User login
Medicare withdraws plans to exclude drugs from Part D protected classes
Proposals that would have allowed Medicare Part D prescription drug plan sponsors to exclude certain drugs in the six protected classes have been withdrawn by the Centers for Medicare & Medicaid Services.
In a final rule that targets drug pricing in Medicare Advantage and Part D – released online May 16 and scheduled for publication in the Federal Register on May 23 – CMS did not finalize a proposal that would have allowed a plan sponsor to exclude a drug in a protected class from a formulary, if the price of that drug increased faster than the rate of inflation.
“In considering whether to propose these exceptions, CMS took our other enrollee access protections into account, which have successfully protected beneficiary access to needed medications in the more than 12 years the Part D program has been operational,” the agency stated in the final rule.
Agency officials cited rules on formulary transparency, formulary requirements, reassignment formulary coverage notices, transition supplies and notices, and the expedited coverage determination and appeals process as policies that have protected beneficiary access.
Agency officials said that they believe the current enrollee access protections are “sufficient,” and they are not finalizing the pricing threshold exception.
The agency also chose not to finalize a plan’s ability to exclude a drug in a protected class if the drug represents a new formulation of an existing single-source product, regardless of whether the older formulation remains on the market.
Part D plan sponsors are required by law to cover “all or substantially all” drugs in six classes: antidepressants, antipsychotics, anticonvulsants, immunosuppressants for the treatment of transplant rejection, antiretrovirals, and antineoplastics.
CMS chose not to finalize this proposal because it was persuaded by comments noting that under the proposed policy, “in a scenario where our other formulary requirements did not require Part D sponsors to have the new formulation on their formulary, a Part D enrollee who is stable on the old formulation could be left without access to the new formulation,” the agency stated in the final rule. “Consequently, we decline to finalize this exception.”
The final rule codifies in regulation a plan’s ability to impose prior authorization and step therapy for beneficiaries initiating therapy in five of the six classes, as has been the policy since 2006 (antiretrovirals are excluded from prior authorization and step therapy).
CMS also finalized a policy implemented in 2019 that allows Medicare Advantage plans to implement step therapy for drugs administered in the physician office under Medicare Part B. Similar to step therapy in Medicare Part D, this applies only to beneficiaries newly starting on treatment and includes an appeals process similar to Part D.
Another proposal finalized is one that prohibits so-called “gag clauses” in Part D contracts, which prevent or penalize pharmacists from discussing lower-cost pharmaceutical options with customers.
CMS also will be requiring Part D plans to adopt tools no later than Jan. 1, 2021, that integrate with a prescriber’s electronic health record or e-prescribing software to inform providers when lower-cost pharmaceutical options are available under a patient’s drug benefit. Similarly, the Part D explanation of benefits statement, effective the same date, will be required to inform beneficiaries of drug price increases and lower-cost alternatives.
Proposals that would have allowed Medicare Part D prescription drug plan sponsors to exclude certain drugs in the six protected classes have been withdrawn by the Centers for Medicare & Medicaid Services.
In a final rule that targets drug pricing in Medicare Advantage and Part D – released online May 16 and scheduled for publication in the Federal Register on May 23 – CMS did not finalize a proposal that would have allowed a plan sponsor to exclude a drug in a protected class from a formulary, if the price of that drug increased faster than the rate of inflation.
“In considering whether to propose these exceptions, CMS took our other enrollee access protections into account, which have successfully protected beneficiary access to needed medications in the more than 12 years the Part D program has been operational,” the agency stated in the final rule.
Agency officials cited rules on formulary transparency, formulary requirements, reassignment formulary coverage notices, transition supplies and notices, and the expedited coverage determination and appeals process as policies that have protected beneficiary access.
Agency officials said that they believe the current enrollee access protections are “sufficient,” and they are not finalizing the pricing threshold exception.
The agency also chose not to finalize a plan’s ability to exclude a drug in a protected class if the drug represents a new formulation of an existing single-source product, regardless of whether the older formulation remains on the market.
Part D plan sponsors are required by law to cover “all or substantially all” drugs in six classes: antidepressants, antipsychotics, anticonvulsants, immunosuppressants for the treatment of transplant rejection, antiretrovirals, and antineoplastics.
CMS chose not to finalize this proposal because it was persuaded by comments noting that under the proposed policy, “in a scenario where our other formulary requirements did not require Part D sponsors to have the new formulation on their formulary, a Part D enrollee who is stable on the old formulation could be left without access to the new formulation,” the agency stated in the final rule. “Consequently, we decline to finalize this exception.”
The final rule codifies in regulation a plan’s ability to impose prior authorization and step therapy for beneficiaries initiating therapy in five of the six classes, as has been the policy since 2006 (antiretrovirals are excluded from prior authorization and step therapy).
CMS also finalized a policy implemented in 2019 that allows Medicare Advantage plans to implement step therapy for drugs administered in the physician office under Medicare Part B. Similar to step therapy in Medicare Part D, this applies only to beneficiaries newly starting on treatment and includes an appeals process similar to Part D.
Another proposal finalized is one that prohibits so-called “gag clauses” in Part D contracts, which prevent or penalize pharmacists from discussing lower-cost pharmaceutical options with customers.
CMS also will be requiring Part D plans to adopt tools no later than Jan. 1, 2021, that integrate with a prescriber’s electronic health record or e-prescribing software to inform providers when lower-cost pharmaceutical options are available under a patient’s drug benefit. Similarly, the Part D explanation of benefits statement, effective the same date, will be required to inform beneficiaries of drug price increases and lower-cost alternatives.
Proposals that would have allowed Medicare Part D prescription drug plan sponsors to exclude certain drugs in the six protected classes have been withdrawn by the Centers for Medicare & Medicaid Services.
In a final rule that targets drug pricing in Medicare Advantage and Part D – released online May 16 and scheduled for publication in the Federal Register on May 23 – CMS did not finalize a proposal that would have allowed a plan sponsor to exclude a drug in a protected class from a formulary, if the price of that drug increased faster than the rate of inflation.
“In considering whether to propose these exceptions, CMS took our other enrollee access protections into account, which have successfully protected beneficiary access to needed medications in the more than 12 years the Part D program has been operational,” the agency stated in the final rule.
Agency officials cited rules on formulary transparency, formulary requirements, reassignment formulary coverage notices, transition supplies and notices, and the expedited coverage determination and appeals process as policies that have protected beneficiary access.
Agency officials said that they believe the current enrollee access protections are “sufficient,” and they are not finalizing the pricing threshold exception.
The agency also chose not to finalize a plan’s ability to exclude a drug in a protected class if the drug represents a new formulation of an existing single-source product, regardless of whether the older formulation remains on the market.
Part D plan sponsors are required by law to cover “all or substantially all” drugs in six classes: antidepressants, antipsychotics, anticonvulsants, immunosuppressants for the treatment of transplant rejection, antiretrovirals, and antineoplastics.
CMS chose not to finalize this proposal because it was persuaded by comments noting that under the proposed policy, “in a scenario where our other formulary requirements did not require Part D sponsors to have the new formulation on their formulary, a Part D enrollee who is stable on the old formulation could be left without access to the new formulation,” the agency stated in the final rule. “Consequently, we decline to finalize this exception.”
The final rule codifies in regulation a plan’s ability to impose prior authorization and step therapy for beneficiaries initiating therapy in five of the six classes, as has been the policy since 2006 (antiretrovirals are excluded from prior authorization and step therapy).
CMS also finalized a policy implemented in 2019 that allows Medicare Advantage plans to implement step therapy for drugs administered in the physician office under Medicare Part B. Similar to step therapy in Medicare Part D, this applies only to beneficiaries newly starting on treatment and includes an appeals process similar to Part D.
Another proposal finalized is one that prohibits so-called “gag clauses” in Part D contracts, which prevent or penalize pharmacists from discussing lower-cost pharmaceutical options with customers.
CMS also will be requiring Part D plans to adopt tools no later than Jan. 1, 2021, that integrate with a prescriber’s electronic health record or e-prescribing software to inform providers when lower-cost pharmaceutical options are available under a patient’s drug benefit. Similarly, the Part D explanation of benefits statement, effective the same date, will be required to inform beneficiaries of drug price increases and lower-cost alternatives.
Key clinical point: A proposal that would have allowed for drugs to be excluded from Medicare Part D protected classes was not finalized by the Centers for Medicare & Medicaid Services.
Major finding: Agency officials wrote that there are “sufficient” enrollee access protections in place, and they were not finalizing the proposal.
Study details: The proposal would have allowed a plan sponsor to exclude a drug in a protected class from a formulary, if the price of that drug increased faster than the rate of inflation.
Disclosures: CMS makes no disclosures in issuing the final rule.
Source: CMS final rule.
Vitamin D levels linked to depression in teens
BALTIMORE – Anna-Lisa Munson, MD, MPH, of Denver Health Medical Center in Colorado, told attendees at the Pediatric Academic Societies annual meeting.

Although several studies in adults have suggested a link between vitamin D deficiency and depression, no large-scale studies have investigated whether such a relationship exists in adolescents, up to half of whom have a vitamin D deficiency, Dr Munson said.
The researchers relied on National Health and Nutrition Examination Survey (NHANES) data from 2005 to 2010 to assess prevalence of major depressive disorder and vitamin D 25-hydroxy levels in teens aged 12-17 years. Serum vitamin D levels of less than 30 nmol/L were considered deficient while 30-50 nmol/L was considered insufficient, and at least 50 nmol/L was sufficient. A score between 10 and 27 on the Patient Health Questionnaire-9 (PHQ-9) qualified as depression.
The researchers adjusted their findings for age and sex, as well as other covariates linked to vitamin D levels or depression in previous research: latitude, season, race/ethnicity, and poverty to income ratio.
Among the 2,815 participants who completed the National Institute of Mental Health Diagnostic Interview Schedule for Children (NIMH-DISC), 8% had major depression. Among the 2,420 of participants with serum vitamin D values, 8% had vitamin D deficiency, 33% had insufficiency, and 59% had sufficiency.
Risk of depression dropped 10% for every additional 10 nmol/L of vitamin D, the analysis showed (odds ratio, 0.90).
Although non-Hispanic white students had about twice the odds of depression as other ethnic groups, risk of depression did not vary according to gender, age, season, latitude, poverty to income ratio, or use of vitamin D supplements.
The findings are limited by the cross-sectional data and lack of data regarding other factors that could affect vitamin D absorption, such as sunscreen use or clothing worn in the sun. The researchers also had only broad – not precise – data on latitude, and the PHQ-9 was used as a proxy for major depression instead of a clinical diagnosis.
The research was funded by the Denver Health Division of General Pediatrics. The authors had no relevant financial disclosures.
BALTIMORE – Anna-Lisa Munson, MD, MPH, of Denver Health Medical Center in Colorado, told attendees at the Pediatric Academic Societies annual meeting.

Although several studies in adults have suggested a link between vitamin D deficiency and depression, no large-scale studies have investigated whether such a relationship exists in adolescents, up to half of whom have a vitamin D deficiency, Dr Munson said.
The researchers relied on National Health and Nutrition Examination Survey (NHANES) data from 2005 to 2010 to assess prevalence of major depressive disorder and vitamin D 25-hydroxy levels in teens aged 12-17 years. Serum vitamin D levels of less than 30 nmol/L were considered deficient while 30-50 nmol/L was considered insufficient, and at least 50 nmol/L was sufficient. A score between 10 and 27 on the Patient Health Questionnaire-9 (PHQ-9) qualified as depression.
The researchers adjusted their findings for age and sex, as well as other covariates linked to vitamin D levels or depression in previous research: latitude, season, race/ethnicity, and poverty to income ratio.
Among the 2,815 participants who completed the National Institute of Mental Health Diagnostic Interview Schedule for Children (NIMH-DISC), 8% had major depression. Among the 2,420 of participants with serum vitamin D values, 8% had vitamin D deficiency, 33% had insufficiency, and 59% had sufficiency.
Risk of depression dropped 10% for every additional 10 nmol/L of vitamin D, the analysis showed (odds ratio, 0.90).
Although non-Hispanic white students had about twice the odds of depression as other ethnic groups, risk of depression did not vary according to gender, age, season, latitude, poverty to income ratio, or use of vitamin D supplements.
The findings are limited by the cross-sectional data and lack of data regarding other factors that could affect vitamin D absorption, such as sunscreen use or clothing worn in the sun. The researchers also had only broad – not precise – data on latitude, and the PHQ-9 was used as a proxy for major depression instead of a clinical diagnosis.
The research was funded by the Denver Health Division of General Pediatrics. The authors had no relevant financial disclosures.
BALTIMORE – Anna-Lisa Munson, MD, MPH, of Denver Health Medical Center in Colorado, told attendees at the Pediatric Academic Societies annual meeting.

Although several studies in adults have suggested a link between vitamin D deficiency and depression, no large-scale studies have investigated whether such a relationship exists in adolescents, up to half of whom have a vitamin D deficiency, Dr Munson said.
The researchers relied on National Health and Nutrition Examination Survey (NHANES) data from 2005 to 2010 to assess prevalence of major depressive disorder and vitamin D 25-hydroxy levels in teens aged 12-17 years. Serum vitamin D levels of less than 30 nmol/L were considered deficient while 30-50 nmol/L was considered insufficient, and at least 50 nmol/L was sufficient. A score between 10 and 27 on the Patient Health Questionnaire-9 (PHQ-9) qualified as depression.
The researchers adjusted their findings for age and sex, as well as other covariates linked to vitamin D levels or depression in previous research: latitude, season, race/ethnicity, and poverty to income ratio.
Among the 2,815 participants who completed the National Institute of Mental Health Diagnostic Interview Schedule for Children (NIMH-DISC), 8% had major depression. Among the 2,420 of participants with serum vitamin D values, 8% had vitamin D deficiency, 33% had insufficiency, and 59% had sufficiency.
Risk of depression dropped 10% for every additional 10 nmol/L of vitamin D, the analysis showed (odds ratio, 0.90).
Although non-Hispanic white students had about twice the odds of depression as other ethnic groups, risk of depression did not vary according to gender, age, season, latitude, poverty to income ratio, or use of vitamin D supplements.
The findings are limited by the cross-sectional data and lack of data regarding other factors that could affect vitamin D absorption, such as sunscreen use or clothing worn in the sun. The researchers also had only broad – not precise – data on latitude, and the PHQ-9 was used as a proxy for major depression instead of a clinical diagnosis.
The research was funded by the Denver Health Division of General Pediatrics. The authors had no relevant financial disclosures.
REPORTING FROM PAS 2019
A primer on cannabis for cosmeceuticals: Research and treatments for particular skin conditions
The relatively recent discovery of the endogenous cannabinoid system and the quickly evolving, yet still convoluted, legal status of cannabis in the United States has spurred excitement over expanded research opportunities. Despite its checkered legal history, marijuana – derived from Cannabis sativa and Cannabis indica – has long been used for medical purposes and is one of the most widely used drugs throughout the world.1 Modern medicine has deployed this dynamic plant to treat chronic pain, glaucoma, and nausea, and continues to investigate its application in a broad array of conditions: anorexia, spasticity, atherosclerosis, autoimmune disorders, inflammatory bowel disease, multiple sclerosis, spasticity, tumorigenesis, and multiple cutaneous disorders, including acne, eczematous disorders, lichen simplex, melanoma and nonmelanoma skin cancer, melasma, prurigo, pruritus, psoriasis, scleroderma and systemic sclerosis, and seborrheic dermatitis.1-4 This .

Acne
Oláh et al. have demonstrated that the nonpsychotropic phytocannabinoid ((-)-cannabidiol [CBD]) imparts anti-acne benefits by diminishing sebaceous lipid synthesis, decreasing proliferation, and easing inflammation in human SZ95 sebocytes.5 In additional investigations of nonpsychotropic phytocannabinoids and their effects on human sebocyte function, they reported in 2016 that the phytocannabinoids (-)-cannabigerol [CBG] and (-)-cannabigerovarin (CBGV) appear to exhibit promise in treating xerotic and seborrheic skin, and ((-)-cannabichromene [CBC], (-)-cannabidivarin [CBDV], and (-)-delta9-tetrahydrocannabivarin [THCV], in particular, display notable potential as anti-acne ingredients. The investigators added that these compounds, due to their substantial anti-inflammatory effects, warrant consideration for use in treating skin inflammation.5 Previously, Ali and Akhtar conducted a single-blinded, 12-week comparative study in healthy male volunteers to evaluate the effects of twice-daily application of 3% cannabis seed extract cream on human cheek skin. The researchers found the base with 3% cannabis seed extract to be safe and effective, with skin sebum and erythema content on the treated side reduced significantly compared with the side treated only with the control base. They concluded that this well-tolerated formulation could be indicated for the treatment of acne and seborrhea to enhance facial appearance.6
Psoriasis
The endocannabinoid system itself is thought to play a potentially important role in the treatment of psoriasis, as interactions between the immune and nervous systems via cholinergic anti-inflammatory pathways are considered to be key in psoriasis etiology and the endocannabinoid system interacts with both systems through the cannabinoid (CB) receptors CB1 and CB2.7 Compared with normal human skin, psoriatic skin is characterized by fewer CB receptors.8
In 2007, Wilkinson and Williamson used a keratinocyte proliferation assay to study the phytocannabinoids delta9-tetrahydrocannabinol (THC), CBD, CBG, and cannabinol (CNB) to assess their capacity to halt the growth of a hyper-proliferating human keratinocyte cell line with an eye toward potential use in treating psoriasis. CB1 and CB2 receptors were confirmed present by Western blot and RT-PCR analyses. All cannabinoids investigated concentration-dependently hindered keratinocyte proliferation, as the authors concluded that these compounds show potential for use in psoriasis treatment.9
In 2013, Ramot et al. found that treating human skin culture with the CB1-specific agonist arachidonoyl-chloro-ethanolamide reduced the expression of keratins K6 and K16 in vitro and in situ, which may have implications for psoriasis treatment as K6 and K16 are upregulated in that disorder.10 The same team has also recently shown that the CB1 agonist arachidonyl-2’-chloroethylamide upregulated K10 protein expression in human epidermis and reduced K1 in human skin culture thus suggesting its potential as a treatment for epidermolytic ichthyosis.11
Notably, the synthetic cannabinoid JWH-133, known for its potent antiangiogenic and anti-inflammatory properties, has been shown in vivo and in vitro to suppress various inflammatory cytokines and angiogenic growth factors involved in psoriasis pathogenesis, including hypoxia inducible factor-1 alpha (HIF-1 alpha), vascular endothelial growth factor (VEGF), matrix metalloproteinases, basic fibroblast growth factor (bFGF), angiopoietin-2, interleukin-8 (IL-8), IL-17, and IL-2. While more research is necessary to determine the safety and efficacy of this product, it appears promising as an anti-psoriatic agent.12
Pruritus
Stimulation of the CB1 receptor has been demonstrated to inhibit histamine-induced pruritus.8
In 2005, Szepietowski et al. conducted a preliminary study to ascertain the efficacy and tolerance of a cream with structured physiological lipids and endogenous cannabinoids in managing pruritus in 21 patients on maintenance dialysis. For 3 weeks, the patients with uremic pruritus applied the test cream twice daily, with eight patients experiencing full eradication of pruritus at the end of this period. Further, xerosis was completely eliminated in 17 patients after the study, and significantly decreased during the 3-week period. The investigators suggested that while more research was needed, the well-tolerated product is thought to have been enhanced by the addition of endocannabinoids.13
A year later, Ständer et al. assessed the effects of the use of the topical cannabinoid agonist N-palmitoyl ethanolamine (PEA), which stimulates the endocannabinoid arachidonoyl ethanolamide (AEA) to activate CB1, in an open application study with 22 patients with prurigo, lichen simplex, and pruritus. Antipruritic benefits were seen in 14 patients, with an average decrease in itch of 86.4%. The treatment was reported to be well tolerated, as no patients complained of adverse effects such as contact dermatitis or a burning sensation.14
Eczematic dermatoses
Atopic dermatitis
In a small pilot study on pediatric atopic dermatitis in 2007, Pulvirenti et al. evaluated the safety and efficacy of the twice-daily application of a topical emulsion containing a synthetic aliamide (adelmidrol 2%), comparable to its parent substance PEA, in the treatment of 11 males and 9 females with atopic dermatitis (AD), whose mean age was 8 years. Among the 20 pediatric patients, 16 experienced complete resolution of symptoms after 4 weeks of treatment and had no relapses at the 8-week follow-up assessment. No improvement was noted in the six patches of AD in six patients with several untreated lesions that served as controls.15 Also in 2007, Del Rosso reported on a trial in which a PEA-containing nonsteroidal cream significantly lowered the mean time between flares in pediatric and adult AD patients.16
One year later, Eberlein et al. evaluated an emollient containing PEA in AD patients, finding that itch severity and sleep loss were improved by an average of 60%, with 38% of participants stopping oral antihistamines, 33.6% discontinuing topical steroid regimens, and 20% ending their use of topical immunomodulators as the study concluded.4,17
In 2018, Río et al. suggested that targeted manipulation of the endocannabinoid system at various AD stages might rein in the inflammatory and immune responses and ensuing alterations in keratinocytes, thus helping to preserve epidermal barrier function.18 As Trusler et al. noted, though, no control groups were used in the latter two studies, so it is unknown what effect the application of the vehicle alone would have had on the pruritus in these patients.19
Allergic contact dermatitis
In 2007, Karsak et al. demonstrated that mice lacking CB1/2 receptors exhibited aggravated contact hypersensitivity, whereas mice with higher levels of AEA evinced lower cutaneous allergic responses.20
Recently, Petrosino et al. provided the first evidence that the nonpsychotropic cannabinoid cannabidiol conferred anti-inflammatory activity in an experimental in vitro model of allergic contact dermatitis.21
Dermatomyositis
Robinson et al. have found that treating blood samples of patients with dermatomyositis with the nonpsychoactive cannabinoid ajulemic acid appears to limit the production of pathogenic cytokines. They suggest that oral administration of this cannabinoid merits consideration for dermatomyositis.22
Skin cancer
In 2015, Glodde et al. used a mouse model to investigate the role of cannabinoids in skin cancer pathogenesis. They considered THC, which binds to CB1 and CB2, and the endogenous cannabinoid system. The researchers found that in a CB receptor-dependent fashion THC significantly hindered the tumor growth of HCmel12 melanomas in vivo, verifying the merit of exogenous cannabinoids in melanoma treatment. They did not identify a role of the endogenous cannabinoid system in skin cancer pathogenesis.23
Additional studies suggest that endocannabinoids, phytocannabinoids, and synthetic cannabinoids diminish skin cancer growth (melanoma and nonmelanoma) in vitro and in vivo through CB receptor-dependent and -independent pathways, though in vivo human studies have not yet been conducted.8,24
Epidermolysis bullosa
In a promising observational study in 2018, Chelliah et al. reported on three cases of self-initiated topical cannabidiol use in patients with epidermolysis bullosa. Each patient experienced more rapid wound healing, less blistering, and reduced pain as a result of cannabidiol treatment, and one was able to discontinue oral opioids. The authors were encouraged by such findings, but cautioned that randomized, double-blind clinical trials are needed to establish cannabidiol as an effective therapy.25
This seems particularly important given the climate of expanding legalization of medical and recreational cannabis use, as well as the increasing use of topical cannabinoids among dermatology patients.26 Nevertheless, it is important to be cognizant of one’s own state laws as topical cannabinoids may be restricted; these products are marketed for pain and pruritus on the Internet but are unavailable by prescription unless the physician has a special license.4
Attitudes about cannabinoid use in dermatology
In an intriguing study last year about the knowledge, cognizance, and perceptions of cannabinoids among dermatologists, Robinson et al. created a 20-question online survey that netted a response rate of 21% (n = 531). In terms of awareness, 29% of respondents did not know that THC is psychoactive and a significant majority (64%) did not know that CBD is not psychoactive. Nevertheless, the majority thought that cannabinoids should be legal for medical treatment (86%), and even more (94%) support researching dermatologic applications of cannabinoids. More responders (86%) would prescribe a Food and Drug Administration–approved cannabinoid-containing topical formulation than an oral product (71%). In also noting that 55% revealed at least one conversation about cannabinoids initiated by a patient in the previous year, while 48% expressed concern about a possible stigma associated with suggesting cannabinoid treatments to patients, Robinson et al. call for further education about the benefits and risks of cutaneous cannabinoids for dermatologists.27
Conclusion
It is important that we educate ourselves as to the effects of orally administered and topical products containing cannabis so that we are prepared for questions from patients. Data on psoriasis, pruritus, eczema, and acne warrant optimism and much additional research. Now that the FDA is allowing research sites to enroll for a special license to investigate schedule I drugs, we stand to learn much more about the various effects on the health benefits of cannabis. Despite the longstanding traditional use of C. sativa and C. indica, we are in the early stages of research on the impact of phytocannabinoids and synthetic cannabinoids on human health and the role that the endocannabinoid system plays. The extant findings provide reasons to consider the endocannabinoid system as a target for therapeutic intervention for various cutaneous disorders as research continues.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. She has no relevant disclosures related to this column. Write to her at dermnews@mdedge.com.
References
1. Russo EB. Chem Biodivers. 2007 Aug;4(8):1614-48.
2. Goldenberg M et al. Drug Alcohol Depend. 2017 May 1;174:80-90.
3. Mounessa JS et al. J Am Acad Dermatol. 2017 Jul;77(1):188-90.
4. Shalaby M et al. Pract Dermatol. 2018;68-70.
5. Oláh A et al. Exp Dermatol. 2016 Sep;25(9):701-7.
6. Ali A et al. Pak J Pharm Sci. 2015 Jul;28(4):1389-95.
7. Derakhshan N et al. Curr Clin Pharmacol. 2016;11(2):146-7.
8. Singh D et al. Clin Dermatol. 2018 May-Jun;36(3):399-419.
9. Wilkinson JD et al. J Dermatol Sci. 2007 Feb;45(2):87-92.
10. Ramot Y et al. PeerJ. 2013 Feb 19;1:e40.
11. Ramot Y et al. Br J Dermatol. 2018 Jun;178(6):1469.
12. Norooznezhad AH et al. Med Hypotheses. 2017 Feb;99:15-18.
13. Szepietowski JC et al. Acta Dermatovenerol Croat. 2005;13(2):97-103.
14. Ständer S et al. Hautarzt. 2006 Sep;57(9):801-7.
15. Pulvirenti N et al. Acta Dermatovenerol Croat. 2007;15(2):80-3.
16. Del Rosso JQ. Cosmetic Dermatol. 2007 Apr; 20(4):208-211.
17. Eberlein B et al. J Eur Acad Dermatol Venereol. 2008 Jan;22(1):73-82.
18. Del Río CD et al. Biochem Pharmacol. 2018 Nov;157:122-133.
19. Trusler AR et al. Dermatitis. 2017 Jan/Feb;28(1):22-32.
20. Karsak M et al. Science. 2007 Jun 8;316(5830):1494-7.
21. Petrosino S et al. J Pharmacol Exp Ther. 2018 Jun;365(3):652-63.
22. Robinson ES et al. J Invest Dermatol. 2017 Nov;137(11):2445-7.
23. Glodde N et al. Life Sci. 2015 Oct 1;138:35-40.
24. Soliman E. et al. J Dermatol Clin Res. 2016;4(2):1069-76.
25. Chelliah MP et al. Pediatr Dermatol. 2018 Jul;35(4):e224-e227.
26. Hashim PW et al. Cutis. 2017 Jul;100(1):50-52.
27. Robinson E et al. J Drugs Dermatol. 2018 Dec 1;17(12):1273-8.
The relatively recent discovery of the endogenous cannabinoid system and the quickly evolving, yet still convoluted, legal status of cannabis in the United States has spurred excitement over expanded research opportunities. Despite its checkered legal history, marijuana – derived from Cannabis sativa and Cannabis indica – has long been used for medical purposes and is one of the most widely used drugs throughout the world.1 Modern medicine has deployed this dynamic plant to treat chronic pain, glaucoma, and nausea, and continues to investigate its application in a broad array of conditions: anorexia, spasticity, atherosclerosis, autoimmune disorders, inflammatory bowel disease, multiple sclerosis, spasticity, tumorigenesis, and multiple cutaneous disorders, including acne, eczematous disorders, lichen simplex, melanoma and nonmelanoma skin cancer, melasma, prurigo, pruritus, psoriasis, scleroderma and systemic sclerosis, and seborrheic dermatitis.1-4 This .

Acne
Oláh et al. have demonstrated that the nonpsychotropic phytocannabinoid ((-)-cannabidiol [CBD]) imparts anti-acne benefits by diminishing sebaceous lipid synthesis, decreasing proliferation, and easing inflammation in human SZ95 sebocytes.5 In additional investigations of nonpsychotropic phytocannabinoids and their effects on human sebocyte function, they reported in 2016 that the phytocannabinoids (-)-cannabigerol [CBG] and (-)-cannabigerovarin (CBGV) appear to exhibit promise in treating xerotic and seborrheic skin, and ((-)-cannabichromene [CBC], (-)-cannabidivarin [CBDV], and (-)-delta9-tetrahydrocannabivarin [THCV], in particular, display notable potential as anti-acne ingredients. The investigators added that these compounds, due to their substantial anti-inflammatory effects, warrant consideration for use in treating skin inflammation.5 Previously, Ali and Akhtar conducted a single-blinded, 12-week comparative study in healthy male volunteers to evaluate the effects of twice-daily application of 3% cannabis seed extract cream on human cheek skin. The researchers found the base with 3% cannabis seed extract to be safe and effective, with skin sebum and erythema content on the treated side reduced significantly compared with the side treated only with the control base. They concluded that this well-tolerated formulation could be indicated for the treatment of acne and seborrhea to enhance facial appearance.6
Psoriasis
The endocannabinoid system itself is thought to play a potentially important role in the treatment of psoriasis, as interactions between the immune and nervous systems via cholinergic anti-inflammatory pathways are considered to be key in psoriasis etiology and the endocannabinoid system interacts with both systems through the cannabinoid (CB) receptors CB1 and CB2.7 Compared with normal human skin, psoriatic skin is characterized by fewer CB receptors.8
In 2007, Wilkinson and Williamson used a keratinocyte proliferation assay to study the phytocannabinoids delta9-tetrahydrocannabinol (THC), CBD, CBG, and cannabinol (CNB) to assess their capacity to halt the growth of a hyper-proliferating human keratinocyte cell line with an eye toward potential use in treating psoriasis. CB1 and CB2 receptors were confirmed present by Western blot and RT-PCR analyses. All cannabinoids investigated concentration-dependently hindered keratinocyte proliferation, as the authors concluded that these compounds show potential for use in psoriasis treatment.9
In 2013, Ramot et al. found that treating human skin culture with the CB1-specific agonist arachidonoyl-chloro-ethanolamide reduced the expression of keratins K6 and K16 in vitro and in situ, which may have implications for psoriasis treatment as K6 and K16 are upregulated in that disorder.10 The same team has also recently shown that the CB1 agonist arachidonyl-2’-chloroethylamide upregulated K10 protein expression in human epidermis and reduced K1 in human skin culture thus suggesting its potential as a treatment for epidermolytic ichthyosis.11
Notably, the synthetic cannabinoid JWH-133, known for its potent antiangiogenic and anti-inflammatory properties, has been shown in vivo and in vitro to suppress various inflammatory cytokines and angiogenic growth factors involved in psoriasis pathogenesis, including hypoxia inducible factor-1 alpha (HIF-1 alpha), vascular endothelial growth factor (VEGF), matrix metalloproteinases, basic fibroblast growth factor (bFGF), angiopoietin-2, interleukin-8 (IL-8), IL-17, and IL-2. While more research is necessary to determine the safety and efficacy of this product, it appears promising as an anti-psoriatic agent.12
Pruritus
Stimulation of the CB1 receptor has been demonstrated to inhibit histamine-induced pruritus.8
In 2005, Szepietowski et al. conducted a preliminary study to ascertain the efficacy and tolerance of a cream with structured physiological lipids and endogenous cannabinoids in managing pruritus in 21 patients on maintenance dialysis. For 3 weeks, the patients with uremic pruritus applied the test cream twice daily, with eight patients experiencing full eradication of pruritus at the end of this period. Further, xerosis was completely eliminated in 17 patients after the study, and significantly decreased during the 3-week period. The investigators suggested that while more research was needed, the well-tolerated product is thought to have been enhanced by the addition of endocannabinoids.13
A year later, Ständer et al. assessed the effects of the use of the topical cannabinoid agonist N-palmitoyl ethanolamine (PEA), which stimulates the endocannabinoid arachidonoyl ethanolamide (AEA) to activate CB1, in an open application study with 22 patients with prurigo, lichen simplex, and pruritus. Antipruritic benefits were seen in 14 patients, with an average decrease in itch of 86.4%. The treatment was reported to be well tolerated, as no patients complained of adverse effects such as contact dermatitis or a burning sensation.14
Eczematic dermatoses
Atopic dermatitis
In a small pilot study on pediatric atopic dermatitis in 2007, Pulvirenti et al. evaluated the safety and efficacy of the twice-daily application of a topical emulsion containing a synthetic aliamide (adelmidrol 2%), comparable to its parent substance PEA, in the treatment of 11 males and 9 females with atopic dermatitis (AD), whose mean age was 8 years. Among the 20 pediatric patients, 16 experienced complete resolution of symptoms after 4 weeks of treatment and had no relapses at the 8-week follow-up assessment. No improvement was noted in the six patches of AD in six patients with several untreated lesions that served as controls.15 Also in 2007, Del Rosso reported on a trial in which a PEA-containing nonsteroidal cream significantly lowered the mean time between flares in pediatric and adult AD patients.16
One year later, Eberlein et al. evaluated an emollient containing PEA in AD patients, finding that itch severity and sleep loss were improved by an average of 60%, with 38% of participants stopping oral antihistamines, 33.6% discontinuing topical steroid regimens, and 20% ending their use of topical immunomodulators as the study concluded.4,17
In 2018, Río et al. suggested that targeted manipulation of the endocannabinoid system at various AD stages might rein in the inflammatory and immune responses and ensuing alterations in keratinocytes, thus helping to preserve epidermal barrier function.18 As Trusler et al. noted, though, no control groups were used in the latter two studies, so it is unknown what effect the application of the vehicle alone would have had on the pruritus in these patients.19
Allergic contact dermatitis
In 2007, Karsak et al. demonstrated that mice lacking CB1/2 receptors exhibited aggravated contact hypersensitivity, whereas mice with higher levels of AEA evinced lower cutaneous allergic responses.20
Recently, Petrosino et al. provided the first evidence that the nonpsychotropic cannabinoid cannabidiol conferred anti-inflammatory activity in an experimental in vitro model of allergic contact dermatitis.21
Dermatomyositis
Robinson et al. have found that treating blood samples of patients with dermatomyositis with the nonpsychoactive cannabinoid ajulemic acid appears to limit the production of pathogenic cytokines. They suggest that oral administration of this cannabinoid merits consideration for dermatomyositis.22
Skin cancer
In 2015, Glodde et al. used a mouse model to investigate the role of cannabinoids in skin cancer pathogenesis. They considered THC, which binds to CB1 and CB2, and the endogenous cannabinoid system. The researchers found that in a CB receptor-dependent fashion THC significantly hindered the tumor growth of HCmel12 melanomas in vivo, verifying the merit of exogenous cannabinoids in melanoma treatment. They did not identify a role of the endogenous cannabinoid system in skin cancer pathogenesis.23
Additional studies suggest that endocannabinoids, phytocannabinoids, and synthetic cannabinoids diminish skin cancer growth (melanoma and nonmelanoma) in vitro and in vivo through CB receptor-dependent and -independent pathways, though in vivo human studies have not yet been conducted.8,24
Epidermolysis bullosa
In a promising observational study in 2018, Chelliah et al. reported on three cases of self-initiated topical cannabidiol use in patients with epidermolysis bullosa. Each patient experienced more rapid wound healing, less blistering, and reduced pain as a result of cannabidiol treatment, and one was able to discontinue oral opioids. The authors were encouraged by such findings, but cautioned that randomized, double-blind clinical trials are needed to establish cannabidiol as an effective therapy.25
This seems particularly important given the climate of expanding legalization of medical and recreational cannabis use, as well as the increasing use of topical cannabinoids among dermatology patients.26 Nevertheless, it is important to be cognizant of one’s own state laws as topical cannabinoids may be restricted; these products are marketed for pain and pruritus on the Internet but are unavailable by prescription unless the physician has a special license.4
Attitudes about cannabinoid use in dermatology
In an intriguing study last year about the knowledge, cognizance, and perceptions of cannabinoids among dermatologists, Robinson et al. created a 20-question online survey that netted a response rate of 21% (n = 531). In terms of awareness, 29% of respondents did not know that THC is psychoactive and a significant majority (64%) did not know that CBD is not psychoactive. Nevertheless, the majority thought that cannabinoids should be legal for medical treatment (86%), and even more (94%) support researching dermatologic applications of cannabinoids. More responders (86%) would prescribe a Food and Drug Administration–approved cannabinoid-containing topical formulation than an oral product (71%). In also noting that 55% revealed at least one conversation about cannabinoids initiated by a patient in the previous year, while 48% expressed concern about a possible stigma associated with suggesting cannabinoid treatments to patients, Robinson et al. call for further education about the benefits and risks of cutaneous cannabinoids for dermatologists.27
Conclusion
It is important that we educate ourselves as to the effects of orally administered and topical products containing cannabis so that we are prepared for questions from patients. Data on psoriasis, pruritus, eczema, and acne warrant optimism and much additional research. Now that the FDA is allowing research sites to enroll for a special license to investigate schedule I drugs, we stand to learn much more about the various effects on the health benefits of cannabis. Despite the longstanding traditional use of C. sativa and C. indica, we are in the early stages of research on the impact of phytocannabinoids and synthetic cannabinoids on human health and the role that the endocannabinoid system plays. The extant findings provide reasons to consider the endocannabinoid system as a target for therapeutic intervention for various cutaneous disorders as research continues.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. She has no relevant disclosures related to this column. Write to her at dermnews@mdedge.com.
References
1. Russo EB. Chem Biodivers. 2007 Aug;4(8):1614-48.
2. Goldenberg M et al. Drug Alcohol Depend. 2017 May 1;174:80-90.
3. Mounessa JS et al. J Am Acad Dermatol. 2017 Jul;77(1):188-90.
4. Shalaby M et al. Pract Dermatol. 2018;68-70.
5. Oláh A et al. Exp Dermatol. 2016 Sep;25(9):701-7.
6. Ali A et al. Pak J Pharm Sci. 2015 Jul;28(4):1389-95.
7. Derakhshan N et al. Curr Clin Pharmacol. 2016;11(2):146-7.
8. Singh D et al. Clin Dermatol. 2018 May-Jun;36(3):399-419.
9. Wilkinson JD et al. J Dermatol Sci. 2007 Feb;45(2):87-92.
10. Ramot Y et al. PeerJ. 2013 Feb 19;1:e40.
11. Ramot Y et al. Br J Dermatol. 2018 Jun;178(6):1469.
12. Norooznezhad AH et al. Med Hypotheses. 2017 Feb;99:15-18.
13. Szepietowski JC et al. Acta Dermatovenerol Croat. 2005;13(2):97-103.
14. Ständer S et al. Hautarzt. 2006 Sep;57(9):801-7.
15. Pulvirenti N et al. Acta Dermatovenerol Croat. 2007;15(2):80-3.
16. Del Rosso JQ. Cosmetic Dermatol. 2007 Apr; 20(4):208-211.
17. Eberlein B et al. J Eur Acad Dermatol Venereol. 2008 Jan;22(1):73-82.
18. Del Río CD et al. Biochem Pharmacol. 2018 Nov;157:122-133.
19. Trusler AR et al. Dermatitis. 2017 Jan/Feb;28(1):22-32.
20. Karsak M et al. Science. 2007 Jun 8;316(5830):1494-7.
21. Petrosino S et al. J Pharmacol Exp Ther. 2018 Jun;365(3):652-63.
22. Robinson ES et al. J Invest Dermatol. 2017 Nov;137(11):2445-7.
23. Glodde N et al. Life Sci. 2015 Oct 1;138:35-40.
24. Soliman E. et al. J Dermatol Clin Res. 2016;4(2):1069-76.
25. Chelliah MP et al. Pediatr Dermatol. 2018 Jul;35(4):e224-e227.
26. Hashim PW et al. Cutis. 2017 Jul;100(1):50-52.
27. Robinson E et al. J Drugs Dermatol. 2018 Dec 1;17(12):1273-8.
The relatively recent discovery of the endogenous cannabinoid system and the quickly evolving, yet still convoluted, legal status of cannabis in the United States has spurred excitement over expanded research opportunities. Despite its checkered legal history, marijuana – derived from Cannabis sativa and Cannabis indica – has long been used for medical purposes and is one of the most widely used drugs throughout the world.1 Modern medicine has deployed this dynamic plant to treat chronic pain, glaucoma, and nausea, and continues to investigate its application in a broad array of conditions: anorexia, spasticity, atherosclerosis, autoimmune disorders, inflammatory bowel disease, multiple sclerosis, spasticity, tumorigenesis, and multiple cutaneous disorders, including acne, eczematous disorders, lichen simplex, melanoma and nonmelanoma skin cancer, melasma, prurigo, pruritus, psoriasis, scleroderma and systemic sclerosis, and seborrheic dermatitis.1-4 This .

Acne
Oláh et al. have demonstrated that the nonpsychotropic phytocannabinoid ((-)-cannabidiol [CBD]) imparts anti-acne benefits by diminishing sebaceous lipid synthesis, decreasing proliferation, and easing inflammation in human SZ95 sebocytes.5 In additional investigations of nonpsychotropic phytocannabinoids and their effects on human sebocyte function, they reported in 2016 that the phytocannabinoids (-)-cannabigerol [CBG] and (-)-cannabigerovarin (CBGV) appear to exhibit promise in treating xerotic and seborrheic skin, and ((-)-cannabichromene [CBC], (-)-cannabidivarin [CBDV], and (-)-delta9-tetrahydrocannabivarin [THCV], in particular, display notable potential as anti-acne ingredients. The investigators added that these compounds, due to their substantial anti-inflammatory effects, warrant consideration for use in treating skin inflammation.5 Previously, Ali and Akhtar conducted a single-blinded, 12-week comparative study in healthy male volunteers to evaluate the effects of twice-daily application of 3% cannabis seed extract cream on human cheek skin. The researchers found the base with 3% cannabis seed extract to be safe and effective, with skin sebum and erythema content on the treated side reduced significantly compared with the side treated only with the control base. They concluded that this well-tolerated formulation could be indicated for the treatment of acne and seborrhea to enhance facial appearance.6
Psoriasis
The endocannabinoid system itself is thought to play a potentially important role in the treatment of psoriasis, as interactions between the immune and nervous systems via cholinergic anti-inflammatory pathways are considered to be key in psoriasis etiology and the endocannabinoid system interacts with both systems through the cannabinoid (CB) receptors CB1 and CB2.7 Compared with normal human skin, psoriatic skin is characterized by fewer CB receptors.8
In 2007, Wilkinson and Williamson used a keratinocyte proliferation assay to study the phytocannabinoids delta9-tetrahydrocannabinol (THC), CBD, CBG, and cannabinol (CNB) to assess their capacity to halt the growth of a hyper-proliferating human keratinocyte cell line with an eye toward potential use in treating psoriasis. CB1 and CB2 receptors were confirmed present by Western blot and RT-PCR analyses. All cannabinoids investigated concentration-dependently hindered keratinocyte proliferation, as the authors concluded that these compounds show potential for use in psoriasis treatment.9
In 2013, Ramot et al. found that treating human skin culture with the CB1-specific agonist arachidonoyl-chloro-ethanolamide reduced the expression of keratins K6 and K16 in vitro and in situ, which may have implications for psoriasis treatment as K6 and K16 are upregulated in that disorder.10 The same team has also recently shown that the CB1 agonist arachidonyl-2’-chloroethylamide upregulated K10 protein expression in human epidermis and reduced K1 in human skin culture thus suggesting its potential as a treatment for epidermolytic ichthyosis.11
Notably, the synthetic cannabinoid JWH-133, known for its potent antiangiogenic and anti-inflammatory properties, has been shown in vivo and in vitro to suppress various inflammatory cytokines and angiogenic growth factors involved in psoriasis pathogenesis, including hypoxia inducible factor-1 alpha (HIF-1 alpha), vascular endothelial growth factor (VEGF), matrix metalloproteinases, basic fibroblast growth factor (bFGF), angiopoietin-2, interleukin-8 (IL-8), IL-17, and IL-2. While more research is necessary to determine the safety and efficacy of this product, it appears promising as an anti-psoriatic agent.12
Pruritus
Stimulation of the CB1 receptor has been demonstrated to inhibit histamine-induced pruritus.8
In 2005, Szepietowski et al. conducted a preliminary study to ascertain the efficacy and tolerance of a cream with structured physiological lipids and endogenous cannabinoids in managing pruritus in 21 patients on maintenance dialysis. For 3 weeks, the patients with uremic pruritus applied the test cream twice daily, with eight patients experiencing full eradication of pruritus at the end of this period. Further, xerosis was completely eliminated in 17 patients after the study, and significantly decreased during the 3-week period. The investigators suggested that while more research was needed, the well-tolerated product is thought to have been enhanced by the addition of endocannabinoids.13
A year later, Ständer et al. assessed the effects of the use of the topical cannabinoid agonist N-palmitoyl ethanolamine (PEA), which stimulates the endocannabinoid arachidonoyl ethanolamide (AEA) to activate CB1, in an open application study with 22 patients with prurigo, lichen simplex, and pruritus. Antipruritic benefits were seen in 14 patients, with an average decrease in itch of 86.4%. The treatment was reported to be well tolerated, as no patients complained of adverse effects such as contact dermatitis or a burning sensation.14
Eczematic dermatoses
Atopic dermatitis
In a small pilot study on pediatric atopic dermatitis in 2007, Pulvirenti et al. evaluated the safety and efficacy of the twice-daily application of a topical emulsion containing a synthetic aliamide (adelmidrol 2%), comparable to its parent substance PEA, in the treatment of 11 males and 9 females with atopic dermatitis (AD), whose mean age was 8 years. Among the 20 pediatric patients, 16 experienced complete resolution of symptoms after 4 weeks of treatment and had no relapses at the 8-week follow-up assessment. No improvement was noted in the six patches of AD in six patients with several untreated lesions that served as controls.15 Also in 2007, Del Rosso reported on a trial in which a PEA-containing nonsteroidal cream significantly lowered the mean time between flares in pediatric and adult AD patients.16
One year later, Eberlein et al. evaluated an emollient containing PEA in AD patients, finding that itch severity and sleep loss were improved by an average of 60%, with 38% of participants stopping oral antihistamines, 33.6% discontinuing topical steroid regimens, and 20% ending their use of topical immunomodulators as the study concluded.4,17
In 2018, Río et al. suggested that targeted manipulation of the endocannabinoid system at various AD stages might rein in the inflammatory and immune responses and ensuing alterations in keratinocytes, thus helping to preserve epidermal barrier function.18 As Trusler et al. noted, though, no control groups were used in the latter two studies, so it is unknown what effect the application of the vehicle alone would have had on the pruritus in these patients.19
Allergic contact dermatitis
In 2007, Karsak et al. demonstrated that mice lacking CB1/2 receptors exhibited aggravated contact hypersensitivity, whereas mice with higher levels of AEA evinced lower cutaneous allergic responses.20
Recently, Petrosino et al. provided the first evidence that the nonpsychotropic cannabinoid cannabidiol conferred anti-inflammatory activity in an experimental in vitro model of allergic contact dermatitis.21
Dermatomyositis
Robinson et al. have found that treating blood samples of patients with dermatomyositis with the nonpsychoactive cannabinoid ajulemic acid appears to limit the production of pathogenic cytokines. They suggest that oral administration of this cannabinoid merits consideration for dermatomyositis.22
Skin cancer
In 2015, Glodde et al. used a mouse model to investigate the role of cannabinoids in skin cancer pathogenesis. They considered THC, which binds to CB1 and CB2, and the endogenous cannabinoid system. The researchers found that in a CB receptor-dependent fashion THC significantly hindered the tumor growth of HCmel12 melanomas in vivo, verifying the merit of exogenous cannabinoids in melanoma treatment. They did not identify a role of the endogenous cannabinoid system in skin cancer pathogenesis.23
Additional studies suggest that endocannabinoids, phytocannabinoids, and synthetic cannabinoids diminish skin cancer growth (melanoma and nonmelanoma) in vitro and in vivo through CB receptor-dependent and -independent pathways, though in vivo human studies have not yet been conducted.8,24
Epidermolysis bullosa
In a promising observational study in 2018, Chelliah et al. reported on three cases of self-initiated topical cannabidiol use in patients with epidermolysis bullosa. Each patient experienced more rapid wound healing, less blistering, and reduced pain as a result of cannabidiol treatment, and one was able to discontinue oral opioids. The authors were encouraged by such findings, but cautioned that randomized, double-blind clinical trials are needed to establish cannabidiol as an effective therapy.25
This seems particularly important given the climate of expanding legalization of medical and recreational cannabis use, as well as the increasing use of topical cannabinoids among dermatology patients.26 Nevertheless, it is important to be cognizant of one’s own state laws as topical cannabinoids may be restricted; these products are marketed for pain and pruritus on the Internet but are unavailable by prescription unless the physician has a special license.4
Attitudes about cannabinoid use in dermatology
In an intriguing study last year about the knowledge, cognizance, and perceptions of cannabinoids among dermatologists, Robinson et al. created a 20-question online survey that netted a response rate of 21% (n = 531). In terms of awareness, 29% of respondents did not know that THC is psychoactive and a significant majority (64%) did not know that CBD is not psychoactive. Nevertheless, the majority thought that cannabinoids should be legal for medical treatment (86%), and even more (94%) support researching dermatologic applications of cannabinoids. More responders (86%) would prescribe a Food and Drug Administration–approved cannabinoid-containing topical formulation than an oral product (71%). In also noting that 55% revealed at least one conversation about cannabinoids initiated by a patient in the previous year, while 48% expressed concern about a possible stigma associated with suggesting cannabinoid treatments to patients, Robinson et al. call for further education about the benefits and risks of cutaneous cannabinoids for dermatologists.27
Conclusion
It is important that we educate ourselves as to the effects of orally administered and topical products containing cannabis so that we are prepared for questions from patients. Data on psoriasis, pruritus, eczema, and acne warrant optimism and much additional research. Now that the FDA is allowing research sites to enroll for a special license to investigate schedule I drugs, we stand to learn much more about the various effects on the health benefits of cannabis. Despite the longstanding traditional use of C. sativa and C. indica, we are in the early stages of research on the impact of phytocannabinoids and synthetic cannabinoids on human health and the role that the endocannabinoid system plays. The extant findings provide reasons to consider the endocannabinoid system as a target for therapeutic intervention for various cutaneous disorders as research continues.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. She has no relevant disclosures related to this column. Write to her at dermnews@mdedge.com.
References
1. Russo EB. Chem Biodivers. 2007 Aug;4(8):1614-48.
2. Goldenberg M et al. Drug Alcohol Depend. 2017 May 1;174:80-90.
3. Mounessa JS et al. J Am Acad Dermatol. 2017 Jul;77(1):188-90.
4. Shalaby M et al. Pract Dermatol. 2018;68-70.
5. Oláh A et al. Exp Dermatol. 2016 Sep;25(9):701-7.
6. Ali A et al. Pak J Pharm Sci. 2015 Jul;28(4):1389-95.
7. Derakhshan N et al. Curr Clin Pharmacol. 2016;11(2):146-7.
8. Singh D et al. Clin Dermatol. 2018 May-Jun;36(3):399-419.
9. Wilkinson JD et al. J Dermatol Sci. 2007 Feb;45(2):87-92.
10. Ramot Y et al. PeerJ. 2013 Feb 19;1:e40.
11. Ramot Y et al. Br J Dermatol. 2018 Jun;178(6):1469.
12. Norooznezhad AH et al. Med Hypotheses. 2017 Feb;99:15-18.
13. Szepietowski JC et al. Acta Dermatovenerol Croat. 2005;13(2):97-103.
14. Ständer S et al. Hautarzt. 2006 Sep;57(9):801-7.
15. Pulvirenti N et al. Acta Dermatovenerol Croat. 2007;15(2):80-3.
16. Del Rosso JQ. Cosmetic Dermatol. 2007 Apr; 20(4):208-211.
17. Eberlein B et al. J Eur Acad Dermatol Venereol. 2008 Jan;22(1):73-82.
18. Del Río CD et al. Biochem Pharmacol. 2018 Nov;157:122-133.
19. Trusler AR et al. Dermatitis. 2017 Jan/Feb;28(1):22-32.
20. Karsak M et al. Science. 2007 Jun 8;316(5830):1494-7.
21. Petrosino S et al. J Pharmacol Exp Ther. 2018 Jun;365(3):652-63.
22. Robinson ES et al. J Invest Dermatol. 2017 Nov;137(11):2445-7.
23. Glodde N et al. Life Sci. 2015 Oct 1;138:35-40.
24. Soliman E. et al. J Dermatol Clin Res. 2016;4(2):1069-76.
25. Chelliah MP et al. Pediatr Dermatol. 2018 Jul;35(4):e224-e227.
26. Hashim PW et al. Cutis. 2017 Jul;100(1):50-52.
27. Robinson E et al. J Drugs Dermatol. 2018 Dec 1;17(12):1273-8.
Methotrexate does not cause rheumatoid interstitial lung disease
BIRMINGHAM, ENGLAND – Data from two early RA inception cohorts provide reassurance that methotrexate does not cause interstitial lung disease and suggest that treatment with methotrexate might even be protective.
In the Early RA Study (ERAS) and Early RA Network (ERAN), which together include 2,701 patients with RA, 101 (3.7%) had interstitial lung disease (ILD). There were 92 patients with RA-ILD who had information available on exposure to any conventional synthetic disease-modifying antirheumatic drug (csDMARD); of these, 39 (2.5%) had been exposed to methotrexate (n = 1,578) and 53 (4.8%) to other csDMARDs (n = 1,114).
Multivariate analysis showed that methotrexate exposure was associated with a reduced risk of developing ILD, with an odds ratio of 0.48 (P = .004). In a separate analysis that excluded 25 patients who had ILD before they received any csDMARD therapy (n = 67), there was no association between methotrexate use and ILD (OR, 0.85; P = .578). In fact, there was a nonsignificant trend for a delayed onset of ILD in patients who had been treated with methotrexate (OR, 0.54; P = .072).
Methotrexate use is associated with an acute hypersensitivity pneumonitis in patients with RA, explained Patrick Kiely, MBBS, PhD, of St. George’s University Hospitals NHS Foundation Trust in London at the British Society for Rheumatology annual conference. “This is well recognized, it’s very rare [0.43%-1.00%], it’s easy to spot, and usually goes away if you stop methotrexate,” said Dr. Kiely, adding that “it’s not benign, and severe cases can be life threatening.”
Because of the association between methotrexate and pneumonitis, there has been concern that methotrexate may exacerbate or even cause ILD in RA but there are sparse data available to confirm this. The bottom line is that you should not start someone on methotrexate if you think their existing lung capacity is not up to treatment with methotrexate, Dr. Kiely said.
ILD is not always symptomatic in RA, but when it is, it is associated with very poor survival. The lung disease can be present before joint symptoms, Dr. Kiely said. Although less than 10% of cases may be symptomatic, this “is a big deal, because it has a high mortality, with death within 5 years. It’s the second-commonest cause of excess mortality in RA after cardiovascular disease.”
To look at the association between incident RA-ILD and the use of methotrexate, Dr. Kiely and associates analyzed data from ERAS (1986-2001) and ERAN (2002-2013), that together have more than 25 years of follow-up data on patients who were recruited at the first sign of RA symptoms. Patients within these cohorts have been treated according to best practice, and a range of outcomes – including RA-ILD – have been assessed at annual intervals.
In the patients who developed ILD after any csDMARD exposure, older age at RA onset (OR, 1.04; P less than .001) and having ever smoked (OR, 1.91; P = .016) were associated with the development of the lung disease. Incident ILD was also associated with being positive for rheumatoid factor (OR, 2.02; P = .029) at baseline. Being male was also associated with a higher risk for developing ILD, Dr. Kiely reported, as was a longer duration of time between the onset of first RA symptoms and the first secondary care visit. Conversely, the presence of nonrespiratory, major comorbidities at baseline appeared to be protective (OR, 0.62; P = .027).
“We found no association between methotrexate treatment and incident RA-ILD and a possibility that it may be protective,” Dr. Kiely concluded, noting that these data were now published in BMJ Open (2019;9:e028466. doi: 10.1136/bmjopen-2018-028466).
Following Dr. Kiely’s presentation, an audience member asked if the protective effect seen with methotrexate could have been caused by better disease control overall.
Dr. Kiely answered that, up until 2001, the time when ERAS was ongoing, standard practice in the United Kingdom was to use sulfasalazine, but then methotrexate started to be used in higher and higher doses, as seen in ERAN.
The interesting thing is that in ERAN more methotrexate was used in higher doses, but less RA-ILD was seen, Dr. Kiely observed. The overall prevalence of RA-ILD in the later early RA cohort was 3.2% and the median dose of methotrexate used was 20 mg. In ERAS, the prevalence was 4.2% and the median dose of methotrexate used was 10 mg.
There was a suggestion that disease control was slightly better in ERAN than ERAS, but that wasn’t statistically significant, Dr. Kiely said.
So, should a patient with RA and ILD be given methotrexate? There’s no reason not to, Dr. Kiely suggested, based on the evidence shown. Part of the challenge will now be convincing chest physician colleagues that methotrexate is not problematic in terms of causing ILD.
These findings are completely on board with the ILD group’s findings that methotrexate doesn’t cause pulmonary fibrosis in patients with RA, commented Julie Dawson, MD, of St. Helens and Knowsley Teaching Hospitals NHS Trust, St. Helens, England. Her own research, which includes a 10-year follow-up of patients with inflammatory arthritis, has shown that methotrexate does not appear to increase the risk of pulmonary fibrosis.
The study had no specific outside funding. Dr. Kiely reported having no conflicts of interest.
SOURCE: Kiely P et al. Rheumatology. 2019;58(suppl 3), Abstract 009.
BIRMINGHAM, ENGLAND – Data from two early RA inception cohorts provide reassurance that methotrexate does not cause interstitial lung disease and suggest that treatment with methotrexate might even be protective.
In the Early RA Study (ERAS) and Early RA Network (ERAN), which together include 2,701 patients with RA, 101 (3.7%) had interstitial lung disease (ILD). There were 92 patients with RA-ILD who had information available on exposure to any conventional synthetic disease-modifying antirheumatic drug (csDMARD); of these, 39 (2.5%) had been exposed to methotrexate (n = 1,578) and 53 (4.8%) to other csDMARDs (n = 1,114).
Multivariate analysis showed that methotrexate exposure was associated with a reduced risk of developing ILD, with an odds ratio of 0.48 (P = .004). In a separate analysis that excluded 25 patients who had ILD before they received any csDMARD therapy (n = 67), there was no association between methotrexate use and ILD (OR, 0.85; P = .578). In fact, there was a nonsignificant trend for a delayed onset of ILD in patients who had been treated with methotrexate (OR, 0.54; P = .072).
Methotrexate use is associated with an acute hypersensitivity pneumonitis in patients with RA, explained Patrick Kiely, MBBS, PhD, of St. George’s University Hospitals NHS Foundation Trust in London at the British Society for Rheumatology annual conference. “This is well recognized, it’s very rare [0.43%-1.00%], it’s easy to spot, and usually goes away if you stop methotrexate,” said Dr. Kiely, adding that “it’s not benign, and severe cases can be life threatening.”
Because of the association between methotrexate and pneumonitis, there has been concern that methotrexate may exacerbate or even cause ILD in RA but there are sparse data available to confirm this. The bottom line is that you should not start someone on methotrexate if you think their existing lung capacity is not up to treatment with methotrexate, Dr. Kiely said.
ILD is not always symptomatic in RA, but when it is, it is associated with very poor survival. The lung disease can be present before joint symptoms, Dr. Kiely said. Although less than 10% of cases may be symptomatic, this “is a big deal, because it has a high mortality, with death within 5 years. It’s the second-commonest cause of excess mortality in RA after cardiovascular disease.”
To look at the association between incident RA-ILD and the use of methotrexate, Dr. Kiely and associates analyzed data from ERAS (1986-2001) and ERAN (2002-2013), that together have more than 25 years of follow-up data on patients who were recruited at the first sign of RA symptoms. Patients within these cohorts have been treated according to best practice, and a range of outcomes – including RA-ILD – have been assessed at annual intervals.
In the patients who developed ILD after any csDMARD exposure, older age at RA onset (OR, 1.04; P less than .001) and having ever smoked (OR, 1.91; P = .016) were associated with the development of the lung disease. Incident ILD was also associated with being positive for rheumatoid factor (OR, 2.02; P = .029) at baseline. Being male was also associated with a higher risk for developing ILD, Dr. Kiely reported, as was a longer duration of time between the onset of first RA symptoms and the first secondary care visit. Conversely, the presence of nonrespiratory, major comorbidities at baseline appeared to be protective (OR, 0.62; P = .027).
“We found no association between methotrexate treatment and incident RA-ILD and a possibility that it may be protective,” Dr. Kiely concluded, noting that these data were now published in BMJ Open (2019;9:e028466. doi: 10.1136/bmjopen-2018-028466).
Following Dr. Kiely’s presentation, an audience member asked if the protective effect seen with methotrexate could have been caused by better disease control overall.
Dr. Kiely answered that, up until 2001, the time when ERAS was ongoing, standard practice in the United Kingdom was to use sulfasalazine, but then methotrexate started to be used in higher and higher doses, as seen in ERAN.
The interesting thing is that in ERAN more methotrexate was used in higher doses, but less RA-ILD was seen, Dr. Kiely observed. The overall prevalence of RA-ILD in the later early RA cohort was 3.2% and the median dose of methotrexate used was 20 mg. In ERAS, the prevalence was 4.2% and the median dose of methotrexate used was 10 mg.
There was a suggestion that disease control was slightly better in ERAN than ERAS, but that wasn’t statistically significant, Dr. Kiely said.
So, should a patient with RA and ILD be given methotrexate? There’s no reason not to, Dr. Kiely suggested, based on the evidence shown. Part of the challenge will now be convincing chest physician colleagues that methotrexate is not problematic in terms of causing ILD.
These findings are completely on board with the ILD group’s findings that methotrexate doesn’t cause pulmonary fibrosis in patients with RA, commented Julie Dawson, MD, of St. Helens and Knowsley Teaching Hospitals NHS Trust, St. Helens, England. Her own research, which includes a 10-year follow-up of patients with inflammatory arthritis, has shown that methotrexate does not appear to increase the risk of pulmonary fibrosis.
The study had no specific outside funding. Dr. Kiely reported having no conflicts of interest.
SOURCE: Kiely P et al. Rheumatology. 2019;58(suppl 3), Abstract 009.
BIRMINGHAM, ENGLAND – Data from two early RA inception cohorts provide reassurance that methotrexate does not cause interstitial lung disease and suggest that treatment with methotrexate might even be protective.
In the Early RA Study (ERAS) and Early RA Network (ERAN), which together include 2,701 patients with RA, 101 (3.7%) had interstitial lung disease (ILD). There were 92 patients with RA-ILD who had information available on exposure to any conventional synthetic disease-modifying antirheumatic drug (csDMARD); of these, 39 (2.5%) had been exposed to methotrexate (n = 1,578) and 53 (4.8%) to other csDMARDs (n = 1,114).
Multivariate analysis showed that methotrexate exposure was associated with a reduced risk of developing ILD, with an odds ratio of 0.48 (P = .004). In a separate analysis that excluded 25 patients who had ILD before they received any csDMARD therapy (n = 67), there was no association between methotrexate use and ILD (OR, 0.85; P = .578). In fact, there was a nonsignificant trend for a delayed onset of ILD in patients who had been treated with methotrexate (OR, 0.54; P = .072).
Methotrexate use is associated with an acute hypersensitivity pneumonitis in patients with RA, explained Patrick Kiely, MBBS, PhD, of St. George’s University Hospitals NHS Foundation Trust in London at the British Society for Rheumatology annual conference. “This is well recognized, it’s very rare [0.43%-1.00%], it’s easy to spot, and usually goes away if you stop methotrexate,” said Dr. Kiely, adding that “it’s not benign, and severe cases can be life threatening.”
Because of the association between methotrexate and pneumonitis, there has been concern that methotrexate may exacerbate or even cause ILD in RA but there are sparse data available to confirm this. The bottom line is that you should not start someone on methotrexate if you think their existing lung capacity is not up to treatment with methotrexate, Dr. Kiely said.
ILD is not always symptomatic in RA, but when it is, it is associated with very poor survival. The lung disease can be present before joint symptoms, Dr. Kiely said. Although less than 10% of cases may be symptomatic, this “is a big deal, because it has a high mortality, with death within 5 years. It’s the second-commonest cause of excess mortality in RA after cardiovascular disease.”
To look at the association between incident RA-ILD and the use of methotrexate, Dr. Kiely and associates analyzed data from ERAS (1986-2001) and ERAN (2002-2013), that together have more than 25 years of follow-up data on patients who were recruited at the first sign of RA symptoms. Patients within these cohorts have been treated according to best practice, and a range of outcomes – including RA-ILD – have been assessed at annual intervals.
In the patients who developed ILD after any csDMARD exposure, older age at RA onset (OR, 1.04; P less than .001) and having ever smoked (OR, 1.91; P = .016) were associated with the development of the lung disease. Incident ILD was also associated with being positive for rheumatoid factor (OR, 2.02; P = .029) at baseline. Being male was also associated with a higher risk for developing ILD, Dr. Kiely reported, as was a longer duration of time between the onset of first RA symptoms and the first secondary care visit. Conversely, the presence of nonrespiratory, major comorbidities at baseline appeared to be protective (OR, 0.62; P = .027).
“We found no association between methotrexate treatment and incident RA-ILD and a possibility that it may be protective,” Dr. Kiely concluded, noting that these data were now published in BMJ Open (2019;9:e028466. doi: 10.1136/bmjopen-2018-028466).
Following Dr. Kiely’s presentation, an audience member asked if the protective effect seen with methotrexate could have been caused by better disease control overall.
Dr. Kiely answered that, up until 2001, the time when ERAS was ongoing, standard practice in the United Kingdom was to use sulfasalazine, but then methotrexate started to be used in higher and higher doses, as seen in ERAN.
The interesting thing is that in ERAN more methotrexate was used in higher doses, but less RA-ILD was seen, Dr. Kiely observed. The overall prevalence of RA-ILD in the later early RA cohort was 3.2% and the median dose of methotrexate used was 20 mg. In ERAS, the prevalence was 4.2% and the median dose of methotrexate used was 10 mg.
There was a suggestion that disease control was slightly better in ERAN than ERAS, but that wasn’t statistically significant, Dr. Kiely said.
So, should a patient with RA and ILD be given methotrexate? There’s no reason not to, Dr. Kiely suggested, based on the evidence shown. Part of the challenge will now be convincing chest physician colleagues that methotrexate is not problematic in terms of causing ILD.
These findings are completely on board with the ILD group’s findings that methotrexate doesn’t cause pulmonary fibrosis in patients with RA, commented Julie Dawson, MD, of St. Helens and Knowsley Teaching Hospitals NHS Trust, St. Helens, England. Her own research, which includes a 10-year follow-up of patients with inflammatory arthritis, has shown that methotrexate does not appear to increase the risk of pulmonary fibrosis.
The study had no specific outside funding. Dr. Kiely reported having no conflicts of interest.
SOURCE: Kiely P et al. Rheumatology. 2019;58(suppl 3), Abstract 009.
REPORTING FROM BSR 2019
Culture: An unseen force in the hospital workplace
Parallels from the airline industry
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.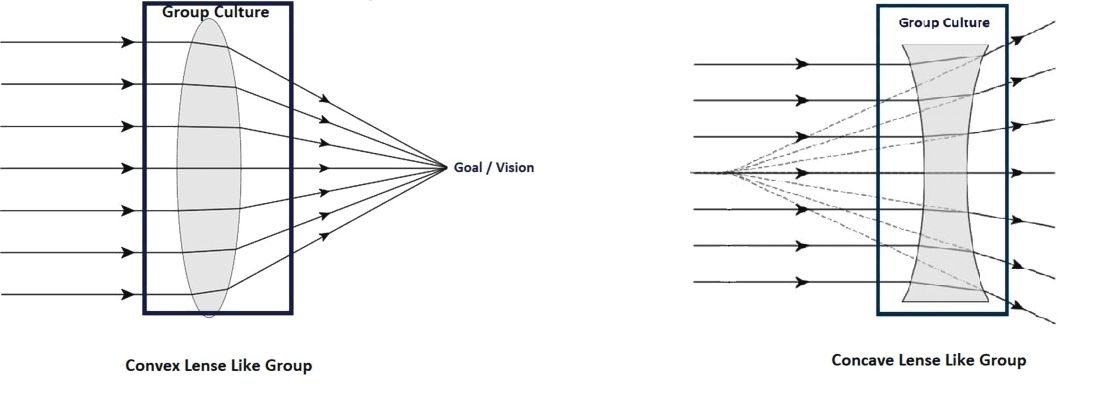
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.
Parallels from the airline industry
Parallels from the airline industry
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.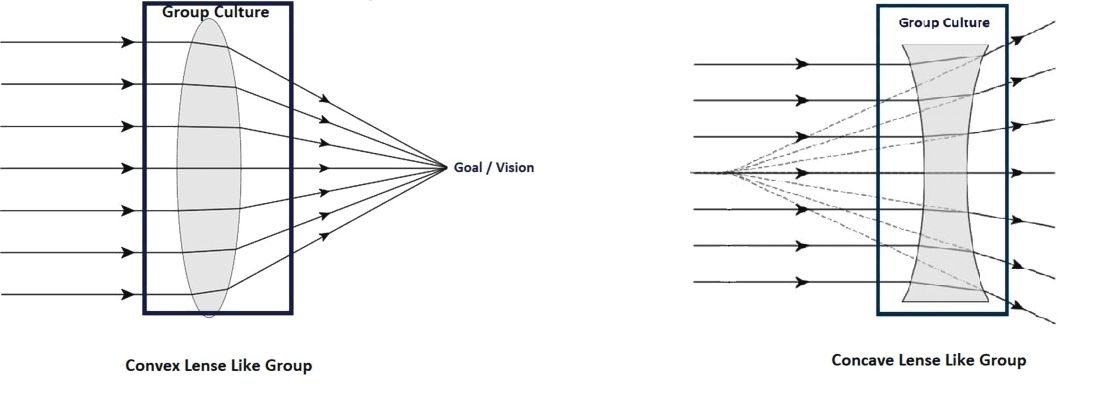
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.
“Workplace culture” has a profound influence on the success or failure of a team in the modern-day work environment, where teamwork and interpersonal interactions have paramount importance. Crew resource management (CRM), a technique developed originally by the airline industry, has been used as a tool to improve safety and quality in ICUs, trauma rooms, and operating rooms.1,2 This article discusses the use of CRM in hospital medicine as a tool for training and maintaining a favorable workplace culture.
Origin and evolution of CRM
United Airlines instituted the airline industry’s first crew resource management for pilots in 1981, following the 1978 crash of United Flight 173 in Portland, Ore. CRM was created based on recommendations from the National Transportation Safety Board and from a NASA workshop held subsequently.3 CRM has since evolved through five generations, and is a required annual training for most major commercial airline companies around the world. It also has been adapted for personnel training by several modern international industries.4
From the airline industry to the hospital
The health care industry is similar to the airline industry in that there is absolutely no margin of error, and that workplace culture plays a very important role. The culture being referred to here is the sum total of values, beliefs, work ethics, work strategies, strengths, and weaknesses of a group of people, and how they interact as a group. In other words, it is the dynamics of a group.
According to Donelson R. Forsyth, a social and personality psychologist at the University of Richmond (Virginia), the two key determinants of successful teamwork are a “shared mental representation of the task,” which refers to an in-depth understanding of the team and the tasks they are attempting; and “group unity/cohesion,” which means that, generally, members of cohesive groups like each other and the group, and they also are united in their pursuit of collective, group-level goals.5
Understanding the culture of a hospitalist team
Analyzing group dynamics and actively managing them toward both the institutional and global goals of health care is critical for the success of an organization. This is the core of successfully managing any team in any industry.
Additionally, the rapidly changing health care climate and insurance payment systems requires hospital medicine groups to rapidly adapt to the constantly changing health care business environment. As a result, there are a couple of ways to evaluate the effectiveness of the team:
- Measure tangible outcomes. The outcomes have to be well defined, important and measurable. These could be cost of care, quality of care, engagement of the team etc. These tangible measures’ outcome over a period of time can be used as a measure of how effective the team is.
- Simply ask your team! It is very important to know what core values the team holds dear. The best way to get that information from the team is to find out the de facto leaders of the team. They should be involved in the decision-making process, thus making them valuable to the management as well as the team.
Culture shapes outcomes
We have used the analogy of a convex and concave lens to help understand this better. A well-developed and well-coordinated team is like convex lens. A lens’ ability to converge or diverge light rays depends on certain characteristics like the curvature of surfaces and refractory index. Likewise, the culture of a group determines its ability to transform all the demands of the collective workload toward a unified goal/outcome. If it is favorable, the group will work as one and success will happen automatically.
Unfortunately, the opposite of this, (the concave lens effect), is more commonplace, where the dynamics of a team prevent the goals being achieved, as there is discordance, poor coordination of ideas and values, and team members not liking each other.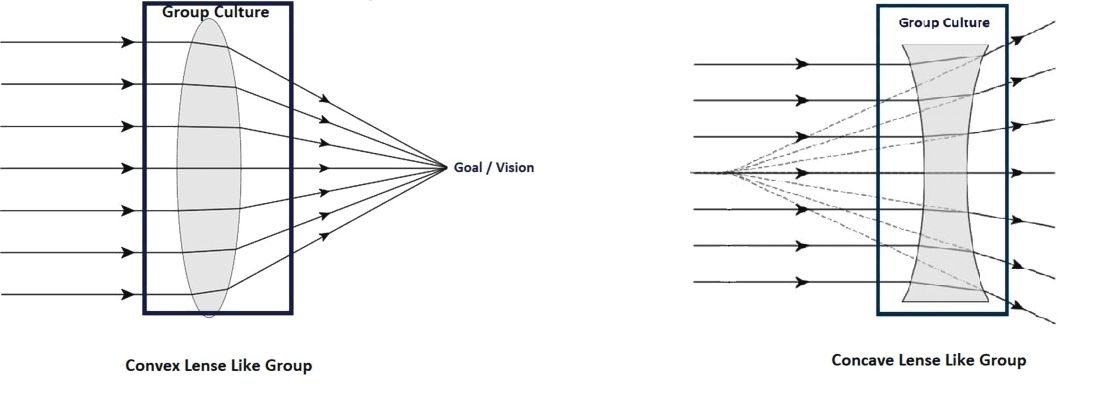
Most teams would fall somewhere within this spectrum, spanning the most favorable convex lens–like group to the least favorable concave lens–like group.
Change team dynamics using CRM principles
The concept of using CRM principles in health care is not entirely new. Such agencies as the Joint Commission and the Agency for Healthcare Research and Quality recommend using principles of CRM to improve communications, and as an error-prevention tool in health care.6
This approach can be broken down into four important steps:
1. Recruit right. It is important to make sure that the new recruit is the right fit for the team and that the de facto leaders and a few other team members are involved in interviewing the candidates. Their assessment should be given due consideration in making the decision to give the new recruit the job.
Every program looks for aspects like clinical competence, interpersonal communication, teamwork, etc., in a candidate, but it is even more important to make sure the candidate has the tenets that would make him/her a part of that particular team.
2. Train well. The newly recruited providers should be given focused training and the seasoned providers should be given refresher training at regular intervals. Care should be taken in designing the training programs in such a way that the providers are trained in skills that they don’t always think about, things that aren’t readily obvious, and in skills that they never get trained in during medical school and residency.
Specifically, they should be trained in:
- Values. These should include the values of both the organization and the team.
- Safety. This should include all the safety protocols that are in place in the organization - where to get help, how to report unsafe events etc.
- Communication.
Within the group: Have a mentor for the new provider, and also develop a culture where he/she feels comfortable to reach out to anyone in the team for help.
With patients and families: This training should ideally be done in a simulated environment if possible.
With other groups in the hospital: Consultants, nurses, other ancillary staff. Give them an idea about the prevailing culture in the organization with regard to these groups, so that they know what to expect when dealing with them.
- Managing perceptions. How the providers are viewed in the hospital, and how to improve it or maintain it.
- Nurturing the good. Use positive reinforcements to solidify the positive aspects of group dynamics these individuals might possess.
- Weeding out the bad. Use training and feedback to alter the negative group dynamic aspects.
3. Intervene. This is necessary either to maintain the positive aspects of a team that is already high-functioning, or to transform a poorly functioning team into a well-coordinated team. This is where the principles of CRM are going to be most useful.
There are five generations of CRM, each with a different focus.6 Only the aspects relevant to hospital medicine training are mentioned here.
- Communication. Address the gaps in communication. It is important to include people who are trusted by the team in designing and executing these sessions.
- Leadership. The goal should be to encourage the team to take ownership of the program. This will make a tremendous change in the ability of a team to deliver and rise up to challenges. The organizational leadership has to be willing to elevate the leaders of the group to positions where they can meaningfully take part in managing the team and making decisions that are critical to the team.
- Burnout management. Providers getting disillusioned: having no work-life balance; not getting enough respect from management, as well as other groups of doctors/nurses/etc. in the hospital; they are subject to bad scheduling and poor pay – all of which can all lead to career-ending burnout. It is important to recognize this and mitigate the factors that cause burnout.
- Organizational culture. If the team feels valued and supported, they will, in turn, work hard toward success. Creative leadership and a willingness to accommodate what matters the most to the team is essential for achieving this.
- Simulated training. These can be done in simulation labs, or in-group sessions with the team, re-creating difficult scenarios or problems in which the whole team can come together and solve them.
- Error containment and management. The team needs to identify possible sources of error and contain them before errors happen. The group should get together if a serious event happens and brainstorm why it happened and take measures to prevent it.
4. Reevaluate. Team dynamics tend to change over time. It is important to constantly re-evaluate the team and make sure that the team’s culture remains favorable. There should be recurrent cycles of retraining and interventions to maintain the positive growth that has been attained, as depicted in the schematic below:
Conclusion
CRM is widely accepted as an effective tool in training individuals in many high performing industries. This article describes a framework in which the principles of CRM can be applied to hospital medicine to maintain positive work culture.
Dr. Prabhakaran is director of hospital medicine transitions of care, Baystate Medical Center, Springfield, Mass., and assistant professor of medicine, University of Massachusetts, Worcester. Dr. Medarametla is medical director, hospital medicine, Baystate Medical Center, and assistant professor of medicine, University of Massachusetts.
References
1. Haerkens MH et al. Crew Resource Management in the ICU: The need for culture change. Ann Intensive Care. 2012 Aug 22;2:39.
2. Haerkens MH et al. Crew Resource Management in the trauma room: A prospective 3-year cohort study. Eur J Emerg Med. 2018 Aug;25(4):281-7.
3. Malcolm Gladwell. The ethnic theory of plane crashes. Outliers: The Story of Success. (Boston: Little, Brown and Company; 2008:177-223).
4. Helmreich RL et al. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19-32.
5. Forsyth DR. The psychology of groups. In R. Biswas-Diener & E. Diener (eds), Noba textbook series: Psychology. Champaign, Ill: DEF publishers; 2017.
6. Crew Resource Management. Available at Aviation Knowledge. Accessed Dec. 20, 2017.
A 5-year-old boy with a papular rash on his arm
Lichen striatus (LS) is a common benign skin condition that presents in children between the ages of 5 and 15 years.1 The rash is typically unilateral and most frequently on the extremities, although it may appear on the face, trunk, or buttocks. The lesions start as pink or skin-colored asymptomatic papules in a linear orientation following the lines of Blaschko. There may be residual postinflammatory hypo- or hyperpigmentation which often improves within a few years.
Of note, there are subsets of lichen striatus: Hypopigmented lichen striatus with minimal papules has been termed “lichen striatus albus.” Nail lichen striatus may present as onycholysis or fissuring of nails, present as an isolated finding, or more commonly in association with concurrent affected skin. Nail lichen striatus typically resolves on its own, however there are case reports of improvement with intralesional steroids.2
There is no established etiology for LS. Autoimmune disease, viruses, immunizations, medications, and hypersensitivity reactions have been associated with triggering LS in various case reports, although strength of the associations is low. Children have been reported to have LS following scarlet fever and Candida vulvitis.3 Diagnosis usually is clinical, although biopsy may be helpful for histopathologic confirmation. No work-up for associated infections or conditions is warranted.
The differential for linear papular lesions includes inflammatory linear verrucous epidermal nevus (ILVEN), blaschkitis, or linear morphea. ILVEN is a hamartoma that usually is congenital or presents in early childhood; presents with linear or whorled, hyperkeratotic papules and plaque in similar linear “line of Blaschko” patterns; and represents cutaneous mosaicism. It is often difficult to differentiate between lichen striatus and ILVEN, however lichen striatus is not congenital, and is a self-limited condition. Under dermoscopy (polarized light systems) findings of LS more frequently demonstrate gray granular pigmentation. ILVEN is more frequently associated with cerebriform pattern.4 Blaschkitis is a term for a blaschkoid inflammation of the skin that presents with more eczematous findings and histology of spongiosis, unlike the lichenoid findings of LS. It is typically accompanied by noticeable pruritus and broader bands of involved area, and has older age of onset than LS. Linear morphea is a deeper inflammatory process of the dermis or subcutaneous fat, presenting with sclerotic skin, and typically has associated atrophy.
Treatment need not be pursued for lichen striatus because it is a benign condition. The lesions typically self-resolve without any residual scarring. If patients have associated pruritus then low- to midpotency topical steroids can be used for symptomatic relief.
Dr. Kaushik is with the division of pediatric and adolescent dermatology at Rady Children’s Hospital-San Diego, and Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. There are no conflicts of interest or financial disclosures for Dr. Kaushik or Dr. Eichenfield. Email them at pdnews@mdedge.com.
References
1. Gupta D, Mathes E. Lichen Striatus. (Levy ML ed.) 2019: UpToDate.
2. Dermatol Ther. 2018 Nov;31(6):e12713.
3. Int J Dermatol. 2018 Sep;57(9):1118-9.
4. J Dermatol. 2017 Dec;44(12):e355-6.
Lichen striatus (LS) is a common benign skin condition that presents in children between the ages of 5 and 15 years.1 The rash is typically unilateral and most frequently on the extremities, although it may appear on the face, trunk, or buttocks. The lesions start as pink or skin-colored asymptomatic papules in a linear orientation following the lines of Blaschko. There may be residual postinflammatory hypo- or hyperpigmentation which often improves within a few years.
Of note, there are subsets of lichen striatus: Hypopigmented lichen striatus with minimal papules has been termed “lichen striatus albus.” Nail lichen striatus may present as onycholysis or fissuring of nails, present as an isolated finding, or more commonly in association with concurrent affected skin. Nail lichen striatus typically resolves on its own, however there are case reports of improvement with intralesional steroids.2
There is no established etiology for LS. Autoimmune disease, viruses, immunizations, medications, and hypersensitivity reactions have been associated with triggering LS in various case reports, although strength of the associations is low. Children have been reported to have LS following scarlet fever and Candida vulvitis.3 Diagnosis usually is clinical, although biopsy may be helpful for histopathologic confirmation. No work-up for associated infections or conditions is warranted.
The differential for linear papular lesions includes inflammatory linear verrucous epidermal nevus (ILVEN), blaschkitis, or linear morphea. ILVEN is a hamartoma that usually is congenital or presents in early childhood; presents with linear or whorled, hyperkeratotic papules and plaque in similar linear “line of Blaschko” patterns; and represents cutaneous mosaicism. It is often difficult to differentiate between lichen striatus and ILVEN, however lichen striatus is not congenital, and is a self-limited condition. Under dermoscopy (polarized light systems) findings of LS more frequently demonstrate gray granular pigmentation. ILVEN is more frequently associated with cerebriform pattern.4 Blaschkitis is a term for a blaschkoid inflammation of the skin that presents with more eczematous findings and histology of spongiosis, unlike the lichenoid findings of LS. It is typically accompanied by noticeable pruritus and broader bands of involved area, and has older age of onset than LS. Linear morphea is a deeper inflammatory process of the dermis or subcutaneous fat, presenting with sclerotic skin, and typically has associated atrophy.
Treatment need not be pursued for lichen striatus because it is a benign condition. The lesions typically self-resolve without any residual scarring. If patients have associated pruritus then low- to midpotency topical steroids can be used for symptomatic relief.
Dr. Kaushik is with the division of pediatric and adolescent dermatology at Rady Children’s Hospital-San Diego, and Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. There are no conflicts of interest or financial disclosures for Dr. Kaushik or Dr. Eichenfield. Email them at pdnews@mdedge.com.
References
1. Gupta D, Mathes E. Lichen Striatus. (Levy ML ed.) 2019: UpToDate.
2. Dermatol Ther. 2018 Nov;31(6):e12713.
3. Int J Dermatol. 2018 Sep;57(9):1118-9.
4. J Dermatol. 2017 Dec;44(12):e355-6.
Lichen striatus (LS) is a common benign skin condition that presents in children between the ages of 5 and 15 years.1 The rash is typically unilateral and most frequently on the extremities, although it may appear on the face, trunk, or buttocks. The lesions start as pink or skin-colored asymptomatic papules in a linear orientation following the lines of Blaschko. There may be residual postinflammatory hypo- or hyperpigmentation which often improves within a few years.
Of note, there are subsets of lichen striatus: Hypopigmented lichen striatus with minimal papules has been termed “lichen striatus albus.” Nail lichen striatus may present as onycholysis or fissuring of nails, present as an isolated finding, or more commonly in association with concurrent affected skin. Nail lichen striatus typically resolves on its own, however there are case reports of improvement with intralesional steroids.2
There is no established etiology for LS. Autoimmune disease, viruses, immunizations, medications, and hypersensitivity reactions have been associated with triggering LS in various case reports, although strength of the associations is low. Children have been reported to have LS following scarlet fever and Candida vulvitis.3 Diagnosis usually is clinical, although biopsy may be helpful for histopathologic confirmation. No work-up for associated infections or conditions is warranted.
The differential for linear papular lesions includes inflammatory linear verrucous epidermal nevus (ILVEN), blaschkitis, or linear morphea. ILVEN is a hamartoma that usually is congenital or presents in early childhood; presents with linear or whorled, hyperkeratotic papules and plaque in similar linear “line of Blaschko” patterns; and represents cutaneous mosaicism. It is often difficult to differentiate between lichen striatus and ILVEN, however lichen striatus is not congenital, and is a self-limited condition. Under dermoscopy (polarized light systems) findings of LS more frequently demonstrate gray granular pigmentation. ILVEN is more frequently associated with cerebriform pattern.4 Blaschkitis is a term for a blaschkoid inflammation of the skin that presents with more eczematous findings and histology of spongiosis, unlike the lichenoid findings of LS. It is typically accompanied by noticeable pruritus and broader bands of involved area, and has older age of onset than LS. Linear morphea is a deeper inflammatory process of the dermis or subcutaneous fat, presenting with sclerotic skin, and typically has associated atrophy.
Treatment need not be pursued for lichen striatus because it is a benign condition. The lesions typically self-resolve without any residual scarring. If patients have associated pruritus then low- to midpotency topical steroids can be used for symptomatic relief.
Dr. Kaushik is with the division of pediatric and adolescent dermatology at Rady Children’s Hospital-San Diego, and Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. There are no conflicts of interest or financial disclosures for Dr. Kaushik or Dr. Eichenfield. Email them at pdnews@mdedge.com.
References
1. Gupta D, Mathes E. Lichen Striatus. (Levy ML ed.) 2019: UpToDate.
2. Dermatol Ther. 2018 Nov;31(6):e12713.
3. Int J Dermatol. 2018 Sep;57(9):1118-9.
4. J Dermatol. 2017 Dec;44(12):e355-6.
Do some EGFR mutation subtypes benefit from immune checkpoint blockade?
Although epidermal growth factor receptor–mutant lung cancers generally don’t benefit from checkpoint inhibitors, there may be some subtypes that do respond, results of a large, multi-institution analysis suggest.
Compared with wild-type lung cancer cases, tumors with epidermal growth factor receptor (EGFR) exon 19 deletion did indeed have worse outcomes after progressive death-1/progressive death–ligand 1 (PD-1/PD-L1) blockade; however, tumors harboring EGFR L858R mutations had comparable response rates and overall survival.
These findings don’t change clinical practice, but do serve as a “foundation” for more research into which patients with EGFR-mutant disease might benefit from immunotherapy, according to Katherine Hastings, PhD, of Yale University, New Haven, Conn., and associates.
“We unequivocally support the guidance that EGFR TKIs should be the preferred first-line treatment option for patients with EGFR-mutant lung cancer,” Dr. Hastings and coauthors wrote in Annals of Oncology.
To date, clinical investigations of immune checkpoint inhibitors in patients with EGFR-mutant lung cancers have largely been discouraging, the authors wrote. However, there have been some exceptions, including a phase 2 study where third-line durvalumab showed activity in some patients with EGFR-positive, PD-L1-expressing advanced non–small cell lung cancer (NSCLC).
Accordingly, the investigators sought to determine whether specific molecular features made a difference. They looked at a total of 171 EGFR-mutant lung cancers that had been treated with PD-1/PD-L1 inhibitors, alone or in combination with a cytotoxic T-lymphocyte antigen 4 inhibitor.
In their analysis, they drilled down on the most common EGFR tyrosine kinase inhibitor–sensitizing alleles: EGFR exon 19 deletions, which represented 76 cases, and EGFR L858R, which represented 44 cases. For comparison, they looked at a cohort of 212 patients with EGFR wild-type NSCLC who had also been treated with immune checkpoint inhibitors.
EGFR exon 19 deletion cases had a significantly lower overall response rate versus EGFR wild-type tumors, at 7% versus 22%, respectively (P = .002), the investigators found. Likewise, overall survival was significantly reduced, with a hazard ratio of 0.69 (95% confidence interval, 0.493-0.965; P = .03).
By contrast, EGFR L858R tumors had similar response rates versus EGFR wild type, at 16% and 22%, respectively (P = .42); overall survival also was similar, with a hazard ratio of 0.917 (95% CI, 0.597-1.409; P = .69).
Of note, progression-free survival was reduced in both EGFR L858R and EGFR exon 19 deletion cases as compared with EGFR wild-type cases, though the investigators wrote that discrepancy might be related to variations in scanning intervals between different institutions that contributed cases to the study.
“Overall, these data suggest that patients with EGFR exon 19–mutant tumors, in particular, have a significantly reduced benefit upon treatment with immune checkpoint inhibitors,” the authors noted.
In a separate but related analysis of 383 patients with EGFR-mutant lung cancer, tumor mutation burden was lower in EGFR exon 19 deletion cases as compared with the EGFR L858R cases. That finding lined up with the immunotherapy response data, the investigators wrote, though it’s unclear what might be driving the differences in tumor burden between these two groups.
There were no differences in response to immune checkpoint blockade based on whether or not tumors harbored the EGFR T790M mutation, the investigators added. Similarly, PD-L1 expression did not impact response.
The study authors reported disclosures related to Astellas Pharma, AstraZeneca, Bristol-Myers Squibb, Calithera Biosciences, Daiichi, Eli Lilly, Merck, Mirati Therapeutics, Novartis, Pfizer, Roche, and Takeda, among others.
SOURCE: Hastings K et al. Ann Oncol. 2019 May 14. doi: 10.1093/annonc/mdz141.
Although epidermal growth factor receptor–mutant lung cancers generally don’t benefit from checkpoint inhibitors, there may be some subtypes that do respond, results of a large, multi-institution analysis suggest.
Compared with wild-type lung cancer cases, tumors with epidermal growth factor receptor (EGFR) exon 19 deletion did indeed have worse outcomes after progressive death-1/progressive death–ligand 1 (PD-1/PD-L1) blockade; however, tumors harboring EGFR L858R mutations had comparable response rates and overall survival.
These findings don’t change clinical practice, but do serve as a “foundation” for more research into which patients with EGFR-mutant disease might benefit from immunotherapy, according to Katherine Hastings, PhD, of Yale University, New Haven, Conn., and associates.
“We unequivocally support the guidance that EGFR TKIs should be the preferred first-line treatment option for patients with EGFR-mutant lung cancer,” Dr. Hastings and coauthors wrote in Annals of Oncology.
To date, clinical investigations of immune checkpoint inhibitors in patients with EGFR-mutant lung cancers have largely been discouraging, the authors wrote. However, there have been some exceptions, including a phase 2 study where third-line durvalumab showed activity in some patients with EGFR-positive, PD-L1-expressing advanced non–small cell lung cancer (NSCLC).
Accordingly, the investigators sought to determine whether specific molecular features made a difference. They looked at a total of 171 EGFR-mutant lung cancers that had been treated with PD-1/PD-L1 inhibitors, alone or in combination with a cytotoxic T-lymphocyte antigen 4 inhibitor.
In their analysis, they drilled down on the most common EGFR tyrosine kinase inhibitor–sensitizing alleles: EGFR exon 19 deletions, which represented 76 cases, and EGFR L858R, which represented 44 cases. For comparison, they looked at a cohort of 212 patients with EGFR wild-type NSCLC who had also been treated with immune checkpoint inhibitors.
EGFR exon 19 deletion cases had a significantly lower overall response rate versus EGFR wild-type tumors, at 7% versus 22%, respectively (P = .002), the investigators found. Likewise, overall survival was significantly reduced, with a hazard ratio of 0.69 (95% confidence interval, 0.493-0.965; P = .03).
By contrast, EGFR L858R tumors had similar response rates versus EGFR wild type, at 16% and 22%, respectively (P = .42); overall survival also was similar, with a hazard ratio of 0.917 (95% CI, 0.597-1.409; P = .69).
Of note, progression-free survival was reduced in both EGFR L858R and EGFR exon 19 deletion cases as compared with EGFR wild-type cases, though the investigators wrote that discrepancy might be related to variations in scanning intervals between different institutions that contributed cases to the study.
“Overall, these data suggest that patients with EGFR exon 19–mutant tumors, in particular, have a significantly reduced benefit upon treatment with immune checkpoint inhibitors,” the authors noted.
In a separate but related analysis of 383 patients with EGFR-mutant lung cancer, tumor mutation burden was lower in EGFR exon 19 deletion cases as compared with the EGFR L858R cases. That finding lined up with the immunotherapy response data, the investigators wrote, though it’s unclear what might be driving the differences in tumor burden between these two groups.
There were no differences in response to immune checkpoint blockade based on whether or not tumors harbored the EGFR T790M mutation, the investigators added. Similarly, PD-L1 expression did not impact response.
The study authors reported disclosures related to Astellas Pharma, AstraZeneca, Bristol-Myers Squibb, Calithera Biosciences, Daiichi, Eli Lilly, Merck, Mirati Therapeutics, Novartis, Pfizer, Roche, and Takeda, among others.
SOURCE: Hastings K et al. Ann Oncol. 2019 May 14. doi: 10.1093/annonc/mdz141.
Although epidermal growth factor receptor–mutant lung cancers generally don’t benefit from checkpoint inhibitors, there may be some subtypes that do respond, results of a large, multi-institution analysis suggest.
Compared with wild-type lung cancer cases, tumors with epidermal growth factor receptor (EGFR) exon 19 deletion did indeed have worse outcomes after progressive death-1/progressive death–ligand 1 (PD-1/PD-L1) blockade; however, tumors harboring EGFR L858R mutations had comparable response rates and overall survival.
These findings don’t change clinical practice, but do serve as a “foundation” for more research into which patients with EGFR-mutant disease might benefit from immunotherapy, according to Katherine Hastings, PhD, of Yale University, New Haven, Conn., and associates.
“We unequivocally support the guidance that EGFR TKIs should be the preferred first-line treatment option for patients with EGFR-mutant lung cancer,” Dr. Hastings and coauthors wrote in Annals of Oncology.
To date, clinical investigations of immune checkpoint inhibitors in patients with EGFR-mutant lung cancers have largely been discouraging, the authors wrote. However, there have been some exceptions, including a phase 2 study where third-line durvalumab showed activity in some patients with EGFR-positive, PD-L1-expressing advanced non–small cell lung cancer (NSCLC).
Accordingly, the investigators sought to determine whether specific molecular features made a difference. They looked at a total of 171 EGFR-mutant lung cancers that had been treated with PD-1/PD-L1 inhibitors, alone or in combination with a cytotoxic T-lymphocyte antigen 4 inhibitor.
In their analysis, they drilled down on the most common EGFR tyrosine kinase inhibitor–sensitizing alleles: EGFR exon 19 deletions, which represented 76 cases, and EGFR L858R, which represented 44 cases. For comparison, they looked at a cohort of 212 patients with EGFR wild-type NSCLC who had also been treated with immune checkpoint inhibitors.
EGFR exon 19 deletion cases had a significantly lower overall response rate versus EGFR wild-type tumors, at 7% versus 22%, respectively (P = .002), the investigators found. Likewise, overall survival was significantly reduced, with a hazard ratio of 0.69 (95% confidence interval, 0.493-0.965; P = .03).
By contrast, EGFR L858R tumors had similar response rates versus EGFR wild type, at 16% and 22%, respectively (P = .42); overall survival also was similar, with a hazard ratio of 0.917 (95% CI, 0.597-1.409; P = .69).
Of note, progression-free survival was reduced in both EGFR L858R and EGFR exon 19 deletion cases as compared with EGFR wild-type cases, though the investigators wrote that discrepancy might be related to variations in scanning intervals between different institutions that contributed cases to the study.
“Overall, these data suggest that patients with EGFR exon 19–mutant tumors, in particular, have a significantly reduced benefit upon treatment with immune checkpoint inhibitors,” the authors noted.
In a separate but related analysis of 383 patients with EGFR-mutant lung cancer, tumor mutation burden was lower in EGFR exon 19 deletion cases as compared with the EGFR L858R cases. That finding lined up with the immunotherapy response data, the investigators wrote, though it’s unclear what might be driving the differences in tumor burden between these two groups.
There were no differences in response to immune checkpoint blockade based on whether or not tumors harbored the EGFR T790M mutation, the investigators added. Similarly, PD-L1 expression did not impact response.
The study authors reported disclosures related to Astellas Pharma, AstraZeneca, Bristol-Myers Squibb, Calithera Biosciences, Daiichi, Eli Lilly, Merck, Mirati Therapeutics, Novartis, Pfizer, Roche, and Takeda, among others.
SOURCE: Hastings K et al. Ann Oncol. 2019 May 14. doi: 10.1093/annonc/mdz141.
FROM ANNALS OF ONCOLOGY
Th17-associated cytokines, CRP fail as biomarkers for ustekinumab success in PsA
Neither baseline Th17-associated cytokines nor C-reactive protein levels were predictive of response to ustekinumab in patients with psoriatic arthritis, despite significant reductions following treatment, according to Stefan Siebert, PhD, of the University of Glasgow (Scotland) and associates.
In a study published in Arthritis & Rheumatology, the authors retrospectively analyzed serum samples collected from 927 patients with psoriatic arthritis who participated in the phase 3 PSUMMIT trials. Patients received ustekinumab (Stelara) or placebo, and samples were collected at baseline, 4 weeks, and 24 weeks.
At baseline, interleukin-17A, -17F, and -23 levels were associated with skin disease scores, but neither these nor C-reactive protein (CRP) were associated with joint disease scores. While IL-17A, IL-17F, and CRP were reduced in patients who responded to ustekinumab, baseline levels of IL-17A, IL-17F, IL-23, and CRP were not associated with ustekinumab response in either skin or joints.
In patients who achieved a 75% reduction in their Psoriasis Area and Severity Index scores or a 20% reduction in their American College of Rheumatology response score after 24 weeks, CRP levels were significantly lower than in patients who did not achieve these scores (51%-58% vs. 32%-33%; P less than .05). However, IL-17A and IL-17F levels were not significantly different in these patients.
“While the biomarkers studied in the PSUMMIT program did not translate into therapeutic utility, it is important that relevant biomarker studies associated with phase 3 clinical trial programs are published in order to increase our understanding of this complex disease and further dissect the role of the IL-23/IL-17 pathway,” the investigators concluded.
The study was funded by Janssen; four coauthors reported being employed with Janssen.
SOURCE: Siebert S et al. Arthritis Rheumatol. 2019 May 9. doi: 10.1002/art.40921.
Neither baseline Th17-associated cytokines nor C-reactive protein levels were predictive of response to ustekinumab in patients with psoriatic arthritis, despite significant reductions following treatment, according to Stefan Siebert, PhD, of the University of Glasgow (Scotland) and associates.
In a study published in Arthritis & Rheumatology, the authors retrospectively analyzed serum samples collected from 927 patients with psoriatic arthritis who participated in the phase 3 PSUMMIT trials. Patients received ustekinumab (Stelara) or placebo, and samples were collected at baseline, 4 weeks, and 24 weeks.
At baseline, interleukin-17A, -17F, and -23 levels were associated with skin disease scores, but neither these nor C-reactive protein (CRP) were associated with joint disease scores. While IL-17A, IL-17F, and CRP were reduced in patients who responded to ustekinumab, baseline levels of IL-17A, IL-17F, IL-23, and CRP were not associated with ustekinumab response in either skin or joints.
In patients who achieved a 75% reduction in their Psoriasis Area and Severity Index scores or a 20% reduction in their American College of Rheumatology response score after 24 weeks, CRP levels were significantly lower than in patients who did not achieve these scores (51%-58% vs. 32%-33%; P less than .05). However, IL-17A and IL-17F levels were not significantly different in these patients.
“While the biomarkers studied in the PSUMMIT program did not translate into therapeutic utility, it is important that relevant biomarker studies associated with phase 3 clinical trial programs are published in order to increase our understanding of this complex disease and further dissect the role of the IL-23/IL-17 pathway,” the investigators concluded.
The study was funded by Janssen; four coauthors reported being employed with Janssen.
SOURCE: Siebert S et al. Arthritis Rheumatol. 2019 May 9. doi: 10.1002/art.40921.
Neither baseline Th17-associated cytokines nor C-reactive protein levels were predictive of response to ustekinumab in patients with psoriatic arthritis, despite significant reductions following treatment, according to Stefan Siebert, PhD, of the University of Glasgow (Scotland) and associates.
In a study published in Arthritis & Rheumatology, the authors retrospectively analyzed serum samples collected from 927 patients with psoriatic arthritis who participated in the phase 3 PSUMMIT trials. Patients received ustekinumab (Stelara) or placebo, and samples were collected at baseline, 4 weeks, and 24 weeks.
At baseline, interleukin-17A, -17F, and -23 levels were associated with skin disease scores, but neither these nor C-reactive protein (CRP) were associated with joint disease scores. While IL-17A, IL-17F, and CRP were reduced in patients who responded to ustekinumab, baseline levels of IL-17A, IL-17F, IL-23, and CRP were not associated with ustekinumab response in either skin or joints.
In patients who achieved a 75% reduction in their Psoriasis Area and Severity Index scores or a 20% reduction in their American College of Rheumatology response score after 24 weeks, CRP levels were significantly lower than in patients who did not achieve these scores (51%-58% vs. 32%-33%; P less than .05). However, IL-17A and IL-17F levels were not significantly different in these patients.
“While the biomarkers studied in the PSUMMIT program did not translate into therapeutic utility, it is important that relevant biomarker studies associated with phase 3 clinical trial programs are published in order to increase our understanding of this complex disease and further dissect the role of the IL-23/IL-17 pathway,” the investigators concluded.
The study was funded by Janssen; four coauthors reported being employed with Janssen.
SOURCE: Siebert S et al. Arthritis Rheumatol. 2019 May 9. doi: 10.1002/art.40921.
FROM ARTHRITIS & RHEUMATOLOGY
Family history plays a large role in bleeding disorder diagnosis in women
Disease severity and family history appear to play a significant role in the age of diagnosis for women with congenital bleeding disorders, according to recent survey findings.
A European multinational survey has identified delays in diagnosis and other challenges faced by girls and women with congenital bleeding disorders.
“The aim of this survey, carried out by the European Haemophilia Consortium (EHC), was to provide the patient voice of their lived experiences with congenital bleeding disorders,” wrote Declan Noone of the EHC in Brussels, and colleagues. The findings were published in Haemophilia.
The researchers conducted a survey of 709 girls and women with various congenital bleeding disorders from 32 countries, primarily located in Western Europe. Most respondents were adults, with just 3.8% under age 18 years.
The questionnaire was administered to eligible patients at various hemophilia treatment centers. More than half of respondents were hemophilia carriers and nearly 28% had von Willebrand disease.
The survey explored the effects of bleeding disorders on several activities of daily life, including symptoms, physical activity, and reproductive ability.
After analysis, the researchers found that overall the median age at diagnosis of a bleeding disorder was 16 years (range, 2-28 years) among respondents. Having a family history of a bleeding disorder resulted in a significantly younger median age at diagnosis (6 years; range, 0-26 years) versus those without a family history (17 years; range 5-28 years; P less than .01).
Disease severity also appears to play a role. Women with type 3 von Willebrand disease had a median age of diagnosis of 1 year old, compared with 19.3 years old for type 2 disease (P less than .01).
Respondents reported a substantial disease burden on activities of daily life, especially for women with platelet function disorders and other factor deficiency.
Women without a known family history of a bleeding disorders reported a significantly greater impact on their physical life, social life, and romantic life (P less than .01 for all domains), compared with women with a family history of bleeding disorders.
There were no statistically significant differences across types of bleeding disorders on questions related to reproductive life. However, the researchers reported that “surprisingly,” 25% of women reported that having a bleeding disorder “has had a severe impact on their decision or has prevented them from having children.
“The bleeding symptom of biggest impact on daily life is [heavy menstrual bleeding], reported by 55% of women,” the researchers wrote.
The researchers acknowledged that a key limitation of the survey was the composition of the sample: predominantly of patients from Western Europe. As a result, the findings may not be generalizable to all patient populations.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Noone D et al. Haemophilia. 2019 Apr 29. doi: 10.1111/hae.13722.
Disease severity and family history appear to play a significant role in the age of diagnosis for women with congenital bleeding disorders, according to recent survey findings.
A European multinational survey has identified delays in diagnosis and other challenges faced by girls and women with congenital bleeding disorders.
“The aim of this survey, carried out by the European Haemophilia Consortium (EHC), was to provide the patient voice of their lived experiences with congenital bleeding disorders,” wrote Declan Noone of the EHC in Brussels, and colleagues. The findings were published in Haemophilia.
The researchers conducted a survey of 709 girls and women with various congenital bleeding disorders from 32 countries, primarily located in Western Europe. Most respondents were adults, with just 3.8% under age 18 years.
The questionnaire was administered to eligible patients at various hemophilia treatment centers. More than half of respondents were hemophilia carriers and nearly 28% had von Willebrand disease.
The survey explored the effects of bleeding disorders on several activities of daily life, including symptoms, physical activity, and reproductive ability.
After analysis, the researchers found that overall the median age at diagnosis of a bleeding disorder was 16 years (range, 2-28 years) among respondents. Having a family history of a bleeding disorder resulted in a significantly younger median age at diagnosis (6 years; range, 0-26 years) versus those without a family history (17 years; range 5-28 years; P less than .01).
Disease severity also appears to play a role. Women with type 3 von Willebrand disease had a median age of diagnosis of 1 year old, compared with 19.3 years old for type 2 disease (P less than .01).
Respondents reported a substantial disease burden on activities of daily life, especially for women with platelet function disorders and other factor deficiency.
Women without a known family history of a bleeding disorders reported a significantly greater impact on their physical life, social life, and romantic life (P less than .01 for all domains), compared with women with a family history of bleeding disorders.
There were no statistically significant differences across types of bleeding disorders on questions related to reproductive life. However, the researchers reported that “surprisingly,” 25% of women reported that having a bleeding disorder “has had a severe impact on their decision or has prevented them from having children.
“The bleeding symptom of biggest impact on daily life is [heavy menstrual bleeding], reported by 55% of women,” the researchers wrote.
The researchers acknowledged that a key limitation of the survey was the composition of the sample: predominantly of patients from Western Europe. As a result, the findings may not be generalizable to all patient populations.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Noone D et al. Haemophilia. 2019 Apr 29. doi: 10.1111/hae.13722.
Disease severity and family history appear to play a significant role in the age of diagnosis for women with congenital bleeding disorders, according to recent survey findings.
A European multinational survey has identified delays in diagnosis and other challenges faced by girls and women with congenital bleeding disorders.
“The aim of this survey, carried out by the European Haemophilia Consortium (EHC), was to provide the patient voice of their lived experiences with congenital bleeding disorders,” wrote Declan Noone of the EHC in Brussels, and colleagues. The findings were published in Haemophilia.
The researchers conducted a survey of 709 girls and women with various congenital bleeding disorders from 32 countries, primarily located in Western Europe. Most respondents were adults, with just 3.8% under age 18 years.
The questionnaire was administered to eligible patients at various hemophilia treatment centers. More than half of respondents were hemophilia carriers and nearly 28% had von Willebrand disease.
The survey explored the effects of bleeding disorders on several activities of daily life, including symptoms, physical activity, and reproductive ability.
After analysis, the researchers found that overall the median age at diagnosis of a bleeding disorder was 16 years (range, 2-28 years) among respondents. Having a family history of a bleeding disorder resulted in a significantly younger median age at diagnosis (6 years; range, 0-26 years) versus those without a family history (17 years; range 5-28 years; P less than .01).
Disease severity also appears to play a role. Women with type 3 von Willebrand disease had a median age of diagnosis of 1 year old, compared with 19.3 years old for type 2 disease (P less than .01).
Respondents reported a substantial disease burden on activities of daily life, especially for women with platelet function disorders and other factor deficiency.
Women without a known family history of a bleeding disorders reported a significantly greater impact on their physical life, social life, and romantic life (P less than .01 for all domains), compared with women with a family history of bleeding disorders.
There were no statistically significant differences across types of bleeding disorders on questions related to reproductive life. However, the researchers reported that “surprisingly,” 25% of women reported that having a bleeding disorder “has had a severe impact on their decision or has prevented them from having children.
“The bleeding symptom of biggest impact on daily life is [heavy menstrual bleeding], reported by 55% of women,” the researchers wrote.
The researchers acknowledged that a key limitation of the survey was the composition of the sample: predominantly of patients from Western Europe. As a result, the findings may not be generalizable to all patient populations.
No funding sources were reported. The authors reported having no conflicts of interest.
SOURCE: Noone D et al. Haemophilia. 2019 Apr 29. doi: 10.1111/hae.13722.
FROM HAEMOPHILIA
NGS comparable to FC for minimal residual disease assessment
NEW ORLEANS – Next-generation sequencing of peripheral blood is at least as effective as flow cytometry of bone marrow for assessing minimal residual disease, according to a new study.
Researchers compared bone marrow flow cytometry (FC) and peripheral blood next-generation sequencing (NGS) for minimal residual disease (MRD) assessment in pediatric and young adult patients with B-cell acute lymphoblastic leukemia (B-ALL) who received treatment with tisagenlecleucel. There was a high level of concordance between the assays, but the NGS assay detected more MRD-positive samples and NGS results provided a longer lead time to relapse.
Michael A. Pulsipher, MD, of the Children’s Hospital Los Angeles, presented these results at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The researchers analyzed samples from pediatric and young adult patients aged 2-25 years who had relapsed or refractory B-ALL and received treatment with tisagenlecleucel on the ELIANA or ENSIGN trials.
The patients had received at least two prior lines of therapy and were ineligible for allogeneic transplant. They received a single dose of tisagenlecleucel. MRD was assessed before tisagenlecleucel infusion, at various time points after infusion, and at relapse.
Dr. Pulsipher and his colleagues compared MRD results from an NGS assay – Adaptive Biotechnologies’ clonoSEQ – using peripheral blood and results from FC of bone marrow. NGS and FC results were available for 237 samples from 83 patients.
After treatment, NGS detected more MRD-positive samples at each sensitivity level tested (10-4, 10-5, and 10-6). At 10-6, NGS detected 18% more MRD-positive samples than did FC – 50% and 32%, respectively.
Detection of MRD positivity prior to relapse was faster with NGS than with FC. In 17 of 34 patients with morphological relapse, NGS provided a median lead time of 67 days. FC provided a median lead time of 39 days in 11 of the 34 patients.
About 80% of patients who had an MRD status of zero by NGS at day 28 remained relapse-free for up to 3 years.
Among complete responders (n = 50), the duration of response was significantly longer in patients who had an MRD status of zero at day 28 by NGS than in patients who had an MRD status greater than zero (P = .0003). Overall survival was significantly better among patients with an MRD status of zero as well (P = .0004).
Dr. Pulsipher said additional studies are needed to confirm these findings and determine the best way to know if a patient has been cured or needs additional therapy after tisagenlecleucel.
Dr. Pulsipher reported relationships with Adaptive Biotech, Novartis, Incyte, Amgen, Bellicum Pharmaceuticals, Medac Pharma, and Miltenyi Biotec. ELIANA and ENSIGN were funded by Novartis, which markets tisagenlecleucel as Kymriah.
SOURCE: Pulsipher MA et al. ASPHO 2019, Abstract 2001.
NEW ORLEANS – Next-generation sequencing of peripheral blood is at least as effective as flow cytometry of bone marrow for assessing minimal residual disease, according to a new study.
Researchers compared bone marrow flow cytometry (FC) and peripheral blood next-generation sequencing (NGS) for minimal residual disease (MRD) assessment in pediatric and young adult patients with B-cell acute lymphoblastic leukemia (B-ALL) who received treatment with tisagenlecleucel. There was a high level of concordance between the assays, but the NGS assay detected more MRD-positive samples and NGS results provided a longer lead time to relapse.
Michael A. Pulsipher, MD, of the Children’s Hospital Los Angeles, presented these results at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The researchers analyzed samples from pediatric and young adult patients aged 2-25 years who had relapsed or refractory B-ALL and received treatment with tisagenlecleucel on the ELIANA or ENSIGN trials.
The patients had received at least two prior lines of therapy and were ineligible for allogeneic transplant. They received a single dose of tisagenlecleucel. MRD was assessed before tisagenlecleucel infusion, at various time points after infusion, and at relapse.
Dr. Pulsipher and his colleagues compared MRD results from an NGS assay – Adaptive Biotechnologies’ clonoSEQ – using peripheral blood and results from FC of bone marrow. NGS and FC results were available for 237 samples from 83 patients.
After treatment, NGS detected more MRD-positive samples at each sensitivity level tested (10-4, 10-5, and 10-6). At 10-6, NGS detected 18% more MRD-positive samples than did FC – 50% and 32%, respectively.
Detection of MRD positivity prior to relapse was faster with NGS than with FC. In 17 of 34 patients with morphological relapse, NGS provided a median lead time of 67 days. FC provided a median lead time of 39 days in 11 of the 34 patients.
About 80% of patients who had an MRD status of zero by NGS at day 28 remained relapse-free for up to 3 years.
Among complete responders (n = 50), the duration of response was significantly longer in patients who had an MRD status of zero at day 28 by NGS than in patients who had an MRD status greater than zero (P = .0003). Overall survival was significantly better among patients with an MRD status of zero as well (P = .0004).
Dr. Pulsipher said additional studies are needed to confirm these findings and determine the best way to know if a patient has been cured or needs additional therapy after tisagenlecleucel.
Dr. Pulsipher reported relationships with Adaptive Biotech, Novartis, Incyte, Amgen, Bellicum Pharmaceuticals, Medac Pharma, and Miltenyi Biotec. ELIANA and ENSIGN were funded by Novartis, which markets tisagenlecleucel as Kymriah.
SOURCE: Pulsipher MA et al. ASPHO 2019, Abstract 2001.
NEW ORLEANS – Next-generation sequencing of peripheral blood is at least as effective as flow cytometry of bone marrow for assessing minimal residual disease, according to a new study.
Researchers compared bone marrow flow cytometry (FC) and peripheral blood next-generation sequencing (NGS) for minimal residual disease (MRD) assessment in pediatric and young adult patients with B-cell acute lymphoblastic leukemia (B-ALL) who received treatment with tisagenlecleucel. There was a high level of concordance between the assays, but the NGS assay detected more MRD-positive samples and NGS results provided a longer lead time to relapse.
Michael A. Pulsipher, MD, of the Children’s Hospital Los Angeles, presented these results at the annual meeting of the American Society of Pediatric Hematology/Oncology.
The researchers analyzed samples from pediatric and young adult patients aged 2-25 years who had relapsed or refractory B-ALL and received treatment with tisagenlecleucel on the ELIANA or ENSIGN trials.
The patients had received at least two prior lines of therapy and were ineligible for allogeneic transplant. They received a single dose of tisagenlecleucel. MRD was assessed before tisagenlecleucel infusion, at various time points after infusion, and at relapse.
Dr. Pulsipher and his colleagues compared MRD results from an NGS assay – Adaptive Biotechnologies’ clonoSEQ – using peripheral blood and results from FC of bone marrow. NGS and FC results were available for 237 samples from 83 patients.
After treatment, NGS detected more MRD-positive samples at each sensitivity level tested (10-4, 10-5, and 10-6). At 10-6, NGS detected 18% more MRD-positive samples than did FC – 50% and 32%, respectively.
Detection of MRD positivity prior to relapse was faster with NGS than with FC. In 17 of 34 patients with morphological relapse, NGS provided a median lead time of 67 days. FC provided a median lead time of 39 days in 11 of the 34 patients.
About 80% of patients who had an MRD status of zero by NGS at day 28 remained relapse-free for up to 3 years.
Among complete responders (n = 50), the duration of response was significantly longer in patients who had an MRD status of zero at day 28 by NGS than in patients who had an MRD status greater than zero (P = .0003). Overall survival was significantly better among patients with an MRD status of zero as well (P = .0004).
Dr. Pulsipher said additional studies are needed to confirm these findings and determine the best way to know if a patient has been cured or needs additional therapy after tisagenlecleucel.
Dr. Pulsipher reported relationships with Adaptive Biotech, Novartis, Incyte, Amgen, Bellicum Pharmaceuticals, Medac Pharma, and Miltenyi Biotec. ELIANA and ENSIGN were funded by Novartis, which markets tisagenlecleucel as Kymriah.
SOURCE: Pulsipher MA et al. ASPHO 2019, Abstract 2001.
REPORTING FROM 2019 ASPHO CONFERENCE
Key clinical point: Major finding: At the highest sensitivity level tested, next-generation sequencing detected 18% more minimal residual disease–positive samples than did flow cytometry – 50% and 32%, respectively.
Study details: An analysis of samples from pediatric and young adult patients with B-cell acute lymphoblastic leukemia who received treatment with tisagenlecleucel on the ELIANA and ENSIGN trials.
Disclosures: The speaker reported relationships with Adaptive Biotech, Novartis, Incyte, Amgen, Bellicum Pharmaceuticals, Medac Pharma, and Miltenyi Biotec. The ELIANA and ENSIGN trials were funded by Novartis, which markets tisagenlecleucel as Kymriah.
Source: Pulsipher MA et al. ASPHO 2019, Abstract 2001.












