User login
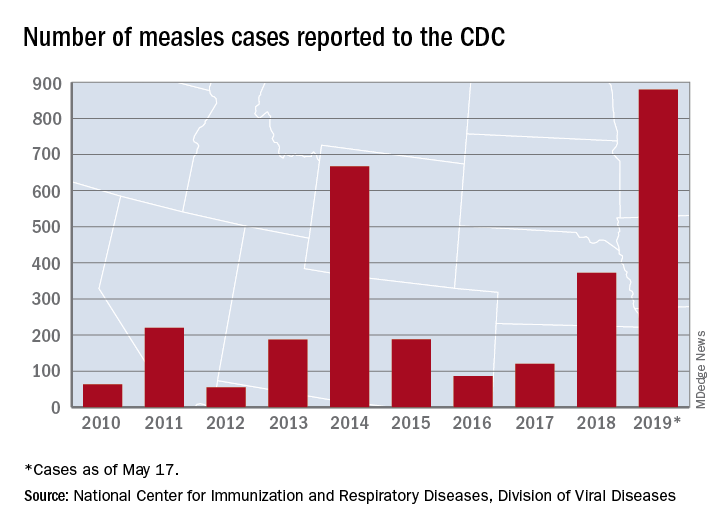
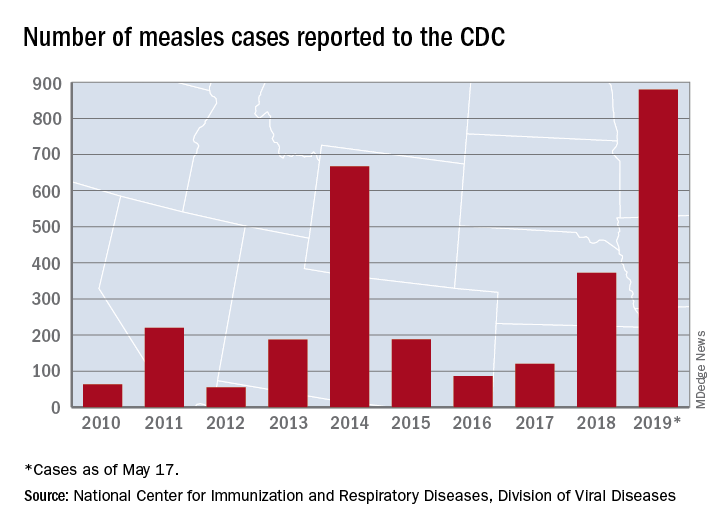
U.S. measles total sees smallest increase in 2 months
according to the Centers for Disease Control and Prevention.
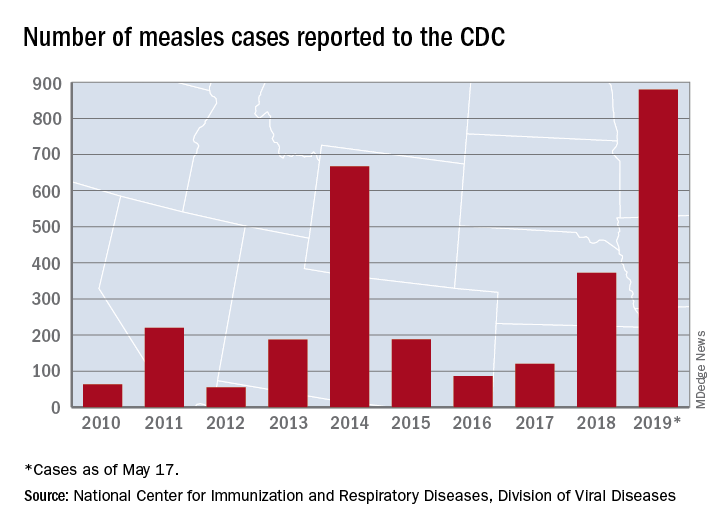
That weekly increase of 41 cases is the smallest since the week ending March 14, when the total rose by 40. The largest 1-week rise of the year came during the week ending April 11, when there were 90 new cases, CDC data show.
A case that has been reported by the media in the last week but not officially through the CDC would make New Mexico the 25th state with a measles case this year. The state’s health department has confirmed measles in a 1-year-old from Sierra County, which is New Mexico’s first case since 2014, the Las Cruces Sun News reported, adding that 4,441 school-aged children had an exemption for vaccination filed with the state in 2018.
Making a return appearance to the CDC’s list of outbreaks is Washington State, which reported six new cases last week in three Puget Sound counties (King, Pierce, and Snohomish). The most likely location and date of exposure was at Seattle-Tacoma International Airport on April 25, the Washington State Department of Health said. In February and March, there were 71 cases in Clark County on the state’s border with Oregon.
The ongoing outbreak in Michigan had been quiet since April, but the state’s Department of Health and Human Services confirmed a measles case in St. Clair County on May 17, bringing the total to 44 for the year. The new case, which is not related to an earlier outbreak that occurred mainly in Oakland County, involves an international traveler visiting Michigan.
according to the Centers for Disease Control and Prevention.
That weekly increase of 41 cases is the smallest since the week ending March 14, when the total rose by 40. The largest 1-week rise of the year came during the week ending April 11, when there were 90 new cases, CDC data show.
A case that has been reported by the media in the last week but not officially through the CDC would make New Mexico the 25th state with a measles case this year. The state’s health department has confirmed measles in a 1-year-old from Sierra County, which is New Mexico’s first case since 2014, the Las Cruces Sun News reported, adding that 4,441 school-aged children had an exemption for vaccination filed with the state in 2018.
Making a return appearance to the CDC’s list of outbreaks is Washington State, which reported six new cases last week in three Puget Sound counties (King, Pierce, and Snohomish). The most likely location and date of exposure was at Seattle-Tacoma International Airport on April 25, the Washington State Department of Health said. In February and March, there were 71 cases in Clark County on the state’s border with Oregon.
The ongoing outbreak in Michigan had been quiet since April, but the state’s Department of Health and Human Services confirmed a measles case in St. Clair County on May 17, bringing the total to 44 for the year. The new case, which is not related to an earlier outbreak that occurred mainly in Oakland County, involves an international traveler visiting Michigan.
according to the Centers for Disease Control and Prevention.
That weekly increase of 41 cases is the smallest since the week ending March 14, when the total rose by 40. The largest 1-week rise of the year came during the week ending April 11, when there were 90 new cases, CDC data show.
A case that has been reported by the media in the last week but not officially through the CDC would make New Mexico the 25th state with a measles case this year. The state’s health department has confirmed measles in a 1-year-old from Sierra County, which is New Mexico’s first case since 2014, the Las Cruces Sun News reported, adding that 4,441 school-aged children had an exemption for vaccination filed with the state in 2018.
Making a return appearance to the CDC’s list of outbreaks is Washington State, which reported six new cases last week in three Puget Sound counties (King, Pierce, and Snohomish). The most likely location and date of exposure was at Seattle-Tacoma International Airport on April 25, the Washington State Department of Health said. In February and March, there were 71 cases in Clark County on the state’s border with Oregon.
The ongoing outbreak in Michigan had been quiet since April, but the state’s Department of Health and Human Services confirmed a measles case in St. Clair County on May 17, bringing the total to 44 for the year. The new case, which is not related to an earlier outbreak that occurred mainly in Oakland County, involves an international traveler visiting Michigan.
Physical activity linked to less cirrhosis-related mortality
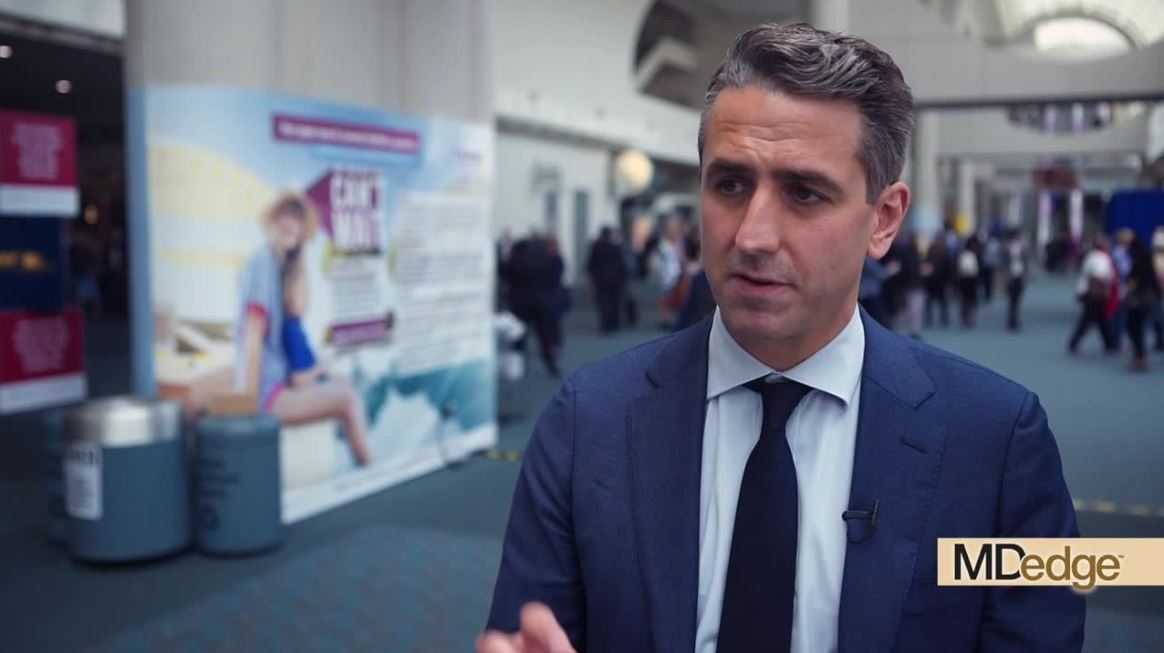
SAN DIEGO – People who were more physically active, including those who did strength training, had significantly reduced risks of cirrhosis-related and liver cancer–related mortality, based on 26 years of prospective data from 113,000 participants in the Nurses Health Study and the Health Professionals Follow-Up Study.
Adults in the highest quintile of physical activity in the study had a 73% lower risk for cirrhosis-related death than did those in the lowest quintile, according to researchers at Massachusetts General Hospital and Harvard Medical School, Boston, who presented the study findings at Digestive Disease Week 2019.
One of the researchers, Tracey Simon, MD, MPH, of Massachusetts General Hospital, Boston, broke down the major take-home messages from the study in this video interview.
For example, vigorous activity was not necessary to improve hepatic health, she said. Walking for 4 hours per week made a big difference.
Dr. Simon has no relevant financial disclosures.
SAN DIEGO – People who were more physically active, including those who did strength training, had significantly reduced risks of cirrhosis-related and liver cancer–related mortality, based on 26 years of prospective data from 113,000 participants in the Nurses Health Study and the Health Professionals Follow-Up Study.
Adults in the highest quintile of physical activity in the study had a 73% lower risk for cirrhosis-related death than did those in the lowest quintile, according to researchers at Massachusetts General Hospital and Harvard Medical School, Boston, who presented the study findings at Digestive Disease Week 2019.
One of the researchers, Tracey Simon, MD, MPH, of Massachusetts General Hospital, Boston, broke down the major take-home messages from the study in this video interview.
For example, vigorous activity was not necessary to improve hepatic health, she said. Walking for 4 hours per week made a big difference.
Dr. Simon has no relevant financial disclosures.
SAN DIEGO – People who were more physically active, including those who did strength training, had significantly reduced risks of cirrhosis-related and liver cancer–related mortality, based on 26 years of prospective data from 113,000 participants in the Nurses Health Study and the Health Professionals Follow-Up Study.
Adults in the highest quintile of physical activity in the study had a 73% lower risk for cirrhosis-related death than did those in the lowest quintile, according to researchers at Massachusetts General Hospital and Harvard Medical School, Boston, who presented the study findings at Digestive Disease Week 2019.
One of the researchers, Tracey Simon, MD, MPH, of Massachusetts General Hospital, Boston, broke down the major take-home messages from the study in this video interview.
For example, vigorous activity was not necessary to improve hepatic health, she said. Walking for 4 hours per week made a big difference.
Dr. Simon has no relevant financial disclosures.
REPORTING FROM DDW 2019
ASTRO survey: Prior authorization delays care, add costs
Nine in 10 radiation oncologists report that prior authorization for treatment is either very challenging (42%) or moderately challenging (48%), according to data from a member survey released by the American Society for Radiation Oncology (ASTRO).
“In 2018, [prior authorization] became the most challenging issue facing radiation oncologists,” Paul Harari, MD, Jack Fowler Professor and chair of oncology at the University of Wisconsin, Madison, and chair of the ASTRO board of directors, said during a press briefing. “Prior authorization is creating multiple obstacles to cancer patient care.”
According to responses from 673 ASTRO members, 31% said seeking prior authorization has caused delays in treatment of 5 or more days, 32% said it causes delays of 4-5 days, and 30% said it causes delays of 1-3 days. Seven percent said the prior authorization requests are resolved within less than a day.
Prior authorization delays forced 32% of respondents to alter treatment plans in more than 10% of their cases, and another 31% said treatment plans were altered in 5%-10% of their cases. For 37% of the respondents, less than 5% of their treatment plans were altered because of delays in the prior authorization process.
Data on initial treatment denials show that few hold up on appeal.
“If there is evidence of large-scale inappropriate utilization or overutilization, then treatment denials should withstand scrutiny on appeal,” Vivek Kavadi, MD, a radiation oncologist with Texas Oncology and vice chair of ASTRO’s Payer Relations Subcommittee, said during the briefing. “However, that is not what we found. This raises serious questions on the justification for the denial in the first place.”
In the survey, 41% of respondents said 76%-100% of denials are overturned, 22% said 51%-75% are overturned, 17% said 26%-50% are overturned, 19% said 0-25% are overturned, and 2% said none of their appeals resulted in a prior authorization denial being overturned.
In addition, 44% of respondents said the peer-to-peer appeals processes are typically not handled by a radiation oncologist on the payer side.
“We very rarely have a case denied following peer-to-peer review or appeal,” Dr. Harari said. “However, the many hours spent by our physician providers and the delays in commencing treatment for these cancer patients can never be recovered.”
To handle the workload generated by the prior authorization process, 63% of those responding to the survey said they have hired staff specifically to handle prior authorization requests.
“In an era of value-based care, where is the value when we are increasing costs without adding clinical benefit?” Dr. Kavadi asked.
Dr. Harari called for legislation to simplify the prior authorization process and make it less burdensome, but individual proposals were not highlighted.
SOURCE: American Society for Radiation Oncology survey.
Nine in 10 radiation oncologists report that prior authorization for treatment is either very challenging (42%) or moderately challenging (48%), according to data from a member survey released by the American Society for Radiation Oncology (ASTRO).
“In 2018, [prior authorization] became the most challenging issue facing radiation oncologists,” Paul Harari, MD, Jack Fowler Professor and chair of oncology at the University of Wisconsin, Madison, and chair of the ASTRO board of directors, said during a press briefing. “Prior authorization is creating multiple obstacles to cancer patient care.”
According to responses from 673 ASTRO members, 31% said seeking prior authorization has caused delays in treatment of 5 or more days, 32% said it causes delays of 4-5 days, and 30% said it causes delays of 1-3 days. Seven percent said the prior authorization requests are resolved within less than a day.
Prior authorization delays forced 32% of respondents to alter treatment plans in more than 10% of their cases, and another 31% said treatment plans were altered in 5%-10% of their cases. For 37% of the respondents, less than 5% of their treatment plans were altered because of delays in the prior authorization process.
Data on initial treatment denials show that few hold up on appeal.
“If there is evidence of large-scale inappropriate utilization or overutilization, then treatment denials should withstand scrutiny on appeal,” Vivek Kavadi, MD, a radiation oncologist with Texas Oncology and vice chair of ASTRO’s Payer Relations Subcommittee, said during the briefing. “However, that is not what we found. This raises serious questions on the justification for the denial in the first place.”
In the survey, 41% of respondents said 76%-100% of denials are overturned, 22% said 51%-75% are overturned, 17% said 26%-50% are overturned, 19% said 0-25% are overturned, and 2% said none of their appeals resulted in a prior authorization denial being overturned.
In addition, 44% of respondents said the peer-to-peer appeals processes are typically not handled by a radiation oncologist on the payer side.
“We very rarely have a case denied following peer-to-peer review or appeal,” Dr. Harari said. “However, the many hours spent by our physician providers and the delays in commencing treatment for these cancer patients can never be recovered.”
To handle the workload generated by the prior authorization process, 63% of those responding to the survey said they have hired staff specifically to handle prior authorization requests.
“In an era of value-based care, where is the value when we are increasing costs without adding clinical benefit?” Dr. Kavadi asked.
Dr. Harari called for legislation to simplify the prior authorization process and make it less burdensome, but individual proposals were not highlighted.
SOURCE: American Society for Radiation Oncology survey.
Nine in 10 radiation oncologists report that prior authorization for treatment is either very challenging (42%) or moderately challenging (48%), according to data from a member survey released by the American Society for Radiation Oncology (ASTRO).
“In 2018, [prior authorization] became the most challenging issue facing radiation oncologists,” Paul Harari, MD, Jack Fowler Professor and chair of oncology at the University of Wisconsin, Madison, and chair of the ASTRO board of directors, said during a press briefing. “Prior authorization is creating multiple obstacles to cancer patient care.”
According to responses from 673 ASTRO members, 31% said seeking prior authorization has caused delays in treatment of 5 or more days, 32% said it causes delays of 4-5 days, and 30% said it causes delays of 1-3 days. Seven percent said the prior authorization requests are resolved within less than a day.
Prior authorization delays forced 32% of respondents to alter treatment plans in more than 10% of their cases, and another 31% said treatment plans were altered in 5%-10% of their cases. For 37% of the respondents, less than 5% of their treatment plans were altered because of delays in the prior authorization process.
Data on initial treatment denials show that few hold up on appeal.
“If there is evidence of large-scale inappropriate utilization or overutilization, then treatment denials should withstand scrutiny on appeal,” Vivek Kavadi, MD, a radiation oncologist with Texas Oncology and vice chair of ASTRO’s Payer Relations Subcommittee, said during the briefing. “However, that is not what we found. This raises serious questions on the justification for the denial in the first place.”
In the survey, 41% of respondents said 76%-100% of denials are overturned, 22% said 51%-75% are overturned, 17% said 26%-50% are overturned, 19% said 0-25% are overturned, and 2% said none of their appeals resulted in a prior authorization denial being overturned.
In addition, 44% of respondents said the peer-to-peer appeals processes are typically not handled by a radiation oncologist on the payer side.
“We very rarely have a case denied following peer-to-peer review or appeal,” Dr. Harari said. “However, the many hours spent by our physician providers and the delays in commencing treatment for these cancer patients can never be recovered.”
To handle the workload generated by the prior authorization process, 63% of those responding to the survey said they have hired staff specifically to handle prior authorization requests.
“In an era of value-based care, where is the value when we are increasing costs without adding clinical benefit?” Dr. Kavadi asked.
Dr. Harari called for legislation to simplify the prior authorization process and make it less burdensome, but individual proposals were not highlighted.
SOURCE: American Society for Radiation Oncology survey.
Violaceous Nodules on the Hard Palate
The Diagnosis: Kaposi Sarcoma
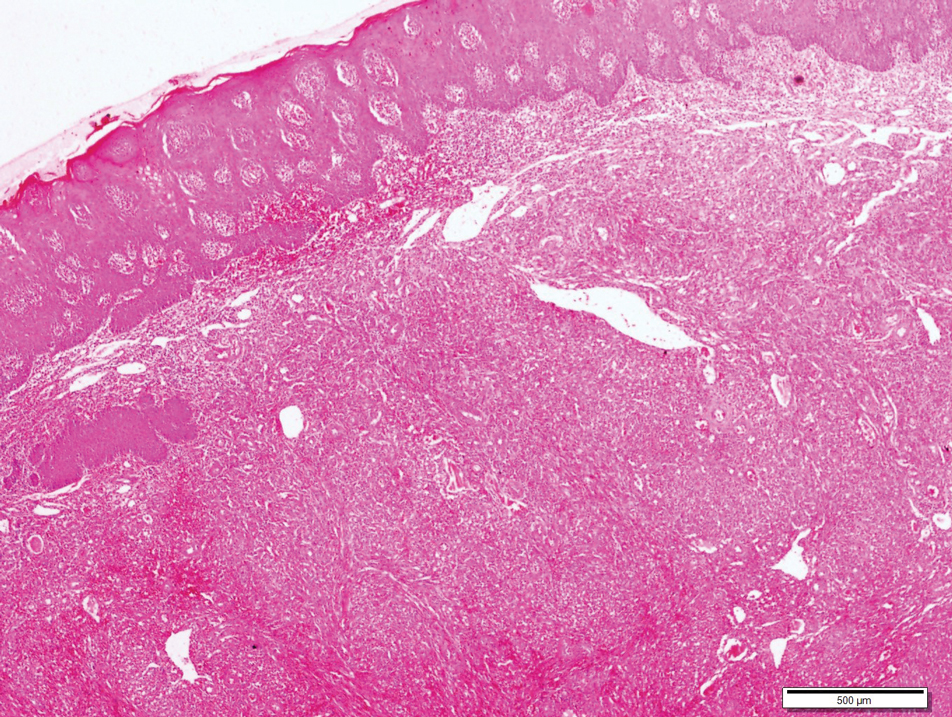
A 4-mm punch biopsy from the border of an ulcerated nodular lesion on the hard palate demonstrated diffusely distributed spindle cells, cleftlike microvascularity with extravasated erythrocytes, and widespread human herpesvirus 8 immunoreactivity on histopathology (Figure 1). Serologic tests were positive for human immunodeficiency virus (HIV) infection; HIV RNA was 14,584 IU/mL and the CD4 count was 254/mm3. The patient was diagnosed with Kaposi sarcoma (KS) and referred to the infectious disease department for initiation of antiviral therapy. Marked regression was detected after 6 months of highly active antiretroviral therapy (HAART) without any additional treatment (Figure 2).
widespread human herpesvirus 8 immunoreactivity (H&E, original magnification ×4).
Kaposi sarcoma is a human herpesvirus 8-associated angioproliferative disorder with low-grade malignant potential. There are 4 well-known clinical types: classic, endemic, iatrogenic, and AIDS associated.1 Involvement of the oral cavity may be seen in all types but mostly is associated with the AIDS-associated type, which also could be a signal for undiagnosed asymptomatic HIV infection.2 Oral KS most often affects the hard and soft palate, gingiva, and dorsal tongue, with plaques or tumors ranging from nonpigmented to brownish red or violaceous. AIDS-associated KS is known to be related to cytokine expression, which is induced by HIV infection causing immune dysregulation by altering the expression of cytokines, including IL-1, tumor necrosis factor α, and IL-6.1 An in vitro study showed that cytokines secrete a number of angiogenic growth factors that, along with HIV proteins, induce and proliferate cells to become sarcoma cells. Integrins and the apoptosis process also are important in proliferation and neovascularization of KS tumor cells.3
Bacillary angiomatosis (BA) is a rare manifestation of infection caused by Bartonella species, which leads to vasoproliferative lesions of the skin and other organs. Bacillary angiomatosis affects individuals with advanced HIV or other immunocompromised individuals and may clinically mimic KS, which is similarly characterized by red-purple papules, nodules, or plaques. Differentiating BA from KS largely depends on histopathologic examination, with BA demonstrating protuberant endothelial cells surrounded by clumps of bacilli that are visible on Warthin-Starry silver stain.
Lymphangioma is a benign hamartomatous hyperplasia of the lymphatic vessels. The majority of lymphangiomas are superficial, but a few may extend deeply into the connective tissue. Intraoral lymphangiomas occur more frequently on the dorsum of the tongue, followed by the palate, buccal mucosa, gingiva, and lips. They may be differentiated with their soft quality, pebblelike surface, and translucent vesicles.
Malignant tumors of the oral cavity are rare, representing only 5% of tumors occurring in the body.4 Among malignant tumors of the oral cavity, squamous cell carcinomas are the most frequent type (90%-98%), and lymphomas and melanoma are the most outstanding among the remaining 2% to 10%. Both for lymphoma and mucosal melanoma, the most common sites of involvement are the soft tissues of the oral cavity, palatal mucosa, gingiva, tongue, cheeks, floor of the mouth, and lips.4 Although mucosal melanoma lesions usually are characterized by pigmented and ulcerated lesions, amelanotic variants also should be kept in mind. Histopathologic examination is mandatory for diagnosis.
Intralesional chemotherapy with vinblastine or bleomycin, radiotherapy, electrochemotherapy, systemic antiretroviral therapy (ie, HAART), and chemotherapy with daunorubicin and pegylated liposomal doxorubicin are the main treatment options.5,6 The immune system activator role of HAART leads to an increased CD4 count and reduces HIV proteins, which helps induction of the proliferation and neovascularization of KS tumor cells.3 This effect may help resolution of KS with localized involvement and allows physicians to utilize HAART without any other additional local and systemic chemotherapy treatment.
- Fatahzadeh M, Schwartz RA. Oral Kaposi's sarcoma: a review and update. Int J Dermatol. 2013;52:666-672.
- Martorano LM, Cannella JD, Lloyd JR. Mucocutaneous presentation of Kaposi sarcoma in an asymptomatic human immunodeficiency virus-positive man. Cutis. 2015;95:E19-E22.
- Stebbing J, Portsmouth S, Gazzard B. How does HAART lead to the resolution of Kaposi's sarcoma? J Antimicrobial Chemother. 2003;51:1095-1098.
- Guevara-Canales JO, Morales-Vadillo R, Sacsaquispe-Contreras SJ, et al. Malignant lymphoma of the oral cavity and the maxillofacial region: overall survivalprognostic factors. Med Oral Patol Oral Cir Bucal. 2013;18:E619-E626.
- Donato V, Guarnaccia R, Dognini J, et al. Radiation therapy in the treatment of HIV-related Kaposi's sarcoma. Anticancer Res. 2013;33:2153-2157.
- Gbabe OF, Okwundu CI, Dedicoat M, et al. Treatment of severe or progressive Kaposi's sarcoma in HIV-infected adults. Cochrane Database Syst Rev. 2014:CD003256.
The Diagnosis: Kaposi Sarcoma
A 4-mm punch biopsy from the border of an ulcerated nodular lesion on the hard palate demonstrated diffusely distributed spindle cells, cleftlike microvascularity with extravasated erythrocytes, and widespread human herpesvirus 8 immunoreactivity on histopathology (Figure 1). Serologic tests were positive for human immunodeficiency virus (HIV) infection; HIV RNA was 14,584 IU/mL and the CD4 count was 254/mm3. The patient was diagnosed with Kaposi sarcoma (KS) and referred to the infectious disease department for initiation of antiviral therapy. Marked regression was detected after 6 months of highly active antiretroviral therapy (HAART) without any additional treatment (Figure 2).
widespread human herpesvirus 8 immunoreactivity (H&E, original magnification ×4).
Kaposi sarcoma is a human herpesvirus 8-associated angioproliferative disorder with low-grade malignant potential. There are 4 well-known clinical types: classic, endemic, iatrogenic, and AIDS associated.1 Involvement of the oral cavity may be seen in all types but mostly is associated with the AIDS-associated type, which also could be a signal for undiagnosed asymptomatic HIV infection.2 Oral KS most often affects the hard and soft palate, gingiva, and dorsal tongue, with plaques or tumors ranging from nonpigmented to brownish red or violaceous. AIDS-associated KS is known to be related to cytokine expression, which is induced by HIV infection causing immune dysregulation by altering the expression of cytokines, including IL-1, tumor necrosis factor α, and IL-6.1 An in vitro study showed that cytokines secrete a number of angiogenic growth factors that, along with HIV proteins, induce and proliferate cells to become sarcoma cells. Integrins and the apoptosis process also are important in proliferation and neovascularization of KS tumor cells.3
Bacillary angiomatosis (BA) is a rare manifestation of infection caused by Bartonella species, which leads to vasoproliferative lesions of the skin and other organs. Bacillary angiomatosis affects individuals with advanced HIV or other immunocompromised individuals and may clinically mimic KS, which is similarly characterized by red-purple papules, nodules, or plaques. Differentiating BA from KS largely depends on histopathologic examination, with BA demonstrating protuberant endothelial cells surrounded by clumps of bacilli that are visible on Warthin-Starry silver stain.
Lymphangioma is a benign hamartomatous hyperplasia of the lymphatic vessels. The majority of lymphangiomas are superficial, but a few may extend deeply into the connective tissue. Intraoral lymphangiomas occur more frequently on the dorsum of the tongue, followed by the palate, buccal mucosa, gingiva, and lips. They may be differentiated with their soft quality, pebblelike surface, and translucent vesicles.
Malignant tumors of the oral cavity are rare, representing only 5% of tumors occurring in the body.4 Among malignant tumors of the oral cavity, squamous cell carcinomas are the most frequent type (90%-98%), and lymphomas and melanoma are the most outstanding among the remaining 2% to 10%. Both for lymphoma and mucosal melanoma, the most common sites of involvement are the soft tissues of the oral cavity, palatal mucosa, gingiva, tongue, cheeks, floor of the mouth, and lips.4 Although mucosal melanoma lesions usually are characterized by pigmented and ulcerated lesions, amelanotic variants also should be kept in mind. Histopathologic examination is mandatory for diagnosis.
Intralesional chemotherapy with vinblastine or bleomycin, radiotherapy, electrochemotherapy, systemic antiretroviral therapy (ie, HAART), and chemotherapy with daunorubicin and pegylated liposomal doxorubicin are the main treatment options.5,6 The immune system activator role of HAART leads to an increased CD4 count and reduces HIV proteins, which helps induction of the proliferation and neovascularization of KS tumor cells.3 This effect may help resolution of KS with localized involvement and allows physicians to utilize HAART without any other additional local and systemic chemotherapy treatment.
The Diagnosis: Kaposi Sarcoma
A 4-mm punch biopsy from the border of an ulcerated nodular lesion on the hard palate demonstrated diffusely distributed spindle cells, cleftlike microvascularity with extravasated erythrocytes, and widespread human herpesvirus 8 immunoreactivity on histopathology (Figure 1). Serologic tests were positive for human immunodeficiency virus (HIV) infection; HIV RNA was 14,584 IU/mL and the CD4 count was 254/mm3. The patient was diagnosed with Kaposi sarcoma (KS) and referred to the infectious disease department for initiation of antiviral therapy. Marked regression was detected after 6 months of highly active antiretroviral therapy (HAART) without any additional treatment (Figure 2).
widespread human herpesvirus 8 immunoreactivity (H&E, original magnification ×4).
Kaposi sarcoma is a human herpesvirus 8-associated angioproliferative disorder with low-grade malignant potential. There are 4 well-known clinical types: classic, endemic, iatrogenic, and AIDS associated.1 Involvement of the oral cavity may be seen in all types but mostly is associated with the AIDS-associated type, which also could be a signal for undiagnosed asymptomatic HIV infection.2 Oral KS most often affects the hard and soft palate, gingiva, and dorsal tongue, with plaques or tumors ranging from nonpigmented to brownish red or violaceous. AIDS-associated KS is known to be related to cytokine expression, which is induced by HIV infection causing immune dysregulation by altering the expression of cytokines, including IL-1, tumor necrosis factor α, and IL-6.1 An in vitro study showed that cytokines secrete a number of angiogenic growth factors that, along with HIV proteins, induce and proliferate cells to become sarcoma cells. Integrins and the apoptosis process also are important in proliferation and neovascularization of KS tumor cells.3
Bacillary angiomatosis (BA) is a rare manifestation of infection caused by Bartonella species, which leads to vasoproliferative lesions of the skin and other organs. Bacillary angiomatosis affects individuals with advanced HIV or other immunocompromised individuals and may clinically mimic KS, which is similarly characterized by red-purple papules, nodules, or plaques. Differentiating BA from KS largely depends on histopathologic examination, with BA demonstrating protuberant endothelial cells surrounded by clumps of bacilli that are visible on Warthin-Starry silver stain.
Lymphangioma is a benign hamartomatous hyperplasia of the lymphatic vessels. The majority of lymphangiomas are superficial, but a few may extend deeply into the connective tissue. Intraoral lymphangiomas occur more frequently on the dorsum of the tongue, followed by the palate, buccal mucosa, gingiva, and lips. They may be differentiated with their soft quality, pebblelike surface, and translucent vesicles.
Malignant tumors of the oral cavity are rare, representing only 5% of tumors occurring in the body.4 Among malignant tumors of the oral cavity, squamous cell carcinomas are the most frequent type (90%-98%), and lymphomas and melanoma are the most outstanding among the remaining 2% to 10%. Both for lymphoma and mucosal melanoma, the most common sites of involvement are the soft tissues of the oral cavity, palatal mucosa, gingiva, tongue, cheeks, floor of the mouth, and lips.4 Although mucosal melanoma lesions usually are characterized by pigmented and ulcerated lesions, amelanotic variants also should be kept in mind. Histopathologic examination is mandatory for diagnosis.
Intralesional chemotherapy with vinblastine or bleomycin, radiotherapy, electrochemotherapy, systemic antiretroviral therapy (ie, HAART), and chemotherapy with daunorubicin and pegylated liposomal doxorubicin are the main treatment options.5,6 The immune system activator role of HAART leads to an increased CD4 count and reduces HIV proteins, which helps induction of the proliferation and neovascularization of KS tumor cells.3 This effect may help resolution of KS with localized involvement and allows physicians to utilize HAART without any other additional local and systemic chemotherapy treatment.
- Fatahzadeh M, Schwartz RA. Oral Kaposi's sarcoma: a review and update. Int J Dermatol. 2013;52:666-672.
- Martorano LM, Cannella JD, Lloyd JR. Mucocutaneous presentation of Kaposi sarcoma in an asymptomatic human immunodeficiency virus-positive man. Cutis. 2015;95:E19-E22.
- Stebbing J, Portsmouth S, Gazzard B. How does HAART lead to the resolution of Kaposi's sarcoma? J Antimicrobial Chemother. 2003;51:1095-1098.
- Guevara-Canales JO, Morales-Vadillo R, Sacsaquispe-Contreras SJ, et al. Malignant lymphoma of the oral cavity and the maxillofacial region: overall survivalprognostic factors. Med Oral Patol Oral Cir Bucal. 2013;18:E619-E626.
- Donato V, Guarnaccia R, Dognini J, et al. Radiation therapy in the treatment of HIV-related Kaposi's sarcoma. Anticancer Res. 2013;33:2153-2157.
- Gbabe OF, Okwundu CI, Dedicoat M, et al. Treatment of severe or progressive Kaposi's sarcoma in HIV-infected adults. Cochrane Database Syst Rev. 2014:CD003256.
- Fatahzadeh M, Schwartz RA. Oral Kaposi's sarcoma: a review and update. Int J Dermatol. 2013;52:666-672.
- Martorano LM, Cannella JD, Lloyd JR. Mucocutaneous presentation of Kaposi sarcoma in an asymptomatic human immunodeficiency virus-positive man. Cutis. 2015;95:E19-E22.
- Stebbing J, Portsmouth S, Gazzard B. How does HAART lead to the resolution of Kaposi's sarcoma? J Antimicrobial Chemother. 2003;51:1095-1098.
- Guevara-Canales JO, Morales-Vadillo R, Sacsaquispe-Contreras SJ, et al. Malignant lymphoma of the oral cavity and the maxillofacial region: overall survivalprognostic factors. Med Oral Patol Oral Cir Bucal. 2013;18:E619-E626.
- Donato V, Guarnaccia R, Dognini J, et al. Radiation therapy in the treatment of HIV-related Kaposi's sarcoma. Anticancer Res. 2013;33:2153-2157.
- Gbabe OF, Okwundu CI, Dedicoat M, et al. Treatment of severe or progressive Kaposi's sarcoma in HIV-infected adults. Cochrane Database Syst Rev. 2014:CD003256.
A 30-year-old man presented to our outpatient clinic with rapidly growing, ulcerated, violaceous lesions on the hard palate of 4 months' duration. Physical examination revealed approximately 2.0×1.5-cm, centrally ulcerated, violaceous, nodular lesions on the hard palate, as well as a 4-mm pinkish papular lesion on the soft palate.
Bundled payment for OA surgery linked to more emergency department visits
And therein lies a key lesson for health policy makers who have embraced bundled payments to reduce rising health care costs, Mayilee Canizares, PhD, observed at the OARSI 2019 World Congress.
In Ontario, with patients discharged sooner and directly to home, there was the negative impact of increased emergency department visits after surgery, Dr. Canizares, of the University Health Network in Toronto, said at OARSI 2019 World Congress, sponsored by the Osteoarthritis Research Society International. “Our findings highlight the importance of coordinating the appropriate support services as well as the need to continue assessing the optimal discharge care plan for osteoarthritis patients undergoing surgery.”
Dr. Canizares’ study of the Ontario-wide experience with orthopedic surgery for osteoarthritis during 2004-2016 received the OARSI 2019 award for the meeting’s top-rated study in clinical epidemiology/health services research.
Using administrative data from Canada’s national health care system, Dr. Canizares and her coinvestigators found that the number of individuals undergoing elective orthopedic surgery for osteoarthritis ballooned from 22,700 in 2004 to 41,900 in 2016, representing an increase from 246 to 381 procedures per 100,000 people. During this time, the mean length of stay declined from about 5 days to just under 3 days, the 30-day readmission rate dropped from 4.2% to 3.4%, and the rate of emergency department visits within 30 days post discharge rose steadily from 8.7% in 2004 to 14.1% in 2016.
Roughly half of the operations were total knee replacements and one-third were hip replacements. The profile of patients undergoing surgery changed little over the course of the 12-year study with the exception that in more recent years patients presented with more comorbidities: Indeed, three or more comorbid conditions were present in 2.9% of the surgical patients in 2004 compared to 4.2% in 2016.
In multivariate logistic regression analyses, patient characteristics didn’t explain the change over time in early readmission or unplanned emergency department visit rates. However, discharge disposition did: By 2014, more patients were being discharged home, and in nearly half of cases that was being done without support.
Dr. Canizares reported having no financial conflicts regarding her study, funded by the Toronto General and Western Hospital Foundation.
SOURCE: Canizares M. OARSI, Abstract 16.
And therein lies a key lesson for health policy makers who have embraced bundled payments to reduce rising health care costs, Mayilee Canizares, PhD, observed at the OARSI 2019 World Congress.
In Ontario, with patients discharged sooner and directly to home, there was the negative impact of increased emergency department visits after surgery, Dr. Canizares, of the University Health Network in Toronto, said at OARSI 2019 World Congress, sponsored by the Osteoarthritis Research Society International. “Our findings highlight the importance of coordinating the appropriate support services as well as the need to continue assessing the optimal discharge care plan for osteoarthritis patients undergoing surgery.”
Dr. Canizares’ study of the Ontario-wide experience with orthopedic surgery for osteoarthritis during 2004-2016 received the OARSI 2019 award for the meeting’s top-rated study in clinical epidemiology/health services research.
Using administrative data from Canada’s national health care system, Dr. Canizares and her coinvestigators found that the number of individuals undergoing elective orthopedic surgery for osteoarthritis ballooned from 22,700 in 2004 to 41,900 in 2016, representing an increase from 246 to 381 procedures per 100,000 people. During this time, the mean length of stay declined from about 5 days to just under 3 days, the 30-day readmission rate dropped from 4.2% to 3.4%, and the rate of emergency department visits within 30 days post discharge rose steadily from 8.7% in 2004 to 14.1% in 2016.
Roughly half of the operations were total knee replacements and one-third were hip replacements. The profile of patients undergoing surgery changed little over the course of the 12-year study with the exception that in more recent years patients presented with more comorbidities: Indeed, three or more comorbid conditions were present in 2.9% of the surgical patients in 2004 compared to 4.2% in 2016.
In multivariate logistic regression analyses, patient characteristics didn’t explain the change over time in early readmission or unplanned emergency department visit rates. However, discharge disposition did: By 2014, more patients were being discharged home, and in nearly half of cases that was being done without support.
Dr. Canizares reported having no financial conflicts regarding her study, funded by the Toronto General and Western Hospital Foundation.
SOURCE: Canizares M. OARSI, Abstract 16.
And therein lies a key lesson for health policy makers who have embraced bundled payments to reduce rising health care costs, Mayilee Canizares, PhD, observed at the OARSI 2019 World Congress.
In Ontario, with patients discharged sooner and directly to home, there was the negative impact of increased emergency department visits after surgery, Dr. Canizares, of the University Health Network in Toronto, said at OARSI 2019 World Congress, sponsored by the Osteoarthritis Research Society International. “Our findings highlight the importance of coordinating the appropriate support services as well as the need to continue assessing the optimal discharge care plan for osteoarthritis patients undergoing surgery.”
Dr. Canizares’ study of the Ontario-wide experience with orthopedic surgery for osteoarthritis during 2004-2016 received the OARSI 2019 award for the meeting’s top-rated study in clinical epidemiology/health services research.
Using administrative data from Canada’s national health care system, Dr. Canizares and her coinvestigators found that the number of individuals undergoing elective orthopedic surgery for osteoarthritis ballooned from 22,700 in 2004 to 41,900 in 2016, representing an increase from 246 to 381 procedures per 100,000 people. During this time, the mean length of stay declined from about 5 days to just under 3 days, the 30-day readmission rate dropped from 4.2% to 3.4%, and the rate of emergency department visits within 30 days post discharge rose steadily from 8.7% in 2004 to 14.1% in 2016.
Roughly half of the operations were total knee replacements and one-third were hip replacements. The profile of patients undergoing surgery changed little over the course of the 12-year study with the exception that in more recent years patients presented with more comorbidities: Indeed, three or more comorbid conditions were present in 2.9% of the surgical patients in 2004 compared to 4.2% in 2016.
In multivariate logistic regression analyses, patient characteristics didn’t explain the change over time in early readmission or unplanned emergency department visit rates. However, discharge disposition did: By 2014, more patients were being discharged home, and in nearly half of cases that was being done without support.
Dr. Canizares reported having no financial conflicts regarding her study, funded by the Toronto General and Western Hospital Foundation.
SOURCE: Canizares M. OARSI, Abstract 16.
REPORTING FROM OARSI 2019
Short Takes
Evidence is uncertain for benefit of short-stay unit hospitalization
A Cochrane review of 14 randomized trials evaluating short-stay unit hospitalization for internal medicine conditions was unable to ascertain any definite benefit or harm, compared with usual care, with concerns for heterogeneity, bias, and random error in the studies. The authors recommended conducting more trials with low risk of bias and low risk of random errors.
Citation: Strøm C et al. Hospitalisation in short-stay units for adults with internal medicine diseases and conditions. Cochrane Database Syst Rev. 2018;8. CD012370. doi: 10.1002/14651858.CD012370.pub2.
Hospice use among Medicare patients with heart failure
Of the 4% percent of Medicare patients discharged to hospice from a hospitalization for heart failure, 25% died within 72 hours of discharge, leading the authors to conclude that hospice is underutilized and initiated too late in the setting of heart failure.
Citation: Warraich HJ et al. Trends in hospice discharge and relative outcomes among Medicare patients in the Get With The Guidelines–Heart Failure Registry. JAMA Cardiol. 2018 Oct 1;3(10):917-26.
Culprit lesion PCI has similar 1-year mortality to immediate multivessel PCI
This is the follow-up study to CULPRIT-SHOCK trial , which examined percutaneous coronary intervention in culprit lesion only vs. multivessel PCI in the setting of cardiogenic shock. The initial trial showed improved 30-day mortality outcomes with culprit lesion PCI only and the follow-up demonstrated no significant difference in 1-year mortality between the two groups.
Citation: Thiele H et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018 Nov 1;379(18):1699-710 .
Evidence is uncertain for benefit of short-stay unit hospitalization
A Cochrane review of 14 randomized trials evaluating short-stay unit hospitalization for internal medicine conditions was unable to ascertain any definite benefit or harm, compared with usual care, with concerns for heterogeneity, bias, and random error in the studies. The authors recommended conducting more trials with low risk of bias and low risk of random errors.
Citation: Strøm C et al. Hospitalisation in short-stay units for adults with internal medicine diseases and conditions. Cochrane Database Syst Rev. 2018;8. CD012370. doi: 10.1002/14651858.CD012370.pub2.
Hospice use among Medicare patients with heart failure
Of the 4% percent of Medicare patients discharged to hospice from a hospitalization for heart failure, 25% died within 72 hours of discharge, leading the authors to conclude that hospice is underutilized and initiated too late in the setting of heart failure.
Citation: Warraich HJ et al. Trends in hospice discharge and relative outcomes among Medicare patients in the Get With The Guidelines–Heart Failure Registry. JAMA Cardiol. 2018 Oct 1;3(10):917-26.
Culprit lesion PCI has similar 1-year mortality to immediate multivessel PCI
This is the follow-up study to CULPRIT-SHOCK trial , which examined percutaneous coronary intervention in culprit lesion only vs. multivessel PCI in the setting of cardiogenic shock. The initial trial showed improved 30-day mortality outcomes with culprit lesion PCI only and the follow-up demonstrated no significant difference in 1-year mortality between the two groups.
Citation: Thiele H et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018 Nov 1;379(18):1699-710 .
Evidence is uncertain for benefit of short-stay unit hospitalization
A Cochrane review of 14 randomized trials evaluating short-stay unit hospitalization for internal medicine conditions was unable to ascertain any definite benefit or harm, compared with usual care, with concerns for heterogeneity, bias, and random error in the studies. The authors recommended conducting more trials with low risk of bias and low risk of random errors.
Citation: Strøm C et al. Hospitalisation in short-stay units for adults with internal medicine diseases and conditions. Cochrane Database Syst Rev. 2018;8. CD012370. doi: 10.1002/14651858.CD012370.pub2.
Hospice use among Medicare patients with heart failure
Of the 4% percent of Medicare patients discharged to hospice from a hospitalization for heart failure, 25% died within 72 hours of discharge, leading the authors to conclude that hospice is underutilized and initiated too late in the setting of heart failure.
Citation: Warraich HJ et al. Trends in hospice discharge and relative outcomes among Medicare patients in the Get With The Guidelines–Heart Failure Registry. JAMA Cardiol. 2018 Oct 1;3(10):917-26.
Culprit lesion PCI has similar 1-year mortality to immediate multivessel PCI
This is the follow-up study to CULPRIT-SHOCK trial , which examined percutaneous coronary intervention in culprit lesion only vs. multivessel PCI in the setting of cardiogenic shock. The initial trial showed improved 30-day mortality outcomes with culprit lesion PCI only and the follow-up demonstrated no significant difference in 1-year mortality between the two groups.
Citation: Thiele H et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018 Nov 1;379(18):1699-710 .
Immunostaining boosts pathologists’ accuracy in Barrett’s esophagus
SAN DIEGO – Years of experience and an academic medical center affiliation predicted the accuracy of pathologists reviewing biopsies from patients with Barrett’s esophagus, according to the results of a multinational study.
Those with 5 or more years of experience were less likely to make major diagnostic errors in reviewing Barrett’s esophagus biopsies (odds ratio [OR], 0.48, 95% confidence interval, 0.31-0.74). Pathologists who worked in nonacademic settings were more likely to make a major diagnostic error (OR, 1.76; 95% CI, 1.15-2.69) when reviewing hematoxylin and eosin-stained slides alone, but the addition of p53 immunostaining greatly improved accuracy.
Current guidelines recommend expert evaluation of Barrett’s esophagus biopsies that show dysplasia, but exact determination of expert review status had been lacking, according to Marnix Jansen, MD, a pathologist at University College London.
“The guidelines say that biopsies with dysplasia need to be reviewed by an expert pathologist, but don’t define what makes an expert pathologist,” Dr. Jansen said in an interview at the annual Digestive Disease Week.
“We wanted to advance the field by for the first time creating objective and quantitative standards” to delineate the characteristics of an expert pathologist in reviewing Barrett’s esophagus tissue samples, said Dr. Jansen. The study’s first author is Myrtle J. van der Wel, MD, of Amsterdam University Medical Center, the Netherlands.
More than 6,000 individual case diagnoses were used in the study, which included pathologists from more than 20 countries. Before the pathologists began reviewing the case set, they answered a questionnaire about training, practice context, years of experience, case volume, and other demographic characteristics.
“We then sent those biopsies around the world to ... 55 pathologists in the U.S., in Europe, Japan, Australia, even some in South America – so really around the whole globe,” explained Dr. Jansen. Biopsies were assessed by each pathologist before and after p53 immunostaining.
“Once we had the final dataset – which is massive, because we had 6,000 case diagnoses within our dataset – we could then regress those variables back onto the consensus data,” providing a first-ever look at “clear predictors of what the pathologist looks like that will score on a par with where the experts are,” said Dr. Jansen.
The results? “You need at least 5 years of experience. On top of that, if you are a pathologist working in a [nonacademic center], you are at a slightly increased risk of making major diagnostic errors,” said Dr. Jansen. However, the analysis convincingly showed that the addition of p53 immunostaining neutralized the risk for these pathologists – a strength of having such a large dataset, he said.
The study also affirmed the safety of digital pathology for expert review, said Dr. Jansen: “One of the reassuring points of our study was that we found that the best concordance was for nondysplastic Barrett’s, and high-grade dysplasia, which really replicates known glass slide characteristics. So we can really say that digital pathology is safe for this application – which is very relevant for pathologists that are taking in cases from outside for expert review.”
Concordance rates for nondysplastic Barrett’s esophagus and high-grade dysplasia were over 70%; for low-grade dysplasia, rates were intermediate at 42%.
Going forward, the study can inform the next iteration of guidelines for pathologist review of Barrett’s dysplasia, said Dr. Jansen. Rather than just recommending expert review, the guidelines can include a quantitative assessment of what’s needed. “You need to have to have at least 5 years of experience, and if you work in a [community hospital], to use a p53, and that is collectively what amounts to expertise in Barrett’s pathology.”
A follow-up study with a similar design is planned within the United Kingdom, the Netherlands, and the United States. This study, which Dr. Jansen said would enroll hundreds of pathologists, will include an intervention arm that administers a tutorial with the aim of improving concordance scoring.
Dr. Jansen reported no relevant conflicts of interest.
SAN DIEGO – Years of experience and an academic medical center affiliation predicted the accuracy of pathologists reviewing biopsies from patients with Barrett’s esophagus, according to the results of a multinational study.
Those with 5 or more years of experience were less likely to make major diagnostic errors in reviewing Barrett’s esophagus biopsies (odds ratio [OR], 0.48, 95% confidence interval, 0.31-0.74). Pathologists who worked in nonacademic settings were more likely to make a major diagnostic error (OR, 1.76; 95% CI, 1.15-2.69) when reviewing hematoxylin and eosin-stained slides alone, but the addition of p53 immunostaining greatly improved accuracy.
Current guidelines recommend expert evaluation of Barrett’s esophagus biopsies that show dysplasia, but exact determination of expert review status had been lacking, according to Marnix Jansen, MD, a pathologist at University College London.
“The guidelines say that biopsies with dysplasia need to be reviewed by an expert pathologist, but don’t define what makes an expert pathologist,” Dr. Jansen said in an interview at the annual Digestive Disease Week.
“We wanted to advance the field by for the first time creating objective and quantitative standards” to delineate the characteristics of an expert pathologist in reviewing Barrett’s esophagus tissue samples, said Dr. Jansen. The study’s first author is Myrtle J. van der Wel, MD, of Amsterdam University Medical Center, the Netherlands.
More than 6,000 individual case diagnoses were used in the study, which included pathologists from more than 20 countries. Before the pathologists began reviewing the case set, they answered a questionnaire about training, practice context, years of experience, case volume, and other demographic characteristics.
“We then sent those biopsies around the world to ... 55 pathologists in the U.S., in Europe, Japan, Australia, even some in South America – so really around the whole globe,” explained Dr. Jansen. Biopsies were assessed by each pathologist before and after p53 immunostaining.
“Once we had the final dataset – which is massive, because we had 6,000 case diagnoses within our dataset – we could then regress those variables back onto the consensus data,” providing a first-ever look at “clear predictors of what the pathologist looks like that will score on a par with where the experts are,” said Dr. Jansen.
The results? “You need at least 5 years of experience. On top of that, if you are a pathologist working in a [nonacademic center], you are at a slightly increased risk of making major diagnostic errors,” said Dr. Jansen. However, the analysis convincingly showed that the addition of p53 immunostaining neutralized the risk for these pathologists – a strength of having such a large dataset, he said.
The study also affirmed the safety of digital pathology for expert review, said Dr. Jansen: “One of the reassuring points of our study was that we found that the best concordance was for nondysplastic Barrett’s, and high-grade dysplasia, which really replicates known glass slide characteristics. So we can really say that digital pathology is safe for this application – which is very relevant for pathologists that are taking in cases from outside for expert review.”
Concordance rates for nondysplastic Barrett’s esophagus and high-grade dysplasia were over 70%; for low-grade dysplasia, rates were intermediate at 42%.
Going forward, the study can inform the next iteration of guidelines for pathologist review of Barrett’s dysplasia, said Dr. Jansen. Rather than just recommending expert review, the guidelines can include a quantitative assessment of what’s needed. “You need to have to have at least 5 years of experience, and if you work in a [community hospital], to use a p53, and that is collectively what amounts to expertise in Barrett’s pathology.”
A follow-up study with a similar design is planned within the United Kingdom, the Netherlands, and the United States. This study, which Dr. Jansen said would enroll hundreds of pathologists, will include an intervention arm that administers a tutorial with the aim of improving concordance scoring.
Dr. Jansen reported no relevant conflicts of interest.
SAN DIEGO – Years of experience and an academic medical center affiliation predicted the accuracy of pathologists reviewing biopsies from patients with Barrett’s esophagus, according to the results of a multinational study.
Those with 5 or more years of experience were less likely to make major diagnostic errors in reviewing Barrett’s esophagus biopsies (odds ratio [OR], 0.48, 95% confidence interval, 0.31-0.74). Pathologists who worked in nonacademic settings were more likely to make a major diagnostic error (OR, 1.76; 95% CI, 1.15-2.69) when reviewing hematoxylin and eosin-stained slides alone, but the addition of p53 immunostaining greatly improved accuracy.
Current guidelines recommend expert evaluation of Barrett’s esophagus biopsies that show dysplasia, but exact determination of expert review status had been lacking, according to Marnix Jansen, MD, a pathologist at University College London.
“The guidelines say that biopsies with dysplasia need to be reviewed by an expert pathologist, but don’t define what makes an expert pathologist,” Dr. Jansen said in an interview at the annual Digestive Disease Week.
“We wanted to advance the field by for the first time creating objective and quantitative standards” to delineate the characteristics of an expert pathologist in reviewing Barrett’s esophagus tissue samples, said Dr. Jansen. The study’s first author is Myrtle J. van der Wel, MD, of Amsterdam University Medical Center, the Netherlands.
More than 6,000 individual case diagnoses were used in the study, which included pathologists from more than 20 countries. Before the pathologists began reviewing the case set, they answered a questionnaire about training, practice context, years of experience, case volume, and other demographic characteristics.
“We then sent those biopsies around the world to ... 55 pathologists in the U.S., in Europe, Japan, Australia, even some in South America – so really around the whole globe,” explained Dr. Jansen. Biopsies were assessed by each pathologist before and after p53 immunostaining.
“Once we had the final dataset – which is massive, because we had 6,000 case diagnoses within our dataset – we could then regress those variables back onto the consensus data,” providing a first-ever look at “clear predictors of what the pathologist looks like that will score on a par with where the experts are,” said Dr. Jansen.
The results? “You need at least 5 years of experience. On top of that, if you are a pathologist working in a [nonacademic center], you are at a slightly increased risk of making major diagnostic errors,” said Dr. Jansen. However, the analysis convincingly showed that the addition of p53 immunostaining neutralized the risk for these pathologists – a strength of having such a large dataset, he said.
The study also affirmed the safety of digital pathology for expert review, said Dr. Jansen: “One of the reassuring points of our study was that we found that the best concordance was for nondysplastic Barrett’s, and high-grade dysplasia, which really replicates known glass slide characteristics. So we can really say that digital pathology is safe for this application – which is very relevant for pathologists that are taking in cases from outside for expert review.”
Concordance rates for nondysplastic Barrett’s esophagus and high-grade dysplasia were over 70%; for low-grade dysplasia, rates were intermediate at 42%.
Going forward, the study can inform the next iteration of guidelines for pathologist review of Barrett’s dysplasia, said Dr. Jansen. Rather than just recommending expert review, the guidelines can include a quantitative assessment of what’s needed. “You need to have to have at least 5 years of experience, and if you work in a [community hospital], to use a p53, and that is collectively what amounts to expertise in Barrett’s pathology.”
A follow-up study with a similar design is planned within the United Kingdom, the Netherlands, and the United States. This study, which Dr. Jansen said would enroll hundreds of pathologists, will include an intervention arm that administers a tutorial with the aim of improving concordance scoring.
Dr. Jansen reported no relevant conflicts of interest.
REPORTING FROM DDW 2019
When the parent is a psychiatrist: How are children affected?
SAN FRANCISCO – Research into how the children of psychiatrists fare psychologically is sparse. But anecdotally, children report that having a psychiatrist parent is a gift – not only for them – but for their friends’ families, Michelle B. Riba, MD, said at the annual meeting of the American Psychiatric Association.

In this video, Dr. Riba is interviewed by Carol A. Bernstein, MD, about what she expected when she helped start the Children of Psychiatrists workshop at the APA meeting with Leah J. Dickstein, MD, and how it draws a standing room–only crowd each year.
“In general ... people feel very appreciative of having an empathic, knowledgeable parent to help guide them – and not overguide them,” Dr. Riba said. Psychiatrists also can provide insight into the causes of societal challenges such as homelessness. One audience member in this year’s workshop discussed the value of having a psychiatrist parent put a school suicide into perspective. Dr. Bernstein said she is viewed by her daughter’s friends as “the psychiatrist in residence.”
The children of psychiatrists who spoke on the panel this year said they liked being able to facilitate care for their friends. “They didn’t feel burdened by [having a psychiatrist parent],” Dr. Riba said. “We asked about that very question today.”
Dr. Riba, a past president of the APA, is professor of psychiatry at the University of Michigan, Ann Arbor. She also serves as director of the consultation-liaison fellowship, and director of the PsychOncology program at the university’s Rogel Cancer Center. She had no disclosures.
Dr. Bernstein, also an APA past president, is professor of psychiatry and obstetrics and gynecology, and vice chair for faculty development in psychiatry at the Albert Einstein College of Medicine, New York. She previously served as vice chair for education in psychiatry and director of residency training in psychiatry at the NYU School of Medicine. Dr. Bernstein had no disclosures.
SAN FRANCISCO – Research into how the children of psychiatrists fare psychologically is sparse. But anecdotally, children report that having a psychiatrist parent is a gift – not only for them – but for their friends’ families, Michelle B. Riba, MD, said at the annual meeting of the American Psychiatric Association.

In this video, Dr. Riba is interviewed by Carol A. Bernstein, MD, about what she expected when she helped start the Children of Psychiatrists workshop at the APA meeting with Leah J. Dickstein, MD, and how it draws a standing room–only crowd each year.
“In general ... people feel very appreciative of having an empathic, knowledgeable parent to help guide them – and not overguide them,” Dr. Riba said. Psychiatrists also can provide insight into the causes of societal challenges such as homelessness. One audience member in this year’s workshop discussed the value of having a psychiatrist parent put a school suicide into perspective. Dr. Bernstein said she is viewed by her daughter’s friends as “the psychiatrist in residence.”
The children of psychiatrists who spoke on the panel this year said they liked being able to facilitate care for their friends. “They didn’t feel burdened by [having a psychiatrist parent],” Dr. Riba said. “We asked about that very question today.”
Dr. Riba, a past president of the APA, is professor of psychiatry at the University of Michigan, Ann Arbor. She also serves as director of the consultation-liaison fellowship, and director of the PsychOncology program at the university’s Rogel Cancer Center. She had no disclosures.
Dr. Bernstein, also an APA past president, is professor of psychiatry and obstetrics and gynecology, and vice chair for faculty development in psychiatry at the Albert Einstein College of Medicine, New York. She previously served as vice chair for education in psychiatry and director of residency training in psychiatry at the NYU School of Medicine. Dr. Bernstein had no disclosures.
SAN FRANCISCO – Research into how the children of psychiatrists fare psychologically is sparse. But anecdotally, children report that having a psychiatrist parent is a gift – not only for them – but for their friends’ families, Michelle B. Riba, MD, said at the annual meeting of the American Psychiatric Association.

In this video, Dr. Riba is interviewed by Carol A. Bernstein, MD, about what she expected when she helped start the Children of Psychiatrists workshop at the APA meeting with Leah J. Dickstein, MD, and how it draws a standing room–only crowd each year.
“In general ... people feel very appreciative of having an empathic, knowledgeable parent to help guide them – and not overguide them,” Dr. Riba said. Psychiatrists also can provide insight into the causes of societal challenges such as homelessness. One audience member in this year’s workshop discussed the value of having a psychiatrist parent put a school suicide into perspective. Dr. Bernstein said she is viewed by her daughter’s friends as “the psychiatrist in residence.”
The children of psychiatrists who spoke on the panel this year said they liked being able to facilitate care for their friends. “They didn’t feel burdened by [having a psychiatrist parent],” Dr. Riba said. “We asked about that very question today.”
Dr. Riba, a past president of the APA, is professor of psychiatry at the University of Michigan, Ann Arbor. She also serves as director of the consultation-liaison fellowship, and director of the PsychOncology program at the university’s Rogel Cancer Center. She had no disclosures.
Dr. Bernstein, also an APA past president, is professor of psychiatry and obstetrics and gynecology, and vice chair for faculty development in psychiatry at the Albert Einstein College of Medicine, New York. She previously served as vice chair for education in psychiatry and director of residency training in psychiatry at the NYU School of Medicine. Dr. Bernstein had no disclosures.
REPORTING FROM APA 2019
Eminently qualified physician
Just how good are you? Are you a pretty good doc? A better-than-average leader? Or, are you truly an eminently qualified physician?
For all the talk about In medicine, we’re careful to show respect to each other and tend to be slow to be critical. This might seem a kind approach to feedback, but I wonder if it is.
There are other professions where evaluations and feedback are more direct. In the military, performance standards are often quite explicit. The Marines, for instance, take performance evaluations seriously. This is evident if you’ve ever completed, or been a recipient of, a U.S. Marine Corps fitness report. Reading it, I realized many of the criteria could apply to us in medicine. Here are a few examples from that form (lightly modified for physicians).
Think about your clinical and technical expertise. Would you grade yourself as “competent. Possesses requisite range of skills and knowledge commensurate with training and experience?” Or maybe the next grade “demonstrates mastery of all required skills. Expertise, education and experience consistently enhance department. Innovative troubleshooter and problem solver. Effectively imparts skills to trainees.” Or perhaps you’re a “true expert in the field. Knowledge and skills impact far beyond those of peers. Translates broad-based education into forward-thinking, innovative actions. Makes immeasurable impact on department. Peerless teacher, selflessly imparts expertise to peers, residents, students.”
What about your effectiveness under stress?
Do you act “commensurate with your training and role?” Or do you have an “uncanny ability to anticipate requirements and quickly formulate original solutions?” Do you always “take decisive, effective action?”
How about your leadership performance?
Are you simply “engaged, providing instruction and direction?” Or do you “achieve a highly effective balance between direction and delegation, effectively tasking subordinates and clearly delineating standards expected?” A few of us even “engender willing loyalty and trust that allow subordinates to overcome their perceived limitations.” And exhibit “leadership that fosters the highest levels of motivation and morale, ensuring accomplishment in the most difficult circumstances.”
We might even mitigate physician burnout better if we had better performance standards. For example, do you simply “deal confidently with issues pertinent to subordinate welfare and recognize suitable courses of action?” Maybe you’re at the next level, “actively fostering the development of and uses of support systems for subordinates which improve their ability to perform.” I’m fortunate to know a few physician leaders who “noticeably enhance subordinate well-being, resulting in measurable increase in department effectiveness and proactively energize team members to ‘take care of their own.’ Widely recognized for techniques and policies that produce results and build morale.” By codifying what the standard should be, we can better hold ourselves accountable for our performance. In doing so, we might be better at recognizing and reducing burnout in our direct reports and peers.
The final question on the Marine fitness report is a comparative assessment. The evaluating officer checks one of the following boxes: 1. Unsatisfactory; 2. A qualified Marine; 3. One of many highly qualified Marines; 4. One of the few exceptionally qualified Marines; or, 5. The eminently qualified Marine.
Which are you? Can you describe yourself as “the eminently qualified physician?” You’ll have to define that standard in order to reach it.
This post was inspired by the “Set Standards. Aspire to Achieve Them” episode of Jocko Podcast.
Dr. Benabio is director of health care transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Just how good are you? Are you a pretty good doc? A better-than-average leader? Or, are you truly an eminently qualified physician?
For all the talk about In medicine, we’re careful to show respect to each other and tend to be slow to be critical. This might seem a kind approach to feedback, but I wonder if it is.
There are other professions where evaluations and feedback are more direct. In the military, performance standards are often quite explicit. The Marines, for instance, take performance evaluations seriously. This is evident if you’ve ever completed, or been a recipient of, a U.S. Marine Corps fitness report. Reading it, I realized many of the criteria could apply to us in medicine. Here are a few examples from that form (lightly modified for physicians).
Think about your clinical and technical expertise. Would you grade yourself as “competent. Possesses requisite range of skills and knowledge commensurate with training and experience?” Or maybe the next grade “demonstrates mastery of all required skills. Expertise, education and experience consistently enhance department. Innovative troubleshooter and problem solver. Effectively imparts skills to trainees.” Or perhaps you’re a “true expert in the field. Knowledge and skills impact far beyond those of peers. Translates broad-based education into forward-thinking, innovative actions. Makes immeasurable impact on department. Peerless teacher, selflessly imparts expertise to peers, residents, students.”
What about your effectiveness under stress?
Do you act “commensurate with your training and role?” Or do you have an “uncanny ability to anticipate requirements and quickly formulate original solutions?” Do you always “take decisive, effective action?”
How about your leadership performance?
Are you simply “engaged, providing instruction and direction?” Or do you “achieve a highly effective balance between direction and delegation, effectively tasking subordinates and clearly delineating standards expected?” A few of us even “engender willing loyalty and trust that allow subordinates to overcome their perceived limitations.” And exhibit “leadership that fosters the highest levels of motivation and morale, ensuring accomplishment in the most difficult circumstances.”
We might even mitigate physician burnout better if we had better performance standards. For example, do you simply “deal confidently with issues pertinent to subordinate welfare and recognize suitable courses of action?” Maybe you’re at the next level, “actively fostering the development of and uses of support systems for subordinates which improve their ability to perform.” I’m fortunate to know a few physician leaders who “noticeably enhance subordinate well-being, resulting in measurable increase in department effectiveness and proactively energize team members to ‘take care of their own.’ Widely recognized for techniques and policies that produce results and build morale.” By codifying what the standard should be, we can better hold ourselves accountable for our performance. In doing so, we might be better at recognizing and reducing burnout in our direct reports and peers.
The final question on the Marine fitness report is a comparative assessment. The evaluating officer checks one of the following boxes: 1. Unsatisfactory; 2. A qualified Marine; 3. One of many highly qualified Marines; 4. One of the few exceptionally qualified Marines; or, 5. The eminently qualified Marine.
Which are you? Can you describe yourself as “the eminently qualified physician?” You’ll have to define that standard in order to reach it.
This post was inspired by the “Set Standards. Aspire to Achieve Them” episode of Jocko Podcast.
Dr. Benabio is director of health care transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Just how good are you? Are you a pretty good doc? A better-than-average leader? Or, are you truly an eminently qualified physician?
For all the talk about In medicine, we’re careful to show respect to each other and tend to be slow to be critical. This might seem a kind approach to feedback, but I wonder if it is.
There are other professions where evaluations and feedback are more direct. In the military, performance standards are often quite explicit. The Marines, for instance, take performance evaluations seriously. This is evident if you’ve ever completed, or been a recipient of, a U.S. Marine Corps fitness report. Reading it, I realized many of the criteria could apply to us in medicine. Here are a few examples from that form (lightly modified for physicians).
Think about your clinical and technical expertise. Would you grade yourself as “competent. Possesses requisite range of skills and knowledge commensurate with training and experience?” Or maybe the next grade “demonstrates mastery of all required skills. Expertise, education and experience consistently enhance department. Innovative troubleshooter and problem solver. Effectively imparts skills to trainees.” Or perhaps you’re a “true expert in the field. Knowledge and skills impact far beyond those of peers. Translates broad-based education into forward-thinking, innovative actions. Makes immeasurable impact on department. Peerless teacher, selflessly imparts expertise to peers, residents, students.”
What about your effectiveness under stress?
Do you act “commensurate with your training and role?” Or do you have an “uncanny ability to anticipate requirements and quickly formulate original solutions?” Do you always “take decisive, effective action?”
How about your leadership performance?
Are you simply “engaged, providing instruction and direction?” Or do you “achieve a highly effective balance between direction and delegation, effectively tasking subordinates and clearly delineating standards expected?” A few of us even “engender willing loyalty and trust that allow subordinates to overcome their perceived limitations.” And exhibit “leadership that fosters the highest levels of motivation and morale, ensuring accomplishment in the most difficult circumstances.”
We might even mitigate physician burnout better if we had better performance standards. For example, do you simply “deal confidently with issues pertinent to subordinate welfare and recognize suitable courses of action?” Maybe you’re at the next level, “actively fostering the development of and uses of support systems for subordinates which improve their ability to perform.” I’m fortunate to know a few physician leaders who “noticeably enhance subordinate well-being, resulting in measurable increase in department effectiveness and proactively energize team members to ‘take care of their own.’ Widely recognized for techniques and policies that produce results and build morale.” By codifying what the standard should be, we can better hold ourselves accountable for our performance. In doing so, we might be better at recognizing and reducing burnout in our direct reports and peers.
The final question on the Marine fitness report is a comparative assessment. The evaluating officer checks one of the following boxes: 1. Unsatisfactory; 2. A qualified Marine; 3. One of many highly qualified Marines; 4. One of the few exceptionally qualified Marines; or, 5. The eminently qualified Marine.
Which are you? Can you describe yourself as “the eminently qualified physician?” You’ll have to define that standard in order to reach it.
This post was inspired by the “Set Standards. Aspire to Achieve Them” episode of Jocko Podcast.
Dr. Benabio is director of health care transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com.
Button batteries that pass to the stomach may warrant rapid endoscopic removal
SAN DIEGO – A button battery lodged in a child’s esophagus is an acknowledged emergency, but there is less evidence about retrieval of button batteries that have passed to the stomach. Observation alone has been recommended when an x-ray determines that the button battery has passed to the stomach within 2 hours of ingestion, when the battery is less than 20 mm, and the child is aged at least 5 years.
At the annual Digestive Disease Week, Racha Khalaf, MD, and Thomas Walker, MD, both of Children’s Hospital Colorado, Aurora, presented data that call this approach into question. Their retrospective cohort study of 4 years’ worth of records from four pediatric centers in the United States identified 68 cases in which a pediatric gastroenterologist had endoscopically removed the button battery. In 60% of those cases, the battery had already caused mucosal damage varying from minor to deep necrosis and perforation.
Further, the degree of injury was not correlated with symptoms, strengthening the recommendation for retrieving the button battery from the stomach.
In our exclusive video interview, Dr. Khalaf and Dr. Walker discussed the impact of their findings for guidelines for pediatric gastroenterologists and Poison Control Center advice to parents about ingestion of button batteries.
Their study was partly supported by a Cystic Fibrosis Foundational Grant Award and by National Institutes of Health Training Grants.
SAN DIEGO – A button battery lodged in a child’s esophagus is an acknowledged emergency, but there is less evidence about retrieval of button batteries that have passed to the stomach. Observation alone has been recommended when an x-ray determines that the button battery has passed to the stomach within 2 hours of ingestion, when the battery is less than 20 mm, and the child is aged at least 5 years.
At the annual Digestive Disease Week, Racha Khalaf, MD, and Thomas Walker, MD, both of Children’s Hospital Colorado, Aurora, presented data that call this approach into question. Their retrospective cohort study of 4 years’ worth of records from four pediatric centers in the United States identified 68 cases in which a pediatric gastroenterologist had endoscopically removed the button battery. In 60% of those cases, the battery had already caused mucosal damage varying from minor to deep necrosis and perforation.
Further, the degree of injury was not correlated with symptoms, strengthening the recommendation for retrieving the button battery from the stomach.
In our exclusive video interview, Dr. Khalaf and Dr. Walker discussed the impact of their findings for guidelines for pediatric gastroenterologists and Poison Control Center advice to parents about ingestion of button batteries.
Their study was partly supported by a Cystic Fibrosis Foundational Grant Award and by National Institutes of Health Training Grants.
SAN DIEGO – A button battery lodged in a child’s esophagus is an acknowledged emergency, but there is less evidence about retrieval of button batteries that have passed to the stomach. Observation alone has been recommended when an x-ray determines that the button battery has passed to the stomach within 2 hours of ingestion, when the battery is less than 20 mm, and the child is aged at least 5 years.
At the annual Digestive Disease Week, Racha Khalaf, MD, and Thomas Walker, MD, both of Children’s Hospital Colorado, Aurora, presented data that call this approach into question. Their retrospective cohort study of 4 years’ worth of records from four pediatric centers in the United States identified 68 cases in which a pediatric gastroenterologist had endoscopically removed the button battery. In 60% of those cases, the battery had already caused mucosal damage varying from minor to deep necrosis and perforation.
Further, the degree of injury was not correlated with symptoms, strengthening the recommendation for retrieving the button battery from the stomach.
In our exclusive video interview, Dr. Khalaf and Dr. Walker discussed the impact of their findings for guidelines for pediatric gastroenterologists and Poison Control Center advice to parents about ingestion of button batteries.
Their study was partly supported by a Cystic Fibrosis Foundational Grant Award and by National Institutes of Health Training Grants.
REPORTING FROM DDW 2019