User login
Anxiety, depression, burnout higher in physician mothers caring for others at home
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
FROM JAMA INTERNAL MEDICINE
Key clinical point:
Major finding: Risk of anxiety and mood disorders is 21% higher and burnout is 25% higher among physician mothers with extra caregiving at home.
Study details: The findings are based on an online cross-sectional survey of 5,613 United States–based physician mothers conducted from June to July 2016.
Disclosures: No single entity directly funded the study, but the authors were supported by a variety of grants from foundations and the National Institutes of Health at the time it was completed. One coauthor is founder of Equity Quotient, a company that provides gender equity culture analytics for institutions, and another has consulted for Amgen and Vizient and receives stock options as an Equity Quotient advisory board member.
Source: Yank V et al. JAMA Internal Medicine. 2018 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
Routine clinical data may predict psychiatric adverse effects from levetiracetam
Among patients with epilepsy, a simple model that incorporates factors such as a patient’s sex and history of depression, anxiety, and recreational drug use may help predict the risk of a psychiatric adverse effect from levetiracetam, according to a study published in JAMA Neurology.
“This study derived 2 simple models that predict the risk of a psychiatric adverse effect from levetiracetam” and can “guide prescription in clinical practice,” said Colin B. Josephson, MD, of the department of clinical neurosciences at the University of Calgary (Canada) and his research colleagues.
Levetiracetam is a commonly used first-line treatment for epilepsy because of its ease of use, broad spectrum of action, and safety profile, the researchers said. Still, psychiatric adverse reactions occur in as many as 16% of patients and frequently require treatment discontinuation.
To evaluate whether routine clinical data can predict which patients with epilepsy will experience a psychiatric adverse event from levetiracetam, the investigators analyzed data from The Health Improvement Network (THIN) database, which includes anonymized patient records from general practices in the United Kingdom. They assessed 21 variables for possible inclusion in prediction models. They identified these variables by searching the literature and weighing input from a panel of experts.
Their analysis included data from Jan. 1, 2000–May 31, 2012. Among the more than 11 million patients in THIN, the researchers identified 7,300 incident cases of epilepsy. The researchers examined when patients received a first prescription for levetiracetam and whether patients experienced a psychiatric symptom or disorder within 2 years of the prescription.
Among 1,173 patients with epilepsy receiving levetiracetam, the median age was 39 years; about half were women. In all, 14.1% experienced a psychiatric symptom or disorder within 2 years of prescription. Women were more likely to report a psychiatric symptom (odds ratio, 1.41), as were patients with a history of social deprivation (OR, 1.15), anxiety (OR, 1.74), recreational drug use (OR, 2.02), or depression (OR, 2.20).
The final model included female sex, history of depression, history of anxiety, and history of recreational drug use. Low socioeconomic status was not included because “it would be challenging to assign this score in clinic,” the authors said.
“There was a gradient in risk probabilities increasing from 8% for 0 risk factors to 11%-17% for 1, 17% to 31% for 2, 30%-42% for 3, and 49% when all risk factors were present,” Dr. Josephson and his colleagues indicated. “The discovered incremental probability of reporting a psychiatric sign can help generate an index of suspicion to counsel patients.”
Using the example of a woman patient with depression, the model “suggests she would be at risk,” with a 22% chance of a psychiatric adverse event in the 2 years after receiving a levetiracetam prescription.
The researchers created a second prediction algorithm based on data from patients without documentation of a mental health sign, symptom, or disorder prior to their levetiracetam prescription. This model incorporated age, sex, recreational drug use, and levetiracetam daily dose; it performed comparably well and might be used to determine safety of prescription, according to Dr. Josephson and his colleagues.
The authors noted that the study was limited by an inability to evaluate medication adherence and seizure type and frequency. One advantage of the study’s design is that it may have circumvented expectation bias because general practitioners were not prone to anticipating psychiatric adverse events or to have a lower threshold for diagnosing them.
The authors disclosed research fellowships and support from foundations and federal agencies.
SOURCE: Josephson CB et al. JAMA Neurol. 2019 Jan 28. doi: 10.1001/jamaneurol.2018.4561.
Among patients with epilepsy, a simple model that incorporates factors such as a patient’s sex and history of depression, anxiety, and recreational drug use may help predict the risk of a psychiatric adverse effect from levetiracetam, according to a study published in JAMA Neurology.
“This study derived 2 simple models that predict the risk of a psychiatric adverse effect from levetiracetam” and can “guide prescription in clinical practice,” said Colin B. Josephson, MD, of the department of clinical neurosciences at the University of Calgary (Canada) and his research colleagues.
Levetiracetam is a commonly used first-line treatment for epilepsy because of its ease of use, broad spectrum of action, and safety profile, the researchers said. Still, psychiatric adverse reactions occur in as many as 16% of patients and frequently require treatment discontinuation.
To evaluate whether routine clinical data can predict which patients with epilepsy will experience a psychiatric adverse event from levetiracetam, the investigators analyzed data from The Health Improvement Network (THIN) database, which includes anonymized patient records from general practices in the United Kingdom. They assessed 21 variables for possible inclusion in prediction models. They identified these variables by searching the literature and weighing input from a panel of experts.
Their analysis included data from Jan. 1, 2000–May 31, 2012. Among the more than 11 million patients in THIN, the researchers identified 7,300 incident cases of epilepsy. The researchers examined when patients received a first prescription for levetiracetam and whether patients experienced a psychiatric symptom or disorder within 2 years of the prescription.
Among 1,173 patients with epilepsy receiving levetiracetam, the median age was 39 years; about half were women. In all, 14.1% experienced a psychiatric symptom or disorder within 2 years of prescription. Women were more likely to report a psychiatric symptom (odds ratio, 1.41), as were patients with a history of social deprivation (OR, 1.15), anxiety (OR, 1.74), recreational drug use (OR, 2.02), or depression (OR, 2.20).
The final model included female sex, history of depression, history of anxiety, and history of recreational drug use. Low socioeconomic status was not included because “it would be challenging to assign this score in clinic,” the authors said.
“There was a gradient in risk probabilities increasing from 8% for 0 risk factors to 11%-17% for 1, 17% to 31% for 2, 30%-42% for 3, and 49% when all risk factors were present,” Dr. Josephson and his colleagues indicated. “The discovered incremental probability of reporting a psychiatric sign can help generate an index of suspicion to counsel patients.”
Using the example of a woman patient with depression, the model “suggests she would be at risk,” with a 22% chance of a psychiatric adverse event in the 2 years after receiving a levetiracetam prescription.
The researchers created a second prediction algorithm based on data from patients without documentation of a mental health sign, symptom, or disorder prior to their levetiracetam prescription. This model incorporated age, sex, recreational drug use, and levetiracetam daily dose; it performed comparably well and might be used to determine safety of prescription, according to Dr. Josephson and his colleagues.
The authors noted that the study was limited by an inability to evaluate medication adherence and seizure type and frequency. One advantage of the study’s design is that it may have circumvented expectation bias because general practitioners were not prone to anticipating psychiatric adverse events or to have a lower threshold for diagnosing them.
The authors disclosed research fellowships and support from foundations and federal agencies.
SOURCE: Josephson CB et al. JAMA Neurol. 2019 Jan 28. doi: 10.1001/jamaneurol.2018.4561.
Among patients with epilepsy, a simple model that incorporates factors such as a patient’s sex and history of depression, anxiety, and recreational drug use may help predict the risk of a psychiatric adverse effect from levetiracetam, according to a study published in JAMA Neurology.
“This study derived 2 simple models that predict the risk of a psychiatric adverse effect from levetiracetam” and can “guide prescription in clinical practice,” said Colin B. Josephson, MD, of the department of clinical neurosciences at the University of Calgary (Canada) and his research colleagues.
Levetiracetam is a commonly used first-line treatment for epilepsy because of its ease of use, broad spectrum of action, and safety profile, the researchers said. Still, psychiatric adverse reactions occur in as many as 16% of patients and frequently require treatment discontinuation.
To evaluate whether routine clinical data can predict which patients with epilepsy will experience a psychiatric adverse event from levetiracetam, the investigators analyzed data from The Health Improvement Network (THIN) database, which includes anonymized patient records from general practices in the United Kingdom. They assessed 21 variables for possible inclusion in prediction models. They identified these variables by searching the literature and weighing input from a panel of experts.
Their analysis included data from Jan. 1, 2000–May 31, 2012. Among the more than 11 million patients in THIN, the researchers identified 7,300 incident cases of epilepsy. The researchers examined when patients received a first prescription for levetiracetam and whether patients experienced a psychiatric symptom or disorder within 2 years of the prescription.
Among 1,173 patients with epilepsy receiving levetiracetam, the median age was 39 years; about half were women. In all, 14.1% experienced a psychiatric symptom or disorder within 2 years of prescription. Women were more likely to report a psychiatric symptom (odds ratio, 1.41), as were patients with a history of social deprivation (OR, 1.15), anxiety (OR, 1.74), recreational drug use (OR, 2.02), or depression (OR, 2.20).
The final model included female sex, history of depression, history of anxiety, and history of recreational drug use. Low socioeconomic status was not included because “it would be challenging to assign this score in clinic,” the authors said.
“There was a gradient in risk probabilities increasing from 8% for 0 risk factors to 11%-17% for 1, 17% to 31% for 2, 30%-42% for 3, and 49% when all risk factors were present,” Dr. Josephson and his colleagues indicated. “The discovered incremental probability of reporting a psychiatric sign can help generate an index of suspicion to counsel patients.”
Using the example of a woman patient with depression, the model “suggests she would be at risk,” with a 22% chance of a psychiatric adverse event in the 2 years after receiving a levetiracetam prescription.
The researchers created a second prediction algorithm based on data from patients without documentation of a mental health sign, symptom, or disorder prior to their levetiracetam prescription. This model incorporated age, sex, recreational drug use, and levetiracetam daily dose; it performed comparably well and might be used to determine safety of prescription, according to Dr. Josephson and his colleagues.
The authors noted that the study was limited by an inability to evaluate medication adherence and seizure type and frequency. One advantage of the study’s design is that it may have circumvented expectation bias because general practitioners were not prone to anticipating psychiatric adverse events or to have a lower threshold for diagnosing them.
The authors disclosed research fellowships and support from foundations and federal agencies.
SOURCE: Josephson CB et al. JAMA Neurol. 2019 Jan 28. doi: 10.1001/jamaneurol.2018.4561.
FROM JAMA NEUROLOGY
Key clinical point: Among patients with epilepsy, a simple model may help predict the risk of a psychiatric adverse effect from levetiracetam.
Major finding: The likelihood of a psychiatric adverse event increases from 8% for patients with no risk factors to 49% with all risk factors present.
Study details: A retrospective open cohort study of 1,173 patients with epilepsy receiving levetiracetam in the United Kingdom.
Disclosures: The authors disclosed research fellowships and support from foundations and federal agencies.
Source: Josephson CB et al. JAMA Neurol. 2019 Jan 28. doi: 10.1001/jamaneurol.2018.4561
Polysomnography beats Fitbit
Also today, there is no evidence for the disease-modifying effect of levodopa in Parkinson’s Disease, and ablation surpassed drugs for raising quality of life for atrial fibrillation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, there is no evidence for the disease-modifying effect of levodopa in Parkinson’s Disease, and ablation surpassed drugs for raising quality of life for atrial fibrillation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, there is no evidence for the disease-modifying effect of levodopa in Parkinson’s Disease, and ablation surpassed drugs for raising quality of life for atrial fibrillation.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Have you paid your 2019 SVS membership dues yet?
To those members who have not yet paid their 2019 dues -- are you planning to attend the Vascular Annual Meeting? Do you find your Journal of Vascular Surgery publications invaluable? Those are just two of the member benefits that will be lost to those who do not pay their dues soon. Others include use of trademarked professional designations and access to the new online communications forum, SVSConnect. Renew today to continue to receive these and all other SVS member benefits.
To those members who have not yet paid their 2019 dues -- are you planning to attend the Vascular Annual Meeting? Do you find your Journal of Vascular Surgery publications invaluable? Those are just two of the member benefits that will be lost to those who do not pay their dues soon. Others include use of trademarked professional designations and access to the new online communications forum, SVSConnect. Renew today to continue to receive these and all other SVS member benefits.
To those members who have not yet paid their 2019 dues -- are you planning to attend the Vascular Annual Meeting? Do you find your Journal of Vascular Surgery publications invaluable? Those are just two of the member benefits that will be lost to those who do not pay their dues soon. Others include use of trademarked professional designations and access to the new online communications forum, SVSConnect. Renew today to continue to receive these and all other SVS member benefits.
Women’s Leadership Training Grant
Because leadership skills are integral to success but are not typically taught in medical school, the SVS Leadership Development and Diversity Committee offers the Women's Leadership Training Grant to help women sharpen their leadership skills. The $5,000 awards (offered at three levels of a woman's career) defray costs to attend leadership courses and activities. Applications are due March 1.
Because leadership skills are integral to success but are not typically taught in medical school, the SVS Leadership Development and Diversity Committee offers the Women's Leadership Training Grant to help women sharpen their leadership skills. The $5,000 awards (offered at three levels of a woman's career) defray costs to attend leadership courses and activities. Applications are due March 1.
Because leadership skills are integral to success but are not typically taught in medical school, the SVS Leadership Development and Diversity Committee offers the Women's Leadership Training Grant to help women sharpen their leadership skills. The $5,000 awards (offered at three levels of a woman's career) defray costs to attend leadership courses and activities. Applications are due March 1.
FDA permits marketing of first M. genitalium diagnostic test
the first test for the diagnoses of sexually transmitted infections (STIs) caused by the M. genitalium bacterium, the agency reported in a press release.
M. genitalium is associated with nongonococcal urethritis in men and cervicitis in women, causing 15%-30% of persistent or recurring urethritis cases and 10%-30% of cervicitis cases, according to the Centers for Disease Control and Prevention. It also can lead to pelvic inflammatory disease (PID) in women. The assay is a nucleic acid amplification test, which can detect the bacterium in urine, as well as urethral, penile meatal, endocervical, or vaginal swab samples.
In a clinical study of 11,774 samples, the Aptima assay correctly identified M. genitalium in about 90% of vaginal, male urethral, male urine, and penile samples. It also correctly identified the bacterium in female urine and endocervical samples 78% and 82% of the time, respectively. The test was even more accurate in identifying samples that did not have M. genitalium present, according to an FDA press release
“In the past, it has been hard to diagnose this organism. By being able to detect it more reliably, doctors may be able to more carefully tailor treatment and use medicines most likely to be effective,” FDA Commissioner Scott Gottlieb, MD, said in the press release. “Having accurate and reliable tests to identify the specific bacteria that’s causing an infection can assist doctors in choosing the right treatment for the right infection, which can reduce overuse of antibiotics and help in the fight against antimicrobial resistance.”
Find the full press release on the FDA website.
the first test for the diagnoses of sexually transmitted infections (STIs) caused by the M. genitalium bacterium, the agency reported in a press release.
M. genitalium is associated with nongonococcal urethritis in men and cervicitis in women, causing 15%-30% of persistent or recurring urethritis cases and 10%-30% of cervicitis cases, according to the Centers for Disease Control and Prevention. It also can lead to pelvic inflammatory disease (PID) in women. The assay is a nucleic acid amplification test, which can detect the bacterium in urine, as well as urethral, penile meatal, endocervical, or vaginal swab samples.
In a clinical study of 11,774 samples, the Aptima assay correctly identified M. genitalium in about 90% of vaginal, male urethral, male urine, and penile samples. It also correctly identified the bacterium in female urine and endocervical samples 78% and 82% of the time, respectively. The test was even more accurate in identifying samples that did not have M. genitalium present, according to an FDA press release
“In the past, it has been hard to diagnose this organism. By being able to detect it more reliably, doctors may be able to more carefully tailor treatment and use medicines most likely to be effective,” FDA Commissioner Scott Gottlieb, MD, said in the press release. “Having accurate and reliable tests to identify the specific bacteria that’s causing an infection can assist doctors in choosing the right treatment for the right infection, which can reduce overuse of antibiotics and help in the fight against antimicrobial resistance.”
Find the full press release on the FDA website.
the first test for the diagnoses of sexually transmitted infections (STIs) caused by the M. genitalium bacterium, the agency reported in a press release.
M. genitalium is associated with nongonococcal urethritis in men and cervicitis in women, causing 15%-30% of persistent or recurring urethritis cases and 10%-30% of cervicitis cases, according to the Centers for Disease Control and Prevention. It also can lead to pelvic inflammatory disease (PID) in women. The assay is a nucleic acid amplification test, which can detect the bacterium in urine, as well as urethral, penile meatal, endocervical, or vaginal swab samples.
In a clinical study of 11,774 samples, the Aptima assay correctly identified M. genitalium in about 90% of vaginal, male urethral, male urine, and penile samples. It also correctly identified the bacterium in female urine and endocervical samples 78% and 82% of the time, respectively. The test was even more accurate in identifying samples that did not have M. genitalium present, according to an FDA press release
“In the past, it has been hard to diagnose this organism. By being able to detect it more reliably, doctors may be able to more carefully tailor treatment and use medicines most likely to be effective,” FDA Commissioner Scott Gottlieb, MD, said in the press release. “Having accurate and reliable tests to identify the specific bacteria that’s causing an infection can assist doctors in choosing the right treatment for the right infection, which can reduce overuse of antibiotics and help in the fight against antimicrobial resistance.”
Find the full press release on the FDA website.
Tamsulosin not effective in promoting stone expulsion in symptomatic patients
Clinical question: Does tamsulosin provide benefit in ureteral stone expulsion for patients who present with a symptomatic stone less than 9 mm?
Background: Treatment of urinary stone disease often includes the use of alpha-blockers such as tamsulosin to promote stone passage, and between 15% and 55% of patients presenting to EDs for renal colic are prescribed alpha-blockers. Current treatment guidelines support the use of tamsulosin, with recent evidence suggesting that this treatment is more effective for larger stones (5-10 mm). However, other prospective trials have called these guidelines into question.
Study design: Double-blind, placebo-controlled study.
Setting: Six emergency departments at U.S. tertiary-care hospitals.
Synopsis: 512 participants with symptomatic ureteral stones were randomized to either tamsulosin or placebo. At the end of a 28-day treatment period, the rate of urinary stone passage was 49.6% in the tamsulosin group vs. 47.3% in the placebo group (95.8% confidence interval, 0.87-1.27; P = .60). The time to stone passage also was not different between treatment groups (P = .92). A second phase of the trial also evaluated stone passage by CT scan at 28 days, with stone passage rates of 83.6% in the tamsulosin group and 77.6% in the placebo group (95% CI, 0.95-1.22; P = .24). This study is the largest of its kind in the United States, with findings similar to those of two recent international multisite trials, increasing the evidence that tamsulosin is not beneficial for larger stone passage.
Bottom line: For patients presenting to the ED for renal colic from ureteral stones smaller than 9 mm, tamsulosin does not appear to promote stone passage.
Citation: Meltzer AC et al. Effect of tamsulosin on passage of symptomatic ureteral stones: A randomized clinical trial. JAMA Intern Med. 2018;178(8):1051-7. Published online June 18, 2018.
Dr. Breviu is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Clinical question: Does tamsulosin provide benefit in ureteral stone expulsion for patients who present with a symptomatic stone less than 9 mm?
Background: Treatment of urinary stone disease often includes the use of alpha-blockers such as tamsulosin to promote stone passage, and between 15% and 55% of patients presenting to EDs for renal colic are prescribed alpha-blockers. Current treatment guidelines support the use of tamsulosin, with recent evidence suggesting that this treatment is more effective for larger stones (5-10 mm). However, other prospective trials have called these guidelines into question.
Study design: Double-blind, placebo-controlled study.
Setting: Six emergency departments at U.S. tertiary-care hospitals.
Synopsis: 512 participants with symptomatic ureteral stones were randomized to either tamsulosin or placebo. At the end of a 28-day treatment period, the rate of urinary stone passage was 49.6% in the tamsulosin group vs. 47.3% in the placebo group (95.8% confidence interval, 0.87-1.27; P = .60). The time to stone passage also was not different between treatment groups (P = .92). A second phase of the trial also evaluated stone passage by CT scan at 28 days, with stone passage rates of 83.6% in the tamsulosin group and 77.6% in the placebo group (95% CI, 0.95-1.22; P = .24). This study is the largest of its kind in the United States, with findings similar to those of two recent international multisite trials, increasing the evidence that tamsulosin is not beneficial for larger stone passage.
Bottom line: For patients presenting to the ED for renal colic from ureteral stones smaller than 9 mm, tamsulosin does not appear to promote stone passage.
Citation: Meltzer AC et al. Effect of tamsulosin on passage of symptomatic ureteral stones: A randomized clinical trial. JAMA Intern Med. 2018;178(8):1051-7. Published online June 18, 2018.
Dr. Breviu is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Clinical question: Does tamsulosin provide benefit in ureteral stone expulsion for patients who present with a symptomatic stone less than 9 mm?
Background: Treatment of urinary stone disease often includes the use of alpha-blockers such as tamsulosin to promote stone passage, and between 15% and 55% of patients presenting to EDs for renal colic are prescribed alpha-blockers. Current treatment guidelines support the use of tamsulosin, with recent evidence suggesting that this treatment is more effective for larger stones (5-10 mm). However, other prospective trials have called these guidelines into question.
Study design: Double-blind, placebo-controlled study.
Setting: Six emergency departments at U.S. tertiary-care hospitals.
Synopsis: 512 participants with symptomatic ureteral stones were randomized to either tamsulosin or placebo. At the end of a 28-day treatment period, the rate of urinary stone passage was 49.6% in the tamsulosin group vs. 47.3% in the placebo group (95.8% confidence interval, 0.87-1.27; P = .60). The time to stone passage also was not different between treatment groups (P = .92). A second phase of the trial also evaluated stone passage by CT scan at 28 days, with stone passage rates of 83.6% in the tamsulosin group and 77.6% in the placebo group (95% CI, 0.95-1.22; P = .24). This study is the largest of its kind in the United States, with findings similar to those of two recent international multisite trials, increasing the evidence that tamsulosin is not beneficial for larger stone passage.
Bottom line: For patients presenting to the ED for renal colic from ureteral stones smaller than 9 mm, tamsulosin does not appear to promote stone passage.
Citation: Meltzer AC et al. Effect of tamsulosin on passage of symptomatic ureteral stones: A randomized clinical trial. JAMA Intern Med. 2018;178(8):1051-7. Published online June 18, 2018.
Dr. Breviu is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Before you refer for AF ablation
SNOWMASS, COLO. – Appropriate in the way of benefit, along with instilling awareness of the warning signals heralding serious late complications, Samuel J. Asirvatham, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Who to steer toward ablation? You have to have a symptomatic patient – that’s a given. For the ones who are paroxysmal, the ones with a relatively normal heart, there’s a much better chance that you’ll help manage their symptoms with ablation than if they have persistent or permanent A-fib. Notice I do not use the word ‘cure’ for A-fib. We talk about controlling symptoms and decreasing frequency, because the longer follow-up you have with intensive monitoring, the more you realize that patients still tend to have some A-fib,” explained Dr. Asirvatham, an electrophysiologist who is professor of medicine and pediatrics at the Mayo Clinic in Rochester, Minn.
The rationale for early atrial fibrillation (AF) ablation in younger patients with troublesome symptoms of paroxysmal AF despite pharmacologic attempts at rate or rhythm control is that it will arrest the progression from an atrial arrhythmia that has just a few triggers readily neutralized by pulmonary vein isolation to persistent AF with a diseased heart and a multitude of arrhythmia trigger points coming from many directions.
A solid candidate for ablation of paroxysmal AF has about a 75% likelihood of having a successful first ablation procedure, with substantial improvement in symptoms and no need for medication. Another 9%-10% will achieve marked reduction in symptom burden upon addition of antiarrhythmic agents that weren’t effective before ablation.
Late complications can be deceptive
Periprocedural stroke/transient ischemic attack, tamponade, or bleeding on the table are infrequent complications readily recognized by the interventionalist. More problematic are several late complications which are often misinterpreted, with the resultant delay causing major harm.
- Pulmonary vein stenosis. This complication of inadvertent ablation inside the pulmonary vein manifests as shortness of breath, typically beginning about 4 weeks post ablation.
“This is very different from the shortness of breath they had with atrial fibrillation. They almost always have a cough that they didn’t have before, and they may have hemoptysis. It’s very important to recognize this promptly, because before it closes completely we can do an angioplasty and stent the vein with good results. But once it closes completely, it becomes an extremely complicated procedure to try to reopen that vein,” according to Dr. Asirvatham.
Very often the patient’s general cardiologist, chest physician, or primary care physician fails to recognize what’s happening. He cited an example: He recently had a patient with a cough who was first referred to an infectious disease specialist, who ordered a bronchoalveolar lavage. The specimen grew atypical actinomycetes. That prompted a referral to thoracic surgery for an open-lung biopsy. But that procedure required cardiac clearance beforehand. It was a cardiologist who said, ‘Wait – all this started after you had an ablation?’
“That patient had pulmonary vein stenosis. And, unfortunately, that complication has not gone away. Being a referral center for pulmonary vein isolation, we see just as many cases of pulmonary vein stenosis today as we did a few years ago,” he said.
- Atrial esophageal fistula. The hallmark of this complication is onset of a plethora of what Dr. Asirvatham called “funny symptoms” more than a month post ablation. These include fever, transient ischemic attacks (TIAs), sepsislike symptoms, discomfort in swallowing, and in some cases hemoptysis.
“The predominant picture is endocarditis/TIA/stroke. If you see this, and the patient has had ablation, immediately refer to surgery to have the fistula between the esophagus and heart fixed. This is not a patient where you say, ‘Nothing by mouth, give some antibiotics, and see what happens.’ I can tell you what will happen: The patient will die,” the cardiologist said.
- Atrial stiffness. This typically occurs about a month after a second or third ablation procedure, when the patient develops shortness of breath that keeps worsening.
“You think ‘pulmonary vein stenosis,’ but the CT scan shows the veins are wide open. Many of these patients will get misdiagnosed as having heart failure with preserved ejection fraction even though they never had it before. The problem here is the atrium has become too stiff from the ablation, and this stiff atrium causes increased pressure, resulting in the shortness of breath. Sometimes patients feel better over time, but sometimes it’s very difficult to treat. But it’s important to recognize atrial stiffness and exclude other causes like pulmonary vein stenosis,” Dr. Asirvatham continued.
- Gastroparesis. This occurs because of injury to the vagus nerve branches located at the top of the esophagus, with resultant delayed gastric emptying.
“It’s an uncomfortable feeling of fullness all the time. The patient will say, ‘It seems like I just ate, even though I ate 8 hours ago,” the electrophysiologist said. “Most of these patients will recover in about 6 months. They may feel better on a gastric motility agent, like a macrolide antibiotic. I personally have not seen a patient who did not feel better within 6-8 months.”
Novel treatment approaches: “A-fib may be an autonomic epilepsy of the heart”
“Patients sometimes will ask you, ‘What is this ablation? What does that mean?’ You have to be truthful and tell them that it’s just a fancy word for burning,” the electrophysiologist said.
Achievement of AF ablation without radiofrequency or cryoablation, instead utilizing nonthermal direct-current pulsed electrical fields, is “the hottest topic in the field of electrophysiology,” according to Dr. Asirvatham.
These electrical fields result in irreversible electroporation of targeted myocardial cell membranes, leading to cell death. It is a tissue-specific intervention, so it’s much less likely than conventional ablation to cause collateral damage to the esophagus and other structures.
“Direct current electroporation has transitioned from proof-of-concept studies to three relatively large patient trials. This is potentially an important breakthrough because if we don’t heat, a lot of the complications of A-fib ablation will probably decrease,” he explained.
Two other promising outside-the-box approaches to the treatment of AF are autonomic nervous system modulation at sites distant from the heart and particle beam ablation without need for cardiac catheters.
“If you put electrodes everywhere in the body to see where A-fib starts, it’s not in the atrium, not in the pulmonary veins, it’s in the nerves behind the pulmonary veins, and before those nerves it’s in some other area of the autonomic nervous system. This has given rise to the notion that A-fib may be an autonomic epilepsy of the heart,” according to the electrophysiologist.
This concept has given rise to a completely different approach to treatment of AF through neurostimulation. That’s how acupuncture works. Also, headphones have been used successfully to terminate and prevent AF by stimulating autonomic nerve centers near the ears. Low-level electrical stimulation of the vagus nerve in order to reduce stellate ganglion activity is under study. So is the application of botulinum toxin at key points in the autonomic nervous system.
“Catheters, drugs, and devices that target these areas, maybe without any ablation in the heart itself, is an exciting area of future management of A-fib,” he said.
Another promising approach is borrowed from radiation oncology: particulate ablation using beams of carbon atoms, protons, or photons.
“The first patients have now been treated for ventricular tachycardia and A-fib. It really is quite amazing how precise the lesion formation is. And with no catheters in the heart, clot can’t form on catheters,” he observed.
Dr. Asirvatham reported having no financial conflicts regarding his presentation, although he serves as a consultant to a handful of medical startup companies and holds patents on intellectual property, the royalties for which go directly to the Mayo Clinic.
SNOWMASS, COLO. – Appropriate in the way of benefit, along with instilling awareness of the warning signals heralding serious late complications, Samuel J. Asirvatham, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Who to steer toward ablation? You have to have a symptomatic patient – that’s a given. For the ones who are paroxysmal, the ones with a relatively normal heart, there’s a much better chance that you’ll help manage their symptoms with ablation than if they have persistent or permanent A-fib. Notice I do not use the word ‘cure’ for A-fib. We talk about controlling symptoms and decreasing frequency, because the longer follow-up you have with intensive monitoring, the more you realize that patients still tend to have some A-fib,” explained Dr. Asirvatham, an electrophysiologist who is professor of medicine and pediatrics at the Mayo Clinic in Rochester, Minn.
The rationale for early atrial fibrillation (AF) ablation in younger patients with troublesome symptoms of paroxysmal AF despite pharmacologic attempts at rate or rhythm control is that it will arrest the progression from an atrial arrhythmia that has just a few triggers readily neutralized by pulmonary vein isolation to persistent AF with a diseased heart and a multitude of arrhythmia trigger points coming from many directions.
A solid candidate for ablation of paroxysmal AF has about a 75% likelihood of having a successful first ablation procedure, with substantial improvement in symptoms and no need for medication. Another 9%-10% will achieve marked reduction in symptom burden upon addition of antiarrhythmic agents that weren’t effective before ablation.
Late complications can be deceptive
Periprocedural stroke/transient ischemic attack, tamponade, or bleeding on the table are infrequent complications readily recognized by the interventionalist. More problematic are several late complications which are often misinterpreted, with the resultant delay causing major harm.
- Pulmonary vein stenosis. This complication of inadvertent ablation inside the pulmonary vein manifests as shortness of breath, typically beginning about 4 weeks post ablation.
“This is very different from the shortness of breath they had with atrial fibrillation. They almost always have a cough that they didn’t have before, and they may have hemoptysis. It’s very important to recognize this promptly, because before it closes completely we can do an angioplasty and stent the vein with good results. But once it closes completely, it becomes an extremely complicated procedure to try to reopen that vein,” according to Dr. Asirvatham.
Very often the patient’s general cardiologist, chest physician, or primary care physician fails to recognize what’s happening. He cited an example: He recently had a patient with a cough who was first referred to an infectious disease specialist, who ordered a bronchoalveolar lavage. The specimen grew atypical actinomycetes. That prompted a referral to thoracic surgery for an open-lung biopsy. But that procedure required cardiac clearance beforehand. It was a cardiologist who said, ‘Wait – all this started after you had an ablation?’
“That patient had pulmonary vein stenosis. And, unfortunately, that complication has not gone away. Being a referral center for pulmonary vein isolation, we see just as many cases of pulmonary vein stenosis today as we did a few years ago,” he said.
- Atrial esophageal fistula. The hallmark of this complication is onset of a plethora of what Dr. Asirvatham called “funny symptoms” more than a month post ablation. These include fever, transient ischemic attacks (TIAs), sepsislike symptoms, discomfort in swallowing, and in some cases hemoptysis.
“The predominant picture is endocarditis/TIA/stroke. If you see this, and the patient has had ablation, immediately refer to surgery to have the fistula between the esophagus and heart fixed. This is not a patient where you say, ‘Nothing by mouth, give some antibiotics, and see what happens.’ I can tell you what will happen: The patient will die,” the cardiologist said.
- Atrial stiffness. This typically occurs about a month after a second or third ablation procedure, when the patient develops shortness of breath that keeps worsening.
“You think ‘pulmonary vein stenosis,’ but the CT scan shows the veins are wide open. Many of these patients will get misdiagnosed as having heart failure with preserved ejection fraction even though they never had it before. The problem here is the atrium has become too stiff from the ablation, and this stiff atrium causes increased pressure, resulting in the shortness of breath. Sometimes patients feel better over time, but sometimes it’s very difficult to treat. But it’s important to recognize atrial stiffness and exclude other causes like pulmonary vein stenosis,” Dr. Asirvatham continued.
- Gastroparesis. This occurs because of injury to the vagus nerve branches located at the top of the esophagus, with resultant delayed gastric emptying.
“It’s an uncomfortable feeling of fullness all the time. The patient will say, ‘It seems like I just ate, even though I ate 8 hours ago,” the electrophysiologist said. “Most of these patients will recover in about 6 months. They may feel better on a gastric motility agent, like a macrolide antibiotic. I personally have not seen a patient who did not feel better within 6-8 months.”
Novel treatment approaches: “A-fib may be an autonomic epilepsy of the heart”
“Patients sometimes will ask you, ‘What is this ablation? What does that mean?’ You have to be truthful and tell them that it’s just a fancy word for burning,” the electrophysiologist said.
Achievement of AF ablation without radiofrequency or cryoablation, instead utilizing nonthermal direct-current pulsed electrical fields, is “the hottest topic in the field of electrophysiology,” according to Dr. Asirvatham.
These electrical fields result in irreversible electroporation of targeted myocardial cell membranes, leading to cell death. It is a tissue-specific intervention, so it’s much less likely than conventional ablation to cause collateral damage to the esophagus and other structures.
“Direct current electroporation has transitioned from proof-of-concept studies to three relatively large patient trials. This is potentially an important breakthrough because if we don’t heat, a lot of the complications of A-fib ablation will probably decrease,” he explained.
Two other promising outside-the-box approaches to the treatment of AF are autonomic nervous system modulation at sites distant from the heart and particle beam ablation without need for cardiac catheters.
“If you put electrodes everywhere in the body to see where A-fib starts, it’s not in the atrium, not in the pulmonary veins, it’s in the nerves behind the pulmonary veins, and before those nerves it’s in some other area of the autonomic nervous system. This has given rise to the notion that A-fib may be an autonomic epilepsy of the heart,” according to the electrophysiologist.
This concept has given rise to a completely different approach to treatment of AF through neurostimulation. That’s how acupuncture works. Also, headphones have been used successfully to terminate and prevent AF by stimulating autonomic nerve centers near the ears. Low-level electrical stimulation of the vagus nerve in order to reduce stellate ganglion activity is under study. So is the application of botulinum toxin at key points in the autonomic nervous system.
“Catheters, drugs, and devices that target these areas, maybe without any ablation in the heart itself, is an exciting area of future management of A-fib,” he said.
Another promising approach is borrowed from radiation oncology: particulate ablation using beams of carbon atoms, protons, or photons.
“The first patients have now been treated for ventricular tachycardia and A-fib. It really is quite amazing how precise the lesion formation is. And with no catheters in the heart, clot can’t form on catheters,” he observed.
Dr. Asirvatham reported having no financial conflicts regarding his presentation, although he serves as a consultant to a handful of medical startup companies and holds patents on intellectual property, the royalties for which go directly to the Mayo Clinic.
SNOWMASS, COLO. – Appropriate in the way of benefit, along with instilling awareness of the warning signals heralding serious late complications, Samuel J. Asirvatham, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Who to steer toward ablation? You have to have a symptomatic patient – that’s a given. For the ones who are paroxysmal, the ones with a relatively normal heart, there’s a much better chance that you’ll help manage their symptoms with ablation than if they have persistent or permanent A-fib. Notice I do not use the word ‘cure’ for A-fib. We talk about controlling symptoms and decreasing frequency, because the longer follow-up you have with intensive monitoring, the more you realize that patients still tend to have some A-fib,” explained Dr. Asirvatham, an electrophysiologist who is professor of medicine and pediatrics at the Mayo Clinic in Rochester, Minn.
The rationale for early atrial fibrillation (AF) ablation in younger patients with troublesome symptoms of paroxysmal AF despite pharmacologic attempts at rate or rhythm control is that it will arrest the progression from an atrial arrhythmia that has just a few triggers readily neutralized by pulmonary vein isolation to persistent AF with a diseased heart and a multitude of arrhythmia trigger points coming from many directions.
A solid candidate for ablation of paroxysmal AF has about a 75% likelihood of having a successful first ablation procedure, with substantial improvement in symptoms and no need for medication. Another 9%-10% will achieve marked reduction in symptom burden upon addition of antiarrhythmic agents that weren’t effective before ablation.
Late complications can be deceptive
Periprocedural stroke/transient ischemic attack, tamponade, or bleeding on the table are infrequent complications readily recognized by the interventionalist. More problematic are several late complications which are often misinterpreted, with the resultant delay causing major harm.
- Pulmonary vein stenosis. This complication of inadvertent ablation inside the pulmonary vein manifests as shortness of breath, typically beginning about 4 weeks post ablation.
“This is very different from the shortness of breath they had with atrial fibrillation. They almost always have a cough that they didn’t have before, and they may have hemoptysis. It’s very important to recognize this promptly, because before it closes completely we can do an angioplasty and stent the vein with good results. But once it closes completely, it becomes an extremely complicated procedure to try to reopen that vein,” according to Dr. Asirvatham.
Very often the patient’s general cardiologist, chest physician, or primary care physician fails to recognize what’s happening. He cited an example: He recently had a patient with a cough who was first referred to an infectious disease specialist, who ordered a bronchoalveolar lavage. The specimen grew atypical actinomycetes. That prompted a referral to thoracic surgery for an open-lung biopsy. But that procedure required cardiac clearance beforehand. It was a cardiologist who said, ‘Wait – all this started after you had an ablation?’
“That patient had pulmonary vein stenosis. And, unfortunately, that complication has not gone away. Being a referral center for pulmonary vein isolation, we see just as many cases of pulmonary vein stenosis today as we did a few years ago,” he said.
- Atrial esophageal fistula. The hallmark of this complication is onset of a plethora of what Dr. Asirvatham called “funny symptoms” more than a month post ablation. These include fever, transient ischemic attacks (TIAs), sepsislike symptoms, discomfort in swallowing, and in some cases hemoptysis.
“The predominant picture is endocarditis/TIA/stroke. If you see this, and the patient has had ablation, immediately refer to surgery to have the fistula between the esophagus and heart fixed. This is not a patient where you say, ‘Nothing by mouth, give some antibiotics, and see what happens.’ I can tell you what will happen: The patient will die,” the cardiologist said.
- Atrial stiffness. This typically occurs about a month after a second or third ablation procedure, when the patient develops shortness of breath that keeps worsening.
“You think ‘pulmonary vein stenosis,’ but the CT scan shows the veins are wide open. Many of these patients will get misdiagnosed as having heart failure with preserved ejection fraction even though they never had it before. The problem here is the atrium has become too stiff from the ablation, and this stiff atrium causes increased pressure, resulting in the shortness of breath. Sometimes patients feel better over time, but sometimes it’s very difficult to treat. But it’s important to recognize atrial stiffness and exclude other causes like pulmonary vein stenosis,” Dr. Asirvatham continued.
- Gastroparesis. This occurs because of injury to the vagus nerve branches located at the top of the esophagus, with resultant delayed gastric emptying.
“It’s an uncomfortable feeling of fullness all the time. The patient will say, ‘It seems like I just ate, even though I ate 8 hours ago,” the electrophysiologist said. “Most of these patients will recover in about 6 months. They may feel better on a gastric motility agent, like a macrolide antibiotic. I personally have not seen a patient who did not feel better within 6-8 months.”
Novel treatment approaches: “A-fib may be an autonomic epilepsy of the heart”
“Patients sometimes will ask you, ‘What is this ablation? What does that mean?’ You have to be truthful and tell them that it’s just a fancy word for burning,” the electrophysiologist said.
Achievement of AF ablation without radiofrequency or cryoablation, instead utilizing nonthermal direct-current pulsed electrical fields, is “the hottest topic in the field of electrophysiology,” according to Dr. Asirvatham.
These electrical fields result in irreversible electroporation of targeted myocardial cell membranes, leading to cell death. It is a tissue-specific intervention, so it’s much less likely than conventional ablation to cause collateral damage to the esophagus and other structures.
“Direct current electroporation has transitioned from proof-of-concept studies to three relatively large patient trials. This is potentially an important breakthrough because if we don’t heat, a lot of the complications of A-fib ablation will probably decrease,” he explained.
Two other promising outside-the-box approaches to the treatment of AF are autonomic nervous system modulation at sites distant from the heart and particle beam ablation without need for cardiac catheters.
“If you put electrodes everywhere in the body to see where A-fib starts, it’s not in the atrium, not in the pulmonary veins, it’s in the nerves behind the pulmonary veins, and before those nerves it’s in some other area of the autonomic nervous system. This has given rise to the notion that A-fib may be an autonomic epilepsy of the heart,” according to the electrophysiologist.
This concept has given rise to a completely different approach to treatment of AF through neurostimulation. That’s how acupuncture works. Also, headphones have been used successfully to terminate and prevent AF by stimulating autonomic nerve centers near the ears. Low-level electrical stimulation of the vagus nerve in order to reduce stellate ganglion activity is under study. So is the application of botulinum toxin at key points in the autonomic nervous system.
“Catheters, drugs, and devices that target these areas, maybe without any ablation in the heart itself, is an exciting area of future management of A-fib,” he said.
Another promising approach is borrowed from radiation oncology: particulate ablation using beams of carbon atoms, protons, or photons.
“The first patients have now been treated for ventricular tachycardia and A-fib. It really is quite amazing how precise the lesion formation is. And with no catheters in the heart, clot can’t form on catheters,” he observed.
Dr. Asirvatham reported having no financial conflicts regarding his presentation, although he serves as a consultant to a handful of medical startup companies and holds patents on intellectual property, the royalties for which go directly to the Mayo Clinic.
REPORTING FROM ACC SNOWMASS 2019
A theory of relativity for rosacea patients
Rosacea has several known comorbidities, but the widespread use of their relative, rather than absolute, risks “may result in overestimation of the clinical importance of exposures,” Leonardo A. Tjahjono and his associates wrote.
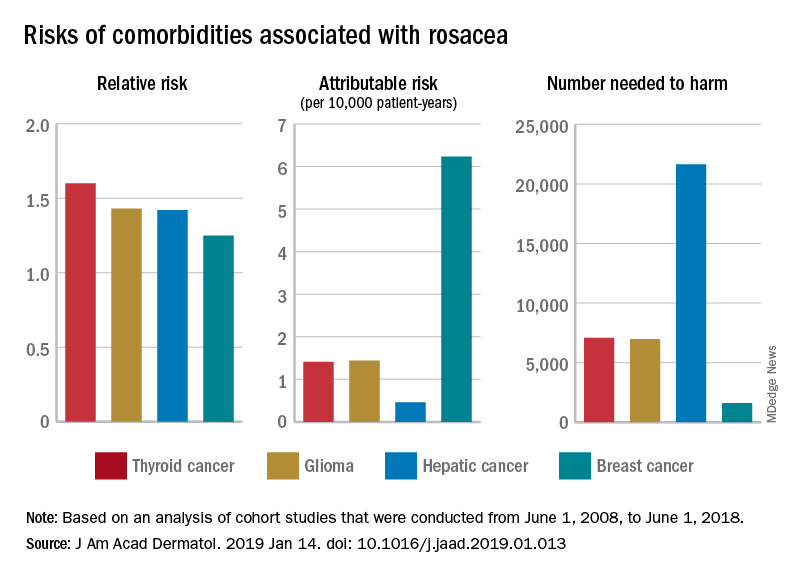
For a patient with rosacea, the relative risk of hepatic cancer is 1.42, but the attributable risk and the number needed to harm (NNH), which provide “a clearer, absolute picture regarding the association” with rosacea, are 0.46 per 10,000 patient-years and 21,645, respectively. The relative risk of comorbid breast cancer is 1.25, compared with an attributable risk of 6.23 per 10,000 patient-years and an NNH of 1,606, Mr. Tjahjono of Wake Forest University in Winston-Salem, N.C., and his associates reported in the Journal of the American Academy of Dermatology.
Physician misconceptions based on patients’ relative risks of comorbidities may lead to increased cancer screenings, which “can provide great benefit in a proper context; however, they are not without consequences. For example, 0.7 % of liver biopsies result in severe intraperitoneal hematoma,” the investigators said.
The absolute risks – calculated by the investigators using cohort studies that were conducted from June 1, 2008, to June 1, 2018 – present “a better understanding regarding rosacea’s impact on public health and clinical settings, “ they wrote.
SOURCE: Tjahjono LA et al. J Am Acad Dermatol. 2019 Jan 14. doi: 10.1016/j.jaad.2019.01.013.
Rosacea has several known comorbidities, but the widespread use of their relative, rather than absolute, risks “may result in overestimation of the clinical importance of exposures,” Leonardo A. Tjahjono and his associates wrote.
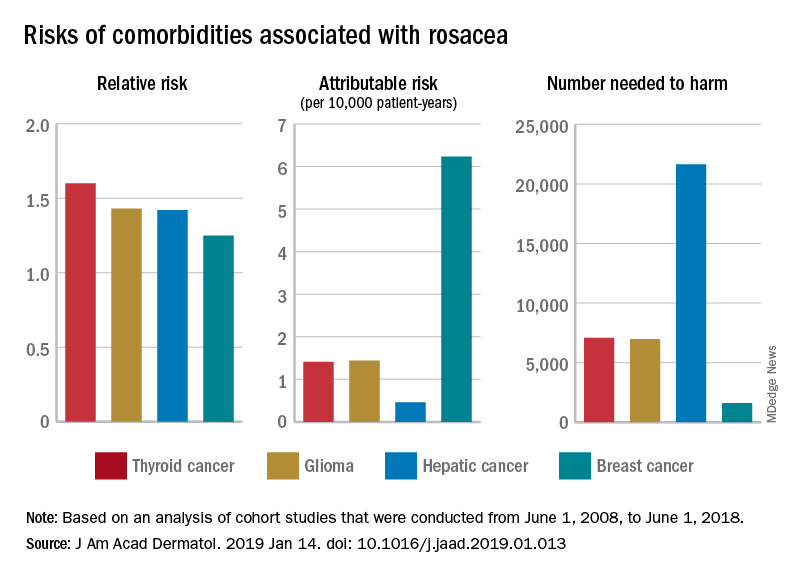
For a patient with rosacea, the relative risk of hepatic cancer is 1.42, but the attributable risk and the number needed to harm (NNH), which provide “a clearer, absolute picture regarding the association” with rosacea, are 0.46 per 10,000 patient-years and 21,645, respectively. The relative risk of comorbid breast cancer is 1.25, compared with an attributable risk of 6.23 per 10,000 patient-years and an NNH of 1,606, Mr. Tjahjono of Wake Forest University in Winston-Salem, N.C., and his associates reported in the Journal of the American Academy of Dermatology.
Physician misconceptions based on patients’ relative risks of comorbidities may lead to increased cancer screenings, which “can provide great benefit in a proper context; however, they are not without consequences. For example, 0.7 % of liver biopsies result in severe intraperitoneal hematoma,” the investigators said.
The absolute risks – calculated by the investigators using cohort studies that were conducted from June 1, 2008, to June 1, 2018 – present “a better understanding regarding rosacea’s impact on public health and clinical settings, “ they wrote.
SOURCE: Tjahjono LA et al. J Am Acad Dermatol. 2019 Jan 14. doi: 10.1016/j.jaad.2019.01.013.
Rosacea has several known comorbidities, but the widespread use of their relative, rather than absolute, risks “may result in overestimation of the clinical importance of exposures,” Leonardo A. Tjahjono and his associates wrote.
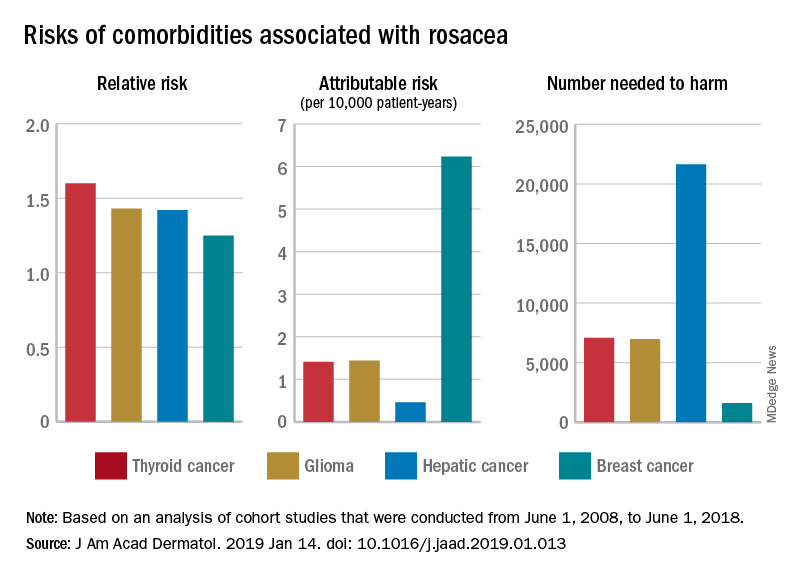
For a patient with rosacea, the relative risk of hepatic cancer is 1.42, but the attributable risk and the number needed to harm (NNH), which provide “a clearer, absolute picture regarding the association” with rosacea, are 0.46 per 10,000 patient-years and 21,645, respectively. The relative risk of comorbid breast cancer is 1.25, compared with an attributable risk of 6.23 per 10,000 patient-years and an NNH of 1,606, Mr. Tjahjono of Wake Forest University in Winston-Salem, N.C., and his associates reported in the Journal of the American Academy of Dermatology.
Physician misconceptions based on patients’ relative risks of comorbidities may lead to increased cancer screenings, which “can provide great benefit in a proper context; however, they are not without consequences. For example, 0.7 % of liver biopsies result in severe intraperitoneal hematoma,” the investigators said.
The absolute risks – calculated by the investigators using cohort studies that were conducted from June 1, 2008, to June 1, 2018 – present “a better understanding regarding rosacea’s impact on public health and clinical settings, “ they wrote.
SOURCE: Tjahjono LA et al. J Am Acad Dermatol. 2019 Jan 14. doi: 10.1016/j.jaad.2019.01.013.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Winter exfoliation: A multicultural approach
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.











