User login
Look No Further
As I follow Mary Jo Gorman, MD, MBA, as president of SHM, it might be tempting for me to simply follow the leading rule of the “organizational” Hippocratic Oath and “First do no harm.”
Put another way, in the context of the success SHM has enjoyed for the past 10 years, there is a case to be made for standing out of the way of our society’s positive momentum. But I believe we can—and will—do better than that. None of us can afford to be spectators in this arena.
We often speak of teamwork in healthcare, but precious few of us intuitively know what this means—much less have any education in its principles. During my training, the idea of teamwork amounted to little more than relying on a medical assistant to obtain daily weights or counting on the pharmacist to calculate and follow the appropriate dosing schedule for gentamicin. Common sense led me to understand that building an amicable relationship with the nursing staff made my working life easier.
Slowly, the advantages of structuring a more organized team in the hospital setting became more evident and helped encourage me to find ways of exploiting this concept further. As I look back, it was Jeff Dichter, MD, past president of SHM and director of the hospitalist program at Ball Memorial Hospital in Muncie, Ind., who emerged as one of the true champions for teamwork as an optimal model for inpatient care. Jeff would talk about it to everyone who would listen, in every venue he could reach. He wrote about it in this very column. He charged our meeting planners and committee chairs with integrating teamwork principles into our educational content as well as our advocacy and membership development initiatives. His vision of a true team galvanized SHM’s commitment to supporting a broad constituency, extending well beyond hospitalist physicians. Jeff knew care is never delivered by an individual; it’s always a team. And he believed this framework to be fully realized by way of building from a strong organizational agenda for quality improvement.
Speaking of quality in healthcare, I look no further than Mark Williams, MD, editor of the Journal of Hospital Medicine, for having built that agenda for our society through his own efforts as well as collaboration with the Institute for Healthcare Improvement (IHI) and other national entities. As another past president of SHM, Mark brought a level of organizational focus and rigor around quality improvement and patient safety that rose to the challenges outlined in two Institute of Medicine reports, “To Err is Human” and “Crossing the Quality Chasm.” He helped move “quality” from something we talk about to something we do. He pushed it from an espoused value to a core commitment of our specialty. Quality improvement is now inseparable from what I consider to be the true promise of hospital medicine: that care organized in well-orchestrated, well-resourced teams can deliver our patients remarkable improvements in the quality, safety, and experience of healthcare.
But how do we get this done? How do we take a relatively abstract notion of a team, channel its activities to drive measurable improvements in quality, and change the arcane systems of inpatient care so as to sustain and hardwire those improvements?
Leadership. Like it or not, each of you is regarded as one of—if not the—most important leaders in the hospital. Nursing, case management, physical therapy, patients, and families look to you to provide leadership for clinical and operational systems. You are the person most able to make meaningful decisions at the front-line level that directly affect the patient experience. You are called upon to lead and manage change in a volatile environment, to resolve the inevitable conflicts that change provokes, and to reconcile hospital business drivers with quality and safety imperatives.
Our immediate past president, Dr. Gorman, emphasized the crucial role we serve as leaders. Recognizing the tremendous development needs for skills and knowledge to effectively lead, SHM has created Leadership Academies and is working on e-discussion forums and mentoring programs to promote longitudinal learning. While we must unlearn some of the behaviors and beliefs seared into our brains during our traditional medical training, we must position ourselves to forge high-performing teams and lead the quality agenda.
At a dinner during the SHM Annual Meeting in May, I sat with a senior leader from the American Medical Association’s Organized Medical Staff Section (AMA OMSS). He had flown in with other AMA representatives to meet with us on common interests. By the end of the evening, the late-career surgeon took me aside and said: “I have to tell you how touched I am by your organization. The passion, drive, and commitment of your membership is what’s missing in so many professional societies today. You must bring this passion to the larger house of medicine.”
As SHM enjoys 10 years of explosive growth and remarkable success, we need to balance the right to celebrate success with the duty not to rest on laurels. Much has been accomplished, but more than a life’s work lies before us. The road is complex and fraught with uncertainty. We might become frustrated with mounting complexity, tired with resistance to change, and fatigued with leading against the status quo. It is hard—and lonely—to confront the systems and issues that desperately need to be confronted on our journey to transform care. And it might be easy for us to become distracted from our core commitments to teamwork and leading quality by allowing our medical society to become more of a guild that defends our professional incomes and way of life. Yet I believe—I know—a much brighter future lies ahead than emerging as a casualty of temptation.
If the best predictor of behavior is past behavior, then our future will mirror the spirit in which SHM was founded. It’s the spirit an invited guest observed in a few short hours at our annual meeting. It’s the spirit that binds teamwork, quality improvement, and leadership into a unified approach to our professional endeavors. That spirit has a name: accountability. It’s the fundamental understanding that we are answerable to others, including patients, families, the community, hospital and medical staff, as well as each other, for the performance of the care systems in which we work.
Being accountable means we must rebuild trust of the broader public in hospital care, and that we follow through on the promise of hospital medicine. It means we own our mistakes, we agree that transparency and measurement will lead to better outcomes, and we commit to being part of the solution.
Accountability also mandates that we eliminate blame and “victimhood.” We cannot first think of ourselves as victims of a broken reimbursement model, or a lack of data or a hospital administration that “just doesn’t get it.” The real questions are: What can I do today about improving management of scarce resources? About the nursing shortage? About incorporating patient-safety principles into a new facility? About access to care and overcrowding? About the needless hospital deaths due to ventilator-assisted pneumonia (VAP), acute myocardial infarction, and methicillin-resistant Staphylococcus aureus? About ensuring seamless transitions of patients throughout the care continuum?
Several years ago I spoke with Brent James, MD, executive director of the Institute for Health Care Delivery Research and vice president of medical research and continuing medical education at InterMountain Healthcare in Salt Lake City, Utah. At the time, I was trying to learn quality improvement methods and practices. He reminded me of a quote Sir William Osler, the father of internal medicine, made at the end of his career when he gave an address at the Phipps Clinic in England to a group of young physicians who had recently completed training. They were about to embark on their careers early in the 20th century. “I am sorry for you young men of this generation,” he told the physicians. “Oh, you’ll do great things. You’ll have great victories, and standing on our shoulders you’ll see far. But you can never have our sensations. To have lived through a revolution, to have seen a new birth of science, new dispensation of health, redesigned medical training, remodeled hospitals, a new outlook for humanity. That is not given to every generation.”
While it seems appropriate in retrospect that these young physicians were indeed entering a time after which tremendous change and transformation had taken place, it seems equally appropriate to consider ourselves one of those generations that must lead and drive change of the magnitude of which Osler spoke. As we lead teams in the hospital to revolutionize the state of healthcare quality, we must begin every thought, every action, by holding ourselves and each other accountable for being part of the solution. To begin, we need look no further than ourselves. TH
Dr. Holman is president of SHM.
As I follow Mary Jo Gorman, MD, MBA, as president of SHM, it might be tempting for me to simply follow the leading rule of the “organizational” Hippocratic Oath and “First do no harm.”
Put another way, in the context of the success SHM has enjoyed for the past 10 years, there is a case to be made for standing out of the way of our society’s positive momentum. But I believe we can—and will—do better than that. None of us can afford to be spectators in this arena.
We often speak of teamwork in healthcare, but precious few of us intuitively know what this means—much less have any education in its principles. During my training, the idea of teamwork amounted to little more than relying on a medical assistant to obtain daily weights or counting on the pharmacist to calculate and follow the appropriate dosing schedule for gentamicin. Common sense led me to understand that building an amicable relationship with the nursing staff made my working life easier.
Slowly, the advantages of structuring a more organized team in the hospital setting became more evident and helped encourage me to find ways of exploiting this concept further. As I look back, it was Jeff Dichter, MD, past president of SHM and director of the hospitalist program at Ball Memorial Hospital in Muncie, Ind., who emerged as one of the true champions for teamwork as an optimal model for inpatient care. Jeff would talk about it to everyone who would listen, in every venue he could reach. He wrote about it in this very column. He charged our meeting planners and committee chairs with integrating teamwork principles into our educational content as well as our advocacy and membership development initiatives. His vision of a true team galvanized SHM’s commitment to supporting a broad constituency, extending well beyond hospitalist physicians. Jeff knew care is never delivered by an individual; it’s always a team. And he believed this framework to be fully realized by way of building from a strong organizational agenda for quality improvement.
Speaking of quality in healthcare, I look no further than Mark Williams, MD, editor of the Journal of Hospital Medicine, for having built that agenda for our society through his own efforts as well as collaboration with the Institute for Healthcare Improvement (IHI) and other national entities. As another past president of SHM, Mark brought a level of organizational focus and rigor around quality improvement and patient safety that rose to the challenges outlined in two Institute of Medicine reports, “To Err is Human” and “Crossing the Quality Chasm.” He helped move “quality” from something we talk about to something we do. He pushed it from an espoused value to a core commitment of our specialty. Quality improvement is now inseparable from what I consider to be the true promise of hospital medicine: that care organized in well-orchestrated, well-resourced teams can deliver our patients remarkable improvements in the quality, safety, and experience of healthcare.
But how do we get this done? How do we take a relatively abstract notion of a team, channel its activities to drive measurable improvements in quality, and change the arcane systems of inpatient care so as to sustain and hardwire those improvements?
Leadership. Like it or not, each of you is regarded as one of—if not the—most important leaders in the hospital. Nursing, case management, physical therapy, patients, and families look to you to provide leadership for clinical and operational systems. You are the person most able to make meaningful decisions at the front-line level that directly affect the patient experience. You are called upon to lead and manage change in a volatile environment, to resolve the inevitable conflicts that change provokes, and to reconcile hospital business drivers with quality and safety imperatives.
Our immediate past president, Dr. Gorman, emphasized the crucial role we serve as leaders. Recognizing the tremendous development needs for skills and knowledge to effectively lead, SHM has created Leadership Academies and is working on e-discussion forums and mentoring programs to promote longitudinal learning. While we must unlearn some of the behaviors and beliefs seared into our brains during our traditional medical training, we must position ourselves to forge high-performing teams and lead the quality agenda.
At a dinner during the SHM Annual Meeting in May, I sat with a senior leader from the American Medical Association’s Organized Medical Staff Section (AMA OMSS). He had flown in with other AMA representatives to meet with us on common interests. By the end of the evening, the late-career surgeon took me aside and said: “I have to tell you how touched I am by your organization. The passion, drive, and commitment of your membership is what’s missing in so many professional societies today. You must bring this passion to the larger house of medicine.”
As SHM enjoys 10 years of explosive growth and remarkable success, we need to balance the right to celebrate success with the duty not to rest on laurels. Much has been accomplished, but more than a life’s work lies before us. The road is complex and fraught with uncertainty. We might become frustrated with mounting complexity, tired with resistance to change, and fatigued with leading against the status quo. It is hard—and lonely—to confront the systems and issues that desperately need to be confronted on our journey to transform care. And it might be easy for us to become distracted from our core commitments to teamwork and leading quality by allowing our medical society to become more of a guild that defends our professional incomes and way of life. Yet I believe—I know—a much brighter future lies ahead than emerging as a casualty of temptation.
If the best predictor of behavior is past behavior, then our future will mirror the spirit in which SHM was founded. It’s the spirit an invited guest observed in a few short hours at our annual meeting. It’s the spirit that binds teamwork, quality improvement, and leadership into a unified approach to our professional endeavors. That spirit has a name: accountability. It’s the fundamental understanding that we are answerable to others, including patients, families, the community, hospital and medical staff, as well as each other, for the performance of the care systems in which we work.
Being accountable means we must rebuild trust of the broader public in hospital care, and that we follow through on the promise of hospital medicine. It means we own our mistakes, we agree that transparency and measurement will lead to better outcomes, and we commit to being part of the solution.
Accountability also mandates that we eliminate blame and “victimhood.” We cannot first think of ourselves as victims of a broken reimbursement model, or a lack of data or a hospital administration that “just doesn’t get it.” The real questions are: What can I do today about improving management of scarce resources? About the nursing shortage? About incorporating patient-safety principles into a new facility? About access to care and overcrowding? About the needless hospital deaths due to ventilator-assisted pneumonia (VAP), acute myocardial infarction, and methicillin-resistant Staphylococcus aureus? About ensuring seamless transitions of patients throughout the care continuum?
Several years ago I spoke with Brent James, MD, executive director of the Institute for Health Care Delivery Research and vice president of medical research and continuing medical education at InterMountain Healthcare in Salt Lake City, Utah. At the time, I was trying to learn quality improvement methods and practices. He reminded me of a quote Sir William Osler, the father of internal medicine, made at the end of his career when he gave an address at the Phipps Clinic in England to a group of young physicians who had recently completed training. They were about to embark on their careers early in the 20th century. “I am sorry for you young men of this generation,” he told the physicians. “Oh, you’ll do great things. You’ll have great victories, and standing on our shoulders you’ll see far. But you can never have our sensations. To have lived through a revolution, to have seen a new birth of science, new dispensation of health, redesigned medical training, remodeled hospitals, a new outlook for humanity. That is not given to every generation.”
While it seems appropriate in retrospect that these young physicians were indeed entering a time after which tremendous change and transformation had taken place, it seems equally appropriate to consider ourselves one of those generations that must lead and drive change of the magnitude of which Osler spoke. As we lead teams in the hospital to revolutionize the state of healthcare quality, we must begin every thought, every action, by holding ourselves and each other accountable for being part of the solution. To begin, we need look no further than ourselves. TH
Dr. Holman is president of SHM.
As I follow Mary Jo Gorman, MD, MBA, as president of SHM, it might be tempting for me to simply follow the leading rule of the “organizational” Hippocratic Oath and “First do no harm.”
Put another way, in the context of the success SHM has enjoyed for the past 10 years, there is a case to be made for standing out of the way of our society’s positive momentum. But I believe we can—and will—do better than that. None of us can afford to be spectators in this arena.
We often speak of teamwork in healthcare, but precious few of us intuitively know what this means—much less have any education in its principles. During my training, the idea of teamwork amounted to little more than relying on a medical assistant to obtain daily weights or counting on the pharmacist to calculate and follow the appropriate dosing schedule for gentamicin. Common sense led me to understand that building an amicable relationship with the nursing staff made my working life easier.
Slowly, the advantages of structuring a more organized team in the hospital setting became more evident and helped encourage me to find ways of exploiting this concept further. As I look back, it was Jeff Dichter, MD, past president of SHM and director of the hospitalist program at Ball Memorial Hospital in Muncie, Ind., who emerged as one of the true champions for teamwork as an optimal model for inpatient care. Jeff would talk about it to everyone who would listen, in every venue he could reach. He wrote about it in this very column. He charged our meeting planners and committee chairs with integrating teamwork principles into our educational content as well as our advocacy and membership development initiatives. His vision of a true team galvanized SHM’s commitment to supporting a broad constituency, extending well beyond hospitalist physicians. Jeff knew care is never delivered by an individual; it’s always a team. And he believed this framework to be fully realized by way of building from a strong organizational agenda for quality improvement.
Speaking of quality in healthcare, I look no further than Mark Williams, MD, editor of the Journal of Hospital Medicine, for having built that agenda for our society through his own efforts as well as collaboration with the Institute for Healthcare Improvement (IHI) and other national entities. As another past president of SHM, Mark brought a level of organizational focus and rigor around quality improvement and patient safety that rose to the challenges outlined in two Institute of Medicine reports, “To Err is Human” and “Crossing the Quality Chasm.” He helped move “quality” from something we talk about to something we do. He pushed it from an espoused value to a core commitment of our specialty. Quality improvement is now inseparable from what I consider to be the true promise of hospital medicine: that care organized in well-orchestrated, well-resourced teams can deliver our patients remarkable improvements in the quality, safety, and experience of healthcare.
But how do we get this done? How do we take a relatively abstract notion of a team, channel its activities to drive measurable improvements in quality, and change the arcane systems of inpatient care so as to sustain and hardwire those improvements?
Leadership. Like it or not, each of you is regarded as one of—if not the—most important leaders in the hospital. Nursing, case management, physical therapy, patients, and families look to you to provide leadership for clinical and operational systems. You are the person most able to make meaningful decisions at the front-line level that directly affect the patient experience. You are called upon to lead and manage change in a volatile environment, to resolve the inevitable conflicts that change provokes, and to reconcile hospital business drivers with quality and safety imperatives.
Our immediate past president, Dr. Gorman, emphasized the crucial role we serve as leaders. Recognizing the tremendous development needs for skills and knowledge to effectively lead, SHM has created Leadership Academies and is working on e-discussion forums and mentoring programs to promote longitudinal learning. While we must unlearn some of the behaviors and beliefs seared into our brains during our traditional medical training, we must position ourselves to forge high-performing teams and lead the quality agenda.
At a dinner during the SHM Annual Meeting in May, I sat with a senior leader from the American Medical Association’s Organized Medical Staff Section (AMA OMSS). He had flown in with other AMA representatives to meet with us on common interests. By the end of the evening, the late-career surgeon took me aside and said: “I have to tell you how touched I am by your organization. The passion, drive, and commitment of your membership is what’s missing in so many professional societies today. You must bring this passion to the larger house of medicine.”
As SHM enjoys 10 years of explosive growth and remarkable success, we need to balance the right to celebrate success with the duty not to rest on laurels. Much has been accomplished, but more than a life’s work lies before us. The road is complex and fraught with uncertainty. We might become frustrated with mounting complexity, tired with resistance to change, and fatigued with leading against the status quo. It is hard—and lonely—to confront the systems and issues that desperately need to be confronted on our journey to transform care. And it might be easy for us to become distracted from our core commitments to teamwork and leading quality by allowing our medical society to become more of a guild that defends our professional incomes and way of life. Yet I believe—I know—a much brighter future lies ahead than emerging as a casualty of temptation.
If the best predictor of behavior is past behavior, then our future will mirror the spirit in which SHM was founded. It’s the spirit an invited guest observed in a few short hours at our annual meeting. It’s the spirit that binds teamwork, quality improvement, and leadership into a unified approach to our professional endeavors. That spirit has a name: accountability. It’s the fundamental understanding that we are answerable to others, including patients, families, the community, hospital and medical staff, as well as each other, for the performance of the care systems in which we work.
Being accountable means we must rebuild trust of the broader public in hospital care, and that we follow through on the promise of hospital medicine. It means we own our mistakes, we agree that transparency and measurement will lead to better outcomes, and we commit to being part of the solution.
Accountability also mandates that we eliminate blame and “victimhood.” We cannot first think of ourselves as victims of a broken reimbursement model, or a lack of data or a hospital administration that “just doesn’t get it.” The real questions are: What can I do today about improving management of scarce resources? About the nursing shortage? About incorporating patient-safety principles into a new facility? About access to care and overcrowding? About the needless hospital deaths due to ventilator-assisted pneumonia (VAP), acute myocardial infarction, and methicillin-resistant Staphylococcus aureus? About ensuring seamless transitions of patients throughout the care continuum?
Several years ago I spoke with Brent James, MD, executive director of the Institute for Health Care Delivery Research and vice president of medical research and continuing medical education at InterMountain Healthcare in Salt Lake City, Utah. At the time, I was trying to learn quality improvement methods and practices. He reminded me of a quote Sir William Osler, the father of internal medicine, made at the end of his career when he gave an address at the Phipps Clinic in England to a group of young physicians who had recently completed training. They were about to embark on their careers early in the 20th century. “I am sorry for you young men of this generation,” he told the physicians. “Oh, you’ll do great things. You’ll have great victories, and standing on our shoulders you’ll see far. But you can never have our sensations. To have lived through a revolution, to have seen a new birth of science, new dispensation of health, redesigned medical training, remodeled hospitals, a new outlook for humanity. That is not given to every generation.”
While it seems appropriate in retrospect that these young physicians were indeed entering a time after which tremendous change and transformation had taken place, it seems equally appropriate to consider ourselves one of those generations that must lead and drive change of the magnitude of which Osler spoke. As we lead teams in the hospital to revolutionize the state of healthcare quality, we must begin every thought, every action, by holding ourselves and each other accountable for being part of the solution. To begin, we need look no further than ourselves. TH
Dr. Holman is president of SHM.
Kindred Spirits
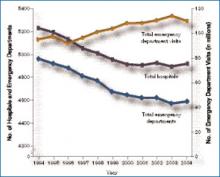
Emergency care in the U.S. has been called a system in crisis, and the data are startling. From 1994 to 2004, the number of hospitals and emergency departments (EDs) decreased, the latter by 9%, but the number of ED visits increased by more than 1 million annually.1 (See Figure 1, p. 17)
According to the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics, between 40% and 50% of U.S. hospitals experience crowded conditions in the ED, with almost two-thirds of metropolitan EDs experiencing crowding at times.2
Hospitalists and emergency medicine physicians asked about their complex relationship—the good, the bad, and the not yet solved—praised their ability to work together.
“In general, our relationship with hospitalists has been fantastic,” says James Hoekstra, MD, president of the Society of Academic Emergency Medicine. “To have physicians who are willing to take patients with a lot of different disease states that are not necessarily procedure oriented, don’t necessarily fit into a specific specialty, or are somewhat undifferentiated in their presentation—for us that is an absolute joy.”
The number of hospitalists and emergency medicine physicians might be said to be running in parallel, says Alpesh Amin, MD, MBA, FACP, executive director of the hospitalist program and vice chair for clinical affairs and quality in the department of medicine at the University of California, Irvine. He tends to refer to this ratio as 30-30, meaning that, within a few years, there will be roughly 30,000 hospitalists, while there are currently that many emergency medicine physicians.3 In addition, emergency medicine and hospital medicine are site-based specialties, says Dr. Amin, so bridging their separateness is crucial to patient care.
“Aside from a small proportion of direct [patient] admissions,” says Jasen W. Gundersen, MD, chief of hospital medicine at the U. Mass. Medical Center in Worcester, “we are an extension of the ER, and the ER is an extension of us. We need to all be on the same page so that what’s said in the ER matches what happens on the floor, which matches what we send out to the primary [care physician].”
Optimizing patient flow is primarily a function of communication, says Marc Newquist, MD, FACEP, a hospitalist, an emergency medicine physician, and program director of the hospitalist division of The Schumacher Group in Lafayette, La. “The better that these communication systems can be standardized, the better hospitalists and their emergency medicine colleagues can promote a seamless integration between the two specialties as patients journey through their hospital stays,” he says.
“As medicine becomes more fragmented and hospital medicine does, let’s face it, fragment care,” adds Dr. Gundersen. “We also have to make sure that information flows from the primary-care physician who may send the patient to the ER. Everybody is a partner, and everybody needs to communicate back and forth and understand that if the ER wants to get someone admitted, timely communication with the hospitalist and understanding how the flow of the hospital works is really important.”
Interactions and Roles
“Far and away the most common type of interaction between hospitalists and ED docs is admissions,” says David M. Pressel, MD, PhD, director, Inpatient Service, General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. The next most common interaction will depend upon the institution and its style, but, primarily, interactions include consults, and—in some institutions—patient discharge.
Dr. Pressel works at a tertiary-care referral center where residents staff the ED and his unit. “But at a community hospital where you generally have ED medicine-trained docs—not pediatricians who have ED
medicine fellowships—they have less experience with pediatrics, so they may be more likely to consult us on a patient,” he says. The development of care pathways to facilitate care is another important interaction between emergency medicine physicians and hospitalists.
An example of a protocol development the hospitalist and the ED should do together, says Dr. Pressel, is when patients come in with certain symptoms that would indicate a possible communicable disease for which the patient might need special isolation on an inpatient unit. That issue may more likely be foremost in hospitalist’s mind, and he or she can perform an evaluation early to determine what isolation may be needed. If the hospitalist suspects a patient has varicella or active pulmonary tuberculosis, for instance, “those kinds of [isolation] rooms are limited,” says Dr. Pressel. “Hospitals don’t have a lot of them, so you have to make sure you’re getting beds assigned well.”
Our interviews say the major roles of the hospitalist in managing relationships with emergency medicine physicians involve professionalism. “The hospitalist needs to understand the needs of the ER physician in terms of the needs of the [overall] ER: timing, flow, and getting patients seen in a prompt manner,” says Dr. Gundersen. “There’s a give and take, and both sides need to understand the other side of the job to maximize that collegiality and to maximize that sense of teamwork.”
Dr. Gundersen, who works full time as a hospitalist and moonlights as an ED physician, says that “what at times the ED doesn’t realize is that the time it takes for them to do something in the ED is not the same as it takes for us to do something on the floor. If they order a CT scan in the ED, it happens right away. If they say, ‘You can just get the CT scan on the floor,’ well, we don’t have as much priority in terms of getting lab draws and diagnostic tests done as fast as they do.”
—Debra L. Burgy, MD, hospitalist, Abbott Northwestern Hospital, Minneapolis, Minn.
Stepping on toes is always a danger.
“One of the key things for the relationship is to realize that you’re not walking in the other person’s shoes,” says Dr. Pressel. “I’ve witnessed [situations] where a hospitalist on the receiving end scoffs at the management in the ED—either because, number one, the patient was perceived to be not sick enough to merit hospitalization according to the hospitalist, or, number two, because of over-workup and overdiagnosis or under-workup and under- or misdiagnosis.”
Both groups need to realize that the patient’s condition evolves over time. “What the ED saw three hours ago may not be what’s being seen now, and that’s true in the reverse,” he says. “If the patient looked great three hours ago, now [their condition may be life-threatening].”
Therefore, feedback between ED doctors and hospitalists should be provided in a “respectful, collegial, follow-up type of manner,” says Dr. Pressel. A beneficial means of communication involves feedback that is “telling it as an evolving story,” he says, as opposed to assuming the ED doctor is wrong. That is, “collaborating and adding to the story and the end diagnosis and recognizing that the ED doc’s job is not necessarily to make the final diagnosis.”
Dr. Pressel thinks it comes down to politeness, plain and simple. “I hope that when I miss something, someone will be kind enough to [be polite] to me, [to phrase it as] ‘I’m sure you were thinking of this but the clues looked this way and we went on to do further evaluation.’ ”
That kind of interaction happens all the time, he says. “And ultimately it’s best for the patient, number one, because everybody learns that way, and, number two, if you make yourself obnoxious with your colleagues, they’re not necessarily going to want to call you.”
The Nature of the Beast
Most interactions with their ED colleagues go smoothly, our hospitalists say, but sometimes there are bumps in the road—most often involving flow and the transfer of care.
Jason R. Orlinick, MD, PhD, chief, Section of Hospital Medicine at Norwalk Hospital, Conn., and clinical instructor of medicine at Yale University (New Haven, Conn.), probably represents the bulk of his hospitalist colleagues when he says he and the emergency medicine physicians with whom he works have a cordial relationship overall. But “there is always some level of tension between the hospitalists and the emergency department—at least at the institutions I’ve been at. To some extent, it depends on the mentality of the ED docs where you’re working.”
Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis, puts it this way: “The interface between hospitalists and the ED is sometimes tense because the ED physicians are regularly bombarded with patients, which is completely unpredictable, and they do not have adequate support staff, such as social workers and psychiatric assessment workers, to create a safe disposition for patients who could otherwise go home.
“The path of least resistance, and the least time-consuming route, is to admit patients. The chain reaction continues with the hospitalist service being overwhelmed.”
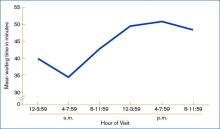
It is common for the ED to get a large volume of patients in the afternoon, our hospitalists remark. (See Figure 2, left) “We sometimes get hit with this huge bolus of patients,” Dr. Gundersen says. The biggest challenges involve “promptly identifying those patients who are identified for admission and maintaining a more open communication because when we get three, four, five admissions at once, we have difficulty working down that backlog.”
In the medical residency program at Dr. Orlinick’s institution, the bolus phenomenon can overwhelm residents’ and attendings’ capacities to see patients in a timely manner. “Unfortunately, we’ve not had a lot of success with that,” he says, and recently, his institution approached the hospitalists to work on a solution.
The timing of handoffs represents a large part of the breakdown in patient flow. “This is because of the ED physician who works until 4 p.m. or 6 p.m. and then tries to get all their patients whom they’re not sending home admitted right away before [the hospitalists] go off service,” Dr. Gundersen says. “It’s not uncommon that I get called or paged every three minutes—if I don’t answer right away—because they are trying to get someone admitted seconds after they call. The ER needs the beds, we haven’t been able to discharge the patients, everything gets bottlenecked.”
Although Dr. Gundersen recognizes that this problem is unavoidable at times, he suggests it would help “if the ED physicians were cognizant that there may be just one or two hospitalists who are admitting for the day, and giving them five admissions all at once, for instance, is going to take time to get through.”
On the other side, “Hospitalists rely on ED physicians to have the patient worked up and know which service they belong to,” explains Dr. Gundersen. “Succinct transfer of care is [paramount] so that critical information is brought to the attention of the accepting physician.” For the most part, he says, his ED colleagues do a good job.
Because the ED is always in a rush to get patients admitted and a disposition made, “there is the tendency to hamstring what’s happening on the floor. I think that big downstream effect from everything that begins in the ER transitions through the patient’s whole length of stay in the hospital,” says Dr. Gundersen.
All the interviewed hospitalists realize that the hospitalists and ED physicians need to have an understanding of what the other group faces. “We have to be understanding of the ER position that there are a lot of patients to be seen, and they’re trying to do the best they can in that period of time,” says Dr. Gundersen. A 2006 study revealed that interruptions within the ED were prevalent and diverse in nature and—on average—there was an interruption every nine and 14 minutes, respectively, for the attending emergency medicine physicians and residents.5
“And ED physicians have to realize that whatever patient they give to us, we then deal with,” says Dr. Gundersen, “and we [continue] to deal with all the issues, moving them through tests and studies [and] getting them discharged, so sometimes there are delays on both ends. It’s just the nature of the beast.”
A Sense of Control
The benefits of maintaining collegiality with ED physicians go beyond the norm, says Jeff Glasheen, MD, director of both the hospital medicine program and inpatient clinical services in the department of medicine at the University of Colorado at Denver Health Sciences Center. Dr. Glasheen has conducted some research on burnout—mostly in residents.6-7
“One of the main things that leads to burnout is lack of control and feeling like you don’t have control over your daily job,” he says. “One of the things that comes out of this relationship with the ER is that it’s no longer like someone’s just dumping on us. They’re very reasonable when we say, ‘That sounds like somebody who could go home; let me come down and see the patient, and let’s see if we can get this patient discharged.’ You begin to feel like you have control over your day, control over the patients who are admitted to you, and—quite honestly—it’s more fun. That kind of professional interaction is hard to put a price on, but I think it’s priceless.”TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006 Sep 28;355(13):1300-1303.
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006 Sep 27;(376):1-23. Available at www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed April 10, 2007.
- Freed DH. Hospitalists: evolution, evidence, and eventualities. Health Care Manag. 2004 Jul-Sep;23(3):238-256;1-38.
- McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2003 emergency department summary. Adv Data. 2005;(358):1-38. Available at www.cdc.gov/nchs/data/ad/ad358.pdf. Last accessed April 10, 2007.
- Laxmisan A, Hakimzada F, Sayan OR, et al. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2006 Oct 21. [Epub ahead of print.]
- Gopal RK, Carreira F, Baker WA, et al. Internal medicine residents reject “longer and gentler” training. J Gen Intern Med. 2007 Jan;22(1):102-106.
- Gopal R, Glasheen JJ, Miyoshi TJ, et al. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005 Dec 12-26;165(22):2595-2600. Comment in Arch Intern Med. 2005 Dec 12-26; 165(22):2561-2562. Arch Intern Med. 2006 Jul 10;166(13):1423; author reply 1423-1425.
Emergency care in the U.S. has been called a system in crisis, and the data are startling. From 1994 to 2004, the number of hospitals and emergency departments (EDs) decreased, the latter by 9%, but the number of ED visits increased by more than 1 million annually.1 (See Figure 1, p. 17)
According to the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics, between 40% and 50% of U.S. hospitals experience crowded conditions in the ED, with almost two-thirds of metropolitan EDs experiencing crowding at times.2
Hospitalists and emergency medicine physicians asked about their complex relationship—the good, the bad, and the not yet solved—praised their ability to work together.
“In general, our relationship with hospitalists has been fantastic,” says James Hoekstra, MD, president of the Society of Academic Emergency Medicine. “To have physicians who are willing to take patients with a lot of different disease states that are not necessarily procedure oriented, don’t necessarily fit into a specific specialty, or are somewhat undifferentiated in their presentation—for us that is an absolute joy.”
The number of hospitalists and emergency medicine physicians might be said to be running in parallel, says Alpesh Amin, MD, MBA, FACP, executive director of the hospitalist program and vice chair for clinical affairs and quality in the department of medicine at the University of California, Irvine. He tends to refer to this ratio as 30-30, meaning that, within a few years, there will be roughly 30,000 hospitalists, while there are currently that many emergency medicine physicians.3 In addition, emergency medicine and hospital medicine are site-based specialties, says Dr. Amin, so bridging their separateness is crucial to patient care.
“Aside from a small proportion of direct [patient] admissions,” says Jasen W. Gundersen, MD, chief of hospital medicine at the U. Mass. Medical Center in Worcester, “we are an extension of the ER, and the ER is an extension of us. We need to all be on the same page so that what’s said in the ER matches what happens on the floor, which matches what we send out to the primary [care physician].”
Optimizing patient flow is primarily a function of communication, says Marc Newquist, MD, FACEP, a hospitalist, an emergency medicine physician, and program director of the hospitalist division of The Schumacher Group in Lafayette, La. “The better that these communication systems can be standardized, the better hospitalists and their emergency medicine colleagues can promote a seamless integration between the two specialties as patients journey through their hospital stays,” he says.
“As medicine becomes more fragmented and hospital medicine does, let’s face it, fragment care,” adds Dr. Gundersen. “We also have to make sure that information flows from the primary-care physician who may send the patient to the ER. Everybody is a partner, and everybody needs to communicate back and forth and understand that if the ER wants to get someone admitted, timely communication with the hospitalist and understanding how the flow of the hospital works is really important.”
Interactions and Roles
“Far and away the most common type of interaction between hospitalists and ED docs is admissions,” says David M. Pressel, MD, PhD, director, Inpatient Service, General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. The next most common interaction will depend upon the institution and its style, but, primarily, interactions include consults, and—in some institutions—patient discharge.
Dr. Pressel works at a tertiary-care referral center where residents staff the ED and his unit. “But at a community hospital where you generally have ED medicine-trained docs—not pediatricians who have ED
medicine fellowships—they have less experience with pediatrics, so they may be more likely to consult us on a patient,” he says. The development of care pathways to facilitate care is another important interaction between emergency medicine physicians and hospitalists.
An example of a protocol development the hospitalist and the ED should do together, says Dr. Pressel, is when patients come in with certain symptoms that would indicate a possible communicable disease for which the patient might need special isolation on an inpatient unit. That issue may more likely be foremost in hospitalist’s mind, and he or she can perform an evaluation early to determine what isolation may be needed. If the hospitalist suspects a patient has varicella or active pulmonary tuberculosis, for instance, “those kinds of [isolation] rooms are limited,” says Dr. Pressel. “Hospitals don’t have a lot of them, so you have to make sure you’re getting beds assigned well.”
Our interviews say the major roles of the hospitalist in managing relationships with emergency medicine physicians involve professionalism. “The hospitalist needs to understand the needs of the ER physician in terms of the needs of the [overall] ER: timing, flow, and getting patients seen in a prompt manner,” says Dr. Gundersen. “There’s a give and take, and both sides need to understand the other side of the job to maximize that collegiality and to maximize that sense of teamwork.”
Dr. Gundersen, who works full time as a hospitalist and moonlights as an ED physician, says that “what at times the ED doesn’t realize is that the time it takes for them to do something in the ED is not the same as it takes for us to do something on the floor. If they order a CT scan in the ED, it happens right away. If they say, ‘You can just get the CT scan on the floor,’ well, we don’t have as much priority in terms of getting lab draws and diagnostic tests done as fast as they do.”
—Debra L. Burgy, MD, hospitalist, Abbott Northwestern Hospital, Minneapolis, Minn.
Stepping on toes is always a danger.
“One of the key things for the relationship is to realize that you’re not walking in the other person’s shoes,” says Dr. Pressel. “I’ve witnessed [situations] where a hospitalist on the receiving end scoffs at the management in the ED—either because, number one, the patient was perceived to be not sick enough to merit hospitalization according to the hospitalist, or, number two, because of over-workup and overdiagnosis or under-workup and under- or misdiagnosis.”
Both groups need to realize that the patient’s condition evolves over time. “What the ED saw three hours ago may not be what’s being seen now, and that’s true in the reverse,” he says. “If the patient looked great three hours ago, now [their condition may be life-threatening].”
Therefore, feedback between ED doctors and hospitalists should be provided in a “respectful, collegial, follow-up type of manner,” says Dr. Pressel. A beneficial means of communication involves feedback that is “telling it as an evolving story,” he says, as opposed to assuming the ED doctor is wrong. That is, “collaborating and adding to the story and the end diagnosis and recognizing that the ED doc’s job is not necessarily to make the final diagnosis.”
Dr. Pressel thinks it comes down to politeness, plain and simple. “I hope that when I miss something, someone will be kind enough to [be polite] to me, [to phrase it as] ‘I’m sure you were thinking of this but the clues looked this way and we went on to do further evaluation.’ ”
That kind of interaction happens all the time, he says. “And ultimately it’s best for the patient, number one, because everybody learns that way, and, number two, if you make yourself obnoxious with your colleagues, they’re not necessarily going to want to call you.”
The Nature of the Beast
Most interactions with their ED colleagues go smoothly, our hospitalists say, but sometimes there are bumps in the road—most often involving flow and the transfer of care.
Jason R. Orlinick, MD, PhD, chief, Section of Hospital Medicine at Norwalk Hospital, Conn., and clinical instructor of medicine at Yale University (New Haven, Conn.), probably represents the bulk of his hospitalist colleagues when he says he and the emergency medicine physicians with whom he works have a cordial relationship overall. But “there is always some level of tension between the hospitalists and the emergency department—at least at the institutions I’ve been at. To some extent, it depends on the mentality of the ED docs where you’re working.”
Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis, puts it this way: “The interface between hospitalists and the ED is sometimes tense because the ED physicians are regularly bombarded with patients, which is completely unpredictable, and they do not have adequate support staff, such as social workers and psychiatric assessment workers, to create a safe disposition for patients who could otherwise go home.
“The path of least resistance, and the least time-consuming route, is to admit patients. The chain reaction continues with the hospitalist service being overwhelmed.”
It is common for the ED to get a large volume of patients in the afternoon, our hospitalists remark. (See Figure 2, left) “We sometimes get hit with this huge bolus of patients,” Dr. Gundersen says. The biggest challenges involve “promptly identifying those patients who are identified for admission and maintaining a more open communication because when we get three, four, five admissions at once, we have difficulty working down that backlog.”
In the medical residency program at Dr. Orlinick’s institution, the bolus phenomenon can overwhelm residents’ and attendings’ capacities to see patients in a timely manner. “Unfortunately, we’ve not had a lot of success with that,” he says, and recently, his institution approached the hospitalists to work on a solution.
The timing of handoffs represents a large part of the breakdown in patient flow. “This is because of the ED physician who works until 4 p.m. or 6 p.m. and then tries to get all their patients whom they’re not sending home admitted right away before [the hospitalists] go off service,” Dr. Gundersen says. “It’s not uncommon that I get called or paged every three minutes—if I don’t answer right away—because they are trying to get someone admitted seconds after they call. The ER needs the beds, we haven’t been able to discharge the patients, everything gets bottlenecked.”
Although Dr. Gundersen recognizes that this problem is unavoidable at times, he suggests it would help “if the ED physicians were cognizant that there may be just one or two hospitalists who are admitting for the day, and giving them five admissions all at once, for instance, is going to take time to get through.”
On the other side, “Hospitalists rely on ED physicians to have the patient worked up and know which service they belong to,” explains Dr. Gundersen. “Succinct transfer of care is [paramount] so that critical information is brought to the attention of the accepting physician.” For the most part, he says, his ED colleagues do a good job.
Because the ED is always in a rush to get patients admitted and a disposition made, “there is the tendency to hamstring what’s happening on the floor. I think that big downstream effect from everything that begins in the ER transitions through the patient’s whole length of stay in the hospital,” says Dr. Gundersen.
All the interviewed hospitalists realize that the hospitalists and ED physicians need to have an understanding of what the other group faces. “We have to be understanding of the ER position that there are a lot of patients to be seen, and they’re trying to do the best they can in that period of time,” says Dr. Gundersen. A 2006 study revealed that interruptions within the ED were prevalent and diverse in nature and—on average—there was an interruption every nine and 14 minutes, respectively, for the attending emergency medicine physicians and residents.5
“And ED physicians have to realize that whatever patient they give to us, we then deal with,” says Dr. Gundersen, “and we [continue] to deal with all the issues, moving them through tests and studies [and] getting them discharged, so sometimes there are delays on both ends. It’s just the nature of the beast.”
A Sense of Control
The benefits of maintaining collegiality with ED physicians go beyond the norm, says Jeff Glasheen, MD, director of both the hospital medicine program and inpatient clinical services in the department of medicine at the University of Colorado at Denver Health Sciences Center. Dr. Glasheen has conducted some research on burnout—mostly in residents.6-7
“One of the main things that leads to burnout is lack of control and feeling like you don’t have control over your daily job,” he says. “One of the things that comes out of this relationship with the ER is that it’s no longer like someone’s just dumping on us. They’re very reasonable when we say, ‘That sounds like somebody who could go home; let me come down and see the patient, and let’s see if we can get this patient discharged.’ You begin to feel like you have control over your day, control over the patients who are admitted to you, and—quite honestly—it’s more fun. That kind of professional interaction is hard to put a price on, but I think it’s priceless.”TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006 Sep 28;355(13):1300-1303.
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006 Sep 27;(376):1-23. Available at www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed April 10, 2007.
- Freed DH. Hospitalists: evolution, evidence, and eventualities. Health Care Manag. 2004 Jul-Sep;23(3):238-256;1-38.
- McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2003 emergency department summary. Adv Data. 2005;(358):1-38. Available at www.cdc.gov/nchs/data/ad/ad358.pdf. Last accessed April 10, 2007.
- Laxmisan A, Hakimzada F, Sayan OR, et al. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2006 Oct 21. [Epub ahead of print.]
- Gopal RK, Carreira F, Baker WA, et al. Internal medicine residents reject “longer and gentler” training. J Gen Intern Med. 2007 Jan;22(1):102-106.
- Gopal R, Glasheen JJ, Miyoshi TJ, et al. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005 Dec 12-26;165(22):2595-2600. Comment in Arch Intern Med. 2005 Dec 12-26; 165(22):2561-2562. Arch Intern Med. 2006 Jul 10;166(13):1423; author reply 1423-1425.
Emergency care in the U.S. has been called a system in crisis, and the data are startling. From 1994 to 2004, the number of hospitals and emergency departments (EDs) decreased, the latter by 9%, but the number of ED visits increased by more than 1 million annually.1 (See Figure 1, p. 17)
According to the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics, between 40% and 50% of U.S. hospitals experience crowded conditions in the ED, with almost two-thirds of metropolitan EDs experiencing crowding at times.2
Hospitalists and emergency medicine physicians asked about their complex relationship—the good, the bad, and the not yet solved—praised their ability to work together.
“In general, our relationship with hospitalists has been fantastic,” says James Hoekstra, MD, president of the Society of Academic Emergency Medicine. “To have physicians who are willing to take patients with a lot of different disease states that are not necessarily procedure oriented, don’t necessarily fit into a specific specialty, or are somewhat undifferentiated in their presentation—for us that is an absolute joy.”
The number of hospitalists and emergency medicine physicians might be said to be running in parallel, says Alpesh Amin, MD, MBA, FACP, executive director of the hospitalist program and vice chair for clinical affairs and quality in the department of medicine at the University of California, Irvine. He tends to refer to this ratio as 30-30, meaning that, within a few years, there will be roughly 30,000 hospitalists, while there are currently that many emergency medicine physicians.3 In addition, emergency medicine and hospital medicine are site-based specialties, says Dr. Amin, so bridging their separateness is crucial to patient care.
“Aside from a small proportion of direct [patient] admissions,” says Jasen W. Gundersen, MD, chief of hospital medicine at the U. Mass. Medical Center in Worcester, “we are an extension of the ER, and the ER is an extension of us. We need to all be on the same page so that what’s said in the ER matches what happens on the floor, which matches what we send out to the primary [care physician].”
Optimizing patient flow is primarily a function of communication, says Marc Newquist, MD, FACEP, a hospitalist, an emergency medicine physician, and program director of the hospitalist division of The Schumacher Group in Lafayette, La. “The better that these communication systems can be standardized, the better hospitalists and their emergency medicine colleagues can promote a seamless integration between the two specialties as patients journey through their hospital stays,” he says.
“As medicine becomes more fragmented and hospital medicine does, let’s face it, fragment care,” adds Dr. Gundersen. “We also have to make sure that information flows from the primary-care physician who may send the patient to the ER. Everybody is a partner, and everybody needs to communicate back and forth and understand that if the ER wants to get someone admitted, timely communication with the hospitalist and understanding how the flow of the hospital works is really important.”
Interactions and Roles
“Far and away the most common type of interaction between hospitalists and ED docs is admissions,” says David M. Pressel, MD, PhD, director, Inpatient Service, General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. The next most common interaction will depend upon the institution and its style, but, primarily, interactions include consults, and—in some institutions—patient discharge.
Dr. Pressel works at a tertiary-care referral center where residents staff the ED and his unit. “But at a community hospital where you generally have ED medicine-trained docs—not pediatricians who have ED
medicine fellowships—they have less experience with pediatrics, so they may be more likely to consult us on a patient,” he says. The development of care pathways to facilitate care is another important interaction between emergency medicine physicians and hospitalists.
An example of a protocol development the hospitalist and the ED should do together, says Dr. Pressel, is when patients come in with certain symptoms that would indicate a possible communicable disease for which the patient might need special isolation on an inpatient unit. That issue may more likely be foremost in hospitalist’s mind, and he or she can perform an evaluation early to determine what isolation may be needed. If the hospitalist suspects a patient has varicella or active pulmonary tuberculosis, for instance, “those kinds of [isolation] rooms are limited,” says Dr. Pressel. “Hospitals don’t have a lot of them, so you have to make sure you’re getting beds assigned well.”
Our interviews say the major roles of the hospitalist in managing relationships with emergency medicine physicians involve professionalism. “The hospitalist needs to understand the needs of the ER physician in terms of the needs of the [overall] ER: timing, flow, and getting patients seen in a prompt manner,” says Dr. Gundersen. “There’s a give and take, and both sides need to understand the other side of the job to maximize that collegiality and to maximize that sense of teamwork.”
Dr. Gundersen, who works full time as a hospitalist and moonlights as an ED physician, says that “what at times the ED doesn’t realize is that the time it takes for them to do something in the ED is not the same as it takes for us to do something on the floor. If they order a CT scan in the ED, it happens right away. If they say, ‘You can just get the CT scan on the floor,’ well, we don’t have as much priority in terms of getting lab draws and diagnostic tests done as fast as they do.”
—Debra L. Burgy, MD, hospitalist, Abbott Northwestern Hospital, Minneapolis, Minn.
Stepping on toes is always a danger.
“One of the key things for the relationship is to realize that you’re not walking in the other person’s shoes,” says Dr. Pressel. “I’ve witnessed [situations] where a hospitalist on the receiving end scoffs at the management in the ED—either because, number one, the patient was perceived to be not sick enough to merit hospitalization according to the hospitalist, or, number two, because of over-workup and overdiagnosis or under-workup and under- or misdiagnosis.”
Both groups need to realize that the patient’s condition evolves over time. “What the ED saw three hours ago may not be what’s being seen now, and that’s true in the reverse,” he says. “If the patient looked great three hours ago, now [their condition may be life-threatening].”
Therefore, feedback between ED doctors and hospitalists should be provided in a “respectful, collegial, follow-up type of manner,” says Dr. Pressel. A beneficial means of communication involves feedback that is “telling it as an evolving story,” he says, as opposed to assuming the ED doctor is wrong. That is, “collaborating and adding to the story and the end diagnosis and recognizing that the ED doc’s job is not necessarily to make the final diagnosis.”
Dr. Pressel thinks it comes down to politeness, plain and simple. “I hope that when I miss something, someone will be kind enough to [be polite] to me, [to phrase it as] ‘I’m sure you were thinking of this but the clues looked this way and we went on to do further evaluation.’ ”
That kind of interaction happens all the time, he says. “And ultimately it’s best for the patient, number one, because everybody learns that way, and, number two, if you make yourself obnoxious with your colleagues, they’re not necessarily going to want to call you.”
The Nature of the Beast
Most interactions with their ED colleagues go smoothly, our hospitalists say, but sometimes there are bumps in the road—most often involving flow and the transfer of care.
Jason R. Orlinick, MD, PhD, chief, Section of Hospital Medicine at Norwalk Hospital, Conn., and clinical instructor of medicine at Yale University (New Haven, Conn.), probably represents the bulk of his hospitalist colleagues when he says he and the emergency medicine physicians with whom he works have a cordial relationship overall. But “there is always some level of tension between the hospitalists and the emergency department—at least at the institutions I’ve been at. To some extent, it depends on the mentality of the ED docs where you’re working.”
Debra L. Burgy, MD, a hospitalist at Abbott Northwestern Hospital in Minneapolis, puts it this way: “The interface between hospitalists and the ED is sometimes tense because the ED physicians are regularly bombarded with patients, which is completely unpredictable, and they do not have adequate support staff, such as social workers and psychiatric assessment workers, to create a safe disposition for patients who could otherwise go home.
“The path of least resistance, and the least time-consuming route, is to admit patients. The chain reaction continues with the hospitalist service being overwhelmed.”
It is common for the ED to get a large volume of patients in the afternoon, our hospitalists remark. (See Figure 2, left) “We sometimes get hit with this huge bolus of patients,” Dr. Gundersen says. The biggest challenges involve “promptly identifying those patients who are identified for admission and maintaining a more open communication because when we get three, four, five admissions at once, we have difficulty working down that backlog.”
In the medical residency program at Dr. Orlinick’s institution, the bolus phenomenon can overwhelm residents’ and attendings’ capacities to see patients in a timely manner. “Unfortunately, we’ve not had a lot of success with that,” he says, and recently, his institution approached the hospitalists to work on a solution.
The timing of handoffs represents a large part of the breakdown in patient flow. “This is because of the ED physician who works until 4 p.m. or 6 p.m. and then tries to get all their patients whom they’re not sending home admitted right away before [the hospitalists] go off service,” Dr. Gundersen says. “It’s not uncommon that I get called or paged every three minutes—if I don’t answer right away—because they are trying to get someone admitted seconds after they call. The ER needs the beds, we haven’t been able to discharge the patients, everything gets bottlenecked.”
Although Dr. Gundersen recognizes that this problem is unavoidable at times, he suggests it would help “if the ED physicians were cognizant that there may be just one or two hospitalists who are admitting for the day, and giving them five admissions all at once, for instance, is going to take time to get through.”
On the other side, “Hospitalists rely on ED physicians to have the patient worked up and know which service they belong to,” explains Dr. Gundersen. “Succinct transfer of care is [paramount] so that critical information is brought to the attention of the accepting physician.” For the most part, he says, his ED colleagues do a good job.
Because the ED is always in a rush to get patients admitted and a disposition made, “there is the tendency to hamstring what’s happening on the floor. I think that big downstream effect from everything that begins in the ER transitions through the patient’s whole length of stay in the hospital,” says Dr. Gundersen.
All the interviewed hospitalists realize that the hospitalists and ED physicians need to have an understanding of what the other group faces. “We have to be understanding of the ER position that there are a lot of patients to be seen, and they’re trying to do the best they can in that period of time,” says Dr. Gundersen. A 2006 study revealed that interruptions within the ED were prevalent and diverse in nature and—on average—there was an interruption every nine and 14 minutes, respectively, for the attending emergency medicine physicians and residents.5
“And ED physicians have to realize that whatever patient they give to us, we then deal with,” says Dr. Gundersen, “and we [continue] to deal with all the issues, moving them through tests and studies [and] getting them discharged, so sometimes there are delays on both ends. It’s just the nature of the beast.”
A Sense of Control
The benefits of maintaining collegiality with ED physicians go beyond the norm, says Jeff Glasheen, MD, director of both the hospital medicine program and inpatient clinical services in the department of medicine at the University of Colorado at Denver Health Sciences Center. Dr. Glasheen has conducted some research on burnout—mostly in residents.6-7
“One of the main things that leads to burnout is lack of control and feeling like you don’t have control over your daily job,” he says. “One of the things that comes out of this relationship with the ER is that it’s no longer like someone’s just dumping on us. They’re very reasonable when we say, ‘That sounds like somebody who could go home; let me come down and see the patient, and let’s see if we can get this patient discharged.’ You begin to feel like you have control over your day, control over the patients who are admitted to you, and—quite honestly—it’s more fun. That kind of professional interaction is hard to put a price on, but I think it’s priceless.”TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006 Sep 28;355(13):1300-1303.
- Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006 Sep 27;(376):1-23. Available at www.cdc.gov/nchs/data/ad/ad376.pdf. Last accessed April 10, 2007.
- Freed DH. Hospitalists: evolution, evidence, and eventualities. Health Care Manag. 2004 Jul-Sep;23(3):238-256;1-38.
- McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2003 emergency department summary. Adv Data. 2005;(358):1-38. Available at www.cdc.gov/nchs/data/ad/ad358.pdf. Last accessed April 10, 2007.
- Laxmisan A, Hakimzada F, Sayan OR, et al. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2006 Oct 21. [Epub ahead of print.]
- Gopal RK, Carreira F, Baker WA, et al. Internal medicine residents reject “longer and gentler” training. J Gen Intern Med. 2007 Jan;22(1):102-106.
- Gopal R, Glasheen JJ, Miyoshi TJ, et al. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005 Dec 12-26;165(22):2595-2600. Comment in Arch Intern Med. 2005 Dec 12-26; 165(22):2561-2562. Arch Intern Med. 2006 Jul 10;166(13):1423; author reply 1423-1425.
Word Gets Around
The online version of the Oxford English Dictionary (OED) is the latest in a string of dictionaries to include the word “hospitalist” among its entries.
“This is just another sign that “hospitalist” has become another part of the landscape, and that we’ve arrived and will be here for a very long time,” says Larry Wellikson, MD, CEO of SHM. “I think SHM has been working on defining what a hospitalist is in textbooks and other reference materials since I got here in 2000.”
Asked if SHM solicited the OED staff to include hospitalist in its entries, Dr. Wellikson said it wasn’t necessary. “No, we didn’t lobby them,” he says. “They did it totally on their own. If you Google hospitalist, you’ll see thousands of stories that have been written during the past 10 years, including by such publications as the The Wall Street Journal.”
Dr. Wellikson noted that CNN’s Larry King mentioned hospitalists during a segment in 2005. “[The word hospitalist] has turned up in so many places,” he says.
To date, “hospitalist” has been included in print editions of The American Heritage Dictionary of the English Language, Merriam-Webster’s collegiate and medical dictionaries, as well as other print medical dictionaries and some online dictionaries. The American Heritage Dictionary appears to be the first to have included the word in a print edition in 2000, according to a spokesman for the publication.
The process of selecting a new word for inclusion in a dictionary appears fairly constant in the industry.
“It can include suggestions from our readership or people in a particular industry who might suggest that a new word unique to their profession should be included,” says Katherine Martin, senior assistant editor at OED’s New York offices. “It also includes our own (staff) study to ascertain if a certain word that is tested over time will have continued longevity.”
Tested over time indeed. Martin and other dictionary staff members say it can sometimes take up to 10 years for a new word to be included in a dictionary.
That’s how long it took to include hospitalist in Merriam-Webster’s Collegiate Dictionary, according to a spokesman for that publication. And while hospitalist was included in the OED’s online version in December 2006, it’s uncertain if it will ever get into the print version, according to Martin.
The OED’s second edition was last printed in 1989, Martin says, and because of the huge cost involved, “We haven’t even begun discussing the possibility of printing a third edition.”
Access to the 20-volume print edition is available to subscribers to the OED’s fee-based online version, Martin says.
The term hospitalist was first introduced in 1996 in an article by Robert M. Wachter, MD, and Lee Goldman, MD, to describe physicians who devote much of their professional time and focus to the care of hospitalized patients.
Merriam-Webster began monitoring the term when the article first appeared in the New England Journal of Medicine, according to Peter Sokolowski, associate editor. He says hospitalist made it into the company’s collegiate dictionary in 2005, and the medical dictionary a year later.
For the most part, both print and online dictionaries give a relatively simple definition of hospitalist: “A physician specializing in the care of hospital in-patients,” says the OED’s online version. Merriam-Webster’s dictionaries define the term as “a physician who specializes in treating hospitalized patients of other physicians in order to minimize the number of hospital visits by other physicians.”
Perhaps the most extensive definition online appears in Wikipedia, the free online encyclopedia. In addition to the definition, Wikipedia also provides information on the specialty under various subtitles, including Training and History. TH
Tom Giordano is a freelance journalist based in Connecticut
The online version of the Oxford English Dictionary (OED) is the latest in a string of dictionaries to include the word “hospitalist” among its entries.
“This is just another sign that “hospitalist” has become another part of the landscape, and that we’ve arrived and will be here for a very long time,” says Larry Wellikson, MD, CEO of SHM. “I think SHM has been working on defining what a hospitalist is in textbooks and other reference materials since I got here in 2000.”
Asked if SHM solicited the OED staff to include hospitalist in its entries, Dr. Wellikson said it wasn’t necessary. “No, we didn’t lobby them,” he says. “They did it totally on their own. If you Google hospitalist, you’ll see thousands of stories that have been written during the past 10 years, including by such publications as the The Wall Street Journal.”
Dr. Wellikson noted that CNN’s Larry King mentioned hospitalists during a segment in 2005. “[The word hospitalist] has turned up in so many places,” he says.
To date, “hospitalist” has been included in print editions of The American Heritage Dictionary of the English Language, Merriam-Webster’s collegiate and medical dictionaries, as well as other print medical dictionaries and some online dictionaries. The American Heritage Dictionary appears to be the first to have included the word in a print edition in 2000, according to a spokesman for the publication.
The process of selecting a new word for inclusion in a dictionary appears fairly constant in the industry.
“It can include suggestions from our readership or people in a particular industry who might suggest that a new word unique to their profession should be included,” says Katherine Martin, senior assistant editor at OED’s New York offices. “It also includes our own (staff) study to ascertain if a certain word that is tested over time will have continued longevity.”
Tested over time indeed. Martin and other dictionary staff members say it can sometimes take up to 10 years for a new word to be included in a dictionary.
That’s how long it took to include hospitalist in Merriam-Webster’s Collegiate Dictionary, according to a spokesman for that publication. And while hospitalist was included in the OED’s online version in December 2006, it’s uncertain if it will ever get into the print version, according to Martin.
The OED’s second edition was last printed in 1989, Martin says, and because of the huge cost involved, “We haven’t even begun discussing the possibility of printing a third edition.”
Access to the 20-volume print edition is available to subscribers to the OED’s fee-based online version, Martin says.
The term hospitalist was first introduced in 1996 in an article by Robert M. Wachter, MD, and Lee Goldman, MD, to describe physicians who devote much of their professional time and focus to the care of hospitalized patients.
Merriam-Webster began monitoring the term when the article first appeared in the New England Journal of Medicine, according to Peter Sokolowski, associate editor. He says hospitalist made it into the company’s collegiate dictionary in 2005, and the medical dictionary a year later.
For the most part, both print and online dictionaries give a relatively simple definition of hospitalist: “A physician specializing in the care of hospital in-patients,” says the OED’s online version. Merriam-Webster’s dictionaries define the term as “a physician who specializes in treating hospitalized patients of other physicians in order to minimize the number of hospital visits by other physicians.”
Perhaps the most extensive definition online appears in Wikipedia, the free online encyclopedia. In addition to the definition, Wikipedia also provides information on the specialty under various subtitles, including Training and History. TH
Tom Giordano is a freelance journalist based in Connecticut
The online version of the Oxford English Dictionary (OED) is the latest in a string of dictionaries to include the word “hospitalist” among its entries.
“This is just another sign that “hospitalist” has become another part of the landscape, and that we’ve arrived and will be here for a very long time,” says Larry Wellikson, MD, CEO of SHM. “I think SHM has been working on defining what a hospitalist is in textbooks and other reference materials since I got here in 2000.”
Asked if SHM solicited the OED staff to include hospitalist in its entries, Dr. Wellikson said it wasn’t necessary. “No, we didn’t lobby them,” he says. “They did it totally on their own. If you Google hospitalist, you’ll see thousands of stories that have been written during the past 10 years, including by such publications as the The Wall Street Journal.”
Dr. Wellikson noted that CNN’s Larry King mentioned hospitalists during a segment in 2005. “[The word hospitalist] has turned up in so many places,” he says.
To date, “hospitalist” has been included in print editions of The American Heritage Dictionary of the English Language, Merriam-Webster’s collegiate and medical dictionaries, as well as other print medical dictionaries and some online dictionaries. The American Heritage Dictionary appears to be the first to have included the word in a print edition in 2000, according to a spokesman for the publication.
The process of selecting a new word for inclusion in a dictionary appears fairly constant in the industry.
“It can include suggestions from our readership or people in a particular industry who might suggest that a new word unique to their profession should be included,” says Katherine Martin, senior assistant editor at OED’s New York offices. “It also includes our own (staff) study to ascertain if a certain word that is tested over time will have continued longevity.”
Tested over time indeed. Martin and other dictionary staff members say it can sometimes take up to 10 years for a new word to be included in a dictionary.
That’s how long it took to include hospitalist in Merriam-Webster’s Collegiate Dictionary, according to a spokesman for that publication. And while hospitalist was included in the OED’s online version in December 2006, it’s uncertain if it will ever get into the print version, according to Martin.
The OED’s second edition was last printed in 1989, Martin says, and because of the huge cost involved, “We haven’t even begun discussing the possibility of printing a third edition.”
Access to the 20-volume print edition is available to subscribers to the OED’s fee-based online version, Martin says.
The term hospitalist was first introduced in 1996 in an article by Robert M. Wachter, MD, and Lee Goldman, MD, to describe physicians who devote much of their professional time and focus to the care of hospitalized patients.
Merriam-Webster began monitoring the term when the article first appeared in the New England Journal of Medicine, according to Peter Sokolowski, associate editor. He says hospitalist made it into the company’s collegiate dictionary in 2005, and the medical dictionary a year later.
For the most part, both print and online dictionaries give a relatively simple definition of hospitalist: “A physician specializing in the care of hospital in-patients,” says the OED’s online version. Merriam-Webster’s dictionaries define the term as “a physician who specializes in treating hospitalized patients of other physicians in order to minimize the number of hospital visits by other physicians.”
Perhaps the most extensive definition online appears in Wikipedia, the free online encyclopedia. In addition to the definition, Wikipedia also provides information on the specialty under various subtitles, including Training and History. TH
Tom Giordano is a freelance journalist based in Connecticut
A Keg in the Garage
It is standard wisdom that when patients say they drink two beers a day, you should double that amount. Possibly triple it. I’ve had patients tell me they “don’t drink anymore,” meaning any more then they did before.
Though we tend to believe our patients when they recite their litany of pains and woes, when it comes to alcohol (and several other topics such as chronic pain, disability exams, and worker’s compensation) our credulity is often tested.
Mr. Q had been my patient for several years. He was a chain-smoking, hard-drinking Korean War veteran. He was a diminutive, cachectic, dyspneic, but extremely pleasant man. He was always accompanied to my clinic (in my prehospitalist days) with his ever-suffering, massive, and markedly less affable wife in tow.
His COPD was progressively worsening, and one day he told me he was going to quit smoking. His wife laughed unpleasantly, and commented that he’d quit just like he’d quit drinking. He prided himself on the keg of beer he kept in his garage. It was this keg that drove his wife most crazy, and perhaps that was the source of his pride. He went from two packs a day to five cigarettes. He said he planned to wake up every morning and load five in an empty pack, and these would be his five for the day. He would smoke the hell out of them, but if he ran out he would wait till the next morning to reload. His wife, as usual, sat and scowled and undermined his efforts.
On a subsequent visit, when he said he was down to five cigarettes, she laughed and said he was lying; he was smoking in the closet, in the car, wherever he could when she wasn’t looking—especially in the garage. Yet, some how I believed him. Maybe.
Before he came under my care Mr. Q also had been diagnosed with cirrhosis. I warned him many times about his need to stop drinking. I gave him lurid descriptions of esophageal varices and exsanguination, and other hepatic complications too fierce to mention. He always asserted that he didn’t drink anymore, with a large wink; his wife squirming in her chair. She snorted and said he should tell that to the keg in the garage. She said he would sit there all night long, drinking and watching the old black and white. I could see him wanting to escape her beady-eyed gaze. Yet I found this harder to believe than the possibility that he’d cut back his smoking.
Over the next year or so I pleaded with him to stop drinking as he developed diabetes. I knew a dozen beers a day couldn’t be helping his condition. I talked about diet and exercise, and he just laughed at me. He said he wasn’t going to exercise much with his lungs and remarked that if I’d tasted his wife’s cooking, diet wouldn’t be an issue. I marveled at what strange, attractive force held these two people together. Mutual hatred seemed the answer.
Two months later I admitted him to the hospital with a cardiac arrhythmia. He’d popped into atrial fibrillation. His wife grumbled that her husband hadn’t been out of the garage in a week. A diagnosis immediately came to mind: holiday heart. He’d drunk himself into an arrhythmia.
I got his heart rate under control but was frustrated with my seemingly fruitless efforts to control his drinking. His wife stormed out of his hospital room. The first time I was alone with him, I asked him why he’d never stopped drinking. He looked at me and laughed bitterly. He said he knew I wouldn’t believe him but that he had not had a drink in three years. The keg had been dry all that time, he just liked to sit in the garage and pretend he was having a few to keep away from his wife. He enjoyed his garage, the tools he was too sick to use, and his old black-and-white television.
How could this be? The history and exam did not jibe with this at all. He looked and acted like an alcoholic. Yet if his story were true, how could I explain his current condition? I wanted to believe him, but his persistent liver dysfunction, diabetes, and new arrhythmia argued against it. I looked at him. He was a gnarled, emphysematous shell of a man. At least he had a nice tan. I commented on this, mentioning that he must spend some time out of the garage to keep his melanocytes so primed. He looked at me quizzically. He said he never went outside, unless it was to get the newspaper; he hated sitting in the sun.
A light bulb lit in my head, then exploded into a million pieces. What if he really hadn’t been drinking? What else could explain this clinical picture? I was sure I knew the answer now, and a lab test quickly confirmed it. To my chagrin, his ferritin was more than 2,000. Bronze diabetes: his liver abnormalities, diabetes, pseudo-tan, and cardiac arrhythmia were due to iron deposition. He had hemochromatosis!
Several years later, Mr. Q died of complications of COPD. His son found him sitting in a lounge chair in his garage, with the old black and white tuned to his favorite station. He did not die from the diagnosis I had missed. Would his clinical outcome have been any different if the diagnosis had been made earlier? Probably not. Further, if his wife had known he wasn’t drinking, he might have lost his place of refuge. I promised myself that the next time a patient told me how much they drank that I would try to be less cynical in my response.
The day he died I went home and opened a fine merlot and poured myself a glass—then didn’t drink it. TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
It is standard wisdom that when patients say they drink two beers a day, you should double that amount. Possibly triple it. I’ve had patients tell me they “don’t drink anymore,” meaning any more then they did before.
Though we tend to believe our patients when they recite their litany of pains and woes, when it comes to alcohol (and several other topics such as chronic pain, disability exams, and worker’s compensation) our credulity is often tested.
Mr. Q had been my patient for several years. He was a chain-smoking, hard-drinking Korean War veteran. He was a diminutive, cachectic, dyspneic, but extremely pleasant man. He was always accompanied to my clinic (in my prehospitalist days) with his ever-suffering, massive, and markedly less affable wife in tow.
His COPD was progressively worsening, and one day he told me he was going to quit smoking. His wife laughed unpleasantly, and commented that he’d quit just like he’d quit drinking. He prided himself on the keg of beer he kept in his garage. It was this keg that drove his wife most crazy, and perhaps that was the source of his pride. He went from two packs a day to five cigarettes. He said he planned to wake up every morning and load five in an empty pack, and these would be his five for the day. He would smoke the hell out of them, but if he ran out he would wait till the next morning to reload. His wife, as usual, sat and scowled and undermined his efforts.
On a subsequent visit, when he said he was down to five cigarettes, she laughed and said he was lying; he was smoking in the closet, in the car, wherever he could when she wasn’t looking—especially in the garage. Yet, some how I believed him. Maybe.
Before he came under my care Mr. Q also had been diagnosed with cirrhosis. I warned him many times about his need to stop drinking. I gave him lurid descriptions of esophageal varices and exsanguination, and other hepatic complications too fierce to mention. He always asserted that he didn’t drink anymore, with a large wink; his wife squirming in her chair. She snorted and said he should tell that to the keg in the garage. She said he would sit there all night long, drinking and watching the old black and white. I could see him wanting to escape her beady-eyed gaze. Yet I found this harder to believe than the possibility that he’d cut back his smoking.
Over the next year or so I pleaded with him to stop drinking as he developed diabetes. I knew a dozen beers a day couldn’t be helping his condition. I talked about diet and exercise, and he just laughed at me. He said he wasn’t going to exercise much with his lungs and remarked that if I’d tasted his wife’s cooking, diet wouldn’t be an issue. I marveled at what strange, attractive force held these two people together. Mutual hatred seemed the answer.
Two months later I admitted him to the hospital with a cardiac arrhythmia. He’d popped into atrial fibrillation. His wife grumbled that her husband hadn’t been out of the garage in a week. A diagnosis immediately came to mind: holiday heart. He’d drunk himself into an arrhythmia.
I got his heart rate under control but was frustrated with my seemingly fruitless efforts to control his drinking. His wife stormed out of his hospital room. The first time I was alone with him, I asked him why he’d never stopped drinking. He looked at me and laughed bitterly. He said he knew I wouldn’t believe him but that he had not had a drink in three years. The keg had been dry all that time, he just liked to sit in the garage and pretend he was having a few to keep away from his wife. He enjoyed his garage, the tools he was too sick to use, and his old black-and-white television.
How could this be? The history and exam did not jibe with this at all. He looked and acted like an alcoholic. Yet if his story were true, how could I explain his current condition? I wanted to believe him, but his persistent liver dysfunction, diabetes, and new arrhythmia argued against it. I looked at him. He was a gnarled, emphysematous shell of a man. At least he had a nice tan. I commented on this, mentioning that he must spend some time out of the garage to keep his melanocytes so primed. He looked at me quizzically. He said he never went outside, unless it was to get the newspaper; he hated sitting in the sun.
A light bulb lit in my head, then exploded into a million pieces. What if he really hadn’t been drinking? What else could explain this clinical picture? I was sure I knew the answer now, and a lab test quickly confirmed it. To my chagrin, his ferritin was more than 2,000. Bronze diabetes: his liver abnormalities, diabetes, pseudo-tan, and cardiac arrhythmia were due to iron deposition. He had hemochromatosis!
Several years later, Mr. Q died of complications of COPD. His son found him sitting in a lounge chair in his garage, with the old black and white tuned to his favorite station. He did not die from the diagnosis I had missed. Would his clinical outcome have been any different if the diagnosis had been made earlier? Probably not. Further, if his wife had known he wasn’t drinking, he might have lost his place of refuge. I promised myself that the next time a patient told me how much they drank that I would try to be less cynical in my response.
The day he died I went home and opened a fine merlot and poured myself a glass—then didn’t drink it. TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
It is standard wisdom that when patients say they drink two beers a day, you should double that amount. Possibly triple it. I’ve had patients tell me they “don’t drink anymore,” meaning any more then they did before.
Though we tend to believe our patients when they recite their litany of pains and woes, when it comes to alcohol (and several other topics such as chronic pain, disability exams, and worker’s compensation) our credulity is often tested.
Mr. Q had been my patient for several years. He was a chain-smoking, hard-drinking Korean War veteran. He was a diminutive, cachectic, dyspneic, but extremely pleasant man. He was always accompanied to my clinic (in my prehospitalist days) with his ever-suffering, massive, and markedly less affable wife in tow.
His COPD was progressively worsening, and one day he told me he was going to quit smoking. His wife laughed unpleasantly, and commented that he’d quit just like he’d quit drinking. He prided himself on the keg of beer he kept in his garage. It was this keg that drove his wife most crazy, and perhaps that was the source of his pride. He went from two packs a day to five cigarettes. He said he planned to wake up every morning and load five in an empty pack, and these would be his five for the day. He would smoke the hell out of them, but if he ran out he would wait till the next morning to reload. His wife, as usual, sat and scowled and undermined his efforts.
On a subsequent visit, when he said he was down to five cigarettes, she laughed and said he was lying; he was smoking in the closet, in the car, wherever he could when she wasn’t looking—especially in the garage. Yet, some how I believed him. Maybe.
Before he came under my care Mr. Q also had been diagnosed with cirrhosis. I warned him many times about his need to stop drinking. I gave him lurid descriptions of esophageal varices and exsanguination, and other hepatic complications too fierce to mention. He always asserted that he didn’t drink anymore, with a large wink; his wife squirming in her chair. She snorted and said he should tell that to the keg in the garage. She said he would sit there all night long, drinking and watching the old black and white. I could see him wanting to escape her beady-eyed gaze. Yet I found this harder to believe than the possibility that he’d cut back his smoking.
Over the next year or so I pleaded with him to stop drinking as he developed diabetes. I knew a dozen beers a day couldn’t be helping his condition. I talked about diet and exercise, and he just laughed at me. He said he wasn’t going to exercise much with his lungs and remarked that if I’d tasted his wife’s cooking, diet wouldn’t be an issue. I marveled at what strange, attractive force held these two people together. Mutual hatred seemed the answer.
Two months later I admitted him to the hospital with a cardiac arrhythmia. He’d popped into atrial fibrillation. His wife grumbled that her husband hadn’t been out of the garage in a week. A diagnosis immediately came to mind: holiday heart. He’d drunk himself into an arrhythmia.
I got his heart rate under control but was frustrated with my seemingly fruitless efforts to control his drinking. His wife stormed out of his hospital room. The first time I was alone with him, I asked him why he’d never stopped drinking. He looked at me and laughed bitterly. He said he knew I wouldn’t believe him but that he had not had a drink in three years. The keg had been dry all that time, he just liked to sit in the garage and pretend he was having a few to keep away from his wife. He enjoyed his garage, the tools he was too sick to use, and his old black-and-white television.
How could this be? The history and exam did not jibe with this at all. He looked and acted like an alcoholic. Yet if his story were true, how could I explain his current condition? I wanted to believe him, but his persistent liver dysfunction, diabetes, and new arrhythmia argued against it. I looked at him. He was a gnarled, emphysematous shell of a man. At least he had a nice tan. I commented on this, mentioning that he must spend some time out of the garage to keep his melanocytes so primed. He looked at me quizzically. He said he never went outside, unless it was to get the newspaper; he hated sitting in the sun.
A light bulb lit in my head, then exploded into a million pieces. What if he really hadn’t been drinking? What else could explain this clinical picture? I was sure I knew the answer now, and a lab test quickly confirmed it. To my chagrin, his ferritin was more than 2,000. Bronze diabetes: his liver abnormalities, diabetes, pseudo-tan, and cardiac arrhythmia were due to iron deposition. He had hemochromatosis!
Several years later, Mr. Q died of complications of COPD. His son found him sitting in a lounge chair in his garage, with the old black and white tuned to his favorite station. He did not die from the diagnosis I had missed. Would his clinical outcome have been any different if the diagnosis had been made earlier? Probably not. Further, if his wife had known he wasn’t drinking, he might have lost his place of refuge. I promised myself that the next time a patient told me how much they drank that I would try to be less cynical in my response.
The day he died I went home and opened a fine merlot and poured myself a glass—then didn’t drink it. TH
Dr. Newman is the physician editor of The Hospitalist. He’s also consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Comp Close-Up
How hard do hospitalists work and how much are they paid? There are several sources of data to answer this question, and each has its strengths and weaknesses. Because these data influence contract negotiations and compliance with federal regulations, it is worth taking the time to understand the differences in each data set.
I’ll focus on the two most common sources of data: the biannual SHM survey of hospitalist productivity and compensation (officially titled “The Authoritative Source on the State of Hospital Medicine”), and the Medical Group Management Association’s (MGMA) annual “Physician Compensation and Production Survey.” There are many other surveys that report hospitalist data such as those by the American Medical Group Association (AMGA), Sullivan & Cotter, Hay Group, and others. Each July, Modern Healthcare magazine publishes the average compensation (but no other data) reported for hospitalists and other specialties by each of these organizations and several others (but not the SHM data). It should be easy to find a copy of Modern Healthcare in your hospital administration or library, or on the Internet.
The SHM and MGMA surveys are the most widely used sources of data for hospitalists, and some of their attributes are described in Table 1 (see below).
I should acknowledge my potential conflict of interest and potential for bias in comparing these surveys. This column is in an SHM publication. I’m very active in SHM, and I’m a past chairman and ongoing member of the Benchmarks Committee, which oversees the design and analysis of the SHM survey. And while I am familiar with and regularly review the MGMA survey, I have no other connection to that organization.
Much of the difference between the surveys is a result of the SHM survey being designed specifically for hospitalists in any type of practice setting (e.g., small hospitalist-only groups, as well as hospitalists with huge organizations like a university faculty group practice). In contrast, the MGMA survey is designed for all physician specialties, so a hospitalist answers the same questions as a traditional primary care doctor, plastic surgeon, and obstetrician.
MGMA data can be adversely affected by the inclusion of primary care office-based encounters. One of the principal ways the two surveys differ is how they address ambulatory visits. The MGMA survey reports inpatient and ambulatory visits separately, but “ambulatory” visits include any for a patient who is not a hospital inpatient. By this definition, hospitalists make ambulatory visits, most commonly to hospitalized patients who are on observation status, and also patients seen in an ED, skilled nursing facility, or pre-op clinic. Thus the MGMA survey doesn’t distinguish between ambulatory encounters a hospitalist would generate in the course of serving as a hospitalist, and those generated while that doctor might be serving in a non-hospitalist role such as office-based primary care or urgent care.
The SHM survey doesn’t include—and isn’t contaminated by—office-based primary care or urgent-care visits.
Of the 3,376 total encounters reported in the MGMA survey, 40% (1,351) are ambulatory encounters. Although the SHM survey does not distinguish between hospital and ambulatory encounters, my experience suggests few, if any, hospitalist practices make 40% of their total encounters with patients on observation status, or in an ED, SNF, or pre-op clinic. Thus, many of the ambulatory encounters reported by MGMA might have been office visits, not hospital-related visits.
Additionally, the median internal medicine hospitalist encounters (ambulatory and hospital combined) in the MGMA survey (3,376) is 42% higher than the median total encounters reported for internal medicine hospitalists in SHM’s survey (2,378). Yet the wRVUs reported in the MGMA survey (3,514) are only 8% higher than those reported in the SHM survey (3,256). Thus the calculated average wRVUs per encounter for the MGMA data is only 1.04, compared with 1.37 for the SHM data. An average of 1.04 wRVUs per encounter is very low for hospitalists, when almost all current procedural terminology (CPT) codes a hospitalist uses have a value of one or more wRVUs. Again, this suggests the MGMA data may be significantly influenced by the inclusion of office-based encounters, some of which have wRVUs of less than one. SHM has approached MGMA to discuss this data definition issue in their survey.
Why It Matters
You can use whichever data set best describes your situation. The MGMA has historically shown higher hospitalist salaries and higher workloads than the SHM data. But because the SHM data is the result of a survey customized for hospitalists and less likely than the MGMA data to be contaminated by non-hospital-related visits, the SHM data probably gives a more accurate picture.
Because the MGMA survey has been conducted for many years (far longer than the SHM survey) it has appropriately become one of the most authoritative sources of data on physician compensation for all specialties. Stark II regulations require hospitals to ensure they aren’t paying physicians above the fair market compensation (which could be seen as an inducement to refer patients to the hospital, among other concerns). And it specifically states that the MGMA survey is one of several approved sources of determining what fair market compensation is.
Even though the SHM data is most likely more representative and provides an important benchmark for hospitalists, the MGMA data has “pre-approved” status and thus is potentially safer to use for the specific purpose of determinations of fair market value.
With each iteration, the SHM survey will be adjusted to more specifically capture hospitalist activity; in many cases it is the best data for hospitalists to use in planning and benchmarking. But the MGMA data are still valuable and may be the most appropriate to refer to in contracts.
Note to readers: In May, SHM contacted MGMA regarding their concerns that MGMA survey data was not representative of hospitalists. MGMA responded with a willingness to discuss these issues with SHM. As this story goes to press, SHM and MGMA continue to have a dialogue about maximizing the accuracy of survey data. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
How hard do hospitalists work and how much are they paid? There are several sources of data to answer this question, and each has its strengths and weaknesses. Because these data influence contract negotiations and compliance with federal regulations, it is worth taking the time to understand the differences in each data set.
I’ll focus on the two most common sources of data: the biannual SHM survey of hospitalist productivity and compensation (officially titled “The Authoritative Source on the State of Hospital Medicine”), and the Medical Group Management Association’s (MGMA) annual “Physician Compensation and Production Survey.” There are many other surveys that report hospitalist data such as those by the American Medical Group Association (AMGA), Sullivan & Cotter, Hay Group, and others. Each July, Modern Healthcare magazine publishes the average compensation (but no other data) reported for hospitalists and other specialties by each of these organizations and several others (but not the SHM data). It should be easy to find a copy of Modern Healthcare in your hospital administration or library, or on the Internet.
The SHM and MGMA surveys are the most widely used sources of data for hospitalists, and some of their attributes are described in Table 1 (see below).
I should acknowledge my potential conflict of interest and potential for bias in comparing these surveys. This column is in an SHM publication. I’m very active in SHM, and I’m a past chairman and ongoing member of the Benchmarks Committee, which oversees the design and analysis of the SHM survey. And while I am familiar with and regularly review the MGMA survey, I have no other connection to that organization.
Much of the difference between the surveys is a result of the SHM survey being designed specifically for hospitalists in any type of practice setting (e.g., small hospitalist-only groups, as well as hospitalists with huge organizations like a university faculty group practice). In contrast, the MGMA survey is designed for all physician specialties, so a hospitalist answers the same questions as a traditional primary care doctor, plastic surgeon, and obstetrician.
MGMA data can be adversely affected by the inclusion of primary care office-based encounters. One of the principal ways the two surveys differ is how they address ambulatory visits. The MGMA survey reports inpatient and ambulatory visits separately, but “ambulatory” visits include any for a patient who is not a hospital inpatient. By this definition, hospitalists make ambulatory visits, most commonly to hospitalized patients who are on observation status, and also patients seen in an ED, skilled nursing facility, or pre-op clinic. Thus the MGMA survey doesn’t distinguish between ambulatory encounters a hospitalist would generate in the course of serving as a hospitalist, and those generated while that doctor might be serving in a non-hospitalist role such as office-based primary care or urgent care.
The SHM survey doesn’t include—and isn’t contaminated by—office-based primary care or urgent-care visits.
Of the 3,376 total encounters reported in the MGMA survey, 40% (1,351) are ambulatory encounters. Although the SHM survey does not distinguish between hospital and ambulatory encounters, my experience suggests few, if any, hospitalist practices make 40% of their total encounters with patients on observation status, or in an ED, SNF, or pre-op clinic. Thus, many of the ambulatory encounters reported by MGMA might have been office visits, not hospital-related visits.
Additionally, the median internal medicine hospitalist encounters (ambulatory and hospital combined) in the MGMA survey (3,376) is 42% higher than the median total encounters reported for internal medicine hospitalists in SHM’s survey (2,378). Yet the wRVUs reported in the MGMA survey (3,514) are only 8% higher than those reported in the SHM survey (3,256). Thus the calculated average wRVUs per encounter for the MGMA data is only 1.04, compared with 1.37 for the SHM data. An average of 1.04 wRVUs per encounter is very low for hospitalists, when almost all current procedural terminology (CPT) codes a hospitalist uses have a value of one or more wRVUs. Again, this suggests the MGMA data may be significantly influenced by the inclusion of office-based encounters, some of which have wRVUs of less than one. SHM has approached MGMA to discuss this data definition issue in their survey.
Why It Matters
You can use whichever data set best describes your situation. The MGMA has historically shown higher hospitalist salaries and higher workloads than the SHM data. But because the SHM data is the result of a survey customized for hospitalists and less likely than the MGMA data to be contaminated by non-hospital-related visits, the SHM data probably gives a more accurate picture.
Because the MGMA survey has been conducted for many years (far longer than the SHM survey) it has appropriately become one of the most authoritative sources of data on physician compensation for all specialties. Stark II regulations require hospitals to ensure they aren’t paying physicians above the fair market compensation (which could be seen as an inducement to refer patients to the hospital, among other concerns). And it specifically states that the MGMA survey is one of several approved sources of determining what fair market compensation is.
Even though the SHM data is most likely more representative and provides an important benchmark for hospitalists, the MGMA data has “pre-approved” status and thus is potentially safer to use for the specific purpose of determinations of fair market value.
With each iteration, the SHM survey will be adjusted to more specifically capture hospitalist activity; in many cases it is the best data for hospitalists to use in planning and benchmarking. But the MGMA data are still valuable and may be the most appropriate to refer to in contracts.
Note to readers: In May, SHM contacted MGMA regarding their concerns that MGMA survey data was not representative of hospitalists. MGMA responded with a willingness to discuss these issues with SHM. As this story goes to press, SHM and MGMA continue to have a dialogue about maximizing the accuracy of survey data. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
How hard do hospitalists work and how much are they paid? There are several sources of data to answer this question, and each has its strengths and weaknesses. Because these data influence contract negotiations and compliance with federal regulations, it is worth taking the time to understand the differences in each data set.
I’ll focus on the two most common sources of data: the biannual SHM survey of hospitalist productivity and compensation (officially titled “The Authoritative Source on the State of Hospital Medicine”), and the Medical Group Management Association’s (MGMA) annual “Physician Compensation and Production Survey.” There are many other surveys that report hospitalist data such as those by the American Medical Group Association (AMGA), Sullivan & Cotter, Hay Group, and others. Each July, Modern Healthcare magazine publishes the average compensation (but no other data) reported for hospitalists and other specialties by each of these organizations and several others (but not the SHM data). It should be easy to find a copy of Modern Healthcare in your hospital administration or library, or on the Internet.
The SHM and MGMA surveys are the most widely used sources of data for hospitalists, and some of their attributes are described in Table 1 (see below).
I should acknowledge my potential conflict of interest and potential for bias in comparing these surveys. This column is in an SHM publication. I’m very active in SHM, and I’m a past chairman and ongoing member of the Benchmarks Committee, which oversees the design and analysis of the SHM survey. And while I am familiar with and regularly review the MGMA survey, I have no other connection to that organization.
Much of the difference between the surveys is a result of the SHM survey being designed specifically for hospitalists in any type of practice setting (e.g., small hospitalist-only groups, as well as hospitalists with huge organizations like a university faculty group practice). In contrast, the MGMA survey is designed for all physician specialties, so a hospitalist answers the same questions as a traditional primary care doctor, plastic surgeon, and obstetrician.
MGMA data can be adversely affected by the inclusion of primary care office-based encounters. One of the principal ways the two surveys differ is how they address ambulatory visits. The MGMA survey reports inpatient and ambulatory visits separately, but “ambulatory” visits include any for a patient who is not a hospital inpatient. By this definition, hospitalists make ambulatory visits, most commonly to hospitalized patients who are on observation status, and also patients seen in an ED, skilled nursing facility, or pre-op clinic. Thus the MGMA survey doesn’t distinguish between ambulatory encounters a hospitalist would generate in the course of serving as a hospitalist, and those generated while that doctor might be serving in a non-hospitalist role such as office-based primary care or urgent care.
The SHM survey doesn’t include—and isn’t contaminated by—office-based primary care or urgent-care visits.
Of the 3,376 total encounters reported in the MGMA survey, 40% (1,351) are ambulatory encounters. Although the SHM survey does not distinguish between hospital and ambulatory encounters, my experience suggests few, if any, hospitalist practices make 40% of their total encounters with patients on observation status, or in an ED, SNF, or pre-op clinic. Thus, many of the ambulatory encounters reported by MGMA might have been office visits, not hospital-related visits.
Additionally, the median internal medicine hospitalist encounters (ambulatory and hospital combined) in the MGMA survey (3,376) is 42% higher than the median total encounters reported for internal medicine hospitalists in SHM’s survey (2,378). Yet the wRVUs reported in the MGMA survey (3,514) are only 8% higher than those reported in the SHM survey (3,256). Thus the calculated average wRVUs per encounter for the MGMA data is only 1.04, compared with 1.37 for the SHM data. An average of 1.04 wRVUs per encounter is very low for hospitalists, when almost all current procedural terminology (CPT) codes a hospitalist uses have a value of one or more wRVUs. Again, this suggests the MGMA data may be significantly influenced by the inclusion of office-based encounters, some of which have wRVUs of less than one. SHM has approached MGMA to discuss this data definition issue in their survey.
Why It Matters
You can use whichever data set best describes your situation. The MGMA has historically shown higher hospitalist salaries and higher workloads than the SHM data. But because the SHM data is the result of a survey customized for hospitalists and less likely than the MGMA data to be contaminated by non-hospital-related visits, the SHM data probably gives a more accurate picture.
Because the MGMA survey has been conducted for many years (far longer than the SHM survey) it has appropriately become one of the most authoritative sources of data on physician compensation for all specialties. Stark II regulations require hospitals to ensure they aren’t paying physicians above the fair market compensation (which could be seen as an inducement to refer patients to the hospital, among other concerns). And it specifically states that the MGMA survey is one of several approved sources of determining what fair market compensation is.
Even though the SHM data is most likely more representative and provides an important benchmark for hospitalists, the MGMA data has “pre-approved” status and thus is potentially safer to use for the specific purpose of determinations of fair market value.
With each iteration, the SHM survey will be adjusted to more specifically capture hospitalist activity; in many cases it is the best data for hospitalists to use in planning and benchmarking. But the MGMA data are still valuable and may be the most appropriate to refer to in contracts.
Note to readers: In May, SHM contacted MGMA regarding their concerns that MGMA survey data was not representative of hospitalists. MGMA responded with a willingness to discuss these issues with SHM. As this story goes to press, SHM and MGMA continue to have a dialogue about maximizing the accuracy of survey data. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
In the Literature
Performance Measures and Outcomes for Heart Patients
Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70
As our population ages, more emphasis will be placed on issues surrounding efficient and evidence-based care. Heart failure, which accounted for 3.6 million hospitalizations in 2003 and has an overall prevalence of 5 million, will be at the forefront of public policy. As pay for performance (P4P) and standards of care become increasingly prevalent, the medical community will need to scrutinize the standards by which we are measured.
The American College of Cardiology and the American Heart Association (ACC/AHA) developed guidelines for the treatment and care of patients with heart failure. These measures include heart failure discharge instructions, evaluation of left ventricle (LV) function, angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor antagonist (ARB) for LV dysfunction, adult smoking cessation counseling, and anticoagulation at discharge for patients with atrial fibrillation. Adherence to these performance measures should be based on evidence.
The authors’ goal was to determine the validity of these guidelines. The Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry allowed for the documentation and follow-up of patients adhering to the heart failure guidelines as set forth by the ACC/AHA. The study assessed the relationship between these guidelines and clinical outcomes, including 60- to 90-day mortality and a composite end point of mortality or rehospitalization.
In this study the OPTIMIZE-HF registry was used as the source of prospective data collection. Ten percent of eligible patients were randomly selected from the registry between March 2003 and December 2004 from 91 hospitals. Eligibility for the OPTIMIZE-HF registry included patients 18 and older admitted for worsening heart failure or significant heart failure during their hospital stay. The performance measure of discharge instruction, smoking cessation, and anticoagulation were measured for all eligible patients. Patients with an ejection fraction of 40% or less, or moderate to severe systolic function, were included for the ACE inhibitor/ARB performance measure. One measure not included was treatment with beta-blockers at discharge. The authors included beta-blockers at discharge with metrics similar to those described for ACE/ARB criteria.
The conformity rates and process-outcome links were then determined for the performance measures and beta-blocker treatment as it related to 60- to 90-day mortality/rehospitalization.
The study focused on a random follow-up cohort of 5,791 patients from 91 hospitals. This was similar to the OPTIMIZE-HF cohort of 48,612 patients in 259 hospitals. Demographically, the average cohort’s age was 72, 51% male and 78% white, with 42% of patients diagnosed with ischemic heart disease and 43% with diabetes mellitus. These results were similar to the demographics of the overall OPTIMIZE-HF registry.
Of the eligible patients in the follow-up cohort, 66% (4,010) received complete discharge instructions. Eighty-nine percent of eligible patients (4,664) had their left ventricular function evaluated. For those patients with documented left ventricular systolic dysfunction (2,181), 83% were given an ACE inhibitor or ARB at discharge. Patients who had a diagnosis of atrial fibrillation were discharged with anticoagulation at a rate of 53%, and 72% of patients were counseled on smoking cessation. As compared with ACE inhibitors/ARB, similar results (84%) were seen for beta-blockers at discharge.
Only two of the five ACC/AHA performance measures were predictive of decreasing morbidity and mortality/rehospitalization in unadjusted analysis: patients discharged on ACE inhibitors/ARBs (odds ratio, 0.51; 95% CI 0.34–0.78; P- .002) and smoking cessation counseling. Beta-blockers, not a formal part of the ACC/AHA guidelines, were also a predictor of lower risk of both mortality and rehospitalization (odds ratio, 0.73; 95% CI, 0.55-0.96; P-0.02)
The OPTIMIZE-HF cohort analysis allowed for an opportunity to determine the degree of conformity for the ACC/AHA performance measures. The ACE inhibitors or ARB use at discharge was shown in the OPTIMIZE-HF cohort to have a relative reduction in one-year post discharge mortality by 17% (risk reduction, 0.83; 95% CI, 0.79-0.88) and a trend to lower 60- to 90-days post-discharge mortality and rehospitalization. Although smoking cessation had an early positive correlation, outcomes did not reach statistical significance. The measure of discharge instruction in the current study did not show a benefit on early mortality/rehospitalization in 60- to 90-days post discharge. It is unclear from this study if discharge instructions given to patients were either rushed or discussed in a comprehensive manner. This factor will need clarification and further research.
The measures of discharge instructions, smoking cessation, LV assessment, and anticoagulation for atrial fibrillation have not been examined as effective performance measures prior to this study. These measures were unable to show an independent decrease in 60- to 90-day mortality and rehospitalization.
Patients discharged with beta-blockers showed an association between lower mortality and rehospitalization. This association was found to be stronger than any of the formal ACC/AHA current performance measures.
The ACC/AHA guidelines are becoming standards of care for reporting to agencies such as Centers for Medicare and Medicaid Services or other P4P programs. To allow for improvement of quality, JCAHO and ACC/AHA designed the above criteria to act as a guide for the post discharge care of coronary heart failure patients. Because these criteria are the measures by which hospitals need to report, it will be necessary for data to show validity and a link between the clinical performance measures and improved outcomes.
Of the five measures stated, only ACE inhibitors/ARB at discharge was associated with a decrease in mortality/rehospitalization. Beta-blockers, currently not a performance measure, also showed this trend. Increased scrutiny needs to be part of the criteria for which hospitals and practitioners are being held accountable, and further research validating their effectiveness is warranted.
Risk Indexes for COPD
Niewoehner DE, Lockhnygina Y, Rice K, et al. Risk indexes for exacerbations and hospitalizations due to COPD. Chest. 2007 Jan;131(1):20-28.
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality in the U.S. and continues to increase its numbers annually.
The cornerstone of COPD diagnosis and key predictor of prognosis is a low level of lung function. Another important predictor of morbidity, mortality, and progression of disease is COPD exacerbations.
Unfortunately, the definition of an exacerbation is varied, ranging from an increase in symptoms to COPD-related hospitalizations and death.1 Therefore, prevention of COPD exacerbations is an important management goal. This study focuses on setting a risk model as a clinical management tool, similar to what exists for cardiovascular events or community acquired pneumonia. No previous study has attempted to identify risk factors for exacerbations using prospective data collection and a clearly stated definition of exacerbation.
The study was a parallel-group, randomized, double-blind, placebo-controlled trial in patients with moderate to severe COPD conducted at 26 Veterans Affairs medical centers in the United States. Subjects were 40 or older, with a cigarette smoking history of 10 packs a year or more, a clinical diagnosis of COPD, and a forced expiratory volume [FEV] of 60% or less predicted and 70% or less of the forced vital capacity [FVC].1 Patients were allocated to receive one capsule of tiotropium (18 mg) or placebo for six months.
Of the 1,829 patients selected, 914 were assigned to the tiotropium arm. Patients kept a daily diary, and the investigators collected data by monthly telephone interviews and by site visits at three and six months with spirometry evaluation. They evaluated the association between baseline characteristics, concomitant medications and the study drug and the time to first COPD exacerbation and the time to first hospitalization due to exacerbation. The authors defined an exacerbation as a complex of respiratory symptoms of more than one of the following: cough, sputum, wheezing, dyspnea, or chest tightness with a duration of at least three days requiring treatment with antibiotics and/or systemic corticosteroids and/or hospital admission.
The investigators found that a statistically significant greater risk for both COPD exacerbations and hospitalizations is associated with being of older age, being a noncurrent smoker, having poorer lung function, using home oxygen, visiting the clinic or emergency department more often, either scheduled or unscheduled, being hospitalized for COPD in the prior year, using either antibiotics or systemic steroids for COPD more often in the prior year, and using short-acting beta agonist, inhaled or oral corticosteroid at a baseline rate.
On the other hand, a statistically significant greater risk of only COPD exacerbation was seen in white patients, with presence of productive cough, longer duration of COPD, use of long-acting beta agonist or theophylline at baseline, and presence of any gastrointestinal or hepatobiliary disease. Lower body-mass index and the presence of cardiovascular comorbidity were associated with statistically significant greater risk for only hospitalization due to COPD.
The investigators also confirmed the previous suggestion that chronic cough is an independent predictor of exacerbation. Interestingly, they found that any cardiovascular comorbidity is a strong and independent predictor of hospitalizations due to COPD. It is unclear if cardiovascular disease truly predisposes subjects to COPD hospitalizations or merely represents a misdiagnosis because both diseases have similar symptoms.
Current smokers were identified as having lower risk of exacerbation and hospitalization, probably due to the “healthy smoker” theory—that deteriorating lung function causes the patient to quit smoking.
This study is the first to gather information about predictors of COPD exacerbations in a prospective fashion using a clear definition of exacerbation. The authors developed a model to assess the risk of COPD exacerbations and hospitalizations due to exacerbations in patients with moderate to severe COPD. Moreover, this model can easily be applied to individual patients and reproduced with simple spirometry and a series of questions.
Though this trial had a reasonable level of statistical significance, it is important to mention that the trial was conducted within a single health system (Veterans Affairs medical centers), there were few women in the study, and the eligibility criteria were very specific.
References
- Mannino DM, Watt G, Hole D, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J. 2006 Mar;27(3):627-643.
Glucose Management in Hospitalized Patients
Leahy JL. Insulin Management of diabetic patients on general medical and surgical floors. Endocr Pract. Jul/Aug 2006;12(Suppl3):86-89.
Although the rationale behind the science for tight control of blood sugar in subsets of hospitalized patient populations is without debate when it comes to the majority of general ward patients, the management of hyperglycemia becomes more of an art. Increasingly we recognize the effect of the relationship between improving glucose management and improving clinical outcomes.
Guidelines for inpatient targeted blood glucose levels exist, but hospitals are moving toward a more individualized approach to subcutaneous insulin protocols for their patients, thus moving beyond the passive sliding scale era.
Institution of an insulin protocol at one such hospital, the University of Vermont, highlights such an approach. The ongoing internal nonrandomized study exemplifies a two-tiered approach initially aimed at expanding the house physician comfort zone to change the culture of hyperglycemic management beyond simply avoiding hypoglycemia to one of an active and—per our current standards—aggressive individualized insulin protocol.
It seems the author envisions a gradual process allowing initial flexibility within the protocol, increasing the intensity of dosing as comfort zones expand. Throughout the process, the principles of determining a patient’s weight-based daily insulin needs are maintained, taking into consideration factors like comorbidities, severity of illness, amount of oral intake, steroid usage, and age. Then, the insulin regimen is physiologically (basal/bolus, basal, continuous) administered according to the route (i.e., total parenteral nutrition) and timing of their nutritional intake.
Adjustments being made to insulin regimens are based on fasting, pre-meal and bedtime glucose as well as the novel approach of bolus insulin after meals with short-acting insulin (i.e., lispro).
Unfortunately although the protocol does perhaps yield itself to being looked at more stringently—in terms of cost effectiveness, improved length of hospital stay, and improved clinical outcomes—the outcome studied here was primarily one of hospitalwide education in advancing the understanding and culture of aggressive individualized insulin protocols. These can often be even more statistically difficult to quantify. As self-reported, improvements were made.
One of the most important aspects of this paper is that it draws attention to the paucity of evidence for improved clinical and monetary outcomes supporting the aggressive hospital management of hyperglycemia in the non-acutely ill patient. Often, the guiding principle is to avoid hypoglycemia. Detailing the specific protocols of one such approach serves as an example for the motivated reader.
Early Switch from IV to Oral Antibiotic in Severe CAP
Oosterheert JJ, Bonten JM, Schneider MME, et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia; multicentre randomised trial. BMJ. 2006 Dec 9; 333:1193.
Community acquired pneumonia (CAP) is a common and potentially fatal infection with high healthcare costs. When patients are first admitted to hospitals, antibiotics are usually given intravenously to provide optimal concentrations in the tissues.
The duration of intravenous treatment is an important determinant of length of hospital stay (LOS). The concept of early transition from intravenous to oral antibiotic in the treatment of CAP has been evaluated before, but only in mild to moderately severe disease—and rarely in randomized trials.
This multicenter random controlled trial from five teaching hospitals and two medical centers in the Netherlands enrolled 302 patients in non-intensive care units with severe CAP. The primary outcome was clinical cure and secondary outcome was LOS. The inclusion criteria were adults 18 or older with severe CAP; mean pneumonia severity index of IV-V, new progressive infiltrate on chest X-ray, plus at least two other criteria (cough, sputum production, rectal temperature >38o C or <36.1o C, auscultative findings consistent with pneumonia, leukocytes >109 WBC/L or >15% bands, positive cultures of blob or pleural fluids, CRP three times greater times upper limit of normal).
Exclusion criteria included the need for mechanical ventilation, cystic fibrosis, a history of colonization with gram-negative bacteria due to structural damage to the respiratory tract, malfunction of the digestive tract, life expectancy of less than one month because of underlying disease, infections other than pneumonia that needed antibiotic treatment, and severe immunosuppression (neutropenia [<0.5 109 neutrophils/liter] or a CD4 count< 200/mm3).
Treatment failure was defined as death, still in hospital at day 28 of the study, or clinical deterioration (increase in temperature after initial improvement or the need for mechanical ventilation, switch back to intravenous antibiotics, or readmission for pulmonary reinfection after discharge).
Clinical cure was defined as discharged in good health without signs and symptoms of pneumonia and no treatment failure during follow-up.
The control group comprised 150 subjects who were to receive a standard course of seven days’ intravenous treatment. Meanwhile, 152 subjects were randomized to the early switch group. Baseline characteristics were similar in both groups. More than 80% of patients were in pneumonia severity class IV or V. Most patients received empirical monotherapy with amoxicillin or amoxicillin plus clavulanic acid (n=174; 58%) or a cephalosporin (n=59; 20%), which is in line with Dutch prescribing policies.
The most frequently identified microorganism was S pneumoniae (n=76; 25%). Atypical pathogens were detected in 33 patients (11%). Before day three, 37 patients (12%) were excluded from analysis, leaving 132 patients for analysis in the intervention group and 133 in the control group.
Reasons for exclusion included when the initial diagnosis of CAP was replaced by another diagnosis (n=9), consent was withdrawn (n=11), the protocol was violated (n=4), the patient was admitted to an intensive-care unit for mechanical ventilation (n=6), and the patient died (n=7). After three days of intravenous treatment, 108 of 132 patients (81%) in the intervention group were switched to oral treatment, of whom 102 (94%) received amoxicillin plus clavulanic acid (500+125 mg every eight hours).
In the control group, five patients did not receive intravenous antibiotics for all seven days because of phlebitis associated with intravenous treatment; none of them needed treatment for line-related sepsis. Overall duration of antibiotic treatment was 10.1 days in the intervention group and 9.3 days in the control group (mean difference 0.8 days, 95% confidence interval -0.6 to 2.0).
The duration of intravenous treatment was significantly shorter in the intervention group (mean 3.6 [SD 1.5] versus 7.0 [2.0] days, mean difference 3.4, 2.8 to 3.9). Average time to meet the discharge criteria was 5.2 (2.9) days in the intervention group and 5.7 (3.1) days in the control group (0.5 days -0.3 to 1.2) Total length of hospital stay was 9.6 (5.0) and 11.5 (4.9) days for patients in the intervention group and control group (1.9 days 0.6 to 3.2).
The authors’ findings provide strong evidence that early transition from intravenous to oral antibiotic is also viable in patients with highly graded Pneumonia Severity Index (PSI) CAP, not only in mild to moderately severe disease. This leads to reduced LOS, cost, and possibly reduced risk of line infections and increased patient satisfaction for early discharge.
Note: This study was done with patients suffering straightforward, uncomplicated CAP. The investigators’ findings cannot be applied to patients with other comorbidities like diabetes, COPD, heart failure, or sickle cell, which might require more days on intravenous antibiotic. One might also wonder what impact would have been seen had 37 patients not dropped off, and if another class of oral antibiotic such as quinolones had been used.
Last, the study sample showed S pneumoniae identified in 25% of cases and atypical pathogens to be 11%. What then are the majority of pathogens identified 64% of the time? This would have been another key factor that might have had a great effect on the result.
Although a larger sampling and further risk stratification (to include patients with other comorbidities) are needed, this study makes a valid point for early transition to oral antibiotics in highly graded, uncomplicated CAP. TH
Performance Measures and Outcomes for Heart Patients
Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70
As our population ages, more emphasis will be placed on issues surrounding efficient and evidence-based care. Heart failure, which accounted for 3.6 million hospitalizations in 2003 and has an overall prevalence of 5 million, will be at the forefront of public policy. As pay for performance (P4P) and standards of care become increasingly prevalent, the medical community will need to scrutinize the standards by which we are measured.
The American College of Cardiology and the American Heart Association (ACC/AHA) developed guidelines for the treatment and care of patients with heart failure. These measures include heart failure discharge instructions, evaluation of left ventricle (LV) function, angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor antagonist (ARB) for LV dysfunction, adult smoking cessation counseling, and anticoagulation at discharge for patients with atrial fibrillation. Adherence to these performance measures should be based on evidence.
The authors’ goal was to determine the validity of these guidelines. The Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry allowed for the documentation and follow-up of patients adhering to the heart failure guidelines as set forth by the ACC/AHA. The study assessed the relationship between these guidelines and clinical outcomes, including 60- to 90-day mortality and a composite end point of mortality or rehospitalization.
In this study the OPTIMIZE-HF registry was used as the source of prospective data collection. Ten percent of eligible patients were randomly selected from the registry between March 2003 and December 2004 from 91 hospitals. Eligibility for the OPTIMIZE-HF registry included patients 18 and older admitted for worsening heart failure or significant heart failure during their hospital stay. The performance measure of discharge instruction, smoking cessation, and anticoagulation were measured for all eligible patients. Patients with an ejection fraction of 40% or less, or moderate to severe systolic function, were included for the ACE inhibitor/ARB performance measure. One measure not included was treatment with beta-blockers at discharge. The authors included beta-blockers at discharge with metrics similar to those described for ACE/ARB criteria.
The conformity rates and process-outcome links were then determined for the performance measures and beta-blocker treatment as it related to 60- to 90-day mortality/rehospitalization.
The study focused on a random follow-up cohort of 5,791 patients from 91 hospitals. This was similar to the OPTIMIZE-HF cohort of 48,612 patients in 259 hospitals. Demographically, the average cohort’s age was 72, 51% male and 78% white, with 42% of patients diagnosed with ischemic heart disease and 43% with diabetes mellitus. These results were similar to the demographics of the overall OPTIMIZE-HF registry.
Of the eligible patients in the follow-up cohort, 66% (4,010) received complete discharge instructions. Eighty-nine percent of eligible patients (4,664) had their left ventricular function evaluated. For those patients with documented left ventricular systolic dysfunction (2,181), 83% were given an ACE inhibitor or ARB at discharge. Patients who had a diagnosis of atrial fibrillation were discharged with anticoagulation at a rate of 53%, and 72% of patients were counseled on smoking cessation. As compared with ACE inhibitors/ARB, similar results (84%) were seen for beta-blockers at discharge.
Only two of the five ACC/AHA performance measures were predictive of decreasing morbidity and mortality/rehospitalization in unadjusted analysis: patients discharged on ACE inhibitors/ARBs (odds ratio, 0.51; 95% CI 0.34–0.78; P- .002) and smoking cessation counseling. Beta-blockers, not a formal part of the ACC/AHA guidelines, were also a predictor of lower risk of both mortality and rehospitalization (odds ratio, 0.73; 95% CI, 0.55-0.96; P-0.02)
The OPTIMIZE-HF cohort analysis allowed for an opportunity to determine the degree of conformity for the ACC/AHA performance measures. The ACE inhibitors or ARB use at discharge was shown in the OPTIMIZE-HF cohort to have a relative reduction in one-year post discharge mortality by 17% (risk reduction, 0.83; 95% CI, 0.79-0.88) and a trend to lower 60- to 90-days post-discharge mortality and rehospitalization. Although smoking cessation had an early positive correlation, outcomes did not reach statistical significance. The measure of discharge instruction in the current study did not show a benefit on early mortality/rehospitalization in 60- to 90-days post discharge. It is unclear from this study if discharge instructions given to patients were either rushed or discussed in a comprehensive manner. This factor will need clarification and further research.
The measures of discharge instructions, smoking cessation, LV assessment, and anticoagulation for atrial fibrillation have not been examined as effective performance measures prior to this study. These measures were unable to show an independent decrease in 60- to 90-day mortality and rehospitalization.
Patients discharged with beta-blockers showed an association between lower mortality and rehospitalization. This association was found to be stronger than any of the formal ACC/AHA current performance measures.
The ACC/AHA guidelines are becoming standards of care for reporting to agencies such as Centers for Medicare and Medicaid Services or other P4P programs. To allow for improvement of quality, JCAHO and ACC/AHA designed the above criteria to act as a guide for the post discharge care of coronary heart failure patients. Because these criteria are the measures by which hospitals need to report, it will be necessary for data to show validity and a link between the clinical performance measures and improved outcomes.
Of the five measures stated, only ACE inhibitors/ARB at discharge was associated with a decrease in mortality/rehospitalization. Beta-blockers, currently not a performance measure, also showed this trend. Increased scrutiny needs to be part of the criteria for which hospitals and practitioners are being held accountable, and further research validating their effectiveness is warranted.
Risk Indexes for COPD
Niewoehner DE, Lockhnygina Y, Rice K, et al. Risk indexes for exacerbations and hospitalizations due to COPD. Chest. 2007 Jan;131(1):20-28.
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality in the U.S. and continues to increase its numbers annually.
The cornerstone of COPD diagnosis and key predictor of prognosis is a low level of lung function. Another important predictor of morbidity, mortality, and progression of disease is COPD exacerbations.
Unfortunately, the definition of an exacerbation is varied, ranging from an increase in symptoms to COPD-related hospitalizations and death.1 Therefore, prevention of COPD exacerbations is an important management goal. This study focuses on setting a risk model as a clinical management tool, similar to what exists for cardiovascular events or community acquired pneumonia. No previous study has attempted to identify risk factors for exacerbations using prospective data collection and a clearly stated definition of exacerbation.
The study was a parallel-group, randomized, double-blind, placebo-controlled trial in patients with moderate to severe COPD conducted at 26 Veterans Affairs medical centers in the United States. Subjects were 40 or older, with a cigarette smoking history of 10 packs a year or more, a clinical diagnosis of COPD, and a forced expiratory volume [FEV] of 60% or less predicted and 70% or less of the forced vital capacity [FVC].1 Patients were allocated to receive one capsule of tiotropium (18 mg) or placebo for six months.
Of the 1,829 patients selected, 914 were assigned to the tiotropium arm. Patients kept a daily diary, and the investigators collected data by monthly telephone interviews and by site visits at three and six months with spirometry evaluation. They evaluated the association between baseline characteristics, concomitant medications and the study drug and the time to first COPD exacerbation and the time to first hospitalization due to exacerbation. The authors defined an exacerbation as a complex of respiratory symptoms of more than one of the following: cough, sputum, wheezing, dyspnea, or chest tightness with a duration of at least three days requiring treatment with antibiotics and/or systemic corticosteroids and/or hospital admission.
The investigators found that a statistically significant greater risk for both COPD exacerbations and hospitalizations is associated with being of older age, being a noncurrent smoker, having poorer lung function, using home oxygen, visiting the clinic or emergency department more often, either scheduled or unscheduled, being hospitalized for COPD in the prior year, using either antibiotics or systemic steroids for COPD more often in the prior year, and using short-acting beta agonist, inhaled or oral corticosteroid at a baseline rate.
On the other hand, a statistically significant greater risk of only COPD exacerbation was seen in white patients, with presence of productive cough, longer duration of COPD, use of long-acting beta agonist or theophylline at baseline, and presence of any gastrointestinal or hepatobiliary disease. Lower body-mass index and the presence of cardiovascular comorbidity were associated with statistically significant greater risk for only hospitalization due to COPD.
The investigators also confirmed the previous suggestion that chronic cough is an independent predictor of exacerbation. Interestingly, they found that any cardiovascular comorbidity is a strong and independent predictor of hospitalizations due to COPD. It is unclear if cardiovascular disease truly predisposes subjects to COPD hospitalizations or merely represents a misdiagnosis because both diseases have similar symptoms.
Current smokers were identified as having lower risk of exacerbation and hospitalization, probably due to the “healthy smoker” theory—that deteriorating lung function causes the patient to quit smoking.
This study is the first to gather information about predictors of COPD exacerbations in a prospective fashion using a clear definition of exacerbation. The authors developed a model to assess the risk of COPD exacerbations and hospitalizations due to exacerbations in patients with moderate to severe COPD. Moreover, this model can easily be applied to individual patients and reproduced with simple spirometry and a series of questions.
Though this trial had a reasonable level of statistical significance, it is important to mention that the trial was conducted within a single health system (Veterans Affairs medical centers), there were few women in the study, and the eligibility criteria were very specific.
References
- Mannino DM, Watt G, Hole D, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J. 2006 Mar;27(3):627-643.
Glucose Management in Hospitalized Patients
Leahy JL. Insulin Management of diabetic patients on general medical and surgical floors. Endocr Pract. Jul/Aug 2006;12(Suppl3):86-89.
Although the rationale behind the science for tight control of blood sugar in subsets of hospitalized patient populations is without debate when it comes to the majority of general ward patients, the management of hyperglycemia becomes more of an art. Increasingly we recognize the effect of the relationship between improving glucose management and improving clinical outcomes.
Guidelines for inpatient targeted blood glucose levels exist, but hospitals are moving toward a more individualized approach to subcutaneous insulin protocols for their patients, thus moving beyond the passive sliding scale era.
Institution of an insulin protocol at one such hospital, the University of Vermont, highlights such an approach. The ongoing internal nonrandomized study exemplifies a two-tiered approach initially aimed at expanding the house physician comfort zone to change the culture of hyperglycemic management beyond simply avoiding hypoglycemia to one of an active and—per our current standards—aggressive individualized insulin protocol.
It seems the author envisions a gradual process allowing initial flexibility within the protocol, increasing the intensity of dosing as comfort zones expand. Throughout the process, the principles of determining a patient’s weight-based daily insulin needs are maintained, taking into consideration factors like comorbidities, severity of illness, amount of oral intake, steroid usage, and age. Then, the insulin regimen is physiologically (basal/bolus, basal, continuous) administered according to the route (i.e., total parenteral nutrition) and timing of their nutritional intake.
Adjustments being made to insulin regimens are based on fasting, pre-meal and bedtime glucose as well as the novel approach of bolus insulin after meals with short-acting insulin (i.e., lispro).
Unfortunately although the protocol does perhaps yield itself to being looked at more stringently—in terms of cost effectiveness, improved length of hospital stay, and improved clinical outcomes—the outcome studied here was primarily one of hospitalwide education in advancing the understanding and culture of aggressive individualized insulin protocols. These can often be even more statistically difficult to quantify. As self-reported, improvements were made.
One of the most important aspects of this paper is that it draws attention to the paucity of evidence for improved clinical and monetary outcomes supporting the aggressive hospital management of hyperglycemia in the non-acutely ill patient. Often, the guiding principle is to avoid hypoglycemia. Detailing the specific protocols of one such approach serves as an example for the motivated reader.
Early Switch from IV to Oral Antibiotic in Severe CAP
Oosterheert JJ, Bonten JM, Schneider MME, et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia; multicentre randomised trial. BMJ. 2006 Dec 9; 333:1193.
Community acquired pneumonia (CAP) is a common and potentially fatal infection with high healthcare costs. When patients are first admitted to hospitals, antibiotics are usually given intravenously to provide optimal concentrations in the tissues.
The duration of intravenous treatment is an important determinant of length of hospital stay (LOS). The concept of early transition from intravenous to oral antibiotic in the treatment of CAP has been evaluated before, but only in mild to moderately severe disease—and rarely in randomized trials.
This multicenter random controlled trial from five teaching hospitals and two medical centers in the Netherlands enrolled 302 patients in non-intensive care units with severe CAP. The primary outcome was clinical cure and secondary outcome was LOS. The inclusion criteria were adults 18 or older with severe CAP; mean pneumonia severity index of IV-V, new progressive infiltrate on chest X-ray, plus at least two other criteria (cough, sputum production, rectal temperature >38o C or <36.1o C, auscultative findings consistent with pneumonia, leukocytes >109 WBC/L or >15% bands, positive cultures of blob or pleural fluids, CRP three times greater times upper limit of normal).
Exclusion criteria included the need for mechanical ventilation, cystic fibrosis, a history of colonization with gram-negative bacteria due to structural damage to the respiratory tract, malfunction of the digestive tract, life expectancy of less than one month because of underlying disease, infections other than pneumonia that needed antibiotic treatment, and severe immunosuppression (neutropenia [<0.5 109 neutrophils/liter] or a CD4 count< 200/mm3).
Treatment failure was defined as death, still in hospital at day 28 of the study, or clinical deterioration (increase in temperature after initial improvement or the need for mechanical ventilation, switch back to intravenous antibiotics, or readmission for pulmonary reinfection after discharge).
Clinical cure was defined as discharged in good health without signs and symptoms of pneumonia and no treatment failure during follow-up.
The control group comprised 150 subjects who were to receive a standard course of seven days’ intravenous treatment. Meanwhile, 152 subjects were randomized to the early switch group. Baseline characteristics were similar in both groups. More than 80% of patients were in pneumonia severity class IV or V. Most patients received empirical monotherapy with amoxicillin or amoxicillin plus clavulanic acid (n=174; 58%) or a cephalosporin (n=59; 20%), which is in line with Dutch prescribing policies.
The most frequently identified microorganism was S pneumoniae (n=76; 25%). Atypical pathogens were detected in 33 patients (11%). Before day three, 37 patients (12%) were excluded from analysis, leaving 132 patients for analysis in the intervention group and 133 in the control group.
Reasons for exclusion included when the initial diagnosis of CAP was replaced by another diagnosis (n=9), consent was withdrawn (n=11), the protocol was violated (n=4), the patient was admitted to an intensive-care unit for mechanical ventilation (n=6), and the patient died (n=7). After three days of intravenous treatment, 108 of 132 patients (81%) in the intervention group were switched to oral treatment, of whom 102 (94%) received amoxicillin plus clavulanic acid (500+125 mg every eight hours).
In the control group, five patients did not receive intravenous antibiotics for all seven days because of phlebitis associated with intravenous treatment; none of them needed treatment for line-related sepsis. Overall duration of antibiotic treatment was 10.1 days in the intervention group and 9.3 days in the control group (mean difference 0.8 days, 95% confidence interval -0.6 to 2.0).
The duration of intravenous treatment was significantly shorter in the intervention group (mean 3.6 [SD 1.5] versus 7.0 [2.0] days, mean difference 3.4, 2.8 to 3.9). Average time to meet the discharge criteria was 5.2 (2.9) days in the intervention group and 5.7 (3.1) days in the control group (0.5 days -0.3 to 1.2) Total length of hospital stay was 9.6 (5.0) and 11.5 (4.9) days for patients in the intervention group and control group (1.9 days 0.6 to 3.2).
The authors’ findings provide strong evidence that early transition from intravenous to oral antibiotic is also viable in patients with highly graded Pneumonia Severity Index (PSI) CAP, not only in mild to moderately severe disease. This leads to reduced LOS, cost, and possibly reduced risk of line infections and increased patient satisfaction for early discharge.
Note: This study was done with patients suffering straightforward, uncomplicated CAP. The investigators’ findings cannot be applied to patients with other comorbidities like diabetes, COPD, heart failure, or sickle cell, which might require more days on intravenous antibiotic. One might also wonder what impact would have been seen had 37 patients not dropped off, and if another class of oral antibiotic such as quinolones had been used.
Last, the study sample showed S pneumoniae identified in 25% of cases and atypical pathogens to be 11%. What then are the majority of pathogens identified 64% of the time? This would have been another key factor that might have had a great effect on the result.
Although a larger sampling and further risk stratification (to include patients with other comorbidities) are needed, this study makes a valid point for early transition to oral antibiotics in highly graded, uncomplicated CAP. TH
Performance Measures and Outcomes for Heart Patients
Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70
As our population ages, more emphasis will be placed on issues surrounding efficient and evidence-based care. Heart failure, which accounted for 3.6 million hospitalizations in 2003 and has an overall prevalence of 5 million, will be at the forefront of public policy. As pay for performance (P4P) and standards of care become increasingly prevalent, the medical community will need to scrutinize the standards by which we are measured.
The American College of Cardiology and the American Heart Association (ACC/AHA) developed guidelines for the treatment and care of patients with heart failure. These measures include heart failure discharge instructions, evaluation of left ventricle (LV) function, angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor antagonist (ARB) for LV dysfunction, adult smoking cessation counseling, and anticoagulation at discharge for patients with atrial fibrillation. Adherence to these performance measures should be based on evidence.
The authors’ goal was to determine the validity of these guidelines. The Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry allowed for the documentation and follow-up of patients adhering to the heart failure guidelines as set forth by the ACC/AHA. The study assessed the relationship between these guidelines and clinical outcomes, including 60- to 90-day mortality and a composite end point of mortality or rehospitalization.
In this study the OPTIMIZE-HF registry was used as the source of prospective data collection. Ten percent of eligible patients were randomly selected from the registry between March 2003 and December 2004 from 91 hospitals. Eligibility for the OPTIMIZE-HF registry included patients 18 and older admitted for worsening heart failure or significant heart failure during their hospital stay. The performance measure of discharge instruction, smoking cessation, and anticoagulation were measured for all eligible patients. Patients with an ejection fraction of 40% or less, or moderate to severe systolic function, were included for the ACE inhibitor/ARB performance measure. One measure not included was treatment with beta-blockers at discharge. The authors included beta-blockers at discharge with metrics similar to those described for ACE/ARB criteria.
The conformity rates and process-outcome links were then determined for the performance measures and beta-blocker treatment as it related to 60- to 90-day mortality/rehospitalization.
The study focused on a random follow-up cohort of 5,791 patients from 91 hospitals. This was similar to the OPTIMIZE-HF cohort of 48,612 patients in 259 hospitals. Demographically, the average cohort’s age was 72, 51% male and 78% white, with 42% of patients diagnosed with ischemic heart disease and 43% with diabetes mellitus. These results were similar to the demographics of the overall OPTIMIZE-HF registry.
Of the eligible patients in the follow-up cohort, 66% (4,010) received complete discharge instructions. Eighty-nine percent of eligible patients (4,664) had their left ventricular function evaluated. For those patients with documented left ventricular systolic dysfunction (2,181), 83% were given an ACE inhibitor or ARB at discharge. Patients who had a diagnosis of atrial fibrillation were discharged with anticoagulation at a rate of 53%, and 72% of patients were counseled on smoking cessation. As compared with ACE inhibitors/ARB, similar results (84%) were seen for beta-blockers at discharge.
Only two of the five ACC/AHA performance measures were predictive of decreasing morbidity and mortality/rehospitalization in unadjusted analysis: patients discharged on ACE inhibitors/ARBs (odds ratio, 0.51; 95% CI 0.34–0.78; P- .002) and smoking cessation counseling. Beta-blockers, not a formal part of the ACC/AHA guidelines, were also a predictor of lower risk of both mortality and rehospitalization (odds ratio, 0.73; 95% CI, 0.55-0.96; P-0.02)
The OPTIMIZE-HF cohort analysis allowed for an opportunity to determine the degree of conformity for the ACC/AHA performance measures. The ACE inhibitors or ARB use at discharge was shown in the OPTIMIZE-HF cohort to have a relative reduction in one-year post discharge mortality by 17% (risk reduction, 0.83; 95% CI, 0.79-0.88) and a trend to lower 60- to 90-days post-discharge mortality and rehospitalization. Although smoking cessation had an early positive correlation, outcomes did not reach statistical significance. The measure of discharge instruction in the current study did not show a benefit on early mortality/rehospitalization in 60- to 90-days post discharge. It is unclear from this study if discharge instructions given to patients were either rushed or discussed in a comprehensive manner. This factor will need clarification and further research.
The measures of discharge instructions, smoking cessation, LV assessment, and anticoagulation for atrial fibrillation have not been examined as effective performance measures prior to this study. These measures were unable to show an independent decrease in 60- to 90-day mortality and rehospitalization.
Patients discharged with beta-blockers showed an association between lower mortality and rehospitalization. This association was found to be stronger than any of the formal ACC/AHA current performance measures.
The ACC/AHA guidelines are becoming standards of care for reporting to agencies such as Centers for Medicare and Medicaid Services or other P4P programs. To allow for improvement of quality, JCAHO and ACC/AHA designed the above criteria to act as a guide for the post discharge care of coronary heart failure patients. Because these criteria are the measures by which hospitals need to report, it will be necessary for data to show validity and a link between the clinical performance measures and improved outcomes.
Of the five measures stated, only ACE inhibitors/ARB at discharge was associated with a decrease in mortality/rehospitalization. Beta-blockers, currently not a performance measure, also showed this trend. Increased scrutiny needs to be part of the criteria for which hospitals and practitioners are being held accountable, and further research validating their effectiveness is warranted.
Risk Indexes for COPD
Niewoehner DE, Lockhnygina Y, Rice K, et al. Risk indexes for exacerbations and hospitalizations due to COPD. Chest. 2007 Jan;131(1):20-28.
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality in the U.S. and continues to increase its numbers annually.
The cornerstone of COPD diagnosis and key predictor of prognosis is a low level of lung function. Another important predictor of morbidity, mortality, and progression of disease is COPD exacerbations.
Unfortunately, the definition of an exacerbation is varied, ranging from an increase in symptoms to COPD-related hospitalizations and death.1 Therefore, prevention of COPD exacerbations is an important management goal. This study focuses on setting a risk model as a clinical management tool, similar to what exists for cardiovascular events or community acquired pneumonia. No previous study has attempted to identify risk factors for exacerbations using prospective data collection and a clearly stated definition of exacerbation.
The study was a parallel-group, randomized, double-blind, placebo-controlled trial in patients with moderate to severe COPD conducted at 26 Veterans Affairs medical centers in the United States. Subjects were 40 or older, with a cigarette smoking history of 10 packs a year or more, a clinical diagnosis of COPD, and a forced expiratory volume [FEV] of 60% or less predicted and 70% or less of the forced vital capacity [FVC].1 Patients were allocated to receive one capsule of tiotropium (18 mg) or placebo for six months.
Of the 1,829 patients selected, 914 were assigned to the tiotropium arm. Patients kept a daily diary, and the investigators collected data by monthly telephone interviews and by site visits at three and six months with spirometry evaluation. They evaluated the association between baseline characteristics, concomitant medications and the study drug and the time to first COPD exacerbation and the time to first hospitalization due to exacerbation. The authors defined an exacerbation as a complex of respiratory symptoms of more than one of the following: cough, sputum, wheezing, dyspnea, or chest tightness with a duration of at least three days requiring treatment with antibiotics and/or systemic corticosteroids and/or hospital admission.
The investigators found that a statistically significant greater risk for both COPD exacerbations and hospitalizations is associated with being of older age, being a noncurrent smoker, having poorer lung function, using home oxygen, visiting the clinic or emergency department more often, either scheduled or unscheduled, being hospitalized for COPD in the prior year, using either antibiotics or systemic steroids for COPD more often in the prior year, and using short-acting beta agonist, inhaled or oral corticosteroid at a baseline rate.
On the other hand, a statistically significant greater risk of only COPD exacerbation was seen in white patients, with presence of productive cough, longer duration of COPD, use of long-acting beta agonist or theophylline at baseline, and presence of any gastrointestinal or hepatobiliary disease. Lower body-mass index and the presence of cardiovascular comorbidity were associated with statistically significant greater risk for only hospitalization due to COPD.
The investigators also confirmed the previous suggestion that chronic cough is an independent predictor of exacerbation. Interestingly, they found that any cardiovascular comorbidity is a strong and independent predictor of hospitalizations due to COPD. It is unclear if cardiovascular disease truly predisposes subjects to COPD hospitalizations or merely represents a misdiagnosis because both diseases have similar symptoms.
Current smokers were identified as having lower risk of exacerbation and hospitalization, probably due to the “healthy smoker” theory—that deteriorating lung function causes the patient to quit smoking.
This study is the first to gather information about predictors of COPD exacerbations in a prospective fashion using a clear definition of exacerbation. The authors developed a model to assess the risk of COPD exacerbations and hospitalizations due to exacerbations in patients with moderate to severe COPD. Moreover, this model can easily be applied to individual patients and reproduced with simple spirometry and a series of questions.
Though this trial had a reasonable level of statistical significance, it is important to mention that the trial was conducted within a single health system (Veterans Affairs medical centers), there were few women in the study, and the eligibility criteria were very specific.
References
- Mannino DM, Watt G, Hole D, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J. 2006 Mar;27(3):627-643.
Glucose Management in Hospitalized Patients
Leahy JL. Insulin Management of diabetic patients on general medical and surgical floors. Endocr Pract. Jul/Aug 2006;12(Suppl3):86-89.
Although the rationale behind the science for tight control of blood sugar in subsets of hospitalized patient populations is without debate when it comes to the majority of general ward patients, the management of hyperglycemia becomes more of an art. Increasingly we recognize the effect of the relationship between improving glucose management and improving clinical outcomes.
Guidelines for inpatient targeted blood glucose levels exist, but hospitals are moving toward a more individualized approach to subcutaneous insulin protocols for their patients, thus moving beyond the passive sliding scale era.
Institution of an insulin protocol at one such hospital, the University of Vermont, highlights such an approach. The ongoing internal nonrandomized study exemplifies a two-tiered approach initially aimed at expanding the house physician comfort zone to change the culture of hyperglycemic management beyond simply avoiding hypoglycemia to one of an active and—per our current standards—aggressive individualized insulin protocol.
It seems the author envisions a gradual process allowing initial flexibility within the protocol, increasing the intensity of dosing as comfort zones expand. Throughout the process, the principles of determining a patient’s weight-based daily insulin needs are maintained, taking into consideration factors like comorbidities, severity of illness, amount of oral intake, steroid usage, and age. Then, the insulin regimen is physiologically (basal/bolus, basal, continuous) administered according to the route (i.e., total parenteral nutrition) and timing of their nutritional intake.
Adjustments being made to insulin regimens are based on fasting, pre-meal and bedtime glucose as well as the novel approach of bolus insulin after meals with short-acting insulin (i.e., lispro).
Unfortunately although the protocol does perhaps yield itself to being looked at more stringently—in terms of cost effectiveness, improved length of hospital stay, and improved clinical outcomes—the outcome studied here was primarily one of hospitalwide education in advancing the understanding and culture of aggressive individualized insulin protocols. These can often be even more statistically difficult to quantify. As self-reported, improvements were made.
One of the most important aspects of this paper is that it draws attention to the paucity of evidence for improved clinical and monetary outcomes supporting the aggressive hospital management of hyperglycemia in the non-acutely ill patient. Often, the guiding principle is to avoid hypoglycemia. Detailing the specific protocols of one such approach serves as an example for the motivated reader.
Early Switch from IV to Oral Antibiotic in Severe CAP
Oosterheert JJ, Bonten JM, Schneider MME, et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia; multicentre randomised trial. BMJ. 2006 Dec 9; 333:1193.
Community acquired pneumonia (CAP) is a common and potentially fatal infection with high healthcare costs. When patients are first admitted to hospitals, antibiotics are usually given intravenously to provide optimal concentrations in the tissues.
The duration of intravenous treatment is an important determinant of length of hospital stay (LOS). The concept of early transition from intravenous to oral antibiotic in the treatment of CAP has been evaluated before, but only in mild to moderately severe disease—and rarely in randomized trials.
This multicenter random controlled trial from five teaching hospitals and two medical centers in the Netherlands enrolled 302 patients in non-intensive care units with severe CAP. The primary outcome was clinical cure and secondary outcome was LOS. The inclusion criteria were adults 18 or older with severe CAP; mean pneumonia severity index of IV-V, new progressive infiltrate on chest X-ray, plus at least two other criteria (cough, sputum production, rectal temperature >38o C or <36.1o C, auscultative findings consistent with pneumonia, leukocytes >109 WBC/L or >15% bands, positive cultures of blob or pleural fluids, CRP three times greater times upper limit of normal).
Exclusion criteria included the need for mechanical ventilation, cystic fibrosis, a history of colonization with gram-negative bacteria due to structural damage to the respiratory tract, malfunction of the digestive tract, life expectancy of less than one month because of underlying disease, infections other than pneumonia that needed antibiotic treatment, and severe immunosuppression (neutropenia [<0.5 109 neutrophils/liter] or a CD4 count< 200/mm3).
Treatment failure was defined as death, still in hospital at day 28 of the study, or clinical deterioration (increase in temperature after initial improvement or the need for mechanical ventilation, switch back to intravenous antibiotics, or readmission for pulmonary reinfection after discharge).
Clinical cure was defined as discharged in good health without signs and symptoms of pneumonia and no treatment failure during follow-up.
The control group comprised 150 subjects who were to receive a standard course of seven days’ intravenous treatment. Meanwhile, 152 subjects were randomized to the early switch group. Baseline characteristics were similar in both groups. More than 80% of patients were in pneumonia severity class IV or V. Most patients received empirical monotherapy with amoxicillin or amoxicillin plus clavulanic acid (n=174; 58%) or a cephalosporin (n=59; 20%), which is in line with Dutch prescribing policies.
The most frequently identified microorganism was S pneumoniae (n=76; 25%). Atypical pathogens were detected in 33 patients (11%). Before day three, 37 patients (12%) were excluded from analysis, leaving 132 patients for analysis in the intervention group and 133 in the control group.
Reasons for exclusion included when the initial diagnosis of CAP was replaced by another diagnosis (n=9), consent was withdrawn (n=11), the protocol was violated (n=4), the patient was admitted to an intensive-care unit for mechanical ventilation (n=6), and the patient died (n=7). After three days of intravenous treatment, 108 of 132 patients (81%) in the intervention group were switched to oral treatment, of whom 102 (94%) received amoxicillin plus clavulanic acid (500+125 mg every eight hours).
In the control group, five patients did not receive intravenous antibiotics for all seven days because of phlebitis associated with intravenous treatment; none of them needed treatment for line-related sepsis. Overall duration of antibiotic treatment was 10.1 days in the intervention group and 9.3 days in the control group (mean difference 0.8 days, 95% confidence interval -0.6 to 2.0).
The duration of intravenous treatment was significantly shorter in the intervention group (mean 3.6 [SD 1.5] versus 7.0 [2.0] days, mean difference 3.4, 2.8 to 3.9). Average time to meet the discharge criteria was 5.2 (2.9) days in the intervention group and 5.7 (3.1) days in the control group (0.5 days -0.3 to 1.2) Total length of hospital stay was 9.6 (5.0) and 11.5 (4.9) days for patients in the intervention group and control group (1.9 days 0.6 to 3.2).
The authors’ findings provide strong evidence that early transition from intravenous to oral antibiotic is also viable in patients with highly graded Pneumonia Severity Index (PSI) CAP, not only in mild to moderately severe disease. This leads to reduced LOS, cost, and possibly reduced risk of line infections and increased patient satisfaction for early discharge.
Note: This study was done with patients suffering straightforward, uncomplicated CAP. The investigators’ findings cannot be applied to patients with other comorbidities like diabetes, COPD, heart failure, or sickle cell, which might require more days on intravenous antibiotic. One might also wonder what impact would have been seen had 37 patients not dropped off, and if another class of oral antibiotic such as quinolones had been used.
Last, the study sample showed S pneumoniae identified in 25% of cases and atypical pathogens to be 11%. What then are the majority of pathogens identified 64% of the time? This would have been another key factor that might have had a great effect on the result.
Although a larger sampling and further risk stratification (to include patients with other comorbidities) are needed, this study makes a valid point for early transition to oral antibiotics in highly graded, uncomplicated CAP. TH
Heal the Whole Hurt
Note: This is Part 3 of The Hospitalist’s series on pain and hospital medicine. Part 1 appeared on p. 45 of the April issue, and Part 2 appeared on p. 33 of the June issue.
Hospitalists face demands for pain care every day. Usually, the general pain principles described in the first two articles in this series and the use of a few opioid analgesics with which the hospitalist has become familiar can supply relief.
But what about the more difficult cases in which psychosocial influences or a history of substance abuse complicates the patient’s pain? Perhaps it is a chronic pain case that has never been adequately addressed, or the patient keeps turning up in the emergency department (ED) complaining of out-of-control pain. Other examples of difficult-to-manage pain include complex regional pain syndrome, post-herpetic neuralgia, other neuropathic pains, sickle cell anemia, and patients at high risk of opioid toxicity.
These cases are like a leaky bucket for the hospital—costly, frustrating, unsatisfying to the patient, and prone to bad outcomes, says Jerry Wesch, PhD, director of the pain service for the Alexian Brothers Health System in greater Chicago. “These are the patients who tend to bedevil everybody in the hospital,” he says.
Dealing with such patients is a demanding task.
“You don’t have chronic pain without a psycho-social-spiritual overlay,” adds Scott Fishman, MD, chief of the Division of Pain Medicine at University of California-Davis in Sacramento. “Their emotional lives are deteriorating. They can’t sleep, they’re depressed, and their physical functioning is also deteriorating. There are all kinds of situations that demand use of a full spectrum of bio-psycho-social interventions in addition to opioid analgesics.”
These complex, unresolved cases are likely to have emotional, social, or spiritual manifestations. But what does that mean to a busy hospitalist with a short window of opportunity to address patients’ pain before pointing them toward discharge? A psychologist, social worker, or chaplain may have something to contribute to pain management. Meanwhile, the rest of the caseload is clamoring for the hospitalist’s attention.
Make Pain Management Multidisciplinary
A dizzying array of pain modalities can be brought to bear on complex pain cases. These range from opioid analgesics to a variety of adjuvant non-opioid medications to interventional techniques involving surgery, spinal injections, nerve blocks, nerve stimulation, and nerve destruction techniques.
There are also complementary methodologies (e.g., acupuncture) that have been shown to reduce the volume of narcotics needed for pain control, even though how they work is not well understood.
But how many hospitalists call on acupuncturists, hypnotists, or teachers of guided-imagery meditation for their patients? Many of these techniques are more appropriately initiated in the outpatient setting, but the hospitalist still has a responsibility to make sure “frequent fliers” with complex pain complaints get connected post-discharge to a pain service that can offer long-term relief. The challenge is applying the acute treatment models of the hospital to chronic pain syndromes that are not optimally addressed in crisis mode.
Jonathan Weston, MD, a hospitalist at Penrose Hospital in Colorado Springs, Colo., says these difficult, chronic pain cases are the bane of the hospitalist’s working life. These patients show up at night in the ED saying, “ ‘I’m in so much pain, please don’t send me home,’ ” he says. “The emergency physician puts them on an IV drip and their pain is relieved for the moment, but only one facet of that pain has been addressed.”
The emergency physician—also under caseload pressure— decides the easiest disposition is to admit the patient and dump the problem on the hospitalist. “They’re out of their pain medications at home, and when you call the attending you are told that they are drug seekers,” Dr. Weston relates. “These patients take a lot of energy. They can be manipulative. We can’t do right for them. It’s not satisfying. We don’t want to round on them. The way we hospitalists manage these patients sometimes reflects not only the patient’s personality, but our personality as well.”
Hospitalists don’t just treat these patients’ pain, they also address their suffering, he says.
High-quality pain management is multidisciplinary, Dr. Weston notes, because pain is multifactorial. The hospitalist occupies an important coordinating position and is charged with responsibility for the whole person during that patient’s brief hospital stay. But there are limits to what the hospitalist can accomplish. A palliative care team or an acute pain service can make important contributions to hospitalized patients’ pain. So can social workers, psychologists, pharmacists, and chaplains. But it is the hospitalist’s responsibility to coordinate these pieces of the pain puzzle for patients on service.
In many hospitals, the palliative care service has been set up to consult on pain, suffering, and clarification of treatment goals for patients nearing the end of life. These services vary from institution to institution in terms of whether they prefer to focus on end-of-life issues or are comfortable fielding other kinds of chronic pain questions. Acute pain services equally vary in terms of whether their focus is primarily on surgical pain “interventions” or on a multidisciplinary approach to pain management.
Ideally, Dr. Weston says, a major hospital would have both services available as resources to the hospitalist. Or, if there is only one of them, it should have a broad approach to pain management. Otherwise, it is up to the hospitalist to pull together a virtual pain team to provide a multidisciplinary response to complex pain.
“I am also board certified in hospice and palliative medicine,” Dr. Weston says. “I can use my medical knowledge to try to get the patient comfortable on oral meds so that they can go home. And I can personally make an appointment for them within 48 hours of discharge with their attending physician or a pain specialist. But for too many patients, this connection never happens.”
“Pain management in general is a hard thing to deal with,” adds Lauren Fraser, MD, regional chief of the department of hospital medicine for Kaiser Permanente Colorado in Denver. “It’s frustrating because you want to do the right thing,” she says. “We need first of all to rule out anything we can fix that might be causing the pain. Then we’re dealing with the patient’s quality of life and the disabling effects of pain. Each patient and family has a different need, and when you meet with them one-on-one you’re dealing with all of it.”
Dr. Fraser doesn’t have access to an acute pain service in her current setting, “although we have interventional folks to put in the PCAs and epidurals. We generally are able to get the services we need, although there would be an advantage to having an identified multidisciplinary pain service to provide the coordination.”
A “Pain Hospitalist”
Jerry Wesch, director of the pain program at Alexian Brothers Hospital Network in Arlington Heights, Ill., recently posted a job listing on the Internet seeking a pain management physician. He is looking for a doctor with an interest in comprehensive, interdisciplinary team management of chronic pain who is “able to function as a pain hospitalist.”
Although the details of this new position are still being finalized and a pain hospitalist would function with a different focus than a generalist hospitalist, Wesch suggests the role has important analogies with what hospitalists like Dr. Weston face in coordinating a virtual team of multidisciplinary pain resources.
Wesch is building an inpatient pain service comprising the pain physician, two nurse practitioners, and a part-time psychologist with full-time presence in two Alexian Brothers acute hospitals. This team would work closely with hospitalists, the palliative care service, and ancillary services such as physical therapy and chaplains.
“This should make us ideal collaborators with the hospitalists, who can just walk down the hall and initiate a pain consult,” he explains. “We’re all working toward the same goal, which is to improve efficiency, medical management, quality of care, and patient satisfaction. A good hospitalist is also my best ally in building a multidisciplinary pain service.”
In other settings, however, it will be the hospitalist’s responsibility to build the relationships that bring these pain resources together.
Deb Gordon, RN, MS, FAAN, senior clinical nurse specialist at the University of Wisconsin Medical Center in Madison, also sees herself functioning like a hospitalist in addressing pain issues. “I manage a clinical pain consultation service. I see patients every day,” she says. “I’m also in staff development, helping professionals in the hospital learn to manage pain better, and using quality improvement techniques to take what we know about pain management to support people like hospitalists at the bedside.”
Since 1990, an interdisciplinary quality improvement pain management group has been meeting at the UW medical center to improve the institution’s response to pain patients. Gordon believes pain is a natural target for hospital quality-improvement activities because it touches on the domains of quality identified by groups such as the Institute of Medicine in Washington, D.C., and the Institute for Healthcare Improvement in Cambridge, Mass.
Limits in the Hospital Setting
Even with a vast array of pain modalities, hospitalists face inherent limitations in addressing pain challenges within the hospital, starting with caseload pressures and short lengths of stay. Many of the approaches that might offer long-term solutions to the patient’s chronic pain syndrome belong in the outpatient setting, adds John Massey, MD, president and medical director of Nebraska Pain Consultants in Lincoln.
Dr. Massey sees chronic pain cases that have been refractory to treatment, both at his clinic and as a consultant in the hospital. Inevitably there is a psychological overlay to these cases, he says. That doesn’t mean the patient’s pain isn’t real, but if high doses of analgesics have failed to bring the pain under control, then a different approach is needed—one that includes behavioral techniques and involves the patient not as a passive recipient of treatment, but an active participant in his or her own pain management and coping strategies.
“There are ways to treat, for example, back pain that require finding a specific nerve in the spine responsible for the pain,” says Dr. Massey. “If I can locate that nerve, there are things that I can do, like radio frequency neuro-ablation. But this requires three separate visits to the pain clinic to make an accurate diagnosis. I’m often consulted by hospitalists and there are things I can do to put a finger in the dike. But I try to add another perspective to my discussion with the hospitalist, pointing out that many of the best pain management modalities are done on an outpatient basis.”
What can be achieved in the hospital often is more of a Band-Aid, sometimes even a step backward in terms of the lifestyle changes necessary to get patients out of their passive response to their chronic pain, Dr. Massey says.
The hospitalist’s job is to see what can be done to make patients more comfortable and then send them home with a referral to the pain service, if that is indicated. “I’m happy to help with an intervention in the hospital but, ultimately, we’d like the patient to be less dependent on opioids to treat their pain,” says Dr. Massey. “I know that nothing I can do will really change the situation until I get them out of the hospital and can initiate physical therapy and behavioral interventions.”
There are no shortcuts to permanent pain relief, which can be long, slow, hard work using evidence-based medicine, Dr. Massey says. But it also involves a frank discussion with the patient, which may be hard in the hospital.
“One of the questions we ask patients is: How many times have you visited the emergency room for pain?” says Dr. Massey. “If the answer is more than four in a year, there are likely to be psychological co-morbidities. The challenge for the hospitalist is, ‘How can I arrest this acute pain episode, and then what can I contribute to helping the patient find the help he or she needs to prevent the next episode?’ That means trying to establish rapport and pointing the person to appropriate follow-up pain resources. If you go too hard too fast, the patient may reject what you’re offering. But if you do nothing, you’re facilitating a continued passive approach that doesn’t lead to meaningful solutions.”
Dr. Massey recently saw a woman who had been in the ED 48 times in the previous year for pain that had a major behavioral component. The hospital hired him after the 48th visit to find a different approach to controlling the patient’s pain.
Make Pain a Priority
“My hospitalist group meets regularly to discuss difficult topics, and pain often comes up,” says Stephen Bekanich, MD, hospitalist and palliative care physician at the University of Utah Medical Center in Salt Lake City. “The more you can focus on pain, the more time you spend making it a priority, you are sending a message: This is important to me. You communicate to nurses and other staff that you take pain seriously.”
Dr. Fishman concurs. “Ultimately, it is an issue of priorities and how to prioritize what gets done in the hospital,” he says. “Why would a health professional ever categorize pain relief as a lower priority? We have wandered far from our compassionate mission as doctors when that happens.
“In the real world, when there is no one else to do it, and no pain clinics available, the responsibility for pain management falls on the provider at the front lines, often the emergency physician and the hospitalist. Hospitalists are becoming de facto pain specialists for patients with chronic and terminal conditions. These patients are looking for support, comfort, and redirection. This can also be one of the most rewarding aspects of hospital practice. It really brings you back to the roots of medicine.” TH
Larry Beresford is a regular contributor to The Hospitalist.
Note: This is Part 3 of The Hospitalist’s series on pain and hospital medicine. Part 1 appeared on p. 45 of the April issue, and Part 2 appeared on p. 33 of the June issue.
Hospitalists face demands for pain care every day. Usually, the general pain principles described in the first two articles in this series and the use of a few opioid analgesics with which the hospitalist has become familiar can supply relief.
But what about the more difficult cases in which psychosocial influences or a history of substance abuse complicates the patient’s pain? Perhaps it is a chronic pain case that has never been adequately addressed, or the patient keeps turning up in the emergency department (ED) complaining of out-of-control pain. Other examples of difficult-to-manage pain include complex regional pain syndrome, post-herpetic neuralgia, other neuropathic pains, sickle cell anemia, and patients at high risk of opioid toxicity.
These cases are like a leaky bucket for the hospital—costly, frustrating, unsatisfying to the patient, and prone to bad outcomes, says Jerry Wesch, PhD, director of the pain service for the Alexian Brothers Health System in greater Chicago. “These are the patients who tend to bedevil everybody in the hospital,” he says.
Dealing with such patients is a demanding task.
“You don’t have chronic pain without a psycho-social-spiritual overlay,” adds Scott Fishman, MD, chief of the Division of Pain Medicine at University of California-Davis in Sacramento. “Their emotional lives are deteriorating. They can’t sleep, they’re depressed, and their physical functioning is also deteriorating. There are all kinds of situations that demand use of a full spectrum of bio-psycho-social interventions in addition to opioid analgesics.”
These complex, unresolved cases are likely to have emotional, social, or spiritual manifestations. But what does that mean to a busy hospitalist with a short window of opportunity to address patients’ pain before pointing them toward discharge? A psychologist, social worker, or chaplain may have something to contribute to pain management. Meanwhile, the rest of the caseload is clamoring for the hospitalist’s attention.
Make Pain Management Multidisciplinary
A dizzying array of pain modalities can be brought to bear on complex pain cases. These range from opioid analgesics to a variety of adjuvant non-opioid medications to interventional techniques involving surgery, spinal injections, nerve blocks, nerve stimulation, and nerve destruction techniques.
There are also complementary methodologies (e.g., acupuncture) that have been shown to reduce the volume of narcotics needed for pain control, even though how they work is not well understood.
But how many hospitalists call on acupuncturists, hypnotists, or teachers of guided-imagery meditation for their patients? Many of these techniques are more appropriately initiated in the outpatient setting, but the hospitalist still has a responsibility to make sure “frequent fliers” with complex pain complaints get connected post-discharge to a pain service that can offer long-term relief. The challenge is applying the acute treatment models of the hospital to chronic pain syndromes that are not optimally addressed in crisis mode.
Jonathan Weston, MD, a hospitalist at Penrose Hospital in Colorado Springs, Colo., says these difficult, chronic pain cases are the bane of the hospitalist’s working life. These patients show up at night in the ED saying, “ ‘I’m in so much pain, please don’t send me home,’ ” he says. “The emergency physician puts them on an IV drip and their pain is relieved for the moment, but only one facet of that pain has been addressed.”
The emergency physician—also under caseload pressure— decides the easiest disposition is to admit the patient and dump the problem on the hospitalist. “They’re out of their pain medications at home, and when you call the attending you are told that they are drug seekers,” Dr. Weston relates. “These patients take a lot of energy. They can be manipulative. We can’t do right for them. It’s not satisfying. We don’t want to round on them. The way we hospitalists manage these patients sometimes reflects not only the patient’s personality, but our personality as well.”
Hospitalists don’t just treat these patients’ pain, they also address their suffering, he says.
High-quality pain management is multidisciplinary, Dr. Weston notes, because pain is multifactorial. The hospitalist occupies an important coordinating position and is charged with responsibility for the whole person during that patient’s brief hospital stay. But there are limits to what the hospitalist can accomplish. A palliative care team or an acute pain service can make important contributions to hospitalized patients’ pain. So can social workers, psychologists, pharmacists, and chaplains. But it is the hospitalist’s responsibility to coordinate these pieces of the pain puzzle for patients on service.
In many hospitals, the palliative care service has been set up to consult on pain, suffering, and clarification of treatment goals for patients nearing the end of life. These services vary from institution to institution in terms of whether they prefer to focus on end-of-life issues or are comfortable fielding other kinds of chronic pain questions. Acute pain services equally vary in terms of whether their focus is primarily on surgical pain “interventions” or on a multidisciplinary approach to pain management.
Ideally, Dr. Weston says, a major hospital would have both services available as resources to the hospitalist. Or, if there is only one of them, it should have a broad approach to pain management. Otherwise, it is up to the hospitalist to pull together a virtual pain team to provide a multidisciplinary response to complex pain.
“I am also board certified in hospice and palliative medicine,” Dr. Weston says. “I can use my medical knowledge to try to get the patient comfortable on oral meds so that they can go home. And I can personally make an appointment for them within 48 hours of discharge with their attending physician or a pain specialist. But for too many patients, this connection never happens.”
“Pain management in general is a hard thing to deal with,” adds Lauren Fraser, MD, regional chief of the department of hospital medicine for Kaiser Permanente Colorado in Denver. “It’s frustrating because you want to do the right thing,” she says. “We need first of all to rule out anything we can fix that might be causing the pain. Then we’re dealing with the patient’s quality of life and the disabling effects of pain. Each patient and family has a different need, and when you meet with them one-on-one you’re dealing with all of it.”
Dr. Fraser doesn’t have access to an acute pain service in her current setting, “although we have interventional folks to put in the PCAs and epidurals. We generally are able to get the services we need, although there would be an advantage to having an identified multidisciplinary pain service to provide the coordination.”
A “Pain Hospitalist”
Jerry Wesch, director of the pain program at Alexian Brothers Hospital Network in Arlington Heights, Ill., recently posted a job listing on the Internet seeking a pain management physician. He is looking for a doctor with an interest in comprehensive, interdisciplinary team management of chronic pain who is “able to function as a pain hospitalist.”
Although the details of this new position are still being finalized and a pain hospitalist would function with a different focus than a generalist hospitalist, Wesch suggests the role has important analogies with what hospitalists like Dr. Weston face in coordinating a virtual team of multidisciplinary pain resources.
Wesch is building an inpatient pain service comprising the pain physician, two nurse practitioners, and a part-time psychologist with full-time presence in two Alexian Brothers acute hospitals. This team would work closely with hospitalists, the palliative care service, and ancillary services such as physical therapy and chaplains.
“This should make us ideal collaborators with the hospitalists, who can just walk down the hall and initiate a pain consult,” he explains. “We’re all working toward the same goal, which is to improve efficiency, medical management, quality of care, and patient satisfaction. A good hospitalist is also my best ally in building a multidisciplinary pain service.”
In other settings, however, it will be the hospitalist’s responsibility to build the relationships that bring these pain resources together.
Deb Gordon, RN, MS, FAAN, senior clinical nurse specialist at the University of Wisconsin Medical Center in Madison, also sees herself functioning like a hospitalist in addressing pain issues. “I manage a clinical pain consultation service. I see patients every day,” she says. “I’m also in staff development, helping professionals in the hospital learn to manage pain better, and using quality improvement techniques to take what we know about pain management to support people like hospitalists at the bedside.”
Since 1990, an interdisciplinary quality improvement pain management group has been meeting at the UW medical center to improve the institution’s response to pain patients. Gordon believes pain is a natural target for hospital quality-improvement activities because it touches on the domains of quality identified by groups such as the Institute of Medicine in Washington, D.C., and the Institute for Healthcare Improvement in Cambridge, Mass.
Limits in the Hospital Setting
Even with a vast array of pain modalities, hospitalists face inherent limitations in addressing pain challenges within the hospital, starting with caseload pressures and short lengths of stay. Many of the approaches that might offer long-term solutions to the patient’s chronic pain syndrome belong in the outpatient setting, adds John Massey, MD, president and medical director of Nebraska Pain Consultants in Lincoln.
Dr. Massey sees chronic pain cases that have been refractory to treatment, both at his clinic and as a consultant in the hospital. Inevitably there is a psychological overlay to these cases, he says. That doesn’t mean the patient’s pain isn’t real, but if high doses of analgesics have failed to bring the pain under control, then a different approach is needed—one that includes behavioral techniques and involves the patient not as a passive recipient of treatment, but an active participant in his or her own pain management and coping strategies.
“There are ways to treat, for example, back pain that require finding a specific nerve in the spine responsible for the pain,” says Dr. Massey. “If I can locate that nerve, there are things that I can do, like radio frequency neuro-ablation. But this requires three separate visits to the pain clinic to make an accurate diagnosis. I’m often consulted by hospitalists and there are things I can do to put a finger in the dike. But I try to add another perspective to my discussion with the hospitalist, pointing out that many of the best pain management modalities are done on an outpatient basis.”
What can be achieved in the hospital often is more of a Band-Aid, sometimes even a step backward in terms of the lifestyle changes necessary to get patients out of their passive response to their chronic pain, Dr. Massey says.
The hospitalist’s job is to see what can be done to make patients more comfortable and then send them home with a referral to the pain service, if that is indicated. “I’m happy to help with an intervention in the hospital but, ultimately, we’d like the patient to be less dependent on opioids to treat their pain,” says Dr. Massey. “I know that nothing I can do will really change the situation until I get them out of the hospital and can initiate physical therapy and behavioral interventions.”
There are no shortcuts to permanent pain relief, which can be long, slow, hard work using evidence-based medicine, Dr. Massey says. But it also involves a frank discussion with the patient, which may be hard in the hospital.
“One of the questions we ask patients is: How many times have you visited the emergency room for pain?” says Dr. Massey. “If the answer is more than four in a year, there are likely to be psychological co-morbidities. The challenge for the hospitalist is, ‘How can I arrest this acute pain episode, and then what can I contribute to helping the patient find the help he or she needs to prevent the next episode?’ That means trying to establish rapport and pointing the person to appropriate follow-up pain resources. If you go too hard too fast, the patient may reject what you’re offering. But if you do nothing, you’re facilitating a continued passive approach that doesn’t lead to meaningful solutions.”
Dr. Massey recently saw a woman who had been in the ED 48 times in the previous year for pain that had a major behavioral component. The hospital hired him after the 48th visit to find a different approach to controlling the patient’s pain.
Make Pain a Priority
“My hospitalist group meets regularly to discuss difficult topics, and pain often comes up,” says Stephen Bekanich, MD, hospitalist and palliative care physician at the University of Utah Medical Center in Salt Lake City. “The more you can focus on pain, the more time you spend making it a priority, you are sending a message: This is important to me. You communicate to nurses and other staff that you take pain seriously.”
Dr. Fishman concurs. “Ultimately, it is an issue of priorities and how to prioritize what gets done in the hospital,” he says. “Why would a health professional ever categorize pain relief as a lower priority? We have wandered far from our compassionate mission as doctors when that happens.
“In the real world, when there is no one else to do it, and no pain clinics available, the responsibility for pain management falls on the provider at the front lines, often the emergency physician and the hospitalist. Hospitalists are becoming de facto pain specialists for patients with chronic and terminal conditions. These patients are looking for support, comfort, and redirection. This can also be one of the most rewarding aspects of hospital practice. It really brings you back to the roots of medicine.” TH
Larry Beresford is a regular contributor to The Hospitalist.
Note: This is Part 3 of The Hospitalist’s series on pain and hospital medicine. Part 1 appeared on p. 45 of the April issue, and Part 2 appeared on p. 33 of the June issue.
Hospitalists face demands for pain care every day. Usually, the general pain principles described in the first two articles in this series and the use of a few opioid analgesics with which the hospitalist has become familiar can supply relief.
But what about the more difficult cases in which psychosocial influences or a history of substance abuse complicates the patient’s pain? Perhaps it is a chronic pain case that has never been adequately addressed, or the patient keeps turning up in the emergency department (ED) complaining of out-of-control pain. Other examples of difficult-to-manage pain include complex regional pain syndrome, post-herpetic neuralgia, other neuropathic pains, sickle cell anemia, and patients at high risk of opioid toxicity.
These cases are like a leaky bucket for the hospital—costly, frustrating, unsatisfying to the patient, and prone to bad outcomes, says Jerry Wesch, PhD, director of the pain service for the Alexian Brothers Health System in greater Chicago. “These are the patients who tend to bedevil everybody in the hospital,” he says.
Dealing with such patients is a demanding task.
“You don’t have chronic pain without a psycho-social-spiritual overlay,” adds Scott Fishman, MD, chief of the Division of Pain Medicine at University of California-Davis in Sacramento. “Their emotional lives are deteriorating. They can’t sleep, they’re depressed, and their physical functioning is also deteriorating. There are all kinds of situations that demand use of a full spectrum of bio-psycho-social interventions in addition to opioid analgesics.”
These complex, unresolved cases are likely to have emotional, social, or spiritual manifestations. But what does that mean to a busy hospitalist with a short window of opportunity to address patients’ pain before pointing them toward discharge? A psychologist, social worker, or chaplain may have something to contribute to pain management. Meanwhile, the rest of the caseload is clamoring for the hospitalist’s attention.
Make Pain Management Multidisciplinary
A dizzying array of pain modalities can be brought to bear on complex pain cases. These range from opioid analgesics to a variety of adjuvant non-opioid medications to interventional techniques involving surgery, spinal injections, nerve blocks, nerve stimulation, and nerve destruction techniques.
There are also complementary methodologies (e.g., acupuncture) that have been shown to reduce the volume of narcotics needed for pain control, even though how they work is not well understood.
But how many hospitalists call on acupuncturists, hypnotists, or teachers of guided-imagery meditation for their patients? Many of these techniques are more appropriately initiated in the outpatient setting, but the hospitalist still has a responsibility to make sure “frequent fliers” with complex pain complaints get connected post-discharge to a pain service that can offer long-term relief. The challenge is applying the acute treatment models of the hospital to chronic pain syndromes that are not optimally addressed in crisis mode.
Jonathan Weston, MD, a hospitalist at Penrose Hospital in Colorado Springs, Colo., says these difficult, chronic pain cases are the bane of the hospitalist’s working life. These patients show up at night in the ED saying, “ ‘I’m in so much pain, please don’t send me home,’ ” he says. “The emergency physician puts them on an IV drip and their pain is relieved for the moment, but only one facet of that pain has been addressed.”
The emergency physician—also under caseload pressure— decides the easiest disposition is to admit the patient and dump the problem on the hospitalist. “They’re out of their pain medications at home, and when you call the attending you are told that they are drug seekers,” Dr. Weston relates. “These patients take a lot of energy. They can be manipulative. We can’t do right for them. It’s not satisfying. We don’t want to round on them. The way we hospitalists manage these patients sometimes reflects not only the patient’s personality, but our personality as well.”
Hospitalists don’t just treat these patients’ pain, they also address their suffering, he says.
High-quality pain management is multidisciplinary, Dr. Weston notes, because pain is multifactorial. The hospitalist occupies an important coordinating position and is charged with responsibility for the whole person during that patient’s brief hospital stay. But there are limits to what the hospitalist can accomplish. A palliative care team or an acute pain service can make important contributions to hospitalized patients’ pain. So can social workers, psychologists, pharmacists, and chaplains. But it is the hospitalist’s responsibility to coordinate these pieces of the pain puzzle for patients on service.
In many hospitals, the palliative care service has been set up to consult on pain, suffering, and clarification of treatment goals for patients nearing the end of life. These services vary from institution to institution in terms of whether they prefer to focus on end-of-life issues or are comfortable fielding other kinds of chronic pain questions. Acute pain services equally vary in terms of whether their focus is primarily on surgical pain “interventions” or on a multidisciplinary approach to pain management.
Ideally, Dr. Weston says, a major hospital would have both services available as resources to the hospitalist. Or, if there is only one of them, it should have a broad approach to pain management. Otherwise, it is up to the hospitalist to pull together a virtual pain team to provide a multidisciplinary response to complex pain.
“I am also board certified in hospice and palliative medicine,” Dr. Weston says. “I can use my medical knowledge to try to get the patient comfortable on oral meds so that they can go home. And I can personally make an appointment for them within 48 hours of discharge with their attending physician or a pain specialist. But for too many patients, this connection never happens.”
“Pain management in general is a hard thing to deal with,” adds Lauren Fraser, MD, regional chief of the department of hospital medicine for Kaiser Permanente Colorado in Denver. “It’s frustrating because you want to do the right thing,” she says. “We need first of all to rule out anything we can fix that might be causing the pain. Then we’re dealing with the patient’s quality of life and the disabling effects of pain. Each patient and family has a different need, and when you meet with them one-on-one you’re dealing with all of it.”
Dr. Fraser doesn’t have access to an acute pain service in her current setting, “although we have interventional folks to put in the PCAs and epidurals. We generally are able to get the services we need, although there would be an advantage to having an identified multidisciplinary pain service to provide the coordination.”
A “Pain Hospitalist”
Jerry Wesch, director of the pain program at Alexian Brothers Hospital Network in Arlington Heights, Ill., recently posted a job listing on the Internet seeking a pain management physician. He is looking for a doctor with an interest in comprehensive, interdisciplinary team management of chronic pain who is “able to function as a pain hospitalist.”
Although the details of this new position are still being finalized and a pain hospitalist would function with a different focus than a generalist hospitalist, Wesch suggests the role has important analogies with what hospitalists like Dr. Weston face in coordinating a virtual team of multidisciplinary pain resources.
Wesch is building an inpatient pain service comprising the pain physician, two nurse practitioners, and a part-time psychologist with full-time presence in two Alexian Brothers acute hospitals. This team would work closely with hospitalists, the palliative care service, and ancillary services such as physical therapy and chaplains.
“This should make us ideal collaborators with the hospitalists, who can just walk down the hall and initiate a pain consult,” he explains. “We’re all working toward the same goal, which is to improve efficiency, medical management, quality of care, and patient satisfaction. A good hospitalist is also my best ally in building a multidisciplinary pain service.”
In other settings, however, it will be the hospitalist’s responsibility to build the relationships that bring these pain resources together.
Deb Gordon, RN, MS, FAAN, senior clinical nurse specialist at the University of Wisconsin Medical Center in Madison, also sees herself functioning like a hospitalist in addressing pain issues. “I manage a clinical pain consultation service. I see patients every day,” she says. “I’m also in staff development, helping professionals in the hospital learn to manage pain better, and using quality improvement techniques to take what we know about pain management to support people like hospitalists at the bedside.”
Since 1990, an interdisciplinary quality improvement pain management group has been meeting at the UW medical center to improve the institution’s response to pain patients. Gordon believes pain is a natural target for hospital quality-improvement activities because it touches on the domains of quality identified by groups such as the Institute of Medicine in Washington, D.C., and the Institute for Healthcare Improvement in Cambridge, Mass.
Limits in the Hospital Setting
Even with a vast array of pain modalities, hospitalists face inherent limitations in addressing pain challenges within the hospital, starting with caseload pressures and short lengths of stay. Many of the approaches that might offer long-term solutions to the patient’s chronic pain syndrome belong in the outpatient setting, adds John Massey, MD, president and medical director of Nebraska Pain Consultants in Lincoln.
Dr. Massey sees chronic pain cases that have been refractory to treatment, both at his clinic and as a consultant in the hospital. Inevitably there is a psychological overlay to these cases, he says. That doesn’t mean the patient’s pain isn’t real, but if high doses of analgesics have failed to bring the pain under control, then a different approach is needed—one that includes behavioral techniques and involves the patient not as a passive recipient of treatment, but an active participant in his or her own pain management and coping strategies.
“There are ways to treat, for example, back pain that require finding a specific nerve in the spine responsible for the pain,” says Dr. Massey. “If I can locate that nerve, there are things that I can do, like radio frequency neuro-ablation. But this requires three separate visits to the pain clinic to make an accurate diagnosis. I’m often consulted by hospitalists and there are things I can do to put a finger in the dike. But I try to add another perspective to my discussion with the hospitalist, pointing out that many of the best pain management modalities are done on an outpatient basis.”
What can be achieved in the hospital often is more of a Band-Aid, sometimes even a step backward in terms of the lifestyle changes necessary to get patients out of their passive response to their chronic pain, Dr. Massey says.
The hospitalist’s job is to see what can be done to make patients more comfortable and then send them home with a referral to the pain service, if that is indicated. “I’m happy to help with an intervention in the hospital but, ultimately, we’d like the patient to be less dependent on opioids to treat their pain,” says Dr. Massey. “I know that nothing I can do will really change the situation until I get them out of the hospital and can initiate physical therapy and behavioral interventions.”
There are no shortcuts to permanent pain relief, which can be long, slow, hard work using evidence-based medicine, Dr. Massey says. But it also involves a frank discussion with the patient, which may be hard in the hospital.
“One of the questions we ask patients is: How many times have you visited the emergency room for pain?” says Dr. Massey. “If the answer is more than four in a year, there are likely to be psychological co-morbidities. The challenge for the hospitalist is, ‘How can I arrest this acute pain episode, and then what can I contribute to helping the patient find the help he or she needs to prevent the next episode?’ That means trying to establish rapport and pointing the person to appropriate follow-up pain resources. If you go too hard too fast, the patient may reject what you’re offering. But if you do nothing, you’re facilitating a continued passive approach that doesn’t lead to meaningful solutions.”
Dr. Massey recently saw a woman who had been in the ED 48 times in the previous year for pain that had a major behavioral component. The hospital hired him after the 48th visit to find a different approach to controlling the patient’s pain.
Make Pain a Priority
“My hospitalist group meets regularly to discuss difficult topics, and pain often comes up,” says Stephen Bekanich, MD, hospitalist and palliative care physician at the University of Utah Medical Center in Salt Lake City. “The more you can focus on pain, the more time you spend making it a priority, you are sending a message: This is important to me. You communicate to nurses and other staff that you take pain seriously.”
Dr. Fishman concurs. “Ultimately, it is an issue of priorities and how to prioritize what gets done in the hospital,” he says. “Why would a health professional ever categorize pain relief as a lower priority? We have wandered far from our compassionate mission as doctors when that happens.
“In the real world, when there is no one else to do it, and no pain clinics available, the responsibility for pain management falls on the provider at the front lines, often the emergency physician and the hospitalist. Hospitalists are becoming de facto pain specialists for patients with chronic and terminal conditions. These patients are looking for support, comfort, and redirection. This can also be one of the most rewarding aspects of hospital practice. It really brings you back to the roots of medicine.” TH
Larry Beresford is a regular contributor to The Hospitalist.
Pray With Me
Early in his career, hospitalist Richard Bailey, MD, encountered a widow from the inner city with no family. She was blind, and had been weakened and debilitated by a very challenging hospital course with many iatrogenic complications. “I was first struck, walking into her room,” recalls Dr. Bailey, “that she had a Bible on the table next to her bed. While making conversation, I mentioned this and instinctively asked her if she needed someone to read it to her. She smiled, and asked if I would oblige. I closed the door, sat down, and read her some of her favorite passages. This went on for several days until I went off service.”
Now medical director of Inpatient Care and Hospitalist Services at Saint Clare’s Hospital, a Catholic hospital in Wausau, Wis., Dr. Bailey says he is not an overtly religious person and that his spiritual life is rather private. “But I do like to have that depth of connection with my patients,” he says.
So if a patient or a family member asks him to pray with them, Dr. Bailey does so. “I cannot separate my humanness, which includes spirituality, from my work,” he explains.
When faced with serious or life-threatening medical conditions, patients and their family members are more likely to invoke their faith to cope with the attendant anxieties.
William D. Atchley Jr., MD, medical director of the Division of Hospital Medicine for Sentara Medical Group in Hampton, Va., believes that joining his patients in prayer, when asked, “helps develop a better relationship with the family and patient.”
Many Americans tend to “live in the here and now,” notes Carol R. Taylor, RN, MSN, PhD, director of the Center for Clinical Bioethics at Georgetown University. “They usually do not ask the bigger questions so long as life is good. But when life as we know it is threatened by illness, the bigger questions can become very important: ‘Is there anything beyond the here and now? And if so, where do I stand in relation to that God or higher power?’ ”
Prayer is a common response when patients face perilous medical situations.
“The vast majority of patients who are feeling imperiled due to a severe diagnosis or potential mortality is going to be praying,” says Stephen G. Post, PhD, professor and associate director for educational programs, department of bioethics at Case Western Reserve University, Cleveland. “In a way, you can’t get away from those requests.”
Are hospitalists and their institutions fully equipped to respond to the spiritual aspect of caregiving? Some researchers note that biomedicine often regards faith and spiritual world views as relevant only when they obstruct implementation of scientifically sound medical care.1 Studies have also shown healthcare professionals are less likely than their patients to actively practice a religion.
“There’s very often a mismatch between patients and families who would value that intervention and our comfort in being able to be responsive,” says Dr. Taylor, who is also an assistant professor of nursing.
Dr. Taylor and other bioethicists increasingly urge medical practitioners to include spiritual needs when they take a patient’s history. Timely referrals to chaplaincy services, knowledge of the dominant faiths and ethnic traditions in their hospitals’ catchment areas, and improvement of interpersonal skills can allow hospitalists to compassionately and ethically address their patients’ spiritual concerns.
Need to Do a Better Job
The holistic view of medicine defines health as a multidimensional construct that includes the physical, emotional, and social aspects of the patient. This view should be matched with a holistic approach to healthcare delivery that encompasses patients’ subjective illness experience, says Dr. Post.
Dr. Taylor concedes that the medical community’s recognition of patients’ spiritual needs is growing. And yet, she says, practitioners are not held accountable for delivering spiritual care, “which I think is a failing of healthcare as it is practiced today.”
Many reports have indicated patients are unhappy with the low referral rates to pastoral clinical care, adds Dr. Post.2
Assessment Essential
Incorporate a spiritual-needs assessment when taking each patient’s history upon admittance, the two bioethicists agree. This assessment usually takes the form of questions such as:
- What is your source of strength?
- Is spirituality/religion important to you? (If the patient answers “yes,” proceed to the next question.)
- How would you like us to facilitate your needs?
- Would you like a referral to pastoral care?
Once patients indicate they would like to speak with a chaplain, referral to appropriate clergy trained in pastoral care is essential.
“All physicians need to be respectful of these kinds of appeals,” says Dr. Post. “But they should feel free to make a referral to those who are, in fact, competently trained to deal with this specific area of life.”
While opposed to professional separatism, Dr. Post does argue for keeping “friendly, knee-high white fences” between physicians and pastoral counselors to maintain professional boundaries.3
Marc B. Westle, DO, FACP, president and managing partner of Asheville Hospitalist Group, PA, in North Carolina, agrees with this approach. “As a professional, I completely respect and empathize with the patient’s and the family’s spiritual needs as part of the total care of the patient,” he says. “Just as in other areas where I may not have expertise, I refer to our in-house professionals. We have an excellent chaplaincy service that we involve all the time, on a routine basis.” He says the chaplaincy service at Mission Hospital is in-house 24/7, just as the hospitalists are, and make rounds as the physicians do.
Availability of trained clergy differs from institution to institution, notes Dr. Taylor. She recently visited a metropolitan research institution where the two staff chaplains estimate there are nearly 1,000 daily patient contacts. With this many patients flowing through the facility, the chaplains rely on medical staff to triage patients’ and families’ needs so they can be referred to families who will benefit most from their help. In busy urban hospitals, pastoral coverage may not always be available, and the burden of addressing spiritual requests can fall to the hospital medicine team.
The Comfort Zone
The question of whether to pray with a patient or family member depends on the physician’s comfort with doing so.
- Rule No. 1 when it comes to the question of prayer with/for a patient or family: Clinicians should never proselytize or initiate the prayer. This can constitute a serious breach of professional boundaries.4
- Balancing the need to support patients’ emotional needs while respecting one’s integrity can be difficult. If a physician feels comfortable, it is appropriate to pray with a patient. Or, a physician can offer to sit quietly while a patient prays. If uncomfortable with this scenario, offering to keep the patient in your thoughts is one way to still be supportive while maintaining the integrity of your beliefs.3
“I think most physicians try to be very sensitive to these matters,” says Dr. Post.
Dr. Westle notes he has provided more companionate care (“hugging family and patients, sitting and talking about the good old days”) than spiritual guidance.
“Some patients and families feel supported simply by their doctor or nurse joining in a moment of silence or even holding hands during a spoken prayer,” adds Dr. Taylor. “Some of us are better than others at identifying and responding to spiritual needs. But I do think it’s a shared responsibility. The more people we can engage in identifying and responding to spiritual needs, the better patient, family, and medical team will be served. Hospitalists are in an excellent position to identify those needs because of their everyday contact. And if they simply make the right referrals, they’ve done a really good job.” TH
Gretchen Henkel writes frequently for The Hospitalist.
References
- Barnes LL, Plotnikoff GA, Fox K, et al. Spirituality, religion, and pediatrics: intersecting worlds of healing. Pediatrics 2000 Oct;106(4 Suppl):899-908.
- Post SG, Puchalski CM, Larson DB. Physicians and Patient Spirituality: Professional Boundaries, Competency, and Ethics. Ann Intern Med. 2000 April 4;132(7):578-583. Comment in: Ann Intern Med. 2000 Dec 5;133(11):920-1; Ann Intern Med. 2000 Nov 7;133(9):748-9.
- Kwiatkowski K, Arnold B, Barnard D. Physicians and Prayer Requests. Fast Fact and Concept #120. Available at www.eperc.mcw.edu/fastFact/ff_120.htm. Last accessed April 5, 2007.
- Taylor C, Lillis C, LeMone P. Fundamentals of Nursing: The Art and Science of Nursing Care, 5th ed. 2005. Philadelphia: Lippincott, Williams & Wilkins; 2005.
Early in his career, hospitalist Richard Bailey, MD, encountered a widow from the inner city with no family. She was blind, and had been weakened and debilitated by a very challenging hospital course with many iatrogenic complications. “I was first struck, walking into her room,” recalls Dr. Bailey, “that she had a Bible on the table next to her bed. While making conversation, I mentioned this and instinctively asked her if she needed someone to read it to her. She smiled, and asked if I would oblige. I closed the door, sat down, and read her some of her favorite passages. This went on for several days until I went off service.”
Now medical director of Inpatient Care and Hospitalist Services at Saint Clare’s Hospital, a Catholic hospital in Wausau, Wis., Dr. Bailey says he is not an overtly religious person and that his spiritual life is rather private. “But I do like to have that depth of connection with my patients,” he says.
So if a patient or a family member asks him to pray with them, Dr. Bailey does so. “I cannot separate my humanness, which includes spirituality, from my work,” he explains.
When faced with serious or life-threatening medical conditions, patients and their family members are more likely to invoke their faith to cope with the attendant anxieties.
William D. Atchley Jr., MD, medical director of the Division of Hospital Medicine for Sentara Medical Group in Hampton, Va., believes that joining his patients in prayer, when asked, “helps develop a better relationship with the family and patient.”
Many Americans tend to “live in the here and now,” notes Carol R. Taylor, RN, MSN, PhD, director of the Center for Clinical Bioethics at Georgetown University. “They usually do not ask the bigger questions so long as life is good. But when life as we know it is threatened by illness, the bigger questions can become very important: ‘Is there anything beyond the here and now? And if so, where do I stand in relation to that God or higher power?’ ”
Prayer is a common response when patients face perilous medical situations.
“The vast majority of patients who are feeling imperiled due to a severe diagnosis or potential mortality is going to be praying,” says Stephen G. Post, PhD, professor and associate director for educational programs, department of bioethics at Case Western Reserve University, Cleveland. “In a way, you can’t get away from those requests.”
Are hospitalists and their institutions fully equipped to respond to the spiritual aspect of caregiving? Some researchers note that biomedicine often regards faith and spiritual world views as relevant only when they obstruct implementation of scientifically sound medical care.1 Studies have also shown healthcare professionals are less likely than their patients to actively practice a religion.
“There’s very often a mismatch between patients and families who would value that intervention and our comfort in being able to be responsive,” says Dr. Taylor, who is also an assistant professor of nursing.
Dr. Taylor and other bioethicists increasingly urge medical practitioners to include spiritual needs when they take a patient’s history. Timely referrals to chaplaincy services, knowledge of the dominant faiths and ethnic traditions in their hospitals’ catchment areas, and improvement of interpersonal skills can allow hospitalists to compassionately and ethically address their patients’ spiritual concerns.
Need to Do a Better Job
The holistic view of medicine defines health as a multidimensional construct that includes the physical, emotional, and social aspects of the patient. This view should be matched with a holistic approach to healthcare delivery that encompasses patients’ subjective illness experience, says Dr. Post.
Dr. Taylor concedes that the medical community’s recognition of patients’ spiritual needs is growing. And yet, she says, practitioners are not held accountable for delivering spiritual care, “which I think is a failing of healthcare as it is practiced today.”
Many reports have indicated patients are unhappy with the low referral rates to pastoral clinical care, adds Dr. Post.2
Assessment Essential
Incorporate a spiritual-needs assessment when taking each patient’s history upon admittance, the two bioethicists agree. This assessment usually takes the form of questions such as:
- What is your source of strength?
- Is spirituality/religion important to you? (If the patient answers “yes,” proceed to the next question.)
- How would you like us to facilitate your needs?
- Would you like a referral to pastoral care?
Once patients indicate they would like to speak with a chaplain, referral to appropriate clergy trained in pastoral care is essential.
“All physicians need to be respectful of these kinds of appeals,” says Dr. Post. “But they should feel free to make a referral to those who are, in fact, competently trained to deal with this specific area of life.”
While opposed to professional separatism, Dr. Post does argue for keeping “friendly, knee-high white fences” between physicians and pastoral counselors to maintain professional boundaries.3
Marc B. Westle, DO, FACP, president and managing partner of Asheville Hospitalist Group, PA, in North Carolina, agrees with this approach. “As a professional, I completely respect and empathize with the patient’s and the family’s spiritual needs as part of the total care of the patient,” he says. “Just as in other areas where I may not have expertise, I refer to our in-house professionals. We have an excellent chaplaincy service that we involve all the time, on a routine basis.” He says the chaplaincy service at Mission Hospital is in-house 24/7, just as the hospitalists are, and make rounds as the physicians do.
Availability of trained clergy differs from institution to institution, notes Dr. Taylor. She recently visited a metropolitan research institution where the two staff chaplains estimate there are nearly 1,000 daily patient contacts. With this many patients flowing through the facility, the chaplains rely on medical staff to triage patients’ and families’ needs so they can be referred to families who will benefit most from their help. In busy urban hospitals, pastoral coverage may not always be available, and the burden of addressing spiritual requests can fall to the hospital medicine team.
The Comfort Zone
The question of whether to pray with a patient or family member depends on the physician’s comfort with doing so.
- Rule No. 1 when it comes to the question of prayer with/for a patient or family: Clinicians should never proselytize or initiate the prayer. This can constitute a serious breach of professional boundaries.4
- Balancing the need to support patients’ emotional needs while respecting one’s integrity can be difficult. If a physician feels comfortable, it is appropriate to pray with a patient. Or, a physician can offer to sit quietly while a patient prays. If uncomfortable with this scenario, offering to keep the patient in your thoughts is one way to still be supportive while maintaining the integrity of your beliefs.3
“I think most physicians try to be very sensitive to these matters,” says Dr. Post.
Dr. Westle notes he has provided more companionate care (“hugging family and patients, sitting and talking about the good old days”) than spiritual guidance.
“Some patients and families feel supported simply by their doctor or nurse joining in a moment of silence or even holding hands during a spoken prayer,” adds Dr. Taylor. “Some of us are better than others at identifying and responding to spiritual needs. But I do think it’s a shared responsibility. The more people we can engage in identifying and responding to spiritual needs, the better patient, family, and medical team will be served. Hospitalists are in an excellent position to identify those needs because of their everyday contact. And if they simply make the right referrals, they’ve done a really good job.” TH
Gretchen Henkel writes frequently for The Hospitalist.
References
- Barnes LL, Plotnikoff GA, Fox K, et al. Spirituality, religion, and pediatrics: intersecting worlds of healing. Pediatrics 2000 Oct;106(4 Suppl):899-908.
- Post SG, Puchalski CM, Larson DB. Physicians and Patient Spirituality: Professional Boundaries, Competency, and Ethics. Ann Intern Med. 2000 April 4;132(7):578-583. Comment in: Ann Intern Med. 2000 Dec 5;133(11):920-1; Ann Intern Med. 2000 Nov 7;133(9):748-9.
- Kwiatkowski K, Arnold B, Barnard D. Physicians and Prayer Requests. Fast Fact and Concept #120. Available at www.eperc.mcw.edu/fastFact/ff_120.htm. Last accessed April 5, 2007.
- Taylor C, Lillis C, LeMone P. Fundamentals of Nursing: The Art and Science of Nursing Care, 5th ed. 2005. Philadelphia: Lippincott, Williams & Wilkins; 2005.
Early in his career, hospitalist Richard Bailey, MD, encountered a widow from the inner city with no family. She was blind, and had been weakened and debilitated by a very challenging hospital course with many iatrogenic complications. “I was first struck, walking into her room,” recalls Dr. Bailey, “that she had a Bible on the table next to her bed. While making conversation, I mentioned this and instinctively asked her if she needed someone to read it to her. She smiled, and asked if I would oblige. I closed the door, sat down, and read her some of her favorite passages. This went on for several days until I went off service.”
Now medical director of Inpatient Care and Hospitalist Services at Saint Clare’s Hospital, a Catholic hospital in Wausau, Wis., Dr. Bailey says he is not an overtly religious person and that his spiritual life is rather private. “But I do like to have that depth of connection with my patients,” he says.
So if a patient or a family member asks him to pray with them, Dr. Bailey does so. “I cannot separate my humanness, which includes spirituality, from my work,” he explains.
When faced with serious or life-threatening medical conditions, patients and their family members are more likely to invoke their faith to cope with the attendant anxieties.
William D. Atchley Jr., MD, medical director of the Division of Hospital Medicine for Sentara Medical Group in Hampton, Va., believes that joining his patients in prayer, when asked, “helps develop a better relationship with the family and patient.”
Many Americans tend to “live in the here and now,” notes Carol R. Taylor, RN, MSN, PhD, director of the Center for Clinical Bioethics at Georgetown University. “They usually do not ask the bigger questions so long as life is good. But when life as we know it is threatened by illness, the bigger questions can become very important: ‘Is there anything beyond the here and now? And if so, where do I stand in relation to that God or higher power?’ ”
Prayer is a common response when patients face perilous medical situations.
“The vast majority of patients who are feeling imperiled due to a severe diagnosis or potential mortality is going to be praying,” says Stephen G. Post, PhD, professor and associate director for educational programs, department of bioethics at Case Western Reserve University, Cleveland. “In a way, you can’t get away from those requests.”
Are hospitalists and their institutions fully equipped to respond to the spiritual aspect of caregiving? Some researchers note that biomedicine often regards faith and spiritual world views as relevant only when they obstruct implementation of scientifically sound medical care.1 Studies have also shown healthcare professionals are less likely than their patients to actively practice a religion.
“There’s very often a mismatch between patients and families who would value that intervention and our comfort in being able to be responsive,” says Dr. Taylor, who is also an assistant professor of nursing.
Dr. Taylor and other bioethicists increasingly urge medical practitioners to include spiritual needs when they take a patient’s history. Timely referrals to chaplaincy services, knowledge of the dominant faiths and ethnic traditions in their hospitals’ catchment areas, and improvement of interpersonal skills can allow hospitalists to compassionately and ethically address their patients’ spiritual concerns.
Need to Do a Better Job
The holistic view of medicine defines health as a multidimensional construct that includes the physical, emotional, and social aspects of the patient. This view should be matched with a holistic approach to healthcare delivery that encompasses patients’ subjective illness experience, says Dr. Post.
Dr. Taylor concedes that the medical community’s recognition of patients’ spiritual needs is growing. And yet, she says, practitioners are not held accountable for delivering spiritual care, “which I think is a failing of healthcare as it is practiced today.”
Many reports have indicated patients are unhappy with the low referral rates to pastoral clinical care, adds Dr. Post.2
Assessment Essential
Incorporate a spiritual-needs assessment when taking each patient’s history upon admittance, the two bioethicists agree. This assessment usually takes the form of questions such as:
- What is your source of strength?
- Is spirituality/religion important to you? (If the patient answers “yes,” proceed to the next question.)
- How would you like us to facilitate your needs?
- Would you like a referral to pastoral care?
Once patients indicate they would like to speak with a chaplain, referral to appropriate clergy trained in pastoral care is essential.
“All physicians need to be respectful of these kinds of appeals,” says Dr. Post. “But they should feel free to make a referral to those who are, in fact, competently trained to deal with this specific area of life.”
While opposed to professional separatism, Dr. Post does argue for keeping “friendly, knee-high white fences” between physicians and pastoral counselors to maintain professional boundaries.3
Marc B. Westle, DO, FACP, president and managing partner of Asheville Hospitalist Group, PA, in North Carolina, agrees with this approach. “As a professional, I completely respect and empathize with the patient’s and the family’s spiritual needs as part of the total care of the patient,” he says. “Just as in other areas where I may not have expertise, I refer to our in-house professionals. We have an excellent chaplaincy service that we involve all the time, on a routine basis.” He says the chaplaincy service at Mission Hospital is in-house 24/7, just as the hospitalists are, and make rounds as the physicians do.
Availability of trained clergy differs from institution to institution, notes Dr. Taylor. She recently visited a metropolitan research institution where the two staff chaplains estimate there are nearly 1,000 daily patient contacts. With this many patients flowing through the facility, the chaplains rely on medical staff to triage patients’ and families’ needs so they can be referred to families who will benefit most from their help. In busy urban hospitals, pastoral coverage may not always be available, and the burden of addressing spiritual requests can fall to the hospital medicine team.
The Comfort Zone
The question of whether to pray with a patient or family member depends on the physician’s comfort with doing so.
- Rule No. 1 when it comes to the question of prayer with/for a patient or family: Clinicians should never proselytize or initiate the prayer. This can constitute a serious breach of professional boundaries.4
- Balancing the need to support patients’ emotional needs while respecting one’s integrity can be difficult. If a physician feels comfortable, it is appropriate to pray with a patient. Or, a physician can offer to sit quietly while a patient prays. If uncomfortable with this scenario, offering to keep the patient in your thoughts is one way to still be supportive while maintaining the integrity of your beliefs.3
“I think most physicians try to be very sensitive to these matters,” says Dr. Post.
Dr. Westle notes he has provided more companionate care (“hugging family and patients, sitting and talking about the good old days”) than spiritual guidance.
“Some patients and families feel supported simply by their doctor or nurse joining in a moment of silence or even holding hands during a spoken prayer,” adds Dr. Taylor. “Some of us are better than others at identifying and responding to spiritual needs. But I do think it’s a shared responsibility. The more people we can engage in identifying and responding to spiritual needs, the better patient, family, and medical team will be served. Hospitalists are in an excellent position to identify those needs because of their everyday contact. And if they simply make the right referrals, they’ve done a really good job.” TH
Gretchen Henkel writes frequently for The Hospitalist.
References
- Barnes LL, Plotnikoff GA, Fox K, et al. Spirituality, religion, and pediatrics: intersecting worlds of healing. Pediatrics 2000 Oct;106(4 Suppl):899-908.
- Post SG, Puchalski CM, Larson DB. Physicians and Patient Spirituality: Professional Boundaries, Competency, and Ethics. Ann Intern Med. 2000 April 4;132(7):578-583. Comment in: Ann Intern Med. 2000 Dec 5;133(11):920-1; Ann Intern Med. 2000 Nov 7;133(9):748-9.
- Kwiatkowski K, Arnold B, Barnard D. Physicians and Prayer Requests. Fast Fact and Concept #120. Available at www.eperc.mcw.edu/fastFact/ff_120.htm. Last accessed April 5, 2007.
- Taylor C, Lillis C, LeMone P. Fundamentals of Nursing: The Art and Science of Nursing Care, 5th ed. 2005. Philadelphia: Lippincott, Williams & Wilkins; 2005.
Googling for Diagnoses
Googling—the use of search-engines such as Google—is a new diagnostic tool in the modern clinician’s armamentarium.
A 2006 study published in The British Medical Journal examined how often searching with Google leads physicians to a correct diagnosis.1 The investigators were blinded to the correct diagnoses and compared the results of diagnostic cases published in the 2005 case records of The New England Journal of Medicine (NEJM) with diagnoses made using Google searches. Their results indicated that Google searches revealed the correct diagnosis in 15 of 26 cases, or 58% of the time. (See Table 1, p. 34.)
The limitations of the study are important to recognize when considering how well a Web-searched diagnosis can compare with one made without Web searching.
In some cases, although Google supplied information that approximated the diagnoses made in NEJM, the researchers thought the diagnoses were not specific enough.
For instance, one case for which Google suggested a diagnosis of extrinsic allergic alveolitis was described in the NEJM case record as extrinsic allergic alveolitis caused by Mycobacterium avium, also known as “hot tub lung.” This exemplifies the point that search engines don’t make diagnoses—people do. Expert knowledge is required to choose the best search words and select among the results.
Experts agree that using search engines for a diagnosis is likely to be more effective for conditions with unique symptoms and most useful in a certain class of diagnostic challenges in which clinical experts are at the helm of diagnostic deliberations.1,2
The choice of search engines is important and will increasingly affect accurate diagnoses as the technology develops.
“Hospitalists may utilize [Google] less; they are often working in environments [hospitals] that have ready access to more thoroughly vetted sources such as UpToDate, Medline, or MDConsult,” says Joshua Lee, MD, a hospitalist and medical director of Information Services at the University of California at San Diego. “Within Google there are variations on a theme, such as GoogleScholar, which accesses many of the same academic journals as Medline. Given that they are accessing the same journals, many would feel that searching with GoogleScholar is just as accurate as [searching with] Medline—at least as far as the source material is concerned.”
Search engines offer an impressive volume of new scientific material that is indexed daily. But, current search engines cannot identify differences of meaning in symptoms, drug names, anatomic features, or diagnoses.
“The key drawback to using open Google is that you cannot guarantee that the information comes from peer-reviewed journals,” Dr. Lee says. “When a search with ‘regular’ Google brings back untested medical information that is not peer reviewed, it gets dicey, and thus less reliable.”
Current Web technologies may merely be a first step in creating a much more powerful infrastructure for Web-based diagnostics. The so-called semantic Web will allow computers to process meaning in documentation.3 Two key elements of this revolution are the resource description framework (RDF) and Web ontology language (OWL) technologies. These next-generation search tools are being beta tested and will be freely available within the next decade.
There are a number of caveats to using and trusting information from search-engine investigations. Google stands up much better than other search engines in simple diagnostic searches. Also, diagnostic problems are not solved on a linear scale of difficulty.2 Research and development of the benefits of the semantic Web in clinical practice will help maximize this tool for diagnostics. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Tang H, Ng JHK. Googling for a diagnosis—use of Google as a diagnostic aid: internet based study. BMJ. 2006 Dec 2;333(7579):1143-1145.
- Gardner M. Diagnosis using search engines. BMJ. 2006 Dec 2;333(7579):1131.
- Berners-Lee T, Hendler J, Lassila O. The semantic web. Sci Am. 2001 May 1;34-43.
Googling—the use of search-engines such as Google—is a new diagnostic tool in the modern clinician’s armamentarium.
A 2006 study published in The British Medical Journal examined how often searching with Google leads physicians to a correct diagnosis.1 The investigators were blinded to the correct diagnoses and compared the results of diagnostic cases published in the 2005 case records of The New England Journal of Medicine (NEJM) with diagnoses made using Google searches. Their results indicated that Google searches revealed the correct diagnosis in 15 of 26 cases, or 58% of the time. (See Table 1, p. 34.)
The limitations of the study are important to recognize when considering how well a Web-searched diagnosis can compare with one made without Web searching.
In some cases, although Google supplied information that approximated the diagnoses made in NEJM, the researchers thought the diagnoses were not specific enough.
For instance, one case for which Google suggested a diagnosis of extrinsic allergic alveolitis was described in the NEJM case record as extrinsic allergic alveolitis caused by Mycobacterium avium, also known as “hot tub lung.” This exemplifies the point that search engines don’t make diagnoses—people do. Expert knowledge is required to choose the best search words and select among the results.
Experts agree that using search engines for a diagnosis is likely to be more effective for conditions with unique symptoms and most useful in a certain class of diagnostic challenges in which clinical experts are at the helm of diagnostic deliberations.1,2
The choice of search engines is important and will increasingly affect accurate diagnoses as the technology develops.
“Hospitalists may utilize [Google] less; they are often working in environments [hospitals] that have ready access to more thoroughly vetted sources such as UpToDate, Medline, or MDConsult,” says Joshua Lee, MD, a hospitalist and medical director of Information Services at the University of California at San Diego. “Within Google there are variations on a theme, such as GoogleScholar, which accesses many of the same academic journals as Medline. Given that they are accessing the same journals, many would feel that searching with GoogleScholar is just as accurate as [searching with] Medline—at least as far as the source material is concerned.”
Search engines offer an impressive volume of new scientific material that is indexed daily. But, current search engines cannot identify differences of meaning in symptoms, drug names, anatomic features, or diagnoses.
“The key drawback to using open Google is that you cannot guarantee that the information comes from peer-reviewed journals,” Dr. Lee says. “When a search with ‘regular’ Google brings back untested medical information that is not peer reviewed, it gets dicey, and thus less reliable.”
Current Web technologies may merely be a first step in creating a much more powerful infrastructure for Web-based diagnostics. The so-called semantic Web will allow computers to process meaning in documentation.3 Two key elements of this revolution are the resource description framework (RDF) and Web ontology language (OWL) technologies. These next-generation search tools are being beta tested and will be freely available within the next decade.
There are a number of caveats to using and trusting information from search-engine investigations. Google stands up much better than other search engines in simple diagnostic searches. Also, diagnostic problems are not solved on a linear scale of difficulty.2 Research and development of the benefits of the semantic Web in clinical practice will help maximize this tool for diagnostics. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Tang H, Ng JHK. Googling for a diagnosis—use of Google as a diagnostic aid: internet based study. BMJ. 2006 Dec 2;333(7579):1143-1145.
- Gardner M. Diagnosis using search engines. BMJ. 2006 Dec 2;333(7579):1131.
- Berners-Lee T, Hendler J, Lassila O. The semantic web. Sci Am. 2001 May 1;34-43.
Googling—the use of search-engines such as Google—is a new diagnostic tool in the modern clinician’s armamentarium.
A 2006 study published in The British Medical Journal examined how often searching with Google leads physicians to a correct diagnosis.1 The investigators were blinded to the correct diagnoses and compared the results of diagnostic cases published in the 2005 case records of The New England Journal of Medicine (NEJM) with diagnoses made using Google searches. Their results indicated that Google searches revealed the correct diagnosis in 15 of 26 cases, or 58% of the time. (See Table 1, p. 34.)
The limitations of the study are important to recognize when considering how well a Web-searched diagnosis can compare with one made without Web searching.
In some cases, although Google supplied information that approximated the diagnoses made in NEJM, the researchers thought the diagnoses were not specific enough.
For instance, one case for which Google suggested a diagnosis of extrinsic allergic alveolitis was described in the NEJM case record as extrinsic allergic alveolitis caused by Mycobacterium avium, also known as “hot tub lung.” This exemplifies the point that search engines don’t make diagnoses—people do. Expert knowledge is required to choose the best search words and select among the results.
Experts agree that using search engines for a diagnosis is likely to be more effective for conditions with unique symptoms and most useful in a certain class of diagnostic challenges in which clinical experts are at the helm of diagnostic deliberations.1,2
The choice of search engines is important and will increasingly affect accurate diagnoses as the technology develops.
“Hospitalists may utilize [Google] less; they are often working in environments [hospitals] that have ready access to more thoroughly vetted sources such as UpToDate, Medline, or MDConsult,” says Joshua Lee, MD, a hospitalist and medical director of Information Services at the University of California at San Diego. “Within Google there are variations on a theme, such as GoogleScholar, which accesses many of the same academic journals as Medline. Given that they are accessing the same journals, many would feel that searching with GoogleScholar is just as accurate as [searching with] Medline—at least as far as the source material is concerned.”
Search engines offer an impressive volume of new scientific material that is indexed daily. But, current search engines cannot identify differences of meaning in symptoms, drug names, anatomic features, or diagnoses.
“The key drawback to using open Google is that you cannot guarantee that the information comes from peer-reviewed journals,” Dr. Lee says. “When a search with ‘regular’ Google brings back untested medical information that is not peer reviewed, it gets dicey, and thus less reliable.”
Current Web technologies may merely be a first step in creating a much more powerful infrastructure for Web-based diagnostics. The so-called semantic Web will allow computers to process meaning in documentation.3 Two key elements of this revolution are the resource description framework (RDF) and Web ontology language (OWL) technologies. These next-generation search tools are being beta tested and will be freely available within the next decade.
There are a number of caveats to using and trusting information from search-engine investigations. Google stands up much better than other search engines in simple diagnostic searches. Also, diagnostic problems are not solved on a linear scale of difficulty.2 Research and development of the benefits of the semantic Web in clinical practice will help maximize this tool for diagnostics. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Tang H, Ng JHK. Googling for a diagnosis—use of Google as a diagnostic aid: internet based study. BMJ. 2006 Dec 2;333(7579):1143-1145.
- Gardner M. Diagnosis using search engines. BMJ. 2006 Dec 2;333(7579):1131.
- Berners-Lee T, Hendler J, Lassila O. The semantic web. Sci Am. 2001 May 1;34-43.
The Telehospitalist
The patient was in the ICU at Saint Clare’s Hospital in Wausau, Wis. An intensivist from St. Louis who had been caring for her remotely through telemedicine technology was helping clinicians manage the end-of-life issue for her and her family.
Subjects like this can be difficult for hospitalists, who may not have as much experience with the protocols involved in end-of-life care. But at Saint Clare’s, which offers remote care and monitoring by intensivists and critical-care nurses through an eICU program, critical-care specialists are there to provide continuous care to the hospital’s sickest patients, as well as support for the onsite clinicians in any number of situations involving ICU patient care.
Dellice Dickhaus, MD, medical director for Advanced ICU Care and a practicing intensivist, helps provide remote care around the clock for patients in Saint Clare’s ICU. Advanced ICU Care’s board-certified intensivists and critical-care nurses remotely care for and monitor patients in multiple sites from their operations center, more than 400 miles away in St. Louis. They use telemedicine technology developed by Baltimore, Md., firm VISICU that combines clinical management software with real-time video feeds and patient data, such as labs, vital signs and medications.
In the case of the critically ill patient, while the hospitalist was driving the patient’s care program and taking care of many of the daily issues, Dr. Dickhaus helped manage the end-of-life issue. She was available at the push of a button to talk with relatives and provide information they needed to make decisions about their family member’s care. She discussed the patient’s prognosis and options with the family, and kept the hospitalist on staff apprised of the conversations.
Because Dr. Dickhaus and other clinicians at Advanced ICU Care had been helping manage the patient’s care in the ICU, the patient’s family gained confidence in the remote intensivists, says Dr. Dickhaus.
Demands of an Aging Population
The aging of America will have a tremendous effect on healthcare, particularly regarding care of the critically ill and in managing such areas as pulmonary disease. Consider that more than half of all ICU stays are incurred by patients older than 65. Further, patients older than 65 account for more than two-thirds of all inpatient pulmonary days.
What does this mean for hospitalists? For one, the aging population will create a demand for care that is projected to outpace the supply of intensivists and pulmonologists.1 With fewer of these specialists, hospitalists may be compelled to take on more responsibilities with critically ill patients, leaving less time for other patients. The expectation of healthcare services provided will likely change, possibly growing in scope and complexity. The time it will take to deliver care is also expected to rise. All these are reasons for the growth in telemedicine technologies, with many designed to improve patient care by delivering limited resources where they are needed most.
Continuity of Care
Richard Bailey, MD, medical director of Inpatient Care and Hospitalist Services at Saint Clare’s, says having remote intensivists lets his staff focus on hospital patients outside the ICU.
“One critical patient can tie you up for hours,” Dr. Bailey says. “Advanced ICU Care’s intensivists are hands-on physicians, helping us round on ICU patients, take patient notes, and handle first-line phone calls.”
There is no difference, he says, between having intensivists in St. Louis, for example, versus on-site. “They are more than a microphone and a camera in the ceiling; they are members of our staff,” he says. “We trust them to take care of our patients.”
He explains that remote intensivists are often good at being the “bug in the ear” for hospitalists, helping with treatment recommendations and asking, “Did you remember to … ?” While stabilizing a just-transferred ICU patient in a near-code situation, Dr. Bailey needed immediate access to the patient’s labs. An intensivist in St. Louis was able to look at the labs and recommend treatment.
Preliminary numbers at Saint Clare’s hint at a reduction of one day in ICU length of stay and two days for total hospitalization, notes Dr. Bailey. Figures like these can mean real savings in hospital costs.
Working together, hospitalists and remote intensivists can provide continuity of care as the patient is admitted through the emergency department and brought into the ICU, explains Dr. Bailey.
William D. Atchley Jr., MD, medical director for the Division of Hospital Medicine for Sentara Medical Group in Norfolk, Va., agrees with Dr. Bailey’s view. Dr. Atchley’s group also uses telemedicine technology for the remote care and monitoring of ICU patients. He is also a member of SHM’s Board of Directors.
“This is a true team effort, creating a seamless continuity from the emergency department to the ICU,” says Dr. Atchley. He cites septic shock patients as an example. He is able to start the septic shock protocols with the patient in the ED, and the intensivist will carry the protocols forward with the patient in the ICU. By morning, Dr. Atchley says he knows the patient has received the care needed, which frees him to care for other patients.
Sentara Healthcare, based in Norfolk, Va., was the first hospital system in the nation to implement VISICU’s technology, which allows hospitals to create a systemwide critical-care program. Using the VISICU eICU, the hospital or healthcare system provides the intensivists to staff the program, helping to leverage scarce clinical resources among the system’s ICUs.
Studies have shown that care by intensivists via telemedicine technology improves patient care and safety in the ICU. In a 2004 study, Sentara documented a 27% decrease in overall ICU and hospital mortality.2
Mobile Telemedicine
Advances in telemedicine technology have come a long way. Take remote robotic systems, for instance, which allow physicians to consult with patients, family members, and on-site caregivers while seated in their office, in another wing of the hospital, or at home.
InTouch Health, a Santa Barbara, Calif., company, uses about 100 robotic systems. While seated at a control station, equipped with video capabilities, a microphone, and a joystick, the physician can “drive” the robot into a patient’s room for consultation. The patient can see the doctor’s face on the monitor and—on the other end—the physician has access to patient data and can see the patient through a live video image.
The robotic system provides added ability for intensivists and other specialists to do another evening round on their patients, explains Tim Wright, vice president of strategic marketing for InTouch. A recent study shows that when physicians use robotic telepresence to make rounds in the ICU in response to nursing pages, physician response is significantly faster. Additionally, the study found a reduced length of stay, particularly for patients with subarachnoid hemorrhage and brain trauma, as well as an ICU cost savings of $1.1 million.3
The idea of robotic telepresence is similar to the telemedicine model of care being used in the ICU. Through the robotic system, an intensivist can log in and perform an evening round, updating hospitalists on new patients and issues that may have arisen.
“The beauty is that the intensivist and the hospitalist can be looking at everything together,” Wright says. “The intensivist can provide the specialist knowledge and training, while the hospitalist provides the ongoing care.”
Not Just the ICU
Of course, telemedicine is not limited to the ICU. It is being used for virtually every medical specialty to help provide greater access to care.
Take the University of Texas Medical Branch at Galveston (UTMB), which has used telemedicine technologies since 1994. Its Electronic Health Network (EHN) utilizes telemedicine to help care for the state’s indigent and rural populations, as well as other groups, such as the elderly, prisoners, and even researchers in Antarctica.
One of the fastest-growing services UTMB operates is the telemedicine-based corporate healthcare programs, allowing employees to “see” a primary care physician without leaving work. Companies see this as a way to help control healthcare costs and make preventive care more accessible, notes Glenn Hammack, OD, assistant vice president and executive director of the UTMB Electronic Health Network. He also pegs the application of telemedicine to psychiatry as another growing service and one that illustrates how the technology is being used to help address a shortage of providers, especially in rural and underserved parts of Texas. Like the eICU programs designed to bring scarce intensivist care to ICU patients, UTMB’s services help distribute rare resources, such as child and adolescent psychiatrists who speak Spanish, to patients.
The telemedicine program at UMTB began in 1994 as a way to help provide cost-effective healthcare for inmates in the Texas prison system. Today, the Correctional Managed Care (CMC) department has telemedicine stations in 120 correctional units throughout Texas and accounts for about half of UTMB’s telemedicine program.
The 11 telemedicine studios at UTMB used for patients across the EHN are equipped with live interactive video links that allow the telemedicine physician to see and hear the patient, located at the remote station with a registered health professional on-site. Digital stethoscopes, hand-held cameras, and other electronic medical devices help the physician treat patients. The telemedicine program also utilizes shared electronic medical records, which are critical to its success, says Dr. Hammack.
Telemedicine can also be used between departments within the hospital. Dr. Hammack notes that hospitals have become large and complicated; the journey from one end to another for a test or procedure can be difficult on patients. “Telemedicine offers the ability for face-to-face interaction, and when used within hospital departments, it can bring some humanity of scale back to the increasingly complicated hospital environment,” he says.
Another Vision
Troy Sybert, MD, medical director for CMC Hospital Medicine and a practicing hospitalist at Texas Department of Criminal Justice (TDCJ) Hospital in Galveston, Texas, was hired a year ago to help create a hospitalist program within the prison system. His is the only health facility dedicated to prisoners and located on a medical school campus.
While his six-member team is not engaged in telemedicine, he sees a number of possibilities for CMC hospitalists to utilize telemedicine technology. For one, hospitalists could use their expertise in admissions to help triage patients via telemedicine. The CMC recently created a network of regional hubs similar to ED observation centers but without a 24/7 physician presence. Telemedicine triage could help the system offload the decision to admit and would likely reduce the number of hospital admissions, says Dr. Sybert.
Telemedicine technology could also provide other possibilities in perioperative care for surgery patients at TDCJ Hospital. In partnership with the surgery and anesthesia departments, pre- and post-operative work up and care could be done remotely with the patient back in the unit, promoting shorter lengths of stay and reducing transportation needs. The hospitalists, trained in correctional care, would provide support and coordinate with surgery—especially on the patient’s transition to and from the prison facility.
“The whole concept of telemedicine is to utilize experience from a centralized location,” says Dr. Sybert. “We have a vision for where we might like to go with telemedicine, bringing our hospitalist group’s experience with managed correctional care to prison units throughout the state.”
Whether it is bringing intensivist care to a critically ill patient, providing therapy sessions to patients in rural areas, or delivering the expertise of hospitalists, telemedicine technology is likely to play an ever-increasing role in healthcare. Dr. Hammack believes telemedicine will be used more and more as care providers and administrators find the right balance between technology and touch.
“It can be difficult to figure out how telemedicine can fit into the way hospitals do things. But it can fit in and does so very well. Technologies like these have the promise to provide support and result in better quality of care for patients,” he says.
Donya Hengehold is freelance medical journalist.
References
- Angus DC, Kelley MA, Schmitz RJ, et al. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease. JAMA. 2000 Dec 6;284(21):2762-2770. Comment in JAMA. 2001 Feb 28;285(8):1016-1017; author reply 1018. JAMA. 2001 Feb 28;285(8):1017-1018.
- Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: an alternative paradigm for intensivist staffing. Crit Care Med. 2004 Jan;32(1):31-38. Erratum in: Crit Care Med. 2004 Jul;32(7):1632.Comment in: Crit Care Med. 2004 Jan;32(1):287-288. Crit Care Med. 2004 Jan;32(1):288-290.
- Vespa PM, Miller C, Hu X, et al. Intensive care unit robotic telepresence facilitates rapid physician response to unstable patients and decreased cost in neurointensive care. Surg Neurol. 2007 April;67(4):331-337.
The patient was in the ICU at Saint Clare’s Hospital in Wausau, Wis. An intensivist from St. Louis who had been caring for her remotely through telemedicine technology was helping clinicians manage the end-of-life issue for her and her family.
Subjects like this can be difficult for hospitalists, who may not have as much experience with the protocols involved in end-of-life care. But at Saint Clare’s, which offers remote care and monitoring by intensivists and critical-care nurses through an eICU program, critical-care specialists are there to provide continuous care to the hospital’s sickest patients, as well as support for the onsite clinicians in any number of situations involving ICU patient care.
Dellice Dickhaus, MD, medical director for Advanced ICU Care and a practicing intensivist, helps provide remote care around the clock for patients in Saint Clare’s ICU. Advanced ICU Care’s board-certified intensivists and critical-care nurses remotely care for and monitor patients in multiple sites from their operations center, more than 400 miles away in St. Louis. They use telemedicine technology developed by Baltimore, Md., firm VISICU that combines clinical management software with real-time video feeds and patient data, such as labs, vital signs and medications.
In the case of the critically ill patient, while the hospitalist was driving the patient’s care program and taking care of many of the daily issues, Dr. Dickhaus helped manage the end-of-life issue. She was available at the push of a button to talk with relatives and provide information they needed to make decisions about their family member’s care. She discussed the patient’s prognosis and options with the family, and kept the hospitalist on staff apprised of the conversations.
Because Dr. Dickhaus and other clinicians at Advanced ICU Care had been helping manage the patient’s care in the ICU, the patient’s family gained confidence in the remote intensivists, says Dr. Dickhaus.
Demands of an Aging Population
The aging of America will have a tremendous effect on healthcare, particularly regarding care of the critically ill and in managing such areas as pulmonary disease. Consider that more than half of all ICU stays are incurred by patients older than 65. Further, patients older than 65 account for more than two-thirds of all inpatient pulmonary days.
What does this mean for hospitalists? For one, the aging population will create a demand for care that is projected to outpace the supply of intensivists and pulmonologists.1 With fewer of these specialists, hospitalists may be compelled to take on more responsibilities with critically ill patients, leaving less time for other patients. The expectation of healthcare services provided will likely change, possibly growing in scope and complexity. The time it will take to deliver care is also expected to rise. All these are reasons for the growth in telemedicine technologies, with many designed to improve patient care by delivering limited resources where they are needed most.
Continuity of Care
Richard Bailey, MD, medical director of Inpatient Care and Hospitalist Services at Saint Clare’s, says having remote intensivists lets his staff focus on hospital patients outside the ICU.
“One critical patient can tie you up for hours,” Dr. Bailey says. “Advanced ICU Care’s intensivists are hands-on physicians, helping us round on ICU patients, take patient notes, and handle first-line phone calls.”
There is no difference, he says, between having intensivists in St. Louis, for example, versus on-site. “They are more than a microphone and a camera in the ceiling; they are members of our staff,” he says. “We trust them to take care of our patients.”
He explains that remote intensivists are often good at being the “bug in the ear” for hospitalists, helping with treatment recommendations and asking, “Did you remember to … ?” While stabilizing a just-transferred ICU patient in a near-code situation, Dr. Bailey needed immediate access to the patient’s labs. An intensivist in St. Louis was able to look at the labs and recommend treatment.
Preliminary numbers at Saint Clare’s hint at a reduction of one day in ICU length of stay and two days for total hospitalization, notes Dr. Bailey. Figures like these can mean real savings in hospital costs.
Working together, hospitalists and remote intensivists can provide continuity of care as the patient is admitted through the emergency department and brought into the ICU, explains Dr. Bailey.
William D. Atchley Jr., MD, medical director for the Division of Hospital Medicine for Sentara Medical Group in Norfolk, Va., agrees with Dr. Bailey’s view. Dr. Atchley’s group also uses telemedicine technology for the remote care and monitoring of ICU patients. He is also a member of SHM’s Board of Directors.
“This is a true team effort, creating a seamless continuity from the emergency department to the ICU,” says Dr. Atchley. He cites septic shock patients as an example. He is able to start the septic shock protocols with the patient in the ED, and the intensivist will carry the protocols forward with the patient in the ICU. By morning, Dr. Atchley says he knows the patient has received the care needed, which frees him to care for other patients.
Sentara Healthcare, based in Norfolk, Va., was the first hospital system in the nation to implement VISICU’s technology, which allows hospitals to create a systemwide critical-care program. Using the VISICU eICU, the hospital or healthcare system provides the intensivists to staff the program, helping to leverage scarce clinical resources among the system’s ICUs.
Studies have shown that care by intensivists via telemedicine technology improves patient care and safety in the ICU. In a 2004 study, Sentara documented a 27% decrease in overall ICU and hospital mortality.2
Mobile Telemedicine
Advances in telemedicine technology have come a long way. Take remote robotic systems, for instance, which allow physicians to consult with patients, family members, and on-site caregivers while seated in their office, in another wing of the hospital, or at home.
InTouch Health, a Santa Barbara, Calif., company, uses about 100 robotic systems. While seated at a control station, equipped with video capabilities, a microphone, and a joystick, the physician can “drive” the robot into a patient’s room for consultation. The patient can see the doctor’s face on the monitor and—on the other end—the physician has access to patient data and can see the patient through a live video image.
The robotic system provides added ability for intensivists and other specialists to do another evening round on their patients, explains Tim Wright, vice president of strategic marketing for InTouch. A recent study shows that when physicians use robotic telepresence to make rounds in the ICU in response to nursing pages, physician response is significantly faster. Additionally, the study found a reduced length of stay, particularly for patients with subarachnoid hemorrhage and brain trauma, as well as an ICU cost savings of $1.1 million.3
The idea of robotic telepresence is similar to the telemedicine model of care being used in the ICU. Through the robotic system, an intensivist can log in and perform an evening round, updating hospitalists on new patients and issues that may have arisen.
“The beauty is that the intensivist and the hospitalist can be looking at everything together,” Wright says. “The intensivist can provide the specialist knowledge and training, while the hospitalist provides the ongoing care.”
Not Just the ICU
Of course, telemedicine is not limited to the ICU. It is being used for virtually every medical specialty to help provide greater access to care.
Take the University of Texas Medical Branch at Galveston (UTMB), which has used telemedicine technologies since 1994. Its Electronic Health Network (EHN) utilizes telemedicine to help care for the state’s indigent and rural populations, as well as other groups, such as the elderly, prisoners, and even researchers in Antarctica.
One of the fastest-growing services UTMB operates is the telemedicine-based corporate healthcare programs, allowing employees to “see” a primary care physician without leaving work. Companies see this as a way to help control healthcare costs and make preventive care more accessible, notes Glenn Hammack, OD, assistant vice president and executive director of the UTMB Electronic Health Network. He also pegs the application of telemedicine to psychiatry as another growing service and one that illustrates how the technology is being used to help address a shortage of providers, especially in rural and underserved parts of Texas. Like the eICU programs designed to bring scarce intensivist care to ICU patients, UTMB’s services help distribute rare resources, such as child and adolescent psychiatrists who speak Spanish, to patients.
The telemedicine program at UMTB began in 1994 as a way to help provide cost-effective healthcare for inmates in the Texas prison system. Today, the Correctional Managed Care (CMC) department has telemedicine stations in 120 correctional units throughout Texas and accounts for about half of UTMB’s telemedicine program.
The 11 telemedicine studios at UTMB used for patients across the EHN are equipped with live interactive video links that allow the telemedicine physician to see and hear the patient, located at the remote station with a registered health professional on-site. Digital stethoscopes, hand-held cameras, and other electronic medical devices help the physician treat patients. The telemedicine program also utilizes shared electronic medical records, which are critical to its success, says Dr. Hammack.
Telemedicine can also be used between departments within the hospital. Dr. Hammack notes that hospitals have become large and complicated; the journey from one end to another for a test or procedure can be difficult on patients. “Telemedicine offers the ability for face-to-face interaction, and when used within hospital departments, it can bring some humanity of scale back to the increasingly complicated hospital environment,” he says.
Another Vision
Troy Sybert, MD, medical director for CMC Hospital Medicine and a practicing hospitalist at Texas Department of Criminal Justice (TDCJ) Hospital in Galveston, Texas, was hired a year ago to help create a hospitalist program within the prison system. His is the only health facility dedicated to prisoners and located on a medical school campus.
While his six-member team is not engaged in telemedicine, he sees a number of possibilities for CMC hospitalists to utilize telemedicine technology. For one, hospitalists could use their expertise in admissions to help triage patients via telemedicine. The CMC recently created a network of regional hubs similar to ED observation centers but without a 24/7 physician presence. Telemedicine triage could help the system offload the decision to admit and would likely reduce the number of hospital admissions, says Dr. Sybert.
Telemedicine technology could also provide other possibilities in perioperative care for surgery patients at TDCJ Hospital. In partnership with the surgery and anesthesia departments, pre- and post-operative work up and care could be done remotely with the patient back in the unit, promoting shorter lengths of stay and reducing transportation needs. The hospitalists, trained in correctional care, would provide support and coordinate with surgery—especially on the patient’s transition to and from the prison facility.
“The whole concept of telemedicine is to utilize experience from a centralized location,” says Dr. Sybert. “We have a vision for where we might like to go with telemedicine, bringing our hospitalist group’s experience with managed correctional care to prison units throughout the state.”
Whether it is bringing intensivist care to a critically ill patient, providing therapy sessions to patients in rural areas, or delivering the expertise of hospitalists, telemedicine technology is likely to play an ever-increasing role in healthcare. Dr. Hammack believes telemedicine will be used more and more as care providers and administrators find the right balance between technology and touch.
“It can be difficult to figure out how telemedicine can fit into the way hospitals do things. But it can fit in and does so very well. Technologies like these have the promise to provide support and result in better quality of care for patients,” he says.
Donya Hengehold is freelance medical journalist.
References
- Angus DC, Kelley MA, Schmitz RJ, et al. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease. JAMA. 2000 Dec 6;284(21):2762-2770. Comment in JAMA. 2001 Feb 28;285(8):1016-1017; author reply 1018. JAMA. 2001 Feb 28;285(8):1017-1018.
- Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: an alternative paradigm for intensivist staffing. Crit Care Med. 2004 Jan;32(1):31-38. Erratum in: Crit Care Med. 2004 Jul;32(7):1632.Comment in: Crit Care Med. 2004 Jan;32(1):287-288. Crit Care Med. 2004 Jan;32(1):288-290.
- Vespa PM, Miller C, Hu X, et al. Intensive care unit robotic telepresence facilitates rapid physician response to unstable patients and decreased cost in neurointensive care. Surg Neurol. 2007 April;67(4):331-337.
The patient was in the ICU at Saint Clare’s Hospital in Wausau, Wis. An intensivist from St. Louis who had been caring for her remotely through telemedicine technology was helping clinicians manage the end-of-life issue for her and her family.
Subjects like this can be difficult for hospitalists, who may not have as much experience with the protocols involved in end-of-life care. But at Saint Clare’s, which offers remote care and monitoring by intensivists and critical-care nurses through an eICU program, critical-care specialists are there to provide continuous care to the hospital’s sickest patients, as well as support for the onsite clinicians in any number of situations involving ICU patient care.
Dellice Dickhaus, MD, medical director for Advanced ICU Care and a practicing intensivist, helps provide remote care around the clock for patients in Saint Clare’s ICU. Advanced ICU Care’s board-certified intensivists and critical-care nurses remotely care for and monitor patients in multiple sites from their operations center, more than 400 miles away in St. Louis. They use telemedicine technology developed by Baltimore, Md., firm VISICU that combines clinical management software with real-time video feeds and patient data, such as labs, vital signs and medications.
In the case of the critically ill patient, while the hospitalist was driving the patient’s care program and taking care of many of the daily issues, Dr. Dickhaus helped manage the end-of-life issue. She was available at the push of a button to talk with relatives and provide information they needed to make decisions about their family member’s care. She discussed the patient’s prognosis and options with the family, and kept the hospitalist on staff apprised of the conversations.
Because Dr. Dickhaus and other clinicians at Advanced ICU Care had been helping manage the patient’s care in the ICU, the patient’s family gained confidence in the remote intensivists, says Dr. Dickhaus.
Demands of an Aging Population
The aging of America will have a tremendous effect on healthcare, particularly regarding care of the critically ill and in managing such areas as pulmonary disease. Consider that more than half of all ICU stays are incurred by patients older than 65. Further, patients older than 65 account for more than two-thirds of all inpatient pulmonary days.
What does this mean for hospitalists? For one, the aging population will create a demand for care that is projected to outpace the supply of intensivists and pulmonologists.1 With fewer of these specialists, hospitalists may be compelled to take on more responsibilities with critically ill patients, leaving less time for other patients. The expectation of healthcare services provided will likely change, possibly growing in scope and complexity. The time it will take to deliver care is also expected to rise. All these are reasons for the growth in telemedicine technologies, with many designed to improve patient care by delivering limited resources where they are needed most.
Continuity of Care
Richard Bailey, MD, medical director of Inpatient Care and Hospitalist Services at Saint Clare’s, says having remote intensivists lets his staff focus on hospital patients outside the ICU.
“One critical patient can tie you up for hours,” Dr. Bailey says. “Advanced ICU Care’s intensivists are hands-on physicians, helping us round on ICU patients, take patient notes, and handle first-line phone calls.”
There is no difference, he says, between having intensivists in St. Louis, for example, versus on-site. “They are more than a microphone and a camera in the ceiling; they are members of our staff,” he says. “We trust them to take care of our patients.”
He explains that remote intensivists are often good at being the “bug in the ear” for hospitalists, helping with treatment recommendations and asking, “Did you remember to … ?” While stabilizing a just-transferred ICU patient in a near-code situation, Dr. Bailey needed immediate access to the patient’s labs. An intensivist in St. Louis was able to look at the labs and recommend treatment.
Preliminary numbers at Saint Clare’s hint at a reduction of one day in ICU length of stay and two days for total hospitalization, notes Dr. Bailey. Figures like these can mean real savings in hospital costs.
Working together, hospitalists and remote intensivists can provide continuity of care as the patient is admitted through the emergency department and brought into the ICU, explains Dr. Bailey.
William D. Atchley Jr., MD, medical director for the Division of Hospital Medicine for Sentara Medical Group in Norfolk, Va., agrees with Dr. Bailey’s view. Dr. Atchley’s group also uses telemedicine technology for the remote care and monitoring of ICU patients. He is also a member of SHM’s Board of Directors.
“This is a true team effort, creating a seamless continuity from the emergency department to the ICU,” says Dr. Atchley. He cites septic shock patients as an example. He is able to start the septic shock protocols with the patient in the ED, and the intensivist will carry the protocols forward with the patient in the ICU. By morning, Dr. Atchley says he knows the patient has received the care needed, which frees him to care for other patients.
Sentara Healthcare, based in Norfolk, Va., was the first hospital system in the nation to implement VISICU’s technology, which allows hospitals to create a systemwide critical-care program. Using the VISICU eICU, the hospital or healthcare system provides the intensivists to staff the program, helping to leverage scarce clinical resources among the system’s ICUs.
Studies have shown that care by intensivists via telemedicine technology improves patient care and safety in the ICU. In a 2004 study, Sentara documented a 27% decrease in overall ICU and hospital mortality.2
Mobile Telemedicine
Advances in telemedicine technology have come a long way. Take remote robotic systems, for instance, which allow physicians to consult with patients, family members, and on-site caregivers while seated in their office, in another wing of the hospital, or at home.
InTouch Health, a Santa Barbara, Calif., company, uses about 100 robotic systems. While seated at a control station, equipped with video capabilities, a microphone, and a joystick, the physician can “drive” the robot into a patient’s room for consultation. The patient can see the doctor’s face on the monitor and—on the other end—the physician has access to patient data and can see the patient through a live video image.
The robotic system provides added ability for intensivists and other specialists to do another evening round on their patients, explains Tim Wright, vice president of strategic marketing for InTouch. A recent study shows that when physicians use robotic telepresence to make rounds in the ICU in response to nursing pages, physician response is significantly faster. Additionally, the study found a reduced length of stay, particularly for patients with subarachnoid hemorrhage and brain trauma, as well as an ICU cost savings of $1.1 million.3
The idea of robotic telepresence is similar to the telemedicine model of care being used in the ICU. Through the robotic system, an intensivist can log in and perform an evening round, updating hospitalists on new patients and issues that may have arisen.
“The beauty is that the intensivist and the hospitalist can be looking at everything together,” Wright says. “The intensivist can provide the specialist knowledge and training, while the hospitalist provides the ongoing care.”
Not Just the ICU
Of course, telemedicine is not limited to the ICU. It is being used for virtually every medical specialty to help provide greater access to care.
Take the University of Texas Medical Branch at Galveston (UTMB), which has used telemedicine technologies since 1994. Its Electronic Health Network (EHN) utilizes telemedicine to help care for the state’s indigent and rural populations, as well as other groups, such as the elderly, prisoners, and even researchers in Antarctica.
One of the fastest-growing services UTMB operates is the telemedicine-based corporate healthcare programs, allowing employees to “see” a primary care physician without leaving work. Companies see this as a way to help control healthcare costs and make preventive care more accessible, notes Glenn Hammack, OD, assistant vice president and executive director of the UTMB Electronic Health Network. He also pegs the application of telemedicine to psychiatry as another growing service and one that illustrates how the technology is being used to help address a shortage of providers, especially in rural and underserved parts of Texas. Like the eICU programs designed to bring scarce intensivist care to ICU patients, UTMB’s services help distribute rare resources, such as child and adolescent psychiatrists who speak Spanish, to patients.
The telemedicine program at UMTB began in 1994 as a way to help provide cost-effective healthcare for inmates in the Texas prison system. Today, the Correctional Managed Care (CMC) department has telemedicine stations in 120 correctional units throughout Texas and accounts for about half of UTMB’s telemedicine program.
The 11 telemedicine studios at UTMB used for patients across the EHN are equipped with live interactive video links that allow the telemedicine physician to see and hear the patient, located at the remote station with a registered health professional on-site. Digital stethoscopes, hand-held cameras, and other electronic medical devices help the physician treat patients. The telemedicine program also utilizes shared electronic medical records, which are critical to its success, says Dr. Hammack.
Telemedicine can also be used between departments within the hospital. Dr. Hammack notes that hospitals have become large and complicated; the journey from one end to another for a test or procedure can be difficult on patients. “Telemedicine offers the ability for face-to-face interaction, and when used within hospital departments, it can bring some humanity of scale back to the increasingly complicated hospital environment,” he says.
Another Vision
Troy Sybert, MD, medical director for CMC Hospital Medicine and a practicing hospitalist at Texas Department of Criminal Justice (TDCJ) Hospital in Galveston, Texas, was hired a year ago to help create a hospitalist program within the prison system. His is the only health facility dedicated to prisoners and located on a medical school campus.
While his six-member team is not engaged in telemedicine, he sees a number of possibilities for CMC hospitalists to utilize telemedicine technology. For one, hospitalists could use their expertise in admissions to help triage patients via telemedicine. The CMC recently created a network of regional hubs similar to ED observation centers but without a 24/7 physician presence. Telemedicine triage could help the system offload the decision to admit and would likely reduce the number of hospital admissions, says Dr. Sybert.
Telemedicine technology could also provide other possibilities in perioperative care for surgery patients at TDCJ Hospital. In partnership with the surgery and anesthesia departments, pre- and post-operative work up and care could be done remotely with the patient back in the unit, promoting shorter lengths of stay and reducing transportation needs. The hospitalists, trained in correctional care, would provide support and coordinate with surgery—especially on the patient’s transition to and from the prison facility.
“The whole concept of telemedicine is to utilize experience from a centralized location,” says Dr. Sybert. “We have a vision for where we might like to go with telemedicine, bringing our hospitalist group’s experience with managed correctional care to prison units throughout the state.”
Whether it is bringing intensivist care to a critically ill patient, providing therapy sessions to patients in rural areas, or delivering the expertise of hospitalists, telemedicine technology is likely to play an ever-increasing role in healthcare. Dr. Hammack believes telemedicine will be used more and more as care providers and administrators find the right balance between technology and touch.
“It can be difficult to figure out how telemedicine can fit into the way hospitals do things. But it can fit in and does so very well. Technologies like these have the promise to provide support and result in better quality of care for patients,” he says.
Donya Hengehold is freelance medical journalist.
References
- Angus DC, Kelley MA, Schmitz RJ, et al. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease. JAMA. 2000 Dec 6;284(21):2762-2770. Comment in JAMA. 2001 Feb 28;285(8):1016-1017; author reply 1018. JAMA. 2001 Feb 28;285(8):1017-1018.
- Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: an alternative paradigm for intensivist staffing. Crit Care Med. 2004 Jan;32(1):31-38. Erratum in: Crit Care Med. 2004 Jul;32(7):1632.Comment in: Crit Care Med. 2004 Jan;32(1):287-288. Crit Care Med. 2004 Jan;32(1):288-290.
- Vespa PM, Miller C, Hu X, et al. Intensive care unit robotic telepresence facilitates rapid physician response to unstable patients and decreased cost in neurointensive care. Surg Neurol. 2007 April;67(4):331-337.