User login
Validation of the Timberlawn Couple and Family Evaluation Scales–Self-Report in Veterans with PTSD
Although about 8.3% of the general adult civilian population will be diagnosed with posttraumatic stress disorder (PTSD) in their lifetime, rates of PTSD are even higher in the veteran population.1,2 PTSD is associated with a number of psychosocial consequences in veterans, including decreased intimate partner relationship functioning.3,4 For example, Cloitre and colleagues reported that PTSD is associated with difficulty with socializing, intimacy, responsibility, and control, all of which increase difficulties in intimate partner relationships.5 Similarly, researchers also have noted that traumatic experiences can affect an individual’s attachment style, resulting in progressive avoidance of interpersonal relationships, which can lead to marked difficulties in maintaining and beginning intimate partner relationships.6,7 Despite these known consequences of PTSD, as Dekel and Monson noted in a review,further research is still needed regarding the mechanisms by which trauma and PTSD result in decreased intimate partner relationship functioning among veterans.8 Nonetheless, as positive interpersonal relationships are associated with decreased PTSD symptom severity9,10 and increased engagement in PTSD treatment,11 determining methods of measuring intimate partner relationship functioning in veterans with PTSD is important to inform future research and aid the provision of care.
To date, limited research has examined the valid measurement of intimate partner relationship functioning among veterans with PTSD. Many existing measures that comprehensively assess intimate partner relationship functioning are time and resource intensive. One such measure, the Timberlawn Couple and Family Evaluation Scales (TCFES), comprehensively assesses multiple pertinent domains of intimate partner relationship functioning (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict).12 By assessing multiple domains, the TCFES offers a method of understanding the specific components of an individual’s intimate partner relationship in need of increased clinical attention.12 However, the TCFES is a time- and labor-intensive observational measure that requires a couple to interact while a blinded, independent rater observes and rates their interactions using an intricate coding process. This survey structure precludes the ability to quickly and comprehensively assess a veteran’s intimate partner functioning in settings such as mental health outpatient clinics where mental health providers engage in brief, time-limited psychotherapy. As such, brief measures of intimate partner relationship functioning are needed to best inform clinical care among veterans with PTSD.
The primary aim of the current study was to create a psychometrically valid, yet brief, self-report version of the TCFES to assess multiple domains of intimate partner relationship functioning. The psychometric properties of this measure were assessed among a sample of US veterans with PTSD who were in an intimate partner relationship. We specifically examined factor structure, reliability, and associations to established measures of specific domains of relational functioning.
Methods
Ninety-four veterans were recruited via posted advertisements, promotion in PTSD therapy groups/staff meetings, and word of mouth at the Dallas Veterans Affairs Medical Center (VAMC). Participants were eligible if they had a documented diagnosis of PTSD as confirmed in the veteran’s electronic medical record and an affirmative response to currently being involved in an intimate partner relationship (ie, legally married, common-law spouse, involved in a relationship/partnership). There were no exclusion criteria.
Interested veterans were invited to complete several study-related self-report measures concerning their intimate partner relationships that would take about an hour. They were informed that the surveys were voluntary and confidential, and that they would be compensated for their participation. All veterans who participated provided written consent and the study was approved by the Dallas VAMC institutional review board.
Of the 94 veterans recruited, 3 veterans’ data were removed from current analyses after informed consent but before completing the surveys when they indicated they were not currently in a relationship or were divorced. After consent, the 91 participants were administered several study-related self-report measures. The measures took between 30 and 55 minutes to complete. Participants were then compensated $25 for their participation.
Intimate Partner Relationship Functioning
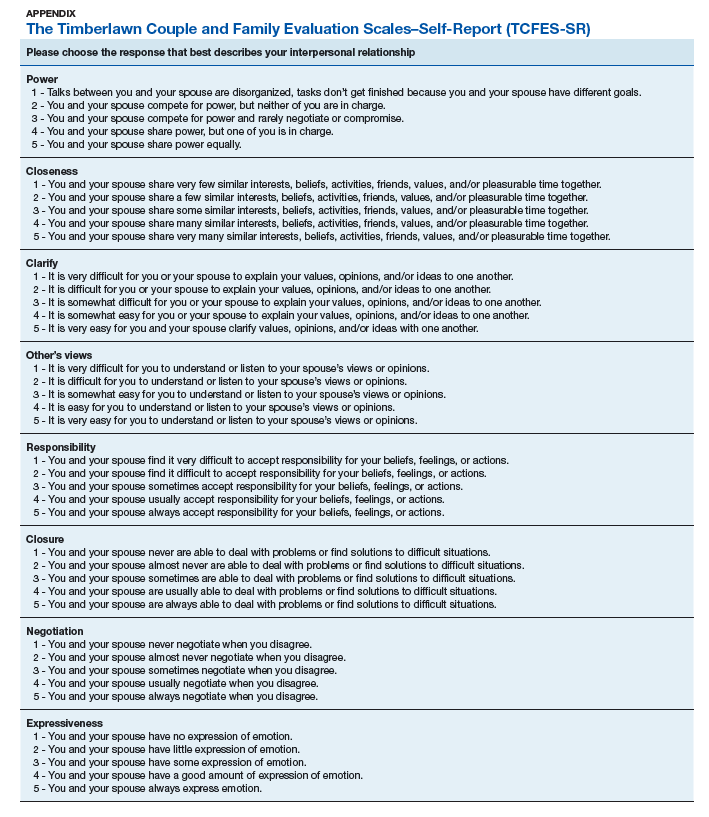
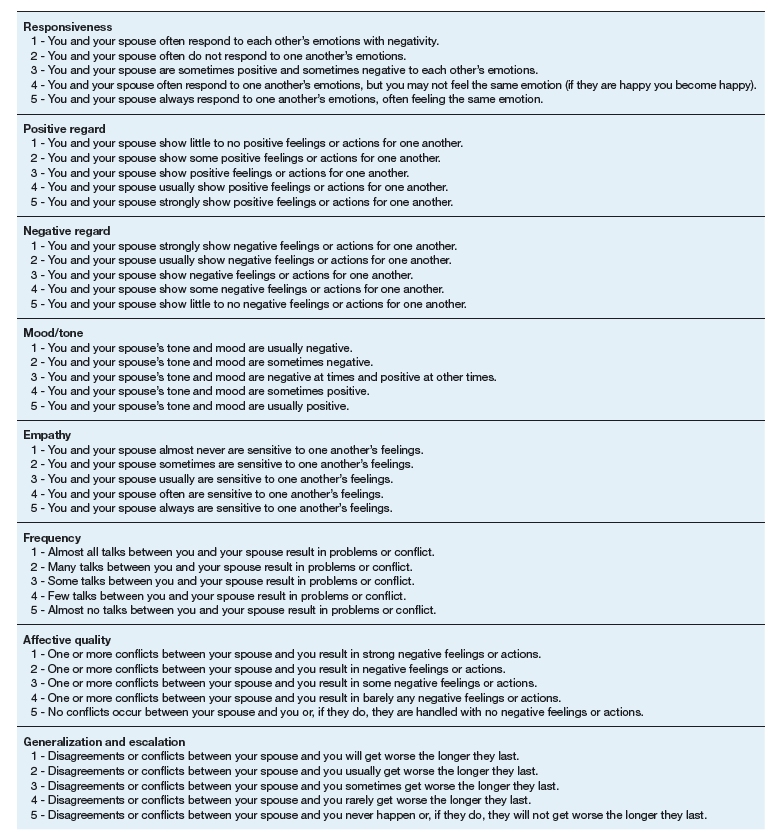
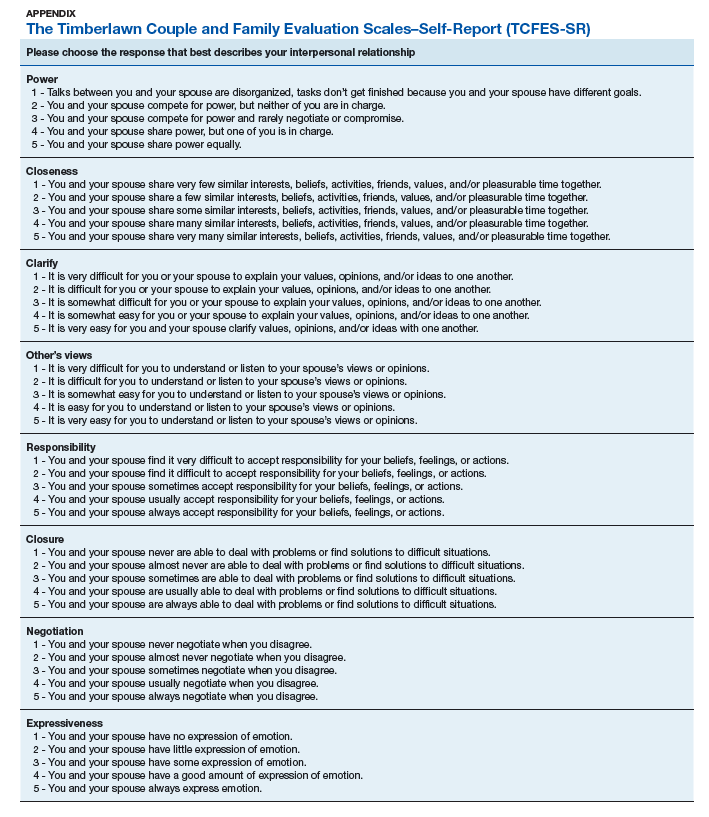
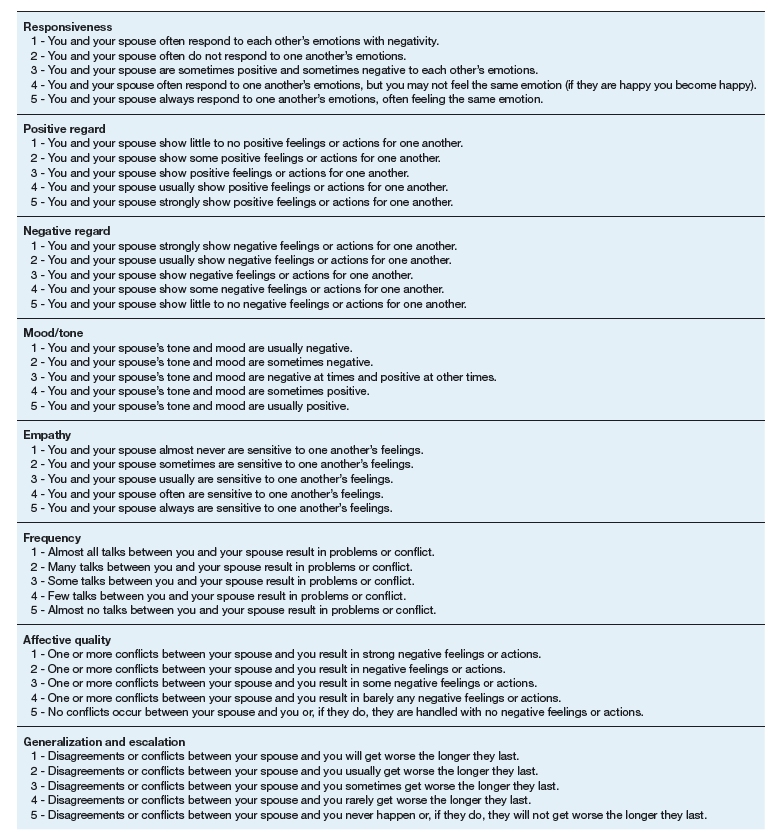
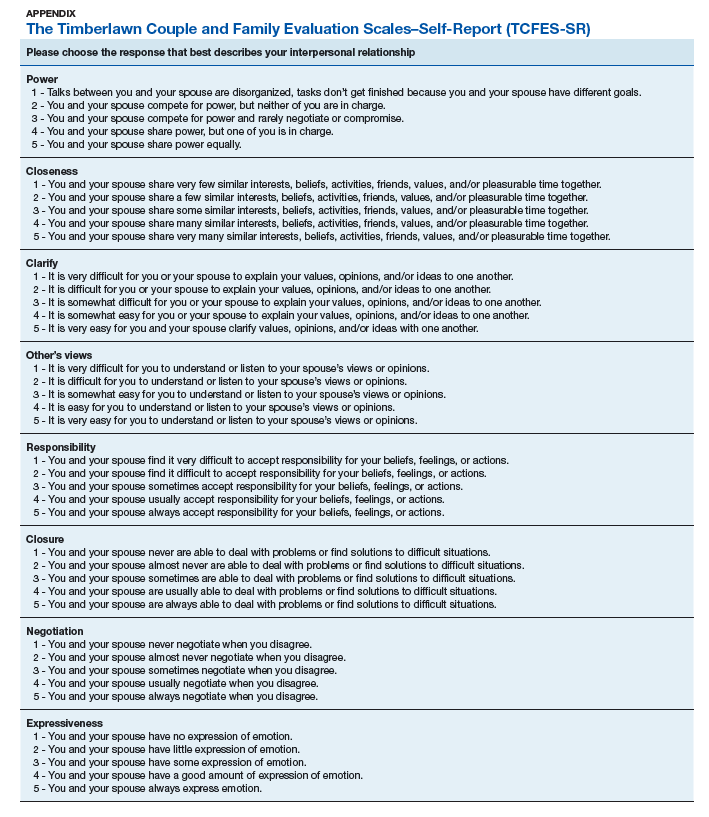
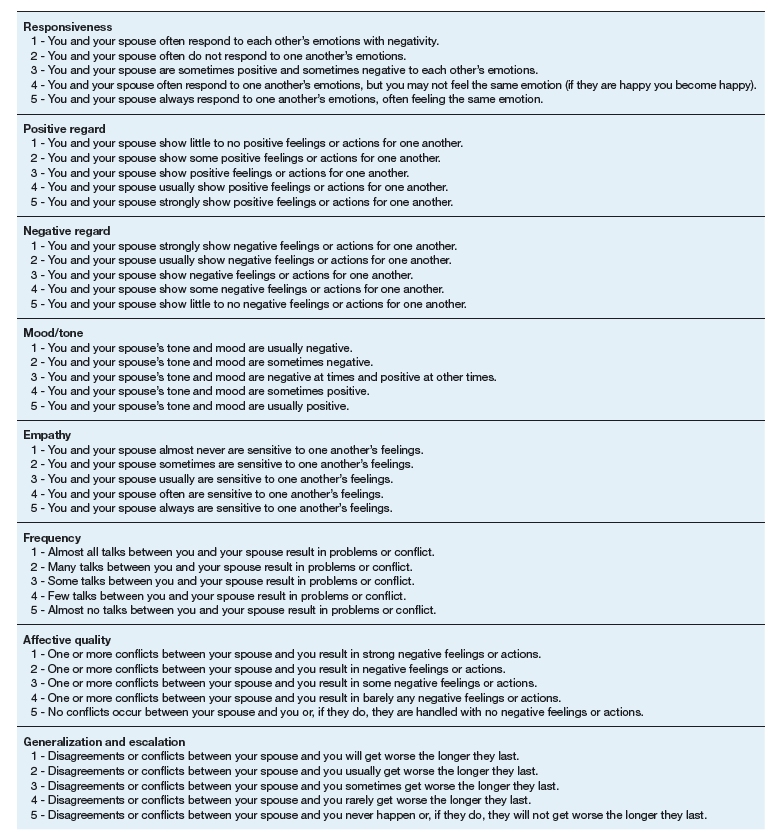
The 16-item TCFES self-report version (TCFES-SR) was developed to assess multiple domains of interpersonal functioning (Appendix). The observational TCFES assesses 5 intimate partner relationship characteristic domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict) during a couple’s interaction by an independent trained rater.12 Each of the 16 TCFES-SR items were modeled after original constructs measured by the TCFES, including power, closeness, clarify, other’s views, responsibility, closure, negotiation, expressiveness, responsiveness, positive regard, negative regard, mood/tone, empathy, frequency, affective quality, and generalization and escalation. To maintain consistency with the TCFES, each item of the TCFES-SR was scored from 1 (severely dysfunctional) to 5 (highly functional). Additionally, all item wording for the TCFES-SR was based on wording in the TCFES manual after consultation with an expert who facilitated the development of the TCFES.12 On average, the TCFES-SR took 5 to 10 minutes to complete.
To measure concurrent validity of the modified TCFES-SR, several additional interpersonal measures were selected and administered based on prior research and established domains of the TCFES. The Positive and Negative Quality in Marriage Scale (PANQIMS) was administered to assess perceived attitudes toward a relationship.13,14 The PANQIMS generates 2 subscales: positive quality and negative quality in the relationship. Because the PANQIMS specifically assesses married relationships and our sample included married and nonmarried participants, wording was modified (eg, “spouse/partner”).
The relative power subscale of the Network Relationships Inventory–Relationship Qualities Version (NRI-RQV) measure was administered to assess the unequal/shared role romantic partners have in power equality (ie, relative power).15
The Revised Dyadic Adjustment Scale (RDAS) is a self-report measure that assesses multiple dimensions of marital adjustment and functioning.16 Six subscales of the RDAS were chosen based on items of the TCFES-SR: decision making, values, affection, conflict, activities, and discussion.
The Interpersonal Reactivity Index (IRI) empathetic concern subscale was administered to assess empathy across multiple contexts and situations17 and the Experiences in Close Relationships-Revised Questionnaire (ECR-R) was administered to assess relational functioning by determining attachment-related anxiety and avoidance.18
Sociodemographic Information
A sociodemographic questionnaire also was administered. The questionnaire assessed gender, age, education, service branch, length of interpersonal relationship, race, and ethnicity of the veteran as well as gender of the veteran’s partner.
Statistical Analysis
Factor structure of the TCFES-SR was determined by conducting an exploratory factor analysis. To allow for correlation between items, the Promax oblique rotation method was chosen.19 Number of factors was determined by agreement between number of eigenvalues ≥ 1, visual inspection of the scree plot, and a parallel analysis. Factor loadings of ≥ 0.3 were used to determine which items loaded on to which factors.
Convergent validity was assessed by conducting Pearson’s bivariate correlations between identified TCFES-SR factor(s) and other administered measures of interpersonal functioning (ie, PANQIMS positive and negative quality; NRI-RQV relative power subscale; RDAS decision making, values, affection, conflict, activities, and discussion subscales; IRI-empathetic concern subscale; and ECR-R attachment-related anxiety and avoidance subscales). Strength of relationship was determined based on the following guidelines: ± 0.3 to 0.49 = small, ± 0.5 to 0.69 = moderate, and ± 0.7 to 1.00 = large. Internal consistency was also determined for TCFES-SR factor(s) using Cronbach’s α. A standard level of significance (α=.05) was used for all statistical analyses.
Results
Eighty-six veterans provided complete data (Table 1). The Kaiser-Meyer-Olkin measure of sampling adequacy was indicative that sample size was adequate (.91), while Bartlett’s test of sphericity found the variables were suitable for structure detection, χ2 (120) = 800.00, P < .001. While 2 eigenvalues were ≥ 1, visual inspection of the scree plot and subsequent parallel analysis identified a unidimensional structure (ie, 1 factor) for the TCFES-SR. All items were found to load to this single factor, with all loadings being ≥ 0.5 (Table 2). Additionally, internal consistency was excellent for the scale (α = .93).
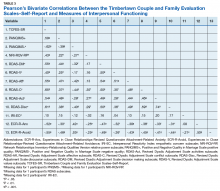
Pearson’s bivariate correlations were significant (P < .05) between TCFES-SR total score, and almost all administered interpersonal functioning measures (Table 3). Interestingly, no significant associations were found between any of the administered measures, including the TCFES-SR total score, and the IRI-empathetic concern subscale (P > .05).
Discussion
These findings provide initial support for the psychometric properties of the TCFES-SR, including excellent internal consistency and the adequate association of its total score to established measures of interpersonal functioning. Contrary to the TCFES, the TCFES-SR was shown to best fit a unidimensional factor rather than a multidimensional measure of relationship functioning. However, the TCFES-SR was also shown to have strong convergent validity with multiple domains of relationship functioning, indicating that the measure of overall intimate partner relationship functioning encompasses a number of relational domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict). Critically, the TCFES-SR is brief and was administered easily in our sample, providing utility as clinical tool to be used in time-sensitive outpatient settings.
A unidimensional factor has particular strength in providing a global portrait of perceived intimate partner relationship functioning, and mental health providers can administer the TCFES-SR to assess for overall perceptions of intimate partner relationship functioning rather than administering a number of measures focusing on specific interpersonal domains (eg, decision making processes or positive/negative attitudes towards one’s relationship). This allows for the quick assessment (ie, 5-10 minutes) of overall intimate partner relationship functioning rather than administration of multiple self-report measures which can be time-intensive and expensive. However, the TCFES-SR also is limited by a lack of nuanced understanding of perceptions of functioning specific to particular domains. For example, the TCFES-SR score cannot describe intimate partner functioning in the domain of problem solving. Therefore, brief screening tools need to be developed that assess multiple intimate partner relationship domains.
Importantly, overall intimate partner relationship functioning as measured by the TCFES-SR may not incorporate perceptions of relationship empathy, as the total score did not correlate with a measure of empathetic concern (ie, the IRI-empathetic concern subscale). As empathy was based on one item in the TCFES-SR vs 7 in the IRI-empathetic concern subscale, it is unclear if the TCFES-SR only captures a portion of the construct of empathy (ie, sensitivity to partner) vs the comprehensive assessment of trait empathy that the IRI subscale measures. Additionally, the IRI-empathetic concern subscale did not significantly correlate with any of the other administered measures of relationship functioning. Given the role of empathy in positive, healthy intimate partner relationships, future research should explore the role of empathetic concern among veterans with PTSD as it relates to overall (eg, TCFES-SR) and specific aspects of intimate partner relationship functioning.20
While the clinical applicability of the TCFES-SR requires further examination, this measure has a number of potential uses. Information captured quickly by the TCFES-SR may help to inform appropriate referral for treatment. For instance, veterans reporting low total scores on the TCFES-SR may indicate a need for a referral for intervention focused on improving overall relationship functioning (eg, Integrative Behavioral Couple Therapy).21,22 Measurement-based care (ie, tracking and discussing changes in symptoms during treatment using validated self-report measures) is now required by the Joint Commission as a standard of care,and has been shown to improve outcomes in couples therapy.23,24 As a brief self-report measure, the TCFES-SR may be able to facilitate measurement-based care and assist providers in tracking changes in overall relationship functioning over the course of treatment. However, the purpose of the current study was to validate the TCFES-SR and not to examine the utility of the TCFES-SR in clinical care; additional research is needed to determine standardized cutoff scores to indicate a need for clinical intervention.
Limitations
Several limitations should be noted. The current study only assessed perceived intimate partner relationship functioning from the perspective of the veteran, thus limiting implications as it pertains to the spouse/partner of the veteran. PTSD diagnosis was based on chart review rather than a psychodiagnostic measure (eg, Clinician Administered PTSD Scale); therefore, whether this diagnosis was current or in remission was unclear. Although our sample was adequate to conduct an exploratory factor analysis,the overall sample size was modest, and results should be considered preliminary with need for further replication.25 The sample was also primarily male, white or black, and non-Hispanic; therefore, results may not generalize to a more sociodemographically diverse population. Finally, given the focus of the study to develop a self-report measure, we did not compare the TCFES-SR to the original TCFES. Thus, further research examining the relationship between the TCFES-SR and TCFES may be needed to better understand overlap and potential incongruence in these measures, and to ascertain any differences in their factor structures.
Conclusion
This study is novel in that it adapted a comprehensive observational measure of relationship functioning to a self-report measure piloted among a sample of veterans with PTSD in an intimate partner relationship, a clinical population that remains largely understudied. Although findings are preliminary, the TCFES-SR was found to be a reliable and valid measure of overall intimate partner relationship functioning. Given the rapid administration of this self-report measure, the TCFES-SR may hold clinical utility as a screen of intimate partner relationship deficits in need of clinical intervention. Replication in a larger, more diverse sample is needed to further examine the generalizability and confirm psychometric properties of the TCFES-SR. Additionally, further understanding of the clinical utility of the TCFES-SR in treatment settings remains critical to promote the development and maintenance of healthy intimate partner relationships among veterans with PTSD. Finally, development of effective self-report measures of intimate partner relationship functioning, such as the TCFES-SR, may help to facilitate needed research to understand the effect of PTSD on establishing and maintaining healthy intimate partner relationships among veterans.
Acknowledgments
The current study was funded by the Timberlawn Psychiatric Research Foundation. This material is the result of work supported in part by the US Department of Veterans Affairs; the Rocky Mountain Mental Illness Research, Education and Clinical Center (MIRECC) for Suicide Prevention; Sierra Pacific MIRECC; and the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
1. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547.
2. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD? Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953.
3. Galovski T, Lyons JA. Psychological sequelae of combat violence: a review of the impact of PTSD on the veteran’s family and possible interventions. Aggress Violent Behav. 2004;9(5):477-501.
4. Ray SL, Vanstone M. The impact of PTSD on veterans’ family relationships: an interpretative phenomenological inquiry. Int J Nurs Stud. 2009;46(6):838-847.
5. Cloitre M, Miranda R, Stovall-McClough KC, Han H. Beyond PTSD: emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behav Ther. 2005;36(2):119-124.
6. McFarlane AC, Bookless C. The effect of PTSD on interpersonal relationships: issues for emergency service works. Sex Relation Ther. 2001;16(3):261-267.
7. Itzhaky L, Stein JY, Levin Y, Solomon Z. Posttraumatic stress symptoms and marital adjustment among Israeli combat veterans: the role of loneliness and attachment. Psychol Trauma. 2017;9(6):655-662.
8. Dekel R, Monson CM. Military-related post-traumatic stress disorder and family relations: current knowledge and future directions. Aggress Violent Behav. 2010;15(4):303-309.
9. Allen ES, Rhoades GK, Stanley SM, Markman HJ. Hitting home: relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. J Fam Psychol. 2010;24(3):280-288.
10. Laffaye C, Cavella S, Drescher K, Rosen C. Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. J Trauma Stress. 2008;21(4):394-401.
11. Meis LA, Noorbaloochi S, Hagel Campbell EM, et al. Sticking it out in trauma-focused treatment for PTSD: it takes a village. J Consult Clin Psychol. 2019;87(3):246-256.
12. Lewis JM, Gossett JT, Housson MM, Owen MT. Timberlawn Couple and Family Evaluation Scales. Dallas, TX: Timberlawn Psychiatric Research Foundation; 1999.
13. Fincham FD, Linfield KJ. A new look at marital quality: can spouses feel positive and negative about their marriage? J Fam Psychol. 1997;11(4):489-502.
14. Kaplan KJ. On the ambivalence-indifference problem in attitude theory and measurement: a suggested modification of the semantic differential technique. Psychol Bull. 1972;77(5):361-372.
15. Buhrmester D, Furman W. The Network of Relationship Inventory: Relationship Qualities Version [unpublished measure]. University of Texas at Dallas; 2008.
16. Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21(3):289-308.
17. Davis MH. A multidimensional approach to individual differences in empathy. JSAS Catalog Sel Doc Psychol. 1980;10:85.
18. Fraley RC, Waller NG, Brennan KA. An item-response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78(2):350-365.
19. Tabachnick BG, Fidell L. Using Multivariate Statistics. 6th ed. Boston, MA: Pearson; 2013.
20. Sautter FJ, Armelie AP, Glynn SM, Wielt DB. The development of a couple-based treatment for PTSD in returning veterans. Prof Psychol Res Pr. 2011;42(1):63-69.
21. Jacobson NS, Christensen A, Prince SE, Cordova J, Eldridge K. Integrative behavioral couple therapy: an acceptance-based, promising new treatment of couple discord. J Consult Clin Psychol. 2000;9(2):351-355.
22. Makin-Byrd K, Gifford E, McCutcheon S, Glynn S. Family and couples treatment for newly returning veterans. Prof Psychol Res Pr. 2011;42(1):47-55.
23. Peterson K, Anderson J, Bourne D. Evidence Brief: Use of Patient Reported Outcome Measures for Measurement Based Care in Mental Health Shared Decision Making. Washington, DC: Department of Veterans Affairs; 2018. https://www.ncbi.nlm.nih.gov/books/NBK536143. Accessed September 13, 2019.
24. Fortney JC, Unützer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68(2):179-188.
25. Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1-9.
Although about 8.3% of the general adult civilian population will be diagnosed with posttraumatic stress disorder (PTSD) in their lifetime, rates of PTSD are even higher in the veteran population.1,2 PTSD is associated with a number of psychosocial consequences in veterans, including decreased intimate partner relationship functioning.3,4 For example, Cloitre and colleagues reported that PTSD is associated with difficulty with socializing, intimacy, responsibility, and control, all of which increase difficulties in intimate partner relationships.5 Similarly, researchers also have noted that traumatic experiences can affect an individual’s attachment style, resulting in progressive avoidance of interpersonal relationships, which can lead to marked difficulties in maintaining and beginning intimate partner relationships.6,7 Despite these known consequences of PTSD, as Dekel and Monson noted in a review,further research is still needed regarding the mechanisms by which trauma and PTSD result in decreased intimate partner relationship functioning among veterans.8 Nonetheless, as positive interpersonal relationships are associated with decreased PTSD symptom severity9,10 and increased engagement in PTSD treatment,11 determining methods of measuring intimate partner relationship functioning in veterans with PTSD is important to inform future research and aid the provision of care.
To date, limited research has examined the valid measurement of intimate partner relationship functioning among veterans with PTSD. Many existing measures that comprehensively assess intimate partner relationship functioning are time and resource intensive. One such measure, the Timberlawn Couple and Family Evaluation Scales (TCFES), comprehensively assesses multiple pertinent domains of intimate partner relationship functioning (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict).12 By assessing multiple domains, the TCFES offers a method of understanding the specific components of an individual’s intimate partner relationship in need of increased clinical attention.12 However, the TCFES is a time- and labor-intensive observational measure that requires a couple to interact while a blinded, independent rater observes and rates their interactions using an intricate coding process. This survey structure precludes the ability to quickly and comprehensively assess a veteran’s intimate partner functioning in settings such as mental health outpatient clinics where mental health providers engage in brief, time-limited psychotherapy. As such, brief measures of intimate partner relationship functioning are needed to best inform clinical care among veterans with PTSD.
The primary aim of the current study was to create a psychometrically valid, yet brief, self-report version of the TCFES to assess multiple domains of intimate partner relationship functioning. The psychometric properties of this measure were assessed among a sample of US veterans with PTSD who were in an intimate partner relationship. We specifically examined factor structure, reliability, and associations to established measures of specific domains of relational functioning.
Methods
Ninety-four veterans were recruited via posted advertisements, promotion in PTSD therapy groups/staff meetings, and word of mouth at the Dallas Veterans Affairs Medical Center (VAMC). Participants were eligible if they had a documented diagnosis of PTSD as confirmed in the veteran’s electronic medical record and an affirmative response to currently being involved in an intimate partner relationship (ie, legally married, common-law spouse, involved in a relationship/partnership). There were no exclusion criteria.
Interested veterans were invited to complete several study-related self-report measures concerning their intimate partner relationships that would take about an hour. They were informed that the surveys were voluntary and confidential, and that they would be compensated for their participation. All veterans who participated provided written consent and the study was approved by the Dallas VAMC institutional review board.
Of the 94 veterans recruited, 3 veterans’ data were removed from current analyses after informed consent but before completing the surveys when they indicated they were not currently in a relationship or were divorced. After consent, the 91 participants were administered several study-related self-report measures. The measures took between 30 and 55 minutes to complete. Participants were then compensated $25 for their participation.
Intimate Partner Relationship Functioning
The 16-item TCFES self-report version (TCFES-SR) was developed to assess multiple domains of interpersonal functioning (Appendix). The observational TCFES assesses 5 intimate partner relationship characteristic domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict) during a couple’s interaction by an independent trained rater.12 Each of the 16 TCFES-SR items were modeled after original constructs measured by the TCFES, including power, closeness, clarify, other’s views, responsibility, closure, negotiation, expressiveness, responsiveness, positive regard, negative regard, mood/tone, empathy, frequency, affective quality, and generalization and escalation. To maintain consistency with the TCFES, each item of the TCFES-SR was scored from 1 (severely dysfunctional) to 5 (highly functional). Additionally, all item wording for the TCFES-SR was based on wording in the TCFES manual after consultation with an expert who facilitated the development of the TCFES.12 On average, the TCFES-SR took 5 to 10 minutes to complete.
To measure concurrent validity of the modified TCFES-SR, several additional interpersonal measures were selected and administered based on prior research and established domains of the TCFES. The Positive and Negative Quality in Marriage Scale (PANQIMS) was administered to assess perceived attitudes toward a relationship.13,14 The PANQIMS generates 2 subscales: positive quality and negative quality in the relationship. Because the PANQIMS specifically assesses married relationships and our sample included married and nonmarried participants, wording was modified (eg, “spouse/partner”).
The relative power subscale of the Network Relationships Inventory–Relationship Qualities Version (NRI-RQV) measure was administered to assess the unequal/shared role romantic partners have in power equality (ie, relative power).15
The Revised Dyadic Adjustment Scale (RDAS) is a self-report measure that assesses multiple dimensions of marital adjustment and functioning.16 Six subscales of the RDAS were chosen based on items of the TCFES-SR: decision making, values, affection, conflict, activities, and discussion.
The Interpersonal Reactivity Index (IRI) empathetic concern subscale was administered to assess empathy across multiple contexts and situations17 and the Experiences in Close Relationships-Revised Questionnaire (ECR-R) was administered to assess relational functioning by determining attachment-related anxiety and avoidance.18
Sociodemographic Information
A sociodemographic questionnaire also was administered. The questionnaire assessed gender, age, education, service branch, length of interpersonal relationship, race, and ethnicity of the veteran as well as gender of the veteran’s partner.
Statistical Analysis
Factor structure of the TCFES-SR was determined by conducting an exploratory factor analysis. To allow for correlation between items, the Promax oblique rotation method was chosen.19 Number of factors was determined by agreement between number of eigenvalues ≥ 1, visual inspection of the scree plot, and a parallel analysis. Factor loadings of ≥ 0.3 were used to determine which items loaded on to which factors.
Convergent validity was assessed by conducting Pearson’s bivariate correlations between identified TCFES-SR factor(s) and other administered measures of interpersonal functioning (ie, PANQIMS positive and negative quality; NRI-RQV relative power subscale; RDAS decision making, values, affection, conflict, activities, and discussion subscales; IRI-empathetic concern subscale; and ECR-R attachment-related anxiety and avoidance subscales). Strength of relationship was determined based on the following guidelines: ± 0.3 to 0.49 = small, ± 0.5 to 0.69 = moderate, and ± 0.7 to 1.00 = large. Internal consistency was also determined for TCFES-SR factor(s) using Cronbach’s α. A standard level of significance (α=.05) was used for all statistical analyses.
Results
Eighty-six veterans provided complete data (Table 1). The Kaiser-Meyer-Olkin measure of sampling adequacy was indicative that sample size was adequate (.91), while Bartlett’s test of sphericity found the variables were suitable for structure detection, χ2 (120) = 800.00, P < .001. While 2 eigenvalues were ≥ 1, visual inspection of the scree plot and subsequent parallel analysis identified a unidimensional structure (ie, 1 factor) for the TCFES-SR. All items were found to load to this single factor, with all loadings being ≥ 0.5 (Table 2). Additionally, internal consistency was excellent for the scale (α = .93).
Pearson’s bivariate correlations were significant (P < .05) between TCFES-SR total score, and almost all administered interpersonal functioning measures (Table 3). Interestingly, no significant associations were found between any of the administered measures, including the TCFES-SR total score, and the IRI-empathetic concern subscale (P > .05).
Discussion
These findings provide initial support for the psychometric properties of the TCFES-SR, including excellent internal consistency and the adequate association of its total score to established measures of interpersonal functioning. Contrary to the TCFES, the TCFES-SR was shown to best fit a unidimensional factor rather than a multidimensional measure of relationship functioning. However, the TCFES-SR was also shown to have strong convergent validity with multiple domains of relationship functioning, indicating that the measure of overall intimate partner relationship functioning encompasses a number of relational domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict). Critically, the TCFES-SR is brief and was administered easily in our sample, providing utility as clinical tool to be used in time-sensitive outpatient settings.
A unidimensional factor has particular strength in providing a global portrait of perceived intimate partner relationship functioning, and mental health providers can administer the TCFES-SR to assess for overall perceptions of intimate partner relationship functioning rather than administering a number of measures focusing on specific interpersonal domains (eg, decision making processes or positive/negative attitudes towards one’s relationship). This allows for the quick assessment (ie, 5-10 minutes) of overall intimate partner relationship functioning rather than administration of multiple self-report measures which can be time-intensive and expensive. However, the TCFES-SR also is limited by a lack of nuanced understanding of perceptions of functioning specific to particular domains. For example, the TCFES-SR score cannot describe intimate partner functioning in the domain of problem solving. Therefore, brief screening tools need to be developed that assess multiple intimate partner relationship domains.
Importantly, overall intimate partner relationship functioning as measured by the TCFES-SR may not incorporate perceptions of relationship empathy, as the total score did not correlate with a measure of empathetic concern (ie, the IRI-empathetic concern subscale). As empathy was based on one item in the TCFES-SR vs 7 in the IRI-empathetic concern subscale, it is unclear if the TCFES-SR only captures a portion of the construct of empathy (ie, sensitivity to partner) vs the comprehensive assessment of trait empathy that the IRI subscale measures. Additionally, the IRI-empathetic concern subscale did not significantly correlate with any of the other administered measures of relationship functioning. Given the role of empathy in positive, healthy intimate partner relationships, future research should explore the role of empathetic concern among veterans with PTSD as it relates to overall (eg, TCFES-SR) and specific aspects of intimate partner relationship functioning.20
While the clinical applicability of the TCFES-SR requires further examination, this measure has a number of potential uses. Information captured quickly by the TCFES-SR may help to inform appropriate referral for treatment. For instance, veterans reporting low total scores on the TCFES-SR may indicate a need for a referral for intervention focused on improving overall relationship functioning (eg, Integrative Behavioral Couple Therapy).21,22 Measurement-based care (ie, tracking and discussing changes in symptoms during treatment using validated self-report measures) is now required by the Joint Commission as a standard of care,and has been shown to improve outcomes in couples therapy.23,24 As a brief self-report measure, the TCFES-SR may be able to facilitate measurement-based care and assist providers in tracking changes in overall relationship functioning over the course of treatment. However, the purpose of the current study was to validate the TCFES-SR and not to examine the utility of the TCFES-SR in clinical care; additional research is needed to determine standardized cutoff scores to indicate a need for clinical intervention.
Limitations
Several limitations should be noted. The current study only assessed perceived intimate partner relationship functioning from the perspective of the veteran, thus limiting implications as it pertains to the spouse/partner of the veteran. PTSD diagnosis was based on chart review rather than a psychodiagnostic measure (eg, Clinician Administered PTSD Scale); therefore, whether this diagnosis was current or in remission was unclear. Although our sample was adequate to conduct an exploratory factor analysis,the overall sample size was modest, and results should be considered preliminary with need for further replication.25 The sample was also primarily male, white or black, and non-Hispanic; therefore, results may not generalize to a more sociodemographically diverse population. Finally, given the focus of the study to develop a self-report measure, we did not compare the TCFES-SR to the original TCFES. Thus, further research examining the relationship between the TCFES-SR and TCFES may be needed to better understand overlap and potential incongruence in these measures, and to ascertain any differences in their factor structures.
Conclusion
This study is novel in that it adapted a comprehensive observational measure of relationship functioning to a self-report measure piloted among a sample of veterans with PTSD in an intimate partner relationship, a clinical population that remains largely understudied. Although findings are preliminary, the TCFES-SR was found to be a reliable and valid measure of overall intimate partner relationship functioning. Given the rapid administration of this self-report measure, the TCFES-SR may hold clinical utility as a screen of intimate partner relationship deficits in need of clinical intervention. Replication in a larger, more diverse sample is needed to further examine the generalizability and confirm psychometric properties of the TCFES-SR. Additionally, further understanding of the clinical utility of the TCFES-SR in treatment settings remains critical to promote the development and maintenance of healthy intimate partner relationships among veterans with PTSD. Finally, development of effective self-report measures of intimate partner relationship functioning, such as the TCFES-SR, may help to facilitate needed research to understand the effect of PTSD on establishing and maintaining healthy intimate partner relationships among veterans.
Acknowledgments
The current study was funded by the Timberlawn Psychiatric Research Foundation. This material is the result of work supported in part by the US Department of Veterans Affairs; the Rocky Mountain Mental Illness Research, Education and Clinical Center (MIRECC) for Suicide Prevention; Sierra Pacific MIRECC; and the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
Although about 8.3% of the general adult civilian population will be diagnosed with posttraumatic stress disorder (PTSD) in their lifetime, rates of PTSD are even higher in the veteran population.1,2 PTSD is associated with a number of psychosocial consequences in veterans, including decreased intimate partner relationship functioning.3,4 For example, Cloitre and colleagues reported that PTSD is associated with difficulty with socializing, intimacy, responsibility, and control, all of which increase difficulties in intimate partner relationships.5 Similarly, researchers also have noted that traumatic experiences can affect an individual’s attachment style, resulting in progressive avoidance of interpersonal relationships, which can lead to marked difficulties in maintaining and beginning intimate partner relationships.6,7 Despite these known consequences of PTSD, as Dekel and Monson noted in a review,further research is still needed regarding the mechanisms by which trauma and PTSD result in decreased intimate partner relationship functioning among veterans.8 Nonetheless, as positive interpersonal relationships are associated with decreased PTSD symptom severity9,10 and increased engagement in PTSD treatment,11 determining methods of measuring intimate partner relationship functioning in veterans with PTSD is important to inform future research and aid the provision of care.
To date, limited research has examined the valid measurement of intimate partner relationship functioning among veterans with PTSD. Many existing measures that comprehensively assess intimate partner relationship functioning are time and resource intensive. One such measure, the Timberlawn Couple and Family Evaluation Scales (TCFES), comprehensively assesses multiple pertinent domains of intimate partner relationship functioning (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict).12 By assessing multiple domains, the TCFES offers a method of understanding the specific components of an individual’s intimate partner relationship in need of increased clinical attention.12 However, the TCFES is a time- and labor-intensive observational measure that requires a couple to interact while a blinded, independent rater observes and rates their interactions using an intricate coding process. This survey structure precludes the ability to quickly and comprehensively assess a veteran’s intimate partner functioning in settings such as mental health outpatient clinics where mental health providers engage in brief, time-limited psychotherapy. As such, brief measures of intimate partner relationship functioning are needed to best inform clinical care among veterans with PTSD.
The primary aim of the current study was to create a psychometrically valid, yet brief, self-report version of the TCFES to assess multiple domains of intimate partner relationship functioning. The psychometric properties of this measure were assessed among a sample of US veterans with PTSD who were in an intimate partner relationship. We specifically examined factor structure, reliability, and associations to established measures of specific domains of relational functioning.
Methods
Ninety-four veterans were recruited via posted advertisements, promotion in PTSD therapy groups/staff meetings, and word of mouth at the Dallas Veterans Affairs Medical Center (VAMC). Participants were eligible if they had a documented diagnosis of PTSD as confirmed in the veteran’s electronic medical record and an affirmative response to currently being involved in an intimate partner relationship (ie, legally married, common-law spouse, involved in a relationship/partnership). There were no exclusion criteria.
Interested veterans were invited to complete several study-related self-report measures concerning their intimate partner relationships that would take about an hour. They were informed that the surveys were voluntary and confidential, and that they would be compensated for their participation. All veterans who participated provided written consent and the study was approved by the Dallas VAMC institutional review board.
Of the 94 veterans recruited, 3 veterans’ data were removed from current analyses after informed consent but before completing the surveys when they indicated they were not currently in a relationship or were divorced. After consent, the 91 participants were administered several study-related self-report measures. The measures took between 30 and 55 minutes to complete. Participants were then compensated $25 for their participation.
Intimate Partner Relationship Functioning
The 16-item TCFES self-report version (TCFES-SR) was developed to assess multiple domains of interpersonal functioning (Appendix). The observational TCFES assesses 5 intimate partner relationship characteristic domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict) during a couple’s interaction by an independent trained rater.12 Each of the 16 TCFES-SR items were modeled after original constructs measured by the TCFES, including power, closeness, clarify, other’s views, responsibility, closure, negotiation, expressiveness, responsiveness, positive regard, negative regard, mood/tone, empathy, frequency, affective quality, and generalization and escalation. To maintain consistency with the TCFES, each item of the TCFES-SR was scored from 1 (severely dysfunctional) to 5 (highly functional). Additionally, all item wording for the TCFES-SR was based on wording in the TCFES manual after consultation with an expert who facilitated the development of the TCFES.12 On average, the TCFES-SR took 5 to 10 minutes to complete.
To measure concurrent validity of the modified TCFES-SR, several additional interpersonal measures were selected and administered based on prior research and established domains of the TCFES. The Positive and Negative Quality in Marriage Scale (PANQIMS) was administered to assess perceived attitudes toward a relationship.13,14 The PANQIMS generates 2 subscales: positive quality and negative quality in the relationship. Because the PANQIMS specifically assesses married relationships and our sample included married and nonmarried participants, wording was modified (eg, “spouse/partner”).
The relative power subscale of the Network Relationships Inventory–Relationship Qualities Version (NRI-RQV) measure was administered to assess the unequal/shared role romantic partners have in power equality (ie, relative power).15
The Revised Dyadic Adjustment Scale (RDAS) is a self-report measure that assesses multiple dimensions of marital adjustment and functioning.16 Six subscales of the RDAS were chosen based on items of the TCFES-SR: decision making, values, affection, conflict, activities, and discussion.
The Interpersonal Reactivity Index (IRI) empathetic concern subscale was administered to assess empathy across multiple contexts and situations17 and the Experiences in Close Relationships-Revised Questionnaire (ECR-R) was administered to assess relational functioning by determining attachment-related anxiety and avoidance.18
Sociodemographic Information
A sociodemographic questionnaire also was administered. The questionnaire assessed gender, age, education, service branch, length of interpersonal relationship, race, and ethnicity of the veteran as well as gender of the veteran’s partner.
Statistical Analysis
Factor structure of the TCFES-SR was determined by conducting an exploratory factor analysis. To allow for correlation between items, the Promax oblique rotation method was chosen.19 Number of factors was determined by agreement between number of eigenvalues ≥ 1, visual inspection of the scree plot, and a parallel analysis. Factor loadings of ≥ 0.3 were used to determine which items loaded on to which factors.
Convergent validity was assessed by conducting Pearson’s bivariate correlations between identified TCFES-SR factor(s) and other administered measures of interpersonal functioning (ie, PANQIMS positive and negative quality; NRI-RQV relative power subscale; RDAS decision making, values, affection, conflict, activities, and discussion subscales; IRI-empathetic concern subscale; and ECR-R attachment-related anxiety and avoidance subscales). Strength of relationship was determined based on the following guidelines: ± 0.3 to 0.49 = small, ± 0.5 to 0.69 = moderate, and ± 0.7 to 1.00 = large. Internal consistency was also determined for TCFES-SR factor(s) using Cronbach’s α. A standard level of significance (α=.05) was used for all statistical analyses.
Results
Eighty-six veterans provided complete data (Table 1). The Kaiser-Meyer-Olkin measure of sampling adequacy was indicative that sample size was adequate (.91), while Bartlett’s test of sphericity found the variables were suitable for structure detection, χ2 (120) = 800.00, P < .001. While 2 eigenvalues were ≥ 1, visual inspection of the scree plot and subsequent parallel analysis identified a unidimensional structure (ie, 1 factor) for the TCFES-SR. All items were found to load to this single factor, with all loadings being ≥ 0.5 (Table 2). Additionally, internal consistency was excellent for the scale (α = .93).
Pearson’s bivariate correlations were significant (P < .05) between TCFES-SR total score, and almost all administered interpersonal functioning measures (Table 3). Interestingly, no significant associations were found between any of the administered measures, including the TCFES-SR total score, and the IRI-empathetic concern subscale (P > .05).
Discussion
These findings provide initial support for the psychometric properties of the TCFES-SR, including excellent internal consistency and the adequate association of its total score to established measures of interpersonal functioning. Contrary to the TCFES, the TCFES-SR was shown to best fit a unidimensional factor rather than a multidimensional measure of relationship functioning. However, the TCFES-SR was also shown to have strong convergent validity with multiple domains of relationship functioning, indicating that the measure of overall intimate partner relationship functioning encompasses a number of relational domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict). Critically, the TCFES-SR is brief and was administered easily in our sample, providing utility as clinical tool to be used in time-sensitive outpatient settings.
A unidimensional factor has particular strength in providing a global portrait of perceived intimate partner relationship functioning, and mental health providers can administer the TCFES-SR to assess for overall perceptions of intimate partner relationship functioning rather than administering a number of measures focusing on specific interpersonal domains (eg, decision making processes or positive/negative attitudes towards one’s relationship). This allows for the quick assessment (ie, 5-10 minutes) of overall intimate partner relationship functioning rather than administration of multiple self-report measures which can be time-intensive and expensive. However, the TCFES-SR also is limited by a lack of nuanced understanding of perceptions of functioning specific to particular domains. For example, the TCFES-SR score cannot describe intimate partner functioning in the domain of problem solving. Therefore, brief screening tools need to be developed that assess multiple intimate partner relationship domains.
Importantly, overall intimate partner relationship functioning as measured by the TCFES-SR may not incorporate perceptions of relationship empathy, as the total score did not correlate with a measure of empathetic concern (ie, the IRI-empathetic concern subscale). As empathy was based on one item in the TCFES-SR vs 7 in the IRI-empathetic concern subscale, it is unclear if the TCFES-SR only captures a portion of the construct of empathy (ie, sensitivity to partner) vs the comprehensive assessment of trait empathy that the IRI subscale measures. Additionally, the IRI-empathetic concern subscale did not significantly correlate with any of the other administered measures of relationship functioning. Given the role of empathy in positive, healthy intimate partner relationships, future research should explore the role of empathetic concern among veterans with PTSD as it relates to overall (eg, TCFES-SR) and specific aspects of intimate partner relationship functioning.20
While the clinical applicability of the TCFES-SR requires further examination, this measure has a number of potential uses. Information captured quickly by the TCFES-SR may help to inform appropriate referral for treatment. For instance, veterans reporting low total scores on the TCFES-SR may indicate a need for a referral for intervention focused on improving overall relationship functioning (eg, Integrative Behavioral Couple Therapy).21,22 Measurement-based care (ie, tracking and discussing changes in symptoms during treatment using validated self-report measures) is now required by the Joint Commission as a standard of care,and has been shown to improve outcomes in couples therapy.23,24 As a brief self-report measure, the TCFES-SR may be able to facilitate measurement-based care and assist providers in tracking changes in overall relationship functioning over the course of treatment. However, the purpose of the current study was to validate the TCFES-SR and not to examine the utility of the TCFES-SR in clinical care; additional research is needed to determine standardized cutoff scores to indicate a need for clinical intervention.
Limitations
Several limitations should be noted. The current study only assessed perceived intimate partner relationship functioning from the perspective of the veteran, thus limiting implications as it pertains to the spouse/partner of the veteran. PTSD diagnosis was based on chart review rather than a psychodiagnostic measure (eg, Clinician Administered PTSD Scale); therefore, whether this diagnosis was current or in remission was unclear. Although our sample was adequate to conduct an exploratory factor analysis,the overall sample size was modest, and results should be considered preliminary with need for further replication.25 The sample was also primarily male, white or black, and non-Hispanic; therefore, results may not generalize to a more sociodemographically diverse population. Finally, given the focus of the study to develop a self-report measure, we did not compare the TCFES-SR to the original TCFES. Thus, further research examining the relationship between the TCFES-SR and TCFES may be needed to better understand overlap and potential incongruence in these measures, and to ascertain any differences in their factor structures.
Conclusion
This study is novel in that it adapted a comprehensive observational measure of relationship functioning to a self-report measure piloted among a sample of veterans with PTSD in an intimate partner relationship, a clinical population that remains largely understudied. Although findings are preliminary, the TCFES-SR was found to be a reliable and valid measure of overall intimate partner relationship functioning. Given the rapid administration of this self-report measure, the TCFES-SR may hold clinical utility as a screen of intimate partner relationship deficits in need of clinical intervention. Replication in a larger, more diverse sample is needed to further examine the generalizability and confirm psychometric properties of the TCFES-SR. Additionally, further understanding of the clinical utility of the TCFES-SR in treatment settings remains critical to promote the development and maintenance of healthy intimate partner relationships among veterans with PTSD. Finally, development of effective self-report measures of intimate partner relationship functioning, such as the TCFES-SR, may help to facilitate needed research to understand the effect of PTSD on establishing and maintaining healthy intimate partner relationships among veterans.
Acknowledgments
The current study was funded by the Timberlawn Psychiatric Research Foundation. This material is the result of work supported in part by the US Department of Veterans Affairs; the Rocky Mountain Mental Illness Research, Education and Clinical Center (MIRECC) for Suicide Prevention; Sierra Pacific MIRECC; and the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
1. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547.
2. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD? Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953.
3. Galovski T, Lyons JA. Psychological sequelae of combat violence: a review of the impact of PTSD on the veteran’s family and possible interventions. Aggress Violent Behav. 2004;9(5):477-501.
4. Ray SL, Vanstone M. The impact of PTSD on veterans’ family relationships: an interpretative phenomenological inquiry. Int J Nurs Stud. 2009;46(6):838-847.
5. Cloitre M, Miranda R, Stovall-McClough KC, Han H. Beyond PTSD: emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behav Ther. 2005;36(2):119-124.
6. McFarlane AC, Bookless C. The effect of PTSD on interpersonal relationships: issues for emergency service works. Sex Relation Ther. 2001;16(3):261-267.
7. Itzhaky L, Stein JY, Levin Y, Solomon Z. Posttraumatic stress symptoms and marital adjustment among Israeli combat veterans: the role of loneliness and attachment. Psychol Trauma. 2017;9(6):655-662.
8. Dekel R, Monson CM. Military-related post-traumatic stress disorder and family relations: current knowledge and future directions. Aggress Violent Behav. 2010;15(4):303-309.
9. Allen ES, Rhoades GK, Stanley SM, Markman HJ. Hitting home: relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. J Fam Psychol. 2010;24(3):280-288.
10. Laffaye C, Cavella S, Drescher K, Rosen C. Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. J Trauma Stress. 2008;21(4):394-401.
11. Meis LA, Noorbaloochi S, Hagel Campbell EM, et al. Sticking it out in trauma-focused treatment for PTSD: it takes a village. J Consult Clin Psychol. 2019;87(3):246-256.
12. Lewis JM, Gossett JT, Housson MM, Owen MT. Timberlawn Couple and Family Evaluation Scales. Dallas, TX: Timberlawn Psychiatric Research Foundation; 1999.
13. Fincham FD, Linfield KJ. A new look at marital quality: can spouses feel positive and negative about their marriage? J Fam Psychol. 1997;11(4):489-502.
14. Kaplan KJ. On the ambivalence-indifference problem in attitude theory and measurement: a suggested modification of the semantic differential technique. Psychol Bull. 1972;77(5):361-372.
15. Buhrmester D, Furman W. The Network of Relationship Inventory: Relationship Qualities Version [unpublished measure]. University of Texas at Dallas; 2008.
16. Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21(3):289-308.
17. Davis MH. A multidimensional approach to individual differences in empathy. JSAS Catalog Sel Doc Psychol. 1980;10:85.
18. Fraley RC, Waller NG, Brennan KA. An item-response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78(2):350-365.
19. Tabachnick BG, Fidell L. Using Multivariate Statistics. 6th ed. Boston, MA: Pearson; 2013.
20. Sautter FJ, Armelie AP, Glynn SM, Wielt DB. The development of a couple-based treatment for PTSD in returning veterans. Prof Psychol Res Pr. 2011;42(1):63-69.
21. Jacobson NS, Christensen A, Prince SE, Cordova J, Eldridge K. Integrative behavioral couple therapy: an acceptance-based, promising new treatment of couple discord. J Consult Clin Psychol. 2000;9(2):351-355.
22. Makin-Byrd K, Gifford E, McCutcheon S, Glynn S. Family and couples treatment for newly returning veterans. Prof Psychol Res Pr. 2011;42(1):47-55.
23. Peterson K, Anderson J, Bourne D. Evidence Brief: Use of Patient Reported Outcome Measures for Measurement Based Care in Mental Health Shared Decision Making. Washington, DC: Department of Veterans Affairs; 2018. https://www.ncbi.nlm.nih.gov/books/NBK536143. Accessed September 13, 2019.
24. Fortney JC, Unützer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68(2):179-188.
25. Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1-9.
1. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547.
2. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD? Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953.
3. Galovski T, Lyons JA. Psychological sequelae of combat violence: a review of the impact of PTSD on the veteran’s family and possible interventions. Aggress Violent Behav. 2004;9(5):477-501.
4. Ray SL, Vanstone M. The impact of PTSD on veterans’ family relationships: an interpretative phenomenological inquiry. Int J Nurs Stud. 2009;46(6):838-847.
5. Cloitre M, Miranda R, Stovall-McClough KC, Han H. Beyond PTSD: emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behav Ther. 2005;36(2):119-124.
6. McFarlane AC, Bookless C. The effect of PTSD on interpersonal relationships: issues for emergency service works. Sex Relation Ther. 2001;16(3):261-267.
7. Itzhaky L, Stein JY, Levin Y, Solomon Z. Posttraumatic stress symptoms and marital adjustment among Israeli combat veterans: the role of loneliness and attachment. Psychol Trauma. 2017;9(6):655-662.
8. Dekel R, Monson CM. Military-related post-traumatic stress disorder and family relations: current knowledge and future directions. Aggress Violent Behav. 2010;15(4):303-309.
9. Allen ES, Rhoades GK, Stanley SM, Markman HJ. Hitting home: relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. J Fam Psychol. 2010;24(3):280-288.
10. Laffaye C, Cavella S, Drescher K, Rosen C. Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. J Trauma Stress. 2008;21(4):394-401.
11. Meis LA, Noorbaloochi S, Hagel Campbell EM, et al. Sticking it out in trauma-focused treatment for PTSD: it takes a village. J Consult Clin Psychol. 2019;87(3):246-256.
12. Lewis JM, Gossett JT, Housson MM, Owen MT. Timberlawn Couple and Family Evaluation Scales. Dallas, TX: Timberlawn Psychiatric Research Foundation; 1999.
13. Fincham FD, Linfield KJ. A new look at marital quality: can spouses feel positive and negative about their marriage? J Fam Psychol. 1997;11(4):489-502.
14. Kaplan KJ. On the ambivalence-indifference problem in attitude theory and measurement: a suggested modification of the semantic differential technique. Psychol Bull. 1972;77(5):361-372.
15. Buhrmester D, Furman W. The Network of Relationship Inventory: Relationship Qualities Version [unpublished measure]. University of Texas at Dallas; 2008.
16. Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21(3):289-308.
17. Davis MH. A multidimensional approach to individual differences in empathy. JSAS Catalog Sel Doc Psychol. 1980;10:85.
18. Fraley RC, Waller NG, Brennan KA. An item-response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78(2):350-365.
19. Tabachnick BG, Fidell L. Using Multivariate Statistics. 6th ed. Boston, MA: Pearson; 2013.
20. Sautter FJ, Armelie AP, Glynn SM, Wielt DB. The development of a couple-based treatment for PTSD in returning veterans. Prof Psychol Res Pr. 2011;42(1):63-69.
21. Jacobson NS, Christensen A, Prince SE, Cordova J, Eldridge K. Integrative behavioral couple therapy: an acceptance-based, promising new treatment of couple discord. J Consult Clin Psychol. 2000;9(2):351-355.
22. Makin-Byrd K, Gifford E, McCutcheon S, Glynn S. Family and couples treatment for newly returning veterans. Prof Psychol Res Pr. 2011;42(1):47-55.
23. Peterson K, Anderson J, Bourne D. Evidence Brief: Use of Patient Reported Outcome Measures for Measurement Based Care in Mental Health Shared Decision Making. Washington, DC: Department of Veterans Affairs; 2018. https://www.ncbi.nlm.nih.gov/books/NBK536143. Accessed September 13, 2019.
24. Fortney JC, Unützer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68(2):179-188.
25. Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1-9.
Understanding the enduring power of caste
Isabel Wilkerson’s naming of the malady facilitates space for a shift in thinking.
America has been struggling to understand its racial dynamics since the arrival of enslaved Africans more than 400 years ago. Today, with much of the world more polarized than ever, and certainly in our United States, there is a need for something to shift us from our fear and survival paranoid schizoid (us-vs.-them) position to an integrated form if we are to come out of this unusual democratic and societal unrest whole.
Yet, we’ve never had the lexicon to adequately describe the sociopolitical dynamics rooted in race and racism and their power to shape the thinking of all who originate in this country and all who enter its self-made borders whether forcefully or voluntarily. Enter Isabel Wilkerson, a Pulitzer Prize–winning, former New York Times Chicago bureau chief, and author of “The Warmth of Other Suns: The Epic Story of America’s Great Migration” (New York: Random House, 2010) with her second book, “Caste: The Origins of Our Discontents” (New York: Random House, 2020).
Ms. Wilkerson quickly gets to work in an engaging storytelling style of weaving past to present with ideas she supports with letters from the past, historians’ impressions, research studies, and data. Her observations and research are bookended by the lead up to the 2016 presidential election and its aftermath on the one end, and the impending 2020 presidential election on the other. In her view, the reemergence of violence that has accelerated in the 21st century and the renewed commitment to promote white supremacy can be understood if we expand our view of race and racism to consider the enduring power of caste. For, in Ms. Wilkerson’s view, the fear of the 2042 U.S. census (which is predicted to reflect for the first time a non-White majority) is a driving force behind the dominant caste’s determination to maintain the status quo power dynamics in the United States.
In an effort to explain American’s racial hierarchy, Ms. Wilkerson explains the need for a new lexicon “that may sound like a foreign language,” but this is intentional on her part. She writes:
“To recalibrate how we see ourselves, I use language that may be more commonly associated with people in other cultures, to suggest a new way of understanding our hierarchy: Dominant caste, ruling majority, favored caste, or upper caste, instead of, or in addition to, white. Middle castes instead of, or in addition to, Asian or Latino. Subordinate caste, lowest caste, bottom caste, disfavored caste, historically stigmatized instead of African-American. Original, conquered, or indigenous peoples instead of, or in addition to, Native American. Marginalized people in addition to, or instead of, women of any race, or minorities of any kind.”
Early in the book Ms. Wilkerson anchors her argument in Rev. Dr. Martin Luther King Jr.’s sojourn to India. Rather than focus on the known history of Dr. King’s admiration of Mohandas Gandhi, Ms. Wilkerson directs our attention to Dr. King’s discovery of his connection to Dalits, those who had been considered “untouchables” until Bhimrao Ramji Ambedkar, the Indian economist, jurist, social reformer, and Dalit leader, fiercely and successfully advocated for a rebranding of his caste of origin; instead of “untouchables” they would be considered Dalits or “broken people.” Dr. King did not meet Mr. Ambedkar, who died 3 years before this journey, but Ms. Wilkerson writes that Dr. King acknowledged the kinship, “And he said unto himself, Yes, I am an untouchable, and every Negro in the United States is an untouchable.” The Dalits and Dr. King recognized in each other their shared positions as subordinates in a global caste system.
In answering the question about the difference between racism and casteism, Ms. Wilkerson writes:
“Because caste and race are interwoven in America, it can be hard to separate the two. ... Casteism is the investment in keeping the hierarchy as it is in order to maintain your own ranking, advantage, privilege, or to elevate yourself above others or to keep others beneath you.”
Reading “Caste: The Origins of Our Discontents” is akin to the experience of gaining relief after struggling for years with a chronic malady that has a fluctuating course: Under the surface is low-grade pain that is compartmentalized and often met with denial or gaslighting when symptoms and systems are reported to members of the dominant caste. Yet, when there are acute flare-ups and increasingly frequent deadly encounters, the defenses of denial are painfully revealed; structures are broken and sometimes burned down. This has been the clinical course of racism, particularly in the United States. In that vein, an early reaction while reading “Caste” might be comparable to hearing an interpretation that educates, clarifies, resonates, and lands perfectly on the right diagnosis at the right moment.
Approach proves clarifying
In conceptualizing the malady as one of caste, Ms. Wilkerson achieves several things simultaneously – she names the malady, thus providing a lexicon, describes its symptoms, and most importantly, in our opinion, shares some of the compelling data from her field studies. By focusing on India, Nazi Germany, and the United States, she describes how easily one system influences another in the global effort to maintain power among the privileged.
This is not a new way of conceptualizing racial hierarchy; however, what is truly persuasive is Ms. Wilkerson’s ability to weave her rigorous research, sociopolitical analysis, and cogent psychological insights and interpretations to explain the 400-year trajectory of racialized caste in the United States. She achieves this exigent task with beautiful prose that motivates the reader to return time and time again to learn gut-wrenching painful historical details. She summarizes truths that have been unearthed (again) about Germany, India, and, in particular, the United States during her research and travels around the world. In doing so, she provides vivid examples of racism layered on caste. Consider the following:
“The Nazis were impressed by the American custom of lynching its subordinate caste of African-Americans, having become aware of the ritual torture and mutilations that typically accompanied them. Hitler especially marveled at the American ‘knack for maintaining an air of robust innocence in the wake of mass death.’ ” Ms. Wilkerson informs us that Hitler sent emissaries to study America’s Jim Crow system and then imported some features to orchestrate the Holocaust in Nazi Germany.
and a corresponding sense of inadequacy in the presence of someone who is considered to be from a higher caste.
A painful account of interpersonal racism is captured as Ms. Wilkerson recounts her experience after a routine business flight from Chicago to Detroit. She details her difficulty leaving a rental car parking lot because she had become so disoriented after being profiled and accosted by Drug Enforcement Administration agents who had intercepted her in the airport terminal and followed her onto the airport shuttle bus as she attempted to reach her destination. She provides a description of “getting turned around in a parking lot that I had been to dozens of times, going in circles, not able to get out, not registering the signs to the exit, not seeing how to get to Interstate 94, when I knew full well how to get to I-94 after all the times I’d driven it. ... This was the thievery of caste, stealing the time and psychic resources of the marginalized, draining energy in an already uphill competition. They were not, like me, frozen and disoriented, trying to make sense of a public violation that seemed all the more menacing now that I could see it in full. The quiet mundanity of that terror has never left me, the scars outliving the cut.”
This account is consistent with the dissociative, disorienting dynamics of race-based trauma. Her experience is not uncommon and helps to explain the activism of those in the subordinate caste who have attained some measure of wealth, power, and influence, and are motivated to expend their resources (energy, time, fame, and/or wealth) to raise awareness about social and political injustices by calling out structural racism in medicine, protesting police use of force by taking a knee, boycotting sporting events, and even demanding that football stadiums be used as polling sites. At the end of the day, all of us who have “made it” know that when we leave our homes, our relegation to the subordinate caste determines how we are perceived and what landmines we must navigate to make it through the day and that determine whether we will make it home.
This tour de force work of art has the potential to be a game changer in the way that we think about racial polarization in the United States. It is hoped that this new language opens up a space that allows each of us to explore this hegemony while identifying our placement and actions we take to maintain it, for each of us undeniably has a position in this caste system.
Having this new lexicon summons to mind the reactions of patients who gain immediate relief from having their illnesses named. In the case of the U.S. malady that has gripped us all, Ms. Wilkerson reiterates the importance of naming the condition. She writes:
“Because, to truly understand America, we must open our eyes to the hidden work of a caste system that has gone unnamed but prevails among us to our collective detriment, to see that we have more in common with each other and with cultures that we might otherwise dismiss, and to summon the courage to consider that therein may lie the answers.”
The naming allows both doctor and patient to have greater insight, understanding its origins and course, as well as having hope that there is a remedy. Naming facilitates the space for a shift in thinking and implementation of treatment protocols, such as Nazi Germany’s “zero tolerance policy” of swastikas in comparison to the ongoing U.S. controversy about the display of Confederate symbols. At this point in history, we welcome a diagnosis that has the potential to shift us from these poles of dominant and subordinate, black and white, good and bad, toward integration and wholeness of the individual psyche and collective global community. This is similar to what Melanie Klein calls the depressive position. Ms. Wilkerson suggests, in relinquishing these polar splits, we increase our capacity to shift to a space where our psychic integration occurs and our inextricable interdependence and responsibility for one another are honored.
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures. Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Isabel Wilkerson’s naming of the malady facilitates space for a shift in thinking.
Isabel Wilkerson’s naming of the malady facilitates space for a shift in thinking.
America has been struggling to understand its racial dynamics since the arrival of enslaved Africans more than 400 years ago. Today, with much of the world more polarized than ever, and certainly in our United States, there is a need for something to shift us from our fear and survival paranoid schizoid (us-vs.-them) position to an integrated form if we are to come out of this unusual democratic and societal unrest whole.
Yet, we’ve never had the lexicon to adequately describe the sociopolitical dynamics rooted in race and racism and their power to shape the thinking of all who originate in this country and all who enter its self-made borders whether forcefully or voluntarily. Enter Isabel Wilkerson, a Pulitzer Prize–winning, former New York Times Chicago bureau chief, and author of “The Warmth of Other Suns: The Epic Story of America’s Great Migration” (New York: Random House, 2010) with her second book, “Caste: The Origins of Our Discontents” (New York: Random House, 2020).
Ms. Wilkerson quickly gets to work in an engaging storytelling style of weaving past to present with ideas she supports with letters from the past, historians’ impressions, research studies, and data. Her observations and research are bookended by the lead up to the 2016 presidential election and its aftermath on the one end, and the impending 2020 presidential election on the other. In her view, the reemergence of violence that has accelerated in the 21st century and the renewed commitment to promote white supremacy can be understood if we expand our view of race and racism to consider the enduring power of caste. For, in Ms. Wilkerson’s view, the fear of the 2042 U.S. census (which is predicted to reflect for the first time a non-White majority) is a driving force behind the dominant caste’s determination to maintain the status quo power dynamics in the United States.
In an effort to explain American’s racial hierarchy, Ms. Wilkerson explains the need for a new lexicon “that may sound like a foreign language,” but this is intentional on her part. She writes:
“To recalibrate how we see ourselves, I use language that may be more commonly associated with people in other cultures, to suggest a new way of understanding our hierarchy: Dominant caste, ruling majority, favored caste, or upper caste, instead of, or in addition to, white. Middle castes instead of, or in addition to, Asian or Latino. Subordinate caste, lowest caste, bottom caste, disfavored caste, historically stigmatized instead of African-American. Original, conquered, or indigenous peoples instead of, or in addition to, Native American. Marginalized people in addition to, or instead of, women of any race, or minorities of any kind.”
Early in the book Ms. Wilkerson anchors her argument in Rev. Dr. Martin Luther King Jr.’s sojourn to India. Rather than focus on the known history of Dr. King’s admiration of Mohandas Gandhi, Ms. Wilkerson directs our attention to Dr. King’s discovery of his connection to Dalits, those who had been considered “untouchables” until Bhimrao Ramji Ambedkar, the Indian economist, jurist, social reformer, and Dalit leader, fiercely and successfully advocated for a rebranding of his caste of origin; instead of “untouchables” they would be considered Dalits or “broken people.” Dr. King did not meet Mr. Ambedkar, who died 3 years before this journey, but Ms. Wilkerson writes that Dr. King acknowledged the kinship, “And he said unto himself, Yes, I am an untouchable, and every Negro in the United States is an untouchable.” The Dalits and Dr. King recognized in each other their shared positions as subordinates in a global caste system.
In answering the question about the difference between racism and casteism, Ms. Wilkerson writes:
“Because caste and race are interwoven in America, it can be hard to separate the two. ... Casteism is the investment in keeping the hierarchy as it is in order to maintain your own ranking, advantage, privilege, or to elevate yourself above others or to keep others beneath you.”
Reading “Caste: The Origins of Our Discontents” is akin to the experience of gaining relief after struggling for years with a chronic malady that has a fluctuating course: Under the surface is low-grade pain that is compartmentalized and often met with denial or gaslighting when symptoms and systems are reported to members of the dominant caste. Yet, when there are acute flare-ups and increasingly frequent deadly encounters, the defenses of denial are painfully revealed; structures are broken and sometimes burned down. This has been the clinical course of racism, particularly in the United States. In that vein, an early reaction while reading “Caste” might be comparable to hearing an interpretation that educates, clarifies, resonates, and lands perfectly on the right diagnosis at the right moment.
Approach proves clarifying
In conceptualizing the malady as one of caste, Ms. Wilkerson achieves several things simultaneously – she names the malady, thus providing a lexicon, describes its symptoms, and most importantly, in our opinion, shares some of the compelling data from her field studies. By focusing on India, Nazi Germany, and the United States, she describes how easily one system influences another in the global effort to maintain power among the privileged.
This is not a new way of conceptualizing racial hierarchy; however, what is truly persuasive is Ms. Wilkerson’s ability to weave her rigorous research, sociopolitical analysis, and cogent psychological insights and interpretations to explain the 400-year trajectory of racialized caste in the United States. She achieves this exigent task with beautiful prose that motivates the reader to return time and time again to learn gut-wrenching painful historical details. She summarizes truths that have been unearthed (again) about Germany, India, and, in particular, the United States during her research and travels around the world. In doing so, she provides vivid examples of racism layered on caste. Consider the following:
“The Nazis were impressed by the American custom of lynching its subordinate caste of African-Americans, having become aware of the ritual torture and mutilations that typically accompanied them. Hitler especially marveled at the American ‘knack for maintaining an air of robust innocence in the wake of mass death.’ ” Ms. Wilkerson informs us that Hitler sent emissaries to study America’s Jim Crow system and then imported some features to orchestrate the Holocaust in Nazi Germany.
and a corresponding sense of inadequacy in the presence of someone who is considered to be from a higher caste.
A painful account of interpersonal racism is captured as Ms. Wilkerson recounts her experience after a routine business flight from Chicago to Detroit. She details her difficulty leaving a rental car parking lot because she had become so disoriented after being profiled and accosted by Drug Enforcement Administration agents who had intercepted her in the airport terminal and followed her onto the airport shuttle bus as she attempted to reach her destination. She provides a description of “getting turned around in a parking lot that I had been to dozens of times, going in circles, not able to get out, not registering the signs to the exit, not seeing how to get to Interstate 94, when I knew full well how to get to I-94 after all the times I’d driven it. ... This was the thievery of caste, stealing the time and psychic resources of the marginalized, draining energy in an already uphill competition. They were not, like me, frozen and disoriented, trying to make sense of a public violation that seemed all the more menacing now that I could see it in full. The quiet mundanity of that terror has never left me, the scars outliving the cut.”
This account is consistent with the dissociative, disorienting dynamics of race-based trauma. Her experience is not uncommon and helps to explain the activism of those in the subordinate caste who have attained some measure of wealth, power, and influence, and are motivated to expend their resources (energy, time, fame, and/or wealth) to raise awareness about social and political injustices by calling out structural racism in medicine, protesting police use of force by taking a knee, boycotting sporting events, and even demanding that football stadiums be used as polling sites. At the end of the day, all of us who have “made it” know that when we leave our homes, our relegation to the subordinate caste determines how we are perceived and what landmines we must navigate to make it through the day and that determine whether we will make it home.
This tour de force work of art has the potential to be a game changer in the way that we think about racial polarization in the United States. It is hoped that this new language opens up a space that allows each of us to explore this hegemony while identifying our placement and actions we take to maintain it, for each of us undeniably has a position in this caste system.
Having this new lexicon summons to mind the reactions of patients who gain immediate relief from having their illnesses named. In the case of the U.S. malady that has gripped us all, Ms. Wilkerson reiterates the importance of naming the condition. She writes:
“Because, to truly understand America, we must open our eyes to the hidden work of a caste system that has gone unnamed but prevails among us to our collective detriment, to see that we have more in common with each other and with cultures that we might otherwise dismiss, and to summon the courage to consider that therein may lie the answers.”
The naming allows both doctor and patient to have greater insight, understanding its origins and course, as well as having hope that there is a remedy. Naming facilitates the space for a shift in thinking and implementation of treatment protocols, such as Nazi Germany’s “zero tolerance policy” of swastikas in comparison to the ongoing U.S. controversy about the display of Confederate symbols. At this point in history, we welcome a diagnosis that has the potential to shift us from these poles of dominant and subordinate, black and white, good and bad, toward integration and wholeness of the individual psyche and collective global community. This is similar to what Melanie Klein calls the depressive position. Ms. Wilkerson suggests, in relinquishing these polar splits, we increase our capacity to shift to a space where our psychic integration occurs and our inextricable interdependence and responsibility for one another are honored.
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures. Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
America has been struggling to understand its racial dynamics since the arrival of enslaved Africans more than 400 years ago. Today, with much of the world more polarized than ever, and certainly in our United States, there is a need for something to shift us from our fear and survival paranoid schizoid (us-vs.-them) position to an integrated form if we are to come out of this unusual democratic and societal unrest whole.
Yet, we’ve never had the lexicon to adequately describe the sociopolitical dynamics rooted in race and racism and their power to shape the thinking of all who originate in this country and all who enter its self-made borders whether forcefully or voluntarily. Enter Isabel Wilkerson, a Pulitzer Prize–winning, former New York Times Chicago bureau chief, and author of “The Warmth of Other Suns: The Epic Story of America’s Great Migration” (New York: Random House, 2010) with her second book, “Caste: The Origins of Our Discontents” (New York: Random House, 2020).
Ms. Wilkerson quickly gets to work in an engaging storytelling style of weaving past to present with ideas she supports with letters from the past, historians’ impressions, research studies, and data. Her observations and research are bookended by the lead up to the 2016 presidential election and its aftermath on the one end, and the impending 2020 presidential election on the other. In her view, the reemergence of violence that has accelerated in the 21st century and the renewed commitment to promote white supremacy can be understood if we expand our view of race and racism to consider the enduring power of caste. For, in Ms. Wilkerson’s view, the fear of the 2042 U.S. census (which is predicted to reflect for the first time a non-White majority) is a driving force behind the dominant caste’s determination to maintain the status quo power dynamics in the United States.
In an effort to explain American’s racial hierarchy, Ms. Wilkerson explains the need for a new lexicon “that may sound like a foreign language,” but this is intentional on her part. She writes:
“To recalibrate how we see ourselves, I use language that may be more commonly associated with people in other cultures, to suggest a new way of understanding our hierarchy: Dominant caste, ruling majority, favored caste, or upper caste, instead of, or in addition to, white. Middle castes instead of, or in addition to, Asian or Latino. Subordinate caste, lowest caste, bottom caste, disfavored caste, historically stigmatized instead of African-American. Original, conquered, or indigenous peoples instead of, or in addition to, Native American. Marginalized people in addition to, or instead of, women of any race, or minorities of any kind.”
Early in the book Ms. Wilkerson anchors her argument in Rev. Dr. Martin Luther King Jr.’s sojourn to India. Rather than focus on the known history of Dr. King’s admiration of Mohandas Gandhi, Ms. Wilkerson directs our attention to Dr. King’s discovery of his connection to Dalits, those who had been considered “untouchables” until Bhimrao Ramji Ambedkar, the Indian economist, jurist, social reformer, and Dalit leader, fiercely and successfully advocated for a rebranding of his caste of origin; instead of “untouchables” they would be considered Dalits or “broken people.” Dr. King did not meet Mr. Ambedkar, who died 3 years before this journey, but Ms. Wilkerson writes that Dr. King acknowledged the kinship, “And he said unto himself, Yes, I am an untouchable, and every Negro in the United States is an untouchable.” The Dalits and Dr. King recognized in each other their shared positions as subordinates in a global caste system.
In answering the question about the difference between racism and casteism, Ms. Wilkerson writes:
“Because caste and race are interwoven in America, it can be hard to separate the two. ... Casteism is the investment in keeping the hierarchy as it is in order to maintain your own ranking, advantage, privilege, or to elevate yourself above others or to keep others beneath you.”
Reading “Caste: The Origins of Our Discontents” is akin to the experience of gaining relief after struggling for years with a chronic malady that has a fluctuating course: Under the surface is low-grade pain that is compartmentalized and often met with denial or gaslighting when symptoms and systems are reported to members of the dominant caste. Yet, when there are acute flare-ups and increasingly frequent deadly encounters, the defenses of denial are painfully revealed; structures are broken and sometimes burned down. This has been the clinical course of racism, particularly in the United States. In that vein, an early reaction while reading “Caste” might be comparable to hearing an interpretation that educates, clarifies, resonates, and lands perfectly on the right diagnosis at the right moment.
Approach proves clarifying
In conceptualizing the malady as one of caste, Ms. Wilkerson achieves several things simultaneously – she names the malady, thus providing a lexicon, describes its symptoms, and most importantly, in our opinion, shares some of the compelling data from her field studies. By focusing on India, Nazi Germany, and the United States, she describes how easily one system influences another in the global effort to maintain power among the privileged.
This is not a new way of conceptualizing racial hierarchy; however, what is truly persuasive is Ms. Wilkerson’s ability to weave her rigorous research, sociopolitical analysis, and cogent psychological insights and interpretations to explain the 400-year trajectory of racialized caste in the United States. She achieves this exigent task with beautiful prose that motivates the reader to return time and time again to learn gut-wrenching painful historical details. She summarizes truths that have been unearthed (again) about Germany, India, and, in particular, the United States during her research and travels around the world. In doing so, she provides vivid examples of racism layered on caste. Consider the following:
“The Nazis were impressed by the American custom of lynching its subordinate caste of African-Americans, having become aware of the ritual torture and mutilations that typically accompanied them. Hitler especially marveled at the American ‘knack for maintaining an air of robust innocence in the wake of mass death.’ ” Ms. Wilkerson informs us that Hitler sent emissaries to study America’s Jim Crow system and then imported some features to orchestrate the Holocaust in Nazi Germany.
and a corresponding sense of inadequacy in the presence of someone who is considered to be from a higher caste.
A painful account of interpersonal racism is captured as Ms. Wilkerson recounts her experience after a routine business flight from Chicago to Detroit. She details her difficulty leaving a rental car parking lot because she had become so disoriented after being profiled and accosted by Drug Enforcement Administration agents who had intercepted her in the airport terminal and followed her onto the airport shuttle bus as she attempted to reach her destination. She provides a description of “getting turned around in a parking lot that I had been to dozens of times, going in circles, not able to get out, not registering the signs to the exit, not seeing how to get to Interstate 94, when I knew full well how to get to I-94 after all the times I’d driven it. ... This was the thievery of caste, stealing the time and psychic resources of the marginalized, draining energy in an already uphill competition. They were not, like me, frozen and disoriented, trying to make sense of a public violation that seemed all the more menacing now that I could see it in full. The quiet mundanity of that terror has never left me, the scars outliving the cut.”
This account is consistent with the dissociative, disorienting dynamics of race-based trauma. Her experience is not uncommon and helps to explain the activism of those in the subordinate caste who have attained some measure of wealth, power, and influence, and are motivated to expend their resources (energy, time, fame, and/or wealth) to raise awareness about social and political injustices by calling out structural racism in medicine, protesting police use of force by taking a knee, boycotting sporting events, and even demanding that football stadiums be used as polling sites. At the end of the day, all of us who have “made it” know that when we leave our homes, our relegation to the subordinate caste determines how we are perceived and what landmines we must navigate to make it through the day and that determine whether we will make it home.
This tour de force work of art has the potential to be a game changer in the way that we think about racial polarization in the United States. It is hoped that this new language opens up a space that allows each of us to explore this hegemony while identifying our placement and actions we take to maintain it, for each of us undeniably has a position in this caste system.
Having this new lexicon summons to mind the reactions of patients who gain immediate relief from having their illnesses named. In the case of the U.S. malady that has gripped us all, Ms. Wilkerson reiterates the importance of naming the condition. She writes:
“Because, to truly understand America, we must open our eyes to the hidden work of a caste system that has gone unnamed but prevails among us to our collective detriment, to see that we have more in common with each other and with cultures that we might otherwise dismiss, and to summon the courage to consider that therein may lie the answers.”
The naming allows both doctor and patient to have greater insight, understanding its origins and course, as well as having hope that there is a remedy. Naming facilitates the space for a shift in thinking and implementation of treatment protocols, such as Nazi Germany’s “zero tolerance policy” of swastikas in comparison to the ongoing U.S. controversy about the display of Confederate symbols. At this point in history, we welcome a diagnosis that has the potential to shift us from these poles of dominant and subordinate, black and white, good and bad, toward integration and wholeness of the individual psyche and collective global community. This is similar to what Melanie Klein calls the depressive position. Ms. Wilkerson suggests, in relinquishing these polar splits, we increase our capacity to shift to a space where our psychic integration occurs and our inextricable interdependence and responsibility for one another are honored.
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures. Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Can experiencing bigotry and racism lead to PTSD?
I have been studying, writing about, and treating posttraumatic stress disorder for many years. Over this time, I have seen PTSD expand to more and more areas of life, including my own view of a “subthreshold” version, which occurs in vulnerable people who experience a job loss, divorce, financial setbacks, or any number of painful life events.
As I noted in my recent book, “Find Freedom Fast,” for some people, PTSD can be triggered in the wake of events that are not life-threatening yet catastrophic for them and not tied to manmade or natural disasters, torture, assault, or war zone experiences.
The expansion of PTSD has led to the disorder being recognized in ICU patients during and after recovery (Crit Care Med. 2015 May;43[5]:1121-9), as well as in people diagnosed with cancer (Lancet Psychiatry. 2017 Apr;4[4]:330-8) and other illnesses that may cause emotional trauma – where one feels that one’s life is threatened. In some instances, the person’s life might indeed be in danger, not unlike what can happen in disasters, wars, torture, and even in some encounters with law enforcement.
This leads me to yet another circumstance that in some, may be tied to PTSD – and that is racial, religious, ethnic, and gender-related bigotry. In these cases, individuals feel threatened just for who they are in a society. Being on the receiving end of a circumstance that threatens a person’s very existence would seem to me to place a person as a potential survivor of PTSD, as well as any number of disorders, including anxiety, depression, or even paranoia.
Yes, discrimination and prejudice have been with us for a long time, and what concerns me is the psychological effect it has on children as well as adults. Friends of Irish descent remind me of hearing stories from parents and grandparents about employment signs reading, “Irish need not apply.” Certainly, those of Italian ancestry will easily recall the prejudice focused against them. And members of the Jewish community also can easily remember the bigotry and exclusion they have been subject to in certain neighborhoods and organizations, in addition to the horrors of the Holocaust during World War II, and the anti-Semitic chants in Charlottesville, Va., from just 3 years ago – with gun-carrying militants doing the chanting.
Obviously, in certain circles, we still have private clubs, plus neighborhoods and residential buildings that exclude people for a variety of reasons.
Coming from a medical family, years ago I heard stories that, if you were Roman Catholic, it would be hard to get into certain medical schools – which might explain the establishment of Catholic medical schools that often were open to people of other faiths. Then we had medical school discrimination toward Jewish students, which was followed by the establishment of medical schools focused on admitting more Jewish students. The African American community also responded to discrimination by establishing medical schools, such as the school at Howard University in Washington.
Furthermore, we cannot forget the discrimination that women faced in institutions of higher learning. My father had two women in his medical school class, I was told. In my era, I would say at least 30% were women, and today, in the United States, medical school classes are more equally balanced with men and women. Some schools have more women than men.
The question I ask, is: How did all those women feel for so many years knowing that, for reasons beyond their control, they were prevented from achieving their chosen goals? Some might have felt badly, and others might have internalized the rejection. Others might have developed PTSD based on feelings of rejection.
However, the question here mainly is: Can PTSD result when exclusion and prejudice induce fear and terror in those on the receiving end – especially innocent children? Children separated from their parents at the U.S.-Mexico border and those who witness their parents being shot immediately come to mind. This trauma can last well beyond childhood.
and make us realize the extent to which the African American community has been traumatized. Perhaps we should not be surprised by a study that found that the prevalence of PTSD among African Americans is 9.1%, compared with 6.8% for Whites (J Anxiety Dis. 2009 Jun;23[5]:573-90). Speaking with Black colleagues, friends, and patients, reading books such “The Warmth of Other Suns,” and watching films such as “Green Book,” give us a sense of how dangerous it was for Black families to travel in certain parts of the country in the recent past. I recall as a child hearing that, in Miami Beach, people of color could not stay overnight. (Even as a child I was surprised – having never heard anything like that. After all, I went to school with people of many religions and backgrounds. My parents thought those practices were terrible, and were appalled when they learned that some hotels were closed to Jews and others closed to Catholics.)
DSM-5, ICD-10 fall short
The DSM-5 describes trauma using a more or less one-dimensional set of guidelines as the focus. Those guidelines include exposure to direct violence, manmade or natural disasters, war, or torture, as well as exposure to a disaster or a life-threatening situation affecting a loved one. The ICD-10 is less restrictive about trauma but still has some limitations.
While considering potential PTSD, I try to use a less rigid diagnostic multidimensional approach, where I assess individual differences and experiences that play a role in those experiences as well as the patient’s vulnerability to the causation of PTSD – which also has to include any exposure to trauma (Curr Opin Psychol. 2017 Apr;14:29-34) before age 11 or 12. The data suggest that such early exposure leaves people more vulnerable to PTSD as adults (Soc Sci Med. 2018 Feb;199:230-40).
In my view, if individuals are frightened because of who they are – be it tied to their religion, race, sexual identity, or ethnicity – and what harm may come to them, and if they live in fear and avoidance of these potential traumatic situations that affect their mental stability and the way they live their lives, they might fit the PTSD model.
If we clinicians focus on what’s currently being brought vividly into the public eye today regarding the African American community, we would see that some of the ongoing fears of racism – whether tied to residential or workplace discrimination, unfair treatment by figures of authority, harassment, health inequities, or microaggressions – may give rise to PTSD. I know we can do better. We should broaden our definition and awareness of this very serious disorder – and be prepared to treat it.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
I have been studying, writing about, and treating posttraumatic stress disorder for many years. Over this time, I have seen PTSD expand to more and more areas of life, including my own view of a “subthreshold” version, which occurs in vulnerable people who experience a job loss, divorce, financial setbacks, or any number of painful life events.
As I noted in my recent book, “Find Freedom Fast,” for some people, PTSD can be triggered in the wake of events that are not life-threatening yet catastrophic for them and not tied to manmade or natural disasters, torture, assault, or war zone experiences.
The expansion of PTSD has led to the disorder being recognized in ICU patients during and after recovery (Crit Care Med. 2015 May;43[5]:1121-9), as well as in people diagnosed with cancer (Lancet Psychiatry. 2017 Apr;4[4]:330-8) and other illnesses that may cause emotional trauma – where one feels that one’s life is threatened. In some instances, the person’s life might indeed be in danger, not unlike what can happen in disasters, wars, torture, and even in some encounters with law enforcement.
This leads me to yet another circumstance that in some, may be tied to PTSD – and that is racial, religious, ethnic, and gender-related bigotry. In these cases, individuals feel threatened just for who they are in a society. Being on the receiving end of a circumstance that threatens a person’s very existence would seem to me to place a person as a potential survivor of PTSD, as well as any number of disorders, including anxiety, depression, or even paranoia.
Yes, discrimination and prejudice have been with us for a long time, and what concerns me is the psychological effect it has on children as well as adults. Friends of Irish descent remind me of hearing stories from parents and grandparents about employment signs reading, “Irish need not apply.” Certainly, those of Italian ancestry will easily recall the prejudice focused against them. And members of the Jewish community also can easily remember the bigotry and exclusion they have been subject to in certain neighborhoods and organizations, in addition to the horrors of the Holocaust during World War II, and the anti-Semitic chants in Charlottesville, Va., from just 3 years ago – with gun-carrying militants doing the chanting.
Obviously, in certain circles, we still have private clubs, plus neighborhoods and residential buildings that exclude people for a variety of reasons.
Coming from a medical family, years ago I heard stories that, if you were Roman Catholic, it would be hard to get into certain medical schools – which might explain the establishment of Catholic medical schools that often were open to people of other faiths. Then we had medical school discrimination toward Jewish students, which was followed by the establishment of medical schools focused on admitting more Jewish students. The African American community also responded to discrimination by establishing medical schools, such as the school at Howard University in Washington.
Furthermore, we cannot forget the discrimination that women faced in institutions of higher learning. My father had two women in his medical school class, I was told. In my era, I would say at least 30% were women, and today, in the United States, medical school classes are more equally balanced with men and women. Some schools have more women than men.
The question I ask, is: How did all those women feel for so many years knowing that, for reasons beyond their control, they were prevented from achieving their chosen goals? Some might have felt badly, and others might have internalized the rejection. Others might have developed PTSD based on feelings of rejection.
However, the question here mainly is: Can PTSD result when exclusion and prejudice induce fear and terror in those on the receiving end – especially innocent children? Children separated from their parents at the U.S.-Mexico border and those who witness their parents being shot immediately come to mind. This trauma can last well beyond childhood.
and make us realize the extent to which the African American community has been traumatized. Perhaps we should not be surprised by a study that found that the prevalence of PTSD among African Americans is 9.1%, compared with 6.8% for Whites (J Anxiety Dis. 2009 Jun;23[5]:573-90). Speaking with Black colleagues, friends, and patients, reading books such “The Warmth of Other Suns,” and watching films such as “Green Book,” give us a sense of how dangerous it was for Black families to travel in certain parts of the country in the recent past. I recall as a child hearing that, in Miami Beach, people of color could not stay overnight. (Even as a child I was surprised – having never heard anything like that. After all, I went to school with people of many religions and backgrounds. My parents thought those practices were terrible, and were appalled when they learned that some hotels were closed to Jews and others closed to Catholics.)
DSM-5, ICD-10 fall short
The DSM-5 describes trauma using a more or less one-dimensional set of guidelines as the focus. Those guidelines include exposure to direct violence, manmade or natural disasters, war, or torture, as well as exposure to a disaster or a life-threatening situation affecting a loved one. The ICD-10 is less restrictive about trauma but still has some limitations.
While considering potential PTSD, I try to use a less rigid diagnostic multidimensional approach, where I assess individual differences and experiences that play a role in those experiences as well as the patient’s vulnerability to the causation of PTSD – which also has to include any exposure to trauma (Curr Opin Psychol. 2017 Apr;14:29-34) before age 11 or 12. The data suggest that such early exposure leaves people more vulnerable to PTSD as adults (Soc Sci Med. 2018 Feb;199:230-40).
In my view, if individuals are frightened because of who they are – be it tied to their religion, race, sexual identity, or ethnicity – and what harm may come to them, and if they live in fear and avoidance of these potential traumatic situations that affect their mental stability and the way they live their lives, they might fit the PTSD model.
If we clinicians focus on what’s currently being brought vividly into the public eye today regarding the African American community, we would see that some of the ongoing fears of racism – whether tied to residential or workplace discrimination, unfair treatment by figures of authority, harassment, health inequities, or microaggressions – may give rise to PTSD. I know we can do better. We should broaden our definition and awareness of this very serious disorder – and be prepared to treat it.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
I have been studying, writing about, and treating posttraumatic stress disorder for many years. Over this time, I have seen PTSD expand to more and more areas of life, including my own view of a “subthreshold” version, which occurs in vulnerable people who experience a job loss, divorce, financial setbacks, or any number of painful life events.
As I noted in my recent book, “Find Freedom Fast,” for some people, PTSD can be triggered in the wake of events that are not life-threatening yet catastrophic for them and not tied to manmade or natural disasters, torture, assault, or war zone experiences.
The expansion of PTSD has led to the disorder being recognized in ICU patients during and after recovery (Crit Care Med. 2015 May;43[5]:1121-9), as well as in people diagnosed with cancer (Lancet Psychiatry. 2017 Apr;4[4]:330-8) and other illnesses that may cause emotional trauma – where one feels that one’s life is threatened. In some instances, the person’s life might indeed be in danger, not unlike what can happen in disasters, wars, torture, and even in some encounters with law enforcement.
This leads me to yet another circumstance that in some, may be tied to PTSD – and that is racial, religious, ethnic, and gender-related bigotry. In these cases, individuals feel threatened just for who they are in a society. Being on the receiving end of a circumstance that threatens a person’s very existence would seem to me to place a person as a potential survivor of PTSD, as well as any number of disorders, including anxiety, depression, or even paranoia.
Yes, discrimination and prejudice have been with us for a long time, and what concerns me is the psychological effect it has on children as well as adults. Friends of Irish descent remind me of hearing stories from parents and grandparents about employment signs reading, “Irish need not apply.” Certainly, those of Italian ancestry will easily recall the prejudice focused against them. And members of the Jewish community also can easily remember the bigotry and exclusion they have been subject to in certain neighborhoods and organizations, in addition to the horrors of the Holocaust during World War II, and the anti-Semitic chants in Charlottesville, Va., from just 3 years ago – with gun-carrying militants doing the chanting.
Obviously, in certain circles, we still have private clubs, plus neighborhoods and residential buildings that exclude people for a variety of reasons.
Coming from a medical family, years ago I heard stories that, if you were Roman Catholic, it would be hard to get into certain medical schools – which might explain the establishment of Catholic medical schools that often were open to people of other faiths. Then we had medical school discrimination toward Jewish students, which was followed by the establishment of medical schools focused on admitting more Jewish students. The African American community also responded to discrimination by establishing medical schools, such as the school at Howard University in Washington.
Furthermore, we cannot forget the discrimination that women faced in institutions of higher learning. My father had two women in his medical school class, I was told. In my era, I would say at least 30% were women, and today, in the United States, medical school classes are more equally balanced with men and women. Some schools have more women than men.
The question I ask, is: How did all those women feel for so many years knowing that, for reasons beyond their control, they were prevented from achieving their chosen goals? Some might have felt badly, and others might have internalized the rejection. Others might have developed PTSD based on feelings of rejection.
However, the question here mainly is: Can PTSD result when exclusion and prejudice induce fear and terror in those on the receiving end – especially innocent children? Children separated from their parents at the U.S.-Mexico border and those who witness their parents being shot immediately come to mind. This trauma can last well beyond childhood.
and make us realize the extent to which the African American community has been traumatized. Perhaps we should not be surprised by a study that found that the prevalence of PTSD among African Americans is 9.1%, compared with 6.8% for Whites (J Anxiety Dis. 2009 Jun;23[5]:573-90). Speaking with Black colleagues, friends, and patients, reading books such “The Warmth of Other Suns,” and watching films such as “Green Book,” give us a sense of how dangerous it was for Black families to travel in certain parts of the country in the recent past. I recall as a child hearing that, in Miami Beach, people of color could not stay overnight. (Even as a child I was surprised – having never heard anything like that. After all, I went to school with people of many religions and backgrounds. My parents thought those practices were terrible, and were appalled when they learned that some hotels were closed to Jews and others closed to Catholics.)
DSM-5, ICD-10 fall short
The DSM-5 describes trauma using a more or less one-dimensional set of guidelines as the focus. Those guidelines include exposure to direct violence, manmade or natural disasters, war, or torture, as well as exposure to a disaster or a life-threatening situation affecting a loved one. The ICD-10 is less restrictive about trauma but still has some limitations.
While considering potential PTSD, I try to use a less rigid diagnostic multidimensional approach, where I assess individual differences and experiences that play a role in those experiences as well as the patient’s vulnerability to the causation of PTSD – which also has to include any exposure to trauma (Curr Opin Psychol. 2017 Apr;14:29-34) before age 11 or 12. The data suggest that such early exposure leaves people more vulnerable to PTSD as adults (Soc Sci Med. 2018 Feb;199:230-40).
In my view, if individuals are frightened because of who they are – be it tied to their religion, race, sexual identity, or ethnicity – and what harm may come to them, and if they live in fear and avoidance of these potential traumatic situations that affect their mental stability and the way they live their lives, they might fit the PTSD model.
If we clinicians focus on what’s currently being brought vividly into the public eye today regarding the African American community, we would see that some of the ongoing fears of racism – whether tied to residential or workplace discrimination, unfair treatment by figures of authority, harassment, health inequities, or microaggressions – may give rise to PTSD. I know we can do better. We should broaden our definition and awareness of this very serious disorder – and be prepared to treat it.
Dr. London has been a practicing psychiatrist for 4 decades and a newspaper columnist for almost as long. He has a private practice in New York and is author of “Find Freedom Fast: Short-Term Therapy That Works” (New York: Kettlehole Publishing, 2019). Dr. London has no conflicts of interest.
Clinical pearls for administering cognitive exams during the pandemic
Patients have often been labeled as “poor historians” if they are not able to recollect their own medical history, whether through illness or difficulties in communication. But Fred Ovsiew, MD, speaking at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sees that label as an excuse on the part of the clinician.
“I strongly advise you to drop that phrase from your vocabulary if you do use it, because the patient is not the historian. The doctor, the clinician is the historian,” Dr. Ovsiew said at the meeting, presented by Global Academy for Medical Education. “It is the clinician’s job to put the story together using the account by the patient as one source, but [also] interviewing a collateral informant and/or reviewing records, which is necessary in almost every case of a neuropsychiatric illness.”
Rather, clinicians taking history at the bedside should focus on why the patients cannot give a narrative account of their illness. Patients can have narrative incapacity on a psychogenic basis, such as in patients with conversion or somatoform disorder, he explained. “I think this is a result of the narrative incapacity that develops in people who have had trauma or adverse experiences in childhood and insecure attachment. This is shown on the adult attachment interview as a disorganized account of their childhoods.”
Other patients might not be able to recount their medical history because they are amnestic, which leaves their account vague because of a lack of access to information. “It may be frozen in time in the sense that, up to a certain point in their life, they can recount the history,” Dr. Ovsiew said. “But in recent years, their account becomes vague.”
Patients with right hemisphere lesions might not know that their account has incongruity and is implausible, while patients with dorsolateral prefrontal lesions might be aspontaneous, use few words to describe their situation, and have poor insight. Those with ventromedial prefrontal lesions can be impulsive and have poor insight, not considering alternative possibilities, Dr. Ovsiew noted.
Asking open-ended questions of the patient is the first step to identifying any potential narrative incapacity, followed by a detailed medical history by the clinician. When taking a medical history, try avoiding what Dr. Ovsiew calls the “anything like that?” problem, where a clinician asks a question about a cluster of symptoms that would make sense to a doctor, but not a patient. For example, a doctor might ask whether a patient is experiencing “chest pain or leg swelling – anything like that?” because he or she knows what those symptoms have in common, but the patient might not know the relationship between those symptoms. “You can’t count on the patient to tell you all the relevant information,” he said. “You have to know what to ask about.”
“Patients with brain disease have subtle personality changes, sometimes more obvious personality changes. These need to be inquired about,” Dr. Ovsiew said. “The patient with apathy has reduced negative as well as positive emotions. The patient with depression has reduced positive emotions, but often tells you very clearly about the negative emotions of sadness, guilt. The patient with depression has diurnal variation in mood, a very telling symptom, especially when it’s disclosed spontaneously,” Dr. Ovsiew explained. “The point is, you need to know to ask about it.”
When taking a sleep history, clinicians should be aware of sleep disturbances apart from insomnia and early waking. REM sleep behavior disorder is a condition that should be inquired about. Obstructive sleep apnea is a condition that might not be immediately apparent to the patient, but a bed partner can identify whether a patient has problems breathing throughout the night.
“This is an important condition to uncover for the neuropsychiatrist because it contributes to treatment resistance and depression, and it contributes to cognitive impairment,” Dr. Ovsiew said. “These patients commonly have mild difficulties with attention and concentration.”
Always ask about head injury in every history, which can be relevant to later onset depression, PTSD, and cognitive impairment. Every head injury follows a trajectory of retrograde amnesia and altered state of consciousness (including coma), followed by a period of posttraumatic amnesia. Duration of these states can be used to assess the severity of brain injury, but the 15-point Glasgow Coma Scale is another way to assess injury severity, Dr. Ovsiew explained.
However, the two do not always overlap, he noted. “Someone may have a Glasgow Coma Scale score that is 9-12, predicting moderate brain injury, but they may have a short duration of amnesia. These don’t always follow the same path. There are many different ways of classifying how severe the brain injury is.”
Keep probes brief, straightforward
Cognitive exams of patients with suspected psychiatric disorders should be simple, easy to administer and focused on a single domain of cognition. “Probes should be brief. They should not require specialized equipment. The Purdue Pegboard Test might be a great neuropsychological instrument, but very few of us carry a pegboard around in our medical bags,” Dr. Ovsiew said.
The probe administered should also be accessible to the patient. The serial sevens clinical test, where a patient is asked to repeatedly subtract 7 from 100, is only effective at testing concentration if the patient is capable of completing the test. “There are going to be patients who can’t do the task, but it’s not because of concentration failure, it’s because of subtraction failure,” he said.
When assessing attention, effective tasks include having the patient perform the digit span test forward and backward, count backward from 20 to 1, listing the months of the year in reverse, and performing the Mental Alternation Test. However, Dr. Ovsiew explained there may be some barriers for patients in completing these tasks. “The person may be aphasic and not know the alphabet. The person may have English as a second language and not be skilled at giving the alphabet in English. In some cases, you may want to check and not assume that the patient can count and does know the alphabet.”
In assessing language, listen for aphasic abnormalities. “The patient, of course, is speaking throughout the interview, but you need to take a moment to listen for prosody, to listen to rate of speech, to listen for paraphasic errors or word-finding problems,” Dr. Ovsiew said. Any abnormalities should be probed further through confrontation naming tasks, which can be done in person and with some success through video, but not by phone. Naming to definition (“What do you call the part of a shirt that covers the arm?”) is one way of administering the test over the phone.
Visuospatial function can be assessed by clock drawing but also carries problems. Patients who do not plan their clock before beginning to draw, for example, may have an executive function problem instead of a visuospatial problem, Dr. Ovsiew noted. Patients in whom a clinician suspects hemineglect should be given a visual search task or line by section task. “I like doing clock drawing. It’s a nice screening test. It’s becoming, I think, less useful as people count on digital clocks and have trouble even imagining what an analog clock looks like.”
An approach that is better suited to in-person assessment, but also works by video, is the Poppelreuter figure visual perceptual function test, which is a prompt for the patient that involves common household items overlaying one another “in atypical positions and atypical configurations” where the patient is instructed to describe the items they see on the card. Another approach that works over video is the interlocking finger test, where the patient is asked to copy the hand positions made by the clinician.
Dr. Ovsiew admitted that visuospatial function is nearly impossible to assess over the phone. Asking topographical questions (“If you’re driving from Chicago to Los Angeles, is the Pacific Ocean in front of you, behind you, to your left, or to your right?”) may help judge visuospatial function, but this relies on the patient having the topographic knowledge to answer the questions. Some patients who are topographically disoriented can’t do them at all,” Dr. Ovsiew said.
Bedside neuropsychiatry assesses encoding of a memory, its retention and its retrieval as well as verbal and visual cues. Each one of these aspects of memory can be impaired on its own and should be explored separately, Dr. Ovsiew explained. “Neuropsychiatric clinicians have a rough-and-ready, seat-of-the-pants way of approaching this that wouldn’t pass muster if you’re a psychologist, but is the best we can do at the bedside.”
To test retrieval and retention, the Three Words–Three Shapes test works well in person, with some difficulty by video, and is not possible to administer over the phone. In lieu of that test, giving the patient a simple word list and asking them to repeat the list in order. Using the word list, “these different stages of memory function can be parsed out pretty well at the bedside or chairside, and even by the phone. Figuring out where the memory failure is diagnostically important,” Dr. Ovsiew said.
Executive function, which involves activation, planning, sequencing, maintaining, self-monitoring, and flexible employment of action and attention, is “complicated to evaluate because there are multiple aspects of executive function, multiple deficits that can be seen with executive dysfunction, and they don’t all correlate with each other.”
Within executive function evaluation, the Mental Alternation Test can assess working memory, motor sequencing can be assessed through the ring/fist, fist/edge/palm, alternating fist, and rampart tests. The Go/No-Go test can be used to assess response inhibition. For effortful retrieval evaluation, spontaneous word-list generation – such as thinking of all the items one can buy at a supermarket– can test category fluency, while a task to name all the words starting with a certain letter can assess letter stimulus.
Executive function “is of crucial importance in the neuropsychiatric evaluation because it’s strongly correlated with how well the person functions outside the office,” Dr. Ovsiew said.
Global Academy and this news organization are owned by the same parent company. Dr. Ovsiew reported relationships with Wolters Kluwer Health in the form of consulting, receiving royalty payments, and related activities.
Patients have often been labeled as “poor historians” if they are not able to recollect their own medical history, whether through illness or difficulties in communication. But Fred Ovsiew, MD, speaking at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sees that label as an excuse on the part of the clinician.
“I strongly advise you to drop that phrase from your vocabulary if you do use it, because the patient is not the historian. The doctor, the clinician is the historian,” Dr. Ovsiew said at the meeting, presented by Global Academy for Medical Education. “It is the clinician’s job to put the story together using the account by the patient as one source, but [also] interviewing a collateral informant and/or reviewing records, which is necessary in almost every case of a neuropsychiatric illness.”
Rather, clinicians taking history at the bedside should focus on why the patients cannot give a narrative account of their illness. Patients can have narrative incapacity on a psychogenic basis, such as in patients with conversion or somatoform disorder, he explained. “I think this is a result of the narrative incapacity that develops in people who have had trauma or adverse experiences in childhood and insecure attachment. This is shown on the adult attachment interview as a disorganized account of their childhoods.”
Other patients might not be able to recount their medical history because they are amnestic, which leaves their account vague because of a lack of access to information. “It may be frozen in time in the sense that, up to a certain point in their life, they can recount the history,” Dr. Ovsiew said. “But in recent years, their account becomes vague.”
Patients with right hemisphere lesions might not know that their account has incongruity and is implausible, while patients with dorsolateral prefrontal lesions might be aspontaneous, use few words to describe their situation, and have poor insight. Those with ventromedial prefrontal lesions can be impulsive and have poor insight, not considering alternative possibilities, Dr. Ovsiew noted.
Asking open-ended questions of the patient is the first step to identifying any potential narrative incapacity, followed by a detailed medical history by the clinician. When taking a medical history, try avoiding what Dr. Ovsiew calls the “anything like that?” problem, where a clinician asks a question about a cluster of symptoms that would make sense to a doctor, but not a patient. For example, a doctor might ask whether a patient is experiencing “chest pain or leg swelling – anything like that?” because he or she knows what those symptoms have in common, but the patient might not know the relationship between those symptoms. “You can’t count on the patient to tell you all the relevant information,” he said. “You have to know what to ask about.”
“Patients with brain disease have subtle personality changes, sometimes more obvious personality changes. These need to be inquired about,” Dr. Ovsiew said. “The patient with apathy has reduced negative as well as positive emotions. The patient with depression has reduced positive emotions, but often tells you very clearly about the negative emotions of sadness, guilt. The patient with depression has diurnal variation in mood, a very telling symptom, especially when it’s disclosed spontaneously,” Dr. Ovsiew explained. “The point is, you need to know to ask about it.”
When taking a sleep history, clinicians should be aware of sleep disturbances apart from insomnia and early waking. REM sleep behavior disorder is a condition that should be inquired about. Obstructive sleep apnea is a condition that might not be immediately apparent to the patient, but a bed partner can identify whether a patient has problems breathing throughout the night.
“This is an important condition to uncover for the neuropsychiatrist because it contributes to treatment resistance and depression, and it contributes to cognitive impairment,” Dr. Ovsiew said. “These patients commonly have mild difficulties with attention and concentration.”
Always ask about head injury in every history, which can be relevant to later onset depression, PTSD, and cognitive impairment. Every head injury follows a trajectory of retrograde amnesia and altered state of consciousness (including coma), followed by a period of posttraumatic amnesia. Duration of these states can be used to assess the severity of brain injury, but the 15-point Glasgow Coma Scale is another way to assess injury severity, Dr. Ovsiew explained.
However, the two do not always overlap, he noted. “Someone may have a Glasgow Coma Scale score that is 9-12, predicting moderate brain injury, but they may have a short duration of amnesia. These don’t always follow the same path. There are many different ways of classifying how severe the brain injury is.”
Keep probes brief, straightforward
Cognitive exams of patients with suspected psychiatric disorders should be simple, easy to administer and focused on a single domain of cognition. “Probes should be brief. They should not require specialized equipment. The Purdue Pegboard Test might be a great neuropsychological instrument, but very few of us carry a pegboard around in our medical bags,” Dr. Ovsiew said.
The probe administered should also be accessible to the patient. The serial sevens clinical test, where a patient is asked to repeatedly subtract 7 from 100, is only effective at testing concentration if the patient is capable of completing the test. “There are going to be patients who can’t do the task, but it’s not because of concentration failure, it’s because of subtraction failure,” he said.
When assessing attention, effective tasks include having the patient perform the digit span test forward and backward, count backward from 20 to 1, listing the months of the year in reverse, and performing the Mental Alternation Test. However, Dr. Ovsiew explained there may be some barriers for patients in completing these tasks. “The person may be aphasic and not know the alphabet. The person may have English as a second language and not be skilled at giving the alphabet in English. In some cases, you may want to check and not assume that the patient can count and does know the alphabet.”
In assessing language, listen for aphasic abnormalities. “The patient, of course, is speaking throughout the interview, but you need to take a moment to listen for prosody, to listen to rate of speech, to listen for paraphasic errors or word-finding problems,” Dr. Ovsiew said. Any abnormalities should be probed further through confrontation naming tasks, which can be done in person and with some success through video, but not by phone. Naming to definition (“What do you call the part of a shirt that covers the arm?”) is one way of administering the test over the phone.
Visuospatial function can be assessed by clock drawing but also carries problems. Patients who do not plan their clock before beginning to draw, for example, may have an executive function problem instead of a visuospatial problem, Dr. Ovsiew noted. Patients in whom a clinician suspects hemineglect should be given a visual search task or line by section task. “I like doing clock drawing. It’s a nice screening test. It’s becoming, I think, less useful as people count on digital clocks and have trouble even imagining what an analog clock looks like.”
An approach that is better suited to in-person assessment, but also works by video, is the Poppelreuter figure visual perceptual function test, which is a prompt for the patient that involves common household items overlaying one another “in atypical positions and atypical configurations” where the patient is instructed to describe the items they see on the card. Another approach that works over video is the interlocking finger test, where the patient is asked to copy the hand positions made by the clinician.
Dr. Ovsiew admitted that visuospatial function is nearly impossible to assess over the phone. Asking topographical questions (“If you’re driving from Chicago to Los Angeles, is the Pacific Ocean in front of you, behind you, to your left, or to your right?”) may help judge visuospatial function, but this relies on the patient having the topographic knowledge to answer the questions. Some patients who are topographically disoriented can’t do them at all,” Dr. Ovsiew said.
Bedside neuropsychiatry assesses encoding of a memory, its retention and its retrieval as well as verbal and visual cues. Each one of these aspects of memory can be impaired on its own and should be explored separately, Dr. Ovsiew explained. “Neuropsychiatric clinicians have a rough-and-ready, seat-of-the-pants way of approaching this that wouldn’t pass muster if you’re a psychologist, but is the best we can do at the bedside.”
To test retrieval and retention, the Three Words–Three Shapes test works well in person, with some difficulty by video, and is not possible to administer over the phone. In lieu of that test, giving the patient a simple word list and asking them to repeat the list in order. Using the word list, “these different stages of memory function can be parsed out pretty well at the bedside or chairside, and even by the phone. Figuring out where the memory failure is diagnostically important,” Dr. Ovsiew said.
Executive function, which involves activation, planning, sequencing, maintaining, self-monitoring, and flexible employment of action and attention, is “complicated to evaluate because there are multiple aspects of executive function, multiple deficits that can be seen with executive dysfunction, and they don’t all correlate with each other.”
Within executive function evaluation, the Mental Alternation Test can assess working memory, motor sequencing can be assessed through the ring/fist, fist/edge/palm, alternating fist, and rampart tests. The Go/No-Go test can be used to assess response inhibition. For effortful retrieval evaluation, spontaneous word-list generation – such as thinking of all the items one can buy at a supermarket– can test category fluency, while a task to name all the words starting with a certain letter can assess letter stimulus.
Executive function “is of crucial importance in the neuropsychiatric evaluation because it’s strongly correlated with how well the person functions outside the office,” Dr. Ovsiew said.
Global Academy and this news organization are owned by the same parent company. Dr. Ovsiew reported relationships with Wolters Kluwer Health in the form of consulting, receiving royalty payments, and related activities.
Patients have often been labeled as “poor historians” if they are not able to recollect their own medical history, whether through illness or difficulties in communication. But Fred Ovsiew, MD, speaking at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sees that label as an excuse on the part of the clinician.
“I strongly advise you to drop that phrase from your vocabulary if you do use it, because the patient is not the historian. The doctor, the clinician is the historian,” Dr. Ovsiew said at the meeting, presented by Global Academy for Medical Education. “It is the clinician’s job to put the story together using the account by the patient as one source, but [also] interviewing a collateral informant and/or reviewing records, which is necessary in almost every case of a neuropsychiatric illness.”
Rather, clinicians taking history at the bedside should focus on why the patients cannot give a narrative account of their illness. Patients can have narrative incapacity on a psychogenic basis, such as in patients with conversion or somatoform disorder, he explained. “I think this is a result of the narrative incapacity that develops in people who have had trauma or adverse experiences in childhood and insecure attachment. This is shown on the adult attachment interview as a disorganized account of their childhoods.”
Other patients might not be able to recount their medical history because they are amnestic, which leaves their account vague because of a lack of access to information. “It may be frozen in time in the sense that, up to a certain point in their life, they can recount the history,” Dr. Ovsiew said. “But in recent years, their account becomes vague.”
Patients with right hemisphere lesions might not know that their account has incongruity and is implausible, while patients with dorsolateral prefrontal lesions might be aspontaneous, use few words to describe their situation, and have poor insight. Those with ventromedial prefrontal lesions can be impulsive and have poor insight, not considering alternative possibilities, Dr. Ovsiew noted.
Asking open-ended questions of the patient is the first step to identifying any potential narrative incapacity, followed by a detailed medical history by the clinician. When taking a medical history, try avoiding what Dr. Ovsiew calls the “anything like that?” problem, where a clinician asks a question about a cluster of symptoms that would make sense to a doctor, but not a patient. For example, a doctor might ask whether a patient is experiencing “chest pain or leg swelling – anything like that?” because he or she knows what those symptoms have in common, but the patient might not know the relationship between those symptoms. “You can’t count on the patient to tell you all the relevant information,” he said. “You have to know what to ask about.”
“Patients with brain disease have subtle personality changes, sometimes more obvious personality changes. These need to be inquired about,” Dr. Ovsiew said. “The patient with apathy has reduced negative as well as positive emotions. The patient with depression has reduced positive emotions, but often tells you very clearly about the negative emotions of sadness, guilt. The patient with depression has diurnal variation in mood, a very telling symptom, especially when it’s disclosed spontaneously,” Dr. Ovsiew explained. “The point is, you need to know to ask about it.”
When taking a sleep history, clinicians should be aware of sleep disturbances apart from insomnia and early waking. REM sleep behavior disorder is a condition that should be inquired about. Obstructive sleep apnea is a condition that might not be immediately apparent to the patient, but a bed partner can identify whether a patient has problems breathing throughout the night.
“This is an important condition to uncover for the neuropsychiatrist because it contributes to treatment resistance and depression, and it contributes to cognitive impairment,” Dr. Ovsiew said. “These patients commonly have mild difficulties with attention and concentration.”
Always ask about head injury in every history, which can be relevant to later onset depression, PTSD, and cognitive impairment. Every head injury follows a trajectory of retrograde amnesia and altered state of consciousness (including coma), followed by a period of posttraumatic amnesia. Duration of these states can be used to assess the severity of brain injury, but the 15-point Glasgow Coma Scale is another way to assess injury severity, Dr. Ovsiew explained.
However, the two do not always overlap, he noted. “Someone may have a Glasgow Coma Scale score that is 9-12, predicting moderate brain injury, but they may have a short duration of amnesia. These don’t always follow the same path. There are many different ways of classifying how severe the brain injury is.”
Keep probes brief, straightforward
Cognitive exams of patients with suspected psychiatric disorders should be simple, easy to administer and focused on a single domain of cognition. “Probes should be brief. They should not require specialized equipment. The Purdue Pegboard Test might be a great neuropsychological instrument, but very few of us carry a pegboard around in our medical bags,” Dr. Ovsiew said.
The probe administered should also be accessible to the patient. The serial sevens clinical test, where a patient is asked to repeatedly subtract 7 from 100, is only effective at testing concentration if the patient is capable of completing the test. “There are going to be patients who can’t do the task, but it’s not because of concentration failure, it’s because of subtraction failure,” he said.
When assessing attention, effective tasks include having the patient perform the digit span test forward and backward, count backward from 20 to 1, listing the months of the year in reverse, and performing the Mental Alternation Test. However, Dr. Ovsiew explained there may be some barriers for patients in completing these tasks. “The person may be aphasic and not know the alphabet. The person may have English as a second language and not be skilled at giving the alphabet in English. In some cases, you may want to check and not assume that the patient can count and does know the alphabet.”
In assessing language, listen for aphasic abnormalities. “The patient, of course, is speaking throughout the interview, but you need to take a moment to listen for prosody, to listen to rate of speech, to listen for paraphasic errors or word-finding problems,” Dr. Ovsiew said. Any abnormalities should be probed further through confrontation naming tasks, which can be done in person and with some success through video, but not by phone. Naming to definition (“What do you call the part of a shirt that covers the arm?”) is one way of administering the test over the phone.
Visuospatial function can be assessed by clock drawing but also carries problems. Patients who do not plan their clock before beginning to draw, for example, may have an executive function problem instead of a visuospatial problem, Dr. Ovsiew noted. Patients in whom a clinician suspects hemineglect should be given a visual search task or line by section task. “I like doing clock drawing. It’s a nice screening test. It’s becoming, I think, less useful as people count on digital clocks and have trouble even imagining what an analog clock looks like.”
An approach that is better suited to in-person assessment, but also works by video, is the Poppelreuter figure visual perceptual function test, which is a prompt for the patient that involves common household items overlaying one another “in atypical positions and atypical configurations” where the patient is instructed to describe the items they see on the card. Another approach that works over video is the interlocking finger test, where the patient is asked to copy the hand positions made by the clinician.
Dr. Ovsiew admitted that visuospatial function is nearly impossible to assess over the phone. Asking topographical questions (“If you’re driving from Chicago to Los Angeles, is the Pacific Ocean in front of you, behind you, to your left, or to your right?”) may help judge visuospatial function, but this relies on the patient having the topographic knowledge to answer the questions. Some patients who are topographically disoriented can’t do them at all,” Dr. Ovsiew said.
Bedside neuropsychiatry assesses encoding of a memory, its retention and its retrieval as well as verbal and visual cues. Each one of these aspects of memory can be impaired on its own and should be explored separately, Dr. Ovsiew explained. “Neuropsychiatric clinicians have a rough-and-ready, seat-of-the-pants way of approaching this that wouldn’t pass muster if you’re a psychologist, but is the best we can do at the bedside.”
To test retrieval and retention, the Three Words–Three Shapes test works well in person, with some difficulty by video, and is not possible to administer over the phone. In lieu of that test, giving the patient a simple word list and asking them to repeat the list in order. Using the word list, “these different stages of memory function can be parsed out pretty well at the bedside or chairside, and even by the phone. Figuring out where the memory failure is diagnostically important,” Dr. Ovsiew said.
Executive function, which involves activation, planning, sequencing, maintaining, self-monitoring, and flexible employment of action and attention, is “complicated to evaluate because there are multiple aspects of executive function, multiple deficits that can be seen with executive dysfunction, and they don’t all correlate with each other.”
Within executive function evaluation, the Mental Alternation Test can assess working memory, motor sequencing can be assessed through the ring/fist, fist/edge/palm, alternating fist, and rampart tests. The Go/No-Go test can be used to assess response inhibition. For effortful retrieval evaluation, spontaneous word-list generation – such as thinking of all the items one can buy at a supermarket– can test category fluency, while a task to name all the words starting with a certain letter can assess letter stimulus.
Executive function “is of crucial importance in the neuropsychiatric evaluation because it’s strongly correlated with how well the person functions outside the office,” Dr. Ovsiew said.
Global Academy and this news organization are owned by the same parent company. Dr. Ovsiew reported relationships with Wolters Kluwer Health in the form of consulting, receiving royalty payments, and related activities.
FROM FOCUS ON NEUROPSYCHIATRY 2020
CDC data confirm mental health is suffering during COVID-19
The ongoing COVID-19 pandemic continues to exact a huge toll on mental health in the United States, according to results of a survey released Aug. 13 by the Centers for Disease Control and Prevention.
During late June, about two in five U.S. adults surveyed said they were struggling with mental health or substance use. Younger adults, racial/ethnic minorities, essential workers, and those with preexisting psychiatric conditions were suffering the most.
“Addressing mental health disparities and preparing support systems to mitigate mental health consequences as the pandemic evolves will continue to be needed urgently,” write Rashon Lane, with the CDC COVID-19 Response Team, and colleagues in an article published online in the CDC’s Morbidity and Mortality Weekly Report.
During the period of June 24-30, 2020, 5,412 U.S. adults aged 18 and older completed online surveys that gauged mental health, substance use, and suicidal ideation.
Overall, 40.9% of respondents reported having at least one adverse mental or behavioral health condition; 31% reported symptoms of anxiety or depressive disorder; and 26% reported symptoms of a trauma- and stressor-related disorder related to the pandemic.
The prevalence of symptoms of anxiety disorder alone was roughly three times that reported in the second quarter of 2019, the authors noted.
In addition, , and nearly 11% reported having seriously considered suicide in the preceding 30 days.
Approximately twice as many respondents reported seriously considering suicide in the prior month compared with adults in the United States in 2018 (referring to the previous 12 months), the authors noted.
Suicidal ideation was significantly higher among younger respondents (aged 18-24 years, 26%), Hispanic persons (19%), non-Hispanic Black persons (15%), unpaid caregivers for adults (31%), and essential workers (22%).
The survey results are in line with recent data from Mental Health America, which indicate dramatic increases in depression, anxiety, and suicidality since the start of the COVID-19 pandemic.
The “markedly elevated” prevalence of adverse mental and behavioral health conditions associated with the COVID-19 pandemic highlights the “broad impact of the pandemic and the need to prevent and treat these conditions,” the researchers wrote.
The survey also highlights populations at increased risk for psychological distress and unhealthy coping.
“Future studies should identify drivers of adverse mental and behavioral health during the COVID-19 pandemic and whether factors such as social isolation, absence of school structure, unemployment and other financial worries, and various forms of violence (e.g., physical, emotional, mental, or sexual abuse) serve as additional stressors,” they suggested.
A version of this article originally appeared on Medscape.com.
The ongoing COVID-19 pandemic continues to exact a huge toll on mental health in the United States, according to results of a survey released Aug. 13 by the Centers for Disease Control and Prevention.
During late June, about two in five U.S. adults surveyed said they were struggling with mental health or substance use. Younger adults, racial/ethnic minorities, essential workers, and those with preexisting psychiatric conditions were suffering the most.
“Addressing mental health disparities and preparing support systems to mitigate mental health consequences as the pandemic evolves will continue to be needed urgently,” write Rashon Lane, with the CDC COVID-19 Response Team, and colleagues in an article published online in the CDC’s Morbidity and Mortality Weekly Report.
During the period of June 24-30, 2020, 5,412 U.S. adults aged 18 and older completed online surveys that gauged mental health, substance use, and suicidal ideation.
Overall, 40.9% of respondents reported having at least one adverse mental or behavioral health condition; 31% reported symptoms of anxiety or depressive disorder; and 26% reported symptoms of a trauma- and stressor-related disorder related to the pandemic.
The prevalence of symptoms of anxiety disorder alone was roughly three times that reported in the second quarter of 2019, the authors noted.
In addition, , and nearly 11% reported having seriously considered suicide in the preceding 30 days.
Approximately twice as many respondents reported seriously considering suicide in the prior month compared with adults in the United States in 2018 (referring to the previous 12 months), the authors noted.
Suicidal ideation was significantly higher among younger respondents (aged 18-24 years, 26%), Hispanic persons (19%), non-Hispanic Black persons (15%), unpaid caregivers for adults (31%), and essential workers (22%).
The survey results are in line with recent data from Mental Health America, which indicate dramatic increases in depression, anxiety, and suicidality since the start of the COVID-19 pandemic.
The “markedly elevated” prevalence of adverse mental and behavioral health conditions associated with the COVID-19 pandemic highlights the “broad impact of the pandemic and the need to prevent and treat these conditions,” the researchers wrote.
The survey also highlights populations at increased risk for psychological distress and unhealthy coping.
“Future studies should identify drivers of adverse mental and behavioral health during the COVID-19 pandemic and whether factors such as social isolation, absence of school structure, unemployment and other financial worries, and various forms of violence (e.g., physical, emotional, mental, or sexual abuse) serve as additional stressors,” they suggested.
A version of this article originally appeared on Medscape.com.
The ongoing COVID-19 pandemic continues to exact a huge toll on mental health in the United States, according to results of a survey released Aug. 13 by the Centers for Disease Control and Prevention.
During late June, about two in five U.S. adults surveyed said they were struggling with mental health or substance use. Younger adults, racial/ethnic minorities, essential workers, and those with preexisting psychiatric conditions were suffering the most.
“Addressing mental health disparities and preparing support systems to mitigate mental health consequences as the pandemic evolves will continue to be needed urgently,” write Rashon Lane, with the CDC COVID-19 Response Team, and colleagues in an article published online in the CDC’s Morbidity and Mortality Weekly Report.
During the period of June 24-30, 2020, 5,412 U.S. adults aged 18 and older completed online surveys that gauged mental health, substance use, and suicidal ideation.
Overall, 40.9% of respondents reported having at least one adverse mental or behavioral health condition; 31% reported symptoms of anxiety or depressive disorder; and 26% reported symptoms of a trauma- and stressor-related disorder related to the pandemic.
The prevalence of symptoms of anxiety disorder alone was roughly three times that reported in the second quarter of 2019, the authors noted.
In addition, , and nearly 11% reported having seriously considered suicide in the preceding 30 days.
Approximately twice as many respondents reported seriously considering suicide in the prior month compared with adults in the United States in 2018 (referring to the previous 12 months), the authors noted.
Suicidal ideation was significantly higher among younger respondents (aged 18-24 years, 26%), Hispanic persons (19%), non-Hispanic Black persons (15%), unpaid caregivers for adults (31%), and essential workers (22%).
The survey results are in line with recent data from Mental Health America, which indicate dramatic increases in depression, anxiety, and suicidality since the start of the COVID-19 pandemic.
The “markedly elevated” prevalence of adverse mental and behavioral health conditions associated with the COVID-19 pandemic highlights the “broad impact of the pandemic and the need to prevent and treat these conditions,” the researchers wrote.
The survey also highlights populations at increased risk for psychological distress and unhealthy coping.
“Future studies should identify drivers of adverse mental and behavioral health during the COVID-19 pandemic and whether factors such as social isolation, absence of school structure, unemployment and other financial worries, and various forms of violence (e.g., physical, emotional, mental, or sexual abuse) serve as additional stressors,” they suggested.
A version of this article originally appeared on Medscape.com.
Meditations in an emergency: Talking through pandemic anxiety with a pioneer of mind-body medicine
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
George Floyd, race, and psychiatry: How to talk to patients
Editor’s Note: This transcript from the June 5 special episode of the Psychcast has been edited for clarity.
Nick Andrews: This is the Psychcast, the official podcast of MDedge Psychiatry. I am the voice of the MDedge podcasts, Nick Andrews. We are bringing this special edition of the Psychcast from MDedge in response to all of the unrest, peaceful or otherwise, in the United States in the aftermath of the shocking murder of George Floyd in late May of 2020.
Dr. Lorenzo Norris agreed to have this “after hours” discussion, believing the most appropriate response would be for us to have a real conversation about it. So welcome aboard.
Lorenzo Norris, MD: I’m happy to be here, Nick, and I’m so pleased to be talking with our guest, Dr. Brandon Newsome, a young black male psychiatrist. Dr. Newsome, sir, tell us a little about yourself and where you’re coming from.
Brandon Newsome, MD: I’m a 4th-year psychiatry resident at Boston Medical Center, so I’m about to graduate and to become a first-year fellow, as of July, at Children’s National Medical Center in Washington, D.C. I was born and raised in the South so I can talk about those experiences, and now I’ve been in the Northeast for the past 4 years.
Dr. Norris: Let’s get right into it. This is a time in our country that we’ve not seen – I shouldn’t say we, because depending on where you live in America, you have seen this and you’ve seen this multiple times.
I see a lot of myself in Dr. Newsome right now, and I am struggling with this: I’m talking to you about the same stuff I was talking about when I was a 4th-year resident. I’m talking to you about the same stuff I was talking about when I was a college student. I’m still talking about the same stuff I was talking about when I was a medical student. I’m still talking about the same things that were the impetus for the hip-hop generation regarding police brutality and violence.
We are still talking about the use of lethal force and abuse of power, particularly by police or law enforcement officers, and how that is perpetrated against African American men in particular, and the unfortunate and tragic murder of Mr. George Floyd. Dr. Newsome, tell me how you’re thinking about this. Before we even get into how our patients or our colleagues are doing, how are you doing with this?
Dr. Newsome: It’s been difficult. Like you, I’ve heard this story time and time again. I was just on a panel, having a conversation about race and policing, and I realized we had the same conversation during my first or second year of residency because there had been another death. But even though all of these unfortunate deaths are triggering us, this one is a little different for me for a few reasons. As you know, this is happening with the backdrop of the COVID-19 crisis and we’re already seeing so many people, especially from black and brown communities, dying from that.
And then I’m witnessing what happened, watching that video and thinking about all the interventions we’ve already tried. We tried body cameras, and the dude was wearing a body camera. We tried to get our police officers to be engaged, to try to check their roles, but people were there, witnessing everything, and nothing happened. An upstander was there, a white upstander, a firefighter who was telling them to check his pulse. Still nothing happened; it didn’t stop them.
I believe the backdrop of the COVID-19 crisis makes it a whole lot more painful for me and many others. I am part of a black physician email group and it’s been triggering for all of us because we all imagine that this could be me one day, especially when you think about the Amy Coopers of the world, among other things.
Dr. Norris: I completely agree. We’re dealing with loss of life due to a virus, including, [personally speaking] that of my departed grandmother Why am I bringing this up? I bring it up because, regardless of one’s socioeconomic strata or title or whatnot, particularly in the black community, this is the kind of mess we’re dealing with. We’re dealing with the stress of COVID-19 that is disproportionately affecting African Americans. We’re dealing with social isolation, we’re dealing with the economic recession and the collapse that everyone else is dealing with, and on top of that we are now dealing with another murder. But this particular murder resonates very differently because, as you said, it seemed like every single thing that could have been done was done.
You will read reports that Mr. Floyd was resisting arrest. But you look at this video; this is not a man resisting arrest. This is a man trying to say, please, you are killing me. These are other people saying the same thing. These are police officers not acting right. This is so many different things going on, and when you hear this and look at this video, you can come to no other conclusion than it is murder.
As psychiatrists, we frequently have to restrain people, and it is always understood that restraint can turn into assault extremely quickly. But in this particular case, there was no thought or concern about this man’s life or his health. There are many good police officers that do think of that, and so this was shocking. It was jarring. It was another thing piled on an already taxed black America. I was talking with my black male colleagues about this, and I think a lot of people don’t actually realize that, while there are black male psychiatrists, there are only a few of us.
Dr. Newsome: True that.
Dr. Norris: There are only so many black male physicians, period, and black male psychiatrists in particular. At different points in time we are called on to take leadership roles, and to talk, to speak on things and be a voice. Well, I have to tell you, after a while, this is pretty goddamn tiring for us to contain our disappointment, our anger, and our rage and still stay hopeful, optimistic, and still be a voice for those who are not able to speak.
Dr. Newsome: I agree that sometimes it can be tiring to have to take leadership roles and continue to talk about all these things, but I also feel that, at least for me, it gives me some sort of route to address the angst and do something with it. I believe all of us are just figuring out how to deal with these feelings that we shouldn’t have to feel because of a murder that was televised.
Dr. Norris: Thank you. For a murder that was televised; that was tweeted; that was broadbanded; that was streamed.
Now we’ve laid the framework, in terms of what we’re feeling. Let’s move on to why you and I are in this profession, and that’s our patients. What are you seeing on the front lines? What are you seeing with our patients?
Dr. Newsome: I was speaking with one of my black male patients, and he was fearful. He had been perfectly fine, even in the COVID crisis, he was doing well. But when you get this milieu of police violence, now he’s feeling this intense fear. Should I be walking alone at night? What happens if I am the one who is at the wrong place at the wrong time?
I also find that some of my nonminority patients sometimes find difficulty making sense of it. Minority individuals already know these things are happening. But some of the nonminorities are wondering how or why would something like this happen in America? This is just how America is for the black folks.
Dr. Norris: Could you elaborate on that? I always found that to be a very interesting dynamic for those who are not minorities or people of color. I will have folks in a psychotherapy session who are just bewildered by events like this. It is not the America they think they know – they are shocked that this is actually what’s going on.
Dr. Newsome: It’s all about experiences. If you didn’t grow up around a lot of minorities, you haven’t necessarily had these conversations. Even speaking for myself, sometimes I don’t want to discuss these things; you never know what you’re going to get. You might find an ally, or you might find someone who isn’t at all supportive. I think the surprise is from lack of exposure. If you don’t have to live through racism, you can most certainly have blinders on and not notice.
Dr. Norris: Can you comment on the fear you’re seeing in some folks? Can it get to the point of reactivating PTSD?
Dr. Newsome: I notice it more with black individuals, a fear that they might be the ones who may die; or with black mothers, wondering, what about my child? Is this what they are going to have to live with for the rest of their lives? Older people would say that we fought already and it’s still going on. What are the fruits of the labor we put in?
Dr. Norris: I agree with you completely. What are the fruits? You’re going to see those strong reactions. You’re going to see fear, you’re going to see anger, and you’re also going to see guilt that they could not stop this. I’m speaking particularly about some of my nonminority patients. It goes along with that confusion. This manifests in a desperate need to do something.
But here’s the problem: You don’t really know what to do because no one is educated on it. And as you said before, race is a very polarized subject. No one even likes to talk about racism because it’s so, oh my goodness. We’ve run away from it so much to the point that we can’t deal with it. We all have to start to own that. You can’t just stay siloed, because eventually, it’s going to come back and affect you.
I could easily be Mr. Floyd, but at the same time, due to my station and things of that nature, I have a certain level of privilege and autonomy. There could be a tendency to put your head under the sand, you know, look at how far we’ve come, Barack Obama. But you’ve got to say, no, we still have enormous amounts of work to do.
We’ve been talking about the patients. What have you noticed in your colleagues and how they’ve been feeling about this?
Dr. Newsome: Again, I see them feeling saddened by the events. One of the other things I’ve noticed is that some people are in environments where they have program directors and chairs who will directly condemn certain behaviors and say, “This is racist, this shouldn’t happen.” But then there are other programs that have been more silent. I’ve had people say that this is the first time that they have felt isolated in a long while.
We all participate in these physician WhatsApp groups, and according to some of the comments, people are realizing that these folks that they were just on the front lines with, fighting COVID, are perhaps not the allies that they originally thought they were, based on the things these people are saying.
Dr. Norris: Wow. It’s good that we’re talking about this from the viewpoint of two different generations. You’ve got the WhatsApp group and Google Hangouts and all that kind of good stuff, and I’m still with pagers and such. That’s interesting – the reality that folks you thought were your allies turn out not to be, because you’re bringing up difficult conversations that we don’t normally talk about.
I have noticed that some people around me have been silent because they don’t know what to say. They’re so concerned that I’m going to be offended or they’re going to hurt me or say the wrong thing, so they stay quiet. As I reflect now, this is the wrong thing to do. Own your concern. I’ve been in two large meetings now, and I’ve had multiple people whom I consider friends say, I wanted to email or text you right then and ask you how you’re doing, but I didn’t because I didn’t know what to say. I have entered meetings recently, and the meeting felt tense, and I’m thinking, what’s going on? And now I realize they did not know what to say or how to approach it.
That’s been a very interesting dynamic and tells us where we are with this. Today, for example, I was pleased to have the support of my dean’s group. I felt I had to speak out, I just had to straight out tell them. Do you want to know what I’m feeling? I’m feeling rage. I’m feeling rage. And you all have to understand that, because I have to speak for those who aren’t necessarily going to be able to express themselves. More importantly, I have to speak for myself and I’m feeling rage.
How our colleagues are processing this and how they’re thinking about this runs the gamut. But I think about people not necessarily knowing what to say or how to approach it. I absolutely agree that with the leadership, you’re going to get many different responses, and sometimes you’re left to wonder, do I have to watch what I say? But I’m definitely supported at my institution.
What else are you seeing out there in terms of your colleagues or how people think about it?
Dr. Newsome: This also spurs some folks to activism. Some have been participating in protests. There will be White Coats for Black Lives protests, among other things. So it’s spurred folks to action, and it’s also spurred folks to try to be part of a community. Of course, with the whole COVID crisis, we can’t necessarily come together, so we’ve been doing Zoom gatherings more than anything else. But it has encouraged folks to want to do that more, too, because they want to check in on their brother or their sister to make sure they are doing well, and also to be able to express what’s going on with them in a community where they know they can get validation.

Dr. Norris: I’m going to push you a bit because I detect in your tone something similar to what I’m feeling. I just got the email, the White Coats For Black Lives email. But I think your feeling is similar to mine – I’ve done this before. I’ve done White Coats for Black Lives. You all may have protested. But this display in Washington, D.C., of the use of military and law enforcement to clear a public square of peaceful protesters is above and beyond the pale of anything I’ve ever seen in my life. We have to label that for the danger it is, for the threat to everything this country and the people that bled for this country stand for.
So while I’m going to participate in White Coats for Black Lives and many other things, I am looking for what is actually going to move the needle. I think the protests are great, but at this point in time I want institutions, I want money, I want lawyers, I want a systematic approach.
Dr. Newsome: I most certainly agree. Of course, the protests are really important, but depending on where you are, you have a different lens. As physicians, especially as black physicians, since there are so few of us, we have a unique opportunity to leverage that, whether that means communicating through op-eds or calling your senators and talking with them to try to move things forward.
Physicians are mobilizing. In the last few days, a physician created a Zoom event and hundreds of physicians joined to try to figure out how we can structurally fix this problem. So I most certainly believe that in this effort to address racism, we physicians will need to lend our voices and our privilege to move the needle as best we can.
Dr. Norris: Some of our colleagues in Black Psychiatrists of America have put out a press release on racism in which they propose some actions that should be taken immediately. I think this is a useful thing to talk about.
The first action: “Declare racism a public health problem and establish national goals for addressing this as a health equity issue. Give priority to addressing the issues of health care disparities, including the mental health needs of historically marginalized communities across the U.S.”
What do you think about that?
Dr. Newsome: Those are two extremely important steps. The question is: How do you make that happen?
Dr. Norris: You’re reading my mind. I love that our colleagues put that out there, but that was my next question.
Dr. Newsome: There is going to be a town hall about this and I’m hoping that we can plan how we envision this happening. I can imagine that 20 or 30 years ago there was also a fear in society that there would be episodes of police brutality. I can imagine that there were similar ideals and hopes. But I think we need to put all of our minds together and ask: How are we going to accomplish this? Is this going to be something we’re going to put our money into? Is this going to be something we’re going to get senators and legislatures onboard with to make policy?
Dr. Norris: Let me read off some of the other action points they put out. There are six of them.
“Establish a governmental multidisciplinary and ethnically diverse commission with representatives from the major health care professional associations in medicine, nursing, psychiatry, public health, psychology, social work, etc., and the faith-based community to provide recommendations to Congress regarding policies on how to best improve the health and well-being of our nation’s black citizens.”
That’s a very solid overall recommendation. My question is, doesn’t that, in some way, shape, or form already exist? Could we not put up policy statements from all of these folks regarding racism and things of that nature? I agree with what they’re saying, but part of me wonders why certain things in the current system aren’t working. That becomes the question. Are we not integrated enough? Do we not have enough cross talk? Do we not have enough money behind it? So I agree with that goal, but I would be curious if that doesn’t already exist. What are your thoughts about that, Dr. Newsome?
Dr. Newsome: I would imagine that the National Institute on Minority Mental Health and Health Disparities would have something similar. I believe one of the things you mentioned is really important. In addition to making these recommendations, we need to be looking at where these leaks are occurring that keep them from working. What is the current structure and why is it the way it is with regard to the governance?
Dr. Norris: Here is another of their action statements: “Declare ‘civic mental health’ a national priority and incorporate it into the educational curriculum from K through college, as well as in the training of local, state, and national officials, law enforcement, and the criminal justice system.”
Let me be clear, I like every single one of these action statements. I encourage everyone to participate in dialogue and discussion. You may agree with some of these, and some of them you may not, but if there is one you agree with, that you really are motivated about, that’s one that you need to explore and dig into a bit more, because it’s too big for us to handle on our own, just like racism and equality.
I’m going to tell you, I like this statement. I do like this. Obviously these are broad points, but I do like the idea of training law enforcement officers about “civic mental health.” For example, Dr. Michael Compton, who has done a lot of great work in the area of mental health and prevention, has worked with police officers to help them interact with those with mental health conditions by modulating their own emotional response. I’m very interested in these types of recommendations that particularly target law enforcement officers, and helping with that ”emotional quotient.” I’m interested in seeing how far that can spread in the country. What do you think, Dr. Newsome?
Dr. Newsome: Educating police officers about how to interact would be quite important. I believe the National Alliance on Mental Illness does some of that work, partnering with law enforcement agencies, talking about mental health and cues to look at. There also are some programs where people ride along with mental health clinicians and police officers, which I find to be really helpful. But clearly, what’s going on right now isn’t working. So I would be open to any reasonable idea.
Dr. Norris: Here’s one last action point: “Establish police community review boards with power to take action in areas of police misconduct pending formal review by the appropriate authorities. This will offer a level of empowerment when communities feel they have a voice that can be heard.”
This is where I want my focus to be, as I move forward to try to do something sustainable. To deal with police brutality and abuse of power in general, but specifically as it relates to African American men and the lethal use of force. We need to work on policies that will enable African American men to make it to court, so that every encounter with a police officer is not literally viewed as a potentially lethal encounter.
A lot of people aren’t going to like me saying that, but it’s the absolute truth. You have to think like that, as an African American male, regardless of your station, regardless of where you live, this is the reality. There are many, many good police officers out there. I have a few friends who are law enforcement officers. I work with security at the George Washington Hospital constantly. But that still does not change the fact that if I get pulled over at a traffic stop, I know precisely certain things I need to do and not do, or the encounter could end badly. By that I mean loss of life.
So I encourage anything where we can start to take a systematic look at law enforcement and empower communities to look at who is doing it right and who is doing it wrong. Information is coming out now about the man who murdered Mr. Floyd, and this was not the first time he was involved in misconduct. There were red flags; we have to start to confront this. We have to learn from every single one of these situations and grow because another one is going to happen next week, it’s just whether or not you hear about it. That’s the reality of the state of America. You may not like to hear it, but that’s just a fact.
To hear the entire conversation, go to mdedge.com/podcasts or listen wherever you find your podcasts.
Editor’s Note: This transcript from the June 5 special episode of the Psychcast has been edited for clarity.
Nick Andrews: This is the Psychcast, the official podcast of MDedge Psychiatry. I am the voice of the MDedge podcasts, Nick Andrews. We are bringing this special edition of the Psychcast from MDedge in response to all of the unrest, peaceful or otherwise, in the United States in the aftermath of the shocking murder of George Floyd in late May of 2020.
Dr. Lorenzo Norris agreed to have this “after hours” discussion, believing the most appropriate response would be for us to have a real conversation about it. So welcome aboard.
Lorenzo Norris, MD: I’m happy to be here, Nick, and I’m so pleased to be talking with our guest, Dr. Brandon Newsome, a young black male psychiatrist. Dr. Newsome, sir, tell us a little about yourself and where you’re coming from.
Brandon Newsome, MD: I’m a 4th-year psychiatry resident at Boston Medical Center, so I’m about to graduate and to become a first-year fellow, as of July, at Children’s National Medical Center in Washington, D.C. I was born and raised in the South so I can talk about those experiences, and now I’ve been in the Northeast for the past 4 years.
Dr. Norris: Let’s get right into it. This is a time in our country that we’ve not seen – I shouldn’t say we, because depending on where you live in America, you have seen this and you’ve seen this multiple times.
I see a lot of myself in Dr. Newsome right now, and I am struggling with this: I’m talking to you about the same stuff I was talking about when I was a 4th-year resident. I’m talking to you about the same stuff I was talking about when I was a college student. I’m still talking about the same stuff I was talking about when I was a medical student. I’m still talking about the same things that were the impetus for the hip-hop generation regarding police brutality and violence.
We are still talking about the use of lethal force and abuse of power, particularly by police or law enforcement officers, and how that is perpetrated against African American men in particular, and the unfortunate and tragic murder of Mr. George Floyd. Dr. Newsome, tell me how you’re thinking about this. Before we even get into how our patients or our colleagues are doing, how are you doing with this?
Dr. Newsome: It’s been difficult. Like you, I’ve heard this story time and time again. I was just on a panel, having a conversation about race and policing, and I realized we had the same conversation during my first or second year of residency because there had been another death. But even though all of these unfortunate deaths are triggering us, this one is a little different for me for a few reasons. As you know, this is happening with the backdrop of the COVID-19 crisis and we’re already seeing so many people, especially from black and brown communities, dying from that.
And then I’m witnessing what happened, watching that video and thinking about all the interventions we’ve already tried. We tried body cameras, and the dude was wearing a body camera. We tried to get our police officers to be engaged, to try to check their roles, but people were there, witnessing everything, and nothing happened. An upstander was there, a white upstander, a firefighter who was telling them to check his pulse. Still nothing happened; it didn’t stop them.
I believe the backdrop of the COVID-19 crisis makes it a whole lot more painful for me and many others. I am part of a black physician email group and it’s been triggering for all of us because we all imagine that this could be me one day, especially when you think about the Amy Coopers of the world, among other things.
Dr. Norris: I completely agree. We’re dealing with loss of life due to a virus, including, [personally speaking] that of my departed grandmother Why am I bringing this up? I bring it up because, regardless of one’s socioeconomic strata or title or whatnot, particularly in the black community, this is the kind of mess we’re dealing with. We’re dealing with the stress of COVID-19 that is disproportionately affecting African Americans. We’re dealing with social isolation, we’re dealing with the economic recession and the collapse that everyone else is dealing with, and on top of that we are now dealing with another murder. But this particular murder resonates very differently because, as you said, it seemed like every single thing that could have been done was done.
You will read reports that Mr. Floyd was resisting arrest. But you look at this video; this is not a man resisting arrest. This is a man trying to say, please, you are killing me. These are other people saying the same thing. These are police officers not acting right. This is so many different things going on, and when you hear this and look at this video, you can come to no other conclusion than it is murder.
As psychiatrists, we frequently have to restrain people, and it is always understood that restraint can turn into assault extremely quickly. But in this particular case, there was no thought or concern about this man’s life or his health. There are many good police officers that do think of that, and so this was shocking. It was jarring. It was another thing piled on an already taxed black America. I was talking with my black male colleagues about this, and I think a lot of people don’t actually realize that, while there are black male psychiatrists, there are only a few of us.
Dr. Newsome: True that.
Dr. Norris: There are only so many black male physicians, period, and black male psychiatrists in particular. At different points in time we are called on to take leadership roles, and to talk, to speak on things and be a voice. Well, I have to tell you, after a while, this is pretty goddamn tiring for us to contain our disappointment, our anger, and our rage and still stay hopeful, optimistic, and still be a voice for those who are not able to speak.
Dr. Newsome: I agree that sometimes it can be tiring to have to take leadership roles and continue to talk about all these things, but I also feel that, at least for me, it gives me some sort of route to address the angst and do something with it. I believe all of us are just figuring out how to deal with these feelings that we shouldn’t have to feel because of a murder that was televised.
Dr. Norris: Thank you. For a murder that was televised; that was tweeted; that was broadbanded; that was streamed.
Now we’ve laid the framework, in terms of what we’re feeling. Let’s move on to why you and I are in this profession, and that’s our patients. What are you seeing on the front lines? What are you seeing with our patients?
Dr. Newsome: I was speaking with one of my black male patients, and he was fearful. He had been perfectly fine, even in the COVID crisis, he was doing well. But when you get this milieu of police violence, now he’s feeling this intense fear. Should I be walking alone at night? What happens if I am the one who is at the wrong place at the wrong time?
I also find that some of my nonminority patients sometimes find difficulty making sense of it. Minority individuals already know these things are happening. But some of the nonminorities are wondering how or why would something like this happen in America? This is just how America is for the black folks.
Dr. Norris: Could you elaborate on that? I always found that to be a very interesting dynamic for those who are not minorities or people of color. I will have folks in a psychotherapy session who are just bewildered by events like this. It is not the America they think they know – they are shocked that this is actually what’s going on.
Dr. Newsome: It’s all about experiences. If you didn’t grow up around a lot of minorities, you haven’t necessarily had these conversations. Even speaking for myself, sometimes I don’t want to discuss these things; you never know what you’re going to get. You might find an ally, or you might find someone who isn’t at all supportive. I think the surprise is from lack of exposure. If you don’t have to live through racism, you can most certainly have blinders on and not notice.
Dr. Norris: Can you comment on the fear you’re seeing in some folks? Can it get to the point of reactivating PTSD?
Dr. Newsome: I notice it more with black individuals, a fear that they might be the ones who may die; or with black mothers, wondering, what about my child? Is this what they are going to have to live with for the rest of their lives? Older people would say that we fought already and it’s still going on. What are the fruits of the labor we put in?
Dr. Norris: I agree with you completely. What are the fruits? You’re going to see those strong reactions. You’re going to see fear, you’re going to see anger, and you’re also going to see guilt that they could not stop this. I’m speaking particularly about some of my nonminority patients. It goes along with that confusion. This manifests in a desperate need to do something.
But here’s the problem: You don’t really know what to do because no one is educated on it. And as you said before, race is a very polarized subject. No one even likes to talk about racism because it’s so, oh my goodness. We’ve run away from it so much to the point that we can’t deal with it. We all have to start to own that. You can’t just stay siloed, because eventually, it’s going to come back and affect you.
I could easily be Mr. Floyd, but at the same time, due to my station and things of that nature, I have a certain level of privilege and autonomy. There could be a tendency to put your head under the sand, you know, look at how far we’ve come, Barack Obama. But you’ve got to say, no, we still have enormous amounts of work to do.
We’ve been talking about the patients. What have you noticed in your colleagues and how they’ve been feeling about this?
Dr. Newsome: Again, I see them feeling saddened by the events. One of the other things I’ve noticed is that some people are in environments where they have program directors and chairs who will directly condemn certain behaviors and say, “This is racist, this shouldn’t happen.” But then there are other programs that have been more silent. I’ve had people say that this is the first time that they have felt isolated in a long while.
We all participate in these physician WhatsApp groups, and according to some of the comments, people are realizing that these folks that they were just on the front lines with, fighting COVID, are perhaps not the allies that they originally thought they were, based on the things these people are saying.
Dr. Norris: Wow. It’s good that we’re talking about this from the viewpoint of two different generations. You’ve got the WhatsApp group and Google Hangouts and all that kind of good stuff, and I’m still with pagers and such. That’s interesting – the reality that folks you thought were your allies turn out not to be, because you’re bringing up difficult conversations that we don’t normally talk about.
I have noticed that some people around me have been silent because they don’t know what to say. They’re so concerned that I’m going to be offended or they’re going to hurt me or say the wrong thing, so they stay quiet. As I reflect now, this is the wrong thing to do. Own your concern. I’ve been in two large meetings now, and I’ve had multiple people whom I consider friends say, I wanted to email or text you right then and ask you how you’re doing, but I didn’t because I didn’t know what to say. I have entered meetings recently, and the meeting felt tense, and I’m thinking, what’s going on? And now I realize they did not know what to say or how to approach it.
That’s been a very interesting dynamic and tells us where we are with this. Today, for example, I was pleased to have the support of my dean’s group. I felt I had to speak out, I just had to straight out tell them. Do you want to know what I’m feeling? I’m feeling rage. I’m feeling rage. And you all have to understand that, because I have to speak for those who aren’t necessarily going to be able to express themselves. More importantly, I have to speak for myself and I’m feeling rage.
How our colleagues are processing this and how they’re thinking about this runs the gamut. But I think about people not necessarily knowing what to say or how to approach it. I absolutely agree that with the leadership, you’re going to get many different responses, and sometimes you’re left to wonder, do I have to watch what I say? But I’m definitely supported at my institution.
What else are you seeing out there in terms of your colleagues or how people think about it?
Dr. Newsome: This also spurs some folks to activism. Some have been participating in protests. There will be White Coats for Black Lives protests, among other things. So it’s spurred folks to action, and it’s also spurred folks to try to be part of a community. Of course, with the whole COVID crisis, we can’t necessarily come together, so we’ve been doing Zoom gatherings more than anything else. But it has encouraged folks to want to do that more, too, because they want to check in on their brother or their sister to make sure they are doing well, and also to be able to express what’s going on with them in a community where they know they can get validation.

Dr. Norris: I’m going to push you a bit because I detect in your tone something similar to what I’m feeling. I just got the email, the White Coats For Black Lives email. But I think your feeling is similar to mine – I’ve done this before. I’ve done White Coats for Black Lives. You all may have protested. But this display in Washington, D.C., of the use of military and law enforcement to clear a public square of peaceful protesters is above and beyond the pale of anything I’ve ever seen in my life. We have to label that for the danger it is, for the threat to everything this country and the people that bled for this country stand for.
So while I’m going to participate in White Coats for Black Lives and many other things, I am looking for what is actually going to move the needle. I think the protests are great, but at this point in time I want institutions, I want money, I want lawyers, I want a systematic approach.
Dr. Newsome: I most certainly agree. Of course, the protests are really important, but depending on where you are, you have a different lens. As physicians, especially as black physicians, since there are so few of us, we have a unique opportunity to leverage that, whether that means communicating through op-eds or calling your senators and talking with them to try to move things forward.
Physicians are mobilizing. In the last few days, a physician created a Zoom event and hundreds of physicians joined to try to figure out how we can structurally fix this problem. So I most certainly believe that in this effort to address racism, we physicians will need to lend our voices and our privilege to move the needle as best we can.
Dr. Norris: Some of our colleagues in Black Psychiatrists of America have put out a press release on racism in which they propose some actions that should be taken immediately. I think this is a useful thing to talk about.
The first action: “Declare racism a public health problem and establish national goals for addressing this as a health equity issue. Give priority to addressing the issues of health care disparities, including the mental health needs of historically marginalized communities across the U.S.”
What do you think about that?
Dr. Newsome: Those are two extremely important steps. The question is: How do you make that happen?
Dr. Norris: You’re reading my mind. I love that our colleagues put that out there, but that was my next question.
Dr. Newsome: There is going to be a town hall about this and I’m hoping that we can plan how we envision this happening. I can imagine that 20 or 30 years ago there was also a fear in society that there would be episodes of police brutality. I can imagine that there were similar ideals and hopes. But I think we need to put all of our minds together and ask: How are we going to accomplish this? Is this going to be something we’re going to put our money into? Is this going to be something we’re going to get senators and legislatures onboard with to make policy?
Dr. Norris: Let me read off some of the other action points they put out. There are six of them.
“Establish a governmental multidisciplinary and ethnically diverse commission with representatives from the major health care professional associations in medicine, nursing, psychiatry, public health, psychology, social work, etc., and the faith-based community to provide recommendations to Congress regarding policies on how to best improve the health and well-being of our nation’s black citizens.”
That’s a very solid overall recommendation. My question is, doesn’t that, in some way, shape, or form already exist? Could we not put up policy statements from all of these folks regarding racism and things of that nature? I agree with what they’re saying, but part of me wonders why certain things in the current system aren’t working. That becomes the question. Are we not integrated enough? Do we not have enough cross talk? Do we not have enough money behind it? So I agree with that goal, but I would be curious if that doesn’t already exist. What are your thoughts about that, Dr. Newsome?
Dr. Newsome: I would imagine that the National Institute on Minority Mental Health and Health Disparities would have something similar. I believe one of the things you mentioned is really important. In addition to making these recommendations, we need to be looking at where these leaks are occurring that keep them from working. What is the current structure and why is it the way it is with regard to the governance?
Dr. Norris: Here is another of their action statements: “Declare ‘civic mental health’ a national priority and incorporate it into the educational curriculum from K through college, as well as in the training of local, state, and national officials, law enforcement, and the criminal justice system.”
Let me be clear, I like every single one of these action statements. I encourage everyone to participate in dialogue and discussion. You may agree with some of these, and some of them you may not, but if there is one you agree with, that you really are motivated about, that’s one that you need to explore and dig into a bit more, because it’s too big for us to handle on our own, just like racism and equality.
I’m going to tell you, I like this statement. I do like this. Obviously these are broad points, but I do like the idea of training law enforcement officers about “civic mental health.” For example, Dr. Michael Compton, who has done a lot of great work in the area of mental health and prevention, has worked with police officers to help them interact with those with mental health conditions by modulating their own emotional response. I’m very interested in these types of recommendations that particularly target law enforcement officers, and helping with that ”emotional quotient.” I’m interested in seeing how far that can spread in the country. What do you think, Dr. Newsome?
Dr. Newsome: Educating police officers about how to interact would be quite important. I believe the National Alliance on Mental Illness does some of that work, partnering with law enforcement agencies, talking about mental health and cues to look at. There also are some programs where people ride along with mental health clinicians and police officers, which I find to be really helpful. But clearly, what’s going on right now isn’t working. So I would be open to any reasonable idea.
Dr. Norris: Here’s one last action point: “Establish police community review boards with power to take action in areas of police misconduct pending formal review by the appropriate authorities. This will offer a level of empowerment when communities feel they have a voice that can be heard.”
This is where I want my focus to be, as I move forward to try to do something sustainable. To deal with police brutality and abuse of power in general, but specifically as it relates to African American men and the lethal use of force. We need to work on policies that will enable African American men to make it to court, so that every encounter with a police officer is not literally viewed as a potentially lethal encounter.
A lot of people aren’t going to like me saying that, but it’s the absolute truth. You have to think like that, as an African American male, regardless of your station, regardless of where you live, this is the reality. There are many, many good police officers out there. I have a few friends who are law enforcement officers. I work with security at the George Washington Hospital constantly. But that still does not change the fact that if I get pulled over at a traffic stop, I know precisely certain things I need to do and not do, or the encounter could end badly. By that I mean loss of life.
So I encourage anything where we can start to take a systematic look at law enforcement and empower communities to look at who is doing it right and who is doing it wrong. Information is coming out now about the man who murdered Mr. Floyd, and this was not the first time he was involved in misconduct. There were red flags; we have to start to confront this. We have to learn from every single one of these situations and grow because another one is going to happen next week, it’s just whether or not you hear about it. That’s the reality of the state of America. You may not like to hear it, but that’s just a fact.
To hear the entire conversation, go to mdedge.com/podcasts or listen wherever you find your podcasts.
Editor’s Note: This transcript from the June 5 special episode of the Psychcast has been edited for clarity.
Nick Andrews: This is the Psychcast, the official podcast of MDedge Psychiatry. I am the voice of the MDedge podcasts, Nick Andrews. We are bringing this special edition of the Psychcast from MDedge in response to all of the unrest, peaceful or otherwise, in the United States in the aftermath of the shocking murder of George Floyd in late May of 2020.
Dr. Lorenzo Norris agreed to have this “after hours” discussion, believing the most appropriate response would be for us to have a real conversation about it. So welcome aboard.
Lorenzo Norris, MD: I’m happy to be here, Nick, and I’m so pleased to be talking with our guest, Dr. Brandon Newsome, a young black male psychiatrist. Dr. Newsome, sir, tell us a little about yourself and where you’re coming from.
Brandon Newsome, MD: I’m a 4th-year psychiatry resident at Boston Medical Center, so I’m about to graduate and to become a first-year fellow, as of July, at Children’s National Medical Center in Washington, D.C. I was born and raised in the South so I can talk about those experiences, and now I’ve been in the Northeast for the past 4 years.
Dr. Norris: Let’s get right into it. This is a time in our country that we’ve not seen – I shouldn’t say we, because depending on where you live in America, you have seen this and you’ve seen this multiple times.
I see a lot of myself in Dr. Newsome right now, and I am struggling with this: I’m talking to you about the same stuff I was talking about when I was a 4th-year resident. I’m talking to you about the same stuff I was talking about when I was a college student. I’m still talking about the same stuff I was talking about when I was a medical student. I’m still talking about the same things that were the impetus for the hip-hop generation regarding police brutality and violence.
We are still talking about the use of lethal force and abuse of power, particularly by police or law enforcement officers, and how that is perpetrated against African American men in particular, and the unfortunate and tragic murder of Mr. George Floyd. Dr. Newsome, tell me how you’re thinking about this. Before we even get into how our patients or our colleagues are doing, how are you doing with this?
Dr. Newsome: It’s been difficult. Like you, I’ve heard this story time and time again. I was just on a panel, having a conversation about race and policing, and I realized we had the same conversation during my first or second year of residency because there had been another death. But even though all of these unfortunate deaths are triggering us, this one is a little different for me for a few reasons. As you know, this is happening with the backdrop of the COVID-19 crisis and we’re already seeing so many people, especially from black and brown communities, dying from that.
And then I’m witnessing what happened, watching that video and thinking about all the interventions we’ve already tried. We tried body cameras, and the dude was wearing a body camera. We tried to get our police officers to be engaged, to try to check their roles, but people were there, witnessing everything, and nothing happened. An upstander was there, a white upstander, a firefighter who was telling them to check his pulse. Still nothing happened; it didn’t stop them.
I believe the backdrop of the COVID-19 crisis makes it a whole lot more painful for me and many others. I am part of a black physician email group and it’s been triggering for all of us because we all imagine that this could be me one day, especially when you think about the Amy Coopers of the world, among other things.
Dr. Norris: I completely agree. We’re dealing with loss of life due to a virus, including, [personally speaking] that of my departed grandmother Why am I bringing this up? I bring it up because, regardless of one’s socioeconomic strata or title or whatnot, particularly in the black community, this is the kind of mess we’re dealing with. We’re dealing with the stress of COVID-19 that is disproportionately affecting African Americans. We’re dealing with social isolation, we’re dealing with the economic recession and the collapse that everyone else is dealing with, and on top of that we are now dealing with another murder. But this particular murder resonates very differently because, as you said, it seemed like every single thing that could have been done was done.
You will read reports that Mr. Floyd was resisting arrest. But you look at this video; this is not a man resisting arrest. This is a man trying to say, please, you are killing me. These are other people saying the same thing. These are police officers not acting right. This is so many different things going on, and when you hear this and look at this video, you can come to no other conclusion than it is murder.
As psychiatrists, we frequently have to restrain people, and it is always understood that restraint can turn into assault extremely quickly. But in this particular case, there was no thought or concern about this man’s life or his health. There are many good police officers that do think of that, and so this was shocking. It was jarring. It was another thing piled on an already taxed black America. I was talking with my black male colleagues about this, and I think a lot of people don’t actually realize that, while there are black male psychiatrists, there are only a few of us.
Dr. Newsome: True that.
Dr. Norris: There are only so many black male physicians, period, and black male psychiatrists in particular. At different points in time we are called on to take leadership roles, and to talk, to speak on things and be a voice. Well, I have to tell you, after a while, this is pretty goddamn tiring for us to contain our disappointment, our anger, and our rage and still stay hopeful, optimistic, and still be a voice for those who are not able to speak.
Dr. Newsome: I agree that sometimes it can be tiring to have to take leadership roles and continue to talk about all these things, but I also feel that, at least for me, it gives me some sort of route to address the angst and do something with it. I believe all of us are just figuring out how to deal with these feelings that we shouldn’t have to feel because of a murder that was televised.
Dr. Norris: Thank you. For a murder that was televised; that was tweeted; that was broadbanded; that was streamed.
Now we’ve laid the framework, in terms of what we’re feeling. Let’s move on to why you and I are in this profession, and that’s our patients. What are you seeing on the front lines? What are you seeing with our patients?
Dr. Newsome: I was speaking with one of my black male patients, and he was fearful. He had been perfectly fine, even in the COVID crisis, he was doing well. But when you get this milieu of police violence, now he’s feeling this intense fear. Should I be walking alone at night? What happens if I am the one who is at the wrong place at the wrong time?
I also find that some of my nonminority patients sometimes find difficulty making sense of it. Minority individuals already know these things are happening. But some of the nonminorities are wondering how or why would something like this happen in America? This is just how America is for the black folks.
Dr. Norris: Could you elaborate on that? I always found that to be a very interesting dynamic for those who are not minorities or people of color. I will have folks in a psychotherapy session who are just bewildered by events like this. It is not the America they think they know – they are shocked that this is actually what’s going on.
Dr. Newsome: It’s all about experiences. If you didn’t grow up around a lot of minorities, you haven’t necessarily had these conversations. Even speaking for myself, sometimes I don’t want to discuss these things; you never know what you’re going to get. You might find an ally, or you might find someone who isn’t at all supportive. I think the surprise is from lack of exposure. If you don’t have to live through racism, you can most certainly have blinders on and not notice.
Dr. Norris: Can you comment on the fear you’re seeing in some folks? Can it get to the point of reactivating PTSD?
Dr. Newsome: I notice it more with black individuals, a fear that they might be the ones who may die; or with black mothers, wondering, what about my child? Is this what they are going to have to live with for the rest of their lives? Older people would say that we fought already and it’s still going on. What are the fruits of the labor we put in?
Dr. Norris: I agree with you completely. What are the fruits? You’re going to see those strong reactions. You’re going to see fear, you’re going to see anger, and you’re also going to see guilt that they could not stop this. I’m speaking particularly about some of my nonminority patients. It goes along with that confusion. This manifests in a desperate need to do something.
But here’s the problem: You don’t really know what to do because no one is educated on it. And as you said before, race is a very polarized subject. No one even likes to talk about racism because it’s so, oh my goodness. We’ve run away from it so much to the point that we can’t deal with it. We all have to start to own that. You can’t just stay siloed, because eventually, it’s going to come back and affect you.
I could easily be Mr. Floyd, but at the same time, due to my station and things of that nature, I have a certain level of privilege and autonomy. There could be a tendency to put your head under the sand, you know, look at how far we’ve come, Barack Obama. But you’ve got to say, no, we still have enormous amounts of work to do.
We’ve been talking about the patients. What have you noticed in your colleagues and how they’ve been feeling about this?
Dr. Newsome: Again, I see them feeling saddened by the events. One of the other things I’ve noticed is that some people are in environments where they have program directors and chairs who will directly condemn certain behaviors and say, “This is racist, this shouldn’t happen.” But then there are other programs that have been more silent. I’ve had people say that this is the first time that they have felt isolated in a long while.
We all participate in these physician WhatsApp groups, and according to some of the comments, people are realizing that these folks that they were just on the front lines with, fighting COVID, are perhaps not the allies that they originally thought they were, based on the things these people are saying.
Dr. Norris: Wow. It’s good that we’re talking about this from the viewpoint of two different generations. You’ve got the WhatsApp group and Google Hangouts and all that kind of good stuff, and I’m still with pagers and such. That’s interesting – the reality that folks you thought were your allies turn out not to be, because you’re bringing up difficult conversations that we don’t normally talk about.
I have noticed that some people around me have been silent because they don’t know what to say. They’re so concerned that I’m going to be offended or they’re going to hurt me or say the wrong thing, so they stay quiet. As I reflect now, this is the wrong thing to do. Own your concern. I’ve been in two large meetings now, and I’ve had multiple people whom I consider friends say, I wanted to email or text you right then and ask you how you’re doing, but I didn’t because I didn’t know what to say. I have entered meetings recently, and the meeting felt tense, and I’m thinking, what’s going on? And now I realize they did not know what to say or how to approach it.
That’s been a very interesting dynamic and tells us where we are with this. Today, for example, I was pleased to have the support of my dean’s group. I felt I had to speak out, I just had to straight out tell them. Do you want to know what I’m feeling? I’m feeling rage. I’m feeling rage. And you all have to understand that, because I have to speak for those who aren’t necessarily going to be able to express themselves. More importantly, I have to speak for myself and I’m feeling rage.
How our colleagues are processing this and how they’re thinking about this runs the gamut. But I think about people not necessarily knowing what to say or how to approach it. I absolutely agree that with the leadership, you’re going to get many different responses, and sometimes you’re left to wonder, do I have to watch what I say? But I’m definitely supported at my institution.
What else are you seeing out there in terms of your colleagues or how people think about it?
Dr. Newsome: This also spurs some folks to activism. Some have been participating in protests. There will be White Coats for Black Lives protests, among other things. So it’s spurred folks to action, and it’s also spurred folks to try to be part of a community. Of course, with the whole COVID crisis, we can’t necessarily come together, so we’ve been doing Zoom gatherings more than anything else. But it has encouraged folks to want to do that more, too, because they want to check in on their brother or their sister to make sure they are doing well, and also to be able to express what’s going on with them in a community where they know they can get validation.

Dr. Norris: I’m going to push you a bit because I detect in your tone something similar to what I’m feeling. I just got the email, the White Coats For Black Lives email. But I think your feeling is similar to mine – I’ve done this before. I’ve done White Coats for Black Lives. You all may have protested. But this display in Washington, D.C., of the use of military and law enforcement to clear a public square of peaceful protesters is above and beyond the pale of anything I’ve ever seen in my life. We have to label that for the danger it is, for the threat to everything this country and the people that bled for this country stand for.
So while I’m going to participate in White Coats for Black Lives and many other things, I am looking for what is actually going to move the needle. I think the protests are great, but at this point in time I want institutions, I want money, I want lawyers, I want a systematic approach.
Dr. Newsome: I most certainly agree. Of course, the protests are really important, but depending on where you are, you have a different lens. As physicians, especially as black physicians, since there are so few of us, we have a unique opportunity to leverage that, whether that means communicating through op-eds or calling your senators and talking with them to try to move things forward.
Physicians are mobilizing. In the last few days, a physician created a Zoom event and hundreds of physicians joined to try to figure out how we can structurally fix this problem. So I most certainly believe that in this effort to address racism, we physicians will need to lend our voices and our privilege to move the needle as best we can.
Dr. Norris: Some of our colleagues in Black Psychiatrists of America have put out a press release on racism in which they propose some actions that should be taken immediately. I think this is a useful thing to talk about.
The first action: “Declare racism a public health problem and establish national goals for addressing this as a health equity issue. Give priority to addressing the issues of health care disparities, including the mental health needs of historically marginalized communities across the U.S.”
What do you think about that?
Dr. Newsome: Those are two extremely important steps. The question is: How do you make that happen?
Dr. Norris: You’re reading my mind. I love that our colleagues put that out there, but that was my next question.
Dr. Newsome: There is going to be a town hall about this and I’m hoping that we can plan how we envision this happening. I can imagine that 20 or 30 years ago there was also a fear in society that there would be episodes of police brutality. I can imagine that there were similar ideals and hopes. But I think we need to put all of our minds together and ask: How are we going to accomplish this? Is this going to be something we’re going to put our money into? Is this going to be something we’re going to get senators and legislatures onboard with to make policy?
Dr. Norris: Let me read off some of the other action points they put out. There are six of them.
“Establish a governmental multidisciplinary and ethnically diverse commission with representatives from the major health care professional associations in medicine, nursing, psychiatry, public health, psychology, social work, etc., and the faith-based community to provide recommendations to Congress regarding policies on how to best improve the health and well-being of our nation’s black citizens.”
That’s a very solid overall recommendation. My question is, doesn’t that, in some way, shape, or form already exist? Could we not put up policy statements from all of these folks regarding racism and things of that nature? I agree with what they’re saying, but part of me wonders why certain things in the current system aren’t working. That becomes the question. Are we not integrated enough? Do we not have enough cross talk? Do we not have enough money behind it? So I agree with that goal, but I would be curious if that doesn’t already exist. What are your thoughts about that, Dr. Newsome?
Dr. Newsome: I would imagine that the National Institute on Minority Mental Health and Health Disparities would have something similar. I believe one of the things you mentioned is really important. In addition to making these recommendations, we need to be looking at where these leaks are occurring that keep them from working. What is the current structure and why is it the way it is with regard to the governance?
Dr. Norris: Here is another of their action statements: “Declare ‘civic mental health’ a national priority and incorporate it into the educational curriculum from K through college, as well as in the training of local, state, and national officials, law enforcement, and the criminal justice system.”
Let me be clear, I like every single one of these action statements. I encourage everyone to participate in dialogue and discussion. You may agree with some of these, and some of them you may not, but if there is one you agree with, that you really are motivated about, that’s one that you need to explore and dig into a bit more, because it’s too big for us to handle on our own, just like racism and equality.
I’m going to tell you, I like this statement. I do like this. Obviously these are broad points, but I do like the idea of training law enforcement officers about “civic mental health.” For example, Dr. Michael Compton, who has done a lot of great work in the area of mental health and prevention, has worked with police officers to help them interact with those with mental health conditions by modulating their own emotional response. I’m very interested in these types of recommendations that particularly target law enforcement officers, and helping with that ”emotional quotient.” I’m interested in seeing how far that can spread in the country. What do you think, Dr. Newsome?
Dr. Newsome: Educating police officers about how to interact would be quite important. I believe the National Alliance on Mental Illness does some of that work, partnering with law enforcement agencies, talking about mental health and cues to look at. There also are some programs where people ride along with mental health clinicians and police officers, which I find to be really helpful. But clearly, what’s going on right now isn’t working. So I would be open to any reasonable idea.
Dr. Norris: Here’s one last action point: “Establish police community review boards with power to take action in areas of police misconduct pending formal review by the appropriate authorities. This will offer a level of empowerment when communities feel they have a voice that can be heard.”
This is where I want my focus to be, as I move forward to try to do something sustainable. To deal with police brutality and abuse of power in general, but specifically as it relates to African American men and the lethal use of force. We need to work on policies that will enable African American men to make it to court, so that every encounter with a police officer is not literally viewed as a potentially lethal encounter.
A lot of people aren’t going to like me saying that, but it’s the absolute truth. You have to think like that, as an African American male, regardless of your station, regardless of where you live, this is the reality. There are many, many good police officers out there. I have a few friends who are law enforcement officers. I work with security at the George Washington Hospital constantly. But that still does not change the fact that if I get pulled over at a traffic stop, I know precisely certain things I need to do and not do, or the encounter could end badly. By that I mean loss of life.
So I encourage anything where we can start to take a systematic look at law enforcement and empower communities to look at who is doing it right and who is doing it wrong. Information is coming out now about the man who murdered Mr. Floyd, and this was not the first time he was involved in misconduct. There were red flags; we have to start to confront this. We have to learn from every single one of these situations and grow because another one is going to happen next week, it’s just whether or not you hear about it. That’s the reality of the state of America. You may not like to hear it, but that’s just a fact.
To hear the entire conversation, go to mdedge.com/podcasts or listen wherever you find your podcasts.
Management of race in psychotherapy and supervision
On the Friday evening after the public execution of George Floyd, we were painfully reminded of the urgency to address the inadequate management of race, racism, and anti-blackness in medical education, residency training, and postgraduate continuing medical education.
The reminder did not originate from the rioting that was occurring in some cities, though we could feel the ground shifting beneath our feet as civic protests that began in U.S. cities spread around the globe. Instead, it occurred during a webinar we were hosting for psychiatry residents focused on techniques for eliminating blind spots in the management of race in clinical psychotherapy supervision. (Dr. Jessica Isom chaired the webinar, Dr. Flavia DeSouza and Dr. Myra Mathis comoderated, and Dr. Ebony Dennis and Dr. Constance E. Dunlap served as discussants.)
Our panel had presented an ambitious agenda that included reviewing how the disavowal of bias, race, racism, and anti-blackness contributes to ineffective psychotherapy, undermines the quality of medical care, and perpetuates mental health disparities. We spent some time exploring how unacknowledged and unexamined conscious and unconscious racial stereotypes affect interpersonal relationships, the psychotherapeutic process, and the supervisory experience. Our presentation included a clinical vignette demonstrating how racism, colorism, and anti-blackness have global impact, influencing the self-esteem, identity formation, and identity consolidation of immigrants as they grapple with the unique form of racism that exists in America. Other clinical vignettes demonstrated blind spots that were retroactively identified though omitted in supervisory discussions. We also discussed alternative interventions and interpretations of the material presented.1-5
Because 21st-century trainees are generally psychologically astute and committed to social justice, we did two things. First, before the webinar, we provided them access to a prerecorded explanation of object relations theorist Melanie Klein’s paranoid-schizoid and depressive positions concepts, which were applied to theoretically explain the development of race, specifically the defenses used by early colonists that contributed to the development of “whiteness” and “blackness” as social constructs, and their influence on the development of the U.S. psyche. For example, as early colonists attempted to develop new and improved identities distinct from those they had in their homelands, they used enslaved black people (and other vulnerable groups) to “other.” What we mean here by othering is the process of using an other to project one’s badness into in order to relieve the self of uncomfortable aspects and feelings originating within the self. If this other accepts the projection (which is often the case with vulnerable parties), the self recognizes, that is, identifies (locates) the bad they just projected in the other, who is now experienced as a bad-other. This is projection in action. If the other accepts the projection and behaves accordingly, for example, in a manner that reflects badness, this becomes projective identification. Conversely, if the other does not accept these projections, the self (who projects) is left to cope with aspects of the self s/he might not have the capacity to manage. By capacity, we are speaking of the Bionian idea of the ability to experience an extreme emotion while also being able to think. Without the ego strength to cope with bad aspects of the self, the ego either collapses (and is unable to think) or further projection is attempted.6-8
We have seen this latter dynamic play out repeatedly when police officers fatally shoot black citizens and then claim that they feared for their lives; these same officers have been exonerated by juries by continuing to portray the deceased victims as threatening, dangerous objects not worthy of living. We are also seeing a global movement of black and nonblack people who are in touch with a justified rage that has motivated them to return these projections by collectively protesting, and in some cases, by rioting.
Back to the webinar
In anticipating the residents’ curiosity, impatience, and anger about the lack of progress, the second thing we did was to show a segment from the “Black Psychoanalysts Speak” trailer. In the clip played, senior psychoanalyst Kirkland C. Vaughans, PhD, shares: “The issue of race so prompts excessive anxiety that it blocks off our ability to think.”
We showed this clip to validate the trainees’ frustrations about the difficulty the broader establishment has had with addressing this serious, longstanding public health problem. We wanted these young psychiatrists to know that there are psychoanalysts, psychiatrists, psychologists, and social workers who have been committed to this work, even though the contributions of this diverse group have curiously been omitted from education and training curricula.9
So, what happened? What was the painful reminder? After the formal panel presentations, a black male psychiatry resident recounted his experience in a clinical supervision meeting that had occurred several days after the murder of George Floyd. In short, a patient had shared his reactions to yet another incident of fatal police use of force and paused to ask how the resident physician, Dr. A., was doing. The question was experienced as sincere concern about the psychiatrist’s mental well-being. The resident was not sure how to answer this question since it was a matter of self-disclosure, which was a reasonable and thoughtful consideration for a seasoned clinician and, certainly, for a novice therapist. The supervisor, Dr. B., seemingly eager to move on, to not think about this, responded to the resident by saying: “Now tell me about the patient.” In other words, what had just been shared by the resident – material that featured a patient’s reaction to another killing of a black man by police and the patient’s expressed concern for his black psychiatrist, and this resident physician appropriately seeking space in supervision to process and receive guidance about how to respond – all of this was considered separate (split off from) and extraneous to the patient’s treatment and the resident’s training. This is a problem. And, unfortunately, this problem or some variation of it is not rare.
Why is this still the state of affairs when we have identified racism as a major health concern and our patients and our trainees are asking for help?
Rethinking a metaphor
Despite calls to action over the last 50 years to encourage medicine to effectively address race and racism, deficits remain in didactic education, clinical rotations, and supervisory experiences of trainees learning how to do psychodynamic psychotherapy.8-10 Earlier that evening, we used the metaphor of a vehicular blind spot to capture what we believe occurs insupervision. Like drivers, supervisors generally have the ability to see. However, there are places (times) and positions (stances) that block their vision (awareness). Racism – whether institutionalized, interpersonally mediated, or internalized – also contributes to this blindness.
As is true of drivers managing a blind spot, what is required is for the drivers – the supervisors – to lean forward or reposition themselves so as to avoid collisions, maintain safety, and continue on course. We use this metaphor because it is understood that any clinician providing psychodynamic supervision to psychiatry residents, regardless of professional discipline, has the requisite skills and training.10-13
Until May 25, we thought eliminating blind spots would be effective. But, in the aftermath of the police killing of George Floyd, our eyes have been opened.
Hiding behind the blue wall of silence is an establishment that has looked the other way while black and brown women, men, and children have come to live in fear as a result of the state-sanctioned violence that repeatedly occurs across the nation. Excessive police use of force is a public health issue of crisis magnitude. However, the house of medicine, like many other established structures in society, has colluded with the societal constructs that have supported law enforcement by remaining willfully blind, often neutral, and by refusing to make the necessary adjustments, including connecting the dots between police violence and physical and mental health.
For example, racism has never been listed even in the index of the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders.14 Being the victim of police use of force is not generally regarded as an adverse childhood experience, even though communities that are heavily policed experience harassment by law enforcement on a regular basis. The 12 causes of trauma listed on the website15 of the National Child Traumatic Stress Network – bullying, community violence, complex trauma, disasters, early childhood trauma, intimate partner violence, medical trauma, physical abuse, refugee trauma, sexual abuse, terrorism and violence, and traumatic grief – do not include maltreatment, abuse, or trauma resulting from interactions with members of law enforcement. Much of the adverse childhood experiences literature focuses on white, upper middle class children and on experiences within the home. When community level experiences, such as discrimination based on race or ethnicity, are included, as in the Philadelphia ACES study,16 as many as 40% reported ACE scores of greater than 4 for community level exposures.
As psychiatrists, we recognize the psychic underpinnings and parallels between the psychic projections onto black and brown people and the actual bullets pumped into the bodies of black and brown people; there is a lurid propensity to use these others as repositories. Those who have the privilege of being protected by law enforcement and the ability to avoid being used as containers for the psychic projections and bullets of some police officers also have the privilege of compartmentalizing and looking the other way when excessive acts of force – projections and projectiles – are used on other human beings. This partly explains why the injuries and deaths of black and brown people caused by police officers’ excessive use of force have continued even though these unjustified deaths are widely televised and disseminated via various social media platforms.
Prior to the death of George Floyd on May 25, other than the American Public Health Association, the National Medical Association (NMA) was the only major medical organization to issue a call to consider police use of force as a public health issue. In its July 2016 press release, provided in the aftermath of the death of Freddie Gray while in the custody of Baltimore police officers, the NMA summarized the scope of injuries citizens sustain during “the pre-custody (commission of a crime, during a fight, chase, and apprehension, during a siege or hostage situation, or during restraint or submission), custody (soon after being admitted to jail, during interrogation, during incarceration, or legal execution), and post-custody (revenge by police or rival criminals or after reentry into the community)” periods. It is noteworthy that the scope of these injuries is comparable to those encountered in a combat zone.17,18 According to the NMA:
“Injuries sustained by civilians at the hands of law enforcement include gunshot wounds, skull fractures, cervical spine injuries, facial fractures, broken legs, blunt trauma orbital floor fractures, laryngeal cartilage fractures, shoulder dislocations, cuts and bruises, concussions, hemorrhage, choking (positional or due to upper body holds), abdominal trauma, hemothorax, and pneumothorax. Complications of such injuries include posttraumatic brain swelling, infections following open fractures and lacerations, hydrocephalus due to blood or infection, as well as subdural and epidural hematomas and, in the most severe cases, death.”
In addition, there are multiple emotional and psychiatric sequelae of these injuries for the victims, families, upstanders, bystanders, and those viewing these images via various social media platforms. Increasingly, many are experiencing retraumatization each time a new death is reported. How do we explain that we are turning away from this as physicians and trainers of physicians? Seeing and not seeing – all of the methods used to avert one’s gaze and look the other way (to protect the psyches of nonmarginalized members of society from being disturbed and possibly traumatized) – these key defense mechanisms creep into consulting rooms and become fertile ground for the enactment described above.
Yet, there is reason to believe in change. It’s not simply because we are mental health professionals and that’s what we do. With the posting of position statements issued by major corporations and a growing number of medical organizations, many of us are experiencing a mixture of hope, anger, and sadness. Hope that widespread awareness will continue to tilt the axis of our country in a manner that opens eyes – and hearts – so that real work can be done; and anger and sadness because it has taken 400 years to receive even this level of validation.
In the meantime, we are encouraged by a joint position statement recently issued by the APA and the NMA, the first joint effort by these two medical organizations to partner and advocate for criminal justice reform. We mention this statement because the NMA has been committed to the needs of the black community since its inception in 1895, and the APA has as its mission a commitment to serve “the needs of evolving, diverse, underrepresented, and underserved patient populations” ... and the resources to do so. This is the kind of partnership that could transform words into meaningful action.19,20
Of course, resident psychiatrist Dr. A. had begun supervision with the discussion of his dyadic experience with his patient, which is set in the context of a global coronavirus pandemic that is disproportionately affecting black and brown people. And, while his peers are marching in protest, he and his fellow trainees deserve our support as they deal with their own psychic pain and prepare to steady themselves. For these psychiatrists will be called to provide care to those who will consult them once they begin to grapple with the experiences and, in some cases, traumas that have compelled them to take action and literally risk their safety and lives while protesting.
That evening, the residents were hungry for methods to fill the gaps in their training and supervision. In some cases, we provided scripts to be taken back to supervision. For example, the following is a potential scripted response for the supervisor in the enactment described above:
Resident speaking to supervisor: This is a black patient who, like many others, is affected by the chronic, repeated televised images of black men killed by police. I am also a black man.
I think what I have shared is pertinent to the patient’s care and my experience as a black male psychiatrist who will need to learn how to address this in my patients who are black and for other racialized groups, as well as with whites who might have rarely been cared for by a black man. Can we discuss this?
We also anticipated that some residents would need to exercise their right to request reassignment to another supervisor. And, until we do better at listening, seeing, and deepening our understanding, outside and inside the consulting room and in supervision, more residents might need to steer around those who have the potential to undermine training and adversely affect treatment. But, as a professional medical community in crisis, do we really want to proceed in such an ad hoc fashion?
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures.
Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Dr. DeSouza is a PGY-4 psychiatry resident and public psychiatry fellow in the department of psychiatry at Yale University, New Haven, Conn. Her professional interests include health services development and delivery in low- and middle-income settings, as well as the intersection of mental health and spirituality. She has no disclosures.
Dr. Isom is a staff psychiatrist at the Codman Square Health Center in Dorchester, Mass., and Boston Medical Center. Her interests include racial mental health equity and population health approaches to community psychiatry. She has no disclosures.
Dr. Mathis is an addictions fellow in the department of psychiatry at Yale University and former programwide chief resident at Yale. Her interests include the intersection of racial justice and mental health, health equity, and spirituality. She has no disclosures.
References
1. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2001.
2. Banaji MR and Greenwald AG. Blindspot: Hidden Biases of Good People. New York: Delacorte Press, 2013.
3. Anekwe ON. Voices in Bioethics. 2014.
4. Soute BJ. The American Psychoanalyst Magazine. 2017 Winter/Spring.
5. Powell DR. J Am Psychoanal Assoc. 2019 Jan 8. doi: 10.1177/000306511881847.
6. Allen TW. The Invention of the White Race. London: Verso, 1994.
7. Klein M. Int J Psychoanal. 1946;27(pt.3-4):99-100.
8. Bion WR. (1962b). Psychoanal Q. 2013 Apr;82(2):301-10.
9. Black Psychoanalysts Speak trailer.
10. Thomas A and Sillen S. Racism and Psychiatry. New York: Brunner/Mazel, 1972.
11. Jones BE et al. Am J Psychiatry. 1970 Dec;127(6):798-803.
12. Sabshin M et al. Am J Psychiatry. 1970 Dec;126(6):787-93.
13. Medlock M et al. Am J Psychiatry. 2017 May 9. doi: 10.1176/appi.ajp-rj.2016.110206.
14. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). Arlington, Va.: American Psychiatric Association, 2013.
15. “What is Child Trauma?” The National Child Traumatic Stress Network.
16. The Philadelphia Project. Philadelphia ACE Survey.
17. “Addressing law enforcement violence as a public health issue.” Washington: American Public Health Association. 2018 Nov 13. Policy# 20811.
18. National Medical Association position statement on police use of force. NMA 2016.
19. “APA and NMA jointly condemn systemic racism in America.” 2020 Jun 16.
20. APA Strategic Plan. 2015 Mar.
On the Friday evening after the public execution of George Floyd, we were painfully reminded of the urgency to address the inadequate management of race, racism, and anti-blackness in medical education, residency training, and postgraduate continuing medical education.
The reminder did not originate from the rioting that was occurring in some cities, though we could feel the ground shifting beneath our feet as civic protests that began in U.S. cities spread around the globe. Instead, it occurred during a webinar we were hosting for psychiatry residents focused on techniques for eliminating blind spots in the management of race in clinical psychotherapy supervision. (Dr. Jessica Isom chaired the webinar, Dr. Flavia DeSouza and Dr. Myra Mathis comoderated, and Dr. Ebony Dennis and Dr. Constance E. Dunlap served as discussants.)
Our panel had presented an ambitious agenda that included reviewing how the disavowal of bias, race, racism, and anti-blackness contributes to ineffective psychotherapy, undermines the quality of medical care, and perpetuates mental health disparities. We spent some time exploring how unacknowledged and unexamined conscious and unconscious racial stereotypes affect interpersonal relationships, the psychotherapeutic process, and the supervisory experience. Our presentation included a clinical vignette demonstrating how racism, colorism, and anti-blackness have global impact, influencing the self-esteem, identity formation, and identity consolidation of immigrants as they grapple with the unique form of racism that exists in America. Other clinical vignettes demonstrated blind spots that were retroactively identified though omitted in supervisory discussions. We also discussed alternative interventions and interpretations of the material presented.1-5
Because 21st-century trainees are generally psychologically astute and committed to social justice, we did two things. First, before the webinar, we provided them access to a prerecorded explanation of object relations theorist Melanie Klein’s paranoid-schizoid and depressive positions concepts, which were applied to theoretically explain the development of race, specifically the defenses used by early colonists that contributed to the development of “whiteness” and “blackness” as social constructs, and their influence on the development of the U.S. psyche. For example, as early colonists attempted to develop new and improved identities distinct from those they had in their homelands, they used enslaved black people (and other vulnerable groups) to “other.” What we mean here by othering is the process of using an other to project one’s badness into in order to relieve the self of uncomfortable aspects and feelings originating within the self. If this other accepts the projection (which is often the case with vulnerable parties), the self recognizes, that is, identifies (locates) the bad they just projected in the other, who is now experienced as a bad-other. This is projection in action. If the other accepts the projection and behaves accordingly, for example, in a manner that reflects badness, this becomes projective identification. Conversely, if the other does not accept these projections, the self (who projects) is left to cope with aspects of the self s/he might not have the capacity to manage. By capacity, we are speaking of the Bionian idea of the ability to experience an extreme emotion while also being able to think. Without the ego strength to cope with bad aspects of the self, the ego either collapses (and is unable to think) or further projection is attempted.6-8
We have seen this latter dynamic play out repeatedly when police officers fatally shoot black citizens and then claim that they feared for their lives; these same officers have been exonerated by juries by continuing to portray the deceased victims as threatening, dangerous objects not worthy of living. We are also seeing a global movement of black and nonblack people who are in touch with a justified rage that has motivated them to return these projections by collectively protesting, and in some cases, by rioting.
Back to the webinar
In anticipating the residents’ curiosity, impatience, and anger about the lack of progress, the second thing we did was to show a segment from the “Black Psychoanalysts Speak” trailer. In the clip played, senior psychoanalyst Kirkland C. Vaughans, PhD, shares: “The issue of race so prompts excessive anxiety that it blocks off our ability to think.”
We showed this clip to validate the trainees’ frustrations about the difficulty the broader establishment has had with addressing this serious, longstanding public health problem. We wanted these young psychiatrists to know that there are psychoanalysts, psychiatrists, psychologists, and social workers who have been committed to this work, even though the contributions of this diverse group have curiously been omitted from education and training curricula.9
So, what happened? What was the painful reminder? After the formal panel presentations, a black male psychiatry resident recounted his experience in a clinical supervision meeting that had occurred several days after the murder of George Floyd. In short, a patient had shared his reactions to yet another incident of fatal police use of force and paused to ask how the resident physician, Dr. A., was doing. The question was experienced as sincere concern about the psychiatrist’s mental well-being. The resident was not sure how to answer this question since it was a matter of self-disclosure, which was a reasonable and thoughtful consideration for a seasoned clinician and, certainly, for a novice therapist. The supervisor, Dr. B., seemingly eager to move on, to not think about this, responded to the resident by saying: “Now tell me about the patient.” In other words, what had just been shared by the resident – material that featured a patient’s reaction to another killing of a black man by police and the patient’s expressed concern for his black psychiatrist, and this resident physician appropriately seeking space in supervision to process and receive guidance about how to respond – all of this was considered separate (split off from) and extraneous to the patient’s treatment and the resident’s training. This is a problem. And, unfortunately, this problem or some variation of it is not rare.
Why is this still the state of affairs when we have identified racism as a major health concern and our patients and our trainees are asking for help?
Rethinking a metaphor
Despite calls to action over the last 50 years to encourage medicine to effectively address race and racism, deficits remain in didactic education, clinical rotations, and supervisory experiences of trainees learning how to do psychodynamic psychotherapy.8-10 Earlier that evening, we used the metaphor of a vehicular blind spot to capture what we believe occurs insupervision. Like drivers, supervisors generally have the ability to see. However, there are places (times) and positions (stances) that block their vision (awareness). Racism – whether institutionalized, interpersonally mediated, or internalized – also contributes to this blindness.
As is true of drivers managing a blind spot, what is required is for the drivers – the supervisors – to lean forward or reposition themselves so as to avoid collisions, maintain safety, and continue on course. We use this metaphor because it is understood that any clinician providing psychodynamic supervision to psychiatry residents, regardless of professional discipline, has the requisite skills and training.10-13
Until May 25, we thought eliminating blind spots would be effective. But, in the aftermath of the police killing of George Floyd, our eyes have been opened.
Hiding behind the blue wall of silence is an establishment that has looked the other way while black and brown women, men, and children have come to live in fear as a result of the state-sanctioned violence that repeatedly occurs across the nation. Excessive police use of force is a public health issue of crisis magnitude. However, the house of medicine, like many other established structures in society, has colluded with the societal constructs that have supported law enforcement by remaining willfully blind, often neutral, and by refusing to make the necessary adjustments, including connecting the dots between police violence and physical and mental health.
For example, racism has never been listed even in the index of the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders.14 Being the victim of police use of force is not generally regarded as an adverse childhood experience, even though communities that are heavily policed experience harassment by law enforcement on a regular basis. The 12 causes of trauma listed on the website15 of the National Child Traumatic Stress Network – bullying, community violence, complex trauma, disasters, early childhood trauma, intimate partner violence, medical trauma, physical abuse, refugee trauma, sexual abuse, terrorism and violence, and traumatic grief – do not include maltreatment, abuse, or trauma resulting from interactions with members of law enforcement. Much of the adverse childhood experiences literature focuses on white, upper middle class children and on experiences within the home. When community level experiences, such as discrimination based on race or ethnicity, are included, as in the Philadelphia ACES study,16 as many as 40% reported ACE scores of greater than 4 for community level exposures.
As psychiatrists, we recognize the psychic underpinnings and parallels between the psychic projections onto black and brown people and the actual bullets pumped into the bodies of black and brown people; there is a lurid propensity to use these others as repositories. Those who have the privilege of being protected by law enforcement and the ability to avoid being used as containers for the psychic projections and bullets of some police officers also have the privilege of compartmentalizing and looking the other way when excessive acts of force – projections and projectiles – are used on other human beings. This partly explains why the injuries and deaths of black and brown people caused by police officers’ excessive use of force have continued even though these unjustified deaths are widely televised and disseminated via various social media platforms.
Prior to the death of George Floyd on May 25, other than the American Public Health Association, the National Medical Association (NMA) was the only major medical organization to issue a call to consider police use of force as a public health issue. In its July 2016 press release, provided in the aftermath of the death of Freddie Gray while in the custody of Baltimore police officers, the NMA summarized the scope of injuries citizens sustain during “the pre-custody (commission of a crime, during a fight, chase, and apprehension, during a siege or hostage situation, or during restraint or submission), custody (soon after being admitted to jail, during interrogation, during incarceration, or legal execution), and post-custody (revenge by police or rival criminals or after reentry into the community)” periods. It is noteworthy that the scope of these injuries is comparable to those encountered in a combat zone.17,18 According to the NMA:
“Injuries sustained by civilians at the hands of law enforcement include gunshot wounds, skull fractures, cervical spine injuries, facial fractures, broken legs, blunt trauma orbital floor fractures, laryngeal cartilage fractures, shoulder dislocations, cuts and bruises, concussions, hemorrhage, choking (positional or due to upper body holds), abdominal trauma, hemothorax, and pneumothorax. Complications of such injuries include posttraumatic brain swelling, infections following open fractures and lacerations, hydrocephalus due to blood or infection, as well as subdural and epidural hematomas and, in the most severe cases, death.”
In addition, there are multiple emotional and psychiatric sequelae of these injuries for the victims, families, upstanders, bystanders, and those viewing these images via various social media platforms. Increasingly, many are experiencing retraumatization each time a new death is reported. How do we explain that we are turning away from this as physicians and trainers of physicians? Seeing and not seeing – all of the methods used to avert one’s gaze and look the other way (to protect the psyches of nonmarginalized members of society from being disturbed and possibly traumatized) – these key defense mechanisms creep into consulting rooms and become fertile ground for the enactment described above.
Yet, there is reason to believe in change. It’s not simply because we are mental health professionals and that’s what we do. With the posting of position statements issued by major corporations and a growing number of medical organizations, many of us are experiencing a mixture of hope, anger, and sadness. Hope that widespread awareness will continue to tilt the axis of our country in a manner that opens eyes – and hearts – so that real work can be done; and anger and sadness because it has taken 400 years to receive even this level of validation.
In the meantime, we are encouraged by a joint position statement recently issued by the APA and the NMA, the first joint effort by these two medical organizations to partner and advocate for criminal justice reform. We mention this statement because the NMA has been committed to the needs of the black community since its inception in 1895, and the APA has as its mission a commitment to serve “the needs of evolving, diverse, underrepresented, and underserved patient populations” ... and the resources to do so. This is the kind of partnership that could transform words into meaningful action.19,20
Of course, resident psychiatrist Dr. A. had begun supervision with the discussion of his dyadic experience with his patient, which is set in the context of a global coronavirus pandemic that is disproportionately affecting black and brown people. And, while his peers are marching in protest, he and his fellow trainees deserve our support as they deal with their own psychic pain and prepare to steady themselves. For these psychiatrists will be called to provide care to those who will consult them once they begin to grapple with the experiences and, in some cases, traumas that have compelled them to take action and literally risk their safety and lives while protesting.
That evening, the residents were hungry for methods to fill the gaps in their training and supervision. In some cases, we provided scripts to be taken back to supervision. For example, the following is a potential scripted response for the supervisor in the enactment described above:
Resident speaking to supervisor: This is a black patient who, like many others, is affected by the chronic, repeated televised images of black men killed by police. I am also a black man.
I think what I have shared is pertinent to the patient’s care and my experience as a black male psychiatrist who will need to learn how to address this in my patients who are black and for other racialized groups, as well as with whites who might have rarely been cared for by a black man. Can we discuss this?
We also anticipated that some residents would need to exercise their right to request reassignment to another supervisor. And, until we do better at listening, seeing, and deepening our understanding, outside and inside the consulting room and in supervision, more residents might need to steer around those who have the potential to undermine training and adversely affect treatment. But, as a professional medical community in crisis, do we really want to proceed in such an ad hoc fashion?
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures.
Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Dr. DeSouza is a PGY-4 psychiatry resident and public psychiatry fellow in the department of psychiatry at Yale University, New Haven, Conn. Her professional interests include health services development and delivery in low- and middle-income settings, as well as the intersection of mental health and spirituality. She has no disclosures.
Dr. Isom is a staff psychiatrist at the Codman Square Health Center in Dorchester, Mass., and Boston Medical Center. Her interests include racial mental health equity and population health approaches to community psychiatry. She has no disclosures.
Dr. Mathis is an addictions fellow in the department of psychiatry at Yale University and former programwide chief resident at Yale. Her interests include the intersection of racial justice and mental health, health equity, and spirituality. She has no disclosures.
References
1. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2001.
2. Banaji MR and Greenwald AG. Blindspot: Hidden Biases of Good People. New York: Delacorte Press, 2013.
3. Anekwe ON. Voices in Bioethics. 2014.
4. Soute BJ. The American Psychoanalyst Magazine. 2017 Winter/Spring.
5. Powell DR. J Am Psychoanal Assoc. 2019 Jan 8. doi: 10.1177/000306511881847.
6. Allen TW. The Invention of the White Race. London: Verso, 1994.
7. Klein M. Int J Psychoanal. 1946;27(pt.3-4):99-100.
8. Bion WR. (1962b). Psychoanal Q. 2013 Apr;82(2):301-10.
9. Black Psychoanalysts Speak trailer.
10. Thomas A and Sillen S. Racism and Psychiatry. New York: Brunner/Mazel, 1972.
11. Jones BE et al. Am J Psychiatry. 1970 Dec;127(6):798-803.
12. Sabshin M et al. Am J Psychiatry. 1970 Dec;126(6):787-93.
13. Medlock M et al. Am J Psychiatry. 2017 May 9. doi: 10.1176/appi.ajp-rj.2016.110206.
14. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). Arlington, Va.: American Psychiatric Association, 2013.
15. “What is Child Trauma?” The National Child Traumatic Stress Network.
16. The Philadelphia Project. Philadelphia ACE Survey.
17. “Addressing law enforcement violence as a public health issue.” Washington: American Public Health Association. 2018 Nov 13. Policy# 20811.
18. National Medical Association position statement on police use of force. NMA 2016.
19. “APA and NMA jointly condemn systemic racism in America.” 2020 Jun 16.
20. APA Strategic Plan. 2015 Mar.
On the Friday evening after the public execution of George Floyd, we were painfully reminded of the urgency to address the inadequate management of race, racism, and anti-blackness in medical education, residency training, and postgraduate continuing medical education.
The reminder did not originate from the rioting that was occurring in some cities, though we could feel the ground shifting beneath our feet as civic protests that began in U.S. cities spread around the globe. Instead, it occurred during a webinar we were hosting for psychiatry residents focused on techniques for eliminating blind spots in the management of race in clinical psychotherapy supervision. (Dr. Jessica Isom chaired the webinar, Dr. Flavia DeSouza and Dr. Myra Mathis comoderated, and Dr. Ebony Dennis and Dr. Constance E. Dunlap served as discussants.)
Our panel had presented an ambitious agenda that included reviewing how the disavowal of bias, race, racism, and anti-blackness contributes to ineffective psychotherapy, undermines the quality of medical care, and perpetuates mental health disparities. We spent some time exploring how unacknowledged and unexamined conscious and unconscious racial stereotypes affect interpersonal relationships, the psychotherapeutic process, and the supervisory experience. Our presentation included a clinical vignette demonstrating how racism, colorism, and anti-blackness have global impact, influencing the self-esteem, identity formation, and identity consolidation of immigrants as they grapple with the unique form of racism that exists in America. Other clinical vignettes demonstrated blind spots that were retroactively identified though omitted in supervisory discussions. We also discussed alternative interventions and interpretations of the material presented.1-5
Because 21st-century trainees are generally psychologically astute and committed to social justice, we did two things. First, before the webinar, we provided them access to a prerecorded explanation of object relations theorist Melanie Klein’s paranoid-schizoid and depressive positions concepts, which were applied to theoretically explain the development of race, specifically the defenses used by early colonists that contributed to the development of “whiteness” and “blackness” as social constructs, and their influence on the development of the U.S. psyche. For example, as early colonists attempted to develop new and improved identities distinct from those they had in their homelands, they used enslaved black people (and other vulnerable groups) to “other.” What we mean here by othering is the process of using an other to project one’s badness into in order to relieve the self of uncomfortable aspects and feelings originating within the self. If this other accepts the projection (which is often the case with vulnerable parties), the self recognizes, that is, identifies (locates) the bad they just projected in the other, who is now experienced as a bad-other. This is projection in action. If the other accepts the projection and behaves accordingly, for example, in a manner that reflects badness, this becomes projective identification. Conversely, if the other does not accept these projections, the self (who projects) is left to cope with aspects of the self s/he might not have the capacity to manage. By capacity, we are speaking of the Bionian idea of the ability to experience an extreme emotion while also being able to think. Without the ego strength to cope with bad aspects of the self, the ego either collapses (and is unable to think) or further projection is attempted.6-8
We have seen this latter dynamic play out repeatedly when police officers fatally shoot black citizens and then claim that they feared for their lives; these same officers have been exonerated by juries by continuing to portray the deceased victims as threatening, dangerous objects not worthy of living. We are also seeing a global movement of black and nonblack people who are in touch with a justified rage that has motivated them to return these projections by collectively protesting, and in some cases, by rioting.
Back to the webinar
In anticipating the residents’ curiosity, impatience, and anger about the lack of progress, the second thing we did was to show a segment from the “Black Psychoanalysts Speak” trailer. In the clip played, senior psychoanalyst Kirkland C. Vaughans, PhD, shares: “The issue of race so prompts excessive anxiety that it blocks off our ability to think.”
We showed this clip to validate the trainees’ frustrations about the difficulty the broader establishment has had with addressing this serious, longstanding public health problem. We wanted these young psychiatrists to know that there are psychoanalysts, psychiatrists, psychologists, and social workers who have been committed to this work, even though the contributions of this diverse group have curiously been omitted from education and training curricula.9
So, what happened? What was the painful reminder? After the formal panel presentations, a black male psychiatry resident recounted his experience in a clinical supervision meeting that had occurred several days after the murder of George Floyd. In short, a patient had shared his reactions to yet another incident of fatal police use of force and paused to ask how the resident physician, Dr. A., was doing. The question was experienced as sincere concern about the psychiatrist’s mental well-being. The resident was not sure how to answer this question since it was a matter of self-disclosure, which was a reasonable and thoughtful consideration for a seasoned clinician and, certainly, for a novice therapist. The supervisor, Dr. B., seemingly eager to move on, to not think about this, responded to the resident by saying: “Now tell me about the patient.” In other words, what had just been shared by the resident – material that featured a patient’s reaction to another killing of a black man by police and the patient’s expressed concern for his black psychiatrist, and this resident physician appropriately seeking space in supervision to process and receive guidance about how to respond – all of this was considered separate (split off from) and extraneous to the patient’s treatment and the resident’s training. This is a problem. And, unfortunately, this problem or some variation of it is not rare.
Why is this still the state of affairs when we have identified racism as a major health concern and our patients and our trainees are asking for help?
Rethinking a metaphor
Despite calls to action over the last 50 years to encourage medicine to effectively address race and racism, deficits remain in didactic education, clinical rotations, and supervisory experiences of trainees learning how to do psychodynamic psychotherapy.8-10 Earlier that evening, we used the metaphor of a vehicular blind spot to capture what we believe occurs insupervision. Like drivers, supervisors generally have the ability to see. However, there are places (times) and positions (stances) that block their vision (awareness). Racism – whether institutionalized, interpersonally mediated, or internalized – also contributes to this blindness.
As is true of drivers managing a blind spot, what is required is for the drivers – the supervisors – to lean forward or reposition themselves so as to avoid collisions, maintain safety, and continue on course. We use this metaphor because it is understood that any clinician providing psychodynamic supervision to psychiatry residents, regardless of professional discipline, has the requisite skills and training.10-13
Until May 25, we thought eliminating blind spots would be effective. But, in the aftermath of the police killing of George Floyd, our eyes have been opened.
Hiding behind the blue wall of silence is an establishment that has looked the other way while black and brown women, men, and children have come to live in fear as a result of the state-sanctioned violence that repeatedly occurs across the nation. Excessive police use of force is a public health issue of crisis magnitude. However, the house of medicine, like many other established structures in society, has colluded with the societal constructs that have supported law enforcement by remaining willfully blind, often neutral, and by refusing to make the necessary adjustments, including connecting the dots between police violence and physical and mental health.
For example, racism has never been listed even in the index of the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders.14 Being the victim of police use of force is not generally regarded as an adverse childhood experience, even though communities that are heavily policed experience harassment by law enforcement on a regular basis. The 12 causes of trauma listed on the website15 of the National Child Traumatic Stress Network – bullying, community violence, complex trauma, disasters, early childhood trauma, intimate partner violence, medical trauma, physical abuse, refugee trauma, sexual abuse, terrorism and violence, and traumatic grief – do not include maltreatment, abuse, or trauma resulting from interactions with members of law enforcement. Much of the adverse childhood experiences literature focuses on white, upper middle class children and on experiences within the home. When community level experiences, such as discrimination based on race or ethnicity, are included, as in the Philadelphia ACES study,16 as many as 40% reported ACE scores of greater than 4 for community level exposures.
As psychiatrists, we recognize the psychic underpinnings and parallels between the psychic projections onto black and brown people and the actual bullets pumped into the bodies of black and brown people; there is a lurid propensity to use these others as repositories. Those who have the privilege of being protected by law enforcement and the ability to avoid being used as containers for the psychic projections and bullets of some police officers also have the privilege of compartmentalizing and looking the other way when excessive acts of force – projections and projectiles – are used on other human beings. This partly explains why the injuries and deaths of black and brown people caused by police officers’ excessive use of force have continued even though these unjustified deaths are widely televised and disseminated via various social media platforms.
Prior to the death of George Floyd on May 25, other than the American Public Health Association, the National Medical Association (NMA) was the only major medical organization to issue a call to consider police use of force as a public health issue. In its July 2016 press release, provided in the aftermath of the death of Freddie Gray while in the custody of Baltimore police officers, the NMA summarized the scope of injuries citizens sustain during “the pre-custody (commission of a crime, during a fight, chase, and apprehension, during a siege or hostage situation, or during restraint or submission), custody (soon after being admitted to jail, during interrogation, during incarceration, or legal execution), and post-custody (revenge by police or rival criminals or after reentry into the community)” periods. It is noteworthy that the scope of these injuries is comparable to those encountered in a combat zone.17,18 According to the NMA:
“Injuries sustained by civilians at the hands of law enforcement include gunshot wounds, skull fractures, cervical spine injuries, facial fractures, broken legs, blunt trauma orbital floor fractures, laryngeal cartilage fractures, shoulder dislocations, cuts and bruises, concussions, hemorrhage, choking (positional or due to upper body holds), abdominal trauma, hemothorax, and pneumothorax. Complications of such injuries include posttraumatic brain swelling, infections following open fractures and lacerations, hydrocephalus due to blood or infection, as well as subdural and epidural hematomas and, in the most severe cases, death.”
In addition, there are multiple emotional and psychiatric sequelae of these injuries for the victims, families, upstanders, bystanders, and those viewing these images via various social media platforms. Increasingly, many are experiencing retraumatization each time a new death is reported. How do we explain that we are turning away from this as physicians and trainers of physicians? Seeing and not seeing – all of the methods used to avert one’s gaze and look the other way (to protect the psyches of nonmarginalized members of society from being disturbed and possibly traumatized) – these key defense mechanisms creep into consulting rooms and become fertile ground for the enactment described above.
Yet, there is reason to believe in change. It’s not simply because we are mental health professionals and that’s what we do. With the posting of position statements issued by major corporations and a growing number of medical organizations, many of us are experiencing a mixture of hope, anger, and sadness. Hope that widespread awareness will continue to tilt the axis of our country in a manner that opens eyes – and hearts – so that real work can be done; and anger and sadness because it has taken 400 years to receive even this level of validation.
In the meantime, we are encouraged by a joint position statement recently issued by the APA and the NMA, the first joint effort by these two medical organizations to partner and advocate for criminal justice reform. We mention this statement because the NMA has been committed to the needs of the black community since its inception in 1895, and the APA has as its mission a commitment to serve “the needs of evolving, diverse, underrepresented, and underserved patient populations” ... and the resources to do so. This is the kind of partnership that could transform words into meaningful action.19,20
Of course, resident psychiatrist Dr. A. had begun supervision with the discussion of his dyadic experience with his patient, which is set in the context of a global coronavirus pandemic that is disproportionately affecting black and brown people. And, while his peers are marching in protest, he and his fellow trainees deserve our support as they deal with their own psychic pain and prepare to steady themselves. For these psychiatrists will be called to provide care to those who will consult them once they begin to grapple with the experiences and, in some cases, traumas that have compelled them to take action and literally risk their safety and lives while protesting.
That evening, the residents were hungry for methods to fill the gaps in their training and supervision. In some cases, we provided scripts to be taken back to supervision. For example, the following is a potential scripted response for the supervisor in the enactment described above:
Resident speaking to supervisor: This is a black patient who, like many others, is affected by the chronic, repeated televised images of black men killed by police. I am also a black man.
I think what I have shared is pertinent to the patient’s care and my experience as a black male psychiatrist who will need to learn how to address this in my patients who are black and for other racialized groups, as well as with whites who might have rarely been cared for by a black man. Can we discuss this?
We also anticipated that some residents would need to exercise their right to request reassignment to another supervisor. And, until we do better at listening, seeing, and deepening our understanding, outside and inside the consulting room and in supervision, more residents might need to steer around those who have the potential to undermine training and adversely affect treatment. But, as a professional medical community in crisis, do we really want to proceed in such an ad hoc fashion?
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures.
Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Dr. DeSouza is a PGY-4 psychiatry resident and public psychiatry fellow in the department of psychiatry at Yale University, New Haven, Conn. Her professional interests include health services development and delivery in low- and middle-income settings, as well as the intersection of mental health and spirituality. She has no disclosures.
Dr. Isom is a staff psychiatrist at the Codman Square Health Center in Dorchester, Mass., and Boston Medical Center. Her interests include racial mental health equity and population health approaches to community psychiatry. She has no disclosures.
Dr. Mathis is an addictions fellow in the department of psychiatry at Yale University and former programwide chief resident at Yale. Her interests include the intersection of racial justice and mental health, health equity, and spirituality. She has no disclosures.
References
1. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2001.
2. Banaji MR and Greenwald AG. Blindspot: Hidden Biases of Good People. New York: Delacorte Press, 2013.
3. Anekwe ON. Voices in Bioethics. 2014.
4. Soute BJ. The American Psychoanalyst Magazine. 2017 Winter/Spring.
5. Powell DR. J Am Psychoanal Assoc. 2019 Jan 8. doi: 10.1177/000306511881847.
6. Allen TW. The Invention of the White Race. London: Verso, 1994.
7. Klein M. Int J Psychoanal. 1946;27(pt.3-4):99-100.
8. Bion WR. (1962b). Psychoanal Q. 2013 Apr;82(2):301-10.
9. Black Psychoanalysts Speak trailer.
10. Thomas A and Sillen S. Racism and Psychiatry. New York: Brunner/Mazel, 1972.
11. Jones BE et al. Am J Psychiatry. 1970 Dec;127(6):798-803.
12. Sabshin M et al. Am J Psychiatry. 1970 Dec;126(6):787-93.
13. Medlock M et al. Am J Psychiatry. 2017 May 9. doi: 10.1176/appi.ajp-rj.2016.110206.
14. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). Arlington, Va.: American Psychiatric Association, 2013.
15. “What is Child Trauma?” The National Child Traumatic Stress Network.
16. The Philadelphia Project. Philadelphia ACE Survey.
17. “Addressing law enforcement violence as a public health issue.” Washington: American Public Health Association. 2018 Nov 13. Policy# 20811.
18. National Medical Association position statement on police use of force. NMA 2016.
19. “APA and NMA jointly condemn systemic racism in America.” 2020 Jun 16.
20. APA Strategic Plan. 2015 Mar.
One-fifth of stem cell transplantation patients develop PTSD
Approximately one-fifth of patients undergoing hematopoietic stem cell transplantation (HSCT) develop posttraumatic stress disorder (PTSD), based on a retrospective analysis.
Patient factors at time of transplantation, such as low quality of life and high anxiety, predicted PTSD 6 months later, reported lead author Sarah Griffith, MD, of Massachusetts General Hospital, Boston, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
“We know that patients admitted for HSCT are often isolated in the hospital for a prolonged period of time, usually about 3-4 weeks, and that they endure substantial toxicities that impact both their physical and psychological well-being,” Dr. Griffith said. “We also know from the literature that HSCT can be considered a traumatic event and that it may lead to clinically significant PTSD symptoms.” But studies evaluating the prevalence and characteristics of PTSD in this patient population have been lacking, she noted.
Dr. Griffith and her colleagues therefore conducted a retrospective analysis involving 250 adults with hematologic malignancies who underwent autologous or allogeneic HSCT during clinical trials conducted from 2014 to 2016. Median patient age was 56 years.
The first objective of the study was to measure the prevalence of PTSD. The second was to characterize features of PTSD such as intrusion, which entails reliving experiences in the form of nightmares or flashbacks, and hypervigilance, which encompasses insomnia, irritability, and hyperarousal for threat. The third objective was to determine risk factors at baseline.
At time of admission for HSCT, after 2 weeks of hospitalization, and again 6 months after transplantation, patients were evaluated using the Functional Assessment of Cancer Therapy–Bone Marrow Transplant (FACT-BMT), and the Hospital Anxiety and Depression Scale (HADS), which measured of quality of life, anxiety, and depression. Six months after HSCT, patients also underwent screening for PTSD with the Post-Traumatic Stress Checklist (PTSD-CL). Multivariate regression models were used to determine predictive risk factors.
Six months after HSCT, 18.9% of patients had clinically significant PTSD symptoms; most common were symptoms of avoidance (92.3%), hypervigilance (92.3%), and intrusion (76.9%). Among those who did not have clinically significant PTSD, almost one-quarter (24.5%) demonstrated significant hypervigilance, while 13.7% showed symptoms of avoidance.
“Clinically significant PTSD symptoms are common in the transplant population,” Dr. Griffith said.
Baseline predictors of PTSD included single status and lower quality of life. More severe PTSD was predicted by single status, younger age, higher baseline scores for anxiety or depression, and increased anxiety during hospitalization.
Concluding her presentation, Dr. Griffith said that the findings, while correlative and not causative, should prompt concern and intervention.
“It is very important to be aware of and to manage PTSD symptoms in these patients,” she said. “There are several baseline factors that can be identified prior to HSCT that may illuminate patients at risk for developing worse PTSD symptoms down the road, and these patients may benefit from tailored supportive care interventions.”
Specifically, Dr. Griffith recommended integrating palliative care into hospitalization, as this has been shown to reduce anxiety.
In a virtual presentation, invited discussant Nirali N. Shah, MD, of the National Cancer Institute, Bethesda, Md., highlighted the importance of the findings, while also noting that the impact of palliative care on risk of PTSD has yet to be demonstrated.
Dr. Shah suggested that future research may be improved through use of a formal diagnosis for PTSD, instead of a PTSD checklist, as was used in the present study.
“And certainly long-term follow-up would be important to evaluate the utility of this tool looking at symptoms beyond 6 months,” she said.
Dr. Shah went on to discuss the relevance of the findings for pediatric populations, as children may face unique risk factors and consequences related to PTSD.
“[PTSD in children] may be impacted by family dynamics and structure,” Dr. Shah said. “Children may also have significant neurocognitive implications as a result of their underlying disease or prior therapy. They may experience chronic pain as they go out into adulthood and long-term survivorship, and may also struggle with symptoms of anxiety and depression.”
According to Dr. Shah, one previous study involving more than 6,000 adult survivors of childhood cancer found that PTSD was relatively common, with prevalence rate of 9%, suggesting that interventional work is necessary.
“Applying the data in the study from Griffith et al. suggests that evaluation in the more proximal posttransplant period for children is needed to specifically evaluate PTSD and symptoms thereof, and to try to use this to identify an opportunity for intervention,” Dr. Shah said.
“Pediatric-specific assessments are essential to optimally capture disease and/or age-specific considerations,” she added.
The study was funded by the Lymphoma and Leukemia Society. The investigators disclosed additional relationships with Vector Oncology, Pfizer, AstraZeneca, and Gaido Health/BCG Digital Ventures.
SOURCE: Griffith et al. ASCO 2020. Abstract # 7505.
Approximately one-fifth of patients undergoing hematopoietic stem cell transplantation (HSCT) develop posttraumatic stress disorder (PTSD), based on a retrospective analysis.
Patient factors at time of transplantation, such as low quality of life and high anxiety, predicted PTSD 6 months later, reported lead author Sarah Griffith, MD, of Massachusetts General Hospital, Boston, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
“We know that patients admitted for HSCT are often isolated in the hospital for a prolonged period of time, usually about 3-4 weeks, and that they endure substantial toxicities that impact both their physical and psychological well-being,” Dr. Griffith said. “We also know from the literature that HSCT can be considered a traumatic event and that it may lead to clinically significant PTSD symptoms.” But studies evaluating the prevalence and characteristics of PTSD in this patient population have been lacking, she noted.
Dr. Griffith and her colleagues therefore conducted a retrospective analysis involving 250 adults with hematologic malignancies who underwent autologous or allogeneic HSCT during clinical trials conducted from 2014 to 2016. Median patient age was 56 years.
The first objective of the study was to measure the prevalence of PTSD. The second was to characterize features of PTSD such as intrusion, which entails reliving experiences in the form of nightmares or flashbacks, and hypervigilance, which encompasses insomnia, irritability, and hyperarousal for threat. The third objective was to determine risk factors at baseline.
At time of admission for HSCT, after 2 weeks of hospitalization, and again 6 months after transplantation, patients were evaluated using the Functional Assessment of Cancer Therapy–Bone Marrow Transplant (FACT-BMT), and the Hospital Anxiety and Depression Scale (HADS), which measured of quality of life, anxiety, and depression. Six months after HSCT, patients also underwent screening for PTSD with the Post-Traumatic Stress Checklist (PTSD-CL). Multivariate regression models were used to determine predictive risk factors.
Six months after HSCT, 18.9% of patients had clinically significant PTSD symptoms; most common were symptoms of avoidance (92.3%), hypervigilance (92.3%), and intrusion (76.9%). Among those who did not have clinically significant PTSD, almost one-quarter (24.5%) demonstrated significant hypervigilance, while 13.7% showed symptoms of avoidance.
“Clinically significant PTSD symptoms are common in the transplant population,” Dr. Griffith said.
Baseline predictors of PTSD included single status and lower quality of life. More severe PTSD was predicted by single status, younger age, higher baseline scores for anxiety or depression, and increased anxiety during hospitalization.
Concluding her presentation, Dr. Griffith said that the findings, while correlative and not causative, should prompt concern and intervention.
“It is very important to be aware of and to manage PTSD symptoms in these patients,” she said. “There are several baseline factors that can be identified prior to HSCT that may illuminate patients at risk for developing worse PTSD symptoms down the road, and these patients may benefit from tailored supportive care interventions.”
Specifically, Dr. Griffith recommended integrating palliative care into hospitalization, as this has been shown to reduce anxiety.
In a virtual presentation, invited discussant Nirali N. Shah, MD, of the National Cancer Institute, Bethesda, Md., highlighted the importance of the findings, while also noting that the impact of palliative care on risk of PTSD has yet to be demonstrated.
Dr. Shah suggested that future research may be improved through use of a formal diagnosis for PTSD, instead of a PTSD checklist, as was used in the present study.
“And certainly long-term follow-up would be important to evaluate the utility of this tool looking at symptoms beyond 6 months,” she said.
Dr. Shah went on to discuss the relevance of the findings for pediatric populations, as children may face unique risk factors and consequences related to PTSD.
“[PTSD in children] may be impacted by family dynamics and structure,” Dr. Shah said. “Children may also have significant neurocognitive implications as a result of their underlying disease or prior therapy. They may experience chronic pain as they go out into adulthood and long-term survivorship, and may also struggle with symptoms of anxiety and depression.”
According to Dr. Shah, one previous study involving more than 6,000 adult survivors of childhood cancer found that PTSD was relatively common, with prevalence rate of 9%, suggesting that interventional work is necessary.
“Applying the data in the study from Griffith et al. suggests that evaluation in the more proximal posttransplant period for children is needed to specifically evaluate PTSD and symptoms thereof, and to try to use this to identify an opportunity for intervention,” Dr. Shah said.
“Pediatric-specific assessments are essential to optimally capture disease and/or age-specific considerations,” she added.
The study was funded by the Lymphoma and Leukemia Society. The investigators disclosed additional relationships with Vector Oncology, Pfizer, AstraZeneca, and Gaido Health/BCG Digital Ventures.
SOURCE: Griffith et al. ASCO 2020. Abstract # 7505.
Approximately one-fifth of patients undergoing hematopoietic stem cell transplantation (HSCT) develop posttraumatic stress disorder (PTSD), based on a retrospective analysis.
Patient factors at time of transplantation, such as low quality of life and high anxiety, predicted PTSD 6 months later, reported lead author Sarah Griffith, MD, of Massachusetts General Hospital, Boston, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
“We know that patients admitted for HSCT are often isolated in the hospital for a prolonged period of time, usually about 3-4 weeks, and that they endure substantial toxicities that impact both their physical and psychological well-being,” Dr. Griffith said. “We also know from the literature that HSCT can be considered a traumatic event and that it may lead to clinically significant PTSD symptoms.” But studies evaluating the prevalence and characteristics of PTSD in this patient population have been lacking, she noted.
Dr. Griffith and her colleagues therefore conducted a retrospective analysis involving 250 adults with hematologic malignancies who underwent autologous or allogeneic HSCT during clinical trials conducted from 2014 to 2016. Median patient age was 56 years.
The first objective of the study was to measure the prevalence of PTSD. The second was to characterize features of PTSD such as intrusion, which entails reliving experiences in the form of nightmares or flashbacks, and hypervigilance, which encompasses insomnia, irritability, and hyperarousal for threat. The third objective was to determine risk factors at baseline.
At time of admission for HSCT, after 2 weeks of hospitalization, and again 6 months after transplantation, patients were evaluated using the Functional Assessment of Cancer Therapy–Bone Marrow Transplant (FACT-BMT), and the Hospital Anxiety and Depression Scale (HADS), which measured of quality of life, anxiety, and depression. Six months after HSCT, patients also underwent screening for PTSD with the Post-Traumatic Stress Checklist (PTSD-CL). Multivariate regression models were used to determine predictive risk factors.
Six months after HSCT, 18.9% of patients had clinically significant PTSD symptoms; most common were symptoms of avoidance (92.3%), hypervigilance (92.3%), and intrusion (76.9%). Among those who did not have clinically significant PTSD, almost one-quarter (24.5%) demonstrated significant hypervigilance, while 13.7% showed symptoms of avoidance.
“Clinically significant PTSD symptoms are common in the transplant population,” Dr. Griffith said.
Baseline predictors of PTSD included single status and lower quality of life. More severe PTSD was predicted by single status, younger age, higher baseline scores for anxiety or depression, and increased anxiety during hospitalization.
Concluding her presentation, Dr. Griffith said that the findings, while correlative and not causative, should prompt concern and intervention.
“It is very important to be aware of and to manage PTSD symptoms in these patients,” she said. “There are several baseline factors that can be identified prior to HSCT that may illuminate patients at risk for developing worse PTSD symptoms down the road, and these patients may benefit from tailored supportive care interventions.”
Specifically, Dr. Griffith recommended integrating palliative care into hospitalization, as this has been shown to reduce anxiety.
In a virtual presentation, invited discussant Nirali N. Shah, MD, of the National Cancer Institute, Bethesda, Md., highlighted the importance of the findings, while also noting that the impact of palliative care on risk of PTSD has yet to be demonstrated.
Dr. Shah suggested that future research may be improved through use of a formal diagnosis for PTSD, instead of a PTSD checklist, as was used in the present study.
“And certainly long-term follow-up would be important to evaluate the utility of this tool looking at symptoms beyond 6 months,” she said.
Dr. Shah went on to discuss the relevance of the findings for pediatric populations, as children may face unique risk factors and consequences related to PTSD.
“[PTSD in children] may be impacted by family dynamics and structure,” Dr. Shah said. “Children may also have significant neurocognitive implications as a result of their underlying disease or prior therapy. They may experience chronic pain as they go out into adulthood and long-term survivorship, and may also struggle with symptoms of anxiety and depression.”
According to Dr. Shah, one previous study involving more than 6,000 adult survivors of childhood cancer found that PTSD was relatively common, with prevalence rate of 9%, suggesting that interventional work is necessary.
“Applying the data in the study from Griffith et al. suggests that evaluation in the more proximal posttransplant period for children is needed to specifically evaluate PTSD and symptoms thereof, and to try to use this to identify an opportunity for intervention,” Dr. Shah said.
“Pediatric-specific assessments are essential to optimally capture disease and/or age-specific considerations,” she added.
The study was funded by the Lymphoma and Leukemia Society. The investigators disclosed additional relationships with Vector Oncology, Pfizer, AstraZeneca, and Gaido Health/BCG Digital Ventures.
SOURCE: Griffith et al. ASCO 2020. Abstract # 7505.
FROM ASCO 2020