User login
The Constant and Familiar Face
Editors’ note: “Alliances” is a series written about the relationships that hospitalists have with members of the clinical care team, from the team members’ points of view. It’s our hope that each installment of “Alliances” will provide valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
Nancy Perovic, RN, BSN, quality improvement and innovations coordinator with the hospitalist program at the University of Chicago Medical Center, says this quote from In Our Hands: How Hospital Leaders Can Build a Thriving Workforce is a statement she refers to often in her work and teaching: “Mutual respect between nurses and physicians for each other’s knowledge and competence, coupled with a mutual concern that quality patient care will be provided, are key organizational elements of work environments that attract and retain nurses.”1
In hospitals around the United States, in efforts to improve patient safety and in other initiatives including nurse recruitment and retention, one consistent element is optimizing communication among providers.2-4 Barbara Blakeney, MS, RN, president of the American Nurses Association, interviewed for the publication Web Morbidity and Mortality by its editor, hospitalist Robert Wachter, MD, says that when nurses are not properly supported in the work environment by other staff, and when there are not enough nurses, “it becomes a catch-22—the fewer nurses you have, the more difficult is the working environment, which leads to fewer nurses.”5
Blakeney recommends mutual training for physicians and nurses to improve patient care and safety focus on a number of key areas:
- Understanding and appreciating each other’s skill sets and knowledge base;
- Properly handing off patients and information; and
- Nurturing “a culture in which safety is considered a problem-solving situation and not a punishment situation.”6
“Nurses comprise the surveillance system in hospitals for errors and adverse occurrences,” emphasizes Blakeney, and “the effectiveness of nurse surveillance is influenced by factors that include the quality of the work environment.”5
As essential members of hospital teams, hospitalists play a big role in nurses’ work environments, and mutual support between hospitalists and nurses affects patient care and outcomes, and physician and nurse job satisfaction.6,7 In general, nurses give hospitalists high marks for communication, nurse support, and teamwork.
“From a communication perspective, working with hospitalists makes patient care a lot safer because you don’t have to think of everything that you need to tell attending physicians when they are making their daily rounds,” says Scarlett Blue, RNC, MSN, administrative director, Hospitalist Services for FirstHealth of the Carolinas, Pinehurst, N.C. “With hospitalists you know you can do real-time communication, real-time information. That’s not saying you can’t do that with other physicians who are not in the hospital, but it certainly does make it a lot easier when they’re right here.”
Make Contact
One way that hospitalists support their nurse colleagues is by their ready availability to answer questions about patient care. Julie Koppel, RN, BSN, patient care manager on the General Medicine floor at the University of California at San Francisco Medical Center, has worked exclusively with the hospitalist model in her five years of nursing. She is complimentary about hospitalists’ communication skills and refers to them as “the constant and familiar face.” Koppel relates an instance where the attending hospitalist was already off service and yet she still paged him. “He got back to me promptly and still addressed the issues even though he wasn’t on service anymore and it was about something that had happened a month ago. I still feel hospitalists are available when they’re not even here.”
Many nurses don’t have a second thought about calling a hospitalist about a patient care issue, but may still be afraid of “bothering” the hospitalist when he or she is busy. Blue says her colleagues have worked with their nursing staff to overcome that reluctance. “Call them because if they’re talking with a family or if they’re in the middle of a physical exam or if it’s something where they can’t talk, they’re going to put the hold button on,” she tells her staff. “So when you hear the Muzak, the elevator music, then you know that you need to call them back. And it’s worked.”
It’s especially important, Blue says, that nurses surmount any reluctance they feel to initiate a call so that they will do so easily in urgent situations such as alerting rapid response teams and reporting medical errors.4 Blue believes the following anecdote illustrates the perspective of most hospitalists about this issue.
“We just started rapid response teams here,” she says, “And I heard one of the hospitalists say, ‘We’ve had five rapid response team calls so far and we were looking at whether or not the calls met the criteria and were appropriate.’ And one of the other hospitalists said, ‘You know, this really wasn’t a rapid response team call, but I want the nurses to feel free to call and I think that when we’re first starting out, we just want them to call. And then we can work on fine tuning it later. I don’t want to stifle them so they feel they cannot call.”
—Mark Williams, MD
Clear and to the Point
What are the best means to improve communication between hospitalists and nurses? Three major areas for attention include developing relationships, defining communication strategies, and packaging information for clarity.7
Blue often advises nurses to speak with clarity. “Probably the best thing from a hospitalist’s perspective is to be real clear about what you are asking or what it is that you need,” she says. “The clearer that you can be in your requests, the better off you’re going to be in the long run.”
But, Blue says “hospitalists have to understand that one of the greatest benefits from a nurse’s perspective about the hospitalist program is access, immediate access, and dealing with a nurse who does not communicate well might sometimes come along with it.”
The mismatched communication styles of most physicians and nurses are well recognized by a committee at the University of Chicago in which Nancy Perovic is involved. Vineet Arora, MD, MA, a hospitalist and associate program director for the Internal Medicine Residency Program at the University of Chicago, is one of the three hospitalist members on a committee working to improve nurse-physician communication.
“We know that nurses and physicians communicate differently,” says Dr. Arora. “Physicians communicate in more of a task-oriented way and nurses are trained to communicate in a descriptive way. And that’s part of the problem, because nurses might report that physicians don’t respond to them when they need to be responded to; they might not prioritize a patient that the nurse believes is very sick. And a physician might say, ‘I didn’t know that patient was really sick’ because he was given a description such as, ‘They’re not doing OK.’”
Also, Dr. Arora says, “part of the problem that nurses and physicians may have in communicating with each other can be traced to a difference in how they were trained. Physicians are trained to interact with other physicians and nurses are trained by other nurses.”
The committee at Chicago has adopted what is referred to as the Situation-Background-Assessment-Recommendation (SBAR) technique, a tool that the U.S. Navy has used to improve communication on aircraft carriers.8 Developed by Michael Leonard, MD, physician coordinator of clinical informatics, and others at Kaiser Permanente of Colorado, the SBAR technique has been implemented widely at health systems to provide a standard framework for members of the healthcare team when communicating about a patient’s condition.
“What nurses are not very good at is being assertive,” says Perovic. “We’re getting better as we’re getting more modern, but sometimes nurses talk in a more holistic, narrative fashion and doctors just want: what’s the problem, pinpoint it, let me know what it is.”
Chicago’s Perovic and her colleagues plan to educate nurses to use the SBAR technique so they can “talk in the way that doctors are trained to accept information and respond,” she says. “For example, this might sound like, ‘This is this patient with this diagnosis and these vital signs; this is what’s happening: they’re going down, their blood pressure’s dropped, I’m really concerned, this is a different change, I suggest that we do this and that, and I need you here in 10 minutes.’”
Perovic says nurses are then instructed to “make a recommendation; so the hospitalist can prioritize from all the other patients he has to see, to answer the questions: What does this patient need right now? When do I need to see this patient? and What can the nurse do until I get there?”
Literature on the SBAR technique and the tool itself are available online at www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.htm.8
Heedful Versus Heedless Interrelating
Exactly how hospitalists affect outcomes and influence system issues is being addressed in research led by Mark V. Williams, MD, and Tracy Scott, PhD, at Emory University Medical Center, Atlanta. Dr. Williams, who is the director of the medicine unit at Emory Hospital, the editor-in-chief of the Journal of Hospital Medicine, and a past president of SHM, spoke to The Hospitalist about the exploratory research his team is doing to assess the impact hospitalists have in nurse-physician relationships in two hospitals in Atlanta, and to particularly examine how these relationships affect patient safety.
High Reliability Organization theory, which elucidates causal pathways between work relationships and reduced error, may provide a framework for how hospitalists affect hospital functioning. “Heedful interrelating,” the theory postulates, creates an organization “mind” and through facilitating teamwork is more alert to and capable of dealing with unexpected occurrences. In fact, says Dr. Williams, data from operating rooms, emergency departments, and ICUs suggest that a lack of teamwork adversely affects patient care and increases medical errors. Research along this vein has been absent on general medical floors.
The research design explores the degree of “heedful interrelating” as opposed to “heedless interrelating” between physicians and nurses and whether hospitalists have different relationships with nurses than do other physicians.
“In heedful interrelating,” explains Dr. Williams, “the physician heeds what the nurse is saying and doing and, likewise, the nurse heeds what the physician is saying and doing.” To date, the investigators have interviewed 45 nurses (half in a university hospital setting and half in a community hospital) and 24 physicians of whom half are hospitalists.
The study examines multiple components, but an example is that “heedful interrelating is based on true mutual respect, which is almost more important over agreement,” says Dr. Williams. “And in heedless interrelating, only one view of the situation is considered correct. It represents your classic arrogant physician.”
Another example of heedful interrelating is that “it advances the goals of the whole team; in heedless interrelating, you think only of your own role,” he says. Nurses in the study reported that compared with other physicians hospitalists are more accessible, more approachable, and more appreciative of the value of the nurse’s role.
The investigators conclude that hospitalists improve the nurse-physician relationship through heedful interrelating and thereby may improve patient safety. In addition, “the nurses emphasized the need for more collaboration and perceived that physicians were not proactive in asking them about their knowledge of the patient, and lacked a holistic view of the patient’s needs. Most importantly, about half the nurses mentioned specific instances where problems in their communication with physicians led directly to problems in patient care.
Dr. Williams believes that the ideal system for communication between hospitalists and nurses would include a means for them to do their patient rounds together. Nurses want hospitalists to develop a system to deliver the patient care plans quickly and reliably, include them in formal and informal educational efforts, and acknowledge them.
Timely Distribution of Care Plans
Blue says that hospitalists at her institution, FirstHealth Moore Regional Hospital (Pinehurst, N.C.), a 385-bed acute care, nonprofit hospital that serves as the referral center for a 15-county region in the mid-Carolinas, work often and closely with the nurses on issues of outcomes. “And outcomes here are like discharge planning utilization review,” she says. “We have a report every morning and there’s a representative from that department who’s online sending out the plans for the patients for the day to the other outcomes managers. That’s already in the works, and we’re not waiting for the hospitalist to get up to the floor to see the patient.”
Overall, however, nurses in other (e.g., larger) settings may not have as good a system in place to distribute care plans. Perovic says that in focus groups she facilitates, she often hears frustration from nurses because “doctors in general—although hospitalists are better at it—do not give nurses the plan of the day or the plan of care in a timely, organized fashion so they can do their care appropriately and prepare themselves and the patient.”
Some of the problem is due to the systems of an academic medical center, Perovic says, where “doctors make rounds at various times of the day and sometimes one team can make four rounds a day. What happens is that the plan for patient care changes each time new rounds are completed because you either get new information or discover you didn’t do something.” But although the team doctors are good at communicating plan modifications among themselves, she says, “what they fail to do is always communicate that well to the nurses.”
Perovic says there is an ideal and then a real solution. “Ideally, it would be great if patient rounds were at a certain time of the day every day so that the nurse can pass her meds and then be available for rounding,” she says. “You could say to nurses, ‘Rounds are between 10 and 11; take care of your patients’ needs and then be on call and ready to go to your rounds when possible.’ Or another solution is what we do in the pediatric hospital: We have a charge nurse who has no patients and she is able to round with all the teams and all the doctors and then give the individual nurse that plan for her patients.”
Hiring a charge nurse in this vein is a human resource issue, Perovic says, and an individual hospital has to decide that it wants to pay a nurse to not have patients. In that case, she says, it is an expensive but good fix. However, accommodating nurses to accompany hospitalists on rounds is logistically almost impossible. “Because if a nurse on the general medicine ward has five patients,” Perovic says, “she might have five different teams of doctors. But depending on the diagnosis of each patient, it won’t be the same team of doctors rounding on them. She might not catch A, B, and C at the same time that D and E are making their rounds. And she could be doing a blood draw on patient D when D team comes, or giving a bath to patient A when team E comes.”
Perovic and her coworkers have tried the call light method, where the doctor comes into the room, the attending presses the call light, and the nurse knows rounds are happening and to join them at that room. But that, as well as other avenues they tried, failed because neither the nurse nor the team can necessarily count on their times of availability coinciding. Still, Dr. Arora says, “we learned a lot about trying to work together and how to understand each other. And we used some of that information to continue thinking about how to best improve physician-nurse communication.”
The team at Chicago is now considering how to design and evaluate “an intervention for more of an interdisciplinary educational process where physicians and nurses would be trained on how to communicate with each other using this standard language,” says Dr. Arora. “Nurses would understand that they could potentially use the SBAR tool to communicate with physicians, and physicians would understand that the nurses need to be included in the plan for the day and would make time to incorporate nurse suggestions and input for the plan.”
Acknowledgment
In some hospital settings what has been described as a two-class system can exist for providers.9 A culture that encourages patient safety is threatened by the nature of the hierarchy or the segregation that is established, even subtly, where nurses are treated as unequals.6,9 In the hospital culture, the “invisibility of nursing” has historically been perpetuated by a number of factors, not the least of which are differences in gender and income.6 In this atmosphere, nurses are not as likely to share from their skills and knowledge. Their lack of assertiveness with hospitalists or other physicians may take its toll in many ways, including increased risks to patient outcomes and to provider morale and satisfaction.7
Linda Aiken, PhD, FAAN, FRCN, RN, the Claire M. Fagin Leadership Professor of Nursing and director of the Center for Health Outcomes and Policy Research at the University of Pennsylvania (Philadelphia), has extensively investigated the dynamics between nurses and their co-workers. “Nurse-physician relationships are one of the most important drivers of the work environment,”9 she writes. There are also data that demonstrate the association of nurse-doctor relationships on cost, lower morbidity and mortality, retention of nurses, higher quality of care, and improved hospital reimbursement and/or market share.9
In other words, “healthy nurse-physician relationships are not just a nice thing to have,” writes Dr. Aiken. “They are a competitive advantage.”
Given the association of these relationships to so many outcomes, it is unfortunate that many nurses crave greater acknowledgment for what they bring to their work. One benefit for nursing is that because hospitalists are around the hospital more than an average attending, they know the nurses better.
“As a nurse, what I need from hospitalists is for them to recognize and teach their residents and interns that the nurse is a constant player at the bedside in the hospital, with many more years of experience,” says Perovic. “Even though she doesn’t have as much medical training as a doctor or resident, she has enough clinical-nursing hospital experience. Doctors need to appreciate that nurses are experts at hospital care and bedside care, and [doctors] need to show that respect when we’re teaching our residents because we can learn a lot from the nurses, and the nurses can actually make the doctors’ lives easier.”
In a study of a multidisciplinary intervention tested on an acute inpatient medical unit, the effect of the intervention—to improve communication and collaboration—was strongest among house staff, who reported significant increases in collaborative efforts with nurses.10 This finding underlines the importance for hospitalists to serve as models to students, interns, and residents because the most effective time to learn collaborative practice is during early training when experienced nurses can assist inexperienced interns.10 Hospitalists can also consciously reject the traditional “doctor-nurse game,” whereby patterns of behavior suggest that doctors are the dominant players and nurses must defer to them.
“Ask nurses for their opinion,” advises Blue. “Treat them like an equal, which is another one of the beauties of this program, because hospitalists certainly do that. When it comes down to it, people want to be appreciated, respected, and acknowledged for their contribution.”
Blue and her team also encourage hospitalists to share with the nurses if they happen to hear news of their patients’ progress. “If we have follow-up on somebody from the primary care provider after that patient has left the hospital, for example, we try to share that with the nursing staff because they’re our patients. They’re not just my patients and they’re not your patients; they’re our patients.”
Conclusion
The quality of the nurse-hospitalist relationship is central to patient care. The methods, means, and styles of individual and team communication all influence the effectiveness of a hospital team. Retraining providers to traverse the gap of different communication styles is a way to approach the issues that exist. Mutual training for physicians and nurses, as well as training nurses to communicate in ways that more approximate how physicians communicate, will better serve patient and provider needs.
Hospitalists can encourage nurses to overcome hesitancies to initiate calls, clarify their preferences for how nurses should contact them, and work with nurses to seek workable ways to perform patient rounds in concert. Most of all, nurses need timely care plan distribution and acknowledgment for their contributions to teamwork and patient care. TH
Writer Andrea Sattinger will write about occupational therapists’ experiences with hospitalists in the January issue.
References
- ANA Commission on Workforce for Hospitals and Health Systems. In our hands: how hospital leaders can build a thriving workforce. American Hospital Association; Chicago; 2002;55:30-31.
- Aiken LH. The unfinished patient safety agenda. In: Wachter R, ed. Morbidity and Mortality Rounds on the Web: Agency for Healthcare Research and Quality; 2005. Accessed August. 29, 2005 at http://webmm.ahrq.gov/perspective.aspx?perspectiveID=7&searchStr=The+unfinished+patient+safety+agenda
- Aiken LH, Clarke SP, Sloane DM. International Hospital Outcomes Research Consortium. Hospital staffing, organization, and quality of care: cross-national findings. Int J Qual Health Care. 2002;14:5-13.
- Friesen MA, Farquhar MB, Hughes R. The nurse’s role in promoting a culture of safety: American Nurses Association Continuing Education, Center for American Nurses; 2005.
- Wachter R. In conversation with … Barbara A. Blakeney, MS, RN. In: Wachter R, ed. Morbidity and Mortality Rounds on the Web. Agency for Healthcare Research and Quality; 2005. Accessed Aug. 29, 2005 at http://webmm.ahrq.gov/perspective.aspx?perspectiveID=8&searchStr=Blakeney
- Lindeke LL, Sieckert AM. Nurse-physician workplace collaboration. Online J Issues Nurs. 2005;10:5.
- Burke M, Boal J, Mitchell R. Communicating for better care: improving nurse-physician communication. Am J Nurs. 2004;104:40-47
- SBAR initiative to improve staff communication. Healthcare Benchmarks Qual Improv. 2005;12:40-41.
- Smith AP. Partners at the bedside: the importance of nurse-physician relationships. Nurs Econ. 2004;22:161-164.
- Vazirani S, Hays RD, Shapiro MF, et al. Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care. 2005;14:71-77.
Editors’ note: “Alliances” is a series written about the relationships that hospitalists have with members of the clinical care team, from the team members’ points of view. It’s our hope that each installment of “Alliances” will provide valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
Nancy Perovic, RN, BSN, quality improvement and innovations coordinator with the hospitalist program at the University of Chicago Medical Center, says this quote from In Our Hands: How Hospital Leaders Can Build a Thriving Workforce is a statement she refers to often in her work and teaching: “Mutual respect between nurses and physicians for each other’s knowledge and competence, coupled with a mutual concern that quality patient care will be provided, are key organizational elements of work environments that attract and retain nurses.”1
In hospitals around the United States, in efforts to improve patient safety and in other initiatives including nurse recruitment and retention, one consistent element is optimizing communication among providers.2-4 Barbara Blakeney, MS, RN, president of the American Nurses Association, interviewed for the publication Web Morbidity and Mortality by its editor, hospitalist Robert Wachter, MD, says that when nurses are not properly supported in the work environment by other staff, and when there are not enough nurses, “it becomes a catch-22—the fewer nurses you have, the more difficult is the working environment, which leads to fewer nurses.”5
Blakeney recommends mutual training for physicians and nurses to improve patient care and safety focus on a number of key areas:
- Understanding and appreciating each other’s skill sets and knowledge base;
- Properly handing off patients and information; and
- Nurturing “a culture in which safety is considered a problem-solving situation and not a punishment situation.”6
“Nurses comprise the surveillance system in hospitals for errors and adverse occurrences,” emphasizes Blakeney, and “the effectiveness of nurse surveillance is influenced by factors that include the quality of the work environment.”5
As essential members of hospital teams, hospitalists play a big role in nurses’ work environments, and mutual support between hospitalists and nurses affects patient care and outcomes, and physician and nurse job satisfaction.6,7 In general, nurses give hospitalists high marks for communication, nurse support, and teamwork.
“From a communication perspective, working with hospitalists makes patient care a lot safer because you don’t have to think of everything that you need to tell attending physicians when they are making their daily rounds,” says Scarlett Blue, RNC, MSN, administrative director, Hospitalist Services for FirstHealth of the Carolinas, Pinehurst, N.C. “With hospitalists you know you can do real-time communication, real-time information. That’s not saying you can’t do that with other physicians who are not in the hospital, but it certainly does make it a lot easier when they’re right here.”
Make Contact
One way that hospitalists support their nurse colleagues is by their ready availability to answer questions about patient care. Julie Koppel, RN, BSN, patient care manager on the General Medicine floor at the University of California at San Francisco Medical Center, has worked exclusively with the hospitalist model in her five years of nursing. She is complimentary about hospitalists’ communication skills and refers to them as “the constant and familiar face.” Koppel relates an instance where the attending hospitalist was already off service and yet she still paged him. “He got back to me promptly and still addressed the issues even though he wasn’t on service anymore and it was about something that had happened a month ago. I still feel hospitalists are available when they’re not even here.”
Many nurses don’t have a second thought about calling a hospitalist about a patient care issue, but may still be afraid of “bothering” the hospitalist when he or she is busy. Blue says her colleagues have worked with their nursing staff to overcome that reluctance. “Call them because if they’re talking with a family or if they’re in the middle of a physical exam or if it’s something where they can’t talk, they’re going to put the hold button on,” she tells her staff. “So when you hear the Muzak, the elevator music, then you know that you need to call them back. And it’s worked.”
It’s especially important, Blue says, that nurses surmount any reluctance they feel to initiate a call so that they will do so easily in urgent situations such as alerting rapid response teams and reporting medical errors.4 Blue believes the following anecdote illustrates the perspective of most hospitalists about this issue.
“We just started rapid response teams here,” she says, “And I heard one of the hospitalists say, ‘We’ve had five rapid response team calls so far and we were looking at whether or not the calls met the criteria and were appropriate.’ And one of the other hospitalists said, ‘You know, this really wasn’t a rapid response team call, but I want the nurses to feel free to call and I think that when we’re first starting out, we just want them to call. And then we can work on fine tuning it later. I don’t want to stifle them so they feel they cannot call.”
—Mark Williams, MD
Clear and to the Point
What are the best means to improve communication between hospitalists and nurses? Three major areas for attention include developing relationships, defining communication strategies, and packaging information for clarity.7
Blue often advises nurses to speak with clarity. “Probably the best thing from a hospitalist’s perspective is to be real clear about what you are asking or what it is that you need,” she says. “The clearer that you can be in your requests, the better off you’re going to be in the long run.”
But, Blue says “hospitalists have to understand that one of the greatest benefits from a nurse’s perspective about the hospitalist program is access, immediate access, and dealing with a nurse who does not communicate well might sometimes come along with it.”
The mismatched communication styles of most physicians and nurses are well recognized by a committee at the University of Chicago in which Nancy Perovic is involved. Vineet Arora, MD, MA, a hospitalist and associate program director for the Internal Medicine Residency Program at the University of Chicago, is one of the three hospitalist members on a committee working to improve nurse-physician communication.
“We know that nurses and physicians communicate differently,” says Dr. Arora. “Physicians communicate in more of a task-oriented way and nurses are trained to communicate in a descriptive way. And that’s part of the problem, because nurses might report that physicians don’t respond to them when they need to be responded to; they might not prioritize a patient that the nurse believes is very sick. And a physician might say, ‘I didn’t know that patient was really sick’ because he was given a description such as, ‘They’re not doing OK.’”
Also, Dr. Arora says, “part of the problem that nurses and physicians may have in communicating with each other can be traced to a difference in how they were trained. Physicians are trained to interact with other physicians and nurses are trained by other nurses.”
The committee at Chicago has adopted what is referred to as the Situation-Background-Assessment-Recommendation (SBAR) technique, a tool that the U.S. Navy has used to improve communication on aircraft carriers.8 Developed by Michael Leonard, MD, physician coordinator of clinical informatics, and others at Kaiser Permanente of Colorado, the SBAR technique has been implemented widely at health systems to provide a standard framework for members of the healthcare team when communicating about a patient’s condition.
“What nurses are not very good at is being assertive,” says Perovic. “We’re getting better as we’re getting more modern, but sometimes nurses talk in a more holistic, narrative fashion and doctors just want: what’s the problem, pinpoint it, let me know what it is.”
Chicago’s Perovic and her colleagues plan to educate nurses to use the SBAR technique so they can “talk in the way that doctors are trained to accept information and respond,” she says. “For example, this might sound like, ‘This is this patient with this diagnosis and these vital signs; this is what’s happening: they’re going down, their blood pressure’s dropped, I’m really concerned, this is a different change, I suggest that we do this and that, and I need you here in 10 minutes.’”
Perovic says nurses are then instructed to “make a recommendation; so the hospitalist can prioritize from all the other patients he has to see, to answer the questions: What does this patient need right now? When do I need to see this patient? and What can the nurse do until I get there?”
Literature on the SBAR technique and the tool itself are available online at www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.htm.8
Heedful Versus Heedless Interrelating
Exactly how hospitalists affect outcomes and influence system issues is being addressed in research led by Mark V. Williams, MD, and Tracy Scott, PhD, at Emory University Medical Center, Atlanta. Dr. Williams, who is the director of the medicine unit at Emory Hospital, the editor-in-chief of the Journal of Hospital Medicine, and a past president of SHM, spoke to The Hospitalist about the exploratory research his team is doing to assess the impact hospitalists have in nurse-physician relationships in two hospitals in Atlanta, and to particularly examine how these relationships affect patient safety.
High Reliability Organization theory, which elucidates causal pathways between work relationships and reduced error, may provide a framework for how hospitalists affect hospital functioning. “Heedful interrelating,” the theory postulates, creates an organization “mind” and through facilitating teamwork is more alert to and capable of dealing with unexpected occurrences. In fact, says Dr. Williams, data from operating rooms, emergency departments, and ICUs suggest that a lack of teamwork adversely affects patient care and increases medical errors. Research along this vein has been absent on general medical floors.
The research design explores the degree of “heedful interrelating” as opposed to “heedless interrelating” between physicians and nurses and whether hospitalists have different relationships with nurses than do other physicians.
“In heedful interrelating,” explains Dr. Williams, “the physician heeds what the nurse is saying and doing and, likewise, the nurse heeds what the physician is saying and doing.” To date, the investigators have interviewed 45 nurses (half in a university hospital setting and half in a community hospital) and 24 physicians of whom half are hospitalists.
The study examines multiple components, but an example is that “heedful interrelating is based on true mutual respect, which is almost more important over agreement,” says Dr. Williams. “And in heedless interrelating, only one view of the situation is considered correct. It represents your classic arrogant physician.”
Another example of heedful interrelating is that “it advances the goals of the whole team; in heedless interrelating, you think only of your own role,” he says. Nurses in the study reported that compared with other physicians hospitalists are more accessible, more approachable, and more appreciative of the value of the nurse’s role.
The investigators conclude that hospitalists improve the nurse-physician relationship through heedful interrelating and thereby may improve patient safety. In addition, “the nurses emphasized the need for more collaboration and perceived that physicians were not proactive in asking them about their knowledge of the patient, and lacked a holistic view of the patient’s needs. Most importantly, about half the nurses mentioned specific instances where problems in their communication with physicians led directly to problems in patient care.
Dr. Williams believes that the ideal system for communication between hospitalists and nurses would include a means for them to do their patient rounds together. Nurses want hospitalists to develop a system to deliver the patient care plans quickly and reliably, include them in formal and informal educational efforts, and acknowledge them.
Timely Distribution of Care Plans
Blue says that hospitalists at her institution, FirstHealth Moore Regional Hospital (Pinehurst, N.C.), a 385-bed acute care, nonprofit hospital that serves as the referral center for a 15-county region in the mid-Carolinas, work often and closely with the nurses on issues of outcomes. “And outcomes here are like discharge planning utilization review,” she says. “We have a report every morning and there’s a representative from that department who’s online sending out the plans for the patients for the day to the other outcomes managers. That’s already in the works, and we’re not waiting for the hospitalist to get up to the floor to see the patient.”
Overall, however, nurses in other (e.g., larger) settings may not have as good a system in place to distribute care plans. Perovic says that in focus groups she facilitates, she often hears frustration from nurses because “doctors in general—although hospitalists are better at it—do not give nurses the plan of the day or the plan of care in a timely, organized fashion so they can do their care appropriately and prepare themselves and the patient.”
Some of the problem is due to the systems of an academic medical center, Perovic says, where “doctors make rounds at various times of the day and sometimes one team can make four rounds a day. What happens is that the plan for patient care changes each time new rounds are completed because you either get new information or discover you didn’t do something.” But although the team doctors are good at communicating plan modifications among themselves, she says, “what they fail to do is always communicate that well to the nurses.”
Perovic says there is an ideal and then a real solution. “Ideally, it would be great if patient rounds were at a certain time of the day every day so that the nurse can pass her meds and then be available for rounding,” she says. “You could say to nurses, ‘Rounds are between 10 and 11; take care of your patients’ needs and then be on call and ready to go to your rounds when possible.’ Or another solution is what we do in the pediatric hospital: We have a charge nurse who has no patients and she is able to round with all the teams and all the doctors and then give the individual nurse that plan for her patients.”
Hiring a charge nurse in this vein is a human resource issue, Perovic says, and an individual hospital has to decide that it wants to pay a nurse to not have patients. In that case, she says, it is an expensive but good fix. However, accommodating nurses to accompany hospitalists on rounds is logistically almost impossible. “Because if a nurse on the general medicine ward has five patients,” Perovic says, “she might have five different teams of doctors. But depending on the diagnosis of each patient, it won’t be the same team of doctors rounding on them. She might not catch A, B, and C at the same time that D and E are making their rounds. And she could be doing a blood draw on patient D when D team comes, or giving a bath to patient A when team E comes.”
Perovic and her coworkers have tried the call light method, where the doctor comes into the room, the attending presses the call light, and the nurse knows rounds are happening and to join them at that room. But that, as well as other avenues they tried, failed because neither the nurse nor the team can necessarily count on their times of availability coinciding. Still, Dr. Arora says, “we learned a lot about trying to work together and how to understand each other. And we used some of that information to continue thinking about how to best improve physician-nurse communication.”
The team at Chicago is now considering how to design and evaluate “an intervention for more of an interdisciplinary educational process where physicians and nurses would be trained on how to communicate with each other using this standard language,” says Dr. Arora. “Nurses would understand that they could potentially use the SBAR tool to communicate with physicians, and physicians would understand that the nurses need to be included in the plan for the day and would make time to incorporate nurse suggestions and input for the plan.”
Acknowledgment
In some hospital settings what has been described as a two-class system can exist for providers.9 A culture that encourages patient safety is threatened by the nature of the hierarchy or the segregation that is established, even subtly, where nurses are treated as unequals.6,9 In the hospital culture, the “invisibility of nursing” has historically been perpetuated by a number of factors, not the least of which are differences in gender and income.6 In this atmosphere, nurses are not as likely to share from their skills and knowledge. Their lack of assertiveness with hospitalists or other physicians may take its toll in many ways, including increased risks to patient outcomes and to provider morale and satisfaction.7
Linda Aiken, PhD, FAAN, FRCN, RN, the Claire M. Fagin Leadership Professor of Nursing and director of the Center for Health Outcomes and Policy Research at the University of Pennsylvania (Philadelphia), has extensively investigated the dynamics between nurses and their co-workers. “Nurse-physician relationships are one of the most important drivers of the work environment,”9 she writes. There are also data that demonstrate the association of nurse-doctor relationships on cost, lower morbidity and mortality, retention of nurses, higher quality of care, and improved hospital reimbursement and/or market share.9
In other words, “healthy nurse-physician relationships are not just a nice thing to have,” writes Dr. Aiken. “They are a competitive advantage.”
Given the association of these relationships to so many outcomes, it is unfortunate that many nurses crave greater acknowledgment for what they bring to their work. One benefit for nursing is that because hospitalists are around the hospital more than an average attending, they know the nurses better.
“As a nurse, what I need from hospitalists is for them to recognize and teach their residents and interns that the nurse is a constant player at the bedside in the hospital, with many more years of experience,” says Perovic. “Even though she doesn’t have as much medical training as a doctor or resident, she has enough clinical-nursing hospital experience. Doctors need to appreciate that nurses are experts at hospital care and bedside care, and [doctors] need to show that respect when we’re teaching our residents because we can learn a lot from the nurses, and the nurses can actually make the doctors’ lives easier.”
In a study of a multidisciplinary intervention tested on an acute inpatient medical unit, the effect of the intervention—to improve communication and collaboration—was strongest among house staff, who reported significant increases in collaborative efforts with nurses.10 This finding underlines the importance for hospitalists to serve as models to students, interns, and residents because the most effective time to learn collaborative practice is during early training when experienced nurses can assist inexperienced interns.10 Hospitalists can also consciously reject the traditional “doctor-nurse game,” whereby patterns of behavior suggest that doctors are the dominant players and nurses must defer to them.
“Ask nurses for their opinion,” advises Blue. “Treat them like an equal, which is another one of the beauties of this program, because hospitalists certainly do that. When it comes down to it, people want to be appreciated, respected, and acknowledged for their contribution.”
Blue and her team also encourage hospitalists to share with the nurses if they happen to hear news of their patients’ progress. “If we have follow-up on somebody from the primary care provider after that patient has left the hospital, for example, we try to share that with the nursing staff because they’re our patients. They’re not just my patients and they’re not your patients; they’re our patients.”
Conclusion
The quality of the nurse-hospitalist relationship is central to patient care. The methods, means, and styles of individual and team communication all influence the effectiveness of a hospital team. Retraining providers to traverse the gap of different communication styles is a way to approach the issues that exist. Mutual training for physicians and nurses, as well as training nurses to communicate in ways that more approximate how physicians communicate, will better serve patient and provider needs.
Hospitalists can encourage nurses to overcome hesitancies to initiate calls, clarify their preferences for how nurses should contact them, and work with nurses to seek workable ways to perform patient rounds in concert. Most of all, nurses need timely care plan distribution and acknowledgment for their contributions to teamwork and patient care. TH
Writer Andrea Sattinger will write about occupational therapists’ experiences with hospitalists in the January issue.
References
- ANA Commission on Workforce for Hospitals and Health Systems. In our hands: how hospital leaders can build a thriving workforce. American Hospital Association; Chicago; 2002;55:30-31.
- Aiken LH. The unfinished patient safety agenda. In: Wachter R, ed. Morbidity and Mortality Rounds on the Web: Agency for Healthcare Research and Quality; 2005. Accessed August. 29, 2005 at http://webmm.ahrq.gov/perspective.aspx?perspectiveID=7&searchStr=The+unfinished+patient+safety+agenda
- Aiken LH, Clarke SP, Sloane DM. International Hospital Outcomes Research Consortium. Hospital staffing, organization, and quality of care: cross-national findings. Int J Qual Health Care. 2002;14:5-13.
- Friesen MA, Farquhar MB, Hughes R. The nurse’s role in promoting a culture of safety: American Nurses Association Continuing Education, Center for American Nurses; 2005.
- Wachter R. In conversation with … Barbara A. Blakeney, MS, RN. In: Wachter R, ed. Morbidity and Mortality Rounds on the Web. Agency for Healthcare Research and Quality; 2005. Accessed Aug. 29, 2005 at http://webmm.ahrq.gov/perspective.aspx?perspectiveID=8&searchStr=Blakeney
- Lindeke LL, Sieckert AM. Nurse-physician workplace collaboration. Online J Issues Nurs. 2005;10:5.
- Burke M, Boal J, Mitchell R. Communicating for better care: improving nurse-physician communication. Am J Nurs. 2004;104:40-47
- SBAR initiative to improve staff communication. Healthcare Benchmarks Qual Improv. 2005;12:40-41.
- Smith AP. Partners at the bedside: the importance of nurse-physician relationships. Nurs Econ. 2004;22:161-164.
- Vazirani S, Hays RD, Shapiro MF, et al. Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care. 2005;14:71-77.
Editors’ note: “Alliances” is a series written about the relationships that hospitalists have with members of the clinical care team, from the team members’ points of view. It’s our hope that each installment of “Alliances” will provide valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
Nancy Perovic, RN, BSN, quality improvement and innovations coordinator with the hospitalist program at the University of Chicago Medical Center, says this quote from In Our Hands: How Hospital Leaders Can Build a Thriving Workforce is a statement she refers to often in her work and teaching: “Mutual respect between nurses and physicians for each other’s knowledge and competence, coupled with a mutual concern that quality patient care will be provided, are key organizational elements of work environments that attract and retain nurses.”1
In hospitals around the United States, in efforts to improve patient safety and in other initiatives including nurse recruitment and retention, one consistent element is optimizing communication among providers.2-4 Barbara Blakeney, MS, RN, president of the American Nurses Association, interviewed for the publication Web Morbidity and Mortality by its editor, hospitalist Robert Wachter, MD, says that when nurses are not properly supported in the work environment by other staff, and when there are not enough nurses, “it becomes a catch-22—the fewer nurses you have, the more difficult is the working environment, which leads to fewer nurses.”5
Blakeney recommends mutual training for physicians and nurses to improve patient care and safety focus on a number of key areas:
- Understanding and appreciating each other’s skill sets and knowledge base;
- Properly handing off patients and information; and
- Nurturing “a culture in which safety is considered a problem-solving situation and not a punishment situation.”6
“Nurses comprise the surveillance system in hospitals for errors and adverse occurrences,” emphasizes Blakeney, and “the effectiveness of nurse surveillance is influenced by factors that include the quality of the work environment.”5
As essential members of hospital teams, hospitalists play a big role in nurses’ work environments, and mutual support between hospitalists and nurses affects patient care and outcomes, and physician and nurse job satisfaction.6,7 In general, nurses give hospitalists high marks for communication, nurse support, and teamwork.
“From a communication perspective, working with hospitalists makes patient care a lot safer because you don’t have to think of everything that you need to tell attending physicians when they are making their daily rounds,” says Scarlett Blue, RNC, MSN, administrative director, Hospitalist Services for FirstHealth of the Carolinas, Pinehurst, N.C. “With hospitalists you know you can do real-time communication, real-time information. That’s not saying you can’t do that with other physicians who are not in the hospital, but it certainly does make it a lot easier when they’re right here.”
Make Contact
One way that hospitalists support their nurse colleagues is by their ready availability to answer questions about patient care. Julie Koppel, RN, BSN, patient care manager on the General Medicine floor at the University of California at San Francisco Medical Center, has worked exclusively with the hospitalist model in her five years of nursing. She is complimentary about hospitalists’ communication skills and refers to them as “the constant and familiar face.” Koppel relates an instance where the attending hospitalist was already off service and yet she still paged him. “He got back to me promptly and still addressed the issues even though he wasn’t on service anymore and it was about something that had happened a month ago. I still feel hospitalists are available when they’re not even here.”
Many nurses don’t have a second thought about calling a hospitalist about a patient care issue, but may still be afraid of “bothering” the hospitalist when he or she is busy. Blue says her colleagues have worked with their nursing staff to overcome that reluctance. “Call them because if they’re talking with a family or if they’re in the middle of a physical exam or if it’s something where they can’t talk, they’re going to put the hold button on,” she tells her staff. “So when you hear the Muzak, the elevator music, then you know that you need to call them back. And it’s worked.”
It’s especially important, Blue says, that nurses surmount any reluctance they feel to initiate a call so that they will do so easily in urgent situations such as alerting rapid response teams and reporting medical errors.4 Blue believes the following anecdote illustrates the perspective of most hospitalists about this issue.
“We just started rapid response teams here,” she says, “And I heard one of the hospitalists say, ‘We’ve had five rapid response team calls so far and we were looking at whether or not the calls met the criteria and were appropriate.’ And one of the other hospitalists said, ‘You know, this really wasn’t a rapid response team call, but I want the nurses to feel free to call and I think that when we’re first starting out, we just want them to call. And then we can work on fine tuning it later. I don’t want to stifle them so they feel they cannot call.”
—Mark Williams, MD
Clear and to the Point
What are the best means to improve communication between hospitalists and nurses? Three major areas for attention include developing relationships, defining communication strategies, and packaging information for clarity.7
Blue often advises nurses to speak with clarity. “Probably the best thing from a hospitalist’s perspective is to be real clear about what you are asking or what it is that you need,” she says. “The clearer that you can be in your requests, the better off you’re going to be in the long run.”
But, Blue says “hospitalists have to understand that one of the greatest benefits from a nurse’s perspective about the hospitalist program is access, immediate access, and dealing with a nurse who does not communicate well might sometimes come along with it.”
The mismatched communication styles of most physicians and nurses are well recognized by a committee at the University of Chicago in which Nancy Perovic is involved. Vineet Arora, MD, MA, a hospitalist and associate program director for the Internal Medicine Residency Program at the University of Chicago, is one of the three hospitalist members on a committee working to improve nurse-physician communication.
“We know that nurses and physicians communicate differently,” says Dr. Arora. “Physicians communicate in more of a task-oriented way and nurses are trained to communicate in a descriptive way. And that’s part of the problem, because nurses might report that physicians don’t respond to them when they need to be responded to; they might not prioritize a patient that the nurse believes is very sick. And a physician might say, ‘I didn’t know that patient was really sick’ because he was given a description such as, ‘They’re not doing OK.’”
Also, Dr. Arora says, “part of the problem that nurses and physicians may have in communicating with each other can be traced to a difference in how they were trained. Physicians are trained to interact with other physicians and nurses are trained by other nurses.”
The committee at Chicago has adopted what is referred to as the Situation-Background-Assessment-Recommendation (SBAR) technique, a tool that the U.S. Navy has used to improve communication on aircraft carriers.8 Developed by Michael Leonard, MD, physician coordinator of clinical informatics, and others at Kaiser Permanente of Colorado, the SBAR technique has been implemented widely at health systems to provide a standard framework for members of the healthcare team when communicating about a patient’s condition.
“What nurses are not very good at is being assertive,” says Perovic. “We’re getting better as we’re getting more modern, but sometimes nurses talk in a more holistic, narrative fashion and doctors just want: what’s the problem, pinpoint it, let me know what it is.”
Chicago’s Perovic and her colleagues plan to educate nurses to use the SBAR technique so they can “talk in the way that doctors are trained to accept information and respond,” she says. “For example, this might sound like, ‘This is this patient with this diagnosis and these vital signs; this is what’s happening: they’re going down, their blood pressure’s dropped, I’m really concerned, this is a different change, I suggest that we do this and that, and I need you here in 10 minutes.’”
Perovic says nurses are then instructed to “make a recommendation; so the hospitalist can prioritize from all the other patients he has to see, to answer the questions: What does this patient need right now? When do I need to see this patient? and What can the nurse do until I get there?”
Literature on the SBAR technique and the tool itself are available online at www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.htm.8
Heedful Versus Heedless Interrelating
Exactly how hospitalists affect outcomes and influence system issues is being addressed in research led by Mark V. Williams, MD, and Tracy Scott, PhD, at Emory University Medical Center, Atlanta. Dr. Williams, who is the director of the medicine unit at Emory Hospital, the editor-in-chief of the Journal of Hospital Medicine, and a past president of SHM, spoke to The Hospitalist about the exploratory research his team is doing to assess the impact hospitalists have in nurse-physician relationships in two hospitals in Atlanta, and to particularly examine how these relationships affect patient safety.
High Reliability Organization theory, which elucidates causal pathways between work relationships and reduced error, may provide a framework for how hospitalists affect hospital functioning. “Heedful interrelating,” the theory postulates, creates an organization “mind” and through facilitating teamwork is more alert to and capable of dealing with unexpected occurrences. In fact, says Dr. Williams, data from operating rooms, emergency departments, and ICUs suggest that a lack of teamwork adversely affects patient care and increases medical errors. Research along this vein has been absent on general medical floors.
The research design explores the degree of “heedful interrelating” as opposed to “heedless interrelating” between physicians and nurses and whether hospitalists have different relationships with nurses than do other physicians.
“In heedful interrelating,” explains Dr. Williams, “the physician heeds what the nurse is saying and doing and, likewise, the nurse heeds what the physician is saying and doing.” To date, the investigators have interviewed 45 nurses (half in a university hospital setting and half in a community hospital) and 24 physicians of whom half are hospitalists.
The study examines multiple components, but an example is that “heedful interrelating is based on true mutual respect, which is almost more important over agreement,” says Dr. Williams. “And in heedless interrelating, only one view of the situation is considered correct. It represents your classic arrogant physician.”
Another example of heedful interrelating is that “it advances the goals of the whole team; in heedless interrelating, you think only of your own role,” he says. Nurses in the study reported that compared with other physicians hospitalists are more accessible, more approachable, and more appreciative of the value of the nurse’s role.
The investigators conclude that hospitalists improve the nurse-physician relationship through heedful interrelating and thereby may improve patient safety. In addition, “the nurses emphasized the need for more collaboration and perceived that physicians were not proactive in asking them about their knowledge of the patient, and lacked a holistic view of the patient’s needs. Most importantly, about half the nurses mentioned specific instances where problems in their communication with physicians led directly to problems in patient care.
Dr. Williams believes that the ideal system for communication between hospitalists and nurses would include a means for them to do their patient rounds together. Nurses want hospitalists to develop a system to deliver the patient care plans quickly and reliably, include them in formal and informal educational efforts, and acknowledge them.
Timely Distribution of Care Plans
Blue says that hospitalists at her institution, FirstHealth Moore Regional Hospital (Pinehurst, N.C.), a 385-bed acute care, nonprofit hospital that serves as the referral center for a 15-county region in the mid-Carolinas, work often and closely with the nurses on issues of outcomes. “And outcomes here are like discharge planning utilization review,” she says. “We have a report every morning and there’s a representative from that department who’s online sending out the plans for the patients for the day to the other outcomes managers. That’s already in the works, and we’re not waiting for the hospitalist to get up to the floor to see the patient.”
Overall, however, nurses in other (e.g., larger) settings may not have as good a system in place to distribute care plans. Perovic says that in focus groups she facilitates, she often hears frustration from nurses because “doctors in general—although hospitalists are better at it—do not give nurses the plan of the day or the plan of care in a timely, organized fashion so they can do their care appropriately and prepare themselves and the patient.”
Some of the problem is due to the systems of an academic medical center, Perovic says, where “doctors make rounds at various times of the day and sometimes one team can make four rounds a day. What happens is that the plan for patient care changes each time new rounds are completed because you either get new information or discover you didn’t do something.” But although the team doctors are good at communicating plan modifications among themselves, she says, “what they fail to do is always communicate that well to the nurses.”
Perovic says there is an ideal and then a real solution. “Ideally, it would be great if patient rounds were at a certain time of the day every day so that the nurse can pass her meds and then be available for rounding,” she says. “You could say to nurses, ‘Rounds are between 10 and 11; take care of your patients’ needs and then be on call and ready to go to your rounds when possible.’ Or another solution is what we do in the pediatric hospital: We have a charge nurse who has no patients and she is able to round with all the teams and all the doctors and then give the individual nurse that plan for her patients.”
Hiring a charge nurse in this vein is a human resource issue, Perovic says, and an individual hospital has to decide that it wants to pay a nurse to not have patients. In that case, she says, it is an expensive but good fix. However, accommodating nurses to accompany hospitalists on rounds is logistically almost impossible. “Because if a nurse on the general medicine ward has five patients,” Perovic says, “she might have five different teams of doctors. But depending on the diagnosis of each patient, it won’t be the same team of doctors rounding on them. She might not catch A, B, and C at the same time that D and E are making their rounds. And she could be doing a blood draw on patient D when D team comes, or giving a bath to patient A when team E comes.”
Perovic and her coworkers have tried the call light method, where the doctor comes into the room, the attending presses the call light, and the nurse knows rounds are happening and to join them at that room. But that, as well as other avenues they tried, failed because neither the nurse nor the team can necessarily count on their times of availability coinciding. Still, Dr. Arora says, “we learned a lot about trying to work together and how to understand each other. And we used some of that information to continue thinking about how to best improve physician-nurse communication.”
The team at Chicago is now considering how to design and evaluate “an intervention for more of an interdisciplinary educational process where physicians and nurses would be trained on how to communicate with each other using this standard language,” says Dr. Arora. “Nurses would understand that they could potentially use the SBAR tool to communicate with physicians, and physicians would understand that the nurses need to be included in the plan for the day and would make time to incorporate nurse suggestions and input for the plan.”
Acknowledgment
In some hospital settings what has been described as a two-class system can exist for providers.9 A culture that encourages patient safety is threatened by the nature of the hierarchy or the segregation that is established, even subtly, where nurses are treated as unequals.6,9 In the hospital culture, the “invisibility of nursing” has historically been perpetuated by a number of factors, not the least of which are differences in gender and income.6 In this atmosphere, nurses are not as likely to share from their skills and knowledge. Their lack of assertiveness with hospitalists or other physicians may take its toll in many ways, including increased risks to patient outcomes and to provider morale and satisfaction.7
Linda Aiken, PhD, FAAN, FRCN, RN, the Claire M. Fagin Leadership Professor of Nursing and director of the Center for Health Outcomes and Policy Research at the University of Pennsylvania (Philadelphia), has extensively investigated the dynamics between nurses and their co-workers. “Nurse-physician relationships are one of the most important drivers of the work environment,”9 she writes. There are also data that demonstrate the association of nurse-doctor relationships on cost, lower morbidity and mortality, retention of nurses, higher quality of care, and improved hospital reimbursement and/or market share.9
In other words, “healthy nurse-physician relationships are not just a nice thing to have,” writes Dr. Aiken. “They are a competitive advantage.”
Given the association of these relationships to so many outcomes, it is unfortunate that many nurses crave greater acknowledgment for what they bring to their work. One benefit for nursing is that because hospitalists are around the hospital more than an average attending, they know the nurses better.
“As a nurse, what I need from hospitalists is for them to recognize and teach their residents and interns that the nurse is a constant player at the bedside in the hospital, with many more years of experience,” says Perovic. “Even though she doesn’t have as much medical training as a doctor or resident, she has enough clinical-nursing hospital experience. Doctors need to appreciate that nurses are experts at hospital care and bedside care, and [doctors] need to show that respect when we’re teaching our residents because we can learn a lot from the nurses, and the nurses can actually make the doctors’ lives easier.”
In a study of a multidisciplinary intervention tested on an acute inpatient medical unit, the effect of the intervention—to improve communication and collaboration—was strongest among house staff, who reported significant increases in collaborative efforts with nurses.10 This finding underlines the importance for hospitalists to serve as models to students, interns, and residents because the most effective time to learn collaborative practice is during early training when experienced nurses can assist inexperienced interns.10 Hospitalists can also consciously reject the traditional “doctor-nurse game,” whereby patterns of behavior suggest that doctors are the dominant players and nurses must defer to them.
“Ask nurses for their opinion,” advises Blue. “Treat them like an equal, which is another one of the beauties of this program, because hospitalists certainly do that. When it comes down to it, people want to be appreciated, respected, and acknowledged for their contribution.”
Blue and her team also encourage hospitalists to share with the nurses if they happen to hear news of their patients’ progress. “If we have follow-up on somebody from the primary care provider after that patient has left the hospital, for example, we try to share that with the nursing staff because they’re our patients. They’re not just my patients and they’re not your patients; they’re our patients.”
Conclusion
The quality of the nurse-hospitalist relationship is central to patient care. The methods, means, and styles of individual and team communication all influence the effectiveness of a hospital team. Retraining providers to traverse the gap of different communication styles is a way to approach the issues that exist. Mutual training for physicians and nurses, as well as training nurses to communicate in ways that more approximate how physicians communicate, will better serve patient and provider needs.
Hospitalists can encourage nurses to overcome hesitancies to initiate calls, clarify their preferences for how nurses should contact them, and work with nurses to seek workable ways to perform patient rounds in concert. Most of all, nurses need timely care plan distribution and acknowledgment for their contributions to teamwork and patient care. TH
Writer Andrea Sattinger will write about occupational therapists’ experiences with hospitalists in the January issue.
References
- ANA Commission on Workforce for Hospitals and Health Systems. In our hands: how hospital leaders can build a thriving workforce. American Hospital Association; Chicago; 2002;55:30-31.
- Aiken LH. The unfinished patient safety agenda. In: Wachter R, ed. Morbidity and Mortality Rounds on the Web: Agency for Healthcare Research and Quality; 2005. Accessed August. 29, 2005 at http://webmm.ahrq.gov/perspective.aspx?perspectiveID=7&searchStr=The+unfinished+patient+safety+agenda
- Aiken LH, Clarke SP, Sloane DM. International Hospital Outcomes Research Consortium. Hospital staffing, organization, and quality of care: cross-national findings. Int J Qual Health Care. 2002;14:5-13.
- Friesen MA, Farquhar MB, Hughes R. The nurse’s role in promoting a culture of safety: American Nurses Association Continuing Education, Center for American Nurses; 2005.
- Wachter R. In conversation with … Barbara A. Blakeney, MS, RN. In: Wachter R, ed. Morbidity and Mortality Rounds on the Web. Agency for Healthcare Research and Quality; 2005. Accessed Aug. 29, 2005 at http://webmm.ahrq.gov/perspective.aspx?perspectiveID=8&searchStr=Blakeney
- Lindeke LL, Sieckert AM. Nurse-physician workplace collaboration. Online J Issues Nurs. 2005;10:5.
- Burke M, Boal J, Mitchell R. Communicating for better care: improving nurse-physician communication. Am J Nurs. 2004;104:40-47
- SBAR initiative to improve staff communication. Healthcare Benchmarks Qual Improv. 2005;12:40-41.
- Smith AP. Partners at the bedside: the importance of nurse-physician relationships. Nurs Econ. 2004;22:161-164.
- Vazirani S, Hays RD, Shapiro MF, et al. Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care. 2005;14:71-77.
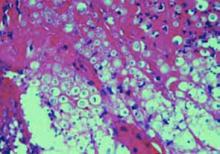
One-Month-Old UTI Patient
Scenario: A 32-day-old female presents with vomiting and jaundice, and the mother reports that the child is irritable and not eating as well as usual. The pediatric hospitalist suspects a UTI and orders a dipstick/urinalysis and urine culture. The dipstick/urinalysis results are positive for nitrite and leukocyte esterase, indicating antibiotic therapy for presumed UTI.
Introduction
UTI is one of the most common bacterial infections in infants and young children. To prevent progression to pyelonephritis and avoid potential renal scarring or failure, early recognition and prompt treatment are critical.
Clinical signs and symptoms of UTI in newborns include jaundice, sepsis, failure to thrive, poor feeding, vomiting, and fever. In infants and preschoolers, hospitalists should also suspect UTI in the presence of diarrhea, strong-smelling urine, abdominal or flank pain, and new onset urinary incontinence.1
Treatment recommendations, which are age-dependent, include antibiotic therapy initiated upon an abnormal dipstick/urinalysis. If a urine culture is positive, a seven- to 14-day course of antibiotic therapy is recommended, followed by prophylactic antibiotics until results of imaging studies are available.1 According to a study by Hoberman and Wald, treatment of UTI with oral antibiotics alone is generally effective, even for young children with pyelonephritis.2
Imaging recommendations for a first UTI include ultrasound, cystogram, and renal cortical scan.
Up to this point, there’s been very little disagreement about the management of UTI. However, the question of whether the one-month-old patient in our scenario should be admitted or sent home with strict instructions on the administration of antibiotics remains controversial. The pediatric UTI guideline from Cincinnati Children’s Hospital Medical Center recommends routine hospital admission if the infant is under 30 days old.1 On the other hand, Santen and Altieri, among others, recommend, “Sick children and infants less than three months should be treated as inpatients, and healthy children and older infants may be treated as outpatients.”3,4
—Jeffrey M. Simmons, MD
The Set-Up
We asked several pediatric hospitalists across the country—including an instructor of pediatrics at Cincinnati Children’s Hospital Medical Center—to respond to this simple scenario, posing the following questions: “What recommendation would you follow? Would you admit the one-month-old infant in our scenario or send her home? Why?”
Predictably, admission criteria varied, but most agreed that this infant should be admitted. No one based their response on age.
Automatic Admission Cut-off Not Well Supported
Jeffrey M. Simmons, MD, instructor of pediatrics, Division of General and Community Pediatrics, Cincinnati Children’s Hospital Medical Center, responds: “My perspective on the UTI scenario is that the only dogma that applies is that the infant needs antibiotics. Because [the scenario] mentions vomiting, I would, therefore, most likely give parenteral antibiotics and admit.
“An issue within this scenario that I don’t believe the literature answers clearly is once a UTI is identified by the U/A, what risk remains of bacteremia or meningitis in the over 30-day-old infant? We are taught that infants don’t ‘localize’ infections well (i.e., a serious bacterial infection in one place can rapidly lead to disseminated infection). I sense a growing consensus that after 30 days or so this concern is less at issue. However, for clarity, I would prefer to obtain blood and CSF cultures on this infant prior to initiating antibiotic therapy. Without those cultures, and the screening tests that go with them (i.e., serum WBC count, CSF cell count, and glucose), I would be uncomfortable sending the infant home.
“However, if the WBC count was between 5 and 15, the CSF reassuring, the parents in agreement and reliable with good primary care follow-up the next morning, I think such an infant could be managed with one dose of IV/IM antibiotics after cultures are obtained and sent home. The following day, depending on culture results and the clinical situation, this infant might either be admitted, given another dose of parenteral antibiotics pending final blood culture, or switched to oral antibiotics.
“Such a plan is complex, so if the primary care physician or family was at all uncomfortable, admission to accomplish that plan would clearly be appropriate.
“A final issue not adequately addressed within the scenario is an assessment of the infant’s hydration—potentially an issue due to the vomiting. If the infant was mildly to moderately dehydrated with persistent vomiting, I would also then admit until this improved.
“In regard to the cited evidence, I would say that clearly an arbitrary cut-off of automatic admission under three months is not well supported by current literature, but is certainly many practitioners’ ‘style.’ Oral antibiotics are clearly efficacious for pyelonephritis, but the clinician needs to be confident the family can give them and the infant will keep them down. I believe most practitioners would agree with admission for an infant under 30 days, but where to precisely draw that line needs to be better established through investigation. Potential concomitant bacteremia and meningitis lead me to support obtaining blood and CSF cultures on any infant under 60 days for which I plan to initiate antibiotics for UTI.”
Possibility of Dehydration Indicates Admission
Michael P. Fullmer, DO, Central Iowa Pediatric Hospitalists, Mercy Medical Center, Des Moines, Iowa, responds: “This patient is not febrile, but does have other systemic symptoms, including poor feeding, irritability, jaundice, and vomiting. These systemic symptoms could be indicative of a serious bacterial infection like UTI, bacteremia, or meningitis. This patient most likely has a UTI. These symptoms may suggest pyelonephritis rather than lower UTI, but the distinction is not necessary for our decision here.
“Bacteremia is present in up to 22.7% of infants less than two months old with a UTI. This adds to the complexity of the issue, and a blood culture is probably indicated. Meningitis should be considered, but a lumbar puncture is probably not indicated in this scenario.
“A one-month-old with a UTI should be admitted to the hospital and started on parenteral antibiotics. There are several reasons for admission. First, the presence of vomiting makes oral antibiotic administration impractical (if not impossible). Intramuscular antibiotic injection may be an option, but the IV route gives the provider more options and is usually better accepted by parents. Next, if the patient is not already dehydrated, the poor feeding and vomiting could lead to dehydration. This alone would be an indication for admission. Finally, admission would give the physician time to observe the infant for clinical improvement. This may be subtle in the absence of fever.
“Another consideration is the recommended imaging for all children less than two years old. The AAP has recommended a renal ultrasound and VCUG for all infants and young children with their first UTI. This is important for discovery of urinary tract anomalies that predispose the patient to recurrent UTIs and eventual renal scarring and dysfunction. The imaging should be performed at the earliest convenient time if the patient is responding to therapy. In our practice, we generally have the renal ultrasound performed while the patient is in the hospital and arrange the VCUG as an outpatient [exam] prior to completion of the course of antibiotics.
“Patients are discharged when they are afebrile for 24 hours, have adequate oral intake and are able to take oral antibiotics. Please refer to the AAP Clinical Practice Guideline for more detail.5,6
—Michael Fullmer, DO
Admission Criteria Must Take Fever Into Account
John W. Graef, MD, chief, Services Office at Children’s Hospital, Harvard Vanguard Services Office, Boston, responds: “The presence or absence of fever is an important variable. Dipstick urines are shortcuts and don’t provide such information as the presence or absence of casts, although the fact that the child is vomiting and irritable is suggestive of pyelonephritis as opposed to a simple UTI/cystitis. [The scenario doesn’t] mention how the urine is obtained. Presumably it is a cath specimen, but that needs to be specified.
“Jaundice can occur with a UTI, but usually in the first week or so of life. A 32-day-old infant with pyelo is unlikely to be jaundiced unless for some other reason.
“I certainly agree with routine admission of a febrile infant up to one month, but not necessarily an otherwise well female infant. The presence of vomiting and irritability with or without fever might prompt a full septic work-up, in which case the decision to admit an afebrile infant would depend on the results of the CBC/UA and probably an LP. A blood culture and CBC should be drawn in the ED.
“In other words, one can’t have it both ways. If the irritability and vomiting are due to pyelo, a septic work-up is warranted. If all parameters are normal, the only reason for admission is hydration of a vomiting infant. If the infant was afebrile and had an uncomplicated UTI, I would not automatically admit an otherwise well 32-day-old.
“Poor PO (per OS, i.e., oral, by mouth) intake in an infant with a UTI warrants IV fluid regardless of age.”
—John W. Graef, MD
True Emesis With Decreased Oral Intake Indicates Admission
Erin R. Stucky, MD, pediatric hospitalist, Children’s Hospital and Health Center San Diego, associate professor, UCSD Pediatrics, responds: “The decision to admit or discharge this one-month-old with vomiting, jaundice, poor eating, and irritability should include consideration of hydration status, toxicity, sepsis potential, and ability to secure close follow-up. We will make the assumption that the infant is term, with no past medical history, family history, or prenatal evaluation that would put the infant at greater risk for sepsis or likelihood of underlying anatomic genitourinary abnormality. In addition we will assume that the urinalysis was performed by catheterization in a non-pretreated infant.
“A careful history should elicit the change in urine output, frequency, and volume of emesis to contrast with small ‘spit-ups,’ and change in feeding duration or volume. Observation of a feeding in the office or emergency department can be of great value in determining likelihood of ability to maintain hydration at home. Feeding type should be confirmed [because] parents may dilute or alternately concentrate formula in response to vomiting. In this scenario, true emesis in an infant with decreased oral intake would be grounds for admission, intravenous hydration, and evaluation of electrolytes.
“A newly irritable infant evokes a visceral sensation for all pediatric hospitalists. An irritable one-month-old may be suffering from a single system infection, electrolyte imbalance, or other insult, but unfortunately may just as easily have multisystem involvement. Vital signs and physical exam findings of toxicity, such as tachycardia and delayed capillary refill, are not known to us. The presence of jaundice raises concern for cholestasis induced by E. coli or possibly rarer metabolic disease, such as galactosemia. Admission would allow for evaluation and monitoring of the more likely causes of irritability in our index patient, which include sepsis, meningitis, and electrolyte and acid-base imbalances.
“The urinalysis in this infant is suggestive of a urinary tract infection, although infants may have no abnormalities noted on initial urinalysis.7,8 The risk of bacteremia in infants under 60 days with documented urinary tract infection is significant. A number of studies support the need to treat infants less than 30 days with parenteral antibiotics.9-14 Addition of C-reactive protein testing at this time does not aid in distinguishing those who are bacteremic in this age group.15 The often quoted study by Hoberman of 306 children included only 13 under the age of two months.16 Of the 13 reported positive blood cultures, 10 were in children under age six months. Daily intramuscular ceftriaxone treatment would cover a majority of the typical neonatal UTI organisms, can be administered in the outpatient setting, and is proven to be as effective as intravenous delivery. The clinical response to bacteremia is, however, unpredictable in young infants. The sepsis potential in this infant requires admission for physiologic monitoring and support as needed.
“Final, but not inconsequential, concerns are barriers to follow-up. These include parental experience and coping skills with feeding and monitoring an ill infant, ability to educate on the illness and reasons for follow-up, transportation, and operational issues, such as weekend clinic hours or holiday office closures. For the index patient these issues are overshadowed by the clinical criteria for admission but would be of great importance for discharge.”
Conclusion
Based on these responses, admitting a suspected UTI patient on the basis of age alone, as suggested by Santen and Altieri, is likely inappropriate. Many other factors must be weighed and would likely indicate admission for the patient in the scenario, regardless of the infant’s age. In short, until there’s better evidence for age-based admission criteria, clinical judgment based on the individual patient presentation must continue to drive care and treatment decisions.
Keri Losavio is a medical journalist with more than 10 years’ experience.
References
- UTI Guideline Team, Cincinnati Children’s Hospital Medical Center. “Evidence based clinical practice guideline for children 12 years of age or less with acute first time urinary tract infection.” www.cincinnatichildrens.org/svc/dept-div/health-policy/ev-based/uti.htm. Guideline 7, pages 1–20, April 2005.
- Hoberman A, Wald ER. Treatment of urinary tract infections. Pediatr Infect Dis J. 1999;18(11):1020–1021.
- Santen SA, Altieri MF. Pediatric urinary tract infection. Emerg Med Clin North Am. 200119(3):675–690.
- Egland AG, Egland TK. Pyelonephritis. eMedicine. www.emedicine.com/emerg/topic769.htm. Accessed Oct. 16, 2005.
- No authors listed. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. American Academy of Pediatrics. Committee on Quality Improvement. Subcommittee on Urinary Tract Infection. Pediatrics. 1999;103(4):843–852.
- Pitetti RD, Choi S. Utility of blood cultures in febrile children with UTI. Am J Emerg Med. 2002;20:271–274.
- Dayan PS, Bennett J, Best R, et al. Test characteristics of the urine Gram stain in infants 60 days of age with fever. Pediatr Emerg Care. 2002;18(1):12–14.
- Huicho L, Campos-Sanchez M, Alamo C. Meta-analysis of urine screening tests for determining the risk of urinary tract infection in children. Pediatr Infect Dis J. 2002;21 (1):1-11.
- Byington C L, Enriquez F, Hoff C, et al. Serious bacterial infections in febrile infants 1 to 90 days old with and without viral infections. Pediatrics. 2004; 113(6):1662–1666.
- Baraff L. Management of fever without source in infants and children. Ann Emerg Med. 2000;36(6):602–614.
- Baraff LJ, Oslund SA, Schriger DL, Stephen ML. Probability of bacterial infections in febrile infants less than three months of age: A meta-analysis. Pediatr Infect Dis J. 1992;11(4):257–264.
- Klein JO. Management of the febrile child without a focus of infection in the era of universal pneumococcal immunization. Pediatr Infect Dis J. 2002;21(6):584–588.
- Syrogiannopoulos G, Grieva I, Anastassiou E, et al. Sterile cerebrospinal fluid pleocytosis in young infants with urinary tract infections. Pediatr Infect Dis J. 2001;20(10):927–930.
- Jaskiewicz JA, McCarthy CA, Richardson AC, et al. Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester criteria and implications for management. Febrile Collaborative Study Group. Pediatrics. 1994;94(3):390–396.
- Malik A, Hui C, Pennie RA, Kirpalani H. Beyond the complete blood cell count and C-reactive protein: A systematic review of modern diagnostic tests for neonatal sepsis. Arch Pediatr Adolesc Med. 2003;157(6):511–516.
- Hoberman A, Wald ER, Hickey RW, et al. Oral versus intravenous therapy for urinary tract Infections in young children. Pediatrics.1999;104:79–86
PEDIATRIC SPECIAL SECTION
IN THE LITERATURE
Utilize Clinical and Demographic Factors to Diagnose UTIs in Young Febrile Infants
Review by Sara E. Gardner, MD
Zorc JJ, Levine DA, Platt SL, et al. Clinical and demographic factors associated with urinary tract infections in young febrile infants. Pediatrics. 2000;116(3):644-648.
UTI is a common cause of serious bacterial infection in the febrile infant <60 days of age. Standard urinalysis and urine dipstick techniques, commonly used to diagnose UTI, have relatively low sensitivity increasing the possibility of a missed diagnosis. An accurate initial diagnosis is critical in this age group for whom complications from UTI include bacteremia and renal scarring.
To describe the demographic and clinical factors associated with UTI in infants ≤60 days of age with fever, these authors conducted a prospective cross sectional study from October 1999 to March 2001. Patients were enrolled at eight different institutions after presentation to an emergency department. One-thousand-twenty-five patients age 60 days or younger (mean age 35.5 days, 60.5% male) were enrolled with either reported or documented fever >38. Routine testing for all children included respiratory syncytial virus (RSV) sampling and bladder catheterization or suprapubic aspiration for urinalysis and culture.
A positive urinalysis was defined as a trace or greater result for leukocyte esterase and/or nitrite on dipstick or greater than or equal to five WBCs per high power field (hpf) on urine microscopy. UTI was defined as growth of a single pathogen of ≥1,000 colony forming units (cfu)/mL for urine cultures obtained by suprapubic catheterization, ≥50,000 cfu/mL from a catheterized specimen, or ≥10,000 cfu/ml from a catheterized specimen with a positive urinalysis.
Of the patients enrolled in the study, 92 were found to have UTI by these diagnostic criteria. Using the chi-squared test and calculated odds ratios with 95% confidence intervals, uncircumcised male (OR: 10.4; 95% CI: 4.7-31.4) and maximum temperature of ≥39º C (OR: 2.4 per degree C; 95% CI: 1.5-3.6) were found to be statistically significant variables for predicting UTI. These risk factors remained statistically significant after multivariable analysis controlling for other factors.
Interestingly of the above 92 patients diagnosed with UTI, 85 grew ≥50,000 cfu of a single pathogen, but six (8%) grew 10,000-49,000 cfu with a positive UA based on the study criteria. Zorc, et al. included these patients with >10,000 cfu and >5 WBC/hpf in this study despite previous studies that have established a definition of positive urinalysis to be ≥10 WBC/hpf. Zorc, et al. acknowledge the conservative definition applied in their current study, but assert that the overall results of the study would have been similar had 10,000 or 50,000 cfu/mL thresholds been chosen. To support this assertion, Zorc, et al. retrospectively applied enhanced urinalysis, a sensitive form of urinalysis including hemocytometric cell count and gram stain described by Hoberman, et al. to study patients with low bacteria counts. Based on Hoberman’s study, enhanced urinalysis can differentiate acute infection from asymptomatic bacteriuria in patients with bacterial growth between 10,000 to 50,000 cfu/mL.
Another significant limitation of this study was failure to enroll one-third of eligible patients to the study. In addition, the authors note that missed patients had a lower rate of UTI compared with enrolled patients.
Although this study design prohibits generalization to patient care areas outside the emergency department, the findings can assist the hospitalist in the evaluation of the febrile infant during RSV season and potentially guide decisions regarding empiric antibiotic therapy as part of evaluations to diagnose or exclude serious bacterial infection. Additionally, this study raises the question of need for better methods of urinalysis for febrile, uncircumcised male infants.
Back to the Basics: A Clinical Approach to Excluding Acute Appendicitis
Review by Jane G. Buss, MD
Kharbanda AB, Taylor GA, Fishman SJ, et al. A clinical decision rule to identify children at low risk for appendicitis. Pediatrics. 2005;116(3):709-16.
Appendicitis is the most common condition requiring emergency abdominal surgery in the pediatric population. To diagnosis appendicitis, clinicians typically utilize clinical findings, imaging studies, and laboratory testing. The use of clinical scoring systems to improve the diagnosis of appendicitis in children has been limited, mostly resulting from unacceptably low sensitivities/specificities, or the lack of validation. The use of CT scan to aid in the evaluation of children with appendicitis has become widespread. Concerns remain, however, regarding long-term radiation effects and increased healthcare costs associated with this approach.
The authors of this study sought to develop clinical scores for children to predict which of those with acute abdominal pain do not have appendicitis. Additionally, they hoped to lessen the use of CT scanning. Their goal was to identify those groups of children who have significant abdominal pain without appendicitis who could be safely observed without CT scan or possible surgery.
This prospective cohort study enrolled 601 eligible children ages three to 18 with suspected appendicitis who presented to the emergency department over a 15-month period. Two low-risk clinical decision rules were developed using logistic regression and recursive partitioning. Using logistic regression, six factors were identified from analysis of 425 patients in the derivation set significantly associated with an increased likelihood of appendicitis. The score components include:
- Nausea (2 points);
- History of focal right lower quadrant pain (RLQ) (2 points);
- Migration of pain (1 point);
- Difficulty walking (1 point);
- Rebound tenderness (2 points); and
- Absolute neutrophil count (ANC) >6.75 x 103/uL (6 points).
When tested with data from the 176 patients in the validation set, a score of less than or equal to five had a sensitivity of 96.3%, and a negative predictive value of 95.6% for excluding appendicitis.
The authors then derived a second clinical low-risk decision rule by recursive partitioning. They determined that a combination of ANC <6.75 X 10 to the third/microliter, absence of nausea (or emesis or anorexia), and absence of maximal tenderness in the RLQ essentially excluded appendicitis in the derivation and validation groups. This rule had a sensitivity of 98.1%, and a negative predictive value of 97.5%.
In summary, these authors derived two clinical decision rules giving the clinician the option of a clinical score (logistic regression) or a decision tree (recursive partitioning) to identify children at low risk for appendicitis. Their findings suggest application of either low-risk rule would lead to decreased reliance on CT scan. Applying these clinical rules to their patients could have reduced the rate of CT scan by 20%. They conclude that pediatric patients who have suspected appendicitis and are at low risk by either model should be considered for observation rather than undergo CT scan or operative care.
Epidemiology of Fungal Infection in the Tertiary Care Inpatient Setting
Review by Brandan P. Kennedy, MD
Abelson, JA, Moore T, Bruckner D, et al. Frequency of fungemia in hospitalized pediatric inpatients over 11 years at a tertiary care institution. Pediatrics. 2005;116(1):611-617.
Fungal organisms are relatively uncommon causes of blood infections in the pediatric population. When they do occur, they cause significant morbidity and mortality. The incidence of fungal blood infections appears to be rising at a faster rate than that of other pathogens. Authors from the University of California performed this study to describe those rate changes, and to evaluate whether treatment has improved in the past 11 years.
This retrospective cohort study involved children admitted to Mattel Children’s Hospital in Los Angeles, California, during an 11-year period from January 1991 to December 2001. Information obtained on all positive fungal cultures from all body sites included date and site of culture, demographics, and fungal etiology. Additionally, data regarding underlying illness, hospital course, outcome, and antimicrobial treatment were considered.
Study results demonstrated a significant increase in diagnosed fungemia in children. There was a 15% increase in overall pediatric admissions in the study period, and a 23% increase in positive fungal cultures in the same period. Of 272 blood cultures, 97 were positive for fungus. Although this is a relatively small number of total infections, data demonstrated a 91% increase in fungemia during the study period. Candida species were the organisms most frequently isolated from any body site with 85% of the total isolates. Of the total positive isolates, it appeared that approximately 78% reflected colonization as opposed to infection.
Outcomes for fungal infections improved only marginally in the study period. Fifty percent of patients with fungemia died between 1991 and 1996, and 45% died between 1997 and 2001. The mortality rate for immunocompromised conditions was 57%. The cost effectiveness of fungal screening cultures was also evaluated, which demonstrated that fungal cultures identified 14 patients independent of bacterial blood cultures at a cost of $560,000, which resulted in a cost of $40,000 per identified patient.
The study reaches several significant conclusions. First there has been a significant increase in fungal infections that exceeds the increase in overall pediatric hospital admissions. However, it is important to recognize the increase in immunocompromised conditions during the study period, which may account for the higher incidence of fungemia.
Second the addition of fungal blood cultures to bacterial blood cultures as part of a routine workup for febrile patients appeared to yield limited clinical information at a very high cost. Third this study highlights the serious threat fungal infections pose to immunocompromised hosts who have a significantly higher incidence of infection, as well as higher morbidity and mortality. Fourth the use of broad spectrum antibiotics may be increasing fungal colonization in patients and consequently increasing the risk for pathologic fungal infection. Finally morbidity and mortality rates for fungal infections did not greatly improve, despite significant improvements in supportive care made during the study period
This study demonstrates a need for better diagnostic markers for fungal infections, especially those that might provide earlier detection and diagnosis at less cost. The importance of judicious use of antibiotics is underscored while the need for a broader base of therapeutic agents is highlighted. These issues may be key ingredients needed to reduce adverse outcomes from fungal infections, especially in the immunocompromised host.
Rotavirus Vaccine Revisited
Salinas B, Perez Schael I, Linhares AC, et al. Evaluation of safety, immunogenicity and efficacy of an attenuated rotavirus vaccine, RIX4414. Ped Infect Dis J. 2005;24(9):807-816.
Rotavirus is the leading cause of severe gastroenteritis among children worldwide. In the United States, rotavirus is responsible for approximately 5%-10% of all diarrhea among children older than five and accounts for approximately 50,000 hospitalizations each year. An estimated one in 200,000 children with rotavirus diarrhea dies from complications of infection. The immunizing effect of rotavirus infection stimulated the development of live attenuated vaccines. In 1998, a three-dose regimen of a tetravalent rhesus-human reassortant vaccine (RotaShield: Wyeth Laboratories,) was licensed for infant immunization in the United States. Within the first year of use, it was withdrawn due to an observed risk of intussusception. The current study was designed to evaluate immunogenicity and efficacy of a live attenuated monovalent human rotavirus vaccine, RIX4414.
A double-blind, randomized, placebo-controlled design was utilized with the RIX4414 rotavirus vaccine administered at three different virus concentrations. Infants were randomly assigned to one of the three study groups or the placebo group. Infants in the vaccine groups received two oral doses of the vaccine at the age of two and four months. An identical placebo containing the same constituents as the vaccine except for the vaccine virus was used as the control. The vaccine was given concomitantly with other routine vaccinations. To determine immunogenicity, blood samples were obtained from all infants immediately before the first vaccination to exclude previous rotavirus infection. Blood samples were obtained two months after the first second vaccine doses and again at one year to measure anti-rotavirus IgA antibodies. Additionally, stool was obtained from 25% of the study sample and tested for rotavirus viral shedding, with differentiation between wild type and vaccine also being performed.
There were 2,155 infants enrolled in this study from three countries in South America, allowing for slightly more than 500 infants in each group. The study began in May 2001, and the final one-year follow-up was completed in April 2003. The anti-rotavirus IgA seroconversion rates two months after first and second doses were 38%-43% and 61%-65%, respectively. This compared with a 5.3% seroconversion rate in the control group, which was determined to be a wild type virus. Vaccine take after two doses was shown in all three vaccine study groups, ranging from 65% to 75% for the lowest to highest vaccine concentration groups. Reactogenicity and safety was evaluated by monitoring incidences of fever, diarrhea, vomiting, irritability, and loss of appetite during the 15 days after vaccine administration. The results were similar for the four study groups suggesting no significant reactogenicity. There were 220 serious adverse events reported including one intussusception. However, none of these events was determined to be related to the vaccine. The RIX4414 vaccine was demonstrated to effectively protect against severe gastroenteritis caused by G1 type rotavirus and also was shown to provide some cross protection to other serotypes.
This well-designed study demonstrated a statistically significant reduction in gastroenteritis due to rotavirus infection, especially of the predominant G1 serotype, after two doses of the RIX4414 human rotavirus vaccine. Objective measures of viral shedding and IgA seroconversion support the efficacy of the vaccine. This study provided a large sample population with good controls.
An important and possibly confounding variable not addressed by the study was breastfeeding status of the infants. There is clinical evidence demonstrating the protective properties of secretory IgA in human milk against rotavirus infection, and this could have influenced the observed severity of disease in the sample population. It would have been interesting to isolate breastfeeding status as a study variable and note any effect on the results of the study.
Aside from this observation, this study appears to show a promising new oral rotavirus vaccine. As further research on the RIX4414 vaccine continues, there is hope that this vaccine could make a significant positive impact on morbidity and hospitalization rates for rotavirus infections worldwide. TH
Scenario: A 32-day-old female presents with vomiting and jaundice, and the mother reports that the child is irritable and not eating as well as usual. The pediatric hospitalist suspects a UTI and orders a dipstick/urinalysis and urine culture. The dipstick/urinalysis results are positive for nitrite and leukocyte esterase, indicating antibiotic therapy for presumed UTI.
Introduction
UTI is one of the most common bacterial infections in infants and young children. To prevent progression to pyelonephritis and avoid potential renal scarring or failure, early recognition and prompt treatment are critical.
Clinical signs and symptoms of UTI in newborns include jaundice, sepsis, failure to thrive, poor feeding, vomiting, and fever. In infants and preschoolers, hospitalists should also suspect UTI in the presence of diarrhea, strong-smelling urine, abdominal or flank pain, and new onset urinary incontinence.1
Treatment recommendations, which are age-dependent, include antibiotic therapy initiated upon an abnormal dipstick/urinalysis. If a urine culture is positive, a seven- to 14-day course of antibiotic therapy is recommended, followed by prophylactic antibiotics until results of imaging studies are available.1 According to a study by Hoberman and Wald, treatment of UTI with oral antibiotics alone is generally effective, even for young children with pyelonephritis.2
Imaging recommendations for a first UTI include ultrasound, cystogram, and renal cortical scan.
Up to this point, there’s been very little disagreement about the management of UTI. However, the question of whether the one-month-old patient in our scenario should be admitted or sent home with strict instructions on the administration of antibiotics remains controversial. The pediatric UTI guideline from Cincinnati Children’s Hospital Medical Center recommends routine hospital admission if the infant is under 30 days old.1 On the other hand, Santen and Altieri, among others, recommend, “Sick children and infants less than three months should be treated as inpatients, and healthy children and older infants may be treated as outpatients.”3,4
—Jeffrey M. Simmons, MD
The Set-Up
We asked several pediatric hospitalists across the country—including an instructor of pediatrics at Cincinnati Children’s Hospital Medical Center—to respond to this simple scenario, posing the following questions: “What recommendation would you follow? Would you admit the one-month-old infant in our scenario or send her home? Why?”
Predictably, admission criteria varied, but most agreed that this infant should be admitted. No one based their response on age.
Automatic Admission Cut-off Not Well Supported
Jeffrey M. Simmons, MD, instructor of pediatrics, Division of General and Community Pediatrics, Cincinnati Children’s Hospital Medical Center, responds: “My perspective on the UTI scenario is that the only dogma that applies is that the infant needs antibiotics. Because [the scenario] mentions vomiting, I would, therefore, most likely give parenteral antibiotics and admit.
“An issue within this scenario that I don’t believe the literature answers clearly is once a UTI is identified by the U/A, what risk remains of bacteremia or meningitis in the over 30-day-old infant? We are taught that infants don’t ‘localize’ infections well (i.e., a serious bacterial infection in one place can rapidly lead to disseminated infection). I sense a growing consensus that after 30 days or so this concern is less at issue. However, for clarity, I would prefer to obtain blood and CSF cultures on this infant prior to initiating antibiotic therapy. Without those cultures, and the screening tests that go with them (i.e., serum WBC count, CSF cell count, and glucose), I would be uncomfortable sending the infant home.
“However, if the WBC count was between 5 and 15, the CSF reassuring, the parents in agreement and reliable with good primary care follow-up the next morning, I think such an infant could be managed with one dose of IV/IM antibiotics after cultures are obtained and sent home. The following day, depending on culture results and the clinical situation, this infant might either be admitted, given another dose of parenteral antibiotics pending final blood culture, or switched to oral antibiotics.
“Such a plan is complex, so if the primary care physician or family was at all uncomfortable, admission to accomplish that plan would clearly be appropriate.
“A final issue not adequately addressed within the scenario is an assessment of the infant’s hydration—potentially an issue due to the vomiting. If the infant was mildly to moderately dehydrated with persistent vomiting, I would also then admit until this improved.
“In regard to the cited evidence, I would say that clearly an arbitrary cut-off of automatic admission under three months is not well supported by current literature, but is certainly many practitioners’ ‘style.’ Oral antibiotics are clearly efficacious for pyelonephritis, but the clinician needs to be confident the family can give them and the infant will keep them down. I believe most practitioners would agree with admission for an infant under 30 days, but where to precisely draw that line needs to be better established through investigation. Potential concomitant bacteremia and meningitis lead me to support obtaining blood and CSF cultures on any infant under 60 days for which I plan to initiate antibiotics for UTI.”
Possibility of Dehydration Indicates Admission
Michael P. Fullmer, DO, Central Iowa Pediatric Hospitalists, Mercy Medical Center, Des Moines, Iowa, responds: “This patient is not febrile, but does have other systemic symptoms, including poor feeding, irritability, jaundice, and vomiting. These systemic symptoms could be indicative of a serious bacterial infection like UTI, bacteremia, or meningitis. This patient most likely has a UTI. These symptoms may suggest pyelonephritis rather than lower UTI, but the distinction is not necessary for our decision here.
“Bacteremia is present in up to 22.7% of infants less than two months old with a UTI. This adds to the complexity of the issue, and a blood culture is probably indicated. Meningitis should be considered, but a lumbar puncture is probably not indicated in this scenario.
“A one-month-old with a UTI should be admitted to the hospital and started on parenteral antibiotics. There are several reasons for admission. First, the presence of vomiting makes oral antibiotic administration impractical (if not impossible). Intramuscular antibiotic injection may be an option, but the IV route gives the provider more options and is usually better accepted by parents. Next, if the patient is not already dehydrated, the poor feeding and vomiting could lead to dehydration. This alone would be an indication for admission. Finally, admission would give the physician time to observe the infant for clinical improvement. This may be subtle in the absence of fever.
“Another consideration is the recommended imaging for all children less than two years old. The AAP has recommended a renal ultrasound and VCUG for all infants and young children with their first UTI. This is important for discovery of urinary tract anomalies that predispose the patient to recurrent UTIs and eventual renal scarring and dysfunction. The imaging should be performed at the earliest convenient time if the patient is responding to therapy. In our practice, we generally have the renal ultrasound performed while the patient is in the hospital and arrange the VCUG as an outpatient [exam] prior to completion of the course of antibiotics.
“Patients are discharged when they are afebrile for 24 hours, have adequate oral intake and are able to take oral antibiotics. Please refer to the AAP Clinical Practice Guideline for more detail.5,6
—Michael Fullmer, DO
Admission Criteria Must Take Fever Into Account
John W. Graef, MD, chief, Services Office at Children’s Hospital, Harvard Vanguard Services Office, Boston, responds: “The presence or absence of fever is an important variable. Dipstick urines are shortcuts and don’t provide such information as the presence or absence of casts, although the fact that the child is vomiting and irritable is suggestive of pyelonephritis as opposed to a simple UTI/cystitis. [The scenario doesn’t] mention how the urine is obtained. Presumably it is a cath specimen, but that needs to be specified.
“Jaundice can occur with a UTI, but usually in the first week or so of life. A 32-day-old infant with pyelo is unlikely to be jaundiced unless for some other reason.
“I certainly agree with routine admission of a febrile infant up to one month, but not necessarily an otherwise well female infant. The presence of vomiting and irritability with or without fever might prompt a full septic work-up, in which case the decision to admit an afebrile infant would depend on the results of the CBC/UA and probably an LP. A blood culture and CBC should be drawn in the ED.
“In other words, one can’t have it both ways. If the irritability and vomiting are due to pyelo, a septic work-up is warranted. If all parameters are normal, the only reason for admission is hydration of a vomiting infant. If the infant was afebrile and had an uncomplicated UTI, I would not automatically admit an otherwise well 32-day-old.
“Poor PO (per OS, i.e., oral, by mouth) intake in an infant with a UTI warrants IV fluid regardless of age.”
—John W. Graef, MD
True Emesis With Decreased Oral Intake Indicates Admission
Erin R. Stucky, MD, pediatric hospitalist, Children’s Hospital and Health Center San Diego, associate professor, UCSD Pediatrics, responds: “The decision to admit or discharge this one-month-old with vomiting, jaundice, poor eating, and irritability should include consideration of hydration status, toxicity, sepsis potential, and ability to secure close follow-up. We will make the assumption that the infant is term, with no past medical history, family history, or prenatal evaluation that would put the infant at greater risk for sepsis or likelihood of underlying anatomic genitourinary abnormality. In addition we will assume that the urinalysis was performed by catheterization in a non-pretreated infant.
“A careful history should elicit the change in urine output, frequency, and volume of emesis to contrast with small ‘spit-ups,’ and change in feeding duration or volume. Observation of a feeding in the office or emergency department can be of great value in determining likelihood of ability to maintain hydration at home. Feeding type should be confirmed [because] parents may dilute or alternately concentrate formula in response to vomiting. In this scenario, true emesis in an infant with decreased oral intake would be grounds for admission, intravenous hydration, and evaluation of electrolytes.
“A newly irritable infant evokes a visceral sensation for all pediatric hospitalists. An irritable one-month-old may be suffering from a single system infection, electrolyte imbalance, or other insult, but unfortunately may just as easily have multisystem involvement. Vital signs and physical exam findings of toxicity, such as tachycardia and delayed capillary refill, are not known to us. The presence of jaundice raises concern for cholestasis induced by E. coli or possibly rarer metabolic disease, such as galactosemia. Admission would allow for evaluation and monitoring of the more likely causes of irritability in our index patient, which include sepsis, meningitis, and electrolyte and acid-base imbalances.
“The urinalysis in this infant is suggestive of a urinary tract infection, although infants may have no abnormalities noted on initial urinalysis.7,8 The risk of bacteremia in infants under 60 days with documented urinary tract infection is significant. A number of studies support the need to treat infants less than 30 days with parenteral antibiotics.9-14 Addition of C-reactive protein testing at this time does not aid in distinguishing those who are bacteremic in this age group.15 The often quoted study by Hoberman of 306 children included only 13 under the age of two months.16 Of the 13 reported positive blood cultures, 10 were in children under age six months. Daily intramuscular ceftriaxone treatment would cover a majority of the typical neonatal UTI organisms, can be administered in the outpatient setting, and is proven to be as effective as intravenous delivery. The clinical response to bacteremia is, however, unpredictable in young infants. The sepsis potential in this infant requires admission for physiologic monitoring and support as needed.
“Final, but not inconsequential, concerns are barriers to follow-up. These include parental experience and coping skills with feeding and monitoring an ill infant, ability to educate on the illness and reasons for follow-up, transportation, and operational issues, such as weekend clinic hours or holiday office closures. For the index patient these issues are overshadowed by the clinical criteria for admission but would be of great importance for discharge.”
Conclusion
Based on these responses, admitting a suspected UTI patient on the basis of age alone, as suggested by Santen and Altieri, is likely inappropriate. Many other factors must be weighed and would likely indicate admission for the patient in the scenario, regardless of the infant’s age. In short, until there’s better evidence for age-based admission criteria, clinical judgment based on the individual patient presentation must continue to drive care and treatment decisions.
Keri Losavio is a medical journalist with more than 10 years’ experience.
References
- UTI Guideline Team, Cincinnati Children’s Hospital Medical Center. “Evidence based clinical practice guideline for children 12 years of age or less with acute first time urinary tract infection.” www.cincinnatichildrens.org/svc/dept-div/health-policy/ev-based/uti.htm. Guideline 7, pages 1–20, April 2005.
- Hoberman A, Wald ER. Treatment of urinary tract infections. Pediatr Infect Dis J. 1999;18(11):1020–1021.
- Santen SA, Altieri MF. Pediatric urinary tract infection. Emerg Med Clin North Am. 200119(3):675–690.
- Egland AG, Egland TK. Pyelonephritis. eMedicine. www.emedicine.com/emerg/topic769.htm. Accessed Oct. 16, 2005.
- No authors listed. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. American Academy of Pediatrics. Committee on Quality Improvement. Subcommittee on Urinary Tract Infection. Pediatrics. 1999;103(4):843–852.
- Pitetti RD, Choi S. Utility of blood cultures in febrile children with UTI. Am J Emerg Med. 2002;20:271–274.
- Dayan PS, Bennett J, Best R, et al. Test characteristics of the urine Gram stain in infants 60 days of age with fever. Pediatr Emerg Care. 2002;18(1):12–14.
- Huicho L, Campos-Sanchez M, Alamo C. Meta-analysis of urine screening tests for determining the risk of urinary tract infection in children. Pediatr Infect Dis J. 2002;21 (1):1-11.
- Byington C L, Enriquez F, Hoff C, et al. Serious bacterial infections in febrile infants 1 to 90 days old with and without viral infections. Pediatrics. 2004; 113(6):1662–1666.
- Baraff L. Management of fever without source in infants and children. Ann Emerg Med. 2000;36(6):602–614.
- Baraff LJ, Oslund SA, Schriger DL, Stephen ML. Probability of bacterial infections in febrile infants less than three months of age: A meta-analysis. Pediatr Infect Dis J. 1992;11(4):257–264.
- Klein JO. Management of the febrile child without a focus of infection in the era of universal pneumococcal immunization. Pediatr Infect Dis J. 2002;21(6):584–588.
- Syrogiannopoulos G, Grieva I, Anastassiou E, et al. Sterile cerebrospinal fluid pleocytosis in young infants with urinary tract infections. Pediatr Infect Dis J. 2001;20(10):927–930.
- Jaskiewicz JA, McCarthy CA, Richardson AC, et al. Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester criteria and implications for management. Febrile Collaborative Study Group. Pediatrics. 1994;94(3):390–396.
- Malik A, Hui C, Pennie RA, Kirpalani H. Beyond the complete blood cell count and C-reactive protein: A systematic review of modern diagnostic tests for neonatal sepsis. Arch Pediatr Adolesc Med. 2003;157(6):511–516.
- Hoberman A, Wald ER, Hickey RW, et al. Oral versus intravenous therapy for urinary tract Infections in young children. Pediatrics.1999;104:79–86
PEDIATRIC SPECIAL SECTION
IN THE LITERATURE
Utilize Clinical and Demographic Factors to Diagnose UTIs in Young Febrile Infants
Review by Sara E. Gardner, MD
Zorc JJ, Levine DA, Platt SL, et al. Clinical and demographic factors associated with urinary tract infections in young febrile infants. Pediatrics. 2000;116(3):644-648.
UTI is a common cause of serious bacterial infection in the febrile infant <60 days of age. Standard urinalysis and urine dipstick techniques, commonly used to diagnose UTI, have relatively low sensitivity increasing the possibility of a missed diagnosis. An accurate initial diagnosis is critical in this age group for whom complications from UTI include bacteremia and renal scarring.
To describe the demographic and clinical factors associated with UTI in infants ≤60 days of age with fever, these authors conducted a prospective cross sectional study from October 1999 to March 2001. Patients were enrolled at eight different institutions after presentation to an emergency department. One-thousand-twenty-five patients age 60 days or younger (mean age 35.5 days, 60.5% male) were enrolled with either reported or documented fever >38. Routine testing for all children included respiratory syncytial virus (RSV) sampling and bladder catheterization or suprapubic aspiration for urinalysis and culture.
A positive urinalysis was defined as a trace or greater result for leukocyte esterase and/or nitrite on dipstick or greater than or equal to five WBCs per high power field (hpf) on urine microscopy. UTI was defined as growth of a single pathogen of ≥1,000 colony forming units (cfu)/mL for urine cultures obtained by suprapubic catheterization, ≥50,000 cfu/mL from a catheterized specimen, or ≥10,000 cfu/ml from a catheterized specimen with a positive urinalysis.
Of the patients enrolled in the study, 92 were found to have UTI by these diagnostic criteria. Using the chi-squared test and calculated odds ratios with 95% confidence intervals, uncircumcised male (OR: 10.4; 95% CI: 4.7-31.4) and maximum temperature of ≥39º C (OR: 2.4 per degree C; 95% CI: 1.5-3.6) were found to be statistically significant variables for predicting UTI. These risk factors remained statistically significant after multivariable analysis controlling for other factors.
Interestingly of the above 92 patients diagnosed with UTI, 85 grew ≥50,000 cfu of a single pathogen, but six (8%) grew 10,000-49,000 cfu with a positive UA based on the study criteria. Zorc, et al. included these patients with >10,000 cfu and >5 WBC/hpf in this study despite previous studies that have established a definition of positive urinalysis to be ≥10 WBC/hpf. Zorc, et al. acknowledge the conservative definition applied in their current study, but assert that the overall results of the study would have been similar had 10,000 or 50,000 cfu/mL thresholds been chosen. To support this assertion, Zorc, et al. retrospectively applied enhanced urinalysis, a sensitive form of urinalysis including hemocytometric cell count and gram stain described by Hoberman, et al. to study patients with low bacteria counts. Based on Hoberman’s study, enhanced urinalysis can differentiate acute infection from asymptomatic bacteriuria in patients with bacterial growth between 10,000 to 50,000 cfu/mL.
Another significant limitation of this study was failure to enroll one-third of eligible patients to the study. In addition, the authors note that missed patients had a lower rate of UTI compared with enrolled patients.
Although this study design prohibits generalization to patient care areas outside the emergency department, the findings can assist the hospitalist in the evaluation of the febrile infant during RSV season and potentially guide decisions regarding empiric antibiotic therapy as part of evaluations to diagnose or exclude serious bacterial infection. Additionally, this study raises the question of need for better methods of urinalysis for febrile, uncircumcised male infants.
Back to the Basics: A Clinical Approach to Excluding Acute Appendicitis
Review by Jane G. Buss, MD
Kharbanda AB, Taylor GA, Fishman SJ, et al. A clinical decision rule to identify children at low risk for appendicitis. Pediatrics. 2005;116(3):709-16.
Appendicitis is the most common condition requiring emergency abdominal surgery in the pediatric population. To diagnosis appendicitis, clinicians typically utilize clinical findings, imaging studies, and laboratory testing. The use of clinical scoring systems to improve the diagnosis of appendicitis in children has been limited, mostly resulting from unacceptably low sensitivities/specificities, or the lack of validation. The use of CT scan to aid in the evaluation of children with appendicitis has become widespread. Concerns remain, however, regarding long-term radiation effects and increased healthcare costs associated with this approach.
The authors of this study sought to develop clinical scores for children to predict which of those with acute abdominal pain do not have appendicitis. Additionally, they hoped to lessen the use of CT scanning. Their goal was to identify those groups of children who have significant abdominal pain without appendicitis who could be safely observed without CT scan or possible surgery.
This prospective cohort study enrolled 601 eligible children ages three to 18 with suspected appendicitis who presented to the emergency department over a 15-month period. Two low-risk clinical decision rules were developed using logistic regression and recursive partitioning. Using logistic regression, six factors were identified from analysis of 425 patients in the derivation set significantly associated with an increased likelihood of appendicitis. The score components include:
- Nausea (2 points);
- History of focal right lower quadrant pain (RLQ) (2 points);
- Migration of pain (1 point);
- Difficulty walking (1 point);
- Rebound tenderness (2 points); and
- Absolute neutrophil count (ANC) >6.75 x 103/uL (6 points).
When tested with data from the 176 patients in the validation set, a score of less than or equal to five had a sensitivity of 96.3%, and a negative predictive value of 95.6% for excluding appendicitis.
The authors then derived a second clinical low-risk decision rule by recursive partitioning. They determined that a combination of ANC <6.75 X 10 to the third/microliter, absence of nausea (or emesis or anorexia), and absence of maximal tenderness in the RLQ essentially excluded appendicitis in the derivation and validation groups. This rule had a sensitivity of 98.1%, and a negative predictive value of 97.5%.
In summary, these authors derived two clinical decision rules giving the clinician the option of a clinical score (logistic regression) or a decision tree (recursive partitioning) to identify children at low risk for appendicitis. Their findings suggest application of either low-risk rule would lead to decreased reliance on CT scan. Applying these clinical rules to their patients could have reduced the rate of CT scan by 20%. They conclude that pediatric patients who have suspected appendicitis and are at low risk by either model should be considered for observation rather than undergo CT scan or operative care.
Epidemiology of Fungal Infection in the Tertiary Care Inpatient Setting
Review by Brandan P. Kennedy, MD
Abelson, JA, Moore T, Bruckner D, et al. Frequency of fungemia in hospitalized pediatric inpatients over 11 years at a tertiary care institution. Pediatrics. 2005;116(1):611-617.
Fungal organisms are relatively uncommon causes of blood infections in the pediatric population. When they do occur, they cause significant morbidity and mortality. The incidence of fungal blood infections appears to be rising at a faster rate than that of other pathogens. Authors from the University of California performed this study to describe those rate changes, and to evaluate whether treatment has improved in the past 11 years.
This retrospective cohort study involved children admitted to Mattel Children’s Hospital in Los Angeles, California, during an 11-year period from January 1991 to December 2001. Information obtained on all positive fungal cultures from all body sites included date and site of culture, demographics, and fungal etiology. Additionally, data regarding underlying illness, hospital course, outcome, and antimicrobial treatment were considered.
Study results demonstrated a significant increase in diagnosed fungemia in children. There was a 15% increase in overall pediatric admissions in the study period, and a 23% increase in positive fungal cultures in the same period. Of 272 blood cultures, 97 were positive for fungus. Although this is a relatively small number of total infections, data demonstrated a 91% increase in fungemia during the study period. Candida species were the organisms most frequently isolated from any body site with 85% of the total isolates. Of the total positive isolates, it appeared that approximately 78% reflected colonization as opposed to infection.
Outcomes for fungal infections improved only marginally in the study period. Fifty percent of patients with fungemia died between 1991 and 1996, and 45% died between 1997 and 2001. The mortality rate for immunocompromised conditions was 57%. The cost effectiveness of fungal screening cultures was also evaluated, which demonstrated that fungal cultures identified 14 patients independent of bacterial blood cultures at a cost of $560,000, which resulted in a cost of $40,000 per identified patient.
The study reaches several significant conclusions. First there has been a significant increase in fungal infections that exceeds the increase in overall pediatric hospital admissions. However, it is important to recognize the increase in immunocompromised conditions during the study period, which may account for the higher incidence of fungemia.
Second the addition of fungal blood cultures to bacterial blood cultures as part of a routine workup for febrile patients appeared to yield limited clinical information at a very high cost. Third this study highlights the serious threat fungal infections pose to immunocompromised hosts who have a significantly higher incidence of infection, as well as higher morbidity and mortality. Fourth the use of broad spectrum antibiotics may be increasing fungal colonization in patients and consequently increasing the risk for pathologic fungal infection. Finally morbidity and mortality rates for fungal infections did not greatly improve, despite significant improvements in supportive care made during the study period
This study demonstrates a need for better diagnostic markers for fungal infections, especially those that might provide earlier detection and diagnosis at less cost. The importance of judicious use of antibiotics is underscored while the need for a broader base of therapeutic agents is highlighted. These issues may be key ingredients needed to reduce adverse outcomes from fungal infections, especially in the immunocompromised host.
Rotavirus Vaccine Revisited
Salinas B, Perez Schael I, Linhares AC, et al. Evaluation of safety, immunogenicity and efficacy of an attenuated rotavirus vaccine, RIX4414. Ped Infect Dis J. 2005;24(9):807-816.
Rotavirus is the leading cause of severe gastroenteritis among children worldwide. In the United States, rotavirus is responsible for approximately 5%-10% of all diarrhea among children older than five and accounts for approximately 50,000 hospitalizations each year. An estimated one in 200,000 children with rotavirus diarrhea dies from complications of infection. The immunizing effect of rotavirus infection stimulated the development of live attenuated vaccines. In 1998, a three-dose regimen of a tetravalent rhesus-human reassortant vaccine (RotaShield: Wyeth Laboratories,) was licensed for infant immunization in the United States. Within the first year of use, it was withdrawn due to an observed risk of intussusception. The current study was designed to evaluate immunogenicity and efficacy of a live attenuated monovalent human rotavirus vaccine, RIX4414.
A double-blind, randomized, placebo-controlled design was utilized with the RIX4414 rotavirus vaccine administered at three different virus concentrations. Infants were randomly assigned to one of the three study groups or the placebo group. Infants in the vaccine groups received two oral doses of the vaccine at the age of two and four months. An identical placebo containing the same constituents as the vaccine except for the vaccine virus was used as the control. The vaccine was given concomitantly with other routine vaccinations. To determine immunogenicity, blood samples were obtained from all infants immediately before the first vaccination to exclude previous rotavirus infection. Blood samples were obtained two months after the first second vaccine doses and again at one year to measure anti-rotavirus IgA antibodies. Additionally, stool was obtained from 25% of the study sample and tested for rotavirus viral shedding, with differentiation between wild type and vaccine also being performed.
There were 2,155 infants enrolled in this study from three countries in South America, allowing for slightly more than 500 infants in each group. The study began in May 2001, and the final one-year follow-up was completed in April 2003. The anti-rotavirus IgA seroconversion rates two months after first and second doses were 38%-43% and 61%-65%, respectively. This compared with a 5.3% seroconversion rate in the control group, which was determined to be a wild type virus. Vaccine take after two doses was shown in all three vaccine study groups, ranging from 65% to 75% for the lowest to highest vaccine concentration groups. Reactogenicity and safety was evaluated by monitoring incidences of fever, diarrhea, vomiting, irritability, and loss of appetite during the 15 days after vaccine administration. The results were similar for the four study groups suggesting no significant reactogenicity. There were 220 serious adverse events reported including one intussusception. However, none of these events was determined to be related to the vaccine. The RIX4414 vaccine was demonstrated to effectively protect against severe gastroenteritis caused by G1 type rotavirus and also was shown to provide some cross protection to other serotypes.
This well-designed study demonstrated a statistically significant reduction in gastroenteritis due to rotavirus infection, especially of the predominant G1 serotype, after two doses of the RIX4414 human rotavirus vaccine. Objective measures of viral shedding and IgA seroconversion support the efficacy of the vaccine. This study provided a large sample population with good controls.
An important and possibly confounding variable not addressed by the study was breastfeeding status of the infants. There is clinical evidence demonstrating the protective properties of secretory IgA in human milk against rotavirus infection, and this could have influenced the observed severity of disease in the sample population. It would have been interesting to isolate breastfeeding status as a study variable and note any effect on the results of the study.
Aside from this observation, this study appears to show a promising new oral rotavirus vaccine. As further research on the RIX4414 vaccine continues, there is hope that this vaccine could make a significant positive impact on morbidity and hospitalization rates for rotavirus infections worldwide. TH
Scenario: A 32-day-old female presents with vomiting and jaundice, and the mother reports that the child is irritable and not eating as well as usual. The pediatric hospitalist suspects a UTI and orders a dipstick/urinalysis and urine culture. The dipstick/urinalysis results are positive for nitrite and leukocyte esterase, indicating antibiotic therapy for presumed UTI.
Introduction
UTI is one of the most common bacterial infections in infants and young children. To prevent progression to pyelonephritis and avoid potential renal scarring or failure, early recognition and prompt treatment are critical.
Clinical signs and symptoms of UTI in newborns include jaundice, sepsis, failure to thrive, poor feeding, vomiting, and fever. In infants and preschoolers, hospitalists should also suspect UTI in the presence of diarrhea, strong-smelling urine, abdominal or flank pain, and new onset urinary incontinence.1
Treatment recommendations, which are age-dependent, include antibiotic therapy initiated upon an abnormal dipstick/urinalysis. If a urine culture is positive, a seven- to 14-day course of antibiotic therapy is recommended, followed by prophylactic antibiotics until results of imaging studies are available.1 According to a study by Hoberman and Wald, treatment of UTI with oral antibiotics alone is generally effective, even for young children with pyelonephritis.2
Imaging recommendations for a first UTI include ultrasound, cystogram, and renal cortical scan.
Up to this point, there’s been very little disagreement about the management of UTI. However, the question of whether the one-month-old patient in our scenario should be admitted or sent home with strict instructions on the administration of antibiotics remains controversial. The pediatric UTI guideline from Cincinnati Children’s Hospital Medical Center recommends routine hospital admission if the infant is under 30 days old.1 On the other hand, Santen and Altieri, among others, recommend, “Sick children and infants less than three months should be treated as inpatients, and healthy children and older infants may be treated as outpatients.”3,4
—Jeffrey M. Simmons, MD
The Set-Up
We asked several pediatric hospitalists across the country—including an instructor of pediatrics at Cincinnati Children’s Hospital Medical Center—to respond to this simple scenario, posing the following questions: “What recommendation would you follow? Would you admit the one-month-old infant in our scenario or send her home? Why?”
Predictably, admission criteria varied, but most agreed that this infant should be admitted. No one based their response on age.
Automatic Admission Cut-off Not Well Supported
Jeffrey M. Simmons, MD, instructor of pediatrics, Division of General and Community Pediatrics, Cincinnati Children’s Hospital Medical Center, responds: “My perspective on the UTI scenario is that the only dogma that applies is that the infant needs antibiotics. Because [the scenario] mentions vomiting, I would, therefore, most likely give parenteral antibiotics and admit.
“An issue within this scenario that I don’t believe the literature answers clearly is once a UTI is identified by the U/A, what risk remains of bacteremia or meningitis in the over 30-day-old infant? We are taught that infants don’t ‘localize’ infections well (i.e., a serious bacterial infection in one place can rapidly lead to disseminated infection). I sense a growing consensus that after 30 days or so this concern is less at issue. However, for clarity, I would prefer to obtain blood and CSF cultures on this infant prior to initiating antibiotic therapy. Without those cultures, and the screening tests that go with them (i.e., serum WBC count, CSF cell count, and glucose), I would be uncomfortable sending the infant home.
“However, if the WBC count was between 5 and 15, the CSF reassuring, the parents in agreement and reliable with good primary care follow-up the next morning, I think such an infant could be managed with one dose of IV/IM antibiotics after cultures are obtained and sent home. The following day, depending on culture results and the clinical situation, this infant might either be admitted, given another dose of parenteral antibiotics pending final blood culture, or switched to oral antibiotics.
“Such a plan is complex, so if the primary care physician or family was at all uncomfortable, admission to accomplish that plan would clearly be appropriate.
“A final issue not adequately addressed within the scenario is an assessment of the infant’s hydration—potentially an issue due to the vomiting. If the infant was mildly to moderately dehydrated with persistent vomiting, I would also then admit until this improved.
“In regard to the cited evidence, I would say that clearly an arbitrary cut-off of automatic admission under three months is not well supported by current literature, but is certainly many practitioners’ ‘style.’ Oral antibiotics are clearly efficacious for pyelonephritis, but the clinician needs to be confident the family can give them and the infant will keep them down. I believe most practitioners would agree with admission for an infant under 30 days, but where to precisely draw that line needs to be better established through investigation. Potential concomitant bacteremia and meningitis lead me to support obtaining blood and CSF cultures on any infant under 60 days for which I plan to initiate antibiotics for UTI.”
Possibility of Dehydration Indicates Admission
Michael P. Fullmer, DO, Central Iowa Pediatric Hospitalists, Mercy Medical Center, Des Moines, Iowa, responds: “This patient is not febrile, but does have other systemic symptoms, including poor feeding, irritability, jaundice, and vomiting. These systemic symptoms could be indicative of a serious bacterial infection like UTI, bacteremia, or meningitis. This patient most likely has a UTI. These symptoms may suggest pyelonephritis rather than lower UTI, but the distinction is not necessary for our decision here.
“Bacteremia is present in up to 22.7% of infants less than two months old with a UTI. This adds to the complexity of the issue, and a blood culture is probably indicated. Meningitis should be considered, but a lumbar puncture is probably not indicated in this scenario.
“A one-month-old with a UTI should be admitted to the hospital and started on parenteral antibiotics. There are several reasons for admission. First, the presence of vomiting makes oral antibiotic administration impractical (if not impossible). Intramuscular antibiotic injection may be an option, but the IV route gives the provider more options and is usually better accepted by parents. Next, if the patient is not already dehydrated, the poor feeding and vomiting could lead to dehydration. This alone would be an indication for admission. Finally, admission would give the physician time to observe the infant for clinical improvement. This may be subtle in the absence of fever.
“Another consideration is the recommended imaging for all children less than two years old. The AAP has recommended a renal ultrasound and VCUG for all infants and young children with their first UTI. This is important for discovery of urinary tract anomalies that predispose the patient to recurrent UTIs and eventual renal scarring and dysfunction. The imaging should be performed at the earliest convenient time if the patient is responding to therapy. In our practice, we generally have the renal ultrasound performed while the patient is in the hospital and arrange the VCUG as an outpatient [exam] prior to completion of the course of antibiotics.
“Patients are discharged when they are afebrile for 24 hours, have adequate oral intake and are able to take oral antibiotics. Please refer to the AAP Clinical Practice Guideline for more detail.5,6
—Michael Fullmer, DO
Admission Criteria Must Take Fever Into Account
John W. Graef, MD, chief, Services Office at Children’s Hospital, Harvard Vanguard Services Office, Boston, responds: “The presence or absence of fever is an important variable. Dipstick urines are shortcuts and don’t provide such information as the presence or absence of casts, although the fact that the child is vomiting and irritable is suggestive of pyelonephritis as opposed to a simple UTI/cystitis. [The scenario doesn’t] mention how the urine is obtained. Presumably it is a cath specimen, but that needs to be specified.
“Jaundice can occur with a UTI, but usually in the first week or so of life. A 32-day-old infant with pyelo is unlikely to be jaundiced unless for some other reason.
“I certainly agree with routine admission of a febrile infant up to one month, but not necessarily an otherwise well female infant. The presence of vomiting and irritability with or without fever might prompt a full septic work-up, in which case the decision to admit an afebrile infant would depend on the results of the CBC/UA and probably an LP. A blood culture and CBC should be drawn in the ED.
“In other words, one can’t have it both ways. If the irritability and vomiting are due to pyelo, a septic work-up is warranted. If all parameters are normal, the only reason for admission is hydration of a vomiting infant. If the infant was afebrile and had an uncomplicated UTI, I would not automatically admit an otherwise well 32-day-old.
“Poor PO (per OS, i.e., oral, by mouth) intake in an infant with a UTI warrants IV fluid regardless of age.”
—John W. Graef, MD
True Emesis With Decreased Oral Intake Indicates Admission
Erin R. Stucky, MD, pediatric hospitalist, Children’s Hospital and Health Center San Diego, associate professor, UCSD Pediatrics, responds: “The decision to admit or discharge this one-month-old with vomiting, jaundice, poor eating, and irritability should include consideration of hydration status, toxicity, sepsis potential, and ability to secure close follow-up. We will make the assumption that the infant is term, with no past medical history, family history, or prenatal evaluation that would put the infant at greater risk for sepsis or likelihood of underlying anatomic genitourinary abnormality. In addition we will assume that the urinalysis was performed by catheterization in a non-pretreated infant.
“A careful history should elicit the change in urine output, frequency, and volume of emesis to contrast with small ‘spit-ups,’ and change in feeding duration or volume. Observation of a feeding in the office or emergency department can be of great value in determining likelihood of ability to maintain hydration at home. Feeding type should be confirmed [because] parents may dilute or alternately concentrate formula in response to vomiting. In this scenario, true emesis in an infant with decreased oral intake would be grounds for admission, intravenous hydration, and evaluation of electrolytes.
“A newly irritable infant evokes a visceral sensation for all pediatric hospitalists. An irritable one-month-old may be suffering from a single system infection, electrolyte imbalance, or other insult, but unfortunately may just as easily have multisystem involvement. Vital signs and physical exam findings of toxicity, such as tachycardia and delayed capillary refill, are not known to us. The presence of jaundice raises concern for cholestasis induced by E. coli or possibly rarer metabolic disease, such as galactosemia. Admission would allow for evaluation and monitoring of the more likely causes of irritability in our index patient, which include sepsis, meningitis, and electrolyte and acid-base imbalances.
“The urinalysis in this infant is suggestive of a urinary tract infection, although infants may have no abnormalities noted on initial urinalysis.7,8 The risk of bacteremia in infants under 60 days with documented urinary tract infection is significant. A number of studies support the need to treat infants less than 30 days with parenteral antibiotics.9-14 Addition of C-reactive protein testing at this time does not aid in distinguishing those who are bacteremic in this age group.15 The often quoted study by Hoberman of 306 children included only 13 under the age of two months.16 Of the 13 reported positive blood cultures, 10 were in children under age six months. Daily intramuscular ceftriaxone treatment would cover a majority of the typical neonatal UTI organisms, can be administered in the outpatient setting, and is proven to be as effective as intravenous delivery. The clinical response to bacteremia is, however, unpredictable in young infants. The sepsis potential in this infant requires admission for physiologic monitoring and support as needed.
“Final, but not inconsequential, concerns are barriers to follow-up. These include parental experience and coping skills with feeding and monitoring an ill infant, ability to educate on the illness and reasons for follow-up, transportation, and operational issues, such as weekend clinic hours or holiday office closures. For the index patient these issues are overshadowed by the clinical criteria for admission but would be of great importance for discharge.”
Conclusion
Based on these responses, admitting a suspected UTI patient on the basis of age alone, as suggested by Santen and Altieri, is likely inappropriate. Many other factors must be weighed and would likely indicate admission for the patient in the scenario, regardless of the infant’s age. In short, until there’s better evidence for age-based admission criteria, clinical judgment based on the individual patient presentation must continue to drive care and treatment decisions.
Keri Losavio is a medical journalist with more than 10 years’ experience.
References
- UTI Guideline Team, Cincinnati Children’s Hospital Medical Center. “Evidence based clinical practice guideline for children 12 years of age or less with acute first time urinary tract infection.” www.cincinnatichildrens.org/svc/dept-div/health-policy/ev-based/uti.htm. Guideline 7, pages 1–20, April 2005.
- Hoberman A, Wald ER. Treatment of urinary tract infections. Pediatr Infect Dis J. 1999;18(11):1020–1021.
- Santen SA, Altieri MF. Pediatric urinary tract infection. Emerg Med Clin North Am. 200119(3):675–690.
- Egland AG, Egland TK. Pyelonephritis. eMedicine. www.emedicine.com/emerg/topic769.htm. Accessed Oct. 16, 2005.
- No authors listed. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. American Academy of Pediatrics. Committee on Quality Improvement. Subcommittee on Urinary Tract Infection. Pediatrics. 1999;103(4):843–852.
- Pitetti RD, Choi S. Utility of blood cultures in febrile children with UTI. Am J Emerg Med. 2002;20:271–274.
- Dayan PS, Bennett J, Best R, et al. Test characteristics of the urine Gram stain in infants 60 days of age with fever. Pediatr Emerg Care. 2002;18(1):12–14.
- Huicho L, Campos-Sanchez M, Alamo C. Meta-analysis of urine screening tests for determining the risk of urinary tract infection in children. Pediatr Infect Dis J. 2002;21 (1):1-11.
- Byington C L, Enriquez F, Hoff C, et al. Serious bacterial infections in febrile infants 1 to 90 days old with and without viral infections. Pediatrics. 2004; 113(6):1662–1666.
- Baraff L. Management of fever without source in infants and children. Ann Emerg Med. 2000;36(6):602–614.
- Baraff LJ, Oslund SA, Schriger DL, Stephen ML. Probability of bacterial infections in febrile infants less than three months of age: A meta-analysis. Pediatr Infect Dis J. 1992;11(4):257–264.
- Klein JO. Management of the febrile child without a focus of infection in the era of universal pneumococcal immunization. Pediatr Infect Dis J. 2002;21(6):584–588.
- Syrogiannopoulos G, Grieva I, Anastassiou E, et al. Sterile cerebrospinal fluid pleocytosis in young infants with urinary tract infections. Pediatr Infect Dis J. 2001;20(10):927–930.
- Jaskiewicz JA, McCarthy CA, Richardson AC, et al. Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester criteria and implications for management. Febrile Collaborative Study Group. Pediatrics. 1994;94(3):390–396.
- Malik A, Hui C, Pennie RA, Kirpalani H. Beyond the complete blood cell count and C-reactive protein: A systematic review of modern diagnostic tests for neonatal sepsis. Arch Pediatr Adolesc Med. 2003;157(6):511–516.
- Hoberman A, Wald ER, Hickey RW, et al. Oral versus intravenous therapy for urinary tract Infections in young children. Pediatrics.1999;104:79–86
PEDIATRIC SPECIAL SECTION
IN THE LITERATURE
Utilize Clinical and Demographic Factors to Diagnose UTIs in Young Febrile Infants
Review by Sara E. Gardner, MD
Zorc JJ, Levine DA, Platt SL, et al. Clinical and demographic factors associated with urinary tract infections in young febrile infants. Pediatrics. 2000;116(3):644-648.
UTI is a common cause of serious bacterial infection in the febrile infant <60 days of age. Standard urinalysis and urine dipstick techniques, commonly used to diagnose UTI, have relatively low sensitivity increasing the possibility of a missed diagnosis. An accurate initial diagnosis is critical in this age group for whom complications from UTI include bacteremia and renal scarring.
To describe the demographic and clinical factors associated with UTI in infants ≤60 days of age with fever, these authors conducted a prospective cross sectional study from October 1999 to March 2001. Patients were enrolled at eight different institutions after presentation to an emergency department. One-thousand-twenty-five patients age 60 days or younger (mean age 35.5 days, 60.5% male) were enrolled with either reported or documented fever >38. Routine testing for all children included respiratory syncytial virus (RSV) sampling and bladder catheterization or suprapubic aspiration for urinalysis and culture.
A positive urinalysis was defined as a trace or greater result for leukocyte esterase and/or nitrite on dipstick or greater than or equal to five WBCs per high power field (hpf) on urine microscopy. UTI was defined as growth of a single pathogen of ≥1,000 colony forming units (cfu)/mL for urine cultures obtained by suprapubic catheterization, ≥50,000 cfu/mL from a catheterized specimen, or ≥10,000 cfu/ml from a catheterized specimen with a positive urinalysis.
Of the patients enrolled in the study, 92 were found to have UTI by these diagnostic criteria. Using the chi-squared test and calculated odds ratios with 95% confidence intervals, uncircumcised male (OR: 10.4; 95% CI: 4.7-31.4) and maximum temperature of ≥39º C (OR: 2.4 per degree C; 95% CI: 1.5-3.6) were found to be statistically significant variables for predicting UTI. These risk factors remained statistically significant after multivariable analysis controlling for other factors.
Interestingly of the above 92 patients diagnosed with UTI, 85 grew ≥50,000 cfu of a single pathogen, but six (8%) grew 10,000-49,000 cfu with a positive UA based on the study criteria. Zorc, et al. included these patients with >10,000 cfu and >5 WBC/hpf in this study despite previous studies that have established a definition of positive urinalysis to be ≥10 WBC/hpf. Zorc, et al. acknowledge the conservative definition applied in their current study, but assert that the overall results of the study would have been similar had 10,000 or 50,000 cfu/mL thresholds been chosen. To support this assertion, Zorc, et al. retrospectively applied enhanced urinalysis, a sensitive form of urinalysis including hemocytometric cell count and gram stain described by Hoberman, et al. to study patients with low bacteria counts. Based on Hoberman’s study, enhanced urinalysis can differentiate acute infection from asymptomatic bacteriuria in patients with bacterial growth between 10,000 to 50,000 cfu/mL.
Another significant limitation of this study was failure to enroll one-third of eligible patients to the study. In addition, the authors note that missed patients had a lower rate of UTI compared with enrolled patients.
Although this study design prohibits generalization to patient care areas outside the emergency department, the findings can assist the hospitalist in the evaluation of the febrile infant during RSV season and potentially guide decisions regarding empiric antibiotic therapy as part of evaluations to diagnose or exclude serious bacterial infection. Additionally, this study raises the question of need for better methods of urinalysis for febrile, uncircumcised male infants.
Back to the Basics: A Clinical Approach to Excluding Acute Appendicitis
Review by Jane G. Buss, MD
Kharbanda AB, Taylor GA, Fishman SJ, et al. A clinical decision rule to identify children at low risk for appendicitis. Pediatrics. 2005;116(3):709-16.
Appendicitis is the most common condition requiring emergency abdominal surgery in the pediatric population. To diagnosis appendicitis, clinicians typically utilize clinical findings, imaging studies, and laboratory testing. The use of clinical scoring systems to improve the diagnosis of appendicitis in children has been limited, mostly resulting from unacceptably low sensitivities/specificities, or the lack of validation. The use of CT scan to aid in the evaluation of children with appendicitis has become widespread. Concerns remain, however, regarding long-term radiation effects and increased healthcare costs associated with this approach.
The authors of this study sought to develop clinical scores for children to predict which of those with acute abdominal pain do not have appendicitis. Additionally, they hoped to lessen the use of CT scanning. Their goal was to identify those groups of children who have significant abdominal pain without appendicitis who could be safely observed without CT scan or possible surgery.
This prospective cohort study enrolled 601 eligible children ages three to 18 with suspected appendicitis who presented to the emergency department over a 15-month period. Two low-risk clinical decision rules were developed using logistic regression and recursive partitioning. Using logistic regression, six factors were identified from analysis of 425 patients in the derivation set significantly associated with an increased likelihood of appendicitis. The score components include:
- Nausea (2 points);
- History of focal right lower quadrant pain (RLQ) (2 points);
- Migration of pain (1 point);
- Difficulty walking (1 point);
- Rebound tenderness (2 points); and
- Absolute neutrophil count (ANC) >6.75 x 103/uL (6 points).
When tested with data from the 176 patients in the validation set, a score of less than or equal to five had a sensitivity of 96.3%, and a negative predictive value of 95.6% for excluding appendicitis.
The authors then derived a second clinical low-risk decision rule by recursive partitioning. They determined that a combination of ANC <6.75 X 10 to the third/microliter, absence of nausea (or emesis or anorexia), and absence of maximal tenderness in the RLQ essentially excluded appendicitis in the derivation and validation groups. This rule had a sensitivity of 98.1%, and a negative predictive value of 97.5%.
In summary, these authors derived two clinical decision rules giving the clinician the option of a clinical score (logistic regression) or a decision tree (recursive partitioning) to identify children at low risk for appendicitis. Their findings suggest application of either low-risk rule would lead to decreased reliance on CT scan. Applying these clinical rules to their patients could have reduced the rate of CT scan by 20%. They conclude that pediatric patients who have suspected appendicitis and are at low risk by either model should be considered for observation rather than undergo CT scan or operative care.
Epidemiology of Fungal Infection in the Tertiary Care Inpatient Setting
Review by Brandan P. Kennedy, MD
Abelson, JA, Moore T, Bruckner D, et al. Frequency of fungemia in hospitalized pediatric inpatients over 11 years at a tertiary care institution. Pediatrics. 2005;116(1):611-617.
Fungal organisms are relatively uncommon causes of blood infections in the pediatric population. When they do occur, they cause significant morbidity and mortality. The incidence of fungal blood infections appears to be rising at a faster rate than that of other pathogens. Authors from the University of California performed this study to describe those rate changes, and to evaluate whether treatment has improved in the past 11 years.
This retrospective cohort study involved children admitted to Mattel Children’s Hospital in Los Angeles, California, during an 11-year period from January 1991 to December 2001. Information obtained on all positive fungal cultures from all body sites included date and site of culture, demographics, and fungal etiology. Additionally, data regarding underlying illness, hospital course, outcome, and antimicrobial treatment were considered.
Study results demonstrated a significant increase in diagnosed fungemia in children. There was a 15% increase in overall pediatric admissions in the study period, and a 23% increase in positive fungal cultures in the same period. Of 272 blood cultures, 97 were positive for fungus. Although this is a relatively small number of total infections, data demonstrated a 91% increase in fungemia during the study period. Candida species were the organisms most frequently isolated from any body site with 85% of the total isolates. Of the total positive isolates, it appeared that approximately 78% reflected colonization as opposed to infection.
Outcomes for fungal infections improved only marginally in the study period. Fifty percent of patients with fungemia died between 1991 and 1996, and 45% died between 1997 and 2001. The mortality rate for immunocompromised conditions was 57%. The cost effectiveness of fungal screening cultures was also evaluated, which demonstrated that fungal cultures identified 14 patients independent of bacterial blood cultures at a cost of $560,000, which resulted in a cost of $40,000 per identified patient.
The study reaches several significant conclusions. First there has been a significant increase in fungal infections that exceeds the increase in overall pediatric hospital admissions. However, it is important to recognize the increase in immunocompromised conditions during the study period, which may account for the higher incidence of fungemia.
Second the addition of fungal blood cultures to bacterial blood cultures as part of a routine workup for febrile patients appeared to yield limited clinical information at a very high cost. Third this study highlights the serious threat fungal infections pose to immunocompromised hosts who have a significantly higher incidence of infection, as well as higher morbidity and mortality. Fourth the use of broad spectrum antibiotics may be increasing fungal colonization in patients and consequently increasing the risk for pathologic fungal infection. Finally morbidity and mortality rates for fungal infections did not greatly improve, despite significant improvements in supportive care made during the study period
This study demonstrates a need for better diagnostic markers for fungal infections, especially those that might provide earlier detection and diagnosis at less cost. The importance of judicious use of antibiotics is underscored while the need for a broader base of therapeutic agents is highlighted. These issues may be key ingredients needed to reduce adverse outcomes from fungal infections, especially in the immunocompromised host.
Rotavirus Vaccine Revisited
Salinas B, Perez Schael I, Linhares AC, et al. Evaluation of safety, immunogenicity and efficacy of an attenuated rotavirus vaccine, RIX4414. Ped Infect Dis J. 2005;24(9):807-816.
Rotavirus is the leading cause of severe gastroenteritis among children worldwide. In the United States, rotavirus is responsible for approximately 5%-10% of all diarrhea among children older than five and accounts for approximately 50,000 hospitalizations each year. An estimated one in 200,000 children with rotavirus diarrhea dies from complications of infection. The immunizing effect of rotavirus infection stimulated the development of live attenuated vaccines. In 1998, a three-dose regimen of a tetravalent rhesus-human reassortant vaccine (RotaShield: Wyeth Laboratories,) was licensed for infant immunization in the United States. Within the first year of use, it was withdrawn due to an observed risk of intussusception. The current study was designed to evaluate immunogenicity and efficacy of a live attenuated monovalent human rotavirus vaccine, RIX4414.
A double-blind, randomized, placebo-controlled design was utilized with the RIX4414 rotavirus vaccine administered at three different virus concentrations. Infants were randomly assigned to one of the three study groups or the placebo group. Infants in the vaccine groups received two oral doses of the vaccine at the age of two and four months. An identical placebo containing the same constituents as the vaccine except for the vaccine virus was used as the control. The vaccine was given concomitantly with other routine vaccinations. To determine immunogenicity, blood samples were obtained from all infants immediately before the first vaccination to exclude previous rotavirus infection. Blood samples were obtained two months after the first second vaccine doses and again at one year to measure anti-rotavirus IgA antibodies. Additionally, stool was obtained from 25% of the study sample and tested for rotavirus viral shedding, with differentiation between wild type and vaccine also being performed.
There were 2,155 infants enrolled in this study from three countries in South America, allowing for slightly more than 500 infants in each group. The study began in May 2001, and the final one-year follow-up was completed in April 2003. The anti-rotavirus IgA seroconversion rates two months after first and second doses were 38%-43% and 61%-65%, respectively. This compared with a 5.3% seroconversion rate in the control group, which was determined to be a wild type virus. Vaccine take after two doses was shown in all three vaccine study groups, ranging from 65% to 75% for the lowest to highest vaccine concentration groups. Reactogenicity and safety was evaluated by monitoring incidences of fever, diarrhea, vomiting, irritability, and loss of appetite during the 15 days after vaccine administration. The results were similar for the four study groups suggesting no significant reactogenicity. There were 220 serious adverse events reported including one intussusception. However, none of these events was determined to be related to the vaccine. The RIX4414 vaccine was demonstrated to effectively protect against severe gastroenteritis caused by G1 type rotavirus and also was shown to provide some cross protection to other serotypes.
This well-designed study demonstrated a statistically significant reduction in gastroenteritis due to rotavirus infection, especially of the predominant G1 serotype, after two doses of the RIX4414 human rotavirus vaccine. Objective measures of viral shedding and IgA seroconversion support the efficacy of the vaccine. This study provided a large sample population with good controls.
An important and possibly confounding variable not addressed by the study was breastfeeding status of the infants. There is clinical evidence demonstrating the protective properties of secretory IgA in human milk against rotavirus infection, and this could have influenced the observed severity of disease in the sample population. It would have been interesting to isolate breastfeeding status as a study variable and note any effect on the results of the study.
Aside from this observation, this study appears to show a promising new oral rotavirus vaccine. As further research on the RIX4414 vaccine continues, there is hope that this vaccine could make a significant positive impact on morbidity and hospitalization rates for rotavirus infections worldwide. TH
Say What?
Mack Lipkin, MD, the founding president of the American Academy on Physician and Patient, a society dedicated to research, education, and professional standards in patient-physician communication, reported some interesting data in a PowerPoint presentation he gave in 2000 at the working conference on Diversity and Communication in Healthcare sponsored in part by the U.S. Office of Minority Health. Dr. Lipkin said that physicians’ lowest level of communication skills are reached during their medical residencies; even medical students’ skills were rated higher. Dr. Lipkin, who is also director of the Division of Primary Care in the Department of Medicine at New York University School of Medicine, New York City, went on to explain that, typically, physicians will recover some capacity with communication as they enter practice and years of experience ensue, but they never reach the level they possessed before they entered medical school.
While some hospitalists may consider this a startling claim, few are likely to find it shocking. Although hospitalists believe using good communication skills is an important part of their work, their skills may not necessarily match their beliefs or intentions. Research in progress by hospitalist Paul Mueller, MD, and his colleagues at the Mayo Clinic College of Medicine, Rochester, Minn., reveals that a majority of new internal medicine faculty—regardless of years in practice or background—believe they could benefit from and desire additional training in communication; yet these individuals teach communication skills to medical students (personal communication, 2005).
Medical education curriculum experts nationwide are pumping up their coverage of physician-patient communication to supply the demand stemming from a surge of interest in this topic in recent decades. Some reasons for this include reports and investigations into medical errors, an explosion of medical and health information easily accessible to patients and families, the rise of a vital consumer advocacy and empowerment movement, the reliance on outcomes assessments that include patient satisfaction ratings, a growing emphasis on patient- or relationship-centered care, and the reduced time for medical encounters caused at least in part by cost-containment initiatives.
The relationship between communication and medical outcomes is being increasingly explored, including the effects on physician satisfaction.1-5 But what are the further, personal effects to the individual hospitalist when he or she perpetuates poor communication skills?
—Robert Trowbridge, MD
Communication With Patients And Families
The work of hospitalists depends acutely on communication.
“It’s part of the role of the hospitalist to explain and help shepherd [patients] through the healthcare system,” says Robert Trowbridge, MD, a hospitalist and assistant professor of medicine, University of Vermont College of Medicine, Maine Medical Center, Portland.
Professionals whose medical practice is based on short clinical visits or performing procedures may or may not be good communicators, but it’s probably not as integral to the way they or the situations their patients are going through will be perceived. The conventional wisdom in professional and lay circles tends to be, “He may be a lousy communicator, but he’s a hellava surgeon,” says Dr. Trowbridge.
But most patients expect good communication from their primary care physician and because they are serving that function when a patient is hospitalized, hospitalists should understand that patients and families expect those skills of them. “And if the [hospitalists] don’t do well [in communicating], there can be much more stress on the patients and physicians,” explains Dr. Trowbridge.
What Constitutes Poor Communication?
“First, on one level, poor communication skills are inefficient in talking with patients,” says Steven Pantilat, MD, SHM president. “So, I think it makes your work harder.”
Some examples of communication inefficiency (or ineffectiveness) for a clinician include:2,4,5,6-8
- Lacking the ability to articulate ideas adequately;
- Transferring insufficient information between the provider and the patient, including inadequate elicitation of key facts from the patient;
- Failing to assess the current level of information before supplying new information;
- Taking too much or too little time in regard to the needs of the situation;
- Overusing medical terms and not recognizing when patients cannot decipher them;
- Using little eye contact and appropriate touch;
- Using closed body language;
- Being inattentive to the patient’s body language;
- Using inappropriately open or closed questions when the circumstance calls for the opposite;
- Not using a patient’s own words when doing so would be helpful to diagnosis or management;
- Exhibiting a lack of empathy, compassion, understanding, and support;
- Being inattentive or insensitive to a patient’s feelings;
- Being inattentive to cognitive, psychosocial, and affective needs;
- Disregarding the need for shared decision-making;
- Lacking the skill for or failing to use active listening;
- Failing to use timeliness in feedback or reporting test results;
- Neglecting to seek feedback regarding whether cultural, regional, or language/accent differences (both the doctor’s and the patient’s) impede communication; or
- Using an angry, anxious, or dominant tone of voice.
The second effect of poor communication that Dr. Pantilat cites is that “patients are less satisfied with their care and … to the extent that the relationship with the physician actually has an impact on how patients feel, patients may not ‘get better,’ ” he says. “And I don’t mean, for instance, that with a patient who has pneumonia, their pneumonia won’t get better; but there are a lot of other conditions where feeling like someone is listening to you, feeling like you’ve been heard, feeling like someone has communicated clearly can make you feel better.”7 (See also The Hospitalist, “Patient Satisfaction: The Hospitalist’s Role,” July/August 2005.)8
Inpatient communication tends to be a different kind of communication than that used in some other medical settings—more intense in a shorter time period and conducted between people who are strangers at the time of the patient’s admission. “It’s not that the stakes are higher, but it’s actually just the intensity of it is different,” says Arpana Vidyarthi, MD, a hospitalist who is the director of quality inpatient medicine at the University of California, San Francisco Medical Center.
“Time constraints are a major reason for poor communication skills happening,” says Dr. Trowbridge, whose hospitalist practice involves 60% clinical work with the Maine Hospitalist Group and 40% administrative work involving medical students and faculty development with the Department of Medicine at Maine Medical Center. “Relationships are really what many physicians most enjoy in medicine: with colleagues, … with patients, … with families. Having poor communication skills has a huge impact on job satisfaction and then personal satisfaction,” in many instances because of the heightened levels of stress.
“People are not here because they’re trying to get their lipids down,” says Dr. Vidyarthi. “They’re here because they’re [acutely ill]. When people are very, very ill, or when they’re having an intense experience, they tend to hang on every word.”
For the physician, she says, “there are so many things to communicate and because it is often very complicated, the relationship and the trust have to be built quickly, and information has to be transferred very quickly. Poor communication will lead to potentially not being able to build that alliance with the patient during that short period of time of their hospital experience.”
Hospitalists must be on the lookout for how the constraints of time affect the way they practice and relate to their patients because every nuance of behavior or tone of voice can make a difference to how a patient perceives his or her doctor.
For example, in a study conducted at Harvard University in 2002, investigators used audiotapes of 57 surgeons, 36 of whom had had two or more malpractice claims filed against them.9 Patients were asked to listen to two 20-second clips of audio between these surgeons and two patients. Those surgeons who were judged by the tone of their voices as “high dominance” and “low concern/anxiety” correlated with those who had had previous malpractice claims.
Because there is no continuity of relationship to help steady what might be an emotional response when things go wrong in the patient’s treatment or when patients and families are upset by circumstances, hospitalists may be subjected to blame, resentment, fear, and displaced anger concerning their communications with patients and families.
“Especially if you’re harried in an incredible time crunch, if you don’t [communicate] with patients and patient families [about] what is going on [in their care], those relationships very quickly can turn antagonistic,” says Dr. Trowbridge. “And then the very thing most of us like about medicine—relationships with patients and families—becomes something that people tend to avoid.”
Dr. Trowbridge says that this can become somewhat of a vicious cycle whereby a certain extent of inadvertently “avoiding the patient and family may lead to further communication faults.” On the flip side, using good communication can be a circular process but in a positive way: A good communicator may experience better well-being, which in turn, leads to better communication skills.2,5 Also, on a practical level, the data are clear that bad communication puts you at risk for malpractice litigation.9,10
Communication with Colleagues
“People that don’t have very good communication skills tend not to be successful,” says Dr. Vidyarthi, who practices with the hospitalist group at UCSF and is also an assistant professor there. Her definition of success is closely linked to the quality of relationships; that is, “being well liked by the nurses, building working relationships with … the nurses,” as well as others, including the hospital administrator. “Hospitalists are almost always … doing quality work or performance improvement,” she explained. “They’re on committees. That is the nature of what we do. … Not learning what those [communication skills] are and [not] being able to communicate at [effective] levels would … be a detriment to one’s personal job advancement, but absolutely to one’s job satisfaction as well.”
Collegiality, in fact, is one component cited as a “powerful engine of socialization” in organizational structures more likely to foster the lifelong learning and commitment that are inherent to medical professionalism.1,3-5,11,12
Many of the components of effective communication with colleagues parallel those that are best used with patients. “Communication is what holds that team together,” says Dr. Vidyarthi, whose interests include information transfer and communication as a form for team-building. “In academic medicine, poor communication can impact the teaching environment, the experience of the students and the residents, and that team cohesion. And that can lead to poor patient care, it can definitely lead to a poor educational experience, and it is not enjoyable, so job satisfaction suffers.”
Dr. Pantilat, who is associate professor of clinical medicine and director, Palliative Care Service and Palliative Care Leadership Center at UCSF, theorizes that when interacting with colleagues such as other hospitalists and physicians, nurses, social workers, case managers, and pharmacists, poor communication skills can make the physician’s work tougher. “Poor communication makes your life difficult with your colleagues,” says Dr. Pantilat. “People don’t like talking to you or interacting with you … and your job can generally be more difficult.”
Post-Discharge Communication
In the traditional medical model, a primary care physician would see patients in her/his office, the hospital, or rehabilitation. With the expansion in hospital medicine, patients are now “handed off” and seen by a number of providers. Hand-off fumbles can mean critical information may be lost, leading to poorer outcomes and greater readmission rates.13-15
Forging and maintaining effective communication with colleagues following the discharge of patients is an area where few in-house physicians do well, says Dr. Vidyarthi, who has it on her agenda to tackle this “huge problem” for her institution in the coming year. There are two pieces to that problem, she says. One is to accurately identify the patients’ primary care physicians and the other is to make contact with them.
“You could page them, but they’re in clinic, and they can’t take five minutes out when you can’t take five minutes out,” says Dr. Vidyarthi. “The communication with the primary care physician is actually a field in and of itself.”15
Part of her plan is to devise some means of “physician-independent generated communication,” perhaps a letter or e-mail sent from the hospital to report to a primary care physician that his/her patient has been admitted to the hospital.
“That raises a flag to that primary so they can try to find the hospitalist, which is usually very easy … because we’re always in the hospital,” says Dr. Vidyarthi. “And it’s the first stage of the communication: Now that person is aware. If I can find them, if I can access them, they’ll be able to take that time out, because they know their patient’s there.”
In her work as a senior fellow at the Center for Health Professions at UCSF, Dr. Vidyarthi strives to “embed communication into the larger framework of organizational change.” And what does a hospitalist do if an institution’s post-discharge communications system is not up to par? There are three basic things you can do to help overcome this source of frustration, she says. The first is to continually build relationships with primary care providers.
“If I send an e-mail to somebody and they know who I am, they are much more likely to respond to that because they know me,” says Dr. Vidyarthi.
Next, find a system that works for you. “Don’t wait for the rest of the systems to be put in place,” she says. “This is about personal practice. And if that means you take five minutes in the morning to send an e-mail or five minutes in the evening, whatever it is, find [a system] that really works and figure out a way to evaluate it.”
A good way to do this, Dr. Vidyarthi suggests, is to take a quick survey in the midst of talking to that primary care physician to ask whether the medium, content, and timing that you used to contact him/her worked well.
“Then,” she says, “if you have five primaries that you talked to [who] maybe said, ‘Yes, that was helpful to me,’ or ‘Not so much really, I had all that info already,’ at least you have data. Asking ‘Do you think this will help your patients when they come to see you in the office?’ is a great question [to solidify] performance improvement. In other words, find out if what you’re doing is being effective.”
The final step to overcome a lack of an effective institutional system for post-discharge communication is to share what you’ve learned with others. “These little pieces can really empower others to make a difference,” says Dr. Vidyarthi. “Trying to change and overhaul an entire system will turn off even the most motivated of people who want to improve the system, so focus on your own personal practice models. Change it, figure out what works, and then try to disseminate it. That makes it feel and seem much more doable.”
Conclusion
Hospitalists who exercise poor communication skills with patients, families, and colleagues can experience multiple negative effects, including poor patient-related outcomes and an increased risk of malpractice litigation. Personally, consistently using poor communication may make work more difficult, reduce job satisfaction, and reduce work success and enjoyment with hospital teams and primary care physicians. TH
Contributor Andrea Sattinger makes good communication a priority every day.
References
- Finset KB, Gude T, Hem E, et al. Which young physicians are satisfied with their work? A prospective nationwide study in Norway. BMC Med Educ. 2005;5:19.
- Roter DL, Stewart M, Putnam SM, et al. Communication patterns of primary care physicians. JAMA. 1997;277:350-356.
- Konrad TR, Williams ES, Linzer M, et al. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Measuring physician job satisfaction in a changing workplace and a challenging environment. Med Care. 1999;37:1174-1182.
- Shanafelt TD, West C, Zhao X, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005;20:559-564.
- Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114:513-519.
- Novack DH, Suchman AL, Clark W, et al. Calibrating the physician. Personal awareness and effective patient care. Working Group on Promoting Physician Personal Awareness, American Academy on Physician and Patient. JAMA. 1997;278:502-509.
- Greenfield S, Kaplan S, Ware WE Jr. Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med. 1985;102:520-528.
- Torcson PJ. Patient satisfaction: the hospitalist’s role. The Hospitalist. 2005;July/Aug:27-30.
- Ambady N, LaPlante D, Nguyen T. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132:5-9.
- Levinson W, Roter DL, Mullooly JP. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277:553-559.
- Frankford DM, Patterson MA, Konrad TR. Transforming practice organizations to foster lifelong learning and commitment to medical professionalism. Acad Med. 2000;75:708-17.
- Falkum E, Vaglum P. The relationship between interpersonal problems and occupational stress in physicians. Gen Hosp Psychiatry. 2005;27:285-291.
- Coleman EA, Smith JD, Min SJ, et al. Post-hospital medicine discrepancies; prevalence, types, and contributing factors. Paper presented at the Society of Hospital Medicine Annual Meeting; April 29-30; Chicago, Illinois: Society of Hospital Medicine 2005.
- Burniske GM, Burnett A, Greenwald J, et al. Post-discharge follow-up telephone call by a pharmacist and impact on patient care. Paper presented at the Society of Hospital Medicine Annual Meeting. April 29-30; Chicago.
- Wachter R, Shojania K. Internal Bleeding: The Truth Behind America's Terrifying Epidemic of Medical Mistakes. New York, NY: Rugged Land; 2004.
Mack Lipkin, MD, the founding president of the American Academy on Physician and Patient, a society dedicated to research, education, and professional standards in patient-physician communication, reported some interesting data in a PowerPoint presentation he gave in 2000 at the working conference on Diversity and Communication in Healthcare sponsored in part by the U.S. Office of Minority Health. Dr. Lipkin said that physicians’ lowest level of communication skills are reached during their medical residencies; even medical students’ skills were rated higher. Dr. Lipkin, who is also director of the Division of Primary Care in the Department of Medicine at New York University School of Medicine, New York City, went on to explain that, typically, physicians will recover some capacity with communication as they enter practice and years of experience ensue, but they never reach the level they possessed before they entered medical school.
While some hospitalists may consider this a startling claim, few are likely to find it shocking. Although hospitalists believe using good communication skills is an important part of their work, their skills may not necessarily match their beliefs or intentions. Research in progress by hospitalist Paul Mueller, MD, and his colleagues at the Mayo Clinic College of Medicine, Rochester, Minn., reveals that a majority of new internal medicine faculty—regardless of years in practice or background—believe they could benefit from and desire additional training in communication; yet these individuals teach communication skills to medical students (personal communication, 2005).
Medical education curriculum experts nationwide are pumping up their coverage of physician-patient communication to supply the demand stemming from a surge of interest in this topic in recent decades. Some reasons for this include reports and investigations into medical errors, an explosion of medical and health information easily accessible to patients and families, the rise of a vital consumer advocacy and empowerment movement, the reliance on outcomes assessments that include patient satisfaction ratings, a growing emphasis on patient- or relationship-centered care, and the reduced time for medical encounters caused at least in part by cost-containment initiatives.
The relationship between communication and medical outcomes is being increasingly explored, including the effects on physician satisfaction.1-5 But what are the further, personal effects to the individual hospitalist when he or she perpetuates poor communication skills?
—Robert Trowbridge, MD
Communication With Patients And Families
The work of hospitalists depends acutely on communication.
“It’s part of the role of the hospitalist to explain and help shepherd [patients] through the healthcare system,” says Robert Trowbridge, MD, a hospitalist and assistant professor of medicine, University of Vermont College of Medicine, Maine Medical Center, Portland.
Professionals whose medical practice is based on short clinical visits or performing procedures may or may not be good communicators, but it’s probably not as integral to the way they or the situations their patients are going through will be perceived. The conventional wisdom in professional and lay circles tends to be, “He may be a lousy communicator, but he’s a hellava surgeon,” says Dr. Trowbridge.
But most patients expect good communication from their primary care physician and because they are serving that function when a patient is hospitalized, hospitalists should understand that patients and families expect those skills of them. “And if the [hospitalists] don’t do well [in communicating], there can be much more stress on the patients and physicians,” explains Dr. Trowbridge.
What Constitutes Poor Communication?
“First, on one level, poor communication skills are inefficient in talking with patients,” says Steven Pantilat, MD, SHM president. “So, I think it makes your work harder.”
Some examples of communication inefficiency (or ineffectiveness) for a clinician include:2,4,5,6-8
- Lacking the ability to articulate ideas adequately;
- Transferring insufficient information between the provider and the patient, including inadequate elicitation of key facts from the patient;
- Failing to assess the current level of information before supplying new information;
- Taking too much or too little time in regard to the needs of the situation;
- Overusing medical terms and not recognizing when patients cannot decipher them;
- Using little eye contact and appropriate touch;
- Using closed body language;
- Being inattentive to the patient’s body language;
- Using inappropriately open or closed questions when the circumstance calls for the opposite;
- Not using a patient’s own words when doing so would be helpful to diagnosis or management;
- Exhibiting a lack of empathy, compassion, understanding, and support;
- Being inattentive or insensitive to a patient’s feelings;
- Being inattentive to cognitive, psychosocial, and affective needs;
- Disregarding the need for shared decision-making;
- Lacking the skill for or failing to use active listening;
- Failing to use timeliness in feedback or reporting test results;
- Neglecting to seek feedback regarding whether cultural, regional, or language/accent differences (both the doctor’s and the patient’s) impede communication; or
- Using an angry, anxious, or dominant tone of voice.
The second effect of poor communication that Dr. Pantilat cites is that “patients are less satisfied with their care and … to the extent that the relationship with the physician actually has an impact on how patients feel, patients may not ‘get better,’ ” he says. “And I don’t mean, for instance, that with a patient who has pneumonia, their pneumonia won’t get better; but there are a lot of other conditions where feeling like someone is listening to you, feeling like you’ve been heard, feeling like someone has communicated clearly can make you feel better.”7 (See also The Hospitalist, “Patient Satisfaction: The Hospitalist’s Role,” July/August 2005.)8
Inpatient communication tends to be a different kind of communication than that used in some other medical settings—more intense in a shorter time period and conducted between people who are strangers at the time of the patient’s admission. “It’s not that the stakes are higher, but it’s actually just the intensity of it is different,” says Arpana Vidyarthi, MD, a hospitalist who is the director of quality inpatient medicine at the University of California, San Francisco Medical Center.
“Time constraints are a major reason for poor communication skills happening,” says Dr. Trowbridge, whose hospitalist practice involves 60% clinical work with the Maine Hospitalist Group and 40% administrative work involving medical students and faculty development with the Department of Medicine at Maine Medical Center. “Relationships are really what many physicians most enjoy in medicine: with colleagues, … with patients, … with families. Having poor communication skills has a huge impact on job satisfaction and then personal satisfaction,” in many instances because of the heightened levels of stress.
“People are not here because they’re trying to get their lipids down,” says Dr. Vidyarthi. “They’re here because they’re [acutely ill]. When people are very, very ill, or when they’re having an intense experience, they tend to hang on every word.”
For the physician, she says, “there are so many things to communicate and because it is often very complicated, the relationship and the trust have to be built quickly, and information has to be transferred very quickly. Poor communication will lead to potentially not being able to build that alliance with the patient during that short period of time of their hospital experience.”
Hospitalists must be on the lookout for how the constraints of time affect the way they practice and relate to their patients because every nuance of behavior or tone of voice can make a difference to how a patient perceives his or her doctor.
For example, in a study conducted at Harvard University in 2002, investigators used audiotapes of 57 surgeons, 36 of whom had had two or more malpractice claims filed against them.9 Patients were asked to listen to two 20-second clips of audio between these surgeons and two patients. Those surgeons who were judged by the tone of their voices as “high dominance” and “low concern/anxiety” correlated with those who had had previous malpractice claims.
Because there is no continuity of relationship to help steady what might be an emotional response when things go wrong in the patient’s treatment or when patients and families are upset by circumstances, hospitalists may be subjected to blame, resentment, fear, and displaced anger concerning their communications with patients and families.
“Especially if you’re harried in an incredible time crunch, if you don’t [communicate] with patients and patient families [about] what is going on [in their care], those relationships very quickly can turn antagonistic,” says Dr. Trowbridge. “And then the very thing most of us like about medicine—relationships with patients and families—becomes something that people tend to avoid.”
Dr. Trowbridge says that this can become somewhat of a vicious cycle whereby a certain extent of inadvertently “avoiding the patient and family may lead to further communication faults.” On the flip side, using good communication can be a circular process but in a positive way: A good communicator may experience better well-being, which in turn, leads to better communication skills.2,5 Also, on a practical level, the data are clear that bad communication puts you at risk for malpractice litigation.9,10
Communication with Colleagues
“People that don’t have very good communication skills tend not to be successful,” says Dr. Vidyarthi, who practices with the hospitalist group at UCSF and is also an assistant professor there. Her definition of success is closely linked to the quality of relationships; that is, “being well liked by the nurses, building working relationships with … the nurses,” as well as others, including the hospital administrator. “Hospitalists are almost always … doing quality work or performance improvement,” she explained. “They’re on committees. That is the nature of what we do. … Not learning what those [communication skills] are and [not] being able to communicate at [effective] levels would … be a detriment to one’s personal job advancement, but absolutely to one’s job satisfaction as well.”
Collegiality, in fact, is one component cited as a “powerful engine of socialization” in organizational structures more likely to foster the lifelong learning and commitment that are inherent to medical professionalism.1,3-5,11,12
Many of the components of effective communication with colleagues parallel those that are best used with patients. “Communication is what holds that team together,” says Dr. Vidyarthi, whose interests include information transfer and communication as a form for team-building. “In academic medicine, poor communication can impact the teaching environment, the experience of the students and the residents, and that team cohesion. And that can lead to poor patient care, it can definitely lead to a poor educational experience, and it is not enjoyable, so job satisfaction suffers.”
Dr. Pantilat, who is associate professor of clinical medicine and director, Palliative Care Service and Palliative Care Leadership Center at UCSF, theorizes that when interacting with colleagues such as other hospitalists and physicians, nurses, social workers, case managers, and pharmacists, poor communication skills can make the physician’s work tougher. “Poor communication makes your life difficult with your colleagues,” says Dr. Pantilat. “People don’t like talking to you or interacting with you … and your job can generally be more difficult.”
Post-Discharge Communication
In the traditional medical model, a primary care physician would see patients in her/his office, the hospital, or rehabilitation. With the expansion in hospital medicine, patients are now “handed off” and seen by a number of providers. Hand-off fumbles can mean critical information may be lost, leading to poorer outcomes and greater readmission rates.13-15
Forging and maintaining effective communication with colleagues following the discharge of patients is an area where few in-house physicians do well, says Dr. Vidyarthi, who has it on her agenda to tackle this “huge problem” for her institution in the coming year. There are two pieces to that problem, she says. One is to accurately identify the patients’ primary care physicians and the other is to make contact with them.
“You could page them, but they’re in clinic, and they can’t take five minutes out when you can’t take five minutes out,” says Dr. Vidyarthi. “The communication with the primary care physician is actually a field in and of itself.”15
Part of her plan is to devise some means of “physician-independent generated communication,” perhaps a letter or e-mail sent from the hospital to report to a primary care physician that his/her patient has been admitted to the hospital.
“That raises a flag to that primary so they can try to find the hospitalist, which is usually very easy … because we’re always in the hospital,” says Dr. Vidyarthi. “And it’s the first stage of the communication: Now that person is aware. If I can find them, if I can access them, they’ll be able to take that time out, because they know their patient’s there.”
In her work as a senior fellow at the Center for Health Professions at UCSF, Dr. Vidyarthi strives to “embed communication into the larger framework of organizational change.” And what does a hospitalist do if an institution’s post-discharge communications system is not up to par? There are three basic things you can do to help overcome this source of frustration, she says. The first is to continually build relationships with primary care providers.
“If I send an e-mail to somebody and they know who I am, they are much more likely to respond to that because they know me,” says Dr. Vidyarthi.
Next, find a system that works for you. “Don’t wait for the rest of the systems to be put in place,” she says. “This is about personal practice. And if that means you take five minutes in the morning to send an e-mail or five minutes in the evening, whatever it is, find [a system] that really works and figure out a way to evaluate it.”
A good way to do this, Dr. Vidyarthi suggests, is to take a quick survey in the midst of talking to that primary care physician to ask whether the medium, content, and timing that you used to contact him/her worked well.
“Then,” she says, “if you have five primaries that you talked to [who] maybe said, ‘Yes, that was helpful to me,’ or ‘Not so much really, I had all that info already,’ at least you have data. Asking ‘Do you think this will help your patients when they come to see you in the office?’ is a great question [to solidify] performance improvement. In other words, find out if what you’re doing is being effective.”
The final step to overcome a lack of an effective institutional system for post-discharge communication is to share what you’ve learned with others. “These little pieces can really empower others to make a difference,” says Dr. Vidyarthi. “Trying to change and overhaul an entire system will turn off even the most motivated of people who want to improve the system, so focus on your own personal practice models. Change it, figure out what works, and then try to disseminate it. That makes it feel and seem much more doable.”
Conclusion
Hospitalists who exercise poor communication skills with patients, families, and colleagues can experience multiple negative effects, including poor patient-related outcomes and an increased risk of malpractice litigation. Personally, consistently using poor communication may make work more difficult, reduce job satisfaction, and reduce work success and enjoyment with hospital teams and primary care physicians. TH
Contributor Andrea Sattinger makes good communication a priority every day.
References
- Finset KB, Gude T, Hem E, et al. Which young physicians are satisfied with their work? A prospective nationwide study in Norway. BMC Med Educ. 2005;5:19.
- Roter DL, Stewart M, Putnam SM, et al. Communication patterns of primary care physicians. JAMA. 1997;277:350-356.
- Konrad TR, Williams ES, Linzer M, et al. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Measuring physician job satisfaction in a changing workplace and a challenging environment. Med Care. 1999;37:1174-1182.
- Shanafelt TD, West C, Zhao X, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005;20:559-564.
- Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114:513-519.
- Novack DH, Suchman AL, Clark W, et al. Calibrating the physician. Personal awareness and effective patient care. Working Group on Promoting Physician Personal Awareness, American Academy on Physician and Patient. JAMA. 1997;278:502-509.
- Greenfield S, Kaplan S, Ware WE Jr. Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med. 1985;102:520-528.
- Torcson PJ. Patient satisfaction: the hospitalist’s role. The Hospitalist. 2005;July/Aug:27-30.
- Ambady N, LaPlante D, Nguyen T. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132:5-9.
- Levinson W, Roter DL, Mullooly JP. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277:553-559.
- Frankford DM, Patterson MA, Konrad TR. Transforming practice organizations to foster lifelong learning and commitment to medical professionalism. Acad Med. 2000;75:708-17.
- Falkum E, Vaglum P. The relationship between interpersonal problems and occupational stress in physicians. Gen Hosp Psychiatry. 2005;27:285-291.
- Coleman EA, Smith JD, Min SJ, et al. Post-hospital medicine discrepancies; prevalence, types, and contributing factors. Paper presented at the Society of Hospital Medicine Annual Meeting; April 29-30; Chicago, Illinois: Society of Hospital Medicine 2005.
- Burniske GM, Burnett A, Greenwald J, et al. Post-discharge follow-up telephone call by a pharmacist and impact on patient care. Paper presented at the Society of Hospital Medicine Annual Meeting. April 29-30; Chicago.
- Wachter R, Shojania K. Internal Bleeding: The Truth Behind America's Terrifying Epidemic of Medical Mistakes. New York, NY: Rugged Land; 2004.
Mack Lipkin, MD, the founding president of the American Academy on Physician and Patient, a society dedicated to research, education, and professional standards in patient-physician communication, reported some interesting data in a PowerPoint presentation he gave in 2000 at the working conference on Diversity and Communication in Healthcare sponsored in part by the U.S. Office of Minority Health. Dr. Lipkin said that physicians’ lowest level of communication skills are reached during their medical residencies; even medical students’ skills were rated higher. Dr. Lipkin, who is also director of the Division of Primary Care in the Department of Medicine at New York University School of Medicine, New York City, went on to explain that, typically, physicians will recover some capacity with communication as they enter practice and years of experience ensue, but they never reach the level they possessed before they entered medical school.
While some hospitalists may consider this a startling claim, few are likely to find it shocking. Although hospitalists believe using good communication skills is an important part of their work, their skills may not necessarily match their beliefs or intentions. Research in progress by hospitalist Paul Mueller, MD, and his colleagues at the Mayo Clinic College of Medicine, Rochester, Minn., reveals that a majority of new internal medicine faculty—regardless of years in practice or background—believe they could benefit from and desire additional training in communication; yet these individuals teach communication skills to medical students (personal communication, 2005).
Medical education curriculum experts nationwide are pumping up their coverage of physician-patient communication to supply the demand stemming from a surge of interest in this topic in recent decades. Some reasons for this include reports and investigations into medical errors, an explosion of medical and health information easily accessible to patients and families, the rise of a vital consumer advocacy and empowerment movement, the reliance on outcomes assessments that include patient satisfaction ratings, a growing emphasis on patient- or relationship-centered care, and the reduced time for medical encounters caused at least in part by cost-containment initiatives.
The relationship between communication and medical outcomes is being increasingly explored, including the effects on physician satisfaction.1-5 But what are the further, personal effects to the individual hospitalist when he or she perpetuates poor communication skills?
—Robert Trowbridge, MD
Communication With Patients And Families
The work of hospitalists depends acutely on communication.
“It’s part of the role of the hospitalist to explain and help shepherd [patients] through the healthcare system,” says Robert Trowbridge, MD, a hospitalist and assistant professor of medicine, University of Vermont College of Medicine, Maine Medical Center, Portland.
Professionals whose medical practice is based on short clinical visits or performing procedures may or may not be good communicators, but it’s probably not as integral to the way they or the situations their patients are going through will be perceived. The conventional wisdom in professional and lay circles tends to be, “He may be a lousy communicator, but he’s a hellava surgeon,” says Dr. Trowbridge.
But most patients expect good communication from their primary care physician and because they are serving that function when a patient is hospitalized, hospitalists should understand that patients and families expect those skills of them. “And if the [hospitalists] don’t do well [in communicating], there can be much more stress on the patients and physicians,” explains Dr. Trowbridge.
What Constitutes Poor Communication?
“First, on one level, poor communication skills are inefficient in talking with patients,” says Steven Pantilat, MD, SHM president. “So, I think it makes your work harder.”
Some examples of communication inefficiency (or ineffectiveness) for a clinician include:2,4,5,6-8
- Lacking the ability to articulate ideas adequately;
- Transferring insufficient information between the provider and the patient, including inadequate elicitation of key facts from the patient;
- Failing to assess the current level of information before supplying new information;
- Taking too much or too little time in regard to the needs of the situation;
- Overusing medical terms and not recognizing when patients cannot decipher them;
- Using little eye contact and appropriate touch;
- Using closed body language;
- Being inattentive to the patient’s body language;
- Using inappropriately open or closed questions when the circumstance calls for the opposite;
- Not using a patient’s own words when doing so would be helpful to diagnosis or management;
- Exhibiting a lack of empathy, compassion, understanding, and support;
- Being inattentive or insensitive to a patient’s feelings;
- Being inattentive to cognitive, psychosocial, and affective needs;
- Disregarding the need for shared decision-making;
- Lacking the skill for or failing to use active listening;
- Failing to use timeliness in feedback or reporting test results;
- Neglecting to seek feedback regarding whether cultural, regional, or language/accent differences (both the doctor’s and the patient’s) impede communication; or
- Using an angry, anxious, or dominant tone of voice.
The second effect of poor communication that Dr. Pantilat cites is that “patients are less satisfied with their care and … to the extent that the relationship with the physician actually has an impact on how patients feel, patients may not ‘get better,’ ” he says. “And I don’t mean, for instance, that with a patient who has pneumonia, their pneumonia won’t get better; but there are a lot of other conditions where feeling like someone is listening to you, feeling like you’ve been heard, feeling like someone has communicated clearly can make you feel better.”7 (See also The Hospitalist, “Patient Satisfaction: The Hospitalist’s Role,” July/August 2005.)8
Inpatient communication tends to be a different kind of communication than that used in some other medical settings—more intense in a shorter time period and conducted between people who are strangers at the time of the patient’s admission. “It’s not that the stakes are higher, but it’s actually just the intensity of it is different,” says Arpana Vidyarthi, MD, a hospitalist who is the director of quality inpatient medicine at the University of California, San Francisco Medical Center.
“Time constraints are a major reason for poor communication skills happening,” says Dr. Trowbridge, whose hospitalist practice involves 60% clinical work with the Maine Hospitalist Group and 40% administrative work involving medical students and faculty development with the Department of Medicine at Maine Medical Center. “Relationships are really what many physicians most enjoy in medicine: with colleagues, … with patients, … with families. Having poor communication skills has a huge impact on job satisfaction and then personal satisfaction,” in many instances because of the heightened levels of stress.
“People are not here because they’re trying to get their lipids down,” says Dr. Vidyarthi. “They’re here because they’re [acutely ill]. When people are very, very ill, or when they’re having an intense experience, they tend to hang on every word.”
For the physician, she says, “there are so many things to communicate and because it is often very complicated, the relationship and the trust have to be built quickly, and information has to be transferred very quickly. Poor communication will lead to potentially not being able to build that alliance with the patient during that short period of time of their hospital experience.”
Hospitalists must be on the lookout for how the constraints of time affect the way they practice and relate to their patients because every nuance of behavior or tone of voice can make a difference to how a patient perceives his or her doctor.
For example, in a study conducted at Harvard University in 2002, investigators used audiotapes of 57 surgeons, 36 of whom had had two or more malpractice claims filed against them.9 Patients were asked to listen to two 20-second clips of audio between these surgeons and two patients. Those surgeons who were judged by the tone of their voices as “high dominance” and “low concern/anxiety” correlated with those who had had previous malpractice claims.
Because there is no continuity of relationship to help steady what might be an emotional response when things go wrong in the patient’s treatment or when patients and families are upset by circumstances, hospitalists may be subjected to blame, resentment, fear, and displaced anger concerning their communications with patients and families.
“Especially if you’re harried in an incredible time crunch, if you don’t [communicate] with patients and patient families [about] what is going on [in their care], those relationships very quickly can turn antagonistic,” says Dr. Trowbridge. “And then the very thing most of us like about medicine—relationships with patients and families—becomes something that people tend to avoid.”
Dr. Trowbridge says that this can become somewhat of a vicious cycle whereby a certain extent of inadvertently “avoiding the patient and family may lead to further communication faults.” On the flip side, using good communication can be a circular process but in a positive way: A good communicator may experience better well-being, which in turn, leads to better communication skills.2,5 Also, on a practical level, the data are clear that bad communication puts you at risk for malpractice litigation.9,10
Communication with Colleagues
“People that don’t have very good communication skills tend not to be successful,” says Dr. Vidyarthi, who practices with the hospitalist group at UCSF and is also an assistant professor there. Her definition of success is closely linked to the quality of relationships; that is, “being well liked by the nurses, building working relationships with … the nurses,” as well as others, including the hospital administrator. “Hospitalists are almost always … doing quality work or performance improvement,” she explained. “They’re on committees. That is the nature of what we do. … Not learning what those [communication skills] are and [not] being able to communicate at [effective] levels would … be a detriment to one’s personal job advancement, but absolutely to one’s job satisfaction as well.”
Collegiality, in fact, is one component cited as a “powerful engine of socialization” in organizational structures more likely to foster the lifelong learning and commitment that are inherent to medical professionalism.1,3-5,11,12
Many of the components of effective communication with colleagues parallel those that are best used with patients. “Communication is what holds that team together,” says Dr. Vidyarthi, whose interests include information transfer and communication as a form for team-building. “In academic medicine, poor communication can impact the teaching environment, the experience of the students and the residents, and that team cohesion. And that can lead to poor patient care, it can definitely lead to a poor educational experience, and it is not enjoyable, so job satisfaction suffers.”
Dr. Pantilat, who is associate professor of clinical medicine and director, Palliative Care Service and Palliative Care Leadership Center at UCSF, theorizes that when interacting with colleagues such as other hospitalists and physicians, nurses, social workers, case managers, and pharmacists, poor communication skills can make the physician’s work tougher. “Poor communication makes your life difficult with your colleagues,” says Dr. Pantilat. “People don’t like talking to you or interacting with you … and your job can generally be more difficult.”
Post-Discharge Communication
In the traditional medical model, a primary care physician would see patients in her/his office, the hospital, or rehabilitation. With the expansion in hospital medicine, patients are now “handed off” and seen by a number of providers. Hand-off fumbles can mean critical information may be lost, leading to poorer outcomes and greater readmission rates.13-15
Forging and maintaining effective communication with colleagues following the discharge of patients is an area where few in-house physicians do well, says Dr. Vidyarthi, who has it on her agenda to tackle this “huge problem” for her institution in the coming year. There are two pieces to that problem, she says. One is to accurately identify the patients’ primary care physicians and the other is to make contact with them.
“You could page them, but they’re in clinic, and they can’t take five minutes out when you can’t take five minutes out,” says Dr. Vidyarthi. “The communication with the primary care physician is actually a field in and of itself.”15
Part of her plan is to devise some means of “physician-independent generated communication,” perhaps a letter or e-mail sent from the hospital to report to a primary care physician that his/her patient has been admitted to the hospital.
“That raises a flag to that primary so they can try to find the hospitalist, which is usually very easy … because we’re always in the hospital,” says Dr. Vidyarthi. “And it’s the first stage of the communication: Now that person is aware. If I can find them, if I can access them, they’ll be able to take that time out, because they know their patient’s there.”
In her work as a senior fellow at the Center for Health Professions at UCSF, Dr. Vidyarthi strives to “embed communication into the larger framework of organizational change.” And what does a hospitalist do if an institution’s post-discharge communications system is not up to par? There are three basic things you can do to help overcome this source of frustration, she says. The first is to continually build relationships with primary care providers.
“If I send an e-mail to somebody and they know who I am, they are much more likely to respond to that because they know me,” says Dr. Vidyarthi.
Next, find a system that works for you. “Don’t wait for the rest of the systems to be put in place,” she says. “This is about personal practice. And if that means you take five minutes in the morning to send an e-mail or five minutes in the evening, whatever it is, find [a system] that really works and figure out a way to evaluate it.”
A good way to do this, Dr. Vidyarthi suggests, is to take a quick survey in the midst of talking to that primary care physician to ask whether the medium, content, and timing that you used to contact him/her worked well.
“Then,” she says, “if you have five primaries that you talked to [who] maybe said, ‘Yes, that was helpful to me,’ or ‘Not so much really, I had all that info already,’ at least you have data. Asking ‘Do you think this will help your patients when they come to see you in the office?’ is a great question [to solidify] performance improvement. In other words, find out if what you’re doing is being effective.”
The final step to overcome a lack of an effective institutional system for post-discharge communication is to share what you’ve learned with others. “These little pieces can really empower others to make a difference,” says Dr. Vidyarthi. “Trying to change and overhaul an entire system will turn off even the most motivated of people who want to improve the system, so focus on your own personal practice models. Change it, figure out what works, and then try to disseminate it. That makes it feel and seem much more doable.”
Conclusion
Hospitalists who exercise poor communication skills with patients, families, and colleagues can experience multiple negative effects, including poor patient-related outcomes and an increased risk of malpractice litigation. Personally, consistently using poor communication may make work more difficult, reduce job satisfaction, and reduce work success and enjoyment with hospital teams and primary care physicians. TH
Contributor Andrea Sattinger makes good communication a priority every day.
References
- Finset KB, Gude T, Hem E, et al. Which young physicians are satisfied with their work? A prospective nationwide study in Norway. BMC Med Educ. 2005;5:19.
- Roter DL, Stewart M, Putnam SM, et al. Communication patterns of primary care physicians. JAMA. 1997;277:350-356.
- Konrad TR, Williams ES, Linzer M, et al. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Measuring physician job satisfaction in a changing workplace and a challenging environment. Med Care. 1999;37:1174-1182.
- Shanafelt TD, West C, Zhao X, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005;20:559-564.
- Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114:513-519.
- Novack DH, Suchman AL, Clark W, et al. Calibrating the physician. Personal awareness and effective patient care. Working Group on Promoting Physician Personal Awareness, American Academy on Physician and Patient. JAMA. 1997;278:502-509.
- Greenfield S, Kaplan S, Ware WE Jr. Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med. 1985;102:520-528.
- Torcson PJ. Patient satisfaction: the hospitalist’s role. The Hospitalist. 2005;July/Aug:27-30.
- Ambady N, LaPlante D, Nguyen T. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132:5-9.
- Levinson W, Roter DL, Mullooly JP. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277:553-559.
- Frankford DM, Patterson MA, Konrad TR. Transforming practice organizations to foster lifelong learning and commitment to medical professionalism. Acad Med. 2000;75:708-17.
- Falkum E, Vaglum P. The relationship between interpersonal problems and occupational stress in physicians. Gen Hosp Psychiatry. 2005;27:285-291.
- Coleman EA, Smith JD, Min SJ, et al. Post-hospital medicine discrepancies; prevalence, types, and contributing factors. Paper presented at the Society of Hospital Medicine Annual Meeting; April 29-30; Chicago, Illinois: Society of Hospital Medicine 2005.
- Burniske GM, Burnett A, Greenwald J, et al. Post-discharge follow-up telephone call by a pharmacist and impact on patient care. Paper presented at the Society of Hospital Medicine Annual Meeting. April 29-30; Chicago.
- Wachter R, Shojania K. Internal Bleeding: The Truth Behind America's Terrifying Epidemic of Medical Mistakes. New York, NY: Rugged Land; 2004.
Evidence Based Medicine for The Hospitalist
The first step in finding an answer to a clinical question is to ask an effective question. This was the subject of the previous installment in this series, in which the PICOT question format was introduced (see The Hospitalist, Nov. 2005, p. 32). This format leads naturally to effective search strategies, so we optimize our chances of finding quality answers if they exist. There are many possible sources of information that can be searched, however, and the type of question asked can provide valuable guidance as to which sources should be first up for review.
Types of Questions and Where to Look for Answers
Many clinical questions pertain to basic medical knowledge rather than cutting-edge current research. These so-called background questions typically involve such issues as the underlying pathophysiology of a disease, the incidence of the disease, the general treatment considerations for the disease, and overall prognosis for patients with the disease. These questions usually do not require evaluation of the most recent medical literature and can often be answered by reviewing sources of established medical knowledge such as medical textbooks, MD Consult, or UpToDate. In fact, searching for basic knowledge in the current research literature can be exhausting because the focus of most papers is necessarily narrow and therefore too restrictive to properly address knowledge of a general nature.
The main limitation of these more general sources is that it takes years for medical knowledge to become established, so the most current results will seldom be incorporated. For background questions this is usually acceptable, but if a major breakthrough in our understanding of a disease occurs it is unlikely to be found in these sources. An additional limitation is that the statements found in these sources are often not truly evidence-based—at least not in a transparent or reproducible manner. These limitations are becoming less problematic as resources such as UpToDate strive to add evidence-based reviews and quality measures to their summaries, and also begin to update information much more rapidly as online materials become more standard.
In contrast to background clinical questions, foreground clinical questions are more likely to relate to the management of an individual patient in a specific clinical setting, and are therefore too narrow in scope to be addressed well by the sources best suited for background questions. For example, consider the question posed in the last installment of this series, “Among men over the age of 65 with Stage II renal cell carcinoma, does post-resection chemotherapy result in greater five-year survival than nephrectomy alone?” No textbook will answer a question with this narrow focus. To find an answer we need to be able to sift through the current medical research literature.

How to Search Research Databases
The number of medical journals has increased dramatically in the past 20 years. As a result, while it may be more likely that your question has been addressed somewhere, it can be more difficult to locate the paper you need. One approach to this problem is to become skilled in developing search strategies. We will return to this, but an alternative is to utilize secondary journals such as ACP Journal Club (www.acponline.org) or prefiltered sources such as the Cochrane Library (www.cochrane.org).
Secondary journals typically screen articles for both clinical relevance and methodologic quality, making them efficient resources for busy clinicians. The Cochrane Library focuses mainly on systematic reviews of controlled trials of therapeutic interventions. The main downside of these sources is that they may not address your particular question. Therefore, one effective search strategy is to first search a secondary journal or prefiltered source and stop if you find what you need. If you don’t find what you are looking for, you will need to enter the world of the large medical research database armed with a search strategy.
Constructing effective search strategies is perhaps even more of an art than constructing effective clinical questions. Luckily, medical librarians are experts at this and should be your first stop. Not only can skilled medical librarians help you with your searches, they can also teach you efficient ways to conduct simple searches yourself. I will mention a few of these strategies, but these are truly only the tip of the iceberg.
The key elements of searching the large medical information databases such as MEDLINE include an understanding of Medical Subject Headings (MeSH), text-word searching, and combining searches. Mapping to a MeSH term and clicking the “explode” option on the search page will gather not just those papers indexed to the term of interest, but also papers referencing more specific aspects of that term. Clicking on the search term itself will reveal the “tree” of terms related to your chosen search term. For example, try searching MEDLINE for “cancer.” You will be mapped to “neoplasms,” and if you click on that term, you will see a tree of related terms. If you select “explode” for your initial search, you will include each of these related terms, expanding your search. You could also narrow your search by selecting “neoplasms by site” or another subheading, and further refining your approach from there.
To begin a search, it is helpful to first enter in relevant keywords from your clinical question. Following our previous example, these could include renal cell carcinoma, chemotherapy, and survival. Then you could perform one search for each term, combining them using the search window options. Alternatively, each term could be linked in one search using the AND/OR operators. Further restrictions such as looking only at randomized controlled trials or for specific authors are also possible. Finally, many MEDLINE sites have a collection of saved search strategies for common clinical question types. For example, a saved search strategy for articles on diagnosis (or therapy, prognosis, or any other question type) can provide an effective searching technique based on the expertise of your resident search professional.
Because many of these approaches rely on the way in which an article has been indexed, searching for synonyms can also be helpful. You may search for temporal arteritis and miss articles indexed only under giant cell arteritis, for example. MEDLINE does a good job of mapping these terms to each other, but this can fall short, particularly if you search by text word alone. Being clever with synonyms can be the difference between finding and missing the one key article that will answer your clinical question.
Searchable Sources of Medical Information
“Overview of Searchable Sources of Medical Information” (p. 18) presents a brief overview of searchable sources of information. Becoming a searching expert takes considerable dedication, but fortunately the basic strategies are not overly complicated. Additionally, significant efforts are being made to simplify the steps needed to answer clinical questions, as can be seen in the growing number of secondary journals available for both general medicine and subspecialties.
Summary
Searching for the answers to well-constructed clinical questions is obviously a crucial step in the EBM process. Well-built questions suggest efficient search strategies, simplifying what can be a complex and daunting process. Many resources are available to help with this step, including medical librarians, prefiltered searches, and saved searches for common query types. Once you locate an article addressing your clinical question, the next step is to critically appraise the article to determine whether its results are applicable to your patient. TH
Dr. West practices in the Division of General Internal Medicine, Mayo Clinic College of Medicine, Rochester, Minn.
The first step in finding an answer to a clinical question is to ask an effective question. This was the subject of the previous installment in this series, in which the PICOT question format was introduced (see The Hospitalist, Nov. 2005, p. 32). This format leads naturally to effective search strategies, so we optimize our chances of finding quality answers if they exist. There are many possible sources of information that can be searched, however, and the type of question asked can provide valuable guidance as to which sources should be first up for review.
Types of Questions and Where to Look for Answers
Many clinical questions pertain to basic medical knowledge rather than cutting-edge current research. These so-called background questions typically involve such issues as the underlying pathophysiology of a disease, the incidence of the disease, the general treatment considerations for the disease, and overall prognosis for patients with the disease. These questions usually do not require evaluation of the most recent medical literature and can often be answered by reviewing sources of established medical knowledge such as medical textbooks, MD Consult, or UpToDate. In fact, searching for basic knowledge in the current research literature can be exhausting because the focus of most papers is necessarily narrow and therefore too restrictive to properly address knowledge of a general nature.
The main limitation of these more general sources is that it takes years for medical knowledge to become established, so the most current results will seldom be incorporated. For background questions this is usually acceptable, but if a major breakthrough in our understanding of a disease occurs it is unlikely to be found in these sources. An additional limitation is that the statements found in these sources are often not truly evidence-based—at least not in a transparent or reproducible manner. These limitations are becoming less problematic as resources such as UpToDate strive to add evidence-based reviews and quality measures to their summaries, and also begin to update information much more rapidly as online materials become more standard.
In contrast to background clinical questions, foreground clinical questions are more likely to relate to the management of an individual patient in a specific clinical setting, and are therefore too narrow in scope to be addressed well by the sources best suited for background questions. For example, consider the question posed in the last installment of this series, “Among men over the age of 65 with Stage II renal cell carcinoma, does post-resection chemotherapy result in greater five-year survival than nephrectomy alone?” No textbook will answer a question with this narrow focus. To find an answer we need to be able to sift through the current medical research literature.

How to Search Research Databases
The number of medical journals has increased dramatically in the past 20 years. As a result, while it may be more likely that your question has been addressed somewhere, it can be more difficult to locate the paper you need. One approach to this problem is to become skilled in developing search strategies. We will return to this, but an alternative is to utilize secondary journals such as ACP Journal Club (www.acponline.org) or prefiltered sources such as the Cochrane Library (www.cochrane.org).
Secondary journals typically screen articles for both clinical relevance and methodologic quality, making them efficient resources for busy clinicians. The Cochrane Library focuses mainly on systematic reviews of controlled trials of therapeutic interventions. The main downside of these sources is that they may not address your particular question. Therefore, one effective search strategy is to first search a secondary journal or prefiltered source and stop if you find what you need. If you don’t find what you are looking for, you will need to enter the world of the large medical research database armed with a search strategy.
Constructing effective search strategies is perhaps even more of an art than constructing effective clinical questions. Luckily, medical librarians are experts at this and should be your first stop. Not only can skilled medical librarians help you with your searches, they can also teach you efficient ways to conduct simple searches yourself. I will mention a few of these strategies, but these are truly only the tip of the iceberg.
The key elements of searching the large medical information databases such as MEDLINE include an understanding of Medical Subject Headings (MeSH), text-word searching, and combining searches. Mapping to a MeSH term and clicking the “explode” option on the search page will gather not just those papers indexed to the term of interest, but also papers referencing more specific aspects of that term. Clicking on the search term itself will reveal the “tree” of terms related to your chosen search term. For example, try searching MEDLINE for “cancer.” You will be mapped to “neoplasms,” and if you click on that term, you will see a tree of related terms. If you select “explode” for your initial search, you will include each of these related terms, expanding your search. You could also narrow your search by selecting “neoplasms by site” or another subheading, and further refining your approach from there.
To begin a search, it is helpful to first enter in relevant keywords from your clinical question. Following our previous example, these could include renal cell carcinoma, chemotherapy, and survival. Then you could perform one search for each term, combining them using the search window options. Alternatively, each term could be linked in one search using the AND/OR operators. Further restrictions such as looking only at randomized controlled trials or for specific authors are also possible. Finally, many MEDLINE sites have a collection of saved search strategies for common clinical question types. For example, a saved search strategy for articles on diagnosis (or therapy, prognosis, or any other question type) can provide an effective searching technique based on the expertise of your resident search professional.
Because many of these approaches rely on the way in which an article has been indexed, searching for synonyms can also be helpful. You may search for temporal arteritis and miss articles indexed only under giant cell arteritis, for example. MEDLINE does a good job of mapping these terms to each other, but this can fall short, particularly if you search by text word alone. Being clever with synonyms can be the difference between finding and missing the one key article that will answer your clinical question.
Searchable Sources of Medical Information
“Overview of Searchable Sources of Medical Information” (p. 18) presents a brief overview of searchable sources of information. Becoming a searching expert takes considerable dedication, but fortunately the basic strategies are not overly complicated. Additionally, significant efforts are being made to simplify the steps needed to answer clinical questions, as can be seen in the growing number of secondary journals available for both general medicine and subspecialties.
Summary
Searching for the answers to well-constructed clinical questions is obviously a crucial step in the EBM process. Well-built questions suggest efficient search strategies, simplifying what can be a complex and daunting process. Many resources are available to help with this step, including medical librarians, prefiltered searches, and saved searches for common query types. Once you locate an article addressing your clinical question, the next step is to critically appraise the article to determine whether its results are applicable to your patient. TH
Dr. West practices in the Division of General Internal Medicine, Mayo Clinic College of Medicine, Rochester, Minn.
The first step in finding an answer to a clinical question is to ask an effective question. This was the subject of the previous installment in this series, in which the PICOT question format was introduced (see The Hospitalist, Nov. 2005, p. 32). This format leads naturally to effective search strategies, so we optimize our chances of finding quality answers if they exist. There are many possible sources of information that can be searched, however, and the type of question asked can provide valuable guidance as to which sources should be first up for review.
Types of Questions and Where to Look for Answers
Many clinical questions pertain to basic medical knowledge rather than cutting-edge current research. These so-called background questions typically involve such issues as the underlying pathophysiology of a disease, the incidence of the disease, the general treatment considerations for the disease, and overall prognosis for patients with the disease. These questions usually do not require evaluation of the most recent medical literature and can often be answered by reviewing sources of established medical knowledge such as medical textbooks, MD Consult, or UpToDate. In fact, searching for basic knowledge in the current research literature can be exhausting because the focus of most papers is necessarily narrow and therefore too restrictive to properly address knowledge of a general nature.
The main limitation of these more general sources is that it takes years for medical knowledge to become established, so the most current results will seldom be incorporated. For background questions this is usually acceptable, but if a major breakthrough in our understanding of a disease occurs it is unlikely to be found in these sources. An additional limitation is that the statements found in these sources are often not truly evidence-based—at least not in a transparent or reproducible manner. These limitations are becoming less problematic as resources such as UpToDate strive to add evidence-based reviews and quality measures to their summaries, and also begin to update information much more rapidly as online materials become more standard.
In contrast to background clinical questions, foreground clinical questions are more likely to relate to the management of an individual patient in a specific clinical setting, and are therefore too narrow in scope to be addressed well by the sources best suited for background questions. For example, consider the question posed in the last installment of this series, “Among men over the age of 65 with Stage II renal cell carcinoma, does post-resection chemotherapy result in greater five-year survival than nephrectomy alone?” No textbook will answer a question with this narrow focus. To find an answer we need to be able to sift through the current medical research literature.

How to Search Research Databases
The number of medical journals has increased dramatically in the past 20 years. As a result, while it may be more likely that your question has been addressed somewhere, it can be more difficult to locate the paper you need. One approach to this problem is to become skilled in developing search strategies. We will return to this, but an alternative is to utilize secondary journals such as ACP Journal Club (www.acponline.org) or prefiltered sources such as the Cochrane Library (www.cochrane.org).
Secondary journals typically screen articles for both clinical relevance and methodologic quality, making them efficient resources for busy clinicians. The Cochrane Library focuses mainly on systematic reviews of controlled trials of therapeutic interventions. The main downside of these sources is that they may not address your particular question. Therefore, one effective search strategy is to first search a secondary journal or prefiltered source and stop if you find what you need. If you don’t find what you are looking for, you will need to enter the world of the large medical research database armed with a search strategy.
Constructing effective search strategies is perhaps even more of an art than constructing effective clinical questions. Luckily, medical librarians are experts at this and should be your first stop. Not only can skilled medical librarians help you with your searches, they can also teach you efficient ways to conduct simple searches yourself. I will mention a few of these strategies, but these are truly only the tip of the iceberg.
The key elements of searching the large medical information databases such as MEDLINE include an understanding of Medical Subject Headings (MeSH), text-word searching, and combining searches. Mapping to a MeSH term and clicking the “explode” option on the search page will gather not just those papers indexed to the term of interest, but also papers referencing more specific aspects of that term. Clicking on the search term itself will reveal the “tree” of terms related to your chosen search term. For example, try searching MEDLINE for “cancer.” You will be mapped to “neoplasms,” and if you click on that term, you will see a tree of related terms. If you select “explode” for your initial search, you will include each of these related terms, expanding your search. You could also narrow your search by selecting “neoplasms by site” or another subheading, and further refining your approach from there.
To begin a search, it is helpful to first enter in relevant keywords from your clinical question. Following our previous example, these could include renal cell carcinoma, chemotherapy, and survival. Then you could perform one search for each term, combining them using the search window options. Alternatively, each term could be linked in one search using the AND/OR operators. Further restrictions such as looking only at randomized controlled trials or for specific authors are also possible. Finally, many MEDLINE sites have a collection of saved search strategies for common clinical question types. For example, a saved search strategy for articles on diagnosis (or therapy, prognosis, or any other question type) can provide an effective searching technique based on the expertise of your resident search professional.
Because many of these approaches rely on the way in which an article has been indexed, searching for synonyms can also be helpful. You may search for temporal arteritis and miss articles indexed only under giant cell arteritis, for example. MEDLINE does a good job of mapping these terms to each other, but this can fall short, particularly if you search by text word alone. Being clever with synonyms can be the difference between finding and missing the one key article that will answer your clinical question.
Searchable Sources of Medical Information
“Overview of Searchable Sources of Medical Information” (p. 18) presents a brief overview of searchable sources of information. Becoming a searching expert takes considerable dedication, but fortunately the basic strategies are not overly complicated. Additionally, significant efforts are being made to simplify the steps needed to answer clinical questions, as can be seen in the growing number of secondary journals available for both general medicine and subspecialties.
Summary
Searching for the answers to well-constructed clinical questions is obviously a crucial step in the EBM process. Well-built questions suggest efficient search strategies, simplifying what can be a complex and daunting process. Many resources are available to help with this step, including medical librarians, prefiltered searches, and saved searches for common query types. Once you locate an article addressing your clinical question, the next step is to critically appraise the article to determine whether its results are applicable to your patient. TH
Dr. West practices in the Division of General Internal Medicine, Mayo Clinic College of Medicine, Rochester, Minn.
The End of General Hospitals
Where will you be in 20 years? If you’re a young hospitalist, you may work in an enormous state-of-the-art hospital complex that includes the latest technologies, the best in amenities, and a well-thought-out design that will meet your needs and those of other staff for years to come.
“There are a lot of different approaches” to designing the hospital facility of the future, says George R. Tingwald, MD, AIA, ACHA, director of healthcare design at Skidmore, Owings, and Merrill in San Francisco. “The difference depends on whether you look at it from a constructability standpoint versus a much more consumer-based focus. Though many think they have the right approach, it’s hard to say that everybody’s decided on a single solution.”
The Future Looks … Big
It’s not just the hospital facility itself that will change in the future. The number of hospitals in each community may change as well—and the hospitals will be considerably larger.
“We will probably see fewer but larger hospitals in the future,” predicts Dr. Tingwald. “We’re in an era where we’re seeing significant growth in the number of inpatients served. Because of the baby boom and increasing longevity in Americans we’re already seeing an increase, and it’s going to continue. We’ll definitely see more hospital beds in the future.”
The type of patients who fill those hospital beds will change as well.
“We’ll continue to see sicker and sicker patients in those hospital beds,” says Dr. Tingwald. “More people will be managed on an outpatient basis as more diagnostic and treatment procedures will be done as outpatients. Look at breast cancer: From initial detection to diagnosis to biopsy to lumpectomy to chemotherapy or radiation treatment, to cure, or end-of-life care, each step can now be done on an outpatient basis.”
What does this mean? “Someone can have a very significant, multiepisodic disease and never stay in the hospital—unless there are complications,” explains Dr. Tingwald. “Therefore, we’ll have only very acute patients in the hospital. The hospital will basically become an intensive care unit.”
In the past, approximately 10% of a hospital’s beds were in the ICU. That percentage is rising—an indication of things to come. That percentage is now around 20% or 30% and growing, especially in major centers. Only seriously ill people will be admitted—but even they won’t spend a lot of time in the hospital. They will die, recover to a point where they can be moved to rehabilitation or other support facility, or be sent home.
What about the prediction that there will be fewer hospitals in the future? Dr. Tingwald predicts that technology and expertise will weed out some facilities.
“We used to have a lot of what I would call general hospitals—meaning every one was the same,” he explains. “That’s changing radically. The institutions with the expertise and wherewithal to develop technical sophistication, such as university hospitals and specialty hospitals, are doing well. Those that don’t have that sophistication can’t keep up. The big centers are growing because they have the equipment and the expertise. The smaller ones are failing.”
This trend may come as a surprise to some in healthcare, in light of previous predictions. “This is different than the futurists were saying 10 or 20 years ago, when predictions were for more home-based and community-based care,” says Dr. Tingwald. “The reverse has happened. The latest equipment is not available to everyone, let alone smaller, unaffiliated hospitals. And the people that can work with that technology are few and far between.”
The addition of new technology will have some effect on the size of the hospital. “You need a lot of physical space for wiring,” admits Dr. Tingwald. “But the ‘brains’ of the technology can be offsite at a separate IT center or data center.”
Focus on Family-Centered Care
Perhaps the most noticeable differences in the hospital facility of the future will be those related to a change in services, design, and attitude toward providing amenities for patients and their families.
“Patient-centered care, or its close cousin—family-centered care—is a significant trend in healthcare design now, and that significantly impacts the design of facilities,” states Dr. Tingwald. “The most important aspect is having all private rooms. Almost no new construction includes shared patient rooms. The key element of this care is family involvement, and that includes families rooming in with patients. You can’t physically or psychologically do this in a shared room.”
He points out that this trend includes all room types: “It started in pediatrics, but has gone into general acute care settings, intensive care settings, and now neonatal intensive care units.”
What are the pros and cons of a move toward all private rooms? “It takes up room, but it’s proving not to be significantly more costly,” says Dr. Tingwald. “Private rooms are more expensive to build, but in the end they’re less expensive to operate. In an all-private room hospital you can increase your occupancy to 80% or even 90% because you’re not trying to match up patients by gender and age. Also, nursing isn’t moving patients to get the bed mixes right. Studies show that nurses spend up to 40% of their time in transfers. And finally, private rooms have increased market share considerably.”
Another aspect of family centered care is the addition of technologies and services that cater to patient comfort and even enjoyment. “Anything someone has at home or wants in a hotel, families and patients are demanding, including room service,” says Dr. Tingwald. “Patients can decide when and what they want to eat [within their prescribed diet], and families can order food. In some hospitals, patients can already order food using a plasma screen in their room. This is showing to be an economically viable alternative. There’s less food waste, and patients are much happier.”
You’ll also see patient rooms with plasma screen televisions and DVD players, equipped for movies on demand, educational content—even the ability for physicians to view X-rays and other diagnostics on screen, and for families waiting in the room to communicate with physicians in the operating room.
“These are consumer-driven things, but they’re not luxuries,” insists Dr. Tingwald. “They’re often things that save time, increase the ability for education, and significantly decrease errors.”
Another argument for adding amenities like plasma screen TVs and room service: “In healthcare you think adding this technology must be too expensive,” says Dr. Tingwald, “but if you walk into a fast-food place, the person behind the counter uses a touch screen. Everybody else has done this already. Facilities that don’t partake in these transitions are not going to survive.”
Other family-centered improvements include major changes in patient registration. “Most registration can be done from home, over the Internet,” he says. “At Northwestern Memorial Hospital [in Chicago], patients have an encoded card they swipe when they drive into the parking garage, and the receptionist knows they’re coming and gets their room ready before they arrive.”
In the future, more facilities will offer options like these to make the registration process easy and fast.
The hospital of the future will feature a friendlier environment, with landscaping and nice views from patient rooms, artwork and amenities that are important in the healing process. They will also include an emphasis on alternative treatments, says Dr. Tingwald, “from massage to aromatherapy to spaces for yoga or meditation.”
Plan for Flexibility
The key to the design of the hospital of the future will be its ability to change without building additions, remodeling, or rehabbing.
“We’re no longer planning a facility in a static way, thinking that things will not change. Flexibility and adaptability are planned from the beginning,” explains Dr. Tingwald. “You’ll see a lot more generic room types—rooms that are all a single size, but adaptable. A private patient room might be initially planned for acute care, but it can be adapted for an ICU room with minimal or no remodeling.”
This holds true for other room types as well. “In diagnostic and treatment spaces, we plan for one, or no more than two, sizes of space,” he says. “You don’t know if in the future more procedures will be surgical or non-invasive, so rooms are planned to handle both functions. Also, the kingdoms are coming down and divisions between diagnostic departments are blending.”
The Johns Hopkins Hospital (Baltimore), the University of California, Los Angeles Medical Center, and California Pacific Medical Center in San Francisco are all designing “platform floors,” where surgery, interventional imaging, cardiac catheterization, and other procedure-based services share preoperative and postoperative areas and have single access.
“These floors provide adjacency of services allowing a lot more flexibility and decreased redundancy,” explains Dr. Tingwald. “Also, there aren’t as many patient transfers, and a key to patient-centered care is less movement of the patient.”
Built-in flexibility is designed to accommodate scalability as well. “In the planning process, we anticipate higher volumes in an emergency or disaster,” he says. “We plan how to expand the emergency room, and we make rooms larger than we used to. That way, if volumes increase quickly, you could put two, three, maybe more patients in a space. Nurses hate when you say that, but we have to have timely solutions that are affordable. This approach can be considered on nursing units as well, with these ‘super singles’ able to handle a second patient during a February flu outbreak, for example. That’s better than having an entire wing of the hospital that’s only used during winter months, patients stuck in the emergency department for days, or patients in the halls.”
A Design with Built-In Patient Safety
The physical design of the hospital of the future will better address and correct issues with patient safety. “Whatever design elements can minimize errors and improve outcomes are being studied intensively right now,” says Dr. Tingwald. “For example, we used to mirror many room types so that walls could share plumbing, etc. One room would be the mirror image of the one next to it, requiring the staff to learn different layouts, which increases time of response and possible errors. Now, we try to make procedure rooms as similar as possible to reduce the potential for error.”
There are design elements that limit the possibility of hospital-borne infection, including ultraviolet light and biologic surfaces. There is also a greater emphasis on including track systems for lifts for getting patients out of bed and moving them without injury to the patient or the staff.
Consider Hospitalists and Other Staff
How will the hospital of the future accommodate hospitalists?
“We’re certainly seeing more hospitalists,” says Dr. Tingwald. “As you have sicker patients in the hospital, it’s harder for their primary care physicians to manage them, so we’re going to see even more hospitalists. This means that we have to provide space for them; both offices, because they don’t have other office space, and sleeping accommodations, which means private rooms with bath, as well as lounge space.”
Hospitals will provide appealing space for physicians because it will help them recruit hospitalists. Improving lounges and other staff spaces will be a goal of future hospital designs.
“There will be a lot more emphasis on good environments for work and for support services,” predicts Dr. Tingwald. “This will increase the attraction and retention of top staff. You’ll see things like fitness centers, and basic additions like enough parking spaces.”
As hospital facilities move toward more patient-centered care, with flexible layouts and space designed for patient safety, the working environment is certain to become more conducive to providing good care and working efficiently. It will also become more comfortable, convenient, and pleasant for hospitalists and other staff. And that is something to look forward to. TH
Writer Jane Jerrard wrote the first three installments of the “Future” series.
Where will you be in 20 years? If you’re a young hospitalist, you may work in an enormous state-of-the-art hospital complex that includes the latest technologies, the best in amenities, and a well-thought-out design that will meet your needs and those of other staff for years to come.
“There are a lot of different approaches” to designing the hospital facility of the future, says George R. Tingwald, MD, AIA, ACHA, director of healthcare design at Skidmore, Owings, and Merrill in San Francisco. “The difference depends on whether you look at it from a constructability standpoint versus a much more consumer-based focus. Though many think they have the right approach, it’s hard to say that everybody’s decided on a single solution.”
The Future Looks … Big
It’s not just the hospital facility itself that will change in the future. The number of hospitals in each community may change as well—and the hospitals will be considerably larger.
“We will probably see fewer but larger hospitals in the future,” predicts Dr. Tingwald. “We’re in an era where we’re seeing significant growth in the number of inpatients served. Because of the baby boom and increasing longevity in Americans we’re already seeing an increase, and it’s going to continue. We’ll definitely see more hospital beds in the future.”
The type of patients who fill those hospital beds will change as well.
“We’ll continue to see sicker and sicker patients in those hospital beds,” says Dr. Tingwald. “More people will be managed on an outpatient basis as more diagnostic and treatment procedures will be done as outpatients. Look at breast cancer: From initial detection to diagnosis to biopsy to lumpectomy to chemotherapy or radiation treatment, to cure, or end-of-life care, each step can now be done on an outpatient basis.”
What does this mean? “Someone can have a very significant, multiepisodic disease and never stay in the hospital—unless there are complications,” explains Dr. Tingwald. “Therefore, we’ll have only very acute patients in the hospital. The hospital will basically become an intensive care unit.”
In the past, approximately 10% of a hospital’s beds were in the ICU. That percentage is rising—an indication of things to come. That percentage is now around 20% or 30% and growing, especially in major centers. Only seriously ill people will be admitted—but even they won’t spend a lot of time in the hospital. They will die, recover to a point where they can be moved to rehabilitation or other support facility, or be sent home.
What about the prediction that there will be fewer hospitals in the future? Dr. Tingwald predicts that technology and expertise will weed out some facilities.
“We used to have a lot of what I would call general hospitals—meaning every one was the same,” he explains. “That’s changing radically. The institutions with the expertise and wherewithal to develop technical sophistication, such as university hospitals and specialty hospitals, are doing well. Those that don’t have that sophistication can’t keep up. The big centers are growing because they have the equipment and the expertise. The smaller ones are failing.”
This trend may come as a surprise to some in healthcare, in light of previous predictions. “This is different than the futurists were saying 10 or 20 years ago, when predictions were for more home-based and community-based care,” says Dr. Tingwald. “The reverse has happened. The latest equipment is not available to everyone, let alone smaller, unaffiliated hospitals. And the people that can work with that technology are few and far between.”
The addition of new technology will have some effect on the size of the hospital. “You need a lot of physical space for wiring,” admits Dr. Tingwald. “But the ‘brains’ of the technology can be offsite at a separate IT center or data center.”
Focus on Family-Centered Care
Perhaps the most noticeable differences in the hospital facility of the future will be those related to a change in services, design, and attitude toward providing amenities for patients and their families.
“Patient-centered care, or its close cousin—family-centered care—is a significant trend in healthcare design now, and that significantly impacts the design of facilities,” states Dr. Tingwald. “The most important aspect is having all private rooms. Almost no new construction includes shared patient rooms. The key element of this care is family involvement, and that includes families rooming in with patients. You can’t physically or psychologically do this in a shared room.”
He points out that this trend includes all room types: “It started in pediatrics, but has gone into general acute care settings, intensive care settings, and now neonatal intensive care units.”
What are the pros and cons of a move toward all private rooms? “It takes up room, but it’s proving not to be significantly more costly,” says Dr. Tingwald. “Private rooms are more expensive to build, but in the end they’re less expensive to operate. In an all-private room hospital you can increase your occupancy to 80% or even 90% because you’re not trying to match up patients by gender and age. Also, nursing isn’t moving patients to get the bed mixes right. Studies show that nurses spend up to 40% of their time in transfers. And finally, private rooms have increased market share considerably.”
Another aspect of family centered care is the addition of technologies and services that cater to patient comfort and even enjoyment. “Anything someone has at home or wants in a hotel, families and patients are demanding, including room service,” says Dr. Tingwald. “Patients can decide when and what they want to eat [within their prescribed diet], and families can order food. In some hospitals, patients can already order food using a plasma screen in their room. This is showing to be an economically viable alternative. There’s less food waste, and patients are much happier.”
You’ll also see patient rooms with plasma screen televisions and DVD players, equipped for movies on demand, educational content—even the ability for physicians to view X-rays and other diagnostics on screen, and for families waiting in the room to communicate with physicians in the operating room.
“These are consumer-driven things, but they’re not luxuries,” insists Dr. Tingwald. “They’re often things that save time, increase the ability for education, and significantly decrease errors.”
Another argument for adding amenities like plasma screen TVs and room service: “In healthcare you think adding this technology must be too expensive,” says Dr. Tingwald, “but if you walk into a fast-food place, the person behind the counter uses a touch screen. Everybody else has done this already. Facilities that don’t partake in these transitions are not going to survive.”
Other family-centered improvements include major changes in patient registration. “Most registration can be done from home, over the Internet,” he says. “At Northwestern Memorial Hospital [in Chicago], patients have an encoded card they swipe when they drive into the parking garage, and the receptionist knows they’re coming and gets their room ready before they arrive.”
In the future, more facilities will offer options like these to make the registration process easy and fast.
The hospital of the future will feature a friendlier environment, with landscaping and nice views from patient rooms, artwork and amenities that are important in the healing process. They will also include an emphasis on alternative treatments, says Dr. Tingwald, “from massage to aromatherapy to spaces for yoga or meditation.”
Plan for Flexibility
The key to the design of the hospital of the future will be its ability to change without building additions, remodeling, or rehabbing.
“We’re no longer planning a facility in a static way, thinking that things will not change. Flexibility and adaptability are planned from the beginning,” explains Dr. Tingwald. “You’ll see a lot more generic room types—rooms that are all a single size, but adaptable. A private patient room might be initially planned for acute care, but it can be adapted for an ICU room with minimal or no remodeling.”
This holds true for other room types as well. “In diagnostic and treatment spaces, we plan for one, or no more than two, sizes of space,” he says. “You don’t know if in the future more procedures will be surgical or non-invasive, so rooms are planned to handle both functions. Also, the kingdoms are coming down and divisions between diagnostic departments are blending.”
The Johns Hopkins Hospital (Baltimore), the University of California, Los Angeles Medical Center, and California Pacific Medical Center in San Francisco are all designing “platform floors,” where surgery, interventional imaging, cardiac catheterization, and other procedure-based services share preoperative and postoperative areas and have single access.
“These floors provide adjacency of services allowing a lot more flexibility and decreased redundancy,” explains Dr. Tingwald. “Also, there aren’t as many patient transfers, and a key to patient-centered care is less movement of the patient.”
Built-in flexibility is designed to accommodate scalability as well. “In the planning process, we anticipate higher volumes in an emergency or disaster,” he says. “We plan how to expand the emergency room, and we make rooms larger than we used to. That way, if volumes increase quickly, you could put two, three, maybe more patients in a space. Nurses hate when you say that, but we have to have timely solutions that are affordable. This approach can be considered on nursing units as well, with these ‘super singles’ able to handle a second patient during a February flu outbreak, for example. That’s better than having an entire wing of the hospital that’s only used during winter months, patients stuck in the emergency department for days, or patients in the halls.”
A Design with Built-In Patient Safety
The physical design of the hospital of the future will better address and correct issues with patient safety. “Whatever design elements can minimize errors and improve outcomes are being studied intensively right now,” says Dr. Tingwald. “For example, we used to mirror many room types so that walls could share plumbing, etc. One room would be the mirror image of the one next to it, requiring the staff to learn different layouts, which increases time of response and possible errors. Now, we try to make procedure rooms as similar as possible to reduce the potential for error.”
There are design elements that limit the possibility of hospital-borne infection, including ultraviolet light and biologic surfaces. There is also a greater emphasis on including track systems for lifts for getting patients out of bed and moving them without injury to the patient or the staff.
Consider Hospitalists and Other Staff
How will the hospital of the future accommodate hospitalists?
“We’re certainly seeing more hospitalists,” says Dr. Tingwald. “As you have sicker patients in the hospital, it’s harder for their primary care physicians to manage them, so we’re going to see even more hospitalists. This means that we have to provide space for them; both offices, because they don’t have other office space, and sleeping accommodations, which means private rooms with bath, as well as lounge space.”
Hospitals will provide appealing space for physicians because it will help them recruit hospitalists. Improving lounges and other staff spaces will be a goal of future hospital designs.
“There will be a lot more emphasis on good environments for work and for support services,” predicts Dr. Tingwald. “This will increase the attraction and retention of top staff. You’ll see things like fitness centers, and basic additions like enough parking spaces.”
As hospital facilities move toward more patient-centered care, with flexible layouts and space designed for patient safety, the working environment is certain to become more conducive to providing good care and working efficiently. It will also become more comfortable, convenient, and pleasant for hospitalists and other staff. And that is something to look forward to. TH
Writer Jane Jerrard wrote the first three installments of the “Future” series.
Where will you be in 20 years? If you’re a young hospitalist, you may work in an enormous state-of-the-art hospital complex that includes the latest technologies, the best in amenities, and a well-thought-out design that will meet your needs and those of other staff for years to come.
“There are a lot of different approaches” to designing the hospital facility of the future, says George R. Tingwald, MD, AIA, ACHA, director of healthcare design at Skidmore, Owings, and Merrill in San Francisco. “The difference depends on whether you look at it from a constructability standpoint versus a much more consumer-based focus. Though many think they have the right approach, it’s hard to say that everybody’s decided on a single solution.”
The Future Looks … Big
It’s not just the hospital facility itself that will change in the future. The number of hospitals in each community may change as well—and the hospitals will be considerably larger.
“We will probably see fewer but larger hospitals in the future,” predicts Dr. Tingwald. “We’re in an era where we’re seeing significant growth in the number of inpatients served. Because of the baby boom and increasing longevity in Americans we’re already seeing an increase, and it’s going to continue. We’ll definitely see more hospital beds in the future.”
The type of patients who fill those hospital beds will change as well.
“We’ll continue to see sicker and sicker patients in those hospital beds,” says Dr. Tingwald. “More people will be managed on an outpatient basis as more diagnostic and treatment procedures will be done as outpatients. Look at breast cancer: From initial detection to diagnosis to biopsy to lumpectomy to chemotherapy or radiation treatment, to cure, or end-of-life care, each step can now be done on an outpatient basis.”
What does this mean? “Someone can have a very significant, multiepisodic disease and never stay in the hospital—unless there are complications,” explains Dr. Tingwald. “Therefore, we’ll have only very acute patients in the hospital. The hospital will basically become an intensive care unit.”
In the past, approximately 10% of a hospital’s beds were in the ICU. That percentage is rising—an indication of things to come. That percentage is now around 20% or 30% and growing, especially in major centers. Only seriously ill people will be admitted—but even they won’t spend a lot of time in the hospital. They will die, recover to a point where they can be moved to rehabilitation or other support facility, or be sent home.
What about the prediction that there will be fewer hospitals in the future? Dr. Tingwald predicts that technology and expertise will weed out some facilities.
“We used to have a lot of what I would call general hospitals—meaning every one was the same,” he explains. “That’s changing radically. The institutions with the expertise and wherewithal to develop technical sophistication, such as university hospitals and specialty hospitals, are doing well. Those that don’t have that sophistication can’t keep up. The big centers are growing because they have the equipment and the expertise. The smaller ones are failing.”
This trend may come as a surprise to some in healthcare, in light of previous predictions. “This is different than the futurists were saying 10 or 20 years ago, when predictions were for more home-based and community-based care,” says Dr. Tingwald. “The reverse has happened. The latest equipment is not available to everyone, let alone smaller, unaffiliated hospitals. And the people that can work with that technology are few and far between.”
The addition of new technology will have some effect on the size of the hospital. “You need a lot of physical space for wiring,” admits Dr. Tingwald. “But the ‘brains’ of the technology can be offsite at a separate IT center or data center.”
Focus on Family-Centered Care
Perhaps the most noticeable differences in the hospital facility of the future will be those related to a change in services, design, and attitude toward providing amenities for patients and their families.
“Patient-centered care, or its close cousin—family-centered care—is a significant trend in healthcare design now, and that significantly impacts the design of facilities,” states Dr. Tingwald. “The most important aspect is having all private rooms. Almost no new construction includes shared patient rooms. The key element of this care is family involvement, and that includes families rooming in with patients. You can’t physically or psychologically do this in a shared room.”
He points out that this trend includes all room types: “It started in pediatrics, but has gone into general acute care settings, intensive care settings, and now neonatal intensive care units.”
What are the pros and cons of a move toward all private rooms? “It takes up room, but it’s proving not to be significantly more costly,” says Dr. Tingwald. “Private rooms are more expensive to build, but in the end they’re less expensive to operate. In an all-private room hospital you can increase your occupancy to 80% or even 90% because you’re not trying to match up patients by gender and age. Also, nursing isn’t moving patients to get the bed mixes right. Studies show that nurses spend up to 40% of their time in transfers. And finally, private rooms have increased market share considerably.”
Another aspect of family centered care is the addition of technologies and services that cater to patient comfort and even enjoyment. “Anything someone has at home or wants in a hotel, families and patients are demanding, including room service,” says Dr. Tingwald. “Patients can decide when and what they want to eat [within their prescribed diet], and families can order food. In some hospitals, patients can already order food using a plasma screen in their room. This is showing to be an economically viable alternative. There’s less food waste, and patients are much happier.”
You’ll also see patient rooms with plasma screen televisions and DVD players, equipped for movies on demand, educational content—even the ability for physicians to view X-rays and other diagnostics on screen, and for families waiting in the room to communicate with physicians in the operating room.
“These are consumer-driven things, but they’re not luxuries,” insists Dr. Tingwald. “They’re often things that save time, increase the ability for education, and significantly decrease errors.”
Another argument for adding amenities like plasma screen TVs and room service: “In healthcare you think adding this technology must be too expensive,” says Dr. Tingwald, “but if you walk into a fast-food place, the person behind the counter uses a touch screen. Everybody else has done this already. Facilities that don’t partake in these transitions are not going to survive.”
Other family-centered improvements include major changes in patient registration. “Most registration can be done from home, over the Internet,” he says. “At Northwestern Memorial Hospital [in Chicago], patients have an encoded card they swipe when they drive into the parking garage, and the receptionist knows they’re coming and gets their room ready before they arrive.”
In the future, more facilities will offer options like these to make the registration process easy and fast.
The hospital of the future will feature a friendlier environment, with landscaping and nice views from patient rooms, artwork and amenities that are important in the healing process. They will also include an emphasis on alternative treatments, says Dr. Tingwald, “from massage to aromatherapy to spaces for yoga or meditation.”
Plan for Flexibility
The key to the design of the hospital of the future will be its ability to change without building additions, remodeling, or rehabbing.
“We’re no longer planning a facility in a static way, thinking that things will not change. Flexibility and adaptability are planned from the beginning,” explains Dr. Tingwald. “You’ll see a lot more generic room types—rooms that are all a single size, but adaptable. A private patient room might be initially planned for acute care, but it can be adapted for an ICU room with minimal or no remodeling.”
This holds true for other room types as well. “In diagnostic and treatment spaces, we plan for one, or no more than two, sizes of space,” he says. “You don’t know if in the future more procedures will be surgical or non-invasive, so rooms are planned to handle both functions. Also, the kingdoms are coming down and divisions between diagnostic departments are blending.”
The Johns Hopkins Hospital (Baltimore), the University of California, Los Angeles Medical Center, and California Pacific Medical Center in San Francisco are all designing “platform floors,” where surgery, interventional imaging, cardiac catheterization, and other procedure-based services share preoperative and postoperative areas and have single access.
“These floors provide adjacency of services allowing a lot more flexibility and decreased redundancy,” explains Dr. Tingwald. “Also, there aren’t as many patient transfers, and a key to patient-centered care is less movement of the patient.”
Built-in flexibility is designed to accommodate scalability as well. “In the planning process, we anticipate higher volumes in an emergency or disaster,” he says. “We plan how to expand the emergency room, and we make rooms larger than we used to. That way, if volumes increase quickly, you could put two, three, maybe more patients in a space. Nurses hate when you say that, but we have to have timely solutions that are affordable. This approach can be considered on nursing units as well, with these ‘super singles’ able to handle a second patient during a February flu outbreak, for example. That’s better than having an entire wing of the hospital that’s only used during winter months, patients stuck in the emergency department for days, or patients in the halls.”
A Design with Built-In Patient Safety
The physical design of the hospital of the future will better address and correct issues with patient safety. “Whatever design elements can minimize errors and improve outcomes are being studied intensively right now,” says Dr. Tingwald. “For example, we used to mirror many room types so that walls could share plumbing, etc. One room would be the mirror image of the one next to it, requiring the staff to learn different layouts, which increases time of response and possible errors. Now, we try to make procedure rooms as similar as possible to reduce the potential for error.”
There are design elements that limit the possibility of hospital-borne infection, including ultraviolet light and biologic surfaces. There is also a greater emphasis on including track systems for lifts for getting patients out of bed and moving them without injury to the patient or the staff.
Consider Hospitalists and Other Staff
How will the hospital of the future accommodate hospitalists?
“We’re certainly seeing more hospitalists,” says Dr. Tingwald. “As you have sicker patients in the hospital, it’s harder for their primary care physicians to manage them, so we’re going to see even more hospitalists. This means that we have to provide space for them; both offices, because they don’t have other office space, and sleeping accommodations, which means private rooms with bath, as well as lounge space.”
Hospitals will provide appealing space for physicians because it will help them recruit hospitalists. Improving lounges and other staff spaces will be a goal of future hospital designs.
“There will be a lot more emphasis on good environments for work and for support services,” predicts Dr. Tingwald. “This will increase the attraction and retention of top staff. You’ll see things like fitness centers, and basic additions like enough parking spaces.”
As hospital facilities move toward more patient-centered care, with flexible layouts and space designed for patient safety, the working environment is certain to become more conducive to providing good care and working efficiently. It will also become more comfortable, convenient, and pleasant for hospitalists and other staff. And that is something to look forward to. TH
Writer Jane Jerrard wrote the first three installments of the “Future” series.
An Itchy Neck
A62-year-old male with a history of a cadaveric renal transplant complains of a three-week history of progressive, slightly pruritic lesions on his head and neck. Physical exam reveals multiple 3-8 mm umbilicated papules with some excoriations distributed on sun-exposed areas of face, scalp, and neck. (See photo above.) He takes tacrolimus 1 mg PO QD, mycophenolate mofetil 750 mg BID and prednisone 10 mg QD. He is otherwise without complaints except for some mild blurry vision that started several days ago.
The most appropriate plan of care is:
- Apply triamcinolone 0.1% cream bid for 10 days; biopsy if no improvement. Instruct him not to scratch these lesions of prurigo nodularis.
- Biopsy a lesion and send half of the material for tissue culture. Watch for development of systemic/central nervous system signs.
- Liquid nitrogen for likely molluscum contagiosum lesions.
- Electrodessication and curettage for these presumed non-melanoma skin cancers.
- Valacyclovir 1,000 mg PO TID for seven days for herpes zoster.
Discussion
The answer is B: Biopsy a lesion and send half of the material for tissue culture. Watch for development of systemic/central nervous system signs.
In this immunosuppressed patient, the differential diagnosis should include molluscum contagiosum, disseminated HSV/VZV, non-melanoma skin cancers, fungal infections (including Cryptococcus, Histoplasma, Coccidioidomycosis, and Penicillium marneffeii), Leishmaniasis, and prurigo nodularis. The appropriate step in the management is to assume a possible opportunistic infection because this may be a sign of systemic infection that can be rapidly fatal.
This case was diagnosed by a Tzanck smear showing multiple narrow-based budding yeast forms consistent with Cryptococcus. (See photo below.) A tissue culture and H&E preparation confirmed the diagnosis. (See photo at right.) The patient was admitted immediately after evaluation by the Tzanck smear and started on liposomal amphotericin B. He developed systemic symptoms within 24 hours of hospitalization and was found to have Cryptococcal antigen in his serum and CSF. He eventually recovered after a 17-day hospitalization and was discharged on lifelong fluconazole.
Cryptococcosis, caused by the yeast Cryptococcus neoformans, is a major source of morbidity and mortality in immunosuppressed patients. It is a ubiquitous fungus primarily associated with bird droppings. The organism is inhaled and uses the lung as a portal of entry. In immunocompromised patients, the decrease in cell-mediated immunity allows the organism to disseminate widely. Although many organs may become affected, there is a predilection for central nervous system involvement and development of a meningoencephalitis. Skin involvement occurs in 10% to 20% of patients. If skin involvement occurs it should alert the physician to underlying disseminated disease. Prompt diagnosis and initiation of treatment are essential to reduce the high mortality (up to 80%) associated with untreated cases. Work-up should be directed toward findings on history and physical exam, but should at least include a chest x-ray, serum cryptococcal Ag, blood and urine cultures, and consideration of a lumbar puncture.
Cutaneous lesions are protean and can be nodules, papules, pustules, acneiform papules and pustules, molluscum contagiosum-like papules, herpetic-like vesicles, ulcers, or cellulitis. Given the non-specific appearance, one should lower the threshold in immunocompromised patients for consideration of deep fungal infections. TH
References
- Vilchez RA, Fung J, Kusne S. Cryptococcosis in organ transplant recipients: an overview. Am J Transplantation. 2002;2:575-580.
- Vincenzo R, Ruocco E. Tzanck smear, an old test for the new millennium: when and how. Int J Derm. 1999;38(11):830-834.
- Perfect JR, Casadevall A. Cryptococcosis. Infect Dis Clin North Am. 2002;16(4):837-874.
A62-year-old male with a history of a cadaveric renal transplant complains of a three-week history of progressive, slightly pruritic lesions on his head and neck. Physical exam reveals multiple 3-8 mm umbilicated papules with some excoriations distributed on sun-exposed areas of face, scalp, and neck. (See photo above.) He takes tacrolimus 1 mg PO QD, mycophenolate mofetil 750 mg BID and prednisone 10 mg QD. He is otherwise without complaints except for some mild blurry vision that started several days ago.
The most appropriate plan of care is:
- Apply triamcinolone 0.1% cream bid for 10 days; biopsy if no improvement. Instruct him not to scratch these lesions of prurigo nodularis.
- Biopsy a lesion and send half of the material for tissue culture. Watch for development of systemic/central nervous system signs.
- Liquid nitrogen for likely molluscum contagiosum lesions.
- Electrodessication and curettage for these presumed non-melanoma skin cancers.
- Valacyclovir 1,000 mg PO TID for seven days for herpes zoster.
Discussion
The answer is B: Biopsy a lesion and send half of the material for tissue culture. Watch for development of systemic/central nervous system signs.
In this immunosuppressed patient, the differential diagnosis should include molluscum contagiosum, disseminated HSV/VZV, non-melanoma skin cancers, fungal infections (including Cryptococcus, Histoplasma, Coccidioidomycosis, and Penicillium marneffeii), Leishmaniasis, and prurigo nodularis. The appropriate step in the management is to assume a possible opportunistic infection because this may be a sign of systemic infection that can be rapidly fatal.
This case was diagnosed by a Tzanck smear showing multiple narrow-based budding yeast forms consistent with Cryptococcus. (See photo below.) A tissue culture and H&E preparation confirmed the diagnosis. (See photo at right.) The patient was admitted immediately after evaluation by the Tzanck smear and started on liposomal amphotericin B. He developed systemic symptoms within 24 hours of hospitalization and was found to have Cryptococcal antigen in his serum and CSF. He eventually recovered after a 17-day hospitalization and was discharged on lifelong fluconazole.
Cryptococcosis, caused by the yeast Cryptococcus neoformans, is a major source of morbidity and mortality in immunosuppressed patients. It is a ubiquitous fungus primarily associated with bird droppings. The organism is inhaled and uses the lung as a portal of entry. In immunocompromised patients, the decrease in cell-mediated immunity allows the organism to disseminate widely. Although many organs may become affected, there is a predilection for central nervous system involvement and development of a meningoencephalitis. Skin involvement occurs in 10% to 20% of patients. If skin involvement occurs it should alert the physician to underlying disseminated disease. Prompt diagnosis and initiation of treatment are essential to reduce the high mortality (up to 80%) associated with untreated cases. Work-up should be directed toward findings on history and physical exam, but should at least include a chest x-ray, serum cryptococcal Ag, blood and urine cultures, and consideration of a lumbar puncture.
Cutaneous lesions are protean and can be nodules, papules, pustules, acneiform papules and pustules, molluscum contagiosum-like papules, herpetic-like vesicles, ulcers, or cellulitis. Given the non-specific appearance, one should lower the threshold in immunocompromised patients for consideration of deep fungal infections. TH
References
- Vilchez RA, Fung J, Kusne S. Cryptococcosis in organ transplant recipients: an overview. Am J Transplantation. 2002;2:575-580.
- Vincenzo R, Ruocco E. Tzanck smear, an old test for the new millennium: when and how. Int J Derm. 1999;38(11):830-834.
- Perfect JR, Casadevall A. Cryptococcosis. Infect Dis Clin North Am. 2002;16(4):837-874.
A62-year-old male with a history of a cadaveric renal transplant complains of a three-week history of progressive, slightly pruritic lesions on his head and neck. Physical exam reveals multiple 3-8 mm umbilicated papules with some excoriations distributed on sun-exposed areas of face, scalp, and neck. (See photo above.) He takes tacrolimus 1 mg PO QD, mycophenolate mofetil 750 mg BID and prednisone 10 mg QD. He is otherwise without complaints except for some mild blurry vision that started several days ago.
The most appropriate plan of care is:
- Apply triamcinolone 0.1% cream bid for 10 days; biopsy if no improvement. Instruct him not to scratch these lesions of prurigo nodularis.
- Biopsy a lesion and send half of the material for tissue culture. Watch for development of systemic/central nervous system signs.
- Liquid nitrogen for likely molluscum contagiosum lesions.
- Electrodessication and curettage for these presumed non-melanoma skin cancers.
- Valacyclovir 1,000 mg PO TID for seven days for herpes zoster.
Discussion
The answer is B: Biopsy a lesion and send half of the material for tissue culture. Watch for development of systemic/central nervous system signs.
In this immunosuppressed patient, the differential diagnosis should include molluscum contagiosum, disseminated HSV/VZV, non-melanoma skin cancers, fungal infections (including Cryptococcus, Histoplasma, Coccidioidomycosis, and Penicillium marneffeii), Leishmaniasis, and prurigo nodularis. The appropriate step in the management is to assume a possible opportunistic infection because this may be a sign of systemic infection that can be rapidly fatal.
This case was diagnosed by a Tzanck smear showing multiple narrow-based budding yeast forms consistent with Cryptococcus. (See photo below.) A tissue culture and H&E preparation confirmed the diagnosis. (See photo at right.) The patient was admitted immediately after evaluation by the Tzanck smear and started on liposomal amphotericin B. He developed systemic symptoms within 24 hours of hospitalization and was found to have Cryptococcal antigen in his serum and CSF. He eventually recovered after a 17-day hospitalization and was discharged on lifelong fluconazole.
Cryptococcosis, caused by the yeast Cryptococcus neoformans, is a major source of morbidity and mortality in immunosuppressed patients. It is a ubiquitous fungus primarily associated with bird droppings. The organism is inhaled and uses the lung as a portal of entry. In immunocompromised patients, the decrease in cell-mediated immunity allows the organism to disseminate widely. Although many organs may become affected, there is a predilection for central nervous system involvement and development of a meningoencephalitis. Skin involvement occurs in 10% to 20% of patients. If skin involvement occurs it should alert the physician to underlying disseminated disease. Prompt diagnosis and initiation of treatment are essential to reduce the high mortality (up to 80%) associated with untreated cases. Work-up should be directed toward findings on history and physical exam, but should at least include a chest x-ray, serum cryptococcal Ag, blood and urine cultures, and consideration of a lumbar puncture.
Cutaneous lesions are protean and can be nodules, papules, pustules, acneiform papules and pustules, molluscum contagiosum-like papules, herpetic-like vesicles, ulcers, or cellulitis. Given the non-specific appearance, one should lower the threshold in immunocompromised patients for consideration of deep fungal infections. TH
References
- Vilchez RA, Fung J, Kusne S. Cryptococcosis in organ transplant recipients: an overview. Am J Transplantation. 2002;2:575-580.
- Vincenzo R, Ruocco E. Tzanck smear, an old test for the new millennium: when and how. Int J Derm. 1999;38(11):830-834.
- Perfect JR, Casadevall A. Cryptococcosis. Infect Dis Clin North Am. 2002;16(4):837-874.
Career Satisfaction Toolkit
Early survey data on hospitalists, which suggest high levels of job engagement and low turnover rates, may not be as relevant as programs mature in a competitive marketplace to meet important needs such as rising census and Accreditation Council for Graduate Medical Education (ACGME) requirements. There is also a paucity of data on how different models of compensation affect hospitalists’ career satisfaction.
In 2005 the role of the hospitalist has evolved from simply improving throughput (average length of stay) to one of leadership, quality improvement, and teaching that extends beyond direct patient care. Compensation for hospitalists should not, therefore, be based solely on billing revenue. Improving the efficiency of the hospitalists work environment, which may include IT support, adequate office space, and administrative support, may not only enhance productivity but also job satisfaction. More research is needed to examine these questions.
Progress Report
One of the Career Satisfaction Task Force’s major initiatives has been developing a toolkit for the SHM membership with the purpose of providing members with an action plan for attaining a long and satisfying career in hospital medicine. The following steps are being taken in the creation of the toolkit:
- Needs assessment—questionnaire at the SHM 2005 Annual Meeting;
- Monthly conference calls;
- Timeline:
- Toolkit draft completion—Sept. 2005;
- Review SHM Membership Committee—Oct. 2005;
- Further revision;
- Submission to SHM Board for review—Nov. 2005;
- Further revision; and
- Dissemination at SHM Annual Meeting—May 2006.
- Content—four workplace domains:
- Control/Autonomy;
- Workload/Schedule;
- Community/Environment; and
- Reward/Recognition.
- Elements comprising each domain:
- Definition: specific description of workplace domain;
- Background: review of literature, expert opinion, experience-based observation, executive summary of background content;
- Guidelines: practical actionable recommendations and educational initiatives;
- Pitfalls: specific examples;
- Examples: application to different settings (community, academic, pediatric); and
- References.
Research and Timeline
In parallel to the development of the work domains for the toolkit, the Career Satisfaction Task Force is developing a questionnaire to survey hospitalist physicians on career satisfaction and “worklife.” The last survey of this type was performed in 1999. This questionnaire will allow us to assess changes in hospitalist quality of working life over time to further explore how hospitalists are faring during this critical time of rapid growth of our specialty.
The task force is developing a list of important aspects of worklife, satisfaction, and stress for hospitalists. This list will be supplemented by semi-structured interviews of SHM members and leaders in hospital medicine to include a representative viewpoint of hospitalist worklife: adult and pediatric medicine, academic and community, gender and age, directors of programs, and different employer types.
The interviews were expected to be completed in the fall of 2005. Qualitative data analysis will allow us to ascertain important themes for job performance and satisfaction to be highlighted in the survey. The questionnaire development will also consider inclusion of aspects from the prior surveys to follow results over time and when possible will use validated questions from the quality of working life literature.
We anticipate completion of the questionnaire in spring 2006 followed by surveying of a random sample of hospitalists from the SHM membership through a Web-based survey. Sampling of groups of hospitalists based on job characteristics will occur because there is significant interest and need for information about hospitalist worklife in certain work settings. The questionnaire dissemination time will overlap with the annual meeting to maximize survey response. The task force will work with SHM annual meeting committee to discuss having a dedicated computer for filling out the Web-based survey on-site.
Any SHM member who would like to participate in the questionnaire on-site, even if they were not selected for the random sample, will be encouraged to do so. Data analysis will occur in mid-late 2006. The task force will use information from the analyses to update the SHM Worklife Toolkit. We will also provide numerous forums for dissemination of the data. In particular, we plan to showcase this data at the 2007 SHM Annual Meeting followed by journal publication and Web site posting. It is our hope that this data will provide key information on the current quality of working life of hospitalist physicians to support worklife recommendations that promote sustainable, enjoyable careers in hospital medicine.
Early survey data on hospitalists, which suggest high levels of job engagement and low turnover rates, may not be as relevant as programs mature in a competitive marketplace to meet important needs such as rising census and Accreditation Council for Graduate Medical Education (ACGME) requirements. There is also a paucity of data on how different models of compensation affect hospitalists’ career satisfaction.
In 2005 the role of the hospitalist has evolved from simply improving throughput (average length of stay) to one of leadership, quality improvement, and teaching that extends beyond direct patient care. Compensation for hospitalists should not, therefore, be based solely on billing revenue. Improving the efficiency of the hospitalists work environment, which may include IT support, adequate office space, and administrative support, may not only enhance productivity but also job satisfaction. More research is needed to examine these questions.
Progress Report
One of the Career Satisfaction Task Force’s major initiatives has been developing a toolkit for the SHM membership with the purpose of providing members with an action plan for attaining a long and satisfying career in hospital medicine. The following steps are being taken in the creation of the toolkit:
- Needs assessment—questionnaire at the SHM 2005 Annual Meeting;
- Monthly conference calls;
- Timeline:
- Toolkit draft completion—Sept. 2005;
- Review SHM Membership Committee—Oct. 2005;
- Further revision;
- Submission to SHM Board for review—Nov. 2005;
- Further revision; and
- Dissemination at SHM Annual Meeting—May 2006.
- Content—four workplace domains:
- Control/Autonomy;
- Workload/Schedule;
- Community/Environment; and
- Reward/Recognition.
- Elements comprising each domain:
- Definition: specific description of workplace domain;
- Background: review of literature, expert opinion, experience-based observation, executive summary of background content;
- Guidelines: practical actionable recommendations and educational initiatives;
- Pitfalls: specific examples;
- Examples: application to different settings (community, academic, pediatric); and
- References.
Research and Timeline
In parallel to the development of the work domains for the toolkit, the Career Satisfaction Task Force is developing a questionnaire to survey hospitalist physicians on career satisfaction and “worklife.” The last survey of this type was performed in 1999. This questionnaire will allow us to assess changes in hospitalist quality of working life over time to further explore how hospitalists are faring during this critical time of rapid growth of our specialty.
The task force is developing a list of important aspects of worklife, satisfaction, and stress for hospitalists. This list will be supplemented by semi-structured interviews of SHM members and leaders in hospital medicine to include a representative viewpoint of hospitalist worklife: adult and pediatric medicine, academic and community, gender and age, directors of programs, and different employer types.
The interviews were expected to be completed in the fall of 2005. Qualitative data analysis will allow us to ascertain important themes for job performance and satisfaction to be highlighted in the survey. The questionnaire development will also consider inclusion of aspects from the prior surveys to follow results over time and when possible will use validated questions from the quality of working life literature.
We anticipate completion of the questionnaire in spring 2006 followed by surveying of a random sample of hospitalists from the SHM membership through a Web-based survey. Sampling of groups of hospitalists based on job characteristics will occur because there is significant interest and need for information about hospitalist worklife in certain work settings. The questionnaire dissemination time will overlap with the annual meeting to maximize survey response. The task force will work with SHM annual meeting committee to discuss having a dedicated computer for filling out the Web-based survey on-site.
Any SHM member who would like to participate in the questionnaire on-site, even if they were not selected for the random sample, will be encouraged to do so. Data analysis will occur in mid-late 2006. The task force will use information from the analyses to update the SHM Worklife Toolkit. We will also provide numerous forums for dissemination of the data. In particular, we plan to showcase this data at the 2007 SHM Annual Meeting followed by journal publication and Web site posting. It is our hope that this data will provide key information on the current quality of working life of hospitalist physicians to support worklife recommendations that promote sustainable, enjoyable careers in hospital medicine.
Early survey data on hospitalists, which suggest high levels of job engagement and low turnover rates, may not be as relevant as programs mature in a competitive marketplace to meet important needs such as rising census and Accreditation Council for Graduate Medical Education (ACGME) requirements. There is also a paucity of data on how different models of compensation affect hospitalists’ career satisfaction.
In 2005 the role of the hospitalist has evolved from simply improving throughput (average length of stay) to one of leadership, quality improvement, and teaching that extends beyond direct patient care. Compensation for hospitalists should not, therefore, be based solely on billing revenue. Improving the efficiency of the hospitalists work environment, which may include IT support, adequate office space, and administrative support, may not only enhance productivity but also job satisfaction. More research is needed to examine these questions.
Progress Report
One of the Career Satisfaction Task Force’s major initiatives has been developing a toolkit for the SHM membership with the purpose of providing members with an action plan for attaining a long and satisfying career in hospital medicine. The following steps are being taken in the creation of the toolkit:
- Needs assessment—questionnaire at the SHM 2005 Annual Meeting;
- Monthly conference calls;
- Timeline:
- Toolkit draft completion—Sept. 2005;
- Review SHM Membership Committee—Oct. 2005;
- Further revision;
- Submission to SHM Board for review—Nov. 2005;
- Further revision; and
- Dissemination at SHM Annual Meeting—May 2006.
- Content—four workplace domains:
- Control/Autonomy;
- Workload/Schedule;
- Community/Environment; and
- Reward/Recognition.
- Elements comprising each domain:
- Definition: specific description of workplace domain;
- Background: review of literature, expert opinion, experience-based observation, executive summary of background content;
- Guidelines: practical actionable recommendations and educational initiatives;
- Pitfalls: specific examples;
- Examples: application to different settings (community, academic, pediatric); and
- References.
Research and Timeline
In parallel to the development of the work domains for the toolkit, the Career Satisfaction Task Force is developing a questionnaire to survey hospitalist physicians on career satisfaction and “worklife.” The last survey of this type was performed in 1999. This questionnaire will allow us to assess changes in hospitalist quality of working life over time to further explore how hospitalists are faring during this critical time of rapid growth of our specialty.
The task force is developing a list of important aspects of worklife, satisfaction, and stress for hospitalists. This list will be supplemented by semi-structured interviews of SHM members and leaders in hospital medicine to include a representative viewpoint of hospitalist worklife: adult and pediatric medicine, academic and community, gender and age, directors of programs, and different employer types.
The interviews were expected to be completed in the fall of 2005. Qualitative data analysis will allow us to ascertain important themes for job performance and satisfaction to be highlighted in the survey. The questionnaire development will also consider inclusion of aspects from the prior surveys to follow results over time and when possible will use validated questions from the quality of working life literature.
We anticipate completion of the questionnaire in spring 2006 followed by surveying of a random sample of hospitalists from the SHM membership through a Web-based survey. Sampling of groups of hospitalists based on job characteristics will occur because there is significant interest and need for information about hospitalist worklife in certain work settings. The questionnaire dissemination time will overlap with the annual meeting to maximize survey response. The task force will work with SHM annual meeting committee to discuss having a dedicated computer for filling out the Web-based survey on-site.
Any SHM member who would like to participate in the questionnaire on-site, even if they were not selected for the random sample, will be encouraged to do so. Data analysis will occur in mid-late 2006. The task force will use information from the analyses to update the SHM Worklife Toolkit. We will also provide numerous forums for dissemination of the data. In particular, we plan to showcase this data at the 2007 SHM Annual Meeting followed by journal publication and Web site posting. It is our hope that this data will provide key information on the current quality of working life of hospitalist physicians to support worklife recommendations that promote sustainable, enjoyable careers in hospital medicine.
Quality Will Be Job One
One of the potential benefits of hospital medicine is the tangible opportunity to change healthcare in a meaningful way. Although much of the initial ballyhoo for hospital medicine has been around service-related issues, that is about to change.
Hospitalists have been willing to take on the inpatient responsibilities for primarily outpatient-based internists, family practitioners, and pediatricians. We have been available to admit and manage the patients who present to emergency rooms with acute illnesses and who have no physician of record. We have actively worked with surgeons and subspecialists to co-manage their patient’s medical problems.
In addition, because hospitalists are much more readily available to acutely ill inpatients, because we have more expertise with these medical problems, and because practice generally makes for better performance, hospitalists have been expected to provide more effective and more efficient care.
But that is just the front end of what is creating the enormous energy behind the hospital medicine movement. We are moving into an era of measurement of defined patient outcomes and expectations from insurance companies, Medicare, the business community, and—yes—even our patients. That era will require us to step up and deliver higher quality healthcare.
This is the driver to the pay-for-performance movement and a shift from just rewarding physicians and hospitals for doing the procedure or “visiting” the patient and moving to where those who can demonstrate expertise and performance are rewarded financially and by reputation.
Hospitalists and SHM take this very seriously and are creating alliances and programs to help hospitalists become leaders in the quality and performance arenas.
Walking through the approach that SHM is taking in improving glycemic control in hospitalized patients (see below) will serve as a template for other activities SHM has planned in heart failure, VTE, hospitalized infections, and other illnesses hospitalists see and treat every day.
In a practical way, hospitals and health professionals finally came into the performance era with the first publication of the individual hospital performance results to performance measures developed by JCAHO and co-promoted with CMS in their Hospital Compare Web site. This was promulgated widely, especially at www.hospitalcompare.hhs.gov.
Because Hospital Compare was picked up by The New York Times, the Los Angeles Times, and many local papers, hospitals were soon trying to explain why their performance in heart failure, pneumonia, and heart attack looked like a failing grade. Now that the public is involved, hospitals are scrambling to quickly improve their performance rather than attacking the data.
Looking to the future, SHM is working with JCAHO to develop performance standards for glycemic control for inpatients as a way to assess how our hospitals and physicians are doing in managing diabetes. SHM is also allying with many other key stakeholders to form a steering committee for this project. These standards will take almost three years to develop, test, and implement. So the first reporting of how every hospital is doing in diabetes is most likely a 2008 or 2009 event.
Expecting that many hospitals will improve their performance in diabetic care during 2008 and 2009, SHM is now developing the tools and the training to allow hospitalists to be ready with practical solutions.
In October 2005 SHM convened a Working Group on Inpatient Glycemic Control in Chicago. This meeting under the leadership of Greg Maynard, MD, associate clinical professor of medicine, chief of the division of hospital medicine, University of California at San Diego, brought together nationally recognized diabetologists and endocrinologists with hospitalist leaders, as well as experts in the field of nursing, case management, pharmacy, risk management, and nutrition. The end result is an understanding of what constitutes an ideal management of inpatient diabetes and what role hospitalists can play.
This work group now is analyzing what resources currently exist and what gaps need to be filled. Next SHM will develop an implementation plan to get this information out to our nation’s hospitalists.
SHM has some experience in developing quality improvement tools, as you can see in our Resource Rooms on the SHM Web site. For a current working example, take a look at the DVT Quality Improvement Resource Room at www.hospitalmedicine.org/AM/Template.cfm?Section=Quality_Improvement_Resource_Rooms1&Template=/CM/HTMLDisplay.cfm&ContentID=6312.
But SHM plans a more aggressive approach with proposed training sessions at the SHM Annual Meeting quality pre-course and taking these tools and approaches out to our hospitalists at local meetings throughout the country. SHM is also looking into creating a network of quality mentors that will work with individual hospitalists groups as they put SHM quality improvement tools into the workflow at their hospitals. SHM will also develop strategies for baseline measurement, ongoing data collection, involvement of team members, and procurement of local resources. SHM hopes to support research to further develop best practices and approaches.
The game plan goes something like this: SHM will develop the resources hospitalists need to improve management of inpatient diabetes in 2006. In 2007 and 2008 SHM will roll out this strategy to as many hospitalists as we can train. By 2008 JCAHO and CMS will have deployed their Performance Measures in Diabetes. When the first scores show the same deficiencies as we have seen this year in MI and heart failure, our nation’s hospitalists will be well armed to provide practical tangible solutions to improve quality.
And the beauty of this approach is that SHM is working on similar strategies right now for heart failure, DVT, pneumonia, and other key clinical conditions.
Those who pay for and receive care in our hospitals are looking at our current performance and demanding improvements. For the first time hospitals and those with resources are ready to make measurable quality a high priority. The presence of hospitalists in more than 2,000 hospitals (and more in the near future) ideally positions hospitalists to be a key change agent. The tools SHM is developing will give hospitalists the strategies and the expertise to make this happen.
This is a watershed moment in American healthcare. There is a palpable swing in the priorities of our patients. Hospitalists can help the healthcare team find real solutions. SHM has the vision and the plan to provide you with as much help as you need. Together we will do great things. TH
Dr. Wellikson has been CEO of SHM since 2000.
One of the potential benefits of hospital medicine is the tangible opportunity to change healthcare in a meaningful way. Although much of the initial ballyhoo for hospital medicine has been around service-related issues, that is about to change.
Hospitalists have been willing to take on the inpatient responsibilities for primarily outpatient-based internists, family practitioners, and pediatricians. We have been available to admit and manage the patients who present to emergency rooms with acute illnesses and who have no physician of record. We have actively worked with surgeons and subspecialists to co-manage their patient’s medical problems.
In addition, because hospitalists are much more readily available to acutely ill inpatients, because we have more expertise with these medical problems, and because practice generally makes for better performance, hospitalists have been expected to provide more effective and more efficient care.
But that is just the front end of what is creating the enormous energy behind the hospital medicine movement. We are moving into an era of measurement of defined patient outcomes and expectations from insurance companies, Medicare, the business community, and—yes—even our patients. That era will require us to step up and deliver higher quality healthcare.
This is the driver to the pay-for-performance movement and a shift from just rewarding physicians and hospitals for doing the procedure or “visiting” the patient and moving to where those who can demonstrate expertise and performance are rewarded financially and by reputation.
Hospitalists and SHM take this very seriously and are creating alliances and programs to help hospitalists become leaders in the quality and performance arenas.
Walking through the approach that SHM is taking in improving glycemic control in hospitalized patients (see below) will serve as a template for other activities SHM has planned in heart failure, VTE, hospitalized infections, and other illnesses hospitalists see and treat every day.
In a practical way, hospitals and health professionals finally came into the performance era with the first publication of the individual hospital performance results to performance measures developed by JCAHO and co-promoted with CMS in their Hospital Compare Web site. This was promulgated widely, especially at www.hospitalcompare.hhs.gov.
Because Hospital Compare was picked up by The New York Times, the Los Angeles Times, and many local papers, hospitals were soon trying to explain why their performance in heart failure, pneumonia, and heart attack looked like a failing grade. Now that the public is involved, hospitals are scrambling to quickly improve their performance rather than attacking the data.
Looking to the future, SHM is working with JCAHO to develop performance standards for glycemic control for inpatients as a way to assess how our hospitals and physicians are doing in managing diabetes. SHM is also allying with many other key stakeholders to form a steering committee for this project. These standards will take almost three years to develop, test, and implement. So the first reporting of how every hospital is doing in diabetes is most likely a 2008 or 2009 event.
Expecting that many hospitals will improve their performance in diabetic care during 2008 and 2009, SHM is now developing the tools and the training to allow hospitalists to be ready with practical solutions.
In October 2005 SHM convened a Working Group on Inpatient Glycemic Control in Chicago. This meeting under the leadership of Greg Maynard, MD, associate clinical professor of medicine, chief of the division of hospital medicine, University of California at San Diego, brought together nationally recognized diabetologists and endocrinologists with hospitalist leaders, as well as experts in the field of nursing, case management, pharmacy, risk management, and nutrition. The end result is an understanding of what constitutes an ideal management of inpatient diabetes and what role hospitalists can play.
This work group now is analyzing what resources currently exist and what gaps need to be filled. Next SHM will develop an implementation plan to get this information out to our nation’s hospitalists.
SHM has some experience in developing quality improvement tools, as you can see in our Resource Rooms on the SHM Web site. For a current working example, take a look at the DVT Quality Improvement Resource Room at www.hospitalmedicine.org/AM/Template.cfm?Section=Quality_Improvement_Resource_Rooms1&Template=/CM/HTMLDisplay.cfm&ContentID=6312.
But SHM plans a more aggressive approach with proposed training sessions at the SHM Annual Meeting quality pre-course and taking these tools and approaches out to our hospitalists at local meetings throughout the country. SHM is also looking into creating a network of quality mentors that will work with individual hospitalists groups as they put SHM quality improvement tools into the workflow at their hospitals. SHM will also develop strategies for baseline measurement, ongoing data collection, involvement of team members, and procurement of local resources. SHM hopes to support research to further develop best practices and approaches.
The game plan goes something like this: SHM will develop the resources hospitalists need to improve management of inpatient diabetes in 2006. In 2007 and 2008 SHM will roll out this strategy to as many hospitalists as we can train. By 2008 JCAHO and CMS will have deployed their Performance Measures in Diabetes. When the first scores show the same deficiencies as we have seen this year in MI and heart failure, our nation’s hospitalists will be well armed to provide practical tangible solutions to improve quality.
And the beauty of this approach is that SHM is working on similar strategies right now for heart failure, DVT, pneumonia, and other key clinical conditions.
Those who pay for and receive care in our hospitals are looking at our current performance and demanding improvements. For the first time hospitals and those with resources are ready to make measurable quality a high priority. The presence of hospitalists in more than 2,000 hospitals (and more in the near future) ideally positions hospitalists to be a key change agent. The tools SHM is developing will give hospitalists the strategies and the expertise to make this happen.
This is a watershed moment in American healthcare. There is a palpable swing in the priorities of our patients. Hospitalists can help the healthcare team find real solutions. SHM has the vision and the plan to provide you with as much help as you need. Together we will do great things. TH
Dr. Wellikson has been CEO of SHM since 2000.
One of the potential benefits of hospital medicine is the tangible opportunity to change healthcare in a meaningful way. Although much of the initial ballyhoo for hospital medicine has been around service-related issues, that is about to change.
Hospitalists have been willing to take on the inpatient responsibilities for primarily outpatient-based internists, family practitioners, and pediatricians. We have been available to admit and manage the patients who present to emergency rooms with acute illnesses and who have no physician of record. We have actively worked with surgeons and subspecialists to co-manage their patient’s medical problems.
In addition, because hospitalists are much more readily available to acutely ill inpatients, because we have more expertise with these medical problems, and because practice generally makes for better performance, hospitalists have been expected to provide more effective and more efficient care.
But that is just the front end of what is creating the enormous energy behind the hospital medicine movement. We are moving into an era of measurement of defined patient outcomes and expectations from insurance companies, Medicare, the business community, and—yes—even our patients. That era will require us to step up and deliver higher quality healthcare.
This is the driver to the pay-for-performance movement and a shift from just rewarding physicians and hospitals for doing the procedure or “visiting” the patient and moving to where those who can demonstrate expertise and performance are rewarded financially and by reputation.
Hospitalists and SHM take this very seriously and are creating alliances and programs to help hospitalists become leaders in the quality and performance arenas.
Walking through the approach that SHM is taking in improving glycemic control in hospitalized patients (see below) will serve as a template for other activities SHM has planned in heart failure, VTE, hospitalized infections, and other illnesses hospitalists see and treat every day.
In a practical way, hospitals and health professionals finally came into the performance era with the first publication of the individual hospital performance results to performance measures developed by JCAHO and co-promoted with CMS in their Hospital Compare Web site. This was promulgated widely, especially at www.hospitalcompare.hhs.gov.
Because Hospital Compare was picked up by The New York Times, the Los Angeles Times, and many local papers, hospitals were soon trying to explain why their performance in heart failure, pneumonia, and heart attack looked like a failing grade. Now that the public is involved, hospitals are scrambling to quickly improve their performance rather than attacking the data.
Looking to the future, SHM is working with JCAHO to develop performance standards for glycemic control for inpatients as a way to assess how our hospitals and physicians are doing in managing diabetes. SHM is also allying with many other key stakeholders to form a steering committee for this project. These standards will take almost three years to develop, test, and implement. So the first reporting of how every hospital is doing in diabetes is most likely a 2008 or 2009 event.
Expecting that many hospitals will improve their performance in diabetic care during 2008 and 2009, SHM is now developing the tools and the training to allow hospitalists to be ready with practical solutions.
In October 2005 SHM convened a Working Group on Inpatient Glycemic Control in Chicago. This meeting under the leadership of Greg Maynard, MD, associate clinical professor of medicine, chief of the division of hospital medicine, University of California at San Diego, brought together nationally recognized diabetologists and endocrinologists with hospitalist leaders, as well as experts in the field of nursing, case management, pharmacy, risk management, and nutrition. The end result is an understanding of what constitutes an ideal management of inpatient diabetes and what role hospitalists can play.
This work group now is analyzing what resources currently exist and what gaps need to be filled. Next SHM will develop an implementation plan to get this information out to our nation’s hospitalists.
SHM has some experience in developing quality improvement tools, as you can see in our Resource Rooms on the SHM Web site. For a current working example, take a look at the DVT Quality Improvement Resource Room at www.hospitalmedicine.org/AM/Template.cfm?Section=Quality_Improvement_Resource_Rooms1&Template=/CM/HTMLDisplay.cfm&ContentID=6312.
But SHM plans a more aggressive approach with proposed training sessions at the SHM Annual Meeting quality pre-course and taking these tools and approaches out to our hospitalists at local meetings throughout the country. SHM is also looking into creating a network of quality mentors that will work with individual hospitalists groups as they put SHM quality improvement tools into the workflow at their hospitals. SHM will also develop strategies for baseline measurement, ongoing data collection, involvement of team members, and procurement of local resources. SHM hopes to support research to further develop best practices and approaches.
The game plan goes something like this: SHM will develop the resources hospitalists need to improve management of inpatient diabetes in 2006. In 2007 and 2008 SHM will roll out this strategy to as many hospitalists as we can train. By 2008 JCAHO and CMS will have deployed their Performance Measures in Diabetes. When the first scores show the same deficiencies as we have seen this year in MI and heart failure, our nation’s hospitalists will be well armed to provide practical tangible solutions to improve quality.
And the beauty of this approach is that SHM is working on similar strategies right now for heart failure, DVT, pneumonia, and other key clinical conditions.
Those who pay for and receive care in our hospitals are looking at our current performance and demanding improvements. For the first time hospitals and those with resources are ready to make measurable quality a high priority. The presence of hospitalists in more than 2,000 hospitals (and more in the near future) ideally positions hospitalists to be a key change agent. The tools SHM is developing will give hospitalists the strategies and the expertise to make this happen.
This is a watershed moment in American healthcare. There is a palpable swing in the priorities of our patients. Hospitalists can help the healthcare team find real solutions. SHM has the vision and the plan to provide you with as much help as you need. Together we will do great things. TH
Dr. Wellikson has been CEO of SHM since 2000.
Hospitalists Defined—Officially
When I was a kid I remember saying that “ain’t ain’t a word because ain’t ain’t in the dictionary.” I just found “ain’t” in my online dictionary, which warned against using “ain’t” because it “does not form a part of standard English and should not be used in formal contexts.”
If the dictionary is the final arbiter of what is and is not a word, then finally “hospitalist” is a word (as we reported last month, see Nov. The Hospitalist, p. 17). Of course we have been using the word since Bob Wachter and Lee Goldman first coined it in their paper in the New England Journal of Medicine in 1996.1 But the 2005 update of the Eleventh Edition of Merriam-Webster’s Collegiate Dictionary defines a “hospitalist” as “a physician who specializes in treating hospitalized patients of other physicians in order to minimize the number of hospital visits by other physicians.”
While I am delighted that our specialty is in the dictionary, I would argue that the role of a hospitalist is about more than saving other physicians’ commute time. In fact SHM published an entire supplement that catalogued the many roles of hospitalists and how we add value.2 But even if the dictionary didn’t get the definition quite right, the presence of the word hospitalist is yet more evidence of the increasing importance and growth of our field. I want to share with you some of the exciting projects that the SHM is working on to further define our field.
Board Certification
We have been in discussion with the American Board of Internal Medicine and other societies that represent important interests in internal medicine regarding board certification for hospitalists. At this point I cannot tell you what certification will look like, how it will be conferred, or when it will come about; however, SHM is committed to developing a process that recognizes the expertise and experience of hospitalists and supports high quality care for patients. As you might imagine, any process of certification for hospitalists has huge implications for all physicians who practice internal medicine, and we are working to consider these issues carefully as we move ahead. Board certification, and the process of making it come about, marks another step along the path in the maturing of our field.
Journal of Hospital Medicine and Research
More evidence of our growth as a field is the coming publication of the Journal of Hospital Medicine. Under the editorship of Mark Williams, MD, the journal will be the first dedicated to hospital medicine and the care of hospitalized patients. I still remember the early discussions at the SHM Board of Directors meetings where we first discussed having a journal. At the time there were only three or four hospitalist researchers and our major concern was whether there would be sufficient content to fill a journal once let alone six or more times a year; however, at the time we also saw where our field was headed. We knew that in order to continue to define the field of hospital medicine a journal was key.
Perhaps our decision several years ago was hubris, perhaps it was blind optimism, but I like to think it was faith in our members and our society and a belief that hospital medicine was here to stay and would only get bigger. Next month SHM will proudly publish the first volume of the Journal of Hospital Medicine. I am happy to report that we have plenty of high quality content to fill the journal. Our field has continued to expand and with it more and more researchers are focusing on hospital medicine. One walk around the poster session at our annual meeting is enough to demonstrate all of the outstanding academic work that hospitalists at academic centers and community hospitals are doing.
Hand in hand with the publication of our journal has been our research initiative. I firmly believe that in order for SHM to lead hospital medicine, we must also lead in the area of research. In order to coordinate and expand our efforts in research, we recently brought Kathleen Kerr on board at SHM as a senior advisor to lead our research initiative. Kathleen brings a new level of rigor and enthusiasm to our research initiative and helps support the outstanding work of our research committee led by Andy Auerbach, MD. At SHM research reflects our members and includes hospitalists from all settings. I invite you to present your work at our annual meeting (we are currently accepting submissions through Jan. 6, 2006, for the Research, Innovations and Clinical Vignettes competition for the 2006 annual meeting) so we can all benefit and learn from the work we are doing. I also invite you to submit your work for publication in the Journal of Hospital Medicine.
Core Competency
Yet another sign of our maturing as a field will be the publication of the Core Competencies in Hospital Medicine as a supplement to the first volume of the Journal of Hospital Medicine. The core competencies reflect hundreds of hours of work by a dedicated group of hospitalists and SHM staff led by Tina Budnitz MPH, to define the core of what hospitalists need to know. Yes, hospitalists are more than just timesavers for other physicians. The core competencies in hospital medicine will outline what hospital medicine is about and serve as the foundation for educational programs, curricula, and initiatives in hospital medicine. The core competencies will also form the basis for certification of hospitalists by defining the key attitudes and skills needed to be a hospitalist. Look for the core competencies in early 2006 along with your first volume of the journal.
Evolution of Other “Ists”
If imitation is the finest form of flattery, then hospitalists should be very flattered by the proliferation of other “-ists.” Within our own field we find “nocurnists,” hospitalists who care for patients in the hospital overnight. Although it is not clear whether being a nocturnist is a permanent state in which you work only nights or a title that you hold temporarily, it is clear that “hospitalist” is leading to a wide use of the “-ist” suffix to describe the practice of physicians.
Even more interesting is the emergence of hospitalists in other fields such as surgery and obstetrics (see our related coverage in The Hospitalist—“What Is a Laborist,” Oct. 2005, p. 6; “Trendwatch: The specialization of hospital medicine,” Oct. 2005, p. 27; and “The Doctor Is In: The role of psychiatric hospitalists,” Oct. 2005, p. 30). Because the “ist” doesn’t work well universally (neither “surgicalist” nor “obstetricist” sounds right and neither does “deliverist”) the terms being used are “surgical hospitalist” or “OB hospitalist.” In either case the idea is that there is a physician, surgeon, or an obstetrician who sees patients in the hospital instead of the patients’ primary physician. Typically these physicians are employed by the hospital to care for unassigned patients admitted through the emergency department. The adoption of “hospitalist” by other fields in medicine to describe clinicians whose professional identity revolves around the hospital is a testament to the acceptance—and even normalization—of hospitalists and to the profound change in the way we care for hospitalized patients brought about by our field.
We certainly have come a long way from the days when our newly formed society decided not to use the word hospitalist or hospital or anything like it in our name for fear of inciting animosity. In just a few short years we find a world where hospitalist is in the dictionary and other physicians begin to use the term to describe themselves. Reflecting this maturing of our field, SHM is involved in several initiatives including certification, research, a journal, and core competencies to further define hospital medicine.
If you have been thinking about getting more involved in the SHM, do so now. Become an active member; volunteer for committees. Help shape our field and the world of hospital medicine in the future. This ride certainly ain’t over. In fact, it’s just beginning. TH
SHM President Dr. Pantilat is an associate professor of clinical medicine at the University of California at San Francisco.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514-517.
- Pile J. How hospitalists add value. The Hospitalist. 2005;9:Supplement 1.
When I was a kid I remember saying that “ain’t ain’t a word because ain’t ain’t in the dictionary.” I just found “ain’t” in my online dictionary, which warned against using “ain’t” because it “does not form a part of standard English and should not be used in formal contexts.”
If the dictionary is the final arbiter of what is and is not a word, then finally “hospitalist” is a word (as we reported last month, see Nov. The Hospitalist, p. 17). Of course we have been using the word since Bob Wachter and Lee Goldman first coined it in their paper in the New England Journal of Medicine in 1996.1 But the 2005 update of the Eleventh Edition of Merriam-Webster’s Collegiate Dictionary defines a “hospitalist” as “a physician who specializes in treating hospitalized patients of other physicians in order to minimize the number of hospital visits by other physicians.”
While I am delighted that our specialty is in the dictionary, I would argue that the role of a hospitalist is about more than saving other physicians’ commute time. In fact SHM published an entire supplement that catalogued the many roles of hospitalists and how we add value.2 But even if the dictionary didn’t get the definition quite right, the presence of the word hospitalist is yet more evidence of the increasing importance and growth of our field. I want to share with you some of the exciting projects that the SHM is working on to further define our field.
Board Certification
We have been in discussion with the American Board of Internal Medicine and other societies that represent important interests in internal medicine regarding board certification for hospitalists. At this point I cannot tell you what certification will look like, how it will be conferred, or when it will come about; however, SHM is committed to developing a process that recognizes the expertise and experience of hospitalists and supports high quality care for patients. As you might imagine, any process of certification for hospitalists has huge implications for all physicians who practice internal medicine, and we are working to consider these issues carefully as we move ahead. Board certification, and the process of making it come about, marks another step along the path in the maturing of our field.
Journal of Hospital Medicine and Research
More evidence of our growth as a field is the coming publication of the Journal of Hospital Medicine. Under the editorship of Mark Williams, MD, the journal will be the first dedicated to hospital medicine and the care of hospitalized patients. I still remember the early discussions at the SHM Board of Directors meetings where we first discussed having a journal. At the time there were only three or four hospitalist researchers and our major concern was whether there would be sufficient content to fill a journal once let alone six or more times a year; however, at the time we also saw where our field was headed. We knew that in order to continue to define the field of hospital medicine a journal was key.
Perhaps our decision several years ago was hubris, perhaps it was blind optimism, but I like to think it was faith in our members and our society and a belief that hospital medicine was here to stay and would only get bigger. Next month SHM will proudly publish the first volume of the Journal of Hospital Medicine. I am happy to report that we have plenty of high quality content to fill the journal. Our field has continued to expand and with it more and more researchers are focusing on hospital medicine. One walk around the poster session at our annual meeting is enough to demonstrate all of the outstanding academic work that hospitalists at academic centers and community hospitals are doing.
Hand in hand with the publication of our journal has been our research initiative. I firmly believe that in order for SHM to lead hospital medicine, we must also lead in the area of research. In order to coordinate and expand our efforts in research, we recently brought Kathleen Kerr on board at SHM as a senior advisor to lead our research initiative. Kathleen brings a new level of rigor and enthusiasm to our research initiative and helps support the outstanding work of our research committee led by Andy Auerbach, MD. At SHM research reflects our members and includes hospitalists from all settings. I invite you to present your work at our annual meeting (we are currently accepting submissions through Jan. 6, 2006, for the Research, Innovations and Clinical Vignettes competition for the 2006 annual meeting) so we can all benefit and learn from the work we are doing. I also invite you to submit your work for publication in the Journal of Hospital Medicine.
Core Competency
Yet another sign of our maturing as a field will be the publication of the Core Competencies in Hospital Medicine as a supplement to the first volume of the Journal of Hospital Medicine. The core competencies reflect hundreds of hours of work by a dedicated group of hospitalists and SHM staff led by Tina Budnitz MPH, to define the core of what hospitalists need to know. Yes, hospitalists are more than just timesavers for other physicians. The core competencies in hospital medicine will outline what hospital medicine is about and serve as the foundation for educational programs, curricula, and initiatives in hospital medicine. The core competencies will also form the basis for certification of hospitalists by defining the key attitudes and skills needed to be a hospitalist. Look for the core competencies in early 2006 along with your first volume of the journal.
Evolution of Other “Ists”
If imitation is the finest form of flattery, then hospitalists should be very flattered by the proliferation of other “-ists.” Within our own field we find “nocurnists,” hospitalists who care for patients in the hospital overnight. Although it is not clear whether being a nocturnist is a permanent state in which you work only nights or a title that you hold temporarily, it is clear that “hospitalist” is leading to a wide use of the “-ist” suffix to describe the practice of physicians.
Even more interesting is the emergence of hospitalists in other fields such as surgery and obstetrics (see our related coverage in The Hospitalist—“What Is a Laborist,” Oct. 2005, p. 6; “Trendwatch: The specialization of hospital medicine,” Oct. 2005, p. 27; and “The Doctor Is In: The role of psychiatric hospitalists,” Oct. 2005, p. 30). Because the “ist” doesn’t work well universally (neither “surgicalist” nor “obstetricist” sounds right and neither does “deliverist”) the terms being used are “surgical hospitalist” or “OB hospitalist.” In either case the idea is that there is a physician, surgeon, or an obstetrician who sees patients in the hospital instead of the patients’ primary physician. Typically these physicians are employed by the hospital to care for unassigned patients admitted through the emergency department. The adoption of “hospitalist” by other fields in medicine to describe clinicians whose professional identity revolves around the hospital is a testament to the acceptance—and even normalization—of hospitalists and to the profound change in the way we care for hospitalized patients brought about by our field.
We certainly have come a long way from the days when our newly formed society decided not to use the word hospitalist or hospital or anything like it in our name for fear of inciting animosity. In just a few short years we find a world where hospitalist is in the dictionary and other physicians begin to use the term to describe themselves. Reflecting this maturing of our field, SHM is involved in several initiatives including certification, research, a journal, and core competencies to further define hospital medicine.
If you have been thinking about getting more involved in the SHM, do so now. Become an active member; volunteer for committees. Help shape our field and the world of hospital medicine in the future. This ride certainly ain’t over. In fact, it’s just beginning. TH
SHM President Dr. Pantilat is an associate professor of clinical medicine at the University of California at San Francisco.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514-517.
- Pile J. How hospitalists add value. The Hospitalist. 2005;9:Supplement 1.
When I was a kid I remember saying that “ain’t ain’t a word because ain’t ain’t in the dictionary.” I just found “ain’t” in my online dictionary, which warned against using “ain’t” because it “does not form a part of standard English and should not be used in formal contexts.”
If the dictionary is the final arbiter of what is and is not a word, then finally “hospitalist” is a word (as we reported last month, see Nov. The Hospitalist, p. 17). Of course we have been using the word since Bob Wachter and Lee Goldman first coined it in their paper in the New England Journal of Medicine in 1996.1 But the 2005 update of the Eleventh Edition of Merriam-Webster’s Collegiate Dictionary defines a “hospitalist” as “a physician who specializes in treating hospitalized patients of other physicians in order to minimize the number of hospital visits by other physicians.”
While I am delighted that our specialty is in the dictionary, I would argue that the role of a hospitalist is about more than saving other physicians’ commute time. In fact SHM published an entire supplement that catalogued the many roles of hospitalists and how we add value.2 But even if the dictionary didn’t get the definition quite right, the presence of the word hospitalist is yet more evidence of the increasing importance and growth of our field. I want to share with you some of the exciting projects that the SHM is working on to further define our field.
Board Certification
We have been in discussion with the American Board of Internal Medicine and other societies that represent important interests in internal medicine regarding board certification for hospitalists. At this point I cannot tell you what certification will look like, how it will be conferred, or when it will come about; however, SHM is committed to developing a process that recognizes the expertise and experience of hospitalists and supports high quality care for patients. As you might imagine, any process of certification for hospitalists has huge implications for all physicians who practice internal medicine, and we are working to consider these issues carefully as we move ahead. Board certification, and the process of making it come about, marks another step along the path in the maturing of our field.
Journal of Hospital Medicine and Research
More evidence of our growth as a field is the coming publication of the Journal of Hospital Medicine. Under the editorship of Mark Williams, MD, the journal will be the first dedicated to hospital medicine and the care of hospitalized patients. I still remember the early discussions at the SHM Board of Directors meetings where we first discussed having a journal. At the time there were only three or four hospitalist researchers and our major concern was whether there would be sufficient content to fill a journal once let alone six or more times a year; however, at the time we also saw where our field was headed. We knew that in order to continue to define the field of hospital medicine a journal was key.
Perhaps our decision several years ago was hubris, perhaps it was blind optimism, but I like to think it was faith in our members and our society and a belief that hospital medicine was here to stay and would only get bigger. Next month SHM will proudly publish the first volume of the Journal of Hospital Medicine. I am happy to report that we have plenty of high quality content to fill the journal. Our field has continued to expand and with it more and more researchers are focusing on hospital medicine. One walk around the poster session at our annual meeting is enough to demonstrate all of the outstanding academic work that hospitalists at academic centers and community hospitals are doing.
Hand in hand with the publication of our journal has been our research initiative. I firmly believe that in order for SHM to lead hospital medicine, we must also lead in the area of research. In order to coordinate and expand our efforts in research, we recently brought Kathleen Kerr on board at SHM as a senior advisor to lead our research initiative. Kathleen brings a new level of rigor and enthusiasm to our research initiative and helps support the outstanding work of our research committee led by Andy Auerbach, MD. At SHM research reflects our members and includes hospitalists from all settings. I invite you to present your work at our annual meeting (we are currently accepting submissions through Jan. 6, 2006, for the Research, Innovations and Clinical Vignettes competition for the 2006 annual meeting) so we can all benefit and learn from the work we are doing. I also invite you to submit your work for publication in the Journal of Hospital Medicine.
Core Competency
Yet another sign of our maturing as a field will be the publication of the Core Competencies in Hospital Medicine as a supplement to the first volume of the Journal of Hospital Medicine. The core competencies reflect hundreds of hours of work by a dedicated group of hospitalists and SHM staff led by Tina Budnitz MPH, to define the core of what hospitalists need to know. Yes, hospitalists are more than just timesavers for other physicians. The core competencies in hospital medicine will outline what hospital medicine is about and serve as the foundation for educational programs, curricula, and initiatives in hospital medicine. The core competencies will also form the basis for certification of hospitalists by defining the key attitudes and skills needed to be a hospitalist. Look for the core competencies in early 2006 along with your first volume of the journal.
Evolution of Other “Ists”
If imitation is the finest form of flattery, then hospitalists should be very flattered by the proliferation of other “-ists.” Within our own field we find “nocurnists,” hospitalists who care for patients in the hospital overnight. Although it is not clear whether being a nocturnist is a permanent state in which you work only nights or a title that you hold temporarily, it is clear that “hospitalist” is leading to a wide use of the “-ist” suffix to describe the practice of physicians.
Even more interesting is the emergence of hospitalists in other fields such as surgery and obstetrics (see our related coverage in The Hospitalist—“What Is a Laborist,” Oct. 2005, p. 6; “Trendwatch: The specialization of hospital medicine,” Oct. 2005, p. 27; and “The Doctor Is In: The role of psychiatric hospitalists,” Oct. 2005, p. 30). Because the “ist” doesn’t work well universally (neither “surgicalist” nor “obstetricist” sounds right and neither does “deliverist”) the terms being used are “surgical hospitalist” or “OB hospitalist.” In either case the idea is that there is a physician, surgeon, or an obstetrician who sees patients in the hospital instead of the patients’ primary physician. Typically these physicians are employed by the hospital to care for unassigned patients admitted through the emergency department. The adoption of “hospitalist” by other fields in medicine to describe clinicians whose professional identity revolves around the hospital is a testament to the acceptance—and even normalization—of hospitalists and to the profound change in the way we care for hospitalized patients brought about by our field.
We certainly have come a long way from the days when our newly formed society decided not to use the word hospitalist or hospital or anything like it in our name for fear of inciting animosity. In just a few short years we find a world where hospitalist is in the dictionary and other physicians begin to use the term to describe themselves. Reflecting this maturing of our field, SHM is involved in several initiatives including certification, research, a journal, and core competencies to further define hospital medicine.
If you have been thinking about getting more involved in the SHM, do so now. Become an active member; volunteer for committees. Help shape our field and the world of hospital medicine in the future. This ride certainly ain’t over. In fact, it’s just beginning. TH
SHM President Dr. Pantilat is an associate professor of clinical medicine at the University of California at San Francisco.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514-517.
- Pile J. How hospitalists add value. The Hospitalist. 2005;9:Supplement 1.
A Malpractice Primer
In a 2001 Hospital Practice article Robert Wachter, MD, named malpractice as one of the top 10 issues that require consideration as it relates to the hospitalist movement.1 There are many areas to consider when looking at malpractice insurance for hospitalists as opposed to other physician specialties. Just one area being reviewed by insurance carriers: Underwriters are grouping hospitalists with internal medicine physicians because hospitalists do not yet have their own classification code.
“When physicians spend 85% to 100% of their time in the office,” wrote Dr. Wachter, “it seems prudent to base assessments of competence on the quality of the office practice rather than that of the hospital practice. As in other situations, the hospitalist movement has exposed the inadequacies of the earlier system.” This assessment seems applicable to the area of insurance as well. There may be a need to create means by which hospitalists can be better protected from malpractice risk and coverage inadequacy. This area, like all others associated with hospital medicine, is evolving.
In this article we highlight malpractice insurance for hospitalists: what you should consider now and in the future regarding policy coverage. policies Available to Hospitalists
The types of malpractice insurance available to hospitalists include:
- Policies provided under your employer’s policy or purchased for yourself;
- Policies that cover you when any event actually occurs or when the claim is filed; and
- Policies purchased by hospitals where the payouts for claims are made either by the insurance company (the carrier) or by the employer (the hospital).
Most hospitalists are covered by institutional or group employers. In most cases, hospitalists are hired directly by hospitals or by an agency that contracts with hospitalists and administrates this relationship with the hospital.
“We recommend that the hospitals employ the hospitalists and that they put them on their hospital malpractice policy,” says Pam Kirks, insurance broker with the Gallagher Health Insurance Company in Raleigh, N.C., “because that’s the cheapest way to go for the hospitalist. There are different types of coverage out there that they can get; they can get their own coverage certainly. But I think the majority of them are becoming hospital employees.”
Occurrence or Claims Made
The types of medical malpractice insurance available to hospitalists are either “occurrence” or “claims-made” policies. An occurrence policy is one in which the policy that responds to a claim is the one that was in effect when the incident actually occurred. A claims-made policy that responds to a claim is the one that is in effect when the claim is made—provided that you also had continuous coverage from the time that the incident occurred.
Joe Zorola, director of underwriting at ProMutual Insurance Company in Boston, further explains the claims-made policy. “For instance, let’s say you have a policy this year and something happens tomorrow and five years down the line [the patient] file[s] a claim because of what happened tomorrow,” he explains. “You should have continued this policy through the next five years so that there’s no lapse of coverage, but the policy that will respond will be the policy five years from now.”
Of the 52 hospitals and 14,000 people that ProMutual insures, half of the policies are individual policies and half are group policies.
“The majority of [policies] are in Massachusetts and so are written under an occurrence basis,” says Zorola. “The ones outside of Massachusetts—and those are the group policies that we do have—are claims made.”
Physicians and insurance carriers each have preferences between the two types. “The occurrence policy is the policy that a lot of physicians like because they understand that if they did something today, [they can think] ‘I never have to worry about having insurance in the future for it,’” says Zorola. “The claims-made policy is the one that we as [insurance] companies like because it allows us to close our books on each policy year much sooner because we know that we aren’t going to have any more claims attached to the policy this year or in another year or two.”
Fully Insured or Self Insured?
Malpractice policies available through employers are either fully insured or self insured. The difference between the two types involves who is responsible for the claims payouts. With fully insured plans, the employer pays a premium to an insurer and the insurer pays claims out of the pool of premiums it collects from everyone it insures. Under a self-insured plan, the employer is responsible for paying all claims out of company assets. The Employee Retirement Income Security Act (ERISA) regulates self-insured plans; the plans are then under the jurisdiction of the U.S. Department of Labor.
“The hospitalists that we do [under]write [fully insured policies] for tend to be in the smaller community hospitals, which may not necessarily have the huge need for hospitalists; whereas the larger institutions may have a larger need for hospitalists [and] they usually tend to be self-insured,” says Zorola.
Controlled Risk Insurance Company of Vermont, known as CRICO and located in Cambridge, Mass, is one example of a self-insured system. “We only have one [malpractice insurance] product for a closed system where our clients are the Harvard teaching hospitals” says Karen O’Rourke, senior vice president of CRICO.
Individual Policies for Certain Circumstances
Hospitalists who take out individual policies are usually practicing part-time or moonlighting and have another policy with a carrier that is covering their primary practice. “And this is true across the country,” says Zorola. “Most carriers will have some sort of part-time credit that they will provide [to] the people who come to them for policies. Now there are some carriers, and these are usually the large hospital carriers, who won’t provide individual policies to physicians. They only provide coverage for the hospital and the hospital’s employees.”
Hospitalists who take out their own individual policies usually get coverage from one of the local Physician Insurers Association of America carriers.
Why Are Hospitalists Sued?
In general, hospitalists are infrequently sued for medical malpractice. They may be named in initial claims, but many are dropped before the case is resolved. However, while experts report that lawsuits against hospitalists are scarce, they also reference the lack of classification code specifically created for the hospitalist and his/her duties. Without it, it’s impossible to distinguish in data to learn when and in how many cases hospitalists were named.
O’Rourke says that internists in ambulatory or outpatient practice settings are usually at risk for claims of failure to diagnose—mostly failure to diagnose cancer or myocardial infarctions. In contrast, “the hospitalists’ failures come in the communication area,” she says, “because that’s primarily what they’re there for is to make sure that the patient receives the medical care that they’re supposed to in a hospital setting.”
O’Rourke, who directs the management of underwriting claims as part of her work at CRICO, believes there is a vast difference between the reasons for claims for internists versus hospitalists.3
“We receive so many failure-to-diagnose cases with internal medicine physicians,” she elaborates. “There have been huge losses associated with them throughout other systems that we’ve seen—some of our own, such as increases in [the rates of] breast cancer or colorectal cancer. You’re not going to see that with a hospitalist unless there’s a post-op complication—bleeding that isn’t caught and failure to diagnose—that kind of issue—soon enough. But they’re still under a surgeon’s care normally.”
O’Rourke recognizes that the care of the hospital patient is a team effort. “So it’s going to be a question of how the hospital defines the hospitalist role for each and every condition or [for] surgical patients,” she says.
If the Hospitalist Sees the Patient
A new claim that ProMutual recently received involves a hospitalist. The allegation is “failure to monitor a patient for suicide.” The claim states that the patient attempted suicide twice by trying to hang herself. The patient was admitted to the psychiatric unit of the hospital. Although a medical consultation must be done any time a patient is admitted, the hospitalist was not consulted to assess for suicide precautions. The hospitalist’s next involvement was after the attempted suicide when she responded to the code and admitted the patient to the ICU.
Given the lines of protocol, it is likely to be decided that the named psychiatrist was responsible for noting the risks with this patient and the hospitalist’s name will be dropped from the claim. The important thing for hospitalists to know is that because the hospitalist was listed as seeing the patient, she was named in the claim and this is customary procedure.
“A lot of times the plaintiff attorney will note every doctor who has seen the patient over the last number of years,” says Zorola, “because they probably don’t know a lot about the claim either, at that point. So until the investigation is done, and you can perform the depositions and find out exactly who was responsible for what,” the hospitalist will be a part of this process.
The Classification of Hospitalists
The growing trend is that insurance underwriters are creating a separate hospitalist classification. ProMutual underwriters established a classification for hospitalist and placed it in the same rate group as internal medicine physicians. But then the underwriters listened to what some of the hospitalists were saying: that because they are more specialized and are seeing patients who are more aware of the care that should be provided in the hospital, being grouped with physicians who spend most of the their time in office practice was not an accurate way to classify them.
Zorola and his colleagues now see that “setting up a separate classification for [hospitalists] allows us in the future to review their experience and determine whether they ought to be grouped with internal medicines or whether they belong in a lower or higher classification.” Hospitalists might belong in a higher, risk-associated classification “because they are seeing sick patients whereas internal medicine and family practice doctors have a mixture of sick and well patients,” he notes.
In fact, the common assumption is that hospitalists are doing riskier work simply because they work in places in which they have more opportunities to encounter risk. O’Rourke can’t say definitively how many hospitalists CRICO insures. But she can say that few claims involve hospitalists.
“We thought they were a riskier group for a while, but we couldn’t find any evidence of that in our data,” she explains. “We had a couple of claims involving people who were hospitalists, but nothing of concern.”
Whether hospitalists prove to be a riskier group in future research will depend on first determining more precisely what hospitalists do.
What Do Hospitalists Really Do?
“I can imagine that some of [the answer to this question] is that you go find out what works best for the systems you already have in place and develop systems that are needed to really quantify what [hospitalists] are supposed to do,” says O’Rourke. “And that will vary from institution to institution depending on whether it’s a teaching hospital or not.”
But there are other factors and issues at play, some of which are entirely out of control of the insured hospitalist. Barry Halpern, an attorney with Snell and Wilmer Law Firm, whose insured clients are spread over the western half of the United States, says “malpractice insurers, for a variety of reasons, … have many, many classifications for underwriting purposes and others [have] not very many at all. There are marketing issues associated with that and they don’t have a lot to do with the aspects of the specialty.”4
Your Policy Type May Matter
“[A]s you look at this from an insurance perspective, there are pros and cons for having separate insurance for hospitalists and the hospital,” says Halpern. “Where there is separate insurance, there is sometimes greater potential for conflict tension among the provider team than when the insurance is provided on an entity basis, particularly when entity claims against hospitals are a [somewhat] growing trend.”
Halpern notes that, in general, the courts are delivering their verdicts without considering the actual relationship between a hospital and a staff physician.3 “Of course,” he adds, “the courts are hunting for ways to make hospitals responsible on an entity basis rather than specifically for negligence in credentialing, or negligence in supervising, or negligence in providing staff and tools.”
Halpern thinks that in lawsuits where any staff physician is considered as part of the entity of the hospital institution, “it may make sense for the hospitalist to be insured under the hospital’s coverage, so that you minimize the potential for finger-pointing within the hospital-based team.” Besides creating potential tension within the group, Halpern says, “there may be indemnity agreements entered into between the hospitalists and the hospital that shift legal responsibility in a way that is sometimes not as carefully considered at the front end of an arrangement than at the back end, when a problem occurs.”
Halpern says that those kinds of situations must be looked at carefully. “[T]hose kinds of indemnity agreements can lead to a whole world of collateral claims litigation and can sometimes compromise insurance coverage,” he says. “For instance, if a hospitalist group signs an indemnity contract with the hospital without clearing it with the hospitalist’s insurer, the insurer might look at that and say, ‘We didn’t underwrite that additional obligation to defend and pay damages for the benefit of the hospital. And therefore, we deny coverage.’”
What Should Hospitalists Do?
If you are an individual hospitalist and your hospital provides your coverage, our experts have some suggestions on how to best protect yourself from surprises later about your liability insurance.
“[Y]ou certainly ought to get a copy of the policy,” says Halpern, and “focus very carefully on several things: 1) what’s covered, 2) what’s excluded, 3) what are the limits, and 4) who’s providing the coverage?”
You need to be able to feel that you can say “yes” to the question, “Is this a company that I can be confident will be there when it’s needed?”
If after a careful review of your policy, you have areas you would like to discuss with the hospital, it’s a matter of negotiation. And when you have the “negotiation muscle” to get what you need for protection, says Halpern, you’re in a better position.
“Frankly, most hospitals are interested in maintaining quality staff, quality relations with physicians—both employed and on the consulting staff,” says Halpern. “[They] are not typically in the business of muscling people and treating them badly. So if the hospitalist finds a legitimate gap in coverage or a concern, by and large hospitals look to be fair in working those things out. If they’re not, there are two basic approaches, and one is to not continue in the relationship.” (In other words, quit). “The second [approach] is to insure over the gap by going to an insurance broker and seeing if you can find coverage.”
Conclusion
Although most hospitalists are covered under their hospital policies, all hospitalists would benefit from understanding the specifics of their malpractice coverage. The dynamics of the hospitalist model will require changes in many areas including malpractice insurance. The trend of insurance carriers to establish a separate classification for hospitalists is likely to provide more precisely written coverage that accounts for the particulars of hospital medicine practice TH
Writer Andrea Sattinger will write about risk management for hospitalists in the Jan. ’06 issue.
References
- Wachter RM. The hospitalist movement: ten issues to consider. Hosp Pract. 1999;34(2):104-106.
- Entman SS, Glass CA, Hickson GB, et al. The relationship between malpractice claims history and subsequent obstetric care JAMA. 1994;272:1588-1591.
- Alpers A. Key legal principles for hospitalists. Am J Med. 2001;111:5-9.
- Pham HH, Devers KJ, Kuo S, et al. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20:101-107.
In a 2001 Hospital Practice article Robert Wachter, MD, named malpractice as one of the top 10 issues that require consideration as it relates to the hospitalist movement.1 There are many areas to consider when looking at malpractice insurance for hospitalists as opposed to other physician specialties. Just one area being reviewed by insurance carriers: Underwriters are grouping hospitalists with internal medicine physicians because hospitalists do not yet have their own classification code.
“When physicians spend 85% to 100% of their time in the office,” wrote Dr. Wachter, “it seems prudent to base assessments of competence on the quality of the office practice rather than that of the hospital practice. As in other situations, the hospitalist movement has exposed the inadequacies of the earlier system.” This assessment seems applicable to the area of insurance as well. There may be a need to create means by which hospitalists can be better protected from malpractice risk and coverage inadequacy. This area, like all others associated with hospital medicine, is evolving.
In this article we highlight malpractice insurance for hospitalists: what you should consider now and in the future regarding policy coverage. policies Available to Hospitalists
The types of malpractice insurance available to hospitalists include:
- Policies provided under your employer’s policy or purchased for yourself;
- Policies that cover you when any event actually occurs or when the claim is filed; and
- Policies purchased by hospitals where the payouts for claims are made either by the insurance company (the carrier) or by the employer (the hospital).
Most hospitalists are covered by institutional or group employers. In most cases, hospitalists are hired directly by hospitals or by an agency that contracts with hospitalists and administrates this relationship with the hospital.
“We recommend that the hospitals employ the hospitalists and that they put them on their hospital malpractice policy,” says Pam Kirks, insurance broker with the Gallagher Health Insurance Company in Raleigh, N.C., “because that’s the cheapest way to go for the hospitalist. There are different types of coverage out there that they can get; they can get their own coverage certainly. But I think the majority of them are becoming hospital employees.”
Occurrence or Claims Made
The types of medical malpractice insurance available to hospitalists are either “occurrence” or “claims-made” policies. An occurrence policy is one in which the policy that responds to a claim is the one that was in effect when the incident actually occurred. A claims-made policy that responds to a claim is the one that is in effect when the claim is made—provided that you also had continuous coverage from the time that the incident occurred.
Joe Zorola, director of underwriting at ProMutual Insurance Company in Boston, further explains the claims-made policy. “For instance, let’s say you have a policy this year and something happens tomorrow and five years down the line [the patient] file[s] a claim because of what happened tomorrow,” he explains. “You should have continued this policy through the next five years so that there’s no lapse of coverage, but the policy that will respond will be the policy five years from now.”
Of the 52 hospitals and 14,000 people that ProMutual insures, half of the policies are individual policies and half are group policies.
“The majority of [policies] are in Massachusetts and so are written under an occurrence basis,” says Zorola. “The ones outside of Massachusetts—and those are the group policies that we do have—are claims made.”
Physicians and insurance carriers each have preferences between the two types. “The occurrence policy is the policy that a lot of physicians like because they understand that if they did something today, [they can think] ‘I never have to worry about having insurance in the future for it,’” says Zorola. “The claims-made policy is the one that we as [insurance] companies like because it allows us to close our books on each policy year much sooner because we know that we aren’t going to have any more claims attached to the policy this year or in another year or two.”
Fully Insured or Self Insured?
Malpractice policies available through employers are either fully insured or self insured. The difference between the two types involves who is responsible for the claims payouts. With fully insured plans, the employer pays a premium to an insurer and the insurer pays claims out of the pool of premiums it collects from everyone it insures. Under a self-insured plan, the employer is responsible for paying all claims out of company assets. The Employee Retirement Income Security Act (ERISA) regulates self-insured plans; the plans are then under the jurisdiction of the U.S. Department of Labor.
“The hospitalists that we do [under]write [fully insured policies] for tend to be in the smaller community hospitals, which may not necessarily have the huge need for hospitalists; whereas the larger institutions may have a larger need for hospitalists [and] they usually tend to be self-insured,” says Zorola.
Controlled Risk Insurance Company of Vermont, known as CRICO and located in Cambridge, Mass, is one example of a self-insured system. “We only have one [malpractice insurance] product for a closed system where our clients are the Harvard teaching hospitals” says Karen O’Rourke, senior vice president of CRICO.
Individual Policies for Certain Circumstances
Hospitalists who take out individual policies are usually practicing part-time or moonlighting and have another policy with a carrier that is covering their primary practice. “And this is true across the country,” says Zorola. “Most carriers will have some sort of part-time credit that they will provide [to] the people who come to them for policies. Now there are some carriers, and these are usually the large hospital carriers, who won’t provide individual policies to physicians. They only provide coverage for the hospital and the hospital’s employees.”
Hospitalists who take out their own individual policies usually get coverage from one of the local Physician Insurers Association of America carriers.
Why Are Hospitalists Sued?
In general, hospitalists are infrequently sued for medical malpractice. They may be named in initial claims, but many are dropped before the case is resolved. However, while experts report that lawsuits against hospitalists are scarce, they also reference the lack of classification code specifically created for the hospitalist and his/her duties. Without it, it’s impossible to distinguish in data to learn when and in how many cases hospitalists were named.
O’Rourke says that internists in ambulatory or outpatient practice settings are usually at risk for claims of failure to diagnose—mostly failure to diagnose cancer or myocardial infarctions. In contrast, “the hospitalists’ failures come in the communication area,” she says, “because that’s primarily what they’re there for is to make sure that the patient receives the medical care that they’re supposed to in a hospital setting.”
O’Rourke, who directs the management of underwriting claims as part of her work at CRICO, believes there is a vast difference between the reasons for claims for internists versus hospitalists.3
“We receive so many failure-to-diagnose cases with internal medicine physicians,” she elaborates. “There have been huge losses associated with them throughout other systems that we’ve seen—some of our own, such as increases in [the rates of] breast cancer or colorectal cancer. You’re not going to see that with a hospitalist unless there’s a post-op complication—bleeding that isn’t caught and failure to diagnose—that kind of issue—soon enough. But they’re still under a surgeon’s care normally.”
O’Rourke recognizes that the care of the hospital patient is a team effort. “So it’s going to be a question of how the hospital defines the hospitalist role for each and every condition or [for] surgical patients,” she says.
If the Hospitalist Sees the Patient
A new claim that ProMutual recently received involves a hospitalist. The allegation is “failure to monitor a patient for suicide.” The claim states that the patient attempted suicide twice by trying to hang herself. The patient was admitted to the psychiatric unit of the hospital. Although a medical consultation must be done any time a patient is admitted, the hospitalist was not consulted to assess for suicide precautions. The hospitalist’s next involvement was after the attempted suicide when she responded to the code and admitted the patient to the ICU.
Given the lines of protocol, it is likely to be decided that the named psychiatrist was responsible for noting the risks with this patient and the hospitalist’s name will be dropped from the claim. The important thing for hospitalists to know is that because the hospitalist was listed as seeing the patient, she was named in the claim and this is customary procedure.
“A lot of times the plaintiff attorney will note every doctor who has seen the patient over the last number of years,” says Zorola, “because they probably don’t know a lot about the claim either, at that point. So until the investigation is done, and you can perform the depositions and find out exactly who was responsible for what,” the hospitalist will be a part of this process.
The Classification of Hospitalists
The growing trend is that insurance underwriters are creating a separate hospitalist classification. ProMutual underwriters established a classification for hospitalist and placed it in the same rate group as internal medicine physicians. But then the underwriters listened to what some of the hospitalists were saying: that because they are more specialized and are seeing patients who are more aware of the care that should be provided in the hospital, being grouped with physicians who spend most of the their time in office practice was not an accurate way to classify them.
Zorola and his colleagues now see that “setting up a separate classification for [hospitalists] allows us in the future to review their experience and determine whether they ought to be grouped with internal medicines or whether they belong in a lower or higher classification.” Hospitalists might belong in a higher, risk-associated classification “because they are seeing sick patients whereas internal medicine and family practice doctors have a mixture of sick and well patients,” he notes.
In fact, the common assumption is that hospitalists are doing riskier work simply because they work in places in which they have more opportunities to encounter risk. O’Rourke can’t say definitively how many hospitalists CRICO insures. But she can say that few claims involve hospitalists.
“We thought they were a riskier group for a while, but we couldn’t find any evidence of that in our data,” she explains. “We had a couple of claims involving people who were hospitalists, but nothing of concern.”
Whether hospitalists prove to be a riskier group in future research will depend on first determining more precisely what hospitalists do.
What Do Hospitalists Really Do?
“I can imagine that some of [the answer to this question] is that you go find out what works best for the systems you already have in place and develop systems that are needed to really quantify what [hospitalists] are supposed to do,” says O’Rourke. “And that will vary from institution to institution depending on whether it’s a teaching hospital or not.”
But there are other factors and issues at play, some of which are entirely out of control of the insured hospitalist. Barry Halpern, an attorney with Snell and Wilmer Law Firm, whose insured clients are spread over the western half of the United States, says “malpractice insurers, for a variety of reasons, … have many, many classifications for underwriting purposes and others [have] not very many at all. There are marketing issues associated with that and they don’t have a lot to do with the aspects of the specialty.”4
Your Policy Type May Matter
“[A]s you look at this from an insurance perspective, there are pros and cons for having separate insurance for hospitalists and the hospital,” says Halpern. “Where there is separate insurance, there is sometimes greater potential for conflict tension among the provider team than when the insurance is provided on an entity basis, particularly when entity claims against hospitals are a [somewhat] growing trend.”
Halpern notes that, in general, the courts are delivering their verdicts without considering the actual relationship between a hospital and a staff physician.3 “Of course,” he adds, “the courts are hunting for ways to make hospitals responsible on an entity basis rather than specifically for negligence in credentialing, or negligence in supervising, or negligence in providing staff and tools.”
Halpern thinks that in lawsuits where any staff physician is considered as part of the entity of the hospital institution, “it may make sense for the hospitalist to be insured under the hospital’s coverage, so that you minimize the potential for finger-pointing within the hospital-based team.” Besides creating potential tension within the group, Halpern says, “there may be indemnity agreements entered into between the hospitalists and the hospital that shift legal responsibility in a way that is sometimes not as carefully considered at the front end of an arrangement than at the back end, when a problem occurs.”
Halpern says that those kinds of situations must be looked at carefully. “[T]hose kinds of indemnity agreements can lead to a whole world of collateral claims litigation and can sometimes compromise insurance coverage,” he says. “For instance, if a hospitalist group signs an indemnity contract with the hospital without clearing it with the hospitalist’s insurer, the insurer might look at that and say, ‘We didn’t underwrite that additional obligation to defend and pay damages for the benefit of the hospital. And therefore, we deny coverage.’”
What Should Hospitalists Do?
If you are an individual hospitalist and your hospital provides your coverage, our experts have some suggestions on how to best protect yourself from surprises later about your liability insurance.
“[Y]ou certainly ought to get a copy of the policy,” says Halpern, and “focus very carefully on several things: 1) what’s covered, 2) what’s excluded, 3) what are the limits, and 4) who’s providing the coverage?”
You need to be able to feel that you can say “yes” to the question, “Is this a company that I can be confident will be there when it’s needed?”
If after a careful review of your policy, you have areas you would like to discuss with the hospital, it’s a matter of negotiation. And when you have the “negotiation muscle” to get what you need for protection, says Halpern, you’re in a better position.
“Frankly, most hospitals are interested in maintaining quality staff, quality relations with physicians—both employed and on the consulting staff,” says Halpern. “[They] are not typically in the business of muscling people and treating them badly. So if the hospitalist finds a legitimate gap in coverage or a concern, by and large hospitals look to be fair in working those things out. If they’re not, there are two basic approaches, and one is to not continue in the relationship.” (In other words, quit). “The second [approach] is to insure over the gap by going to an insurance broker and seeing if you can find coverage.”
Conclusion
Although most hospitalists are covered under their hospital policies, all hospitalists would benefit from understanding the specifics of their malpractice coverage. The dynamics of the hospitalist model will require changes in many areas including malpractice insurance. The trend of insurance carriers to establish a separate classification for hospitalists is likely to provide more precisely written coverage that accounts for the particulars of hospital medicine practice TH
Writer Andrea Sattinger will write about risk management for hospitalists in the Jan. ’06 issue.
References
- Wachter RM. The hospitalist movement: ten issues to consider. Hosp Pract. 1999;34(2):104-106.
- Entman SS, Glass CA, Hickson GB, et al. The relationship between malpractice claims history and subsequent obstetric care JAMA. 1994;272:1588-1591.
- Alpers A. Key legal principles for hospitalists. Am J Med. 2001;111:5-9.
- Pham HH, Devers KJ, Kuo S, et al. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20:101-107.
In a 2001 Hospital Practice article Robert Wachter, MD, named malpractice as one of the top 10 issues that require consideration as it relates to the hospitalist movement.1 There are many areas to consider when looking at malpractice insurance for hospitalists as opposed to other physician specialties. Just one area being reviewed by insurance carriers: Underwriters are grouping hospitalists with internal medicine physicians because hospitalists do not yet have their own classification code.
“When physicians spend 85% to 100% of their time in the office,” wrote Dr. Wachter, “it seems prudent to base assessments of competence on the quality of the office practice rather than that of the hospital practice. As in other situations, the hospitalist movement has exposed the inadequacies of the earlier system.” This assessment seems applicable to the area of insurance as well. There may be a need to create means by which hospitalists can be better protected from malpractice risk and coverage inadequacy. This area, like all others associated with hospital medicine, is evolving.
In this article we highlight malpractice insurance for hospitalists: what you should consider now and in the future regarding policy coverage. policies Available to Hospitalists
The types of malpractice insurance available to hospitalists include:
- Policies provided under your employer’s policy or purchased for yourself;
- Policies that cover you when any event actually occurs or when the claim is filed; and
- Policies purchased by hospitals where the payouts for claims are made either by the insurance company (the carrier) or by the employer (the hospital).
Most hospitalists are covered by institutional or group employers. In most cases, hospitalists are hired directly by hospitals or by an agency that contracts with hospitalists and administrates this relationship with the hospital.
“We recommend that the hospitals employ the hospitalists and that they put them on their hospital malpractice policy,” says Pam Kirks, insurance broker with the Gallagher Health Insurance Company in Raleigh, N.C., “because that’s the cheapest way to go for the hospitalist. There are different types of coverage out there that they can get; they can get their own coverage certainly. But I think the majority of them are becoming hospital employees.”
Occurrence or Claims Made
The types of medical malpractice insurance available to hospitalists are either “occurrence” or “claims-made” policies. An occurrence policy is one in which the policy that responds to a claim is the one that was in effect when the incident actually occurred. A claims-made policy that responds to a claim is the one that is in effect when the claim is made—provided that you also had continuous coverage from the time that the incident occurred.
Joe Zorola, director of underwriting at ProMutual Insurance Company in Boston, further explains the claims-made policy. “For instance, let’s say you have a policy this year and something happens tomorrow and five years down the line [the patient] file[s] a claim because of what happened tomorrow,” he explains. “You should have continued this policy through the next five years so that there’s no lapse of coverage, but the policy that will respond will be the policy five years from now.”
Of the 52 hospitals and 14,000 people that ProMutual insures, half of the policies are individual policies and half are group policies.
“The majority of [policies] are in Massachusetts and so are written under an occurrence basis,” says Zorola. “The ones outside of Massachusetts—and those are the group policies that we do have—are claims made.”
Physicians and insurance carriers each have preferences between the two types. “The occurrence policy is the policy that a lot of physicians like because they understand that if they did something today, [they can think] ‘I never have to worry about having insurance in the future for it,’” says Zorola. “The claims-made policy is the one that we as [insurance] companies like because it allows us to close our books on each policy year much sooner because we know that we aren’t going to have any more claims attached to the policy this year or in another year or two.”
Fully Insured or Self Insured?
Malpractice policies available through employers are either fully insured or self insured. The difference between the two types involves who is responsible for the claims payouts. With fully insured plans, the employer pays a premium to an insurer and the insurer pays claims out of the pool of premiums it collects from everyone it insures. Under a self-insured plan, the employer is responsible for paying all claims out of company assets. The Employee Retirement Income Security Act (ERISA) regulates self-insured plans; the plans are then under the jurisdiction of the U.S. Department of Labor.
“The hospitalists that we do [under]write [fully insured policies] for tend to be in the smaller community hospitals, which may not necessarily have the huge need for hospitalists; whereas the larger institutions may have a larger need for hospitalists [and] they usually tend to be self-insured,” says Zorola.
Controlled Risk Insurance Company of Vermont, known as CRICO and located in Cambridge, Mass, is one example of a self-insured system. “We only have one [malpractice insurance] product for a closed system where our clients are the Harvard teaching hospitals” says Karen O’Rourke, senior vice president of CRICO.
Individual Policies for Certain Circumstances
Hospitalists who take out individual policies are usually practicing part-time or moonlighting and have another policy with a carrier that is covering their primary practice. “And this is true across the country,” says Zorola. “Most carriers will have some sort of part-time credit that they will provide [to] the people who come to them for policies. Now there are some carriers, and these are usually the large hospital carriers, who won’t provide individual policies to physicians. They only provide coverage for the hospital and the hospital’s employees.”
Hospitalists who take out their own individual policies usually get coverage from one of the local Physician Insurers Association of America carriers.
Why Are Hospitalists Sued?
In general, hospitalists are infrequently sued for medical malpractice. They may be named in initial claims, but many are dropped before the case is resolved. However, while experts report that lawsuits against hospitalists are scarce, they also reference the lack of classification code specifically created for the hospitalist and his/her duties. Without it, it’s impossible to distinguish in data to learn when and in how many cases hospitalists were named.
O’Rourke says that internists in ambulatory or outpatient practice settings are usually at risk for claims of failure to diagnose—mostly failure to diagnose cancer or myocardial infarctions. In contrast, “the hospitalists’ failures come in the communication area,” she says, “because that’s primarily what they’re there for is to make sure that the patient receives the medical care that they’re supposed to in a hospital setting.”
O’Rourke, who directs the management of underwriting claims as part of her work at CRICO, believes there is a vast difference between the reasons for claims for internists versus hospitalists.3
“We receive so many failure-to-diagnose cases with internal medicine physicians,” she elaborates. “There have been huge losses associated with them throughout other systems that we’ve seen—some of our own, such as increases in [the rates of] breast cancer or colorectal cancer. You’re not going to see that with a hospitalist unless there’s a post-op complication—bleeding that isn’t caught and failure to diagnose—that kind of issue—soon enough. But they’re still under a surgeon’s care normally.”
O’Rourke recognizes that the care of the hospital patient is a team effort. “So it’s going to be a question of how the hospital defines the hospitalist role for each and every condition or [for] surgical patients,” she says.
If the Hospitalist Sees the Patient
A new claim that ProMutual recently received involves a hospitalist. The allegation is “failure to monitor a patient for suicide.” The claim states that the patient attempted suicide twice by trying to hang herself. The patient was admitted to the psychiatric unit of the hospital. Although a medical consultation must be done any time a patient is admitted, the hospitalist was not consulted to assess for suicide precautions. The hospitalist’s next involvement was after the attempted suicide when she responded to the code and admitted the patient to the ICU.
Given the lines of protocol, it is likely to be decided that the named psychiatrist was responsible for noting the risks with this patient and the hospitalist’s name will be dropped from the claim. The important thing for hospitalists to know is that because the hospitalist was listed as seeing the patient, she was named in the claim and this is customary procedure.
“A lot of times the plaintiff attorney will note every doctor who has seen the patient over the last number of years,” says Zorola, “because they probably don’t know a lot about the claim either, at that point. So until the investigation is done, and you can perform the depositions and find out exactly who was responsible for what,” the hospitalist will be a part of this process.
The Classification of Hospitalists
The growing trend is that insurance underwriters are creating a separate hospitalist classification. ProMutual underwriters established a classification for hospitalist and placed it in the same rate group as internal medicine physicians. But then the underwriters listened to what some of the hospitalists were saying: that because they are more specialized and are seeing patients who are more aware of the care that should be provided in the hospital, being grouped with physicians who spend most of the their time in office practice was not an accurate way to classify them.
Zorola and his colleagues now see that “setting up a separate classification for [hospitalists] allows us in the future to review their experience and determine whether they ought to be grouped with internal medicines or whether they belong in a lower or higher classification.” Hospitalists might belong in a higher, risk-associated classification “because they are seeing sick patients whereas internal medicine and family practice doctors have a mixture of sick and well patients,” he notes.
In fact, the common assumption is that hospitalists are doing riskier work simply because they work in places in which they have more opportunities to encounter risk. O’Rourke can’t say definitively how many hospitalists CRICO insures. But she can say that few claims involve hospitalists.
“We thought they were a riskier group for a while, but we couldn’t find any evidence of that in our data,” she explains. “We had a couple of claims involving people who were hospitalists, but nothing of concern.”
Whether hospitalists prove to be a riskier group in future research will depend on first determining more precisely what hospitalists do.
What Do Hospitalists Really Do?
“I can imagine that some of [the answer to this question] is that you go find out what works best for the systems you already have in place and develop systems that are needed to really quantify what [hospitalists] are supposed to do,” says O’Rourke. “And that will vary from institution to institution depending on whether it’s a teaching hospital or not.”
But there are other factors and issues at play, some of which are entirely out of control of the insured hospitalist. Barry Halpern, an attorney with Snell and Wilmer Law Firm, whose insured clients are spread over the western half of the United States, says “malpractice insurers, for a variety of reasons, … have many, many classifications for underwriting purposes and others [have] not very many at all. There are marketing issues associated with that and they don’t have a lot to do with the aspects of the specialty.”4
Your Policy Type May Matter
“[A]s you look at this from an insurance perspective, there are pros and cons for having separate insurance for hospitalists and the hospital,” says Halpern. “Where there is separate insurance, there is sometimes greater potential for conflict tension among the provider team than when the insurance is provided on an entity basis, particularly when entity claims against hospitals are a [somewhat] growing trend.”
Halpern notes that, in general, the courts are delivering their verdicts without considering the actual relationship between a hospital and a staff physician.3 “Of course,” he adds, “the courts are hunting for ways to make hospitals responsible on an entity basis rather than specifically for negligence in credentialing, or negligence in supervising, or negligence in providing staff and tools.”
Halpern thinks that in lawsuits where any staff physician is considered as part of the entity of the hospital institution, “it may make sense for the hospitalist to be insured under the hospital’s coverage, so that you minimize the potential for finger-pointing within the hospital-based team.” Besides creating potential tension within the group, Halpern says, “there may be indemnity agreements entered into between the hospitalists and the hospital that shift legal responsibility in a way that is sometimes not as carefully considered at the front end of an arrangement than at the back end, when a problem occurs.”
Halpern says that those kinds of situations must be looked at carefully. “[T]hose kinds of indemnity agreements can lead to a whole world of collateral claims litigation and can sometimes compromise insurance coverage,” he says. “For instance, if a hospitalist group signs an indemnity contract with the hospital without clearing it with the hospitalist’s insurer, the insurer might look at that and say, ‘We didn’t underwrite that additional obligation to defend and pay damages for the benefit of the hospital. And therefore, we deny coverage.’”
What Should Hospitalists Do?
If you are an individual hospitalist and your hospital provides your coverage, our experts have some suggestions on how to best protect yourself from surprises later about your liability insurance.
“[Y]ou certainly ought to get a copy of the policy,” says Halpern, and “focus very carefully on several things: 1) what’s covered, 2) what’s excluded, 3) what are the limits, and 4) who’s providing the coverage?”
You need to be able to feel that you can say “yes” to the question, “Is this a company that I can be confident will be there when it’s needed?”
If after a careful review of your policy, you have areas you would like to discuss with the hospital, it’s a matter of negotiation. And when you have the “negotiation muscle” to get what you need for protection, says Halpern, you’re in a better position.
“Frankly, most hospitals are interested in maintaining quality staff, quality relations with physicians—both employed and on the consulting staff,” says Halpern. “[They] are not typically in the business of muscling people and treating them badly. So if the hospitalist finds a legitimate gap in coverage or a concern, by and large hospitals look to be fair in working those things out. If they’re not, there are two basic approaches, and one is to not continue in the relationship.” (In other words, quit). “The second [approach] is to insure over the gap by going to an insurance broker and seeing if you can find coverage.”
Conclusion
Although most hospitalists are covered under their hospital policies, all hospitalists would benefit from understanding the specifics of their malpractice coverage. The dynamics of the hospitalist model will require changes in many areas including malpractice insurance. The trend of insurance carriers to establish a separate classification for hospitalists is likely to provide more precisely written coverage that accounts for the particulars of hospital medicine practice TH
Writer Andrea Sattinger will write about risk management for hospitalists in the Jan. ’06 issue.
References
- Wachter RM. The hospitalist movement: ten issues to consider. Hosp Pract. 1999;34(2):104-106.
- Entman SS, Glass CA, Hickson GB, et al. The relationship between malpractice claims history and subsequent obstetric care JAMA. 1994;272:1588-1591.
- Alpers A. Key legal principles for hospitalists. Am J Med. 2001;111:5-9.
- Pham HH, Devers KJ, Kuo S, et al. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20:101-107.