User login
The future of medicine is RNA
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Every once in a while, medicine changes in a fundamental way, and we may not realize it while it’s happening. I wasn’t around in 1928 when Fleming discovered penicillin; or in 1953 when Watson, Crick, and Franklin characterized the double-helical structure of DNA.
But looking at medicine today, there are essentially two places where I think we will see, in retrospect, that we were at a fundamental turning point. One is artificial intelligence, which gets so much attention and hype that I will simply say yes, this will change things, stay tuned.
The other is a bit more obscure, but I suspect it may be just as impactful. That other thing is
I want to start with the idea that many diseases are, fundamentally, a problem of proteins. In some cases, like hypercholesterolemia, the body produces too much protein; in others, like hemophilia, too little.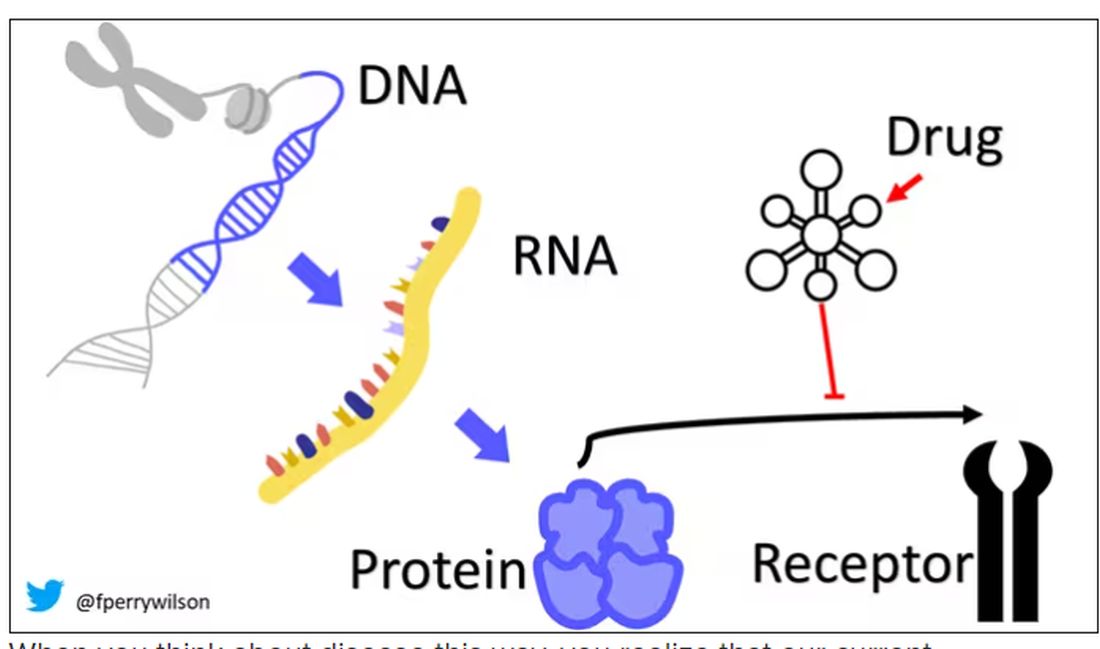
When you think about disease this way, you realize that our current medications take effect late in the disease game. We have these molecules that try to block a protein from its receptor, prevent a protein from cleaving another protein, or increase the rate that a protein is broken down. It’s all distal to the fundamental problem: the production of the bad protein in the first place.
Enter small inhibitory RNAs, or siRNAs for short, discovered in 1998 by Andrew Fire and Craig Mello at UMass Worcester. The two won the Nobel prize in medicine just 8 years later; that’s a really short time, highlighting just how important this discovery was. In contrast, Karikó and Weissman won the Nobel for mRNA vaccines this year, after inventing them 18 years ago.
siRNAs are the body’s way of targeting proteins for destruction before they are ever created. About 20 base pairs long, siRNAs seek out a complementary target mRNA, attach to it, and call in a group of proteins to destroy it. With the target mRNA gone, no protein can be created.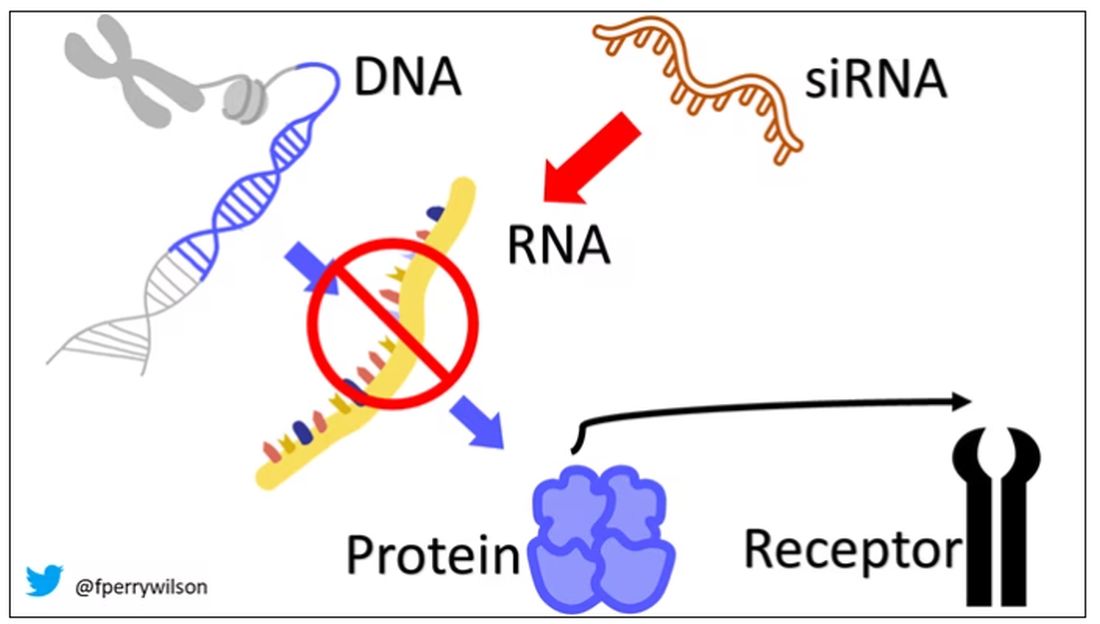
You see where this is going, right? How does high cholesterol kill you? Proteins. How does Staphylococcus aureus kill you? Proteins. Even viruses can’t replicate if their RNA is prevented from being turned into proteins.
So, how do we use siRNAs? A new paper appearing in JAMA describes a fairly impressive use case.
The background here is that higher levels of lipoprotein(a), an LDL-like protein, are associated with cardiovascular disease, heart attack, and stroke. But unfortunately, statins really don’t have any effect on lipoprotein(a) levels. Neither does diet. Your lipoprotein(a) level seems to be more or less hard-coded genetically.
So, what if we stop the genetic machinery from working? Enter lepodisiran, a drug from Eli Lilly. Unlike so many other medications, which are usually found in nature, purified, and synthesized, lepodisiran was created from scratch. It’s not hard. Thanks to the Human Genome Project, we know the genetic code for lipoprotein(a), so inventing an siRNA to target it specifically is trivial. That’s one of the key features of siRNA – you don’t have to find a chemical that binds strongly to some protein receptor, and worry about the off-target effects and all that nonsense. You just pick a protein you want to suppress and you suppress it.
Okay, it’s not that simple. siRNA is broken down very quickly by the body, so it needs to be targeted to the organ of interest – in this case, the liver, since that is where lipoprotein(a) is synthesized. Lepodisiran is targeted to the liver by this special targeting label here.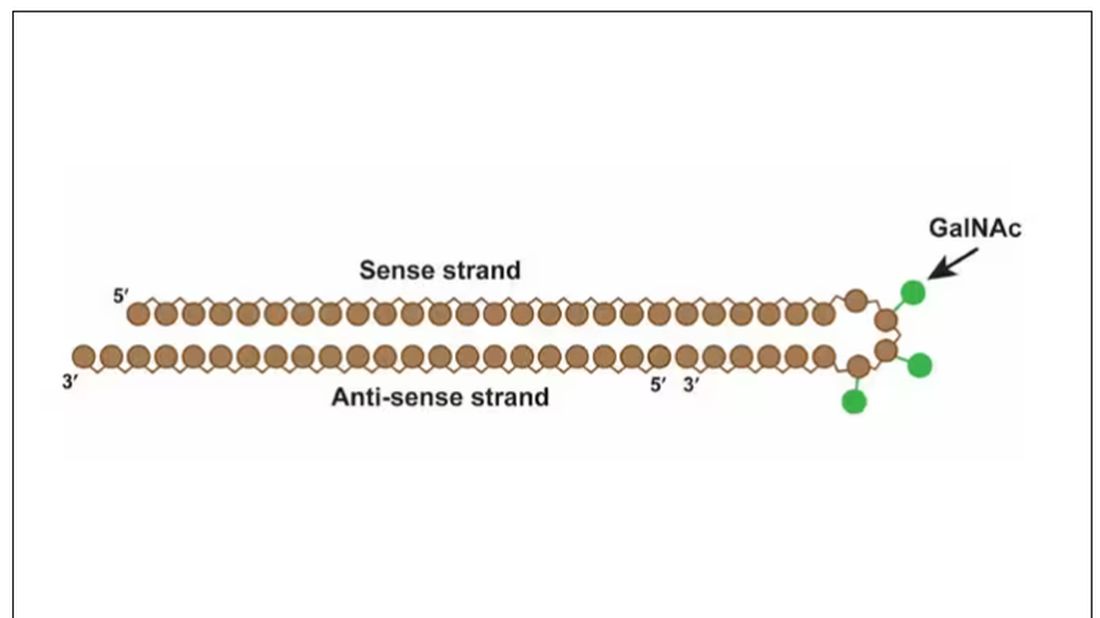
The report is a standard dose-escalation trial. Six patients, all with elevated lipoprotein(a) levels, were started with a 4-mg dose (two additional individuals got placebo). They were intensely monitored, spending 3 days in a research unit for multiple blood draws followed by weekly, and then biweekly outpatient visits. Once they had done well, the next group of six people received a higher dose (two more got placebo), and the process was repeated – six times total – until the highest dose, 608 mg, was reached.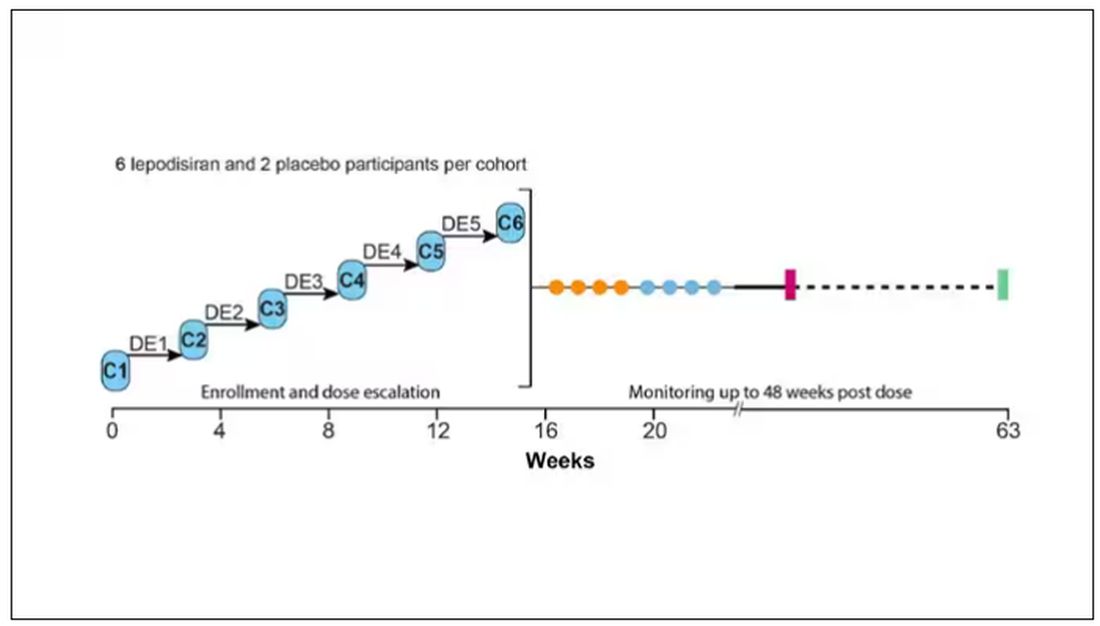
This is an injection, of course; siRNA wouldn’t withstand the harshness of the digestive system. And it’s only one injection. You can see from the blood concentration curves that within about 48 hours, circulating lepodisiran was not detectable.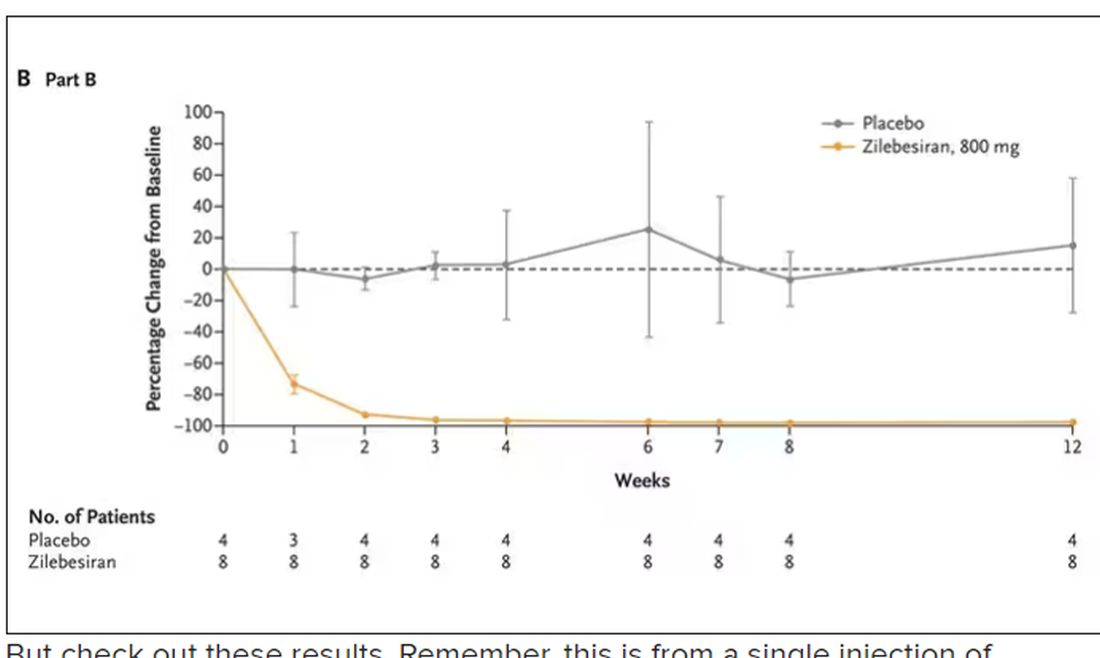
But check out these results. Remember, this is from a single injection of lepodisiran.
Lipoprotein(a) levels start to drop within a week of administration, and they stay down. In the higher-dose groups, levels are nearly undetectable a year after that injection.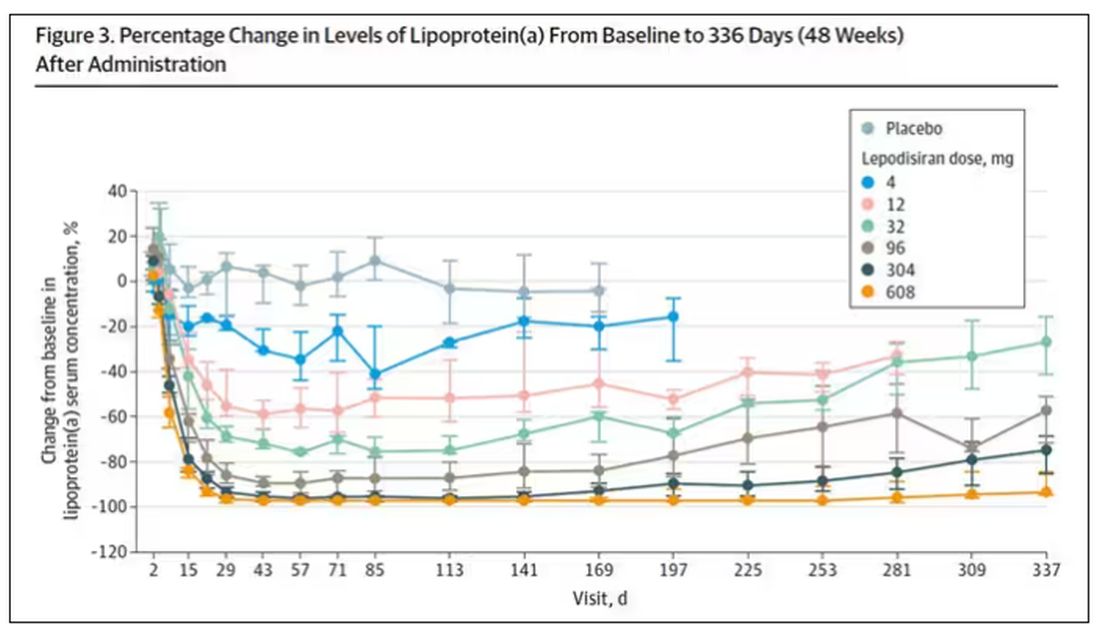
It was this graph that made me sit back and think that there might be something new under the sun. A single injection that can suppress protein synthesis for an entire year? If it really works, it changes the game.
Of course, this study wasn’t powered to look at important outcomes like heart attacks and strokes. It was primarily designed to assess safety, and the drug was pretty well tolerated, with similar rates of adverse events in the drug and placebo groups.
As crazy as it sounds, the real concern here might be that this drug is too good; is it safe to drop your lipoprotein(a) levels to zero for a year? I don’t know. But lower doses don’t have quite as strong an effect.
Trust me, these drugs are going to change things. They already are. In July, The New England Journal of Medicine published a study of zilebesiran, an siRNA that inhibits the production of angiotensinogen, to control blood pressure. Similar story: One injection led to a basically complete suppression of angiotensinogen and a sustained decrease in blood pressure.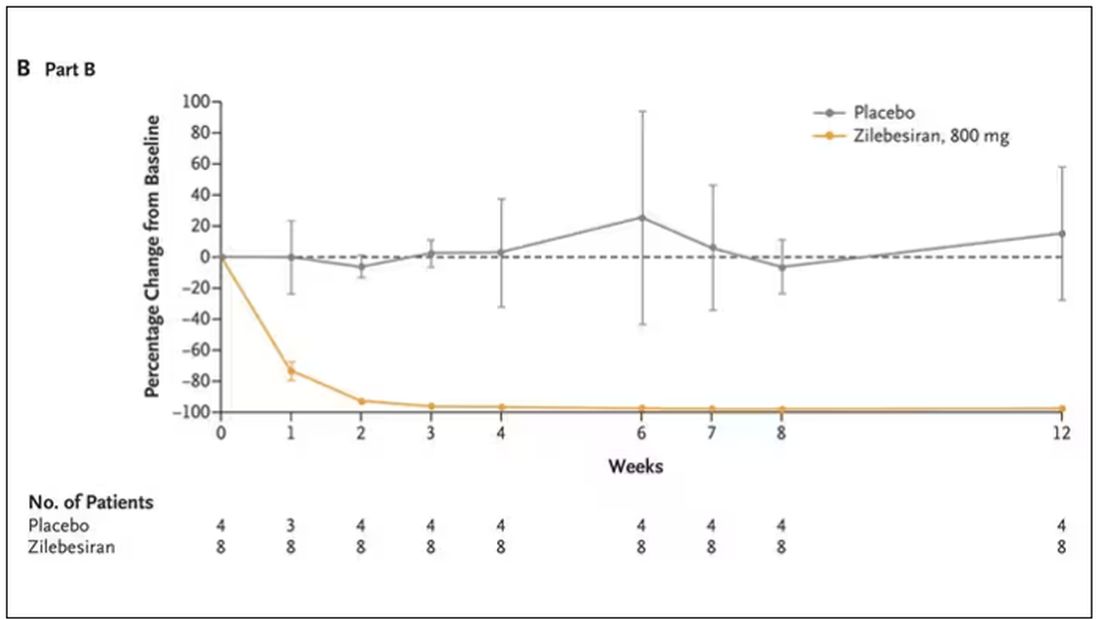
I’m not exaggerating when I say that there may come a time when you go to your doctor once a year, get your RNA shots, and don’t have to take any other medication from that point on. And that time may be, like, 5 years from now. It’s wild.
Seems to me that that rapid Nobel Prize was very well deserved.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships. This transcript has been edited for clarity.
A version of this article appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Every once in a while, medicine changes in a fundamental way, and we may not realize it while it’s happening. I wasn’t around in 1928 when Fleming discovered penicillin; or in 1953 when Watson, Crick, and Franklin characterized the double-helical structure of DNA.
But looking at medicine today, there are essentially two places where I think we will see, in retrospect, that we were at a fundamental turning point. One is artificial intelligence, which gets so much attention and hype that I will simply say yes, this will change things, stay tuned.
The other is a bit more obscure, but I suspect it may be just as impactful. That other thing is
I want to start with the idea that many diseases are, fundamentally, a problem of proteins. In some cases, like hypercholesterolemia, the body produces too much protein; in others, like hemophilia, too little.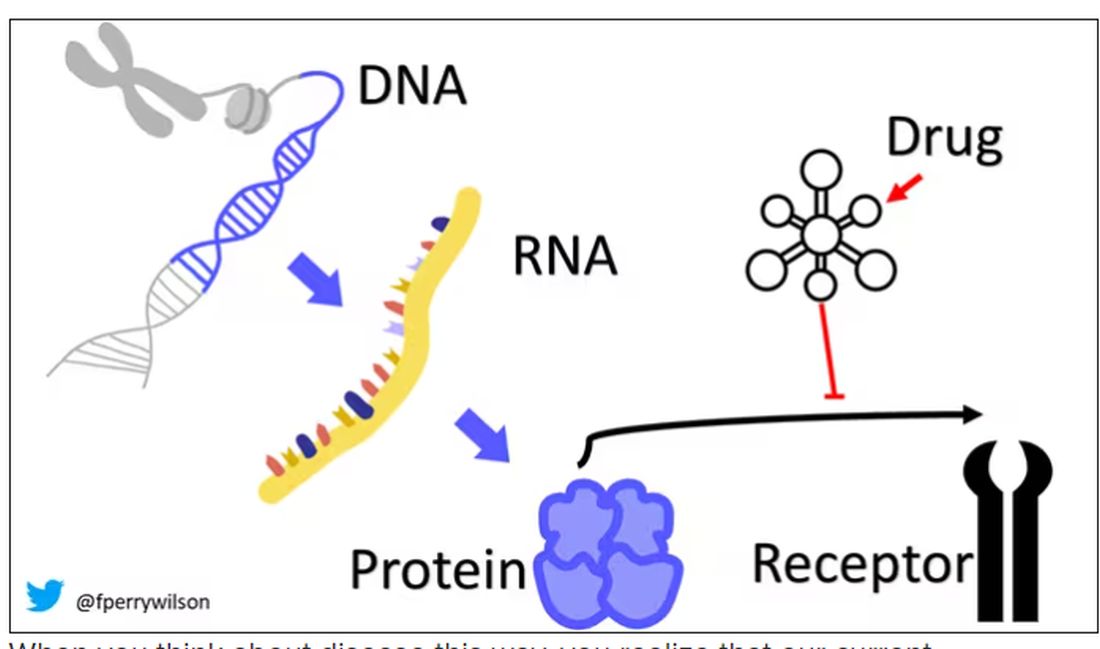
When you think about disease this way, you realize that our current medications take effect late in the disease game. We have these molecules that try to block a protein from its receptor, prevent a protein from cleaving another protein, or increase the rate that a protein is broken down. It’s all distal to the fundamental problem: the production of the bad protein in the first place.
Enter small inhibitory RNAs, or siRNAs for short, discovered in 1998 by Andrew Fire and Craig Mello at UMass Worcester. The two won the Nobel prize in medicine just 8 years later; that’s a really short time, highlighting just how important this discovery was. In contrast, Karikó and Weissman won the Nobel for mRNA vaccines this year, after inventing them 18 years ago.
siRNAs are the body’s way of targeting proteins for destruction before they are ever created. About 20 base pairs long, siRNAs seek out a complementary target mRNA, attach to it, and call in a group of proteins to destroy it. With the target mRNA gone, no protein can be created.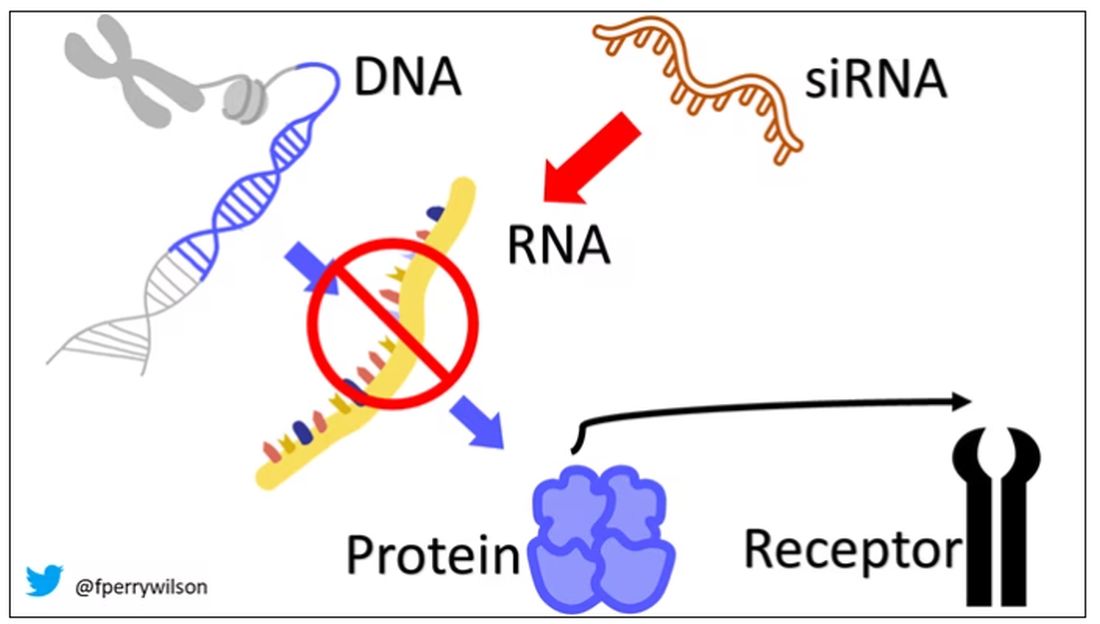
You see where this is going, right? How does high cholesterol kill you? Proteins. How does Staphylococcus aureus kill you? Proteins. Even viruses can’t replicate if their RNA is prevented from being turned into proteins.
So, how do we use siRNAs? A new paper appearing in JAMA describes a fairly impressive use case.
The background here is that higher levels of lipoprotein(a), an LDL-like protein, are associated with cardiovascular disease, heart attack, and stroke. But unfortunately, statins really don’t have any effect on lipoprotein(a) levels. Neither does diet. Your lipoprotein(a) level seems to be more or less hard-coded genetically.
So, what if we stop the genetic machinery from working? Enter lepodisiran, a drug from Eli Lilly. Unlike so many other medications, which are usually found in nature, purified, and synthesized, lepodisiran was created from scratch. It’s not hard. Thanks to the Human Genome Project, we know the genetic code for lipoprotein(a), so inventing an siRNA to target it specifically is trivial. That’s one of the key features of siRNA – you don’t have to find a chemical that binds strongly to some protein receptor, and worry about the off-target effects and all that nonsense. You just pick a protein you want to suppress and you suppress it.
Okay, it’s not that simple. siRNA is broken down very quickly by the body, so it needs to be targeted to the organ of interest – in this case, the liver, since that is where lipoprotein(a) is synthesized. Lepodisiran is targeted to the liver by this special targeting label here.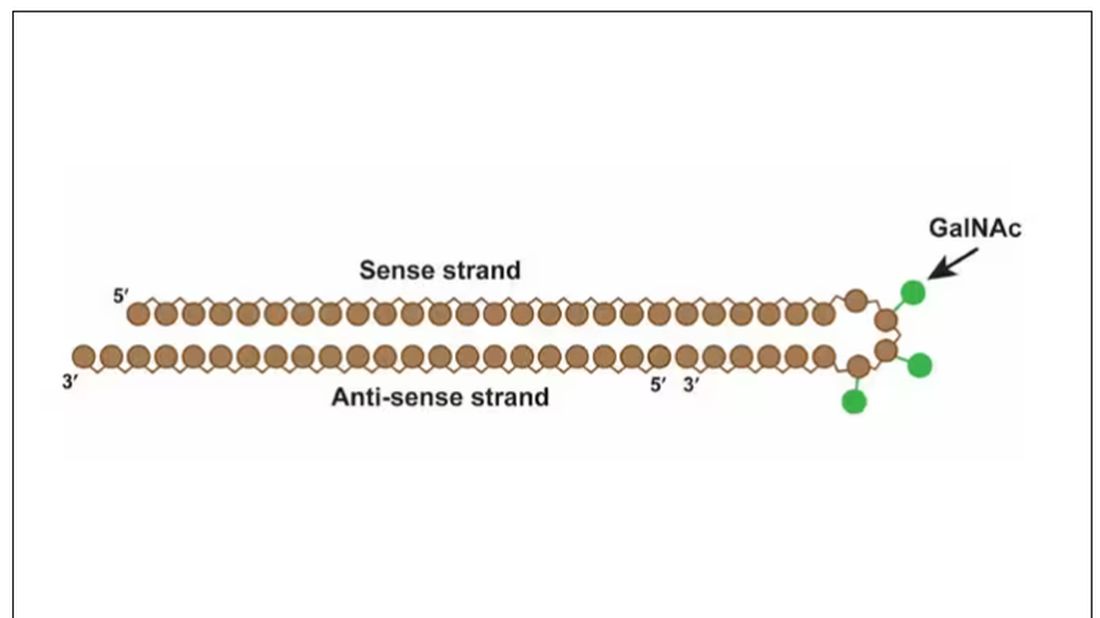
The report is a standard dose-escalation trial. Six patients, all with elevated lipoprotein(a) levels, were started with a 4-mg dose (two additional individuals got placebo). They were intensely monitored, spending 3 days in a research unit for multiple blood draws followed by weekly, and then biweekly outpatient visits. Once they had done well, the next group of six people received a higher dose (two more got placebo), and the process was repeated – six times total – until the highest dose, 608 mg, was reached.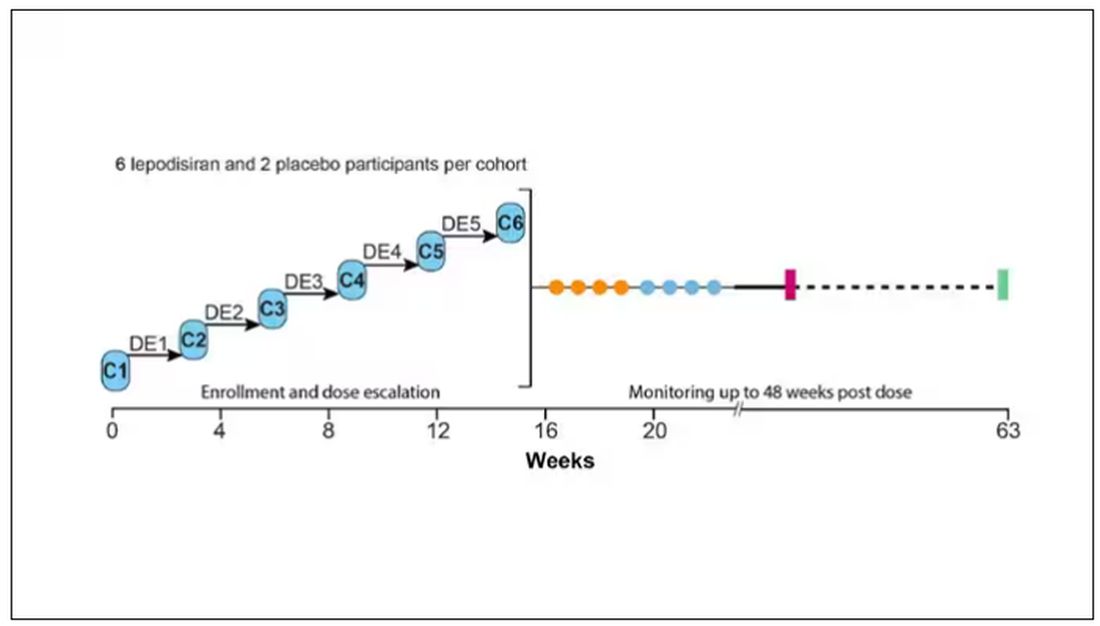
This is an injection, of course; siRNA wouldn’t withstand the harshness of the digestive system. And it’s only one injection. You can see from the blood concentration curves that within about 48 hours, circulating lepodisiran was not detectable.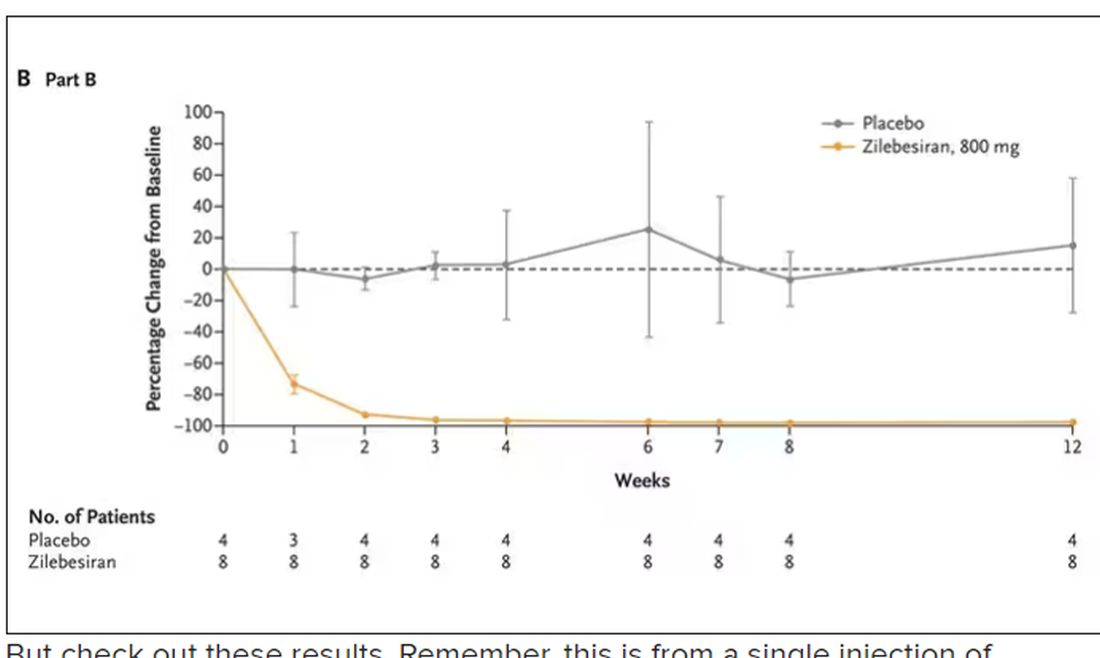
But check out these results. Remember, this is from a single injection of lepodisiran.
Lipoprotein(a) levels start to drop within a week of administration, and they stay down. In the higher-dose groups, levels are nearly undetectable a year after that injection.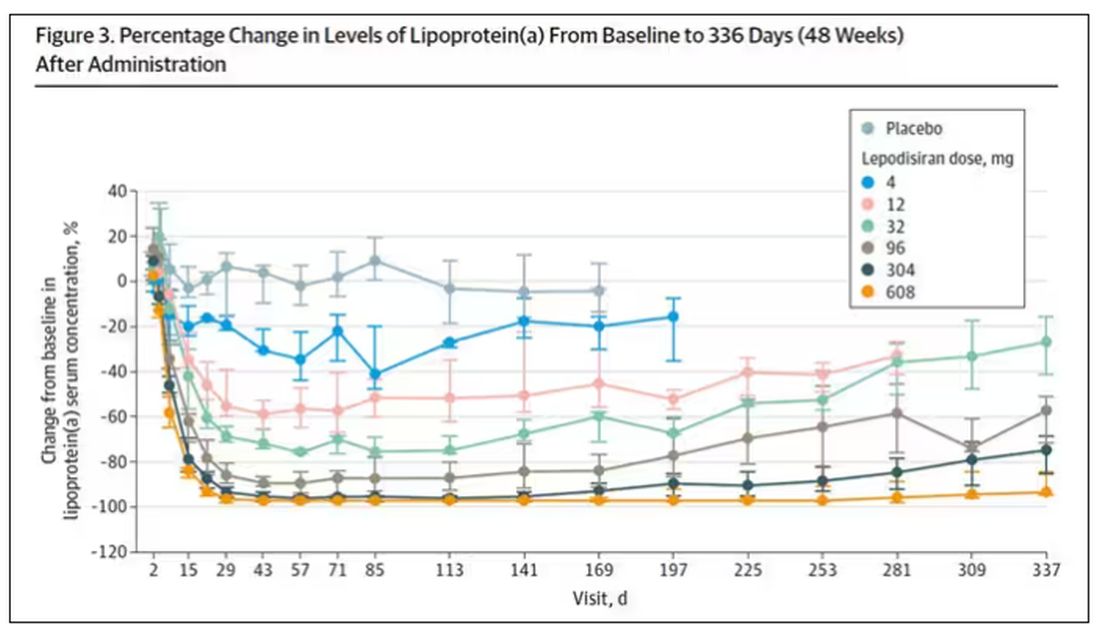
It was this graph that made me sit back and think that there might be something new under the sun. A single injection that can suppress protein synthesis for an entire year? If it really works, it changes the game.
Of course, this study wasn’t powered to look at important outcomes like heart attacks and strokes. It was primarily designed to assess safety, and the drug was pretty well tolerated, with similar rates of adverse events in the drug and placebo groups.
As crazy as it sounds, the real concern here might be that this drug is too good; is it safe to drop your lipoprotein(a) levels to zero for a year? I don’t know. But lower doses don’t have quite as strong an effect.
Trust me, these drugs are going to change things. They already are. In July, The New England Journal of Medicine published a study of zilebesiran, an siRNA that inhibits the production of angiotensinogen, to control blood pressure. Similar story: One injection led to a basically complete suppression of angiotensinogen and a sustained decrease in blood pressure.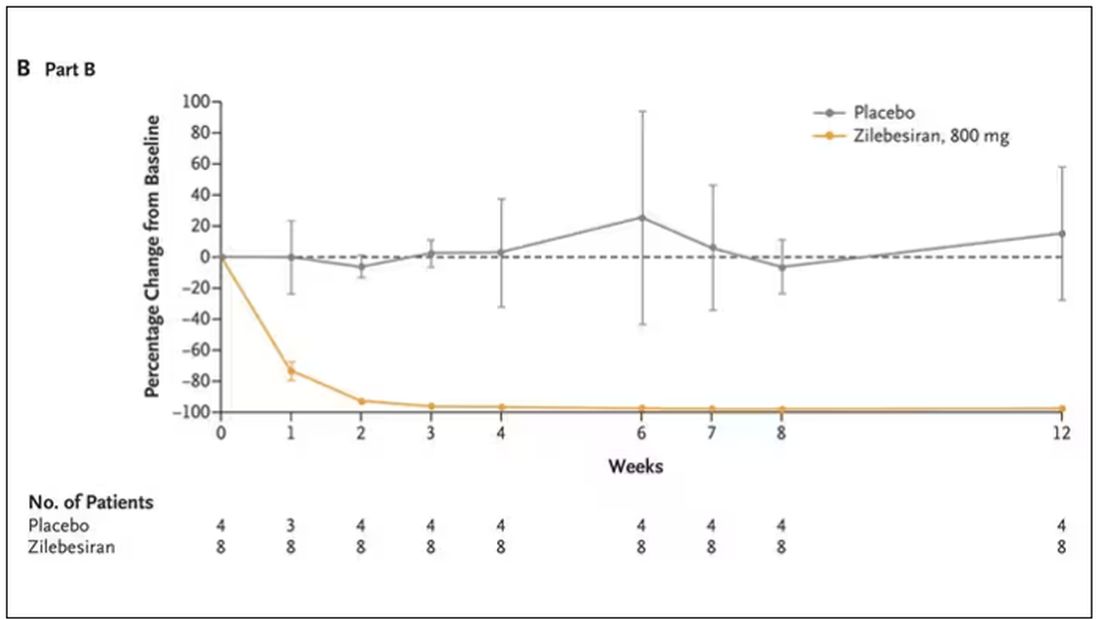
I’m not exaggerating when I say that there may come a time when you go to your doctor once a year, get your RNA shots, and don’t have to take any other medication from that point on. And that time may be, like, 5 years from now. It’s wild.
Seems to me that that rapid Nobel Prize was very well deserved.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships. This transcript has been edited for clarity.
A version of this article appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
Every once in a while, medicine changes in a fundamental way, and we may not realize it while it’s happening. I wasn’t around in 1928 when Fleming discovered penicillin; or in 1953 when Watson, Crick, and Franklin characterized the double-helical structure of DNA.
But looking at medicine today, there are essentially two places where I think we will see, in retrospect, that we were at a fundamental turning point. One is artificial intelligence, which gets so much attention and hype that I will simply say yes, this will change things, stay tuned.
The other is a bit more obscure, but I suspect it may be just as impactful. That other thing is
I want to start with the idea that many diseases are, fundamentally, a problem of proteins. In some cases, like hypercholesterolemia, the body produces too much protein; in others, like hemophilia, too little.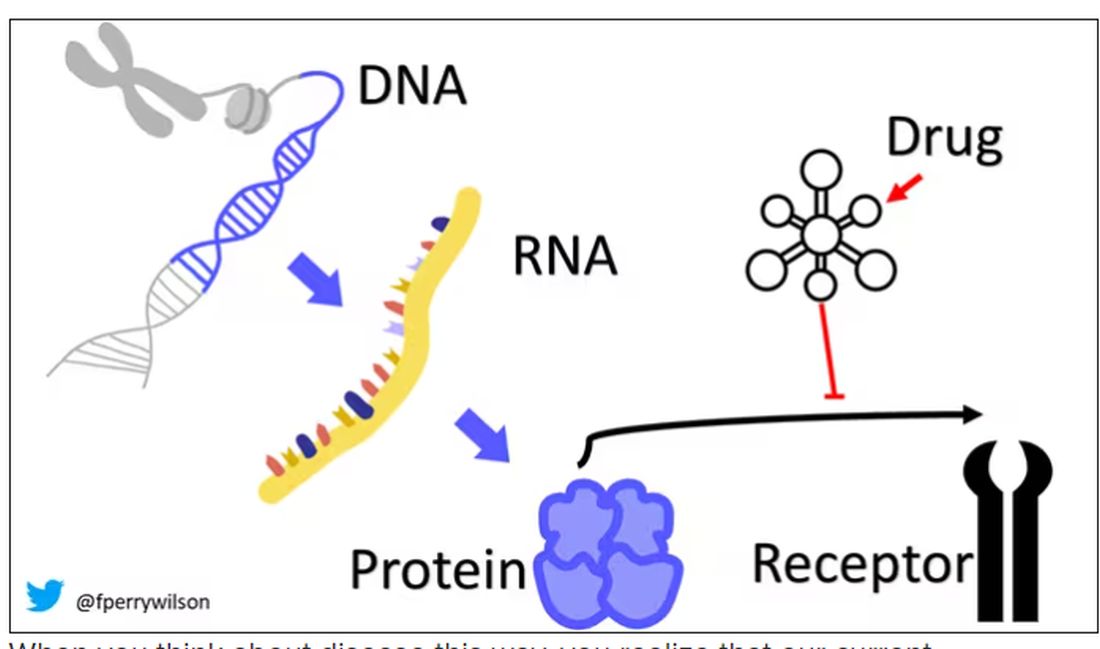
When you think about disease this way, you realize that our current medications take effect late in the disease game. We have these molecules that try to block a protein from its receptor, prevent a protein from cleaving another protein, or increase the rate that a protein is broken down. It’s all distal to the fundamental problem: the production of the bad protein in the first place.
Enter small inhibitory RNAs, or siRNAs for short, discovered in 1998 by Andrew Fire and Craig Mello at UMass Worcester. The two won the Nobel prize in medicine just 8 years later; that’s a really short time, highlighting just how important this discovery was. In contrast, Karikó and Weissman won the Nobel for mRNA vaccines this year, after inventing them 18 years ago.
siRNAs are the body’s way of targeting proteins for destruction before they are ever created. About 20 base pairs long, siRNAs seek out a complementary target mRNA, attach to it, and call in a group of proteins to destroy it. With the target mRNA gone, no protein can be created.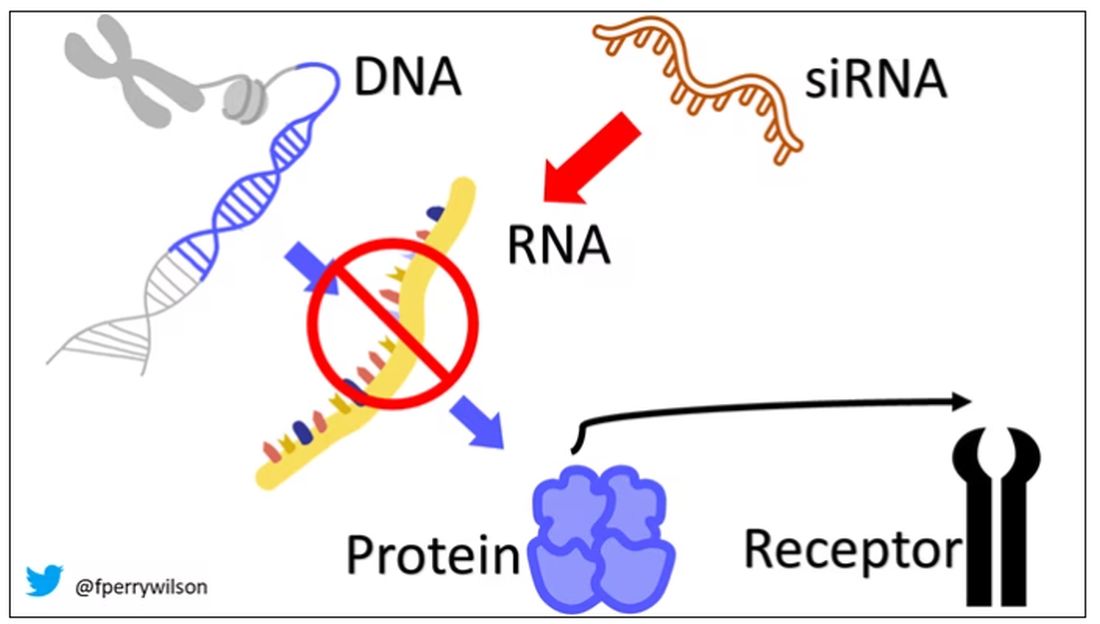
You see where this is going, right? How does high cholesterol kill you? Proteins. How does Staphylococcus aureus kill you? Proteins. Even viruses can’t replicate if their RNA is prevented from being turned into proteins.
So, how do we use siRNAs? A new paper appearing in JAMA describes a fairly impressive use case.
The background here is that higher levels of lipoprotein(a), an LDL-like protein, are associated with cardiovascular disease, heart attack, and stroke. But unfortunately, statins really don’t have any effect on lipoprotein(a) levels. Neither does diet. Your lipoprotein(a) level seems to be more or less hard-coded genetically.
So, what if we stop the genetic machinery from working? Enter lepodisiran, a drug from Eli Lilly. Unlike so many other medications, which are usually found in nature, purified, and synthesized, lepodisiran was created from scratch. It’s not hard. Thanks to the Human Genome Project, we know the genetic code for lipoprotein(a), so inventing an siRNA to target it specifically is trivial. That’s one of the key features of siRNA – you don’t have to find a chemical that binds strongly to some protein receptor, and worry about the off-target effects and all that nonsense. You just pick a protein you want to suppress and you suppress it.
Okay, it’s not that simple. siRNA is broken down very quickly by the body, so it needs to be targeted to the organ of interest – in this case, the liver, since that is where lipoprotein(a) is synthesized. Lepodisiran is targeted to the liver by this special targeting label here.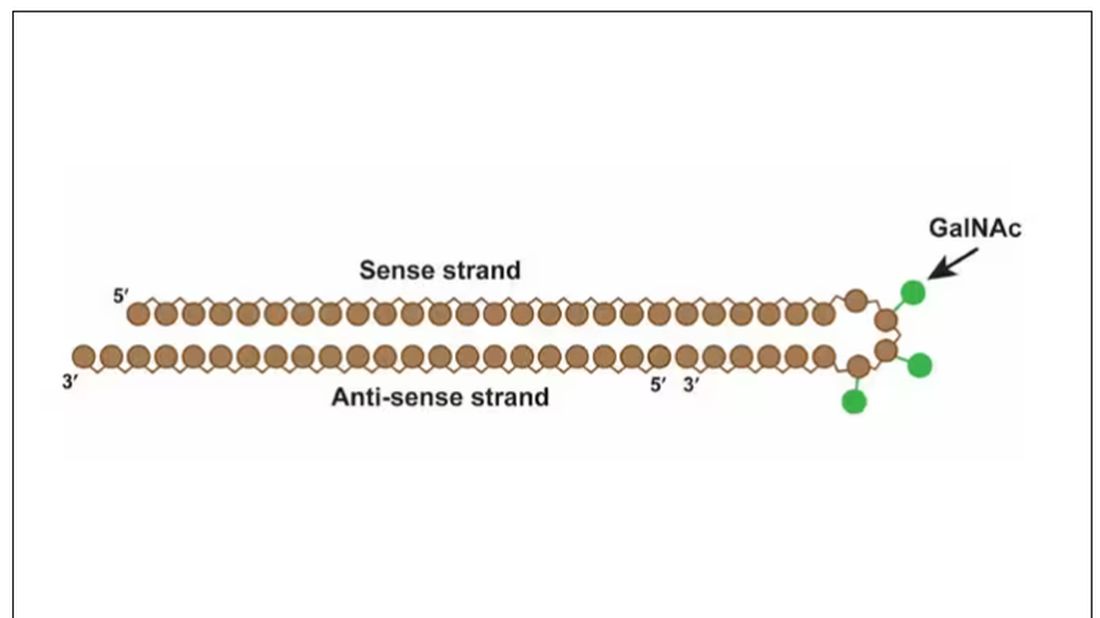
The report is a standard dose-escalation trial. Six patients, all with elevated lipoprotein(a) levels, were started with a 4-mg dose (two additional individuals got placebo). They were intensely monitored, spending 3 days in a research unit for multiple blood draws followed by weekly, and then biweekly outpatient visits. Once they had done well, the next group of six people received a higher dose (two more got placebo), and the process was repeated – six times total – until the highest dose, 608 mg, was reached.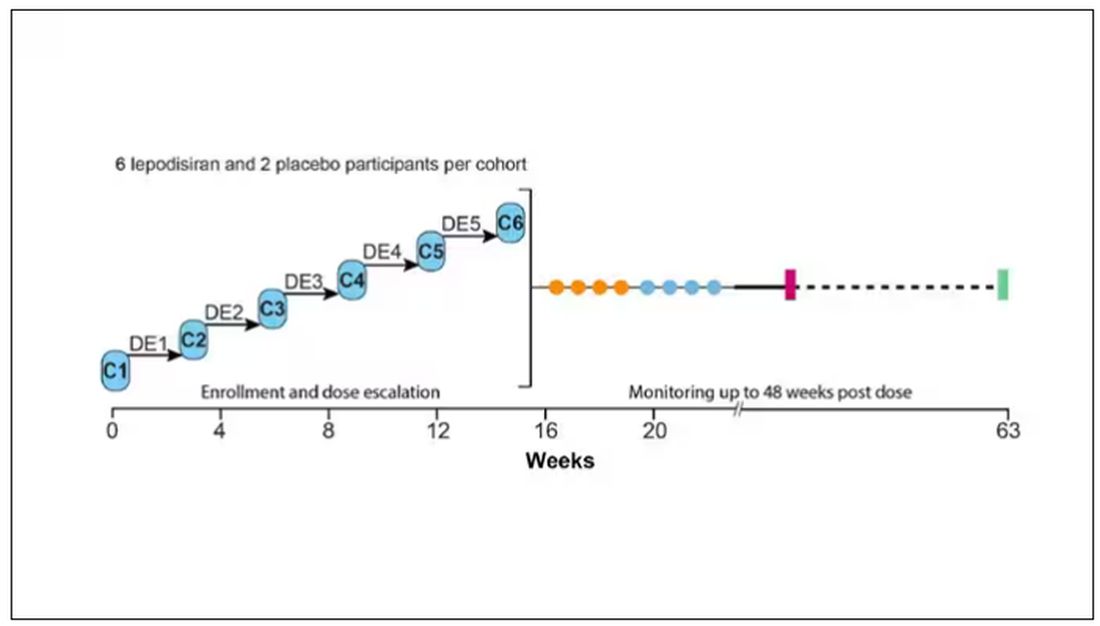
This is an injection, of course; siRNA wouldn’t withstand the harshness of the digestive system. And it’s only one injection. You can see from the blood concentration curves that within about 48 hours, circulating lepodisiran was not detectable.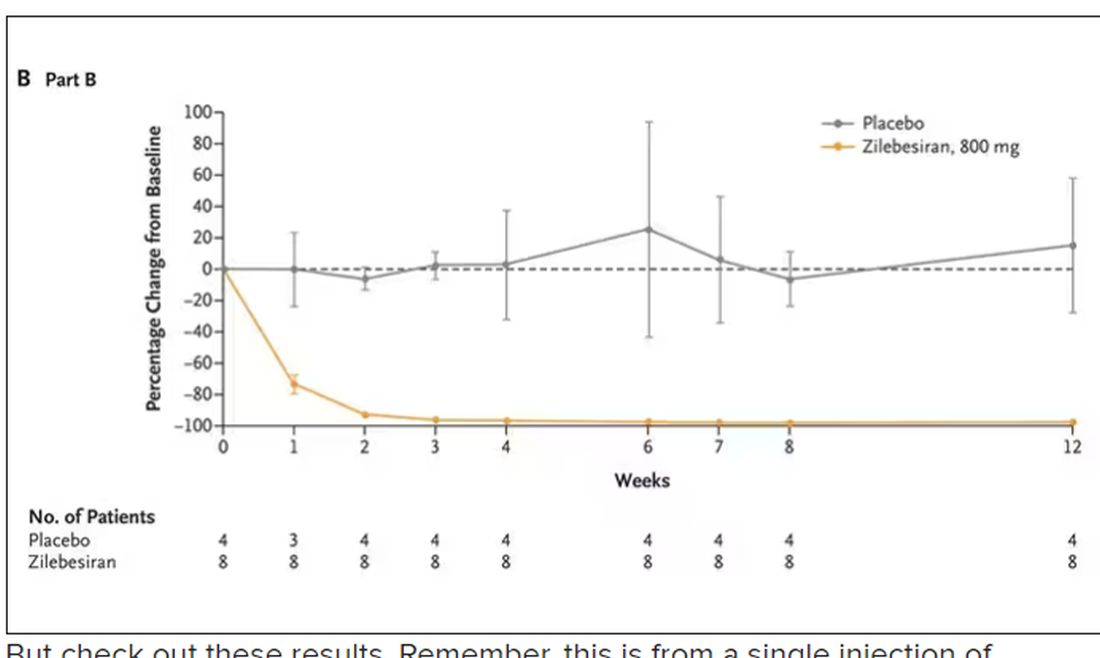
But check out these results. Remember, this is from a single injection of lepodisiran.
Lipoprotein(a) levels start to drop within a week of administration, and they stay down. In the higher-dose groups, levels are nearly undetectable a year after that injection.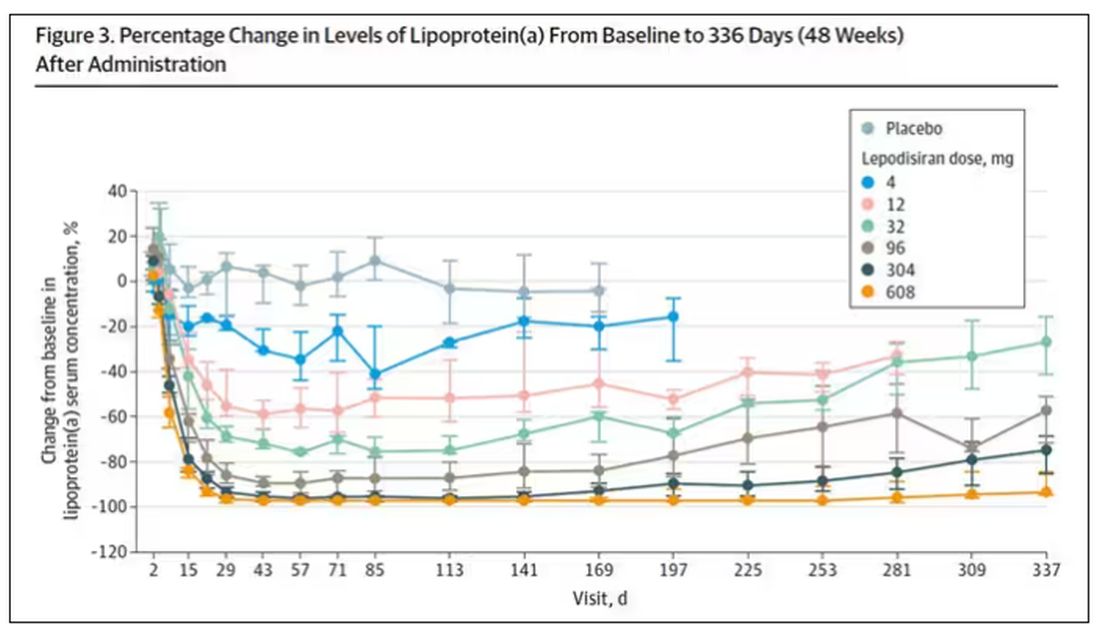
It was this graph that made me sit back and think that there might be something new under the sun. A single injection that can suppress protein synthesis for an entire year? If it really works, it changes the game.
Of course, this study wasn’t powered to look at important outcomes like heart attacks and strokes. It was primarily designed to assess safety, and the drug was pretty well tolerated, with similar rates of adverse events in the drug and placebo groups.
As crazy as it sounds, the real concern here might be that this drug is too good; is it safe to drop your lipoprotein(a) levels to zero for a year? I don’t know. But lower doses don’t have quite as strong an effect.
Trust me, these drugs are going to change things. They already are. In July, The New England Journal of Medicine published a study of zilebesiran, an siRNA that inhibits the production of angiotensinogen, to control blood pressure. Similar story: One injection led to a basically complete suppression of angiotensinogen and a sustained decrease in blood pressure.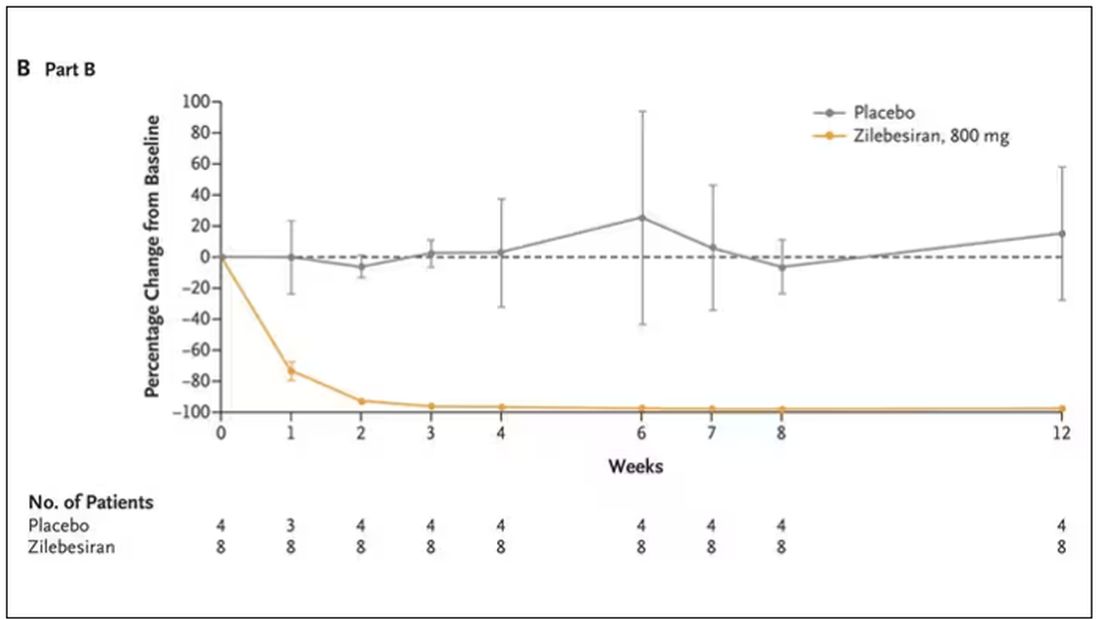
I’m not exaggerating when I say that there may come a time when you go to your doctor once a year, get your RNA shots, and don’t have to take any other medication from that point on. And that time may be, like, 5 years from now. It’s wild.
Seems to me that that rapid Nobel Prize was very well deserved.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships. This transcript has been edited for clarity.
A version of this article appeared on Medscape.com.
Can vitamin and mineral supplementation prevent cancer or cardiovascular disease?
Patients often come to us with questions about vitamin and mineral supplements. Sometimes they come to us with bags full of the things they are taking. The Internet is full of the wonders these nutritional supplements can do, from turmeric curing cancer to vitamin D curing COVID. It is hard to keep up with medicine itself without learning a whole new field of nutritional supplements.
However, for cardiovascular disease (CVD) and cancer prevention, the answer is pretty easy according to USPSTF (United States Preventative Services Task Force) guidelines. They evaluated 17,459 unique citations as well as 379 full-text articles that included randomized clinical trials and observational cohort studies. The conclusions of their research showed that there was little to no benefit in taking vitamin or mineral supplements to prevent CVD, cancer, or death. In fact, beta-carotene supplementation was associated with increased risk of lung cancer and other adverse outcomes in patients at increased risk of lung cancer.
Although they are often marketed like drugs, nutritional supplements are regulated as foods, with less stringent standards.* Our current medical culture pushes us to practice evidence-based medicine. Without evidence, we simply cannot counsel patients about supplements because there is little evidence to support their use.
Additionally, many patients assume that they are safe. While this may be true for many of them, some of them can be harmful in several ways. They can interact with medications the patient may be taking for medical conditions. Some of them have been shown to cause liver and other organ damage. When they are used to replace traditional medicine, they can also lead to harm by delaying appropriate medical care. For example, a patient who believes a supplement can treat cancer when it does nothing is delaying care that might save their life. By the time they realize it is not working, the cancer may have advanced too far to be treatable.
While there may be a few studies that do show some efficacy for vitamins and minerals in certain diseases, these guidelines are looking only at use in terms of preventing cancer and CVD. As primary care physicians, we all know the screening guidelines for cancer prevention. We are better off recommending screening mammograms and colon cancer screening tests. And we all know the risk factors for CVD and how to mitigate these risks.
What can we do when patients come to us with false claims regarding supplements?
- Hear what they are saying. They don’t know who to trust. We will never become their trusted source of medical information if we don’t listen to their concerns.
- Answer their questions, no matter how ridiculous they may seem to us. Many people who sell supplements sound convincing. That is how they sell their products. Our advice may seem just as ridiculous to them. We need to explain the facts clearly and be sure the patient understands.
- Give the patient resources. Know what websites to direct them to so that they can get accurate information.
- Know what’s out there. I was once surprised when a patient told me she was going to try turmeric as a treatment for uterine cancer. We cannot combat misinformation when we don’t know what’s being said.
- Become a voice for medical information. There is so much misinformation being spread. We need more doctors to speak up about the right medical information.
Currently, patients often look for medical information online. We do them a disservice when we brush aside their questions regarding supplements, no matter how trivial they seem. We need to take a firm stand and tell them the evidence regarding these supplements: They are neither FDA approved nor studied for safety and efficacy. Anyone can sell a supplement and make any claim regarding it that they want. It is much better to eat a healthy, balanced diet to get the vitamins and minerals that you need. Not only do we need to show them the evidence, we need to convince them that it is true.
*Correction, 12/4: An earlier version of this article misstated the regulatory requirements for nutritional supplements.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. She was paid by Pfizer as a consultant on Paxlovid and is the editor in chief of Physician’s Weekly.
Patients often come to us with questions about vitamin and mineral supplements. Sometimes they come to us with bags full of the things they are taking. The Internet is full of the wonders these nutritional supplements can do, from turmeric curing cancer to vitamin D curing COVID. It is hard to keep up with medicine itself without learning a whole new field of nutritional supplements.
However, for cardiovascular disease (CVD) and cancer prevention, the answer is pretty easy according to USPSTF (United States Preventative Services Task Force) guidelines. They evaluated 17,459 unique citations as well as 379 full-text articles that included randomized clinical trials and observational cohort studies. The conclusions of their research showed that there was little to no benefit in taking vitamin or mineral supplements to prevent CVD, cancer, or death. In fact, beta-carotene supplementation was associated with increased risk of lung cancer and other adverse outcomes in patients at increased risk of lung cancer.
Although they are often marketed like drugs, nutritional supplements are regulated as foods, with less stringent standards.* Our current medical culture pushes us to practice evidence-based medicine. Without evidence, we simply cannot counsel patients about supplements because there is little evidence to support their use.
Additionally, many patients assume that they are safe. While this may be true for many of them, some of them can be harmful in several ways. They can interact with medications the patient may be taking for medical conditions. Some of them have been shown to cause liver and other organ damage. When they are used to replace traditional medicine, they can also lead to harm by delaying appropriate medical care. For example, a patient who believes a supplement can treat cancer when it does nothing is delaying care that might save their life. By the time they realize it is not working, the cancer may have advanced too far to be treatable.
While there may be a few studies that do show some efficacy for vitamins and minerals in certain diseases, these guidelines are looking only at use in terms of preventing cancer and CVD. As primary care physicians, we all know the screening guidelines for cancer prevention. We are better off recommending screening mammograms and colon cancer screening tests. And we all know the risk factors for CVD and how to mitigate these risks.
What can we do when patients come to us with false claims regarding supplements?
- Hear what they are saying. They don’t know who to trust. We will never become their trusted source of medical information if we don’t listen to their concerns.
- Answer their questions, no matter how ridiculous they may seem to us. Many people who sell supplements sound convincing. That is how they sell their products. Our advice may seem just as ridiculous to them. We need to explain the facts clearly and be sure the patient understands.
- Give the patient resources. Know what websites to direct them to so that they can get accurate information.
- Know what’s out there. I was once surprised when a patient told me she was going to try turmeric as a treatment for uterine cancer. We cannot combat misinformation when we don’t know what’s being said.
- Become a voice for medical information. There is so much misinformation being spread. We need more doctors to speak up about the right medical information.
Currently, patients often look for medical information online. We do them a disservice when we brush aside their questions regarding supplements, no matter how trivial they seem. We need to take a firm stand and tell them the evidence regarding these supplements: They are neither FDA approved nor studied for safety and efficacy. Anyone can sell a supplement and make any claim regarding it that they want. It is much better to eat a healthy, balanced diet to get the vitamins and minerals that you need. Not only do we need to show them the evidence, we need to convince them that it is true.
*Correction, 12/4: An earlier version of this article misstated the regulatory requirements for nutritional supplements.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. She was paid by Pfizer as a consultant on Paxlovid and is the editor in chief of Physician’s Weekly.
Patients often come to us with questions about vitamin and mineral supplements. Sometimes they come to us with bags full of the things they are taking. The Internet is full of the wonders these nutritional supplements can do, from turmeric curing cancer to vitamin D curing COVID. It is hard to keep up with medicine itself without learning a whole new field of nutritional supplements.
However, for cardiovascular disease (CVD) and cancer prevention, the answer is pretty easy according to USPSTF (United States Preventative Services Task Force) guidelines. They evaluated 17,459 unique citations as well as 379 full-text articles that included randomized clinical trials and observational cohort studies. The conclusions of their research showed that there was little to no benefit in taking vitamin or mineral supplements to prevent CVD, cancer, or death. In fact, beta-carotene supplementation was associated with increased risk of lung cancer and other adverse outcomes in patients at increased risk of lung cancer.
Although they are often marketed like drugs, nutritional supplements are regulated as foods, with less stringent standards.* Our current medical culture pushes us to practice evidence-based medicine. Without evidence, we simply cannot counsel patients about supplements because there is little evidence to support their use.
Additionally, many patients assume that they are safe. While this may be true for many of them, some of them can be harmful in several ways. They can interact with medications the patient may be taking for medical conditions. Some of them have been shown to cause liver and other organ damage. When they are used to replace traditional medicine, they can also lead to harm by delaying appropriate medical care. For example, a patient who believes a supplement can treat cancer when it does nothing is delaying care that might save their life. By the time they realize it is not working, the cancer may have advanced too far to be treatable.
While there may be a few studies that do show some efficacy for vitamins and minerals in certain diseases, these guidelines are looking only at use in terms of preventing cancer and CVD. As primary care physicians, we all know the screening guidelines for cancer prevention. We are better off recommending screening mammograms and colon cancer screening tests. And we all know the risk factors for CVD and how to mitigate these risks.
What can we do when patients come to us with false claims regarding supplements?
- Hear what they are saying. They don’t know who to trust. We will never become their trusted source of medical information if we don’t listen to their concerns.
- Answer their questions, no matter how ridiculous they may seem to us. Many people who sell supplements sound convincing. That is how they sell their products. Our advice may seem just as ridiculous to them. We need to explain the facts clearly and be sure the patient understands.
- Give the patient resources. Know what websites to direct them to so that they can get accurate information.
- Know what’s out there. I was once surprised when a patient told me she was going to try turmeric as a treatment for uterine cancer. We cannot combat misinformation when we don’t know what’s being said.
- Become a voice for medical information. There is so much misinformation being spread. We need more doctors to speak up about the right medical information.
Currently, patients often look for medical information online. We do them a disservice when we brush aside their questions regarding supplements, no matter how trivial they seem. We need to take a firm stand and tell them the evidence regarding these supplements: They are neither FDA approved nor studied for safety and efficacy. Anyone can sell a supplement and make any claim regarding it that they want. It is much better to eat a healthy, balanced diet to get the vitamins and minerals that you need. Not only do we need to show them the evidence, we need to convince them that it is true.
*Correction, 12/4: An earlier version of this article misstated the regulatory requirements for nutritional supplements.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. She was paid by Pfizer as a consultant on Paxlovid and is the editor in chief of Physician’s Weekly.
A nurse’s view: Women desperately need information about pelvic floor disorders
Pelvic floor disorders are embarrassing, annoying, painful, and extremely disruptive to a woman’s life, often resulting in depression, anxiety, and a poor self-image. According to a 2021 study, approximately 75% of peripartum women and 68% of postmenopausal women feel insufficiently informed about pelvic floor disorders.1
Consequently, a large majority of women are not seeking care for these disorders. This drives health care costs higher as women wait until their symptoms are unbearable until finally seeking help. Many of these women don’t know they have options.
Who is at risk?
To understand the scope of this growing problem, it is vital to see who is most at risk. Parity, age, body mass index, and race are significant factors, although any woman can have a pelvic floor disorder (PFD).
Urinary incontinence (UI), pelvic floor prolapses (POP), and fecal incontinence (FI) are three of the most common pelvic floor disorders. Pregnancy and childbirth, specifically a vaginal birth, greatly contribute to this population’s risk. In pregnancy, the increase in plasma volume and glomerular filtration rate, along with hormone changes impacting urethral pressure and the growing gravid uterus, cause urinary frequency and nocturia. This can result in urinary incontinence during and after pregnancy.
Indeed, 76% of women with urinary incontinence at 3 months postpartum report it 12 years later.1 Third- and fourth-degree lacerations during delivery are uncommon (3.3%), but can cause fecal incontinence, often requiring surgery.1 Independently, all of these symptoms have been correlated with sexual dysfunction and postpartum depression.
One-third of all women and 50% of women over the age of 55 are currently affected by a PFD. Contributing factors include hormone changes with menopause that affect the pelvic floor muscles and connective tissue, prior childbirth and pregnancy, constipation, heavy lifting, prior pelvic surgery, and obesity. These women are vulnerable to pelvic organ prolapse from the weakened pelvic floor muscles. They will often present with a vague complaint of “something is protruding out of my vagina.” These women also present with urinary incontinence or leakage, proclaiming they have to wear a diaper or a pad. Without proper knowledge, aging women think these issues are normal and nothing can be done.
The woman with a BMI above 30 may have damaged tissues supporting the uterus and bladder, weakening those organs, and causing a prolapse. Incontinence is a result of poor muscle and connective tissue of the vagina that support the urethra. Obese women can suffer from both urinary and bowel incontinence. By the year 2030, it is projected that one in two adults will be obese.2 This will greatly impact health care costs.
To date, there is little conclusive evidence on the impact of race on pelvic floor disorders. A study in Scientific Reports did find that Asian women have a significantly lower risk for any PFD.2 Some research has found that Black and Hispanic women have less risk for UI but are at higher risk for FI and other PFDs.3 Understandably, women of certain cultures and demographics may be less likely to report incontinence to their clinicians and may be less informed as well.
What can we do?
The American College of Obstetricians and Gynecologists (ACOG) has acknowledged the deficiencies and lack of standard care of pelvic health in pregnancy and postpartum.1 There are differences in definitions across clinical practice and in the medical literature. Inconsistent patient reporting of PFD symptoms occurs due to nonstandard methods (questionnaire, interview, physical exam). With the often-short time allotted for visits with health care providers, women may neglect to discuss their symptoms, especially if they have other more pressing matters to address.
At the first OB appointment, a pregnant woman should be given information on what are normal and abnormal symptoms, from the beginning through postpartum. At each visit, she should be given ample opportunity to discuss symptoms of pelvic health. Clinicians should continue assessing, questioning, and discussing treatment options as applicable. Women need to know that early recognition and treatment can have a positive affect on their pelvic health for years to come.
ACOG recommends all postpartum patients see an obstetric provider within 3 weeks of delivery.1 Most are seen at 6 weeks. Pelvic health should be discussed at this final postpartum appointment, including normal and abnormal symptoms within the next few months and beyond.
Regardless of pregnancy status, women need a safe and supportive place to describe their pelvic floor issues. There is a validated questionnaire tool available for postpartum, but one is desperately needed for all women, especially women at risk. A pelvic health assessment must be included in every annual exam.
Women need to know there are multiple treatment modalities including simple exercises, physical therapy, a variety of pessaries, medications, and surgery. Sometimes, all that is needed are a few lifestyle changes: avoiding pushing or straining while urinating or having a bowel movement, maintaining a healthy diet rich in high fiber foods, and drinking plenty of fluids.
The National Public Health Service in the United Kingdom recently announced a government-funded program for pelvic health services to begin in April 2024.4 This program will address the pelvic floor needs, assessment, education and treatment for women after childbirth.
There are multiple clinics in the United States focusing on women’s health that feature urogynecologists – specialists in pelvic floor disorders. These specialists do a thorough health and physical assessment, explain types of pelvic floor disorders, and suggest appropriate treatment options. Most importantly, urogynecologists listen and address a woman’s concerns and fears.
There is no reason for women to feel compromised at any age. We, as health care providers, just need to assess, educate, treat, and follow up.
Ms. Barnett is a registered nurse in the department of obstetrics, Mills-Peninsula Medical Center, Burlingame, Calif. She has disclosed no relevant financial relationships.
References
1. Madsen AM et al. Recognition and management of pelvic floor disorders in pregnancy and the postpartum period. Obstet Gynecol Clin North Am. 2021 Sep;48(3):571-84. doi: 10.1016/j.ogc.2021.05.009.
2. Kenne KA et al. Prevalence of pelvic floor disorders in adult women being seen in a primary care setting and associated risk factors. Sci Rep. 2022 June; (12):9878. doi: 10.1038/s41598-022-13501-w.
3. Nygaard I et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311-6. doi: 10.1001/jama.300.11.1311.
4. United Kingdom Department of Health and Social Care. “National pelvic health service to support women.” 2023 Oct 19.
Pelvic floor disorders are embarrassing, annoying, painful, and extremely disruptive to a woman’s life, often resulting in depression, anxiety, and a poor self-image. According to a 2021 study, approximately 75% of peripartum women and 68% of postmenopausal women feel insufficiently informed about pelvic floor disorders.1
Consequently, a large majority of women are not seeking care for these disorders. This drives health care costs higher as women wait until their symptoms are unbearable until finally seeking help. Many of these women don’t know they have options.
Who is at risk?
To understand the scope of this growing problem, it is vital to see who is most at risk. Parity, age, body mass index, and race are significant factors, although any woman can have a pelvic floor disorder (PFD).
Urinary incontinence (UI), pelvic floor prolapses (POP), and fecal incontinence (FI) are three of the most common pelvic floor disorders. Pregnancy and childbirth, specifically a vaginal birth, greatly contribute to this population’s risk. In pregnancy, the increase in plasma volume and glomerular filtration rate, along with hormone changes impacting urethral pressure and the growing gravid uterus, cause urinary frequency and nocturia. This can result in urinary incontinence during and after pregnancy.
Indeed, 76% of women with urinary incontinence at 3 months postpartum report it 12 years later.1 Third- and fourth-degree lacerations during delivery are uncommon (3.3%), but can cause fecal incontinence, often requiring surgery.1 Independently, all of these symptoms have been correlated with sexual dysfunction and postpartum depression.
One-third of all women and 50% of women over the age of 55 are currently affected by a PFD. Contributing factors include hormone changes with menopause that affect the pelvic floor muscles and connective tissue, prior childbirth and pregnancy, constipation, heavy lifting, prior pelvic surgery, and obesity. These women are vulnerable to pelvic organ prolapse from the weakened pelvic floor muscles. They will often present with a vague complaint of “something is protruding out of my vagina.” These women also present with urinary incontinence or leakage, proclaiming they have to wear a diaper or a pad. Without proper knowledge, aging women think these issues are normal and nothing can be done.
The woman with a BMI above 30 may have damaged tissues supporting the uterus and bladder, weakening those organs, and causing a prolapse. Incontinence is a result of poor muscle and connective tissue of the vagina that support the urethra. Obese women can suffer from both urinary and bowel incontinence. By the year 2030, it is projected that one in two adults will be obese.2 This will greatly impact health care costs.
To date, there is little conclusive evidence on the impact of race on pelvic floor disorders. A study in Scientific Reports did find that Asian women have a significantly lower risk for any PFD.2 Some research has found that Black and Hispanic women have less risk for UI but are at higher risk for FI and other PFDs.3 Understandably, women of certain cultures and demographics may be less likely to report incontinence to their clinicians and may be less informed as well.
What can we do?
The American College of Obstetricians and Gynecologists (ACOG) has acknowledged the deficiencies and lack of standard care of pelvic health in pregnancy and postpartum.1 There are differences in definitions across clinical practice and in the medical literature. Inconsistent patient reporting of PFD symptoms occurs due to nonstandard methods (questionnaire, interview, physical exam). With the often-short time allotted for visits with health care providers, women may neglect to discuss their symptoms, especially if they have other more pressing matters to address.
At the first OB appointment, a pregnant woman should be given information on what are normal and abnormal symptoms, from the beginning through postpartum. At each visit, she should be given ample opportunity to discuss symptoms of pelvic health. Clinicians should continue assessing, questioning, and discussing treatment options as applicable. Women need to know that early recognition and treatment can have a positive affect on their pelvic health for years to come.
ACOG recommends all postpartum patients see an obstetric provider within 3 weeks of delivery.1 Most are seen at 6 weeks. Pelvic health should be discussed at this final postpartum appointment, including normal and abnormal symptoms within the next few months and beyond.
Regardless of pregnancy status, women need a safe and supportive place to describe their pelvic floor issues. There is a validated questionnaire tool available for postpartum, but one is desperately needed for all women, especially women at risk. A pelvic health assessment must be included in every annual exam.
Women need to know there are multiple treatment modalities including simple exercises, physical therapy, a variety of pessaries, medications, and surgery. Sometimes, all that is needed are a few lifestyle changes: avoiding pushing or straining while urinating or having a bowel movement, maintaining a healthy diet rich in high fiber foods, and drinking plenty of fluids.
The National Public Health Service in the United Kingdom recently announced a government-funded program for pelvic health services to begin in April 2024.4 This program will address the pelvic floor needs, assessment, education and treatment for women after childbirth.
There are multiple clinics in the United States focusing on women’s health that feature urogynecologists – specialists in pelvic floor disorders. These specialists do a thorough health and physical assessment, explain types of pelvic floor disorders, and suggest appropriate treatment options. Most importantly, urogynecologists listen and address a woman’s concerns and fears.
There is no reason for women to feel compromised at any age. We, as health care providers, just need to assess, educate, treat, and follow up.
Ms. Barnett is a registered nurse in the department of obstetrics, Mills-Peninsula Medical Center, Burlingame, Calif. She has disclosed no relevant financial relationships.
References
1. Madsen AM et al. Recognition and management of pelvic floor disorders in pregnancy and the postpartum period. Obstet Gynecol Clin North Am. 2021 Sep;48(3):571-84. doi: 10.1016/j.ogc.2021.05.009.
2. Kenne KA et al. Prevalence of pelvic floor disorders in adult women being seen in a primary care setting and associated risk factors. Sci Rep. 2022 June; (12):9878. doi: 10.1038/s41598-022-13501-w.
3. Nygaard I et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311-6. doi: 10.1001/jama.300.11.1311.
4. United Kingdom Department of Health and Social Care. “National pelvic health service to support women.” 2023 Oct 19.
Pelvic floor disorders are embarrassing, annoying, painful, and extremely disruptive to a woman’s life, often resulting in depression, anxiety, and a poor self-image. According to a 2021 study, approximately 75% of peripartum women and 68% of postmenopausal women feel insufficiently informed about pelvic floor disorders.1
Consequently, a large majority of women are not seeking care for these disorders. This drives health care costs higher as women wait until their symptoms are unbearable until finally seeking help. Many of these women don’t know they have options.
Who is at risk?
To understand the scope of this growing problem, it is vital to see who is most at risk. Parity, age, body mass index, and race are significant factors, although any woman can have a pelvic floor disorder (PFD).
Urinary incontinence (UI), pelvic floor prolapses (POP), and fecal incontinence (FI) are three of the most common pelvic floor disorders. Pregnancy and childbirth, specifically a vaginal birth, greatly contribute to this population’s risk. In pregnancy, the increase in plasma volume and glomerular filtration rate, along with hormone changes impacting urethral pressure and the growing gravid uterus, cause urinary frequency and nocturia. This can result in urinary incontinence during and after pregnancy.
Indeed, 76% of women with urinary incontinence at 3 months postpartum report it 12 years later.1 Third- and fourth-degree lacerations during delivery are uncommon (3.3%), but can cause fecal incontinence, often requiring surgery.1 Independently, all of these symptoms have been correlated with sexual dysfunction and postpartum depression.
One-third of all women and 50% of women over the age of 55 are currently affected by a PFD. Contributing factors include hormone changes with menopause that affect the pelvic floor muscles and connective tissue, prior childbirth and pregnancy, constipation, heavy lifting, prior pelvic surgery, and obesity. These women are vulnerable to pelvic organ prolapse from the weakened pelvic floor muscles. They will often present with a vague complaint of “something is protruding out of my vagina.” These women also present with urinary incontinence or leakage, proclaiming they have to wear a diaper or a pad. Without proper knowledge, aging women think these issues are normal and nothing can be done.
The woman with a BMI above 30 may have damaged tissues supporting the uterus and bladder, weakening those organs, and causing a prolapse. Incontinence is a result of poor muscle and connective tissue of the vagina that support the urethra. Obese women can suffer from both urinary and bowel incontinence. By the year 2030, it is projected that one in two adults will be obese.2 This will greatly impact health care costs.
To date, there is little conclusive evidence on the impact of race on pelvic floor disorders. A study in Scientific Reports did find that Asian women have a significantly lower risk for any PFD.2 Some research has found that Black and Hispanic women have less risk for UI but are at higher risk for FI and other PFDs.3 Understandably, women of certain cultures and demographics may be less likely to report incontinence to their clinicians and may be less informed as well.
What can we do?
The American College of Obstetricians and Gynecologists (ACOG) has acknowledged the deficiencies and lack of standard care of pelvic health in pregnancy and postpartum.1 There are differences in definitions across clinical practice and in the medical literature. Inconsistent patient reporting of PFD symptoms occurs due to nonstandard methods (questionnaire, interview, physical exam). With the often-short time allotted for visits with health care providers, women may neglect to discuss their symptoms, especially if they have other more pressing matters to address.
At the first OB appointment, a pregnant woman should be given information on what are normal and abnormal symptoms, from the beginning through postpartum. At each visit, she should be given ample opportunity to discuss symptoms of pelvic health. Clinicians should continue assessing, questioning, and discussing treatment options as applicable. Women need to know that early recognition and treatment can have a positive affect on their pelvic health for years to come.
ACOG recommends all postpartum patients see an obstetric provider within 3 weeks of delivery.1 Most are seen at 6 weeks. Pelvic health should be discussed at this final postpartum appointment, including normal and abnormal symptoms within the next few months and beyond.
Regardless of pregnancy status, women need a safe and supportive place to describe their pelvic floor issues. There is a validated questionnaire tool available for postpartum, but one is desperately needed for all women, especially women at risk. A pelvic health assessment must be included in every annual exam.
Women need to know there are multiple treatment modalities including simple exercises, physical therapy, a variety of pessaries, medications, and surgery. Sometimes, all that is needed are a few lifestyle changes: avoiding pushing or straining while urinating or having a bowel movement, maintaining a healthy diet rich in high fiber foods, and drinking plenty of fluids.
The National Public Health Service in the United Kingdom recently announced a government-funded program for pelvic health services to begin in April 2024.4 This program will address the pelvic floor needs, assessment, education and treatment for women after childbirth.
There are multiple clinics in the United States focusing on women’s health that feature urogynecologists – specialists in pelvic floor disorders. These specialists do a thorough health and physical assessment, explain types of pelvic floor disorders, and suggest appropriate treatment options. Most importantly, urogynecologists listen and address a woman’s concerns and fears.
There is no reason for women to feel compromised at any age. We, as health care providers, just need to assess, educate, treat, and follow up.
Ms. Barnett is a registered nurse in the department of obstetrics, Mills-Peninsula Medical Center, Burlingame, Calif. She has disclosed no relevant financial relationships.
References
1. Madsen AM et al. Recognition and management of pelvic floor disorders in pregnancy and the postpartum period. Obstet Gynecol Clin North Am. 2021 Sep;48(3):571-84. doi: 10.1016/j.ogc.2021.05.009.
2. Kenne KA et al. Prevalence of pelvic floor disorders in adult women being seen in a primary care setting and associated risk factors. Sci Rep. 2022 June; (12):9878. doi: 10.1038/s41598-022-13501-w.
3. Nygaard I et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311-6. doi: 10.1001/jama.300.11.1311.
4. United Kingdom Department of Health and Social Care. “National pelvic health service to support women.” 2023 Oct 19.
Marketing the meds
I am not a marketing person. I never will be. I don’t think like one.
A current article on FiercePharma talked about Boehringer Ingelheim’s recent “rebranding,” which involved (among other things) changing the blues in its logo and ads to greens.
Maybe someone else out there would notice that change, but I wouldn’t have if I hadn’t read about it. Nor am I sure what affect it would have on me, if any. But I’m sure they paid psychologists and marketing teams quite a bit to make sure it was a good idea.
Likewise, when AbbVie repackaged Ubrelvy from 10 to a package to 16, the company felt the need to change the design of the sample boxes (which are also now green). I’m pretty sure none of my patients noticed. The only reason I did is because I’m the one who stocks my sample shelf here.
Abbvie and Boehringer aren’t alone in this, of course. Pharmaceutical marketing is big business. I understand the companies want doctors and patients to know about their products. In that respect they’re no different from General Motors or Kellogg’s.
But pharmaceuticals fall into a different area. Kellogg’s products don’t require a middleman handing you a script allowing you to buy corn flakes, so although the products are sold to the public, they also have to be sold to a person who isn’t buying them – the prescriber.
Not all these ads are bad, of course. At best they raise public awareness of different health conditions and the options to treat them. At worst ... well, currently there are several movies out there about the results of marketing done by the Sackler family and Purdue.
To me, most pharmaceutical ads look the same. They show happy people going about their lives, with the impression being that they couldn’t have done this without the benefit of the drug being marketed.
To a large extent I can’t knock that. Pharmaceuticals are amazing things. They’ve contributed dramatically to human health, life quality, and longevity.
But would I, or most people, notice if the lettering in the ads were blue, green, or yellow? Probably not. Someone with a background in the psychology of marketing would be able to show me data on how different colors affect our perceptions, but I still look at this and wonder if the money could have been better spent.
Maybe that’s why I’m not in marketing. I tend to be on the practical side. The idea of hiring a celebrity to endorse a migraine (or pretty much any) medication would never have occurred to me. I have no idea how much Pfizer paid Lady Gaga to sell Nurtec, but I’m pretty sure it’s a lot more than I’ll earn this year. Probably ever.
Like most neurologists I’m hopelessly left-brained. But I still wonder how much things like this really make a difference.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I am not a marketing person. I never will be. I don’t think like one.
A current article on FiercePharma talked about Boehringer Ingelheim’s recent “rebranding,” which involved (among other things) changing the blues in its logo and ads to greens.
Maybe someone else out there would notice that change, but I wouldn’t have if I hadn’t read about it. Nor am I sure what affect it would have on me, if any. But I’m sure they paid psychologists and marketing teams quite a bit to make sure it was a good idea.
Likewise, when AbbVie repackaged Ubrelvy from 10 to a package to 16, the company felt the need to change the design of the sample boxes (which are also now green). I’m pretty sure none of my patients noticed. The only reason I did is because I’m the one who stocks my sample shelf here.
Abbvie and Boehringer aren’t alone in this, of course. Pharmaceutical marketing is big business. I understand the companies want doctors and patients to know about their products. In that respect they’re no different from General Motors or Kellogg’s.
But pharmaceuticals fall into a different area. Kellogg’s products don’t require a middleman handing you a script allowing you to buy corn flakes, so although the products are sold to the public, they also have to be sold to a person who isn’t buying them – the prescriber.
Not all these ads are bad, of course. At best they raise public awareness of different health conditions and the options to treat them. At worst ... well, currently there are several movies out there about the results of marketing done by the Sackler family and Purdue.
To me, most pharmaceutical ads look the same. They show happy people going about their lives, with the impression being that they couldn’t have done this without the benefit of the drug being marketed.
To a large extent I can’t knock that. Pharmaceuticals are amazing things. They’ve contributed dramatically to human health, life quality, and longevity.
But would I, or most people, notice if the lettering in the ads were blue, green, or yellow? Probably not. Someone with a background in the psychology of marketing would be able to show me data on how different colors affect our perceptions, but I still look at this and wonder if the money could have been better spent.
Maybe that’s why I’m not in marketing. I tend to be on the practical side. The idea of hiring a celebrity to endorse a migraine (or pretty much any) medication would never have occurred to me. I have no idea how much Pfizer paid Lady Gaga to sell Nurtec, but I’m pretty sure it’s a lot more than I’ll earn this year. Probably ever.
Like most neurologists I’m hopelessly left-brained. But I still wonder how much things like this really make a difference.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I am not a marketing person. I never will be. I don’t think like one.
A current article on FiercePharma talked about Boehringer Ingelheim’s recent “rebranding,” which involved (among other things) changing the blues in its logo and ads to greens.
Maybe someone else out there would notice that change, but I wouldn’t have if I hadn’t read about it. Nor am I sure what affect it would have on me, if any. But I’m sure they paid psychologists and marketing teams quite a bit to make sure it was a good idea.
Likewise, when AbbVie repackaged Ubrelvy from 10 to a package to 16, the company felt the need to change the design of the sample boxes (which are also now green). I’m pretty sure none of my patients noticed. The only reason I did is because I’m the one who stocks my sample shelf here.
Abbvie and Boehringer aren’t alone in this, of course. Pharmaceutical marketing is big business. I understand the companies want doctors and patients to know about their products. In that respect they’re no different from General Motors or Kellogg’s.
But pharmaceuticals fall into a different area. Kellogg’s products don’t require a middleman handing you a script allowing you to buy corn flakes, so although the products are sold to the public, they also have to be sold to a person who isn’t buying them – the prescriber.
Not all these ads are bad, of course. At best they raise public awareness of different health conditions and the options to treat them. At worst ... well, currently there are several movies out there about the results of marketing done by the Sackler family and Purdue.
To me, most pharmaceutical ads look the same. They show happy people going about their lives, with the impression being that they couldn’t have done this without the benefit of the drug being marketed.
To a large extent I can’t knock that. Pharmaceuticals are amazing things. They’ve contributed dramatically to human health, life quality, and longevity.
But would I, or most people, notice if the lettering in the ads were blue, green, or yellow? Probably not. Someone with a background in the psychology of marketing would be able to show me data on how different colors affect our perceptions, but I still look at this and wonder if the money could have been better spent.
Maybe that’s why I’m not in marketing. I tend to be on the practical side. The idea of hiring a celebrity to endorse a migraine (or pretty much any) medication would never have occurred to me. I have no idea how much Pfizer paid Lady Gaga to sell Nurtec, but I’m pretty sure it’s a lot more than I’ll earn this year. Probably ever.
Like most neurologists I’m hopelessly left-brained. But I still wonder how much things like this really make a difference.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The easy way to talk about penises
This transcript has been edited for clarity.
I mean it. Penis problems are very common and are an early sign that patients could have a cardiac event. Think about it: Clogging the arteries of the heart is called a heart attack; clogging the arteries to the penis is a penis attack, or as doctors like to call it, erectile dysfunction.
The arteries to the penis are only 1 mm in diameter. They develop plaque and clog the circulation long before the 3-mm cardiac arteries. So, it’s very important for primary care doctors to talk to their patients about erection health. And I’ll be honest: It’s easier to talk to patients about how lifestyle is affecting their penis health than it is to discuss how lifestyle affects longevity or prevents cancer. I get a lot of men to quit smoking because I tell them what it’s doing to their penises.
It can be challenging for doctors and patients to talk about penises. It doesn’t come naturally for many of us. If a 20-year-old comes in to my office with his 85-year-old grandfather and they both say their penises aren’t working, how do you figure out what’s going on? Do they even have the same thing wrong with them?
Here’s a fun and helpful tool that I use in my office. It’s called the Erection Hardness Score. It was developed around the time that Viagra came out, in 1998. It’s been game-changing for me to get patients more comfortable talking about their erection issues.
I tell them it’s a 4-number scale. A “1” is no erection at all. A “2” is when it gets harder and larger, but it’s not going to penetrate. A “3” will penetrate, but it’s pretty wobbly. A “4” is that perfect cucumber–porn star erection that everyone is seeking. I have the patient tell me a story. They may say, “When I wake up in the morning, I’m at a 2. When I stimulate myself, I can get up to a 3. When I’m with my partner, sometimes I can get up to a 4.”
This is really helpful because they can talk in numbers. And after I give them treatments such as lifestyle changes, sex therapy, testosterone, a PDE5 inhibitor such as Viagra or Cialis, or an injection, they can come back and tell me how the story has changed. I have an objective measure that shows me how the treatment is affecting their erections. Not only do I feel more confident having those objective measures, but my patients feel more confident in the care that they’re getting, and they feel more comfortable talking to me about the changes. So, I encourage all of you to bring that EHS tool into your office. Show it to patients and get them more comfortable talking about erections.
Dr. Rubin is assistant clinical professor, department of urology, Georgetown University, Washington. She disclosed financial relationships with Absorption Pharmaceuticals, GlaxoSmithKline, and Endo Pharmaceuticals; has served as a speaker for Sprout; and has received research grant from Maternal Medical.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I mean it. Penis problems are very common and are an early sign that patients could have a cardiac event. Think about it: Clogging the arteries of the heart is called a heart attack; clogging the arteries to the penis is a penis attack, or as doctors like to call it, erectile dysfunction.
The arteries to the penis are only 1 mm in diameter. They develop plaque and clog the circulation long before the 3-mm cardiac arteries. So, it’s very important for primary care doctors to talk to their patients about erection health. And I’ll be honest: It’s easier to talk to patients about how lifestyle is affecting their penis health than it is to discuss how lifestyle affects longevity or prevents cancer. I get a lot of men to quit smoking because I tell them what it’s doing to their penises.
It can be challenging for doctors and patients to talk about penises. It doesn’t come naturally for many of us. If a 20-year-old comes in to my office with his 85-year-old grandfather and they both say their penises aren’t working, how do you figure out what’s going on? Do they even have the same thing wrong with them?
Here’s a fun and helpful tool that I use in my office. It’s called the Erection Hardness Score. It was developed around the time that Viagra came out, in 1998. It’s been game-changing for me to get patients more comfortable talking about their erection issues.
I tell them it’s a 4-number scale. A “1” is no erection at all. A “2” is when it gets harder and larger, but it’s not going to penetrate. A “3” will penetrate, but it’s pretty wobbly. A “4” is that perfect cucumber–porn star erection that everyone is seeking. I have the patient tell me a story. They may say, “When I wake up in the morning, I’m at a 2. When I stimulate myself, I can get up to a 3. When I’m with my partner, sometimes I can get up to a 4.”
This is really helpful because they can talk in numbers. And after I give them treatments such as lifestyle changes, sex therapy, testosterone, a PDE5 inhibitor such as Viagra or Cialis, or an injection, they can come back and tell me how the story has changed. I have an objective measure that shows me how the treatment is affecting their erections. Not only do I feel more confident having those objective measures, but my patients feel more confident in the care that they’re getting, and they feel more comfortable talking to me about the changes. So, I encourage all of you to bring that EHS tool into your office. Show it to patients and get them more comfortable talking about erections.
Dr. Rubin is assistant clinical professor, department of urology, Georgetown University, Washington. She disclosed financial relationships with Absorption Pharmaceuticals, GlaxoSmithKline, and Endo Pharmaceuticals; has served as a speaker for Sprout; and has received research grant from Maternal Medical.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I mean it. Penis problems are very common and are an early sign that patients could have a cardiac event. Think about it: Clogging the arteries of the heart is called a heart attack; clogging the arteries to the penis is a penis attack, or as doctors like to call it, erectile dysfunction.
The arteries to the penis are only 1 mm in diameter. They develop plaque and clog the circulation long before the 3-mm cardiac arteries. So, it’s very important for primary care doctors to talk to their patients about erection health. And I’ll be honest: It’s easier to talk to patients about how lifestyle is affecting their penis health than it is to discuss how lifestyle affects longevity or prevents cancer. I get a lot of men to quit smoking because I tell them what it’s doing to their penises.
It can be challenging for doctors and patients to talk about penises. It doesn’t come naturally for many of us. If a 20-year-old comes in to my office with his 85-year-old grandfather and they both say their penises aren’t working, how do you figure out what’s going on? Do they even have the same thing wrong with them?
Here’s a fun and helpful tool that I use in my office. It’s called the Erection Hardness Score. It was developed around the time that Viagra came out, in 1998. It’s been game-changing for me to get patients more comfortable talking about their erection issues.
I tell them it’s a 4-number scale. A “1” is no erection at all. A “2” is when it gets harder and larger, but it’s not going to penetrate. A “3” will penetrate, but it’s pretty wobbly. A “4” is that perfect cucumber–porn star erection that everyone is seeking. I have the patient tell me a story. They may say, “When I wake up in the morning, I’m at a 2. When I stimulate myself, I can get up to a 3. When I’m with my partner, sometimes I can get up to a 4.”
This is really helpful because they can talk in numbers. And after I give them treatments such as lifestyle changes, sex therapy, testosterone, a PDE5 inhibitor such as Viagra or Cialis, or an injection, they can come back and tell me how the story has changed. I have an objective measure that shows me how the treatment is affecting their erections. Not only do I feel more confident having those objective measures, but my patients feel more confident in the care that they’re getting, and they feel more comfortable talking to me about the changes. So, I encourage all of you to bring that EHS tool into your office. Show it to patients and get them more comfortable talking about erections.
Dr. Rubin is assistant clinical professor, department of urology, Georgetown University, Washington. She disclosed financial relationships with Absorption Pharmaceuticals, GlaxoSmithKline, and Endo Pharmaceuticals; has served as a speaker for Sprout; and has received research grant from Maternal Medical.
A version of this article appeared on Medscape.com.
The steep costs of disrupting gut-barrier harmony
An interview with Elena Ivanina, DO, MPH
From Ayurveda to the teachings of Hippocrates, medicine’s earliest traditions advanced a belief that the gut was the foundation of all health and disease. It wasn’t until recently, however, that Western medicine has adopted the notion of gut-barrier dysfunction as a pathologic phenomenon critical to not only digestive health but also chronic allergic, inflammatory, and autoimmune disease.
To learn more, Medscape contributor Akash Goel, MD, interviewed Elena Ivanina, DO, MPH, an integrative gastroenterologist, on the role of the gut barrier. Dr. Ivanina is the founder of the Center for Integrative Gut Health and the former director of Neurogastroenterology and Motility at Lenox Hill Hospital in New York. She runs the educational platform for all things gut health, gutlove.com.
What is the role of the gut barrier in overall health and disease?
The gut contains the human body’s largest interface between a person and their external environment. The actual interface is at the gut barrier, where there needs to be an ideal homeostasis and selectivity mechanism to allow the absorption of healthy nutrients, but on the other hand prevent the penetration of harmful microbes, food antigens, and other proinflammatory factors and toxins.
The gut barrier is made up of the mucus layer, gut microbiome, epithelial cells, and immune cells in the lamina propria. When this apparatus is disrupted by factors such as infection, low-fiber diet, antibiotics, and alcohol, then it cannot function normally to selectively keep out the harmful intraluminal substances.
Gut-barrier disruption leads to translocation of dangerous intraluminal components, such as bacteria and their components, into the gut wall and, most importantly, exposes the immune system to them. This causes improper immune activation and dysregulation, which has been shown to lead to various diseases, including gastrointestinal inflammatory disorders such as inflammatory bowel disease (IBD) and celiac disease, systemic autoimmune diseases such as multiple sclerosis and rheumatoid arthritis, and metabolic diseases such as obesity and diabetes.
Is disruption of this barrier what is usually referred to as “leaky gut”?
Leaky gut is a colloquial term for increased intestinal permeability or intestinal hyperpermeability. In a 2019 review article, Dr. Michael Camilleri exposes leaky gut as a term that can be misleading and confusing to the general population. It calls upon clinicians to have an increased awareness of the potential of barrier dysfunction in diseases, and to consider the barrier as a target for treatment.
Is leaky gut more of a mechanism of underlying chronic disease or is it a disease of its own?
Intestinal permeability is a pathophysiologic process in the gut with certain risk factors that in some conditions has been shown to precede chronic disease. There has not been any convincing evidence that it can be diagnosed and treated as its own entity, but research is ongoing.
In IBD, the Crohn’s and Colitis Canada Genetic, Environmental, Microbial Project research consortium has been studying individuals at increased risk for Crohn’s disease because of a first-degree family member with Crohn’s disease. They found an increased abundance of Ruminococcus torques in the microbiomes of at-risk individuals who went on to develop the disease. R. torques are mucin degraders that induce an increase in other mucin-using bacteria, which can contribute to gut-barrier compromise.
In other studies, patients have been found to have asymptomatic intestinal hyperpermeability years before their diagnosis of Crohn’s disease. This supports understanding more about the potential of intestinal hyperpermeability as its own diagnosis that, if addressed, could possibly prevent disease development.
The many possible sources of gut-barrier disruption
What causes leaky gut, and when should physicians and patients be suspicious if they have it?
There are many risk factors that have been associated with leaky gut in both human studies and animal studies, including acrolein (food toxin), aging, alcohol, antacid drugs, antibiotics, burn injury, chemotherapy, circadian rhythm disruption, corticosteroids, emulsifiers (food additives), strenuous exercise (≥ 2 hours) at 60% VO2 max, starvation, fructose, fructans, gliadin (wheat protein), high-fat diet, high-salt diet, high-sugar diet, hyperglycemia, low-fiber diet, nonsteroidal anti-inflammatory drugs, pesticide, proinflammatory cytokines, psychological stress, radiation, sleep deprivation, smoking, and sweeteners.
Patients may be completely asymptomatic with leaky gut. Physicians should be suspicious if there is a genetic predisposition to chronic disease or if any risk factors are unveiled after assessing diet and lifestyle exposures.
What is the role of the Western diet and processed food consumption in driving disruptions of the gut barrier?
The Western diet reduces gut-barrier mucus thickness, leading to increased gut permeability. People who consume a Western diet typically eat less than 15 grams of fiber per day, which is significantly less than many other cultures, including the hunter-gatherers of Tanzania (Hadza), who get 100 or more grams of fiber a day in their food.
With a fiber-depleted diet, gut microbiota that normally feed on fiber gradually disappear and other commensals shift their metabolism to degrade the gut-barrier mucus layer.
A low-fiber diet also decreases short-chain fatty acid production, which reduces production of mucus and affects tight junction regulation.
Emerging evidence on causality
New evidence is demonstrating that previous functional conditions of the gastrointestinal tract, like functional dyspepsia, are associated with abnormalities to the intestinal barrier. What is the association between conditions like functional dyspepsia and irritable bowel syndrome (IBS) with gut-barrier disruption?
Conditions such as functional dyspepsia and IBS are similar in that their pathophysiology is incompletely understood and likely attributable to contributions from many different underlying mechanisms. This makes it difficult for clinicians to explain the condition to patients and often to treat without specific therapeutic targets.
Emerging evidence with new diagnostic tools, such as confocal laser endomicroscopy, has demonstrated altered mucosal barrier function in both conditions.
In patients with IBS who have a suspected food intolerance, studies looking at exposure to the food antigens found that the food caused immediate breaks, increased intervillous spaces, and increased inflammatory cells in the gut mucosa. These changes were associated with patient responses to exclusion diets.
In functional dyspepsia, another study, using confocal laser endomicroscopy, has shown that affected patients have significantly greater epithelial gap density in the duodenum, compared with healthy controls. There was also impaired duodenal-epithelial barrier integrity and evidence of increased cellular pyroptosis in the duodenal mucosa.
These findings suggest that while IBS and functional dyspepsia are still likely multifactorial, there may be a common preclinical state that can be further investigated as far as preventing its development and using it as a therapeutic target.
What diagnostic testing are you using to determine whether patients have disruptions to the gut barrier? Are they validated or more experimental?
There are various testing strategies that have been used in research to diagnose intestinal hyperpermeability. In a 2021 analysis, Dr. Michael Camilleri found that the optimal probes for measuring small intestinal and colonic permeability are the mass excreted of 13C-mannitol at 0-2 hours and lactulose during 2-8 hours or sucralose during 8-24 hours. Studies looking at postinfectious IBS have incorporated elevated urinary lactulose/mannitol ratios. Dr. Alessio Fasano and others have looked at using zonulin as a biomarker of impaired gut-barrier function. These tests are still considered experimental.
Is there an association between alterations in the gut microbiome and gut-barrier disruption?
There is an integral relationship between the gut microbiome and gut-barrier function, and dysbiosis can disrupt gut-barrier functionality.
The microbiota produce a variety of metabolites in close proximity to the gut epithelium, impacting gut-barrier function and immune response. For example, short-chain fatty acids produced by Bifidobacterium, Bacteroides, Enterobacter, Faecalibacterium, and Roseburia species impact host immune cell differentiation and metabolism as well as influence susceptibility to pathogens.
Studies have shown that sodium butyrate significantly improves epithelial-barrier function. Other experiments have used transplantation of the intestinal microbiota to show that introduction of certain microbial phenotypes can significantly increase gut permeability.
Practical advice for clinicians and patients
How do you advise patients to avoid gut-barrier disruption?
It is important to educate and counsel patients about the long list of risk factors, many of which are closely related to a Western diet and lifestyle, which can increase their risk for leaky gut.
Once one has it, can it be repaired? Can you share a bit about your protocols in general terms?
Many interventions have been shown to improve intestinal permeability. They include berberine, butyrate, caloric restriction and fasting, curcumin, dietary fiber (prebiotics), moderate exercise, fermented food, fish oil, glutamine, quercetin, probiotics, vagus nerve stimulation, vitamin D, and zinc.
Protocols have to be tailored to patients and their risk factors, diet, and lifestyle.
What are some tips from a nutrition and lifestyle standpoint that patients can follow to ensure a robust gut barrier?
It is important to emphasize a high-fiber diet with naturally fermented food, incorporating time-restricted eating, such as eating an early dinner and nothing else before bedtime, a moderate exercise routine, and gut-brain modulation with techniques such as acupuncture that can incorporate vagus nerve stimulation. Limited safe precision supplementation can be discussed on an individual basis based on the patient’s interest, additional testing, and other existing health conditions.
Dr. Akash Goel is a clinical assistant professor of medicine at Weill Cornell in gastroenterology and hepatology. He has disclosed no relevant financial relationships. His work has appeared on networks and publications such as CNN, The New York Times, Time Magazine, and Financial Times. He has a deep interest in nutrition, food as medicine, and the intersection between the gut microbiome and human health.
A version of this article appeared on Medscape.com.
An interview with Elena Ivanina, DO, MPH
An interview with Elena Ivanina, DO, MPH
From Ayurveda to the teachings of Hippocrates, medicine’s earliest traditions advanced a belief that the gut was the foundation of all health and disease. It wasn’t until recently, however, that Western medicine has adopted the notion of gut-barrier dysfunction as a pathologic phenomenon critical to not only digestive health but also chronic allergic, inflammatory, and autoimmune disease.
To learn more, Medscape contributor Akash Goel, MD, interviewed Elena Ivanina, DO, MPH, an integrative gastroenterologist, on the role of the gut barrier. Dr. Ivanina is the founder of the Center for Integrative Gut Health and the former director of Neurogastroenterology and Motility at Lenox Hill Hospital in New York. She runs the educational platform for all things gut health, gutlove.com.
What is the role of the gut barrier in overall health and disease?
The gut contains the human body’s largest interface between a person and their external environment. The actual interface is at the gut barrier, where there needs to be an ideal homeostasis and selectivity mechanism to allow the absorption of healthy nutrients, but on the other hand prevent the penetration of harmful microbes, food antigens, and other proinflammatory factors and toxins.
The gut barrier is made up of the mucus layer, gut microbiome, epithelial cells, and immune cells in the lamina propria. When this apparatus is disrupted by factors such as infection, low-fiber diet, antibiotics, and alcohol, then it cannot function normally to selectively keep out the harmful intraluminal substances.
Gut-barrier disruption leads to translocation of dangerous intraluminal components, such as bacteria and their components, into the gut wall and, most importantly, exposes the immune system to them. This causes improper immune activation and dysregulation, which has been shown to lead to various diseases, including gastrointestinal inflammatory disorders such as inflammatory bowel disease (IBD) and celiac disease, systemic autoimmune diseases such as multiple sclerosis and rheumatoid arthritis, and metabolic diseases such as obesity and diabetes.
Is disruption of this barrier what is usually referred to as “leaky gut”?
Leaky gut is a colloquial term for increased intestinal permeability or intestinal hyperpermeability. In a 2019 review article, Dr. Michael Camilleri exposes leaky gut as a term that can be misleading and confusing to the general population. It calls upon clinicians to have an increased awareness of the potential of barrier dysfunction in diseases, and to consider the barrier as a target for treatment.
Is leaky gut more of a mechanism of underlying chronic disease or is it a disease of its own?
Intestinal permeability is a pathophysiologic process in the gut with certain risk factors that in some conditions has been shown to precede chronic disease. There has not been any convincing evidence that it can be diagnosed and treated as its own entity, but research is ongoing.
In IBD, the Crohn’s and Colitis Canada Genetic, Environmental, Microbial Project research consortium has been studying individuals at increased risk for Crohn’s disease because of a first-degree family member with Crohn’s disease. They found an increased abundance of Ruminococcus torques in the microbiomes of at-risk individuals who went on to develop the disease. R. torques are mucin degraders that induce an increase in other mucin-using bacteria, which can contribute to gut-barrier compromise.
In other studies, patients have been found to have asymptomatic intestinal hyperpermeability years before their diagnosis of Crohn’s disease. This supports understanding more about the potential of intestinal hyperpermeability as its own diagnosis that, if addressed, could possibly prevent disease development.
The many possible sources of gut-barrier disruption
What causes leaky gut, and when should physicians and patients be suspicious if they have it?
There are many risk factors that have been associated with leaky gut in both human studies and animal studies, including acrolein (food toxin), aging, alcohol, antacid drugs, antibiotics, burn injury, chemotherapy, circadian rhythm disruption, corticosteroids, emulsifiers (food additives), strenuous exercise (≥ 2 hours) at 60% VO2 max, starvation, fructose, fructans, gliadin (wheat protein), high-fat diet, high-salt diet, high-sugar diet, hyperglycemia, low-fiber diet, nonsteroidal anti-inflammatory drugs, pesticide, proinflammatory cytokines, psychological stress, radiation, sleep deprivation, smoking, and sweeteners.
Patients may be completely asymptomatic with leaky gut. Physicians should be suspicious if there is a genetic predisposition to chronic disease or if any risk factors are unveiled after assessing diet and lifestyle exposures.
What is the role of the Western diet and processed food consumption in driving disruptions of the gut barrier?
The Western diet reduces gut-barrier mucus thickness, leading to increased gut permeability. People who consume a Western diet typically eat less than 15 grams of fiber per day, which is significantly less than many other cultures, including the hunter-gatherers of Tanzania (Hadza), who get 100 or more grams of fiber a day in their food.
With a fiber-depleted diet, gut microbiota that normally feed on fiber gradually disappear and other commensals shift their metabolism to degrade the gut-barrier mucus layer.
A low-fiber diet also decreases short-chain fatty acid production, which reduces production of mucus and affects tight junction regulation.
Emerging evidence on causality
New evidence is demonstrating that previous functional conditions of the gastrointestinal tract, like functional dyspepsia, are associated with abnormalities to the intestinal barrier. What is the association between conditions like functional dyspepsia and irritable bowel syndrome (IBS) with gut-barrier disruption?
Conditions such as functional dyspepsia and IBS are similar in that their pathophysiology is incompletely understood and likely attributable to contributions from many different underlying mechanisms. This makes it difficult for clinicians to explain the condition to patients and often to treat without specific therapeutic targets.
Emerging evidence with new diagnostic tools, such as confocal laser endomicroscopy, has demonstrated altered mucosal barrier function in both conditions.
In patients with IBS who have a suspected food intolerance, studies looking at exposure to the food antigens found that the food caused immediate breaks, increased intervillous spaces, and increased inflammatory cells in the gut mucosa. These changes were associated with patient responses to exclusion diets.
In functional dyspepsia, another study, using confocal laser endomicroscopy, has shown that affected patients have significantly greater epithelial gap density in the duodenum, compared with healthy controls. There was also impaired duodenal-epithelial barrier integrity and evidence of increased cellular pyroptosis in the duodenal mucosa.
These findings suggest that while IBS and functional dyspepsia are still likely multifactorial, there may be a common preclinical state that can be further investigated as far as preventing its development and using it as a therapeutic target.
What diagnostic testing are you using to determine whether patients have disruptions to the gut barrier? Are they validated or more experimental?
There are various testing strategies that have been used in research to diagnose intestinal hyperpermeability. In a 2021 analysis, Dr. Michael Camilleri found that the optimal probes for measuring small intestinal and colonic permeability are the mass excreted of 13C-mannitol at 0-2 hours and lactulose during 2-8 hours or sucralose during 8-24 hours. Studies looking at postinfectious IBS have incorporated elevated urinary lactulose/mannitol ratios. Dr. Alessio Fasano and others have looked at using zonulin as a biomarker of impaired gut-barrier function. These tests are still considered experimental.
Is there an association between alterations in the gut microbiome and gut-barrier disruption?
There is an integral relationship between the gut microbiome and gut-barrier function, and dysbiosis can disrupt gut-barrier functionality.
The microbiota produce a variety of metabolites in close proximity to the gut epithelium, impacting gut-barrier function and immune response. For example, short-chain fatty acids produced by Bifidobacterium, Bacteroides, Enterobacter, Faecalibacterium, and Roseburia species impact host immune cell differentiation and metabolism as well as influence susceptibility to pathogens.
Studies have shown that sodium butyrate significantly improves epithelial-barrier function. Other experiments have used transplantation of the intestinal microbiota to show that introduction of certain microbial phenotypes can significantly increase gut permeability.
Practical advice for clinicians and patients
How do you advise patients to avoid gut-barrier disruption?
It is important to educate and counsel patients about the long list of risk factors, many of which are closely related to a Western diet and lifestyle, which can increase their risk for leaky gut.
Once one has it, can it be repaired? Can you share a bit about your protocols in general terms?
Many interventions have been shown to improve intestinal permeability. They include berberine, butyrate, caloric restriction and fasting, curcumin, dietary fiber (prebiotics), moderate exercise, fermented food, fish oil, glutamine, quercetin, probiotics, vagus nerve stimulation, vitamin D, and zinc.
Protocols have to be tailored to patients and their risk factors, diet, and lifestyle.
What are some tips from a nutrition and lifestyle standpoint that patients can follow to ensure a robust gut barrier?
It is important to emphasize a high-fiber diet with naturally fermented food, incorporating time-restricted eating, such as eating an early dinner and nothing else before bedtime, a moderate exercise routine, and gut-brain modulation with techniques such as acupuncture that can incorporate vagus nerve stimulation. Limited safe precision supplementation can be discussed on an individual basis based on the patient’s interest, additional testing, and other existing health conditions.
Dr. Akash Goel is a clinical assistant professor of medicine at Weill Cornell in gastroenterology and hepatology. He has disclosed no relevant financial relationships. His work has appeared on networks and publications such as CNN, The New York Times, Time Magazine, and Financial Times. He has a deep interest in nutrition, food as medicine, and the intersection between the gut microbiome and human health.
A version of this article appeared on Medscape.com.
From Ayurveda to the teachings of Hippocrates, medicine’s earliest traditions advanced a belief that the gut was the foundation of all health and disease. It wasn’t until recently, however, that Western medicine has adopted the notion of gut-barrier dysfunction as a pathologic phenomenon critical to not only digestive health but also chronic allergic, inflammatory, and autoimmune disease.
To learn more, Medscape contributor Akash Goel, MD, interviewed Elena Ivanina, DO, MPH, an integrative gastroenterologist, on the role of the gut barrier. Dr. Ivanina is the founder of the Center for Integrative Gut Health and the former director of Neurogastroenterology and Motility at Lenox Hill Hospital in New York. She runs the educational platform for all things gut health, gutlove.com.
What is the role of the gut barrier in overall health and disease?
The gut contains the human body’s largest interface between a person and their external environment. The actual interface is at the gut barrier, where there needs to be an ideal homeostasis and selectivity mechanism to allow the absorption of healthy nutrients, but on the other hand prevent the penetration of harmful microbes, food antigens, and other proinflammatory factors and toxins.
The gut barrier is made up of the mucus layer, gut microbiome, epithelial cells, and immune cells in the lamina propria. When this apparatus is disrupted by factors such as infection, low-fiber diet, antibiotics, and alcohol, then it cannot function normally to selectively keep out the harmful intraluminal substances.
Gut-barrier disruption leads to translocation of dangerous intraluminal components, such as bacteria and their components, into the gut wall and, most importantly, exposes the immune system to them. This causes improper immune activation and dysregulation, which has been shown to lead to various diseases, including gastrointestinal inflammatory disorders such as inflammatory bowel disease (IBD) and celiac disease, systemic autoimmune diseases such as multiple sclerosis and rheumatoid arthritis, and metabolic diseases such as obesity and diabetes.
Is disruption of this barrier what is usually referred to as “leaky gut”?
Leaky gut is a colloquial term for increased intestinal permeability or intestinal hyperpermeability. In a 2019 review article, Dr. Michael Camilleri exposes leaky gut as a term that can be misleading and confusing to the general population. It calls upon clinicians to have an increased awareness of the potential of barrier dysfunction in diseases, and to consider the barrier as a target for treatment.
Is leaky gut more of a mechanism of underlying chronic disease or is it a disease of its own?
Intestinal permeability is a pathophysiologic process in the gut with certain risk factors that in some conditions has been shown to precede chronic disease. There has not been any convincing evidence that it can be diagnosed and treated as its own entity, but research is ongoing.
In IBD, the Crohn’s and Colitis Canada Genetic, Environmental, Microbial Project research consortium has been studying individuals at increased risk for Crohn’s disease because of a first-degree family member with Crohn’s disease. They found an increased abundance of Ruminococcus torques in the microbiomes of at-risk individuals who went on to develop the disease. R. torques are mucin degraders that induce an increase in other mucin-using bacteria, which can contribute to gut-barrier compromise.
In other studies, patients have been found to have asymptomatic intestinal hyperpermeability years before their diagnosis of Crohn’s disease. This supports understanding more about the potential of intestinal hyperpermeability as its own diagnosis that, if addressed, could possibly prevent disease development.
The many possible sources of gut-barrier disruption
What causes leaky gut, and when should physicians and patients be suspicious if they have it?
There are many risk factors that have been associated with leaky gut in both human studies and animal studies, including acrolein (food toxin), aging, alcohol, antacid drugs, antibiotics, burn injury, chemotherapy, circadian rhythm disruption, corticosteroids, emulsifiers (food additives), strenuous exercise (≥ 2 hours) at 60% VO2 max, starvation, fructose, fructans, gliadin (wheat protein), high-fat diet, high-salt diet, high-sugar diet, hyperglycemia, low-fiber diet, nonsteroidal anti-inflammatory drugs, pesticide, proinflammatory cytokines, psychological stress, radiation, sleep deprivation, smoking, and sweeteners.
Patients may be completely asymptomatic with leaky gut. Physicians should be suspicious if there is a genetic predisposition to chronic disease or if any risk factors are unveiled after assessing diet and lifestyle exposures.
What is the role of the Western diet and processed food consumption in driving disruptions of the gut barrier?
The Western diet reduces gut-barrier mucus thickness, leading to increased gut permeability. People who consume a Western diet typically eat less than 15 grams of fiber per day, which is significantly less than many other cultures, including the hunter-gatherers of Tanzania (Hadza), who get 100 or more grams of fiber a day in their food.
With a fiber-depleted diet, gut microbiota that normally feed on fiber gradually disappear and other commensals shift their metabolism to degrade the gut-barrier mucus layer.
A low-fiber diet also decreases short-chain fatty acid production, which reduces production of mucus and affects tight junction regulation.
Emerging evidence on causality
New evidence is demonstrating that previous functional conditions of the gastrointestinal tract, like functional dyspepsia, are associated with abnormalities to the intestinal barrier. What is the association between conditions like functional dyspepsia and irritable bowel syndrome (IBS) with gut-barrier disruption?
Conditions such as functional dyspepsia and IBS are similar in that their pathophysiology is incompletely understood and likely attributable to contributions from many different underlying mechanisms. This makes it difficult for clinicians to explain the condition to patients and often to treat without specific therapeutic targets.
Emerging evidence with new diagnostic tools, such as confocal laser endomicroscopy, has demonstrated altered mucosal barrier function in both conditions.
In patients with IBS who have a suspected food intolerance, studies looking at exposure to the food antigens found that the food caused immediate breaks, increased intervillous spaces, and increased inflammatory cells in the gut mucosa. These changes were associated with patient responses to exclusion diets.
In functional dyspepsia, another study, using confocal laser endomicroscopy, has shown that affected patients have significantly greater epithelial gap density in the duodenum, compared with healthy controls. There was also impaired duodenal-epithelial barrier integrity and evidence of increased cellular pyroptosis in the duodenal mucosa.
These findings suggest that while IBS and functional dyspepsia are still likely multifactorial, there may be a common preclinical state that can be further investigated as far as preventing its development and using it as a therapeutic target.
What diagnostic testing are you using to determine whether patients have disruptions to the gut barrier? Are they validated or more experimental?
There are various testing strategies that have been used in research to diagnose intestinal hyperpermeability. In a 2021 analysis, Dr. Michael Camilleri found that the optimal probes for measuring small intestinal and colonic permeability are the mass excreted of 13C-mannitol at 0-2 hours and lactulose during 2-8 hours or sucralose during 8-24 hours. Studies looking at postinfectious IBS have incorporated elevated urinary lactulose/mannitol ratios. Dr. Alessio Fasano and others have looked at using zonulin as a biomarker of impaired gut-barrier function. These tests are still considered experimental.
Is there an association between alterations in the gut microbiome and gut-barrier disruption?
There is an integral relationship between the gut microbiome and gut-barrier function, and dysbiosis can disrupt gut-barrier functionality.
The microbiota produce a variety of metabolites in close proximity to the gut epithelium, impacting gut-barrier function and immune response. For example, short-chain fatty acids produced by Bifidobacterium, Bacteroides, Enterobacter, Faecalibacterium, and Roseburia species impact host immune cell differentiation and metabolism as well as influence susceptibility to pathogens.
Studies have shown that sodium butyrate significantly improves epithelial-barrier function. Other experiments have used transplantation of the intestinal microbiota to show that introduction of certain microbial phenotypes can significantly increase gut permeability.
Practical advice for clinicians and patients
How do you advise patients to avoid gut-barrier disruption?
It is important to educate and counsel patients about the long list of risk factors, many of which are closely related to a Western diet and lifestyle, which can increase their risk for leaky gut.
Once one has it, can it be repaired? Can you share a bit about your protocols in general terms?
Many interventions have been shown to improve intestinal permeability. They include berberine, butyrate, caloric restriction and fasting, curcumin, dietary fiber (prebiotics), moderate exercise, fermented food, fish oil, glutamine, quercetin, probiotics, vagus nerve stimulation, vitamin D, and zinc.
Protocols have to be tailored to patients and their risk factors, diet, and lifestyle.
What are some tips from a nutrition and lifestyle standpoint that patients can follow to ensure a robust gut barrier?
It is important to emphasize a high-fiber diet with naturally fermented food, incorporating time-restricted eating, such as eating an early dinner and nothing else before bedtime, a moderate exercise routine, and gut-brain modulation with techniques such as acupuncture that can incorporate vagus nerve stimulation. Limited safe precision supplementation can be discussed on an individual basis based on the patient’s interest, additional testing, and other existing health conditions.
Dr. Akash Goel is a clinical assistant professor of medicine at Weill Cornell in gastroenterology and hepatology. He has disclosed no relevant financial relationships. His work has appeared on networks and publications such as CNN, The New York Times, Time Magazine, and Financial Times. He has a deep interest in nutrition, food as medicine, and the intersection between the gut microbiome and human health.
A version of this article appeared on Medscape.com.
An 88-year-old Black woman presented with 3 months duration of asymptomatic, violaceous patches on the left breast
Angiosarcomas are uncommon, high-grade malignant tumors of endothelial cell origin that can arise via the lymphatics or vasculature. They typically occur spontaneously; however, there have been cases reported of benign vascular transformation. These tumors are more commonly found in elderly men on the head and neck in sun-damaged skin. . This is a late complication, typically occurring about 5-10 years after radiation. Stewart-Treves syndrome, chronic lymphedema occurring after breast cancer treatment with axillary node dissection, increases the risk of angiosarcoma. As a vascular tumor, angiosarcoma spreads hematogenously and carries a poor prognosis if not caught early. Differential diagnoses include other vascular tumors such as retiform hemangioendothelioma. In this specific patient, the differential diagnosis includes Paget’s disease, chronic radiation skin changes, and eczema.
Histopathologically, angiosarcomas exhibit abnormal, pleomorphic, malignant endothelial cells. As the tumor progresses, the cell architecture becomes more distorted and cells form layers with papillary projections into the vascular lumen. Malignant cells may stain positive for CD31, CD34, the oncogene ERG and the proto-oncogene FLI-1. Histology in this patient revealed radiation changes in the dermis, as well as few vascular channels lined by large endothelial cells with marked nuclear atypia, in the form of large nucleoli and variably coarse chromatin. The cells were positive for MYC.
Treatment of angiosarcoma involves a multidisciplinary approach. Resection with wide margins is generally the treatment of choice. However, recurrence is relatively common, which may be a result of microsatellite deposits of the tumor. Perioperative radiation is recommended, and adjuvant chemotherapy often is recommended for metastatic disease. Specifically, paclitaxel has been found to promote survival in some cases of cutaneous angiosarcoma. Metastatic disease may be treated with cytotoxic drugs such as anthracyclines and taxanes. Additionally, targeted therapy including anti-VEGF drugs and tyrosine kinase inhibitors have been tested.
The case and photo were submitted by Mr. Shapiro of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Fla., and Dr. Bilu Martin. The column was edited by Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Cohen-Hallaleh RB et al. Clin Sarcoma Res. 2017 Aug 7:7:15.
Cozzi S et al. Rep Pract Oncol Radiother. 2021 Sep 30;26(5):827-32.
Spiker AM, Mangla A, Ramsey ML. Angiosarcoma. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing; 2023 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK441983/
Angiosarcomas are uncommon, high-grade malignant tumors of endothelial cell origin that can arise via the lymphatics or vasculature. They typically occur spontaneously; however, there have been cases reported of benign vascular transformation. These tumors are more commonly found in elderly men on the head and neck in sun-damaged skin. . This is a late complication, typically occurring about 5-10 years after radiation. Stewart-Treves syndrome, chronic lymphedema occurring after breast cancer treatment with axillary node dissection, increases the risk of angiosarcoma. As a vascular tumor, angiosarcoma spreads hematogenously and carries a poor prognosis if not caught early. Differential diagnoses include other vascular tumors such as retiform hemangioendothelioma. In this specific patient, the differential diagnosis includes Paget’s disease, chronic radiation skin changes, and eczema.
Histopathologically, angiosarcomas exhibit abnormal, pleomorphic, malignant endothelial cells. As the tumor progresses, the cell architecture becomes more distorted and cells form layers with papillary projections into the vascular lumen. Malignant cells may stain positive for CD31, CD34, the oncogene ERG and the proto-oncogene FLI-1. Histology in this patient revealed radiation changes in the dermis, as well as few vascular channels lined by large endothelial cells with marked nuclear atypia, in the form of large nucleoli and variably coarse chromatin. The cells were positive for MYC.
Treatment of angiosarcoma involves a multidisciplinary approach. Resection with wide margins is generally the treatment of choice. However, recurrence is relatively common, which may be a result of microsatellite deposits of the tumor. Perioperative radiation is recommended, and adjuvant chemotherapy often is recommended for metastatic disease. Specifically, paclitaxel has been found to promote survival in some cases of cutaneous angiosarcoma. Metastatic disease may be treated with cytotoxic drugs such as anthracyclines and taxanes. Additionally, targeted therapy including anti-VEGF drugs and tyrosine kinase inhibitors have been tested.
The case and photo were submitted by Mr. Shapiro of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Fla., and Dr. Bilu Martin. The column was edited by Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Cohen-Hallaleh RB et al. Clin Sarcoma Res. 2017 Aug 7:7:15.
Cozzi S et al. Rep Pract Oncol Radiother. 2021 Sep 30;26(5):827-32.
Spiker AM, Mangla A, Ramsey ML. Angiosarcoma. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing; 2023 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK441983/
Angiosarcomas are uncommon, high-grade malignant tumors of endothelial cell origin that can arise via the lymphatics or vasculature. They typically occur spontaneously; however, there have been cases reported of benign vascular transformation. These tumors are more commonly found in elderly men on the head and neck in sun-damaged skin. . This is a late complication, typically occurring about 5-10 years after radiation. Stewart-Treves syndrome, chronic lymphedema occurring after breast cancer treatment with axillary node dissection, increases the risk of angiosarcoma. As a vascular tumor, angiosarcoma spreads hematogenously and carries a poor prognosis if not caught early. Differential diagnoses include other vascular tumors such as retiform hemangioendothelioma. In this specific patient, the differential diagnosis includes Paget’s disease, chronic radiation skin changes, and eczema.
Histopathologically, angiosarcomas exhibit abnormal, pleomorphic, malignant endothelial cells. As the tumor progresses, the cell architecture becomes more distorted and cells form layers with papillary projections into the vascular lumen. Malignant cells may stain positive for CD31, CD34, the oncogene ERG and the proto-oncogene FLI-1. Histology in this patient revealed radiation changes in the dermis, as well as few vascular channels lined by large endothelial cells with marked nuclear atypia, in the form of large nucleoli and variably coarse chromatin. The cells were positive for MYC.
Treatment of angiosarcoma involves a multidisciplinary approach. Resection with wide margins is generally the treatment of choice. However, recurrence is relatively common, which may be a result of microsatellite deposits of the tumor. Perioperative radiation is recommended, and adjuvant chemotherapy often is recommended for metastatic disease. Specifically, paclitaxel has been found to promote survival in some cases of cutaneous angiosarcoma. Metastatic disease may be treated with cytotoxic drugs such as anthracyclines and taxanes. Additionally, targeted therapy including anti-VEGF drugs and tyrosine kinase inhibitors have been tested.
The case and photo were submitted by Mr. Shapiro of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Fla., and Dr. Bilu Martin. The column was edited by Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Cohen-Hallaleh RB et al. Clin Sarcoma Res. 2017 Aug 7:7:15.
Cozzi S et al. Rep Pract Oncol Radiother. 2021 Sep 30;26(5):827-32.
Spiker AM, Mangla A, Ramsey ML. Angiosarcoma. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing; 2023 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK441983/
A letter from Michael Camilleri, MD, DSc, AGAF, AGA Research Foundation chair and past AGA Institute president
And you understand the tremendous value of research to advance patient care.
We are in a time of major scientific breakthroughs; however, there is a growing gap in federal funding for research. Without gastroenterology and hepatology research, there would be no discoveries to develop new diagnostic and therapeutic approaches and to improve our understanding of the pathogenesis of digestive diseases.
The AGA Research Foundation funds promising GI investigators who don’t receive funding at crucial times in their early careers. The research of these talented individuals, while important to the field, could end prematurely if they are left unfunded. That’s something the fields of gastroenterology and hepatology can’t afford, and that’s why, as an AGA member, I’m making a year-end donation to the AGA Research Foundation. You can help fill the funding gap and protect the next generation of investigators by joining me in supporting the AGA Research Foundation through a personal year-end gift.
Gifts to the AGA Research Foundation this past year directly supported 71 investigators. Despite this success, close to 245 other promising research proposals were not funded.
We must continue to foster the careers of talented scientists and clinicians, and protect the GI research pipeline. A financial contribution to the AGA Research Foundation is the opportunity for you to help foster the careers of talented scientists and protect the GI research pipeline.
Help make a difference. You can make your tax-deductible donation online at www.gastro.org/donateonline; by phone at 301-222-4002; or, by mail:
AGA Research Foundation
4930 Del Ray Avenue
Bethesda, MD 20814
All gifts are tax-deductible to the fullest extent of U.S. law.
Thank you for your support and best wishes for a happy, healthy holiday season and prosperous New Year.
And you understand the tremendous value of research to advance patient care.
We are in a time of major scientific breakthroughs; however, there is a growing gap in federal funding for research. Without gastroenterology and hepatology research, there would be no discoveries to develop new diagnostic and therapeutic approaches and to improve our understanding of the pathogenesis of digestive diseases.
The AGA Research Foundation funds promising GI investigators who don’t receive funding at crucial times in their early careers. The research of these talented individuals, while important to the field, could end prematurely if they are left unfunded. That’s something the fields of gastroenterology and hepatology can’t afford, and that’s why, as an AGA member, I’m making a year-end donation to the AGA Research Foundation. You can help fill the funding gap and protect the next generation of investigators by joining me in supporting the AGA Research Foundation through a personal year-end gift.
Gifts to the AGA Research Foundation this past year directly supported 71 investigators. Despite this success, close to 245 other promising research proposals were not funded.
We must continue to foster the careers of talented scientists and clinicians, and protect the GI research pipeline. A financial contribution to the AGA Research Foundation is the opportunity for you to help foster the careers of talented scientists and protect the GI research pipeline.
Help make a difference. You can make your tax-deductible donation online at www.gastro.org/donateonline; by phone at 301-222-4002; or, by mail:
AGA Research Foundation
4930 Del Ray Avenue
Bethesda, MD 20814
All gifts are tax-deductible to the fullest extent of U.S. law.
Thank you for your support and best wishes for a happy, healthy holiday season and prosperous New Year.
And you understand the tremendous value of research to advance patient care.
We are in a time of major scientific breakthroughs; however, there is a growing gap in federal funding for research. Without gastroenterology and hepatology research, there would be no discoveries to develop new diagnostic and therapeutic approaches and to improve our understanding of the pathogenesis of digestive diseases.
The AGA Research Foundation funds promising GI investigators who don’t receive funding at crucial times in their early careers. The research of these talented individuals, while important to the field, could end prematurely if they are left unfunded. That’s something the fields of gastroenterology and hepatology can’t afford, and that’s why, as an AGA member, I’m making a year-end donation to the AGA Research Foundation. You can help fill the funding gap and protect the next generation of investigators by joining me in supporting the AGA Research Foundation through a personal year-end gift.
Gifts to the AGA Research Foundation this past year directly supported 71 investigators. Despite this success, close to 245 other promising research proposals were not funded.
We must continue to foster the careers of talented scientists and clinicians, and protect the GI research pipeline. A financial contribution to the AGA Research Foundation is the opportunity for you to help foster the careers of talented scientists and protect the GI research pipeline.
Help make a difference. You can make your tax-deductible donation online at www.gastro.org/donateonline; by phone at 301-222-4002; or, by mail:
AGA Research Foundation
4930 Del Ray Avenue
Bethesda, MD 20814
All gifts are tax-deductible to the fullest extent of U.S. law.
Thank you for your support and best wishes for a happy, healthy holiday season and prosperous New Year.
What not to prescribe to older adults and what to use instead
This transcript has been edited for clarity.
These criteria have been updated and revised approximately every 5 years since 1991 and serve to alert us to medications for which the risk-benefit ratio is not as good in older adults as in the rest of the population.
These are important criteria because medications are metabolized differently in older adults and have different effects compared with younger patients. For the sake of these criteria, older adults are 65 years of age or older. That said, we know that everyone from 65 to 100 is not the same. As people age, they develop more comorbidities, they become more frail, and they are more sensitive to the effects and side effects of drugs.
The guidance covers potentially inappropriate medications for older adults. The word “potentially” is important because this is guidance. As clinicians, we make decisions involving individuals. This guidance should be used with judgment, integrating the clinical context of the individual patient.
There is a lot in this guidance. I am going to try to cover what I feel are the most important points.
Aspirin. Since the risk for major bleeding increases with age, for primary prevention of atherosclerotic cardiovascular disease, the harm can be greater than the benefit in older adults, so aspirin should not be used for primary prevention. Aspirin remains indicated for secondary prevention in individuals with established cardiovascular disease.
Warfarin. For treatment of atrial fibrillation or venous thromboembolism (deep vein thrombosis or pulmonary embolism), warfarin should be avoided if possible. Warfarin has a higher risk for major bleeding, particularly intracranial bleeding, than direct oral anticoagulants (DOACs); therefore the latter are preferred. Rivaroxaban should be avoided, as it has a higher risk for major bleeding in older adults than the other DOACs. Apixaban is preferred over dabigatran. If a patient is well controlled on warfarin, you can consider continuing that treatment.
Antipsychotics. These include first- and second-generation antipsychotics such as aripiprazole, haloperidol, olanzapine, quetiapine, risperidone, and others. The guidance says to avoid these agents except for FDA-approved indications such as schizophrenia, bipolar disorder, and adjuvant treatment of depression. Use of these antipsychotics can increase risk for stroke, heart attack, and mortality. Essentially, the guidance says do not use these medications lightly for the treatment of agitated dementia. For those of us with older patients, this can get tricky because agitated dementia is a difficult issue for which there are no good effective medications. The Beers guidance recognizes this in saying that these medications should be avoided unless behavioral interventions have failed. So, there are times where you may need to use these medicines, but use them judiciously.
For patients with dementia, anticholinergics, antipsychotics, and benzodiazepines should be avoided if possible.
Benzodiazepines. Benzodiazepines should also be avoided because older adults have increased sensitivity to their effects due to slower metabolism and clearance of these medications, which can lead to a much longer half-life and higher serum level. In older adults, benzodiazepines increase the risk for cognitive impairment, delirium, falls, fractures, and even motor accidents. The same concerns affect the group of non-benzodiazepine sleeping medicines known as “Z-drugs.”
Nonsteroidal anti-inflammatory drugs (NSAIDs). Used frequently in our practices, NSAIDs are nevertheless on the list. As we think through the risk-benefit ratio of using NSAIDs in older adults, we often underappreciate the risks of these agents. Upper gastrointestinal ulcers with bleeding occur in approximately 1% of patients treated for 3-6 months with an NSAID and in 2%-4% of patients treated for a year. NSAIDs also increase the risk for renal impairment and cardiovascular disease.
Other medications to avoid (if possible). These include:
Sulfonylureas, due to a high risk for hypoglycemia. A short-acting sulfonylurea, such as glipizide, should be used if one is needed.
Proton pump inhibitors should not be used long-term if it can be avoided.
Digoxin should not be first-line treatment for atrial fibrillation or heart failure. Decreased renal clearance in older adults can lead to toxic levels of digoxin, particularly during acute illnesses. Avoid doses > 0.125 mg/day.
Nitrofurantoin should be avoided when the patient’s creatinine clearance is < 30 or for long-term suppressive therapy.
Avoid combining medications that have high anticholinergic side effects, such as scopolamine, diphenhydramine, oxybutynin, cyclobenzaprine, and others.
It is always important to understand the benefits and the risks of the drugs we prescribe. It is also important to remember that older adults are a particularly vulnerable population. The Beers criteria provide important guidance, which we can then use to make decisions about medicines for individual patients.
Dr. Skolnik is a professor in the department of family medicine at Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director in the department of family medicine at Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GSK, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
These criteria have been updated and revised approximately every 5 years since 1991 and serve to alert us to medications for which the risk-benefit ratio is not as good in older adults as in the rest of the population.
These are important criteria because medications are metabolized differently in older adults and have different effects compared with younger patients. For the sake of these criteria, older adults are 65 years of age or older. That said, we know that everyone from 65 to 100 is not the same. As people age, they develop more comorbidities, they become more frail, and they are more sensitive to the effects and side effects of drugs.
The guidance covers potentially inappropriate medications for older adults. The word “potentially” is important because this is guidance. As clinicians, we make decisions involving individuals. This guidance should be used with judgment, integrating the clinical context of the individual patient.
There is a lot in this guidance. I am going to try to cover what I feel are the most important points.
Aspirin. Since the risk for major bleeding increases with age, for primary prevention of atherosclerotic cardiovascular disease, the harm can be greater than the benefit in older adults, so aspirin should not be used for primary prevention. Aspirin remains indicated for secondary prevention in individuals with established cardiovascular disease.
Warfarin. For treatment of atrial fibrillation or venous thromboembolism (deep vein thrombosis or pulmonary embolism), warfarin should be avoided if possible. Warfarin has a higher risk for major bleeding, particularly intracranial bleeding, than direct oral anticoagulants (DOACs); therefore the latter are preferred. Rivaroxaban should be avoided, as it has a higher risk for major bleeding in older adults than the other DOACs. Apixaban is preferred over dabigatran. If a patient is well controlled on warfarin, you can consider continuing that treatment.
Antipsychotics. These include first- and second-generation antipsychotics such as aripiprazole, haloperidol, olanzapine, quetiapine, risperidone, and others. The guidance says to avoid these agents except for FDA-approved indications such as schizophrenia, bipolar disorder, and adjuvant treatment of depression. Use of these antipsychotics can increase risk for stroke, heart attack, and mortality. Essentially, the guidance says do not use these medications lightly for the treatment of agitated dementia. For those of us with older patients, this can get tricky because agitated dementia is a difficult issue for which there are no good effective medications. The Beers guidance recognizes this in saying that these medications should be avoided unless behavioral interventions have failed. So, there are times where you may need to use these medicines, but use them judiciously.
For patients with dementia, anticholinergics, antipsychotics, and benzodiazepines should be avoided if possible.
Benzodiazepines. Benzodiazepines should also be avoided because older adults have increased sensitivity to their effects due to slower metabolism and clearance of these medications, which can lead to a much longer half-life and higher serum level. In older adults, benzodiazepines increase the risk for cognitive impairment, delirium, falls, fractures, and even motor accidents. The same concerns affect the group of non-benzodiazepine sleeping medicines known as “Z-drugs.”
Nonsteroidal anti-inflammatory drugs (NSAIDs). Used frequently in our practices, NSAIDs are nevertheless on the list. As we think through the risk-benefit ratio of using NSAIDs in older adults, we often underappreciate the risks of these agents. Upper gastrointestinal ulcers with bleeding occur in approximately 1% of patients treated for 3-6 months with an NSAID and in 2%-4% of patients treated for a year. NSAIDs also increase the risk for renal impairment and cardiovascular disease.
Other medications to avoid (if possible). These include:
Sulfonylureas, due to a high risk for hypoglycemia. A short-acting sulfonylurea, such as glipizide, should be used if one is needed.
Proton pump inhibitors should not be used long-term if it can be avoided.
Digoxin should not be first-line treatment for atrial fibrillation or heart failure. Decreased renal clearance in older adults can lead to toxic levels of digoxin, particularly during acute illnesses. Avoid doses > 0.125 mg/day.
Nitrofurantoin should be avoided when the patient’s creatinine clearance is < 30 or for long-term suppressive therapy.
Avoid combining medications that have high anticholinergic side effects, such as scopolamine, diphenhydramine, oxybutynin, cyclobenzaprine, and others.
It is always important to understand the benefits and the risks of the drugs we prescribe. It is also important to remember that older adults are a particularly vulnerable population. The Beers criteria provide important guidance, which we can then use to make decisions about medicines for individual patients.
Dr. Skolnik is a professor in the department of family medicine at Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director in the department of family medicine at Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GSK, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
These criteria have been updated and revised approximately every 5 years since 1991 and serve to alert us to medications for which the risk-benefit ratio is not as good in older adults as in the rest of the population.
These are important criteria because medications are metabolized differently in older adults and have different effects compared with younger patients. For the sake of these criteria, older adults are 65 years of age or older. That said, we know that everyone from 65 to 100 is not the same. As people age, they develop more comorbidities, they become more frail, and they are more sensitive to the effects and side effects of drugs.
The guidance covers potentially inappropriate medications for older adults. The word “potentially” is important because this is guidance. As clinicians, we make decisions involving individuals. This guidance should be used with judgment, integrating the clinical context of the individual patient.
There is a lot in this guidance. I am going to try to cover what I feel are the most important points.
Aspirin. Since the risk for major bleeding increases with age, for primary prevention of atherosclerotic cardiovascular disease, the harm can be greater than the benefit in older adults, so aspirin should not be used for primary prevention. Aspirin remains indicated for secondary prevention in individuals with established cardiovascular disease.
Warfarin. For treatment of atrial fibrillation or venous thromboembolism (deep vein thrombosis or pulmonary embolism), warfarin should be avoided if possible. Warfarin has a higher risk for major bleeding, particularly intracranial bleeding, than direct oral anticoagulants (DOACs); therefore the latter are preferred. Rivaroxaban should be avoided, as it has a higher risk for major bleeding in older adults than the other DOACs. Apixaban is preferred over dabigatran. If a patient is well controlled on warfarin, you can consider continuing that treatment.
Antipsychotics. These include first- and second-generation antipsychotics such as aripiprazole, haloperidol, olanzapine, quetiapine, risperidone, and others. The guidance says to avoid these agents except for FDA-approved indications such as schizophrenia, bipolar disorder, and adjuvant treatment of depression. Use of these antipsychotics can increase risk for stroke, heart attack, and mortality. Essentially, the guidance says do not use these medications lightly for the treatment of agitated dementia. For those of us with older patients, this can get tricky because agitated dementia is a difficult issue for which there are no good effective medications. The Beers guidance recognizes this in saying that these medications should be avoided unless behavioral interventions have failed. So, there are times where you may need to use these medicines, but use them judiciously.
For patients with dementia, anticholinergics, antipsychotics, and benzodiazepines should be avoided if possible.
Benzodiazepines. Benzodiazepines should also be avoided because older adults have increased sensitivity to their effects due to slower metabolism and clearance of these medications, which can lead to a much longer half-life and higher serum level. In older adults, benzodiazepines increase the risk for cognitive impairment, delirium, falls, fractures, and even motor accidents. The same concerns affect the group of non-benzodiazepine sleeping medicines known as “Z-drugs.”
Nonsteroidal anti-inflammatory drugs (NSAIDs). Used frequently in our practices, NSAIDs are nevertheless on the list. As we think through the risk-benefit ratio of using NSAIDs in older adults, we often underappreciate the risks of these agents. Upper gastrointestinal ulcers with bleeding occur in approximately 1% of patients treated for 3-6 months with an NSAID and in 2%-4% of patients treated for a year. NSAIDs also increase the risk for renal impairment and cardiovascular disease.
Other medications to avoid (if possible). These include:
Sulfonylureas, due to a high risk for hypoglycemia. A short-acting sulfonylurea, such as glipizide, should be used if one is needed.
Proton pump inhibitors should not be used long-term if it can be avoided.
Digoxin should not be first-line treatment for atrial fibrillation or heart failure. Decreased renal clearance in older adults can lead to toxic levels of digoxin, particularly during acute illnesses. Avoid doses > 0.125 mg/day.
Nitrofurantoin should be avoided when the patient’s creatinine clearance is < 30 or for long-term suppressive therapy.
Avoid combining medications that have high anticholinergic side effects, such as scopolamine, diphenhydramine, oxybutynin, cyclobenzaprine, and others.
It is always important to understand the benefits and the risks of the drugs we prescribe. It is also important to remember that older adults are a particularly vulnerable population. The Beers criteria provide important guidance, which we can then use to make decisions about medicines for individual patients.
Dr. Skolnik is a professor in the department of family medicine at Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and associate director in the department of family medicine at Abington (Pa.) Jefferson Health. He disclosed ties with AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, GSK, Merck, Sanofi, Sanofi Pasteur, and Teva.
A version of this article appeared on Medscape.com.
MOC: An ‘insult to oncologists’ engaged in patient care
This transcript has been edited for clarity.
I am far from the only doctor, and certainly far from the only oncologist, to recently comment on the topic of Maintenance of Certification. Of course, this is happening in a wider debate about our relationship as subspecialists to the American Board of Internal Medicine, and what they deem acceptable for the recertification of doctors in practice.
One of the things I tell my patients is that if I practiced exactly the way I was trained to practice — and I had a very good fellowship program with superb faculty – if I practiced the way they taught me, it would now be malpractice. I finished my fellowship in 2012, just over a decade ago. The rate of progress in the interim is simply staggering. It looks so different now than it did then.
For instance, 2011 was my first experience ever using a form of immunotherapy. It was an anti-CTLA4 agent, ipilimumab, and I was treating metastatic melanoma. I learned in that instance just how effective these drugs can be, but also how toxic they can be. Ever since then, I’ve been refining my use of immunotherapy. We do that iteratively. We do that as we encounter patients and as we try to meet their needs.
I do understand that the ABIM is saying they want an independent governing body to legislate that process. I think the reason this is stuck in the craw of so many oncologists is that we demonstrate our commitment to continuing medical education all the time.
I’m recording this in my office, which is separate from the space where I see patients. I see patients in a different group of exam rooms for their privacy and it’s a better setup for aspects of the physical encounter. Not a single patient has ever asked to come into my office and see my diplomas, and I sometimes wonder if I keep them here mostly as a visual cue to myself, sort of an antidote to ward off imposter syndrome and remind myself, Oh yeah – I earned these. I earned these through formal training.
Then something happens once you finish your training, whether it’s residency or fellowship, and you become an attending. I think you feel a weight of responsibility, the responsibility of independent learning. All of us are doing this. We have to do this. The field is moving along at such a rapid clip that it’s essentially built into what we do that we are going to keep up. In fact, channels such as the various aspects of social media are a way I curate my own information feed so I can stay up to speed and not feel like I’m drowning in a deluge of new data.
But what’s hard to demonstrate to the ABIM is that [this learning] is already happening. I think we can do it if we submit our records of CME credits that we formally accrue. The reason this is such an almost insult to oncologists in practice is because it is a necessary part of our day-to-day existence to keep apprised of developments so we can apply them to patient care.
One litmus test of attending a medical conference like the annual meeting of the American Society of Clinical Oncology is to ask oneself, When I go back to clinic, is this meeting going to change the way that I take care of patients? The answer almost invariably these days is yes. I go to multiple meetings per year, and I think it’s the exception, not the rule, that I return home and nothing changes in my management patterns. Again, this process is happening whether the ABIM recognizes it or not.
Lastly, I sat down in the fall of 2022 and I did my recertification. I looked at the span of all the things that had happened between 2012, when I first sat for my board examination in medical oncology, and 2022. It was staggering. I think the reason that it wasn’t such an overwhelming amount of information to review is that I had actually been accreting it slowly and gradually, month by month, year by year throughout that decade.
Again, it’s necessary that the ABIM hear us, hear oncologists, and know that of all the medical subspecialties they govern, it is basically already an essential task of our day-to-day professional existence that we engage in lifelong learning. To suggest otherwise really paints us as outdated. The reason that matters so much is that if we’re not up-to-date, then we are underserving our patients.
Mark A. Lewis, MD, is director of gastrointestinal oncology at Intermountain Healthcare in Salt Lake City. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I am far from the only doctor, and certainly far from the only oncologist, to recently comment on the topic of Maintenance of Certification. Of course, this is happening in a wider debate about our relationship as subspecialists to the American Board of Internal Medicine, and what they deem acceptable for the recertification of doctors in practice.
One of the things I tell my patients is that if I practiced exactly the way I was trained to practice — and I had a very good fellowship program with superb faculty – if I practiced the way they taught me, it would now be malpractice. I finished my fellowship in 2012, just over a decade ago. The rate of progress in the interim is simply staggering. It looks so different now than it did then.
For instance, 2011 was my first experience ever using a form of immunotherapy. It was an anti-CTLA4 agent, ipilimumab, and I was treating metastatic melanoma. I learned in that instance just how effective these drugs can be, but also how toxic they can be. Ever since then, I’ve been refining my use of immunotherapy. We do that iteratively. We do that as we encounter patients and as we try to meet their needs.
I do understand that the ABIM is saying they want an independent governing body to legislate that process. I think the reason this is stuck in the craw of so many oncologists is that we demonstrate our commitment to continuing medical education all the time.
I’m recording this in my office, which is separate from the space where I see patients. I see patients in a different group of exam rooms for their privacy and it’s a better setup for aspects of the physical encounter. Not a single patient has ever asked to come into my office and see my diplomas, and I sometimes wonder if I keep them here mostly as a visual cue to myself, sort of an antidote to ward off imposter syndrome and remind myself, Oh yeah – I earned these. I earned these through formal training.
Then something happens once you finish your training, whether it’s residency or fellowship, and you become an attending. I think you feel a weight of responsibility, the responsibility of independent learning. All of us are doing this. We have to do this. The field is moving along at such a rapid clip that it’s essentially built into what we do that we are going to keep up. In fact, channels such as the various aspects of social media are a way I curate my own information feed so I can stay up to speed and not feel like I’m drowning in a deluge of new data.
But what’s hard to demonstrate to the ABIM is that [this learning] is already happening. I think we can do it if we submit our records of CME credits that we formally accrue. The reason this is such an almost insult to oncologists in practice is because it is a necessary part of our day-to-day existence to keep apprised of developments so we can apply them to patient care.
One litmus test of attending a medical conference like the annual meeting of the American Society of Clinical Oncology is to ask oneself, When I go back to clinic, is this meeting going to change the way that I take care of patients? The answer almost invariably these days is yes. I go to multiple meetings per year, and I think it’s the exception, not the rule, that I return home and nothing changes in my management patterns. Again, this process is happening whether the ABIM recognizes it or not.
Lastly, I sat down in the fall of 2022 and I did my recertification. I looked at the span of all the things that had happened between 2012, when I first sat for my board examination in medical oncology, and 2022. It was staggering. I think the reason that it wasn’t such an overwhelming amount of information to review is that I had actually been accreting it slowly and gradually, month by month, year by year throughout that decade.
Again, it’s necessary that the ABIM hear us, hear oncologists, and know that of all the medical subspecialties they govern, it is basically already an essential task of our day-to-day professional existence that we engage in lifelong learning. To suggest otherwise really paints us as outdated. The reason that matters so much is that if we’re not up-to-date, then we are underserving our patients.
Mark A. Lewis, MD, is director of gastrointestinal oncology at Intermountain Healthcare in Salt Lake City. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I am far from the only doctor, and certainly far from the only oncologist, to recently comment on the topic of Maintenance of Certification. Of course, this is happening in a wider debate about our relationship as subspecialists to the American Board of Internal Medicine, and what they deem acceptable for the recertification of doctors in practice.
One of the things I tell my patients is that if I practiced exactly the way I was trained to practice — and I had a very good fellowship program with superb faculty – if I practiced the way they taught me, it would now be malpractice. I finished my fellowship in 2012, just over a decade ago. The rate of progress in the interim is simply staggering. It looks so different now than it did then.
For instance, 2011 was my first experience ever using a form of immunotherapy. It was an anti-CTLA4 agent, ipilimumab, and I was treating metastatic melanoma. I learned in that instance just how effective these drugs can be, but also how toxic they can be. Ever since then, I’ve been refining my use of immunotherapy. We do that iteratively. We do that as we encounter patients and as we try to meet their needs.
I do understand that the ABIM is saying they want an independent governing body to legislate that process. I think the reason this is stuck in the craw of so many oncologists is that we demonstrate our commitment to continuing medical education all the time.
I’m recording this in my office, which is separate from the space where I see patients. I see patients in a different group of exam rooms for their privacy and it’s a better setup for aspects of the physical encounter. Not a single patient has ever asked to come into my office and see my diplomas, and I sometimes wonder if I keep them here mostly as a visual cue to myself, sort of an antidote to ward off imposter syndrome and remind myself, Oh yeah – I earned these. I earned these through formal training.
Then something happens once you finish your training, whether it’s residency or fellowship, and you become an attending. I think you feel a weight of responsibility, the responsibility of independent learning. All of us are doing this. We have to do this. The field is moving along at such a rapid clip that it’s essentially built into what we do that we are going to keep up. In fact, channels such as the various aspects of social media are a way I curate my own information feed so I can stay up to speed and not feel like I’m drowning in a deluge of new data.
But what’s hard to demonstrate to the ABIM is that [this learning] is already happening. I think we can do it if we submit our records of CME credits that we formally accrue. The reason this is such an almost insult to oncologists in practice is because it is a necessary part of our day-to-day existence to keep apprised of developments so we can apply them to patient care.
One litmus test of attending a medical conference like the annual meeting of the American Society of Clinical Oncology is to ask oneself, When I go back to clinic, is this meeting going to change the way that I take care of patients? The answer almost invariably these days is yes. I go to multiple meetings per year, and I think it’s the exception, not the rule, that I return home and nothing changes in my management patterns. Again, this process is happening whether the ABIM recognizes it or not.
Lastly, I sat down in the fall of 2022 and I did my recertification. I looked at the span of all the things that had happened between 2012, when I first sat for my board examination in medical oncology, and 2022. It was staggering. I think the reason that it wasn’t such an overwhelming amount of information to review is that I had actually been accreting it slowly and gradually, month by month, year by year throughout that decade.
Again, it’s necessary that the ABIM hear us, hear oncologists, and know that of all the medical subspecialties they govern, it is basically already an essential task of our day-to-day professional existence that we engage in lifelong learning. To suggest otherwise really paints us as outdated. The reason that matters so much is that if we’re not up-to-date, then we are underserving our patients.
Mark A. Lewis, MD, is director of gastrointestinal oncology at Intermountain Healthcare in Salt Lake City. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.









