User login
A Call to Address Sexual Harassment and Gender Discrimination in Medicine
PART I
Reports of sexual harassment and gender discrimination have dominated news headlines, and the #MeToo movement has brought the scope and severity of discriminatory behavior to the forefront of public consciousness. The #MeToo movement has raised national and global awareness of gender discrimination and sexual harassment in all industries and has given rise to Time’s Up initiative within health care.
Academic medicine has not been immune to workplace gender discrimination and sexual harassment as has been vastly reported in the literature and clearly documented in the 2018 National Academies of Sciences, Engineering, and Medicine report, which points out that … “the cumulative effect of sexual harassment is a significant and costly loss of talent in academic science, engineering, and medicine, which has consequences for advancing the nation’s economic and social well-being and its overall public health.”1
With the increasing recognition that healthcare is an environment especially prone to inequality, gender discrimination and sexual discrimination, the Time’s Up national organization, supported by the Time’s Up Legal Defense Fund, launched the Time’s Up initiative for health care workers on March 1, 2019.2,3 The overarching goal of this initiative is to expose workplace inequalities; drive policy and legislative changes focused on equal pay, equal opportunity, and equal work environments; and support safe, fair, and dignified work for women in health care. 2,3
This article, presented over the next three issues of Vascular Specialist, will present data on the ongoing problem of sexual harassment in medicine, discuss why the problem is prevalent in academic medicine, and provide recommendations for mitigating the problem in our workplace.
Defining & Measuring Sexual Harassment
Although commonly referred to as “sex discrimination,” sexual harassment differs from sexual discrimination. Sex discrimination refers to an employees’ denial of civil rights, raises, job opportunities, employment or a demotion or other mistreatments based on sex. On the other hand, sexual harassment relates to behavior that is inappropriate or offensive. A 2018 report from the National Academies Press defined sexual harassment (a form of discrimination) as comprising three categories of behavior: gender harassment – verbal and nonverbal behaviors that convey hostility, objectification, exclusion, or second-class status about members of one sex; unwanted sexual attention – verbal or physical unwelcome sexual advances, which can include assault; and sexual coercion – when favorable professional or educational treatment is conditional based on sexual activity.1
During 1995-2016, more than 7,000 health care service employees filed claims of sexual harassment with the Equal Employment Opportunity Commission. While this number may seem large, the number of official reports severely undervalues the prevalence of sexual discrimination in U.S. health care.1 Prevalence is best determined using representative validated surveys that rely on firsthand experience or observation of the behavior(s) without requiring the respondent to label those behaviors.
Environments at Risk for Sexual Harassment
Research reveals that academic settings in the fields of science exhibit characteristics that create high levels of risk for sexual harassment to occur. These environments historically are male dominated, tolerate sexually harassing behavior, and create a hierarchy in which men hold most of the positions of power and authority. Moreover, dependent relationships often exist between these gatekeepers and those subordinate to them, with gatekeepers directly influencing the career advancement of those subordinates.1
The greatest predictor of sexual harassment in the workplace is the organizational climate, which refers to the tolerance for sexual harassment and is measured on three elements: a lack of sanctions against offenders; a perceived risk to those who report sexually harassing behavior; and the perception that one’s report of sexually harassing behavior will not be taken seriously.1 Women are less likely to be directly harassed in environments that do not tolerate harassing behaviors or have a strong, clear, transparent consequence for these behaviors.
Sexual Harassment in Academic Medicine
Academic medicine has the highest rate of gender and sexual harassment in the health care industry, with about 50% of female academic physicians reporting incidents of sexual harassment.1 A recent survey suggests that more than half (58%) of women surgeons experienced sexual harassment within just the previous year alone.4 The conditions that increase the risk of sexual harassment against women – male-dominated hierarchical environments and organizational tolerance of sexual harassment – still prevail in academic medicine.
Higher-education environments are perceived as permissive environments in part because when targets report sexual harassment, they are retaliated against or there are few consequences for the perpetrator. Academic institutions are replete with cases in which the conduct of offenders is regarded as an open secret, but there are no sanctions for that bad behavior. These offenders often are perceived as superstars in their particular substantive area. Because they hold valued grants or national status within their specialty area, they often receive preferential treatment and are not held accountable for gender-biased and sexually harassing behavior. Interview data regarding sexual harassment in academic medicine reveals that interview respondents and other colleagues often know which individuals have a history of sexually harassing behavior. Both men and women warn colleagues of these perpetrators – knowing that calling out or reporting these behaviors is fruitless – and that the best manner for dealing with their behavior is to avoid or ignore it. This normalization of sexual harassment and gender bias was noted, unfortunately, to fuel similar behavior in new cohorts of medicine faculty.1
Sexual harassment of women in academic medicine starts in medical school. Female medical students are significantly more likely to experience sexual harassment by faculty and staff than are graduate or undergraduate students. Sexual harassment continues into residency training with residency described as “breeding grounds for abusive behavior by superiors.”1 Interview studies report that both men and women trainees widely accept harassing behavior at this stage of their training. The expectation of abusive and grueling conditions during residency caused several respondents to view sexual harassment as part of a continuum that they were expected to endure. Female residents in surgery and emergency medicine are more likely to be harassed than those in other specialties because of the high value placed on a hierarchical and authoritative workplace. Once out of residency, the sexual harassment of women in the workplace continues. A recent meta-analysis reveals that 58% of women faculty experience sexual harassment at work. Academic medicine has the second-highest rate of sexual harassment, behind the military (69%), as compared with all other workplaces. Women physicians of color experience more harassment (as a combination of sexual and racial harassment) than do white women physicians.1
Why Women Are Not Likely to Report Sexual Harassment
Only 25% of targets file formal reports with their employer, with even fewer taking claims to court. These numbers are even lower for women in the military and academic medicine, where formal reporting is the last resort for the victims. The reluctance to use formal reporting mechanisms is rooted in the “fear of blame, disbelief, inaction, retaliation, humiliation, ostracism, and the damage to one’s career and reputation.”1 Targets may perceive that there seem to be few benefits and high costs for reporting. Women and nonwhites often resist calling bad behavior “discrimination” because that increases their loss of control and victimhood.1 Women frequently perceive that grievance procedures favor the institution over the individual, and research has proven that women face retaliation, both professional and social, for speaking out. Furthermore, stark power differentials between the target and the perpetrator exacerbate the reluctance to report and the fear of retaliation. The overall effects can be long lasting.
References:
1. National Academies of Sciences, Engineering, and Medicine. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine. The National Academies Press, Washington, DC; 2018. doi. 10.17226/24994.
2. Choo EK et al. From #MeToo to #TimesUp in Health Care: Can a Culture of Accountability End Inequity and Harassment? Lancet. 2019 Feb 9;393(10171):499-502.
3. Choo EK et al. Time’s Up for Medicine? Only Time Will Tell. N Engl J Med. 2018 Oct 25;379(17):1592-3.
4. Medicine Has Its Own #MeToo Problems. Can Time’s Up Healthcare Fix It?
Dr. Mitchell is a vascular surgeon at Salem (Ore.) Hospital; Dr. Drudi is as vascular surgery resident at McGill University, Montreal; Dr. Brown is a professor of surgery at the Medical College of Wisconsin. Milwaukee; Dr. Sachdev-Ost is an associate professor of surgery at the University of Pittsburgh Medical Center.
PART I
Reports of sexual harassment and gender discrimination have dominated news headlines, and the #MeToo movement has brought the scope and severity of discriminatory behavior to the forefront of public consciousness. The #MeToo movement has raised national and global awareness of gender discrimination and sexual harassment in all industries and has given rise to Time’s Up initiative within health care.
Academic medicine has not been immune to workplace gender discrimination and sexual harassment as has been vastly reported in the literature and clearly documented in the 2018 National Academies of Sciences, Engineering, and Medicine report, which points out that … “the cumulative effect of sexual harassment is a significant and costly loss of talent in academic science, engineering, and medicine, which has consequences for advancing the nation’s economic and social well-being and its overall public health.”1
With the increasing recognition that healthcare is an environment especially prone to inequality, gender discrimination and sexual discrimination, the Time’s Up national organization, supported by the Time’s Up Legal Defense Fund, launched the Time’s Up initiative for health care workers on March 1, 2019.2,3 The overarching goal of this initiative is to expose workplace inequalities; drive policy and legislative changes focused on equal pay, equal opportunity, and equal work environments; and support safe, fair, and dignified work for women in health care. 2,3
This article, presented over the next three issues of Vascular Specialist, will present data on the ongoing problem of sexual harassment in medicine, discuss why the problem is prevalent in academic medicine, and provide recommendations for mitigating the problem in our workplace.
Defining & Measuring Sexual Harassment
Although commonly referred to as “sex discrimination,” sexual harassment differs from sexual discrimination. Sex discrimination refers to an employees’ denial of civil rights, raises, job opportunities, employment or a demotion or other mistreatments based on sex. On the other hand, sexual harassment relates to behavior that is inappropriate or offensive. A 2018 report from the National Academies Press defined sexual harassment (a form of discrimination) as comprising three categories of behavior: gender harassment – verbal and nonverbal behaviors that convey hostility, objectification, exclusion, or second-class status about members of one sex; unwanted sexual attention – verbal or physical unwelcome sexual advances, which can include assault; and sexual coercion – when favorable professional or educational treatment is conditional based on sexual activity.1
During 1995-2016, more than 7,000 health care service employees filed claims of sexual harassment with the Equal Employment Opportunity Commission. While this number may seem large, the number of official reports severely undervalues the prevalence of sexual discrimination in U.S. health care.1 Prevalence is best determined using representative validated surveys that rely on firsthand experience or observation of the behavior(s) without requiring the respondent to label those behaviors.
Environments at Risk for Sexual Harassment
Research reveals that academic settings in the fields of science exhibit characteristics that create high levels of risk for sexual harassment to occur. These environments historically are male dominated, tolerate sexually harassing behavior, and create a hierarchy in which men hold most of the positions of power and authority. Moreover, dependent relationships often exist between these gatekeepers and those subordinate to them, with gatekeepers directly influencing the career advancement of those subordinates.1
The greatest predictor of sexual harassment in the workplace is the organizational climate, which refers to the tolerance for sexual harassment and is measured on three elements: a lack of sanctions against offenders; a perceived risk to those who report sexually harassing behavior; and the perception that one’s report of sexually harassing behavior will not be taken seriously.1 Women are less likely to be directly harassed in environments that do not tolerate harassing behaviors or have a strong, clear, transparent consequence for these behaviors.
Sexual Harassment in Academic Medicine
Academic medicine has the highest rate of gender and sexual harassment in the health care industry, with about 50% of female academic physicians reporting incidents of sexual harassment.1 A recent survey suggests that more than half (58%) of women surgeons experienced sexual harassment within just the previous year alone.4 The conditions that increase the risk of sexual harassment against women – male-dominated hierarchical environments and organizational tolerance of sexual harassment – still prevail in academic medicine.
Higher-education environments are perceived as permissive environments in part because when targets report sexual harassment, they are retaliated against or there are few consequences for the perpetrator. Academic institutions are replete with cases in which the conduct of offenders is regarded as an open secret, but there are no sanctions for that bad behavior. These offenders often are perceived as superstars in their particular substantive area. Because they hold valued grants or national status within their specialty area, they often receive preferential treatment and are not held accountable for gender-biased and sexually harassing behavior. Interview data regarding sexual harassment in academic medicine reveals that interview respondents and other colleagues often know which individuals have a history of sexually harassing behavior. Both men and women warn colleagues of these perpetrators – knowing that calling out or reporting these behaviors is fruitless – and that the best manner for dealing with their behavior is to avoid or ignore it. This normalization of sexual harassment and gender bias was noted, unfortunately, to fuel similar behavior in new cohorts of medicine faculty.1
Sexual harassment of women in academic medicine starts in medical school. Female medical students are significantly more likely to experience sexual harassment by faculty and staff than are graduate or undergraduate students. Sexual harassment continues into residency training with residency described as “breeding grounds for abusive behavior by superiors.”1 Interview studies report that both men and women trainees widely accept harassing behavior at this stage of their training. The expectation of abusive and grueling conditions during residency caused several respondents to view sexual harassment as part of a continuum that they were expected to endure. Female residents in surgery and emergency medicine are more likely to be harassed than those in other specialties because of the high value placed on a hierarchical and authoritative workplace. Once out of residency, the sexual harassment of women in the workplace continues. A recent meta-analysis reveals that 58% of women faculty experience sexual harassment at work. Academic medicine has the second-highest rate of sexual harassment, behind the military (69%), as compared with all other workplaces. Women physicians of color experience more harassment (as a combination of sexual and racial harassment) than do white women physicians.1
Why Women Are Not Likely to Report Sexual Harassment
Only 25% of targets file formal reports with their employer, with even fewer taking claims to court. These numbers are even lower for women in the military and academic medicine, where formal reporting is the last resort for the victims. The reluctance to use formal reporting mechanisms is rooted in the “fear of blame, disbelief, inaction, retaliation, humiliation, ostracism, and the damage to one’s career and reputation.”1 Targets may perceive that there seem to be few benefits and high costs for reporting. Women and nonwhites often resist calling bad behavior “discrimination” because that increases their loss of control and victimhood.1 Women frequently perceive that grievance procedures favor the institution over the individual, and research has proven that women face retaliation, both professional and social, for speaking out. Furthermore, stark power differentials between the target and the perpetrator exacerbate the reluctance to report and the fear of retaliation. The overall effects can be long lasting.
References:
1. National Academies of Sciences, Engineering, and Medicine. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine. The National Academies Press, Washington, DC; 2018. doi. 10.17226/24994.
2. Choo EK et al. From #MeToo to #TimesUp in Health Care: Can a Culture of Accountability End Inequity and Harassment? Lancet. 2019 Feb 9;393(10171):499-502.
3. Choo EK et al. Time’s Up for Medicine? Only Time Will Tell. N Engl J Med. 2018 Oct 25;379(17):1592-3.
4. Medicine Has Its Own #MeToo Problems. Can Time’s Up Healthcare Fix It?
Dr. Mitchell is a vascular surgeon at Salem (Ore.) Hospital; Dr. Drudi is as vascular surgery resident at McGill University, Montreal; Dr. Brown is a professor of surgery at the Medical College of Wisconsin. Milwaukee; Dr. Sachdev-Ost is an associate professor of surgery at the University of Pittsburgh Medical Center.
PART I
Reports of sexual harassment and gender discrimination have dominated news headlines, and the #MeToo movement has brought the scope and severity of discriminatory behavior to the forefront of public consciousness. The #MeToo movement has raised national and global awareness of gender discrimination and sexual harassment in all industries and has given rise to Time’s Up initiative within health care.
Academic medicine has not been immune to workplace gender discrimination and sexual harassment as has been vastly reported in the literature and clearly documented in the 2018 National Academies of Sciences, Engineering, and Medicine report, which points out that … “the cumulative effect of sexual harassment is a significant and costly loss of talent in academic science, engineering, and medicine, which has consequences for advancing the nation’s economic and social well-being and its overall public health.”1
With the increasing recognition that healthcare is an environment especially prone to inequality, gender discrimination and sexual discrimination, the Time’s Up national organization, supported by the Time’s Up Legal Defense Fund, launched the Time’s Up initiative for health care workers on March 1, 2019.2,3 The overarching goal of this initiative is to expose workplace inequalities; drive policy and legislative changes focused on equal pay, equal opportunity, and equal work environments; and support safe, fair, and dignified work for women in health care. 2,3
This article, presented over the next three issues of Vascular Specialist, will present data on the ongoing problem of sexual harassment in medicine, discuss why the problem is prevalent in academic medicine, and provide recommendations for mitigating the problem in our workplace.
Defining & Measuring Sexual Harassment
Although commonly referred to as “sex discrimination,” sexual harassment differs from sexual discrimination. Sex discrimination refers to an employees’ denial of civil rights, raises, job opportunities, employment or a demotion or other mistreatments based on sex. On the other hand, sexual harassment relates to behavior that is inappropriate or offensive. A 2018 report from the National Academies Press defined sexual harassment (a form of discrimination) as comprising three categories of behavior: gender harassment – verbal and nonverbal behaviors that convey hostility, objectification, exclusion, or second-class status about members of one sex; unwanted sexual attention – verbal or physical unwelcome sexual advances, which can include assault; and sexual coercion – when favorable professional or educational treatment is conditional based on sexual activity.1
During 1995-2016, more than 7,000 health care service employees filed claims of sexual harassment with the Equal Employment Opportunity Commission. While this number may seem large, the number of official reports severely undervalues the prevalence of sexual discrimination in U.S. health care.1 Prevalence is best determined using representative validated surveys that rely on firsthand experience or observation of the behavior(s) without requiring the respondent to label those behaviors.
Environments at Risk for Sexual Harassment
Research reveals that academic settings in the fields of science exhibit characteristics that create high levels of risk for sexual harassment to occur. These environments historically are male dominated, tolerate sexually harassing behavior, and create a hierarchy in which men hold most of the positions of power and authority. Moreover, dependent relationships often exist between these gatekeepers and those subordinate to them, with gatekeepers directly influencing the career advancement of those subordinates.1
The greatest predictor of sexual harassment in the workplace is the organizational climate, which refers to the tolerance for sexual harassment and is measured on three elements: a lack of sanctions against offenders; a perceived risk to those who report sexually harassing behavior; and the perception that one’s report of sexually harassing behavior will not be taken seriously.1 Women are less likely to be directly harassed in environments that do not tolerate harassing behaviors or have a strong, clear, transparent consequence for these behaviors.
Sexual Harassment in Academic Medicine
Academic medicine has the highest rate of gender and sexual harassment in the health care industry, with about 50% of female academic physicians reporting incidents of sexual harassment.1 A recent survey suggests that more than half (58%) of women surgeons experienced sexual harassment within just the previous year alone.4 The conditions that increase the risk of sexual harassment against women – male-dominated hierarchical environments and organizational tolerance of sexual harassment – still prevail in academic medicine.
Higher-education environments are perceived as permissive environments in part because when targets report sexual harassment, they are retaliated against or there are few consequences for the perpetrator. Academic institutions are replete with cases in which the conduct of offenders is regarded as an open secret, but there are no sanctions for that bad behavior. These offenders often are perceived as superstars in their particular substantive area. Because they hold valued grants or national status within their specialty area, they often receive preferential treatment and are not held accountable for gender-biased and sexually harassing behavior. Interview data regarding sexual harassment in academic medicine reveals that interview respondents and other colleagues often know which individuals have a history of sexually harassing behavior. Both men and women warn colleagues of these perpetrators – knowing that calling out or reporting these behaviors is fruitless – and that the best manner for dealing with their behavior is to avoid or ignore it. This normalization of sexual harassment and gender bias was noted, unfortunately, to fuel similar behavior in new cohorts of medicine faculty.1
Sexual harassment of women in academic medicine starts in medical school. Female medical students are significantly more likely to experience sexual harassment by faculty and staff than are graduate or undergraduate students. Sexual harassment continues into residency training with residency described as “breeding grounds for abusive behavior by superiors.”1 Interview studies report that both men and women trainees widely accept harassing behavior at this stage of their training. The expectation of abusive and grueling conditions during residency caused several respondents to view sexual harassment as part of a continuum that they were expected to endure. Female residents in surgery and emergency medicine are more likely to be harassed than those in other specialties because of the high value placed on a hierarchical and authoritative workplace. Once out of residency, the sexual harassment of women in the workplace continues. A recent meta-analysis reveals that 58% of women faculty experience sexual harassment at work. Academic medicine has the second-highest rate of sexual harassment, behind the military (69%), as compared with all other workplaces. Women physicians of color experience more harassment (as a combination of sexual and racial harassment) than do white women physicians.1
Why Women Are Not Likely to Report Sexual Harassment
Only 25% of targets file formal reports with their employer, with even fewer taking claims to court. These numbers are even lower for women in the military and academic medicine, where formal reporting is the last resort for the victims. The reluctance to use formal reporting mechanisms is rooted in the “fear of blame, disbelief, inaction, retaliation, humiliation, ostracism, and the damage to one’s career and reputation.”1 Targets may perceive that there seem to be few benefits and high costs for reporting. Women and nonwhites often resist calling bad behavior “discrimination” because that increases their loss of control and victimhood.1 Women frequently perceive that grievance procedures favor the institution over the individual, and research has proven that women face retaliation, both professional and social, for speaking out. Furthermore, stark power differentials between the target and the perpetrator exacerbate the reluctance to report and the fear of retaliation. The overall effects can be long lasting.
References:
1. National Academies of Sciences, Engineering, and Medicine. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine. The National Academies Press, Washington, DC; 2018. doi. 10.17226/24994.
2. Choo EK et al. From #MeToo to #TimesUp in Health Care: Can a Culture of Accountability End Inequity and Harassment? Lancet. 2019 Feb 9;393(10171):499-502.
3. Choo EK et al. Time’s Up for Medicine? Only Time Will Tell. N Engl J Med. 2018 Oct 25;379(17):1592-3.
4. Medicine Has Its Own #MeToo Problems. Can Time’s Up Healthcare Fix It?
Dr. Mitchell is a vascular surgeon at Salem (Ore.) Hospital; Dr. Drudi is as vascular surgery resident at McGill University, Montreal; Dr. Brown is a professor of surgery at the Medical College of Wisconsin. Milwaukee; Dr. Sachdev-Ost is an associate professor of surgery at the University of Pittsburgh Medical Center.
Coordination of Care Between Primary Care and Oncology for Patients With Prostate Cancer (FULL)
The following is a lightly edited transcript of a teleconference recorded in July 2018. The teleconference brought together health care providers from the Greater Los Angeles VA Health Care System (GLAVAHCS) to discuss the real-world processes for managing the treatment of patients with prostate cancer as they move between primary and specialist care.
William J. Aronson, MD. We are fortunate in having a superb medical record system at the Department of Veterans Affairs (VA) where we can all communicate with each other through a number of methods. Let’s start our discussion by reviewing an index patient that we see in our practice who has been treated with either radical prostatectomy or radiation therapy. One question to address is: Is there a point when the Urology or Radiation Oncology service can transition the patient’s entire care back to the primary care team? And if so, what would be the optimal way to accomplish this?
Nick, is there some point at which you discharge the patient from the radiation oncology service and give specific directions to primary care, or is it primarily just back to urology in your case?
Nicholas G. Nickols, MD, PhD. I have not discharged any patient from my clinic after definitive prostate cancer treatment. During treatment, patients are seen every week. Subsequently, I see them 6 weeks posttreatment, and then every 4 months for the first year, then every 6 months for the next 4 years, and then yearly after that. Although I never formally discharged a patient from my clinic, you can see based on the frequency of visits, that the patient will see more often than their primary care provider (PCP) toward the beginning. And then, after some years, the patient sees their primary more than they me. So it’s not an immediate hand off but rather a gradual transition. It’s important that the PCP is aware of what to look for especially for the late recurrences, late potential side effects, probably more significantly than the early side effects, how to manage them when appropriate, and when to ask the patient to see our team more frequently in follow-up.
William Aronson. We have a number of patients who travel tremendous distances to see us, and I tend to think that many of our follow-up patients, once things are stabilized with regards to management of their side effects, really could see their primary care doctors if we can give them specific instructions on, for example, when to get a prostate-specific antigen (PSA) test and when to refer back to us.
Alison, can you think of some specific cases where you feel like we’ve successfully done that?
Alison Neymark, MS. For the most part we haven’t discharged people, either. What we have done is transitioned them over to a phone clinic. In our department, we have 4 nurse practitioners (NPs) who each have a half-day of phone clinic where they call patients with their test results. Some of those patients are prostate cancer patients that we have been following for years. We schedule them for a phone call, whether it’s every 3 months, every 6 months or every year, to review the updated PSA level and to just check in with them by phone. It’s a win-win because it’s a really quick phone call to reassure the veteran that the PSA level is being followed, and it frees up an in-person appointment slot for another veteran.
We still have patients that prefer face-to-face visits, even though they know we’re not doing anything except discussing a PSA level with them—they just want that security of seeing our face. Some patients are very nervous, and they don’t necessarily want to be discharged, so to speak, back to primary care. Also, for those patients that travel a long distance to clinic, we offer an appointment in the video chat clinic, with the community-based outpatient clinics in Bakersfield and Santa Maria, California.
PSA Levels
William Aronson. I probably see a patient about every 4 to 6 weeks who has a low PSA after about 10 years and has a long distance to travel and mobility and other problems that make it difficult to come in.
The challenge that I have is, what is that specific guideline to give with regards to the rise in PSA? I think it all depends on the patients prostate cancer clinical features and comorbidities.
Nicholas Nickols. If a patient has been seen by me in follow-up a number of times and there’s really no active issues and there’s a low suspicion of recurrence, then I offer the patient the option of a phone follow-up as an alternative to face to face. Some of them accept that, but I ask that they agree to also see either urology or their PCP face to face. I will also remotely ensure that they’re getting the right laboratory tests, and if not, I’ll put those orders in.
With regard to when to refer a patient back for a suspected recurrence after definitive radiation therapy, there is an accepted definition of biochemical failure called the Phoenix definition, which is an absolute rise in 2 ng/mL of PSA over their posttreatment nadir. Often the posttreatment nadir, especially if they were on hormone therapy, will be close to 0. If the PSA gets to 2, that is a good trigger for a referral back to me and/or urology to discuss restaging and workup for a suspected recurrence.
For patients that are postsurgery and then subsequently get salvage radiation, it is not as clear when a restaging workup should be initiated. Currently, the imaging that is routine care is not very sensitive for detecting PSA in that setting until the PSA is around 0.8 ng/mL, and that’s with the most modern imaging available. Over time that may improve.
William Aronson. The other index patient to think about would be the patient who is on watchful waiting for their prostate cancer, which is to be distinguished from active surveillance. If someone’s on active surveillance, we’re regularly doing prostate biopsies and doing very close monitoring; but we also have patients who have multiple other medical problems, have a limited life expectancy, don’t have aggressive prostate cancer, and it’s extremely reasonable not to do a biopsy in those patients.
Again, those are patients where we do follow the PSA generally every 6 months. And I think there’s also scenarios there where it’s reasonable to refer back to primary care with specific instructions. These, again, are patients who had difficulty getting in to see us or have mobility issues, but it is also a way to limit patient visits if that’s their desire.
Peter Glassman, MBBS, MSc: I’m trained as both a general internist and board certified in hospice and palliative medicine. I currently provide primary care as well as palliative care. I view prostate cancer from the diagnosis through the treatment spectrum as a continuum. It starts with the PCP with an elevated PSA level or if the digital rectal exam has an abnormality, and then the role of the genitourinary (GU) practitioner becomes more significant during the active treatment and diagnostic phases.
Primary care doesn’t disappear, and I think there are 2 major issues that go along with that. First of all, we in primary care, because we take care of patients that often have other comorbidities, need to work with the patient on those comorbidities. Secondly, we need the information shared between the GU and primary care providers so that we can answer questions from our patients and have an understanding of what they’re going through and when.
As time goes on, we go through various phases: We may reach a cure, a quiescent period, active therapy, watchful waiting, or recurrence. Primary care gets involved as time goes on when the disease either becomes quiescent, is just being followed, or is considered cured. Clearly when you have watchful waiting, active treatment, or are in a recurrence, then GU takes the forefront.
I view it as a wave function. Primary care to GU with primary in smaller letters and then primary, if you will, in larger letters, GU becomes a lesser participant unless there is active therapy, watchful waiting or recurrence.
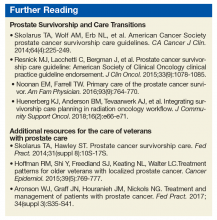
In doing a little bit of research, I found 2 very good and very helpful documents. One is the American Cancer Society (ACS) prostate cancer survivorship care guidelines (Box). And the other is a synopsis of the guidelines. What I liked was that the guidelines focused not only on what should be done for the initial period of prostate cancer, but also for many of the ancillary issues which we often don’t give voice to. The guidelines provide a structure, a foundation to work with our patients over time on their prostate cancer-related issues while, at the same time, being cognizant that we need to deal with their other comorbid conditions.
Modes of Communication
Alison Neymark. We find that including parameters for PSA monitoring in our Progress Notes in the electronic health record (EHR) the best way to communicate with other providers. We’ll say, “If PSA gets to this level, please refer back.” We try to make it clear because with the VA being a training facility, it could be a different resident/attending physician team that’s going to see the patient the next time he is in primary care.
Peter Glassman. Yes, we’re very lucky, as Bill talked about earlier and Alison just mentioned. We have the EHR, and Bill may remember this. Before the EHR, we were constantly fishing to find the most relevant notes. If a patient saw a GU practitioner the day before they saw me, I was often asking the patient what was said. Now we can just review the notes.
It’s a double-edged sword though because there are, of course, many notes in a medical record; and you have to look for the specific items. The EHR and documenting the medical record probably plays the primary role in getting information across. When you want to have an active handoff, or you need to communicate with each other, we have a variety of mechanisms, ranging from the phone to the Microsoft Skype Link (Redmond, WA) system that allows us to tap a message to a colleague.
And I’ve been here long enough that I’ve seen most permutations of how prostate cancer is diagnosed as well as shared among providers. Bill and I have shared patients. Alison and I have shared patients, not necessarily with prostate cancer, although that too. But we know how to communicate with each other. And of course, there’s paging if you need something more urgently.
William Aronson. We also use Microsoft Outlook e-mail, and encrypt the messages to keep them confidential and private. The other nice thing we have is there is a nationwide urology Outlook e-mail, so if any of us have any specific questions, through one e-mail we can send it around the country; and there’s usually multiple very useful responses. That’s another real strength of our system within the VA that helps patient care enormously.
Nicholas Nickols. Sometimes, if there’s a critical note that I absolutely want someone on the care team to read, I’ll add them as a cosigner; and that will pop up when they log in to the Computerized Patient Record System (CPRS) as something that they need to read.
If the patient lives particularly far or gets his care at another VA medical center and laboratory tests are needed, then I will reach out to their PCP via e-mail. If contact is not confirmed, I will reach out via phone or Skype.
Peter Glassman. The most helpful notes are those that are very specific as to what primary care is being asked to do and/or what urology is going to be doing. So, the more specific we get in the notes as to what is being addressed, I think that’s very helpful.
I have been here long enough that I’ve known both Alison and Bill; and if they have an issue, they will tap me a message. It wasn’t long ago that Bill sent a message to me, and we worked on a patient with prostate cancer who was going to be on long-term hormone therapy. We talked about osteoporosis management, and between us we worked out who was going to do what. Those are the kind of shared decision-making situations that are very, very helpful.
Alison Neymark. Also, GLAVAHCS has a home-based primary care team (HBPC), and a lot of the PCPs for that team are NPs. They know that they can contact me for their patients because a lot of those patients are on watchful waiting, and we do not necessarily need to see them face to face in clinic. Our urology team just needs to review updated lab results and how they are doing clinically. The HBPC NP who knows them best can contact me every 6 months or so, and we’ll discuss the case, which avoids making the patient come in, especially when they’re homebound. Those of us that have been working at the VA for many years have established good relationships. We feel very comfortable reaching out and talking to each other about these patients
Peter Glassman. Alison, I agree. When I can talk to my patients and say, “You know, we had that question about,” whatever the question might be, “and I contacted urology, and this is what they said.” It gives the patient confidence that we’re following up on the issues that they have and that we’re communicating with each other in a way that is to their benefit. And I think it’s very appreciated both by the provider as well as the patient.
William Aronson. Not infrequently I’ll have patients who have nonurologic issues, which I may first detect, or who have specific issues with their prostate cancer that can be comanaged. And I have found that when I send an encrypted e-mail to the PCP, it has been an extremely satisfying interaction; and we really get to the heart of the matter quickly for the sake of the veteran.
Veterans With Comorbidities
William Aronson. Posttraumatic stress disorder (PTSD) is a very significant and unique aspect of our patients, which is enormously important to recognize. For example, the side effects of prostate treatments can be very significant, whether radiation or surgery. Our patients understandably can be very fearful of the prostate cancer diagnosis and treatment side effects.
We know, for example, after a patient gets a diagnosis of prostate cancer, they’re at increased risk of cardiac death. That’s an especially important issue for our patients that there be an ongoing interaction between urology and primary care.
The ACS guidelines that Dr. Glassman referred to were enlightening. In many cases, primary care can look at the whole patient and their circumstances better than we can and may detect, for example, specific psychological issues that either they can manage or refer to other specialists.
Peter Glassman. One of the things that was highlighted in the ACS guideline is that in any population of men who have this disease, there’s going to be distress, anxiety, and full-fledged depression. Of course, there are psychosocial aspects of prostate cancer, such as sexual activity and intimacy with a partner that we often don’t explore but are probably playing an important role in the overall health of our patients. We need to be mindful of these psychosocial aspects and at least periodically ask them, “How are you doing with this? How are things at home?” And of course, we already use screeners for depression. As the article noted, distress and anxiety and other factors can make somebody’s life less optimal with poorer quality of life.
Dual Care Patients
Alison Neymark. Many patients whether they have Medicare, insurance through their spouse, or Kaiser Permanente through their job, choose to go to both places. The challenge is communicating with the non-VA providers because here at the VA we can communicate easily through Skype, Outlook e-mail, or CPRS, but for dual care patients who’s in charge? I encourage the veterans to choose whom they want to manage their care; we’re always here and happy to treat them, but they need to decide who’s in charge because I don’t want them to get into a situation where the differing opinions lead to a delay in care.
Nicholas Nickols. The communication when the patient is receiving care outside VA, either on a continuous basis or temporarily, is more of a challenge. We obviously can’t rely upon the messaging system, face-to-face contact is difficult, and they may not be able to use e-mail as well. So in those situations, usually a phone call is the best approach. I have found that the outside providers are happy to speak on the phone to coordinate care.
Peter Glassman. I agree, it does add a layer of complexity because we don’t readily have the notes, any information in front of us. That said, a lot of our patients can and do bring in information from outside specialists, and I’m hopeful that they share the information that we provide back to their outside doctors as well.
William Aronson. Some patient get nervous. They might decide they want care elsewhere, but they still want the VA available for them. I always let them know they should proceed in whatever way they prefer, but we’re always available and here for them. I try to empower them to make their own decisions and feel comfortable with them.
Nicholas Nickols. Notes from the outside, if they’re being referred for VA Choice or community care, do get uploaded into VistA Imaging and can be accessed, although it’s not instantaneous. Sometimes there’s a delay, but I have been able to access outside notes most of the time. If a patient goes through a clinic at the VA, the note is written in real time, and you can read it immediately.
Peter Glassman. That is true for patients that are within the VA system who receive contracted care either through Choice or through non-VA care that is contracted through VA. For somebody who is choosing to use 2 health care systems, that can provide more of a challenge because those notes don’t come to us. Over time, most of my patients have brought test results to me.
The thing with oncologic care, of course, is it’s a lot more complex. And it’s hard to know without reasonable documentation what’s been going on. At some level, you have to trust that the outside provider is doing whatever they need to do, or you have to take it upon yourself to do it within the system.
Alison Neymark. In my experience with the Choice Program, it really depends on the outside providers and how comfortable they are with the system that has been established to share records. Not all providers are going into that system and accessing it. I have had cases where I will see the non-VA provider’s note and it’ll say, “No documentation available for this consultation.” It just happens that they didn’t go into the system to review it. So it can be a challenge.
I’ve had good communication with the providers who use the system correctly. In some cases, just to make it easier, I will go ahead and communicate with them through encrypted e-mail, or I’ll talk to their care coordinators directly by phone.
Peter Glassman. Many, if not most, PCPs are going to take care of these patients, certainly within the VA, with their GU colleagues. And most of us feel comfortable using the current documentation system in a way that allows us to share information or at least to gather information about these patients.
One of the things that I think came out for me in looking at this was that there are guidelines or there are ideas out there on how to take better care of these patients. And I for one learned a fair bit just by going through these documents, which I’m very appreciative of. But it does highlight to me that we can give good care and provide good shared care for prostate cancer survivors. I think that is something that perhaps this discussion will highlight that not only are people doing that, but there are resources they can utilize that will help them get a more comprehensive picture of taking care of prostate cancer survivors in the primary care clinic.
The beauty of the VA system as a system is that as these issues come up that might affect the overall health of the veteran with prostate cancer, for example, psychosocial issues, we have many people that can address this that are experts in their area. And one of the great beauties of having an all-encompassing healthcare system is being able to use resources within the system, whether that be for other medical problems or other social or other psychological issues, that we ourselves are not expert in. We can reach out to our other colleagues and ask them for assistance. We have that available to help the patients. It’s really holistic.
We even have integrated medicine where we can help patients, hopefully, get back into a healthy lifestyle, for example, whereas we may not have that expertise or knowledge. We often think of this as sort of a shared decision between GU and primary care. But, in fact, it’s really the responsibility of many, many people of the system at large. We are very lucky to have that.
The following is a lightly edited transcript of a teleconference recorded in July 2018. The teleconference brought together health care providers from the Greater Los Angeles VA Health Care System (GLAVAHCS) to discuss the real-world processes for managing the treatment of patients with prostate cancer as they move between primary and specialist care.
William J. Aronson, MD. We are fortunate in having a superb medical record system at the Department of Veterans Affairs (VA) where we can all communicate with each other through a number of methods. Let’s start our discussion by reviewing an index patient that we see in our practice who has been treated with either radical prostatectomy or radiation therapy. One question to address is: Is there a point when the Urology or Radiation Oncology service can transition the patient’s entire care back to the primary care team? And if so, what would be the optimal way to accomplish this?
Nick, is there some point at which you discharge the patient from the radiation oncology service and give specific directions to primary care, or is it primarily just back to urology in your case?
Nicholas G. Nickols, MD, PhD. I have not discharged any patient from my clinic after definitive prostate cancer treatment. During treatment, patients are seen every week. Subsequently, I see them 6 weeks posttreatment, and then every 4 months for the first year, then every 6 months for the next 4 years, and then yearly after that. Although I never formally discharged a patient from my clinic, you can see based on the frequency of visits, that the patient will see more often than their primary care provider (PCP) toward the beginning. And then, after some years, the patient sees their primary more than they me. So it’s not an immediate hand off but rather a gradual transition. It’s important that the PCP is aware of what to look for especially for the late recurrences, late potential side effects, probably more significantly than the early side effects, how to manage them when appropriate, and when to ask the patient to see our team more frequently in follow-up.
William Aronson. We have a number of patients who travel tremendous distances to see us, and I tend to think that many of our follow-up patients, once things are stabilized with regards to management of their side effects, really could see their primary care doctors if we can give them specific instructions on, for example, when to get a prostate-specific antigen (PSA) test and when to refer back to us.
Alison, can you think of some specific cases where you feel like we’ve successfully done that?
Alison Neymark, MS. For the most part we haven’t discharged people, either. What we have done is transitioned them over to a phone clinic. In our department, we have 4 nurse practitioners (NPs) who each have a half-day of phone clinic where they call patients with their test results. Some of those patients are prostate cancer patients that we have been following for years. We schedule them for a phone call, whether it’s every 3 months, every 6 months or every year, to review the updated PSA level and to just check in with them by phone. It’s a win-win because it’s a really quick phone call to reassure the veteran that the PSA level is being followed, and it frees up an in-person appointment slot for another veteran.
We still have patients that prefer face-to-face visits, even though they know we’re not doing anything except discussing a PSA level with them—they just want that security of seeing our face. Some patients are very nervous, and they don’t necessarily want to be discharged, so to speak, back to primary care. Also, for those patients that travel a long distance to clinic, we offer an appointment in the video chat clinic, with the community-based outpatient clinics in Bakersfield and Santa Maria, California.
PSA Levels
William Aronson. I probably see a patient about every 4 to 6 weeks who has a low PSA after about 10 years and has a long distance to travel and mobility and other problems that make it difficult to come in.
The challenge that I have is, what is that specific guideline to give with regards to the rise in PSA? I think it all depends on the patients prostate cancer clinical features and comorbidities.
Nicholas Nickols. If a patient has been seen by me in follow-up a number of times and there’s really no active issues and there’s a low suspicion of recurrence, then I offer the patient the option of a phone follow-up as an alternative to face to face. Some of them accept that, but I ask that they agree to also see either urology or their PCP face to face. I will also remotely ensure that they’re getting the right laboratory tests, and if not, I’ll put those orders in.
With regard to when to refer a patient back for a suspected recurrence after definitive radiation therapy, there is an accepted definition of biochemical failure called the Phoenix definition, which is an absolute rise in 2 ng/mL of PSA over their posttreatment nadir. Often the posttreatment nadir, especially if they were on hormone therapy, will be close to 0. If the PSA gets to 2, that is a good trigger for a referral back to me and/or urology to discuss restaging and workup for a suspected recurrence.
For patients that are postsurgery and then subsequently get salvage radiation, it is not as clear when a restaging workup should be initiated. Currently, the imaging that is routine care is not very sensitive for detecting PSA in that setting until the PSA is around 0.8 ng/mL, and that’s with the most modern imaging available. Over time that may improve.
William Aronson. The other index patient to think about would be the patient who is on watchful waiting for their prostate cancer, which is to be distinguished from active surveillance. If someone’s on active surveillance, we’re regularly doing prostate biopsies and doing very close monitoring; but we also have patients who have multiple other medical problems, have a limited life expectancy, don’t have aggressive prostate cancer, and it’s extremely reasonable not to do a biopsy in those patients.
Again, those are patients where we do follow the PSA generally every 6 months. And I think there’s also scenarios there where it’s reasonable to refer back to primary care with specific instructions. These, again, are patients who had difficulty getting in to see us or have mobility issues, but it is also a way to limit patient visits if that’s their desire.
Peter Glassman, MBBS, MSc: I’m trained as both a general internist and board certified in hospice and palliative medicine. I currently provide primary care as well as palliative care. I view prostate cancer from the diagnosis through the treatment spectrum as a continuum. It starts with the PCP with an elevated PSA level or if the digital rectal exam has an abnormality, and then the role of the genitourinary (GU) practitioner becomes more significant during the active treatment and diagnostic phases.
Primary care doesn’t disappear, and I think there are 2 major issues that go along with that. First of all, we in primary care, because we take care of patients that often have other comorbidities, need to work with the patient on those comorbidities. Secondly, we need the information shared between the GU and primary care providers so that we can answer questions from our patients and have an understanding of what they’re going through and when.
As time goes on, we go through various phases: We may reach a cure, a quiescent period, active therapy, watchful waiting, or recurrence. Primary care gets involved as time goes on when the disease either becomes quiescent, is just being followed, or is considered cured. Clearly when you have watchful waiting, active treatment, or are in a recurrence, then GU takes the forefront.
I view it as a wave function. Primary care to GU with primary in smaller letters and then primary, if you will, in larger letters, GU becomes a lesser participant unless there is active therapy, watchful waiting or recurrence.
In doing a little bit of research, I found 2 very good and very helpful documents. One is the American Cancer Society (ACS) prostate cancer survivorship care guidelines (Box). And the other is a synopsis of the guidelines. What I liked was that the guidelines focused not only on what should be done for the initial period of prostate cancer, but also for many of the ancillary issues which we often don’t give voice to. The guidelines provide a structure, a foundation to work with our patients over time on their prostate cancer-related issues while, at the same time, being cognizant that we need to deal with their other comorbid conditions.
Modes of Communication
Alison Neymark. We find that including parameters for PSA monitoring in our Progress Notes in the electronic health record (EHR) the best way to communicate with other providers. We’ll say, “If PSA gets to this level, please refer back.” We try to make it clear because with the VA being a training facility, it could be a different resident/attending physician team that’s going to see the patient the next time he is in primary care.
Peter Glassman. Yes, we’re very lucky, as Bill talked about earlier and Alison just mentioned. We have the EHR, and Bill may remember this. Before the EHR, we were constantly fishing to find the most relevant notes. If a patient saw a GU practitioner the day before they saw me, I was often asking the patient what was said. Now we can just review the notes.
It’s a double-edged sword though because there are, of course, many notes in a medical record; and you have to look for the specific items. The EHR and documenting the medical record probably plays the primary role in getting information across. When you want to have an active handoff, or you need to communicate with each other, we have a variety of mechanisms, ranging from the phone to the Microsoft Skype Link (Redmond, WA) system that allows us to tap a message to a colleague.
And I’ve been here long enough that I’ve seen most permutations of how prostate cancer is diagnosed as well as shared among providers. Bill and I have shared patients. Alison and I have shared patients, not necessarily with prostate cancer, although that too. But we know how to communicate with each other. And of course, there’s paging if you need something more urgently.
William Aronson. We also use Microsoft Outlook e-mail, and encrypt the messages to keep them confidential and private. The other nice thing we have is there is a nationwide urology Outlook e-mail, so if any of us have any specific questions, through one e-mail we can send it around the country; and there’s usually multiple very useful responses. That’s another real strength of our system within the VA that helps patient care enormously.
Nicholas Nickols. Sometimes, if there’s a critical note that I absolutely want someone on the care team to read, I’ll add them as a cosigner; and that will pop up when they log in to the Computerized Patient Record System (CPRS) as something that they need to read.
If the patient lives particularly far or gets his care at another VA medical center and laboratory tests are needed, then I will reach out to their PCP via e-mail. If contact is not confirmed, I will reach out via phone or Skype.
Peter Glassman. The most helpful notes are those that are very specific as to what primary care is being asked to do and/or what urology is going to be doing. So, the more specific we get in the notes as to what is being addressed, I think that’s very helpful.
I have been here long enough that I’ve known both Alison and Bill; and if they have an issue, they will tap me a message. It wasn’t long ago that Bill sent a message to me, and we worked on a patient with prostate cancer who was going to be on long-term hormone therapy. We talked about osteoporosis management, and between us we worked out who was going to do what. Those are the kind of shared decision-making situations that are very, very helpful.
Alison Neymark. Also, GLAVAHCS has a home-based primary care team (HBPC), and a lot of the PCPs for that team are NPs. They know that they can contact me for their patients because a lot of those patients are on watchful waiting, and we do not necessarily need to see them face to face in clinic. Our urology team just needs to review updated lab results and how they are doing clinically. The HBPC NP who knows them best can contact me every 6 months or so, and we’ll discuss the case, which avoids making the patient come in, especially when they’re homebound. Those of us that have been working at the VA for many years have established good relationships. We feel very comfortable reaching out and talking to each other about these patients
Peter Glassman. Alison, I agree. When I can talk to my patients and say, “You know, we had that question about,” whatever the question might be, “and I contacted urology, and this is what they said.” It gives the patient confidence that we’re following up on the issues that they have and that we’re communicating with each other in a way that is to their benefit. And I think it’s very appreciated both by the provider as well as the patient.
William Aronson. Not infrequently I’ll have patients who have nonurologic issues, which I may first detect, or who have specific issues with their prostate cancer that can be comanaged. And I have found that when I send an encrypted e-mail to the PCP, it has been an extremely satisfying interaction; and we really get to the heart of the matter quickly for the sake of the veteran.
Veterans With Comorbidities
William Aronson. Posttraumatic stress disorder (PTSD) is a very significant and unique aspect of our patients, which is enormously important to recognize. For example, the side effects of prostate treatments can be very significant, whether radiation or surgery. Our patients understandably can be very fearful of the prostate cancer diagnosis and treatment side effects.
We know, for example, after a patient gets a diagnosis of prostate cancer, they’re at increased risk of cardiac death. That’s an especially important issue for our patients that there be an ongoing interaction between urology and primary care.
The ACS guidelines that Dr. Glassman referred to were enlightening. In many cases, primary care can look at the whole patient and their circumstances better than we can and may detect, for example, specific psychological issues that either they can manage or refer to other specialists.
Peter Glassman. One of the things that was highlighted in the ACS guideline is that in any population of men who have this disease, there’s going to be distress, anxiety, and full-fledged depression. Of course, there are psychosocial aspects of prostate cancer, such as sexual activity and intimacy with a partner that we often don’t explore but are probably playing an important role in the overall health of our patients. We need to be mindful of these psychosocial aspects and at least periodically ask them, “How are you doing with this? How are things at home?” And of course, we already use screeners for depression. As the article noted, distress and anxiety and other factors can make somebody’s life less optimal with poorer quality of life.
Dual Care Patients
Alison Neymark. Many patients whether they have Medicare, insurance through their spouse, or Kaiser Permanente through their job, choose to go to both places. The challenge is communicating with the non-VA providers because here at the VA we can communicate easily through Skype, Outlook e-mail, or CPRS, but for dual care patients who’s in charge? I encourage the veterans to choose whom they want to manage their care; we’re always here and happy to treat them, but they need to decide who’s in charge because I don’t want them to get into a situation where the differing opinions lead to a delay in care.
Nicholas Nickols. The communication when the patient is receiving care outside VA, either on a continuous basis or temporarily, is more of a challenge. We obviously can’t rely upon the messaging system, face-to-face contact is difficult, and they may not be able to use e-mail as well. So in those situations, usually a phone call is the best approach. I have found that the outside providers are happy to speak on the phone to coordinate care.
Peter Glassman. I agree, it does add a layer of complexity because we don’t readily have the notes, any information in front of us. That said, a lot of our patients can and do bring in information from outside specialists, and I’m hopeful that they share the information that we provide back to their outside doctors as well.
William Aronson. Some patient get nervous. They might decide they want care elsewhere, but they still want the VA available for them. I always let them know they should proceed in whatever way they prefer, but we’re always available and here for them. I try to empower them to make their own decisions and feel comfortable with them.
Nicholas Nickols. Notes from the outside, if they’re being referred for VA Choice or community care, do get uploaded into VistA Imaging and can be accessed, although it’s not instantaneous. Sometimes there’s a delay, but I have been able to access outside notes most of the time. If a patient goes through a clinic at the VA, the note is written in real time, and you can read it immediately.
Peter Glassman. That is true for patients that are within the VA system who receive contracted care either through Choice or through non-VA care that is contracted through VA. For somebody who is choosing to use 2 health care systems, that can provide more of a challenge because those notes don’t come to us. Over time, most of my patients have brought test results to me.
The thing with oncologic care, of course, is it’s a lot more complex. And it’s hard to know without reasonable documentation what’s been going on. At some level, you have to trust that the outside provider is doing whatever they need to do, or you have to take it upon yourself to do it within the system.
Alison Neymark. In my experience with the Choice Program, it really depends on the outside providers and how comfortable they are with the system that has been established to share records. Not all providers are going into that system and accessing it. I have had cases where I will see the non-VA provider’s note and it’ll say, “No documentation available for this consultation.” It just happens that they didn’t go into the system to review it. So it can be a challenge.
I’ve had good communication with the providers who use the system correctly. In some cases, just to make it easier, I will go ahead and communicate with them through encrypted e-mail, or I’ll talk to their care coordinators directly by phone.
Peter Glassman. Many, if not most, PCPs are going to take care of these patients, certainly within the VA, with their GU colleagues. And most of us feel comfortable using the current documentation system in a way that allows us to share information or at least to gather information about these patients.
One of the things that I think came out for me in looking at this was that there are guidelines or there are ideas out there on how to take better care of these patients. And I for one learned a fair bit just by going through these documents, which I’m very appreciative of. But it does highlight to me that we can give good care and provide good shared care for prostate cancer survivors. I think that is something that perhaps this discussion will highlight that not only are people doing that, but there are resources they can utilize that will help them get a more comprehensive picture of taking care of prostate cancer survivors in the primary care clinic.
The beauty of the VA system as a system is that as these issues come up that might affect the overall health of the veteran with prostate cancer, for example, psychosocial issues, we have many people that can address this that are experts in their area. And one of the great beauties of having an all-encompassing healthcare system is being able to use resources within the system, whether that be for other medical problems or other social or other psychological issues, that we ourselves are not expert in. We can reach out to our other colleagues and ask them for assistance. We have that available to help the patients. It’s really holistic.
We even have integrated medicine where we can help patients, hopefully, get back into a healthy lifestyle, for example, whereas we may not have that expertise or knowledge. We often think of this as sort of a shared decision between GU and primary care. But, in fact, it’s really the responsibility of many, many people of the system at large. We are very lucky to have that.
The following is a lightly edited transcript of a teleconference recorded in July 2018. The teleconference brought together health care providers from the Greater Los Angeles VA Health Care System (GLAVAHCS) to discuss the real-world processes for managing the treatment of patients with prostate cancer as they move between primary and specialist care.
William J. Aronson, MD. We are fortunate in having a superb medical record system at the Department of Veterans Affairs (VA) where we can all communicate with each other through a number of methods. Let’s start our discussion by reviewing an index patient that we see in our practice who has been treated with either radical prostatectomy or radiation therapy. One question to address is: Is there a point when the Urology or Radiation Oncology service can transition the patient’s entire care back to the primary care team? And if so, what would be the optimal way to accomplish this?
Nick, is there some point at which you discharge the patient from the radiation oncology service and give specific directions to primary care, or is it primarily just back to urology in your case?
Nicholas G. Nickols, MD, PhD. I have not discharged any patient from my clinic after definitive prostate cancer treatment. During treatment, patients are seen every week. Subsequently, I see them 6 weeks posttreatment, and then every 4 months for the first year, then every 6 months for the next 4 years, and then yearly after that. Although I never formally discharged a patient from my clinic, you can see based on the frequency of visits, that the patient will see more often than their primary care provider (PCP) toward the beginning. And then, after some years, the patient sees their primary more than they me. So it’s not an immediate hand off but rather a gradual transition. It’s important that the PCP is aware of what to look for especially for the late recurrences, late potential side effects, probably more significantly than the early side effects, how to manage them when appropriate, and when to ask the patient to see our team more frequently in follow-up.
William Aronson. We have a number of patients who travel tremendous distances to see us, and I tend to think that many of our follow-up patients, once things are stabilized with regards to management of their side effects, really could see their primary care doctors if we can give them specific instructions on, for example, when to get a prostate-specific antigen (PSA) test and when to refer back to us.
Alison, can you think of some specific cases where you feel like we’ve successfully done that?
Alison Neymark, MS. For the most part we haven’t discharged people, either. What we have done is transitioned them over to a phone clinic. In our department, we have 4 nurse practitioners (NPs) who each have a half-day of phone clinic where they call patients with their test results. Some of those patients are prostate cancer patients that we have been following for years. We schedule them for a phone call, whether it’s every 3 months, every 6 months or every year, to review the updated PSA level and to just check in with them by phone. It’s a win-win because it’s a really quick phone call to reassure the veteran that the PSA level is being followed, and it frees up an in-person appointment slot for another veteran.
We still have patients that prefer face-to-face visits, even though they know we’re not doing anything except discussing a PSA level with them—they just want that security of seeing our face. Some patients are very nervous, and they don’t necessarily want to be discharged, so to speak, back to primary care. Also, for those patients that travel a long distance to clinic, we offer an appointment in the video chat clinic, with the community-based outpatient clinics in Bakersfield and Santa Maria, California.
PSA Levels
William Aronson. I probably see a patient about every 4 to 6 weeks who has a low PSA after about 10 years and has a long distance to travel and mobility and other problems that make it difficult to come in.
The challenge that I have is, what is that specific guideline to give with regards to the rise in PSA? I think it all depends on the patients prostate cancer clinical features and comorbidities.
Nicholas Nickols. If a patient has been seen by me in follow-up a number of times and there’s really no active issues and there’s a low suspicion of recurrence, then I offer the patient the option of a phone follow-up as an alternative to face to face. Some of them accept that, but I ask that they agree to also see either urology or their PCP face to face. I will also remotely ensure that they’re getting the right laboratory tests, and if not, I’ll put those orders in.
With regard to when to refer a patient back for a suspected recurrence after definitive radiation therapy, there is an accepted definition of biochemical failure called the Phoenix definition, which is an absolute rise in 2 ng/mL of PSA over their posttreatment nadir. Often the posttreatment nadir, especially if they were on hormone therapy, will be close to 0. If the PSA gets to 2, that is a good trigger for a referral back to me and/or urology to discuss restaging and workup for a suspected recurrence.
For patients that are postsurgery and then subsequently get salvage radiation, it is not as clear when a restaging workup should be initiated. Currently, the imaging that is routine care is not very sensitive for detecting PSA in that setting until the PSA is around 0.8 ng/mL, and that’s with the most modern imaging available. Over time that may improve.
William Aronson. The other index patient to think about would be the patient who is on watchful waiting for their prostate cancer, which is to be distinguished from active surveillance. If someone’s on active surveillance, we’re regularly doing prostate biopsies and doing very close monitoring; but we also have patients who have multiple other medical problems, have a limited life expectancy, don’t have aggressive prostate cancer, and it’s extremely reasonable not to do a biopsy in those patients.
Again, those are patients where we do follow the PSA generally every 6 months. And I think there’s also scenarios there where it’s reasonable to refer back to primary care with specific instructions. These, again, are patients who had difficulty getting in to see us or have mobility issues, but it is also a way to limit patient visits if that’s their desire.
Peter Glassman, MBBS, MSc: I’m trained as both a general internist and board certified in hospice and palliative medicine. I currently provide primary care as well as palliative care. I view prostate cancer from the diagnosis through the treatment spectrum as a continuum. It starts with the PCP with an elevated PSA level or if the digital rectal exam has an abnormality, and then the role of the genitourinary (GU) practitioner becomes more significant during the active treatment and diagnostic phases.
Primary care doesn’t disappear, and I think there are 2 major issues that go along with that. First of all, we in primary care, because we take care of patients that often have other comorbidities, need to work with the patient on those comorbidities. Secondly, we need the information shared between the GU and primary care providers so that we can answer questions from our patients and have an understanding of what they’re going through and when.
As time goes on, we go through various phases: We may reach a cure, a quiescent period, active therapy, watchful waiting, or recurrence. Primary care gets involved as time goes on when the disease either becomes quiescent, is just being followed, or is considered cured. Clearly when you have watchful waiting, active treatment, or are in a recurrence, then GU takes the forefront.
I view it as a wave function. Primary care to GU with primary in smaller letters and then primary, if you will, in larger letters, GU becomes a lesser participant unless there is active therapy, watchful waiting or recurrence.
In doing a little bit of research, I found 2 very good and very helpful documents. One is the American Cancer Society (ACS) prostate cancer survivorship care guidelines (Box). And the other is a synopsis of the guidelines. What I liked was that the guidelines focused not only on what should be done for the initial period of prostate cancer, but also for many of the ancillary issues which we often don’t give voice to. The guidelines provide a structure, a foundation to work with our patients over time on their prostate cancer-related issues while, at the same time, being cognizant that we need to deal with their other comorbid conditions.
Modes of Communication
Alison Neymark. We find that including parameters for PSA monitoring in our Progress Notes in the electronic health record (EHR) the best way to communicate with other providers. We’ll say, “If PSA gets to this level, please refer back.” We try to make it clear because with the VA being a training facility, it could be a different resident/attending physician team that’s going to see the patient the next time he is in primary care.
Peter Glassman. Yes, we’re very lucky, as Bill talked about earlier and Alison just mentioned. We have the EHR, and Bill may remember this. Before the EHR, we were constantly fishing to find the most relevant notes. If a patient saw a GU practitioner the day before they saw me, I was often asking the patient what was said. Now we can just review the notes.
It’s a double-edged sword though because there are, of course, many notes in a medical record; and you have to look for the specific items. The EHR and documenting the medical record probably plays the primary role in getting information across. When you want to have an active handoff, or you need to communicate with each other, we have a variety of mechanisms, ranging from the phone to the Microsoft Skype Link (Redmond, WA) system that allows us to tap a message to a colleague.
And I’ve been here long enough that I’ve seen most permutations of how prostate cancer is diagnosed as well as shared among providers. Bill and I have shared patients. Alison and I have shared patients, not necessarily with prostate cancer, although that too. But we know how to communicate with each other. And of course, there’s paging if you need something more urgently.
William Aronson. We also use Microsoft Outlook e-mail, and encrypt the messages to keep them confidential and private. The other nice thing we have is there is a nationwide urology Outlook e-mail, so if any of us have any specific questions, through one e-mail we can send it around the country; and there’s usually multiple very useful responses. That’s another real strength of our system within the VA that helps patient care enormously.
Nicholas Nickols. Sometimes, if there’s a critical note that I absolutely want someone on the care team to read, I’ll add them as a cosigner; and that will pop up when they log in to the Computerized Patient Record System (CPRS) as something that they need to read.
If the patient lives particularly far or gets his care at another VA medical center and laboratory tests are needed, then I will reach out to their PCP via e-mail. If contact is not confirmed, I will reach out via phone or Skype.
Peter Glassman. The most helpful notes are those that are very specific as to what primary care is being asked to do and/or what urology is going to be doing. So, the more specific we get in the notes as to what is being addressed, I think that’s very helpful.
I have been here long enough that I’ve known both Alison and Bill; and if they have an issue, they will tap me a message. It wasn’t long ago that Bill sent a message to me, and we worked on a patient with prostate cancer who was going to be on long-term hormone therapy. We talked about osteoporosis management, and between us we worked out who was going to do what. Those are the kind of shared decision-making situations that are very, very helpful.
Alison Neymark. Also, GLAVAHCS has a home-based primary care team (HBPC), and a lot of the PCPs for that team are NPs. They know that they can contact me for their patients because a lot of those patients are on watchful waiting, and we do not necessarily need to see them face to face in clinic. Our urology team just needs to review updated lab results and how they are doing clinically. The HBPC NP who knows them best can contact me every 6 months or so, and we’ll discuss the case, which avoids making the patient come in, especially when they’re homebound. Those of us that have been working at the VA for many years have established good relationships. We feel very comfortable reaching out and talking to each other about these patients
Peter Glassman. Alison, I agree. When I can talk to my patients and say, “You know, we had that question about,” whatever the question might be, “and I contacted urology, and this is what they said.” It gives the patient confidence that we’re following up on the issues that they have and that we’re communicating with each other in a way that is to their benefit. And I think it’s very appreciated both by the provider as well as the patient.
William Aronson. Not infrequently I’ll have patients who have nonurologic issues, which I may first detect, or who have specific issues with their prostate cancer that can be comanaged. And I have found that when I send an encrypted e-mail to the PCP, it has been an extremely satisfying interaction; and we really get to the heart of the matter quickly for the sake of the veteran.
Veterans With Comorbidities
William Aronson. Posttraumatic stress disorder (PTSD) is a very significant and unique aspect of our patients, which is enormously important to recognize. For example, the side effects of prostate treatments can be very significant, whether radiation or surgery. Our patients understandably can be very fearful of the prostate cancer diagnosis and treatment side effects.
We know, for example, after a patient gets a diagnosis of prostate cancer, they’re at increased risk of cardiac death. That’s an especially important issue for our patients that there be an ongoing interaction between urology and primary care.
The ACS guidelines that Dr. Glassman referred to were enlightening. In many cases, primary care can look at the whole patient and their circumstances better than we can and may detect, for example, specific psychological issues that either they can manage or refer to other specialists.
Peter Glassman. One of the things that was highlighted in the ACS guideline is that in any population of men who have this disease, there’s going to be distress, anxiety, and full-fledged depression. Of course, there are psychosocial aspects of prostate cancer, such as sexual activity and intimacy with a partner that we often don’t explore but are probably playing an important role in the overall health of our patients. We need to be mindful of these psychosocial aspects and at least periodically ask them, “How are you doing with this? How are things at home?” And of course, we already use screeners for depression. As the article noted, distress and anxiety and other factors can make somebody’s life less optimal with poorer quality of life.
Dual Care Patients
Alison Neymark. Many patients whether they have Medicare, insurance through their spouse, or Kaiser Permanente through their job, choose to go to both places. The challenge is communicating with the non-VA providers because here at the VA we can communicate easily through Skype, Outlook e-mail, or CPRS, but for dual care patients who’s in charge? I encourage the veterans to choose whom they want to manage their care; we’re always here and happy to treat them, but they need to decide who’s in charge because I don’t want them to get into a situation where the differing opinions lead to a delay in care.
Nicholas Nickols. The communication when the patient is receiving care outside VA, either on a continuous basis or temporarily, is more of a challenge. We obviously can’t rely upon the messaging system, face-to-face contact is difficult, and they may not be able to use e-mail as well. So in those situations, usually a phone call is the best approach. I have found that the outside providers are happy to speak on the phone to coordinate care.
Peter Glassman. I agree, it does add a layer of complexity because we don’t readily have the notes, any information in front of us. That said, a lot of our patients can and do bring in information from outside specialists, and I’m hopeful that they share the information that we provide back to their outside doctors as well.
William Aronson. Some patient get nervous. They might decide they want care elsewhere, but they still want the VA available for them. I always let them know they should proceed in whatever way they prefer, but we’re always available and here for them. I try to empower them to make their own decisions and feel comfortable with them.
Nicholas Nickols. Notes from the outside, if they’re being referred for VA Choice or community care, do get uploaded into VistA Imaging and can be accessed, although it’s not instantaneous. Sometimes there’s a delay, but I have been able to access outside notes most of the time. If a patient goes through a clinic at the VA, the note is written in real time, and you can read it immediately.
Peter Glassman. That is true for patients that are within the VA system who receive contracted care either through Choice or through non-VA care that is contracted through VA. For somebody who is choosing to use 2 health care systems, that can provide more of a challenge because those notes don’t come to us. Over time, most of my patients have brought test results to me.
The thing with oncologic care, of course, is it’s a lot more complex. And it’s hard to know without reasonable documentation what’s been going on. At some level, you have to trust that the outside provider is doing whatever they need to do, or you have to take it upon yourself to do it within the system.
Alison Neymark. In my experience with the Choice Program, it really depends on the outside providers and how comfortable they are with the system that has been established to share records. Not all providers are going into that system and accessing it. I have had cases where I will see the non-VA provider’s note and it’ll say, “No documentation available for this consultation.” It just happens that they didn’t go into the system to review it. So it can be a challenge.
I’ve had good communication with the providers who use the system correctly. In some cases, just to make it easier, I will go ahead and communicate with them through encrypted e-mail, or I’ll talk to their care coordinators directly by phone.
Peter Glassman. Many, if not most, PCPs are going to take care of these patients, certainly within the VA, with their GU colleagues. And most of us feel comfortable using the current documentation system in a way that allows us to share information or at least to gather information about these patients.
One of the things that I think came out for me in looking at this was that there are guidelines or there are ideas out there on how to take better care of these patients. And I for one learned a fair bit just by going through these documents, which I’m very appreciative of. But it does highlight to me that we can give good care and provide good shared care for prostate cancer survivors. I think that is something that perhaps this discussion will highlight that not only are people doing that, but there are resources they can utilize that will help them get a more comprehensive picture of taking care of prostate cancer survivors in the primary care clinic.
The beauty of the VA system as a system is that as these issues come up that might affect the overall health of the veteran with prostate cancer, for example, psychosocial issues, we have many people that can address this that are experts in their area. And one of the great beauties of having an all-encompassing healthcare system is being able to use resources within the system, whether that be for other medical problems or other social or other psychological issues, that we ourselves are not expert in. We can reach out to our other colleagues and ask them for assistance. We have that available to help the patients. It’s really holistic.
We even have integrated medicine where we can help patients, hopefully, get back into a healthy lifestyle, for example, whereas we may not have that expertise or knowledge. We often think of this as sort of a shared decision between GU and primary care. But, in fact, it’s really the responsibility of many, many people of the system at large. We are very lucky to have that.
First death from severe lung illness associated with vaping reported in Illinois
The first death to occur in a patient with severe lung illness associated with e-cigarette product use has been reported in Illinois, officials announced at a Centers for Disease Control and Prevention telebriefing.
The cause for the mysterious lung illnesses has not been determined, but an infectious disease does not appear to be implicated. As of yesterday, 193 potential cases have been identified in 22 states since June 28.
No specific product has been implicated in all cases, and it is unclear if there is a common cause or if these are several diseases with a similar presentation.
Wisconsin and Illinois have asked the CDC to directly assist them in their investigations of cases. Other states are handling their own investigations. Further information is available from the CDC at cdc.gov/e-cigarettes.
There have been 22 cases of the illness in Illinois and an additional 12 individuals are being evaluated as possible cases, according to Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist, Illinois Department of Public Health.
Illinois is working with the CDC and the Food and Drug Administration to investigate devices that affected patients have used. No specific product has been implicated across all cases; all patients have reported vaping in recent months Several patients in Illinois have reported using tetrahydrocannabinol (THC) product oils, but Dr. Layden reiterated the investigations are reliant on information reported by affected patients only.
Mitch Zeller, JD, director, Center for Tobacco Products at the FDA, said product samples from a number of states are being evaluated to determine their contents. The FDA is examining samples sent and trying to identify product contents.
The cases reported to date have been in adults aged 17-38 years and have occurred primarily men. The investigation is in a relatively early stage and is working with incomplete case reports. These will become standardized to include more specific information, such as the name of the product, where it was purchased, and whether it was used as intended or whether other products were added, he said.
As e-cigarettes are not a new product, it’s possible that cases of this illness has been occurring but that the link was not recognized, and the cases were neither captured nor reported, said Brian King, PhD, MPH, deputy director, Research Translation, Office on Smoking and Health, CDC. He noted that e-cigarettes may contain “a variety of constituents that could be problematic in terms of pulmonary illness,” such as ingredients in certain flavorings and ultrafine particulates.
The agencies are now trying to harmonize reporting across all states so cases can be evaluated in a more standardized way. Information on standardized reporting on a national level will be issued in the next few days, according to the CDC.
The CDC notified U.S. health care systems and clinicians about the illnesses and what to watch for via a Clinician Outreach and Communication Activity Clinical Action Message.
In general, patients have reported a gradual onset of symptoms including shortness of breath or chest pain that increased over days or weeks before hospital admission. Gastrointestinal symptoms including vomiting, diarrhea, and fatigue have been reported by some.
The first death to occur in a patient with severe lung illness associated with e-cigarette product use has been reported in Illinois, officials announced at a Centers for Disease Control and Prevention telebriefing.
The cause for the mysterious lung illnesses has not been determined, but an infectious disease does not appear to be implicated. As of yesterday, 193 potential cases have been identified in 22 states since June 28.
No specific product has been implicated in all cases, and it is unclear if there is a common cause or if these are several diseases with a similar presentation.
Wisconsin and Illinois have asked the CDC to directly assist them in their investigations of cases. Other states are handling their own investigations. Further information is available from the CDC at cdc.gov/e-cigarettes.
There have been 22 cases of the illness in Illinois and an additional 12 individuals are being evaluated as possible cases, according to Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist, Illinois Department of Public Health.
Illinois is working with the CDC and the Food and Drug Administration to investigate devices that affected patients have used. No specific product has been implicated across all cases; all patients have reported vaping in recent months Several patients in Illinois have reported using tetrahydrocannabinol (THC) product oils, but Dr. Layden reiterated the investigations are reliant on information reported by affected patients only.
Mitch Zeller, JD, director, Center for Tobacco Products at the FDA, said product samples from a number of states are being evaluated to determine their contents. The FDA is examining samples sent and trying to identify product contents.
The cases reported to date have been in adults aged 17-38 years and have occurred primarily men. The investigation is in a relatively early stage and is working with incomplete case reports. These will become standardized to include more specific information, such as the name of the product, where it was purchased, and whether it was used as intended or whether other products were added, he said.
As e-cigarettes are not a new product, it’s possible that cases of this illness has been occurring but that the link was not recognized, and the cases were neither captured nor reported, said Brian King, PhD, MPH, deputy director, Research Translation, Office on Smoking and Health, CDC. He noted that e-cigarettes may contain “a variety of constituents that could be problematic in terms of pulmonary illness,” such as ingredients in certain flavorings and ultrafine particulates.
The agencies are now trying to harmonize reporting across all states so cases can be evaluated in a more standardized way. Information on standardized reporting on a national level will be issued in the next few days, according to the CDC.
The CDC notified U.S. health care systems and clinicians about the illnesses and what to watch for via a Clinician Outreach and Communication Activity Clinical Action Message.
In general, patients have reported a gradual onset of symptoms including shortness of breath or chest pain that increased over days or weeks before hospital admission. Gastrointestinal symptoms including vomiting, diarrhea, and fatigue have been reported by some.
The first death to occur in a patient with severe lung illness associated with e-cigarette product use has been reported in Illinois, officials announced at a Centers for Disease Control and Prevention telebriefing.
The cause for the mysterious lung illnesses has not been determined, but an infectious disease does not appear to be implicated. As of yesterday, 193 potential cases have been identified in 22 states since June 28.
No specific product has been implicated in all cases, and it is unclear if there is a common cause or if these are several diseases with a similar presentation.
Wisconsin and Illinois have asked the CDC to directly assist them in their investigations of cases. Other states are handling their own investigations. Further information is available from the CDC at cdc.gov/e-cigarettes.
There have been 22 cases of the illness in Illinois and an additional 12 individuals are being evaluated as possible cases, according to Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist, Illinois Department of Public Health.
Illinois is working with the CDC and the Food and Drug Administration to investigate devices that affected patients have used. No specific product has been implicated across all cases; all patients have reported vaping in recent months Several patients in Illinois have reported using tetrahydrocannabinol (THC) product oils, but Dr. Layden reiterated the investigations are reliant on information reported by affected patients only.
Mitch Zeller, JD, director, Center for Tobacco Products at the FDA, said product samples from a number of states are being evaluated to determine their contents. The FDA is examining samples sent and trying to identify product contents.
The cases reported to date have been in adults aged 17-38 years and have occurred primarily men. The investigation is in a relatively early stage and is working with incomplete case reports. These will become standardized to include more specific information, such as the name of the product, where it was purchased, and whether it was used as intended or whether other products were added, he said.
As e-cigarettes are not a new product, it’s possible that cases of this illness has been occurring but that the link was not recognized, and the cases were neither captured nor reported, said Brian King, PhD, MPH, deputy director, Research Translation, Office on Smoking and Health, CDC. He noted that e-cigarettes may contain “a variety of constituents that could be problematic in terms of pulmonary illness,” such as ingredients in certain flavorings and ultrafine particulates.
The agencies are now trying to harmonize reporting across all states so cases can be evaluated in a more standardized way. Information on standardized reporting on a national level will be issued in the next few days, according to the CDC.
The CDC notified U.S. health care systems and clinicians about the illnesses and what to watch for via a Clinician Outreach and Communication Activity Clinical Action Message.
In general, patients have reported a gradual onset of symptoms including shortness of breath or chest pain that increased over days or weeks before hospital admission. Gastrointestinal symptoms including vomiting, diarrhea, and fatigue have been reported by some.
Pediatric hospitalist certification beset by gender bias concerns
Are women unfairly penalized?
More than 1,625 pediatricians have applied to take the first pediatric hospitalist certification exam in November 2019, and approximately 93% of them have been accepted, according to a statement from the American Board of Pediatrics.
It was the rejection of the 7%, however, that set off a firestorm on the electronic discussion board for American Academy of Pediatrics (AAP) hospital medicine this summer, and led to a petition to the board to revise its eligibility requirements, ensure that the requirements are fair to women, and bring transparency to its decision process. The petition has more than 1,400 signatures.
Seattle Children’s Hospital and Yale New Haven (Conn.) Children’s Hospital have both said they will not consider board certification in hiring decisions until the situation is resolved.
The American Board of Pediatrics (ABP) declined an interview request pending its formal response to the Aug. 6 petition, but in a statement to this news organization, executive vice president Suzanne Woods, MD, said, “The percentage of women and men meeting the eligibility requirements for the exam did not differ. We stress this point because a concern about possible gender bias appears to have been the principal reason for this ... petition, and we wanted to offer immediate reassurance that no unintended bias has occurred.”
“We are carefully considering the requests and will release detailed data to hospitalists on the AAP’s [pediatric hospital medicine (PHM) electronic discussion board] ... and on the ABP’s website. We are conferring with ABP PHM subboard members as well as leaders from our volunteer community. We expect to provide a thoughtful response within the next 3 weeks,” Dr. Woods said in the Aug. 15 statement.
“Case-by-case” exceptions
The backstory is that, for better or worse depending on who you talk to, pediatric hospital medicine is becoming a board certified subspecialty. A fellowship will be required to sit for the exam after a few years, which is standard for subspecialties.
What’s generated concern is how the board is grandfathering current pediatric hospitalists into certification via a “practice pathway” until the fellowship requirement takes hold after 2023.
To qualify for the November test, hospitalists had to complete 4 years of full-time practice by June 30, 2019, which has been understood to mean 48 months of continual employment. At least 50% of that time had to be devoted to “professional activities ... related to the care of hospitalized children,” and at least 25% of that “devoted to direct patient care.” Assuming about 2,000 work hours per year, it translated to “450-500 hours” of direct patient care “per year over the most recent four years” to sit for the test, the board said.
“For individuals who have interrupted practice during the most recent four years for family leave or other such circumstances, an exception may be considered if there is substantial prior experience in pediatric hospital medicine. ... Such exceptions are made at the discretion of the ABP and will be considered on a case-by-case basis.” Specific criteria for exceptions were not spelled out.
In the end, there were more than a few surprises when denial letters went out in recent months, and scores of appeals have been filed. There’s “a lot of tension and a lot of confusion” about why some people with practice gaps during the 4 years were approved, but others were denied. There’s been “a lack of transparency on the ABP’s part,” said H. Barrett Fromme, MD, section chief of pediatric hospital medicine and a professor of pediatrics at the University of Chicago.
“The standard has to be reasonable”
There are concerns about the availability of fellowship slots and other issues, but the 4-year rule – instead of averaging clinical hours over 4 or 5 years, for instance – is the main sticking point. It’s a gender issue because “women take maternity; women move with their spouse; women take care of elders; women tend to be in these roles that require time off” more than men do, Dr. Fromme said.
Until the board releases its data, the gender breakdown of the denials and the degree to which practice gaps due to such issues led to them is unknown. There’s concern that women have been unfairly penalized.
The storm was set off on the discussion board this summer by stories from physicians such as Chandani DeZure, MD, a pediatric hospitalist currently working in the neonatal ICU at Stanford (Calif.) University. She was denied a seat at the table in November, appealed, and was denied again.
She was a full-time pediatric hospitalist at Children’s National Medical Center in Washington, from 2014, when she graduated residency, until Oct. 2018, when her husband, also a doctor, was offered a promising research position in California, and “we decided to take it,” Dr. DeZure said.
They moved to California with their young son in November. Dr. DeZure got her California medical license in 6 weeks, was hired by Stanford in January, and started her new postion in mid-April.
Because of the move, she worked only 3.5 years in the board’s 4 year practice window, but, as is common with young physicians, that time was spent in direct patient care, for a total of over 6,000 hours.
“How is that not good enough? How is a person that worked 500 hours with patients for 4 years” – for a total of 2,000 hours – “better qualified than someone who worked 100% for 3 and a half years? Nobody is saying there shouldn’t be a standard, but the standard has to be reasonable,” Dr. DeZure said.
“Illegal regardless of intent”
It’s situations like Dr. DeZure’s that led to the petition. One of demands is that ABP “revise the practice pathway criteria to be more inclusive of applicants with interrupted practice and varied clinical experience, to include clear-cut parameters rather than considering these applications on a closed-door ‘case-by-case basis...at the discretion of the ABP.’ ” Also, the petition asks the board to “clarify the appeals process and improve responsiveness to appeals and inquiries regarding denials.”
As ABP noted in its statement, however, the major demand is that the board “facilitate a timely analysis to determine if gender bias is present.” The petition noted that signers “do not suspect intentional bias on the part of the ABP; however, if gender bias is present it is unethical and potentially illegal regardless of intent.”
For now, the perception is that the board has “a hard 48-month rule” with not many exceptions; there are people who are “very concerned that, ‘Oh my gosh, I can’t have children for 4 years because I won’t be able to sit for the boards.’ No one should ever have to have that in their head,” Dr. Fromme said. At this point, it seems that 3 months off for maternity is being grandfathered in, but perhaps not 6 months for a second child; no one knows for sure.
Dr. DeZure, meanwhile, continues to study for the board exam, just in case.
Looking back over the past year, she said “I could have somehow picked up one shift a week moonlighting that would have kept me eligible, but the [board] didn’t respond to me” when contacted about her situation during the California move.
“The other option was for me was to live cross country from my husband with a small child,” she said.
Are women unfairly penalized?
Are women unfairly penalized?
More than 1,625 pediatricians have applied to take the first pediatric hospitalist certification exam in November 2019, and approximately 93% of them have been accepted, according to a statement from the American Board of Pediatrics.
It was the rejection of the 7%, however, that set off a firestorm on the electronic discussion board for American Academy of Pediatrics (AAP) hospital medicine this summer, and led to a petition to the board to revise its eligibility requirements, ensure that the requirements are fair to women, and bring transparency to its decision process. The petition has more than 1,400 signatures.
Seattle Children’s Hospital and Yale New Haven (Conn.) Children’s Hospital have both said they will not consider board certification in hiring decisions until the situation is resolved.
The American Board of Pediatrics (ABP) declined an interview request pending its formal response to the Aug. 6 petition, but in a statement to this news organization, executive vice president Suzanne Woods, MD, said, “The percentage of women and men meeting the eligibility requirements for the exam did not differ. We stress this point because a concern about possible gender bias appears to have been the principal reason for this ... petition, and we wanted to offer immediate reassurance that no unintended bias has occurred.”
“We are carefully considering the requests and will release detailed data to hospitalists on the AAP’s [pediatric hospital medicine (PHM) electronic discussion board] ... and on the ABP’s website. We are conferring with ABP PHM subboard members as well as leaders from our volunteer community. We expect to provide a thoughtful response within the next 3 weeks,” Dr. Woods said in the Aug. 15 statement.
“Case-by-case” exceptions
The backstory is that, for better or worse depending on who you talk to, pediatric hospital medicine is becoming a board certified subspecialty. A fellowship will be required to sit for the exam after a few years, which is standard for subspecialties.
What’s generated concern is how the board is grandfathering current pediatric hospitalists into certification via a “practice pathway” until the fellowship requirement takes hold after 2023.
To qualify for the November test, hospitalists had to complete 4 years of full-time practice by June 30, 2019, which has been understood to mean 48 months of continual employment. At least 50% of that time had to be devoted to “professional activities ... related to the care of hospitalized children,” and at least 25% of that “devoted to direct patient care.” Assuming about 2,000 work hours per year, it translated to “450-500 hours” of direct patient care “per year over the most recent four years” to sit for the test, the board said.
“For individuals who have interrupted practice during the most recent four years for family leave or other such circumstances, an exception may be considered if there is substantial prior experience in pediatric hospital medicine. ... Such exceptions are made at the discretion of the ABP and will be considered on a case-by-case basis.” Specific criteria for exceptions were not spelled out.
In the end, there were more than a few surprises when denial letters went out in recent months, and scores of appeals have been filed. There’s “a lot of tension and a lot of confusion” about why some people with practice gaps during the 4 years were approved, but others were denied. There’s been “a lack of transparency on the ABP’s part,” said H. Barrett Fromme, MD, section chief of pediatric hospital medicine and a professor of pediatrics at the University of Chicago.
“The standard has to be reasonable”
There are concerns about the availability of fellowship slots and other issues, but the 4-year rule – instead of averaging clinical hours over 4 or 5 years, for instance – is the main sticking point. It’s a gender issue because “women take maternity; women move with their spouse; women take care of elders; women tend to be in these roles that require time off” more than men do, Dr. Fromme said.
Until the board releases its data, the gender breakdown of the denials and the degree to which practice gaps due to such issues led to them is unknown. There’s concern that women have been unfairly penalized.
The storm was set off on the discussion board this summer by stories from physicians such as Chandani DeZure, MD, a pediatric hospitalist currently working in the neonatal ICU at Stanford (Calif.) University. She was denied a seat at the table in November, appealed, and was denied again.
She was a full-time pediatric hospitalist at Children’s National Medical Center in Washington, from 2014, when she graduated residency, until Oct. 2018, when her husband, also a doctor, was offered a promising research position in California, and “we decided to take it,” Dr. DeZure said.
They moved to California with their young son in November. Dr. DeZure got her California medical license in 6 weeks, was hired by Stanford in January, and started her new postion in mid-April.
Because of the move, she worked only 3.5 years in the board’s 4 year practice window, but, as is common with young physicians, that time was spent in direct patient care, for a total of over 6,000 hours.
“How is that not good enough? How is a person that worked 500 hours with patients for 4 years” – for a total of 2,000 hours – “better qualified than someone who worked 100% for 3 and a half years? Nobody is saying there shouldn’t be a standard, but the standard has to be reasonable,” Dr. DeZure said.
“Illegal regardless of intent”
It’s situations like Dr. DeZure’s that led to the petition. One of demands is that ABP “revise the practice pathway criteria to be more inclusive of applicants with interrupted practice and varied clinical experience, to include clear-cut parameters rather than considering these applications on a closed-door ‘case-by-case basis...at the discretion of the ABP.’ ” Also, the petition asks the board to “clarify the appeals process and improve responsiveness to appeals and inquiries regarding denials.”
As ABP noted in its statement, however, the major demand is that the board “facilitate a timely analysis to determine if gender bias is present.” The petition noted that signers “do not suspect intentional bias on the part of the ABP; however, if gender bias is present it is unethical and potentially illegal regardless of intent.”
For now, the perception is that the board has “a hard 48-month rule” with not many exceptions; there are people who are “very concerned that, ‘Oh my gosh, I can’t have children for 4 years because I won’t be able to sit for the boards.’ No one should ever have to have that in their head,” Dr. Fromme said. At this point, it seems that 3 months off for maternity is being grandfathered in, but perhaps not 6 months for a second child; no one knows for sure.
Dr. DeZure, meanwhile, continues to study for the board exam, just in case.
Looking back over the past year, she said “I could have somehow picked up one shift a week moonlighting that would have kept me eligible, but the [board] didn’t respond to me” when contacted about her situation during the California move.
“The other option was for me was to live cross country from my husband with a small child,” she said.
More than 1,625 pediatricians have applied to take the first pediatric hospitalist certification exam in November 2019, and approximately 93% of them have been accepted, according to a statement from the American Board of Pediatrics.
It was the rejection of the 7%, however, that set off a firestorm on the electronic discussion board for American Academy of Pediatrics (AAP) hospital medicine this summer, and led to a petition to the board to revise its eligibility requirements, ensure that the requirements are fair to women, and bring transparency to its decision process. The petition has more than 1,400 signatures.
Seattle Children’s Hospital and Yale New Haven (Conn.) Children’s Hospital have both said they will not consider board certification in hiring decisions until the situation is resolved.
The American Board of Pediatrics (ABP) declined an interview request pending its formal response to the Aug. 6 petition, but in a statement to this news organization, executive vice president Suzanne Woods, MD, said, “The percentage of women and men meeting the eligibility requirements for the exam did not differ. We stress this point because a concern about possible gender bias appears to have been the principal reason for this ... petition, and we wanted to offer immediate reassurance that no unintended bias has occurred.”
“We are carefully considering the requests and will release detailed data to hospitalists on the AAP’s [pediatric hospital medicine (PHM) electronic discussion board] ... and on the ABP’s website. We are conferring with ABP PHM subboard members as well as leaders from our volunteer community. We expect to provide a thoughtful response within the next 3 weeks,” Dr. Woods said in the Aug. 15 statement.
“Case-by-case” exceptions
The backstory is that, for better or worse depending on who you talk to, pediatric hospital medicine is becoming a board certified subspecialty. A fellowship will be required to sit for the exam after a few years, which is standard for subspecialties.
What’s generated concern is how the board is grandfathering current pediatric hospitalists into certification via a “practice pathway” until the fellowship requirement takes hold after 2023.
To qualify for the November test, hospitalists had to complete 4 years of full-time practice by June 30, 2019, which has been understood to mean 48 months of continual employment. At least 50% of that time had to be devoted to “professional activities ... related to the care of hospitalized children,” and at least 25% of that “devoted to direct patient care.” Assuming about 2,000 work hours per year, it translated to “450-500 hours” of direct patient care “per year over the most recent four years” to sit for the test, the board said.
“For individuals who have interrupted practice during the most recent four years for family leave or other such circumstances, an exception may be considered if there is substantial prior experience in pediatric hospital medicine. ... Such exceptions are made at the discretion of the ABP and will be considered on a case-by-case basis.” Specific criteria for exceptions were not spelled out.
In the end, there were more than a few surprises when denial letters went out in recent months, and scores of appeals have been filed. There’s “a lot of tension and a lot of confusion” about why some people with practice gaps during the 4 years were approved, but others were denied. There’s been “a lack of transparency on the ABP’s part,” said H. Barrett Fromme, MD, section chief of pediatric hospital medicine and a professor of pediatrics at the University of Chicago.
“The standard has to be reasonable”
There are concerns about the availability of fellowship slots and other issues, but the 4-year rule – instead of averaging clinical hours over 4 or 5 years, for instance – is the main sticking point. It’s a gender issue because “women take maternity; women move with their spouse; women take care of elders; women tend to be in these roles that require time off” more than men do, Dr. Fromme said.
Until the board releases its data, the gender breakdown of the denials and the degree to which practice gaps due to such issues led to them is unknown. There’s concern that women have been unfairly penalized.
The storm was set off on the discussion board this summer by stories from physicians such as Chandani DeZure, MD, a pediatric hospitalist currently working in the neonatal ICU at Stanford (Calif.) University. She was denied a seat at the table in November, appealed, and was denied again.
She was a full-time pediatric hospitalist at Children’s National Medical Center in Washington, from 2014, when she graduated residency, until Oct. 2018, when her husband, also a doctor, was offered a promising research position in California, and “we decided to take it,” Dr. DeZure said.
They moved to California with their young son in November. Dr. DeZure got her California medical license in 6 weeks, was hired by Stanford in January, and started her new postion in mid-April.
Because of the move, she worked only 3.5 years in the board’s 4 year practice window, but, as is common with young physicians, that time was spent in direct patient care, for a total of over 6,000 hours.
“How is that not good enough? How is a person that worked 500 hours with patients for 4 years” – for a total of 2,000 hours – “better qualified than someone who worked 100% for 3 and a half years? Nobody is saying there shouldn’t be a standard, but the standard has to be reasonable,” Dr. DeZure said.
“Illegal regardless of intent”
It’s situations like Dr. DeZure’s that led to the petition. One of demands is that ABP “revise the practice pathway criteria to be more inclusive of applicants with interrupted practice and varied clinical experience, to include clear-cut parameters rather than considering these applications on a closed-door ‘case-by-case basis...at the discretion of the ABP.’ ” Also, the petition asks the board to “clarify the appeals process and improve responsiveness to appeals and inquiries regarding denials.”
As ABP noted in its statement, however, the major demand is that the board “facilitate a timely analysis to determine if gender bias is present.” The petition noted that signers “do not suspect intentional bias on the part of the ABP; however, if gender bias is present it is unethical and potentially illegal regardless of intent.”
For now, the perception is that the board has “a hard 48-month rule” with not many exceptions; there are people who are “very concerned that, ‘Oh my gosh, I can’t have children for 4 years because I won’t be able to sit for the boards.’ No one should ever have to have that in their head,” Dr. Fromme said. At this point, it seems that 3 months off for maternity is being grandfathered in, but perhaps not 6 months for a second child; no one knows for sure.
Dr. DeZure, meanwhile, continues to study for the board exam, just in case.
Looking back over the past year, she said “I could have somehow picked up one shift a week moonlighting that would have kept me eligible, but the [board] didn’t respond to me” when contacted about her situation during the California move.
“The other option was for me was to live cross country from my husband with a small child,” she said.
Anticoagulant therapy for AFib in patients with end-stage renal disease
Warfarin or apixaban are sensible options
Case
A 78-year-old woman with end-stage renal disease (ESRD) is hospitalized with cellulitis and is incidentally found to be in atrial fibrillation. She does not have a history of mitral stenosis, nor does she have a prosthetic valve. She does have a history of hypertension, diabetes, and prior stroke without residual deficits.
After counseling her about the risk of stroke associated with atrial fibrillation (AFib) she makes it clear she is interested in pharmacologic therapy to minimize her risk of stroke and asks what medication you would recommend for anticoagulation.
Brief overview of the issue
Anticoagulation for AFib is indicated for stroke prophylaxis in patients with an elevated risk of stroke. The CHA2DS2-VASc score is useful in calculating an individual patient’s risk of stroke and as a decision tool to determine who would benefit from anticoagulation, and it is recommended in the American Heart Association guidelines.1
Low-risk patients (CHA2DS2-VASc score of 0 in men or 1 in women) should not be started on anticoagulation for stroke prophylaxis. For anyone with a risk factor, other than being female, anticoagulation is indicated and should be considered.
The guideline recommends anticoagulant therapy, not antiplatelet agents. For most of the recent past, this has meant a vitamin K antagonist (warfarin) or sometimes a low-molecular-weight heparin injected subcutaneously. Over the past decade, however, with the approval of multiple direct oral anticoagulants (DOACs), nonwarfarin oral anticoagulation has grown in popularity as the prophylactic medication of choice.2
While the data for patients with preserved renal function is robust, there is far less data to guide decision making for patients with end-stage renal disease.
Overview of the data
Until the introduction of DOACs, warfarin was the main agent used for stroke prophylaxis in patients with end-stage kidney disease and AFib. Professional guidelines favored warfarin for these patients who were mostly excluded from DOAC trials. Specialized conferences also looked at this issue.
The Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference, which reviewed chronic kidney disease and arrhythmias, noted that there were no randomized controlled trials that examined the efficacy and safety of anticoagulation in chronic kidney disease patients with estimated creatinine clearance less than 30 mL/min. They remarked that there was insufficient high-quality evidence to recommend warfarin for the prevention of stroke in patients with AFib and dialysis-dependent chronic kidney disease.
Since, according to other trials, DOACs had better safety profiles in other populations, the conference noted that lower-dose apixaban (2.5 mg orally twice daily) or rivaroxaban (15 mg daily) may be considered in this population until clinical safety data were available. Furthermore, the conference recommended that these patients be treated with a multidisciplinary approach in regards to anticoagulation and have an annual reevaluation of treatment goals, along with a risk-benefit assessment.3
Since the publication of the 2018 AHA guidelines and the guidance document that resulted from the KDIGO conference, additional research has been published comparing anticoagulation with a DOAC versus warfarin for AFib in patients with ESRD.
“Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States” was an observational, retrospective, cohort study that compared outcomes in dialysis patients who took warfarin for AFib with those who took apixaban.4 Patients’ data was taken from the U.S. Renal Data System database and were included in the final analysis if they had ESRD, a recent diagnosis of AFib or atrial flutter, and a new prescription for either warfarin or apixaban. Outcome measures were stroke or systemic embolism, major bleeding (critical site, transfusion, or death), gastrointestinal bleeding, intracranial bleeding, or death. Drug usage and compliance were assessed using Medicare Part D prescription information.
A total of 25,523 patients met the inclusion/exclusion criteria and had taken either warfarin (n = 23,172) or apixaban (n = 2,351). To account for selection bias in these cohorts, a subset of the warfarin patients was selected based on prognostic score matching. The prognostic score was calculated from the baseline characteristics (which included age, stroke history, diabetes, smoking, antiplatelet medication, liver disease, prior bleeding, and CHA2DS2-VASc score). Kaplan-Meier and Cox regression analysis were used to give hazard ratios and 95% confidence intervals for each outcome measure. Prespecified subgroup analyses were conducted to compare apixaban doses, where 44% were prescribed 5 mg b.i.d. and 56% were prescribed 2.5 mg b.i.d..
In the study, patients in the apixaban group had a significantly lower risk of major bleeding as compared with the warfarin group (HR, 0.72; 95% CI, 0.59-0.87; P less than .001) with overall high rates of major bleeding in both groups at 19.7 and 22.9 per 100 patient-years in the apixaban group and warfarin group, respectively. There was no difference in the rate of stroke/systemic embolism between patients receiving apixaban and warfarin (HR, 0.88; 95% CI, 0.69-1.12; P = .29). There was a nonsignificant trend toward decreased risk of GI bleeding in the apixaban group and no significant differences between the groups in the rates of intracranial bleeding. Apixaban was also associated with a nonsignificant trend toward lower risk of mortality (HR, 0.85; 95% CI, 0.71-1.01; P = .06).
Notably, censoring rates because of expired prescriptions or a 1-month gap between prescriptions were high in both groups and the majority of censoring occurred within the first 12 months. Additionally, in dose specific analyses, patients receiving the 5-mg, twice-daily dose were found to have statistically significant decreases in risk of stroke/systemic embolism (P = .035) and mortality (P = .005) as compared with the 2.5-mg, twice-daily dose without significant differences in GI or intracranial bleeding.
There are three ongoing, open-label, randomized, controlled trials examining anticoagulation for nonvalvular AFib in patients with ESRD on hemodialysis with two comparing apixaban to warfarin (or derivative) and the other warfarin versus no anticoagulation.5 All trials are in adult patients with documented AFib and CHA2DS2-VASc score of at least 2. AKADIA (Germany based) plans to enroll 222 patients and compares a vitamin K antagonist (INR goal, 2-3) with 2.5-mg b.i.d. apixaban patients with ESRD on hemodialysis for at least 3 months with primary outcome of major and clinically relevant nonmajor bleeding and secondary outcome of thromboembolic events, as well as apixaban levels pre- and post hemodialysis.
RENAL-AF (U.S. based) plans to enrolled 762 patients and compares 5-mg b.i.d. apixaban (with 2.5 mg for selected patients) with warfarin in people of chronic hemodialysis with primary outcome of days to first major or clinically relevant nonmajor bleeding event and secondary outcome of stroke, systemic embolism, mortality, adherence and plasma apixaban levels. AVKDIAL (France based) plans to enroll 855 patients and compares no anticoagulation with vitamin K antagonists in patients on hemodialysis for at least 1 month, with primary outcome of cumulative incidence of severe bleeding and thrombosis.
Application of the data to our original case
Our patient is Medicare age with ESRD and newly diagnosed nonvalvular AFib. Recent data suggests apixaban could be used for stroke prevention instead of the prior standard of care, warfarin. This approach is supported in the 2019 guidelines.1
Patients with ESRD have an increased risk of bleeding and apixaban was shown to have less bleeding complications than warfarin in this analysis. However, only standard-dose apixaban was associated with a statistically significant lower risk of stroke/systemic embolism, major bleeding, and death. Reduced-dose apixaban had a lower risk of major bleeding but no difference for stroke/systemic embolism or death. Reduced-dose apixaban is used for patients who have two out of the following three criteria: aged at least 80 years, weight of at least 60 kg, and creatinine of at least 1.5 mg/dL. Therefore, many Medicare-age patients with ESRD would not be indicated for the dose of apixaban that was shown to improve the most important outcomes of stroke/SE and death.
It may still be beneficial to use apixaban in this patient since it appears to work as well as warfarin for stroke/systemic embolism prevention with less bleeding complications.
Bottom line
For patients who have decided to pursue an anticoagulation strategy for stroke prevention in AFib and have end-stage renal disease, either warfarin or apixaban are sensible options.
Dr. Farber is a medical instructor at Duke University Health System in Durham, N.C. Dr. Stafford is a medical instructor at Duke University. Dr. Sata is assistant professor of medicine at Duke University. Dr. Abdo and Dr. Menon are hospitalists at Duke University. Dr. Brooks is assistant professor of medicine at Duke University. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor of medicine at Duke University. Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and assistant professor of medicine at Duke University.
References
1. January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
2. Lippi G et al. Direct oral anticoagulants: Analysis of worldwide use and popularity using Google Trends. Ann Transl Med. 2017 Aug; 5(16):322. doi: 10.21037/atm.2017.06.65.
3. Turakhia MP et al. Chronic kidney disease and arrhythmias: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Eur Heart J. 2018 Jun 21;39(24):2314-25. doi: 10.1093/eurheartj/ehy060.
4. Siontis KC et al. Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States. Circulation. 2018 Oct 9;138(15):1519-29. doi: 10.1161/CIRCULATIONAHA.118.035418.
5. Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit-to-risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Key points
- According to 2019 American Heart Association guidelines, warfarin or apixaban are reasonable options for stroke prevention for patients who have end-stage renal disease and who plan for anticoagulation because of atrial fibrillation.
- Recent observational data suggests that apixaban may be safer than warfarin in this population.
- Several randomized, controlled trials are ongoing that may help determine the optimal agent to use in this setting.
- Until more definitive data is available, a reasonable approach is to discuss the risks and benefits of various treatment strategies with patients, and engage a multidisciplinary team (cardiologist, nephrologist, primary care provider, pharmacist) in the decision making process.
Additional reading
January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit to risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Garlo KG et al. Demystifying the benefits and harms of anticoagulation for atrial fibrillation in chronic kidney disease. Clin J Am Soc Nephrol 2019;14:125-36. doi: 10.2215/CJN.06430518.
Quiz
Two days ago you admitted a 72-year-old woman with end-stage renal disease on dialysis who had developed new-onset atrial fibrillation causing a mild acute diastolic congestive heart failure exacerbation. Transthoracic ECG showed a preserved left ventricular ejection fraction and no significant valvular disease. After two sessions of dialysis in the hospital and initiation of a beta-blocker for control of her heart rate, she is stable and ready for discharge. Her discharge weight is 75 kg.
Which of the following recommendations should you make to this patient regarding anticoagulation for prevention of stroke and systemic embolism from atrial fibrillation?
A. Take warfarin with a international normalized ratio goal of 2.5.
B. Take apixaban 2.5 mg twice a day.
C. Take apixaban 5 mg twice a day.
D. Discuss the risks/benefits of various treatment approaches with the patient, and involve the hospital pharmacist as well as the patient’s nephrologist, cardiologist, and/or primary care provider in the decision making process to reach a consensus and to ensure a safe follow-up plan.
The best answer is D. While A, B, and C are all reasonable approaches based on the available data and current guidelines, the best approach is to involve the patient and the multidisciplinary team in the decision making process. When more clinical trial data becomes available in the future, the optimal approach to managing patients such as this one may become clearer, but until then it makes sense to take into account individual patient characteristics and patient preferences.
Warfarin or apixaban are sensible options
Warfarin or apixaban are sensible options
Case
A 78-year-old woman with end-stage renal disease (ESRD) is hospitalized with cellulitis and is incidentally found to be in atrial fibrillation. She does not have a history of mitral stenosis, nor does she have a prosthetic valve. She does have a history of hypertension, diabetes, and prior stroke without residual deficits.
After counseling her about the risk of stroke associated with atrial fibrillation (AFib) she makes it clear she is interested in pharmacologic therapy to minimize her risk of stroke and asks what medication you would recommend for anticoagulation.
Brief overview of the issue
Anticoagulation for AFib is indicated for stroke prophylaxis in patients with an elevated risk of stroke. The CHA2DS2-VASc score is useful in calculating an individual patient’s risk of stroke and as a decision tool to determine who would benefit from anticoagulation, and it is recommended in the American Heart Association guidelines.1
Low-risk patients (CHA2DS2-VASc score of 0 in men or 1 in women) should not be started on anticoagulation for stroke prophylaxis. For anyone with a risk factor, other than being female, anticoagulation is indicated and should be considered.
The guideline recommends anticoagulant therapy, not antiplatelet agents. For most of the recent past, this has meant a vitamin K antagonist (warfarin) or sometimes a low-molecular-weight heparin injected subcutaneously. Over the past decade, however, with the approval of multiple direct oral anticoagulants (DOACs), nonwarfarin oral anticoagulation has grown in popularity as the prophylactic medication of choice.2
While the data for patients with preserved renal function is robust, there is far less data to guide decision making for patients with end-stage renal disease.
Overview of the data
Until the introduction of DOACs, warfarin was the main agent used for stroke prophylaxis in patients with end-stage kidney disease and AFib. Professional guidelines favored warfarin for these patients who were mostly excluded from DOAC trials. Specialized conferences also looked at this issue.
The Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference, which reviewed chronic kidney disease and arrhythmias, noted that there were no randomized controlled trials that examined the efficacy and safety of anticoagulation in chronic kidney disease patients with estimated creatinine clearance less than 30 mL/min. They remarked that there was insufficient high-quality evidence to recommend warfarin for the prevention of stroke in patients with AFib and dialysis-dependent chronic kidney disease.
Since, according to other trials, DOACs had better safety profiles in other populations, the conference noted that lower-dose apixaban (2.5 mg orally twice daily) or rivaroxaban (15 mg daily) may be considered in this population until clinical safety data were available. Furthermore, the conference recommended that these patients be treated with a multidisciplinary approach in regards to anticoagulation and have an annual reevaluation of treatment goals, along with a risk-benefit assessment.3
Since the publication of the 2018 AHA guidelines and the guidance document that resulted from the KDIGO conference, additional research has been published comparing anticoagulation with a DOAC versus warfarin for AFib in patients with ESRD.
“Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States” was an observational, retrospective, cohort study that compared outcomes in dialysis patients who took warfarin for AFib with those who took apixaban.4 Patients’ data was taken from the U.S. Renal Data System database and were included in the final analysis if they had ESRD, a recent diagnosis of AFib or atrial flutter, and a new prescription for either warfarin or apixaban. Outcome measures were stroke or systemic embolism, major bleeding (critical site, transfusion, or death), gastrointestinal bleeding, intracranial bleeding, or death. Drug usage and compliance were assessed using Medicare Part D prescription information.
A total of 25,523 patients met the inclusion/exclusion criteria and had taken either warfarin (n = 23,172) or apixaban (n = 2,351). To account for selection bias in these cohorts, a subset of the warfarin patients was selected based on prognostic score matching. The prognostic score was calculated from the baseline characteristics (which included age, stroke history, diabetes, smoking, antiplatelet medication, liver disease, prior bleeding, and CHA2DS2-VASc score). Kaplan-Meier and Cox regression analysis were used to give hazard ratios and 95% confidence intervals for each outcome measure. Prespecified subgroup analyses were conducted to compare apixaban doses, where 44% were prescribed 5 mg b.i.d. and 56% were prescribed 2.5 mg b.i.d..
In the study, patients in the apixaban group had a significantly lower risk of major bleeding as compared with the warfarin group (HR, 0.72; 95% CI, 0.59-0.87; P less than .001) with overall high rates of major bleeding in both groups at 19.7 and 22.9 per 100 patient-years in the apixaban group and warfarin group, respectively. There was no difference in the rate of stroke/systemic embolism between patients receiving apixaban and warfarin (HR, 0.88; 95% CI, 0.69-1.12; P = .29). There was a nonsignificant trend toward decreased risk of GI bleeding in the apixaban group and no significant differences between the groups in the rates of intracranial bleeding. Apixaban was also associated with a nonsignificant trend toward lower risk of mortality (HR, 0.85; 95% CI, 0.71-1.01; P = .06).
Notably, censoring rates because of expired prescriptions or a 1-month gap between prescriptions were high in both groups and the majority of censoring occurred within the first 12 months. Additionally, in dose specific analyses, patients receiving the 5-mg, twice-daily dose were found to have statistically significant decreases in risk of stroke/systemic embolism (P = .035) and mortality (P = .005) as compared with the 2.5-mg, twice-daily dose without significant differences in GI or intracranial bleeding.
There are three ongoing, open-label, randomized, controlled trials examining anticoagulation for nonvalvular AFib in patients with ESRD on hemodialysis with two comparing apixaban to warfarin (or derivative) and the other warfarin versus no anticoagulation.5 All trials are in adult patients with documented AFib and CHA2DS2-VASc score of at least 2. AKADIA (Germany based) plans to enroll 222 patients and compares a vitamin K antagonist (INR goal, 2-3) with 2.5-mg b.i.d. apixaban patients with ESRD on hemodialysis for at least 3 months with primary outcome of major and clinically relevant nonmajor bleeding and secondary outcome of thromboembolic events, as well as apixaban levels pre- and post hemodialysis.
RENAL-AF (U.S. based) plans to enrolled 762 patients and compares 5-mg b.i.d. apixaban (with 2.5 mg for selected patients) with warfarin in people of chronic hemodialysis with primary outcome of days to first major or clinically relevant nonmajor bleeding event and secondary outcome of stroke, systemic embolism, mortality, adherence and plasma apixaban levels. AVKDIAL (France based) plans to enroll 855 patients and compares no anticoagulation with vitamin K antagonists in patients on hemodialysis for at least 1 month, with primary outcome of cumulative incidence of severe bleeding and thrombosis.
Application of the data to our original case
Our patient is Medicare age with ESRD and newly diagnosed nonvalvular AFib. Recent data suggests apixaban could be used for stroke prevention instead of the prior standard of care, warfarin. This approach is supported in the 2019 guidelines.1
Patients with ESRD have an increased risk of bleeding and apixaban was shown to have less bleeding complications than warfarin in this analysis. However, only standard-dose apixaban was associated with a statistically significant lower risk of stroke/systemic embolism, major bleeding, and death. Reduced-dose apixaban had a lower risk of major bleeding but no difference for stroke/systemic embolism or death. Reduced-dose apixaban is used for patients who have two out of the following three criteria: aged at least 80 years, weight of at least 60 kg, and creatinine of at least 1.5 mg/dL. Therefore, many Medicare-age patients with ESRD would not be indicated for the dose of apixaban that was shown to improve the most important outcomes of stroke/SE and death.
It may still be beneficial to use apixaban in this patient since it appears to work as well as warfarin for stroke/systemic embolism prevention with less bleeding complications.
Bottom line
For patients who have decided to pursue an anticoagulation strategy for stroke prevention in AFib and have end-stage renal disease, either warfarin or apixaban are sensible options.
Dr. Farber is a medical instructor at Duke University Health System in Durham, N.C. Dr. Stafford is a medical instructor at Duke University. Dr. Sata is assistant professor of medicine at Duke University. Dr. Abdo and Dr. Menon are hospitalists at Duke University. Dr. Brooks is assistant professor of medicine at Duke University. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor of medicine at Duke University. Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and assistant professor of medicine at Duke University.
References
1. January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
2. Lippi G et al. Direct oral anticoagulants: Analysis of worldwide use and popularity using Google Trends. Ann Transl Med. 2017 Aug; 5(16):322. doi: 10.21037/atm.2017.06.65.
3. Turakhia MP et al. Chronic kidney disease and arrhythmias: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Eur Heart J. 2018 Jun 21;39(24):2314-25. doi: 10.1093/eurheartj/ehy060.
4. Siontis KC et al. Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States. Circulation. 2018 Oct 9;138(15):1519-29. doi: 10.1161/CIRCULATIONAHA.118.035418.
5. Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit-to-risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Key points
- According to 2019 American Heart Association guidelines, warfarin or apixaban are reasonable options for stroke prevention for patients who have end-stage renal disease and who plan for anticoagulation because of atrial fibrillation.
- Recent observational data suggests that apixaban may be safer than warfarin in this population.
- Several randomized, controlled trials are ongoing that may help determine the optimal agent to use in this setting.
- Until more definitive data is available, a reasonable approach is to discuss the risks and benefits of various treatment strategies with patients, and engage a multidisciplinary team (cardiologist, nephrologist, primary care provider, pharmacist) in the decision making process.
Additional reading
January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit to risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Garlo KG et al. Demystifying the benefits and harms of anticoagulation for atrial fibrillation in chronic kidney disease. Clin J Am Soc Nephrol 2019;14:125-36. doi: 10.2215/CJN.06430518.
Quiz
Two days ago you admitted a 72-year-old woman with end-stage renal disease on dialysis who had developed new-onset atrial fibrillation causing a mild acute diastolic congestive heart failure exacerbation. Transthoracic ECG showed a preserved left ventricular ejection fraction and no significant valvular disease. After two sessions of dialysis in the hospital and initiation of a beta-blocker for control of her heart rate, she is stable and ready for discharge. Her discharge weight is 75 kg.
Which of the following recommendations should you make to this patient regarding anticoagulation for prevention of stroke and systemic embolism from atrial fibrillation?
A. Take warfarin with a international normalized ratio goal of 2.5.
B. Take apixaban 2.5 mg twice a day.
C. Take apixaban 5 mg twice a day.
D. Discuss the risks/benefits of various treatment approaches with the patient, and involve the hospital pharmacist as well as the patient’s nephrologist, cardiologist, and/or primary care provider in the decision making process to reach a consensus and to ensure a safe follow-up plan.
The best answer is D. While A, B, and C are all reasonable approaches based on the available data and current guidelines, the best approach is to involve the patient and the multidisciplinary team in the decision making process. When more clinical trial data becomes available in the future, the optimal approach to managing patients such as this one may become clearer, but until then it makes sense to take into account individual patient characteristics and patient preferences.
Case
A 78-year-old woman with end-stage renal disease (ESRD) is hospitalized with cellulitis and is incidentally found to be in atrial fibrillation. She does not have a history of mitral stenosis, nor does she have a prosthetic valve. She does have a history of hypertension, diabetes, and prior stroke without residual deficits.
After counseling her about the risk of stroke associated with atrial fibrillation (AFib) she makes it clear she is interested in pharmacologic therapy to minimize her risk of stroke and asks what medication you would recommend for anticoagulation.
Brief overview of the issue
Anticoagulation for AFib is indicated for stroke prophylaxis in patients with an elevated risk of stroke. The CHA2DS2-VASc score is useful in calculating an individual patient’s risk of stroke and as a decision tool to determine who would benefit from anticoagulation, and it is recommended in the American Heart Association guidelines.1
Low-risk patients (CHA2DS2-VASc score of 0 in men or 1 in women) should not be started on anticoagulation for stroke prophylaxis. For anyone with a risk factor, other than being female, anticoagulation is indicated and should be considered.
The guideline recommends anticoagulant therapy, not antiplatelet agents. For most of the recent past, this has meant a vitamin K antagonist (warfarin) or sometimes a low-molecular-weight heparin injected subcutaneously. Over the past decade, however, with the approval of multiple direct oral anticoagulants (DOACs), nonwarfarin oral anticoagulation has grown in popularity as the prophylactic medication of choice.2
While the data for patients with preserved renal function is robust, there is far less data to guide decision making for patients with end-stage renal disease.
Overview of the data
Until the introduction of DOACs, warfarin was the main agent used for stroke prophylaxis in patients with end-stage kidney disease and AFib. Professional guidelines favored warfarin for these patients who were mostly excluded from DOAC trials. Specialized conferences also looked at this issue.
The Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference, which reviewed chronic kidney disease and arrhythmias, noted that there were no randomized controlled trials that examined the efficacy and safety of anticoagulation in chronic kidney disease patients with estimated creatinine clearance less than 30 mL/min. They remarked that there was insufficient high-quality evidence to recommend warfarin for the prevention of stroke in patients with AFib and dialysis-dependent chronic kidney disease.
Since, according to other trials, DOACs had better safety profiles in other populations, the conference noted that lower-dose apixaban (2.5 mg orally twice daily) or rivaroxaban (15 mg daily) may be considered in this population until clinical safety data were available. Furthermore, the conference recommended that these patients be treated with a multidisciplinary approach in regards to anticoagulation and have an annual reevaluation of treatment goals, along with a risk-benefit assessment.3
Since the publication of the 2018 AHA guidelines and the guidance document that resulted from the KDIGO conference, additional research has been published comparing anticoagulation with a DOAC versus warfarin for AFib in patients with ESRD.
“Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States” was an observational, retrospective, cohort study that compared outcomes in dialysis patients who took warfarin for AFib with those who took apixaban.4 Patients’ data was taken from the U.S. Renal Data System database and were included in the final analysis if they had ESRD, a recent diagnosis of AFib or atrial flutter, and a new prescription for either warfarin or apixaban. Outcome measures were stroke or systemic embolism, major bleeding (critical site, transfusion, or death), gastrointestinal bleeding, intracranial bleeding, or death. Drug usage and compliance were assessed using Medicare Part D prescription information.
A total of 25,523 patients met the inclusion/exclusion criteria and had taken either warfarin (n = 23,172) or apixaban (n = 2,351). To account for selection bias in these cohorts, a subset of the warfarin patients was selected based on prognostic score matching. The prognostic score was calculated from the baseline characteristics (which included age, stroke history, diabetes, smoking, antiplatelet medication, liver disease, prior bleeding, and CHA2DS2-VASc score). Kaplan-Meier and Cox regression analysis were used to give hazard ratios and 95% confidence intervals for each outcome measure. Prespecified subgroup analyses were conducted to compare apixaban doses, where 44% were prescribed 5 mg b.i.d. and 56% were prescribed 2.5 mg b.i.d..
In the study, patients in the apixaban group had a significantly lower risk of major bleeding as compared with the warfarin group (HR, 0.72; 95% CI, 0.59-0.87; P less than .001) with overall high rates of major bleeding in both groups at 19.7 and 22.9 per 100 patient-years in the apixaban group and warfarin group, respectively. There was no difference in the rate of stroke/systemic embolism between patients receiving apixaban and warfarin (HR, 0.88; 95% CI, 0.69-1.12; P = .29). There was a nonsignificant trend toward decreased risk of GI bleeding in the apixaban group and no significant differences between the groups in the rates of intracranial bleeding. Apixaban was also associated with a nonsignificant trend toward lower risk of mortality (HR, 0.85; 95% CI, 0.71-1.01; P = .06).
Notably, censoring rates because of expired prescriptions or a 1-month gap between prescriptions were high in both groups and the majority of censoring occurred within the first 12 months. Additionally, in dose specific analyses, patients receiving the 5-mg, twice-daily dose were found to have statistically significant decreases in risk of stroke/systemic embolism (P = .035) and mortality (P = .005) as compared with the 2.5-mg, twice-daily dose without significant differences in GI or intracranial bleeding.
There are three ongoing, open-label, randomized, controlled trials examining anticoagulation for nonvalvular AFib in patients with ESRD on hemodialysis with two comparing apixaban to warfarin (or derivative) and the other warfarin versus no anticoagulation.5 All trials are in adult patients with documented AFib and CHA2DS2-VASc score of at least 2. AKADIA (Germany based) plans to enroll 222 patients and compares a vitamin K antagonist (INR goal, 2-3) with 2.5-mg b.i.d. apixaban patients with ESRD on hemodialysis for at least 3 months with primary outcome of major and clinically relevant nonmajor bleeding and secondary outcome of thromboembolic events, as well as apixaban levels pre- and post hemodialysis.
RENAL-AF (U.S. based) plans to enrolled 762 patients and compares 5-mg b.i.d. apixaban (with 2.5 mg for selected patients) with warfarin in people of chronic hemodialysis with primary outcome of days to first major or clinically relevant nonmajor bleeding event and secondary outcome of stroke, systemic embolism, mortality, adherence and plasma apixaban levels. AVKDIAL (France based) plans to enroll 855 patients and compares no anticoagulation with vitamin K antagonists in patients on hemodialysis for at least 1 month, with primary outcome of cumulative incidence of severe bleeding and thrombosis.
Application of the data to our original case
Our patient is Medicare age with ESRD and newly diagnosed nonvalvular AFib. Recent data suggests apixaban could be used for stroke prevention instead of the prior standard of care, warfarin. This approach is supported in the 2019 guidelines.1
Patients with ESRD have an increased risk of bleeding and apixaban was shown to have less bleeding complications than warfarin in this analysis. However, only standard-dose apixaban was associated with a statistically significant lower risk of stroke/systemic embolism, major bleeding, and death. Reduced-dose apixaban had a lower risk of major bleeding but no difference for stroke/systemic embolism or death. Reduced-dose apixaban is used for patients who have two out of the following three criteria: aged at least 80 years, weight of at least 60 kg, and creatinine of at least 1.5 mg/dL. Therefore, many Medicare-age patients with ESRD would not be indicated for the dose of apixaban that was shown to improve the most important outcomes of stroke/SE and death.
It may still be beneficial to use apixaban in this patient since it appears to work as well as warfarin for stroke/systemic embolism prevention with less bleeding complications.
Bottom line
For patients who have decided to pursue an anticoagulation strategy for stroke prevention in AFib and have end-stage renal disease, either warfarin or apixaban are sensible options.
Dr. Farber is a medical instructor at Duke University Health System in Durham, N.C. Dr. Stafford is a medical instructor at Duke University. Dr. Sata is assistant professor of medicine at Duke University. Dr. Abdo and Dr. Menon are hospitalists at Duke University. Dr. Brooks is assistant professor of medicine at Duke University. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor of medicine at Duke University. Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and assistant professor of medicine at Duke University.
References
1. January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
2. Lippi G et al. Direct oral anticoagulants: Analysis of worldwide use and popularity using Google Trends. Ann Transl Med. 2017 Aug; 5(16):322. doi: 10.21037/atm.2017.06.65.
3. Turakhia MP et al. Chronic kidney disease and arrhythmias: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Eur Heart J. 2018 Jun 21;39(24):2314-25. doi: 10.1093/eurheartj/ehy060.
4. Siontis KC et al. Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States. Circulation. 2018 Oct 9;138(15):1519-29. doi: 10.1161/CIRCULATIONAHA.118.035418.
5. Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit-to-risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Key points
- According to 2019 American Heart Association guidelines, warfarin or apixaban are reasonable options for stroke prevention for patients who have end-stage renal disease and who plan for anticoagulation because of atrial fibrillation.
- Recent observational data suggests that apixaban may be safer than warfarin in this population.
- Several randomized, controlled trials are ongoing that may help determine the optimal agent to use in this setting.
- Until more definitive data is available, a reasonable approach is to discuss the risks and benefits of various treatment strategies with patients, and engage a multidisciplinary team (cardiologist, nephrologist, primary care provider, pharmacist) in the decision making process.
Additional reading
January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit to risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Garlo KG et al. Demystifying the benefits and harms of anticoagulation for atrial fibrillation in chronic kidney disease. Clin J Am Soc Nephrol 2019;14:125-36. doi: 10.2215/CJN.06430518.
Quiz
Two days ago you admitted a 72-year-old woman with end-stage renal disease on dialysis who had developed new-onset atrial fibrillation causing a mild acute diastolic congestive heart failure exacerbation. Transthoracic ECG showed a preserved left ventricular ejection fraction and no significant valvular disease. After two sessions of dialysis in the hospital and initiation of a beta-blocker for control of her heart rate, she is stable and ready for discharge. Her discharge weight is 75 kg.
Which of the following recommendations should you make to this patient regarding anticoagulation for prevention of stroke and systemic embolism from atrial fibrillation?
A. Take warfarin with a international normalized ratio goal of 2.5.
B. Take apixaban 2.5 mg twice a day.
C. Take apixaban 5 mg twice a day.
D. Discuss the risks/benefits of various treatment approaches with the patient, and involve the hospital pharmacist as well as the patient’s nephrologist, cardiologist, and/or primary care provider in the decision making process to reach a consensus and to ensure a safe follow-up plan.
The best answer is D. While A, B, and C are all reasonable approaches based on the available data and current guidelines, the best approach is to involve the patient and the multidisciplinary team in the decision making process. When more clinical trial data becomes available in the future, the optimal approach to managing patients such as this one may become clearer, but until then it makes sense to take into account individual patient characteristics and patient preferences.
Years ago, this doctor linked a mysterious lung disease to vaping
John E. Parker, MD, was working at a West Virginia hospital in 2015 when a 31-year-old female patient was admitted with acute respiratory problems. A team of doctors ultimately suspected that her mysterious case of lipoid pneumonia might be related to vaping and weren’t sure they had seen anything like it before. They were intrigued enough to submit the case for presentation at the CHEST Annual Meeting that year (Chest. 2015;148:382A. doi: 10.1378/chest.2274860).
Now, almost 4 years later, federal officials have begun investigating a national outbreak of severe lung illnesses linked to vaping that has struck more than 150 patients in 16 states. In an interview, Dr. Parker, a professor of pulmonary critical care and sleep medicine at West Virginia University, Morgantown, described what happened.
Q: Can you describe what the patient’s symptoms were when she arrived?
We would view them as classic for what is getting to be called vaping-associated lung disease. She was very, very short of breath and had a cough, and we were, of course, very worried that she might have pneumonia or some other acute respiratory illness. And then she was so sick she needed to be intubated.
Q: What happens next in cases like this?
We look for things like a [hemorrhage] or an active infection. And then for lipid-containing macrophages. And then we usually start some antibiotics [and a] low-dose steroid and then support the patient with a ventilator and oxygen and nutrition. And then just kind of wait and see if any other cultures come back to prove anything different than what you might be thinking.
Early on, we just felt like it was an unusual case and may not be a common viral or bacterial infection.
Q: How did you figure out the cause of her lipoid pneumonia was e-cigarettes?
It’s a diagnosis of exclusion. We excluded other [options], and it became the most likely cause.
We were convinced enough that the case was submitted for [presentation at the CHEST annual meeting] and was accepted.
Q: Once you figured out the cause could be e-cigarettes, did you contact the Centers for Disease Control and Prevention or the Food and Drug Administration or any other regulatory agency to tell them about this?
We did not. We felt at the time that putting it in the medical literature was appropriate. And if other case reports from other parts of the country came forward, then we’d have more of a clustering of findings that might then warrant research agencies [getting a] better understanding [about] the cause of the disease.
Q: Which federal agency would you report it to, if you did?
In 2015, the FDA, of course, was still regulating cigarettes, but I don’t think the government had yet decided who would regulate vaping products. So I’m sure it was unclear who we should call.
Q: So did you or your team think this was a one-off event when you witnessed it?
We really felt that it wasn’t going to be a one-off event and that it was what we usually called in public health a “sentinel” health event … that it was an example of a respiratory illness that can be caused by this exposure and that it probably wasn’t the first case ever seen nor would it be the last.
Q: Was it the first case that you had seen at your institution?
To our knowledge it was our first case, but we are humble enough clinicians to realize we may have missed some other cases that we interpreted [as] viral pneumonia or bacterial pneumonia.
Q: Have you seen more cases since then?
I know we’ve seen a case [of alveolar hemorrhage syndrome] that we published, and in polling some colleagues, we think we’ve probably also seen [cases of] cryptogenic organizing pneumonia as well as lipoid pneumonia and acute eosinophilic pneumonia. Yeah, we’ve certainly seen at least probably four forms of lung disease from vaping.
Q: If your team was seeing this back in 2015, is it possible that it’s been happening in the four years since then and people just don’t know about it?
I really have every reason to think we were not the first ones to see it, by any means.
And I don’t think we were even the first ones to report it. I think that there were some clusters in Wisconsin and some other places in the United States. I also know that the Japanese have been very interested. They’ve probably got four or five papers at least in the medical literature about vaping-related lung injury.
Q: Do you have a theory of what might be causing the lipoid pneumonia cases? Do you think there may be certain chemicals that are irritants?
We need a strong multidisciplinary team to understand the real etiology and cause of lung injury from inhalation. I think it could be any number of components in the mixtures. Lungs don’t like oil, in general, and probably the most specific agent that’s been studied recently is diacetyl, which was studied in popcorn-flavoring lung disease.
Q: Have these kinds of cases changed the way you approach patients?
Yeah, we search very carefully for a history of vaping. … I think it’s quite important to understand if they might be using inhaled agents or vaping that might present new toxicities to the lung.
Q: Will these illnesses have long-term health effects?
An inhalational injury may cause an acute lung injury that’s life-threatening and that someone may survive from and have no long-term sequelae [condition]. But there also is the possibility that long-term [e-cigarette] use may cause more insidious or chronic diseases from which there may not be a full recovery.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
John E. Parker, MD, was working at a West Virginia hospital in 2015 when a 31-year-old female patient was admitted with acute respiratory problems. A team of doctors ultimately suspected that her mysterious case of lipoid pneumonia might be related to vaping and weren’t sure they had seen anything like it before. They were intrigued enough to submit the case for presentation at the CHEST Annual Meeting that year (Chest. 2015;148:382A. doi: 10.1378/chest.2274860).
Now, almost 4 years later, federal officials have begun investigating a national outbreak of severe lung illnesses linked to vaping that has struck more than 150 patients in 16 states. In an interview, Dr. Parker, a professor of pulmonary critical care and sleep medicine at West Virginia University, Morgantown, described what happened.
Q: Can you describe what the patient’s symptoms were when she arrived?
We would view them as classic for what is getting to be called vaping-associated lung disease. She was very, very short of breath and had a cough, and we were, of course, very worried that she might have pneumonia or some other acute respiratory illness. And then she was so sick she needed to be intubated.
Q: What happens next in cases like this?
We look for things like a [hemorrhage] or an active infection. And then for lipid-containing macrophages. And then we usually start some antibiotics [and a] low-dose steroid and then support the patient with a ventilator and oxygen and nutrition. And then just kind of wait and see if any other cultures come back to prove anything different than what you might be thinking.
Early on, we just felt like it was an unusual case and may not be a common viral or bacterial infection.
Q: How did you figure out the cause of her lipoid pneumonia was e-cigarettes?
It’s a diagnosis of exclusion. We excluded other [options], and it became the most likely cause.
We were convinced enough that the case was submitted for [presentation at the CHEST annual meeting] and was accepted.
Q: Once you figured out the cause could be e-cigarettes, did you contact the Centers for Disease Control and Prevention or the Food and Drug Administration or any other regulatory agency to tell them about this?
We did not. We felt at the time that putting it in the medical literature was appropriate. And if other case reports from other parts of the country came forward, then we’d have more of a clustering of findings that might then warrant research agencies [getting a] better understanding [about] the cause of the disease.
Q: Which federal agency would you report it to, if you did?
In 2015, the FDA, of course, was still regulating cigarettes, but I don’t think the government had yet decided who would regulate vaping products. So I’m sure it was unclear who we should call.
Q: So did you or your team think this was a one-off event when you witnessed it?
We really felt that it wasn’t going to be a one-off event and that it was what we usually called in public health a “sentinel” health event … that it was an example of a respiratory illness that can be caused by this exposure and that it probably wasn’t the first case ever seen nor would it be the last.
Q: Was it the first case that you had seen at your institution?
To our knowledge it was our first case, but we are humble enough clinicians to realize we may have missed some other cases that we interpreted [as] viral pneumonia or bacterial pneumonia.
Q: Have you seen more cases since then?
I know we’ve seen a case [of alveolar hemorrhage syndrome] that we published, and in polling some colleagues, we think we’ve probably also seen [cases of] cryptogenic organizing pneumonia as well as lipoid pneumonia and acute eosinophilic pneumonia. Yeah, we’ve certainly seen at least probably four forms of lung disease from vaping.
Q: If your team was seeing this back in 2015, is it possible that it’s been happening in the four years since then and people just don’t know about it?
I really have every reason to think we were not the first ones to see it, by any means.
And I don’t think we were even the first ones to report it. I think that there were some clusters in Wisconsin and some other places in the United States. I also know that the Japanese have been very interested. They’ve probably got four or five papers at least in the medical literature about vaping-related lung injury.
Q: Do you have a theory of what might be causing the lipoid pneumonia cases? Do you think there may be certain chemicals that are irritants?
We need a strong multidisciplinary team to understand the real etiology and cause of lung injury from inhalation. I think it could be any number of components in the mixtures. Lungs don’t like oil, in general, and probably the most specific agent that’s been studied recently is diacetyl, which was studied in popcorn-flavoring lung disease.
Q: Have these kinds of cases changed the way you approach patients?
Yeah, we search very carefully for a history of vaping. … I think it’s quite important to understand if they might be using inhaled agents or vaping that might present new toxicities to the lung.
Q: Will these illnesses have long-term health effects?
An inhalational injury may cause an acute lung injury that’s life-threatening and that someone may survive from and have no long-term sequelae [condition]. But there also is the possibility that long-term [e-cigarette] use may cause more insidious or chronic diseases from which there may not be a full recovery.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
John E. Parker, MD, was working at a West Virginia hospital in 2015 when a 31-year-old female patient was admitted with acute respiratory problems. A team of doctors ultimately suspected that her mysterious case of lipoid pneumonia might be related to vaping and weren’t sure they had seen anything like it before. They were intrigued enough to submit the case for presentation at the CHEST Annual Meeting that year (Chest. 2015;148:382A. doi: 10.1378/chest.2274860).
Now, almost 4 years later, federal officials have begun investigating a national outbreak of severe lung illnesses linked to vaping that has struck more than 150 patients in 16 states. In an interview, Dr. Parker, a professor of pulmonary critical care and sleep medicine at West Virginia University, Morgantown, described what happened.
Q: Can you describe what the patient’s symptoms were when she arrived?
We would view them as classic for what is getting to be called vaping-associated lung disease. She was very, very short of breath and had a cough, and we were, of course, very worried that she might have pneumonia or some other acute respiratory illness. And then she was so sick she needed to be intubated.
Q: What happens next in cases like this?
We look for things like a [hemorrhage] or an active infection. And then for lipid-containing macrophages. And then we usually start some antibiotics [and a] low-dose steroid and then support the patient with a ventilator and oxygen and nutrition. And then just kind of wait and see if any other cultures come back to prove anything different than what you might be thinking.
Early on, we just felt like it was an unusual case and may not be a common viral or bacterial infection.
Q: How did you figure out the cause of her lipoid pneumonia was e-cigarettes?
It’s a diagnosis of exclusion. We excluded other [options], and it became the most likely cause.
We were convinced enough that the case was submitted for [presentation at the CHEST annual meeting] and was accepted.
Q: Once you figured out the cause could be e-cigarettes, did you contact the Centers for Disease Control and Prevention or the Food and Drug Administration or any other regulatory agency to tell them about this?
We did not. We felt at the time that putting it in the medical literature was appropriate. And if other case reports from other parts of the country came forward, then we’d have more of a clustering of findings that might then warrant research agencies [getting a] better understanding [about] the cause of the disease.
Q: Which federal agency would you report it to, if you did?
In 2015, the FDA, of course, was still regulating cigarettes, but I don’t think the government had yet decided who would regulate vaping products. So I’m sure it was unclear who we should call.
Q: So did you or your team think this was a one-off event when you witnessed it?
We really felt that it wasn’t going to be a one-off event and that it was what we usually called in public health a “sentinel” health event … that it was an example of a respiratory illness that can be caused by this exposure and that it probably wasn’t the first case ever seen nor would it be the last.
Q: Was it the first case that you had seen at your institution?
To our knowledge it was our first case, but we are humble enough clinicians to realize we may have missed some other cases that we interpreted [as] viral pneumonia or bacterial pneumonia.
Q: Have you seen more cases since then?
I know we’ve seen a case [of alveolar hemorrhage syndrome] that we published, and in polling some colleagues, we think we’ve probably also seen [cases of] cryptogenic organizing pneumonia as well as lipoid pneumonia and acute eosinophilic pneumonia. Yeah, we’ve certainly seen at least probably four forms of lung disease from vaping.
Q: If your team was seeing this back in 2015, is it possible that it’s been happening in the four years since then and people just don’t know about it?
I really have every reason to think we were not the first ones to see it, by any means.
And I don’t think we were even the first ones to report it. I think that there were some clusters in Wisconsin and some other places in the United States. I also know that the Japanese have been very interested. They’ve probably got four or five papers at least in the medical literature about vaping-related lung injury.
Q: Do you have a theory of what might be causing the lipoid pneumonia cases? Do you think there may be certain chemicals that are irritants?
We need a strong multidisciplinary team to understand the real etiology and cause of lung injury from inhalation. I think it could be any number of components in the mixtures. Lungs don’t like oil, in general, and probably the most specific agent that’s been studied recently is diacetyl, which was studied in popcorn-flavoring lung disease.
Q: Have these kinds of cases changed the way you approach patients?
Yeah, we search very carefully for a history of vaping. … I think it’s quite important to understand if they might be using inhaled agents or vaping that might present new toxicities to the lung.
Q: Will these illnesses have long-term health effects?
An inhalational injury may cause an acute lung injury that’s life-threatening and that someone may survive from and have no long-term sequelae [condition]. But there also is the possibility that long-term [e-cigarette] use may cause more insidious or chronic diseases from which there may not be a full recovery.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.
Severe lipodystrophy linked to pembrolizumab
according to a case study.
A 47-year-old woman received pembrolizumab to treat metastatic melanoma and developed immune-related generalized acquired lipodystrophy. The condition has persisted 12 months after she stopped taking pembrolizumab.
Julie Delyon, MD, PhD, of Saint-Louis Hospital in Paris, and colleagues described this case in the British Journal of Dermatology.
The patient was diagnosed with BRAF-mutated, stage IV melanoma with bone and lymph node metastases. She received pembrolizumab at 2 mg/kg every 3 weeks as first-line treatment. She achieved a complete response and was still in remission at last follow-up.
The patient was obese at baseline, with a body mass index of 40 kg/m2, but she did not have diabetes, hepatic steatosis, or dyslipidemia.
Within 2 months of starting pembrolizumab, the patient observed “some major changes to her physical appearance,” according to Dr. Delyon and colleagues. At 10 months, the patient had severe lipodystrophy.
The patient experienced a change in fat distribution – namely, severe peripheral lipoatrophy and an accumulation of trunk fat. Imaging revealed a decrease in subcutaneous adipose tissue, which contrasted with an increase in visceral fat observed from baseline.
The patient also developed “moderate hirsutism, facial and limb atrophy, and prominent forearm and leg muscles and veins,” according to the authors. She had impaired glucose tolerance with insulin resistance, reduced concentrations of leptin and adiponectin, hypertriglyceridemia, a low level of HDL cholesterol, and hepatic steatosis.
Analyses of subcutaneous fat revealed adipose tissue atrophy with edema, lipophages, and CD3+/CD4+ T-cell infiltration of the fat and vessel walls. This suggested that the lipodystrophy had an autoimmune origin, according to the authors.
The patient had no family history of autoimmune disease or lipodystrophy. She tested negative for mutations in 23 genes associated with generalized lipodystrophy.
The patient also tested negative for HIV, antinuclear antibodies, native anti-DNA, and anti-insulin receptor antibodies. There were no signs of panniculitis, and the authors noted that “there were no arguments in favor of hyperthyroidism, Cushing syndrome, or acromegaly.”
In an attempt to reverse the lipodystrophy, the researchers stopped pembrolizumab treatment. The patient was treated for diabetes and hypertriglyceridemia as well. She could not receive corticosteroids because of the risk of severe metabolic complications, and she didn’t receive metreleptin because it wasn’t available. The patient still had lipodystrophy 12 months after stopping pembrolizumab.
Dr. Delyon and colleagues wrote that this case suggests pembrolizumab, and perhaps other anti–programmed death 1 therapies, may cause lipodystrophy with severe metabolic complications. “The long-term side effects of such metabolic adverse events, although rare, are unknown and will probably become a topic of utmost importance, considering the increasing rate of remission following ICIs and their use in the adjuvant setting.”
Two coauthors reported relationships with Merck, which markets pembrolizumab as Keytruda. The authors also reported relationships with Bristol-Myers Squibb, Pierre Fabre, Takeda, Innate Pharma, LEO Pharma, Roche, GlaxoSmithKline, Novartis, and Amgen.
SOURCE: Delyon J et al. Br J Dermatol. 2019 May 11. doi: 10.1111/bjd.18124.
according to a case study.
A 47-year-old woman received pembrolizumab to treat metastatic melanoma and developed immune-related generalized acquired lipodystrophy. The condition has persisted 12 months after she stopped taking pembrolizumab.
Julie Delyon, MD, PhD, of Saint-Louis Hospital in Paris, and colleagues described this case in the British Journal of Dermatology.
The patient was diagnosed with BRAF-mutated, stage IV melanoma with bone and lymph node metastases. She received pembrolizumab at 2 mg/kg every 3 weeks as first-line treatment. She achieved a complete response and was still in remission at last follow-up.
The patient was obese at baseline, with a body mass index of 40 kg/m2, but she did not have diabetes, hepatic steatosis, or dyslipidemia.
Within 2 months of starting pembrolizumab, the patient observed “some major changes to her physical appearance,” according to Dr. Delyon and colleagues. At 10 months, the patient had severe lipodystrophy.
The patient experienced a change in fat distribution – namely, severe peripheral lipoatrophy and an accumulation of trunk fat. Imaging revealed a decrease in subcutaneous adipose tissue, which contrasted with an increase in visceral fat observed from baseline.
The patient also developed “moderate hirsutism, facial and limb atrophy, and prominent forearm and leg muscles and veins,” according to the authors. She had impaired glucose tolerance with insulin resistance, reduced concentrations of leptin and adiponectin, hypertriglyceridemia, a low level of HDL cholesterol, and hepatic steatosis.
Analyses of subcutaneous fat revealed adipose tissue atrophy with edema, lipophages, and CD3+/CD4+ T-cell infiltration of the fat and vessel walls. This suggested that the lipodystrophy had an autoimmune origin, according to the authors.
The patient had no family history of autoimmune disease or lipodystrophy. She tested negative for mutations in 23 genes associated with generalized lipodystrophy.
The patient also tested negative for HIV, antinuclear antibodies, native anti-DNA, and anti-insulin receptor antibodies. There were no signs of panniculitis, and the authors noted that “there were no arguments in favor of hyperthyroidism, Cushing syndrome, or acromegaly.”
In an attempt to reverse the lipodystrophy, the researchers stopped pembrolizumab treatment. The patient was treated for diabetes and hypertriglyceridemia as well. She could not receive corticosteroids because of the risk of severe metabolic complications, and she didn’t receive metreleptin because it wasn’t available. The patient still had lipodystrophy 12 months after stopping pembrolizumab.
Dr. Delyon and colleagues wrote that this case suggests pembrolizumab, and perhaps other anti–programmed death 1 therapies, may cause lipodystrophy with severe metabolic complications. “The long-term side effects of such metabolic adverse events, although rare, are unknown and will probably become a topic of utmost importance, considering the increasing rate of remission following ICIs and their use in the adjuvant setting.”
Two coauthors reported relationships with Merck, which markets pembrolizumab as Keytruda. The authors also reported relationships with Bristol-Myers Squibb, Pierre Fabre, Takeda, Innate Pharma, LEO Pharma, Roche, GlaxoSmithKline, Novartis, and Amgen.
SOURCE: Delyon J et al. Br J Dermatol. 2019 May 11. doi: 10.1111/bjd.18124.
according to a case study.
A 47-year-old woman received pembrolizumab to treat metastatic melanoma and developed immune-related generalized acquired lipodystrophy. The condition has persisted 12 months after she stopped taking pembrolizumab.
Julie Delyon, MD, PhD, of Saint-Louis Hospital in Paris, and colleagues described this case in the British Journal of Dermatology.
The patient was diagnosed with BRAF-mutated, stage IV melanoma with bone and lymph node metastases. She received pembrolizumab at 2 mg/kg every 3 weeks as first-line treatment. She achieved a complete response and was still in remission at last follow-up.
The patient was obese at baseline, with a body mass index of 40 kg/m2, but she did not have diabetes, hepatic steatosis, or dyslipidemia.
Within 2 months of starting pembrolizumab, the patient observed “some major changes to her physical appearance,” according to Dr. Delyon and colleagues. At 10 months, the patient had severe lipodystrophy.
The patient experienced a change in fat distribution – namely, severe peripheral lipoatrophy and an accumulation of trunk fat. Imaging revealed a decrease in subcutaneous adipose tissue, which contrasted with an increase in visceral fat observed from baseline.
The patient also developed “moderate hirsutism, facial and limb atrophy, and prominent forearm and leg muscles and veins,” according to the authors. She had impaired glucose tolerance with insulin resistance, reduced concentrations of leptin and adiponectin, hypertriglyceridemia, a low level of HDL cholesterol, and hepatic steatosis.
Analyses of subcutaneous fat revealed adipose tissue atrophy with edema, lipophages, and CD3+/CD4+ T-cell infiltration of the fat and vessel walls. This suggested that the lipodystrophy had an autoimmune origin, according to the authors.
The patient had no family history of autoimmune disease or lipodystrophy. She tested negative for mutations in 23 genes associated with generalized lipodystrophy.
The patient also tested negative for HIV, antinuclear antibodies, native anti-DNA, and anti-insulin receptor antibodies. There were no signs of panniculitis, and the authors noted that “there were no arguments in favor of hyperthyroidism, Cushing syndrome, or acromegaly.”
In an attempt to reverse the lipodystrophy, the researchers stopped pembrolizumab treatment. The patient was treated for diabetes and hypertriglyceridemia as well. She could not receive corticosteroids because of the risk of severe metabolic complications, and she didn’t receive metreleptin because it wasn’t available. The patient still had lipodystrophy 12 months after stopping pembrolizumab.
Dr. Delyon and colleagues wrote that this case suggests pembrolizumab, and perhaps other anti–programmed death 1 therapies, may cause lipodystrophy with severe metabolic complications. “The long-term side effects of such metabolic adverse events, although rare, are unknown and will probably become a topic of utmost importance, considering the increasing rate of remission following ICIs and their use in the adjuvant setting.”
Two coauthors reported relationships with Merck, which markets pembrolizumab as Keytruda. The authors also reported relationships with Bristol-Myers Squibb, Pierre Fabre, Takeda, Innate Pharma, LEO Pharma, Roche, GlaxoSmithKline, Novartis, and Amgen.
SOURCE: Delyon J et al. Br J Dermatol. 2019 May 11. doi: 10.1111/bjd.18124.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
September 2019 - Quick Quiz Question 2
Q2. Correct Answer: A
Rationale:
In a patient with chronic pancreatitis and a pancreatic mass, the most likely etiology is adenocarcinoma. This patient has radiologically resectable pancreas cancer. There is no evidence of lymphadenopathy or vascular invasion. Performing an ERCP with stent placement to relieve biliary obstruction has not been shown to be of benefit in patients with a resectable pancreatic mass. In fact, surgical outcomes are worse if a stent is placed in the bile duct. Surgical consultation should be obtained and the patient should undergo pancreaticoduodenectomy. EUS is sometimes done, but most cases of resectable disease should go straight to surgery.
Reference
Ghaneh P, et al. Biology and management of pancreatic cancer. Gut 2007;56(8)1134-52.
ginews@gastro.org
Q2. Correct Answer: A
Rationale:
In a patient with chronic pancreatitis and a pancreatic mass, the most likely etiology is adenocarcinoma. This patient has radiologically resectable pancreas cancer. There is no evidence of lymphadenopathy or vascular invasion. Performing an ERCP with stent placement to relieve biliary obstruction has not been shown to be of benefit in patients with a resectable pancreatic mass. In fact, surgical outcomes are worse if a stent is placed in the bile duct. Surgical consultation should be obtained and the patient should undergo pancreaticoduodenectomy. EUS is sometimes done, but most cases of resectable disease should go straight to surgery.
Reference
Ghaneh P, et al. Biology and management of pancreatic cancer. Gut 2007;56(8)1134-52.
ginews@gastro.org
Q2. Correct Answer: A
Rationale:
In a patient with chronic pancreatitis and a pancreatic mass, the most likely etiology is adenocarcinoma. This patient has radiologically resectable pancreas cancer. There is no evidence of lymphadenopathy or vascular invasion. Performing an ERCP with stent placement to relieve biliary obstruction has not been shown to be of benefit in patients with a resectable pancreatic mass. In fact, surgical outcomes are worse if a stent is placed in the bile duct. Surgical consultation should be obtained and the patient should undergo pancreaticoduodenectomy. EUS is sometimes done, but most cases of resectable disease should go straight to surgery.
Reference
Ghaneh P, et al. Biology and management of pancreatic cancer. Gut 2007;56(8)1134-52.
ginews@gastro.org
Q2. A 56-year-old male with known chronic pancreatitis presents with progressive abdominal pain, weight loss, and obstructive jaundice and a bilirubin of eight. A CT scan with contrast reveals a 4-cm mass in the pancreas head. There is no lymphadenopathy and vascular architecture is maintained.
September 2019 - Quick Quiz Question 1
Q1. Correct Answer: B
Rationale:
Risk factors for gallstone formation include increased age, female gender, pregnancy, dyslipidemia, diabetes, obesity and rapid weight loss - especially after gastric bypass surgery. Medications such as hormone replacement therapies/ oral contraceptive agents, fibrates, somatostatin analogues also increase gallstone risk. Currently, there is evidence suggesting potential benefit of prophylactic cholecystectomy during Roux-en-Y gastric bypass, given the potential risk of gallstone formation with rapid weight loss following surgery. However, there is also data from randomized controlled trials that the use of ursodeoxycholic acid following surgery may help reduce risk of gallstone formation for this group of patients.
Reference:
Stokes et al. Ursodeoxycholic acid and diets higher in fat prevent gallbladder Stones during weight loss: A meta-analysis of randomized controlled trials. 2014. Clin Gastroenterol Hepatol. 2014;12:1090-100.
Q1. Correct Answer: B
Rationale:
Risk factors for gallstone formation include increased age, female gender, pregnancy, dyslipidemia, diabetes, obesity and rapid weight loss - especially after gastric bypass surgery. Medications such as hormone replacement therapies/ oral contraceptive agents, fibrates, somatostatin analogues also increase gallstone risk. Currently, there is evidence suggesting potential benefit of prophylactic cholecystectomy during Roux-en-Y gastric bypass, given the potential risk of gallstone formation with rapid weight loss following surgery. However, there is also data from randomized controlled trials that the use of ursodeoxycholic acid following surgery may help reduce risk of gallstone formation for this group of patients.
Reference:
Stokes et al. Ursodeoxycholic acid and diets higher in fat prevent gallbladder Stones during weight loss: A meta-analysis of randomized controlled trials. 2014. Clin Gastroenterol Hepatol. 2014;12:1090-100.
Q1. Correct Answer: B
Rationale:
Risk factors for gallstone formation include increased age, female gender, pregnancy, dyslipidemia, diabetes, obesity and rapid weight loss - especially after gastric bypass surgery. Medications such as hormone replacement therapies/ oral contraceptive agents, fibrates, somatostatin analogues also increase gallstone risk. Currently, there is evidence suggesting potential benefit of prophylactic cholecystectomy during Roux-en-Y gastric bypass, given the potential risk of gallstone formation with rapid weight loss following surgery. However, there is also data from randomized controlled trials that the use of ursodeoxycholic acid following surgery may help reduce risk of gallstone formation for this group of patients.
Reference:
Stokes et al. Ursodeoxycholic acid and diets higher in fat prevent gallbladder Stones during weight loss: A meta-analysis of randomized controlled trials. 2014. Clin Gastroenterol Hepatol. 2014;12:1090-100.
Q1. A 43-year-old woman presents to the office after Roux-en-Y surgery for weight loss. She has a strong family history of gallstones, and asks about measures to prevent gallstone formation after her surgery.
Local treatment boosts survival for some with oligometastatic lung cancer
Adding local treatment to systemic therapy may extend survival among certain patients with oligometastatic non–small cell lung cancer (NSCLC), according to a retrospective look at more than 34,000 patients.
Surgical resection provided the greatest survival benefit, followed by external beam radiotherapy or thermal ablation (EBRT/TA), reported lead author Johannes Uhlig, MD, of University Medical Center Göttingen (Germany) and colleagues.
NSCLC patients with five or fewer metastatic sites (oligometastatic disease) are thought to achieve better outcomes than patients with more widely disseminated disease, the investigators noted in JAMA Network Open, but the benefit of local therapy for this population is unclear.
“A recent randomized, prospective study of 74 patients with oligometastatic NSCLC identified superior progression-free survival with local control after hypofractionated radiotherapy or surgical resection and radiotherapy compared with systemic therapy alone, suggesting an important application of local treatment options for patients with metastatic disease,” the investigators wrote.
To build on these findings, the investigators retrospectively evaluated 34,887 patients with stage IV NSCLC who had up to one distant metastatic lesion in the liver, lung, brain, or bone, as documented in the National Cancer Database. Treatment groups were divided into patients who received systemic therapy alone, surgical resection plus systemic therapy, or EBRT/TA plus systemic therapy. Multivariable Cox proportional hazards models were used to compare overall survival among the three groups.
Including a median follow-up of 39.4 months, data analysis showed that patients who underwent surgery and systemic therapy fared the best. Adding surgery reduced mortality risk by 38% and 41%, compared with EBRT/TA plus systemic therapy and systemic therapy alone, respectively (P less than .001 for both). Compared with systemic therapy alone, adding EBRT/TA reduced mortality risk by 5% (P = .002).
The impact of EBRT/TA varied among subgroups. For those with squamous cell carcinoma who had limited nodal disease, adding EBRT/TA resulted in a clear benefit, reducing mortality risk by 32% (P less than .001). Compared with systemic therapy alone, this benefit translated to higher survival rates for up to 3 years. Conversely, adding EBRT/TA increased risk of death by 39% among patients with extended local and distant adenocarcinoma (P less than .001). In this subgroup, survival rates over the next 3 years were higher among patients treated with systemic therapy alone.
“The present study supports a combined approach of local therapy in addition to systemic treatment for select patients with oligometastatic NSCLC,” the investigators concluded.
The study was funded by the U.S. Department of Defense. The investigators disclosed additional relationships with Bayer, AstraZeneca, Bristol-Myers Squibb, and others.
SOURCE: Uhlig et al. JAMA Netw Open. 2019 Aug 21. doi: 10.1001/jamanetworkopen.2019.9702.
Adding local treatment to systemic therapy may extend survival among certain patients with oligometastatic non–small cell lung cancer (NSCLC), according to a retrospective look at more than 34,000 patients.
Surgical resection provided the greatest survival benefit, followed by external beam radiotherapy or thermal ablation (EBRT/TA), reported lead author Johannes Uhlig, MD, of University Medical Center Göttingen (Germany) and colleagues.
NSCLC patients with five or fewer metastatic sites (oligometastatic disease) are thought to achieve better outcomes than patients with more widely disseminated disease, the investigators noted in JAMA Network Open, but the benefit of local therapy for this population is unclear.
“A recent randomized, prospective study of 74 patients with oligometastatic NSCLC identified superior progression-free survival with local control after hypofractionated radiotherapy or surgical resection and radiotherapy compared with systemic therapy alone, suggesting an important application of local treatment options for patients with metastatic disease,” the investigators wrote.
To build on these findings, the investigators retrospectively evaluated 34,887 patients with stage IV NSCLC who had up to one distant metastatic lesion in the liver, lung, brain, or bone, as documented in the National Cancer Database. Treatment groups were divided into patients who received systemic therapy alone, surgical resection plus systemic therapy, or EBRT/TA plus systemic therapy. Multivariable Cox proportional hazards models were used to compare overall survival among the three groups.
Including a median follow-up of 39.4 months, data analysis showed that patients who underwent surgery and systemic therapy fared the best. Adding surgery reduced mortality risk by 38% and 41%, compared with EBRT/TA plus systemic therapy and systemic therapy alone, respectively (P less than .001 for both). Compared with systemic therapy alone, adding EBRT/TA reduced mortality risk by 5% (P = .002).
The impact of EBRT/TA varied among subgroups. For those with squamous cell carcinoma who had limited nodal disease, adding EBRT/TA resulted in a clear benefit, reducing mortality risk by 32% (P less than .001). Compared with systemic therapy alone, this benefit translated to higher survival rates for up to 3 years. Conversely, adding EBRT/TA increased risk of death by 39% among patients with extended local and distant adenocarcinoma (P less than .001). In this subgroup, survival rates over the next 3 years were higher among patients treated with systemic therapy alone.
“The present study supports a combined approach of local therapy in addition to systemic treatment for select patients with oligometastatic NSCLC,” the investigators concluded.
The study was funded by the U.S. Department of Defense. The investigators disclosed additional relationships with Bayer, AstraZeneca, Bristol-Myers Squibb, and others.
SOURCE: Uhlig et al. JAMA Netw Open. 2019 Aug 21. doi: 10.1001/jamanetworkopen.2019.9702.
Adding local treatment to systemic therapy may extend survival among certain patients with oligometastatic non–small cell lung cancer (NSCLC), according to a retrospective look at more than 34,000 patients.
Surgical resection provided the greatest survival benefit, followed by external beam radiotherapy or thermal ablation (EBRT/TA), reported lead author Johannes Uhlig, MD, of University Medical Center Göttingen (Germany) and colleagues.
NSCLC patients with five or fewer metastatic sites (oligometastatic disease) are thought to achieve better outcomes than patients with more widely disseminated disease, the investigators noted in JAMA Network Open, but the benefit of local therapy for this population is unclear.
“A recent randomized, prospective study of 74 patients with oligometastatic NSCLC identified superior progression-free survival with local control after hypofractionated radiotherapy or surgical resection and radiotherapy compared with systemic therapy alone, suggesting an important application of local treatment options for patients with metastatic disease,” the investigators wrote.
To build on these findings, the investigators retrospectively evaluated 34,887 patients with stage IV NSCLC who had up to one distant metastatic lesion in the liver, lung, brain, or bone, as documented in the National Cancer Database. Treatment groups were divided into patients who received systemic therapy alone, surgical resection plus systemic therapy, or EBRT/TA plus systemic therapy. Multivariable Cox proportional hazards models were used to compare overall survival among the three groups.
Including a median follow-up of 39.4 months, data analysis showed that patients who underwent surgery and systemic therapy fared the best. Adding surgery reduced mortality risk by 38% and 41%, compared with EBRT/TA plus systemic therapy and systemic therapy alone, respectively (P less than .001 for both). Compared with systemic therapy alone, adding EBRT/TA reduced mortality risk by 5% (P = .002).
The impact of EBRT/TA varied among subgroups. For those with squamous cell carcinoma who had limited nodal disease, adding EBRT/TA resulted in a clear benefit, reducing mortality risk by 32% (P less than .001). Compared with systemic therapy alone, this benefit translated to higher survival rates for up to 3 years. Conversely, adding EBRT/TA increased risk of death by 39% among patients with extended local and distant adenocarcinoma (P less than .001). In this subgroup, survival rates over the next 3 years were higher among patients treated with systemic therapy alone.
“The present study supports a combined approach of local therapy in addition to systemic treatment for select patients with oligometastatic NSCLC,” the investigators concluded.
The study was funded by the U.S. Department of Defense. The investigators disclosed additional relationships with Bayer, AstraZeneca, Bristol-Myers Squibb, and others.
SOURCE: Uhlig et al. JAMA Netw Open. 2019 Aug 21. doi: 10.1001/jamanetworkopen.2019.9702.
FROM JAMA NETWORK OPEN
Key clinical point: Adding local treatment to systemic therapy may extend survival among certain patients with oligometastatic non–small cell lung cancer (NSCLC).
Major finding: Patients treated with a combination of surgical resection and systemic therapy had better overall survival than patients treated with systemic therapy alone (hazard ratio, 0.59).
Study details: A retrospective analysis of 34,887 patients with stage IV NSCLC.
Disclosures: The study was funded by the U.S. Department of Defense. The investigators disclosed additional relationships with Bayer, AstraZeneca, Bristol-Myers Squibb, and others.
Source: Uhlig J et al. JAMA Netw Open. 2019 Aug 21. doi: 10.1001/jamanetworkopen.2019.9702.