User login
The power of the turkey sandwich
A relatively high proportion of pediatric visits to the emergency department are related to psychiatric symptoms, oftentimes with suicidal or violent ideation.1 Given that pediatric emergencies related to psychiatric symptoms are on the increase, clinicians frequently are called to assess children and adolescents with symptoms of aggression and violence. Management of these cases can be tricky.
Case presentation
Henry is a 6-year-old boy with mild developmental delays and possible anxiety who was brought to the emergency department because of concerns on the bus. For about a month, Henry, who is repeating his kindergarten year, had been struggling with getting on and off the bus and with other transitions at school. These struggles had been attributed to anxiety. He was started on sertraline and the dose was increased about 2 weeks later. Soon thereafter he complained of stomach upset with the sertraline, refused to take the medicine, and had a very hard day at school. He required one-on-one attention for unsafe behavior most of that day, and he missed most of his lunch and recess. His school support team was able to get him onto the bus at the end of the day, but he refused to get off of the bus at home. He became violent with the bus driver, kicking and biting him until the police were called. The police called EMS and he was brought into the emergency department after fighting to get on the transport stretcher. He was eventually brought into a secure exam room in the emergency department, but was unable to be fully assessed because he would only make animal noises when approached. His father already had been called, but was unable to calm him down. The emergency department physician was unable to approach Henry because he began swinging at him as soon as the physician entered the room. An emergent psychiatric consultation was called to determine what medication to give to Henry to calm him down and to assess him for possible psychosis.
Case discussion
It sounds like Henry was having a severe tantrum exacerbated by a number of factors. First of all, this is a child who struggles with transitions. That day had been loaded with transitions, eventually leading him to be in an unfamiliar environment with many unfamiliar faces. Even the familiar face of his father wasn’t enough to help because he was overly stimulated and scared. Next, he was probably hungry. We know for certain that he missed lunch, and several hours into his presentation there were no breaks to deal with his basic needs. The first approach to assessment of aggressive behavior in the emergency setting is to try to care for the basic needs of the individual to deescalate the situation. Finally, he had recently been started on sertraline, a selective serotonin reuptake inhibitor. He had been having some dyspepsia and/or nausea with the sertraline, leading to his having missed some doses. Some children and adolescents have a discontinuation syndrome, which can be more severe in younger children and with medications that have shorter half-lives.2 In Henry’s case, a missed dose or two can be enough to trigger this discontinuation response leading to more aggressive behavior.
Case follow-up
The child and adolescent psychiatrist called to the case received a history from the primary team. When he started to try to talk with the parent outside of the room, the child became upset. He was able to gather the information that Henry also had skipped breakfast. In an attempt to calm the patient down, the psychiatrist addressed Henry using a nonjudgmental, nonconfrontational, collaborative approach, incorporating play. Henry responded to this approach and allowed the psychiatrist to ask a few questions about basic needs, and admitted that he was hungry. He was offered a turkey sandwich, which was rapidly ingested. The tantrum slowly subsided. Within about 30 minutes (and with some more food), the child was able to sit on his parent’s lap and finish the interview. The decision was made to have him follow up with his primary care provider to change to an SSRI with a longer half-life, such as fluoxetine, as he did seem to be experiencing some discontinuation even after missing just a dose or two of sertraline.
When dealing with emergent, aggressive behavior, food isn’t always the best medicine, but sometimes it is. Environmental barriers to the child’s regaining control include hunger, thirst, a full bladder, constipation, or other pain. Attending to these issues first sometimes can help avoid sedating medications, which can prolong emergency visits and lead to unwelcome side effects.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at pdnews@mdedge.com.
References
1. Pediatrics. 2011 May;127(5):e1356-66.
2. J Can Acad Child Adolesc Psychiatry. 2011 Feb;20(1):60-7.
A relatively high proportion of pediatric visits to the emergency department are related to psychiatric symptoms, oftentimes with suicidal or violent ideation.1 Given that pediatric emergencies related to psychiatric symptoms are on the increase, clinicians frequently are called to assess children and adolescents with symptoms of aggression and violence. Management of these cases can be tricky.
Case presentation
Henry is a 6-year-old boy with mild developmental delays and possible anxiety who was brought to the emergency department because of concerns on the bus. For about a month, Henry, who is repeating his kindergarten year, had been struggling with getting on and off the bus and with other transitions at school. These struggles had been attributed to anxiety. He was started on sertraline and the dose was increased about 2 weeks later. Soon thereafter he complained of stomach upset with the sertraline, refused to take the medicine, and had a very hard day at school. He required one-on-one attention for unsafe behavior most of that day, and he missed most of his lunch and recess. His school support team was able to get him onto the bus at the end of the day, but he refused to get off of the bus at home. He became violent with the bus driver, kicking and biting him until the police were called. The police called EMS and he was brought into the emergency department after fighting to get on the transport stretcher. He was eventually brought into a secure exam room in the emergency department, but was unable to be fully assessed because he would only make animal noises when approached. His father already had been called, but was unable to calm him down. The emergency department physician was unable to approach Henry because he began swinging at him as soon as the physician entered the room. An emergent psychiatric consultation was called to determine what medication to give to Henry to calm him down and to assess him for possible psychosis.
Case discussion
It sounds like Henry was having a severe tantrum exacerbated by a number of factors. First of all, this is a child who struggles with transitions. That day had been loaded with transitions, eventually leading him to be in an unfamiliar environment with many unfamiliar faces. Even the familiar face of his father wasn’t enough to help because he was overly stimulated and scared. Next, he was probably hungry. We know for certain that he missed lunch, and several hours into his presentation there were no breaks to deal with his basic needs. The first approach to assessment of aggressive behavior in the emergency setting is to try to care for the basic needs of the individual to deescalate the situation. Finally, he had recently been started on sertraline, a selective serotonin reuptake inhibitor. He had been having some dyspepsia and/or nausea with the sertraline, leading to his having missed some doses. Some children and adolescents have a discontinuation syndrome, which can be more severe in younger children and with medications that have shorter half-lives.2 In Henry’s case, a missed dose or two can be enough to trigger this discontinuation response leading to more aggressive behavior.
Case follow-up
The child and adolescent psychiatrist called to the case received a history from the primary team. When he started to try to talk with the parent outside of the room, the child became upset. He was able to gather the information that Henry also had skipped breakfast. In an attempt to calm the patient down, the psychiatrist addressed Henry using a nonjudgmental, nonconfrontational, collaborative approach, incorporating play. Henry responded to this approach and allowed the psychiatrist to ask a few questions about basic needs, and admitted that he was hungry. He was offered a turkey sandwich, which was rapidly ingested. The tantrum slowly subsided. Within about 30 minutes (and with some more food), the child was able to sit on his parent’s lap and finish the interview. The decision was made to have him follow up with his primary care provider to change to an SSRI with a longer half-life, such as fluoxetine, as he did seem to be experiencing some discontinuation even after missing just a dose or two of sertraline.
When dealing with emergent, aggressive behavior, food isn’t always the best medicine, but sometimes it is. Environmental barriers to the child’s regaining control include hunger, thirst, a full bladder, constipation, or other pain. Attending to these issues first sometimes can help avoid sedating medications, which can prolong emergency visits and lead to unwelcome side effects.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at pdnews@mdedge.com.
References
1. Pediatrics. 2011 May;127(5):e1356-66.
2. J Can Acad Child Adolesc Psychiatry. 2011 Feb;20(1):60-7.
A relatively high proportion of pediatric visits to the emergency department are related to psychiatric symptoms, oftentimes with suicidal or violent ideation.1 Given that pediatric emergencies related to psychiatric symptoms are on the increase, clinicians frequently are called to assess children and adolescents with symptoms of aggression and violence. Management of these cases can be tricky.
Case presentation
Henry is a 6-year-old boy with mild developmental delays and possible anxiety who was brought to the emergency department because of concerns on the bus. For about a month, Henry, who is repeating his kindergarten year, had been struggling with getting on and off the bus and with other transitions at school. These struggles had been attributed to anxiety. He was started on sertraline and the dose was increased about 2 weeks later. Soon thereafter he complained of stomach upset with the sertraline, refused to take the medicine, and had a very hard day at school. He required one-on-one attention for unsafe behavior most of that day, and he missed most of his lunch and recess. His school support team was able to get him onto the bus at the end of the day, but he refused to get off of the bus at home. He became violent with the bus driver, kicking and biting him until the police were called. The police called EMS and he was brought into the emergency department after fighting to get on the transport stretcher. He was eventually brought into a secure exam room in the emergency department, but was unable to be fully assessed because he would only make animal noises when approached. His father already had been called, but was unable to calm him down. The emergency department physician was unable to approach Henry because he began swinging at him as soon as the physician entered the room. An emergent psychiatric consultation was called to determine what medication to give to Henry to calm him down and to assess him for possible psychosis.
Case discussion
It sounds like Henry was having a severe tantrum exacerbated by a number of factors. First of all, this is a child who struggles with transitions. That day had been loaded with transitions, eventually leading him to be in an unfamiliar environment with many unfamiliar faces. Even the familiar face of his father wasn’t enough to help because he was overly stimulated and scared. Next, he was probably hungry. We know for certain that he missed lunch, and several hours into his presentation there were no breaks to deal with his basic needs. The first approach to assessment of aggressive behavior in the emergency setting is to try to care for the basic needs of the individual to deescalate the situation. Finally, he had recently been started on sertraline, a selective serotonin reuptake inhibitor. He had been having some dyspepsia and/or nausea with the sertraline, leading to his having missed some doses. Some children and adolescents have a discontinuation syndrome, which can be more severe in younger children and with medications that have shorter half-lives.2 In Henry’s case, a missed dose or two can be enough to trigger this discontinuation response leading to more aggressive behavior.
Case follow-up
The child and adolescent psychiatrist called to the case received a history from the primary team. When he started to try to talk with the parent outside of the room, the child became upset. He was able to gather the information that Henry also had skipped breakfast. In an attempt to calm the patient down, the psychiatrist addressed Henry using a nonjudgmental, nonconfrontational, collaborative approach, incorporating play. Henry responded to this approach and allowed the psychiatrist to ask a few questions about basic needs, and admitted that he was hungry. He was offered a turkey sandwich, which was rapidly ingested. The tantrum slowly subsided. Within about 30 minutes (and with some more food), the child was able to sit on his parent’s lap and finish the interview. The decision was made to have him follow up with his primary care provider to change to an SSRI with a longer half-life, such as fluoxetine, as he did seem to be experiencing some discontinuation even after missing just a dose or two of sertraline.
When dealing with emergent, aggressive behavior, food isn’t always the best medicine, but sometimes it is. Environmental barriers to the child’s regaining control include hunger, thirst, a full bladder, constipation, or other pain. Attending to these issues first sometimes can help avoid sedating medications, which can prolong emergency visits and lead to unwelcome side effects.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at pdnews@mdedge.com.
References
1. Pediatrics. 2011 May;127(5):e1356-66.
2. J Can Acad Child Adolesc Psychiatry. 2011 Feb;20(1):60-7.
Phase 3 data support apixaban for cancer-associated VTE
SAN DIEGO – according to the Phase 3 ADAM VTE trial.
The rates of major bleeding and clinically relevant nonmajor bleeding in patients who received apixaban were similar to those in patients who received dalteparin. However, the rate of VTE recurrence was significantly lower with apixaban than it was with dalteparin.
“[A]pixaban was associated with very low bleeding rates and venous thrombosis recurrence rates compared to dalteparin,” said Robert D. McBane II, MD, of the Mayo Clinic in Rochester, Minn., at the annual meeting of the American Society of Hematology.
The trial included 300 adults (aged 18 years and older) with active cancer and acute VTE who were randomized to receive apixaban (n = 150) or dalteparin (n = 150). The dose and schedule for oral apixaban was 10 mg twice daily for 7 days followed by 5 mg twice daily for 6 months. Dalteparin was given subcutaneously at 200 IU/kg per day for 1 month followed by 150 IU/kg daily for 6 months. Among the patients in the study, 145 patients in the apixaban arm and 142 in the dalteparin arm ultimately received their assigned treatment.
Every month, patients completed an anticoagulation satisfaction survey and bruise survey (a modification of the Duke Anticoagulation Satisfaction Scale). They also underwent lab testing (complete blood count, liver and renal function testing) and were assessed for outcomes, medication reconciliation, drug compliance, and ECOG status on a monthly basis.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The mean age was 64 years in both arms, and roughly half of patients in both arms were female. Hematologic malignancies were present in 9% of patients in the apixaban arm and 11% in the dalteparin arm. Others included lung, colorectal,
pancreatic/hepatobiliary, gynecologic, breast, genitourinary, upper gastrointestinal, and brain cancers.
Of patients in the study, 65% of those in the apixaban arm and 66% in the dalteparin arm had distant metastasis, and 74% of patients in both arms were receiving chemotherapy while on study.
Patients had the following qualifying thrombotic events:
- Any pulmonary embolism (PE) – 55% of patients in the apixaban arm and 51% in the dalteparin arm
- Any deep vein thrombosis (DVT) – 48% and 47%, respectively
- PE only – 44% and 39%, respectively
- PE with DVT – 12% in both arms
- DVT only – 37% and 35%, respectively
- Lower extremity DVT – 31% and 34%, respectively
- Upper extremity DVT – 17% and 14%, respectively
- Cerebral venous thrombosis (VT) – 1% and 0%, respectively
- Splanchnic VT – 8% and 18%, respectively.
Bleeding, thrombosis, and death
The study’s primary endpoint was major bleeding, which did not occur in any of the apixaban-treated patients. However, major bleeding did occur in two (1.4%) patients in the dalteparin arm (P = .14).
A secondary endpoint was major bleeding plus clinically relevant nonmajor bleeding. This occurred in nine (6.2%) patients in the apixaban arm and nine (6.3%) in the dalteparin arm (P = .88).
The researchers also assessed VTE recurrence. One patient in the apixaban arm (0.7%) and nine in the dalteparin arm (6.3%) had VTE recurrence (P = .03).
The patient in the apixaban arm experienced cerebral VT, and the patients with recurrence in the dalteparin arm had leg (n = 4) or arm (n = 2) VTE, PE (n = 1), or splanchnic VT (n = 2).
One patient in each arm (0.7%) had arterial thrombosis.
There was no significant difference in cumulative mortality between the treatment arms (hazard ratio, 1.40; P = .3078).
Satisfaction and discontinuation
Overall, apixaban fared better than dalteparin in the monthly patient satisfaction surveys. At various time points, apixaban-treated patients were significantly less likely to be concerned about excessive bruising, find anticoagulant treatment a burden or difficult to carry out, or say anticoagulant treatment added stress to their lives, negatively impacted their quality of life, or caused them “a great deal” of worry, irritation, or frustration.
However, apixaban-treated patients were less likely than dalteparin recipients to have confidence that their drug protected them from VTE recurrence, while the apixaban recipients were more likely than the dalteparin group to report overall satisfaction with their treatment.
In addition, premature treatment discontinuation was more common in the dalteparin group than in the apixaban group – 15% and 4%, respectively (P = .0012).
“Apixaban was well tolerated with superior patient safety satisfaction, as well as significantly fewer study drug discontinuations compared to dalteparin,” Dr. McBane said. “I believe that these data support the use of apixaban for the acute treatment of cancer-associated venous thromboembolism.”
This study was funded by BMS/Pfizer Alliance. Dr. McBane declared no other conflicts of interest.
jensmith@mdedge.com
SOURCE: McBane RD et al. ASH 2018, Abstract 421.
SAN DIEGO – according to the Phase 3 ADAM VTE trial.
The rates of major bleeding and clinically relevant nonmajor bleeding in patients who received apixaban were similar to those in patients who received dalteparin. However, the rate of VTE recurrence was significantly lower with apixaban than it was with dalteparin.
“[A]pixaban was associated with very low bleeding rates and venous thrombosis recurrence rates compared to dalteparin,” said Robert D. McBane II, MD, of the Mayo Clinic in Rochester, Minn., at the annual meeting of the American Society of Hematology.
The trial included 300 adults (aged 18 years and older) with active cancer and acute VTE who were randomized to receive apixaban (n = 150) or dalteparin (n = 150). The dose and schedule for oral apixaban was 10 mg twice daily for 7 days followed by 5 mg twice daily for 6 months. Dalteparin was given subcutaneously at 200 IU/kg per day for 1 month followed by 150 IU/kg daily for 6 months. Among the patients in the study, 145 patients in the apixaban arm and 142 in the dalteparin arm ultimately received their assigned treatment.
Every month, patients completed an anticoagulation satisfaction survey and bruise survey (a modification of the Duke Anticoagulation Satisfaction Scale). They also underwent lab testing (complete blood count, liver and renal function testing) and were assessed for outcomes, medication reconciliation, drug compliance, and ECOG status on a monthly basis.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The mean age was 64 years in both arms, and roughly half of patients in both arms were female. Hematologic malignancies were present in 9% of patients in the apixaban arm and 11% in the dalteparin arm. Others included lung, colorectal,
pancreatic/hepatobiliary, gynecologic, breast, genitourinary, upper gastrointestinal, and brain cancers.
Of patients in the study, 65% of those in the apixaban arm and 66% in the dalteparin arm had distant metastasis, and 74% of patients in both arms were receiving chemotherapy while on study.
Patients had the following qualifying thrombotic events:
- Any pulmonary embolism (PE) – 55% of patients in the apixaban arm and 51% in the dalteparin arm
- Any deep vein thrombosis (DVT) – 48% and 47%, respectively
- PE only – 44% and 39%, respectively
- PE with DVT – 12% in both arms
- DVT only – 37% and 35%, respectively
- Lower extremity DVT – 31% and 34%, respectively
- Upper extremity DVT – 17% and 14%, respectively
- Cerebral venous thrombosis (VT) – 1% and 0%, respectively
- Splanchnic VT – 8% and 18%, respectively.
Bleeding, thrombosis, and death
The study’s primary endpoint was major bleeding, which did not occur in any of the apixaban-treated patients. However, major bleeding did occur in two (1.4%) patients in the dalteparin arm (P = .14).
A secondary endpoint was major bleeding plus clinically relevant nonmajor bleeding. This occurred in nine (6.2%) patients in the apixaban arm and nine (6.3%) in the dalteparin arm (P = .88).
The researchers also assessed VTE recurrence. One patient in the apixaban arm (0.7%) and nine in the dalteparin arm (6.3%) had VTE recurrence (P = .03).
The patient in the apixaban arm experienced cerebral VT, and the patients with recurrence in the dalteparin arm had leg (n = 4) or arm (n = 2) VTE, PE (n = 1), or splanchnic VT (n = 2).
One patient in each arm (0.7%) had arterial thrombosis.
There was no significant difference in cumulative mortality between the treatment arms (hazard ratio, 1.40; P = .3078).
Satisfaction and discontinuation
Overall, apixaban fared better than dalteparin in the monthly patient satisfaction surveys. At various time points, apixaban-treated patients were significantly less likely to be concerned about excessive bruising, find anticoagulant treatment a burden or difficult to carry out, or say anticoagulant treatment added stress to their lives, negatively impacted their quality of life, or caused them “a great deal” of worry, irritation, or frustration.
However, apixaban-treated patients were less likely than dalteparin recipients to have confidence that their drug protected them from VTE recurrence, while the apixaban recipients were more likely than the dalteparin group to report overall satisfaction with their treatment.
In addition, premature treatment discontinuation was more common in the dalteparin group than in the apixaban group – 15% and 4%, respectively (P = .0012).
“Apixaban was well tolerated with superior patient safety satisfaction, as well as significantly fewer study drug discontinuations compared to dalteparin,” Dr. McBane said. “I believe that these data support the use of apixaban for the acute treatment of cancer-associated venous thromboembolism.”
This study was funded by BMS/Pfizer Alliance. Dr. McBane declared no other conflicts of interest.
jensmith@mdedge.com
SOURCE: McBane RD et al. ASH 2018, Abstract 421.
SAN DIEGO – according to the Phase 3 ADAM VTE trial.
The rates of major bleeding and clinically relevant nonmajor bleeding in patients who received apixaban were similar to those in patients who received dalteparin. However, the rate of VTE recurrence was significantly lower with apixaban than it was with dalteparin.
“[A]pixaban was associated with very low bleeding rates and venous thrombosis recurrence rates compared to dalteparin,” said Robert D. McBane II, MD, of the Mayo Clinic in Rochester, Minn., at the annual meeting of the American Society of Hematology.
The trial included 300 adults (aged 18 years and older) with active cancer and acute VTE who were randomized to receive apixaban (n = 150) or dalteparin (n = 150). The dose and schedule for oral apixaban was 10 mg twice daily for 7 days followed by 5 mg twice daily for 6 months. Dalteparin was given subcutaneously at 200 IU/kg per day for 1 month followed by 150 IU/kg daily for 6 months. Among the patients in the study, 145 patients in the apixaban arm and 142 in the dalteparin arm ultimately received their assigned treatment.
Every month, patients completed an anticoagulation satisfaction survey and bruise survey (a modification of the Duke Anticoagulation Satisfaction Scale). They also underwent lab testing (complete blood count, liver and renal function testing) and were assessed for outcomes, medication reconciliation, drug compliance, and ECOG status on a monthly basis.
Patient characteristics
Baseline characteristics were similar between the treatment arms. The mean age was 64 years in both arms, and roughly half of patients in both arms were female. Hematologic malignancies were present in 9% of patients in the apixaban arm and 11% in the dalteparin arm. Others included lung, colorectal,
pancreatic/hepatobiliary, gynecologic, breast, genitourinary, upper gastrointestinal, and brain cancers.
Of patients in the study, 65% of those in the apixaban arm and 66% in the dalteparin arm had distant metastasis, and 74% of patients in both arms were receiving chemotherapy while on study.
Patients had the following qualifying thrombotic events:
- Any pulmonary embolism (PE) – 55% of patients in the apixaban arm and 51% in the dalteparin arm
- Any deep vein thrombosis (DVT) – 48% and 47%, respectively
- PE only – 44% and 39%, respectively
- PE with DVT – 12% in both arms
- DVT only – 37% and 35%, respectively
- Lower extremity DVT – 31% and 34%, respectively
- Upper extremity DVT – 17% and 14%, respectively
- Cerebral venous thrombosis (VT) – 1% and 0%, respectively
- Splanchnic VT – 8% and 18%, respectively.
Bleeding, thrombosis, and death
The study’s primary endpoint was major bleeding, which did not occur in any of the apixaban-treated patients. However, major bleeding did occur in two (1.4%) patients in the dalteparin arm (P = .14).
A secondary endpoint was major bleeding plus clinically relevant nonmajor bleeding. This occurred in nine (6.2%) patients in the apixaban arm and nine (6.3%) in the dalteparin arm (P = .88).
The researchers also assessed VTE recurrence. One patient in the apixaban arm (0.7%) and nine in the dalteparin arm (6.3%) had VTE recurrence (P = .03).
The patient in the apixaban arm experienced cerebral VT, and the patients with recurrence in the dalteparin arm had leg (n = 4) or arm (n = 2) VTE, PE (n = 1), or splanchnic VT (n = 2).
One patient in each arm (0.7%) had arterial thrombosis.
There was no significant difference in cumulative mortality between the treatment arms (hazard ratio, 1.40; P = .3078).
Satisfaction and discontinuation
Overall, apixaban fared better than dalteparin in the monthly patient satisfaction surveys. At various time points, apixaban-treated patients were significantly less likely to be concerned about excessive bruising, find anticoagulant treatment a burden or difficult to carry out, or say anticoagulant treatment added stress to their lives, negatively impacted their quality of life, or caused them “a great deal” of worry, irritation, or frustration.
However, apixaban-treated patients were less likely than dalteparin recipients to have confidence that their drug protected them from VTE recurrence, while the apixaban recipients were more likely than the dalteparin group to report overall satisfaction with their treatment.
In addition, premature treatment discontinuation was more common in the dalteparin group than in the apixaban group – 15% and 4%, respectively (P = .0012).
“Apixaban was well tolerated with superior patient safety satisfaction, as well as significantly fewer study drug discontinuations compared to dalteparin,” Dr. McBane said. “I believe that these data support the use of apixaban for the acute treatment of cancer-associated venous thromboembolism.”
This study was funded by BMS/Pfizer Alliance. Dr. McBane declared no other conflicts of interest.
jensmith@mdedge.com
SOURCE: McBane RD et al. ASH 2018, Abstract 421.
REPORTING FROM ASH 2018
Key clinical point: Apixaban is associated with a similar risk of major bleeding and a lower risk of VTE recurrence when compared with dalteparin in patients with cancer-associated VTE.
Major finding: There were no major bleeding events in the apixaban arm and two in the dalteparin arm (P = .14).
Study details: Phase 3 study of 300 patients.
Disclosures: This study was funded by BMS/Pfizer Alliance.
Source: McBane RD et al. ASH 2018, Abstract 421.
Open enrollment 2019: Busiest week so far at HealthCare.gov
but the weekly and cumulative totals for plans selected continued to run below last year’s levels, according to the Centers for Medicare & Medicaid Services.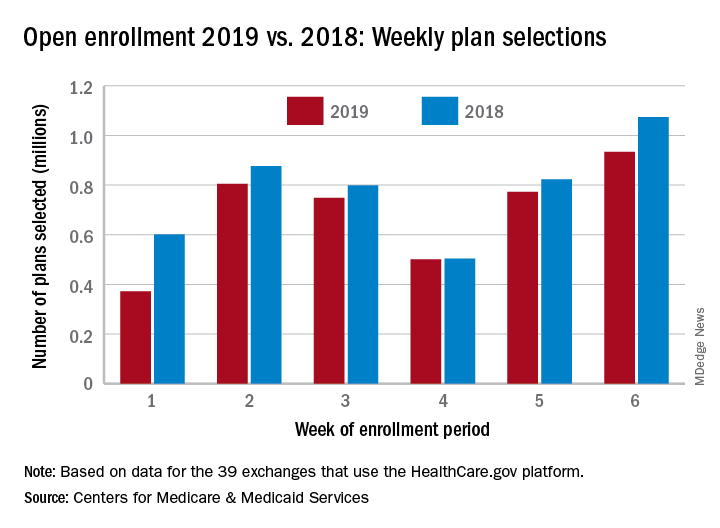
Over 934,000 plans were selected from Dec. 2 to Dec. 8, which puts the total at 4.13 million plans for the 2019 coverage year in the 39 states that use the HealthCare.gov platform, the CMS reported. Consumers renewing their coverage make up the majority of plans selected during week 6 (640,000) and cumulatively for the season (3.03 million), with new applications running at 295,000 for week 6 and 1.1 million overall.
Those numbers are down from last year, when 1.07 million plans (685,000 renewals and 389,000 new applications) were selected during week 6 of open enrollment for the 2018 coverage year, which brought the total for the season at the time to 4.68 million (3.30 million/1.38 million), CMS data show.
The deadline to enroll in a plan for 2019 is Dec. 15.
but the weekly and cumulative totals for plans selected continued to run below last year’s levels, according to the Centers for Medicare & Medicaid Services.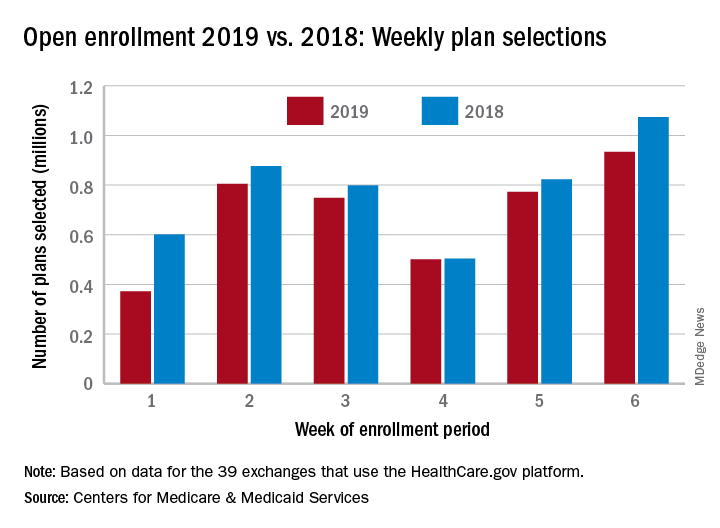
Over 934,000 plans were selected from Dec. 2 to Dec. 8, which puts the total at 4.13 million plans for the 2019 coverage year in the 39 states that use the HealthCare.gov platform, the CMS reported. Consumers renewing their coverage make up the majority of plans selected during week 6 (640,000) and cumulatively for the season (3.03 million), with new applications running at 295,000 for week 6 and 1.1 million overall.
Those numbers are down from last year, when 1.07 million plans (685,000 renewals and 389,000 new applications) were selected during week 6 of open enrollment for the 2018 coverage year, which brought the total for the season at the time to 4.68 million (3.30 million/1.38 million), CMS data show.
The deadline to enroll in a plan for 2019 is Dec. 15.
but the weekly and cumulative totals for plans selected continued to run below last year’s levels, according to the Centers for Medicare & Medicaid Services.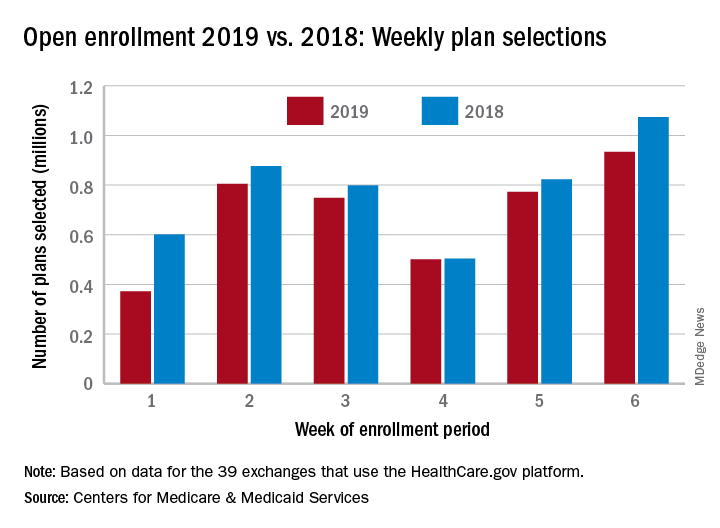
Over 934,000 plans were selected from Dec. 2 to Dec. 8, which puts the total at 4.13 million plans for the 2019 coverage year in the 39 states that use the HealthCare.gov platform, the CMS reported. Consumers renewing their coverage make up the majority of plans selected during week 6 (640,000) and cumulatively for the season (3.03 million), with new applications running at 295,000 for week 6 and 1.1 million overall.
Those numbers are down from last year, when 1.07 million plans (685,000 renewals and 389,000 new applications) were selected during week 6 of open enrollment for the 2018 coverage year, which brought the total for the season at the time to 4.68 million (3.30 million/1.38 million), CMS data show.
The deadline to enroll in a plan for 2019 is Dec. 15.
FDA issues alert over e-liquids with undeclared drugs
The Food and Drug Administration has issued an alert regarding two . E-liquid is the flavored mixture used in electronic cigarettes.
In a laboratory analysis, the FDA found that “E-Cialis HelloCig E-Liquid” contained both sildenafil and tadalafil, and that “E-Rimonabant HelloCig E-Liquid” contained sildenafil. Sildenafil and tadalafil are approved for the treatment of erectile dysfunction. Unapproved usage of these drugs in over-the-counter e-liquids is therefore illegal.
Both sildenafil and tadalafil can interact with nitrates found in some prescription drugs and can cause a dangerous lowering of blood pressure. Conditions commonly treated with nitrates include diabetes, high blood pressure, high cholesterol, or heart disease.
“FDA recently warned HelloCig of these issues and contacted the company several times to recommend they recall these products due to the risks to consumers. However, HelloCig has not responded to the agency’s recommendation. Therefore, FDA urges consumers to stop using these products and to contact their health care professional with any concerns associated with their use,” the FDA said in the press release.
Find the full press release on the FDA website.
The Food and Drug Administration has issued an alert regarding two . E-liquid is the flavored mixture used in electronic cigarettes.
In a laboratory analysis, the FDA found that “E-Cialis HelloCig E-Liquid” contained both sildenafil and tadalafil, and that “E-Rimonabant HelloCig E-Liquid” contained sildenafil. Sildenafil and tadalafil are approved for the treatment of erectile dysfunction. Unapproved usage of these drugs in over-the-counter e-liquids is therefore illegal.
Both sildenafil and tadalafil can interact with nitrates found in some prescription drugs and can cause a dangerous lowering of blood pressure. Conditions commonly treated with nitrates include diabetes, high blood pressure, high cholesterol, or heart disease.
“FDA recently warned HelloCig of these issues and contacted the company several times to recommend they recall these products due to the risks to consumers. However, HelloCig has not responded to the agency’s recommendation. Therefore, FDA urges consumers to stop using these products and to contact their health care professional with any concerns associated with their use,” the FDA said in the press release.
Find the full press release on the FDA website.
The Food and Drug Administration has issued an alert regarding two . E-liquid is the flavored mixture used in electronic cigarettes.
In a laboratory analysis, the FDA found that “E-Cialis HelloCig E-Liquid” contained both sildenafil and tadalafil, and that “E-Rimonabant HelloCig E-Liquid” contained sildenafil. Sildenafil and tadalafil are approved for the treatment of erectile dysfunction. Unapproved usage of these drugs in over-the-counter e-liquids is therefore illegal.
Both sildenafil and tadalafil can interact with nitrates found in some prescription drugs and can cause a dangerous lowering of blood pressure. Conditions commonly treated with nitrates include diabetes, high blood pressure, high cholesterol, or heart disease.
“FDA recently warned HelloCig of these issues and contacted the company several times to recommend they recall these products due to the risks to consumers. However, HelloCig has not responded to the agency’s recommendation. Therefore, FDA urges consumers to stop using these products and to contact their health care professional with any concerns associated with their use,” the FDA said in the press release.
Find the full press release on the FDA website.
Severe adverse events seen in placebo arm of cancer clinical trials
A significant number of patients who receive only a placebo in a clinical trial of cancer immunotherapy still experience grade three or grade four adverse events, research suggests.
Writing in JAMA Network Open, researchers reported the outcomes of a systematic review and meta-analysis of 10 randomized, double-blind, placebo-controlled, phase 3 trials of targeted therapy or immunotherapy drugs for cancer, in which patients in the placebo group were treated only with placebo and no other anticancer drugs.
Among the 4,873 patients who were randomized to placebo, a mean of 85.1% experienced some sort of placebo adverse event. The overall incidence of grade 3-4 placebo adverse events was 18% but was as high as 25% in two trials – one in renal cell carcinoma and one in melanoma – and as low as 11% in one trial.
Hypertension was the most frequent grade 3-4 adverse event among patients on placebo, experienced by a mean of 2.8% of patients, followed by fatigue (1%) and diarrhea (0.8%).
Neither route of administration nor cancer type made a significant difference in terms of the rate of placebo adverse events. No deaths attributed to the placebo were reported, but the mean rate of discontinuation due to placebo adverse events was 3.9%, and was higher than 5% for four trials.
The median duration of placebo administration ranged from 10 to 15 months for all but one study, and the authors noted that the longer the placebo exposure, the higher the proportion of grade 3-4 adverse events.
The investigators – Matías Rodrigo Chacón, MD, and his colleagues in the research department at the Argentine Association of Clinical Oncology – said that studies with a lower incidence of grade 3-4 adverse events in the treatment arm also had a lower incidence of grade 3-4 placebo adverse events, while the higher incidences of placebo adverse events were seen in studies that also had a higher incidence of treatment-related adverse events.
They suggested that “contextual factors,” such as the information given during the informed consent process, could contribute to negative expectations of adverse events.
“To illustrate this point, in an RCT [randomized controlled trial] of aspirin as a treatment for unstable angina, a higher incidence of gastrointestinal irritation was reported in centers that specified its potential occurrence in the informed consent compared with research units that did not include that risk,” they wrote.
They also suggested that patients may experience anxiety associated with the uncertainty about whether they had received active treatment or placebo, and this could also affect their distress levels.
No conflicts of interest were declared.
SOURCE: Chacón M et al. JAMA Network Open. 2018 Dec 7. doi: 10.1001/jamanetworkopen.2018.5617.
A significant number of patients who receive only a placebo in a clinical trial of cancer immunotherapy still experience grade three or grade four adverse events, research suggests.
Writing in JAMA Network Open, researchers reported the outcomes of a systematic review and meta-analysis of 10 randomized, double-blind, placebo-controlled, phase 3 trials of targeted therapy or immunotherapy drugs for cancer, in which patients in the placebo group were treated only with placebo and no other anticancer drugs.
Among the 4,873 patients who were randomized to placebo, a mean of 85.1% experienced some sort of placebo adverse event. The overall incidence of grade 3-4 placebo adverse events was 18% but was as high as 25% in two trials – one in renal cell carcinoma and one in melanoma – and as low as 11% in one trial.
Hypertension was the most frequent grade 3-4 adverse event among patients on placebo, experienced by a mean of 2.8% of patients, followed by fatigue (1%) and diarrhea (0.8%).
Neither route of administration nor cancer type made a significant difference in terms of the rate of placebo adverse events. No deaths attributed to the placebo were reported, but the mean rate of discontinuation due to placebo adverse events was 3.9%, and was higher than 5% for four trials.
The median duration of placebo administration ranged from 10 to 15 months for all but one study, and the authors noted that the longer the placebo exposure, the higher the proportion of grade 3-4 adverse events.
The investigators – Matías Rodrigo Chacón, MD, and his colleagues in the research department at the Argentine Association of Clinical Oncology – said that studies with a lower incidence of grade 3-4 adverse events in the treatment arm also had a lower incidence of grade 3-4 placebo adverse events, while the higher incidences of placebo adverse events were seen in studies that also had a higher incidence of treatment-related adverse events.
They suggested that “contextual factors,” such as the information given during the informed consent process, could contribute to negative expectations of adverse events.
“To illustrate this point, in an RCT [randomized controlled trial] of aspirin as a treatment for unstable angina, a higher incidence of gastrointestinal irritation was reported in centers that specified its potential occurrence in the informed consent compared with research units that did not include that risk,” they wrote.
They also suggested that patients may experience anxiety associated with the uncertainty about whether they had received active treatment or placebo, and this could also affect their distress levels.
No conflicts of interest were declared.
SOURCE: Chacón M et al. JAMA Network Open. 2018 Dec 7. doi: 10.1001/jamanetworkopen.2018.5617.
A significant number of patients who receive only a placebo in a clinical trial of cancer immunotherapy still experience grade three or grade four adverse events, research suggests.
Writing in JAMA Network Open, researchers reported the outcomes of a systematic review and meta-analysis of 10 randomized, double-blind, placebo-controlled, phase 3 trials of targeted therapy or immunotherapy drugs for cancer, in which patients in the placebo group were treated only with placebo and no other anticancer drugs.
Among the 4,873 patients who were randomized to placebo, a mean of 85.1% experienced some sort of placebo adverse event. The overall incidence of grade 3-4 placebo adverse events was 18% but was as high as 25% in two trials – one in renal cell carcinoma and one in melanoma – and as low as 11% in one trial.
Hypertension was the most frequent grade 3-4 adverse event among patients on placebo, experienced by a mean of 2.8% of patients, followed by fatigue (1%) and diarrhea (0.8%).
Neither route of administration nor cancer type made a significant difference in terms of the rate of placebo adverse events. No deaths attributed to the placebo were reported, but the mean rate of discontinuation due to placebo adverse events was 3.9%, and was higher than 5% for four trials.
The median duration of placebo administration ranged from 10 to 15 months for all but one study, and the authors noted that the longer the placebo exposure, the higher the proportion of grade 3-4 adverse events.
The investigators – Matías Rodrigo Chacón, MD, and his colleagues in the research department at the Argentine Association of Clinical Oncology – said that studies with a lower incidence of grade 3-4 adverse events in the treatment arm also had a lower incidence of grade 3-4 placebo adverse events, while the higher incidences of placebo adverse events were seen in studies that also had a higher incidence of treatment-related adverse events.
They suggested that “contextual factors,” such as the information given during the informed consent process, could contribute to negative expectations of adverse events.
“To illustrate this point, in an RCT [randomized controlled trial] of aspirin as a treatment for unstable angina, a higher incidence of gastrointestinal irritation was reported in centers that specified its potential occurrence in the informed consent compared with research units that did not include that risk,” they wrote.
They also suggested that patients may experience anxiety associated with the uncertainty about whether they had received active treatment or placebo, and this could also affect their distress levels.
No conflicts of interest were declared.
SOURCE: Chacón M et al. JAMA Network Open. 2018 Dec 7. doi: 10.1001/jamanetworkopen.2018.5617.
FROM JAMA NETWORK OPEN
Key clinical point: Serious adverse events can occur in patients treated only with placebo in cancer clinical trials.
Major finding: The incidence of grade 3-4 placebo adverse events was 18% in cancer clinical trials.
Study details: Systematic review and meta-analysis of 10 randomized, placebo-controlled, double-blind trials.
Disclosures: No conflicts of interest were declared.
Source: Chacón M et al. JAMA Network Open. 2018 Dec 7. doi: 10.1001/jamanetworkopen.2018.5617.
Wasp-stung lung bugs, fat clay, Botoxed Vulcans, and ‘GOT’ mortality risk
The wonderful world of wasps
Never thought you’d be thankful for wasps, did you? Neither did we. Using mice as test subjects, scientists at MIT found that a tiny peptide in the venom was able to completely eliminate Pseudomonas aeruginosa, which causes respiratory infections and is often resistant to antibiotics. Now if you’re sick, all you have to do is go outside and get stung by a bunch of wasps!
Wait, no, that’s not right. The researchers at MIT engineered a molecule that can be used to create an antibiotic that’s safe for humans. While most insect venom is chock full of compounds that are toxic to humans, the scientists were able to transform their tiny peptide into a bacteria-defeating machine. This is a big victory in the war against antibiotic-resistant bacteria. Go, wasps!
Live long and Botox
Talk about highly illogical! Botox patients sometimes return for follow-up visits with dermatologist Kelly Stankiewicz, MD, and haven’t noticed they’ve “Spocked,” even though it may be obvious to just about everyone else.
But other Botox patients are most certainly aware that their eyebrows have arched up on the right and left sides – just like those of a certain Vulcan character on “Star Trek.” And they want to be beamed out of that uncomfortable situation pronto.
Dr. Stankiewicz, who works in Park City, Utah, explained the “Spocking” phenomenon in a presentation about facial treatments at the recent Las Vegas Dermatology Symposium. Spocking can occur in patents who get Botox treatment to eliminate the “11 line” – two vertical wrinkles – between the eyebrows, Dr. Stankiewicz said. It occurs “when the middle of the forehead doesn’t move but the outside does,” she said, causing an unsightly outwardly arched eyebrow look.
The solution to Spocking is easy, she said: “Put a tiny bit of Botox in the forehead muscle right where the eyebrow is peaking the most.”
Leonard Nimoy, the original Mr. Spock, is not available for comment, given that he died in 2015. But Dr. Stankiewicz does have a perspective on Mr. Spock’s trademark look: “It’s like the people who drew his brow knew that Botox was on the horizon.”
Add the dirt, lose the fat
Lots of things are supposed to be stronger than dirt, but it looks like obesity might not be one of them. Investigators who were trying to improve drug delivery using a type of clay – spray-dried smectite clay particles, to be exact – discovered that it has “a unique ability to ‘soak up’ fat droplets in the gut,” according to a statement from the University of South Australia, Adelaide.
“Not only were the clay materials trapping the fats within their particle structure, but they were also preventing them from being absorbed by the body, ensuring that fat simply passed through the digestive system,” researcher Tahnee J. Dening said.
In the study, the smectite outperformed the weight-loss drug orlistat in rats fed a high-fat diet for 2 weeks (Pharm Res. 2019;36:21 doi: 10.1007/s11095-018-2552-9). Even better, smectite is already widely used in foods and nutraceuticals and is considered to be safe. Even even better, smectite is a really fun word to say. And with the prevalence of obesity such as it is, we’re sure that physicians will prescribe smectite just so they can say “smectite” to their patients. Smectite.
When you play the game of thrones …
… You conduct an evidence-based analysis of mortality across the Seven Kingdoms. In celebration of the approaching final season, two researchers published a study of mortality and survival in HBO’s “Game of Thrones” series. They examined data on sociodemographic factors and circumstances of death to identify predictors of mortality.
After looking at 330 characters from the show (186 who suffered death), the authors determined that being male, lowborn, and loyal had the highest correlation with mortality. Poor men who never switched their allegiance from one side to the other had the lowest chance of survival. In addition, the probability of dying in the first hour after appearing on screen was 14%. Not a good statistic if you’re trying to become famous in Westeros. And a mortality risk rivaling even that of Mr. Spock’s red-shirted shipmates down in engineering.
Nurse, sand wedge, STAT!
There really is no sport like golf. The wide green spaces, the fresh air, the thrill of launching a 300-yard drive down the fairway, the fun of double-bogeying the last three holes to shoot yet another 93; golf is a noble pursuit, indeed. And a sport everyone knows doctors love. Right?
In research published in the Christmas edition of the BMJ, a group of doctors from Massachusetts sought to find out just how accurate the stereotype was. Their answer? Doctors really do enjoy teeing it up.
Well, male doctors.
Well, old male doctors.
Using a database of about a million physicians, the researchers found that 5.5% of male physicians and 1.3% of female physicians – or 4.1% overall – maintained an official United States Golf Association handicap. Male physicians aged 61-70 years were most likely to play, and female physicians aged 31-35 years were least likely.
However, while golf is certainly a common pastime among doctors, they aren’t exactly very good at it, as the average doctor is actually slightly worse than the average nondoctor. Surgeons presented a notable exception, possessing significantly lower handicaps than their colleagues while, perhaps not coincidentally, also playing more often. We’re sure there’s a joke about overpaid surgeons in narrow specialties having too much time on their hands, and we’ll get right back to you with it after our 12 o’clock tee time.
The wonderful world of wasps
Never thought you’d be thankful for wasps, did you? Neither did we. Using mice as test subjects, scientists at MIT found that a tiny peptide in the venom was able to completely eliminate Pseudomonas aeruginosa, which causes respiratory infections and is often resistant to antibiotics. Now if you’re sick, all you have to do is go outside and get stung by a bunch of wasps!
Wait, no, that’s not right. The researchers at MIT engineered a molecule that can be used to create an antibiotic that’s safe for humans. While most insect venom is chock full of compounds that are toxic to humans, the scientists were able to transform their tiny peptide into a bacteria-defeating machine. This is a big victory in the war against antibiotic-resistant bacteria. Go, wasps!
Live long and Botox
Talk about highly illogical! Botox patients sometimes return for follow-up visits with dermatologist Kelly Stankiewicz, MD, and haven’t noticed they’ve “Spocked,” even though it may be obvious to just about everyone else.
But other Botox patients are most certainly aware that their eyebrows have arched up on the right and left sides – just like those of a certain Vulcan character on “Star Trek.” And they want to be beamed out of that uncomfortable situation pronto.
Dr. Stankiewicz, who works in Park City, Utah, explained the “Spocking” phenomenon in a presentation about facial treatments at the recent Las Vegas Dermatology Symposium. Spocking can occur in patents who get Botox treatment to eliminate the “11 line” – two vertical wrinkles – between the eyebrows, Dr. Stankiewicz said. It occurs “when the middle of the forehead doesn’t move but the outside does,” she said, causing an unsightly outwardly arched eyebrow look.
The solution to Spocking is easy, she said: “Put a tiny bit of Botox in the forehead muscle right where the eyebrow is peaking the most.”
Leonard Nimoy, the original Mr. Spock, is not available for comment, given that he died in 2015. But Dr. Stankiewicz does have a perspective on Mr. Spock’s trademark look: “It’s like the people who drew his brow knew that Botox was on the horizon.”
Add the dirt, lose the fat
Lots of things are supposed to be stronger than dirt, but it looks like obesity might not be one of them. Investigators who were trying to improve drug delivery using a type of clay – spray-dried smectite clay particles, to be exact – discovered that it has “a unique ability to ‘soak up’ fat droplets in the gut,” according to a statement from the University of South Australia, Adelaide.
“Not only were the clay materials trapping the fats within their particle structure, but they were also preventing them from being absorbed by the body, ensuring that fat simply passed through the digestive system,” researcher Tahnee J. Dening said.
In the study, the smectite outperformed the weight-loss drug orlistat in rats fed a high-fat diet for 2 weeks (Pharm Res. 2019;36:21 doi: 10.1007/s11095-018-2552-9). Even better, smectite is already widely used in foods and nutraceuticals and is considered to be safe. Even even better, smectite is a really fun word to say. And with the prevalence of obesity such as it is, we’re sure that physicians will prescribe smectite just so they can say “smectite” to their patients. Smectite.
When you play the game of thrones …
… You conduct an evidence-based analysis of mortality across the Seven Kingdoms. In celebration of the approaching final season, two researchers published a study of mortality and survival in HBO’s “Game of Thrones” series. They examined data on sociodemographic factors and circumstances of death to identify predictors of mortality.
After looking at 330 characters from the show (186 who suffered death), the authors determined that being male, lowborn, and loyal had the highest correlation with mortality. Poor men who never switched their allegiance from one side to the other had the lowest chance of survival. In addition, the probability of dying in the first hour after appearing on screen was 14%. Not a good statistic if you’re trying to become famous in Westeros. And a mortality risk rivaling even that of Mr. Spock’s red-shirted shipmates down in engineering.
Nurse, sand wedge, STAT!
There really is no sport like golf. The wide green spaces, the fresh air, the thrill of launching a 300-yard drive down the fairway, the fun of double-bogeying the last three holes to shoot yet another 93; golf is a noble pursuit, indeed. And a sport everyone knows doctors love. Right?
In research published in the Christmas edition of the BMJ, a group of doctors from Massachusetts sought to find out just how accurate the stereotype was. Their answer? Doctors really do enjoy teeing it up.
Well, male doctors.
Well, old male doctors.
Using a database of about a million physicians, the researchers found that 5.5% of male physicians and 1.3% of female physicians – or 4.1% overall – maintained an official United States Golf Association handicap. Male physicians aged 61-70 years were most likely to play, and female physicians aged 31-35 years were least likely.
However, while golf is certainly a common pastime among doctors, they aren’t exactly very good at it, as the average doctor is actually slightly worse than the average nondoctor. Surgeons presented a notable exception, possessing significantly lower handicaps than their colleagues while, perhaps not coincidentally, also playing more often. We’re sure there’s a joke about overpaid surgeons in narrow specialties having too much time on their hands, and we’ll get right back to you with it after our 12 o’clock tee time.
The wonderful world of wasps
Never thought you’d be thankful for wasps, did you? Neither did we. Using mice as test subjects, scientists at MIT found that a tiny peptide in the venom was able to completely eliminate Pseudomonas aeruginosa, which causes respiratory infections and is often resistant to antibiotics. Now if you’re sick, all you have to do is go outside and get stung by a bunch of wasps!
Wait, no, that’s not right. The researchers at MIT engineered a molecule that can be used to create an antibiotic that’s safe for humans. While most insect venom is chock full of compounds that are toxic to humans, the scientists were able to transform their tiny peptide into a bacteria-defeating machine. This is a big victory in the war against antibiotic-resistant bacteria. Go, wasps!
Live long and Botox
Talk about highly illogical! Botox patients sometimes return for follow-up visits with dermatologist Kelly Stankiewicz, MD, and haven’t noticed they’ve “Spocked,” even though it may be obvious to just about everyone else.
But other Botox patients are most certainly aware that their eyebrows have arched up on the right and left sides – just like those of a certain Vulcan character on “Star Trek.” And they want to be beamed out of that uncomfortable situation pronto.
Dr. Stankiewicz, who works in Park City, Utah, explained the “Spocking” phenomenon in a presentation about facial treatments at the recent Las Vegas Dermatology Symposium. Spocking can occur in patents who get Botox treatment to eliminate the “11 line” – two vertical wrinkles – between the eyebrows, Dr. Stankiewicz said. It occurs “when the middle of the forehead doesn’t move but the outside does,” she said, causing an unsightly outwardly arched eyebrow look.
The solution to Spocking is easy, she said: “Put a tiny bit of Botox in the forehead muscle right where the eyebrow is peaking the most.”
Leonard Nimoy, the original Mr. Spock, is not available for comment, given that he died in 2015. But Dr. Stankiewicz does have a perspective on Mr. Spock’s trademark look: “It’s like the people who drew his brow knew that Botox was on the horizon.”
Add the dirt, lose the fat
Lots of things are supposed to be stronger than dirt, but it looks like obesity might not be one of them. Investigators who were trying to improve drug delivery using a type of clay – spray-dried smectite clay particles, to be exact – discovered that it has “a unique ability to ‘soak up’ fat droplets in the gut,” according to a statement from the University of South Australia, Adelaide.
“Not only were the clay materials trapping the fats within their particle structure, but they were also preventing them from being absorbed by the body, ensuring that fat simply passed through the digestive system,” researcher Tahnee J. Dening said.
In the study, the smectite outperformed the weight-loss drug orlistat in rats fed a high-fat diet for 2 weeks (Pharm Res. 2019;36:21 doi: 10.1007/s11095-018-2552-9). Even better, smectite is already widely used in foods and nutraceuticals and is considered to be safe. Even even better, smectite is a really fun word to say. And with the prevalence of obesity such as it is, we’re sure that physicians will prescribe smectite just so they can say “smectite” to their patients. Smectite.
When you play the game of thrones …
… You conduct an evidence-based analysis of mortality across the Seven Kingdoms. In celebration of the approaching final season, two researchers published a study of mortality and survival in HBO’s “Game of Thrones” series. They examined data on sociodemographic factors and circumstances of death to identify predictors of mortality.
After looking at 330 characters from the show (186 who suffered death), the authors determined that being male, lowborn, and loyal had the highest correlation with mortality. Poor men who never switched their allegiance from one side to the other had the lowest chance of survival. In addition, the probability of dying in the first hour after appearing on screen was 14%. Not a good statistic if you’re trying to become famous in Westeros. And a mortality risk rivaling even that of Mr. Spock’s red-shirted shipmates down in engineering.
Nurse, sand wedge, STAT!
There really is no sport like golf. The wide green spaces, the fresh air, the thrill of launching a 300-yard drive down the fairway, the fun of double-bogeying the last three holes to shoot yet another 93; golf is a noble pursuit, indeed. And a sport everyone knows doctors love. Right?
In research published in the Christmas edition of the BMJ, a group of doctors from Massachusetts sought to find out just how accurate the stereotype was. Their answer? Doctors really do enjoy teeing it up.
Well, male doctors.
Well, old male doctors.
Using a database of about a million physicians, the researchers found that 5.5% of male physicians and 1.3% of female physicians – or 4.1% overall – maintained an official United States Golf Association handicap. Male physicians aged 61-70 years were most likely to play, and female physicians aged 31-35 years were least likely.
However, while golf is certainly a common pastime among doctors, they aren’t exactly very good at it, as the average doctor is actually slightly worse than the average nondoctor. Surgeons presented a notable exception, possessing significantly lower handicaps than their colleagues while, perhaps not coincidentally, also playing more often. We’re sure there’s a joke about overpaid surgeons in narrow specialties having too much time on their hands, and we’ll get right back to you with it after our 12 o’clock tee time.
‘Optimal’ pazopanib levels linked to lower toxicity in RCC patients
In patients with renal cell carcinoma, trough concentrations of pazopanib in a specific target range were associated with better safety and comparable efficacy, versus higher concentrations of the drug, authors of an exploratory investigation have reported.
Fewer serious toxicities were seen in patients with pazopanib concentrations in the 20- to 50-mcg/mL range, yet overall response rate was similar compared to patients with concentrations over 50 mcg/mL, according to results of the retrospective study.
The findings suggest therapeutic drug monitoring to achieve a specific trough concentration may be useful to optimize pazopanib dosing, according to investigator Tomohiro Terada, PhD, of Shiga University of Medical Science Hospital, Japan, and coinvestigators.
Therapeutic drug monitoring for sunitinib in RCC patients was recently covered by medical insurance in Japan, Dr. Terada and colleagues wrote in Clinical Genitourinary Cancer.
The strategy may be especially suited to adjusting the dose of pazopanib, which is often associated with severe toxicities and has pharmacokinetics that suggest a wide variation between individuals, they added.
The retrospective study by Dr. Terada and colleagues included 27 renal cell carcinoma patients who received pazopanib at doses of 400, 600, or 800 mg daily based on the recommendation of the treating physician, with doses reduced or discontinued based on adverse events or progression.
Trough concentrations of pazopanib 3 months after starting the treatment ranged from a low of 10.6 mcg/mL to a high of 106 mcg/mL, with a median of 49.1 mcg/mL, according to the report.
One-third of patients experienced grade 3 or greater toxicities, including anorexia, hypertension, anemia, and thrombocytopenia, among others. The median pazopanib concentration for those nine patients was 69.3 mcg/mL, compared with 41.2 mcg/mL for those not experiencing serious toxicities (P less than .05).
A concentration over 50.3 mcg/mL predicted grade 3 or greater toxicity, statistical analysis showed, with 8 out of 13 patients with concentrations above that threshold experiencing serious toxicities. By contrast, 1 of 14 patients below that threshold experienced grade 3 or greater toxicities.
No responses were observed in three patients with pazopanib concentrations below 20.5 mcg/mL, a concentration level considered to be subtherapeutic based on previous investigations.
Overall response rates were similar for patients with concentrations in the “optimal” 20.5- and 50.3-mcg/mL range and those with concentrations over 50.3 mcg/mL, according to the investigators.
Among 11 patients in that “optimal” range, partial responses were seen in 5, they reported, while for the 13 patients with high concentrations of the drug, partial responses were seen in 4 patients and a complete response was seen in 1 patient.
Trough concentrations may not predict all types of toxicities, according to the investigators, who said that the results of their small, retrospective analysis should be validated in a large, prospective study.
In particular, there was no significant relationship between trough concentration of pazopanib and development of grade 2 or greater hepatotoxicity, a common and specific side effect of the drug.
“Based on these findings, pazopanib-induced hepatotoxicity may not be related to the pharmacokinetics of pazopanib,” they wrote. “Therefore, pharmacogenomics testing is needed to predict pazopanib-induced hepatotoxicity.”
Dr. Terada and coauthors said they had no conflicts of interest to report.
SOURCE: Noda S et al. Clin Genitourin Cancer. 2018 Dec 7. doi: 10.1016/j.clgc.2018.12.001.
In patients with renal cell carcinoma, trough concentrations of pazopanib in a specific target range were associated with better safety and comparable efficacy, versus higher concentrations of the drug, authors of an exploratory investigation have reported.
Fewer serious toxicities were seen in patients with pazopanib concentrations in the 20- to 50-mcg/mL range, yet overall response rate was similar compared to patients with concentrations over 50 mcg/mL, according to results of the retrospective study.
The findings suggest therapeutic drug monitoring to achieve a specific trough concentration may be useful to optimize pazopanib dosing, according to investigator Tomohiro Terada, PhD, of Shiga University of Medical Science Hospital, Japan, and coinvestigators.
Therapeutic drug monitoring for sunitinib in RCC patients was recently covered by medical insurance in Japan, Dr. Terada and colleagues wrote in Clinical Genitourinary Cancer.
The strategy may be especially suited to adjusting the dose of pazopanib, which is often associated with severe toxicities and has pharmacokinetics that suggest a wide variation between individuals, they added.
The retrospective study by Dr. Terada and colleagues included 27 renal cell carcinoma patients who received pazopanib at doses of 400, 600, or 800 mg daily based on the recommendation of the treating physician, with doses reduced or discontinued based on adverse events or progression.
Trough concentrations of pazopanib 3 months after starting the treatment ranged from a low of 10.6 mcg/mL to a high of 106 mcg/mL, with a median of 49.1 mcg/mL, according to the report.
One-third of patients experienced grade 3 or greater toxicities, including anorexia, hypertension, anemia, and thrombocytopenia, among others. The median pazopanib concentration for those nine patients was 69.3 mcg/mL, compared with 41.2 mcg/mL for those not experiencing serious toxicities (P less than .05).
A concentration over 50.3 mcg/mL predicted grade 3 or greater toxicity, statistical analysis showed, with 8 out of 13 patients with concentrations above that threshold experiencing serious toxicities. By contrast, 1 of 14 patients below that threshold experienced grade 3 or greater toxicities.
No responses were observed in three patients with pazopanib concentrations below 20.5 mcg/mL, a concentration level considered to be subtherapeutic based on previous investigations.
Overall response rates were similar for patients with concentrations in the “optimal” 20.5- and 50.3-mcg/mL range and those with concentrations over 50.3 mcg/mL, according to the investigators.
Among 11 patients in that “optimal” range, partial responses were seen in 5, they reported, while for the 13 patients with high concentrations of the drug, partial responses were seen in 4 patients and a complete response was seen in 1 patient.
Trough concentrations may not predict all types of toxicities, according to the investigators, who said that the results of their small, retrospective analysis should be validated in a large, prospective study.
In particular, there was no significant relationship between trough concentration of pazopanib and development of grade 2 or greater hepatotoxicity, a common and specific side effect of the drug.
“Based on these findings, pazopanib-induced hepatotoxicity may not be related to the pharmacokinetics of pazopanib,” they wrote. “Therefore, pharmacogenomics testing is needed to predict pazopanib-induced hepatotoxicity.”
Dr. Terada and coauthors said they had no conflicts of interest to report.
SOURCE: Noda S et al. Clin Genitourin Cancer. 2018 Dec 7. doi: 10.1016/j.clgc.2018.12.001.
In patients with renal cell carcinoma, trough concentrations of pazopanib in a specific target range were associated with better safety and comparable efficacy, versus higher concentrations of the drug, authors of an exploratory investigation have reported.
Fewer serious toxicities were seen in patients with pazopanib concentrations in the 20- to 50-mcg/mL range, yet overall response rate was similar compared to patients with concentrations over 50 mcg/mL, according to results of the retrospective study.
The findings suggest therapeutic drug monitoring to achieve a specific trough concentration may be useful to optimize pazopanib dosing, according to investigator Tomohiro Terada, PhD, of Shiga University of Medical Science Hospital, Japan, and coinvestigators.
Therapeutic drug monitoring for sunitinib in RCC patients was recently covered by medical insurance in Japan, Dr. Terada and colleagues wrote in Clinical Genitourinary Cancer.
The strategy may be especially suited to adjusting the dose of pazopanib, which is often associated with severe toxicities and has pharmacokinetics that suggest a wide variation between individuals, they added.
The retrospective study by Dr. Terada and colleagues included 27 renal cell carcinoma patients who received pazopanib at doses of 400, 600, or 800 mg daily based on the recommendation of the treating physician, with doses reduced or discontinued based on adverse events or progression.
Trough concentrations of pazopanib 3 months after starting the treatment ranged from a low of 10.6 mcg/mL to a high of 106 mcg/mL, with a median of 49.1 mcg/mL, according to the report.
One-third of patients experienced grade 3 or greater toxicities, including anorexia, hypertension, anemia, and thrombocytopenia, among others. The median pazopanib concentration for those nine patients was 69.3 mcg/mL, compared with 41.2 mcg/mL for those not experiencing serious toxicities (P less than .05).
A concentration over 50.3 mcg/mL predicted grade 3 or greater toxicity, statistical analysis showed, with 8 out of 13 patients with concentrations above that threshold experiencing serious toxicities. By contrast, 1 of 14 patients below that threshold experienced grade 3 or greater toxicities.
No responses were observed in three patients with pazopanib concentrations below 20.5 mcg/mL, a concentration level considered to be subtherapeutic based on previous investigations.
Overall response rates were similar for patients with concentrations in the “optimal” 20.5- and 50.3-mcg/mL range and those with concentrations over 50.3 mcg/mL, according to the investigators.
Among 11 patients in that “optimal” range, partial responses were seen in 5, they reported, while for the 13 patients with high concentrations of the drug, partial responses were seen in 4 patients and a complete response was seen in 1 patient.
Trough concentrations may not predict all types of toxicities, according to the investigators, who said that the results of their small, retrospective analysis should be validated in a large, prospective study.
In particular, there was no significant relationship between trough concentration of pazopanib and development of grade 2 or greater hepatotoxicity, a common and specific side effect of the drug.
“Based on these findings, pazopanib-induced hepatotoxicity may not be related to the pharmacokinetics of pazopanib,” they wrote. “Therefore, pharmacogenomics testing is needed to predict pazopanib-induced hepatotoxicity.”
Dr. Terada and coauthors said they had no conflicts of interest to report.
SOURCE: Noda S et al. Clin Genitourin Cancer. 2018 Dec 7. doi: 10.1016/j.clgc.2018.12.001.
FROM CLINICAL GENITOURINARY CANCER
Key clinical point: Trough concentrations of pazopanib in approximately the 20- to 50-mcg/mL range were associated with less toxicity but a similar overall response rate, versus higher concentrations.
Major finding: The overall response rate was about 46% in patients with pazopanib concentrations in that range, and in patients with higher concentrations. One patient in the “optimal” range experienced a grade 3 or greater toxicity.
Study details: An exploratory analysis including 27 patients with renal cell carcinoma.
Disclosures: The authors reported no conflicts of interest.
Source: Noda S et al. Clin Genitourin Cancer. 2018 Dec 7. doi: 10.1016/j.clgc.2018.12.001.
Bioequivalents lamotrigine, levetiracetam control new-onset focal seizures equally well
NEW ORLEANS – Bioequivalent generic formulations of levetiracetam and lamotrigine reduced seizures by a similar extent over 2 years in a retrospective study of patients with newly diagnosed focal epilepsy.
Each drug had a specific adverse event profile, with lamotrigine associated with rash and levetiracetam with mood disorders, Sirichai Chayasirisobhon, MD, said at the annual meeting of the American Epilepsy Society. This finding can play into the initial therapeutic decision, said Dr. Chayasirisobhon of Kaiser Permanente Southern California. “If someone comes in with depression or mood disorder, I will start on lamotrigine, not levetiracetam. And we can decrease the chance of rash with a very slow titration, as we did here, starting with just 5 mg/kg and working up over 6 months.”
Although the drugs have a somewhat similar teratogenic profile, Dr. Chayasirisobhon added that he favors lamotrigine for women of childbearing years. “It’s a little bit better choice for them I think.”
His retrospective analysis followed 442 patients from first seizure and medical therapy for 2 years. The generic medications came from Kaiser Permanente’s central pharmacy. They were single-source, with a proven 95% bioequivalence. The main outcome was the percentage of patients who became seizure free and remained so. Any seizure, whether febrile, breakthroughs, or from titration, was considered a failure. These patients were dropped from the study. Any patient who developed a drug-related rash was dropped from the study and started on another medication.
More women than men took lamotrigine (113 vs. 75), whereas more men took levetiracetam (148 vs. 106). Those taking lamotrigine were younger than were those taking levetiracetam (30 vs. 40 years).
At the end of 2 years, there was no statistically significant difference in the primary outcome of being free from seizures (66.5% with lamotrigine vs. 72.4% with levetiracetam). In the lamotrigine group, 33.5% were eliminated from the study, 24% because they had a seizure, and the rest due to an adverse event. In the levetiracetam group, 27.6% were eliminated, 13% because they had a seizure and the rest because of an adverse event.
Adverse events in the lamotrigine group included rash (12), dizziness (3), lethargy (1), and mood changes (2). Among the levetiracetam group, adverse events included dizziness (3), lethargy (7), mood changes (20), slowed thinking (4), depression (2) and headache (1).
“Rash was the main event we saw in this group, and this was even when we did a very slow titration of 5 mg/kg per week,” Dr. Chayasirisobhon said. “Any sign of rash or itching at all, we told them to stop immediately and call us. Fortunately, we had no cases of Steven-Johnson syndrome and all our cases of rash were transient. But in the levetiracetam group, the mood changes are the major thing. Some of the patients became very agitated and aggressive. Whenever we see a patient for the first time, we always ask about mood changes, and we instruct the family to call and report any changes in mood immediately.”
Aside from reproductive age, however, Dr. Chayasirisobhon generally prefers to start new patients on levetiracetam. Its safety profile is remarkable, he said, recounting a case report he published in 2010 (Acta Neurol Taiwan. 2010;19:292-5).
The paper describes a male patient who decided to commit suicide after an argument with his wife. He took his levetiracetam and walked to his father’s grave, swallowing pills the entire time. When he arrived at the grave, he had taken around 65 grams of the medication. “The amazing thing was, he’s still walking, just a little unsteady. Then he decided he’s not ready to die,” Dr. Chayasirisobhon said. “He was able to call 911, so he’s still talking fine. When they checked his level it was so high, but he remained unimpaired except for the unsteady gait and some nystagmus.”
The study did not receive outside funding. Dr. Chayasirisobhon had no financial disclosures.
NEW ORLEANS – Bioequivalent generic formulations of levetiracetam and lamotrigine reduced seizures by a similar extent over 2 years in a retrospective study of patients with newly diagnosed focal epilepsy.
Each drug had a specific adverse event profile, with lamotrigine associated with rash and levetiracetam with mood disorders, Sirichai Chayasirisobhon, MD, said at the annual meeting of the American Epilepsy Society. This finding can play into the initial therapeutic decision, said Dr. Chayasirisobhon of Kaiser Permanente Southern California. “If someone comes in with depression or mood disorder, I will start on lamotrigine, not levetiracetam. And we can decrease the chance of rash with a very slow titration, as we did here, starting with just 5 mg/kg and working up over 6 months.”
Although the drugs have a somewhat similar teratogenic profile, Dr. Chayasirisobhon added that he favors lamotrigine for women of childbearing years. “It’s a little bit better choice for them I think.”
His retrospective analysis followed 442 patients from first seizure and medical therapy for 2 years. The generic medications came from Kaiser Permanente’s central pharmacy. They were single-source, with a proven 95% bioequivalence. The main outcome was the percentage of patients who became seizure free and remained so. Any seizure, whether febrile, breakthroughs, or from titration, was considered a failure. These patients were dropped from the study. Any patient who developed a drug-related rash was dropped from the study and started on another medication.
More women than men took lamotrigine (113 vs. 75), whereas more men took levetiracetam (148 vs. 106). Those taking lamotrigine were younger than were those taking levetiracetam (30 vs. 40 years).
At the end of 2 years, there was no statistically significant difference in the primary outcome of being free from seizures (66.5% with lamotrigine vs. 72.4% with levetiracetam). In the lamotrigine group, 33.5% were eliminated from the study, 24% because they had a seizure, and the rest due to an adverse event. In the levetiracetam group, 27.6% were eliminated, 13% because they had a seizure and the rest because of an adverse event.
Adverse events in the lamotrigine group included rash (12), dizziness (3), lethargy (1), and mood changes (2). Among the levetiracetam group, adverse events included dizziness (3), lethargy (7), mood changes (20), slowed thinking (4), depression (2) and headache (1).
“Rash was the main event we saw in this group, and this was even when we did a very slow titration of 5 mg/kg per week,” Dr. Chayasirisobhon said. “Any sign of rash or itching at all, we told them to stop immediately and call us. Fortunately, we had no cases of Steven-Johnson syndrome and all our cases of rash were transient. But in the levetiracetam group, the mood changes are the major thing. Some of the patients became very agitated and aggressive. Whenever we see a patient for the first time, we always ask about mood changes, and we instruct the family to call and report any changes in mood immediately.”
Aside from reproductive age, however, Dr. Chayasirisobhon generally prefers to start new patients on levetiracetam. Its safety profile is remarkable, he said, recounting a case report he published in 2010 (Acta Neurol Taiwan. 2010;19:292-5).
The paper describes a male patient who decided to commit suicide after an argument with his wife. He took his levetiracetam and walked to his father’s grave, swallowing pills the entire time. When he arrived at the grave, he had taken around 65 grams of the medication. “The amazing thing was, he’s still walking, just a little unsteady. Then he decided he’s not ready to die,” Dr. Chayasirisobhon said. “He was able to call 911, so he’s still talking fine. When they checked his level it was so high, but he remained unimpaired except for the unsteady gait and some nystagmus.”
The study did not receive outside funding. Dr. Chayasirisobhon had no financial disclosures.
NEW ORLEANS – Bioequivalent generic formulations of levetiracetam and lamotrigine reduced seizures by a similar extent over 2 years in a retrospective study of patients with newly diagnosed focal epilepsy.
Each drug had a specific adverse event profile, with lamotrigine associated with rash and levetiracetam with mood disorders, Sirichai Chayasirisobhon, MD, said at the annual meeting of the American Epilepsy Society. This finding can play into the initial therapeutic decision, said Dr. Chayasirisobhon of Kaiser Permanente Southern California. “If someone comes in with depression or mood disorder, I will start on lamotrigine, not levetiracetam. And we can decrease the chance of rash with a very slow titration, as we did here, starting with just 5 mg/kg and working up over 6 months.”
Although the drugs have a somewhat similar teratogenic profile, Dr. Chayasirisobhon added that he favors lamotrigine for women of childbearing years. “It’s a little bit better choice for them I think.”
His retrospective analysis followed 442 patients from first seizure and medical therapy for 2 years. The generic medications came from Kaiser Permanente’s central pharmacy. They were single-source, with a proven 95% bioequivalence. The main outcome was the percentage of patients who became seizure free and remained so. Any seizure, whether febrile, breakthroughs, or from titration, was considered a failure. These patients were dropped from the study. Any patient who developed a drug-related rash was dropped from the study and started on another medication.
More women than men took lamotrigine (113 vs. 75), whereas more men took levetiracetam (148 vs. 106). Those taking lamotrigine were younger than were those taking levetiracetam (30 vs. 40 years).
At the end of 2 years, there was no statistically significant difference in the primary outcome of being free from seizures (66.5% with lamotrigine vs. 72.4% with levetiracetam). In the lamotrigine group, 33.5% were eliminated from the study, 24% because they had a seizure, and the rest due to an adverse event. In the levetiracetam group, 27.6% were eliminated, 13% because they had a seizure and the rest because of an adverse event.
Adverse events in the lamotrigine group included rash (12), dizziness (3), lethargy (1), and mood changes (2). Among the levetiracetam group, adverse events included dizziness (3), lethargy (7), mood changes (20), slowed thinking (4), depression (2) and headache (1).
“Rash was the main event we saw in this group, and this was even when we did a very slow titration of 5 mg/kg per week,” Dr. Chayasirisobhon said. “Any sign of rash or itching at all, we told them to stop immediately and call us. Fortunately, we had no cases of Steven-Johnson syndrome and all our cases of rash were transient. But in the levetiracetam group, the mood changes are the major thing. Some of the patients became very agitated and aggressive. Whenever we see a patient for the first time, we always ask about mood changes, and we instruct the family to call and report any changes in mood immediately.”
Aside from reproductive age, however, Dr. Chayasirisobhon generally prefers to start new patients on levetiracetam. Its safety profile is remarkable, he said, recounting a case report he published in 2010 (Acta Neurol Taiwan. 2010;19:292-5).
The paper describes a male patient who decided to commit suicide after an argument with his wife. He took his levetiracetam and walked to his father’s grave, swallowing pills the entire time. When he arrived at the grave, he had taken around 65 grams of the medication. “The amazing thing was, he’s still walking, just a little unsteady. Then he decided he’s not ready to die,” Dr. Chayasirisobhon said. “He was able to call 911, so he’s still talking fine. When they checked his level it was so high, but he remained unimpaired except for the unsteady gait and some nystagmus.”
The study did not receive outside funding. Dr. Chayasirisobhon had no financial disclosures.
REPORTING FROM AES 2018
Key clinical point:
Major finding: At 2 years, 66.5% of the lamotrigine group and 72.4% of the levetiracetam group were seizure free.
Study details: The retrospective study comprised 442 patients.
Disclosures: The study did not receive outside funding. Dr. Chayasirisobhon had no financial disclosures.
Source: Chayasirisobhon S et al. AES 2018, Abstract 2.147.
Rural teleprescribing for opioid use disorder shows success
BONITA SPRINGS, FLA. – Clinician shortages and alarming opioid overdose rates are prompting rural health care centers to turn to telemedicine for delivering treatments for opioid use disorder (OUD). Several studies suggest that these treatments are being delivered effectively, experts said at the annual meeting of the American Academy of Addiction Psychiatry.
In both Maryland and West Virginia, for example, success using a telehealth approach has been reported recently, said David Moore, MD, PhD, assistant professor of psychiatry at Yale University, New Haven, Conn.
Specifically, in rural Maryland, physicians used telemedicine to provide buprenorphine treatment for OUD at a treatment center in August 2015. Researchers at the University of Maryland, Baltimore, looked at the first 177 of the patients treated with the approach. They found that retention in treatment was 91% at 1 month and 57% at 3 months. Of patients still in treatment at 3 months, 86% had urine that was opioid negative, researchers said (Am J Addict. 2018 Dec;27[8]:612-17).
And in West Virginia, researchers reviewed the records of 100 patients receiving buprenorphine treatment to compare outcomes of those treated with telemedicine and those treated face-to-face. They found no significant differences between the groups in additional substance use, time to achieve 30 days and 90 days of abstinence, or retention rates at 3 months and 1 year (J Addict Med. 2017 Mar-Apr;11[2]:138-44).
In addition, Dr. Moore said, he has had success with home inductions in the northern reaches of Maine. His first home induction involved a 55-year-old veteran with a history of oxycodone and hydrocodone use who used illicit buprenorphine when he could. Dr. Moore said the man was referred to him on a Monday. He called in a prescription for the drug the next day and gave the patient a handout on how to do a home induction. “Then he had a phone check-in, and we followed up on Thursday. It actually worked really well,” Dr. Moore said.
The dearth of buprenorphine providers in northern Maine makes those kinds of arrangements attractive, he said. In Maine’s Piscataquis County, he said, there is one buprenorphine provider for every 2,000 square miles. “We have about 1 in every 5 square miles in New Haven,” he said. “Thinking about the distance you have to travel, it gets to be pretty daunting.”
The ability of clinicians to provide buprenorphine with telemedicine varies by state. Among the resources needed to provide telemedicine services are reliable Internet access and an ability for a patient to consent to the treatment.
Nationwide, 56.3% of rural counties have no buprenorphine provider, according to a recent study, said Lewei (Allison) Lin, MD, assistant professor of psychiatry at the University of Michigan, Ann Arbor. A survey of 1,100 rural providers, results of which were included in that study, found that 48% of them said concerns about substance diversion or misuse were a barrier to providing buprenorphine, and 44% cited a lack of mental health or psychosocial support services.
“Although this country still has a major issue with access to treatment, we see that the access problem is about double in rural areas,” she said. “If you add on the distance issue and time, this becomes an even greater challenge.”
Nurse practitioners and physician assistants are now able to obtain a Drug Enforcement Administration waiver that will allow them to prescribe OUD, thanks to the Comprehensive Addiction and Recovery Act of 2016.
BONITA SPRINGS, FLA. – Clinician shortages and alarming opioid overdose rates are prompting rural health care centers to turn to telemedicine for delivering treatments for opioid use disorder (OUD). Several studies suggest that these treatments are being delivered effectively, experts said at the annual meeting of the American Academy of Addiction Psychiatry.
In both Maryland and West Virginia, for example, success using a telehealth approach has been reported recently, said David Moore, MD, PhD, assistant professor of psychiatry at Yale University, New Haven, Conn.
Specifically, in rural Maryland, physicians used telemedicine to provide buprenorphine treatment for OUD at a treatment center in August 2015. Researchers at the University of Maryland, Baltimore, looked at the first 177 of the patients treated with the approach. They found that retention in treatment was 91% at 1 month and 57% at 3 months. Of patients still in treatment at 3 months, 86% had urine that was opioid negative, researchers said (Am J Addict. 2018 Dec;27[8]:612-17).
And in West Virginia, researchers reviewed the records of 100 patients receiving buprenorphine treatment to compare outcomes of those treated with telemedicine and those treated face-to-face. They found no significant differences between the groups in additional substance use, time to achieve 30 days and 90 days of abstinence, or retention rates at 3 months and 1 year (J Addict Med. 2017 Mar-Apr;11[2]:138-44).
In addition, Dr. Moore said, he has had success with home inductions in the northern reaches of Maine. His first home induction involved a 55-year-old veteran with a history of oxycodone and hydrocodone use who used illicit buprenorphine when he could. Dr. Moore said the man was referred to him on a Monday. He called in a prescription for the drug the next day and gave the patient a handout on how to do a home induction. “Then he had a phone check-in, and we followed up on Thursday. It actually worked really well,” Dr. Moore said.
The dearth of buprenorphine providers in northern Maine makes those kinds of arrangements attractive, he said. In Maine’s Piscataquis County, he said, there is one buprenorphine provider for every 2,000 square miles. “We have about 1 in every 5 square miles in New Haven,” he said. “Thinking about the distance you have to travel, it gets to be pretty daunting.”
The ability of clinicians to provide buprenorphine with telemedicine varies by state. Among the resources needed to provide telemedicine services are reliable Internet access and an ability for a patient to consent to the treatment.
Nationwide, 56.3% of rural counties have no buprenorphine provider, according to a recent study, said Lewei (Allison) Lin, MD, assistant professor of psychiatry at the University of Michigan, Ann Arbor. A survey of 1,100 rural providers, results of which were included in that study, found that 48% of them said concerns about substance diversion or misuse were a barrier to providing buprenorphine, and 44% cited a lack of mental health or psychosocial support services.
“Although this country still has a major issue with access to treatment, we see that the access problem is about double in rural areas,” she said. “If you add on the distance issue and time, this becomes an even greater challenge.”
Nurse practitioners and physician assistants are now able to obtain a Drug Enforcement Administration waiver that will allow them to prescribe OUD, thanks to the Comprehensive Addiction and Recovery Act of 2016.
BONITA SPRINGS, FLA. – Clinician shortages and alarming opioid overdose rates are prompting rural health care centers to turn to telemedicine for delivering treatments for opioid use disorder (OUD). Several studies suggest that these treatments are being delivered effectively, experts said at the annual meeting of the American Academy of Addiction Psychiatry.
In both Maryland and West Virginia, for example, success using a telehealth approach has been reported recently, said David Moore, MD, PhD, assistant professor of psychiatry at Yale University, New Haven, Conn.
Specifically, in rural Maryland, physicians used telemedicine to provide buprenorphine treatment for OUD at a treatment center in August 2015. Researchers at the University of Maryland, Baltimore, looked at the first 177 of the patients treated with the approach. They found that retention in treatment was 91% at 1 month and 57% at 3 months. Of patients still in treatment at 3 months, 86% had urine that was opioid negative, researchers said (Am J Addict. 2018 Dec;27[8]:612-17).
And in West Virginia, researchers reviewed the records of 100 patients receiving buprenorphine treatment to compare outcomes of those treated with telemedicine and those treated face-to-face. They found no significant differences between the groups in additional substance use, time to achieve 30 days and 90 days of abstinence, or retention rates at 3 months and 1 year (J Addict Med. 2017 Mar-Apr;11[2]:138-44).
In addition, Dr. Moore said, he has had success with home inductions in the northern reaches of Maine. His first home induction involved a 55-year-old veteran with a history of oxycodone and hydrocodone use who used illicit buprenorphine when he could. Dr. Moore said the man was referred to him on a Monday. He called in a prescription for the drug the next day and gave the patient a handout on how to do a home induction. “Then he had a phone check-in, and we followed up on Thursday. It actually worked really well,” Dr. Moore said.
The dearth of buprenorphine providers in northern Maine makes those kinds of arrangements attractive, he said. In Maine’s Piscataquis County, he said, there is one buprenorphine provider for every 2,000 square miles. “We have about 1 in every 5 square miles in New Haven,” he said. “Thinking about the distance you have to travel, it gets to be pretty daunting.”
The ability of clinicians to provide buprenorphine with telemedicine varies by state. Among the resources needed to provide telemedicine services are reliable Internet access and an ability for a patient to consent to the treatment.
Nationwide, 56.3% of rural counties have no buprenorphine provider, according to a recent study, said Lewei (Allison) Lin, MD, assistant professor of psychiatry at the University of Michigan, Ann Arbor. A survey of 1,100 rural providers, results of which were included in that study, found that 48% of them said concerns about substance diversion or misuse were a barrier to providing buprenorphine, and 44% cited a lack of mental health or psychosocial support services.
“Although this country still has a major issue with access to treatment, we see that the access problem is about double in rural areas,” she said. “If you add on the distance issue and time, this becomes an even greater challenge.”
Nurse practitioners and physician assistants are now able to obtain a Drug Enforcement Administration waiver that will allow them to prescribe OUD, thanks to the Comprehensive Addiction and Recovery Act of 2016.
REPORTING FROM AAAP 2018
Brazil sees first live birth from deceased-donor uterus transplant
The healthy 2,550-g infant girl was born in December 2017 via a planned cesarean delivery at about 36 weeks’ gestation. Her mother, the transplant recipient, has congenital absence of the uterus from Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Removal of the transplanted uterus at the time of delivery allowed the woman to stop taking the immunosuppressive medications that she’d been on since the transplantation, which had been performed less than a year and a half previously.
The uterus had been retrieved from a 45-year-old donor who experienced a subarachnoid hemorrhage and subsequent brain death. The donor had three vaginal deliveries, and no history of reproductive issues or sexually transmitted infection, wrote Dani Ejzenberg, MD, and his colleagues at the University of São Paolo, Brazil.
The retrieval and transplantation procedures were done at the university’s hospital, in accordance with a research protocol approved by the university, a Brazilian national ethics committee, and the country’s national transplantation system. Thorough psychological evaluation was part of the research protocol, and the patient and her partner had monthly psychological counseling from therapists with expertise in transplant and fertility, wrote Dr. Ejzenberg and his colleagues.
In preparation for the transplantation, which occurred when the recipient was 32 years old, she had in vitro fertilization several months before the procedure. Eight “good-quality” blastocysts were retrieved and cryopreserved, said Dr. Ejzenberg and his coauthors. The recipient’s menstrual cycle resumed 37 days after transplantation, and one of the cryopreserved embryos was transferred about 7 months after the uterine transplantation procedure, resulting in the pregnancy.
The donor and recipient were matched only by ABO blood type, with no further tissue typing being done, wrote Dr. Ejzenberg and his colleagues. The immunosuppressive regimen paralleled that used in previous successful uterine transplantations from live donors in Sweden, with induction via 1 g intraoperative methylprednisolone and 1.5 mg/kg of thymoglobulin. Thereafter, the recipient received tacrolimus titrated to a trough of 8-10 ng/mL, along with mycophenolate mofetil 720 mg twice daily. Five months after her transplantation, the mycophenolate mofetil was replaced with 100 mg azathioprine and 10 mg prednisone daily, a regimen that she stayed on until cesarean delivery.
Broad-spectrum antibiotics, antifungals, and anthelmintics were administered during the patient’s hospital stay. Prophylactic antibiotics were continued for 6 months, and antiviral medication was given prophylactically for 3 months. The recipient had one episode of vaginal discharge, treated with antifungal medication, and one episode of pyelonephritis during pregnancy, treated during a brief inpatient stay.
Enoxaparin and aspirin were used for inpatient venous thromboembolism prophylaxis, and heparin and aspirin thereafter. Aspirin was discontinued at 34 weeks, and heparin the day before delivery.
Swedish and American teams involved in uterine transplantation are working to develop standardization of surgical techniques, immunosuppression protocol, and methods to monitor rejection.
However, pointed out Dr. Ejzenberg and his coauthors, some technical aspects were unique to the deceased donor transplantation. These included managing total ischemic time for the donor tissue because heart, liver, and kidney retrieval all were given priority.
One downstream effect of this was longer-than-expected procedure and anesthesia time for the recipient, because coordinating donor uterus retrieval and preparation of the surgical bed in the live recipient was tricky; surgery time was about 10.5 hours. Also, there was prolonged warm-ischemia time because six small-vessel anastomoses needed to be performed, wrote the investigators.
After reperfusion of the implanted uterus, there was brisk bleeding from a number of small vessels that had not been ligated on retrieval because of concerns about ischemic time. These were identified and sutured or cauterized, but the total estimated blood loss during the procedures was 1,200 mL, with most of that coming from the uterus, said Dr. Ejzenberg and his coauthors.
The donor uterus had a total of almost 8 hours of ischemic time, exceeding the previously published live donor maximum uterine ischemic time of 3 hours, 25 minutes. This experience can inform surgical teams considering future uterine transplantations.
Dr. Ejzenberg and his colleagues also said that they cast a broad net with immunosuppression, erring on the side of caution. With more experience may come the ability to scale back immunosuppressive regimens, they noted.
The explantation of the uterus and associated blood vessels after delivery afforded the opportunity for pathological examination of the uterus and other tissues, which showed no signs of rejection. The uterine arteries did have mild intimal fibrous hyperplasia that was likely related to the age of the donor, said Dr. Ejzenberg and his coauthors.
This successful completion of a deceased-donor uterine transplantation demonstrates the feasibility of accessing “a much wider potential donor population, as the numbers of people willing and committed to donate organs upon their own deaths are far larger than those of potential live donors,” wrote Dr. Ejzenberg and his colleagues. “Further incidental but substantial benefits of the use of deceased donors include lower costs and avoidance of live donors’ surgical risks.”
In 2011, a uterine transplantation from a deceased donor resulted in pregnancy, but ended in miscarriage.
Funding was provided by Fundação de Amparo à Pesquisa do Estado de São Paulo and the Hospital das Clínicas of University of São Paulo School of Medicine. Dr. Ejzenberg and his colleagues reported that they had no conflicts of interest.
SOURCE: Ejzenberg D. et al. Lancet. 2018 Dec. doi: 10.1015/S0140-6736(18)31766-5.
Among the advances seen in this deceased-donor uterus transplant is a demonstration that ischemic time of nearly 8 hours – four times the average seen in live donation – does not preclude a successful transplantation.
Also, the timetable for transplantation seen here did not involve the year-long waiting period between transplantation and pregnancy that has been the norm in live uterine transplantation.
However, uterine transplantation, whether from a living or deceased donor, is still in its early stages. Among the many unsettled questions are whether live or deceased donor transplantations yield superior results. Additional technical aspects to be further studied include best surgical approach for the donor uterus, best anastomosis technique, and optimal immunosuppression and antimicrobial/antifungal/antiviral regimens.
Continued work needs to be done to standardize these and other aspects of the peri- and postoperative care of women undergoing uterine transplantation.
In addition, long-term tracking of children born from transplanted uteri is needed, so outcomes can be assessed over the lifespan.
Going forward, it could be that uterine transplantation may be offered to an expanded cohort of women, including those with bulky, nonoperable uterine fibroids, those who have received pelvic radiotherapy, and even those who have had multiple unexplained problems with implantation during fertility treatments. In all cases, researchers should work toward achieving the highest live birth rate at the lowest risk to donors and patients, while also working to make more organs available; establishing registries, and encouraging prospective registration and transparent reporting of uterus transplantation procedures.
Cesar Diaz-Garcia, MD, is medical director of IVI-London, and Antonio Pellicer, MD, is professor of obstetrics and gynecology at the University of Valencia, Spain. These remarks were drawn from their editorial accompanying the report by Ejzenberg et al. (Lancet. 2018 Dec. doi: 10.1016/50140-6736(18)32106-8).
Among the advances seen in this deceased-donor uterus transplant is a demonstration that ischemic time of nearly 8 hours – four times the average seen in live donation – does not preclude a successful transplantation.
Also, the timetable for transplantation seen here did not involve the year-long waiting period between transplantation and pregnancy that has been the norm in live uterine transplantation.
However, uterine transplantation, whether from a living or deceased donor, is still in its early stages. Among the many unsettled questions are whether live or deceased donor transplantations yield superior results. Additional technical aspects to be further studied include best surgical approach for the donor uterus, best anastomosis technique, and optimal immunosuppression and antimicrobial/antifungal/antiviral regimens.
Continued work needs to be done to standardize these and other aspects of the peri- and postoperative care of women undergoing uterine transplantation.
In addition, long-term tracking of children born from transplanted uteri is needed, so outcomes can be assessed over the lifespan.
Going forward, it could be that uterine transplantation may be offered to an expanded cohort of women, including those with bulky, nonoperable uterine fibroids, those who have received pelvic radiotherapy, and even those who have had multiple unexplained problems with implantation during fertility treatments. In all cases, researchers should work toward achieving the highest live birth rate at the lowest risk to donors and patients, while also working to make more organs available; establishing registries, and encouraging prospective registration and transparent reporting of uterus transplantation procedures.
Cesar Diaz-Garcia, MD, is medical director of IVI-London, and Antonio Pellicer, MD, is professor of obstetrics and gynecology at the University of Valencia, Spain. These remarks were drawn from their editorial accompanying the report by Ejzenberg et al. (Lancet. 2018 Dec. doi: 10.1016/50140-6736(18)32106-8).
Among the advances seen in this deceased-donor uterus transplant is a demonstration that ischemic time of nearly 8 hours – four times the average seen in live donation – does not preclude a successful transplantation.
Also, the timetable for transplantation seen here did not involve the year-long waiting period between transplantation and pregnancy that has been the norm in live uterine transplantation.
However, uterine transplantation, whether from a living or deceased donor, is still in its early stages. Among the many unsettled questions are whether live or deceased donor transplantations yield superior results. Additional technical aspects to be further studied include best surgical approach for the donor uterus, best anastomosis technique, and optimal immunosuppression and antimicrobial/antifungal/antiviral regimens.
Continued work needs to be done to standardize these and other aspects of the peri- and postoperative care of women undergoing uterine transplantation.
In addition, long-term tracking of children born from transplanted uteri is needed, so outcomes can be assessed over the lifespan.
Going forward, it could be that uterine transplantation may be offered to an expanded cohort of women, including those with bulky, nonoperable uterine fibroids, those who have received pelvic radiotherapy, and even those who have had multiple unexplained problems with implantation during fertility treatments. In all cases, researchers should work toward achieving the highest live birth rate at the lowest risk to donors and patients, while also working to make more organs available; establishing registries, and encouraging prospective registration and transparent reporting of uterus transplantation procedures.
Cesar Diaz-Garcia, MD, is medical director of IVI-London, and Antonio Pellicer, MD, is professor of obstetrics and gynecology at the University of Valencia, Spain. These remarks were drawn from their editorial accompanying the report by Ejzenberg et al. (Lancet. 2018 Dec. doi: 10.1016/50140-6736(18)32106-8).
The healthy 2,550-g infant girl was born in December 2017 via a planned cesarean delivery at about 36 weeks’ gestation. Her mother, the transplant recipient, has congenital absence of the uterus from Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Removal of the transplanted uterus at the time of delivery allowed the woman to stop taking the immunosuppressive medications that she’d been on since the transplantation, which had been performed less than a year and a half previously.
The uterus had been retrieved from a 45-year-old donor who experienced a subarachnoid hemorrhage and subsequent brain death. The donor had three vaginal deliveries, and no history of reproductive issues or sexually transmitted infection, wrote Dani Ejzenberg, MD, and his colleagues at the University of São Paolo, Brazil.
The retrieval and transplantation procedures were done at the university’s hospital, in accordance with a research protocol approved by the university, a Brazilian national ethics committee, and the country’s national transplantation system. Thorough psychological evaluation was part of the research protocol, and the patient and her partner had monthly psychological counseling from therapists with expertise in transplant and fertility, wrote Dr. Ejzenberg and his colleagues.
In preparation for the transplantation, which occurred when the recipient was 32 years old, she had in vitro fertilization several months before the procedure. Eight “good-quality” blastocysts were retrieved and cryopreserved, said Dr. Ejzenberg and his coauthors. The recipient’s menstrual cycle resumed 37 days after transplantation, and one of the cryopreserved embryos was transferred about 7 months after the uterine transplantation procedure, resulting in the pregnancy.
The donor and recipient were matched only by ABO blood type, with no further tissue typing being done, wrote Dr. Ejzenberg and his colleagues. The immunosuppressive regimen paralleled that used in previous successful uterine transplantations from live donors in Sweden, with induction via 1 g intraoperative methylprednisolone and 1.5 mg/kg of thymoglobulin. Thereafter, the recipient received tacrolimus titrated to a trough of 8-10 ng/mL, along with mycophenolate mofetil 720 mg twice daily. Five months after her transplantation, the mycophenolate mofetil was replaced with 100 mg azathioprine and 10 mg prednisone daily, a regimen that she stayed on until cesarean delivery.
Broad-spectrum antibiotics, antifungals, and anthelmintics were administered during the patient’s hospital stay. Prophylactic antibiotics were continued for 6 months, and antiviral medication was given prophylactically for 3 months. The recipient had one episode of vaginal discharge, treated with antifungal medication, and one episode of pyelonephritis during pregnancy, treated during a brief inpatient stay.
Enoxaparin and aspirin were used for inpatient venous thromboembolism prophylaxis, and heparin and aspirin thereafter. Aspirin was discontinued at 34 weeks, and heparin the day before delivery.
Swedish and American teams involved in uterine transplantation are working to develop standardization of surgical techniques, immunosuppression protocol, and methods to monitor rejection.
However, pointed out Dr. Ejzenberg and his coauthors, some technical aspects were unique to the deceased donor transplantation. These included managing total ischemic time for the donor tissue because heart, liver, and kidney retrieval all were given priority.
One downstream effect of this was longer-than-expected procedure and anesthesia time for the recipient, because coordinating donor uterus retrieval and preparation of the surgical bed in the live recipient was tricky; surgery time was about 10.5 hours. Also, there was prolonged warm-ischemia time because six small-vessel anastomoses needed to be performed, wrote the investigators.
After reperfusion of the implanted uterus, there was brisk bleeding from a number of small vessels that had not been ligated on retrieval because of concerns about ischemic time. These were identified and sutured or cauterized, but the total estimated blood loss during the procedures was 1,200 mL, with most of that coming from the uterus, said Dr. Ejzenberg and his coauthors.
The donor uterus had a total of almost 8 hours of ischemic time, exceeding the previously published live donor maximum uterine ischemic time of 3 hours, 25 minutes. This experience can inform surgical teams considering future uterine transplantations.
Dr. Ejzenberg and his colleagues also said that they cast a broad net with immunosuppression, erring on the side of caution. With more experience may come the ability to scale back immunosuppressive regimens, they noted.
The explantation of the uterus and associated blood vessels after delivery afforded the opportunity for pathological examination of the uterus and other tissues, which showed no signs of rejection. The uterine arteries did have mild intimal fibrous hyperplasia that was likely related to the age of the donor, said Dr. Ejzenberg and his coauthors.
This successful completion of a deceased-donor uterine transplantation demonstrates the feasibility of accessing “a much wider potential donor population, as the numbers of people willing and committed to donate organs upon their own deaths are far larger than those of potential live donors,” wrote Dr. Ejzenberg and his colleagues. “Further incidental but substantial benefits of the use of deceased donors include lower costs and avoidance of live donors’ surgical risks.”
In 2011, a uterine transplantation from a deceased donor resulted in pregnancy, but ended in miscarriage.
Funding was provided by Fundação de Amparo à Pesquisa do Estado de São Paulo and the Hospital das Clínicas of University of São Paulo School of Medicine. Dr. Ejzenberg and his colleagues reported that they had no conflicts of interest.
SOURCE: Ejzenberg D. et al. Lancet. 2018 Dec. doi: 10.1015/S0140-6736(18)31766-5.
The healthy 2,550-g infant girl was born in December 2017 via a planned cesarean delivery at about 36 weeks’ gestation. Her mother, the transplant recipient, has congenital absence of the uterus from Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Removal of the transplanted uterus at the time of delivery allowed the woman to stop taking the immunosuppressive medications that she’d been on since the transplantation, which had been performed less than a year and a half previously.
The uterus had been retrieved from a 45-year-old donor who experienced a subarachnoid hemorrhage and subsequent brain death. The donor had three vaginal deliveries, and no history of reproductive issues or sexually transmitted infection, wrote Dani Ejzenberg, MD, and his colleagues at the University of São Paolo, Brazil.
The retrieval and transplantation procedures were done at the university’s hospital, in accordance with a research protocol approved by the university, a Brazilian national ethics committee, and the country’s national transplantation system. Thorough psychological evaluation was part of the research protocol, and the patient and her partner had monthly psychological counseling from therapists with expertise in transplant and fertility, wrote Dr. Ejzenberg and his colleagues.
In preparation for the transplantation, which occurred when the recipient was 32 years old, she had in vitro fertilization several months before the procedure. Eight “good-quality” blastocysts were retrieved and cryopreserved, said Dr. Ejzenberg and his coauthors. The recipient’s menstrual cycle resumed 37 days after transplantation, and one of the cryopreserved embryos was transferred about 7 months after the uterine transplantation procedure, resulting in the pregnancy.
The donor and recipient were matched only by ABO blood type, with no further tissue typing being done, wrote Dr. Ejzenberg and his colleagues. The immunosuppressive regimen paralleled that used in previous successful uterine transplantations from live donors in Sweden, with induction via 1 g intraoperative methylprednisolone and 1.5 mg/kg of thymoglobulin. Thereafter, the recipient received tacrolimus titrated to a trough of 8-10 ng/mL, along with mycophenolate mofetil 720 mg twice daily. Five months after her transplantation, the mycophenolate mofetil was replaced with 100 mg azathioprine and 10 mg prednisone daily, a regimen that she stayed on until cesarean delivery.
Broad-spectrum antibiotics, antifungals, and anthelmintics were administered during the patient’s hospital stay. Prophylactic antibiotics were continued for 6 months, and antiviral medication was given prophylactically for 3 months. The recipient had one episode of vaginal discharge, treated with antifungal medication, and one episode of pyelonephritis during pregnancy, treated during a brief inpatient stay.
Enoxaparin and aspirin were used for inpatient venous thromboembolism prophylaxis, and heparin and aspirin thereafter. Aspirin was discontinued at 34 weeks, and heparin the day before delivery.
Swedish and American teams involved in uterine transplantation are working to develop standardization of surgical techniques, immunosuppression protocol, and methods to monitor rejection.
However, pointed out Dr. Ejzenberg and his coauthors, some technical aspects were unique to the deceased donor transplantation. These included managing total ischemic time for the donor tissue because heart, liver, and kidney retrieval all were given priority.
One downstream effect of this was longer-than-expected procedure and anesthesia time for the recipient, because coordinating donor uterus retrieval and preparation of the surgical bed in the live recipient was tricky; surgery time was about 10.5 hours. Also, there was prolonged warm-ischemia time because six small-vessel anastomoses needed to be performed, wrote the investigators.
After reperfusion of the implanted uterus, there was brisk bleeding from a number of small vessels that had not been ligated on retrieval because of concerns about ischemic time. These were identified and sutured or cauterized, but the total estimated blood loss during the procedures was 1,200 mL, with most of that coming from the uterus, said Dr. Ejzenberg and his coauthors.
The donor uterus had a total of almost 8 hours of ischemic time, exceeding the previously published live donor maximum uterine ischemic time of 3 hours, 25 minutes. This experience can inform surgical teams considering future uterine transplantations.
Dr. Ejzenberg and his colleagues also said that they cast a broad net with immunosuppression, erring on the side of caution. With more experience may come the ability to scale back immunosuppressive regimens, they noted.
The explantation of the uterus and associated blood vessels after delivery afforded the opportunity for pathological examination of the uterus and other tissues, which showed no signs of rejection. The uterine arteries did have mild intimal fibrous hyperplasia that was likely related to the age of the donor, said Dr. Ejzenberg and his coauthors.
This successful completion of a deceased-donor uterine transplantation demonstrates the feasibility of accessing “a much wider potential donor population, as the numbers of people willing and committed to donate organs upon their own deaths are far larger than those of potential live donors,” wrote Dr. Ejzenberg and his colleagues. “Further incidental but substantial benefits of the use of deceased donors include lower costs and avoidance of live donors’ surgical risks.”
In 2011, a uterine transplantation from a deceased donor resulted in pregnancy, but ended in miscarriage.
Funding was provided by Fundação de Amparo à Pesquisa do Estado de São Paulo and the Hospital das Clínicas of University of São Paulo School of Medicine. Dr. Ejzenberg and his colleagues reported that they had no conflicts of interest.
SOURCE: Ejzenberg D. et al. Lancet. 2018 Dec. doi: 10.1015/S0140-6736(18)31766-5.
FROM THE LANCET