User login
Scientific doubt tempers COVID-19 vaccine optimism
US government and industry projections that a COVID-19 vaccine will be ready by this fall or even January would take compressing what usually takes at least a decade into months, with little room for error or safety surprises.
“If all the cards fall into the right place and all the stars are aligned, you definitely could get a vaccine by December or January,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said last week.
But Fauci said a more realistic timeline is still 12 to 18 months, and experts interviewed by Medscape Medical News agree. They say that although recent developments are encouraging, history and scientific reason say the day when a COVID-19 vaccine is widely available will not come this year and may not come by the end of 2021.
The encouraging signals come primarily from two recent announcements: the $1.2 billion United States backing last week of one vaccine platform and the announcement on May 18 that the first human trials of another have produced some positive phase 1 results.
Recent developments
On May 21, the US Department of Health and Human Services (HHS) under “Operation Warp Speed” announced that the US will give AstraZeneca $1.2 billion “to make available at least 300 million doses of a coronavirus vaccine called AZD1222, with the first doses delivered as early as October 2020.”
On May 18, the Massachusetts-based biotechnology company Moderna announced that phase 1 clinical results showed that its vaccine candidate, which uses a new messenger RNA (mRNA) technology, appeared safe. Eight participants in the human trials were able to produce neutralizing antibodies that researchers believe are important in developing protection from the virus.
Moderna Chief Medical Officer Tal Zaks, MD, PhD told CNN that if the vaccine candidate does well in phase 2, “it could be ready by January 2021.”
The two candidates are among 10 in clinical trials for the SARS-CoV-2 virus, according to the World Health Organization (WHO). The AstraZeneca/ AZD1222 candidate (also called ChAdOx1 nCoV-19, in collaboration with the University of Oxford) has entered phase 2/3.
Moderna’s candidate and another being developed in Beijing, China, are in phase 2, WHO reports. As of yesterday, 115 other candidates are in preclinical evaluation.
Maria Elena Bottazzi, PhD, associate dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, Texas, told Medscape Medical News it’s important to realize that, in the case of the $1.2 billion US investment, “what they’re talking about is manufacturing.”
The idea, she said, is to pay AstraZeneca up front so that manufacturing can start before it is known whether the vaccine candidate is safe or effective, the reverse of how the clinical trial process usually works.
That way, if the candidate is deemed safe and effective, time is not lost by then deciding how to make it and distribute it.
By the end of this year, she said, “Maybe we will have many vaccines made and stored in a refrigerator somewhere. But between now and December, there’s absolutely no way you can show efficacy of the vaccine at the same time you confirm that it’s safe.”
“Take these things with a grain of salt”
Animal testing for the AstraZeneca candidate, made in partnership with the University of Oxford in the United Kingdom, has yielded lackluster results, according to results on the preprint server BioRxiv, which have not been peer-reviewed.
“The results were not bad, but they were not gangbusters,” Bottazzi said. The results show the vaccine offered only partial protection.
“Partial protection is better than no protection,” she noted. “You have to take these things with a grain of salt. We don’t know what’s going to happen in humans.”
As for the Moderna candidate, Bottazzi said, “the good news is they found an appropriate safety profile. But from an eight-person group to make the extrapolation that they have efficacy — it’s unrealistic.”
Nicole Lurie, MD, MSPH, is senior adviser to the CEO for the Coalition for Epidemic Preparedness Innovation (CEPI), a nongovernmental organization funded by the Wellcome Trust, the Bill and Melinda Gates Foundation, the European Commission, and eight countries (Australia, Belgium, Canada, Ethiopia, Germany, Japan, Norway, and the United Kingdom) charged with supporting development of vaccines for pathogens on WHO’s priority list.
She and her colleagues write in a paper published online in the New England Journal of Medicine on March 30 that “it typically takes multiple candidates and many years to produce a licensed vaccine.”
The fastest time for developing a vaccine to date is 4 years, for the mumps vaccine, licensed in 1967.
As to whether she would expect a rollout of any vaccine by the end of the year, Lurie told Medscape Medical News, “If everything goes according to plan in every way, shape or form, well then maybe you can get there. But I wouldn’t hold my breath.”
Lurie and her colleagues write that “it’s far from certain that these new platforms will be scalable or that existing capacity can provide sufficient quantities of vaccine fast enough.”
On a call with reporters today, leaders of some of the words largest pharmaceutical companies said that one of the key bottlenecks is the sheer number of vials needed in order to distribute billions of doses of a successful vaccine.
Pfizer CEO Albert Bourla, DVM, PhD, said, “Typically we are producing vaccines in single-dose vials. We are exploring with governments right now if it would be more convenient if there were 5-dose vials or 10-dose vials. I think we can resolve a significant part of the bottleneck.”
Despite the challenges, experts interviewed for this article agree that it will be possible to make a vaccine for COVID-19. They don’t expect attempts to meet the same complications that HIV researchers have seen over decades as the virus continues to confound with mutations.
Fred Ledley, MD, director of the Center for Integration of Science and Industry at Bentley University in Waltham, Massachusetts, told Medscape Medical News, “There doesn’t appear to be anything terribly diabolical about this virus. The mutation rate doesn’t appear to be anything like HIV. It appears to have some big, ugly proteins on the surface, which is good for vaccines — proteins with a lot of physical features look distinguishable from healthy cells. Signs all point to that it should be possible to make a vaccine.”
History raises safety concerns
However, Ledley said, “The idea of doing it in 6 months is largely unrealistic.”
He says 18 months is more realistic, primarily because of the sheer number of people that would have to be enrolled in a phase 3 study to truly test whether the endpoints are being met.
Vaccines are given to healthy volunteers. If safety signals arise, they may not be apparent until massive numbers of people are tested in phase 3.
“You’re never going to see the rates cut to 0%, but to see the difference between 10 people getting sick and seven people getting sick, takes very, very large numbers,” Ledley said. “There’s no way that can be done in 6 months. You’re talking about tens of thousands of people enrolled.”
He notes at this point it’s unclear what the endpoints will be and what the safety thresholds will be after consideration of risks and benefit.
Another big question for Ledley: “We don’t know what type of immunity we need to protect us against the virus. Do you just need the antibodies in your blood or do you need cells that are primed to attack the virus? Is it more of a chemical clearance or do the cells need to physically go in and digest the virus?”
History also points to the need for rigorous safety precautions that scientists fear could be compromised as trial phases overlap and processes are run in parallel instead of one step at a time.
An early batch of the Salk vaccine for polio in 1955, for example, turned out to be contaminated and caused paralysis in some children and 10 deaths, he points out.
CEPI’s Lurie adds that early candidates for another coronavirus, severe acute respiratory syndrome (SARS), “caused a reaction in the lungs that was very dangerous” before development was halted.
She also pointed to previous findings that a vaccine for dengue fever could worsen the disease in some people through a phenomenon called antibody-dependent enhancement.
Lurie and colleagues write in their paper that “it’s critical that vaccines also be developed using the tried-and-true methods, even if they may take longer to enter clinical trials or to result in large numbers of doses.”
Live attenuated vaccine
Raul Andino, PhD, a virologist at the University of California San Francisco, is among the scientists working with a tried-and-true method — a live attenuated vaccine — and he told Medscape Medical News he’s predicting it will take 2 years to develop.
He said it is cheaper to produce because scientists just have to learn how to grow the virus. Because the technology is already proven, a live attenuated vaccine could be rapidly produced on a worldwide scale.
The hope is also that a live attenuated vaccine would be given once in a lifetime and therefore be more affordable, especially in poorer countries.
“While a Moderna vaccine might be good for Europe and the United States,” he said, “It’s not going to be good for Africa, India, Brazil.”
Andino said, “I would bet money” that the front-runner vaccines so far will not be one-time vaccines.
He points out that most of the vaccine candidates are trying to protect people from disease. While there’s nothing wrong with that, he said, “In my opinion that is the lower-hanging fruit.”
“In my mind we need something that interrupts the chain of transmission and induces protection,” Andino said, important for developing herd immunity.
The reason this type of approach takes longer is because you are introducing a weakened form of the virus to the body and you have to make sure it doesn’t cause disease, not just in a small test population, but in populations who may be more susceptible to the disease, Andino said.
A call for unified strategies
Universities, countries, international consortiums, and public-private partnerships are all racing to find several safe and effective vaccines as no one entity will likely be able to provide the global solution.
Some of the efforts involve overlap of entities but with different focuses.
Along with “Operation Warp Speed” and CEPI, other collaborations include Gavi the Vaccine Alliance, whose core partners include WHO, UNICEF, the World Bank, and the Gates Foundation; and “Accelerating Therapeutic Interventions and Vaccines (ACTIV) partnership,” led by the National Institutes of Health.
Industry partners in ACTIV (18 biopharmaceutical companies), according to a May 18 article published online in the Journal of the American Medical Association, have said they will contribute their respective clinical trial capacities, regardless of which agent is studied.
Some, however, have called for more streamlining of efforts.
“Ideally we’d be working together,” Lurie told Medscape Medical News.
“I’m hopeful we will find ways to collaborate scientifically,” she said. “The US government’s responsibility is to make doses for the US. CEPI’s responsibility is to make doses for the world. A big focus of CEPI is to make sure we have manufacturing capacity outside of the US so those doses can be available to the world and they don’t get seized by wealthy countries.”
Bottazzi, Ledley, Lurie, and Andino report no relevant financial relationships.
This article first appeared on Medscape.com.
US government and industry projections that a COVID-19 vaccine will be ready by this fall or even January would take compressing what usually takes at least a decade into months, with little room for error or safety surprises.
“If all the cards fall into the right place and all the stars are aligned, you definitely could get a vaccine by December or January,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said last week.
But Fauci said a more realistic timeline is still 12 to 18 months, and experts interviewed by Medscape Medical News agree. They say that although recent developments are encouraging, history and scientific reason say the day when a COVID-19 vaccine is widely available will not come this year and may not come by the end of 2021.
The encouraging signals come primarily from two recent announcements: the $1.2 billion United States backing last week of one vaccine platform and the announcement on May 18 that the first human trials of another have produced some positive phase 1 results.
Recent developments
On May 21, the US Department of Health and Human Services (HHS) under “Operation Warp Speed” announced that the US will give AstraZeneca $1.2 billion “to make available at least 300 million doses of a coronavirus vaccine called AZD1222, with the first doses delivered as early as October 2020.”
On May 18, the Massachusetts-based biotechnology company Moderna announced that phase 1 clinical results showed that its vaccine candidate, which uses a new messenger RNA (mRNA) technology, appeared safe. Eight participants in the human trials were able to produce neutralizing antibodies that researchers believe are important in developing protection from the virus.
Moderna Chief Medical Officer Tal Zaks, MD, PhD told CNN that if the vaccine candidate does well in phase 2, “it could be ready by January 2021.”
The two candidates are among 10 in clinical trials for the SARS-CoV-2 virus, according to the World Health Organization (WHO). The AstraZeneca/ AZD1222 candidate (also called ChAdOx1 nCoV-19, in collaboration with the University of Oxford) has entered phase 2/3.
Moderna’s candidate and another being developed in Beijing, China, are in phase 2, WHO reports. As of yesterday, 115 other candidates are in preclinical evaluation.
Maria Elena Bottazzi, PhD, associate dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, Texas, told Medscape Medical News it’s important to realize that, in the case of the $1.2 billion US investment, “what they’re talking about is manufacturing.”
The idea, she said, is to pay AstraZeneca up front so that manufacturing can start before it is known whether the vaccine candidate is safe or effective, the reverse of how the clinical trial process usually works.
That way, if the candidate is deemed safe and effective, time is not lost by then deciding how to make it and distribute it.
By the end of this year, she said, “Maybe we will have many vaccines made and stored in a refrigerator somewhere. But between now and December, there’s absolutely no way you can show efficacy of the vaccine at the same time you confirm that it’s safe.”
“Take these things with a grain of salt”
Animal testing for the AstraZeneca candidate, made in partnership with the University of Oxford in the United Kingdom, has yielded lackluster results, according to results on the preprint server BioRxiv, which have not been peer-reviewed.
“The results were not bad, but they were not gangbusters,” Bottazzi said. The results show the vaccine offered only partial protection.
“Partial protection is better than no protection,” she noted. “You have to take these things with a grain of salt. We don’t know what’s going to happen in humans.”
As for the Moderna candidate, Bottazzi said, “the good news is they found an appropriate safety profile. But from an eight-person group to make the extrapolation that they have efficacy — it’s unrealistic.”
Nicole Lurie, MD, MSPH, is senior adviser to the CEO for the Coalition for Epidemic Preparedness Innovation (CEPI), a nongovernmental organization funded by the Wellcome Trust, the Bill and Melinda Gates Foundation, the European Commission, and eight countries (Australia, Belgium, Canada, Ethiopia, Germany, Japan, Norway, and the United Kingdom) charged with supporting development of vaccines for pathogens on WHO’s priority list.
She and her colleagues write in a paper published online in the New England Journal of Medicine on March 30 that “it typically takes multiple candidates and many years to produce a licensed vaccine.”
The fastest time for developing a vaccine to date is 4 years, for the mumps vaccine, licensed in 1967.
As to whether she would expect a rollout of any vaccine by the end of the year, Lurie told Medscape Medical News, “If everything goes according to plan in every way, shape or form, well then maybe you can get there. But I wouldn’t hold my breath.”
Lurie and her colleagues write that “it’s far from certain that these new platforms will be scalable or that existing capacity can provide sufficient quantities of vaccine fast enough.”
On a call with reporters today, leaders of some of the words largest pharmaceutical companies said that one of the key bottlenecks is the sheer number of vials needed in order to distribute billions of doses of a successful vaccine.
Pfizer CEO Albert Bourla, DVM, PhD, said, “Typically we are producing vaccines in single-dose vials. We are exploring with governments right now if it would be more convenient if there were 5-dose vials or 10-dose vials. I think we can resolve a significant part of the bottleneck.”
Despite the challenges, experts interviewed for this article agree that it will be possible to make a vaccine for COVID-19. They don’t expect attempts to meet the same complications that HIV researchers have seen over decades as the virus continues to confound with mutations.
Fred Ledley, MD, director of the Center for Integration of Science and Industry at Bentley University in Waltham, Massachusetts, told Medscape Medical News, “There doesn’t appear to be anything terribly diabolical about this virus. The mutation rate doesn’t appear to be anything like HIV. It appears to have some big, ugly proteins on the surface, which is good for vaccines — proteins with a lot of physical features look distinguishable from healthy cells. Signs all point to that it should be possible to make a vaccine.”
History raises safety concerns
However, Ledley said, “The idea of doing it in 6 months is largely unrealistic.”
He says 18 months is more realistic, primarily because of the sheer number of people that would have to be enrolled in a phase 3 study to truly test whether the endpoints are being met.
Vaccines are given to healthy volunteers. If safety signals arise, they may not be apparent until massive numbers of people are tested in phase 3.
“You’re never going to see the rates cut to 0%, but to see the difference between 10 people getting sick and seven people getting sick, takes very, very large numbers,” Ledley said. “There’s no way that can be done in 6 months. You’re talking about tens of thousands of people enrolled.”
He notes at this point it’s unclear what the endpoints will be and what the safety thresholds will be after consideration of risks and benefit.
Another big question for Ledley: “We don’t know what type of immunity we need to protect us against the virus. Do you just need the antibodies in your blood or do you need cells that are primed to attack the virus? Is it more of a chemical clearance or do the cells need to physically go in and digest the virus?”
History also points to the need for rigorous safety precautions that scientists fear could be compromised as trial phases overlap and processes are run in parallel instead of one step at a time.
An early batch of the Salk vaccine for polio in 1955, for example, turned out to be contaminated and caused paralysis in some children and 10 deaths, he points out.
CEPI’s Lurie adds that early candidates for another coronavirus, severe acute respiratory syndrome (SARS), “caused a reaction in the lungs that was very dangerous” before development was halted.
She also pointed to previous findings that a vaccine for dengue fever could worsen the disease in some people through a phenomenon called antibody-dependent enhancement.
Lurie and colleagues write in their paper that “it’s critical that vaccines also be developed using the tried-and-true methods, even if they may take longer to enter clinical trials or to result in large numbers of doses.”
Live attenuated vaccine
Raul Andino, PhD, a virologist at the University of California San Francisco, is among the scientists working with a tried-and-true method — a live attenuated vaccine — and he told Medscape Medical News he’s predicting it will take 2 years to develop.
He said it is cheaper to produce because scientists just have to learn how to grow the virus. Because the technology is already proven, a live attenuated vaccine could be rapidly produced on a worldwide scale.
The hope is also that a live attenuated vaccine would be given once in a lifetime and therefore be more affordable, especially in poorer countries.
“While a Moderna vaccine might be good for Europe and the United States,” he said, “It’s not going to be good for Africa, India, Brazil.”
Andino said, “I would bet money” that the front-runner vaccines so far will not be one-time vaccines.
He points out that most of the vaccine candidates are trying to protect people from disease. While there’s nothing wrong with that, he said, “In my opinion that is the lower-hanging fruit.”
“In my mind we need something that interrupts the chain of transmission and induces protection,” Andino said, important for developing herd immunity.
The reason this type of approach takes longer is because you are introducing a weakened form of the virus to the body and you have to make sure it doesn’t cause disease, not just in a small test population, but in populations who may be more susceptible to the disease, Andino said.
A call for unified strategies
Universities, countries, international consortiums, and public-private partnerships are all racing to find several safe and effective vaccines as no one entity will likely be able to provide the global solution.
Some of the efforts involve overlap of entities but with different focuses.
Along with “Operation Warp Speed” and CEPI, other collaborations include Gavi the Vaccine Alliance, whose core partners include WHO, UNICEF, the World Bank, and the Gates Foundation; and “Accelerating Therapeutic Interventions and Vaccines (ACTIV) partnership,” led by the National Institutes of Health.
Industry partners in ACTIV (18 biopharmaceutical companies), according to a May 18 article published online in the Journal of the American Medical Association, have said they will contribute their respective clinical trial capacities, regardless of which agent is studied.
Some, however, have called for more streamlining of efforts.
“Ideally we’d be working together,” Lurie told Medscape Medical News.
“I’m hopeful we will find ways to collaborate scientifically,” she said. “The US government’s responsibility is to make doses for the US. CEPI’s responsibility is to make doses for the world. A big focus of CEPI is to make sure we have manufacturing capacity outside of the US so those doses can be available to the world and they don’t get seized by wealthy countries.”
Bottazzi, Ledley, Lurie, and Andino report no relevant financial relationships.
This article first appeared on Medscape.com.
US government and industry projections that a COVID-19 vaccine will be ready by this fall or even January would take compressing what usually takes at least a decade into months, with little room for error or safety surprises.
“If all the cards fall into the right place and all the stars are aligned, you definitely could get a vaccine by December or January,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said last week.
But Fauci said a more realistic timeline is still 12 to 18 months, and experts interviewed by Medscape Medical News agree. They say that although recent developments are encouraging, history and scientific reason say the day when a COVID-19 vaccine is widely available will not come this year and may not come by the end of 2021.
The encouraging signals come primarily from two recent announcements: the $1.2 billion United States backing last week of one vaccine platform and the announcement on May 18 that the first human trials of another have produced some positive phase 1 results.
Recent developments
On May 21, the US Department of Health and Human Services (HHS) under “Operation Warp Speed” announced that the US will give AstraZeneca $1.2 billion “to make available at least 300 million doses of a coronavirus vaccine called AZD1222, with the first doses delivered as early as October 2020.”
On May 18, the Massachusetts-based biotechnology company Moderna announced that phase 1 clinical results showed that its vaccine candidate, which uses a new messenger RNA (mRNA) technology, appeared safe. Eight participants in the human trials were able to produce neutralizing antibodies that researchers believe are important in developing protection from the virus.
Moderna Chief Medical Officer Tal Zaks, MD, PhD told CNN that if the vaccine candidate does well in phase 2, “it could be ready by January 2021.”
The two candidates are among 10 in clinical trials for the SARS-CoV-2 virus, according to the World Health Organization (WHO). The AstraZeneca/ AZD1222 candidate (also called ChAdOx1 nCoV-19, in collaboration with the University of Oxford) has entered phase 2/3.
Moderna’s candidate and another being developed in Beijing, China, are in phase 2, WHO reports. As of yesterday, 115 other candidates are in preclinical evaluation.
Maria Elena Bottazzi, PhD, associate dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, Texas, told Medscape Medical News it’s important to realize that, in the case of the $1.2 billion US investment, “what they’re talking about is manufacturing.”
The idea, she said, is to pay AstraZeneca up front so that manufacturing can start before it is known whether the vaccine candidate is safe or effective, the reverse of how the clinical trial process usually works.
That way, if the candidate is deemed safe and effective, time is not lost by then deciding how to make it and distribute it.
By the end of this year, she said, “Maybe we will have many vaccines made and stored in a refrigerator somewhere. But between now and December, there’s absolutely no way you can show efficacy of the vaccine at the same time you confirm that it’s safe.”
“Take these things with a grain of salt”
Animal testing for the AstraZeneca candidate, made in partnership with the University of Oxford in the United Kingdom, has yielded lackluster results, according to results on the preprint server BioRxiv, which have not been peer-reviewed.
“The results were not bad, but they were not gangbusters,” Bottazzi said. The results show the vaccine offered only partial protection.
“Partial protection is better than no protection,” she noted. “You have to take these things with a grain of salt. We don’t know what’s going to happen in humans.”
As for the Moderna candidate, Bottazzi said, “the good news is they found an appropriate safety profile. But from an eight-person group to make the extrapolation that they have efficacy — it’s unrealistic.”
Nicole Lurie, MD, MSPH, is senior adviser to the CEO for the Coalition for Epidemic Preparedness Innovation (CEPI), a nongovernmental organization funded by the Wellcome Trust, the Bill and Melinda Gates Foundation, the European Commission, and eight countries (Australia, Belgium, Canada, Ethiopia, Germany, Japan, Norway, and the United Kingdom) charged with supporting development of vaccines for pathogens on WHO’s priority list.
She and her colleagues write in a paper published online in the New England Journal of Medicine on March 30 that “it typically takes multiple candidates and many years to produce a licensed vaccine.”
The fastest time for developing a vaccine to date is 4 years, for the mumps vaccine, licensed in 1967.
As to whether she would expect a rollout of any vaccine by the end of the year, Lurie told Medscape Medical News, “If everything goes according to plan in every way, shape or form, well then maybe you can get there. But I wouldn’t hold my breath.”
Lurie and her colleagues write that “it’s far from certain that these new platforms will be scalable or that existing capacity can provide sufficient quantities of vaccine fast enough.”
On a call with reporters today, leaders of some of the words largest pharmaceutical companies said that one of the key bottlenecks is the sheer number of vials needed in order to distribute billions of doses of a successful vaccine.
Pfizer CEO Albert Bourla, DVM, PhD, said, “Typically we are producing vaccines in single-dose vials. We are exploring with governments right now if it would be more convenient if there were 5-dose vials or 10-dose vials. I think we can resolve a significant part of the bottleneck.”
Despite the challenges, experts interviewed for this article agree that it will be possible to make a vaccine for COVID-19. They don’t expect attempts to meet the same complications that HIV researchers have seen over decades as the virus continues to confound with mutations.
Fred Ledley, MD, director of the Center for Integration of Science and Industry at Bentley University in Waltham, Massachusetts, told Medscape Medical News, “There doesn’t appear to be anything terribly diabolical about this virus. The mutation rate doesn’t appear to be anything like HIV. It appears to have some big, ugly proteins on the surface, which is good for vaccines — proteins with a lot of physical features look distinguishable from healthy cells. Signs all point to that it should be possible to make a vaccine.”
History raises safety concerns
However, Ledley said, “The idea of doing it in 6 months is largely unrealistic.”
He says 18 months is more realistic, primarily because of the sheer number of people that would have to be enrolled in a phase 3 study to truly test whether the endpoints are being met.
Vaccines are given to healthy volunteers. If safety signals arise, they may not be apparent until massive numbers of people are tested in phase 3.
“You’re never going to see the rates cut to 0%, but to see the difference between 10 people getting sick and seven people getting sick, takes very, very large numbers,” Ledley said. “There’s no way that can be done in 6 months. You’re talking about tens of thousands of people enrolled.”
He notes at this point it’s unclear what the endpoints will be and what the safety thresholds will be after consideration of risks and benefit.
Another big question for Ledley: “We don’t know what type of immunity we need to protect us against the virus. Do you just need the antibodies in your blood or do you need cells that are primed to attack the virus? Is it more of a chemical clearance or do the cells need to physically go in and digest the virus?”
History also points to the need for rigorous safety precautions that scientists fear could be compromised as trial phases overlap and processes are run in parallel instead of one step at a time.
An early batch of the Salk vaccine for polio in 1955, for example, turned out to be contaminated and caused paralysis in some children and 10 deaths, he points out.
CEPI’s Lurie adds that early candidates for another coronavirus, severe acute respiratory syndrome (SARS), “caused a reaction in the lungs that was very dangerous” before development was halted.
She also pointed to previous findings that a vaccine for dengue fever could worsen the disease in some people through a phenomenon called antibody-dependent enhancement.
Lurie and colleagues write in their paper that “it’s critical that vaccines also be developed using the tried-and-true methods, even if they may take longer to enter clinical trials or to result in large numbers of doses.”
Live attenuated vaccine
Raul Andino, PhD, a virologist at the University of California San Francisco, is among the scientists working with a tried-and-true method — a live attenuated vaccine — and he told Medscape Medical News he’s predicting it will take 2 years to develop.
He said it is cheaper to produce because scientists just have to learn how to grow the virus. Because the technology is already proven, a live attenuated vaccine could be rapidly produced on a worldwide scale.
The hope is also that a live attenuated vaccine would be given once in a lifetime and therefore be more affordable, especially in poorer countries.
“While a Moderna vaccine might be good for Europe and the United States,” he said, “It’s not going to be good for Africa, India, Brazil.”
Andino said, “I would bet money” that the front-runner vaccines so far will not be one-time vaccines.
He points out that most of the vaccine candidates are trying to protect people from disease. While there’s nothing wrong with that, he said, “In my opinion that is the lower-hanging fruit.”
“In my mind we need something that interrupts the chain of transmission and induces protection,” Andino said, important for developing herd immunity.
The reason this type of approach takes longer is because you are introducing a weakened form of the virus to the body and you have to make sure it doesn’t cause disease, not just in a small test population, but in populations who may be more susceptible to the disease, Andino said.
A call for unified strategies
Universities, countries, international consortiums, and public-private partnerships are all racing to find several safe and effective vaccines as no one entity will likely be able to provide the global solution.
Some of the efforts involve overlap of entities but with different focuses.
Along with “Operation Warp Speed” and CEPI, other collaborations include Gavi the Vaccine Alliance, whose core partners include WHO, UNICEF, the World Bank, and the Gates Foundation; and “Accelerating Therapeutic Interventions and Vaccines (ACTIV) partnership,” led by the National Institutes of Health.
Industry partners in ACTIV (18 biopharmaceutical companies), according to a May 18 article published online in the Journal of the American Medical Association, have said they will contribute their respective clinical trial capacities, regardless of which agent is studied.
Some, however, have called for more streamlining of efforts.
“Ideally we’d be working together,” Lurie told Medscape Medical News.
“I’m hopeful we will find ways to collaborate scientifically,” she said. “The US government’s responsibility is to make doses for the US. CEPI’s responsibility is to make doses for the world. A big focus of CEPI is to make sure we have manufacturing capacity outside of the US so those doses can be available to the world and they don’t get seized by wealthy countries.”
Bottazzi, Ledley, Lurie, and Andino report no relevant financial relationships.
This article first appeared on Medscape.com.
Clinicians still unaware of need for genetic testing in NSCLC
Moreover, the majority of these clinicians believe that fewer than 50% of patients in their country undergo molecular testing, the same survey showed.
The survey was conducted by the International Association for the Study of Lung Cancer (IASLC); 2537 questionnaires from 102 countries were returned and analyzed.
It was published online May 20 in the Journal of Thoracic Oncology.
The results are concerning because “the risk of death for patients with NSCLC is substantially reduced when a gene alteration is identified and the available targeted therapy is administered,” the authors emphasize.
“Specific protocols to initiate reflex testing for guideline-recommended molecular markers would help providers consider molecular testing earlier and optimize tissue,” they suggest.
Surprised that clinicians were unaware of guidelines
“I was not surprised that we found suboptimal testing rates based on other research that has demonstrated the need to improve the quality of lung cancer in some areas,” corresponding author Matthew Smeltzer, PhD, University of Memphis, Tennessee, told Medscape Medical News in an email.
“However, I was surprised that so many respondents were unaware of guidelines,” he said.
The College of American Pathologists, IASLC, and Association for Molecular Pathology established evidence-based standards for the selection of NSCLC patients for molecular testing in 2013, and these guidelines were subsequently endorsed by the American Society of Clinical Oncology.
“We suspect that the level of access a provider has to targeted therapies does affect molecular testing rates,” Smeltzer acknowledged.
Molecular testing survey
“The survey included a seven-question introduction for all respondents and then divided respondents into one of three tracks,” the authors explain.
These tracks included respondents who requested tests and who treated patients (medical oncologists), those who analyzed and interpreted assays (pathologists), and those who acquired tissue samples (surgeons, pulmonologists, radiologists).
Countries were also grouped into five geographic regions — Asia, Europe, Latin America, United States, and Canada — and the rest of the world (ROW).
“Overall, respondents reported that molecular testing rates were lower than we would like but they were not satisfied with the current state of testing, and they reported higher testing rates in their own clinics,” Smeltzer noted.
However, when tests were ordered, “we found 99% of respondents in the requesting/treating track ordered tests for EGFR, 95% for ALK, 79% for ROS1, and < 50% ordered other tests,” the authors observe.
Indeed, EGFR, ALK, and ROS1 were the top three tests ordered across all regions, though less frequently so in the ROW, they add.
More than half of requesting/treating track respondents also order multiplex assays, although Latin America and the ROW did this less frequently than other regions.
Over 90% of respondents who perform or interpret assays indicated that they perform EGFR testing, while 83% of the same group do ALK testing; 69% tested for KRAS; 68% for BRAF, 64% for ROS1, and 56% for HER2. Fewer than half of them performed other tests.
Survey results also showed that EGFR, ALK, and KRAS are the top three tests performed across all regions, with no regional differences.
“Respondents also reported on the acquisition and testing of liquid biopsies,” survey authors point out.
Here, 87% of requesting/treating track respondents indicated that they “sometimes” request molecular testing on liquid biopsies, but the proportions of those who sometimes use liquid biopsy varied by region and were lowest in Latin America and the ROW.
A lower proportion of those who perform and interpret assays, at 69%, also offer tests on liquid biopsies, but this percentage, too, varied significantly by region, being the least frequently done in the United States and Canada, as well as in the ROW.
All the above tests are for genetic mutations or alterations that guide clinicians on use of targeted therapy directed at particular mutations, for example, drugs like erlotinib for EGFR and crizotinib for ALK.
However, immunotherapy with checkpoint inhibitors has also made a big impact on the treatment of NSCLC, and the use of these agents is sometimes guided by testing for programmed cell-death ligand (PD-L1).
PD-L1 is not a molecular marker per se, the authors note.
Nevertheless, “we found that 84% of respondents in the requesting/treating track ordered PD-L1 and 68% of respondents who perform or interpret assays report PD-L1 is offered in their own lab,” the authors observe.
Smeltzer commented that both approaches — targeted therapies and immunotherapy — have made inroads into the treatment of NSCLC, in some cases replacing chemotherapy.
He emphasized that “it is important to know if a specific oncogene driver is present before initiating immunotherapy treatment,” and noted that when tissue is sent out for both types of testing, the results for PD-L1 are usually available before the results for the full molecular testing panel are back.
Barriers to testing
“The most frequent barrier to molecular testing in every region was cost,” the survey authors note.
Insufficient amount of tumor cells was the main reason for molecular testing failures along with inadequate tissue quality.
The majority of respondents who order tests and treat patients were sure that the laboratories they use perform appropriate validation of molecular tests, while almost all of those who perform or interpret assays said they perform validation tests in their labs.
Only 30% of respondents who request tests and treat patients have access to molecular testing labs within their own institutions; the remaining respondents have to outsource testing completely or partially.
Most respondents who test and treat patients also have multidisciplinary tumor boards to discuss patients with NSCLC, but almost one quarter of the same group indicated their board met less than once a month.
“Turnaround time is a barrier to molecular testing across the world,” the authors continue, with 29% of those who request tests and treat patients reporting that it typically takes 10 days or more to receive molecular testing results.
Interestingly, the highest percentage of respondents who reported this long turnaround time were in North America.
Perhaps encouragingly, 41% of respondents who perform or interpret assays indicated they were dissatisfied with the condition of molecular testing in their country, although in this regard, the United States and Canada had the lowest rates of dissatisfaction.
In fact, 39% of those who request tests and treat patients ranked the conditions of molecular testing in their country as “average or below,” while 42% of respondents in the tissue acquisition track ranked the conditions of molecular testing as average or below, the worst rankings coming from Latin America and the ROW.
Low quality of tissue samples was another reason respondents expressed dissatisfaction with the current state of molecular testing in their country.
Smeltzer is a research consultant for the Association of Community Cancer Centers.
This article first appeared on Medscape.com.
Moreover, the majority of these clinicians believe that fewer than 50% of patients in their country undergo molecular testing, the same survey showed.
The survey was conducted by the International Association for the Study of Lung Cancer (IASLC); 2537 questionnaires from 102 countries were returned and analyzed.
It was published online May 20 in the Journal of Thoracic Oncology.
The results are concerning because “the risk of death for patients with NSCLC is substantially reduced when a gene alteration is identified and the available targeted therapy is administered,” the authors emphasize.
“Specific protocols to initiate reflex testing for guideline-recommended molecular markers would help providers consider molecular testing earlier and optimize tissue,” they suggest.
Surprised that clinicians were unaware of guidelines
“I was not surprised that we found suboptimal testing rates based on other research that has demonstrated the need to improve the quality of lung cancer in some areas,” corresponding author Matthew Smeltzer, PhD, University of Memphis, Tennessee, told Medscape Medical News in an email.
“However, I was surprised that so many respondents were unaware of guidelines,” he said.
The College of American Pathologists, IASLC, and Association for Molecular Pathology established evidence-based standards for the selection of NSCLC patients for molecular testing in 2013, and these guidelines were subsequently endorsed by the American Society of Clinical Oncology.
“We suspect that the level of access a provider has to targeted therapies does affect molecular testing rates,” Smeltzer acknowledged.
Molecular testing survey
“The survey included a seven-question introduction for all respondents and then divided respondents into one of three tracks,” the authors explain.
These tracks included respondents who requested tests and who treated patients (medical oncologists), those who analyzed and interpreted assays (pathologists), and those who acquired tissue samples (surgeons, pulmonologists, radiologists).
Countries were also grouped into five geographic regions — Asia, Europe, Latin America, United States, and Canada — and the rest of the world (ROW).
“Overall, respondents reported that molecular testing rates were lower than we would like but they were not satisfied with the current state of testing, and they reported higher testing rates in their own clinics,” Smeltzer noted.
However, when tests were ordered, “we found 99% of respondents in the requesting/treating track ordered tests for EGFR, 95% for ALK, 79% for ROS1, and < 50% ordered other tests,” the authors observe.
Indeed, EGFR, ALK, and ROS1 were the top three tests ordered across all regions, though less frequently so in the ROW, they add.
More than half of requesting/treating track respondents also order multiplex assays, although Latin America and the ROW did this less frequently than other regions.
Over 90% of respondents who perform or interpret assays indicated that they perform EGFR testing, while 83% of the same group do ALK testing; 69% tested for KRAS; 68% for BRAF, 64% for ROS1, and 56% for HER2. Fewer than half of them performed other tests.
Survey results also showed that EGFR, ALK, and KRAS are the top three tests performed across all regions, with no regional differences.
“Respondents also reported on the acquisition and testing of liquid biopsies,” survey authors point out.
Here, 87% of requesting/treating track respondents indicated that they “sometimes” request molecular testing on liquid biopsies, but the proportions of those who sometimes use liquid biopsy varied by region and were lowest in Latin America and the ROW.
A lower proportion of those who perform and interpret assays, at 69%, also offer tests on liquid biopsies, but this percentage, too, varied significantly by region, being the least frequently done in the United States and Canada, as well as in the ROW.
All the above tests are for genetic mutations or alterations that guide clinicians on use of targeted therapy directed at particular mutations, for example, drugs like erlotinib for EGFR and crizotinib for ALK.
However, immunotherapy with checkpoint inhibitors has also made a big impact on the treatment of NSCLC, and the use of these agents is sometimes guided by testing for programmed cell-death ligand (PD-L1).
PD-L1 is not a molecular marker per se, the authors note.
Nevertheless, “we found that 84% of respondents in the requesting/treating track ordered PD-L1 and 68% of respondents who perform or interpret assays report PD-L1 is offered in their own lab,” the authors observe.
Smeltzer commented that both approaches — targeted therapies and immunotherapy — have made inroads into the treatment of NSCLC, in some cases replacing chemotherapy.
He emphasized that “it is important to know if a specific oncogene driver is present before initiating immunotherapy treatment,” and noted that when tissue is sent out for both types of testing, the results for PD-L1 are usually available before the results for the full molecular testing panel are back.
Barriers to testing
“The most frequent barrier to molecular testing in every region was cost,” the survey authors note.
Insufficient amount of tumor cells was the main reason for molecular testing failures along with inadequate tissue quality.
The majority of respondents who order tests and treat patients were sure that the laboratories they use perform appropriate validation of molecular tests, while almost all of those who perform or interpret assays said they perform validation tests in their labs.
Only 30% of respondents who request tests and treat patients have access to molecular testing labs within their own institutions; the remaining respondents have to outsource testing completely or partially.
Most respondents who test and treat patients also have multidisciplinary tumor boards to discuss patients with NSCLC, but almost one quarter of the same group indicated their board met less than once a month.
“Turnaround time is a barrier to molecular testing across the world,” the authors continue, with 29% of those who request tests and treat patients reporting that it typically takes 10 days or more to receive molecular testing results.
Interestingly, the highest percentage of respondents who reported this long turnaround time were in North America.
Perhaps encouragingly, 41% of respondents who perform or interpret assays indicated they were dissatisfied with the condition of molecular testing in their country, although in this regard, the United States and Canada had the lowest rates of dissatisfaction.
In fact, 39% of those who request tests and treat patients ranked the conditions of molecular testing in their country as “average or below,” while 42% of respondents in the tissue acquisition track ranked the conditions of molecular testing as average or below, the worst rankings coming from Latin America and the ROW.
Low quality of tissue samples was another reason respondents expressed dissatisfaction with the current state of molecular testing in their country.
Smeltzer is a research consultant for the Association of Community Cancer Centers.
This article first appeared on Medscape.com.
Moreover, the majority of these clinicians believe that fewer than 50% of patients in their country undergo molecular testing, the same survey showed.
The survey was conducted by the International Association for the Study of Lung Cancer (IASLC); 2537 questionnaires from 102 countries were returned and analyzed.
It was published online May 20 in the Journal of Thoracic Oncology.
The results are concerning because “the risk of death for patients with NSCLC is substantially reduced when a gene alteration is identified and the available targeted therapy is administered,” the authors emphasize.
“Specific protocols to initiate reflex testing for guideline-recommended molecular markers would help providers consider molecular testing earlier and optimize tissue,” they suggest.
Surprised that clinicians were unaware of guidelines
“I was not surprised that we found suboptimal testing rates based on other research that has demonstrated the need to improve the quality of lung cancer in some areas,” corresponding author Matthew Smeltzer, PhD, University of Memphis, Tennessee, told Medscape Medical News in an email.
“However, I was surprised that so many respondents were unaware of guidelines,” he said.
The College of American Pathologists, IASLC, and Association for Molecular Pathology established evidence-based standards for the selection of NSCLC patients for molecular testing in 2013, and these guidelines were subsequently endorsed by the American Society of Clinical Oncology.
“We suspect that the level of access a provider has to targeted therapies does affect molecular testing rates,” Smeltzer acknowledged.
Molecular testing survey
“The survey included a seven-question introduction for all respondents and then divided respondents into one of three tracks,” the authors explain.
These tracks included respondents who requested tests and who treated patients (medical oncologists), those who analyzed and interpreted assays (pathologists), and those who acquired tissue samples (surgeons, pulmonologists, radiologists).
Countries were also grouped into five geographic regions — Asia, Europe, Latin America, United States, and Canada — and the rest of the world (ROW).
“Overall, respondents reported that molecular testing rates were lower than we would like but they were not satisfied with the current state of testing, and they reported higher testing rates in their own clinics,” Smeltzer noted.
However, when tests were ordered, “we found 99% of respondents in the requesting/treating track ordered tests for EGFR, 95% for ALK, 79% for ROS1, and < 50% ordered other tests,” the authors observe.
Indeed, EGFR, ALK, and ROS1 were the top three tests ordered across all regions, though less frequently so in the ROW, they add.
More than half of requesting/treating track respondents also order multiplex assays, although Latin America and the ROW did this less frequently than other regions.
Over 90% of respondents who perform or interpret assays indicated that they perform EGFR testing, while 83% of the same group do ALK testing; 69% tested for KRAS; 68% for BRAF, 64% for ROS1, and 56% for HER2. Fewer than half of them performed other tests.
Survey results also showed that EGFR, ALK, and KRAS are the top three tests performed across all regions, with no regional differences.
“Respondents also reported on the acquisition and testing of liquid biopsies,” survey authors point out.
Here, 87% of requesting/treating track respondents indicated that they “sometimes” request molecular testing on liquid biopsies, but the proportions of those who sometimes use liquid biopsy varied by region and were lowest in Latin America and the ROW.
A lower proportion of those who perform and interpret assays, at 69%, also offer tests on liquid biopsies, but this percentage, too, varied significantly by region, being the least frequently done in the United States and Canada, as well as in the ROW.
All the above tests are for genetic mutations or alterations that guide clinicians on use of targeted therapy directed at particular mutations, for example, drugs like erlotinib for EGFR and crizotinib for ALK.
However, immunotherapy with checkpoint inhibitors has also made a big impact on the treatment of NSCLC, and the use of these agents is sometimes guided by testing for programmed cell-death ligand (PD-L1).
PD-L1 is not a molecular marker per se, the authors note.
Nevertheless, “we found that 84% of respondents in the requesting/treating track ordered PD-L1 and 68% of respondents who perform or interpret assays report PD-L1 is offered in their own lab,” the authors observe.
Smeltzer commented that both approaches — targeted therapies and immunotherapy — have made inroads into the treatment of NSCLC, in some cases replacing chemotherapy.
He emphasized that “it is important to know if a specific oncogene driver is present before initiating immunotherapy treatment,” and noted that when tissue is sent out for both types of testing, the results for PD-L1 are usually available before the results for the full molecular testing panel are back.
Barriers to testing
“The most frequent barrier to molecular testing in every region was cost,” the survey authors note.
Insufficient amount of tumor cells was the main reason for molecular testing failures along with inadequate tissue quality.
The majority of respondents who order tests and treat patients were sure that the laboratories they use perform appropriate validation of molecular tests, while almost all of those who perform or interpret assays said they perform validation tests in their labs.
Only 30% of respondents who request tests and treat patients have access to molecular testing labs within their own institutions; the remaining respondents have to outsource testing completely or partially.
Most respondents who test and treat patients also have multidisciplinary tumor boards to discuss patients with NSCLC, but almost one quarter of the same group indicated their board met less than once a month.
“Turnaround time is a barrier to molecular testing across the world,” the authors continue, with 29% of those who request tests and treat patients reporting that it typically takes 10 days or more to receive molecular testing results.
Interestingly, the highest percentage of respondents who reported this long turnaround time were in North America.
Perhaps encouragingly, 41% of respondents who perform or interpret assays indicated they were dissatisfied with the condition of molecular testing in their country, although in this regard, the United States and Canada had the lowest rates of dissatisfaction.
In fact, 39% of those who request tests and treat patients ranked the conditions of molecular testing in their country as “average or below,” while 42% of respondents in the tissue acquisition track ranked the conditions of molecular testing as average or below, the worst rankings coming from Latin America and the ROW.
Low quality of tissue samples was another reason respondents expressed dissatisfaction with the current state of molecular testing in their country.
Smeltzer is a research consultant for the Association of Community Cancer Centers.
This article first appeared on Medscape.com.
Nilotinib is safe in moderate and advanced Parkinson’s disease
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
FROM AAN 2020
Early or delayed cardioversion in recent-onset atrial fibrillation
Background: Often atrial fibrillation terminates spontaneously and occasionally recurs; therefore, the advantage of immediate electric or pharmacologic cardioversion over watchful waiting and subsequent delayed cardioversion is not clear.
Study design: Multicenter, randomized, open-label, noninferiority trial.
Setting: 15 hospitals in the Netherlands (3 academic, 8 nonacademic teaching, and 4 nonteaching).
Synopsis: Randomizing 437 patients with early-onset (less than 36 hours) symptomatic AFib presenting to 15 hospitals, the authors showed that, at 4 weeks’ follow-up, a similar number of patients remained in sinus rhythm whether they were assigned to an immediate cardioversion strategy or to a delayed one where rate control was attempted first and cardioversion was done if patients remained in fibrillation after 48 hours. Specifically the presence of sinus rhythm occurred in 94% in the early cardioversion group and in 91% of the delayed one (95% confidence interval, –8.2 to 2.2; P = .005 for noninferiority). Both groups received anticoagulation per current standards.
This was a noninferiority, open-label study that was not powered enough to study harm between the two strategies. It showed a 30% incidence of recurrence of AFib regardless of study assignment. Hospitalists should not feel pressured to initiate early cardioversion for new-onset AFib. Rate control, anticoagulation (if applicable), prompt follow-up, and early discharge (even from the ED) seem to be a safe and practical approach.
Bottom line: In patients presenting with symptomatic recent-onset AFib, delayed cardioversion in a wait-and-see approach was noninferior to early cardioversion in achieving sinus rhythm at 4 weeks’ follow-up.
Citation: Pluymaekers NA et al. Early or delayed cardioversion in recent-onset atrial fibrillation. N Engl J Med.
Dr. Abdo is a hospitalist at Duke University Health System.
Background: Often atrial fibrillation terminates spontaneously and occasionally recurs; therefore, the advantage of immediate electric or pharmacologic cardioversion over watchful waiting and subsequent delayed cardioversion is not clear.
Study design: Multicenter, randomized, open-label, noninferiority trial.
Setting: 15 hospitals in the Netherlands (3 academic, 8 nonacademic teaching, and 4 nonteaching).
Synopsis: Randomizing 437 patients with early-onset (less than 36 hours) symptomatic AFib presenting to 15 hospitals, the authors showed that, at 4 weeks’ follow-up, a similar number of patients remained in sinus rhythm whether they were assigned to an immediate cardioversion strategy or to a delayed one where rate control was attempted first and cardioversion was done if patients remained in fibrillation after 48 hours. Specifically the presence of sinus rhythm occurred in 94% in the early cardioversion group and in 91% of the delayed one (95% confidence interval, –8.2 to 2.2; P = .005 for noninferiority). Both groups received anticoagulation per current standards.
This was a noninferiority, open-label study that was not powered enough to study harm between the two strategies. It showed a 30% incidence of recurrence of AFib regardless of study assignment. Hospitalists should not feel pressured to initiate early cardioversion for new-onset AFib. Rate control, anticoagulation (if applicable), prompt follow-up, and early discharge (even from the ED) seem to be a safe and practical approach.
Bottom line: In patients presenting with symptomatic recent-onset AFib, delayed cardioversion in a wait-and-see approach was noninferior to early cardioversion in achieving sinus rhythm at 4 weeks’ follow-up.
Citation: Pluymaekers NA et al. Early or delayed cardioversion in recent-onset atrial fibrillation. N Engl J Med.
Dr. Abdo is a hospitalist at Duke University Health System.
Background: Often atrial fibrillation terminates spontaneously and occasionally recurs; therefore, the advantage of immediate electric or pharmacologic cardioversion over watchful waiting and subsequent delayed cardioversion is not clear.
Study design: Multicenter, randomized, open-label, noninferiority trial.
Setting: 15 hospitals in the Netherlands (3 academic, 8 nonacademic teaching, and 4 nonteaching).
Synopsis: Randomizing 437 patients with early-onset (less than 36 hours) symptomatic AFib presenting to 15 hospitals, the authors showed that, at 4 weeks’ follow-up, a similar number of patients remained in sinus rhythm whether they were assigned to an immediate cardioversion strategy or to a delayed one where rate control was attempted first and cardioversion was done if patients remained in fibrillation after 48 hours. Specifically the presence of sinus rhythm occurred in 94% in the early cardioversion group and in 91% of the delayed one (95% confidence interval, –8.2 to 2.2; P = .005 for noninferiority). Both groups received anticoagulation per current standards.
This was a noninferiority, open-label study that was not powered enough to study harm between the two strategies. It showed a 30% incidence of recurrence of AFib regardless of study assignment. Hospitalists should not feel pressured to initiate early cardioversion for new-onset AFib. Rate control, anticoagulation (if applicable), prompt follow-up, and early discharge (even from the ED) seem to be a safe and practical approach.
Bottom line: In patients presenting with symptomatic recent-onset AFib, delayed cardioversion in a wait-and-see approach was noninferior to early cardioversion in achieving sinus rhythm at 4 weeks’ follow-up.
Citation: Pluymaekers NA et al. Early or delayed cardioversion in recent-onset atrial fibrillation. N Engl J Med.
Dr. Abdo is a hospitalist at Duke University Health System.
Improving care for women who have experienced stillbirth
Think of the current standard of care and do the opposite
One of hardest parts of being an obstetrician is taking care of patients who experience a stillbirth. I am very comfortable with the care of a grieving patient and I always have been, although I am not sure why. I have a model of care that I have evolved in my 16 years since medical school graduation. This model is not based on formal instruction because I received none, but on my natural instincts of what a grieving mom and her family need to hear and receive in the worst moments of their lives. All obstetrics providers grieve the loss of the baby, but often not with the patient but on our own. We may do this because we want to respect the patient’s privacy or because we are not sure of the words to say. I hope I can provide some guidance for those who struggle with what to do.
I delivered my first stillborn baby as a third-year medical student. My mentor, a chief resident, saw something in me and encouraged me to care for this mother. She had twins and one baby was still living, but the prognosis was poor since this was the surviving twin from a monochorionic diamniotic pregnancy. On the day of the mom’s induction, I just pulled up a chair and talked with her. We talked about her life, the loss of the first baby several weeks before, and her hope that her surviving son would be okay. She felt so bonded to me that she refused to push until I was there. Her delivery is still firm in my mind. I still remember 17 years later the room she delivered in.
My first loss (stillbirth) as a resident was my intern year – a beautiful baby named Jude, who was stillborn at 39 weeks. After delivering Jude, I asked the family about the funeral arrangements. Three days later, I attended his funeral. I looked all around for the mother’s attending doctors but none of them were there. I remember thinking then that it was a given that they would be there, but now I know that it is rare. I also learned a lot about the grief a stillborn baby brings while listening to Jude’s father’s eulogy. He talked about how Jude would never bake cookies with Aunt Jane, ride the slide with cousin Chris, or put on a yellow backpack and ride the bus on the first day of school. Because of this eulogy, I understood this unique kind of grief that these losses bring early in my training.
I delivered many losses in my residency. The attendings left soon after the birth and I stayed behind with the family. I sat and counseled the families, and I helped them make memories. I realized that to care for these patients, I would need to trust my instincts because there was no formal and little informal training on how to care for families who lost their babies.
Once I completed residency, I was really able to do my “thing.” At loss deliveries, I was able to model for residents my method of care. I showed them that families want and need attention, support, and guidance. I modeled for them how to deliver and greet the baby. That it is not necessary to leave the room right after the birth, and it is okay to grieve and help families meet their babies. I modeled commenting on the baby’s features, on who they looked like. I showed how laughing about how the baby has grandma’s nose is okay. I showed them that it is okay to ask to hold and get a picture taken with the baby. I showed them that these are the only moments these families will get with their babies, and it is our job to help them do this. The family will have many moments alone in the days and weeks to come. They need our support and guidance. It is a part of being an ob.gyn. to care for families after stillbirths, and we do not want our patients to feel abandoned during this time by those they entrust to care for them.
I also was able to create a model for aftercare. I call my families often after they go home. Sometimes I catch them in the anger stage of the grief process and I let them vent. I work through this with them, and I answer their hardest and sometimes accusatory questions regarding care leading up to the diagnosis. I am not saying this is easy for me or for them. I think fear of these tough conversations is a barrier to giving the emotional support that these families need. I work through this with them in an honest and open manner. I also call to check on the patients as much as possible, especially on anniversaries. I am not saying that all providers must follow this model. This is my passion and is natural for me, but data clearly show that the standard of emotional care we provide is not what patients need at this time. Thankfully, there is an amazing resource of grief counselors, social workers, online resources, and support groups for these families to help them get through the tragedy. These resources, however, are not the provider who spent this precious time with them and their beloved baby, and our emotional support is invaluable.
This past year has been very eventful for me. One of my patients delivered a new baby, after a prior loss, and asked if we could teach together. I had mentioned that everything I do with stillbirths is not based on my residency education, but on my experience and instinctual feeling of what families need. She knew from friends in bereavement circles that they felt that their care was different. We started teaching last summer and have done 10 training sessions to date; hopefully we will continue to teach new groups of nurses, residents, medical students, doulas, and physician assistant students each year.
This year also was eventful because I discovered the Star Legacy Foundation, a national not-for-profit organization with the goal of spreading awareness, education, and prevention regarding stillbirth. I attended their 2019 Summit in Minnesota. I thought I would meet many more doctors and midwives like myself, and I would learn even more about care for bereaved patients. However, that summer I learned preventing stillbirth may be possible from the then chief medical officer of Scotland, Catherine Calderwood, MB ChB. She talked about the preventive protocol she had created that had reduced the stillbirth rate by 23%. Because I was one of only five ob.gyn. nonspeaker attendees in a room of 400, I realized I had a real opportunity to try to bring some model for prevention to the United States. I brought the U.K. protocol to my practice and we have been doing it now for 9 months. (See “Decreased fetal movement: Time to educate patients and ourselves” at mdedge.com/pediatrics.)
I have had a year to think about why the U.S. stillbirth rate is higher than that of many high-income nations and why we have the lowest annual rate of reduction in the 2016 Lancet series among high resource nations.1 I think it is due to lack of education and training for providers in stillbirth prevention and care, which has led to further marginalization and stigmatization of bereaved moms. This has pushed them further into the shadows and makes it taboo to share their stories. It is providers being fearful to even mention to patients that stillbirth still happens. It is the lack of any protocol on how to educate patients and providers about fetal movement, and what to do if pregnant women complain about a decrease or change in fetal movement. I think a lot of this stems from an innate discomfort that obstetric providers have in the care of these patients. That if women felt cared for and empowered to tell their stories, there would be more efforts at stillbirth education and prevention.
I often think of an experience that the founder of Star Legacy, Lindsey Wimmer, experienced when she lost her son, Garrett, 16 years ago. She told a story in the documentary, “Don’t talk about the baby.” She tells that on the first night of the induction, the nurse came in and told her that the attending wanted to turn off the oxytocin so “she could get her rest.” I heard this and immediately knew the attending’s true reason for turning off the oxytocin. Lindsey then said she knew it was because the attending did not want to wake up to deliver a dead baby. I wrote Lindsey that day and told her I completely agreed and apologized on behalf of my profession for that care. She wrote me back that she had waited 16 years to have a provider validate her feelings about this. I told her I think her doctor was fearful and uncomfortable with this birth and was avoiding it, but I believe with better education and training this can change. I want to deliver babies like Garrett during my shift, because it is giving this vital care that reminds me why I became a doctor in the first place.
I know there are many providers out there who follow a similar model, but I want more providers to do so, and so does the bereavement community. In one study of 20 parents, all but 2 were frustrated about how the ob.gyn. and staff handled their deliveries.2 I truly believe that every person who delivers babies does it because they love it. Part of doing this job we love is realizing there will be times of great sadness. I also believe if this model of care is attempted by wary providers, they will quickly realize that this is what patients and their families need. With this care, stillbirth may become less of a taboo subject, and our stillbirth rate may fall.
Dr. Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, N.Y. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures. Email her a obnews@mdedge.com.
References
1. “Stillbirths 2016: ending preventable stillbirths.” Series from The Lancet journals. Published: Jan. 20, 2016.
2. BMC Pregnancy Childbirth. 2012 Nov 27. doi: 10.1186/1471-2393-12-137.
Think of the current standard of care and do the opposite
Think of the current standard of care and do the opposite
One of hardest parts of being an obstetrician is taking care of patients who experience a stillbirth. I am very comfortable with the care of a grieving patient and I always have been, although I am not sure why. I have a model of care that I have evolved in my 16 years since medical school graduation. This model is not based on formal instruction because I received none, but on my natural instincts of what a grieving mom and her family need to hear and receive in the worst moments of their lives. All obstetrics providers grieve the loss of the baby, but often not with the patient but on our own. We may do this because we want to respect the patient’s privacy or because we are not sure of the words to say. I hope I can provide some guidance for those who struggle with what to do.
I delivered my first stillborn baby as a third-year medical student. My mentor, a chief resident, saw something in me and encouraged me to care for this mother. She had twins and one baby was still living, but the prognosis was poor since this was the surviving twin from a monochorionic diamniotic pregnancy. On the day of the mom’s induction, I just pulled up a chair and talked with her. We talked about her life, the loss of the first baby several weeks before, and her hope that her surviving son would be okay. She felt so bonded to me that she refused to push until I was there. Her delivery is still firm in my mind. I still remember 17 years later the room she delivered in.
My first loss (stillbirth) as a resident was my intern year – a beautiful baby named Jude, who was stillborn at 39 weeks. After delivering Jude, I asked the family about the funeral arrangements. Three days later, I attended his funeral. I looked all around for the mother’s attending doctors but none of them were there. I remember thinking then that it was a given that they would be there, but now I know that it is rare. I also learned a lot about the grief a stillborn baby brings while listening to Jude’s father’s eulogy. He talked about how Jude would never bake cookies with Aunt Jane, ride the slide with cousin Chris, or put on a yellow backpack and ride the bus on the first day of school. Because of this eulogy, I understood this unique kind of grief that these losses bring early in my training.
I delivered many losses in my residency. The attendings left soon after the birth and I stayed behind with the family. I sat and counseled the families, and I helped them make memories. I realized that to care for these patients, I would need to trust my instincts because there was no formal and little informal training on how to care for families who lost their babies.
Once I completed residency, I was really able to do my “thing.” At loss deliveries, I was able to model for residents my method of care. I showed them that families want and need attention, support, and guidance. I modeled for them how to deliver and greet the baby. That it is not necessary to leave the room right after the birth, and it is okay to grieve and help families meet their babies. I modeled commenting on the baby’s features, on who they looked like. I showed how laughing about how the baby has grandma’s nose is okay. I showed them that it is okay to ask to hold and get a picture taken with the baby. I showed them that these are the only moments these families will get with their babies, and it is our job to help them do this. The family will have many moments alone in the days and weeks to come. They need our support and guidance. It is a part of being an ob.gyn. to care for families after stillbirths, and we do not want our patients to feel abandoned during this time by those they entrust to care for them.
I also was able to create a model for aftercare. I call my families often after they go home. Sometimes I catch them in the anger stage of the grief process and I let them vent. I work through this with them, and I answer their hardest and sometimes accusatory questions regarding care leading up to the diagnosis. I am not saying this is easy for me or for them. I think fear of these tough conversations is a barrier to giving the emotional support that these families need. I work through this with them in an honest and open manner. I also call to check on the patients as much as possible, especially on anniversaries. I am not saying that all providers must follow this model. This is my passion and is natural for me, but data clearly show that the standard of emotional care we provide is not what patients need at this time. Thankfully, there is an amazing resource of grief counselors, social workers, online resources, and support groups for these families to help them get through the tragedy. These resources, however, are not the provider who spent this precious time with them and their beloved baby, and our emotional support is invaluable.
This past year has been very eventful for me. One of my patients delivered a new baby, after a prior loss, and asked if we could teach together. I had mentioned that everything I do with stillbirths is not based on my residency education, but on my experience and instinctual feeling of what families need. She knew from friends in bereavement circles that they felt that their care was different. We started teaching last summer and have done 10 training sessions to date; hopefully we will continue to teach new groups of nurses, residents, medical students, doulas, and physician assistant students each year.
This year also was eventful because I discovered the Star Legacy Foundation, a national not-for-profit organization with the goal of spreading awareness, education, and prevention regarding stillbirth. I attended their 2019 Summit in Minnesota. I thought I would meet many more doctors and midwives like myself, and I would learn even more about care for bereaved patients. However, that summer I learned preventing stillbirth may be possible from the then chief medical officer of Scotland, Catherine Calderwood, MB ChB. She talked about the preventive protocol she had created that had reduced the stillbirth rate by 23%. Because I was one of only five ob.gyn. nonspeaker attendees in a room of 400, I realized I had a real opportunity to try to bring some model for prevention to the United States. I brought the U.K. protocol to my practice and we have been doing it now for 9 months. (See “Decreased fetal movement: Time to educate patients and ourselves” at mdedge.com/pediatrics.)
I have had a year to think about why the U.S. stillbirth rate is higher than that of many high-income nations and why we have the lowest annual rate of reduction in the 2016 Lancet series among high resource nations.1 I think it is due to lack of education and training for providers in stillbirth prevention and care, which has led to further marginalization and stigmatization of bereaved moms. This has pushed them further into the shadows and makes it taboo to share their stories. It is providers being fearful to even mention to patients that stillbirth still happens. It is the lack of any protocol on how to educate patients and providers about fetal movement, and what to do if pregnant women complain about a decrease or change in fetal movement. I think a lot of this stems from an innate discomfort that obstetric providers have in the care of these patients. That if women felt cared for and empowered to tell their stories, there would be more efforts at stillbirth education and prevention.
I often think of an experience that the founder of Star Legacy, Lindsey Wimmer, experienced when she lost her son, Garrett, 16 years ago. She told a story in the documentary, “Don’t talk about the baby.” She tells that on the first night of the induction, the nurse came in and told her that the attending wanted to turn off the oxytocin so “she could get her rest.” I heard this and immediately knew the attending’s true reason for turning off the oxytocin. Lindsey then said she knew it was because the attending did not want to wake up to deliver a dead baby. I wrote Lindsey that day and told her I completely agreed and apologized on behalf of my profession for that care. She wrote me back that she had waited 16 years to have a provider validate her feelings about this. I told her I think her doctor was fearful and uncomfortable with this birth and was avoiding it, but I believe with better education and training this can change. I want to deliver babies like Garrett during my shift, because it is giving this vital care that reminds me why I became a doctor in the first place.
I know there are many providers out there who follow a similar model, but I want more providers to do so, and so does the bereavement community. In one study of 20 parents, all but 2 were frustrated about how the ob.gyn. and staff handled their deliveries.2 I truly believe that every person who delivers babies does it because they love it. Part of doing this job we love is realizing there will be times of great sadness. I also believe if this model of care is attempted by wary providers, they will quickly realize that this is what patients and their families need. With this care, stillbirth may become less of a taboo subject, and our stillbirth rate may fall.
Dr. Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, N.Y. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures. Email her a obnews@mdedge.com.
References
1. “Stillbirths 2016: ending preventable stillbirths.” Series from The Lancet journals. Published: Jan. 20, 2016.
2. BMC Pregnancy Childbirth. 2012 Nov 27. doi: 10.1186/1471-2393-12-137.
One of hardest parts of being an obstetrician is taking care of patients who experience a stillbirth. I am very comfortable with the care of a grieving patient and I always have been, although I am not sure why. I have a model of care that I have evolved in my 16 years since medical school graduation. This model is not based on formal instruction because I received none, but on my natural instincts of what a grieving mom and her family need to hear and receive in the worst moments of their lives. All obstetrics providers grieve the loss of the baby, but often not with the patient but on our own. We may do this because we want to respect the patient’s privacy or because we are not sure of the words to say. I hope I can provide some guidance for those who struggle with what to do.
I delivered my first stillborn baby as a third-year medical student. My mentor, a chief resident, saw something in me and encouraged me to care for this mother. She had twins and one baby was still living, but the prognosis was poor since this was the surviving twin from a monochorionic diamniotic pregnancy. On the day of the mom’s induction, I just pulled up a chair and talked with her. We talked about her life, the loss of the first baby several weeks before, and her hope that her surviving son would be okay. She felt so bonded to me that she refused to push until I was there. Her delivery is still firm in my mind. I still remember 17 years later the room she delivered in.
My first loss (stillbirth) as a resident was my intern year – a beautiful baby named Jude, who was stillborn at 39 weeks. After delivering Jude, I asked the family about the funeral arrangements. Three days later, I attended his funeral. I looked all around for the mother’s attending doctors but none of them were there. I remember thinking then that it was a given that they would be there, but now I know that it is rare. I also learned a lot about the grief a stillborn baby brings while listening to Jude’s father’s eulogy. He talked about how Jude would never bake cookies with Aunt Jane, ride the slide with cousin Chris, or put on a yellow backpack and ride the bus on the first day of school. Because of this eulogy, I understood this unique kind of grief that these losses bring early in my training.
I delivered many losses in my residency. The attendings left soon after the birth and I stayed behind with the family. I sat and counseled the families, and I helped them make memories. I realized that to care for these patients, I would need to trust my instincts because there was no formal and little informal training on how to care for families who lost their babies.
Once I completed residency, I was really able to do my “thing.” At loss deliveries, I was able to model for residents my method of care. I showed them that families want and need attention, support, and guidance. I modeled for them how to deliver and greet the baby. That it is not necessary to leave the room right after the birth, and it is okay to grieve and help families meet their babies. I modeled commenting on the baby’s features, on who they looked like. I showed how laughing about how the baby has grandma’s nose is okay. I showed them that it is okay to ask to hold and get a picture taken with the baby. I showed them that these are the only moments these families will get with their babies, and it is our job to help them do this. The family will have many moments alone in the days and weeks to come. They need our support and guidance. It is a part of being an ob.gyn. to care for families after stillbirths, and we do not want our patients to feel abandoned during this time by those they entrust to care for them.
I also was able to create a model for aftercare. I call my families often after they go home. Sometimes I catch them in the anger stage of the grief process and I let them vent. I work through this with them, and I answer their hardest and sometimes accusatory questions regarding care leading up to the diagnosis. I am not saying this is easy for me or for them. I think fear of these tough conversations is a barrier to giving the emotional support that these families need. I work through this with them in an honest and open manner. I also call to check on the patients as much as possible, especially on anniversaries. I am not saying that all providers must follow this model. This is my passion and is natural for me, but data clearly show that the standard of emotional care we provide is not what patients need at this time. Thankfully, there is an amazing resource of grief counselors, social workers, online resources, and support groups for these families to help them get through the tragedy. These resources, however, are not the provider who spent this precious time with them and their beloved baby, and our emotional support is invaluable.
This past year has been very eventful for me. One of my patients delivered a new baby, after a prior loss, and asked if we could teach together. I had mentioned that everything I do with stillbirths is not based on my residency education, but on my experience and instinctual feeling of what families need. She knew from friends in bereavement circles that they felt that their care was different. We started teaching last summer and have done 10 training sessions to date; hopefully we will continue to teach new groups of nurses, residents, medical students, doulas, and physician assistant students each year.
This year also was eventful because I discovered the Star Legacy Foundation, a national not-for-profit organization with the goal of spreading awareness, education, and prevention regarding stillbirth. I attended their 2019 Summit in Minnesota. I thought I would meet many more doctors and midwives like myself, and I would learn even more about care for bereaved patients. However, that summer I learned preventing stillbirth may be possible from the then chief medical officer of Scotland, Catherine Calderwood, MB ChB. She talked about the preventive protocol she had created that had reduced the stillbirth rate by 23%. Because I was one of only five ob.gyn. nonspeaker attendees in a room of 400, I realized I had a real opportunity to try to bring some model for prevention to the United States. I brought the U.K. protocol to my practice and we have been doing it now for 9 months. (See “Decreased fetal movement: Time to educate patients and ourselves” at mdedge.com/pediatrics.)
I have had a year to think about why the U.S. stillbirth rate is higher than that of many high-income nations and why we have the lowest annual rate of reduction in the 2016 Lancet series among high resource nations.1 I think it is due to lack of education and training for providers in stillbirth prevention and care, which has led to further marginalization and stigmatization of bereaved moms. This has pushed them further into the shadows and makes it taboo to share their stories. It is providers being fearful to even mention to patients that stillbirth still happens. It is the lack of any protocol on how to educate patients and providers about fetal movement, and what to do if pregnant women complain about a decrease or change in fetal movement. I think a lot of this stems from an innate discomfort that obstetric providers have in the care of these patients. That if women felt cared for and empowered to tell their stories, there would be more efforts at stillbirth education and prevention.
I often think of an experience that the founder of Star Legacy, Lindsey Wimmer, experienced when she lost her son, Garrett, 16 years ago. She told a story in the documentary, “Don’t talk about the baby.” She tells that on the first night of the induction, the nurse came in and told her that the attending wanted to turn off the oxytocin so “she could get her rest.” I heard this and immediately knew the attending’s true reason for turning off the oxytocin. Lindsey then said she knew it was because the attending did not want to wake up to deliver a dead baby. I wrote Lindsey that day and told her I completely agreed and apologized on behalf of my profession for that care. She wrote me back that she had waited 16 years to have a provider validate her feelings about this. I told her I think her doctor was fearful and uncomfortable with this birth and was avoiding it, but I believe with better education and training this can change. I want to deliver babies like Garrett during my shift, because it is giving this vital care that reminds me why I became a doctor in the first place.
I know there are many providers out there who follow a similar model, but I want more providers to do so, and so does the bereavement community. In one study of 20 parents, all but 2 were frustrated about how the ob.gyn. and staff handled their deliveries.2 I truly believe that every person who delivers babies does it because they love it. Part of doing this job we love is realizing there will be times of great sadness. I also believe if this model of care is attempted by wary providers, they will quickly realize that this is what patients and their families need. With this care, stillbirth may become less of a taboo subject, and our stillbirth rate may fall.
Dr. Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, N.Y. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures. Email her a obnews@mdedge.com.
References
1. “Stillbirths 2016: ending preventable stillbirths.” Series from The Lancet journals. Published: Jan. 20, 2016.
2. BMC Pregnancy Childbirth. 2012 Nov 27. doi: 10.1186/1471-2393-12-137.
Ofatumumab shows high elimination of disease activity in MS
, a new study shows.
The drug, which is already approved for the treatment of chronic lymphocytic leukemia, is currently under review for relapsing MS as a once-per-month self-injected therapy that could offer a convenient alternative to DMTs that require in-office infusion.
The new findings are from a pooled analysis from the phase 3 ASCLEPIOS I/II trials of the use of ofatumumab for patients with relapsing MS. There were 927 patients in the ASCLEPIOS I trial and 955 in the ASCLEPIOS II trial. The trials were conducted in 37 countries and involved patients aged 18-55 years.
The late-breaking research was presented at the virtual meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
The studies compared patients who were treated with subcutaneous ofatumumab 20 mg with patients treated with oral teriflunomide 14 mg once daily for up to 30 months. The average duration of follow-up was 18 months.
NEDA-3, commonly used to determine treatment outcomes for patients with relapsing MS, was defined as a composite of having no worsening of disability over a 6-month period (6mCDW), no confirmed MS relapse, no new/enlarging T2 lesions, and no gadolinium-enhancing T1 lesions.
The pooled results showed that the odds of achieving NEDA-3 during the first 12 months were three times greater with ofatumumab than with teriflunomide (47.0% vs. 24.5%; odds ratio [OR], 3.36; P < .001) and were more than eight times greater from months 12 to 24 (87.8% vs. 48.2%; OR, 8.09; P < .001).
In addition, compared with patients who received teriflunomide, a higher proportion of patients who received ofatumumab were free from 6mCDW over 2 years (91.9% vs. 88.9%), as well as from relapses (82.3% vs 69.2%) and lesion activity (54.1% vs. 27.5%).
There was a significantly greater reduction in annualized relapse rate with ofatumumab compared with teriflunomide at all cumulative time intervals, including months 0 to 3 (P = .011), and at all subsequent time intervals from month 0 to 27 (P < .001).
The pooled findings further showed that ofatumumab reduced the mean number of gadolinium-enhancing T1 lesions per scan by 95.9% compared with teriflunomide (P < .001).
“Ofatumumab increased the probability of achieving NEDA-3 and demonstrated superior efficacy vs teriflunomide in patients with relapsing MS,” said the authors, led by Stephen L. Hauser, MD, of the department of neurology, UCSF Weill Institute for Neurosciences, University of California, San Francisco.
Ofatumumab superior in primary, secondary outcomes
As previously reported, subcutaneous ofatumumab also demonstrated superior efficacy over oral teriflunomide in the primary and secondary endpoints in the ASCLEPIOS I/II trials. The annualized relapse rate was reduced by 0.22 in the teriflunomide group, vs 0.11 in the ofatumumab group (50.5% relative reduction; P < .001) in the ASCLEPIOS I trial, and by 0.25 vs. 0.10 (58.5% relative reduction P < .001) in ASCLEPIOS II.
Ofatumumab also reduced the number of gadolinium-enhancing T1 lesions and new or enlarging T2 lesions compared with teriflunomide (all P < .001). It reduced the risk for disability progression by 34.4% over 3 months and by 32.5% over 6 months.
In the studies, the rate of serious infection with ofatumumab was 2.5%, compared with 1.8% with teriflunomide. Rates of malignancies were 0.5% and 0.3%, respectively.
“Ofatumumab demonstrated superior efficacy versus teriflunomide, with an acceptable safety profile, in patients with relapsing MS,” the authors reported.
Adherence rates with self-injection encouraging
An additional analysis from the two trials presented virtually in a separate abstract at the CMSC showed greater adherence to the self-administered regimen.
The analysis shows that in the ASCLEPIOS I study, 86.0% patients who were randomly assigned to receive ofatumumab and 77.7% who received teriflunomide completed the study on the assigned study drug. The proportion of patients who received ofatumumab and who discontinued treatment was 14.0%, versus 21.2% for those in the teriflunomide group. The most common reasons for discontinuation were patient/guardian decision (ofatumumab, 4.9%; teriflunomide, 8.2%), adverse event (ofatumumab, 5.2%; teriflunomide, 5.0%), and physician decision (ofatumumab, 2.2%; teriflunomide, 6.5%).
In the ASCLEPIOS II study, the rates were similar in all measures.
“In ASCLEPIOS trials, compliance with home-administered subcutaneous ofatumumab was high, and fewer patients discontinued ofatumumab as compared to teriflunomide,” the authors concluded.
Comparator drug a weak choice?
In commenting on the research, Stephen Kamin, MD, professor, vice chair, and chief of service, department of neurology, New Jersey Medical School, in Newark, noted that a limitation of the ASCLEPIOS trials is the comparison with teriflunomide.
“The comparator drug, teriflunomide, is one of the least effective DMTs, and one that some clinicians, including myself, don’t use,” he said.
Previously, when asked in an interview about the choice of teriflunomide as the comparator, Dr. Hauser noted that considerable discussion had gone into the decision. “The rationale was that we wanted to have a comparator that would be present not only against focal disease activity but also potentially against progression, and we were also able to blind the study successfully,” he said at the time.
Dr. Kamin said that ofatumumab will nevertheless likely represent a welcome addition to the tool kit of treatment options for MS. “Any new drug is helpful in adding to our choices as a general rule,” he said. “Subcutaneous injection does have increased convenience.”
It is not likely that the drug will be a game changer, he added, although the treatment’s efficacy compared with other drugs remains to be seen. “It all depends upon the relative efficacy of ofatumumab versus ocrelizumab or siponimod,” Dr. Kamin said.
“There has been another subcutaneous monoclonal for MS, daclizumab, although this was withdrawn from the market due to severe adverse effects not related to route of administration,” he added.
Dr. Hauser has relationships with Alector, Annexon, Bionure, Molecular Stethoscope, Symbiotix, and F. Hoffmann-La Roche. Dr. Kamin has received research support from Biogen, Novartis and CMSC.
A version of this article originally appeared on Medscape.com.
, a new study shows.
The drug, which is already approved for the treatment of chronic lymphocytic leukemia, is currently under review for relapsing MS as a once-per-month self-injected therapy that could offer a convenient alternative to DMTs that require in-office infusion.
The new findings are from a pooled analysis from the phase 3 ASCLEPIOS I/II trials of the use of ofatumumab for patients with relapsing MS. There were 927 patients in the ASCLEPIOS I trial and 955 in the ASCLEPIOS II trial. The trials were conducted in 37 countries and involved patients aged 18-55 years.
The late-breaking research was presented at the virtual meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
The studies compared patients who were treated with subcutaneous ofatumumab 20 mg with patients treated with oral teriflunomide 14 mg once daily for up to 30 months. The average duration of follow-up was 18 months.
NEDA-3, commonly used to determine treatment outcomes for patients with relapsing MS, was defined as a composite of having no worsening of disability over a 6-month period (6mCDW), no confirmed MS relapse, no new/enlarging T2 lesions, and no gadolinium-enhancing T1 lesions.
The pooled results showed that the odds of achieving NEDA-3 during the first 12 months were three times greater with ofatumumab than with teriflunomide (47.0% vs. 24.5%; odds ratio [OR], 3.36; P < .001) and were more than eight times greater from months 12 to 24 (87.8% vs. 48.2%; OR, 8.09; P < .001).
In addition, compared with patients who received teriflunomide, a higher proportion of patients who received ofatumumab were free from 6mCDW over 2 years (91.9% vs. 88.9%), as well as from relapses (82.3% vs 69.2%) and lesion activity (54.1% vs. 27.5%).
There was a significantly greater reduction in annualized relapse rate with ofatumumab compared with teriflunomide at all cumulative time intervals, including months 0 to 3 (P = .011), and at all subsequent time intervals from month 0 to 27 (P < .001).
The pooled findings further showed that ofatumumab reduced the mean number of gadolinium-enhancing T1 lesions per scan by 95.9% compared with teriflunomide (P < .001).
“Ofatumumab increased the probability of achieving NEDA-3 and demonstrated superior efficacy vs teriflunomide in patients with relapsing MS,” said the authors, led by Stephen L. Hauser, MD, of the department of neurology, UCSF Weill Institute for Neurosciences, University of California, San Francisco.
Ofatumumab superior in primary, secondary outcomes
As previously reported, subcutaneous ofatumumab also demonstrated superior efficacy over oral teriflunomide in the primary and secondary endpoints in the ASCLEPIOS I/II trials. The annualized relapse rate was reduced by 0.22 in the teriflunomide group, vs 0.11 in the ofatumumab group (50.5% relative reduction; P < .001) in the ASCLEPIOS I trial, and by 0.25 vs. 0.10 (58.5% relative reduction P < .001) in ASCLEPIOS II.
Ofatumumab also reduced the number of gadolinium-enhancing T1 lesions and new or enlarging T2 lesions compared with teriflunomide (all P < .001). It reduced the risk for disability progression by 34.4% over 3 months and by 32.5% over 6 months.
In the studies, the rate of serious infection with ofatumumab was 2.5%, compared with 1.8% with teriflunomide. Rates of malignancies were 0.5% and 0.3%, respectively.
“Ofatumumab demonstrated superior efficacy versus teriflunomide, with an acceptable safety profile, in patients with relapsing MS,” the authors reported.
Adherence rates with self-injection encouraging
An additional analysis from the two trials presented virtually in a separate abstract at the CMSC showed greater adherence to the self-administered regimen.
The analysis shows that in the ASCLEPIOS I study, 86.0% patients who were randomly assigned to receive ofatumumab and 77.7% who received teriflunomide completed the study on the assigned study drug. The proportion of patients who received ofatumumab and who discontinued treatment was 14.0%, versus 21.2% for those in the teriflunomide group. The most common reasons for discontinuation were patient/guardian decision (ofatumumab, 4.9%; teriflunomide, 8.2%), adverse event (ofatumumab, 5.2%; teriflunomide, 5.0%), and physician decision (ofatumumab, 2.2%; teriflunomide, 6.5%).
In the ASCLEPIOS II study, the rates were similar in all measures.
“In ASCLEPIOS trials, compliance with home-administered subcutaneous ofatumumab was high, and fewer patients discontinued ofatumumab as compared to teriflunomide,” the authors concluded.
Comparator drug a weak choice?
In commenting on the research, Stephen Kamin, MD, professor, vice chair, and chief of service, department of neurology, New Jersey Medical School, in Newark, noted that a limitation of the ASCLEPIOS trials is the comparison with teriflunomide.
“The comparator drug, teriflunomide, is one of the least effective DMTs, and one that some clinicians, including myself, don’t use,” he said.
Previously, when asked in an interview about the choice of teriflunomide as the comparator, Dr. Hauser noted that considerable discussion had gone into the decision. “The rationale was that we wanted to have a comparator that would be present not only against focal disease activity but also potentially against progression, and we were also able to blind the study successfully,” he said at the time.
Dr. Kamin said that ofatumumab will nevertheless likely represent a welcome addition to the tool kit of treatment options for MS. “Any new drug is helpful in adding to our choices as a general rule,” he said. “Subcutaneous injection does have increased convenience.”
It is not likely that the drug will be a game changer, he added, although the treatment’s efficacy compared with other drugs remains to be seen. “It all depends upon the relative efficacy of ofatumumab versus ocrelizumab or siponimod,” Dr. Kamin said.
“There has been another subcutaneous monoclonal for MS, daclizumab, although this was withdrawn from the market due to severe adverse effects not related to route of administration,” he added.
Dr. Hauser has relationships with Alector, Annexon, Bionure, Molecular Stethoscope, Symbiotix, and F. Hoffmann-La Roche. Dr. Kamin has received research support from Biogen, Novartis and CMSC.
A version of this article originally appeared on Medscape.com.
, a new study shows.
The drug, which is already approved for the treatment of chronic lymphocytic leukemia, is currently under review for relapsing MS as a once-per-month self-injected therapy that could offer a convenient alternative to DMTs that require in-office infusion.
The new findings are from a pooled analysis from the phase 3 ASCLEPIOS I/II trials of the use of ofatumumab for patients with relapsing MS. There were 927 patients in the ASCLEPIOS I trial and 955 in the ASCLEPIOS II trial. The trials were conducted in 37 countries and involved patients aged 18-55 years.
The late-breaking research was presented at the virtual meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
The studies compared patients who were treated with subcutaneous ofatumumab 20 mg with patients treated with oral teriflunomide 14 mg once daily for up to 30 months. The average duration of follow-up was 18 months.
NEDA-3, commonly used to determine treatment outcomes for patients with relapsing MS, was defined as a composite of having no worsening of disability over a 6-month period (6mCDW), no confirmed MS relapse, no new/enlarging T2 lesions, and no gadolinium-enhancing T1 lesions.
The pooled results showed that the odds of achieving NEDA-3 during the first 12 months were three times greater with ofatumumab than with teriflunomide (47.0% vs. 24.5%; odds ratio [OR], 3.36; P < .001) and were more than eight times greater from months 12 to 24 (87.8% vs. 48.2%; OR, 8.09; P < .001).
In addition, compared with patients who received teriflunomide, a higher proportion of patients who received ofatumumab were free from 6mCDW over 2 years (91.9% vs. 88.9%), as well as from relapses (82.3% vs 69.2%) and lesion activity (54.1% vs. 27.5%).
There was a significantly greater reduction in annualized relapse rate with ofatumumab compared with teriflunomide at all cumulative time intervals, including months 0 to 3 (P = .011), and at all subsequent time intervals from month 0 to 27 (P < .001).
The pooled findings further showed that ofatumumab reduced the mean number of gadolinium-enhancing T1 lesions per scan by 95.9% compared with teriflunomide (P < .001).
“Ofatumumab increased the probability of achieving NEDA-3 and demonstrated superior efficacy vs teriflunomide in patients with relapsing MS,” said the authors, led by Stephen L. Hauser, MD, of the department of neurology, UCSF Weill Institute for Neurosciences, University of California, San Francisco.
Ofatumumab superior in primary, secondary outcomes
As previously reported, subcutaneous ofatumumab also demonstrated superior efficacy over oral teriflunomide in the primary and secondary endpoints in the ASCLEPIOS I/II trials. The annualized relapse rate was reduced by 0.22 in the teriflunomide group, vs 0.11 in the ofatumumab group (50.5% relative reduction; P < .001) in the ASCLEPIOS I trial, and by 0.25 vs. 0.10 (58.5% relative reduction P < .001) in ASCLEPIOS II.
Ofatumumab also reduced the number of gadolinium-enhancing T1 lesions and new or enlarging T2 lesions compared with teriflunomide (all P < .001). It reduced the risk for disability progression by 34.4% over 3 months and by 32.5% over 6 months.
In the studies, the rate of serious infection with ofatumumab was 2.5%, compared with 1.8% with teriflunomide. Rates of malignancies were 0.5% and 0.3%, respectively.
“Ofatumumab demonstrated superior efficacy versus teriflunomide, with an acceptable safety profile, in patients with relapsing MS,” the authors reported.
Adherence rates with self-injection encouraging
An additional analysis from the two trials presented virtually in a separate abstract at the CMSC showed greater adherence to the self-administered regimen.
The analysis shows that in the ASCLEPIOS I study, 86.0% patients who were randomly assigned to receive ofatumumab and 77.7% who received teriflunomide completed the study on the assigned study drug. The proportion of patients who received ofatumumab and who discontinued treatment was 14.0%, versus 21.2% for those in the teriflunomide group. The most common reasons for discontinuation were patient/guardian decision (ofatumumab, 4.9%; teriflunomide, 8.2%), adverse event (ofatumumab, 5.2%; teriflunomide, 5.0%), and physician decision (ofatumumab, 2.2%; teriflunomide, 6.5%).
In the ASCLEPIOS II study, the rates were similar in all measures.
“In ASCLEPIOS trials, compliance with home-administered subcutaneous ofatumumab was high, and fewer patients discontinued ofatumumab as compared to teriflunomide,” the authors concluded.
Comparator drug a weak choice?
In commenting on the research, Stephen Kamin, MD, professor, vice chair, and chief of service, department of neurology, New Jersey Medical School, in Newark, noted that a limitation of the ASCLEPIOS trials is the comparison with teriflunomide.
“The comparator drug, teriflunomide, is one of the least effective DMTs, and one that some clinicians, including myself, don’t use,” he said.
Previously, when asked in an interview about the choice of teriflunomide as the comparator, Dr. Hauser noted that considerable discussion had gone into the decision. “The rationale was that we wanted to have a comparator that would be present not only against focal disease activity but also potentially against progression, and we were also able to blind the study successfully,” he said at the time.
Dr. Kamin said that ofatumumab will nevertheless likely represent a welcome addition to the tool kit of treatment options for MS. “Any new drug is helpful in adding to our choices as a general rule,” he said. “Subcutaneous injection does have increased convenience.”
It is not likely that the drug will be a game changer, he added, although the treatment’s efficacy compared with other drugs remains to be seen. “It all depends upon the relative efficacy of ofatumumab versus ocrelizumab or siponimod,” Dr. Kamin said.
“There has been another subcutaneous monoclonal for MS, daclizumab, although this was withdrawn from the market due to severe adverse effects not related to route of administration,” he added.
Dr. Hauser has relationships with Alector, Annexon, Bionure, Molecular Stethoscope, Symbiotix, and F. Hoffmann-La Roche. Dr. Kamin has received research support from Biogen, Novartis and CMSC.
A version of this article originally appeared on Medscape.com.
From CMSC 2020
Moving on up: Maintenance therapy extends OS in bladder cancer
Is maintenance therapy with an immune checkpoint inhibitor a good idea for patients with advanced bladder cancer who do not progress after initial chemotherapy?
Yes, and furthermore this approach offers “a new first-line standard of care for advanced urothelial cancer,” said Thomas Powles, MD, professor of genitourinary oncology and director of the Barts Cancer Centre in London.
Dr. Powles was discussing “first-line maintenance therapy” with avelumab (Bavencio, EMD Serono and Pfizer) from the JAVELIN Bladder 100 trial.
Results from this trial will be presented at the plenary session of the 2020 annual meeting of the American Society of Clinical Oncology, held virtually because the coronavirus pandemic. ASCO chief medical officer Richard Schilsky, MD, PhD, highlighted this abstract as one of three from the plenary session that were “practice changing.”
Dr. Powles provided a glimpse of the results at a premeeting press briefing.
The trial involved 700 patients who had not progressed after at least four cycles of first-line, platinum-based chemotherapy. Maintenance therapy with avelumab improved overall survival by 7.1 months when compared with best supportive care (BSC) alone.
The median OS was 21.4 months for avelumab plus BSC versus 14.3 months for BSC alone (hazard ratio, 0.69; P = .0005).
An expert not involved with the study was impressed with the outcome.
“The data are encouraging and we look forward to FDA review, and hopefully approval [in this setting],” said Padmanee Sharma, MD, PhD, a genitourinary medical oncologist at the University of Texas MD Anderson Cancer Center, Houston.
Avelumab is already approved for use in advanced urothelial cancer, but in a second-line setting, like a number of other immune checkpoint inhibitors.
“Instead of waiting for cancer to return”
Dr. Powles commented that about 65%-75% of patients with advanced urothelial cancer have disease control with first-line chemotherapy, but that progression-free survival (PFS) and OS are “short” because of chemoresistance.
Many patients do not receive second-line treatment with immunotherapy and only a “minority” achieve durable clinical benefit, he added.
“Instead of waiting for the cancer to return,” which it will do “quickly,” Dr. Powles suggested that maintenance with immunotherapy should become the standard of care.
“Our findings should give hope to many patients with advanced urothelial cancer who face a very challenging and difficult condition,” coauthor Petros Grivas, MD, PhD, clinical director of the Genitourinary Cancers Program at the Seattle Cancer Care Alliance, said in a statement. He was the global coprincipal investigator of the JAVELIN Bladder 100 trial.
“People with advanced urothelial cancer generally have a poor prognosis, and most experience cancer progression (growth) within 8 months after initiation of first-line chemotherapy,” he said.
“We are very excited with these results, which indicate that immunotherapy with avelumab first-line maintenance could offer a new treatment option that helps patients live longer. Even if this is likely not a complete cure and may cause potential side effects in some patients, the significant prolongation of overall survival is clearly a remarkable improvement, while many treated patients may not experience significant side effects from this approach,” he added.
The safety profile was “manageable” and consistent with other studies of avelumab, Dr. Powles reported.
All-causality adverse events (AEs) were reported at any grade in 98% versus 77.7% in the avelumab plus BSC versus BSC-alone groups; AEs of grade 3 or higher were 47.4% vs 25.2%. The most frequent grade ≥3 AEs were urinary tract infection (4.4% vs. 2.6%), anemia (3.8% vs. 2.9%), hematuria (1.7% vs. 1.4%), fatigue (1.7% vs. 0.6%), and back pain (1.2% vs. 2.3%).
The results from JAVELIN with avelumab show the “largest survival benefit” seen so far in advanced urothelial cancer in the maintenance setting, according to ASCO press materials.
Has there ever been a survival benefit found with maintenance therapy?
No, according to a 2019 review in Future Oncology. Three prospective, randomized, controlled trials (of vinflunine, sunitinib, and lapatinib, respectively) did not reveal any significant oncologic benefit vs placebo.
But in a phase 2, randomized, controlled trial involving 107 patients, maintenance pembrolizumab provided longer PFS, compared with placebo (5.4 vs 3.2 months, HR, 0.64; 95% confidence interval, 0.41-0.98).
This pembrolizumab trial showed a “similar PFS hazard ratio” to that seen with avelumab in JAVELIN, Dr. Powles commented, noting however that the pembrolizumab trial was not designed to look at survival.
Even better response among PD-L1-positive patients
JAVELIN patients had unresectable locally advanced or metastatic urothelial carcinoma and were treated with gemcitabine with either cisplatin or carboplatin.
Just over half (51%) of these patients had tumors that were PD-L1 positive.
The maintenance therapy strategy was even more effective in these patients. Avelumab plus BSC significantly prolonged OS versus BSC alone in patients with PD-L1-positive tumors (HR, 0.56; 1-sided P = .0003). Median OS was not reached versus 17.1 months, respectively.
An OS benefit was also observed across all prespecified subgroups, including those patients with visceral metastases.
Commenting on the study, Dr. Sharma said she would like to see more detailed outcome data related to the number of chemotherapy cycles administered (the range was 4 to 6) and information on the amount of time between the end of chemo to the start of avelumab. Dr. Powles commented that his international team has not looked at number of cycles and outcome, nor the time from completion of chemotherapy and randomization. “They are both valid questions for the future,” he said.
The study was funded by Pfizer. Dr. Powles and many of the coauthors have financial relationships with Pfizer and other pharmaceuticals. Dr. Sharma has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Is maintenance therapy with an immune checkpoint inhibitor a good idea for patients with advanced bladder cancer who do not progress after initial chemotherapy?
Yes, and furthermore this approach offers “a new first-line standard of care for advanced urothelial cancer,” said Thomas Powles, MD, professor of genitourinary oncology and director of the Barts Cancer Centre in London.
Dr. Powles was discussing “first-line maintenance therapy” with avelumab (Bavencio, EMD Serono and Pfizer) from the JAVELIN Bladder 100 trial.
Results from this trial will be presented at the plenary session of the 2020 annual meeting of the American Society of Clinical Oncology, held virtually because the coronavirus pandemic. ASCO chief medical officer Richard Schilsky, MD, PhD, highlighted this abstract as one of three from the plenary session that were “practice changing.”
Dr. Powles provided a glimpse of the results at a premeeting press briefing.
The trial involved 700 patients who had not progressed after at least four cycles of first-line, platinum-based chemotherapy. Maintenance therapy with avelumab improved overall survival by 7.1 months when compared with best supportive care (BSC) alone.
The median OS was 21.4 months for avelumab plus BSC versus 14.3 months for BSC alone (hazard ratio, 0.69; P = .0005).
An expert not involved with the study was impressed with the outcome.
“The data are encouraging and we look forward to FDA review, and hopefully approval [in this setting],” said Padmanee Sharma, MD, PhD, a genitourinary medical oncologist at the University of Texas MD Anderson Cancer Center, Houston.
Avelumab is already approved for use in advanced urothelial cancer, but in a second-line setting, like a number of other immune checkpoint inhibitors.
“Instead of waiting for cancer to return”
Dr. Powles commented that about 65%-75% of patients with advanced urothelial cancer have disease control with first-line chemotherapy, but that progression-free survival (PFS) and OS are “short” because of chemoresistance.
Many patients do not receive second-line treatment with immunotherapy and only a “minority” achieve durable clinical benefit, he added.
“Instead of waiting for the cancer to return,” which it will do “quickly,” Dr. Powles suggested that maintenance with immunotherapy should become the standard of care.
“Our findings should give hope to many patients with advanced urothelial cancer who face a very challenging and difficult condition,” coauthor Petros Grivas, MD, PhD, clinical director of the Genitourinary Cancers Program at the Seattle Cancer Care Alliance, said in a statement. He was the global coprincipal investigator of the JAVELIN Bladder 100 trial.
“People with advanced urothelial cancer generally have a poor prognosis, and most experience cancer progression (growth) within 8 months after initiation of first-line chemotherapy,” he said.
“We are very excited with these results, which indicate that immunotherapy with avelumab first-line maintenance could offer a new treatment option that helps patients live longer. Even if this is likely not a complete cure and may cause potential side effects in some patients, the significant prolongation of overall survival is clearly a remarkable improvement, while many treated patients may not experience significant side effects from this approach,” he added.
The safety profile was “manageable” and consistent with other studies of avelumab, Dr. Powles reported.
All-causality adverse events (AEs) were reported at any grade in 98% versus 77.7% in the avelumab plus BSC versus BSC-alone groups; AEs of grade 3 or higher were 47.4% vs 25.2%. The most frequent grade ≥3 AEs were urinary tract infection (4.4% vs. 2.6%), anemia (3.8% vs. 2.9%), hematuria (1.7% vs. 1.4%), fatigue (1.7% vs. 0.6%), and back pain (1.2% vs. 2.3%).
The results from JAVELIN with avelumab show the “largest survival benefit” seen so far in advanced urothelial cancer in the maintenance setting, according to ASCO press materials.
Has there ever been a survival benefit found with maintenance therapy?
No, according to a 2019 review in Future Oncology. Three prospective, randomized, controlled trials (of vinflunine, sunitinib, and lapatinib, respectively) did not reveal any significant oncologic benefit vs placebo.
But in a phase 2, randomized, controlled trial involving 107 patients, maintenance pembrolizumab provided longer PFS, compared with placebo (5.4 vs 3.2 months, HR, 0.64; 95% confidence interval, 0.41-0.98).
This pembrolizumab trial showed a “similar PFS hazard ratio” to that seen with avelumab in JAVELIN, Dr. Powles commented, noting however that the pembrolizumab trial was not designed to look at survival.
Even better response among PD-L1-positive patients
JAVELIN patients had unresectable locally advanced or metastatic urothelial carcinoma and were treated with gemcitabine with either cisplatin or carboplatin.
Just over half (51%) of these patients had tumors that were PD-L1 positive.
The maintenance therapy strategy was even more effective in these patients. Avelumab plus BSC significantly prolonged OS versus BSC alone in patients with PD-L1-positive tumors (HR, 0.56; 1-sided P = .0003). Median OS was not reached versus 17.1 months, respectively.
An OS benefit was also observed across all prespecified subgroups, including those patients with visceral metastases.
Commenting on the study, Dr. Sharma said she would like to see more detailed outcome data related to the number of chemotherapy cycles administered (the range was 4 to 6) and information on the amount of time between the end of chemo to the start of avelumab. Dr. Powles commented that his international team has not looked at number of cycles and outcome, nor the time from completion of chemotherapy and randomization. “They are both valid questions for the future,” he said.
The study was funded by Pfizer. Dr. Powles and many of the coauthors have financial relationships with Pfizer and other pharmaceuticals. Dr. Sharma has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Is maintenance therapy with an immune checkpoint inhibitor a good idea for patients with advanced bladder cancer who do not progress after initial chemotherapy?
Yes, and furthermore this approach offers “a new first-line standard of care for advanced urothelial cancer,” said Thomas Powles, MD, professor of genitourinary oncology and director of the Barts Cancer Centre in London.
Dr. Powles was discussing “first-line maintenance therapy” with avelumab (Bavencio, EMD Serono and Pfizer) from the JAVELIN Bladder 100 trial.
Results from this trial will be presented at the plenary session of the 2020 annual meeting of the American Society of Clinical Oncology, held virtually because the coronavirus pandemic. ASCO chief medical officer Richard Schilsky, MD, PhD, highlighted this abstract as one of three from the plenary session that were “practice changing.”
Dr. Powles provided a glimpse of the results at a premeeting press briefing.
The trial involved 700 patients who had not progressed after at least four cycles of first-line, platinum-based chemotherapy. Maintenance therapy with avelumab improved overall survival by 7.1 months when compared with best supportive care (BSC) alone.
The median OS was 21.4 months for avelumab plus BSC versus 14.3 months for BSC alone (hazard ratio, 0.69; P = .0005).
An expert not involved with the study was impressed with the outcome.
“The data are encouraging and we look forward to FDA review, and hopefully approval [in this setting],” said Padmanee Sharma, MD, PhD, a genitourinary medical oncologist at the University of Texas MD Anderson Cancer Center, Houston.
Avelumab is already approved for use in advanced urothelial cancer, but in a second-line setting, like a number of other immune checkpoint inhibitors.
“Instead of waiting for cancer to return”
Dr. Powles commented that about 65%-75% of patients with advanced urothelial cancer have disease control with first-line chemotherapy, but that progression-free survival (PFS) and OS are “short” because of chemoresistance.
Many patients do not receive second-line treatment with immunotherapy and only a “minority” achieve durable clinical benefit, he added.
“Instead of waiting for the cancer to return,” which it will do “quickly,” Dr. Powles suggested that maintenance with immunotherapy should become the standard of care.
“Our findings should give hope to many patients with advanced urothelial cancer who face a very challenging and difficult condition,” coauthor Petros Grivas, MD, PhD, clinical director of the Genitourinary Cancers Program at the Seattle Cancer Care Alliance, said in a statement. He was the global coprincipal investigator of the JAVELIN Bladder 100 trial.
“People with advanced urothelial cancer generally have a poor prognosis, and most experience cancer progression (growth) within 8 months after initiation of first-line chemotherapy,” he said.
“We are very excited with these results, which indicate that immunotherapy with avelumab first-line maintenance could offer a new treatment option that helps patients live longer. Even if this is likely not a complete cure and may cause potential side effects in some patients, the significant prolongation of overall survival is clearly a remarkable improvement, while many treated patients may not experience significant side effects from this approach,” he added.
The safety profile was “manageable” and consistent with other studies of avelumab, Dr. Powles reported.
All-causality adverse events (AEs) were reported at any grade in 98% versus 77.7% in the avelumab plus BSC versus BSC-alone groups; AEs of grade 3 or higher were 47.4% vs 25.2%. The most frequent grade ≥3 AEs were urinary tract infection (4.4% vs. 2.6%), anemia (3.8% vs. 2.9%), hematuria (1.7% vs. 1.4%), fatigue (1.7% vs. 0.6%), and back pain (1.2% vs. 2.3%).
The results from JAVELIN with avelumab show the “largest survival benefit” seen so far in advanced urothelial cancer in the maintenance setting, according to ASCO press materials.
Has there ever been a survival benefit found with maintenance therapy?
No, according to a 2019 review in Future Oncology. Three prospective, randomized, controlled trials (of vinflunine, sunitinib, and lapatinib, respectively) did not reveal any significant oncologic benefit vs placebo.
But in a phase 2, randomized, controlled trial involving 107 patients, maintenance pembrolizumab provided longer PFS, compared with placebo (5.4 vs 3.2 months, HR, 0.64; 95% confidence interval, 0.41-0.98).
This pembrolizumab trial showed a “similar PFS hazard ratio” to that seen with avelumab in JAVELIN, Dr. Powles commented, noting however that the pembrolizumab trial was not designed to look at survival.
Even better response among PD-L1-positive patients
JAVELIN patients had unresectable locally advanced or metastatic urothelial carcinoma and were treated with gemcitabine with either cisplatin or carboplatin.
Just over half (51%) of these patients had tumors that were PD-L1 positive.
The maintenance therapy strategy was even more effective in these patients. Avelumab plus BSC significantly prolonged OS versus BSC alone in patients with PD-L1-positive tumors (HR, 0.56; 1-sided P = .0003). Median OS was not reached versus 17.1 months, respectively.
An OS benefit was also observed across all prespecified subgroups, including those patients with visceral metastases.
Commenting on the study, Dr. Sharma said she would like to see more detailed outcome data related to the number of chemotherapy cycles administered (the range was 4 to 6) and information on the amount of time between the end of chemo to the start of avelumab. Dr. Powles commented that his international team has not looked at number of cycles and outcome, nor the time from completion of chemotherapy and randomization. “They are both valid questions for the future,” he said.
The study was funded by Pfizer. Dr. Powles and many of the coauthors have financial relationships with Pfizer and other pharmaceuticals. Dr. Sharma has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
FROM ASCO 2020
COVID-19: Putting distance between projection and reality
When it comes to COVID-19, studies show that social distancing flattened the curve.
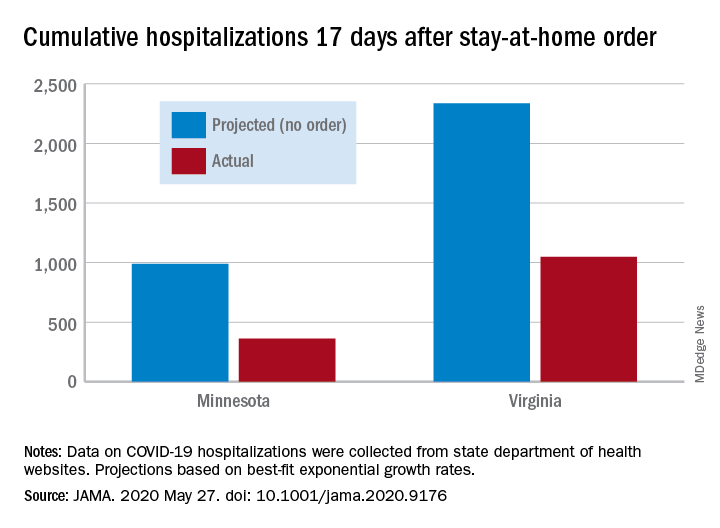
Cumulative hospitalizations in four states with stay-at-home orders were well short of the projected exponential growth curves, Soumya Sen, PhD, of the University of Minnesota, Minneapolis, and associates reported May 27 in a research letter in JAMA. All states were observed through April 28.
The deviations between observed cases and worst-case projections in the four states – Colorado, Minnesota, Ohio, and Virginia – all began within 8-10 days of the stay-at-home orders. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In Virginia, the corresponding numbers were 1,048 observed and 2,335 projected, they reported.
“Observed hospitalizations consistently fell outside of the 95% prediction bands of the projected exponential growth curve,” Dr. Sen and associates noted.
In a separate Canadian study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention, Ashleigh R. Tuite, PhD, MPH, of the University of Toronto and associates wrote May 27 in a letter in Annals of Internal Medicine.
Their model, based on a 70% reduction in physical contacts for March 19–May 3, projected 2.0 cases per 100,000 population with physical distancing and 37.4 per 100,000 without. Deaths among those ICU patients were projected at 2.5 per 100,000 with distancing and 12.7 per 100,000 without intervention, they reported.
“Our modeling also shows the challenges associated with relaxation of physical distancing measures without a concomitant increase in other public health measures. Specifically, when the number of contacts between persons returns to more than 50% of normal, we expect disease activity to resurge rapidly and ICUs to quickly reach capacity,” they wrote.
The study published in JAMA used publicly available data from the University of Minnesota COVID-19 Hospitalization Project, which is partially funded by the University of Minnesota Office of Academic Clinical Affairs and United Health Foundation.
SOURCES: Sen S et al. JAMA. 2020 May 27. doi: 10.1001/jama.2020.9176; Tuite AR et al. Ann Intern Med. 2020 May 27. doi: 10.7326/M20-2945.
When it comes to COVID-19, studies show that social distancing flattened the curve.
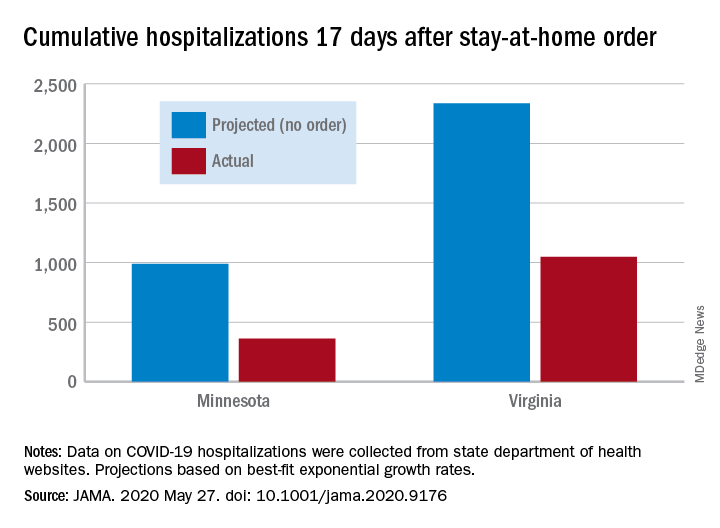
Cumulative hospitalizations in four states with stay-at-home orders were well short of the projected exponential growth curves, Soumya Sen, PhD, of the University of Minnesota, Minneapolis, and associates reported May 27 in a research letter in JAMA. All states were observed through April 28.
The deviations between observed cases and worst-case projections in the four states – Colorado, Minnesota, Ohio, and Virginia – all began within 8-10 days of the stay-at-home orders. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In Virginia, the corresponding numbers were 1,048 observed and 2,335 projected, they reported.
“Observed hospitalizations consistently fell outside of the 95% prediction bands of the projected exponential growth curve,” Dr. Sen and associates noted.
In a separate Canadian study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention, Ashleigh R. Tuite, PhD, MPH, of the University of Toronto and associates wrote May 27 in a letter in Annals of Internal Medicine.
Their model, based on a 70% reduction in physical contacts for March 19–May 3, projected 2.0 cases per 100,000 population with physical distancing and 37.4 per 100,000 without. Deaths among those ICU patients were projected at 2.5 per 100,000 with distancing and 12.7 per 100,000 without intervention, they reported.
“Our modeling also shows the challenges associated with relaxation of physical distancing measures without a concomitant increase in other public health measures. Specifically, when the number of contacts between persons returns to more than 50% of normal, we expect disease activity to resurge rapidly and ICUs to quickly reach capacity,” they wrote.
The study published in JAMA used publicly available data from the University of Minnesota COVID-19 Hospitalization Project, which is partially funded by the University of Minnesota Office of Academic Clinical Affairs and United Health Foundation.
SOURCES: Sen S et al. JAMA. 2020 May 27. doi: 10.1001/jama.2020.9176; Tuite AR et al. Ann Intern Med. 2020 May 27. doi: 10.7326/M20-2945.
When it comes to COVID-19, studies show that social distancing flattened the curve.
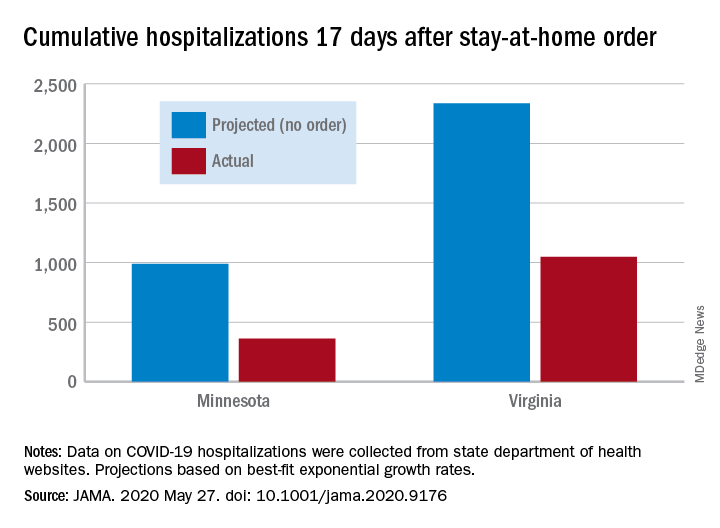
Cumulative hospitalizations in four states with stay-at-home orders were well short of the projected exponential growth curves, Soumya Sen, PhD, of the University of Minnesota, Minneapolis, and associates reported May 27 in a research letter in JAMA. All states were observed through April 28.
The deviations between observed cases and worst-case projections in the four states – Colorado, Minnesota, Ohio, and Virginia – all began within 8-10 days of the stay-at-home orders. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In Virginia, the corresponding numbers were 1,048 observed and 2,335 projected, they reported.
“Observed hospitalizations consistently fell outside of the 95% prediction bands of the projected exponential growth curve,” Dr. Sen and associates noted.
In a separate Canadian study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention, Ashleigh R. Tuite, PhD, MPH, of the University of Toronto and associates wrote May 27 in a letter in Annals of Internal Medicine.
Their model, based on a 70% reduction in physical contacts for March 19–May 3, projected 2.0 cases per 100,000 population with physical distancing and 37.4 per 100,000 without. Deaths among those ICU patients were projected at 2.5 per 100,000 with distancing and 12.7 per 100,000 without intervention, they reported.
“Our modeling also shows the challenges associated with relaxation of physical distancing measures without a concomitant increase in other public health measures. Specifically, when the number of contacts between persons returns to more than 50% of normal, we expect disease activity to resurge rapidly and ICUs to quickly reach capacity,” they wrote.
The study published in JAMA used publicly available data from the University of Minnesota COVID-19 Hospitalization Project, which is partially funded by the University of Minnesota Office of Academic Clinical Affairs and United Health Foundation.
SOURCES: Sen S et al. JAMA. 2020 May 27. doi: 10.1001/jama.2020.9176; Tuite AR et al. Ann Intern Med. 2020 May 27. doi: 10.7326/M20-2945.
Patients find CAC more persuasive than ASCVD risk score for statin decisions
Patients who received a protocol-driven recommendation to initiate statin therapy for primary prevention of cardiovascular disease based upon their CT angiography coronary artery calcium score were twice as likely to actually start on the drug than those whose recommendation was guided by the American College of Cardiology/American Heart Association Pooled Cohort Equations Risk Calculator, according to the results of the randomized CorCal Vanguard study.
These results suggest that patients – and their primary care physicians – find the conventional method of screening for cardiovascular risk using the Pooled Cohort Equations to estimate the 10-year risk of MI or stroke, as recommended in ACC/AHA guidelines, to be less persuasive than screening for the presence or absence of actual disease as captured by CT angiography images and the associated coronary artery calcium (CAC) score, Joseph B. Muhlestein, MD, said at the joint scientific sessions of the ACC and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
The CorCal Vanguard study included 601 patients with an average baseline LDL cholesterol of 120 mg/dL, an average age of 60 years, and no history of cardiovascular disease, diabetes, or prior statin therapy. They were randomized to decision-making regarding statin therapy based on either the ACC/AHA guideline–endorsed Pooled Cohort Equations, which use an estimated 10-year risk of 7.5% or more as the threshold for statin initiation, or their CAC score.
If a patient’s CAC score was 0, the recommendation was against starting a statin. Everyone with a CAC greater than 100 received a recommendation for high-intensity statin therapy. And for those with a CAC of 1-100, the decision defaulted to the results of the Pooled Cohort Equations. The screening results were provided to a patient’s primary physician so they could engage in joint decision-making regarding initiation of statin therapy. Adherence to a screening-based recommendation to start on a statin was assessed at 3 and 12 months of follow-up, explained Dr. Muhlestein, a cardiologist at the Intermountain Medical Center Heart Institute in Salt Lake City.
He noted that CorCal Vanguard was merely a feasibility study. Based on the study results he presented at ACC 2020, the full 9,000-patient CorCal primary prevention trial is now enrolling participants. CorCal is the first randomized trial to pit the Pooled Cohort Equations against the CAC score in a large study looking for differences in downstream clinical outcomes.
The rationale for this line of clinical research lies in the known limitations of the ACC/AHA risk calculator. “It may overestimate risk in some populations, patients aren’t always adherent to Pooled Cohort Equations Risk Calculator recommendations, and it doesn’t include novel risk markers such as C-reactive protein that some consider important for risk assessment. And the big question: Should we continue risk screening to determine potential benefit from drug therapy, or should we switch to disease screening?” the cardiologist commented.
The CorCal Vanguard results
A recommendation to start statin therapy was made in 48% of patients in the Pooled Cohort Equations group, versus 36% of the group randomized to CAC. However, only 17% of patients in the Pooled Cohort Equations group actually initiated a statin, a significantly lower rate than the 26% figure in the CAC arm. Fully 70% of patients who received a recommendation to start taking a statin on the basis of their CAC score actually did so, compared to just 36% of those whose recommendation was based upon their Pooled Cohort Equations Risk Calculator.
At 3 months of follow-up, 61% of patients who received an initial recommendation to start statin therapy based upon their CAC screening were actually taking a statin, compared with 41% of those whose recommendation was based upon the Pooled Cohort Equations. At 12 months, the figures were 64% and 49%.
In both groups, at 12 months of follow-up, the No. 1 reason patients weren’t taking a statin as recommended was that their personal physician had advised against it or never prescribed it. That accounted for roughly half of the nonadherence. Another quarter was because of a preference to try lifestyle change first. Fear of drug side effects was a less common reason.
Putting the CorCal Vanguard study results in perspective, Dr. Muhlestein observed that, prior to the screening study, none of the participants had ever been on a statin, yet 37% of them were found by one screening method or the other to be at high cardiovascular risk. Of those high-risk patients, 51% actually initiated statin therapy and the majority of them were still taking their medication 12 months later.
“That has to be a good thing. It emphasizes what can be done when proactive primary prevention is practiced,” the cardiologist said.
He reported having no financial conflicts regarding the CorCal study, which was funded by a grant from the Dell Loy Hansen Cardiovascular Research Fund.
SOURCE: Muhlestein JB et al. ACC 2020, Abstract 909-12.
Patients who received a protocol-driven recommendation to initiate statin therapy for primary prevention of cardiovascular disease based upon their CT angiography coronary artery calcium score were twice as likely to actually start on the drug than those whose recommendation was guided by the American College of Cardiology/American Heart Association Pooled Cohort Equations Risk Calculator, according to the results of the randomized CorCal Vanguard study.
These results suggest that patients – and their primary care physicians – find the conventional method of screening for cardiovascular risk using the Pooled Cohort Equations to estimate the 10-year risk of MI or stroke, as recommended in ACC/AHA guidelines, to be less persuasive than screening for the presence or absence of actual disease as captured by CT angiography images and the associated coronary artery calcium (CAC) score, Joseph B. Muhlestein, MD, said at the joint scientific sessions of the ACC and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
The CorCal Vanguard study included 601 patients with an average baseline LDL cholesterol of 120 mg/dL, an average age of 60 years, and no history of cardiovascular disease, diabetes, or prior statin therapy. They were randomized to decision-making regarding statin therapy based on either the ACC/AHA guideline–endorsed Pooled Cohort Equations, which use an estimated 10-year risk of 7.5% or more as the threshold for statin initiation, or their CAC score.
If a patient’s CAC score was 0, the recommendation was against starting a statin. Everyone with a CAC greater than 100 received a recommendation for high-intensity statin therapy. And for those with a CAC of 1-100, the decision defaulted to the results of the Pooled Cohort Equations. The screening results were provided to a patient’s primary physician so they could engage in joint decision-making regarding initiation of statin therapy. Adherence to a screening-based recommendation to start on a statin was assessed at 3 and 12 months of follow-up, explained Dr. Muhlestein, a cardiologist at the Intermountain Medical Center Heart Institute in Salt Lake City.
He noted that CorCal Vanguard was merely a feasibility study. Based on the study results he presented at ACC 2020, the full 9,000-patient CorCal primary prevention trial is now enrolling participants. CorCal is the first randomized trial to pit the Pooled Cohort Equations against the CAC score in a large study looking for differences in downstream clinical outcomes.
The rationale for this line of clinical research lies in the known limitations of the ACC/AHA risk calculator. “It may overestimate risk in some populations, patients aren’t always adherent to Pooled Cohort Equations Risk Calculator recommendations, and it doesn’t include novel risk markers such as C-reactive protein that some consider important for risk assessment. And the big question: Should we continue risk screening to determine potential benefit from drug therapy, or should we switch to disease screening?” the cardiologist commented.
The CorCal Vanguard results
A recommendation to start statin therapy was made in 48% of patients in the Pooled Cohort Equations group, versus 36% of the group randomized to CAC. However, only 17% of patients in the Pooled Cohort Equations group actually initiated a statin, a significantly lower rate than the 26% figure in the CAC arm. Fully 70% of patients who received a recommendation to start taking a statin on the basis of their CAC score actually did so, compared to just 36% of those whose recommendation was based upon their Pooled Cohort Equations Risk Calculator.
At 3 months of follow-up, 61% of patients who received an initial recommendation to start statin therapy based upon their CAC screening were actually taking a statin, compared with 41% of those whose recommendation was based upon the Pooled Cohort Equations. At 12 months, the figures were 64% and 49%.
In both groups, at 12 months of follow-up, the No. 1 reason patients weren’t taking a statin as recommended was that their personal physician had advised against it or never prescribed it. That accounted for roughly half of the nonadherence. Another quarter was because of a preference to try lifestyle change first. Fear of drug side effects was a less common reason.
Putting the CorCal Vanguard study results in perspective, Dr. Muhlestein observed that, prior to the screening study, none of the participants had ever been on a statin, yet 37% of them were found by one screening method or the other to be at high cardiovascular risk. Of those high-risk patients, 51% actually initiated statin therapy and the majority of them were still taking their medication 12 months later.
“That has to be a good thing. It emphasizes what can be done when proactive primary prevention is practiced,” the cardiologist said.
He reported having no financial conflicts regarding the CorCal study, which was funded by a grant from the Dell Loy Hansen Cardiovascular Research Fund.
SOURCE: Muhlestein JB et al. ACC 2020, Abstract 909-12.
Patients who received a protocol-driven recommendation to initiate statin therapy for primary prevention of cardiovascular disease based upon their CT angiography coronary artery calcium score were twice as likely to actually start on the drug than those whose recommendation was guided by the American College of Cardiology/American Heart Association Pooled Cohort Equations Risk Calculator, according to the results of the randomized CorCal Vanguard study.
These results suggest that patients – and their primary care physicians – find the conventional method of screening for cardiovascular risk using the Pooled Cohort Equations to estimate the 10-year risk of MI or stroke, as recommended in ACC/AHA guidelines, to be less persuasive than screening for the presence or absence of actual disease as captured by CT angiography images and the associated coronary artery calcium (CAC) score, Joseph B. Muhlestein, MD, said at the joint scientific sessions of the ACC and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
The CorCal Vanguard study included 601 patients with an average baseline LDL cholesterol of 120 mg/dL, an average age of 60 years, and no history of cardiovascular disease, diabetes, or prior statin therapy. They were randomized to decision-making regarding statin therapy based on either the ACC/AHA guideline–endorsed Pooled Cohort Equations, which use an estimated 10-year risk of 7.5% or more as the threshold for statin initiation, or their CAC score.
If a patient’s CAC score was 0, the recommendation was against starting a statin. Everyone with a CAC greater than 100 received a recommendation for high-intensity statin therapy. And for those with a CAC of 1-100, the decision defaulted to the results of the Pooled Cohort Equations. The screening results were provided to a patient’s primary physician so they could engage in joint decision-making regarding initiation of statin therapy. Adherence to a screening-based recommendation to start on a statin was assessed at 3 and 12 months of follow-up, explained Dr. Muhlestein, a cardiologist at the Intermountain Medical Center Heart Institute in Salt Lake City.
He noted that CorCal Vanguard was merely a feasibility study. Based on the study results he presented at ACC 2020, the full 9,000-patient CorCal primary prevention trial is now enrolling participants. CorCal is the first randomized trial to pit the Pooled Cohort Equations against the CAC score in a large study looking for differences in downstream clinical outcomes.
The rationale for this line of clinical research lies in the known limitations of the ACC/AHA risk calculator. “It may overestimate risk in some populations, patients aren’t always adherent to Pooled Cohort Equations Risk Calculator recommendations, and it doesn’t include novel risk markers such as C-reactive protein that some consider important for risk assessment. And the big question: Should we continue risk screening to determine potential benefit from drug therapy, or should we switch to disease screening?” the cardiologist commented.
The CorCal Vanguard results
A recommendation to start statin therapy was made in 48% of patients in the Pooled Cohort Equations group, versus 36% of the group randomized to CAC. However, only 17% of patients in the Pooled Cohort Equations group actually initiated a statin, a significantly lower rate than the 26% figure in the CAC arm. Fully 70% of patients who received a recommendation to start taking a statin on the basis of their CAC score actually did so, compared to just 36% of those whose recommendation was based upon their Pooled Cohort Equations Risk Calculator.
At 3 months of follow-up, 61% of patients who received an initial recommendation to start statin therapy based upon their CAC screening were actually taking a statin, compared with 41% of those whose recommendation was based upon the Pooled Cohort Equations. At 12 months, the figures were 64% and 49%.
In both groups, at 12 months of follow-up, the No. 1 reason patients weren’t taking a statin as recommended was that their personal physician had advised against it or never prescribed it. That accounted for roughly half of the nonadherence. Another quarter was because of a preference to try lifestyle change first. Fear of drug side effects was a less common reason.
Putting the CorCal Vanguard study results in perspective, Dr. Muhlestein observed that, prior to the screening study, none of the participants had ever been on a statin, yet 37% of them were found by one screening method or the other to be at high cardiovascular risk. Of those high-risk patients, 51% actually initiated statin therapy and the majority of them were still taking their medication 12 months later.
“That has to be a good thing. It emphasizes what can be done when proactive primary prevention is practiced,” the cardiologist said.
He reported having no financial conflicts regarding the CorCal study, which was funded by a grant from the Dell Loy Hansen Cardiovascular Research Fund.
SOURCE: Muhlestein JB et al. ACC 2020, Abstract 909-12.
FROM ACC 2020
Cardiologists’ pay increases; most satisfied with profession
Cardiologists remain among the top earners in medicine in 2020 and their annual pay has increased over 2019, although female cardiologists continue to earn less than their male peers, according to the 2020 Medscape Cardiologist Compensation Report.
However, an important caveat is that the data for this year’s report were collected prior to Feb. 10 and therefore reflect physician salary and income prior to the COVID-19 crisis, which has had a huge impact on physicians.
For example, since the start of the crisis, data show that physician practices have seen a 55% dip in revenue and a 60% drop in patient volume on average. Hospitals and physician groups nationwide have implemented layoffs, furloughs, and pay cuts.
In March, 43,000 health care workers were laid off; 9% of independent medical practices reported that they have closed their practices, at least temporarily. With this in mind, the Medscape 2020 report shows that annual compensation for cardiologists increased to $438,000 in 2020, up from $430,000 in 2019.
Cardiologist pay is the fourth highest of all specialties in the overall Medscape Physician Compensation Report 2020, which covers U.S. physicians as a whole and more than 17,000 physicians in more than 30 specialties.
Nearly two-thirds of cardiologists (61%) report that they feel fairly compensated, somewhat higher than last year’s percentage (54%).
On average, cardiologists are eligible for an average incentive bonus of $63,000. Average incentive bonuses are highest among orthopedists ($96,000) and lowest among family medicine physicians ($24,000).
More than half of cardiologists (55%) say they receive three-quarters of their potential annual incentive bonus.
But COVID-19 may change that. Experts interviewed recently by this news organization noted that productivity benchmarks for physicians are likely to be lowered in light of plunging patient numbers from COVID-19, and bonuses are expected to take a hit.
Most cardiologists happy at work
On average, male cardiologists spend 42.6 hours per week seeing patients, somewhat higher than female cardiologists (36.9 hours); the average for all physicians is 37.9 hours per week.
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 16.9 hours per week on paperwork and administration, similar to physicians overall (15.6 hours).
Intensivists top the list regarding such tasks (19.1 hours), followed by internists (18.5), infectious disease physicians (18.5), and psychiatrists (18.3). Anesthesiologists and ophthalmologists spend the least amount of time on paperwork/administration (10.0 and 9.8 hours per week, respectively).
What is most rewarding about being a cardiologist? Relationships with and gratitude from patients (31%) tops the list, followed by being good at what they do/finding answers, diagnoses (26%), making the world a better place (18%), and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (3%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (30%), respondents report. Other challenges include having to work long hours (21%), working with electronic health records (17%), dealing with difficult patients (8%), and trouble getting fair reimbursement (7%).
Despite the challenges, 82% of cardiologists said they would choose medicine again, and 92% would choose cardiology again.
Other key findings from the latest report regarding cardiologists include the following:
- At 15%, cardiologists rank at the lower end of physicians potentially losing money on denied or resubmitted claims. Plastic surgery and emergency medicine have the highest percentage of claims denied or resubmitted (28% and 22%, respectively). One study found that, on average, 63% of denied claims are recoverable, but health care professionals spend about $118 per claim on appeals.
- 41% of cardiologists say they use physician assistants to treat patients in their practices, while two-thirds use nurse practitioners; 26% use neither for patient care. Half of cardiologists who work with physician assistants and nurse practitioners in their offices say these employees have helped boost profitability.
- 84% of cardiologists say they will continue taking new and current Medicare/Medicaid patients; only 1% say they won’t take new Medicare patients, and 13% are undecided, roughly the same as last year.
- The large majority of cardiologists rely on payers; 44% rely on fee-for-service arrangements and 29% on accountable care organizations for patient-based income.
- 42% of cardiologists expect to participate in merit-based incentive payment system, but only 9% expect to participate in alternative payment models.
This article first appeared on Medscape.com.
Cardiologists remain among the top earners in medicine in 2020 and their annual pay has increased over 2019, although female cardiologists continue to earn less than their male peers, according to the 2020 Medscape Cardiologist Compensation Report.
However, an important caveat is that the data for this year’s report were collected prior to Feb. 10 and therefore reflect physician salary and income prior to the COVID-19 crisis, which has had a huge impact on physicians.
For example, since the start of the crisis, data show that physician practices have seen a 55% dip in revenue and a 60% drop in patient volume on average. Hospitals and physician groups nationwide have implemented layoffs, furloughs, and pay cuts.
In March, 43,000 health care workers were laid off; 9% of independent medical practices reported that they have closed their practices, at least temporarily. With this in mind, the Medscape 2020 report shows that annual compensation for cardiologists increased to $438,000 in 2020, up from $430,000 in 2019.
Cardiologist pay is the fourth highest of all specialties in the overall Medscape Physician Compensation Report 2020, which covers U.S. physicians as a whole and more than 17,000 physicians in more than 30 specialties.
Nearly two-thirds of cardiologists (61%) report that they feel fairly compensated, somewhat higher than last year’s percentage (54%).
On average, cardiologists are eligible for an average incentive bonus of $63,000. Average incentive bonuses are highest among orthopedists ($96,000) and lowest among family medicine physicians ($24,000).
More than half of cardiologists (55%) say they receive three-quarters of their potential annual incentive bonus.
But COVID-19 may change that. Experts interviewed recently by this news organization noted that productivity benchmarks for physicians are likely to be lowered in light of plunging patient numbers from COVID-19, and bonuses are expected to take a hit.
Most cardiologists happy at work
On average, male cardiologists spend 42.6 hours per week seeing patients, somewhat higher than female cardiologists (36.9 hours); the average for all physicians is 37.9 hours per week.
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 16.9 hours per week on paperwork and administration, similar to physicians overall (15.6 hours).
Intensivists top the list regarding such tasks (19.1 hours), followed by internists (18.5), infectious disease physicians (18.5), and psychiatrists (18.3). Anesthesiologists and ophthalmologists spend the least amount of time on paperwork/administration (10.0 and 9.8 hours per week, respectively).
What is most rewarding about being a cardiologist? Relationships with and gratitude from patients (31%) tops the list, followed by being good at what they do/finding answers, diagnoses (26%), making the world a better place (18%), and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (3%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (30%), respondents report. Other challenges include having to work long hours (21%), working with electronic health records (17%), dealing with difficult patients (8%), and trouble getting fair reimbursement (7%).
Despite the challenges, 82% of cardiologists said they would choose medicine again, and 92% would choose cardiology again.
Other key findings from the latest report regarding cardiologists include the following:
- At 15%, cardiologists rank at the lower end of physicians potentially losing money on denied or resubmitted claims. Plastic surgery and emergency medicine have the highest percentage of claims denied or resubmitted (28% and 22%, respectively). One study found that, on average, 63% of denied claims are recoverable, but health care professionals spend about $118 per claim on appeals.
- 41% of cardiologists say they use physician assistants to treat patients in their practices, while two-thirds use nurse practitioners; 26% use neither for patient care. Half of cardiologists who work with physician assistants and nurse practitioners in their offices say these employees have helped boost profitability.
- 84% of cardiologists say they will continue taking new and current Medicare/Medicaid patients; only 1% say they won’t take new Medicare patients, and 13% are undecided, roughly the same as last year.
- The large majority of cardiologists rely on payers; 44% rely on fee-for-service arrangements and 29% on accountable care organizations for patient-based income.
- 42% of cardiologists expect to participate in merit-based incentive payment system, but only 9% expect to participate in alternative payment models.
This article first appeared on Medscape.com.
Cardiologists remain among the top earners in medicine in 2020 and their annual pay has increased over 2019, although female cardiologists continue to earn less than their male peers, according to the 2020 Medscape Cardiologist Compensation Report.
However, an important caveat is that the data for this year’s report were collected prior to Feb. 10 and therefore reflect physician salary and income prior to the COVID-19 crisis, which has had a huge impact on physicians.
For example, since the start of the crisis, data show that physician practices have seen a 55% dip in revenue and a 60% drop in patient volume on average. Hospitals and physician groups nationwide have implemented layoffs, furloughs, and pay cuts.
In March, 43,000 health care workers were laid off; 9% of independent medical practices reported that they have closed their practices, at least temporarily. With this in mind, the Medscape 2020 report shows that annual compensation for cardiologists increased to $438,000 in 2020, up from $430,000 in 2019.
Cardiologist pay is the fourth highest of all specialties in the overall Medscape Physician Compensation Report 2020, which covers U.S. physicians as a whole and more than 17,000 physicians in more than 30 specialties.
Nearly two-thirds of cardiologists (61%) report that they feel fairly compensated, somewhat higher than last year’s percentage (54%).
On average, cardiologists are eligible for an average incentive bonus of $63,000. Average incentive bonuses are highest among orthopedists ($96,000) and lowest among family medicine physicians ($24,000).
More than half of cardiologists (55%) say they receive three-quarters of their potential annual incentive bonus.
But COVID-19 may change that. Experts interviewed recently by this news organization noted that productivity benchmarks for physicians are likely to be lowered in light of plunging patient numbers from COVID-19, and bonuses are expected to take a hit.
Most cardiologists happy at work
On average, male cardiologists spend 42.6 hours per week seeing patients, somewhat higher than female cardiologists (36.9 hours); the average for all physicians is 37.9 hours per week.
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, cardiologists spend 16.9 hours per week on paperwork and administration, similar to physicians overall (15.6 hours).
Intensivists top the list regarding such tasks (19.1 hours), followed by internists (18.5), infectious disease physicians (18.5), and psychiatrists (18.3). Anesthesiologists and ophthalmologists spend the least amount of time on paperwork/administration (10.0 and 9.8 hours per week, respectively).
What is most rewarding about being a cardiologist? Relationships with and gratitude from patients (31%) tops the list, followed by being good at what they do/finding answers, diagnoses (26%), making the world a better place (18%), and making good money at a job they like (12%). A few cited pride in their profession (6%) and teaching (3%). These figures are in line with last year’s responses.
The most challenging part of practicing cardiology is having so many rules and regulations (30%), respondents report. Other challenges include having to work long hours (21%), working with electronic health records (17%), dealing with difficult patients (8%), and trouble getting fair reimbursement (7%).
Despite the challenges, 82% of cardiologists said they would choose medicine again, and 92% would choose cardiology again.
Other key findings from the latest report regarding cardiologists include the following:
- At 15%, cardiologists rank at the lower end of physicians potentially losing money on denied or resubmitted claims. Plastic surgery and emergency medicine have the highest percentage of claims denied or resubmitted (28% and 22%, respectively). One study found that, on average, 63% of denied claims are recoverable, but health care professionals spend about $118 per claim on appeals.
- 41% of cardiologists say they use physician assistants to treat patients in their practices, while two-thirds use nurse practitioners; 26% use neither for patient care. Half of cardiologists who work with physician assistants and nurse practitioners in their offices say these employees have helped boost profitability.
- 84% of cardiologists say they will continue taking new and current Medicare/Medicaid patients; only 1% say they won’t take new Medicare patients, and 13% are undecided, roughly the same as last year.
- The large majority of cardiologists rely on payers; 44% rely on fee-for-service arrangements and 29% on accountable care organizations for patient-based income.
- 42% of cardiologists expect to participate in merit-based incentive payment system, but only 9% expect to participate in alternative payment models.
This article first appeared on Medscape.com.