Although today’s young physicians are cross-trained in multiple disciplines, the current job market may not directly match these skill sets. Of the 7,235 jobs listed by the New England Journal of Medicine (NEJM) career center (www.nejmcareercenter.org/jobs), only 54 were targeted at those with combined training, the majority of which were aimed at those trained in internal medicine/pediatrics. Of the combined specialties in the Table, formal positions were listed for only 6.24 A search of nearly 1,500 federal medical positions on USAJOBS (www.usajobs.gov) found only 4 jobs that combined specialties, all restricted to internal medicine/pediatrics.25 When searching for jobs containing the terms MBA, MPH, and public health there were only 8 such positions on NEJM and 7 on USAJOBS.24,25 Although the totality of the medical marketplace may not be best encompassed by these sources, the authors believe NEJM and USAJOBS are somewhat representative of the opportunities for physicians in the US.
Medical jobs tailored to cross-trained physicians do not appear to have kept pace with the numbers of such specialists currently in medical school and residency training. Though millennials are cross-training in increasing numbers, we surmise that they are not doing so as a direct result of the job market.
Future Medicine
Regardless of the mismatch between cross-trained physicians and the current job market, millennials may be well suited for future health systems. In 2001, the National Academies of Sciences, Engineering and Medicine (NASEM) called for increasing interdisciplinary training and improving cross-functional team performance as a major goal for health care providers in twenty-first century health systems.26 NASEM also recommended that academic medical centers develop medical leaders who can manage systems changes required to enhance health, a proposal supported by the fact that hospitals with medically trained CEOs outperform others.27,28
Public Health 3.0, a federal initiative to improve and integrate public health efforts, also emphasizes cross-disciplinary teams and cross-sector partnerships,29 while the Centers for Medicare and Medicaid Services (CMS) has incentivized the development of interprofessional health care teams.30 While cross-training does not automatically connote interdisciplinary training, we believe that cross-training may reveal or develop an interdisciplinary mind-set that may support and embrace interdisciplinary performance. Finally, the US Department of Health and Human Services’ (HHS) Strategic Goals emphasize integrated care for vulnerable populations, something that cross-trained physicians may be especially poised to accomplish.31
A Path Forward
The education, training, and priorities of young physicians demonstrates career interests that diverge from mainstream, traditional options. Data provided herein describe the increasing rates at which millennial physicians are cross-training and have suggested that the current marketplace may not match the interests of this population. The ultimate question is where such cross-trained physicians fit into today’s (or tomorrow’s) health system?
It may be easiest to deploy cross-trained physicians in their respective clinical departments (eg, having a physician trained in internal medicine and pediatrics perform clinical duties in both a medicine department and a pediatrics department). But < 40% of dual-boarded physicians practice both specialties in which they’re trained, so other opportunities should be pursued.32,33 One strategy may be to embrace the promise of interdisciplinary care, as supported by Public Health 3.0 and NASEM.26,29 Our evidence may demonstrate that the interdisciplinary mind-set may be more readily evident in the millennial generation, and that this mind-set may improve interdisciplinary care.
As health is impacted both by direct clinical care as well as programs designed to address population health, cross-trained physicians may be better equipped to integrate aspects of clinical care spanning a variety of clinical fields as well as orchestrating programs designed to improve health at the population level. This mind-set may be best captured by organizations willing to adapt their medical positions to emphasize multidisciplinary training, skills, and capabilities. For example, a physician trained in internal medicine and psychiatry may have the unique training and skill-set to establish an integrated behavioral health clinic that crosses boundaries between traditional departments, emphasizing the whole health of the clinic’s population and not simply focusing on providing services of a particular specialty. Hiring cross-trained physicians throughout such a clinic may benefit the operations of the clinic and improve not only the services provided, but ultimately, the health of that clinic’s patients. By embracing cross-trained physicians, health care organizations and educators may better meet the needs of their employees, likely resulting in a more cost-effective investment for employers, employees, and the health system as a whole.4 Additionally, patient health may also improve.
There is evidence that cross-trained physicians are already likely to hold leadership positions compared with their categorically-trained counterparts, and this may reflect the benefits of an interdisciplinary mind-set.33 Perhaps a cross-trained physician is more likely to see beyond standard, specialty-based institutional barriers and develop processes and programs designed for overall patient benefit. Leadership is a skill that many millennials clearly wish to enhance throughout their career.34 Recruiting cross-trained physicians for leadership positions may reveal synergies between such training and an ability to lead health care organizations into the future.
Many millennial physicians are bringing a new set of skills into the medical marketplace. Health organizations should identify ways to recruit for these skills and deploy them within their systems in order to have more dedicated, engaged employees, more effective health systems, and ultimately, healthier patients.
Acknowledgments
Data from this analysis were presented at the 10th Consortium of Universities for Global Health conference in 2019.35
1. Dimock M. Defining generations: where millennials end and generation Z begins. http://www.pewresearch.org/fact-tank/2018/03/01/defining-generations-where-millennials-end-and-post-millennials-begin/. Published January 17, 2019. Accessed November 7, 2019.
2. IHS Inc. The complexities of physician supply and demand: projections from 2014 to 2025. Final report. https://www.modernhealthcare.com/assets/pdf/CH10888123.pdf. Published April 5, 2016. Accessed November 7, 2019.
3. Miller RN. Millennial physicians sound off on state of medicine today. https://wire.ama-assn.org/life-career/millennial-physicians-sound-state-medicine-today. Published March 27, 2017. Accessed November 7, 2019.
4. World Economic Forum. Matching skills and labour market needs: building social partnerships for better skills and better jobs. http://www3.weforum.org/docs/GAC/2014/WEF_GAC_Employment_MatchingSkillsLabourMarket_Report_2014.pdf. Published January 2014. Accessed November 7, 2019.
5. Brint SG, Turk-Bicakci L, Proctor K, Murphy SP. Expanding the social frame of knowledge: interdisciplinary, degree-granting fields in American Colleges and Universities, 1975–2000. Rev High Ed. 2009;32(2):155-183.
6. National Science Foundation. National survey of college graduates. https://www.nsf.gov/statistics/srvygrads. Updated February 2019. Accessed November 7, 2019.
7. Simon CC. Major decisions. New York Times. November 2, 2012. http://www.nytimes.com/2012/11/04/education/edlife/choosing-one-college-major-out-of-hundreds.html. Accessed November 7, 2019.
8. Berry SL, Erin GL, Therese J. Health humanities baccalaureate programs in the United States. http://www.hiram.edu/wp-content/uploads/2017/09/HHBP2017.pdf. Published September 2017. Accessed November 7, 2019.
9. Sorensen NE, Jackson JR. Science majors and nonscience majors entering medical school: acceptance rates and academic performance. NACADA J. 1997;17(1):32-41.
10. Association of American Medical Colleges. Table A-17: MCAT and GPAs for applicants and matriculants to U.S. medical schools by primary undergraduate major, 2019-2020. https://www.aamc.org/download/321496/data/factstablea17.pdf. Published October 16, 2019. Accessed November 7, 2019.
11. University of Michigan Medical School. Many paths, one destination: medical school welcomes its 170th class of medical students. https://medicine.umich.edu/medschool/news/many-paths-one-destination-medical-school-welcomes-its-170th-class-medical-students. Updated July 29, 2016. Accessed November 7, 2019.
12. Harding CV, Akabas MH, Andersen OS. History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad Med. 2017; 92(10):1390-1398.
13. Association of American Medical Colleges. MD-PhD in “social sciences or humanities” and “other non-traditional fields of graduate study” - by school. https://students-residents.aamc.org/choosing-medical-career/careers-medical-research/md-phd-dual-degree-training/non-basic-science-phd-training-school/. Accessed November 8, 2019.
14. Holmes SM, Karlin J, Stonington SD, Gottheil DL. The first nationwide survey of MD-PhDs in the social sciences and humanities: training patterns and career choices. BMC Med Educ. 2017;17(1):60.
15. Association of American Medical Colleges Combined degrees and early acceptance programs. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/combined-degrees-and-early-acceptance-programs. Accessed November 8, 2019.
16. Tufts University School of Medicine. 2023 class profile. http://medicine.tufts.edu/Education/MD-Programs/Doctor-of-Medicine/Class-Profile. Published 2015. Accessed November 8, 2019.
17. Zweifler J, Evan R. Development of a residency/MPH program. Family Med. 2001;33(6):453-458.
18. American Medical Association. The AMA residency and fellowship database. http://freida.ama-assn.org/Freida. Accessed November 7, 2019.
19. National Resident Matching Program. NRMP data. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata1996.pdf. Published March 1996. Accessed November 7, 2019.
20. Brotherton SE, Etzel SI. Graduate medical education, 2016-2017. JAMA. 2017;318(23):2368-2387.
21. American Board of Psychiatry and Neurology. Update for psychiatry GME programs on combined training program accreditation/approval February 2012. https://www.umassmed.edu/globalassets/neuropsychiatry/files/combined-program-letter.pdf. Accessed November 7, 2019.
22. Massachusetts General Hospital. Surgical residency program. https://www.massgeneral.org/surgery/education/residency.aspx?id=77. Accessed November 7, 2019.
23. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
24. New England Journal of Medicine. NEJM CareerCenter. http://www.nejmcareercenter.org. Accessed November 7, 2019.
25. US Office of Personnel Management. USAJOBS. https://www.usajobs.gov. Accessed November 7, 2019.
26. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Published March 2001. Accessed November 7, 2019.
27. Kohn LT, ed; Committee on the Roles of Academic Health Centers in the 21st Century; Institute of Medicine of the National Academies. Academic Health Centers: Leading Change in the 21st Century. National Academy Press: Washington, DC; 2004.
28. Goodall AH. Physician-leaders and hospital performance: is there an association? http://ftp.iza.org/dp5830.pdf. Published July 2011. Accessed November 7, 2019.
29. US Department of Health and Human Services, Office of the Assistant Secretary for Health. Public health 3.0: a call to action to create a 21st century public health infrastructure. https://www.healthypeople.gov/sites/default/files/Public-Health-3.0-White-Paper.pdf. Accessed November 7, 2019.
30. Centers for Medicare and Medicaid Services. Health care innovation awards round one project profiles. http://innovation.cms.gov/files/x/hcia-project-profiles.pdf. Updated December 2013. Accessed November 7, 2019.
31. US Department of Health and Human Services. Strategic Objective 1.3: Improve Americans’ access to healthcare and expand choices of care and service options. https://www.hhs.gov/about/strategic-plan/strategic-goal-1/index.html#obj_1_3. Updated March 18, 2019. Accessed November 7, 2019.
32. Kessler CS, Stallings LA, Gonzalez AA, Templeman TA. Combined residency training in emergency medicine and internal medicine: an update on career outcomes and job satisfaction. Acad Emerg Med. 2009;16(9):894-899.
33. Summergrad P, Silberman E, Price LL. Practice and career outcomes of double-boarded psychiatrists. Psychosomatics. 2011;52(6):537-543.
34. Rigoni B, Adkins A. What millennials want from a new job. Harvard Business Rev. May 11, 2016. https://hbr.org/2016/05/what-millennials-want-from-a-new-job. Accessed November 7, 2019.
35. Jung P, Smith C. Medical millennials: a mismatch between training preferences and employment opportunities. Lancet Glob Health. 2019;7(suppl 1):S38.
Millennials, defined as those born between 1981 and 1996, currently comprise 15% of all active physicians in the US.1,2 A recent survey found that nearly 4 of 5 US millennial physicians have a desire for cross-sectional work in areas beyond patient care, such as academic research, health care consulting, entrepreneurship, and health care administration.3
For employers and educators, a better understanding of these preferences, through consideration of the unique education and skill set of the millennial physician workforce, may lead to more effective recruitment of young physicians and improved health systems, avoiding a mismatch between health care provider skills and available jobs that can be costly for both employers and employees.4
This article describes how US millennial physicians are choosing to cross-train (obtaining multiple degrees and/or completing combined medical residency training) throughout undergraduate, medical, and graduate medical education. We also outline ways in which the current physician marketplace may not match the skills of this population and suggest some ways that health care organizations could capitalize on this trend toward more cross-trained personnel in order to effectively recruit and retain the next generation of physicians.
Millennial Education
Undergraduates
The number of interdisciplinary undergraduate majors increased by almost 250% from 1975 to 2000.5 In 2010, nearly 20% of US college students graduated with 2 majors, representing a 70% increase in double majors between 2001 and 2011.6,7 One emerging category of interdisciplinary majors in US colleges is health humanities programs, which have quadrupled since 2000.8
Medical school applicants and matriculants reflect this trend. Whereas in 1994, only 19% of applicants to medical school held nonscience degrees, about one-third of applicants now hold such degrees.9,10 We have found no aggregated data on double majors entering US medical schools, but public class profiles suggest that medical school matriculants mirror their undergraduate counterparts in their tendency to hold double majors. In 2016, for example, 15% of the incoming class at the University of Michigan Medical School was composed of double majors, increasing to over 25% in 2017.11
Medical Students
Early dual-degree programs in undergraduate medical training were reserved for MD/PhD programs.12 Most US MD/PhD programs (90 out of 151) now offer doctorates in social sciences, humanities, or other nontraditional fields of graduate medical study, reflecting a shift in interests of those seeking dual-degree training in undergraduate medical education.13 While only 3 MD/PhD programs in the 1970s included trainees in the social sciences, 17 such programs exist today.14
Interest in dual-degree programs offering master’s level study has also increased over the past decade. In 2017, 87 medical schools offered programs for students to pursue a master of public health (MPH) and 41 offered master of science degrees in various fields, up from 52 and 37 institutions, respectively in 2006.15 The number of schools offering combined training in nonscience fields has also grown, with 63 institutions now offering a master of business administration (MBA), nearly double the number offered in 2006.15 At some institutions more than 20% of students are earning a master’s degree or doctorate in addition to their MD degree.16
Residents
The authors found no documentation of US residency training programs, outside of those in the specialty of preventive medicine, providing trainees with formal opportunities to obtain an MBA or MPH prior to 2001.17 However, of the 510 internal medicine residency programs listed on the American Medical Association residency and fellowship database (freida.ama-assn.org), 45 identified as having established a pathway for residents to pursue an MBA, MPH, or PhD during residency.18
Over the past 20 years, combined residency programs have increased 49% (from 128 to 191), which is triple the 16% rate (1,350 to 1,562) of increase in programs in internal medicine, pediatrics, family medicine, psychiatry, and emergency medicine.19,20 A 2009 moratorium on the creation of new combined residency programs in psychiatry and neurology was lifted in 2016and is likely to increase the rate of total combined programs.21
The Table shows the number of categorical and combined residency programs available in 1996 and in 2016. Over 2 decades, 17 new specialty combinations became available for residency training. While there were no combined training programs within these 17 new combinations in 1996,there were 66 programs with these combinations in 2016.19,20
Although surgical specialties are notably absent from the list of combined residency options, likely due to the duration of surgical training, some surgical training programs do offer pathways that culminate in combined degrees,22 and a high number of surgery program directors agree that residents should receive formal training in business and practice management.23
The Medical Job Market
Although today’s young physicians are cross-trained in multiple disciplines, the current job market may not directly match these skill sets. Of the 7,235 jobs listed by the New England Journal of Medicine (NEJM) career center (www.nejmcareercenter.org/jobs), only 54 were targeted at those with combined training, the majority of which were aimed at those trained in internal medicine/pediatrics. Of the combined specialties in the Table, formal positions were listed for only 6.24 A search of nearly 1,500 federal medical positions on USAJOBS (www.usajobs.gov) found only 4 jobs that combined specialties, all restricted to internal medicine/pediatrics.25 When searching for jobs containing the terms MBA, MPH, and public health there were only 8 such positions on NEJM and 7 on USAJOBS.24,25 Although the totality of the medical marketplace may not be best encompassed by these sources, the authors believe NEJM and USAJOBS are somewhat representative of the opportunities for physicians in the US.
Medical jobs tailored to cross-trained physicians do not appear to have kept pace with the numbers of such specialists currently in medical school and residency training. Though millennials are cross-training in increasing numbers, we surmise that they are not doing so as a direct result of the job market.
Future Medicine
Regardless of the mismatch between cross-trained physicians and the current job market, millennials may be well suited for future health systems. In 2001, the National Academies of Sciences, Engineering and Medicine (NASEM) called for increasing interdisciplinary training and improving cross-functional team performance as a major goal for health care providers in twenty-first century health systems.26 NASEM also recommended that academic medical centers develop medical leaders who can manage systems changes required to enhance health, a proposal supported by the fact that hospitals with medically trained CEOs outperform others.27,28
Public Health 3.0, a federal initiative to improve and integrate public health efforts, also emphasizes cross-disciplinary teams and cross-sector partnerships,29 while the Centers for Medicare and Medicaid Services (CMS) has incentivized the development of interprofessional health care teams.30 While cross-training does not automatically connote interdisciplinary training, we believe that cross-training may reveal or develop an interdisciplinary mind-set that may support and embrace interdisciplinary performance. Finally, the US Department of Health and Human Services’ (HHS) Strategic Goals emphasize integrated care for vulnerable populations, something that cross-trained physicians may be especially poised to accomplish.31
A Path Forward
The education, training, and priorities of young physicians demonstrates career interests that diverge from mainstream, traditional options. Data provided herein describe the increasing rates at which millennial physicians are cross-training and have suggested that the current marketplace may not match the interests of this population. The ultimate question is where such cross-trained physicians fit into today’s (or tomorrow’s) health system?
It may be easiest to deploy cross-trained physicians in their respective clinical departments (eg, having a physician trained in internal medicine and pediatrics perform clinical duties in both a medicine department and a pediatrics department). But < 40% of dual-boarded physicians practice both specialties in which they’re trained, so other opportunities should be pursued.32,33 One strategy may be to embrace the promise of interdisciplinary care, as supported by Public Health 3.0 and NASEM.26,29 Our evidence may demonstrate that the interdisciplinary mind-set may be more readily evident in the millennial generation, and that this mind-set may improve interdisciplinary care.
As health is impacted both by direct clinical care as well as programs designed to address population health, cross-trained physicians may be better equipped to integrate aspects of clinical care spanning a variety of clinical fields as well as orchestrating programs designed to improve health at the population level. This mind-set may be best captured by organizations willing to adapt their medical positions to emphasize multidisciplinary training, skills, and capabilities. For example, a physician trained in internal medicine and psychiatry may have the unique training and skill-set to establish an integrated behavioral health clinic that crosses boundaries between traditional departments, emphasizing the whole health of the clinic’s population and not simply focusing on providing services of a particular specialty. Hiring cross-trained physicians throughout such a clinic may benefit the operations of the clinic and improve not only the services provided, but ultimately, the health of that clinic’s patients. By embracing cross-trained physicians, health care organizations and educators may better meet the needs of their employees, likely resulting in a more cost-effective investment for employers, employees, and the health system as a whole.4 Additionally, patient health may also improve.
There is evidence that cross-trained physicians are already likely to hold leadership positions compared with their categorically-trained counterparts, and this may reflect the benefits of an interdisciplinary mind-set.33 Perhaps a cross-trained physician is more likely to see beyond standard, specialty-based institutional barriers and develop processes and programs designed for overall patient benefit. Leadership is a skill that many millennials clearly wish to enhance throughout their career.34 Recruiting cross-trained physicians for leadership positions may reveal synergies between such training and an ability to lead health care organizations into the future.
Many millennial physicians are bringing a new set of skills into the medical marketplace. Health organizations should identify ways to recruit for these skills and deploy them within their systems in order to have more dedicated, engaged employees, more effective health systems, and ultimately, healthier patients.
Acknowledgments
Data from this analysis were presented at the 10th Consortium of Universities for Global Health conference in 2019.35
Millennials, defined as those born between 1981 and 1996, currently comprise 15% of all active physicians in the US.1,2 A recent survey found that nearly 4 of 5 US millennial physicians have a desire for cross-sectional work in areas beyond patient care, such as academic research, health care consulting, entrepreneurship, and health care administration.3
For employers and educators, a better understanding of these preferences, through consideration of the unique education and skill set of the millennial physician workforce, may lead to more effective recruitment of young physicians and improved health systems, avoiding a mismatch between health care provider skills and available jobs that can be costly for both employers and employees.4
This article describes how US millennial physicians are choosing to cross-train (obtaining multiple degrees and/or completing combined medical residency training) throughout undergraduate, medical, and graduate medical education. We also outline ways in which the current physician marketplace may not match the skills of this population and suggest some ways that health care organizations could capitalize on this trend toward more cross-trained personnel in order to effectively recruit and retain the next generation of physicians.
Millennial Education
Undergraduates
The number of interdisciplinary undergraduate majors increased by almost 250% from 1975 to 2000.5 In 2010, nearly 20% of US college students graduated with 2 majors, representing a 70% increase in double majors between 2001 and 2011.6,7 One emerging category of interdisciplinary majors in US colleges is health humanities programs, which have quadrupled since 2000.8
Medical school applicants and matriculants reflect this trend. Whereas in 1994, only 19% of applicants to medical school held nonscience degrees, about one-third of applicants now hold such degrees.9,10 We have found no aggregated data on double majors entering US medical schools, but public class profiles suggest that medical school matriculants mirror their undergraduate counterparts in their tendency to hold double majors. In 2016, for example, 15% of the incoming class at the University of Michigan Medical School was composed of double majors, increasing to over 25% in 2017.11
Medical Students
Early dual-degree programs in undergraduate medical training were reserved for MD/PhD programs.12 Most US MD/PhD programs (90 out of 151) now offer doctorates in social sciences, humanities, or other nontraditional fields of graduate medical study, reflecting a shift in interests of those seeking dual-degree training in undergraduate medical education.13 While only 3 MD/PhD programs in the 1970s included trainees in the social sciences, 17 such programs exist today.14
Interest in dual-degree programs offering master’s level study has also increased over the past decade. In 2017, 87 medical schools offered programs for students to pursue a master of public health (MPH) and 41 offered master of science degrees in various fields, up from 52 and 37 institutions, respectively in 2006.15 The number of schools offering combined training in nonscience fields has also grown, with 63 institutions now offering a master of business administration (MBA), nearly double the number offered in 2006.15 At some institutions more than 20% of students are earning a master’s degree or doctorate in addition to their MD degree.16
Residents
The authors found no documentation of US residency training programs, outside of those in the specialty of preventive medicine, providing trainees with formal opportunities to obtain an MBA or MPH prior to 2001.17 However, of the 510 internal medicine residency programs listed on the American Medical Association residency and fellowship database (freida.ama-assn.org), 45 identified as having established a pathway for residents to pursue an MBA, MPH, or PhD during residency.18
Over the past 20 years, combined residency programs have increased 49% (from 128 to 191), which is triple the 16% rate (1,350 to 1,562) of increase in programs in internal medicine, pediatrics, family medicine, psychiatry, and emergency medicine.19,20 A 2009 moratorium on the creation of new combined residency programs in psychiatry and neurology was lifted in 2016and is likely to increase the rate of total combined programs.21
The Table shows the number of categorical and combined residency programs available in 1996 and in 2016. Over 2 decades, 17 new specialty combinations became available for residency training. While there were no combined training programs within these 17 new combinations in 1996,there were 66 programs with these combinations in 2016.19,20
Although surgical specialties are notably absent from the list of combined residency options, likely due to the duration of surgical training, some surgical training programs do offer pathways that culminate in combined degrees,22 and a high number of surgery program directors agree that residents should receive formal training in business and practice management.23
The Medical Job Market
Although today’s young physicians are cross-trained in multiple disciplines, the current job market may not directly match these skill sets. Of the 7,235 jobs listed by the New England Journal of Medicine (NEJM) career center (www.nejmcareercenter.org/jobs), only 54 were targeted at those with combined training, the majority of which were aimed at those trained in internal medicine/pediatrics. Of the combined specialties in the Table, formal positions were listed for only 6.24 A search of nearly 1,500 federal medical positions on USAJOBS (www.usajobs.gov) found only 4 jobs that combined specialties, all restricted to internal medicine/pediatrics.25 When searching for jobs containing the terms MBA, MPH, and public health there were only 8 such positions on NEJM and 7 on USAJOBS.24,25 Although the totality of the medical marketplace may not be best encompassed by these sources, the authors believe NEJM and USAJOBS are somewhat representative of the opportunities for physicians in the US.
Medical jobs tailored to cross-trained physicians do not appear to have kept pace with the numbers of such specialists currently in medical school and residency training. Though millennials are cross-training in increasing numbers, we surmise that they are not doing so as a direct result of the job market.
Future Medicine
Regardless of the mismatch between cross-trained physicians and the current job market, millennials may be well suited for future health systems. In 2001, the National Academies of Sciences, Engineering and Medicine (NASEM) called for increasing interdisciplinary training and improving cross-functional team performance as a major goal for health care providers in twenty-first century health systems.26 NASEM also recommended that academic medical centers develop medical leaders who can manage systems changes required to enhance health, a proposal supported by the fact that hospitals with medically trained CEOs outperform others.27,28
Public Health 3.0, a federal initiative to improve and integrate public health efforts, also emphasizes cross-disciplinary teams and cross-sector partnerships,29 while the Centers for Medicare and Medicaid Services (CMS) has incentivized the development of interprofessional health care teams.30 While cross-training does not automatically connote interdisciplinary training, we believe that cross-training may reveal or develop an interdisciplinary mind-set that may support and embrace interdisciplinary performance. Finally, the US Department of Health and Human Services’ (HHS) Strategic Goals emphasize integrated care for vulnerable populations, something that cross-trained physicians may be especially poised to accomplish.31
A Path Forward
The education, training, and priorities of young physicians demonstrates career interests that diverge from mainstream, traditional options. Data provided herein describe the increasing rates at which millennial physicians are cross-training and have suggested that the current marketplace may not match the interests of this population. The ultimate question is where such cross-trained physicians fit into today’s (or tomorrow’s) health system?
It may be easiest to deploy cross-trained physicians in their respective clinical departments (eg, having a physician trained in internal medicine and pediatrics perform clinical duties in both a medicine department and a pediatrics department). But < 40% of dual-boarded physicians practice both specialties in which they’re trained, so other opportunities should be pursued.32,33 One strategy may be to embrace the promise of interdisciplinary care, as supported by Public Health 3.0 and NASEM.26,29 Our evidence may demonstrate that the interdisciplinary mind-set may be more readily evident in the millennial generation, and that this mind-set may improve interdisciplinary care.
As health is impacted both by direct clinical care as well as programs designed to address population health, cross-trained physicians may be better equipped to integrate aspects of clinical care spanning a variety of clinical fields as well as orchestrating programs designed to improve health at the population level. This mind-set may be best captured by organizations willing to adapt their medical positions to emphasize multidisciplinary training, skills, and capabilities. For example, a physician trained in internal medicine and psychiatry may have the unique training and skill-set to establish an integrated behavioral health clinic that crosses boundaries between traditional departments, emphasizing the whole health of the clinic’s population and not simply focusing on providing services of a particular specialty. Hiring cross-trained physicians throughout such a clinic may benefit the operations of the clinic and improve not only the services provided, but ultimately, the health of that clinic’s patients. By embracing cross-trained physicians, health care organizations and educators may better meet the needs of their employees, likely resulting in a more cost-effective investment for employers, employees, and the health system as a whole.4 Additionally, patient health may also improve.
There is evidence that cross-trained physicians are already likely to hold leadership positions compared with their categorically-trained counterparts, and this may reflect the benefits of an interdisciplinary mind-set.33 Perhaps a cross-trained physician is more likely to see beyond standard, specialty-based institutional barriers and develop processes and programs designed for overall patient benefit. Leadership is a skill that many millennials clearly wish to enhance throughout their career.34 Recruiting cross-trained physicians for leadership positions may reveal synergies between such training and an ability to lead health care organizations into the future.
Many millennial physicians are bringing a new set of skills into the medical marketplace. Health organizations should identify ways to recruit for these skills and deploy them within their systems in order to have more dedicated, engaged employees, more effective health systems, and ultimately, healthier patients.
Acknowledgments
Data from this analysis were presented at the 10th Consortium of Universities for Global Health conference in 2019.35
1. Dimock M. Defining generations: where millennials end and generation Z begins. http://www.pewresearch.org/fact-tank/2018/03/01/defining-generations-where-millennials-end-and-post-millennials-begin/. Published January 17, 2019. Accessed November 7, 2019.
2. IHS Inc. The complexities of physician supply and demand: projections from 2014 to 2025. Final report. https://www.modernhealthcare.com/assets/pdf/CH10888123.pdf. Published April 5, 2016. Accessed November 7, 2019.
3. Miller RN. Millennial physicians sound off on state of medicine today. https://wire.ama-assn.org/life-career/millennial-physicians-sound-state-medicine-today. Published March 27, 2017. Accessed November 7, 2019.
4. World Economic Forum. Matching skills and labour market needs: building social partnerships for better skills and better jobs. http://www3.weforum.org/docs/GAC/2014/WEF_GAC_Employment_MatchingSkillsLabourMarket_Report_2014.pdf. Published January 2014. Accessed November 7, 2019.
5. Brint SG, Turk-Bicakci L, Proctor K, Murphy SP. Expanding the social frame of knowledge: interdisciplinary, degree-granting fields in American Colleges and Universities, 1975–2000. Rev High Ed. 2009;32(2):155-183.
6. National Science Foundation. National survey of college graduates. https://www.nsf.gov/statistics/srvygrads. Updated February 2019. Accessed November 7, 2019.
7. Simon CC. Major decisions. New York Times. November 2, 2012. http://www.nytimes.com/2012/11/04/education/edlife/choosing-one-college-major-out-of-hundreds.html. Accessed November 7, 2019.
8. Berry SL, Erin GL, Therese J. Health humanities baccalaureate programs in the United States. http://www.hiram.edu/wp-content/uploads/2017/09/HHBP2017.pdf. Published September 2017. Accessed November 7, 2019.
9. Sorensen NE, Jackson JR. Science majors and nonscience majors entering medical school: acceptance rates and academic performance. NACADA J. 1997;17(1):32-41.
10. Association of American Medical Colleges. Table A-17: MCAT and GPAs for applicants and matriculants to U.S. medical schools by primary undergraduate major, 2019-2020. https://www.aamc.org/download/321496/data/factstablea17.pdf. Published October 16, 2019. Accessed November 7, 2019.
11. University of Michigan Medical School. Many paths, one destination: medical school welcomes its 170th class of medical students. https://medicine.umich.edu/medschool/news/many-paths-one-destination-medical-school-welcomes-its-170th-class-medical-students. Updated July 29, 2016. Accessed November 7, 2019.
12. Harding CV, Akabas MH, Andersen OS. History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad Med. 2017; 92(10):1390-1398.
13. Association of American Medical Colleges. MD-PhD in “social sciences or humanities” and “other non-traditional fields of graduate study” - by school. https://students-residents.aamc.org/choosing-medical-career/careers-medical-research/md-phd-dual-degree-training/non-basic-science-phd-training-school/. Accessed November 8, 2019.
14. Holmes SM, Karlin J, Stonington SD, Gottheil DL. The first nationwide survey of MD-PhDs in the social sciences and humanities: training patterns and career choices. BMC Med Educ. 2017;17(1):60.
15. Association of American Medical Colleges Combined degrees and early acceptance programs. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/combined-degrees-and-early-acceptance-programs. Accessed November 8, 2019.
16. Tufts University School of Medicine. 2023 class profile. http://medicine.tufts.edu/Education/MD-Programs/Doctor-of-Medicine/Class-Profile. Published 2015. Accessed November 8, 2019.
17. Zweifler J, Evan R. Development of a residency/MPH program. Family Med. 2001;33(6):453-458.
18. American Medical Association. The AMA residency and fellowship database. http://freida.ama-assn.org/Freida. Accessed November 7, 2019.
19. National Resident Matching Program. NRMP data. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata1996.pdf. Published March 1996. Accessed November 7, 2019.
20. Brotherton SE, Etzel SI. Graduate medical education, 2016-2017. JAMA. 2017;318(23):2368-2387.
21. American Board of Psychiatry and Neurology. Update for psychiatry GME programs on combined training program accreditation/approval February 2012. https://www.umassmed.edu/globalassets/neuropsychiatry/files/combined-program-letter.pdf. Accessed November 7, 2019.
22. Massachusetts General Hospital. Surgical residency program. https://www.massgeneral.org/surgery/education/residency.aspx?id=77. Accessed November 7, 2019.
23. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
24. New England Journal of Medicine. NEJM CareerCenter. http://www.nejmcareercenter.org. Accessed November 7, 2019.
25. US Office of Personnel Management. USAJOBS. https://www.usajobs.gov. Accessed November 7, 2019.
26. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Published March 2001. Accessed November 7, 2019.
27. Kohn LT, ed; Committee on the Roles of Academic Health Centers in the 21st Century; Institute of Medicine of the National Academies. Academic Health Centers: Leading Change in the 21st Century. National Academy Press: Washington, DC; 2004.
28. Goodall AH. Physician-leaders and hospital performance: is there an association? http://ftp.iza.org/dp5830.pdf. Published July 2011. Accessed November 7, 2019.
29. US Department of Health and Human Services, Office of the Assistant Secretary for Health. Public health 3.0: a call to action to create a 21st century public health infrastructure. https://www.healthypeople.gov/sites/default/files/Public-Health-3.0-White-Paper.pdf. Accessed November 7, 2019.
30. Centers for Medicare and Medicaid Services. Health care innovation awards round one project profiles. http://innovation.cms.gov/files/x/hcia-project-profiles.pdf. Updated December 2013. Accessed November 7, 2019.
31. US Department of Health and Human Services. Strategic Objective 1.3: Improve Americans’ access to healthcare and expand choices of care and service options. https://www.hhs.gov/about/strategic-plan/strategic-goal-1/index.html#obj_1_3. Updated March 18, 2019. Accessed November 7, 2019.
32. Kessler CS, Stallings LA, Gonzalez AA, Templeman TA. Combined residency training in emergency medicine and internal medicine: an update on career outcomes and job satisfaction. Acad Emerg Med. 2009;16(9):894-899.
33. Summergrad P, Silberman E, Price LL. Practice and career outcomes of double-boarded psychiatrists. Psychosomatics. 2011;52(6):537-543.
34. Rigoni B, Adkins A. What millennials want from a new job. Harvard Business Rev. May 11, 2016. https://hbr.org/2016/05/what-millennials-want-from-a-new-job. Accessed November 7, 2019.
35. Jung P, Smith C. Medical millennials: a mismatch between training preferences and employment opportunities. Lancet Glob Health. 2019;7(suppl 1):S38.
1. Dimock M. Defining generations: where millennials end and generation Z begins. http://www.pewresearch.org/fact-tank/2018/03/01/defining-generations-where-millennials-end-and-post-millennials-begin/. Published January 17, 2019. Accessed November 7, 2019.
2. IHS Inc. The complexities of physician supply and demand: projections from 2014 to 2025. Final report. https://www.modernhealthcare.com/assets/pdf/CH10888123.pdf. Published April 5, 2016. Accessed November 7, 2019.
3. Miller RN. Millennial physicians sound off on state of medicine today. https://wire.ama-assn.org/life-career/millennial-physicians-sound-state-medicine-today. Published March 27, 2017. Accessed November 7, 2019.
4. World Economic Forum. Matching skills and labour market needs: building social partnerships for better skills and better jobs. http://www3.weforum.org/docs/GAC/2014/WEF_GAC_Employment_MatchingSkillsLabourMarket_Report_2014.pdf. Published January 2014. Accessed November 7, 2019.
5. Brint SG, Turk-Bicakci L, Proctor K, Murphy SP. Expanding the social frame of knowledge: interdisciplinary, degree-granting fields in American Colleges and Universities, 1975–2000. Rev High Ed. 2009;32(2):155-183.
6. National Science Foundation. National survey of college graduates. https://www.nsf.gov/statistics/srvygrads. Updated February 2019. Accessed November 7, 2019.
7. Simon CC. Major decisions. New York Times. November 2, 2012. http://www.nytimes.com/2012/11/04/education/edlife/choosing-one-college-major-out-of-hundreds.html. Accessed November 7, 2019.
8. Berry SL, Erin GL, Therese J. Health humanities baccalaureate programs in the United States. http://www.hiram.edu/wp-content/uploads/2017/09/HHBP2017.pdf. Published September 2017. Accessed November 7, 2019.
9. Sorensen NE, Jackson JR. Science majors and nonscience majors entering medical school: acceptance rates and academic performance. NACADA J. 1997;17(1):32-41.
10. Association of American Medical Colleges. Table A-17: MCAT and GPAs for applicants and matriculants to U.S. medical schools by primary undergraduate major, 2019-2020. https://www.aamc.org/download/321496/data/factstablea17.pdf. Published October 16, 2019. Accessed November 7, 2019.
11. University of Michigan Medical School. Many paths, one destination: medical school welcomes its 170th class of medical students. https://medicine.umich.edu/medschool/news/many-paths-one-destination-medical-school-welcomes-its-170th-class-medical-students. Updated July 29, 2016. Accessed November 7, 2019.
12. Harding CV, Akabas MH, Andersen OS. History and outcomes of 50 years of physician-scientist training in medical scientist training programs. Acad Med. 2017; 92(10):1390-1398.
13. Association of American Medical Colleges. MD-PhD in “social sciences or humanities” and “other non-traditional fields of graduate study” - by school. https://students-residents.aamc.org/choosing-medical-career/careers-medical-research/md-phd-dual-degree-training/non-basic-science-phd-training-school/. Accessed November 8, 2019.
14. Holmes SM, Karlin J, Stonington SD, Gottheil DL. The first nationwide survey of MD-PhDs in the social sciences and humanities: training patterns and career choices. BMC Med Educ. 2017;17(1):60.
15. Association of American Medical Colleges Combined degrees and early acceptance programs. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/combined-degrees-and-early-acceptance-programs. Accessed November 8, 2019.
16. Tufts University School of Medicine. 2023 class profile. http://medicine.tufts.edu/Education/MD-Programs/Doctor-of-Medicine/Class-Profile. Published 2015. Accessed November 8, 2019.
17. Zweifler J, Evan R. Development of a residency/MPH program. Family Med. 2001;33(6):453-458.
18. American Medical Association. The AMA residency and fellowship database. http://freida.ama-assn.org/Freida. Accessed November 7, 2019.
19. National Resident Matching Program. NRMP data. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata1996.pdf. Published March 1996. Accessed November 7, 2019.
20. Brotherton SE, Etzel SI. Graduate medical education, 2016-2017. JAMA. 2017;318(23):2368-2387.
21. American Board of Psychiatry and Neurology. Update for psychiatry GME programs on combined training program accreditation/approval February 2012. https://www.umassmed.edu/globalassets/neuropsychiatry/files/combined-program-letter.pdf. Accessed November 7, 2019.
22. Massachusetts General Hospital. Surgical residency program. https://www.massgeneral.org/surgery/education/residency.aspx?id=77. Accessed November 7, 2019.
23. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
24. New England Journal of Medicine. NEJM CareerCenter. http://www.nejmcareercenter.org. Accessed November 7, 2019.
25. US Office of Personnel Management. USAJOBS. https://www.usajobs.gov. Accessed November 7, 2019.
26. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf. Published March 2001. Accessed November 7, 2019.
27. Kohn LT, ed; Committee on the Roles of Academic Health Centers in the 21st Century; Institute of Medicine of the National Academies. Academic Health Centers: Leading Change in the 21st Century. National Academy Press: Washington, DC; 2004.
28. Goodall AH. Physician-leaders and hospital performance: is there an association? http://ftp.iza.org/dp5830.pdf. Published July 2011. Accessed November 7, 2019.
29. US Department of Health and Human Services, Office of the Assistant Secretary for Health. Public health 3.0: a call to action to create a 21st century public health infrastructure. https://www.healthypeople.gov/sites/default/files/Public-Health-3.0-White-Paper.pdf. Accessed November 7, 2019.
30. Centers for Medicare and Medicaid Services. Health care innovation awards round one project profiles. http://innovation.cms.gov/files/x/hcia-project-profiles.pdf. Updated December 2013. Accessed November 7, 2019.
31. US Department of Health and Human Services. Strategic Objective 1.3: Improve Americans’ access to healthcare and expand choices of care and service options. https://www.hhs.gov/about/strategic-plan/strategic-goal-1/index.html#obj_1_3. Updated March 18, 2019. Accessed November 7, 2019.
32. Kessler CS, Stallings LA, Gonzalez AA, Templeman TA. Combined residency training in emergency medicine and internal medicine: an update on career outcomes and job satisfaction. Acad Emerg Med. 2009;16(9):894-899.
33. Summergrad P, Silberman E, Price LL. Practice and career outcomes of double-boarded psychiatrists. Psychosomatics. 2011;52(6):537-543.
34. Rigoni B, Adkins A. What millennials want from a new job. Harvard Business Rev. May 11, 2016. https://hbr.org/2016/05/what-millennials-want-from-a-new-job. Accessed November 7, 2019.
35. Jung P, Smith C. Medical millennials: a mismatch between training preferences and employment opportunities. Lancet Glob Health. 2019;7(suppl 1):S38.
Understanding Principles of High Reliability Organizations Through the Eyes of VIONE, A Clinical Program to Improve Patient Safety by Deprescribing Potentially Inappropriate Medications and Reducing Polypharmacy
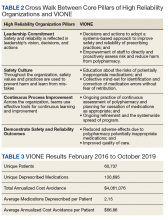
High reliability organizations (HROs) incorporate continuous process improvement through leadership commitment to create a safety culture that works toward creating a zero-harm environment.1 The Veterans Health Administration (VHA) has set transformational goals for becoming an HRO. In this article, we describe VIONE, an expanding medication deprescribing clinical program, which exemplifies the translation of HRO principles into health care system models. Both VIONE and HRO are globally relevant.
Reducing medication errors and related adverse drug events are important for achieving zero harm. Preventable medical errors rank behind heart disease and cancer as the third leading cause of death in the US.2 The simultaneous use of multiple medications can lead to dangerous drug interactions, adverse outcomes, and challenges with adherence. When a person is taking multiple medicines, known as polypharmacy, it is more likely that some are potentially inappropriate medications (PIM). Current literature highlights the prevalence and dangers of polypharmacy, which ranks among the top 10 common causes of death in the US, as well as suggestions to address preventable adverse outcomes from polypharmacy and PIM.3-5
Deprescribing of PIM frequently results in better disease management with improved health outcomes and quality of life.4 Many health care settings lack standardized approaches or set expectations to proactively deprescribe PIM. There has been insufficient emphasis on how to make decisions for deprescribing medications when therapeutic benefits are not clear and/or when the adverse effects may outweigh the therapeutic benefits.5
It is imperative to provide practice guidance for deprescribing nonessential medications along with systems-based infrastructure to enable integrated and effective assessments during opportune moments in the health care continuum. Multimodal approaches that include education, risk stratification, population health management interventions, research and resource allocation can help transform organizational culture in health care facilities toward HRO models of care, aiming at zero harm to patients.
The practical lessons learned from VIONE implementation science experiences on various scales and under diverse circumstances, cumulative wisdom from hindsight, foresight and critical insights gathered during nationwide spread of VIONE over the past 3 years continues to propel us toward the desirable direction and core concepts of an HRO.
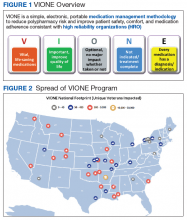
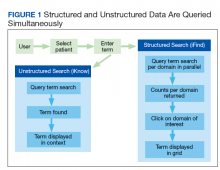
The VIONE program facilitates practical, real-time interventions that could be tailored to various health care settings, organizational needs, and available resources. VIONE implements an electronic Computerized Patient Record System (CPRS) tool to enable planned cessation of nonessential medications that are potentially harmful, inappropriate, not indicated, or not necessary. The VIONE tool supports systematic, individualized assessment and adjustment through 5 filters (Figure 1). It prompts providers to assign 1 of these filters intuitively and objectively. VIONE combines clinical evidence for best practices, an interprofessional team approach, patient engagement, adapted use of existing medical records systems, and HRO principles for effective implementation.
As a tool to support safer prescribing practices, VIONE aligns closely with HRO principles (Table 1) and core pillars (Table 2).6-8 A zero-harm safety culture necessitates that medications be used for correct reasons, over a correct duration of time, and following a correct schedule while monitoring for adverse outcomes. However, reality generally falls significantly short of this for a myriad of reasons, such as compromised health literacy, functional limitations, affordability, communication gaps, patients seen by multiple providers, and an accumulation of prescriptions due to comorbidities, symptom progression, and management of adverse effects. Through a sharpened focus on both precision medicine and competent prescription management, VIONE is a viable opportunity for investing in the zero-harm philosophy that is integral to an HRO.
Design and Implementation
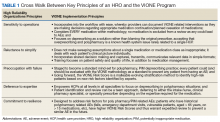
Initially launched in 2016 in a 15-bed inpatient, subacute rehabilitation unit within a VHA tertiary care facility, VIONE has been sustained and gradually expanded to 38 other VHA facility programs (Figure 2). Recognizing the potential value if adopted into widespread use, VIONE was a Gold Status winner in the VHA Under Secretary for Health Shark Tank-style competition in 2017 and was selected by the VHA Diffusion of Excellence as an innovation worthy of scale and spread through national dissemination.9 A toolkit for VIONE implementation, patient and provider brochures, VIONE vignette, and National Dialog template also have been created.10
Implementing VIONE in a new facility requires an actively engaged core team committed to patient safety and reduction of polypharmacy and PIM, interest and availability to lead project implementation strategies, along with meaningful local organizational support. The current structure for VIONE spread is as follows:
- Interested VHA participants review information and contact vavione@va.gov.
- The VIONE team orients implementing champions, mainly pharmacists, physicians, nurse practitioners, and physician assistants at a facility program level, offering guidance and available resources.
- Clinical Application Coordinators at Central Arkansas VA Healthcare System and participating facilities collaborate to add deprescribing menu options in CPRS and install the VIONE Polypharmacy Reminder Dialog template.
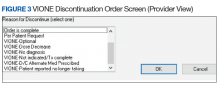
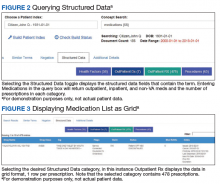
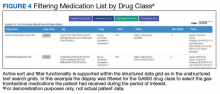
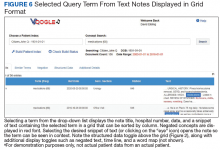
- Through close and ongoing collaborations, medical providers and clinical pharmacists proceed with deprescribing, aiming at planned cessation of nonessential and PIM, using the mnemonic prompt of VIONE. Vital and Important medications are continued and consolidated while a methodical plan is developed to deprescribe any medications that could lead to more harm than benefit and qualify based on the filters of Optional, Not indicated, and Every medicine has a diagnosis/reason. They select the proper discontinuation reasons in the CPRS medication menu (Figure 3) and document the rationale in the progress notes. It is highly encouraged that the collaborating pharmacists and health care providers add each other as cosigners and communicate effectively. Clinical pharmacy specialists also use the VIONE Polypharmacy Reminder Dialog Template (RDT) to document complete medication reviews with veterans to include deprescribing rationale and document shared decision making.
- A VIONE national dashboard captures deprescribing data in real time and automates reporting with daily updates that are readily accessible to all implementing facilities. Minimum data captured include the number of unique veterans impacted, number of medications deprescribed, cumulative cost avoidance to date, and number of prescriptions deprescribed per veteran. The dashboard facilitates real-time use of individual patient data and has also been designed to capture data from VHA administrative data portals and Corporate Data Warehouse.
Results
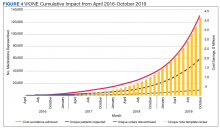
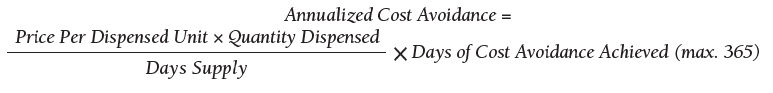
As of October 31, 2019, the assessment of polypharmacy using the VIONE tool across VHA sites has benefited > 60,000 unique veterans, of whom 49.2% were in urban areas, 47.7% in rural areas, and 3.1% in highly rural areas. Elderly male veterans comprised a clear majority. More than 128,000 medications have been deprescribed. The top classes of medications deprescribed are antihypertensives, over-the-counter medications, and antidiabetic medications. An annualized cost avoidance of > $4.0 million has been achieved. Cost avoidance is the cost of medications that otherwise would have continued to be filled and paid for by the VHA if they had not been deprescribed, projected for a maximum of 365 days. The calculation methodology can be summarized as follows:
The calculations reported in Table 3 and Figure 4 are conservative and include only chronic outpatient prescriptions and do not account for medications deprescribed in inpatient units, nursing home, community living centers, or domiciliary populations. Data tracked separately from inpatient and community living center patient populations indicated an additional 25,536 deprescribed medications, across 28 VA facilities, impacting 7,076 veterans with an average 2.15 medications deprescribed per veteran. The additional achieved cost avoidance was $370,272 (based on $14.50 average cost per prescription). Medications restarted within 30 days of deprescribing are not included in these calculations.
The cost avoidance calculation further excludes the effects of VIONE implementation on many other types of interventions. These interventions include, but are not limited to, changing from aggressive care to end of life, comfort care when strongly indicated; reduced emergency department visits or invasive diagnostic and therapeutic approaches, when not indicated; medical supplies, antimicrobial preparations; labor costs related to packaging, mailing, and administering prescriptions; reduced/prevented clinical waste; reduced decompensation of systemic illnesses and subsequent health care needs precipitated by iatrogenic disturbances and prolonged convalescence; and overall changes to prescribing practices through purposeful and targeted interactions with colleagues across various disciplines and various hierarchical levels.
Discussion
The VIONE clinical program exemplifies the translation of HRO principles into health care system practices. VIONE offers a systematic approach to improve medication management with an emphasis on deprescribing nonessential medications across various health care settings, facilitating VHA efforts toward zero harm. It demonstrates close alignment with the key building blocks of an HRO. Effective VIONE incorporation into an organizational culture reflects leadership commitment to safety and reliability in their vision and actions. By empowering staff to proactively reduce inappropriate medications and thereby prevent patient harm, VIONE contributes to enhancing an enterprise-wide culture of safety, with fewer errors and greater reliability. As a standardized decision support tool for the ongoing practice of assessment and planned cessation of potentially inappropriate medications, VIONE illustrates how continuous process improvement can be a part of staff-engaged, veteran-centered, highly reliable care. The standardization of the VIONE tool promotes achievement and sustainment of desired HRO principles and practices within health care delivery systems.
Conclusions
The VIONE program was launched not as a cost savings or research program but as a practical, real-time bedside or ambulatory care intervention to improve patient safety. Its value is reflected in the overwhelming response from scholarly and well-engaged colleagues expressing serious interests in expanding collaborations and tailoring efforts to add more depth and breadth to VIONE related efforts.
Acknowledgments
The authors express their gratitude to Central Arkansas VA Healthcare System leadership, Clinical Applications Coordinators, and colleagues for their unconditional support, to the Diffusion of Excellence programs at US Department of Veterans Affairs Central Office for their endorsement, and to the many VHA participants who renew our optimism and energy as we continue this exciting journey. We also thank Bridget B. Kelly for her assistance in writing and editing of the manuscript.
1. Chassin MR, Jerod ML. High-reliability health care: getting there from here. The Joint Commission. Milbank Q. 2013;91(3):459-490.
2. Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139.
3. Quinn KJ, Shah NH. A dataset quantifying polypharmacy in the United States. Sci Data. 2017;4:170167.
4. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834.
5. Steinman MA. Polypharmacy—time to get beyond numbers. JAMA Intern Med. 2016;176(4):482-483.
6. US Department of Veterans Affairs. High reliability. https://dvagov.sharepoint.com/sites/OHT-PMO/high-reliability/Pages/default.aspx. [Nonpublic source, not verified.]
7. Gordon S, Mendenhall P, O’Connor BB. Beyond the Checklist: What Else Health Care Can Learn from Aviation Teamwork and Safety. Ithaca, NY: Cornell University Press; 2013.
8. Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press; 2000.
9. US Department of Veterans Affairs. Diffusion of Excellence. https://www.va.gov/HEALTHCAREEXCELLENCE/diffusion-of-excellence/. Updated August 10, 2018. Accessed June 26, 2019.
10. US Department of Veterans Affairs. VIONE program toolkit. https://www.vapulse.net/docs/DOC-259375. [Nonpublic source, not verified.]
High reliability organizations (HROs) incorporate continuous process improvement through leadership commitment to create a safety culture that works toward creating a zero-harm environment.1 The Veterans Health Administration (VHA) has set transformational goals for becoming an HRO. In this article, we describe VIONE, an expanding medication deprescribing clinical program, which exemplifies the translation of HRO principles into health care system models. Both VIONE and HRO are globally relevant.
Reducing medication errors and related adverse drug events are important for achieving zero harm. Preventable medical errors rank behind heart disease and cancer as the third leading cause of death in the US.2 The simultaneous use of multiple medications can lead to dangerous drug interactions, adverse outcomes, and challenges with adherence. When a person is taking multiple medicines, known as polypharmacy, it is more likely that some are potentially inappropriate medications (PIM). Current literature highlights the prevalence and dangers of polypharmacy, which ranks among the top 10 common causes of death in the US, as well as suggestions to address preventable adverse outcomes from polypharmacy and PIM.3-5
Deprescribing of PIM frequently results in better disease management with improved health outcomes and quality of life.4 Many health care settings lack standardized approaches or set expectations to proactively deprescribe PIM. There has been insufficient emphasis on how to make decisions for deprescribing medications when therapeutic benefits are not clear and/or when the adverse effects may outweigh the therapeutic benefits.5
It is imperative to provide practice guidance for deprescribing nonessential medications along with systems-based infrastructure to enable integrated and effective assessments during opportune moments in the health care continuum. Multimodal approaches that include education, risk stratification, population health management interventions, research and resource allocation can help transform organizational culture in health care facilities toward HRO models of care, aiming at zero harm to patients.
The practical lessons learned from VIONE implementation science experiences on various scales and under diverse circumstances, cumulative wisdom from hindsight, foresight and critical insights gathered during nationwide spread of VIONE over the past 3 years continues to propel us toward the desirable direction and core concepts of an HRO.
The VIONE program facilitates practical, real-time interventions that could be tailored to various health care settings, organizational needs, and available resources. VIONE implements an electronic Computerized Patient Record System (CPRS) tool to enable planned cessation of nonessential medications that are potentially harmful, inappropriate, not indicated, or not necessary. The VIONE tool supports systematic, individualized assessment and adjustment through 5 filters (Figure 1). It prompts providers to assign 1 of these filters intuitively and objectively. VIONE combines clinical evidence for best practices, an interprofessional team approach, patient engagement, adapted use of existing medical records systems, and HRO principles for effective implementation.
As a tool to support safer prescribing practices, VIONE aligns closely with HRO principles (Table 1) and core pillars (Table 2).6-8 A zero-harm safety culture necessitates that medications be used for correct reasons, over a correct duration of time, and following a correct schedule while monitoring for adverse outcomes. However, reality generally falls significantly short of this for a myriad of reasons, such as compromised health literacy, functional limitations, affordability, communication gaps, patients seen by multiple providers, and an accumulation of prescriptions due to comorbidities, symptom progression, and management of adverse effects. Through a sharpened focus on both precision medicine and competent prescription management, VIONE is a viable opportunity for investing in the zero-harm philosophy that is integral to an HRO.
Design and Implementation
Initially launched in 2016 in a 15-bed inpatient, subacute rehabilitation unit within a VHA tertiary care facility, VIONE has been sustained and gradually expanded to 38 other VHA facility programs (Figure 2). Recognizing the potential value if adopted into widespread use, VIONE was a Gold Status winner in the VHA Under Secretary for Health Shark Tank-style competition in 2017 and was selected by the VHA Diffusion of Excellence as an innovation worthy of scale and spread through national dissemination.9 A toolkit for VIONE implementation, patient and provider brochures, VIONE vignette, and National Dialog template also have been created.10
Implementing VIONE in a new facility requires an actively engaged core team committed to patient safety and reduction of polypharmacy and PIM, interest and availability to lead project implementation strategies, along with meaningful local organizational support. The current structure for VIONE spread is as follows:
- Interested VHA participants review information and contact vavione@va.gov.
- The VIONE team orients implementing champions, mainly pharmacists, physicians, nurse practitioners, and physician assistants at a facility program level, offering guidance and available resources.
- Clinical Application Coordinators at Central Arkansas VA Healthcare System and participating facilities collaborate to add deprescribing menu options in CPRS and install the VIONE Polypharmacy Reminder Dialog template.
- Through close and ongoing collaborations, medical providers and clinical pharmacists proceed with deprescribing, aiming at planned cessation of nonessential and PIM, using the mnemonic prompt of VIONE. Vital and Important medications are continued and consolidated while a methodical plan is developed to deprescribe any medications that could lead to more harm than benefit and qualify based on the filters of Optional, Not indicated, and Every medicine has a diagnosis/reason. They select the proper discontinuation reasons in the CPRS medication menu (Figure 3) and document the rationale in the progress notes. It is highly encouraged that the collaborating pharmacists and health care providers add each other as cosigners and communicate effectively. Clinical pharmacy specialists also use the VIONE Polypharmacy Reminder Dialog Template (RDT) to document complete medication reviews with veterans to include deprescribing rationale and document shared decision making.
- A VIONE national dashboard captures deprescribing data in real time and automates reporting with daily updates that are readily accessible to all implementing facilities. Minimum data captured include the number of unique veterans impacted, number of medications deprescribed, cumulative cost avoidance to date, and number of prescriptions deprescribed per veteran. The dashboard facilitates real-time use of individual patient data and has also been designed to capture data from VHA administrative data portals and Corporate Data Warehouse.
Results
As of October 31, 2019, the assessment of polypharmacy using the VIONE tool across VHA sites has benefited > 60,000 unique veterans, of whom 49.2% were in urban areas, 47.7% in rural areas, and 3.1% in highly rural areas. Elderly male veterans comprised a clear majority. More than 128,000 medications have been deprescribed. The top classes of medications deprescribed are antihypertensives, over-the-counter medications, and antidiabetic medications. An annualized cost avoidance of > $4.0 million has been achieved. Cost avoidance is the cost of medications that otherwise would have continued to be filled and paid for by the VHA if they had not been deprescribed, projected for a maximum of 365 days. The calculation methodology can be summarized as follows:
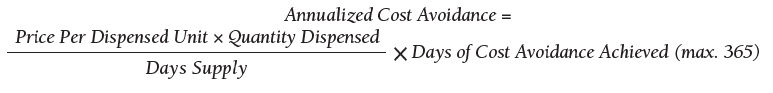
The calculations reported in Table 3 and Figure 4 are conservative and include only chronic outpatient prescriptions and do not account for medications deprescribed in inpatient units, nursing home, community living centers, or domiciliary populations. Data tracked separately from inpatient and community living center patient populations indicated an additional 25,536 deprescribed medications, across 28 VA facilities, impacting 7,076 veterans with an average 2.15 medications deprescribed per veteran. The additional achieved cost avoidance was $370,272 (based on $14.50 average cost per prescription). Medications restarted within 30 days of deprescribing are not included in these calculations.
The cost avoidance calculation further excludes the effects of VIONE implementation on many other types of interventions. These interventions include, but are not limited to, changing from aggressive care to end of life, comfort care when strongly indicated; reduced emergency department visits or invasive diagnostic and therapeutic approaches, when not indicated; medical supplies, antimicrobial preparations; labor costs related to packaging, mailing, and administering prescriptions; reduced/prevented clinical waste; reduced decompensation of systemic illnesses and subsequent health care needs precipitated by iatrogenic disturbances and prolonged convalescence; and overall changes to prescribing practices through purposeful and targeted interactions with colleagues across various disciplines and various hierarchical levels.
Discussion
The VIONE clinical program exemplifies the translation of HRO principles into health care system practices. VIONE offers a systematic approach to improve medication management with an emphasis on deprescribing nonessential medications across various health care settings, facilitating VHA efforts toward zero harm. It demonstrates close alignment with the key building blocks of an HRO. Effective VIONE incorporation into an organizational culture reflects leadership commitment to safety and reliability in their vision and actions. By empowering staff to proactively reduce inappropriate medications and thereby prevent patient harm, VIONE contributes to enhancing an enterprise-wide culture of safety, with fewer errors and greater reliability. As a standardized decision support tool for the ongoing practice of assessment and planned cessation of potentially inappropriate medications, VIONE illustrates how continuous process improvement can be a part of staff-engaged, veteran-centered, highly reliable care. The standardization of the VIONE tool promotes achievement and sustainment of desired HRO principles and practices within health care delivery systems.
Conclusions
The VIONE program was launched not as a cost savings or research program but as a practical, real-time bedside or ambulatory care intervention to improve patient safety. Its value is reflected in the overwhelming response from scholarly and well-engaged colleagues expressing serious interests in expanding collaborations and tailoring efforts to add more depth and breadth to VIONE related efforts.
Acknowledgments
The authors express their gratitude to Central Arkansas VA Healthcare System leadership, Clinical Applications Coordinators, and colleagues for their unconditional support, to the Diffusion of Excellence programs at US Department of Veterans Affairs Central Office for their endorsement, and to the many VHA participants who renew our optimism and energy as we continue this exciting journey. We also thank Bridget B. Kelly for her assistance in writing and editing of the manuscript.
High reliability organizations (HROs) incorporate continuous process improvement through leadership commitment to create a safety culture that works toward creating a zero-harm environment.1 The Veterans Health Administration (VHA) has set transformational goals for becoming an HRO. In this article, we describe VIONE, an expanding medication deprescribing clinical program, which exemplifies the translation of HRO principles into health care system models. Both VIONE and HRO are globally relevant.
Reducing medication errors and related adverse drug events are important for achieving zero harm. Preventable medical errors rank behind heart disease and cancer as the third leading cause of death in the US.2 The simultaneous use of multiple medications can lead to dangerous drug interactions, adverse outcomes, and challenges with adherence. When a person is taking multiple medicines, known as polypharmacy, it is more likely that some are potentially inappropriate medications (PIM). Current literature highlights the prevalence and dangers of polypharmacy, which ranks among the top 10 common causes of death in the US, as well as suggestions to address preventable adverse outcomes from polypharmacy and PIM.3-5
Deprescribing of PIM frequently results in better disease management with improved health outcomes and quality of life.4 Many health care settings lack standardized approaches or set expectations to proactively deprescribe PIM. There has been insufficient emphasis on how to make decisions for deprescribing medications when therapeutic benefits are not clear and/or when the adverse effects may outweigh the therapeutic benefits.5
It is imperative to provide practice guidance for deprescribing nonessential medications along with systems-based infrastructure to enable integrated and effective assessments during opportune moments in the health care continuum. Multimodal approaches that include education, risk stratification, population health management interventions, research and resource allocation can help transform organizational culture in health care facilities toward HRO models of care, aiming at zero harm to patients.
The practical lessons learned from VIONE implementation science experiences on various scales and under diverse circumstances, cumulative wisdom from hindsight, foresight and critical insights gathered during nationwide spread of VIONE over the past 3 years continues to propel us toward the desirable direction and core concepts of an HRO.
The VIONE program facilitates practical, real-time interventions that could be tailored to various health care settings, organizational needs, and available resources. VIONE implements an electronic Computerized Patient Record System (CPRS) tool to enable planned cessation of nonessential medications that are potentially harmful, inappropriate, not indicated, or not necessary. The VIONE tool supports systematic, individualized assessment and adjustment through 5 filters (Figure 1). It prompts providers to assign 1 of these filters intuitively and objectively. VIONE combines clinical evidence for best practices, an interprofessional team approach, patient engagement, adapted use of existing medical records systems, and HRO principles for effective implementation.
As a tool to support safer prescribing practices, VIONE aligns closely with HRO principles (Table 1) and core pillars (Table 2).6-8 A zero-harm safety culture necessitates that medications be used for correct reasons, over a correct duration of time, and following a correct schedule while monitoring for adverse outcomes. However, reality generally falls significantly short of this for a myriad of reasons, such as compromised health literacy, functional limitations, affordability, communication gaps, patients seen by multiple providers, and an accumulation of prescriptions due to comorbidities, symptom progression, and management of adverse effects. Through a sharpened focus on both precision medicine and competent prescription management, VIONE is a viable opportunity for investing in the zero-harm philosophy that is integral to an HRO.
Design and Implementation
Initially launched in 2016 in a 15-bed inpatient, subacute rehabilitation unit within a VHA tertiary care facility, VIONE has been sustained and gradually expanded to 38 other VHA facility programs (Figure 2). Recognizing the potential value if adopted into widespread use, VIONE was a Gold Status winner in the VHA Under Secretary for Health Shark Tank-style competition in 2017 and was selected by the VHA Diffusion of Excellence as an innovation worthy of scale and spread through national dissemination.9 A toolkit for VIONE implementation, patient and provider brochures, VIONE vignette, and National Dialog template also have been created.10
Implementing VIONE in a new facility requires an actively engaged core team committed to patient safety and reduction of polypharmacy and PIM, interest and availability to lead project implementation strategies, along with meaningful local organizational support. The current structure for VIONE spread is as follows:
- Interested VHA participants review information and contact vavione@va.gov.
- The VIONE team orients implementing champions, mainly pharmacists, physicians, nurse practitioners, and physician assistants at a facility program level, offering guidance and available resources.
- Clinical Application Coordinators at Central Arkansas VA Healthcare System and participating facilities collaborate to add deprescribing menu options in CPRS and install the VIONE Polypharmacy Reminder Dialog template.
- Through close and ongoing collaborations, medical providers and clinical pharmacists proceed with deprescribing, aiming at planned cessation of nonessential and PIM, using the mnemonic prompt of VIONE. Vital and Important medications are continued and consolidated while a methodical plan is developed to deprescribe any medications that could lead to more harm than benefit and qualify based on the filters of Optional, Not indicated, and Every medicine has a diagnosis/reason. They select the proper discontinuation reasons in the CPRS medication menu (Figure 3) and document the rationale in the progress notes. It is highly encouraged that the collaborating pharmacists and health care providers add each other as cosigners and communicate effectively. Clinical pharmacy specialists also use the VIONE Polypharmacy Reminder Dialog Template (RDT) to document complete medication reviews with veterans to include deprescribing rationale and document shared decision making.
- A VIONE national dashboard captures deprescribing data in real time and automates reporting with daily updates that are readily accessible to all implementing facilities. Minimum data captured include the number of unique veterans impacted, number of medications deprescribed, cumulative cost avoidance to date, and number of prescriptions deprescribed per veteran. The dashboard facilitates real-time use of individual patient data and has also been designed to capture data from VHA administrative data portals and Corporate Data Warehouse.
Results
As of October 31, 2019, the assessment of polypharmacy using the VIONE tool across VHA sites has benefited > 60,000 unique veterans, of whom 49.2% were in urban areas, 47.7% in rural areas, and 3.1% in highly rural areas. Elderly male veterans comprised a clear majority. More than 128,000 medications have been deprescribed. The top classes of medications deprescribed are antihypertensives, over-the-counter medications, and antidiabetic medications. An annualized cost avoidance of > $4.0 million has been achieved. Cost avoidance is the cost of medications that otherwise would have continued to be filled and paid for by the VHA if they had not been deprescribed, projected for a maximum of 365 days. The calculation methodology can be summarized as follows:
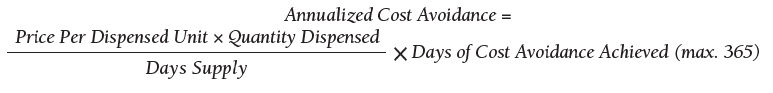
The calculations reported in Table 3 and Figure 4 are conservative and include only chronic outpatient prescriptions and do not account for medications deprescribed in inpatient units, nursing home, community living centers, or domiciliary populations. Data tracked separately from inpatient and community living center patient populations indicated an additional 25,536 deprescribed medications, across 28 VA facilities, impacting 7,076 veterans with an average 2.15 medications deprescribed per veteran. The additional achieved cost avoidance was $370,272 (based on $14.50 average cost per prescription). Medications restarted within 30 days of deprescribing are not included in these calculations.
The cost avoidance calculation further excludes the effects of VIONE implementation on many other types of interventions. These interventions include, but are not limited to, changing from aggressive care to end of life, comfort care when strongly indicated; reduced emergency department visits or invasive diagnostic and therapeutic approaches, when not indicated; medical supplies, antimicrobial preparations; labor costs related to packaging, mailing, and administering prescriptions; reduced/prevented clinical waste; reduced decompensation of systemic illnesses and subsequent health care needs precipitated by iatrogenic disturbances and prolonged convalescence; and overall changes to prescribing practices through purposeful and targeted interactions with colleagues across various disciplines and various hierarchical levels.
Discussion
The VIONE clinical program exemplifies the translation of HRO principles into health care system practices. VIONE offers a systematic approach to improve medication management with an emphasis on deprescribing nonessential medications across various health care settings, facilitating VHA efforts toward zero harm. It demonstrates close alignment with the key building blocks of an HRO. Effective VIONE incorporation into an organizational culture reflects leadership commitment to safety and reliability in their vision and actions. By empowering staff to proactively reduce inappropriate medications and thereby prevent patient harm, VIONE contributes to enhancing an enterprise-wide culture of safety, with fewer errors and greater reliability. As a standardized decision support tool for the ongoing practice of assessment and planned cessation of potentially inappropriate medications, VIONE illustrates how continuous process improvement can be a part of staff-engaged, veteran-centered, highly reliable care. The standardization of the VIONE tool promotes achievement and sustainment of desired HRO principles and practices within health care delivery systems.
Conclusions
The VIONE program was launched not as a cost savings or research program but as a practical, real-time bedside or ambulatory care intervention to improve patient safety. Its value is reflected in the overwhelming response from scholarly and well-engaged colleagues expressing serious interests in expanding collaborations and tailoring efforts to add more depth and breadth to VIONE related efforts.
Acknowledgments
The authors express their gratitude to Central Arkansas VA Healthcare System leadership, Clinical Applications Coordinators, and colleagues for their unconditional support, to the Diffusion of Excellence programs at US Department of Veterans Affairs Central Office for their endorsement, and to the many VHA participants who renew our optimism and energy as we continue this exciting journey. We also thank Bridget B. Kelly for her assistance in writing and editing of the manuscript.
1. Chassin MR, Jerod ML. High-reliability health care: getting there from here. The Joint Commission. Milbank Q. 2013;91(3):459-490.
2. Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139.
3. Quinn KJ, Shah NH. A dataset quantifying polypharmacy in the United States. Sci Data. 2017;4:170167.
4. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834.
5. Steinman MA. Polypharmacy—time to get beyond numbers. JAMA Intern Med. 2016;176(4):482-483.
6. US Department of Veterans Affairs. High reliability. https://dvagov.sharepoint.com/sites/OHT-PMO/high-reliability/Pages/default.aspx. [Nonpublic source, not verified.]
7. Gordon S, Mendenhall P, O’Connor BB. Beyond the Checklist: What Else Health Care Can Learn from Aviation Teamwork and Safety. Ithaca, NY: Cornell University Press; 2013.
8. Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press; 2000.
9. US Department of Veterans Affairs. Diffusion of Excellence. https://www.va.gov/HEALTHCAREEXCELLENCE/diffusion-of-excellence/. Updated August 10, 2018. Accessed June 26, 2019.
10. US Department of Veterans Affairs. VIONE program toolkit. https://www.vapulse.net/docs/DOC-259375. [Nonpublic source, not verified.]
1. Chassin MR, Jerod ML. High-reliability health care: getting there from here. The Joint Commission. Milbank Q. 2013;91(3):459-490.
2. Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139.
3. Quinn KJ, Shah NH. A dataset quantifying polypharmacy in the United States. Sci Data. 2017;4:170167.
4. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834.
5. Steinman MA. Polypharmacy—time to get beyond numbers. JAMA Intern Med. 2016;176(4):482-483.
6. US Department of Veterans Affairs. High reliability. https://dvagov.sharepoint.com/sites/OHT-PMO/high-reliability/Pages/default.aspx. [Nonpublic source, not verified.]
7. Gordon S, Mendenhall P, O’Connor BB. Beyond the Checklist: What Else Health Care Can Learn from Aviation Teamwork and Safety. Ithaca, NY: Cornell University Press; 2013.
8. Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press; 2000.
9. US Department of Veterans Affairs. Diffusion of Excellence. https://www.va.gov/HEALTHCAREEXCELLENCE/diffusion-of-excellence/. Updated August 10, 2018. Accessed June 26, 2019.
10. US Department of Veterans Affairs. VIONE program toolkit. https://www.vapulse.net/docs/DOC-259375. [Nonpublic source, not verified.]
VA Ketamine Controversies
To the Editor: We read with interest the editorial on the clinical use of intranasal esketamine in treatment-resistant depression by Editor-in-Chief Cynthia Geppert in the October 2019 issue of Federal Practitioner.1 A recent case report published in your journal illustrated the success of IV ketamine in alleviating refractory chronic pain caused by a rare disease.2 Ketamine has been well established as an appropriate adjuvant as well as an alternative to opioids in attenuating acute postoperative pain and in certain chronic pain syndromes.3 We write out of concern for the rapidity of adoption of intranasal esketamine without considering the merits of IV ketamine.
When adopting new treatments or extending established drugs for newer indications, clinicians must balance beneficence and nonmaleficence. There is an urgent need for better treatment options for depression, suicidality, posttraumatic stress disorder (PTSD), and chronic pain in the veteran population. However, one must proceed with caution before wide adoption of a treatment that lacks real-world data on sustained or long-term benefits.4 Enthusiasm for this drug must also be tempered by the documented adverse effect (AE) of hepatic injury and the lack of data tracking this AE from repeated, long-term use.5 With these considerations in mind, reliable dosing and predictable pharmacokinetics are of great importance.
In addition to outpatient esketamine, outpatient IV administration of racemic ketamine remains an advantageous option with unique benefits compared with esketamine. Pharmacokinetically, IV ketamine is superior to intranasal esketamine. The bioavailability of intranasal esketamine is likely to be variable. A patient with a poor intranasal application or poor absorption might be falsely labeled an esketamine nonresponder. Increasing intranasal esketamine dosage to avoid false nonresponders may place other patients at risk for overdose and undesired AEs, including dysphoria and hallucinations. The variable bioavailability of intranasal ketamine adds complexity to the examination of its clinical effectiveness. IV ketamine should provide a predictable drug level and more reliable data. One might retort that esketamine is not the same as ketamine. True, esketamine is the S-enantiomer of ketamine, whereas ketamine is a racemic mixture of S- and R-ketamine. However, there is no clear evidence of clinically relevant differences between these formulations.5
Psychomimetic effects and cardiovascular changes are the most common short-term AEs resulting from ketamine.5 An IV infusion allows the treating physician to slowly titrate the administered ketamine to reach an effective concentration at the target site. Unlike an all-or-none intranasal administration, an infusion can be stopped at the first appearance of an AE. Psychomimetic effects, such as hallucinations, visual disturbances, and dysphoria are thought to occur in a dose-dependent fashion and remit once a ketamine infusion is stopped.5 Furthermore, cardiovascular AEs, such as hypertension and tachycardia, are commonly in patients with a body mass index > 30, with IV administration on a mg/kg basis. This suggests that calculated ideal body weight is a safer denominator, and reliable dosing is important to mitigating AEs.6
We urge caution with the widespread adoption of intranasal esketamine and suggest the advantages of the IV route, which offers predictability of AEs and titratability of dose. Questions remain regarding the appropriate dose and formulation of ketamine, rate of infusion, and route of administration for chronic pain and psychiatric indications.5,7 It is our responsibility to further study the long-term safety profile of ketamine and determine an appropriate dose of ketamine. The IV route allows many veterans to be helped in a safe and controllable manner.
Eugene Raggi, MD; and Srikantha L. Rao, MD, MS, FAS
1. Geppert CMA. The VA ketamine controversies. Fed Pract. 2019;36(10):446-447.
2. Eliason AH, Seo Y, Murphy D, Beal C. Adiposis dolorosa pain management. Fed Pract. 2019;36(11):530-533.
3. Orhurhu V, Orhurhu MS, Bhatia A, Cohen SP. Ketamine infusions for chronic pain: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2019;129(1):241-254.
4. Talbot J, Phillips JL, Blier P. Ketamine for chronic depression: two cautionary tales. J Psychiatry Neurosci. 2019;44(6):384-385.
5. Cohen SP, Bhatia A, Buvanendran A, et al. Consensus guidelines on the use of intravenous ketamine infusions for chronic pain from the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018;43(5):521-546.
6. Sanacora G, Frye MA, McDonald W, et al; American Psychiatric Association (APA) Council of Research Task Force on Novel Biomarkers and Treatments. A consensus statement on the use of ketamine in the treatment of mood disorders. JAMA Psychiatry. 2017;74(4):399-405.
7. Andrade C. Ketamine for depression, 4: in what dose, at what rate, by what route, for how long, and at what frequency? J Clin Psychiatry. 2017;78(7):e852-e857.
To the Editor: We read with interest the editorial on the clinical use of intranasal esketamine in treatment-resistant depression by Editor-in-Chief Cynthia Geppert in the October 2019 issue of Federal Practitioner.1 A recent case report published in your journal illustrated the success of IV ketamine in alleviating refractory chronic pain caused by a rare disease.2 Ketamine has been well established as an appropriate adjuvant as well as an alternative to opioids in attenuating acute postoperative pain and in certain chronic pain syndromes.3 We write out of concern for the rapidity of adoption of intranasal esketamine without considering the merits of IV ketamine.
When adopting new treatments or extending established drugs for newer indications, clinicians must balance beneficence and nonmaleficence. There is an urgent need for better treatment options for depression, suicidality, posttraumatic stress disorder (PTSD), and chronic pain in the veteran population. However, one must proceed with caution before wide adoption of a treatment that lacks real-world data on sustained or long-term benefits.4 Enthusiasm for this drug must also be tempered by the documented adverse effect (AE) of hepatic injury and the lack of data tracking this AE from repeated, long-term use.5 With these considerations in mind, reliable dosing and predictable pharmacokinetics are of great importance.
In addition to outpatient esketamine, outpatient IV administration of racemic ketamine remains an advantageous option with unique benefits compared with esketamine. Pharmacokinetically, IV ketamine is superior to intranasal esketamine. The bioavailability of intranasal esketamine is likely to be variable. A patient with a poor intranasal application or poor absorption might be falsely labeled an esketamine nonresponder. Increasing intranasal esketamine dosage to avoid false nonresponders may place other patients at risk for overdose and undesired AEs, including dysphoria and hallucinations. The variable bioavailability of intranasal ketamine adds complexity to the examination of its clinical effectiveness. IV ketamine should provide a predictable drug level and more reliable data. One might retort that esketamine is not the same as ketamine. True, esketamine is the S-enantiomer of ketamine, whereas ketamine is a racemic mixture of S- and R-ketamine. However, there is no clear evidence of clinically relevant differences between these formulations.5
Psychomimetic effects and cardiovascular changes are the most common short-term AEs resulting from ketamine.5 An IV infusion allows the treating physician to slowly titrate the administered ketamine to reach an effective concentration at the target site. Unlike an all-or-none intranasal administration, an infusion can be stopped at the first appearance of an AE. Psychomimetic effects, such as hallucinations, visual disturbances, and dysphoria are thought to occur in a dose-dependent fashion and remit once a ketamine infusion is stopped.5 Furthermore, cardiovascular AEs, such as hypertension and tachycardia, are commonly in patients with a body mass index > 30, with IV administration on a mg/kg basis. This suggests that calculated ideal body weight is a safer denominator, and reliable dosing is important to mitigating AEs.6
We urge caution with the widespread adoption of intranasal esketamine and suggest the advantages of the IV route, which offers predictability of AEs and titratability of dose. Questions remain regarding the appropriate dose and formulation of ketamine, rate of infusion, and route of administration for chronic pain and psychiatric indications.5,7 It is our responsibility to further study the long-term safety profile of ketamine and determine an appropriate dose of ketamine. The IV route allows many veterans to be helped in a safe and controllable manner.
Eugene Raggi, MD; and Srikantha L. Rao, MD, MS, FAS
To the Editor: We read with interest the editorial on the clinical use of intranasal esketamine in treatment-resistant depression by Editor-in-Chief Cynthia Geppert in the October 2019 issue of Federal Practitioner.1 A recent case report published in your journal illustrated the success of IV ketamine in alleviating refractory chronic pain caused by a rare disease.2 Ketamine has been well established as an appropriate adjuvant as well as an alternative to opioids in attenuating acute postoperative pain and in certain chronic pain syndromes.3 We write out of concern for the rapidity of adoption of intranasal esketamine without considering the merits of IV ketamine.
When adopting new treatments or extending established drugs for newer indications, clinicians must balance beneficence and nonmaleficence. There is an urgent need for better treatment options for depression, suicidality, posttraumatic stress disorder (PTSD), and chronic pain in the veteran population. However, one must proceed with caution before wide adoption of a treatment that lacks real-world data on sustained or long-term benefits.4 Enthusiasm for this drug must also be tempered by the documented adverse effect (AE) of hepatic injury and the lack of data tracking this AE from repeated, long-term use.5 With these considerations in mind, reliable dosing and predictable pharmacokinetics are of great importance.
In addition to outpatient esketamine, outpatient IV administration of racemic ketamine remains an advantageous option with unique benefits compared with esketamine. Pharmacokinetically, IV ketamine is superior to intranasal esketamine. The bioavailability of intranasal esketamine is likely to be variable. A patient with a poor intranasal application or poor absorption might be falsely labeled an esketamine nonresponder. Increasing intranasal esketamine dosage to avoid false nonresponders may place other patients at risk for overdose and undesired AEs, including dysphoria and hallucinations. The variable bioavailability of intranasal ketamine adds complexity to the examination of its clinical effectiveness. IV ketamine should provide a predictable drug level and more reliable data. One might retort that esketamine is not the same as ketamine. True, esketamine is the S-enantiomer of ketamine, whereas ketamine is a racemic mixture of S- and R-ketamine. However, there is no clear evidence of clinically relevant differences between these formulations.5
Psychomimetic effects and cardiovascular changes are the most common short-term AEs resulting from ketamine.5 An IV infusion allows the treating physician to slowly titrate the administered ketamine to reach an effective concentration at the target site. Unlike an all-or-none intranasal administration, an infusion can be stopped at the first appearance of an AE. Psychomimetic effects, such as hallucinations, visual disturbances, and dysphoria are thought to occur in a dose-dependent fashion and remit once a ketamine infusion is stopped.5 Furthermore, cardiovascular AEs, such as hypertension and tachycardia, are commonly in patients with a body mass index > 30, with IV administration on a mg/kg basis. This suggests that calculated ideal body weight is a safer denominator, and reliable dosing is important to mitigating AEs.6
We urge caution with the widespread adoption of intranasal esketamine and suggest the advantages of the IV route, which offers predictability of AEs and titratability of dose. Questions remain regarding the appropriate dose and formulation of ketamine, rate of infusion, and route of administration for chronic pain and psychiatric indications.5,7 It is our responsibility to further study the long-term safety profile of ketamine and determine an appropriate dose of ketamine. The IV route allows many veterans to be helped in a safe and controllable manner.
Eugene Raggi, MD; and Srikantha L. Rao, MD, MS, FAS
1. Geppert CMA. The VA ketamine controversies. Fed Pract. 2019;36(10):446-447.
2. Eliason AH, Seo Y, Murphy D, Beal C. Adiposis dolorosa pain management. Fed Pract. 2019;36(11):530-533.
3. Orhurhu V, Orhurhu MS, Bhatia A, Cohen SP. Ketamine infusions for chronic pain: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2019;129(1):241-254.
4. Talbot J, Phillips JL, Blier P. Ketamine for chronic depression: two cautionary tales. J Psychiatry Neurosci. 2019;44(6):384-385.
5. Cohen SP, Bhatia A, Buvanendran A, et al. Consensus guidelines on the use of intravenous ketamine infusions for chronic pain from the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018;43(5):521-546.
6. Sanacora G, Frye MA, McDonald W, et al; American Psychiatric Association (APA) Council of Research Task Force on Novel Biomarkers and Treatments. A consensus statement on the use of ketamine in the treatment of mood disorders. JAMA Psychiatry. 2017;74(4):399-405.
7. Andrade C. Ketamine for depression, 4: in what dose, at what rate, by what route, for how long, and at what frequency? J Clin Psychiatry. 2017;78(7):e852-e857.
1. Geppert CMA. The VA ketamine controversies. Fed Pract. 2019;36(10):446-447.
2. Eliason AH, Seo Y, Murphy D, Beal C. Adiposis dolorosa pain management. Fed Pract. 2019;36(11):530-533.
3. Orhurhu V, Orhurhu MS, Bhatia A, Cohen SP. Ketamine infusions for chronic pain: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2019;129(1):241-254.
4. Talbot J, Phillips JL, Blier P. Ketamine for chronic depression: two cautionary tales. J Psychiatry Neurosci. 2019;44(6):384-385.
5. Cohen SP, Bhatia A, Buvanendran A, et al. Consensus guidelines on the use of intravenous ketamine infusions for chronic pain from the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018;43(5):521-546.
6. Sanacora G, Frye MA, McDonald W, et al; American Psychiatric Association (APA) Council of Research Task Force on Novel Biomarkers and Treatments. A consensus statement on the use of ketamine in the treatment of mood disorders. JAMA Psychiatry. 2017;74(4):399-405.
7. Andrade C. Ketamine for depression, 4: in what dose, at what rate, by what route, for how long, and at what frequency? J Clin Psychiatry. 2017;78(7):e852-e857.
Improving Veteran Care With the Mission Act
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”
OTC hormonal contraception: An important goal in the fight for reproductive justice
A new American College of Obstetricians and Gynecologists (ACOG) committee opinion addresses how contraception access can be improved through over-the-counter (OTC) hormonal contraception for people of all ages—including oral contraceptive pills (OCPs), progesterone-only pills, the patch, vaginal rings, and depot medroxyprogesterone acetate (DMPA). Although ACOG endorses OTC contraception, some health care providers may be hesitant to support the increase in accessibility for a variety of reasons. We are hopeful that we address these concerns and that all clinicians can move to support ACOG’s position.
Easing access to hormonal contraception is a first step
OCPs are the most widely used contraception among teens and women of reproductive age in the United States.1 Although the Affordable Care Act (ACA) mandated health insurance coverage for contraception, many barriers continue to exist, including obtaining a prescription. Only 13 states have made it legal to obtain hormonal contraception through a pharmacist.2 There also has been an increase in the number of telemedicine and online services that deliver contraceptives to individuals’ homes. While these efforts have helped to decrease barriers to hormonal contraception access for some patients, they only reach a small segment of the population. As clinicians, we should strive to make contraception universally accessible and affordable to everyone who desires to use it. OTC provision can bring us closer to this goal.
Addressing the misconceptions about contraception
Adverse events with hormonal contraception are rarer than one may think. There are few risks associated with hormonal contraception. Venous thromboembolus (VTE) is a serious, although rare, adverse effect (AE) of hormonal contraception. The rate of VTE with combined oral contraception is estimated at 3 to 8 events per 10,000 patient-years, and VTE is even less common with progestin-only contraception (1 to 5 per 10,000 patient-years). For both types of hormonal contraception, the risk of VTE is smaller than with pregnancy, which is 5 to 20 per 10,000 patient-years.3 There are comorbidities that increase the risk of VTE and other AEs of hormonal contraception. In the setting of OTC hormonal contraception, individuals would self-screen for contraindications in order to reduce these complications.
Patients have the aptitude to self-screen for contraindications. Studies looking at the ability of patients over the age of 18 to self-screen for contraindications to hormonal contraception have found that patients do appropriately screen themselves. In fact, they are often more conservative than a physician in avoiding hormonal contraceptive methods.4 Patients younger than age 18 rarely have contraindications to hormonal contraception, but limited studies have shown that they too are able to successfully self-screen.5 ACOG recommends self-screening tools be provided with all OTC combined hormonal contraceptive methods to aid an individual’s contraceptive choice.
Most patients continue their well person care. Some opponents to ACOG’s position also have expressed concern that people who access their contraception OTC will forego their annual exam with their provider. However, studies have shown that the majority of people will continue to make their preventative health care visits.6,7
We need to invest in preventing unplanned pregnancy
Currently, hormonal contraception is covered by health insurance under the ACA, with some caveats. Without a prescription, patients may have to pay full price for their contraception. However, one can find generic OCPs for less than $10 per pack out of pocket. Any cost can be prohibitive to many patients; thus, transition to OTC access to contraception also should ensure limiting the cost to the patient. One possible solution to mitigate costs is to require insurance companies to cover the cost of OTC hormonal contraceptives. (See action item below.)
Reduction in unplanned pregnancies improves public health and public expense, and broadening access to effective forms of contraception is imperative in reducing unplanned pregnancies. Every $1 invested in contraception access realizes $7.09 in savings.8 By making hormonal contraception widely available OTC, access could be improved dramatically—although pharmacist provision of hormonal contraception may be a necessary intermediate step. ACOG’s most recent committee opinion encourages all reproductive health care providers to be strong advocates for this improvement in access. As women’s health providers, we should work to decrease access barriers for our patients; working toward OTC contraception is a critical step in equal access to birth control methods for all of our patients.
Action items
Remember, before a pill can move to OTC access, the manufacturing (pharmaceutical) company must submit an application to the US Food and Drug Administration to obtain this status. Once submitted, the process may take 3 to 4 years to be completed. Currently, no company has submitted an OTC application and no hormonal birth control is available OTC. Find resources for OTC birth control access here: http://ocsotc.org/ and www.freethepill.org.
- Talk to your state representatives about why both OTC birth control access and direct pharmacy availability are important to increasing access and decreasing disparities in reproductive health care. Find your local and federal representatives here and check the status of OCP access in your state here.
- Representative Ayanna Pressley (D-MA) and Senator Patty Murray (D-WA) both have introduced legislation—the Affordability is Access Act (HR 3296/S1847)—to ensure insurance coverage for OTC contraception. Call your representative and ask them to cosponsor this legislation.
- Be mindful of legislation that promotes OTC OCPs but limits access to some populations (minors) and increases cost sharing to the patient. This type of legislation can create harmful barriers to access for some of our patients
- Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Rep. 2012;(60):1-25.
- Free the pill. What’s the law in your state? Ibis Reproductive Health website. http://freethepill.org/statepolicies. Accessed November 15, 2019.
- U.S. Food and Drug Administration. FDA Drug Safety Communication: updated information about the risk of blood clots in women taking birth control pills containing drospirenone. https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed November 15, 2019.
- Grossman D, Fernandez L, Hopkins K, et al. Accuracy of self-screening for contraindications to combined oral contraceptive use. Obstet Gynecol. 2008;112:572e8.
- Williams R, Hensel D, Lehmann A, et al. Adolescent self-screening for contraindications to combined oral contraceptive pills [abstract]. Contraception. 2015;92:380.
- Hopkins K, Grossman D, White K, et al. Reproductive health preventive screening among clinic vs. over-the-counter oral contraceptive users. Contraception. 2012;86:376-382.
- Grindlay K, Grossman D. Interest in over-the-counter access to a progestin-only pill among women in the United States. Womens Health Issues. 2018;28:144-151.
- Frost JJ, Sonfield A, Zolna MR, et al. Return on investment: a fuller assessment of the benefits and cost savings of the US publicly funded family planning program. Milbank Q. 2014;92:696-749.
A new American College of Obstetricians and Gynecologists (ACOG) committee opinion addresses how contraception access can be improved through over-the-counter (OTC) hormonal contraception for people of all ages—including oral contraceptive pills (OCPs), progesterone-only pills, the patch, vaginal rings, and depot medroxyprogesterone acetate (DMPA). Although ACOG endorses OTC contraception, some health care providers may be hesitant to support the increase in accessibility for a variety of reasons. We are hopeful that we address these concerns and that all clinicians can move to support ACOG’s position.
Easing access to hormonal contraception is a first step
OCPs are the most widely used contraception among teens and women of reproductive age in the United States.1 Although the Affordable Care Act (ACA) mandated health insurance coverage for contraception, many barriers continue to exist, including obtaining a prescription. Only 13 states have made it legal to obtain hormonal contraception through a pharmacist.2 There also has been an increase in the number of telemedicine and online services that deliver contraceptives to individuals’ homes. While these efforts have helped to decrease barriers to hormonal contraception access for some patients, they only reach a small segment of the population. As clinicians, we should strive to make contraception universally accessible and affordable to everyone who desires to use it. OTC provision can bring us closer to this goal.
Addressing the misconceptions about contraception
Adverse events with hormonal contraception are rarer than one may think. There are few risks associated with hormonal contraception. Venous thromboembolus (VTE) is a serious, although rare, adverse effect (AE) of hormonal contraception. The rate of VTE with combined oral contraception is estimated at 3 to 8 events per 10,000 patient-years, and VTE is even less common with progestin-only contraception (1 to 5 per 10,000 patient-years). For both types of hormonal contraception, the risk of VTE is smaller than with pregnancy, which is 5 to 20 per 10,000 patient-years.3 There are comorbidities that increase the risk of VTE and other AEs of hormonal contraception. In the setting of OTC hormonal contraception, individuals would self-screen for contraindications in order to reduce these complications.
Patients have the aptitude to self-screen for contraindications. Studies looking at the ability of patients over the age of 18 to self-screen for contraindications to hormonal contraception have found that patients do appropriately screen themselves. In fact, they are often more conservative than a physician in avoiding hormonal contraceptive methods.4 Patients younger than age 18 rarely have contraindications to hormonal contraception, but limited studies have shown that they too are able to successfully self-screen.5 ACOG recommends self-screening tools be provided with all OTC combined hormonal contraceptive methods to aid an individual’s contraceptive choice.
Most patients continue their well person care. Some opponents to ACOG’s position also have expressed concern that people who access their contraception OTC will forego their annual exam with their provider. However, studies have shown that the majority of people will continue to make their preventative health care visits.6,7
We need to invest in preventing unplanned pregnancy
Currently, hormonal contraception is covered by health insurance under the ACA, with some caveats. Without a prescription, patients may have to pay full price for their contraception. However, one can find generic OCPs for less than $10 per pack out of pocket. Any cost can be prohibitive to many patients; thus, transition to OTC access to contraception also should ensure limiting the cost to the patient. One possible solution to mitigate costs is to require insurance companies to cover the cost of OTC hormonal contraceptives. (See action item below.)
Reduction in unplanned pregnancies improves public health and public expense, and broadening access to effective forms of contraception is imperative in reducing unplanned pregnancies. Every $1 invested in contraception access realizes $7.09 in savings.8 By making hormonal contraception widely available OTC, access could be improved dramatically—although pharmacist provision of hormonal contraception may be a necessary intermediate step. ACOG’s most recent committee opinion encourages all reproductive health care providers to be strong advocates for this improvement in access. As women’s health providers, we should work to decrease access barriers for our patients; working toward OTC contraception is a critical step in equal access to birth control methods for all of our patients.
Action items
Remember, before a pill can move to OTC access, the manufacturing (pharmaceutical) company must submit an application to the US Food and Drug Administration to obtain this status. Once submitted, the process may take 3 to 4 years to be completed. Currently, no company has submitted an OTC application and no hormonal birth control is available OTC. Find resources for OTC birth control access here: http://ocsotc.org/ and www.freethepill.org.
- Talk to your state representatives about why both OTC birth control access and direct pharmacy availability are important to increasing access and decreasing disparities in reproductive health care. Find your local and federal representatives here and check the status of OCP access in your state here.
- Representative Ayanna Pressley (D-MA) and Senator Patty Murray (D-WA) both have introduced legislation—the Affordability is Access Act (HR 3296/S1847)—to ensure insurance coverage for OTC contraception. Call your representative and ask them to cosponsor this legislation.
- Be mindful of legislation that promotes OTC OCPs but limits access to some populations (minors) and increases cost sharing to the patient. This type of legislation can create harmful barriers to access for some of our patients
A new American College of Obstetricians and Gynecologists (ACOG) committee opinion addresses how contraception access can be improved through over-the-counter (OTC) hormonal contraception for people of all ages—including oral contraceptive pills (OCPs), progesterone-only pills, the patch, vaginal rings, and depot medroxyprogesterone acetate (DMPA). Although ACOG endorses OTC contraception, some health care providers may be hesitant to support the increase in accessibility for a variety of reasons. We are hopeful that we address these concerns and that all clinicians can move to support ACOG’s position.
Easing access to hormonal contraception is a first step
OCPs are the most widely used contraception among teens and women of reproductive age in the United States.1 Although the Affordable Care Act (ACA) mandated health insurance coverage for contraception, many barriers continue to exist, including obtaining a prescription. Only 13 states have made it legal to obtain hormonal contraception through a pharmacist.2 There also has been an increase in the number of telemedicine and online services that deliver contraceptives to individuals’ homes. While these efforts have helped to decrease barriers to hormonal contraception access for some patients, they only reach a small segment of the population. As clinicians, we should strive to make contraception universally accessible and affordable to everyone who desires to use it. OTC provision can bring us closer to this goal.
Addressing the misconceptions about contraception
Adverse events with hormonal contraception are rarer than one may think. There are few risks associated with hormonal contraception. Venous thromboembolus (VTE) is a serious, although rare, adverse effect (AE) of hormonal contraception. The rate of VTE with combined oral contraception is estimated at 3 to 8 events per 10,000 patient-years, and VTE is even less common with progestin-only contraception (1 to 5 per 10,000 patient-years). For both types of hormonal contraception, the risk of VTE is smaller than with pregnancy, which is 5 to 20 per 10,000 patient-years.3 There are comorbidities that increase the risk of VTE and other AEs of hormonal contraception. In the setting of OTC hormonal contraception, individuals would self-screen for contraindications in order to reduce these complications.
Patients have the aptitude to self-screen for contraindications. Studies looking at the ability of patients over the age of 18 to self-screen for contraindications to hormonal contraception have found that patients do appropriately screen themselves. In fact, they are often more conservative than a physician in avoiding hormonal contraceptive methods.4 Patients younger than age 18 rarely have contraindications to hormonal contraception, but limited studies have shown that they too are able to successfully self-screen.5 ACOG recommends self-screening tools be provided with all OTC combined hormonal contraceptive methods to aid an individual’s contraceptive choice.
Most patients continue their well person care. Some opponents to ACOG’s position also have expressed concern that people who access their contraception OTC will forego their annual exam with their provider. However, studies have shown that the majority of people will continue to make their preventative health care visits.6,7
We need to invest in preventing unplanned pregnancy
Currently, hormonal contraception is covered by health insurance under the ACA, with some caveats. Without a prescription, patients may have to pay full price for their contraception. However, one can find generic OCPs for less than $10 per pack out of pocket. Any cost can be prohibitive to many patients; thus, transition to OTC access to contraception also should ensure limiting the cost to the patient. One possible solution to mitigate costs is to require insurance companies to cover the cost of OTC hormonal contraceptives. (See action item below.)
Reduction in unplanned pregnancies improves public health and public expense, and broadening access to effective forms of contraception is imperative in reducing unplanned pregnancies. Every $1 invested in contraception access realizes $7.09 in savings.8 By making hormonal contraception widely available OTC, access could be improved dramatically—although pharmacist provision of hormonal contraception may be a necessary intermediate step. ACOG’s most recent committee opinion encourages all reproductive health care providers to be strong advocates for this improvement in access. As women’s health providers, we should work to decrease access barriers for our patients; working toward OTC contraception is a critical step in equal access to birth control methods for all of our patients.
Action items
Remember, before a pill can move to OTC access, the manufacturing (pharmaceutical) company must submit an application to the US Food and Drug Administration to obtain this status. Once submitted, the process may take 3 to 4 years to be completed. Currently, no company has submitted an OTC application and no hormonal birth control is available OTC. Find resources for OTC birth control access here: http://ocsotc.org/ and www.freethepill.org.
- Talk to your state representatives about why both OTC birth control access and direct pharmacy availability are important to increasing access and decreasing disparities in reproductive health care. Find your local and federal representatives here and check the status of OCP access in your state here.
- Representative Ayanna Pressley (D-MA) and Senator Patty Murray (D-WA) both have introduced legislation—the Affordability is Access Act (HR 3296/S1847)—to ensure insurance coverage for OTC contraception. Call your representative and ask them to cosponsor this legislation.
- Be mindful of legislation that promotes OTC OCPs but limits access to some populations (minors) and increases cost sharing to the patient. This type of legislation can create harmful barriers to access for some of our patients
- Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Rep. 2012;(60):1-25.
- Free the pill. What’s the law in your state? Ibis Reproductive Health website. http://freethepill.org/statepolicies. Accessed November 15, 2019.
- U.S. Food and Drug Administration. FDA Drug Safety Communication: updated information about the risk of blood clots in women taking birth control pills containing drospirenone. https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed November 15, 2019.
- Grossman D, Fernandez L, Hopkins K, et al. Accuracy of self-screening for contraindications to combined oral contraceptive use. Obstet Gynecol. 2008;112:572e8.
- Williams R, Hensel D, Lehmann A, et al. Adolescent self-screening for contraindications to combined oral contraceptive pills [abstract]. Contraception. 2015;92:380.
- Hopkins K, Grossman D, White K, et al. Reproductive health preventive screening among clinic vs. over-the-counter oral contraceptive users. Contraception. 2012;86:376-382.
- Grindlay K, Grossman D. Interest in over-the-counter access to a progestin-only pill among women in the United States. Womens Health Issues. 2018;28:144-151.
- Frost JJ, Sonfield A, Zolna MR, et al. Return on investment: a fuller assessment of the benefits and cost savings of the US publicly funded family planning program. Milbank Q. 2014;92:696-749.
- Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Rep. 2012;(60):1-25.
- Free the pill. What’s the law in your state? Ibis Reproductive Health website. http://freethepill.org/statepolicies. Accessed November 15, 2019.
- U.S. Food and Drug Administration. FDA Drug Safety Communication: updated information about the risk of blood clots in women taking birth control pills containing drospirenone. https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed November 15, 2019.
- Grossman D, Fernandez L, Hopkins K, et al. Accuracy of self-screening for contraindications to combined oral contraceptive use. Obstet Gynecol. 2008;112:572e8.
- Williams R, Hensel D, Lehmann A, et al. Adolescent self-screening for contraindications to combined oral contraceptive pills [abstract]. Contraception. 2015;92:380.
- Hopkins K, Grossman D, White K, et al. Reproductive health preventive screening among clinic vs. over-the-counter oral contraceptive users. Contraception. 2012;86:376-382.
- Grindlay K, Grossman D. Interest in over-the-counter access to a progestin-only pill among women in the United States. Womens Health Issues. 2018;28:144-151.
- Frost JJ, Sonfield A, Zolna MR, et al. Return on investment: a fuller assessment of the benefits and cost savings of the US publicly funded family planning program. Milbank Q. 2014;92:696-749.
Court strikes down Trump’s conscience rule
A federal court has struck down a Trump administration rule that would have allowed clinicians to refuse to provide medical care to patients for religious or moral reasons.
In a Nov. 6 decision, the U.S. District Court for the Southern District of New York vacated President Trump’s rule in its entirety, concluding that the rule had no justification and that its provisions were arbitrary and capricious. In his 147-page opinion, District Judge Paul Engelmayer wrote that the U.S. Department of Health & Human Services did not have the authority to enact such an expansive rule and that the measure conflicts with the Administrative Procedure Act, Title VII of the Civil Rights Act, and the Emergency Medical Treatment & Labor Act, among other laws.
“Had the court found only narrow parts of the rule infirm, a remedy tailoring the vacatur to only the problematic provision might well have been viable,” Judge Engelmayer wrote. “The [Administrative Procedure Act] violations that the court has found, however, are numerous, fundamental, and far reaching ... In these circumstances, a decision to leave standing isolated shards of the rule that have not been found specifically infirm would ignore the big picture: that the rulemaking exercise here was sufficiently shot through with glaring legal defects as to not justify a search for survivors [and] leaving stray nonsubstantive provisions intact would not serve a useful purpose.”
At press time, the Trump administration had not indicated whether they plan to file an appeal.
Clare Coleman, president & CEO for the National Family Planning & Reproductive Health Association, a plaintiff in the case, said the organization was heartened by the ruling and that the judge’s decision protects health care for millions of Americans.
“The court safeguarded the public’s health by striking down the Trump administration’s health care refusal rule,” Ms. Coleman said in a statement. “This unlawful rule is an outright attack on the health and wellness of millions of people across the country, and the court heard clear and compelling arguments about the harm communities face when our health care system is distorted to the point in which a patient’s health care needs are not paramount.”
The conscience rule, finalized in May 2019 by HHS, would have allowed clinicians to refuse care to patients if they deemed that care was in conflict with their religious or moral beliefs. The provisions principally – although not exclusively – addressed objections to abortion, sterilization, and assisted suicide, as well as counseling and referrals associated with these services.
According to HHS, the final rule fulfills President Trump’s promise to promote and protect rights of conscience and religious liberty. “This rule ensures that health care entities and professionals won’t be bullied out of the health care field because they decline to participate in actions that violate their conscience, including the taking of human life,” Roger Severino, director of the Office for Civil Rights, said in a statement. “Protecting conscience and religious freedom not only fosters greater diversity in health care, it’s the law.”
The judge’s order invalidating the rule consolidated three legal challenges against HHS over the rule. Plaintiffs included more than 15 states, Planned Parenthood Federation of America, and the National Family Planning & Reproductive Health Association, among others. The plaintiffs argued that the rule, scheduled to take effect on Nov. 22, would have threatened the ability of clinicians to provide essential, potentially life-saving medical care and would have exacerbated health disparities.
Stephanie Taub, senior counsel at the First Liberty Institute, an organization that represents religious freedom cases, said the court’s decision leaves health care professionals across America vulnerable to being forced “to perform, facilitate, or refer for procedures that violate their conscience.”
“The Trump administration’s HHS protections would ensure that health care professionals are free to work consistent with their religious beliefs while providing the best care to their patients,” Ms. Taub said in a statement.
The court’s decision comes less than a week after another district judge temporarily blocked an order by President Trump that would make having health insurance, or the ability to pay for medical care, a requirement for immigrants seeking U.S. visas. In that case, the judge said there are serious questions about whether President Trump’s immigration rule was arbitrary and capricious and, therefore, a violation of the Administrative Procedure Act. The order is on hold while the case continues through the courts.
A federal court has struck down a Trump administration rule that would have allowed clinicians to refuse to provide medical care to patients for religious or moral reasons.
In a Nov. 6 decision, the U.S. District Court for the Southern District of New York vacated President Trump’s rule in its entirety, concluding that the rule had no justification and that its provisions were arbitrary and capricious. In his 147-page opinion, District Judge Paul Engelmayer wrote that the U.S. Department of Health & Human Services did not have the authority to enact such an expansive rule and that the measure conflicts with the Administrative Procedure Act, Title VII of the Civil Rights Act, and the Emergency Medical Treatment & Labor Act, among other laws.
“Had the court found only narrow parts of the rule infirm, a remedy tailoring the vacatur to only the problematic provision might well have been viable,” Judge Engelmayer wrote. “The [Administrative Procedure Act] violations that the court has found, however, are numerous, fundamental, and far reaching ... In these circumstances, a decision to leave standing isolated shards of the rule that have not been found specifically infirm would ignore the big picture: that the rulemaking exercise here was sufficiently shot through with glaring legal defects as to not justify a search for survivors [and] leaving stray nonsubstantive provisions intact would not serve a useful purpose.”
At press time, the Trump administration had not indicated whether they plan to file an appeal.
Clare Coleman, president & CEO for the National Family Planning & Reproductive Health Association, a plaintiff in the case, said the organization was heartened by the ruling and that the judge’s decision protects health care for millions of Americans.
“The court safeguarded the public’s health by striking down the Trump administration’s health care refusal rule,” Ms. Coleman said in a statement. “This unlawful rule is an outright attack on the health and wellness of millions of people across the country, and the court heard clear and compelling arguments about the harm communities face when our health care system is distorted to the point in which a patient’s health care needs are not paramount.”
The conscience rule, finalized in May 2019 by HHS, would have allowed clinicians to refuse care to patients if they deemed that care was in conflict with their religious or moral beliefs. The provisions principally – although not exclusively – addressed objections to abortion, sterilization, and assisted suicide, as well as counseling and referrals associated with these services.
According to HHS, the final rule fulfills President Trump’s promise to promote and protect rights of conscience and religious liberty. “This rule ensures that health care entities and professionals won’t be bullied out of the health care field because they decline to participate in actions that violate their conscience, including the taking of human life,” Roger Severino, director of the Office for Civil Rights, said in a statement. “Protecting conscience and religious freedom not only fosters greater diversity in health care, it’s the law.”
The judge’s order invalidating the rule consolidated three legal challenges against HHS over the rule. Plaintiffs included more than 15 states, Planned Parenthood Federation of America, and the National Family Planning & Reproductive Health Association, among others. The plaintiffs argued that the rule, scheduled to take effect on Nov. 22, would have threatened the ability of clinicians to provide essential, potentially life-saving medical care and would have exacerbated health disparities.
Stephanie Taub, senior counsel at the First Liberty Institute, an organization that represents religious freedom cases, said the court’s decision leaves health care professionals across America vulnerable to being forced “to perform, facilitate, or refer for procedures that violate their conscience.”
“The Trump administration’s HHS protections would ensure that health care professionals are free to work consistent with their religious beliefs while providing the best care to their patients,” Ms. Taub said in a statement.
The court’s decision comes less than a week after another district judge temporarily blocked an order by President Trump that would make having health insurance, or the ability to pay for medical care, a requirement for immigrants seeking U.S. visas. In that case, the judge said there are serious questions about whether President Trump’s immigration rule was arbitrary and capricious and, therefore, a violation of the Administrative Procedure Act. The order is on hold while the case continues through the courts.
A federal court has struck down a Trump administration rule that would have allowed clinicians to refuse to provide medical care to patients for religious or moral reasons.
In a Nov. 6 decision, the U.S. District Court for the Southern District of New York vacated President Trump’s rule in its entirety, concluding that the rule had no justification and that its provisions were arbitrary and capricious. In his 147-page opinion, District Judge Paul Engelmayer wrote that the U.S. Department of Health & Human Services did not have the authority to enact such an expansive rule and that the measure conflicts with the Administrative Procedure Act, Title VII of the Civil Rights Act, and the Emergency Medical Treatment & Labor Act, among other laws.
“Had the court found only narrow parts of the rule infirm, a remedy tailoring the vacatur to only the problematic provision might well have been viable,” Judge Engelmayer wrote. “The [Administrative Procedure Act] violations that the court has found, however, are numerous, fundamental, and far reaching ... In these circumstances, a decision to leave standing isolated shards of the rule that have not been found specifically infirm would ignore the big picture: that the rulemaking exercise here was sufficiently shot through with glaring legal defects as to not justify a search for survivors [and] leaving stray nonsubstantive provisions intact would not serve a useful purpose.”
At press time, the Trump administration had not indicated whether they plan to file an appeal.
Clare Coleman, president & CEO for the National Family Planning & Reproductive Health Association, a plaintiff in the case, said the organization was heartened by the ruling and that the judge’s decision protects health care for millions of Americans.
“The court safeguarded the public’s health by striking down the Trump administration’s health care refusal rule,” Ms. Coleman said in a statement. “This unlawful rule is an outright attack on the health and wellness of millions of people across the country, and the court heard clear and compelling arguments about the harm communities face when our health care system is distorted to the point in which a patient’s health care needs are not paramount.”
The conscience rule, finalized in May 2019 by HHS, would have allowed clinicians to refuse care to patients if they deemed that care was in conflict with their religious or moral beliefs. The provisions principally – although not exclusively – addressed objections to abortion, sterilization, and assisted suicide, as well as counseling and referrals associated with these services.
According to HHS, the final rule fulfills President Trump’s promise to promote and protect rights of conscience and religious liberty. “This rule ensures that health care entities and professionals won’t be bullied out of the health care field because they decline to participate in actions that violate their conscience, including the taking of human life,” Roger Severino, director of the Office for Civil Rights, said in a statement. “Protecting conscience and religious freedom not only fosters greater diversity in health care, it’s the law.”
The judge’s order invalidating the rule consolidated three legal challenges against HHS over the rule. Plaintiffs included more than 15 states, Planned Parenthood Federation of America, and the National Family Planning & Reproductive Health Association, among others. The plaintiffs argued that the rule, scheduled to take effect on Nov. 22, would have threatened the ability of clinicians to provide essential, potentially life-saving medical care and would have exacerbated health disparities.
Stephanie Taub, senior counsel at the First Liberty Institute, an organization that represents religious freedom cases, said the court’s decision leaves health care professionals across America vulnerable to being forced “to perform, facilitate, or refer for procedures that violate their conscience.”
“The Trump administration’s HHS protections would ensure that health care professionals are free to work consistent with their religious beliefs while providing the best care to their patients,” Ms. Taub said in a statement.
The court’s decision comes less than a week after another district judge temporarily blocked an order by President Trump that would make having health insurance, or the ability to pay for medical care, a requirement for immigrants seeking U.S. visas. In that case, the judge said there are serious questions about whether President Trump’s immigration rule was arbitrary and capricious and, therefore, a violation of the Administrative Procedure Act. The order is on hold while the case continues through the courts.
Using Voogle to Search Within Patient Records in the VA Corporate Data Warehouse
Digitalization of patient-specific information over the past 2 decades has dramatically altered health care delivery. Nonetheless, this technology has yet to live up to its promise of improving patient outcomes, in part due to data storage challenges as well as the emphasis on data entry to support administrative and financial goals of the institution.1-4 Substantially less emphasis has been placed on the retrieval of information required for accurate diagnosis.
A new search engine, Voogle, is now available through Microsoft Internet Explorer (Redmond, WA) to all providers in the US Department of Veterans Affairs (VA) on any intranet-enabled computer behind the VA firewall. Voogle facilitates rapid query-based search and retrieval of patient-specific data in the VA Corporate Data Warehouse (CDW).
Case Example
A veteran presented requesting consideration for implantation of a new device for obstructive sleep apnea. Guidelines for implantation of the new device specify a narrow therapeutic window, so determination of his apnea-hypopnea index (AHI) was critical. The patient had received care at more than 20 VA facilities and knew the approximate year the test had been performed at a non-VA facility.
A health care provider (HCP) using Voogle from his VA computer indexed all Veterans Information Systems and Technology Architecture (VistA) notes for the desired date range. The indexing of > 200 notes was completed in seconds. The HCP opened the indexed records with Voogle and entered a query for “sleep apnea,” which displayed multiple instances of the term within the patient record notes. A VA HCP had previously entered the data from the outside sleep study into a note shortly after the study.
This information was found immediately by sorting the indexed notes by date. The total time required by Voogle to find and display the critical information from the sleep study entered at a different VA more than a dozen years earlier was about 1 minute. These data provided the information needed for decision making at the time of the current patient encounter, without which repeat (and unnecessary) testing would have been required.
Information Overload
Electronic health records (EHRs) such as VistA, upload, store, collate, and present data in near real-time across multiple locations. Although the availability of these data can potentially reduce the risk of error due to missing critical information, its sheer volume limits its utility for point-of-care decision making. Much patient-specific text data found in clinical notes are recorded for administrative, financial, and business purposes rather than to support patient care decision making.1-3 The majority of data documents processes of care rather than HCP observations, assessment of current status, or plans for care. Much of this text is inserted into templates, consists of imported structured data elements, and may contain repeated copy-and-paste free text.
Data uploaded to the CDW are aggregated from multiple hospitals, each with its own “instance” of VistA. Often the CDW contains thousands of text notes for a single patient. This volume of text may conceal critical historical information needed for patient care mixed with a plethora of duplicated or extraneous text entered to satisfy administrative requirements. The effects of information overload and poor system usability have been studied extensively in other disciplines, but this science has largely not been incorporated into EHR design.1,3,4
A position paper published recently by the American College of Physicians notes that physician cognitive work is adversely impacted by the incorporation of nonclinical information into the EHR for use by other administrative and financial functions.2
Information Chaos
Beasley and colleagues noted that information in an EHR needed for optimal care may be unavailable, inadequate, scattered, conflicting, lost, or inaccurate, a condition they term information chaos.5 Smith and colleagues reported that decision making in 1 of 7 primary care visits was impaired by missing critical information. Surveyed HCPs estimated that 44% of patients with missing information may receive compromised care as a result, including delayed or erroneous diagnosis and increased costs due to duplication of diagnostic testing.6
Even when technically available, the usability of patient-specific data needed for accurate diagnosis is compromised if the HCP cannot find the information. In most systems data storage paradigms mirror database design rather than provider cognitive models. Ultimately, the design of current EHR interaction paradigms squanders precious cognitive resources and time, particularly during patient encounters, leaving little available for the cognitive tasks necessary for accurate diagnosis and treatment decisions.1,3,4,7
VA Corporate Data Warehouse
VistA was implemented as a decentralized system with 130 instances, each of which is a freestanding EHR. However, as all systems share common data structures, the data can be combined from multiple instances when needed. The VA established a CDW more than 15 years ago in order to collate information from multiple sites to support operations as well as to seek new insights. The CDW currently updates nightly from all 130 EHR instances and is the only location in which patient information from all treating sites is combined. Voogle can access the CDW through the Veterans Informatics and Computing Infrastructure (VINCI), which is a mirror of the CDW databases and was established as a secure research environment.
The CDW contains information on 25 million veterans, with about 15 terabytes of text data. Approximately 4 billion data points, including 1 million text notes, are accrued nightly. The Integrated Control Number (ICN), a unique patient identifier, is assigned to each CDW record and is cross-indexed in the master patient index. All CDW data are tied to the ICN, facilitating access to and attribution of all patient data from all VA sites. Voogle relies on this identifier to build indexed files, or domains (which are document collections), of requested specific patient information to support its search algorithm.
Structured Data
Most of the data accrued in an EHR are structured data (such as laboratory test results and vital signs) and stored in a defined database framework. Voogle uses iFind (Intersystems Inc, Cambridge, MA) to index, count, and then search for requested information within structured data fields.
Unstructured Text
In contrast to structured data, text notes are stored as documents that are retrievable by patient, author, date, clinic, as well as numerous other fields. Unstructured (free) text notes are more information rich than either structured data or templated notes since their narrative format more closely parallels providers’ cognitive processes.1,7 The value of the narrative becomes even more critical in understanding complex clinical scenarios with multiple interacting disease processes. Narratives emphasize important details, reducing cognitive overload by reducing the salience of detail the author deems to be less critical. Narrative notes simultaneously assure availability through the use of unstandardized language, often including specialty and disease-specific abbreviations.1 Information needed for decision making in the illustrative case in this report was present only in HCP-entered free-text notes, as the structured data from which the free text was derived were not available.
Search
The introduction of search engines can be considered one of the major technologic disruptors of the 21st century.8 However, this advance has not yet made significant inroads into health care, despite advances in other domains. As of 2019, EHR users are still required to be familiar with the system’s data and menu structure in order to find needed information (or enter orders, code visits, or any of a number of tasks). Anecdotally, one of the authors (David Eibling) observed that the most common question from his trainees is “How do you . . .?” referring not to the care of the patient but rather to interaction with the EHR.
What is needed is a simple query-based application that finds the data on request. In addition to Voogle, other advances are being made in this arena such as the EMERSE, medical record search engine (project-emerse.org). Voogle was released to VA providers in 2017 and is available through the Internet Explorer browser on VA computers with VA intranet access. The goal of Voogle is to reduce HCP cognitive load by reducing the time and effort needed to seek relevant information for the care of a specific patient.
Natural Language Processing
Linguistic analysis of text seeking to understand its meaning constitutes a rapidly expanding field, with current heavy emphasis on the role of artificial intelligence and machine learning.1 Advances in processing both structured data and free-text notes in the health care domain is in its infancy, despite the investment of considerable resources. Undoubtedly, advances in this arena will dramatically change provider cognitive work in the next decades.
VistA is coded in MUMPS (Massachusetts General Hospital Utility Multi-Programming System, also known as M), which has been in use for more than 50 years. Voogle employs iKnow, a novel natural language processing (NLP) application that resides in Caché (Intersystems, Boston, MA), the vendor-supported MUMPS infrastructure VistA uses to perform text analysis. iKnow does not attempt to interpret the meaning of text as do other common NLP applications, but instead relies on the expert user to interpret the meaning of the analyzed text. iKnow initially divides sentences into relations (usually verbs) and concepts, and then generates an index of these entities. The efficiency of iKnow results in very rapid indexing—often several thousand notes (not an uncommon number) can be indexed in 20 to 30 seconds. iKnow responds to a user query by searching for specific terms or similar terms within the indexed text, and then displays these terms within the original source documents, similar to well-known commercial search engines. Structured data are indexed by the iFind program simultaneously with free-text indexing (Figure 1).
Security
Maintaining high levels of security of Health Insurance Portability and Accountability (HIPAA)-compliant information in an online application such as Voogle is critical to ensure trust of veterans and HCPs. All patient data accessed by Voogle reside within the secure firewall-protected VINCI environment. All moving information is protected with high-level encryption protocols (transport layer security [TLS]), and data at rest are also encrypted. As the application is online, no data are stored on the accessing device. Voogle uses a secure Microsoft Windows logon using VA Active Directory coupled with VistA authorization to regulate who can see the data and use the application. All access is audited, not only for “sensitive patients,” but also for specific data types. Users are reminded of this Voogle attribute on the home screen.
Accessing Voogle
Voogle is available on the VA intranet to all authorized users at https://voogle.vha.med.va.gov/voogle. To assure high-level security the application can only be accessed with the Internet Explorer browser using established user identification protocols to avoid unauthorized access or duplicative log-in tasks.
Indexing
Indexing is user-driven and is required prior to patient selection and term query. The user is prompted for a patient identifier and a date range. The CDW unique patient identifier is used for all internal processing. However, a social security number look-up table is incorporated to facilitate patient selection. The date field defaults to 3 years but can be extended to approximately the year 2000.
Queries
Entering the patient name in Lastname, Firstname (no space) format will yield a list of indexed patients. All access is audited in order to deter unauthorized queries. Data from a demonstration patient are displayed in Figures 2, 3, 4, 5,
and 6.
Structured Data Searches
Structured data categories that contain the queried term, as well as a term count, are displayed after the “Structured Data” toggle is selected (Figure 2). After the desired category (Figure 2: “Outpatient Rx”) is selected, Voogle accesses the data file and displays it as a grid (medication list, Figure 3). Filter and sort functions enable display of specific medications, drug classes, or date ranges (Figure 4).
Display of Terms Within Text Notes
Selecting a term from the drop-down list (Figure 5) opens a grid with the term highlighted in a snippet of text (Figure 6). Opening the document displays the context of the term, along with negation terms (ie, not, denies, no, etc) in red font if present. Voogle, unlike other NLP tools that attempt to interpret medical notes, relies on interpretation by the HCP user. Duplicate note fragments will be displayed in multiple notes, often across multiple screens, vividly demonstrating the pervasive use of the copy-and-paste text-entry strategy. Voogle satisfies 2 of the 4 recommendations of the recent report on copy-and-paste by Tsou and colleagues.9 The Voogle text display grid identifies copy-and-pasted text as well as establishes the provenance of the text (by sorting on the date column). Text can be copied from Voogle into an active Computerized Patient Record System (CPRS) note if needed for active patient care. Reindexing the following day and then repeating the search will demonstrate the newly copied-and-pasted text appended to the sequence.
Limitations
Voogle is unable to access all VA patient data currently. There are a dozen or so clinical domains that are indexed by Voogle that include prescriptions, problem lists, health factors, and others. More domains can be added with minimal effort and would then be available for fast search. The most critical deficiency is its inability to access, index, or query text reports stored as images within VistA Imaging. This includes nearly all reports from outside HCPs, emergency department visits or discharge summaries from unlinked hospitals, anesthesia reports, intensive care unit flow sheets, electrocardiograms, as well as numerous other text reports such as pulmonary function reports or sleep studies. Information that is transcribed by the provider into VistA as text (as in the case presented) is available within the CDW and can be found and displayed by Voogle search.
Voogle requires that the user initiates the indexing process prior to initiating the search process. Although Voogle defaults to 3 years prior to the current date, the user can specify a start date extending to close to the year 2000. The volume of data flowing into the CDW precludes automatic indexing of all patient data, as well as automatic updating of previously indexed data. We have explored the feasibility of queueing scheduled appointments for the following day, and although the strategy shows some promise, avoiding conflict with user-requested on-demand indexing remains challenging.
The current VA network architecture updates the CDW every night, resulting in up to a 24-hour delay in data availability. However, this delay should be reduced to several minutes after implementation of real-time data feeds accompanying the coming transition to a new EHR platform.
Conclusions
The recent introduction of the Joint Legacy Viewer (JLV) to the VA EHR desktop has enhanced the breadth of patient-specific information available to any VHA clinician, with recent enhancements providing access to some community care notes from outside HCPs. Voogle builds on this capability by enabling rapid search of text notes and structured data from multiple VA sites, over an extended time frame, and perhaps entered by hundreds of authors, as demonstrated in the case example. Formal usability and workload studies have not been performed; however, anecdotal reports indicate the application dramatically reduces the time required to search for critical information needed for care of complex patients who have been treated in multiple different VA hospitals and clinics.
The Voogle paradigm of leveraging patient information stored within a large enterprise-wide data warehouse through NLP techniques may be applicable to other systems as well, and warrants exploration. We believe that replacing traditional data search paradigms that require knowledge of data structure with a true query-based paradigm is a potential game changer for health information systems. Ultimately this strategy may help provide an antidote for the information chaos impacting HCP cognition. Moreover, reducing HCP cognitive load and time on task may lessen overall health care costs, reduce provider burn-out, and improve the quality of care received by patients.
Near real-time data feeds and adding additional clinical domains will potentially provide other benefits to patient care. For example, the authors plan to investigate whether sampling incoming data may assist with behind-the-scenes continuous monitoring of indicators of patient status to facilitate early warning of impending physiologic collapse.10 Other possible applications could include real-time scans for biosurveillance or other population screening requirements.
Acknowledgments
The authors express their sincere appreciation to Leslie DeYoung for documentation and Justin Wilson who constructed much of the graphical user interface for the Voogle application and design. Without their expertise, passion, and commitment the application would not be available as it is now.
1. Wachter RM. The Digital Doctor: Hope, Hype and Harm at the Dawn of the Computer Age New York: McGraw-Hill Education; 2017.
2. Erickson SM, Rockwern B, Koltov M, McLean RM; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med. 2017;166(9):659-661.
3. Woods DD, Patterson ES, Roth EM. Can we ever escape from data overload? A cognitive systems diagnosis. Cogn Technol Work. 2002;4(1):22-36.
4. Gupta A, Harrod M, Quinn M, et al. Mind the overlap: how system problems contribute to cognitive failure and diagnostic errors. Diagnosis (Berl). 2018;5(3):151-156.
5. Beasley JW, Wetterneck TB, Temte J, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med. 2011;24(6):745-751.
6. Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA. 2005;293(5):565-571.
7. Papadakos PJ, Berman E, eds. Distracted Doctoring: Returning to Patient-Centered Care in the Digital Age. New York: Springer International Publishing; 2017.
8. Battelle J. Search: How Google and its Rivals Rewrote the Rules of Business and Transformed Our Culture. New York: Penguin Group; 2005.
9. Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the EHR. Systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017;8(1):12-34.
10. Rothman MJ, Rothman SI, Beals J 4th. Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46(5):837-848.
Digitalization of patient-specific information over the past 2 decades has dramatically altered health care delivery. Nonetheless, this technology has yet to live up to its promise of improving patient outcomes, in part due to data storage challenges as well as the emphasis on data entry to support administrative and financial goals of the institution.1-4 Substantially less emphasis has been placed on the retrieval of information required for accurate diagnosis.
A new search engine, Voogle, is now available through Microsoft Internet Explorer (Redmond, WA) to all providers in the US Department of Veterans Affairs (VA) on any intranet-enabled computer behind the VA firewall. Voogle facilitates rapid query-based search and retrieval of patient-specific data in the VA Corporate Data Warehouse (CDW).
Case Example
A veteran presented requesting consideration for implantation of a new device for obstructive sleep apnea. Guidelines for implantation of the new device specify a narrow therapeutic window, so determination of his apnea-hypopnea index (AHI) was critical. The patient had received care at more than 20 VA facilities and knew the approximate year the test had been performed at a non-VA facility.
A health care provider (HCP) using Voogle from his VA computer indexed all Veterans Information Systems and Technology Architecture (VistA) notes for the desired date range. The indexing of > 200 notes was completed in seconds. The HCP opened the indexed records with Voogle and entered a query for “sleep apnea,” which displayed multiple instances of the term within the patient record notes. A VA HCP had previously entered the data from the outside sleep study into a note shortly after the study.
This information was found immediately by sorting the indexed notes by date. The total time required by Voogle to find and display the critical information from the sleep study entered at a different VA more than a dozen years earlier was about 1 minute. These data provided the information needed for decision making at the time of the current patient encounter, without which repeat (and unnecessary) testing would have been required.
Information Overload
Electronic health records (EHRs) such as VistA, upload, store, collate, and present data in near real-time across multiple locations. Although the availability of these data can potentially reduce the risk of error due to missing critical information, its sheer volume limits its utility for point-of-care decision making. Much patient-specific text data found in clinical notes are recorded for administrative, financial, and business purposes rather than to support patient care decision making.1-3 The majority of data documents processes of care rather than HCP observations, assessment of current status, or plans for care. Much of this text is inserted into templates, consists of imported structured data elements, and may contain repeated copy-and-paste free text.
Data uploaded to the CDW are aggregated from multiple hospitals, each with its own “instance” of VistA. Often the CDW contains thousands of text notes for a single patient. This volume of text may conceal critical historical information needed for patient care mixed with a plethora of duplicated or extraneous text entered to satisfy administrative requirements. The effects of information overload and poor system usability have been studied extensively in other disciplines, but this science has largely not been incorporated into EHR design.1,3,4
A position paper published recently by the American College of Physicians notes that physician cognitive work is adversely impacted by the incorporation of nonclinical information into the EHR for use by other administrative and financial functions.2
Information Chaos
Beasley and colleagues noted that information in an EHR needed for optimal care may be unavailable, inadequate, scattered, conflicting, lost, or inaccurate, a condition they term information chaos.5 Smith and colleagues reported that decision making in 1 of 7 primary care visits was impaired by missing critical information. Surveyed HCPs estimated that 44% of patients with missing information may receive compromised care as a result, including delayed or erroneous diagnosis and increased costs due to duplication of diagnostic testing.6
Even when technically available, the usability of patient-specific data needed for accurate diagnosis is compromised if the HCP cannot find the information. In most systems data storage paradigms mirror database design rather than provider cognitive models. Ultimately, the design of current EHR interaction paradigms squanders precious cognitive resources and time, particularly during patient encounters, leaving little available for the cognitive tasks necessary for accurate diagnosis and treatment decisions.1,3,4,7
VA Corporate Data Warehouse
VistA was implemented as a decentralized system with 130 instances, each of which is a freestanding EHR. However, as all systems share common data structures, the data can be combined from multiple instances when needed. The VA established a CDW more than 15 years ago in order to collate information from multiple sites to support operations as well as to seek new insights. The CDW currently updates nightly from all 130 EHR instances and is the only location in which patient information from all treating sites is combined. Voogle can access the CDW through the Veterans Informatics and Computing Infrastructure (VINCI), which is a mirror of the CDW databases and was established as a secure research environment.
The CDW contains information on 25 million veterans, with about 15 terabytes of text data. Approximately 4 billion data points, including 1 million text notes, are accrued nightly. The Integrated Control Number (ICN), a unique patient identifier, is assigned to each CDW record and is cross-indexed in the master patient index. All CDW data are tied to the ICN, facilitating access to and attribution of all patient data from all VA sites. Voogle relies on this identifier to build indexed files, or domains (which are document collections), of requested specific patient information to support its search algorithm.
Structured Data
Most of the data accrued in an EHR are structured data (such as laboratory test results and vital signs) and stored in a defined database framework. Voogle uses iFind (Intersystems Inc, Cambridge, MA) to index, count, and then search for requested information within structured data fields.
Unstructured Text
In contrast to structured data, text notes are stored as documents that are retrievable by patient, author, date, clinic, as well as numerous other fields. Unstructured (free) text notes are more information rich than either structured data or templated notes since their narrative format more closely parallels providers’ cognitive processes.1,7 The value of the narrative becomes even more critical in understanding complex clinical scenarios with multiple interacting disease processes. Narratives emphasize important details, reducing cognitive overload by reducing the salience of detail the author deems to be less critical. Narrative notes simultaneously assure availability through the use of unstandardized language, often including specialty and disease-specific abbreviations.1 Information needed for decision making in the illustrative case in this report was present only in HCP-entered free-text notes, as the structured data from which the free text was derived were not available.
Search
The introduction of search engines can be considered one of the major technologic disruptors of the 21st century.8 However, this advance has not yet made significant inroads into health care, despite advances in other domains. As of 2019, EHR users are still required to be familiar with the system’s data and menu structure in order to find needed information (or enter orders, code visits, or any of a number of tasks). Anecdotally, one of the authors (David Eibling) observed that the most common question from his trainees is “How do you . . .?” referring not to the care of the patient but rather to interaction with the EHR.
What is needed is a simple query-based application that finds the data on request. In addition to Voogle, other advances are being made in this arena such as the EMERSE, medical record search engine (project-emerse.org). Voogle was released to VA providers in 2017 and is available through the Internet Explorer browser on VA computers with VA intranet access. The goal of Voogle is to reduce HCP cognitive load by reducing the time and effort needed to seek relevant information for the care of a specific patient.
Natural Language Processing
Linguistic analysis of text seeking to understand its meaning constitutes a rapidly expanding field, with current heavy emphasis on the role of artificial intelligence and machine learning.1 Advances in processing both structured data and free-text notes in the health care domain is in its infancy, despite the investment of considerable resources. Undoubtedly, advances in this arena will dramatically change provider cognitive work in the next decades.
VistA is coded in MUMPS (Massachusetts General Hospital Utility Multi-Programming System, also known as M), which has been in use for more than 50 years. Voogle employs iKnow, a novel natural language processing (NLP) application that resides in Caché (Intersystems, Boston, MA), the vendor-supported MUMPS infrastructure VistA uses to perform text analysis. iKnow does not attempt to interpret the meaning of text as do other common NLP applications, but instead relies on the expert user to interpret the meaning of the analyzed text. iKnow initially divides sentences into relations (usually verbs) and concepts, and then generates an index of these entities. The efficiency of iKnow results in very rapid indexing—often several thousand notes (not an uncommon number) can be indexed in 20 to 30 seconds. iKnow responds to a user query by searching for specific terms or similar terms within the indexed text, and then displays these terms within the original source documents, similar to well-known commercial search engines. Structured data are indexed by the iFind program simultaneously with free-text indexing (Figure 1).
Security
Maintaining high levels of security of Health Insurance Portability and Accountability (HIPAA)-compliant information in an online application such as Voogle is critical to ensure trust of veterans and HCPs. All patient data accessed by Voogle reside within the secure firewall-protected VINCI environment. All moving information is protected with high-level encryption protocols (transport layer security [TLS]), and data at rest are also encrypted. As the application is online, no data are stored on the accessing device. Voogle uses a secure Microsoft Windows logon using VA Active Directory coupled with VistA authorization to regulate who can see the data and use the application. All access is audited, not only for “sensitive patients,” but also for specific data types. Users are reminded of this Voogle attribute on the home screen.
Accessing Voogle
Voogle is available on the VA intranet to all authorized users at https://voogle.vha.med.va.gov/voogle. To assure high-level security the application can only be accessed with the Internet Explorer browser using established user identification protocols to avoid unauthorized access or duplicative log-in tasks.
Indexing
Indexing is user-driven and is required prior to patient selection and term query. The user is prompted for a patient identifier and a date range. The CDW unique patient identifier is used for all internal processing. However, a social security number look-up table is incorporated to facilitate patient selection. The date field defaults to 3 years but can be extended to approximately the year 2000.
Queries
Entering the patient name in Lastname, Firstname (no space) format will yield a list of indexed patients. All access is audited in order to deter unauthorized queries. Data from a demonstration patient are displayed in Figures 2, 3, 4, 5,
and 6.
Structured Data Searches
Structured data categories that contain the queried term, as well as a term count, are displayed after the “Structured Data” toggle is selected (Figure 2). After the desired category (Figure 2: “Outpatient Rx”) is selected, Voogle accesses the data file and displays it as a grid (medication list, Figure 3). Filter and sort functions enable display of specific medications, drug classes, or date ranges (Figure 4).
Display of Terms Within Text Notes
Selecting a term from the drop-down list (Figure 5) opens a grid with the term highlighted in a snippet of text (Figure 6). Opening the document displays the context of the term, along with negation terms (ie, not, denies, no, etc) in red font if present. Voogle, unlike other NLP tools that attempt to interpret medical notes, relies on interpretation by the HCP user. Duplicate note fragments will be displayed in multiple notes, often across multiple screens, vividly demonstrating the pervasive use of the copy-and-paste text-entry strategy. Voogle satisfies 2 of the 4 recommendations of the recent report on copy-and-paste by Tsou and colleagues.9 The Voogle text display grid identifies copy-and-pasted text as well as establishes the provenance of the text (by sorting on the date column). Text can be copied from Voogle into an active Computerized Patient Record System (CPRS) note if needed for active patient care. Reindexing the following day and then repeating the search will demonstrate the newly copied-and-pasted text appended to the sequence.
Limitations
Voogle is unable to access all VA patient data currently. There are a dozen or so clinical domains that are indexed by Voogle that include prescriptions, problem lists, health factors, and others. More domains can be added with minimal effort and would then be available for fast search. The most critical deficiency is its inability to access, index, or query text reports stored as images within VistA Imaging. This includes nearly all reports from outside HCPs, emergency department visits or discharge summaries from unlinked hospitals, anesthesia reports, intensive care unit flow sheets, electrocardiograms, as well as numerous other text reports such as pulmonary function reports or sleep studies. Information that is transcribed by the provider into VistA as text (as in the case presented) is available within the CDW and can be found and displayed by Voogle search.
Voogle requires that the user initiates the indexing process prior to initiating the search process. Although Voogle defaults to 3 years prior to the current date, the user can specify a start date extending to close to the year 2000. The volume of data flowing into the CDW precludes automatic indexing of all patient data, as well as automatic updating of previously indexed data. We have explored the feasibility of queueing scheduled appointments for the following day, and although the strategy shows some promise, avoiding conflict with user-requested on-demand indexing remains challenging.
The current VA network architecture updates the CDW every night, resulting in up to a 24-hour delay in data availability. However, this delay should be reduced to several minutes after implementation of real-time data feeds accompanying the coming transition to a new EHR platform.
Conclusions
The recent introduction of the Joint Legacy Viewer (JLV) to the VA EHR desktop has enhanced the breadth of patient-specific information available to any VHA clinician, with recent enhancements providing access to some community care notes from outside HCPs. Voogle builds on this capability by enabling rapid search of text notes and structured data from multiple VA sites, over an extended time frame, and perhaps entered by hundreds of authors, as demonstrated in the case example. Formal usability and workload studies have not been performed; however, anecdotal reports indicate the application dramatically reduces the time required to search for critical information needed for care of complex patients who have been treated in multiple different VA hospitals and clinics.
The Voogle paradigm of leveraging patient information stored within a large enterprise-wide data warehouse through NLP techniques may be applicable to other systems as well, and warrants exploration. We believe that replacing traditional data search paradigms that require knowledge of data structure with a true query-based paradigm is a potential game changer for health information systems. Ultimately this strategy may help provide an antidote for the information chaos impacting HCP cognition. Moreover, reducing HCP cognitive load and time on task may lessen overall health care costs, reduce provider burn-out, and improve the quality of care received by patients.
Near real-time data feeds and adding additional clinical domains will potentially provide other benefits to patient care. For example, the authors plan to investigate whether sampling incoming data may assist with behind-the-scenes continuous monitoring of indicators of patient status to facilitate early warning of impending physiologic collapse.10 Other possible applications could include real-time scans for biosurveillance or other population screening requirements.
Acknowledgments
The authors express their sincere appreciation to Leslie DeYoung for documentation and Justin Wilson who constructed much of the graphical user interface for the Voogle application and design. Without their expertise, passion, and commitment the application would not be available as it is now.
Digitalization of patient-specific information over the past 2 decades has dramatically altered health care delivery. Nonetheless, this technology has yet to live up to its promise of improving patient outcomes, in part due to data storage challenges as well as the emphasis on data entry to support administrative and financial goals of the institution.1-4 Substantially less emphasis has been placed on the retrieval of information required for accurate diagnosis.
A new search engine, Voogle, is now available through Microsoft Internet Explorer (Redmond, WA) to all providers in the US Department of Veterans Affairs (VA) on any intranet-enabled computer behind the VA firewall. Voogle facilitates rapid query-based search and retrieval of patient-specific data in the VA Corporate Data Warehouse (CDW).
Case Example
A veteran presented requesting consideration for implantation of a new device for obstructive sleep apnea. Guidelines for implantation of the new device specify a narrow therapeutic window, so determination of his apnea-hypopnea index (AHI) was critical. The patient had received care at more than 20 VA facilities and knew the approximate year the test had been performed at a non-VA facility.
A health care provider (HCP) using Voogle from his VA computer indexed all Veterans Information Systems and Technology Architecture (VistA) notes for the desired date range. The indexing of > 200 notes was completed in seconds. The HCP opened the indexed records with Voogle and entered a query for “sleep apnea,” which displayed multiple instances of the term within the patient record notes. A VA HCP had previously entered the data from the outside sleep study into a note shortly after the study.
This information was found immediately by sorting the indexed notes by date. The total time required by Voogle to find and display the critical information from the sleep study entered at a different VA more than a dozen years earlier was about 1 minute. These data provided the information needed for decision making at the time of the current patient encounter, without which repeat (and unnecessary) testing would have been required.
Information Overload
Electronic health records (EHRs) such as VistA, upload, store, collate, and present data in near real-time across multiple locations. Although the availability of these data can potentially reduce the risk of error due to missing critical information, its sheer volume limits its utility for point-of-care decision making. Much patient-specific text data found in clinical notes are recorded for administrative, financial, and business purposes rather than to support patient care decision making.1-3 The majority of data documents processes of care rather than HCP observations, assessment of current status, or plans for care. Much of this text is inserted into templates, consists of imported structured data elements, and may contain repeated copy-and-paste free text.
Data uploaded to the CDW are aggregated from multiple hospitals, each with its own “instance” of VistA. Often the CDW contains thousands of text notes for a single patient. This volume of text may conceal critical historical information needed for patient care mixed with a plethora of duplicated or extraneous text entered to satisfy administrative requirements. The effects of information overload and poor system usability have been studied extensively in other disciplines, but this science has largely not been incorporated into EHR design.1,3,4
A position paper published recently by the American College of Physicians notes that physician cognitive work is adversely impacted by the incorporation of nonclinical information into the EHR for use by other administrative and financial functions.2
Information Chaos
Beasley and colleagues noted that information in an EHR needed for optimal care may be unavailable, inadequate, scattered, conflicting, lost, or inaccurate, a condition they term information chaos.5 Smith and colleagues reported that decision making in 1 of 7 primary care visits was impaired by missing critical information. Surveyed HCPs estimated that 44% of patients with missing information may receive compromised care as a result, including delayed or erroneous diagnosis and increased costs due to duplication of diagnostic testing.6
Even when technically available, the usability of patient-specific data needed for accurate diagnosis is compromised if the HCP cannot find the information. In most systems data storage paradigms mirror database design rather than provider cognitive models. Ultimately, the design of current EHR interaction paradigms squanders precious cognitive resources and time, particularly during patient encounters, leaving little available for the cognitive tasks necessary for accurate diagnosis and treatment decisions.1,3,4,7
VA Corporate Data Warehouse
VistA was implemented as a decentralized system with 130 instances, each of which is a freestanding EHR. However, as all systems share common data structures, the data can be combined from multiple instances when needed. The VA established a CDW more than 15 years ago in order to collate information from multiple sites to support operations as well as to seek new insights. The CDW currently updates nightly from all 130 EHR instances and is the only location in which patient information from all treating sites is combined. Voogle can access the CDW through the Veterans Informatics and Computing Infrastructure (VINCI), which is a mirror of the CDW databases and was established as a secure research environment.
The CDW contains information on 25 million veterans, with about 15 terabytes of text data. Approximately 4 billion data points, including 1 million text notes, are accrued nightly. The Integrated Control Number (ICN), a unique patient identifier, is assigned to each CDW record and is cross-indexed in the master patient index. All CDW data are tied to the ICN, facilitating access to and attribution of all patient data from all VA sites. Voogle relies on this identifier to build indexed files, or domains (which are document collections), of requested specific patient information to support its search algorithm.
Structured Data
Most of the data accrued in an EHR are structured data (such as laboratory test results and vital signs) and stored in a defined database framework. Voogle uses iFind (Intersystems Inc, Cambridge, MA) to index, count, and then search for requested information within structured data fields.
Unstructured Text
In contrast to structured data, text notes are stored as documents that are retrievable by patient, author, date, clinic, as well as numerous other fields. Unstructured (free) text notes are more information rich than either structured data or templated notes since their narrative format more closely parallels providers’ cognitive processes.1,7 The value of the narrative becomes even more critical in understanding complex clinical scenarios with multiple interacting disease processes. Narratives emphasize important details, reducing cognitive overload by reducing the salience of detail the author deems to be less critical. Narrative notes simultaneously assure availability through the use of unstandardized language, often including specialty and disease-specific abbreviations.1 Information needed for decision making in the illustrative case in this report was present only in HCP-entered free-text notes, as the structured data from which the free text was derived were not available.
Search
The introduction of search engines can be considered one of the major technologic disruptors of the 21st century.8 However, this advance has not yet made significant inroads into health care, despite advances in other domains. As of 2019, EHR users are still required to be familiar with the system’s data and menu structure in order to find needed information (or enter orders, code visits, or any of a number of tasks). Anecdotally, one of the authors (David Eibling) observed that the most common question from his trainees is “How do you . . .?” referring not to the care of the patient but rather to interaction with the EHR.
What is needed is a simple query-based application that finds the data on request. In addition to Voogle, other advances are being made in this arena such as the EMERSE, medical record search engine (project-emerse.org). Voogle was released to VA providers in 2017 and is available through the Internet Explorer browser on VA computers with VA intranet access. The goal of Voogle is to reduce HCP cognitive load by reducing the time and effort needed to seek relevant information for the care of a specific patient.
Natural Language Processing
Linguistic analysis of text seeking to understand its meaning constitutes a rapidly expanding field, with current heavy emphasis on the role of artificial intelligence and machine learning.1 Advances in processing both structured data and free-text notes in the health care domain is in its infancy, despite the investment of considerable resources. Undoubtedly, advances in this arena will dramatically change provider cognitive work in the next decades.
VistA is coded in MUMPS (Massachusetts General Hospital Utility Multi-Programming System, also known as M), which has been in use for more than 50 years. Voogle employs iKnow, a novel natural language processing (NLP) application that resides in Caché (Intersystems, Boston, MA), the vendor-supported MUMPS infrastructure VistA uses to perform text analysis. iKnow does not attempt to interpret the meaning of text as do other common NLP applications, but instead relies on the expert user to interpret the meaning of the analyzed text. iKnow initially divides sentences into relations (usually verbs) and concepts, and then generates an index of these entities. The efficiency of iKnow results in very rapid indexing—often several thousand notes (not an uncommon number) can be indexed in 20 to 30 seconds. iKnow responds to a user query by searching for specific terms or similar terms within the indexed text, and then displays these terms within the original source documents, similar to well-known commercial search engines. Structured data are indexed by the iFind program simultaneously with free-text indexing (Figure 1).
Security
Maintaining high levels of security of Health Insurance Portability and Accountability (HIPAA)-compliant information in an online application such as Voogle is critical to ensure trust of veterans and HCPs. All patient data accessed by Voogle reside within the secure firewall-protected VINCI environment. All moving information is protected with high-level encryption protocols (transport layer security [TLS]), and data at rest are also encrypted. As the application is online, no data are stored on the accessing device. Voogle uses a secure Microsoft Windows logon using VA Active Directory coupled with VistA authorization to regulate who can see the data and use the application. All access is audited, not only for “sensitive patients,” but also for specific data types. Users are reminded of this Voogle attribute on the home screen.
Accessing Voogle
Voogle is available on the VA intranet to all authorized users at https://voogle.vha.med.va.gov/voogle. To assure high-level security the application can only be accessed with the Internet Explorer browser using established user identification protocols to avoid unauthorized access or duplicative log-in tasks.
Indexing
Indexing is user-driven and is required prior to patient selection and term query. The user is prompted for a patient identifier and a date range. The CDW unique patient identifier is used for all internal processing. However, a social security number look-up table is incorporated to facilitate patient selection. The date field defaults to 3 years but can be extended to approximately the year 2000.
Queries
Entering the patient name in Lastname, Firstname (no space) format will yield a list of indexed patients. All access is audited in order to deter unauthorized queries. Data from a demonstration patient are displayed in Figures 2, 3, 4, 5,
and 6.
Structured Data Searches
Structured data categories that contain the queried term, as well as a term count, are displayed after the “Structured Data” toggle is selected (Figure 2). After the desired category (Figure 2: “Outpatient Rx”) is selected, Voogle accesses the data file and displays it as a grid (medication list, Figure 3). Filter and sort functions enable display of specific medications, drug classes, or date ranges (Figure 4).
Display of Terms Within Text Notes
Selecting a term from the drop-down list (Figure 5) opens a grid with the term highlighted in a snippet of text (Figure 6). Opening the document displays the context of the term, along with negation terms (ie, not, denies, no, etc) in red font if present. Voogle, unlike other NLP tools that attempt to interpret medical notes, relies on interpretation by the HCP user. Duplicate note fragments will be displayed in multiple notes, often across multiple screens, vividly demonstrating the pervasive use of the copy-and-paste text-entry strategy. Voogle satisfies 2 of the 4 recommendations of the recent report on copy-and-paste by Tsou and colleagues.9 The Voogle text display grid identifies copy-and-pasted text as well as establishes the provenance of the text (by sorting on the date column). Text can be copied from Voogle into an active Computerized Patient Record System (CPRS) note if needed for active patient care. Reindexing the following day and then repeating the search will demonstrate the newly copied-and-pasted text appended to the sequence.
Limitations
Voogle is unable to access all VA patient data currently. There are a dozen or so clinical domains that are indexed by Voogle that include prescriptions, problem lists, health factors, and others. More domains can be added with minimal effort and would then be available for fast search. The most critical deficiency is its inability to access, index, or query text reports stored as images within VistA Imaging. This includes nearly all reports from outside HCPs, emergency department visits or discharge summaries from unlinked hospitals, anesthesia reports, intensive care unit flow sheets, electrocardiograms, as well as numerous other text reports such as pulmonary function reports or sleep studies. Information that is transcribed by the provider into VistA as text (as in the case presented) is available within the CDW and can be found and displayed by Voogle search.
Voogle requires that the user initiates the indexing process prior to initiating the search process. Although Voogle defaults to 3 years prior to the current date, the user can specify a start date extending to close to the year 2000. The volume of data flowing into the CDW precludes automatic indexing of all patient data, as well as automatic updating of previously indexed data. We have explored the feasibility of queueing scheduled appointments for the following day, and although the strategy shows some promise, avoiding conflict with user-requested on-demand indexing remains challenging.
The current VA network architecture updates the CDW every night, resulting in up to a 24-hour delay in data availability. However, this delay should be reduced to several minutes after implementation of real-time data feeds accompanying the coming transition to a new EHR platform.
Conclusions
The recent introduction of the Joint Legacy Viewer (JLV) to the VA EHR desktop has enhanced the breadth of patient-specific information available to any VHA clinician, with recent enhancements providing access to some community care notes from outside HCPs. Voogle builds on this capability by enabling rapid search of text notes and structured data from multiple VA sites, over an extended time frame, and perhaps entered by hundreds of authors, as demonstrated in the case example. Formal usability and workload studies have not been performed; however, anecdotal reports indicate the application dramatically reduces the time required to search for critical information needed for care of complex patients who have been treated in multiple different VA hospitals and clinics.
The Voogle paradigm of leveraging patient information stored within a large enterprise-wide data warehouse through NLP techniques may be applicable to other systems as well, and warrants exploration. We believe that replacing traditional data search paradigms that require knowledge of data structure with a true query-based paradigm is a potential game changer for health information systems. Ultimately this strategy may help provide an antidote for the information chaos impacting HCP cognition. Moreover, reducing HCP cognitive load and time on task may lessen overall health care costs, reduce provider burn-out, and improve the quality of care received by patients.
Near real-time data feeds and adding additional clinical domains will potentially provide other benefits to patient care. For example, the authors plan to investigate whether sampling incoming data may assist with behind-the-scenes continuous monitoring of indicators of patient status to facilitate early warning of impending physiologic collapse.10 Other possible applications could include real-time scans for biosurveillance or other population screening requirements.
Acknowledgments
The authors express their sincere appreciation to Leslie DeYoung for documentation and Justin Wilson who constructed much of the graphical user interface for the Voogle application and design. Without their expertise, passion, and commitment the application would not be available as it is now.
1. Wachter RM. The Digital Doctor: Hope, Hype and Harm at the Dawn of the Computer Age New York: McGraw-Hill Education; 2017.
2. Erickson SM, Rockwern B, Koltov M, McLean RM; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med. 2017;166(9):659-661.
3. Woods DD, Patterson ES, Roth EM. Can we ever escape from data overload? A cognitive systems diagnosis. Cogn Technol Work. 2002;4(1):22-36.
4. Gupta A, Harrod M, Quinn M, et al. Mind the overlap: how system problems contribute to cognitive failure and diagnostic errors. Diagnosis (Berl). 2018;5(3):151-156.
5. Beasley JW, Wetterneck TB, Temte J, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med. 2011;24(6):745-751.
6. Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA. 2005;293(5):565-571.
7. Papadakos PJ, Berman E, eds. Distracted Doctoring: Returning to Patient-Centered Care in the Digital Age. New York: Springer International Publishing; 2017.
8. Battelle J. Search: How Google and its Rivals Rewrote the Rules of Business and Transformed Our Culture. New York: Penguin Group; 2005.
9. Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the EHR. Systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017;8(1):12-34.
10. Rothman MJ, Rothman SI, Beals J 4th. Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46(5):837-848.
1. Wachter RM. The Digital Doctor: Hope, Hype and Harm at the Dawn of the Computer Age New York: McGraw-Hill Education; 2017.
2. Erickson SM, Rockwern B, Koltov M, McLean RM; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med. 2017;166(9):659-661.
3. Woods DD, Patterson ES, Roth EM. Can we ever escape from data overload? A cognitive systems diagnosis. Cogn Technol Work. 2002;4(1):22-36.
4. Gupta A, Harrod M, Quinn M, et al. Mind the overlap: how system problems contribute to cognitive failure and diagnostic errors. Diagnosis (Berl). 2018;5(3):151-156.
5. Beasley JW, Wetterneck TB, Temte J, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med. 2011;24(6):745-751.
6. Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA. 2005;293(5):565-571.
7. Papadakos PJ, Berman E, eds. Distracted Doctoring: Returning to Patient-Centered Care in the Digital Age. New York: Springer International Publishing; 2017.
8. Battelle J. Search: How Google and its Rivals Rewrote the Rules of Business and Transformed Our Culture. New York: Penguin Group; 2005.
9. Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the EHR. Systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017;8(1):12-34.
10. Rothman MJ, Rothman SI, Beals J 4th. Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46(5):837-848.
Letters: Reframing Clinician Distress: Moral Injury Not Burnout
To the Editor: In the September 2019 guest editorial “Reframing Clinician Distress: Moral Injury Not Burnout,” the authors have advanced a thoughtful and provocative hypothesis addressing a salient issue.1 Their argument is that burnout does not accurately capture physician distress. Furthermore, they posit the term burnout focuses remediation strategies at the individual provider level, thereby discounting the contribution of the larger health care system. This is not the first effort to argue that burnout is not a syndrome of mental illness (eg, depression) located within the person but rather a disrupted physician-work relationship.2
As the authors cite, population and practice changes have contributed significantly to physician distress and dissatisfaction. Indeed, recent findings indicate that female physicians may suffer increased prevalence of burnout, which represents a challenge given the growing numbers of women in medicine.3 Unfortunately, by shifting focus almost exclusively to the system level to address burnout, the authors discount a large body of literature examining associations and contributors at the individual and clinic level.
Burnout is conceptualized as consisting of 3 domains: depersonalization, emotional exhaustion, and personal accomplishment.4 While this conceptualization may not capture the totality of physician distress, it has provided a body of literature focused on decreasing symptoms of burnout. Successful interventions have been targeted at the individual provider level (ie, stress management, small group discussion, mindfulness) as well as the organizational level (ie, reduction in duty hours, scribes).5,6 Recent studies have also suggested that increasing the occurrence of social encounters that are civil and respectful decreases reported physician burnout.7
Frustration, the annoyance or anger at being unable to change or achieve something, also can be a leading cause of burnout and moral injury. The inability to deal with unresolvable issues due to a lack of skills or inability to create a positive reframe can lead to a constellation of symptoms that are detrimental to the individual provider. Nevertheless, system rigidity, inability to recognitize pain and pressure, and goals perceived as unachievable can also lead to frustration. Physicians may experience growing frustration if they are unable to influence their systems. Thus, experiencing personal frustration, combined with an inability or lack of energy or time to influence a system can snowball.
Just as we counsel our patients that good medical care involves not only engagement with the medical system, but also individual engagement in their care (eg, nutrition, exercise), this problem requires a multicomponent solution. While advocating and working for a system that induces less moral injury, frustration, and burnout, physicians need to examine the resources available to them and their colleagues in a more immediate way.
Physician distress is a serious problem with both personal, patient, occupational, and public health costs. Thus, it is important that we grapple with the complexity of a multiconstruct definition amenable to multilevel interventions. The concept of moral injury is an important component and opens additional lines of both clinical inquiry and intervention. However, in our view, to subsume all burnout under this construct is overly reductive.
In closing, this topic is too important not to discuss. Let the conversations continue!
Lynne Padgett, PhD; and Joao L. Ascensao, MD, PhD
Author affiliations: Departments of Medicine and Mental Health, Washington DC VA Medical Center and Department of Medicine, George Washington University School of Medicine
Correspondence: Lynne Padgett (lynne.padgett@va.gov)
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Epstein RM, Privitera MR. Doing something about physician burnout. Lancet. 2016;388(10057):2216-2217.
3. Templeton K, Bernstein CA, Sukhera J, et al. Gender-based differences in burnout: issues faced by women physicians. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2019. https://nam.edu/wp-content/uploads/2019/05/Gender-Based-Differences-in-Burnout.pdf. Published May 28, 2019. Accessed October 10, 2019.
4. Eckleberry-Hunt J Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93(3):367-370.
5. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
6. Squiers JJ, Lobdell KW, Fann JI, DiMaio JM. Physician burnout: are we treating the symptom instead of the disease? Ann Thorac Surg. 2017;104(4):1117-1122.
7. Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160-163.
To the Editor: We applaud Dean and her colleagues for their thought-provoking commentary on clinicians’ distress, a problem that has surged in recent years and has now reached epidemic proportions.1 Their argument focuses on the language used to define and frame clinical distress. Do we label this distress as burnout, as moral injury, or as something else? Moral injury occurs any time clinicians are impeded from doing the right thing at the right time in the right way; or even worse, doing the wrong thing to serve the needs of health system stakeholders other than the patient. These other stakeholders may include administrators, corporations, insurance adjusters, and others.
Naming the problem correctly is crucial to finding the solution. The name frames the discussion and impacts the solution. Burnout implies difficulty coping with the many stresses of health care and of personal responsibility for the problem. The solution would therefore be to help individuals to cope with their stresses. Moral injury on the other hand implies a corrupt system; thereby, reframing the discussion to systems issues and suggesting solutions by changing the business of health care delivery.
These authors state that current clinical distress is due to moral injury and not to burnout. Therefore, the business in which health care is performed needs to change.
The authors define the drivers of moral injury in our current system, mostly as (1) a massive information technology overload that has largely overtaken the patient as center of attention; and (2) the profit motive of the health care corporation and its shareholders. A focus on making profits has increased in the wake of falling reimbursements; the result is pressure on clinicians to see more patients more quickly and to do more even when not necessary. This has diverted the focus on healing patients to a focus on making profits. These major drivers of clinician distress—the electronic health record and the pressure to bill more—are fundamentally driven by the corporatization of American medicine in which profit is the measured outcome.
Thus rather than having their highest loyalty to patients and their families, clinicians now have other loyalties—the electronic health record, insurers, the hospital, the health care system, and even their own salaries.
Therein lies the moral injury felt by increasing numbers of clinicians, leading to soaring rates of clinical distress. Many physicians are now recognizing moral injury as the basis of their pain. For example, Gawande has described unceasing computer data entry as a cause of physician distress and physician loneliness in the interesting essay, “Why Doctors Hate Their Computers.”2 Topol has suggested that corporate interference and attention away from patient care is a reason doctors should unite and organize for a more healthful environment.3 Ofri has gone so far as to suggest that the health care system is surviving because it can exploit its physicians for every drop of energy, diverting the focus of clinical encounters on billing rather than healing.4 However, it may be simplistic to imply or state that all clinical distress is related to moral injury. Other factors in caring for the sick and dying also can cause distress to health care providers. Physicians work long, hard hours and listen to many stories of distress and suffering from patients. Some of this is internalized and processed as one’s own suffering. Clinicians also have enormous amounts of information to absorb and assimilate, keep long hours, and are often sleep deprived, all of which may harm their well-being. In addition, clinicians may have work/life imbalances, be hesitant to reveal their weaknesses, and have perfectionist personalities. Still other factors may also be involved, such as a hostile environment in which managers can overuse their power; racism that can limit opportunities for advancement; and/or a family-unfriendly environment.
Just as the treatment of cancer depends on good surgery, radiation and/or chemotherapy as well as reducing underlying predisposing cause (ie, smoking, drinking, obesity, antiviral therapy) and leading a healthy lifestyle, so too treatment of clinical distress needs a multipronged approach. Fixing the business framework is an important step forward but may not always be enough. We agree with the authors’ suggestions for improvement: bringing administrators and clinicians into conversation with each other, making clinician satisfaction a financial priority, assuring that physician leaders have cell phone numbers of their legislators, and reestablishing a sense of community among clinicians. However, none of these goals will be easy to accomplish and some may be impossible to realize in some settings.
A necessary corollary to the suggestions by Dean and colleagues is research. Much research is needed to discover all of the factors of clinician distress, whatever we name the problem. We need to know vulnerabilities of different populations of clinicians and differences in prevalence in different types of health care systems.
It is likely that physicians in a government-owned health care system, such as the US Department of Veterans Affairs (VA) hospitals, have lower distress since there are no corporate interests or profit motives. In our experience, we have noted that many VA providers are expatriates of private health care systems due to their moral distress. If profit making and corporatization are important factors in distress, then clinicians in the VA system should have much lower distress; however, this is not known.
We also need research in pilot projects that relieve clinician distress. These could relate to collegial activities to bring physicians—and administrators—together in community, allowing more time with patients than the usual 15-minute allotments, allowing more time for creative, narrative experiences in medicine, developing forums for discussion and resolution of distress-inducing situations, etc.
An important yet overlooked issue in this discussion is that clinician distress, regardless of its name or cause, is a public health crisis. Clinician distress not only affects the clinician most directly and most crucially, but also affects every person in his/her community. Physicians who are distressed for whatever reason deliver less adequate care, make more medical errors, and are less invested in their patients. Patients of distressed clinicians have less favorable outcomes and suffer more. Medical errors are now the third leading cause of death in the US. Much of this is due to inadequate care by focusing attention on profit-making over health improvement and to clinician distress. Clinician distress due to moral injury or any other factor is a public health crisis and needs much more attention, research, and prioritization of clinician satisfaction.
Paulette Mehta, MD, MPH; and Jay Mehta, PhD
Author Affiliations: Central Arkansas Veterans Health Care System; University of Arkansas for Medical Sciences
Correspondence: Paulette Mehta (paulette.mehta@va.gov)
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Gawande A. Why doctors hate their computers. New Yorker. November 12, 2018. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers. Accessed October 16, 2019.
3. Topol E. Why doctors should organize. New Yorker. August 5, 2019. https://www.newyorker.com/culture/annals-of-inquiry/why-doctors-should-organize. Accessed October 16, 2019.
4. Ofri D. The business of healthcare depends on exploiting doctors and nurses. The New York Times. June 8, 2019. https://www.nytimes.com/2019/06/08/opinion/sunday/hospitals-doctors-nurses-burnout.html. Accessed October 16, 2019.
To the Editor: The September 2019 editorial “Reframing clinician distress: moral injury not burnout” argues for a renaming of what has been called burnout to moral injury.1 The article by Dean, Talbot, and Dean compares the experience of health care providers to soldiers and other service members who have served in combat and suffer as a result of their experiences. I would like to comment on 2 areas: Whether the term burnout should be replaced with moral injury; and the adequacy of the recommendations made by Dean, Talbot, and Dean.
Briefly, my own credentials to opine on the topic include being both a physician and a soldier. I served in the US Army as a psychiatrist from 1986 to 2010 and deployed to various hazardous locations, including South Korea, Somalia, Iraq, and Guantanamo Bay, Cuba. Since my retirement from the Army I have worked as a psychiatrist on different front lines, with both veterans and the chronically mentally ill and often homeless population.
Moral injury is a term that was popularized by Johnathan Shay after the Vietnam War, especially in his masterful book Achilles in Vietnam.1 Most authors who have written on the subject of moral injury, including myself, think of it as feelings of guilt and shame related to (1) killing civilians (especially children or innocents); (2) surviving while other comrades did not; and/or (3) feeling betrayed by the government they served.2,3
While also arising in combat settings, moral injury is related but separate from posttraumatic stress disorder (PTSD). It comes from an affront to our morals rather than our physical well-being. It is not considered a medical diagnosis, treatments are experimental, and the literature is anecdotal.
I have mixed feelings about equating the moral injury from combat to working as a physician or other health care provider. On the one hand, certainly health care providers may sacrifice health and safety to taking care of patients. They may feel guilty when they cannot do enough for their patients. But does it rise to the same level as actually combat and having numerous comrades killed or maimed?
On the other hand, working on an inpatient psychiatry ward with an inner-city population who generally have severe mental illness and are often on phencyclidine and related drugs, has its own share of risks. Unfortunately, physical attacks on staff are way too common.
The term burnout also has a robust background of research into both causes and possible solutions. Indeed, there was even a journal devoted to it: Burnout Research.4 Moral injury research is on different populations, and generally the remedies are focused more on spiritual and existential support.
Which brings me to the recommendations and solutions part of the editorial. I agree that yoga and meditation, while beneficial, do not curb the feelings of frustration and betrayal that often arise when you cannot treat patients the way you feel they deserve. The recommendations listed in the editorial are a start, but much more should be done.
Now comes the hard part. Specifically, what more should be done? All the easy solutions have already been tried. Ones that would really make a difference, such as making an electronic health record that allows you to still look at and connect to the patient, seem to elude us. Many of us in the health care industry would love to have a single payer system across the board, to avoid all the inequities cited in the article. But health care, like climate change, is mired in our political deadlocks.
Therefore, I will finish by focusing on one of their recommendations, which is achievable: tie the incentives for the executive leadership to the satisfaction of health care providers, as is done for patient satisfaction. That is both doable and will benefit various institutions in the long run. Health care providers will be more likely to stay in a health care system and thus patient satisfaction improves. Win-win.
COL (Ret) Elspeth Cameron Ritchie, MD, MPH, USA
Author Affiliation: Uniformed Services University of the Health Sciences
Correspondence: Elspeth Cameron Ritchie (elspethcameronritchie@gmail.com)
Disclosures: The author reports no conflict of interest with regard to this article.
References
1. Shay J. Achilles in Vietnam: Combat Trauma and the Undoing of Character. New York: Atheneum; 1994.
2. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin. Psychol Rev. 2009;29(8):695-706.
3. Ritchie EC. Moral injury: a profound sense of alienation and abject shame. Time. April 17, 2013. http://nation.time.com/2013/04/17/moral-injury-a-profound-sense-of-alienation-and-abject-shame.
4. Burnout Research. 2014;1(1):1-56. https://www.sciencedirect.com/journal/burnout-research/vol/1/issue/1. Accessed October 17, 2019.
Response: We appreciate the very thoughtful and thorough responses of Mehta. Mehta, Padgett, Ascensao, and Ritchie. Common themes in the responses were the suggestion that supplanting the term burnout with moral injury may not be appropriate and that changing the underlying drivers of distress requires a multifaceted approach, which is likely to require prolonged effort. We agree with both of these themes, believing the concept of moral injury and mitigation strategies do not benefit from reductionism.
Burnout is a nonspecific symptom constellation of emotional exhaustion, depersonalization, and a lack of a sense of accomplishment.1 Because it is nonspecific, the symptoms can arise from any number of situations, not only moral injury. However, from our conversations over the past 15 months, moral injury fuels a large percentage of burnout in health care. In a recent informal survey conducted at the ORExcellence meeting, almost all respondents believed they were experiencing moral injury rather than burnout when both terms were explained. When clinicians are physically and emotionally exhausted with battling a broken system in their efforts to provide good care—when they have incurred innumerable moral insults, amassing to a moral injury—many give up. This is the end stage of moral injury, or burnout.We absolutely agree research is necessary to validate this concept, which has been applied only to health care since July 2018. We are pursuing various avenues of inquiry and are validating a new assessment tool. But we do not believe that intervention must wait until there are data to support what resonates so profoundly with so many and, as we have heard dozens of times, “finally gives language to my experience.”Finally, we would not suggest that civilian physician experience is equivalent to combat experience. But just as there are multiple etiologies for posttraumatic stress disorder (PTSD), such as combat exposure, physical abuse, sexual assault, there are likely multiple ways one can incur moral injury. Witnessing or participating in a situation that transgresses deeply held moral beliefs is the prerequisite for moral injury rather than physical danger. In different contexts, physicians and service members may ultimately face similar accumulated risk to their moral integrity, though of widely disparate intensity, frequency, and duration. Physicians face low-intensity, high-frequency threats over years; service members more often face high-intensity, less frequent threats during time-limited deployments. Just because moral injury was first applied to combat veterans—as was PTSD—does not mean we should limit the use of a powerfully resonant concept to a military population any more than we limited the use of Letterman’s ambulances or Morel’s tourniquets to the battlefield.2,3
Wendy Dean, MD; and Simon Talbot, MD
Author affiliations: Wendy Dean is President and co-founder of Moral Injury of Healthcare. Simon Talbot is a reconstructive plastic surgeon at Brigham and Women’s Hospital and associate professor of surgery at Harvard Medical School, Boston, Massachusetts.
Correspondence: Wendy Dean (wdean@moralinjury. Healthcare,@WDeanMD)
Disclosures: Wendy Dean and Simon Talbot founded Moral Injury of Healthcare, a nonprofit organization; they report no other actual or potential conflicts of interest with regard to this article.
References
1. Freudenberger HJ. The staff burn-out syndrome in alternative institutions. Psychother Theory Res Pract. 1975;12(1):73-82.
2. Place RJ. The strategic genius of Jonathan Letterman: the relevancy of the American Civil War to current health care policy makers. Mil Med. 2015;180(3):259-262.
3. Welling DR, McKay PL, Rasmussen TE, Rich NM. A brief history of the tourniquet. J Vasc Surg. 2012;55(1):286-290.
To the Editor: In the September 2019 guest editorial “Reframing Clinician Distress: Moral Injury Not Burnout,” the authors have advanced a thoughtful and provocative hypothesis addressing a salient issue.1 Their argument is that burnout does not accurately capture physician distress. Furthermore, they posit the term burnout focuses remediation strategies at the individual provider level, thereby discounting the contribution of the larger health care system. This is not the first effort to argue that burnout is not a syndrome of mental illness (eg, depression) located within the person but rather a disrupted physician-work relationship.2
As the authors cite, population and practice changes have contributed significantly to physician distress and dissatisfaction. Indeed, recent findings indicate that female physicians may suffer increased prevalence of burnout, which represents a challenge given the growing numbers of women in medicine.3 Unfortunately, by shifting focus almost exclusively to the system level to address burnout, the authors discount a large body of literature examining associations and contributors at the individual and clinic level.
Burnout is conceptualized as consisting of 3 domains: depersonalization, emotional exhaustion, and personal accomplishment.4 While this conceptualization may not capture the totality of physician distress, it has provided a body of literature focused on decreasing symptoms of burnout. Successful interventions have been targeted at the individual provider level (ie, stress management, small group discussion, mindfulness) as well as the organizational level (ie, reduction in duty hours, scribes).5,6 Recent studies have also suggested that increasing the occurrence of social encounters that are civil and respectful decreases reported physician burnout.7
Frustration, the annoyance or anger at being unable to change or achieve something, also can be a leading cause of burnout and moral injury. The inability to deal with unresolvable issues due to a lack of skills or inability to create a positive reframe can lead to a constellation of symptoms that are detrimental to the individual provider. Nevertheless, system rigidity, inability to recognitize pain and pressure, and goals perceived as unachievable can also lead to frustration. Physicians may experience growing frustration if they are unable to influence their systems. Thus, experiencing personal frustration, combined with an inability or lack of energy or time to influence a system can snowball.
Just as we counsel our patients that good medical care involves not only engagement with the medical system, but also individual engagement in their care (eg, nutrition, exercise), this problem requires a multicomponent solution. While advocating and working for a system that induces less moral injury, frustration, and burnout, physicians need to examine the resources available to them and their colleagues in a more immediate way.
Physician distress is a serious problem with both personal, patient, occupational, and public health costs. Thus, it is important that we grapple with the complexity of a multiconstruct definition amenable to multilevel interventions. The concept of moral injury is an important component and opens additional lines of both clinical inquiry and intervention. However, in our view, to subsume all burnout under this construct is overly reductive.
In closing, this topic is too important not to discuss. Let the conversations continue!
Lynne Padgett, PhD; and Joao L. Ascensao, MD, PhD
Author affiliations: Departments of Medicine and Mental Health, Washington DC VA Medical Center and Department of Medicine, George Washington University School of Medicine
Correspondence: Lynne Padgett (lynne.padgett@va.gov)
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Epstein RM, Privitera MR. Doing something about physician burnout. Lancet. 2016;388(10057):2216-2217.
3. Templeton K, Bernstein CA, Sukhera J, et al. Gender-based differences in burnout: issues faced by women physicians. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2019. https://nam.edu/wp-content/uploads/2019/05/Gender-Based-Differences-in-Burnout.pdf. Published May 28, 2019. Accessed October 10, 2019.
4. Eckleberry-Hunt J Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93(3):367-370.
5. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
6. Squiers JJ, Lobdell KW, Fann JI, DiMaio JM. Physician burnout: are we treating the symptom instead of the disease? Ann Thorac Surg. 2017;104(4):1117-1122.
7. Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160-163.
To the Editor: We applaud Dean and her colleagues for their thought-provoking commentary on clinicians’ distress, a problem that has surged in recent years and has now reached epidemic proportions.1 Their argument focuses on the language used to define and frame clinical distress. Do we label this distress as burnout, as moral injury, or as something else? Moral injury occurs any time clinicians are impeded from doing the right thing at the right time in the right way; or even worse, doing the wrong thing to serve the needs of health system stakeholders other than the patient. These other stakeholders may include administrators, corporations, insurance adjusters, and others.
Naming the problem correctly is crucial to finding the solution. The name frames the discussion and impacts the solution. Burnout implies difficulty coping with the many stresses of health care and of personal responsibility for the problem. The solution would therefore be to help individuals to cope with their stresses. Moral injury on the other hand implies a corrupt system; thereby, reframing the discussion to systems issues and suggesting solutions by changing the business of health care delivery.
These authors state that current clinical distress is due to moral injury and not to burnout. Therefore, the business in which health care is performed needs to change.
The authors define the drivers of moral injury in our current system, mostly as (1) a massive information technology overload that has largely overtaken the patient as center of attention; and (2) the profit motive of the health care corporation and its shareholders. A focus on making profits has increased in the wake of falling reimbursements; the result is pressure on clinicians to see more patients more quickly and to do more even when not necessary. This has diverted the focus on healing patients to a focus on making profits. These major drivers of clinician distress—the electronic health record and the pressure to bill more—are fundamentally driven by the corporatization of American medicine in which profit is the measured outcome.
Thus rather than having their highest loyalty to patients and their families, clinicians now have other loyalties—the electronic health record, insurers, the hospital, the health care system, and even their own salaries.
Therein lies the moral injury felt by increasing numbers of clinicians, leading to soaring rates of clinical distress. Many physicians are now recognizing moral injury as the basis of their pain. For example, Gawande has described unceasing computer data entry as a cause of physician distress and physician loneliness in the interesting essay, “Why Doctors Hate Their Computers.”2 Topol has suggested that corporate interference and attention away from patient care is a reason doctors should unite and organize for a more healthful environment.3 Ofri has gone so far as to suggest that the health care system is surviving because it can exploit its physicians for every drop of energy, diverting the focus of clinical encounters on billing rather than healing.4 However, it may be simplistic to imply or state that all clinical distress is related to moral injury. Other factors in caring for the sick and dying also can cause distress to health care providers. Physicians work long, hard hours and listen to many stories of distress and suffering from patients. Some of this is internalized and processed as one’s own suffering. Clinicians also have enormous amounts of information to absorb and assimilate, keep long hours, and are often sleep deprived, all of which may harm their well-being. In addition, clinicians may have work/life imbalances, be hesitant to reveal their weaknesses, and have perfectionist personalities. Still other factors may also be involved, such as a hostile environment in which managers can overuse their power; racism that can limit opportunities for advancement; and/or a family-unfriendly environment.
Just as the treatment of cancer depends on good surgery, radiation and/or chemotherapy as well as reducing underlying predisposing cause (ie, smoking, drinking, obesity, antiviral therapy) and leading a healthy lifestyle, so too treatment of clinical distress needs a multipronged approach. Fixing the business framework is an important step forward but may not always be enough. We agree with the authors’ suggestions for improvement: bringing administrators and clinicians into conversation with each other, making clinician satisfaction a financial priority, assuring that physician leaders have cell phone numbers of their legislators, and reestablishing a sense of community among clinicians. However, none of these goals will be easy to accomplish and some may be impossible to realize in some settings.
A necessary corollary to the suggestions by Dean and colleagues is research. Much research is needed to discover all of the factors of clinician distress, whatever we name the problem. We need to know vulnerabilities of different populations of clinicians and differences in prevalence in different types of health care systems.
It is likely that physicians in a government-owned health care system, such as the US Department of Veterans Affairs (VA) hospitals, have lower distress since there are no corporate interests or profit motives. In our experience, we have noted that many VA providers are expatriates of private health care systems due to their moral distress. If profit making and corporatization are important factors in distress, then clinicians in the VA system should have much lower distress; however, this is not known.
We also need research in pilot projects that relieve clinician distress. These could relate to collegial activities to bring physicians—and administrators—together in community, allowing more time with patients than the usual 15-minute allotments, allowing more time for creative, narrative experiences in medicine, developing forums for discussion and resolution of distress-inducing situations, etc.
An important yet overlooked issue in this discussion is that clinician distress, regardless of its name or cause, is a public health crisis. Clinician distress not only affects the clinician most directly and most crucially, but also affects every person in his/her community. Physicians who are distressed for whatever reason deliver less adequate care, make more medical errors, and are less invested in their patients. Patients of distressed clinicians have less favorable outcomes and suffer more. Medical errors are now the third leading cause of death in the US. Much of this is due to inadequate care by focusing attention on profit-making over health improvement and to clinician distress. Clinician distress due to moral injury or any other factor is a public health crisis and needs much more attention, research, and prioritization of clinician satisfaction.
Paulette Mehta, MD, MPH; and Jay Mehta, PhD
Author Affiliations: Central Arkansas Veterans Health Care System; University of Arkansas for Medical Sciences
Correspondence: Paulette Mehta (paulette.mehta@va.gov)
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Gawande A. Why doctors hate their computers. New Yorker. November 12, 2018. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers. Accessed October 16, 2019.
3. Topol E. Why doctors should organize. New Yorker. August 5, 2019. https://www.newyorker.com/culture/annals-of-inquiry/why-doctors-should-organize. Accessed October 16, 2019.
4. Ofri D. The business of healthcare depends on exploiting doctors and nurses. The New York Times. June 8, 2019. https://www.nytimes.com/2019/06/08/opinion/sunday/hospitals-doctors-nurses-burnout.html. Accessed October 16, 2019.
To the Editor: The September 2019 editorial “Reframing clinician distress: moral injury not burnout” argues for a renaming of what has been called burnout to moral injury.1 The article by Dean, Talbot, and Dean compares the experience of health care providers to soldiers and other service members who have served in combat and suffer as a result of their experiences. I would like to comment on 2 areas: Whether the term burnout should be replaced with moral injury; and the adequacy of the recommendations made by Dean, Talbot, and Dean.
Briefly, my own credentials to opine on the topic include being both a physician and a soldier. I served in the US Army as a psychiatrist from 1986 to 2010 and deployed to various hazardous locations, including South Korea, Somalia, Iraq, and Guantanamo Bay, Cuba. Since my retirement from the Army I have worked as a psychiatrist on different front lines, with both veterans and the chronically mentally ill and often homeless population.
Moral injury is a term that was popularized by Johnathan Shay after the Vietnam War, especially in his masterful book Achilles in Vietnam.1 Most authors who have written on the subject of moral injury, including myself, think of it as feelings of guilt and shame related to (1) killing civilians (especially children or innocents); (2) surviving while other comrades did not; and/or (3) feeling betrayed by the government they served.2,3
While also arising in combat settings, moral injury is related but separate from posttraumatic stress disorder (PTSD). It comes from an affront to our morals rather than our physical well-being. It is not considered a medical diagnosis, treatments are experimental, and the literature is anecdotal.
I have mixed feelings about equating the moral injury from combat to working as a physician or other health care provider. On the one hand, certainly health care providers may sacrifice health and safety to taking care of patients. They may feel guilty when they cannot do enough for their patients. But does it rise to the same level as actually combat and having numerous comrades killed or maimed?
On the other hand, working on an inpatient psychiatry ward with an inner-city population who generally have severe mental illness and are often on phencyclidine and related drugs, has its own share of risks. Unfortunately, physical attacks on staff are way too common.
The term burnout also has a robust background of research into both causes and possible solutions. Indeed, there was even a journal devoted to it: Burnout Research.4 Moral injury research is on different populations, and generally the remedies are focused more on spiritual and existential support.
Which brings me to the recommendations and solutions part of the editorial. I agree that yoga and meditation, while beneficial, do not curb the feelings of frustration and betrayal that often arise when you cannot treat patients the way you feel they deserve. The recommendations listed in the editorial are a start, but much more should be done.
Now comes the hard part. Specifically, what more should be done? All the easy solutions have already been tried. Ones that would really make a difference, such as making an electronic health record that allows you to still look at and connect to the patient, seem to elude us. Many of us in the health care industry would love to have a single payer system across the board, to avoid all the inequities cited in the article. But health care, like climate change, is mired in our political deadlocks.
Therefore, I will finish by focusing on one of their recommendations, which is achievable: tie the incentives for the executive leadership to the satisfaction of health care providers, as is done for patient satisfaction. That is both doable and will benefit various institutions in the long run. Health care providers will be more likely to stay in a health care system and thus patient satisfaction improves. Win-win.
COL (Ret) Elspeth Cameron Ritchie, MD, MPH, USA
Author Affiliation: Uniformed Services University of the Health Sciences
Correspondence: Elspeth Cameron Ritchie (elspethcameronritchie@gmail.com)
Disclosures: The author reports no conflict of interest with regard to this article.
References
1. Shay J. Achilles in Vietnam: Combat Trauma and the Undoing of Character. New York: Atheneum; 1994.
2. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin. Psychol Rev. 2009;29(8):695-706.
3. Ritchie EC. Moral injury: a profound sense of alienation and abject shame. Time. April 17, 2013. http://nation.time.com/2013/04/17/moral-injury-a-profound-sense-of-alienation-and-abject-shame.
4. Burnout Research. 2014;1(1):1-56. https://www.sciencedirect.com/journal/burnout-research/vol/1/issue/1. Accessed October 17, 2019.
Response: We appreciate the very thoughtful and thorough responses of Mehta. Mehta, Padgett, Ascensao, and Ritchie. Common themes in the responses were the suggestion that supplanting the term burnout with moral injury may not be appropriate and that changing the underlying drivers of distress requires a multifaceted approach, which is likely to require prolonged effort. We agree with both of these themes, believing the concept of moral injury and mitigation strategies do not benefit from reductionism.
Burnout is a nonspecific symptom constellation of emotional exhaustion, depersonalization, and a lack of a sense of accomplishment.1 Because it is nonspecific, the symptoms can arise from any number of situations, not only moral injury. However, from our conversations over the past 15 months, moral injury fuels a large percentage of burnout in health care. In a recent informal survey conducted at the ORExcellence meeting, almost all respondents believed they were experiencing moral injury rather than burnout when both terms were explained. When clinicians are physically and emotionally exhausted with battling a broken system in their efforts to provide good care—when they have incurred innumerable moral insults, amassing to a moral injury—many give up. This is the end stage of moral injury, or burnout.We absolutely agree research is necessary to validate this concept, which has been applied only to health care since July 2018. We are pursuing various avenues of inquiry and are validating a new assessment tool. But we do not believe that intervention must wait until there are data to support what resonates so profoundly with so many and, as we have heard dozens of times, “finally gives language to my experience.”Finally, we would not suggest that civilian physician experience is equivalent to combat experience. But just as there are multiple etiologies for posttraumatic stress disorder (PTSD), such as combat exposure, physical abuse, sexual assault, there are likely multiple ways one can incur moral injury. Witnessing or participating in a situation that transgresses deeply held moral beliefs is the prerequisite for moral injury rather than physical danger. In different contexts, physicians and service members may ultimately face similar accumulated risk to their moral integrity, though of widely disparate intensity, frequency, and duration. Physicians face low-intensity, high-frequency threats over years; service members more often face high-intensity, less frequent threats during time-limited deployments. Just because moral injury was first applied to combat veterans—as was PTSD—does not mean we should limit the use of a powerfully resonant concept to a military population any more than we limited the use of Letterman’s ambulances or Morel’s tourniquets to the battlefield.2,3
Wendy Dean, MD; and Simon Talbot, MD
Author affiliations: Wendy Dean is President and co-founder of Moral Injury of Healthcare. Simon Talbot is a reconstructive plastic surgeon at Brigham and Women’s Hospital and associate professor of surgery at Harvard Medical School, Boston, Massachusetts.
Correspondence: Wendy Dean (wdean@moralinjury. Healthcare,@WDeanMD)
Disclosures: Wendy Dean and Simon Talbot founded Moral Injury of Healthcare, a nonprofit organization; they report no other actual or potential conflicts of interest with regard to this article.
References
1. Freudenberger HJ. The staff burn-out syndrome in alternative institutions. Psychother Theory Res Pract. 1975;12(1):73-82.
2. Place RJ. The strategic genius of Jonathan Letterman: the relevancy of the American Civil War to current health care policy makers. Mil Med. 2015;180(3):259-262.
3. Welling DR, McKay PL, Rasmussen TE, Rich NM. A brief history of the tourniquet. J Vasc Surg. 2012;55(1):286-290.
To the Editor: In the September 2019 guest editorial “Reframing Clinician Distress: Moral Injury Not Burnout,” the authors have advanced a thoughtful and provocative hypothesis addressing a salient issue.1 Their argument is that burnout does not accurately capture physician distress. Furthermore, they posit the term burnout focuses remediation strategies at the individual provider level, thereby discounting the contribution of the larger health care system. This is not the first effort to argue that burnout is not a syndrome of mental illness (eg, depression) located within the person but rather a disrupted physician-work relationship.2
As the authors cite, population and practice changes have contributed significantly to physician distress and dissatisfaction. Indeed, recent findings indicate that female physicians may suffer increased prevalence of burnout, which represents a challenge given the growing numbers of women in medicine.3 Unfortunately, by shifting focus almost exclusively to the system level to address burnout, the authors discount a large body of literature examining associations and contributors at the individual and clinic level.
Burnout is conceptualized as consisting of 3 domains: depersonalization, emotional exhaustion, and personal accomplishment.4 While this conceptualization may not capture the totality of physician distress, it has provided a body of literature focused on decreasing symptoms of burnout. Successful interventions have been targeted at the individual provider level (ie, stress management, small group discussion, mindfulness) as well as the organizational level (ie, reduction in duty hours, scribes).5,6 Recent studies have also suggested that increasing the occurrence of social encounters that are civil and respectful decreases reported physician burnout.7
Frustration, the annoyance or anger at being unable to change or achieve something, also can be a leading cause of burnout and moral injury. The inability to deal with unresolvable issues due to a lack of skills or inability to create a positive reframe can lead to a constellation of symptoms that are detrimental to the individual provider. Nevertheless, system rigidity, inability to recognitize pain and pressure, and goals perceived as unachievable can also lead to frustration. Physicians may experience growing frustration if they are unable to influence their systems. Thus, experiencing personal frustration, combined with an inability or lack of energy or time to influence a system can snowball.
Just as we counsel our patients that good medical care involves not only engagement with the medical system, but also individual engagement in their care (eg, nutrition, exercise), this problem requires a multicomponent solution. While advocating and working for a system that induces less moral injury, frustration, and burnout, physicians need to examine the resources available to them and their colleagues in a more immediate way.
Physician distress is a serious problem with both personal, patient, occupational, and public health costs. Thus, it is important that we grapple with the complexity of a multiconstruct definition amenable to multilevel interventions. The concept of moral injury is an important component and opens additional lines of both clinical inquiry and intervention. However, in our view, to subsume all burnout under this construct is overly reductive.
In closing, this topic is too important not to discuss. Let the conversations continue!
Lynne Padgett, PhD; and Joao L. Ascensao, MD, PhD
Author affiliations: Departments of Medicine and Mental Health, Washington DC VA Medical Center and Department of Medicine, George Washington University School of Medicine
Correspondence: Lynne Padgett (lynne.padgett@va.gov)
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Epstein RM, Privitera MR. Doing something about physician burnout. Lancet. 2016;388(10057):2216-2217.
3. Templeton K, Bernstein CA, Sukhera J, et al. Gender-based differences in burnout: issues faced by women physicians. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2019. https://nam.edu/wp-content/uploads/2019/05/Gender-Based-Differences-in-Burnout.pdf. Published May 28, 2019. Accessed October 10, 2019.
4. Eckleberry-Hunt J Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93(3):367-370.
5. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281.
6. Squiers JJ, Lobdell KW, Fann JI, DiMaio JM. Physician burnout: are we treating the symptom instead of the disease? Ann Thorac Surg. 2017;104(4):1117-1122.
7. Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160-163.
To the Editor: We applaud Dean and her colleagues for their thought-provoking commentary on clinicians’ distress, a problem that has surged in recent years and has now reached epidemic proportions.1 Their argument focuses on the language used to define and frame clinical distress. Do we label this distress as burnout, as moral injury, or as something else? Moral injury occurs any time clinicians are impeded from doing the right thing at the right time in the right way; or even worse, doing the wrong thing to serve the needs of health system stakeholders other than the patient. These other stakeholders may include administrators, corporations, insurance adjusters, and others.
Naming the problem correctly is crucial to finding the solution. The name frames the discussion and impacts the solution. Burnout implies difficulty coping with the many stresses of health care and of personal responsibility for the problem. The solution would therefore be to help individuals to cope with their stresses. Moral injury on the other hand implies a corrupt system; thereby, reframing the discussion to systems issues and suggesting solutions by changing the business of health care delivery.
These authors state that current clinical distress is due to moral injury and not to burnout. Therefore, the business in which health care is performed needs to change.
The authors define the drivers of moral injury in our current system, mostly as (1) a massive information technology overload that has largely overtaken the patient as center of attention; and (2) the profit motive of the health care corporation and its shareholders. A focus on making profits has increased in the wake of falling reimbursements; the result is pressure on clinicians to see more patients more quickly and to do more even when not necessary. This has diverted the focus on healing patients to a focus on making profits. These major drivers of clinician distress—the electronic health record and the pressure to bill more—are fundamentally driven by the corporatization of American medicine in which profit is the measured outcome.
Thus rather than having their highest loyalty to patients and their families, clinicians now have other loyalties—the electronic health record, insurers, the hospital, the health care system, and even their own salaries.
Therein lies the moral injury felt by increasing numbers of clinicians, leading to soaring rates of clinical distress. Many physicians are now recognizing moral injury as the basis of their pain. For example, Gawande has described unceasing computer data entry as a cause of physician distress and physician loneliness in the interesting essay, “Why Doctors Hate Their Computers.”2 Topol has suggested that corporate interference and attention away from patient care is a reason doctors should unite and organize for a more healthful environment.3 Ofri has gone so far as to suggest that the health care system is surviving because it can exploit its physicians for every drop of energy, diverting the focus of clinical encounters on billing rather than healing.4 However, it may be simplistic to imply or state that all clinical distress is related to moral injury. Other factors in caring for the sick and dying also can cause distress to health care providers. Physicians work long, hard hours and listen to many stories of distress and suffering from patients. Some of this is internalized and processed as one’s own suffering. Clinicians also have enormous amounts of information to absorb and assimilate, keep long hours, and are often sleep deprived, all of which may harm their well-being. In addition, clinicians may have work/life imbalances, be hesitant to reveal their weaknesses, and have perfectionist personalities. Still other factors may also be involved, such as a hostile environment in which managers can overuse their power; racism that can limit opportunities for advancement; and/or a family-unfriendly environment.
Just as the treatment of cancer depends on good surgery, radiation and/or chemotherapy as well as reducing underlying predisposing cause (ie, smoking, drinking, obesity, antiviral therapy) and leading a healthy lifestyle, so too treatment of clinical distress needs a multipronged approach. Fixing the business framework is an important step forward but may not always be enough. We agree with the authors’ suggestions for improvement: bringing administrators and clinicians into conversation with each other, making clinician satisfaction a financial priority, assuring that physician leaders have cell phone numbers of their legislators, and reestablishing a sense of community among clinicians. However, none of these goals will be easy to accomplish and some may be impossible to realize in some settings.
A necessary corollary to the suggestions by Dean and colleagues is research. Much research is needed to discover all of the factors of clinician distress, whatever we name the problem. We need to know vulnerabilities of different populations of clinicians and differences in prevalence in different types of health care systems.
It is likely that physicians in a government-owned health care system, such as the US Department of Veterans Affairs (VA) hospitals, have lower distress since there are no corporate interests or profit motives. In our experience, we have noted that many VA providers are expatriates of private health care systems due to their moral distress. If profit making and corporatization are important factors in distress, then clinicians in the VA system should have much lower distress; however, this is not known.
We also need research in pilot projects that relieve clinician distress. These could relate to collegial activities to bring physicians—and administrators—together in community, allowing more time with patients than the usual 15-minute allotments, allowing more time for creative, narrative experiences in medicine, developing forums for discussion and resolution of distress-inducing situations, etc.
An important yet overlooked issue in this discussion is that clinician distress, regardless of its name or cause, is a public health crisis. Clinician distress not only affects the clinician most directly and most crucially, but also affects every person in his/her community. Physicians who are distressed for whatever reason deliver less adequate care, make more medical errors, and are less invested in their patients. Patients of distressed clinicians have less favorable outcomes and suffer more. Medical errors are now the third leading cause of death in the US. Much of this is due to inadequate care by focusing attention on profit-making over health improvement and to clinician distress. Clinician distress due to moral injury or any other factor is a public health crisis and needs much more attention, research, and prioritization of clinician satisfaction.
Paulette Mehta, MD, MPH; and Jay Mehta, PhD
Author Affiliations: Central Arkansas Veterans Health Care System; University of Arkansas for Medical Sciences
Correspondence: Paulette Mehta (paulette.mehta@va.gov)
Disclosures: The authors report no conflict of interest with regard to this article.
References
1. Dean W, Talbot S, Dean A. Reframing clinical distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
2. Gawande A. Why doctors hate their computers. New Yorker. November 12, 2018. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers. Accessed October 16, 2019.
3. Topol E. Why doctors should organize. New Yorker. August 5, 2019. https://www.newyorker.com/culture/annals-of-inquiry/why-doctors-should-organize. Accessed October 16, 2019.
4. Ofri D. The business of healthcare depends on exploiting doctors and nurses. The New York Times. June 8, 2019. https://www.nytimes.com/2019/06/08/opinion/sunday/hospitals-doctors-nurses-burnout.html. Accessed October 16, 2019.
To the Editor: The September 2019 editorial “Reframing clinician distress: moral injury not burnout” argues for a renaming of what has been called burnout to moral injury.1 The article by Dean, Talbot, and Dean compares the experience of health care providers to soldiers and other service members who have served in combat and suffer as a result of their experiences. I would like to comment on 2 areas: Whether the term burnout should be replaced with moral injury; and the adequacy of the recommendations made by Dean, Talbot, and Dean.
Briefly, my own credentials to opine on the topic include being both a physician and a soldier. I served in the US Army as a psychiatrist from 1986 to 2010 and deployed to various hazardous locations, including South Korea, Somalia, Iraq, and Guantanamo Bay, Cuba. Since my retirement from the Army I have worked as a psychiatrist on different front lines, with both veterans and the chronically mentally ill and often homeless population.
Moral injury is a term that was popularized by Johnathan Shay after the Vietnam War, especially in his masterful book Achilles in Vietnam.1 Most authors who have written on the subject of moral injury, including myself, think of it as feelings of guilt and shame related to (1) killing civilians (especially children or innocents); (2) surviving while other comrades did not; and/or (3) feeling betrayed by the government they served.2,3
While also arising in combat settings, moral injury is related but separate from posttraumatic stress disorder (PTSD). It comes from an affront to our morals rather than our physical well-being. It is not considered a medical diagnosis, treatments are experimental, and the literature is anecdotal.
I have mixed feelings about equating the moral injury from combat to working as a physician or other health care provider. On the one hand, certainly health care providers may sacrifice health and safety to taking care of patients. They may feel guilty when they cannot do enough for their patients. But does it rise to the same level as actually combat and having numerous comrades killed or maimed?
On the other hand, working on an inpatient psychiatry ward with an inner-city population who generally have severe mental illness and are often on phencyclidine and related drugs, has its own share of risks. Unfortunately, physical attacks on staff are way too common.
The term burnout also has a robust background of research into both causes and possible solutions. Indeed, there was even a journal devoted to it: Burnout Research.4 Moral injury research is on different populations, and generally the remedies are focused more on spiritual and existential support.
Which brings me to the recommendations and solutions part of the editorial. I agree that yoga and meditation, while beneficial, do not curb the feelings of frustration and betrayal that often arise when you cannot treat patients the way you feel they deserve. The recommendations listed in the editorial are a start, but much more should be done.
Now comes the hard part. Specifically, what more should be done? All the easy solutions have already been tried. Ones that would really make a difference, such as making an electronic health record that allows you to still look at and connect to the patient, seem to elude us. Many of us in the health care industry would love to have a single payer system across the board, to avoid all the inequities cited in the article. But health care, like climate change, is mired in our political deadlocks.
Therefore, I will finish by focusing on one of their recommendations, which is achievable: tie the incentives for the executive leadership to the satisfaction of health care providers, as is done for patient satisfaction. That is both doable and will benefit various institutions in the long run. Health care providers will be more likely to stay in a health care system and thus patient satisfaction improves. Win-win.
COL (Ret) Elspeth Cameron Ritchie, MD, MPH, USA
Author Affiliation: Uniformed Services University of the Health Sciences
Correspondence: Elspeth Cameron Ritchie (elspethcameronritchie@gmail.com)
Disclosures: The author reports no conflict of interest with regard to this article.
References
1. Shay J. Achilles in Vietnam: Combat Trauma and the Undoing of Character. New York: Atheneum; 1994.
2. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin. Psychol Rev. 2009;29(8):695-706.
3. Ritchie EC. Moral injury: a profound sense of alienation and abject shame. Time. April 17, 2013. http://nation.time.com/2013/04/17/moral-injury-a-profound-sense-of-alienation-and-abject-shame.
4. Burnout Research. 2014;1(1):1-56. https://www.sciencedirect.com/journal/burnout-research/vol/1/issue/1. Accessed October 17, 2019.
Response: We appreciate the very thoughtful and thorough responses of Mehta. Mehta, Padgett, Ascensao, and Ritchie. Common themes in the responses were the suggestion that supplanting the term burnout with moral injury may not be appropriate and that changing the underlying drivers of distress requires a multifaceted approach, which is likely to require prolonged effort. We agree with both of these themes, believing the concept of moral injury and mitigation strategies do not benefit from reductionism.
Burnout is a nonspecific symptom constellation of emotional exhaustion, depersonalization, and a lack of a sense of accomplishment.1 Because it is nonspecific, the symptoms can arise from any number of situations, not only moral injury. However, from our conversations over the past 15 months, moral injury fuels a large percentage of burnout in health care. In a recent informal survey conducted at the ORExcellence meeting, almost all respondents believed they were experiencing moral injury rather than burnout when both terms were explained. When clinicians are physically and emotionally exhausted with battling a broken system in their efforts to provide good care—when they have incurred innumerable moral insults, amassing to a moral injury—many give up. This is the end stage of moral injury, or burnout.We absolutely agree research is necessary to validate this concept, which has been applied only to health care since July 2018. We are pursuing various avenues of inquiry and are validating a new assessment tool. But we do not believe that intervention must wait until there are data to support what resonates so profoundly with so many and, as we have heard dozens of times, “finally gives language to my experience.”Finally, we would not suggest that civilian physician experience is equivalent to combat experience. But just as there are multiple etiologies for posttraumatic stress disorder (PTSD), such as combat exposure, physical abuse, sexual assault, there are likely multiple ways one can incur moral injury. Witnessing or participating in a situation that transgresses deeply held moral beliefs is the prerequisite for moral injury rather than physical danger. In different contexts, physicians and service members may ultimately face similar accumulated risk to their moral integrity, though of widely disparate intensity, frequency, and duration. Physicians face low-intensity, high-frequency threats over years; service members more often face high-intensity, less frequent threats during time-limited deployments. Just because moral injury was first applied to combat veterans—as was PTSD—does not mean we should limit the use of a powerfully resonant concept to a military population any more than we limited the use of Letterman’s ambulances or Morel’s tourniquets to the battlefield.2,3
Wendy Dean, MD; and Simon Talbot, MD
Author affiliations: Wendy Dean is President and co-founder of Moral Injury of Healthcare. Simon Talbot is a reconstructive plastic surgeon at Brigham and Women’s Hospital and associate professor of surgery at Harvard Medical School, Boston, Massachusetts.
Correspondence: Wendy Dean (wdean@moralinjury. Healthcare,@WDeanMD)
Disclosures: Wendy Dean and Simon Talbot founded Moral Injury of Healthcare, a nonprofit organization; they report no other actual or potential conflicts of interest with regard to this article.
References
1. Freudenberger HJ. The staff burn-out syndrome in alternative institutions. Psychother Theory Res Pract. 1975;12(1):73-82.
2. Place RJ. The strategic genius of Jonathan Letterman: the relevancy of the American Civil War to current health care policy makers. Mil Med. 2015;180(3):259-262.
3. Welling DR, McKay PL, Rasmussen TE, Rich NM. A brief history of the tourniquet. J Vasc Surg. 2012;55(1):286-290.
Moroccan Health Care: A Link to Radicalization and Proposed Solution
The relationship between the Kingdom of Morocco and the US began just after the US declared its own independence. It is one of the oldest of US partnerships with a foreign country, and since the end of the First Barbary War in 1805 it has remained one of the most stable. The Utah National Guard (UTNG) has an active state partnership program (SPP) with Morocco, which helps maintain that stability and fosters the relationship. The SPP provides the Kingdom of Morocco assistance in the areas of disaster medicine, prehospital medicine, and rural access to health care.
The objective of this review is to highlight the role the SPP plays in ensuring Morocco’s continued stability, enhancing its role as a leader among African nations, aiding its medically vulnerable rural populations to prevent recruitment by terrorist organizations, and maintaining its long-term relationship with the US.
Background
The Kingdom of Morocco resides in a geologically and politically unstable part of the world, yet it has been a stable constitutional monarchy. Like California, Morocco has a long coastline of more than 1,000 miles. It sits along an active earthquake fault line with a disaster response program that is only in its infancy. The Kingdom has a high youth unemployment rate and lacks adequate public education opportunities, which exacerbate feelings of government indifference. Morocco’s medical system is highly centralized, and large parts of the rural population lack access to basic medical care—potentially alienating the population. The Moroccan current disaster plan ORSEC (plan d’ Organization des Secours) was established in 1966 and updated in 2005 but does not provide a comprehensive, unified disaster response. The ORSEC plan is of French derivation and is not a list of actions but a general plan of organization and supply. 1
When governments fail to provide basic services—health care being just one—those services may be filled by groups seeking to influence the government and population by threatening acts of violence to achieve political, religious, and ideologic gain; for example, the Taliban in Afghanistan, the Muslim brotherhood in Egypt and in the West Bank, and the Islamic State in Iraq and Syria (ISIS) in Syria.2-5 These groups gain a foothold and legitimacy by providing mosques, youth groups, clinics, hospitals, and schools. 2-5
Identified Needs
Morocco is at risk of experiencing an earthquake and possible subsequent tsunami. In 1755, Morocco was impacted by the Great Lisbon earthquake and tsunami. Witnesses reported 15-meter waves with 24-meter crests.6 Building codes and architecture laws have changed little since the 1960 Agadir earthquake, which killed 12,000 people. The disaster response program—although improved since the 1960s—is still in the early stages of development, and another earthquake and possible subsequent tsunami would result in a disaster that could overwhelm the medical community of Morocco.
Perceived Government Indifference
The Moroccan constitutional monarchy is more stable than are the governments of its North African neighbors. King Mohammed VI presides over the government, and regular elections are held for members of Parliament, which names a prime minister. However, in August 2019, overall unemployment was at 8.5%, and youth unemployment was 22.3%.7 A United Nations report in August 2019 stated that literacy rates for Morocco were 71.7%. These data were from a 2015 census, the last year data were collected.8 These deficits in employment and education can foster anger toward the Moroccan government for not adequately providing these services and possibly introduce radicalization as a result of the population’s perceived government indifference and lack of economic mobility.
Access to Medical Care
Morocco has a 2-tiered medical system for providing services: urban and rural. In 2018 the Legatum Prosperity Index ranked Morocco 103 of 149 countries in health care. The prosperity index measures health variables, which include but were not limited to basic physical and mental health, health infrastructure, and preventive care.9 Outside the metropolitan areas, emergency medical care is nonexistent, primary care is sporadic, and there is little modern technology available.
Despite humanitarian efforts over many years, there is little to no medical care in the rural “medical desert.” A 2017 study from the University of Washington Institute for Health Metrics and Evaluation compared the global burden of disease in similar countries. The study found that Morocco was significantly higher than the mean in the prevalence of ischemic heart disease and Alzheimer disease, lower than the mean in the areas of neonatal disorders, lower respiratory infections, and tuberculosis, and statistically indistinct from the mean in stroke, congenital defects, road injuries, diabetes mellitus, and hypertensive heart disease compared with the disease prevalence of other countries of similar size and economic measures.10 The study also found a particularly acute disparity in access to health care in rural areas. In 2016, the Oxford Business Group reported staff shortages and disproportionate distribution of resources in the Moroccan health care system.11
Additionally, the lack of trained health care personnel has added to an already overstressed health care system. A chief stressor in a health care system is an insufficient replacement rate. Health employees working for the Moroccan Ministry of Health retire at a rate of 1,500 per year.10,11 These shortages may serve to further the feelings of frustration and government indifference. This frustration is momentarily decreased by humanitarian efforts that have taken place in the African continent in the past decades, but this band-aid approach to assisting the population that is medically underserved has done little to alleviate the long-term problem of access to care. And feelings of government abandonment can sow the seeds of discontent in the rural population, creating fertile ground for recruitment by terrorist organizations.2,3
Lack of Health Care and Radicalism
It has been postulated that there is a link between radicalization and lack of medical care. Depression and perceived government indifference are considered contributors to radicalization.12-16 In 2005, Victoroff suggested that there are certain psychological traits characteristic of “typical" terrorists: these include high affective valence regarding an ideologic issue, a personal stake (perceived oppression, persecution or humiliation, need for identity, glory, or vengeance), low cognitive ability, low tolerance for ambiguity, and a capacity to suppress instinctive and learned moral constraints against harming innocents.15 In 2009, Lafree and Ackerman suggested that terrorism feeds on the ability of groups to portray governments and their agents as illegitimate.16 It is possible that part of the illegitimacy campaign of radicalization and terrorist recruitment may be identification of the lack of health care by the government thus magnifying feelings of government abandonment in a vulnerable population.
In 2011, the new Moroccan constitution identified access to basic health care as a right of the Moroccan people.17 Additionally, in 2013, a government white paper was produced outlining the need to increase access to health care, particularly in rural areas, including a focus on infant and maternal mortality, diabetes mellitus (DM), heart disease, and respiratory problems.17,18
Proposed Solutions, A Beginning
A health outreach program with a regional health professional training center in a relatively stable country within the African Union (AU) would be a step toward delivering health care to Morocco and interested AU members. Interested nations have been and will continue to be invited to train at the Moroccan center and return to their countries and start training programs. This idea was echoed by the World Bank in a 2015 loan proposal to Morocco, which suggested that addressing disparities in access to health care is a social justice issue, with other benefits such as increased productivity, employment, lower out-of-pocket expenditures, and promotion of good governance.17
In 2012, Buhi reported that a positive regard for authorities and healthier influences seemed to be a protective factor against radicalization. He also suggested a public health approach to understanding and preventing violent radicalization.19 The solutions are complex, especially in rural areas and in vulnerable nations common to Africa.
Medical training efforts by the US Department of Defense (DoD), Medical Readiness Training Institute (DMRT), and international health specialists working with the military and civilian entities in neighboring African countries have improved response to regional disasters. However, to address the broader issues, a more permanent, cooperative possible solution may begin with the establishment in Morocco of a regional education center for disaster preparedness and for health care providers (HCPs). This would serve as a training program for disaster first responders. Graduates of the program would receive additional training to become HCPs similar to physician assistant (PA) and nurse practitioner (NP) programs in the US. Morocco is uniquely positioned to accomplish this due to its location, political stability, and ties with other African nations.
The goal of the Moroccan regional education center (within the King Mohammed V Hospital) is to bring together global health experts and increase the intellectual infrastructure of not only Morocco, but also offer this training program to interested countries within the AU. Advancement of the regional education center will require legislative changes to expand prescriptive privileges and scope of practice within each country. The medical element of the SPP as presently constituted without the regional education center will continue its humanitarian goals, but the proposed creation of the regional education center will educate participants to serve the rural communities within each participating country. Eventually the entire educational program will be the responsibility of the Moroccan military and the AU participants. This will require reprioritizing resources from the provision of humanitarian health care services to an HCP education approach.
Disaster Response
Deficits in disaster response capabilities have been identified by members of the Moroccan military with the assistance of the UTNG. The most glaring deficit identified was the disparity in training between military and civilian first responders. Thus, a training program was initiated by the Moroccan military and the UTNG that combined internationally recognized, durable, robust emergency training programs. These programs consisted of, but were not limited to, parts or entire programs of the following: basic disaster life support, advanced disaster life support, disaster casualty care, and advanced trauma life support. The goal of this training was to improve communication, reduce mortality, and create strike teams, which can quickly provide health care independent of a hospital during a disaster.
Patients can overwhelm hospitals in a disaster when need exceeds resources. In 1996, Mallonee reported that at least 67% of the patients who sought care at a hospital during the Oklahoma City bombing disaster did not need advanced medical treatment.20 Such patients could be seen at an identified casualty collection point by a strike team and treated and released rather than traveling to the hospital and using staff and resources that could be used more judiciously for the more seriously injured.21 These teams consist of trained first responders with an experienced HCP (physician, PA, NP) and a nurse and are trained to operate for up to 72 hours in a predetermined location and serve as a “filter” for the hospital. Their role is to treat and release the less severely injured and refer only the more severely injured to the hospital after basic stabilization, thus preserving precious resources necessary for the more seriously injured.
This disaster response training program was offered to the Moroccan military, ministry of health and ministry of tourism, and quickly turned into an Africa-wide interest. A regional training center was proposed. This was assisted with the cooperation of Weber State University in Ogden Utah, Utah Valley University in Orem, and private interests in a public/private/military state partnership. Program supplies and didactic instruction were and will be provided by the UTNG and supplemented through the DoD Africa command. Instruction will be a cooperative effort agreed on between the UTNG and the Moroccan military medical specialists within their specific area of expertise.
Underserved Communities
Finally, from this pool of interested strike team members, a health care provider school will be formed to educate, certify, and service the needs of the underserved communities in Morocco and interested AU countries. This program will be similar to the PA and NP programs in the US and will be geared to those graduates from the previous programs with intense classroom instruction for one year followed by a year of one-on-one preceptorship with an experienced physician. The goal of the program is to prepare individuals with patient care experience to fulfill a bigger role in health care in an underserved (usually austere, rural) area that currently has minimal health care presence. This fills a need identified by the World Bank in 2015 that the Moroccan government needs to respond to the demand for improved access to and quality of health care services—particularly to the rural poor.17
The Moroccan military has a presence in many medically underserved areas. The logical fit for the HCP program will be drawn from a pool of active-duty military individuals who express an interest and qualify through attendance in all phases of the training.
Conclusion
This program of disaster medical education, strike teams, and HCPs is currently training more than 200 students a year throughout Morocco. The proposed direction of this cooperative program to produce HCPs in rural areas will increase access to health care for the Moroccan people who are now underserved. Morocco, as a health care training hub in Africa, will increase access to health care for interested African countries. The goal politically will be to reduce feelings of government indifference in vulnerable populations and reduce recruitment into radical ideologies.
1. Nahon M, Michaloux M. L’organisation de la réponse de la sécurité civile: le dispositif ORSEC Organisation of civilian emergency services: The ORSEC plan. https://www.sciencedirect.com/science/article/pii/S2211423816300499#! Published July 2016. Accessed October 7, 2019.
2. Berman E. Hamas, Taliban and the Jewish underground: an economist's view of radical religious militias. NBER Working Paper No. w10004. https://ssrn.com/abstract=450885. Published September 2003. Accessed October 7, 2019.
3. Jordan J. Attacking the leader. Missing the mark; why terrorist groups survive decapitation strikes. Int Secur. 2014;38(4):7-38.
4. Grynkewich A. Welfare as warfare: how violent non-state groups use social services to attack the state. Stud Conflict Terrorism. 2008;31(4):350-370.
5. Marin M, Solomon H. Islamic State: understanding the nature of the beast and its funding. Contemp Rev Middle East. 2017;4(1):18-49.
6. Bressan D. November 1, 1755: the earthquake of Lisbon: wrath of god or natural disaster? Scientific American, History of Geology. https://blogs.scientificamerican.com/history-of-geology/november-1-1755-the-earthquake-of-lisbon-wraith-of-god-or-natural-disaster. Published November 2011. Accessed October 7, 2019.
7. Trading Economics. Morocco unemployment rate. Second quarter statistics. August 2019. https://tradingeconomics.com/morocco/unemployment-rate. Accessed October 7, 2019.
8. Knoema World Data Atlas 2015. Morocco adult literacy rates. https://knoema.com/atlas/Morocco/topics/Education/Literacy/Adult-literacy-rate. Accessed October 4, 2019.
9. The Legatum Prosperity Index 2018. Morocco. https://www.prosperity.com/globe/morocco. Accessed October 7, 2019.
10. University of Washington, Institute for Health Metrics and Evaluation. Morocco. http://www.healthdata.org/morocco. Published 2018. Accessed October 7, 2019.
11. Oxford Business Group. Access to health care broadens in Morocco. https://oxfordbusinessgroup.com/overview/forward-steps-access-care-has-broadened-and-infrastructure-improved-challenges-remain. Accessed September 12. 2019.
12. Wright NMJ, Hankins FM. Preventing radicalization and terrorism: Is there a GP response? Br J Gen Pract. 2016;66(647):288-289.
13. Buhi K, Everitt K, Jones E. Might depression psychosocial adversity, and limited social assets explain vulnerability to and resistance against violent radicalization? PlosOne. 2014;9(9):e105918.
14. DeAngelis T. Understanding terrorism. apa.org/monitor/2009/11/terrorism. Published November 2009. Accessed October 14, 2019.
15. Victoroff J. The mind of the terrorist: a review and critique of psychological approaches. J Conflict Resolut. 2005;49(1):3-42.
16. Lafree G, Ackerman G. The empirical study of terrorism: social and legal research. Ann Rev Law Soc Sci. 2009;5:347-374.
17. World Bank. Morocco—improving primary health in rural areas program-for-results project (English). http://documents.worldbank.org/curated/en/716821468274482723/Morocco-Improving-Primary-Health-in-Rural-Areas-Program-for-Results-Project. Published 2015. Accessed September 16, 2019.
18. Royaume du Maroc, Ministère de la Santé. Livre blanc: pour une nouvelle gouvernance du secteur de la santé. Paper presented at: 2nd National Health Conference; July 1-3, 2013; Marrakesh, Morocco.
19. Buhi K, Hicks MH, Lashley M, Jones E. A public health approach to understanding and preventing violent radicalization. BMC Med. 2012;10:16.
20. Mallonee S, Sahriat S, Stennies G, Waxweiler R, Hogan D, Jordan F. Physical injuries and fatalities resulting from the Oklahoma City bombing. JAMA. 1996;276(5):382-387.
21. Ushizawa H, Foxwell AR, Bice S, et al. Needs for disaster medicine: lessons from the field of the Great East Japan Earthquake. Western Pac Surveil Response J. 2013;4(1):51-55.
The relationship between the Kingdom of Morocco and the US began just after the US declared its own independence. It is one of the oldest of US partnerships with a foreign country, and since the end of the First Barbary War in 1805 it has remained one of the most stable. The Utah National Guard (UTNG) has an active state partnership program (SPP) with Morocco, which helps maintain that stability and fosters the relationship. The SPP provides the Kingdom of Morocco assistance in the areas of disaster medicine, prehospital medicine, and rural access to health care.
The objective of this review is to highlight the role the SPP plays in ensuring Morocco’s continued stability, enhancing its role as a leader among African nations, aiding its medically vulnerable rural populations to prevent recruitment by terrorist organizations, and maintaining its long-term relationship with the US.
Background
The Kingdom of Morocco resides in a geologically and politically unstable part of the world, yet it has been a stable constitutional monarchy. Like California, Morocco has a long coastline of more than 1,000 miles. It sits along an active earthquake fault line with a disaster response program that is only in its infancy. The Kingdom has a high youth unemployment rate and lacks adequate public education opportunities, which exacerbate feelings of government indifference. Morocco’s medical system is highly centralized, and large parts of the rural population lack access to basic medical care—potentially alienating the population. The Moroccan current disaster plan ORSEC (plan d’ Organization des Secours) was established in 1966 and updated in 2005 but does not provide a comprehensive, unified disaster response. The ORSEC plan is of French derivation and is not a list of actions but a general plan of organization and supply. 1
When governments fail to provide basic services—health care being just one—those services may be filled by groups seeking to influence the government and population by threatening acts of violence to achieve political, religious, and ideologic gain; for example, the Taliban in Afghanistan, the Muslim brotherhood in Egypt and in the West Bank, and the Islamic State in Iraq and Syria (ISIS) in Syria.2-5 These groups gain a foothold and legitimacy by providing mosques, youth groups, clinics, hospitals, and schools. 2-5
Identified Needs
Morocco is at risk of experiencing an earthquake and possible subsequent tsunami. In 1755, Morocco was impacted by the Great Lisbon earthquake and tsunami. Witnesses reported 15-meter waves with 24-meter crests.6 Building codes and architecture laws have changed little since the 1960 Agadir earthquake, which killed 12,000 people. The disaster response program—although improved since the 1960s—is still in the early stages of development, and another earthquake and possible subsequent tsunami would result in a disaster that could overwhelm the medical community of Morocco.
Perceived Government Indifference
The Moroccan constitutional monarchy is more stable than are the governments of its North African neighbors. King Mohammed VI presides over the government, and regular elections are held for members of Parliament, which names a prime minister. However, in August 2019, overall unemployment was at 8.5%, and youth unemployment was 22.3%.7 A United Nations report in August 2019 stated that literacy rates for Morocco were 71.7%. These data were from a 2015 census, the last year data were collected.8 These deficits in employment and education can foster anger toward the Moroccan government for not adequately providing these services and possibly introduce radicalization as a result of the population’s perceived government indifference and lack of economic mobility.
Access to Medical Care
Morocco has a 2-tiered medical system for providing services: urban and rural. In 2018 the Legatum Prosperity Index ranked Morocco 103 of 149 countries in health care. The prosperity index measures health variables, which include but were not limited to basic physical and mental health, health infrastructure, and preventive care.9 Outside the metropolitan areas, emergency medical care is nonexistent, primary care is sporadic, and there is little modern technology available.
Despite humanitarian efforts over many years, there is little to no medical care in the rural “medical desert.” A 2017 study from the University of Washington Institute for Health Metrics and Evaluation compared the global burden of disease in similar countries. The study found that Morocco was significantly higher than the mean in the prevalence of ischemic heart disease and Alzheimer disease, lower than the mean in the areas of neonatal disorders, lower respiratory infections, and tuberculosis, and statistically indistinct from the mean in stroke, congenital defects, road injuries, diabetes mellitus, and hypertensive heart disease compared with the disease prevalence of other countries of similar size and economic measures.10 The study also found a particularly acute disparity in access to health care in rural areas. In 2016, the Oxford Business Group reported staff shortages and disproportionate distribution of resources in the Moroccan health care system.11
Additionally, the lack of trained health care personnel has added to an already overstressed health care system. A chief stressor in a health care system is an insufficient replacement rate. Health employees working for the Moroccan Ministry of Health retire at a rate of 1,500 per year.10,11 These shortages may serve to further the feelings of frustration and government indifference. This frustration is momentarily decreased by humanitarian efforts that have taken place in the African continent in the past decades, but this band-aid approach to assisting the population that is medically underserved has done little to alleviate the long-term problem of access to care. And feelings of government abandonment can sow the seeds of discontent in the rural population, creating fertile ground for recruitment by terrorist organizations.2,3
Lack of Health Care and Radicalism
It has been postulated that there is a link between radicalization and lack of medical care. Depression and perceived government indifference are considered contributors to radicalization.12-16 In 2005, Victoroff suggested that there are certain psychological traits characteristic of “typical" terrorists: these include high affective valence regarding an ideologic issue, a personal stake (perceived oppression, persecution or humiliation, need for identity, glory, or vengeance), low cognitive ability, low tolerance for ambiguity, and a capacity to suppress instinctive and learned moral constraints against harming innocents.15 In 2009, Lafree and Ackerman suggested that terrorism feeds on the ability of groups to portray governments and their agents as illegitimate.16 It is possible that part of the illegitimacy campaign of radicalization and terrorist recruitment may be identification of the lack of health care by the government thus magnifying feelings of government abandonment in a vulnerable population.
In 2011, the new Moroccan constitution identified access to basic health care as a right of the Moroccan people.17 Additionally, in 2013, a government white paper was produced outlining the need to increase access to health care, particularly in rural areas, including a focus on infant and maternal mortality, diabetes mellitus (DM), heart disease, and respiratory problems.17,18
Proposed Solutions, A Beginning
A health outreach program with a regional health professional training center in a relatively stable country within the African Union (AU) would be a step toward delivering health care to Morocco and interested AU members. Interested nations have been and will continue to be invited to train at the Moroccan center and return to their countries and start training programs. This idea was echoed by the World Bank in a 2015 loan proposal to Morocco, which suggested that addressing disparities in access to health care is a social justice issue, with other benefits such as increased productivity, employment, lower out-of-pocket expenditures, and promotion of good governance.17
In 2012, Buhi reported that a positive regard for authorities and healthier influences seemed to be a protective factor against radicalization. He also suggested a public health approach to understanding and preventing violent radicalization.19 The solutions are complex, especially in rural areas and in vulnerable nations common to Africa.
Medical training efforts by the US Department of Defense (DoD), Medical Readiness Training Institute (DMRT), and international health specialists working with the military and civilian entities in neighboring African countries have improved response to regional disasters. However, to address the broader issues, a more permanent, cooperative possible solution may begin with the establishment in Morocco of a regional education center for disaster preparedness and for health care providers (HCPs). This would serve as a training program for disaster first responders. Graduates of the program would receive additional training to become HCPs similar to physician assistant (PA) and nurse practitioner (NP) programs in the US. Morocco is uniquely positioned to accomplish this due to its location, political stability, and ties with other African nations.
The goal of the Moroccan regional education center (within the King Mohammed V Hospital) is to bring together global health experts and increase the intellectual infrastructure of not only Morocco, but also offer this training program to interested countries within the AU. Advancement of the regional education center will require legislative changes to expand prescriptive privileges and scope of practice within each country. The medical element of the SPP as presently constituted without the regional education center will continue its humanitarian goals, but the proposed creation of the regional education center will educate participants to serve the rural communities within each participating country. Eventually the entire educational program will be the responsibility of the Moroccan military and the AU participants. This will require reprioritizing resources from the provision of humanitarian health care services to an HCP education approach.
Disaster Response
Deficits in disaster response capabilities have been identified by members of the Moroccan military with the assistance of the UTNG. The most glaring deficit identified was the disparity in training between military and civilian first responders. Thus, a training program was initiated by the Moroccan military and the UTNG that combined internationally recognized, durable, robust emergency training programs. These programs consisted of, but were not limited to, parts or entire programs of the following: basic disaster life support, advanced disaster life support, disaster casualty care, and advanced trauma life support. The goal of this training was to improve communication, reduce mortality, and create strike teams, which can quickly provide health care independent of a hospital during a disaster.
Patients can overwhelm hospitals in a disaster when need exceeds resources. In 1996, Mallonee reported that at least 67% of the patients who sought care at a hospital during the Oklahoma City bombing disaster did not need advanced medical treatment.20 Such patients could be seen at an identified casualty collection point by a strike team and treated and released rather than traveling to the hospital and using staff and resources that could be used more judiciously for the more seriously injured.21 These teams consist of trained first responders with an experienced HCP (physician, PA, NP) and a nurse and are trained to operate for up to 72 hours in a predetermined location and serve as a “filter” for the hospital. Their role is to treat and release the less severely injured and refer only the more severely injured to the hospital after basic stabilization, thus preserving precious resources necessary for the more seriously injured.
This disaster response training program was offered to the Moroccan military, ministry of health and ministry of tourism, and quickly turned into an Africa-wide interest. A regional training center was proposed. This was assisted with the cooperation of Weber State University in Ogden Utah, Utah Valley University in Orem, and private interests in a public/private/military state partnership. Program supplies and didactic instruction were and will be provided by the UTNG and supplemented through the DoD Africa command. Instruction will be a cooperative effort agreed on between the UTNG and the Moroccan military medical specialists within their specific area of expertise.
Underserved Communities
Finally, from this pool of interested strike team members, a health care provider school will be formed to educate, certify, and service the needs of the underserved communities in Morocco and interested AU countries. This program will be similar to the PA and NP programs in the US and will be geared to those graduates from the previous programs with intense classroom instruction for one year followed by a year of one-on-one preceptorship with an experienced physician. The goal of the program is to prepare individuals with patient care experience to fulfill a bigger role in health care in an underserved (usually austere, rural) area that currently has minimal health care presence. This fills a need identified by the World Bank in 2015 that the Moroccan government needs to respond to the demand for improved access to and quality of health care services—particularly to the rural poor.17
The Moroccan military has a presence in many medically underserved areas. The logical fit for the HCP program will be drawn from a pool of active-duty military individuals who express an interest and qualify through attendance in all phases of the training.
Conclusion
This program of disaster medical education, strike teams, and HCPs is currently training more than 200 students a year throughout Morocco. The proposed direction of this cooperative program to produce HCPs in rural areas will increase access to health care for the Moroccan people who are now underserved. Morocco, as a health care training hub in Africa, will increase access to health care for interested African countries. The goal politically will be to reduce feelings of government indifference in vulnerable populations and reduce recruitment into radical ideologies.
The relationship between the Kingdom of Morocco and the US began just after the US declared its own independence. It is one of the oldest of US partnerships with a foreign country, and since the end of the First Barbary War in 1805 it has remained one of the most stable. The Utah National Guard (UTNG) has an active state partnership program (SPP) with Morocco, which helps maintain that stability and fosters the relationship. The SPP provides the Kingdom of Morocco assistance in the areas of disaster medicine, prehospital medicine, and rural access to health care.
The objective of this review is to highlight the role the SPP plays in ensuring Morocco’s continued stability, enhancing its role as a leader among African nations, aiding its medically vulnerable rural populations to prevent recruitment by terrorist organizations, and maintaining its long-term relationship with the US.
Background
The Kingdom of Morocco resides in a geologically and politically unstable part of the world, yet it has been a stable constitutional monarchy. Like California, Morocco has a long coastline of more than 1,000 miles. It sits along an active earthquake fault line with a disaster response program that is only in its infancy. The Kingdom has a high youth unemployment rate and lacks adequate public education opportunities, which exacerbate feelings of government indifference. Morocco’s medical system is highly centralized, and large parts of the rural population lack access to basic medical care—potentially alienating the population. The Moroccan current disaster plan ORSEC (plan d’ Organization des Secours) was established in 1966 and updated in 2005 but does not provide a comprehensive, unified disaster response. The ORSEC plan is of French derivation and is not a list of actions but a general plan of organization and supply. 1
When governments fail to provide basic services—health care being just one—those services may be filled by groups seeking to influence the government and population by threatening acts of violence to achieve political, religious, and ideologic gain; for example, the Taliban in Afghanistan, the Muslim brotherhood in Egypt and in the West Bank, and the Islamic State in Iraq and Syria (ISIS) in Syria.2-5 These groups gain a foothold and legitimacy by providing mosques, youth groups, clinics, hospitals, and schools. 2-5
Identified Needs
Morocco is at risk of experiencing an earthquake and possible subsequent tsunami. In 1755, Morocco was impacted by the Great Lisbon earthquake and tsunami. Witnesses reported 15-meter waves with 24-meter crests.6 Building codes and architecture laws have changed little since the 1960 Agadir earthquake, which killed 12,000 people. The disaster response program—although improved since the 1960s—is still in the early stages of development, and another earthquake and possible subsequent tsunami would result in a disaster that could overwhelm the medical community of Morocco.
Perceived Government Indifference
The Moroccan constitutional monarchy is more stable than are the governments of its North African neighbors. King Mohammed VI presides over the government, and regular elections are held for members of Parliament, which names a prime minister. However, in August 2019, overall unemployment was at 8.5%, and youth unemployment was 22.3%.7 A United Nations report in August 2019 stated that literacy rates for Morocco were 71.7%. These data were from a 2015 census, the last year data were collected.8 These deficits in employment and education can foster anger toward the Moroccan government for not adequately providing these services and possibly introduce radicalization as a result of the population’s perceived government indifference and lack of economic mobility.
Access to Medical Care
Morocco has a 2-tiered medical system for providing services: urban and rural. In 2018 the Legatum Prosperity Index ranked Morocco 103 of 149 countries in health care. The prosperity index measures health variables, which include but were not limited to basic physical and mental health, health infrastructure, and preventive care.9 Outside the metropolitan areas, emergency medical care is nonexistent, primary care is sporadic, and there is little modern technology available.
Despite humanitarian efforts over many years, there is little to no medical care in the rural “medical desert.” A 2017 study from the University of Washington Institute for Health Metrics and Evaluation compared the global burden of disease in similar countries. The study found that Morocco was significantly higher than the mean in the prevalence of ischemic heart disease and Alzheimer disease, lower than the mean in the areas of neonatal disorders, lower respiratory infections, and tuberculosis, and statistically indistinct from the mean in stroke, congenital defects, road injuries, diabetes mellitus, and hypertensive heart disease compared with the disease prevalence of other countries of similar size and economic measures.10 The study also found a particularly acute disparity in access to health care in rural areas. In 2016, the Oxford Business Group reported staff shortages and disproportionate distribution of resources in the Moroccan health care system.11
Additionally, the lack of trained health care personnel has added to an already overstressed health care system. A chief stressor in a health care system is an insufficient replacement rate. Health employees working for the Moroccan Ministry of Health retire at a rate of 1,500 per year.10,11 These shortages may serve to further the feelings of frustration and government indifference. This frustration is momentarily decreased by humanitarian efforts that have taken place in the African continent in the past decades, but this band-aid approach to assisting the population that is medically underserved has done little to alleviate the long-term problem of access to care. And feelings of government abandonment can sow the seeds of discontent in the rural population, creating fertile ground for recruitment by terrorist organizations.2,3
Lack of Health Care and Radicalism
It has been postulated that there is a link between radicalization and lack of medical care. Depression and perceived government indifference are considered contributors to radicalization.12-16 In 2005, Victoroff suggested that there are certain psychological traits characteristic of “typical" terrorists: these include high affective valence regarding an ideologic issue, a personal stake (perceived oppression, persecution or humiliation, need for identity, glory, or vengeance), low cognitive ability, low tolerance for ambiguity, and a capacity to suppress instinctive and learned moral constraints against harming innocents.15 In 2009, Lafree and Ackerman suggested that terrorism feeds on the ability of groups to portray governments and their agents as illegitimate.16 It is possible that part of the illegitimacy campaign of radicalization and terrorist recruitment may be identification of the lack of health care by the government thus magnifying feelings of government abandonment in a vulnerable population.
In 2011, the new Moroccan constitution identified access to basic health care as a right of the Moroccan people.17 Additionally, in 2013, a government white paper was produced outlining the need to increase access to health care, particularly in rural areas, including a focus on infant and maternal mortality, diabetes mellitus (DM), heart disease, and respiratory problems.17,18
Proposed Solutions, A Beginning
A health outreach program with a regional health professional training center in a relatively stable country within the African Union (AU) would be a step toward delivering health care to Morocco and interested AU members. Interested nations have been and will continue to be invited to train at the Moroccan center and return to their countries and start training programs. This idea was echoed by the World Bank in a 2015 loan proposal to Morocco, which suggested that addressing disparities in access to health care is a social justice issue, with other benefits such as increased productivity, employment, lower out-of-pocket expenditures, and promotion of good governance.17
In 2012, Buhi reported that a positive regard for authorities and healthier influences seemed to be a protective factor against radicalization. He also suggested a public health approach to understanding and preventing violent radicalization.19 The solutions are complex, especially in rural areas and in vulnerable nations common to Africa.
Medical training efforts by the US Department of Defense (DoD), Medical Readiness Training Institute (DMRT), and international health specialists working with the military and civilian entities in neighboring African countries have improved response to regional disasters. However, to address the broader issues, a more permanent, cooperative possible solution may begin with the establishment in Morocco of a regional education center for disaster preparedness and for health care providers (HCPs). This would serve as a training program for disaster first responders. Graduates of the program would receive additional training to become HCPs similar to physician assistant (PA) and nurse practitioner (NP) programs in the US. Morocco is uniquely positioned to accomplish this due to its location, political stability, and ties with other African nations.
The goal of the Moroccan regional education center (within the King Mohammed V Hospital) is to bring together global health experts and increase the intellectual infrastructure of not only Morocco, but also offer this training program to interested countries within the AU. Advancement of the regional education center will require legislative changes to expand prescriptive privileges and scope of practice within each country. The medical element of the SPP as presently constituted without the regional education center will continue its humanitarian goals, but the proposed creation of the regional education center will educate participants to serve the rural communities within each participating country. Eventually the entire educational program will be the responsibility of the Moroccan military and the AU participants. This will require reprioritizing resources from the provision of humanitarian health care services to an HCP education approach.
Disaster Response
Deficits in disaster response capabilities have been identified by members of the Moroccan military with the assistance of the UTNG. The most glaring deficit identified was the disparity in training between military and civilian first responders. Thus, a training program was initiated by the Moroccan military and the UTNG that combined internationally recognized, durable, robust emergency training programs. These programs consisted of, but were not limited to, parts or entire programs of the following: basic disaster life support, advanced disaster life support, disaster casualty care, and advanced trauma life support. The goal of this training was to improve communication, reduce mortality, and create strike teams, which can quickly provide health care independent of a hospital during a disaster.
Patients can overwhelm hospitals in a disaster when need exceeds resources. In 1996, Mallonee reported that at least 67% of the patients who sought care at a hospital during the Oklahoma City bombing disaster did not need advanced medical treatment.20 Such patients could be seen at an identified casualty collection point by a strike team and treated and released rather than traveling to the hospital and using staff and resources that could be used more judiciously for the more seriously injured.21 These teams consist of trained first responders with an experienced HCP (physician, PA, NP) and a nurse and are trained to operate for up to 72 hours in a predetermined location and serve as a “filter” for the hospital. Their role is to treat and release the less severely injured and refer only the more severely injured to the hospital after basic stabilization, thus preserving precious resources necessary for the more seriously injured.
This disaster response training program was offered to the Moroccan military, ministry of health and ministry of tourism, and quickly turned into an Africa-wide interest. A regional training center was proposed. This was assisted with the cooperation of Weber State University in Ogden Utah, Utah Valley University in Orem, and private interests in a public/private/military state partnership. Program supplies and didactic instruction were and will be provided by the UTNG and supplemented through the DoD Africa command. Instruction will be a cooperative effort agreed on between the UTNG and the Moroccan military medical specialists within their specific area of expertise.
Underserved Communities
Finally, from this pool of interested strike team members, a health care provider school will be formed to educate, certify, and service the needs of the underserved communities in Morocco and interested AU countries. This program will be similar to the PA and NP programs in the US and will be geared to those graduates from the previous programs with intense classroom instruction for one year followed by a year of one-on-one preceptorship with an experienced physician. The goal of the program is to prepare individuals with patient care experience to fulfill a bigger role in health care in an underserved (usually austere, rural) area that currently has minimal health care presence. This fills a need identified by the World Bank in 2015 that the Moroccan government needs to respond to the demand for improved access to and quality of health care services—particularly to the rural poor.17
The Moroccan military has a presence in many medically underserved areas. The logical fit for the HCP program will be drawn from a pool of active-duty military individuals who express an interest and qualify through attendance in all phases of the training.
Conclusion
This program of disaster medical education, strike teams, and HCPs is currently training more than 200 students a year throughout Morocco. The proposed direction of this cooperative program to produce HCPs in rural areas will increase access to health care for the Moroccan people who are now underserved. Morocco, as a health care training hub in Africa, will increase access to health care for interested African countries. The goal politically will be to reduce feelings of government indifference in vulnerable populations and reduce recruitment into radical ideologies.
1. Nahon M, Michaloux M. L’organisation de la réponse de la sécurité civile: le dispositif ORSEC Organisation of civilian emergency services: The ORSEC plan. https://www.sciencedirect.com/science/article/pii/S2211423816300499#! Published July 2016. Accessed October 7, 2019.
2. Berman E. Hamas, Taliban and the Jewish underground: an economist's view of radical religious militias. NBER Working Paper No. w10004. https://ssrn.com/abstract=450885. Published September 2003. Accessed October 7, 2019.
3. Jordan J. Attacking the leader. Missing the mark; why terrorist groups survive decapitation strikes. Int Secur. 2014;38(4):7-38.
4. Grynkewich A. Welfare as warfare: how violent non-state groups use social services to attack the state. Stud Conflict Terrorism. 2008;31(4):350-370.
5. Marin M, Solomon H. Islamic State: understanding the nature of the beast and its funding. Contemp Rev Middle East. 2017;4(1):18-49.
6. Bressan D. November 1, 1755: the earthquake of Lisbon: wrath of god or natural disaster? Scientific American, History of Geology. https://blogs.scientificamerican.com/history-of-geology/november-1-1755-the-earthquake-of-lisbon-wraith-of-god-or-natural-disaster. Published November 2011. Accessed October 7, 2019.
7. Trading Economics. Morocco unemployment rate. Second quarter statistics. August 2019. https://tradingeconomics.com/morocco/unemployment-rate. Accessed October 7, 2019.
8. Knoema World Data Atlas 2015. Morocco adult literacy rates. https://knoema.com/atlas/Morocco/topics/Education/Literacy/Adult-literacy-rate. Accessed October 4, 2019.
9. The Legatum Prosperity Index 2018. Morocco. https://www.prosperity.com/globe/morocco. Accessed October 7, 2019.
10. University of Washington, Institute for Health Metrics and Evaluation. Morocco. http://www.healthdata.org/morocco. Published 2018. Accessed October 7, 2019.
11. Oxford Business Group. Access to health care broadens in Morocco. https://oxfordbusinessgroup.com/overview/forward-steps-access-care-has-broadened-and-infrastructure-improved-challenges-remain. Accessed September 12. 2019.
12. Wright NMJ, Hankins FM. Preventing radicalization and terrorism: Is there a GP response? Br J Gen Pract. 2016;66(647):288-289.
13. Buhi K, Everitt K, Jones E. Might depression psychosocial adversity, and limited social assets explain vulnerability to and resistance against violent radicalization? PlosOne. 2014;9(9):e105918.
14. DeAngelis T. Understanding terrorism. apa.org/monitor/2009/11/terrorism. Published November 2009. Accessed October 14, 2019.
15. Victoroff J. The mind of the terrorist: a review and critique of psychological approaches. J Conflict Resolut. 2005;49(1):3-42.
16. Lafree G, Ackerman G. The empirical study of terrorism: social and legal research. Ann Rev Law Soc Sci. 2009;5:347-374.
17. World Bank. Morocco—improving primary health in rural areas program-for-results project (English). http://documents.worldbank.org/curated/en/716821468274482723/Morocco-Improving-Primary-Health-in-Rural-Areas-Program-for-Results-Project. Published 2015. Accessed September 16, 2019.
18. Royaume du Maroc, Ministère de la Santé. Livre blanc: pour une nouvelle gouvernance du secteur de la santé. Paper presented at: 2nd National Health Conference; July 1-3, 2013; Marrakesh, Morocco.
19. Buhi K, Hicks MH, Lashley M, Jones E. A public health approach to understanding and preventing violent radicalization. BMC Med. 2012;10:16.
20. Mallonee S, Sahriat S, Stennies G, Waxweiler R, Hogan D, Jordan F. Physical injuries and fatalities resulting from the Oklahoma City bombing. JAMA. 1996;276(5):382-387.
21. Ushizawa H, Foxwell AR, Bice S, et al. Needs for disaster medicine: lessons from the field of the Great East Japan Earthquake. Western Pac Surveil Response J. 2013;4(1):51-55.
1. Nahon M, Michaloux M. L’organisation de la réponse de la sécurité civile: le dispositif ORSEC Organisation of civilian emergency services: The ORSEC plan. https://www.sciencedirect.com/science/article/pii/S2211423816300499#! Published July 2016. Accessed October 7, 2019.
2. Berman E. Hamas, Taliban and the Jewish underground: an economist's view of radical religious militias. NBER Working Paper No. w10004. https://ssrn.com/abstract=450885. Published September 2003. Accessed October 7, 2019.
3. Jordan J. Attacking the leader. Missing the mark; why terrorist groups survive decapitation strikes. Int Secur. 2014;38(4):7-38.
4. Grynkewich A. Welfare as warfare: how violent non-state groups use social services to attack the state. Stud Conflict Terrorism. 2008;31(4):350-370.
5. Marin M, Solomon H. Islamic State: understanding the nature of the beast and its funding. Contemp Rev Middle East. 2017;4(1):18-49.
6. Bressan D. November 1, 1755: the earthquake of Lisbon: wrath of god or natural disaster? Scientific American, History of Geology. https://blogs.scientificamerican.com/history-of-geology/november-1-1755-the-earthquake-of-lisbon-wraith-of-god-or-natural-disaster. Published November 2011. Accessed October 7, 2019.
7. Trading Economics. Morocco unemployment rate. Second quarter statistics. August 2019. https://tradingeconomics.com/morocco/unemployment-rate. Accessed October 7, 2019.
8. Knoema World Data Atlas 2015. Morocco adult literacy rates. https://knoema.com/atlas/Morocco/topics/Education/Literacy/Adult-literacy-rate. Accessed October 4, 2019.
9. The Legatum Prosperity Index 2018. Morocco. https://www.prosperity.com/globe/morocco. Accessed October 7, 2019.
10. University of Washington, Institute for Health Metrics and Evaluation. Morocco. http://www.healthdata.org/morocco. Published 2018. Accessed October 7, 2019.
11. Oxford Business Group. Access to health care broadens in Morocco. https://oxfordbusinessgroup.com/overview/forward-steps-access-care-has-broadened-and-infrastructure-improved-challenges-remain. Accessed September 12. 2019.
12. Wright NMJ, Hankins FM. Preventing radicalization and terrorism: Is there a GP response? Br J Gen Pract. 2016;66(647):288-289.
13. Buhi K, Everitt K, Jones E. Might depression psychosocial adversity, and limited social assets explain vulnerability to and resistance against violent radicalization? PlosOne. 2014;9(9):e105918.
14. DeAngelis T. Understanding terrorism. apa.org/monitor/2009/11/terrorism. Published November 2009. Accessed October 14, 2019.
15. Victoroff J. The mind of the terrorist: a review and critique of psychological approaches. J Conflict Resolut. 2005;49(1):3-42.
16. Lafree G, Ackerman G. The empirical study of terrorism: social and legal research. Ann Rev Law Soc Sci. 2009;5:347-374.
17. World Bank. Morocco—improving primary health in rural areas program-for-results project (English). http://documents.worldbank.org/curated/en/716821468274482723/Morocco-Improving-Primary-Health-in-Rural-Areas-Program-for-Results-Project. Published 2015. Accessed September 16, 2019.
18. Royaume du Maroc, Ministère de la Santé. Livre blanc: pour une nouvelle gouvernance du secteur de la santé. Paper presented at: 2nd National Health Conference; July 1-3, 2013; Marrakesh, Morocco.
19. Buhi K, Hicks MH, Lashley M, Jones E. A public health approach to understanding and preventing violent radicalization. BMC Med. 2012;10:16.
20. Mallonee S, Sahriat S, Stennies G, Waxweiler R, Hogan D, Jordan F. Physical injuries and fatalities resulting from the Oklahoma City bombing. JAMA. 1996;276(5):382-387.
21. Ushizawa H, Foxwell AR, Bice S, et al. Needs for disaster medicine: lessons from the field of the Great East Japan Earthquake. Western Pac Surveil Response J. 2013;4(1):51-55.