User login
Health insurance rates among cancer survivors increased after ACA
The introduction of the Affordable Care Act was associated with an increase in health insurance among cancer survivors, but cost still remains a barrier to insurance, particularly among certain groups, research suggests.
Researchers conducted an analysis of National Health Interview Survey data from 17,806 survey participants who reported a cancer diagnosis. The findings are in JAMA Oncology.
Around one in ten of those surveyed did not have health insurance, but this rate was significantly higher before the introduction of the Affordable Care Act compared to the 3-year period after its implementation in 2014 (10.6% vs. 6.2%, P less than .001).
While cost was the most common reason for not having health insurance, the survey showed that the proportion of noninsured cancer survivors who cited cost as the reason for noninsurance decreased significantly after implementation of the Affordable Care Act (49.6% vs. 37.6%, P = .003).
Unemployment was the second-most common reason for noninsurance, but this also decreased in the 2014-2017 period compared with 2000-2013 (37.1% vs. 28.5%, P = .005).
Younger cancer survivors – aged below the mean age of 50.9 years – were 84% more likely to be uninsured, compared with those above the mean age of the study population, and those with a family income below the poverty threshold were nearly twice as likely not to be insured.
Participants of Hispanic ethnicity, noncitizens, and current smokers were significantly more likely to be uninsured.
Before the implementation of the Affordable Care Act, black patients were 29% more likely to be uninsured compared with nonblack patients. But after the ACA was introduced, this difference disappeared.
Nina N. Sanford, MD, of the University of Texas, Dallas, and coauthors wrote that, to their knowledge, this was the first study to look at reasons for noninsurance among cancer survivors, and highlighted that efforts to improve insurance coverage would require “diverse policy initiatives.
“Despite these improvements [after the Affordable Care Act], our study identified several demographic subgroups who appear to continue to be at risk for not having insurance even after the ACA, which may contribute to worse cancer-specific outcomes, decreased quality of life, and greater mortality,” they wrote. “Policymakers should be aware of these disparities when proposing legislation to either augment or limit health care coverage.”
They expressed concern about the association between smoking and a lack of health insurance, noting that the Affordable Care Act allows insurers to impose a surcharge premium on smokers. However they pointed out that this initiative has not decreased rates of smoking, and may instead have led to higher rates of noninsurance among cancer survivors who continue to smoke.
One author was supported by the American Society of Radiation Oncology and the Prostate Cancer Foundation, and one author declared funding from the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Sanford N et al. JAMA Oncology 2019, May 15. doi: 10.1001/jamaoncol.2019.1973.
The introduction of the Affordable Care Act was associated with an increase in health insurance among cancer survivors, but cost still remains a barrier to insurance, particularly among certain groups, research suggests.
Researchers conducted an analysis of National Health Interview Survey data from 17,806 survey participants who reported a cancer diagnosis. The findings are in JAMA Oncology.
Around one in ten of those surveyed did not have health insurance, but this rate was significantly higher before the introduction of the Affordable Care Act compared to the 3-year period after its implementation in 2014 (10.6% vs. 6.2%, P less than .001).
While cost was the most common reason for not having health insurance, the survey showed that the proportion of noninsured cancer survivors who cited cost as the reason for noninsurance decreased significantly after implementation of the Affordable Care Act (49.6% vs. 37.6%, P = .003).
Unemployment was the second-most common reason for noninsurance, but this also decreased in the 2014-2017 period compared with 2000-2013 (37.1% vs. 28.5%, P = .005).
Younger cancer survivors – aged below the mean age of 50.9 years – were 84% more likely to be uninsured, compared with those above the mean age of the study population, and those with a family income below the poverty threshold were nearly twice as likely not to be insured.
Participants of Hispanic ethnicity, noncitizens, and current smokers were significantly more likely to be uninsured.
Before the implementation of the Affordable Care Act, black patients were 29% more likely to be uninsured compared with nonblack patients. But after the ACA was introduced, this difference disappeared.
Nina N. Sanford, MD, of the University of Texas, Dallas, and coauthors wrote that, to their knowledge, this was the first study to look at reasons for noninsurance among cancer survivors, and highlighted that efforts to improve insurance coverage would require “diverse policy initiatives.
“Despite these improvements [after the Affordable Care Act], our study identified several demographic subgroups who appear to continue to be at risk for not having insurance even after the ACA, which may contribute to worse cancer-specific outcomes, decreased quality of life, and greater mortality,” they wrote. “Policymakers should be aware of these disparities when proposing legislation to either augment or limit health care coverage.”
They expressed concern about the association between smoking and a lack of health insurance, noting that the Affordable Care Act allows insurers to impose a surcharge premium on smokers. However they pointed out that this initiative has not decreased rates of smoking, and may instead have led to higher rates of noninsurance among cancer survivors who continue to smoke.
One author was supported by the American Society of Radiation Oncology and the Prostate Cancer Foundation, and one author declared funding from the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Sanford N et al. JAMA Oncology 2019, May 15. doi: 10.1001/jamaoncol.2019.1973.
The introduction of the Affordable Care Act was associated with an increase in health insurance among cancer survivors, but cost still remains a barrier to insurance, particularly among certain groups, research suggests.
Researchers conducted an analysis of National Health Interview Survey data from 17,806 survey participants who reported a cancer diagnosis. The findings are in JAMA Oncology.
Around one in ten of those surveyed did not have health insurance, but this rate was significantly higher before the introduction of the Affordable Care Act compared to the 3-year period after its implementation in 2014 (10.6% vs. 6.2%, P less than .001).
While cost was the most common reason for not having health insurance, the survey showed that the proportion of noninsured cancer survivors who cited cost as the reason for noninsurance decreased significantly after implementation of the Affordable Care Act (49.6% vs. 37.6%, P = .003).
Unemployment was the second-most common reason for noninsurance, but this also decreased in the 2014-2017 period compared with 2000-2013 (37.1% vs. 28.5%, P = .005).
Younger cancer survivors – aged below the mean age of 50.9 years – were 84% more likely to be uninsured, compared with those above the mean age of the study population, and those with a family income below the poverty threshold were nearly twice as likely not to be insured.
Participants of Hispanic ethnicity, noncitizens, and current smokers were significantly more likely to be uninsured.
Before the implementation of the Affordable Care Act, black patients were 29% more likely to be uninsured compared with nonblack patients. But after the ACA was introduced, this difference disappeared.
Nina N. Sanford, MD, of the University of Texas, Dallas, and coauthors wrote that, to their knowledge, this was the first study to look at reasons for noninsurance among cancer survivors, and highlighted that efforts to improve insurance coverage would require “diverse policy initiatives.
“Despite these improvements [after the Affordable Care Act], our study identified several demographic subgroups who appear to continue to be at risk for not having insurance even after the ACA, which may contribute to worse cancer-specific outcomes, decreased quality of life, and greater mortality,” they wrote. “Policymakers should be aware of these disparities when proposing legislation to either augment or limit health care coverage.”
They expressed concern about the association between smoking and a lack of health insurance, noting that the Affordable Care Act allows insurers to impose a surcharge premium on smokers. However they pointed out that this initiative has not decreased rates of smoking, and may instead have led to higher rates of noninsurance among cancer survivors who continue to smoke.
One author was supported by the American Society of Radiation Oncology and the Prostate Cancer Foundation, and one author declared funding from the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Sanford N et al. JAMA Oncology 2019, May 15. doi: 10.1001/jamaoncol.2019.1973.
FROM JAMA ONCOLOGY
Anomalous RT dose linked to lower survival in uterine cancer
As many as one in eight patients with uterine cancer who undergo adjuvant radiation therapy may have been treated with doses that are inconsistent with standard practice, a new study suggests.
Writing in JCO Clinical Cancer Informatics, Corbin D. Jacobs, MD, of Duke University, Durham, N.C., and coauthors analyzed National Cancer Database data from 14,298 women with stage IIIC1-C2 uterine cancer who underwent adjuvant radiation therapy after hysterectomy. The analysis included information on radiation therapy site, modality, dose, fractions, timing, duration, and stage, as well as details about the facilities at which the treatment was given.
Overall, 16% of the women had at least one ‘anomalous’ entry in their records of radiation therapy. The most common anomalies were that the combined total radiation therapy dose was insufficient, or there was an insufficient number of external beam radiation therapy fractions, both of which may have represented an incomplete course of radiation therapy.
Other anomalies were excessive brachytherapy fractions, inconsistency in the staging, and less than 100 days of radiation therapy.
The study showed that the 5-year overall survival rate in individuals who had at least one anomalous data entry was 51.3% compared with 58% among individuals without any anomalous entries (P less than .001). The difference in survival rates was entirely accounted for by insufficient, excessive, or unknown radiation therapy dose.
More than half of patients in the study had missing or unknown data for at least one entry, and this was associated with lower 5-year survival compared with patients with complete data entries.
The researchers also looked at facility-specific factors, such as the type of facility, its location, and its distance from the patient’s home, and how these impacted the frequency of anomalous data. They found that comprehensive community cancer programs had the lowest incidence of anomalous data (14.7%) compared with non–comprehensive community cancer programs, which had an incidence of 17.1%.
The incidence of anomalous data was highest in facilities in the south Atlantic, east south central and west south central regions of the United States. The further away from a patient’s home the reporting facility was, the higher the presence of anomalous data.
“Because an insufficient RT dose or fewer than 20 fractions accounted for such a large proportion of the anomalies, patients may potentially be more likely to have an incomplete RT course or complete RT in a hypofractionated manner when the facility is farther from their home,” the authors wrote.
One author was an employee of Bioventus, and three declared research funding from the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Jacobs C et al. JCO Clin Cancer Inform. 2019, May 3. doi: 10.1200/CCI.18.00118.
As many as one in eight patients with uterine cancer who undergo adjuvant radiation therapy may have been treated with doses that are inconsistent with standard practice, a new study suggests.
Writing in JCO Clinical Cancer Informatics, Corbin D. Jacobs, MD, of Duke University, Durham, N.C., and coauthors analyzed National Cancer Database data from 14,298 women with stage IIIC1-C2 uterine cancer who underwent adjuvant radiation therapy after hysterectomy. The analysis included information on radiation therapy site, modality, dose, fractions, timing, duration, and stage, as well as details about the facilities at which the treatment was given.
Overall, 16% of the women had at least one ‘anomalous’ entry in their records of radiation therapy. The most common anomalies were that the combined total radiation therapy dose was insufficient, or there was an insufficient number of external beam radiation therapy fractions, both of which may have represented an incomplete course of radiation therapy.
Other anomalies were excessive brachytherapy fractions, inconsistency in the staging, and less than 100 days of radiation therapy.
The study showed that the 5-year overall survival rate in individuals who had at least one anomalous data entry was 51.3% compared with 58% among individuals without any anomalous entries (P less than .001). The difference in survival rates was entirely accounted for by insufficient, excessive, or unknown radiation therapy dose.
More than half of patients in the study had missing or unknown data for at least one entry, and this was associated with lower 5-year survival compared with patients with complete data entries.
The researchers also looked at facility-specific factors, such as the type of facility, its location, and its distance from the patient’s home, and how these impacted the frequency of anomalous data. They found that comprehensive community cancer programs had the lowest incidence of anomalous data (14.7%) compared with non–comprehensive community cancer programs, which had an incidence of 17.1%.
The incidence of anomalous data was highest in facilities in the south Atlantic, east south central and west south central regions of the United States. The further away from a patient’s home the reporting facility was, the higher the presence of anomalous data.
“Because an insufficient RT dose or fewer than 20 fractions accounted for such a large proportion of the anomalies, patients may potentially be more likely to have an incomplete RT course or complete RT in a hypofractionated manner when the facility is farther from their home,” the authors wrote.
One author was an employee of Bioventus, and three declared research funding from the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Jacobs C et al. JCO Clin Cancer Inform. 2019, May 3. doi: 10.1200/CCI.18.00118.
As many as one in eight patients with uterine cancer who undergo adjuvant radiation therapy may have been treated with doses that are inconsistent with standard practice, a new study suggests.
Writing in JCO Clinical Cancer Informatics, Corbin D. Jacobs, MD, of Duke University, Durham, N.C., and coauthors analyzed National Cancer Database data from 14,298 women with stage IIIC1-C2 uterine cancer who underwent adjuvant radiation therapy after hysterectomy. The analysis included information on radiation therapy site, modality, dose, fractions, timing, duration, and stage, as well as details about the facilities at which the treatment was given.
Overall, 16% of the women had at least one ‘anomalous’ entry in their records of radiation therapy. The most common anomalies were that the combined total radiation therapy dose was insufficient, or there was an insufficient number of external beam radiation therapy fractions, both of which may have represented an incomplete course of radiation therapy.
Other anomalies were excessive brachytherapy fractions, inconsistency in the staging, and less than 100 days of radiation therapy.
The study showed that the 5-year overall survival rate in individuals who had at least one anomalous data entry was 51.3% compared with 58% among individuals without any anomalous entries (P less than .001). The difference in survival rates was entirely accounted for by insufficient, excessive, or unknown radiation therapy dose.
More than half of patients in the study had missing or unknown data for at least one entry, and this was associated with lower 5-year survival compared with patients with complete data entries.
The researchers also looked at facility-specific factors, such as the type of facility, its location, and its distance from the patient’s home, and how these impacted the frequency of anomalous data. They found that comprehensive community cancer programs had the lowest incidence of anomalous data (14.7%) compared with non–comprehensive community cancer programs, which had an incidence of 17.1%.
The incidence of anomalous data was highest in facilities in the south Atlantic, east south central and west south central regions of the United States. The further away from a patient’s home the reporting facility was, the higher the presence of anomalous data.
“Because an insufficient RT dose or fewer than 20 fractions accounted for such a large proportion of the anomalies, patients may potentially be more likely to have an incomplete RT course or complete RT in a hypofractionated manner when the facility is farther from their home,” the authors wrote.
One author was an employee of Bioventus, and three declared research funding from the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Jacobs C et al. JCO Clin Cancer Inform. 2019, May 3. doi: 10.1200/CCI.18.00118.
FROM JCO CLINICAL CANCER INFORMATICS
Low-dose chemo feasible for older, frail patients with advanced gastroesophageal cancer
A low-dose chemotherapy regimen appears safe and effective for older and frail patients with advanced gastroesophageal cancer.
In a phase 3 trial, progression-free survival in patients who received the lowest dose of oxaliplatin and capecitabine was noninferior to progression-free survival in patients who received two higher doses of the combination.
The lowest dose also was associated with better overall treatment utility, which is a composite of clinical benefit, tolerability, quality of life, and patient value.
“[T]his is the largest randomized, controlled trial to date specifically investigating frail or elderly patients with advanced gastroesophageal cancer,” said study investigator Peter S. Hall, PhD, of the University of Edinburgh. “We found that the lowest dose tested was noninferior in terms of progression-free survival, it produced less toxicity, and it had better overall treatment utility.”
These findings are scheduled to be presented at the annual meeting of the American Society of Clinical Oncology. Dr. Hall discussed the findings during a press briefing in advance of the meeting.
The phase 3 trial (ISRCTN44687907) enrolled older and frail patients, aged 51-96 years, with advanced gastroesophageal cancer. Dr. Hall presented data on 514 patients randomized to receive oxaliplatin and capecitabine at one of three dose levels. Dose level A consisted of oxaliplatin given at 130 mg/m2 once every 21 days and capecitabine given at 625 mg/m2 twice a day every day. Dose level B was 80% of the level A dosage, and dose level C was 60% of the level A dosage. Patients with decreased kidney function received 75% of the allocated capecitabine dose.
The trial’s primary endpoint was noninferiority of progression-free survival at 12 months. Noninferiority was confirmed for level B, compared with level A, with a hazard ratio of 1.09, and for level C, compared with level A, with a hazard ratio of 1.10.
“The lowest dose, the level C dose, had the best overall treatment utility … compared to patients either on level A or level B, and this was due to lower side effects and better quality of life,” Dr. Hall said.
Overall treatment utility outcomes were “good” in 35% of the dose A group, 36% of the dose B group, and 43% of the dose C group. Outcomes were “poor” in 31%, 38%, and 29%, respectively, and outcomes were “intermediate” in 34%, 26%, and 27%, respectively.
To achieve “good” overall treatment utility, patients had to achieve the following six domains: cancer doesn’t progress on scans, oncologist assesses a benefit of treatment, lack of severe toxicity, patient’s global quality of life scores aren’t deteriorating, patient scores the treatment as worthwhile, and the patient says the treatment doesn’t interfere with daily activities.
These results suggest low-dose chemotherapy is feasible for older and frail patients with advanced gastroesophageal cancer, according to Dr. Hall.
“[L]ow-dose treatment may be offered to patients who are suitable for chemotherapy but considered too frail or elderly for a full-dose standard regime, in the confidence that it can produce superior outcomes without compromising cancer control or survival,” Dr. Hall said.
Dr. Hall reported relationships with Eisai, Pfizer, Roche, AstraZeneca, Daiichi Sankyo, and Novartis. The trial was funded by Cancer Research UK and sponsored by the University of Leeds (England).
SOURCE: Hall PS et al. ASCO 2019, Abstract 4006.
A low-dose chemotherapy regimen appears safe and effective for older and frail patients with advanced gastroesophageal cancer.
In a phase 3 trial, progression-free survival in patients who received the lowest dose of oxaliplatin and capecitabine was noninferior to progression-free survival in patients who received two higher doses of the combination.
The lowest dose also was associated with better overall treatment utility, which is a composite of clinical benefit, tolerability, quality of life, and patient value.
“[T]his is the largest randomized, controlled trial to date specifically investigating frail or elderly patients with advanced gastroesophageal cancer,” said study investigator Peter S. Hall, PhD, of the University of Edinburgh. “We found that the lowest dose tested was noninferior in terms of progression-free survival, it produced less toxicity, and it had better overall treatment utility.”
These findings are scheduled to be presented at the annual meeting of the American Society of Clinical Oncology. Dr. Hall discussed the findings during a press briefing in advance of the meeting.
The phase 3 trial (ISRCTN44687907) enrolled older and frail patients, aged 51-96 years, with advanced gastroesophageal cancer. Dr. Hall presented data on 514 patients randomized to receive oxaliplatin and capecitabine at one of three dose levels. Dose level A consisted of oxaliplatin given at 130 mg/m2 once every 21 days and capecitabine given at 625 mg/m2 twice a day every day. Dose level B was 80% of the level A dosage, and dose level C was 60% of the level A dosage. Patients with decreased kidney function received 75% of the allocated capecitabine dose.
The trial’s primary endpoint was noninferiority of progression-free survival at 12 months. Noninferiority was confirmed for level B, compared with level A, with a hazard ratio of 1.09, and for level C, compared with level A, with a hazard ratio of 1.10.
“The lowest dose, the level C dose, had the best overall treatment utility … compared to patients either on level A or level B, and this was due to lower side effects and better quality of life,” Dr. Hall said.
Overall treatment utility outcomes were “good” in 35% of the dose A group, 36% of the dose B group, and 43% of the dose C group. Outcomes were “poor” in 31%, 38%, and 29%, respectively, and outcomes were “intermediate” in 34%, 26%, and 27%, respectively.
To achieve “good” overall treatment utility, patients had to achieve the following six domains: cancer doesn’t progress on scans, oncologist assesses a benefit of treatment, lack of severe toxicity, patient’s global quality of life scores aren’t deteriorating, patient scores the treatment as worthwhile, and the patient says the treatment doesn’t interfere with daily activities.
These results suggest low-dose chemotherapy is feasible for older and frail patients with advanced gastroesophageal cancer, according to Dr. Hall.
“[L]ow-dose treatment may be offered to patients who are suitable for chemotherapy but considered too frail or elderly for a full-dose standard regime, in the confidence that it can produce superior outcomes without compromising cancer control or survival,” Dr. Hall said.
Dr. Hall reported relationships with Eisai, Pfizer, Roche, AstraZeneca, Daiichi Sankyo, and Novartis. The trial was funded by Cancer Research UK and sponsored by the University of Leeds (England).
SOURCE: Hall PS et al. ASCO 2019, Abstract 4006.
A low-dose chemotherapy regimen appears safe and effective for older and frail patients with advanced gastroesophageal cancer.
In a phase 3 trial, progression-free survival in patients who received the lowest dose of oxaliplatin and capecitabine was noninferior to progression-free survival in patients who received two higher doses of the combination.
The lowest dose also was associated with better overall treatment utility, which is a composite of clinical benefit, tolerability, quality of life, and patient value.
“[T]his is the largest randomized, controlled trial to date specifically investigating frail or elderly patients with advanced gastroesophageal cancer,” said study investigator Peter S. Hall, PhD, of the University of Edinburgh. “We found that the lowest dose tested was noninferior in terms of progression-free survival, it produced less toxicity, and it had better overall treatment utility.”
These findings are scheduled to be presented at the annual meeting of the American Society of Clinical Oncology. Dr. Hall discussed the findings during a press briefing in advance of the meeting.
The phase 3 trial (ISRCTN44687907) enrolled older and frail patients, aged 51-96 years, with advanced gastroesophageal cancer. Dr. Hall presented data on 514 patients randomized to receive oxaliplatin and capecitabine at one of three dose levels. Dose level A consisted of oxaliplatin given at 130 mg/m2 once every 21 days and capecitabine given at 625 mg/m2 twice a day every day. Dose level B was 80% of the level A dosage, and dose level C was 60% of the level A dosage. Patients with decreased kidney function received 75% of the allocated capecitabine dose.
The trial’s primary endpoint was noninferiority of progression-free survival at 12 months. Noninferiority was confirmed for level B, compared with level A, with a hazard ratio of 1.09, and for level C, compared with level A, with a hazard ratio of 1.10.
“The lowest dose, the level C dose, had the best overall treatment utility … compared to patients either on level A or level B, and this was due to lower side effects and better quality of life,” Dr. Hall said.
Overall treatment utility outcomes were “good” in 35% of the dose A group, 36% of the dose B group, and 43% of the dose C group. Outcomes were “poor” in 31%, 38%, and 29%, respectively, and outcomes were “intermediate” in 34%, 26%, and 27%, respectively.
To achieve “good” overall treatment utility, patients had to achieve the following six domains: cancer doesn’t progress on scans, oncologist assesses a benefit of treatment, lack of severe toxicity, patient’s global quality of life scores aren’t deteriorating, patient scores the treatment as worthwhile, and the patient says the treatment doesn’t interfere with daily activities.
These results suggest low-dose chemotherapy is feasible for older and frail patients with advanced gastroesophageal cancer, according to Dr. Hall.
“[L]ow-dose treatment may be offered to patients who are suitable for chemotherapy but considered too frail or elderly for a full-dose standard regime, in the confidence that it can produce superior outcomes without compromising cancer control or survival,” Dr. Hall said.
Dr. Hall reported relationships with Eisai, Pfizer, Roche, AstraZeneca, Daiichi Sankyo, and Novartis. The trial was funded by Cancer Research UK and sponsored by the University of Leeds (England).
SOURCE: Hall PS et al. ASCO 2019, Abstract 4006.
FROM ASCO 2019
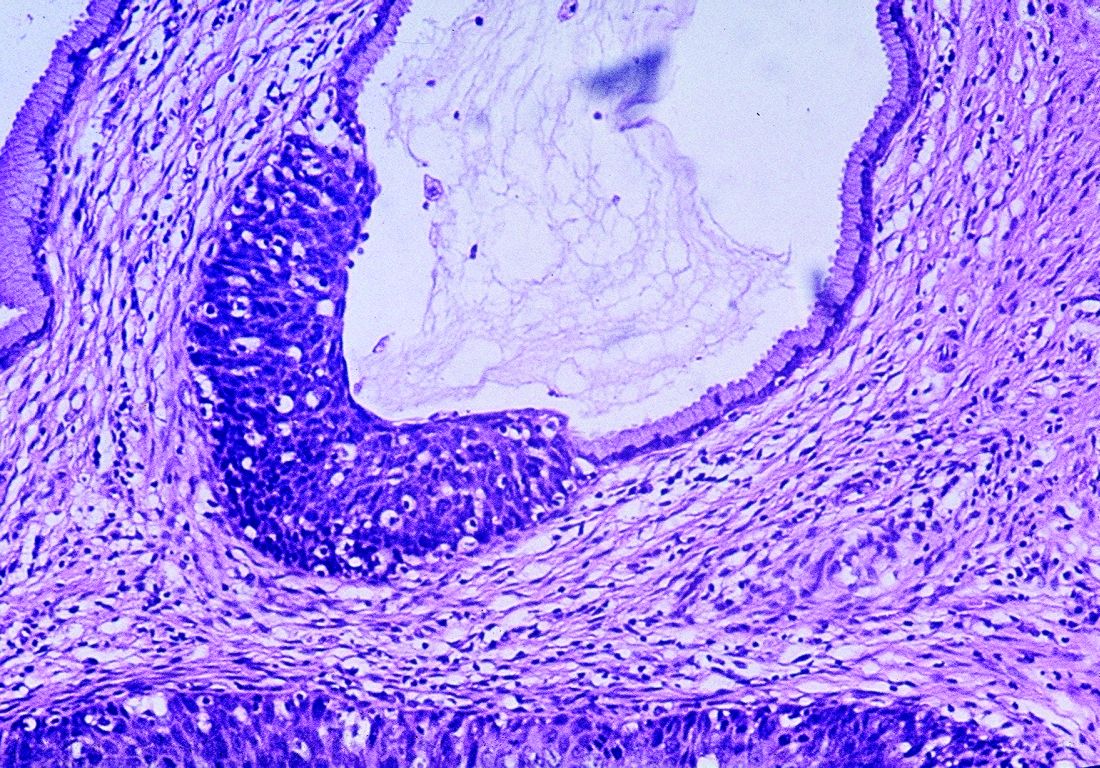
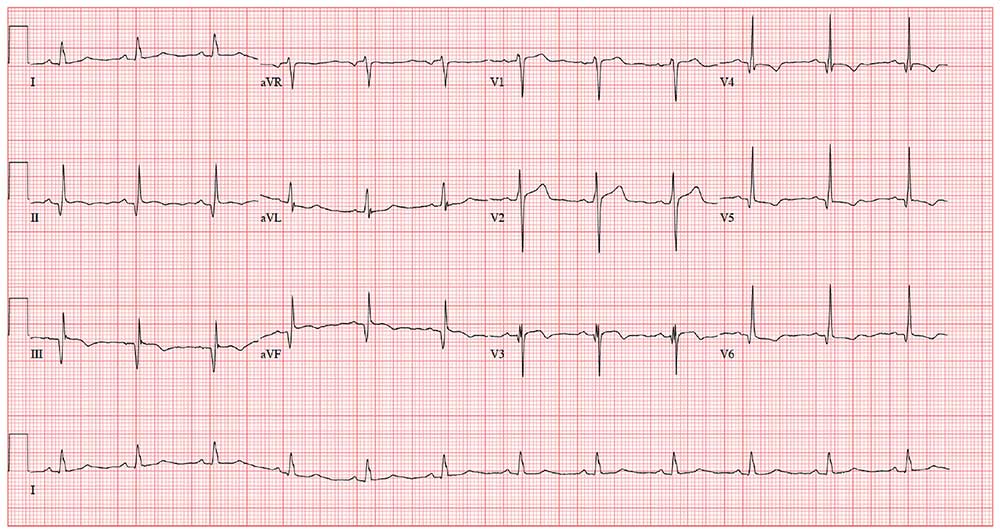
Ultrasound’s arrhythmia localization surpassed ECG’s accuracy
SAN FRANCISCO – A new type of echocardiography that uses a high frame rate to track tissue motion allowed researchers to noninvasively map the source of cardiac arrhythmias in patients with significantly more precision than did standard 12-lead ECG recordings in a pilot, single-center study with 55 patients.
Electromechanical wave imaging (EWI) correctly identified the arrhythmia source in 53 of 55 (96%) patients scheduled to undergo arrhythmia ablation, whereas only 39 of the same 55 patients (71%) were correctly mapped using recordings from a standard 12-lead ECG read by several trained electrophysiologists. The findings from this pilot study suggested that EWI performed with noninvasive ultrasound can provide useful, added information to 12-lead ECG tracings to localize cardiac arrhythmias of various types prior to invasive procedures, Elaine Y. Wan, MD, said at the annual scientific sessions of the Heart Rhythm Society.
She cautioned, however, that future studies must still establish that adding EWI to standard preprocedural assessment can benefit patients by, for example, reducing their radiation dosages or shortening their procedure times.
Patients at Columbia University Medical Center in New York scheduled to undergo ablation for a cardiac arrhythmia first had noninvasive assessment with EWI and 12-lead ECG. Patients averaged 56 years old; 45% had an atrial flutter, 22% had Wolff-Parkinson-White syndrome accessory pathways, 20% had premature ventricular complexes, and 13% had an atrial tachycardia. The researchers used 3D electroanatomic arrhythmia mapping performed during ablation as the arrhythmia-localization standard against which they compared both the EWI and ECG results.
EWI can map cardiac electromechanical activity in all four heart chambers by tracking, with high temporal and spatial resolution, transient tissue deformations that occur in response to local electrical activation of cardiac myocytes, the depolarizations in cardiac muscle that produce tissue movement. The technique captures 2,000 image frames per second, creating a “video of tissue movement that lets us see where the movement started,” explained Dr. Wan, a cardiac electrophysiologist at Columbia.
Dr. Wan and associates previously reported use of EWI to successfully map accessory pathways in all 14 children with Wolff-Parkinson-White syndrome they tested versus success in 11 of these 14 patients (79%) when using expert interpretation of 12-lead ECG recordings (JACC Clin Electrophysiol. 2019 Apr;5[4]:427-37).
The new study is the first report on using EWI in adults, Dr. Wan noted. Advantages of EWI over 12-lead ECG include its lack of dependence on correct lead placement, and EWI does not share the inherent limitation of 12-lead ECG for localizing arrhythmias on the heart’s posterior wall, she said in a video interview.
SOURCE: Wan EY et al. Heart Rhythm 2019, Abstract S-LCT04-03.
SAN FRANCISCO – A new type of echocardiography that uses a high frame rate to track tissue motion allowed researchers to noninvasively map the source of cardiac arrhythmias in patients with significantly more precision than did standard 12-lead ECG recordings in a pilot, single-center study with 55 patients.
Electromechanical wave imaging (EWI) correctly identified the arrhythmia source in 53 of 55 (96%) patients scheduled to undergo arrhythmia ablation, whereas only 39 of the same 55 patients (71%) were correctly mapped using recordings from a standard 12-lead ECG read by several trained electrophysiologists. The findings from this pilot study suggested that EWI performed with noninvasive ultrasound can provide useful, added information to 12-lead ECG tracings to localize cardiac arrhythmias of various types prior to invasive procedures, Elaine Y. Wan, MD, said at the annual scientific sessions of the Heart Rhythm Society.
She cautioned, however, that future studies must still establish that adding EWI to standard preprocedural assessment can benefit patients by, for example, reducing their radiation dosages or shortening their procedure times.
Patients at Columbia University Medical Center in New York scheduled to undergo ablation for a cardiac arrhythmia first had noninvasive assessment with EWI and 12-lead ECG. Patients averaged 56 years old; 45% had an atrial flutter, 22% had Wolff-Parkinson-White syndrome accessory pathways, 20% had premature ventricular complexes, and 13% had an atrial tachycardia. The researchers used 3D electroanatomic arrhythmia mapping performed during ablation as the arrhythmia-localization standard against which they compared both the EWI and ECG results.
EWI can map cardiac electromechanical activity in all four heart chambers by tracking, with high temporal and spatial resolution, transient tissue deformations that occur in response to local electrical activation of cardiac myocytes, the depolarizations in cardiac muscle that produce tissue movement. The technique captures 2,000 image frames per second, creating a “video of tissue movement that lets us see where the movement started,” explained Dr. Wan, a cardiac electrophysiologist at Columbia.
Dr. Wan and associates previously reported use of EWI to successfully map accessory pathways in all 14 children with Wolff-Parkinson-White syndrome they tested versus success in 11 of these 14 patients (79%) when using expert interpretation of 12-lead ECG recordings (JACC Clin Electrophysiol. 2019 Apr;5[4]:427-37).
The new study is the first report on using EWI in adults, Dr. Wan noted. Advantages of EWI over 12-lead ECG include its lack of dependence on correct lead placement, and EWI does not share the inherent limitation of 12-lead ECG for localizing arrhythmias on the heart’s posterior wall, she said in a video interview.
SOURCE: Wan EY et al. Heart Rhythm 2019, Abstract S-LCT04-03.
SAN FRANCISCO – A new type of echocardiography that uses a high frame rate to track tissue motion allowed researchers to noninvasively map the source of cardiac arrhythmias in patients with significantly more precision than did standard 12-lead ECG recordings in a pilot, single-center study with 55 patients.
Electromechanical wave imaging (EWI) correctly identified the arrhythmia source in 53 of 55 (96%) patients scheduled to undergo arrhythmia ablation, whereas only 39 of the same 55 patients (71%) were correctly mapped using recordings from a standard 12-lead ECG read by several trained electrophysiologists. The findings from this pilot study suggested that EWI performed with noninvasive ultrasound can provide useful, added information to 12-lead ECG tracings to localize cardiac arrhythmias of various types prior to invasive procedures, Elaine Y. Wan, MD, said at the annual scientific sessions of the Heart Rhythm Society.
She cautioned, however, that future studies must still establish that adding EWI to standard preprocedural assessment can benefit patients by, for example, reducing their radiation dosages or shortening their procedure times.
Patients at Columbia University Medical Center in New York scheduled to undergo ablation for a cardiac arrhythmia first had noninvasive assessment with EWI and 12-lead ECG. Patients averaged 56 years old; 45% had an atrial flutter, 22% had Wolff-Parkinson-White syndrome accessory pathways, 20% had premature ventricular complexes, and 13% had an atrial tachycardia. The researchers used 3D electroanatomic arrhythmia mapping performed during ablation as the arrhythmia-localization standard against which they compared both the EWI and ECG results.
EWI can map cardiac electromechanical activity in all four heart chambers by tracking, with high temporal and spatial resolution, transient tissue deformations that occur in response to local electrical activation of cardiac myocytes, the depolarizations in cardiac muscle that produce tissue movement. The technique captures 2,000 image frames per second, creating a “video of tissue movement that lets us see where the movement started,” explained Dr. Wan, a cardiac electrophysiologist at Columbia.
Dr. Wan and associates previously reported use of EWI to successfully map accessory pathways in all 14 children with Wolff-Parkinson-White syndrome they tested versus success in 11 of these 14 patients (79%) when using expert interpretation of 12-lead ECG recordings (JACC Clin Electrophysiol. 2019 Apr;5[4]:427-37).
The new study is the first report on using EWI in adults, Dr. Wan noted. Advantages of EWI over 12-lead ECG include its lack of dependence on correct lead placement, and EWI does not share the inherent limitation of 12-lead ECG for localizing arrhythmias on the heart’s posterior wall, she said in a video interview.
SOURCE: Wan EY et al. Heart Rhythm 2019, Abstract S-LCT04-03.
REPORTING FROM HEART RHYTHM 2019
EMA: Stop high-dose Xeljanz in certain patients
The Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency has recommended that patients at high risk of blood clots in the lungs should not be prescribed the 10-mg, twice-daily dose of tofacitinib (Xeljanz).
The PRAC recommendation is based on results from an ongoing study of patients with rheumatoid arthritis (RA), which has shown that patients receiving the 10-mg, twice-daily dose – twice the approved dose for RA – are at an increased risk of blood clots in the lungs and death.
Patients at risk include those with heart failure, cancer, inherited blood clotting disorders, or a history of blood clots, as well as patients who take combined hormonal contraceptives, are receiving hormone replacement therapy, or are undergoing major surgery. In addition, age, obesity, smoking, or immobilization should also be considered as risk factors.
In Europe, tofacitinib is indicated for the treatment of RA, psoriatic arthritis, and severe ulcerative colitis. Because the 10-mg dose is the only indicated treatment for ulcerative colitis, patients with the disease and who are at high risk should not be started on tofacitinib, and patients who are already taking the drug should be switched to a different treatment.
“The new recommendations are temporary and follow previous PRAC advice not to exceed the recommended 5-mg, twice-daily dose when treating rheumatoid arthritis. The PRAC will now carry out a review of all available evidence, and updated guidance will be provided to patients and healthcare professionals once the review is concluded,” according to the European Medicines Agency.
Find the full press release on the European Medicines Agency website.
The Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency has recommended that patients at high risk of blood clots in the lungs should not be prescribed the 10-mg, twice-daily dose of tofacitinib (Xeljanz).
The PRAC recommendation is based on results from an ongoing study of patients with rheumatoid arthritis (RA), which has shown that patients receiving the 10-mg, twice-daily dose – twice the approved dose for RA – are at an increased risk of blood clots in the lungs and death.
Patients at risk include those with heart failure, cancer, inherited blood clotting disorders, or a history of blood clots, as well as patients who take combined hormonal contraceptives, are receiving hormone replacement therapy, or are undergoing major surgery. In addition, age, obesity, smoking, or immobilization should also be considered as risk factors.
In Europe, tofacitinib is indicated for the treatment of RA, psoriatic arthritis, and severe ulcerative colitis. Because the 10-mg dose is the only indicated treatment for ulcerative colitis, patients with the disease and who are at high risk should not be started on tofacitinib, and patients who are already taking the drug should be switched to a different treatment.
“The new recommendations are temporary and follow previous PRAC advice not to exceed the recommended 5-mg, twice-daily dose when treating rheumatoid arthritis. The PRAC will now carry out a review of all available evidence, and updated guidance will be provided to patients and healthcare professionals once the review is concluded,” according to the European Medicines Agency.
Find the full press release on the European Medicines Agency website.
The Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency has recommended that patients at high risk of blood clots in the lungs should not be prescribed the 10-mg, twice-daily dose of tofacitinib (Xeljanz).
The PRAC recommendation is based on results from an ongoing study of patients with rheumatoid arthritis (RA), which has shown that patients receiving the 10-mg, twice-daily dose – twice the approved dose for RA – are at an increased risk of blood clots in the lungs and death.
Patients at risk include those with heart failure, cancer, inherited blood clotting disorders, or a history of blood clots, as well as patients who take combined hormonal contraceptives, are receiving hormone replacement therapy, or are undergoing major surgery. In addition, age, obesity, smoking, or immobilization should also be considered as risk factors.
In Europe, tofacitinib is indicated for the treatment of RA, psoriatic arthritis, and severe ulcerative colitis. Because the 10-mg dose is the only indicated treatment for ulcerative colitis, patients with the disease and who are at high risk should not be started on tofacitinib, and patients who are already taking the drug should be switched to a different treatment.
“The new recommendations are temporary and follow previous PRAC advice not to exceed the recommended 5-mg, twice-daily dose when treating rheumatoid arthritis. The PRAC will now carry out a review of all available evidence, and updated guidance will be provided to patients and healthcare professionals once the review is concluded,” according to the European Medicines Agency.
Find the full press release on the European Medicines Agency website.
Atopic dermatitis in adults associated with increased risk of dementia
CHICAGO – Atopic dermatitis in adulthood was associated with a twofold increase in the risk of developing dementia late in life, based on results from a large longitudinal cohort study presented at the annual meeting of the Society for Investigative Dermatology.
“After adjusting for potential mediators such as smoking status, depression, cardiovascular disease, and asthma or rhinitis, the effect was decreased slightly but still remained strongly statistically significant,” reported Katrina Abuabara, MD, of the University of California, San Francisco.
Atopic dermatitis is the latest in growing list of chronic inflammatory conditions that have been associated with an increased risk of dementia, according to Dr. Abuabara, who cited a body of evidence suggesting that inflammation triggers or exacerbates the processes that drive risk of developing dementia late in life.
Interest in the potential association of atopic dermatitis and dementia has been triggered “by a paradigm shift in which we now think of atopic dermatitis as a systemic inflammatory condition.” Dr. Abuabara reported.
In a primary care database of more than 1 million patients, both atopic dermatitis and dementia were common in those aged 60 years or older. The two disorders were identified in 6.75% and 6.49% of patients, respectively.
Cox proportional hazard ratios were employed to determine the relationship between the presence of atopic dermatitis and subsequent development of dementia. The median follow-up was 8 years. Atopic dermatitis was classified as mild, moderate, or severe involvement based on treatment records.
Patients with dementia associated with infectious diseases such as HIV, alcoholism, and other exogenous toxins were excluded from the analysis.
For those with atopic dermatitis relative to those without, the unadjusted hazard ratios were 1.91 for dementia of any type, 2.14 for Alzheimer’s dementia, and 2.25 for vascular-related dementia. After adjustment for confounders such as age, sex, and socioeconomic status, these hazard ratios, respectively, were only somewhat lower and remained statistically significant.
There was a trend for greater dementia risk with greater atopic dermatitis severity, rising from 2.07 in those with mild atopic dermatitis to 2.72 to those with severe disease, according to Dr. Abuabara.
“The important next step is to determine if better control of atopic dermatitis results in a lower risk of dementia,” she said.
According to Dr. Abuabara, some experimental studies have supported the hypothesis that downregulation of systemic markers of inflammation may be protective.
“Even if you reduced risk by a small amount, it would translate into a large health impact because of the large and growing prevalence of dementia,” she said.
Dr. Abuabara is a consultant for the TARGET-DERM study, sponsored by Target PharmaSolutions.
CHICAGO – Atopic dermatitis in adulthood was associated with a twofold increase in the risk of developing dementia late in life, based on results from a large longitudinal cohort study presented at the annual meeting of the Society for Investigative Dermatology.
“After adjusting for potential mediators such as smoking status, depression, cardiovascular disease, and asthma or rhinitis, the effect was decreased slightly but still remained strongly statistically significant,” reported Katrina Abuabara, MD, of the University of California, San Francisco.
Atopic dermatitis is the latest in growing list of chronic inflammatory conditions that have been associated with an increased risk of dementia, according to Dr. Abuabara, who cited a body of evidence suggesting that inflammation triggers or exacerbates the processes that drive risk of developing dementia late in life.
Interest in the potential association of atopic dermatitis and dementia has been triggered “by a paradigm shift in which we now think of atopic dermatitis as a systemic inflammatory condition.” Dr. Abuabara reported.
In a primary care database of more than 1 million patients, both atopic dermatitis and dementia were common in those aged 60 years or older. The two disorders were identified in 6.75% and 6.49% of patients, respectively.
Cox proportional hazard ratios were employed to determine the relationship between the presence of atopic dermatitis and subsequent development of dementia. The median follow-up was 8 years. Atopic dermatitis was classified as mild, moderate, or severe involvement based on treatment records.
Patients with dementia associated with infectious diseases such as HIV, alcoholism, and other exogenous toxins were excluded from the analysis.
For those with atopic dermatitis relative to those without, the unadjusted hazard ratios were 1.91 for dementia of any type, 2.14 for Alzheimer’s dementia, and 2.25 for vascular-related dementia. After adjustment for confounders such as age, sex, and socioeconomic status, these hazard ratios, respectively, were only somewhat lower and remained statistically significant.
There was a trend for greater dementia risk with greater atopic dermatitis severity, rising from 2.07 in those with mild atopic dermatitis to 2.72 to those with severe disease, according to Dr. Abuabara.
“The important next step is to determine if better control of atopic dermatitis results in a lower risk of dementia,” she said.
According to Dr. Abuabara, some experimental studies have supported the hypothesis that downregulation of systemic markers of inflammation may be protective.
“Even if you reduced risk by a small amount, it would translate into a large health impact because of the large and growing prevalence of dementia,” she said.
Dr. Abuabara is a consultant for the TARGET-DERM study, sponsored by Target PharmaSolutions.
CHICAGO – Atopic dermatitis in adulthood was associated with a twofold increase in the risk of developing dementia late in life, based on results from a large longitudinal cohort study presented at the annual meeting of the Society for Investigative Dermatology.
“After adjusting for potential mediators such as smoking status, depression, cardiovascular disease, and asthma or rhinitis, the effect was decreased slightly but still remained strongly statistically significant,” reported Katrina Abuabara, MD, of the University of California, San Francisco.
Atopic dermatitis is the latest in growing list of chronic inflammatory conditions that have been associated with an increased risk of dementia, according to Dr. Abuabara, who cited a body of evidence suggesting that inflammation triggers or exacerbates the processes that drive risk of developing dementia late in life.
Interest in the potential association of atopic dermatitis and dementia has been triggered “by a paradigm shift in which we now think of atopic dermatitis as a systemic inflammatory condition.” Dr. Abuabara reported.
In a primary care database of more than 1 million patients, both atopic dermatitis and dementia were common in those aged 60 years or older. The two disorders were identified in 6.75% and 6.49% of patients, respectively.
Cox proportional hazard ratios were employed to determine the relationship between the presence of atopic dermatitis and subsequent development of dementia. The median follow-up was 8 years. Atopic dermatitis was classified as mild, moderate, or severe involvement based on treatment records.
Patients with dementia associated with infectious diseases such as HIV, alcoholism, and other exogenous toxins were excluded from the analysis.
For those with atopic dermatitis relative to those without, the unadjusted hazard ratios were 1.91 for dementia of any type, 2.14 for Alzheimer’s dementia, and 2.25 for vascular-related dementia. After adjustment for confounders such as age, sex, and socioeconomic status, these hazard ratios, respectively, were only somewhat lower and remained statistically significant.
There was a trend for greater dementia risk with greater atopic dermatitis severity, rising from 2.07 in those with mild atopic dermatitis to 2.72 to those with severe disease, according to Dr. Abuabara.
“The important next step is to determine if better control of atopic dermatitis results in a lower risk of dementia,” she said.
According to Dr. Abuabara, some experimental studies have supported the hypothesis that downregulation of systemic markers of inflammation may be protective.
“Even if you reduced risk by a small amount, it would translate into a large health impact because of the large and growing prevalence of dementia,” she said.
Dr. Abuabara is a consultant for the TARGET-DERM study, sponsored by Target PharmaSolutions.
REPORTING FROM SID 2019
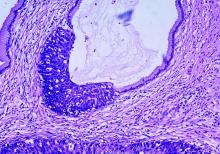
Thrice yearly cytologic testing may best annual cervical screenings
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Current ways of testing women for cervical testing may be replaced in the near future.
Major finding: Two studies challenge existing recommendations on when women should be screened for cervical cancer and explore how to manage abnormal results.
Study details: It is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment, compared with Papanicolaou cytologic testing.
Disclosures: Five authors from Sawaya et al. reported receiving grants from the National Cancer Institute and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or National Institutes of Health. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
Sources: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
CD23 expression linked to improved survival in MCL
In a large cohort of patients with mantle cell lymphoma (MCL), CD23 expression was associated with significantly improved survival outcomes, according to a retrospective analysis.
“Mantle cell lymphoma has a distinctive immunophenotype, typically positive for pan B-cell markers, CD5 and cyclin D1, but negative for CD10, CD23, and CD200. Although most cases show this immunophenotype, some MCL cases have atypical immunophenotypic features, such as expression of CD10, CD23, or rarely CD200 or lack of expression of CD5,” wrote Annapurna Saksena, MD, of MD Anderson Cancer Center, Houston, and colleagues. Their report is in Human Pathology.
They retrospectively reviewed medical records from a pathology database at MD Anderson from the period of 2008-2016. In all, 798 patients with MCL were identified, of which 103 were classified as CD23-positive via flow cytometry.
The team collected data related to the immunophenotypic and clinicopathologic characteristics of the disease, in addition to survival-related outcomes, including progression-free survival (PFS) and overall survival (OS). They compared outcomes for the CD23-positive group against 240 patients with CD23-negative MCL.
After analysis, Dr. Saksena and colleagues found that patients with CD23-positive MCL more frequently had bone marrow involvement (89% vs. 78%, P = .02), a leukemic nonnodal presentation (42% vs. 11%, P = .0001), an elevated leukocyte count (33% vs. 18%, P = .009), and stage 4 disease (87% vs. 77%, P = .03).
The researchers reported that CD23 expression was associated with significantly improved PFS and OS (P = .029 and P = .02, respectively) in the univariate analysis.
However, the prognostic significance was partially lost when leukemic nonnodal cases were excluded, the researchers reported.
In addition to the higher frequency of leukemic nonnodal presentation with CD23-positive MCL cases, there was a higher frequency of CD200 expression and a lower frequency of SOX11 expression.
The researchers acknowledged that a key limitation of the study was the loss of prognostic significance in the multivariate analysis. Further studies are needed to fully understand the links between CD23 expression and MCL survival, they noted.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Saksena A et al. Hum Pathol. 2019 May 2. doi: 10.1016/j.humpath.2019.04.010.
In a large cohort of patients with mantle cell lymphoma (MCL), CD23 expression was associated with significantly improved survival outcomes, according to a retrospective analysis.
“Mantle cell lymphoma has a distinctive immunophenotype, typically positive for pan B-cell markers, CD5 and cyclin D1, but negative for CD10, CD23, and CD200. Although most cases show this immunophenotype, some MCL cases have atypical immunophenotypic features, such as expression of CD10, CD23, or rarely CD200 or lack of expression of CD5,” wrote Annapurna Saksena, MD, of MD Anderson Cancer Center, Houston, and colleagues. Their report is in Human Pathology.
They retrospectively reviewed medical records from a pathology database at MD Anderson from the period of 2008-2016. In all, 798 patients with MCL were identified, of which 103 were classified as CD23-positive via flow cytometry.
The team collected data related to the immunophenotypic and clinicopathologic characteristics of the disease, in addition to survival-related outcomes, including progression-free survival (PFS) and overall survival (OS). They compared outcomes for the CD23-positive group against 240 patients with CD23-negative MCL.
After analysis, Dr. Saksena and colleagues found that patients with CD23-positive MCL more frequently had bone marrow involvement (89% vs. 78%, P = .02), a leukemic nonnodal presentation (42% vs. 11%, P = .0001), an elevated leukocyte count (33% vs. 18%, P = .009), and stage 4 disease (87% vs. 77%, P = .03).
The researchers reported that CD23 expression was associated with significantly improved PFS and OS (P = .029 and P = .02, respectively) in the univariate analysis.
However, the prognostic significance was partially lost when leukemic nonnodal cases were excluded, the researchers reported.
In addition to the higher frequency of leukemic nonnodal presentation with CD23-positive MCL cases, there was a higher frequency of CD200 expression and a lower frequency of SOX11 expression.
The researchers acknowledged that a key limitation of the study was the loss of prognostic significance in the multivariate analysis. Further studies are needed to fully understand the links between CD23 expression and MCL survival, they noted.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Saksena A et al. Hum Pathol. 2019 May 2. doi: 10.1016/j.humpath.2019.04.010.
In a large cohort of patients with mantle cell lymphoma (MCL), CD23 expression was associated with significantly improved survival outcomes, according to a retrospective analysis.
“Mantle cell lymphoma has a distinctive immunophenotype, typically positive for pan B-cell markers, CD5 and cyclin D1, but negative for CD10, CD23, and CD200. Although most cases show this immunophenotype, some MCL cases have atypical immunophenotypic features, such as expression of CD10, CD23, or rarely CD200 or lack of expression of CD5,” wrote Annapurna Saksena, MD, of MD Anderson Cancer Center, Houston, and colleagues. Their report is in Human Pathology.
They retrospectively reviewed medical records from a pathology database at MD Anderson from the period of 2008-2016. In all, 798 patients with MCL were identified, of which 103 were classified as CD23-positive via flow cytometry.
The team collected data related to the immunophenotypic and clinicopathologic characteristics of the disease, in addition to survival-related outcomes, including progression-free survival (PFS) and overall survival (OS). They compared outcomes for the CD23-positive group against 240 patients with CD23-negative MCL.
After analysis, Dr. Saksena and colleagues found that patients with CD23-positive MCL more frequently had bone marrow involvement (89% vs. 78%, P = .02), a leukemic nonnodal presentation (42% vs. 11%, P = .0001), an elevated leukocyte count (33% vs. 18%, P = .009), and stage 4 disease (87% vs. 77%, P = .03).
The researchers reported that CD23 expression was associated with significantly improved PFS and OS (P = .029 and P = .02, respectively) in the univariate analysis.
However, the prognostic significance was partially lost when leukemic nonnodal cases were excluded, the researchers reported.
In addition to the higher frequency of leukemic nonnodal presentation with CD23-positive MCL cases, there was a higher frequency of CD200 expression and a lower frequency of SOX11 expression.
The researchers acknowledged that a key limitation of the study was the loss of prognostic significance in the multivariate analysis. Further studies are needed to fully understand the links between CD23 expression and MCL survival, they noted.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Saksena A et al. Hum Pathol. 2019 May 2. doi: 10.1016/j.humpath.2019.04.010.
FROM HUMAN PATHOLOGY
Youth suicide: Rates rising more rapidly in girls
Youth suicide rates appear to be increasing faster in girls than in boys, narrowing the historical gap between the two, according to research published in JAMA Network Open.
From 1999 to 2014, suicide rates in the United States have increased by 33%, but the incidence always has been higher among men than women in all age groups.
Recent reports suggesting that suicide rates were increasing in girls prompted Donna A. Ruch, PhD, from the the Research Institute at Nationwide Children’s Hospital in Columbus, Ohio, and her coauthors to undertake a cross-sectional study of all suicides in the United States among individuals aged 10-19 years, between 1975 and 2016.
During that time there were a total of 85,051 suicide deaths in youth aged 10-19 years; approximately 80% of the deaths were in males, representing a nearly fourfold higher rate in males than females (incidence rate ratio [IRR], 3.82).
From 1975 to 1993, researchers noted a 5.4% increase each year in suicide rates among girls aged 10-14 years and a 4.5% increase among boys in the same age group. From 2003-2007, suicide rates among both sexes declined until 2007, at which point the suicide rates among girls increased annually by 12.7%, compared with 7.1% among boys.
Overall, the male to female incidence rate ratio among youth aged 10-14 decreased from 3.14 in 1975-1991 to 1.80 from 2007-2016, a statistically significant difference.
“The narrowing gap between male and female rates of suicide was most pronounced among youth aged 10 to 14 years, underscoring the importance of early prevention efforts that take both sex and developmental level into consideration,” the authors wrote.
Ethnicity was an influence, with the most consistent declining trend in male to female incidence rate ratio seen in non-Hispanic white youth, and also was significant in non-Hispanic youth of other races. There was no significant change in the male to female incidence rate ratio seen with younger non-Hispanic black youth or Hispanic youth.
Among youth aged 15-19, the differences between male and female suicide rates decreased significantly in non-Hispanic youth of other race, and a significant downward trend also was seen in Hispanic youth.
The analysis also looked at method of suicide. The results showed that while the male to female incidence rate ratio for shooting suicides increased significantly in youth aged 15-19 years, it decreased for suicide by hanging or suffocation across all ages groups.
“Future research to identify sex-specific risk factors for youth suicide and distinct mechanisms of suicide in male and female individuals within racial/ethnic groups could lead to improved suicide prevention strategies and interventions,” the authors wrote.
One author was supported by a grant from the National Institute of Mental Health, and declared unpaid board membership for the scientific advisory board of a mental health company. No other conflicts of interest were declared.
SOURCE: Ruch D et al. JAMA Network Open. 2019, May 17. doi:10.1001/jamanetworkopen.2019.3886.
Rates of suicide among girls aged 10-14 have tripled between 1999-2014, and this new study raises questions about what is driving this trend. Fingers have been pointed at the rise of social media use, particularly among this age group, as a clear and powerful social change that has occurred over the same period. But social media use has risen among both sexes, so why is it disproportionately impacting girls?
It may be that girls’ social media use is more likely to result in interpersonal stress, but also that girls are known to use social media more frequently and are more likely to experience cyberbullying. Research also suggests that girls with depression experience more negative comments from peers on social media compared to boys with depression, suggesting that increasing social media use may make young girls more vulnerable to suicide.
Joan Luby, MD, and Sarah Kertz, PhD, are from the department of psychiatry at Washington University in St. Louis. These comments are adapted from an editorial accompanying the article by Ruch et al. (JAMA Network Open. 2019, May 17. doi: 10.1001/jamanetworkopen.2019.3916). Dr Luby reported grants from the National Institute of Mental Health. No other disclosures were reported.
Rates of suicide among girls aged 10-14 have tripled between 1999-2014, and this new study raises questions about what is driving this trend. Fingers have been pointed at the rise of social media use, particularly among this age group, as a clear and powerful social change that has occurred over the same period. But social media use has risen among both sexes, so why is it disproportionately impacting girls?
It may be that girls’ social media use is more likely to result in interpersonal stress, but also that girls are known to use social media more frequently and are more likely to experience cyberbullying. Research also suggests that girls with depression experience more negative comments from peers on social media compared to boys with depression, suggesting that increasing social media use may make young girls more vulnerable to suicide.
Joan Luby, MD, and Sarah Kertz, PhD, are from the department of psychiatry at Washington University in St. Louis. These comments are adapted from an editorial accompanying the article by Ruch et al. (JAMA Network Open. 2019, May 17. doi: 10.1001/jamanetworkopen.2019.3916). Dr Luby reported grants from the National Institute of Mental Health. No other disclosures were reported.
Rates of suicide among girls aged 10-14 have tripled between 1999-2014, and this new study raises questions about what is driving this trend. Fingers have been pointed at the rise of social media use, particularly among this age group, as a clear and powerful social change that has occurred over the same period. But social media use has risen among both sexes, so why is it disproportionately impacting girls?
It may be that girls’ social media use is more likely to result in interpersonal stress, but also that girls are known to use social media more frequently and are more likely to experience cyberbullying. Research also suggests that girls with depression experience more negative comments from peers on social media compared to boys with depression, suggesting that increasing social media use may make young girls more vulnerable to suicide.
Joan Luby, MD, and Sarah Kertz, PhD, are from the department of psychiatry at Washington University in St. Louis. These comments are adapted from an editorial accompanying the article by Ruch et al. (JAMA Network Open. 2019, May 17. doi: 10.1001/jamanetworkopen.2019.3916). Dr Luby reported grants from the National Institute of Mental Health. No other disclosures were reported.
Youth suicide rates appear to be increasing faster in girls than in boys, narrowing the historical gap between the two, according to research published in JAMA Network Open.
From 1999 to 2014, suicide rates in the United States have increased by 33%, but the incidence always has been higher among men than women in all age groups.
Recent reports suggesting that suicide rates were increasing in girls prompted Donna A. Ruch, PhD, from the the Research Institute at Nationwide Children’s Hospital in Columbus, Ohio, and her coauthors to undertake a cross-sectional study of all suicides in the United States among individuals aged 10-19 years, between 1975 and 2016.
During that time there were a total of 85,051 suicide deaths in youth aged 10-19 years; approximately 80% of the deaths were in males, representing a nearly fourfold higher rate in males than females (incidence rate ratio [IRR], 3.82).
From 1975 to 1993, researchers noted a 5.4% increase each year in suicide rates among girls aged 10-14 years and a 4.5% increase among boys in the same age group. From 2003-2007, suicide rates among both sexes declined until 2007, at which point the suicide rates among girls increased annually by 12.7%, compared with 7.1% among boys.
Overall, the male to female incidence rate ratio among youth aged 10-14 decreased from 3.14 in 1975-1991 to 1.80 from 2007-2016, a statistically significant difference.
“The narrowing gap between male and female rates of suicide was most pronounced among youth aged 10 to 14 years, underscoring the importance of early prevention efforts that take both sex and developmental level into consideration,” the authors wrote.
Ethnicity was an influence, with the most consistent declining trend in male to female incidence rate ratio seen in non-Hispanic white youth, and also was significant in non-Hispanic youth of other races. There was no significant change in the male to female incidence rate ratio seen with younger non-Hispanic black youth or Hispanic youth.
Among youth aged 15-19, the differences between male and female suicide rates decreased significantly in non-Hispanic youth of other race, and a significant downward trend also was seen in Hispanic youth.
The analysis also looked at method of suicide. The results showed that while the male to female incidence rate ratio for shooting suicides increased significantly in youth aged 15-19 years, it decreased for suicide by hanging or suffocation across all ages groups.
“Future research to identify sex-specific risk factors for youth suicide and distinct mechanisms of suicide in male and female individuals within racial/ethnic groups could lead to improved suicide prevention strategies and interventions,” the authors wrote.
One author was supported by a grant from the National Institute of Mental Health, and declared unpaid board membership for the scientific advisory board of a mental health company. No other conflicts of interest were declared.
SOURCE: Ruch D et al. JAMA Network Open. 2019, May 17. doi:10.1001/jamanetworkopen.2019.3886.
Youth suicide rates appear to be increasing faster in girls than in boys, narrowing the historical gap between the two, according to research published in JAMA Network Open.
From 1999 to 2014, suicide rates in the United States have increased by 33%, but the incidence always has been higher among men than women in all age groups.
Recent reports suggesting that suicide rates were increasing in girls prompted Donna A. Ruch, PhD, from the the Research Institute at Nationwide Children’s Hospital in Columbus, Ohio, and her coauthors to undertake a cross-sectional study of all suicides in the United States among individuals aged 10-19 years, between 1975 and 2016.
During that time there were a total of 85,051 suicide deaths in youth aged 10-19 years; approximately 80% of the deaths were in males, representing a nearly fourfold higher rate in males than females (incidence rate ratio [IRR], 3.82).
From 1975 to 1993, researchers noted a 5.4% increase each year in suicide rates among girls aged 10-14 years and a 4.5% increase among boys in the same age group. From 2003-2007, suicide rates among both sexes declined until 2007, at which point the suicide rates among girls increased annually by 12.7%, compared with 7.1% among boys.
Overall, the male to female incidence rate ratio among youth aged 10-14 decreased from 3.14 in 1975-1991 to 1.80 from 2007-2016, a statistically significant difference.
“The narrowing gap between male and female rates of suicide was most pronounced among youth aged 10 to 14 years, underscoring the importance of early prevention efforts that take both sex and developmental level into consideration,” the authors wrote.
Ethnicity was an influence, with the most consistent declining trend in male to female incidence rate ratio seen in non-Hispanic white youth, and also was significant in non-Hispanic youth of other races. There was no significant change in the male to female incidence rate ratio seen with younger non-Hispanic black youth or Hispanic youth.
Among youth aged 15-19, the differences between male and female suicide rates decreased significantly in non-Hispanic youth of other race, and a significant downward trend also was seen in Hispanic youth.
The analysis also looked at method of suicide. The results showed that while the male to female incidence rate ratio for shooting suicides increased significantly in youth aged 15-19 years, it decreased for suicide by hanging or suffocation across all ages groups.
“Future research to identify sex-specific risk factors for youth suicide and distinct mechanisms of suicide in male and female individuals within racial/ethnic groups could lead to improved suicide prevention strategies and interventions,” the authors wrote.
One author was supported by a grant from the National Institute of Mental Health, and declared unpaid board membership for the scientific advisory board of a mental health company. No other conflicts of interest were declared.
SOURCE: Ruch D et al. JAMA Network Open. 2019, May 17. doi:10.1001/jamanetworkopen.2019.3886.
FROM JAMA NETWORK OPEN
Key clinical point: Suicide rates are rising faster among girls than boys.
Major finding: Suicide rates in girls have increased annually by 12.7% since 2007, compared with 7.1% among boys.
Study details: Cross-sectional study of 85,051 suicide deaths in youth aged 10-19 years.
Disclosures: One author was supported by a grant from the National Institute of Mental Health, and declared unpaid board membership for the scientific advisory board of a mental health company. No other conflicts of interest were declared.
Source: Ruch D et al. JAMA Network Open 2019, May 17. doi: 10.1001/jamanetworkopen.2019.3886.
Hanging by a Thread
ANSWER
The correct interpretation incudes normal sinus rhythm, inferior MI, possible anterior MI, and ST-T wave abnormalit
Normal sinus rhythm is evidenced by a P wave for every QRS and a QRS for every P wave with a normal PR interval and a rate > 60 and < 100 beats/min.
An old inferior MI is indicated by the Q waves in inferior leads II, III, and aVF. The absence of ST-segment elevation in these leads also contributes to the diagnosis of an old rather than new MI. Possible anterior MI can be inferred from the poor R-wave progression in leads V1 through V3 with the absence of ST elevation.
ST-T wave abnormalities are evidenced by the chronic ST-segment elevation in V1 and V2 with T-wave inversions in leads V3 through V6 and in aVF. These may be due to remodeling and/or ECG lead placement.
The patient was subsequently cleared for his shoulder repair.
ANSWER
The correct interpretation incudes normal sinus rhythm, inferior MI, possible anterior MI, and ST-T wave abnormalit
Normal sinus rhythm is evidenced by a P wave for every QRS and a QRS for every P wave with a normal PR interval and a rate > 60 and < 100 beats/min.
An old inferior MI is indicated by the Q waves in inferior leads II, III, and aVF. The absence of ST-segment elevation in these leads also contributes to the diagnosis of an old rather than new MI. Possible anterior MI can be inferred from the poor R-wave progression in leads V1 through V3 with the absence of ST elevation.
ST-T wave abnormalities are evidenced by the chronic ST-segment elevation in V1 and V2 with T-wave inversions in leads V3 through V6 and in aVF. These may be due to remodeling and/or ECG lead placement.
The patient was subsequently cleared for his shoulder repair.
ANSWER
The correct interpretation incudes normal sinus rhythm, inferior MI, possible anterior MI, and ST-T wave abnormalit
Normal sinus rhythm is evidenced by a P wave for every QRS and a QRS for every P wave with a normal PR interval and a rate > 60 and < 100 beats/min.
An old inferior MI is indicated by the Q waves in inferior leads II, III, and aVF. The absence of ST-segment elevation in these leads also contributes to the diagnosis of an old rather than new MI. Possible anterior MI can be inferred from the poor R-wave progression in leads V1 through V3 with the absence of ST elevation.
ST-T wave abnormalities are evidenced by the chronic ST-segment elevation in V1 and V2 with T-wave inversions in leads V3 through V6 and in aVF. These may be due to remodeling and/or ECG lead placement.
The patient was subsequently cleared for his shoulder repair.
A 54-year-old man presents for preoperative workup for surgical repair of a partial tear of his right rotator cuff. He sustained the injury about 8 months ago, while rock climbing. His clinical work-up included MRI, magnetic resonance arthrogram, and dynamic musculoskeletal ultrasound. Initial treatment included physical therapy and 2 corticosteroid injections, without relief. A repeat arthrogram showed no resolution of the tear and revealed tendon retraction and muscular atrophy. The patient declined further physical therapy and opted for surgical intervention instead, because the injury is in his dominant shoulder and the pain continues to interfere with his job as a general contractor.
His medical history is positive for hypertension and hypercholesterolemia, which have been managed with medications. There is also a history of myocardial infarction (MI), which occurred 3 years ago when he was lifting a heavy truss at a job site; it manifested as acute chest pain, shortness of breath, and diaphoresis. He waited 3 days before seeking medical care because he “needed to get that project done.” He has had no further chest pain, but he‘s felt “a twinge” now and again in the past 2 months. He denies shortness of breath, dyspnea on exertion, or exertional chest pain. He has had no palpitations, syncope, or near-syncope.
His current medications include diltiazem, atorvastatin, and isosorbide. He tried metoprolol but did not like how he felt when taking it. He has no known drug allergies.
Family history is positive for familial hyperlipidemia on his father’s side. His father died of a heart attack at age 51. His mother has type 2 diabetes mellitus. His 2 older brothers have had MIs; his younger sister has no known health issues.
The patient is a self-employed general contractor. He has been married for 20 years and has a 21-year-old son who works for him. He smokes 1 to 1.5 packs a day and takes a shot of bourbon every night before dinner.
A review of systems reveals an 8-lb weight gain over the past 6 months. He denies fever, chills, and gastrointestinal and urologic symptoms. He believes he is depressed because his rotator cuff injury prevents him from doing what he would like.
Vital signs include a blood pressure of 138/88 mm Hg; pulse, 72 beats/min; respiratory rate, 14 breaths/min; O2 saturation, 98% on room air; and temperature, 97.4°F. His height is 70 in and his weight, 208 lb.
Physical exam reveals an anxious male in no distress wearing a sling on his right upper extremity. The HEENT exam is remarkable for corrective lenses. There are no lesions in the oropharynx, and his tobacco-stained teeth are in otherwise good repair. The neck is supple, and there are no carotid bruits, jugular venous distention, or thyromegaly. The pulmonary exam reveals coarse, scattered crackles with end-expiratory wheezing that clears with coughing.
Cardiac exam reveals a regular rate and rhythm of 72 beats/min. There are no murmurs, extra heart sounds, or rubs.
The abdomen is soft and nontender without palpable organomegaly or pulsatile masses. The lower extremities reveal no edema. The right upper extremity exam is deferred because the patient is very apprehensive about any movement of his shoulder. Peripheral pulses are strong and equal bilaterally. The neurologic exam is grossly intact.
As part of the preoperative workup, an ECG is ordered. It shows a ventricular rate of 72 beats/min; PR interval, 158 ms; QRS duration, 106 ms; QT/QTc interval, 400/438 ms; P axis, 33°; R axis, 38°; and T axis, –15°. What is your interpretation of this ECG?