User login
Frequent lab testing is common, but low-yield, for isotretinoin patients
Abnormalities in lipids, liver enzymes, and blood counts were rare, and
In a review of 1,863 patients receiving isotretinoin, there were no cases of grade 4 abnormalities of lipids, liver enzymes, or complete blood count (CBC). Further, fewer than 1% of patients had grade 2-3 laboratory abnormalities, and no patients had cholesterol or CBC abnormalities of grade 3 or higher.
The retrospective cohort study used an electronic database to identify patients who were prescribed isotretinoin for acne from 2007 to 2017, with inclusion criteria structured to “increase the likelihood of capturing a complete course of isotretinoin therapy,” wrote John Barbieri, MD, and coauthors. The database allowed the investigators to group lab values into baseline testing, and testing by month of therapy for individual deidentified patient records.
Dr. Barbieri, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, and coinvestigators found that over half of all patients had baseline triglyceride, total cholesterol, AST, ALT, and platelet and white blood cell count levels.
Though the number of patients who had any of these levels checked in a given month of treatment declined over time, as did the total number of patients still on isotretinoin therapy, monthly AST and ALT monitoring occurred in 37.6%-58.5% of patients. Monthly triglyceride monitoring was conducted in between 39.6% and 61.4% of participants, and CBCs were obtained in 26.8%-37.4% of participants.
In terms of the abnormalities that were seen, grade 1 triglyceride elevations of 150-300 mg/dL were present in about 13% of patients at baseline, rising to 39% of participants who were still receiving isotretinoin at month 6. However, grade 2 elevations of up to 500 mg/dL were seen in 1.4% of patients at baseline and 2.4%-5.6% of patients during subsequent months.
Grade 1 liver enzyme abnormalities of less than three times the upper limit of normal values were seen at baseline in under 4% of patients, and in no more than 6.7% of patients through the course of treatment.
Leukopenia of between 3 x 103/mcL and the lower limit of normal occurred in 4.1% of baseline tests and in 6.6%-10.1% of tests in subsequent months. Grade 1 thrombocytopenia (values between 75 x 103/mcL and the lower limit of normal) occurred in 1.9% of baseline tests and no more than 2.9% of tests in the following months.
The results, wrote Dr. Barbieri and coauthors, affirm that most patients fare well on isotretinoin, and frequent laboratory testing is likely to be low-yield. Even using relatively low Medicare reimbursement rates for these tests yielded an estimated $134 in per-patient charges for the studied population. If baseline lipid and liver functions were followed only by repeat testing when peak isotretinoin dose was reached, charges would drop to about $87 per patient. Using the iPLEDGE database figures, this would save $17.4 million in monitoring costs annually, they wrote.
They also calculated that the monitoring regimen they observed puts the cost of detecting one single grade 3 hepatic enzyme elevation at $6,000; one grade 3 triglyceride elevation would cost $7,750.
Of the patients, 49% were female, the median age was 18.2 years, and the median duration of isotretinoin therapy was under 5 months (148 days). Nearly 90% of patients were white and non-Hispanic; 2.5% were black.
The data used for the analysis did not give the investigators access to clinician notes, but they did observe that, even when abnormal test values were seen, isotretinoin prescribing continued. This, they added, pointed toward reassuring clinical scenarios, even in cases of abnormal lab values.
“These findings are consistent with prior studies and suggest that extensive laboratory monitoring observed in this population may be of low value,” concluded Dr. Barbieri and colleagues. “In addition, changes to lipid levels observed in this study typically occurred during the first 2-3 months of therapy before stabilizing, which is consistent with findings in prior studies.”
The investigators noted that, despite mounting evidence of isotretinoin’s safety, there was no trend toward decreased CBC testing over the decade-long period of the study, and there were only “modest” decreases in hepatic enzyme and lipid monitoring. They called for an awareness campaign on the part of professional societies, and consideration for “more specific guideline recommendations” that may ease the testing burden on the adolescent and young adult population receiving isotretinoin.
The study was funded in part by the National Institutes of Health, and Dr. Barbieri receives partial salary support from Pfizer through a grant to the University of Pennsylvania. He has received support for unrelated work from Eli Lilly and Novartis. The other authors reported no conflicts of interest.
SOURCE: Barbieri J et al. J Am Acad Dermatol. 2020 Jan;82(1):72-9.
Abnormalities in lipids, liver enzymes, and blood counts were rare, and
In a review of 1,863 patients receiving isotretinoin, there were no cases of grade 4 abnormalities of lipids, liver enzymes, or complete blood count (CBC). Further, fewer than 1% of patients had grade 2-3 laboratory abnormalities, and no patients had cholesterol or CBC abnormalities of grade 3 or higher.
The retrospective cohort study used an electronic database to identify patients who were prescribed isotretinoin for acne from 2007 to 2017, with inclusion criteria structured to “increase the likelihood of capturing a complete course of isotretinoin therapy,” wrote John Barbieri, MD, and coauthors. The database allowed the investigators to group lab values into baseline testing, and testing by month of therapy for individual deidentified patient records.
Dr. Barbieri, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, and coinvestigators found that over half of all patients had baseline triglyceride, total cholesterol, AST, ALT, and platelet and white blood cell count levels.
Though the number of patients who had any of these levels checked in a given month of treatment declined over time, as did the total number of patients still on isotretinoin therapy, monthly AST and ALT monitoring occurred in 37.6%-58.5% of patients. Monthly triglyceride monitoring was conducted in between 39.6% and 61.4% of participants, and CBCs were obtained in 26.8%-37.4% of participants.
In terms of the abnormalities that were seen, grade 1 triglyceride elevations of 150-300 mg/dL were present in about 13% of patients at baseline, rising to 39% of participants who were still receiving isotretinoin at month 6. However, grade 2 elevations of up to 500 mg/dL were seen in 1.4% of patients at baseline and 2.4%-5.6% of patients during subsequent months.
Grade 1 liver enzyme abnormalities of less than three times the upper limit of normal values were seen at baseline in under 4% of patients, and in no more than 6.7% of patients through the course of treatment.
Leukopenia of between 3 x 103/mcL and the lower limit of normal occurred in 4.1% of baseline tests and in 6.6%-10.1% of tests in subsequent months. Grade 1 thrombocytopenia (values between 75 x 103/mcL and the lower limit of normal) occurred in 1.9% of baseline tests and no more than 2.9% of tests in the following months.
The results, wrote Dr. Barbieri and coauthors, affirm that most patients fare well on isotretinoin, and frequent laboratory testing is likely to be low-yield. Even using relatively low Medicare reimbursement rates for these tests yielded an estimated $134 in per-patient charges for the studied population. If baseline lipid and liver functions were followed only by repeat testing when peak isotretinoin dose was reached, charges would drop to about $87 per patient. Using the iPLEDGE database figures, this would save $17.4 million in monitoring costs annually, they wrote.
They also calculated that the monitoring regimen they observed puts the cost of detecting one single grade 3 hepatic enzyme elevation at $6,000; one grade 3 triglyceride elevation would cost $7,750.
Of the patients, 49% were female, the median age was 18.2 years, and the median duration of isotretinoin therapy was under 5 months (148 days). Nearly 90% of patients were white and non-Hispanic; 2.5% were black.
The data used for the analysis did not give the investigators access to clinician notes, but they did observe that, even when abnormal test values were seen, isotretinoin prescribing continued. This, they added, pointed toward reassuring clinical scenarios, even in cases of abnormal lab values.
“These findings are consistent with prior studies and suggest that extensive laboratory monitoring observed in this population may be of low value,” concluded Dr. Barbieri and colleagues. “In addition, changes to lipid levels observed in this study typically occurred during the first 2-3 months of therapy before stabilizing, which is consistent with findings in prior studies.”
The investigators noted that, despite mounting evidence of isotretinoin’s safety, there was no trend toward decreased CBC testing over the decade-long period of the study, and there were only “modest” decreases in hepatic enzyme and lipid monitoring. They called for an awareness campaign on the part of professional societies, and consideration for “more specific guideline recommendations” that may ease the testing burden on the adolescent and young adult population receiving isotretinoin.
The study was funded in part by the National Institutes of Health, and Dr. Barbieri receives partial salary support from Pfizer through a grant to the University of Pennsylvania. He has received support for unrelated work from Eli Lilly and Novartis. The other authors reported no conflicts of interest.
SOURCE: Barbieri J et al. J Am Acad Dermatol. 2020 Jan;82(1):72-9.
Abnormalities in lipids, liver enzymes, and blood counts were rare, and
In a review of 1,863 patients receiving isotretinoin, there were no cases of grade 4 abnormalities of lipids, liver enzymes, or complete blood count (CBC). Further, fewer than 1% of patients had grade 2-3 laboratory abnormalities, and no patients had cholesterol or CBC abnormalities of grade 3 or higher.
The retrospective cohort study used an electronic database to identify patients who were prescribed isotretinoin for acne from 2007 to 2017, with inclusion criteria structured to “increase the likelihood of capturing a complete course of isotretinoin therapy,” wrote John Barbieri, MD, and coauthors. The database allowed the investigators to group lab values into baseline testing, and testing by month of therapy for individual deidentified patient records.
Dr. Barbieri, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, and coinvestigators found that over half of all patients had baseline triglyceride, total cholesterol, AST, ALT, and platelet and white blood cell count levels.
Though the number of patients who had any of these levels checked in a given month of treatment declined over time, as did the total number of patients still on isotretinoin therapy, monthly AST and ALT monitoring occurred in 37.6%-58.5% of patients. Monthly triglyceride monitoring was conducted in between 39.6% and 61.4% of participants, and CBCs were obtained in 26.8%-37.4% of participants.
In terms of the abnormalities that were seen, grade 1 triglyceride elevations of 150-300 mg/dL were present in about 13% of patients at baseline, rising to 39% of participants who were still receiving isotretinoin at month 6. However, grade 2 elevations of up to 500 mg/dL were seen in 1.4% of patients at baseline and 2.4%-5.6% of patients during subsequent months.
Grade 1 liver enzyme abnormalities of less than three times the upper limit of normal values were seen at baseline in under 4% of patients, and in no more than 6.7% of patients through the course of treatment.
Leukopenia of between 3 x 103/mcL and the lower limit of normal occurred in 4.1% of baseline tests and in 6.6%-10.1% of tests in subsequent months. Grade 1 thrombocytopenia (values between 75 x 103/mcL and the lower limit of normal) occurred in 1.9% of baseline tests and no more than 2.9% of tests in the following months.
The results, wrote Dr. Barbieri and coauthors, affirm that most patients fare well on isotretinoin, and frequent laboratory testing is likely to be low-yield. Even using relatively low Medicare reimbursement rates for these tests yielded an estimated $134 in per-patient charges for the studied population. If baseline lipid and liver functions were followed only by repeat testing when peak isotretinoin dose was reached, charges would drop to about $87 per patient. Using the iPLEDGE database figures, this would save $17.4 million in monitoring costs annually, they wrote.
They also calculated that the monitoring regimen they observed puts the cost of detecting one single grade 3 hepatic enzyme elevation at $6,000; one grade 3 triglyceride elevation would cost $7,750.
Of the patients, 49% were female, the median age was 18.2 years, and the median duration of isotretinoin therapy was under 5 months (148 days). Nearly 90% of patients were white and non-Hispanic; 2.5% were black.
The data used for the analysis did not give the investigators access to clinician notes, but they did observe that, even when abnormal test values were seen, isotretinoin prescribing continued. This, they added, pointed toward reassuring clinical scenarios, even in cases of abnormal lab values.
“These findings are consistent with prior studies and suggest that extensive laboratory monitoring observed in this population may be of low value,” concluded Dr. Barbieri and colleagues. “In addition, changes to lipid levels observed in this study typically occurred during the first 2-3 months of therapy before stabilizing, which is consistent with findings in prior studies.”
The investigators noted that, despite mounting evidence of isotretinoin’s safety, there was no trend toward decreased CBC testing over the decade-long period of the study, and there were only “modest” decreases in hepatic enzyme and lipid monitoring. They called for an awareness campaign on the part of professional societies, and consideration for “more specific guideline recommendations” that may ease the testing burden on the adolescent and young adult population receiving isotretinoin.
The study was funded in part by the National Institutes of Health, and Dr. Barbieri receives partial salary support from Pfizer through a grant to the University of Pennsylvania. He has received support for unrelated work from Eli Lilly and Novartis. The other authors reported no conflicts of interest.
SOURCE: Barbieri J et al. J Am Acad Dermatol. 2020 Jan;82(1):72-9.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
February 2020 – ICYMI
Gastroenterology
November 2019
Clip closure after resection of large colorectal lesions with substantial risk of bleeding. Albéniz E et al. 2019 Nov;157(5):1213-21.e4. doi. 10.1053/j.gastro.2019.07.037.
Tumor seeding during colonoscopy as a possible cause for metachronous colorectal cancer. Backes Y et al. 2019 Nov;157(5):1222-32.e4. doi. 10.1053/j.gastro.2019.07.062.
December 2019
How to “DEAL” with disruptive physician behavior. Junga Z et al. 2019 Dec;157(6):1469-72. doi. 10.1053/j.gastro.2019.10.021.
Effect of sex, age, and positivity threshold on fecal immunochemical test accuracy: A systematic review and meta-analysis. Selby K et al. 2019 Dec;(6):1494-505. doi. 10.1053/j.gastro.2019.08.023.
January 2020
How to approach burnout among gastroenterology fellows. DeCross AJ 2020 Jan;158(1):32-5. doi. 10.1053/j.gastro.2019.11.032.
Efficacy and safety of peppermint oil in a randomized, double-blind trial of patients with irritable bowel syndrome. Weerts ZZRM et al. 2020 Jan;158(1):123-36. doi. 10.1053/j.gastro.2019.08.026.
Validation of a machine learning model that outperforms clinical risk scoring systems for upper gastrointestinal bleeding. Shung DL et al. 2020 Jan;158(1):160-7. doi. 10.1053/j.gastro.2019.09.009.
Efficacy and safety of early vs elective colonoscopy for acute lower gastrointestinal bleeding. Niikura R et al. 2020 Jan;158(1):168-75.e6. doi. 10.1053/j.gastro.2019.09.010.
Clinical Gastroenterology and Hepatology
November 2019
Medical professional liability in gastroenterology: Understanding the claims landscape and proposed mechanisms for reform. Adams MA and John I. Allen. 2019 Nov;17(12):2392-6.e1. doi. 10.1016/j.cgh.2019.07.002.
Optimizing use of nonalcoholic fatty liver disease fibrosis score, Fibrosis-4 score, and liver stiffness measurement to identify patients with advanced fibrosis. Chan W-K et al. 2019 Nov;17(12):2570-80.e37. doi. 10.1016/j.cgh.2019.03.006.
December 2019
Clinical and molecular features of post-colonoscopy colorectal cancers. Samadder NJ et al. 2019 Dec;17(12):2731-9.e2. doi. 10.1016/j.cgh.2019.02.040.
Neurologic deficits in patients with newly diagnosed celiac disease are frequent and linked with autoimmunity to transglutaminase 6. Hadjivassiliou M et al. 2019 Dec;17(12):2678-86.e2. doi. 10.1016/j.cgh.2019.03.014.
Increased risk of death in first year after liver transplantation among patients with nonalcoholic steatohepatitis vs liver disease of other etiologies. Nagai S et al. 2019 Dec;17(12):2759-68.e5. doi. 10.1016/j.cgh.2019.04.033.
January 2020
Incorporating high value care into gastroenterology fellowship training. Shah BJ and Janice H. Jou. 2020 Jan;18(1):11-3. doi. 10.1016/j.cgh.2019.10.040.
Association of obesity with colonic diverticulosis in women. Peery AF et al. 2020 Jan;18(1):107-14.e1. doi. 10.1016/j.cgh.2019.04.058.
Endocuff vision reduces inspection time without decreasing lesion detection: A clinical randomized trial. Rex DK et al. 2020 Jan;18(1):158-62.e1 doi. 10.1016/j.cgh.2019.01.015.
Gastroenterology
November 2019
Clip closure after resection of large colorectal lesions with substantial risk of bleeding. Albéniz E et al. 2019 Nov;157(5):1213-21.e4. doi. 10.1053/j.gastro.2019.07.037.
Tumor seeding during colonoscopy as a possible cause for metachronous colorectal cancer. Backes Y et al. 2019 Nov;157(5):1222-32.e4. doi. 10.1053/j.gastro.2019.07.062.
December 2019
How to “DEAL” with disruptive physician behavior. Junga Z et al. 2019 Dec;157(6):1469-72. doi. 10.1053/j.gastro.2019.10.021.
Effect of sex, age, and positivity threshold on fecal immunochemical test accuracy: A systematic review and meta-analysis. Selby K et al. 2019 Dec;(6):1494-505. doi. 10.1053/j.gastro.2019.08.023.
January 2020
How to approach burnout among gastroenterology fellows. DeCross AJ 2020 Jan;158(1):32-5. doi. 10.1053/j.gastro.2019.11.032.
Efficacy and safety of peppermint oil in a randomized, double-blind trial of patients with irritable bowel syndrome. Weerts ZZRM et al. 2020 Jan;158(1):123-36. doi. 10.1053/j.gastro.2019.08.026.
Validation of a machine learning model that outperforms clinical risk scoring systems for upper gastrointestinal bleeding. Shung DL et al. 2020 Jan;158(1):160-7. doi. 10.1053/j.gastro.2019.09.009.
Efficacy and safety of early vs elective colonoscopy for acute lower gastrointestinal bleeding. Niikura R et al. 2020 Jan;158(1):168-75.e6. doi. 10.1053/j.gastro.2019.09.010.
Clinical Gastroenterology and Hepatology
November 2019
Medical professional liability in gastroenterology: Understanding the claims landscape and proposed mechanisms for reform. Adams MA and John I. Allen. 2019 Nov;17(12):2392-6.e1. doi. 10.1016/j.cgh.2019.07.002.
Optimizing use of nonalcoholic fatty liver disease fibrosis score, Fibrosis-4 score, and liver stiffness measurement to identify patients with advanced fibrosis. Chan W-K et al. 2019 Nov;17(12):2570-80.e37. doi. 10.1016/j.cgh.2019.03.006.
December 2019
Clinical and molecular features of post-colonoscopy colorectal cancers. Samadder NJ et al. 2019 Dec;17(12):2731-9.e2. doi. 10.1016/j.cgh.2019.02.040.
Neurologic deficits in patients with newly diagnosed celiac disease are frequent and linked with autoimmunity to transglutaminase 6. Hadjivassiliou M et al. 2019 Dec;17(12):2678-86.e2. doi. 10.1016/j.cgh.2019.03.014.
Increased risk of death in first year after liver transplantation among patients with nonalcoholic steatohepatitis vs liver disease of other etiologies. Nagai S et al. 2019 Dec;17(12):2759-68.e5. doi. 10.1016/j.cgh.2019.04.033.
January 2020
Incorporating high value care into gastroenterology fellowship training. Shah BJ and Janice H. Jou. 2020 Jan;18(1):11-3. doi. 10.1016/j.cgh.2019.10.040.
Association of obesity with colonic diverticulosis in women. Peery AF et al. 2020 Jan;18(1):107-14.e1. doi. 10.1016/j.cgh.2019.04.058.
Endocuff vision reduces inspection time without decreasing lesion detection: A clinical randomized trial. Rex DK et al. 2020 Jan;18(1):158-62.e1 doi. 10.1016/j.cgh.2019.01.015.
Gastroenterology
November 2019
Clip closure after resection of large colorectal lesions with substantial risk of bleeding. Albéniz E et al. 2019 Nov;157(5):1213-21.e4. doi. 10.1053/j.gastro.2019.07.037.
Tumor seeding during colonoscopy as a possible cause for metachronous colorectal cancer. Backes Y et al. 2019 Nov;157(5):1222-32.e4. doi. 10.1053/j.gastro.2019.07.062.
December 2019
How to “DEAL” with disruptive physician behavior. Junga Z et al. 2019 Dec;157(6):1469-72. doi. 10.1053/j.gastro.2019.10.021.
Effect of sex, age, and positivity threshold on fecal immunochemical test accuracy: A systematic review and meta-analysis. Selby K et al. 2019 Dec;(6):1494-505. doi. 10.1053/j.gastro.2019.08.023.
January 2020
How to approach burnout among gastroenterology fellows. DeCross AJ 2020 Jan;158(1):32-5. doi. 10.1053/j.gastro.2019.11.032.
Efficacy and safety of peppermint oil in a randomized, double-blind trial of patients with irritable bowel syndrome. Weerts ZZRM et al. 2020 Jan;158(1):123-36. doi. 10.1053/j.gastro.2019.08.026.
Validation of a machine learning model that outperforms clinical risk scoring systems for upper gastrointestinal bleeding. Shung DL et al. 2020 Jan;158(1):160-7. doi. 10.1053/j.gastro.2019.09.009.
Efficacy and safety of early vs elective colonoscopy for acute lower gastrointestinal bleeding. Niikura R et al. 2020 Jan;158(1):168-75.e6. doi. 10.1053/j.gastro.2019.09.010.
Clinical Gastroenterology and Hepatology
November 2019
Medical professional liability in gastroenterology: Understanding the claims landscape and proposed mechanisms for reform. Adams MA and John I. Allen. 2019 Nov;17(12):2392-6.e1. doi. 10.1016/j.cgh.2019.07.002.
Optimizing use of nonalcoholic fatty liver disease fibrosis score, Fibrosis-4 score, and liver stiffness measurement to identify patients with advanced fibrosis. Chan W-K et al. 2019 Nov;17(12):2570-80.e37. doi. 10.1016/j.cgh.2019.03.006.
December 2019
Clinical and molecular features of post-colonoscopy colorectal cancers. Samadder NJ et al. 2019 Dec;17(12):2731-9.e2. doi. 10.1016/j.cgh.2019.02.040.
Neurologic deficits in patients with newly diagnosed celiac disease are frequent and linked with autoimmunity to transglutaminase 6. Hadjivassiliou M et al. 2019 Dec;17(12):2678-86.e2. doi. 10.1016/j.cgh.2019.03.014.
Increased risk of death in first year after liver transplantation among patients with nonalcoholic steatohepatitis vs liver disease of other etiologies. Nagai S et al. 2019 Dec;17(12):2759-68.e5. doi. 10.1016/j.cgh.2019.04.033.
January 2020
Incorporating high value care into gastroenterology fellowship training. Shah BJ and Janice H. Jou. 2020 Jan;18(1):11-3. doi. 10.1016/j.cgh.2019.10.040.
Association of obesity with colonic diverticulosis in women. Peery AF et al. 2020 Jan;18(1):107-14.e1. doi. 10.1016/j.cgh.2019.04.058.
Endocuff vision reduces inspection time without decreasing lesion detection: A clinical randomized trial. Rex DK et al. 2020 Jan;18(1):158-62.e1 doi. 10.1016/j.cgh.2019.01.015.
Rash on legs and abdomen
The rash was consistent with nonblanching purpura. Two punch biopsies were performed for hematoxylin and eosin stain and direct immunofluorescence, which were consistent with IgA mediated small vessel vasculitis, or Henoch-Schoenlein purpura.
IgA small vessel vasculitis commonly occurs in children after a transient viral illness or as an allergic reaction to a medication. Nonblanching purpura occurs because small vessels have been cracked open by neutrophils and lymphocytes and leaked blood cells outside of the vascular circulation. Pressure fails to move these cells downstream, and thus, the skin does not blanch.
Joint pain is common, as is a self-resolving IgA mediated nephropathy. Approximately 1% to 3% of children will progress to end stage renal disease. IgA vasculitis also occurs in adults, with a higher portion developing nephropathy. In adults, lesions that present on the abdomen are suspected to correspond with gravity dependency and the total burden of IgA, leading to a higher risk for nephropathy.
The differential diagnosis of purpura is broad, but includes leukocytoclastic vasculitis, antineutrophil cytoplasmic antibodies-associated vasculitis, capillaritis, and disseminated intravascular coagulation.
The patient in this case was given topical triamcinolone 0.1% ointment to treat the rash. She returned 3 weeks later and her blood pressure was 160/105 mm Hg and she had protein and blood in her urine. The FP recommended a renal biopsy, which confirmed severe IgA nephropathy and end stage renal failure. She was given systemic steroids and ultimately received a renal transplant. Her outcome was atypical and unfortunate. Usually IgA vasculitis is benign and self-resolves with rest. Even when nephropathy is present, it typically resolves over weeks to months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Audemard-Verger A, Terrier B, Dechartres A, et al. French Vasculitis Study Group. Characteristics and management of IgA vasculitis (Henoch-Schönlein) in adults: data from 260 patients included in a French multicenter retrospective survey. Arthritis Rheumatol. 2017;69:1862-1870.
The rash was consistent with nonblanching purpura. Two punch biopsies were performed for hematoxylin and eosin stain and direct immunofluorescence, which were consistent with IgA mediated small vessel vasculitis, or Henoch-Schoenlein purpura.
IgA small vessel vasculitis commonly occurs in children after a transient viral illness or as an allergic reaction to a medication. Nonblanching purpura occurs because small vessels have been cracked open by neutrophils and lymphocytes and leaked blood cells outside of the vascular circulation. Pressure fails to move these cells downstream, and thus, the skin does not blanch.
Joint pain is common, as is a self-resolving IgA mediated nephropathy. Approximately 1% to 3% of children will progress to end stage renal disease. IgA vasculitis also occurs in adults, with a higher portion developing nephropathy. In adults, lesions that present on the abdomen are suspected to correspond with gravity dependency and the total burden of IgA, leading to a higher risk for nephropathy.
The differential diagnosis of purpura is broad, but includes leukocytoclastic vasculitis, antineutrophil cytoplasmic antibodies-associated vasculitis, capillaritis, and disseminated intravascular coagulation.
The patient in this case was given topical triamcinolone 0.1% ointment to treat the rash. She returned 3 weeks later and her blood pressure was 160/105 mm Hg and she had protein and blood in her urine. The FP recommended a renal biopsy, which confirmed severe IgA nephropathy and end stage renal failure. She was given systemic steroids and ultimately received a renal transplant. Her outcome was atypical and unfortunate. Usually IgA vasculitis is benign and self-resolves with rest. Even when nephropathy is present, it typically resolves over weeks to months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
The rash was consistent with nonblanching purpura. Two punch biopsies were performed for hematoxylin and eosin stain and direct immunofluorescence, which were consistent with IgA mediated small vessel vasculitis, or Henoch-Schoenlein purpura.
IgA small vessel vasculitis commonly occurs in children after a transient viral illness or as an allergic reaction to a medication. Nonblanching purpura occurs because small vessels have been cracked open by neutrophils and lymphocytes and leaked blood cells outside of the vascular circulation. Pressure fails to move these cells downstream, and thus, the skin does not blanch.
Joint pain is common, as is a self-resolving IgA mediated nephropathy. Approximately 1% to 3% of children will progress to end stage renal disease. IgA vasculitis also occurs in adults, with a higher portion developing nephropathy. In adults, lesions that present on the abdomen are suspected to correspond with gravity dependency and the total burden of IgA, leading to a higher risk for nephropathy.
The differential diagnosis of purpura is broad, but includes leukocytoclastic vasculitis, antineutrophil cytoplasmic antibodies-associated vasculitis, capillaritis, and disseminated intravascular coagulation.
The patient in this case was given topical triamcinolone 0.1% ointment to treat the rash. She returned 3 weeks later and her blood pressure was 160/105 mm Hg and she had protein and blood in her urine. The FP recommended a renal biopsy, which confirmed severe IgA nephropathy and end stage renal failure. She was given systemic steroids and ultimately received a renal transplant. Her outcome was atypical and unfortunate. Usually IgA vasculitis is benign and self-resolves with rest. Even when nephropathy is present, it typically resolves over weeks to months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Audemard-Verger A, Terrier B, Dechartres A, et al. French Vasculitis Study Group. Characteristics and management of IgA vasculitis (Henoch-Schönlein) in adults: data from 260 patients included in a French multicenter retrospective survey. Arthritis Rheumatol. 2017;69:1862-1870.
Audemard-Verger A, Terrier B, Dechartres A, et al. French Vasculitis Study Group. Characteristics and management of IgA vasculitis (Henoch-Schönlein) in adults: data from 260 patients included in a French multicenter retrospective survey. Arthritis Rheumatol. 2017;69:1862-1870.
Cherry concentrate fails for gout flares
Tart cherry concentrate had no impact on gout flares over a 28-day period, based on data from 50 adult patients.
Urate-lowering therapy is part of gout management, and previous studies have suggested that tart cherry concentrate lowers sodium urate within hours in healthy volunteers and to a nonsignificant extent over 120 days in patients with gout, but “the optimal dose of tart cherry concentrate for either a serum urate effect on or flare prevention is unknown,” wrote Lisa K. Stamp, MD, of the University of Otago, Christchurch, New Zealand, and colleagues.
In a study published in Rheumatology, the researchers randomized 50 adults with gout and baseline serum urate levels greater than 0.36 mmol/L (6 mg/dL) to receive one of four doses of tart cherry juice concentrate (7.5 mL, 15 mL, 22.5 mL, or 30 mL) or a placebo twice daily for 28 days. Half of the participants were taking allopurinol and half were not taking any urate-lowering therapy.
After 28 days, patients who received cherry juice showed no significant changes in serum urate regardless of whether they were also taking allopurinol. In addition, cherry juice at any dose had no significant effect on reducing the serum urate area under the curve and no apparent impact on measures including urine urate excretion, change in urinary anthocyanins, and frequency of gout flares, compared with placebo. However, the cherry juice was well tolerated, and 84% of the study participants said they would recommend it to a friend as a method of gout prevention.
The researchers collected blood samples at baseline, and at 1, 3, and 5 hours after consuming cherry juice, and on days 1, 3, 7, 14, 21, and 28. “If there is an effect of cherry concentrate on gout flares over a longer time period, it is not likely to be mediated by reduction in serum urate,” the researchers said.
Of 24 adverse events reported during the study, 18 occurred in patients taking cherry juice at all dosage levels, and one case of hyperglycemia was potentially related to cherry concentrate. No serious adverse events associated with tart cherry concentrate occurred during the study period.
The study findings were limited by several factors including the inability to blind the study because participants prepared their doses at home, and the lack of data on the exact contents of the cherry juice concentrate used in the study, the researchers noted. However, the results suggest that tart cherry concentrate has no effect on serum urate concentration or urinary urate excretion, which make it unlikely to be useful in reducing gout flares, they concluded.
The study was supported by the Health Research Council of New Zealand. The researchers had no financial conflicts to disclose.
SOURCE: Stamp LK et al. Rheumatology. 2019 Dec 31. doi: 10.1093/rheumatology/kez606.
Tart cherry concentrate had no impact on gout flares over a 28-day period, based on data from 50 adult patients.
Urate-lowering therapy is part of gout management, and previous studies have suggested that tart cherry concentrate lowers sodium urate within hours in healthy volunteers and to a nonsignificant extent over 120 days in patients with gout, but “the optimal dose of tart cherry concentrate for either a serum urate effect on or flare prevention is unknown,” wrote Lisa K. Stamp, MD, of the University of Otago, Christchurch, New Zealand, and colleagues.
In a study published in Rheumatology, the researchers randomized 50 adults with gout and baseline serum urate levels greater than 0.36 mmol/L (6 mg/dL) to receive one of four doses of tart cherry juice concentrate (7.5 mL, 15 mL, 22.5 mL, or 30 mL) or a placebo twice daily for 28 days. Half of the participants were taking allopurinol and half were not taking any urate-lowering therapy.
After 28 days, patients who received cherry juice showed no significant changes in serum urate regardless of whether they were also taking allopurinol. In addition, cherry juice at any dose had no significant effect on reducing the serum urate area under the curve and no apparent impact on measures including urine urate excretion, change in urinary anthocyanins, and frequency of gout flares, compared with placebo. However, the cherry juice was well tolerated, and 84% of the study participants said they would recommend it to a friend as a method of gout prevention.
The researchers collected blood samples at baseline, and at 1, 3, and 5 hours after consuming cherry juice, and on days 1, 3, 7, 14, 21, and 28. “If there is an effect of cherry concentrate on gout flares over a longer time period, it is not likely to be mediated by reduction in serum urate,” the researchers said.
Of 24 adverse events reported during the study, 18 occurred in patients taking cherry juice at all dosage levels, and one case of hyperglycemia was potentially related to cherry concentrate. No serious adverse events associated with tart cherry concentrate occurred during the study period.
The study findings were limited by several factors including the inability to blind the study because participants prepared their doses at home, and the lack of data on the exact contents of the cherry juice concentrate used in the study, the researchers noted. However, the results suggest that tart cherry concentrate has no effect on serum urate concentration or urinary urate excretion, which make it unlikely to be useful in reducing gout flares, they concluded.
The study was supported by the Health Research Council of New Zealand. The researchers had no financial conflicts to disclose.
SOURCE: Stamp LK et al. Rheumatology. 2019 Dec 31. doi: 10.1093/rheumatology/kez606.
Tart cherry concentrate had no impact on gout flares over a 28-day period, based on data from 50 adult patients.
Urate-lowering therapy is part of gout management, and previous studies have suggested that tart cherry concentrate lowers sodium urate within hours in healthy volunteers and to a nonsignificant extent over 120 days in patients with gout, but “the optimal dose of tart cherry concentrate for either a serum urate effect on or flare prevention is unknown,” wrote Lisa K. Stamp, MD, of the University of Otago, Christchurch, New Zealand, and colleagues.
In a study published in Rheumatology, the researchers randomized 50 adults with gout and baseline serum urate levels greater than 0.36 mmol/L (6 mg/dL) to receive one of four doses of tart cherry juice concentrate (7.5 mL, 15 mL, 22.5 mL, or 30 mL) or a placebo twice daily for 28 days. Half of the participants were taking allopurinol and half were not taking any urate-lowering therapy.
After 28 days, patients who received cherry juice showed no significant changes in serum urate regardless of whether they were also taking allopurinol. In addition, cherry juice at any dose had no significant effect on reducing the serum urate area under the curve and no apparent impact on measures including urine urate excretion, change in urinary anthocyanins, and frequency of gout flares, compared with placebo. However, the cherry juice was well tolerated, and 84% of the study participants said they would recommend it to a friend as a method of gout prevention.
The researchers collected blood samples at baseline, and at 1, 3, and 5 hours after consuming cherry juice, and on days 1, 3, 7, 14, 21, and 28. “If there is an effect of cherry concentrate on gout flares over a longer time period, it is not likely to be mediated by reduction in serum urate,” the researchers said.
Of 24 adverse events reported during the study, 18 occurred in patients taking cherry juice at all dosage levels, and one case of hyperglycemia was potentially related to cherry concentrate. No serious adverse events associated with tart cherry concentrate occurred during the study period.
The study findings were limited by several factors including the inability to blind the study because participants prepared their doses at home, and the lack of data on the exact contents of the cherry juice concentrate used in the study, the researchers noted. However, the results suggest that tart cherry concentrate has no effect on serum urate concentration or urinary urate excretion, which make it unlikely to be useful in reducing gout flares, they concluded.
The study was supported by the Health Research Council of New Zealand. The researchers had no financial conflicts to disclose.
SOURCE: Stamp LK et al. Rheumatology. 2019 Dec 31. doi: 10.1093/rheumatology/kez606.
FROM RHEUMATOLOGY
UKALL14: Rituximab improves EFS in B-ALL, but four doses not enough
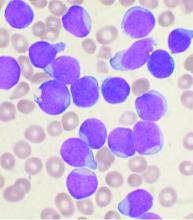
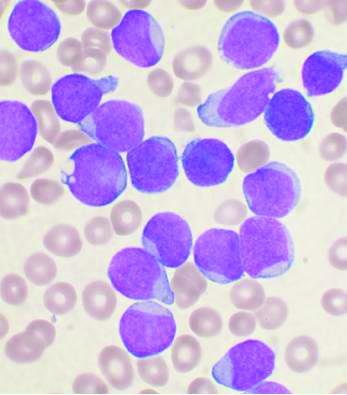
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
REPORTING FROM ASH 2019
Medicaid spending on MS drugs rose despite introduction of generic glatiramer
Prescription pricing is a primary reason why Medicaid spending on multiple sclerosis disease-modifying therapies (DMTs) has more than doubled between 2011 and 2017 and the introduction of a generic glatiramer acetate is having nominal effect on pricing and utilization within the class, new research is showing.
“Gross spending on self-administered and infusible MS DMTs in the Medicaid program increased 2.9-fold from $453 million in 2011 to $1.32 billion in 2017,” Daniel Hartung, PharmD, of Oregon Health and Science University, Portland, and his colleagues wrote in a research report published Jan. 15 in Neurology. Net spending after accounting for rebates during this period showed a doubling of spending from $278 million per year to $600 million per year.
Use of MS DMTs during this period overall remained stable, but there was a shift from injectable DMTs to oral DMTs during this time window, the researchers found, with the plurality of utilization attributed to glatiramer acetate.
Sandoz began marketing a generic version of glatiramer acetate 20 mg in the second quarter of 2015, which led to an immediate increase in the cost per prescription of $441 for the branded version of glatiramer acetate 20 mg, although that cost has come down gradually by $52 per prescription over time. Other DMTs saw minimal price changes at that time, Dr. Hartung and his colleagues noted.
The researchers attributed the increased Medicaid spending to rising prices of DMTs.
“Although some of this increase is attributable to the 2014 Medicaid expansion, the primary driver was rising DMT costs per prescription, which doubled over the period,” the researchers wrote. “Thus, we assert that rising prices, not increasing use, are the primary driver of spending for DMTs in the Medicaid program.”
In addition, the introduction of the first generic DMT “appeared to have little effect on the overall trajectory of DMT costs,” they continued. “In fact, the cost of Teva’s 20-mg glatiramer acetate increased significantly following the release of Sandoz’s generic. ... The increase possibly signified efforts to both retain revenue and further push market share to the 40-mg version. Although the costs for generic glatiramer acetate declined over time, its introduction appears not to have fundamentally affected the overall trend in DMT costs.”
Indeed, the researchers’ examination of utilization trends found that Teva executed a successful preemptive strategy of converting 20-mg users of glatiramer acetate to 40-mg users, something that is not interchangeable with the generic product.
“Low generic penetration is also due to the fact that Sandoz’s product was only 15% less expensive than branded glatiramer acetate 20 mg and approximately the same cost as the 40-mg version at launch,” Dr. Hartung and his colleagues stated. “This difference may have been further diminished by rebates that Teva may have provided to maintain preferred status on state Medicaid formularies.”
These factors reflect an “urgent need for robust generic competition within the DMT class,” the authors wrote.
The study was supported by the National Multiple Sclerosis Society. Lead author Dr. Hartung reported receiving research support from AbbVie.
SOURCE: Hartung D et al. Neurology. Jan 15. doi: 10.1212/WNL.0000000000008936.
Prescription pricing is a primary reason why Medicaid spending on multiple sclerosis disease-modifying therapies (DMTs) has more than doubled between 2011 and 2017 and the introduction of a generic glatiramer acetate is having nominal effect on pricing and utilization within the class, new research is showing.
“Gross spending on self-administered and infusible MS DMTs in the Medicaid program increased 2.9-fold from $453 million in 2011 to $1.32 billion in 2017,” Daniel Hartung, PharmD, of Oregon Health and Science University, Portland, and his colleagues wrote in a research report published Jan. 15 in Neurology. Net spending after accounting for rebates during this period showed a doubling of spending from $278 million per year to $600 million per year.
Use of MS DMTs during this period overall remained stable, but there was a shift from injectable DMTs to oral DMTs during this time window, the researchers found, with the plurality of utilization attributed to glatiramer acetate.
Sandoz began marketing a generic version of glatiramer acetate 20 mg in the second quarter of 2015, which led to an immediate increase in the cost per prescription of $441 for the branded version of glatiramer acetate 20 mg, although that cost has come down gradually by $52 per prescription over time. Other DMTs saw minimal price changes at that time, Dr. Hartung and his colleagues noted.
The researchers attributed the increased Medicaid spending to rising prices of DMTs.
“Although some of this increase is attributable to the 2014 Medicaid expansion, the primary driver was rising DMT costs per prescription, which doubled over the period,” the researchers wrote. “Thus, we assert that rising prices, not increasing use, are the primary driver of spending for DMTs in the Medicaid program.”
In addition, the introduction of the first generic DMT “appeared to have little effect on the overall trajectory of DMT costs,” they continued. “In fact, the cost of Teva’s 20-mg glatiramer acetate increased significantly following the release of Sandoz’s generic. ... The increase possibly signified efforts to both retain revenue and further push market share to the 40-mg version. Although the costs for generic glatiramer acetate declined over time, its introduction appears not to have fundamentally affected the overall trend in DMT costs.”
Indeed, the researchers’ examination of utilization trends found that Teva executed a successful preemptive strategy of converting 20-mg users of glatiramer acetate to 40-mg users, something that is not interchangeable with the generic product.
“Low generic penetration is also due to the fact that Sandoz’s product was only 15% less expensive than branded glatiramer acetate 20 mg and approximately the same cost as the 40-mg version at launch,” Dr. Hartung and his colleagues stated. “This difference may have been further diminished by rebates that Teva may have provided to maintain preferred status on state Medicaid formularies.”
These factors reflect an “urgent need for robust generic competition within the DMT class,” the authors wrote.
The study was supported by the National Multiple Sclerosis Society. Lead author Dr. Hartung reported receiving research support from AbbVie.
SOURCE: Hartung D et al. Neurology. Jan 15. doi: 10.1212/WNL.0000000000008936.
Prescription pricing is a primary reason why Medicaid spending on multiple sclerosis disease-modifying therapies (DMTs) has more than doubled between 2011 and 2017 and the introduction of a generic glatiramer acetate is having nominal effect on pricing and utilization within the class, new research is showing.
“Gross spending on self-administered and infusible MS DMTs in the Medicaid program increased 2.9-fold from $453 million in 2011 to $1.32 billion in 2017,” Daniel Hartung, PharmD, of Oregon Health and Science University, Portland, and his colleagues wrote in a research report published Jan. 15 in Neurology. Net spending after accounting for rebates during this period showed a doubling of spending from $278 million per year to $600 million per year.
Use of MS DMTs during this period overall remained stable, but there was a shift from injectable DMTs to oral DMTs during this time window, the researchers found, with the plurality of utilization attributed to glatiramer acetate.
Sandoz began marketing a generic version of glatiramer acetate 20 mg in the second quarter of 2015, which led to an immediate increase in the cost per prescription of $441 for the branded version of glatiramer acetate 20 mg, although that cost has come down gradually by $52 per prescription over time. Other DMTs saw minimal price changes at that time, Dr. Hartung and his colleagues noted.
The researchers attributed the increased Medicaid spending to rising prices of DMTs.
“Although some of this increase is attributable to the 2014 Medicaid expansion, the primary driver was rising DMT costs per prescription, which doubled over the period,” the researchers wrote. “Thus, we assert that rising prices, not increasing use, are the primary driver of spending for DMTs in the Medicaid program.”
In addition, the introduction of the first generic DMT “appeared to have little effect on the overall trajectory of DMT costs,” they continued. “In fact, the cost of Teva’s 20-mg glatiramer acetate increased significantly following the release of Sandoz’s generic. ... The increase possibly signified efforts to both retain revenue and further push market share to the 40-mg version. Although the costs for generic glatiramer acetate declined over time, its introduction appears not to have fundamentally affected the overall trend in DMT costs.”
Indeed, the researchers’ examination of utilization trends found that Teva executed a successful preemptive strategy of converting 20-mg users of glatiramer acetate to 40-mg users, something that is not interchangeable with the generic product.
“Low generic penetration is also due to the fact that Sandoz’s product was only 15% less expensive than branded glatiramer acetate 20 mg and approximately the same cost as the 40-mg version at launch,” Dr. Hartung and his colleagues stated. “This difference may have been further diminished by rebates that Teva may have provided to maintain preferred status on state Medicaid formularies.”
These factors reflect an “urgent need for robust generic competition within the DMT class,” the authors wrote.
The study was supported by the National Multiple Sclerosis Society. Lead author Dr. Hartung reported receiving research support from AbbVie.
SOURCE: Hartung D et al. Neurology. Jan 15. doi: 10.1212/WNL.0000000000008936.
FROM NEUROLOGY
Key clinical point: Medicaid spending on MS DMTs continues to rise in spite of generic introduction.
Major finding: Cost is the major factor in spending as utilization has remained stable.
Study details: Researchers examined quarterly Medicaid State Drug Utilization Data from 2011 to 2017, examining spending, utilization and cost per prescription for 15 MS DMTs, including brand and generic versions of glatiramer acetate.
Disclosures: The study was supported by the National Multiple Sclerosis Society. Lead author Dr. Hartung reported receiving research support from AbbVie.
Source: Hartung D et al. Neurology. Jan 15. doi: 10.1212/WNL.0000000000008936.
Fewer interventions after sleeve gastrectomy vs. Roux-en-Y, real-world data show
Sleeve gastrectomy was associated with significantly fewer postsurgical interventions and operations than was Roux-en-Y gastric bypass over longer-term follow-up in a recent cohort study based on real-world clinical data, according to investigators.
Interventions, operations, and hospitalizations were “relatively common” for both procedures over the 5-year follow-up, though significantly less so with sleeve gastrectomy, which has become the most common bariatric operation, the investigators said in a recent report on the study.
The benefit of sleeve gastrectomy seemed to be most pronounced in patients with lower body mass index and those with fewer comorbidities, according to the authors of the report, led by bariatric and general surgeon Anita Courcoulas, MD, of the University of Pittsburgh Medical Center.
That finding is counterintuitive, since in clinical practice, sleeve gastrectomy is frequently thought of as the preferred procedure for individuals with higher BMI or more comorbidities, though Dr. Courcoulas and colleagues cautioned that the findings were “exploratory” and require further investigation. Historically, Roux-en-Y gastric bypass provided more weight loss.
Safety results from this study, balanced by weight loss and health outcomes data, will “help inform procedure-specific decision making for prospective patients and physicians,” said Dr. Courcoulas and coauthors of the report, which appears in JAMA Surgery.
The study included 33,560 adults who had undergone the Roux-en-Y procedure or sleeve gastrectomy, making it one of the largest bariatric cohort studies ever to be done, according to the investigators.
The majority of patients in the study (54%) underwent Roux-en-Y gastric bypass, though the number of sleeve gastrectomy procedures increased each year in the study, which included patients who underwent a primary bariatric surgery procedure between January 2005 and September 2015 at 1 of 10 sites in the National Patient-Centered Clinical Research Network.
Most of the patients were female (80%) and white (66%), and 26% were Hispanic, according to the researchers, who said their study was more racially diverse than other bariatric studies, and therefore potentially more generalizable to real-world clinical practice.
Over the 5-year follow-up period, patients who underwent sleeve gastrectomy were less likely to subsequently undergo operations involving the abdomen, or interventions for enteral access, such as placement of gastrostomy tubes, according to the investigators, who reported a hazard ratio (HR) of 0.72 (95% confidence interval [CI], 0.65-0.79; P less than .001).
The estimated cumulative rate of operations or interventions at 5 years was 8.94% (95% CI, 8.23%-9.65%) for the patients who underwent sleeve gastrectomy, compared with 12.27% (95% CI, 11.49%-13.05%) for those who underwent the Roux-en-Y procedure, according to the report.
Hospitalization was also less likely for sleeve gastrectomy versus Roux-en-Y gastric bypass, with a hazard ratio of 0.82 and estimated cumulative incidence rates of 32.79% and 38.33%, respectively. Likewise, endoscopy was less likely in the sleeve gastrectomy group.
All-cause mortality did not differ between the groups at this 5-year follow-up, the investigators said.
“The present data were gathered from clinical care in the real world, yet the results are comparable to controlled studies and therefore lend additional support to the findings of these other types of studies that operation and intervention occur less commonly after sleeve gastrectomy than after Roux-en-Y gastric bypass for up to 5 years,” Dr. Courcoulas and coauthors noted in a discussion of their results.
This work was funded by the Patient-Centered Outcomes Research Institute. Dr. Courcoulas reported receiving a grant from Allurion. Coauthors provided disclosures related to the National Institutes of Health, IFSO Latin America Chapter, and the Food and Drug Administration.
*This story was updated on January 16, 2020.
SOURCE: Courcoulas A et al. JAMA Surg. 2020 Jan 15. doi: 10.1001/jamasurg.2019.5470.
This study by Courcoulas and colleagues adds to an established body of data showing that bariatric surgery is safe, according to authors of an invited commentary on the study.
More specifically, the study provides data that sleeve gastrectomy – which has become the most common bariatric procedure in the United States – is safe in the long term, said Anne P. Ehlers, MD, MPH, and Amir A. Ghaferi, MD, MS.
Barriers to surgery need to come down in response to the worsening public health crisis that these procedures address, according to Dr. Ehlers and Dr. Ghaferi.
“It is time we stop questioning the safety or efficacy of surgery and begin advocating for comprehensive obesity care for patients,” they said in their invited commentary.
Less than 1% of patients eligible for bariatric surgery undergo this “life-saving” treatment, they said, adding that obesity bias delays surgical referrals, while some “continue to fear” surgical risks, and decades-old guidelines restrict procedures to patients with higher body mass index.
The present study shows that sleeve gastrectomy is at least as safe, if not safer, than the Roux-en-Y gastric bypass procedure, said Dr. Ehlers and Dr. Ghaferi.
The study also answers the question of whether sleeve gastrectomy has an “unacceptably high” rate of gastroesophageal reflux disease (GERD) prompting revision surgeries, they said.
On the contrary, sleeve gastrectomy was associated with lower rates of reoperation, and lower rates of endoscopies, which almost always come before reoperations related to GERD, they explained.
Anne P. Ehlers, MD, MPH, and Amir A. Ghaferi, MD, MS, are with the department of surgery at the University of Michigan in Ann Arbor. They reported no conflicts of interests related to their invited commentary, which appears in JAMA Surgery .
This study by Courcoulas and colleagues adds to an established body of data showing that bariatric surgery is safe, according to authors of an invited commentary on the study.
More specifically, the study provides data that sleeve gastrectomy – which has become the most common bariatric procedure in the United States – is safe in the long term, said Anne P. Ehlers, MD, MPH, and Amir A. Ghaferi, MD, MS.
Barriers to surgery need to come down in response to the worsening public health crisis that these procedures address, according to Dr. Ehlers and Dr. Ghaferi.
“It is time we stop questioning the safety or efficacy of surgery and begin advocating for comprehensive obesity care for patients,” they said in their invited commentary.
Less than 1% of patients eligible for bariatric surgery undergo this “life-saving” treatment, they said, adding that obesity bias delays surgical referrals, while some “continue to fear” surgical risks, and decades-old guidelines restrict procedures to patients with higher body mass index.
The present study shows that sleeve gastrectomy is at least as safe, if not safer, than the Roux-en-Y gastric bypass procedure, said Dr. Ehlers and Dr. Ghaferi.
The study also answers the question of whether sleeve gastrectomy has an “unacceptably high” rate of gastroesophageal reflux disease (GERD) prompting revision surgeries, they said.
On the contrary, sleeve gastrectomy was associated with lower rates of reoperation, and lower rates of endoscopies, which almost always come before reoperations related to GERD, they explained.
Anne P. Ehlers, MD, MPH, and Amir A. Ghaferi, MD, MS, are with the department of surgery at the University of Michigan in Ann Arbor. They reported no conflicts of interests related to their invited commentary, which appears in JAMA Surgery .
This study by Courcoulas and colleagues adds to an established body of data showing that bariatric surgery is safe, according to authors of an invited commentary on the study.
More specifically, the study provides data that sleeve gastrectomy – which has become the most common bariatric procedure in the United States – is safe in the long term, said Anne P. Ehlers, MD, MPH, and Amir A. Ghaferi, MD, MS.
Barriers to surgery need to come down in response to the worsening public health crisis that these procedures address, according to Dr. Ehlers and Dr. Ghaferi.
“It is time we stop questioning the safety or efficacy of surgery and begin advocating for comprehensive obesity care for patients,” they said in their invited commentary.
Less than 1% of patients eligible for bariatric surgery undergo this “life-saving” treatment, they said, adding that obesity bias delays surgical referrals, while some “continue to fear” surgical risks, and decades-old guidelines restrict procedures to patients with higher body mass index.
The present study shows that sleeve gastrectomy is at least as safe, if not safer, than the Roux-en-Y gastric bypass procedure, said Dr. Ehlers and Dr. Ghaferi.
The study also answers the question of whether sleeve gastrectomy has an “unacceptably high” rate of gastroesophageal reflux disease (GERD) prompting revision surgeries, they said.
On the contrary, sleeve gastrectomy was associated with lower rates of reoperation, and lower rates of endoscopies, which almost always come before reoperations related to GERD, they explained.
Anne P. Ehlers, MD, MPH, and Amir A. Ghaferi, MD, MS, are with the department of surgery at the University of Michigan in Ann Arbor. They reported no conflicts of interests related to their invited commentary, which appears in JAMA Surgery .
Sleeve gastrectomy was associated with significantly fewer postsurgical interventions and operations than was Roux-en-Y gastric bypass over longer-term follow-up in a recent cohort study based on real-world clinical data, according to investigators.
Interventions, operations, and hospitalizations were “relatively common” for both procedures over the 5-year follow-up, though significantly less so with sleeve gastrectomy, which has become the most common bariatric operation, the investigators said in a recent report on the study.
The benefit of sleeve gastrectomy seemed to be most pronounced in patients with lower body mass index and those with fewer comorbidities, according to the authors of the report, led by bariatric and general surgeon Anita Courcoulas, MD, of the University of Pittsburgh Medical Center.
That finding is counterintuitive, since in clinical practice, sleeve gastrectomy is frequently thought of as the preferred procedure for individuals with higher BMI or more comorbidities, though Dr. Courcoulas and colleagues cautioned that the findings were “exploratory” and require further investigation. Historically, Roux-en-Y gastric bypass provided more weight loss.
Safety results from this study, balanced by weight loss and health outcomes data, will “help inform procedure-specific decision making for prospective patients and physicians,” said Dr. Courcoulas and coauthors of the report, which appears in JAMA Surgery.
The study included 33,560 adults who had undergone the Roux-en-Y procedure or sleeve gastrectomy, making it one of the largest bariatric cohort studies ever to be done, according to the investigators.
The majority of patients in the study (54%) underwent Roux-en-Y gastric bypass, though the number of sleeve gastrectomy procedures increased each year in the study, which included patients who underwent a primary bariatric surgery procedure between January 2005 and September 2015 at 1 of 10 sites in the National Patient-Centered Clinical Research Network.
Most of the patients were female (80%) and white (66%), and 26% were Hispanic, according to the researchers, who said their study was more racially diverse than other bariatric studies, and therefore potentially more generalizable to real-world clinical practice.
Over the 5-year follow-up period, patients who underwent sleeve gastrectomy were less likely to subsequently undergo operations involving the abdomen, or interventions for enteral access, such as placement of gastrostomy tubes, according to the investigators, who reported a hazard ratio (HR) of 0.72 (95% confidence interval [CI], 0.65-0.79; P less than .001).
The estimated cumulative rate of operations or interventions at 5 years was 8.94% (95% CI, 8.23%-9.65%) for the patients who underwent sleeve gastrectomy, compared with 12.27% (95% CI, 11.49%-13.05%) for those who underwent the Roux-en-Y procedure, according to the report.
Hospitalization was also less likely for sleeve gastrectomy versus Roux-en-Y gastric bypass, with a hazard ratio of 0.82 and estimated cumulative incidence rates of 32.79% and 38.33%, respectively. Likewise, endoscopy was less likely in the sleeve gastrectomy group.
All-cause mortality did not differ between the groups at this 5-year follow-up, the investigators said.
“The present data were gathered from clinical care in the real world, yet the results are comparable to controlled studies and therefore lend additional support to the findings of these other types of studies that operation and intervention occur less commonly after sleeve gastrectomy than after Roux-en-Y gastric bypass for up to 5 years,” Dr. Courcoulas and coauthors noted in a discussion of their results.
This work was funded by the Patient-Centered Outcomes Research Institute. Dr. Courcoulas reported receiving a grant from Allurion. Coauthors provided disclosures related to the National Institutes of Health, IFSO Latin America Chapter, and the Food and Drug Administration.
*This story was updated on January 16, 2020.
SOURCE: Courcoulas A et al. JAMA Surg. 2020 Jan 15. doi: 10.1001/jamasurg.2019.5470.
Sleeve gastrectomy was associated with significantly fewer postsurgical interventions and operations than was Roux-en-Y gastric bypass over longer-term follow-up in a recent cohort study based on real-world clinical data, according to investigators.
Interventions, operations, and hospitalizations were “relatively common” for both procedures over the 5-year follow-up, though significantly less so with sleeve gastrectomy, which has become the most common bariatric operation, the investigators said in a recent report on the study.
The benefit of sleeve gastrectomy seemed to be most pronounced in patients with lower body mass index and those with fewer comorbidities, according to the authors of the report, led by bariatric and general surgeon Anita Courcoulas, MD, of the University of Pittsburgh Medical Center.
That finding is counterintuitive, since in clinical practice, sleeve gastrectomy is frequently thought of as the preferred procedure for individuals with higher BMI or more comorbidities, though Dr. Courcoulas and colleagues cautioned that the findings were “exploratory” and require further investigation. Historically, Roux-en-Y gastric bypass provided more weight loss.
Safety results from this study, balanced by weight loss and health outcomes data, will “help inform procedure-specific decision making for prospective patients and physicians,” said Dr. Courcoulas and coauthors of the report, which appears in JAMA Surgery.
The study included 33,560 adults who had undergone the Roux-en-Y procedure or sleeve gastrectomy, making it one of the largest bariatric cohort studies ever to be done, according to the investigators.
The majority of patients in the study (54%) underwent Roux-en-Y gastric bypass, though the number of sleeve gastrectomy procedures increased each year in the study, which included patients who underwent a primary bariatric surgery procedure between January 2005 and September 2015 at 1 of 10 sites in the National Patient-Centered Clinical Research Network.
Most of the patients were female (80%) and white (66%), and 26% were Hispanic, according to the researchers, who said their study was more racially diverse than other bariatric studies, and therefore potentially more generalizable to real-world clinical practice.
Over the 5-year follow-up period, patients who underwent sleeve gastrectomy were less likely to subsequently undergo operations involving the abdomen, or interventions for enteral access, such as placement of gastrostomy tubes, according to the investigators, who reported a hazard ratio (HR) of 0.72 (95% confidence interval [CI], 0.65-0.79; P less than .001).
The estimated cumulative rate of operations or interventions at 5 years was 8.94% (95% CI, 8.23%-9.65%) for the patients who underwent sleeve gastrectomy, compared with 12.27% (95% CI, 11.49%-13.05%) for those who underwent the Roux-en-Y procedure, according to the report.
Hospitalization was also less likely for sleeve gastrectomy versus Roux-en-Y gastric bypass, with a hazard ratio of 0.82 and estimated cumulative incidence rates of 32.79% and 38.33%, respectively. Likewise, endoscopy was less likely in the sleeve gastrectomy group.
All-cause mortality did not differ between the groups at this 5-year follow-up, the investigators said.
“The present data were gathered from clinical care in the real world, yet the results are comparable to controlled studies and therefore lend additional support to the findings of these other types of studies that operation and intervention occur less commonly after sleeve gastrectomy than after Roux-en-Y gastric bypass for up to 5 years,” Dr. Courcoulas and coauthors noted in a discussion of their results.
This work was funded by the Patient-Centered Outcomes Research Institute. Dr. Courcoulas reported receiving a grant from Allurion. Coauthors provided disclosures related to the National Institutes of Health, IFSO Latin America Chapter, and the Food and Drug Administration.
*This story was updated on January 16, 2020.
SOURCE: Courcoulas A et al. JAMA Surg. 2020 Jan 15. doi: 10.1001/jamasurg.2019.5470.
FROM JAMA SURGERY
Synaptic pruning deficits may cause tremor in essential tremor
according to an investigation published January 15 in Science Translational Medicine. These synaptic pruning deficits result from insufficiency of glutamate receptor delta 2 (GluR[delta]2) protein. The findings indicate molecular, structural, physiological, and behavioral factors that contribute to tremor and might influence future treatment of essential tremor, the authors wrote.

Essential tremor has a complex etiology that includes genetic and environmental factors. Its pathophysiology is poorly understood. First author Ming-Kai Pan, MD, assistant professor of medical research and neurology at National Taiwan University Hospital in Taipei, and colleagues previously observed pruning deficits of CF-PC synapses in the cerebellum of deceased patients with essential tremor. An excess of CF-PC synapses are a prominent feature of essential tremor, but not of other cerebellar degenerative disorders. Researchers have observed this pathology consistently in patients with essential tremor who have diverse clinical features. Dr. Pan and colleagues therefore chose to examine these synaptic changes to clarify the pathophysiology of essential tremor.
Patients had more CF synapses than did controls
The investigators performed a pathological examination of postmortem cerebellar tissue from patients with essential tremor and controls to identify microstructural changes in essential tremor. Next, they applied these changes to mouse models of essential tremor and examined the corresponding structural, electrophysiologic, and behavioral changes. Finally, Dr. Pan and colleagues used cerebellar EEG to validate their findings in patients with essential tremor.
Compared with age-matched controls, patients with essential tremor had more CF synapses in the parallel-fiber synaptic territory on PC dendrites. Patients also had an approximately 75% reduction in mean GluR(delta)2 expression, compared with controls. The amount of GluR(delta)2 was inversely correlated with the percentage of CFs extending to parallel-fiber synaptic territory. The findings suggest that PC synaptic pathology in essential tremor might be related to reduced GluR(delta)2 expression, Dr. Pan and colleagues wrote.
The investigators examined a mouse model that produces 10% of full-length GluR(delta)2 protein. These mice had significant reduction of GluR(delta)2 in the cerebellar cortex and the PC dendrites. In addition, the mice consistently developed CF synapses innervating distal, thin PC dendrites. The investigators observed a 20-Hz tremor in the mice that occurred mainly during action and rarely during rest.
Dr. Pan and colleagues injected a virus containing GluR(delta)2 protein into the mice’s brains to test the protein’s relationship to tremor. Five days after the injection, the mice’s brains were expressing GluR(delta)2 protein reliably. By 4-6 days after injection, the mice’s tremor had been reduced. It returned to baseline levels at 12-14 days after injection. Injecting a control virus did not affect tremor.
Cerebellar oscillatory indexes were correlated with tremor scores
When the researchers examined local field potentials in mouse cerebellum, they found cerebellar oscillations at 20 Hz that were consistent with the observed tremor. “Putting the evidence together, GluR(delta)2 insufficiency causes CF synaptic pruning deficits, and the surplus CF-PC synaptic activity generates excessive cerebellar oscillations, which drive tremor,” Dr. Pan and colleagues reported.
Next, the researchers performed cerebellar EEG in 10 patients with essential tremor and 10 age-matched controls. Patients had cerebellar oscillations at 4-12 Hz, which are the human tremor frequencies. In an expanded cohort of 20 patients with essential tremor and 20 controls, the cerebellar oscillatory indexes were correlated with tremor scores in patients, which showed that the former could be an index of tremor severity. “Currently, diagnosis of essential tremor is based on pure clinical tremor phenomenology and direct tremor measurement, without a physiological marker indicating the underlying brain circuitry abnormalities,” they wrote. “Cerebellar oscillations can be a physiological signature and a therapeutic target for essential tremor.”
The research was funded by grants from the National Institutes of Health, the Parkinson’s Foundation, the International Essential Tremor Foundation, the Ministry of Science and Technology in Taiwan, and the National Taiwan University Hospital. The authors declared that they had no competing interests.
SOURCE: Pan M-K et al. Sci Transl Med. 2020;12:eaay1769. doi: 10.1126/scitranslmed.aay1769.
according to an investigation published January 15 in Science Translational Medicine. These synaptic pruning deficits result from insufficiency of glutamate receptor delta 2 (GluR[delta]2) protein. The findings indicate molecular, structural, physiological, and behavioral factors that contribute to tremor and might influence future treatment of essential tremor, the authors wrote.

Essential tremor has a complex etiology that includes genetic and environmental factors. Its pathophysiology is poorly understood. First author Ming-Kai Pan, MD, assistant professor of medical research and neurology at National Taiwan University Hospital in Taipei, and colleagues previously observed pruning deficits of CF-PC synapses in the cerebellum of deceased patients with essential tremor. An excess of CF-PC synapses are a prominent feature of essential tremor, but not of other cerebellar degenerative disorders. Researchers have observed this pathology consistently in patients with essential tremor who have diverse clinical features. Dr. Pan and colleagues therefore chose to examine these synaptic changes to clarify the pathophysiology of essential tremor.
Patients had more CF synapses than did controls
The investigators performed a pathological examination of postmortem cerebellar tissue from patients with essential tremor and controls to identify microstructural changes in essential tremor. Next, they applied these changes to mouse models of essential tremor and examined the corresponding structural, electrophysiologic, and behavioral changes. Finally, Dr. Pan and colleagues used cerebellar EEG to validate their findings in patients with essential tremor.
Compared with age-matched controls, patients with essential tremor had more CF synapses in the parallel-fiber synaptic territory on PC dendrites. Patients also had an approximately 75% reduction in mean GluR(delta)2 expression, compared with controls. The amount of GluR(delta)2 was inversely correlated with the percentage of CFs extending to parallel-fiber synaptic territory. The findings suggest that PC synaptic pathology in essential tremor might be related to reduced GluR(delta)2 expression, Dr. Pan and colleagues wrote.
The investigators examined a mouse model that produces 10% of full-length GluR(delta)2 protein. These mice had significant reduction of GluR(delta)2 in the cerebellar cortex and the PC dendrites. In addition, the mice consistently developed CF synapses innervating distal, thin PC dendrites. The investigators observed a 20-Hz tremor in the mice that occurred mainly during action and rarely during rest.
Dr. Pan and colleagues injected a virus containing GluR(delta)2 protein into the mice’s brains to test the protein’s relationship to tremor. Five days after the injection, the mice’s brains were expressing GluR(delta)2 protein reliably. By 4-6 days after injection, the mice’s tremor had been reduced. It returned to baseline levels at 12-14 days after injection. Injecting a control virus did not affect tremor.
Cerebellar oscillatory indexes were correlated with tremor scores
When the researchers examined local field potentials in mouse cerebellum, they found cerebellar oscillations at 20 Hz that were consistent with the observed tremor. “Putting the evidence together, GluR(delta)2 insufficiency causes CF synaptic pruning deficits, and the surplus CF-PC synaptic activity generates excessive cerebellar oscillations, which drive tremor,” Dr. Pan and colleagues reported.
Next, the researchers performed cerebellar EEG in 10 patients with essential tremor and 10 age-matched controls. Patients had cerebellar oscillations at 4-12 Hz, which are the human tremor frequencies. In an expanded cohort of 20 patients with essential tremor and 20 controls, the cerebellar oscillatory indexes were correlated with tremor scores in patients, which showed that the former could be an index of tremor severity. “Currently, diagnosis of essential tremor is based on pure clinical tremor phenomenology and direct tremor measurement, without a physiological marker indicating the underlying brain circuitry abnormalities,” they wrote. “Cerebellar oscillations can be a physiological signature and a therapeutic target for essential tremor.”
The research was funded by grants from the National Institutes of Health, the Parkinson’s Foundation, the International Essential Tremor Foundation, the Ministry of Science and Technology in Taiwan, and the National Taiwan University Hospital. The authors declared that they had no competing interests.
SOURCE: Pan M-K et al. Sci Transl Med. 2020;12:eaay1769. doi: 10.1126/scitranslmed.aay1769.
according to an investigation published January 15 in Science Translational Medicine. These synaptic pruning deficits result from insufficiency of glutamate receptor delta 2 (GluR[delta]2) protein. The findings indicate molecular, structural, physiological, and behavioral factors that contribute to tremor and might influence future treatment of essential tremor, the authors wrote.

Essential tremor has a complex etiology that includes genetic and environmental factors. Its pathophysiology is poorly understood. First author Ming-Kai Pan, MD, assistant professor of medical research and neurology at National Taiwan University Hospital in Taipei, and colleagues previously observed pruning deficits of CF-PC synapses in the cerebellum of deceased patients with essential tremor. An excess of CF-PC synapses are a prominent feature of essential tremor, but not of other cerebellar degenerative disorders. Researchers have observed this pathology consistently in patients with essential tremor who have diverse clinical features. Dr. Pan and colleagues therefore chose to examine these synaptic changes to clarify the pathophysiology of essential tremor.
Patients had more CF synapses than did controls
The investigators performed a pathological examination of postmortem cerebellar tissue from patients with essential tremor and controls to identify microstructural changes in essential tremor. Next, they applied these changes to mouse models of essential tremor and examined the corresponding structural, electrophysiologic, and behavioral changes. Finally, Dr. Pan and colleagues used cerebellar EEG to validate their findings in patients with essential tremor.
Compared with age-matched controls, patients with essential tremor had more CF synapses in the parallel-fiber synaptic territory on PC dendrites. Patients also had an approximately 75% reduction in mean GluR(delta)2 expression, compared with controls. The amount of GluR(delta)2 was inversely correlated with the percentage of CFs extending to parallel-fiber synaptic territory. The findings suggest that PC synaptic pathology in essential tremor might be related to reduced GluR(delta)2 expression, Dr. Pan and colleagues wrote.
The investigators examined a mouse model that produces 10% of full-length GluR(delta)2 protein. These mice had significant reduction of GluR(delta)2 in the cerebellar cortex and the PC dendrites. In addition, the mice consistently developed CF synapses innervating distal, thin PC dendrites. The investigators observed a 20-Hz tremor in the mice that occurred mainly during action and rarely during rest.
Dr. Pan and colleagues injected a virus containing GluR(delta)2 protein into the mice’s brains to test the protein’s relationship to tremor. Five days after the injection, the mice’s brains were expressing GluR(delta)2 protein reliably. By 4-6 days after injection, the mice’s tremor had been reduced. It returned to baseline levels at 12-14 days after injection. Injecting a control virus did not affect tremor.
Cerebellar oscillatory indexes were correlated with tremor scores
When the researchers examined local field potentials in mouse cerebellum, they found cerebellar oscillations at 20 Hz that were consistent with the observed tremor. “Putting the evidence together, GluR(delta)2 insufficiency causes CF synaptic pruning deficits, and the surplus CF-PC synaptic activity generates excessive cerebellar oscillations, which drive tremor,” Dr. Pan and colleagues reported.
Next, the researchers performed cerebellar EEG in 10 patients with essential tremor and 10 age-matched controls. Patients had cerebellar oscillations at 4-12 Hz, which are the human tremor frequencies. In an expanded cohort of 20 patients with essential tremor and 20 controls, the cerebellar oscillatory indexes were correlated with tremor scores in patients, which showed that the former could be an index of tremor severity. “Currently, diagnosis of essential tremor is based on pure clinical tremor phenomenology and direct tremor measurement, without a physiological marker indicating the underlying brain circuitry abnormalities,” they wrote. “Cerebellar oscillations can be a physiological signature and a therapeutic target for essential tremor.”
The research was funded by grants from the National Institutes of Health, the Parkinson’s Foundation, the International Essential Tremor Foundation, the Ministry of Science and Technology in Taiwan, and the National Taiwan University Hospital. The authors declared that they had no competing interests.
SOURCE: Pan M-K et al. Sci Transl Med. 2020;12:eaay1769. doi: 10.1126/scitranslmed.aay1769.
FROM SCIENCE TRANSLATIONAL MEDICINE
Sleep apnea’s got your tongue, and singin’ in the kerosene rain
On the tip of my tongue
The greatest risk factor for obstructive sleep apnea is obesity, and unsurprisingly, people who are obese and have sleep apnea very often improve their breathing when they lose weight.
But what if you’re secretly a hobbit named Peregrin Took, and you absolutely have to have both first and second breakfast? Is there any way to ease your sleep apnea?
According to a study published in the American Journal of Respiratory and Critical Care Medicine, weight loss in and of itself isn’t what improves sleep apnea symptoms. No, it’s something more targeted.
The secret to improving sleep apnea is ... tongue fat.
The patients in the study lost about 10% of their body weight over 6 months, and experienced a 31% improvement in sleep apnea scores. MRIs done before and after the intervention showed that, while reductions in pterygoid and pharyngeal lateral wall volumes helped, the reduction of tongue fat volume was the primary link between weight loss and sleep apnea improvement.
The Livin’ on the MDedge team eagerly awaits the dawning of the tongue weight-loss industry, thanks to this new research. Tongue diets. Tongue exercise. Pretty soon you’ll be able to buy “Sweatin’ to the Oldies” DVDs featuring tongues in bad ’80s Spandex flopping all over the place. Have your cake and eat it too – just don’t let your tongue know.
The rain falls mainly from the plane
Why does rain inspire music? Gene Kelly sang in it. Prince crooned about its purple hue. The Weather Girls gave vocal thanks for a downpour of men. And kids will joyfully create a symphony of mud in a summer shower.
But what if it rains on the playground? On a sunny day? Kids will definitely sing the blues, right?
Especially when the shower’s not water.
Shortly after takeoff from Los Angeles International Airport this week, Delta Air Lines Flight 89 to Shanghai developed engine problems. Which sent Flight 89 right back to LAX. Not wanting to land a distressed Boeing 777 with wings full of explosive aviation fuel, the pilot began dumping his Jet A-1 kerosene as he circled back to the airport.
Which fell to earth as a mist ... that blanketed five elementary schools in the middle of the school day.
The plane rain led to minor lung and skin irritation in 56 kids and adults below. But the Los Angeles County Fire Department said injuries were minor, and the drizzling jet fuel evaporated quickly.
Given the absence of serious injuries, it’s clear the Los Angeles students heeded at least one public health message during the kerosene shower: Nobody was engaged in outdoor underage smoking.
And the Inventing Oscar goes to ...
For many people, the new year means the announcement of the Oscar nominations.
We here at LOTME have been waiting for an announcement that comes at the beginning of each year, but it has nothing to do with who got snubbed by the Academy. We’re talking about something really big: the National Inventors Hall of Fame class of 2020.
As usual, we were not disappointed. The world of health care was well represented among this year’s inductees.
At the head of the class, at least alphabetically, is R. Rox Anderson, who developed groundbreaking laser technology (patent number 5,595,568) used in medical treatments and procedures. Then there’s James McEwen, who invented the first microprocessor-controlled automatic surgical tourniquet system (patent number 4,469,099).
Posthumous NIHF nominations went to Stewart Adams and John Nicholson, the codevelopers of 2-(4-isobutylphenyl) propionic acid, which we know as ibuprofen (patent number 3,228,831). Adams, a pharmacologist, and Nicholson, an organic chemist, worked for Boots Pure Drug Co. in England during the 1950s and 1960s while they collaborated on the drug’s creation.
Several other nominees have somewhat-less-direct medical connections. Edward W. Bullard invented the hard hat (patent number 1,699,133), which has undoubtedly saved lives and prevented injuries. Lisa Lindahl, Hinda Miller, and Polly Smith invented the sports bra (patent number 4,174,717), which “has enabled women’s participation in athletic activities and advanced women’s health and well-being,” the NIHF said in a written statement.
And finally – for those of you who thought this would never end – there’s Floyd Smith, the trapeze artist turned aviator who invented the modern parachute (patent numbers 1,340,423 and 1,462,456) and kept many sky divers out of the emergency department.
On the tip of my tongue
The greatest risk factor for obstructive sleep apnea is obesity, and unsurprisingly, people who are obese and have sleep apnea very often improve their breathing when they lose weight.
But what if you’re secretly a hobbit named Peregrin Took, and you absolutely have to have both first and second breakfast? Is there any way to ease your sleep apnea?
According to a study published in the American Journal of Respiratory and Critical Care Medicine, weight loss in and of itself isn’t what improves sleep apnea symptoms. No, it’s something more targeted.
The secret to improving sleep apnea is ... tongue fat.
The patients in the study lost about 10% of their body weight over 6 months, and experienced a 31% improvement in sleep apnea scores. MRIs done before and after the intervention showed that, while reductions in pterygoid and pharyngeal lateral wall volumes helped, the reduction of tongue fat volume was the primary link between weight loss and sleep apnea improvement.
The Livin’ on the MDedge team eagerly awaits the dawning of the tongue weight-loss industry, thanks to this new research. Tongue diets. Tongue exercise. Pretty soon you’ll be able to buy “Sweatin’ to the Oldies” DVDs featuring tongues in bad ’80s Spandex flopping all over the place. Have your cake and eat it too – just don’t let your tongue know.
The rain falls mainly from the plane
Why does rain inspire music? Gene Kelly sang in it. Prince crooned about its purple hue. The Weather Girls gave vocal thanks for a downpour of men. And kids will joyfully create a symphony of mud in a summer shower.
But what if it rains on the playground? On a sunny day? Kids will definitely sing the blues, right?
Especially when the shower’s not water.
Shortly after takeoff from Los Angeles International Airport this week, Delta Air Lines Flight 89 to Shanghai developed engine problems. Which sent Flight 89 right back to LAX. Not wanting to land a distressed Boeing 777 with wings full of explosive aviation fuel, the pilot began dumping his Jet A-1 kerosene as he circled back to the airport.
Which fell to earth as a mist ... that blanketed five elementary schools in the middle of the school day.
The plane rain led to minor lung and skin irritation in 56 kids and adults below. But the Los Angeles County Fire Department said injuries were minor, and the drizzling jet fuel evaporated quickly.
Given the absence of serious injuries, it’s clear the Los Angeles students heeded at least one public health message during the kerosene shower: Nobody was engaged in outdoor underage smoking.
And the Inventing Oscar goes to ...
For many people, the new year means the announcement of the Oscar nominations.
We here at LOTME have been waiting for an announcement that comes at the beginning of each year, but it has nothing to do with who got snubbed by the Academy. We’re talking about something really big: the National Inventors Hall of Fame class of 2020.
As usual, we were not disappointed. The world of health care was well represented among this year’s inductees.
At the head of the class, at least alphabetically, is R. Rox Anderson, who developed groundbreaking laser technology (patent number 5,595,568) used in medical treatments and procedures. Then there’s James McEwen, who invented the first microprocessor-controlled automatic surgical tourniquet system (patent number 4,469,099).
Posthumous NIHF nominations went to Stewart Adams and John Nicholson, the codevelopers of 2-(4-isobutylphenyl) propionic acid, which we know as ibuprofen (patent number 3,228,831). Adams, a pharmacologist, and Nicholson, an organic chemist, worked for Boots Pure Drug Co. in England during the 1950s and 1960s while they collaborated on the drug’s creation.
Several other nominees have somewhat-less-direct medical connections. Edward W. Bullard invented the hard hat (patent number 1,699,133), which has undoubtedly saved lives and prevented injuries. Lisa Lindahl, Hinda Miller, and Polly Smith invented the sports bra (patent number 4,174,717), which “has enabled women’s participation in athletic activities and advanced women’s health and well-being,” the NIHF said in a written statement.
And finally – for those of you who thought this would never end – there’s Floyd Smith, the trapeze artist turned aviator who invented the modern parachute (patent numbers 1,340,423 and 1,462,456) and kept many sky divers out of the emergency department.
On the tip of my tongue
The greatest risk factor for obstructive sleep apnea is obesity, and unsurprisingly, people who are obese and have sleep apnea very often improve their breathing when they lose weight.
But what if you’re secretly a hobbit named Peregrin Took, and you absolutely have to have both first and second breakfast? Is there any way to ease your sleep apnea?
According to a study published in the American Journal of Respiratory and Critical Care Medicine, weight loss in and of itself isn’t what improves sleep apnea symptoms. No, it’s something more targeted.
The secret to improving sleep apnea is ... tongue fat.
The patients in the study lost about 10% of their body weight over 6 months, and experienced a 31% improvement in sleep apnea scores. MRIs done before and after the intervention showed that, while reductions in pterygoid and pharyngeal lateral wall volumes helped, the reduction of tongue fat volume was the primary link between weight loss and sleep apnea improvement.
The Livin’ on the MDedge team eagerly awaits the dawning of the tongue weight-loss industry, thanks to this new research. Tongue diets. Tongue exercise. Pretty soon you’ll be able to buy “Sweatin’ to the Oldies” DVDs featuring tongues in bad ’80s Spandex flopping all over the place. Have your cake and eat it too – just don’t let your tongue know.
The rain falls mainly from the plane
Why does rain inspire music? Gene Kelly sang in it. Prince crooned about its purple hue. The Weather Girls gave vocal thanks for a downpour of men. And kids will joyfully create a symphony of mud in a summer shower.
But what if it rains on the playground? On a sunny day? Kids will definitely sing the blues, right?
Especially when the shower’s not water.
Shortly after takeoff from Los Angeles International Airport this week, Delta Air Lines Flight 89 to Shanghai developed engine problems. Which sent Flight 89 right back to LAX. Not wanting to land a distressed Boeing 777 with wings full of explosive aviation fuel, the pilot began dumping his Jet A-1 kerosene as he circled back to the airport.
Which fell to earth as a mist ... that blanketed five elementary schools in the middle of the school day.
The plane rain led to minor lung and skin irritation in 56 kids and adults below. But the Los Angeles County Fire Department said injuries were minor, and the drizzling jet fuel evaporated quickly.
Given the absence of serious injuries, it’s clear the Los Angeles students heeded at least one public health message during the kerosene shower: Nobody was engaged in outdoor underage smoking.
And the Inventing Oscar goes to ...
For many people, the new year means the announcement of the Oscar nominations.
We here at LOTME have been waiting for an announcement that comes at the beginning of each year, but it has nothing to do with who got snubbed by the Academy. We’re talking about something really big: the National Inventors Hall of Fame class of 2020.
As usual, we were not disappointed. The world of health care was well represented among this year’s inductees.
At the head of the class, at least alphabetically, is R. Rox Anderson, who developed groundbreaking laser technology (patent number 5,595,568) used in medical treatments and procedures. Then there’s James McEwen, who invented the first microprocessor-controlled automatic surgical tourniquet system (patent number 4,469,099).
Posthumous NIHF nominations went to Stewart Adams and John Nicholson, the codevelopers of 2-(4-isobutylphenyl) propionic acid, which we know as ibuprofen (patent number 3,228,831). Adams, a pharmacologist, and Nicholson, an organic chemist, worked for Boots Pure Drug Co. in England during the 1950s and 1960s while they collaborated on the drug’s creation.
Several other nominees have somewhat-less-direct medical connections. Edward W. Bullard invented the hard hat (patent number 1,699,133), which has undoubtedly saved lives and prevented injuries. Lisa Lindahl, Hinda Miller, and Polly Smith invented the sports bra (patent number 4,174,717), which “has enabled women’s participation in athletic activities and advanced women’s health and well-being,” the NIHF said in a written statement.
And finally – for those of you who thought this would never end – there’s Floyd Smith, the trapeze artist turned aviator who invented the modern parachute (patent numbers 1,340,423 and 1,462,456) and kept many sky divers out of the emergency department.
Bariatric surgery is most effective early in the diabetes trajectory
LOS ANGELES – In the clinical experience of Kurt GMM Alberti, DPhil, FRCP, FRCPath, The problem is, far fewer people with diabetes are being referred for the surgery than would benefit from it.
At the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease, Dr. Alberti said that only about 1% of eligible patients in the United States undergo bariatric surgery, compared with just 0.22% of eligible patients in the United Kingdom.
“Obesity is an increasing problem,” said Dr. Alberti, a senior research investigator in the section of diabetes, endocrinology, and metabolism at Imperial College, London. “The United States is leading the field [in obesity], and it doesn’t seem to be going away. This is in parallel with diabetes. According to the 2019 International Diabetes Federation’s Diabetes Atlas, the diabetes prevalence worldwide is now 463 million. It’s projected to reach 578 million by 2030 and 700 million by 2045. We have a major problem.”
Lifestyle modification with diet and exercise have been the cornerstone of diabetes therapy for more than 100 years, with only modest success. “A range of oral agents have been added [and they] certainly improve glycemic control, but few achieve lasting success, and few achieve remission,” Dr. Alberti said. Findings from DiRECT (Lancet. 2018;391:541-51) and the Look AHEAD (Action for Health in Diabetes) study (N Engl J Med. 2013;369:145-54) have shown dramatic improvements in glycemia, but only in the minority of patients who achieved weight loss of 10 kg or more. “In this group, 80% achieved remission after 2 years in DiRECT,” he said. “It is uncertain whether this can be sustained long term in real life, and how many people will respond. Major community prevention programs are under way in the U.S. and [United Kingdom], but many target individuals with prediabetes. Currently, it is unknown how successful these programs will be.”
The 2018 American Diabetes Association/European Association for the Study of Diabetes clinical guidelines state that bariatric surgery is a recommended treatment option for adults with type 2 diabetes and a body mass index of either 40.0 kg/m2 or higher (or 37.5 kg/m2 or higher in people of Asian ancestry) or 35.0-39.9 kg/m2 (32.5-37.4 kg/m2 in people of Asian ancestry) and who do not achieve durable weight loss and improvement in comorbidities with reasonable nonsurgical methods. According to Dr. Alberti, surgery should be an accepted option in people who have type 2 diabetes and a body mass index of 30 kg/m2 or higher, and priority should be given to adolescents, young adults, and those with a shorter duration of diabetes.
The main suggestive evidence in favor of bariatric surgery having an impact on diabetes comes from the Swedish Obese Subjects Study, which had a median follow-up of 10 years (J Intern Med. 2013;273[3]:219-34). In patients with diabetes at baseline, 30% were still in remission at 15 years after surgery. After 18 years, cumulative microvascular disease had fallen from 42 to 21 per 1,000 person-years, and macrovascular complications had fallen by 25%. “This was not a randomized, controlled trial, however,” Dr. Alberti said. Several of these studies have now been performed, including the STAMPEDE trial (N Engl J Med. 2017;376:641-51) and recent studies led by Geltrude Mingrone, MD, PhD, which show major glycemic benefit (Lancet. 2015;386[9997]:P964-73) with bariatric surgery.
According to Dr. Alberti, laparoscopic adjustable gastric lap band is the easiest bariatric surgery to perform but it has fallen out of favor because of lower diabetes remission rates, compared with the other procedures. Roux-en-Y gastric bypass, sleeve gastrectomy, and biliary pancreatic diversion are all in use. Slightly higher remission rates have been shown with biliary pancreatic diversion. “There have also been consistent improvements in quality of life and cardiovascular risk factors,” he said. “Long-term follow-up is still [needed], but, in general, it seems that diabetic complications are lower than in medically treated control groups, and mortality may also be lower. The real question is, what is the impact on complications? There we have a problem, because we do not have any good randomized, controlled trials covering a 10- to 20-year period, which would give us clear evidence. There is reasonable evidence from cohort studies, though.”
Added benefits of bariatric surgery include improved quality of life, decreased blood pressure, less sleep apnea, improved cardiovascular risk factors, and better musculoskeletal function. For now, though, an unmet need persists. “The problem is that far fewer people are referred for bariatric surgery than would benefit,” Dr. Alberti said. “There are several barriers to greater use of bariatric surgery in those with diabetes. These include physician attitudes, inadequate referrals, patient perceptions, lack of awareness among patients, inadequate insurance coverage, and particularly health system capacity. There is also a lack of sympathy for overweight people in some places.”
Dr. Alberti reported having no financial disclosures.
LOS ANGELES – In the clinical experience of Kurt GMM Alberti, DPhil, FRCP, FRCPath, The problem is, far fewer people with diabetes are being referred for the surgery than would benefit from it.
At the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease, Dr. Alberti said that only about 1% of eligible patients in the United States undergo bariatric surgery, compared with just 0.22% of eligible patients in the United Kingdom.
“Obesity is an increasing problem,” said Dr. Alberti, a senior research investigator in the section of diabetes, endocrinology, and metabolism at Imperial College, London. “The United States is leading the field [in obesity], and it doesn’t seem to be going away. This is in parallel with diabetes. According to the 2019 International Diabetes Federation’s Diabetes Atlas, the diabetes prevalence worldwide is now 463 million. It’s projected to reach 578 million by 2030 and 700 million by 2045. We have a major problem.”
Lifestyle modification with diet and exercise have been the cornerstone of diabetes therapy for more than 100 years, with only modest success. “A range of oral agents have been added [and they] certainly improve glycemic control, but few achieve lasting success, and few achieve remission,” Dr. Alberti said. Findings from DiRECT (Lancet. 2018;391:541-51) and the Look AHEAD (Action for Health in Diabetes) study (N Engl J Med. 2013;369:145-54) have shown dramatic improvements in glycemia, but only in the minority of patients who achieved weight loss of 10 kg or more. “In this group, 80% achieved remission after 2 years in DiRECT,” he said. “It is uncertain whether this can be sustained long term in real life, and how many people will respond. Major community prevention programs are under way in the U.S. and [United Kingdom], but many target individuals with prediabetes. Currently, it is unknown how successful these programs will be.”
The 2018 American Diabetes Association/European Association for the Study of Diabetes clinical guidelines state that bariatric surgery is a recommended treatment option for adults with type 2 diabetes and a body mass index of either 40.0 kg/m2 or higher (or 37.5 kg/m2 or higher in people of Asian ancestry) or 35.0-39.9 kg/m2 (32.5-37.4 kg/m2 in people of Asian ancestry) and who do not achieve durable weight loss and improvement in comorbidities with reasonable nonsurgical methods. According to Dr. Alberti, surgery should be an accepted option in people who have type 2 diabetes and a body mass index of 30 kg/m2 or higher, and priority should be given to adolescents, young adults, and those with a shorter duration of diabetes.
The main suggestive evidence in favor of bariatric surgery having an impact on diabetes comes from the Swedish Obese Subjects Study, which had a median follow-up of 10 years (J Intern Med. 2013;273[3]:219-34). In patients with diabetes at baseline, 30% were still in remission at 15 years after surgery. After 18 years, cumulative microvascular disease had fallen from 42 to 21 per 1,000 person-years, and macrovascular complications had fallen by 25%. “This was not a randomized, controlled trial, however,” Dr. Alberti said. Several of these studies have now been performed, including the STAMPEDE trial (N Engl J Med. 2017;376:641-51) and recent studies led by Geltrude Mingrone, MD, PhD, which show major glycemic benefit (Lancet. 2015;386[9997]:P964-73) with bariatric surgery.
According to Dr. Alberti, laparoscopic adjustable gastric lap band is the easiest bariatric surgery to perform but it has fallen out of favor because of lower diabetes remission rates, compared with the other procedures. Roux-en-Y gastric bypass, sleeve gastrectomy, and biliary pancreatic diversion are all in use. Slightly higher remission rates have been shown with biliary pancreatic diversion. “There have also been consistent improvements in quality of life and cardiovascular risk factors,” he said. “Long-term follow-up is still [needed], but, in general, it seems that diabetic complications are lower than in medically treated control groups, and mortality may also be lower. The real question is, what is the impact on complications? There we have a problem, because we do not have any good randomized, controlled trials covering a 10- to 20-year period, which would give us clear evidence. There is reasonable evidence from cohort studies, though.”
Added benefits of bariatric surgery include improved quality of life, decreased blood pressure, less sleep apnea, improved cardiovascular risk factors, and better musculoskeletal function. For now, though, an unmet need persists. “The problem is that far fewer people are referred for bariatric surgery than would benefit,” Dr. Alberti said. “There are several barriers to greater use of bariatric surgery in those with diabetes. These include physician attitudes, inadequate referrals, patient perceptions, lack of awareness among patients, inadequate insurance coverage, and particularly health system capacity. There is also a lack of sympathy for overweight people in some places.”
Dr. Alberti reported having no financial disclosures.
LOS ANGELES – In the clinical experience of Kurt GMM Alberti, DPhil, FRCP, FRCPath, The problem is, far fewer people with diabetes are being referred for the surgery than would benefit from it.
At the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease, Dr. Alberti said that only about 1% of eligible patients in the United States undergo bariatric surgery, compared with just 0.22% of eligible patients in the United Kingdom.
“Obesity is an increasing problem,” said Dr. Alberti, a senior research investigator in the section of diabetes, endocrinology, and metabolism at Imperial College, London. “The United States is leading the field [in obesity], and it doesn’t seem to be going away. This is in parallel with diabetes. According to the 2019 International Diabetes Federation’s Diabetes Atlas, the diabetes prevalence worldwide is now 463 million. It’s projected to reach 578 million by 2030 and 700 million by 2045. We have a major problem.”
Lifestyle modification with diet and exercise have been the cornerstone of diabetes therapy for more than 100 years, with only modest success. “A range of oral agents have been added [and they] certainly improve glycemic control, but few achieve lasting success, and few achieve remission,” Dr. Alberti said. Findings from DiRECT (Lancet. 2018;391:541-51) and the Look AHEAD (Action for Health in Diabetes) study (N Engl J Med. 2013;369:145-54) have shown dramatic improvements in glycemia, but only in the minority of patients who achieved weight loss of 10 kg or more. “In this group, 80% achieved remission after 2 years in DiRECT,” he said. “It is uncertain whether this can be sustained long term in real life, and how many people will respond. Major community prevention programs are under way in the U.S. and [United Kingdom], but many target individuals with prediabetes. Currently, it is unknown how successful these programs will be.”
The 2018 American Diabetes Association/European Association for the Study of Diabetes clinical guidelines state that bariatric surgery is a recommended treatment option for adults with type 2 diabetes and a body mass index of either 40.0 kg/m2 or higher (or 37.5 kg/m2 or higher in people of Asian ancestry) or 35.0-39.9 kg/m2 (32.5-37.4 kg/m2 in people of Asian ancestry) and who do not achieve durable weight loss and improvement in comorbidities with reasonable nonsurgical methods. According to Dr. Alberti, surgery should be an accepted option in people who have type 2 diabetes and a body mass index of 30 kg/m2 or higher, and priority should be given to adolescents, young adults, and those with a shorter duration of diabetes.
The main suggestive evidence in favor of bariatric surgery having an impact on diabetes comes from the Swedish Obese Subjects Study, which had a median follow-up of 10 years (J Intern Med. 2013;273[3]:219-34). In patients with diabetes at baseline, 30% were still in remission at 15 years after surgery. After 18 years, cumulative microvascular disease had fallen from 42 to 21 per 1,000 person-years, and macrovascular complications had fallen by 25%. “This was not a randomized, controlled trial, however,” Dr. Alberti said. Several of these studies have now been performed, including the STAMPEDE trial (N Engl J Med. 2017;376:641-51) and recent studies led by Geltrude Mingrone, MD, PhD, which show major glycemic benefit (Lancet. 2015;386[9997]:P964-73) with bariatric surgery.
According to Dr. Alberti, laparoscopic adjustable gastric lap band is the easiest bariatric surgery to perform but it has fallen out of favor because of lower diabetes remission rates, compared with the other procedures. Roux-en-Y gastric bypass, sleeve gastrectomy, and biliary pancreatic diversion are all in use. Slightly higher remission rates have been shown with biliary pancreatic diversion. “There have also been consistent improvements in quality of life and cardiovascular risk factors,” he said. “Long-term follow-up is still [needed], but, in general, it seems that diabetic complications are lower than in medically treated control groups, and mortality may also be lower. The real question is, what is the impact on complications? There we have a problem, because we do not have any good randomized, controlled trials covering a 10- to 20-year period, which would give us clear evidence. There is reasonable evidence from cohort studies, though.”
Added benefits of bariatric surgery include improved quality of life, decreased blood pressure, less sleep apnea, improved cardiovascular risk factors, and better musculoskeletal function. For now, though, an unmet need persists. “The problem is that far fewer people are referred for bariatric surgery than would benefit,” Dr. Alberti said. “There are several barriers to greater use of bariatric surgery in those with diabetes. These include physician attitudes, inadequate referrals, patient perceptions, lack of awareness among patients, inadequate insurance coverage, and particularly health system capacity. There is also a lack of sympathy for overweight people in some places.”
Dr. Alberti reported having no financial disclosures.
EXPERT ANALYSIS FROM WCIRDC 2019