User login
Top 10 tips community hospitalists need to know for implementing a QI project
Consider low-cost, high-impact projects
Quality improvement (QI) is essential to the advancement of medicine. QI differs from research as it focuses on already proven knowledge and aims to make quick, sustainable change in local health care systems. Community hospitals may not have organized quality improvement initiatives and often rely on individual hospitalists to be their champions.
Although there are resources for quality improvement projects, initiating a project can seem daunting to a hospitalist. Our aim is to equip the community hospitalist with basic skills to initiate their own successful project. We present our “Top 10” tips to review.
1. Start small: Many quality improvement ideas include grandiose changes that require a large buy-in or worse, more money. When starting a QI project, you need to consider low-cost, high-impact projects. Even the smallest projects can make considerable change. Focus on ideas that require only one or two improvement cycles to implement. Understand your hospital culture, flow, and processes, and then pick a project that is reasonable.
Projects can be as simple as decreasing the number of daily labs ordered by your hospitalist group. Projects that are small could still improve patient satisfaction and decrease costs. Listen to your colleagues, if they are discussing an issue, turn this into an idea! As you learn the culture of your hospital you will be able to tackle larger projects. Plus, it gets your name out there!
2. Establish buy-in: Surround yourself with champions of your cause. Properly identifying and engaging key players is paramount to a successful QI project. First, start with your hospital administration, and garner their support by aligning your project with the goals and objectives that the administration leaders have identified to be important for your institution. Next, select a motivated multidisciplinary team. When choosing your team, be sure to include a representative from the various stakeholders, that is, the individuals who have a variety of hospital roles likely to be affected by the outcome of the project. Stakeholders ensure the success of the project because they have a fundamental understanding of how the project will influence workflow, can predict issues before they arise, and often become empowered to make changes that directly influence their work.
Lastly, include at least one well-respected and highly influential member on your team. Change is always hard, and this person’s support and endorsement of the project, can often move mountains when challenges arise.
3. Know the data collector: It is important to understand what data can be collected because, without data, you cannot measure your success. Arrange a meeting and develop a partnership with the data collector. Obtain a general understanding of how and what specific data is collected. Be sure the data collector has a clear understanding of the project design and the specific details of the project. Include the overall project mission, specific aims of the project, the time frame in which data should be collected, and specific inclusion and exclusion criteria.
Often, data collectors prefer to collect extra data points upfront, even if you end up not using some of them, rather than having to find missing data after the fact. Communication is key, so be available for questions and open to the suggestions of the data collector.
4. Don’t reinvent the wheel: Prior to starting any QI projects, evaluate available resources for project ideas and implementation. The Society of Hospital Medicine and the American College of Physicians outline multiple projects on their websites. Reach out to colleagues at other institutions and obtain their input as they are likely struggling with similar issues and/or have worked on similar project ideas. Use these resources as scaffolding and edit them to fit your institution’s processes and culture, and use their metrics as your measures of success.
5. Remove waste: When determining QI projects, consider focusing on health care waste. Many of the current processes at our institutions have redundancies that add unhealthy time, effort, and inefficiency to our days that can not only impede patient care but also can lead to burnout. When outlining a project idea, consider mapping the process in your interested area to identify those redundancies and inefficiencies. Consider focusing on these instead of building an entirely new process. Improving inefficiencies also can help with provider buy-in with process changes, especially if this helps in improving their everyday frustrations.
6. Express your values: Create a sense of urgency around the problem you are trying to solve. Educate your colleagues to understand the depth of the QI initiative and its impact on their ability to care for patients and patient safety. Express genuine interest in improving your colleagues’ ability to care for patients and improve their days.
Sharing your passion about your project allows people to understand your vested interest in improving the system. This will inspire team members to lead the way to change and encourage colleagues to adopt the recommended changes.
7. Recognize and reward your team: Involve “champions” in every process change. Identify people who are part of your team and ensure they feel valued. Recognition and acknowledgment will allow people to feel more involved and to gain their buy-in. When it comes to results or progress, consider your group’s dynamics. If they are competitive, consider posting progress results on a publicly displayed run chart. If your group is less likely to be motivated by competition, hold individual meetings to help show progress. This is a crucial dynamic to understand, because creating a competitive environment may alienate some members of your group. Remember, the final result is not to blame those lagging behind but to encourage everyone to find the best pathway to success.
8. Be okay with failure: Celebrate your failures because failure is a chance to learn. Every failure is an educational opportunity to understand what not to do, or a chance to gain insight into a process that did not work.
Be a divergent thinker. Start considering problems as part of the path to solution, rather than a barrier in the way. Be open to change and learn from your mistakes. Don’t just be okay with your failures, own them. This will lead to trust with your team members and show your commitment.
9. Finish: This is key. You must finish your project. Even if you anticipate that the project will fail, you should see the project through to its completion. This proves both you and the process of QI are valid and worthwhile; you have to see results and share them with others.
Completing your project also shows your colleagues that you are resilient, committed, and dedicated. Completing a QI project, even with disappointing results, is a success in and of itself. In the end, it is most important to remember to show progress, not perfection.
10. Create sustainability: When your QI project is finished, you need to decide if the changes are sustainable. Some projects show small change and do not need permanent implementation, rather reminders over time. Other projects may be sustainable with EHR or organizational changes. Once you have successful results, your goal should be to find a way to ensure that the process stays in place over time. This is where all your hard work establishing buy-in comes in handy. Your team is more likely to create sustainable change with the hard work you forged through following these key tips.
These Top 10 tips are a hospitalist’s starting point to begin making changes at their own community hospital. Your motivation and effort in making quality change will not go unnoticed. Small ideas will open doors for larger, more sustainable QI projects. Remember, a failure just means a new idea for the next cycle! Enjoy the process of working collaboratively with your hospital on improving quality. Good luck!
Dr. Astik is a hospitalist and instructor of medicine at Northwestern Memorial Hospital, Chicago. Dr. Corbett is a hospitalist and assistant professor at the University of Oklahoma, Tulsa. Dr. Patel is a hospitalist and assistant professor at the University of Colorado, Denver. Dr. Ronan is a hospitalist and associate professor at Christus St. Vincent Regional Medical Center, Santa Fe, NM.
Consider low-cost, high-impact projects
Consider low-cost, high-impact projects
Quality improvement (QI) is essential to the advancement of medicine. QI differs from research as it focuses on already proven knowledge and aims to make quick, sustainable change in local health care systems. Community hospitals may not have organized quality improvement initiatives and often rely on individual hospitalists to be their champions.
Although there are resources for quality improvement projects, initiating a project can seem daunting to a hospitalist. Our aim is to equip the community hospitalist with basic skills to initiate their own successful project. We present our “Top 10” tips to review.
1. Start small: Many quality improvement ideas include grandiose changes that require a large buy-in or worse, more money. When starting a QI project, you need to consider low-cost, high-impact projects. Even the smallest projects can make considerable change. Focus on ideas that require only one or two improvement cycles to implement. Understand your hospital culture, flow, and processes, and then pick a project that is reasonable.
Projects can be as simple as decreasing the number of daily labs ordered by your hospitalist group. Projects that are small could still improve patient satisfaction and decrease costs. Listen to your colleagues, if they are discussing an issue, turn this into an idea! As you learn the culture of your hospital you will be able to tackle larger projects. Plus, it gets your name out there!
2. Establish buy-in: Surround yourself with champions of your cause. Properly identifying and engaging key players is paramount to a successful QI project. First, start with your hospital administration, and garner their support by aligning your project with the goals and objectives that the administration leaders have identified to be important for your institution. Next, select a motivated multidisciplinary team. When choosing your team, be sure to include a representative from the various stakeholders, that is, the individuals who have a variety of hospital roles likely to be affected by the outcome of the project. Stakeholders ensure the success of the project because they have a fundamental understanding of how the project will influence workflow, can predict issues before they arise, and often become empowered to make changes that directly influence their work.
Lastly, include at least one well-respected and highly influential member on your team. Change is always hard, and this person’s support and endorsement of the project, can often move mountains when challenges arise.
3. Know the data collector: It is important to understand what data can be collected because, without data, you cannot measure your success. Arrange a meeting and develop a partnership with the data collector. Obtain a general understanding of how and what specific data is collected. Be sure the data collector has a clear understanding of the project design and the specific details of the project. Include the overall project mission, specific aims of the project, the time frame in which data should be collected, and specific inclusion and exclusion criteria.
Often, data collectors prefer to collect extra data points upfront, even if you end up not using some of them, rather than having to find missing data after the fact. Communication is key, so be available for questions and open to the suggestions of the data collector.
4. Don’t reinvent the wheel: Prior to starting any QI projects, evaluate available resources for project ideas and implementation. The Society of Hospital Medicine and the American College of Physicians outline multiple projects on their websites. Reach out to colleagues at other institutions and obtain their input as they are likely struggling with similar issues and/or have worked on similar project ideas. Use these resources as scaffolding and edit them to fit your institution’s processes and culture, and use their metrics as your measures of success.
5. Remove waste: When determining QI projects, consider focusing on health care waste. Many of the current processes at our institutions have redundancies that add unhealthy time, effort, and inefficiency to our days that can not only impede patient care but also can lead to burnout. When outlining a project idea, consider mapping the process in your interested area to identify those redundancies and inefficiencies. Consider focusing on these instead of building an entirely new process. Improving inefficiencies also can help with provider buy-in with process changes, especially if this helps in improving their everyday frustrations.
6. Express your values: Create a sense of urgency around the problem you are trying to solve. Educate your colleagues to understand the depth of the QI initiative and its impact on their ability to care for patients and patient safety. Express genuine interest in improving your colleagues’ ability to care for patients and improve their days.
Sharing your passion about your project allows people to understand your vested interest in improving the system. This will inspire team members to lead the way to change and encourage colleagues to adopt the recommended changes.
7. Recognize and reward your team: Involve “champions” in every process change. Identify people who are part of your team and ensure they feel valued. Recognition and acknowledgment will allow people to feel more involved and to gain their buy-in. When it comes to results or progress, consider your group’s dynamics. If they are competitive, consider posting progress results on a publicly displayed run chart. If your group is less likely to be motivated by competition, hold individual meetings to help show progress. This is a crucial dynamic to understand, because creating a competitive environment may alienate some members of your group. Remember, the final result is not to blame those lagging behind but to encourage everyone to find the best pathway to success.
8. Be okay with failure: Celebrate your failures because failure is a chance to learn. Every failure is an educational opportunity to understand what not to do, or a chance to gain insight into a process that did not work.
Be a divergent thinker. Start considering problems as part of the path to solution, rather than a barrier in the way. Be open to change and learn from your mistakes. Don’t just be okay with your failures, own them. This will lead to trust with your team members and show your commitment.
9. Finish: This is key. You must finish your project. Even if you anticipate that the project will fail, you should see the project through to its completion. This proves both you and the process of QI are valid and worthwhile; you have to see results and share them with others.
Completing your project also shows your colleagues that you are resilient, committed, and dedicated. Completing a QI project, even with disappointing results, is a success in and of itself. In the end, it is most important to remember to show progress, not perfection.
10. Create sustainability: When your QI project is finished, you need to decide if the changes are sustainable. Some projects show small change and do not need permanent implementation, rather reminders over time. Other projects may be sustainable with EHR or organizational changes. Once you have successful results, your goal should be to find a way to ensure that the process stays in place over time. This is where all your hard work establishing buy-in comes in handy. Your team is more likely to create sustainable change with the hard work you forged through following these key tips.
These Top 10 tips are a hospitalist’s starting point to begin making changes at their own community hospital. Your motivation and effort in making quality change will not go unnoticed. Small ideas will open doors for larger, more sustainable QI projects. Remember, a failure just means a new idea for the next cycle! Enjoy the process of working collaboratively with your hospital on improving quality. Good luck!
Dr. Astik is a hospitalist and instructor of medicine at Northwestern Memorial Hospital, Chicago. Dr. Corbett is a hospitalist and assistant professor at the University of Oklahoma, Tulsa. Dr. Patel is a hospitalist and assistant professor at the University of Colorado, Denver. Dr. Ronan is a hospitalist and associate professor at Christus St. Vincent Regional Medical Center, Santa Fe, NM.
Quality improvement (QI) is essential to the advancement of medicine. QI differs from research as it focuses on already proven knowledge and aims to make quick, sustainable change in local health care systems. Community hospitals may not have organized quality improvement initiatives and often rely on individual hospitalists to be their champions.
Although there are resources for quality improvement projects, initiating a project can seem daunting to a hospitalist. Our aim is to equip the community hospitalist with basic skills to initiate their own successful project. We present our “Top 10” tips to review.
1. Start small: Many quality improvement ideas include grandiose changes that require a large buy-in or worse, more money. When starting a QI project, you need to consider low-cost, high-impact projects. Even the smallest projects can make considerable change. Focus on ideas that require only one or two improvement cycles to implement. Understand your hospital culture, flow, and processes, and then pick a project that is reasonable.
Projects can be as simple as decreasing the number of daily labs ordered by your hospitalist group. Projects that are small could still improve patient satisfaction and decrease costs. Listen to your colleagues, if they are discussing an issue, turn this into an idea! As you learn the culture of your hospital you will be able to tackle larger projects. Plus, it gets your name out there!
2. Establish buy-in: Surround yourself with champions of your cause. Properly identifying and engaging key players is paramount to a successful QI project. First, start with your hospital administration, and garner their support by aligning your project with the goals and objectives that the administration leaders have identified to be important for your institution. Next, select a motivated multidisciplinary team. When choosing your team, be sure to include a representative from the various stakeholders, that is, the individuals who have a variety of hospital roles likely to be affected by the outcome of the project. Stakeholders ensure the success of the project because they have a fundamental understanding of how the project will influence workflow, can predict issues before they arise, and often become empowered to make changes that directly influence their work.
Lastly, include at least one well-respected and highly influential member on your team. Change is always hard, and this person’s support and endorsement of the project, can often move mountains when challenges arise.
3. Know the data collector: It is important to understand what data can be collected because, without data, you cannot measure your success. Arrange a meeting and develop a partnership with the data collector. Obtain a general understanding of how and what specific data is collected. Be sure the data collector has a clear understanding of the project design and the specific details of the project. Include the overall project mission, specific aims of the project, the time frame in which data should be collected, and specific inclusion and exclusion criteria.
Often, data collectors prefer to collect extra data points upfront, even if you end up not using some of them, rather than having to find missing data after the fact. Communication is key, so be available for questions and open to the suggestions of the data collector.
4. Don’t reinvent the wheel: Prior to starting any QI projects, evaluate available resources for project ideas and implementation. The Society of Hospital Medicine and the American College of Physicians outline multiple projects on their websites. Reach out to colleagues at other institutions and obtain their input as they are likely struggling with similar issues and/or have worked on similar project ideas. Use these resources as scaffolding and edit them to fit your institution’s processes and culture, and use their metrics as your measures of success.
5. Remove waste: When determining QI projects, consider focusing on health care waste. Many of the current processes at our institutions have redundancies that add unhealthy time, effort, and inefficiency to our days that can not only impede patient care but also can lead to burnout. When outlining a project idea, consider mapping the process in your interested area to identify those redundancies and inefficiencies. Consider focusing on these instead of building an entirely new process. Improving inefficiencies also can help with provider buy-in with process changes, especially if this helps in improving their everyday frustrations.
6. Express your values: Create a sense of urgency around the problem you are trying to solve. Educate your colleagues to understand the depth of the QI initiative and its impact on their ability to care for patients and patient safety. Express genuine interest in improving your colleagues’ ability to care for patients and improve their days.
Sharing your passion about your project allows people to understand your vested interest in improving the system. This will inspire team members to lead the way to change and encourage colleagues to adopt the recommended changes.
7. Recognize and reward your team: Involve “champions” in every process change. Identify people who are part of your team and ensure they feel valued. Recognition and acknowledgment will allow people to feel more involved and to gain their buy-in. When it comes to results or progress, consider your group’s dynamics. If they are competitive, consider posting progress results on a publicly displayed run chart. If your group is less likely to be motivated by competition, hold individual meetings to help show progress. This is a crucial dynamic to understand, because creating a competitive environment may alienate some members of your group. Remember, the final result is not to blame those lagging behind but to encourage everyone to find the best pathway to success.
8. Be okay with failure: Celebrate your failures because failure is a chance to learn. Every failure is an educational opportunity to understand what not to do, or a chance to gain insight into a process that did not work.
Be a divergent thinker. Start considering problems as part of the path to solution, rather than a barrier in the way. Be open to change and learn from your mistakes. Don’t just be okay with your failures, own them. This will lead to trust with your team members and show your commitment.
9. Finish: This is key. You must finish your project. Even if you anticipate that the project will fail, you should see the project through to its completion. This proves both you and the process of QI are valid and worthwhile; you have to see results and share them with others.
Completing your project also shows your colleagues that you are resilient, committed, and dedicated. Completing a QI project, even with disappointing results, is a success in and of itself. In the end, it is most important to remember to show progress, not perfection.
10. Create sustainability: When your QI project is finished, you need to decide if the changes are sustainable. Some projects show small change and do not need permanent implementation, rather reminders over time. Other projects may be sustainable with EHR or organizational changes. Once you have successful results, your goal should be to find a way to ensure that the process stays in place over time. This is where all your hard work establishing buy-in comes in handy. Your team is more likely to create sustainable change with the hard work you forged through following these key tips.
These Top 10 tips are a hospitalist’s starting point to begin making changes at their own community hospital. Your motivation and effort in making quality change will not go unnoticed. Small ideas will open doors for larger, more sustainable QI projects. Remember, a failure just means a new idea for the next cycle! Enjoy the process of working collaboratively with your hospital on improving quality. Good luck!
Dr. Astik is a hospitalist and instructor of medicine at Northwestern Memorial Hospital, Chicago. Dr. Corbett is a hospitalist and assistant professor at the University of Oklahoma, Tulsa. Dr. Patel is a hospitalist and assistant professor at the University of Colorado, Denver. Dr. Ronan is a hospitalist and associate professor at Christus St. Vincent Regional Medical Center, Santa Fe, NM.
Top 10 things physician advisors want hospitalists to know
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
Hospitalist and Internal Medicine Leaders’ Perspectives of Early Discharge Challenges at Academic Medical Centers
The discharge process is a critical bottleneck for efficient patient flow through the hospital. Delayed discharges translate into delays in admissions and other patient transitions, often leading to excess costs, patient dissatisfaction, and even patient harm.1-3 The emergency department is particularly impacted by these delays; bottlenecks there lead to overcrowding, increased overall hospital length of stay, and increased risks for bad outcomes during hospitalization.2
Academic medical centers in particular may struggle with delayed discharges. In a typical teaching hospital, a team composed of an attending physician and housestaff share responsibility for determining the discharge plan. Additionally, clinical teaching activities may affect the process and quality of discharge.4-6
The prevalence and causes of delayed discharges vary greatly.7-9 To improve efficiency around discharge, many hospitals have launched initiatives designed to discharge patients earlier in the day, including goal setting (“discharge by noon”), scheduling discharge appointments, and using quality-improvement methods, such as Lean Methodology (LEAN), to remove inefficiencies within discharge processes.10-12 However, there are few data on the prevalence and effectiveness of different strategies.
The aim of this study was to survey academic hospitalist and general internal medicine physician leaders to elicit their perspectives on the factors contributing to discharge timing and the relative importance and effectiveness of early-discharge initiatives.
METHODS
Study Design, Participants, and Oversight
We obtained a list of 115 university-affiliated hospitals associated with a residency program and, in most cases, a medical school from Vizient Inc. (formerly University HealthSystem Consortium), an alliance of academic medical centers and affiliated hospitals. Each member institution submits clinical data to allow for the benchmarking of outcomes to drive transparency and quality improvement.13 More than 95% of the nation’s academic medical centers and affiliated hospitals participate in this collaborative. Vizient works with members but does not set nor promote quality metrics, such as discharge timeliness. E-mail addresses for hospital medicine physician leaders (eg, division chief) of major academic medical centers were obtained from each institution via publicly available data (eg, the institution’s website). When an institution did not have a hospital medicine section, we identified the division chief of general internal medicine. The University of California, San Francisco Institutional Review Board approved this study.
Survey Development and Domains
We developed a 30-item survey to evaluate 5 main domains of interest: current discharge practices, degree of prioritization of early discharge on the inpatient service, barriers to timely discharge, prevalence and perceived effectiveness of implemented early-discharge initiatives, and barriers to implementation of early-discharge initiatives.
Respondents were first asked to identify their institutions’ goals for discharge time. They were then asked to compare the priority of early-discharge initiatives to other departmental quality-improvement initiatives, such as reducing 30-day readmissions, improving interpreter use, and improving patient satisfaction. Next, respondents were asked to estimate the degree to which clinical or patient factors contributed to delays in discharge. Respondents were then asked whether specific early-discharge initiatives, such as changes to rounding practices or communication interventions, were implemented at their institutions and, if so, the perceived effectiveness of these initiatives at meeting discharge targets. We piloted the questions locally with physicians and researchers prior to finalizing the survey.
Data Collection
We sent surveys via an online platform (Research Electronic Data Capture).14 Nonresponders were sent 2 e-mail reminders and then a follow-up telephone call asking them to complete the survey. Only 1 survey per academic medical center was collected. Any respondent who completed the survey within 2 weeks of receiving it was entered to win a Kindle Fire.
Data Analysis
We summarized survey responses using descriptive statistics. Analysis was completed in IBM SPSS version 22 (Armonk, NY).
RESULTS
Survey Respondent and Institutional Characteristics
Of the 115 institutions surveyed, we received 61 responses (response rate of 53%), with 39 (64%) respondents from divisions of hospital medicine and 22 (36%) from divisions of general internal medicine. A majority (n = 53; 87%) stated their medicine services have a combination of teaching (with residents) and nonteaching (without residents) teams. Thirty-nine (64%) reported having daily multidisciplinary rounds.
Early Discharge as a Priority
Forty-seven (77%) institutional representatives strongly agreed or agreed that early discharge was a priority, with discharge by noon being the most common target time (n = 23; 38%). Thirty (50%) respondents rated early discharge as more important than improving interpreter use for non-English-speaking patients and equally important as reducing 30-day readmissions (n = 29; 48%) and improving patient satisfaction (n = 27; 44%).
Factors Delaying Discharge
The most common factors perceived as delaying discharge were considered external to the hospital, such as postacute care bed availability or scheduled (eg, ambulance) transport delays (n = 48; 79%), followed by patient factors such as patient transport issues (n = 44; 72%). Less commonly reported were workflow issues, such as competing primary team priorities or case manager bandwidth (n = 38; 62%; Table 1).
Initiatives to Improve Discharge
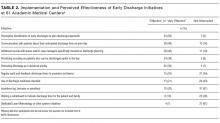
The most commonly implemented initiatives perceived as effective at improving discharge times were the preemptive identification of early discharges to plan discharge paperwork (n = 34; 56%), communication with patients about anticipated discharge time on the day prior to discharge (n = 29; 48%), and the implementation of additional rounds between physician teams and case managers specifically around discharge planning (n = 28; 46%). Initiatives not commonly implemented included regular audit of and feedback on discharge times to providers and teams (n = 21; 34%), the use of a discharge readiness checklist (n = 26; 43%), incentives such as bonuses or penalties (n = 37; 61%), the use of a whiteboard to indicate discharge times (n = 23; 38%), and dedicated quality-improvement approaches such as LEAN (n = 37; 61%; Table 2).
DISCUSSION
Our study suggests early discharge for medicine patients is a priority among academic institutions. Hospitalist and general internal medicine physician leaders in our study generally attributed delayed discharges to external factors, particularly unavailability of postacute care facilities and transportation delays. Having issues with finding postacute care placements is consistent with previous findings by Selker et al.15 and Carey et al.8 This is despite the 20-year difference between Selker et al.’s study and the current study, reflecting a continued opportunity for improvement, including stronger partnerships with local and regional postacute care facilities to expedite care transition and stronger discharge-planning efforts early in the admission process. Efforts in postacute care placement may be particularly important for Medicaid-insured and uninsured patients.
Our responders, hospitalist and internal medicine physician leaders, did not perceive the additional responsibilities of teaching and supervising trainees to be factors that significantly delayed patient discharge. This is in contrast to previous studies, which attributed delays in discharge to prolonged clinical decision-making related to teaching and supervision.4-6,8 This discrepancy may be due to the fact that we only surveyed single physician leaders at each institution and not residents. Our finding warrants further investigation to understand the degree to which resident skills may impact discharge planning and processes.
Institutions represented in our study have attempted a variety of initiatives promoting earlier discharge, with varying levels of perceived success. Initiatives perceived to be the most effective by hospital leaders centered on 2 main areas: (1) changing individual provider practice and (2) anticipatory discharge preparation. Interestingly, this is in discordance with the main factors labeled as causing delays in discharges, such as obtaining postacute care beds, busy case managers, and competing demands on primary teams. We hypothesize this may be because such changes require organization- or system-level changes and are perceived as more arduous than changes at the individual level. In addition, changes to individual provider behavior may be more cost- and time-effective than more systemic initiatives.
Our findings are consistent with the work published by Wertheimer and colleagues,11 who show that additional afternoon interdisciplinary rounds can help identify patients who may be discharged before noon the next day. In their study, identifying such patients in advance improved the overall early-discharge rate the following day.
Our findings should be interpreted in light of several limitations. Our survey only considers the perspectives of hospitalist and general internal medicine physician leaders at academic medical centers that are part of the Vizient Inc. collaborative. They do not represent all academic or community-based medical centers. Although the perceived effectiveness of some initiatives was high, we did not collect empirical data to support these claims or to determine which initiative had the greatest relative impact on discharge timeliness. Lastly, we did not obtain resident, nursing, or case manager perspectives on discharge practices. Given their roles as frontline providers, we may have missed these alternative perspectives.
Our study shows there is a strong interest in increasing early discharges in an effort to improve hospital throughput and patient flow.
Acknowledgments
The authors thank all participants who completed the survey and Danielle Carrier at Vizient Inc. (formally University HealthSystem Consortium) for her assistance in obtaining data.
Disclosures
Hemali Patel, Margaret Fang, Michelle Mourad, Adrienne Green, Ryan Murphy, and James Harrison report no conflicts of interest. At the time the research was conducted, Robert Wachter reported that he is a member of the Lucian Leape Institute at the National Patient Safety Foundation (no compensation except travel expenses); recently chaired an advisory board to England’s National Health Service (NHS) reviewing the NHS’s digital health strategy (no compensation except travel expenses); has a contract with UCSF from the Agency for Healthcare Research and Quality to edit a patient-safety website; receives compensation from John Wiley & Sons for writing a blog; receives royalties from Lippincott Williams & Wilkins and McGraw-Hill Education for writing and/or editing several books; receives stock options for serving on the board of Acuity Medical Management Systems; receives a yearly stipend for serving on the board of The Doctors Company; serves on the scientific advisory boards for amino.com, PatientSafe Solutions Inc., Twine, and EarlySense (for which he receives stock options); has a small royalty stake in CareWeb, a hospital communication tool developed at UCSF; and holds the Marc and Lynne Benioff Endowed Chair in Hospital Medicine and the Holly Smith Distinguished Professorship in Science and Medicine at UCSF.
1. Khanna S, Boyle J, Good N, Lind J. Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82-88. PubMed
2. White BA, Biddinger PD, Chang Y, Grabowski B, Carignan S, Brown DFM. Boarding Inpatients in the Emergency Department Increases Discharged Patient Length of Stay. J Emerg Med. 2013;44(1):230-235. doi:10.1016/j.jemermed.2012.05.007. PubMed
3. Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63-68. PubMed
4. da Silva SA, Valácio RA, Botelho FC, Amaral CFS. Reasons for discharge delays in teaching hospitals. Rev Saúde Pública. 2014;48(2):314-321. doi:10.1590/S0034-8910.2014048004971. PubMed
5. Greysen SR, Schiliro D, Horwitz LI, Curry L, Bradley EH. “Out of Sight, Out of Mind”: Housestaff Perceptions of Quality-Limiting Factors in Discharge Care at Teaching Hospitals. J Hosp Med Off Publ Soc Hosp Med. 2012;7(5):376-381. doi:10.1002/jhm.1928. PubMed
6. Goldman J, Reeves S, Wu R, Silver I, MacMillan K, Kitto S. Medical Residents and Interprofessional Interactions in Discharge: An Ethnographic Exploration of Factors That Affect Negotiation. J Gen Intern Med. 2015;30(10):1454-1460. doi:10.1007/s11606-015-3306-6. PubMed
7. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. doi:10.2147/JMDH.S72633. PubMed
8. Carey MR, Sheth H, Scott Braithwaite R. A Prospective Study of Reasons for Prolonged Hospitalizations on a General Medicine Teaching Service. J Gen Intern Med. 2005;20(2):108-115. doi:10.1111/j.1525-1497.2005.40269.x. PubMed
9. Kim CS, Hart AL, Paretti RF, et al. Excess Hospitalization Days in an Academic Medical Center: Perceptions of Hospitalists and Discharge Planners. Am J Manag Care. 2011;17(2):e34-e42. http://www.ajmc.com/journals/issue/2011/2011-2-vol17-n2/AJMC_11feb_Kim_WebX_e34to42/. Accessed on October 26, 2016.
10. Gershengorn HB, Kocher R, Factor P. Management Strategies to Effect Change in Intensive Care Units: Lessons from the World of Business. Part II. Quality-Improvement Strategies. Ann Am Thorac Soc. 2014;11(3):444-453. doi:10.1513/AnnalsATS.201311-392AS. PubMed
11. Wertheimer B, Jacobs REA, Bailey M, et al. Discharge before noon: An achievable hospital goal. J Hosp Med. 2014;9(4):210-214. doi:10.1002/jhm.2154. PubMed
12. Manning DM, Tammel KJ, Blegen RN, et al. In-room display of day and time patient is anticipated to leave hospital: a “discharge appointment.” J Hosp Med. 2007;2(1):13-16. doi:10.1002/jhm.146. PubMed
13. Networks for academic medical centers. https://www.vizientinc.com/Our-networks/Networks-for-academic-medical-centers. Accessed on July 13, 2017.
14. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010. PubMed
15. Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in a teaching hospital. The development and use of a tool that detects unnecessary hospital days. Med Care. 1989;27(2):112-129. PubMed
The discharge process is a critical bottleneck for efficient patient flow through the hospital. Delayed discharges translate into delays in admissions and other patient transitions, often leading to excess costs, patient dissatisfaction, and even patient harm.1-3 The emergency department is particularly impacted by these delays; bottlenecks there lead to overcrowding, increased overall hospital length of stay, and increased risks for bad outcomes during hospitalization.2
Academic medical centers in particular may struggle with delayed discharges. In a typical teaching hospital, a team composed of an attending physician and housestaff share responsibility for determining the discharge plan. Additionally, clinical teaching activities may affect the process and quality of discharge.4-6
The prevalence and causes of delayed discharges vary greatly.7-9 To improve efficiency around discharge, many hospitals have launched initiatives designed to discharge patients earlier in the day, including goal setting (“discharge by noon”), scheduling discharge appointments, and using quality-improvement methods, such as Lean Methodology (LEAN), to remove inefficiencies within discharge processes.10-12 However, there are few data on the prevalence and effectiveness of different strategies.
The aim of this study was to survey academic hospitalist and general internal medicine physician leaders to elicit their perspectives on the factors contributing to discharge timing and the relative importance and effectiveness of early-discharge initiatives.
METHODS
Study Design, Participants, and Oversight
We obtained a list of 115 university-affiliated hospitals associated with a residency program and, in most cases, a medical school from Vizient Inc. (formerly University HealthSystem Consortium), an alliance of academic medical centers and affiliated hospitals. Each member institution submits clinical data to allow for the benchmarking of outcomes to drive transparency and quality improvement.13 More than 95% of the nation’s academic medical centers and affiliated hospitals participate in this collaborative. Vizient works with members but does not set nor promote quality metrics, such as discharge timeliness. E-mail addresses for hospital medicine physician leaders (eg, division chief) of major academic medical centers were obtained from each institution via publicly available data (eg, the institution’s website). When an institution did not have a hospital medicine section, we identified the division chief of general internal medicine. The University of California, San Francisco Institutional Review Board approved this study.
Survey Development and Domains
We developed a 30-item survey to evaluate 5 main domains of interest: current discharge practices, degree of prioritization of early discharge on the inpatient service, barriers to timely discharge, prevalence and perceived effectiveness of implemented early-discharge initiatives, and barriers to implementation of early-discharge initiatives.
Respondents were first asked to identify their institutions’ goals for discharge time. They were then asked to compare the priority of early-discharge initiatives to other departmental quality-improvement initiatives, such as reducing 30-day readmissions, improving interpreter use, and improving patient satisfaction. Next, respondents were asked to estimate the degree to which clinical or patient factors contributed to delays in discharge. Respondents were then asked whether specific early-discharge initiatives, such as changes to rounding practices or communication interventions, were implemented at their institutions and, if so, the perceived effectiveness of these initiatives at meeting discharge targets. We piloted the questions locally with physicians and researchers prior to finalizing the survey.
Data Collection
We sent surveys via an online platform (Research Electronic Data Capture).14 Nonresponders were sent 2 e-mail reminders and then a follow-up telephone call asking them to complete the survey. Only 1 survey per academic medical center was collected. Any respondent who completed the survey within 2 weeks of receiving it was entered to win a Kindle Fire.
Data Analysis
We summarized survey responses using descriptive statistics. Analysis was completed in IBM SPSS version 22 (Armonk, NY).
RESULTS
Survey Respondent and Institutional Characteristics
Of the 115 institutions surveyed, we received 61 responses (response rate of 53%), with 39 (64%) respondents from divisions of hospital medicine and 22 (36%) from divisions of general internal medicine. A majority (n = 53; 87%) stated their medicine services have a combination of teaching (with residents) and nonteaching (without residents) teams. Thirty-nine (64%) reported having daily multidisciplinary rounds.
Early Discharge as a Priority
Forty-seven (77%) institutional representatives strongly agreed or agreed that early discharge was a priority, with discharge by noon being the most common target time (n = 23; 38%). Thirty (50%) respondents rated early discharge as more important than improving interpreter use for non-English-speaking patients and equally important as reducing 30-day readmissions (n = 29; 48%) and improving patient satisfaction (n = 27; 44%).
Factors Delaying Discharge
The most common factors perceived as delaying discharge were considered external to the hospital, such as postacute care bed availability or scheduled (eg, ambulance) transport delays (n = 48; 79%), followed by patient factors such as patient transport issues (n = 44; 72%). Less commonly reported were workflow issues, such as competing primary team priorities or case manager bandwidth (n = 38; 62%; Table 1).
Initiatives to Improve Discharge
The most commonly implemented initiatives perceived as effective at improving discharge times were the preemptive identification of early discharges to plan discharge paperwork (n = 34; 56%), communication with patients about anticipated discharge time on the day prior to discharge (n = 29; 48%), and the implementation of additional rounds between physician teams and case managers specifically around discharge planning (n = 28; 46%). Initiatives not commonly implemented included regular audit of and feedback on discharge times to providers and teams (n = 21; 34%), the use of a discharge readiness checklist (n = 26; 43%), incentives such as bonuses or penalties (n = 37; 61%), the use of a whiteboard to indicate discharge times (n = 23; 38%), and dedicated quality-improvement approaches such as LEAN (n = 37; 61%; Table 2).
DISCUSSION
Our study suggests early discharge for medicine patients is a priority among academic institutions. Hospitalist and general internal medicine physician leaders in our study generally attributed delayed discharges to external factors, particularly unavailability of postacute care facilities and transportation delays. Having issues with finding postacute care placements is consistent with previous findings by Selker et al.15 and Carey et al.8 This is despite the 20-year difference between Selker et al.’s study and the current study, reflecting a continued opportunity for improvement, including stronger partnerships with local and regional postacute care facilities to expedite care transition and stronger discharge-planning efforts early in the admission process. Efforts in postacute care placement may be particularly important for Medicaid-insured and uninsured patients.
Our responders, hospitalist and internal medicine physician leaders, did not perceive the additional responsibilities of teaching and supervising trainees to be factors that significantly delayed patient discharge. This is in contrast to previous studies, which attributed delays in discharge to prolonged clinical decision-making related to teaching and supervision.4-6,8 This discrepancy may be due to the fact that we only surveyed single physician leaders at each institution and not residents. Our finding warrants further investigation to understand the degree to which resident skills may impact discharge planning and processes.
Institutions represented in our study have attempted a variety of initiatives promoting earlier discharge, with varying levels of perceived success. Initiatives perceived to be the most effective by hospital leaders centered on 2 main areas: (1) changing individual provider practice and (2) anticipatory discharge preparation. Interestingly, this is in discordance with the main factors labeled as causing delays in discharges, such as obtaining postacute care beds, busy case managers, and competing demands on primary teams. We hypothesize this may be because such changes require organization- or system-level changes and are perceived as more arduous than changes at the individual level. In addition, changes to individual provider behavior may be more cost- and time-effective than more systemic initiatives.
Our findings are consistent with the work published by Wertheimer and colleagues,11 who show that additional afternoon interdisciplinary rounds can help identify patients who may be discharged before noon the next day. In their study, identifying such patients in advance improved the overall early-discharge rate the following day.
Our findings should be interpreted in light of several limitations. Our survey only considers the perspectives of hospitalist and general internal medicine physician leaders at academic medical centers that are part of the Vizient Inc. collaborative. They do not represent all academic or community-based medical centers. Although the perceived effectiveness of some initiatives was high, we did not collect empirical data to support these claims or to determine which initiative had the greatest relative impact on discharge timeliness. Lastly, we did not obtain resident, nursing, or case manager perspectives on discharge practices. Given their roles as frontline providers, we may have missed these alternative perspectives.
Our study shows there is a strong interest in increasing early discharges in an effort to improve hospital throughput and patient flow.
Acknowledgments
The authors thank all participants who completed the survey and Danielle Carrier at Vizient Inc. (formally University HealthSystem Consortium) for her assistance in obtaining data.
Disclosures
Hemali Patel, Margaret Fang, Michelle Mourad, Adrienne Green, Ryan Murphy, and James Harrison report no conflicts of interest. At the time the research was conducted, Robert Wachter reported that he is a member of the Lucian Leape Institute at the National Patient Safety Foundation (no compensation except travel expenses); recently chaired an advisory board to England’s National Health Service (NHS) reviewing the NHS’s digital health strategy (no compensation except travel expenses); has a contract with UCSF from the Agency for Healthcare Research and Quality to edit a patient-safety website; receives compensation from John Wiley & Sons for writing a blog; receives royalties from Lippincott Williams & Wilkins and McGraw-Hill Education for writing and/or editing several books; receives stock options for serving on the board of Acuity Medical Management Systems; receives a yearly stipend for serving on the board of The Doctors Company; serves on the scientific advisory boards for amino.com, PatientSafe Solutions Inc., Twine, and EarlySense (for which he receives stock options); has a small royalty stake in CareWeb, a hospital communication tool developed at UCSF; and holds the Marc and Lynne Benioff Endowed Chair in Hospital Medicine and the Holly Smith Distinguished Professorship in Science and Medicine at UCSF.
The discharge process is a critical bottleneck for efficient patient flow through the hospital. Delayed discharges translate into delays in admissions and other patient transitions, often leading to excess costs, patient dissatisfaction, and even patient harm.1-3 The emergency department is particularly impacted by these delays; bottlenecks there lead to overcrowding, increased overall hospital length of stay, and increased risks for bad outcomes during hospitalization.2
Academic medical centers in particular may struggle with delayed discharges. In a typical teaching hospital, a team composed of an attending physician and housestaff share responsibility for determining the discharge plan. Additionally, clinical teaching activities may affect the process and quality of discharge.4-6
The prevalence and causes of delayed discharges vary greatly.7-9 To improve efficiency around discharge, many hospitals have launched initiatives designed to discharge patients earlier in the day, including goal setting (“discharge by noon”), scheduling discharge appointments, and using quality-improvement methods, such as Lean Methodology (LEAN), to remove inefficiencies within discharge processes.10-12 However, there are few data on the prevalence and effectiveness of different strategies.
The aim of this study was to survey academic hospitalist and general internal medicine physician leaders to elicit their perspectives on the factors contributing to discharge timing and the relative importance and effectiveness of early-discharge initiatives.
METHODS
Study Design, Participants, and Oversight
We obtained a list of 115 university-affiliated hospitals associated with a residency program and, in most cases, a medical school from Vizient Inc. (formerly University HealthSystem Consortium), an alliance of academic medical centers and affiliated hospitals. Each member institution submits clinical data to allow for the benchmarking of outcomes to drive transparency and quality improvement.13 More than 95% of the nation’s academic medical centers and affiliated hospitals participate in this collaborative. Vizient works with members but does not set nor promote quality metrics, such as discharge timeliness. E-mail addresses for hospital medicine physician leaders (eg, division chief) of major academic medical centers were obtained from each institution via publicly available data (eg, the institution’s website). When an institution did not have a hospital medicine section, we identified the division chief of general internal medicine. The University of California, San Francisco Institutional Review Board approved this study.
Survey Development and Domains
We developed a 30-item survey to evaluate 5 main domains of interest: current discharge practices, degree of prioritization of early discharge on the inpatient service, barriers to timely discharge, prevalence and perceived effectiveness of implemented early-discharge initiatives, and barriers to implementation of early-discharge initiatives.
Respondents were first asked to identify their institutions’ goals for discharge time. They were then asked to compare the priority of early-discharge initiatives to other departmental quality-improvement initiatives, such as reducing 30-day readmissions, improving interpreter use, and improving patient satisfaction. Next, respondents were asked to estimate the degree to which clinical or patient factors contributed to delays in discharge. Respondents were then asked whether specific early-discharge initiatives, such as changes to rounding practices or communication interventions, were implemented at their institutions and, if so, the perceived effectiveness of these initiatives at meeting discharge targets. We piloted the questions locally with physicians and researchers prior to finalizing the survey.
Data Collection
We sent surveys via an online platform (Research Electronic Data Capture).14 Nonresponders were sent 2 e-mail reminders and then a follow-up telephone call asking them to complete the survey. Only 1 survey per academic medical center was collected. Any respondent who completed the survey within 2 weeks of receiving it was entered to win a Kindle Fire.
Data Analysis
We summarized survey responses using descriptive statistics. Analysis was completed in IBM SPSS version 22 (Armonk, NY).
RESULTS
Survey Respondent and Institutional Characteristics
Of the 115 institutions surveyed, we received 61 responses (response rate of 53%), with 39 (64%) respondents from divisions of hospital medicine and 22 (36%) from divisions of general internal medicine. A majority (n = 53; 87%) stated their medicine services have a combination of teaching (with residents) and nonteaching (without residents) teams. Thirty-nine (64%) reported having daily multidisciplinary rounds.
Early Discharge as a Priority
Forty-seven (77%) institutional representatives strongly agreed or agreed that early discharge was a priority, with discharge by noon being the most common target time (n = 23; 38%). Thirty (50%) respondents rated early discharge as more important than improving interpreter use for non-English-speaking patients and equally important as reducing 30-day readmissions (n = 29; 48%) and improving patient satisfaction (n = 27; 44%).
Factors Delaying Discharge
The most common factors perceived as delaying discharge were considered external to the hospital, such as postacute care bed availability or scheduled (eg, ambulance) transport delays (n = 48; 79%), followed by patient factors such as patient transport issues (n = 44; 72%). Less commonly reported were workflow issues, such as competing primary team priorities or case manager bandwidth (n = 38; 62%; Table 1).
Initiatives to Improve Discharge
The most commonly implemented initiatives perceived as effective at improving discharge times were the preemptive identification of early discharges to plan discharge paperwork (n = 34; 56%), communication with patients about anticipated discharge time on the day prior to discharge (n = 29; 48%), and the implementation of additional rounds between physician teams and case managers specifically around discharge planning (n = 28; 46%). Initiatives not commonly implemented included regular audit of and feedback on discharge times to providers and teams (n = 21; 34%), the use of a discharge readiness checklist (n = 26; 43%), incentives such as bonuses or penalties (n = 37; 61%), the use of a whiteboard to indicate discharge times (n = 23; 38%), and dedicated quality-improvement approaches such as LEAN (n = 37; 61%; Table 2).
DISCUSSION
Our study suggests early discharge for medicine patients is a priority among academic institutions. Hospitalist and general internal medicine physician leaders in our study generally attributed delayed discharges to external factors, particularly unavailability of postacute care facilities and transportation delays. Having issues with finding postacute care placements is consistent with previous findings by Selker et al.15 and Carey et al.8 This is despite the 20-year difference between Selker et al.’s study and the current study, reflecting a continued opportunity for improvement, including stronger partnerships with local and regional postacute care facilities to expedite care transition and stronger discharge-planning efforts early in the admission process. Efforts in postacute care placement may be particularly important for Medicaid-insured and uninsured patients.
Our responders, hospitalist and internal medicine physician leaders, did not perceive the additional responsibilities of teaching and supervising trainees to be factors that significantly delayed patient discharge. This is in contrast to previous studies, which attributed delays in discharge to prolonged clinical decision-making related to teaching and supervision.4-6,8 This discrepancy may be due to the fact that we only surveyed single physician leaders at each institution and not residents. Our finding warrants further investigation to understand the degree to which resident skills may impact discharge planning and processes.
Institutions represented in our study have attempted a variety of initiatives promoting earlier discharge, with varying levels of perceived success. Initiatives perceived to be the most effective by hospital leaders centered on 2 main areas: (1) changing individual provider practice and (2) anticipatory discharge preparation. Interestingly, this is in discordance with the main factors labeled as causing delays in discharges, such as obtaining postacute care beds, busy case managers, and competing demands on primary teams. We hypothesize this may be because such changes require organization- or system-level changes and are perceived as more arduous than changes at the individual level. In addition, changes to individual provider behavior may be more cost- and time-effective than more systemic initiatives.
Our findings are consistent with the work published by Wertheimer and colleagues,11 who show that additional afternoon interdisciplinary rounds can help identify patients who may be discharged before noon the next day. In their study, identifying such patients in advance improved the overall early-discharge rate the following day.
Our findings should be interpreted in light of several limitations. Our survey only considers the perspectives of hospitalist and general internal medicine physician leaders at academic medical centers that are part of the Vizient Inc. collaborative. They do not represent all academic or community-based medical centers. Although the perceived effectiveness of some initiatives was high, we did not collect empirical data to support these claims or to determine which initiative had the greatest relative impact on discharge timeliness. Lastly, we did not obtain resident, nursing, or case manager perspectives on discharge practices. Given their roles as frontline providers, we may have missed these alternative perspectives.
Our study shows there is a strong interest in increasing early discharges in an effort to improve hospital throughput and patient flow.
Acknowledgments
The authors thank all participants who completed the survey and Danielle Carrier at Vizient Inc. (formally University HealthSystem Consortium) for her assistance in obtaining data.
Disclosures
Hemali Patel, Margaret Fang, Michelle Mourad, Adrienne Green, Ryan Murphy, and James Harrison report no conflicts of interest. At the time the research was conducted, Robert Wachter reported that he is a member of the Lucian Leape Institute at the National Patient Safety Foundation (no compensation except travel expenses); recently chaired an advisory board to England’s National Health Service (NHS) reviewing the NHS’s digital health strategy (no compensation except travel expenses); has a contract with UCSF from the Agency for Healthcare Research and Quality to edit a patient-safety website; receives compensation from John Wiley & Sons for writing a blog; receives royalties from Lippincott Williams & Wilkins and McGraw-Hill Education for writing and/or editing several books; receives stock options for serving on the board of Acuity Medical Management Systems; receives a yearly stipend for serving on the board of The Doctors Company; serves on the scientific advisory boards for amino.com, PatientSafe Solutions Inc., Twine, and EarlySense (for which he receives stock options); has a small royalty stake in CareWeb, a hospital communication tool developed at UCSF; and holds the Marc and Lynne Benioff Endowed Chair in Hospital Medicine and the Holly Smith Distinguished Professorship in Science and Medicine at UCSF.
1. Khanna S, Boyle J, Good N, Lind J. Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82-88. PubMed
2. White BA, Biddinger PD, Chang Y, Grabowski B, Carignan S, Brown DFM. Boarding Inpatients in the Emergency Department Increases Discharged Patient Length of Stay. J Emerg Med. 2013;44(1):230-235. doi:10.1016/j.jemermed.2012.05.007. PubMed
3. Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63-68. PubMed
4. da Silva SA, Valácio RA, Botelho FC, Amaral CFS. Reasons for discharge delays in teaching hospitals. Rev Saúde Pública. 2014;48(2):314-321. doi:10.1590/S0034-8910.2014048004971. PubMed
5. Greysen SR, Schiliro D, Horwitz LI, Curry L, Bradley EH. “Out of Sight, Out of Mind”: Housestaff Perceptions of Quality-Limiting Factors in Discharge Care at Teaching Hospitals. J Hosp Med Off Publ Soc Hosp Med. 2012;7(5):376-381. doi:10.1002/jhm.1928. PubMed
6. Goldman J, Reeves S, Wu R, Silver I, MacMillan K, Kitto S. Medical Residents and Interprofessional Interactions in Discharge: An Ethnographic Exploration of Factors That Affect Negotiation. J Gen Intern Med. 2015;30(10):1454-1460. doi:10.1007/s11606-015-3306-6. PubMed
7. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. doi:10.2147/JMDH.S72633. PubMed
8. Carey MR, Sheth H, Scott Braithwaite R. A Prospective Study of Reasons for Prolonged Hospitalizations on a General Medicine Teaching Service. J Gen Intern Med. 2005;20(2):108-115. doi:10.1111/j.1525-1497.2005.40269.x. PubMed
9. Kim CS, Hart AL, Paretti RF, et al. Excess Hospitalization Days in an Academic Medical Center: Perceptions of Hospitalists and Discharge Planners. Am J Manag Care. 2011;17(2):e34-e42. http://www.ajmc.com/journals/issue/2011/2011-2-vol17-n2/AJMC_11feb_Kim_WebX_e34to42/. Accessed on October 26, 2016.
10. Gershengorn HB, Kocher R, Factor P. Management Strategies to Effect Change in Intensive Care Units: Lessons from the World of Business. Part II. Quality-Improvement Strategies. Ann Am Thorac Soc. 2014;11(3):444-453. doi:10.1513/AnnalsATS.201311-392AS. PubMed
11. Wertheimer B, Jacobs REA, Bailey M, et al. Discharge before noon: An achievable hospital goal. J Hosp Med. 2014;9(4):210-214. doi:10.1002/jhm.2154. PubMed
12. Manning DM, Tammel KJ, Blegen RN, et al. In-room display of day and time patient is anticipated to leave hospital: a “discharge appointment.” J Hosp Med. 2007;2(1):13-16. doi:10.1002/jhm.146. PubMed
13. Networks for academic medical centers. https://www.vizientinc.com/Our-networks/Networks-for-academic-medical-centers. Accessed on July 13, 2017.
14. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010. PubMed
15. Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in a teaching hospital. The development and use of a tool that detects unnecessary hospital days. Med Care. 1989;27(2):112-129. PubMed
1. Khanna S, Boyle J, Good N, Lind J. Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82-88. PubMed
2. White BA, Biddinger PD, Chang Y, Grabowski B, Carignan S, Brown DFM. Boarding Inpatients in the Emergency Department Increases Discharged Patient Length of Stay. J Emerg Med. 2013;44(1):230-235. doi:10.1016/j.jemermed.2012.05.007. PubMed
3. Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63-68. PubMed
4. da Silva SA, Valácio RA, Botelho FC, Amaral CFS. Reasons for discharge delays in teaching hospitals. Rev Saúde Pública. 2014;48(2):314-321. doi:10.1590/S0034-8910.2014048004971. PubMed
5. Greysen SR, Schiliro D, Horwitz LI, Curry L, Bradley EH. “Out of Sight, Out of Mind”: Housestaff Perceptions of Quality-Limiting Factors in Discharge Care at Teaching Hospitals. J Hosp Med Off Publ Soc Hosp Med. 2012;7(5):376-381. doi:10.1002/jhm.1928. PubMed
6. Goldman J, Reeves S, Wu R, Silver I, MacMillan K, Kitto S. Medical Residents and Interprofessional Interactions in Discharge: An Ethnographic Exploration of Factors That Affect Negotiation. J Gen Intern Med. 2015;30(10):1454-1460. doi:10.1007/s11606-015-3306-6. PubMed
7. Okoniewska B, Santana MJ, Groshaus H, et al. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. J Multidiscip Healthc. 2015;8:83-89. doi:10.2147/JMDH.S72633. PubMed
8. Carey MR, Sheth H, Scott Braithwaite R. A Prospective Study of Reasons for Prolonged Hospitalizations on a General Medicine Teaching Service. J Gen Intern Med. 2005;20(2):108-115. doi:10.1111/j.1525-1497.2005.40269.x. PubMed
9. Kim CS, Hart AL, Paretti RF, et al. Excess Hospitalization Days in an Academic Medical Center: Perceptions of Hospitalists and Discharge Planners. Am J Manag Care. 2011;17(2):e34-e42. http://www.ajmc.com/journals/issue/2011/2011-2-vol17-n2/AJMC_11feb_Kim_WebX_e34to42/. Accessed on October 26, 2016.
10. Gershengorn HB, Kocher R, Factor P. Management Strategies to Effect Change in Intensive Care Units: Lessons from the World of Business. Part II. Quality-Improvement Strategies. Ann Am Thorac Soc. 2014;11(3):444-453. doi:10.1513/AnnalsATS.201311-392AS. PubMed
11. Wertheimer B, Jacobs REA, Bailey M, et al. Discharge before noon: An achievable hospital goal. J Hosp Med. 2014;9(4):210-214. doi:10.1002/jhm.2154. PubMed
12. Manning DM, Tammel KJ, Blegen RN, et al. In-room display of day and time patient is anticipated to leave hospital: a “discharge appointment.” J Hosp Med. 2007;2(1):13-16. doi:10.1002/jhm.146. PubMed
13. Networks for academic medical centers. https://www.vizientinc.com/Our-networks/Networks-for-academic-medical-centers. Accessed on July 13, 2017.
14. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010. PubMed
15. Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in a teaching hospital. The development and use of a tool that detects unnecessary hospital days. Med Care. 1989;27(2):112-129. PubMed
© 2017 Society of Hospital Medicine
Promoting Scholarship for Hospitalists
Academic hospital medicine is a fast‐growing specialty and has a strong emphasis on high‐value care, efficiency, and quality improvement (QI).[1] Developing scholarly work in these areas and describing findings in peer‐reviewed publications can help disseminate ideas and innovations more widely. In addition, success in academic medicine, at least in part, continues to be measured by traditional academic benchmarks, including the production of scholarly publications, conference presentations, and abstracts.[2]
Hospital medicine, however, faces challenges in providing an academic environment conducive to fostering scholarly work. As a relatively young specialty, there may be a dearth of senior mentors and experienced researchers; lack of structured mentorship can be associated with failure to produce publications or lead national teaching sessions.[3] Relatively few hospitalists undergo fellowships or other specialized training that provides a clinical research background, and internal medicine residency programs rarely provide the comprehensive research skill set required to design, implement, or disseminate academic work.[4, 5, 6] Finally, heavy clinical responsibilities may hinder efforts to conduct and sustain research.
A works‐in‐progress (WIP) session, commonly employed in clinical research groups, can provide a forum to discuss and receive feedback on evolving projects and can foster mentorship, motivation, and training.[7] Although a WIP session may stimulate discussion and advance project ideas, academic hospitalist groups do not commonly employ this model, and it is not known if a regularly scheduled WIP session can provide the mentorship, training, and motivation necessary to assist junior faculty in advancing scholarly project to completion.[8] In this article, we describe how we developed a regular WIP series to promote scholarship activities within our rapidly growing, primarily clinically focused Division of Hospital Medicine (DHM) at the University of California, San Francisco (UCSF), and the results of a survey of WIP participants. We hope that our experience can help illustrate key features of such a model, as well as describe inherent challenges and lessons learned to help promote successful academic efforts at other institutions.
METHODS
Program Setting
During years 2010 to 2013, the time period captured by our survey, the DHM at UCSF grew from 37 to 46 full‐time hospitalists, with 76% primarily clinical faculty (nonresearchers) and 24% primarily clinician‐investigators (researchers), defined as individuals having completed a 2‐year clinical research fellowship and/or dedicating 70% time in their faculty position to clinical research. In addition, there were between 1 and 3 hospitalist fellows per year. In 2012, a PhD researcher joined the division to support research and academic activities within the division as well as to pursue an independent research career.
Program Description
The DHM WIP, named the Incubator, was initially developed in 2007 when researchers recognized the need and desire for a forum where scholarly projects could be reviewed and evaluated. In the first year, the Incubator was primarily utilized by junior research‐trained mentees applying for National Institutes of Health career development awards. However, it soon became clear that nonresearch trained junior fellow and faculty members were pursuing scholarly projects needing additional guidance and input. In particular, the Incubator became frequently utilized by academic hospital medicine fellows and resident trainees pursuing QI and education projects. Over time, more DHM faculty, and junior faculty in particular, began to present their projects and receive structured feedback from researchers as well as other senior members of the group.
Incubator is structured as a 50‐minute session held from 1:10 to 2:00 pm on Thursdays in a DHM conference room. The time was selected because it did not conflict with other divisional conferences and to reserve mornings for clinical responsibilities. Incubator is held on most weeks of the year except for holidays or when there is no scheduled presenter. Presenting at Incubator is voluntary, and presenters sign up for open spots in advance with the upcoming presenter schedule sent out to the division in advance of the conference. Incubator is also used as a forum to provide feedback on anticipated abstract submissions for professional society meetings. For the purposes of the survey described in this article, we did not include Incubator sessions on reviewing abstracts/posters. Trainees and hospitalists present a broad range of projects at any stage of preparation. These include project ideas, grant applications, manuscripts, abstracts, and oral presentations at any stage of completion for feedback. Our mission was to create a forum where researchers, clinicians, and educators meet to provide the tools and guidance necessary to promote scholarly projects across the range of the division's activities by connecting individuals with complementary skills and interests and providing necessary mentorship and peer support. We have defined scholarship broadly, including evaluation of QI, global health, or other health system innovations, as well as advancements in medical education and traditional clinical research.
All faculty are invited to Incubator, and attendees include senior and junior faculty, researchers in the division, fellows, and occasionally residents and medical students. One week prior to the session, an administrative assistant solicits project information, including any related materials and questions the presenter may have for the group using a prespecified template, and emails this information to division members for review. In addition, the same materials are also printed prior to Incubator for any attendees who may not have reviewed the material in advance. Also, prior to the session, a physician is specified to serve as moderator of the discussion, and another physician is assigned the role of primary reviewer to provide the initial specific feedback and recommendations. The role of the moderator is to manage the discussion and keep the focus on time, and is assigned to a researcher or senior clinical faculty member. The role of primary reviewer is assigned to provide more junior faculty (both researchers and nonresearchers) the opportunity to practice their editing and critiquing skills by providing the initial feedback. Presenters and moderators receive worksheets outlining the structure of Incubator and their respective roles (see Supporting Information, Appendix 1, in the online version of this article).
Incubator begins with the presenter providing a brief synopsis of their project and their specific goals and objectives for the session. The moderator then leads the discussion and guides the format, often starting with any questions the group may have for the presenter followed by the specific feedback from the primary reviewer. The primary reviewer, having reviewed the materials in advance of the session, answers the prespecified questions as listed by the presenter, occasionally providing additional targeted feedback. The session is then opened to the rest of the group for feedback and suggestions. Meanwhile, the presenter is encouraged to wait until the end of the hour to summarize their take on the feedback and what their initial thoughts on the next to do items would be (Table 1).
| Presenter | Administrative assistant |
| 2‐ to 3‐sentence summary of career focus | Schedule session and conference room |
| Distribute short set of materials in advance | Collect presenters' materials in advance |
| Summarize feedback at end of session | Prepare materials for Incubator |
| Brainstorm on next steps at end of session | Monitor attendance and topics of presentation |
| Primary reviewer | Moderator |
| Junior faculty (24 years) | Senior or research faculty |
| Provide brief overview of project | Keep session on time |
| Reiterate key questions | Give additional input |
| Provide 2 major, 3 minor suggestions | Summarize comments from group at the end |
| Constructive, outside the box feedback | Allow last 10 minutes for presenter to discuss plans |
Program Evaluation
Survey Respondents and Process
We retrospectively surveyed the lead presenter for each Incubator session held between May 2010 through November 2013. Surveys were administered through the Research Electronic Data Capture application (REDCap).[9] Participants who were lead presenters at Incubator for more than 1 Incubator session completed a survey for each individual presentation. Therefore, some presenters completed more than 1 survey. The presenters included resident physicians, hospital medicine fellows, junior faculty, and researchers. We defined researchers as hospitalists who had completed a 2‐year research fellowship and/or devoted at least 70% time in their faculty position to research.
Survey Development and Domains
We developed a survey questionnaire using the Kirkpatrick 4‐level model to evaluate the educational experience of the primary presenters and to determine how the session impacted their progress on the project, with each model component graded according to a Likert scale.[10] The 4 major components of the model are: (1) Reaction: participants' estimates of satisfaction with Incubator; (2) Learning: extent of knowledge acquisition achieved at Incubator; (3) Behavior: extent to which learning has been applied or transfer of skills through participation in Incubator; and (4) Results: results of the project, wider changes in organizational scholarship as impacted by Incubator.
We also collected information on the presenter's status at time of presentation including career paths (researcher or nonresearcher), their job description (faculty, fellow, resident), and the total number of years on faculty (if applicable). Hospitalists in their first 2 years on the faculty were considered junior physicians. We also collected information on the number of times they had presented at the Incubator sessions and stage of progress of the project, whether in the early, mid, or late phase at the time of presentation. Early phase was defined as presenting an initial project idea or brainstorming possible project options and/or directions. Mid phase was defined as presenting initial results, data, and initial drafts prior to completion of analysis. Late phase was defined as presenting a project nearing completion such as a written abstract, oral presentation, paper, or grant application. Respondents were also asked to identify the main focus of their projects, selecting the categories based on the interests of the division, including medical education, clinical research, QI, high‐value care, and global health.
Survey Data Analysis
We converted Likert scale data into dichotomous variables, with paring of positive responses versus the negative options. We summarized survey responses using descriptive statistics and determined if there were any differences in responses between career researchers and nonresearchers using 2 tests. All analysis was performed using StataSE version 13.1 (StataCorp, College Station, TX).
RESULTS
Survey Respondent Characteristics
We received 51 completed surveys from presenters at an Incubator session, for a total survey response rate of 70%. Of the 51 presentations, 26 (51%) of the projects were led by physicians in training or junior faculty, and 35 (69%) of the presenters were nonresearchers.
Project Characteristics
The most frequently presented topic areas were QI (N = 20), clinical research (N = 14), medical education (N = 6), and global health (N = 6). Whereas researchers were more likely to present clinical research topics and grant applications, nonresearchers more often presented on QI or medical education projects (Table 2). Projects were presented at all stages of development, with the middle stage, where presenters presented initial results, being the most common phase.
| All | Nonresearcher, No. (%) | Researcher, No. (%) | P Value | |
|---|---|---|---|---|
| ||||
| Total | 51 | 35 | 16 | |
| Trainee or junior faculty | 19 (54%) | 7 (44%) | 0.49 | |
| Topic of project | 0.02 | |||
| Quality improvement | 20 (39%) | 15 (43%) | 5 (31%) | |
| Clinical research | 14 (27%) | 8 (23%) | 6 (38%) | |
| Medical education | 6 (12%) | 5 (14%) | 1 (6%) | |
| Health technology | 4 (8%) | 0 (0%) | 4 (25%) | |
| High‐value care | 1 (2%) | 1 (3%) | 0 (0%) | |
| Global health | 6 (12%) | 6 (12%) | 0 (0%) | |
| Stage of project | 0.31 | |||
| Early* | 12 (23%) | 7 (20%) | 5 (31%) | |
| Middle | 24 (47%) | 19 (54%) | 5 (31%) | |
| Late | 15 (29%) | 9 (26%) | 6 (38%) | |
Impact of Incubator
The reaction to the session was very positive, with 100% of respondents recommending Incubator to others (Table 3), and 35% reported learning as a result of the session. Twenty‐three (45%) of respondents reported that the session helped reframe the project idea and changed the study design, and 20 (39%) reported improved written or oral presentation style. A majority (45, 88%) reported that Incubator was valuable in advancing the project to completion.
| All | Nonresearcher, No. (%) | Researcher, No. (%) | P Value | |
|---|---|---|---|---|
| ||||
| Trainee or junior faculty | 51 | 35 (69%) | 16 (31%) | 0.49 |
| Reaction | ||||
| Satisfied with their WIP session | 50 (98%) | 35 (100%) | 15 (94%) | 0.25 |
| Would recommend WIP to others | 51 (100%) | 35 (100%) | 16 (100%) | 1.00 |
| Any of the above | 35 (100%) | 16 (100%) | 1.00 | |
| Learning | ||||
| Advanced research methodology | 18 (35%) | 12 (34%) | 6 (38%) | 0.82 |
| Advanced knowledge in the area | 9 (18%) | 5 (14%) | 4 (25%) | 0.35 |
| Any of the above | 14 (40%) | 9 (56%) | 0.28 | |
| Behavior | ||||
| Current project | ||||
| Reframed project idea | 23 (45%) | 15 (43%) | 8 (50%) | 0.63 |
| Changed study design or methodology | 23 (45%) | 16 (46%) | 7 (44%) | 0.9 |
| Improved written or oral presentation style | 20 (39%) | 15 (43%) | 5 (31%) | 0.43 |
| Future projects | ||||
| Changed approach to future projects | 19 (37%) | 17 (49%) | 2 (13%) | 0.01 |
| Any of the above | 34 (97%) | 14 (88%) | 0.17 | |
| Results | ||||
| Valuable in advancing project to completion | 45 (88%) | 31 (89%) | 14 (88%) | 0.18 |
| Provided mentoring and peer support | 29 (57%) | 24 (69%) | 5 (31%) | 0.01 |
| Connected individuals with similar results | 13 (13%) | 9 (26%) | 4 (25%) | 0.96 |
| Any of the above | 34 (97%) | 14 (88%) | 0.17 | |
Survey results of researchers compared to nonresearchers were similar overall, although nonresearchers were more likely to report changes in behavior and in improved mentoring as a result of presenting at Incubator. Notably, 17 (49%) of nonresearchers reported that Incubator changed their approach to future projects as opposed to only 2 (13%) researchers (P = 0.01). In addition, 24 (69%) nonresearchers reported value in mentorship and peer support compared to 5 (31%) researchers (P = 0.01). A reasonably large proportion of projects originally presented during the Incubator sessions became published articles at the time of survey completion (N = 19, 37%) or were publications in progress (N = 14, 27%). For all remaining items, there were no statistically significant differences in the survey responses among junior faculty/trainees (N = 26) compared to nonjunior faculty (N = 25) presenters (P > 0.05).
Attendance at Incubator During the Study Period
Attendance at Incubator was open and voluntary for all DHM faculty, fellows, and collaborating UCSF trainees. From July 2012, when we began tracking attendance, through the end of the survey period in November 2013, the average number of attendees for each session was 10.7 (standard deviation [SD] 3.8). On average, 50% (SD 16%) of attendees at Incubator were career researchers.
DISCUSSION
The results of this program evaluation suggest that a WIP session employed by an academic division of hospital medicine, consisting of a weekly moderated session, can help advance scholarly work. Our evaluation found that presenters, both researchers and nonresearchers, favorably viewed the regular WIP sessions and reported that feedback in the Incubator helped them advance their project to completion. Importantly, nonresearch‐focused faculty and fellows reported the biggest gains in learning from presenting at Incubator. Whereas half the Incubator attendees were career researchers, consistent with the observation that researchers within the division were most committed to attending Incubator regularly, 69% of the presenters were nonresearchers, demonstrating strong participation among both researchers and nonresearchers within the division.
WIP sessions, though informal, are interactive, inspire critical self‐reflection, and encourage physicians to act on generated ideas, as evidenced by the change in behavior of the participants after the session. These sessions allow for transformative learning by encouraging physicians to be open to alternative viewpoints and engage in discourse, boosting learning beyond just content knowledge. Prior assessments of WIP seminars similarly found high satisfaction with these formats.[11]
Although we cannot identify specifically which features made Incubator effective, we believe that our WIP had some characteristics that may have contributed to its success and may aid in implementation at other institutions: holding the session regularly, voluntary participation, distributing the materials and questions for the group in advance, and designating a moderator for the session in advance to facilitate discussion.
A potential strength of the Incubator is that both researchers and nonresearchers attend. We hypothesize that combining these groups provides improved mentorship and learning for nonresearchers, in particular. In addition, it creates a mutually beneficial environment where each group is able to witness the diversity of projects within the division and learn to provide focused, constructive feedback on the presented work. Not only did this create a transparent environment with better understanding of divisional activities, but also fostered collaboration among hospitalists with similar interests and complementary skills.
Challenges, Setbacks, Updated Approaches
The creation of a successful Incubator session, however, was not without its challenges. At initial inception, the WIP was attended primarily by researchers and had low overall attendance. Members of the division who were primarily clinicians initially perceived the conferences as largely inapplicable to their career objectives and had competing demands from patient care, educational, or administrative responsibilities. However, over time and with encouragement from divisional leaders and service line directors, increasing numbers of hospitalists began to participate in Incubator. The timing of Incubator during afternoons after the Department of Medicine Grand Rounds was chosen specifically to allow clinicians to complete their responsibilities, including morning rounds and teaching, to allow better attendance.
In addition, the results of our survey informed changes to the structure of Incubator. The efficacy of assigning a primary reviewer for each session was not clear, so this component was eventually dropped. The finding that nonresearchers in particular reported a benefit from mentoring and peer‐support at Incubator led to the implementation of querying the presenter for a wish list of faculty attendees at their Incubator session. We then sent a special invitation to those faculty members thought to have special insights on the project. This gave junior faculty the opportunity to present their projects to more senior faculty members within their areas of research, as well as to receive focused expert feedback.
Finally, we have initiated special Incubator sessions focused more on didactics to teach the process of writing manuscripts and brainstorming workshop ideas for national meetings.
Limitations
Our study has limitations. It is a single‐center study based on a small overall sample size, and it is not certain whether a similar innovation would have comparable effects at another institution. In addition, generalizability of our results may be limited for hospital medicine groups without a robust research program. We did not have a control group nor do we know whether participants would have been equally successful without Incubator. We also were unable to assess how Incubator affected long‐term outcomes such as promotion and overall publication record, as we do not have detailed data on productivity prior to the survey period. Finally, we are unable to quantify the effect of Incubator on scholarly success in the division. Although the numbers of published articles and grant funding has increased since the Incubator began (data not shown), the division also grew both in number of research‐focused and nonresearch‐focused faculty, and this study does not account for other temporal changes that may have contributed to improvements in the scholarly output of the division.
CONCLUSIONS
In summary, the Incubator has been a successful program that fostered progress on scholarly projects within a largely clinically focused DHM. Given the importance of scholarship in academic hospital medicine, a WIP session such as the one we describe is a valuable way to support and mentor junior hospitalists and nonresearchers.
Acknowledgements
The authors extend special thanks to Oralia Schatzman, divisional administrative assistant, who organized and arranged the Incubator sessions and recorded attendance, and to Katherine Li, who collected data on numbers of faculty within the division over the duration of the study.
Disclosures: Dr. Hemali Patel, Dr. Margaret Fang, and Mr. James Harrison report no conflicts of interest. At the time the research was conducted, Dr. Kangelaris was supported by the National Heart, Lung, and Blood Institute (1K23HL116800‐01). Dr. Auerbach was supported by the National Heart, Lung, and Blood Institute (K24 K24HL098372).
- , , , . Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161–166.
- , , , , . Tried and true: a survey of successfully promoted academic hospitalists. J Hosp Med. 2011;6(7):411–415.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23–27.
- , , , , , . The PRIME curriculum. J Gen Intern Med. 2006;21(5):506–509.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–7.
- , , . Instituting systems‐based practice and practice‐based learning and improvement: a curriculum of inquiry. Med Educ Online. 2013;18:21612.
- , , , et al. A physician peer support writing group. Fam Med. 2003;35(3):195–201.
- , , , . Research in progress conference for hospitalists provides valuable peer mentoring. J Hosp Med. 2011;6(1):43–46.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , . Evaluating Training Programs: The Four Levels. 3rd ed. San Francisco, CA: Berrett‐Koehler; 2006.
- , , . Works‐in‐progress: guiding junior scientists through career development applications. J Cancer Educ. 2008;23(3):142–148.
Academic hospital medicine is a fast‐growing specialty and has a strong emphasis on high‐value care, efficiency, and quality improvement (QI).[1] Developing scholarly work in these areas and describing findings in peer‐reviewed publications can help disseminate ideas and innovations more widely. In addition, success in academic medicine, at least in part, continues to be measured by traditional academic benchmarks, including the production of scholarly publications, conference presentations, and abstracts.[2]
Hospital medicine, however, faces challenges in providing an academic environment conducive to fostering scholarly work. As a relatively young specialty, there may be a dearth of senior mentors and experienced researchers; lack of structured mentorship can be associated with failure to produce publications or lead national teaching sessions.[3] Relatively few hospitalists undergo fellowships or other specialized training that provides a clinical research background, and internal medicine residency programs rarely provide the comprehensive research skill set required to design, implement, or disseminate academic work.[4, 5, 6] Finally, heavy clinical responsibilities may hinder efforts to conduct and sustain research.
A works‐in‐progress (WIP) session, commonly employed in clinical research groups, can provide a forum to discuss and receive feedback on evolving projects and can foster mentorship, motivation, and training.[7] Although a WIP session may stimulate discussion and advance project ideas, academic hospitalist groups do not commonly employ this model, and it is not known if a regularly scheduled WIP session can provide the mentorship, training, and motivation necessary to assist junior faculty in advancing scholarly project to completion.[8] In this article, we describe how we developed a regular WIP series to promote scholarship activities within our rapidly growing, primarily clinically focused Division of Hospital Medicine (DHM) at the University of California, San Francisco (UCSF), and the results of a survey of WIP participants. We hope that our experience can help illustrate key features of such a model, as well as describe inherent challenges and lessons learned to help promote successful academic efforts at other institutions.
METHODS
Program Setting
During years 2010 to 2013, the time period captured by our survey, the DHM at UCSF grew from 37 to 46 full‐time hospitalists, with 76% primarily clinical faculty (nonresearchers) and 24% primarily clinician‐investigators (researchers), defined as individuals having completed a 2‐year clinical research fellowship and/or dedicating 70% time in their faculty position to clinical research. In addition, there were between 1 and 3 hospitalist fellows per year. In 2012, a PhD researcher joined the division to support research and academic activities within the division as well as to pursue an independent research career.
Program Description
The DHM WIP, named the Incubator, was initially developed in 2007 when researchers recognized the need and desire for a forum where scholarly projects could be reviewed and evaluated. In the first year, the Incubator was primarily utilized by junior research‐trained mentees applying for National Institutes of Health career development awards. However, it soon became clear that nonresearch trained junior fellow and faculty members were pursuing scholarly projects needing additional guidance and input. In particular, the Incubator became frequently utilized by academic hospital medicine fellows and resident trainees pursuing QI and education projects. Over time, more DHM faculty, and junior faculty in particular, began to present their projects and receive structured feedback from researchers as well as other senior members of the group.
Incubator is structured as a 50‐minute session held from 1:10 to 2:00 pm on Thursdays in a DHM conference room. The time was selected because it did not conflict with other divisional conferences and to reserve mornings for clinical responsibilities. Incubator is held on most weeks of the year except for holidays or when there is no scheduled presenter. Presenting at Incubator is voluntary, and presenters sign up for open spots in advance with the upcoming presenter schedule sent out to the division in advance of the conference. Incubator is also used as a forum to provide feedback on anticipated abstract submissions for professional society meetings. For the purposes of the survey described in this article, we did not include Incubator sessions on reviewing abstracts/posters. Trainees and hospitalists present a broad range of projects at any stage of preparation. These include project ideas, grant applications, manuscripts, abstracts, and oral presentations at any stage of completion for feedback. Our mission was to create a forum where researchers, clinicians, and educators meet to provide the tools and guidance necessary to promote scholarly projects across the range of the division's activities by connecting individuals with complementary skills and interests and providing necessary mentorship and peer support. We have defined scholarship broadly, including evaluation of QI, global health, or other health system innovations, as well as advancements in medical education and traditional clinical research.
All faculty are invited to Incubator, and attendees include senior and junior faculty, researchers in the division, fellows, and occasionally residents and medical students. One week prior to the session, an administrative assistant solicits project information, including any related materials and questions the presenter may have for the group using a prespecified template, and emails this information to division members for review. In addition, the same materials are also printed prior to Incubator for any attendees who may not have reviewed the material in advance. Also, prior to the session, a physician is specified to serve as moderator of the discussion, and another physician is assigned the role of primary reviewer to provide the initial specific feedback and recommendations. The role of the moderator is to manage the discussion and keep the focus on time, and is assigned to a researcher or senior clinical faculty member. The role of primary reviewer is assigned to provide more junior faculty (both researchers and nonresearchers) the opportunity to practice their editing and critiquing skills by providing the initial feedback. Presenters and moderators receive worksheets outlining the structure of Incubator and their respective roles (see Supporting Information, Appendix 1, in the online version of this article).
Incubator begins with the presenter providing a brief synopsis of their project and their specific goals and objectives for the session. The moderator then leads the discussion and guides the format, often starting with any questions the group may have for the presenter followed by the specific feedback from the primary reviewer. The primary reviewer, having reviewed the materials in advance of the session, answers the prespecified questions as listed by the presenter, occasionally providing additional targeted feedback. The session is then opened to the rest of the group for feedback and suggestions. Meanwhile, the presenter is encouraged to wait until the end of the hour to summarize their take on the feedback and what their initial thoughts on the next to do items would be (Table 1).
| Presenter | Administrative assistant |
| 2‐ to 3‐sentence summary of career focus | Schedule session and conference room |
| Distribute short set of materials in advance | Collect presenters' materials in advance |
| Summarize feedback at end of session | Prepare materials for Incubator |
| Brainstorm on next steps at end of session | Monitor attendance and topics of presentation |
| Primary reviewer | Moderator |
| Junior faculty (24 years) | Senior or research faculty |
| Provide brief overview of project | Keep session on time |
| Reiterate key questions | Give additional input |
| Provide 2 major, 3 minor suggestions | Summarize comments from group at the end |
| Constructive, outside the box feedback | Allow last 10 minutes for presenter to discuss plans |
Program Evaluation
Survey Respondents and Process
We retrospectively surveyed the lead presenter for each Incubator session held between May 2010 through November 2013. Surveys were administered through the Research Electronic Data Capture application (REDCap).[9] Participants who were lead presenters at Incubator for more than 1 Incubator session completed a survey for each individual presentation. Therefore, some presenters completed more than 1 survey. The presenters included resident physicians, hospital medicine fellows, junior faculty, and researchers. We defined researchers as hospitalists who had completed a 2‐year research fellowship and/or devoted at least 70% time in their faculty position to research.
Survey Development and Domains
We developed a survey questionnaire using the Kirkpatrick 4‐level model to evaluate the educational experience of the primary presenters and to determine how the session impacted their progress on the project, with each model component graded according to a Likert scale.[10] The 4 major components of the model are: (1) Reaction: participants' estimates of satisfaction with Incubator; (2) Learning: extent of knowledge acquisition achieved at Incubator; (3) Behavior: extent to which learning has been applied or transfer of skills through participation in Incubator; and (4) Results: results of the project, wider changes in organizational scholarship as impacted by Incubator.
We also collected information on the presenter's status at time of presentation including career paths (researcher or nonresearcher), their job description (faculty, fellow, resident), and the total number of years on faculty (if applicable). Hospitalists in their first 2 years on the faculty were considered junior physicians. We also collected information on the number of times they had presented at the Incubator sessions and stage of progress of the project, whether in the early, mid, or late phase at the time of presentation. Early phase was defined as presenting an initial project idea or brainstorming possible project options and/or directions. Mid phase was defined as presenting initial results, data, and initial drafts prior to completion of analysis. Late phase was defined as presenting a project nearing completion such as a written abstract, oral presentation, paper, or grant application. Respondents were also asked to identify the main focus of their projects, selecting the categories based on the interests of the division, including medical education, clinical research, QI, high‐value care, and global health.
Survey Data Analysis
We converted Likert scale data into dichotomous variables, with paring of positive responses versus the negative options. We summarized survey responses using descriptive statistics and determined if there were any differences in responses between career researchers and nonresearchers using 2 tests. All analysis was performed using StataSE version 13.1 (StataCorp, College Station, TX).
RESULTS
Survey Respondent Characteristics
We received 51 completed surveys from presenters at an Incubator session, for a total survey response rate of 70%. Of the 51 presentations, 26 (51%) of the projects were led by physicians in training or junior faculty, and 35 (69%) of the presenters were nonresearchers.
Project Characteristics
The most frequently presented topic areas were QI (N = 20), clinical research (N = 14), medical education (N = 6), and global health (N = 6). Whereas researchers were more likely to present clinical research topics and grant applications, nonresearchers more often presented on QI or medical education projects (Table 2). Projects were presented at all stages of development, with the middle stage, where presenters presented initial results, being the most common phase.
| All | Nonresearcher, No. (%) | Researcher, No. (%) | P Value | |
|---|---|---|---|---|
| ||||
| Total | 51 | 35 | 16 | |
| Trainee or junior faculty | 19 (54%) | 7 (44%) | 0.49 | |
| Topic of project | 0.02 | |||
| Quality improvement | 20 (39%) | 15 (43%) | 5 (31%) | |
| Clinical research | 14 (27%) | 8 (23%) | 6 (38%) | |
| Medical education | 6 (12%) | 5 (14%) | 1 (6%) | |
| Health technology | 4 (8%) | 0 (0%) | 4 (25%) | |
| High‐value care | 1 (2%) | 1 (3%) | 0 (0%) | |
| Global health | 6 (12%) | 6 (12%) | 0 (0%) | |
| Stage of project | 0.31 | |||
| Early* | 12 (23%) | 7 (20%) | 5 (31%) | |
| Middle | 24 (47%) | 19 (54%) | 5 (31%) | |
| Late | 15 (29%) | 9 (26%) | 6 (38%) | |
Impact of Incubator
The reaction to the session was very positive, with 100% of respondents recommending Incubator to others (Table 3), and 35% reported learning as a result of the session. Twenty‐three (45%) of respondents reported that the session helped reframe the project idea and changed the study design, and 20 (39%) reported improved written or oral presentation style. A majority (45, 88%) reported that Incubator was valuable in advancing the project to completion.
| All | Nonresearcher, No. (%) | Researcher, No. (%) | P Value | |
|---|---|---|---|---|
| ||||
| Trainee or junior faculty | 51 | 35 (69%) | 16 (31%) | 0.49 |
| Reaction | ||||
| Satisfied with their WIP session | 50 (98%) | 35 (100%) | 15 (94%) | 0.25 |
| Would recommend WIP to others | 51 (100%) | 35 (100%) | 16 (100%) | 1.00 |
| Any of the above | 35 (100%) | 16 (100%) | 1.00 | |
| Learning | ||||
| Advanced research methodology | 18 (35%) | 12 (34%) | 6 (38%) | 0.82 |
| Advanced knowledge in the area | 9 (18%) | 5 (14%) | 4 (25%) | 0.35 |
| Any of the above | 14 (40%) | 9 (56%) | 0.28 | |
| Behavior | ||||
| Current project | ||||
| Reframed project idea | 23 (45%) | 15 (43%) | 8 (50%) | 0.63 |
| Changed study design or methodology | 23 (45%) | 16 (46%) | 7 (44%) | 0.9 |
| Improved written or oral presentation style | 20 (39%) | 15 (43%) | 5 (31%) | 0.43 |
| Future projects | ||||
| Changed approach to future projects | 19 (37%) | 17 (49%) | 2 (13%) | 0.01 |
| Any of the above | 34 (97%) | 14 (88%) | 0.17 | |
| Results | ||||
| Valuable in advancing project to completion | 45 (88%) | 31 (89%) | 14 (88%) | 0.18 |
| Provided mentoring and peer support | 29 (57%) | 24 (69%) | 5 (31%) | 0.01 |
| Connected individuals with similar results | 13 (13%) | 9 (26%) | 4 (25%) | 0.96 |
| Any of the above | 34 (97%) | 14 (88%) | 0.17 | |
Survey results of researchers compared to nonresearchers were similar overall, although nonresearchers were more likely to report changes in behavior and in improved mentoring as a result of presenting at Incubator. Notably, 17 (49%) of nonresearchers reported that Incubator changed their approach to future projects as opposed to only 2 (13%) researchers (P = 0.01). In addition, 24 (69%) nonresearchers reported value in mentorship and peer support compared to 5 (31%) researchers (P = 0.01). A reasonably large proportion of projects originally presented during the Incubator sessions became published articles at the time of survey completion (N = 19, 37%) or were publications in progress (N = 14, 27%). For all remaining items, there were no statistically significant differences in the survey responses among junior faculty/trainees (N = 26) compared to nonjunior faculty (N = 25) presenters (P > 0.05).
Attendance at Incubator During the Study Period
Attendance at Incubator was open and voluntary for all DHM faculty, fellows, and collaborating UCSF trainees. From July 2012, when we began tracking attendance, through the end of the survey period in November 2013, the average number of attendees for each session was 10.7 (standard deviation [SD] 3.8). On average, 50% (SD 16%) of attendees at Incubator were career researchers.
DISCUSSION
The results of this program evaluation suggest that a WIP session employed by an academic division of hospital medicine, consisting of a weekly moderated session, can help advance scholarly work. Our evaluation found that presenters, both researchers and nonresearchers, favorably viewed the regular WIP sessions and reported that feedback in the Incubator helped them advance their project to completion. Importantly, nonresearch‐focused faculty and fellows reported the biggest gains in learning from presenting at Incubator. Whereas half the Incubator attendees were career researchers, consistent with the observation that researchers within the division were most committed to attending Incubator regularly, 69% of the presenters were nonresearchers, demonstrating strong participation among both researchers and nonresearchers within the division.
WIP sessions, though informal, are interactive, inspire critical self‐reflection, and encourage physicians to act on generated ideas, as evidenced by the change in behavior of the participants after the session. These sessions allow for transformative learning by encouraging physicians to be open to alternative viewpoints and engage in discourse, boosting learning beyond just content knowledge. Prior assessments of WIP seminars similarly found high satisfaction with these formats.[11]
Although we cannot identify specifically which features made Incubator effective, we believe that our WIP had some characteristics that may have contributed to its success and may aid in implementation at other institutions: holding the session regularly, voluntary participation, distributing the materials and questions for the group in advance, and designating a moderator for the session in advance to facilitate discussion.
A potential strength of the Incubator is that both researchers and nonresearchers attend. We hypothesize that combining these groups provides improved mentorship and learning for nonresearchers, in particular. In addition, it creates a mutually beneficial environment where each group is able to witness the diversity of projects within the division and learn to provide focused, constructive feedback on the presented work. Not only did this create a transparent environment with better understanding of divisional activities, but also fostered collaboration among hospitalists with similar interests and complementary skills.
Challenges, Setbacks, Updated Approaches
The creation of a successful Incubator session, however, was not without its challenges. At initial inception, the WIP was attended primarily by researchers and had low overall attendance. Members of the division who were primarily clinicians initially perceived the conferences as largely inapplicable to their career objectives and had competing demands from patient care, educational, or administrative responsibilities. However, over time and with encouragement from divisional leaders and service line directors, increasing numbers of hospitalists began to participate in Incubator. The timing of Incubator during afternoons after the Department of Medicine Grand Rounds was chosen specifically to allow clinicians to complete their responsibilities, including morning rounds and teaching, to allow better attendance.
In addition, the results of our survey informed changes to the structure of Incubator. The efficacy of assigning a primary reviewer for each session was not clear, so this component was eventually dropped. The finding that nonresearchers in particular reported a benefit from mentoring and peer‐support at Incubator led to the implementation of querying the presenter for a wish list of faculty attendees at their Incubator session. We then sent a special invitation to those faculty members thought to have special insights on the project. This gave junior faculty the opportunity to present their projects to more senior faculty members within their areas of research, as well as to receive focused expert feedback.
Finally, we have initiated special Incubator sessions focused more on didactics to teach the process of writing manuscripts and brainstorming workshop ideas for national meetings.
Limitations
Our study has limitations. It is a single‐center study based on a small overall sample size, and it is not certain whether a similar innovation would have comparable effects at another institution. In addition, generalizability of our results may be limited for hospital medicine groups without a robust research program. We did not have a control group nor do we know whether participants would have been equally successful without Incubator. We also were unable to assess how Incubator affected long‐term outcomes such as promotion and overall publication record, as we do not have detailed data on productivity prior to the survey period. Finally, we are unable to quantify the effect of Incubator on scholarly success in the division. Although the numbers of published articles and grant funding has increased since the Incubator began (data not shown), the division also grew both in number of research‐focused and nonresearch‐focused faculty, and this study does not account for other temporal changes that may have contributed to improvements in the scholarly output of the division.
CONCLUSIONS
In summary, the Incubator has been a successful program that fostered progress on scholarly projects within a largely clinically focused DHM. Given the importance of scholarship in academic hospital medicine, a WIP session such as the one we describe is a valuable way to support and mentor junior hospitalists and nonresearchers.
Acknowledgements
The authors extend special thanks to Oralia Schatzman, divisional administrative assistant, who organized and arranged the Incubator sessions and recorded attendance, and to Katherine Li, who collected data on numbers of faculty within the division over the duration of the study.
Disclosures: Dr. Hemali Patel, Dr. Margaret Fang, and Mr. James Harrison report no conflicts of interest. At the time the research was conducted, Dr. Kangelaris was supported by the National Heart, Lung, and Blood Institute (1K23HL116800‐01). Dr. Auerbach was supported by the National Heart, Lung, and Blood Institute (K24 K24HL098372).
Academic hospital medicine is a fast‐growing specialty and has a strong emphasis on high‐value care, efficiency, and quality improvement (QI).[1] Developing scholarly work in these areas and describing findings in peer‐reviewed publications can help disseminate ideas and innovations more widely. In addition, success in academic medicine, at least in part, continues to be measured by traditional academic benchmarks, including the production of scholarly publications, conference presentations, and abstracts.[2]
Hospital medicine, however, faces challenges in providing an academic environment conducive to fostering scholarly work. As a relatively young specialty, there may be a dearth of senior mentors and experienced researchers; lack of structured mentorship can be associated with failure to produce publications or lead national teaching sessions.[3] Relatively few hospitalists undergo fellowships or other specialized training that provides a clinical research background, and internal medicine residency programs rarely provide the comprehensive research skill set required to design, implement, or disseminate academic work.[4, 5, 6] Finally, heavy clinical responsibilities may hinder efforts to conduct and sustain research.
A works‐in‐progress (WIP) session, commonly employed in clinical research groups, can provide a forum to discuss and receive feedback on evolving projects and can foster mentorship, motivation, and training.[7] Although a WIP session may stimulate discussion and advance project ideas, academic hospitalist groups do not commonly employ this model, and it is not known if a regularly scheduled WIP session can provide the mentorship, training, and motivation necessary to assist junior faculty in advancing scholarly project to completion.[8] In this article, we describe how we developed a regular WIP series to promote scholarship activities within our rapidly growing, primarily clinically focused Division of Hospital Medicine (DHM) at the University of California, San Francisco (UCSF), and the results of a survey of WIP participants. We hope that our experience can help illustrate key features of such a model, as well as describe inherent challenges and lessons learned to help promote successful academic efforts at other institutions.
METHODS
Program Setting
During years 2010 to 2013, the time period captured by our survey, the DHM at UCSF grew from 37 to 46 full‐time hospitalists, with 76% primarily clinical faculty (nonresearchers) and 24% primarily clinician‐investigators (researchers), defined as individuals having completed a 2‐year clinical research fellowship and/or dedicating 70% time in their faculty position to clinical research. In addition, there were between 1 and 3 hospitalist fellows per year. In 2012, a PhD researcher joined the division to support research and academic activities within the division as well as to pursue an independent research career.
Program Description
The DHM WIP, named the Incubator, was initially developed in 2007 when researchers recognized the need and desire for a forum where scholarly projects could be reviewed and evaluated. In the first year, the Incubator was primarily utilized by junior research‐trained mentees applying for National Institutes of Health career development awards. However, it soon became clear that nonresearch trained junior fellow and faculty members were pursuing scholarly projects needing additional guidance and input. In particular, the Incubator became frequently utilized by academic hospital medicine fellows and resident trainees pursuing QI and education projects. Over time, more DHM faculty, and junior faculty in particular, began to present their projects and receive structured feedback from researchers as well as other senior members of the group.
Incubator is structured as a 50‐minute session held from 1:10 to 2:00 pm on Thursdays in a DHM conference room. The time was selected because it did not conflict with other divisional conferences and to reserve mornings for clinical responsibilities. Incubator is held on most weeks of the year except for holidays or when there is no scheduled presenter. Presenting at Incubator is voluntary, and presenters sign up for open spots in advance with the upcoming presenter schedule sent out to the division in advance of the conference. Incubator is also used as a forum to provide feedback on anticipated abstract submissions for professional society meetings. For the purposes of the survey described in this article, we did not include Incubator sessions on reviewing abstracts/posters. Trainees and hospitalists present a broad range of projects at any stage of preparation. These include project ideas, grant applications, manuscripts, abstracts, and oral presentations at any stage of completion for feedback. Our mission was to create a forum where researchers, clinicians, and educators meet to provide the tools and guidance necessary to promote scholarly projects across the range of the division's activities by connecting individuals with complementary skills and interests and providing necessary mentorship and peer support. We have defined scholarship broadly, including evaluation of QI, global health, or other health system innovations, as well as advancements in medical education and traditional clinical research.
All faculty are invited to Incubator, and attendees include senior and junior faculty, researchers in the division, fellows, and occasionally residents and medical students. One week prior to the session, an administrative assistant solicits project information, including any related materials and questions the presenter may have for the group using a prespecified template, and emails this information to division members for review. In addition, the same materials are also printed prior to Incubator for any attendees who may not have reviewed the material in advance. Also, prior to the session, a physician is specified to serve as moderator of the discussion, and another physician is assigned the role of primary reviewer to provide the initial specific feedback and recommendations. The role of the moderator is to manage the discussion and keep the focus on time, and is assigned to a researcher or senior clinical faculty member. The role of primary reviewer is assigned to provide more junior faculty (both researchers and nonresearchers) the opportunity to practice their editing and critiquing skills by providing the initial feedback. Presenters and moderators receive worksheets outlining the structure of Incubator and their respective roles (see Supporting Information, Appendix 1, in the online version of this article).
Incubator begins with the presenter providing a brief synopsis of their project and their specific goals and objectives for the session. The moderator then leads the discussion and guides the format, often starting with any questions the group may have for the presenter followed by the specific feedback from the primary reviewer. The primary reviewer, having reviewed the materials in advance of the session, answers the prespecified questions as listed by the presenter, occasionally providing additional targeted feedback. The session is then opened to the rest of the group for feedback and suggestions. Meanwhile, the presenter is encouraged to wait until the end of the hour to summarize their take on the feedback and what their initial thoughts on the next to do items would be (Table 1).
| Presenter | Administrative assistant |
| 2‐ to 3‐sentence summary of career focus | Schedule session and conference room |
| Distribute short set of materials in advance | Collect presenters' materials in advance |
| Summarize feedback at end of session | Prepare materials for Incubator |
| Brainstorm on next steps at end of session | Monitor attendance and topics of presentation |
| Primary reviewer | Moderator |
| Junior faculty (24 years) | Senior or research faculty |
| Provide brief overview of project | Keep session on time |
| Reiterate key questions | Give additional input |
| Provide 2 major, 3 minor suggestions | Summarize comments from group at the end |
| Constructive, outside the box feedback | Allow last 10 minutes for presenter to discuss plans |
Program Evaluation
Survey Respondents and Process
We retrospectively surveyed the lead presenter for each Incubator session held between May 2010 through November 2013. Surveys were administered through the Research Electronic Data Capture application (REDCap).[9] Participants who were lead presenters at Incubator for more than 1 Incubator session completed a survey for each individual presentation. Therefore, some presenters completed more than 1 survey. The presenters included resident physicians, hospital medicine fellows, junior faculty, and researchers. We defined researchers as hospitalists who had completed a 2‐year research fellowship and/or devoted at least 70% time in their faculty position to research.
Survey Development and Domains
We developed a survey questionnaire using the Kirkpatrick 4‐level model to evaluate the educational experience of the primary presenters and to determine how the session impacted their progress on the project, with each model component graded according to a Likert scale.[10] The 4 major components of the model are: (1) Reaction: participants' estimates of satisfaction with Incubator; (2) Learning: extent of knowledge acquisition achieved at Incubator; (3) Behavior: extent to which learning has been applied or transfer of skills through participation in Incubator; and (4) Results: results of the project, wider changes in organizational scholarship as impacted by Incubator.
We also collected information on the presenter's status at time of presentation including career paths (researcher or nonresearcher), their job description (faculty, fellow, resident), and the total number of years on faculty (if applicable). Hospitalists in their first 2 years on the faculty were considered junior physicians. We also collected information on the number of times they had presented at the Incubator sessions and stage of progress of the project, whether in the early, mid, or late phase at the time of presentation. Early phase was defined as presenting an initial project idea or brainstorming possible project options and/or directions. Mid phase was defined as presenting initial results, data, and initial drafts prior to completion of analysis. Late phase was defined as presenting a project nearing completion such as a written abstract, oral presentation, paper, or grant application. Respondents were also asked to identify the main focus of their projects, selecting the categories based on the interests of the division, including medical education, clinical research, QI, high‐value care, and global health.
Survey Data Analysis
We converted Likert scale data into dichotomous variables, with paring of positive responses versus the negative options. We summarized survey responses using descriptive statistics and determined if there were any differences in responses between career researchers and nonresearchers using 2 tests. All analysis was performed using StataSE version 13.1 (StataCorp, College Station, TX).
RESULTS
Survey Respondent Characteristics
We received 51 completed surveys from presenters at an Incubator session, for a total survey response rate of 70%. Of the 51 presentations, 26 (51%) of the projects were led by physicians in training or junior faculty, and 35 (69%) of the presenters were nonresearchers.
Project Characteristics
The most frequently presented topic areas were QI (N = 20), clinical research (N = 14), medical education (N = 6), and global health (N = 6). Whereas researchers were more likely to present clinical research topics and grant applications, nonresearchers more often presented on QI or medical education projects (Table 2). Projects were presented at all stages of development, with the middle stage, where presenters presented initial results, being the most common phase.
| All | Nonresearcher, No. (%) | Researcher, No. (%) | P Value | |
|---|---|---|---|---|
| ||||
| Total | 51 | 35 | 16 | |
| Trainee or junior faculty | 19 (54%) | 7 (44%) | 0.49 | |
| Topic of project | 0.02 | |||
| Quality improvement | 20 (39%) | 15 (43%) | 5 (31%) | |
| Clinical research | 14 (27%) | 8 (23%) | 6 (38%) | |
| Medical education | 6 (12%) | 5 (14%) | 1 (6%) | |
| Health technology | 4 (8%) | 0 (0%) | 4 (25%) | |
| High‐value care | 1 (2%) | 1 (3%) | 0 (0%) | |
| Global health | 6 (12%) | 6 (12%) | 0 (0%) | |
| Stage of project | 0.31 | |||
| Early* | 12 (23%) | 7 (20%) | 5 (31%) | |
| Middle | 24 (47%) | 19 (54%) | 5 (31%) | |
| Late | 15 (29%) | 9 (26%) | 6 (38%) | |
Impact of Incubator
The reaction to the session was very positive, with 100% of respondents recommending Incubator to others (Table 3), and 35% reported learning as a result of the session. Twenty‐three (45%) of respondents reported that the session helped reframe the project idea and changed the study design, and 20 (39%) reported improved written or oral presentation style. A majority (45, 88%) reported that Incubator was valuable in advancing the project to completion.
| All | Nonresearcher, No. (%) | Researcher, No. (%) | P Value | |
|---|---|---|---|---|
| ||||
| Trainee or junior faculty | 51 | 35 (69%) | 16 (31%) | 0.49 |
| Reaction | ||||
| Satisfied with their WIP session | 50 (98%) | 35 (100%) | 15 (94%) | 0.25 |
| Would recommend WIP to others | 51 (100%) | 35 (100%) | 16 (100%) | 1.00 |
| Any of the above | 35 (100%) | 16 (100%) | 1.00 | |
| Learning | ||||
| Advanced research methodology | 18 (35%) | 12 (34%) | 6 (38%) | 0.82 |
| Advanced knowledge in the area | 9 (18%) | 5 (14%) | 4 (25%) | 0.35 |
| Any of the above | 14 (40%) | 9 (56%) | 0.28 | |
| Behavior | ||||
| Current project | ||||
| Reframed project idea | 23 (45%) | 15 (43%) | 8 (50%) | 0.63 |
| Changed study design or methodology | 23 (45%) | 16 (46%) | 7 (44%) | 0.9 |
| Improved written or oral presentation style | 20 (39%) | 15 (43%) | 5 (31%) | 0.43 |
| Future projects | ||||
| Changed approach to future projects | 19 (37%) | 17 (49%) | 2 (13%) | 0.01 |
| Any of the above | 34 (97%) | 14 (88%) | 0.17 | |
| Results | ||||
| Valuable in advancing project to completion | 45 (88%) | 31 (89%) | 14 (88%) | 0.18 |
| Provided mentoring and peer support | 29 (57%) | 24 (69%) | 5 (31%) | 0.01 |
| Connected individuals with similar results | 13 (13%) | 9 (26%) | 4 (25%) | 0.96 |
| Any of the above | 34 (97%) | 14 (88%) | 0.17 | |
Survey results of researchers compared to nonresearchers were similar overall, although nonresearchers were more likely to report changes in behavior and in improved mentoring as a result of presenting at Incubator. Notably, 17 (49%) of nonresearchers reported that Incubator changed their approach to future projects as opposed to only 2 (13%) researchers (P = 0.01). In addition, 24 (69%) nonresearchers reported value in mentorship and peer support compared to 5 (31%) researchers (P = 0.01). A reasonably large proportion of projects originally presented during the Incubator sessions became published articles at the time of survey completion (N = 19, 37%) or were publications in progress (N = 14, 27%). For all remaining items, there were no statistically significant differences in the survey responses among junior faculty/trainees (N = 26) compared to nonjunior faculty (N = 25) presenters (P > 0.05).
Attendance at Incubator During the Study Period
Attendance at Incubator was open and voluntary for all DHM faculty, fellows, and collaborating UCSF trainees. From July 2012, when we began tracking attendance, through the end of the survey period in November 2013, the average number of attendees for each session was 10.7 (standard deviation [SD] 3.8). On average, 50% (SD 16%) of attendees at Incubator were career researchers.
DISCUSSION
The results of this program evaluation suggest that a WIP session employed by an academic division of hospital medicine, consisting of a weekly moderated session, can help advance scholarly work. Our evaluation found that presenters, both researchers and nonresearchers, favorably viewed the regular WIP sessions and reported that feedback in the Incubator helped them advance their project to completion. Importantly, nonresearch‐focused faculty and fellows reported the biggest gains in learning from presenting at Incubator. Whereas half the Incubator attendees were career researchers, consistent with the observation that researchers within the division were most committed to attending Incubator regularly, 69% of the presenters were nonresearchers, demonstrating strong participation among both researchers and nonresearchers within the division.
WIP sessions, though informal, are interactive, inspire critical self‐reflection, and encourage physicians to act on generated ideas, as evidenced by the change in behavior of the participants after the session. These sessions allow for transformative learning by encouraging physicians to be open to alternative viewpoints and engage in discourse, boosting learning beyond just content knowledge. Prior assessments of WIP seminars similarly found high satisfaction with these formats.[11]
Although we cannot identify specifically which features made Incubator effective, we believe that our WIP had some characteristics that may have contributed to its success and may aid in implementation at other institutions: holding the session regularly, voluntary participation, distributing the materials and questions for the group in advance, and designating a moderator for the session in advance to facilitate discussion.
A potential strength of the Incubator is that both researchers and nonresearchers attend. We hypothesize that combining these groups provides improved mentorship and learning for nonresearchers, in particular. In addition, it creates a mutually beneficial environment where each group is able to witness the diversity of projects within the division and learn to provide focused, constructive feedback on the presented work. Not only did this create a transparent environment with better understanding of divisional activities, but also fostered collaboration among hospitalists with similar interests and complementary skills.
Challenges, Setbacks, Updated Approaches
The creation of a successful Incubator session, however, was not without its challenges. At initial inception, the WIP was attended primarily by researchers and had low overall attendance. Members of the division who were primarily clinicians initially perceived the conferences as largely inapplicable to their career objectives and had competing demands from patient care, educational, or administrative responsibilities. However, over time and with encouragement from divisional leaders and service line directors, increasing numbers of hospitalists began to participate in Incubator. The timing of Incubator during afternoons after the Department of Medicine Grand Rounds was chosen specifically to allow clinicians to complete their responsibilities, including morning rounds and teaching, to allow better attendance.
In addition, the results of our survey informed changes to the structure of Incubator. The efficacy of assigning a primary reviewer for each session was not clear, so this component was eventually dropped. The finding that nonresearchers in particular reported a benefit from mentoring and peer‐support at Incubator led to the implementation of querying the presenter for a wish list of faculty attendees at their Incubator session. We then sent a special invitation to those faculty members thought to have special insights on the project. This gave junior faculty the opportunity to present their projects to more senior faculty members within their areas of research, as well as to receive focused expert feedback.
Finally, we have initiated special Incubator sessions focused more on didactics to teach the process of writing manuscripts and brainstorming workshop ideas for national meetings.
Limitations
Our study has limitations. It is a single‐center study based on a small overall sample size, and it is not certain whether a similar innovation would have comparable effects at another institution. In addition, generalizability of our results may be limited for hospital medicine groups without a robust research program. We did not have a control group nor do we know whether participants would have been equally successful without Incubator. We also were unable to assess how Incubator affected long‐term outcomes such as promotion and overall publication record, as we do not have detailed data on productivity prior to the survey period. Finally, we are unable to quantify the effect of Incubator on scholarly success in the division. Although the numbers of published articles and grant funding has increased since the Incubator began (data not shown), the division also grew both in number of research‐focused and nonresearch‐focused faculty, and this study does not account for other temporal changes that may have contributed to improvements in the scholarly output of the division.
CONCLUSIONS
In summary, the Incubator has been a successful program that fostered progress on scholarly projects within a largely clinically focused DHM. Given the importance of scholarship in academic hospital medicine, a WIP session such as the one we describe is a valuable way to support and mentor junior hospitalists and nonresearchers.
Acknowledgements
The authors extend special thanks to Oralia Schatzman, divisional administrative assistant, who organized and arranged the Incubator sessions and recorded attendance, and to Katherine Li, who collected data on numbers of faculty within the division over the duration of the study.
Disclosures: Dr. Hemali Patel, Dr. Margaret Fang, and Mr. James Harrison report no conflicts of interest. At the time the research was conducted, Dr. Kangelaris was supported by the National Heart, Lung, and Blood Institute (1K23HL116800‐01). Dr. Auerbach was supported by the National Heart, Lung, and Blood Institute (K24 K24HL098372).
- , , , . Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161–166.
- , , , , . Tried and true: a survey of successfully promoted academic hospitalists. J Hosp Med. 2011;6(7):411–415.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23–27.
- , , , , , . The PRIME curriculum. J Gen Intern Med. 2006;21(5):506–509.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–7.
- , , . Instituting systems‐based practice and practice‐based learning and improvement: a curriculum of inquiry. Med Educ Online. 2013;18:21612.
- , , , et al. A physician peer support writing group. Fam Med. 2003;35(3):195–201.
- , , , . Research in progress conference for hospitalists provides valuable peer mentoring. J Hosp Med. 2011;6(1):43–46.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , . Evaluating Training Programs: The Four Levels. 3rd ed. San Francisco, CA: Berrett‐Koehler; 2006.
- , , . Works‐in‐progress: guiding junior scientists through career development applications. J Cancer Educ. 2008;23(3):142–148.
- , , , . Investing in the future: building an academic hospitalist faculty development program. J Hosp Med. 2011;6(3):161–166.
- , , , , . Tried and true: a survey of successfully promoted academic hospitalists. J Hosp Med. 2011;6(7):411–415.
- , , , , , . Mentorship, productivity, and promotion among academic hospitalists. J Gen Intern Med. 2012;27(1):23–27.
- , , , , , . The PRIME curriculum. J Gen Intern Med. 2006;21(5):506–509.
- , , , . Hospital medicine fellowships: works in progress. Am J Med. 2006;119(1):72.e1–7.
- , , . Instituting systems‐based practice and practice‐based learning and improvement: a curriculum of inquiry. Med Educ Online. 2013;18:21612.
- , , , et al. A physician peer support writing group. Fam Med. 2003;35(3):195–201.
- , , , . Research in progress conference for hospitalists provides valuable peer mentoring. J Hosp Med. 2011;6(1):43–46.
- , , , , , . Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- , . Evaluating Training Programs: The Four Levels. 3rd ed. San Francisco, CA: Berrett‐Koehler; 2006.
- , , . Works‐in‐progress: guiding junior scientists through career development applications. J Cancer Educ. 2008;23(3):142–148.
© 2016 Society of Hospital Medicine
Assessing Discharge Readiness
Widespread evidence suggests that the period around hospitalization remains a vulnerable time for patients. Nearly 20% of patients experience adverse events, including medication errors and hospital readmissions, within 3 weeks of discharge.[1] Multiple factors contribute to adverse events, including the overwhelming volume of information patients receive on their last day in the hospital and fragmented interdisciplinary communication, both among hospital‐based providers and with community providers.[2, 3, 4] A growing body of literature suggests that to ensure patient understanding and a safe transition, discharge planning should start at time of admission. Yet, in the context of high patient volumes and competing priorities, clinicians often postpone discharge planning until they perceive a patient's discharge is imminent. Discharge bundles, designed to improve the safety of hospital discharge, such as those developed by Project BOOST (Better Outcomes by Optimizing Safe Transitions) or Project RED (Re‐Engineered Discharge), are not designed to help providers determine when a patient might be approaching discharge.[5, 6] Early identification of a patient's probable discharge date can provide vital information to inpatient and outpatient teams as they establish comprehensive discharge plans. Accurate discharge‐date predictions allow for effective discharge planning, serving to reduce length of stay (LOS) and consequently improving patient satisfaction and patient safety.[7] However, in the complex world of internal medicine, can clinicians accurately predict the timing of discharge?
A study by Sullivan and colleagues[8] in this issue of the Journal of Hospital Medicine explores a physician's ability to predict hospital discharge. Trainees and attending physicians on general internal medicine wards were asked to predict whether each patient under their care would be discharged on the next day, on the same day, or neither. Discharge predictions were recorded at 3 time points: mornings (79 am), midday (122 pm), or afternoons (57 pm). For predictions of next‐day discharges, the sensitivity (SN) and positive predictive value (PPV) were highest in the afternoon (SN 67%, PPV 69%), whereas for same‐day discharges, accuracy was highest midday (SN 88%, PPV 79%). The authors note that physicians' ability to correctly predict discharges continually improved as time to actual discharge fell.
This study is novel; to our knowledge, no other studies have evaluated the accuracy with which physicians can predict the actual day of discharge. Although this study is particular to a trainee setting and more specific to a single academic medical center, the results are thought provoking. Why are attendings and trainees unable to predict next‐day discharges more accurately? Can we do better? The majority of medical patients are not electively admitted and therefore may have complex and unpredictable courses compared to elective or surgical admissions. Subspecialty consultants may be guiding clinical care and potentially even determining readiness for discharge. Furthermore, the additional responsibilities of teaching and supervising trainees in academic medical centers may further delay discussions and decisions about patient discharges. Another plausible hypothesis, however, is that determination of barriers to discharge and discharge readiness is a clinical skill that is underappreciated and not taught or modeled sufficiently.
If we are to do better at predicting and planning for discharge, we need to build prompts for discharge readiness assessment into our daily work and education of trainees. Although interdisciplinary rounds are typically held in the morning, Wertheimer and colleagues show that additional afternoon interdisciplinary rounds can help identify patients who might be discharged before noon the next day.[9] In their study, identifying such patients in advance improved the overall early discharge rate, moved the average discharge time to earlier in the day, and decreased the observed‐to‐expected LOS, all without any adverse effects on readmissions. We also need more communication between members of the physician care team, especially with subspecialists helping manage care. The authors describe moderate agreement with next‐day and substantial agreement with same‐day discharges between trainees and attendings. Although the authors do not reveal whether trainees or attendings were more accurate, the discrepancy with next‐day discharges is notable. The disagreement suggests a lack of communication between team members about discharge barriers that can hinder planning efforts. Assessing a patient's readiness for and needs upon discharge, and anticipating a patient's disease trajectory, are important clinical skills. Trainees may lack clinical judgment and experience to accurately predict a patient's clinical evolution. As hospitalists, we can role model how to continuously assess patients' discharge needs throughout hospitalization by discussing discharge barriers during daily rounds. As part of transitions of care curricula, in addition to learning about best practices in discharge planning (eg, medication reconciliation, teach back, follow‐up appointments, effective discharge summaries), trainees should be encouraged to conduct structured, daily assessment of discharge readiness and anticipated day of discharge.
Starting the discharge planning process earlier in an admission has the potential to create more thoughtful, efficient, and ultimately safer discharges for our patients. By building discharge readiness assessments into the daily workflow and education curricula, we can prompt trainees and attendings to communicate with interdisciplinary team members and address potential challenges that patients may face in managing their health after discharge. Adequately preparing patients for safe discharges has readmission implications. With Centers for Medicare and Medicaid Services reducing payments to facilities with high rates of readmissions, reducing avoidable readmissions is a priority for all institutions.[10]
We can accomplish safe and early discharges. However, we must get better at accurately assessing our patients' readiness for discharge if we are to take the first step.
Disclosure
Nothing to report.
Widespread evidence suggests that the period around hospitalization remains a vulnerable time for patients. Nearly 20% of patients experience adverse events, including medication errors and hospital readmissions, within 3 weeks of discharge.[1] Multiple factors contribute to adverse events, including the overwhelming volume of information patients receive on their last day in the hospital and fragmented interdisciplinary communication, both among hospital‐based providers and with community providers.[2, 3, 4] A growing body of literature suggests that to ensure patient understanding and a safe transition, discharge planning should start at time of admission. Yet, in the context of high patient volumes and competing priorities, clinicians often postpone discharge planning until they perceive a patient's discharge is imminent. Discharge bundles, designed to improve the safety of hospital discharge, such as those developed by Project BOOST (Better Outcomes by Optimizing Safe Transitions) or Project RED (Re‐Engineered Discharge), are not designed to help providers determine when a patient might be approaching discharge.[5, 6] Early identification of a patient's probable discharge date can provide vital information to inpatient and outpatient teams as they establish comprehensive discharge plans. Accurate discharge‐date predictions allow for effective discharge planning, serving to reduce length of stay (LOS) and consequently improving patient satisfaction and patient safety.[7] However, in the complex world of internal medicine, can clinicians accurately predict the timing of discharge?
A study by Sullivan and colleagues[8] in this issue of the Journal of Hospital Medicine explores a physician's ability to predict hospital discharge. Trainees and attending physicians on general internal medicine wards were asked to predict whether each patient under their care would be discharged on the next day, on the same day, or neither. Discharge predictions were recorded at 3 time points: mornings (79 am), midday (122 pm), or afternoons (57 pm). For predictions of next‐day discharges, the sensitivity (SN) and positive predictive value (PPV) were highest in the afternoon (SN 67%, PPV 69%), whereas for same‐day discharges, accuracy was highest midday (SN 88%, PPV 79%). The authors note that physicians' ability to correctly predict discharges continually improved as time to actual discharge fell.
This study is novel; to our knowledge, no other studies have evaluated the accuracy with which physicians can predict the actual day of discharge. Although this study is particular to a trainee setting and more specific to a single academic medical center, the results are thought provoking. Why are attendings and trainees unable to predict next‐day discharges more accurately? Can we do better? The majority of medical patients are not electively admitted and therefore may have complex and unpredictable courses compared to elective or surgical admissions. Subspecialty consultants may be guiding clinical care and potentially even determining readiness for discharge. Furthermore, the additional responsibilities of teaching and supervising trainees in academic medical centers may further delay discussions and decisions about patient discharges. Another plausible hypothesis, however, is that determination of barriers to discharge and discharge readiness is a clinical skill that is underappreciated and not taught or modeled sufficiently.
If we are to do better at predicting and planning for discharge, we need to build prompts for discharge readiness assessment into our daily work and education of trainees. Although interdisciplinary rounds are typically held in the morning, Wertheimer and colleagues show that additional afternoon interdisciplinary rounds can help identify patients who might be discharged before noon the next day.[9] In their study, identifying such patients in advance improved the overall early discharge rate, moved the average discharge time to earlier in the day, and decreased the observed‐to‐expected LOS, all without any adverse effects on readmissions. We also need more communication between members of the physician care team, especially with subspecialists helping manage care. The authors describe moderate agreement with next‐day and substantial agreement with same‐day discharges between trainees and attendings. Although the authors do not reveal whether trainees or attendings were more accurate, the discrepancy with next‐day discharges is notable. The disagreement suggests a lack of communication between team members about discharge barriers that can hinder planning efforts. Assessing a patient's readiness for and needs upon discharge, and anticipating a patient's disease trajectory, are important clinical skills. Trainees may lack clinical judgment and experience to accurately predict a patient's clinical evolution. As hospitalists, we can role model how to continuously assess patients' discharge needs throughout hospitalization by discussing discharge barriers during daily rounds. As part of transitions of care curricula, in addition to learning about best practices in discharge planning (eg, medication reconciliation, teach back, follow‐up appointments, effective discharge summaries), trainees should be encouraged to conduct structured, daily assessment of discharge readiness and anticipated day of discharge.
Starting the discharge planning process earlier in an admission has the potential to create more thoughtful, efficient, and ultimately safer discharges for our patients. By building discharge readiness assessments into the daily workflow and education curricula, we can prompt trainees and attendings to communicate with interdisciplinary team members and address potential challenges that patients may face in managing their health after discharge. Adequately preparing patients for safe discharges has readmission implications. With Centers for Medicare and Medicaid Services reducing payments to facilities with high rates of readmissions, reducing avoidable readmissions is a priority for all institutions.[10]
We can accomplish safe and early discharges. However, we must get better at accurately assessing our patients' readiness for discharge if we are to take the first step.
Disclosure
Nothing to report.
Widespread evidence suggests that the period around hospitalization remains a vulnerable time for patients. Nearly 20% of patients experience adverse events, including medication errors and hospital readmissions, within 3 weeks of discharge.[1] Multiple factors contribute to adverse events, including the overwhelming volume of information patients receive on their last day in the hospital and fragmented interdisciplinary communication, both among hospital‐based providers and with community providers.[2, 3, 4] A growing body of literature suggests that to ensure patient understanding and a safe transition, discharge planning should start at time of admission. Yet, in the context of high patient volumes and competing priorities, clinicians often postpone discharge planning until they perceive a patient's discharge is imminent. Discharge bundles, designed to improve the safety of hospital discharge, such as those developed by Project BOOST (Better Outcomes by Optimizing Safe Transitions) or Project RED (Re‐Engineered Discharge), are not designed to help providers determine when a patient might be approaching discharge.[5, 6] Early identification of a patient's probable discharge date can provide vital information to inpatient and outpatient teams as they establish comprehensive discharge plans. Accurate discharge‐date predictions allow for effective discharge planning, serving to reduce length of stay (LOS) and consequently improving patient satisfaction and patient safety.[7] However, in the complex world of internal medicine, can clinicians accurately predict the timing of discharge?
A study by Sullivan and colleagues[8] in this issue of the Journal of Hospital Medicine explores a physician's ability to predict hospital discharge. Trainees and attending physicians on general internal medicine wards were asked to predict whether each patient under their care would be discharged on the next day, on the same day, or neither. Discharge predictions were recorded at 3 time points: mornings (79 am), midday (122 pm), or afternoons (57 pm). For predictions of next‐day discharges, the sensitivity (SN) and positive predictive value (PPV) were highest in the afternoon (SN 67%, PPV 69%), whereas for same‐day discharges, accuracy was highest midday (SN 88%, PPV 79%). The authors note that physicians' ability to correctly predict discharges continually improved as time to actual discharge fell.
This study is novel; to our knowledge, no other studies have evaluated the accuracy with which physicians can predict the actual day of discharge. Although this study is particular to a trainee setting and more specific to a single academic medical center, the results are thought provoking. Why are attendings and trainees unable to predict next‐day discharges more accurately? Can we do better? The majority of medical patients are not electively admitted and therefore may have complex and unpredictable courses compared to elective or surgical admissions. Subspecialty consultants may be guiding clinical care and potentially even determining readiness for discharge. Furthermore, the additional responsibilities of teaching and supervising trainees in academic medical centers may further delay discussions and decisions about patient discharges. Another plausible hypothesis, however, is that determination of barriers to discharge and discharge readiness is a clinical skill that is underappreciated and not taught or modeled sufficiently.
If we are to do better at predicting and planning for discharge, we need to build prompts for discharge readiness assessment into our daily work and education of trainees. Although interdisciplinary rounds are typically held in the morning, Wertheimer and colleagues show that additional afternoon interdisciplinary rounds can help identify patients who might be discharged before noon the next day.[9] In their study, identifying such patients in advance improved the overall early discharge rate, moved the average discharge time to earlier in the day, and decreased the observed‐to‐expected LOS, all without any adverse effects on readmissions. We also need more communication between members of the physician care team, especially with subspecialists helping manage care. The authors describe moderate agreement with next‐day and substantial agreement with same‐day discharges between trainees and attendings. Although the authors do not reveal whether trainees or attendings were more accurate, the discrepancy with next‐day discharges is notable. The disagreement suggests a lack of communication between team members about discharge barriers that can hinder planning efforts. Assessing a patient's readiness for and needs upon discharge, and anticipating a patient's disease trajectory, are important clinical skills. Trainees may lack clinical judgment and experience to accurately predict a patient's clinical evolution. As hospitalists, we can role model how to continuously assess patients' discharge needs throughout hospitalization by discussing discharge barriers during daily rounds. As part of transitions of care curricula, in addition to learning about best practices in discharge planning (eg, medication reconciliation, teach back, follow‐up appointments, effective discharge summaries), trainees should be encouraged to conduct structured, daily assessment of discharge readiness and anticipated day of discharge.
Starting the discharge planning process earlier in an admission has the potential to create more thoughtful, efficient, and ultimately safer discharges for our patients. By building discharge readiness assessments into the daily workflow and education curricula, we can prompt trainees and attendings to communicate with interdisciplinary team members and address potential challenges that patients may face in managing their health after discharge. Adequately preparing patients for safe discharges has readmission implications. With Centers for Medicare and Medicaid Services reducing payments to facilities with high rates of readmissions, reducing avoidable readmissions is a priority for all institutions.[10]
We can accomplish safe and early discharges. However, we must get better at accurately assessing our patients' readiness for discharge if we are to take the first step.
Disclosure
Nothing to report.
Fondaparinux for Treatment of Heparin-Induced Thrombocytopenia
Clinical question: Is fondaparinux as safe and effective as argatroban and danaparoid in treating heparin-induced thrombocytopenia (HIT)?
Background: Guidelines for the treatment of HIT recommend using danaparoid (factor Xa inhibitor), argatroban, or lepirudin (both direct thrombin inhibitors). Reduced availability, cost, and complexity of administration limit these options, and fondaparinux is often used off label in the treatment of HIT.
Study design: Retrospective cohort study.
Setting: London Health Sciences Centre, Ontario, Canada.
Synopsis: Investigators analyzed 133 patients receiving fondaparinux for HIT against unmatched (n=106) and matched (n=60) cohorts receiving either argatroban or danaparoid. Using a composite of new thrombotic events, amputation, gangrene, thrombosis-related death, or death in which thrombosis cannot be excluded as the primary outcome, there was no difference between fondaparinux (16.5%) and the unmatched (19.8%) or matched (16.5%) cohorts of argatroban/danaparoid.
There also was no difference in major bleeding events between fondaparinux (21.1%) and the unmatched (25.5%) and matched (20.0%) argatroban/danaparoid cohorts, though major bleeding rates in this group were higher than in other studies, possibly reflecting a greater proportion of patients with renal dysfunction.
The single-site study was underpowered, and generalizability is limited, as the authors could not review all potential patient files. The risk of confounding effects is increased in the absence of randomization and universal gold standard confirmatory testing among the cohort. Prospective trials are needed to establish the safety and efficacy of treating HIT with fondaparinux.
Bottom line: In this underpowered and retrospective cohort study, fondaparinux was as effective in treating HIT as argatroban and danaparoid, with a similar safety profile.
Citation: Kang M, Alahmadi M, Sawh S, Kovacs MJ, Lazo-Langner A. Fondaparinux for the treatment of suspected heparin-induced thrombocytopenia: a propensity score-matched study. Blood. 2015;125(6):924-929.
Clinical question: Is fondaparinux as safe and effective as argatroban and danaparoid in treating heparin-induced thrombocytopenia (HIT)?
Background: Guidelines for the treatment of HIT recommend using danaparoid (factor Xa inhibitor), argatroban, or lepirudin (both direct thrombin inhibitors). Reduced availability, cost, and complexity of administration limit these options, and fondaparinux is often used off label in the treatment of HIT.
Study design: Retrospective cohort study.
Setting: London Health Sciences Centre, Ontario, Canada.
Synopsis: Investigators analyzed 133 patients receiving fondaparinux for HIT against unmatched (n=106) and matched (n=60) cohorts receiving either argatroban or danaparoid. Using a composite of new thrombotic events, amputation, gangrene, thrombosis-related death, or death in which thrombosis cannot be excluded as the primary outcome, there was no difference between fondaparinux (16.5%) and the unmatched (19.8%) or matched (16.5%) cohorts of argatroban/danaparoid.
There also was no difference in major bleeding events between fondaparinux (21.1%) and the unmatched (25.5%) and matched (20.0%) argatroban/danaparoid cohorts, though major bleeding rates in this group were higher than in other studies, possibly reflecting a greater proportion of patients with renal dysfunction.
The single-site study was underpowered, and generalizability is limited, as the authors could not review all potential patient files. The risk of confounding effects is increased in the absence of randomization and universal gold standard confirmatory testing among the cohort. Prospective trials are needed to establish the safety and efficacy of treating HIT with fondaparinux.
Bottom line: In this underpowered and retrospective cohort study, fondaparinux was as effective in treating HIT as argatroban and danaparoid, with a similar safety profile.
Citation: Kang M, Alahmadi M, Sawh S, Kovacs MJ, Lazo-Langner A. Fondaparinux for the treatment of suspected heparin-induced thrombocytopenia: a propensity score-matched study. Blood. 2015;125(6):924-929.
Clinical question: Is fondaparinux as safe and effective as argatroban and danaparoid in treating heparin-induced thrombocytopenia (HIT)?
Background: Guidelines for the treatment of HIT recommend using danaparoid (factor Xa inhibitor), argatroban, or lepirudin (both direct thrombin inhibitors). Reduced availability, cost, and complexity of administration limit these options, and fondaparinux is often used off label in the treatment of HIT.
Study design: Retrospective cohort study.
Setting: London Health Sciences Centre, Ontario, Canada.
Synopsis: Investigators analyzed 133 patients receiving fondaparinux for HIT against unmatched (n=106) and matched (n=60) cohorts receiving either argatroban or danaparoid. Using a composite of new thrombotic events, amputation, gangrene, thrombosis-related death, or death in which thrombosis cannot be excluded as the primary outcome, there was no difference between fondaparinux (16.5%) and the unmatched (19.8%) or matched (16.5%) cohorts of argatroban/danaparoid.
There also was no difference in major bleeding events between fondaparinux (21.1%) and the unmatched (25.5%) and matched (20.0%) argatroban/danaparoid cohorts, though major bleeding rates in this group were higher than in other studies, possibly reflecting a greater proportion of patients with renal dysfunction.
The single-site study was underpowered, and generalizability is limited, as the authors could not review all potential patient files. The risk of confounding effects is increased in the absence of randomization and universal gold standard confirmatory testing among the cohort. Prospective trials are needed to establish the safety and efficacy of treating HIT with fondaparinux.
Bottom line: In this underpowered and retrospective cohort study, fondaparinux was as effective in treating HIT as argatroban and danaparoid, with a similar safety profile.
Citation: Kang M, Alahmadi M, Sawh S, Kovacs MJ, Lazo-Langner A. Fondaparinux for the treatment of suspected heparin-induced thrombocytopenia: a propensity score-matched study. Blood. 2015;125(6):924-929.
Rapid Response Teams Increase Perception of Education without Reducing Autonomy
Clinical question: Does the presence of a rapid response team (RRT) affect the perception of resident education and autonomy?
Background: Studies on the perception of RRTs, which can generally be activated by any concerned staff member, have been primarily limited to nurses. No studies to date have evaluated resident perception of the effects of RRTs on education or autonomy.
Study design: Survey study measure on a five-point Likert scale.
Setting: Moffitt-Long Hospital, a 600-bed acute care hospital and tertiary academic medical center of the University of California San Francisco.
Synopsis: Among 342 potential respondents, 246 surveys were completed, 10 of which were excluded due a lack of experience with RRTs. Overall, 78% of respondents felt that working with RRTs creates a valuable educational experience, though this was seen more commonly in the responses of medical residents (83.2%) than in those of surgical residents (70.4%). There was no significant difference between interns (82.9%) and upper-level residents (77.3%).
Additionally, 75.8% of respondents did not feel that the presence of an RRT decreased resident autonomy, and there was no statistically significant difference between the responses of interns (77.8%) and upper-level residents (76.8%), or between those of medical (79.9%) and surgical (71.2%) residents.
The survey design increases the risk of response bias, and the single-site nature limits generalizability. Additionally, no objective measurements of education or autonomy were evaluated.
Bottom line: The presence of RRTs is perceived as having educational value and is not perceived by residents as reducing resident autonomy.
Citation: Butcher BW, Quist CE, Harrison JD, Ranji SR. The effect of a rapid response team on resident perceptions of education and autonomy. J Hosp Med. 2015;10(1):8-12.
Clinical question: Does the presence of a rapid response team (RRT) affect the perception of resident education and autonomy?
Background: Studies on the perception of RRTs, which can generally be activated by any concerned staff member, have been primarily limited to nurses. No studies to date have evaluated resident perception of the effects of RRTs on education or autonomy.
Study design: Survey study measure on a five-point Likert scale.
Setting: Moffitt-Long Hospital, a 600-bed acute care hospital and tertiary academic medical center of the University of California San Francisco.
Synopsis: Among 342 potential respondents, 246 surveys were completed, 10 of which were excluded due a lack of experience with RRTs. Overall, 78% of respondents felt that working with RRTs creates a valuable educational experience, though this was seen more commonly in the responses of medical residents (83.2%) than in those of surgical residents (70.4%). There was no significant difference between interns (82.9%) and upper-level residents (77.3%).
Additionally, 75.8% of respondents did not feel that the presence of an RRT decreased resident autonomy, and there was no statistically significant difference between the responses of interns (77.8%) and upper-level residents (76.8%), or between those of medical (79.9%) and surgical (71.2%) residents.
The survey design increases the risk of response bias, and the single-site nature limits generalizability. Additionally, no objective measurements of education or autonomy were evaluated.
Bottom line: The presence of RRTs is perceived as having educational value and is not perceived by residents as reducing resident autonomy.
Citation: Butcher BW, Quist CE, Harrison JD, Ranji SR. The effect of a rapid response team on resident perceptions of education and autonomy. J Hosp Med. 2015;10(1):8-12.
Clinical question: Does the presence of a rapid response team (RRT) affect the perception of resident education and autonomy?
Background: Studies on the perception of RRTs, which can generally be activated by any concerned staff member, have been primarily limited to nurses. No studies to date have evaluated resident perception of the effects of RRTs on education or autonomy.
Study design: Survey study measure on a five-point Likert scale.
Setting: Moffitt-Long Hospital, a 600-bed acute care hospital and tertiary academic medical center of the University of California San Francisco.
Synopsis: Among 342 potential respondents, 246 surveys were completed, 10 of which were excluded due a lack of experience with RRTs. Overall, 78% of respondents felt that working with RRTs creates a valuable educational experience, though this was seen more commonly in the responses of medical residents (83.2%) than in those of surgical residents (70.4%). There was no significant difference between interns (82.9%) and upper-level residents (77.3%).
Additionally, 75.8% of respondents did not feel that the presence of an RRT decreased resident autonomy, and there was no statistically significant difference between the responses of interns (77.8%) and upper-level residents (76.8%), or between those of medical (79.9%) and surgical (71.2%) residents.
The survey design increases the risk of response bias, and the single-site nature limits generalizability. Additionally, no objective measurements of education or autonomy were evaluated.
Bottom line: The presence of RRTs is perceived as having educational value and is not perceived by residents as reducing resident autonomy.
Citation: Butcher BW, Quist CE, Harrison JD, Ranji SR. The effect of a rapid response team on resident perceptions of education and autonomy. J Hosp Med. 2015;10(1):8-12.
Physician Dashboard, Pay-for-Performance Improve Rate of Appropriate VTE Prophylaxis
Clinical question: Do individual provider feedback and a pay-for-performance incentive program improve the use of guideline-compliant VTE prophylaxis?
Background: The appropriate use of VTE prophylaxis is a Joint Commission core measure set, a publicly reported performance metric for quality care, and part of the hospital value-based purchasing component of healthcare reform. Despite guidelines on effective and safe measures to prevent VTE, compliance rates are often below 50%.
Study design: Retrospective analysis.
Setting: Academic hospitalists at a tertiary care medical center.
Synopsis: Using a web-based, transparent dashboard and a pay-for-performance program with graduated payouts, this analysis showed a significant improvement in VTE compliance rates by providers. Specifically, the combination of both interventions yielded the highest rate. The monthly compliance rate increased from a baseline of 86% (95% confidence interval [CI], 85-88%) to 90% (95% CI, 88-93%) with the dashboard alone (P=0.001) and was further augmented to 94% (95% CI, 93-96%) with the combined dashboard and payment incentive program (P=0.001).
This study highlights the impact of both intrinsic (peer norms) and extrinsic (payments) motivation, as they work synergistically to improve VTE compliance rates.
Bottom line: Transparent feedback through real-time dashboards and performance-based payment incentives can be used to bring about significant improvement in patient safety and quality benchmarks.
Citation: Michtalik HJ, Carolan HT, Haut ER, et al. Use of provider-level dashboards and pay-for-performance in venous thromboembolism prophylaxis. J Hosp Med. 2015;10(3):172-178.
Clinical question: Do individual provider feedback and a pay-for-performance incentive program improve the use of guideline-compliant VTE prophylaxis?
Background: The appropriate use of VTE prophylaxis is a Joint Commission core measure set, a publicly reported performance metric for quality care, and part of the hospital value-based purchasing component of healthcare reform. Despite guidelines on effective and safe measures to prevent VTE, compliance rates are often below 50%.
Study design: Retrospective analysis.
Setting: Academic hospitalists at a tertiary care medical center.
Synopsis: Using a web-based, transparent dashboard and a pay-for-performance program with graduated payouts, this analysis showed a significant improvement in VTE compliance rates by providers. Specifically, the combination of both interventions yielded the highest rate. The monthly compliance rate increased from a baseline of 86% (95% confidence interval [CI], 85-88%) to 90% (95% CI, 88-93%) with the dashboard alone (P=0.001) and was further augmented to 94% (95% CI, 93-96%) with the combined dashboard and payment incentive program (P=0.001).
This study highlights the impact of both intrinsic (peer norms) and extrinsic (payments) motivation, as they work synergistically to improve VTE compliance rates.
Bottom line: Transparent feedback through real-time dashboards and performance-based payment incentives can be used to bring about significant improvement in patient safety and quality benchmarks.
Citation: Michtalik HJ, Carolan HT, Haut ER, et al. Use of provider-level dashboards and pay-for-performance in venous thromboembolism prophylaxis. J Hosp Med. 2015;10(3):172-178.
Clinical question: Do individual provider feedback and a pay-for-performance incentive program improve the use of guideline-compliant VTE prophylaxis?
Background: The appropriate use of VTE prophylaxis is a Joint Commission core measure set, a publicly reported performance metric for quality care, and part of the hospital value-based purchasing component of healthcare reform. Despite guidelines on effective and safe measures to prevent VTE, compliance rates are often below 50%.
Study design: Retrospective analysis.
Setting: Academic hospitalists at a tertiary care medical center.
Synopsis: Using a web-based, transparent dashboard and a pay-for-performance program with graduated payouts, this analysis showed a significant improvement in VTE compliance rates by providers. Specifically, the combination of both interventions yielded the highest rate. The monthly compliance rate increased from a baseline of 86% (95% confidence interval [CI], 85-88%) to 90% (95% CI, 88-93%) with the dashboard alone (P=0.001) and was further augmented to 94% (95% CI, 93-96%) with the combined dashboard and payment incentive program (P=0.001).
This study highlights the impact of both intrinsic (peer norms) and extrinsic (payments) motivation, as they work synergistically to improve VTE compliance rates.
Bottom line: Transparent feedback through real-time dashboards and performance-based payment incentives can be used to bring about significant improvement in patient safety and quality benchmarks.
Citation: Michtalik HJ, Carolan HT, Haut ER, et al. Use of provider-level dashboards and pay-for-performance in venous thromboembolism prophylaxis. J Hosp Med. 2015;10(3):172-178.
Intercepting Wrong-Patient Orders in a Computerized Provider Order Entry System
Clinical question: Does implementing a patient verification dialog that appears at the beginning of each ordering session, accompanied by a 2.5-second delay, decrease wrong-patient orders?
Background: Computerized provider order entry (CPOE) is known to increase the rate of wrong-patient order entry and, although the rate in the ED has not been well characterized, CPOE wrong-patient order entry has been known to lead to fatalities in the emergency setting.
Study design: A parallel-controlled, experimental, before-after design.
Setting: Five teaching hospital EDs were included in New York City: two adult EDs, two pediatric EDs, and a combined ED, all totaling 250,000 annual visits.
Synopsis: The EDs in this study implemented a patient verification module into their Allscripts system. This verification included three identifiers: full name, birth date, and medical record number. A 2.5-second delay in ability to close the alert was implemented. All patients in the ED rooms were included in the analysis. The primary outcome was intercepted wrong-patient orders, as measured by number of retract and re-order events.
A baseline data set over four months was compared to immediate post-intervention data, as well as data two years post-intervention, with 30% and 25% reductions in the rate of wrong-patient orders, respectively. Of all retractions, 41% were for diagnostic procedures, 21% for medications, and 38% were nursing and miscellaneous orders. The majority of orders were placed by resident physicians (51%), followed by attending physicians (34%), physician assistants (12%), and others (3%).
This method of observation is limited to identified and corrected wrong-patient orders.
Bottom line: Implementing a patient verification alert can significantly decrease the number of order retractions and re-orders due to wrong-patient order entry in the ED setting.
Citation: Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system [published online ahead of print December 17, 2014]. Ann Emerg Med.
Clinical question: Does implementing a patient verification dialog that appears at the beginning of each ordering session, accompanied by a 2.5-second delay, decrease wrong-patient orders?
Background: Computerized provider order entry (CPOE) is known to increase the rate of wrong-patient order entry and, although the rate in the ED has not been well characterized, CPOE wrong-patient order entry has been known to lead to fatalities in the emergency setting.
Study design: A parallel-controlled, experimental, before-after design.
Setting: Five teaching hospital EDs were included in New York City: two adult EDs, two pediatric EDs, and a combined ED, all totaling 250,000 annual visits.
Synopsis: The EDs in this study implemented a patient verification module into their Allscripts system. This verification included three identifiers: full name, birth date, and medical record number. A 2.5-second delay in ability to close the alert was implemented. All patients in the ED rooms were included in the analysis. The primary outcome was intercepted wrong-patient orders, as measured by number of retract and re-order events.
A baseline data set over four months was compared to immediate post-intervention data, as well as data two years post-intervention, with 30% and 25% reductions in the rate of wrong-patient orders, respectively. Of all retractions, 41% were for diagnostic procedures, 21% for medications, and 38% were nursing and miscellaneous orders. The majority of orders were placed by resident physicians (51%), followed by attending physicians (34%), physician assistants (12%), and others (3%).
This method of observation is limited to identified and corrected wrong-patient orders.
Bottom line: Implementing a patient verification alert can significantly decrease the number of order retractions and re-orders due to wrong-patient order entry in the ED setting.
Citation: Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system [published online ahead of print December 17, 2014]. Ann Emerg Med.
Clinical question: Does implementing a patient verification dialog that appears at the beginning of each ordering session, accompanied by a 2.5-second delay, decrease wrong-patient orders?
Background: Computerized provider order entry (CPOE) is known to increase the rate of wrong-patient order entry and, although the rate in the ED has not been well characterized, CPOE wrong-patient order entry has been known to lead to fatalities in the emergency setting.
Study design: A parallel-controlled, experimental, before-after design.
Setting: Five teaching hospital EDs were included in New York City: two adult EDs, two pediatric EDs, and a combined ED, all totaling 250,000 annual visits.
Synopsis: The EDs in this study implemented a patient verification module into their Allscripts system. This verification included three identifiers: full name, birth date, and medical record number. A 2.5-second delay in ability to close the alert was implemented. All patients in the ED rooms were included in the analysis. The primary outcome was intercepted wrong-patient orders, as measured by number of retract and re-order events.
A baseline data set over four months was compared to immediate post-intervention data, as well as data two years post-intervention, with 30% and 25% reductions in the rate of wrong-patient orders, respectively. Of all retractions, 41% were for diagnostic procedures, 21% for medications, and 38% were nursing and miscellaneous orders. The majority of orders were placed by resident physicians (51%), followed by attending physicians (34%), physician assistants (12%), and others (3%).
This method of observation is limited to identified and corrected wrong-patient orders.
Bottom line: Implementing a patient verification alert can significantly decrease the number of order retractions and re-orders due to wrong-patient order entry in the ED setting.
Citation: Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system [published online ahead of print December 17, 2014]. Ann Emerg Med.
Epidemiology of Peri-Operative, Transfusion-Associated, Circulatory Overload
Clinical question: What is the incidence of transfusion-associated circulatory overload (TACO) as it relates to specific characteristics of patients and transfusion situations?
Background: TACO is the second-leading cause of transfusion-related fatalities; however, the epidemiology of TACO is centered mostly on patients in the ICU, and the epidemiology for noncardiac surgical patients is not well characterized. This might result in suboptimal care delivery and unfavorable outcomes in peri-operative patients.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Using an electronic algorithm, 2,162 and 1,908 patients in 2004 and 2011, respectively, were screened for TACO if they received intra-operative transfusions during noncardiac surgery with general anesthesia. Analyses evaluated associations between patient and transfusion characteristics with TACO rates. Patients with TACO were compared to complication-free transfused counterparts.
The incidence of TACO increased significantly with the volume of blood product transfused, advanced age, and total intra-operative fluid balance. Mixed blood products had highest incidence of TACO, followed by fresh frozen plasma. Vascular, transplant, and thoracic surgeries had the highest, and obstetric and gynecologic surgeries the lowest TACO rates. Patients with TACO, compared with their counterparts, had a longer ICU and hospital length of stay.
The study population is derived from a single tertiary care referral center and confounded by referral bias, and, therefore, not easily generalizable. Also, results cannot be generalized to nongeneral anesthesia patients.
Although associations were noted between certain characteristics and the development of TACO, more robust and definitive evaluations of TACO risk factors are needed, as many rates were not adjusted for confounding factors.
Bottom line: Understanding characteristics of at-risk patients may facilitate improved decision making regarding transfusion strategies for peri-operative noncardiac surgical patients.
Citation: Clifford L, Jia Q, Yadav H, et al. Characterizing the epidemiology of perioperative transfusion-associated circulatory overload. Anesthesiology. 2015;122(1):21-28.
Clinical question: What is the incidence of transfusion-associated circulatory overload (TACO) as it relates to specific characteristics of patients and transfusion situations?
Background: TACO is the second-leading cause of transfusion-related fatalities; however, the epidemiology of TACO is centered mostly on patients in the ICU, and the epidemiology for noncardiac surgical patients is not well characterized. This might result in suboptimal care delivery and unfavorable outcomes in peri-operative patients.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Using an electronic algorithm, 2,162 and 1,908 patients in 2004 and 2011, respectively, were screened for TACO if they received intra-operative transfusions during noncardiac surgery with general anesthesia. Analyses evaluated associations between patient and transfusion characteristics with TACO rates. Patients with TACO were compared to complication-free transfused counterparts.
The incidence of TACO increased significantly with the volume of blood product transfused, advanced age, and total intra-operative fluid balance. Mixed blood products had highest incidence of TACO, followed by fresh frozen plasma. Vascular, transplant, and thoracic surgeries had the highest, and obstetric and gynecologic surgeries the lowest TACO rates. Patients with TACO, compared with their counterparts, had a longer ICU and hospital length of stay.
The study population is derived from a single tertiary care referral center and confounded by referral bias, and, therefore, not easily generalizable. Also, results cannot be generalized to nongeneral anesthesia patients.
Although associations were noted between certain characteristics and the development of TACO, more robust and definitive evaluations of TACO risk factors are needed, as many rates were not adjusted for confounding factors.
Bottom line: Understanding characteristics of at-risk patients may facilitate improved decision making regarding transfusion strategies for peri-operative noncardiac surgical patients.
Citation: Clifford L, Jia Q, Yadav H, et al. Characterizing the epidemiology of perioperative transfusion-associated circulatory overload. Anesthesiology. 2015;122(1):21-28.
Clinical question: What is the incidence of transfusion-associated circulatory overload (TACO) as it relates to specific characteristics of patients and transfusion situations?
Background: TACO is the second-leading cause of transfusion-related fatalities; however, the epidemiology of TACO is centered mostly on patients in the ICU, and the epidemiology for noncardiac surgical patients is not well characterized. This might result in suboptimal care delivery and unfavorable outcomes in peri-operative patients.
Study design: Retrospective cohort study.
Setting: Mayo Clinic, Rochester, Minn.
Synopsis: Using an electronic algorithm, 2,162 and 1,908 patients in 2004 and 2011, respectively, were screened for TACO if they received intra-operative transfusions during noncardiac surgery with general anesthesia. Analyses evaluated associations between patient and transfusion characteristics with TACO rates. Patients with TACO were compared to complication-free transfused counterparts.
The incidence of TACO increased significantly with the volume of blood product transfused, advanced age, and total intra-operative fluid balance. Mixed blood products had highest incidence of TACO, followed by fresh frozen plasma. Vascular, transplant, and thoracic surgeries had the highest, and obstetric and gynecologic surgeries the lowest TACO rates. Patients with TACO, compared with their counterparts, had a longer ICU and hospital length of stay.
The study population is derived from a single tertiary care referral center and confounded by referral bias, and, therefore, not easily generalizable. Also, results cannot be generalized to nongeneral anesthesia patients.
Although associations were noted between certain characteristics and the development of TACO, more robust and definitive evaluations of TACO risk factors are needed, as many rates were not adjusted for confounding factors.
Bottom line: Understanding characteristics of at-risk patients may facilitate improved decision making regarding transfusion strategies for peri-operative noncardiac surgical patients.
Citation: Clifford L, Jia Q, Yadav H, et al. Characterizing the epidemiology of perioperative transfusion-associated circulatory overload. Anesthesiology. 2015;122(1):21-28.