User login
Trauma-Informed Telehealth in the COVID-19 Era and Beyond
COVID-19 has created stressors that are unprecedented in our modern era, prompting health care systems to adapt rapidly. Demand for telehealth has skyrocketed, and clinicians, many of whom had planned to adopt virtual practices in the future, have been pressured to do so immediately.1 In March 2020, the Centers for Medicare and Medicaid Services (CMS) expanded telehealth services, removing many barriers to virtual care.2 Similar remedy was not necessary for the Veterans Health Administration (VHA) which reported more than 2.6 million episodes of telehealth care in 2019.3 By the time the pandemic was underway in the US, use of telehealth was widespread across the agency. In late March 2020, VHA released a COVID-19 Response Plan, in which telehealth played a critical role in safe, uninterrupted delivery of services.4 While telehealth has been widely used in VHA, the call for replacement of most in-person outpatient visits with telehealth visits was a fundamental paradigm shift for many patients and clinicians.4
The Coronavirus Aid, Relief, and Economic Security (CARES) Act (HR 748) gave the US Department of Veterans Affairs (VA) funding to expand coronavirus-related telehealth services, including the purchase of mobile devices and broadband expansion. CARES authorized the agency to expand telemental health services, enter into short-term agreements with telecommunications companies to provide temporary broadband services to veterans, temporarily waived an in-person home visit requirement (accepting video and phone calls as an alternative), and provided means to make telehealth available for homeless veterans and case managers through the HUD-VASH (US Department of Housing and Urban Development-VA Supportive Housing) program.
VHA is a national telehealth exemplar, initiating telehealth by use of closed-circuit televisions as early as 1968, and continuing to expand through 2017 with the implementation of the Veterans Video Connect (VVC) platform.5 VVC has enabled veterans to participate in virtual visits from distant locations, including their homes. VVC was used successfully during hurricanes Sandy, Harvey, Irma, and Maria and is being widely deployed in the current crisis.6-8
While telehealth can take many forms, the current discussion will focus on live (synchronous) videoconferencing: a 2-way audiovisual link between a patient and clinician, such as VVC, which enables patients to maintain a safe and social distance from others while connecting with the health care team and receiving urgent as well as ongoing medical care for both new and established conditions.9 VHA has developed multiple training resources for use of VVC across many settings, including primary care, mental health, and specialties. In this review, we will make the novel case for applying a trauma-informed lens to telehealth care across VHA and beyond to other health care systems.
Trauma-Informed Care
Although our current focus is rightly on mitigating the health effects of a pandemic, we must recognize that stressful phenomena like COVID-19 occur against a backdrop of widespread physical, sexual, psychological, and racial trauma in our communities. The Substance Abuse and Mental Health Services Administration (SAMHSA) describes trauma as resulting from “an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.”10 Trauma exposure is both ubiquitous worldwide and inequitably distributed, with vulnerable populations disproportionately impacted.11,12
Veterans as a population are often highly trauma exposed, and while VHA routinely screens for experiences of trauma, such as military sexual trauma (MST) and intimate partner violence (IPV), and potential mental health sequelae of trauma, including posttraumatic stress disorder (PTSD) and suicidality, veterans may experience other forms of trauma or be unwilling or unable to talk about past exposures.13 One common example is that of adverse childhood experiences (ACEs), which include household dysfunction, neglect, and physical and sexual abuse before the age of 18 years.14 ACEs have been associated with a wide range of risk behaviors and poor health outcomes in adulthood.14 In population-based data, both male and female veterans have reported higher ACE scores.15 In addition, ACE scores are higher overall for those serving in the all-volunteer era (after July 1, 1973).16 Because trauma may be unseen, unmeasured, and unnamed, it is important to deliver all medical care with sensitivity to its potential presence.
It is important to distinguish the concept of trauma-informed care (TIC) from trauma-focused services. Trauma-focused or trauma-specific treatment refers to evidence-based and best practice treatment models that have been proven to facilitate recovery from problems resulting from the experience of trauma, such as PTSD.17 These treatments directly address the emotional, behavioral, and physiologic impact of trauma on an individual’s life and facilitate improvement in related symptoms and functioning: They are designed to treat the consequences of trauma. VHA offers a wide range of trauma-specific treatments, and considerable experience in delivering evidence-based trauma-focused treatment through telehealth exists.18,19 Given the range of possible responses to the experience of trauma, not all veterans with trauma histories need to, chose to, or feel ready to access trauma-specific treatments.20
In contrast, TIC is a global, universal precautions approach to providing quality care that can be applied to all aspects of health care and to all patients.21 TIC is a strengths-based service delivery framework that is grounded in an understanding of, and responsiveness to, the disempowering impact of experiencing trauma. It seeks to maximize physical, psychological, and emotional safety in all health care encounters, not just those that are specifically trauma-focused, and creates opportunities to rebuild a sense of control and empowerment while fostering healing through safe and collaborative patient-clinician relationships.22 TIC is not accomplished through any single technique or checklist but through continuous appraisal of approaches to care delivery. SAMHSA has elucidated 6 fundamental principles of TIC: safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment; voice and choice; and sensitivity to cultural, historical, and gender issues.10
TIC is based on the understanding that often traditional service delivery models of care may trigger, silence, or disempower survivors of trauma, exacerbating physical and mental health symptoms and potentially increasing disengagement from care and poorer outcomes.23 Currier and colleagues aptly noted, “TIC assumes that trustworthiness is not something that an organization creates in a veteran client, but something that he or she will freely grant to an organization.”24 Given the global prevalence of trauma, its well-established and deleterious impact on lifelong health, and the potential for health care itself to be traumatizing, TIC is a fundamental construct to apply universally with any patient at any time, especially in the context of a large-scale community trauma, such as a pandemic.12
Trauma-Informed COVID-19 Care
Catastrophic events, such as natural disasters and pandemics, may serve as both newly traumatic and as potential triggers for survivors who have endured prior trauma.25,26 Increases in depression, PTSD, and substance use disorder (SUD) are common sequalae, occurring during the event, the immediate aftermath, and beyond.25,27 In 2003, quarantine contained the spread of Severe acute respiratory syndrome (SARS) but resulted in a high prevalence of psychological distress, including PTSD and depression.27 Many veterans may have deployed in support of humanitarian assistance/disaster relief missions, which typically do not involve armed combat but may expose service members to warlike situations, including social insecurity and suffering populations.28 COVID-19 may be reminiscent of some of these deployments as well.
The impact of the current COVID-19 pandemic on patients is pervasive. Those with preexisting financial insecurity now face additional economic hardship and health challenges, which are amplified by loneliness and loss of social support networks.26 Widespread unemployment and closures of many businesses add to stress and may exacerbate preexisting mental and physical health concerns for many; some veterans also may be at increased risk.29 While previous postdisaster research suggests that psychopathology in the general population will significantly remit over time, high-risk groups remain vulnerable to PTSD and bear the brunt of social and economic consequences associated with the crisis.25 Veterans with preexisting trauma histories and mental health conditions are at increased risk for being retraumatized by the current pandemic and impacted by isolation and unplanned job or wage loss from it.29 Compounding this, social distancing serves to protect communities but may amplify isolation and danger in abusive relationships or exacerbate underlying mental illness.26,30
Thus, as we expand our use of telehealth, replacing our face-to-face visits with virtual encounters, it is critical for clinicians to be mindful that the pandemic and public health responses to it may result in trauma and retraumatization for veterans and other vulnerable patients, which in turn can impact both access and response to care. The application of trauma-informed principles to our virtual encounters has the potential to mitigate some of these health impacts, increase engagement in care, and provide opportunities for protective, healing connections.
In the setting of the continued fear and uncertainty of the COVID-19 pandemic, we believe that application of a trauma-informed lens to telehealth efforts is timely. While virtual visits may seem to lack the warmth and immediacy of traditional medical encounters, accumulated experience suggests otherwise.19 Telehealth is fundamentally more patient-focused than traditional encounters, overcomes service delivery barriers, offers a greater range of options for treatment engagement, and can enhance clinician-patient partnerships.6,31,32 Although the rapid transition to telehealth may be challenging for those new to it, experienced clinicians and patients express high degrees of satisfaction with virtual care because direct communication is unhampered by in-office challenges and travel logistics.33
While it may feel daunting to integrate principles of TIC into telehealth during a crisis-driven scale-up, a growing practice and body of research can inform these efforts. To help better understand how trauma-exposed patients respond to telehealth, we reviewed findings from trauma-focused telemental health (TMH) treatment. This research demonstrates that telehealth promotes safety and collaboration—fundamental principles of TIC—that can, in turn, be applied to telehealth visits in primary care and other medical and surgical specialties. When compared with traditional in-person treatment, studies of both individual and group formats of TMH found no significant differences in satisfaction, acceptability, or outcomes (such as reduction in PTSD symptom severity scores34), and TMH did not impede development of rapport.19,35
Although counterintuitive, the virtual space created by the combined physical and psychological distance of videoconferencing has been shown to promote safety and transparency. In TMH, patients have reported greater honesty due to the protection afforded by this virtual space.31 Engaging in telehealth visits from the comfort of one’s home can feel emotionally safer than having to travel to a medical office, resulting in feeling more at ease during encounters.31 In one TMH study, veterans with PTSD described high comfort levels and ability to let their guard down during virtual treatment.19 Similarly, in palliative telehealth care, patients reported that clinicians successfully nurtured an experience of intimacy, expressed empathy verbally and nonverbally, and responded to the patient’s unique situation and emotions.33
Trauma-Informed Telehealth
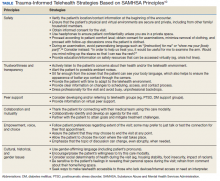
We have discussed how telehealth’s greater flexibility may create an ideal environment in which to implement principles of TIC. It may allow increased collaboration and closeness between patients and clinicians, empowering patients to codesign their care.31,33 The Table reviews 6 core SAMHSA principles of TIC and offers examples of their application to telehealth visits. The following case illustrates the application of trauma-informed telehealth care.
Case Presentation
S is a 45-year-old male veteran of Operation Enduring Freedom (OEF) who served as a combat medic. He has a history of osteoarthritis and PTSD related to combat experiences like caring for traumatic amputees. Before the pandemic began, he was employed as a server at a local restaurant but was laid off as the business transitioned to takeout orders only. The patient worked near a VA primary care clinic and frequently dropped by to see the staff and to pick up prescriptions. He had never agreed to video visits despite receiving encouragement from his medical team. He was reluctant to try telehealth, but he had developed a painful, itchy rash on his lower leg and was concerned about getting care.
For patients like S who may be reluctant to try telehealth, it is important to understand the cause. Potential barriers to telehealth may include lack of Internet access or familiarity with technology, discomfort with being on video, shame about the appearance of one’s home, or a strong cultural preference for face-to-face medical visits. Some may miss the social support benefit of coming into a clinic, particularly in VHA, which is designed specifically for veteran patients. For these reasons it is important to offer the patient a choice and to begin with a supportive phone call that explores and strives to address the patient’s concerns about videoconferencing.
The clinic nurse called S who agreed to try a VVC visit with gentle encouragement. He shared that he was embarrassed about the appearance of his apartment and fearful about pictures being recorded of his body due to “a bad experience in my past.” The patient was reassured that visits are private and will not be recorded. The nurse also reminded him that he can choose the location in which the visit will take place and can turn his camera off at any time. Importantly, the nurse did not ask him to recount additional details of what happened in his past. Next, the nurse verified his location and contact information and explained why obtaining this information was necessary. Next, she asked his consent to proceed with the visit, reminding him that the visit can end at any point if he feels uncomfortable. After finishing this initial discussion, the nurse told him that his primary care physician (PCP) would join the visit and address his concerns with his leg.
S was happy to see his PCP despite his hesitations about video care. The PCP noticed that he seemed anxious and was avoiding talking about the rash. Knowing that he was anxious about this VVC visit, the PCP was careful to look directly at the camera to make eye contact and to be sure her face was well lit and not in shadows. She gave him some time to acclimate to the virtual environment and thanked him for joining the visit. Knowing that he was a combat veteran, she warned him that there have been sudden, loud construction noises outside her window. Although the PCP was pressed for time, she was aware that S may have had a previous difficult experience around images of his body or even combat-related trauma. She gently brought up the rash and asked for permission to examine it, avoiding commands or personalizing language such as “show me your leg” or “take off your pants for me.”36After some hesitation, the patient revealed his leg that appeared to have multiple excoriations and old scars from picking. After the examination, the PCP waited until the patient’s leg was fully covered before beginning a discussion of the care plan. Together they collaboratively reviewed treatments that would soothe the skin. They decided to virtually consult a social worker to obtain emergency economic assistance and to speak with the patient’s care team psychologist to reduce some of the anxiety that may be leading to his leg scratching.
Case Discussion
This case illustrates the ways in which TIC can be applied to telehealth for a veteran with combat-related PTSD who may have experienced additional interpersonal trauma. It was not necessary to know more detail about the veteran’s trauma history to conduct the visit in a trauma-informed manner. Connecting to patients at home while considering these principles may thus foster mutuality, mitigate retraumatization, and cultivate enhanced collaboration with health care teams in this era of social distancing.
While a virtual physical examination creates both limitations and opportunity in telehealth, patients may find the greater degree of choice over their clothing and surroundings to be empowering. Telehealth also can allow for a greater portion of time to be dedicated to quality discussion and collaborative planning, with the clinician hearing and responding to the patient’s needs with reduced distraction. This may include opportunities to discuss mental health concerns openly, normalize emotional reactions, and offer connection to mental health and support services available through telehealth, including for patients who have not previously engaged in such care.
Conclusions
1. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957-962. doi:10.1093/jamia/ocaa067
2. Centers for Medicare and Medicaid Services. Medicare and Medicaid programs; policy and regulatory revisions in response to the COVID-19 public health emergency. CMS-1744-IFC. https://www.cms.gov/files/document/covid-final-ifc.pdf. Published March 24, 2020. Accessed April 8, 2020.
3. Eddy N. VA sees a surge in veterans’ use of telehealth services. https://www.healthcareitnews.com/news/va-sees-surge-veterans-use-telehealth-services. Published November 25, 2019. Accessed June 17, 2020.
4. Veterans Health Administration, Office of Emergency Management. COVID-19 response plan. Version 1.6. Published March 23, 2020. Accessed June 17, 2020.
5. Caudill RL, Sager Z. Institutionally based videoconferencing. Int Rev Psychiatry. 2015;27(6):496-503. doi:10.3109/09540261.2015.1085369
6. Heyworth L. Sharing Connections [published correction appears in JAMA. 2018 May 8;319(18):1939]. JAMA. 2018;319(13):1323-1324. doi:10.1001/jama.2018.2717
7. Dobalian A. U.S. Department of Veterans Affairs’ (VA’s) response to the 2017 hurricanes. Presented at: American Public Health Association 2019 Annual Meeting and Exposition; November 2-6, 2019; Philadelphia, PA. https://apha.confex.com/apha/2019/meetingapp.cgi/Session/58543. Accessed June 16, 2020.
8. Der-Martirosian C, Griffin AR, Chu K, Dobalian A. Telehealth at the US Department of Veterans Affairs after Hurricane Sandy. J Telemed Telecare. 2019;25(5):310-317. doi:10.1177/1357633X17751005
9. The Office of the National Coordinator for Health Information Technology. Telemedicine and telehealth. https://www.healthit.gov/topic/health-it-initiatives/telemedicine-and-telehealth. Updated September 28, 2017. Accessed June 16, 2020.
10. Substance Abuse and Mental Health Services Administration, Trauma and Justice Strategic Initiative. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. https://ncsacw.samhsa.gov/userfiles/files/SAMHSA_Trauma.pdf. Published July 2014. Accessed June 16, 2020.
11. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547. doi:10.1002/jts.21848
12. Kimberg L, Wheeler M. Trauma and Trauma-informed Care. In: Gerber MR, ed. Trauma-informed Healthcare Approaches: A Guide for Primary Care. Cham, Switzerland: Springer Nature; 2019:25-56.
13. Gerber MR. Trauma-informed care of veterans. In: Gerber MR, ed. Trauma-informed Healthcare Approaches: A Guide for Primary Care. Cham, Switzerland: Springer Nature; 2019:25-56.
14. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245-258. doi:10.1016/s0749-3797(98)00017-8
15. Katon JG, Lehavot K, Simpson TL, et al. Adverse childhood experiences, Military service, and adult health. Am J Prev Med. 2015;49(4):573-582. doi:10.1016/j.amepre.2015.03.020
16. Blosnich JR, Dichter ME, Cerulli C, Batten SV, Bossarte RM. Disparities in adverse childhood experiences among individuals with a history of military service. JAMA Psychiatry. 2014;71(9):1041-1048. doi:10.1001/jamapsychiatry.2014.724
17. Center for Substance Abuse Treatment. Treatment improvement protocol (TIP). Series, No. 57. In: SAMHSA, ed. Trauma-Informed Care in Behavioral Health Services. SAMHSA: Rockville, MD; 2014:137-155.
18. US Department of Veterans Affairs, Veterans Health Administration, National Center for PTSD. Trauma, PTSD and treatment. https://www.ptsd.va.gov/PTSD/professional/treat/index.asp. Updated July 5, 2019. Accessed June 17, 2020.
19. Turgoose D, Ashwick R, Murphy D. Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. J Telemed Telecare. 2018;24(9):575-585. doi:10.1177/1357633X17730443
20. Cook JM, Simiola V, Hamblen JL, Bernardy N, Schnurr PP. The influence of patient readiness on implementation of evidence-based PTSD treatments in Veterans Affairs residential programs. Psychol Trauma. 2017;9(suppl 1):51-58. doi:10.1037/tra0000162
21. Raja S, Hasnain M, Hoersch M, Gove-Yin S, Rajagopalan C. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health. 2015;38(3):216-226. doi:10.1097/FCH.0000000000000071
22. Hopper EK, Bassuk EL, Olivet J. Shelter from the storm: trauma-informed care in homeless service settings. Open Health Serv Policy J. 2009;2:131-151.
23. Kelly U, Boyd MA, Valente SM, Czekanski E. Trauma-informed care: keeping mental health settings safe for veterans [published correction appears in Issues Ment Health Nurs. 2015 Jun;36(6):482]. Issues Ment Health Nurs. 2014;35(6):413-419. doi:10.3109/01612840.2014.881941
24. Currier JM, Stefurak T, Carroll TD, Shatto EH. Applying trauma-informed care to community-based mental health services for military veterans. Best Pract Ment Health. 2017;13(1):47-64.
25. Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38(4):467-480. doi:10.1017/S0033291707001353
26. Galea S, Merchant RM, Lurie N. the mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention [published online ahead of print, 2020 Apr 10]. JAMA Intern Med. 2020;10.1001/jamainternmed.2020.1562. doi:10.1001/jamainternmed.2020.1562
27. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10(7):1206-1212. doi:10.3201/eid1007.030703
28. Cunha JM, Shen YC, Burke ZR. Contrasting the impacts of combat and humanitarian assistance/disaster relief missions on the mental health of military service members. Def Peace Economics. 2018;29(1):62-77. doi: 10.1080/10242694.2017.1349365
29. Ramchand R, Harrell MC, Berglass N, Lauck M. Veterans and COVID-19: Projecting the Economic, Social and Mental Health Needs of America’s Veterans. New York, NY: The Bob Woodruff Foundation; 2020.
30. van Gelder N, Peterman A, Potts A, et al. COVID-19: reducing the risk of infection might increase the risk of intimate partner violence [published online ahead of print, 2020 Apr 11]. EClinicalMedicine. 2020;21:100348. doi:10.1016/j.eclinm.2020.100348
31. Azarang A, Pakyurek M, Giroux C, Nordahl TE, Yellowlees P. Information technologies: an augmentation to post-traumatic stress disorder treatment among trauma survivors. Telemed J E Health. 2019;25(4):263-271. doi:10.1089/tmj.2018.0068.
32. Gilmore AK, Davis MT, Grubaugh A, et al. “Do you expect me to receive PTSD care in a setting where most of the other patients remind me of the perpetrator?”: Home-based telemedicine to address barriers to care unique to military sexual trauma and veterans affairs hospitals. Contemp Clin Trials. 2016;48:59-64. doi:10.1016/j.cct.2016.03.004.
33. van Gurp J, van Selm M, Vissers K, van Leeuwen E, Hasselaar J. How outpatient palliative care teleconsultation facilitates empathic patient-professional relationships: a qualitative study. PLoS One. 2015;10(4):e0124387. Published 2015 Apr 22. doi:10.1371/journal.pone.0124387
34. Morland LA, Mackintosh MA, Glassman LH, et al. Home-based delivery of variable length prolonged exposure therapy: a comparison of clinical efficacy between service modalities. Depress Anxiety. 2020;37(4):346-355. doi:10.1002/da.22979
35. Morland LA, Hynes AK, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress. 2011;24(4):465-469. doi:10.1002/jts.20661
36. Elisseou S, Puranam S, Nandi M. A novel, trauma-informed physical examination curriculum. Med Educ. 2018;52(5):555-556. doi:10.1111/medu.13569
COVID-19 has created stressors that are unprecedented in our modern era, prompting health care systems to adapt rapidly. Demand for telehealth has skyrocketed, and clinicians, many of whom had planned to adopt virtual practices in the future, have been pressured to do so immediately.1 In March 2020, the Centers for Medicare and Medicaid Services (CMS) expanded telehealth services, removing many barriers to virtual care.2 Similar remedy was not necessary for the Veterans Health Administration (VHA) which reported more than 2.6 million episodes of telehealth care in 2019.3 By the time the pandemic was underway in the US, use of telehealth was widespread across the agency. In late March 2020, VHA released a COVID-19 Response Plan, in which telehealth played a critical role in safe, uninterrupted delivery of services.4 While telehealth has been widely used in VHA, the call for replacement of most in-person outpatient visits with telehealth visits was a fundamental paradigm shift for many patients and clinicians.4
The Coronavirus Aid, Relief, and Economic Security (CARES) Act (HR 748) gave the US Department of Veterans Affairs (VA) funding to expand coronavirus-related telehealth services, including the purchase of mobile devices and broadband expansion. CARES authorized the agency to expand telemental health services, enter into short-term agreements with telecommunications companies to provide temporary broadband services to veterans, temporarily waived an in-person home visit requirement (accepting video and phone calls as an alternative), and provided means to make telehealth available for homeless veterans and case managers through the HUD-VASH (US Department of Housing and Urban Development-VA Supportive Housing) program.
VHA is a national telehealth exemplar, initiating telehealth by use of closed-circuit televisions as early as 1968, and continuing to expand through 2017 with the implementation of the Veterans Video Connect (VVC) platform.5 VVC has enabled veterans to participate in virtual visits from distant locations, including their homes. VVC was used successfully during hurricanes Sandy, Harvey, Irma, and Maria and is being widely deployed in the current crisis.6-8
While telehealth can take many forms, the current discussion will focus on live (synchronous) videoconferencing: a 2-way audiovisual link between a patient and clinician, such as VVC, which enables patients to maintain a safe and social distance from others while connecting with the health care team and receiving urgent as well as ongoing medical care for both new and established conditions.9 VHA has developed multiple training resources for use of VVC across many settings, including primary care, mental health, and specialties. In this review, we will make the novel case for applying a trauma-informed lens to telehealth care across VHA and beyond to other health care systems.
Trauma-Informed Care
Although our current focus is rightly on mitigating the health effects of a pandemic, we must recognize that stressful phenomena like COVID-19 occur against a backdrop of widespread physical, sexual, psychological, and racial trauma in our communities. The Substance Abuse and Mental Health Services Administration (SAMHSA) describes trauma as resulting from “an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.”10 Trauma exposure is both ubiquitous worldwide and inequitably distributed, with vulnerable populations disproportionately impacted.11,12
Veterans as a population are often highly trauma exposed, and while VHA routinely screens for experiences of trauma, such as military sexual trauma (MST) and intimate partner violence (IPV), and potential mental health sequelae of trauma, including posttraumatic stress disorder (PTSD) and suicidality, veterans may experience other forms of trauma or be unwilling or unable to talk about past exposures.13 One common example is that of adverse childhood experiences (ACEs), which include household dysfunction, neglect, and physical and sexual abuse before the age of 18 years.14 ACEs have been associated with a wide range of risk behaviors and poor health outcomes in adulthood.14 In population-based data, both male and female veterans have reported higher ACE scores.15 In addition, ACE scores are higher overall for those serving in the all-volunteer era (after July 1, 1973).16 Because trauma may be unseen, unmeasured, and unnamed, it is important to deliver all medical care with sensitivity to its potential presence.
It is important to distinguish the concept of trauma-informed care (TIC) from trauma-focused services. Trauma-focused or trauma-specific treatment refers to evidence-based and best practice treatment models that have been proven to facilitate recovery from problems resulting from the experience of trauma, such as PTSD.17 These treatments directly address the emotional, behavioral, and physiologic impact of trauma on an individual’s life and facilitate improvement in related symptoms and functioning: They are designed to treat the consequences of trauma. VHA offers a wide range of trauma-specific treatments, and considerable experience in delivering evidence-based trauma-focused treatment through telehealth exists.18,19 Given the range of possible responses to the experience of trauma, not all veterans with trauma histories need to, chose to, or feel ready to access trauma-specific treatments.20
In contrast, TIC is a global, universal precautions approach to providing quality care that can be applied to all aspects of health care and to all patients.21 TIC is a strengths-based service delivery framework that is grounded in an understanding of, and responsiveness to, the disempowering impact of experiencing trauma. It seeks to maximize physical, psychological, and emotional safety in all health care encounters, not just those that are specifically trauma-focused, and creates opportunities to rebuild a sense of control and empowerment while fostering healing through safe and collaborative patient-clinician relationships.22 TIC is not accomplished through any single technique or checklist but through continuous appraisal of approaches to care delivery. SAMHSA has elucidated 6 fundamental principles of TIC: safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment; voice and choice; and sensitivity to cultural, historical, and gender issues.10
TIC is based on the understanding that often traditional service delivery models of care may trigger, silence, or disempower survivors of trauma, exacerbating physical and mental health symptoms and potentially increasing disengagement from care and poorer outcomes.23 Currier and colleagues aptly noted, “TIC assumes that trustworthiness is not something that an organization creates in a veteran client, but something that he or she will freely grant to an organization.”24 Given the global prevalence of trauma, its well-established and deleterious impact on lifelong health, and the potential for health care itself to be traumatizing, TIC is a fundamental construct to apply universally with any patient at any time, especially in the context of a large-scale community trauma, such as a pandemic.12
Trauma-Informed COVID-19 Care
Catastrophic events, such as natural disasters and pandemics, may serve as both newly traumatic and as potential triggers for survivors who have endured prior trauma.25,26 Increases in depression, PTSD, and substance use disorder (SUD) are common sequalae, occurring during the event, the immediate aftermath, and beyond.25,27 In 2003, quarantine contained the spread of Severe acute respiratory syndrome (SARS) but resulted in a high prevalence of psychological distress, including PTSD and depression.27 Many veterans may have deployed in support of humanitarian assistance/disaster relief missions, which typically do not involve armed combat but may expose service members to warlike situations, including social insecurity and suffering populations.28 COVID-19 may be reminiscent of some of these deployments as well.
The impact of the current COVID-19 pandemic on patients is pervasive. Those with preexisting financial insecurity now face additional economic hardship and health challenges, which are amplified by loneliness and loss of social support networks.26 Widespread unemployment and closures of many businesses add to stress and may exacerbate preexisting mental and physical health concerns for many; some veterans also may be at increased risk.29 While previous postdisaster research suggests that psychopathology in the general population will significantly remit over time, high-risk groups remain vulnerable to PTSD and bear the brunt of social and economic consequences associated with the crisis.25 Veterans with preexisting trauma histories and mental health conditions are at increased risk for being retraumatized by the current pandemic and impacted by isolation and unplanned job or wage loss from it.29 Compounding this, social distancing serves to protect communities but may amplify isolation and danger in abusive relationships or exacerbate underlying mental illness.26,30
Thus, as we expand our use of telehealth, replacing our face-to-face visits with virtual encounters, it is critical for clinicians to be mindful that the pandemic and public health responses to it may result in trauma and retraumatization for veterans and other vulnerable patients, which in turn can impact both access and response to care. The application of trauma-informed principles to our virtual encounters has the potential to mitigate some of these health impacts, increase engagement in care, and provide opportunities for protective, healing connections.
In the setting of the continued fear and uncertainty of the COVID-19 pandemic, we believe that application of a trauma-informed lens to telehealth efforts is timely. While virtual visits may seem to lack the warmth and immediacy of traditional medical encounters, accumulated experience suggests otherwise.19 Telehealth is fundamentally more patient-focused than traditional encounters, overcomes service delivery barriers, offers a greater range of options for treatment engagement, and can enhance clinician-patient partnerships.6,31,32 Although the rapid transition to telehealth may be challenging for those new to it, experienced clinicians and patients express high degrees of satisfaction with virtual care because direct communication is unhampered by in-office challenges and travel logistics.33
While it may feel daunting to integrate principles of TIC into telehealth during a crisis-driven scale-up, a growing practice and body of research can inform these efforts. To help better understand how trauma-exposed patients respond to telehealth, we reviewed findings from trauma-focused telemental health (TMH) treatment. This research demonstrates that telehealth promotes safety and collaboration—fundamental principles of TIC—that can, in turn, be applied to telehealth visits in primary care and other medical and surgical specialties. When compared with traditional in-person treatment, studies of both individual and group formats of TMH found no significant differences in satisfaction, acceptability, or outcomes (such as reduction in PTSD symptom severity scores34), and TMH did not impede development of rapport.19,35
Although counterintuitive, the virtual space created by the combined physical and psychological distance of videoconferencing has been shown to promote safety and transparency. In TMH, patients have reported greater honesty due to the protection afforded by this virtual space.31 Engaging in telehealth visits from the comfort of one’s home can feel emotionally safer than having to travel to a medical office, resulting in feeling more at ease during encounters.31 In one TMH study, veterans with PTSD described high comfort levels and ability to let their guard down during virtual treatment.19 Similarly, in palliative telehealth care, patients reported that clinicians successfully nurtured an experience of intimacy, expressed empathy verbally and nonverbally, and responded to the patient’s unique situation and emotions.33
Trauma-Informed Telehealth
We have discussed how telehealth’s greater flexibility may create an ideal environment in which to implement principles of TIC. It may allow increased collaboration and closeness between patients and clinicians, empowering patients to codesign their care.31,33 The Table reviews 6 core SAMHSA principles of TIC and offers examples of their application to telehealth visits. The following case illustrates the application of trauma-informed telehealth care.
Case Presentation
S is a 45-year-old male veteran of Operation Enduring Freedom (OEF) who served as a combat medic. He has a history of osteoarthritis and PTSD related to combat experiences like caring for traumatic amputees. Before the pandemic began, he was employed as a server at a local restaurant but was laid off as the business transitioned to takeout orders only. The patient worked near a VA primary care clinic and frequently dropped by to see the staff and to pick up prescriptions. He had never agreed to video visits despite receiving encouragement from his medical team. He was reluctant to try telehealth, but he had developed a painful, itchy rash on his lower leg and was concerned about getting care.
For patients like S who may be reluctant to try telehealth, it is important to understand the cause. Potential barriers to telehealth may include lack of Internet access or familiarity with technology, discomfort with being on video, shame about the appearance of one’s home, or a strong cultural preference for face-to-face medical visits. Some may miss the social support benefit of coming into a clinic, particularly in VHA, which is designed specifically for veteran patients. For these reasons it is important to offer the patient a choice and to begin with a supportive phone call that explores and strives to address the patient’s concerns about videoconferencing.
The clinic nurse called S who agreed to try a VVC visit with gentle encouragement. He shared that he was embarrassed about the appearance of his apartment and fearful about pictures being recorded of his body due to “a bad experience in my past.” The patient was reassured that visits are private and will not be recorded. The nurse also reminded him that he can choose the location in which the visit will take place and can turn his camera off at any time. Importantly, the nurse did not ask him to recount additional details of what happened in his past. Next, the nurse verified his location and contact information and explained why obtaining this information was necessary. Next, she asked his consent to proceed with the visit, reminding him that the visit can end at any point if he feels uncomfortable. After finishing this initial discussion, the nurse told him that his primary care physician (PCP) would join the visit and address his concerns with his leg.
S was happy to see his PCP despite his hesitations about video care. The PCP noticed that he seemed anxious and was avoiding talking about the rash. Knowing that he was anxious about this VVC visit, the PCP was careful to look directly at the camera to make eye contact and to be sure her face was well lit and not in shadows. She gave him some time to acclimate to the virtual environment and thanked him for joining the visit. Knowing that he was a combat veteran, she warned him that there have been sudden, loud construction noises outside her window. Although the PCP was pressed for time, she was aware that S may have had a previous difficult experience around images of his body or even combat-related trauma. She gently brought up the rash and asked for permission to examine it, avoiding commands or personalizing language such as “show me your leg” or “take off your pants for me.”36After some hesitation, the patient revealed his leg that appeared to have multiple excoriations and old scars from picking. After the examination, the PCP waited until the patient’s leg was fully covered before beginning a discussion of the care plan. Together they collaboratively reviewed treatments that would soothe the skin. They decided to virtually consult a social worker to obtain emergency economic assistance and to speak with the patient’s care team psychologist to reduce some of the anxiety that may be leading to his leg scratching.
Case Discussion
This case illustrates the ways in which TIC can be applied to telehealth for a veteran with combat-related PTSD who may have experienced additional interpersonal trauma. It was not necessary to know more detail about the veteran’s trauma history to conduct the visit in a trauma-informed manner. Connecting to patients at home while considering these principles may thus foster mutuality, mitigate retraumatization, and cultivate enhanced collaboration with health care teams in this era of social distancing.
While a virtual physical examination creates both limitations and opportunity in telehealth, patients may find the greater degree of choice over their clothing and surroundings to be empowering. Telehealth also can allow for a greater portion of time to be dedicated to quality discussion and collaborative planning, with the clinician hearing and responding to the patient’s needs with reduced distraction. This may include opportunities to discuss mental health concerns openly, normalize emotional reactions, and offer connection to mental health and support services available through telehealth, including for patients who have not previously engaged in such care.
Conclusions
COVID-19 has created stressors that are unprecedented in our modern era, prompting health care systems to adapt rapidly. Demand for telehealth has skyrocketed, and clinicians, many of whom had planned to adopt virtual practices in the future, have been pressured to do so immediately.1 In March 2020, the Centers for Medicare and Medicaid Services (CMS) expanded telehealth services, removing many barriers to virtual care.2 Similar remedy was not necessary for the Veterans Health Administration (VHA) which reported more than 2.6 million episodes of telehealth care in 2019.3 By the time the pandemic was underway in the US, use of telehealth was widespread across the agency. In late March 2020, VHA released a COVID-19 Response Plan, in which telehealth played a critical role in safe, uninterrupted delivery of services.4 While telehealth has been widely used in VHA, the call for replacement of most in-person outpatient visits with telehealth visits was a fundamental paradigm shift for many patients and clinicians.4
The Coronavirus Aid, Relief, and Economic Security (CARES) Act (HR 748) gave the US Department of Veterans Affairs (VA) funding to expand coronavirus-related telehealth services, including the purchase of mobile devices and broadband expansion. CARES authorized the agency to expand telemental health services, enter into short-term agreements with telecommunications companies to provide temporary broadband services to veterans, temporarily waived an in-person home visit requirement (accepting video and phone calls as an alternative), and provided means to make telehealth available for homeless veterans and case managers through the HUD-VASH (US Department of Housing and Urban Development-VA Supportive Housing) program.
VHA is a national telehealth exemplar, initiating telehealth by use of closed-circuit televisions as early as 1968, and continuing to expand through 2017 with the implementation of the Veterans Video Connect (VVC) platform.5 VVC has enabled veterans to participate in virtual visits from distant locations, including their homes. VVC was used successfully during hurricanes Sandy, Harvey, Irma, and Maria and is being widely deployed in the current crisis.6-8
While telehealth can take many forms, the current discussion will focus on live (synchronous) videoconferencing: a 2-way audiovisual link between a patient and clinician, such as VVC, which enables patients to maintain a safe and social distance from others while connecting with the health care team and receiving urgent as well as ongoing medical care for both new and established conditions.9 VHA has developed multiple training resources for use of VVC across many settings, including primary care, mental health, and specialties. In this review, we will make the novel case for applying a trauma-informed lens to telehealth care across VHA and beyond to other health care systems.
Trauma-Informed Care
Although our current focus is rightly on mitigating the health effects of a pandemic, we must recognize that stressful phenomena like COVID-19 occur against a backdrop of widespread physical, sexual, psychological, and racial trauma in our communities. The Substance Abuse and Mental Health Services Administration (SAMHSA) describes trauma as resulting from “an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.”10 Trauma exposure is both ubiquitous worldwide and inequitably distributed, with vulnerable populations disproportionately impacted.11,12
Veterans as a population are often highly trauma exposed, and while VHA routinely screens for experiences of trauma, such as military sexual trauma (MST) and intimate partner violence (IPV), and potential mental health sequelae of trauma, including posttraumatic stress disorder (PTSD) and suicidality, veterans may experience other forms of trauma or be unwilling or unable to talk about past exposures.13 One common example is that of adverse childhood experiences (ACEs), which include household dysfunction, neglect, and physical and sexual abuse before the age of 18 years.14 ACEs have been associated with a wide range of risk behaviors and poor health outcomes in adulthood.14 In population-based data, both male and female veterans have reported higher ACE scores.15 In addition, ACE scores are higher overall for those serving in the all-volunteer era (after July 1, 1973).16 Because trauma may be unseen, unmeasured, and unnamed, it is important to deliver all medical care with sensitivity to its potential presence.
It is important to distinguish the concept of trauma-informed care (TIC) from trauma-focused services. Trauma-focused or trauma-specific treatment refers to evidence-based and best practice treatment models that have been proven to facilitate recovery from problems resulting from the experience of trauma, such as PTSD.17 These treatments directly address the emotional, behavioral, and physiologic impact of trauma on an individual’s life and facilitate improvement in related symptoms and functioning: They are designed to treat the consequences of trauma. VHA offers a wide range of trauma-specific treatments, and considerable experience in delivering evidence-based trauma-focused treatment through telehealth exists.18,19 Given the range of possible responses to the experience of trauma, not all veterans with trauma histories need to, chose to, or feel ready to access trauma-specific treatments.20
In contrast, TIC is a global, universal precautions approach to providing quality care that can be applied to all aspects of health care and to all patients.21 TIC is a strengths-based service delivery framework that is grounded in an understanding of, and responsiveness to, the disempowering impact of experiencing trauma. It seeks to maximize physical, psychological, and emotional safety in all health care encounters, not just those that are specifically trauma-focused, and creates opportunities to rebuild a sense of control and empowerment while fostering healing through safe and collaborative patient-clinician relationships.22 TIC is not accomplished through any single technique or checklist but through continuous appraisal of approaches to care delivery. SAMHSA has elucidated 6 fundamental principles of TIC: safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment; voice and choice; and sensitivity to cultural, historical, and gender issues.10
TIC is based on the understanding that often traditional service delivery models of care may trigger, silence, or disempower survivors of trauma, exacerbating physical and mental health symptoms and potentially increasing disengagement from care and poorer outcomes.23 Currier and colleagues aptly noted, “TIC assumes that trustworthiness is not something that an organization creates in a veteran client, but something that he or she will freely grant to an organization.”24 Given the global prevalence of trauma, its well-established and deleterious impact on lifelong health, and the potential for health care itself to be traumatizing, TIC is a fundamental construct to apply universally with any patient at any time, especially in the context of a large-scale community trauma, such as a pandemic.12
Trauma-Informed COVID-19 Care
Catastrophic events, such as natural disasters and pandemics, may serve as both newly traumatic and as potential triggers for survivors who have endured prior trauma.25,26 Increases in depression, PTSD, and substance use disorder (SUD) are common sequalae, occurring during the event, the immediate aftermath, and beyond.25,27 In 2003, quarantine contained the spread of Severe acute respiratory syndrome (SARS) but resulted in a high prevalence of psychological distress, including PTSD and depression.27 Many veterans may have deployed in support of humanitarian assistance/disaster relief missions, which typically do not involve armed combat but may expose service members to warlike situations, including social insecurity and suffering populations.28 COVID-19 may be reminiscent of some of these deployments as well.
The impact of the current COVID-19 pandemic on patients is pervasive. Those with preexisting financial insecurity now face additional economic hardship and health challenges, which are amplified by loneliness and loss of social support networks.26 Widespread unemployment and closures of many businesses add to stress and may exacerbate preexisting mental and physical health concerns for many; some veterans also may be at increased risk.29 While previous postdisaster research suggests that psychopathology in the general population will significantly remit over time, high-risk groups remain vulnerable to PTSD and bear the brunt of social and economic consequences associated with the crisis.25 Veterans with preexisting trauma histories and mental health conditions are at increased risk for being retraumatized by the current pandemic and impacted by isolation and unplanned job or wage loss from it.29 Compounding this, social distancing serves to protect communities but may amplify isolation and danger in abusive relationships or exacerbate underlying mental illness.26,30
Thus, as we expand our use of telehealth, replacing our face-to-face visits with virtual encounters, it is critical for clinicians to be mindful that the pandemic and public health responses to it may result in trauma and retraumatization for veterans and other vulnerable patients, which in turn can impact both access and response to care. The application of trauma-informed principles to our virtual encounters has the potential to mitigate some of these health impacts, increase engagement in care, and provide opportunities for protective, healing connections.
In the setting of the continued fear and uncertainty of the COVID-19 pandemic, we believe that application of a trauma-informed lens to telehealth efforts is timely. While virtual visits may seem to lack the warmth and immediacy of traditional medical encounters, accumulated experience suggests otherwise.19 Telehealth is fundamentally more patient-focused than traditional encounters, overcomes service delivery barriers, offers a greater range of options for treatment engagement, and can enhance clinician-patient partnerships.6,31,32 Although the rapid transition to telehealth may be challenging for those new to it, experienced clinicians and patients express high degrees of satisfaction with virtual care because direct communication is unhampered by in-office challenges and travel logistics.33
While it may feel daunting to integrate principles of TIC into telehealth during a crisis-driven scale-up, a growing practice and body of research can inform these efforts. To help better understand how trauma-exposed patients respond to telehealth, we reviewed findings from trauma-focused telemental health (TMH) treatment. This research demonstrates that telehealth promotes safety and collaboration—fundamental principles of TIC—that can, in turn, be applied to telehealth visits in primary care and other medical and surgical specialties. When compared with traditional in-person treatment, studies of both individual and group formats of TMH found no significant differences in satisfaction, acceptability, or outcomes (such as reduction in PTSD symptom severity scores34), and TMH did not impede development of rapport.19,35
Although counterintuitive, the virtual space created by the combined physical and psychological distance of videoconferencing has been shown to promote safety and transparency. In TMH, patients have reported greater honesty due to the protection afforded by this virtual space.31 Engaging in telehealth visits from the comfort of one’s home can feel emotionally safer than having to travel to a medical office, resulting in feeling more at ease during encounters.31 In one TMH study, veterans with PTSD described high comfort levels and ability to let their guard down during virtual treatment.19 Similarly, in palliative telehealth care, patients reported that clinicians successfully nurtured an experience of intimacy, expressed empathy verbally and nonverbally, and responded to the patient’s unique situation and emotions.33
Trauma-Informed Telehealth
We have discussed how telehealth’s greater flexibility may create an ideal environment in which to implement principles of TIC. It may allow increased collaboration and closeness between patients and clinicians, empowering patients to codesign their care.31,33 The Table reviews 6 core SAMHSA principles of TIC and offers examples of their application to telehealth visits. The following case illustrates the application of trauma-informed telehealth care.
Case Presentation
S is a 45-year-old male veteran of Operation Enduring Freedom (OEF) who served as a combat medic. He has a history of osteoarthritis and PTSD related to combat experiences like caring for traumatic amputees. Before the pandemic began, he was employed as a server at a local restaurant but was laid off as the business transitioned to takeout orders only. The patient worked near a VA primary care clinic and frequently dropped by to see the staff and to pick up prescriptions. He had never agreed to video visits despite receiving encouragement from his medical team. He was reluctant to try telehealth, but he had developed a painful, itchy rash on his lower leg and was concerned about getting care.
For patients like S who may be reluctant to try telehealth, it is important to understand the cause. Potential barriers to telehealth may include lack of Internet access or familiarity with technology, discomfort with being on video, shame about the appearance of one’s home, or a strong cultural preference for face-to-face medical visits. Some may miss the social support benefit of coming into a clinic, particularly in VHA, which is designed specifically for veteran patients. For these reasons it is important to offer the patient a choice and to begin with a supportive phone call that explores and strives to address the patient’s concerns about videoconferencing.
The clinic nurse called S who agreed to try a VVC visit with gentle encouragement. He shared that he was embarrassed about the appearance of his apartment and fearful about pictures being recorded of his body due to “a bad experience in my past.” The patient was reassured that visits are private and will not be recorded. The nurse also reminded him that he can choose the location in which the visit will take place and can turn his camera off at any time. Importantly, the nurse did not ask him to recount additional details of what happened in his past. Next, the nurse verified his location and contact information and explained why obtaining this information was necessary. Next, she asked his consent to proceed with the visit, reminding him that the visit can end at any point if he feels uncomfortable. After finishing this initial discussion, the nurse told him that his primary care physician (PCP) would join the visit and address his concerns with his leg.
S was happy to see his PCP despite his hesitations about video care. The PCP noticed that he seemed anxious and was avoiding talking about the rash. Knowing that he was anxious about this VVC visit, the PCP was careful to look directly at the camera to make eye contact and to be sure her face was well lit and not in shadows. She gave him some time to acclimate to the virtual environment and thanked him for joining the visit. Knowing that he was a combat veteran, she warned him that there have been sudden, loud construction noises outside her window. Although the PCP was pressed for time, she was aware that S may have had a previous difficult experience around images of his body or even combat-related trauma. She gently brought up the rash and asked for permission to examine it, avoiding commands or personalizing language such as “show me your leg” or “take off your pants for me.”36After some hesitation, the patient revealed his leg that appeared to have multiple excoriations and old scars from picking. After the examination, the PCP waited until the patient’s leg was fully covered before beginning a discussion of the care plan. Together they collaboratively reviewed treatments that would soothe the skin. They decided to virtually consult a social worker to obtain emergency economic assistance and to speak with the patient’s care team psychologist to reduce some of the anxiety that may be leading to his leg scratching.
Case Discussion
This case illustrates the ways in which TIC can be applied to telehealth for a veteran with combat-related PTSD who may have experienced additional interpersonal trauma. It was not necessary to know more detail about the veteran’s trauma history to conduct the visit in a trauma-informed manner. Connecting to patients at home while considering these principles may thus foster mutuality, mitigate retraumatization, and cultivate enhanced collaboration with health care teams in this era of social distancing.
While a virtual physical examination creates both limitations and opportunity in telehealth, patients may find the greater degree of choice over their clothing and surroundings to be empowering. Telehealth also can allow for a greater portion of time to be dedicated to quality discussion and collaborative planning, with the clinician hearing and responding to the patient’s needs with reduced distraction. This may include opportunities to discuss mental health concerns openly, normalize emotional reactions, and offer connection to mental health and support services available through telehealth, including for patients who have not previously engaged in such care.
Conclusions
1. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957-962. doi:10.1093/jamia/ocaa067
2. Centers for Medicare and Medicaid Services. Medicare and Medicaid programs; policy and regulatory revisions in response to the COVID-19 public health emergency. CMS-1744-IFC. https://www.cms.gov/files/document/covid-final-ifc.pdf. Published March 24, 2020. Accessed April 8, 2020.
3. Eddy N. VA sees a surge in veterans’ use of telehealth services. https://www.healthcareitnews.com/news/va-sees-surge-veterans-use-telehealth-services. Published November 25, 2019. Accessed June 17, 2020.
4. Veterans Health Administration, Office of Emergency Management. COVID-19 response plan. Version 1.6. Published March 23, 2020. Accessed June 17, 2020.
5. Caudill RL, Sager Z. Institutionally based videoconferencing. Int Rev Psychiatry. 2015;27(6):496-503. doi:10.3109/09540261.2015.1085369
6. Heyworth L. Sharing Connections [published correction appears in JAMA. 2018 May 8;319(18):1939]. JAMA. 2018;319(13):1323-1324. doi:10.1001/jama.2018.2717
7. Dobalian A. U.S. Department of Veterans Affairs’ (VA’s) response to the 2017 hurricanes. Presented at: American Public Health Association 2019 Annual Meeting and Exposition; November 2-6, 2019; Philadelphia, PA. https://apha.confex.com/apha/2019/meetingapp.cgi/Session/58543. Accessed June 16, 2020.
8. Der-Martirosian C, Griffin AR, Chu K, Dobalian A. Telehealth at the US Department of Veterans Affairs after Hurricane Sandy. J Telemed Telecare. 2019;25(5):310-317. doi:10.1177/1357633X17751005
9. The Office of the National Coordinator for Health Information Technology. Telemedicine and telehealth. https://www.healthit.gov/topic/health-it-initiatives/telemedicine-and-telehealth. Updated September 28, 2017. Accessed June 16, 2020.
10. Substance Abuse and Mental Health Services Administration, Trauma and Justice Strategic Initiative. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. https://ncsacw.samhsa.gov/userfiles/files/SAMHSA_Trauma.pdf. Published July 2014. Accessed June 16, 2020.
11. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547. doi:10.1002/jts.21848
12. Kimberg L, Wheeler M. Trauma and Trauma-informed Care. In: Gerber MR, ed. Trauma-informed Healthcare Approaches: A Guide for Primary Care. Cham, Switzerland: Springer Nature; 2019:25-56.
13. Gerber MR. Trauma-informed care of veterans. In: Gerber MR, ed. Trauma-informed Healthcare Approaches: A Guide for Primary Care. Cham, Switzerland: Springer Nature; 2019:25-56.
14. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245-258. doi:10.1016/s0749-3797(98)00017-8
15. Katon JG, Lehavot K, Simpson TL, et al. Adverse childhood experiences, Military service, and adult health. Am J Prev Med. 2015;49(4):573-582. doi:10.1016/j.amepre.2015.03.020
16. Blosnich JR, Dichter ME, Cerulli C, Batten SV, Bossarte RM. Disparities in adverse childhood experiences among individuals with a history of military service. JAMA Psychiatry. 2014;71(9):1041-1048. doi:10.1001/jamapsychiatry.2014.724
17. Center for Substance Abuse Treatment. Treatment improvement protocol (TIP). Series, No. 57. In: SAMHSA, ed. Trauma-Informed Care in Behavioral Health Services. SAMHSA: Rockville, MD; 2014:137-155.
18. US Department of Veterans Affairs, Veterans Health Administration, National Center for PTSD. Trauma, PTSD and treatment. https://www.ptsd.va.gov/PTSD/professional/treat/index.asp. Updated July 5, 2019. Accessed June 17, 2020.
19. Turgoose D, Ashwick R, Murphy D. Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. J Telemed Telecare. 2018;24(9):575-585. doi:10.1177/1357633X17730443
20. Cook JM, Simiola V, Hamblen JL, Bernardy N, Schnurr PP. The influence of patient readiness on implementation of evidence-based PTSD treatments in Veterans Affairs residential programs. Psychol Trauma. 2017;9(suppl 1):51-58. doi:10.1037/tra0000162
21. Raja S, Hasnain M, Hoersch M, Gove-Yin S, Rajagopalan C. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health. 2015;38(3):216-226. doi:10.1097/FCH.0000000000000071
22. Hopper EK, Bassuk EL, Olivet J. Shelter from the storm: trauma-informed care in homeless service settings. Open Health Serv Policy J. 2009;2:131-151.
23. Kelly U, Boyd MA, Valente SM, Czekanski E. Trauma-informed care: keeping mental health settings safe for veterans [published correction appears in Issues Ment Health Nurs. 2015 Jun;36(6):482]. Issues Ment Health Nurs. 2014;35(6):413-419. doi:10.3109/01612840.2014.881941
24. Currier JM, Stefurak T, Carroll TD, Shatto EH. Applying trauma-informed care to community-based mental health services for military veterans. Best Pract Ment Health. 2017;13(1):47-64.
25. Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38(4):467-480. doi:10.1017/S0033291707001353
26. Galea S, Merchant RM, Lurie N. the mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention [published online ahead of print, 2020 Apr 10]. JAMA Intern Med. 2020;10.1001/jamainternmed.2020.1562. doi:10.1001/jamainternmed.2020.1562
27. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10(7):1206-1212. doi:10.3201/eid1007.030703
28. Cunha JM, Shen YC, Burke ZR. Contrasting the impacts of combat and humanitarian assistance/disaster relief missions on the mental health of military service members. Def Peace Economics. 2018;29(1):62-77. doi: 10.1080/10242694.2017.1349365
29. Ramchand R, Harrell MC, Berglass N, Lauck M. Veterans and COVID-19: Projecting the Economic, Social and Mental Health Needs of America’s Veterans. New York, NY: The Bob Woodruff Foundation; 2020.
30. van Gelder N, Peterman A, Potts A, et al. COVID-19: reducing the risk of infection might increase the risk of intimate partner violence [published online ahead of print, 2020 Apr 11]. EClinicalMedicine. 2020;21:100348. doi:10.1016/j.eclinm.2020.100348
31. Azarang A, Pakyurek M, Giroux C, Nordahl TE, Yellowlees P. Information technologies: an augmentation to post-traumatic stress disorder treatment among trauma survivors. Telemed J E Health. 2019;25(4):263-271. doi:10.1089/tmj.2018.0068.
32. Gilmore AK, Davis MT, Grubaugh A, et al. “Do you expect me to receive PTSD care in a setting where most of the other patients remind me of the perpetrator?”: Home-based telemedicine to address barriers to care unique to military sexual trauma and veterans affairs hospitals. Contemp Clin Trials. 2016;48:59-64. doi:10.1016/j.cct.2016.03.004.
33. van Gurp J, van Selm M, Vissers K, van Leeuwen E, Hasselaar J. How outpatient palliative care teleconsultation facilitates empathic patient-professional relationships: a qualitative study. PLoS One. 2015;10(4):e0124387. Published 2015 Apr 22. doi:10.1371/journal.pone.0124387
34. Morland LA, Mackintosh MA, Glassman LH, et al. Home-based delivery of variable length prolonged exposure therapy: a comparison of clinical efficacy between service modalities. Depress Anxiety. 2020;37(4):346-355. doi:10.1002/da.22979
35. Morland LA, Hynes AK, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress. 2011;24(4):465-469. doi:10.1002/jts.20661
36. Elisseou S, Puranam S, Nandi M. A novel, trauma-informed physical examination curriculum. Med Educ. 2018;52(5):555-556. doi:10.1111/medu.13569
1. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957-962. doi:10.1093/jamia/ocaa067
2. Centers for Medicare and Medicaid Services. Medicare and Medicaid programs; policy and regulatory revisions in response to the COVID-19 public health emergency. CMS-1744-IFC. https://www.cms.gov/files/document/covid-final-ifc.pdf. Published March 24, 2020. Accessed April 8, 2020.
3. Eddy N. VA sees a surge in veterans’ use of telehealth services. https://www.healthcareitnews.com/news/va-sees-surge-veterans-use-telehealth-services. Published November 25, 2019. Accessed June 17, 2020.
4. Veterans Health Administration, Office of Emergency Management. COVID-19 response plan. Version 1.6. Published March 23, 2020. Accessed June 17, 2020.
5. Caudill RL, Sager Z. Institutionally based videoconferencing. Int Rev Psychiatry. 2015;27(6):496-503. doi:10.3109/09540261.2015.1085369
6. Heyworth L. Sharing Connections [published correction appears in JAMA. 2018 May 8;319(18):1939]. JAMA. 2018;319(13):1323-1324. doi:10.1001/jama.2018.2717
7. Dobalian A. U.S. Department of Veterans Affairs’ (VA’s) response to the 2017 hurricanes. Presented at: American Public Health Association 2019 Annual Meeting and Exposition; November 2-6, 2019; Philadelphia, PA. https://apha.confex.com/apha/2019/meetingapp.cgi/Session/58543. Accessed June 16, 2020.
8. Der-Martirosian C, Griffin AR, Chu K, Dobalian A. Telehealth at the US Department of Veterans Affairs after Hurricane Sandy. J Telemed Telecare. 2019;25(5):310-317. doi:10.1177/1357633X17751005
9. The Office of the National Coordinator for Health Information Technology. Telemedicine and telehealth. https://www.healthit.gov/topic/health-it-initiatives/telemedicine-and-telehealth. Updated September 28, 2017. Accessed June 16, 2020.
10. Substance Abuse and Mental Health Services Administration, Trauma and Justice Strategic Initiative. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. https://ncsacw.samhsa.gov/userfiles/files/SAMHSA_Trauma.pdf. Published July 2014. Accessed June 16, 2020.
11. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547. doi:10.1002/jts.21848
12. Kimberg L, Wheeler M. Trauma and Trauma-informed Care. In: Gerber MR, ed. Trauma-informed Healthcare Approaches: A Guide for Primary Care. Cham, Switzerland: Springer Nature; 2019:25-56.
13. Gerber MR. Trauma-informed care of veterans. In: Gerber MR, ed. Trauma-informed Healthcare Approaches: A Guide for Primary Care. Cham, Switzerland: Springer Nature; 2019:25-56.
14. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245-258. doi:10.1016/s0749-3797(98)00017-8
15. Katon JG, Lehavot K, Simpson TL, et al. Adverse childhood experiences, Military service, and adult health. Am J Prev Med. 2015;49(4):573-582. doi:10.1016/j.amepre.2015.03.020
16. Blosnich JR, Dichter ME, Cerulli C, Batten SV, Bossarte RM. Disparities in adverse childhood experiences among individuals with a history of military service. JAMA Psychiatry. 2014;71(9):1041-1048. doi:10.1001/jamapsychiatry.2014.724
17. Center for Substance Abuse Treatment. Treatment improvement protocol (TIP). Series, No. 57. In: SAMHSA, ed. Trauma-Informed Care in Behavioral Health Services. SAMHSA: Rockville, MD; 2014:137-155.
18. US Department of Veterans Affairs, Veterans Health Administration, National Center for PTSD. Trauma, PTSD and treatment. https://www.ptsd.va.gov/PTSD/professional/treat/index.asp. Updated July 5, 2019. Accessed June 17, 2020.
19. Turgoose D, Ashwick R, Murphy D. Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. J Telemed Telecare. 2018;24(9):575-585. doi:10.1177/1357633X17730443
20. Cook JM, Simiola V, Hamblen JL, Bernardy N, Schnurr PP. The influence of patient readiness on implementation of evidence-based PTSD treatments in Veterans Affairs residential programs. Psychol Trauma. 2017;9(suppl 1):51-58. doi:10.1037/tra0000162
21. Raja S, Hasnain M, Hoersch M, Gove-Yin S, Rajagopalan C. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health. 2015;38(3):216-226. doi:10.1097/FCH.0000000000000071
22. Hopper EK, Bassuk EL, Olivet J. Shelter from the storm: trauma-informed care in homeless service settings. Open Health Serv Policy J. 2009;2:131-151.
23. Kelly U, Boyd MA, Valente SM, Czekanski E. Trauma-informed care: keeping mental health settings safe for veterans [published correction appears in Issues Ment Health Nurs. 2015 Jun;36(6):482]. Issues Ment Health Nurs. 2014;35(6):413-419. doi:10.3109/01612840.2014.881941
24. Currier JM, Stefurak T, Carroll TD, Shatto EH. Applying trauma-informed care to community-based mental health services for military veterans. Best Pract Ment Health. 2017;13(1):47-64.
25. Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38(4):467-480. doi:10.1017/S0033291707001353
26. Galea S, Merchant RM, Lurie N. the mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention [published online ahead of print, 2020 Apr 10]. JAMA Intern Med. 2020;10.1001/jamainternmed.2020.1562. doi:10.1001/jamainternmed.2020.1562
27. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10(7):1206-1212. doi:10.3201/eid1007.030703
28. Cunha JM, Shen YC, Burke ZR. Contrasting the impacts of combat and humanitarian assistance/disaster relief missions on the mental health of military service members. Def Peace Economics. 2018;29(1):62-77. doi: 10.1080/10242694.2017.1349365
29. Ramchand R, Harrell MC, Berglass N, Lauck M. Veterans and COVID-19: Projecting the Economic, Social and Mental Health Needs of America’s Veterans. New York, NY: The Bob Woodruff Foundation; 2020.
30. van Gelder N, Peterman A, Potts A, et al. COVID-19: reducing the risk of infection might increase the risk of intimate partner violence [published online ahead of print, 2020 Apr 11]. EClinicalMedicine. 2020;21:100348. doi:10.1016/j.eclinm.2020.100348
31. Azarang A, Pakyurek M, Giroux C, Nordahl TE, Yellowlees P. Information technologies: an augmentation to post-traumatic stress disorder treatment among trauma survivors. Telemed J E Health. 2019;25(4):263-271. doi:10.1089/tmj.2018.0068.
32. Gilmore AK, Davis MT, Grubaugh A, et al. “Do you expect me to receive PTSD care in a setting where most of the other patients remind me of the perpetrator?”: Home-based telemedicine to address barriers to care unique to military sexual trauma and veterans affairs hospitals. Contemp Clin Trials. 2016;48:59-64. doi:10.1016/j.cct.2016.03.004.
33. van Gurp J, van Selm M, Vissers K, van Leeuwen E, Hasselaar J. How outpatient palliative care teleconsultation facilitates empathic patient-professional relationships: a qualitative study. PLoS One. 2015;10(4):e0124387. Published 2015 Apr 22. doi:10.1371/journal.pone.0124387
34. Morland LA, Mackintosh MA, Glassman LH, et al. Home-based delivery of variable length prolonged exposure therapy: a comparison of clinical efficacy between service modalities. Depress Anxiety. 2020;37(4):346-355. doi:10.1002/da.22979
35. Morland LA, Hynes AK, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress. 2011;24(4):465-469. doi:10.1002/jts.20661
36. Elisseou S, Puranam S, Nandi M. A novel, trauma-informed physical examination curriculum. Med Educ. 2018;52(5):555-556. doi:10.1111/medu.13569
The Dog Days of COVID-19
The editorials I have written so far in this series on COVID-19 have been on weighty topics as befits the serious situation of the pandemic, which as of June 30, 2020 had taken more than 500,000 lives across the globe and caused anguish and sorrow such as the world has not known since the 1918 influenza pandemic.2
The human spirit can bear only so much distress and tragedy before it is bowed and unable to stand. Stand though we must; not just against the inanimate invasion of viruses from the outside, but also our own endemic national tensions and conflicts. A periodic lifting of our burdens and a recharging of our psychological and spiritual energies are crucial to the resilience and flexibility that are necessary to walk the long difficult road ahead of us as a nation and as public servants in health care. This column takes a lighter look at COVID-19 and considers the restorative role companion animals, especially, for me, my beloved canines, have played in caring for and about us humans during the pandemic.
You will likely read this editorial during the official dog days of summer, which run from July 22 to August 22. We all may imagine a big dog laying on a porch in the American South while his owners drink lemonade and quietly rock in chairs watching the long lazy days pass in a simpler time.
However pleasant this bucolic picture, it has little to do with the origin of the expression, which dates back to ancient Greece. The dog refers not to our literal furry friends but, according to National Geographic (and who should know better), to the position of the “dog star” in a constellation in the night sky.3 Unfortunately, we cannot completely get away from the sobering theme of the pandemic: The rise of the star to prominence during the peak of the Mediterranean summer’s heat was a period associated with disaster and illness.
Real dogs, cats, and assorted other so-called pandemic pets, though, have been another type of star in this difficult period. Early in the shelter-in-place, pet adoptions from city and county animal shelters and rescue organizations skyrocketed.4 Although animal welfare experts have legitimate concerns that some of these adoptees will be surrendered if there is ever a return to normal. For now many people feel it is the perfect time to adopt, precisely because they now have space to bring a new member into the family. Before adopting, as a recent National Public Radio report emphasized, individuals should consider whether they truly have the resources both material and emotional to care for a pet.5 For those who take stock honestly and believe they have the room in their heart and budget, rescuing a companion is good psychological news, arguably even more for the human than for the animal.
Sheltering-in-place has reduced the transmission of the virus, which scientists estimate has saved thousands of lives.6 But it also has triggered a second health crisis, this time of mental health with an unprecedented increase in rates of depression, anxiety, suicide attempts, and substance use that is expected to worsen over the coming months and years.7 Companion animals certainly cannot solve this complex and mammoth public health problem; however, they can contribute in simple and small yet very significant ways to the mental health of individuals.8
Caring for a pet who shows unconditional love and loyalty to you can reduce isolation; foster hope; provide meaning, comfort, and cheer to you when you are down or afraid; and offer a routine and reason to get out of bed every day and take a walk outside. Research shows that those positive effects can decrease the risk of the very mental health conditions that are now plaguing us in such alarming numbers.9,10
“How many more lives are we willing to sacrifice in the name of containing the virus?” Elinore McCance-Katz, MD, PhD, the nation’s top mental health official ominously asked about the potential effects of another shutdown during a cabinet meeting.11 For some of us, a companion animal who does not require physical distancing (at least when you are healthy) may permit us to prevent the spread of the virus while protecting our mental health.
Nor is emotional support the only clinical way in which animals are helping pandemic- beleaguered humans. There is a low risk we can infect household pets, and dogs are not likely to transmit the virus. In fact, they even can be trained to serve as highly efficient virus testers who don’t need scarce reagents or carry high price tags—just a pat on the head and an occasional treat.12 Medscape reported that clinical trials starting in the United Kingdom are set to evaluate the accuracy of these “bio-detection” dogs. The story quotes a leading British public health official as saying, “Properly trained sniffer dogs could revolutionise our approach to this whole pandemic, screening 250 people an hour for the virus.”13
Canines are not only healers who can ease our troubles through the pandemic but also peacemakers. As injustice and violence rock the country, we would do well to imitate their attitudes of nonjudgmental acceptance. “Dogs are our link to paradise. They do not know evil or jealousy or discontent,” wrote novelist Milan Kundera. “To sit with a dog on a hillside on a glorious afternoon is to be back in Eden, where doing nothing was not boring—it was peace.”14 Those indeed would be dog days as when better nature we sometimes share with animals prevailed.
1. Buber M. I and Thou . Kaufmann W, trans. New York: Charles Scribner’s Sons: 1970:144.
2. World Health Organization. Coronavirus disease (COVID-19). Situation report-153. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200621-covid-19-sitrep-153.pdf?sfvrsn=c896464d_2. Published June 21, 2020. Accessed June 22, 2020.
3. Little B. Why do we call them the ‘dog days’ of summer. National Geographic . July 10, 2015. https://www.nationalgeographic.com/news/2015/07/150710-dog-days-summer-sirius-star-astronomy-weather-language. Accessed June 21, 2020.
4. Ellis EG. Thanks to sheltering in place, animal shelters are empty. https://www.wired.com/story/coronavirus-pet-adoption-boom. Published April 10, 2020. Accessed June 21, 2020.
5. Balaban S. Should I adopt a dog during the coronavirus crisis? Read this first. https://www.npr.org/2020/05/08/853088872/should-i-adopt-a-dog-during-the-coronavirus-crisis-read-this-first. Published May 11, 2020. Accessed June 21, 2020
6. Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic [published online ahead of print, 2020 Jun 8]. Nature. 2020;10.1038/s41586-020-2404-8. doi:10.1038/s41586-020-2404-8
7. Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention [published online ahead of print, 2020 Apr 10]. JAMA Intern Med. 2020;10.1001/jamainternmed.2020.1562. doi:10.1001/jamainternmed.2020.1562
8. Rajewski G. How animals help us during the COVID-19 pandemic. https://now.tufts.edu/articles/how-animals-help-us-during-covid-19-pandemic. Published Mach 30, 2020. Accessed June 21, 2020
9. Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America [published online ahead of print, 2020 Jun 4]. Psychol Trauma . 2020;10.1037/tra0000924. doi:10.1037/tra0000924
10. Rajkumar RP. COVID-19 and mental health: A review of the existing literature [published online ahead of print, 2020 Apr 10]. Asian J Psychiatr. 2020;52:102066. doi:10.1016/j.ajp.2020.102066
11. The White House. Remarks by President Trump in cabinet meeting. https://www.whitehouse.gov/briefings-statements/remarks-president-trump-cabinet-meeting-17. Published May 19, 2020. Accessed June 21, 2020
12. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). COVID -19 and animals. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/animals.html. Updated June 22, 2020. Accessed June 24, 2020.
13. Russell P. Could bio-detection dogs sniff out COVID-19 infection. https://www.medscape.com/viewarticle/930652. Published May 17, 2020. Accessed June 21, 2020.
14. Kundera M. The Unbearable Lightness of Being . New York: Harper & Row; 1984.
The editorials I have written so far in this series on COVID-19 have been on weighty topics as befits the serious situation of the pandemic, which as of June 30, 2020 had taken more than 500,000 lives across the globe and caused anguish and sorrow such as the world has not known since the 1918 influenza pandemic.2
The human spirit can bear only so much distress and tragedy before it is bowed and unable to stand. Stand though we must; not just against the inanimate invasion of viruses from the outside, but also our own endemic national tensions and conflicts. A periodic lifting of our burdens and a recharging of our psychological and spiritual energies are crucial to the resilience and flexibility that are necessary to walk the long difficult road ahead of us as a nation and as public servants in health care. This column takes a lighter look at COVID-19 and considers the restorative role companion animals, especially, for me, my beloved canines, have played in caring for and about us humans during the pandemic.
You will likely read this editorial during the official dog days of summer, which run from July 22 to August 22. We all may imagine a big dog laying on a porch in the American South while his owners drink lemonade and quietly rock in chairs watching the long lazy days pass in a simpler time.
However pleasant this bucolic picture, it has little to do with the origin of the expression, which dates back to ancient Greece. The dog refers not to our literal furry friends but, according to National Geographic (and who should know better), to the position of the “dog star” in a constellation in the night sky.3 Unfortunately, we cannot completely get away from the sobering theme of the pandemic: The rise of the star to prominence during the peak of the Mediterranean summer’s heat was a period associated with disaster and illness.
Real dogs, cats, and assorted other so-called pandemic pets, though, have been another type of star in this difficult period. Early in the shelter-in-place, pet adoptions from city and county animal shelters and rescue organizations skyrocketed.4 Although animal welfare experts have legitimate concerns that some of these adoptees will be surrendered if there is ever a return to normal. For now many people feel it is the perfect time to adopt, precisely because they now have space to bring a new member into the family. Before adopting, as a recent National Public Radio report emphasized, individuals should consider whether they truly have the resources both material and emotional to care for a pet.5 For those who take stock honestly and believe they have the room in their heart and budget, rescuing a companion is good psychological news, arguably even more for the human than for the animal.
Sheltering-in-place has reduced the transmission of the virus, which scientists estimate has saved thousands of lives.6 But it also has triggered a second health crisis, this time of mental health with an unprecedented increase in rates of depression, anxiety, suicide attempts, and substance use that is expected to worsen over the coming months and years.7 Companion animals certainly cannot solve this complex and mammoth public health problem; however, they can contribute in simple and small yet very significant ways to the mental health of individuals.8
Caring for a pet who shows unconditional love and loyalty to you can reduce isolation; foster hope; provide meaning, comfort, and cheer to you when you are down or afraid; and offer a routine and reason to get out of bed every day and take a walk outside. Research shows that those positive effects can decrease the risk of the very mental health conditions that are now plaguing us in such alarming numbers.9,10
“How many more lives are we willing to sacrifice in the name of containing the virus?” Elinore McCance-Katz, MD, PhD, the nation’s top mental health official ominously asked about the potential effects of another shutdown during a cabinet meeting.11 For some of us, a companion animal who does not require physical distancing (at least when you are healthy) may permit us to prevent the spread of the virus while protecting our mental health.
Nor is emotional support the only clinical way in which animals are helping pandemic- beleaguered humans. There is a low risk we can infect household pets, and dogs are not likely to transmit the virus. In fact, they even can be trained to serve as highly efficient virus testers who don’t need scarce reagents or carry high price tags—just a pat on the head and an occasional treat.12 Medscape reported that clinical trials starting in the United Kingdom are set to evaluate the accuracy of these “bio-detection” dogs. The story quotes a leading British public health official as saying, “Properly trained sniffer dogs could revolutionise our approach to this whole pandemic, screening 250 people an hour for the virus.”13
Canines are not only healers who can ease our troubles through the pandemic but also peacemakers. As injustice and violence rock the country, we would do well to imitate their attitudes of nonjudgmental acceptance. “Dogs are our link to paradise. They do not know evil or jealousy or discontent,” wrote novelist Milan Kundera. “To sit with a dog on a hillside on a glorious afternoon is to be back in Eden, where doing nothing was not boring—it was peace.”14 Those indeed would be dog days as when better nature we sometimes share with animals prevailed.
The editorials I have written so far in this series on COVID-19 have been on weighty topics as befits the serious situation of the pandemic, which as of June 30, 2020 had taken more than 500,000 lives across the globe and caused anguish and sorrow such as the world has not known since the 1918 influenza pandemic.2
The human spirit can bear only so much distress and tragedy before it is bowed and unable to stand. Stand though we must; not just against the inanimate invasion of viruses from the outside, but also our own endemic national tensions and conflicts. A periodic lifting of our burdens and a recharging of our psychological and spiritual energies are crucial to the resilience and flexibility that are necessary to walk the long difficult road ahead of us as a nation and as public servants in health care. This column takes a lighter look at COVID-19 and considers the restorative role companion animals, especially, for me, my beloved canines, have played in caring for and about us humans during the pandemic.
You will likely read this editorial during the official dog days of summer, which run from July 22 to August 22. We all may imagine a big dog laying on a porch in the American South while his owners drink lemonade and quietly rock in chairs watching the long lazy days pass in a simpler time.
However pleasant this bucolic picture, it has little to do with the origin of the expression, which dates back to ancient Greece. The dog refers not to our literal furry friends but, according to National Geographic (and who should know better), to the position of the “dog star” in a constellation in the night sky.3 Unfortunately, we cannot completely get away from the sobering theme of the pandemic: The rise of the star to prominence during the peak of the Mediterranean summer’s heat was a period associated with disaster and illness.
Real dogs, cats, and assorted other so-called pandemic pets, though, have been another type of star in this difficult period. Early in the shelter-in-place, pet adoptions from city and county animal shelters and rescue organizations skyrocketed.4 Although animal welfare experts have legitimate concerns that some of these adoptees will be surrendered if there is ever a return to normal. For now many people feel it is the perfect time to adopt, precisely because they now have space to bring a new member into the family. Before adopting, as a recent National Public Radio report emphasized, individuals should consider whether they truly have the resources both material and emotional to care for a pet.5 For those who take stock honestly and believe they have the room in their heart and budget, rescuing a companion is good psychological news, arguably even more for the human than for the animal.
Sheltering-in-place has reduced the transmission of the virus, which scientists estimate has saved thousands of lives.6 But it also has triggered a second health crisis, this time of mental health with an unprecedented increase in rates of depression, anxiety, suicide attempts, and substance use that is expected to worsen over the coming months and years.7 Companion animals certainly cannot solve this complex and mammoth public health problem; however, they can contribute in simple and small yet very significant ways to the mental health of individuals.8
Caring for a pet who shows unconditional love and loyalty to you can reduce isolation; foster hope; provide meaning, comfort, and cheer to you when you are down or afraid; and offer a routine and reason to get out of bed every day and take a walk outside. Research shows that those positive effects can decrease the risk of the very mental health conditions that are now plaguing us in such alarming numbers.9,10
“How many more lives are we willing to sacrifice in the name of containing the virus?” Elinore McCance-Katz, MD, PhD, the nation’s top mental health official ominously asked about the potential effects of another shutdown during a cabinet meeting.11 For some of us, a companion animal who does not require physical distancing (at least when you are healthy) may permit us to prevent the spread of the virus while protecting our mental health.
Nor is emotional support the only clinical way in which animals are helping pandemic- beleaguered humans. There is a low risk we can infect household pets, and dogs are not likely to transmit the virus. In fact, they even can be trained to serve as highly efficient virus testers who don’t need scarce reagents or carry high price tags—just a pat on the head and an occasional treat.12 Medscape reported that clinical trials starting in the United Kingdom are set to evaluate the accuracy of these “bio-detection” dogs. The story quotes a leading British public health official as saying, “Properly trained sniffer dogs could revolutionise our approach to this whole pandemic, screening 250 people an hour for the virus.”13
Canines are not only healers who can ease our troubles through the pandemic but also peacemakers. As injustice and violence rock the country, we would do well to imitate their attitudes of nonjudgmental acceptance. “Dogs are our link to paradise. They do not know evil or jealousy or discontent,” wrote novelist Milan Kundera. “To sit with a dog on a hillside on a glorious afternoon is to be back in Eden, where doing nothing was not boring—it was peace.”14 Those indeed would be dog days as when better nature we sometimes share with animals prevailed.
1. Buber M. I and Thou . Kaufmann W, trans. New York: Charles Scribner’s Sons: 1970:144.
2. World Health Organization. Coronavirus disease (COVID-19). Situation report-153. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200621-covid-19-sitrep-153.pdf?sfvrsn=c896464d_2. Published June 21, 2020. Accessed June 22, 2020.
3. Little B. Why do we call them the ‘dog days’ of summer. National Geographic . July 10, 2015. https://www.nationalgeographic.com/news/2015/07/150710-dog-days-summer-sirius-star-astronomy-weather-language. Accessed June 21, 2020.
4. Ellis EG. Thanks to sheltering in place, animal shelters are empty. https://www.wired.com/story/coronavirus-pet-adoption-boom. Published April 10, 2020. Accessed June 21, 2020.
5. Balaban S. Should I adopt a dog during the coronavirus crisis? Read this first. https://www.npr.org/2020/05/08/853088872/should-i-adopt-a-dog-during-the-coronavirus-crisis-read-this-first. Published May 11, 2020. Accessed June 21, 2020
6. Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic [published online ahead of print, 2020 Jun 8]. Nature. 2020;10.1038/s41586-020-2404-8. doi:10.1038/s41586-020-2404-8
7. Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention [published online ahead of print, 2020 Apr 10]. JAMA Intern Med. 2020;10.1001/jamainternmed.2020.1562. doi:10.1001/jamainternmed.2020.1562
8. Rajewski G. How animals help us during the COVID-19 pandemic. https://now.tufts.edu/articles/how-animals-help-us-during-covid-19-pandemic. Published Mach 30, 2020. Accessed June 21, 2020
9. Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America [published online ahead of print, 2020 Jun 4]. Psychol Trauma . 2020;10.1037/tra0000924. doi:10.1037/tra0000924
10. Rajkumar RP. COVID-19 and mental health: A review of the existing literature [published online ahead of print, 2020 Apr 10]. Asian J Psychiatr. 2020;52:102066. doi:10.1016/j.ajp.2020.102066
11. The White House. Remarks by President Trump in cabinet meeting. https://www.whitehouse.gov/briefings-statements/remarks-president-trump-cabinet-meeting-17. Published May 19, 2020. Accessed June 21, 2020
12. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). COVID -19 and animals. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/animals.html. Updated June 22, 2020. Accessed June 24, 2020.
13. Russell P. Could bio-detection dogs sniff out COVID-19 infection. https://www.medscape.com/viewarticle/930652. Published May 17, 2020. Accessed June 21, 2020.
14. Kundera M. The Unbearable Lightness of Being . New York: Harper & Row; 1984.
1. Buber M. I and Thou . Kaufmann W, trans. New York: Charles Scribner’s Sons: 1970:144.
2. World Health Organization. Coronavirus disease (COVID-19). Situation report-153. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200621-covid-19-sitrep-153.pdf?sfvrsn=c896464d_2. Published June 21, 2020. Accessed June 22, 2020.
3. Little B. Why do we call them the ‘dog days’ of summer. National Geographic . July 10, 2015. https://www.nationalgeographic.com/news/2015/07/150710-dog-days-summer-sirius-star-astronomy-weather-language. Accessed June 21, 2020.
4. Ellis EG. Thanks to sheltering in place, animal shelters are empty. https://www.wired.com/story/coronavirus-pet-adoption-boom. Published April 10, 2020. Accessed June 21, 2020.
5. Balaban S. Should I adopt a dog during the coronavirus crisis? Read this first. https://www.npr.org/2020/05/08/853088872/should-i-adopt-a-dog-during-the-coronavirus-crisis-read-this-first. Published May 11, 2020. Accessed June 21, 2020
6. Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic [published online ahead of print, 2020 Jun 8]. Nature. 2020;10.1038/s41586-020-2404-8. doi:10.1038/s41586-020-2404-8
7. Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention [published online ahead of print, 2020 Apr 10]. JAMA Intern Med. 2020;10.1001/jamainternmed.2020.1562. doi:10.1001/jamainternmed.2020.1562
8. Rajewski G. How animals help us during the COVID-19 pandemic. https://now.tufts.edu/articles/how-animals-help-us-during-covid-19-pandemic. Published Mach 30, 2020. Accessed June 21, 2020
9. Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America [published online ahead of print, 2020 Jun 4]. Psychol Trauma . 2020;10.1037/tra0000924. doi:10.1037/tra0000924
10. Rajkumar RP. COVID-19 and mental health: A review of the existing literature [published online ahead of print, 2020 Apr 10]. Asian J Psychiatr. 2020;52:102066. doi:10.1016/j.ajp.2020.102066
11. The White House. Remarks by President Trump in cabinet meeting. https://www.whitehouse.gov/briefings-statements/remarks-president-trump-cabinet-meeting-17. Published May 19, 2020. Accessed June 21, 2020
12. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). COVID -19 and animals. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/animals.html. Updated June 22, 2020. Accessed June 24, 2020.
13. Russell P. Could bio-detection dogs sniff out COVID-19 infection. https://www.medscape.com/viewarticle/930652. Published May 17, 2020. Accessed June 21, 2020.
14. Kundera M. The Unbearable Lightness of Being . New York: Harper & Row; 1984.
Wear N95 masks during endoscopy
COVID-19 guideline update
Nausea, vomiting, and diarrhea are gastrointestinal symptoms that COVID-19 patients have had, and up to 30% have been reported to have liver symptoms. Because patients with these symptoms may require endoscopy, the American Gastroenterological Association has issued a rapid recommendation document that advises physicians and health care workers to use N95 masks, double gloves, and negative-pressure rooms when performing GI procedures during the COVID-19 pandemic.
The recommendations, published in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.03.072), also cover non–COVID-19 patients and situations where N95 masks should be used, offer guidelines for triaging patients for endoscopy and timing of nonurgent procedures, and evaluate the latest evidence in the incidence of GI and liver manifestations of COVID-19. The guideline panel met in March.
The document includes seven recommendations for use of personal protective equipment by physicians and nurses performing GI procedures. The recommendations and the level of evidence supporting them fall under four categories:
1. Masks, comprising four recommendations: use of N95 masks for upper and lower GI procedures regardless of a patient’s COVID-19 status; no use of only surgical masks in confirmed COVID-19 patients or suspected cases; and use of reused N95 masks when fresh ones aren’t available instead of using a surgical mask only (very low to moderate level of evidence depending on the recommendation).
2. Double-gloving when performing any GI procedure regardless of the patient’s COVID-19 status (moderate quality evidence).
3. When available, a negative-pressure room for any COVID-19 patient or suspect rather than a regular endoscopy room (very low certainty of evidence).
4. Standard cleaning, endoscopic disinfection, and reprocessing protocols regardless of a patient’s COVID-19 status (good practice statement).
For decontamination, the panel noted that commonly used biocidal agents, such as hydrogen peroxide, alcohols, sodium hypochlorite, or benzalkonium chloride have proved effective for decontaminating of coronavirus.
For implementing the PPE recommendations, the panel stated that personnel still need to practice don and doff standard protocols, and that N95 masks should be fitted for each individual.
Other steps include banning personal belongings in the procedure area; minimizing the number of personnel in the room; avoiding change of personnel and keeping nonprocedural personnel out during the procedure; considering use of nursing teams that follow the patient through preprocedure, procedure, and recovery, and considering having endoscopy teams remain together during the day to minimize exposure.
The triage recommendations stated that “trained medical personnel” should review all procedures and categorize them as time-sensitive or not time-sensitive, based on a framework the recommendation includes. In “an open-access endoscopy system” when there isn’t enough information to determine timing for the procedure, the recommendation provides a three-step approach: a phone consult with the referring physician, a telehealth visit with the patient, or a multidisciplinary team approach or virtual disease/tumor board.
“The proposed framework of separating procedures into time-sensitive and non–time-sensitive cases may be useful in determining which procedures if delayed may negatively impact on patient-important outcomes,” wrote Shahnaz Sultan, MD, AGAF, of the University of Minnesota, Minneapolis, and colleagues. The panel noted decision-making should focus on “patient-important outcomes.”
For nonurgent procedures, the panel arrived at a consensus that 8 weeks was an appropriate window for reassessment of deferred procedures, depending on the availability of resources and if the time-sensitivity of the procedure changes.
The panel also attempted to determine the likelihood of GI and liver manifestations of COVID-19 by evaluating published cohort studies. They found that 2%-13.8% of patients had diarrhea, 1%-10.1% had nausea or vomiting, and one study reported 2% had abdominal pain (Am J Gastroenterol. 2020 May;115[5]766-73). What’s more, some studies have shown stool samples positive for SARS-CoV-2 RNA even after respiratory samples were negative.
The evidence on liver manifestations isn’t as robust, but one study reported that 20%-30% of patients had liver injury upon diagnosis of COVID-19 (Gastroenterology. 2020;158:1518-9), and that severe hepatitis has been reported but liver failure seems rare (Lancet. 2020 Feb 15;395[10223]:507-13). “The pattern of liver injury appears to be predominantly hepatocellular, and the etiology remains uncertain but may represent a secondary effect of the systemic inflammatory response observed with COVID-19 disease, although direct viral infection and drug-induced liver injury cannot be excluded,” Dr. Sultan and colleagues noted.
There were no relevant author conflicts of interest. The American Gastroenterological Association (AGA) Institute funded the study.
SOURCE: Sultan S et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.072.
Check out the AGA COVID-19 Resource Library for new clinical guidance, education, research and physician resources, including recent guidance on how to treat patients with IBD during the pandemic, at www.gastro.org/covid.
COVID-19 guideline update
COVID-19 guideline update
Nausea, vomiting, and diarrhea are gastrointestinal symptoms that COVID-19 patients have had, and up to 30% have been reported to have liver symptoms. Because patients with these symptoms may require endoscopy, the American Gastroenterological Association has issued a rapid recommendation document that advises physicians and health care workers to use N95 masks, double gloves, and negative-pressure rooms when performing GI procedures during the COVID-19 pandemic.
The recommendations, published in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.03.072), also cover non–COVID-19 patients and situations where N95 masks should be used, offer guidelines for triaging patients for endoscopy and timing of nonurgent procedures, and evaluate the latest evidence in the incidence of GI and liver manifestations of COVID-19. The guideline panel met in March.
The document includes seven recommendations for use of personal protective equipment by physicians and nurses performing GI procedures. The recommendations and the level of evidence supporting them fall under four categories:
1. Masks, comprising four recommendations: use of N95 masks for upper and lower GI procedures regardless of a patient’s COVID-19 status; no use of only surgical masks in confirmed COVID-19 patients or suspected cases; and use of reused N95 masks when fresh ones aren’t available instead of using a surgical mask only (very low to moderate level of evidence depending on the recommendation).
2. Double-gloving when performing any GI procedure regardless of the patient’s COVID-19 status (moderate quality evidence).
3. When available, a negative-pressure room for any COVID-19 patient or suspect rather than a regular endoscopy room (very low certainty of evidence).
4. Standard cleaning, endoscopic disinfection, and reprocessing protocols regardless of a patient’s COVID-19 status (good practice statement).
For decontamination, the panel noted that commonly used biocidal agents, such as hydrogen peroxide, alcohols, sodium hypochlorite, or benzalkonium chloride have proved effective for decontaminating of coronavirus.
For implementing the PPE recommendations, the panel stated that personnel still need to practice don and doff standard protocols, and that N95 masks should be fitted for each individual.
Other steps include banning personal belongings in the procedure area; minimizing the number of personnel in the room; avoiding change of personnel and keeping nonprocedural personnel out during the procedure; considering use of nursing teams that follow the patient through preprocedure, procedure, and recovery, and considering having endoscopy teams remain together during the day to minimize exposure.
The triage recommendations stated that “trained medical personnel” should review all procedures and categorize them as time-sensitive or not time-sensitive, based on a framework the recommendation includes. In “an open-access endoscopy system” when there isn’t enough information to determine timing for the procedure, the recommendation provides a three-step approach: a phone consult with the referring physician, a telehealth visit with the patient, or a multidisciplinary team approach or virtual disease/tumor board.
“The proposed framework of separating procedures into time-sensitive and non–time-sensitive cases may be useful in determining which procedures if delayed may negatively impact on patient-important outcomes,” wrote Shahnaz Sultan, MD, AGAF, of the University of Minnesota, Minneapolis, and colleagues. The panel noted decision-making should focus on “patient-important outcomes.”
For nonurgent procedures, the panel arrived at a consensus that 8 weeks was an appropriate window for reassessment of deferred procedures, depending on the availability of resources and if the time-sensitivity of the procedure changes.
The panel also attempted to determine the likelihood of GI and liver manifestations of COVID-19 by evaluating published cohort studies. They found that 2%-13.8% of patients had diarrhea, 1%-10.1% had nausea or vomiting, and one study reported 2% had abdominal pain (Am J Gastroenterol. 2020 May;115[5]766-73). What’s more, some studies have shown stool samples positive for SARS-CoV-2 RNA even after respiratory samples were negative.
The evidence on liver manifestations isn’t as robust, but one study reported that 20%-30% of patients had liver injury upon diagnosis of COVID-19 (Gastroenterology. 2020;158:1518-9), and that severe hepatitis has been reported but liver failure seems rare (Lancet. 2020 Feb 15;395[10223]:507-13). “The pattern of liver injury appears to be predominantly hepatocellular, and the etiology remains uncertain but may represent a secondary effect of the systemic inflammatory response observed with COVID-19 disease, although direct viral infection and drug-induced liver injury cannot be excluded,” Dr. Sultan and colleagues noted.
There were no relevant author conflicts of interest. The American Gastroenterological Association (AGA) Institute funded the study.
SOURCE: Sultan S et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.072.
Check out the AGA COVID-19 Resource Library for new clinical guidance, education, research and physician resources, including recent guidance on how to treat patients with IBD during the pandemic, at www.gastro.org/covid.
Nausea, vomiting, and diarrhea are gastrointestinal symptoms that COVID-19 patients have had, and up to 30% have been reported to have liver symptoms. Because patients with these symptoms may require endoscopy, the American Gastroenterological Association has issued a rapid recommendation document that advises physicians and health care workers to use N95 masks, double gloves, and negative-pressure rooms when performing GI procedures during the COVID-19 pandemic.
The recommendations, published in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.03.072), also cover non–COVID-19 patients and situations where N95 masks should be used, offer guidelines for triaging patients for endoscopy and timing of nonurgent procedures, and evaluate the latest evidence in the incidence of GI and liver manifestations of COVID-19. The guideline panel met in March.
The document includes seven recommendations for use of personal protective equipment by physicians and nurses performing GI procedures. The recommendations and the level of evidence supporting them fall under four categories:
1. Masks, comprising four recommendations: use of N95 masks for upper and lower GI procedures regardless of a patient’s COVID-19 status; no use of only surgical masks in confirmed COVID-19 patients or suspected cases; and use of reused N95 masks when fresh ones aren’t available instead of using a surgical mask only (very low to moderate level of evidence depending on the recommendation).
2. Double-gloving when performing any GI procedure regardless of the patient’s COVID-19 status (moderate quality evidence).
3. When available, a negative-pressure room for any COVID-19 patient or suspect rather than a regular endoscopy room (very low certainty of evidence).
4. Standard cleaning, endoscopic disinfection, and reprocessing protocols regardless of a patient’s COVID-19 status (good practice statement).
For decontamination, the panel noted that commonly used biocidal agents, such as hydrogen peroxide, alcohols, sodium hypochlorite, or benzalkonium chloride have proved effective for decontaminating of coronavirus.
For implementing the PPE recommendations, the panel stated that personnel still need to practice don and doff standard protocols, and that N95 masks should be fitted for each individual.
Other steps include banning personal belongings in the procedure area; minimizing the number of personnel in the room; avoiding change of personnel and keeping nonprocedural personnel out during the procedure; considering use of nursing teams that follow the patient through preprocedure, procedure, and recovery, and considering having endoscopy teams remain together during the day to minimize exposure.
The triage recommendations stated that “trained medical personnel” should review all procedures and categorize them as time-sensitive or not time-sensitive, based on a framework the recommendation includes. In “an open-access endoscopy system” when there isn’t enough information to determine timing for the procedure, the recommendation provides a three-step approach: a phone consult with the referring physician, a telehealth visit with the patient, or a multidisciplinary team approach or virtual disease/tumor board.
“The proposed framework of separating procedures into time-sensitive and non–time-sensitive cases may be useful in determining which procedures if delayed may negatively impact on patient-important outcomes,” wrote Shahnaz Sultan, MD, AGAF, of the University of Minnesota, Minneapolis, and colleagues. The panel noted decision-making should focus on “patient-important outcomes.”
For nonurgent procedures, the panel arrived at a consensus that 8 weeks was an appropriate window for reassessment of deferred procedures, depending on the availability of resources and if the time-sensitivity of the procedure changes.
The panel also attempted to determine the likelihood of GI and liver manifestations of COVID-19 by evaluating published cohort studies. They found that 2%-13.8% of patients had diarrhea, 1%-10.1% had nausea or vomiting, and one study reported 2% had abdominal pain (Am J Gastroenterol. 2020 May;115[5]766-73). What’s more, some studies have shown stool samples positive for SARS-CoV-2 RNA even after respiratory samples were negative.
The evidence on liver manifestations isn’t as robust, but one study reported that 20%-30% of patients had liver injury upon diagnosis of COVID-19 (Gastroenterology. 2020;158:1518-9), and that severe hepatitis has been reported but liver failure seems rare (Lancet. 2020 Feb 15;395[10223]:507-13). “The pattern of liver injury appears to be predominantly hepatocellular, and the etiology remains uncertain but may represent a secondary effect of the systemic inflammatory response observed with COVID-19 disease, although direct viral infection and drug-induced liver injury cannot be excluded,” Dr. Sultan and colleagues noted.
There were no relevant author conflicts of interest. The American Gastroenterological Association (AGA) Institute funded the study.
SOURCE: Sultan S et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.072.
Check out the AGA COVID-19 Resource Library for new clinical guidance, education, research and physician resources, including recent guidance on how to treat patients with IBD during the pandemic, at www.gastro.org/covid.
A 72-year-old with an acute, pruritic, bullous eruption involving his right pretibial extremity
Localized bullous pemphigoid
with a predilection in the elderly population.1
Localized variants of bullous pemphigoid (BP) are rare and have been reported to arise at sites of mechanical trauma, prior radiation, lymphedema, surgical scars, burns, fistulas, and ostomies.1-3 Although the mechanism remains unclear, the Koebner phenomenon is thought to induce dysregulation of immunologic and vascular factors in sites of mechanical shear and trauma in susceptible individuals.3
Localized BP is an important entity for the dermatologist to be familiar with, as the diagnosis is often delayed. The localized, well-defined skin lesions frequently mimic contact dermatitis. In fact, previous reports have shown the most likely misdiagnosis of localized BP is acute allergic contact dermatitis, stasis dermatitis, and eczematous dermatitis.4,5
In this patient, histopathologic examination of a biopsy revealed a subepidermal blister with numerous eosinophils. Direct immunofluorescence study of perilesional skin showed strong linear IgG and C3 deposits at the basal membrane level. Serum level of autoantibody to BP180 antigen was elevated. Bacterial culture was positive for Staphylococcus aureus. These findings were suggestive of unilateral, localized BP with superimposed bacterial infection. Initial treatment with an extended course of doxycycline 200 mg twice daily, topical triamcinolone 0.1% ointment twice daily with compression therapy, and leg elevation led to clinical improvement with healing of previous lesions on the leg. At follow-up 3 weeks later, the patient had continued to develop new bullous lesions on the trunk and upper thighs. He was subsequently started on systemic immunosuppressive therapy for generalized bullous pemphigoid.
Importantly, localized BP generally follows a more benign disease course, although long-term follow-up is recommended for monitoring given the potential risk of developing the generalized form of BP of approximately 15%.3 Topical corticosteroids and oral antibiotics are recommended as the first-line therapy in these patients, with an escalated systemic therapy if needed for disease progression.3,5
Our case represents an important differential diagnosis to consider when evaluating an acute localized bullous eruption in an elderly patient.
Dr. Cusick and Dr. Dolohanty are with the department of dermatology, University of Rochester (N.Y.), and provided the case and photo. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Kohroh K et al. J Dermatol. 2007 Jul;34(7):482-5.
2. Nguyen T et al. Dermatology 2014;229(2):88-96.
3. Sen BB et al. Indian J Dermatol Venereol Leprol. 2013;79(4):554.
4. Salomon RJ et al. Arch Dermatol. 1987 Mar;123(3):389-92.
5. Tran JT, Mutasim DF. Int J Dermatol. 2005 Nov;44(11):942-5.
Localized bullous pemphigoid
with a predilection in the elderly population.1
Localized variants of bullous pemphigoid (BP) are rare and have been reported to arise at sites of mechanical trauma, prior radiation, lymphedema, surgical scars, burns, fistulas, and ostomies.1-3 Although the mechanism remains unclear, the Koebner phenomenon is thought to induce dysregulation of immunologic and vascular factors in sites of mechanical shear and trauma in susceptible individuals.3
Localized BP is an important entity for the dermatologist to be familiar with, as the diagnosis is often delayed. The localized, well-defined skin lesions frequently mimic contact dermatitis. In fact, previous reports have shown the most likely misdiagnosis of localized BP is acute allergic contact dermatitis, stasis dermatitis, and eczematous dermatitis.4,5
In this patient, histopathologic examination of a biopsy revealed a subepidermal blister with numerous eosinophils. Direct immunofluorescence study of perilesional skin showed strong linear IgG and C3 deposits at the basal membrane level. Serum level of autoantibody to BP180 antigen was elevated. Bacterial culture was positive for Staphylococcus aureus. These findings were suggestive of unilateral, localized BP with superimposed bacterial infection. Initial treatment with an extended course of doxycycline 200 mg twice daily, topical triamcinolone 0.1% ointment twice daily with compression therapy, and leg elevation led to clinical improvement with healing of previous lesions on the leg. At follow-up 3 weeks later, the patient had continued to develop new bullous lesions on the trunk and upper thighs. He was subsequently started on systemic immunosuppressive therapy for generalized bullous pemphigoid.
Importantly, localized BP generally follows a more benign disease course, although long-term follow-up is recommended for monitoring given the potential risk of developing the generalized form of BP of approximately 15%.3 Topical corticosteroids and oral antibiotics are recommended as the first-line therapy in these patients, with an escalated systemic therapy if needed for disease progression.3,5
Our case represents an important differential diagnosis to consider when evaluating an acute localized bullous eruption in an elderly patient.
Dr. Cusick and Dr. Dolohanty are with the department of dermatology, University of Rochester (N.Y.), and provided the case and photo. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Kohroh K et al. J Dermatol. 2007 Jul;34(7):482-5.
2. Nguyen T et al. Dermatology 2014;229(2):88-96.
3. Sen BB et al. Indian J Dermatol Venereol Leprol. 2013;79(4):554.
4. Salomon RJ et al. Arch Dermatol. 1987 Mar;123(3):389-92.
5. Tran JT, Mutasim DF. Int J Dermatol. 2005 Nov;44(11):942-5.
Localized bullous pemphigoid
with a predilection in the elderly population.1
Localized variants of bullous pemphigoid (BP) are rare and have been reported to arise at sites of mechanical trauma, prior radiation, lymphedema, surgical scars, burns, fistulas, and ostomies.1-3 Although the mechanism remains unclear, the Koebner phenomenon is thought to induce dysregulation of immunologic and vascular factors in sites of mechanical shear and trauma in susceptible individuals.3
Localized BP is an important entity for the dermatologist to be familiar with, as the diagnosis is often delayed. The localized, well-defined skin lesions frequently mimic contact dermatitis. In fact, previous reports have shown the most likely misdiagnosis of localized BP is acute allergic contact dermatitis, stasis dermatitis, and eczematous dermatitis.4,5
In this patient, histopathologic examination of a biopsy revealed a subepidermal blister with numerous eosinophils. Direct immunofluorescence study of perilesional skin showed strong linear IgG and C3 deposits at the basal membrane level. Serum level of autoantibody to BP180 antigen was elevated. Bacterial culture was positive for Staphylococcus aureus. These findings were suggestive of unilateral, localized BP with superimposed bacterial infection. Initial treatment with an extended course of doxycycline 200 mg twice daily, topical triamcinolone 0.1% ointment twice daily with compression therapy, and leg elevation led to clinical improvement with healing of previous lesions on the leg. At follow-up 3 weeks later, the patient had continued to develop new bullous lesions on the trunk and upper thighs. He was subsequently started on systemic immunosuppressive therapy for generalized bullous pemphigoid.
Importantly, localized BP generally follows a more benign disease course, although long-term follow-up is recommended for monitoring given the potential risk of developing the generalized form of BP of approximately 15%.3 Topical corticosteroids and oral antibiotics are recommended as the first-line therapy in these patients, with an escalated systemic therapy if needed for disease progression.3,5
Our case represents an important differential diagnosis to consider when evaluating an acute localized bullous eruption in an elderly patient.
Dr. Cusick and Dr. Dolohanty are with the department of dermatology, University of Rochester (N.Y.), and provided the case and photo. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Kohroh K et al. J Dermatol. 2007 Jul;34(7):482-5.
2. Nguyen T et al. Dermatology 2014;229(2):88-96.
3. Sen BB et al. Indian J Dermatol Venereol Leprol. 2013;79(4):554.
4. Salomon RJ et al. Arch Dermatol. 1987 Mar;123(3):389-92.
5. Tran JT, Mutasim DF. Int J Dermatol. 2005 Nov;44(11):942-5.
International medical graduates facing challenges amid COVID-19
International medical graduates (IMGs) constitute more than 24% of the total percentage of active physicians, 30% of active psychiatrists, and 33% of psychiatry residents in the United States.1 IMGs serve in various medical specialties and provide medical care to socioeconomically disadvantaged patients in underserved communities.2 Evidence suggests that patient outcomes among elderly patients admitted in U.S. hospitals for those treated by IMGs were on par with outcomes of U.S. graduates. Moreover, patients who were treated by IMGs had a lower mortality rates.3
IMGs trained in the United States make considerable contributions to psychiatry and have been very successful as educators, researchers, and leaders. Over the last 3 decades, for example, three American Psychiatric Association (APA) presidents and one past president of the American Academy of Child and Adolescent Psychiatry were IMGs. Many of them also hold department chair positions at many academic institutions.4,5
In short, IMGs are an important part of the U.S. health care system – particularly in psychiatry.
In addition to participating in psychiatry residency programs, IMG physicians are heavily represented in subspecialties, including geriatric psychiatry (45%), addiction psychiatry (42%), child and adolescent psychiatry (36%), psychosomatic medicine (32%), and forensic psychiatry (25%).6 IMG trainees face multiple challenges that begin as they transition to psychiatry residency in the United States, including understanding the American health care system, electronic medical records and documentation, and evidence-based medicine. In addition, they need to adapt to cultural changes, and work on language barriers, communication skills, and social isolation.7,8 Training programs account for these challenges and proactively take essential steps to facilitate the transition of IMGs into the U.S. system.9,10
As training programs prepare for the new academic year starting from July 2020 and continue to provide educational experiences to current trainees, the COVID-19 pandemic has brought additional challenges for the training programs. The gravity of the novel coronavirus pandemic continues to deepen, causing immense fear and uncertainty globally. An APA poll of more than 1,000 adults conducted early in the pandemic showed that about 40% of Americans were anxious about becoming seriously ill or dying with COVID-19. Nearly half of the respondents (48%) were anxious about the possibility of getting COVID-19, and even more (62%) were anxious about the possibility of their loved ones getting infected by this virus. Also, one-third of Americans reported a serious impact on their mental health.
Furthermore, the ailing economy and increasing unemployment are raising financial concerns for individuals and families. This pandemic also has had an impact on our patients’ sleep hygiene, relationships with their loved ones, and consumption of alcohol or other drugs/substances.11 Deteriorating mental health raises concerns about increased suicide risk as a secondary consequence.12
Physicians and other frontline teams who are taking care of these patients and their families continue to provide unexcelled, compassionate care in these unprecedented times. Selfless care continues despite awareness of the high probability of getting exposed to the virus and spreading it further to family members. Physicians involved in direct patient care for COVID-19 patients are at high risk for demoralization, burnout, depression, and anxiety.13
Struggles experienced by IMGs
On the personal front, IMGs often struggle with multiple stressors, such as lack of social support, ethnic-minority prejudice, and the need to understand financial structures such as mortgages in the new countries even after extended periods of residence.14 This virus has killed many health care professionals, including physicians around the world. There was a report of suicide by an emergency medicine physician who was treating patients with COVID-19 and ended up contracting the virus. That news was devastating and overwhelming for everyone, especially health care clinicians. It also adds to the stress and worries of IMGs who are still on nonimmigrant visas.
Bigger concerns exist if there is a demise of a nonimmigrant IMG and the implications of that loss for dependent families – who might face deportation. Even for those who were recently granted permanent residency status, worries about limited support systems and financial hardships to their families can be stressors.
Also, a large number of IMGs represent the geographical area where the pandemic began. Fortunately, the World Health Organization has taken a firm stance against possible discrimination by calling for global solidarity in these times. Furthermore, the WHO has emphasized the importance of referring to the disease caused by SARS-CoV-2 as “COVID-19” only – and not by the name of a particular country or city.15 Despite those official positions, people continue to express racially discriminatory opinions related to the virus, and those comments are not only disturbing to IMGs, they also are demoralizing.
Travel restrictions
In addition to the worries that IMGs might have about their own health and that of their families residing with them, the well-being of their extended families, including their aging parents back in their countries of origin, is unsettling as well. It is even more unnerving during the pandemic because the Centers for Disease Control and Prevention and the State Department advised avoiding all international travel at this time. Under these circumstances, IMGs are concerned about travel to their countries of origin in the event of a family emergency and the quarantine protocols in place, at both the country of origin and at residences.
Immigration issues
The U.S. administration temporarily suspended all immigration for 60 days, starting from April 2020. Recently, an executive order was signed suspending entry in the country on several visas, including the J-1 and the H1-B. Those are two categories that allow physicians to train and work in the United States.
IMGs in the United States reside and practice here under different types of immigrant and nonimmigrant visas (J-1, H1-B). This year, the Match results coincided with the timeline of those new immigration restrictions. Many IMGs are currently in the process of renewing their H1-B visas. They are worried because their visas will expire in the coming months. During the pandemic, U.S. Citizenship and Immigration Services suspended routine visa services and premium processing for visa renewals. This halt led to a delay in visa processing for graduating residents in June and practicing physicians seeking visa renewal. Those delays add to personal stress, and furthermore, distract these immigrant physicians from fighting this pandemic.
Another complication is that rules for J-1 visa holders have changed so that trainees must return to their countries of origin for at least 2 years after completing their training. If they decide to continue practicing medicine in the United States, they need a specific type of J-1 waiver and must gain a pathway to be a lawful permanent resident (Green Card). Many IMGs who are on waiver positions might not be able to treat patients ailing from COVID-19 to the full extent because waivers restrict them to practicing only in certain identified health systems.
IMGs who are coming from a country such India have to wait for more than 11 years after completing their accredited training to get permanent residency because of backlog for the permanent residency process.16 While waiting for a Green Card, they must continue to work on an H1-B visa, which requires periodic renewal.
Potential impact on training
Non-U.S. citizen IMGs accounted for 13% of the total of first-year positions in the 2020 Match. They will start medical training in residency programs in the United States in the coming months. The numbers for psychiatry residency matches are higher; about 16% of total first-year positions are filled by non-U.S. IMGs.17 At this time, when they should be celebrating their successful Match after many years of hard work and persistence, there is increased anxiety. They wonder whether they will be able to enter the United States to begin their training program on time. Their concerns are multifold, but the main concern is related to uncertainties around getting visas on time. With the recent executive order in place, physicians only working actively with COVID-19 patients will be able to enter the country on visas. As mental health concerns continue to rise during these times, incoming residents might not be able to start training if they are out of the country.
Furthermore, because of travel/air restrictions, there are worries about whether physicians will be able to get flights to the United States, given the lockdown in many countries around the world. Conversely, IMGs who will be graduating from residency and fellowship programs this summer and have accepted new positions also are dealing with similar uncertainty. Their new jobs will require visa processing, and the current scenario provides limited insight, so far, about whether they will be able to start their respective jobs or whether they will have to return to their home countries until their visa processing is completed.
The American Medical Association has advised the Secretary of State and acting Secretary of Homeland Security to expedite physician workforce expansion in an effort to meet the growing need for health care services during this pandemic.18 It is encouraging that, recently, the State Department declared that visa processing will continue for medical professionals and that cases would be expedited for those who meet the criteria. However, the requirement for in-person interviews remains for individuals who are seeking a U.S. visa outside the country.
As residency programs are trying their best to continue to provide educational experiences to trainees during this phase, if psychiatry residents are placed on quarantine because of either getting exposed or contracting the illness, there is a possibility that they might need to extend their training. This would bring another challenge for IMGs, requiring them to extend their visas to complete their training. Future J-1 waiver jobs could be compromised.
Investment in physician wellness critical
Psychiatrists, along with other health care workers, are front-line soldiers in the fight against COVID-19. All physicians are at high risk for demoralization, burnout, depression, anxiety, and suicide. It is of utmost importance that we invest immediately in physicians’ wellness. As noted, significant numbers of psychiatrists are IMGs who are dealing with additional challenges while responding to the pandemic. There are certain challenges for IMGs, such as the well-being of their extended families in other countries, and travel bans put in place because of the pandemic. Those issues are not easy to resolve. However, addressing visa issues and providing support to their families in the event that something happens to physicians during the pandemic would be reassuring and would help alleviate additional stress. Those kinds of actions also would allow immigrant physicians to focus on clinical work and to improve their overall well-being. Given the health risks and numerous other insecurities that go along with living amid a pandemic, IMGs should not have the additional pressure of visa uncertainty.
Public health crises such as COVID-19 are associated with increased rates of anxiety,19 depression,20 illicit substance use,21 and an increased rate of suicide.22 Patients with serious mental illness might be among the hardest hit both physically and mentally during the pandemic.23 Even in the absence of a pandemic, there is already a shortage of psychiatrists at the national level, and it is expected that this shortage will grow in the future. Rural and underserved areas are expected to experience the physician deficit more acutely.24
The pandemic is likely to resolve gradually and unpredictably – and might recur along the way over the next 1-2 years. However, the psychiatrist shortage will escalate more, as the mental health needs in the United States increase further in coming months. We need psychiatrists now more than ever, and it will be crucial that prospective residents, graduating residents, and fellows are able to come on board to join the American health care system promptly. In addition to national-level interventions, residency programs, potential employers, and communities must be aware of and do whatever they can to address the challenges faced by IMGs during these times.
Dr. Raman Baweja is affiliated with the department of psychiatry and behavioral health at Penn State University, Hershey. He has no conflicts of interest. Dr. Verma is affiliated with Rogers Behavioral Health in Kenosha County, Wis., and the department of psychiatry and behavioral health at Rosalind Franklin University of Medicine and Science in North Chicago. She has no conflicts of interest. Dr. Ritika Baweja is affiliated with the department of psychiatry and behavioral health at Penn State. Dr. Ritika Baweja is the spouse of Dr. Raman Baweja. Dr. Adam is affiliated with the department of psychiatry at the University of Missouri, Columbia.
References
1. American Psychiatric Association. Navigating psychiatry residency in the United States. A Guide for IMG Physicians.
2. Berg S. 5 IMG physicians who speak up for patients and fellow doctors. American Medical Association. 2019 Oct 22.
3. Tsugawa Y et al. BMJ. 2017 Feb 3;256. doi: 10.1136/bmj.j273.
4. Gogineni RR et al. Child Adolesc Psychiatr Clin N Am. 2010 Oct 1;19(4):833-53.
5. Majeed MH et al. Academic Psychiatry. 2017 Dec 1;41(6):849-51.
6. Brotherton SE and Etzel SI. JAMA. 2018 Sep 11;320(10):1051-70.
7. Sockalingam S et al. Acad Psychiatry. 2012 Jul 1;36(4):277-81.
8. Singareddy R et al. Acad Psychiatry. 2008 Jul-Aug;32(4):343-4.
9. Kramer MN. Acad Psychiatry. 2005 Jul-Aug;29(3):322-4.
10. Rao NR and Kotapati VP. Pathways for success in academic medicine for an international medical graduate: Challenges and opportunities. In “Roberts Academic Medicine Handbook” 2020. Springer:163-70.
11. American Psychiatric Association. New poll: COVID-19 impacting mental well-being: Americans feeling anxious, especially for loved ones; older adults are less anxious. 2020 Mar 25.
12. Reger MA et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
13. Lai J et al. JAMA Netw Open. 2020 Mar 23;3(3):e203976-e203976. doi: 10.1001/jamanetworkopen.2020.3976.
14. Kalra G et al. Acad Psychiatry. 2012 Jul;36(4):323-9.
15. WHO best practices for the naming of new human infectious diseases. World Health Organization. 2015.
16. U.S. Department of State. Bureau of Consular Affairs. Visa Bulletin for March 2020.
17. National Resident Matching Program® (NRMP®). Thousands of medical students and graduates celebrate NRMP Match results.
18. American Medical Association. AMA: U.S. should open visas to international physicians amid COVID-19. AMA press release. 2020 Mar 25.
19. McKay D et al. J Anxiety Disord. 2020 Jun;73:02233. doi: 10.1016/j.janxdis.2020.102233.
20. Tang W et al. J Affect Disord. 2020 May 13;274:1-7.
21. Collins F et al. NIH Director’s Blog. NIH.gov. 2020 Apr 21.
22. Reger M et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
23. Druss BG. JAMA Psychiatry. 2020 Apr 3. doi: 10.1001/jamapsychiatry.2020.0894.
24. American Association of Medical Colleges. “The complexities of physician supply and demand: Projections from 2018-2033.” 2020 Jun.
International medical graduates (IMGs) constitute more than 24% of the total percentage of active physicians, 30% of active psychiatrists, and 33% of psychiatry residents in the United States.1 IMGs serve in various medical specialties and provide medical care to socioeconomically disadvantaged patients in underserved communities.2 Evidence suggests that patient outcomes among elderly patients admitted in U.S. hospitals for those treated by IMGs were on par with outcomes of U.S. graduates. Moreover, patients who were treated by IMGs had a lower mortality rates.3
IMGs trained in the United States make considerable contributions to psychiatry and have been very successful as educators, researchers, and leaders. Over the last 3 decades, for example, three American Psychiatric Association (APA) presidents and one past president of the American Academy of Child and Adolescent Psychiatry were IMGs. Many of them also hold department chair positions at many academic institutions.4,5
In short, IMGs are an important part of the U.S. health care system – particularly in psychiatry.
In addition to participating in psychiatry residency programs, IMG physicians are heavily represented in subspecialties, including geriatric psychiatry (45%), addiction psychiatry (42%), child and adolescent psychiatry (36%), psychosomatic medicine (32%), and forensic psychiatry (25%).6 IMG trainees face multiple challenges that begin as they transition to psychiatry residency in the United States, including understanding the American health care system, electronic medical records and documentation, and evidence-based medicine. In addition, they need to adapt to cultural changes, and work on language barriers, communication skills, and social isolation.7,8 Training programs account for these challenges and proactively take essential steps to facilitate the transition of IMGs into the U.S. system.9,10
As training programs prepare for the new academic year starting from July 2020 and continue to provide educational experiences to current trainees, the COVID-19 pandemic has brought additional challenges for the training programs. The gravity of the novel coronavirus pandemic continues to deepen, causing immense fear and uncertainty globally. An APA poll of more than 1,000 adults conducted early in the pandemic showed that about 40% of Americans were anxious about becoming seriously ill or dying with COVID-19. Nearly half of the respondents (48%) were anxious about the possibility of getting COVID-19, and even more (62%) were anxious about the possibility of their loved ones getting infected by this virus. Also, one-third of Americans reported a serious impact on their mental health.
Furthermore, the ailing economy and increasing unemployment are raising financial concerns for individuals and families. This pandemic also has had an impact on our patients’ sleep hygiene, relationships with their loved ones, and consumption of alcohol or other drugs/substances.11 Deteriorating mental health raises concerns about increased suicide risk as a secondary consequence.12
Physicians and other frontline teams who are taking care of these patients and their families continue to provide unexcelled, compassionate care in these unprecedented times. Selfless care continues despite awareness of the high probability of getting exposed to the virus and spreading it further to family members. Physicians involved in direct patient care for COVID-19 patients are at high risk for demoralization, burnout, depression, and anxiety.13
Struggles experienced by IMGs
On the personal front, IMGs often struggle with multiple stressors, such as lack of social support, ethnic-minority prejudice, and the need to understand financial structures such as mortgages in the new countries even after extended periods of residence.14 This virus has killed many health care professionals, including physicians around the world. There was a report of suicide by an emergency medicine physician who was treating patients with COVID-19 and ended up contracting the virus. That news was devastating and overwhelming for everyone, especially health care clinicians. It also adds to the stress and worries of IMGs who are still on nonimmigrant visas.
Bigger concerns exist if there is a demise of a nonimmigrant IMG and the implications of that loss for dependent families – who might face deportation. Even for those who were recently granted permanent residency status, worries about limited support systems and financial hardships to their families can be stressors.
Also, a large number of IMGs represent the geographical area where the pandemic began. Fortunately, the World Health Organization has taken a firm stance against possible discrimination by calling for global solidarity in these times. Furthermore, the WHO has emphasized the importance of referring to the disease caused by SARS-CoV-2 as “COVID-19” only – and not by the name of a particular country or city.15 Despite those official positions, people continue to express racially discriminatory opinions related to the virus, and those comments are not only disturbing to IMGs, they also are demoralizing.
Travel restrictions
In addition to the worries that IMGs might have about their own health and that of their families residing with them, the well-being of their extended families, including their aging parents back in their countries of origin, is unsettling as well. It is even more unnerving during the pandemic because the Centers for Disease Control and Prevention and the State Department advised avoiding all international travel at this time. Under these circumstances, IMGs are concerned about travel to their countries of origin in the event of a family emergency and the quarantine protocols in place, at both the country of origin and at residences.
Immigration issues
The U.S. administration temporarily suspended all immigration for 60 days, starting from April 2020. Recently, an executive order was signed suspending entry in the country on several visas, including the J-1 and the H1-B. Those are two categories that allow physicians to train and work in the United States.
IMGs in the United States reside and practice here under different types of immigrant and nonimmigrant visas (J-1, H1-B). This year, the Match results coincided with the timeline of those new immigration restrictions. Many IMGs are currently in the process of renewing their H1-B visas. They are worried because their visas will expire in the coming months. During the pandemic, U.S. Citizenship and Immigration Services suspended routine visa services and premium processing for visa renewals. This halt led to a delay in visa processing for graduating residents in June and practicing physicians seeking visa renewal. Those delays add to personal stress, and furthermore, distract these immigrant physicians from fighting this pandemic.
Another complication is that rules for J-1 visa holders have changed so that trainees must return to their countries of origin for at least 2 years after completing their training. If they decide to continue practicing medicine in the United States, they need a specific type of J-1 waiver and must gain a pathway to be a lawful permanent resident (Green Card). Many IMGs who are on waiver positions might not be able to treat patients ailing from COVID-19 to the full extent because waivers restrict them to practicing only in certain identified health systems.
IMGs who are coming from a country such India have to wait for more than 11 years after completing their accredited training to get permanent residency because of backlog for the permanent residency process.16 While waiting for a Green Card, they must continue to work on an H1-B visa, which requires periodic renewal.
Potential impact on training
Non-U.S. citizen IMGs accounted for 13% of the total of first-year positions in the 2020 Match. They will start medical training in residency programs in the United States in the coming months. The numbers for psychiatry residency matches are higher; about 16% of total first-year positions are filled by non-U.S. IMGs.17 At this time, when they should be celebrating their successful Match after many years of hard work and persistence, there is increased anxiety. They wonder whether they will be able to enter the United States to begin their training program on time. Their concerns are multifold, but the main concern is related to uncertainties around getting visas on time. With the recent executive order in place, physicians only working actively with COVID-19 patients will be able to enter the country on visas. As mental health concerns continue to rise during these times, incoming residents might not be able to start training if they are out of the country.
Furthermore, because of travel/air restrictions, there are worries about whether physicians will be able to get flights to the United States, given the lockdown in many countries around the world. Conversely, IMGs who will be graduating from residency and fellowship programs this summer and have accepted new positions also are dealing with similar uncertainty. Their new jobs will require visa processing, and the current scenario provides limited insight, so far, about whether they will be able to start their respective jobs or whether they will have to return to their home countries until their visa processing is completed.
The American Medical Association has advised the Secretary of State and acting Secretary of Homeland Security to expedite physician workforce expansion in an effort to meet the growing need for health care services during this pandemic.18 It is encouraging that, recently, the State Department declared that visa processing will continue for medical professionals and that cases would be expedited for those who meet the criteria. However, the requirement for in-person interviews remains for individuals who are seeking a U.S. visa outside the country.
As residency programs are trying their best to continue to provide educational experiences to trainees during this phase, if psychiatry residents are placed on quarantine because of either getting exposed or contracting the illness, there is a possibility that they might need to extend their training. This would bring another challenge for IMGs, requiring them to extend their visas to complete their training. Future J-1 waiver jobs could be compromised.
Investment in physician wellness critical
Psychiatrists, along with other health care workers, are front-line soldiers in the fight against COVID-19. All physicians are at high risk for demoralization, burnout, depression, anxiety, and suicide. It is of utmost importance that we invest immediately in physicians’ wellness. As noted, significant numbers of psychiatrists are IMGs who are dealing with additional challenges while responding to the pandemic. There are certain challenges for IMGs, such as the well-being of their extended families in other countries, and travel bans put in place because of the pandemic. Those issues are not easy to resolve. However, addressing visa issues and providing support to their families in the event that something happens to physicians during the pandemic would be reassuring and would help alleviate additional stress. Those kinds of actions also would allow immigrant physicians to focus on clinical work and to improve their overall well-being. Given the health risks and numerous other insecurities that go along with living amid a pandemic, IMGs should not have the additional pressure of visa uncertainty.
Public health crises such as COVID-19 are associated with increased rates of anxiety,19 depression,20 illicit substance use,21 and an increased rate of suicide.22 Patients with serious mental illness might be among the hardest hit both physically and mentally during the pandemic.23 Even in the absence of a pandemic, there is already a shortage of psychiatrists at the national level, and it is expected that this shortage will grow in the future. Rural and underserved areas are expected to experience the physician deficit more acutely.24
The pandemic is likely to resolve gradually and unpredictably – and might recur along the way over the next 1-2 years. However, the psychiatrist shortage will escalate more, as the mental health needs in the United States increase further in coming months. We need psychiatrists now more than ever, and it will be crucial that prospective residents, graduating residents, and fellows are able to come on board to join the American health care system promptly. In addition to national-level interventions, residency programs, potential employers, and communities must be aware of and do whatever they can to address the challenges faced by IMGs during these times.
Dr. Raman Baweja is affiliated with the department of psychiatry and behavioral health at Penn State University, Hershey. He has no conflicts of interest. Dr. Verma is affiliated with Rogers Behavioral Health in Kenosha County, Wis., and the department of psychiatry and behavioral health at Rosalind Franklin University of Medicine and Science in North Chicago. She has no conflicts of interest. Dr. Ritika Baweja is affiliated with the department of psychiatry and behavioral health at Penn State. Dr. Ritika Baweja is the spouse of Dr. Raman Baweja. Dr. Adam is affiliated with the department of psychiatry at the University of Missouri, Columbia.
References
1. American Psychiatric Association. Navigating psychiatry residency in the United States. A Guide for IMG Physicians.
2. Berg S. 5 IMG physicians who speak up for patients and fellow doctors. American Medical Association. 2019 Oct 22.
3. Tsugawa Y et al. BMJ. 2017 Feb 3;256. doi: 10.1136/bmj.j273.
4. Gogineni RR et al. Child Adolesc Psychiatr Clin N Am. 2010 Oct 1;19(4):833-53.
5. Majeed MH et al. Academic Psychiatry. 2017 Dec 1;41(6):849-51.
6. Brotherton SE and Etzel SI. JAMA. 2018 Sep 11;320(10):1051-70.
7. Sockalingam S et al. Acad Psychiatry. 2012 Jul 1;36(4):277-81.
8. Singareddy R et al. Acad Psychiatry. 2008 Jul-Aug;32(4):343-4.
9. Kramer MN. Acad Psychiatry. 2005 Jul-Aug;29(3):322-4.
10. Rao NR and Kotapati VP. Pathways for success in academic medicine for an international medical graduate: Challenges and opportunities. In “Roberts Academic Medicine Handbook” 2020. Springer:163-70.
11. American Psychiatric Association. New poll: COVID-19 impacting mental well-being: Americans feeling anxious, especially for loved ones; older adults are less anxious. 2020 Mar 25.
12. Reger MA et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
13. Lai J et al. JAMA Netw Open. 2020 Mar 23;3(3):e203976-e203976. doi: 10.1001/jamanetworkopen.2020.3976.
14. Kalra G et al. Acad Psychiatry. 2012 Jul;36(4):323-9.
15. WHO best practices for the naming of new human infectious diseases. World Health Organization. 2015.
16. U.S. Department of State. Bureau of Consular Affairs. Visa Bulletin for March 2020.
17. National Resident Matching Program® (NRMP®). Thousands of medical students and graduates celebrate NRMP Match results.
18. American Medical Association. AMA: U.S. should open visas to international physicians amid COVID-19. AMA press release. 2020 Mar 25.
19. McKay D et al. J Anxiety Disord. 2020 Jun;73:02233. doi: 10.1016/j.janxdis.2020.102233.
20. Tang W et al. J Affect Disord. 2020 May 13;274:1-7.
21. Collins F et al. NIH Director’s Blog. NIH.gov. 2020 Apr 21.
22. Reger M et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
23. Druss BG. JAMA Psychiatry. 2020 Apr 3. doi: 10.1001/jamapsychiatry.2020.0894.
24. American Association of Medical Colleges. “The complexities of physician supply and demand: Projections from 2018-2033.” 2020 Jun.
International medical graduates (IMGs) constitute more than 24% of the total percentage of active physicians, 30% of active psychiatrists, and 33% of psychiatry residents in the United States.1 IMGs serve in various medical specialties and provide medical care to socioeconomically disadvantaged patients in underserved communities.2 Evidence suggests that patient outcomes among elderly patients admitted in U.S. hospitals for those treated by IMGs were on par with outcomes of U.S. graduates. Moreover, patients who were treated by IMGs had a lower mortality rates.3
IMGs trained in the United States make considerable contributions to psychiatry and have been very successful as educators, researchers, and leaders. Over the last 3 decades, for example, three American Psychiatric Association (APA) presidents and one past president of the American Academy of Child and Adolescent Psychiatry were IMGs. Many of them also hold department chair positions at many academic institutions.4,5
In short, IMGs are an important part of the U.S. health care system – particularly in psychiatry.
In addition to participating in psychiatry residency programs, IMG physicians are heavily represented in subspecialties, including geriatric psychiatry (45%), addiction psychiatry (42%), child and adolescent psychiatry (36%), psychosomatic medicine (32%), and forensic psychiatry (25%).6 IMG trainees face multiple challenges that begin as they transition to psychiatry residency in the United States, including understanding the American health care system, electronic medical records and documentation, and evidence-based medicine. In addition, they need to adapt to cultural changes, and work on language barriers, communication skills, and social isolation.7,8 Training programs account for these challenges and proactively take essential steps to facilitate the transition of IMGs into the U.S. system.9,10
As training programs prepare for the new academic year starting from July 2020 and continue to provide educational experiences to current trainees, the COVID-19 pandemic has brought additional challenges for the training programs. The gravity of the novel coronavirus pandemic continues to deepen, causing immense fear and uncertainty globally. An APA poll of more than 1,000 adults conducted early in the pandemic showed that about 40% of Americans were anxious about becoming seriously ill or dying with COVID-19. Nearly half of the respondents (48%) were anxious about the possibility of getting COVID-19, and even more (62%) were anxious about the possibility of their loved ones getting infected by this virus. Also, one-third of Americans reported a serious impact on their mental health.
Furthermore, the ailing economy and increasing unemployment are raising financial concerns for individuals and families. This pandemic also has had an impact on our patients’ sleep hygiene, relationships with their loved ones, and consumption of alcohol or other drugs/substances.11 Deteriorating mental health raises concerns about increased suicide risk as a secondary consequence.12
Physicians and other frontline teams who are taking care of these patients and their families continue to provide unexcelled, compassionate care in these unprecedented times. Selfless care continues despite awareness of the high probability of getting exposed to the virus and spreading it further to family members. Physicians involved in direct patient care for COVID-19 patients are at high risk for demoralization, burnout, depression, and anxiety.13
Struggles experienced by IMGs
On the personal front, IMGs often struggle with multiple stressors, such as lack of social support, ethnic-minority prejudice, and the need to understand financial structures such as mortgages in the new countries even after extended periods of residence.14 This virus has killed many health care professionals, including physicians around the world. There was a report of suicide by an emergency medicine physician who was treating patients with COVID-19 and ended up contracting the virus. That news was devastating and overwhelming for everyone, especially health care clinicians. It also adds to the stress and worries of IMGs who are still on nonimmigrant visas.
Bigger concerns exist if there is a demise of a nonimmigrant IMG and the implications of that loss for dependent families – who might face deportation. Even for those who were recently granted permanent residency status, worries about limited support systems and financial hardships to their families can be stressors.
Also, a large number of IMGs represent the geographical area where the pandemic began. Fortunately, the World Health Organization has taken a firm stance against possible discrimination by calling for global solidarity in these times. Furthermore, the WHO has emphasized the importance of referring to the disease caused by SARS-CoV-2 as “COVID-19” only – and not by the name of a particular country or city.15 Despite those official positions, people continue to express racially discriminatory opinions related to the virus, and those comments are not only disturbing to IMGs, they also are demoralizing.
Travel restrictions
In addition to the worries that IMGs might have about their own health and that of their families residing with them, the well-being of their extended families, including their aging parents back in their countries of origin, is unsettling as well. It is even more unnerving during the pandemic because the Centers for Disease Control and Prevention and the State Department advised avoiding all international travel at this time. Under these circumstances, IMGs are concerned about travel to their countries of origin in the event of a family emergency and the quarantine protocols in place, at both the country of origin and at residences.
Immigration issues
The U.S. administration temporarily suspended all immigration for 60 days, starting from April 2020. Recently, an executive order was signed suspending entry in the country on several visas, including the J-1 and the H1-B. Those are two categories that allow physicians to train and work in the United States.
IMGs in the United States reside and practice here under different types of immigrant and nonimmigrant visas (J-1, H1-B). This year, the Match results coincided with the timeline of those new immigration restrictions. Many IMGs are currently in the process of renewing their H1-B visas. They are worried because their visas will expire in the coming months. During the pandemic, U.S. Citizenship and Immigration Services suspended routine visa services and premium processing for visa renewals. This halt led to a delay in visa processing for graduating residents in June and practicing physicians seeking visa renewal. Those delays add to personal stress, and furthermore, distract these immigrant physicians from fighting this pandemic.
Another complication is that rules for J-1 visa holders have changed so that trainees must return to their countries of origin for at least 2 years after completing their training. If they decide to continue practicing medicine in the United States, they need a specific type of J-1 waiver and must gain a pathway to be a lawful permanent resident (Green Card). Many IMGs who are on waiver positions might not be able to treat patients ailing from COVID-19 to the full extent because waivers restrict them to practicing only in certain identified health systems.
IMGs who are coming from a country such India have to wait for more than 11 years after completing their accredited training to get permanent residency because of backlog for the permanent residency process.16 While waiting for a Green Card, they must continue to work on an H1-B visa, which requires periodic renewal.
Potential impact on training
Non-U.S. citizen IMGs accounted for 13% of the total of first-year positions in the 2020 Match. They will start medical training in residency programs in the United States in the coming months. The numbers for psychiatry residency matches are higher; about 16% of total first-year positions are filled by non-U.S. IMGs.17 At this time, when they should be celebrating their successful Match after many years of hard work and persistence, there is increased anxiety. They wonder whether they will be able to enter the United States to begin their training program on time. Their concerns are multifold, but the main concern is related to uncertainties around getting visas on time. With the recent executive order in place, physicians only working actively with COVID-19 patients will be able to enter the country on visas. As mental health concerns continue to rise during these times, incoming residents might not be able to start training if they are out of the country.
Furthermore, because of travel/air restrictions, there are worries about whether physicians will be able to get flights to the United States, given the lockdown in many countries around the world. Conversely, IMGs who will be graduating from residency and fellowship programs this summer and have accepted new positions also are dealing with similar uncertainty. Their new jobs will require visa processing, and the current scenario provides limited insight, so far, about whether they will be able to start their respective jobs or whether they will have to return to their home countries until their visa processing is completed.
The American Medical Association has advised the Secretary of State and acting Secretary of Homeland Security to expedite physician workforce expansion in an effort to meet the growing need for health care services during this pandemic.18 It is encouraging that, recently, the State Department declared that visa processing will continue for medical professionals and that cases would be expedited for those who meet the criteria. However, the requirement for in-person interviews remains for individuals who are seeking a U.S. visa outside the country.
As residency programs are trying their best to continue to provide educational experiences to trainees during this phase, if psychiatry residents are placed on quarantine because of either getting exposed or contracting the illness, there is a possibility that they might need to extend their training. This would bring another challenge for IMGs, requiring them to extend their visas to complete their training. Future J-1 waiver jobs could be compromised.
Investment in physician wellness critical
Psychiatrists, along with other health care workers, are front-line soldiers in the fight against COVID-19. All physicians are at high risk for demoralization, burnout, depression, anxiety, and suicide. It is of utmost importance that we invest immediately in physicians’ wellness. As noted, significant numbers of psychiatrists are IMGs who are dealing with additional challenges while responding to the pandemic. There are certain challenges for IMGs, such as the well-being of their extended families in other countries, and travel bans put in place because of the pandemic. Those issues are not easy to resolve. However, addressing visa issues and providing support to their families in the event that something happens to physicians during the pandemic would be reassuring and would help alleviate additional stress. Those kinds of actions also would allow immigrant physicians to focus on clinical work and to improve their overall well-being. Given the health risks and numerous other insecurities that go along with living amid a pandemic, IMGs should not have the additional pressure of visa uncertainty.
Public health crises such as COVID-19 are associated with increased rates of anxiety,19 depression,20 illicit substance use,21 and an increased rate of suicide.22 Patients with serious mental illness might be among the hardest hit both physically and mentally during the pandemic.23 Even in the absence of a pandemic, there is already a shortage of psychiatrists at the national level, and it is expected that this shortage will grow in the future. Rural and underserved areas are expected to experience the physician deficit more acutely.24
The pandemic is likely to resolve gradually and unpredictably – and might recur along the way over the next 1-2 years. However, the psychiatrist shortage will escalate more, as the mental health needs in the United States increase further in coming months. We need psychiatrists now more than ever, and it will be crucial that prospective residents, graduating residents, and fellows are able to come on board to join the American health care system promptly. In addition to national-level interventions, residency programs, potential employers, and communities must be aware of and do whatever they can to address the challenges faced by IMGs during these times.
Dr. Raman Baweja is affiliated with the department of psychiatry and behavioral health at Penn State University, Hershey. He has no conflicts of interest. Dr. Verma is affiliated with Rogers Behavioral Health in Kenosha County, Wis., and the department of psychiatry and behavioral health at Rosalind Franklin University of Medicine and Science in North Chicago. She has no conflicts of interest. Dr. Ritika Baweja is affiliated with the department of psychiatry and behavioral health at Penn State. Dr. Ritika Baweja is the spouse of Dr. Raman Baweja. Dr. Adam is affiliated with the department of psychiatry at the University of Missouri, Columbia.
References
1. American Psychiatric Association. Navigating psychiatry residency in the United States. A Guide for IMG Physicians.
2. Berg S. 5 IMG physicians who speak up for patients and fellow doctors. American Medical Association. 2019 Oct 22.
3. Tsugawa Y et al. BMJ. 2017 Feb 3;256. doi: 10.1136/bmj.j273.
4. Gogineni RR et al. Child Adolesc Psychiatr Clin N Am. 2010 Oct 1;19(4):833-53.
5. Majeed MH et al. Academic Psychiatry. 2017 Dec 1;41(6):849-51.
6. Brotherton SE and Etzel SI. JAMA. 2018 Sep 11;320(10):1051-70.
7. Sockalingam S et al. Acad Psychiatry. 2012 Jul 1;36(4):277-81.
8. Singareddy R et al. Acad Psychiatry. 2008 Jul-Aug;32(4):343-4.
9. Kramer MN. Acad Psychiatry. 2005 Jul-Aug;29(3):322-4.
10. Rao NR and Kotapati VP. Pathways for success in academic medicine for an international medical graduate: Challenges and opportunities. In “Roberts Academic Medicine Handbook” 2020. Springer:163-70.
11. American Psychiatric Association. New poll: COVID-19 impacting mental well-being: Americans feeling anxious, especially for loved ones; older adults are less anxious. 2020 Mar 25.
12. Reger MA et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
13. Lai J et al. JAMA Netw Open. 2020 Mar 23;3(3):e203976-e203976. doi: 10.1001/jamanetworkopen.2020.3976.
14. Kalra G et al. Acad Psychiatry. 2012 Jul;36(4):323-9.
15. WHO best practices for the naming of new human infectious diseases. World Health Organization. 2015.
16. U.S. Department of State. Bureau of Consular Affairs. Visa Bulletin for March 2020.
17. National Resident Matching Program® (NRMP®). Thousands of medical students and graduates celebrate NRMP Match results.
18. American Medical Association. AMA: U.S. should open visas to international physicians amid COVID-19. AMA press release. 2020 Mar 25.
19. McKay D et al. J Anxiety Disord. 2020 Jun;73:02233. doi: 10.1016/j.janxdis.2020.102233.
20. Tang W et al. J Affect Disord. 2020 May 13;274:1-7.
21. Collins F et al. NIH Director’s Blog. NIH.gov. 2020 Apr 21.
22. Reger M et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
23. Druss BG. JAMA Psychiatry. 2020 Apr 3. doi: 10.1001/jamapsychiatry.2020.0894.
24. American Association of Medical Colleges. “The complexities of physician supply and demand: Projections from 2018-2033.” 2020 Jun.
Family environment important in early psychosis outcomes
Family environment may influence subsequent functional outcomes in patients with first-episode psychosis, new research suggests.
A study of more than 300 patients with first-episode psychosis (FEP) showed that although family environment was not associated with functioning at initial presentation, an interaction developed over time that could have “important implications for early interventions for both patients and caregivers,” investigators reported.
study coinvestigator Norma Verdolini, MD, PhD, bipolar and depressive disorders unit, hospital Clinic Barcelona, University of Barcelona, said in an interview.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
FAST measures
Previous research has shown that family environment influences the development of psychotic symptoms, with negative family environmental factors associated with poor prognoses.
Conversely, one study indicated that a positive family environment is linked to greater improvement in negative and disorganized symptoms in adolescents at imminent risk for psychosis onset.
However, the current investigators noted that the impact of family environment on longitudinal functioning in individuals presenting with FEP is unclear.
To investigate further, they conducted an analysis as part of the PEPs study, which included 335 patients with FEP and 253 healthy controls. Functioning was measured using the Functional Assessment Short Test (FAST), and family environmental styles were evaluated using the Family Environment Scale (FES), which assesses “emotional climate” of a family across 10 domains.
At baseline, the mean total FAST score was 27.8 in patients with FEP versus 3.5 in the healthy controls, indicating substantially worse functioning among the patients. Linear regression analysis indicated that at baseline there was no significant association between aspects of family environment on the FES and functional scores.
Patients were assessed again at 2 years, by which point 283 had been diagnosed with psychotic disorders and 52 with bipolar disorder. The mean total FAST scores were 20.98 among patients with psychotic disorders and 13.8 in those with bipolar disorder.
Family conflict
Results showed that, among those with bipolar disorder, worse functioning on FAST at 2 years was significantly associated with higher rates of open expression of conflict in the family (P = .004).
In patients with psychotic disorders, worse functioning was significantly associated with lower rates of participation in social activities (P = .006) and an achievement-oriented family environment (P = .039). Worse functioning in patients with psychotic disorders was also significantly associated with higher rates of religious practice and values (P = .003).
Dr. Verdolini noted the reason family environment does not appear to have an impact at initial FEP presentation may be that the “first kick” is given by an individual’s genetic liability for psychiatric disorders in combination with the family environment. In reality, the two are intertwined, especially when considering what it means to a family to have one member with a psychiatric disorder, which “will have an impact on the family environment.”
Dr. Verdolini added: “This is not actually the objective family environment,” but the perceived family environment.
“So maybe in the following 2 years the patient who experiences a first episode of psychosis may change their idea of the family environment itself,” she noted. She added that at her institution psychoeducation is offered to FEP patients’ families.
‘Interesting’ findings
Commenting on the study, Nicole Kozloff, MD, from the child, youth, and emerging adult program at the Centre for Addiction and Mental Health in Toronto, said one limitation of the study is that it’s not clear what care patients received – or who in the family completed the FES.
It is also important to note that “measures of association do not necessarily imply that one factor caused the other factor,” said Dr. Kozloff, who was not involved in the research. “For example, it may be that, among people with bipolar disorder, open expression of conflict in the family can lead to worse functioning, or that worse functioning can lead to more conflict in the family.”
Nevertheless, Dr. Kozloff described the finding of an emerging association between the family environment and functioning over time as “interesting.”
When young people with FEP enter treatment, “they have reached a crisis point and are functioning poorly,” she noted.
“It could be that there is less to differentiate among levels of functioning at treatment entry but, after 2 years, the individuals have separated into those who have been responsive to treatment and are functioning well, and those who continue to have functional challenges. And this is where we start to see a relationship with family environment emerge,” Dr. Kozloff said.
She also agreed with Dr. Verdolini’s take on the findings, and that family psychoeducation “can reduce relapse rates in schizophrenia and the emotional burden on the family.”
“We also know that having family involvement in care is one of the most robust predictors that young people with psychosis will remain engaged in mental health services,” she said.
Teaching families about psychosis and its treatment, about problem-solving and communication skills, and providing support to ensure that family members know how to get help in a crisis, “is a key part of comprehensive early psychosis intervention,” Dr. Kozloff said. “It is good for the patient and good for the family, and allows the clinicians to provide better care.”
Articulates clinical practice findings
Also commenting on the results, Brian O’Donoghue, MD, PhD, senior clinical research fellow at Orygen, the National Centre of Excellence in Youth Mental Health in Melbourne, described the research as important, adding that the study highlights the need for sufficient follow-up.
“It makes sense that the involvement of family over time has a strong impact upon outcome and functioning,” he said in an interview.
“These research findings articulate what we see in clinical practice, so it is good to see that it is captured,” added Dr. O’Donoghue, who was not associated with the study.
He noted that it is common for family involvement to influence outcome, especially if the family is positively involved. “It is invaluable toward their recovery. However, conversely, if there are ongoing family stressors, then this can be a trigger for relapse or lack of improvement.”
Overall, the results “really emphasize that the family needs to be involved in care.”
The Early Psychosis Prevention and Intervention Centre where Dr. O’Donoghue is a consultant psychiatrist offers a psychoeducational course “to inform families about psychosis, treatment, and how they can support their family members.”
“We also have family peer support workers and family therapists, which are essential to the service and for the young person’s recovery,” Dr. O’Donoghue said.
The investigators and Dr. O’Donoghue disclosed no relevant financial relationships. Dr. Kozloff reported receiving research funding from the CAMH Foundation, Brain & Behavior Research Foundation, Canadian Institutes of Health Research, and AFP Innovation Fund; honoraria from Humber River Hospital, the University of Calgary (Alta.), and the Canadian Consortium for Early Intervention in Psychosis; and salary support from Inner City Health Associates.
A version of this article originally appeared on Medscape.com.
Family environment may influence subsequent functional outcomes in patients with first-episode psychosis, new research suggests.
A study of more than 300 patients with first-episode psychosis (FEP) showed that although family environment was not associated with functioning at initial presentation, an interaction developed over time that could have “important implications for early interventions for both patients and caregivers,” investigators reported.
study coinvestigator Norma Verdolini, MD, PhD, bipolar and depressive disorders unit, hospital Clinic Barcelona, University of Barcelona, said in an interview.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
FAST measures
Previous research has shown that family environment influences the development of psychotic symptoms, with negative family environmental factors associated with poor prognoses.
Conversely, one study indicated that a positive family environment is linked to greater improvement in negative and disorganized symptoms in adolescents at imminent risk for psychosis onset.
However, the current investigators noted that the impact of family environment on longitudinal functioning in individuals presenting with FEP is unclear.
To investigate further, they conducted an analysis as part of the PEPs study, which included 335 patients with FEP and 253 healthy controls. Functioning was measured using the Functional Assessment Short Test (FAST), and family environmental styles were evaluated using the Family Environment Scale (FES), which assesses “emotional climate” of a family across 10 domains.
At baseline, the mean total FAST score was 27.8 in patients with FEP versus 3.5 in the healthy controls, indicating substantially worse functioning among the patients. Linear regression analysis indicated that at baseline there was no significant association between aspects of family environment on the FES and functional scores.
Patients were assessed again at 2 years, by which point 283 had been diagnosed with psychotic disorders and 52 with bipolar disorder. The mean total FAST scores were 20.98 among patients with psychotic disorders and 13.8 in those with bipolar disorder.
Family conflict
Results showed that, among those with bipolar disorder, worse functioning on FAST at 2 years was significantly associated with higher rates of open expression of conflict in the family (P = .004).
In patients with psychotic disorders, worse functioning was significantly associated with lower rates of participation in social activities (P = .006) and an achievement-oriented family environment (P = .039). Worse functioning in patients with psychotic disorders was also significantly associated with higher rates of religious practice and values (P = .003).
Dr. Verdolini noted the reason family environment does not appear to have an impact at initial FEP presentation may be that the “first kick” is given by an individual’s genetic liability for psychiatric disorders in combination with the family environment. In reality, the two are intertwined, especially when considering what it means to a family to have one member with a psychiatric disorder, which “will have an impact on the family environment.”
Dr. Verdolini added: “This is not actually the objective family environment,” but the perceived family environment.
“So maybe in the following 2 years the patient who experiences a first episode of psychosis may change their idea of the family environment itself,” she noted. She added that at her institution psychoeducation is offered to FEP patients’ families.
‘Interesting’ findings
Commenting on the study, Nicole Kozloff, MD, from the child, youth, and emerging adult program at the Centre for Addiction and Mental Health in Toronto, said one limitation of the study is that it’s not clear what care patients received – or who in the family completed the FES.
It is also important to note that “measures of association do not necessarily imply that one factor caused the other factor,” said Dr. Kozloff, who was not involved in the research. “For example, it may be that, among people with bipolar disorder, open expression of conflict in the family can lead to worse functioning, or that worse functioning can lead to more conflict in the family.”
Nevertheless, Dr. Kozloff described the finding of an emerging association between the family environment and functioning over time as “interesting.”
When young people with FEP enter treatment, “they have reached a crisis point and are functioning poorly,” she noted.
“It could be that there is less to differentiate among levels of functioning at treatment entry but, after 2 years, the individuals have separated into those who have been responsive to treatment and are functioning well, and those who continue to have functional challenges. And this is where we start to see a relationship with family environment emerge,” Dr. Kozloff said.
She also agreed with Dr. Verdolini’s take on the findings, and that family psychoeducation “can reduce relapse rates in schizophrenia and the emotional burden on the family.”
“We also know that having family involvement in care is one of the most robust predictors that young people with psychosis will remain engaged in mental health services,” she said.
Teaching families about psychosis and its treatment, about problem-solving and communication skills, and providing support to ensure that family members know how to get help in a crisis, “is a key part of comprehensive early psychosis intervention,” Dr. Kozloff said. “It is good for the patient and good for the family, and allows the clinicians to provide better care.”
Articulates clinical practice findings
Also commenting on the results, Brian O’Donoghue, MD, PhD, senior clinical research fellow at Orygen, the National Centre of Excellence in Youth Mental Health in Melbourne, described the research as important, adding that the study highlights the need for sufficient follow-up.
“It makes sense that the involvement of family over time has a strong impact upon outcome and functioning,” he said in an interview.
“These research findings articulate what we see in clinical practice, so it is good to see that it is captured,” added Dr. O’Donoghue, who was not associated with the study.
He noted that it is common for family involvement to influence outcome, especially if the family is positively involved. “It is invaluable toward their recovery. However, conversely, if there are ongoing family stressors, then this can be a trigger for relapse or lack of improvement.”
Overall, the results “really emphasize that the family needs to be involved in care.”
The Early Psychosis Prevention and Intervention Centre where Dr. O’Donoghue is a consultant psychiatrist offers a psychoeducational course “to inform families about psychosis, treatment, and how they can support their family members.”
“We also have family peer support workers and family therapists, which are essential to the service and for the young person’s recovery,” Dr. O’Donoghue said.
The investigators and Dr. O’Donoghue disclosed no relevant financial relationships. Dr. Kozloff reported receiving research funding from the CAMH Foundation, Brain & Behavior Research Foundation, Canadian Institutes of Health Research, and AFP Innovation Fund; honoraria from Humber River Hospital, the University of Calgary (Alta.), and the Canadian Consortium for Early Intervention in Psychosis; and salary support from Inner City Health Associates.
A version of this article originally appeared on Medscape.com.
Family environment may influence subsequent functional outcomes in patients with first-episode psychosis, new research suggests.
A study of more than 300 patients with first-episode psychosis (FEP) showed that although family environment was not associated with functioning at initial presentation, an interaction developed over time that could have “important implications for early interventions for both patients and caregivers,” investigators reported.
study coinvestigator Norma Verdolini, MD, PhD, bipolar and depressive disorders unit, hospital Clinic Barcelona, University of Barcelona, said in an interview.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
FAST measures
Previous research has shown that family environment influences the development of psychotic symptoms, with negative family environmental factors associated with poor prognoses.
Conversely, one study indicated that a positive family environment is linked to greater improvement in negative and disorganized symptoms in adolescents at imminent risk for psychosis onset.
However, the current investigators noted that the impact of family environment on longitudinal functioning in individuals presenting with FEP is unclear.
To investigate further, they conducted an analysis as part of the PEPs study, which included 335 patients with FEP and 253 healthy controls. Functioning was measured using the Functional Assessment Short Test (FAST), and family environmental styles were evaluated using the Family Environment Scale (FES), which assesses “emotional climate” of a family across 10 domains.
At baseline, the mean total FAST score was 27.8 in patients with FEP versus 3.5 in the healthy controls, indicating substantially worse functioning among the patients. Linear regression analysis indicated that at baseline there was no significant association between aspects of family environment on the FES and functional scores.
Patients were assessed again at 2 years, by which point 283 had been diagnosed with psychotic disorders and 52 with bipolar disorder. The mean total FAST scores were 20.98 among patients with psychotic disorders and 13.8 in those with bipolar disorder.
Family conflict
Results showed that, among those with bipolar disorder, worse functioning on FAST at 2 years was significantly associated with higher rates of open expression of conflict in the family (P = .004).
In patients with psychotic disorders, worse functioning was significantly associated with lower rates of participation in social activities (P = .006) and an achievement-oriented family environment (P = .039). Worse functioning in patients with psychotic disorders was also significantly associated with higher rates of religious practice and values (P = .003).
Dr. Verdolini noted the reason family environment does not appear to have an impact at initial FEP presentation may be that the “first kick” is given by an individual’s genetic liability for psychiatric disorders in combination with the family environment. In reality, the two are intertwined, especially when considering what it means to a family to have one member with a psychiatric disorder, which “will have an impact on the family environment.”
Dr. Verdolini added: “This is not actually the objective family environment,” but the perceived family environment.
“So maybe in the following 2 years the patient who experiences a first episode of psychosis may change their idea of the family environment itself,” she noted. She added that at her institution psychoeducation is offered to FEP patients’ families.
‘Interesting’ findings
Commenting on the study, Nicole Kozloff, MD, from the child, youth, and emerging adult program at the Centre for Addiction and Mental Health in Toronto, said one limitation of the study is that it’s not clear what care patients received – or who in the family completed the FES.
It is also important to note that “measures of association do not necessarily imply that one factor caused the other factor,” said Dr. Kozloff, who was not involved in the research. “For example, it may be that, among people with bipolar disorder, open expression of conflict in the family can lead to worse functioning, or that worse functioning can lead to more conflict in the family.”
Nevertheless, Dr. Kozloff described the finding of an emerging association between the family environment and functioning over time as “interesting.”
When young people with FEP enter treatment, “they have reached a crisis point and are functioning poorly,” she noted.
“It could be that there is less to differentiate among levels of functioning at treatment entry but, after 2 years, the individuals have separated into those who have been responsive to treatment and are functioning well, and those who continue to have functional challenges. And this is where we start to see a relationship with family environment emerge,” Dr. Kozloff said.
She also agreed with Dr. Verdolini’s take on the findings, and that family psychoeducation “can reduce relapse rates in schizophrenia and the emotional burden on the family.”
“We also know that having family involvement in care is one of the most robust predictors that young people with psychosis will remain engaged in mental health services,” she said.
Teaching families about psychosis and its treatment, about problem-solving and communication skills, and providing support to ensure that family members know how to get help in a crisis, “is a key part of comprehensive early psychosis intervention,” Dr. Kozloff said. “It is good for the patient and good for the family, and allows the clinicians to provide better care.”
Articulates clinical practice findings
Also commenting on the results, Brian O’Donoghue, MD, PhD, senior clinical research fellow at Orygen, the National Centre of Excellence in Youth Mental Health in Melbourne, described the research as important, adding that the study highlights the need for sufficient follow-up.
“It makes sense that the involvement of family over time has a strong impact upon outcome and functioning,” he said in an interview.
“These research findings articulate what we see in clinical practice, so it is good to see that it is captured,” added Dr. O’Donoghue, who was not associated with the study.
He noted that it is common for family involvement to influence outcome, especially if the family is positively involved. “It is invaluable toward their recovery. However, conversely, if there are ongoing family stressors, then this can be a trigger for relapse or lack of improvement.”
Overall, the results “really emphasize that the family needs to be involved in care.”
The Early Psychosis Prevention and Intervention Centre where Dr. O’Donoghue is a consultant psychiatrist offers a psychoeducational course “to inform families about psychosis, treatment, and how they can support their family members.”
“We also have family peer support workers and family therapists, which are essential to the service and for the young person’s recovery,” Dr. O’Donoghue said.
The investigators and Dr. O’Donoghue disclosed no relevant financial relationships. Dr. Kozloff reported receiving research funding from the CAMH Foundation, Brain & Behavior Research Foundation, Canadian Institutes of Health Research, and AFP Innovation Fund; honoraria from Humber River Hospital, the University of Calgary (Alta.), and the Canadian Consortium for Early Intervention in Psychosis; and salary support from Inner City Health Associates.
A version of this article originally appeared on Medscape.com.
FROM SIRS 2020
Could being active reduce cancer death risk from alcohol?
Moderate drinking not a problem
concludes a new observational study involving 50,000-plus British adults.
Being physically active – for example, by walking, house cleaning, or playing a sport – could be promoted as a risk-minimization measure for alcohol-related cancers, say the authors, led by Emmanuel Stamatakis, PhD, professor of Physical Activity, Lifestyle, and Population Health, University of Sydney, Australia.
The researchers found a “strong direct association between alcohol consumption and mortality risk of [10] alcohol-related cancers.”
Specifically, when compared with never drinkers, there was a significantly higher risk of dying from such cancers among drinkers who consumed “hazardous” and “harmful” amounts of alcohol, and also for ex-drinkers.
Notably, occasional drinkers and drinkers within guidelines did not have statistically significantly higher risks for alcohol-related cancer mortality.
But the analysis also found that among the bigger drinkers, the risks were “substantially attenuated” in physically active participants who met at least the lower recommended limit of activity (>7.5 metabolic equivalent task [MET]–hours/week).
That’s not a taxing amount of activity because, for example, general household cleaning results in 3 METs/hour and walking slowly translates into 2 METs/hour. However, nearly a quarter of survey participants reported no physical activity.
The study was published online May 14 in the International Journal of Cancer.
The new results require confirmation because the findings “are limited in their statistical power,” with small numbers of cases in several categories, said Alpa Patel, PhD, an epidemiologist at the American Cancer Society, who was not involved in the study. For example, there were only 55 alcohol-related cancer deaths among the 1540 harmful drinkers.
Patel stressed that, “based on the collective evidence to date, it is best to both avoid alcohol consumption and engage in sufficient amounts of physical activity.” That amount is 150-300 minutes of moderate or 75-150 minutes of vigorous activity per week for cancer prevention.
Her message about abstinence is in-line with new ACS guidelines issued last month, as reported by Medscape Medical News. The ACS’s guidance was criticized by many readers in the comments section, who repeatedly encouraged “moderation.”
However, the ACS also recommended moderation, saying, for those adults who do drink, intake should be no more than 1 drink/day for women or 2 drinks/day for men.
Study author Dr. Stamatakis commented on the alcohol debate.
“Any advice for complete abstinence is bound to alienate many people,” he told Medscape Medical News in an email. “Alcohol drinking has been an integral part of many societies for thousands of years.”
Dr. Stamatakis, who is an occasional beer drinker, also said, “there is no healthy level of alcohol drinking.”
This was also the conclusion of a 2018 study published in the Lancet, which stated that there is “no safe limit,” as even one drink a day increases the risk of cancer. A few years earlier, the 2014 World Cancer Report found a dose-response relationship between alcohol consumption and certain cancers.
However, epidemiological findings are not necessarily “clinically relevant,” commented Jennifer Ligibel, MD, a medical oncologist at the Dana-Farber Cancer Institute, Boston, Massachusetts, in a 2018 interview with Medscape Medical News.
Dr. Ligibel explained that there are 50 years of studies linking alcohol and cancers. “With the huge amount of data we have, even small differences [in consumption] are statistically significant.”
Dr. Ligibel cited an often-repeated statistic: for the average woman, there is a 12% lifetime risk of breast cancer. “If a woman consumes a drink a day, which is considered a low-level intake, that risk may become about 13% – which is statistically significant,” Dr. Ligibel explained.
But that risk increase is not clinically relevant, she added.
Mean 10 years of follow-up
The new study is the first to examine physical activity, drinking, and the 10 cancers that have been linked to alcohol consumption (oral cavity, throat, larynx, esophagus, liver, colorectal, stomach, breast, pancreas, and lung).
The authors used data from 10 British population-based health surveys from 1994-2008 and looked at adults aged 30 years and older. The mean follow-up period was 9.9 years.
Among 54,686 participants, there were 2039 alcohol-related site-specific cancer deaths.
Alcohol consumption categories were based on U.K. guidelines, with 1 unit equal to 8 grams (about 2 ounces) of pure alcohol. The categories were as follows: drinking within guidelines (<14 units/week for women, <21 units/week for men), hazardous level (14-35 units/week for women, 21-49 units/week for men), and harmful level (> 35 units/week for women, >49 units/week for men). The survey also queried participants about being ex-drinkers, occasional drinkers, and never drinkers.
Physical activity was assessed using self-reported accounts of the 4 weeks preceding the health survey and intensity of activity (light, moderate, or vigorous) was queried. Physical activity was categorized using the upper (15 MET-hours/week) and lower (the aforementioned <7 MET-hours/week) recommended limits.
The median age of participants was 51 years; 7.9% were never drinkers and 14.7% exceeded guideline amounts. For physical activity, 23% reported none. The median level of activity was 9 MET-hours/week.
The authors say that the “increased risks [among the harmful, hazardous, and ex-drinker categories] were eliminated” among the individuals who reported physical activity >7.5 MET-hours/week. That meant the hazard ratios for cancer mortality for each category were reduced to the point that they were no longer statistically significant.
For example, for all drinkers in the “hazardous” category, the risk of cancer-related mortality was significantly higher than for nondrinkers (with a hazard ratio of 1.39), but in the subgroup of these participants who were physically active at the lower recommended limit, the hazard ratio dropped to 1.21.
These “broad patterns of effect modification by physical activity persisted when the upper physical activity limit [15 MET-hours/week] was used,” write the authors.
The new study adds to the literature on cancer mortality and alcohol consumption. In another recent study, researchers looked at eight British cohorts and reported overall cancer mortality associated with alcohol consumption was eliminated among those meeting physical activity recommendations (Br J Sports Med. 2017;51:651-7). The new study added two more cohorts to this base of eight and only focused on cancers that have been linked to alcohol consumption. The earlier study included deaths from all types of cancer.
The refinement of focus in the current study is important, say Dr. Stamatakis and colleagues.
“This specificity adds biological plausibility and permits a more immediate translation of our findings into policy and practice,” they write.
Dr. Stamatakis practices what he advocates, but is not a teetotaler.
“I exercise (e.g., dynamic yoga, HIIT cardio workouts, run, cycle, lift weights) for 45-60 minutes a day and I walk 8,000-14,000 steps daily. That would categorize me perhaps in the top 3%-5% for my age/sex group. And I enjoy 1-2 cans of craft beer a couple of times a week,” he said in an email.
Dr. Stamatakis and Dr. Patel have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Moderate drinking not a problem
Moderate drinking not a problem
concludes a new observational study involving 50,000-plus British adults.
Being physically active – for example, by walking, house cleaning, or playing a sport – could be promoted as a risk-minimization measure for alcohol-related cancers, say the authors, led by Emmanuel Stamatakis, PhD, professor of Physical Activity, Lifestyle, and Population Health, University of Sydney, Australia.
The researchers found a “strong direct association between alcohol consumption and mortality risk of [10] alcohol-related cancers.”
Specifically, when compared with never drinkers, there was a significantly higher risk of dying from such cancers among drinkers who consumed “hazardous” and “harmful” amounts of alcohol, and also for ex-drinkers.
Notably, occasional drinkers and drinkers within guidelines did not have statistically significantly higher risks for alcohol-related cancer mortality.
But the analysis also found that among the bigger drinkers, the risks were “substantially attenuated” in physically active participants who met at least the lower recommended limit of activity (>7.5 metabolic equivalent task [MET]–hours/week).
That’s not a taxing amount of activity because, for example, general household cleaning results in 3 METs/hour and walking slowly translates into 2 METs/hour. However, nearly a quarter of survey participants reported no physical activity.
The study was published online May 14 in the International Journal of Cancer.
The new results require confirmation because the findings “are limited in their statistical power,” with small numbers of cases in several categories, said Alpa Patel, PhD, an epidemiologist at the American Cancer Society, who was not involved in the study. For example, there were only 55 alcohol-related cancer deaths among the 1540 harmful drinkers.
Patel stressed that, “based on the collective evidence to date, it is best to both avoid alcohol consumption and engage in sufficient amounts of physical activity.” That amount is 150-300 minutes of moderate or 75-150 minutes of vigorous activity per week for cancer prevention.
Her message about abstinence is in-line with new ACS guidelines issued last month, as reported by Medscape Medical News. The ACS’s guidance was criticized by many readers in the comments section, who repeatedly encouraged “moderation.”
However, the ACS also recommended moderation, saying, for those adults who do drink, intake should be no more than 1 drink/day for women or 2 drinks/day for men.
Study author Dr. Stamatakis commented on the alcohol debate.
“Any advice for complete abstinence is bound to alienate many people,” he told Medscape Medical News in an email. “Alcohol drinking has been an integral part of many societies for thousands of years.”
Dr. Stamatakis, who is an occasional beer drinker, also said, “there is no healthy level of alcohol drinking.”
This was also the conclusion of a 2018 study published in the Lancet, which stated that there is “no safe limit,” as even one drink a day increases the risk of cancer. A few years earlier, the 2014 World Cancer Report found a dose-response relationship between alcohol consumption and certain cancers.
However, epidemiological findings are not necessarily “clinically relevant,” commented Jennifer Ligibel, MD, a medical oncologist at the Dana-Farber Cancer Institute, Boston, Massachusetts, in a 2018 interview with Medscape Medical News.
Dr. Ligibel explained that there are 50 years of studies linking alcohol and cancers. “With the huge amount of data we have, even small differences [in consumption] are statistically significant.”
Dr. Ligibel cited an often-repeated statistic: for the average woman, there is a 12% lifetime risk of breast cancer. “If a woman consumes a drink a day, which is considered a low-level intake, that risk may become about 13% – which is statistically significant,” Dr. Ligibel explained.
But that risk increase is not clinically relevant, she added.
Mean 10 years of follow-up
The new study is the first to examine physical activity, drinking, and the 10 cancers that have been linked to alcohol consumption (oral cavity, throat, larynx, esophagus, liver, colorectal, stomach, breast, pancreas, and lung).
The authors used data from 10 British population-based health surveys from 1994-2008 and looked at adults aged 30 years and older. The mean follow-up period was 9.9 years.
Among 54,686 participants, there were 2039 alcohol-related site-specific cancer deaths.
Alcohol consumption categories were based on U.K. guidelines, with 1 unit equal to 8 grams (about 2 ounces) of pure alcohol. The categories were as follows: drinking within guidelines (<14 units/week for women, <21 units/week for men), hazardous level (14-35 units/week for women, 21-49 units/week for men), and harmful level (> 35 units/week for women, >49 units/week for men). The survey also queried participants about being ex-drinkers, occasional drinkers, and never drinkers.
Physical activity was assessed using self-reported accounts of the 4 weeks preceding the health survey and intensity of activity (light, moderate, or vigorous) was queried. Physical activity was categorized using the upper (15 MET-hours/week) and lower (the aforementioned <7 MET-hours/week) recommended limits.
The median age of participants was 51 years; 7.9% were never drinkers and 14.7% exceeded guideline amounts. For physical activity, 23% reported none. The median level of activity was 9 MET-hours/week.
The authors say that the “increased risks [among the harmful, hazardous, and ex-drinker categories] were eliminated” among the individuals who reported physical activity >7.5 MET-hours/week. That meant the hazard ratios for cancer mortality for each category were reduced to the point that they were no longer statistically significant.
For example, for all drinkers in the “hazardous” category, the risk of cancer-related mortality was significantly higher than for nondrinkers (with a hazard ratio of 1.39), but in the subgroup of these participants who were physically active at the lower recommended limit, the hazard ratio dropped to 1.21.
These “broad patterns of effect modification by physical activity persisted when the upper physical activity limit [15 MET-hours/week] was used,” write the authors.
The new study adds to the literature on cancer mortality and alcohol consumption. In another recent study, researchers looked at eight British cohorts and reported overall cancer mortality associated with alcohol consumption was eliminated among those meeting physical activity recommendations (Br J Sports Med. 2017;51:651-7). The new study added two more cohorts to this base of eight and only focused on cancers that have been linked to alcohol consumption. The earlier study included deaths from all types of cancer.
The refinement of focus in the current study is important, say Dr. Stamatakis and colleagues.
“This specificity adds biological plausibility and permits a more immediate translation of our findings into policy and practice,” they write.
Dr. Stamatakis practices what he advocates, but is not a teetotaler.
“I exercise (e.g., dynamic yoga, HIIT cardio workouts, run, cycle, lift weights) for 45-60 minutes a day and I walk 8,000-14,000 steps daily. That would categorize me perhaps in the top 3%-5% for my age/sex group. And I enjoy 1-2 cans of craft beer a couple of times a week,” he said in an email.
Dr. Stamatakis and Dr. Patel have reported no relevant financial relationships.
This article first appeared on Medscape.com.
concludes a new observational study involving 50,000-plus British adults.
Being physically active – for example, by walking, house cleaning, or playing a sport – could be promoted as a risk-minimization measure for alcohol-related cancers, say the authors, led by Emmanuel Stamatakis, PhD, professor of Physical Activity, Lifestyle, and Population Health, University of Sydney, Australia.
The researchers found a “strong direct association between alcohol consumption and mortality risk of [10] alcohol-related cancers.”
Specifically, when compared with never drinkers, there was a significantly higher risk of dying from such cancers among drinkers who consumed “hazardous” and “harmful” amounts of alcohol, and also for ex-drinkers.
Notably, occasional drinkers and drinkers within guidelines did not have statistically significantly higher risks for alcohol-related cancer mortality.
But the analysis also found that among the bigger drinkers, the risks were “substantially attenuated” in physically active participants who met at least the lower recommended limit of activity (>7.5 metabolic equivalent task [MET]–hours/week).
That’s not a taxing amount of activity because, for example, general household cleaning results in 3 METs/hour and walking slowly translates into 2 METs/hour. However, nearly a quarter of survey participants reported no physical activity.
The study was published online May 14 in the International Journal of Cancer.
The new results require confirmation because the findings “are limited in their statistical power,” with small numbers of cases in several categories, said Alpa Patel, PhD, an epidemiologist at the American Cancer Society, who was not involved in the study. For example, there were only 55 alcohol-related cancer deaths among the 1540 harmful drinkers.
Patel stressed that, “based on the collective evidence to date, it is best to both avoid alcohol consumption and engage in sufficient amounts of physical activity.” That amount is 150-300 minutes of moderate or 75-150 minutes of vigorous activity per week for cancer prevention.
Her message about abstinence is in-line with new ACS guidelines issued last month, as reported by Medscape Medical News. The ACS’s guidance was criticized by many readers in the comments section, who repeatedly encouraged “moderation.”
However, the ACS also recommended moderation, saying, for those adults who do drink, intake should be no more than 1 drink/day for women or 2 drinks/day for men.
Study author Dr. Stamatakis commented on the alcohol debate.
“Any advice for complete abstinence is bound to alienate many people,” he told Medscape Medical News in an email. “Alcohol drinking has been an integral part of many societies for thousands of years.”
Dr. Stamatakis, who is an occasional beer drinker, also said, “there is no healthy level of alcohol drinking.”
This was also the conclusion of a 2018 study published in the Lancet, which stated that there is “no safe limit,” as even one drink a day increases the risk of cancer. A few years earlier, the 2014 World Cancer Report found a dose-response relationship between alcohol consumption and certain cancers.
However, epidemiological findings are not necessarily “clinically relevant,” commented Jennifer Ligibel, MD, a medical oncologist at the Dana-Farber Cancer Institute, Boston, Massachusetts, in a 2018 interview with Medscape Medical News.
Dr. Ligibel explained that there are 50 years of studies linking alcohol and cancers. “With the huge amount of data we have, even small differences [in consumption] are statistically significant.”
Dr. Ligibel cited an often-repeated statistic: for the average woman, there is a 12% lifetime risk of breast cancer. “If a woman consumes a drink a day, which is considered a low-level intake, that risk may become about 13% – which is statistically significant,” Dr. Ligibel explained.
But that risk increase is not clinically relevant, she added.
Mean 10 years of follow-up
The new study is the first to examine physical activity, drinking, and the 10 cancers that have been linked to alcohol consumption (oral cavity, throat, larynx, esophagus, liver, colorectal, stomach, breast, pancreas, and lung).
The authors used data from 10 British population-based health surveys from 1994-2008 and looked at adults aged 30 years and older. The mean follow-up period was 9.9 years.
Among 54,686 participants, there were 2039 alcohol-related site-specific cancer deaths.
Alcohol consumption categories were based on U.K. guidelines, with 1 unit equal to 8 grams (about 2 ounces) of pure alcohol. The categories were as follows: drinking within guidelines (<14 units/week for women, <21 units/week for men), hazardous level (14-35 units/week for women, 21-49 units/week for men), and harmful level (> 35 units/week for women, >49 units/week for men). The survey also queried participants about being ex-drinkers, occasional drinkers, and never drinkers.
Physical activity was assessed using self-reported accounts of the 4 weeks preceding the health survey and intensity of activity (light, moderate, or vigorous) was queried. Physical activity was categorized using the upper (15 MET-hours/week) and lower (the aforementioned <7 MET-hours/week) recommended limits.
The median age of participants was 51 years; 7.9% were never drinkers and 14.7% exceeded guideline amounts. For physical activity, 23% reported none. The median level of activity was 9 MET-hours/week.
The authors say that the “increased risks [among the harmful, hazardous, and ex-drinker categories] were eliminated” among the individuals who reported physical activity >7.5 MET-hours/week. That meant the hazard ratios for cancer mortality for each category were reduced to the point that they were no longer statistically significant.
For example, for all drinkers in the “hazardous” category, the risk of cancer-related mortality was significantly higher than for nondrinkers (with a hazard ratio of 1.39), but in the subgroup of these participants who were physically active at the lower recommended limit, the hazard ratio dropped to 1.21.
These “broad patterns of effect modification by physical activity persisted when the upper physical activity limit [15 MET-hours/week] was used,” write the authors.
The new study adds to the literature on cancer mortality and alcohol consumption. In another recent study, researchers looked at eight British cohorts and reported overall cancer mortality associated with alcohol consumption was eliminated among those meeting physical activity recommendations (Br J Sports Med. 2017;51:651-7). The new study added two more cohorts to this base of eight and only focused on cancers that have been linked to alcohol consumption. The earlier study included deaths from all types of cancer.
The refinement of focus in the current study is important, say Dr. Stamatakis and colleagues.
“This specificity adds biological plausibility and permits a more immediate translation of our findings into policy and practice,” they write.
Dr. Stamatakis practices what he advocates, but is not a teetotaler.
“I exercise (e.g., dynamic yoga, HIIT cardio workouts, run, cycle, lift weights) for 45-60 minutes a day and I walk 8,000-14,000 steps daily. That would categorize me perhaps in the top 3%-5% for my age/sex group. And I enjoy 1-2 cans of craft beer a couple of times a week,” he said in an email.
Dr. Stamatakis and Dr. Patel have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Drug-drug interactions to avoid in patients with GI cancer
warned a leading expert in the field.
Rachel P. Riechelmann, MD, AC Camargo Cancer Center, São Paulo, Brazil, was delivering a keynote speech during the ESMO 22nd World Congress on Gastrointestinal Cancer Virtual Experience on July 4.
One of the drug-drug interactions that can have a deleterious effect on patients with GI cancers is that occurring between proton pump inhibitors (PPIs), such as omeprazole, and chemotherapy regimens containing capecitabine, she said.
She cited clinical trial data showing that the use of PPIs can increase the risk for progression in colorectal cancer patients being treated with adjuvant CapeOx (capecitabine with oxaliplatin) or FOLFOX (leucovorin calcium [folinic acid], fluorouracil, and oxaliplatin). Further clinical trial data from the LOGIC trial show that PPIs have a significant effect on both progression-free and overall survival in HER2+ gastric cancer patients being treated with CapOx with or without lapatinib.
Commenting on the presentation on Twitter, Jose Fernando Moura, MD, PhD, Medical Oncology, Real Hospital Português, Recife, Brazil, agreed that it is better to avoid PPIs during chemotherapy for colorectal and gastrointestinal tumors.
Benedikt Westphalen, MD, PhD, coordinator, molecular oncology, University of Munich Comprehensive Cancer Center, Munich, Germany, replied that the data presented by Dr. Riechelmann are “clearly interesting.”
He added his own checklist of things to consider in regard to drug-drug interactions, including changes in drug levels, the effect on the microbiome, and gender differences.
Previous studies, including many from Dr. Riechelmann’s group, have indicated that potential drug-drug interactions occur in about two thirds of inpatients and in approximately one third of outpatients.
The frequency of clinically relevant drug interactions in oncology patients enrolled in clinical trials is “not that high,” however, at between 3% and 17%, depending on the mechanism of interaction, she commented.
“But it should be zero, because all clinical trials have a list of combinations that should not be prescribed and drugs that should be avoided,” she added.
There have been very few studies on the occurrence of drug-drug interactions in oncology patients in the real world, Dr. Riechelmann commented.
One study suggested that 4% of oncology deaths in hospitals were due to adverse drug reactions or interactions. Another study, conducted by Dr. Riechelmann’s team, suggested that 2% of nonelective hospitalizations among oncology patients were for drug-drug interactions.
She said that common potential drug interactions in oncology involve the use of aspirin, warfarin, beta blockers, and corticosteroids.
She also singled out olaparib (Lynparza, AstraZeneca) as an interesting case. Coadministration of drugs that act as CYP3A4 inhibitors or inducers can effect exposure to this drug; itraconazole significantly increases exposure, and rifampin significantly reduces exposure.
Avoiding interactions
In conclusion, Dr. Riechelmann made a series of recommendations for avoiding dangerous drug-drug interactions in cancer patients, the first of which is to avoid polypharmacy in the first place.
She also suggested that high-risk patients, such as those taking many drugs and who have comorbid illness, should be screened for potential drug interactions, and attention should be paid to “dangerous” combinations.
Combinations to avoid include those of two drugs that each prolong the QT interval. These include quinolones, azithromycin, and clarithromycin.
“I think every one of us has to develop our own list of dangerous combinations” that should be avoided if possible, she said. If their use is necessary, patients should be informed of the potential risk and should be monitored closely for adverse events.
No funding for the study has been reported. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
warned a leading expert in the field.
Rachel P. Riechelmann, MD, AC Camargo Cancer Center, São Paulo, Brazil, was delivering a keynote speech during the ESMO 22nd World Congress on Gastrointestinal Cancer Virtual Experience on July 4.
One of the drug-drug interactions that can have a deleterious effect on patients with GI cancers is that occurring between proton pump inhibitors (PPIs), such as omeprazole, and chemotherapy regimens containing capecitabine, she said.
She cited clinical trial data showing that the use of PPIs can increase the risk for progression in colorectal cancer patients being treated with adjuvant CapeOx (capecitabine with oxaliplatin) or FOLFOX (leucovorin calcium [folinic acid], fluorouracil, and oxaliplatin). Further clinical trial data from the LOGIC trial show that PPIs have a significant effect on both progression-free and overall survival in HER2+ gastric cancer patients being treated with CapOx with or without lapatinib.
Commenting on the presentation on Twitter, Jose Fernando Moura, MD, PhD, Medical Oncology, Real Hospital Português, Recife, Brazil, agreed that it is better to avoid PPIs during chemotherapy for colorectal and gastrointestinal tumors.
Benedikt Westphalen, MD, PhD, coordinator, molecular oncology, University of Munich Comprehensive Cancer Center, Munich, Germany, replied that the data presented by Dr. Riechelmann are “clearly interesting.”
He added his own checklist of things to consider in regard to drug-drug interactions, including changes in drug levels, the effect on the microbiome, and gender differences.
Previous studies, including many from Dr. Riechelmann’s group, have indicated that potential drug-drug interactions occur in about two thirds of inpatients and in approximately one third of outpatients.
The frequency of clinically relevant drug interactions in oncology patients enrolled in clinical trials is “not that high,” however, at between 3% and 17%, depending on the mechanism of interaction, she commented.
“But it should be zero, because all clinical trials have a list of combinations that should not be prescribed and drugs that should be avoided,” she added.
There have been very few studies on the occurrence of drug-drug interactions in oncology patients in the real world, Dr. Riechelmann commented.
One study suggested that 4% of oncology deaths in hospitals were due to adverse drug reactions or interactions. Another study, conducted by Dr. Riechelmann’s team, suggested that 2% of nonelective hospitalizations among oncology patients were for drug-drug interactions.
She said that common potential drug interactions in oncology involve the use of aspirin, warfarin, beta blockers, and corticosteroids.
She also singled out olaparib (Lynparza, AstraZeneca) as an interesting case. Coadministration of drugs that act as CYP3A4 inhibitors or inducers can effect exposure to this drug; itraconazole significantly increases exposure, and rifampin significantly reduces exposure.
Avoiding interactions
In conclusion, Dr. Riechelmann made a series of recommendations for avoiding dangerous drug-drug interactions in cancer patients, the first of which is to avoid polypharmacy in the first place.
She also suggested that high-risk patients, such as those taking many drugs and who have comorbid illness, should be screened for potential drug interactions, and attention should be paid to “dangerous” combinations.
Combinations to avoid include those of two drugs that each prolong the QT interval. These include quinolones, azithromycin, and clarithromycin.
“I think every one of us has to develop our own list of dangerous combinations” that should be avoided if possible, she said. If their use is necessary, patients should be informed of the potential risk and should be monitored closely for adverse events.
No funding for the study has been reported. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
warned a leading expert in the field.
Rachel P. Riechelmann, MD, AC Camargo Cancer Center, São Paulo, Brazil, was delivering a keynote speech during the ESMO 22nd World Congress on Gastrointestinal Cancer Virtual Experience on July 4.
One of the drug-drug interactions that can have a deleterious effect on patients with GI cancers is that occurring between proton pump inhibitors (PPIs), such as omeprazole, and chemotherapy regimens containing capecitabine, she said.
She cited clinical trial data showing that the use of PPIs can increase the risk for progression in colorectal cancer patients being treated with adjuvant CapeOx (capecitabine with oxaliplatin) or FOLFOX (leucovorin calcium [folinic acid], fluorouracil, and oxaliplatin). Further clinical trial data from the LOGIC trial show that PPIs have a significant effect on both progression-free and overall survival in HER2+ gastric cancer patients being treated with CapOx with or without lapatinib.
Commenting on the presentation on Twitter, Jose Fernando Moura, MD, PhD, Medical Oncology, Real Hospital Português, Recife, Brazil, agreed that it is better to avoid PPIs during chemotherapy for colorectal and gastrointestinal tumors.
Benedikt Westphalen, MD, PhD, coordinator, molecular oncology, University of Munich Comprehensive Cancer Center, Munich, Germany, replied that the data presented by Dr. Riechelmann are “clearly interesting.”
He added his own checklist of things to consider in regard to drug-drug interactions, including changes in drug levels, the effect on the microbiome, and gender differences.
Previous studies, including many from Dr. Riechelmann’s group, have indicated that potential drug-drug interactions occur in about two thirds of inpatients and in approximately one third of outpatients.
The frequency of clinically relevant drug interactions in oncology patients enrolled in clinical trials is “not that high,” however, at between 3% and 17%, depending on the mechanism of interaction, she commented.
“But it should be zero, because all clinical trials have a list of combinations that should not be prescribed and drugs that should be avoided,” she added.
There have been very few studies on the occurrence of drug-drug interactions in oncology patients in the real world, Dr. Riechelmann commented.
One study suggested that 4% of oncology deaths in hospitals were due to adverse drug reactions or interactions. Another study, conducted by Dr. Riechelmann’s team, suggested that 2% of nonelective hospitalizations among oncology patients were for drug-drug interactions.
She said that common potential drug interactions in oncology involve the use of aspirin, warfarin, beta blockers, and corticosteroids.
She also singled out olaparib (Lynparza, AstraZeneca) as an interesting case. Coadministration of drugs that act as CYP3A4 inhibitors or inducers can effect exposure to this drug; itraconazole significantly increases exposure, and rifampin significantly reduces exposure.
Avoiding interactions
In conclusion, Dr. Riechelmann made a series of recommendations for avoiding dangerous drug-drug interactions in cancer patients, the first of which is to avoid polypharmacy in the first place.
She also suggested that high-risk patients, such as those taking many drugs and who have comorbid illness, should be screened for potential drug interactions, and attention should be paid to “dangerous” combinations.
Combinations to avoid include those of two drugs that each prolong the QT interval. These include quinolones, azithromycin, and clarithromycin.
“I think every one of us has to develop our own list of dangerous combinations” that should be avoided if possible, she said. If their use is necessary, patients should be informed of the potential risk and should be monitored closely for adverse events.
No funding for the study has been reported. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Nail discoloration
The clinical findings and medical history were consistent with drug-induced hyperpigmentation and minocycline was the likely culprit. Other medications commonly implicated in drug-induced hyperpigmentation include heavy metals (eg, gold, iron, silver), anticonvulsants, hydroxychloroquine, and amiodarone.
Common sites for minocycline pigment deposition—besides the fingernails—include the gingiva, dorsal hands, shins, and old scars. The diagnosis of drug-induced hyperpigmentation is clinical and does not require a biopsy.
While the use of antibiotics for chronic disease can lead to antimicrobial resistance (and should be avoided when possible), certain cases of rosacea may require chronic therapy, and tetracyclines most commonly are used. When minocycline is chosen as a chronic therapy, part of the treatment surveillance should include monitoring for drug-induced hyperpigmentation.
When drug-induced hyperpigmentation does occur, treatment involves discontinuing the offending agent. It can take years for pigment to develop and years for it to resolve—if it completely resolves at all.
In this case, the physician was concerned about the pigmentation worsening or spreading to other sites, so he discontinued the minocycline and prescribed a topical agent for the patient’s rosacea. Ultimately, the patient required occasional use of doxycycline for flares.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Nisar MS, Iyer K, Brodell RT, et al. Minocycline-induced hyperpigmentation: comparison of 3 Q-switched lasers to reverse its effects. Clin Cosmet Investig Dermatol. 2013;6:159-162.
The clinical findings and medical history were consistent with drug-induced hyperpigmentation and minocycline was the likely culprit. Other medications commonly implicated in drug-induced hyperpigmentation include heavy metals (eg, gold, iron, silver), anticonvulsants, hydroxychloroquine, and amiodarone.
Common sites for minocycline pigment deposition—besides the fingernails—include the gingiva, dorsal hands, shins, and old scars. The diagnosis of drug-induced hyperpigmentation is clinical and does not require a biopsy.
While the use of antibiotics for chronic disease can lead to antimicrobial resistance (and should be avoided when possible), certain cases of rosacea may require chronic therapy, and tetracyclines most commonly are used. When minocycline is chosen as a chronic therapy, part of the treatment surveillance should include monitoring for drug-induced hyperpigmentation.
When drug-induced hyperpigmentation does occur, treatment involves discontinuing the offending agent. It can take years for pigment to develop and years for it to resolve—if it completely resolves at all.
In this case, the physician was concerned about the pigmentation worsening or spreading to other sites, so he discontinued the minocycline and prescribed a topical agent for the patient’s rosacea. Ultimately, the patient required occasional use of doxycycline for flares.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
The clinical findings and medical history were consistent with drug-induced hyperpigmentation and minocycline was the likely culprit. Other medications commonly implicated in drug-induced hyperpigmentation include heavy metals (eg, gold, iron, silver), anticonvulsants, hydroxychloroquine, and amiodarone.
Common sites for minocycline pigment deposition—besides the fingernails—include the gingiva, dorsal hands, shins, and old scars. The diagnosis of drug-induced hyperpigmentation is clinical and does not require a biopsy.
While the use of antibiotics for chronic disease can lead to antimicrobial resistance (and should be avoided when possible), certain cases of rosacea may require chronic therapy, and tetracyclines most commonly are used. When minocycline is chosen as a chronic therapy, part of the treatment surveillance should include monitoring for drug-induced hyperpigmentation.
When drug-induced hyperpigmentation does occur, treatment involves discontinuing the offending agent. It can take years for pigment to develop and years for it to resolve—if it completely resolves at all.
In this case, the physician was concerned about the pigmentation worsening or spreading to other sites, so he discontinued the minocycline and prescribed a topical agent for the patient’s rosacea. Ultimately, the patient required occasional use of doxycycline for flares.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Nisar MS, Iyer K, Brodell RT, et al. Minocycline-induced hyperpigmentation: comparison of 3 Q-switched lasers to reverse its effects. Clin Cosmet Investig Dermatol. 2013;6:159-162.
Nisar MS, Iyer K, Brodell RT, et al. Minocycline-induced hyperpigmentation: comparison of 3 Q-switched lasers to reverse its effects. Clin Cosmet Investig Dermatol. 2013;6:159-162.
Pediatric hospitalists convene virtually to discuss PHM designation
A recent teleconference brought together an ad hoc panel of pediatric hospitalists, with more than 100 diverse voices discussing whether there ought to be an additional professional recognition or designation for the subspecialty, apart from the new pediatric hospital medicine (PHM) board certification that was launched in 2019.
The heterogeneity of PHM was on display during the discussion, as participants included university-based pediatric hospitalists and those from community hospitals, physicians trained in combined medicine and pediatrics or in family medicine, doctors who completed a general pediatric residency before going straight into PHM, niche practitioners such as newborn hospitalists, trainees, and a small but growing number of graduates of PHM fellowship programs. There are 61 PHM fellowships, and these programs graduate approximately 70 new fellows per year.
Although a route to some kind of professional designation for PHM – separate from board certification – was the centerpiece of the conference call, there is no proposal actively under consideration for developing such a designation, said Weijen W. Chang, MD, FAAP, SFHM, chief of pediatric hospital medicine at Baystate Medical Center in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts–Baystate Campus.
Who might develop such a proposal? “The hope is that the three major professional societies involved in pediatric hospital medicine – the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association – would jointly develop such a designation,” Dr. Chang said. However, it is not clear whether the three societies could agree on this. An online survey of 551 pediatric hospitalists, shared during the conference call, found that the majority would like to see some kind of alternate designation.
The reality of the boards
The pediatric subspecialty of PHM was recognized by the American Board of Medical Specialties in 2015 following a petition by a group of PHM leaders seeking a way to credential their unique skill set. The first PHM board certification exam was offered by the American Board of Pediatrics on Nov. 12, 2019, with 1,491 hospitalists sitting for the exam and 84% passing. An estimated 4,000 pediatric hospitalists currently work in the field.
Certification as a subspecialty typically requires completing a fellowship, but new subspecialties often offer a “practice pathway” allowing those who already have experience working in the field to sit for the exam. A PHM practice pathway, and a combined fellowship and experience option for those whose fellowship training was less than 2 years, was offered for last year’s exam and will be offered again in 2021 and 2023. After that, board certification will only be available to graduates of recognized fellowships.
But concerns began to emerge last summer in advance of ABM’s initial PHM board exam, when some applicants were told that they weren’t eligible to sit for it, said H. Barrett Fromme, MD, associate dean for faculty development in medical education and section chief for pediatric hospital medicine at the University of Chicago. She also chairs the section of hospital medicine for the AAP.
Concerns including unintended gender bias against women, such as those hospitalists whose training is interrupted for maternity leave, were raised in a petition to ABP. The board promptly responded that gender bias was not supported by the facts, although its response did not account for selection bias in the data. But the ABP removed its practice interruption criteria.1,2
There are various reasons why a pediatric hospitalist might not be able or willing to pursue a 2-year fellowship or otherwise qualify for certification, Dr. Fromme said, including time and cost. For some, the practice pathway’s requirements, including a minimum number of hours worked in pediatrics in the previous 4 years, may be impossible to meet. Pediatric hospitalists boarded in family medicine are not eligible.
For hospitalists who can’t achieve board certification, what might that mean in terms of their future salary, employment opportunities, reimbursement, other career goals? Might they find themselves unable to qualify for PHM jobs at some university-based medical centers? The answers are not yet known.
What might self-designation look like?
PHM is distinct from adult hospital medicine by virtue of its designation as a board-certified subspecialty. But it can look to the broader HM field for examples of designations that bestow a kind of professional recognition, Dr. Chang said. These include SHM’s merit-based Fellow in Hospital Medicine program and the American Board of Medical Specialties’ Focused Practice in Hospital Medicine, a pathway for board recertification in internal medicine and family medicine, he said.
But PHM self-designation is not necessarily a pathway to hospital privileges. “If we build it, will they come? If they come, will it mean anything to them? That’s the million-dollar question?” Dr. Chang said.
Hospitalists need to appreciate that this issue is important to all three PHM professional societies, SHM, AAP, and APA, Dr. Fromme said. “We are concerned about how to support all of our members – certified, noncertified, nonphysician. Alternate designation is one idea, but we need time to understand it. We need a lot more conversations and a lot of people thinking about it.”
Dr. Fromme is part of the Council on Pediatric Hospital Medicine, a small circle of leaders of PHM interest groups within the three professional associations. It meets quarterly and will be reviewing the results of the conference call.
“I personally think we don’t understand the scope of the problem or the needs of pediatric hospitalists who are not able to sit for boards or pursue a fellowship,” she said. “We have empathy and concern for our colleagues who can’t take the boards. We don’t want them to feel excluded, and that includes advanced practice nurses and residents. But does an alternative designation actually provide what people think it provides?”
There are other ways to demonstrate that professionals are engaged with and serious about developing their practice. If they are looking to better themselves at quality improvement, leadership, education, and other elements of PHM practice, the associations can endeavor to provide more educational opportunities, Dr. Fromme said. “But if it’s about how they look as a candidate for hire, relative to board-certified candidates, that’s a different beast, and we need to think about what can help them the most.”
References
1. American Board of Pediatrics, Response to the Pediatric Hospital Medicine Petition. 2019 Aug 20. https://www.abp.org/sites/abp/files/phm-petition-response.pdf.
2. Chang WW et al. J Hosp Med. 2019 Oct;14(10):589-90.
A recent teleconference brought together an ad hoc panel of pediatric hospitalists, with more than 100 diverse voices discussing whether there ought to be an additional professional recognition or designation for the subspecialty, apart from the new pediatric hospital medicine (PHM) board certification that was launched in 2019.
The heterogeneity of PHM was on display during the discussion, as participants included university-based pediatric hospitalists and those from community hospitals, physicians trained in combined medicine and pediatrics or in family medicine, doctors who completed a general pediatric residency before going straight into PHM, niche practitioners such as newborn hospitalists, trainees, and a small but growing number of graduates of PHM fellowship programs. There are 61 PHM fellowships, and these programs graduate approximately 70 new fellows per year.
Although a route to some kind of professional designation for PHM – separate from board certification – was the centerpiece of the conference call, there is no proposal actively under consideration for developing such a designation, said Weijen W. Chang, MD, FAAP, SFHM, chief of pediatric hospital medicine at Baystate Medical Center in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts–Baystate Campus.
Who might develop such a proposal? “The hope is that the three major professional societies involved in pediatric hospital medicine – the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association – would jointly develop such a designation,” Dr. Chang said. However, it is not clear whether the three societies could agree on this. An online survey of 551 pediatric hospitalists, shared during the conference call, found that the majority would like to see some kind of alternate designation.
The reality of the boards
The pediatric subspecialty of PHM was recognized by the American Board of Medical Specialties in 2015 following a petition by a group of PHM leaders seeking a way to credential their unique skill set. The first PHM board certification exam was offered by the American Board of Pediatrics on Nov. 12, 2019, with 1,491 hospitalists sitting for the exam and 84% passing. An estimated 4,000 pediatric hospitalists currently work in the field.
Certification as a subspecialty typically requires completing a fellowship, but new subspecialties often offer a “practice pathway” allowing those who already have experience working in the field to sit for the exam. A PHM practice pathway, and a combined fellowship and experience option for those whose fellowship training was less than 2 years, was offered for last year’s exam and will be offered again in 2021 and 2023. After that, board certification will only be available to graduates of recognized fellowships.
But concerns began to emerge last summer in advance of ABM’s initial PHM board exam, when some applicants were told that they weren’t eligible to sit for it, said H. Barrett Fromme, MD, associate dean for faculty development in medical education and section chief for pediatric hospital medicine at the University of Chicago. She also chairs the section of hospital medicine for the AAP.
Concerns including unintended gender bias against women, such as those hospitalists whose training is interrupted for maternity leave, were raised in a petition to ABP. The board promptly responded that gender bias was not supported by the facts, although its response did not account for selection bias in the data. But the ABP removed its practice interruption criteria.1,2
There are various reasons why a pediatric hospitalist might not be able or willing to pursue a 2-year fellowship or otherwise qualify for certification, Dr. Fromme said, including time and cost. For some, the practice pathway’s requirements, including a minimum number of hours worked in pediatrics in the previous 4 years, may be impossible to meet. Pediatric hospitalists boarded in family medicine are not eligible.
For hospitalists who can’t achieve board certification, what might that mean in terms of their future salary, employment opportunities, reimbursement, other career goals? Might they find themselves unable to qualify for PHM jobs at some university-based medical centers? The answers are not yet known.
What might self-designation look like?
PHM is distinct from adult hospital medicine by virtue of its designation as a board-certified subspecialty. But it can look to the broader HM field for examples of designations that bestow a kind of professional recognition, Dr. Chang said. These include SHM’s merit-based Fellow in Hospital Medicine program and the American Board of Medical Specialties’ Focused Practice in Hospital Medicine, a pathway for board recertification in internal medicine and family medicine, he said.
But PHM self-designation is not necessarily a pathway to hospital privileges. “If we build it, will they come? If they come, will it mean anything to them? That’s the million-dollar question?” Dr. Chang said.
Hospitalists need to appreciate that this issue is important to all three PHM professional societies, SHM, AAP, and APA, Dr. Fromme said. “We are concerned about how to support all of our members – certified, noncertified, nonphysician. Alternate designation is one idea, but we need time to understand it. We need a lot more conversations and a lot of people thinking about it.”
Dr. Fromme is part of the Council on Pediatric Hospital Medicine, a small circle of leaders of PHM interest groups within the three professional associations. It meets quarterly and will be reviewing the results of the conference call.
“I personally think we don’t understand the scope of the problem or the needs of pediatric hospitalists who are not able to sit for boards or pursue a fellowship,” she said. “We have empathy and concern for our colleagues who can’t take the boards. We don’t want them to feel excluded, and that includes advanced practice nurses and residents. But does an alternative designation actually provide what people think it provides?”
There are other ways to demonstrate that professionals are engaged with and serious about developing their practice. If they are looking to better themselves at quality improvement, leadership, education, and other elements of PHM practice, the associations can endeavor to provide more educational opportunities, Dr. Fromme said. “But if it’s about how they look as a candidate for hire, relative to board-certified candidates, that’s a different beast, and we need to think about what can help them the most.”
References
1. American Board of Pediatrics, Response to the Pediatric Hospital Medicine Petition. 2019 Aug 20. https://www.abp.org/sites/abp/files/phm-petition-response.pdf.
2. Chang WW et al. J Hosp Med. 2019 Oct;14(10):589-90.
A recent teleconference brought together an ad hoc panel of pediatric hospitalists, with more than 100 diverse voices discussing whether there ought to be an additional professional recognition or designation for the subspecialty, apart from the new pediatric hospital medicine (PHM) board certification that was launched in 2019.
The heterogeneity of PHM was on display during the discussion, as participants included university-based pediatric hospitalists and those from community hospitals, physicians trained in combined medicine and pediatrics or in family medicine, doctors who completed a general pediatric residency before going straight into PHM, niche practitioners such as newborn hospitalists, trainees, and a small but growing number of graduates of PHM fellowship programs. There are 61 PHM fellowships, and these programs graduate approximately 70 new fellows per year.
Although a route to some kind of professional designation for PHM – separate from board certification – was the centerpiece of the conference call, there is no proposal actively under consideration for developing such a designation, said Weijen W. Chang, MD, FAAP, SFHM, chief of pediatric hospital medicine at Baystate Medical Center in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts–Baystate Campus.
Who might develop such a proposal? “The hope is that the three major professional societies involved in pediatric hospital medicine – the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association – would jointly develop such a designation,” Dr. Chang said. However, it is not clear whether the three societies could agree on this. An online survey of 551 pediatric hospitalists, shared during the conference call, found that the majority would like to see some kind of alternate designation.
The reality of the boards
The pediatric subspecialty of PHM was recognized by the American Board of Medical Specialties in 2015 following a petition by a group of PHM leaders seeking a way to credential their unique skill set. The first PHM board certification exam was offered by the American Board of Pediatrics on Nov. 12, 2019, with 1,491 hospitalists sitting for the exam and 84% passing. An estimated 4,000 pediatric hospitalists currently work in the field.
Certification as a subspecialty typically requires completing a fellowship, but new subspecialties often offer a “practice pathway” allowing those who already have experience working in the field to sit for the exam. A PHM practice pathway, and a combined fellowship and experience option for those whose fellowship training was less than 2 years, was offered for last year’s exam and will be offered again in 2021 and 2023. After that, board certification will only be available to graduates of recognized fellowships.
But concerns began to emerge last summer in advance of ABM’s initial PHM board exam, when some applicants were told that they weren’t eligible to sit for it, said H. Barrett Fromme, MD, associate dean for faculty development in medical education and section chief for pediatric hospital medicine at the University of Chicago. She also chairs the section of hospital medicine for the AAP.
Concerns including unintended gender bias against women, such as those hospitalists whose training is interrupted for maternity leave, were raised in a petition to ABP. The board promptly responded that gender bias was not supported by the facts, although its response did not account for selection bias in the data. But the ABP removed its practice interruption criteria.1,2
There are various reasons why a pediatric hospitalist might not be able or willing to pursue a 2-year fellowship or otherwise qualify for certification, Dr. Fromme said, including time and cost. For some, the practice pathway’s requirements, including a minimum number of hours worked in pediatrics in the previous 4 years, may be impossible to meet. Pediatric hospitalists boarded in family medicine are not eligible.
For hospitalists who can’t achieve board certification, what might that mean in terms of their future salary, employment opportunities, reimbursement, other career goals? Might they find themselves unable to qualify for PHM jobs at some university-based medical centers? The answers are not yet known.
What might self-designation look like?
PHM is distinct from adult hospital medicine by virtue of its designation as a board-certified subspecialty. But it can look to the broader HM field for examples of designations that bestow a kind of professional recognition, Dr. Chang said. These include SHM’s merit-based Fellow in Hospital Medicine program and the American Board of Medical Specialties’ Focused Practice in Hospital Medicine, a pathway for board recertification in internal medicine and family medicine, he said.
But PHM self-designation is not necessarily a pathway to hospital privileges. “If we build it, will they come? If they come, will it mean anything to them? That’s the million-dollar question?” Dr. Chang said.
Hospitalists need to appreciate that this issue is important to all three PHM professional societies, SHM, AAP, and APA, Dr. Fromme said. “We are concerned about how to support all of our members – certified, noncertified, nonphysician. Alternate designation is one idea, but we need time to understand it. We need a lot more conversations and a lot of people thinking about it.”
Dr. Fromme is part of the Council on Pediatric Hospital Medicine, a small circle of leaders of PHM interest groups within the three professional associations. It meets quarterly and will be reviewing the results of the conference call.
“I personally think we don’t understand the scope of the problem or the needs of pediatric hospitalists who are not able to sit for boards or pursue a fellowship,” she said. “We have empathy and concern for our colleagues who can’t take the boards. We don’t want them to feel excluded, and that includes advanced practice nurses and residents. But does an alternative designation actually provide what people think it provides?”
There are other ways to demonstrate that professionals are engaged with and serious about developing their practice. If they are looking to better themselves at quality improvement, leadership, education, and other elements of PHM practice, the associations can endeavor to provide more educational opportunities, Dr. Fromme said. “But if it’s about how they look as a candidate for hire, relative to board-certified candidates, that’s a different beast, and we need to think about what can help them the most.”
References
1. American Board of Pediatrics, Response to the Pediatric Hospital Medicine Petition. 2019 Aug 20. https://www.abp.org/sites/abp/files/phm-petition-response.pdf.
2. Chang WW et al. J Hosp Med. 2019 Oct;14(10):589-90.