User login
Duodenoscopes contain more bacteria than expected
Reprocessed duodenoscopes are more contaminated than expected, with up to 3% of samples testing positive for disease-causing bacteria including Escherichia coli and Staphylococcus aureus, according to an updated safety communication issued by the Food and Drug Administration on December 10.
“Because of the higher-than-expected contamination rates and to help protect patients from bacterial infections associated with the use of duodenoscopes, we have included in today’s safety communication updated recommendations regarding steps that health care providers can take to enhance duodenoscope reprocessing,” Jeff Shuren, MD, director of the Center for Devices and Radiological Health, wrote in the statement.
The FDA advised clinicians to follow additional cleaning measures including microbiological culturing, sterilization, use of a liquid chemical sterilant processing system, and repeated high-level disinfection beyond what is recommended by duodenoscope manufacturers.
The interim data cited in the safety communication come from postmarket surveillance studies conducted by duodenoscope manufacturers at the FDA’s request as part of the agency’s ongoing efforts to prevent patient infections caused by contaminated duodenoscopes. In addition to the positive tests for disease-causing bacteria, up to 3% of properly collected samples contained more than 100 colony-forming units of other organisms unlikely to cause infection. However, the presence of such organisms further highlights the failure of the current reprocessing protocol to adequately clean the devices, according to the FDA.
Dr. Shuren emphasized that the risk of infection from a duodenoscope for an individual patient remains low and that infection rates have declined in recent years in response to the FDA’s enhanced safety measures and stated that the agency remains “committed to enhancing the safety margin of procedures with reprocessed medical devices.”
Read the full safety communication here: https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm628020.htm.
Reprocessed duodenoscopes are more contaminated than expected, with up to 3% of samples testing positive for disease-causing bacteria including Escherichia coli and Staphylococcus aureus, according to an updated safety communication issued by the Food and Drug Administration on December 10.
“Because of the higher-than-expected contamination rates and to help protect patients from bacterial infections associated with the use of duodenoscopes, we have included in today’s safety communication updated recommendations regarding steps that health care providers can take to enhance duodenoscope reprocessing,” Jeff Shuren, MD, director of the Center for Devices and Radiological Health, wrote in the statement.
The FDA advised clinicians to follow additional cleaning measures including microbiological culturing, sterilization, use of a liquid chemical sterilant processing system, and repeated high-level disinfection beyond what is recommended by duodenoscope manufacturers.
The interim data cited in the safety communication come from postmarket surveillance studies conducted by duodenoscope manufacturers at the FDA’s request as part of the agency’s ongoing efforts to prevent patient infections caused by contaminated duodenoscopes. In addition to the positive tests for disease-causing bacteria, up to 3% of properly collected samples contained more than 100 colony-forming units of other organisms unlikely to cause infection. However, the presence of such organisms further highlights the failure of the current reprocessing protocol to adequately clean the devices, according to the FDA.
Dr. Shuren emphasized that the risk of infection from a duodenoscope for an individual patient remains low and that infection rates have declined in recent years in response to the FDA’s enhanced safety measures and stated that the agency remains “committed to enhancing the safety margin of procedures with reprocessed medical devices.”
Read the full safety communication here: https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm628020.htm.
Reprocessed duodenoscopes are more contaminated than expected, with up to 3% of samples testing positive for disease-causing bacteria including Escherichia coli and Staphylococcus aureus, according to an updated safety communication issued by the Food and Drug Administration on December 10.
“Because of the higher-than-expected contamination rates and to help protect patients from bacterial infections associated with the use of duodenoscopes, we have included in today’s safety communication updated recommendations regarding steps that health care providers can take to enhance duodenoscope reprocessing,” Jeff Shuren, MD, director of the Center for Devices and Radiological Health, wrote in the statement.
The FDA advised clinicians to follow additional cleaning measures including microbiological culturing, sterilization, use of a liquid chemical sterilant processing system, and repeated high-level disinfection beyond what is recommended by duodenoscope manufacturers.
The interim data cited in the safety communication come from postmarket surveillance studies conducted by duodenoscope manufacturers at the FDA’s request as part of the agency’s ongoing efforts to prevent patient infections caused by contaminated duodenoscopes. In addition to the positive tests for disease-causing bacteria, up to 3% of properly collected samples contained more than 100 colony-forming units of other organisms unlikely to cause infection. However, the presence of such organisms further highlights the failure of the current reprocessing protocol to adequately clean the devices, according to the FDA.
Dr. Shuren emphasized that the risk of infection from a duodenoscope for an individual patient remains low and that infection rates have declined in recent years in response to the FDA’s enhanced safety measures and stated that the agency remains “committed to enhancing the safety margin of procedures with reprocessed medical devices.”
Read the full safety communication here: https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm628020.htm.
Designing a better EHR
Hospitals can create a more effective system
It’s well known that overuse is an enormous problem in medicine, and when it comes to antibiotics, the problem is even more striking.
“Half of all inpatient antibiotic use is inappropriate,” says Valerie Vaughn, MD, MSc, a hospitalist at the University of Michigan, Ann Arbor, and coauthor of a BMJ editorial about EHRs and antibiotic overuse.
“This has led to an increase in antibiotic-related adverse events (~20% of all hospitalized patients on antibiotics), Clostridium difficile infections (half a million infections and 29,000 deaths in U.S. annually), and resistant bacteria (which now account for nearly 12% of all bacterial infections, costing $2.2 billion annually).”
EHRs can be a tool to combat that trend – if they are well designed. Clinicians are influenced by the design of their electronic health record, Dr. Vaughn said. “Rather than leave its influence to chance, we should capitalize on what is known about design to promote appropriate testing and treatment through the EHR.” Hospitalists – integral to quality improvement – can have a role in making these changes.
“These improvements will be the most effective if behavioral economics and nudging are considered while designing,” Dr. Vaughn said. “For example, when creating order sets, list recommended options first and when possible make them the default,” she said. “This little change will greatly improve appropriate use.”
For every hour physicians spend on direct patient care, they spend another two with the EHR, Dr. Vaughn wrote. “Given this degree of attention, it is not surprising that the EHR influences physician behavior, especially the overuse of low-value medical care. … Displaying brand-name instead of generic options leads to more expensive prescribing. Allowing labs to be ordered recurrently increases unnecessary phlebotomy. Even individually listing inappropriate antibiotics (rather than grouping them) can make them more noticeable, resulting in more broad-spectrum use.”
“All hospitalists – and humans – are affected by knee-jerk responses. One of the most common in medicine is the urge to treat a positive culture or any positive test. Recognize this urge and resist!” she said. “Antibiotics may be the correct response, but clinicians should first think about whether treatment is necessary based on that patient’s symptoms and comorbidities. Resist the knee-jerk urge to give antibiotics for every positive culture.”
Reference
Vaughn VM et al. Thoughtless design of the electronic health record drives overuse, but purposeful design can nudge improved patient care. BMJ Qual Saf. 24 Mar 2018. doi: 10.1136/bmjqs-2017-007578.
Hospitals can create a more effective system
Hospitals can create a more effective system
It’s well known that overuse is an enormous problem in medicine, and when it comes to antibiotics, the problem is even more striking.
“Half of all inpatient antibiotic use is inappropriate,” says Valerie Vaughn, MD, MSc, a hospitalist at the University of Michigan, Ann Arbor, and coauthor of a BMJ editorial about EHRs and antibiotic overuse.
“This has led to an increase in antibiotic-related adverse events (~20% of all hospitalized patients on antibiotics), Clostridium difficile infections (half a million infections and 29,000 deaths in U.S. annually), and resistant bacteria (which now account for nearly 12% of all bacterial infections, costing $2.2 billion annually).”
EHRs can be a tool to combat that trend – if they are well designed. Clinicians are influenced by the design of their electronic health record, Dr. Vaughn said. “Rather than leave its influence to chance, we should capitalize on what is known about design to promote appropriate testing and treatment through the EHR.” Hospitalists – integral to quality improvement – can have a role in making these changes.
“These improvements will be the most effective if behavioral economics and nudging are considered while designing,” Dr. Vaughn said. “For example, when creating order sets, list recommended options first and when possible make them the default,” she said. “This little change will greatly improve appropriate use.”
For every hour physicians spend on direct patient care, they spend another two with the EHR, Dr. Vaughn wrote. “Given this degree of attention, it is not surprising that the EHR influences physician behavior, especially the overuse of low-value medical care. … Displaying brand-name instead of generic options leads to more expensive prescribing. Allowing labs to be ordered recurrently increases unnecessary phlebotomy. Even individually listing inappropriate antibiotics (rather than grouping them) can make them more noticeable, resulting in more broad-spectrum use.”
“All hospitalists – and humans – are affected by knee-jerk responses. One of the most common in medicine is the urge to treat a positive culture or any positive test. Recognize this urge and resist!” she said. “Antibiotics may be the correct response, but clinicians should first think about whether treatment is necessary based on that patient’s symptoms and comorbidities. Resist the knee-jerk urge to give antibiotics for every positive culture.”
Reference
Vaughn VM et al. Thoughtless design of the electronic health record drives overuse, but purposeful design can nudge improved patient care. BMJ Qual Saf. 24 Mar 2018. doi: 10.1136/bmjqs-2017-007578.
It’s well known that overuse is an enormous problem in medicine, and when it comes to antibiotics, the problem is even more striking.
“Half of all inpatient antibiotic use is inappropriate,” says Valerie Vaughn, MD, MSc, a hospitalist at the University of Michigan, Ann Arbor, and coauthor of a BMJ editorial about EHRs and antibiotic overuse.
“This has led to an increase in antibiotic-related adverse events (~20% of all hospitalized patients on antibiotics), Clostridium difficile infections (half a million infections and 29,000 deaths in U.S. annually), and resistant bacteria (which now account for nearly 12% of all bacterial infections, costing $2.2 billion annually).”
EHRs can be a tool to combat that trend – if they are well designed. Clinicians are influenced by the design of their electronic health record, Dr. Vaughn said. “Rather than leave its influence to chance, we should capitalize on what is known about design to promote appropriate testing and treatment through the EHR.” Hospitalists – integral to quality improvement – can have a role in making these changes.
“These improvements will be the most effective if behavioral economics and nudging are considered while designing,” Dr. Vaughn said. “For example, when creating order sets, list recommended options first and when possible make them the default,” she said. “This little change will greatly improve appropriate use.”
For every hour physicians spend on direct patient care, they spend another two with the EHR, Dr. Vaughn wrote. “Given this degree of attention, it is not surprising that the EHR influences physician behavior, especially the overuse of low-value medical care. … Displaying brand-name instead of generic options leads to more expensive prescribing. Allowing labs to be ordered recurrently increases unnecessary phlebotomy. Even individually listing inappropriate antibiotics (rather than grouping them) can make them more noticeable, resulting in more broad-spectrum use.”
“All hospitalists – and humans – are affected by knee-jerk responses. One of the most common in medicine is the urge to treat a positive culture or any positive test. Recognize this urge and resist!” she said. “Antibiotics may be the correct response, but clinicians should first think about whether treatment is necessary based on that patient’s symptoms and comorbidities. Resist the knee-jerk urge to give antibiotics for every positive culture.”
Reference
Vaughn VM et al. Thoughtless design of the electronic health record drives overuse, but purposeful design can nudge improved patient care. BMJ Qual Saf. 24 Mar 2018. doi: 10.1136/bmjqs-2017-007578.
Biomarker algorithm may offer noninvasive look at liver fibrosis
Serum biomarkers may enable a noninvasive method of detecting advanced hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD), according to results from a recent study.
An algorithm created by the investigators distinguished NAFLD patients with advanced liver fibrosis from those with mild to moderate fibrosis, reported lead author Rohit Loomba, MD, of the University of California at San Diego and his colleagues.
“Liver biopsy is currently the gold standard for diagnosing NASH [nonalcoholic steatohepatitis] and staging liver fibrosis,” the investigators wrote in Clinical Gastroenterology and Hepatology. “However, it is a costly and invasive procedure with an all-cause mortality risk of approximately 0.2%. Liver biopsy typically samples only 1/50,000th of the organ, and it is liable to sampling error with an error rate of 25% for diagnosis of hepatic fibrosis.”
Existing serum-based tests are reliable for diagnosing nonfibrotic NAFLD, but they may misdiagnosis patients with advanced fibrosis. Although imaging-based techniques may provide better diagnostic accuracy, some are available only for subgroups of patients, while others come with a high financial burden. Diagnostic shortcomings may have a major effect on patient outcomes, particularly when risk groups are considered.
“Fibrosis stages F3 and F4 (advanced fibrosis) are primary predictors of liver-related morbidity and mortality, with 11%-22% of NASH patients reported to have advanced fibrosis,” the investigators noted.
The investigators therefore aimed to distinguish such high-risk NAFLD patients from those with mild or moderate liver fibrosis. Three biomarkers were included: hyaluronic acid (HA), TIMP metallopeptidase inhibitor 1 (TIMP-1), and alpha2-macroglobulin (A2M). Each biomarker has documented associations with liver fibrosis. For instance, higher A2M concentrations inhibit fibrinolysis, HA is associated with excessive extracellular matrix and fibrotic tissue, and TIMP-1 is a known liver fibrosis marker and inhibitor of extracellular matrix degradation. The relative strengths of each in detecting advanced liver fibrosis was determined through an algorithm.
The investigators relied on archived serum samples from Duke University, Durham, N.C., (n = 792) and University of California at San Diego (n = 244) that were collected within 11 days of liver biopsy. Biopsies were performed with 15- to 16-gauge needles using at least eight portal tracts, and these samples were used to diagnose NAFLD. Patients with alcoholic liver disease or hepatitis C virus were excluded.
Algorithm training was based on serum measurements from 396 patients treated at Duke University. Samples were divided into mild to moderate (F0-F2) or advanced (F3-F4) fibrosis and split into 10 subsets. The logical regression model was trained on nine subsets and tested on the 10th, with iterations 10 times through this sequence until all 10 samples were tested. This process was repeated 10,000 times. Using the median coefficients from 100,000 logistical regression models, the samples were scored using the algorithm from 0 to 100, with higher numbers representing more advanced fibrosis, and the relative weights of each biomarker measurement were determined.
A noninferiority protocol was used to validate the algorithm, through which the area under the receiver operating characteristic (AUROC) curve was calculated. The AUROC curve of the validation samples was 0.856, with 0.5 being the score for a random algorithm. The algorithm correctly classified 90.0% of F0 cases, 75.0% of F1 cases, 53.8% of F2 cases, 77.4% of F3 cases, and 94.4% of F4 cases. The sensitivity was 79.7% and the specificity was 75.7%.
The algorithm was superior to Fibrosis-4 (FIB-4) and NAFLD Fibrosis Score (NFS) in two validation cohorts. In a combination of validation cohorts, the algorithm correctly identified 79.5% of F3-F4 patients, compared with rates of 25.8% and 28.0% from FIB-4 and NFS, respectively. The investigators noted that the algorithm was unaffected by sex or age. In contrast, FIB-4 is biased toward females, and both FIB-4 and NFS are less accurate with patients aged 35 years or younger.
“Performance of the training and validation sets was robust and well matched, enabling the reliable differentiation of NAFLD patients with and without advanced fibrosis,” the investigators concluded.
The study was supported by Prometheus Laboratories. Authors not employed by Prometheus Laboratories were employed by Duke University or the University of California, San Diego; each institution received funding from Prometheus Laboratories.
SOURCE: Loomba R et al. Clin Gastroenterol Hepatol. 2018 Nov 15. doi: 10.1016/j.cgh.2018.11.004.
Serum biomarkers may enable a noninvasive method of detecting advanced hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD), according to results from a recent study.
An algorithm created by the investigators distinguished NAFLD patients with advanced liver fibrosis from those with mild to moderate fibrosis, reported lead author Rohit Loomba, MD, of the University of California at San Diego and his colleagues.
“Liver biopsy is currently the gold standard for diagnosing NASH [nonalcoholic steatohepatitis] and staging liver fibrosis,” the investigators wrote in Clinical Gastroenterology and Hepatology. “However, it is a costly and invasive procedure with an all-cause mortality risk of approximately 0.2%. Liver biopsy typically samples only 1/50,000th of the organ, and it is liable to sampling error with an error rate of 25% for diagnosis of hepatic fibrosis.”
Existing serum-based tests are reliable for diagnosing nonfibrotic NAFLD, but they may misdiagnosis patients with advanced fibrosis. Although imaging-based techniques may provide better diagnostic accuracy, some are available only for subgroups of patients, while others come with a high financial burden. Diagnostic shortcomings may have a major effect on patient outcomes, particularly when risk groups are considered.
“Fibrosis stages F3 and F4 (advanced fibrosis) are primary predictors of liver-related morbidity and mortality, with 11%-22% of NASH patients reported to have advanced fibrosis,” the investigators noted.
The investigators therefore aimed to distinguish such high-risk NAFLD patients from those with mild or moderate liver fibrosis. Three biomarkers were included: hyaluronic acid (HA), TIMP metallopeptidase inhibitor 1 (TIMP-1), and alpha2-macroglobulin (A2M). Each biomarker has documented associations with liver fibrosis. For instance, higher A2M concentrations inhibit fibrinolysis, HA is associated with excessive extracellular matrix and fibrotic tissue, and TIMP-1 is a known liver fibrosis marker and inhibitor of extracellular matrix degradation. The relative strengths of each in detecting advanced liver fibrosis was determined through an algorithm.
The investigators relied on archived serum samples from Duke University, Durham, N.C., (n = 792) and University of California at San Diego (n = 244) that were collected within 11 days of liver biopsy. Biopsies were performed with 15- to 16-gauge needles using at least eight portal tracts, and these samples were used to diagnose NAFLD. Patients with alcoholic liver disease or hepatitis C virus were excluded.
Algorithm training was based on serum measurements from 396 patients treated at Duke University. Samples were divided into mild to moderate (F0-F2) or advanced (F3-F4) fibrosis and split into 10 subsets. The logical regression model was trained on nine subsets and tested on the 10th, with iterations 10 times through this sequence until all 10 samples were tested. This process was repeated 10,000 times. Using the median coefficients from 100,000 logistical regression models, the samples were scored using the algorithm from 0 to 100, with higher numbers representing more advanced fibrosis, and the relative weights of each biomarker measurement were determined.
A noninferiority protocol was used to validate the algorithm, through which the area under the receiver operating characteristic (AUROC) curve was calculated. The AUROC curve of the validation samples was 0.856, with 0.5 being the score for a random algorithm. The algorithm correctly classified 90.0% of F0 cases, 75.0% of F1 cases, 53.8% of F2 cases, 77.4% of F3 cases, and 94.4% of F4 cases. The sensitivity was 79.7% and the specificity was 75.7%.
The algorithm was superior to Fibrosis-4 (FIB-4) and NAFLD Fibrosis Score (NFS) in two validation cohorts. In a combination of validation cohorts, the algorithm correctly identified 79.5% of F3-F4 patients, compared with rates of 25.8% and 28.0% from FIB-4 and NFS, respectively. The investigators noted that the algorithm was unaffected by sex or age. In contrast, FIB-4 is biased toward females, and both FIB-4 and NFS are less accurate with patients aged 35 years or younger.
“Performance of the training and validation sets was robust and well matched, enabling the reliable differentiation of NAFLD patients with and without advanced fibrosis,” the investigators concluded.
The study was supported by Prometheus Laboratories. Authors not employed by Prometheus Laboratories were employed by Duke University or the University of California, San Diego; each institution received funding from Prometheus Laboratories.
SOURCE: Loomba R et al. Clin Gastroenterol Hepatol. 2018 Nov 15. doi: 10.1016/j.cgh.2018.11.004.
Serum biomarkers may enable a noninvasive method of detecting advanced hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD), according to results from a recent study.
An algorithm created by the investigators distinguished NAFLD patients with advanced liver fibrosis from those with mild to moderate fibrosis, reported lead author Rohit Loomba, MD, of the University of California at San Diego and his colleagues.
“Liver biopsy is currently the gold standard for diagnosing NASH [nonalcoholic steatohepatitis] and staging liver fibrosis,” the investigators wrote in Clinical Gastroenterology and Hepatology. “However, it is a costly and invasive procedure with an all-cause mortality risk of approximately 0.2%. Liver biopsy typically samples only 1/50,000th of the organ, and it is liable to sampling error with an error rate of 25% for diagnosis of hepatic fibrosis.”
Existing serum-based tests are reliable for diagnosing nonfibrotic NAFLD, but they may misdiagnosis patients with advanced fibrosis. Although imaging-based techniques may provide better diagnostic accuracy, some are available only for subgroups of patients, while others come with a high financial burden. Diagnostic shortcomings may have a major effect on patient outcomes, particularly when risk groups are considered.
“Fibrosis stages F3 and F4 (advanced fibrosis) are primary predictors of liver-related morbidity and mortality, with 11%-22% of NASH patients reported to have advanced fibrosis,” the investigators noted.
The investigators therefore aimed to distinguish such high-risk NAFLD patients from those with mild or moderate liver fibrosis. Three biomarkers were included: hyaluronic acid (HA), TIMP metallopeptidase inhibitor 1 (TIMP-1), and alpha2-macroglobulin (A2M). Each biomarker has documented associations with liver fibrosis. For instance, higher A2M concentrations inhibit fibrinolysis, HA is associated with excessive extracellular matrix and fibrotic tissue, and TIMP-1 is a known liver fibrosis marker and inhibitor of extracellular matrix degradation. The relative strengths of each in detecting advanced liver fibrosis was determined through an algorithm.
The investigators relied on archived serum samples from Duke University, Durham, N.C., (n = 792) and University of California at San Diego (n = 244) that were collected within 11 days of liver biopsy. Biopsies were performed with 15- to 16-gauge needles using at least eight portal tracts, and these samples were used to diagnose NAFLD. Patients with alcoholic liver disease or hepatitis C virus were excluded.
Algorithm training was based on serum measurements from 396 patients treated at Duke University. Samples were divided into mild to moderate (F0-F2) or advanced (F3-F4) fibrosis and split into 10 subsets. The logical regression model was trained on nine subsets and tested on the 10th, with iterations 10 times through this sequence until all 10 samples were tested. This process was repeated 10,000 times. Using the median coefficients from 100,000 logistical regression models, the samples were scored using the algorithm from 0 to 100, with higher numbers representing more advanced fibrosis, and the relative weights of each biomarker measurement were determined.
A noninferiority protocol was used to validate the algorithm, through which the area under the receiver operating characteristic (AUROC) curve was calculated. The AUROC curve of the validation samples was 0.856, with 0.5 being the score for a random algorithm. The algorithm correctly classified 90.0% of F0 cases, 75.0% of F1 cases, 53.8% of F2 cases, 77.4% of F3 cases, and 94.4% of F4 cases. The sensitivity was 79.7% and the specificity was 75.7%.
The algorithm was superior to Fibrosis-4 (FIB-4) and NAFLD Fibrosis Score (NFS) in two validation cohorts. In a combination of validation cohorts, the algorithm correctly identified 79.5% of F3-F4 patients, compared with rates of 25.8% and 28.0% from FIB-4 and NFS, respectively. The investigators noted that the algorithm was unaffected by sex or age. In contrast, FIB-4 is biased toward females, and both FIB-4 and NFS are less accurate with patients aged 35 years or younger.
“Performance of the training and validation sets was robust and well matched, enabling the reliable differentiation of NAFLD patients with and without advanced fibrosis,” the investigators concluded.
The study was supported by Prometheus Laboratories. Authors not employed by Prometheus Laboratories were employed by Duke University or the University of California, San Diego; each institution received funding from Prometheus Laboratories.
SOURCE: Loomba R et al. Clin Gastroenterol Hepatol. 2018 Nov 15. doi: 10.1016/j.cgh.2018.11.004.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A serum biomarker–based algorithm may provide a noninvasive method of detecting advanced hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD).
Major finding: The area under the receiver operator characteristic (AUROC) curve for a combination of validation samples was 0.856.
Study details: A retrospective study of liver fibrosis serum markers and clinical data from 396 patients with NAFLD and various stages of fibrosis.
Disclosures: The study was supported by Prometheus Laboratories. Authors not employed by Prometheus Laboratories were employed by Duke University or the University of California, San Diego; each institution received funding from Prometheus Laboratories.
Source: Loomba R et al. Clin Gastroenterol Hepatol. 2018 Nov 15. doi: 10.1016/j.cgh.2018.11.004.
AHA statement on statin risks, app that diagnoses STEMI, and more
This week, the American Heart Association says that statins’ benefits far outweigh the risks, a smartphone app is nearly as good as an ECG at diagnosing STEMI, stroke thrombolysis appears safe in patients prone to GI bleeding, and a new strategy for pausing DOAC therapy works in A-fib patients.
Subscribe to Cardiocast wherever you get your podcasts.
Amazon Alexa
Apple Podcasts
This week, the American Heart Association says that statins’ benefits far outweigh the risks, a smartphone app is nearly as good as an ECG at diagnosing STEMI, stroke thrombolysis appears safe in patients prone to GI bleeding, and a new strategy for pausing DOAC therapy works in A-fib patients.
Subscribe to Cardiocast wherever you get your podcasts.
Amazon Alexa
Apple Podcasts
This week, the American Heart Association says that statins’ benefits far outweigh the risks, a smartphone app is nearly as good as an ECG at diagnosing STEMI, stroke thrombolysis appears safe in patients prone to GI bleeding, and a new strategy for pausing DOAC therapy works in A-fib patients.
Subscribe to Cardiocast wherever you get your podcasts.
Amazon Alexa
Apple Podcasts
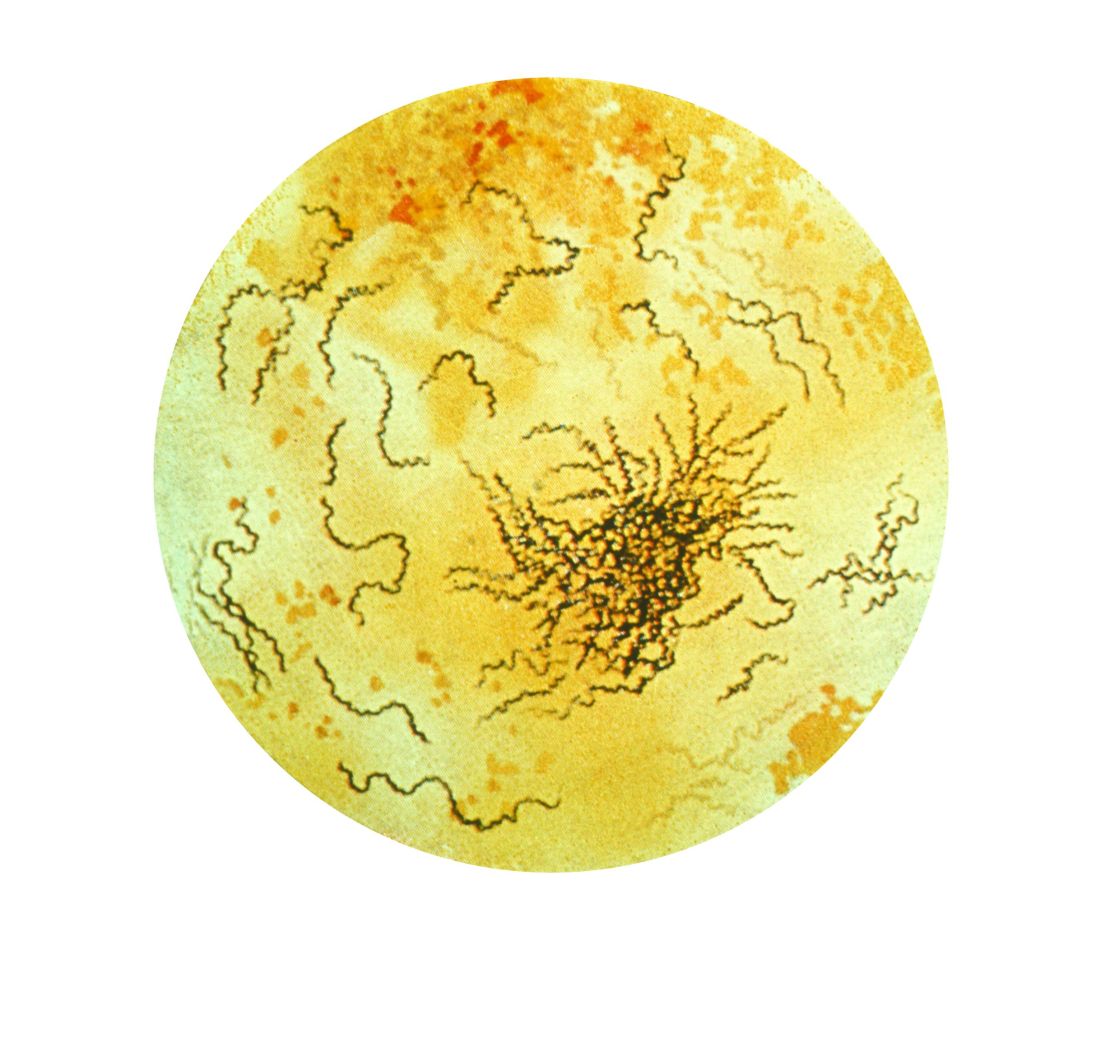
New syphilis cases for pregnant women rose 61% over 5 years
Syphilis cases increased by 61% between 2012 and 2016 among pregnant women, and the proportion of syphilis cases was higher for women who were non-Hispanic black race and Hispanic ethnicity, according to research in Obstetrics & Gynecology.
“These findings support current recommendations for universal syphilis screening at the first prenatal visit and indicate that it may be necessary to include population context when determining whether to implement repeat screening during pregnancy,” Shivika Trivedi, MD, MSc, of the CDC Foundation and the Division of STD Prevention at the Centers for Disease Control and Prevention and colleagues wrote.
Dr. Trivedi and colleagues identified 9,883 pregnant women with reported syphilis in the CDC National Notifiable Diseases Surveillance System during 2012-2016. During that time, there was an increase in the number of female syphilis cases from 9,551 cases in 2012 to 14,838 cases in 2016 (55%), while there was an increase in the number of syphilis cases for pregnant women from 1,561 cases in 2012 to 2,508 cases in 2016 (61%). Of the risk factors reported for syphilis, 49% reported no risk factors within 12 priors before diagnosis, 43% said they had had at least one sexually transmitted disease, and 30% reported more than one sexual partner within the last year.
The greatest prevalence for syphilis was among women who were in their 20s (59%), located in the South (56%), and were non-Hispanic black (49%) or Hispanic (28%). However, researchers noted the rates of syphilis increased among all women between 18 years and 45 years and in every race and ethnicity group between 2012 and 2016. Early syphilis cases increased from 35% in 2012 to 58% in 2016, while late latent cases decreased from 65% in 2012 to 42% in 2016.
Researchers noted several limitations in the study, including case-based surveillance data, which potentially underreported the rates of syphilis, and a lack of pregnancy outcomes for pregnant women with syphilitic infections. However, they noted the data do show a trend of syphilis infections in pregnant women because the live birth rate “was relatively stable and did not fluctuate more than” 1.5% between 2012 and 2016.
“Through an increased awareness of the rising syphilis cases among pregnant women as well as these trend data, health care providers can be better informed to ensure they are following national guidelines and state policies for syphilis screening in pregnancy,” Dr. Trivedi and colleagues concluded.
The authors reported no relevant conflicts of interest.
SOURCE: Trivedi S et al. Obstet Gynecol. 2018. doi: 10.1097/AOG.0000000000003000.
I think this is an important topic of which pregnant women and their providers should be aware. It is possible the rising incidence is a result of increased screening and awareness; however, regardless of whether this is the case, it is important to identify the cases of congenital syphilis as preventable.
It is important for providers to be aware of their local syphilis prevalence and regulations on prenatal syphilis screening because given the effects of congenital syphilis and the ease of treatment.
Martina L. Badell, MD, is an assistant professor in the department of gynecology and obstetrics and maternal-fetal medicine at Emory University in Atlanta. She reported no relevant conflicts of interest.
I think this is an important topic of which pregnant women and their providers should be aware. It is possible the rising incidence is a result of increased screening and awareness; however, regardless of whether this is the case, it is important to identify the cases of congenital syphilis as preventable.
It is important for providers to be aware of their local syphilis prevalence and regulations on prenatal syphilis screening because given the effects of congenital syphilis and the ease of treatment.
Martina L. Badell, MD, is an assistant professor in the department of gynecology and obstetrics and maternal-fetal medicine at Emory University in Atlanta. She reported no relevant conflicts of interest.
I think this is an important topic of which pregnant women and their providers should be aware. It is possible the rising incidence is a result of increased screening and awareness; however, regardless of whether this is the case, it is important to identify the cases of congenital syphilis as preventable.
It is important for providers to be aware of their local syphilis prevalence and regulations on prenatal syphilis screening because given the effects of congenital syphilis and the ease of treatment.
Martina L. Badell, MD, is an assistant professor in the department of gynecology and obstetrics and maternal-fetal medicine at Emory University in Atlanta. She reported no relevant conflicts of interest.
Syphilis cases increased by 61% between 2012 and 2016 among pregnant women, and the proportion of syphilis cases was higher for women who were non-Hispanic black race and Hispanic ethnicity, according to research in Obstetrics & Gynecology.
“These findings support current recommendations for universal syphilis screening at the first prenatal visit and indicate that it may be necessary to include population context when determining whether to implement repeat screening during pregnancy,” Shivika Trivedi, MD, MSc, of the CDC Foundation and the Division of STD Prevention at the Centers for Disease Control and Prevention and colleagues wrote.
Dr. Trivedi and colleagues identified 9,883 pregnant women with reported syphilis in the CDC National Notifiable Diseases Surveillance System during 2012-2016. During that time, there was an increase in the number of female syphilis cases from 9,551 cases in 2012 to 14,838 cases in 2016 (55%), while there was an increase in the number of syphilis cases for pregnant women from 1,561 cases in 2012 to 2,508 cases in 2016 (61%). Of the risk factors reported for syphilis, 49% reported no risk factors within 12 priors before diagnosis, 43% said they had had at least one sexually transmitted disease, and 30% reported more than one sexual partner within the last year.
The greatest prevalence for syphilis was among women who were in their 20s (59%), located in the South (56%), and were non-Hispanic black (49%) or Hispanic (28%). However, researchers noted the rates of syphilis increased among all women between 18 years and 45 years and in every race and ethnicity group between 2012 and 2016. Early syphilis cases increased from 35% in 2012 to 58% in 2016, while late latent cases decreased from 65% in 2012 to 42% in 2016.
Researchers noted several limitations in the study, including case-based surveillance data, which potentially underreported the rates of syphilis, and a lack of pregnancy outcomes for pregnant women with syphilitic infections. However, they noted the data do show a trend of syphilis infections in pregnant women because the live birth rate “was relatively stable and did not fluctuate more than” 1.5% between 2012 and 2016.
“Through an increased awareness of the rising syphilis cases among pregnant women as well as these trend data, health care providers can be better informed to ensure they are following national guidelines and state policies for syphilis screening in pregnancy,” Dr. Trivedi and colleagues concluded.
The authors reported no relevant conflicts of interest.
SOURCE: Trivedi S et al. Obstet Gynecol. 2018. doi: 10.1097/AOG.0000000000003000.
Syphilis cases increased by 61% between 2012 and 2016 among pregnant women, and the proportion of syphilis cases was higher for women who were non-Hispanic black race and Hispanic ethnicity, according to research in Obstetrics & Gynecology.
“These findings support current recommendations for universal syphilis screening at the first prenatal visit and indicate that it may be necessary to include population context when determining whether to implement repeat screening during pregnancy,” Shivika Trivedi, MD, MSc, of the CDC Foundation and the Division of STD Prevention at the Centers for Disease Control and Prevention and colleagues wrote.
Dr. Trivedi and colleagues identified 9,883 pregnant women with reported syphilis in the CDC National Notifiable Diseases Surveillance System during 2012-2016. During that time, there was an increase in the number of female syphilis cases from 9,551 cases in 2012 to 14,838 cases in 2016 (55%), while there was an increase in the number of syphilis cases for pregnant women from 1,561 cases in 2012 to 2,508 cases in 2016 (61%). Of the risk factors reported for syphilis, 49% reported no risk factors within 12 priors before diagnosis, 43% said they had had at least one sexually transmitted disease, and 30% reported more than one sexual partner within the last year.
The greatest prevalence for syphilis was among women who were in their 20s (59%), located in the South (56%), and were non-Hispanic black (49%) or Hispanic (28%). However, researchers noted the rates of syphilis increased among all women between 18 years and 45 years and in every race and ethnicity group between 2012 and 2016. Early syphilis cases increased from 35% in 2012 to 58% in 2016, while late latent cases decreased from 65% in 2012 to 42% in 2016.
Researchers noted several limitations in the study, including case-based surveillance data, which potentially underreported the rates of syphilis, and a lack of pregnancy outcomes for pregnant women with syphilitic infections. However, they noted the data do show a trend of syphilis infections in pregnant women because the live birth rate “was relatively stable and did not fluctuate more than” 1.5% between 2012 and 2016.
“Through an increased awareness of the rising syphilis cases among pregnant women as well as these trend data, health care providers can be better informed to ensure they are following national guidelines and state policies for syphilis screening in pregnancy,” Dr. Trivedi and colleagues concluded.
The authors reported no relevant conflicts of interest.
SOURCE: Trivedi S et al. Obstet Gynecol. 2018. doi: 10.1097/AOG.0000000000003000.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Syphilis rates rose more in pregnant women between 2012 and 2016, compared with women in the general population.
Major finding: There was an increase of syphilis cases by 61% among pregnant women, compared with a 55% increase among women overall.
Study details: A study of national case report data from 9,883 pregnant women with reported syphilis during 2012-2016.
Disclosures: The authors reported no relevant conflicts of interest.
Source: Trivedi S et al. Obstet Gynecol. 2018. doi: 10.1097/AOG.0000000000003000.
Drug test results ‘should not dictate treatment’
BONITA SPRINGS, FLA. – Urine drug screening is a vital part of clinical care, but many clinicians say they do not know enough about how the tests work, an expert said at the annual meeting of the American Academy of Addiction Psychiatry.
Rebecca Ann Payne, MD, said clinicians, including residents, tend to cite little training as a reason for their uncertainty about how to interpret urine drug screen results. Also, primary care clinicians say they need more education on implementing and interpreting the screens.
The good news is that medicine and pediatric residents said they felt that a 30-minute educational program significantly boosted their knowledge base and comfort in interpreting urine drug screens, said Dr. Payne, assistant professor of neuropsychiatry and behavioral science at Palmetto Health–University of South Carolina Medical Group. She offered several points that addiction psychiatrists should be aware of:
“A positive test doesn’t necessarily mean there’s a substance use disorder,” she said. “You still need to walk through those criteria with your patients. And a positive test doesn’t mean they’re physically dependent upon it.” She said she sometimes hears from patients who say that they’d been on a certain treatment – then failed a test given by their clinician – and had their treatment stripped away.
“Drug testing is meant to be a source of information and should not dictate treatment,” she said. “I have found it’s not unusual to hear from the community that decisions are being made solely on the results of these tests, which can be problematic.”
- Point-of-care tests, which sometimes can be bought in drug stores, she said, are “much less than perfect.”
The false-positive rate for benzodiazepines has been found to be 61%; and for methadone, it is 46%; for opioids, 22%; and for amphetamines, 21%.
- Know what your lab is actually testing for, because “it’s not universal.”
She emphasized knowing the particulars of opiate testing.
“A lot of times in a hospital setting, your lab is really only testing those opiates that are directly derived from the poppy – we’re talking about things like codeine, heroin, morphine. They’re not testing for things like your semi-synthetics or your full-synthetic opiates.”
- Know the answer to the question: “Can you get a positive result on a marijuana drug screen just from passive inhalation?”
Physicians often will be confronted by patients who insist they were only in the car or in the same room with someone who was smoking marijuana. How likely is it that their test could be positive?
“Possible,” she said, “but not probable.”
Dr. Payne’s key interest areas include teaching medical students and residents, treating substance use and psychiatric disorders that are comorbid, and conducting research in addiction psychiatry.
BONITA SPRINGS, FLA. – Urine drug screening is a vital part of clinical care, but many clinicians say they do not know enough about how the tests work, an expert said at the annual meeting of the American Academy of Addiction Psychiatry.
Rebecca Ann Payne, MD, said clinicians, including residents, tend to cite little training as a reason for their uncertainty about how to interpret urine drug screen results. Also, primary care clinicians say they need more education on implementing and interpreting the screens.
The good news is that medicine and pediatric residents said they felt that a 30-minute educational program significantly boosted their knowledge base and comfort in interpreting urine drug screens, said Dr. Payne, assistant professor of neuropsychiatry and behavioral science at Palmetto Health–University of South Carolina Medical Group. She offered several points that addiction psychiatrists should be aware of:
“A positive test doesn’t necessarily mean there’s a substance use disorder,” she said. “You still need to walk through those criteria with your patients. And a positive test doesn’t mean they’re physically dependent upon it.” She said she sometimes hears from patients who say that they’d been on a certain treatment – then failed a test given by their clinician – and had their treatment stripped away.
“Drug testing is meant to be a source of information and should not dictate treatment,” she said. “I have found it’s not unusual to hear from the community that decisions are being made solely on the results of these tests, which can be problematic.”
- Point-of-care tests, which sometimes can be bought in drug stores, she said, are “much less than perfect.”
The false-positive rate for benzodiazepines has been found to be 61%; and for methadone, it is 46%; for opioids, 22%; and for amphetamines, 21%.
- Know what your lab is actually testing for, because “it’s not universal.”
She emphasized knowing the particulars of opiate testing.
“A lot of times in a hospital setting, your lab is really only testing those opiates that are directly derived from the poppy – we’re talking about things like codeine, heroin, morphine. They’re not testing for things like your semi-synthetics or your full-synthetic opiates.”
- Know the answer to the question: “Can you get a positive result on a marijuana drug screen just from passive inhalation?”
Physicians often will be confronted by patients who insist they were only in the car or in the same room with someone who was smoking marijuana. How likely is it that their test could be positive?
“Possible,” she said, “but not probable.”
Dr. Payne’s key interest areas include teaching medical students and residents, treating substance use and psychiatric disorders that are comorbid, and conducting research in addiction psychiatry.
BONITA SPRINGS, FLA. – Urine drug screening is a vital part of clinical care, but many clinicians say they do not know enough about how the tests work, an expert said at the annual meeting of the American Academy of Addiction Psychiatry.
Rebecca Ann Payne, MD, said clinicians, including residents, tend to cite little training as a reason for their uncertainty about how to interpret urine drug screen results. Also, primary care clinicians say they need more education on implementing and interpreting the screens.
The good news is that medicine and pediatric residents said they felt that a 30-minute educational program significantly boosted their knowledge base and comfort in interpreting urine drug screens, said Dr. Payne, assistant professor of neuropsychiatry and behavioral science at Palmetto Health–University of South Carolina Medical Group. She offered several points that addiction psychiatrists should be aware of:
“A positive test doesn’t necessarily mean there’s a substance use disorder,” she said. “You still need to walk through those criteria with your patients. And a positive test doesn’t mean they’re physically dependent upon it.” She said she sometimes hears from patients who say that they’d been on a certain treatment – then failed a test given by their clinician – and had their treatment stripped away.
“Drug testing is meant to be a source of information and should not dictate treatment,” she said. “I have found it’s not unusual to hear from the community that decisions are being made solely on the results of these tests, which can be problematic.”
- Point-of-care tests, which sometimes can be bought in drug stores, she said, are “much less than perfect.”
The false-positive rate for benzodiazepines has been found to be 61%; and for methadone, it is 46%; for opioids, 22%; and for amphetamines, 21%.
- Know what your lab is actually testing for, because “it’s not universal.”
She emphasized knowing the particulars of opiate testing.
“A lot of times in a hospital setting, your lab is really only testing those opiates that are directly derived from the poppy – we’re talking about things like codeine, heroin, morphine. They’re not testing for things like your semi-synthetics or your full-synthetic opiates.”
- Know the answer to the question: “Can you get a positive result on a marijuana drug screen just from passive inhalation?”
Physicians often will be confronted by patients who insist they were only in the car or in the same room with someone who was smoking marijuana. How likely is it that their test could be positive?
“Possible,” she said, “but not probable.”
Dr. Payne’s key interest areas include teaching medical students and residents, treating substance use and psychiatric disorders that are comorbid, and conducting research in addiction psychiatry.
REPORTING FROM AAAP 2018
HCC screening linked with improved tumor detection
“Our study’s aim was to characterize utilization of HCC screening receipt and its association with early tumor detection and improved survival in a nationally representative cohort of patients in the United States,” wrote Debra T. Choi, PhD, MPH, of Baylor College of Medicine, Houston, and her colleagues.
The researchers retrospectively studied a cohort of 13,174 patients with HCC from 2003 to 2013 included in the Surveillance, Epidemiology, and End Results Program–Medicare database. They examined the acquisition of HCC in the 3 years leading up to HCC diagnosis using three separate categories: consistent, inconsistent, or no screening. Dr. Choi and her colleagues studied the associations between receiving HCC screening and subsequent effects on overall survival.
“HCC prognosis depends on tumor stage at the time of diagnosis, with curative treatment options only available for patients diagnosed at an early stage,” the researchers wrote. “Patients with early-stage HCC can achieve 5-year survival rates of 70% if they undergo surgical resection or liver transplantation, compared to a median survival of 1 year for patients with advanced HCC,” they added.
After multivariable analysis, the investigators found that 51.1% of patients with cirrhosis did not receive screening in the 3 years leading up to HCC diagnosis. In addition, they went on to report that only 6.8% of patients were consistently screened on an annual basis.
“HCC screening receipt was associated with early tumor detection and potentially improved overall survival, with attenuated benefits in those with inconsistent screening compared to those who had received consistent screening,” they explained.
In terms of efficacy, consistent screening was associated with an increased rate of early-stage tumor detection (odds ratio, 1.98, 95% confidence interval, 1.68-2.33) and decreased risk of death (hazard ratio, 0.76, 95% CI, 0.70-0.83) after adjustment for lead time bias. Given these results, Dr. Choi and her colleagues said that early HCC screening may help with hepatic tumor detection at later disease stages.
“Given the demonstrated benefits of HCC screening, [it] is an important step to reverse the high rates of late stage diagnosis and poor survival,” they added.
The investigators noted that several patient-specific factors may be driving these associations. In particular, they found a link between female sex and receiving HCC screening. Dr. Choi and her colleagues suggested this association is not related to the perceived benefits from screening.
“Studies have suggested females may be more likely to adhere to screening recommendations; however, patient adherence is not a common barrier to HCC screening completion and therefore it is unclear if this is the sole driver of this association,” they acknowledged.
Moving forward, the researchers highlighted the importance of educating primary care providers about the benefits of screening. Moreover, they said that screening receipt is currently on the rise, which has shown positive effects on overall survival.
The Center for Innovations in Quality, Effectiveness, and Safety funded the study. Additional support was provided by the Texas A&M Health Science Center Engineering Experiment Station big data seed grant program. The authors reported no conflicts of interest.
SOURCE: Choi DT et al. Clin Gastroenterol Hepatol. 2018 Oct 25. doi: 10.1016/j.cgh.2018.10.031.
“Our study’s aim was to characterize utilization of HCC screening receipt and its association with early tumor detection and improved survival in a nationally representative cohort of patients in the United States,” wrote Debra T. Choi, PhD, MPH, of Baylor College of Medicine, Houston, and her colleagues.
The researchers retrospectively studied a cohort of 13,174 patients with HCC from 2003 to 2013 included in the Surveillance, Epidemiology, and End Results Program–Medicare database. They examined the acquisition of HCC in the 3 years leading up to HCC diagnosis using three separate categories: consistent, inconsistent, or no screening. Dr. Choi and her colleagues studied the associations between receiving HCC screening and subsequent effects on overall survival.
“HCC prognosis depends on tumor stage at the time of diagnosis, with curative treatment options only available for patients diagnosed at an early stage,” the researchers wrote. “Patients with early-stage HCC can achieve 5-year survival rates of 70% if they undergo surgical resection or liver transplantation, compared to a median survival of 1 year for patients with advanced HCC,” they added.
After multivariable analysis, the investigators found that 51.1% of patients with cirrhosis did not receive screening in the 3 years leading up to HCC diagnosis. In addition, they went on to report that only 6.8% of patients were consistently screened on an annual basis.
“HCC screening receipt was associated with early tumor detection and potentially improved overall survival, with attenuated benefits in those with inconsistent screening compared to those who had received consistent screening,” they explained.
In terms of efficacy, consistent screening was associated with an increased rate of early-stage tumor detection (odds ratio, 1.98, 95% confidence interval, 1.68-2.33) and decreased risk of death (hazard ratio, 0.76, 95% CI, 0.70-0.83) after adjustment for lead time bias. Given these results, Dr. Choi and her colleagues said that early HCC screening may help with hepatic tumor detection at later disease stages.
“Given the demonstrated benefits of HCC screening, [it] is an important step to reverse the high rates of late stage diagnosis and poor survival,” they added.
The investigators noted that several patient-specific factors may be driving these associations. In particular, they found a link between female sex and receiving HCC screening. Dr. Choi and her colleagues suggested this association is not related to the perceived benefits from screening.
“Studies have suggested females may be more likely to adhere to screening recommendations; however, patient adherence is not a common barrier to HCC screening completion and therefore it is unclear if this is the sole driver of this association,” they acknowledged.
Moving forward, the researchers highlighted the importance of educating primary care providers about the benefits of screening. Moreover, they said that screening receipt is currently on the rise, which has shown positive effects on overall survival.
The Center for Innovations in Quality, Effectiveness, and Safety funded the study. Additional support was provided by the Texas A&M Health Science Center Engineering Experiment Station big data seed grant program. The authors reported no conflicts of interest.
SOURCE: Choi DT et al. Clin Gastroenterol Hepatol. 2018 Oct 25. doi: 10.1016/j.cgh.2018.10.031.
“Our study’s aim was to characterize utilization of HCC screening receipt and its association with early tumor detection and improved survival in a nationally representative cohort of patients in the United States,” wrote Debra T. Choi, PhD, MPH, of Baylor College of Medicine, Houston, and her colleagues.
The researchers retrospectively studied a cohort of 13,174 patients with HCC from 2003 to 2013 included in the Surveillance, Epidemiology, and End Results Program–Medicare database. They examined the acquisition of HCC in the 3 years leading up to HCC diagnosis using three separate categories: consistent, inconsistent, or no screening. Dr. Choi and her colleagues studied the associations between receiving HCC screening and subsequent effects on overall survival.
“HCC prognosis depends on tumor stage at the time of diagnosis, with curative treatment options only available for patients diagnosed at an early stage,” the researchers wrote. “Patients with early-stage HCC can achieve 5-year survival rates of 70% if they undergo surgical resection or liver transplantation, compared to a median survival of 1 year for patients with advanced HCC,” they added.
After multivariable analysis, the investigators found that 51.1% of patients with cirrhosis did not receive screening in the 3 years leading up to HCC diagnosis. In addition, they went on to report that only 6.8% of patients were consistently screened on an annual basis.
“HCC screening receipt was associated with early tumor detection and potentially improved overall survival, with attenuated benefits in those with inconsistent screening compared to those who had received consistent screening,” they explained.
In terms of efficacy, consistent screening was associated with an increased rate of early-stage tumor detection (odds ratio, 1.98, 95% confidence interval, 1.68-2.33) and decreased risk of death (hazard ratio, 0.76, 95% CI, 0.70-0.83) after adjustment for lead time bias. Given these results, Dr. Choi and her colleagues said that early HCC screening may help with hepatic tumor detection at later disease stages.
“Given the demonstrated benefits of HCC screening, [it] is an important step to reverse the high rates of late stage diagnosis and poor survival,” they added.
The investigators noted that several patient-specific factors may be driving these associations. In particular, they found a link between female sex and receiving HCC screening. Dr. Choi and her colleagues suggested this association is not related to the perceived benefits from screening.
“Studies have suggested females may be more likely to adhere to screening recommendations; however, patient adherence is not a common barrier to HCC screening completion and therefore it is unclear if this is the sole driver of this association,” they acknowledged.
Moving forward, the researchers highlighted the importance of educating primary care providers about the benefits of screening. Moreover, they said that screening receipt is currently on the rise, which has shown positive effects on overall survival.
The Center for Innovations in Quality, Effectiveness, and Safety funded the study. Additional support was provided by the Texas A&M Health Science Center Engineering Experiment Station big data seed grant program. The authors reported no conflicts of interest.
SOURCE: Choi DT et al. Clin Gastroenterol Hepatol. 2018 Oct 25. doi: 10.1016/j.cgh.2018.10.031.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Hepatocellular carcinoma (HCC) screening for patients with cirrhosis remains an underutilized technique to detect early-stage malignancy.
Major finding: Regular HCC screening was associated with an increased rate of early-stage tumor detection (odds ratio, 1.98).
Study details: Retrospective analysis of 13,174 patients with HCC who were screened 3 years prior to cancer diagnosis.
Disclosures: The Center for Innovations in Quality, Effectiveness, and Safety funded the study. Additional support was provided by the Texas A&M Health Science Center Engineering Experiment Station big data seed grant program. The authors reported no conflicts of interest.
Source: Choi DT et al. Clin Gastroenterol Hepatol. 2018 Oct 25. doi: 10.1016/j.cgh.2018.10.031.
Calciphylaxis: Diagnostic and Treatment Pearls
Weight loss medications may have a role after bariatric surgery
NASHVILLE – .
Phentermine and topiramate were each prescribed to between 10% and 12.5% of bariatric surgery patients at Boston Medical Center in recent years. That figure had been steadily increasing since 2004, when data collection began, Nawfal W. Istfan, MD, PhD, said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
However, the center didn’t know how patients who had received medication fared for long-term maintenance of weight loss, compared with those who had surgery alone; also, there were no clinical guidelines for prescribing weight loss medications (WLMs). “Have we done those patients any benefit by prescribing weight loss medications after gastric bypass surgery?” asked Dr. Istfan. The answer from the Boston Medical Center data is a qualified “yes;” patients with the highest rates of weight regain who were adherent to their medication did see lower rates of regain, and fewer rapid weight regain events.
Comparing patients who received prescriptions with those who did not, patients with less weight loss at nadir were more likely to receive a prescription. “This could very well be the reason they were prescribed a medication: They did not lose as much weight, and they are more likely to ask us” for WLMs, said Dr. Istfan, an endocrinologist at Boston University. However, for those who were prescribed WLMs, the slope of regain was flatter than for those who didn’t receive medication. Of the 626 patients included in the study, 91 received phentermine alone, 54 topiramate alone, and 113 were prescribed both phentermine and topiramate. Three received lorcaserin.
Those receiving medication were similar to the total bariatric surgery population in terms of age, sex, comorbidities, socioeconomic status, and preoperative body mass index, said Dr. Istfan, the senior author in the study. However, Hispanic individuals were more likely to receive WLMs, he said.
Recognizing that “the ratio of weight regain to nadir weight is more indicative of overfeeding than other parameters,” Dr. Istfan said that he and his colleagues divided patients into quartiles of regain, based on this ratio. The quartiles fell out so that those who had the least regain either lost weight or regained less than 1.4%, to make up the first quartile. The second quartile included those who regained from 1.5% to 6.26%, while the third quartile ranged up to 14.29% regain. Those who regained 14.3% or more were in the highest quartile of weight regain.
In comparing characteristics of the quartiles, there were more African Americans in the two higher quartiles (P = .017). More patients had achieved maximal weight loss in the highest quartile of regain (P less than .0001), though preoperative BMI had also been higher in this group (P = .0008).
After statistical adjustment, the investigators found that for individuals who had the highest quartile of regain, patients who were adherent to their WLMs had significantly less weight regain than those who took no medication (P = .014). However, patients considered nonadherent saw no medication effect on weight regain. The differences were small overall, with adherent patients regaining about 27% of weight relative to their nadir and those who didn’t take WLMs regaining about 30%. These significant results were seen long after bariatric surgery, at about 7 years post surgery.
In another analysis that looked just at the quartile of patients with the highest regain rate, weight regain was significantly delayed among those who were prescribed – and were adherent to – WLMs (P = .023). The analysis used a threshold weight regain rate of 1.22% per month; levels lower than that did not see a significant drug effect, and the effect was not seen for those not adherent to their WLMs.
Finally, an adjusted statistical analysis compared those taking and not taking WLMs to see whether WLMs were effective at preventing weight regain in rolling 90-day intervals throughout the study period. Again, in the highest quartile, those who were adherent to WLMs had a lower odds ratio of hitting the 1.22%/month regain rate, compared with those not taking medication (OR, 0.570; 95% confidence interval, 0.371-0.877; P = .01). The effect was not significant for the nonadherent group (OR, 0.872; 95% CI, 0.593-1.284; P = .489).
As more bariatric procedures are being done, and as more patients are living with their surgeries, physicians are seeing more weight regain, said Dr. Istfan, noting that it’s important to assess efficacy of WLMs in the postsurgical population. “Recent work showed that by 5 years after gastric bypass, half of patients had regained more than 15% of their nadir weight, and two-thirds of patients had regained more than 20% of their total maximum weight loss, said Dr. Istfan (King WC et al. JAMA.2018;320:1560).
Typically, patients will see about a 35% weight loss at their nadir, with a gradual increase in weight gain beginning about 2 years after surgery. Though it’s true that a net weight loss of 25% is still good, it can be a misleading way to look at the data, “because it does not focus on the process of weight regain itself,” said Dr. Istfan.
“Despite the maintenance of substantial weight loss, weight regain is concerning: It’s the present and future, not the past,” he said.
Regaining weight necessarily means that patients are having excess nutrient intake and a net-positive energy balance; this state can be associated with oxidative stress, inflammation, and insulin resistance – all potential contributors to the recurrence of comorbidities.
What’s to be done about weight regain, if it’s a point of concern? One option, said Dr. Istfan, is to consider more surgery. Patients might want a “re-do;” techniques that have been tried include reshaping the pouch and doing an anastomosis plication. If a gastro-gastric fistula’s developed, that can be corrected, he said.
Some factors influencing regain can be targeted by behavioral therapy. These include addressing alcohol consumption, discouraging grazing, encouraging exercise, and assessing and modifying diet quality in general.
“There is a general reluctance on the part of physicians to use weight loss medications after bariatric surgery,” said Dr. Istfan. Reasons can include concern about further nutritional compromise, especially when thinking about long-term use of appetite-suppressing medications. Importantly, there aren’t clinical guidelines for prescribing WLMs after bariatric surgery, nor is there a strong body of prospective studies in this area.
Dr. Istfan noted that the medical and surgical bariatric teams collaborate closely at Boston Medical Center to provide pre- and postoperative assessment and management.
The long observational interval and ethnic and socioeconomic diversity of the study population are strengths, said Dr. Istfan. Also, the three different multivariable models converged to similar findings.
However, the study was retrospective, with some confounding likely, and each prescriber involved in the study may have varying prescribing practices. Also, adherence was assessed by follow-up medication appointments, a measure that likely introduced some inaccuracy.
“Weight loss medications are potentially effective tools to counter weight regain after bariatric surgery; prospective studies are needed to optimize the use of weight loss medications after bariatric surgery,” said Dr. Istfan.
Dr. Istfan reported no outside sources of funding, and no conflicts of interest.
AGA provides GIs with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at http://ow.ly/fFA330mWKCn.
SOURCE: Anderson W et al. Obesity Week 2018, Abstract T-OR-2016.
NASHVILLE – .
Phentermine and topiramate were each prescribed to between 10% and 12.5% of bariatric surgery patients at Boston Medical Center in recent years. That figure had been steadily increasing since 2004, when data collection began, Nawfal W. Istfan, MD, PhD, said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
However, the center didn’t know how patients who had received medication fared for long-term maintenance of weight loss, compared with those who had surgery alone; also, there were no clinical guidelines for prescribing weight loss medications (WLMs). “Have we done those patients any benefit by prescribing weight loss medications after gastric bypass surgery?” asked Dr. Istfan. The answer from the Boston Medical Center data is a qualified “yes;” patients with the highest rates of weight regain who were adherent to their medication did see lower rates of regain, and fewer rapid weight regain events.
Comparing patients who received prescriptions with those who did not, patients with less weight loss at nadir were more likely to receive a prescription. “This could very well be the reason they were prescribed a medication: They did not lose as much weight, and they are more likely to ask us” for WLMs, said Dr. Istfan, an endocrinologist at Boston University. However, for those who were prescribed WLMs, the slope of regain was flatter than for those who didn’t receive medication. Of the 626 patients included in the study, 91 received phentermine alone, 54 topiramate alone, and 113 were prescribed both phentermine and topiramate. Three received lorcaserin.
Those receiving medication were similar to the total bariatric surgery population in terms of age, sex, comorbidities, socioeconomic status, and preoperative body mass index, said Dr. Istfan, the senior author in the study. However, Hispanic individuals were more likely to receive WLMs, he said.
Recognizing that “the ratio of weight regain to nadir weight is more indicative of overfeeding than other parameters,” Dr. Istfan said that he and his colleagues divided patients into quartiles of regain, based on this ratio. The quartiles fell out so that those who had the least regain either lost weight or regained less than 1.4%, to make up the first quartile. The second quartile included those who regained from 1.5% to 6.26%, while the third quartile ranged up to 14.29% regain. Those who regained 14.3% or more were in the highest quartile of weight regain.
In comparing characteristics of the quartiles, there were more African Americans in the two higher quartiles (P = .017). More patients had achieved maximal weight loss in the highest quartile of regain (P less than .0001), though preoperative BMI had also been higher in this group (P = .0008).
After statistical adjustment, the investigators found that for individuals who had the highest quartile of regain, patients who were adherent to their WLMs had significantly less weight regain than those who took no medication (P = .014). However, patients considered nonadherent saw no medication effect on weight regain. The differences were small overall, with adherent patients regaining about 27% of weight relative to their nadir and those who didn’t take WLMs regaining about 30%. These significant results were seen long after bariatric surgery, at about 7 years post surgery.
In another analysis that looked just at the quartile of patients with the highest regain rate, weight regain was significantly delayed among those who were prescribed – and were adherent to – WLMs (P = .023). The analysis used a threshold weight regain rate of 1.22% per month; levels lower than that did not see a significant drug effect, and the effect was not seen for those not adherent to their WLMs.
Finally, an adjusted statistical analysis compared those taking and not taking WLMs to see whether WLMs were effective at preventing weight regain in rolling 90-day intervals throughout the study period. Again, in the highest quartile, those who were adherent to WLMs had a lower odds ratio of hitting the 1.22%/month regain rate, compared with those not taking medication (OR, 0.570; 95% confidence interval, 0.371-0.877; P = .01). The effect was not significant for the nonadherent group (OR, 0.872; 95% CI, 0.593-1.284; P = .489).
As more bariatric procedures are being done, and as more patients are living with their surgeries, physicians are seeing more weight regain, said Dr. Istfan, noting that it’s important to assess efficacy of WLMs in the postsurgical population. “Recent work showed that by 5 years after gastric bypass, half of patients had regained more than 15% of their nadir weight, and two-thirds of patients had regained more than 20% of their total maximum weight loss, said Dr. Istfan (King WC et al. JAMA.2018;320:1560).
Typically, patients will see about a 35% weight loss at their nadir, with a gradual increase in weight gain beginning about 2 years after surgery. Though it’s true that a net weight loss of 25% is still good, it can be a misleading way to look at the data, “because it does not focus on the process of weight regain itself,” said Dr. Istfan.
“Despite the maintenance of substantial weight loss, weight regain is concerning: It’s the present and future, not the past,” he said.
Regaining weight necessarily means that patients are having excess nutrient intake and a net-positive energy balance; this state can be associated with oxidative stress, inflammation, and insulin resistance – all potential contributors to the recurrence of comorbidities.
What’s to be done about weight regain, if it’s a point of concern? One option, said Dr. Istfan, is to consider more surgery. Patients might want a “re-do;” techniques that have been tried include reshaping the pouch and doing an anastomosis plication. If a gastro-gastric fistula’s developed, that can be corrected, he said.
Some factors influencing regain can be targeted by behavioral therapy. These include addressing alcohol consumption, discouraging grazing, encouraging exercise, and assessing and modifying diet quality in general.
“There is a general reluctance on the part of physicians to use weight loss medications after bariatric surgery,” said Dr. Istfan. Reasons can include concern about further nutritional compromise, especially when thinking about long-term use of appetite-suppressing medications. Importantly, there aren’t clinical guidelines for prescribing WLMs after bariatric surgery, nor is there a strong body of prospective studies in this area.
Dr. Istfan noted that the medical and surgical bariatric teams collaborate closely at Boston Medical Center to provide pre- and postoperative assessment and management.
The long observational interval and ethnic and socioeconomic diversity of the study population are strengths, said Dr. Istfan. Also, the three different multivariable models converged to similar findings.
However, the study was retrospective, with some confounding likely, and each prescriber involved in the study may have varying prescribing practices. Also, adherence was assessed by follow-up medication appointments, a measure that likely introduced some inaccuracy.
“Weight loss medications are potentially effective tools to counter weight regain after bariatric surgery; prospective studies are needed to optimize the use of weight loss medications after bariatric surgery,” said Dr. Istfan.
Dr. Istfan reported no outside sources of funding, and no conflicts of interest.
AGA provides GIs with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at http://ow.ly/fFA330mWKCn.
SOURCE: Anderson W et al. Obesity Week 2018, Abstract T-OR-2016.
NASHVILLE – .
Phentermine and topiramate were each prescribed to between 10% and 12.5% of bariatric surgery patients at Boston Medical Center in recent years. That figure had been steadily increasing since 2004, when data collection began, Nawfal W. Istfan, MD, PhD, said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
However, the center didn’t know how patients who had received medication fared for long-term maintenance of weight loss, compared with those who had surgery alone; also, there were no clinical guidelines for prescribing weight loss medications (WLMs). “Have we done those patients any benefit by prescribing weight loss medications after gastric bypass surgery?” asked Dr. Istfan. The answer from the Boston Medical Center data is a qualified “yes;” patients with the highest rates of weight regain who were adherent to their medication did see lower rates of regain, and fewer rapid weight regain events.
Comparing patients who received prescriptions with those who did not, patients with less weight loss at nadir were more likely to receive a prescription. “This could very well be the reason they were prescribed a medication: They did not lose as much weight, and they are more likely to ask us” for WLMs, said Dr. Istfan, an endocrinologist at Boston University. However, for those who were prescribed WLMs, the slope of regain was flatter than for those who didn’t receive medication. Of the 626 patients included in the study, 91 received phentermine alone, 54 topiramate alone, and 113 were prescribed both phentermine and topiramate. Three received lorcaserin.
Those receiving medication were similar to the total bariatric surgery population in terms of age, sex, comorbidities, socioeconomic status, and preoperative body mass index, said Dr. Istfan, the senior author in the study. However, Hispanic individuals were more likely to receive WLMs, he said.
Recognizing that “the ratio of weight regain to nadir weight is more indicative of overfeeding than other parameters,” Dr. Istfan said that he and his colleagues divided patients into quartiles of regain, based on this ratio. The quartiles fell out so that those who had the least regain either lost weight or regained less than 1.4%, to make up the first quartile. The second quartile included those who regained from 1.5% to 6.26%, while the third quartile ranged up to 14.29% regain. Those who regained 14.3% or more were in the highest quartile of weight regain.
In comparing characteristics of the quartiles, there were more African Americans in the two higher quartiles (P = .017). More patients had achieved maximal weight loss in the highest quartile of regain (P less than .0001), though preoperative BMI had also been higher in this group (P = .0008).
After statistical adjustment, the investigators found that for individuals who had the highest quartile of regain, patients who were adherent to their WLMs had significantly less weight regain than those who took no medication (P = .014). However, patients considered nonadherent saw no medication effect on weight regain. The differences were small overall, with adherent patients regaining about 27% of weight relative to their nadir and those who didn’t take WLMs regaining about 30%. These significant results were seen long after bariatric surgery, at about 7 years post surgery.
In another analysis that looked just at the quartile of patients with the highest regain rate, weight regain was significantly delayed among those who were prescribed – and were adherent to – WLMs (P = .023). The analysis used a threshold weight regain rate of 1.22% per month; levels lower than that did not see a significant drug effect, and the effect was not seen for those not adherent to their WLMs.
Finally, an adjusted statistical analysis compared those taking and not taking WLMs to see whether WLMs were effective at preventing weight regain in rolling 90-day intervals throughout the study period. Again, in the highest quartile, those who were adherent to WLMs had a lower odds ratio of hitting the 1.22%/month regain rate, compared with those not taking medication (OR, 0.570; 95% confidence interval, 0.371-0.877; P = .01). The effect was not significant for the nonadherent group (OR, 0.872; 95% CI, 0.593-1.284; P = .489).
As more bariatric procedures are being done, and as more patients are living with their surgeries, physicians are seeing more weight regain, said Dr. Istfan, noting that it’s important to assess efficacy of WLMs in the postsurgical population. “Recent work showed that by 5 years after gastric bypass, half of patients had regained more than 15% of their nadir weight, and two-thirds of patients had regained more than 20% of their total maximum weight loss, said Dr. Istfan (King WC et al. JAMA.2018;320:1560).
Typically, patients will see about a 35% weight loss at their nadir, with a gradual increase in weight gain beginning about 2 years after surgery. Though it’s true that a net weight loss of 25% is still good, it can be a misleading way to look at the data, “because it does not focus on the process of weight regain itself,” said Dr. Istfan.
“Despite the maintenance of substantial weight loss, weight regain is concerning: It’s the present and future, not the past,” he said.
Regaining weight necessarily means that patients are having excess nutrient intake and a net-positive energy balance; this state can be associated with oxidative stress, inflammation, and insulin resistance – all potential contributors to the recurrence of comorbidities.
What’s to be done about weight regain, if it’s a point of concern? One option, said Dr. Istfan, is to consider more surgery. Patients might want a “re-do;” techniques that have been tried include reshaping the pouch and doing an anastomosis plication. If a gastro-gastric fistula’s developed, that can be corrected, he said.
Some factors influencing regain can be targeted by behavioral therapy. These include addressing alcohol consumption, discouraging grazing, encouraging exercise, and assessing and modifying diet quality in general.
“There is a general reluctance on the part of physicians to use weight loss medications after bariatric surgery,” said Dr. Istfan. Reasons can include concern about further nutritional compromise, especially when thinking about long-term use of appetite-suppressing medications. Importantly, there aren’t clinical guidelines for prescribing WLMs after bariatric surgery, nor is there a strong body of prospective studies in this area.
Dr. Istfan noted that the medical and surgical bariatric teams collaborate closely at Boston Medical Center to provide pre- and postoperative assessment and management.
The long observational interval and ethnic and socioeconomic diversity of the study population are strengths, said Dr. Istfan. Also, the three different multivariable models converged to similar findings.
However, the study was retrospective, with some confounding likely, and each prescriber involved in the study may have varying prescribing practices. Also, adherence was assessed by follow-up medication appointments, a measure that likely introduced some inaccuracy.
“Weight loss medications are potentially effective tools to counter weight regain after bariatric surgery; prospective studies are needed to optimize the use of weight loss medications after bariatric surgery,” said Dr. Istfan.
Dr. Istfan reported no outside sources of funding, and no conflicts of interest.
AGA provides GIs with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at http://ow.ly/fFA330mWKCn.
SOURCE: Anderson W et al. Obesity Week 2018, Abstract T-OR-2016.
REPORTING FROM OBESITY WEEK 2018
Key clinical point: Weight loss medication flattened the curve of weight regain after bariatric surgery – for some patients.
Major finding: Weight loss medicine reduced regain among those who had the most weight regain (P =.014).
Study details: Retrospective single-center cohort study of 626 bariatric surgery patients.
Disclosures: The study authors reported no external sources of funding. Dr. Istfan reported no conflicts of interest.
Source: Anderson W et al. Obesity Week 2018, Abstract T-OR-2016.
Cortical Thickness Changes in Chronic Migraine
Chronic migraine (CM) patients have significantly greater cortical covariance compared to controls, according to a recent study. Cortical thickness in CM patients was predominantly accounted for by CM duration, posttraumatic stress disorder (PTSD), and poor sleep quality, while improved pain self‐efficacy buffered cortical thickness. Thirty CM cases (mean age 40 years; male‐to‐female 1:4) and 30 sex‐matched healthy controls (mean age 40 years) were enrolled. Participants completed self‐administered and standardized questionnaires assessing headache‐related clinical features and common psychological comorbidities. T1‐weighted brain images were acquired on a 3T MRI and a whole‐brain cortical thickness analysis was performed.
Researchers found:
- The whole brain cortical thickness analysis revealed no significant differences between CM patients and controls.
- However, significant associations between clinical features and cortical thickness were observed for the patients only.
- These associations included the right superior temporal sulcus (R2 = 0.72) and the right insula (R2= 0.71) with distinct clinical variables (ie, longer history of CM, PTSD, sleep quality, pain self‐efficacy, and somatic symptoms).
Woldeamanuel YW, DeSouza DD, Sanjanwala BM, Cowan RP. Clinical features contributing to cortical thickness changes in chronic migraine–A pilot study. [Published online ahead of print November 23, 2018]. Headache. doi:10.1111/head.13452.
Chronic migraine (CM) patients have significantly greater cortical covariance compared to controls, according to a recent study. Cortical thickness in CM patients was predominantly accounted for by CM duration, posttraumatic stress disorder (PTSD), and poor sleep quality, while improved pain self‐efficacy buffered cortical thickness. Thirty CM cases (mean age 40 years; male‐to‐female 1:4) and 30 sex‐matched healthy controls (mean age 40 years) were enrolled. Participants completed self‐administered and standardized questionnaires assessing headache‐related clinical features and common psychological comorbidities. T1‐weighted brain images were acquired on a 3T MRI and a whole‐brain cortical thickness analysis was performed.
Researchers found:
- The whole brain cortical thickness analysis revealed no significant differences between CM patients and controls.
- However, significant associations between clinical features and cortical thickness were observed for the patients only.
- These associations included the right superior temporal sulcus (R2 = 0.72) and the right insula (R2= 0.71) with distinct clinical variables (ie, longer history of CM, PTSD, sleep quality, pain self‐efficacy, and somatic symptoms).
Woldeamanuel YW, DeSouza DD, Sanjanwala BM, Cowan RP. Clinical features contributing to cortical thickness changes in chronic migraine–A pilot study. [Published online ahead of print November 23, 2018]. Headache. doi:10.1111/head.13452.
Chronic migraine (CM) patients have significantly greater cortical covariance compared to controls, according to a recent study. Cortical thickness in CM patients was predominantly accounted for by CM duration, posttraumatic stress disorder (PTSD), and poor sleep quality, while improved pain self‐efficacy buffered cortical thickness. Thirty CM cases (mean age 40 years; male‐to‐female 1:4) and 30 sex‐matched healthy controls (mean age 40 years) were enrolled. Participants completed self‐administered and standardized questionnaires assessing headache‐related clinical features and common psychological comorbidities. T1‐weighted brain images were acquired on a 3T MRI and a whole‐brain cortical thickness analysis was performed.
Researchers found:
- The whole brain cortical thickness analysis revealed no significant differences between CM patients and controls.
- However, significant associations between clinical features and cortical thickness were observed for the patients only.
- These associations included the right superior temporal sulcus (R2 = 0.72) and the right insula (R2= 0.71) with distinct clinical variables (ie, longer history of CM, PTSD, sleep quality, pain self‐efficacy, and somatic symptoms).
Woldeamanuel YW, DeSouza DD, Sanjanwala BM, Cowan RP. Clinical features contributing to cortical thickness changes in chronic migraine–A pilot study. [Published online ahead of print November 23, 2018]. Headache. doi:10.1111/head.13452.