User login
The rise of U.S. dermatology: A brief history from the 1800s to 1970
As Dermatology News (formerly Skin and Allergy News) reaches its 50th-year milestone, a reflection on the history of the discipline, especially in the United States, up to the time of the launch of this publication is in order. Such an overview must, of course, be cursory in this context. Yet, for those who want to learn more, a large body of historical references and research has been created to fill in the gaps, as modern dermatology has always been cognizant of the importance of its history, with many individuals and groups drawn to the subject.
Two excellent sources for the history of the field can be found in work by William Allen Pusey, MD (1865-1940), and Herbert Rattner, MD (1900-1962), “The History of Dermatology” published in 1933 and research by members of the History of Dermatology Society, founded in 1973 in New York.
Modern dermatology
The development of the field of modern dermatology can be traced back to the early to mid-19th century. During the first half of the 19th century, England and France dominated the study of dermatology, but by the middle of the century, the German revolution in microparasitology shifted that focus “with remarkable German discoveries,” according to Bernard S. Potter, MD, in his review of bibliographic landmarks of the history of dermatology (J Am Acad Dermatol 2003;48:919-32). For example, Johann Lucas Schoenlein (1793-1864) in 1839 discovered the fungal origin of favus, and in 1841 Jacob Henle (1809-1885) discovered Demodex folliculorum. Karl Ferdinand Eichstedt (1816-1892) in 1846 followed with the discovery of the causative agent of pityriasis versicolor, and Friedrich Wilhelm Felix von Barensprung (1822-1864) in 1862 coined the term erythrasma and named the organism responsible for this condition Microsporum minutissimum.
Dr. Potter described how American dermatology originated in New York City in 1836 when Henry Daggett Bulkley, MD, (1803-1872) opened the first dispensary for skin diseases, the Broome Street Infirmary for Diseases of the Skin, thus creating the first institution in the United States for the treatment of cutaneous disease. As the first American dermatologist, he was also the first in the United States to lecture on and to exclusively practice dermatology.
The rise of interest in the importance of dermatology led to the organization of the early American Dermatological Association in 1886.
However, the state of dermatology as a science in the 19th century was not always looked upon favorably, even by its practitioners, especially in the United States. In 1871, in a “Review on Modern Dermatology,” given as a series of lectures on skin disease at Harvard University, James C. White, MD (1833-1916) of Massachusetts General Hospital, stated that: “Were the literature of skin diseases previous to that of the last half-century absolutely annihilated, and with it, the influence it has exercised upon that of the present day, it would be an immense gain to dermatology, although much of real value would perish.” He lamented that America had contributed little so far to the study of dermatology, and that the discipline was only taught in some of its largest schools, and he urged that this be changed. He also lamented that The American Journal of Syphilography and Dermatology, established the year before, had so far proved itself heavy on syphilis, but light on dermatology, a situation he also hoped would change dramatically.
By the late-19th century, the conviction that diseases of the skin needed to be connected to the overall metabolism and physiology of the patient as a whole was becoming more mainstream.
“It has been, and still is, too much the custom to study diseases of the skin in the light of pathological pictures, to name the local manifestation and to so label it as disease. It is much easier to give the disease name and to label it than it is to comprehend the process at work. The former is comparatively unimportant for the patient, the latter point upon which recovery may depend. The nature and meaning of the process in connection with the cutaneous symptoms has not received enough attention, and I believe this to be one reason why the treatment of many of these diseases in the past has been so notoriously unsatisfactory,” Louis A. Duhring, MD (1845-1913) chided his colleagues in the Section of Dermatology and Syphilography, at the Forty-fourth Annual Meeting of the American Medical Association in 1894. (collections.nlm.nih.gov/ext/dw/101489447/PDF/101489447.pdf)
In the early-20th century, German dermatology influenced American dermatology more than any other, according to Karl Holubar, MD, of the Institute for the History of Medicine, University of Vienna, in his lecture on the history of European dermatopathology.
He stated that, with regard to dermatopathology, it was Oscar Gans, MD (1888-1983) who brought the latest knowledge into the United States by delivering a series of lectures at Mayo Clinic in the late 1920s upon the invitation of Paul A. O’Leary, MD, (1891-1955) who then headed the Mayo section of dermatology.
By the 1930s, a flurry of organizational activity overtook American dermatology. In 1932, the American Board of Dermatology was established, with its first exams given in 1933 (20 students passed, 7 failed). The Society for Investigative Dermatology was founded in 1937, and the American Academy of Dermatology and Syphilology (now the American Academy of Dermatology), founded in 1938.
The 1930s also saw a major influx of German and other European Jews fleeing Nazi oppression who would forever change the face of American dermatology. “Between 1933 and 1938, a series of repressive measures eliminated them from the practice of medicine in Germany and other countries. Although some died in concentration camps and others committed suicide, many were able to emigrate from Europe. Dermatology in the United States particularly benefited from the influx of several stellar Jewish dermatologists who were major contributors to the subsequent flowering of academic dermatology in the United States” (JAMA Derm. 2013;149[9]:1090-4).
“The overtures of the holocaust and the rising power of Hitler in Europe finally brought over to the United States the flower of dermatologists and investigators of the German School, e.g., Alexander and Walter Lever, Felix and Hermann Pinkus, the Epsteins, Erich Auerbach, Stephen Rothman, to name just a few. With this exodus and transfer of brain power, Europe lost its leading role to never again regain it,” according to Dr. Holubar. Walter F. Lever, MD (1909-1992) was especially well-known for his landmark textbook on dermatology, “Histopathology of the Skin,” published in the United States in 1949.
The therapeutic era
Throughout the 19th century, a variety of soaps and patent medicines were touted as cure-alls for a host of skin diseases. Other than their benefits to surface cleanliness and their antiseptic properties, however, they were of little effect.
It wasn’t until the 20th century that truly effective therapeutics entered the dermatologic pharmacopoeia. In their 1989 review, Diane Quintal, MD, and Robert Jackson, MD, discussed the origins of the most important of these drugs and pointed out that, “Until this century, the essence of dermatology resided in the realm of morphology. Early contributors largely confined their activities to the classification of skin diseases and to the elaboration of clinical dermatologic entities based on morphologic features. ... but “in the last 50 years, there have been significant scientific discoveries in the field of therapeutics that have revolutionized the practice of dermatology.“ (Clin Dermatol. 1989;7[3]38-47).
These key drugs comprised:
- Quinacrine was introduced in 1932 by Walter Kikuth, MD, as an antimalarial drug. But it was not until 1940, that A.J. Prokoptchouksi, MD, reported on its effectiveness 35 patients with lupus erythematosus.
- Para-aminobenzoic acid (PABA) came into prominence in 1942, when Stephen Rothman, MD, and Jack Rubin, MD, at the University of Chicago, published the results of their experiment, showing that when PABA was incorporated in an ointment base and applied to the skin, it could protect against sunburn.
- Dapsone. The effectiveness of sulfapyridine was demonstrated in 1947 by M.J. Costello, MD, who reported its usefulness in a patient with dermatitis herpetiformis, which he believed to be caused by a bacterial allergy. Sulfapyridine controlled the disease, but gastrointestinal intolerance and sulfonamide sensitivity were side effects. Ultimately, in 1951, Theodore Cornbleet, MD, introduced the use of sulfoxones in his article entitled “Sulfoxone (diasones) sodium for dermatitis herpetiformis,” considered more effective than sulfapyridine. Dapsone is the active principal ingredient.
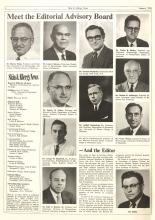
- Hydrocortisone. In August 1952, Marion Sulzberger, MD, and Victor H. Witten, MD (both members of the first Skin & Allergy News editorial advisory board), described use of Compound F (17-hydroxycorticosterone-21-acetate, hydrocortisone) in seven cases of atopic dermatitis and one case of discoid or subacute lupus erythematosus, reporting improvement in all of these cases.
- Benzoyl peroxide. Canadian dermatologist William E. Pace, MD, reported on the beneficial effects of benzoyl peroxide on acne in 1953. The product had originally been used for chronic Staphylococcus aureus folliculitis of the beard.
- Griseofulvin, a metabolic byproduct of a number of species of Penicillium, was first isolated in 1939. But in 1958, Harvey Blank, MD, at the University of Miami (also on the first Skin & Allergy News editorial advisory board), and Stanley I. Cullen, MD, administered the drug to a patient with Trichophyton rubrum granuloma, in the first human trial. In 1959, they reported the drug’s benefits on 31 patients with various fungal infections.
- Methotrexate. In 1951, R. Gubner, MD, and colleagues noticed the rapid clearing of skin lesions in a patient with rheumatoid arthritis who had been treated with the folic acid antagonist, aminopterin. And in 1958, W.F. Edmundson, MD, and W.B. Guy, MD, reported on the oral use of the folic acid antagonist, methotrexate. This was followed by multiple reports on the successful use of methotrexate in psoriasis.
- 5-fluorouracil (5-FU). In 1957, 5-FU, an antimetabolite of uracil, was first synthesized. In 1962, G. Falkson, MD, and E.J. Schulz, MD, reported on skin changes observed in 85 patients being treated with systemic 5-FU for advanced carcinomatosis. They found that 31 of the 85 patients developed sensitivity to sunlight and subsequent disappearance of actinic keratoses in these same patients.
Technology in skin care also was developing in the era just before the launch of Skin & Allergy News. For example, Leon Goldman, MD, then chairman of the department of dermatology at the University of Cincinnati, was the first physician to use a laser for tattoo removal. His publication in 1965 helped to solidify its use, leading him to be “regarded by many in the dermatologic community as the ‘godfather of lasers in medicine and surgery’ ” (Clin Dermatol. 2007;25:434-42).
So, by 1970, dermatology as a field had established itself fully with a strong societal infrastructure, a vibrant base of journals and books, and an evolving set of scientific and technical tools. The launch of Skin & Allergy News (now Dermatology News) that year would chronicle dermatology’s commitment to the development of new therapeutics and technologies in service of patient needs – the stories of which would grace the newspaper’s pages for 5 decades and counting.
As Dermatology News (formerly Skin and Allergy News) reaches its 50th-year milestone, a reflection on the history of the discipline, especially in the United States, up to the time of the launch of this publication is in order. Such an overview must, of course, be cursory in this context. Yet, for those who want to learn more, a large body of historical references and research has been created to fill in the gaps, as modern dermatology has always been cognizant of the importance of its history, with many individuals and groups drawn to the subject.
Two excellent sources for the history of the field can be found in work by William Allen Pusey, MD (1865-1940), and Herbert Rattner, MD (1900-1962), “The History of Dermatology” published in 1933 and research by members of the History of Dermatology Society, founded in 1973 in New York.
Modern dermatology
The development of the field of modern dermatology can be traced back to the early to mid-19th century. During the first half of the 19th century, England and France dominated the study of dermatology, but by the middle of the century, the German revolution in microparasitology shifted that focus “with remarkable German discoveries,” according to Bernard S. Potter, MD, in his review of bibliographic landmarks of the history of dermatology (J Am Acad Dermatol 2003;48:919-32). For example, Johann Lucas Schoenlein (1793-1864) in 1839 discovered the fungal origin of favus, and in 1841 Jacob Henle (1809-1885) discovered Demodex folliculorum. Karl Ferdinand Eichstedt (1816-1892) in 1846 followed with the discovery of the causative agent of pityriasis versicolor, and Friedrich Wilhelm Felix von Barensprung (1822-1864) in 1862 coined the term erythrasma and named the organism responsible for this condition Microsporum minutissimum.
Dr. Potter described how American dermatology originated in New York City in 1836 when Henry Daggett Bulkley, MD, (1803-1872) opened the first dispensary for skin diseases, the Broome Street Infirmary for Diseases of the Skin, thus creating the first institution in the United States for the treatment of cutaneous disease. As the first American dermatologist, he was also the first in the United States to lecture on and to exclusively practice dermatology.
The rise of interest in the importance of dermatology led to the organization of the early American Dermatological Association in 1886.
However, the state of dermatology as a science in the 19th century was not always looked upon favorably, even by its practitioners, especially in the United States. In 1871, in a “Review on Modern Dermatology,” given as a series of lectures on skin disease at Harvard University, James C. White, MD (1833-1916) of Massachusetts General Hospital, stated that: “Were the literature of skin diseases previous to that of the last half-century absolutely annihilated, and with it, the influence it has exercised upon that of the present day, it would be an immense gain to dermatology, although much of real value would perish.” He lamented that America had contributed little so far to the study of dermatology, and that the discipline was only taught in some of its largest schools, and he urged that this be changed. He also lamented that The American Journal of Syphilography and Dermatology, established the year before, had so far proved itself heavy on syphilis, but light on dermatology, a situation he also hoped would change dramatically.
By the late-19th century, the conviction that diseases of the skin needed to be connected to the overall metabolism and physiology of the patient as a whole was becoming more mainstream.
“It has been, and still is, too much the custom to study diseases of the skin in the light of pathological pictures, to name the local manifestation and to so label it as disease. It is much easier to give the disease name and to label it than it is to comprehend the process at work. The former is comparatively unimportant for the patient, the latter point upon which recovery may depend. The nature and meaning of the process in connection with the cutaneous symptoms has not received enough attention, and I believe this to be one reason why the treatment of many of these diseases in the past has been so notoriously unsatisfactory,” Louis A. Duhring, MD (1845-1913) chided his colleagues in the Section of Dermatology and Syphilography, at the Forty-fourth Annual Meeting of the American Medical Association in 1894. (collections.nlm.nih.gov/ext/dw/101489447/PDF/101489447.pdf)
In the early-20th century, German dermatology influenced American dermatology more than any other, according to Karl Holubar, MD, of the Institute for the History of Medicine, University of Vienna, in his lecture on the history of European dermatopathology.
He stated that, with regard to dermatopathology, it was Oscar Gans, MD (1888-1983) who brought the latest knowledge into the United States by delivering a series of lectures at Mayo Clinic in the late 1920s upon the invitation of Paul A. O’Leary, MD, (1891-1955) who then headed the Mayo section of dermatology.
By the 1930s, a flurry of organizational activity overtook American dermatology. In 1932, the American Board of Dermatology was established, with its first exams given in 1933 (20 students passed, 7 failed). The Society for Investigative Dermatology was founded in 1937, and the American Academy of Dermatology and Syphilology (now the American Academy of Dermatology), founded in 1938.
The 1930s also saw a major influx of German and other European Jews fleeing Nazi oppression who would forever change the face of American dermatology. “Between 1933 and 1938, a series of repressive measures eliminated them from the practice of medicine in Germany and other countries. Although some died in concentration camps and others committed suicide, many were able to emigrate from Europe. Dermatology in the United States particularly benefited from the influx of several stellar Jewish dermatologists who were major contributors to the subsequent flowering of academic dermatology in the United States” (JAMA Derm. 2013;149[9]:1090-4).
“The overtures of the holocaust and the rising power of Hitler in Europe finally brought over to the United States the flower of dermatologists and investigators of the German School, e.g., Alexander and Walter Lever, Felix and Hermann Pinkus, the Epsteins, Erich Auerbach, Stephen Rothman, to name just a few. With this exodus and transfer of brain power, Europe lost its leading role to never again regain it,” according to Dr. Holubar. Walter F. Lever, MD (1909-1992) was especially well-known for his landmark textbook on dermatology, “Histopathology of the Skin,” published in the United States in 1949.
The therapeutic era
Throughout the 19th century, a variety of soaps and patent medicines were touted as cure-alls for a host of skin diseases. Other than their benefits to surface cleanliness and their antiseptic properties, however, they were of little effect.
It wasn’t until the 20th century that truly effective therapeutics entered the dermatologic pharmacopoeia. In their 1989 review, Diane Quintal, MD, and Robert Jackson, MD, discussed the origins of the most important of these drugs and pointed out that, “Until this century, the essence of dermatology resided in the realm of morphology. Early contributors largely confined their activities to the classification of skin diseases and to the elaboration of clinical dermatologic entities based on morphologic features. ... but “in the last 50 years, there have been significant scientific discoveries in the field of therapeutics that have revolutionized the practice of dermatology.“ (Clin Dermatol. 1989;7[3]38-47).
These key drugs comprised:
- Quinacrine was introduced in 1932 by Walter Kikuth, MD, as an antimalarial drug. But it was not until 1940, that A.J. Prokoptchouksi, MD, reported on its effectiveness 35 patients with lupus erythematosus.
- Para-aminobenzoic acid (PABA) came into prominence in 1942, when Stephen Rothman, MD, and Jack Rubin, MD, at the University of Chicago, published the results of their experiment, showing that when PABA was incorporated in an ointment base and applied to the skin, it could protect against sunburn.
- Dapsone. The effectiveness of sulfapyridine was demonstrated in 1947 by M.J. Costello, MD, who reported its usefulness in a patient with dermatitis herpetiformis, which he believed to be caused by a bacterial allergy. Sulfapyridine controlled the disease, but gastrointestinal intolerance and sulfonamide sensitivity were side effects. Ultimately, in 1951, Theodore Cornbleet, MD, introduced the use of sulfoxones in his article entitled “Sulfoxone (diasones) sodium for dermatitis herpetiformis,” considered more effective than sulfapyridine. Dapsone is the active principal ingredient.
- Hydrocortisone. In August 1952, Marion Sulzberger, MD, and Victor H. Witten, MD (both members of the first Skin & Allergy News editorial advisory board), described use of Compound F (17-hydroxycorticosterone-21-acetate, hydrocortisone) in seven cases of atopic dermatitis and one case of discoid or subacute lupus erythematosus, reporting improvement in all of these cases.
- Benzoyl peroxide. Canadian dermatologist William E. Pace, MD, reported on the beneficial effects of benzoyl peroxide on acne in 1953. The product had originally been used for chronic Staphylococcus aureus folliculitis of the beard.
- Griseofulvin, a metabolic byproduct of a number of species of Penicillium, was first isolated in 1939. But in 1958, Harvey Blank, MD, at the University of Miami (also on the first Skin & Allergy News editorial advisory board), and Stanley I. Cullen, MD, administered the drug to a patient with Trichophyton rubrum granuloma, in the first human trial. In 1959, they reported the drug’s benefits on 31 patients with various fungal infections.
- Methotrexate. In 1951, R. Gubner, MD, and colleagues noticed the rapid clearing of skin lesions in a patient with rheumatoid arthritis who had been treated with the folic acid antagonist, aminopterin. And in 1958, W.F. Edmundson, MD, and W.B. Guy, MD, reported on the oral use of the folic acid antagonist, methotrexate. This was followed by multiple reports on the successful use of methotrexate in psoriasis.
- 5-fluorouracil (5-FU). In 1957, 5-FU, an antimetabolite of uracil, was first synthesized. In 1962, G. Falkson, MD, and E.J. Schulz, MD, reported on skin changes observed in 85 patients being treated with systemic 5-FU for advanced carcinomatosis. They found that 31 of the 85 patients developed sensitivity to sunlight and subsequent disappearance of actinic keratoses in these same patients.
Technology in skin care also was developing in the era just before the launch of Skin & Allergy News. For example, Leon Goldman, MD, then chairman of the department of dermatology at the University of Cincinnati, was the first physician to use a laser for tattoo removal. His publication in 1965 helped to solidify its use, leading him to be “regarded by many in the dermatologic community as the ‘godfather of lasers in medicine and surgery’ ” (Clin Dermatol. 2007;25:434-42).
So, by 1970, dermatology as a field had established itself fully with a strong societal infrastructure, a vibrant base of journals and books, and an evolving set of scientific and technical tools. The launch of Skin & Allergy News (now Dermatology News) that year would chronicle dermatology’s commitment to the development of new therapeutics and technologies in service of patient needs – the stories of which would grace the newspaper’s pages for 5 decades and counting.
As Dermatology News (formerly Skin and Allergy News) reaches its 50th-year milestone, a reflection on the history of the discipline, especially in the United States, up to the time of the launch of this publication is in order. Such an overview must, of course, be cursory in this context. Yet, for those who want to learn more, a large body of historical references and research has been created to fill in the gaps, as modern dermatology has always been cognizant of the importance of its history, with many individuals and groups drawn to the subject.
Two excellent sources for the history of the field can be found in work by William Allen Pusey, MD (1865-1940), and Herbert Rattner, MD (1900-1962), “The History of Dermatology” published in 1933 and research by members of the History of Dermatology Society, founded in 1973 in New York.
Modern dermatology
The development of the field of modern dermatology can be traced back to the early to mid-19th century. During the first half of the 19th century, England and France dominated the study of dermatology, but by the middle of the century, the German revolution in microparasitology shifted that focus “with remarkable German discoveries,” according to Bernard S. Potter, MD, in his review of bibliographic landmarks of the history of dermatology (J Am Acad Dermatol 2003;48:919-32). For example, Johann Lucas Schoenlein (1793-1864) in 1839 discovered the fungal origin of favus, and in 1841 Jacob Henle (1809-1885) discovered Demodex folliculorum. Karl Ferdinand Eichstedt (1816-1892) in 1846 followed with the discovery of the causative agent of pityriasis versicolor, and Friedrich Wilhelm Felix von Barensprung (1822-1864) in 1862 coined the term erythrasma and named the organism responsible for this condition Microsporum minutissimum.
Dr. Potter described how American dermatology originated in New York City in 1836 when Henry Daggett Bulkley, MD, (1803-1872) opened the first dispensary for skin diseases, the Broome Street Infirmary for Diseases of the Skin, thus creating the first institution in the United States for the treatment of cutaneous disease. As the first American dermatologist, he was also the first in the United States to lecture on and to exclusively practice dermatology.
The rise of interest in the importance of dermatology led to the organization of the early American Dermatological Association in 1886.
However, the state of dermatology as a science in the 19th century was not always looked upon favorably, even by its practitioners, especially in the United States. In 1871, in a “Review on Modern Dermatology,” given as a series of lectures on skin disease at Harvard University, James C. White, MD (1833-1916) of Massachusetts General Hospital, stated that: “Were the literature of skin diseases previous to that of the last half-century absolutely annihilated, and with it, the influence it has exercised upon that of the present day, it would be an immense gain to dermatology, although much of real value would perish.” He lamented that America had contributed little so far to the study of dermatology, and that the discipline was only taught in some of its largest schools, and he urged that this be changed. He also lamented that The American Journal of Syphilography and Dermatology, established the year before, had so far proved itself heavy on syphilis, but light on dermatology, a situation he also hoped would change dramatically.
By the late-19th century, the conviction that diseases of the skin needed to be connected to the overall metabolism and physiology of the patient as a whole was becoming more mainstream.
“It has been, and still is, too much the custom to study diseases of the skin in the light of pathological pictures, to name the local manifestation and to so label it as disease. It is much easier to give the disease name and to label it than it is to comprehend the process at work. The former is comparatively unimportant for the patient, the latter point upon which recovery may depend. The nature and meaning of the process in connection with the cutaneous symptoms has not received enough attention, and I believe this to be one reason why the treatment of many of these diseases in the past has been so notoriously unsatisfactory,” Louis A. Duhring, MD (1845-1913) chided his colleagues in the Section of Dermatology and Syphilography, at the Forty-fourth Annual Meeting of the American Medical Association in 1894. (collections.nlm.nih.gov/ext/dw/101489447/PDF/101489447.pdf)
In the early-20th century, German dermatology influenced American dermatology more than any other, according to Karl Holubar, MD, of the Institute for the History of Medicine, University of Vienna, in his lecture on the history of European dermatopathology.
He stated that, with regard to dermatopathology, it was Oscar Gans, MD (1888-1983) who brought the latest knowledge into the United States by delivering a series of lectures at Mayo Clinic in the late 1920s upon the invitation of Paul A. O’Leary, MD, (1891-1955) who then headed the Mayo section of dermatology.
By the 1930s, a flurry of organizational activity overtook American dermatology. In 1932, the American Board of Dermatology was established, with its first exams given in 1933 (20 students passed, 7 failed). The Society for Investigative Dermatology was founded in 1937, and the American Academy of Dermatology and Syphilology (now the American Academy of Dermatology), founded in 1938.
The 1930s also saw a major influx of German and other European Jews fleeing Nazi oppression who would forever change the face of American dermatology. “Between 1933 and 1938, a series of repressive measures eliminated them from the practice of medicine in Germany and other countries. Although some died in concentration camps and others committed suicide, many were able to emigrate from Europe. Dermatology in the United States particularly benefited from the influx of several stellar Jewish dermatologists who were major contributors to the subsequent flowering of academic dermatology in the United States” (JAMA Derm. 2013;149[9]:1090-4).
“The overtures of the holocaust and the rising power of Hitler in Europe finally brought over to the United States the flower of dermatologists and investigators of the German School, e.g., Alexander and Walter Lever, Felix and Hermann Pinkus, the Epsteins, Erich Auerbach, Stephen Rothman, to name just a few. With this exodus and transfer of brain power, Europe lost its leading role to never again regain it,” according to Dr. Holubar. Walter F. Lever, MD (1909-1992) was especially well-known for his landmark textbook on dermatology, “Histopathology of the Skin,” published in the United States in 1949.
The therapeutic era
Throughout the 19th century, a variety of soaps and patent medicines were touted as cure-alls for a host of skin diseases. Other than their benefits to surface cleanliness and their antiseptic properties, however, they were of little effect.
It wasn’t until the 20th century that truly effective therapeutics entered the dermatologic pharmacopoeia. In their 1989 review, Diane Quintal, MD, and Robert Jackson, MD, discussed the origins of the most important of these drugs and pointed out that, “Until this century, the essence of dermatology resided in the realm of morphology. Early contributors largely confined their activities to the classification of skin diseases and to the elaboration of clinical dermatologic entities based on morphologic features. ... but “in the last 50 years, there have been significant scientific discoveries in the field of therapeutics that have revolutionized the practice of dermatology.“ (Clin Dermatol. 1989;7[3]38-47).
These key drugs comprised:
- Quinacrine was introduced in 1932 by Walter Kikuth, MD, as an antimalarial drug. But it was not until 1940, that A.J. Prokoptchouksi, MD, reported on its effectiveness 35 patients with lupus erythematosus.
- Para-aminobenzoic acid (PABA) came into prominence in 1942, when Stephen Rothman, MD, and Jack Rubin, MD, at the University of Chicago, published the results of their experiment, showing that when PABA was incorporated in an ointment base and applied to the skin, it could protect against sunburn.
- Dapsone. The effectiveness of sulfapyridine was demonstrated in 1947 by M.J. Costello, MD, who reported its usefulness in a patient with dermatitis herpetiformis, which he believed to be caused by a bacterial allergy. Sulfapyridine controlled the disease, but gastrointestinal intolerance and sulfonamide sensitivity were side effects. Ultimately, in 1951, Theodore Cornbleet, MD, introduced the use of sulfoxones in his article entitled “Sulfoxone (diasones) sodium for dermatitis herpetiformis,” considered more effective than sulfapyridine. Dapsone is the active principal ingredient.
- Hydrocortisone. In August 1952, Marion Sulzberger, MD, and Victor H. Witten, MD (both members of the first Skin & Allergy News editorial advisory board), described use of Compound F (17-hydroxycorticosterone-21-acetate, hydrocortisone) in seven cases of atopic dermatitis and one case of discoid or subacute lupus erythematosus, reporting improvement in all of these cases.
- Benzoyl peroxide. Canadian dermatologist William E. Pace, MD, reported on the beneficial effects of benzoyl peroxide on acne in 1953. The product had originally been used for chronic Staphylococcus aureus folliculitis of the beard.
- Griseofulvin, a metabolic byproduct of a number of species of Penicillium, was first isolated in 1939. But in 1958, Harvey Blank, MD, at the University of Miami (also on the first Skin & Allergy News editorial advisory board), and Stanley I. Cullen, MD, administered the drug to a patient with Trichophyton rubrum granuloma, in the first human trial. In 1959, they reported the drug’s benefits on 31 patients with various fungal infections.
- Methotrexate. In 1951, R. Gubner, MD, and colleagues noticed the rapid clearing of skin lesions in a patient with rheumatoid arthritis who had been treated with the folic acid antagonist, aminopterin. And in 1958, W.F. Edmundson, MD, and W.B. Guy, MD, reported on the oral use of the folic acid antagonist, methotrexate. This was followed by multiple reports on the successful use of methotrexate in psoriasis.
- 5-fluorouracil (5-FU). In 1957, 5-FU, an antimetabolite of uracil, was first synthesized. In 1962, G. Falkson, MD, and E.J. Schulz, MD, reported on skin changes observed in 85 patients being treated with systemic 5-FU for advanced carcinomatosis. They found that 31 of the 85 patients developed sensitivity to sunlight and subsequent disappearance of actinic keratoses in these same patients.
Technology in skin care also was developing in the era just before the launch of Skin & Allergy News. For example, Leon Goldman, MD, then chairman of the department of dermatology at the University of Cincinnati, was the first physician to use a laser for tattoo removal. His publication in 1965 helped to solidify its use, leading him to be “regarded by many in the dermatologic community as the ‘godfather of lasers in medicine and surgery’ ” (Clin Dermatol. 2007;25:434-42).
So, by 1970, dermatology as a field had established itself fully with a strong societal infrastructure, a vibrant base of journals and books, and an evolving set of scientific and technical tools. The launch of Skin & Allergy News (now Dermatology News) that year would chronicle dermatology’s commitment to the development of new therapeutics and technologies in service of patient needs – the stories of which would grace the newspaper’s pages for 5 decades and counting.
IHS and AAP Issue Recommendations on Prenatal Exposure to Opioids
The opioid crisis has hit the American Indian and Alaska Native (AI/AN) communities particularly hard, and “[i]nfants born withdrawing from opioids represent one of the most heartbreaking aspects,” says US Department of Health and Human Services Secretary Alex Azar.
Intrauterine exposure to opioids can induce symptoms that may result in spontaneous abortion, placental injury, and reduced nutrients for the fetus. Moreover, as many as 55% to 94% of infants prenatally exposed to opioids develop neonatal opioid withdrawal syndrome (NOWS), which can vary in severity from mild to life-threatening.
AI/AN women face significant barriers to obtaining appropriate care for substance use disorders, which may delay early interventions for the newborn’s health, said Shaquita Bell, MD, FAAP, chair of the American Academy of Pediatrics (AAP) Committee on Native American Child Health. The Indian Health Service (IHS) and the AAP have recently released clinical recommendations on NOWS for IHS, tribal, and urban Indian organization health care facilities.
The recommendations describe supportive, culturally appropriate standards of care for screening, diagnosing, and treating pregnant mothers and infants affected by prenatal opioid exposure. Management of NOWS begins with identifying women at risk, says the multidisciplinary panel responsible for the recommendations. Among other things, the experts advise screening a pregnant woman at the initial presentation for risk of substance use disorder, as well as for prescription opioid use for treatment of pain, and other risk factors for NOWS.
The panel notes that early application of nonpharmacologic treatment and support can reduce the need for pharmacologic treatment and transfer. Patient education should be a “key component of every prenatal care visit,” the panel says, provided in a nonjudgmental, culturally competent way to increase engagement, involving the partner and other family members if possible. Discussion topics may include the physical effects of continued substance use on both the woman and her infant, but also may include social and legal consequences of continued use.
The recommendations are also a companion guide to clinical recommendations for improving care of AI/AN pregnant women and women of childbearing age with opioid use disorder, which were announced by IHS and the American College of Obstetricians and Gynecologists in March 2019.
The opioid crisis has hit the American Indian and Alaska Native (AI/AN) communities particularly hard, and “[i]nfants born withdrawing from opioids represent one of the most heartbreaking aspects,” says US Department of Health and Human Services Secretary Alex Azar.
Intrauterine exposure to opioids can induce symptoms that may result in spontaneous abortion, placental injury, and reduced nutrients for the fetus. Moreover, as many as 55% to 94% of infants prenatally exposed to opioids develop neonatal opioid withdrawal syndrome (NOWS), which can vary in severity from mild to life-threatening.
AI/AN women face significant barriers to obtaining appropriate care for substance use disorders, which may delay early interventions for the newborn’s health, said Shaquita Bell, MD, FAAP, chair of the American Academy of Pediatrics (AAP) Committee on Native American Child Health. The Indian Health Service (IHS) and the AAP have recently released clinical recommendations on NOWS for IHS, tribal, and urban Indian organization health care facilities.
The recommendations describe supportive, culturally appropriate standards of care for screening, diagnosing, and treating pregnant mothers and infants affected by prenatal opioid exposure. Management of NOWS begins with identifying women at risk, says the multidisciplinary panel responsible for the recommendations. Among other things, the experts advise screening a pregnant woman at the initial presentation for risk of substance use disorder, as well as for prescription opioid use for treatment of pain, and other risk factors for NOWS.
The panel notes that early application of nonpharmacologic treatment and support can reduce the need for pharmacologic treatment and transfer. Patient education should be a “key component of every prenatal care visit,” the panel says, provided in a nonjudgmental, culturally competent way to increase engagement, involving the partner and other family members if possible. Discussion topics may include the physical effects of continued substance use on both the woman and her infant, but also may include social and legal consequences of continued use.
The recommendations are also a companion guide to clinical recommendations for improving care of AI/AN pregnant women and women of childbearing age with opioid use disorder, which were announced by IHS and the American College of Obstetricians and Gynecologists in March 2019.
The opioid crisis has hit the American Indian and Alaska Native (AI/AN) communities particularly hard, and “[i]nfants born withdrawing from opioids represent one of the most heartbreaking aspects,” says US Department of Health and Human Services Secretary Alex Azar.
Intrauterine exposure to opioids can induce symptoms that may result in spontaneous abortion, placental injury, and reduced nutrients for the fetus. Moreover, as many as 55% to 94% of infants prenatally exposed to opioids develop neonatal opioid withdrawal syndrome (NOWS), which can vary in severity from mild to life-threatening.
AI/AN women face significant barriers to obtaining appropriate care for substance use disorders, which may delay early interventions for the newborn’s health, said Shaquita Bell, MD, FAAP, chair of the American Academy of Pediatrics (AAP) Committee on Native American Child Health. The Indian Health Service (IHS) and the AAP have recently released clinical recommendations on NOWS for IHS, tribal, and urban Indian organization health care facilities.
The recommendations describe supportive, culturally appropriate standards of care for screening, diagnosing, and treating pregnant mothers and infants affected by prenatal opioid exposure. Management of NOWS begins with identifying women at risk, says the multidisciplinary panel responsible for the recommendations. Among other things, the experts advise screening a pregnant woman at the initial presentation for risk of substance use disorder, as well as for prescription opioid use for treatment of pain, and other risk factors for NOWS.
The panel notes that early application of nonpharmacologic treatment and support can reduce the need for pharmacologic treatment and transfer. Patient education should be a “key component of every prenatal care visit,” the panel says, provided in a nonjudgmental, culturally competent way to increase engagement, involving the partner and other family members if possible. Discussion topics may include the physical effects of continued substance use on both the woman and her infant, but also may include social and legal consequences of continued use.
The recommendations are also a companion guide to clinical recommendations for improving care of AI/AN pregnant women and women of childbearing age with opioid use disorder, which were announced by IHS and the American College of Obstetricians and Gynecologists in March 2019.
Sevuparin failed for acute VOC in sickle cell, but may have preventive potential
ORLANDO – Sevuparin, a novel nonanticoagulant heparinoid drug, showed no efficacy for acute vaso-occlusive crisis (VOC) in patients with sickle cell disease (SCD) in the randomized, controlled, phase 2 TVOC01 trial, but its promising safety and broad mechanism of action warrant further exploration in the prodromal VOC setting, according to investigators.
Time to VOC resolution – the primary study endpoint – was similar at about 168 hours in 71 hospitalized patients randomized to receive sevuparin and in 76 who received placebo (intention-to-treat hazard ratio, 0.89), Bart J. Biemond, MD, explained during a presentation of the findings at the annual meeting of the American Society of Hematology.
A per-protocol analysis based on the 69 and 75 patients dosed in the treatment and placebo arms, respectively, showed a similar result (HR, 0.81), said Dr. Biemond of the department of clinical hematology, Amsterdam UMC, Academic Medical Center, the Netherlands.
Secondary endpoints, including mean change in pain intensity from baseline on a visual analogue scale (VAS), duration of severest pain measured as time to achieve a 30% reduction in VAS score from baseline, and cumulative use of parenteral opioids, also did not differ between the treatment and placebo arms, he added.
Patients in the global, double-blind, multicenter trial were aged 12-50 years (median, 22 years) with any type of SCD. They were enrolled from 16 sites in 7 countries to receive a loading dose of 3 mg/kg of sevuparin and continuous 18 mg/kg per day infusions or placebo. Patients in both arms also received standard-of-care and parenteral opioid therapy.
The groups were generally balanced with respect to demographic and baseline characteristics, Dr. Biemond said, noting that the treatment was safe: No serious adverse events occurred, and any mild-to-moderate adverse events were transient.
The findings were disappointing given the lack of approved treatment options other than pain management for acute VOC in hospitalized patients with SCD, and they were somewhat surprising given that preclinical and clinical data in recent years have demonstrated that “you can actually prevent those crises by antiadhesive strategies,” he said.
“So we hypothesized that, if you perform such an antiadhesive strategy in a patient already having a crisis and admitted in the hospital, you may shorten their period of admission and perhaps also shorten the severity of their pain,” he said.
In fact, a single-center, randomized, controlled trial conducted by Qari et al. in 2007 (Thromb Haemost. 2007 Aug;98[2]:392-6) showed that full-dose tinzaparin reduced pain severity and duration of admission among sickle cell patients with acute VOC – perhaps because of the antiadhesive properties of heparin – but that study was never repeated, Dr. Biemond said, noting that those antiadhesive properties have been well documented in animal studies.
“Heparin is able to inhibit P-selectin, L-selectin, thrombospondin, fibronectin, and von Willebrand activity, which are all involved in vaso-occlusion in patients with sickle cell disease, and very likely also involved during a vaso-occlusive crisis,” he explained, adding that sevuparin, a low-molecular-weight heparin without functional antithrombin binding domain, seemed to be a good candidate for testing that hypothesis.
“It has no anticoagulant effects on factor Xa and IIa,” he said. “It retains, however, its antiadhesive and antiaggregation properties.”
Since it has no anticoagulation activity, it can be dosed at up to 20-fold the therapeutic dose of low-molecular-weight heparin to optimize the antiadhesive effects, he noted.
However, the data indicate that “antiadhesive therapies are clearly not effective in patients with vaso-occlusive crisis,” he said, noting that this was also affirmed by a similar 2019 study of the investigational panselectin inhibitor rivipansel, as reported in a Pfizer press release.
Intriguingly, the difference between the current study and the 2007 study by Qari et al. raises questions about whether anticoagulation, rather than antiadhesion, helped resolve VOC in that study, he said, noting that future studies should focus on whether that is the case.
As for the role of antiadhesive therapy, the mode of action of sevuparin and the current findings taken together suggest that future studies should also assess whether it can be used to prevent VOC.
“Perhaps sevuparin could be administered to patients in a prodromal phase – just before a real vaso-occlusive crisis appears – to prevent such a crisis from happening,” he said. “It would be interesting to use the drug that way.”
Dr. Biemond reported research funding from Sanquin and honoraria from Novartis and GBT.
SOURCE: Biemond B et al. ASH 2019, Abstract 614.
ORLANDO – Sevuparin, a novel nonanticoagulant heparinoid drug, showed no efficacy for acute vaso-occlusive crisis (VOC) in patients with sickle cell disease (SCD) in the randomized, controlled, phase 2 TVOC01 trial, but its promising safety and broad mechanism of action warrant further exploration in the prodromal VOC setting, according to investigators.
Time to VOC resolution – the primary study endpoint – was similar at about 168 hours in 71 hospitalized patients randomized to receive sevuparin and in 76 who received placebo (intention-to-treat hazard ratio, 0.89), Bart J. Biemond, MD, explained during a presentation of the findings at the annual meeting of the American Society of Hematology.
A per-protocol analysis based on the 69 and 75 patients dosed in the treatment and placebo arms, respectively, showed a similar result (HR, 0.81), said Dr. Biemond of the department of clinical hematology, Amsterdam UMC, Academic Medical Center, the Netherlands.
Secondary endpoints, including mean change in pain intensity from baseline on a visual analogue scale (VAS), duration of severest pain measured as time to achieve a 30% reduction in VAS score from baseline, and cumulative use of parenteral opioids, also did not differ between the treatment and placebo arms, he added.
Patients in the global, double-blind, multicenter trial were aged 12-50 years (median, 22 years) with any type of SCD. They were enrolled from 16 sites in 7 countries to receive a loading dose of 3 mg/kg of sevuparin and continuous 18 mg/kg per day infusions or placebo. Patients in both arms also received standard-of-care and parenteral opioid therapy.
The groups were generally balanced with respect to demographic and baseline characteristics, Dr. Biemond said, noting that the treatment was safe: No serious adverse events occurred, and any mild-to-moderate adverse events were transient.
The findings were disappointing given the lack of approved treatment options other than pain management for acute VOC in hospitalized patients with SCD, and they were somewhat surprising given that preclinical and clinical data in recent years have demonstrated that “you can actually prevent those crises by antiadhesive strategies,” he said.
“So we hypothesized that, if you perform such an antiadhesive strategy in a patient already having a crisis and admitted in the hospital, you may shorten their period of admission and perhaps also shorten the severity of their pain,” he said.
In fact, a single-center, randomized, controlled trial conducted by Qari et al. in 2007 (Thromb Haemost. 2007 Aug;98[2]:392-6) showed that full-dose tinzaparin reduced pain severity and duration of admission among sickle cell patients with acute VOC – perhaps because of the antiadhesive properties of heparin – but that study was never repeated, Dr. Biemond said, noting that those antiadhesive properties have been well documented in animal studies.
“Heparin is able to inhibit P-selectin, L-selectin, thrombospondin, fibronectin, and von Willebrand activity, which are all involved in vaso-occlusion in patients with sickle cell disease, and very likely also involved during a vaso-occlusive crisis,” he explained, adding that sevuparin, a low-molecular-weight heparin without functional antithrombin binding domain, seemed to be a good candidate for testing that hypothesis.
“It has no anticoagulant effects on factor Xa and IIa,” he said. “It retains, however, its antiadhesive and antiaggregation properties.”
Since it has no anticoagulation activity, it can be dosed at up to 20-fold the therapeutic dose of low-molecular-weight heparin to optimize the antiadhesive effects, he noted.
However, the data indicate that “antiadhesive therapies are clearly not effective in patients with vaso-occlusive crisis,” he said, noting that this was also affirmed by a similar 2019 study of the investigational panselectin inhibitor rivipansel, as reported in a Pfizer press release.
Intriguingly, the difference between the current study and the 2007 study by Qari et al. raises questions about whether anticoagulation, rather than antiadhesion, helped resolve VOC in that study, he said, noting that future studies should focus on whether that is the case.
As for the role of antiadhesive therapy, the mode of action of sevuparin and the current findings taken together suggest that future studies should also assess whether it can be used to prevent VOC.
“Perhaps sevuparin could be administered to patients in a prodromal phase – just before a real vaso-occlusive crisis appears – to prevent such a crisis from happening,” he said. “It would be interesting to use the drug that way.”
Dr. Biemond reported research funding from Sanquin and honoraria from Novartis and GBT.
SOURCE: Biemond B et al. ASH 2019, Abstract 614.
ORLANDO – Sevuparin, a novel nonanticoagulant heparinoid drug, showed no efficacy for acute vaso-occlusive crisis (VOC) in patients with sickle cell disease (SCD) in the randomized, controlled, phase 2 TVOC01 trial, but its promising safety and broad mechanism of action warrant further exploration in the prodromal VOC setting, according to investigators.
Time to VOC resolution – the primary study endpoint – was similar at about 168 hours in 71 hospitalized patients randomized to receive sevuparin and in 76 who received placebo (intention-to-treat hazard ratio, 0.89), Bart J. Biemond, MD, explained during a presentation of the findings at the annual meeting of the American Society of Hematology.
A per-protocol analysis based on the 69 and 75 patients dosed in the treatment and placebo arms, respectively, showed a similar result (HR, 0.81), said Dr. Biemond of the department of clinical hematology, Amsterdam UMC, Academic Medical Center, the Netherlands.
Secondary endpoints, including mean change in pain intensity from baseline on a visual analogue scale (VAS), duration of severest pain measured as time to achieve a 30% reduction in VAS score from baseline, and cumulative use of parenteral opioids, also did not differ between the treatment and placebo arms, he added.
Patients in the global, double-blind, multicenter trial were aged 12-50 years (median, 22 years) with any type of SCD. They were enrolled from 16 sites in 7 countries to receive a loading dose of 3 mg/kg of sevuparin and continuous 18 mg/kg per day infusions or placebo. Patients in both arms also received standard-of-care and parenteral opioid therapy.
The groups were generally balanced with respect to demographic and baseline characteristics, Dr. Biemond said, noting that the treatment was safe: No serious adverse events occurred, and any mild-to-moderate adverse events were transient.
The findings were disappointing given the lack of approved treatment options other than pain management for acute VOC in hospitalized patients with SCD, and they were somewhat surprising given that preclinical and clinical data in recent years have demonstrated that “you can actually prevent those crises by antiadhesive strategies,” he said.
“So we hypothesized that, if you perform such an antiadhesive strategy in a patient already having a crisis and admitted in the hospital, you may shorten their period of admission and perhaps also shorten the severity of their pain,” he said.
In fact, a single-center, randomized, controlled trial conducted by Qari et al. in 2007 (Thromb Haemost. 2007 Aug;98[2]:392-6) showed that full-dose tinzaparin reduced pain severity and duration of admission among sickle cell patients with acute VOC – perhaps because of the antiadhesive properties of heparin – but that study was never repeated, Dr. Biemond said, noting that those antiadhesive properties have been well documented in animal studies.
“Heparin is able to inhibit P-selectin, L-selectin, thrombospondin, fibronectin, and von Willebrand activity, which are all involved in vaso-occlusion in patients with sickle cell disease, and very likely also involved during a vaso-occlusive crisis,” he explained, adding that sevuparin, a low-molecular-weight heparin without functional antithrombin binding domain, seemed to be a good candidate for testing that hypothesis.
“It has no anticoagulant effects on factor Xa and IIa,” he said. “It retains, however, its antiadhesive and antiaggregation properties.”
Since it has no anticoagulation activity, it can be dosed at up to 20-fold the therapeutic dose of low-molecular-weight heparin to optimize the antiadhesive effects, he noted.
However, the data indicate that “antiadhesive therapies are clearly not effective in patients with vaso-occlusive crisis,” he said, noting that this was also affirmed by a similar 2019 study of the investigational panselectin inhibitor rivipansel, as reported in a Pfizer press release.
Intriguingly, the difference between the current study and the 2007 study by Qari et al. raises questions about whether anticoagulation, rather than antiadhesion, helped resolve VOC in that study, he said, noting that future studies should focus on whether that is the case.
As for the role of antiadhesive therapy, the mode of action of sevuparin and the current findings taken together suggest that future studies should also assess whether it can be used to prevent VOC.
“Perhaps sevuparin could be administered to patients in a prodromal phase – just before a real vaso-occlusive crisis appears – to prevent such a crisis from happening,” he said. “It would be interesting to use the drug that way.”
Dr. Biemond reported research funding from Sanquin and honoraria from Novartis and GBT.
SOURCE: Biemond B et al. ASH 2019, Abstract 614.
REPORTING FROM ASH 2019
Common drug with lots of surprising side effects
A 55-year-old woman comes to clinic for follow-up. She reports her family is worried that she isn’t getting enough sleep and is more tired than usual. The patient reports she is sleeping 8 hours a night and wakes up feeling rested, but she has noticed she has been yawning much more frequently than she remembers in the past.
Past medical history: gastroesophageal reflux disease, hypertension, generalized anxiety disorder, hypothyroidism, and osteoporosis. Medications: amlodipine, lansoprazole, irbesartan, escitalopram, levothyroxine, and alendronate. Physical examination: blood pressure 110/70 mm Hg, pulse 60 bpm. Lower extremities: 1+ edema.
What is the likely cause of her increased yawning?
A. Amlodipine.
B. Alendronate.
C. Irbesartan.
D. Escitalopram.
E. Lansoprazole.
The correct answer here is escitalopram. Selective serotonin reuptake inhibitors in general are well tolerated. Given how commonly these drugs are used, however, there are a number of lesser-known side effects that you are likely to see.
In the above case, this patient has yawning caused by her SSRI. Roncero et al. described a case of yawning in a patient on escitalopram that resolved when the dose of escitalopram was reduced.1 Paroxetine has been reported to cause yawning at both low and high doses.2
In a review of drug-induced yawning, SSRIs as a class were most frequently involved, and sertraline and fluoxetine were implicated in addition to paroxetine.3 The serotonin-norepinephrine reuptake inhibitors duloxetine and venlafaxine have also been associated with yawning.4,5
Hyperhydrosis has also been linked to SSRIs and SNRIs, and both yawning and hyperhidrosis may occur because of an underlying thermoregulatory dysfunction.6
SSRIs have been linked to increased bleeding risk, especially increased risk of upper gastrointestinal hemorrhage. Laporte and colleagues showed an association of SSRI use and risk of bleeding in a meta-analysis of 42 observational studies, with an odds ratio of 1.41 (95% confidence interval, 1.27-1.57; P less than .0001).7 The risk of upper gastrointestinal (UGI) bleeding is further increased if patients are also taking NSAIDs.
Anglin et al. looked at 15 case-control studies and 4 cohort studies and found an OR of 1.66 for UGI bleeding with SSRI use, and an OR of 4.25 for UGI bleeding if SSRI use was combined with NSAID use.8 The number needed to harm is 3,177 for NSAID use in populations at low risk for GI bleeding, but it is much lower (881) in higher-risk populations.8 Make sure to think about patients’ bleeding risks when starting SSRIs.
An issue that comes up frequently is: What is the risk of bleeding in patients on SSRIs who are also on anticoagulants? Dr. Quinn and colleagues looked at the bleeding risk of anticoagulated patients also taking SSRIs in the ROCKET AF trial.9 They found 737 patients who received SSRIs and matched them with other patients not on SSRIs in the trial. All patients in the trial were either receiving rivaroxaban or warfarin for stroke prophylaxis. They found no significant increase risk in bleeding in the patients on SSRIs and anticoagulants.
Take-home points:
- Yawning and hyperhidrosis are interesting side effects of SSRIs.
- Bleeding risk is increased in patients on SSRIs, especially when combined with NSAIDs.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. Neurologia. 2013 Nov-Dec;28(9):589-90.
2. Psychiatry Clin Neurosci. 2006 Apr;60(2):260.
3. Presse Med. 2014 Oct;43(10 Pt 1):1135-6.
4. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Jun 15;33(4):747.
5. Ann Pharmacother. 2011 Oct;45(10):1297-301.
6. Depress Anxiety. 2017 Dec;34(12):1134-46.
7. Pharmacol Res. 2017 Apr;118:19-32.
8. Am J Gastroenterol. 2014 Jun;109(6):811-9.
9. J Am Heart Assoc. 2018 Aug 7;7(15):e008755.
A 55-year-old woman comes to clinic for follow-up. She reports her family is worried that she isn’t getting enough sleep and is more tired than usual. The patient reports she is sleeping 8 hours a night and wakes up feeling rested, but she has noticed she has been yawning much more frequently than she remembers in the past.
Past medical history: gastroesophageal reflux disease, hypertension, generalized anxiety disorder, hypothyroidism, and osteoporosis. Medications: amlodipine, lansoprazole, irbesartan, escitalopram, levothyroxine, and alendronate. Physical examination: blood pressure 110/70 mm Hg, pulse 60 bpm. Lower extremities: 1+ edema.
What is the likely cause of her increased yawning?
A. Amlodipine.
B. Alendronate.
C. Irbesartan.
D. Escitalopram.
E. Lansoprazole.
The correct answer here is escitalopram. Selective serotonin reuptake inhibitors in general are well tolerated. Given how commonly these drugs are used, however, there are a number of lesser-known side effects that you are likely to see.
In the above case, this patient has yawning caused by her SSRI. Roncero et al. described a case of yawning in a patient on escitalopram that resolved when the dose of escitalopram was reduced.1 Paroxetine has been reported to cause yawning at both low and high doses.2
In a review of drug-induced yawning, SSRIs as a class were most frequently involved, and sertraline and fluoxetine were implicated in addition to paroxetine.3 The serotonin-norepinephrine reuptake inhibitors duloxetine and venlafaxine have also been associated with yawning.4,5
Hyperhydrosis has also been linked to SSRIs and SNRIs, and both yawning and hyperhidrosis may occur because of an underlying thermoregulatory dysfunction.6
SSRIs have been linked to increased bleeding risk, especially increased risk of upper gastrointestinal hemorrhage. Laporte and colleagues showed an association of SSRI use and risk of bleeding in a meta-analysis of 42 observational studies, with an odds ratio of 1.41 (95% confidence interval, 1.27-1.57; P less than .0001).7 The risk of upper gastrointestinal (UGI) bleeding is further increased if patients are also taking NSAIDs.
Anglin et al. looked at 15 case-control studies and 4 cohort studies and found an OR of 1.66 for UGI bleeding with SSRI use, and an OR of 4.25 for UGI bleeding if SSRI use was combined with NSAID use.8 The number needed to harm is 3,177 for NSAID use in populations at low risk for GI bleeding, but it is much lower (881) in higher-risk populations.8 Make sure to think about patients’ bleeding risks when starting SSRIs.
An issue that comes up frequently is: What is the risk of bleeding in patients on SSRIs who are also on anticoagulants? Dr. Quinn and colleagues looked at the bleeding risk of anticoagulated patients also taking SSRIs in the ROCKET AF trial.9 They found 737 patients who received SSRIs and matched them with other patients not on SSRIs in the trial. All patients in the trial were either receiving rivaroxaban or warfarin for stroke prophylaxis. They found no significant increase risk in bleeding in the patients on SSRIs and anticoagulants.
Take-home points:
- Yawning and hyperhidrosis are interesting side effects of SSRIs.
- Bleeding risk is increased in patients on SSRIs, especially when combined with NSAIDs.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. Neurologia. 2013 Nov-Dec;28(9):589-90.
2. Psychiatry Clin Neurosci. 2006 Apr;60(2):260.
3. Presse Med. 2014 Oct;43(10 Pt 1):1135-6.
4. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Jun 15;33(4):747.
5. Ann Pharmacother. 2011 Oct;45(10):1297-301.
6. Depress Anxiety. 2017 Dec;34(12):1134-46.
7. Pharmacol Res. 2017 Apr;118:19-32.
8. Am J Gastroenterol. 2014 Jun;109(6):811-9.
9. J Am Heart Assoc. 2018 Aug 7;7(15):e008755.
A 55-year-old woman comes to clinic for follow-up. She reports her family is worried that she isn’t getting enough sleep and is more tired than usual. The patient reports she is sleeping 8 hours a night and wakes up feeling rested, but she has noticed she has been yawning much more frequently than she remembers in the past.
Past medical history: gastroesophageal reflux disease, hypertension, generalized anxiety disorder, hypothyroidism, and osteoporosis. Medications: amlodipine, lansoprazole, irbesartan, escitalopram, levothyroxine, and alendronate. Physical examination: blood pressure 110/70 mm Hg, pulse 60 bpm. Lower extremities: 1+ edema.
What is the likely cause of her increased yawning?
A. Amlodipine.
B. Alendronate.
C. Irbesartan.
D. Escitalopram.
E. Lansoprazole.
The correct answer here is escitalopram. Selective serotonin reuptake inhibitors in general are well tolerated. Given how commonly these drugs are used, however, there are a number of lesser-known side effects that you are likely to see.
In the above case, this patient has yawning caused by her SSRI. Roncero et al. described a case of yawning in a patient on escitalopram that resolved when the dose of escitalopram was reduced.1 Paroxetine has been reported to cause yawning at both low and high doses.2
In a review of drug-induced yawning, SSRIs as a class were most frequently involved, and sertraline and fluoxetine were implicated in addition to paroxetine.3 The serotonin-norepinephrine reuptake inhibitors duloxetine and venlafaxine have also been associated with yawning.4,5
Hyperhydrosis has also been linked to SSRIs and SNRIs, and both yawning and hyperhidrosis may occur because of an underlying thermoregulatory dysfunction.6
SSRIs have been linked to increased bleeding risk, especially increased risk of upper gastrointestinal hemorrhage. Laporte and colleagues showed an association of SSRI use and risk of bleeding in a meta-analysis of 42 observational studies, with an odds ratio of 1.41 (95% confidence interval, 1.27-1.57; P less than .0001).7 The risk of upper gastrointestinal (UGI) bleeding is further increased if patients are also taking NSAIDs.
Anglin et al. looked at 15 case-control studies and 4 cohort studies and found an OR of 1.66 for UGI bleeding with SSRI use, and an OR of 4.25 for UGI bleeding if SSRI use was combined with NSAID use.8 The number needed to harm is 3,177 for NSAID use in populations at low risk for GI bleeding, but it is much lower (881) in higher-risk populations.8 Make sure to think about patients’ bleeding risks when starting SSRIs.
An issue that comes up frequently is: What is the risk of bleeding in patients on SSRIs who are also on anticoagulants? Dr. Quinn and colleagues looked at the bleeding risk of anticoagulated patients also taking SSRIs in the ROCKET AF trial.9 They found 737 patients who received SSRIs and matched them with other patients not on SSRIs in the trial. All patients in the trial were either receiving rivaroxaban or warfarin for stroke prophylaxis. They found no significant increase risk in bleeding in the patients on SSRIs and anticoagulants.
Take-home points:
- Yawning and hyperhidrosis are interesting side effects of SSRIs.
- Bleeding risk is increased in patients on SSRIs, especially when combined with NSAIDs.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. Neurologia. 2013 Nov-Dec;28(9):589-90.
2. Psychiatry Clin Neurosci. 2006 Apr;60(2):260.
3. Presse Med. 2014 Oct;43(10 Pt 1):1135-6.
4. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Jun 15;33(4):747.
5. Ann Pharmacother. 2011 Oct;45(10):1297-301.
6. Depress Anxiety. 2017 Dec;34(12):1134-46.
7. Pharmacol Res. 2017 Apr;118:19-32.
8. Am J Gastroenterol. 2014 Jun;109(6):811-9.
9. J Am Heart Assoc. 2018 Aug 7;7(15):e008755.
Should a normal-appearing hippocampus be resected in a patient with temporal lobe epilepsy?
BALTIMORE – according to an analysis presented at the annual meeting of the American Epilepsy Society. Long-term seizure outcomes, however, are similar between resected and nonresected patients. In addition, sparing a normal-appearing hippocampus is correlated with a lower risk of verbal deficits, but long-term outcomes are unclear.
Neurologists have not arrived at a consensus about the best surgical management of patients with temporal lobe epilepsy and a hippocampus that appears normal on MRI. Few studies have examined seizure and neuropsychologic outcomes in this population, and this scarcity of data makes counseling patients difficult.
A review of data for surgical patients
To investigate this question, Marcia E. Morita-Sherman, MD, from the Cleveland Clinic, and colleagues retrospectively reviewed data for 152 patients who underwent surgery for temporal lobe epilepsy at the Cleveland Clinic during 2010-2018. Eligible participants were older than 16 years, and the researchers excluded patients with MRI or pathologic signs of hippocampal sclerosis and those with prior surgeries from the analysis.
To examine neuropsychological outcomes, Dr. Morita-Sherman and colleagues compared measures of verbal memory, visual memory, and confrontation naming that had been obtained before surgery and at 6 months after surgery. They measured hippocampal volume using Neuroquant. They categorized resections as dominant or nondominant according to patients’ handedness or language lateralization. The investigators classified 74 patients as having a spared hippocampus and 78 patients as having a resected hippocampus. They classified neuropsychological outcomes as showing decline or no decline using epilepsy-specific reliable change indexes.
Type of surgery affected memory and naming
Approximately 40% of patients had seizure recurrence within 1 year after surgery, and 63% had seizure recurrence within 6 years after surgery. The rate of invasive EEG was similar between patients with a spared hippocampus (50%) and those with a resected hippocampus (47%). In a univariate analysis, male sex, longer epilepsy duration, normal MRI, history of invasive evaluation, and acute postoperative seizures were associated with a higher risk of seizure recurrence. Patients with a spared hippocampus had a higher risk of early seizure recurrence, compared with patients with a resected hippocampus, but the difference was not statistically significant. Long-term seizure outcomes were similar between the two groups.
Neuropsychological outcomes were available for 86 patients. Among 56 patients who underwent surgery on the dominant side, those with spared-hippocampal surgery, compared with those with resected-hippocampal surgery, had lower rates of clinically meaningful declines in verbal memory (39.7% vs. 70.4%) and naming (40.7% vs. 79.2%). The investigators found no significant difference in the 30 patients with nondominant surgeries.
“Sparing the hippocampus in a tailored temporal lobe resection doesn’t necessarily prevent any memory decline. Close to 40% of our patients where the hippocampus was spared had a clinically significant memory loss,” said Lara E. Jehi, MD, an epileptologist at the Cleveland Clinic and one of the investigators. “Including the hippocampus in the resection seems to correlate with better odds of seizure freedom, at least in the short term. We need more research to study the long-term memory and naming implications of hippocampal sparing versus resection.”
The study was funded by a grant from the National Institutes of Health. The investigators reported no conflicts of interest. egreb@mdedge.com
SOURCE: Morita-Sherman ME et al. AES 2019, Abstract 1.336.
BALTIMORE – according to an analysis presented at the annual meeting of the American Epilepsy Society. Long-term seizure outcomes, however, are similar between resected and nonresected patients. In addition, sparing a normal-appearing hippocampus is correlated with a lower risk of verbal deficits, but long-term outcomes are unclear.
Neurologists have not arrived at a consensus about the best surgical management of patients with temporal lobe epilepsy and a hippocampus that appears normal on MRI. Few studies have examined seizure and neuropsychologic outcomes in this population, and this scarcity of data makes counseling patients difficult.
A review of data for surgical patients
To investigate this question, Marcia E. Morita-Sherman, MD, from the Cleveland Clinic, and colleagues retrospectively reviewed data for 152 patients who underwent surgery for temporal lobe epilepsy at the Cleveland Clinic during 2010-2018. Eligible participants were older than 16 years, and the researchers excluded patients with MRI or pathologic signs of hippocampal sclerosis and those with prior surgeries from the analysis.
To examine neuropsychological outcomes, Dr. Morita-Sherman and colleagues compared measures of verbal memory, visual memory, and confrontation naming that had been obtained before surgery and at 6 months after surgery. They measured hippocampal volume using Neuroquant. They categorized resections as dominant or nondominant according to patients’ handedness or language lateralization. The investigators classified 74 patients as having a spared hippocampus and 78 patients as having a resected hippocampus. They classified neuropsychological outcomes as showing decline or no decline using epilepsy-specific reliable change indexes.
Type of surgery affected memory and naming
Approximately 40% of patients had seizure recurrence within 1 year after surgery, and 63% had seizure recurrence within 6 years after surgery. The rate of invasive EEG was similar between patients with a spared hippocampus (50%) and those with a resected hippocampus (47%). In a univariate analysis, male sex, longer epilepsy duration, normal MRI, history of invasive evaluation, and acute postoperative seizures were associated with a higher risk of seizure recurrence. Patients with a spared hippocampus had a higher risk of early seizure recurrence, compared with patients with a resected hippocampus, but the difference was not statistically significant. Long-term seizure outcomes were similar between the two groups.
Neuropsychological outcomes were available for 86 patients. Among 56 patients who underwent surgery on the dominant side, those with spared-hippocampal surgery, compared with those with resected-hippocampal surgery, had lower rates of clinically meaningful declines in verbal memory (39.7% vs. 70.4%) and naming (40.7% vs. 79.2%). The investigators found no significant difference in the 30 patients with nondominant surgeries.
“Sparing the hippocampus in a tailored temporal lobe resection doesn’t necessarily prevent any memory decline. Close to 40% of our patients where the hippocampus was spared had a clinically significant memory loss,” said Lara E. Jehi, MD, an epileptologist at the Cleveland Clinic and one of the investigators. “Including the hippocampus in the resection seems to correlate with better odds of seizure freedom, at least in the short term. We need more research to study the long-term memory and naming implications of hippocampal sparing versus resection.”
The study was funded by a grant from the National Institutes of Health. The investigators reported no conflicts of interest. egreb@mdedge.com
SOURCE: Morita-Sherman ME et al. AES 2019, Abstract 1.336.
BALTIMORE – according to an analysis presented at the annual meeting of the American Epilepsy Society. Long-term seizure outcomes, however, are similar between resected and nonresected patients. In addition, sparing a normal-appearing hippocampus is correlated with a lower risk of verbal deficits, but long-term outcomes are unclear.
Neurologists have not arrived at a consensus about the best surgical management of patients with temporal lobe epilepsy and a hippocampus that appears normal on MRI. Few studies have examined seizure and neuropsychologic outcomes in this population, and this scarcity of data makes counseling patients difficult.
A review of data for surgical patients
To investigate this question, Marcia E. Morita-Sherman, MD, from the Cleveland Clinic, and colleagues retrospectively reviewed data for 152 patients who underwent surgery for temporal lobe epilepsy at the Cleveland Clinic during 2010-2018. Eligible participants were older than 16 years, and the researchers excluded patients with MRI or pathologic signs of hippocampal sclerosis and those with prior surgeries from the analysis.
To examine neuropsychological outcomes, Dr. Morita-Sherman and colleagues compared measures of verbal memory, visual memory, and confrontation naming that had been obtained before surgery and at 6 months after surgery. They measured hippocampal volume using Neuroquant. They categorized resections as dominant or nondominant according to patients’ handedness or language lateralization. The investigators classified 74 patients as having a spared hippocampus and 78 patients as having a resected hippocampus. They classified neuropsychological outcomes as showing decline or no decline using epilepsy-specific reliable change indexes.
Type of surgery affected memory and naming
Approximately 40% of patients had seizure recurrence within 1 year after surgery, and 63% had seizure recurrence within 6 years after surgery. The rate of invasive EEG was similar between patients with a spared hippocampus (50%) and those with a resected hippocampus (47%). In a univariate analysis, male sex, longer epilepsy duration, normal MRI, history of invasive evaluation, and acute postoperative seizures were associated with a higher risk of seizure recurrence. Patients with a spared hippocampus had a higher risk of early seizure recurrence, compared with patients with a resected hippocampus, but the difference was not statistically significant. Long-term seizure outcomes were similar between the two groups.
Neuropsychological outcomes were available for 86 patients. Among 56 patients who underwent surgery on the dominant side, those with spared-hippocampal surgery, compared with those with resected-hippocampal surgery, had lower rates of clinically meaningful declines in verbal memory (39.7% vs. 70.4%) and naming (40.7% vs. 79.2%). The investigators found no significant difference in the 30 patients with nondominant surgeries.
“Sparing the hippocampus in a tailored temporal lobe resection doesn’t necessarily prevent any memory decline. Close to 40% of our patients where the hippocampus was spared had a clinically significant memory loss,” said Lara E. Jehi, MD, an epileptologist at the Cleveland Clinic and one of the investigators. “Including the hippocampus in the resection seems to correlate with better odds of seizure freedom, at least in the short term. We need more research to study the long-term memory and naming implications of hippocampal sparing versus resection.”
The study was funded by a grant from the National Institutes of Health. The investigators reported no conflicts of interest. egreb@mdedge.com
SOURCE: Morita-Sherman ME et al. AES 2019, Abstract 1.336.
REPORTING FROM AES 2019
Anxiety may be a part of healthy development, sometimes
Anxiety is probably the most common behavioral health complaint that presents in the pediatrician’s office. The prevalence of anxiety is going up every year, and we do not have a good understanding why. Is it the pressure to perform at earlier and earlier ages? Is it the press of information or rapid communication of every disaster on Earth? Or are children not developing appropriate coping skills for the expectable challenges and stresses they will face through development? We do not know.
Anxiety disorders are most likely to present in the early school years – latency – between the ages of 6 and 12 years. Teenagers may present with new anxiety disorders or may disclose symptoms that they have been quietly managing since they were younger, when they were thought to be “shy.” These disorders include separation anxiety disorder, social phobia, selective mutism, specific phobia, and generalized anxiety disorder. This age period also is marked by high levels of normal anxiety because children’s cognitive development has advanced beyond their emotional development. They are capable of logic, can understand cause and effect, and can appreciate the passage of time and serious matters such as the permanence of death. Gone is the magical thinking of the preschool years! When an elementary student learns about global warming or a refugee crisis, they can fully appreciate the serious implications of the subject. What they lack is experience with tolerating uncertainty and worry and proceeding with life, focusing on what they might address or even bearing the fact that life is sometimes unfair. This mismatch of relative cognitive maturity with emotional immaturity can lead to anxiety and distress. This is particularly true as they face these challenges while they have new independence, spending longer days at school and less time with parents. Bearing this distress with caring adults, learning to focus on what they can do, and discovering that they and the world can go on even when something very unfair has happened is central to how they develop emotional maturity.
How a child learns to manage anxiety is very much determined by how their parents manage anxiety and how well their parents can tolerate their children’s distress. A parent who becomes overwhelmed when their child is upset about missing a goal in soccer will have a difficult time helping their child learn how to manage distress. And children who are facing chronic severe stress, such as poverty, domestic violence, or chronic illness in a parent, are facing the double challenge of managing persistent anxiety that may be impairing their parents’ ability to support them. When the child and their family are connected to a community that has not been able to effectively respond to larger problems, such as creating safe schools or neighborhoods, anxiety can become entrenched in despair.
It often is tempting to jump in with reassurance when your patient or their parents present with anxiety. But when you calmly show curiosity, you model tolerance of their distress. Are they fearful about very specific situations, such as being called on in class? Or do they become dysregulated when facing a separation from their parents, such as at bedtime or before school, seeking contact with their parents with endless questions? Find out how the parents are managing separations and whether they may be inadvertently rewarding by staying with them to negotiate or answer endless questions. Find out if parents may be accommodating anxiety by allowing their children to avoid normal situations that are stirring anxiety. Do they give in anytime their child shows resistance or have they learned to pick their battles and help their children face more-modest stress while avoiding only the most intensely anxious situations? Are the parents able to speak calmly and with good humor about these challenges or do they become very stressed and defensive? Is there a family history of anxiety? Managing a child’s anxiety every day can be exhausting, and parents might need a referral in addition to a discussion about how anxiety is developmentally normal.
For those parents that can manage this discussion, suggest that, like you, if they can remain calm during these times with their child (even if they don’t feel calm), it will help their child get better at managing anxiety, even if their child has an anxiety disorder. They also should be curious about their child’s worries, learning about the details and scenarios their children may be anticipating. They should express compassion about how uncomfortable anxiety is, coupled with their confident belief that the child will be able to tolerate and manage the situation even though it’s uncomfortable. This acknowledgment should not be a dismissal of the anxiety, instead it should be confidence that the child will learn to bear it.
When your patient is a teenager describing anxiety, unpack. Are they anxious about their performance on their five Advanced Placement exams? If their anxiety sounds more like appropriate stress, be compassionate and then curious about how they are learning to relax. Are they using drugs and alcohol? Or have they found healthy ways to unwind and recharge? Focusing on ways in which they are learning to care for themselves, making time for sleep and exercise, live time with friends, and senseless fun is therapeutic. Find out if their parents are supportive of their self-care. You might even give them a prescription!
Anxiety is often a private experience, and parents might not know about it until it presents with an explosion of distress or obstinacy when an anxious child is pushed into scary territory. Asking questions about specific worries (something happening to parents, germs, weather events) can illuminate the extent of anxiety. It also is worth exploring if there are rituals that help them manage their worries, whether they are common (finding a parent, hugging a pet, prayer) or more compulsive (repetitive undoing, hair pulling). Find out if there has recently been any serious stress or change for the family, such as the loss of a job or illness in a grandparent, that may be contributing to a child’s anxiety.
Anytime you see anxieties that are broad or extreme, disrupt their ability to function (go to school, participate in activities, build friendships), or if their parents are clearly struggling with managing their child’s distress, it is worthwhile to find a referral to a psychiatrist or psychologist for evaluation and further treatment. School avoidance constitutes an urgent need for evaluation, as every day of school missed makes it harder for the child to return to school. For all of your anxious patients, even when you make a referral to a psychiatrist for evaluation, teach your patients and parents about how critical adequate sleep and regular exercise are to managing anxiety. Remind them that an appropriate level of anxiety is normal and promotes performance and grit, despite the discomfort, and that learning how to manage anxiety is essential to growing up and building mental health.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Anxiety is probably the most common behavioral health complaint that presents in the pediatrician’s office. The prevalence of anxiety is going up every year, and we do not have a good understanding why. Is it the pressure to perform at earlier and earlier ages? Is it the press of information or rapid communication of every disaster on Earth? Or are children not developing appropriate coping skills for the expectable challenges and stresses they will face through development? We do not know.
Anxiety disorders are most likely to present in the early school years – latency – between the ages of 6 and 12 years. Teenagers may present with new anxiety disorders or may disclose symptoms that they have been quietly managing since they were younger, when they were thought to be “shy.” These disorders include separation anxiety disorder, social phobia, selective mutism, specific phobia, and generalized anxiety disorder. This age period also is marked by high levels of normal anxiety because children’s cognitive development has advanced beyond their emotional development. They are capable of logic, can understand cause and effect, and can appreciate the passage of time and serious matters such as the permanence of death. Gone is the magical thinking of the preschool years! When an elementary student learns about global warming or a refugee crisis, they can fully appreciate the serious implications of the subject. What they lack is experience with tolerating uncertainty and worry and proceeding with life, focusing on what they might address or even bearing the fact that life is sometimes unfair. This mismatch of relative cognitive maturity with emotional immaturity can lead to anxiety and distress. This is particularly true as they face these challenges while they have new independence, spending longer days at school and less time with parents. Bearing this distress with caring adults, learning to focus on what they can do, and discovering that they and the world can go on even when something very unfair has happened is central to how they develop emotional maturity.
How a child learns to manage anxiety is very much determined by how their parents manage anxiety and how well their parents can tolerate their children’s distress. A parent who becomes overwhelmed when their child is upset about missing a goal in soccer will have a difficult time helping their child learn how to manage distress. And children who are facing chronic severe stress, such as poverty, domestic violence, or chronic illness in a parent, are facing the double challenge of managing persistent anxiety that may be impairing their parents’ ability to support them. When the child and their family are connected to a community that has not been able to effectively respond to larger problems, such as creating safe schools or neighborhoods, anxiety can become entrenched in despair.
It often is tempting to jump in with reassurance when your patient or their parents present with anxiety. But when you calmly show curiosity, you model tolerance of their distress. Are they fearful about very specific situations, such as being called on in class? Or do they become dysregulated when facing a separation from their parents, such as at bedtime or before school, seeking contact with their parents with endless questions? Find out how the parents are managing separations and whether they may be inadvertently rewarding by staying with them to negotiate or answer endless questions. Find out if parents may be accommodating anxiety by allowing their children to avoid normal situations that are stirring anxiety. Do they give in anytime their child shows resistance or have they learned to pick their battles and help their children face more-modest stress while avoiding only the most intensely anxious situations? Are the parents able to speak calmly and with good humor about these challenges or do they become very stressed and defensive? Is there a family history of anxiety? Managing a child’s anxiety every day can be exhausting, and parents might need a referral in addition to a discussion about how anxiety is developmentally normal.
For those parents that can manage this discussion, suggest that, like you, if they can remain calm during these times with their child (even if they don’t feel calm), it will help their child get better at managing anxiety, even if their child has an anxiety disorder. They also should be curious about their child’s worries, learning about the details and scenarios their children may be anticipating. They should express compassion about how uncomfortable anxiety is, coupled with their confident belief that the child will be able to tolerate and manage the situation even though it’s uncomfortable. This acknowledgment should not be a dismissal of the anxiety, instead it should be confidence that the child will learn to bear it.
When your patient is a teenager describing anxiety, unpack. Are they anxious about their performance on their five Advanced Placement exams? If their anxiety sounds more like appropriate stress, be compassionate and then curious about how they are learning to relax. Are they using drugs and alcohol? Or have they found healthy ways to unwind and recharge? Focusing on ways in which they are learning to care for themselves, making time for sleep and exercise, live time with friends, and senseless fun is therapeutic. Find out if their parents are supportive of their self-care. You might even give them a prescription!
Anxiety is often a private experience, and parents might not know about it until it presents with an explosion of distress or obstinacy when an anxious child is pushed into scary territory. Asking questions about specific worries (something happening to parents, germs, weather events) can illuminate the extent of anxiety. It also is worth exploring if there are rituals that help them manage their worries, whether they are common (finding a parent, hugging a pet, prayer) or more compulsive (repetitive undoing, hair pulling). Find out if there has recently been any serious stress or change for the family, such as the loss of a job or illness in a grandparent, that may be contributing to a child’s anxiety.
Anytime you see anxieties that are broad or extreme, disrupt their ability to function (go to school, participate in activities, build friendships), or if their parents are clearly struggling with managing their child’s distress, it is worthwhile to find a referral to a psychiatrist or psychologist for evaluation and further treatment. School avoidance constitutes an urgent need for evaluation, as every day of school missed makes it harder for the child to return to school. For all of your anxious patients, even when you make a referral to a psychiatrist for evaluation, teach your patients and parents about how critical adequate sleep and regular exercise are to managing anxiety. Remind them that an appropriate level of anxiety is normal and promotes performance and grit, despite the discomfort, and that learning how to manage anxiety is essential to growing up and building mental health.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Anxiety is probably the most common behavioral health complaint that presents in the pediatrician’s office. The prevalence of anxiety is going up every year, and we do not have a good understanding why. Is it the pressure to perform at earlier and earlier ages? Is it the press of information or rapid communication of every disaster on Earth? Or are children not developing appropriate coping skills for the expectable challenges and stresses they will face through development? We do not know.
Anxiety disorders are most likely to present in the early school years – latency – between the ages of 6 and 12 years. Teenagers may present with new anxiety disorders or may disclose symptoms that they have been quietly managing since they were younger, when they were thought to be “shy.” These disorders include separation anxiety disorder, social phobia, selective mutism, specific phobia, and generalized anxiety disorder. This age period also is marked by high levels of normal anxiety because children’s cognitive development has advanced beyond their emotional development. They are capable of logic, can understand cause and effect, and can appreciate the passage of time and serious matters such as the permanence of death. Gone is the magical thinking of the preschool years! When an elementary student learns about global warming or a refugee crisis, they can fully appreciate the serious implications of the subject. What they lack is experience with tolerating uncertainty and worry and proceeding with life, focusing on what they might address or even bearing the fact that life is sometimes unfair. This mismatch of relative cognitive maturity with emotional immaturity can lead to anxiety and distress. This is particularly true as they face these challenges while they have new independence, spending longer days at school and less time with parents. Bearing this distress with caring adults, learning to focus on what they can do, and discovering that they and the world can go on even when something very unfair has happened is central to how they develop emotional maturity.
How a child learns to manage anxiety is very much determined by how their parents manage anxiety and how well their parents can tolerate their children’s distress. A parent who becomes overwhelmed when their child is upset about missing a goal in soccer will have a difficult time helping their child learn how to manage distress. And children who are facing chronic severe stress, such as poverty, domestic violence, or chronic illness in a parent, are facing the double challenge of managing persistent anxiety that may be impairing their parents’ ability to support them. When the child and their family are connected to a community that has not been able to effectively respond to larger problems, such as creating safe schools or neighborhoods, anxiety can become entrenched in despair.
It often is tempting to jump in with reassurance when your patient or their parents present with anxiety. But when you calmly show curiosity, you model tolerance of their distress. Are they fearful about very specific situations, such as being called on in class? Or do they become dysregulated when facing a separation from their parents, such as at bedtime or before school, seeking contact with their parents with endless questions? Find out how the parents are managing separations and whether they may be inadvertently rewarding by staying with them to negotiate or answer endless questions. Find out if parents may be accommodating anxiety by allowing their children to avoid normal situations that are stirring anxiety. Do they give in anytime their child shows resistance or have they learned to pick their battles and help their children face more-modest stress while avoiding only the most intensely anxious situations? Are the parents able to speak calmly and with good humor about these challenges or do they become very stressed and defensive? Is there a family history of anxiety? Managing a child’s anxiety every day can be exhausting, and parents might need a referral in addition to a discussion about how anxiety is developmentally normal.
For those parents that can manage this discussion, suggest that, like you, if they can remain calm during these times with their child (even if they don’t feel calm), it will help their child get better at managing anxiety, even if their child has an anxiety disorder. They also should be curious about their child’s worries, learning about the details and scenarios their children may be anticipating. They should express compassion about how uncomfortable anxiety is, coupled with their confident belief that the child will be able to tolerate and manage the situation even though it’s uncomfortable. This acknowledgment should not be a dismissal of the anxiety, instead it should be confidence that the child will learn to bear it.
When your patient is a teenager describing anxiety, unpack. Are they anxious about their performance on their five Advanced Placement exams? If their anxiety sounds more like appropriate stress, be compassionate and then curious about how they are learning to relax. Are they using drugs and alcohol? Or have they found healthy ways to unwind and recharge? Focusing on ways in which they are learning to care for themselves, making time for sleep and exercise, live time with friends, and senseless fun is therapeutic. Find out if their parents are supportive of their self-care. You might even give them a prescription!
Anxiety is often a private experience, and parents might not know about it until it presents with an explosion of distress or obstinacy when an anxious child is pushed into scary territory. Asking questions about specific worries (something happening to parents, germs, weather events) can illuminate the extent of anxiety. It also is worth exploring if there are rituals that help them manage their worries, whether they are common (finding a parent, hugging a pet, prayer) or more compulsive (repetitive undoing, hair pulling). Find out if there has recently been any serious stress or change for the family, such as the loss of a job or illness in a grandparent, that may be contributing to a child’s anxiety.
Anytime you see anxieties that are broad or extreme, disrupt their ability to function (go to school, participate in activities, build friendships), or if their parents are clearly struggling with managing their child’s distress, it is worthwhile to find a referral to a psychiatrist or psychologist for evaluation and further treatment. School avoidance constitutes an urgent need for evaluation, as every day of school missed makes it harder for the child to return to school. For all of your anxious patients, even when you make a referral to a psychiatrist for evaluation, teach your patients and parents about how critical adequate sleep and regular exercise are to managing anxiety. Remind them that an appropriate level of anxiety is normal and promotes performance and grit, despite the discomfort, and that learning how to manage anxiety is essential to growing up and building mental health.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Runaway youth: Knowing the risk factors and care needs
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
FROM PEDIATRICS
ACP maps two potential paths to universal health care
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
FROM ANNALS OF INTERNAL MEDICINE
CD1a and cosmetic-related contact dermatitis
As industries develop more chemical extraction techniques for synthetic or purified botanical ingredients to include in cosmetic and personal care products, the incidence of contact dermatitis is rising. Contact dermatitis (irritant or allergic) is the most common occupational skin disease, with current lifetime incidence exceeding 50%. For allergic contact dermatitis, type IV hypersensitivity (or delayed-type hypersensitivity) is thought to be the immunologic mediated pathway in which a T cell–mediated response occurs approximately 72 hours after exposure to the contact allergen. Diagnosis currently is predominately made clinically, after identifying the potential allergen or via patch testing. Treatment typically involves topical steroids or anti-inflammatories should a rash occur, and avoidance of the identified allergen.
In delayed-type hypersensitivity, most T-cell receptors recognize a peptide antigen bound to major histocompatibility complex (MHC) I or MHC II proteins, which stimulates a subsequent inflammatory immune response. However, in a recently published study, the authors wrote that “most known contact allergens are nonpeptidic small molecules, cations, or metals that are typically delivered to skin as drugs, oils, cosmetics, skin creams, or fragrances.” The chemical nature and structure of contact allergens “does not match the chemical structures of most antigens commonly recognized within the TCR-peptide-MHC axis,” they added. Thus, the mechanism by which nonpeptide molecules found in cosmetics cause a T cell–mediated hypersensitivity is poorly understood.
In that study, investigators from Brigham and Women’s Hospital, Boston; Columbia University, New York; and Monash University, Melbourne, looked at whether a protein found in immune cells – CD1a – could be involved in these allergic reactions. In a press release describing the results, cosenior author D. Branch Moody, MD, a principal investigator and physician in Brigham and Women’s division of rheumatology, inflammation, and immunity, noted that they “questioned the prevailing paradigm that T cell–mediated allergic reaction is only triggered when T cells respond to proteins or peptide antigens,” and found “a mechanism through which fragrance can initiate a T-cell response through a protein called CD1a.”
In their study, CD1a was identified as the and personal care products. Specifically, balsam of Peru (a tree oil commonly found in cosmetics and toothpaste), benzyl benzoate, benzyl cinnamate, and farnesol (often present in “fragrance”) after positive patch tests were found to elicit a CD1a-mediated immune response. Their findings suggest that, for these hydrophobic contact allergens, in forming CD1a-farnesol (or other) complexes, displacement of self-lipids normally bound to CD1a occurs, exposing T cell–stimulatory surface regions of CD1a that are normally hidden, thereby eliciting T cell–mediated hypersensitivity reactions.
The authors note that having a better understanding of how these ingredients elicit an immune response on a molecular level can help us potentially identify other molecules that can potentially block this response in humans, thereby treating or potentially mitigating allergic skin disease from these ingredients.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
Resource
Nicolai S et al. Sci Immunol. 2020 Jan 3. doi: 10.1126/sciimmunol.aax5430.
As industries develop more chemical extraction techniques for synthetic or purified botanical ingredients to include in cosmetic and personal care products, the incidence of contact dermatitis is rising. Contact dermatitis (irritant or allergic) is the most common occupational skin disease, with current lifetime incidence exceeding 50%. For allergic contact dermatitis, type IV hypersensitivity (or delayed-type hypersensitivity) is thought to be the immunologic mediated pathway in which a T cell–mediated response occurs approximately 72 hours after exposure to the contact allergen. Diagnosis currently is predominately made clinically, after identifying the potential allergen or via patch testing. Treatment typically involves topical steroids or anti-inflammatories should a rash occur, and avoidance of the identified allergen.
In delayed-type hypersensitivity, most T-cell receptors recognize a peptide antigen bound to major histocompatibility complex (MHC) I or MHC II proteins, which stimulates a subsequent inflammatory immune response. However, in a recently published study, the authors wrote that “most known contact allergens are nonpeptidic small molecules, cations, or metals that are typically delivered to skin as drugs, oils, cosmetics, skin creams, or fragrances.” The chemical nature and structure of contact allergens “does not match the chemical structures of most antigens commonly recognized within the TCR-peptide-MHC axis,” they added. Thus, the mechanism by which nonpeptide molecules found in cosmetics cause a T cell–mediated hypersensitivity is poorly understood.
In that study, investigators from Brigham and Women’s Hospital, Boston; Columbia University, New York; and Monash University, Melbourne, looked at whether a protein found in immune cells – CD1a – could be involved in these allergic reactions. In a press release describing the results, cosenior author D. Branch Moody, MD, a principal investigator and physician in Brigham and Women’s division of rheumatology, inflammation, and immunity, noted that they “questioned the prevailing paradigm that T cell–mediated allergic reaction is only triggered when T cells respond to proteins or peptide antigens,” and found “a mechanism through which fragrance can initiate a T-cell response through a protein called CD1a.”
In their study, CD1a was identified as the and personal care products. Specifically, balsam of Peru (a tree oil commonly found in cosmetics and toothpaste), benzyl benzoate, benzyl cinnamate, and farnesol (often present in “fragrance”) after positive patch tests were found to elicit a CD1a-mediated immune response. Their findings suggest that, for these hydrophobic contact allergens, in forming CD1a-farnesol (or other) complexes, displacement of self-lipids normally bound to CD1a occurs, exposing T cell–stimulatory surface regions of CD1a that are normally hidden, thereby eliciting T cell–mediated hypersensitivity reactions.
The authors note that having a better understanding of how these ingredients elicit an immune response on a molecular level can help us potentially identify other molecules that can potentially block this response in humans, thereby treating or potentially mitigating allergic skin disease from these ingredients.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
Resource
Nicolai S et al. Sci Immunol. 2020 Jan 3. doi: 10.1126/sciimmunol.aax5430.
As industries develop more chemical extraction techniques for synthetic or purified botanical ingredients to include in cosmetic and personal care products, the incidence of contact dermatitis is rising. Contact dermatitis (irritant or allergic) is the most common occupational skin disease, with current lifetime incidence exceeding 50%. For allergic contact dermatitis, type IV hypersensitivity (or delayed-type hypersensitivity) is thought to be the immunologic mediated pathway in which a T cell–mediated response occurs approximately 72 hours after exposure to the contact allergen. Diagnosis currently is predominately made clinically, after identifying the potential allergen or via patch testing. Treatment typically involves topical steroids or anti-inflammatories should a rash occur, and avoidance of the identified allergen.
In delayed-type hypersensitivity, most T-cell receptors recognize a peptide antigen bound to major histocompatibility complex (MHC) I or MHC II proteins, which stimulates a subsequent inflammatory immune response. However, in a recently published study, the authors wrote that “most known contact allergens are nonpeptidic small molecules, cations, or metals that are typically delivered to skin as drugs, oils, cosmetics, skin creams, or fragrances.” The chemical nature and structure of contact allergens “does not match the chemical structures of most antigens commonly recognized within the TCR-peptide-MHC axis,” they added. Thus, the mechanism by which nonpeptide molecules found in cosmetics cause a T cell–mediated hypersensitivity is poorly understood.
In that study, investigators from Brigham and Women’s Hospital, Boston; Columbia University, New York; and Monash University, Melbourne, looked at whether a protein found in immune cells – CD1a – could be involved in these allergic reactions. In a press release describing the results, cosenior author D. Branch Moody, MD, a principal investigator and physician in Brigham and Women’s division of rheumatology, inflammation, and immunity, noted that they “questioned the prevailing paradigm that T cell–mediated allergic reaction is only triggered when T cells respond to proteins or peptide antigens,” and found “a mechanism through which fragrance can initiate a T-cell response through a protein called CD1a.”
In their study, CD1a was identified as the and personal care products. Specifically, balsam of Peru (a tree oil commonly found in cosmetics and toothpaste), benzyl benzoate, benzyl cinnamate, and farnesol (often present in “fragrance”) after positive patch tests were found to elicit a CD1a-mediated immune response. Their findings suggest that, for these hydrophobic contact allergens, in forming CD1a-farnesol (or other) complexes, displacement of self-lipids normally bound to CD1a occurs, exposing T cell–stimulatory surface regions of CD1a that are normally hidden, thereby eliciting T cell–mediated hypersensitivity reactions.
The authors note that having a better understanding of how these ingredients elicit an immune response on a molecular level can help us potentially identify other molecules that can potentially block this response in humans, thereby treating or potentially mitigating allergic skin disease from these ingredients.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
Resource
Nicolai S et al. Sci Immunol. 2020 Jan 3. doi: 10.1126/sciimmunol.aax5430.
A quick guide to PrEP: Steps to take & insurance coverage changes to watch for
References
- Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2010–2016. HIV Surveillance Supplemental Report. 2019;24. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published February 2019. Accessed January 17, 2020.
- US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. CDC Web Site. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Published March 2018. Accessed January 17, 2020.
- US Preventive Services Task Force. Final recommendation statement: prevention of human immunodeficiency virus (HIV) infection: preexposure prophylaxis. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis. Published June 2019. Accessed January 17, 2020.
- Campos-Outcalt D. A look at new guidelines for HIV treatment and prevention. J Fam Pract. 2018;67:768-772.
References
- Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2010–2016. HIV Surveillance Supplemental Report. 2019;24. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published February 2019. Accessed January 17, 2020.
- US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. CDC Web Site. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Published March 2018. Accessed January 17, 2020.
- US Preventive Services Task Force. Final recommendation statement: prevention of human immunodeficiency virus (HIV) infection: preexposure prophylaxis. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis. Published June 2019. Accessed January 17, 2020.
- Campos-Outcalt D. A look at new guidelines for HIV treatment and prevention. J Fam Pract. 2018;67:768-772.
References
- Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2010–2016. HIV Surveillance Supplemental Report. 2019;24. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published February 2019. Accessed January 17, 2020.
- US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. CDC Web Site. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Published March 2018. Accessed January 17, 2020.
- US Preventive Services Task Force. Final recommendation statement: prevention of human immunodeficiency virus (HIV) infection: preexposure prophylaxis. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prevention-of-human-immunodeficiency-virus-hiv-infection-pre-exposure-prophylaxis. Published June 2019. Accessed January 17, 2020.
- Campos-Outcalt D. A look at new guidelines for HIV treatment and prevention. J Fam Pract. 2018;67:768-772.