User login
Most CBT delivery methods effective for depression
Most modes of delivery for cognitive-behavioral therapy appear to be effective interventions for the acute symptoms of depression, with the exception of unguided self-help therapy, a study has found.
In the study, published in JAMA Psychiatry, : individual, group, telephone, guided, and unguided self-help.
In general, CBT delivered individually, in a group, by guided self-help, or by telephone were all significantly more effective at improving the severity of depression than unguided, self-administered CBT, and significantly more effective than the controls of waiting list or usual care.
However, even unguided self-help CBT was more effective than the waiting list, although not more effective than care as usual.
“This study suggests that group, telephone, and guided self-help treatments are effective interventions that may be considered as alternatives to individual CBT,” wrote Pim Cuijpers, PhD, who is affiliated with the Amsterdam Public Health Research Institute at the Vrije Universiteit Amsterdam, and his coauthors. “Applying effective and acceptable CBT in a range of different formats will make CBT easier to implement, disseminate, and deliver across different settings and diverse patient populations.”
In terms of acceptability, individual-, group-, and telephone-delivered CBT were all equally acceptable. The analysis showed that guided self-help had lower acceptability than individual or group therapy, care as usual, and the waiting list, while unguided self-help therapy was less acceptable than being on a waiting list.
The authors said it was not clear why guided self-help CBT showed lower acceptability, compared with the other CBT formats.
“Maybe the absence of direct contact with a professional makes it easier to stop the treatment because there is less personal relationship pressure to continue with the treatment or the study,” they wrote.
The analysis also explored the long-term effectiveness of different delivery methods, although the authors cautioned that this was based on small numbers of comparisons. They found significantly greater long-term effectiveness associated with individual, group, guided self-help, and telephone CBT, compared with usual care, but telephone CBT was less effective than individual CBT.
Two authors reported receiving personal fees from private industry outside of the submitted work, and one reported receiving grants and support from the National Institute for Health Research.
SOURCE: Cuijpers P et al. JAMA Psychiatry. 2019 Apr 17. doi: 10.1001/jamapsychiatry.2019.0268.
Most modes of delivery for cognitive-behavioral therapy appear to be effective interventions for the acute symptoms of depression, with the exception of unguided self-help therapy, a study has found.
In the study, published in JAMA Psychiatry, : individual, group, telephone, guided, and unguided self-help.
In general, CBT delivered individually, in a group, by guided self-help, or by telephone were all significantly more effective at improving the severity of depression than unguided, self-administered CBT, and significantly more effective than the controls of waiting list or usual care.
However, even unguided self-help CBT was more effective than the waiting list, although not more effective than care as usual.
“This study suggests that group, telephone, and guided self-help treatments are effective interventions that may be considered as alternatives to individual CBT,” wrote Pim Cuijpers, PhD, who is affiliated with the Amsterdam Public Health Research Institute at the Vrije Universiteit Amsterdam, and his coauthors. “Applying effective and acceptable CBT in a range of different formats will make CBT easier to implement, disseminate, and deliver across different settings and diverse patient populations.”
In terms of acceptability, individual-, group-, and telephone-delivered CBT were all equally acceptable. The analysis showed that guided self-help had lower acceptability than individual or group therapy, care as usual, and the waiting list, while unguided self-help therapy was less acceptable than being on a waiting list.
The authors said it was not clear why guided self-help CBT showed lower acceptability, compared with the other CBT formats.
“Maybe the absence of direct contact with a professional makes it easier to stop the treatment because there is less personal relationship pressure to continue with the treatment or the study,” they wrote.
The analysis also explored the long-term effectiveness of different delivery methods, although the authors cautioned that this was based on small numbers of comparisons. They found significantly greater long-term effectiveness associated with individual, group, guided self-help, and telephone CBT, compared with usual care, but telephone CBT was less effective than individual CBT.
Two authors reported receiving personal fees from private industry outside of the submitted work, and one reported receiving grants and support from the National Institute for Health Research.
SOURCE: Cuijpers P et al. JAMA Psychiatry. 2019 Apr 17. doi: 10.1001/jamapsychiatry.2019.0268.
Most modes of delivery for cognitive-behavioral therapy appear to be effective interventions for the acute symptoms of depression, with the exception of unguided self-help therapy, a study has found.
In the study, published in JAMA Psychiatry, : individual, group, telephone, guided, and unguided self-help.
In general, CBT delivered individually, in a group, by guided self-help, or by telephone were all significantly more effective at improving the severity of depression than unguided, self-administered CBT, and significantly more effective than the controls of waiting list or usual care.
However, even unguided self-help CBT was more effective than the waiting list, although not more effective than care as usual.
“This study suggests that group, telephone, and guided self-help treatments are effective interventions that may be considered as alternatives to individual CBT,” wrote Pim Cuijpers, PhD, who is affiliated with the Amsterdam Public Health Research Institute at the Vrije Universiteit Amsterdam, and his coauthors. “Applying effective and acceptable CBT in a range of different formats will make CBT easier to implement, disseminate, and deliver across different settings and diverse patient populations.”
In terms of acceptability, individual-, group-, and telephone-delivered CBT were all equally acceptable. The analysis showed that guided self-help had lower acceptability than individual or group therapy, care as usual, and the waiting list, while unguided self-help therapy was less acceptable than being on a waiting list.
The authors said it was not clear why guided self-help CBT showed lower acceptability, compared with the other CBT formats.
“Maybe the absence of direct contact with a professional makes it easier to stop the treatment because there is less personal relationship pressure to continue with the treatment or the study,” they wrote.
The analysis also explored the long-term effectiveness of different delivery methods, although the authors cautioned that this was based on small numbers of comparisons. They found significantly greater long-term effectiveness associated with individual, group, guided self-help, and telephone CBT, compared with usual care, but telephone CBT was less effective than individual CBT.
Two authors reported receiving personal fees from private industry outside of the submitted work, and one reported receiving grants and support from the National Institute for Health Research.
SOURCE: Cuijpers P et al. JAMA Psychiatry. 2019 Apr 17. doi: 10.1001/jamapsychiatry.2019.0268.
FROM JAMA PSYCHIATRY
Diagnostic test helps clinicians identify IPF with nonsurgical biopsy
, according to recent research published in the Lancet Respiratory Medicine.
The results of the molecular test, called the Envisia Genomic Classifier (Veracyte; San Francisco), had a high positive predictive value of proven usual interstitial pneumonia, and could be used in place of surgical lung biopsy to confirm a diagnosis of idiopathic pulmonary fibrosis (IPF), wrote Ganesh Raghu, MD, director at the Center for Interstitial Lung Diseases and professor of medicine at the University of Washington, Seattle, and his colleagues.* The Envisia Genomic Classifier recently received final Medicare local coverage determination for IPF diagnosis, according to a recent press release by Veracyte.
“IPF is often challenging to distinguish from other [interstitial lung disease], but timely and accurate diagnosis is critical so that patients with IPF can access therapies that may slow progression of the disease, while avoiding potentially harmful treatments,” Dr. Raghu stated in a press release. “Our results with molecular classification through machine learning [the Envisia classifier] are promising and, along with clinical information and radiological features in high-resolution CT imaging, physicians through multidisciplinary discussions, may be able to utilize the molecular classification as a diagnostic tool to make a more informed and confident diagnoses.”
The researchers prospectively recruited 237 patients from 29 centers in the United States and Europe who were evaluated with the Bronchial Sample Collection for a Novel Genomic Test for suspected interstitial lung disease and who underwent surgical biopsy, transbronchial biopsy, or cryobiopsy for sample collection. They used histopathology and RNA sequence data from 90 patients to create a training data set of an unusual interstitial pneumonia pattern for the machine learning algorithm.
The classifier found usual interstitial pneumonia diagnoses in 49 patients; the test had a specificity of 88% (95% confidence interval, 70%-98%) and a sensitivity of 70% (95% CI, 47%-87%). Of 42 patients with inconsistent or possible usual interstitial pneumonia identified from high-resolution CT imaging, there was a positive predictive value of 81% (95% CI, 54%-96%). When multidisciplinary teams made diagnoses with the molecular classifier data, there was a clinical agreement of 86% (95% CI, 78%-92%) with diagnoses made using histopathology data. In 18 cases of IPF, there was an improvement in diagnostic confidence using the molecular classifier data, with 89% of diagnoses designated as high confidence, compared with 56% of cases based on histopathologic data (P = .0339). In 48 patients with nondiagnostic pathology or nonclassifiable fibrosis histopathology, 63% of diagnoses with the molecular classifier data were high confidence, compared with 42% using histopathologic data (P = .0412).
This study was funded by Veracyte, creator of the Envisia Genomic Classifier. Some authors reported relationships with Veracyte and other companies.
SOURCE: Raghu G et al. Lancet Respir Med. 2019 Apr 1. doi: 10.1016/S2213-8587(19)300.
Correction, 4/25/19: An earlier version of this article misstated how the Envisia Genomic Classifier could be used. The Envisia test is not intended to replace high-resolution chest CT (HRCT). It is used when HRCT is inconclusive to help prevent patients from having to undergo invasive diagnostic procedures.
Use of a molecular classifier could be most helpful in situations where patients have atypical radiology results or in cases where multidisciplinary teams disagree on the diagnosis, Simon Hart, PhD, wrote in a related editorial.
According to the 2018 international guidelines for idiopathic pulmonary fibrosis, usual interstitial pneumonia certainty is defined as honeycombing seen on high-resolution CT (HRCT), probable if there is presence of traction bronchiectasis but not honeycombing, and indeterminate if there is no presence of usual interstitial pneumonia or another diagnosis. As radiologists “often disagree on HRCT patterns,” IPF sometimes becomes a working diagnosis based on progression of disease, Dr. Hart wrote. In these cases, molecular classifier samples could help identify IPF in patients who have undergone less invasive transbronchial lung biopsy.
Among patients for whom diagnoses using identical clinical features have different results, HRCT and pathology data, particularly in cases of nonspecific interstitial pneumonia and chronic hypersensitivity pneumonitis that follow a similar disease course to idiopathic pulmonary fibrosis, molecular classifier testing could help identify patients with these diseases so treatments such as to avoid treating these patients with anti-inflammatory or immunosuppressive therapy.
“It seems conceivable that in future interstitial lung diseases could be classified by a simple dichotomy: primarily scarring diseases characterized by molecular usual interstitial pneumonia to be treated with antifibrotics versus immune-driven conditions without usual interstitial pneumonia that need an anti-inflammatory approach,” he wrote.
Dr. Hart is from the respiratory research group at Castle Hill Hospital in Cottingham, England. These comments summarize his editorial in response to Raghu et al. (Lancet Respir Med. 2019 Apr 1. doi 10.1016/S2213-2600[19]30058-X). He reported receiving grants and support to attend conferences, and consultancy fees from Boehringer Ingelheim.
Use of a molecular classifier could be most helpful in situations where patients have atypical radiology results or in cases where multidisciplinary teams disagree on the diagnosis, Simon Hart, PhD, wrote in a related editorial.
According to the 2018 international guidelines for idiopathic pulmonary fibrosis, usual interstitial pneumonia certainty is defined as honeycombing seen on high-resolution CT (HRCT), probable if there is presence of traction bronchiectasis but not honeycombing, and indeterminate if there is no presence of usual interstitial pneumonia or another diagnosis. As radiologists “often disagree on HRCT patterns,” IPF sometimes becomes a working diagnosis based on progression of disease, Dr. Hart wrote. In these cases, molecular classifier samples could help identify IPF in patients who have undergone less invasive transbronchial lung biopsy.
Among patients for whom diagnoses using identical clinical features have different results, HRCT and pathology data, particularly in cases of nonspecific interstitial pneumonia and chronic hypersensitivity pneumonitis that follow a similar disease course to idiopathic pulmonary fibrosis, molecular classifier testing could help identify patients with these diseases so treatments such as to avoid treating these patients with anti-inflammatory or immunosuppressive therapy.
“It seems conceivable that in future interstitial lung diseases could be classified by a simple dichotomy: primarily scarring diseases characterized by molecular usual interstitial pneumonia to be treated with antifibrotics versus immune-driven conditions without usual interstitial pneumonia that need an anti-inflammatory approach,” he wrote.
Dr. Hart is from the respiratory research group at Castle Hill Hospital in Cottingham, England. These comments summarize his editorial in response to Raghu et al. (Lancet Respir Med. 2019 Apr 1. doi 10.1016/S2213-2600[19]30058-X). He reported receiving grants and support to attend conferences, and consultancy fees from Boehringer Ingelheim.
Use of a molecular classifier could be most helpful in situations where patients have atypical radiology results or in cases where multidisciplinary teams disagree on the diagnosis, Simon Hart, PhD, wrote in a related editorial.
According to the 2018 international guidelines for idiopathic pulmonary fibrosis, usual interstitial pneumonia certainty is defined as honeycombing seen on high-resolution CT (HRCT), probable if there is presence of traction bronchiectasis but not honeycombing, and indeterminate if there is no presence of usual interstitial pneumonia or another diagnosis. As radiologists “often disagree on HRCT patterns,” IPF sometimes becomes a working diagnosis based on progression of disease, Dr. Hart wrote. In these cases, molecular classifier samples could help identify IPF in patients who have undergone less invasive transbronchial lung biopsy.
Among patients for whom diagnoses using identical clinical features have different results, HRCT and pathology data, particularly in cases of nonspecific interstitial pneumonia and chronic hypersensitivity pneumonitis that follow a similar disease course to idiopathic pulmonary fibrosis, molecular classifier testing could help identify patients with these diseases so treatments such as to avoid treating these patients with anti-inflammatory or immunosuppressive therapy.
“It seems conceivable that in future interstitial lung diseases could be classified by a simple dichotomy: primarily scarring diseases characterized by molecular usual interstitial pneumonia to be treated with antifibrotics versus immune-driven conditions without usual interstitial pneumonia that need an anti-inflammatory approach,” he wrote.
Dr. Hart is from the respiratory research group at Castle Hill Hospital in Cottingham, England. These comments summarize his editorial in response to Raghu et al. (Lancet Respir Med. 2019 Apr 1. doi 10.1016/S2213-2600[19]30058-X). He reported receiving grants and support to attend conferences, and consultancy fees from Boehringer Ingelheim.
, according to recent research published in the Lancet Respiratory Medicine.
The results of the molecular test, called the Envisia Genomic Classifier (Veracyte; San Francisco), had a high positive predictive value of proven usual interstitial pneumonia, and could be used in place of surgical lung biopsy to confirm a diagnosis of idiopathic pulmonary fibrosis (IPF), wrote Ganesh Raghu, MD, director at the Center for Interstitial Lung Diseases and professor of medicine at the University of Washington, Seattle, and his colleagues.* The Envisia Genomic Classifier recently received final Medicare local coverage determination for IPF diagnosis, according to a recent press release by Veracyte.
“IPF is often challenging to distinguish from other [interstitial lung disease], but timely and accurate diagnosis is critical so that patients with IPF can access therapies that may slow progression of the disease, while avoiding potentially harmful treatments,” Dr. Raghu stated in a press release. “Our results with molecular classification through machine learning [the Envisia classifier] are promising and, along with clinical information and radiological features in high-resolution CT imaging, physicians through multidisciplinary discussions, may be able to utilize the molecular classification as a diagnostic tool to make a more informed and confident diagnoses.”
The researchers prospectively recruited 237 patients from 29 centers in the United States and Europe who were evaluated with the Bronchial Sample Collection for a Novel Genomic Test for suspected interstitial lung disease and who underwent surgical biopsy, transbronchial biopsy, or cryobiopsy for sample collection. They used histopathology and RNA sequence data from 90 patients to create a training data set of an unusual interstitial pneumonia pattern for the machine learning algorithm.
The classifier found usual interstitial pneumonia diagnoses in 49 patients; the test had a specificity of 88% (95% confidence interval, 70%-98%) and a sensitivity of 70% (95% CI, 47%-87%). Of 42 patients with inconsistent or possible usual interstitial pneumonia identified from high-resolution CT imaging, there was a positive predictive value of 81% (95% CI, 54%-96%). When multidisciplinary teams made diagnoses with the molecular classifier data, there was a clinical agreement of 86% (95% CI, 78%-92%) with diagnoses made using histopathology data. In 18 cases of IPF, there was an improvement in diagnostic confidence using the molecular classifier data, with 89% of diagnoses designated as high confidence, compared with 56% of cases based on histopathologic data (P = .0339). In 48 patients with nondiagnostic pathology or nonclassifiable fibrosis histopathology, 63% of diagnoses with the molecular classifier data were high confidence, compared with 42% using histopathologic data (P = .0412).
This study was funded by Veracyte, creator of the Envisia Genomic Classifier. Some authors reported relationships with Veracyte and other companies.
SOURCE: Raghu G et al. Lancet Respir Med. 2019 Apr 1. doi: 10.1016/S2213-8587(19)300.
Correction, 4/25/19: An earlier version of this article misstated how the Envisia Genomic Classifier could be used. The Envisia test is not intended to replace high-resolution chest CT (HRCT). It is used when HRCT is inconclusive to help prevent patients from having to undergo invasive diagnostic procedures.
, according to recent research published in the Lancet Respiratory Medicine.
The results of the molecular test, called the Envisia Genomic Classifier (Veracyte; San Francisco), had a high positive predictive value of proven usual interstitial pneumonia, and could be used in place of surgical lung biopsy to confirm a diagnosis of idiopathic pulmonary fibrosis (IPF), wrote Ganesh Raghu, MD, director at the Center for Interstitial Lung Diseases and professor of medicine at the University of Washington, Seattle, and his colleagues.* The Envisia Genomic Classifier recently received final Medicare local coverage determination for IPF diagnosis, according to a recent press release by Veracyte.
“IPF is often challenging to distinguish from other [interstitial lung disease], but timely and accurate diagnosis is critical so that patients with IPF can access therapies that may slow progression of the disease, while avoiding potentially harmful treatments,” Dr. Raghu stated in a press release. “Our results with molecular classification through machine learning [the Envisia classifier] are promising and, along with clinical information and radiological features in high-resolution CT imaging, physicians through multidisciplinary discussions, may be able to utilize the molecular classification as a diagnostic tool to make a more informed and confident diagnoses.”
The researchers prospectively recruited 237 patients from 29 centers in the United States and Europe who were evaluated with the Bronchial Sample Collection for a Novel Genomic Test for suspected interstitial lung disease and who underwent surgical biopsy, transbronchial biopsy, or cryobiopsy for sample collection. They used histopathology and RNA sequence data from 90 patients to create a training data set of an unusual interstitial pneumonia pattern for the machine learning algorithm.
The classifier found usual interstitial pneumonia diagnoses in 49 patients; the test had a specificity of 88% (95% confidence interval, 70%-98%) and a sensitivity of 70% (95% CI, 47%-87%). Of 42 patients with inconsistent or possible usual interstitial pneumonia identified from high-resolution CT imaging, there was a positive predictive value of 81% (95% CI, 54%-96%). When multidisciplinary teams made diagnoses with the molecular classifier data, there was a clinical agreement of 86% (95% CI, 78%-92%) with diagnoses made using histopathology data. In 18 cases of IPF, there was an improvement in diagnostic confidence using the molecular classifier data, with 89% of diagnoses designated as high confidence, compared with 56% of cases based on histopathologic data (P = .0339). In 48 patients with nondiagnostic pathology or nonclassifiable fibrosis histopathology, 63% of diagnoses with the molecular classifier data were high confidence, compared with 42% using histopathologic data (P = .0412).
This study was funded by Veracyte, creator of the Envisia Genomic Classifier. Some authors reported relationships with Veracyte and other companies.
SOURCE: Raghu G et al. Lancet Respir Med. 2019 Apr 1. doi: 10.1016/S2213-8587(19)300.
Correction, 4/25/19: An earlier version of this article misstated how the Envisia Genomic Classifier could be used. The Envisia test is not intended to replace high-resolution chest CT (HRCT). It is used when HRCT is inconclusive to help prevent patients from having to undergo invasive diagnostic procedures.
FROM THE LANCET RESPIRATORY MEDICINE
Definition of Family Medicine as an Academic Disipline: A Current Controversy
Young lupus patients need more than medications
SAN FRANCISCO – – and therein lies the importance of introducing interventions beyond simply prescribing appropriate medications, Hermine I. Brunner, MD, asserted at an international congress on systemic lupus erythematosus.
Pilot studies conducted by her research group as well as others suggest that brief cognitive-behavioral interventions, web-based patient and caregiver education, and social media interactions significantly improve the fatigue and depression, poor quality of life, and lack of adherence to medication that are pervasive in young patients with SLE, according to Dr. Brunner, director of the division of rheumatology and professor of pediatrics at the University of Cincinnati and scientific director of the Pediatric Rheumatology Collaborative Study Group.
“Don’t misunderstand: I don’t think we can treat lupus simply with a psychological intervention at the bedside. However, I think doctors would be well advised to offer both psychological interventions and medication when they see young lupus patients, because without the psychological intervention the patients may not feel sufficiently at ease to take their medication. They will not get the benefit of the medications you’ve prescribed,” she said.
Patients with SLE take an average of eight medications daily. Their medication adherence rate is comparable to that of patients with diabetes or many other chronic diseases: that is to say, lousy. When investigators at the University of Texas MD Anderson Cancer Center, Houston, utilized an electronic monitoring system to chart adherence to prescribed oral medications in adults with SLE, they found that over the course of 2 years of follow-up only one-fourth of them had an adherence rate of 80% or better, which is the standard definition of adherence (Lupus. 2012 Oct;21[11]:1158-65).
Treatment adherence is particularly problematic in adolescents and young adults with SLE. They often have great difficulty in mastering the self-management skills required to stay on top of their disease when they have so much else going on during what is a vulnerable and challenging period of development, even for healthy youths.
The texting intervention
Dr. Brunner and her colleagues at Cincinnati Children’s Hospital Medical Center recognized the scope of the nonadherence problem early on. Years ago they started sending text messaging reminders of pending clinic visits to their patients who had a poor track record of showing up for appointments.
“We texted patients 2 weeks before their scheduled visit, 1 week before, and then again the day before the visit,” she explained.
This simple intervention resulted in a 47% reduction in missed appointments, compared with a control group. Also, text recipients were more likely to cancel appointments instead of simply not showing up, an important benefit from a practice management and scheduling standpoint (J Rheumatol. 2012 Jan;39[1]:174-9). Disappointingly, however, the text messaging intervention had no impact on adherence to prescribed use of hydroxychloroquine. This led the investigators to conduct a deeper dive into the roots of the nonadherence problem in childhood-onset lupus.
Disease control, quality of life
Dr. Brunner and her coworkers conducted an in-depth assessment of health-related quality of life in 50 patients with childhood-onset SLE over the course of 6 months. The results were surprising.
“When we looked at the correlation between disease control and quality of life, actually there was none,” according to the pediatric rheumatologist.
Instead, the investigators found that young patients with persistently low quality of life despite objectively measured good disease control scored high for fatigue and depressive symptoms (Lupus. 2018 Jan;27[1]:124-33). This led Dr. Brunner and her coinvestigators to consider developing a practical behavioral intervention to address these potentially modifiable predictors of impaired health-related quality of life in their patient population.
The need for novel approaches was highlighted in focus groups conducted by the investigators, in which patients and their primary caregivers emphasized that current therapeutic strategies don’t adequately address key problems of living with lupus, especially the prominent fatigue, pain, and depressed mood that hamper daily function and personal relationships. Patients said they don’t feel an immediate benefit from taking their medications, so why bother? And parents expressed frustration about how difficult it is to get their teenagers to understand the consequences of nonadherence when they’re at an age when they don’t yet even grasp the concept of their own mortality (Lupus. 2019 Mar. doi: 10.1177/0961203319839478. These observations spurred the Cincinnati investigators to develop a modified cognitive-behavioral therapy (CBT) protocol, known as TEACH, which they believe is the first CBT intervention to specifically target psychological problems in young people with childhood-onset SLE.
The TEACH program
TEACH (Treatment and Education Approach for Childhood-Onset Lupus) is a six-session program that teaches patients and caregivers self-advocacy, relaxation techniques, how to improve sleep hygiene, the importance of engaging in planned pleasant activities, and why taking medications matters. The program content differs depending upon whether the patient is an adolescent or young adult.
Results of a recently published small feasibility study were highly encouraging, showing that 83% of people who enrolled in the program completed it. Posttreatment assessment showed that patients had a marked decrease in depressive symptoms as measured by both the Children’s Depression Inventory and the Beck Depression Inventory. They also showed a significant reduction in fatigue. However, while favorable trends in terms of reduced pain and anxiety symptoms were noted, they didn’t achieve statistical significance (Pediatr Rheumatol Online J. 2019 Feb 18. doi: 10.1186/s12969-019-0307-8). The next step in this project is a planned controlled randomized trial.
A web-based medication adherence program
Researchers at Pennsylvania State University took a different approach. They created a publicly available educational website, www.facinglupustogether.com, aimed at improving self-management skills – and especially medication adherence – in teens and young adults with SLE.
The website contains eight modules: Making the transition and taking charge of my medications, Learning about lupus, Learning about lupus medications, Managing symptoms of lupus, How do I handle lupus and my family, How do I handle lupus and my friends, Lupus and stress, and My personal goals and how I will achieve them. Each takes about 10 minutes to complete.
In a pilot study, 37 patients tackled one module per week and were randomized to respond to questions about the weekly topic either in a journal or by discussing the key points in an online social media forum with other young people with SLE. The idea was to create an intervention that capitalizes on the excellent social media skills possessed by today’s youth. And indeed, incorporation of social media proved to be a winning strategy. Medication adherence for hydroxychloroquine in the group randomized to social media participation jumped from 50% in the 3 months prior to starting the program to 92% in the first 3 months post completion, whereas medication adherence didn’t change significantly in the other study arm. The social media group also experienced significant improvements in self-efficacy, sense of community, acceptance of illness, optimism and control over the future, and other measures of empowerment. The control group did not show significant change in any of these domains (Pediatr Rheumatol Online J. 2018 Mar 14. doi: 10.1186/s12969-018-0232-2).
The TEACH study was sponsored by the National Institutes of Health. The web-based medication adherence program pilot study was supported by the Lupus Foundation of America. What the two approaches share in common is a conviction that, when it comes to addressing pain, fatigue, diminished quality of life, and poor medication adherence in young patients with SLE: “Our medication prescription alone doesn’t do it,” Dr. Brunner said.
She reported having no financial conflicts regarding her presentation.
SAN FRANCISCO – – and therein lies the importance of introducing interventions beyond simply prescribing appropriate medications, Hermine I. Brunner, MD, asserted at an international congress on systemic lupus erythematosus.
Pilot studies conducted by her research group as well as others suggest that brief cognitive-behavioral interventions, web-based patient and caregiver education, and social media interactions significantly improve the fatigue and depression, poor quality of life, and lack of adherence to medication that are pervasive in young patients with SLE, according to Dr. Brunner, director of the division of rheumatology and professor of pediatrics at the University of Cincinnati and scientific director of the Pediatric Rheumatology Collaborative Study Group.
“Don’t misunderstand: I don’t think we can treat lupus simply with a psychological intervention at the bedside. However, I think doctors would be well advised to offer both psychological interventions and medication when they see young lupus patients, because without the psychological intervention the patients may not feel sufficiently at ease to take their medication. They will not get the benefit of the medications you’ve prescribed,” she said.
Patients with SLE take an average of eight medications daily. Their medication adherence rate is comparable to that of patients with diabetes or many other chronic diseases: that is to say, lousy. When investigators at the University of Texas MD Anderson Cancer Center, Houston, utilized an electronic monitoring system to chart adherence to prescribed oral medications in adults with SLE, they found that over the course of 2 years of follow-up only one-fourth of them had an adherence rate of 80% or better, which is the standard definition of adherence (Lupus. 2012 Oct;21[11]:1158-65).
Treatment adherence is particularly problematic in adolescents and young adults with SLE. They often have great difficulty in mastering the self-management skills required to stay on top of their disease when they have so much else going on during what is a vulnerable and challenging period of development, even for healthy youths.
The texting intervention
Dr. Brunner and her colleagues at Cincinnati Children’s Hospital Medical Center recognized the scope of the nonadherence problem early on. Years ago they started sending text messaging reminders of pending clinic visits to their patients who had a poor track record of showing up for appointments.
“We texted patients 2 weeks before their scheduled visit, 1 week before, and then again the day before the visit,” she explained.
This simple intervention resulted in a 47% reduction in missed appointments, compared with a control group. Also, text recipients were more likely to cancel appointments instead of simply not showing up, an important benefit from a practice management and scheduling standpoint (J Rheumatol. 2012 Jan;39[1]:174-9). Disappointingly, however, the text messaging intervention had no impact on adherence to prescribed use of hydroxychloroquine. This led the investigators to conduct a deeper dive into the roots of the nonadherence problem in childhood-onset lupus.
Disease control, quality of life
Dr. Brunner and her coworkers conducted an in-depth assessment of health-related quality of life in 50 patients with childhood-onset SLE over the course of 6 months. The results were surprising.
“When we looked at the correlation between disease control and quality of life, actually there was none,” according to the pediatric rheumatologist.
Instead, the investigators found that young patients with persistently low quality of life despite objectively measured good disease control scored high for fatigue and depressive symptoms (Lupus. 2018 Jan;27[1]:124-33). This led Dr. Brunner and her coinvestigators to consider developing a practical behavioral intervention to address these potentially modifiable predictors of impaired health-related quality of life in their patient population.
The need for novel approaches was highlighted in focus groups conducted by the investigators, in which patients and their primary caregivers emphasized that current therapeutic strategies don’t adequately address key problems of living with lupus, especially the prominent fatigue, pain, and depressed mood that hamper daily function and personal relationships. Patients said they don’t feel an immediate benefit from taking their medications, so why bother? And parents expressed frustration about how difficult it is to get their teenagers to understand the consequences of nonadherence when they’re at an age when they don’t yet even grasp the concept of their own mortality (Lupus. 2019 Mar. doi: 10.1177/0961203319839478. These observations spurred the Cincinnati investigators to develop a modified cognitive-behavioral therapy (CBT) protocol, known as TEACH, which they believe is the first CBT intervention to specifically target psychological problems in young people with childhood-onset SLE.
The TEACH program
TEACH (Treatment and Education Approach for Childhood-Onset Lupus) is a six-session program that teaches patients and caregivers self-advocacy, relaxation techniques, how to improve sleep hygiene, the importance of engaging in planned pleasant activities, and why taking medications matters. The program content differs depending upon whether the patient is an adolescent or young adult.
Results of a recently published small feasibility study were highly encouraging, showing that 83% of people who enrolled in the program completed it. Posttreatment assessment showed that patients had a marked decrease in depressive symptoms as measured by both the Children’s Depression Inventory and the Beck Depression Inventory. They also showed a significant reduction in fatigue. However, while favorable trends in terms of reduced pain and anxiety symptoms were noted, they didn’t achieve statistical significance (Pediatr Rheumatol Online J. 2019 Feb 18. doi: 10.1186/s12969-019-0307-8). The next step in this project is a planned controlled randomized trial.
A web-based medication adherence program
Researchers at Pennsylvania State University took a different approach. They created a publicly available educational website, www.facinglupustogether.com, aimed at improving self-management skills – and especially medication adherence – in teens and young adults with SLE.
The website contains eight modules: Making the transition and taking charge of my medications, Learning about lupus, Learning about lupus medications, Managing symptoms of lupus, How do I handle lupus and my family, How do I handle lupus and my friends, Lupus and stress, and My personal goals and how I will achieve them. Each takes about 10 minutes to complete.
In a pilot study, 37 patients tackled one module per week and were randomized to respond to questions about the weekly topic either in a journal or by discussing the key points in an online social media forum with other young people with SLE. The idea was to create an intervention that capitalizes on the excellent social media skills possessed by today’s youth. And indeed, incorporation of social media proved to be a winning strategy. Medication adherence for hydroxychloroquine in the group randomized to social media participation jumped from 50% in the 3 months prior to starting the program to 92% in the first 3 months post completion, whereas medication adherence didn’t change significantly in the other study arm. The social media group also experienced significant improvements in self-efficacy, sense of community, acceptance of illness, optimism and control over the future, and other measures of empowerment. The control group did not show significant change in any of these domains (Pediatr Rheumatol Online J. 2018 Mar 14. doi: 10.1186/s12969-018-0232-2).
The TEACH study was sponsored by the National Institutes of Health. The web-based medication adherence program pilot study was supported by the Lupus Foundation of America. What the two approaches share in common is a conviction that, when it comes to addressing pain, fatigue, diminished quality of life, and poor medication adherence in young patients with SLE: “Our medication prescription alone doesn’t do it,” Dr. Brunner said.
She reported having no financial conflicts regarding her presentation.
SAN FRANCISCO – – and therein lies the importance of introducing interventions beyond simply prescribing appropriate medications, Hermine I. Brunner, MD, asserted at an international congress on systemic lupus erythematosus.
Pilot studies conducted by her research group as well as others suggest that brief cognitive-behavioral interventions, web-based patient and caregiver education, and social media interactions significantly improve the fatigue and depression, poor quality of life, and lack of adherence to medication that are pervasive in young patients with SLE, according to Dr. Brunner, director of the division of rheumatology and professor of pediatrics at the University of Cincinnati and scientific director of the Pediatric Rheumatology Collaborative Study Group.
“Don’t misunderstand: I don’t think we can treat lupus simply with a psychological intervention at the bedside. However, I think doctors would be well advised to offer both psychological interventions and medication when they see young lupus patients, because without the psychological intervention the patients may not feel sufficiently at ease to take their medication. They will not get the benefit of the medications you’ve prescribed,” she said.
Patients with SLE take an average of eight medications daily. Their medication adherence rate is comparable to that of patients with diabetes or many other chronic diseases: that is to say, lousy. When investigators at the University of Texas MD Anderson Cancer Center, Houston, utilized an electronic monitoring system to chart adherence to prescribed oral medications in adults with SLE, they found that over the course of 2 years of follow-up only one-fourth of them had an adherence rate of 80% or better, which is the standard definition of adherence (Lupus. 2012 Oct;21[11]:1158-65).
Treatment adherence is particularly problematic in adolescents and young adults with SLE. They often have great difficulty in mastering the self-management skills required to stay on top of their disease when they have so much else going on during what is a vulnerable and challenging period of development, even for healthy youths.
The texting intervention
Dr. Brunner and her colleagues at Cincinnati Children’s Hospital Medical Center recognized the scope of the nonadherence problem early on. Years ago they started sending text messaging reminders of pending clinic visits to their patients who had a poor track record of showing up for appointments.
“We texted patients 2 weeks before their scheduled visit, 1 week before, and then again the day before the visit,” she explained.
This simple intervention resulted in a 47% reduction in missed appointments, compared with a control group. Also, text recipients were more likely to cancel appointments instead of simply not showing up, an important benefit from a practice management and scheduling standpoint (J Rheumatol. 2012 Jan;39[1]:174-9). Disappointingly, however, the text messaging intervention had no impact on adherence to prescribed use of hydroxychloroquine. This led the investigators to conduct a deeper dive into the roots of the nonadherence problem in childhood-onset lupus.
Disease control, quality of life
Dr. Brunner and her coworkers conducted an in-depth assessment of health-related quality of life in 50 patients with childhood-onset SLE over the course of 6 months. The results were surprising.
“When we looked at the correlation between disease control and quality of life, actually there was none,” according to the pediatric rheumatologist.
Instead, the investigators found that young patients with persistently low quality of life despite objectively measured good disease control scored high for fatigue and depressive symptoms (Lupus. 2018 Jan;27[1]:124-33). This led Dr. Brunner and her coinvestigators to consider developing a practical behavioral intervention to address these potentially modifiable predictors of impaired health-related quality of life in their patient population.
The need for novel approaches was highlighted in focus groups conducted by the investigators, in which patients and their primary caregivers emphasized that current therapeutic strategies don’t adequately address key problems of living with lupus, especially the prominent fatigue, pain, and depressed mood that hamper daily function and personal relationships. Patients said they don’t feel an immediate benefit from taking their medications, so why bother? And parents expressed frustration about how difficult it is to get their teenagers to understand the consequences of nonadherence when they’re at an age when they don’t yet even grasp the concept of their own mortality (Lupus. 2019 Mar. doi: 10.1177/0961203319839478. These observations spurred the Cincinnati investigators to develop a modified cognitive-behavioral therapy (CBT) protocol, known as TEACH, which they believe is the first CBT intervention to specifically target psychological problems in young people with childhood-onset SLE.
The TEACH program
TEACH (Treatment and Education Approach for Childhood-Onset Lupus) is a six-session program that teaches patients and caregivers self-advocacy, relaxation techniques, how to improve sleep hygiene, the importance of engaging in planned pleasant activities, and why taking medications matters. The program content differs depending upon whether the patient is an adolescent or young adult.
Results of a recently published small feasibility study were highly encouraging, showing that 83% of people who enrolled in the program completed it. Posttreatment assessment showed that patients had a marked decrease in depressive symptoms as measured by both the Children’s Depression Inventory and the Beck Depression Inventory. They also showed a significant reduction in fatigue. However, while favorable trends in terms of reduced pain and anxiety symptoms were noted, they didn’t achieve statistical significance (Pediatr Rheumatol Online J. 2019 Feb 18. doi: 10.1186/s12969-019-0307-8). The next step in this project is a planned controlled randomized trial.
A web-based medication adherence program
Researchers at Pennsylvania State University took a different approach. They created a publicly available educational website, www.facinglupustogether.com, aimed at improving self-management skills – and especially medication adherence – in teens and young adults with SLE.
The website contains eight modules: Making the transition and taking charge of my medications, Learning about lupus, Learning about lupus medications, Managing symptoms of lupus, How do I handle lupus and my family, How do I handle lupus and my friends, Lupus and stress, and My personal goals and how I will achieve them. Each takes about 10 minutes to complete.
In a pilot study, 37 patients tackled one module per week and were randomized to respond to questions about the weekly topic either in a journal or by discussing the key points in an online social media forum with other young people with SLE. The idea was to create an intervention that capitalizes on the excellent social media skills possessed by today’s youth. And indeed, incorporation of social media proved to be a winning strategy. Medication adherence for hydroxychloroquine in the group randomized to social media participation jumped from 50% in the 3 months prior to starting the program to 92% in the first 3 months post completion, whereas medication adherence didn’t change significantly in the other study arm. The social media group also experienced significant improvements in self-efficacy, sense of community, acceptance of illness, optimism and control over the future, and other measures of empowerment. The control group did not show significant change in any of these domains (Pediatr Rheumatol Online J. 2018 Mar 14. doi: 10.1186/s12969-018-0232-2).
The TEACH study was sponsored by the National Institutes of Health. The web-based medication adherence program pilot study was supported by the Lupus Foundation of America. What the two approaches share in common is a conviction that, when it comes to addressing pain, fatigue, diminished quality of life, and poor medication adherence in young patients with SLE: “Our medication prescription alone doesn’t do it,” Dr. Brunner said.
She reported having no financial conflicts regarding her presentation.
REPORTING FROM LUPUS 2019
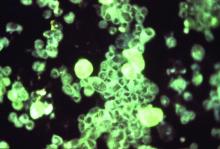
Identifying CMV infection in asymptomatic newborns – one step closer?
Cytomegalovirus (CMV) infection is the most common congenital viral infection in U.S. children, with a frequency between 0.5% and 1% of newborn infants resulting in approximately 30,000 infected children annually. A small minority (approximately 10%) can be identified in the neonatal period as symptomatic with jaundice (from direct hyperbilirubinemia), petechiae (from thrombocytopenia), hepatosplenomegaly, microcephaly, or other manifestations. The vast majority are asymptomatic at birth, yet 15% will have or develop sensorineural hearing loss (SNHL) during the first few years of life; others (1%-2%) will develop vision loss associated with retinal scars. Congenital CMV accounts for 20% of those with SNHL detected at birth and 25% of children with SNHL at 4 years of age.
Screening for congenital CMV has been an ongoing subject of debate. The challenges of implementing screening programs are related both to the diagnostics (collecting urine samples on newborns) as well as with the question of whether we have treatment and interventions to offer babies diagnosed with congenital CMV across the complete spectrum of clinical presentations.
Current screening programs implemented in some hospitals, called “targeted screening,” in which babies who fail newborn screening programs are tested for CMV, are not sufficient to achieve the goal of identifying babies who will need follow-up for early detection of SNHL or vision abnormalities, or possibly early antiviral therapy (Valcyte; valganciclovir), because only a small portion of those who eventually develop SNHL are currently identified by the targeted screening programs.1
However, its availability only has added to the debate as to whether the time has arrived for universal screening.
Vertical transmission of CMV occurs in utero (during any of the trimesters), at birth by passage through the birth canal, or postnatally by ingestion of breast milk. Neonatal infection (in utero and postnatal) occurs in both mothers with primary CMV infection during gestation and in those with recurrent infection (from a different viral strain) or reactivation of infection. Severe clinically symptomatic disease and sequelae is associated with primary maternal infection and early transmission to the fetus. However, it is estimated that nonprimary maternal infection accounts for 75% of neonatal infections. Transmission by breast milk to full-term, healthy infants does not appear to be associated with clinical illness or sequelae; however, preterm infants or those with birth weights less than 1,500 g have a small risk of developing clinical disease.
The polymerase chain reaction–based saliva CMV test (Alethia CMV Assay Test System) was licensed by the Food and Drug Administration in November 2018 after studies demonstrated high sensitivity and specificity, compared with viral culture (the gold standard). In one study, 17,327 infants were screened with the liquid-saliva PCR assay, and 0.5% tested positive for CMV on both the saliva test and culture. Sensitivity and specificity of the liquid-saliva PCR assay were 100% and 99.9%, respectively.2 The availability of an approved saliva-based assay that is both highly sensitive and specific overcomes the challenge of collecting urine, which has been a limiting factor in development of pragmatic universal screening programs. To date, most of the focus in identification of congenital CMV infection has been linking newborn hearing testing programs with CMV testing. For some, these have been labeled “targeted screening programs for CMV.” To us, these appear to be best practice for medical evaluations of an infant with identified SNHL. The availability of saliva-based CMV testing should enable virtually all children who fail newborn screening to be tested for CMV. In multiple studies,3,4 6% of infants with confirmed hearing screen failure tested positive for CMV. A recent study5 identified only 1 infant among the 171 infants who failed newborn screening, however only approximately 15% of the infants were eventually confirmed as hearing impaired at audiology follow-up, suggesting that programmatically testing for CMV might be limited to those with confirmed hearing loss if such can be accomplished within a narrow window of time.
The major challenge with linking CMV testing with newborn hearing screening is whether treatment with valganciclovir would be of value in congenital CMV infection and isolated hearing loss. Studies of children with symptomatic central nervous system congenital CMV disease provide evidence of improvement (or lack of progression) in hearing loss in those treated with valganciclovir. Few, if any of these children had isolated hearing loss in this pivotal study.6 An observational study reported improved outcomes in 55 of 59 (93%) children with congenital CMV and isolated SNHL treated with valganciclovir between birth to 12 weeks of life.7 Hearing improved in nearly 70% of ears, 27% showed no change, and only 3% demonstrated progression of hearing loss; most of the improved ears returned to normal hearing. Currently, a National Institutes of Health study (ValEAR) is recruiting CMV-infected infants with isolated SNHL and randomizing them to treatment with valganciclovir or placebo. The goal is to determine if infants treated with valganciclovir will have better hearing and language outcomes.
Linking CMV testing to those who fail newborn hearing screening programs is an important step, as it appears such children are at least five times more likely to be infected with CMV than is the overall birth cohort. However, such strategies fall short of identifying the majority of newborns with congenital CMV infection, who are completely asymptomatic yet are at risk for development of complications that potentially have substantial impact on their quality of life. Although the availability of sensitive and specific PCR testing in saliva provides a pragmatic approach to identify infected children, many questions remain. First, would a confirmatory test be necessary, such as urine PCR (now considered the gold standard by many CMV experts)? Second, once identified, what regimen for follow-up testing would be indicated to identify those with early SNHL or retinopathy, and until what age? Third, is there a role for treatment in asymptomatic infection? Would that treatment be prophylactic, prior to the development of clinical signs, or implemented once early evidence of SNHL or retinopathy is present?
The Valgan Toddler study – sponsored by NIH and the University of Alabama as part of the Collaborative Antiviral Study Group – will enroll children who are aged 1 month through 3 years and who had a recent diagnosis of hearing loss (within the prior 12 weeks) and evidence of congenital CMV infection. The purpose of this study is to compare the effect on hearing and neurologic outcomes in infants aged 1 month through 4 years with recent onset SNHL who receive 6 weeks of valganciclovir versus children who do not receive this drug. The results of such studies will be critical for the development of best practices.
In summary, the licensure of a rapid PCR-based tool for diagnosis of CMV infection from saliva adds to our ability to develop screening programs to detect asymptomatic infants with congenital CMV infection. The ability to link newborns who fail hearing screening programs with CMV testing will lead to more detection of CMV-infected neonates, both with isolated hearing loss, and subsequently with no signs or symptoms of infection. There is an urgent need for evidence from randomized clinical trials to enable the development of best practices for such infants.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Dr. Lapidot is a senior fellow in pediatric infectious diseases, Boston Medical Center. Neither Dr. Pelton nor Dr. Lapidot have any relevant financial disclosures. Email them at pdnews@mdedge.com.
References
1. J Pediatric Infect Dis Soc. 2019 Mar 28;8(1):55-9.
2. N Engl J Med 2011 Jun 2; 364:2111-8.
3. Pediatrics. 2008 May;121(5):970-5
4. J Clin Virol. 2018 May;102:110-5.
5. J Pediatric Infect Dis Soc. 2019 Mar;8(1):55-9.
6. J Pediatr. 2003 Jul;143(1):16-25.
7. J Pediatr. 2018 Aug;199:166-70.
Cytomegalovirus (CMV) infection is the most common congenital viral infection in U.S. children, with a frequency between 0.5% and 1% of newborn infants resulting in approximately 30,000 infected children annually. A small minority (approximately 10%) can be identified in the neonatal period as symptomatic with jaundice (from direct hyperbilirubinemia), petechiae (from thrombocytopenia), hepatosplenomegaly, microcephaly, or other manifestations. The vast majority are asymptomatic at birth, yet 15% will have or develop sensorineural hearing loss (SNHL) during the first few years of life; others (1%-2%) will develop vision loss associated with retinal scars. Congenital CMV accounts for 20% of those with SNHL detected at birth and 25% of children with SNHL at 4 years of age.
Screening for congenital CMV has been an ongoing subject of debate. The challenges of implementing screening programs are related both to the diagnostics (collecting urine samples on newborns) as well as with the question of whether we have treatment and interventions to offer babies diagnosed with congenital CMV across the complete spectrum of clinical presentations.
Current screening programs implemented in some hospitals, called “targeted screening,” in which babies who fail newborn screening programs are tested for CMV, are not sufficient to achieve the goal of identifying babies who will need follow-up for early detection of SNHL or vision abnormalities, or possibly early antiviral therapy (Valcyte; valganciclovir), because only a small portion of those who eventually develop SNHL are currently identified by the targeted screening programs.1
However, its availability only has added to the debate as to whether the time has arrived for universal screening.
Vertical transmission of CMV occurs in utero (during any of the trimesters), at birth by passage through the birth canal, or postnatally by ingestion of breast milk. Neonatal infection (in utero and postnatal) occurs in both mothers with primary CMV infection during gestation and in those with recurrent infection (from a different viral strain) or reactivation of infection. Severe clinically symptomatic disease and sequelae is associated with primary maternal infection and early transmission to the fetus. However, it is estimated that nonprimary maternal infection accounts for 75% of neonatal infections. Transmission by breast milk to full-term, healthy infants does not appear to be associated with clinical illness or sequelae; however, preterm infants or those with birth weights less than 1,500 g have a small risk of developing clinical disease.
The polymerase chain reaction–based saliva CMV test (Alethia CMV Assay Test System) was licensed by the Food and Drug Administration in November 2018 after studies demonstrated high sensitivity and specificity, compared with viral culture (the gold standard). In one study, 17,327 infants were screened with the liquid-saliva PCR assay, and 0.5% tested positive for CMV on both the saliva test and culture. Sensitivity and specificity of the liquid-saliva PCR assay were 100% and 99.9%, respectively.2 The availability of an approved saliva-based assay that is both highly sensitive and specific overcomes the challenge of collecting urine, which has been a limiting factor in development of pragmatic universal screening programs. To date, most of the focus in identification of congenital CMV infection has been linking newborn hearing testing programs with CMV testing. For some, these have been labeled “targeted screening programs for CMV.” To us, these appear to be best practice for medical evaluations of an infant with identified SNHL. The availability of saliva-based CMV testing should enable virtually all children who fail newborn screening to be tested for CMV. In multiple studies,3,4 6% of infants with confirmed hearing screen failure tested positive for CMV. A recent study5 identified only 1 infant among the 171 infants who failed newborn screening, however only approximately 15% of the infants were eventually confirmed as hearing impaired at audiology follow-up, suggesting that programmatically testing for CMV might be limited to those with confirmed hearing loss if such can be accomplished within a narrow window of time.
The major challenge with linking CMV testing with newborn hearing screening is whether treatment with valganciclovir would be of value in congenital CMV infection and isolated hearing loss. Studies of children with symptomatic central nervous system congenital CMV disease provide evidence of improvement (or lack of progression) in hearing loss in those treated with valganciclovir. Few, if any of these children had isolated hearing loss in this pivotal study.6 An observational study reported improved outcomes in 55 of 59 (93%) children with congenital CMV and isolated SNHL treated with valganciclovir between birth to 12 weeks of life.7 Hearing improved in nearly 70% of ears, 27% showed no change, and only 3% demonstrated progression of hearing loss; most of the improved ears returned to normal hearing. Currently, a National Institutes of Health study (ValEAR) is recruiting CMV-infected infants with isolated SNHL and randomizing them to treatment with valganciclovir or placebo. The goal is to determine if infants treated with valganciclovir will have better hearing and language outcomes.
Linking CMV testing to those who fail newborn hearing screening programs is an important step, as it appears such children are at least five times more likely to be infected with CMV than is the overall birth cohort. However, such strategies fall short of identifying the majority of newborns with congenital CMV infection, who are completely asymptomatic yet are at risk for development of complications that potentially have substantial impact on their quality of life. Although the availability of sensitive and specific PCR testing in saliva provides a pragmatic approach to identify infected children, many questions remain. First, would a confirmatory test be necessary, such as urine PCR (now considered the gold standard by many CMV experts)? Second, once identified, what regimen for follow-up testing would be indicated to identify those with early SNHL or retinopathy, and until what age? Third, is there a role for treatment in asymptomatic infection? Would that treatment be prophylactic, prior to the development of clinical signs, or implemented once early evidence of SNHL or retinopathy is present?
The Valgan Toddler study – sponsored by NIH and the University of Alabama as part of the Collaborative Antiviral Study Group – will enroll children who are aged 1 month through 3 years and who had a recent diagnosis of hearing loss (within the prior 12 weeks) and evidence of congenital CMV infection. The purpose of this study is to compare the effect on hearing and neurologic outcomes in infants aged 1 month through 4 years with recent onset SNHL who receive 6 weeks of valganciclovir versus children who do not receive this drug. The results of such studies will be critical for the development of best practices.
In summary, the licensure of a rapid PCR-based tool for diagnosis of CMV infection from saliva adds to our ability to develop screening programs to detect asymptomatic infants with congenital CMV infection. The ability to link newborns who fail hearing screening programs with CMV testing will lead to more detection of CMV-infected neonates, both with isolated hearing loss, and subsequently with no signs or symptoms of infection. There is an urgent need for evidence from randomized clinical trials to enable the development of best practices for such infants.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Dr. Lapidot is a senior fellow in pediatric infectious diseases, Boston Medical Center. Neither Dr. Pelton nor Dr. Lapidot have any relevant financial disclosures. Email them at pdnews@mdedge.com.
References
1. J Pediatric Infect Dis Soc. 2019 Mar 28;8(1):55-9.
2. N Engl J Med 2011 Jun 2; 364:2111-8.
3. Pediatrics. 2008 May;121(5):970-5
4. J Clin Virol. 2018 May;102:110-5.
5. J Pediatric Infect Dis Soc. 2019 Mar;8(1):55-9.
6. J Pediatr. 2003 Jul;143(1):16-25.
7. J Pediatr. 2018 Aug;199:166-70.
Cytomegalovirus (CMV) infection is the most common congenital viral infection in U.S. children, with a frequency between 0.5% and 1% of newborn infants resulting in approximately 30,000 infected children annually. A small minority (approximately 10%) can be identified in the neonatal period as symptomatic with jaundice (from direct hyperbilirubinemia), petechiae (from thrombocytopenia), hepatosplenomegaly, microcephaly, or other manifestations. The vast majority are asymptomatic at birth, yet 15% will have or develop sensorineural hearing loss (SNHL) during the first few years of life; others (1%-2%) will develop vision loss associated with retinal scars. Congenital CMV accounts for 20% of those with SNHL detected at birth and 25% of children with SNHL at 4 years of age.
Screening for congenital CMV has been an ongoing subject of debate. The challenges of implementing screening programs are related both to the diagnostics (collecting urine samples on newborns) as well as with the question of whether we have treatment and interventions to offer babies diagnosed with congenital CMV across the complete spectrum of clinical presentations.
Current screening programs implemented in some hospitals, called “targeted screening,” in which babies who fail newborn screening programs are tested for CMV, are not sufficient to achieve the goal of identifying babies who will need follow-up for early detection of SNHL or vision abnormalities, or possibly early antiviral therapy (Valcyte; valganciclovir), because only a small portion of those who eventually develop SNHL are currently identified by the targeted screening programs.1
However, its availability only has added to the debate as to whether the time has arrived for universal screening.
Vertical transmission of CMV occurs in utero (during any of the trimesters), at birth by passage through the birth canal, or postnatally by ingestion of breast milk. Neonatal infection (in utero and postnatal) occurs in both mothers with primary CMV infection during gestation and in those with recurrent infection (from a different viral strain) or reactivation of infection. Severe clinically symptomatic disease and sequelae is associated with primary maternal infection and early transmission to the fetus. However, it is estimated that nonprimary maternal infection accounts for 75% of neonatal infections. Transmission by breast milk to full-term, healthy infants does not appear to be associated with clinical illness or sequelae; however, preterm infants or those with birth weights less than 1,500 g have a small risk of developing clinical disease.
The polymerase chain reaction–based saliva CMV test (Alethia CMV Assay Test System) was licensed by the Food and Drug Administration in November 2018 after studies demonstrated high sensitivity and specificity, compared with viral culture (the gold standard). In one study, 17,327 infants were screened with the liquid-saliva PCR assay, and 0.5% tested positive for CMV on both the saliva test and culture. Sensitivity and specificity of the liquid-saliva PCR assay were 100% and 99.9%, respectively.2 The availability of an approved saliva-based assay that is both highly sensitive and specific overcomes the challenge of collecting urine, which has been a limiting factor in development of pragmatic universal screening programs. To date, most of the focus in identification of congenital CMV infection has been linking newborn hearing testing programs with CMV testing. For some, these have been labeled “targeted screening programs for CMV.” To us, these appear to be best practice for medical evaluations of an infant with identified SNHL. The availability of saliva-based CMV testing should enable virtually all children who fail newborn screening to be tested for CMV. In multiple studies,3,4 6% of infants with confirmed hearing screen failure tested positive for CMV. A recent study5 identified only 1 infant among the 171 infants who failed newborn screening, however only approximately 15% of the infants were eventually confirmed as hearing impaired at audiology follow-up, suggesting that programmatically testing for CMV might be limited to those with confirmed hearing loss if such can be accomplished within a narrow window of time.
The major challenge with linking CMV testing with newborn hearing screening is whether treatment with valganciclovir would be of value in congenital CMV infection and isolated hearing loss. Studies of children with symptomatic central nervous system congenital CMV disease provide evidence of improvement (or lack of progression) in hearing loss in those treated with valganciclovir. Few, if any of these children had isolated hearing loss in this pivotal study.6 An observational study reported improved outcomes in 55 of 59 (93%) children with congenital CMV and isolated SNHL treated with valganciclovir between birth to 12 weeks of life.7 Hearing improved in nearly 70% of ears, 27% showed no change, and only 3% demonstrated progression of hearing loss; most of the improved ears returned to normal hearing. Currently, a National Institutes of Health study (ValEAR) is recruiting CMV-infected infants with isolated SNHL and randomizing them to treatment with valganciclovir or placebo. The goal is to determine if infants treated with valganciclovir will have better hearing and language outcomes.
Linking CMV testing to those who fail newborn hearing screening programs is an important step, as it appears such children are at least five times more likely to be infected with CMV than is the overall birth cohort. However, such strategies fall short of identifying the majority of newborns with congenital CMV infection, who are completely asymptomatic yet are at risk for development of complications that potentially have substantial impact on their quality of life. Although the availability of sensitive and specific PCR testing in saliva provides a pragmatic approach to identify infected children, many questions remain. First, would a confirmatory test be necessary, such as urine PCR (now considered the gold standard by many CMV experts)? Second, once identified, what regimen for follow-up testing would be indicated to identify those with early SNHL or retinopathy, and until what age? Third, is there a role for treatment in asymptomatic infection? Would that treatment be prophylactic, prior to the development of clinical signs, or implemented once early evidence of SNHL or retinopathy is present?
The Valgan Toddler study – sponsored by NIH and the University of Alabama as part of the Collaborative Antiviral Study Group – will enroll children who are aged 1 month through 3 years and who had a recent diagnosis of hearing loss (within the prior 12 weeks) and evidence of congenital CMV infection. The purpose of this study is to compare the effect on hearing and neurologic outcomes in infants aged 1 month through 4 years with recent onset SNHL who receive 6 weeks of valganciclovir versus children who do not receive this drug. The results of such studies will be critical for the development of best practices.
In summary, the licensure of a rapid PCR-based tool for diagnosis of CMV infection from saliva adds to our ability to develop screening programs to detect asymptomatic infants with congenital CMV infection. The ability to link newborns who fail hearing screening programs with CMV testing will lead to more detection of CMV-infected neonates, both with isolated hearing loss, and subsequently with no signs or symptoms of infection. There is an urgent need for evidence from randomized clinical trials to enable the development of best practices for such infants.
Dr. Pelton is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Dr. Lapidot is a senior fellow in pediatric infectious diseases, Boston Medical Center. Neither Dr. Pelton nor Dr. Lapidot have any relevant financial disclosures. Email them at pdnews@mdedge.com.
References
1. J Pediatric Infect Dis Soc. 2019 Mar 28;8(1):55-9.
2. N Engl J Med 2011 Jun 2; 364:2111-8.
3. Pediatrics. 2008 May;121(5):970-5
4. J Clin Virol. 2018 May;102:110-5.
5. J Pediatric Infect Dis Soc. 2019 Mar;8(1):55-9.
6. J Pediatr. 2003 Jul;143(1):16-25.
7. J Pediatr. 2018 Aug;199:166-70.
Depression, antidepressant use may be common among patients with OSA
About a quarter of patients with obstructive sleep apnea also had clinical depression and used antidepressants, recent research has shown.
Although patients in the study associated their sleep disorder with poorer quality of life as well as symptoms of anxiety and depression, it is unclear whether treating their obstructive sleep apnea (OSA) with continuous positive airway pressure (CPAP) would alleviate these symptoms, said Melinda L. Jackson, PhD, from Monash University in Clayton, Victoria, Australia, and her colleagues.
“OSA is a modifiable factor that, if treated, may reduce the economic, health care, and personal burden of depression,” Dr. Jackson and her colleagues wrote in their study, recently published in the journal Sleep Medicine. “Findings from the treatment phase of this study will help us determine whether clinical depression is alleviated with CPAP use, taking into account antidepressant use; whether there are subgroups of patients who respond better to treatment; and what are the characteristics of patients who respond compared to those who remain depressed.”
The researchers used baseline data from 109 patients in the CPAP for OSA and Depression trial who were diagnosed with OSA. Participants (mean age, 52.6 years; 43.1% female) consecutively presented to a sleep laboratory where they answered interview questions to assess clinical depression and sleep habits. Data were collected using the structured clinical interview for depression (SCID-IV), Hospital Anxiety and Depression Scale, Pittsburgh Sleep Quality Index (PSQI), Functional Outcomes of Sleep Questionnaire (FOSQ), Epworth Sleepiness Scale, and Assessment of Quality of Life questionnaire. In addition, the researchers performed a meta-analysis of seven studies, including the current study, to determine the prevalence of clinical depression among patients with untreated OSA.
Overall, SCID-IV scores identified clinical depression in 25 participants (22.7%), and these participants said they had greater sleep disturbance and reported higher depressive, anxiety and stress as well as lower quality of life as a result of their clinical depression. Researchers found these participants also had significantly worse quality of sleep (P less than .05) and daytime dysfunction (P less than .05) as identified by PSQI scores, while FOSQ results showed participants with clinical depression had significantly lower activity levels, social outcomes, and general productivity, compared with patients without clinical depression (P less than .05). In a meta-analysis, Dr. Jackson and her colleagues found a pooled prevalence of 23% for clinical depression among participants with OSA.
Participants using antidepressants were examined separately from participants who had clinical depression. The researchers found 27 participants (24.8%) using antidepressants who also had reported higher symptoms of anxiety, depression and stress, lower quality of life, and poorer sleep outcomes. Participants using antidepressants also were more likely to have bipolar disorder or a condition such as hypertension, chronic obstructive pulmonary disease, high cholesterol, or type 2 diabetes, and 75% of these participants reported having some type of comorbid condition.
Dr. Jackson and her colleagues noted they were uncertain whether depression or OSA occurred first, or whether depression exacerbated symptoms of OSA through other factors such as weight gain, sleep disruption, inactivity, or alcohol use. Depression and OSA may also present independently of one another, they added.
“Development of scales to better capture information about when symptoms commenced and the length of time an individual has experienced OSA will provide a clearer understanding of the consequences of OSA on psychological and medical conditions,” the researchers said.
This study was funded by the Austin Medical Research Fund, and one authors reported support from an National Health and Medical Research Council Early Career Fellowship. The authors report no relevant conflicts of interest.
SOURCE: Jackson ML et al. Sleep Med. 2019 Mar 27. doi: 10.1016/j.sleep.2019.03.011.
About a quarter of patients with obstructive sleep apnea also had clinical depression and used antidepressants, recent research has shown.
Although patients in the study associated their sleep disorder with poorer quality of life as well as symptoms of anxiety and depression, it is unclear whether treating their obstructive sleep apnea (OSA) with continuous positive airway pressure (CPAP) would alleviate these symptoms, said Melinda L. Jackson, PhD, from Monash University in Clayton, Victoria, Australia, and her colleagues.
“OSA is a modifiable factor that, if treated, may reduce the economic, health care, and personal burden of depression,” Dr. Jackson and her colleagues wrote in their study, recently published in the journal Sleep Medicine. “Findings from the treatment phase of this study will help us determine whether clinical depression is alleviated with CPAP use, taking into account antidepressant use; whether there are subgroups of patients who respond better to treatment; and what are the characteristics of patients who respond compared to those who remain depressed.”
The researchers used baseline data from 109 patients in the CPAP for OSA and Depression trial who were diagnosed with OSA. Participants (mean age, 52.6 years; 43.1% female) consecutively presented to a sleep laboratory where they answered interview questions to assess clinical depression and sleep habits. Data were collected using the structured clinical interview for depression (SCID-IV), Hospital Anxiety and Depression Scale, Pittsburgh Sleep Quality Index (PSQI), Functional Outcomes of Sleep Questionnaire (FOSQ), Epworth Sleepiness Scale, and Assessment of Quality of Life questionnaire. In addition, the researchers performed a meta-analysis of seven studies, including the current study, to determine the prevalence of clinical depression among patients with untreated OSA.
Overall, SCID-IV scores identified clinical depression in 25 participants (22.7%), and these participants said they had greater sleep disturbance and reported higher depressive, anxiety and stress as well as lower quality of life as a result of their clinical depression. Researchers found these participants also had significantly worse quality of sleep (P less than .05) and daytime dysfunction (P less than .05) as identified by PSQI scores, while FOSQ results showed participants with clinical depression had significantly lower activity levels, social outcomes, and general productivity, compared with patients without clinical depression (P less than .05). In a meta-analysis, Dr. Jackson and her colleagues found a pooled prevalence of 23% for clinical depression among participants with OSA.
Participants using antidepressants were examined separately from participants who had clinical depression. The researchers found 27 participants (24.8%) using antidepressants who also had reported higher symptoms of anxiety, depression and stress, lower quality of life, and poorer sleep outcomes. Participants using antidepressants also were more likely to have bipolar disorder or a condition such as hypertension, chronic obstructive pulmonary disease, high cholesterol, or type 2 diabetes, and 75% of these participants reported having some type of comorbid condition.
Dr. Jackson and her colleagues noted they were uncertain whether depression or OSA occurred first, or whether depression exacerbated symptoms of OSA through other factors such as weight gain, sleep disruption, inactivity, or alcohol use. Depression and OSA may also present independently of one another, they added.
“Development of scales to better capture information about when symptoms commenced and the length of time an individual has experienced OSA will provide a clearer understanding of the consequences of OSA on psychological and medical conditions,” the researchers said.
This study was funded by the Austin Medical Research Fund, and one authors reported support from an National Health and Medical Research Council Early Career Fellowship. The authors report no relevant conflicts of interest.
SOURCE: Jackson ML et al. Sleep Med. 2019 Mar 27. doi: 10.1016/j.sleep.2019.03.011.
About a quarter of patients with obstructive sleep apnea also had clinical depression and used antidepressants, recent research has shown.
Although patients in the study associated their sleep disorder with poorer quality of life as well as symptoms of anxiety and depression, it is unclear whether treating their obstructive sleep apnea (OSA) with continuous positive airway pressure (CPAP) would alleviate these symptoms, said Melinda L. Jackson, PhD, from Monash University in Clayton, Victoria, Australia, and her colleagues.
“OSA is a modifiable factor that, if treated, may reduce the economic, health care, and personal burden of depression,” Dr. Jackson and her colleagues wrote in their study, recently published in the journal Sleep Medicine. “Findings from the treatment phase of this study will help us determine whether clinical depression is alleviated with CPAP use, taking into account antidepressant use; whether there are subgroups of patients who respond better to treatment; and what are the characteristics of patients who respond compared to those who remain depressed.”
The researchers used baseline data from 109 patients in the CPAP for OSA and Depression trial who were diagnosed with OSA. Participants (mean age, 52.6 years; 43.1% female) consecutively presented to a sleep laboratory where they answered interview questions to assess clinical depression and sleep habits. Data were collected using the structured clinical interview for depression (SCID-IV), Hospital Anxiety and Depression Scale, Pittsburgh Sleep Quality Index (PSQI), Functional Outcomes of Sleep Questionnaire (FOSQ), Epworth Sleepiness Scale, and Assessment of Quality of Life questionnaire. In addition, the researchers performed a meta-analysis of seven studies, including the current study, to determine the prevalence of clinical depression among patients with untreated OSA.
Overall, SCID-IV scores identified clinical depression in 25 participants (22.7%), and these participants said they had greater sleep disturbance and reported higher depressive, anxiety and stress as well as lower quality of life as a result of their clinical depression. Researchers found these participants also had significantly worse quality of sleep (P less than .05) and daytime dysfunction (P less than .05) as identified by PSQI scores, while FOSQ results showed participants with clinical depression had significantly lower activity levels, social outcomes, and general productivity, compared with patients without clinical depression (P less than .05). In a meta-analysis, Dr. Jackson and her colleagues found a pooled prevalence of 23% for clinical depression among participants with OSA.
Participants using antidepressants were examined separately from participants who had clinical depression. The researchers found 27 participants (24.8%) using antidepressants who also had reported higher symptoms of anxiety, depression and stress, lower quality of life, and poorer sleep outcomes. Participants using antidepressants also were more likely to have bipolar disorder or a condition such as hypertension, chronic obstructive pulmonary disease, high cholesterol, or type 2 diabetes, and 75% of these participants reported having some type of comorbid condition.
Dr. Jackson and her colleagues noted they were uncertain whether depression or OSA occurred first, or whether depression exacerbated symptoms of OSA through other factors such as weight gain, sleep disruption, inactivity, or alcohol use. Depression and OSA may also present independently of one another, they added.
“Development of scales to better capture information about when symptoms commenced and the length of time an individual has experienced OSA will provide a clearer understanding of the consequences of OSA on psychological and medical conditions,” the researchers said.
This study was funded by the Austin Medical Research Fund, and one authors reported support from an National Health and Medical Research Council Early Career Fellowship. The authors report no relevant conflicts of interest.
SOURCE: Jackson ML et al. Sleep Med. 2019 Mar 27. doi: 10.1016/j.sleep.2019.03.011.
FROM SLEEP MEDICINE
Focus on Science, Not Format: Introducing No Hassle Submissions to the Journal of Hospital Medicine
The Journal of Hospital Medicine® is committed to continually improving the author experience. Our goal is to allow authors to focus more time on communicating their message and less time on navigating the submission and publication process. We commit to three initial areas of emphasis: (1) Make it easy for authors to submit their work; (2) Make timely disposition decisions; and (3) Facilitate dissemination of work that we publish.
We are pleased to introduce a new “No hassle” process for initial original research and brief report manuscript submissions. There is no universally followed format for manuscript submission to medical journals.1-3 As a result, authors spend considerable time reformatting manuscripts for submission to meet each journal’s unique requirements before knowing whether or not their manuscript will be accepted for publication—or even sent for peer review. To streamline the submission process and eliminate unnecessary and burdensome reformatting, we have eased formatting requirements for initial manuscript submissions. We will even accept all manuscript elements in a single PDF (portable document format) file in another journal’s format if your manuscript was submitted elsewhere first but not accepted for publication. Tables and figures can be included in the single document or uploaded separately, depending on your preference. Of course, common elements necessary to assess a manuscript, including declaration of funding sources and conflicts of interest, are required on the title page.1 Journal-specific formatting and signed disclosure and copyright forms will be deferred until a revision request.
We also seek to make timely decisions. Our rapid turnaround allows authors to submit elsewhere expeditiously if not accepted by the Journal of Hospital Medicine. We reject approximately 50% of original research and brief report manuscripts without formal peer review. The rationale for this approach is two-fold. We want to be respectful of how we engage our peer reviewers and we would rather not have them spend time reviewing manuscripts that we are unlikely to publish. We also want to be respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by the Editor-in-Chief and other journal editors, we prefer to return the manuscript to authors for timely submission elsewhere. Our average time from submission to rejection without formal peer review is 1.3 days (median, <1 day). If we send a manuscript out for peer review, our time from submission to first decision is 23 days. Further, if we request a manuscript revision, we sincerely hope to publish the manuscript. Thus, most manuscripts for which we request a revision are ultimately accepted for publication. We are also tracking how quickly we can publish accepted manuscripts with a goal of 120 or fewer days from submission to publication and 60 or fewer days from acceptance to publication.
We highlight our published research in many ways to facilitate dissemination. We promote articles through formal press releases, tweets, visual abstracts, and, more recently, graphic medicine abstracts or comics. Select articles are discussed through our online journal club (#JHMChat).4 Other synergistic methods of dissemination are being planned and we’ll share these ideas with you in the coming year.
We are grateful to receive a large number of submissions and are honored that authors view the Journal of Hospital Medicine as an important venue to showcase their work. We continually strive to improve the author experience and welcome your input.
1. International Committee of Medical Journal Editors. Recommendations for the conduct, reporting, editing, and publication of scholarly work in medical journals. Updated December 2018. www.icmje.org/recommendations/browse/. Accessed April 2, 2019. PubMed
2. Schriger DL, Arora S, Altman DG. The content of medical journal instructions for authors. Ann Emerg Med. 2006;48(6):743-749. doi: 10.1016/j.annemergmed.2006.03.028 PubMed
3. Barron JP. The uniform requirements for manuscripts submitted to biomedical journals recommended by the International Committee of Medical Journal Editors. Chest. 2006;129(4):1098-1099. doi: 10.1378/chest.129.4.1098. PubMed
4. Wray CM, Auerbach AD, Arora VM. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018;13(11):764-769. doi: 10.12788/jhm.2987. PubMed
The Journal of Hospital Medicine® is committed to continually improving the author experience. Our goal is to allow authors to focus more time on communicating their message and less time on navigating the submission and publication process. We commit to three initial areas of emphasis: (1) Make it easy for authors to submit their work; (2) Make timely disposition decisions; and (3) Facilitate dissemination of work that we publish.
We are pleased to introduce a new “No hassle” process for initial original research and brief report manuscript submissions. There is no universally followed format for manuscript submission to medical journals.1-3 As a result, authors spend considerable time reformatting manuscripts for submission to meet each journal’s unique requirements before knowing whether or not their manuscript will be accepted for publication—or even sent for peer review. To streamline the submission process and eliminate unnecessary and burdensome reformatting, we have eased formatting requirements for initial manuscript submissions. We will even accept all manuscript elements in a single PDF (portable document format) file in another journal’s format if your manuscript was submitted elsewhere first but not accepted for publication. Tables and figures can be included in the single document or uploaded separately, depending on your preference. Of course, common elements necessary to assess a manuscript, including declaration of funding sources and conflicts of interest, are required on the title page.1 Journal-specific formatting and signed disclosure and copyright forms will be deferred until a revision request.
We also seek to make timely decisions. Our rapid turnaround allows authors to submit elsewhere expeditiously if not accepted by the Journal of Hospital Medicine. We reject approximately 50% of original research and brief report manuscripts without formal peer review. The rationale for this approach is two-fold. We want to be respectful of how we engage our peer reviewers and we would rather not have them spend time reviewing manuscripts that we are unlikely to publish. We also want to be respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by the Editor-in-Chief and other journal editors, we prefer to return the manuscript to authors for timely submission elsewhere. Our average time from submission to rejection without formal peer review is 1.3 days (median, <1 day). If we send a manuscript out for peer review, our time from submission to first decision is 23 days. Further, if we request a manuscript revision, we sincerely hope to publish the manuscript. Thus, most manuscripts for which we request a revision are ultimately accepted for publication. We are also tracking how quickly we can publish accepted manuscripts with a goal of 120 or fewer days from submission to publication and 60 or fewer days from acceptance to publication.
We highlight our published research in many ways to facilitate dissemination. We promote articles through formal press releases, tweets, visual abstracts, and, more recently, graphic medicine abstracts or comics. Select articles are discussed through our online journal club (#JHMChat).4 Other synergistic methods of dissemination are being planned and we’ll share these ideas with you in the coming year.
We are grateful to receive a large number of submissions and are honored that authors view the Journal of Hospital Medicine as an important venue to showcase their work. We continually strive to improve the author experience and welcome your input.
The Journal of Hospital Medicine® is committed to continually improving the author experience. Our goal is to allow authors to focus more time on communicating their message and less time on navigating the submission and publication process. We commit to three initial areas of emphasis: (1) Make it easy for authors to submit their work; (2) Make timely disposition decisions; and (3) Facilitate dissemination of work that we publish.
We are pleased to introduce a new “No hassle” process for initial original research and brief report manuscript submissions. There is no universally followed format for manuscript submission to medical journals.1-3 As a result, authors spend considerable time reformatting manuscripts for submission to meet each journal’s unique requirements before knowing whether or not their manuscript will be accepted for publication—or even sent for peer review. To streamline the submission process and eliminate unnecessary and burdensome reformatting, we have eased formatting requirements for initial manuscript submissions. We will even accept all manuscript elements in a single PDF (portable document format) file in another journal’s format if your manuscript was submitted elsewhere first but not accepted for publication. Tables and figures can be included in the single document or uploaded separately, depending on your preference. Of course, common elements necessary to assess a manuscript, including declaration of funding sources and conflicts of interest, are required on the title page.1 Journal-specific formatting and signed disclosure and copyright forms will be deferred until a revision request.
We also seek to make timely decisions. Our rapid turnaround allows authors to submit elsewhere expeditiously if not accepted by the Journal of Hospital Medicine. We reject approximately 50% of original research and brief report manuscripts without formal peer review. The rationale for this approach is two-fold. We want to be respectful of how we engage our peer reviewers and we would rather not have them spend time reviewing manuscripts that we are unlikely to publish. We also want to be respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by the Editor-in-Chief and other journal editors, we prefer to return the manuscript to authors for timely submission elsewhere. Our average time from submission to rejection without formal peer review is 1.3 days (median, <1 day). If we send a manuscript out for peer review, our time from submission to first decision is 23 days. Further, if we request a manuscript revision, we sincerely hope to publish the manuscript. Thus, most manuscripts for which we request a revision are ultimately accepted for publication. We are also tracking how quickly we can publish accepted manuscripts with a goal of 120 or fewer days from submission to publication and 60 or fewer days from acceptance to publication.
We highlight our published research in many ways to facilitate dissemination. We promote articles through formal press releases, tweets, visual abstracts, and, more recently, graphic medicine abstracts or comics. Select articles are discussed through our online journal club (#JHMChat).4 Other synergistic methods of dissemination are being planned and we’ll share these ideas with you in the coming year.
We are grateful to receive a large number of submissions and are honored that authors view the Journal of Hospital Medicine as an important venue to showcase their work. We continually strive to improve the author experience and welcome your input.
1. International Committee of Medical Journal Editors. Recommendations for the conduct, reporting, editing, and publication of scholarly work in medical journals. Updated December 2018. www.icmje.org/recommendations/browse/. Accessed April 2, 2019. PubMed
2. Schriger DL, Arora S, Altman DG. The content of medical journal instructions for authors. Ann Emerg Med. 2006;48(6):743-749. doi: 10.1016/j.annemergmed.2006.03.028 PubMed
3. Barron JP. The uniform requirements for manuscripts submitted to biomedical journals recommended by the International Committee of Medical Journal Editors. Chest. 2006;129(4):1098-1099. doi: 10.1378/chest.129.4.1098. PubMed
4. Wray CM, Auerbach AD, Arora VM. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018;13(11):764-769. doi: 10.12788/jhm.2987. PubMed
1. International Committee of Medical Journal Editors. Recommendations for the conduct, reporting, editing, and publication of scholarly work in medical journals. Updated December 2018. www.icmje.org/recommendations/browse/. Accessed April 2, 2019. PubMed
2. Schriger DL, Arora S, Altman DG. The content of medical journal instructions for authors. Ann Emerg Med. 2006;48(6):743-749. doi: 10.1016/j.annemergmed.2006.03.028 PubMed
3. Barron JP. The uniform requirements for manuscripts submitted to biomedical journals recommended by the International Committee of Medical Journal Editors. Chest. 2006;129(4):1098-1099. doi: 10.1378/chest.129.4.1098. PubMed
4. Wray CM, Auerbach AD, Arora VM. The adoption of an online journal club to improve research dissemination and social media engagement among hospitalists. J Hosp Med. 2018;13(11):764-769. doi: 10.12788/jhm.2987. PubMed
© 2019 Society of Hospital Medicine
Restless Legs Syndrome Among Veterans With Spinal Cord Lesions (FULL)
Spinal cord injuries (SCI) are common in veteran populations.1 Veterans with spinal cord injuries and disorders (SCI/D) also may have concurrent sleep disturbances. Spinal cord injury typically causes spasticity.2,3 Hypersensitivity of the flexor reflex pathways is believed to cause painful muscle spasms in patients with SCI.4 Neuropathic pain at or below the level of the lesion also is common.
Restless legs syndrome (RLS) is a common sleep disorder that affects sleep quality and can occur concomitantly with spinal cord lesions.5 In about 80% of RLS cases, involuntary movements of legs across hip, knee, and ankle joints during sleep, known as periodic limb movement during sleep (PLMS), occurs.6 Several studies showed increased prevalence of PLMS in patients with SCI, and some case reports suggest an increased prevalence of RLS in this population.7,8 One small study showed that 100% of patients with SCI had symptoms of RLS.6 Another study found that SCI could trigger PLMS.8
The pathophysiology of RLS and PLMS in patients with SCI is not fully understood, but case reports describing PLM in SCI patients points to a possible role of central pattern generators and the flexor reflex afferents in the pathophysiology of PLMS.9,10 Changes of the tissue microstructure in the midbrain and upper cervical spinal cord have been described in patients with RLS.11The objective of this study was to assess the prevalence of RLS in a veteran population with SCI/D and
Methods
The institutional review and ethical approval boards of the Minneapolis VA Health Care System approved the study. Within the VA system, 666 patients with SCI/D were identified using a national database. Of the 666 people, 316 were excluded, 199 were included, and 151 were deceased.
Patients aged between 18 and 65 years were included in the study. Charts of patients who had been discharged with the diagnosis of SCI from 2002 to 2008 were studied. All patients met the inclusion criteria of the International Restless Legs Syndrome Study Group diagnosis.
Exclusion criteria were as follows: Patients with evidence of brain pathology (eg, stroke), concurrent neurologic condition associated with RLS (Parkinson disease, spinocerebellar ataxia, peripheral neuropathy), concurrent psychiatric condition within the setting of treatment with dopamine antagonists, secondary causes of RLS (renal failure/uremia, iron deficiency, rheumatoid arthritis, and pregnancy) and a recent history of alcohol or drug misuse or current evidence of substance use of < 1 year.
A patient list was compiled that included the etiology of the SCI (vascular injury, multiple sclerosis [MS], trauma, unknown, and other), the level(s) and completeness of the SCI per radiology report, RLS pharmacotherapies, and pertinent medical history.
Axial T2-weighted images on magnetic resonance imaging (MRI) scans were retrospectively reviewed. Sagittal T1/T2-weighted and axial T2-weighted sequences were performed routinely on all patients with spinal cord lesions. The analysis included the extension of the lesion on both sagittal and axial distributions. The anatomic location of the cord lesion was categorized by the following: (1) pure gray matter (central cord); (2) white matter (dorsal [D], dorsolateral [DL], ventral [V], ventrolateral areas [VL]).
A questionnaire using standard diagnostic criteria for RLS was mailed to the 199 patients who met the inclusion criteria (Appendix A).
All analyses were carried out using StataCorp STATA 13 (College Station, TX). Descriptive statistics were used. The analyses were carried out using chi-square and Fisher exact tests. Differences between the groups were considered statistically significant at P < .05. The data were analyzed to obtain point prevalence among patients with SCI, and comparisons were made among the different subgroups.
Results
Of the 162 patients who chose to participate in the study, the sleep specialists confirmed 31 (19%) to have RLS, 112 (69%) were confirmed negative for RLS, and an additional 19 (12%) screened positive for RLS but were not confirmed to have RLS by the sleep specialists (Figure 1).
The etiology of SCI was subdivided into 4 groups: MS, trauma, vascular, and other/unknown. Within each group (– RLS vs + RLS), MS and trauma were the most common etiologies with 55% MS and 36% trauma in the + RLS group.
When comparing RLS among the spinal cord levels (cervical, thoracic, lumbar and cervical + thoracic), only the cervical + thoracic subgroup (18% + RLS vs 5% – RLS) showed a significant difference (Figure 2).
There was no significant difference found with the prevalence of RLS in the axial plane of the spinal cord lesions (ventral/ventro-lateral/central cord vs dorsal/dorsolateral) or by the completeness of spinal cord lesions, P = .76. There was a higher prevalence of incomplete cord injury, however, within each subgroup of RLS.
The Mann-Whitney test was used to analyze the burden of disease in both groups (+ RLS vs – RLS). Moderate level of burden was most frequently reported with a higher prevalence within the + RLS group. Of those receiving treatment for RLS, 71% were + RLS vs 46% – RLS with a P value of .01. Symptoms of RLS after cord injury were 89% + RLS vs 55% – RLS with a P value of .03.
Discussion
This study represents one of the first studies to determine the prevalence of RLS in veterans with spinal cord disease. Research in this area is important to raise awareness of RLS among the veteran population with and without SCI and disorders. Restless legs syndrome often escapes diagnosis because of difficulty understanding the patient’s descriptions of their sensations. In addition, RLS may cause debilitating symptoms of sleep deprivation, daytime sleepiness, discomfort, and fatigue, which often results in decreased quality of life (QOL). Proper screening and treatment may improve QOL.
A study by Kumru and colleagues showed a similar rate of RLS in patients with SCI and RLS symptoms presented in the first year after SCI as did this study (18% vs 19%, respectively).4 In that study, RLS was more common in patients with lesions in lumbosacral area. Kumru and colleagues also showed that a dopaminergic medication improved symptoms of RLS in this population, whereas this study did not explore treatment outcomes.4
The pathogenesis of RLS is not fully known, but hereditary factors, iron metabolism, and the brain dopaminergic system are thought to be involved.11 It is hypothesized that spinal cord lesions allow the appearance of RLS symptoms and spinal leg movement generator by blocking descending inhibitory spinal pathways.12 One hypothesis is that damage to A11 nuclei (the main source of dopamine in the spinal cord or its diencephalospinal tract in animals) causes hyperexcitability of the spinal cord and leads to PLM and RLS symptoms.13 As the axons of A11 nuclei are present along the whole span of the spinal cord, SCI/D in patients with RLS might interrupt this dopaminergic tract and produce the RLS symptoms.
Limitations
This study included only veterans, so the prevalence may not apply to the nonveteran SCI population. Also, the population mainly was male, and there was no accurate information on race. Ferritin levels of the patients were not checked and is a major factor in RLS. The reported onset of RLS after the SCI could be due to recall bias.
Conclusion
The prevalence of RLS in veterans with SCI is above that reported in the general population (19% vs 10%, respectively). Furthermore, those with RLS have symptoms that often started after the SCI (suggesting causality) and required therapy due to their level of RLS symptom burden. A spectrum of severity of symptoms is present among those with RLS, with 83% having moderate-to-severe RLS affecting their QOL.
Although there was not a statistically significant relationship between RLS and spinal cord lesion level, there was a slightly higher prevalence of RLS at the cervical and thoracic levels, which may be relevant for future studies. There was no difference found between the RLS subgroups with respect to the location of the lesion within the spinal cord; however, a larger sample size may be needed to determine whether this would reach statistical significance. Prompt search for symptoms of RLS in veterans with SCI is warranted to provide adequate treatment to improve sleep health and QOL in this population.
1. Lasfargues JE, Custis D, Morrone F, Carswell J, Nguyen T. A model for estimating spinal cord injury prevalence in the United States. Paraplegia. 1995;33(2):62-68.
2. Sjölund BH. Pain and rehabilitation after spinal cord injury: the case of sensory spasticity? Brain Res Brain Res Rev. 2002;40(1-3):250-256.
3. Adams MM, Hicks AL. Spasticity after spinal cord injury. Spinal Cord. 2005;43(10):577-586.
4. Kumru H, Vidal J, Benito J, et al. Restless leg syndrome in patients with spinal cord injury. Parkinsonism Relat Disord. 2015;21(12):1461-1464.
5. Wilt TJ, MacDonald R, Ouellette J, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496-505.
6. American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic and Coding Manual. (AASM ICSD-3). 3rd ed. Westchester, IL: American Academy of Sleep Medicine; 2014.
7. Telles SC, Alves RC, Chadi G. Periodic limb movements during sleep and restless legs syndrome in patients with ASIA A spinal cord injury. J Neurol Sci. 2011;303(1-2):119-123.
8. Telles SC, Alves RS, Chadi G. Spinal cord injury as a trigger to develop periodic leg movements during sleep: an evolutionary perspective. Arq Neuropsiquiatr. 2012;70(11):880-884.
9. Tings T, Baier PC, Paulus W, Trenkwalder C. Restless legs syndrome induced by impairment of sensory spinal pathways. J Neurol. 2003;250(4):499-500.
10. Paulus W, Trenkwalder C. Less is more: pathophysiology of dopaminergic-therapy-related augmentation in restless legs syndrome. Lancet Neurol. 2006;5(10):878-886.
11. Silber MH, Ehrenberg BL, Allen RP, et al; Medical Advisory Board of the Restless Legs Syndrome Foundation. An algorithm for the management of restless legs syndrome. Mayo Clin Proc. 2004;79(7):916-922.
12. Hartmann M, Pfister R, Pfadenhauer K. Restless legs syndrome associated with spinal cord lesions. J Neurol Neurosurg Psychiatry. 1999;66(5):688-689.
13. Clemens S, Rye D, Hochman S. Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology. 2006;67(1):125-130.
Spinal cord injuries (SCI) are common in veteran populations.1 Veterans with spinal cord injuries and disorders (SCI/D) also may have concurrent sleep disturbances. Spinal cord injury typically causes spasticity.2,3 Hypersensitivity of the flexor reflex pathways is believed to cause painful muscle spasms in patients with SCI.4 Neuropathic pain at or below the level of the lesion also is common.
Restless legs syndrome (RLS) is a common sleep disorder that affects sleep quality and can occur concomitantly with spinal cord lesions.5 In about 80% of RLS cases, involuntary movements of legs across hip, knee, and ankle joints during sleep, known as periodic limb movement during sleep (PLMS), occurs.6 Several studies showed increased prevalence of PLMS in patients with SCI, and some case reports suggest an increased prevalence of RLS in this population.7,8 One small study showed that 100% of patients with SCI had symptoms of RLS.6 Another study found that SCI could trigger PLMS.8
The pathophysiology of RLS and PLMS in patients with SCI is not fully understood, but case reports describing PLM in SCI patients points to a possible role of central pattern generators and the flexor reflex afferents in the pathophysiology of PLMS.9,10 Changes of the tissue microstructure in the midbrain and upper cervical spinal cord have been described in patients with RLS.11The objective of this study was to assess the prevalence of RLS in a veteran population with SCI/D and
Methods
The institutional review and ethical approval boards of the Minneapolis VA Health Care System approved the study. Within the VA system, 666 patients with SCI/D were identified using a national database. Of the 666 people, 316 were excluded, 199 were included, and 151 were deceased.
Patients aged between 18 and 65 years were included in the study. Charts of patients who had been discharged with the diagnosis of SCI from 2002 to 2008 were studied. All patients met the inclusion criteria of the International Restless Legs Syndrome Study Group diagnosis.
Exclusion criteria were as follows: Patients with evidence of brain pathology (eg, stroke), concurrent neurologic condition associated with RLS (Parkinson disease, spinocerebellar ataxia, peripheral neuropathy), concurrent psychiatric condition within the setting of treatment with dopamine antagonists, secondary causes of RLS (renal failure/uremia, iron deficiency, rheumatoid arthritis, and pregnancy) and a recent history of alcohol or drug misuse or current evidence of substance use of < 1 year.
A patient list was compiled that included the etiology of the SCI (vascular injury, multiple sclerosis [MS], trauma, unknown, and other), the level(s) and completeness of the SCI per radiology report, RLS pharmacotherapies, and pertinent medical history.
Axial T2-weighted images on magnetic resonance imaging (MRI) scans were retrospectively reviewed. Sagittal T1/T2-weighted and axial T2-weighted sequences were performed routinely on all patients with spinal cord lesions. The analysis included the extension of the lesion on both sagittal and axial distributions. The anatomic location of the cord lesion was categorized by the following: (1) pure gray matter (central cord); (2) white matter (dorsal [D], dorsolateral [DL], ventral [V], ventrolateral areas [VL]).
A questionnaire using standard diagnostic criteria for RLS was mailed to the 199 patients who met the inclusion criteria (Appendix A).
All analyses were carried out using StataCorp STATA 13 (College Station, TX). Descriptive statistics were used. The analyses were carried out using chi-square and Fisher exact tests. Differences between the groups were considered statistically significant at P < .05. The data were analyzed to obtain point prevalence among patients with SCI, and comparisons were made among the different subgroups.
Results
Of the 162 patients who chose to participate in the study, the sleep specialists confirmed 31 (19%) to have RLS, 112 (69%) were confirmed negative for RLS, and an additional 19 (12%) screened positive for RLS but were not confirmed to have RLS by the sleep specialists (Figure 1).
The etiology of SCI was subdivided into 4 groups: MS, trauma, vascular, and other/unknown. Within each group (– RLS vs + RLS), MS and trauma were the most common etiologies with 55% MS and 36% trauma in the + RLS group.
When comparing RLS among the spinal cord levels (cervical, thoracic, lumbar and cervical + thoracic), only the cervical + thoracic subgroup (18% + RLS vs 5% – RLS) showed a significant difference (Figure 2).
There was no significant difference found with the prevalence of RLS in the axial plane of the spinal cord lesions (ventral/ventro-lateral/central cord vs dorsal/dorsolateral) or by the completeness of spinal cord lesions, P = .76. There was a higher prevalence of incomplete cord injury, however, within each subgroup of RLS.
The Mann-Whitney test was used to analyze the burden of disease in both groups (+ RLS vs – RLS). Moderate level of burden was most frequently reported with a higher prevalence within the + RLS group. Of those receiving treatment for RLS, 71% were + RLS vs 46% – RLS with a P value of .01. Symptoms of RLS after cord injury were 89% + RLS vs 55% – RLS with a P value of .03.
Discussion
This study represents one of the first studies to determine the prevalence of RLS in veterans with spinal cord disease. Research in this area is important to raise awareness of RLS among the veteran population with and without SCI and disorders. Restless legs syndrome often escapes diagnosis because of difficulty understanding the patient’s descriptions of their sensations. In addition, RLS may cause debilitating symptoms of sleep deprivation, daytime sleepiness, discomfort, and fatigue, which often results in decreased quality of life (QOL). Proper screening and treatment may improve QOL.
A study by Kumru and colleagues showed a similar rate of RLS in patients with SCI and RLS symptoms presented in the first year after SCI as did this study (18% vs 19%, respectively).4 In that study, RLS was more common in patients with lesions in lumbosacral area. Kumru and colleagues also showed that a dopaminergic medication improved symptoms of RLS in this population, whereas this study did not explore treatment outcomes.4
The pathogenesis of RLS is not fully known, but hereditary factors, iron metabolism, and the brain dopaminergic system are thought to be involved.11 It is hypothesized that spinal cord lesions allow the appearance of RLS symptoms and spinal leg movement generator by blocking descending inhibitory spinal pathways.12 One hypothesis is that damage to A11 nuclei (the main source of dopamine in the spinal cord or its diencephalospinal tract in animals) causes hyperexcitability of the spinal cord and leads to PLM and RLS symptoms.13 As the axons of A11 nuclei are present along the whole span of the spinal cord, SCI/D in patients with RLS might interrupt this dopaminergic tract and produce the RLS symptoms.
Limitations
This study included only veterans, so the prevalence may not apply to the nonveteran SCI population. Also, the population mainly was male, and there was no accurate information on race. Ferritin levels of the patients were not checked and is a major factor in RLS. The reported onset of RLS after the SCI could be due to recall bias.
Conclusion
The prevalence of RLS in veterans with SCI is above that reported in the general population (19% vs 10%, respectively). Furthermore, those with RLS have symptoms that often started after the SCI (suggesting causality) and required therapy due to their level of RLS symptom burden. A spectrum of severity of symptoms is present among those with RLS, with 83% having moderate-to-severe RLS affecting their QOL.
Although there was not a statistically significant relationship between RLS and spinal cord lesion level, there was a slightly higher prevalence of RLS at the cervical and thoracic levels, which may be relevant for future studies. There was no difference found between the RLS subgroups with respect to the location of the lesion within the spinal cord; however, a larger sample size may be needed to determine whether this would reach statistical significance. Prompt search for symptoms of RLS in veterans with SCI is warranted to provide adequate treatment to improve sleep health and QOL in this population.
Spinal cord injuries (SCI) are common in veteran populations.1 Veterans with spinal cord injuries and disorders (SCI/D) also may have concurrent sleep disturbances. Spinal cord injury typically causes spasticity.2,3 Hypersensitivity of the flexor reflex pathways is believed to cause painful muscle spasms in patients with SCI.4 Neuropathic pain at or below the level of the lesion also is common.
Restless legs syndrome (RLS) is a common sleep disorder that affects sleep quality and can occur concomitantly with spinal cord lesions.5 In about 80% of RLS cases, involuntary movements of legs across hip, knee, and ankle joints during sleep, known as periodic limb movement during sleep (PLMS), occurs.6 Several studies showed increased prevalence of PLMS in patients with SCI, and some case reports suggest an increased prevalence of RLS in this population.7,8 One small study showed that 100% of patients with SCI had symptoms of RLS.6 Another study found that SCI could trigger PLMS.8
The pathophysiology of RLS and PLMS in patients with SCI is not fully understood, but case reports describing PLM in SCI patients points to a possible role of central pattern generators and the flexor reflex afferents in the pathophysiology of PLMS.9,10 Changes of the tissue microstructure in the midbrain and upper cervical spinal cord have been described in patients with RLS.11The objective of this study was to assess the prevalence of RLS in a veteran population with SCI/D and
Methods
The institutional review and ethical approval boards of the Minneapolis VA Health Care System approved the study. Within the VA system, 666 patients with SCI/D were identified using a national database. Of the 666 people, 316 were excluded, 199 were included, and 151 were deceased.
Patients aged between 18 and 65 years were included in the study. Charts of patients who had been discharged with the diagnosis of SCI from 2002 to 2008 were studied. All patients met the inclusion criteria of the International Restless Legs Syndrome Study Group diagnosis.
Exclusion criteria were as follows: Patients with evidence of brain pathology (eg, stroke), concurrent neurologic condition associated with RLS (Parkinson disease, spinocerebellar ataxia, peripheral neuropathy), concurrent psychiatric condition within the setting of treatment with dopamine antagonists, secondary causes of RLS (renal failure/uremia, iron deficiency, rheumatoid arthritis, and pregnancy) and a recent history of alcohol or drug misuse or current evidence of substance use of < 1 year.
A patient list was compiled that included the etiology of the SCI (vascular injury, multiple sclerosis [MS], trauma, unknown, and other), the level(s) and completeness of the SCI per radiology report, RLS pharmacotherapies, and pertinent medical history.
Axial T2-weighted images on magnetic resonance imaging (MRI) scans were retrospectively reviewed. Sagittal T1/T2-weighted and axial T2-weighted sequences were performed routinely on all patients with spinal cord lesions. The analysis included the extension of the lesion on both sagittal and axial distributions. The anatomic location of the cord lesion was categorized by the following: (1) pure gray matter (central cord); (2) white matter (dorsal [D], dorsolateral [DL], ventral [V], ventrolateral areas [VL]).
A questionnaire using standard diagnostic criteria for RLS was mailed to the 199 patients who met the inclusion criteria (Appendix A).
All analyses were carried out using StataCorp STATA 13 (College Station, TX). Descriptive statistics were used. The analyses were carried out using chi-square and Fisher exact tests. Differences between the groups were considered statistically significant at P < .05. The data were analyzed to obtain point prevalence among patients with SCI, and comparisons were made among the different subgroups.
Results
Of the 162 patients who chose to participate in the study, the sleep specialists confirmed 31 (19%) to have RLS, 112 (69%) were confirmed negative for RLS, and an additional 19 (12%) screened positive for RLS but were not confirmed to have RLS by the sleep specialists (Figure 1).
The etiology of SCI was subdivided into 4 groups: MS, trauma, vascular, and other/unknown. Within each group (– RLS vs + RLS), MS and trauma were the most common etiologies with 55% MS and 36% trauma in the + RLS group.
When comparing RLS among the spinal cord levels (cervical, thoracic, lumbar and cervical + thoracic), only the cervical + thoracic subgroup (18% + RLS vs 5% – RLS) showed a significant difference (Figure 2).
There was no significant difference found with the prevalence of RLS in the axial plane of the spinal cord lesions (ventral/ventro-lateral/central cord vs dorsal/dorsolateral) or by the completeness of spinal cord lesions, P = .76. There was a higher prevalence of incomplete cord injury, however, within each subgroup of RLS.
The Mann-Whitney test was used to analyze the burden of disease in both groups (+ RLS vs – RLS). Moderate level of burden was most frequently reported with a higher prevalence within the + RLS group. Of those receiving treatment for RLS, 71% were + RLS vs 46% – RLS with a P value of .01. Symptoms of RLS after cord injury were 89% + RLS vs 55% – RLS with a P value of .03.
Discussion
This study represents one of the first studies to determine the prevalence of RLS in veterans with spinal cord disease. Research in this area is important to raise awareness of RLS among the veteran population with and without SCI and disorders. Restless legs syndrome often escapes diagnosis because of difficulty understanding the patient’s descriptions of their sensations. In addition, RLS may cause debilitating symptoms of sleep deprivation, daytime sleepiness, discomfort, and fatigue, which often results in decreased quality of life (QOL). Proper screening and treatment may improve QOL.
A study by Kumru and colleagues showed a similar rate of RLS in patients with SCI and RLS symptoms presented in the first year after SCI as did this study (18% vs 19%, respectively).4 In that study, RLS was more common in patients with lesions in lumbosacral area. Kumru and colleagues also showed that a dopaminergic medication improved symptoms of RLS in this population, whereas this study did not explore treatment outcomes.4
The pathogenesis of RLS is not fully known, but hereditary factors, iron metabolism, and the brain dopaminergic system are thought to be involved.11 It is hypothesized that spinal cord lesions allow the appearance of RLS symptoms and spinal leg movement generator by blocking descending inhibitory spinal pathways.12 One hypothesis is that damage to A11 nuclei (the main source of dopamine in the spinal cord or its diencephalospinal tract in animals) causes hyperexcitability of the spinal cord and leads to PLM and RLS symptoms.13 As the axons of A11 nuclei are present along the whole span of the spinal cord, SCI/D in patients with RLS might interrupt this dopaminergic tract and produce the RLS symptoms.
Limitations
This study included only veterans, so the prevalence may not apply to the nonveteran SCI population. Also, the population mainly was male, and there was no accurate information on race. Ferritin levels of the patients were not checked and is a major factor in RLS. The reported onset of RLS after the SCI could be due to recall bias.
Conclusion
The prevalence of RLS in veterans with SCI is above that reported in the general population (19% vs 10%, respectively). Furthermore, those with RLS have symptoms that often started after the SCI (suggesting causality) and required therapy due to their level of RLS symptom burden. A spectrum of severity of symptoms is present among those with RLS, with 83% having moderate-to-severe RLS affecting their QOL.
Although there was not a statistically significant relationship between RLS and spinal cord lesion level, there was a slightly higher prevalence of RLS at the cervical and thoracic levels, which may be relevant for future studies. There was no difference found between the RLS subgroups with respect to the location of the lesion within the spinal cord; however, a larger sample size may be needed to determine whether this would reach statistical significance. Prompt search for symptoms of RLS in veterans with SCI is warranted to provide adequate treatment to improve sleep health and QOL in this population.
1. Lasfargues JE, Custis D, Morrone F, Carswell J, Nguyen T. A model for estimating spinal cord injury prevalence in the United States. Paraplegia. 1995;33(2):62-68.
2. Sjölund BH. Pain and rehabilitation after spinal cord injury: the case of sensory spasticity? Brain Res Brain Res Rev. 2002;40(1-3):250-256.
3. Adams MM, Hicks AL. Spasticity after spinal cord injury. Spinal Cord. 2005;43(10):577-586.
4. Kumru H, Vidal J, Benito J, et al. Restless leg syndrome in patients with spinal cord injury. Parkinsonism Relat Disord. 2015;21(12):1461-1464.
5. Wilt TJ, MacDonald R, Ouellette J, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496-505.
6. American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic and Coding Manual. (AASM ICSD-3). 3rd ed. Westchester, IL: American Academy of Sleep Medicine; 2014.
7. Telles SC, Alves RC, Chadi G. Periodic limb movements during sleep and restless legs syndrome in patients with ASIA A spinal cord injury. J Neurol Sci. 2011;303(1-2):119-123.
8. Telles SC, Alves RS, Chadi G. Spinal cord injury as a trigger to develop periodic leg movements during sleep: an evolutionary perspective. Arq Neuropsiquiatr. 2012;70(11):880-884.
9. Tings T, Baier PC, Paulus W, Trenkwalder C. Restless legs syndrome induced by impairment of sensory spinal pathways. J Neurol. 2003;250(4):499-500.
10. Paulus W, Trenkwalder C. Less is more: pathophysiology of dopaminergic-therapy-related augmentation in restless legs syndrome. Lancet Neurol. 2006;5(10):878-886.
11. Silber MH, Ehrenberg BL, Allen RP, et al; Medical Advisory Board of the Restless Legs Syndrome Foundation. An algorithm for the management of restless legs syndrome. Mayo Clin Proc. 2004;79(7):916-922.
12. Hartmann M, Pfister R, Pfadenhauer K. Restless legs syndrome associated with spinal cord lesions. J Neurol Neurosurg Psychiatry. 1999;66(5):688-689.
13. Clemens S, Rye D, Hochman S. Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology. 2006;67(1):125-130.
1. Lasfargues JE, Custis D, Morrone F, Carswell J, Nguyen T. A model for estimating spinal cord injury prevalence in the United States. Paraplegia. 1995;33(2):62-68.
2. Sjölund BH. Pain and rehabilitation after spinal cord injury: the case of sensory spasticity? Brain Res Brain Res Rev. 2002;40(1-3):250-256.
3. Adams MM, Hicks AL. Spasticity after spinal cord injury. Spinal Cord. 2005;43(10):577-586.
4. Kumru H, Vidal J, Benito J, et al. Restless leg syndrome in patients with spinal cord injury. Parkinsonism Relat Disord. 2015;21(12):1461-1464.
5. Wilt TJ, MacDonald R, Ouellette J, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496-505.
6. American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic and Coding Manual. (AASM ICSD-3). 3rd ed. Westchester, IL: American Academy of Sleep Medicine; 2014.
7. Telles SC, Alves RC, Chadi G. Periodic limb movements during sleep and restless legs syndrome in patients with ASIA A spinal cord injury. J Neurol Sci. 2011;303(1-2):119-123.
8. Telles SC, Alves RS, Chadi G. Spinal cord injury as a trigger to develop periodic leg movements during sleep: an evolutionary perspective. Arq Neuropsiquiatr. 2012;70(11):880-884.
9. Tings T, Baier PC, Paulus W, Trenkwalder C. Restless legs syndrome induced by impairment of sensory spinal pathways. J Neurol. 2003;250(4):499-500.
10. Paulus W, Trenkwalder C. Less is more: pathophysiology of dopaminergic-therapy-related augmentation in restless legs syndrome. Lancet Neurol. 2006;5(10):878-886.
11. Silber MH, Ehrenberg BL, Allen RP, et al; Medical Advisory Board of the Restless Legs Syndrome Foundation. An algorithm for the management of restless legs syndrome. Mayo Clin Proc. 2004;79(7):916-922.
12. Hartmann M, Pfister R, Pfadenhauer K. Restless legs syndrome associated with spinal cord lesions. J Neurol Neurosurg Psychiatry. 1999;66(5):688-689.
13. Clemens S, Rye D, Hochman S. Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology. 2006;67(1):125-130.
Part 3: Getting to the Scope of the Problem
Nurse practitioners (and PAs, I would submit) have been the most researched group of health care professionals since the inception of the role. Much of that research has focused on evaluating our contributions to primary care. Numerous studies of NP performance in various settings have concluded that we perform as well as physicians with respect to patient outcomes, proper diagnosis, management of specific medical conditions, and patient satisfaction.1
Over the past 10 years, however, the interest in our roles has shifted from the primary care arena to the emergency department (ED). Even before the introduction of the Affordable Care Act (ACA), two-thirds of all EDs utilized NPs and PAs.2 The ACA increased the number of Americans with insurance coverage, resulting in a greater demand for health care services—including ED utilization. Faced with an already strained system, hospital administrators looked for a solution and found one: hiring NPs and PAs to augment the clinician workforce.
This decision to (increasingly) employ NPs and PAs in ED settings was based on a desire to reduce wait times, increase throughput, improve access to care, and control costs. For the most part, these goals have been achieved. A systematic review of the impact of NPs in the ED on quality of care and patient satisfaction demonstrated a reduction in wait times.3 Moreover, in a national survey that included a review of the types of visits made to the ED, NPs and PAs were comparable to MDs in terms of reasons for care, diagnosis, and treatment.4
Given these results, I again ask: What was the intent of the research by Bai et al?5 Surely proper and prompt care is the goal of every ED provider. So the decision to examine only the billing is confounding.
Are the authors suggesting that hospital administrators prefer employing NPs and PAs over MDs? Are we replacing physicians in certain areas or filling voids where the physician workforce is inadequate to meet the community demands? Maybe yes to both. But, if the goal is to improve access, then we should focus on meeting the needs and on the quality of the care, not on who bills for it.
My cynical self says the goal of Bai et al was to establish that NPs and PAs are taking the jobs of ED physicians, and we must be stopped! Am I tilting at windmills with this train of thought? Next week, we’ll conclude our examination and draw our own conclusions! You can join the conversation by writing to NPEditor@mdedge.com.
1. Congressional Budget Office. Physician extenders: their current and future role in medical care delivery. Washington, DC: US Government Printing Office; 1979.
2. Wiler JL, Rooks, SP, Ginde AA. Update on midlevel provider utilization in US emergency departments, 2006 to 2009. Academic Emerg Med. 2012;19(8):986-989.
3. Carter A, Chochinov A. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction, and wait times in the emergency department. Can J Emerg Med. 2007;9(4):286-295.
4. Hooker RS, McCaig L. Emergency department uses of physician assistants and nurse practitioners: a national survey. Am J Emerg Med. 1996;14:245-249.
5. Bai G, Kelen GD, Frick KD, Anderson GF. Nurse practitioners and physician assistants in emergency medical services who billed independently, 2012-2016. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2019.01.052. Accessed April 1, 2019.
Nurse practitioners (and PAs, I would submit) have been the most researched group of health care professionals since the inception of the role. Much of that research has focused on evaluating our contributions to primary care. Numerous studies of NP performance in various settings have concluded that we perform as well as physicians with respect to patient outcomes, proper diagnosis, management of specific medical conditions, and patient satisfaction.1
Over the past 10 years, however, the interest in our roles has shifted from the primary care arena to the emergency department (ED). Even before the introduction of the Affordable Care Act (ACA), two-thirds of all EDs utilized NPs and PAs.2 The ACA increased the number of Americans with insurance coverage, resulting in a greater demand for health care services—including ED utilization. Faced with an already strained system, hospital administrators looked for a solution and found one: hiring NPs and PAs to augment the clinician workforce.
This decision to (increasingly) employ NPs and PAs in ED settings was based on a desire to reduce wait times, increase throughput, improve access to care, and control costs. For the most part, these goals have been achieved. A systematic review of the impact of NPs in the ED on quality of care and patient satisfaction demonstrated a reduction in wait times.3 Moreover, in a national survey that included a review of the types of visits made to the ED, NPs and PAs were comparable to MDs in terms of reasons for care, diagnosis, and treatment.4
Given these results, I again ask: What was the intent of the research by Bai et al?5 Surely proper and prompt care is the goal of every ED provider. So the decision to examine only the billing is confounding.
Are the authors suggesting that hospital administrators prefer employing NPs and PAs over MDs? Are we replacing physicians in certain areas or filling voids where the physician workforce is inadequate to meet the community demands? Maybe yes to both. But, if the goal is to improve access, then we should focus on meeting the needs and on the quality of the care, not on who bills for it.
My cynical self says the goal of Bai et al was to establish that NPs and PAs are taking the jobs of ED physicians, and we must be stopped! Am I tilting at windmills with this train of thought? Next week, we’ll conclude our examination and draw our own conclusions! You can join the conversation by writing to NPEditor@mdedge.com.
Nurse practitioners (and PAs, I would submit) have been the most researched group of health care professionals since the inception of the role. Much of that research has focused on evaluating our contributions to primary care. Numerous studies of NP performance in various settings have concluded that we perform as well as physicians with respect to patient outcomes, proper diagnosis, management of specific medical conditions, and patient satisfaction.1
Over the past 10 years, however, the interest in our roles has shifted from the primary care arena to the emergency department (ED). Even before the introduction of the Affordable Care Act (ACA), two-thirds of all EDs utilized NPs and PAs.2 The ACA increased the number of Americans with insurance coverage, resulting in a greater demand for health care services—including ED utilization. Faced with an already strained system, hospital administrators looked for a solution and found one: hiring NPs and PAs to augment the clinician workforce.
This decision to (increasingly) employ NPs and PAs in ED settings was based on a desire to reduce wait times, increase throughput, improve access to care, and control costs. For the most part, these goals have been achieved. A systematic review of the impact of NPs in the ED on quality of care and patient satisfaction demonstrated a reduction in wait times.3 Moreover, in a national survey that included a review of the types of visits made to the ED, NPs and PAs were comparable to MDs in terms of reasons for care, diagnosis, and treatment.4
Given these results, I again ask: What was the intent of the research by Bai et al?5 Surely proper and prompt care is the goal of every ED provider. So the decision to examine only the billing is confounding.
Are the authors suggesting that hospital administrators prefer employing NPs and PAs over MDs? Are we replacing physicians in certain areas or filling voids where the physician workforce is inadequate to meet the community demands? Maybe yes to both. But, if the goal is to improve access, then we should focus on meeting the needs and on the quality of the care, not on who bills for it.
My cynical self says the goal of Bai et al was to establish that NPs and PAs are taking the jobs of ED physicians, and we must be stopped! Am I tilting at windmills with this train of thought? Next week, we’ll conclude our examination and draw our own conclusions! You can join the conversation by writing to NPEditor@mdedge.com.
1. Congressional Budget Office. Physician extenders: their current and future role in medical care delivery. Washington, DC: US Government Printing Office; 1979.
2. Wiler JL, Rooks, SP, Ginde AA. Update on midlevel provider utilization in US emergency departments, 2006 to 2009. Academic Emerg Med. 2012;19(8):986-989.
3. Carter A, Chochinov A. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction, and wait times in the emergency department. Can J Emerg Med. 2007;9(4):286-295.
4. Hooker RS, McCaig L. Emergency department uses of physician assistants and nurse practitioners: a national survey. Am J Emerg Med. 1996;14:245-249.
5. Bai G, Kelen GD, Frick KD, Anderson GF. Nurse practitioners and physician assistants in emergency medical services who billed independently, 2012-2016. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2019.01.052. Accessed April 1, 2019.
1. Congressional Budget Office. Physician extenders: their current and future role in medical care delivery. Washington, DC: US Government Printing Office; 1979.
2. Wiler JL, Rooks, SP, Ginde AA. Update on midlevel provider utilization in US emergency departments, 2006 to 2009. Academic Emerg Med. 2012;19(8):986-989.
3. Carter A, Chochinov A. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction, and wait times in the emergency department. Can J Emerg Med. 2007;9(4):286-295.
4. Hooker RS, McCaig L. Emergency department uses of physician assistants and nurse practitioners: a national survey. Am J Emerg Med. 1996;14:245-249.
5. Bai G, Kelen GD, Frick KD, Anderson GF. Nurse practitioners and physician assistants in emergency medical services who billed independently, 2012-2016. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2019.01.052. Accessed April 1, 2019.
No difference in GI cancer outcomes with vitamin D supplementation
The findings of two randomized clinical trials indicate that vitamin D supplementation does not improve clinical outcomes in patients with advanced or metastatic colorectal cancer or gastrointestinal cancer. The results of the SUNSHINE and AMATERASU trials were published in JAMA.
The SUNSHINE clinical trial was a double-blind, multicenter, phase 2 study that included 139 patients with metastatic or unresectable advanced colorectal cancer. Participants were randomized to receive either high-dose (8000 IU/day for 2 weeks and 4000 IU/day afterward) or standard-dose (400 IU/day) oral vitamin D3 that was given concomitantly with standard chemotherapy.
The primary outcome measured was median progression-free survival, while overall survival was measured as a secondary endpoint.
“Participants continued to receive treatment until disease progression, intolerable toxicity, or decision to discontinue treatment,” wrote Kimmie Ng, MD, MPH, of the Dana-Farber Cancer Institute in Boston and her colleagues.
The AMATERASU clinical trial was a double-blind, placebo-controlled study of 417 patients with digestive tract cancers conducted at a single center in Japan. Participants were randomized to receive either oral vitamin D (2000 IU/day) or placebo over a maximum duration of 7.6 years.
The primary outcome measured was relapse-free survival (time to cancer relapse or death); overall survival (time to death of any cause) was also included as a secondary endpoint.
“Safety outcomes comprised bone fractures, urinary stones, serious events requiring admission, and new (de novo) cancer,” Mitsuyoshi Urashima, MD, of Jikei University in Tokyo, Japan, wrote with his colleagues.
After analysis, the results of both trials were found to be comparable because the adjusted measures for progression- or relapse-free survival were similar. In addition, both studies showed no differences in overall survival.
Dr. Ng and her colleagues reported that there was a statistically nonsignificant rise in median progression-free survival in participants given high-dose versus standard dose vitamin D3 (13 vs. 11 months, respectively; P = .07), according to results from the SUNSHINE study. The overall survival was the same in both arms (median survival, 24.3 months; P = .43).
Dr. Urashima and his colleagues reported that there was no significant improvement in relapse-free survival in patients treated with vitamin D versus those treated with placebo (hazard ratio, 0.76; 95% confidence interval, 0.50-1.14; P = .18), according to results from the AMATERASU study. In addition, no benefit was seen for overall survival (HR, 0.95; 95% CI, 0.57-1.57).
With respect to safety, neither study reported an increase in toxicity from vitamin D supplementation, and a possible benefit of reduced diarrhea was seen in the SUNSHINE study. Given the preliminary nature of these results, further confirmatory studies that include longer follow-up periods and improved measures of survival are necessary.
“These findings warrant further evaluation in a larger multicenter randomized clinical trial,” Dr. Ng and her colleagues wrote.
“Vitamin D supplementation did not improve relapse-free survival among patients with digestive tract cancer,” Dr. Urashima and his colleagues concluded.
The SUNSHINE clinical trial was supported by grant funding from the National Institutes of Health’s National Cancer Institute. Additional funding was provided by the Gloria Spivak Faculty Advancement Award, Friends of Dana-Farber Cancer Institute Award, Project P Fund, Consano, Pharmavite, and Genentech.
The AMATERASU clinical trial was supported by funding from the Japan-Supported Program for the Strategic Research Foundation at Private Universities, the International University of Health and Welfare Hospital, and the Jikei University School of Medicine.
The authors of both studies reported multiple associations with pharmaceutical companies.
SOURCE: Ng K et al. JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2402; Urashima M et al. JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2210.
In recent decades, numerous observational studies have shown potential benefit of vitamin D supplementation in patients with various forms of cancer. As a result, several randomized trials are currently underway examining the use of the supplement in patients with colorectal cancer.
The SUNSHINE and AMATERASU randomized clinical trials evaluated the use of vitamin D3 supplementation in patients with advanced or metastatic colorectal cancer and gastrointestinal cancer, respectively. In contrast to observational data, both of these trials failed to show significant improvements in pertinent clinical endpoints, including progression-free and relapse-free survival.
However, many questions remain unanswered because of certain quantitative considerations in the studies, such as sample size and the use of one-sided versus two-sided statistical testing. Other potential contributing factors include patient or tumor parameters that could alter the effects of supplementation.
Another important consideration is that these findings may not reflect the potential benefits of supplementation in other forms of malignancy. Increased levels of vitamin D have been linked with significantly reduced morbidity and mortality among hospitalized patients with certain nonmalignant conditions, in addition to other types of cancer.
Additional confirmatory studies that include longer follow-up periods are needed to better understand these preliminary results.
Elizabeth L. Barry, PhD, and Michael N. Passarelli, PhD, are with the department of epidemiology at the Geisel School of Medicine at Dartmouth, Hanover, N.H. John A. Baron, MD, MS, MSc, is with the department of epidemiology at the University of North Carolina at Chapel Hill. No conflicts of interest were reported. These comments are adapted from her editorial (JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2589 ).
In recent decades, numerous observational studies have shown potential benefit of vitamin D supplementation in patients with various forms of cancer. As a result, several randomized trials are currently underway examining the use of the supplement in patients with colorectal cancer.
The SUNSHINE and AMATERASU randomized clinical trials evaluated the use of vitamin D3 supplementation in patients with advanced or metastatic colorectal cancer and gastrointestinal cancer, respectively. In contrast to observational data, both of these trials failed to show significant improvements in pertinent clinical endpoints, including progression-free and relapse-free survival.
However, many questions remain unanswered because of certain quantitative considerations in the studies, such as sample size and the use of one-sided versus two-sided statistical testing. Other potential contributing factors include patient or tumor parameters that could alter the effects of supplementation.
Another important consideration is that these findings may not reflect the potential benefits of supplementation in other forms of malignancy. Increased levels of vitamin D have been linked with significantly reduced morbidity and mortality among hospitalized patients with certain nonmalignant conditions, in addition to other types of cancer.
Additional confirmatory studies that include longer follow-up periods are needed to better understand these preliminary results.
Elizabeth L. Barry, PhD, and Michael N. Passarelli, PhD, are with the department of epidemiology at the Geisel School of Medicine at Dartmouth, Hanover, N.H. John A. Baron, MD, MS, MSc, is with the department of epidemiology at the University of North Carolina at Chapel Hill. No conflicts of interest were reported. These comments are adapted from her editorial (JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2589 ).
In recent decades, numerous observational studies have shown potential benefit of vitamin D supplementation in patients with various forms of cancer. As a result, several randomized trials are currently underway examining the use of the supplement in patients with colorectal cancer.
The SUNSHINE and AMATERASU randomized clinical trials evaluated the use of vitamin D3 supplementation in patients with advanced or metastatic colorectal cancer and gastrointestinal cancer, respectively. In contrast to observational data, both of these trials failed to show significant improvements in pertinent clinical endpoints, including progression-free and relapse-free survival.
However, many questions remain unanswered because of certain quantitative considerations in the studies, such as sample size and the use of one-sided versus two-sided statistical testing. Other potential contributing factors include patient or tumor parameters that could alter the effects of supplementation.
Another important consideration is that these findings may not reflect the potential benefits of supplementation in other forms of malignancy. Increased levels of vitamin D have been linked with significantly reduced morbidity and mortality among hospitalized patients with certain nonmalignant conditions, in addition to other types of cancer.
Additional confirmatory studies that include longer follow-up periods are needed to better understand these preliminary results.
Elizabeth L. Barry, PhD, and Michael N. Passarelli, PhD, are with the department of epidemiology at the Geisel School of Medicine at Dartmouth, Hanover, N.H. John A. Baron, MD, MS, MSc, is with the department of epidemiology at the University of North Carolina at Chapel Hill. No conflicts of interest were reported. These comments are adapted from her editorial (JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2589 ).
The findings of two randomized clinical trials indicate that vitamin D supplementation does not improve clinical outcomes in patients with advanced or metastatic colorectal cancer or gastrointestinal cancer. The results of the SUNSHINE and AMATERASU trials were published in JAMA.
The SUNSHINE clinical trial was a double-blind, multicenter, phase 2 study that included 139 patients with metastatic or unresectable advanced colorectal cancer. Participants were randomized to receive either high-dose (8000 IU/day for 2 weeks and 4000 IU/day afterward) or standard-dose (400 IU/day) oral vitamin D3 that was given concomitantly with standard chemotherapy.
The primary outcome measured was median progression-free survival, while overall survival was measured as a secondary endpoint.
“Participants continued to receive treatment until disease progression, intolerable toxicity, or decision to discontinue treatment,” wrote Kimmie Ng, MD, MPH, of the Dana-Farber Cancer Institute in Boston and her colleagues.
The AMATERASU clinical trial was a double-blind, placebo-controlled study of 417 patients with digestive tract cancers conducted at a single center in Japan. Participants were randomized to receive either oral vitamin D (2000 IU/day) or placebo over a maximum duration of 7.6 years.
The primary outcome measured was relapse-free survival (time to cancer relapse or death); overall survival (time to death of any cause) was also included as a secondary endpoint.
“Safety outcomes comprised bone fractures, urinary stones, serious events requiring admission, and new (de novo) cancer,” Mitsuyoshi Urashima, MD, of Jikei University in Tokyo, Japan, wrote with his colleagues.
After analysis, the results of both trials were found to be comparable because the adjusted measures for progression- or relapse-free survival were similar. In addition, both studies showed no differences in overall survival.
Dr. Ng and her colleagues reported that there was a statistically nonsignificant rise in median progression-free survival in participants given high-dose versus standard dose vitamin D3 (13 vs. 11 months, respectively; P = .07), according to results from the SUNSHINE study. The overall survival was the same in both arms (median survival, 24.3 months; P = .43).
Dr. Urashima and his colleagues reported that there was no significant improvement in relapse-free survival in patients treated with vitamin D versus those treated with placebo (hazard ratio, 0.76; 95% confidence interval, 0.50-1.14; P = .18), according to results from the AMATERASU study. In addition, no benefit was seen for overall survival (HR, 0.95; 95% CI, 0.57-1.57).
With respect to safety, neither study reported an increase in toxicity from vitamin D supplementation, and a possible benefit of reduced diarrhea was seen in the SUNSHINE study. Given the preliminary nature of these results, further confirmatory studies that include longer follow-up periods and improved measures of survival are necessary.
“These findings warrant further evaluation in a larger multicenter randomized clinical trial,” Dr. Ng and her colleagues wrote.
“Vitamin D supplementation did not improve relapse-free survival among patients with digestive tract cancer,” Dr. Urashima and his colleagues concluded.
The SUNSHINE clinical trial was supported by grant funding from the National Institutes of Health’s National Cancer Institute. Additional funding was provided by the Gloria Spivak Faculty Advancement Award, Friends of Dana-Farber Cancer Institute Award, Project P Fund, Consano, Pharmavite, and Genentech.
The AMATERASU clinical trial was supported by funding from the Japan-Supported Program for the Strategic Research Foundation at Private Universities, the International University of Health and Welfare Hospital, and the Jikei University School of Medicine.
The authors of both studies reported multiple associations with pharmaceutical companies.
SOURCE: Ng K et al. JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2402; Urashima M et al. JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2210.
The findings of two randomized clinical trials indicate that vitamin D supplementation does not improve clinical outcomes in patients with advanced or metastatic colorectal cancer or gastrointestinal cancer. The results of the SUNSHINE and AMATERASU trials were published in JAMA.
The SUNSHINE clinical trial was a double-blind, multicenter, phase 2 study that included 139 patients with metastatic or unresectable advanced colorectal cancer. Participants were randomized to receive either high-dose (8000 IU/day for 2 weeks and 4000 IU/day afterward) or standard-dose (400 IU/day) oral vitamin D3 that was given concomitantly with standard chemotherapy.
The primary outcome measured was median progression-free survival, while overall survival was measured as a secondary endpoint.
“Participants continued to receive treatment until disease progression, intolerable toxicity, or decision to discontinue treatment,” wrote Kimmie Ng, MD, MPH, of the Dana-Farber Cancer Institute in Boston and her colleagues.
The AMATERASU clinical trial was a double-blind, placebo-controlled study of 417 patients with digestive tract cancers conducted at a single center in Japan. Participants were randomized to receive either oral vitamin D (2000 IU/day) or placebo over a maximum duration of 7.6 years.
The primary outcome measured was relapse-free survival (time to cancer relapse or death); overall survival (time to death of any cause) was also included as a secondary endpoint.
“Safety outcomes comprised bone fractures, urinary stones, serious events requiring admission, and new (de novo) cancer,” Mitsuyoshi Urashima, MD, of Jikei University in Tokyo, Japan, wrote with his colleagues.
After analysis, the results of both trials were found to be comparable because the adjusted measures for progression- or relapse-free survival were similar. In addition, both studies showed no differences in overall survival.
Dr. Ng and her colleagues reported that there was a statistically nonsignificant rise in median progression-free survival in participants given high-dose versus standard dose vitamin D3 (13 vs. 11 months, respectively; P = .07), according to results from the SUNSHINE study. The overall survival was the same in both arms (median survival, 24.3 months; P = .43).
Dr. Urashima and his colleagues reported that there was no significant improvement in relapse-free survival in patients treated with vitamin D versus those treated with placebo (hazard ratio, 0.76; 95% confidence interval, 0.50-1.14; P = .18), according to results from the AMATERASU study. In addition, no benefit was seen for overall survival (HR, 0.95; 95% CI, 0.57-1.57).
With respect to safety, neither study reported an increase in toxicity from vitamin D supplementation, and a possible benefit of reduced diarrhea was seen in the SUNSHINE study. Given the preliminary nature of these results, further confirmatory studies that include longer follow-up periods and improved measures of survival are necessary.
“These findings warrant further evaluation in a larger multicenter randomized clinical trial,” Dr. Ng and her colleagues wrote.
“Vitamin D supplementation did not improve relapse-free survival among patients with digestive tract cancer,” Dr. Urashima and his colleagues concluded.
The SUNSHINE clinical trial was supported by grant funding from the National Institutes of Health’s National Cancer Institute. Additional funding was provided by the Gloria Spivak Faculty Advancement Award, Friends of Dana-Farber Cancer Institute Award, Project P Fund, Consano, Pharmavite, and Genentech.
The AMATERASU clinical trial was supported by funding from the Japan-Supported Program for the Strategic Research Foundation at Private Universities, the International University of Health and Welfare Hospital, and the Jikei University School of Medicine.
The authors of both studies reported multiple associations with pharmaceutical companies.
SOURCE: Ng K et al. JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2402; Urashima M et al. JAMA. 2019 Apr 9. doi: 10.1001/jama.2019.2210.
FROM JAMA